User login
FDA approves emapalumab for primary HLH
The (HLH).
Emapalumab, an interferon gamma-blocking antibody, is approved to treat patients of all ages (newborn and older) with primary HLH who have refractory, recurrent, or progressive disease or who cannot tolerate conventional HLH therapy. Emapalumab is the first treatment to be FDA approved for primary HLH, and it is expected to be available in the United States in the first quarter of 2019. The FDA previously granted emapalumab priority review, breakthrough therapy designation, orphan drug designation, and rare pediatric disease designation. The FDA’s approval of emapalumab is based on results from a phase 2/3 trial (NCT01818492).
The trial included 34 patients, 27 of whom had refractory, recurrent, or progressive disease or could not tolerate conventional HLH therapy. Patients received emapalumab in combination with dexamethasone. At the end of treatment, 63% (17/27) of patients had achieved a response, which was defined as complete response (n = 7), partial response (n=8), or HLH improvement (n = 2). A total of 70% (n=19) of patients went on to hematopoietic stem cell transplant. The most common adverse events were infections (56%), hypertension (41%), infusion-related reactions (27%), and pyrexia (24%).
Results also are scheduled to be presented at the 2018 annual meeting of the American Society of Hematology in the late-breaker abstract session (Abstract LBA-6).
Emapalumab was developed by Novimmune SA. Sobi acquired global rights to the drug in August 2018.
The (HLH).
Emapalumab, an interferon gamma-blocking antibody, is approved to treat patients of all ages (newborn and older) with primary HLH who have refractory, recurrent, or progressive disease or who cannot tolerate conventional HLH therapy. Emapalumab is the first treatment to be FDA approved for primary HLH, and it is expected to be available in the United States in the first quarter of 2019. The FDA previously granted emapalumab priority review, breakthrough therapy designation, orphan drug designation, and rare pediatric disease designation. The FDA’s approval of emapalumab is based on results from a phase 2/3 trial (NCT01818492).
The trial included 34 patients, 27 of whom had refractory, recurrent, or progressive disease or could not tolerate conventional HLH therapy. Patients received emapalumab in combination with dexamethasone. At the end of treatment, 63% (17/27) of patients had achieved a response, which was defined as complete response (n = 7), partial response (n=8), or HLH improvement (n = 2). A total of 70% (n=19) of patients went on to hematopoietic stem cell transplant. The most common adverse events were infections (56%), hypertension (41%), infusion-related reactions (27%), and pyrexia (24%).
Results also are scheduled to be presented at the 2018 annual meeting of the American Society of Hematology in the late-breaker abstract session (Abstract LBA-6).
Emapalumab was developed by Novimmune SA. Sobi acquired global rights to the drug in August 2018.
The (HLH).
Emapalumab, an interferon gamma-blocking antibody, is approved to treat patients of all ages (newborn and older) with primary HLH who have refractory, recurrent, or progressive disease or who cannot tolerate conventional HLH therapy. Emapalumab is the first treatment to be FDA approved for primary HLH, and it is expected to be available in the United States in the first quarter of 2019. The FDA previously granted emapalumab priority review, breakthrough therapy designation, orphan drug designation, and rare pediatric disease designation. The FDA’s approval of emapalumab is based on results from a phase 2/3 trial (NCT01818492).
The trial included 34 patients, 27 of whom had refractory, recurrent, or progressive disease or could not tolerate conventional HLH therapy. Patients received emapalumab in combination with dexamethasone. At the end of treatment, 63% (17/27) of patients had achieved a response, which was defined as complete response (n = 7), partial response (n=8), or HLH improvement (n = 2). A total of 70% (n=19) of patients went on to hematopoietic stem cell transplant. The most common adverse events were infections (56%), hypertension (41%), infusion-related reactions (27%), and pyrexia (24%).
Results also are scheduled to be presented at the 2018 annual meeting of the American Society of Hematology in the late-breaker abstract session (Abstract LBA-6).
Emapalumab was developed by Novimmune SA. Sobi acquired global rights to the drug in August 2018.
‘Phenomenal’ REDUCE-IT establishes triglyceride theory
CHICAGO – REDUCE-IT is a phenomenal trial and a game changer because it has shown for the first time that triglyceride reduction with an appropriate therapy – in this case icosapent ethyl – when used in appropriate doses can make a significant difference.
That’s according to Prakash C. Deedwania, MD, chief of the cardiology division at the Veterans Affairs Medical Center/University of California San Francisco Program in Fresno, who joined MDedge reporter Richard Mark Kirkner for a video interview at the American Heart Association scientific sessions.
In the large, placebo-controlled REDUCE-IT trial in patients with or at high risk for cardiovascular disease received who received 2 g of icosapent ethyl (Vascepa) twice daily or placebo saw a 25% lower risk of cardiovascular death or an ischemic event, compared with placebo.
CHICAGO – REDUCE-IT is a phenomenal trial and a game changer because it has shown for the first time that triglyceride reduction with an appropriate therapy – in this case icosapent ethyl – when used in appropriate doses can make a significant difference.
That’s according to Prakash C. Deedwania, MD, chief of the cardiology division at the Veterans Affairs Medical Center/University of California San Francisco Program in Fresno, who joined MDedge reporter Richard Mark Kirkner for a video interview at the American Heart Association scientific sessions.
In the large, placebo-controlled REDUCE-IT trial in patients with or at high risk for cardiovascular disease received who received 2 g of icosapent ethyl (Vascepa) twice daily or placebo saw a 25% lower risk of cardiovascular death or an ischemic event, compared with placebo.
CHICAGO – REDUCE-IT is a phenomenal trial and a game changer because it has shown for the first time that triglyceride reduction with an appropriate therapy – in this case icosapent ethyl – when used in appropriate doses can make a significant difference.
That’s according to Prakash C. Deedwania, MD, chief of the cardiology division at the Veterans Affairs Medical Center/University of California San Francisco Program in Fresno, who joined MDedge reporter Richard Mark Kirkner for a video interview at the American Heart Association scientific sessions.
In the large, placebo-controlled REDUCE-IT trial in patients with or at high risk for cardiovascular disease received who received 2 g of icosapent ethyl (Vascepa) twice daily or placebo saw a 25% lower risk of cardiovascular death or an ischemic event, compared with placebo.
REPORTING FROM THE AHA SCIENTIFIC SESSIONS
TMB measured by NGS may ID SCLC patients who will benefit from immunotherapy
WASHINGTON – and targeted next-generation sequencing may help identify those likely to benefit from immunotherapy, findings from a case series suggest.
Of 113 small cell lung cancer (SCLC) patients who had successful next-generation sequencing (NGS) with tumor mutational burden (TMB) assessment at the Dana-Farber Cancer Institute (DFCI) in Boston, 52 were treated with immune checkpoint inhibitors and 61 received chemotherapy but never received subsequent immunotherapy, Biagio Ricciuti, MD, of DFCI said at the annual meeting of the Society for the Immunotherapy of Cancer.
Median TMB for all patients was 9.68 mutations/megabase, with those with TMB above the median considered TMB high, and those with TMB below the median considered TMB low. Median progression-free survival (PFS) was significantly longer among TMB-high versus TMB-low patients (3.3 vs. 1.2 months; hazard ratio, 0.37), as was median overall survival (OS, 10.4 vs. 2.5 months; HR, 0.38), he said.
“To confirm that TMB was a predictive biomarker for immunotherapy only, we also looked at the outcome with chemotherapy according to tumor mutational burden, and as expected we found no difference in terms of median progression-free survival or median overall survival according to TMB-high versus TMB-low groups,” he said.
Additionally, patients with SCLC who were treated with immune checkpoint inhibitors and experienced at least one immune-related adverse event had significantly better median PFS and OS than did patients who experienced no immune-related adverse events (6.7 vs. 1.3 months; HR, 0.25; and 17.9 vs. 2.9 months; HR, 0.27, respectively), he said, noting that, in a 12-week landmark analysis, the differences in PFS and OS between the groups were “nearly double” but did not reach statistical significance.
TMB in the SCLC patients in this study was assessed using the DFCI NGS OncoPanel platform of more than 450 genes, and the TMB-high and TMB-low groups were similar with respect to baseline clinical and pathological features and known prognostic factors, Dr. Ricciuti said.
