User login
AI algorithm on par with radiologists as mammogram reader
The algorithm – from the company Lunit, which was not involved in the study – had an area under the curve of 0.956 for detection of pathologically confirmed breast cancer.
When operating at a specificity of 96.6%, the sensitivity was 81.9% for the algorithm, 77.4% for first-reader radiologists, and 80.1% for second-reader radiologists. Combining the algorithm with first-reader radiologists identified more cases than combining first- and second-reader radiologists.
These findings were published in JAMA Oncology.
The study’s authors wrote that the algorithm results are a “considerable” achievement because, unlike the radiologists, the algorithm had no access to prior mammograms or information about hormonal medications or breast symptoms.
“We believe that the time has come to evaluate AI CAD [computer-aided detection] algorithms as independent readers in prospective clinical studies,” Mattie Salim, MD, of Karolinska Institute/Karolinska University Hospital in Stockholm, and colleagues wrote.
“The authors are to be commended for providing data that support this next critical phase of discovery,” Constance Dobbins Lehman, MD, PhD, of Massachusetts General Hospital and Harvard Medical School, both in Boston, wrote in a related editorial. She added that “it is time to move beyond simulation and reader studies and enter the critical phase of rigorous, prospective clinical evaluation.”
Study rationale and details
Routine mammograms save lives, but the workload for radiologists is high, and the quality of assessments varies widely, Dr. Salim and colleagues wrote. There are also problems with access in areas with few radiologists.
To address these issues, academic and commercial researchers have worked hard to apply AI – specifically, deep neural networks – to computer programs that read mammograms.
For this study, the investigators conducted the first third-party external validation of three competing algorithms. The three algorithms were not named in the report, but Lunit announced that its algorithm was the best-performing algorithm after the study was published. The other two algorithms did not perform as well and remain anonymous.
The investigators compared the algorithms’ assessments with the original radiology reports for 739 women who were diagnosed with breast cancer within 12 months of their mammogram and 8,066 women with negative mammograms who remained cancer free at a 2-year follow-up.
The women, aged 40-74 years, had conventional two-dimensional imaging read by two radiologists at the Karolinska University Hospital during 2008-2015. The subjects’ median age at screening was 54.5 years.
The algorithms gave a prediction score between 0 and 1 for each breast, with 1 denoting the highest level of cancer suspicion. To enable a comparison with the binary decisions of the radiologists, the output of each algorithm was dichotomized (normal or abnormal) at a cut point defined by the mean specificity of the first-reader radiologists, 96.6%.
At a specificity of 96.6%, the sensitivity was 81.9% for the Lunit algorithm, 67.0% for one anonymous algorithm (AI-2), 67.4% for the other anonymous algorithm (AI-3), 77.4% for first-reader radiologists, and 80.1% for second-reader radiologists
The investigators also ran their analysis at a cut point of 88.9% specificity. The sensitivity was 88.6% for the Lunit algorithm, 80.0% for AI-2, and 80.2% for AI-3.
“This can be compared with the Breast Cancer Surveillance Consortium benchmarks of 86.9% sensitivity at 88.9% specificity,” the authors wrote.
The most potent screening strategy was combining the Lunit algorithm with the first reader, which increased cancer detection by 8% but came at the cost of a 77% increase in abnormal assessments.
“More true-positive cases would likely be found, but a much larger proportion of false-positive examinations would have to be handled in the ensuing consensus discussion,” the authors wrote. “[A] cost-benefit analysis is required ... to determine the economic implications of adding a human reader at all.”
The team noted that the Lunit algorithm was trained on images of South Korean women from GE equipment.
“Although we do not have ethnic descriptors of our study population, the vast majority of women in Stockholm are White, and all images in our study were acquired on Hologic equipment,” the authors wrote. “In training AI algorithms for mammographic cancer detection, matching ethnic and equipment distributions between the training population and the clinical test population may not be of highest importance.”
As for why the Lunit algorithm outperformed the other two algorithms, one explanation may be that the Lunit algorithm was trained on more mammograms – 72,000 cancer and 680,000 normal images (vs. 10,000 cancer and 229,000 normal images for AI-2; 6,000 cancer and 106,000 normal images for AI-3).
As for next steps, the investigators are planning a prospective clinical study to see how AI works as an independent reviewer of mammograms in a day-to-day clinical environment, both as a third reviewer and to help select women for follow-up MRI.
The current study was funded by the Stockholm County Council. The investigators disclosed financial relationships with the Swedish Research Council, the Swedish Cancer Society, Stockholm City Council, Collective Minds Radiology, and Pfizer. Dr Lehman’s institution receives grants from GE Healthcare.
SOURCE: Salim M et al. JAMA Oncol. 2020 Aug 27. doi: 10.1001/jamaoncol.2020.3321.
The algorithm – from the company Lunit, which was not involved in the study – had an area under the curve of 0.956 for detection of pathologically confirmed breast cancer.
When operating at a specificity of 96.6%, the sensitivity was 81.9% for the algorithm, 77.4% for first-reader radiologists, and 80.1% for second-reader radiologists. Combining the algorithm with first-reader radiologists identified more cases than combining first- and second-reader radiologists.
These findings were published in JAMA Oncology.
The study’s authors wrote that the algorithm results are a “considerable” achievement because, unlike the radiologists, the algorithm had no access to prior mammograms or information about hormonal medications or breast symptoms.
“We believe that the time has come to evaluate AI CAD [computer-aided detection] algorithms as independent readers in prospective clinical studies,” Mattie Salim, MD, of Karolinska Institute/Karolinska University Hospital in Stockholm, and colleagues wrote.
“The authors are to be commended for providing data that support this next critical phase of discovery,” Constance Dobbins Lehman, MD, PhD, of Massachusetts General Hospital and Harvard Medical School, both in Boston, wrote in a related editorial. She added that “it is time to move beyond simulation and reader studies and enter the critical phase of rigorous, prospective clinical evaluation.”
Study rationale and details
Routine mammograms save lives, but the workload for radiologists is high, and the quality of assessments varies widely, Dr. Salim and colleagues wrote. There are also problems with access in areas with few radiologists.
To address these issues, academic and commercial researchers have worked hard to apply AI – specifically, deep neural networks – to computer programs that read mammograms.
For this study, the investigators conducted the first third-party external validation of three competing algorithms. The three algorithms were not named in the report, but Lunit announced that its algorithm was the best-performing algorithm after the study was published. The other two algorithms did not perform as well and remain anonymous.
The investigators compared the algorithms’ assessments with the original radiology reports for 739 women who were diagnosed with breast cancer within 12 months of their mammogram and 8,066 women with negative mammograms who remained cancer free at a 2-year follow-up.
The women, aged 40-74 years, had conventional two-dimensional imaging read by two radiologists at the Karolinska University Hospital during 2008-2015. The subjects’ median age at screening was 54.5 years.
The algorithms gave a prediction score between 0 and 1 for each breast, with 1 denoting the highest level of cancer suspicion. To enable a comparison with the binary decisions of the radiologists, the output of each algorithm was dichotomized (normal or abnormal) at a cut point defined by the mean specificity of the first-reader radiologists, 96.6%.
At a specificity of 96.6%, the sensitivity was 81.9% for the Lunit algorithm, 67.0% for one anonymous algorithm (AI-2), 67.4% for the other anonymous algorithm (AI-3), 77.4% for first-reader radiologists, and 80.1% for second-reader radiologists
The investigators also ran their analysis at a cut point of 88.9% specificity. The sensitivity was 88.6% for the Lunit algorithm, 80.0% for AI-2, and 80.2% for AI-3.
“This can be compared with the Breast Cancer Surveillance Consortium benchmarks of 86.9% sensitivity at 88.9% specificity,” the authors wrote.
The most potent screening strategy was combining the Lunit algorithm with the first reader, which increased cancer detection by 8% but came at the cost of a 77% increase in abnormal assessments.
“More true-positive cases would likely be found, but a much larger proportion of false-positive examinations would have to be handled in the ensuing consensus discussion,” the authors wrote. “[A] cost-benefit analysis is required ... to determine the economic implications of adding a human reader at all.”
The team noted that the Lunit algorithm was trained on images of South Korean women from GE equipment.
“Although we do not have ethnic descriptors of our study population, the vast majority of women in Stockholm are White, and all images in our study were acquired on Hologic equipment,” the authors wrote. “In training AI algorithms for mammographic cancer detection, matching ethnic and equipment distributions between the training population and the clinical test population may not be of highest importance.”
As for why the Lunit algorithm outperformed the other two algorithms, one explanation may be that the Lunit algorithm was trained on more mammograms – 72,000 cancer and 680,000 normal images (vs. 10,000 cancer and 229,000 normal images for AI-2; 6,000 cancer and 106,000 normal images for AI-3).
As for next steps, the investigators are planning a prospective clinical study to see how AI works as an independent reviewer of mammograms in a day-to-day clinical environment, both as a third reviewer and to help select women for follow-up MRI.
The current study was funded by the Stockholm County Council. The investigators disclosed financial relationships with the Swedish Research Council, the Swedish Cancer Society, Stockholm City Council, Collective Minds Radiology, and Pfizer. Dr Lehman’s institution receives grants from GE Healthcare.
SOURCE: Salim M et al. JAMA Oncol. 2020 Aug 27. doi: 10.1001/jamaoncol.2020.3321.
The algorithm – from the company Lunit, which was not involved in the study – had an area under the curve of 0.956 for detection of pathologically confirmed breast cancer.
When operating at a specificity of 96.6%, the sensitivity was 81.9% for the algorithm, 77.4% for first-reader radiologists, and 80.1% for second-reader radiologists. Combining the algorithm with first-reader radiologists identified more cases than combining first- and second-reader radiologists.
These findings were published in JAMA Oncology.
The study’s authors wrote that the algorithm results are a “considerable” achievement because, unlike the radiologists, the algorithm had no access to prior mammograms or information about hormonal medications or breast symptoms.
“We believe that the time has come to evaluate AI CAD [computer-aided detection] algorithms as independent readers in prospective clinical studies,” Mattie Salim, MD, of Karolinska Institute/Karolinska University Hospital in Stockholm, and colleagues wrote.
“The authors are to be commended for providing data that support this next critical phase of discovery,” Constance Dobbins Lehman, MD, PhD, of Massachusetts General Hospital and Harvard Medical School, both in Boston, wrote in a related editorial. She added that “it is time to move beyond simulation and reader studies and enter the critical phase of rigorous, prospective clinical evaluation.”
Study rationale and details
Routine mammograms save lives, but the workload for radiologists is high, and the quality of assessments varies widely, Dr. Salim and colleagues wrote. There are also problems with access in areas with few radiologists.
To address these issues, academic and commercial researchers have worked hard to apply AI – specifically, deep neural networks – to computer programs that read mammograms.
For this study, the investigators conducted the first third-party external validation of three competing algorithms. The three algorithms were not named in the report, but Lunit announced that its algorithm was the best-performing algorithm after the study was published. The other two algorithms did not perform as well and remain anonymous.
The investigators compared the algorithms’ assessments with the original radiology reports for 739 women who were diagnosed with breast cancer within 12 months of their mammogram and 8,066 women with negative mammograms who remained cancer free at a 2-year follow-up.
The women, aged 40-74 years, had conventional two-dimensional imaging read by two radiologists at the Karolinska University Hospital during 2008-2015. The subjects’ median age at screening was 54.5 years.
The algorithms gave a prediction score between 0 and 1 for each breast, with 1 denoting the highest level of cancer suspicion. To enable a comparison with the binary decisions of the radiologists, the output of each algorithm was dichotomized (normal or abnormal) at a cut point defined by the mean specificity of the first-reader radiologists, 96.6%.
At a specificity of 96.6%, the sensitivity was 81.9% for the Lunit algorithm, 67.0% for one anonymous algorithm (AI-2), 67.4% for the other anonymous algorithm (AI-3), 77.4% for first-reader radiologists, and 80.1% for second-reader radiologists
The investigators also ran their analysis at a cut point of 88.9% specificity. The sensitivity was 88.6% for the Lunit algorithm, 80.0% for AI-2, and 80.2% for AI-3.
“This can be compared with the Breast Cancer Surveillance Consortium benchmarks of 86.9% sensitivity at 88.9% specificity,” the authors wrote.
The most potent screening strategy was combining the Lunit algorithm with the first reader, which increased cancer detection by 8% but came at the cost of a 77% increase in abnormal assessments.
“More true-positive cases would likely be found, but a much larger proportion of false-positive examinations would have to be handled in the ensuing consensus discussion,” the authors wrote. “[A] cost-benefit analysis is required ... to determine the economic implications of adding a human reader at all.”
The team noted that the Lunit algorithm was trained on images of South Korean women from GE equipment.
“Although we do not have ethnic descriptors of our study population, the vast majority of women in Stockholm are White, and all images in our study were acquired on Hologic equipment,” the authors wrote. “In training AI algorithms for mammographic cancer detection, matching ethnic and equipment distributions between the training population and the clinical test population may not be of highest importance.”
As for why the Lunit algorithm outperformed the other two algorithms, one explanation may be that the Lunit algorithm was trained on more mammograms – 72,000 cancer and 680,000 normal images (vs. 10,000 cancer and 229,000 normal images for AI-2; 6,000 cancer and 106,000 normal images for AI-3).
As for next steps, the investigators are planning a prospective clinical study to see how AI works as an independent reviewer of mammograms in a day-to-day clinical environment, both as a third reviewer and to help select women for follow-up MRI.
The current study was funded by the Stockholm County Council. The investigators disclosed financial relationships with the Swedish Research Council, the Swedish Cancer Society, Stockholm City Council, Collective Minds Radiology, and Pfizer. Dr Lehman’s institution receives grants from GE Healthcare.
SOURCE: Salim M et al. JAMA Oncol. 2020 Aug 27. doi: 10.1001/jamaoncol.2020.3321.
FROM JAMA ONCOLOGY
Reassuring findings on SSRIs and diabetes risk in children
SSRIs are associated with a much lower risk of type 2 diabetes (T2D) in children and adolescents than previously reported, new research shows.
Investigators found publicly insured patients treated with SSRIs had a 13% increased risk for T2D, compared with those not treated with these agents. In addition, those taking SSRIs continuously (defined as receiving one or more prescriptions every 3 months) had a 33% increased risk of T2D.
On the other hand, privately insured youth had a much lower increased risk – a finding that may be attributable to a lower prevalence of risk factors for T2D in this group.
“We cannot exclude that children and adolescents treated with SSRIs may be at a small increased risk of developing T2D, particularly publicly insured patients, but the magnitude of association was weaker than previous thought and much smaller than other known risk factors for T2DM, such as obesity, race, and poverty,” lead investigator Jenny Sun, PhD, said in an interview.
“When weighing the known benefits and risks of SSRI treatment in children and adolescents, our findings provide reassurance that the risk of T2DM is not as substantial as initially reported,” said Dr. Sun, a postdoctoral research fellow in the department of population medicine at Harvard Medical School’s Harvard Pilgrim Health Care Institute, Boston.
The study was published online Sept. 2 in JAMA Psychiatry.
Limited evidence
Previous research suggested that SSRIs increase the risk of T2D by up to 90% in children and adolescents.
However, the investigators noted, the study reporting this finding was too small to draw conclusions about the SSRI class as a whole also did not examine specific SSRIs.
In addition, although “several studies have reported that antidepressant use may be a risk factor for T2D in adults, evidence was limited in children and adolescents,” said Dr. Sun.
“Rapid changes in growth during childhood and adolescents can alter drugs’ pharmacokinetics and pharmacodynamics, so high-quality, age-specific data are needed to inform prescribing decisions,” she said.
For the current study, the researchers analyzed claims data on almost 1.6 million patients aged 10-19 years (58.3% female; mean age, 15.1 years) from two large claims databases.
The analysis focused on those with a diagnosis warranting treatment with an SSRI, including depression, generalized or social anxiety disorder, obsessive compulsive disorder, PTSD, panic disorder, or bulimia nervosa.
The Medicaid Analytic Extract database consisted of 316,178 patients insured through Medicaid or the Children’s Health Insurance Program. The IBM MarketScan database consisted of 211,460 privately insured patients. Patients were followed up for a mean of 2.3 and 2.2 years, respectively.
Patients who initiated SSRI treatment were compared with those with a similar indication but who were not taking an SSRI. Secondary analyses compared new SSRI users with patients who recently initiated treatment with bupropion, which has no metabolic side effects, or with patients who recently initiated psychotherapy.
“In observational data, it is difficult to mimic a placebo group, often used in RCTs [randomized, controlled trials], therefore several comparator groups were explored to broaden our understanding,” said Dr. Sun.
In addition, the researchers compared the individual SSRI medications, using fluoxetine as a comparator.
