User login
What Turns Acute Pain Into Chronic Pain?
One of the major challenges in treating pain is to keep an acute event from becoming chronic. What is more, “[o]ur lack of understanding of how acute pain becomes chronic pain has limited our ability to target effective preventive and treatment strategies to patients,” said NIH Director Francis Collins, MD, PhD. So the NIH has launched the Acute to Chronic Pain Signatures (A2CPS) program.
The A2CPS researchers hope to identify individual patient features that will provide clinically meaningful, predictive “signatures” of transition or resilience to chronic pain. They will collect data from patients with acute pain associated with surgery or musculoskeletal trauma. Using neuroimaging, high-throughput biomedical measurements, sensory testing, and psychosocial assessments, they will form a dataset to help predict which patients will develop chronic pain. Those signatures could be valuable in guiding precision medicine and perhaps reducing reliance on opioids, the NIH says.
A2CPS will have an anticipated $40.4 million 4-year budget supplied by the NIH Common Fund.
One of the major challenges in treating pain is to keep an acute event from becoming chronic. What is more, “[o]ur lack of understanding of how acute pain becomes chronic pain has limited our ability to target effective preventive and treatment strategies to patients,” said NIH Director Francis Collins, MD, PhD. So the NIH has launched the Acute to Chronic Pain Signatures (A2CPS) program.
The A2CPS researchers hope to identify individual patient features that will provide clinically meaningful, predictive “signatures” of transition or resilience to chronic pain. They will collect data from patients with acute pain associated with surgery or musculoskeletal trauma. Using neuroimaging, high-throughput biomedical measurements, sensory testing, and psychosocial assessments, they will form a dataset to help predict which patients will develop chronic pain. Those signatures could be valuable in guiding precision medicine and perhaps reducing reliance on opioids, the NIH says.
A2CPS will have an anticipated $40.4 million 4-year budget supplied by the NIH Common Fund.
One of the major challenges in treating pain is to keep an acute event from becoming chronic. What is more, “[o]ur lack of understanding of how acute pain becomes chronic pain has limited our ability to target effective preventive and treatment strategies to patients,” said NIH Director Francis Collins, MD, PhD. So the NIH has launched the Acute to Chronic Pain Signatures (A2CPS) program.
The A2CPS researchers hope to identify individual patient features that will provide clinically meaningful, predictive “signatures” of transition or resilience to chronic pain. They will collect data from patients with acute pain associated with surgery or musculoskeletal trauma. Using neuroimaging, high-throughput biomedical measurements, sensory testing, and psychosocial assessments, they will form a dataset to help predict which patients will develop chronic pain. Those signatures could be valuable in guiding precision medicine and perhaps reducing reliance on opioids, the NIH says.
A2CPS will have an anticipated $40.4 million 4-year budget supplied by the NIH Common Fund.
Optimizing use of TKIs in CML
DUBROVNIK, CROATIA—Long-term efficacy and toxicity should inform decisions about tyrosine kinase inhibitors (TKIs) in chronic myeloid leukemia (CML), according to the keynote presenter at Leukemia and Lymphoma: Europe and the USA, Linking Knowledge and Practice.
Studies have indicated that long-term survival rates are similar whether CML patients receive frontline treatment with imatinib or second-generation TKIs.
However, the newer TKIs pose a higher risk of uncommon toxicities, said Hagop Kantarjian, MD, a professor at MD Anderson Cancer Center in Houston, Texas, who gave the meeting’s keynote speech.
Dr. Kantarjian said most CML patients should receive daily treatment with TKIs—even if they are in complete cytogenetic response or 100% Ph-positive—because they will live longer.
Frontline treatment options for CML that are approved by the U.S. Food and Drug Administration include imatinib, dasatinib, nilotinib, and bosutinib.
Dr. Kantarjian noted that dasatinib and nilotinib bested imatinib in early analyses from clinical trials, but all three TKIs produced similar rates of overall survival (OS) and progression-free survival (PFS) at extended follow-up.
Dasatinib and imatinib produced similar rates of 5-year OS and PFS in the DASISION trial.1 In ENESTnd, 5-year OS and PFS rates were similar with nilotinib and imatinib.2
However, Dr. Kantarjian said the higher incidence of uncommon toxicities with the newer TKIs must be taken into account.
Choosing a TKI
Dr. Kantarjian recommends frontline imatinib for older patients (≥ 65 to 70) and those who are low-risk according to Sokal score.
Second-generation TKIs should be given upfront to patients who are higher-risk by Sokal and for “very young patients in whom early treatment discontinuation is important,” according to Dr. Kantarjian.
“In accelerated or blast phase, I always use the second-generation TKIs,” he said. “If there’s no binding mutation, I prefer dasatinib. I think it’s the most potent of them. If there are toxicities with dasatinib, bosutinib is equivalent in efficacy, so they are interchangeable.”
Dr. Kantarjian also said a TKI should not be discarded unless there is loss of complete cytogenetic response (not major molecular response) at the maximum tolerated adjusted dose that does not cause grade 3-4 toxicities or chronic grade 2 toxicities.
“[W]e have to remember that we can go down on the dosages of, for example, imatinib down to 200 mg a day, dasatinib as low as 20 mg a day, nilotinib as low as 150 mg twice a day or even 200 mg daily, and bosutinib down to 200 mg daily,” Dr. Kantarjian said.
“So if we have a patient who’s responding with side effects, we should not abandon the particular TKI, we should try to manipulate the dose schedule if they are having a good response.”
Dr. Kantarjian noted that pleural effusion is a toxicity of particular concern with dasatinib, but lowering the dose to 50 mg daily results in similar efficacy and significantly less toxicity than 100 mg daily. For patients over the age of 70, a 20 mg dose can be used.
Dr. Kantarjian said vaso-occlusive and vasospastic reactions are increasingly observed in patients treated with nilotinib. Therefore, he prefers to forgo upfront nilotinib, particularly in patients who have cardiovascular or neurotoxic problems.
“The incidence of vaso-occlusive and vasospastic reactions is now close to 10% to 15% at about 10 years with nilotinib,” Dr. Kantarjian said. “So it is not a trivial toxicity.”
For patients with vaso-occlusive/vasospastic reactions, “bosutinib is probably the safest drug,” Dr. Kantarjian said.
For second- or third-line therapy, patients can receive ponatinib or a second-generation TKI (dasatinib, nilotinib, or bosutinib) as well as omacetaxine or allogeneic stem cell transplant.
“If you disregard toxicities, I think ponatinib is the most powerful TKI, and I think that’s because we are using it at a higher dose that produces so many toxicities,” Dr. Kantarjian said.
He added that the reason ponatinib is not used upfront is because of these toxicities, particularly pancreatitis, skin rashes, vaso-occlusive disorders, and hypertension.
Dr. Kantarjian suggests giving ponatinib at 30 mg daily in patients with T315I mutation and those without guiding mutations who are resistant to second-generation TKIs.
When to discontinue TKIs
Dr. Kantarjian said patients can discontinue TKI therapy if they:
- Are low- or intermediate-risk by Sokal
- Have quantifiable BCR-ABL transcripts—B2A2, B3A2 (e13a2 or e14a2)
- Are in chronic phase
- Achieved an optimal response to their first TKI
- Have been on TKI therapy for more than 8 years
- Achieved a complete molecular response (MR4.5)
- Have had a molecular response for more than 2 to 3 years
- Are available for monitoring every other month for the first 2 years.
Dr. Kantarjian did not report any conflicts of interest at the meeting. However, he has previously reported relationships with Novartis (makers of imatinib and nilotinib), Bristol-Myers Squibb (makers of dasatinib), Pfizer (makers of bosutinib), and Ariad Pharmaceuticals (makers of ponatinib, now owned by Takeda Pharmaceutical Company Limited).
1. Cortes JE et al. J Clin Oncol. 2016 Jul 10; 34(20): 2333–2340. doi: 10.1200/JCO.2015.64.8899
2. Hochhaus A et al. Leukemia. 2016 May; 30(5): 1044–1054. doi: 10.1038/leu.2016.5
DUBROVNIK, CROATIA—Long-term efficacy and toxicity should inform decisions about tyrosine kinase inhibitors (TKIs) in chronic myeloid leukemia (CML), according to the keynote presenter at Leukemia and Lymphoma: Europe and the USA, Linking Knowledge and Practice.
Studies have indicated that long-term survival rates are similar whether CML patients receive frontline treatment with imatinib or second-generation TKIs.
However, the newer TKIs pose a higher risk of uncommon toxicities, said Hagop Kantarjian, MD, a professor at MD Anderson Cancer Center in Houston, Texas, who gave the meeting’s keynote speech.
Dr. Kantarjian said most CML patients should receive daily treatment with TKIs—even if they are in complete cytogenetic response or 100% Ph-positive—because they will live longer.
Frontline treatment options for CML that are approved by the U.S. Food and Drug Administration include imatinib, dasatinib, nilotinib, and bosutinib.
Dr. Kantarjian noted that dasatinib and nilotinib bested imatinib in early analyses from clinical trials, but all three TKIs produced similar rates of overall survival (OS) and progression-free survival (PFS) at extended follow-up.
Dasatinib and imatinib produced similar rates of 5-year OS and PFS in the DASISION trial.1 In ENESTnd, 5-year OS and PFS rates were similar with nilotinib and imatinib.2
However, Dr. Kantarjian said the higher incidence of uncommon toxicities with the newer TKIs must be taken into account.
Choosing a TKI
Dr. Kantarjian recommends frontline imatinib for older patients (≥ 65 to 70) and those who are low-risk according to Sokal score.
Second-generation TKIs should be given upfront to patients who are higher-risk by Sokal and for “very young patients in whom early treatment discontinuation is important,” according to Dr. Kantarjian.
“In accelerated or blast phase, I always use the second-generation TKIs,” he said. “If there’s no binding mutation, I prefer dasatinib. I think it’s the most potent of them. If there are toxicities with dasatinib, bosutinib is equivalent in efficacy, so they are interchangeable.”
Dr. Kantarjian also said a TKI should not be discarded unless there is loss of complete cytogenetic response (not major molecular response) at the maximum tolerated adjusted dose that does not cause grade 3-4 toxicities or chronic grade 2 toxicities.
“[W]e have to remember that we can go down on the dosages of, for example, imatinib down to 200 mg a day, dasatinib as low as 20 mg a day, nilotinib as low as 150 mg twice a day or even 200 mg daily, and bosutinib down to 200 mg daily,” Dr. Kantarjian said.
“So if we have a patient who’s responding with side effects, we should not abandon the particular TKI, we should try to manipulate the dose schedule if they are having a good response.”
Dr. Kantarjian noted that pleural effusion is a toxicity of particular concern with dasatinib, but lowering the dose to 50 mg daily results in similar efficacy and significantly less toxicity than 100 mg daily. For patients over the age of 70, a 20 mg dose can be used.
Dr. Kantarjian said vaso-occlusive and vasospastic reactions are increasingly observed in patients treated with nilotinib. Therefore, he prefers to forgo upfront nilotinib, particularly in patients who have cardiovascular or neurotoxic problems.
