User login
FDA approves new drug for thrombocytopenia
with chronic immune thrombocytopenia (ITP).
The Food and Drug Administration approved the oral spleen tyrosine kinase (SYK) inhibitor, which works by impeding platelet destruction, on April 17. Its approval was based on data from FIT clinical program, including two randomized placebo-controlled phase 3 trials.
Physicians are advised to monitor blood pressure and liver function with the drug. Fostamatinib may interact with CYP3A4 inhibitors and inducers. Concomitant use of fostamatinib with CYP3A4 inhibitors increases exposure to R406 – the drug’s major metabolite – and may increase the risk of adverse reactions. Use with strong CYP3A4 inducers is not recommended because it reduces exposure to R406.
Women of reproductive potential should be advised to use appropriate contraception while using fostamatinib and for a month after stopping the drug; pregnant women should be told of potential risk to the fetus. Advise women not to breastfeed during treatment and for at least 1 month after the last dose, according to a press statement.
Rigel Pharmaceuticals plans to release the drug in the United States in late May 2018.
with chronic immune thrombocytopenia (ITP).
The Food and Drug Administration approved the oral spleen tyrosine kinase (SYK) inhibitor, which works by impeding platelet destruction, on April 17. Its approval was based on data from FIT clinical program, including two randomized placebo-controlled phase 3 trials.
Physicians are advised to monitor blood pressure and liver function with the drug. Fostamatinib may interact with CYP3A4 inhibitors and inducers. Concomitant use of fostamatinib with CYP3A4 inhibitors increases exposure to R406 – the drug’s major metabolite – and may increase the risk of adverse reactions. Use with strong CYP3A4 inducers is not recommended because it reduces exposure to R406.
Women of reproductive potential should be advised to use appropriate contraception while using fostamatinib and for a month after stopping the drug; pregnant women should be told of potential risk to the fetus. Advise women not to breastfeed during treatment and for at least 1 month after the last dose, according to a press statement.
Rigel Pharmaceuticals plans to release the drug in the United States in late May 2018.
with chronic immune thrombocytopenia (ITP).
The Food and Drug Administration approved the oral spleen tyrosine kinase (SYK) inhibitor, which works by impeding platelet destruction, on April 17. Its approval was based on data from FIT clinical program, including two randomized placebo-controlled phase 3 trials.
Physicians are advised to monitor blood pressure and liver function with the drug. Fostamatinib may interact with CYP3A4 inhibitors and inducers. Concomitant use of fostamatinib with CYP3A4 inhibitors increases exposure to R406 – the drug’s major metabolite – and may increase the risk of adverse reactions. Use with strong CYP3A4 inducers is not recommended because it reduces exposure to R406.
Women of reproductive potential should be advised to use appropriate contraception while using fostamatinib and for a month after stopping the drug; pregnant women should be told of potential risk to the fetus. Advise women not to breastfeed during treatment and for at least 1 month after the last dose, according to a press statement.
Rigel Pharmaceuticals plans to release the drug in the United States in late May 2018.
Clinical Guidelines: Testosterone therapy in men with hypogonadism
Guidelines issued jointly by the Endocrine Society and the European Society for Endocrinology provide clinicians with a clear consensus approach to male hypogonadism, commonly referred to by patients as “low T.” Hypogonadism results from “the failure of the testes to produce physiological concentrations of testosterone and/or a normal number of spermatozoa due to pathology at one or more levels of the hypothalamic-pituitary-testicular axis,” according to the definition that serves as the basis for the guidelines.
The causes of hypogonadism can also be divided into irreversible and reversible disorders. Irreversible disorders include congenital, structural, or destructive disorders that lead to permanent organ dysfunction. Reversible hypogonadism includes causes, such as obesity, opioids, or systemic illness, that can suppress gonadotropin and testosterone concentrations but that may be reversible.
Diagnosis
The signs and symptoms of hypogonadism are often nonspecific and include decreased energy, depressed mood, poor concentration and memory, sleep disturbance, mild normocytic normochromic anemia, reduced muscle bulk and strength, increased body fat, reduced libido, decreased erections, gynecomastia, low-trauma fractures, and loss of body hair. The diagnosis of hypogonadism is made when there are signs and symptoms of testosterone deficiency and of unequivocally and consistently low serum total testosterone and/or free testosterone concentrations.
Serum testosterone concentrations have diurnal variations, with values peaking in the morning. In addition, food intake suppresses testosterone concentrations. Therefore, testosterone levels should be measured in the morning after an overnight fast. Low testosterone concentrations need to be confirmed before making the diagnosis of hypogonadism because 30% of men with an initial testosterone concentration in the hypogonadal range have a normal testosterone concentration on repeat measurement. In addition, testosterone concentrations are not accurate in patients recovering from acute illness or taking medications known to suppress testosterone.
Testing of free testosterone and sex hormone–binding globulin (SHBG) may be considered in patients at risk for increased or decreased SHBG, including the obese, men with diabetes, the elderly, those with HIV or liver disease, or those taking estrogens and medications that may affect SHBG.
In individuals with low testosterone levels, a serum FSH and LH should be ordered to differentiate primary from secondary hypogonadism. Middle-aged and older men with secondary hypogonadism have a low prevalence of hypothalamic/pituitary abnormalities.
Treatment
In patients found to have low testosterone with signs and symptoms of testosterone deficiency, testosterone therapy is recommended to induce and maintain secondary sex characteristics and correct the symptoms of testosterone deficiency. Testosterone-replacement therapy in men with low testosterone levels leads to a small but statistically significant improvement in libido, erectile function, sexual activity or satisfaction, muscle mass, and bone density but does not lead to improvements in energy and mood.
Testosterone replacement should not be done in patient’s planning fertility in the near future, those with prostate or breast cancer, a palpable prostate nodule, a prostate-specific antigen (PSA) level greater than 4 ng/mL, a PSA greater than 3 ng/mL with high risk for prostate cancer, high hematocrit, untreated obstructive sleep apnea, severe lower urinary tract symptoms, uncontrolled heart failure, MI or stroke within the last 6 months, or thrombophilia.
In men undergoing therapy, there is a higher frequency of erythrocytosis (hematocrit greater than 54%; relative risk, 8.14) but no increase in lower urinary tract symptoms. The benefit and risk of regular prostate cancer screening should be discussed prior to starting therapy with men aged 40-69 years with an increased risk of prostate cancer and with all men aged 55-69 years. For those who desire prostate cancer screening, PSA levels should be checked prior to starting therapy, and a digital prostate examination should be done at baseline and at 3-12 months after starting testosterone treatment. After 1 year, prostate cancer screening can be done per standard guidelines.
The decision about therapy in men older than 65 years is challenging because testosterone levels normally decline with age. It is not necessary to prescribe testosterone routinely to men older than 65 years with only low testosterone, and treatment should be reserved for those with symptoms along with low testosterone concentrations.
Men with HIV with low testosterone concentrations and weight loss can be treated with testosterone to induce and maintain body weight and lean muscle mass.
Monitoring
Patients should be evaluated 3-6 months after initiating treatment to see whether symptoms have improved, to see whether there have been adverse reactions, and to check labs.
Serum testosterone should be checked and the dose of testosterone replacement should be adjusted to maintain the serum testosterone level in the mid-normal range for healthy young men. Serum testosterone should be drawn at different times for different formulations – for instance, it should be checked 2-8 hours following a gel application.
Hematocrit should be checked at baseline and 3-6 months into treatment. If hematocrit is greater than 54%, therapy should be held until hematocrit decreases and then restarted at a reduced dose. Screening for prostate cancer should be done if that was decided upon during discussion with the patient. Further urologic evaluation is indicated in men who, during the first year of treatment, develop an increase from baseline PSA greater than 1.4 ng/mL, have a repeat PSA over 4 ng/mL, or have a prostatic abnormality on digital rectal exam.
The bottom line
Hypogonadism is common and presents diagnostic challenges because of nonspecific signs and symptoms. Serum testosterone should be checked on a first-morning fasting specimen. Low testosterone concentrations need to be confirmed before making the diagnosis and should be followed by checking FSH and LH. For those with signs and symptoms of hypogonadism and persistently low testosterone, testosterone replacement therapy can be beneficial, with a goal of maintaining serum testosterone in the mid-range of normal.
Reference
Bhasin S et al. Testosterone therapy in men with hypogonadism: An Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2018 May;103(5):1-30.
Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Hurchick is a third-year resident in the family medicine residency program at Abington Jefferson Health.
Guidelines issued jointly by the Endocrine Society and the European Society for Endocrinology provide clinicians with a clear consensus approach to male hypogonadism, commonly referred to by patients as “low T.” Hypogonadism results from “the failure of the testes to produce physiological concentrations of testosterone and/or a normal number of spermatozoa due to pathology at one or more levels of the hypothalamic-pituitary-testicular axis,” according to the definition that serves as the basis for the guidelines.
The causes of hypogonadism can also be divided into irreversible and reversible disorders. Irreversible disorders include congenital, structural, or destructive disorders that lead to permanent organ dysfunction. Reversible hypogonadism includes causes, such as obesity, opioids, or systemic illness, that can suppress gonadotropin and testosterone concentrations but that may be reversible.
Diagnosis
The signs and symptoms of hypogonadism are often nonspecific and include decreased energy, depressed mood, poor concentration and memory, sleep disturbance, mild normocytic normochromic anemia, reduced muscle bulk and strength, increased body fat, reduced libido, decreased erections, gynecomastia, low-trauma fractures, and loss of body hair. The diagnosis of hypogonadism is made when there are signs and symptoms of testosterone deficiency and of unequivocally and consistently low serum total testosterone and/or free testosterone concentrations.
Serum testosterone concentrations have diurnal variations, with values peaking in the morning. In addition, food intake suppresses testosterone concentrations. Therefore, testosterone levels should be measured in the morning after an overnight fast. Low testosterone concentrations need to be confirmed before making the diagnosis of hypogonadism because 30% of men with an initial testosterone concentration in the hypogonadal range have a normal testosterone concentration on repeat measurement. In addition, testosterone concentrations are not accurate in patients recovering from acute illness or taking medications known to suppress testosterone.
Testing of free testosterone and sex hormone–binding globulin (SHBG) may be considered in patients at risk for increased or decreased SHBG, including the obese, men with diabetes, the elderly, those with HIV or liver disease, or those taking estrogens and medications that may affect SHBG.
In individuals with low testosterone levels, a serum FSH and LH should be ordered to differentiate primary from secondary hypogonadism. Middle-aged and older men with secondary hypogonadism have a low prevalence of hypothalamic/pituitary abnormalities.
Treatment
In patients found to have low testosterone with signs and symptoms of testosterone deficiency, testosterone therapy is recommended to induce and maintain secondary sex characteristics and correct the symptoms of testosterone deficiency. Testosterone-replacement therapy in men with low testosterone levels leads to a small but statistically significant improvement in libido, erectile function, sexual activity or satisfaction, muscle mass, and bone density but does not lead to improvements in energy and mood.
Testosterone replacement should not be done in patient’s planning fertility in the near future, those with prostate or breast cancer, a palpable prostate nodule, a prostate-specific antigen (PSA) level greater than 4 ng/mL, a PSA greater than 3 ng/mL with high risk for prostate cancer, high hematocrit, untreated obstructive sleep apnea, severe lower urinary tract symptoms, uncontrolled heart failure, MI or stroke within the last 6 months, or thrombophilia.
In men undergoing therapy, there is a higher frequency of erythrocytosis (hematocrit greater than 54%; relative risk, 8.14) but no increase in lower urinary tract symptoms. The benefit and risk of regular prostate cancer screening should be discussed prior to starting therapy with men aged 40-69 years with an increased risk of prostate cancer and with all men aged 55-69 years. For those who desire prostate cancer screening, PSA levels should be checked prior to starting therapy, and a digital prostate examination should be done at baseline and at 3-12 months after starting testosterone treatment. After 1 year, prostate cancer screening can be done per standard guidelines.
The decision about therapy in men older than 65 years is challenging because testosterone levels normally decline with age. It is not necessary to prescribe testosterone routinely to men older than 65 years with only low testosterone, and treatment should be reserved for those with symptoms along with low testosterone concentrations.
Men with HIV with low testosterone concentrations and weight loss can be treated with testosterone to induce and maintain body weight and lean muscle mass.
Monitoring
Patients should be evaluated 3-6 months after initiating treatment to see whether symptoms have improved, to see whether there have been adverse reactions, and to check labs.
Serum testosterone should be checked and the dose of testosterone replacement should be adjusted to maintain the serum testosterone level in the mid-normal range for healthy young men. Serum testosterone should be drawn at different times for different formulations – for instance, it should be checked 2-8 hours following a gel application.
Hematocrit should be checked at baseline and 3-6 months into treatment. If hematocrit is greater than 54%, therapy should be held until hematocrit decreases and then restarted at a reduced dose. Screening for prostate cancer should be done if that was decided upon during discussion with the patient. Further urologic evaluation is indicated in men who, during the first year of treatment, develop an increase from baseline PSA greater than 1.4 ng/mL, have a repeat PSA over 4 ng/mL, or have a prostatic abnormality on digital rectal exam.
The bottom line
Hypogonadism is common and presents diagnostic challenges because of nonspecific signs and symptoms. Serum testosterone should be checked on a first-morning fasting specimen. Low testosterone concentrations need to be confirmed before making the diagnosis and should be followed by checking FSH and LH. For those with signs and symptoms of hypogonadism and persistently low testosterone, testosterone replacement therapy can be beneficial, with a goal of maintaining serum testosterone in the mid-range of normal.
Reference
Bhasin S et al. Testosterone therapy in men with hypogonadism: An Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2018 May;103(5):1-30.
Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Hurchick is a third-year resident in the family medicine residency program at Abington Jefferson Health.
Guidelines issued jointly by the Endocrine Society and the European Society for Endocrinology provide clinicians with a clear consensus approach to male hypogonadism, commonly referred to by patients as “low T.” Hypogonadism results from “the failure of the testes to produce physiological concentrations of testosterone and/or a normal number of spermatozoa due to pathology at one or more levels of the hypothalamic-pituitary-testicular axis,” according to the definition that serves as the basis for the guidelines.
