User login
TissueGene-C effects on knee OA seen at 3 years
LIVERPOOL, ENGLAND – TissueGene-C continues to show promise as a potential disease-modifying osteoarthritis drug, according to the long-term follow-up data of a phase 3 trial.
Within 2-3 years of receiving a single injection of the novel cell-gene therapy, patients with moderate knee OA were still experiencing significant improvement in the coprimary endpoints of knee symptoms, function, sports activity, and knee pain versus baseline values.
Differences in International Knee Documentation Committee (IKDC) scores from baseline to 2 and 3 years were a respective 15.3 and 14.8 points (both P less than .05 vs. baseline). Pain, assessed on a visual analog scale, was also significantly improved from baseline to 2 and 3 years (score changes –23.5 and –23.3; P less than .05 vs. baseline).
There were also significant improvements in the secondary endpoint of pain, stiffness, and physical function measured by the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), with changes in scores of –19.8 and –17.4 versus baseline at 2 and 3 years, respectively (both P less than .05 vs. baseline).
“INVOISSA-K [TissueGene-C] is the first-in-class cell and gene therapy for the treatment of knee OA,” Dr. Lee reminded delegates at the congress, which is sponsored by the Osteoarthritis Research Society International. The novel treatment was made by collecting chondrocytes from a subject with polydactyl hands and then culturing these to create two subpopulations of cells, one with allogenic chondrocytes and the other with genetically modified chondrocytes that overexpress transforming growth factor-beta1. These subpopulations are then mixed in the ratio of 3:1 and delivered in a single intra-articular injection.
Dr. Lee, who is the president and chief executive officer of Kolon TissueGene, Rockville, Md., reported new findings of a phase 3 trial conducted exclusively in Korea at 12 study centers, the results of which were first presented at OARSI 2016.
At that time only the 12-month primary endpoint data were available, which showed that TissueGene-C improved IKDC scores from baseline by a significantly greater amount than a saline placebo, with changes in scores of 15.1 and 5 points, respectively, versus baseline values. Improvements in IKDC scores were seen as early as 3 months but only became significantly better than placebo at 6 months.
Similarly, visual analog scale pain scores had improved from baseline as early as 3 months but were only significantly different from placebo at 6 months (–23.4 change from baseline for TissueGene-C vs. –14.6 for placebo) and out to 12 months (–24.5 vs. –10.3). WOMAC scores with TissueGene-C were only significantly different from placebo at 12 months (–13.5 vs. –6.2 from baseline, respectively).
The 12-month OMERACT-OARSI responder rate was 84% for TissueGene-C and 45% for placebo. The most common adverse events seen with TissueGene-C were related to the injection site, with peripheral edema (9%), arthralgia (8%), joint swelling (6%), and injection-site pain (5%) reported.
A total of 163 patients were recruited into the study, all had Kellgren-Lawrence grade 3 knee OA, which was also graded as 3 or 4 on the International Cartilage Regeneration & Joint Preservation Society scale. Major lesions had be 6 cm2 or smaller. Active treatment was given to 78 patients, and 81 received placebo. The primary assessment period was at 12 months, but patients continued to be followed out to 5 years.
At OARSI 2018, Dr. Lee presented the findings of 12-month structural modification analyses for the first time. These showed that while the osteophyte score on MRI was not significantly different from baseline in the active-treatment arm, there was a significantly increased osteophyte score and total cartilage defect in the placebo-treated patients versus baseline values.
Subchondral bone changes at 12 months showed a trend for less bone area change with TissueGene-C than placebo and a trend for increased cartilage thickness. Greater reductions in serum CTX-1 and urine CTX-II were seen with active treatment than placebo, relative to screening values.
X-ray evaluation of joint-space narrowing showed that nonprogression was more likely in patients treated with TissueGene-C than with placebo (77% vs. 57%), although this was not significant. In addition, fewer patients treated with TissueGene-C than placebo who needed a total knee replacement at 2 years (0% and 7.5%) and at 3 years (2% and 14%).
TissueGene-C “has great potential” for being the first disease-modifying osteoarthritis drug to get to market, Dr. Lee suggested.
The clinical development program for TissueGene-C is further advanced in Korea than in the United States, where a phase 3 trial is about to start recruitment soon.
“We started our clinical trials in 2005 in Korea and in the U.S. simultaneously,” Dr. Lee said, noting that a biologics license application submitted in Korea in 2016 had been accepted by the Ministry of Food and Drug Safety on July 12, 2017, while only phase 1 and 2 trials have been completed in the United States
The study was funded by Kolon Life Science and TissueGene. Dr. Lee is an employee of TissueGene.
SOURCE: Lee B et al. Osteoarthritis Cartilage. 2018 Apr;26(1):S43-4.
LIVERPOOL, ENGLAND – TissueGene-C continues to show promise as a potential disease-modifying osteoarthritis drug, according to the long-term follow-up data of a phase 3 trial.
Within 2-3 years of receiving a single injection of the novel cell-gene therapy, patients with moderate knee OA were still experiencing significant improvement in the coprimary endpoints of knee symptoms, function, sports activity, and knee pain versus baseline values.
Differences in International Knee Documentation Committee (IKDC) scores from baseline to 2 and 3 years were a respective 15.3 and 14.8 points (both P less than .05 vs. baseline). Pain, assessed on a visual analog scale, was also significantly improved from baseline to 2 and 3 years (score changes –23.5 and –23.3; P less than .05 vs. baseline).
There were also significant improvements in the secondary endpoint of pain, stiffness, and physical function measured by the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), with changes in scores of –19.8 and –17.4 versus baseline at 2 and 3 years, respectively (both P less than .05 vs. baseline).
“INVOISSA-K [TissueGene-C] is the first-in-class cell and gene therapy for the treatment of knee OA,” Dr. Lee reminded delegates at the congress, which is sponsored by the Osteoarthritis Research Society International. The novel treatment was made by collecting chondrocytes from a subject with polydactyl hands and then culturing these to create two subpopulations of cells, one with allogenic chondrocytes and the other with genetically modified chondrocytes that overexpress transforming growth factor-beta1. These subpopulations are then mixed in the ratio of 3:1 and delivered in a single intra-articular injection.
Dr. Lee, who is the president and chief executive officer of Kolon TissueGene, Rockville, Md., reported new findings of a phase 3 trial conducted exclusively in Korea at 12 study centers, the results of which were first presented at OARSI 2016.
At that time only the 12-month primary endpoint data were available, which showed that TissueGene-C improved IKDC scores from baseline by a significantly greater amount than a saline placebo, with changes in scores of 15.1 and 5 points, respectively, versus baseline values. Improvements in IKDC scores were seen as early as 3 months but only became significantly better than placebo at 6 months.
Similarly, visual analog scale pain scores had improved from baseline as early as 3 months but were only significantly different from placebo at 6 months (–23.4 change from baseline for TissueGene-C vs. –14.6 for placebo) and out to 12 months (–24.5 vs. –10.3). WOMAC scores with TissueGene-C were only significantly different from placebo at 12 months (–13.5 vs. –6.2 from baseline, respectively).
The 12-month OMERACT-OARSI responder rate was 84% for TissueGene-C and 45% for placebo. The most common adverse events seen with TissueGene-C were related to the injection site, with peripheral edema (9%), arthralgia (8%), joint swelling (6%), and injection-site pain (5%) reported.
A total of 163 patients were recruited into the study, all had Kellgren-Lawrence grade 3 knee OA, which was also graded as 3 or 4 on the International Cartilage Regeneration & Joint Preservation Society scale. Major lesions had be 6 cm2 or smaller. Active treatment was given to 78 patients, and 81 received placebo. The primary assessment period was at 12 months, but patients continued to be followed out to 5 years.
At OARSI 2018, Dr. Lee presented the findings of 12-month structural modification analyses for the first time. These showed that while the osteophyte score on MRI was not significantly different from baseline in the active-treatment arm, there was a significantly increased osteophyte score and total cartilage defect in the placebo-treated patients versus baseline values.
Subchondral bone changes at 12 months showed a trend for less bone area change with TissueGene-C than placebo and a trend for increased cartilage thickness. Greater reductions in serum CTX-1 and urine CTX-II were seen with active treatment than placebo, relative to screening values.
X-ray evaluation of joint-space narrowing showed that nonprogression was more likely in patients treated with TissueGene-C than with placebo (77% vs. 57%), although this was not significant. In addition, fewer patients treated with TissueGene-C than placebo who needed a total knee replacement at 2 years (0% and 7.5%) and at 3 years (2% and 14%).
TissueGene-C “has great potential” for being the first disease-modifying osteoarthritis drug to get to market, Dr. Lee suggested.
The clinical development program for TissueGene-C is further advanced in Korea than in the United States, where a phase 3 trial is about to start recruitment soon.
“We started our clinical trials in 2005 in Korea and in the U.S. simultaneously,” Dr. Lee said, noting that a biologics license application submitted in Korea in 2016 had been accepted by the Ministry of Food and Drug Safety on July 12, 2017, while only phase 1 and 2 trials have been completed in the United States
The study was funded by Kolon Life Science and TissueGene. Dr. Lee is an employee of TissueGene.
SOURCE: Lee B et al. Osteoarthritis Cartilage. 2018 Apr;26(1):S43-4.
LIVERPOOL, ENGLAND – TissueGene-C continues to show promise as a potential disease-modifying osteoarthritis drug, according to the long-term follow-up data of a phase 3 trial.
Within 2-3 years of receiving a single injection of the novel cell-gene therapy, patients with moderate knee OA were still experiencing significant improvement in the coprimary endpoints of knee symptoms, function, sports activity, and knee pain versus baseline values.
Differences in International Knee Documentation Committee (IKDC) scores from baseline to 2 and 3 years were a respective 15.3 and 14.8 points (both P less than .05 vs. baseline). Pain, assessed on a visual analog scale, was also significantly improved from baseline to 2 and 3 years (score changes –23.5 and –23.3; P less than .05 vs. baseline).
There were also significant improvements in the secondary endpoint of pain, stiffness, and physical function measured by the Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), with changes in scores of –19.8 and –17.4 versus baseline at 2 and 3 years, respectively (both P less than .05 vs. baseline).
“INVOISSA-K [TissueGene-C] is the first-in-class cell and gene therapy for the treatment of knee OA,” Dr. Lee reminded delegates at the congress, which is sponsored by the Osteoarthritis Research Society International. The novel treatment was made by collecting chondrocytes from a subject with polydactyl hands and then culturing these to create two subpopulations of cells, one with allogenic chondrocytes and the other with genetically modified chondrocytes that overexpress transforming growth factor-beta1. These subpopulations are then mixed in the ratio of 3:1 and delivered in a single intra-articular injection.
Dr. Lee, who is the president and chief executive officer of Kolon TissueGene, Rockville, Md., reported new findings of a phase 3 trial conducted exclusively in Korea at 12 study centers, the results of which were first presented at OARSI 2016.
At that time only the 12-month primary endpoint data were available, which showed that TissueGene-C improved IKDC scores from baseline by a significantly greater amount than a saline placebo, with changes in scores of 15.1 and 5 points, respectively, versus baseline values. Improvements in IKDC scores were seen as early as 3 months but only became significantly better than placebo at 6 months.
Similarly, visual analog scale pain scores had improved from baseline as early as 3 months but were only significantly different from placebo at 6 months (–23.4 change from baseline for TissueGene-C vs. –14.6 for placebo) and out to 12 months (–24.5 vs. –10.3). WOMAC scores with TissueGene-C were only significantly different from placebo at 12 months (–13.5 vs. –6.2 from baseline, respectively).
The 12-month OMERACT-OARSI responder rate was 84% for TissueGene-C and 45% for placebo. The most common adverse events seen with TissueGene-C were related to the injection site, with peripheral edema (9%), arthralgia (8%), joint swelling (6%), and injection-site pain (5%) reported.
A total of 163 patients were recruited into the study, all had Kellgren-Lawrence grade 3 knee OA, which was also graded as 3 or 4 on the International Cartilage Regeneration & Joint Preservation Society scale. Major lesions had be 6 cm2 or smaller. Active treatment was given to 78 patients, and 81 received placebo. The primary assessment period was at 12 months, but patients continued to be followed out to 5 years.
At OARSI 2018, Dr. Lee presented the findings of 12-month structural modification analyses for the first time. These showed that while the osteophyte score on MRI was not significantly different from baseline in the active-treatment arm, there was a significantly increased osteophyte score and total cartilage defect in the placebo-treated patients versus baseline values.
Subchondral bone changes at 12 months showed a trend for less bone area change with TissueGene-C than placebo and a trend for increased cartilage thickness. Greater reductions in serum CTX-1 and urine CTX-II were seen with active treatment than placebo, relative to screening values.
X-ray evaluation of joint-space narrowing showed that nonprogression was more likely in patients treated with TissueGene-C than with placebo (77% vs. 57%), although this was not significant. In addition, fewer patients treated with TissueGene-C than placebo who needed a total knee replacement at 2 years (0% and 7.5%) and at 3 years (2% and 14%).
TissueGene-C “has great potential” for being the first disease-modifying osteoarthritis drug to get to market, Dr. Lee suggested.
The clinical development program for TissueGene-C is further advanced in Korea than in the United States, where a phase 3 trial is about to start recruitment soon.
“We started our clinical trials in 2005 in Korea and in the U.S. simultaneously,” Dr. Lee said, noting that a biologics license application submitted in Korea in 2016 had been accepted by the Ministry of Food and Drug Safety on July 12, 2017, while only phase 1 and 2 trials have been completed in the United States
The study was funded by Kolon Life Science and TissueGene. Dr. Lee is an employee of TissueGene.
SOURCE: Lee B et al. Osteoarthritis Cartilage. 2018 Apr;26(1):S43-4.
REPORTING FROM OARSI 2018
Key clinical point: A single intra-articular injection of TissueGene C produced significant and long-term relief of knee osteoarthritis.
Major finding: Changes in baseline International Knee Documentation Committee and visual analog scale pain scores from baseline to 2 and 3 years were 15.3 and 14.8 points (P less than .05), and –23.5 and –23.3 (P less than .05), respectively.
Study details: A multicenter, phase 3, randomized, double-blind, placebo-controlled trial of 163 patients with knee osteoarthritis.