“The incidence of vaso-occlusive and vasospastic reactions is now close to 10% to 15% at about 10 years with nilotinib,” Dr. Kantarjian said. “So it is not a trivial toxicity.”
For patients with vaso-occlusive/vasospastic reactions, “bosutinib is probably the safest drug,” Dr. Kantarjian said.
For second- or third-line therapy, patients can receive ponatinib or a second-generation TKI (dasatinib, nilotinib, or bosutinib) as well as omacetaxine or allogeneic stem cell transplant.
“If you disregard toxicities, I think ponatinib is the most powerful TKI, and I think that’s because we are using it at a higher dose that produces so many toxicities,” Dr. Kantarjian said.
He added that the reason ponatinib is not used upfront is because of these toxicities, particularly pancreatitis, skin rashes, vaso-occlusive disorders, and hypertension.
Dr. Kantarjian suggests giving ponatinib at 30 mg daily in patients with T315I mutation and those without guiding mutations who are resistant to second-generation TKIs.
When to discontinue TKIs
Dr. Kantarjian said patients can discontinue TKI therapy if they:
- Are low- or intermediate-risk by Sokal
- Have quantifiable BCR-ABL transcripts—B2A2, B3A2 (e13a2 or e14a2)
- Are in chronic phase
- Achieved an optimal response to their first TKI
- Have been on TKI therapy for more than 8 years
- Achieved a complete molecular response (MR4.5)
- Have had a molecular response for more than 2 to 3 years
- Are available for monitoring every other month for the first 2 years.
Dr. Kantarjian did not report any conflicts of interest at the meeting. However, he has previously reported relationships with Novartis (makers of imatinib and nilotinib), Bristol-Myers Squibb (makers of dasatinib), Pfizer (makers of bosutinib), and Ariad Pharmaceuticals (makers of ponatinib, now owned by Takeda Pharmaceutical Company Limited).
1. Cortes JE et al. J Clin Oncol. 2016 Jul 10; 34(20): 2333–2340. doi: 10.1200/JCO.2015.64.8899
2. Hochhaus A et al. Leukemia. 2016 May; 30(5): 1044–1054. doi: 10.1038/leu.2016.5
DUBROVNIK, CROATIA—Long-term efficacy and toxicity should inform decisions about tyrosine kinase inhibitors (TKIs) in chronic myeloid leukemia (CML), according to the keynote presenter at Leukemia and Lymphoma: Europe and the USA, Linking Knowledge and Practice.
Studies have indicated that long-term survival rates are similar whether CML patients receive frontline treatment with imatinib or second-generation TKIs.
However, the newer TKIs pose a higher risk of uncommon toxicities, said Hagop Kantarjian, MD, a professor at MD Anderson Cancer Center in Houston, Texas, who gave the meeting’s keynote speech.
Dr. Kantarjian said most CML patients should receive daily treatment with TKIs—even if they are in complete cytogenetic response or 100% Ph-positive—because they will live longer.
Frontline treatment options for CML that are approved by the U.S. Food and Drug Administration include imatinib, dasatinib, nilotinib, and bosutinib.
Dr. Kantarjian noted that dasatinib and nilotinib bested imatinib in early analyses from clinical trials, but all three TKIs produced similar rates of overall survival (OS) and progression-free survival (PFS) at extended follow-up.
Dasatinib and imatinib produced similar rates of 5-year OS and PFS in the DASISION trial.1 In ENESTnd, 5-year OS and PFS rates were similar with nilotinib and imatinib.2
However, Dr. Kantarjian said the higher incidence of uncommon toxicities with the newer TKIs must be taken into account.
Choosing a TKI
Dr. Kantarjian recommends frontline imatinib for older patients (≥ 65 to 70) and those who are low-risk according to Sokal score.
Second-generation TKIs should be given upfront to patients who are higher-risk by Sokal and for “very young patients in whom early treatment discontinuation is important,” according to Dr. Kantarjian.
“In accelerated or blast phase, I always use the second-generation TKIs,” he said. “If there’s no binding mutation, I prefer dasatinib. I think it’s the most potent of them. If there are toxicities with dasatinib, bosutinib is equivalent in efficacy, so they are interchangeable.”
Dr. Kantarjian also said a TKI should not be discarded unless there is loss of complete cytogenetic response (not major molecular response) at the maximum tolerated adjusted dose that does not cause grade 3-4 toxicities or chronic grade 2 toxicities.
“[W]e have to remember that we can go down on the dosages of, for example, imatinib down to 200 mg a day, dasatinib as low as 20 mg a day, nilotinib as low as 150 mg twice a day or even 200 mg daily, and bosutinib down to 200 mg daily,” Dr. Kantarjian said.
“So if we have a patient who’s responding with side effects, we should not abandon the particular TKI, we should try to manipulate the dose schedule if they are having a good response.”
Dr. Kantarjian noted that pleural effusion is a toxicity of particular concern with dasatinib, but lowering the dose to 50 mg daily results in similar efficacy and significantly less toxicity than 100 mg daily. For patients over the age of 70, a 20 mg dose can be used.
Dr. Kantarjian said vaso-occlusive and vasospastic reactions are increasingly observed in patients treated with nilotinib. Therefore, he prefers to forgo upfront nilotinib, particularly in patients who have cardiovascular or neurotoxic problems.
“The incidence of vaso-occlusive and vasospastic reactions is now close to 10% to 15% at about 10 years with nilotinib,” Dr. Kantarjian said. “So it is not a trivial toxicity.”
For patients with vaso-occlusive/vasospastic reactions, “bosutinib is probably the safest drug,” Dr. Kantarjian said.
For second- or third-line therapy, patients can receive ponatinib or a second-generation TKI (dasatinib, nilotinib, or bosutinib) as well as omacetaxine or allogeneic stem cell transplant.
“If you disregard toxicities, I think ponatinib is the most powerful TKI, and I think that’s because we are using it at a higher dose that produces so many toxicities,” Dr. Kantarjian said.
He added that the reason ponatinib is not used upfront is because of these toxicities, particularly pancreatitis, skin rashes, vaso-occlusive disorders, and hypertension.
Dr. Kantarjian suggests giving ponatinib at 30 mg daily in patients with T315I mutation and those without guiding mutations who are resistant to second-generation TKIs.
When to discontinue TKIs
Dr. Kantarjian said patients can discontinue TKI therapy if they:
- Are low- or intermediate-risk by Sokal
- Have quantifiable BCR-ABL transcripts—B2A2, B3A2 (e13a2 or e14a2)
- Are in chronic phase
- Achieved an optimal response to their first TKI
- Have been on TKI therapy for more than 8 years
- Achieved a complete molecular response (MR4.5)
- Have had a molecular response for more than 2 to 3 years
- Are available for monitoring every other month for the first 2 years.
Dr. Kantarjian did not report any conflicts of interest at the meeting. However, he has previously reported relationships with Novartis (makers of imatinib and nilotinib), Bristol-Myers Squibb (makers of dasatinib), Pfizer (makers of bosutinib), and Ariad Pharmaceuticals (makers of ponatinib, now owned by Takeda Pharmaceutical Company Limited).
1. Cortes JE et al. J Clin Oncol. 2016 Jul 10; 34(20): 2333–2340. doi: 10.1200/JCO.2015.64.8899
2. Hochhaus A et al. Leukemia. 2016 May; 30(5): 1044–1054. doi: 10.1038/leu.2016.5
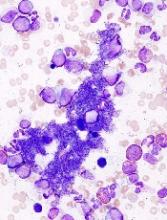
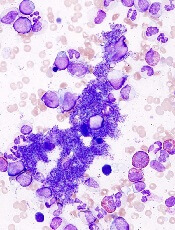
Genomic findings may predict outcomes in MPN patients
New research suggests genomic characteristics of patients with myeloproliferative neoplasms (MPNs) can predict clinical outcomes.
Investigators defined eight genomic subgroups of MPNs, each with distinct clinical features, including event-free survival, risk of leukemic transformation, and blood counts.
Jacob Grinfeld, MD, of the University of Cambridge in the U.K., and his colleagues described these findings in The New England Journal of Medicine.
This study included 2,035 patients with MPNs, including essential thrombocythemia, polycythemia vera, myelofibrosis, and other diagnoses.
The investigators performed targeted sequencing for the full coding sequence of 69 genes and genome-wide copy number information in 1,887 patients. Whole-exome sequencing was performed in another 148 patients.
By sequencing coding exons from 69 myeloid cancer genes, the investigators were able to survey the diversity of mutations across MPN patients and identify mutation-associated clinical outcomes.
The results showed that slightly less than half (45%) of the patients had a solitary abnormality in CALR, MPL, or JAK2, while the remaining patients had additional driver mutations.
In some instances, additional mutations were numerous, particularly in older patients with advanced disease. In at least five cases, 33 genes had driver mutations.
Further analysis revealed eight genomic subgroups that could predict clinical outcomes based on shared chromosomal abnormalities and mutations.
For example, one subgroup included patients with TP53 mutations. These individuals had a “dismal prognosis” and were 15.5 times more likely to transform to acute myeloid leukemia, compared with the JAK2-heterozygous subgroup (P<0.001).
Because prognosis is “a key determinant” of MPN treatment, genomic subgrouping may one day guide clinical decision-making, the investigators concluded.
To further this cause, they have made available an online calculator of individualized patient outcomes, which can be accessed at https://cancer.sanger.ac.uk/mpn-multistage/.
This study was funded by the Wellcome Trust, the National Institute for Health Research Cambridge Biomedical Research Centre, Cancer Research UK, and others. Some study authors reported fees from Celgene, Novartis, Gilead, Shire, and others outside of the study.
New research suggests genomic characteristics of patients with myeloproliferative neoplasms (MPNs) can predict clinical outcomes.
Investigators defined eight genomic subgroups of MPNs, each with distinct clinical features, including event-free survival, risk of leukemic transformation, and blood counts.
Jacob Grinfeld, MD, of the University of Cambridge in the U.K., and his colleagues described these findings in The New England Journal of Medicine.
This study included 2,035 patients with MPNs, including essential thrombocythemia, polycythemia vera, myelofibrosis, and other diagnoses.
The investigators performed targeted sequencing for the full coding sequence of 69 genes and genome-wide copy number information in 1,887 patients. Whole-exome sequencing was performed in another 148 patients.
By sequencing coding exons from 69 myeloid cancer genes, the investigators were able to survey the diversity of mutations across MPN patients and identify mutation-associated clinical outcomes.
The results showed that slightly less than half (45%) of the patients had a solitary abnormality in CALR, MPL, or JAK2, while the remaining patients had additional driver mutations.
In some instances, additional mutations were numerous, particularly in older patients with advanced disease. In at least five cases, 33 genes had driver mutations.
Further analysis revealed eight genomic subgroups that could predict clinical outcomes based on shared chromosomal abnormalities and mutations.
For example, one subgroup included patients with TP53 mutations. These individuals had a “dismal prognosis” and were 15.5 times more likely to transform to acute myeloid leukemia, compared with the JAK2-heterozygous subgroup (P<0.001).