A wide range of more than 100 potential confounders or “proxies of confounders,” were taken into account, including demographic characteristics, psychiatric diagnoses, metabolic conditions, concomitant medications, and use of health care services.
The researchers conducted two analyses. They included an intention-to-treat (ITT) analysis that was restricted to patients with one or more additional SSRI prescriptions during the 6 months following the index exposure assessment period.
Close monitoring required
An as-treated analysis estimated the association of continuous SSRI treatment (vs. untreated, bupropion treatment, and psychotherapy), with adherence assessed at 3-month intervals.
Initiation and continuation of SSRI treatment in publicly insured patients were both associated with a considerably higher risk of T2D, compared with untreated patients, and a steeper risk, compared with their privately insured counterparts.
For newly treated publicly insured patients initiated on SSRI treatment, the ITT adjusted hazard ratio was 1.13 (95% confidence interval, 1.04-1.22).
There was an even stronger association among continuously treated publicly insured patients, with an as-treated aHR of 1.33 (95% CI, 1.21-1.47). The authors noted that this corresponds to 6.6 additional T2D cases per 10,000 patients continuously treated for at least 2 years.
The association was weaker in privately insured patients (ITT aHR, 1.01; 95% CI, 0.84-1.23; as-treated aHR, 1.10; 95% CI, 0.88-1.36).
The secondary analyses yielded similar findings: When SSRI treatment was compared with psychotherapy, the as-treated aHR for publicly insured patients was 1.44 (95% CI, 1.25-1.65), whereas the aHR for privately insured patients was lower at 1.21 (95% CI, 0.93-1.57)
The investigators found no increased risk when SSRIs were compared with bupropion, and the within-class analysis showed that none of the SSRIs carried an increased hazard of T2D, compared with fluoxetine.
“Publicly insured patients are enrolled in Medicaid and the Children’s Health Insurance Program, whereas privately insured patients are generally covered by their parent’s employer-sponsored insurance,” said Dr. Sun.
“Publicly insured patients are of lower socioeconomic status and represent a population with greater overall medical burden, more comorbidities, and a higher prevalence of risk factors for T2D, such as obesity, at the time of treatment initiation,” she said.
She added that high-risk children and youth should be closely monitored and clinicians should also consider recommending dietary modifications and increased exercise to offset T2D risk.
Useful ‘real-world data’
William Cooper, MD, MPH, professor of pediatrics and health policy at Vanderbilt University Medical Center in Nashville, Tenn., said that the study “provides a fascinating look at risks of SSRI medications in children and adolescents.”
Dr. Cooper, who was not involved with the study, said that the authors “draw from real-world data representing two different populations and carefully consider factors which might confound the associations.”
The results, he said, “provide important benefits for patients, families, and clinicians as they weigh the risks and benefits of using SSRIs for children who need treatment for depression and anxiety disorders.
The study was supported by a training grant from the program in pharmacoepidemiology at the Harvard School of Public Health. Dr. Sun disclosed no relevant financial relationships. Dr. Cooper disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
SSRIs are associated with a much lower risk of type 2 diabetes (T2D) in children and adolescents than previously reported, new research shows.
Investigators found publicly insured patients treated with SSRIs had a 13% increased risk for T2D, compared with those not treated with these agents. In addition, those taking SSRIs continuously (defined as receiving one or more prescriptions every 3 months) had a 33% increased risk of T2D.
On the other hand, privately insured youth had a much lower increased risk – a finding that may be attributable to a lower prevalence of risk factors for T2D in this group.
“We cannot exclude that children and adolescents treated with SSRIs may be at a small increased risk of developing T2D, particularly publicly insured patients, but the magnitude of association was weaker than previous thought and much smaller than other known risk factors for T2DM, such as obesity, race, and poverty,” lead investigator Jenny Sun, PhD, said in an interview.
“When weighing the known benefits and risks of SSRI treatment in children and adolescents, our findings provide reassurance that the risk of T2DM is not as substantial as initially reported,” said Dr. Sun, a postdoctoral research fellow in the department of population medicine at Harvard Medical School’s Harvard Pilgrim Health Care Institute, Boston.
The study was published online Sept. 2 in JAMA Psychiatry.
Limited evidence
Previous research suggested that SSRIs increase the risk of T2D by up to 90% in children and adolescents.
However, the investigators noted, the study reporting this finding was too small to draw conclusions about the SSRI class as a whole also did not examine specific SSRIs.
In addition, although “several studies have reported that antidepressant use may be a risk factor for T2D in adults, evidence was limited in children and adolescents,” said Dr. Sun.
“Rapid changes in growth during childhood and adolescents can alter drugs’ pharmacokinetics and pharmacodynamics, so high-quality, age-specific data are needed to inform prescribing decisions,” she said.
For the current study, the researchers analyzed claims data on almost 1.6 million patients aged 10-19 years (58.3% female; mean age, 15.1 years) from two large claims databases.
The analysis focused on those with a diagnosis warranting treatment with an SSRI, including depression, generalized or social anxiety disorder, obsessive compulsive disorder, PTSD, panic disorder, or bulimia nervosa.
The Medicaid Analytic Extract database consisted of 316,178 patients insured through Medicaid or the Children’s Health Insurance Program. The IBM MarketScan database consisted of 211,460 privately insured patients. Patients were followed up for a mean of 2.3 and 2.2 years, respectively.
Patients who initiated SSRI treatment were compared with those with a similar indication but who were not taking an SSRI. Secondary analyses compared new SSRI users with patients who recently initiated treatment with bupropion, which has no metabolic side effects, or with patients who recently initiated psychotherapy.
“In observational data, it is difficult to mimic a placebo group, often used in RCTs [randomized, controlled trials], therefore several comparator groups were explored to broaden our understanding,” said Dr. Sun.
In addition, the researchers compared the individual SSRI medications, using fluoxetine as a comparator.
A wide range of more than 100 potential confounders or “proxies of confounders,” were taken into account, including demographic characteristics, psychiatric diagnoses, metabolic conditions, concomitant medications, and use of health care services.
The researchers conducted two analyses. They included an intention-to-treat (ITT) analysis that was restricted to patients with one or more additional SSRI prescriptions during the 6 months following the index exposure assessment period.
Close monitoring required
An as-treated analysis estimated the association of continuous SSRI treatment (vs. untreated, bupropion treatment, and psychotherapy), with adherence assessed at 3-month intervals.
Initiation and continuation of SSRI treatment in publicly insured patients were both associated with a considerably higher risk of T2D, compared with untreated patients, and a steeper risk, compared with their privately insured counterparts.
For newly treated publicly insured patients initiated on SSRI treatment, the ITT adjusted hazard ratio was 1.13 (95% confidence interval, 1.04-1.22).
There was an even stronger association among continuously treated publicly insured patients, with an as-treated aHR of 1.33 (95% CI, 1.21-1.47). The authors noted that this corresponds to 6.6 additional T2D cases per 10,000 patients continuously treated for at least 2 years.
The association was weaker in privately insured patients (ITT aHR, 1.01; 95% CI, 0.84-1.23; as-treated aHR, 1.10; 95% CI, 0.88-1.36).
The secondary analyses yielded similar findings: When SSRI treatment was compared with psychotherapy, the as-treated aHR for publicly insured patients was 1.44 (95% CI, 1.25-1.65), whereas the aHR for privately insured patients was lower at 1.21 (95% CI, 0.93-1.57)
The investigators found no increased risk when SSRIs were compared with bupropion, and the within-class analysis showed that none of the SSRIs carried an increased hazard of T2D, compared with fluoxetine.
“Publicly insured patients are enrolled in Medicaid and the Children’s Health Insurance Program, whereas privately insured patients are generally covered by their parent’s employer-sponsored insurance,” said Dr. Sun.
“Publicly insured patients are of lower socioeconomic status and represent a population with greater overall medical burden, more comorbidities, and a higher prevalence of risk factors for T2D, such as obesity, at the time of treatment initiation,” she said.
She added that high-risk children and youth should be closely monitored and clinicians should also consider recommending dietary modifications and increased exercise to offset T2D risk.
Useful ‘real-world data’
William Cooper, MD, MPH, professor of pediatrics and health policy at Vanderbilt University Medical Center in Nashville, Tenn., said that the study “provides a fascinating look at risks of SSRI medications in children and adolescents.”
Dr. Cooper, who was not involved with the study, said that the authors “draw from real-world data representing two different populations and carefully consider factors which might confound the associations.”
The results, he said, “provide important benefits for patients, families, and clinicians as they weigh the risks and benefits of using SSRIs for children who need treatment for depression and anxiety disorders.
The study was supported by a training grant from the program in pharmacoepidemiology at the Harvard School of Public Health. Dr. Sun disclosed no relevant financial relationships. Dr. Cooper disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
SSRIs are associated with a much lower risk of type 2 diabetes (T2D) in children and adolescents than previously reported, new research shows.
Investigators found publicly insured patients treated with SSRIs had a 13% increased risk for T2D, compared with those not treated with these agents. In addition, those taking SSRIs continuously (defined as receiving one or more prescriptions every 3 months) had a 33% increased risk of T2D.
On the other hand, privately insured youth had a much lower increased risk – a finding that may be attributable to a lower prevalence of risk factors for T2D in this group.
“We cannot exclude that children and adolescents treated with SSRIs may be at a small increased risk of developing T2D, particularly publicly insured patients, but the magnitude of association was weaker than previous thought and much smaller than other known risk factors for T2DM, such as obesity, race, and poverty,” lead investigator Jenny Sun, PhD, said in an interview.
“When weighing the known benefits and risks of SSRI treatment in children and adolescents, our findings provide reassurance that the risk of T2DM is not as substantial as initially reported,” said Dr. Sun, a postdoctoral research fellow in the department of population medicine at Harvard Medical School’s Harvard Pilgrim Health Care Institute, Boston.
The study was published online Sept. 2 in JAMA Psychiatry.
Limited evidence
Previous research suggested that SSRIs increase the risk of T2D by up to 90% in children and adolescents.
However, the investigators noted, the study reporting this finding was too small to draw conclusions about the SSRI class as a whole also did not examine specific SSRIs.
In addition, although “several studies have reported that antidepressant use may be a risk factor for T2D in adults, evidence was limited in children and adolescents,” said Dr. Sun.
“Rapid changes in growth during childhood and adolescents can alter drugs’ pharmacokinetics and pharmacodynamics, so high-quality, age-specific data are needed to inform prescribing decisions,” she said.
For the current study, the researchers analyzed claims data on almost 1.6 million patients aged 10-19 years (58.3% female; mean age, 15.1 years) from two large claims databases.
The analysis focused on those with a diagnosis warranting treatment with an SSRI, including depression, generalized or social anxiety disorder, obsessive compulsive disorder, PTSD, panic disorder, or bulimia nervosa.
The Medicaid Analytic Extract database consisted of 316,178 patients insured through Medicaid or the Children’s Health Insurance Program. The IBM MarketScan database consisted of 211,460 privately insured patients. Patients were followed up for a mean of 2.3 and 2.2 years, respectively.
Patients who initiated SSRI treatment were compared with those with a similar indication but who were not taking an SSRI. Secondary analyses compared new SSRI users with patients who recently initiated treatment with bupropion, which has no metabolic side effects, or with patients who recently initiated psychotherapy.
“In observational data, it is difficult to mimic a placebo group, often used in RCTs [randomized, controlled trials], therefore several comparator groups were explored to broaden our understanding,” said Dr. Sun.
In addition, the researchers compared the individual SSRI medications, using fluoxetine as a comparator.
A wide range of more than 100 potential confounders or “proxies of confounders,” were taken into account, including demographic characteristics, psychiatric diagnoses, metabolic conditions, concomitant medications, and use of health care services.
The researchers conducted two analyses. They included an intention-to-treat (ITT) analysis that was restricted to patients with one or more additional SSRI prescriptions during the 6 months following the index exposure assessment period.
Close monitoring required
An as-treated analysis estimated the association of continuous SSRI treatment (vs. untreated, bupropion treatment, and psychotherapy), with adherence assessed at 3-month intervals.
Initiation and continuation of SSRI treatment in publicly insured patients were both associated with a considerably higher risk of T2D, compared with untreated patients, and a steeper risk, compared with their privately insured counterparts.
For newly treated publicly insured patients initiated on SSRI treatment, the ITT adjusted hazard ratio was 1.13 (95% confidence interval, 1.04-1.22).
There was an even stronger association among continuously treated publicly insured patients, with an as-treated aHR of 1.33 (95% CI, 1.21-1.47). The authors noted that this corresponds to 6.6 additional T2D cases per 10,000 patients continuously treated for at least 2 years.
The association was weaker in privately insured patients (ITT aHR, 1.01; 95% CI, 0.84-1.23; as-treated aHR, 1.10; 95% CI, 0.88-1.36).
The secondary analyses yielded similar findings: When SSRI treatment was compared with psychotherapy, the as-treated aHR for publicly insured patients was 1.44 (95% CI, 1.25-1.65), whereas the aHR for privately insured patients was lower at 1.21 (95% CI, 0.93-1.57)
The investigators found no increased risk when SSRIs were compared with bupropion, and the within-class analysis showed that none of the SSRIs carried an increased hazard of T2D, compared with fluoxetine.
“Publicly insured patients are enrolled in Medicaid and the Children’s Health Insurance Program, whereas privately insured patients are generally covered by their parent’s employer-sponsored insurance,” said Dr. Sun.
“Publicly insured patients are of lower socioeconomic status and represent a population with greater overall medical burden, more comorbidities, and a higher prevalence of risk factors for T2D, such as obesity, at the time of treatment initiation,” she said.
She added that high-risk children and youth should be closely monitored and clinicians should also consider recommending dietary modifications and increased exercise to offset T2D risk.
Useful ‘real-world data’
William Cooper, MD, MPH, professor of pediatrics and health policy at Vanderbilt University Medical Center in Nashville, Tenn., said that the study “provides a fascinating look at risks of SSRI medications in children and adolescents.”
Dr. Cooper, who was not involved with the study, said that the authors “draw from real-world data representing two different populations and carefully consider factors which might confound the associations.”
The results, he said, “provide important benefits for patients, families, and clinicians as they weigh the risks and benefits of using SSRIs for children who need treatment for depression and anxiety disorders.
The study was supported by a training grant from the program in pharmacoepidemiology at the Harvard School of Public Health. Dr. Sun disclosed no relevant financial relationships. Dr. Cooper disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The gut a new therapeutic target for major depression?
The gut microbiota differs significantly between patients with major depressive disorder (MDD) and healthy individuals and may be modifiable with a probiotic diet to improve stress and depression scores, two new studies suggest.
In one study, investigators compared stool samples between patients with MDD and healthy controls. They found significant differences in bacterial profiles between the two groups, as well as between patients who responded vs those who were resistant to treatment.
“This finding further supports the relevance of an altered composition of the gut microbiota in the etiopathogenesis of MDD and suggests a role in response to antidepressants,” coinvestigator Andrea Fontana, MSc, Fondazione IRCCS Casa Sollievo della Sofferenza, San Giovanni Rotondo, Italy, said in an interview.
Results from the second study showed significant improvements in self-reported stress, anxiety, and depression scores in healthy individuals following a “psychobiotic” diet (using probiotics or prebiotics to manipulate the microbiota to improve mental health) that was rich in fruit, vegetables, and fermented foods vs. those who received dietary advice alone.
The investigators, led by Kirsten Berding, PhD, APC Microbiome Ireland, University College Cork, Ireland, now plan on testing their psychobiotic diet in patients with MDD and hope the findings could be helpful in “the development of adjuvant therapeutic opportunities” where pharmacologic treatment is not effective.
Both studies were presented at the virtual congress of the European College of Neuropsychopharmacology, held online this year because of the COVID-19 pandemic.
A “hallmark” of major depression
Mr. Fontana and colleagues note that the mostly suboptimal response to pharmacologic treatments among patients with MDD is one of the factors that “contributes to the large socioeconomic burden” of the disease.
Previous research shows patients with MDD have gut dysbiosis, or an imbalance in the natural flora; that antidepressants have antimicrobial properties; and that probiotics have an antibiotic effect. However, the correlation between the composition of the gut microbiota and antidepressant response is poorly understood.
The investigators recruited 34 patients with MDD (aged 18-70 years) who were in a euthymic phase and who did not have comorbid conditions that could affect the gut microbiota.
Eight patients were treatment resistant, defined as a poor response to at least two adequate trials of different antidepressant classes, while 19 were treatment responsive and seven were treatment naive.
The researchers also recruited 20 healthy individuals via word of mouth to act as the control group. There were no significant differences between patients and the control group in terms of baseline characteristics.
Genomic sequencing of bacteria obtained from stool samples showed that it was possible to distinguish between patients with MDD and the healthy individuals, especially at the family, genus, and species levels.