Prior studies have demonstrated that high TMB as assessed by whole exome sequencing correlates with benefits from immunotherapy. However, “whole exome sequencing is a very expensive technique, it’s challenging ... and it’s not really available to oncologists across countries,” he said.
Whether the more readily available targeted NGS could help identify the small fraction of SCLC patients who are likely to benefit from immunotherapy has been unclear, as has the relationship between the development of irAEs and immunotherapy response in SCLC; factors associated with clinical benefit from immunotherapy have not previously been well characterized, Dr. Ricciuti noted.
The current findings, though limited by the retrospective study design and small sample size, provide the first evidence for the use of targeted NGS panels to identify patients with advanced SCLC who are most likely to benefit from immunotherapy, he said, adding that, when compared with whole genome sequencing, TMB as assessed using targeted NGS “may offer a very useful tool for clinicians to optimize small cell lung cancer patient selection for immunotherapy.
“Our study also suggests that immune-related adverse events might be associated with improved efficacy of immunotherapy, although larger studies with longer follow-up are required to confirm this finding,” he concluded.
Dr. Ricciuti reported having no disclosures.
WASHINGTON – and targeted next-generation sequencing may help identify those likely to benefit from immunotherapy, findings from a case series suggest.
Of 113 small cell lung cancer (SCLC) patients who had successful next-generation sequencing (NGS) with tumor mutational burden (TMB) assessment at the Dana-Farber Cancer Institute (DFCI) in Boston, 52 were treated with immune checkpoint inhibitors and 61 received chemotherapy but never received subsequent immunotherapy, Biagio Ricciuti, MD, of DFCI said at the annual meeting of the Society for the Immunotherapy of Cancer.
Median TMB for all patients was 9.68 mutations/megabase, with those with TMB above the median considered TMB high, and those with TMB below the median considered TMB low. Median progression-free survival (PFS) was significantly longer among TMB-high versus TMB-low patients (3.3 vs. 1.2 months; hazard ratio, 0.37), as was median overall survival (OS, 10.4 vs. 2.5 months; HR, 0.38), he said.
“To confirm that TMB was a predictive biomarker for immunotherapy only, we also looked at the outcome with chemotherapy according to tumor mutational burden, and as expected we found no difference in terms of median progression-free survival or median overall survival according to TMB-high versus TMB-low groups,” he said.
Additionally, patients with SCLC who were treated with immune checkpoint inhibitors and experienced at least one immune-related adverse event had significantly better median PFS and OS than did patients who experienced no immune-related adverse events (6.7 vs. 1.3 months; HR, 0.25; and 17.9 vs. 2.9 months; HR, 0.27, respectively), he said, noting that, in a 12-week landmark analysis, the differences in PFS and OS between the groups were “nearly double” but did not reach statistical significance.
TMB in the SCLC patients in this study was assessed using the DFCI NGS OncoPanel platform of more than 450 genes, and the TMB-high and TMB-low groups were similar with respect to baseline clinical and pathological features and known prognostic factors, Dr. Ricciuti said.
Prior studies have demonstrated that high TMB as assessed by whole exome sequencing correlates with benefits from immunotherapy. However, “whole exome sequencing is a very expensive technique, it’s challenging ... and it’s not really available to oncologists across countries,” he said.
Whether the more readily available targeted NGS could help identify the small fraction of SCLC patients who are likely to benefit from immunotherapy has been unclear, as has the relationship between the development of irAEs and immunotherapy response in SCLC; factors associated with clinical benefit from immunotherapy have not previously been well characterized, Dr. Ricciuti noted.
The current findings, though limited by the retrospective study design and small sample size, provide the first evidence for the use of targeted NGS panels to identify patients with advanced SCLC who are most likely to benefit from immunotherapy, he said, adding that, when compared with whole genome sequencing, TMB as assessed using targeted NGS “may offer a very useful tool for clinicians to optimize small cell lung cancer patient selection for immunotherapy.
“Our study also suggests that immune-related adverse events might be associated with improved efficacy of immunotherapy, although larger studies with longer follow-up are required to confirm this finding,” he concluded.
Dr. Ricciuti reported having no disclosures.
WASHINGTON – and targeted next-generation sequencing may help identify those likely to benefit from immunotherapy, findings from a case series suggest.
Of 113 small cell lung cancer (SCLC) patients who had successful next-generation sequencing (NGS) with tumor mutational burden (TMB) assessment at the Dana-Farber Cancer Institute (DFCI) in Boston, 52 were treated with immune checkpoint inhibitors and 61 received chemotherapy but never received subsequent immunotherapy, Biagio Ricciuti, MD, of DFCI said at the annual meeting of the Society for the Immunotherapy of Cancer.
Median TMB for all patients was 9.68 mutations/megabase, with those with TMB above the median considered TMB high, and those with TMB below the median considered TMB low. Median progression-free survival (PFS) was significantly longer among TMB-high versus TMB-low patients (3.3 vs. 1.2 months; hazard ratio, 0.37), as was median overall survival (OS, 10.4 vs. 2.5 months; HR, 0.38), he said.
“To confirm that TMB was a predictive biomarker for immunotherapy only, we also looked at the outcome with chemotherapy according to tumor mutational burden, and as expected we found no difference in terms of median progression-free survival or median overall survival according to TMB-high versus TMB-low groups,” he said.
Additionally, patients with SCLC who were treated with immune checkpoint inhibitors and experienced at least one immune-related adverse event had significantly better median PFS and OS than did patients who experienced no immune-related adverse events (6.7 vs. 1.3 months; HR, 0.25; and 17.9 vs. 2.9 months; HR, 0.27, respectively), he said, noting that, in a 12-week landmark analysis, the differences in PFS and OS between the groups were “nearly double” but did not reach statistical significance.
TMB in the SCLC patients in this study was assessed using the DFCI NGS OncoPanel platform of more than 450 genes, and the TMB-high and TMB-low groups were similar with respect to baseline clinical and pathological features and known prognostic factors, Dr. Ricciuti said.
Prior studies have demonstrated that high TMB as assessed by whole exome sequencing correlates with benefits from immunotherapy. However, “whole exome sequencing is a very expensive technique, it’s challenging ... and it’s not really available to oncologists across countries,” he said.
Whether the more readily available targeted NGS could help identify the small fraction of SCLC patients who are likely to benefit from immunotherapy has been unclear, as has the relationship between the development of irAEs and immunotherapy response in SCLC; factors associated with clinical benefit from immunotherapy have not previously been well characterized, Dr. Ricciuti noted.
The current findings, though limited by the retrospective study design and small sample size, provide the first evidence for the use of targeted NGS panels to identify patients with advanced SCLC who are most likely to benefit from immunotherapy, he said, adding that, when compared with whole genome sequencing, TMB as assessed using targeted NGS “may offer a very useful tool for clinicians to optimize small cell lung cancer patient selection for immunotherapy.
“Our study also suggests that immune-related adverse events might be associated with improved efficacy of immunotherapy, although larger studies with longer follow-up are required to confirm this finding,” he concluded.
Dr. Ricciuti reported having no disclosures.
REPORTING FROM SITC 2018
Key clinical point: Next-generation sequencing may help identify small cell lung cancer patients who will benefit from immunotherapy.
Major finding: Median progression-free survival and overall survival were significantly better among tumor mutational burden–high versus tumor mutational burden–low patients (3.3 vs. 1.2 months; hazard ratio, 0.37; and 10.4 vs. 2.5 months; HR, 0.38, respectively).
Study details: A series of 113 patients.
Disclosures: Dr. Ricciuti reported having no disclosures.
MOC update: GI societies and ABIM explore new recertification pathway
AGA is committed to making recertification less burdensome for GIs. After a productive meeting between the GI societies and ABIM, we’re hopeful a new, more flexible pathway is on the horizon.
We heard you
The four major physician organizations in gastroenterology and hepatology — AGA, AASLD, ACG and ASGE — share a fundamental commitment to an efficient, clinically relevant and impactful process for the demonstration of ongoing learning and maintenance of specialty board certification for gastroenterologists and hepatologists.