Because prognosis is “a key determinant” of MPN treatment, genomic subgrouping may one day guide clinical decision-making, the investigators concluded.
To further this cause, they have made available an online calculator of individualized patient outcomes, which can be accessed at https://cancer.sanger.ac.uk/mpn-multistage/.
This study was funded by the Wellcome Trust, the National Institute for Health Research Cambridge Biomedical Research Centre, Cancer Research UK, and others. Some study authors reported fees from Celgene, Novartis, Gilead, Shire, and others outside of the study.
New research suggests genomic characteristics of patients with myeloproliferative neoplasms (MPNs) can predict clinical outcomes.
Investigators defined eight genomic subgroups of MPNs, each with distinct clinical features, including event-free survival, risk of leukemic transformation, and blood counts.
Jacob Grinfeld, MD, of the University of Cambridge in the U.K., and his colleagues described these findings in The New England Journal of Medicine.
This study included 2,035 patients with MPNs, including essential thrombocythemia, polycythemia vera, myelofibrosis, and other diagnoses.
The investigators performed targeted sequencing for the full coding sequence of 69 genes and genome-wide copy number information in 1,887 patients. Whole-exome sequencing was performed in another 148 patients.
By sequencing coding exons from 69 myeloid cancer genes, the investigators were able to survey the diversity of mutations across MPN patients and identify mutation-associated clinical outcomes.
The results showed that slightly less than half (45%) of the patients had a solitary abnormality in CALR, MPL, or JAK2, while the remaining patients had additional driver mutations.
In some instances, additional mutations were numerous, particularly in older patients with advanced disease. In at least five cases, 33 genes had driver mutations.
Further analysis revealed eight genomic subgroups that could predict clinical outcomes based on shared chromosomal abnormalities and mutations.
For example, one subgroup included patients with TP53 mutations. These individuals had a “dismal prognosis” and were 15.5 times more likely to transform to acute myeloid leukemia, compared with the JAK2-heterozygous subgroup (P<0.001).
Because prognosis is “a key determinant” of MPN treatment, genomic subgrouping may one day guide clinical decision-making, the investigators concluded.
To further this cause, they have made available an online calculator of individualized patient outcomes, which can be accessed at https://cancer.sanger.ac.uk/mpn-multistage/.
This study was funded by the Wellcome Trust, the National Institute for Health Research Cambridge Biomedical Research Centre, Cancer Research UK, and others. Some study authors reported fees from Celgene, Novartis, Gilead, Shire, and others outside of the study.
Inhibitor receives orphan designation for PTCL
The U.S. Food and Drug Administration (FDA) has granted orphan drug designation to cerdulatinib for the treatment of peripheral T-cell lymphoma (PTCL).
Cerdulatinib is an oral Syk/JAK inhibitor being developed by Portola Pharmaceuticals, Inc.
Preclinical data have suggested an important role for Syk and JAK in PTCL tumor survival, and cerdulatinib is currently under evaluation in a phase 2a study of patients with PTCL and other non-Hodgkin lymphomas.
Results from this trial were presented at the 23rd Congress of the European Hematology Association (EHA) earlier this year.
At that time, the trial had enrolled 114 patients, 25 of them with PTCL. The patients received cerdulatinib at 25, 30, or 35 mg twice daily.
The objective response rate was 35% among the PTCL patients. All seven responders had a complete response, and 11 PTCL patients were still on cerdulatinib at the time of the presentation.
Grade 3 or higher adverse events observed in all evaluable patients included lipase increase (18%), neutropenia (17%), pneumonia/lung infection (11%), diarrhea (8%), fatigue (6%), amylase increase (5%), sepsis/septic shock (4%), hypertension (4%), anemia (4%), thrombocytopenia (4%), and hypophosphatemia (4%).
There were five deaths due to sepsis or septic shock (three of which were concomitant with pneumonia) that were considered related to cerdulatinib.
Three of the deaths occurred in patients with chronic lymphocytic leukemia, one in a patient with diffuse large B-cell lymphoma, and one in a patient with follicular lymphoma.
The deaths occurred early on in the trial, and researchers have since taken steps—dose reductions, monitoring, and antibiotic prophylaxis—to prevent additional deaths.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the United States.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The U.S. Food and Drug Administration (FDA) has granted orphan drug designation to cerdulatinib for the treatment of peripheral T-cell lymphoma (PTCL).
Cerdulatinib is an oral Syk/JAK inhibitor being developed by Portola Pharmaceuticals, Inc.
Preclinical data have suggested an important role for Syk and JAK in PTCL tumor survival, and cerdulatinib is currently under evaluation in a phase 2a study of patients with PTCL and other non-Hodgkin lymphomas.
Results from this trial were presented at the 23rd Congress of the European Hematology Association (EHA) earlier this year.
At that time, the trial had enrolled 114 patients, 25 of them with PTCL. The patients received cerdulatinib at 25, 30, or 35 mg twice daily.
The objective response rate was 35% among the PTCL patients. All seven responders had a complete response, and 11 PTCL patients were still on cerdulatinib at the time of the presentation.
Grade 3 or higher adverse events observed in all evaluable patients included lipase increase (18%), neutropenia (17%), pneumonia/lung infection (11%), diarrhea (8%), fatigue (6%), amylase increase (5%), sepsis/septic shock (4%), hypertension (4%), anemia (4%), thrombocytopenia (4%), and hypophosphatemia (4%).
There were five deaths due to sepsis or septic shock (three of which were concomitant with pneumonia) that were considered related to cerdulatinib.
Three of the deaths occurred in patients with chronic lymphocytic leukemia, one in a patient with diffuse large B-cell lymphoma, and one in a patient with follicular lymphoma.
The deaths occurred early on in the trial, and researchers have since taken steps—dose reductions, monitoring, and antibiotic prophylaxis—to prevent additional deaths.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the United States.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
The U.S. Food and Drug Administration (FDA) has granted orphan drug designation to cerdulatinib for the treatment of peripheral T-cell lymphoma (PTCL).
Cerdulatinib is an oral Syk/JAK inhibitor being developed by Portola Pharmaceuticals, Inc.
Preclinical data have suggested an important role for Syk and JAK in PTCL tumor survival, and cerdulatinib is currently under evaluation in a phase 2a study of patients with PTCL and other non-Hodgkin lymphomas.
Results from this trial were presented at the 23rd Congress of the European Hematology Association (EHA) earlier this year.
At that time, the trial had enrolled 114 patients, 25 of them with PTCL. The patients received cerdulatinib at 25, 30, or 35 mg twice daily.
The objective response rate was 35% among the PTCL patients. All seven responders had a complete response, and 11 PTCL patients were still on cerdulatinib at the time of the presentation.
Grade 3 or higher adverse events observed in all evaluable patients included lipase increase (18%), neutropenia (17%), pneumonia/lung infection (11%), diarrhea (8%), fatigue (6%), amylase increase (5%), sepsis/septic shock (4%), hypertension (4%), anemia (4%), thrombocytopenia (4%), and hypophosphatemia (4%).
There were five deaths due to sepsis or septic shock (three of which were concomitant with pneumonia) that were considered related to cerdulatinib.
Three of the deaths occurred in patients with chronic lymphocytic leukemia, one in a patient with diffuse large B-cell lymphoma, and one in a patient with follicular lymphoma.
The deaths occurred early on in the trial, and researchers have since taken steps—dose reductions, monitoring, and antibiotic prophylaxis—to prevent additional deaths.
About orphan designation
The FDA grants orphan designation to products intended to treat, diagnose, or prevent diseases/disorders that affect fewer than 200,000 people in the United States.
The designation provides incentives for sponsors to develop products for rare diseases. This may include tax credits toward the cost of clinical trials, prescription drug user fee waivers, and 7 years of market exclusivity if the product is approved.
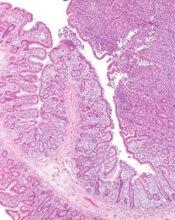
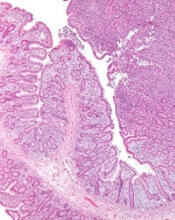
Rash on arm

The FP looked closely at the so-called rash and realized that while it could be nummular eczema it could also be a superficial basal cell carcinoma (BCC).
He explained the differential diagnosis to the patient and suggested that he perform a shave biopsy that day. The patient consented to the biopsy, and the physician numbed the area with 1% lidocaine and epinephrine. He used a DermaBlade and obtained hemostasis with aluminum chloride in water. (See the Watch & Learn video on “Shave biopsy.”) The biopsy result confirmed the FP’s suspicion: The lesion was a superficial BCC.
On the follow-up visit the FP explained the options for treatment, including electrodesiccation and curettage, cryosurgery, or an elliptical excision. He told the patient that the cure rates are about the same, regardless of which of these treatments were chosen. He also explained that either of the 2 destructive methods could be performed immediately, whereas the elliptical excision would require scheduling a longer appointment.
The patient chose the cryosurgery. (See the Watch & Learn video on cryosurgery.) After numbing the area with 1% lidocaine and epinephrine, the physician froze the lesion with a 3 mm halo for 30 seconds using liquid nitrogen spray. At follow-up 3 months later, there was some hypopigmentation, but no evidence of the BCC.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Karnes J, Usatine R. Basal cell carcinoma. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:989-998.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/.
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com.

The FP looked closely at the so-called rash and realized that while it could be nummular eczema it could also be a superficial basal cell carcinoma (BCC).
He explained the differential diagnosis to the patient and suggested that he perform a shave biopsy that day. The patient consented to the biopsy, and the physician numbed the area with 1% lidocaine and epinephrine. He used a DermaBlade and obtained hemostasis with aluminum chloride in water. (See the Watch & Learn video on “Shave biopsy.”) The biopsy result confirmed the FP’s suspicion: The lesion was a superficial BCC.
On the follow-up visit the FP explained the options for treatment, including electrodesiccation and curettage, cryosurgery, or an elliptical excision. He told the patient that the cure rates are about the same, regardless of which of these treatments were chosen. He also explained that either of the 2 destructive methods could be performed immediately, whereas the elliptical excision would require scheduling a longer appointment.
The patient chose the cryosurgery. (See the Watch & Learn video on cryosurgery.) After numbing the area with 1% lidocaine and epinephrine, the physician froze the lesion with a 3 mm halo for 30 seconds using liquid nitrogen spray. At follow-up 3 months later, there was some hypopigmentation, but no evidence of the BCC.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Karnes J, Usatine R. Basal cell carcinoma. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:989-998.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/.
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com.

The FP looked closely at the so-called rash and realized that while it could be nummular eczema it could also be a superficial basal cell carcinoma (BCC).
He explained the differential diagnosis to the patient and suggested that he perform a shave biopsy that day. The patient consented to the biopsy, and the physician numbed the area with 1% lidocaine and epinephrine. He used a DermaBlade and obtained hemostasis with aluminum chloride in water. (See the Watch & Learn video on “Shave biopsy.”) The biopsy result confirmed the FP’s suspicion: The lesion was a superficial BCC.