Disclosures: The study was funded by Kolon Life Science and TissueGene. Dr. Lee is an employee of TissueGene.
Source: Lee B et al. Osteoarthritis Cartilage. 2018 Apr;26(1):S43-4.
Fewer preterm deliveries, and perinatal mortality down
Fewer infants are being delivered early, and there has been a decline in neonatal mortality, according to a retrospective cohort study of more than 34 million singleton live births.
Researchers presented the results of a study in the May 14 online edition of JAMA Pediatrics that attempted to quantify changes in gestational age distribution and gestational age–specific perinatal mortality in the United States between 2007 and 2015.
However the proportion of births at a gestational age of 39-40 weeks increased from 54.5% to 60.2% in that same time period.
“The decreasing proportion of births at gestational ages of 34-36 and 37-38 weeks may be associated with changes in the timing of elective delivery, with hospital policies and quality initiatives effectively reducing unindicated deliveries before 39 completed weeks of gestation,” wrote Cande V. Ananth, PhD, of Columbia University, New York, and coauthors.
“Increased use of low-dose aspirin in women with ischemic placental disease may additionally have resulted in decreased need for indicated delivery before 39 weeks.”
At the same time, perinatal mortality rates decreased overall, from 9 per 1,000 births in 2007 to 8.6 per 1,000 births in 2015, but increased significantly in gestational ages 32-33 weeks (7%), 34-36 weeks (15%), and 37-38 weeks (23%) over that period. There was also a significant 31% increase in perinatal mortality at gestational age 42-44 weeks, but decreases at 20-27 weeks and 39-40 weeks.
Stillbirth rates also increased for gestational ages of 20-27 weeks, 28-31 weeks, 32-33 weeks, 34-36 weeks, 37-38 weeks, and 42-44 weeks.
Commenting on the changes in perinatal and neonatal mortality rates at gestational ages of 34-36 weeks and 37-38 weeks, the authors suggested this may have been the result of recommendations to postpone elective deliveries until 39 weeks.
“A possible reason for the increased mortality at a gestational age of 37-38 weeks could be that physicians may be more likely to defer to 39 weeks for delivery for women at moderately increased risk for adverse perinatal outcomes,” they wrote.
“We found that the decrease in neonatal mortality rates from 2007 to 2015 in the United States was largely associated with changes in the underlying gestational age distribution and less associated with changes in gestational age–specific mortality.”
The researchers reported that they had no conflicts of interest.
SOURCE: Ananth C et al. JAMA Pediatrics. 2018 May 14. doi: 10.1001/jamapediatrics.2018.0249.
Fewer infants are being delivered early, and there has been a decline in neonatal mortality, according to a retrospective cohort study of more than 34 million singleton live births.
Researchers presented the results of a study in the May 14 online edition of JAMA Pediatrics that attempted to quantify changes in gestational age distribution and gestational age–specific perinatal mortality in the United States between 2007 and 2015.
However the proportion of births at a gestational age of 39-40 weeks increased from 54.5% to 60.2% in that same time period.
“The decreasing proportion of births at gestational ages of 34-36 and 37-38 weeks may be associated with changes in the timing of elective delivery, with hospital policies and quality initiatives effectively reducing unindicated deliveries before 39 completed weeks of gestation,” wrote Cande V. Ananth, PhD, of Columbia University, New York, and coauthors.
“Increased use of low-dose aspirin in women with ischemic placental disease may additionally have resulted in decreased need for indicated delivery before 39 weeks.”
At the same time, perinatal mortality rates decreased overall, from 9 per 1,000 births in 2007 to 8.6 per 1,000 births in 2015, but increased significantly in gestational ages 32-33 weeks (7%), 34-36 weeks (15%), and 37-38 weeks (23%) over that period. There was also a significant 31% increase in perinatal mortality at gestational age 42-44 weeks, but decreases at 20-27 weeks and 39-40 weeks.
Stillbirth rates also increased for gestational ages of 20-27 weeks, 28-31 weeks, 32-33 weeks, 34-36 weeks, 37-38 weeks, and 42-44 weeks.
Commenting on the changes in perinatal and neonatal mortality rates at gestational ages of 34-36 weeks and 37-38 weeks, the authors suggested this may have been the result of recommendations to postpone elective deliveries until 39 weeks.
“A possible reason for the increased mortality at a gestational age of 37-38 weeks could be that physicians may be more likely to defer to 39 weeks for delivery for women at moderately increased risk for adverse perinatal outcomes,” they wrote.
“We found that the decrease in neonatal mortality rates from 2007 to 2015 in the United States was largely associated with changes in the underlying gestational age distribution and less associated with changes in gestational age–specific mortality.”
The researchers reported that they had no conflicts of interest.
SOURCE: Ananth C et al. JAMA Pediatrics. 2018 May 14. doi: 10.1001/jamapediatrics.2018.0249.
Fewer infants are being delivered early, and there has been a decline in neonatal mortality, according to a retrospective cohort study of more than 34 million singleton live births.
Researchers presented the results of a study in the May 14 online edition of JAMA Pediatrics that attempted to quantify changes in gestational age distribution and gestational age–specific perinatal mortality in the United States between 2007 and 2015.
However the proportion of births at a gestational age of 39-40 weeks increased from 54.5% to 60.2% in that same time period.
“The decreasing proportion of births at gestational ages of 34-36 and 37-38 weeks may be associated with changes in the timing of elective delivery, with hospital policies and quality initiatives effectively reducing unindicated deliveries before 39 completed weeks of gestation,” wrote Cande V. Ananth, PhD, of Columbia University, New York, and coauthors.
“Increased use of low-dose aspirin in women with ischemic placental disease may additionally have resulted in decreased need for indicated delivery before 39 weeks.”
At the same time, perinatal mortality rates decreased overall, from 9 per 1,000 births in 2007 to 8.6 per 1,000 births in 2015, but increased significantly in gestational ages 32-33 weeks (7%), 34-36 weeks (15%), and 37-38 weeks (23%) over that period. There was also a significant 31% increase in perinatal mortality at gestational age 42-44 weeks, but decreases at 20-27 weeks and 39-40 weeks.
Stillbirth rates also increased for gestational ages of 20-27 weeks, 28-31 weeks, 32-33 weeks, 34-36 weeks, 37-38 weeks, and 42-44 weeks.
Commenting on the changes in perinatal and neonatal mortality rates at gestational ages of 34-36 weeks and 37-38 weeks, the authors suggested this may have been the result of recommendations to postpone elective deliveries until 39 weeks.
“A possible reason for the increased mortality at a gestational age of 37-38 weeks could be that physicians may be more likely to defer to 39 weeks for delivery for women at moderately increased risk for adverse perinatal outcomes,” they wrote.
“We found that the decrease in neonatal mortality rates from 2007 to 2015 in the United States was largely associated with changes in the underlying gestational age distribution and less associated with changes in gestational age–specific mortality.”
The researchers reported that they had no conflicts of interest.
SOURCE: Ananth C et al. JAMA Pediatrics. 2018 May 14. doi: 10.1001/jamapediatrics.2018.0249.
FROM JAMA PEDIATRICS
Key clinical point: Preterm births and perinatal mortality decreased from 2007 to 2015.
Major finding: The proportion of births at 39-40 weeks increased from 54.5% to 60.2% between 2007 and 2015.
Study details: A retrospective cohort study of nearly 35 million singleton births.
Disclosures: The researchers reported that they had no conflicts of interest.
Source: Ananth C et al. JAMA Pediatrics. 2018 May 14. doi: 10.1001/jamapediatrics.2018.0249.
Marketing perks increased opioid prescriptions
, according to a study published in JAMA Internal Medicine.
With 40% of opioid-related deaths still coming from prescription opioids, understanding how marketing influences prescriber habits could lead to the creation of specific policies to lower the number of prescription drugs exchanging hands and save lives.
Dr. Hadland and his colleagues conducted a comparative analysis of opioid prescriptions from 2014 and 2015, retrieved from the Medicare Part D Opioid Prescriber Summary File and cross referenced that information with all recorded transactions from companies to physicians in 2014 from the Open Payments database.
In 2015, a total of 369,139 physicians were recorded prescribing opioids to Medicare patients. About 25,767 (7%) received a combined total of 105,368 “nonresearch opioid-related payments” with a sum total of $9,071,976 in 2014.
While Medicare opioid claims went down in 2015, physicians who received these payments, on average, prescribed 9.3% more opioids than those who did not, according to investigators.
INSYS Therapeutics, Teva Pharmaceuticals USA, and Janssen Pharmaceuticals were the three highest-paying companies, contributing $4.5 million, $869,155, and $854,251, respectively.
Payments included speaking fees ($6.2 million), meals ($1.8 million), travel ($730,824), consulting fees ($290,395), and education ($79,660). Investigators estimated that, with each meal a physician received, there was an associated 0.7% increase in opioid claims.
Dr. Hadland and fellow investigators do acknowledge the possibility of reverse causality, with physicians who already prescribe more opioids being more likely to receive industry payments.
Dr. Hadland and his team report no relevant financial disclosures.
SOURCE: S Hadland et al. JAMA Intern Med. 2018 May 14. doi: 10.1001/jamainternmed.2018.1999.
, according to a study published in JAMA Internal Medicine.
With 40% of opioid-related deaths still coming from prescription opioids, understanding how marketing influences prescriber habits could lead to the creation of specific policies to lower the number of prescription drugs exchanging hands and save lives.
Dr. Hadland and his colleagues conducted a comparative analysis of opioid prescriptions from 2014 and 2015, retrieved from the Medicare Part D Opioid Prescriber Summary File and cross referenced that information with all recorded transactions from companies to physicians in 2014 from the Open Payments database.
In 2015, a total of 369,139 physicians were recorded prescribing opioids to Medicare patients. About 25,767 (7%) received a combined total of 105,368 “nonresearch opioid-related payments” with a sum total of $9,071,976 in 2014.
While Medicare opioid claims went down in 2015, physicians who received these payments, on average, prescribed 9.3% more opioids than those who did not, according to investigators.
INSYS Therapeutics, Teva Pharmaceuticals USA, and Janssen Pharmaceuticals were the three highest-paying companies, contributing $4.5 million, $869,155, and $854,251, respectively.
Payments included speaking fees ($6.2 million), meals ($1.8 million), travel ($730,824), consulting fees ($290,395), and education ($79,660). Investigators estimated that, with each meal a physician received, there was an associated 0.7% increase in opioid claims.
Dr. Hadland and fellow investigators do acknowledge the possibility of reverse causality, with physicians who already prescribe more opioids being more likely to receive industry payments.
Dr. Hadland and his team report no relevant financial disclosures.
SOURCE: S Hadland et al. JAMA Intern Med. 2018 May 14. doi: 10.1001/jamainternmed.2018.1999.
, according to a study published in JAMA Internal Medicine.
With 40% of opioid-related deaths still coming from prescription opioids, understanding how marketing influences prescriber habits could lead to the creation of specific policies to lower the number of prescription drugs exchanging hands and save lives.
Dr. Hadland and his colleagues conducted a comparative analysis of opioid prescriptions from 2014 and 2015, retrieved from the Medicare Part D Opioid Prescriber Summary File and cross referenced that information with all recorded transactions from companies to physicians in 2014 from the Open Payments database.
In 2015, a total of 369,139 physicians were recorded prescribing opioids to Medicare patients. About 25,767 (7%) received a combined total of 105,368 “nonresearch opioid-related payments” with a sum total of $9,071,976 in 2014.
While Medicare opioid claims went down in 2015, physicians who received these payments, on average, prescribed 9.3% more opioids than those who did not, according to investigators.
INSYS Therapeutics, Teva Pharmaceuticals USA, and Janssen Pharmaceuticals were the three highest-paying companies, contributing $4.5 million, $869,155, and $854,251, respectively.
Payments included speaking fees ($6.2 million), meals ($1.8 million), travel ($730,824), consulting fees ($290,395), and education ($79,660). Investigators estimated that, with each meal a physician received, there was an associated 0.7% increase in opioid claims.
Dr. Hadland and fellow investigators do acknowledge the possibility of reverse causality, with physicians who already prescribe more opioids being more likely to receive industry payments.
Dr. Hadland and his team report no relevant financial disclosures.
SOURCE: S Hadland et al. JAMA Intern Med. 2018 May 14. doi: 10.1001/jamainternmed.2018.1999.
FROM JAMA INTERNAL MEDICINE
Key clinical point: Doctors who received nonresearch payments on average had a higher number of opioid prescriptions than those who did not.
Major finding: Receiving a nonresearch payment from a pharmaceutical company was associated with about 9.3% more opioid claims.
Study details: Record analysis of 369,139 physicians collected from the Open Payments database and the Medicare Part D Opioid Prescriber Summary File for the years 2014 and 2015.
Disclosures: Dr. Hadland and his team report no relevant financial disclosures.
Source: S Hadland et al. JAMA Intern Med. 2018 May 14. doi: 10.1001/jamainternmed.2018.1999.