The causes of hypogonadism can also be divided into irreversible and reversible disorders. Irreversible disorders include congenital, structural, or destructive disorders that lead to permanent organ dysfunction. Reversible hypogonadism includes causes, such as obesity, opioids, or systemic illness, that can suppress gonadotropin and testosterone concentrations but that may be reversible.
Diagnosis
The signs and symptoms of hypogonadism are often nonspecific and include decreased energy, depressed mood, poor concentration and memory, sleep disturbance, mild normocytic normochromic anemia, reduced muscle bulk and strength, increased body fat, reduced libido, decreased erections, gynecomastia, low-trauma fractures, and loss of body hair. The diagnosis of hypogonadism is made when there are signs and symptoms of testosterone deficiency and of unequivocally and consistently low serum total testosterone and/or free testosterone concentrations.
Serum testosterone concentrations have diurnal variations, with values peaking in the morning. In addition, food intake suppresses testosterone concentrations. Therefore, testosterone levels should be measured in the morning after an overnight fast. Low testosterone concentrations need to be confirmed before making the diagnosis of hypogonadism because 30% of men with an initial testosterone concentration in the hypogonadal range have a normal testosterone concentration on repeat measurement. In addition, testosterone concentrations are not accurate in patients recovering from acute illness or taking medications known to suppress testosterone.
Testing of free testosterone and sex hormone–binding globulin (SHBG) may be considered in patients at risk for increased or decreased SHBG, including the obese, men with diabetes, the elderly, those with HIV or liver disease, or those taking estrogens and medications that may affect SHBG.
In individuals with low testosterone levels, a serum FSH and LH should be ordered to differentiate primary from secondary hypogonadism. Middle-aged and older men with secondary hypogonadism have a low prevalence of hypothalamic/pituitary abnormalities.
Treatment
In patients found to have low testosterone with signs and symptoms of testosterone deficiency, testosterone therapy is recommended to induce and maintain secondary sex characteristics and correct the symptoms of testosterone deficiency. Testosterone-replacement therapy in men with low testosterone levels leads to a small but statistically significant improvement in libido, erectile function, sexual activity or satisfaction, muscle mass, and bone density but does not lead to improvements in energy and mood.
Testosterone replacement should not be done in patient’s planning fertility in the near future, those with prostate or breast cancer, a palpable prostate nodule, a prostate-specific antigen (PSA) level greater than 4 ng/mL, a PSA greater than 3 ng/mL with high risk for prostate cancer, high hematocrit, untreated obstructive sleep apnea, severe lower urinary tract symptoms, uncontrolled heart failure, MI or stroke within the last 6 months, or thrombophilia.
In men undergoing therapy, there is a higher frequency of erythrocytosis (hematocrit greater than 54%; relative risk, 8.14) but no increase in lower urinary tract symptoms. The benefit and risk of regular prostate cancer screening should be discussed prior to starting therapy with men aged 40-69 years with an increased risk of prostate cancer and with all men aged 55-69 years. For those who desire prostate cancer screening, PSA levels should be checked prior to starting therapy, and a digital prostate examination should be done at baseline and at 3-12 months after starting testosterone treatment. After 1 year, prostate cancer screening can be done per standard guidelines.
The decision about therapy in men older than 65 years is challenging because testosterone levels normally decline with age. It is not necessary to prescribe testosterone routinely to men older than 65 years with only low testosterone, and treatment should be reserved for those with symptoms along with low testosterone concentrations.
Men with HIV with low testosterone concentrations and weight loss can be treated with testosterone to induce and maintain body weight and lean muscle mass.
Monitoring
Patients should be evaluated 3-6 months after initiating treatment to see whether symptoms have improved, to see whether there have been adverse reactions, and to check labs.
Serum testosterone should be checked and the dose of testosterone replacement should be adjusted to maintain the serum testosterone level in the mid-normal range for healthy young men. Serum testosterone should be drawn at different times for different formulations – for instance, it should be checked 2-8 hours following a gel application.
Hematocrit should be checked at baseline and 3-6 months into treatment. If hematocrit is greater than 54%, therapy should be held until hematocrit decreases and then restarted at a reduced dose. Screening for prostate cancer should be done if that was decided upon during discussion with the patient. Further urologic evaluation is indicated in men who, during the first year of treatment, develop an increase from baseline PSA greater than 1.4 ng/mL, have a repeat PSA over 4 ng/mL, or have a prostatic abnormality on digital rectal exam.
The bottom line
Hypogonadism is common and presents diagnostic challenges because of nonspecific signs and symptoms. Serum testosterone should be checked on a first-morning fasting specimen. Low testosterone concentrations need to be confirmed before making the diagnosis and should be followed by checking FSH and LH. For those with signs and symptoms of hypogonadism and persistently low testosterone, testosterone replacement therapy can be beneficial, with a goal of maintaining serum testosterone in the mid-range of normal.
Reference
Bhasin S et al. Testosterone therapy in men with hypogonadism: An Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2018 May;103(5):1-30.
Dr. Skolnik is a professor of family and community medicine at Jefferson Medical College, Philadelphia, and an associate director of the family medicine residency program at Abington (Pa.) Jefferson Health. Dr. Hurchick is a third-year resident in the family medicine residency program at Abington Jefferson Health.
What does burnout cost?
How are you feeling today? Simple words but a bit of introspection can go a long way. P It affects a physician’s well-being, effectiveness, productivity, and the ability to provide quality care. It also carries personal consequences for physicians including broken relationships, substance abuse, suicide, and depression.
Burnout may affect at least one-third of gastroenterologists. At greater risk are younger physicians, physicians performing high-risk procedures, and physicians experiencing work-life conflicts.
While the root cause of physician burnout varies from provider to provider, an overarching theme is work stress. Work stress may develop for a number of reasons, including issues at the level of the health care system (shifts in reimbursement or payment models, increasing clerical burden of the electronic medical record), organizational issues (e.g., dysfunctional administration, system-wide communication issues), and personal issues.
The key to preventing burnout is to first recognize that it can happen. Because initial symptoms build up internally, it can be easy to overlook. These seven steps can help you prevent burnout:
- Be self-aware and stay vigilant.
- Take care of yourself first.
- Stay connected to family, friends, and coworkers.
- Exercise.
- Ensure adequate sleep.
- Use your vacation time and ensure you disconnect yourself from work.
- Learn to say no.
A case study published in Clinical Gastroenterology and Hepatology delves deeper into how burnout develops, why it matters, and provides pathways to successfully combat it.
How are you feeling today? Simple words but a bit of introspection can go a long way. P It affects a physician’s well-being, effectiveness, productivity, and the ability to provide quality care. It also carries personal consequences for physicians including broken relationships, substance abuse, suicide, and depression.
Burnout may affect at least one-third of gastroenterologists. At greater risk are younger physicians, physicians performing high-risk procedures, and physicians experiencing work-life conflicts.
While the root cause of physician burnout varies from provider to provider, an overarching theme is work stress. Work stress may develop for a number of reasons, including issues at the level of the health care system (shifts in reimbursement or payment models, increasing clerical burden of the electronic medical record), organizational issues (e.g., dysfunctional administration, system-wide communication issues), and personal issues.
The key to preventing burnout is to first recognize that it can happen. Because initial symptoms build up internally, it can be easy to overlook. These seven steps can help you prevent burnout:
- Be self-aware and stay vigilant.
- Take care of yourself first.
- Stay connected to family, friends, and coworkers.
- Exercise.
- Ensure adequate sleep.
- Use your vacation time and ensure you disconnect yourself from work.
- Learn to say no.
A case study published in Clinical Gastroenterology and Hepatology delves deeper into how burnout develops, why it matters, and provides pathways to successfully combat it.
How are you feeling today? Simple words but a bit of introspection can go a long way. P It affects a physician’s well-being, effectiveness, productivity, and the ability to provide quality care. It also carries personal consequences for physicians including broken relationships, substance abuse, suicide, and depression.
Burnout may affect at least one-third of gastroenterologists. At greater risk are younger physicians, physicians performing high-risk procedures, and physicians experiencing work-life conflicts.
While the root cause of physician burnout varies from provider to provider, an overarching theme is work stress. Work stress may develop for a number of reasons, including issues at the level of the health care system (shifts in reimbursement or payment models, increasing clerical burden of the electronic medical record), organizational issues (e.g., dysfunctional administration, system-wide communication issues), and personal issues.
The key to preventing burnout is to first recognize that it can happen. Because initial symptoms build up internally, it can be easy to overlook. These seven steps can help you prevent burnout:
- Be self-aware and stay vigilant.
- Take care of yourself first.
- Stay connected to family, friends, and coworkers.
- Exercise.
- Ensure adequate sleep.
- Use your vacation time and ensure you disconnect yourself from work.
- Learn to say no.
A case study published in Clinical Gastroenterology and Hepatology delves deeper into how burnout develops, why it matters, and provides pathways to successfully combat it.
Sessions at DDW® 2018 designed for trainees and early career GIs
Participants will learn about all aspects of starting a career in clinical practice or research, have the opportunity to network with mentors and peers, and review board material.
With the exception of the AGA Postgraduate Course, all of the sessions are free, but you must register for DDW to attend. Registration is open and is complimentary for AGA member trainees, students, medical residents, and postdoctoral fellows until April 18. Visit the AGA website for additional details about these sessions.
Saturday, June 2, and Sunday, June 3
- Difficult Conversations: Navigating People, Negotiations, Promotions, and Complications
Sunday, June 3, 4-5:30 p.m.
- Advancing Clinical Practice: GI Fellow-Directed Quality Improvement Projects
Monday, June 4, 4-5:30 p.m.
- Board Review Course
Tuesday, June 5, 1:30-5:30 p.m.
Participants will learn about all aspects of starting a career in clinical practice or research, have the opportunity to network with mentors and peers, and review board material.
With the exception of the AGA Postgraduate Course, all of the sessions are free, but you must register for DDW to attend. Registration is open and is complimentary for AGA member trainees, students, medical residents, and postdoctoral fellows until April 18. Visit the AGA website for additional details about these sessions.
Saturday, June 2, and Sunday, June 3
- Difficult Conversations: Navigating People, Negotiations, Promotions, and Complications
Sunday, June 3, 4-5:30 p.m.
- Advancing Clinical Practice: GI Fellow-Directed Quality Improvement Projects
Monday, June 4, 4-5:30 p.m.
- Board Review Course
Tuesday, June 5, 1:30-5:30 p.m.
Participants will learn about all aspects of starting a career in clinical practice or research, have the opportunity to network with mentors and peers, and review board material.
With the exception of the AGA Postgraduate Course, all of the sessions are free, but you must register for DDW to attend. Registration is open and is complimentary for AGA member trainees, students, medical residents, and postdoctoral fellows until April 18. Visit the AGA website for additional details about these sessions.
Saturday, June 2, and Sunday, June 3
- Difficult Conversations: Navigating People, Negotiations, Promotions, and Complications
Sunday, June 3, 4-5:30 p.m.
- Advancing Clinical Practice: GI Fellow-Directed Quality Improvement Projects
Monday, June 4, 4-5:30 p.m.
- Board Review Course
Tuesday, June 5, 1:30-5:30 p.m.
Making the most of your DDW experience
It’s that time of the year again: Digestive Disease Week (DDW®)! This event evolved out of the AGA annual meetings and was first advertised as DDW in the January 1969 issue of Gastroenterology.1 Since that time, it has grown into a truly international event with over 14,000 attendees, 41% of whom attend from abroad.2
DDW is a collaborative event that is jointly sponsored by four professional GI/hepatology-related societies – the AGA, the American Association for the Study of Liver Diseases, the American Society for Gastrointestinal Endoscopy, and the Society for Surgery of the Alimentary Tract. The conference topics cover the gamut of GI and hepatology conditions and participants represent all types of professional settings, including private practice (37%), hospitals (33%), and academic medical centers (28%).2 Whether you’re a first-time attendee or a seasoned participant, DDW offers something for everyone.
Plan ahead
Is there a new treatment or condition you’ve wanted to learn more about? Are you interested in testing the latest endoscopic devices or learning a new procedural technique? Experts from around the world come to DDW to showcase the latest developments in GI. However, with over 5,000 abstracts and lectures and almost 300 exhibition booths, it’s easy to feel overwhelmed by all the offerings. To make the most of your experience, plan ahead.
In the months prior to the conference, visit the DDW website to download the Preliminary Program. Pick out your can’t-miss lectures and events, and put them on your calendar right away. As DDW approaches, invitations from colleagues, societies, and industry grow, so preplanning is a necessity.
Approximately 1 month before DDW, the DDW Mobile App will become available for free download in the Apple and Google Play stores. You can highlight events of interest and place them on a personalized calendar. Allow for push notifications to get the latest updates and schedule changes throughout the event. In addition, the in-app maps of the venue are a fantastic way to locate where scheduled events will take place. Try to attend talks that are located close to one another. The conference center is expansive and you may miss your intended presentations by trying to catch overlapping sessions situated far from each other. If you prefer planning on a desktop or laptop, use the DDW Online Planner (available mid-April) to create your schedule. The information can then be synced to your mobile device through the app.
Upon arrival, be sure to pick up your attendee conference bag. Before recycling the contents, look for any product theaters, satellite symposia, exhibitor booths, or other advertised activities you may want to add to your schedule.
Practical tips
a) Register ahead of time and pick up your conference bag during off-hours to avoid long lines.
b) Book your hotel early. Most have generous cancellation policies. Registration is required before booking housing.
c) Pack comfortable shoes and dress in layers to accommodate both unpredictable weather and indoor climate control.
Make new connections and nurture old ones
Is your professional hero giving a talk? Are you looking to land your first job or make a move? Do you need some face time with a mentor outside your institution? DDW is a wonderful opportunity to connect with advisers and possible employers as well as potential and established collaborators. Schedules fill up quickly though, so try your best to email requests for meetings well ahead of time. The app also has a messaging feature you can use to communicate with other attendees.