On the follow-up visit the FP explained the options for treatment, including electrodesiccation and curettage, cryosurgery, or an elliptical excision. He told the patient that the cure rates are about the same, regardless of which of these treatments were chosen. He also explained that either of the 2 destructive methods could be performed immediately, whereas the elliptical excision would require scheduling a longer appointment.
The patient chose the cryosurgery. (See the Watch & Learn video on cryosurgery.) After numbing the area with 1% lidocaine and epinephrine, the physician froze the lesion with a 3 mm halo for 30 seconds using liquid nitrogen spray. At follow-up 3 months later, there was some hypopigmentation, but no evidence of the BCC.
Photos and text for Photo Rounds Friday courtesy of Richard P. Usatine, MD. This case was adapted from: Karnes J, Usatine R. Basal cell carcinoma. In: Usatine R, Smith M, Mayeaux EJ, et al. Color Atlas of Family Medicine. 2nd ed. New York, NY: McGraw-Hill; 2013:989-998.
To learn more about the Color Atlas of Family Medicine, see: www.amazon.com/Color-Family-Medicine-Richard-Usatine/dp/0071769641/.
You can now get the second edition of the Color Atlas of Family Medicine as an app by clicking on this link: usatinemedia.com.
Readmissions after GI bleeds
Clinical question: What is the rate of hospital readmission within 30 days of nonvariceal upper GI hemorrhage, and what are its effects on mortality, morbidity, and health care use in the United States?
Background: Nonvariceal upper GI hemorrhage is the most common GI emergency that leads to hospital admission (approximately 300,000 admissions/year in the United States). Because of the advances in endoscopic therapy and overall medical care, associated in-hospital mortality has been steadily decreasing. As a result of Medicare and Medicaid shifts toward an alternative payment model, quantifying hospital readmission rate after an episode of nonvariceal upper GI hemorrhage and measuring its effects on patient outcomes and resource use have become a key step in both improving treatment outcomes and health care reimbursement.
Study design: Retrospective study.
Setting: The Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project Nationwide Readmission Database for the year 2014.
Synopsis: The study collected data on hospital readmissions for 203,220 adults who were hospitalized for urgent nonvariceal upper gastrointestinal hemorrhage and discharged. The primary outcome was rate of all-cause readmission within 30 days of discharge. Secondary outcomes were reasons for readmission, readmission mortality rate, morbidity (shock and prolonged mechanical ventilation), and resource use (length of stay and total hospitalization costs and charges).
The rate of readmission was determined to be 13%, with only 18% caused by recurrent nonvariceal upper gastrointestinal bleeding. The rate of death among readmissions was higher than that among index admissions, and a higher proportion of readmitted patients had morbidities requiring prolonged mechanical ventilation. The total economic in-hospital burden was $30.3 million in costs and $108 million in charges over the span of readmission-associated 133,368 hospital days. Independent predictors of readmission were having Medicaid insurance, having a higher comorbidity score, having a lower income, residence in a metropolitan area, hemorrhagic shock, and longer stays in the hospital.
Bottom line: Readmissions within 30 days of discharge for upper GI hemorrhage are associated with higher morbidity and mortality and lead to higher resource use.
Citation: Abougergi M et al. Thirty-day readmission among patients with nonvariceal upper gastrointestinal hemorrhage and effects on outcomes. Gastroenterology. 2018 Jul;155(1):38-46.
Dr. White is a hospitalist in the division of hospital medicine in the department of medicine at Loyola University Chicago, Maywood, Ill.
Clinical question: What is the rate of hospital readmission within 30 days of nonvariceal upper GI hemorrhage, and what are its effects on mortality, morbidity, and health care use in the United States?
Background: Nonvariceal upper GI hemorrhage is the most common GI emergency that leads to hospital admission (approximately 300,000 admissions/year in the United States). Because of the advances in endoscopic therapy and overall medical care, associated in-hospital mortality has been steadily decreasing. As a result of Medicare and Medicaid shifts toward an alternative payment model, quantifying hospital readmission rate after an episode of nonvariceal upper GI hemorrhage and measuring its effects on patient outcomes and resource use have become a key step in both improving treatment outcomes and health care reimbursement.
Study design: Retrospective study.
Setting: The Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project Nationwide Readmission Database for the year 2014.
Synopsis: The study collected data on hospital readmissions for 203,220 adults who were hospitalized for urgent nonvariceal upper gastrointestinal hemorrhage and discharged. The primary outcome was rate of all-cause readmission within 30 days of discharge. Secondary outcomes were reasons for readmission, readmission mortality rate, morbidity (shock and prolonged mechanical ventilation), and resource use (length of stay and total hospitalization costs and charges).
The rate of readmission was determined to be 13%, with only 18% caused by recurrent nonvariceal upper gastrointestinal bleeding. The rate of death among readmissions was higher than that among index admissions, and a higher proportion of readmitted patients had morbidities requiring prolonged mechanical ventilation. The total economic in-hospital burden was $30.3 million in costs and $108 million in charges over the span of readmission-associated 133,368 hospital days. Independent predictors of readmission were having Medicaid insurance, having a higher comorbidity score, having a lower income, residence in a metropolitan area, hemorrhagic shock, and longer stays in the hospital.
Bottom line: Readmissions within 30 days of discharge for upper GI hemorrhage are associated with higher morbidity and mortality and lead to higher resource use.
Citation: Abougergi M et al. Thirty-day readmission among patients with nonvariceal upper gastrointestinal hemorrhage and effects on outcomes. Gastroenterology. 2018 Jul;155(1):38-46.
Dr. White is a hospitalist in the division of hospital medicine in the department of medicine at Loyola University Chicago, Maywood, Ill.
Clinical question: What is the rate of hospital readmission within 30 days of nonvariceal upper GI hemorrhage, and what are its effects on mortality, morbidity, and health care use in the United States?
Background: Nonvariceal upper GI hemorrhage is the most common GI emergency that leads to hospital admission (approximately 300,000 admissions/year in the United States). Because of the advances in endoscopic therapy and overall medical care, associated in-hospital mortality has been steadily decreasing. As a result of Medicare and Medicaid shifts toward an alternative payment model, quantifying hospital readmission rate after an episode of nonvariceal upper GI hemorrhage and measuring its effects on patient outcomes and resource use have become a key step in both improving treatment outcomes and health care reimbursement.
Study design: Retrospective study.
Setting: The Agency for Healthcare Research and Quality’s Healthcare Cost and Utilization Project Nationwide Readmission Database for the year 2014.
Synopsis: The study collected data on hospital readmissions for 203,220 adults who were hospitalized for urgent nonvariceal upper gastrointestinal hemorrhage and discharged. The primary outcome was rate of all-cause readmission within 30 days of discharge. Secondary outcomes were reasons for readmission, readmission mortality rate, morbidity (shock and prolonged mechanical ventilation), and resource use (length of stay and total hospitalization costs and charges).
The rate of readmission was determined to be 13%, with only 18% caused by recurrent nonvariceal upper gastrointestinal bleeding. The rate of death among readmissions was higher than that among index admissions, and a higher proportion of readmitted patients had morbidities requiring prolonged mechanical ventilation. The total economic in-hospital burden was $30.3 million in costs and $108 million in charges over the span of readmission-associated 133,368 hospital days. Independent predictors of readmission were having Medicaid insurance, having a higher comorbidity score, having a lower income, residence in a metropolitan area, hemorrhagic shock, and longer stays in the hospital.
Bottom line: Readmissions within 30 days of discharge for upper GI hemorrhage are associated with higher morbidity and mortality and lead to higher resource use.
Citation: Abougergi M et al. Thirty-day readmission among patients with nonvariceal upper gastrointestinal hemorrhage and effects on outcomes. Gastroenterology. 2018 Jul;155(1):38-46.
Dr. White is a hospitalist in the division of hospital medicine in the department of medicine at Loyola University Chicago, Maywood, Ill.
Virus-specific T-cell infusion may resolve progressive multifocal leukoencephalopathy
, according to investigators from the University of Texas MD Anderson Cancer Center, Houston.
The infusion cleared JC virus from the cerebrospinal fluid (CSF) of two patients and reduced viral load in the third, reported lead author Muharrem Muftuoglu, MD, of MD Anderson’s department of stem cell transplantation and cellular therapy and colleagues. One of the patients completely recovered and returned to work.
“Several approaches for the treatment of PML, including the use of antiviral medications and mirtazapine, have been tested, with poor results,” the investigators wrote in the New England Journal of Medicine. Although virus-specific T-cell infusion is a novel approach to treating PML, this method has been used for other conditions.
“Several groups, including ours, have successfully used viral-specific T cells to treat BK virus infection after stem-cell transplantation,” the investigators wrote. “Because BK virus and JC virus are genetically similar to one another and share a number of immunogenic proteins with a substantial degree of sequence homology ... we hypothesized that T cells developed against BK virus may also be effective against JC virus infection.”
This hypothesis proved accurate. The investigators infused three PML patients with “cryopreserved, third-party–produced, viral-specific T cells that had been designed for the treatment of patients with BK virus infection after stem-cell transplantation.” Each patient presented with a different condition and PML-precipitating therapy. The first patient was a 32-year-old woman with high-risk acute myeloid leukemia who had received a cord-blood transplantation, the second a 73-year-old woman with JAK2-positive myeloproliferative neoplasia on ruxolitinib (Jakafi) therapy, and the third a 35-year-old man with HIV who had received highly active antiretroviral therapy.
T-cell infusions cleared JC virus from the CSF of the woman with leukemia (three infusions) and the man with HIV (four infusions). These patients recovered to different degrees: The woman had full resolution of symptoms, while the man had slurred speech and walked with a cane. Treatment reduced JC viral load in the elderly woman with myeloproliferative neoplasia (two infusions), but she did not clear the virus and died about 8 months later.
No adverse events occurred, but two patients developed immune reconstitution inflammatory syndrome. This was likely caused by the T-cell infusion, since absolute T-cell counts remained steady and white matter enhancement was detected on MRI within 4 weeks of treatment. Still, the investigators were optimistic about future potential.
“Third-party–produced, ‘off-the-shelf,’ partially HLA-matched, BK virus–specific T cells may serve as therapy for PML,” the investigators concluded. “Further study in a larger group of patients is required to determine the success rate, durability, and longer-term adverse events associated with this treatment.”
The study was funded by the MD Anderson Cancer Center Moon Shots Program and the National Institutes of Health.
SOURCE: Muftuoglu M et al. N Engl J Med. 2018 Oct 11;379:1443-51
This article was updated 3/22/19.
, according to investigators from the University of Texas MD Anderson Cancer Center, Houston.
The infusion cleared JC virus from the cerebrospinal fluid (CSF) of two patients and reduced viral load in the third, reported lead author Muharrem Muftuoglu, MD, of MD Anderson’s department of stem cell transplantation and cellular therapy and colleagues. One of the patients completely recovered and returned to work.
“Several approaches for the treatment of PML, including the use of antiviral medications and mirtazapine, have been tested, with poor results,” the investigators wrote in the New England Journal of Medicine. Although virus-specific T-cell infusion is a novel approach to treating PML, this method has been used for other conditions.