MDedge Daily News: Many moms with postpartum depression go untreated
Progressive Widespread Telangiectasias
The Diagnosis: Cutaneous Collagenous Vasculopathy
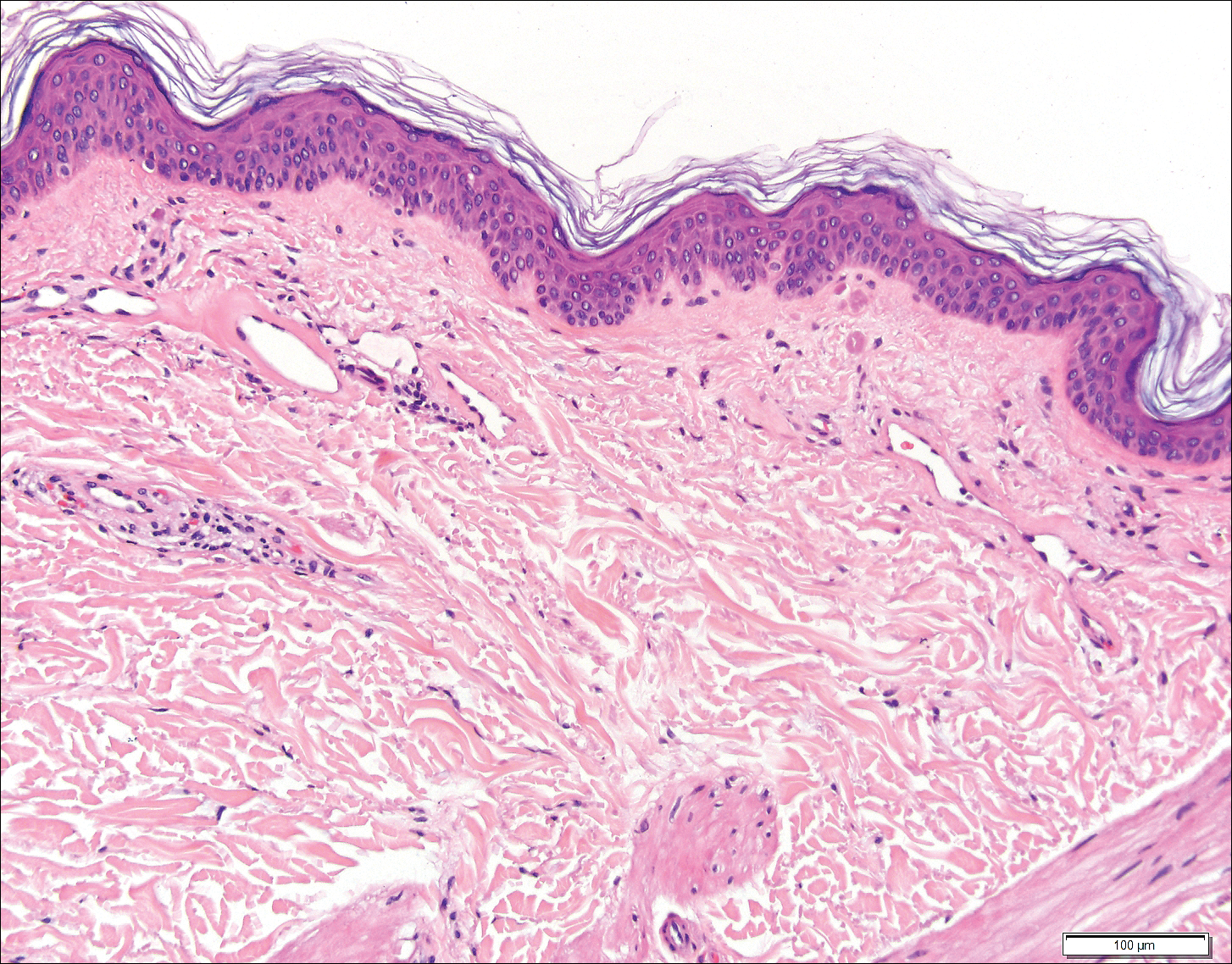
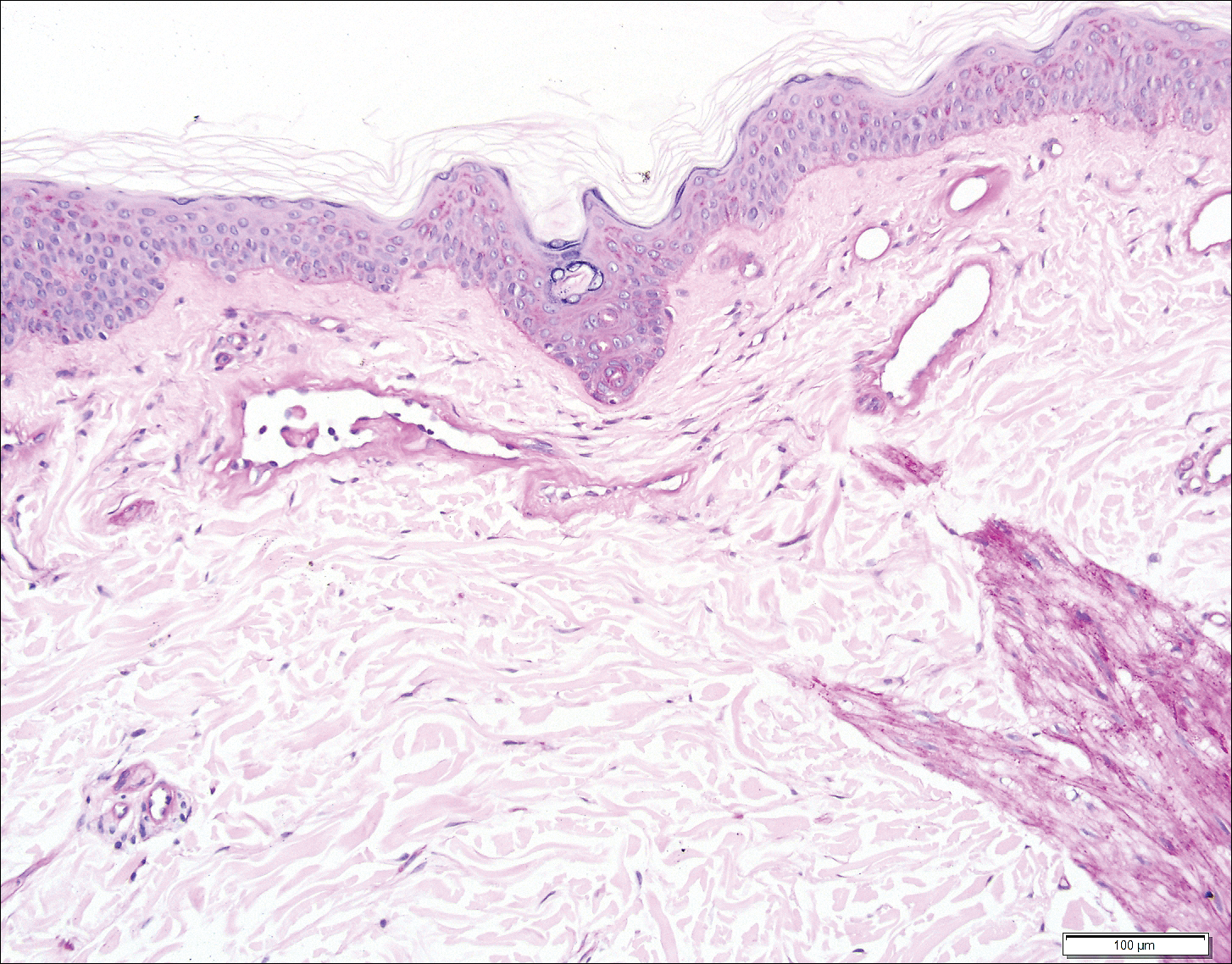
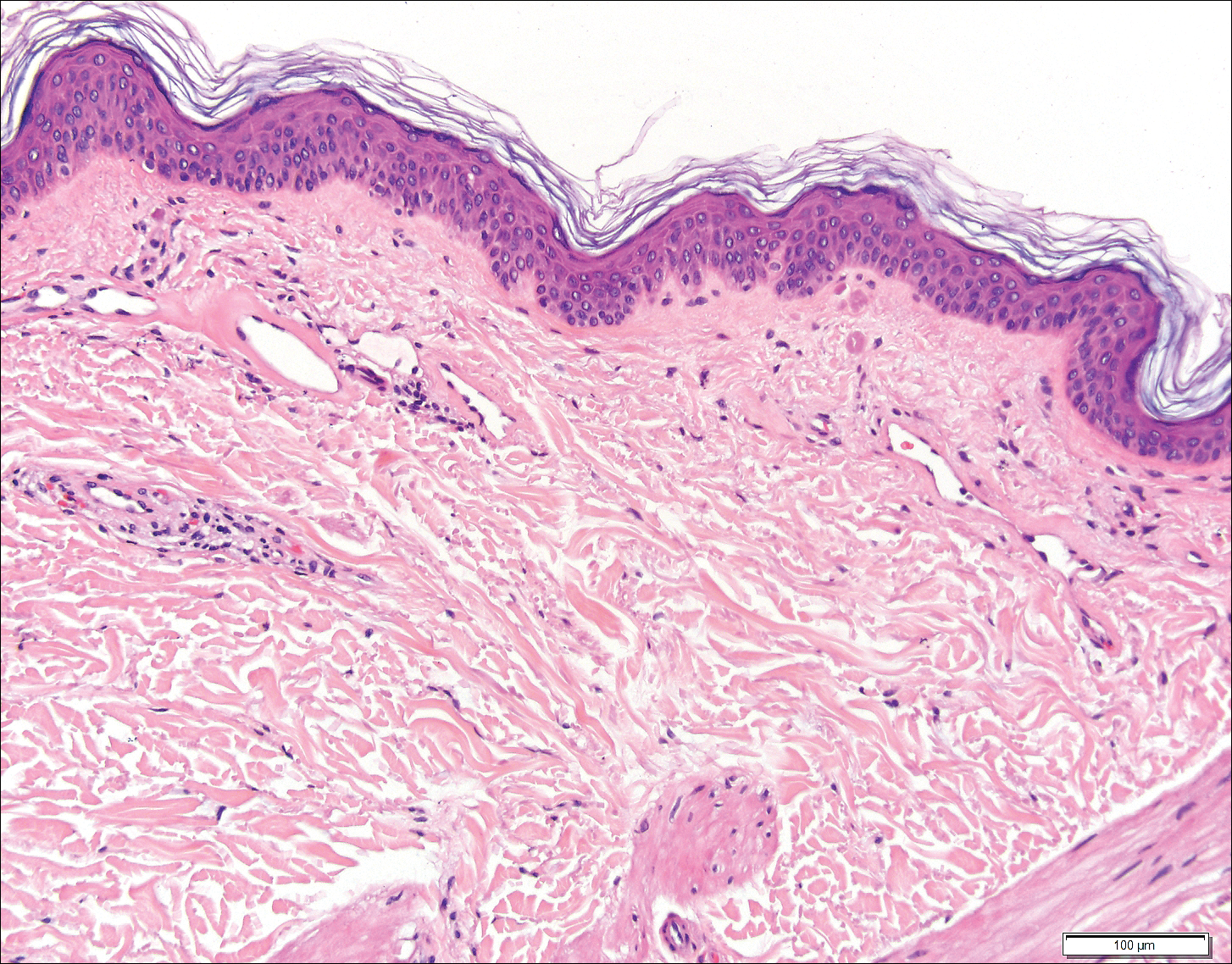
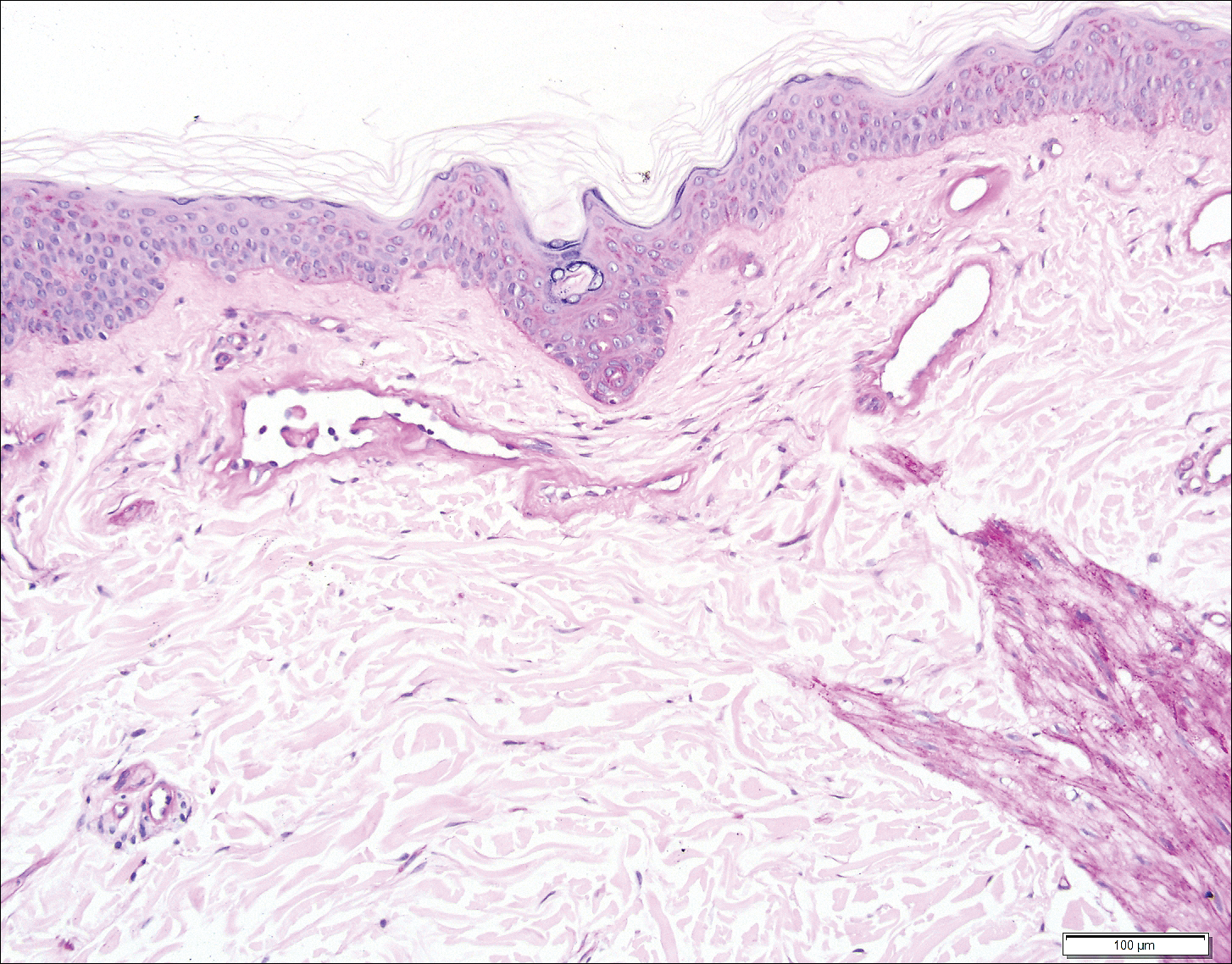
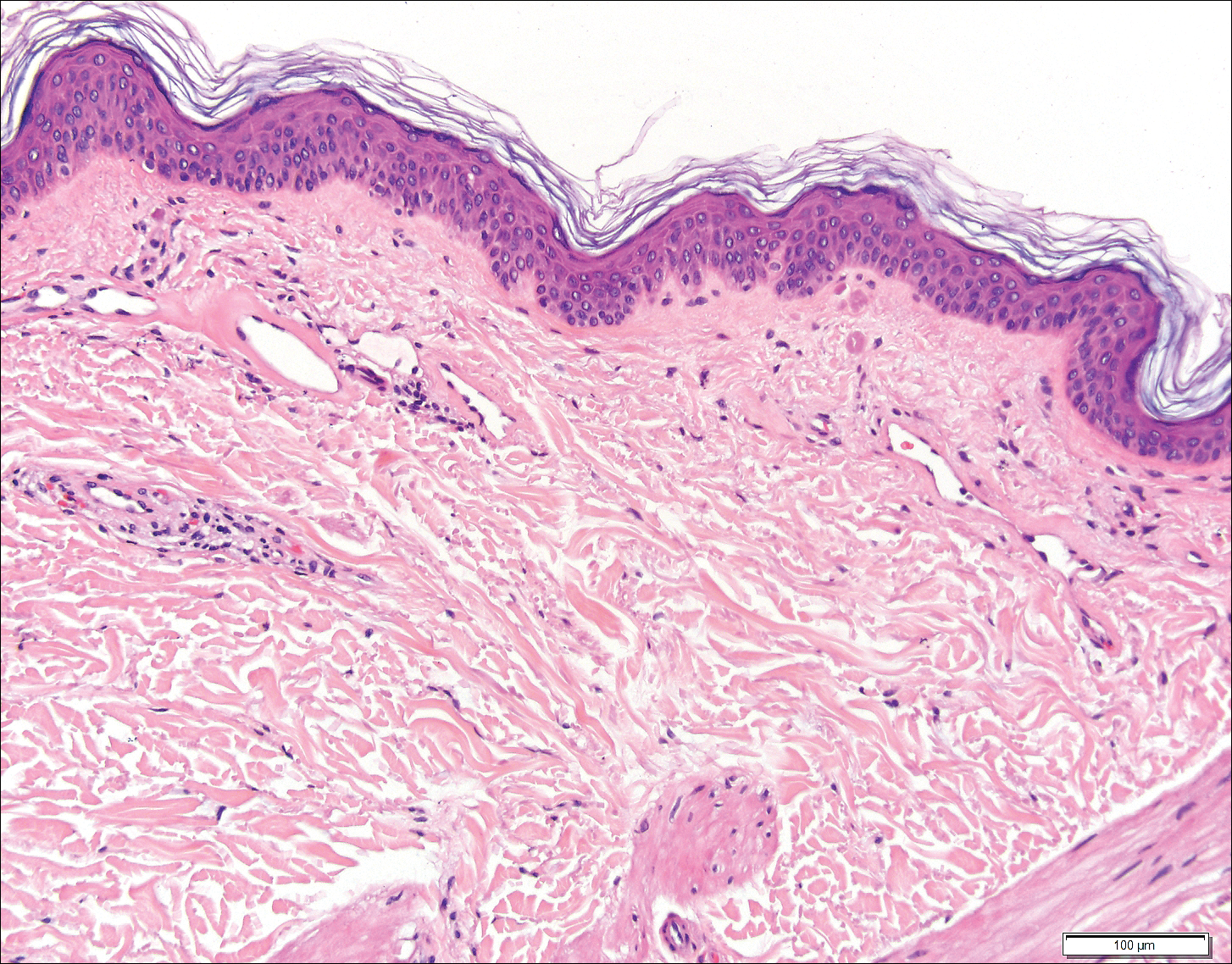
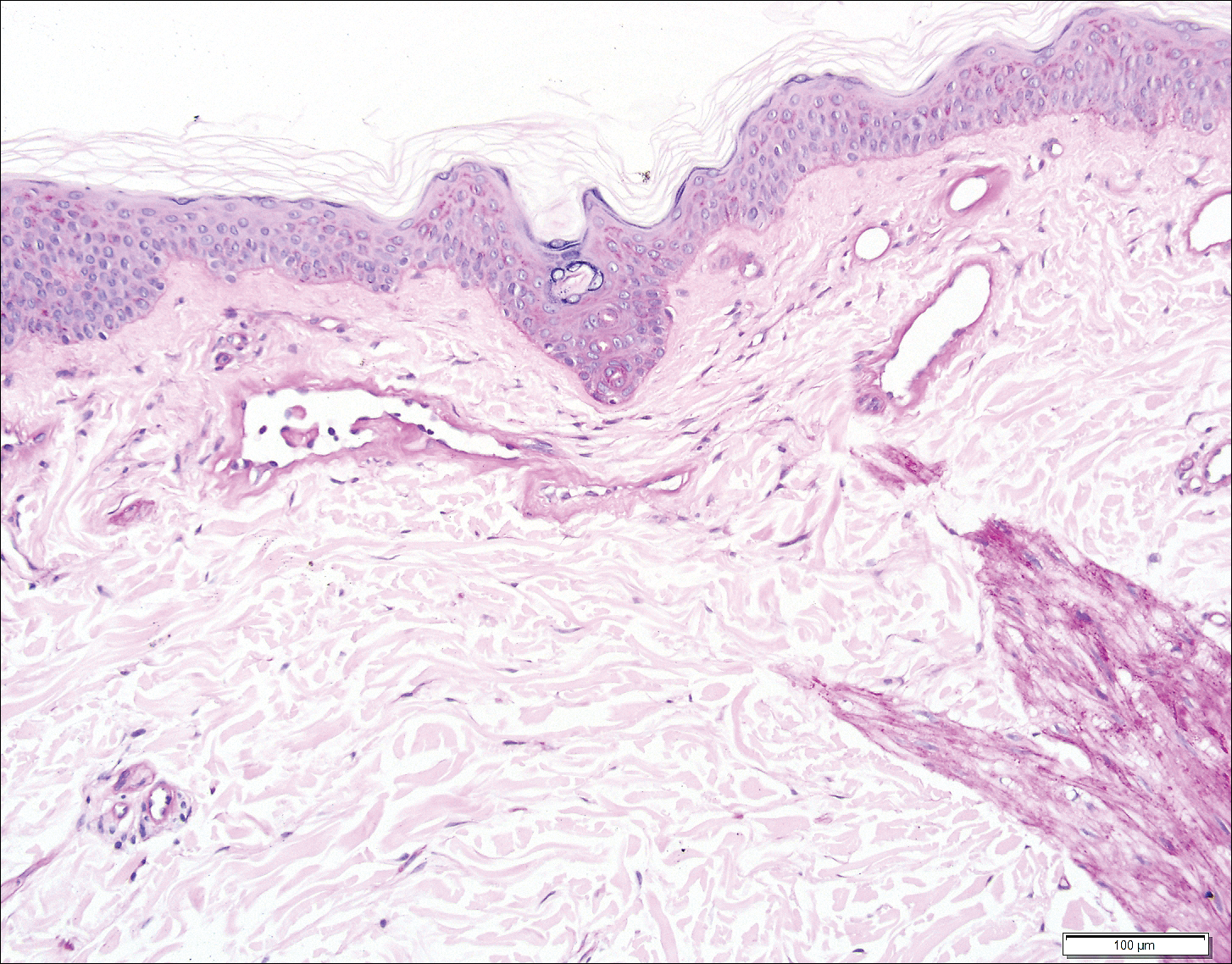
Histopathologic examination revealed ectatic blood vessels lined with unremarkable endothelial cells and thickened, hyalinized vessel walls scattered within the papillary dermis (Figure 1). The epidermis was unremarkable. There was minimal associated inflammation and no extravasation of erythrocytes. The hyalinized material was weakly positive on periodic acid-Schiff staining (Figure 2) and negative on Congo red staining, which supported of a diagnosis of cutaneous collagenous vasculopathy (CCV).
The patient previously had been given a suspected diagnosis of generalized essential telangiectasia by an outside dermatologist several years prior to the current presentation, as CCV had yet to be recognized as its own entity and therefore few cases had been described in the literature. She had a known history of obesity, hypertension, hyperlipidemia, and type 2 diabetes mellitus, which are associated with the condition. Multiple specialists concluded that the disease was too extensive for laser treatment. A review of PubMed articles indexed for MEDLINE yielded no established treatment options.
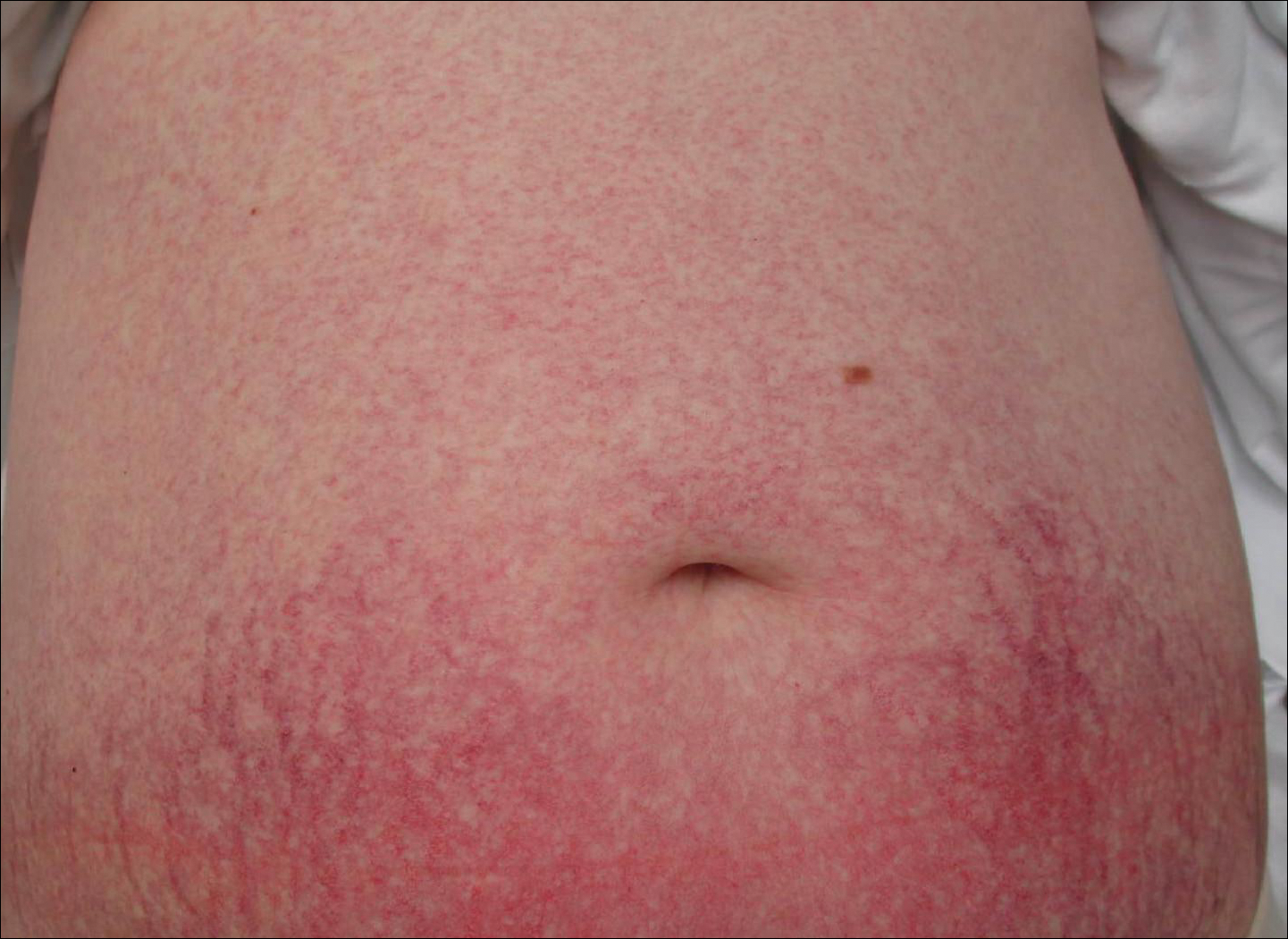
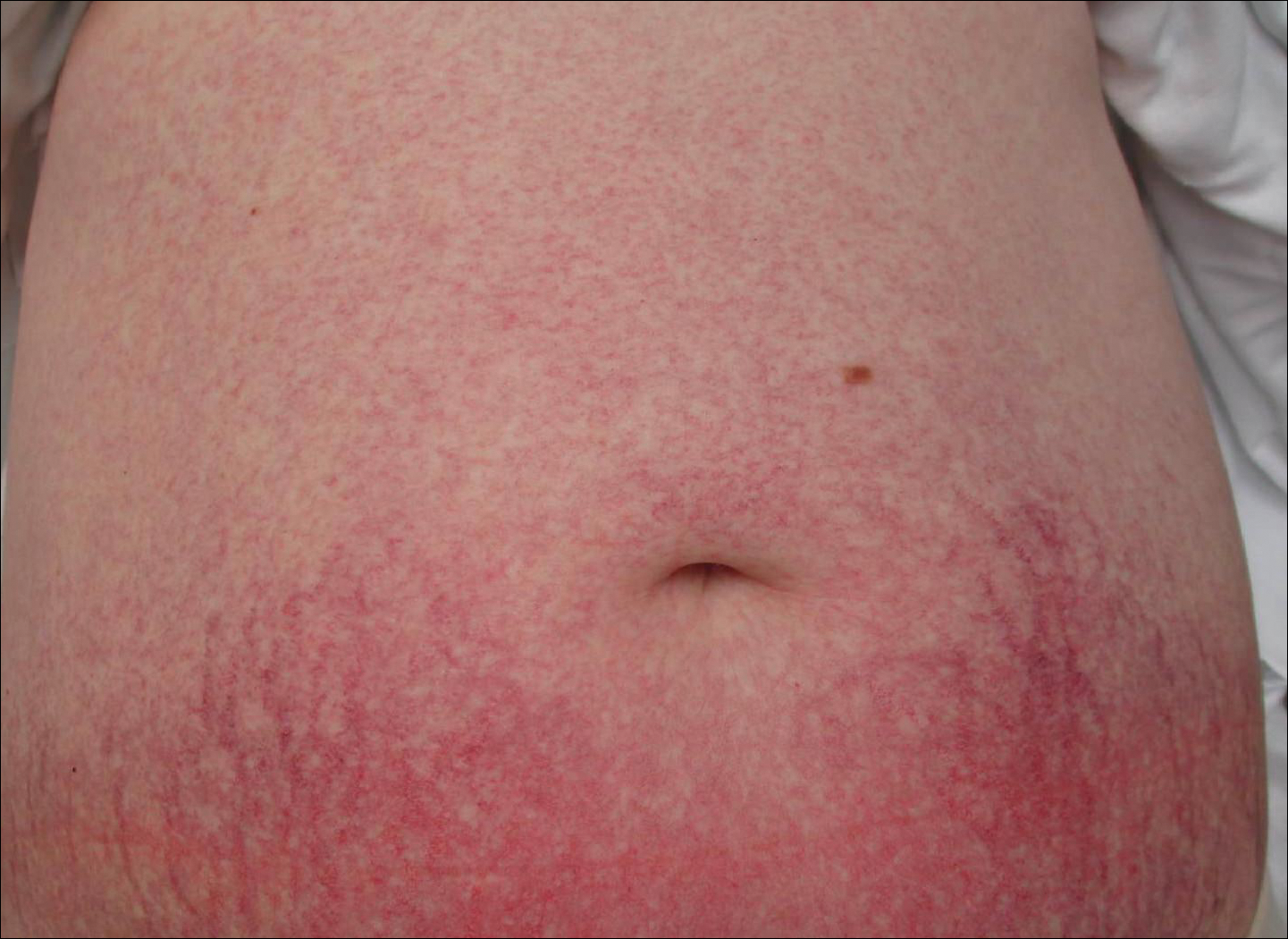
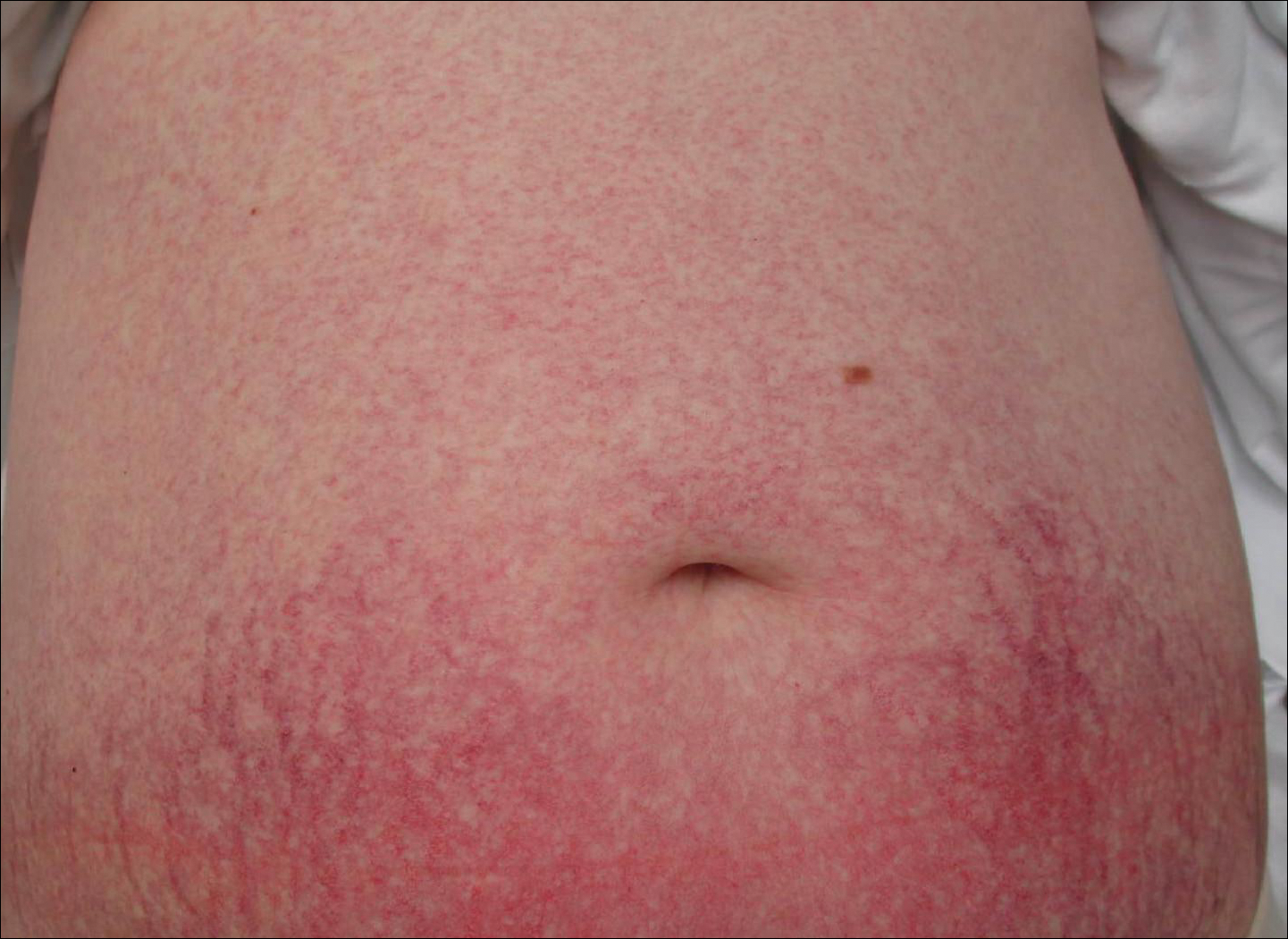
Cutaneous collagenous vasculopathy is a rare acquired microangiopathy involving the small vessels of the skin. Its clinical presentation is indistinguishable from that of generalized essential telangiectasia (GET). Patients generally present with asymptomatic, widespread, blanching, symmetric telangiectasias that classically begin on the legs and steadily progress upward with classic sparing of the face (Figure 3). Whereas GET has been reported to involve the oral and conjunctival mucosa, mucosal involvement is not typically observed in CCV and is considered to be a distinguishing factor between the 2 conditions.1,2 However, our patient reported oral symptoms, and oral erosions were seen on multiple physical examinations; therefore, ours is a rare case of mucosal involvement in conjunction with CCV. Given this finding, it is possible that more cases of CCV with mucosal involvement may exist but have been clinically misdiagnosed as GET.
First described by Salama and Rosenthal3 in 2000, CCV remains a rarely reported entity, with approximately 33 reported cases in the worldwide literature.2,4-7 The condition typically arises in adults with an equal predilection for males and females.2 The true incidence of CCV is unknown and likely is underreported given its close similarities to GET, which often is diagnosed clinically. The unique histopathologic finding of superficial ectatic vascular spaces with eosinophilic hyalinized vessel walls in CCV is key to distinguishing these similar entities, and even this finding can be subtle and is easily overlooked. Inflammation is sparse to absent. Deposited material is positive on periodic acid-Schiff and cytokeratin IV staining (representing reduplicated basement membrane-type collagen) and is diastase resistant. Smooth muscle actin staining is diminished or absent. Ultrastructural examination reveals reduplicated, laminated basement membrane; Luse bodies (abnormally long, widely spaced collagen fibers); and a decrease in or loss of pericytes. Of note, Luse bodies are nonspecific and their absence does not exclude a diagnosis of CCV.1