At the meeting, be an active participant and ask questions. One of the greatest benefits of attending the conference is the opportunity to interact with others. For trainees and early career attendees, DDW is your debutante ball! Introduce yourself and your work to the broader GI community. Bring your business cards as well as a notebook to write down questions and comments about your study. Look engaging when standing by your poster and offer to walk visitors through your research. There will also be an opportunity to have free headshots taken in the Early Career area this year.
Also take advantage of DDW’s big draw to reconnect with old friends and colleagues from around the U.S. and the world. Schedule a time to catch up and swap stories. Learn from each other’s successes and mistakes. It’s good for the soul and your career.
Post-DDW
Attending DDW is only the start! The most important part of the conference is what happens afterward. Send an email to individuals you met to establish a line of communication and thank them for their advice or insight. Did someone offer to share a protocol, start a collaboration, or introduce you to a colleague? Take them up on the offer! Notes that were taken in the app can also be emailed. In addition, registration includes 2 years of access to DDW On Demand, an online library of sessions. If there were any nonticketed presentations that you missed, you can watch them upon your return. Similarly, access missed posters at the DDW ePosters archive, where you can read poster abstracts and view ePosters, if submitted. Abstracts will still be viewable through the app and online planner as well. Reach out to colleagues if you have questions about their work!
Also, don’t forget to take what you learned back to your community. Share your new knowledge with your colleagues and trainees, and consider if there are any new concepts or approaches that should be implemented in your practice.
Practical tip
Before it falls off your radar, submit for CME credits for the sessions you attended. To claim CME, you may flag sessions for CME using the DDW Mobile App, visit a CME kiosk on site or access the DDW CME Claim Site after the meeting. Visit the DDW website for more information on claiming CME.
Refine, refocus, and recharge
DDW is the most comprehensive GI event in the world. Take advantage of the learning opportunities to improve your own work. Note how the landscape of GI is evolving and use it to reevaluate your own career development strategy and how you want to contribute to the field. Most importantly, get inspired. After exploring the most up-to-date advances and connecting with colleagues and thought leaders at DDW, you will hopefully return to your home institution feeling reinvigorated, refreshed, and ready to apply your newfound insights to your patient care or to your research.
See you at DDW!
References
1. Notices. Gastroenterology. 1969;569(1):188-9. http://www.gastrojournal.org/article/S0016-5085(69)80085-5/pdf.
2. Exhibitor Prospectus | Digestive Disease Week® 2018. https://higherlogicdownload.s3.amazonaws.com/GASTRO/44b1f1fd-aaed-44c8-954f-b0eaea6b0462/UploadedFiles/B4KUryNTNS5lEaFk6jBQ_DDW%202018%20Exhibitor%20Prospectus_Staffchanges.pdf
Dr. Chen is assistant professor of medicine, New York University School of Medicine.
It’s that time of the year again: Digestive Disease Week (DDW®)! This event evolved out of the AGA annual meetings and was first advertised as DDW in the January 1969 issue of Gastroenterology.1 Since that time, it has grown into a truly international event with over 14,000 attendees, 41% of whom attend from abroad.2
DDW is a collaborative event that is jointly sponsored by four professional GI/hepatology-related societies – the AGA, the American Association for the Study of Liver Diseases, the American Society for Gastrointestinal Endoscopy, and the Society for Surgery of the Alimentary Tract. The conference topics cover the gamut of GI and hepatology conditions and participants represent all types of professional settings, including private practice (37%), hospitals (33%), and academic medical centers (28%).2 Whether you’re a first-time attendee or a seasoned participant, DDW offers something for everyone.
Plan ahead
Is there a new treatment or condition you’ve wanted to learn more about? Are you interested in testing the latest endoscopic devices or learning a new procedural technique? Experts from around the world come to DDW to showcase the latest developments in GI. However, with over 5,000 abstracts and lectures and almost 300 exhibition booths, it’s easy to feel overwhelmed by all the offerings. To make the most of your experience, plan ahead.
In the months prior to the conference, visit the DDW website to download the Preliminary Program. Pick out your can’t-miss lectures and events, and put them on your calendar right away. As DDW approaches, invitations from colleagues, societies, and industry grow, so preplanning is a necessity.
Approximately 1 month before DDW, the DDW Mobile App will become available for free download in the Apple and Google Play stores. You can highlight events of interest and place them on a personalized calendar. Allow for push notifications to get the latest updates and schedule changes throughout the event. In addition, the in-app maps of the venue are a fantastic way to locate where scheduled events will take place. Try to attend talks that are located close to one another. The conference center is expansive and you may miss your intended presentations by trying to catch overlapping sessions situated far from each other. If you prefer planning on a desktop or laptop, use the DDW Online Planner (available mid-April) to create your schedule. The information can then be synced to your mobile device through the app.
Upon arrival, be sure to pick up your attendee conference bag. Before recycling the contents, look for any product theaters, satellite symposia, exhibitor booths, or other advertised activities you may want to add to your schedule.
Practical tips
a) Register ahead of time and pick up your conference bag during off-hours to avoid long lines.
b) Book your hotel early. Most have generous cancellation policies. Registration is required before booking housing.
c) Pack comfortable shoes and dress in layers to accommodate both unpredictable weather and indoor climate control.
Make new connections and nurture old ones
Is your professional hero giving a talk? Are you looking to land your first job or make a move? Do you need some face time with a mentor outside your institution? DDW is a wonderful opportunity to connect with advisers and possible employers as well as potential and established collaborators. Schedules fill up quickly though, so try your best to email requests for meetings well ahead of time. The app also has a messaging feature you can use to communicate with other attendees.
At the meeting, be an active participant and ask questions. One of the greatest benefits of attending the conference is the opportunity to interact with others. For trainees and early career attendees, DDW is your debutante ball! Introduce yourself and your work to the broader GI community. Bring your business cards as well as a notebook to write down questions and comments about your study. Look engaging when standing by your poster and offer to walk visitors through your research. There will also be an opportunity to have free headshots taken in the Early Career area this year.
Also take advantage of DDW’s big draw to reconnect with old friends and colleagues from around the U.S. and the world. Schedule a time to catch up and swap stories. Learn from each other’s successes and mistakes. It’s good for the soul and your career.
Post-DDW
Attending DDW is only the start! The most important part of the conference is what happens afterward. Send an email to individuals you met to establish a line of communication and thank them for their advice or insight. Did someone offer to share a protocol, start a collaboration, or introduce you to a colleague? Take them up on the offer! Notes that were taken in the app can also be emailed. In addition, registration includes 2 years of access to DDW On Demand, an online library of sessions. If there were any nonticketed presentations that you missed, you can watch them upon your return. Similarly, access missed posters at the DDW ePosters archive, where you can read poster abstracts and view ePosters, if submitted. Abstracts will still be viewable through the app and online planner as well. Reach out to colleagues if you have questions about their work!
Also, don’t forget to take what you learned back to your community. Share your new knowledge with your colleagues and trainees, and consider if there are any new concepts or approaches that should be implemented in your practice.
Practical tip
Before it falls off your radar, submit for CME credits for the sessions you attended. To claim CME, you may flag sessions for CME using the DDW Mobile App, visit a CME kiosk on site or access the DDW CME Claim Site after the meeting. Visit the DDW website for more information on claiming CME.
Refine, refocus, and recharge
DDW is the most comprehensive GI event in the world. Take advantage of the learning opportunities to improve your own work. Note how the landscape of GI is evolving and use it to reevaluate your own career development strategy and how you want to contribute to the field. Most importantly, get inspired. After exploring the most up-to-date advances and connecting with colleagues and thought leaders at DDW, you will hopefully return to your home institution feeling reinvigorated, refreshed, and ready to apply your newfound insights to your patient care or to your research.
See you at DDW!
References
1. Notices. Gastroenterology. 1969;569(1):188-9. http://www.gastrojournal.org/article/S0016-5085(69)80085-5/pdf.
2. Exhibitor Prospectus | Digestive Disease Week® 2018. https://higherlogicdownload.s3.amazonaws.com/GASTRO/44b1f1fd-aaed-44c8-954f-b0eaea6b0462/UploadedFiles/B4KUryNTNS5lEaFk6jBQ_DDW%202018%20Exhibitor%20Prospectus_Staffchanges.pdf
Dr. Chen is assistant professor of medicine, New York University School of Medicine.
It’s that time of the year again: Digestive Disease Week (DDW®)! This event evolved out of the AGA annual meetings and was first advertised as DDW in the January 1969 issue of Gastroenterology.1 Since that time, it has grown into a truly international event with over 14,000 attendees, 41% of whom attend from abroad.2
DDW is a collaborative event that is jointly sponsored by four professional GI/hepatology-related societies – the AGA, the American Association for the Study of Liver Diseases, the American Society for Gastrointestinal Endoscopy, and the Society for Surgery of the Alimentary Tract. The conference topics cover the gamut of GI and hepatology conditions and participants represent all types of professional settings, including private practice (37%), hospitals (33%), and academic medical centers (28%).2 Whether you’re a first-time attendee or a seasoned participant, DDW offers something for everyone.
Plan ahead
Is there a new treatment or condition you’ve wanted to learn more about? Are you interested in testing the latest endoscopic devices or learning a new procedural technique? Experts from around the world come to DDW to showcase the latest developments in GI. However, with over 5,000 abstracts and lectures and almost 300 exhibition booths, it’s easy to feel overwhelmed by all the offerings. To make the most of your experience, plan ahead.
In the months prior to the conference, visit the DDW website to download the Preliminary Program. Pick out your can’t-miss lectures and events, and put them on your calendar right away. As DDW approaches, invitations from colleagues, societies, and industry grow, so preplanning is a necessity.
Approximately 1 month before DDW, the DDW Mobile App will become available for free download in the Apple and Google Play stores. You can highlight events of interest and place them on a personalized calendar. Allow for push notifications to get the latest updates and schedule changes throughout the event. In addition, the in-app maps of the venue are a fantastic way to locate where scheduled events will take place. Try to attend talks that are located close to one another. The conference center is expansive and you may miss your intended presentations by trying to catch overlapping sessions situated far from each other. If you prefer planning on a desktop or laptop, use the DDW Online Planner (available mid-April) to create your schedule. The information can then be synced to your mobile device through the app.
Upon arrival, be sure to pick up your attendee conference bag. Before recycling the contents, look for any product theaters, satellite symposia, exhibitor booths, or other advertised activities you may want to add to your schedule.
Practical tips
a) Register ahead of time and pick up your conference bag during off-hours to avoid long lines.
b) Book your hotel early. Most have generous cancellation policies. Registration is required before booking housing.
c) Pack comfortable shoes and dress in layers to accommodate both unpredictable weather and indoor climate control.
Make new connections and nurture old ones
Is your professional hero giving a talk? Are you looking to land your first job or make a move? Do you need some face time with a mentor outside your institution? DDW is a wonderful opportunity to connect with advisers and possible employers as well as potential and established collaborators. Schedules fill up quickly though, so try your best to email requests for meetings well ahead of time. The app also has a messaging feature you can use to communicate with other attendees.
At the meeting, be an active participant and ask questions. One of the greatest benefits of attending the conference is the opportunity to interact with others. For trainees and early career attendees, DDW is your debutante ball! Introduce yourself and your work to the broader GI community. Bring your business cards as well as a notebook to write down questions and comments about your study. Look engaging when standing by your poster and offer to walk visitors through your research. There will also be an opportunity to have free headshots taken in the Early Career area this year.
Also take advantage of DDW’s big draw to reconnect with old friends and colleagues from around the U.S. and the world. Schedule a time to catch up and swap stories. Learn from each other’s successes and mistakes. It’s good for the soul and your career.
Post-DDW
Attending DDW is only the start! The most important part of the conference is what happens afterward. Send an email to individuals you met to establish a line of communication and thank them for their advice or insight. Did someone offer to share a protocol, start a collaboration, or introduce you to a colleague? Take them up on the offer! Notes that were taken in the app can also be emailed. In addition, registration includes 2 years of access to DDW On Demand, an online library of sessions. If there were any nonticketed presentations that you missed, you can watch them upon your return. Similarly, access missed posters at the DDW ePosters archive, where you can read poster abstracts and view ePosters, if submitted. Abstracts will still be viewable through the app and online planner as well. Reach out to colleagues if you have questions about their work!
Also, don’t forget to take what you learned back to your community. Share your new knowledge with your colleagues and trainees, and consider if there are any new concepts or approaches that should be implemented in your practice.
Practical tip
Before it falls off your radar, submit for CME credits for the sessions you attended. To claim CME, you may flag sessions for CME using the DDW Mobile App, visit a CME kiosk on site or access the DDW CME Claim Site after the meeting. Visit the DDW website for more information on claiming CME.
Refine, refocus, and recharge
DDW is the most comprehensive GI event in the world. Take advantage of the learning opportunities to improve your own work. Note how the landscape of GI is evolving and use it to reevaluate your own career development strategy and how you want to contribute to the field. Most importantly, get inspired. After exploring the most up-to-date advances and connecting with colleagues and thought leaders at DDW, you will hopefully return to your home institution feeling reinvigorated, refreshed, and ready to apply your newfound insights to your patient care or to your research.
See you at DDW!
References
1. Notices. Gastroenterology. 1969;569(1):188-9. http://www.gastrojournal.org/article/S0016-5085(69)80085-5/pdf.
2. Exhibitor Prospectus | Digestive Disease Week® 2018. https://higherlogicdownload.s3.amazonaws.com/GASTRO/44b1f1fd-aaed-44c8-954f-b0eaea6b0462/UploadedFiles/B4KUryNTNS5lEaFk6jBQ_DDW%202018%20Exhibitor%20Prospectus_Staffchanges.pdf
Dr. Chen is assistant professor of medicine, New York University School of Medicine.
