User login
CDC launches new center to watch for future outbreaks
The Centers for Disease Control and Prevention is setting up a new hub to watch for early warning signs of future infectious outbreaks, the agency announced on Aug. 18.
Epidemiologists learn about emerging outbreaks by tracking information, and the quality of their analysis depends on their access to high-quality data. Gaps in existing systems became obvious during the COVID-19 pandemic as experts were challenged by the crisis.
The new Center for Forecasting and Outbreak Analytics will, in part, work like a meteorological office that tracks weather-related changes, only the center will track possible flareups in infectious disease.
The day after he took office, President Joe Biden pledged to modernize the country’s system for public health data. First funding for the initiative will come from the American Rescue Plan.
“We are excited to have the expertise and ability to model and forecast public health concerns and share information in real-time to activate governmental, private sector, and public actions in anticipation of threats both domestically and abroad,” CDC Director Rochelle Walensky, MD, said in a statement.
Devastating toll of COVID-19
Many world leaders are now responding to the destruction of the health crisis and are investing in new infrastructure. A July report from a G-20 panel calls for $75 billion in international financing for pandemic prevention and preparedness –twice as much as current spending levels.
Testifying in a congressional hearing, epidemiologist Caitlin Rivers, PhD, from the Johns Hopkins Center for Health Security, Baltimore, voiced the importance of never being caught unprepared again.
“We were unprepared to manage the emergence and swift global spread of the novel coronavirus, and we were late to recognize when it reached our shores. Those delays set us on a worse trajectory than we might have otherwise faced,” she said.
Dr. Rivers will join the new center’s leadership team as associate director working alongside Marc Lipsitch, PhD, director for science.
“The new center will meet a longstanding need for a national focal point to analyze data and forecast the trajectory of pandemics with the express goal of informing and improving decisions with the best available evidence,” Dr. Lipsitch said in the CDC’s news release announcing the new center.
Experts will map what data sources are needed to assist disease modelers and public health emergency responders tracking emerging problems that they can share with decision-makers. They will expand tracking capability and data sharing using open-source software and application programming with existing and new data streams from the public health ecosystem and elsewhere.
Dylan George, PhD, who will be the center’s director for operations, said in the CDC news release that the center will provide critical information to communities so they can respond.
“Pandemics threaten our families and communities at speed and scale – our response needs to move at speed and scale, too,” he said.
A version of this article first appeared on WebMD.com.
The Centers for Disease Control and Prevention is setting up a new hub to watch for early warning signs of future infectious outbreaks, the agency announced on Aug. 18.
Epidemiologists learn about emerging outbreaks by tracking information, and the quality of their analysis depends on their access to high-quality data. Gaps in existing systems became obvious during the COVID-19 pandemic as experts were challenged by the crisis.
The new Center for Forecasting and Outbreak Analytics will, in part, work like a meteorological office that tracks weather-related changes, only the center will track possible flareups in infectious disease.
The day after he took office, President Joe Biden pledged to modernize the country’s system for public health data. First funding for the initiative will come from the American Rescue Plan.
“We are excited to have the expertise and ability to model and forecast public health concerns and share information in real-time to activate governmental, private sector, and public actions in anticipation of threats both domestically and abroad,” CDC Director Rochelle Walensky, MD, said in a statement.
Devastating toll of COVID-19
Many world leaders are now responding to the destruction of the health crisis and are investing in new infrastructure. A July report from a G-20 panel calls for $75 billion in international financing for pandemic prevention and preparedness –twice as much as current spending levels.
Testifying in a congressional hearing, epidemiologist Caitlin Rivers, PhD, from the Johns Hopkins Center for Health Security, Baltimore, voiced the importance of never being caught unprepared again.
“We were unprepared to manage the emergence and swift global spread of the novel coronavirus, and we were late to recognize when it reached our shores. Those delays set us on a worse trajectory than we might have otherwise faced,” she said.
Dr. Rivers will join the new center’s leadership team as associate director working alongside Marc Lipsitch, PhD, director for science.
“The new center will meet a longstanding need for a national focal point to analyze data and forecast the trajectory of pandemics with the express goal of informing and improving decisions with the best available evidence,” Dr. Lipsitch said in the CDC’s news release announcing the new center.
Experts will map what data sources are needed to assist disease modelers and public health emergency responders tracking emerging problems that they can share with decision-makers. They will expand tracking capability and data sharing using open-source software and application programming with existing and new data streams from the public health ecosystem and elsewhere.
Dylan George, PhD, who will be the center’s director for operations, said in the CDC news release that the center will provide critical information to communities so they can respond.
“Pandemics threaten our families and communities at speed and scale – our response needs to move at speed and scale, too,” he said.
A version of this article first appeared on WebMD.com.
The Centers for Disease Control and Prevention is setting up a new hub to watch for early warning signs of future infectious outbreaks, the agency announced on Aug. 18.
Epidemiologists learn about emerging outbreaks by tracking information, and the quality of their analysis depends on their access to high-quality data. Gaps in existing systems became obvious during the COVID-19 pandemic as experts were challenged by the crisis.
The new Center for Forecasting and Outbreak Analytics will, in part, work like a meteorological office that tracks weather-related changes, only the center will track possible flareups in infectious disease.
The day after he took office, President Joe Biden pledged to modernize the country’s system for public health data. First funding for the initiative will come from the American Rescue Plan.
“We are excited to have the expertise and ability to model and forecast public health concerns and share information in real-time to activate governmental, private sector, and public actions in anticipation of threats both domestically and abroad,” CDC Director Rochelle Walensky, MD, said in a statement.
Devastating toll of COVID-19
Many world leaders are now responding to the destruction of the health crisis and are investing in new infrastructure. A July report from a G-20 panel calls for $75 billion in international financing for pandemic prevention and preparedness –twice as much as current spending levels.
Testifying in a congressional hearing, epidemiologist Caitlin Rivers, PhD, from the Johns Hopkins Center for Health Security, Baltimore, voiced the importance of never being caught unprepared again.
“We were unprepared to manage the emergence and swift global spread of the novel coronavirus, and we were late to recognize when it reached our shores. Those delays set us on a worse trajectory than we might have otherwise faced,” she said.
Dr. Rivers will join the new center’s leadership team as associate director working alongside Marc Lipsitch, PhD, director for science.
“The new center will meet a longstanding need for a national focal point to analyze data and forecast the trajectory of pandemics with the express goal of informing and improving decisions with the best available evidence,” Dr. Lipsitch said in the CDC’s news release announcing the new center.
Experts will map what data sources are needed to assist disease modelers and public health emergency responders tracking emerging problems that they can share with decision-makers. They will expand tracking capability and data sharing using open-source software and application programming with existing and new data streams from the public health ecosystem and elsewhere.
Dylan George, PhD, who will be the center’s director for operations, said in the CDC news release that the center will provide critical information to communities so they can respond.
“Pandemics threaten our families and communities at speed and scale – our response needs to move at speed and scale, too,” he said.
A version of this article first appeared on WebMD.com.
How to pick the best face masks for children, according to the experts
One essential back-to-school item for children this fall is a face mask – the Centers for Disease Control and Prevention and the American Academy of Pediatrics both recommend them – but finding one that’s actually protective for a child is not a straightforward task, as many parents can attest.
There’s little in the way of official guidance or research to inform evidence-based recommendations on what type of face masks works best for children.
Search for children’s face masks on Amazon and you’ll run into a smorgasbord of options: masks with three, four, or five layers, different designs, and different materials. There’s one company selling a mask it calls an m95 model, a term the company devised.
It’s almost impossible to verify many of the claims being made by the manufacturers, or to know if they will fit your child’s face until you order some, which can get expensive.
But it’s worth looking for a good mask. A large study of more than 1 million people being conducted online by Facebook and Carnegie Mellon University found that students who wore face masks in school had a reduced risk for testing positive for the virus and getting sick with COVID-19 symptoms. The study was published in June in the journal Science.
Delta more contagious
The Delta variant of the new coronavirus is much more contagious than previous versions of the virus. Studies have shown that infected people carry 1,000 times more virus in their noses and throats than with the viruses that circulated last winter and spring. They shed more viral particles into the air when they talk or yell or sing, making this COVID-19–causing virus much more transmissible than in the past.
What that means, says Kimberly Prather, PhD, an aerosol scientist and distinguished professor at the Scripps Institution of Oceanography in La Jolla, California, is that if it once took about 15 minutes of proximity to an infected person to catch the infection, that window of risk is now much shorter.
“If you believe the 15-minute magical number, now if you take 1,000 times the viral load, basically in 1 second you could inhale that same amount of virus. So it’s gone from 15 minutes to 1 second,” Dr. Prather said in an online seminar on school safety she helped to organize.
A better mask
What that means is that we need to upgrade our face masks, switching away from ill-fitting fabric masks, which can offer varying degrees of protection depending on the number of layers and type of fabric that’s used, to more highly protective surgical masks or better yet, N95 respirators, which provide the highest level of filtration.
That’s harder to do for children, who have much smaller faces.
Any masks that gapes around the edges isn’t going to work well, no matter how well it filters.
“N95s are not made to fit kids. They do not come in kid sizes, so I do not recommend N95s for kids,” said Linsey Marr, an environmental engineer at Virginia Tech, who tests face masks in her lab.
Ms. Marr says parents need to consider the attributes masks in this order of priority:
Comfort: “If your kid won’t wear it, it’s not helping at all,” she said.
Fit: “Leaks around the sides are like having a hole in your mask and aerosols carrying the virus can get right through,” Ms. Marr said.
Filtration: How well the mask blocks small particles.
One option to improve fit is to layer a fabric mask over a surgical mask. The fabric mask helps to hold the edges of the surgical mask more tightly to a person’s face. The surgical mask creates better filtration.
Ms. Marr said KN94 or KN95 masks, which are being manufactured in China and Korea, are good choices. They offer nearly the same degree of filtration as an N95, and they fit closely to the face, to minimize leaks.
Check for counterfeits
The KN94 and KN95 masks for children are widely available, but Ms. Marr said parents do need to watch out for counterfeits, which don’t perform as well.
The National Institute for Occupational Safety and Health gives examples of counterfeit products here.
There’s also a type of cloth mask that has a built-in, edge-to-edge filter layer that is made for children.
“Some of these filter out more than 99% of particles and those can be very effective, if they fit well,” Ms. Marr said.
She has compiled and publicly posted a list of her recommendations for masks for children.
There’s also a new standard for face masks. It’s called ASTM F3502-21, and it’s published by an international organization that sets voluntary standards for thousands of products. To claim that a mask meets this standard, a manufacturer has to have its mask tested and demonstrate that it provides a certain level of filtration and breathability.