“Several groups, including ours, have successfully used viral-specific T cells to treat BK virus infection after stem-cell transplantation,” the investigators wrote. “Because BK virus and JC virus are genetically similar to one another and share a number of immunogenic proteins with a substantial degree of sequence homology ... we hypothesized that T cells developed against BK virus may also be effective against JC virus infection.”
This hypothesis proved accurate. The investigators infused three PML patients with “cryopreserved, third-party–produced, viral-specific T cells that had been designed for the treatment of patients with BK virus infection after stem-cell transplantation.” Each patient presented with a different condition and PML-precipitating therapy. The first patient was a 32-year-old woman with high-risk acute myeloid leukemia who had received a cord-blood transplantation, the second a 73-year-old woman with JAK2-positive myeloproliferative neoplasia on ruxolitinib (Jakafi) therapy, and the third a 35-year-old man with HIV who had received highly active antiretroviral therapy.
T-cell infusions cleared JC virus from the CSF of the woman with leukemia (three infusions) and the man with HIV (four infusions). These patients recovered to different degrees: The woman had full resolution of symptoms, while the man had slurred speech and walked with a cane. Treatment reduced JC viral load in the elderly woman with myeloproliferative neoplasia (two infusions), but she did not clear the virus and died about 8 months later.
No adverse events occurred, but two patients developed immune reconstitution inflammatory syndrome. This was likely caused by the T-cell infusion, since absolute T-cell counts remained steady and white matter enhancement was detected on MRI within 4 weeks of treatment. Still, the investigators were optimistic about future potential.
“Third-party–produced, ‘off-the-shelf,’ partially HLA-matched, BK virus–specific T cells may serve as therapy for PML,” the investigators concluded. “Further study in a larger group of patients is required to determine the success rate, durability, and longer-term adverse events associated with this treatment.”
The study was funded by the MD Anderson Cancer Center Moon Shots Program and the National Institutes of Health.
SOURCE: Muftuoglu M et al. N Engl J Med. 2018 Oct 11;379:1443-51
This article was updated 3/22/19.
, according to investigators from the University of Texas MD Anderson Cancer Center, Houston.
The infusion cleared JC virus from the cerebrospinal fluid (CSF) of two patients and reduced viral load in the third, reported lead author Muharrem Muftuoglu, MD, of MD Anderson’s department of stem cell transplantation and cellular therapy and colleagues. One of the patients completely recovered and returned to work.
“Several approaches for the treatment of PML, including the use of antiviral medications and mirtazapine, have been tested, with poor results,” the investigators wrote in the New England Journal of Medicine. Although virus-specific T-cell infusion is a novel approach to treating PML, this method has been used for other conditions.
“Several groups, including ours, have successfully used viral-specific T cells to treat BK virus infection after stem-cell transplantation,” the investigators wrote. “Because BK virus and JC virus are genetically similar to one another and share a number of immunogenic proteins with a substantial degree of sequence homology ... we hypothesized that T cells developed against BK virus may also be effective against JC virus infection.”
This hypothesis proved accurate. The investigators infused three PML patients with “cryopreserved, third-party–produced, viral-specific T cells that had been designed for the treatment of patients with BK virus infection after stem-cell transplantation.” Each patient presented with a different condition and PML-precipitating therapy. The first patient was a 32-year-old woman with high-risk acute myeloid leukemia who had received a cord-blood transplantation, the second a 73-year-old woman with JAK2-positive myeloproliferative neoplasia on ruxolitinib (Jakafi) therapy, and the third a 35-year-old man with HIV who had received highly active antiretroviral therapy.
T-cell infusions cleared JC virus from the CSF of the woman with leukemia (three infusions) and the man with HIV (four infusions). These patients recovered to different degrees: The woman had full resolution of symptoms, while the man had slurred speech and walked with a cane. Treatment reduced JC viral load in the elderly woman with myeloproliferative neoplasia (two infusions), but she did not clear the virus and died about 8 months later.
No adverse events occurred, but two patients developed immune reconstitution inflammatory syndrome. This was likely caused by the T-cell infusion, since absolute T-cell counts remained steady and white matter enhancement was detected on MRI within 4 weeks of treatment. Still, the investigators were optimistic about future potential.
“Third-party–produced, ‘off-the-shelf,’ partially HLA-matched, BK virus–specific T cells may serve as therapy for PML,” the investigators concluded. “Further study in a larger group of patients is required to determine the success rate, durability, and longer-term adverse events associated with this treatment.”
The study was funded by the MD Anderson Cancer Center Moon Shots Program and the National Institutes of Health.
SOURCE: Muftuoglu M et al. N Engl J Med. 2018 Oct 11;379:1443-51
This article was updated 3/22/19.
FROM NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Infusion of allogeneic BK virus-specific T cells may be an effective treatment for patients with PML.
Major finding: Two of three patients cleared JC virus from cerebrospinal fluid after infusion.
Study details: A case series involving three patients with PML.
Disclosures: The study was funded by the MD Anderson Cancer Center Moon Shots Program and the National Institutes of Health.
Source: Muftuoglu M et al. N Engl J Med. 2018 Oct 11;379:1443-51.
Snake bite detox, kidney stone coaster cure, soporific speakers
At least opioids don’t bite
Remember that song about the old lady who “swallowed” a fly? Well, what if the fly were actually a poisonous snake? And what if she didn’t really swallow it? And what if we stopped asking so many questions? A 33-year-old Indian man who was addicted to alcohol, tobacco, and opioids in the form of raw opium and “puppy husk” (we’re thinking it’s poppy husk, but the case report clearly said “puppy”) heard about something new: letting a poisonous snake bite you on the tongue.
He found some nomadic snake charmers to provide the snake (possibly a cobra, but he’s not sure), and the snake’s bite provides him with an hour of jerky body movements, blurred vision, and unresponsiveness, followed by 3-4 weeks of heightened arousal and a sense of well-being that is “more intense tha[n] the state of high experienced … with any dose of alcohol or opioids,” according to the Indian Journal of Psychological Medicine (2018;40[3]:269-71). Plus, he doesn’t use nearly as much alcohol and opium. (Yes, he has done this more than once. You’re rude to ask.)
The old lady in the song, of course, dies after “swallowing” a horse. Fortunately for this guy, there’s no such thing as a poisonous horse.
Ride out the kidney stones
Disney World, the happiest place on earth – unless you’re a kidney stone. A professor from the College of Osteopathic Medicine at Michigan State University, East Lansing, was inspired when one of his patients told him a recent trip to the Magic Kingdom had successfully dislodged a kidney stone. Armed with a silicone model of the renal system, David Wartinger, DO, spent many grueling hours atop various theme park rides. And, one can only assume, many more grueling hours exploring Cinderella’s Castle.
Dr. Wartinger discovered that the Big Thunder Mountain Railroad was more effective than Space Mountain or the Rock ‘n’ Roller Coaster at rattling around the rider and thus shaking out those kidney stones.
The brave professor’s tireless work has earned him one of 2018’s Ig Nobel prizes. We salute you.
In Russia, bear cures YOU
They do things a bit differently in Russia. Who else but a group of Russians would stare a freshly caught and presumably very angry Siberian brown bear in the mouth and think, “Hmm, yes – the perfect source for new and exciting antibiotics!”
Somehow, they managed to make it work. In an article published in Proceedings of the National Academy of Sciences, Russian scientists demonstrated a new technology that rapidly tests the microbiota within bear saliva for potential antibiotics to use against antibiotic-resistant infections such as Staphylococcus aureus. In one of the thousands of samples taken, all introduced S. aureus bacteria had been eliminated, and further analysis showed the presence of amicoumacin, a previously known antibiotic.
And this is just one bear. Who knows what new and exciting goodies lie in the mouths of other bears? Now, we feel it’s important to note that the saliva of any sufficiently wild animal would have sufficed. But when in Russia, if you can think of an excuse to catch a bear, then by God you had better go catch a bear. Anything less would be an insult to the Motherland!
I need a hug
Don’t we all. A new study from the department of psychology at Carnegie Mellon University in Pittsburgh examined whether hugs actually do anything to improve a bad mood. Unverified rumors purport that the study was commissioned by a cuddly red monster named Elmo.
Researchers concluded that consensual hugs are beneficial after some sort of conflict or negative event during the day and that they positively affect the hug-receiver. Researchers also concluded that hugs given by teddy bears or red pandas are the most beneficial, but human hugs will do if those aren’t available. Despite their bactericidal qualities, hugs from Russian bears aren’t encouraged.
Next slide, pleazzzzzzz
Picture a world in which your smartwatch counted backward. In which the room WiFi is a black hole. In which space-time’s zipper seems hopelessly stuck, with a loose string – or, in fact, PowerPoint slide #14 – wedged into its interlocking teeth. That’s right: You’re in a session at a medical conference.
Now, one meeting attendee has boldly researched what many an attendee has wondered before: Do boring speakers really talk for longer? Taking one for all humanity, that intrepid time traveler endured an inhumane, institutional review board–unapproved study design of 50 12-minute meeting sessions. After 4 minutes, he determined whether the speaker was, scientifically speaking, “boring” or “not boring.” He then clocked the time each speaker took to wrap it up.
Spoiler alert: “Not boring” also meant “done sooner” – in a mean time of 11 minutes and 42 seconds versus 13 minutes and 12 seconds for those oscillating in the dullness duality’s boring state. So, if the 4-minute marker heralds a soporific session? There’s more schwag and better WiFi in the exhibit hall.
At least opioids don’t bite
Remember that song about the old lady who “swallowed” a fly? Well, what if the fly were actually a poisonous snake? And what if she didn’t really swallow it? And what if we stopped asking so many questions? A 33-year-old Indian man who was addicted to alcohol, tobacco, and opioids in the form of raw opium and “puppy husk” (we’re thinking it’s poppy husk, but the case report clearly said “puppy”) heard about something new: letting a poisonous snake bite you on the tongue.
He found some nomadic snake charmers to provide the snake (possibly a cobra, but he’s not sure), and the snake’s bite provides him with an hour of jerky body movements, blurred vision, and unresponsiveness, followed by 3-4 weeks of heightened arousal and a sense of well-being that is “more intense tha[n] the state of high experienced … with any dose of alcohol or opioids,” according to the Indian Journal of Psychological Medicine (2018;40[3]:269-71). Plus, he doesn’t use nearly as much alcohol and opium. (Yes, he has done this more than once. You’re rude to ask.)
The old lady in the song, of course, dies after “swallowing” a horse. Fortunately for this guy, there’s no such thing as a poisonous horse.
Ride out the kidney stones
Disney World, the happiest place on earth – unless you’re a kidney stone. A professor from the College of Osteopathic Medicine at Michigan State University, East Lansing, was inspired when one of his patients told him a recent trip to the Magic Kingdom had successfully dislodged a kidney stone. Armed with a silicone model of the renal system, David Wartinger, DO, spent many grueling hours atop various theme park rides. And, one can only assume, many more grueling hours exploring Cinderella’s Castle.