In particular, there were significant differences in the Paenibacillaceae and Flavobacteriaceaea families, for the genus Fenollaria, and the species Flintibacter butyricus, Christensenella timonensis, and Eisenbergiella massiliensis, among others.
Results also showed that the phyla Proteobacteria, Tenericutes, and the family Peptostreptococcaceae were more common in patients with treatment-resistant MDD, whereas the phylum Actinobacteria was more abundant in treatment responders.
Moreover, several bacteria were found only in the microbiota of patients with treatment-resistant MDD, while others were seen only in treatment-responsive patients. This made it possible to discriminate not only between treatment-resistant and -responsive patients but also between those two patient groups and healthy controls.
“The results of our study confirm that gut dysbiosis is a hallmark of MDD, and suggests that the gut microbiota of patients with treatment-resistant MDD significantly differs from responders to antidepressants,” Mr. Fontana said.
Psychobiotic diet
For the second study, Dr. Berding and colleagues note that “psychobiotics” has previously achieved “promising results.”
In addition, diet is both “one of the most influential modifying factors” for the gut microbiota and an easily accessible strategy, they wrote. However, there is also a paucity of studies in this area, they added.
The researchers randomly assigned healthy volunteers with relatively poor dietary habits to either a 4-week psychobiotic diet group (n = 21) or a control group (n = 19).
Individuals in the psychobiotic group were told to eat a diet rich in prebiotics, such as fruit and vegetables, fiber including whole grains and legumes, and fermented foods. The control group was educated on Irish healthy-eating guidelines.
Stool and saliva samples were collected and the participants completed several self-reported mental health questionnaires, as well as a 7-day food diary. They also took the socially evaluated cold-pressor test (SECPT) to measure acute stress responses.
Results showed that total daily energy intake decreased significantly in both the diet and control groups over the study period (P = .04 for both) but did not differ significantly between the groups.
In contrast, dietary fiber intake increased significantly in the diet group (P < .001) and was significantly higher than in the control group at the end of the intervention (P = .03).
Individuals in the diet group showed significant decreases in scores on the Perceived Stress Scale (P = .002) and the Beck Depression Inventory (P = .007) during the study, an effect that was not found in the control group.
Dietary intervention
There were no significant effects of diet on the acute stress response, but both groups showed improvements in self-concept, or perceived ability to cope, on the Primary Appraisal, Secondary Appraisal index (P = .03 for the diet group, P = .04 for the control group).
The results show that a dietary intervention targeted at the microbiota “can improve subjective feelings of stress and depression in a healthy population,” the investigators wrote.
However, elucidating the “contribution of the microbiota-gut-brain axis on the signaling response to dietary interventions” will require further studies on microbiota sequencing and biological measures of stress, they added.
This will “contribute to the understanding of the benefits of a psychobiotic diet on stress and anxiety,” wrote the researchers.
Dr. Berding said in an interview that while the consumption of dietary fiber changed the most in the diet group, “it would not be the only nutrient” that had an impact on the results, with fermented foods a likely candidate.
She said the next step is to test the dietary intervention in patients with MDD; however, “doing nutritional interventions in diseased populations is always difficult.”
Dr. Berding suggested that the best approach would be to study inpatients in a clinic, as “we would be able to provide every meal and only provide foods that are part of the dietary intervention.”
Although another option would be to conduct the study in outpatients, she noted that assessing inpatients “would give us the best control over compliance.”
“Brilliant ideas”
Commenting on the findings, Sergueï Fetissov, MD, PhD, professor of physiology at Rouen University, Mont-Saint-Aignan, France, said that although both studies bring attention to a possible role for the gut microbiota in MDD, neither “provide any experimental evidence of a causative nature.”
Dr. Fetissov, who was not involved in either study, noted that this topic has been the subject of clinical nutritional research for many years.
However, “we still need some strong evidence to prove that some bacteria can influence the regulation of mood and anxiety and stress,” he said.
In addition, researchers currently do not know what actually causes MDD. “How we can say the gut bacteria regulates something if we don’t know what really causes the altered mood?” said Dr. Fetissov.
He noted that over the last 50 years, there have been great advances in the development of drugs that alleviate depression and anxiety by regulating dopamine, serotonin, and other neurotransmitters. However, it is still unknown whether these reflect primary or secondary aspects of mood disorders.
Furthermore, it is not clear “how probiotics to bacteria can influence these neuronal pathways,” he said.
The research by Dr. Berding and colleagues is funded by a postdoctoral fellowship grant from the Irish Research Council. The study authors and Dr. Fetissov have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The gut microbiota differs significantly between patients with major depressive disorder (MDD) and healthy individuals and may be modifiable with a probiotic diet to improve stress and depression scores, two new studies suggest.
In one study, investigators compared stool samples between patients with MDD and healthy controls. They found significant differences in bacterial profiles between the two groups, as well as between patients who responded vs those who were resistant to treatment.
“This finding further supports the relevance of an altered composition of the gut microbiota in the etiopathogenesis of MDD and suggests a role in response to antidepressants,” coinvestigator Andrea Fontana, MSc, Fondazione IRCCS Casa Sollievo della Sofferenza, San Giovanni Rotondo, Italy, said in an interview.
Results from the second study showed significant improvements in self-reported stress, anxiety, and depression scores in healthy individuals following a “psychobiotic” diet (using probiotics or prebiotics to manipulate the microbiota to improve mental health) that was rich in fruit, vegetables, and fermented foods vs. those who received dietary advice alone.
The investigators, led by Kirsten Berding, PhD, APC Microbiome Ireland, University College Cork, Ireland, now plan on testing their psychobiotic diet in patients with MDD and hope the findings could be helpful in “the development of adjuvant therapeutic opportunities” where pharmacologic treatment is not effective.
Both studies were presented at the virtual congress of the European College of Neuropsychopharmacology, held online this year because of the COVID-19 pandemic.
A “hallmark” of major depression
Mr. Fontana and colleagues note that the mostly suboptimal response to pharmacologic treatments among patients with MDD is one of the factors that “contributes to the large socioeconomic burden” of the disease.
Previous research shows patients with MDD have gut dysbiosis, or an imbalance in the natural flora; that antidepressants have antimicrobial properties; and that probiotics have an antibiotic effect. However, the correlation between the composition of the gut microbiota and antidepressant response is poorly understood.
The investigators recruited 34 patients with MDD (aged 18-70 years) who were in a euthymic phase and who did not have comorbid conditions that could affect the gut microbiota.
Eight patients were treatment resistant, defined as a poor response to at least two adequate trials of different antidepressant classes, while 19 were treatment responsive and seven were treatment naive.
The researchers also recruited 20 healthy individuals via word of mouth to act as the control group. There were no significant differences between patients and the control group in terms of baseline characteristics.
Genomic sequencing of bacteria obtained from stool samples showed that it was possible to distinguish between patients with MDD and the healthy individuals, especially at the family, genus, and species levels.
In particular, there were significant differences in the Paenibacillaceae and Flavobacteriaceaea families, for the genus Fenollaria, and the species Flintibacter butyricus, Christensenella timonensis, and Eisenbergiella massiliensis, among others.
Results also showed that the phyla Proteobacteria, Tenericutes, and the family Peptostreptococcaceae were more common in patients with treatment-resistant MDD, whereas the phylum Actinobacteria was more abundant in treatment responders.
Moreover, several bacteria were found only in the microbiota of patients with treatment-resistant MDD, while others were seen only in treatment-responsive patients. This made it possible to discriminate not only between treatment-resistant and -responsive patients but also between those two patient groups and healthy controls.
“The results of our study confirm that gut dysbiosis is a hallmark of MDD, and suggests that the gut microbiota of patients with treatment-resistant MDD significantly differs from responders to antidepressants,” Mr. Fontana said.
Psychobiotic diet
For the second study, Dr. Berding and colleagues note that “psychobiotics” has previously achieved “promising results.”
In addition, diet is both “one of the most influential modifying factors” for the gut microbiota and an easily accessible strategy, they wrote. However, there is also a paucity of studies in this area, they added.
The researchers randomly assigned healthy volunteers with relatively poor dietary habits to either a 4-week psychobiotic diet group (n = 21) or a control group (n = 19).
Individuals in the psychobiotic group were told to eat a diet rich in prebiotics, such as fruit and vegetables, fiber including whole grains and legumes, and fermented foods. The control group was educated on Irish healthy-eating guidelines.
Stool and saliva samples were collected and the participants completed several self-reported mental health questionnaires, as well as a 7-day food diary. They also took the socially evaluated cold-pressor test (SECPT) to measure acute stress responses.
Results showed that total daily energy intake decreased significantly in both the diet and control groups over the study period (P = .04 for both) but did not differ significantly between the groups.
In contrast, dietary fiber intake increased significantly in the diet group (P < .001) and was significantly higher than in the control group at the end of the intervention (P = .03).
Individuals in the diet group showed significant decreases in scores on the Perceived Stress Scale (P = .002) and the Beck Depression Inventory (P = .007) during the study, an effect that was not found in the control group.
Dietary intervention
There were no significant effects of diet on the acute stress response, but both groups showed improvements in self-concept, or perceived ability to cope, on the Primary Appraisal, Secondary Appraisal index (P = .03 for the diet group, P = .04 for the control group).
The results show that a dietary intervention targeted at the microbiota “can improve subjective feelings of stress and depression in a healthy population,” the investigators wrote.
However, elucidating the “contribution of the microbiota-gut-brain axis on the signaling response to dietary interventions” will require further studies on microbiota sequencing and biological measures of stress, they added.
This will “contribute to the understanding of the benefits of a psychobiotic diet on stress and anxiety,” wrote the researchers.
Dr. Berding said in an interview that while the consumption of dietary fiber changed the most in the diet group, “it would not be the only nutrient” that had an impact on the results, with fermented foods a likely candidate.
She said the next step is to test the dietary intervention in patients with MDD; however, “doing nutritional interventions in diseased populations is always difficult.”
Dr. Berding suggested that the best approach would be to study inpatients in a clinic, as “we would be able to provide every meal and only provide foods that are part of the dietary intervention.”
Although another option would be to conduct the study in outpatients, she noted that assessing inpatients “would give us the best control over compliance.”
“Brilliant ideas”
Commenting on the findings, Sergueï Fetissov, MD, PhD, professor of physiology at Rouen University, Mont-Saint-Aignan, France, said that although both studies bring attention to a possible role for the gut microbiota in MDD, neither “provide any experimental evidence of a causative nature.”
Dr. Fetissov, who was not involved in either study, noted that this topic has been the subject of clinical nutritional research for many years.
However, “we still need some strong evidence to prove that some bacteria can influence the regulation of mood and anxiety and stress,” he said.
In addition, researchers currently do not know what actually causes MDD. “How we can say the gut bacteria regulates something if we don’t know what really causes the altered mood?” said Dr. Fetissov.
He noted that over the last 50 years, there have been great advances in the development of drugs that alleviate depression and anxiety by regulating dopamine, serotonin, and other neurotransmitters. However, it is still unknown whether these reflect primary or secondary aspects of mood disorders.
Furthermore, it is not clear “how probiotics to bacteria can influence these neuronal pathways,” he said.
The research by Dr. Berding and colleagues is funded by a postdoctoral fellowship grant from the Irish Research Council. The study authors and Dr. Fetissov have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
The gut microbiota differs significantly between patients with major depressive disorder (MDD) and healthy individuals and may be modifiable with a probiotic diet to improve stress and depression scores, two new studies suggest.
In one study, investigators compared stool samples between patients with MDD and healthy controls. They found significant differences in bacterial profiles between the two groups, as well as between patients who responded vs those who were resistant to treatment.
“This finding further supports the relevance of an altered composition of the gut microbiota in the etiopathogenesis of MDD and suggests a role in response to antidepressants,” coinvestigator Andrea Fontana, MSc, Fondazione IRCCS Casa Sollievo della Sofferenza, San Giovanni Rotondo, Italy, said in an interview.
Results from the second study showed significant improvements in self-reported stress, anxiety, and depression scores in healthy individuals following a “psychobiotic” diet (using probiotics or prebiotics to manipulate the microbiota to improve mental health) that was rich in fruit, vegetables, and fermented foods vs. those who received dietary advice alone.
The investigators, led by Kirsten Berding, PhD, APC Microbiome Ireland, University College Cork, Ireland, now plan on testing their psychobiotic diet in patients with MDD and hope the findings could be helpful in “the development of adjuvant therapeutic opportunities” where pharmacologic treatment is not effective.
Both studies were presented at the virtual congress of the European College of Neuropsychopharmacology, held online this year because of the COVID-19 pandemic.
A “hallmark” of major depression
Mr. Fontana and colleagues note that the mostly suboptimal response to pharmacologic treatments among patients with MDD is one of the factors that “contributes to the large socioeconomic burden” of the disease.
Previous research shows patients with MDD have gut dysbiosis, or an imbalance in the natural flora; that antidepressants have antimicrobial properties; and that probiotics have an antibiotic effect. However, the correlation between the composition of the gut microbiota and antidepressant response is poorly understood.
The investigators recruited 34 patients with MDD (aged 18-70 years) who were in a euthymic phase and who did not have comorbid conditions that could affect the gut microbiota.
Eight patients were treatment resistant, defined as a poor response to at least two adequate trials of different antidepressant classes, while 19 were treatment responsive and seven were treatment naive.
The researchers also recruited 20 healthy individuals via word of mouth to act as the control group. There were no significant differences between patients and the control group in terms of baseline characteristics.
Genomic sequencing of bacteria obtained from stool samples showed that it was possible to distinguish between patients with MDD and the healthy individuals, especially at the family, genus, and species levels.
In particular, there were significant differences in the Paenibacillaceae and Flavobacteriaceaea families, for the genus Fenollaria, and the species Flintibacter butyricus, Christensenella timonensis, and Eisenbergiella massiliensis, among others.
Results also showed that the phyla Proteobacteria, Tenericutes, and the family Peptostreptococcaceae were more common in patients with treatment-resistant MDD, whereas the phylum Actinobacteria was more abundant in treatment responders.
Moreover, several bacteria were found only in the microbiota of patients with treatment-resistant MDD, while others were seen only in treatment-responsive patients. This made it possible to discriminate not only between treatment-resistant and -responsive patients but also between those two patient groups and healthy controls.
“The results of our study confirm that gut dysbiosis is a hallmark of MDD, and suggests that the gut microbiota of patients with treatment-resistant MDD significantly differs from responders to antidepressants,” Mr. Fontana said.
Psychobiotic diet
For the second study, Dr. Berding and colleagues note that “psychobiotics” has previously achieved “promising results.”
In addition, diet is both “one of the most influential modifying factors” for the gut microbiota and an easily accessible strategy, they wrote. However, there is also a paucity of studies in this area, they added.
The researchers randomly assigned healthy volunteers with relatively poor dietary habits to either a 4-week psychobiotic diet group (n = 21) or a control group (n = 19).
Individuals in the psychobiotic group were told to eat a diet rich in prebiotics, such as fruit and vegetables, fiber including whole grains and legumes, and fermented foods. The control group was educated on Irish healthy-eating guidelines.
Stool and saliva samples were collected and the participants completed several self-reported mental health questionnaires, as well as a 7-day food diary. They also took the socially evaluated cold-pressor test (SECPT) to measure acute stress responses.
Results showed that total daily energy intake decreased significantly in both the diet and control groups over the study period (P = .04 for both) but did not differ significantly between the groups.
In contrast, dietary fiber intake increased significantly in the diet group (P < .001) and was significantly higher than in the control group at the end of the intervention (P = .03).
Individuals in the diet group showed significant decreases in scores on the Perceived Stress Scale (P = .002) and the Beck Depression Inventory (P = .007) during the study, an effect that was not found in the control group.
Dietary intervention
There were no significant effects of diet on the acute stress response, but both groups showed improvements in self-concept, or perceived ability to cope, on the Primary Appraisal, Secondary Appraisal index (P = .03 for the diet group, P = .04 for the control group).
The results show that a dietary intervention targeted at the microbiota “can improve subjective feelings of stress and depression in a healthy population,” the investigators wrote.
However, elucidating the “contribution of the microbiota-gut-brain axis on the signaling response to dietary interventions” will require further studies on microbiota sequencing and biological measures of stress, they added.
This will “contribute to the understanding of the benefits of a psychobiotic diet on stress and anxiety,” wrote the researchers.
Dr. Berding said in an interview that while the consumption of dietary fiber changed the most in the diet group, “it would not be the only nutrient” that had an impact on the results, with fermented foods a likely candidate.
She said the next step is to test the dietary intervention in patients with MDD; however, “doing nutritional interventions in diseased populations is always difficult.”
Dr. Berding suggested that the best approach would be to study inpatients in a clinic, as “we would be able to provide every meal and only provide foods that are part of the dietary intervention.”
Although another option would be to conduct the study in outpatients, she noted that assessing inpatients “would give us the best control over compliance.”