A version of this article first appeared on Medscape.com.
One essential back-to-school item for children this fall is a face mask – the Centers for Disease Control and Prevention and the American Academy of Pediatrics both recommend them – but finding one that’s actually protective for a child is not a straightforward task, as many parents can attest.
There’s little in the way of official guidance or research to inform evidence-based recommendations on what type of face masks works best for children.
Search for children’s face masks on Amazon and you’ll run into a smorgasbord of options: masks with three, four, or five layers, different designs, and different materials. There’s one company selling a mask it calls an m95 model, a term the company devised.
It’s almost impossible to verify many of the claims being made by the manufacturers, or to know if they will fit your child’s face until you order some, which can get expensive.
But it’s worth looking for a good mask. A large study of more than 1 million people being conducted online by Facebook and Carnegie Mellon University found that students who wore face masks in school had a reduced risk for testing positive for the virus and getting sick with COVID-19 symptoms. The study was published in June in the journal Science.
Delta more contagious
The Delta variant of the new coronavirus is much more contagious than previous versions of the virus. Studies have shown that infected people carry 1,000 times more virus in their noses and throats than with the viruses that circulated last winter and spring. They shed more viral particles into the air when they talk or yell or sing, making this COVID-19–causing virus much more transmissible than in the past.
What that means, says Kimberly Prather, PhD, an aerosol scientist and distinguished professor at the Scripps Institution of Oceanography in La Jolla, California, is that if it once took about 15 minutes of proximity to an infected person to catch the infection, that window of risk is now much shorter.
“If you believe the 15-minute magical number, now if you take 1,000 times the viral load, basically in 1 second you could inhale that same amount of virus. So it’s gone from 15 minutes to 1 second,” Dr. Prather said in an online seminar on school safety she helped to organize.
A better mask
What that means is that we need to upgrade our face masks, switching away from ill-fitting fabric masks, which can offer varying degrees of protection depending on the number of layers and type of fabric that’s used, to more highly protective surgical masks or better yet, N95 respirators, which provide the highest level of filtration.
That’s harder to do for children, who have much smaller faces.
Any masks that gapes around the edges isn’t going to work well, no matter how well it filters.
“N95s are not made to fit kids. They do not come in kid sizes, so I do not recommend N95s for kids,” said Linsey Marr, an environmental engineer at Virginia Tech, who tests face masks in her lab.
Ms. Marr says parents need to consider the attributes masks in this order of priority:
Comfort: “If your kid won’t wear it, it’s not helping at all,” she said.
Fit: “Leaks around the sides are like having a hole in your mask and aerosols carrying the virus can get right through,” Ms. Marr said.
Filtration: How well the mask blocks small particles.
One option to improve fit is to layer a fabric mask over a surgical mask. The fabric mask helps to hold the edges of the surgical mask more tightly to a person’s face. The surgical mask creates better filtration.
Ms. Marr said KN94 or KN95 masks, which are being manufactured in China and Korea, are good choices. They offer nearly the same degree of filtration as an N95, and they fit closely to the face, to minimize leaks.
Check for counterfeits
The KN94 and KN95 masks for children are widely available, but Ms. Marr said parents do need to watch out for counterfeits, which don’t perform as well.
The National Institute for Occupational Safety and Health gives examples of counterfeit products here.
There’s also a type of cloth mask that has a built-in, edge-to-edge filter layer that is made for children.
“Some of these filter out more than 99% of particles and those can be very effective, if they fit well,” Ms. Marr said.
She has compiled and publicly posted a list of her recommendations for masks for children.
There’s also a new standard for face masks. It’s called ASTM F3502-21, and it’s published by an international organization that sets voluntary standards for thousands of products. To claim that a mask meets this standard, a manufacturer has to have its mask tested and demonstrate that it provides a certain level of filtration and breathability.
A version of this article first appeared on Medscape.com.
One essential back-to-school item for children this fall is a face mask – the Centers for Disease Control and Prevention and the American Academy of Pediatrics both recommend them – but finding one that’s actually protective for a child is not a straightforward task, as many parents can attest.
There’s little in the way of official guidance or research to inform evidence-based recommendations on what type of face masks works best for children.
Search for children’s face masks on Amazon and you’ll run into a smorgasbord of options: masks with three, four, or five layers, different designs, and different materials. There’s one company selling a mask it calls an m95 model, a term the company devised.
It’s almost impossible to verify many of the claims being made by the manufacturers, or to know if they will fit your child’s face until you order some, which can get expensive.
But it’s worth looking for a good mask. A large study of more than 1 million people being conducted online by Facebook and Carnegie Mellon University found that students who wore face masks in school had a reduced risk for testing positive for the virus and getting sick with COVID-19 symptoms. The study was published in June in the journal Science.
Delta more contagious
The Delta variant of the new coronavirus is much more contagious than previous versions of the virus. Studies have shown that infected people carry 1,000 times more virus in their noses and throats than with the viruses that circulated last winter and spring. They shed more viral particles into the air when they talk or yell or sing, making this COVID-19–causing virus much more transmissible than in the past.
What that means, says Kimberly Prather, PhD, an aerosol scientist and distinguished professor at the Scripps Institution of Oceanography in La Jolla, California, is that if it once took about 15 minutes of proximity to an infected person to catch the infection, that window of risk is now much shorter.
“If you believe the 15-minute magical number, now if you take 1,000 times the viral load, basically in 1 second you could inhale that same amount of virus. So it’s gone from 15 minutes to 1 second,” Dr. Prather said in an online seminar on school safety she helped to organize.
A better mask
What that means is that we need to upgrade our face masks, switching away from ill-fitting fabric masks, which can offer varying degrees of protection depending on the number of layers and type of fabric that’s used, to more highly protective surgical masks or better yet, N95 respirators, which provide the highest level of filtration.
That’s harder to do for children, who have much smaller faces.
Any masks that gapes around the edges isn’t going to work well, no matter how well it filters.
“N95s are not made to fit kids. They do not come in kid sizes, so I do not recommend N95s for kids,” said Linsey Marr, an environmental engineer at Virginia Tech, who tests face masks in her lab.
Ms. Marr says parents need to consider the attributes masks in this order of priority:
Comfort: “If your kid won’t wear it, it’s not helping at all,” she said.
Fit: “Leaks around the sides are like having a hole in your mask and aerosols carrying the virus can get right through,” Ms. Marr said.
Filtration: How well the mask blocks small particles.
One option to improve fit is to layer a fabric mask over a surgical mask. The fabric mask helps to hold the edges of the surgical mask more tightly to a person’s face. The surgical mask creates better filtration.
Ms. Marr said KN94 or KN95 masks, which are being manufactured in China and Korea, are good choices. They offer nearly the same degree of filtration as an N95, and they fit closely to the face, to minimize leaks.
Check for counterfeits
The KN94 and KN95 masks for children are widely available, but Ms. Marr said parents do need to watch out for counterfeits, which don’t perform as well.
The National Institute for Occupational Safety and Health gives examples of counterfeit products here.
There’s also a type of cloth mask that has a built-in, edge-to-edge filter layer that is made for children.
“Some of these filter out more than 99% of particles and those can be very effective, if they fit well,” Ms. Marr said.
She has compiled and publicly posted a list of her recommendations for masks for children.
There’s also a new standard for face masks. It’s called ASTM F3502-21, and it’s published by an international organization that sets voluntary standards for thousands of products. To claim that a mask meets this standard, a manufacturer has to have its mask tested and demonstrate that it provides a certain level of filtration and breathability.
A version of this article first appeared on Medscape.com.
Antibiotics, microbiome may affect immunogenicity in IBD
The use fluoroquinolones or macrolides reduced immunogenicity risk in inflammatory bowel disease (IBD) patients on anti–tumor necrosis factor (anti-TNF) therapy, according to data from nearly 2,000 individuals.
Anti-TNF therapy with monoclonal antibodies is an established treatment for Crohn’s disease and ulcerative colitis, but approximately 40% of patients fail to respond initially and even more fail to achieve complete remission, wrote Yuri Gorelik, MD, of Rambam Health Care Campus, Haifa, Israel, and colleagues.
“Immunogenicity, which refers to the development of antidrug antibodies [ADA] is considered as the main factor driving secondary loss of response and is likely involved in primary nonresponse as well,” but data on how to predict the risk for ADA formation are limited, they said.
In a study published in Gut, the researchers identified data from 1,946 IBD patients using the epi-IIRN (epidemiology group of the Israeli IBD research nucleus), a nationwide registry of all IBD patients in Israel.
A total of 363 patients had positive ADA after a median follow-up period of 651 days after starting therapy. Overall, the risk of ADA development was significantly higher in patients on cephalosporins (adjusted hazard ratio, 1.97; 95% confidence interval, 1.58-2.44) or penicillin with beta-lactamase inhibitors (BLIs) (aHR, 1.38; 95% CI, 1.13-1.74) during anti-TNF therapy, and it was higher still for patients using both. By contrast, the risk was lower in patients on macrolides (aHR, 0.36; 95% CI, 0.16-0.82) or fluoroquinolones (aHR, 0.20; 95% CI; 95% CI, 0.12-0.35). All P values were less than .05 when compared with nontreated groups.
In the same study, the researchers reported data on mice treated with antibiotics and challenged with infliximab to evaluate the causative effect of antibiotics and the associated disruption to the gut microbiome on the formation of ADA. After 14 days, the researchers found significantly increased ADA production in mice treated with cephalosporins, compared with those treated with macrolides, but germ-free mice produced no ADA, which supports the role of microbial composition on ADA production.
The investigators cited previous research into the microbiome as a biomarker for prediction response to anti-TNF therapy; past results have also suggested that the effect of cephalosporins and penicillin-BLIs could be explained by the particular dysbiosis induced by those agents.
The study findings were limited by several factors including the retrospective design and potential for selection bias, as well as the inability to adjust antibiotic exposure according to type and severity of infection, they noted. However, “this is the first large scale study that extensively evaluated the effect of different antibiotic classes on immunogenicity of anti-TNF therapy,” and the results suggest that ADA development during anti-TNF therapy may to reduced by the use of fluoroquinolones and macrolides.
“Specific microbial manipulation may serve as a tool to modify immunogenicity which is preferably turned on for protective immunizations and off for biological therapy,” they noted. “Further studies involving detailed analysis of the antibiotic effects on the human microbiome and immune milieu are needed, as well as comparative experiments with other medications used to reduce immunogenicity.”