Inspired by our shared objective to create an alternative to the current ABIM 10-year exam and upcoming two-year check-in, the four societies have collaborated to explore alternatives that are less onerous, more relevant, less costly and less time consuming. We look forward to working to achieve this objective for all of GI and hepatology.
Finding a path forward on MOC for GI & hepatology
On Oct. 4, the four societies met with the leadership of ABIM in Philadelphia, Pennsylvania, and presented concepts focusing on a flexible model that can provide a path forward, allowing members of our specialties and subspecialties to focus on knowledge that is relevant to their practice and choose the path that best fits their personal needs.
The GI societies and ABIM agreed to work together to explore the development of a third option for MOC.
Guided by core principles
In working together to develop an alternative to MOC, the four GI societies are guided by these core principles embraced by our organizations several years ago:
• MOC needs to be simpler, less intrusive and less expensive.
• We continue to support alternatives to the high-stakes, every-10-year recertification exam.
• We do not support single source or time-limited assessments, as they do not represent the current realities of medicine in the digital age.
• We support the concept that, for the many diplomates who specialize within certain areas of gastroenterology and hepatology, MOC should not include high-stakes assessments of areas in which the diplomate may not practice.
• We support the principles of lifelong learning, as evidenced by ongoing CME activities, rather than lifelong testing.
AGA is committed to making recertification less burdensome for GIs. After a productive meeting between the GI societies and ABIM, we’re hopeful a new, more flexible pathway is on the horizon.
We heard you
The four major physician organizations in gastroenterology and hepatology — AGA, AASLD, ACG and ASGE — share a fundamental commitment to an efficient, clinically relevant and impactful process for the demonstration of ongoing learning and maintenance of specialty board certification for gastroenterologists and hepatologists.
Inspired by our shared objective to create an alternative to the current ABIM 10-year exam and upcoming two-year check-in, the four societies have collaborated to explore alternatives that are less onerous, more relevant, less costly and less time consuming. We look forward to working to achieve this objective for all of GI and hepatology.
Finding a path forward on MOC for GI & hepatology
On Oct. 4, the four societies met with the leadership of ABIM in Philadelphia, Pennsylvania, and presented concepts focusing on a flexible model that can provide a path forward, allowing members of our specialties and subspecialties to focus on knowledge that is relevant to their practice and choose the path that best fits their personal needs.
The GI societies and ABIM agreed to work together to explore the development of a third option for MOC.
Guided by core principles
In working together to develop an alternative to MOC, the four GI societies are guided by these core principles embraced by our organizations several years ago:
• MOC needs to be simpler, less intrusive and less expensive.
• We continue to support alternatives to the high-stakes, every-10-year recertification exam.
• We do not support single source or time-limited assessments, as they do not represent the current realities of medicine in the digital age.
• We support the concept that, for the many diplomates who specialize within certain areas of gastroenterology and hepatology, MOC should not include high-stakes assessments of areas in which the diplomate may not practice.
• We support the principles of lifelong learning, as evidenced by ongoing CME activities, rather than lifelong testing.
AGA is committed to making recertification less burdensome for GIs. After a productive meeting between the GI societies and ABIM, we’re hopeful a new, more flexible pathway is on the horizon.
We heard you
The four major physician organizations in gastroenterology and hepatology — AGA, AASLD, ACG and ASGE — share a fundamental commitment to an efficient, clinically relevant and impactful process for the demonstration of ongoing learning and maintenance of specialty board certification for gastroenterologists and hepatologists.
Inspired by our shared objective to create an alternative to the current ABIM 10-year exam and upcoming two-year check-in, the four societies have collaborated to explore alternatives that are less onerous, more relevant, less costly and less time consuming. We look forward to working to achieve this objective for all of GI and hepatology.
Finding a path forward on MOC for GI & hepatology
On Oct. 4, the four societies met with the leadership of ABIM in Philadelphia, Pennsylvania, and presented concepts focusing on a flexible model that can provide a path forward, allowing members of our specialties and subspecialties to focus on knowledge that is relevant to their practice and choose the path that best fits their personal needs.
The GI societies and ABIM agreed to work together to explore the development of a third option for MOC.
Guided by core principles
In working together to develop an alternative to MOC, the four GI societies are guided by these core principles embraced by our organizations several years ago:
• MOC needs to be simpler, less intrusive and less expensive.
• We continue to support alternatives to the high-stakes, every-10-year recertification exam.
• We do not support single source or time-limited assessments, as they do not represent the current realities of medicine in the digital age.
• We support the concept that, for the many diplomates who specialize within certain areas of gastroenterology and hepatology, MOC should not include high-stakes assessments of areas in which the diplomate may not practice.
• We support the principles of lifelong learning, as evidenced by ongoing CME activities, rather than lifelong testing.
DDW® 2019 abstract submission site is now open
Digestive Disease Week® (DDW) will be accepting abstracts for DDW 2019 from now through Dec. 1, 2018.
Since 1969, Digestive Disease Week has been the most important venue for sharing research and breakthroughs in digestive disease. What better way to commemorate DDW’s legacy than to make sure your research is included to help promote basic, clinical, and translational research on a global scale?
For DDW 2019, AGA is planning a program filled with cutting-edge advances in the field. To help you match your abstract(s) to the best descriptor for submission to AGA, the AGA Institute Council released an expanded descriptor document, gastro.org/Descriptors, to indicate what the abstract review committee is looking for in submitted abstracts.
Mark your calendar with the important abstract submission dates below and visit the DDW website for more information on submitting your research.
Important dates
Dec. 1, 2018, at 9 p.m. ET: Abstract submission site closes. No abstract edits, author additions or changes to author information will be accepted after this deadline.
Dec. 14, 2018, at 3 p.m. ET: Co-author disclosures due.
Feb. 12, 2019: Acceptance notifications sent by email to presenting authors.
Take advantage of this opportunity to make sure your research is included.
Digestive Disease Week® (DDW) will be accepting abstracts for DDW 2019 from now through Dec. 1, 2018.
Since 1969, Digestive Disease Week has been the most important venue for sharing research and breakthroughs in digestive disease. What better way to commemorate DDW’s legacy than to make sure your research is included to help promote basic, clinical, and translational research on a global scale?
For DDW 2019, AGA is planning a program filled with cutting-edge advances in the field. To help you match your abstract(s) to the best descriptor for submission to AGA, the AGA Institute Council released an expanded descriptor document, gastro.org/Descriptors, to indicate what the abstract review committee is looking for in submitted abstracts.
Mark your calendar with the important abstract submission dates below and visit the DDW website for more information on submitting your research.
Important dates
Dec. 1, 2018, at 9 p.m. ET: Abstract submission site closes. No abstract edits, author additions or changes to author information will be accepted after this deadline.
Dec. 14, 2018, at 3 p.m. ET: Co-author disclosures due.
Feb. 12, 2019: Acceptance notifications sent by email to presenting authors.
Take advantage of this opportunity to make sure your research is included.
Digestive Disease Week® (DDW) will be accepting abstracts for DDW 2019 from now through Dec. 1, 2018.
Since 1969, Digestive Disease Week has been the most important venue for sharing research and breakthroughs in digestive disease. What better way to commemorate DDW’s legacy than to make sure your research is included to help promote basic, clinical, and translational research on a global scale?
For DDW 2019, AGA is planning a program filled with cutting-edge advances in the field. To help you match your abstract(s) to the best descriptor for submission to AGA, the AGA Institute Council released an expanded descriptor document, gastro.org/Descriptors, to indicate what the abstract review committee is looking for in submitted abstracts.
Mark your calendar with the important abstract submission dates below and visit the DDW website for more information on submitting your research.
Important dates
Dec. 1, 2018, at 9 p.m. ET: Abstract submission site closes. No abstract edits, author additions or changes to author information will be accepted after this deadline.
Dec. 14, 2018, at 3 p.m. ET: Co-author disclosures due.
Feb. 12, 2019: Acceptance notifications sent by email to presenting authors.
Take advantage of this opportunity to make sure your research is included.
AGA’s Future Leaders Program receives stellar reviews
Future Leaders alumni and past mentors took to the AGA Community recently to share their experiences with the award-winning program. Now in its third year, the program continues to have an impact on the careers of its participants and AGA.