The etiology of CCV is unclear, and multiple pathogenetic mechanisms have been proposed. Ultimately, this entity is thought to arise from repeated endothelial cell damage, although the trigger for the endothelial cell injury is not completely understood. Diabetes mellitus sometimes is associated with microangiopathy and may be a confounding but not causative factor in some cases.1 Some investigators believe CCV is caused by a genetic defect that alters collagen production in the small vessels of the skin.5 Others have hypothesized that it is a secondary manifestation of an underlying disease or is associated with a medication; however, no disease or drug has been convincingly implicated in CCV.8
Cutaneous collagenous vasculopathy is limited to the skin, with no known reports of systemic involvement in the literature.7 There are no recommended laboratory studies to aid in diagnosis.1 It is critical to exclude hereditary hemorrhagic telangiectasia (HHT), as these patients can have life-threatening systemic involvement. Patients with CCV generally have no history of a bleeding diathesis, patients with HHT classically report recurrent epistaxis and gastrointestinal bleeding.7 A family history of HHT also is helpful for diagnosis, as the condition is autosomal dominant.1 Neither HHT or telangiectasia macularis eruptiva perstans, which also can be included in the differential diagnosis, demonstrate vessel wall hyalinization.
Treatment options for CCV are limited. Basso et al6 reported notable improvement in a patient with CCV treated with a combined 595-nm pulsed dye laser and 1064-nm Nd:YAG laser and optimized pulsed light. In one patient, treatment with a 585-nm pulsed dye laser produced a blanching response, suggesting that this may be a potential treatment option.7 Treatment with sclerotherapy has been ineffective.2
It is critical for both dermatologists and dermatopathologists to recognize and report this newly described entity, as the unique finding of vessel wall hyalinization in CCV may be indicative of a certain pathogenetic mechanism and effective treatment avenue that has yet to be established due to the relatively few number of reports that currently exist in the literature.
- Burdick LM, Lohser S, Somach SC, et al. Cutaneous collagenous vasculopathy: a rare cutaneous microangiopathy. J Cutan Pathol. 2012;39:741-746.
- Brady BG, Ortleb M, Boyd AS, et al. Cutaneous collagenous vasculopathy. J Clin Aesthet Dermatol. 2015;8:49-52.
- Salama S, Rosenthal D. Cutaneous collagenous vasculopathy with generalized telangiectasia: an immunohistochemical and structural study. J Cutan Pathol. 2000;27:40-48.
- Toda-Brito H, Resende C, Catorze G, et al. Cutaneous collagenous vasculopathy: a rare cause of generalised cutaneous telangiectasia. BMJ Case Rep. 2015. doi: 10.1136/bcr-2015-210635.
- Ma DL, Vano-Galvan S. Images in clinical medicine: cutaneous collagenous vasculopathy. N Engl J Med. 2015;373:E14.
- Basso D, Ribero S, Blazek C, et al. Cutaneous collagenous vasculopathy: a rare form of microangiopathy successfully treated with a combination of multiplex laser and optimized pulsed light with a review of the literature. Dermatology. 2016;232:107-111.
- Moteqi SI, Yasuda M, Yamanaka M, et al. Cutaneous collagenous vasculopathy: report of first Japanese case and review of the literature. Australas J Dermatol. 2017;58:145-149.
- González Fernández D, Gómez Bernal S, Vivanco Allende B, et al. Cutaneous collagenous vasculopathy: description of two new cases in elderly women and review of the literature. Dermatology. 2012;225:1-8.
The Diagnosis: Cutaneous Collagenous Vasculopathy
Histopathologic examination revealed ectatic blood vessels lined with unremarkable endothelial cells and thickened, hyalinized vessel walls scattered within the papillary dermis (Figure 1). The epidermis was unremarkable. There was minimal associated inflammation and no extravasation of erythrocytes. The hyalinized material was weakly positive on periodic acid-Schiff staining (Figure 2) and negative on Congo red staining, which supported of a diagnosis of cutaneous collagenous vasculopathy (CCV).