Unexpected findings may drive future drug choices
“Development of antidrug antibodies in patients on biologics for inflammatory bowel disease is an important mechanism for loss of response to a therapeutic agent,” Kim L. Isaacs, MD, AGAF, of the University of North Carolina at Chapel Hill, said in an interview. “To date the causes of development of ADAs is relatively understudied. Our approach to prevent ADA includes increasing immunosuppression in patients most commonly with combination therapy with thiopurines. If factors that provoke or prevent antibody formation are elucidated, therapy can be tailored to prevent ADAs and maximize the duration of response of many of our biologic therapies.”
A prior study performed by the ABIRISK European consortium demonstrated associations with antibiotics. “In the current study, there was a differential effect of cephalosporins/penicillins (increased immunogenicity) and macrolides (decreased immunogenicity),” she said. “These studies suggest that the microbiome may be important in ADA formation to biologics – this is a concept that is novel and unexpected.
“The rationale for the choice of antibiotics in the population studied is not known, and it is possible that different infections may have led to different antibiotic choices, which in turn may have affected immunogenicity,” said Dr. Isaacs. However, clinicians might be able to tailor antibiotic choice in the future if the microbiome is playing a major role in risk for development of ADA.
“Further research is needed to further correlate microbiome changes with immunogenicity, to look at other classes of antibiotics and their role in immunogenicity, and to clarify the infections or reasons that these patients are receiving antibiotics,” Dr. Isaacs concluded.
Understanding the microbiome
Recent observations have shown associations between clinical response to anti-TNF and gut microbiota composition, noted Jatin Roper, MD, of Duke University, Durham, N.C. “More broadly, a growing body of evidence suggests that the gut microbiota modulates the metabolism of many therapeutic agents, as well as immune responses to infections.”
That said, Dr. Roper was surprised that “clinical use of different antibiotics, often short term, had such distinct effects on ADA levels.” Furthermore, “these findings suggest that distinct microbiota or microbial metabolic products impact antibody development to common immunomodulatory therapies in opposite ways,” which is itself a surprising finding.
Such antibodies to anti-TNF therapy are common in IBD, he said, but one implication of the study is how antibiotics could be carefully used “to reduce risk of ADAs and enhance efficacy of anti-TNF therapy.”
However, because any antibiotic therapy will modify the gut microbiome and lead to unwanted effects, “further research is needed on how these agents impact the gut microbiome, with the ultimate goal of identifying specific microbiota or microbial metabolic products that can reproduce the intriguing findings of this paper.”
The study was supported in part by the Leona M. and Harry B. Helmsley Charitable Trust and the Israeli Ministry of Science and Technology. Dr. Gorelik had no financial conflicts to disclose. Several coauthors disclosed relationships with multiple pharmaceutical companies including AbbVie, CytoReason, Takeda, and Pfizer. Dr. Isaacs had no financial conflicts to disclose, but serves on the GI&Hepatology News board of editors. Dr. Roper had no relevant disclosures.
Help your patients better understand their IBD treatment options by sharing AGA’s patient education, “Living with IBD,” in the AGA GI Patient Center at www.gastro.org/IBD.
The use fluoroquinolones or macrolides reduced immunogenicity risk in inflammatory bowel disease (IBD) patients on anti–tumor necrosis factor (anti-TNF) therapy, according to data from nearly 2,000 individuals.
Anti-TNF therapy with monoclonal antibodies is an established treatment for Crohn’s disease and ulcerative colitis, but approximately 40% of patients fail to respond initially and even more fail to achieve complete remission, wrote Yuri Gorelik, MD, of Rambam Health Care Campus, Haifa, Israel, and colleagues.
“Immunogenicity, which refers to the development of antidrug antibodies [ADA] is considered as the main factor driving secondary loss of response and is likely involved in primary nonresponse as well,” but data on how to predict the risk for ADA formation are limited, they said.
In a study published in Gut, the researchers identified data from 1,946 IBD patients using the epi-IIRN (epidemiology group of the Israeli IBD research nucleus), a nationwide registry of all IBD patients in Israel.
A total of 363 patients had positive ADA after a median follow-up period of 651 days after starting therapy. Overall, the risk of ADA development was significantly higher in patients on cephalosporins (adjusted hazard ratio, 1.97; 95% confidence interval, 1.58-2.44) or penicillin with beta-lactamase inhibitors (BLIs) (aHR, 1.38; 95% CI, 1.13-1.74) during anti-TNF therapy, and it was higher still for patients using both. By contrast, the risk was lower in patients on macrolides (aHR, 0.36; 95% CI, 0.16-0.82) or fluoroquinolones (aHR, 0.20; 95% CI; 95% CI, 0.12-0.35). All P values were less than .05 when compared with nontreated groups.
In the same study, the researchers reported data on mice treated with antibiotics and challenged with infliximab to evaluate the causative effect of antibiotics and the associated disruption to the gut microbiome on the formation of ADA. After 14 days, the researchers found significantly increased ADA production in mice treated with cephalosporins, compared with those treated with macrolides, but germ-free mice produced no ADA, which supports the role of microbial composition on ADA production.
The investigators cited previous research into the microbiome as a biomarker for prediction response to anti-TNF therapy; past results have also suggested that the effect of cephalosporins and penicillin-BLIs could be explained by the particular dysbiosis induced by those agents.
The study findings were limited by several factors including the retrospective design and potential for selection bias, as well as the inability to adjust antibiotic exposure according to type and severity of infection, they noted. However, “this is the first large scale study that extensively evaluated the effect of different antibiotic classes on immunogenicity of anti-TNF therapy,” and the results suggest that ADA development during anti-TNF therapy may to reduced by the use of fluoroquinolones and macrolides.
“Specific microbial manipulation may serve as a tool to modify immunogenicity which is preferably turned on for protective immunizations and off for biological therapy,” they noted. “Further studies involving detailed analysis of the antibiotic effects on the human microbiome and immune milieu are needed, as well as comparative experiments with other medications used to reduce immunogenicity.”
Unexpected findings may drive future drug choices
“Development of antidrug antibodies in patients on biologics for inflammatory bowel disease is an important mechanism for loss of response to a therapeutic agent,” Kim L. Isaacs, MD, AGAF, of the University of North Carolina at Chapel Hill, said in an interview. “To date the causes of development of ADAs is relatively understudied. Our approach to prevent ADA includes increasing immunosuppression in patients most commonly with combination therapy with thiopurines. If factors that provoke or prevent antibody formation are elucidated, therapy can be tailored to prevent ADAs and maximize the duration of response of many of our biologic therapies.”
A prior study performed by the ABIRISK European consortium demonstrated associations with antibiotics. “In the current study, there was a differential effect of cephalosporins/penicillins (increased immunogenicity) and macrolides (decreased immunogenicity),” she said. “These studies suggest that the microbiome may be important in ADA formation to biologics – this is a concept that is novel and unexpected.
“The rationale for the choice of antibiotics in the population studied is not known, and it is possible that different infections may have led to different antibiotic choices, which in turn may have affected immunogenicity,” said Dr. Isaacs. However, clinicians might be able to tailor antibiotic choice in the future if the microbiome is playing a major role in risk for development of ADA.
“Further research is needed to further correlate microbiome changes with immunogenicity, to look at other classes of antibiotics and their role in immunogenicity, and to clarify the infections or reasons that these patients are receiving antibiotics,” Dr. Isaacs concluded.
Understanding the microbiome
Recent observations have shown associations between clinical response to anti-TNF and gut microbiota composition, noted Jatin Roper, MD, of Duke University, Durham, N.C. “More broadly, a growing body of evidence suggests that the gut microbiota modulates the metabolism of many therapeutic agents, as well as immune responses to infections.”
That said, Dr. Roper was surprised that “clinical use of different antibiotics, often short term, had such distinct effects on ADA levels.” Furthermore, “these findings suggest that distinct microbiota or microbial metabolic products impact antibody development to common immunomodulatory therapies in opposite ways,” which is itself a surprising finding.
Such antibodies to anti-TNF therapy are common in IBD, he said, but one implication of the study is how antibiotics could be carefully used “to reduce risk of ADAs and enhance efficacy of anti-TNF therapy.”
However, because any antibiotic therapy will modify the gut microbiome and lead to unwanted effects, “further research is needed on how these agents impact the gut microbiome, with the ultimate goal of identifying specific microbiota or microbial metabolic products that can reproduce the intriguing findings of this paper.”
The study was supported in part by the Leona M. and Harry B. Helmsley Charitable Trust and the Israeli Ministry of Science and Technology. Dr. Gorelik had no financial conflicts to disclose. Several coauthors disclosed relationships with multiple pharmaceutical companies including AbbVie, CytoReason, Takeda, and Pfizer. Dr. Isaacs had no financial conflicts to disclose, but serves on the GI&Hepatology News board of editors. Dr. Roper had no relevant disclosures.
Help your patients better understand their IBD treatment options by sharing AGA’s patient education, “Living with IBD,” in the AGA GI Patient Center at www.gastro.org/IBD.
The use fluoroquinolones or macrolides reduced immunogenicity risk in inflammatory bowel disease (IBD) patients on anti–tumor necrosis factor (anti-TNF) therapy, according to data from nearly 2,000 individuals.
Anti-TNF therapy with monoclonal antibodies is an established treatment for Crohn’s disease and ulcerative colitis, but approximately 40% of patients fail to respond initially and even more fail to achieve complete remission, wrote Yuri Gorelik, MD, of Rambam Health Care Campus, Haifa, Israel, and colleagues.
“Immunogenicity, which refers to the development of antidrug antibodies [ADA] is considered as the main factor driving secondary loss of response and is likely involved in primary nonresponse as well,” but data on how to predict the risk for ADA formation are limited, they said.
In a study published in Gut, the researchers identified data from 1,946 IBD patients using the epi-IIRN (epidemiology group of the Israeli IBD research nucleus), a nationwide registry of all IBD patients in Israel.
A total of 363 patients had positive ADA after a median follow-up period of 651 days after starting therapy. Overall, the risk of ADA development was significantly higher in patients on cephalosporins (adjusted hazard ratio, 1.97; 95% confidence interval, 1.58-2.44) or penicillin with beta-lactamase inhibitors (BLIs) (aHR, 1.38; 95% CI, 1.13-1.74) during anti-TNF therapy, and it was higher still for patients using both. By contrast, the risk was lower in patients on macrolides (aHR, 0.36; 95% CI, 0.16-0.82) or fluoroquinolones (aHR, 0.20; 95% CI; 95% CI, 0.12-0.35). All P values were less than .05 when compared with nontreated groups.