“Brilliant ideas”
Commenting on the findings, Sergueï Fetissov, MD, PhD, professor of physiology at Rouen University, Mont-Saint-Aignan, France, said that although both studies bring attention to a possible role for the gut microbiota in MDD, neither “provide any experimental evidence of a causative nature.”
Dr. Fetissov, who was not involved in either study, noted that this topic has been the subject of clinical nutritional research for many years.
However, “we still need some strong evidence to prove that some bacteria can influence the regulation of mood and anxiety and stress,” he said.
In addition, researchers currently do not know what actually causes MDD. “How we can say the gut bacteria regulates something if we don’t know what really causes the altered mood?” said Dr. Fetissov.
He noted that over the last 50 years, there have been great advances in the development of drugs that alleviate depression and anxiety by regulating dopamine, serotonin, and other neurotransmitters. However, it is still unknown whether these reflect primary or secondary aspects of mood disorders.
Furthermore, it is not clear “how probiotics to bacteria can influence these neuronal pathways,” he said.
The research by Dr. Berding and colleagues is funded by a postdoctoral fellowship grant from the Irish Research Council. The study authors and Dr. Fetissov have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
If PPIs are onboard, atezolizumab may not work for bladder cancer
according to a post hoc analysis of 1,360 subjects from two atezolizumab trials.
Proton pump inhibitor (PPI) use was associated with worse overall and progression-free survival among patients on atezolizumab, but there was no such association in a matched cohort receiving chemotherapy alone. In short, concomitant “PPI users had no atezolizumab benefit,” wrote the investigators led by Ashley Hopkins, PhD, a research fellow at Flinders University in Adelaide, Australia.
This is the first time that PPI use has been shown to be an independent prognostic factor for worse survival in this setting with atezolizumab use – but not with chemotherapy, wrote the authors of the study, published online in Clinical Cancer Research.
“PPIs are overused, or inappropriately used, in patients with cancer by up to 50%, seemingly from a perspective that they will cause no harm. The findings from this study suggest that noncritical PPI use needs to be approached very cautiously, particularly when an immune checkpoint inhibitor is being used to treat urothelial cancer,” Hopkins said in a press release.
Although about one third of cancer patients use PPIs, there has been growing evidence that the changes they induce in the gut microbiome impact immune checkpoint inhibitor (ICI) effectiveness. A similar study of pooled trial data recently found that PPIs, as well as antibiotics, were associated with worse survival in advanced non–small cell lung cancer treated with atezolizumab, while no such tie was found with chemotherapy (Ann Oncol. 2020;31:525-31. doi: 10.1016/j.annonc.2020.01.006).
The mechanism is uncertain. PPIs have been associated with T-cell tolerance, pharmacokinetic changes, and decreased gut microbiota diversity. High diversity, the investigators noted, has been associated with stronger ICI responses in melanoma. Antibiotics have been associated with similar gut dysbiosis.
“It is increasingly evident that altered gut microbiota impacts homeostasis, immune response, cancer prognosis, and ICI efficacy. The hypothetical basis of [our] research is that PPIs are associated with marked changes to the gut microbiota, driven by both altered stomach acidity and direct compound effects, and these changes may impact immunotherapy,” Hopkins said in an email to Medscape.
The associations with urothelial cancer hadn’t been investigated before, so Hopkins and his team pooled patient-level data from the single-arm IMvigor210 trial of atezolizumab for urothelial cancer and the randomized IMvigor211 trial, which pitted atezolizumab against chemotherapy for the indication.
The investigators compared the outcomes of the 471 subjects who were on a PPI from 30 days before to 30 days after starting atezolizumab with the outcomes of 889 subjects who were not on a PPI. Findings were adjusted for tumor histology and the number of prior treatments and metastases sites, as well as age, body mass index, performance status, and other potential confounders.
PPI use was associated with markedly worse overall survival (hazard ratio, 1.52; 95% confidence interval, 1.27-1.83; P < .001) and progression-free survival (HR, 1.38; 95% CI, 1.18-1.62; P < .001) in patients on atezolizumab but not chemotherapy. PPI use was also associated with worse objective response to the ICI (HR, 0.51; 95% CI, 0.32-0.82; P = .006).
In the randomized trial, atezolizumab seemed to offer no overall survival benefit versus chemotherapy when PPIs were onboard (HR, 1.04; 95% CI, 0.81-1.34), but atezolizumab offered a substantial benefit when PPIs were not in use (HR, 0.69; 95% CI, 0.56-0.84). Findings were consistent when limited to the PD-L1 IC2/3 population.
It seems that PPIs negate “the magnitude of atezolizumab efficacy,” the investigators wrote.
Concomitant antibiotics made the effect of PPIs on overall survival with atezolizumab even worse (antibiotics plus PPI: HR 2.51; 95% CI, 1.12-5.59; versus no antibiotics with PPI: HR, 1.44; 95% CI, 1.19-1.74).
The investigators cautioned that, although “the conducted analyses have been adjusted, there is the potential that PPI use constitutes a surrogate marker for an unfit or immunodeficient patient.” They called for further investigation with other ICIs, cancer types, and chemotherapy regimens.
The dose and compliance with PPI therapy were unknown, but the team noted that over 90% of the PPI subjects were on PPIs for long-term reasons, most commonly gastric protection and gastroesophageal reflux disease (GERD). Omeprazole, pantoprazole, and esomeprazole were the most frequently used.
There were no significant associations between PPI use and the first occurrence of atezolizumab-induced adverse events.
The study was funded by the National Breast Cancer Foundation (Australia) and the Cancer Council South Australia. Hopkins has disclosed no relevant financial relationships. Multiple study authors have financial ties to industry, including makers of ICIs. The full list can be found with the original article.
This article first appeared on Medscape.com.
according to a post hoc analysis of 1,360 subjects from two atezolizumab trials.
Proton pump inhibitor (PPI) use was associated with worse overall and progression-free survival among patients on atezolizumab, but there was no such association in a matched cohort receiving chemotherapy alone. In short, concomitant “PPI users had no atezolizumab benefit,” wrote the investigators led by Ashley Hopkins, PhD, a research fellow at Flinders University in Adelaide, Australia.
This is the first time that PPI use has been shown to be an independent prognostic factor for worse survival in this setting with atezolizumab use – but not with chemotherapy, wrote the authors of the study, published online in Clinical Cancer Research.
“PPIs are overused, or inappropriately used, in patients with cancer by up to 50%, seemingly from a perspective that they will cause no harm. The findings from this study suggest that noncritical PPI use needs to be approached very cautiously, particularly when an immune checkpoint inhibitor is being used to treat urothelial cancer,” Hopkins said in a press release.
Although about one third of cancer patients use PPIs, there has been growing evidence that the changes they induce in the gut microbiome impact immune checkpoint inhibitor (ICI) effectiveness. A similar study of pooled trial data recently found that PPIs, as well as antibiotics, were associated with worse survival in advanced non–small cell lung cancer treated with atezolizumab, while no such tie was found with chemotherapy (Ann Oncol. 2020;31:525-31. doi: 10.1016/j.annonc.2020.01.006).
The mechanism is uncertain. PPIs have been associated with T-cell tolerance, pharmacokinetic changes, and decreased gut microbiota diversity. High diversity, the investigators noted, has been associated with stronger ICI responses in melanoma. Antibiotics have been associated with similar gut dysbiosis.
“It is increasingly evident that altered gut microbiota impacts homeostasis, immune response, cancer prognosis, and ICI efficacy. The hypothetical basis of [our] research is that PPIs are associated with marked changes to the gut microbiota, driven by both altered stomach acidity and direct compound effects, and these changes may impact immunotherapy,” Hopkins said in an email to Medscape.
The associations with urothelial cancer hadn’t been investigated before, so Hopkins and his team pooled patient-level data from the single-arm IMvigor210 trial of atezolizumab for urothelial cancer and the randomized IMvigor211 trial, which pitted atezolizumab against chemotherapy for the indication.
The investigators compared the outcomes of the 471 subjects who were on a PPI from 30 days before to 30 days after starting atezolizumab with the outcomes of 889 subjects who were not on a PPI. Findings were adjusted for tumor histology and the number of prior treatments and metastases sites, as well as age, body mass index, performance status, and other potential confounders.
PPI use was associated with markedly worse overall survival (hazard ratio, 1.52; 95% confidence interval, 1.27-1.83; P < .001) and progression-free survival (HR, 1.38; 95% CI, 1.18-1.62; P < .001) in patients on atezolizumab but not chemotherapy. PPI use was also associated with worse objective response to the ICI (HR, 0.51; 95% CI, 0.32-0.82; P = .006).
In the randomized trial, atezolizumab seemed to offer no overall survival benefit versus chemotherapy when PPIs were onboard (HR, 1.04; 95% CI, 0.81-1.34), but atezolizumab offered a substantial benefit when PPIs were not in use (HR, 0.69; 95% CI, 0.56-0.84). Findings were consistent when limited to the PD-L1 IC2/3 population.
It seems that PPIs negate “the magnitude of atezolizumab efficacy,” the investigators wrote.
Concomitant antibiotics made the effect of PPIs on overall survival with atezolizumab even worse (antibiotics plus PPI: HR 2.51; 95% CI, 1.12-5.59; versus no antibiotics with PPI: HR, 1.44; 95% CI, 1.19-1.74).
The investigators cautioned that, although “the conducted analyses have been adjusted, there is the potential that PPI use constitutes a surrogate marker for an unfit or immunodeficient patient.” They called for further investigation with other ICIs, cancer types, and chemotherapy regimens.
The dose and compliance with PPI therapy were unknown, but the team noted that over 90% of the PPI subjects were on PPIs for long-term reasons, most commonly gastric protection and gastroesophageal reflux disease (GERD). Omeprazole, pantoprazole, and esomeprazole were the most frequently used.
There were no significant associations between PPI use and the first occurrence of atezolizumab-induced adverse events.
The study was funded by the National Breast Cancer Foundation (Australia) and the Cancer Council South Australia. Hopkins has disclosed no relevant financial relationships. Multiple study authors have financial ties to industry, including makers of ICIs. The full list can be found with the original article.
This article first appeared on Medscape.com.
according to a post hoc analysis of 1,360 subjects from two atezolizumab trials.
Proton pump inhibitor (PPI) use was associated with worse overall and progression-free survival among patients on atezolizumab, but there was no such association in a matched cohort receiving chemotherapy alone. In short, concomitant “PPI users had no atezolizumab benefit,” wrote the investigators led by Ashley Hopkins, PhD, a research fellow at Flinders University in Adelaide, Australia.
This is the first time that PPI use has been shown to be an independent prognostic factor for worse survival in this setting with atezolizumab use – but not with chemotherapy, wrote the authors of the study, published online in Clinical Cancer Research.
“PPIs are overused, or inappropriately used, in patients with cancer by up to 50%, seemingly from a perspective that they will cause no harm. The findings from this study suggest that noncritical PPI use needs to be approached very cautiously, particularly when an immune checkpoint inhibitor is being used to treat urothelial cancer,” Hopkins said in a press release.
Although about one third of cancer patients use PPIs, there has been growing evidence that the changes they induce in the gut microbiome impact immune checkpoint inhibitor (ICI) effectiveness. A similar study of pooled trial data recently found that PPIs, as well as antibiotics, were associated with worse survival in advanced non–small cell lung cancer treated with atezolizumab, while no such tie was found with chemotherapy (Ann Oncol. 2020;31:525-31. doi: 10.1016/j.annonc.2020.01.006).
The mechanism is uncertain. PPIs have been associated with T-cell tolerance, pharmacokinetic changes, and decreased gut microbiota diversity. High diversity, the investigators noted, has been associated with stronger ICI responses in melanoma. Antibiotics have been associated with similar gut dysbiosis.
“It is increasingly evident that altered gut microbiota impacts homeostasis, immune response, cancer prognosis, and ICI efficacy. The hypothetical basis of [our] research is that PPIs are associated with marked changes to the gut microbiota, driven by both altered stomach acidity and direct compound effects, and these changes may impact immunotherapy,” Hopkins said in an email to Medscape.
The associations with urothelial cancer hadn’t been investigated before, so Hopkins and his team pooled patient-level data from the single-arm IMvigor210 trial of atezolizumab for urothelial cancer and the randomized IMvigor211 trial, which pitted atezolizumab against chemotherapy for the indication.
The investigators compared the outcomes of the 471 subjects who were on a PPI from 30 days before to 30 days after starting atezolizumab with the outcomes of 889 subjects who were not on a PPI. Findings were adjusted for tumor histology and the number of prior treatments and metastases sites, as well as age, body mass index, performance status, and other potential confounders.
PPI use was associated with markedly worse overall survival (hazard ratio, 1.52; 95% confidence interval, 1.27-1.83; P < .001) and progression-free survival (HR, 1.38; 95% CI, 1.18-1.62; P < .001) in patients on atezolizumab but not chemotherapy. PPI use was also associated with worse objective response to the ICI (HR, 0.51; 95% CI, 0.32-0.82; P = .006).
In the randomized trial, atezolizumab seemed to offer no overall survival benefit versus chemotherapy when PPIs were onboard (HR, 1.04; 95% CI, 0.81-1.34), but atezolizumab offered a substantial benefit when PPIs were not in use (HR, 0.69; 95% CI, 0.56-0.84). Findings were consistent when limited to the PD-L1 IC2/3 population.
It seems that PPIs negate “the magnitude of atezolizumab efficacy,” the investigators wrote.
Concomitant antibiotics made the effect of PPIs on overall survival with atezolizumab even worse (antibiotics plus PPI: HR 2.51; 95% CI, 1.12-5.59; versus no antibiotics with PPI: HR, 1.44; 95% CI, 1.19-1.74).
The investigators cautioned that, although “the conducted analyses have been adjusted, there is the potential that PPI use constitutes a surrogate marker for an unfit or immunodeficient patient.” They called for further investigation with other ICIs, cancer types, and chemotherapy regimens.
The dose and compliance with PPI therapy were unknown, but the team noted that over 90% of the PPI subjects were on PPIs for long-term reasons, most commonly gastric protection and gastroesophageal reflux disease (GERD). Omeprazole, pantoprazole, and esomeprazole were the most frequently used.
There were no significant associations between PPI use and the first occurrence of atezolizumab-induced adverse events.
The study was funded by the National Breast Cancer Foundation (Australia) and the Cancer Council South Australia. Hopkins has disclosed no relevant financial relationships. Multiple study authors have financial ties to industry, including makers of ICIs. The full list can be found with the original article.
This article first appeared on Medscape.com.
Dr. Fauci: ‘About 40%-45% of infections are asymptomatic’
Anthony Fauci, MD, highlighting the latest COVID-19 developments on Friday, said, “It is now clear that about 40%-45% of infections are asymptomatic.”
Asymptomatic carriers can account for a large proportion — up to 50% — of virus transmissions, Fauci, director of the National Institute of Allergy and Infectious Diseases, told a virtual crowd of critical care clinicians gathered by the Society of Critical Care Medicine.
Such transmissions have made response strategies, such as contact tracing, extremely difficult, he said.
Lew Kaplan, MD, president of SCCM, told Medscape Medical News after the presentation: “That really supports the universal wearing of masks and the capstone message from that – you should protect one another.
“That kind of social responsibility that sits within the public health domain to me is as important as the vaccine candidates and the science behind the receptors. It underpins the necessary relationship and the interdependence of the medical community with the public,” Kaplan added.
Fauci’s plenary led the SCCM’s conference, “COVID-19: What’s Next/Preparing for the Second Wave,” running today and Saturday.
Why U.S. response lags behind Spain and Italy
“This virus has literally exploded upon the planet in a pandemic manner which is unparalleled to anything we’ve seen in the last 102 years since the pandemic of 1918,” Fauci said.
“Unfortunately, the United States has been hit harder than any other country in the world, with 6 million reported cases.”
He explained that in the European Union countries the disease spiked early on and returned to a low baseline. “Unfortunately for them,” Fauci said, “as they’re trying to open up their economy, it’s coming back up.”
The United States, he explained, plateaued at about 20,000 cases a day, then a surge of cases in Florida, California, Texas, and Arizona brought the cases to 70,000 a day. Now cases have returned to 35,000-40,000 a day.
The difference in the trajectory of the response, he said, is that, compared with Spain and Italy for example, the United States has not shut down mobility in parks, outdoor spaces, and grocery stores nearly as much as some European countries did.
He pointed to numerous clusters of cases, spread from social or work gatherings, including the well-known Skagit County Washington state choir practice in March, in which a symptomatic choir member infected 87% of the 61 people rehearsing.
Vaccine by end of the year
As for a vaccine timeline, Fauci told SCCM members, “We project that by the end of this year, namely November/December, we will know if we have a safe and effective vaccine and we are cautiously optimistic that we will be successful, based on promising data in the animal model as well as good immunological data that we see from the phase 1 and phase 2 trials.”