Here’s what they had to say
“The Future Leaders Program provided robust leadership training, valuable mentorship, and invaluable networking with AGA leaders and other AGA members.” – Bryson Katona, MD, MS, PhD, editor of The New Gastroenterologist, University of Pennsylvania
“Through the Future Leaders Program I gained leadership skills, problem-solving skills, and even new research collaborations.” – Jennifer Weiss MD, MS, AGAF, University of Wisconsin School of Medicine and Public Health
“The program not only introduced Future Leaders Program members to the AGA inner circle and provided a deep insight into AGA governance, but also placed participants into meaningful, actionable projects that had the potential to generate real benefits for the AGA itself.” – David Levinthal, MD, PhD, University of Pittsburgh Medical Center
“I think I learned as much from the two outstanding faculty whom I mentored, Jennifer Weiss and Art Beyder, as they did from me!” – Kim Barrett, PhD, AGAF, University of California, San Diego (Mentor)
The program is designed for GIs who aspire to further develop their leadership skills with an eye toward serving in a key leadership position both within the field and AGA. Participation from experienced GIs is also critical to the program’s success. They are needed to serve as mentors and help develop the next generation of leaders. This is the opportunity to help drive AGA’s strategic plan and advance in the field.
Members can access the full discussion: A Fantastic Opportunity: AGA Future Leaders Program in community.gastro.org. Stay tuned to see the list of members selected for the 2019 AGA Future Leaders Program.
Future Leaders alumni and past mentors took to the AGA Community recently to share their experiences with the award-winning program. Now in its third year, the program continues to have an impact on the careers of its participants and AGA.
Here’s what they had to say
“The Future Leaders Program provided robust leadership training, valuable mentorship, and invaluable networking with AGA leaders and other AGA members.” – Bryson Katona, MD, MS, PhD, editor of The New Gastroenterologist, University of Pennsylvania
“Through the Future Leaders Program I gained leadership skills, problem-solving skills, and even new research collaborations.” – Jennifer Weiss MD, MS, AGAF, University of Wisconsin School of Medicine and Public Health
“The program not only introduced Future Leaders Program members to the AGA inner circle and provided a deep insight into AGA governance, but also placed participants into meaningful, actionable projects that had the potential to generate real benefits for the AGA itself.” – David Levinthal, MD, PhD, University of Pittsburgh Medical Center
“I think I learned as much from the two outstanding faculty whom I mentored, Jennifer Weiss and Art Beyder, as they did from me!” – Kim Barrett, PhD, AGAF, University of California, San Diego (Mentor)
The program is designed for GIs who aspire to further develop their leadership skills with an eye toward serving in a key leadership position both within the field and AGA. Participation from experienced GIs is also critical to the program’s success. They are needed to serve as mentors and help develop the next generation of leaders. This is the opportunity to help drive AGA’s strategic plan and advance in the field.
Members can access the full discussion: A Fantastic Opportunity: AGA Future Leaders Program in community.gastro.org. Stay tuned to see the list of members selected for the 2019 AGA Future Leaders Program.
Future Leaders alumni and past mentors took to the AGA Community recently to share their experiences with the award-winning program. Now in its third year, the program continues to have an impact on the careers of its participants and AGA.
Here’s what they had to say
“The Future Leaders Program provided robust leadership training, valuable mentorship, and invaluable networking with AGA leaders and other AGA members.” – Bryson Katona, MD, MS, PhD, editor of The New Gastroenterologist, University of Pennsylvania
“Through the Future Leaders Program I gained leadership skills, problem-solving skills, and even new research collaborations.” – Jennifer Weiss MD, MS, AGAF, University of Wisconsin School of Medicine and Public Health
“The program not only introduced Future Leaders Program members to the AGA inner circle and provided a deep insight into AGA governance, but also placed participants into meaningful, actionable projects that had the potential to generate real benefits for the AGA itself.” – David Levinthal, MD, PhD, University of Pittsburgh Medical Center
“I think I learned as much from the two outstanding faculty whom I mentored, Jennifer Weiss and Art Beyder, as they did from me!” – Kim Barrett, PhD, AGAF, University of California, San Diego (Mentor)
The program is designed for GIs who aspire to further develop their leadership skills with an eye toward serving in a key leadership position both within the field and AGA. Participation from experienced GIs is also critical to the program’s success. They are needed to serve as mentors and help develop the next generation of leaders. This is the opportunity to help drive AGA’s strategic plan and advance in the field.
Members can access the full discussion: A Fantastic Opportunity: AGA Future Leaders Program in community.gastro.org. Stay tuned to see the list of members selected for the 2019 AGA Future Leaders Program.
FDA approves first treatment for primary HLH
The U.S. Food and Drug Administration (FDA) has approved emapalumab-lzsg (Gamifant®) to treat primary hemophagocytic lymphohistiocytosis (HLH).
Emapalumab, an interferon gamma-blocking antibody, is approved to treat to treat patients of all ages (newborn and older) with primary HLH who have refractory, recurrent, or progressive disease or who cannot tolerate conventional HLH therapy.
Emapalumab is the first treatment to be FDA-approved for primary HLH, and it is expected to be available in the United States in the first quarter of 2019.
The FDA previously granted emapalumab priority review, breakthrough therapy designation, orphan drug designation, and rare pediatric disease designation.
The FDA’s approval of emapalumab is based on results from a phase 2/3 trial (NCT01818492).
The trial included 34 patients, 27 of whom had refractory, recurrent, or progressive disease or could not tolerate conventional HLH therapy.
Patients received emapalumab in combination with dexamethasone.
At the end of treatment, 63% (17/27) of patients had achieved a response, which was defined as complete response (n=7), partial response (n=8), or HLH improvement (n=2).
Seventy percent (n=19) of patients went on to hematopoietic stem cell transplant.
The most common adverse events were infections (56%), hypertension (41%), infusion-related reactions (27%), and pyrexia (24%).
Additional results from this study can be found in the prescribing information for emapalumab, which is available at www.gamifant.com.
Results are also scheduled to be presented at the 2018 ASH Annual Meeting (abstract LBA-6).
Emapalumab was developed by Novimmune SA. Sobi acquired global rights to the drug in August 2018.
The U.S. Food and Drug Administration (FDA) has approved emapalumab-lzsg (Gamifant®) to treat primary hemophagocytic lymphohistiocytosis (HLH).
Emapalumab, an interferon gamma-blocking antibody, is approved to treat to treat patients of all ages (newborn and older) with primary HLH who have refractory, recurrent, or progressive disease or who cannot tolerate conventional HLH therapy.
Emapalumab is the first treatment to be FDA-approved for primary HLH, and it is expected to be available in the United States in the first quarter of 2019.
The FDA previously granted emapalumab priority review, breakthrough therapy designation, orphan drug designation, and rare pediatric disease designation.
The FDA’s approval of emapalumab is based on results from a phase 2/3 trial (NCT01818492).
The trial included 34 patients, 27 of whom had refractory, recurrent, or progressive disease or could not tolerate conventional HLH therapy.
Patients received emapalumab in combination with dexamethasone.
At the end of treatment, 63% (17/27) of patients had achieved a response, which was defined as complete response (n=7), partial response (n=8), or HLH improvement (n=2).
Seventy percent (n=19) of patients went on to hematopoietic stem cell transplant.
The most common adverse events were infections (56%), hypertension (41%), infusion-related reactions (27%), and pyrexia (24%).
Additional results from this study can be found in the prescribing information for emapalumab, which is available at www.gamifant.com.
Results are also scheduled to be presented at the 2018 ASH Annual Meeting (abstract LBA-6).
Emapalumab was developed by Novimmune SA. Sobi acquired global rights to the drug in August 2018.
The U.S. Food and Drug Administration (FDA) has approved emapalumab-lzsg (Gamifant®) to treat primary hemophagocytic lymphohistiocytosis (HLH).
Emapalumab, an interferon gamma-blocking antibody, is approved to treat to treat patients of all ages (newborn and older) with primary HLH who have refractory, recurrent, or progressive disease or who cannot tolerate conventional HLH therapy.
Emapalumab is the first treatment to be FDA-approved for primary HLH, and it is expected to be available in the United States in the first quarter of 2019.
The FDA previously granted emapalumab priority review, breakthrough therapy designation, orphan drug designation, and rare pediatric disease designation.