In the same study, the researchers reported data on mice treated with antibiotics and challenged with infliximab to evaluate the causative effect of antibiotics and the associated disruption to the gut microbiome on the formation of ADA. After 14 days, the researchers found significantly increased ADA production in mice treated with cephalosporins, compared with those treated with macrolides, but germ-free mice produced no ADA, which supports the role of microbial composition on ADA production.
The investigators cited previous research into the microbiome as a biomarker for prediction response to anti-TNF therapy; past results have also suggested that the effect of cephalosporins and penicillin-BLIs could be explained by the particular dysbiosis induced by those agents.
The study findings were limited by several factors including the retrospective design and potential for selection bias, as well as the inability to adjust antibiotic exposure according to type and severity of infection, they noted. However, “this is the first large scale study that extensively evaluated the effect of different antibiotic classes on immunogenicity of anti-TNF therapy,” and the results suggest that ADA development during anti-TNF therapy may to reduced by the use of fluoroquinolones and macrolides.
“Specific microbial manipulation may serve as a tool to modify immunogenicity which is preferably turned on for protective immunizations and off for biological therapy,” they noted. “Further studies involving detailed analysis of the antibiotic effects on the human microbiome and immune milieu are needed, as well as comparative experiments with other medications used to reduce immunogenicity.”
Unexpected findings may drive future drug choices
“Development of antidrug antibodies in patients on biologics for inflammatory bowel disease is an important mechanism for loss of response to a therapeutic agent,” Kim L. Isaacs, MD, AGAF, of the University of North Carolina at Chapel Hill, said in an interview. “To date the causes of development of ADAs is relatively understudied. Our approach to prevent ADA includes increasing immunosuppression in patients most commonly with combination therapy with thiopurines. If factors that provoke or prevent antibody formation are elucidated, therapy can be tailored to prevent ADAs and maximize the duration of response of many of our biologic therapies.”
A prior study performed by the ABIRISK European consortium demonstrated associations with antibiotics. “In the current study, there was a differential effect of cephalosporins/penicillins (increased immunogenicity) and macrolides (decreased immunogenicity),” she said. “These studies suggest that the microbiome may be important in ADA formation to biologics – this is a concept that is novel and unexpected.
“The rationale for the choice of antibiotics in the population studied is not known, and it is possible that different infections may have led to different antibiotic choices, which in turn may have affected immunogenicity,” said Dr. Isaacs. However, clinicians might be able to tailor antibiotic choice in the future if the microbiome is playing a major role in risk for development of ADA.
“Further research is needed to further correlate microbiome changes with immunogenicity, to look at other classes of antibiotics and their role in immunogenicity, and to clarify the infections or reasons that these patients are receiving antibiotics,” Dr. Isaacs concluded.
Understanding the microbiome
Recent observations have shown associations between clinical response to anti-TNF and gut microbiota composition, noted Jatin Roper, MD, of Duke University, Durham, N.C. “More broadly, a growing body of evidence suggests that the gut microbiota modulates the metabolism of many therapeutic agents, as well as immune responses to infections.”
That said, Dr. Roper was surprised that “clinical use of different antibiotics, often short term, had such distinct effects on ADA levels.” Furthermore, “these findings suggest that distinct microbiota or microbial metabolic products impact antibody development to common immunomodulatory therapies in opposite ways,” which is itself a surprising finding.
Such antibodies to anti-TNF therapy are common in IBD, he said, but one implication of the study is how antibiotics could be carefully used “to reduce risk of ADAs and enhance efficacy of anti-TNF therapy.”
However, because any antibiotic therapy will modify the gut microbiome and lead to unwanted effects, “further research is needed on how these agents impact the gut microbiome, with the ultimate goal of identifying specific microbiota or microbial metabolic products that can reproduce the intriguing findings of this paper.”
The study was supported in part by the Leona M. and Harry B. Helmsley Charitable Trust and the Israeli Ministry of Science and Technology. Dr. Gorelik had no financial conflicts to disclose. Several coauthors disclosed relationships with multiple pharmaceutical companies including AbbVie, CytoReason, Takeda, and Pfizer. Dr. Isaacs had no financial conflicts to disclose, but serves on the GI&Hepatology News board of editors. Dr. Roper had no relevant disclosures.
Help your patients better understand their IBD treatment options by sharing AGA’s patient education, “Living with IBD,” in the AGA GI Patient Center at www.gastro.org/IBD.
FROM GUT
At-home fecal calprotectin test for IBD shows real-world efficacy
In a real-life setting, fecal calprotectin (FC) home testing performed well at predicting disease endoscopic activity in patients with inflammatory bowel disease (IBD) being treated with adalimumab.
The study, published in the European Journal of Gastroenterology & Hepatology, could be a boon to patients and physicians employing the treat-to-target (T2T) strategy, which relies on disease monitoring through methods like endoscopy, histology, and serum and fecal biomarkers.
One goal of T2T is to identify patients who are asymptomatic in order to prevent or minimize flare-ups. Colonoscopy is the preferred approach for achieving this, but cost, risk, and patient reluctance limit its use. FC has gained attention in recent years, as it outperforms serum biomarkers in its correlation with clinical, endoscopic, and histological disease activity. Consecutive FC measurements predict disease relapse among asymptomatic patients with high specificity and sensitivity. There’s also evidence that it could be useful for perioperative monitoring.
FC is typically assessed in a lab, but the recent availability of smartphone-based tests has allowed patients to collect and test their stool at home. The method has been tested through clinical research, but real-world data have so far been lacking.
First real-life results
In what they described as the first real-life study of its kind, researchers offered at-home FC testing every 4 months to all 72 current IBD patients taking adalimumab at the University Hospital of Heraklion, University of Crete, Irakleio, Greece; seven patients (10%) declined to take part in at-home FC testing. Of the remaining 65, the mean age was 42.3 years, and 58% were male; 89% had a diagnosis of Crohn’s disease. The mean disease duration was 13.3 years.
Abnormal FC values were confirmed with a follow-up test 1 month later, after which point a colonoscopy was scheduled to inform treatment modification. Twenty-four patients (37% of the population) had two positive tests, and 19 who were able underwent colonoscopy. Twelve patients (19%) underwent adalimumab dose intensification, 9 (14%) switched to a different biologic, and 2 (3%) had surgery.
The group of patients who required treatment modification had a significantly higher median FC concentration of 761 mcg/g (37% had values ≥ 1,000 mcg/g), compared with a median concentration of 108 mcg/g for those who did not have their dose modified (P < .0001). With a cutoff of 250 mcg/g, FC correctly identified a need for treatment with an area under the receiver operating characteristic curve (AUC) value of 0.90 (95% confidence interval, 0.80-0.96).
FC was significantly correlated to endoscopic activity (r = 0.543, P < .001), and patients with endoscopic disease had higher median FC concentrations (689 vs. 99 mcg/g; P < .001).
The researchers calculated that a cutoff value of FC levels greater than 413 mcg/g is optimal for predicting endoscopic disease, with a sensitivity of 75%, a specificity of 76%, a positive likelihood ratio of 3.12, and a negative likelihood ratio of 0.33.
Diabeteslike home monitoring for IBD?
“Home monitoring of disease activity and drug levels will be a paradigm shift in management of IBD, because it will place in the patient’s hands the opportunity to assess their disease activity and to have a better understanding of what’s going on when they have symptoms or concerns about their disease control,” commented David Rubin, MD, who did not participate in the study.
He noted that patients are often unsure whether a new symptom is the beginning of another episode of IBD or something unrelated.
“One of the biggest challenges of having IBD is just the perception of loss of control of the disease and knowing when things are going to happen,” said Dr. Rubin, a professor of medicine and the codirector of the digestive diseases center at the University of Chicago, and the chair of the scientific advisory committee for the Crohn’s & Colitis Foundation. “I often explain to people that using a tool like this would be similar to patients with diabetes checking their blood sugar – getting a feel for what’s actually happening closer to the time that it’s happening, rather than waiting for it to progress. I really think that the general idea of home monitoring is going to be a major advance in our field.”
Although the new study proved the technique’s acceptability and efficacy, it isn’t without pitfalls, according to Dr. Rubin. False positives or negatives are a concern, and other factors might influence the results. For example, proton pump inhibitors can increase FC levels. Another concern is that some patients can become obsessed with their FC levels, and may want to test themselves at any sign of illness. They may develop unrealistic expectations about the impact of medications on their FC levels.
“That’s going to open up a whole dialogue with people, so that we all are on the same page about it. But I think that the benefits of having this far outweigh those potential risks,” said Dr. Rubin.
The authors reported no conflicts of interest. Dr. Rubin has consulted for TECHLAB.
Help your patients better understand their IBD treatment options by sharing AGA’s patient education, “Living with IBD,” in the AGA GI Patient Center at www.gastro.org/IBD.
In a real-life setting, fecal calprotectin (FC) home testing performed well at predicting disease endoscopic activity in patients with inflammatory bowel disease (IBD) being treated with adalimumab.
The study, published in the European Journal of Gastroenterology & Hepatology, could be a boon to patients and physicians employing the treat-to-target (T2T) strategy, which relies on disease monitoring through methods like endoscopy, histology, and serum and fecal biomarkers.
One goal of T2T is to identify patients who are asymptomatic in order to prevent or minimize flare-ups. Colonoscopy is the preferred approach for achieving this, but cost, risk, and patient reluctance limit its use. FC has gained attention in recent years, as it outperforms serum biomarkers in its correlation with clinical, endoscopic, and histological disease activity. Consecutive FC measurements predict disease relapse among asymptomatic patients with high specificity and sensitivity. There’s also evidence that it could be useful for perioperative monitoring.
FC is typically assessed in a lab, but the recent availability of smartphone-based tests has allowed patients to collect and test their stool at home. The method has been tested through clinical research, but real-world data have so far been lacking.
First real-life results
In what they described as the first real-life study of its kind, researchers offered at-home FC testing every 4 months to all 72 current IBD patients taking adalimumab at the University Hospital of Heraklion, University of Crete, Irakleio, Greece; seven patients (10%) declined to take part in at-home FC testing. Of the remaining 65, the mean age was 42.3 years, and 58% were male; 89% had a diagnosis of Crohn’s disease. The mean disease duration was 13.3 years.
Abnormal FC values were confirmed with a follow-up test 1 month later, after which point a colonoscopy was scheduled to inform treatment modification. Twenty-four patients (37% of the population) had two positive tests, and 19 who were able underwent colonoscopy. Twelve patients (19%) underwent adalimumab dose intensification, 9 (14%) switched to a different biologic, and 2 (3%) had surgery.