However, also on Friday, Fauci told MSNBC’s Andrea Mitchell that a sense of normalcy is not likely before the middle of next year.
“By the time you mobilize the distribution of the vaccinations, and you get the majority, or more, of the population vaccinated and protected, that’s likely not going to happen [until] the mid- or end of 2021,” he said.
According to the Centers for Disease Control and Prevention (CDC) case tracker, as of Thursday, COVID-19 had resulted in more than 190,000 deaths overall and more than 256,000 new cases in the United States in the past 7 days.
Fauci has warned that the next few months will be critical in the virus’ trajectory, with the double onslaught of COVID-19 and the flu season.
On Thursday, Fauci said, “We need to hunker down and get through this fall and winter because it’s not going to be easy.”
Fauci remains a top trusted source in COVID-19 information, poll numbers show.
A Kaiser Family Foundation poll released Thursday found that 68% of US adults had a fair amount or a great deal of trust that Fauci would provide reliable information on COVID-19, just slightly more that the 67% who said they trust the CDC information. About half (53%) say they trust Deborah Birx, MD, the coordinator for the White House Coronavirus Task Force, as a reliable source of information.
The poll also found that 54% of Americans said they would not get a COVID-19 vaccine if one was approved by the US Food and Drug Administration before the November election and was made available and free to all who wanted it.
Kaplan and Fauci report no relevant financial relationships.
This article first appeared on Medscape.com.
Anthony Fauci, MD, highlighting the latest COVID-19 developments on Friday, said, “It is now clear that about 40%-45% of infections are asymptomatic.”
Asymptomatic carriers can account for a large proportion — up to 50% — of virus transmissions, Fauci, director of the National Institute of Allergy and Infectious Diseases, told a virtual crowd of critical care clinicians gathered by the Society of Critical Care Medicine.
Such transmissions have made response strategies, such as contact tracing, extremely difficult, he said.
Lew Kaplan, MD, president of SCCM, told Medscape Medical News after the presentation: “That really supports the universal wearing of masks and the capstone message from that – you should protect one another.
“That kind of social responsibility that sits within the public health domain to me is as important as the vaccine candidates and the science behind the receptors. It underpins the necessary relationship and the interdependence of the medical community with the public,” Kaplan added.
Fauci’s plenary led the SCCM’s conference, “COVID-19: What’s Next/Preparing for the Second Wave,” running today and Saturday.
Why U.S. response lags behind Spain and Italy
“This virus has literally exploded upon the planet in a pandemic manner which is unparalleled to anything we’ve seen in the last 102 years since the pandemic of 1918,” Fauci said.
“Unfortunately, the United States has been hit harder than any other country in the world, with 6 million reported cases.”
He explained that in the European Union countries the disease spiked early on and returned to a low baseline. “Unfortunately for them,” Fauci said, “as they’re trying to open up their economy, it’s coming back up.”
The United States, he explained, plateaued at about 20,000 cases a day, then a surge of cases in Florida, California, Texas, and Arizona brought the cases to 70,000 a day. Now cases have returned to 35,000-40,000 a day.
The difference in the trajectory of the response, he said, is that, compared with Spain and Italy for example, the United States has not shut down mobility in parks, outdoor spaces, and grocery stores nearly as much as some European countries did.
He pointed to numerous clusters of cases, spread from social or work gatherings, including the well-known Skagit County Washington state choir practice in March, in which a symptomatic choir member infected 87% of the 61 people rehearsing.
Vaccine by end of the year
As for a vaccine timeline, Fauci told SCCM members, “We project that by the end of this year, namely November/December, we will know if we have a safe and effective vaccine and we are cautiously optimistic that we will be successful, based on promising data in the animal model as well as good immunological data that we see from the phase 1 and phase 2 trials.”
However, also on Friday, Fauci told MSNBC’s Andrea Mitchell that a sense of normalcy is not likely before the middle of next year.
“By the time you mobilize the distribution of the vaccinations, and you get the majority, or more, of the population vaccinated and protected, that’s likely not going to happen [until] the mid- or end of 2021,” he said.
According to the Centers for Disease Control and Prevention (CDC) case tracker, as of Thursday, COVID-19 had resulted in more than 190,000 deaths overall and more than 256,000 new cases in the United States in the past 7 days.
Fauci has warned that the next few months will be critical in the virus’ trajectory, with the double onslaught of COVID-19 and the flu season.
On Thursday, Fauci said, “We need to hunker down and get through this fall and winter because it’s not going to be easy.”
Fauci remains a top trusted source in COVID-19 information, poll numbers show.
A Kaiser Family Foundation poll released Thursday found that 68% of US adults had a fair amount or a great deal of trust that Fauci would provide reliable information on COVID-19, just slightly more that the 67% who said they trust the CDC information. About half (53%) say they trust Deborah Birx, MD, the coordinator for the White House Coronavirus Task Force, as a reliable source of information.
The poll also found that 54% of Americans said they would not get a COVID-19 vaccine if one was approved by the US Food and Drug Administration before the November election and was made available and free to all who wanted it.
Kaplan and Fauci report no relevant financial relationships.
This article first appeared on Medscape.com.
Anthony Fauci, MD, highlighting the latest COVID-19 developments on Friday, said, “It is now clear that about 40%-45% of infections are asymptomatic.”
Asymptomatic carriers can account for a large proportion — up to 50% — of virus transmissions, Fauci, director of the National Institute of Allergy and Infectious Diseases, told a virtual crowd of critical care clinicians gathered by the Society of Critical Care Medicine.
Such transmissions have made response strategies, such as contact tracing, extremely difficult, he said.
Lew Kaplan, MD, president of SCCM, told Medscape Medical News after the presentation: “That really supports the universal wearing of masks and the capstone message from that – you should protect one another.
“That kind of social responsibility that sits within the public health domain to me is as important as the vaccine candidates and the science behind the receptors. It underpins the necessary relationship and the interdependence of the medical community with the public,” Kaplan added.
Fauci’s plenary led the SCCM’s conference, “COVID-19: What’s Next/Preparing for the Second Wave,” running today and Saturday.
Why U.S. response lags behind Spain and Italy
“This virus has literally exploded upon the planet in a pandemic manner which is unparalleled to anything we’ve seen in the last 102 years since the pandemic of 1918,” Fauci said.
“Unfortunately, the United States has been hit harder than any other country in the world, with 6 million reported cases.”
He explained that in the European Union countries the disease spiked early on and returned to a low baseline. “Unfortunately for them,” Fauci said, “as they’re trying to open up their economy, it’s coming back up.”
The United States, he explained, plateaued at about 20,000 cases a day, then a surge of cases in Florida, California, Texas, and Arizona brought the cases to 70,000 a day. Now cases have returned to 35,000-40,000 a day.
The difference in the trajectory of the response, he said, is that, compared with Spain and Italy for example, the United States has not shut down mobility in parks, outdoor spaces, and grocery stores nearly as much as some European countries did.
He pointed to numerous clusters of cases, spread from social or work gatherings, including the well-known Skagit County Washington state choir practice in March, in which a symptomatic choir member infected 87% of the 61 people rehearsing.
Vaccine by end of the year
As for a vaccine timeline, Fauci told SCCM members, “We project that by the end of this year, namely November/December, we will know if we have a safe and effective vaccine and we are cautiously optimistic that we will be successful, based on promising data in the animal model as well as good immunological data that we see from the phase 1 and phase 2 trials.”
However, also on Friday, Fauci told MSNBC’s Andrea Mitchell that a sense of normalcy is not likely before the middle of next year.
“By the time you mobilize the distribution of the vaccinations, and you get the majority, or more, of the population vaccinated and protected, that’s likely not going to happen [until] the mid- or end of 2021,” he said.
According to the Centers for Disease Control and Prevention (CDC) case tracker, as of Thursday, COVID-19 had resulted in more than 190,000 deaths overall and more than 256,000 new cases in the United States in the past 7 days.
Fauci has warned that the next few months will be critical in the virus’ trajectory, with the double onslaught of COVID-19 and the flu season.
On Thursday, Fauci said, “We need to hunker down and get through this fall and winter because it’s not going to be easy.”
Fauci remains a top trusted source in COVID-19 information, poll numbers show.
A Kaiser Family Foundation poll released Thursday found that 68% of US adults had a fair amount or a great deal of trust that Fauci would provide reliable information on COVID-19, just slightly more that the 67% who said they trust the CDC information. About half (53%) say they trust Deborah Birx, MD, the coordinator for the White House Coronavirus Task Force, as a reliable source of information.
The poll also found that 54% of Americans said they would not get a COVID-19 vaccine if one was approved by the US Food and Drug Administration before the November election and was made available and free to all who wanted it.
Kaplan and Fauci report no relevant financial relationships.
This article first appeared on Medscape.com.
Liberalized European sports cardiology guidelines break new ground
New guidelines on sports cardiology from the European Society of Cardiology break fresh ground by green-lighting participation in vigorous competitive sports by selected patients with stable coronary artery disease, heart failure, or mild arrhythmias.
These liberalized guidelines, released at the virtual annual congress of the European Society of Cardiology, thus move well beyond the standard exercise advice to engage in about 150 minutes per week of moderate physical activity, typically defined as brisk walking or its equivalent.
The guidelines reflect a conviction that exercise is powerful medicine for patients with cardiovascular disease and also affords a means to help curb the epidemics of diabetes and obesity that drive cardiovascular risk, according to Antonio Pelliccia, MD, who cochaired the 24-member task force of European and American experts that developed the guidelines.
In a session highlighting the new sports cardiology guidelines, Mats Borjesson, MD, head of the Center for Health and Performance at Gothenburg (Sweden) University, summarized the section devoted to patients with stable coronary artery disease: “If you have established CAD and a low risk of adverse events during exercise, you are eligible for high-intensity exercise and competitive sports. But if you have persistent ischemia despite medical treatment, or symptoms, then you’re only eligible for leisure-time subthreshold activity.”
Dr. Pelliccia put this new recommendation into context.
“We are not talking anymore in this particular disease just about cardiac rehabilitation or leisure-time activity, but we are also opening the border and talking about competitive sports activity in selected patients where you have the evidence for low risk of exercise-induced adverse events. This is a major achievement now for what is the major disease in our adult population,” said Dr. Pelliccia, chief of cardiology at the Institute of Sports Medicine and Science at the Italian National Olympic Committee and professor of sports cardiology at La Sapienza University of Rome.
The recommendation for individualized consideration of all types of exercise, even including vigorous competitive sports, in low-risk patients with CAD gets a class IIa, level of evidence (LOE) C recommendation in the new guidelines. That’s a big step down from a ringing class Ia endorsement, but since sports cardiology is a relatively young field with little evidence that’s based on randomized trials, the guidelines are rife with many other class IIa, LOE C recommendations as well.
“The level of evidence is rather low, so these guidelines are very much the personal perspective of the expert panel,” explained Martin Halle, MD, professor and head of the department of prevention, rehabilitation, and sports cardiology at Technical University of Munich.
The high-risk features for exercise-induced cardiac adverse events in patients with longstanding stable CAD, as cited in the guidelines, include a critical coronary stenosis, defined as a more than 70% lesion in a major coronary artery or a greater than 50% stenosis in the left main, and/or a fractional flow reserve score of less than 0.8; a left ventricular ejection fraction of 50% or less with wall-motion abnormalities; inducible myocardial ischemia on maximal exercise testing; nonsustained ventricular tachycardia; polymorphic or very frequent ventricular premature beats at rest and during maximum stress; and a recent acute coronary syndrome (ACS). These features call for an exercise prescription tailored to remain below the patient’s angina and ischemia thresholds.
“It’s important for cardiologists out there to understand that we definitely need a maximal exercise test. In somebody who is running and has an ACS and then wants to start running again, 200 watts on an ergometer is too low. We have to push them up to the end, and then if everything is okay – left ventricular function is okay, no ischemia, no arrhythmias under exercise testing – then it’s fine,” Dr. Halle said.
Dr. Pelliccia added that close follow-up is needed, because this is an evolving disease.”
Exercise and heart failure
Massimo F. Piepoli, MD, PhD, noted that the guidelines give a class IIb, LOE C recommendation for consideration of high-intensity recreational endurance and power sports in patients with heart failure with either midrange or preserved ejection fraction, provided they are stable, asymptomatic, on optimal guideline-directed medical therapy, and without abnormalities on a maximal exercise stress test.
However, such intense physical activity is not recommended in patients with heart failure with reduced ejection fraction, regardless of their symptom status, added Dr. Piepoli of Guglielmo da Saliceto Hospital in Placenza, Italy.
“We’re talking here, I think for the first time, about possible competitive sports participation in individuals with heart failure, depending on their clinical condition. We are really opening the barriers to sports participation, even in these patients in whom we never thought of it before,” Dr. Pelliccia observed.
Valvular heart disease and exercise
Guidelines panelist Sabiha Gati, MRCP, PhD, said asymptomatic individuals with mild valvular abnormalities can participate in all recreational and competitive sports; that’s a class I, LOE C recommendation.
“Moderate regurgitant lesions are better tolerated than stenotic lesions, and those with preserved systolic function, good functional capacity, without any exercise-induced arrhythmias or ischemia or abnormal hemodynamic response are considered to be low risk and can participate in all sports,” added Dr. Gati, a cardiologist at Royal Brompton Hospital, London.
The two most common valvular abnormalities encountered in clinical practice are bicuspid aortic valve and mitral valve prolapse. Dr. Gati noted that, while mitral valve prolapse has a benign prognosis in the great majority of affected individuals, the presence of specific features indicative of increased risk for sudden cardiac death precludes participation in strenuous exercise. These include T-wave inversion in the inferior leads on a 12-lead ECG, long QT, bileaflet mitral valve prolapse, basal inferolateral wall fibrosis, severe mitral regurgitation, or a family history of sudden cardiac death.
Bicuspid aortic valve has a prevalence of 1%-2% in the general population. It can be associated with aortic stenosis, aortic regurgitation, and increased risk of ascending aortic aneurysm and dissection. Since it remains unclear whether intensive exercise accelerates aortic dilatation, a cautious approach to sports participation is recommended in patients with an ascending aorta above the normal limit of 40 mm, she said.
The 80-page ESC sports cardiology guidelines, published online simultaneously with their presentation, cover a broad range of additional topics, including exercise recommendations for the general public, for the elderly, as well as for patients with cardiomyopathies, adult congenital heart disease, arrhythmias, and channelopathies. Gaps in evidence are also highlighted.
SOURCE: Pelliccia A. ESC 2020 and Eur Heart J. 2020 Aug 29. doi: 10.1093/eurheartj/ehaa605.
New guidelines on sports cardiology from the European Society of Cardiology break fresh ground by green-lighting participation in vigorous competitive sports by selected patients with stable coronary artery disease, heart failure, or mild arrhythmias.
These liberalized guidelines, released at the virtual annual congress of the European Society of Cardiology, thus move well beyond the standard exercise advice to engage in about 150 minutes per week of moderate physical activity, typically defined as brisk walking or its equivalent.
The guidelines reflect a conviction that exercise is powerful medicine for patients with cardiovascular disease and also affords a means to help curb the epidemics of diabetes and obesity that drive cardiovascular risk, according to Antonio Pelliccia, MD, who cochaired the 24-member task force of European and American experts that developed the guidelines.
In a session highlighting the new sports cardiology guidelines, Mats Borjesson, MD, head of the Center for Health and Performance at Gothenburg (Sweden) University, summarized the section devoted to patients with stable coronary artery disease: “If you have established CAD and a low risk of adverse events during exercise, you are eligible for high-intensity exercise and competitive sports. But if you have persistent ischemia despite medical treatment, or symptoms, then you’re only eligible for leisure-time subthreshold activity.”
Dr. Pelliccia put this new recommendation into context.
“We are not talking anymore in this particular disease just about cardiac rehabilitation or leisure-time activity, but we are also opening the border and talking about competitive sports activity in selected patients where you have the evidence for low risk of exercise-induced adverse events. This is a major achievement now for what is the major disease in our adult population,” said Dr. Pelliccia, chief of cardiology at the Institute of Sports Medicine and Science at the Italian National Olympic Committee and professor of sports cardiology at La Sapienza University of Rome.
The recommendation for individualized consideration of all types of exercise, even including vigorous competitive sports, in low-risk patients with CAD gets a class IIa, level of evidence (LOE) C recommendation in the new guidelines. That’s a big step down from a ringing class Ia endorsement, but since sports cardiology is a relatively young field with little evidence that’s based on randomized trials, the guidelines are rife with many other class IIa, LOE C recommendations as well.
“The level of evidence is rather low, so these guidelines are very much the personal perspective of the expert panel,” explained Martin Halle, MD, professor and head of the department of prevention, rehabilitation, and sports cardiology at Technical University of Munich.