Dr. Wartinger discovered that the Big Thunder Mountain Railroad was more effective than Space Mountain or the Rock ‘n’ Roller Coaster at rattling around the rider and thus shaking out those kidney stones.
The brave professor’s tireless work has earned him one of 2018’s Ig Nobel prizes. We salute you.
In Russia, bear cures YOU
They do things a bit differently in Russia. Who else but a group of Russians would stare a freshly caught and presumably very angry Siberian brown bear in the mouth and think, “Hmm, yes – the perfect source for new and exciting antibiotics!”
Somehow, they managed to make it work. In an article published in Proceedings of the National Academy of Sciences, Russian scientists demonstrated a new technology that rapidly tests the microbiota within bear saliva for potential antibiotics to use against antibiotic-resistant infections such as Staphylococcus aureus. In one of the thousands of samples taken, all introduced S. aureus bacteria had been eliminated, and further analysis showed the presence of amicoumacin, a previously known antibiotic.
And this is just one bear. Who knows what new and exciting goodies lie in the mouths of other bears? Now, we feel it’s important to note that the saliva of any sufficiently wild animal would have sufficed. But when in Russia, if you can think of an excuse to catch a bear, then by God you had better go catch a bear. Anything less would be an insult to the Motherland!
I need a hug
Don’t we all. A new study from the department of psychology at Carnegie Mellon University in Pittsburgh examined whether hugs actually do anything to improve a bad mood. Unverified rumors purport that the study was commissioned by a cuddly red monster named Elmo.
Researchers concluded that consensual hugs are beneficial after some sort of conflict or negative event during the day and that they positively affect the hug-receiver. Researchers also concluded that hugs given by teddy bears or red pandas are the most beneficial, but human hugs will do if those aren’t available. Despite their bactericidal qualities, hugs from Russian bears aren’t encouraged.
Next slide, pleazzzzzzz
Picture a world in which your smartwatch counted backward. In which the room WiFi is a black hole. In which space-time’s zipper seems hopelessly stuck, with a loose string – or, in fact, PowerPoint slide #14 – wedged into its interlocking teeth. That’s right: You’re in a session at a medical conference.
Now, one meeting attendee has boldly researched what many an attendee has wondered before: Do boring speakers really talk for longer? Taking one for all humanity, that intrepid time traveler endured an inhumane, institutional review board–unapproved study design of 50 12-minute meeting sessions. After 4 minutes, he determined whether the speaker was, scientifically speaking, “boring” or “not boring.” He then clocked the time each speaker took to wrap it up.
Spoiler alert: “Not boring” also meant “done sooner” – in a mean time of 11 minutes and 42 seconds versus 13 minutes and 12 seconds for those oscillating in the dullness duality’s boring state. So, if the 4-minute marker heralds a soporific session? There’s more schwag and better WiFi in the exhibit hall.
At least opioids don’t bite
Remember that song about the old lady who “swallowed” a fly? Well, what if the fly were actually a poisonous snake? And what if she didn’t really swallow it? And what if we stopped asking so many questions? A 33-year-old Indian man who was addicted to alcohol, tobacco, and opioids in the form of raw opium and “puppy husk” (we’re thinking it’s poppy husk, but the case report clearly said “puppy”) heard about something new: letting a poisonous snake bite you on the tongue.
He found some nomadic snake charmers to provide the snake (possibly a cobra, but he’s not sure), and the snake’s bite provides him with an hour of jerky body movements, blurred vision, and unresponsiveness, followed by 3-4 weeks of heightened arousal and a sense of well-being that is “more intense tha[n] the state of high experienced … with any dose of alcohol or opioids,” according to the Indian Journal of Psychological Medicine (2018;40[3]:269-71). Plus, he doesn’t use nearly as much alcohol and opium. (Yes, he has done this more than once. You’re rude to ask.)
The old lady in the song, of course, dies after “swallowing” a horse. Fortunately for this guy, there’s no such thing as a poisonous horse.
Ride out the kidney stones
Disney World, the happiest place on earth – unless you’re a kidney stone. A professor from the College of Osteopathic Medicine at Michigan State University, East Lansing, was inspired when one of his patients told him a recent trip to the Magic Kingdom had successfully dislodged a kidney stone. Armed with a silicone model of the renal system, David Wartinger, DO, spent many grueling hours atop various theme park rides. And, one can only assume, many more grueling hours exploring Cinderella’s Castle.
Dr. Wartinger discovered that the Big Thunder Mountain Railroad was more effective than Space Mountain or the Rock ‘n’ Roller Coaster at rattling around the rider and thus shaking out those kidney stones.
The brave professor’s tireless work has earned him one of 2018’s Ig Nobel prizes. We salute you.
In Russia, bear cures YOU
They do things a bit differently in Russia. Who else but a group of Russians would stare a freshly caught and presumably very angry Siberian brown bear in the mouth and think, “Hmm, yes – the perfect source for new and exciting antibiotics!”
Somehow, they managed to make it work. In an article published in Proceedings of the National Academy of Sciences, Russian scientists demonstrated a new technology that rapidly tests the microbiota within bear saliva for potential antibiotics to use against antibiotic-resistant infections such as Staphylococcus aureus. In one of the thousands of samples taken, all introduced S. aureus bacteria had been eliminated, and further analysis showed the presence of amicoumacin, a previously known antibiotic.
And this is just one bear. Who knows what new and exciting goodies lie in the mouths of other bears? Now, we feel it’s important to note that the saliva of any sufficiently wild animal would have sufficed. But when in Russia, if you can think of an excuse to catch a bear, then by God you had better go catch a bear. Anything less would be an insult to the Motherland!
I need a hug
Don’t we all. A new study from the department of psychology at Carnegie Mellon University in Pittsburgh examined whether hugs actually do anything to improve a bad mood. Unverified rumors purport that the study was commissioned by a cuddly red monster named Elmo.
Researchers concluded that consensual hugs are beneficial after some sort of conflict or negative event during the day and that they positively affect the hug-receiver. Researchers also concluded that hugs given by teddy bears or red pandas are the most beneficial, but human hugs will do if those aren’t available. Despite their bactericidal qualities, hugs from Russian bears aren’t encouraged.
Next slide, pleazzzzzzz
Picture a world in which your smartwatch counted backward. In which the room WiFi is a black hole. In which space-time’s zipper seems hopelessly stuck, with a loose string – or, in fact, PowerPoint slide #14 – wedged into its interlocking teeth. That’s right: You’re in a session at a medical conference.
Now, one meeting attendee has boldly researched what many an attendee has wondered before: Do boring speakers really talk for longer? Taking one for all humanity, that intrepid time traveler endured an inhumane, institutional review board–unapproved study design of 50 12-minute meeting sessions. After 4 minutes, he determined whether the speaker was, scientifically speaking, “boring” or “not boring.” He then clocked the time each speaker took to wrap it up.
Spoiler alert: “Not boring” also meant “done sooner” – in a mean time of 11 minutes and 42 seconds versus 13 minutes and 12 seconds for those oscillating in the dullness duality’s boring state. So, if the 4-minute marker heralds a soporific session? There’s more schwag and better WiFi in the exhibit hall.
Genomic profiling predicts outcomes in patients with MPN
Genomic characteristics of patients with myeloproliferative neoplasms (MPN) can predict clinical outcomes, a recent study found.
Eight genomic subgroups of MPN were recognized, each with distinct clinical features, including event-free survival, risk of leukemic transformation, and blood counts, according to Jacob Grinfeld, MD, of the Wellcome-MRC Cambridge (England) Stem Cell Institute and Cambridge Institute for Medical Research and his colleagues.
“Current classification schemes distinguish among the subtypes of myeloproliferative neoplasms according to clinical and laboratory features, but uncertainty clouds where and how to draw dividing lines among them,” the investigators wrote in the New England Journal of Medicine. “In blood cancers, a progressive shift is under way, from clinical and morphologic classification schemes to those that are based on genomics.”
MPNs are often driven by mutations in CALR, MPL, or JAK2 genes, but classification is not confined to just three genomic types; many patients have additional driver mutations throughout a variety of cancer genes, and it is these additional mutations that are responsible for the wide range of disease phenotypes and clinical outcomes.
This study included 2,035 patients with MPNs, including essential thrombocythemia, polycythemia vera, myelofibrosis, and other MPN diagnoses. The investigators performed targeted sequencing for the full coding sequence of 69 genes and genomewide copy-number information in 1,887 patients. Another 148 patients underwent whole-exome sequencing.
By sequencing coding exons from 69 myeloid cancer genes, the investigators were able to survey the diversity of mutations across a population of patients with MPNs and identify mutation-associated clinical outcomes.
The results showed that slightly less than half (45%) of the patients had a solitary abnormality in CALR, MPL, or JAK2, while the remaining patients had additional driver mutations. In some instances, additional mutations were numerous, particularly in older patients with advanced disease. In at least five cases, 33 genes had driver mutations.
Further analysis identified eight genomic subgroups that could predict clinical outcomes based on shared chromosomal abnormalities and mutations. For example, one subgroup included patients with TP53 mutations; these individuals had a “dismal prognosis” and were 15.5 times more likely to transform to acute myeloid leukemia (AML), compared with the JAK2-heterozygous subgroup (P less than .001).
Because prognosis is “a key determinant of the treatment of patients with MPNs,” genomic subgrouping may one day guide clinical decision making, the investigators concluded.
To further this cause, the investigators have made available an online calculator of individualized patient outcomes, which can be accessed at https://cancer.sanger.ac.uk/mpn-multistage/.
The study was funded by the Wellcome Trust, the National Institute for Health Research Cambridge Biomedical Research Centre, Cancer Research UK, and others. Some study authors reported fees from Celgene, Novartis, Gilead, Shire, and others outside of the study.
SOURCE: Grinfeld J et al. N Engl J Med. 2018;379:1416-30.
Genomic characteristics of patients with myeloproliferative neoplasms (MPN) can predict clinical outcomes, a recent study found.
Eight genomic subgroups of MPN were recognized, each with distinct clinical features, including event-free survival, risk of leukemic transformation, and blood counts, according to Jacob Grinfeld, MD, of the Wellcome-MRC Cambridge (England) Stem Cell Institute and Cambridge Institute for Medical Research and his colleagues.
“Current classification schemes distinguish among the subtypes of myeloproliferative neoplasms according to clinical and laboratory features, but uncertainty clouds where and how to draw dividing lines among them,” the investigators wrote in the New England Journal of Medicine. “In blood cancers, a progressive shift is under way, from clinical and morphologic classification schemes to those that are based on genomics.”
MPNs are often driven by mutations in CALR, MPL, or JAK2 genes, but classification is not confined to just three genomic types; many patients have additional driver mutations throughout a variety of cancer genes, and it is these additional mutations that are responsible for the wide range of disease phenotypes and clinical outcomes.
This study included 2,035 patients with MPNs, including essential thrombocythemia, polycythemia vera, myelofibrosis, and other MPN diagnoses. The investigators performed targeted sequencing for the full coding sequence of 69 genes and genomewide copy-number information in 1,887 patients. Another 148 patients underwent whole-exome sequencing.