The group of patients who required treatment modification had a significantly higher median FC concentration of 761 mcg/g (37% had values ≥ 1,000 mcg/g), compared with a median concentration of 108 mcg/g for those who did not have their dose modified (P < .0001). With a cutoff of 250 mcg/g, FC correctly identified a need for treatment with an area under the receiver operating characteristic curve (AUC) value of 0.90 (95% confidence interval, 0.80-0.96).
FC was significantly correlated to endoscopic activity (r = 0.543, P < .001), and patients with endoscopic disease had higher median FC concentrations (689 vs. 99 mcg/g; P < .001).
The researchers calculated that a cutoff value of FC levels greater than 413 mcg/g is optimal for predicting endoscopic disease, with a sensitivity of 75%, a specificity of 76%, a positive likelihood ratio of 3.12, and a negative likelihood ratio of 0.33.
Diabeteslike home monitoring for IBD?
“Home monitoring of disease activity and drug levels will be a paradigm shift in management of IBD, because it will place in the patient’s hands the opportunity to assess their disease activity and to have a better understanding of what’s going on when they have symptoms or concerns about their disease control,” commented David Rubin, MD, who did not participate in the study.
He noted that patients are often unsure whether a new symptom is the beginning of another episode of IBD or something unrelated.
“One of the biggest challenges of having IBD is just the perception of loss of control of the disease and knowing when things are going to happen,” said Dr. Rubin, a professor of medicine and the codirector of the digestive diseases center at the University of Chicago, and the chair of the scientific advisory committee for the Crohn’s & Colitis Foundation. “I often explain to people that using a tool like this would be similar to patients with diabetes checking their blood sugar – getting a feel for what’s actually happening closer to the time that it’s happening, rather than waiting for it to progress. I really think that the general idea of home monitoring is going to be a major advance in our field.”
Although the new study proved the technique’s acceptability and efficacy, it isn’t without pitfalls, according to Dr. Rubin. False positives or negatives are a concern, and other factors might influence the results. For example, proton pump inhibitors can increase FC levels. Another concern is that some patients can become obsessed with their FC levels, and may want to test themselves at any sign of illness. They may develop unrealistic expectations about the impact of medications on their FC levels.
“That’s going to open up a whole dialogue with people, so that we all are on the same page about it. But I think that the benefits of having this far outweigh those potential risks,” said Dr. Rubin.
The authors reported no conflicts of interest. Dr. Rubin has consulted for TECHLAB.
Help your patients better understand their IBD treatment options by sharing AGA’s patient education, “Living with IBD,” in the AGA GI Patient Center at www.gastro.org/IBD.
In a real-life setting, fecal calprotectin (FC) home testing performed well at predicting disease endoscopic activity in patients with inflammatory bowel disease (IBD) being treated with adalimumab.
The study, published in the European Journal of Gastroenterology & Hepatology, could be a boon to patients and physicians employing the treat-to-target (T2T) strategy, which relies on disease monitoring through methods like endoscopy, histology, and serum and fecal biomarkers.
One goal of T2T is to identify patients who are asymptomatic in order to prevent or minimize flare-ups. Colonoscopy is the preferred approach for achieving this, but cost, risk, and patient reluctance limit its use. FC has gained attention in recent years, as it outperforms serum biomarkers in its correlation with clinical, endoscopic, and histological disease activity. Consecutive FC measurements predict disease relapse among asymptomatic patients with high specificity and sensitivity. There’s also evidence that it could be useful for perioperative monitoring.
FC is typically assessed in a lab, but the recent availability of smartphone-based tests has allowed patients to collect and test their stool at home. The method has been tested through clinical research, but real-world data have so far been lacking.
First real-life results
In what they described as the first real-life study of its kind, researchers offered at-home FC testing every 4 months to all 72 current IBD patients taking adalimumab at the University Hospital of Heraklion, University of Crete, Irakleio, Greece; seven patients (10%) declined to take part in at-home FC testing. Of the remaining 65, the mean age was 42.3 years, and 58% were male; 89% had a diagnosis of Crohn’s disease. The mean disease duration was 13.3 years.
Abnormal FC values were confirmed with a follow-up test 1 month later, after which point a colonoscopy was scheduled to inform treatment modification. Twenty-four patients (37% of the population) had two positive tests, and 19 who were able underwent colonoscopy. Twelve patients (19%) underwent adalimumab dose intensification, 9 (14%) switched to a different biologic, and 2 (3%) had surgery.
The group of patients who required treatment modification had a significantly higher median FC concentration of 761 mcg/g (37% had values ≥ 1,000 mcg/g), compared with a median concentration of 108 mcg/g for those who did not have their dose modified (P < .0001). With a cutoff of 250 mcg/g, FC correctly identified a need for treatment with an area under the receiver operating characteristic curve (AUC) value of 0.90 (95% confidence interval, 0.80-0.96).
FC was significantly correlated to endoscopic activity (r = 0.543, P < .001), and patients with endoscopic disease had higher median FC concentrations (689 vs. 99 mcg/g; P < .001).
The researchers calculated that a cutoff value of FC levels greater than 413 mcg/g is optimal for predicting endoscopic disease, with a sensitivity of 75%, a specificity of 76%, a positive likelihood ratio of 3.12, and a negative likelihood ratio of 0.33.
Diabeteslike home monitoring for IBD?
“Home monitoring of disease activity and drug levels will be a paradigm shift in management of IBD, because it will place in the patient’s hands the opportunity to assess their disease activity and to have a better understanding of what’s going on when they have symptoms or concerns about their disease control,” commented David Rubin, MD, who did not participate in the study.
He noted that patients are often unsure whether a new symptom is the beginning of another episode of IBD or something unrelated.
“One of the biggest challenges of having IBD is just the perception of loss of control of the disease and knowing when things are going to happen,” said Dr. Rubin, a professor of medicine and the codirector of the digestive diseases center at the University of Chicago, and the chair of the scientific advisory committee for the Crohn’s & Colitis Foundation. “I often explain to people that using a tool like this would be similar to patients with diabetes checking their blood sugar – getting a feel for what’s actually happening closer to the time that it’s happening, rather than waiting for it to progress. I really think that the general idea of home monitoring is going to be a major advance in our field.”
Although the new study proved the technique’s acceptability and efficacy, it isn’t without pitfalls, according to Dr. Rubin. False positives or negatives are a concern, and other factors might influence the results. For example, proton pump inhibitors can increase FC levels. Another concern is that some patients can become obsessed with their FC levels, and may want to test themselves at any sign of illness. They may develop unrealistic expectations about the impact of medications on their FC levels.
“That’s going to open up a whole dialogue with people, so that we all are on the same page about it. But I think that the benefits of having this far outweigh those potential risks,” said Dr. Rubin.
The authors reported no conflicts of interest. Dr. Rubin has consulted for TECHLAB.
Help your patients better understand their IBD treatment options by sharing AGA’s patient education, “Living with IBD,” in the AGA GI Patient Center at www.gastro.org/IBD.
FROM THE EUROPEAN JOURNAL OF GASTROENTEROLOGY & HEPATOLOGY
Weathering this storm and the next
Perspectives on disaster preparedness amid COVID-19
The COVID-19 pandemic has tested disaster preparedness in hospitals across the nation. The pandemic brought many unique disaster planning challenges not commonly seen with other emergencies disasters. These included an uncertain and prolonged time frame, the implementation of physical distancing, and the challenges of preserving the health care work force.
But how do we prepare for the next disaster when the health care system and staff are already stretched thin? Here, we discuss the concept of maintaining a state of preparedness through and beyond COVID-19, using a disaster preparedness cycle – including continuous assessments of vulnerabilities, dynamic staffing adjustments to support patient and hospital needs, and broadening of the pandemic response to incorporate planning for the next disaster.
Disaster preparedness and assessing ongoing needs
Disaster preparedness cycle and Hazard Vulnerability Assessment
The disaster preparedness cycle illustrates that disaster preparedness is continuous. Disaster preparedness is achieved with the non-stop cycle of planning, coordinating, and recognizing vulnerable areas.1-5 Hazard vulnerability analysis (HVA) can play a critical role in recognizing areas in which a hospital system has strengths and weaknesses for different disaster scenarios. There are several tools available, but the overarching goal is to provide an objective and systematic approach to evaluate the potential damage and impact a disaster could have on the health care system and surrounding community.
The HVA can also be utilized to reassess system or personnel vulnerabilities that may have been exposed or highlighted during the pandemic.6,7 These vulnerabilities must be addressed during preparations for the next disaster while concurrently “assuming the incident happens at the worst possible time.”7
Disaster preparedness staffing considerations
Management, communication, and staffing issues are critical to disaster response. Key leadership responses during COVID-19 included providing frequent and transparent communication, down-staffing for physical distancing during low census, and prioritizing staff well-being. These measures serve as a strong foundation moving into preparations for the next disaster.8
To ensure adequate staffing during an unexpected natural disaster, we recommend creating “ride-out” and “relief teams” as part of disaster staffing preparedness.9,10 The ride-out team provides the initial care and these providers are expected to stay in the hospital during the primary impact of the event. Once the initial threat of disaster is over and it is deemed safe to travel, the relief team is activated and offers reprieve to the ride-out team. Leaders and backup leaders within these teams should be identified in the event teams are activated. These assignments should be made at the start of the year and updated yearly or more frequently, if needed.
While the COVID-19 pandemic did not significantly affect children, our ride-out and relief teams would have played a significant role in case a surge of pediatric cases had occurred.
Other considerations for disaster staffing include expanding backup coverage and for multisite groups, identifying site leads to help field specific questions or concerns. Lastly, understanding the staffing needs of the hospital during a disaster is vital – bidirectional communication between physicians and hospital leadership optimizes preparedness plans. These measures will help staff feel supported before, during, and after a disaster.
Dynamic disaster response
Supporting patient and hospital needs
The next step in the disaster preparedness cycle is adjusting to changing needs during the disaster. The pediatric inpatient population was less affected initially by COVID-19, allowing hospitalists to support the unpredicted needs of the pandemic. A dynamic and flexible physician response is important to disaster preparedness.
As there has been a continued shift to telehealth during the pandemic, our group has engaged in telehealth calls related to COVID-19. Seizing these new opportunities not only provided additional services to our patients, but also strengthened community support, physician worth, and the hospital’s financial state. This is also an opportunity for higher-risk clinicians or quarantined faculty to offer patient care during the pandemic.
Cram et al. describe the importance of “unspecializing” during the COVID-19 pandemic.11 Starting discussions early with adult and pediatric critical care colleagues is vital. Hospitalists take care of a broad patient population, and therefore, can adapt to where the clinical need may be. Optimizing and expanding our skill sets can bring value to the hospital system during uncertain times.