The patient previously had been given a suspected diagnosis of generalized essential telangiectasia by an outside dermatologist several years prior to the current presentation, as CCV had yet to be recognized as its own entity and therefore few cases had been described in the literature. She had a known history of obesity, hypertension, hyperlipidemia, and type 2 diabetes mellitus, which are associated with the condition. Multiple specialists concluded that the disease was too extensive for laser treatment. A review of PubMed articles indexed for MEDLINE yielded no established treatment options.
Cutaneous collagenous vasculopathy is a rare acquired microangiopathy involving the small vessels of the skin. Its clinical presentation is indistinguishable from that of generalized essential telangiectasia (GET). Patients generally present with asymptomatic, widespread, blanching, symmetric telangiectasias that classically begin on the legs and steadily progress upward with classic sparing of the face (Figure 3). Whereas GET has been reported to involve the oral and conjunctival mucosa, mucosal involvement is not typically observed in CCV and is considered to be a distinguishing factor between the 2 conditions.1,2 However, our patient reported oral symptoms, and oral erosions were seen on multiple physical examinations; therefore, ours is a rare case of mucosal involvement in conjunction with CCV. Given this finding, it is possible that more cases of CCV with mucosal involvement may exist but have been clinically misdiagnosed as GET.
First described by Salama and Rosenthal3 in 2000, CCV remains a rarely reported entity, with approximately 33 reported cases in the worldwide literature.2,4-7 The condition typically arises in adults with an equal predilection for males and females.2 The true incidence of CCV is unknown and likely is underreported given its close similarities to GET, which often is diagnosed clinically. The unique histopathologic finding of superficial ectatic vascular spaces with eosinophilic hyalinized vessel walls in CCV is key to distinguishing these similar entities, and even this finding can be subtle and is easily overlooked. Inflammation is sparse to absent. Deposited material is positive on periodic acid-Schiff and cytokeratin IV staining (representing reduplicated basement membrane-type collagen) and is diastase resistant. Smooth muscle actin staining is diminished or absent. Ultrastructural examination reveals reduplicated, laminated basement membrane; Luse bodies (abnormally long, widely spaced collagen fibers); and a decrease in or loss of pericytes. Of note, Luse bodies are nonspecific and their absence does not exclude a diagnosis of CCV.1
The etiology of CCV is unclear, and multiple pathogenetic mechanisms have been proposed. Ultimately, this entity is thought to arise from repeated endothelial cell damage, although the trigger for the endothelial cell injury is not completely understood. Diabetes mellitus sometimes is associated with microangiopathy and may be a confounding but not causative factor in some cases.1 Some investigators believe CCV is caused by a genetic defect that alters collagen production in the small vessels of the skin.5 Others have hypothesized that it is a secondary manifestation of an underlying disease or is associated with a medication; however, no disease or drug has been convincingly implicated in CCV.8
Cutaneous collagenous vasculopathy is limited to the skin, with no known reports of systemic involvement in the literature.7 There are no recommended laboratory studies to aid in diagnosis.1 It is critical to exclude hereditary hemorrhagic telangiectasia (HHT), as these patients can have life-threatening systemic involvement. Patients with CCV generally have no history of a bleeding diathesis, patients with HHT classically report recurrent epistaxis and gastrointestinal bleeding.7 A family history of HHT also is helpful for diagnosis, as the condition is autosomal dominant.1 Neither HHT or telangiectasia macularis eruptiva perstans, which also can be included in the differential diagnosis, demonstrate vessel wall hyalinization.