The high-risk features for exercise-induced cardiac adverse events in patients with longstanding stable CAD, as cited in the guidelines, include a critical coronary stenosis, defined as a more than 70% lesion in a major coronary artery or a greater than 50% stenosis in the left main, and/or a fractional flow reserve score of less than 0.8; a left ventricular ejection fraction of 50% or less with wall-motion abnormalities; inducible myocardial ischemia on maximal exercise testing; nonsustained ventricular tachycardia; polymorphic or very frequent ventricular premature beats at rest and during maximum stress; and a recent acute coronary syndrome (ACS). These features call for an exercise prescription tailored to remain below the patient’s angina and ischemia thresholds.
“It’s important for cardiologists out there to understand that we definitely need a maximal exercise test. In somebody who is running and has an ACS and then wants to start running again, 200 watts on an ergometer is too low. We have to push them up to the end, and then if everything is okay – left ventricular function is okay, no ischemia, no arrhythmias under exercise testing – then it’s fine,” Dr. Halle said.
Dr. Pelliccia added that close follow-up is needed, because this is an evolving disease.”
Exercise and heart failure
Massimo F. Piepoli, MD, PhD, noted that the guidelines give a class IIb, LOE C recommendation for consideration of high-intensity recreational endurance and power sports in patients with heart failure with either midrange or preserved ejection fraction, provided they are stable, asymptomatic, on optimal guideline-directed medical therapy, and without abnormalities on a maximal exercise stress test.
However, such intense physical activity is not recommended in patients with heart failure with reduced ejection fraction, regardless of their symptom status, added Dr. Piepoli of Guglielmo da Saliceto Hospital in Placenza, Italy.
“We’re talking here, I think for the first time, about possible competitive sports participation in individuals with heart failure, depending on their clinical condition. We are really opening the barriers to sports participation, even in these patients in whom we never thought of it before,” Dr. Pelliccia observed.
Valvular heart disease and exercise
Guidelines panelist Sabiha Gati, MRCP, PhD, said asymptomatic individuals with mild valvular abnormalities can participate in all recreational and competitive sports; that’s a class I, LOE C recommendation.
“Moderate regurgitant lesions are better tolerated than stenotic lesions, and those with preserved systolic function, good functional capacity, without any exercise-induced arrhythmias or ischemia or abnormal hemodynamic response are considered to be low risk and can participate in all sports,” added Dr. Gati, a cardiologist at Royal Brompton Hospital, London.
The two most common valvular abnormalities encountered in clinical practice are bicuspid aortic valve and mitral valve prolapse. Dr. Gati noted that, while mitral valve prolapse has a benign prognosis in the great majority of affected individuals, the presence of specific features indicative of increased risk for sudden cardiac death precludes participation in strenuous exercise. These include T-wave inversion in the inferior leads on a 12-lead ECG, long QT, bileaflet mitral valve prolapse, basal inferolateral wall fibrosis, severe mitral regurgitation, or a family history of sudden cardiac death.
Bicuspid aortic valve has a prevalence of 1%-2% in the general population. It can be associated with aortic stenosis, aortic regurgitation, and increased risk of ascending aortic aneurysm and dissection. Since it remains unclear whether intensive exercise accelerates aortic dilatation, a cautious approach to sports participation is recommended in patients with an ascending aorta above the normal limit of 40 mm, she said.
The 80-page ESC sports cardiology guidelines, published online simultaneously with their presentation, cover a broad range of additional topics, including exercise recommendations for the general public, for the elderly, as well as for patients with cardiomyopathies, adult congenital heart disease, arrhythmias, and channelopathies. Gaps in evidence are also highlighted.
SOURCE: Pelliccia A. ESC 2020 and Eur Heart J. 2020 Aug 29. doi: 10.1093/eurheartj/ehaa605.
New guidelines on sports cardiology from the European Society of Cardiology break fresh ground by green-lighting participation in vigorous competitive sports by selected patients with stable coronary artery disease, heart failure, or mild arrhythmias.
These liberalized guidelines, released at the virtual annual congress of the European Society of Cardiology, thus move well beyond the standard exercise advice to engage in about 150 minutes per week of moderate physical activity, typically defined as brisk walking or its equivalent.
The guidelines reflect a conviction that exercise is powerful medicine for patients with cardiovascular disease and also affords a means to help curb the epidemics of diabetes and obesity that drive cardiovascular risk, according to Antonio Pelliccia, MD, who cochaired the 24-member task force of European and American experts that developed the guidelines.
In a session highlighting the new sports cardiology guidelines, Mats Borjesson, MD, head of the Center for Health and Performance at Gothenburg (Sweden) University, summarized the section devoted to patients with stable coronary artery disease: “If you have established CAD and a low risk of adverse events during exercise, you are eligible for high-intensity exercise and competitive sports. But if you have persistent ischemia despite medical treatment, or symptoms, then you’re only eligible for leisure-time subthreshold activity.”
Dr. Pelliccia put this new recommendation into context.
“We are not talking anymore in this particular disease just about cardiac rehabilitation or leisure-time activity, but we are also opening the border and talking about competitive sports activity in selected patients where you have the evidence for low risk of exercise-induced adverse events. This is a major achievement now for what is the major disease in our adult population,” said Dr. Pelliccia, chief of cardiology at the Institute of Sports Medicine and Science at the Italian National Olympic Committee and professor of sports cardiology at La Sapienza University of Rome.
The recommendation for individualized consideration of all types of exercise, even including vigorous competitive sports, in low-risk patients with CAD gets a class IIa, level of evidence (LOE) C recommendation in the new guidelines. That’s a big step down from a ringing class Ia endorsement, but since sports cardiology is a relatively young field with little evidence that’s based on randomized trials, the guidelines are rife with many other class IIa, LOE C recommendations as well.
“The level of evidence is rather low, so these guidelines are very much the personal perspective of the expert panel,” explained Martin Halle, MD, professor and head of the department of prevention, rehabilitation, and sports cardiology at Technical University of Munich.
The high-risk features for exercise-induced cardiac adverse events in patients with longstanding stable CAD, as cited in the guidelines, include a critical coronary stenosis, defined as a more than 70% lesion in a major coronary artery or a greater than 50% stenosis in the left main, and/or a fractional flow reserve score of less than 0.8; a left ventricular ejection fraction of 50% or less with wall-motion abnormalities; inducible myocardial ischemia on maximal exercise testing; nonsustained ventricular tachycardia; polymorphic or very frequent ventricular premature beats at rest and during maximum stress; and a recent acute coronary syndrome (ACS). These features call for an exercise prescription tailored to remain below the patient’s angina and ischemia thresholds.
“It’s important for cardiologists out there to understand that we definitely need a maximal exercise test. In somebody who is running and has an ACS and then wants to start running again, 200 watts on an ergometer is too low. We have to push them up to the end, and then if everything is okay – left ventricular function is okay, no ischemia, no arrhythmias under exercise testing – then it’s fine,” Dr. Halle said.
Dr. Pelliccia added that close follow-up is needed, because this is an evolving disease.”
Exercise and heart failure
Massimo F. Piepoli, MD, PhD, noted that the guidelines give a class IIb, LOE C recommendation for consideration of high-intensity recreational endurance and power sports in patients with heart failure with either midrange or preserved ejection fraction, provided they are stable, asymptomatic, on optimal guideline-directed medical therapy, and without abnormalities on a maximal exercise stress test.
However, such intense physical activity is not recommended in patients with heart failure with reduced ejection fraction, regardless of their symptom status, added Dr. Piepoli of Guglielmo da Saliceto Hospital in Placenza, Italy.
“We’re talking here, I think for the first time, about possible competitive sports participation in individuals with heart failure, depending on their clinical condition. We are really opening the barriers to sports participation, even in these patients in whom we never thought of it before,” Dr. Pelliccia observed.
Valvular heart disease and exercise
Guidelines panelist Sabiha Gati, MRCP, PhD, said asymptomatic individuals with mild valvular abnormalities can participate in all recreational and competitive sports; that’s a class I, LOE C recommendation.
“Moderate regurgitant lesions are better tolerated than stenotic lesions, and those with preserved systolic function, good functional capacity, without any exercise-induced arrhythmias or ischemia or abnormal hemodynamic response are considered to be low risk and can participate in all sports,” added Dr. Gati, a cardiologist at Royal Brompton Hospital, London.
The two most common valvular abnormalities encountered in clinical practice are bicuspid aortic valve and mitral valve prolapse. Dr. Gati noted that, while mitral valve prolapse has a benign prognosis in the great majority of affected individuals, the presence of specific features indicative of increased risk for sudden cardiac death precludes participation in strenuous exercise. These include T-wave inversion in the inferior leads on a 12-lead ECG, long QT, bileaflet mitral valve prolapse, basal inferolateral wall fibrosis, severe mitral regurgitation, or a family history of sudden cardiac death.
Bicuspid aortic valve has a prevalence of 1%-2% in the general population. It can be associated with aortic stenosis, aortic regurgitation, and increased risk of ascending aortic aneurysm and dissection. Since it remains unclear whether intensive exercise accelerates aortic dilatation, a cautious approach to sports participation is recommended in patients with an ascending aorta above the normal limit of 40 mm, she said.
The 80-page ESC sports cardiology guidelines, published online simultaneously with their presentation, cover a broad range of additional topics, including exercise recommendations for the general public, for the elderly, as well as for patients with cardiomyopathies, adult congenital heart disease, arrhythmias, and channelopathies. Gaps in evidence are also highlighted.
SOURCE: Pelliccia A. ESC 2020 and Eur Heart J. 2020 Aug 29. doi: 10.1093/eurheartj/ehaa605.
FROM ESC CONGRESS 2020
Biologics for psoriasis may also reduce coronary plaque
Biologics used as treatment for psoriasis may also help reduce lipid-rich necrotic core (LRNC), a high-risk plaque associated with cardiovascular events, recent research from a prospective, observational study suggests.
Cardiac CT scans performed on patients with psoriasis 1 year after starting biologic therapy revealed a reduction in LRNC, compared with patients who were not receiving biologics, according to Harry Choi, MD, of the National Heart, Lung, and Blood Institute at the National Institutes of Health and colleagues. The association with reduction in LRNC and biologic therapy remained significant when adjusted for type of biologic. “These findings demonstrate that LRNC may be modulated by the control of systemic inflammation,” the researchers wrote in their study, published Sept. 15 in Circulation: Cardiovascular Imaging.
Dr. Choi and colleagues evaluated 289 patients with psoriasis within the Psoriasis Atherosclerosis and Cardiometabolic Disease Initiative cohort. The patients had a mean age of 50 years and a mean body mass index of 29.4 kg/m2, as well as a mean Psoriasis Area and Severity Index (PASI) score of 6.0. At baseline, 29% of patients had hypertension, 41% had hyperlipidemia, their mean Framingham risk score was 1.9, and a three-quarters (212 of 289) had mild to moderate psoriasis.
Changes in LRNC were observed at 1 year, compared with baseline prior to and after receiving biologic therapy (124 patients) in comparison with patients who did not undergo biologic therapy (85 patients). Biologic therapies were grouped by type, which included anti–tumor necrosis factor (anti-TNF), anti–interleukin (IL)–12/23, and anti–IL-17 biologics.
There were a significant associations between LRNC and Framingham risk score (standardized beta coefficient, 0.12; 95% confidence interval, 0.00-0.15; P = .045) and severity of psoriasis (beta, 0.13; 95% CI, 0.01-0.26; P = .029) at baseline.
Key findings
The researchers found a significant reduction in LRNC 1 year after patients began biologic therapy (median, 2.97 mm2; interquartile range, 1.99-4.66), compared with baseline (median, 3.12 mm2; IQR, 1.84-4.35) (P = .028), while patients who did not receive biologic therapy had nonsignificantly higher LRNC after 1 year (median, 3.12 mm2; IQR, 1.82-4.60), compared with baseline measurements (median, 3.34 mm2; IQR, 2.04–4.74) (P = .06).
The results remained significant after the researchers adjusted for psoriasis severity, Framingham risk score, BMI, use of statins (beta, −0.09; 95% CI, −0.01 to −0.18; P = .033). Significant reductions in LRNC also remained when analyzing patients receiving anti-TNF, anti–IL-12/23, and anti–IL-17 biologics independently, and there were no significant between-group differences in reduction of LRNC.
The potential of biologics for improving vascular health
Discussing the study results in a press release from the American Heart Association, senior author Nehal N. Mehta, MD, MSCE, FAHA, chief of the Lab of Inflammation and Cardiometabolic Diseases at the NHLBI at NIH, compared the effect biologic therapy had on coronary plaque reduction with that of statins.
“There is approximately 6%-8% reduction in coronary plaque following therapy with statins. Similarly, our treatment with biologic therapy reduced coronary plaque by the same amount after one year. These findings suggest that biologic therapy to treat psoriasis may be just as beneficial as statin therapy on heart arteries,” Dr. Mehta said in the release.
In an interview, Nieca Goldberg, MD, medical director of NYU Women’s Heart Program at NYU Langone Health, echoed Dr. Mehta’s commments and said psoriasis carries the “potential to treat two conditions with the same drug.”
“We know conditions such as psoriatic arthritis and rheumatoid arthritis cause chronic inflammation. Chronic inflammation causes injury to blood vessels and high-risk coronary plaque. Individuals with these inflammatory conditions are at high risk for heart attack,” she said. “This study shows that biologic treatment for psoriatic arthritis can reduce the presence of high-risk plaque. It shows the potential to treat chronic inflammation and high-risk coronary plaque.”
While the results show an association between use of biologics and LRNC reduction, the study design was observational and patients had a short follow-up period. Dr. Goldberg noted more studies are needed to evaluate the effect of biologics on reducing cardiovascular events such as a myocardial infarction.
“We have never before been able to show healing of an inflamed plaque like this in humans. Biologic therapy reduces systemic inflammation and immune activation, and it has a favorable impact on improving overall vascular health,” Dr. Mehta said in the press release. “Imagine if we can treat both psoriasis and coronary heart disease with one therapy – that is the question to be asked in future studies.”
This study was funded with support from the NHLBI Intramural Research Program and the NIH Medical Research Scholars Program at the National Institutes of Health. One investigator reports financial relationships with numerous pharmaceutical companies. The other authors report no relevant conflicts of interest. Dr. Mehta also reports numerous such relationships. Dr. Goldberg reports no relevant conflicts of interest.
SOURCE: Choi H et al. Circ Cardiovasc Imaging. 2020 Sep;13(9):e011199.
Biologics used as treatment for psoriasis may also help reduce lipid-rich necrotic core (LRNC), a high-risk plaque associated with cardiovascular events, recent research from a prospective, observational study suggests.
Cardiac CT scans performed on patients with psoriasis 1 year after starting biologic therapy revealed a reduction in LRNC, compared with patients who were not receiving biologics, according to Harry Choi, MD, of the National Heart, Lung, and Blood Institute at the National Institutes of Health and colleagues. The association with reduction in LRNC and biologic therapy remained significant when adjusted for type of biologic. “These findings demonstrate that LRNC may be modulated by the control of systemic inflammation,” the researchers wrote in their study, published Sept. 15 in Circulation: Cardiovascular Imaging.
Dr. Choi and colleagues evaluated 289 patients with psoriasis within the Psoriasis Atherosclerosis and Cardiometabolic Disease Initiative cohort. The patients had a mean age of 50 years and a mean body mass index of 29.4 kg/m2, as well as a mean Psoriasis Area and Severity Index (PASI) score of 6.0. At baseline, 29% of patients had hypertension, 41% had hyperlipidemia, their mean Framingham risk score was 1.9, and a three-quarters (212 of 289) had mild to moderate psoriasis.
Changes in LRNC were observed at 1 year, compared with baseline prior to and after receiving biologic therapy (124 patients) in comparison with patients who did not undergo biologic therapy (85 patients). Biologic therapies were grouped by type, which included anti–tumor necrosis factor (anti-TNF), anti–interleukin (IL)–12/23, and anti–IL-17 biologics.
There were a significant associations between LRNC and Framingham risk score (standardized beta coefficient, 0.12; 95% confidence interval, 0.00-0.15; P = .045) and severity of psoriasis (beta, 0.13; 95% CI, 0.01-0.26; P = .029) at baseline.
Key findings
The researchers found a significant reduction in LRNC 1 year after patients began biologic therapy (median, 2.97 mm2; interquartile range, 1.99-4.66), compared with baseline (median, 3.12 mm2; IQR, 1.84-4.35) (P = .028), while patients who did not receive biologic therapy had nonsignificantly higher LRNC after 1 year (median, 3.12 mm2; IQR, 1.82-4.60), compared with baseline measurements (median, 3.34 mm2; IQR, 2.04–4.74) (P = .06).