Adopting new evidence into practice – a guide for the new gastroenterologist
The transition from gastroenterology fellowship to independent practice can be daunting. There may be concerns about procedural competency and increased levels of responsibility. Recent trainees have to manage their newly busy clinical schedules while trying to integrate evidence from a rapidly evolving landscape of medical literature into daily practice. Many recent graduates also are expected to participate in financial decisions or contribute to assessments about resource allocation regarding new technologies. These are challenges faced by those in both community and academic positions but may be more keenly felt in the first years of practice regardless of setting.
Without the benefit of experience, incorporating pertinent evidence from both within and outside of the field of gastroenterology as well as identifying disruptive technologies can be particularly difficult. There is scant guidance in this area, either during fellowship or from the existing literature1. Yet these are skills that, when properly developed, can be lifelong assets and, as a result, an evaluation of this process is warranted. Herein, we identify recent developments relevant to gastroenterologists to illustrate a conceptual framework for judging novel information.
A practical concern for the new gastroenterologist is learning to efficiently evaluate the merits of the latest research and then implement this knowledge in the clinic. Maintaining active society membership often includes access to scholarly journals. For example, AGA members receive Gastroenterology, Clinical Gastroenterology and Hepatology, and Cellular and Molecular Gastroenterology and Hepatology as part of their member benefits and have the opportunity to receive alerts when new content is published. Social media outlets such as Twitter and Facebook also simplify the process for readers to identify high-impact studies2 (see social media urls at the end of the story). In addition to reading, however, a critical review of these studies can prevent premature enthusiasm for modifying practice. The evolving evidence base for understanding proton pump inhibitor (PPI) risks is illustrative. Several studies attracted widespread media attention describing serious associated side effects, ranging from MI3 to dementia4 and stroke5. These studies were provocative but a decision to withhold PPIs from patients based on these concerns alone could lead to unintended consequences with poor outcomes. Ultimately, subsequent studies published only months later challenged these associations.6-8 Instead, thoughtful disclosure to patients of known risks and appropriate indications for PPI therapy based on resources such as the AGA Best Practice Advice9 is prudent. Reading more may be necessary but is insufficient; finding a forum to discuss novel research topics, such as in a monthly journal club10 or group practice meeting, can lead to stimulating discussion about how to apply pertinent research to change practice. The AGA Community is an excellent venue for this kind of interaction.
In many situations, keeping informed of updates about the risks and safety of medications prescribed by nongastroenterologists, particularly as they relate to GI conditions, can be even more difficult. A prime example of this is the rapidly expanding literature on indications and risks of direct oral anticoagulants. Rotating on the inpatient consultation service, with the chance to interact with multiple non-GI providers, affords an excellent opportunity to stay up to date. With the increased prevalence of atrial fibrillation as well as the potential expanded indications for direct oral anticoagulants based on recent randomized, controlled trials11,12, practicing gastroenterologists will be comanaging increasing numbers of patients hospitalized with gastrointestinal bleeding (GIB). Our understanding of the availability and indication for targeted reversal agents, such as idarucizumab, as well as nonspecific reversal agents, such as prothrombin complex concentrates, for those with life-threatening GIB is critical to optimal management of these patients. Multidisciplinary collaborations, such as with cardiogastroenterology clinics13, can be leveraged for optimal management of direct oral anticoagulants in the periendoscopy period.
Traditional outpatient consultative approaches are sometimes necessary but frequent reference to consensus societal guidelines on endoscopy in patients on antithrombotics14 should be made, particularly if they are printed and readily available in the ambulatory clinic and endoscopy suites. When information may be too new or sparse to utilize a national guideline, employing local data or experience to create a hospital-specific algorithm can ensure the delivery of high-quality, collaborative patient care.
Much like reviewing the literature, evaluating new technologies poses its own challenges. Changes in clinical practice may be slow, as in the adoption of noninvasive methods for Barrett’s esophagus screening.15 But in an age when news of advances and updates in management spreads at tremendous speed through the use of social media, the ability to pivot or assimilate new discoveries and techniques will become increasingly relevant and important. A professional society’s endorsement can provide a framework for a decision, but other principles at play include sensible, critical analyses of the outcomes and costs as well as a balance of organizational and societal perspectives.16 The use of impedance planimetry is one such example. This is a relatively new technology, but it has received increasing interest recently.17 The first questions when considering adopting this type of device likely will be about its supporting evidence and the risk for causing harm. The pace of publications regarding its use for measuring esophageal distensibility has accelerated18. But good data does not necessarily translate into extensive uptake. Other important factors also are practical, e.g., whether a technology committee’s approval is needed and what is the learning curve, available technical support, need for capital purchases, reimbursement, etc. Functional luminal imaging probe (FLIP®) technology was developed to assess compliance in primary esophageal disorders and now has been applied to several other areas including anorectal disease, bariatric surgery, and therapeutic endoscopy19,20. Although seemingly a niche market, there is potential widespread application and an opportunity for collaborations that might not have been evident at first blush. Ultimately, any evaluation of new technology is to a certain extent speculation. Is the technology mature or novel? If it is the latter, this may provide a marketing advantage and facilitate a relationship that could lead to academic partnerships.
Embracing new devices and modifications to existing practice paradigms happens on a spectrum21. We are reminded of the maxim, “never be the first or last to adopt change.” One must be on the lookout for revolutionary or game-changing advances but be cautious to avoid irresponsible enthusiasm. Whether it is incorporating evidence from a recent study into everyday practice or judging the potential of new equipment, a balance must be achieved between detailed evaluation of the literature and understanding the practical consequences and feasibility of implementing change. Although these may be competing interests, achieving this is a pivotal step in success for the new gastroenterologist.
AGA journals' social media accounts
http://twitter.com/aga_cgh
http://twitter.com/aga_cmgh
https://www.facebook.com/gastrojournal/
https://www.facebook.com/cghjournal/
https://www.facebook.com/cmghjournal/
References
1. Arora V et al. Closing the gap between internal medicine training and practice: Recommendations from recent graduates. Am J Med. 2005 Jun;118(6):685-7.
2. Gray DM et al. Making social media work for your practice. Clin Gastroenterol Hepatol. 2017 Nov;15:1651-4.
3. Shah NH et al. Proton pump inhibitor usage and the risk of myocardial infarction in the general population. PLoS One. 2015 Jun 10;10:e0124653.
4. Gomm W et al. Association of proton pump inhibitors with risk of dementia: A pharmacoepidemiological claims data analysis. JAMA Neurol. 2016 Apr;73(4):410-6.
5. Wang YF et al. Proton-pump inhibitor use and the risk of first-time ischemic stroke in the general population: A nationwide population-based study. Am J Gastroenterol. 2017 Jul;112:1084-93.
6. Nguyen LH et al. No significant association between proton pump inhibitor use and risk of stroke after adjustment for lifestyle factors and indication. Gastroenterology. 2018 Apr; 154(5):1290-7.
7. Lochhead P et al. Association between proton pump inhibitor use and cognitive function in women. Gastroenterology. 2017 Oct;153(4):971-9.
8. Landi SN et al. No increase in risk of acute myocardial infarction in privately insured adults prescribed proton pump inhibitors vs histamine-2 receptor antagonists (2002-2014). Gastroenterology 2018 Mar;154(4):861-73.
9. Freedberg DE et al. The risks and benefits of long-term use of proton pump inhibitors: Expert review and best practice advise from the American Gastroenterological Association. Gastroenterology. 2017 Mar;152:706-15.
10. Judd S et al. Approach to presenting a clinical journal club. Gastroenterology. 2014 Jun;146(7):1591-3.
11. Weitz JI et al. Rivaroxaban or aspirin for extended treatment of venous thromboembolism. N Engl J Med. 2017 Mar 30;376:1211-22.
12. Eikelboom JW et al. Rivaroxaban with or without aspirin in stable cardiovascular disease. N Engl J Med. 2017 Oct. 5;377:1319-30.
13. Abraham NS. Novel oral anticoagulants and gastrointestinal bleeding: a case for cardiogastroenterology. Clin Gastroenterol Hepatol. 2013;11(4):324-8.
14. Acosta RD et al. The management of antithrombotic agents for patients undergoing GI endoscopy. Gastrointest Endosc. 2016;83:3-16.
15. Sami SS et al. Screening for Barrett’s esophagus and esophageal adenocarcinoma: rationale, recent progress, challenges and future directions. Clin Gastroenterol Hepatol. 2015 Apr;13:623-34.
16. Laupacis A et al. How attractive does a new technology need to be to warrant adoption and utilization? Tentative guidelines for using clinical and economic evaluations. CMAJ. 1992 Feb 15;146:473-81.
17. Hirano I et al. Functional lumen imaging probe for the management of esophageal disorders: Expert review from the clinical practice updates committee of the AGA Institute. Clin Gastroenterol Hepatol. 2017 Mar;15:325-34.
18. Kwiatek MA et al. Esophagogastric junction distensibility assessed with an endoscopic functional luminal imaging probe (EndoFLIP). Gastrointest Endosc. 2010 Aug;72:272-82.
19. Leroi AM et al. The diagnostic value of the functional lumen imaging probe versus high-resolution anorectal manometry in patients with fecal incontinence. Neurogastroenterol Motil. 2018 Jan 18; doi: 10.1111/nmo.13291.
20. Reynolds JL et al. Intraoperative assessment of the effects of laparoscopic sleeve gastrectomy on the distensibility of the lower esophageal sphincter using impedance planimetry. Surg Endosc. 2016 Nov;30:4904-9.
21. Aisenberg J. Optical biopsy for colorectal polyps: moving along the S-shaped curve. Gastrointest Endosc. 2014 Mar;79:399-401.
Dr. Leiman, assistant professor of medicine, division of gastroenterology, Duke University, Durham, N.C.; Dr. Sengupta, assistant professor of medicine, section of gastroenterology, hepatology, and nutrition, University of Chicago Medical Center.
The transition from gastroenterology fellowship to independent practice can be daunting. There may be concerns about procedural competency and increased levels of responsibility. Recent trainees have to manage their newly busy clinical schedules while trying to integrate evidence from a rapidly evolving landscape of medical literature into daily practice. Many recent graduates also are expected to participate in financial decisions or contribute to assessments about resource allocation regarding new technologies. These are challenges faced by those in both community and academic positions but may be more keenly felt in the first years of practice regardless of setting.
Without the benefit of experience, incorporating pertinent evidence from both within and outside of the field of gastroenterology as well as identifying disruptive technologies can be particularly difficult. There is scant guidance in this area, either during fellowship or from the existing literature1. Yet these are skills that, when properly developed, can be lifelong assets and, as a result, an evaluation of this process is warranted. Herein, we identify recent developments relevant to gastroenterologists to illustrate a conceptual framework for judging novel information.
A practical concern for the new gastroenterologist is learning to efficiently evaluate the merits of the latest research and then implement this knowledge in the clinic. Maintaining active society membership often includes access to scholarly journals. For example, AGA members receive Gastroenterology, Clinical Gastroenterology and Hepatology, and Cellular and Molecular Gastroenterology and Hepatology as part of their member benefits and have the opportunity to receive alerts when new content is published. Social media outlets such as Twitter and Facebook also simplify the process for readers to identify high-impact studies2 (see social media urls at the end of the story). In addition to reading, however, a critical review of these studies can prevent premature enthusiasm for modifying practice. The evolving evidence base for understanding proton pump inhibitor (PPI) risks is illustrative. Several studies attracted widespread media attention describing serious associated side effects, ranging from MI3 to dementia4 and stroke5. These studies were provocative but a decision to withhold PPIs from patients based on these concerns alone could lead to unintended consequences with poor outcomes. Ultimately, subsequent studies published only months later challenged these associations.6-8 Instead, thoughtful disclosure to patients of known risks and appropriate indications for PPI therapy based on resources such as the AGA Best Practice Advice9 is prudent. Reading more may be necessary but is insufficient; finding a forum to discuss novel research topics, such as in a monthly journal club10 or group practice meeting, can lead to stimulating discussion about how to apply pertinent research to change practice. The AGA Community is an excellent venue for this kind of interaction.
In many situations, keeping informed of updates about the risks and safety of medications prescribed by nongastroenterologists, particularly as they relate to GI conditions, can be even more difficult. A prime example of this is the rapidly expanding literature on indications and risks of direct oral anticoagulants. Rotating on the inpatient consultation service, with the chance to interact with multiple non-GI providers, affords an excellent opportunity to stay up to date. With the increased prevalence of atrial fibrillation as well as the potential expanded indications for direct oral anticoagulants based on recent randomized, controlled trials11,12, practicing gastroenterologists will be comanaging increasing numbers of patients hospitalized with gastrointestinal bleeding (GIB). Our understanding of the availability and indication for targeted reversal agents, such as idarucizumab, as well as nonspecific reversal agents, such as prothrombin complex concentrates, for those with life-threatening GIB is critical to optimal management of these patients. Multidisciplinary collaborations, such as with cardiogastroenterology clinics13, can be leveraged for optimal management of direct oral anticoagulants in the periendoscopy period.
Traditional outpatient consultative approaches are sometimes necessary but frequent reference to consensus societal guidelines on endoscopy in patients on antithrombotics14 should be made, particularly if they are printed and readily available in the ambulatory clinic and endoscopy suites. When information may be too new or sparse to utilize a national guideline, employing local data or experience to create a hospital-specific algorithm can ensure the delivery of high-quality, collaborative patient care.
Much like reviewing the literature, evaluating new technologies poses its own challenges. Changes in clinical practice may be slow, as in the adoption of noninvasive methods for Barrett’s esophagus screening.15 But in an age when news of advances and updates in management spreads at tremendous speed through the use of social media, the ability to pivot or assimilate new discoveries and techniques will become increasingly relevant and important. A professional society’s endorsement can provide a framework for a decision, but other principles at play include sensible, critical analyses of the outcomes and costs as well as a balance of organizational and societal perspectives.16 The use of impedance planimetry is one such example. This is a relatively new technology, but it has received increasing interest recently.17 The first questions when considering adopting this type of device likely will be about its supporting evidence and the risk for causing harm. The pace of publications regarding its use for measuring esophageal distensibility has accelerated18. But good data does not necessarily translate into extensive uptake. Other important factors also are practical, e.g., whether a technology committee’s approval is needed and what is the learning curve, available technical support, need for capital purchases, reimbursement, etc. Functional luminal imaging probe (FLIP®) technology was developed to assess compliance in primary esophageal disorders and now has been applied to several other areas including anorectal disease, bariatric surgery, and therapeutic endoscopy19,20. Although seemingly a niche market, there is potential widespread application and an opportunity for collaborations that might not have been evident at first blush. Ultimately, any evaluation of new technology is to a certain extent speculation. Is the technology mature or novel? If it is the latter, this may provide a marketing advantage and facilitate a relationship that could lead to academic partnerships.