Treatment options for CCV are limited. Basso et al6 reported notable improvement in a patient with CCV treated with a combined 595-nm pulsed dye laser and 1064-nm Nd:YAG laser and optimized pulsed light. In one patient, treatment with a 585-nm pulsed dye laser produced a blanching response, suggesting that this may be a potential treatment option.7 Treatment with sclerotherapy has been ineffective.2
It is critical for both dermatologists and dermatopathologists to recognize and report this newly described entity, as the unique finding of vessel wall hyalinization in CCV may be indicative of a certain pathogenetic mechanism and effective treatment avenue that has yet to be established due to the relatively few number of reports that currently exist in the literature.
The Diagnosis: Cutaneous Collagenous Vasculopathy
Histopathologic examination revealed ectatic blood vessels lined with unremarkable endothelial cells and thickened, hyalinized vessel walls scattered within the papillary dermis (Figure 1). The epidermis was unremarkable. There was minimal associated inflammation and no extravasation of erythrocytes. The hyalinized material was weakly positive on periodic acid-Schiff staining (Figure 2) and negative on Congo red staining, which supported of a diagnosis of cutaneous collagenous vasculopathy (CCV).
The patient previously had been given a suspected diagnosis of generalized essential telangiectasia by an outside dermatologist several years prior to the current presentation, as CCV had yet to be recognized as its own entity and therefore few cases had been described in the literature. She had a known history of obesity, hypertension, hyperlipidemia, and type 2 diabetes mellitus, which are associated with the condition. Multiple specialists concluded that the disease was too extensive for laser treatment. A review of PubMed articles indexed for MEDLINE yielded no established treatment options.
Cutaneous collagenous vasculopathy is a rare acquired microangiopathy involving the small vessels of the skin. Its clinical presentation is indistinguishable from that of generalized essential telangiectasia (GET). Patients generally present with asymptomatic, widespread, blanching, symmetric telangiectasias that classically begin on the legs and steadily progress upward with classic sparing of the face (Figure 3). Whereas GET has been reported to involve the oral and conjunctival mucosa, mucosal involvement is not typically observed in CCV and is considered to be a distinguishing factor between the 2 conditions.1,2 However, our patient reported oral symptoms, and oral erosions were seen on multiple physical examinations; therefore, ours is a rare case of mucosal involvement in conjunction with CCV. Given this finding, it is possible that more cases of CCV with mucosal involvement may exist but have been clinically misdiagnosed as GET.
First described by Salama and Rosenthal3 in 2000, CCV remains a rarely reported entity, with approximately 33 reported cases in the worldwide literature.2,4-7 The condition typically arises in adults with an equal predilection for males and females.2 The true incidence of CCV is unknown and likely is underreported given its close similarities to GET, which often is diagnosed clinically. The unique histopathologic finding of superficial ectatic vascular spaces with eosinophilic hyalinized vessel walls in CCV is key to distinguishing these similar entities, and even this finding can be subtle and is easily overlooked. Inflammation is sparse to absent. Deposited material is positive on periodic acid-Schiff and cytokeratin IV staining (representing reduplicated basement membrane-type collagen) and is diastase resistant. Smooth muscle actin staining is diminished or absent. Ultrastructural examination reveals reduplicated, laminated basement membrane; Luse bodies (abnormally long, widely spaced collagen fibers); and a decrease in or loss of pericytes. Of note, Luse bodies are nonspecific and their absence does not exclude a diagnosis of CCV.1
The etiology of CCV is unclear, and multiple pathogenetic mechanisms have been proposed. Ultimately, this entity is thought to arise from repeated endothelial cell damage, although the trigger for the endothelial cell injury is not completely understood. Diabetes mellitus sometimes is associated with microangiopathy and may be a confounding but not causative factor in some cases.1 Some investigators believe CCV is caused by a genetic defect that alters collagen production in the small vessels of the skin.5 Others have hypothesized that it is a secondary manifestation of an underlying disease or is associated with a medication; however, no disease or drug has been convincingly implicated in CCV.8
Cutaneous collagenous vasculopathy is limited to the skin, with no known reports of systemic involvement in the literature.7 There are no recommended laboratory studies to aid in diagnosis.1 It is critical to exclude hereditary hemorrhagic telangiectasia (HHT), as these patients can have life-threatening systemic involvement. Patients with CCV generally have no history of a bleeding diathesis, patients with HHT classically report recurrent epistaxis and gastrointestinal bleeding.7 A family history of HHT also is helpful for diagnosis, as the condition is autosomal dominant.1 Neither HHT or telangiectasia macularis eruptiva perstans, which also can be included in the differential diagnosis, demonstrate vessel wall hyalinization.
Treatment options for CCV are limited. Basso et al6 reported notable improvement in a patient with CCV treated with a combined 595-nm pulsed dye laser and 1064-nm Nd:YAG laser and optimized pulsed light. In one patient, treatment with a 585-nm pulsed dye laser produced a blanching response, suggesting that this may be a potential treatment option.7 Treatment with sclerotherapy has been ineffective.2
It is critical for both dermatologists and dermatopathologists to recognize and report this newly described entity, as the unique finding of vessel wall hyalinization in CCV may be indicative of a certain pathogenetic mechanism and effective treatment avenue that has yet to be established due to the relatively few number of reports that currently exist in the literature.
- Burdick LM, Lohser S, Somach SC, et al. Cutaneous collagenous vasculopathy: a rare cutaneous microangiopathy. J Cutan Pathol. 2012;39:741-746.
- Brady BG, Ortleb M, Boyd AS, et al. Cutaneous collagenous vasculopathy. J Clin Aesthet Dermatol. 2015;8:49-52.
- Salama S, Rosenthal D. Cutaneous collagenous vasculopathy with generalized telangiectasia: an immunohistochemical and structural study. J Cutan Pathol. 2000;27:40-48.
- Toda-Brito H, Resende C, Catorze G, et al. Cutaneous collagenous vasculopathy: a rare cause of generalised cutaneous telangiectasia. BMJ Case Rep. 2015. doi: 10.1136/bcr-2015-210635.
- Ma DL, Vano-Galvan S. Images in clinical medicine: cutaneous collagenous vasculopathy. N Engl J Med. 2015;373:E14.
- Basso D, Ribero S, Blazek C, et al. Cutaneous collagenous vasculopathy: a rare form of microangiopathy successfully treated with a combination of multiplex laser and optimized pulsed light with a review of the literature. Dermatology. 2016;232:107-111.
- Moteqi SI, Yasuda M, Yamanaka M, et al. Cutaneous collagenous vasculopathy: report of first Japanese case and review of the literature. Australas J Dermatol. 2017;58:145-149.
- González Fernández D, Gómez Bernal S, Vivanco Allende B, et al. Cutaneous collagenous vasculopathy: description of two new cases in elderly women and review of the literature. Dermatology. 2012;225:1-8.
- Burdick LM, Lohser S, Somach SC, et al. Cutaneous collagenous vasculopathy: a rare cutaneous microangiopathy. J Cutan Pathol. 2012;39:741-746.
- Brady BG, Ortleb M, Boyd AS, et al. Cutaneous collagenous vasculopathy. J Clin Aesthet Dermatol. 2015;8:49-52.
- Salama S, Rosenthal D. Cutaneous collagenous vasculopathy with generalized telangiectasia: an immunohistochemical and structural study. J Cutan Pathol. 2000;27:40-48.
- Toda-Brito H, Resende C, Catorze G, et al. Cutaneous collagenous vasculopathy: a rare cause of generalised cutaneous telangiectasia. BMJ Case Rep. 2015. doi: 10.1136/bcr-2015-210635.
- Ma DL, Vano-Galvan S. Images in clinical medicine: cutaneous collagenous vasculopathy. N Engl J Med. 2015;373:E14.
- Basso D, Ribero S, Blazek C, et al. Cutaneous collagenous vasculopathy: a rare form of microangiopathy successfully treated with a combination of multiplex laser and optimized pulsed light with a review of the literature. Dermatology. 2016;232:107-111.
- Moteqi SI, Yasuda M, Yamanaka M, et al. Cutaneous collagenous vasculopathy: report of first Japanese case and review of the literature. Australas J Dermatol. 2017;58:145-149.
- González Fernández D, Gómez Bernal S, Vivanco Allende B, et al. Cutaneous collagenous vasculopathy: description of two new cases in elderly women and review of the literature. Dermatology. 2012;225:1-8.
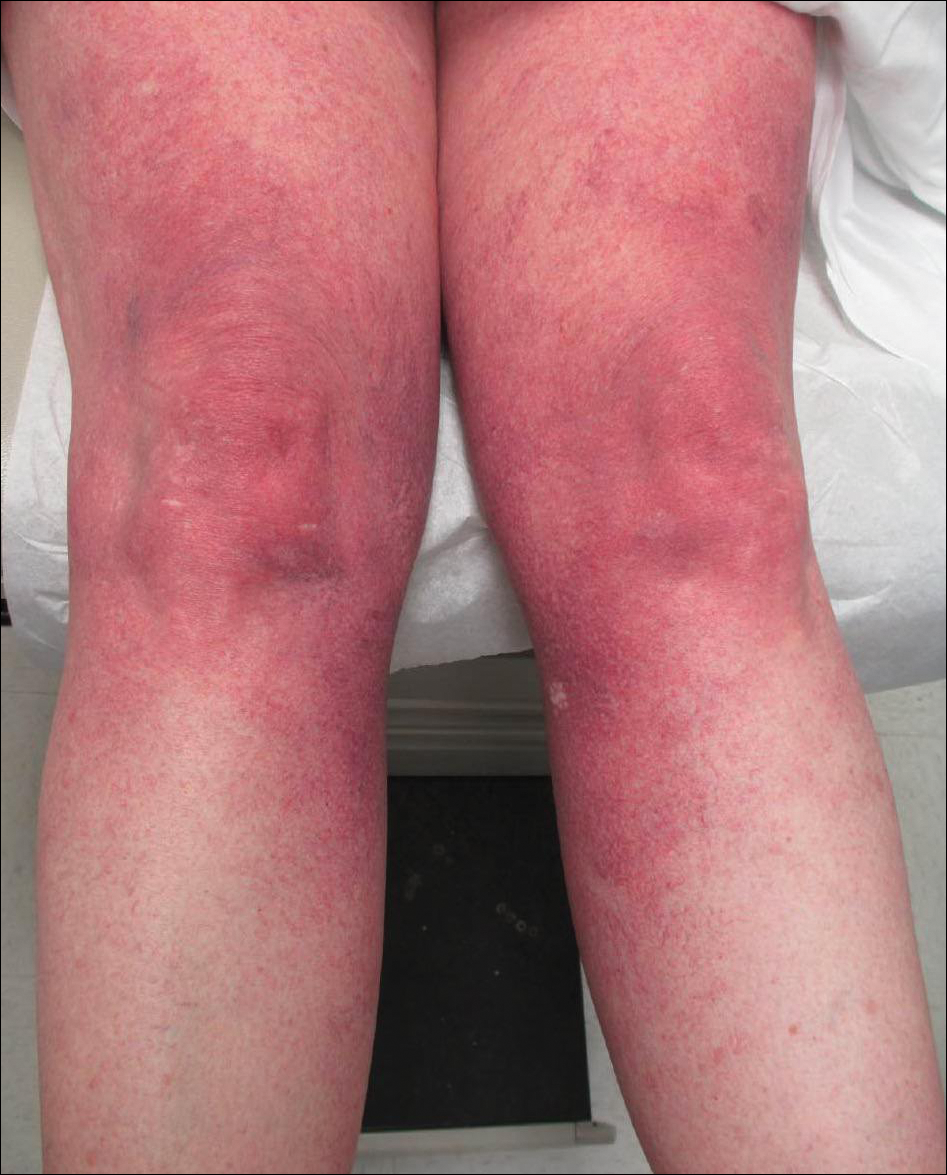
A 55-year-old woman presented for evaluation of widespread asymptomatic telangiectasias of several years' duration that first appeared on the legs and steadily progressed to involve the trunk and arms. A review of systems was remarkable for episodic glossitis and oral erosions that developed at the same time as the eruption. The patient had no history of bleeding diasthesis, and her family history was unremarkable. A laboratory workup (including autoimmune screening) and a malignancy workup were negative. Physical examination revealed confluent sheets of erythematous and purple blanching telangiectasias scattered symmetrically on the trunk, bilateral arms and legs, buttocks, and dorsal aspects of the feet with sparing of the palms, soles, and head and neck regions. A small, shallow erosion was present on the lateral aspect of the tongue. A 4-mm punch biopsy of a thigh lesion revealed ectatic blood vessels with hyalinized walls.
Keep pushing the envelope
By the time this column is published, we will have wrapped up Hospital Medicine 2018 in Orlando, it will be well into spring, and I will have completed my year as past president as well as my 6-year tenure on the Society of Hospital Medicine board of directors.
I can imagine that will feel like a relief and a milestone, and it also will feel like a loss to no longer be part of something that I have contributed my time, energy, passion, and emotion to for so long. I will retire at the ripe age of 48 – a pretty typical age for ending SHM board tenure, and it’s terribly important for SHM that I do so.
If you attended HM18, I hope you appreciated, as I do every year, the energy, enthusiasm, and youth – if not in years, then in spirit – of the event and of hospitalists. As a society and a profession, we take risks. We have set standards for excellence in hospital medicine programs. We have recognized a unique set of competencies and then not only attempted to expand them with education but also defined a specialty around them. We have welcomed practitioners and administrators as equals into our fold. These and many other accomplishments are the work of a board, committees, chapter leaders, and members who look for opportunity to expand our work into new and necessary domains, and not be limited by precedent.