The results remained significant after the researchers adjusted for psoriasis severity, Framingham risk score, BMI, use of statins (beta, −0.09; 95% CI, −0.01 to −0.18; P = .033). Significant reductions in LRNC also remained when analyzing patients receiving anti-TNF, anti–IL-12/23, and anti–IL-17 biologics independently, and there were no significant between-group differences in reduction of LRNC.
The potential of biologics for improving vascular health
Discussing the study results in a press release from the American Heart Association, senior author Nehal N. Mehta, MD, MSCE, FAHA, chief of the Lab of Inflammation and Cardiometabolic Diseases at the NHLBI at NIH, compared the effect biologic therapy had on coronary plaque reduction with that of statins.
“There is approximately 6%-8% reduction in coronary plaque following therapy with statins. Similarly, our treatment with biologic therapy reduced coronary plaque by the same amount after one year. These findings suggest that biologic therapy to treat psoriasis may be just as beneficial as statin therapy on heart arteries,” Dr. Mehta said in the release.
In an interview, Nieca Goldberg, MD, medical director of NYU Women’s Heart Program at NYU Langone Health, echoed Dr. Mehta’s commments and said psoriasis carries the “potential to treat two conditions with the same drug.”
“We know conditions such as psoriatic arthritis and rheumatoid arthritis cause chronic inflammation. Chronic inflammation causes injury to blood vessels and high-risk coronary plaque. Individuals with these inflammatory conditions are at high risk for heart attack,” she said. “This study shows that biologic treatment for psoriatic arthritis can reduce the presence of high-risk plaque. It shows the potential to treat chronic inflammation and high-risk coronary plaque.”
While the results show an association between use of biologics and LRNC reduction, the study design was observational and patients had a short follow-up period. Dr. Goldberg noted more studies are needed to evaluate the effect of biologics on reducing cardiovascular events such as a myocardial infarction.
“We have never before been able to show healing of an inflamed plaque like this in humans. Biologic therapy reduces systemic inflammation and immune activation, and it has a favorable impact on improving overall vascular health,” Dr. Mehta said in the press release. “Imagine if we can treat both psoriasis and coronary heart disease with one therapy – that is the question to be asked in future studies.”
This study was funded with support from the NHLBI Intramural Research Program and the NIH Medical Research Scholars Program at the National Institutes of Health. One investigator reports financial relationships with numerous pharmaceutical companies. The other authors report no relevant conflicts of interest. Dr. Mehta also reports numerous such relationships. Dr. Goldberg reports no relevant conflicts of interest.
SOURCE: Choi H et al. Circ Cardiovasc Imaging. 2020 Sep;13(9):e011199.
Biologics used as treatment for psoriasis may also help reduce lipid-rich necrotic core (LRNC), a high-risk plaque associated with cardiovascular events, recent research from a prospective, observational study suggests.
Cardiac CT scans performed on patients with psoriasis 1 year after starting biologic therapy revealed a reduction in LRNC, compared with patients who were not receiving biologics, according to Harry Choi, MD, of the National Heart, Lung, and Blood Institute at the National Institutes of Health and colleagues. The association with reduction in LRNC and biologic therapy remained significant when adjusted for type of biologic. “These findings demonstrate that LRNC may be modulated by the control of systemic inflammation,” the researchers wrote in their study, published Sept. 15 in Circulation: Cardiovascular Imaging.
Dr. Choi and colleagues evaluated 289 patients with psoriasis within the Psoriasis Atherosclerosis and Cardiometabolic Disease Initiative cohort. The patients had a mean age of 50 years and a mean body mass index of 29.4 kg/m2, as well as a mean Psoriasis Area and Severity Index (PASI) score of 6.0. At baseline, 29% of patients had hypertension, 41% had hyperlipidemia, their mean Framingham risk score was 1.9, and a three-quarters (212 of 289) had mild to moderate psoriasis.
Changes in LRNC were observed at 1 year, compared with baseline prior to and after receiving biologic therapy (124 patients) in comparison with patients who did not undergo biologic therapy (85 patients). Biologic therapies were grouped by type, which included anti–tumor necrosis factor (anti-TNF), anti–interleukin (IL)–12/23, and anti–IL-17 biologics.
There were a significant associations between LRNC and Framingham risk score (standardized beta coefficient, 0.12; 95% confidence interval, 0.00-0.15; P = .045) and severity of psoriasis (beta, 0.13; 95% CI, 0.01-0.26; P = .029) at baseline.
Key findings
The researchers found a significant reduction in LRNC 1 year after patients began biologic therapy (median, 2.97 mm2; interquartile range, 1.99-4.66), compared with baseline (median, 3.12 mm2; IQR, 1.84-4.35) (P = .028), while patients who did not receive biologic therapy had nonsignificantly higher LRNC after 1 year (median, 3.12 mm2; IQR, 1.82-4.60), compared with baseline measurements (median, 3.34 mm2; IQR, 2.04–4.74) (P = .06).
The results remained significant after the researchers adjusted for psoriasis severity, Framingham risk score, BMI, use of statins (beta, −0.09; 95% CI, −0.01 to −0.18; P = .033). Significant reductions in LRNC also remained when analyzing patients receiving anti-TNF, anti–IL-12/23, and anti–IL-17 biologics independently, and there were no significant between-group differences in reduction of LRNC.
The potential of biologics for improving vascular health
Discussing the study results in a press release from the American Heart Association, senior author Nehal N. Mehta, MD, MSCE, FAHA, chief of the Lab of Inflammation and Cardiometabolic Diseases at the NHLBI at NIH, compared the effect biologic therapy had on coronary plaque reduction with that of statins.
“There is approximately 6%-8% reduction in coronary plaque following therapy with statins. Similarly, our treatment with biologic therapy reduced coronary plaque by the same amount after one year. These findings suggest that biologic therapy to treat psoriasis may be just as beneficial as statin therapy on heart arteries,” Dr. Mehta said in the release.
In an interview, Nieca Goldberg, MD, medical director of NYU Women’s Heart Program at NYU Langone Health, echoed Dr. Mehta’s commments and said psoriasis carries the “potential to treat two conditions with the same drug.”
“We know conditions such as psoriatic arthritis and rheumatoid arthritis cause chronic inflammation. Chronic inflammation causes injury to blood vessels and high-risk coronary plaque. Individuals with these inflammatory conditions are at high risk for heart attack,” she said. “This study shows that biologic treatment for psoriatic arthritis can reduce the presence of high-risk plaque. It shows the potential to treat chronic inflammation and high-risk coronary plaque.”
While the results show an association between use of biologics and LRNC reduction, the study design was observational and patients had a short follow-up period. Dr. Goldberg noted more studies are needed to evaluate the effect of biologics on reducing cardiovascular events such as a myocardial infarction.
“We have never before been able to show healing of an inflamed plaque like this in humans. Biologic therapy reduces systemic inflammation and immune activation, and it has a favorable impact on improving overall vascular health,” Dr. Mehta said in the press release. “Imagine if we can treat both psoriasis and coronary heart disease with one therapy – that is the question to be asked in future studies.”
This study was funded with support from the NHLBI Intramural Research Program and the NIH Medical Research Scholars Program at the National Institutes of Health. One investigator reports financial relationships with numerous pharmaceutical companies. The other authors report no relevant conflicts of interest. Dr. Mehta also reports numerous such relationships. Dr. Goldberg reports no relevant conflicts of interest.
SOURCE: Choi H et al. Circ Cardiovasc Imaging. 2020 Sep;13(9):e011199.
FROM CIRCULATION: CARDIOVASCULAR IMAGING
Many providers don’t follow hypertension guidelines
Many health care professionals are not following current, evidence-based guidelines to screen for and diagnose hypertension, and appear to have substantial gaps in knowledge, beliefs, and use of recommended practices, results from a large survey suggest.
“One surprising finding was that there was so much trust in the stethoscope, because the automated monitors are a better way to take blood pressure,” lead author Beverly Green, MD, of Kaiser Permanente Washington Health Research Institute, Seattle, said in an interview.
The results of the survey were presented Sept. 10 at the virtual joint scientific sessions of the American Heart Association Council on Hypertension, AHA Council on Kidney in Cardiovascular Disease, and American Society of Hypertension.
The U.S. Preventive Services Task Force (USPSTF) and the American Heart Association/American College of Cardiology recommend out-of-office blood pressure measurements – via ambulatory blood pressure monitoring (ABPM) or home BP monitoring – before making a new diagnosis of hypertension.
To gauge provider knowledge, beliefs, and practices related to BP diagnostic tests, the researchers surveyed 282 providers: 102 medical assistants (MA), 28 licensed practical nurses (LPNs), 33 registered nurses (RNs), 86 primary care physicians, and 33 advanced practitioners (APs).
More than three-quarters of providers (79%) felt that BP measured manually with a stethoscope and ABPM were “very or highly” accurate ways to measure BP when making a new diagnosis of hypertension.
Most did not think that automated clinic BPs, home BP, or kiosk BP measurements were very or highly accurate.
Nearly all providers surveyed (96%) reported that they “always or almost always” rely on clinic BP measurements when diagnosing hypertension, but the majority of physicians/APs would prefer using ABPM (61%) if available.
The problem with ABPM, said Dr. Green, is “it’s just not very available or convenient for patients, and a lot of providers think that patients won’t tolerate it.” Yet, without it, there is a risk for misclassification, she said.
Karen A. Griffin, MD, who chairs the AHA Council on Hypertension, said it became “customary to use clinic BP since ABPM was not previously reimbursed for the routine diagnosis of hypertension.
“Now that the payment for ABPM has been expanded, the number of machines at most institutions is not adequate for the need. Consequently, it will take some time to catch up with the current guidelines for diagnosing hypertension,” she said in an interview.
The provider survey by Dr. Green and colleagues also shows slow uptake of updated thresholds for high blood pressure.
Eighty-four percent of physicians/APs and 68% of MA/LPN/RNs said they used a clinic BP threshold of at least 140/90 mm Hg for making a new diagnosis of hypertension.
Only 3.5% and 9.0%, respectively, reported using the updated threshold of at least 130/80 mm Hg put forth in 2017.
Dr. Griffin said part of this stems from the fact that the survey began before the updated guidelines were released in 2017, “not to mention the fact that some societies have opposed the new threshold of 130/80 mm Hg.”
“I think, with time, the data on morbidity and mortality associated with the goal of 130/80 mm Hg will hopefully convince those who have not yet implemented these new guidelines that it is a safe and effective BP goal,” Dr. Griffin said.
This research had no specific funding. Dr. Green and Dr. Griffin have no relevant disclosures.
A version of this article originally appeared on Medscape.com.
Many health care professionals are not following current, evidence-based guidelines to screen for and diagnose hypertension, and appear to have substantial gaps in knowledge, beliefs, and use of recommended practices, results from a large survey suggest.
“One surprising finding was that there was so much trust in the stethoscope, because the automated monitors are a better way to take blood pressure,” lead author Beverly Green, MD, of Kaiser Permanente Washington Health Research Institute, Seattle, said in an interview.
The results of the survey were presented Sept. 10 at the virtual joint scientific sessions of the American Heart Association Council on Hypertension, AHA Council on Kidney in Cardiovascular Disease, and American Society of Hypertension.
The U.S. Preventive Services Task Force (USPSTF) and the American Heart Association/American College of Cardiology recommend out-of-office blood pressure measurements – via ambulatory blood pressure monitoring (ABPM) or home BP monitoring – before making a new diagnosis of hypertension.
To gauge provider knowledge, beliefs, and practices related to BP diagnostic tests, the researchers surveyed 282 providers: 102 medical assistants (MA), 28 licensed practical nurses (LPNs), 33 registered nurses (RNs), 86 primary care physicians, and 33 advanced practitioners (APs).
More than three-quarters of providers (79%) felt that BP measured manually with a stethoscope and ABPM were “very or highly” accurate ways to measure BP when making a new diagnosis of hypertension.
Most did not think that automated clinic BPs, home BP, or kiosk BP measurements were very or highly accurate.
Nearly all providers surveyed (96%) reported that they “always or almost always” rely on clinic BP measurements when diagnosing hypertension, but the majority of physicians/APs would prefer using ABPM (61%) if available.
The problem with ABPM, said Dr. Green, is “it’s just not very available or convenient for patients, and a lot of providers think that patients won’t tolerate it.” Yet, without it, there is a risk for misclassification, she said.
Karen A. Griffin, MD, who chairs the AHA Council on Hypertension, said it became “customary to use clinic BP since ABPM was not previously reimbursed for the routine diagnosis of hypertension.
“Now that the payment for ABPM has been expanded, the number of machines at most institutions is not adequate for the need. Consequently, it will take some time to catch up with the current guidelines for diagnosing hypertension,” she said in an interview.
The provider survey by Dr. Green and colleagues also shows slow uptake of updated thresholds for high blood pressure.
Eighty-four percent of physicians/APs and 68% of MA/LPN/RNs said they used a clinic BP threshold of at least 140/90 mm Hg for making a new diagnosis of hypertension.
Only 3.5% and 9.0%, respectively, reported using the updated threshold of at least 130/80 mm Hg put forth in 2017.
Dr. Griffin said part of this stems from the fact that the survey began before the updated guidelines were released in 2017, “not to mention the fact that some societies have opposed the new threshold of 130/80 mm Hg.”
“I think, with time, the data on morbidity and mortality associated with the goal of 130/80 mm Hg will hopefully convince those who have not yet implemented these new guidelines that it is a safe and effective BP goal,” Dr. Griffin said.
This research had no specific funding. Dr. Green and Dr. Griffin have no relevant disclosures.
A version of this article originally appeared on Medscape.com.
Many health care professionals are not following current, evidence-based guidelines to screen for and diagnose hypertension, and appear to have substantial gaps in knowledge, beliefs, and use of recommended practices, results from a large survey suggest.
“One surprising finding was that there was so much trust in the stethoscope, because the automated monitors are a better way to take blood pressure,” lead author Beverly Green, MD, of Kaiser Permanente Washington Health Research Institute, Seattle, said in an interview.
The results of the survey were presented Sept. 10 at the virtual joint scientific sessions of the American Heart Association Council on Hypertension, AHA Council on Kidney in Cardiovascular Disease, and American Society of Hypertension.
The U.S. Preventive Services Task Force (USPSTF) and the American Heart Association/American College of Cardiology recommend out-of-office blood pressure measurements – via ambulatory blood pressure monitoring (ABPM) or home BP monitoring – before making a new diagnosis of hypertension.
To gauge provider knowledge, beliefs, and practices related to BP diagnostic tests, the researchers surveyed 282 providers: 102 medical assistants (MA), 28 licensed practical nurses (LPNs), 33 registered nurses (RNs), 86 primary care physicians, and 33 advanced practitioners (APs).
More than three-quarters of providers (79%) felt that BP measured manually with a stethoscope and ABPM were “very or highly” accurate ways to measure BP when making a new diagnosis of hypertension.
Most did not think that automated clinic BPs, home BP, or kiosk BP measurements were very or highly accurate.
Nearly all providers surveyed (96%) reported that they “always or almost always” rely on clinic BP measurements when diagnosing hypertension, but the majority of physicians/APs would prefer using ABPM (61%) if available.
The problem with ABPM, said Dr. Green, is “it’s just not very available or convenient for patients, and a lot of providers think that patients won’t tolerate it.” Yet, without it, there is a risk for misclassification, she said.
Karen A. Griffin, MD, who chairs the AHA Council on Hypertension, said it became “customary to use clinic BP since ABPM was not previously reimbursed for the routine diagnosis of hypertension.
“Now that the payment for ABPM has been expanded, the number of machines at most institutions is not adequate for the need. Consequently, it will take some time to catch up with the current guidelines for diagnosing hypertension,” she said in an interview.
The provider survey by Dr. Green and colleagues also shows slow uptake of updated thresholds for high blood pressure.
Eighty-four percent of physicians/APs and 68% of MA/LPN/RNs said they used a clinic BP threshold of at least 140/90 mm Hg for making a new diagnosis of hypertension.
Only 3.5% and 9.0%, respectively, reported using the updated threshold of at least 130/80 mm Hg put forth in 2017.
Dr. Griffin said part of this stems from the fact that the survey began before the updated guidelines were released in 2017, “not to mention the fact that some societies have opposed the new threshold of 130/80 mm Hg.”
“I think, with time, the data on morbidity and mortality associated with the goal of 130/80 mm Hg will hopefully convince those who have not yet implemented these new guidelines that it is a safe and effective BP goal,” Dr. Griffin said.
This research had no specific funding. Dr. Green and Dr. Griffin have no relevant disclosures.
A version of this article originally appeared on Medscape.com.
COVID-19 and the psychological side effects of PPE
A few months ago, I published a short thought piece on the use of “sitters” with patients who were COVID-19 positive, or patients under investigation. In it, I recommended the use of telesitters for those who normally would warrant a human sitter, to decrease the discomfort of sitting in full personal protective equipment (PPE) (gown, mask, gloves, etc.) while monitoring a suicidal patient.