Embracing new devices and modifications to existing practice paradigms happens on a spectrum21. We are reminded of the maxim, “never be the first or last to adopt change.” One must be on the lookout for revolutionary or game-changing advances but be cautious to avoid irresponsible enthusiasm. Whether it is incorporating evidence from a recent study into everyday practice or judging the potential of new equipment, a balance must be achieved between detailed evaluation of the literature and understanding the practical consequences and feasibility of implementing change. Although these may be competing interests, achieving this is a pivotal step in success for the new gastroenterologist.
AGA journals' social media accounts
http://twitter.com/aga_cgh
http://twitter.com/aga_cmgh
https://www.facebook.com/gastrojournal/
https://www.facebook.com/cghjournal/
https://www.facebook.com/cmghjournal/
References
1. Arora V et al. Closing the gap between internal medicine training and practice: Recommendations from recent graduates. Am J Med. 2005 Jun;118(6):685-7.
2. Gray DM et al. Making social media work for your practice. Clin Gastroenterol Hepatol. 2017 Nov;15:1651-4.
3. Shah NH et al. Proton pump inhibitor usage and the risk of myocardial infarction in the general population. PLoS One. 2015 Jun 10;10:e0124653.
4. Gomm W et al. Association of proton pump inhibitors with risk of dementia: A pharmacoepidemiological claims data analysis. JAMA Neurol. 2016 Apr;73(4):410-6.
5. Wang YF et al. Proton-pump inhibitor use and the risk of first-time ischemic stroke in the general population: A nationwide population-based study. Am J Gastroenterol. 2017 Jul;112:1084-93.
6. Nguyen LH et al. No significant association between proton pump inhibitor use and risk of stroke after adjustment for lifestyle factors and indication. Gastroenterology. 2018 Apr; 154(5):1290-7.
7. Lochhead P et al. Association between proton pump inhibitor use and cognitive function in women. Gastroenterology. 2017 Oct;153(4):971-9.
8. Landi SN et al. No increase in risk of acute myocardial infarction in privately insured adults prescribed proton pump inhibitors vs histamine-2 receptor antagonists (2002-2014). Gastroenterology 2018 Mar;154(4):861-73.
9. Freedberg DE et al. The risks and benefits of long-term use of proton pump inhibitors: Expert review and best practice advise from the American Gastroenterological Association. Gastroenterology. 2017 Mar;152:706-15.
10. Judd S et al. Approach to presenting a clinical journal club. Gastroenterology. 2014 Jun;146(7):1591-3.
11. Weitz JI et al. Rivaroxaban or aspirin for extended treatment of venous thromboembolism. N Engl J Med. 2017 Mar 30;376:1211-22.
12. Eikelboom JW et al. Rivaroxaban with or without aspirin in stable cardiovascular disease. N Engl J Med. 2017 Oct. 5;377:1319-30.
13. Abraham NS. Novel oral anticoagulants and gastrointestinal bleeding: a case for cardiogastroenterology. Clin Gastroenterol Hepatol. 2013;11(4):324-8.
14. Acosta RD et al. The management of antithrombotic agents for patients undergoing GI endoscopy. Gastrointest Endosc. 2016;83:3-16.
15. Sami SS et al. Screening for Barrett’s esophagus and esophageal adenocarcinoma: rationale, recent progress, challenges and future directions. Clin Gastroenterol Hepatol. 2015 Apr;13:623-34.
16. Laupacis A et al. How attractive does a new technology need to be to warrant adoption and utilization? Tentative guidelines for using clinical and economic evaluations. CMAJ. 1992 Feb 15;146:473-81.
17. Hirano I et al. Functional lumen imaging probe for the management of esophageal disorders: Expert review from the clinical practice updates committee of the AGA Institute. Clin Gastroenterol Hepatol. 2017 Mar;15:325-34.
18. Kwiatek MA et al. Esophagogastric junction distensibility assessed with an endoscopic functional luminal imaging probe (EndoFLIP). Gastrointest Endosc. 2010 Aug;72:272-82.
19. Leroi AM et al. The diagnostic value of the functional lumen imaging probe versus high-resolution anorectal manometry in patients with fecal incontinence. Neurogastroenterol Motil. 2018 Jan 18; doi: 10.1111/nmo.13291.
20. Reynolds JL et al. Intraoperative assessment of the effects of laparoscopic sleeve gastrectomy on the distensibility of the lower esophageal sphincter using impedance planimetry. Surg Endosc. 2016 Nov;30:4904-9.
21. Aisenberg J. Optical biopsy for colorectal polyps: moving along the S-shaped curve. Gastrointest Endosc. 2014 Mar;79:399-401.
Dr. Leiman, assistant professor of medicine, division of gastroenterology, Duke University, Durham, N.C.; Dr. Sengupta, assistant professor of medicine, section of gastroenterology, hepatology, and nutrition, University of Chicago Medical Center.
The transition from gastroenterology fellowship to independent practice can be daunting. There may be concerns about procedural competency and increased levels of responsibility. Recent trainees have to manage their newly busy clinical schedules while trying to integrate evidence from a rapidly evolving landscape of medical literature into daily practice. Many recent graduates also are expected to participate in financial decisions or contribute to assessments about resource allocation regarding new technologies. These are challenges faced by those in both community and academic positions but may be more keenly felt in the first years of practice regardless of setting.
Without the benefit of experience, incorporating pertinent evidence from both within and outside of the field of gastroenterology as well as identifying disruptive technologies can be particularly difficult. There is scant guidance in this area, either during fellowship or from the existing literature1. Yet these are skills that, when properly developed, can be lifelong assets and, as a result, an evaluation of this process is warranted. Herein, we identify recent developments relevant to gastroenterologists to illustrate a conceptual framework for judging novel information.
A practical concern for the new gastroenterologist is learning to efficiently evaluate the merits of the latest research and then implement this knowledge in the clinic. Maintaining active society membership often includes access to scholarly journals. For example, AGA members receive Gastroenterology, Clinical Gastroenterology and Hepatology, and Cellular and Molecular Gastroenterology and Hepatology as part of their member benefits and have the opportunity to receive alerts when new content is published. Social media outlets such as Twitter and Facebook also simplify the process for readers to identify high-impact studies2 (see social media urls at the end of the story). In addition to reading, however, a critical review of these studies can prevent premature enthusiasm for modifying practice. The evolving evidence base for understanding proton pump inhibitor (PPI) risks is illustrative. Several studies attracted widespread media attention describing serious associated side effects, ranging from MI3 to dementia4 and stroke5. These studies were provocative but a decision to withhold PPIs from patients based on these concerns alone could lead to unintended consequences with poor outcomes. Ultimately, subsequent studies published only months later challenged these associations.6-8 Instead, thoughtful disclosure to patients of known risks and appropriate indications for PPI therapy based on resources such as the AGA Best Practice Advice9 is prudent. Reading more may be necessary but is insufficient; finding a forum to discuss novel research topics, such as in a monthly journal club10 or group practice meeting, can lead to stimulating discussion about how to apply pertinent research to change practice. The AGA Community is an excellent venue for this kind of interaction.
In many situations, keeping informed of updates about the risks and safety of medications prescribed by nongastroenterologists, particularly as they relate to GI conditions, can be even more difficult. A prime example of this is the rapidly expanding literature on indications and risks of direct oral anticoagulants. Rotating on the inpatient consultation service, with the chance to interact with multiple non-GI providers, affords an excellent opportunity to stay up to date. With the increased prevalence of atrial fibrillation as well as the potential expanded indications for direct oral anticoagulants based on recent randomized, controlled trials11,12, practicing gastroenterologists will be comanaging increasing numbers of patients hospitalized with gastrointestinal bleeding (GIB). Our understanding of the availability and indication for targeted reversal agents, such as idarucizumab, as well as nonspecific reversal agents, such as prothrombin complex concentrates, for those with life-threatening GIB is critical to optimal management of these patients. Multidisciplinary collaborations, such as with cardiogastroenterology clinics13, can be leveraged for optimal management of direct oral anticoagulants in the periendoscopy period.
Traditional outpatient consultative approaches are sometimes necessary but frequent reference to consensus societal guidelines on endoscopy in patients on antithrombotics14 should be made, particularly if they are printed and readily available in the ambulatory clinic and endoscopy suites. When information may be too new or sparse to utilize a national guideline, employing local data or experience to create a hospital-specific algorithm can ensure the delivery of high-quality, collaborative patient care.
Much like reviewing the literature, evaluating new technologies poses its own challenges. Changes in clinical practice may be slow, as in the adoption of noninvasive methods for Barrett’s esophagus screening.15 But in an age when news of advances and updates in management spreads at tremendous speed through the use of social media, the ability to pivot or assimilate new discoveries and techniques will become increasingly relevant and important. A professional society’s endorsement can provide a framework for a decision, but other principles at play include sensible, critical analyses of the outcomes and costs as well as a balance of organizational and societal perspectives.16 The use of impedance planimetry is one such example. This is a relatively new technology, but it has received increasing interest recently.17 The first questions when considering adopting this type of device likely will be about its supporting evidence and the risk for causing harm. The pace of publications regarding its use for measuring esophageal distensibility has accelerated18. But good data does not necessarily translate into extensive uptake. Other important factors also are practical, e.g., whether a technology committee’s approval is needed and what is the learning curve, available technical support, need for capital purchases, reimbursement, etc. Functional luminal imaging probe (FLIP®) technology was developed to assess compliance in primary esophageal disorders and now has been applied to several other areas including anorectal disease, bariatric surgery, and therapeutic endoscopy19,20. Although seemingly a niche market, there is potential widespread application and an opportunity for collaborations that might not have been evident at first blush. Ultimately, any evaluation of new technology is to a certain extent speculation. Is the technology mature or novel? If it is the latter, this may provide a marketing advantage and facilitate a relationship that could lead to academic partnerships.
Embracing new devices and modifications to existing practice paradigms happens on a spectrum21. We are reminded of the maxim, “never be the first or last to adopt change.” One must be on the lookout for revolutionary or game-changing advances but be cautious to avoid irresponsible enthusiasm. Whether it is incorporating evidence from a recent study into everyday practice or judging the potential of new equipment, a balance must be achieved between detailed evaluation of the literature and understanding the practical consequences and feasibility of implementing change. Although these may be competing interests, achieving this is a pivotal step in success for the new gastroenterologist.
AGA journals' social media accounts
http://twitter.com/aga_cgh
http://twitter.com/aga_cmgh
https://www.facebook.com/gastrojournal/
https://www.facebook.com/cghjournal/
https://www.facebook.com/cmghjournal/
References
1. Arora V et al. Closing the gap between internal medicine training and practice: Recommendations from recent graduates. Am J Med. 2005 Jun;118(6):685-7.
2. Gray DM et al. Making social media work for your practice. Clin Gastroenterol Hepatol. 2017 Nov;15:1651-4.
3. Shah NH et al. Proton pump inhibitor usage and the risk of myocardial infarction in the general population. PLoS One. 2015 Jun 10;10:e0124653.
4. Gomm W et al. Association of proton pump inhibitors with risk of dementia: A pharmacoepidemiological claims data analysis. JAMA Neurol. 2016 Apr;73(4):410-6.
5. Wang YF et al. Proton-pump inhibitor use and the risk of first-time ischemic stroke in the general population: A nationwide population-based study. Am J Gastroenterol. 2017 Jul;112:1084-93.
6. Nguyen LH et al. No significant association between proton pump inhibitor use and risk of stroke after adjustment for lifestyle factors and indication. Gastroenterology. 2018 Apr; 154(5):1290-7.
7. Lochhead P et al. Association between proton pump inhibitor use and cognitive function in women. Gastroenterology. 2017 Oct;153(4):971-9.
8. Landi SN et al. No increase in risk of acute myocardial infarction in privately insured adults prescribed proton pump inhibitors vs histamine-2 receptor antagonists (2002-2014). Gastroenterology 2018 Mar;154(4):861-73.
9. Freedberg DE et al. The risks and benefits of long-term use of proton pump inhibitors: Expert review and best practice advise from the American Gastroenterological Association. Gastroenterology. 2017 Mar;152:706-15.
10. Judd S et al. Approach to presenting a clinical journal club. Gastroenterology. 2014 Jun;146(7):1591-3.
11. Weitz JI et al. Rivaroxaban or aspirin for extended treatment of venous thromboembolism. N Engl J Med. 2017 Mar 30;376:1211-22.
12. Eikelboom JW et al. Rivaroxaban with or without aspirin in stable cardiovascular disease. N Engl J Med. 2017 Oct. 5;377:1319-30.
13. Abraham NS. Novel oral anticoagulants and gastrointestinal bleeding: a case for cardiogastroenterology. Clin Gastroenterol Hepatol. 2013;11(4):324-8.
14. Acosta RD et al. The management of antithrombotic agents for patients undergoing GI endoscopy. Gastrointest Endosc. 2016;83:3-16.
15. Sami SS et al. Screening for Barrett’s esophagus and esophageal adenocarcinoma: rationale, recent progress, challenges and future directions. Clin Gastroenterol Hepatol. 2015 Apr;13:623-34.
16. Laupacis A et al. How attractive does a new technology need to be to warrant adoption and utilization? Tentative guidelines for using clinical and economic evaluations. CMAJ. 1992 Feb 15;146:473-81.
17. Hirano I et al. Functional lumen imaging probe for the management of esophageal disorders: Expert review from the clinical practice updates committee of the AGA Institute. Clin Gastroenterol Hepatol. 2017 Mar;15:325-34.