By sequencing coding exons from 69 myeloid cancer genes, the investigators were able to survey the diversity of mutations across a population of patients with MPNs and identify mutation-associated clinical outcomes.
The results showed that slightly less than half (45%) of the patients had a solitary abnormality in CALR, MPL, or JAK2, while the remaining patients had additional driver mutations. In some instances, additional mutations were numerous, particularly in older patients with advanced disease. In at least five cases, 33 genes had driver mutations.
Further analysis identified eight genomic subgroups that could predict clinical outcomes based on shared chromosomal abnormalities and mutations. For example, one subgroup included patients with TP53 mutations; these individuals had a “dismal prognosis” and were 15.5 times more likely to transform to acute myeloid leukemia (AML), compared with the JAK2-heterozygous subgroup (P less than .001).
Because prognosis is “a key determinant of the treatment of patients with MPNs,” genomic subgrouping may one day guide clinical decision making, the investigators concluded.
To further this cause, the investigators have made available an online calculator of individualized patient outcomes, which can be accessed at https://cancer.sanger.ac.uk/mpn-multistage/.
The study was funded by the Wellcome Trust, the National Institute for Health Research Cambridge Biomedical Research Centre, Cancer Research UK, and others. Some study authors reported fees from Celgene, Novartis, Gilead, Shire, and others outside of the study.
SOURCE: Grinfeld J et al. N Engl J Med. 2018;379:1416-30.
Genomic characteristics of patients with myeloproliferative neoplasms (MPN) can predict clinical outcomes, a recent study found.
Eight genomic subgroups of MPN were recognized, each with distinct clinical features, including event-free survival, risk of leukemic transformation, and blood counts, according to Jacob Grinfeld, MD, of the Wellcome-MRC Cambridge (England) Stem Cell Institute and Cambridge Institute for Medical Research and his colleagues.
“Current classification schemes distinguish among the subtypes of myeloproliferative neoplasms according to clinical and laboratory features, but uncertainty clouds where and how to draw dividing lines among them,” the investigators wrote in the New England Journal of Medicine. “In blood cancers, a progressive shift is under way, from clinical and morphologic classification schemes to those that are based on genomics.”
MPNs are often driven by mutations in CALR, MPL, or JAK2 genes, but classification is not confined to just three genomic types; many patients have additional driver mutations throughout a variety of cancer genes, and it is these additional mutations that are responsible for the wide range of disease phenotypes and clinical outcomes.
This study included 2,035 patients with MPNs, including essential thrombocythemia, polycythemia vera, myelofibrosis, and other MPN diagnoses. The investigators performed targeted sequencing for the full coding sequence of 69 genes and genomewide copy-number information in 1,887 patients. Another 148 patients underwent whole-exome sequencing.
By sequencing coding exons from 69 myeloid cancer genes, the investigators were able to survey the diversity of mutations across a population of patients with MPNs and identify mutation-associated clinical outcomes.
The results showed that slightly less than half (45%) of the patients had a solitary abnormality in CALR, MPL, or JAK2, while the remaining patients had additional driver mutations. In some instances, additional mutations were numerous, particularly in older patients with advanced disease. In at least five cases, 33 genes had driver mutations.
Further analysis identified eight genomic subgroups that could predict clinical outcomes based on shared chromosomal abnormalities and mutations. For example, one subgroup included patients with TP53 mutations; these individuals had a “dismal prognosis” and were 15.5 times more likely to transform to acute myeloid leukemia (AML), compared with the JAK2-heterozygous subgroup (P less than .001).
Because prognosis is “a key determinant of the treatment of patients with MPNs,” genomic subgrouping may one day guide clinical decision making, the investigators concluded.
To further this cause, the investigators have made available an online calculator of individualized patient outcomes, which can be accessed at https://cancer.sanger.ac.uk/mpn-multistage/.
The study was funded by the Wellcome Trust, the National Institute for Health Research Cambridge Biomedical Research Centre, Cancer Research UK, and others. Some study authors reported fees from Celgene, Novartis, Gilead, Shire, and others outside of the study.
SOURCE: Grinfeld J et al. N Engl J Med. 2018;379:1416-30.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point:
Major finding: Eight genomic subgroups of MPN were recognized, each with distinct clinical features, including event-free survival, risk of leukemic transformation, and blood counts.
Study details: A gene sequencing study involving 2,035 patients with MPN.
Disclosures: The study was funded by the Wellcome Trust, the National Institute for Health Research Cambridge Biomedical Research Centre, Cancer Research UK, and others. Some study authors reported fees from Celgene, Novartis, Gilead, Shire, and others outside of the study.
Source: Grinfeld J et al. N Engl J Med. 2018;379:1416-30.
Some dubious of proposal on e-cigarettes; World Mental Health Day takes spotlight
Traditional cigarettes are addictive, and they kill. Now it appears that e-cigarettes, which electronically deliver nicotine in the absence of the lung-damaging smoke, might be a healthier alternative.
The American Cancer Society noted in June that, although the long-term effects of e-cigarettes are “not known,” they are “markedly less harmful” than traditional smoking. Sensing the changing tide, tobacco companies are going all in on e-cigarettes. And, as reported on CBS Sunday Morning, Dr. Gottlieb points out that in light of the impact of nicotine on the developing brain, a “strong regulatory process” is needed that puts new products “through an appropriate series of regulatory gates.”
Still, however, some people are dubious. The tobacco companies that are leading the transition are the same companies that once espoused the healthy benefits of smoking and suppressed counter information. Seeking greater profits, some products are marketed with enticing colors and flavors, with the goal of appealing to consumers – including teens. San Francisco has banned the sale of such products.
Dr. Gottlieb and others are quick to point out that what might be helpful for adults looking to quit also is enticing to teenagers. Using e-cigarettes would seem to be better than cigarette smoking. However, whether e-cigarettes are benign remains unknown.
Mental health takes center stage
An article in The Guardian by Tedros Adhanom Ghebreyesus, PhD, director general of the World Health Organization, and Lady Gaga, musician and cofounder of Born This Way Foundation, cited some sobering facts: 800,000 people kill themselves every year, a rate of six people every minute. Some are famous (Kate Spade and Anthony Bourdain). Others are not. But all leave people who love them and are often devastated by the passing.
For the 25% of people who will experience mental health issues during their lives, admitting their need for help risks being stigmatized, and gaining that help is difficult. This is changing; however, according to the article, funding for mental health constitutes less than 1% of global aid funding.
But there is cause for optimism. WHO is working with countries on a global action plan on mental health. Community-based mental health care initiatives are providing help for those in need. The authors cite the success of the HIV/AIDS efforts as an example of what can be achieved. “That movement helped save millions of lives and is an illustration of the potential for collective human action to tackle seemingly insurmountable problems,” they wrote on the eve of World Mental Health Day, which is Oct. 10.
“The two of us have taken different paths in life. But both of us have seen how political leadership, funding, innovation, and individual acts of bravery and compassion can change the world. It is time to do the same for mental health.”
Navigating the pain of stillbirth
The impending birth of a child can be a time of happy anticipation and planning. But when the pregnancy ends in stillbirth, a person’s world is shattered. The experience is not rare – in the United Kingdom, for example, about nine babies are stillborn every day. When this horror happened to BBC journalist Fiona Crack, she channeled her grief into a chronicle of her journey and those of five other women with some hope and optimism.
“My arms ached. I thought I had a blood clot, but the doctors told me it was normal – a biological response to the shock that there was no living child for me to hold. I sobbed. My milk came through, marking my T-shirt, and I was too exhausted to be embarrassed,” Ms. Crack wrote.
There came a year of first events that would never be shared with her child, Willow – Christmas, Mother’s Day, and the dreaded first birthday. Slowly she mustered resolve. She also connected with five women around the United Kingdom who had faced the same horror.
Some solace has been found. But the scar will always remain. “Over the past year, my need to remember and memorialize Willow has jostled with my need for self-preservation. A year on, grief can still occasionally floor me, slicing behind my knees, but I can feel it coming and I can prepare, knowing I can survive its brief but powerful kick. Willow’s birth made me a Mum and Tim a Dad. My arms no longer ache like those first hours, but they are still empty. I am a mother without a baby,” Ms. Crack writes.
In the United States, about 24,000 stillbirths are reported each year, research shows. Mindfulness therapies have been shown to reduce posttraumatic stress symptoms among women after experiencing stillbirth.
Polygraph tests and employment
Jobs are not always easy to find. Once employed, there can be fear that job security is transient, as well as pressure to please the employer. How far is too far in efforts to gain this pleasure? An article on the BBC website explores the issue.
In some countries, including the United States, the issue is theoretical, since polygraph testing of employees is illegal. But elsewhere, such as in South Africa, there is no legal protection. And polygraph testing has been used in Kenya for prospective politicians. According to polygraph expert Doug Williams, polygraph testing is fallible and is mainly used as a means of intimidation.
“It’s a psychological billy club that coerces and intimidates a person into a confession. It scares the hell out of people. I would never work for a company that requires polygraphs because they’re starting the entire relationship off as an adversarial proceeding,” Mr. Williams said in an interview. The presumption of distrust can be toxic to a workplace.
“If most employees agree to take a lie detection test, then there would naturally come to be some suspicion of those who refuse to take it,” says Nick Bostrom, PhD, ethics professor at the University of Oxford (England). “Refusal would send a bad signal – it suggests you have something to hide.”
In a world where personal information can be just a few mouse clicks away, the issue is worth thinking about.
Music as a healing force
The first album from musician Cat Power (stage name of Chan Marshall) comes after a hiatus of 6 years. The intervening time has been spent as a mom and in other pursuits. The album, “Wanderer,” reflects the stabilizing influence of being a parent and the need to keep striving in life.
“I think I’ve found what I never thought I would have. I’ve found what I never thought I would see, which is becoming a parent. There are no words for what I have now in my heart. But I’m still myself. The psychospiritual parts of me are always looking for truth, always looking for beauty in all that truth,” Ms. Power said in an interview with NPR.
Music also is a way to deal with a life that included a parent who had substance abuse problems and her own bouts of depression. “There’s so much pain that people carry and try to avoid. … That’s why music is so incredible,” she said.
Ms. Power hopes that people who listen to her album will realize that they are not alone. “We’re all on this ball of mud, this tiny speck, a ball of mud together,” she said. “We all feel all the same things. Maybe we don’t know how to communicate well. Maybe we’re learning. Maybe this lifetime, for all of us, is just a learning spell.”
Traditional cigarettes are addictive, and they kill. Now it appears that e-cigarettes, which electronically deliver nicotine in the absence of the lung-damaging smoke, might be a healthier alternative.
The American Cancer Society noted in June that, although the long-term effects of e-cigarettes are “not known,” they are “markedly less harmful” than traditional smoking. Sensing the changing tide, tobacco companies are going all in on e-cigarettes. And, as reported on CBS Sunday Morning, Dr. Gottlieb points out that in light of the impact of nicotine on the developing brain, a “strong regulatory process” is needed that puts new products “through an appropriate series of regulatory gates.”