I received several queries, which I want to address here. In addition, I want to draw from my Army days in terms of the claustrophobia often experienced with PPE.
The first of the questions was about evidence-based practices. The second was about the discomfort of having sitters sit for many hours in the full gear.
I do not know of any evidence-based practices, but I hope we will develop them.
I agree that spending many hours in full PPE can be discomforting, which is why I wrote the essay.
As far as lessons learned from the Army time, I briefly learned how to wear a “gas mask” or Mission-Oriented Protective Posture (MOPP gear) while at Fort Bragg. We were run through the “gas chamber,” where sergeants released tear gas while we had the mask on. We were then asked to lift it up, and then tearing and sputtering, we could leave the small wooden building.
We wore the mask as part of our Army gear, usually on the right leg. After that, I mainly used the protective mask in its bag as a pillow when I was in the field.
Fast forward to August 1990. I arrived at Camp Casey, near the Korean demilitarized zone. Four days later, Saddam Hussein invaded Kuwait. The gas mask moved from a pillow to something we had to wear while doing 12-mile road marches in “full ruck.” In full ruck, you have your uniform on, with TA-50, knapsack, and weapon. No, I do not remember any more what TA-50 stands for, but essentially it is the webbing that holds your bullets and bandages.
Many could not tolerate it. They developed claustrophobia – sweating, air hunger, and panic. If stationed in the Gulf for Operation Desert Storm, they were evacuated home.
I wrote a couple of short articles on treatment of gas mask phobia.1,2 I basically advised desensitization. Start by watching TV in it for 5 minutes. Graduate to ironing your uniform in the mask. Go then to shorter runs. Work up to the 12-mile road march.
In my second tour in Korea, we had exercises where we simulated being hit by nerve agents and had to operate the hospital for days at a time in partial or full PPE. It was tough but we did it, and felt more confident about surviving attacks from North Korea.
So back to the pandemic present. I have gotten more used to my constant wearing of a surgical mask. I get anxious when I see others with masks below their noses.
The pandemic is not going away anytime soon, in my opinion. Furthermore, there are other viruses that are worse, such as Ebola. It is only a matter of time.
So, let us train with our PPE. If health care workers cannot tolerate them, use desensitization- and anxiety-reducing techniques to help them.
There are no easy answers here, in the time of the COVID pandemic. However, we owe it to ourselves, our patients, and society to do the best we can.
References
1. Ritchie EC. Milit Med. 1992 Feb;157(2):104-6.
2. Ritchie EC. Milit Med. 2001 Dec;166. Suppl. 2(1)83-4.
Dr. Ritchie is chair of psychiatry at Medstar Washington Hospital Center and professor of psychiatry at Georgetown University, Washington. She has no disclosures and can be reached at [email protected].
A few months ago, I published a short thought piece on the use of “sitters” with patients who were COVID-19 positive, or patients under investigation. In it, I recommended the use of telesitters for those who normally would warrant a human sitter, to decrease the discomfort of sitting in full personal protective equipment (PPE) (gown, mask, gloves, etc.) while monitoring a suicidal patient.
I received several queries, which I want to address here. In addition, I want to draw from my Army days in terms of the claustrophobia often experienced with PPE.
The first of the questions was about evidence-based practices. The second was about the discomfort of having sitters sit for many hours in the full gear.
I do not know of any evidence-based practices, but I hope we will develop them.
I agree that spending many hours in full PPE can be discomforting, which is why I wrote the essay.
As far as lessons learned from the Army time, I briefly learned how to wear a “gas mask” or Mission-Oriented Protective Posture (MOPP gear) while at Fort Bragg. We were run through the “gas chamber,” where sergeants released tear gas while we had the mask on. We were then asked to lift it up, and then tearing and sputtering, we could leave the small wooden building.
We wore the mask as part of our Army gear, usually on the right leg. After that, I mainly used the protective mask in its bag as a pillow when I was in the field.
Fast forward to August 1990. I arrived at Camp Casey, near the Korean demilitarized zone. Four days later, Saddam Hussein invaded Kuwait. The gas mask moved from a pillow to something we had to wear while doing 12-mile road marches in “full ruck.” In full ruck, you have your uniform on, with TA-50, knapsack, and weapon. No, I do not remember any more what TA-50 stands for, but essentially it is the webbing that holds your bullets and bandages.
Many could not tolerate it. They developed claustrophobia – sweating, air hunger, and panic. If stationed in the Gulf for Operation Desert Storm, they were evacuated home.
I wrote a couple of short articles on treatment of gas mask phobia.1,2 I basically advised desensitization. Start by watching TV in it for 5 minutes. Graduate to ironing your uniform in the mask. Go then to shorter runs. Work up to the 12-mile road march.
In my second tour in Korea, we had exercises where we simulated being hit by nerve agents and had to operate the hospital for days at a time in partial or full PPE. It was tough but we did it, and felt more confident about surviving attacks from North Korea.
So back to the pandemic present. I have gotten more used to my constant wearing of a surgical mask. I get anxious when I see others with masks below their noses.
The pandemic is not going away anytime soon, in my opinion. Furthermore, there are other viruses that are worse, such as Ebola. It is only a matter of time.
So, let us train with our PPE. If health care workers cannot tolerate them, use desensitization- and anxiety-reducing techniques to help them.
There are no easy answers here, in the time of the COVID pandemic. However, we owe it to ourselves, our patients, and society to do the best we can.
References
1. Ritchie EC. Milit Med. 1992 Feb;157(2):104-6.
2. Ritchie EC. Milit Med. 2001 Dec;166. Suppl. 2(1)83-4.
Dr. Ritchie is chair of psychiatry at Medstar Washington Hospital Center and professor of psychiatry at Georgetown University, Washington. She has no disclosures and can be reached at [email protected].
A few months ago, I published a short thought piece on the use of “sitters” with patients who were COVID-19 positive, or patients under investigation. In it, I recommended the use of telesitters for those who normally would warrant a human sitter, to decrease the discomfort of sitting in full personal protective equipment (PPE) (gown, mask, gloves, etc.) while monitoring a suicidal patient.
I received several queries, which I want to address here. In addition, I want to draw from my Army days in terms of the claustrophobia often experienced with PPE.
The first of the questions was about evidence-based practices. The second was about the discomfort of having sitters sit for many hours in the full gear.
I do not know of any evidence-based practices, but I hope we will develop them.
I agree that spending many hours in full PPE can be discomforting, which is why I wrote the essay.
As far as lessons learned from the Army time, I briefly learned how to wear a “gas mask” or Mission-Oriented Protective Posture (MOPP gear) while at Fort Bragg. We were run through the “gas chamber,” where sergeants released tear gas while we had the mask on. We were then asked to lift it up, and then tearing and sputtering, we could leave the small wooden building.
We wore the mask as part of our Army gear, usually on the right leg. After that, I mainly used the protective mask in its bag as a pillow when I was in the field.
Fast forward to August 1990. I arrived at Camp Casey, near the Korean demilitarized zone. Four days later, Saddam Hussein invaded Kuwait. The gas mask moved from a pillow to something we had to wear while doing 12-mile road marches in “full ruck.” In full ruck, you have your uniform on, with TA-50, knapsack, and weapon. No, I do not remember any more what TA-50 stands for, but essentially it is the webbing that holds your bullets and bandages.
Many could not tolerate it. They developed claustrophobia – sweating, air hunger, and panic. If stationed in the Gulf for Operation Desert Storm, they were evacuated home.
I wrote a couple of short articles on treatment of gas mask phobia.1,2 I basically advised desensitization. Start by watching TV in it for 5 minutes. Graduate to ironing your uniform in the mask. Go then to shorter runs. Work up to the 12-mile road march.
In my second tour in Korea, we had exercises where we simulated being hit by nerve agents and had to operate the hospital for days at a time in partial or full PPE. It was tough but we did it, and felt more confident about surviving attacks from North Korea.
So back to the pandemic present. I have gotten more used to my constant wearing of a surgical mask. I get anxious when I see others with masks below their noses.
The pandemic is not going away anytime soon, in my opinion. Furthermore, there are other viruses that are worse, such as Ebola. It is only a matter of time.
So, let us train with our PPE. If health care workers cannot tolerate them, use desensitization- and anxiety-reducing techniques to help them.
There are no easy answers here, in the time of the COVID pandemic. However, we owe it to ourselves, our patients, and society to do the best we can.
References
1. Ritchie EC. Milit Med. 1992 Feb;157(2):104-6.
2. Ritchie EC. Milit Med. 2001 Dec;166. Suppl. 2(1)83-4.
Dr. Ritchie is chair of psychiatry at Medstar Washington Hospital Center and professor of psychiatry at Georgetown University, Washington. She has no disclosures and can be reached at [email protected].
Children and COVID-19: New cases may be leveling off
Growth in new pediatric COVID-19 cases has evened out in recent weeks, but children now represent 10% of all COVID-19 cases in the United States, and that measurement has been rising throughout the pandemic, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
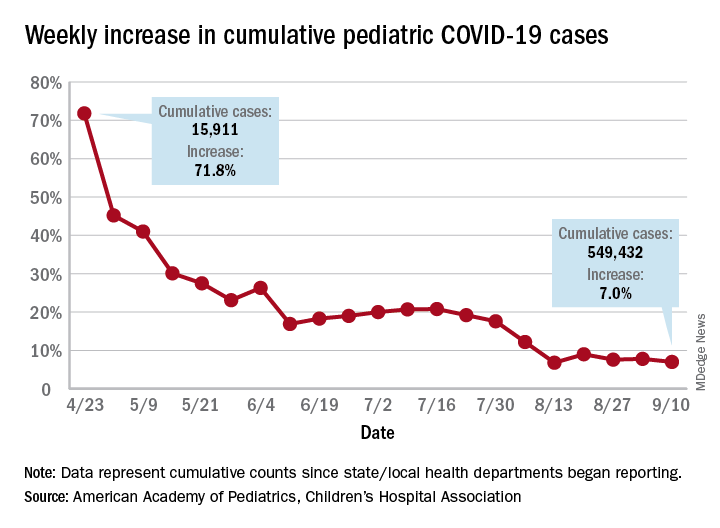
the AAP and the CHA said in the report, based on data from 49 states (New York City is included but not New York state), the District of Columbia, Puerto Rico, and Guam.
The weekly percentage of increase in the number of new cases has not reached double digits since early August and has been no higher than 7.8% over the last 3 weeks. The number of child COVID-19 cases, however, has finally reached 10% of the total for Americans of all ages, which stands at 5.49 million in the jurisdictions included in the report, the AHA and CHA reported.
Measures, however, continue to show low levels of severe illness in children, they noted, including the following:
- Child cases as a proportion of all COVID-19 hospitalizations: 1.7%.
- Hospitalization rate for children: 1.8%.
- Child deaths as a proportion of all deaths: 0.07%.
- Percent of child cases resulting in death: 0.01%.
The number of cumulative cases per 100,000 children is now up to 728.5 nationally, with a range by state that goes from 154.0 in Vermont to 1,670.3 in Tennessee, which is one of only two states reporting cases in those aged 0-20 years as children (the other is South Carolina). The age range for children is 0-17 or 0-19 for most other states, although Florida uses a range of 0-14, the report notes.
Other than Tennessee, there are 10 states with overall rates higher than 1,000 COVID-19 cases per 100,000 children, and there are nine states with cumulative totals over 15,000 cases (California is the highest with just over 75,000), according to the report.
Growth in new pediatric COVID-19 cases has evened out in recent weeks, but children now represent 10% of all COVID-19 cases in the United States, and that measurement has been rising throughout the pandemic, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
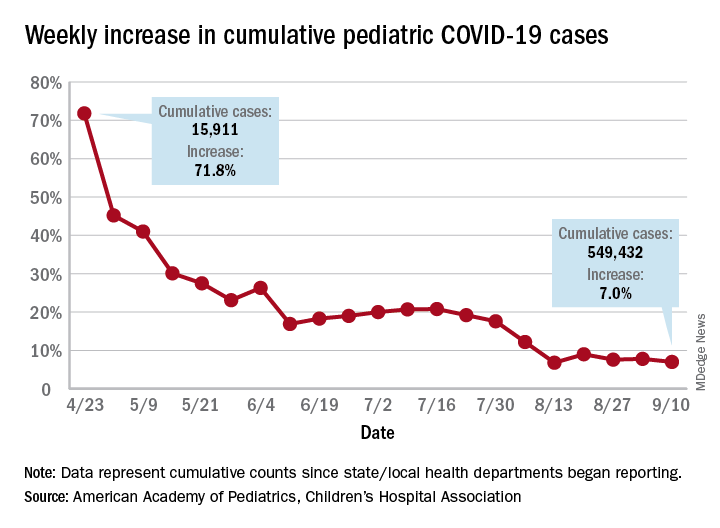
the AAP and the CHA said in the report, based on data from 49 states (New York City is included but not New York state), the District of Columbia, Puerto Rico, and Guam.
The weekly percentage of increase in the number of new cases has not reached double digits since early August and has been no higher than 7.8% over the last 3 weeks. The number of child COVID-19 cases, however, has finally reached 10% of the total for Americans of all ages, which stands at 5.49 million in the jurisdictions included in the report, the AHA and CHA reported.
Measures, however, continue to show low levels of severe illness in children, they noted, including the following:
- Child cases as a proportion of all COVID-19 hospitalizations: 1.7%.
- Hospitalization rate for children: 1.8%.
- Child deaths as a proportion of all deaths: 0.07%.
- Percent of child cases resulting in death: 0.01%.
The number of cumulative cases per 100,000 children is now up to 728.5 nationally, with a range by state that goes from 154.0 in Vermont to 1,670.3 in Tennessee, which is one of only two states reporting cases in those aged 0-20 years as children (the other is South Carolina). The age range for children is 0-17 or 0-19 for most other states, although Florida uses a range of 0-14, the report notes.
Other than Tennessee, there are 10 states with overall rates higher than 1,000 COVID-19 cases per 100,000 children, and there are nine states with cumulative totals over 15,000 cases (California is the highest with just over 75,000), according to the report.
Growth in new pediatric COVID-19 cases has evened out in recent weeks, but children now represent 10% of all COVID-19 cases in the United States, and that measurement has been rising throughout the pandemic, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
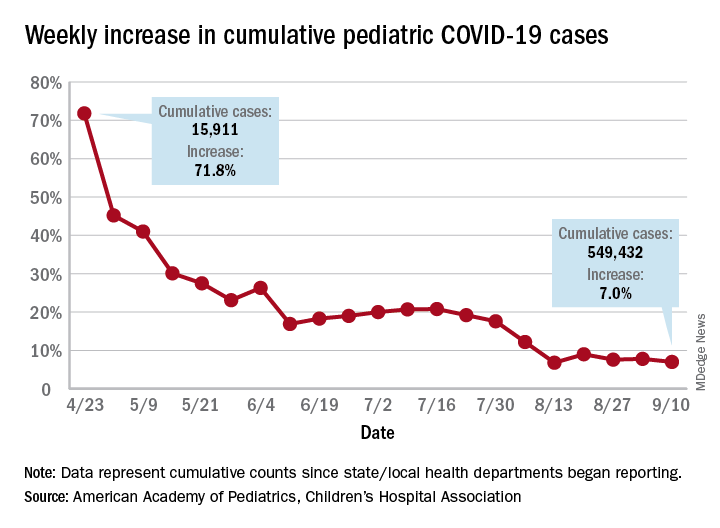
the AAP and the CHA said in the report, based on data from 49 states (New York City is included but not New York state), the District of Columbia, Puerto Rico, and Guam.
The weekly percentage of increase in the number of new cases has not reached double digits since early August and has been no higher than 7.8% over the last 3 weeks. The number of child COVID-19 cases, however, has finally reached 10% of the total for Americans of all ages, which stands at 5.49 million in the jurisdictions included in the report, the AHA and CHA reported.
Measures, however, continue to show low levels of severe illness in children, they noted, including the following:
- Child cases as a proportion of all COVID-19 hospitalizations: 1.7%.
- Hospitalization rate for children: 1.8%.
- Child deaths as a proportion of all deaths: 0.07%.
- Percent of child cases resulting in death: 0.01%.
The number of cumulative cases per 100,000 children is now up to 728.5 nationally, with a range by state that goes from 154.0 in Vermont to 1,670.3 in Tennessee, which is one of only two states reporting cases in those aged 0-20 years as children (the other is South Carolina). The age range for children is 0-17 or 0-19 for most other states, although Florida uses a range of 0-14, the report notes.
Other than Tennessee, there are 10 states with overall rates higher than 1,000 COVID-19 cases per 100,000 children, and there are nine states with cumulative totals over 15,000 cases (California is the highest with just over 75,000), according to the report.