On the SHM board and committees, we tackle issues of governance and strategy. For most of us, the SHM board is our first exposure to nonprofit oversight. And, to be sure, there is a steep learning curve as new members discover the issues and substance of the work of the society. I recall that I barely spoke the first year on the board, uncertain that I understood items fully, and I also was burned once or twice by making suggestions that reflected my lack of knowledge. While ignorance slowly gave way to experience, we also matured as a group as we found ways to debate and resolve tough, sometimes ambiguous, issues.
I came to appreciate that the strength of the board – and of SHM – is that we join the board naive to much of the past. After 6 years, while I may have come to understand issues with greater depth, I also see that the newer members bring fresher thinking, more creative energy, and even thoughts about how the group could function differently and perhaps better. Over the last few years, I realized that we veterans had developed a cadence and predictability to our work, and every year’s new members disrupt that rhythm. This disruption forces us to challenge each other and to be a better board – and hopefully – represent and advocate for you, our membership, better.
So, it’s time for me to move on. Even though I certainly feel like I still could contribute, it’s time to retire my own way of thinking from the leadership of SHM. The fact that we term-limit out at a (relatively) young age is, I believe, an extraordinary aspect of our organization, which is reflected in the work that our staff, our committees, and our members do.
SHM is an organization that, from the top down, embraces change in ways that few other organizations do. I believe we owe it to you to keep pushing the envelope of creativity – of what our goals are, of what a society can accomplish, of what an annual meeting can consist of. My ask of all of you is that you continue to challenge the leadership of SHM to be disruptive, to push the profession to better places, and to always strive to be more diverse, more inclusive, more communicative, more visible – and to stay young. In spirit and attitude if not in age. Thank you for giving me the opportunity to work on your behalf. It has been the greatest privilege of my career.
Dr. Harte is a past president of SHM and president of Cleveland Clinic Akron General and Southern Region.
By the time this column is published, we will have wrapped up Hospital Medicine 2018 in Orlando, it will be well into spring, and I will have completed my year as past president as well as my 6-year tenure on the Society of Hospital Medicine board of directors.
I can imagine that will feel like a relief and a milestone, and it also will feel like a loss to no longer be part of something that I have contributed my time, energy, passion, and emotion to for so long. I will retire at the ripe age of 48 – a pretty typical age for ending SHM board tenure, and it’s terribly important for SHM that I do so.
If you attended HM18, I hope you appreciated, as I do every year, the energy, enthusiasm, and youth – if not in years, then in spirit – of the event and of hospitalists. As a society and a profession, we take risks. We have set standards for excellence in hospital medicine programs. We have recognized a unique set of competencies and then not only attempted to expand them with education but also defined a specialty around them. We have welcomed practitioners and administrators as equals into our fold. These and many other accomplishments are the work of a board, committees, chapter leaders, and members who look for opportunity to expand our work into new and necessary domains, and not be limited by precedent.
On the SHM board and committees, we tackle issues of governance and strategy. For most of us, the SHM board is our first exposure to nonprofit oversight. And, to be sure, there is a steep learning curve as new members discover the issues and substance of the work of the society. I recall that I barely spoke the first year on the board, uncertain that I understood items fully, and I also was burned once or twice by making suggestions that reflected my lack of knowledge. While ignorance slowly gave way to experience, we also matured as a group as we found ways to debate and resolve tough, sometimes ambiguous, issues.
I came to appreciate that the strength of the board – and of SHM – is that we join the board naive to much of the past. After 6 years, while I may have come to understand issues with greater depth, I also see that the newer members bring fresher thinking, more creative energy, and even thoughts about how the group could function differently and perhaps better. Over the last few years, I realized that we veterans had developed a cadence and predictability to our work, and every year’s new members disrupt that rhythm. This disruption forces us to challenge each other and to be a better board – and hopefully – represent and advocate for you, our membership, better.
So, it’s time for me to move on. Even though I certainly feel like I still could contribute, it’s time to retire my own way of thinking from the leadership of SHM. The fact that we term-limit out at a (relatively) young age is, I believe, an extraordinary aspect of our organization, which is reflected in the work that our staff, our committees, and our members do.
SHM is an organization that, from the top down, embraces change in ways that few other organizations do. I believe we owe it to you to keep pushing the envelope of creativity – of what our goals are, of what a society can accomplish, of what an annual meeting can consist of. My ask of all of you is that you continue to challenge the leadership of SHM to be disruptive, to push the profession to better places, and to always strive to be more diverse, more inclusive, more communicative, more visible – and to stay young. In spirit and attitude if not in age. Thank you for giving me the opportunity to work on your behalf. It has been the greatest privilege of my career.
Dr. Harte is a past president of SHM and president of Cleveland Clinic Akron General and Southern Region.
By the time this column is published, we will have wrapped up Hospital Medicine 2018 in Orlando, it will be well into spring, and I will have completed my year as past president as well as my 6-year tenure on the Society of Hospital Medicine board of directors.
I can imagine that will feel like a relief and a milestone, and it also will feel like a loss to no longer be part of something that I have contributed my time, energy, passion, and emotion to for so long. I will retire at the ripe age of 48 – a pretty typical age for ending SHM board tenure, and it’s terribly important for SHM that I do so.
If you attended HM18, I hope you appreciated, as I do every year, the energy, enthusiasm, and youth – if not in years, then in spirit – of the event and of hospitalists. As a society and a profession, we take risks. We have set standards for excellence in hospital medicine programs. We have recognized a unique set of competencies and then not only attempted to expand them with education but also defined a specialty around them. We have welcomed practitioners and administrators as equals into our fold. These and many other accomplishments are the work of a board, committees, chapter leaders, and members who look for opportunity to expand our work into new and necessary domains, and not be limited by precedent.
On the SHM board and committees, we tackle issues of governance and strategy. For most of us, the SHM board is our first exposure to nonprofit oversight. And, to be sure, there is a steep learning curve as new members discover the issues and substance of the work of the society. I recall that I barely spoke the first year on the board, uncertain that I understood items fully, and I also was burned once or twice by making suggestions that reflected my lack of knowledge. While ignorance slowly gave way to experience, we also matured as a group as we found ways to debate and resolve tough, sometimes ambiguous, issues.
I came to appreciate that the strength of the board – and of SHM – is that we join the board naive to much of the past. After 6 years, while I may have come to understand issues with greater depth, I also see that the newer members bring fresher thinking, more creative energy, and even thoughts about how the group could function differently and perhaps better. Over the last few years, I realized that we veterans had developed a cadence and predictability to our work, and every year’s new members disrupt that rhythm. This disruption forces us to challenge each other and to be a better board – and hopefully – represent and advocate for you, our membership, better.
So, it’s time for me to move on. Even though I certainly feel like I still could contribute, it’s time to retire my own way of thinking from the leadership of SHM. The fact that we term-limit out at a (relatively) young age is, I believe, an extraordinary aspect of our organization, which is reflected in the work that our staff, our committees, and our members do.
SHM is an organization that, from the top down, embraces change in ways that few other organizations do. I believe we owe it to you to keep pushing the envelope of creativity – of what our goals are, of what a society can accomplish, of what an annual meeting can consist of. My ask of all of you is that you continue to challenge the leadership of SHM to be disruptive, to push the profession to better places, and to always strive to be more diverse, more inclusive, more communicative, more visible – and to stay young. In spirit and attitude if not in age. Thank you for giving me the opportunity to work on your behalf. It has been the greatest privilege of my career.
Dr. Harte is a past president of SHM and president of Cleveland Clinic Akron General and Southern Region.
Check SVS Website for New Research Opportunities
Looking for a research opportunity? Check our updated website for current programs in your area. If your institution has an opportunity to promote, let us know at [email protected].
Looking for a research opportunity? Check our updated website for current programs in your area. If your institution has an opportunity to promote, let us know at [email protected].
Looking for a research opportunity? Check our updated website for current programs in your area. If your institution has an opportunity to promote, let us know at [email protected].
Submit a case to VAM's “Ask the Experts"
Help build the Vascular Annual Meeting educational program for the new “Ask the Experts” sessions, to be held daily, Wednesday through Saturday. Topics are coding, aortic care for occlusive disease, hemodialysis and PAD. Learn more about case submission here.
And if you haven’t registered for VAM yet, do so! The premier meeting for vascular surgeons is just five weeks (and one day) away. Learn more and register here. And obtain a hotel room here.
Help build the Vascular Annual Meeting educational program for the new “Ask the Experts” sessions, to be held daily, Wednesday through Saturday. Topics are coding, aortic care for occlusive disease, hemodialysis and PAD. Learn more about case submission here.
And if you haven’t registered for VAM yet, do so! The premier meeting for vascular surgeons is just five weeks (and one day) away. Learn more and register here. And obtain a hotel room here.
Help build the Vascular Annual Meeting educational program for the new “Ask the Experts” sessions, to be held daily, Wednesday through Saturday. Topics are coding, aortic care for occlusive disease, hemodialysis and PAD. Learn more about case submission here.
And if you haven’t registered for VAM yet, do so! The premier meeting for vascular surgeons is just five weeks (and one day) away. Learn more and register here. And obtain a hotel room here.
For Members Only: View “Negotiations” Webinar Materials
Did you miss the April 30 webinar on "Negotiating Physician Employment Contracts," presented by the SVS and the SVS Community Practice Committee? Materials -- available only to SVS members -- can be viewed here. Topics include benefits, call pay, termination rights, non-compete clauses, tenure opportunities and more.
Did you miss the April 30 webinar on "Negotiating Physician Employment Contracts," presented by the SVS and the SVS Community Practice Committee? Materials -- available only to SVS members -- can be viewed here. Topics include benefits, call pay, termination rights, non-compete clauses, tenure opportunities and more.
Did you miss the April 30 webinar on "Negotiating Physician Employment Contracts," presented by the SVS and the SVS Community Practice Committee? Materials -- available only to SVS members -- can be viewed here. Topics include benefits, call pay, termination rights, non-compete clauses, tenure opportunities and more.
Device-related thrombus associated with ischemic events
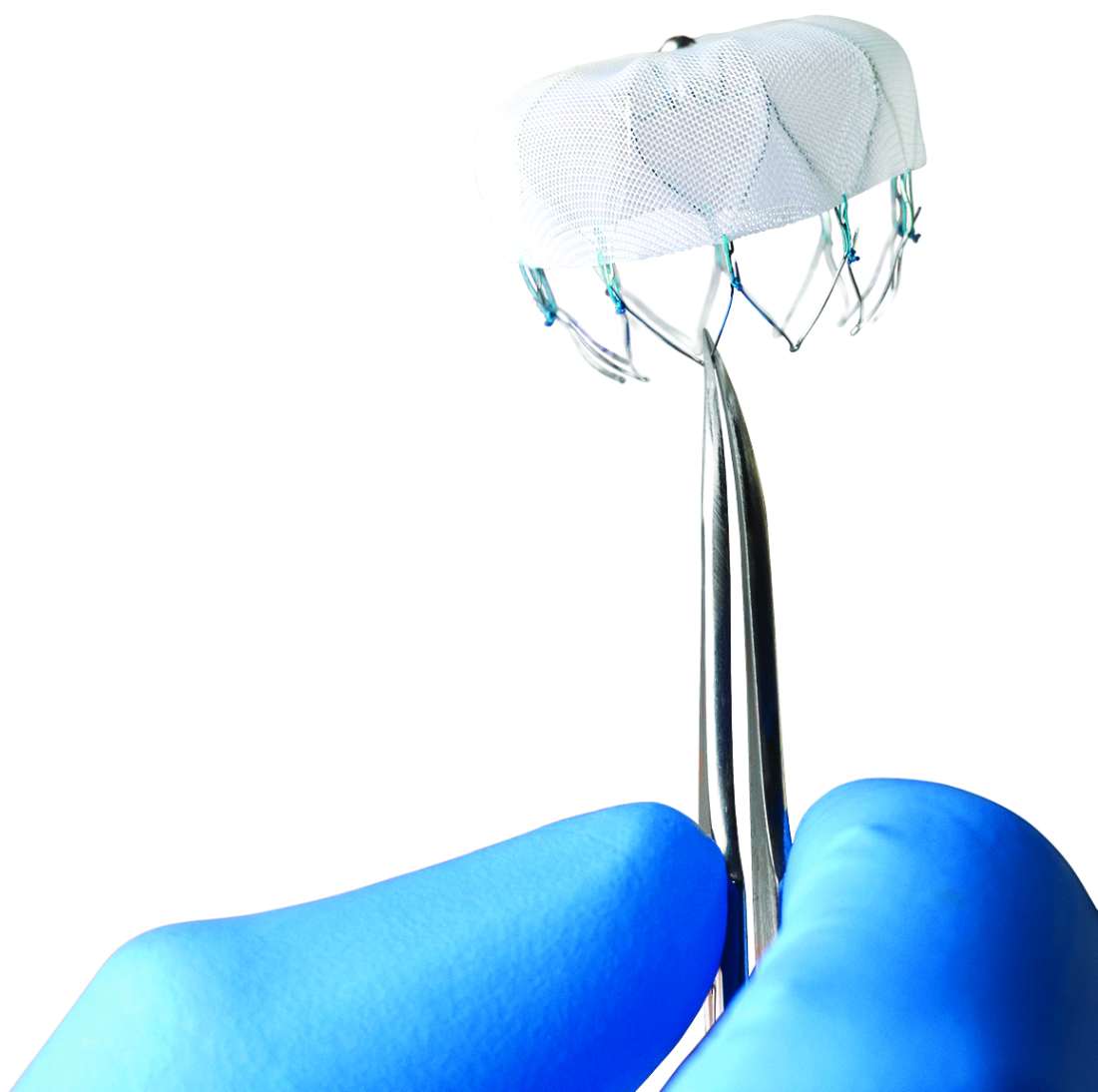
BOSTON – Device-related thrombus (DRT) does not occur often after left atrial appendage closure with the Watchman device. When it does, however, it is associated with a significantly higher rate of stroke and systemic embolism compared with that of patients with no DRT, according to a recent analysis presented at the annual scientific sessions of the Heart Rhythm Society.
Given the negative implications of DRT, a judicious surveillance strategy should be considered, especially when DRT risk factors are present, investigators said in a report on the study, which was published simultaneously in Circulation.