18. Kwiatek MA et al. Esophagogastric junction distensibility assessed with an endoscopic functional luminal imaging probe (EndoFLIP). Gastrointest Endosc. 2010 Aug;72:272-82.
19. Leroi AM et al. The diagnostic value of the functional lumen imaging probe versus high-resolution anorectal manometry in patients with fecal incontinence. Neurogastroenterol Motil. 2018 Jan 18; doi: 10.1111/nmo.13291.
20. Reynolds JL et al. Intraoperative assessment of the effects of laparoscopic sleeve gastrectomy on the distensibility of the lower esophageal sphincter using impedance planimetry. Surg Endosc. 2016 Nov;30:4904-9.
21. Aisenberg J. Optical biopsy for colorectal polyps: moving along the S-shaped curve. Gastrointest Endosc. 2014 Mar;79:399-401.
Dr. Leiman, assistant professor of medicine, division of gastroenterology, Duke University, Durham, N.C.; Dr. Sengupta, assistant professor of medicine, section of gastroenterology, hepatology, and nutrition, University of Chicago Medical Center.
Noninvasive 1060-nm diode laser found effective for axillary hyperhidrosis
DALLAS – , a condition that affects an estimated 1.4% people in the United States.
“Newer treatments such as microwave technology, botulinum toxin injections, and lasers have emerged as effective methods,” lead study author Bruce E. Katz, MD, who directs the Juva Skin & Laser Center in New York, said at the annual conference of the American Society for Laser Medicine and Surgery Inc.
In a prospective pilot study, Dr. Katz and his associates examined the use of a noninvasive 1060-nm diode laser (SculpSure, Cynosure) in 10 subjects with moderate to severe hyperhidrosis of the axilla, which was defined as having Hyperhidrosis Disease Severity Scale (HDSS) scores of 3 or 4. The subjects, whose mean age was 42 years, received two laser treatments on the axillary area at 6-week intervals, and the researchers performed starch iodine tests and took two-dimensional photography of the axilla before and after treatment. Subjects were asked to rate their conditions on the HDSS and satisfaction with treatment. Two blinded dermatologist evaluators graded the reduction in sweat production on photos of starch iodine tests. The researchers also performed a retrospective analysis on all subjects to assess safety and efficacy of treatment.
The 1060-nm diode laser used for the study features four flat, nonsuction applicators. Dr. Katz and his associates positioned two applicators on the axilla simultaneously for 25 minutes. “The 1060-nm wavelength has minimal absorption in the melanin, so we can really treat any skin type,” he said. “It has a high affinity for adipose tissue, and we believe that its targeted effect at the level of the eccrine and apocrine glands should help improve hyperhidrosis. It works by elevating the tissue temperature to about 42 to 47 degrees Centigrade, without damaging surrounding tissue. The device has a sapphire cooling plate, so it’s comfortable for the patient.”
The retrospective analysis revealed minimal adverse events such as pain, mild erythema, and edema, which were transient and resolved without intervention in a day or two. To date, no cases have recurred, “which we were surprised by,” Dr. Katz said. “We were surprised that the effect lasted that long.”
SOURCE: Katz et. al. ASLMS 2018.
DALLAS – , a condition that affects an estimated 1.4% people in the United States.
“Newer treatments such as microwave technology, botulinum toxin injections, and lasers have emerged as effective methods,” lead study author Bruce E. Katz, MD, who directs the Juva Skin & Laser Center in New York, said at the annual conference of the American Society for Laser Medicine and Surgery Inc.
In a prospective pilot study, Dr. Katz and his associates examined the use of a noninvasive 1060-nm diode laser (SculpSure, Cynosure) in 10 subjects with moderate to severe hyperhidrosis of the axilla, which was defined as having Hyperhidrosis Disease Severity Scale (HDSS) scores of 3 or 4. The subjects, whose mean age was 42 years, received two laser treatments on the axillary area at 6-week intervals, and the researchers performed starch iodine tests and took two-dimensional photography of the axilla before and after treatment. Subjects were asked to rate their conditions on the HDSS and satisfaction with treatment. Two blinded dermatologist evaluators graded the reduction in sweat production on photos of starch iodine tests. The researchers also performed a retrospective analysis on all subjects to assess safety and efficacy of treatment.
The 1060-nm diode laser used for the study features four flat, nonsuction applicators. Dr. Katz and his associates positioned two applicators on the axilla simultaneously for 25 minutes. “The 1060-nm wavelength has minimal absorption in the melanin, so we can really treat any skin type,” he said. “It has a high affinity for adipose tissue, and we believe that its targeted effect at the level of the eccrine and apocrine glands should help improve hyperhidrosis. It works by elevating the tissue temperature to about 42 to 47 degrees Centigrade, without damaging surrounding tissue. The device has a sapphire cooling plate, so it’s comfortable for the patient.”
The retrospective analysis revealed minimal adverse events such as pain, mild erythema, and edema, which were transient and resolved without intervention in a day or two. To date, no cases have recurred, “which we were surprised by,” Dr. Katz said. “We were surprised that the effect lasted that long.”
SOURCE: Katz et. al. ASLMS 2018.
DALLAS – , a condition that affects an estimated 1.4% people in the United States.
“Newer treatments such as microwave technology, botulinum toxin injections, and lasers have emerged as effective methods,” lead study author Bruce E. Katz, MD, who directs the Juva Skin & Laser Center in New York, said at the annual conference of the American Society for Laser Medicine and Surgery Inc.
In a prospective pilot study, Dr. Katz and his associates examined the use of a noninvasive 1060-nm diode laser (SculpSure, Cynosure) in 10 subjects with moderate to severe hyperhidrosis of the axilla, which was defined as having Hyperhidrosis Disease Severity Scale (HDSS) scores of 3 or 4. The subjects, whose mean age was 42 years, received two laser treatments on the axillary area at 6-week intervals, and the researchers performed starch iodine tests and took two-dimensional photography of the axilla before and after treatment. Subjects were asked to rate their conditions on the HDSS and satisfaction with treatment. Two blinded dermatologist evaluators graded the reduction in sweat production on photos of starch iodine tests. The researchers also performed a retrospective analysis on all subjects to assess safety and efficacy of treatment.
The 1060-nm diode laser used for the study features four flat, nonsuction applicators. Dr. Katz and his associates positioned two applicators on the axilla simultaneously for 25 minutes. “The 1060-nm wavelength has minimal absorption in the melanin, so we can really treat any skin type,” he said. “It has a high affinity for adipose tissue, and we believe that its targeted effect at the level of the eccrine and apocrine glands should help improve hyperhidrosis. It works by elevating the tissue temperature to about 42 to 47 degrees Centigrade, without damaging surrounding tissue. The device has a sapphire cooling plate, so it’s comfortable for the patient.”
The retrospective analysis revealed minimal adverse events such as pain, mild erythema, and edema, which were transient and resolved without intervention in a day or two. To date, no cases have recurred, “which we were surprised by,” Dr. Katz said. “We were surprised that the effect lasted that long.”
SOURCE: Katz et. al. ASLMS 2018.
REPORTING FROM ASLMS 2018
Advanced training in hepatology
Unlike previous hepatologists, who were trained through gastroenterology programs, most new practitioners seek advanced training in a fellowship year focused exclusively on hepatology.
Like practitioners in many medical subspecialties, transplant hepatologists have varied career goals and responsibilities. Hepatologists who continue to specifically practice transplant hepatology are affiliated with a liver transplant center, which is generally a hospital-based practice. However, most hepatologists also treat nontransplant hepatology patients and some who have completed advanced hepatology training focus exclusively on these patients or provide community-based care for transplant recipients from other centers. Caring for patients with end-stage liver disease and liver transplant recipients can be clinically demanding but also very rewarding. There are also many opportunities for academic pursuits within a hepatology career including areas in urgent need of clinical and basic investigation, clinical trials for novel agents to treat common diseases, education (including leadership in advanced hepatology training), and involvement in professional societies such as the American Gastroenterological Association (AGA) and American Association for the Study of Liver Disease (AASLD).
What are the opportunities for advanced hepatology training?
In 1999, the AASLD determined that the practice of transplant hepatology required its own specialized knowledge and that most practicing gastroenterologists did not consider themselves adequately prepared to care for patients with advanced liver disease.1,2 The following year, the AASLD applied to the American Board of Internal Medicine (ABIM) to develop formalized liver transplant training. After several years of debate and development, the first ABIM certification exam in transplant hepatology was held in 2006 and is now offered every 2 years.2
There are currently three pathways to achieve advanced training in hepatology. The traditional pathway is a 1-year Accreditation Council for Graduate Medical Education (ACGME) transplant fellowship that is separate from, and must follow completion of, a gastroenterology fellowship. There are currently 51 ACGME-accredited 1-year transplant hepatology fellowships in the United States. These fellowships are only at institutions with ACGME-accredited training in internal medicine and gastroenterology as well. The full and updated list of programs can be found on the ACGME website.3 The second pathway is the relatively new ABIM “pilot” program during which the transplant hepatology fellowship year is combined with the third year of gastroenterology fellowship (discussed in detail below). Finally, there remain many 1-year training programs that are not ACGME-accredited, may not be associated with a gastroenterology fellowship program, and do have not regulated requirements for entry. Trainees who complete non-ACGME programs are not candidates for ABIM board certification.
How does one apply for transplant hepatology fellowship?
Transplant hepatology fellowships do not participate in a match system. Therefore, the interviews and offers for training spots may occur at different times depending on the program and the region of the country. In general, fellows apply by the fall of their second year of gastroenterology fellowship in order to begin training after graduating from the third year of fellowship. Each program has its individual approach to the application process and most have this information available on a website as to how to apply. A complete list of ACGME-accredited programs along with the program directors and contact information is available on the ABIM website.3
What is the gastroenterology/transplant hepatology pilot training program?
The AASLD and ABIM have developed a combined gastroenterology and transplant hepatology pilot fellowship training program that allows eligible gastroenterology fellows to spend their third year training in transplant hepatology. This approach has the potential to shorten the total training from 4 years to 3. In addition, if all gastroenterology and transplant hepatology competencies are achieved by the end of the third year, fellows approved to be in this program are eligible to take both gastroenterology and transplant hepatology ABIM certification exams.
Any ACGME-accredited gastroenterology fellowship program that has an accredited hepatology counterpart is eligible to participate in this pilot. Eligible programs and fellows must apply to AASLD during the fellow’s second year. The fellow applicant must complete all clinical gastroenterology requirements before the end of the second year of fellowship and be on a trajectory to meet competency milestones, as the majority of the third year will focus on hepatology.
Since 2012, 59 fellows from 31 programs have participated in this pilot program.4 If you are interested in participating in this pilot program at your institution, it is important to confer with program directors as early as possible to meet all training requirements. In addition, applications are submitted to the Pilot Steering Taskforce during the fellow’s second year for review. This is not meant to be a competitive process and all fellows who meet the criteria are approved.
This track may not be ideal for all fellows interested in advanced and transplant hepatology. In particular, there may be a trade-off between achieving clinical competency in a shortened training period and pursuing scholarly activity. This pilot program is designed to be an intensive clinical track, so fellows who wish to focus on research should discuss with their program directors whether this is the best approach.
What has been your career path after advanced training in hepatology?
I first became interested in hepatology during my inpatient rotations as a medical student. This interest led me to become involved in research in this area very early in my career. The current structure of the fellowship as well as the board certification exam were both developed while I was in training and I adjusted my plans to complete 3 years of gastroenterology fellowship followed by an ACGME-accredited liver transplant fellowship year. Since completing training, I have worked as an attending at an academic medical center in a large liver transplant program and continue to care for patients with all forms of liver disease. In addition, I continued to pursue research as a large component of my job and now have NIH funding and direct the Transplant Clinical Research Center at Columbia University. Finally, I have always been devoted to education and am the program director for the transplant hepatology fellowship at our institution.
What is the future of advanced hepatology training?
The current transplant hepatology training system has evolved significantly since its inception, including development of curricula, ongoing modification of training requirements, and the development of the innovative pilot program. However, there are issues that continue to be debated by the community. For example, it is not certain when or if the combined gastroenterology and transplant hepatology pilot program will become a permanent pathway for training or how best to select fellows for this approach.
Hepatology continues to be a very dynamic area of medicine. With diseases such as nonalcoholic fatty liver disease and hepatocellular carcinoma on the rise, the urgent need for training in HCV treatment to combat the global epidemic of viral hepatitis, and the growing number of patients on the liver transplant waiting list, there has never been a more exciting time to choose hepatology as a career.
References
1. Luxon BA. So you want to be a hepatologist? Gastroenterology. 2013;145(6):1182-5.
2. Bacon BR, Grosso LJ, Freedman N, Althouse LA. Subspecialty certification in transplant hepatology. Liver Transpl. 2007;13(11):1479-81.
3. https://apps.acgme.org/ads/public/reports/report/1.
4. https://www.aasld.org/events-professional-development/educational-learning-faq.
Dr. Verna is assistant professor of medicine, program director, transplant hepatology fellowship, director of clinical research, Transplant Clinical Research Center, Columbia University Medical Center, New York.
Unlike previous hepatologists, who were trained through gastroenterology programs, most new practitioners seek advanced training in a fellowship year focused exclusively on hepatology.
Like practitioners in many medical subspecialties, transplant hepatologists have varied career goals and responsibilities. Hepatologists who continue to specifically practice transplant hepatology are affiliated with a liver transplant center, which is generally a hospital-based practice. However, most hepatologists also treat nontransplant hepatology patients and some who have completed advanced hepatology training focus exclusively on these patients or provide community-based care for transplant recipients from other centers. Caring for patients with end-stage liver disease and liver transplant recipients can be clinically demanding but also very rewarding. There are also many opportunities for academic pursuits within a hepatology career including areas in urgent need of clinical and basic investigation, clinical trials for novel agents to treat common diseases, education (including leadership in advanced hepatology training), and involvement in professional societies such as the American Gastroenterological Association (AGA) and American Association for the Study of Liver Disease (AASLD).