The FDA’s approval of emapalumab is based on results from a phase 2/3 trial (NCT01818492).
The trial included 34 patients, 27 of whom had refractory, recurrent, or progressive disease or could not tolerate conventional HLH therapy.
Patients received emapalumab in combination with dexamethasone.
At the end of treatment, 63% (17/27) of patients had achieved a response, which was defined as complete response (n=7), partial response (n=8), or HLH improvement (n=2).
Seventy percent (n=19) of patients went on to hematopoietic stem cell transplant.
The most common adverse events were infections (56%), hypertension (41%), infusion-related reactions (27%), and pyrexia (24%).
Additional results from this study can be found in the prescribing information for emapalumab, which is available at www.gamifant.com.
Results are also scheduled to be presented at the 2018 ASH Annual Meeting (abstract LBA-6).
Emapalumab was developed by Novimmune SA. Sobi acquired global rights to the drug in August 2018.
ADA releases guidelines for type 2 diabetes in children, youth
The American Diabetes Association’s guidelines for the evaluation and management of pediatric patients with type 2 diabetes differ from those for adults.
“Puberty-related physiologic insulin resistance, particularly in obese youth, may play a role” in the fact that youth are more insulin resistant than adults. Also, type 2 diabetes apparently is “more aggressive in youth than adults, with a faster rate of deterioration of beta-cell function and poorer response to glucose-lowering medications,” wrote Silva Arslanian, MD, from the division of pediatric endocrinology, metabolism, and diabetes mellitus at the University of Pittsburgh, and her colleagues. “Even though our knowledge of youth-onset type 2 diabetes has increased tremendously over the last 2 decades, robust and evidence-based data are still limited regarding diagnostic and therapeutic approaches and prevention of complications.”
The ADA position statement by Dr. Arslanian and her colleagues outlines management of type 2 diabetes in children and youth.
Diagnosis
and repeat testing should occur at least every 3 years for these patients. Pancreatic autoantibody tests should also be considered in this patient population to rule out autoimmune type 1 diabetes, and genetic evaluation should be performed to test for monogenic diabetes, “based on clinical characteristics and presentation,” they wrote.
Use fasting plasma glucose, 2-hour fasting plasma glucose after a 75-g oral glucose tolerance test, or glycosylated hemoglobin (HbA1C) to test for diabetes or prediabetes. Also consider factors like medication adherence and treatment effects when prescribing glucose-lowering or other medications for overweight or obese children and adolescents with type 2 diabetes.
Lifestyle management
With regard to lifestyle management programs, the intervention should be introduced as a part of diabetes care – aimed at reducing between 7% and 10% of body weight – and be based on a chronic care model. The intervention should include 30-60 minutes of moderate to intense physical activity for 5 days each week, strength training 3 days per week, and incorporate healthy eating plans. Dr. Arslanian and her associates noted there was limited evidence for pharmacotherapy for weight reduction in children and adolescents with type 2 diabetes.
Pharmacologic therapy
Pharmacologic therapy should be started together with lifestyle therapy once a diagnosis is made, according to the recommendations.
Metformin is the preferred initial pharmacologic treatment for patients with normal renal function who are asymptomatic and with HbA1C levels of less than 8.5%.
Patients with blood glucose greater than or equal to 250 mg/dL and HbA1C greater than or equal to 8.5% with symptoms such as weight loss, polydipsia, polyuria, or nocturia should receive basal insulin during initiation and titration of metformin.
Patients with ketosis or ketoacidosis should receive intravenous insulin to address hyperglycemia. Once the acidosis is corrected, initiate metformin with subcutaneous insulin therapy. For patients who are reaching home-based glucose monitoring targets, consider tapering the dose over 2-6 weeks with a 10%-30% reduction in insulin every few days.
In patients where metformin alone is not meeting the glycemic target, consider basal insulin therapy and, if that fails to help achieve glycemic targets, more intensive approaches should be considered, such as metabolic surgery.
Jay Cohen, MD, FACE, medical director at the Endocrine Clinic in Memphis, said in an interview that he agreed with the ADA position statement except for the pharmacologic therapy recommendations.
“The pharmacology therapy is 4 years outdated,” he said. “We routinely use all of the medications that are not Food and Drug Administration [approved] for kids, but are FDA approved for adults.”
He also questioned the ADA’s recommendation to give basal insulin to patients who are insulin resistant.
“Why give insulin if these people are insulin resistant?” said Dr. Cohen, who also is a Clinical Endocrinology News editorial board member. “The oral and injectable noninsulins work fabulously with less weight gain – already a problem for these patients – and less hypoglycemia, less side effects, and better compliance.”
Treatment goals
The HbA1C goal for children and adolescents with type 2 diabetes is less than 7% when treated with oral agents alone. HbA1C should be tested every 3 months and should be individualized, according to the ADA recommendations. In some patients, such as those with a shorter diabetes duration, lesser degrees of beta-cell dysfunction, and those who achieve significant weight improvement through lifestyle changes or taking metformin, consider lowering the HbA1C goal to less than 6.5%.
Give individualized care with regard to home self-monitoring of blood glucose. Also provide patients and their families with “culturally competent” diabetes self-management tools and lifestyle programs. Consider social factors such as housing stability, food insecurity, and financial barriers when making treatment decisions.
Screening for complications
To screen for nephropathy, take BP measurements at every visit and promote lifestyle management to reduce risk of diabetic kidney disease and improve weight loss. After 6 months, if a patient’s BP remains greater than the 95th percentile for their age, gender, and height, ACE inhibitors, or angiotensin receptor blockers are initial therapeutic options, according to the position statement. Other BP-lowering treatments may be added as necessary.
Also monitor protein intake (0.8 g/kg per day) as well as urine albumin/creatinine ratio (UACR) and estimated glomerular filtration rate (eGFR) annually. Patients with diabetes and hypertension who are not pregnant should receive an ACE inhibitor or angiotensin receptor blocker if their UACR is modestly elevated (30-299 mg/g creatinine). Such a regimen is strongly recommended if their UACR is above 300 mg/g creatinine and/or if their eGFR is less than 60 mL/min per 1.73 m2.
Screening issues
When considering diabetes distress and mental or behavioral health in children and adolescents with type 2 diabetes, use standardized and validated tools to assess symptoms such as depression and disordered eating behaviors. Regularly screen for smoking and alcohol use and provide preconception counseling for female patients of child-bearing age.
Screen for neuropathy, retinopathy, and nonalcoholic fatty liver disease annually and for obstructive sleep apnea at each visit. Lipid testing should be performed annually once patients have achieved glycemic control. Polycystic ovary syndrome should be considered in female patients with type 2 diabetes and treated with metformin together with lifestyle changes to address menstrual cyclicity and hyperandrogenism, the authors recommended.
Dr. Arslanian is on a data monitoring committee for AstraZeneca; data safety monitoring board for Boehringer Ingelheim; and advisory boards for Eli Lilly, Novo Nordisk, and Sanofi-Aventis; and has received research grants from Eli Lilly and Novo Nordisk. Other authors reported various relationships with a number of pharmaceutical companies.
SOURCE: Arslanian S et al. Diabetes Care. 2018 Nov 13. doi: 10.2337/dci18-0052.
The American Diabetes Association’s guidelines for the evaluation and management of pediatric patients with type 2 diabetes differ from those for adults.
“Puberty-related physiologic insulin resistance, particularly in obese youth, may play a role” in the fact that youth are more insulin resistant than adults. Also, type 2 diabetes apparently is “more aggressive in youth than adults, with a faster rate of deterioration of beta-cell function and poorer response to glucose-lowering medications,” wrote Silva Arslanian, MD, from the division of pediatric endocrinology, metabolism, and diabetes mellitus at the University of Pittsburgh, and her colleagues. “Even though our knowledge of youth-onset type 2 diabetes has increased tremendously over the last 2 decades, robust and evidence-based data are still limited regarding diagnostic and therapeutic approaches and prevention of complications.”
The ADA position statement by Dr. Arslanian and her colleagues outlines management of type 2 diabetes in children and youth.
Diagnosis
and repeat testing should occur at least every 3 years for these patients. Pancreatic autoantibody tests should also be considered in this patient population to rule out autoimmune type 1 diabetes, and genetic evaluation should be performed to test for monogenic diabetes, “based on clinical characteristics and presentation,” they wrote.