Still, however, some people are dubious. The tobacco companies that are leading the transition are the same companies that once espoused the healthy benefits of smoking and suppressed counter information. Seeking greater profits, some products are marketed with enticing colors and flavors, with the goal of appealing to consumers – including teens. San Francisco has banned the sale of such products.
Dr. Gottlieb and others are quick to point out that what might be helpful for adults looking to quit also is enticing to teenagers. Using e-cigarettes would seem to be better than cigarette smoking. However, whether e-cigarettes are benign remains unknown.
Mental health takes center stage
An article in The Guardian by Tedros Adhanom Ghebreyesus, PhD, director general of the World Health Organization, and Lady Gaga, musician and cofounder of Born This Way Foundation, cited some sobering facts: 800,000 people kill themselves every year, a rate of six people every minute. Some are famous (Kate Spade and Anthony Bourdain). Others are not. But all leave people who love them and are often devastated by the passing.
For the 25% of people who will experience mental health issues during their lives, admitting their need for help risks being stigmatized, and gaining that help is difficult. This is changing; however, according to the article, funding for mental health constitutes less than 1% of global aid funding.
But there is cause for optimism. WHO is working with countries on a global action plan on mental health. Community-based mental health care initiatives are providing help for those in need. The authors cite the success of the HIV/AIDS efforts as an example of what can be achieved. “That movement helped save millions of lives and is an illustration of the potential for collective human action to tackle seemingly insurmountable problems,” they wrote on the eve of World Mental Health Day, which is Oct. 10.
“The two of us have taken different paths in life. But both of us have seen how political leadership, funding, innovation, and individual acts of bravery and compassion can change the world. It is time to do the same for mental health.”
Navigating the pain of stillbirth
The impending birth of a child can be a time of happy anticipation and planning. But when the pregnancy ends in stillbirth, a person’s world is shattered. The experience is not rare – in the United Kingdom, for example, about nine babies are stillborn every day. When this horror happened to BBC journalist Fiona Crack, she channeled her grief into a chronicle of her journey and those of five other women with some hope and optimism.
“My arms ached. I thought I had a blood clot, but the doctors told me it was normal – a biological response to the shock that there was no living child for me to hold. I sobbed. My milk came through, marking my T-shirt, and I was too exhausted to be embarrassed,” Ms. Crack wrote.
There came a year of first events that would never be shared with her child, Willow – Christmas, Mother’s Day, and the dreaded first birthday. Slowly she mustered resolve. She also connected with five women around the United Kingdom who had faced the same horror.
Some solace has been found. But the scar will always remain. “Over the past year, my need to remember and memorialize Willow has jostled with my need for self-preservation. A year on, grief can still occasionally floor me, slicing behind my knees, but I can feel it coming and I can prepare, knowing I can survive its brief but powerful kick. Willow’s birth made me a Mum and Tim a Dad. My arms no longer ache like those first hours, but they are still empty. I am a mother without a baby,” Ms. Crack writes.
In the United States, about 24,000 stillbirths are reported each year, research shows. Mindfulness therapies have been shown to reduce posttraumatic stress symptoms among women after experiencing stillbirth.
Polygraph tests and employment
Jobs are not always easy to find. Once employed, there can be fear that job security is transient, as well as pressure to please the employer. How far is too far in efforts to gain this pleasure? An article on the BBC website explores the issue.
In some countries, including the United States, the issue is theoretical, since polygraph testing of employees is illegal. But elsewhere, such as in South Africa, there is no legal protection. And polygraph testing has been used in Kenya for prospective politicians. According to polygraph expert Doug Williams, polygraph testing is fallible and is mainly used as a means of intimidation.
“It’s a psychological billy club that coerces and intimidates a person into a confession. It scares the hell out of people. I would never work for a company that requires polygraphs because they’re starting the entire relationship off as an adversarial proceeding,” Mr. Williams said in an interview. The presumption of distrust can be toxic to a workplace.
“If most employees agree to take a lie detection test, then there would naturally come to be some suspicion of those who refuse to take it,” says Nick Bostrom, PhD, ethics professor at the University of Oxford (England). “Refusal would send a bad signal – it suggests you have something to hide.”
In a world where personal information can be just a few mouse clicks away, the issue is worth thinking about.
Music as a healing force
The first album from musician Cat Power (stage name of Chan Marshall) comes after a hiatus of 6 years. The intervening time has been spent as a mom and in other pursuits. The album, “Wanderer,” reflects the stabilizing influence of being a parent and the need to keep striving in life.
“I think I’ve found what I never thought I would have. I’ve found what I never thought I would see, which is becoming a parent. There are no words for what I have now in my heart. But I’m still myself. The psychospiritual parts of me are always looking for truth, always looking for beauty in all that truth,” Ms. Power said in an interview with NPR.
Music also is a way to deal with a life that included a parent who had substance abuse problems and her own bouts of depression. “There’s so much pain that people carry and try to avoid. … That’s why music is so incredible,” she said.
Ms. Power hopes that people who listen to her album will realize that they are not alone. “We’re all on this ball of mud, this tiny speck, a ball of mud together,” she said. “We all feel all the same things. Maybe we don’t know how to communicate well. Maybe we’re learning. Maybe this lifetime, for all of us, is just a learning spell.”
Traditional cigarettes are addictive, and they kill. Now it appears that e-cigarettes, which electronically deliver nicotine in the absence of the lung-damaging smoke, might be a healthier alternative.
The American Cancer Society noted in June that, although the long-term effects of e-cigarettes are “not known,” they are “markedly less harmful” than traditional smoking. Sensing the changing tide, tobacco companies are going all in on e-cigarettes. And, as reported on CBS Sunday Morning, Dr. Gottlieb points out that in light of the impact of nicotine on the developing brain, a “strong regulatory process” is needed that puts new products “through an appropriate series of regulatory gates.”
Still, however, some people are dubious. The tobacco companies that are leading the transition are the same companies that once espoused the healthy benefits of smoking and suppressed counter information. Seeking greater profits, some products are marketed with enticing colors and flavors, with the goal of appealing to consumers – including teens. San Francisco has banned the sale of such products.
Dr. Gottlieb and others are quick to point out that what might be helpful for adults looking to quit also is enticing to teenagers. Using e-cigarettes would seem to be better than cigarette smoking. However, whether e-cigarettes are benign remains unknown.
Mental health takes center stage
An article in The Guardian by Tedros Adhanom Ghebreyesus, PhD, director general of the World Health Organization, and Lady Gaga, musician and cofounder of Born This Way Foundation, cited some sobering facts: 800,000 people kill themselves every year, a rate of six people every minute. Some are famous (Kate Spade and Anthony Bourdain). Others are not. But all leave people who love them and are often devastated by the passing.
For the 25% of people who will experience mental health issues during their lives, admitting their need for help risks being stigmatized, and gaining that help is difficult. This is changing; however, according to the article, funding for mental health constitutes less than 1% of global aid funding.
But there is cause for optimism. WHO is working with countries on a global action plan on mental health. Community-based mental health care initiatives are providing help for those in need. The authors cite the success of the HIV/AIDS efforts as an example of what can be achieved. “That movement helped save millions of lives and is an illustration of the potential for collective human action to tackle seemingly insurmountable problems,” they wrote on the eve of World Mental Health Day, which is Oct. 10.
“The two of us have taken different paths in life. But both of us have seen how political leadership, funding, innovation, and individual acts of bravery and compassion can change the world. It is time to do the same for mental health.”
Navigating the pain of stillbirth
The impending birth of a child can be a time of happy anticipation and planning. But when the pregnancy ends in stillbirth, a person’s world is shattered. The experience is not rare – in the United Kingdom, for example, about nine babies are stillborn every day. When this horror happened to BBC journalist Fiona Crack, she channeled her grief into a chronicle of her journey and those of five other women with some hope and optimism.
“My arms ached. I thought I had a blood clot, but the doctors told me it was normal – a biological response to the shock that there was no living child for me to hold. I sobbed. My milk came through, marking my T-shirt, and I was too exhausted to be embarrassed,” Ms. Crack wrote.
There came a year of first events that would never be shared with her child, Willow – Christmas, Mother’s Day, and the dreaded first birthday. Slowly she mustered resolve. She also connected with five women around the United Kingdom who had faced the same horror.
Some solace has been found. But the scar will always remain. “Over the past year, my need to remember and memorialize Willow has jostled with my need for self-preservation. A year on, grief can still occasionally floor me, slicing behind my knees, but I can feel it coming and I can prepare, knowing I can survive its brief but powerful kick. Willow’s birth made me a Mum and Tim a Dad. My arms no longer ache like those first hours, but they are still empty. I am a mother without a baby,” Ms. Crack writes.
In the United States, about 24,000 stillbirths are reported each year, research shows. Mindfulness therapies have been shown to reduce posttraumatic stress symptoms among women after experiencing stillbirth.
Polygraph tests and employment
Jobs are not always easy to find. Once employed, there can be fear that job security is transient, as well as pressure to please the employer. How far is too far in efforts to gain this pleasure? An article on the BBC website explores the issue.
In some countries, including the United States, the issue is theoretical, since polygraph testing of employees is illegal. But elsewhere, such as in South Africa, there is no legal protection. And polygraph testing has been used in Kenya for prospective politicians. According to polygraph expert Doug Williams, polygraph testing is fallible and is mainly used as a means of intimidation.
“It’s a psychological billy club that coerces and intimidates a person into a confession. It scares the hell out of people. I would never work for a company that requires polygraphs because they’re starting the entire relationship off as an adversarial proceeding,” Mr. Williams said in an interview. The presumption of distrust can be toxic to a workplace.
“If most employees agree to take a lie detection test, then there would naturally come to be some suspicion of those who refuse to take it,” says Nick Bostrom, PhD, ethics professor at the University of Oxford (England). “Refusal would send a bad signal – it suggests you have something to hide.”
In a world where personal information can be just a few mouse clicks away, the issue is worth thinking about.
Music as a healing force
The first album from musician Cat Power (stage name of Chan Marshall) comes after a hiatus of 6 years. The intervening time has been spent as a mom and in other pursuits. The album, “Wanderer,” reflects the stabilizing influence of being a parent and the need to keep striving in life.
“I think I’ve found what I never thought I would have. I’ve found what I never thought I would see, which is becoming a parent. There are no words for what I have now in my heart. But I’m still myself. The psychospiritual parts of me are always looking for truth, always looking for beauty in all that truth,” Ms. Power said in an interview with NPR.
Music also is a way to deal with a life that included a parent who had substance abuse problems and her own bouts of depression. “There’s so much pain that people carry and try to avoid. … That’s why music is so incredible,” she said.
Ms. Power hopes that people who listen to her album will realize that they are not alone. “We’re all on this ball of mud, this tiny speck, a ball of mud together,” she said. “We all feel all the same things. Maybe we don’t know how to communicate well. Maybe we’re learning. Maybe this lifetime, for all of us, is just a learning spell.”