“Certainly, DRT is associated with an increased risk of stroke, and therapeutic anticoagulation should be resumed when discovered with rigorous transesophageal echocardiography follow-up to ensure resolution,” noted senior investigator Vivek Y. Reddy, MD.
Despite the higher rates of all strokes, ischemic strokes, and hemorrhagic strokes linked with DRT, the complication did not link with a higher rate of all-cause mortality compared with patients who never had a DRT. The results also suggested a causal link between DRT and subsequent stroke in about half the patients with DRT because their strokes occurred within a month following DRT diagnosis.
Despite these findings, a majority – 74% – of patients with an identified DRT did not have a stroke, and 87% of the strokes that occurred in the patients who received the Watchman device occurred in the absence of a DRT, reported Dr. Reddy, who presented the findings at the meeting.
The most immediate implication of the findings is the strong case they make for rethinking the timing of planned follow-up transesophageal echocardiography (TEE) examinations of patients after they receive a Watchman device. The current, standard protocol schedules a TEE at 45 days after Watchman placement, when routine anticoagulation usually stops, and then a second TEE 12 months after placement. A better schedule might be to perform the first TEE 3-4 months after Watchman placement to give a potential DRT time to form once oral anticoagulant therapy stops, suggested Dr. Reddy, professor and director of the cardiac arrhythmia service at Mount Sinai Hospital and Health System in New York.
“Surveillance is very important. I don’t think DRT usually occurs unless anticoagulation is suboptimal or stops.” Dr. Reddy noted that he and his associates are analyzing the best time for TEE surveillance in other large databases of patients treated with left atrial appendage (LAA) closure. Newer models of LAA closure devices structurally modified to reduce thrombus formation are nearing clinical use, he added.
The analysis, believed to be the largest to date of DRT following left atrial appendage closure, was based on prospective data from four clinical trials. That included two randomized controlled trials, PROTECT AF and PREVAIL, as well as the CAP and CAP2 prospective registries.
Among 1,739 patients in those studies receiving an implant, 65 (3.74%) had DRT, the investigators found.
Over 1 year of follow-up, 25% of patients with DRT had an ischemic stroke or systemic embolism, versus 6.8% of patients without DRTs (P less than .001), they reported. That worked out to an event rate of 6.28 and 1.65 events per 100 patient years, respectively.
The strongest predictors of DRT in multivariable analysis included vascular disease, history of stroke or transient ischemic attack, permanent atrial fibrillation, and left atrial appendage diameter, according to the report. Conversely, increasing left ventricular ejection fraction was protective against DRT.
Taken together, these data support reevaluating the transesophageal echocardiography strategy, according to Dr. Reddy and his coauthors. Those approaches might include targeting patients with DRT risk factors, routine additional surveillance at 6 months, or delaying the first transesophageal echocardiography to 4 months.
“Importantly, none of these strategies have been rigorously compared, so these suggestions are subject to future studies,” the researchers wrote.
“DRT remains a problem despite increased operator experience with LAA occlusion and improved occluding devices,” commented David B. De Lurgio, MD, a cardiac electrophysiologist at Emory Healthcare in Atlanta. “What is a little alarming is that the risk for DRT extends beyond the period of prescribed anticoagulation. Although the risk from DRT mitigates the benefit of LAA closure compared with warfarin, it does not mitigate the benefit from occlusion compared with no treatment,” said Dr. De Lurgio, designated discussant for the report. “Prevention and management of DRT may require that each patient receive a tailored regimen of anticoagulation and surveillance.”
The Watchman studies were funded by Boston Scientific, the company that markets the device. Dr. Reddy has been a consultant to and has received research funding from Boston Scientific and from Abbott and Biosense-Webster, and he reported having an equity interest in Javelin and Surecor. Coauthors reported disclosures related to Boston Scientific, Johnson & Johnson, Abbott, and other medical device companies. Dr. De Lurgio has been a consultant to Boston Scientific.
Updated, 5/17/18: This article has been updated with reporting from Mitchel L. Zoler at the meeting, and has been revised for clarity and to reflect that the results were presented by Dr. Reddy.
SOURCE: Dukkipati SR et al. Circulation. 2018 May 11. doi: 10.1161/CIRCULATIONAHA.118.035090.
BOSTON – Device-related thrombus (DRT) does not occur often after left atrial appendage closure with the Watchman device. When it does, however, it is associated with a significantly higher rate of stroke and systemic embolism compared with that of patients with no DRT, according to a recent analysis presented at the annual scientific sessions of the Heart Rhythm Society.
Given the negative implications of DRT, a judicious surveillance strategy should be considered, especially when DRT risk factors are present, investigators said in a report on the study, which was published simultaneously in Circulation.
“Certainly, DRT is associated with an increased risk of stroke, and therapeutic anticoagulation should be resumed when discovered with rigorous transesophageal echocardiography follow-up to ensure resolution,” noted senior investigator Vivek Y. Reddy, MD.
Despite the higher rates of all strokes, ischemic strokes, and hemorrhagic strokes linked with DRT, the complication did not link with a higher rate of all-cause mortality compared with patients who never had a DRT. The results also suggested a causal link between DRT and subsequent stroke in about half the patients with DRT because their strokes occurred within a month following DRT diagnosis.
Despite these findings, a majority – 74% – of patients with an identified DRT did not have a stroke, and 87% of the strokes that occurred in the patients who received the Watchman device occurred in the absence of a DRT, reported Dr. Reddy, who presented the findings at the meeting.
The most immediate implication of the findings is the strong case they make for rethinking the timing of planned follow-up transesophageal echocardiography (TEE) examinations of patients after they receive a Watchman device. The current, standard protocol schedules a TEE at 45 days after Watchman placement, when routine anticoagulation usually stops, and then a second TEE 12 months after placement. A better schedule might be to perform the first TEE 3-4 months after Watchman placement to give a potential DRT time to form once oral anticoagulant therapy stops, suggested Dr. Reddy, professor and director of the cardiac arrhythmia service at Mount Sinai Hospital and Health System in New York.
“Surveillance is very important. I don’t think DRT usually occurs unless anticoagulation is suboptimal or stops.” Dr. Reddy noted that he and his associates are analyzing the best time for TEE surveillance in other large databases of patients treated with left atrial appendage (LAA) closure. Newer models of LAA closure devices structurally modified to reduce thrombus formation are nearing clinical use, he added.
The analysis, believed to be the largest to date of DRT following left atrial appendage closure, was based on prospective data from four clinical trials. That included two randomized controlled trials, PROTECT AF and PREVAIL, as well as the CAP and CAP2 prospective registries.
Among 1,739 patients in those studies receiving an implant, 65 (3.74%) had DRT, the investigators found.
Over 1 year of follow-up, 25% of patients with DRT had an ischemic stroke or systemic embolism, versus 6.8% of patients without DRTs (P less than .001), they reported. That worked out to an event rate of 6.28 and 1.65 events per 100 patient years, respectively.
The strongest predictors of DRT in multivariable analysis included vascular disease, history of stroke or transient ischemic attack, permanent atrial fibrillation, and left atrial appendage diameter, according to the report. Conversely, increasing left ventricular ejection fraction was protective against DRT.
Taken together, these data support reevaluating the transesophageal echocardiography strategy, according to Dr. Reddy and his coauthors. Those approaches might include targeting patients with DRT risk factors, routine additional surveillance at 6 months, or delaying the first transesophageal echocardiography to 4 months.
“Importantly, none of these strategies have been rigorously compared, so these suggestions are subject to future studies,” the researchers wrote.
“DRT remains a problem despite increased operator experience with LAA occlusion and improved occluding devices,” commented David B. De Lurgio, MD, a cardiac electrophysiologist at Emory Healthcare in Atlanta. “What is a little alarming is that the risk for DRT extends beyond the period of prescribed anticoagulation. Although the risk from DRT mitigates the benefit of LAA closure compared with warfarin, it does not mitigate the benefit from occlusion compared with no treatment,” said Dr. De Lurgio, designated discussant for the report. “Prevention and management of DRT may require that each patient receive a tailored regimen of anticoagulation and surveillance.”
The Watchman studies were funded by Boston Scientific, the company that markets the device. Dr. Reddy has been a consultant to and has received research funding from Boston Scientific and from Abbott and Biosense-Webster, and he reported having an equity interest in Javelin and Surecor. Coauthors reported disclosures related to Boston Scientific, Johnson & Johnson, Abbott, and other medical device companies. Dr. De Lurgio has been a consultant to Boston Scientific.
Updated, 5/17/18: This article has been updated with reporting from Mitchel L. Zoler at the meeting, and has been revised for clarity and to reflect that the results were presented by Dr. Reddy.
SOURCE: Dukkipati SR et al. Circulation. 2018 May 11. doi: 10.1161/CIRCULATIONAHA.118.035090.
BOSTON – Device-related thrombus (DRT) does not occur often after left atrial appendage closure with the Watchman device. When it does, however, it is associated with a significantly higher rate of stroke and systemic embolism compared with that of patients with no DRT, according to a recent analysis presented at the annual scientific sessions of the Heart Rhythm Society.
Given the negative implications of DRT, a judicious surveillance strategy should be considered, especially when DRT risk factors are present, investigators said in a report on the study, which was published simultaneously in Circulation.
“Certainly, DRT is associated with an increased risk of stroke, and therapeutic anticoagulation should be resumed when discovered with rigorous transesophageal echocardiography follow-up to ensure resolution,” noted senior investigator Vivek Y. Reddy, MD.
Despite the higher rates of all strokes, ischemic strokes, and hemorrhagic strokes linked with DRT, the complication did not link with a higher rate of all-cause mortality compared with patients who never had a DRT. The results also suggested a causal link between DRT and subsequent stroke in about half the patients with DRT because their strokes occurred within a month following DRT diagnosis.
Despite these findings, a majority – 74% – of patients with an identified DRT did not have a stroke, and 87% of the strokes that occurred in the patients who received the Watchman device occurred in the absence of a DRT, reported Dr. Reddy, who presented the findings at the meeting.
The most immediate implication of the findings is the strong case they make for rethinking the timing of planned follow-up transesophageal echocardiography (TEE) examinations of patients after they receive a Watchman device. The current, standard protocol schedules a TEE at 45 days after Watchman placement, when routine anticoagulation usually stops, and then a second TEE 12 months after placement. A better schedule might be to perform the first TEE 3-4 months after Watchman placement to give a potential DRT time to form once oral anticoagulant therapy stops, suggested Dr. Reddy, professor and director of the cardiac arrhythmia service at Mount Sinai Hospital and Health System in New York.
“Surveillance is very important. I don’t think DRT usually occurs unless anticoagulation is suboptimal or stops.” Dr. Reddy noted that he and his associates are analyzing the best time for TEE surveillance in other large databases of patients treated with left atrial appendage (LAA) closure. Newer models of LAA closure devices structurally modified to reduce thrombus formation are nearing clinical use, he added.
The analysis, believed to be the largest to date of DRT following left atrial appendage closure, was based on prospective data from four clinical trials. That included two randomized controlled trials, PROTECT AF and PREVAIL, as well as the CAP and CAP2 prospective registries.
Among 1,739 patients in those studies receiving an implant, 65 (3.74%) had DRT, the investigators found.
Over 1 year of follow-up, 25% of patients with DRT had an ischemic stroke or systemic embolism, versus 6.8% of patients without DRTs (P less than .001), they reported. That worked out to an event rate of 6.28 and 1.65 events per 100 patient years, respectively.
The strongest predictors of DRT in multivariable analysis included vascular disease, history of stroke or transient ischemic attack, permanent atrial fibrillation, and left atrial appendage diameter, according to the report. Conversely, increasing left ventricular ejection fraction was protective against DRT.
Taken together, these data support reevaluating the transesophageal echocardiography strategy, according to Dr. Reddy and his coauthors. Those approaches might include targeting patients with DRT risk factors, routine additional surveillance at 6 months, or delaying the first transesophageal echocardiography to 4 months.
“Importantly, none of these strategies have been rigorously compared, so these suggestions are subject to future studies,” the researchers wrote.
“DRT remains a problem despite increased operator experience with LAA occlusion and improved occluding devices,” commented David B. De Lurgio, MD, a cardiac electrophysiologist at Emory Healthcare in Atlanta. “What is a little alarming is that the risk for DRT extends beyond the period of prescribed anticoagulation. Although the risk from DRT mitigates the benefit of LAA closure compared with warfarin, it does not mitigate the benefit from occlusion compared with no treatment,” said Dr. De Lurgio, designated discussant for the report. “Prevention and management of DRT may require that each patient receive a tailored regimen of anticoagulation and surveillance.”
The Watchman studies were funded by Boston Scientific, the company that markets the device. Dr. Reddy has been a consultant to and has received research funding from Boston Scientific and from Abbott and Biosense-Webster, and he reported having an equity interest in Javelin and Surecor. Coauthors reported disclosures related to Boston Scientific, Johnson & Johnson, Abbott, and other medical device companies. Dr. De Lurgio has been a consultant to Boston Scientific.
Updated, 5/17/18: This article has been updated with reporting from Mitchel L. Zoler at the meeting, and has been revised for clarity and to reflect that the results were presented by Dr. Reddy.
SOURCE: Dukkipati SR et al. Circulation. 2018 May 11. doi: 10.1161/CIRCULATIONAHA.118.035090.
REPORTING FROM HEART RHYTHM 2018
Key clinical point: Device-related thrombus (DRT) following left atrial appendage closure occurs in less than 4% of patients but is associated with a higher rate of stroke and systemic embolism vs. no DRT.
Major finding: The rate of ischemic stroke and systemic embolism was 6.28 and 1.65 per 100 patient years for patients with DRT and with no DRT, respectively (P less than .001).
Study details: Analysis of data from the device arms of four prospective clinical trials.
Disclosures: The Watchman studies were funded by Boston Scientific, the company that markets the device. Dr. Reddy has been a consultant to and has received research funding from Boston Scientific and from Abbott and Biosense-Webster, and he reported having an equity interest in Javelin and Surecor. Coauthors reported disclosures related to Boston Scientific, Johnson & Johnson, Abbott, and other medical device companies. Dr. De Lurgio has been a consultant to Boston Scientific.
Source: Dukkipati SR et al. Circulation. 2018 May 11. doi: 10.1161/CIRCULATIONAHA.118.035090.