Use fasting plasma glucose, 2-hour fasting plasma glucose after a 75-g oral glucose tolerance test, or glycosylated hemoglobin (HbA1C) to test for diabetes or prediabetes. Also consider factors like medication adherence and treatment effects when prescribing glucose-lowering or other medications for overweight or obese children and adolescents with type 2 diabetes.
Lifestyle management
With regard to lifestyle management programs, the intervention should be introduced as a part of diabetes care – aimed at reducing between 7% and 10% of body weight – and be based on a chronic care model. The intervention should include 30-60 minutes of moderate to intense physical activity for 5 days each week, strength training 3 days per week, and incorporate healthy eating plans. Dr. Arslanian and her associates noted there was limited evidence for pharmacotherapy for weight reduction in children and adolescents with type 2 diabetes.
Pharmacologic therapy
Pharmacologic therapy should be started together with lifestyle therapy once a diagnosis is made, according to the recommendations.
Metformin is the preferred initial pharmacologic treatment for patients with normal renal function who are asymptomatic and with HbA1C levels of less than 8.5%.
Patients with blood glucose greater than or equal to 250 mg/dL and HbA1C greater than or equal to 8.5% with symptoms such as weight loss, polydipsia, polyuria, or nocturia should receive basal insulin during initiation and titration of metformin.
Patients with ketosis or ketoacidosis should receive intravenous insulin to address hyperglycemia. Once the acidosis is corrected, initiate metformin with subcutaneous insulin therapy. For patients who are reaching home-based glucose monitoring targets, consider tapering the dose over 2-6 weeks with a 10%-30% reduction in insulin every few days.
In patients where metformin alone is not meeting the glycemic target, consider basal insulin therapy and, if that fails to help achieve glycemic targets, more intensive approaches should be considered, such as metabolic surgery.
Jay Cohen, MD, FACE, medical director at the Endocrine Clinic in Memphis, said in an interview that he agreed with the ADA position statement except for the pharmacologic therapy recommendations.
“The pharmacology therapy is 4 years outdated,” he said. “We routinely use all of the medications that are not Food and Drug Administration [approved] for kids, but are FDA approved for adults.”
He also questioned the ADA’s recommendation to give basal insulin to patients who are insulin resistant.
“Why give insulin if these people are insulin resistant?” said Dr. Cohen, who also is a Clinical Endocrinology News editorial board member. “The oral and injectable noninsulins work fabulously with less weight gain – already a problem for these patients – and less hypoglycemia, less side effects, and better compliance.”
Treatment goals
The HbA1C goal for children and adolescents with type 2 diabetes is less than 7% when treated with oral agents alone. HbA1C should be tested every 3 months and should be individualized, according to the ADA recommendations. In some patients, such as those with a shorter diabetes duration, lesser degrees of beta-cell dysfunction, and those who achieve significant weight improvement through lifestyle changes or taking metformin, consider lowering the HbA1C goal to less than 6.5%.
Give individualized care with regard to home self-monitoring of blood glucose. Also provide patients and their families with “culturally competent” diabetes self-management tools and lifestyle programs. Consider social factors such as housing stability, food insecurity, and financial barriers when making treatment decisions.
Screening for complications
To screen for nephropathy, take BP measurements at every visit and promote lifestyle management to reduce risk of diabetic kidney disease and improve weight loss. After 6 months, if a patient’s BP remains greater than the 95th percentile for their age, gender, and height, ACE inhibitors, or angiotensin receptor blockers are initial therapeutic options, according to the position statement. Other BP-lowering treatments may be added as necessary.
Also monitor protein intake (0.8 g/kg per day) as well as urine albumin/creatinine ratio (UACR) and estimated glomerular filtration rate (eGFR) annually. Patients with diabetes and hypertension who are not pregnant should receive an ACE inhibitor or angiotensin receptor blocker if their UACR is modestly elevated (30-299 mg/g creatinine). Such a regimen is strongly recommended if their UACR is above 300 mg/g creatinine and/or if their eGFR is less than 60 mL/min per 1.73 m2.
Screening issues
When considering diabetes distress and mental or behavioral health in children and adolescents with type 2 diabetes, use standardized and validated tools to assess symptoms such as depression and disordered eating behaviors. Regularly screen for smoking and alcohol use and provide preconception counseling for female patients of child-bearing age.
Screen for neuropathy, retinopathy, and nonalcoholic fatty liver disease annually and for obstructive sleep apnea at each visit. Lipid testing should be performed annually once patients have achieved glycemic control. Polycystic ovary syndrome should be considered in female patients with type 2 diabetes and treated with metformin together with lifestyle changes to address menstrual cyclicity and hyperandrogenism, the authors recommended.
Dr. Arslanian is on a data monitoring committee for AstraZeneca; data safety monitoring board for Boehringer Ingelheim; and advisory boards for Eli Lilly, Novo Nordisk, and Sanofi-Aventis; and has received research grants from Eli Lilly and Novo Nordisk. Other authors reported various relationships with a number of pharmaceutical companies.
SOURCE: Arslanian S et al. Diabetes Care. 2018 Nov 13. doi: 10.2337/dci18-0052.
The American Diabetes Association’s guidelines for the evaluation and management of pediatric patients with type 2 diabetes differ from those for adults.
“Puberty-related physiologic insulin resistance, particularly in obese youth, may play a role” in the fact that youth are more insulin resistant than adults. Also, type 2 diabetes apparently is “more aggressive in youth than adults, with a faster rate of deterioration of beta-cell function and poorer response to glucose-lowering medications,” wrote Silva Arslanian, MD, from the division of pediatric endocrinology, metabolism, and diabetes mellitus at the University of Pittsburgh, and her colleagues. “Even though our knowledge of youth-onset type 2 diabetes has increased tremendously over the last 2 decades, robust and evidence-based data are still limited regarding diagnostic and therapeutic approaches and prevention of complications.”
The ADA position statement by Dr. Arslanian and her colleagues outlines management of type 2 diabetes in children and youth.
Diagnosis
and repeat testing should occur at least every 3 years for these patients. Pancreatic autoantibody tests should also be considered in this patient population to rule out autoimmune type 1 diabetes, and genetic evaluation should be performed to test for monogenic diabetes, “based on clinical characteristics and presentation,” they wrote.
Use fasting plasma glucose, 2-hour fasting plasma glucose after a 75-g oral glucose tolerance test, or glycosylated hemoglobin (HbA1C) to test for diabetes or prediabetes. Also consider factors like medication adherence and treatment effects when prescribing glucose-lowering or other medications for overweight or obese children and adolescents with type 2 diabetes.
Lifestyle management
With regard to lifestyle management programs, the intervention should be introduced as a part of diabetes care – aimed at reducing between 7% and 10% of body weight – and be based on a chronic care model. The intervention should include 30-60 minutes of moderate to intense physical activity for 5 days each week, strength training 3 days per week, and incorporate healthy eating plans. Dr. Arslanian and her associates noted there was limited evidence for pharmacotherapy for weight reduction in children and adolescents with type 2 diabetes.
Pharmacologic therapy
Pharmacologic therapy should be started together with lifestyle therapy once a diagnosis is made, according to the recommendations.
Metformin is the preferred initial pharmacologic treatment for patients with normal renal function who are asymptomatic and with HbA1C levels of less than 8.5%.
Patients with blood glucose greater than or equal to 250 mg/dL and HbA1C greater than or equal to 8.5% with symptoms such as weight loss, polydipsia, polyuria, or nocturia should receive basal insulin during initiation and titration of metformin.
Patients with ketosis or ketoacidosis should receive intravenous insulin to address hyperglycemia. Once the acidosis is corrected, initiate metformin with subcutaneous insulin therapy. For patients who are reaching home-based glucose monitoring targets, consider tapering the dose over 2-6 weeks with a 10%-30% reduction in insulin every few days.
In patients where metformin alone is not meeting the glycemic target, consider basal insulin therapy and, if that fails to help achieve glycemic targets, more intensive approaches should be considered, such as metabolic surgery.