Hospitalists are also instrumental for patient flow during the pandemic. To address this, our group partnered with hospital leadership from many different areas including administration, nursing, emergency medicine, critical care, and ancillary services. By collaborating as one cohesive hospital unit, we were able to efficiently develop, implement, and update best clinical care guidelines and algorithms for COVID-19–related topics such as testing indications, admission criteria, infection control, and proper personal protective equipment use. Lastly, working with specialists to consolidate teams during a pandemic presents an opportunity for hospitalists to highlight expertise while bringing value to the hospital.
Unique staffing situations related to COVID-19
Different from other disasters, the COVID-19 pandemic affected older or immunocompromised staff in a unique way. Beauhaus et al. note that 20% of the physician workforce in the United Sates is between 55 and 64 years of age, and 9% are 65 years and older.12 Hospitalist groups should focus on how to optimize and preserve their workforce, specifically those that are higher risk due to age or other health conditions.
We used a tiered guide to safely accommodate our physicians that were determined to be at higher-risk for complications of COVID-19; these recommendations included limiting exposure to patients with acute respiratory illnesses and shifting some providers to a different clinical environments with a lower exposure risk, such as telemedicine visits.
Other COVID-19 preparedness considerations that affected our group in particular include the changes in learner staffing. Similar to attending down-staffing to encourage physical distancing during low census, learners (residents, medical students, and physician assistant students) also experienced decreased hours or suspension of rotations. To maintain optimal patient care, adjusting to changing disaster needs may include assessing attendings’ capacity to assume responsibilities typically supported by learners.
Due to the ongoing nature of the pandemic, we have had to maintain a dynamic response while adjusting to changing and ongoing needs during recovery. Creating a measured and staggered approach helps facilitate a smooth transition back to nonemergent activities. The education of learners, academic and scholarly work, and administrative duties will resume, but likely in a different steady state. Also, awareness of physician burnout and fatigue is critical as an institution enters a phase of recovery.
Preparing for the next disaster during the pandemic
This brings us back to the beginning of the disaster preparedness cycle and the need to plan for the next disaster. Current disaster preparedness plans among physician groups and hospitals are likely focused on an individual disaster scenario, but adjusting current disaster plans to account for the uncertain time frame of an event like the COVID-19 pandemic is critical. Several articles in the national news posed similar questions, although these publications focused mainly on the Federal Emergency Management Agency and the governmental response to prepare for the next disaster when resources are already stretched.13-15
How do we adequately plan, maintain a dynamic response, and continue to efficiently move through the disaster staffing cycle during an event like the COVID-19 pandemic? Being aware of current vulnerabilities and addressing gaps at the department and hospital level are vital to disaster preparedness. For example, we reassessed disaster (ride-out/relief) teams and the minimum number of staff needed to maintain safe and quality care, and what in-house arrangements would be needed (food, supplies, sleeping arrangements) while having to maintain physical distance.
Newman et al. explain “in disaster planning, having as many physicians as possible on hand may seem like an advantage, but being overstaffed in tight quarters was almost as bad as being understaffed.”9 This has been particularly true during the COVID-19 pandemic. It is crucial to have backup plans for faculty that are unable to serve ride-out duties from unexpected issues – such as availability, illnesses/quarantines, childcare/dependents. Also, it is important to be aware that some supply chains are already strained because of the pandemic and how this may play a role in the availability of certain supplies. Being aware and proactive about specific constraints allows for a better level of preparedness. Continued collaboration and communication with other services to provide care should be ongoing throughout the disaster preparedness cycle.
Conclusion
Providing and maintaining optimal and safe patient care should be the overarching goal throughout disaster preparedness. Being aware of group and institutional vulnerabilities, collaboration with hospital leadership, and remaining flexible as hospitalists are critical components for successful preparedness amid disasters. A dynamic and responsive disaster plan has been vital amid COVID-19, and for the next disasters we will certainly encounter.
Dr. Hadvani is assistant professor of pediatrics in the section of hospital medicine at Baylor College of Medicine, Texas Children’s Hospital. Dr. Uremovich is assistant professor of pediatrics in the section of hospital medicine at Baylor College of Medicine, Texas Children’s Hospital. Dr. Quinonez is associate professor of pediatrics and chief of pediatric hospital medicine at Baylor College of Medicine, Texas Children’s Hospital. Dr. Lopez is assistant professor of pediatrics in the section of hospital medicine at Baylor College of Medicine, Texas Children’s Hospital. Dr. Mothner is associate professor of pediatrics in the section of hospital medicine at Baylor College of Medicine, Texas Children’s Hospital and is the pediatric hospital medicine medical director for the main campus.
References
1. Malilay J et al. The role of applied epidemiology methods in the disaster management cycle. Am J Public Health. 2014;104(11):2092-102. doi: 10.2105/AJPH.2014.302010.
2. Federal Emergency Management Agency. Developing and maintaining emergency operations plans. 2010 Nov.
3. Federal Emergency Management Agency. National preparedness system. 2020 Jul 31.
4. Federal Emergency Management Agency. National preparedness goal. 2011 Sep.
5. Environmental health in emergencies and disasters: A practical guide. World Health Organization, Geneva. 2002:9-24. Edited by B. Wisner and J. Adams.
6. U.S. Department of Health and Human Services. Topic collection: Hazard vulnerability/risk assessment.
7. Hospital Association of Southern California. Hazard and vulnerability analysis.
8. Meier K et al. Pediatric hospital medicine management, staffing, and well-being in the face of COVID-19. J Hosp Med. 2020 May;15(5):308-10. doi: 10.12788/jhm.3435.
9. Newman B and Gallion C. Hurricane Harvey: Firsthand preparedness in graduate medical education. Acad Med. 2019 Sep;94(9):1267-69. doi: 10.1097/ACM.0000000000002696.
10. Brevard S et al. Analysis of disaster response plans and the aftermath of Hurricane Katrina: Lessons learned from a level I trauma center. J Trauma. 2008 Nov;65(5):1126-32. doi: 10.1097/TA.0b013e318188d6e5.
11. Cram P et al. All hands on deck learning to “un-specialize” in the COVID-19 pandemic. J Hosp Med. 2020 May;15(5):314-5. doi: 10.12788/jhm.3426.
12. Buerhaus P et al. Older clinicians and the surge in novel coronavirus disease 2019 (COVID-19). JAMA. 2020 May 12;323(18):1777-8. doi: 10.1001/jama.2020.4978.
13. VOX Media. Imagine Hurricane Katrina during a pandemic. The US needs to prepare for that – now. 2020 May 27.
14. The Hill. Democratic lawmakers ask how FEMA is planning to balance natural disasters, COVID-19 response. 2020 Apr 20.
15. The Atlantic. What happens if a ‘big one’ strikes during the pandemic? 2020 May 9.
Perspectives on disaster preparedness amid COVID-19
Perspectives on disaster preparedness amid COVID-19
The COVID-19 pandemic has tested disaster preparedness in hospitals across the nation. The pandemic brought many unique disaster planning challenges not commonly seen with other emergencies disasters. These included an uncertain and prolonged time frame, the implementation of physical distancing, and the challenges of preserving the health care work force.
But how do we prepare for the next disaster when the health care system and staff are already stretched thin? Here, we discuss the concept of maintaining a state of preparedness through and beyond COVID-19, using a disaster preparedness cycle – including continuous assessments of vulnerabilities, dynamic staffing adjustments to support patient and hospital needs, and broadening of the pandemic response to incorporate planning for the next disaster.
Disaster preparedness and assessing ongoing needs
Disaster preparedness cycle and Hazard Vulnerability Assessment
The disaster preparedness cycle illustrates that disaster preparedness is continuous. Disaster preparedness is achieved with the non-stop cycle of planning, coordinating, and recognizing vulnerable areas.1-5 Hazard vulnerability analysis (HVA) can play a critical role in recognizing areas in which a hospital system has strengths and weaknesses for different disaster scenarios. There are several tools available, but the overarching goal is to provide an objective and systematic approach to evaluate the potential damage and impact a disaster could have on the health care system and surrounding community.
The HVA can also be utilized to reassess system or personnel vulnerabilities that may have been exposed or highlighted during the pandemic.6,7 These vulnerabilities must be addressed during preparations for the next disaster while concurrently “assuming the incident happens at the worst possible time.”7
Disaster preparedness staffing considerations
Management, communication, and staffing issues are critical to disaster response. Key leadership responses during COVID-19 included providing frequent and transparent communication, down-staffing for physical distancing during low census, and prioritizing staff well-being. These measures serve as a strong foundation moving into preparations for the next disaster.8
To ensure adequate staffing during an unexpected natural disaster, we recommend creating “ride-out” and “relief teams” as part of disaster staffing preparedness.9,10 The ride-out team provides the initial care and these providers are expected to stay in the hospital during the primary impact of the event. Once the initial threat of disaster is over and it is deemed safe to travel, the relief team is activated and offers reprieve to the ride-out team. Leaders and backup leaders within these teams should be identified in the event teams are activated. These assignments should be made at the start of the year and updated yearly or more frequently, if needed.
While the COVID-19 pandemic did not significantly affect children, our ride-out and relief teams would have played a significant role in case a surge of pediatric cases had occurred.
Other considerations for disaster staffing include expanding backup coverage and for multisite groups, identifying site leads to help field specific questions or concerns. Lastly, understanding the staffing needs of the hospital during a disaster is vital – bidirectional communication between physicians and hospital leadership optimizes preparedness plans. These measures will help staff feel supported before, during, and after a disaster.
Dynamic disaster response
Supporting patient and hospital needs
The next step in the disaster preparedness cycle is adjusting to changing needs during the disaster. The pediatric inpatient population was less affected initially by COVID-19, allowing hospitalists to support the unpredicted needs of the pandemic. A dynamic and flexible physician response is important to disaster preparedness.
As there has been a continued shift to telehealth during the pandemic, our group has engaged in telehealth calls related to COVID-19. Seizing these new opportunities not only provided additional services to our patients, but also strengthened community support, physician worth, and the hospital’s financial state. This is also an opportunity for higher-risk clinicians or quarantined faculty to offer patient care during the pandemic.
Cram et al. describe the importance of “unspecializing” during the COVID-19 pandemic.11 Starting discussions early with adult and pediatric critical care colleagues is vital. Hospitalists take care of a broad patient population, and therefore, can adapt to where the clinical need may be. Optimizing and expanding our skill sets can bring value to the hospital system during uncertain times.