What are the opportunities for advanced hepatology training?
In 1999, the AASLD determined that the practice of transplant hepatology required its own specialized knowledge and that most practicing gastroenterologists did not consider themselves adequately prepared to care for patients with advanced liver disease.1,2 The following year, the AASLD applied to the American Board of Internal Medicine (ABIM) to develop formalized liver transplant training. After several years of debate and development, the first ABIM certification exam in transplant hepatology was held in 2006 and is now offered every 2 years.2
There are currently three pathways to achieve advanced training in hepatology. The traditional pathway is a 1-year Accreditation Council for Graduate Medical Education (ACGME) transplant fellowship that is separate from, and must follow completion of, a gastroenterology fellowship. There are currently 51 ACGME-accredited 1-year transplant hepatology fellowships in the United States. These fellowships are only at institutions with ACGME-accredited training in internal medicine and gastroenterology as well. The full and updated list of programs can be found on the ACGME website.3 The second pathway is the relatively new ABIM “pilot” program during which the transplant hepatology fellowship year is combined with the third year of gastroenterology fellowship (discussed in detail below). Finally, there remain many 1-year training programs that are not ACGME-accredited, may not be associated with a gastroenterology fellowship program, and do have not regulated requirements for entry. Trainees who complete non-ACGME programs are not candidates for ABIM board certification.
How does one apply for transplant hepatology fellowship?
Transplant hepatology fellowships do not participate in a match system. Therefore, the interviews and offers for training spots may occur at different times depending on the program and the region of the country. In general, fellows apply by the fall of their second year of gastroenterology fellowship in order to begin training after graduating from the third year of fellowship. Each program has its individual approach to the application process and most have this information available on a website as to how to apply. A complete list of ACGME-accredited programs along with the program directors and contact information is available on the ABIM website.3
What is the gastroenterology/transplant hepatology pilot training program?
The AASLD and ABIM have developed a combined gastroenterology and transplant hepatology pilot fellowship training program that allows eligible gastroenterology fellows to spend their third year training in transplant hepatology. This approach has the potential to shorten the total training from 4 years to 3. In addition, if all gastroenterology and transplant hepatology competencies are achieved by the end of the third year, fellows approved to be in this program are eligible to take both gastroenterology and transplant hepatology ABIM certification exams.
Any ACGME-accredited gastroenterology fellowship program that has an accredited hepatology counterpart is eligible to participate in this pilot. Eligible programs and fellows must apply to AASLD during the fellow’s second year. The fellow applicant must complete all clinical gastroenterology requirements before the end of the second year of fellowship and be on a trajectory to meet competency milestones, as the majority of the third year will focus on hepatology.
Since 2012, 59 fellows from 31 programs have participated in this pilot program.4 If you are interested in participating in this pilot program at your institution, it is important to confer with program directors as early as possible to meet all training requirements. In addition, applications are submitted to the Pilot Steering Taskforce during the fellow’s second year for review. This is not meant to be a competitive process and all fellows who meet the criteria are approved.
This track may not be ideal for all fellows interested in advanced and transplant hepatology. In particular, there may be a trade-off between achieving clinical competency in a shortened training period and pursuing scholarly activity. This pilot program is designed to be an intensive clinical track, so fellows who wish to focus on research should discuss with their program directors whether this is the best approach.
What has been your career path after advanced training in hepatology?
I first became interested in hepatology during my inpatient rotations as a medical student. This interest led me to become involved in research in this area very early in my career. The current structure of the fellowship as well as the board certification exam were both developed while I was in training and I adjusted my plans to complete 3 years of gastroenterology fellowship followed by an ACGME-accredited liver transplant fellowship year. Since completing training, I have worked as an attending at an academic medical center in a large liver transplant program and continue to care for patients with all forms of liver disease. In addition, I continued to pursue research as a large component of my job and now have NIH funding and direct the Transplant Clinical Research Center at Columbia University. Finally, I have always been devoted to education and am the program director for the transplant hepatology fellowship at our institution.
What is the future of advanced hepatology training?
The current transplant hepatology training system has evolved significantly since its inception, including development of curricula, ongoing modification of training requirements, and the development of the innovative pilot program. However, there are issues that continue to be debated by the community. For example, it is not certain when or if the combined gastroenterology and transplant hepatology pilot program will become a permanent pathway for training or how best to select fellows for this approach.
Hepatology continues to be a very dynamic area of medicine. With diseases such as nonalcoholic fatty liver disease and hepatocellular carcinoma on the rise, the urgent need for training in HCV treatment to combat the global epidemic of viral hepatitis, and the growing number of patients on the liver transplant waiting list, there has never been a more exciting time to choose hepatology as a career.
References
1. Luxon BA. So you want to be a hepatologist? Gastroenterology. 2013;145(6):1182-5.
2. Bacon BR, Grosso LJ, Freedman N, Althouse LA. Subspecialty certification in transplant hepatology. Liver Transpl. 2007;13(11):1479-81.
3. https://apps.acgme.org/ads/public/reports/report/1.
4. https://www.aasld.org/events-professional-development/educational-learning-faq.
Dr. Verna is assistant professor of medicine, program director, transplant hepatology fellowship, director of clinical research, Transplant Clinical Research Center, Columbia University Medical Center, New York.
Unlike previous hepatologists, who were trained through gastroenterology programs, most new practitioners seek advanced training in a fellowship year focused exclusively on hepatology.
Like practitioners in many medical subspecialties, transplant hepatologists have varied career goals and responsibilities. Hepatologists who continue to specifically practice transplant hepatology are affiliated with a liver transplant center, which is generally a hospital-based practice. However, most hepatologists also treat nontransplant hepatology patients and some who have completed advanced hepatology training focus exclusively on these patients or provide community-based care for transplant recipients from other centers. Caring for patients with end-stage liver disease and liver transplant recipients can be clinically demanding but also very rewarding. There are also many opportunities for academic pursuits within a hepatology career including areas in urgent need of clinical and basic investigation, clinical trials for novel agents to treat common diseases, education (including leadership in advanced hepatology training), and involvement in professional societies such as the American Gastroenterological Association (AGA) and American Association for the Study of Liver Disease (AASLD).
What are the opportunities for advanced hepatology training?
In 1999, the AASLD determined that the practice of transplant hepatology required its own specialized knowledge and that most practicing gastroenterologists did not consider themselves adequately prepared to care for patients with advanced liver disease.1,2 The following year, the AASLD applied to the American Board of Internal Medicine (ABIM) to develop formalized liver transplant training. After several years of debate and development, the first ABIM certification exam in transplant hepatology was held in 2006 and is now offered every 2 years.2
There are currently three pathways to achieve advanced training in hepatology. The traditional pathway is a 1-year Accreditation Council for Graduate Medical Education (ACGME) transplant fellowship that is separate from, and must follow completion of, a gastroenterology fellowship. There are currently 51 ACGME-accredited 1-year transplant hepatology fellowships in the United States. These fellowships are only at institutions with ACGME-accredited training in internal medicine and gastroenterology as well. The full and updated list of programs can be found on the ACGME website.3 The second pathway is the relatively new ABIM “pilot” program during which the transplant hepatology fellowship year is combined with the third year of gastroenterology fellowship (discussed in detail below). Finally, there remain many 1-year training programs that are not ACGME-accredited, may not be associated with a gastroenterology fellowship program, and do have not regulated requirements for entry. Trainees who complete non-ACGME programs are not candidates for ABIM board certification.
How does one apply for transplant hepatology fellowship?
Transplant hepatology fellowships do not participate in a match system. Therefore, the interviews and offers for training spots may occur at different times depending on the program and the region of the country. In general, fellows apply by the fall of their second year of gastroenterology fellowship in order to begin training after graduating from the third year of fellowship. Each program has its individual approach to the application process and most have this information available on a website as to how to apply. A complete list of ACGME-accredited programs along with the program directors and contact information is available on the ABIM website.3
What is the gastroenterology/transplant hepatology pilot training program?
The AASLD and ABIM have developed a combined gastroenterology and transplant hepatology pilot fellowship training program that allows eligible gastroenterology fellows to spend their third year training in transplant hepatology. This approach has the potential to shorten the total training from 4 years to 3. In addition, if all gastroenterology and transplant hepatology competencies are achieved by the end of the third year, fellows approved to be in this program are eligible to take both gastroenterology and transplant hepatology ABIM certification exams.
Any ACGME-accredited gastroenterology fellowship program that has an accredited hepatology counterpart is eligible to participate in this pilot. Eligible programs and fellows must apply to AASLD during the fellow’s second year. The fellow applicant must complete all clinical gastroenterology requirements before the end of the second year of fellowship and be on a trajectory to meet competency milestones, as the majority of the third year will focus on hepatology.
Since 2012, 59 fellows from 31 programs have participated in this pilot program.4 If you are interested in participating in this pilot program at your institution, it is important to confer with program directors as early as possible to meet all training requirements. In addition, applications are submitted to the Pilot Steering Taskforce during the fellow’s second year for review. This is not meant to be a competitive process and all fellows who meet the criteria are approved.
This track may not be ideal for all fellows interested in advanced and transplant hepatology. In particular, there may be a trade-off between achieving clinical competency in a shortened training period and pursuing scholarly activity. This pilot program is designed to be an intensive clinical track, so fellows who wish to focus on research should discuss with their program directors whether this is the best approach.
What has been your career path after advanced training in hepatology?
I first became interested in hepatology during my inpatient rotations as a medical student. This interest led me to become involved in research in this area very early in my career. The current structure of the fellowship as well as the board certification exam were both developed while I was in training and I adjusted my plans to complete 3 years of gastroenterology fellowship followed by an ACGME-accredited liver transplant fellowship year. Since completing training, I have worked as an attending at an academic medical center in a large liver transplant program and continue to care for patients with all forms of liver disease. In addition, I continued to pursue research as a large component of my job and now have NIH funding and direct the Transplant Clinical Research Center at Columbia University. Finally, I have always been devoted to education and am the program director for the transplant hepatology fellowship at our institution.
What is the future of advanced hepatology training?
The current transplant hepatology training system has evolved significantly since its inception, including development of curricula, ongoing modification of training requirements, and the development of the innovative pilot program. However, there are issues that continue to be debated by the community. For example, it is not certain when or if the combined gastroenterology and transplant hepatology pilot program will become a permanent pathway for training or how best to select fellows for this approach.
Hepatology continues to be a very dynamic area of medicine. With diseases such as nonalcoholic fatty liver disease and hepatocellular carcinoma on the rise, the urgent need for training in HCV treatment to combat the global epidemic of viral hepatitis, and the growing number of patients on the liver transplant waiting list, there has never been a more exciting time to choose hepatology as a career.
References
1. Luxon BA. So you want to be a hepatologist? Gastroenterology. 2013;145(6):1182-5.
2. Bacon BR, Grosso LJ, Freedman N, Althouse LA. Subspecialty certification in transplant hepatology. Liver Transpl. 2007;13(11):1479-81.
3. https://apps.acgme.org/ads/public/reports/report/1.
4. https://www.aasld.org/events-professional-development/educational-learning-faq.
Dr. Verna is assistant professor of medicine, program director, transplant hepatology fellowship, director of clinical research, Transplant Clinical Research Center, Columbia University Medical Center, New York.
Time for a facelift?
A few weeks ago I visited my primary care physician in her new office. As the first patient of the day I was immediately ushered into the examining room by a woman I assume was a medical assistant. She didn’t introduce herself, but her name tag read “Marcy” (not her real name). Her demeanor could best be described as cheerless. She efficiently took my vital signs, asked me my height, and weighed me. She ran through the usual list of screening questions without the slightest hint of a smile despite my efforts to gently inject a bit of levity into my answers.
With her work completed, she left me to wait for “the doctor” without a clue about who I was. She knew that I had one beer and one glass of wine each evening, and that I always wore a seatbelt and didn’t have gun. But she hadn’t provided any outward evidence that she cared about the person who had been providing the answers.
There was a welcome lifting of the chill when my former colleague and current physician entered the exam room. After we had done some catching up about our families and before we started talking about my blood pressure I said, “Marcy really needs to lighten up a bit.”
My observation came as no surprise to my doctor. The transition to a new hospital-owned group practice still had some rough edges including the struggle to instill a more customer-friendly culture among the support staff that she had inherited. She thanked me for my unsolicited feedback.
When Marcy returned to administer my “pneumonia shot” she was wearing a smile. And she was more than willing to engage in the kind of banter that may not have much substance, but is the currency that most of us use to ease the tension in potentially uncomfortable situations. Obviously, while I was waiting she had been given a quick course in customer service.
Marcy and the receptionists are the face of that office, and it certainly wasn’t a welcoming or friendly face. No one was rude. On the other hand, no one was trying to treat the patients as they would like to be treated themselves. You could accuse me of being a nit picky curmudgeon. You could ask if the addition of a smiling face or two would have made a difference in the quality of care coming out of that office. It may not have, but it wouldn’t have hurt, and it would be the nice thing to do.
But and take some of the edge off the anger of patients who are unhappy about the care they have been receiving. There is some evidence that hospitalized patients in customer-friendly situations do better. And I bet that patients seen in customer-friendly offices staff get better more quickly.
If you are aware of staff members whose behavior could be more customer friendly, have you said something to them? It can be touchy. You probably aren’t their supervisor. They may not being doing anything wrong. But their failure to make a pleasant and caring first impression may be making your job more difficult.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
A few weeks ago I visited my primary care physician in her new office. As the first patient of the day I was immediately ushered into the examining room by a woman I assume was a medical assistant. She didn’t introduce herself, but her name tag read “Marcy” (not her real name). Her demeanor could best be described as cheerless. She efficiently took my vital signs, asked me my height, and weighed me. She ran through the usual list of screening questions without the slightest hint of a smile despite my efforts to gently inject a bit of levity into my answers.
With her work completed, she left me to wait for “the doctor” without a clue about who I was. She knew that I had one beer and one glass of wine each evening, and that I always wore a seatbelt and didn’t have gun. But she hadn’t provided any outward evidence that she cared about the person who had been providing the answers.