Jay Cohen, MD, FACE, medical director at the Endocrine Clinic in Memphis, said in an interview that he agreed with the ADA position statement except for the pharmacologic therapy recommendations.
“The pharmacology therapy is 4 years outdated,” he said. “We routinely use all of the medications that are not Food and Drug Administration [approved] for kids, but are FDA approved for adults.”
He also questioned the ADA’s recommendation to give basal insulin to patients who are insulin resistant.
“Why give insulin if these people are insulin resistant?” said Dr. Cohen, who also is a Clinical Endocrinology News editorial board member. “The oral and injectable noninsulins work fabulously with less weight gain – already a problem for these patients – and less hypoglycemia, less side effects, and better compliance.”
Treatment goals
The HbA1C goal for children and adolescents with type 2 diabetes is less than 7% when treated with oral agents alone. HbA1C should be tested every 3 months and should be individualized, according to the ADA recommendations. In some patients, such as those with a shorter diabetes duration, lesser degrees of beta-cell dysfunction, and those who achieve significant weight improvement through lifestyle changes or taking metformin, consider lowering the HbA1C goal to less than 6.5%.
Give individualized care with regard to home self-monitoring of blood glucose. Also provide patients and their families with “culturally competent” diabetes self-management tools and lifestyle programs. Consider social factors such as housing stability, food insecurity, and financial barriers when making treatment decisions.
Screening for complications
To screen for nephropathy, take BP measurements at every visit and promote lifestyle management to reduce risk of diabetic kidney disease and improve weight loss. After 6 months, if a patient’s BP remains greater than the 95th percentile for their age, gender, and height, ACE inhibitors, or angiotensin receptor blockers are initial therapeutic options, according to the position statement. Other BP-lowering treatments may be added as necessary.
Also monitor protein intake (0.8 g/kg per day) as well as urine albumin/creatinine ratio (UACR) and estimated glomerular filtration rate (eGFR) annually. Patients with diabetes and hypertension who are not pregnant should receive an ACE inhibitor or angiotensin receptor blocker if their UACR is modestly elevated (30-299 mg/g creatinine). Such a regimen is strongly recommended if their UACR is above 300 mg/g creatinine and/or if their eGFR is less than 60 mL/min per 1.73 m2.
Screening issues
When considering diabetes distress and mental or behavioral health in children and adolescents with type 2 diabetes, use standardized and validated tools to assess symptoms such as depression and disordered eating behaviors. Regularly screen for smoking and alcohol use and provide preconception counseling for female patients of child-bearing age.
Screen for neuropathy, retinopathy, and nonalcoholic fatty liver disease annually and for obstructive sleep apnea at each visit. Lipid testing should be performed annually once patients have achieved glycemic control. Polycystic ovary syndrome should be considered in female patients with type 2 diabetes and treated with metformin together with lifestyle changes to address menstrual cyclicity and hyperandrogenism, the authors recommended.
Dr. Arslanian is on a data monitoring committee for AstraZeneca; data safety monitoring board for Boehringer Ingelheim; and advisory boards for Eli Lilly, Novo Nordisk, and Sanofi-Aventis; and has received research grants from Eli Lilly and Novo Nordisk. Other authors reported various relationships with a number of pharmaceutical companies.
SOURCE: Arslanian S et al. Diabetes Care. 2018 Nov 13. doi: 10.2337/dci18-0052.
FROM DIABETES CARE
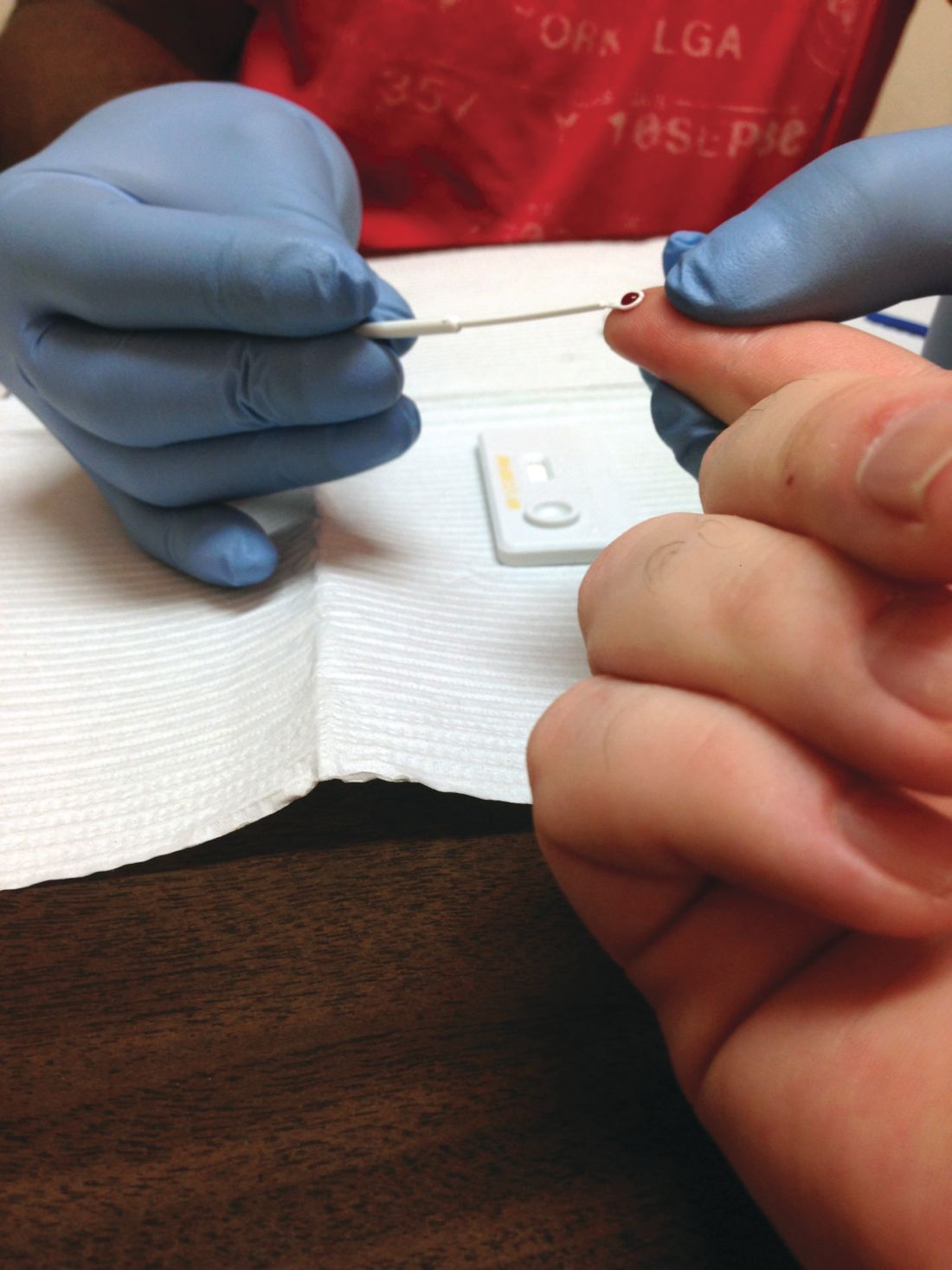
Draft guidelines advise HIV screening for most teens and adults
Individuals aged 15-65 years, including pregnant women, should be screened for HIV infection, and those at risk should be given prophylaxis, according to draft recommendations issued by the U.S. Preventive Services Task Force. The screening recommendation extends to younger adolescents and older adults at increased risk for HIV infection. The recommendations are level A.
HIV remains a significant public health issue in the United States, with rates rising among individuals aged 25-29 years, although the overall number of cases has dropped slightly, according to the USPSTF report.
HIV prevention is a multistep process that includes not only screening but also wearing condoms during sex and using clean needles and syringes if injecting drugs, the researchers noted.
However, those at high risk for HIV, such as intravenous drug users, can help reduce their risk by taking a daily pill, the researchers wrote.
In an evidence report submitted to the Agency for Healthcare Research and Quality, researchers reviewed the Cochrane databases, MEDLINE, and Embase for studies up to June 2018. Based on data from 11 trials, pre-exposure prophylaxis (PrEP) consisting of antiretroviral therapy was associated with decreased risk of HIV infection, compared with placebo or no PrEP, with consistent effects across risk categories, the investigators noted.