Hospitalists are also instrumental for patient flow during the pandemic. To address this, our group partnered with hospital leadership from many different areas including administration, nursing, emergency medicine, critical care, and ancillary services. By collaborating as one cohesive hospital unit, we were able to efficiently develop, implement, and update best clinical care guidelines and algorithms for COVID-19–related topics such as testing indications, admission criteria, infection control, and proper personal protective equipment use. Lastly, working with specialists to consolidate teams during a pandemic presents an opportunity for hospitalists to highlight expertise while bringing value to the hospital.
Unique staffing situations related to COVID-19
Different from other disasters, the COVID-19 pandemic affected older or immunocompromised staff in a unique way. Beauhaus et al. note that 20% of the physician workforce in the United Sates is between 55 and 64 years of age, and 9% are 65 years and older.12 Hospitalist groups should focus on how to optimize and preserve their workforce, specifically those that are higher risk due to age or other health conditions.
We used a tiered guide to safely accommodate our physicians that were determined to be at higher-risk for complications of COVID-19; these recommendations included limiting exposure to patients with acute respiratory illnesses and shifting some providers to a different clinical environments with a lower exposure risk, such as telemedicine visits.
Other COVID-19 preparedness considerations that affected our group in particular include the changes in learner staffing. Similar to attending down-staffing to encourage physical distancing during low census, learners (residents, medical students, and physician assistant students) also experienced decreased hours or suspension of rotations. To maintain optimal patient care, adjusting to changing disaster needs may include assessing attendings’ capacity to assume responsibilities typically supported by learners.
Due to the ongoing nature of the pandemic, we have had to maintain a dynamic response while adjusting to changing and ongoing needs during recovery. Creating a measured and staggered approach helps facilitate a smooth transition back to nonemergent activities. The education of learners, academic and scholarly work, and administrative duties will resume, but likely in a different steady state. Also, awareness of physician burnout and fatigue is critical as an institution enters a phase of recovery.
Preparing for the next disaster during the pandemic
This brings us back to the beginning of the disaster preparedness cycle and the need to plan for the next disaster. Current disaster preparedness plans among physician groups and hospitals are likely focused on an individual disaster scenario, but adjusting current disaster plans to account for the uncertain time frame of an event like the COVID-19 pandemic is critical. Several articles in the national news posed similar questions, although these publications focused mainly on the Federal Emergency Management Agency and the governmental response to prepare for the next disaster when resources are already stretched.13-15
How do we adequately plan, maintain a dynamic response, and continue to efficiently move through the disaster staffing cycle during an event like the COVID-19 pandemic? Being aware of current vulnerabilities and addressing gaps at the department and hospital level are vital to disaster preparedness. For example, we reassessed disaster (ride-out/relief) teams and the minimum number of staff needed to maintain safe and quality care, and what in-house arrangements would be needed (food, supplies, sleeping arrangements) while having to maintain physical distance.
Newman et al. explain “in disaster planning, having as many physicians as possible on hand may seem like an advantage, but being overstaffed in tight quarters was almost as bad as being understaffed.”9 This has been particularly true during the COVID-19 pandemic. It is crucial to have backup plans for faculty that are unable to serve ride-out duties from unexpected issues – such as availability, illnesses/quarantines, childcare/dependents. Also, it is important to be aware that some supply chains are already strained because of the pandemic and how this may play a role in the availability of certain supplies. Being aware and proactive about specific constraints allows for a better level of preparedness. Continued collaboration and communication with other services to provide care should be ongoing throughout the disaster preparedness cycle.
Conclusion
Providing and maintaining optimal and safe patient care should be the overarching goal throughout disaster preparedness. Being aware of group and institutional vulnerabilities, collaboration with hospital leadership, and remaining flexible as hospitalists are critical components for successful preparedness amid disasters. A dynamic and responsive disaster plan has been vital amid COVID-19, and for the next disasters we will certainly encounter.
Dr. Hadvani is assistant professor of pediatrics in the section of hospital medicine at Baylor College of Medicine, Texas Children’s Hospital. Dr. Uremovich is assistant professor of pediatrics in the section of hospital medicine at Baylor College of Medicine, Texas Children’s Hospital. Dr. Quinonez is associate professor of pediatrics and chief of pediatric hospital medicine at Baylor College of Medicine, Texas Children’s Hospital. Dr. Lopez is assistant professor of pediatrics in the section of hospital medicine at Baylor College of Medicine, Texas Children’s Hospital. Dr. Mothner is associate professor of pediatrics in the section of hospital medicine at Baylor College of Medicine, Texas Children’s Hospital and is the pediatric hospital medicine medical director for the main campus.
References
1. Malilay J et al. The role of applied epidemiology methods in the disaster management cycle. Am J Public Health. 2014;104(11):2092-102. doi: 10.2105/AJPH.2014.302010.
2. Federal Emergency Management Agency. Developing and maintaining emergency operations plans. 2010 Nov.
3. Federal Emergency Management Agency. National preparedness system. 2020 Jul 31.
4. Federal Emergency Management Agency. National preparedness goal. 2011 Sep.
5. Environmental health in emergencies and disasters: A practical guide. World Health Organization, Geneva. 2002:9-24. Edited by B. Wisner and J. Adams.
6. U.S. Department of Health and Human Services. Topic collection: Hazard vulnerability/risk assessment.
7. Hospital Association of Southern California. Hazard and vulnerability analysis.
8. Meier K et al. Pediatric hospital medicine management, staffing, and well-being in the face of COVID-19. J Hosp Med. 2020 May;15(5):308-10. doi: 10.12788/jhm.3435.
9. Newman B and Gallion C. Hurricane Harvey: Firsthand preparedness in graduate medical education. Acad Med. 2019 Sep;94(9):1267-69. doi: 10.1097/ACM.0000000000002696.
10. Brevard S et al. Analysis of disaster response plans and the aftermath of Hurricane Katrina: Lessons learned from a level I trauma center. J Trauma. 2008 Nov;65(5):1126-32. doi: 10.1097/TA.0b013e318188d6e5.
11. Cram P et al. All hands on deck learning to “un-specialize” in the COVID-19 pandemic. J Hosp Med. 2020 May;15(5):314-5. doi: 10.12788/jhm.3426.
12. Buerhaus P et al. Older clinicians and the surge in novel coronavirus disease 2019 (COVID-19). JAMA. 2020 May 12;323(18):1777-8. doi: 10.1001/jama.2020.4978.
13. VOX Media. Imagine Hurricane Katrina during a pandemic. The US needs to prepare for that – now. 2020 May 27.
14. The Hill. Democratic lawmakers ask how FEMA is planning to balance natural disasters, COVID-19 response. 2020 Apr 20.
15. The Atlantic. What happens if a ‘big one’ strikes during the pandemic? 2020 May 9.
The COVID-19 pandemic has tested disaster preparedness in hospitals across the nation. The pandemic brought many unique disaster planning challenges not commonly seen with other emergencies disasters. These included an uncertain and prolonged time frame, the implementation of physical distancing, and the challenges of preserving the health care work force.
But how do we prepare for the next disaster when the health care system and staff are already stretched thin? Here, we discuss the concept of maintaining a state of preparedness through and beyond COVID-19, using a disaster preparedness cycle – including continuous assessments of vulnerabilities, dynamic staffing adjustments to support patient and hospital needs, and broadening of the pandemic response to incorporate planning for the next disaster.
Disaster preparedness and assessing ongoing needs
Disaster preparedness cycle and Hazard Vulnerability Assessment
The disaster preparedness cycle illustrates that disaster preparedness is continuous. Disaster preparedness is achieved with the non-stop cycle of planning, coordinating, and recognizing vulnerable areas.1-5 Hazard vulnerability analysis (HVA) can play a critical role in recognizing areas in which a hospital system has strengths and weaknesses for different disaster scenarios. There are several tools available, but the overarching goal is to provide an objective and systematic approach to evaluate the potential damage and impact a disaster could have on the health care system and surrounding community.
The HVA can also be utilized to reassess system or personnel vulnerabilities that may have been exposed or highlighted during the pandemic.6,7 These vulnerabilities must be addressed during preparations for the next disaster while concurrently “assuming the incident happens at the worst possible time.”7
Disaster preparedness staffing considerations
Management, communication, and staffing issues are critical to disaster response. Key leadership responses during COVID-19 included providing frequent and transparent communication, down-staffing for physical distancing during low census, and prioritizing staff well-being. These measures serve as a strong foundation moving into preparations for the next disaster.8
To ensure adequate staffing during an unexpected natural disaster, we recommend creating “ride-out” and “relief teams” as part of disaster staffing preparedness.9,10 The ride-out team provides the initial care and these providers are expected to stay in the hospital during the primary impact of the event. Once the initial threat of disaster is over and it is deemed safe to travel, the relief team is activated and offers reprieve to the ride-out team. Leaders and backup leaders within these teams should be identified in the event teams are activated. These assignments should be made at the start of the year and updated yearly or more frequently, if needed.
While the COVID-19 pandemic did not significantly affect children, our ride-out and relief teams would have played a significant role in case a surge of pediatric cases had occurred.
Other considerations for disaster staffing include expanding backup coverage and for multisite groups, identifying site leads to help field specific questions or concerns. Lastly, understanding the staffing needs of the hospital during a disaster is vital – bidirectional communication between physicians and hospital leadership optimizes preparedness plans. These measures will help staff feel supported before, during, and after a disaster.
Dynamic disaster response
Supporting patient and hospital needs
The next step in the disaster preparedness cycle is adjusting to changing needs during the disaster. The pediatric inpatient population was less affected initially by COVID-19, allowing hospitalists to support the unpredicted needs of the pandemic. A dynamic and flexible physician response is important to disaster preparedness.
As there has been a continued shift to telehealth during the pandemic, our group has engaged in telehealth calls related to COVID-19. Seizing these new opportunities not only provided additional services to our patients, but also strengthened community support, physician worth, and the hospital’s financial state. This is also an opportunity for higher-risk clinicians or quarantined faculty to offer patient care during the pandemic.
Cram et al. describe the importance of “unspecializing” during the COVID-19 pandemic.11 Starting discussions early with adult and pediatric critical care colleagues is vital. Hospitalists take care of a broad patient population, and therefore, can adapt to where the clinical need may be. Optimizing and expanding our skill sets can bring value to the hospital system during uncertain times.
Hospitalists are also instrumental for patient flow during the pandemic. To address this, our group partnered with hospital leadership from many different areas including administration, nursing, emergency medicine, critical care, and ancillary services. By collaborating as one cohesive hospital unit, we were able to efficiently develop, implement, and update best clinical care guidelines and algorithms for COVID-19–related topics such as testing indications, admission criteria, infection control, and proper personal protective equipment use. Lastly, working with specialists to consolidate teams during a pandemic presents an opportunity for hospitalists to highlight expertise while bringing value to the hospital.