There was a welcome lifting of the chill when my former colleague and current physician entered the exam room. After we had done some catching up about our families and before we started talking about my blood pressure I said, “Marcy really needs to lighten up a bit.”
My observation came as no surprise to my doctor. The transition to a new hospital-owned group practice still had some rough edges including the struggle to instill a more customer-friendly culture among the support staff that she had inherited. She thanked me for my unsolicited feedback.
When Marcy returned to administer my “pneumonia shot” she was wearing a smile. And she was more than willing to engage in the kind of banter that may not have much substance, but is the currency that most of us use to ease the tension in potentially uncomfortable situations. Obviously, while I was waiting she had been given a quick course in customer service.
Marcy and the receptionists are the face of that office, and it certainly wasn’t a welcoming or friendly face. No one was rude. On the other hand, no one was trying to treat the patients as they would like to be treated themselves. You could accuse me of being a nit picky curmudgeon. You could ask if the addition of a smiling face or two would have made a difference in the quality of care coming out of that office. It may not have, but it wouldn’t have hurt, and it would be the nice thing to do.
But and take some of the edge off the anger of patients who are unhappy about the care they have been receiving. There is some evidence that hospitalized patients in customer-friendly situations do better. And I bet that patients seen in customer-friendly offices staff get better more quickly.
If you are aware of staff members whose behavior could be more customer friendly, have you said something to them? It can be touchy. You probably aren’t their supervisor. They may not being doing anything wrong. But their failure to make a pleasant and caring first impression may be making your job more difficult.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
A few weeks ago I visited my primary care physician in her new office. As the first patient of the day I was immediately ushered into the examining room by a woman I assume was a medical assistant. She didn’t introduce herself, but her name tag read “Marcy” (not her real name). Her demeanor could best be described as cheerless. She efficiently took my vital signs, asked me my height, and weighed me. She ran through the usual list of screening questions without the slightest hint of a smile despite my efforts to gently inject a bit of levity into my answers.
With her work completed, she left me to wait for “the doctor” without a clue about who I was. She knew that I had one beer and one glass of wine each evening, and that I always wore a seatbelt and didn’t have gun. But she hadn’t provided any outward evidence that she cared about the person who had been providing the answers.
There was a welcome lifting of the chill when my former colleague and current physician entered the exam room. After we had done some catching up about our families and before we started talking about my blood pressure I said, “Marcy really needs to lighten up a bit.”
My observation came as no surprise to my doctor. The transition to a new hospital-owned group practice still had some rough edges including the struggle to instill a more customer-friendly culture among the support staff that she had inherited. She thanked me for my unsolicited feedback.
When Marcy returned to administer my “pneumonia shot” she was wearing a smile. And she was more than willing to engage in the kind of banter that may not have much substance, but is the currency that most of us use to ease the tension in potentially uncomfortable situations. Obviously, while I was waiting she had been given a quick course in customer service.
Marcy and the receptionists are the face of that office, and it certainly wasn’t a welcoming or friendly face. No one was rude. On the other hand, no one was trying to treat the patients as they would like to be treated themselves. You could accuse me of being a nit picky curmudgeon. You could ask if the addition of a smiling face or two would have made a difference in the quality of care coming out of that office. It may not have, but it wouldn’t have hurt, and it would be the nice thing to do.
But and take some of the edge off the anger of patients who are unhappy about the care they have been receiving. There is some evidence that hospitalized patients in customer-friendly situations do better. And I bet that patients seen in customer-friendly offices staff get better more quickly.
If you are aware of staff members whose behavior could be more customer friendly, have you said something to them? It can be touchy. You probably aren’t their supervisor. They may not being doing anything wrong. But their failure to make a pleasant and caring first impression may be making your job more difficult.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
New rankings focus on child health care
a personal finance website.
The District of Columbia joined the party and finished second to Vermont, which pushed Nevada down to 51st place, according to WalletHub’s “Best & Worst States for Children’s Health Care” for 2018.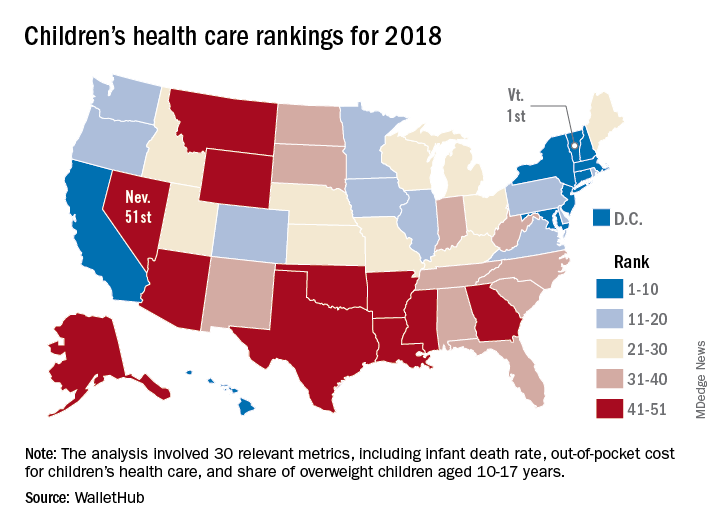
Louisiana’s 50th-ranked health system was just ahead of Nevada’s, and those two were below Texas in 49th, Mississippi in 48th, Arkansas in 47th, and Montana in 46th. The top five had a strong New England flavor (think maple syrup and cranberries), with Vermont joined by Massachusetts in third and Connecticut in fourth, followed by New England’s neighbor New York in fifth, the report showed.
The analysis involved a 100-point system covering three broad areas of health care: health and access to health care (55 points); nutrition, physical activity, and obesity (40 points); and oral health (5 points). Those categories were divided into a total of 30 relevant metrics, including the share of children aged 0-17 years who were in excellent to very good health, pediatricians and family physicians per capita, share of obese children aged 10-17 years, and share of children aged 1-17 years with excellent or very good teeth.
Vermont’s strong showing in WalletHub’s metric system was driven by first-place finishes in lowest infant death rate, pediatricians and family physicians per capita, and percentage of children with recent medical and dental checkups, along with being in third place for percentage of uninsured children and for percentage of overweight children. D.C. had the lowest percentage of children with unaffordable medical bills, and Massachusetts had the lowest percentage of uninsured children, according to data collected by WalletHub from such sources as the U.S. Census Bureau, the Council for Community and Economic research, and the Trust for America’s Health.
“Parents should be supported to learn about and be active in [their] children’s development. … Since our safety net is anemic and our idea of health is about lack of symptoms, this answer challenges us to think more critically about our living conditions and those of our children,” Michael Montoya, PhD, associate professor emeritus in the departments of anthropology, public health, and the program in medical education for the Latino community at the University of California, Irvine, said in the report.
Another respondent to the report, Christina M. Dalton, PhD, of the department of economics at Wake Forest University, Winston-Salem, N.C., said, “Children’s health coverage has important potential to improve health and economic outcomes in the future since early good health enables children to learn better in school. However, any expansion of public options needs to take into account the idea that public insurance can end up taking enrollees away from the private market. … It’s always a trade-off of increasing coverage while not attracting too many of the enrollees that would have already bought insurance without government funding.”
a personal finance website.
The District of Columbia joined the party and finished second to Vermont, which pushed Nevada down to 51st place, according to WalletHub’s “Best & Worst States for Children’s Health Care” for 2018.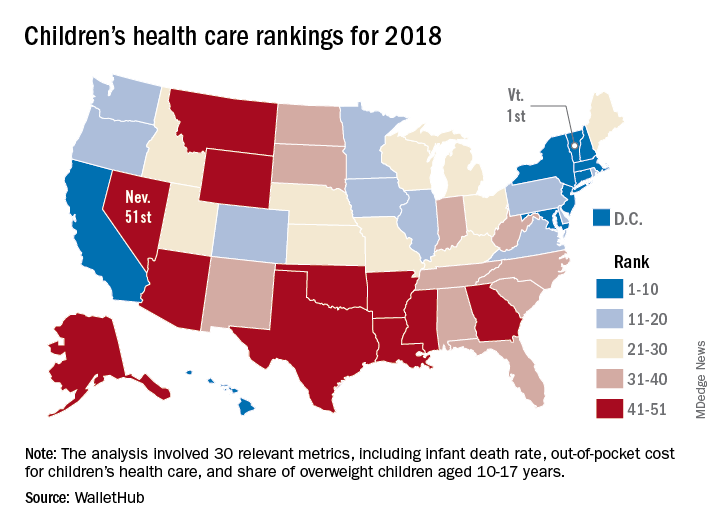
Louisiana’s 50th-ranked health system was just ahead of Nevada’s, and those two were below Texas in 49th, Mississippi in 48th, Arkansas in 47th, and Montana in 46th. The top five had a strong New England flavor (think maple syrup and cranberries), with Vermont joined by Massachusetts in third and Connecticut in fourth, followed by New England’s neighbor New York in fifth, the report showed.
The analysis involved a 100-point system covering three broad areas of health care: health and access to health care (55 points); nutrition, physical activity, and obesity (40 points); and oral health (5 points). Those categories were divided into a total of 30 relevant metrics, including the share of children aged 0-17 years who were in excellent to very good health, pediatricians and family physicians per capita, share of obese children aged 10-17 years, and share of children aged 1-17 years with excellent or very good teeth.
Vermont’s strong showing in WalletHub’s metric system was driven by first-place finishes in lowest infant death rate, pediatricians and family physicians per capita, and percentage of children with recent medical and dental checkups, along with being in third place for percentage of uninsured children and for percentage of overweight children. D.C. had the lowest percentage of children with unaffordable medical bills, and Massachusetts had the lowest percentage of uninsured children, according to data collected by WalletHub from such sources as the U.S. Census Bureau, the Council for Community and Economic research, and the Trust for America’s Health.
“Parents should be supported to learn about and be active in [their] children’s development. … Since our safety net is anemic and our idea of health is about lack of symptoms, this answer challenges us to think more critically about our living conditions and those of our children,” Michael Montoya, PhD, associate professor emeritus in the departments of anthropology, public health, and the program in medical education for the Latino community at the University of California, Irvine, said in the report.
Another respondent to the report, Christina M. Dalton, PhD, of the department of economics at Wake Forest University, Winston-Salem, N.C., said, “Children’s health coverage has important potential to improve health and economic outcomes in the future since early good health enables children to learn better in school. However, any expansion of public options needs to take into account the idea that public insurance can end up taking enrollees away from the private market. … It’s always a trade-off of increasing coverage while not attracting too many of the enrollees that would have already bought insurance without government funding.”
a personal finance website.
The District of Columbia joined the party and finished second to Vermont, which pushed Nevada down to 51st place, according to WalletHub’s “Best & Worst States for Children’s Health Care” for 2018.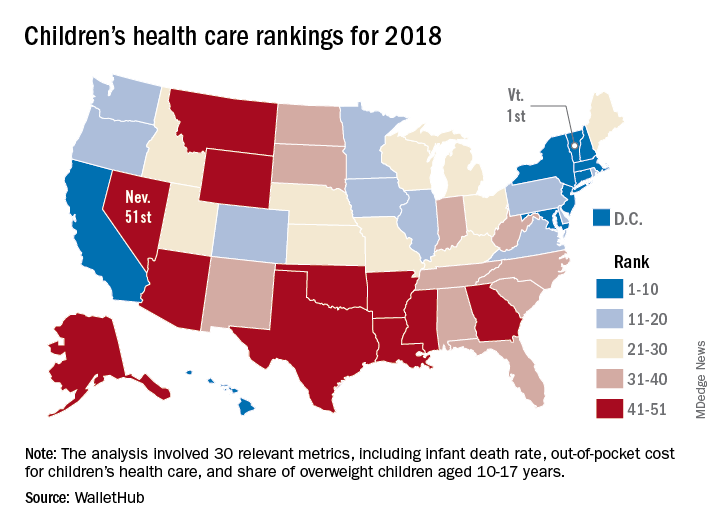
Louisiana’s 50th-ranked health system was just ahead of Nevada’s, and those two were below Texas in 49th, Mississippi in 48th, Arkansas in 47th, and Montana in 46th. The top five had a strong New England flavor (think maple syrup and cranberries), with Vermont joined by Massachusetts in third and Connecticut in fourth, followed by New England’s neighbor New York in fifth, the report showed.
The analysis involved a 100-point system covering three broad areas of health care: health and access to health care (55 points); nutrition, physical activity, and obesity (40 points); and oral health (5 points). Those categories were divided into a total of 30 relevant metrics, including the share of children aged 0-17 years who were in excellent to very good health, pediatricians and family physicians per capita, share of obese children aged 10-17 years, and share of children aged 1-17 years with excellent or very good teeth.
Vermont’s strong showing in WalletHub’s metric system was driven by first-place finishes in lowest infant death rate, pediatricians and family physicians per capita, and percentage of children with recent medical and dental checkups, along with being in third place for percentage of uninsured children and for percentage of overweight children. D.C. had the lowest percentage of children with unaffordable medical bills, and Massachusetts had the lowest percentage of uninsured children, according to data collected by WalletHub from such sources as the U.S. Census Bureau, the Council for Community and Economic research, and the Trust for America’s Health.
“Parents should be supported to learn about and be active in [their] children’s development. … Since our safety net is anemic and our idea of health is about lack of symptoms, this answer challenges us to think more critically about our living conditions and those of our children,” Michael Montoya, PhD, associate professor emeritus in the departments of anthropology, public health, and the program in medical education for the Latino community at the University of California, Irvine, said in the report.
Another respondent to the report, Christina M. Dalton, PhD, of the department of economics at Wake Forest University, Winston-Salem, N.C., said, “Children’s health coverage has important potential to improve health and economic outcomes in the future since early good health enables children to learn better in school. However, any expansion of public options needs to take into account the idea that public insurance can end up taking enrollees away from the private market. … It’s always a trade-off of increasing coverage while not attracting too many of the enrollees that would have already bought insurance without government funding.”