The most common HIV risk factors include man-to-man sexual contact, injection drug use, having sex without a condom, exchanging sex for drugs or money, and having sex with an HIV-infected partner, according to the USPSTF report.
Although PrEP was associated with renal and gastrointestinal adverse effects, most were mild and resolved when the therapy either ended or continued long term. The use of PrEP does not absolve high-risk individuals from observing safety in sex activity and intravenous drug use, the researchers noted.
The Task Force’s draft recommendation statements and draft evidence reviews are available for public comment and are posted on the Task Force website at www.uspreventiveservicestaskforce.org. Comments can be submitted from Nov. 20, 2018, to Dec. 26, 2018, at www.uspreventiveservicestaskforce.org/tfcomment.htm.
Individuals aged 15-65 years, including pregnant women, should be screened for HIV infection, and those at risk should be given prophylaxis, according to draft recommendations issued by the U.S. Preventive Services Task Force. The screening recommendation extends to younger adolescents and older adults at increased risk for HIV infection. The recommendations are level A.
HIV remains a significant public health issue in the United States, with rates rising among individuals aged 25-29 years, although the overall number of cases has dropped slightly, according to the USPSTF report.
HIV prevention is a multistep process that includes not only screening but also wearing condoms during sex and using clean needles and syringes if injecting drugs, the researchers noted.
However, those at high risk for HIV, such as intravenous drug users, can help reduce their risk by taking a daily pill, the researchers wrote.
In an evidence report submitted to the Agency for Healthcare Research and Quality, researchers reviewed the Cochrane databases, MEDLINE, and Embase for studies up to June 2018. Based on data from 11 trials, pre-exposure prophylaxis (PrEP) consisting of antiretroviral therapy was associated with decreased risk of HIV infection, compared with placebo or no PrEP, with consistent effects across risk categories, the investigators noted.
The most common HIV risk factors include man-to-man sexual contact, injection drug use, having sex without a condom, exchanging sex for drugs or money, and having sex with an HIV-infected partner, according to the USPSTF report.
Although PrEP was associated with renal and gastrointestinal adverse effects, most were mild and resolved when the therapy either ended or continued long term. The use of PrEP does not absolve high-risk individuals from observing safety in sex activity and intravenous drug use, the researchers noted.
The Task Force’s draft recommendation statements and draft evidence reviews are available for public comment and are posted on the Task Force website at www.uspreventiveservicestaskforce.org. Comments can be submitted from Nov. 20, 2018, to Dec. 26, 2018, at www.uspreventiveservicestaskforce.org/tfcomment.htm.
Individuals aged 15-65 years, including pregnant women, should be screened for HIV infection, and those at risk should be given prophylaxis, according to draft recommendations issued by the U.S. Preventive Services Task Force. The screening recommendation extends to younger adolescents and older adults at increased risk for HIV infection. The recommendations are level A.
HIV remains a significant public health issue in the United States, with rates rising among individuals aged 25-29 years, although the overall number of cases has dropped slightly, according to the USPSTF report.
HIV prevention is a multistep process that includes not only screening but also wearing condoms during sex and using clean needles and syringes if injecting drugs, the researchers noted.
However, those at high risk for HIV, such as intravenous drug users, can help reduce their risk by taking a daily pill, the researchers wrote.
In an evidence report submitted to the Agency for Healthcare Research and Quality, researchers reviewed the Cochrane databases, MEDLINE, and Embase for studies up to June 2018. Based on data from 11 trials, pre-exposure prophylaxis (PrEP) consisting of antiretroviral therapy was associated with decreased risk of HIV infection, compared with placebo or no PrEP, with consistent effects across risk categories, the investigators noted.
The most common HIV risk factors include man-to-man sexual contact, injection drug use, having sex without a condom, exchanging sex for drugs or money, and having sex with an HIV-infected partner, according to the USPSTF report.
Although PrEP was associated with renal and gastrointestinal adverse effects, most were mild and resolved when the therapy either ended or continued long term. The use of PrEP does not absolve high-risk individuals from observing safety in sex activity and intravenous drug use, the researchers noted.
The Task Force’s draft recommendation statements and draft evidence reviews are available for public comment and are posted on the Task Force website at www.uspreventiveservicestaskforce.org. Comments can be submitted from Nov. 20, 2018, to Dec. 26, 2018, at www.uspreventiveservicestaskforce.org/tfcomment.htm.
FDA approves rifamycin for treatment of traveler’s diarrhea
The Food and Drug Administration has approved rifamycin (Aemcolo) for the treatment of traveler’s diarrhea caused by noninvasive strains of Escherichia coli.
FDA approval was based on results of three clinical trials. The efficacy of rifamycin was shown in a trial of 264 adults with traveler’s diarrhea in Guatemala and Mexico. Compared with placebo, rifamycin significantly reduced symptoms of the condition. The safety of rifamycin was illustrated in a pair of studies including 619 adults with traveler’s diarrhea who took rifamycin orally for 3-4 days. The most common adverse events were headache and constipation.
Traveler’s diarrhea is the most common travel-related illness, affecting 10%-40% of travelers. It can be caused by a multitude of pathogens, but bacteria from food or water is the most common source. High-risk areas include much of Asia, the Middle East, Mexico, Central and South America, and Africa.
Rifamycin was not effective in patients with diarrhea complicated by fever and/or bloody stool or in diarrhea caused by a pathogen other than E. coli.
“Travelers’ diarrhea affects millions of people each year, and having treatment options for this condition can help reduce symptoms of the condition,” Edward Cox, MD, MPH, director of the Office of Antimicrobial Products in the FDA’s Center for Drug Evaluation and Research, said in the press release.
Find the full press release on the FDA website.
The Food and Drug Administration has approved rifamycin (Aemcolo) for the treatment of traveler’s diarrhea caused by noninvasive strains of Escherichia coli.
FDA approval was based on results of three clinical trials. The efficacy of rifamycin was shown in a trial of 264 adults with traveler’s diarrhea in Guatemala and Mexico. Compared with placebo, rifamycin significantly reduced symptoms of the condition. The safety of rifamycin was illustrated in a pair of studies including 619 adults with traveler’s diarrhea who took rifamycin orally for 3-4 days. The most common adverse events were headache and constipation.
Traveler’s diarrhea is the most common travel-related illness, affecting 10%-40% of travelers. It can be caused by a multitude of pathogens, but bacteria from food or water is the most common source. High-risk areas include much of Asia, the Middle East, Mexico, Central and South America, and Africa.
Rifamycin was not effective in patients with diarrhea complicated by fever and/or bloody stool or in diarrhea caused by a pathogen other than E. coli.
“Travelers’ diarrhea affects millions of people each year, and having treatment options for this condition can help reduce symptoms of the condition,” Edward Cox, MD, MPH, director of the Office of Antimicrobial Products in the FDA’s Center for Drug Evaluation and Research, said in the press release.
Find the full press release on the FDA website.
The Food and Drug Administration has approved rifamycin (Aemcolo) for the treatment of traveler’s diarrhea caused by noninvasive strains of Escherichia coli.
FDA approval was based on results of three clinical trials. The efficacy of rifamycin was shown in a trial of 264 adults with traveler’s diarrhea in Guatemala and Mexico. Compared with placebo, rifamycin significantly reduced symptoms of the condition. The safety of rifamycin was illustrated in a pair of studies including 619 adults with traveler’s diarrhea who took rifamycin orally for 3-4 days. The most common adverse events were headache and constipation.
Traveler’s diarrhea is the most common travel-related illness, affecting 10%-40% of travelers. It can be caused by a multitude of pathogens, but bacteria from food or water is the most common source. High-risk areas include much of Asia, the Middle East, Mexico, Central and South America, and Africa.
Rifamycin was not effective in patients with diarrhea complicated by fever and/or bloody stool or in diarrhea caused by a pathogen other than E. coli.
“Travelers’ diarrhea affects millions of people each year, and having treatment options for this condition can help reduce symptoms of the condition,” Edward Cox, MD, MPH, director of the Office of Antimicrobial Products in the FDA’s Center for Drug Evaluation and Research, said in the press release.
Find the full press release on the FDA website.