Unique staffing situations related to COVID-19
Different from other disasters, the COVID-19 pandemic affected older or immunocompromised staff in a unique way. Beauhaus et al. note that 20% of the physician workforce in the United Sates is between 55 and 64 years of age, and 9% are 65 years and older.12 Hospitalist groups should focus on how to optimize and preserve their workforce, specifically those that are higher risk due to age or other health conditions.
We used a tiered guide to safely accommodate our physicians that were determined to be at higher-risk for complications of COVID-19; these recommendations included limiting exposure to patients with acute respiratory illnesses and shifting some providers to a different clinical environments with a lower exposure risk, such as telemedicine visits.
Other COVID-19 preparedness considerations that affected our group in particular include the changes in learner staffing. Similar to attending down-staffing to encourage physical distancing during low census, learners (residents, medical students, and physician assistant students) also experienced decreased hours or suspension of rotations. To maintain optimal patient care, adjusting to changing disaster needs may include assessing attendings’ capacity to assume responsibilities typically supported by learners.
Due to the ongoing nature of the pandemic, we have had to maintain a dynamic response while adjusting to changing and ongoing needs during recovery. Creating a measured and staggered approach helps facilitate a smooth transition back to nonemergent activities. The education of learners, academic and scholarly work, and administrative duties will resume, but likely in a different steady state. Also, awareness of physician burnout and fatigue is critical as an institution enters a phase of recovery.
Preparing for the next disaster during the pandemic
This brings us back to the beginning of the disaster preparedness cycle and the need to plan for the next disaster. Current disaster preparedness plans among physician groups and hospitals are likely focused on an individual disaster scenario, but adjusting current disaster plans to account for the uncertain time frame of an event like the COVID-19 pandemic is critical. Several articles in the national news posed similar questions, although these publications focused mainly on the Federal Emergency Management Agency and the governmental response to prepare for the next disaster when resources are already stretched.13-15
How do we adequately plan, maintain a dynamic response, and continue to efficiently move through the disaster staffing cycle during an event like the COVID-19 pandemic? Being aware of current vulnerabilities and addressing gaps at the department and hospital level are vital to disaster preparedness. For example, we reassessed disaster (ride-out/relief) teams and the minimum number of staff needed to maintain safe and quality care, and what in-house arrangements would be needed (food, supplies, sleeping arrangements) while having to maintain physical distance.
Newman et al. explain “in disaster planning, having as many physicians as possible on hand may seem like an advantage, but being overstaffed in tight quarters was almost as bad as being understaffed.”9 This has been particularly true during the COVID-19 pandemic. It is crucial to have backup plans for faculty that are unable to serve ride-out duties from unexpected issues – such as availability, illnesses/quarantines, childcare/dependents. Also, it is important to be aware that some supply chains are already strained because of the pandemic and how this may play a role in the availability of certain supplies. Being aware and proactive about specific constraints allows for a better level of preparedness. Continued collaboration and communication with other services to provide care should be ongoing throughout the disaster preparedness cycle.
Conclusion
Providing and maintaining optimal and safe patient care should be the overarching goal throughout disaster preparedness. Being aware of group and institutional vulnerabilities, collaboration with hospital leadership, and remaining flexible as hospitalists are critical components for successful preparedness amid disasters. A dynamic and responsive disaster plan has been vital amid COVID-19, and for the next disasters we will certainly encounter.
Dr. Hadvani is assistant professor of pediatrics in the section of hospital medicine at Baylor College of Medicine, Texas Children’s Hospital. Dr. Uremovich is assistant professor of pediatrics in the section of hospital medicine at Baylor College of Medicine, Texas Children’s Hospital. Dr. Quinonez is associate professor of pediatrics and chief of pediatric hospital medicine at Baylor College of Medicine, Texas Children’s Hospital. Dr. Lopez is assistant professor of pediatrics in the section of hospital medicine at Baylor College of Medicine, Texas Children’s Hospital. Dr. Mothner is associate professor of pediatrics in the section of hospital medicine at Baylor College of Medicine, Texas Children’s Hospital and is the pediatric hospital medicine medical director for the main campus.
References
1. Malilay J et al. The role of applied epidemiology methods in the disaster management cycle. Am J Public Health. 2014;104(11):2092-102. doi: 10.2105/AJPH.2014.302010.
2. Federal Emergency Management Agency. Developing and maintaining emergency operations plans. 2010 Nov.
3. Federal Emergency Management Agency. National preparedness system. 2020 Jul 31.
4. Federal Emergency Management Agency. National preparedness goal. 2011 Sep.
5. Environmental health in emergencies and disasters: A practical guide. World Health Organization, Geneva. 2002:9-24. Edited by B. Wisner and J. Adams.
6. U.S. Department of Health and Human Services. Topic collection: Hazard vulnerability/risk assessment.
7. Hospital Association of Southern California. Hazard and vulnerability analysis.
8. Meier K et al. Pediatric hospital medicine management, staffing, and well-being in the face of COVID-19. J Hosp Med. 2020 May;15(5):308-10. doi: 10.12788/jhm.3435.
9. Newman B and Gallion C. Hurricane Harvey: Firsthand preparedness in graduate medical education. Acad Med. 2019 Sep;94(9):1267-69. doi: 10.1097/ACM.0000000000002696.
10. Brevard S et al. Analysis of disaster response plans and the aftermath of Hurricane Katrina: Lessons learned from a level I trauma center. J Trauma. 2008 Nov;65(5):1126-32. doi: 10.1097/TA.0b013e318188d6e5.
11. Cram P et al. All hands on deck learning to “un-specialize” in the COVID-19 pandemic. J Hosp Med. 2020 May;15(5):314-5. doi: 10.12788/jhm.3426.
12. Buerhaus P et al. Older clinicians and the surge in novel coronavirus disease 2019 (COVID-19). JAMA. 2020 May 12;323(18):1777-8. doi: 10.1001/jama.2020.4978.
13. VOX Media. Imagine Hurricane Katrina during a pandemic. The US needs to prepare for that – now. 2020 May 27.
14. The Hill. Democratic lawmakers ask how FEMA is planning to balance natural disasters, COVID-19 response. 2020 Apr 20.
15. The Atlantic. What happens if a ‘big one’ strikes during the pandemic? 2020 May 9.
Low depression scores may miss seniors with suicidal intent
Older adults may have a high degree of suicidal intent yet still have low scores on scales measuring psychiatric symptoms, such as depression, new research suggests.
In a cross-sectional cohort study of more than 800 adults who presented with self-harm to psychiatric EDs in Sweden, participants aged 65 years and older scored higher than younger and middle-aged adults on measures of suicidal intent.
However, only half of the older group fulfilled criteria for major depression, compared with three-quarters of both the middle-aged and young adult–aged groups.
“Suicidal older persons show a somewhat different clinical picture with relatively low levels of psychopathology but with high suicide intent compared to younger persons,” lead author Stefan Wiktorsson, PhD, University of Gothenburg (Sweden), said in an interview.
“It is therefore of importance for clinicians to carefully evaluate suicidal thinking in this age group. he said.
The findings were published online Aug. 9, 2021, in the American Journal of Geriatric Psychiatry.
Research by age groups ‘lacking’
“While there are large age differences in the prevalence of suicidal behavior, research studies that compare symptomatology and diagnostics in different age groups are lacking,” Dr. Wiktorsson said.
He and his colleagues “wanted to compare psychopathology in young, middle-aged, and older adults in order to increase knowledge about potential differences in symptomatology related to suicidal behavior over the life span.”
The researchers recruited patients aged 18 years and older who had sought or had been referred to emergency psychiatric services for self-harm at three psychiatric hospitals in Sweden between April 2012 and March 2016.
Among all patients, 821 fit inclusion criteria and agreed to participate. The researchers excluded participants who had engaged in nonsuicidal self-injury (NNSI), as determined on the basis of the Columbia Suicide Severity Rating Scale (C-SSRS). The remaining 683 participants, who had attempted suicide, were included in the analysis.
The participants were then divided into the following three groups: older (n = 96; age, 65-97 years; mean age, 77.2 years; 57% women), middle-aged (n = 164; age, 45-64 years; mean age, 53.4 years; 57% women), and younger (n = 423; age, 18-44 years; mean age, 28.3 years; 64% women)
Mental health staff interviewed participants within 7 days of the index episode. They collected information about sociodemographics, health, and contact with health care professionals. They used the C-SSRS to identify characteristics of the suicide attempts, and they used the Suicide Intent Scale (SIS) to evaluate circumstances surrounding the suicide attempt, such as active preparation.
Investigators also used the Mini International Neuropsychiatric Interview (MINI), the Suicide Assessment Scale (SUAS), and the Karolinska Affective and Borderline Symptoms Scale.
Greater disability, pain
Of the older patients, 75% lived alone; 88% of the middle-aged and 48% of the younger participants lived alone. A higher proportion of older participants had severe physical illness/disability and severe chronic pain compared with younger participants (all comparisons, P < .001).
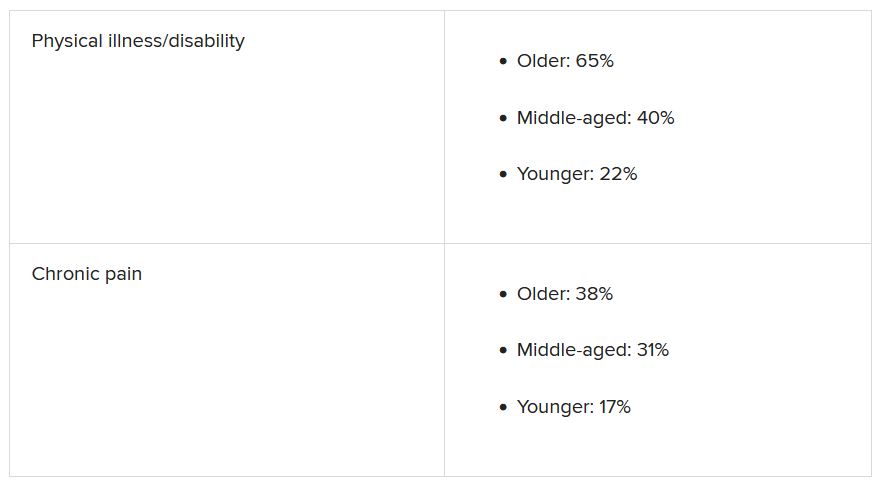
Older adults had less contact with psychiatric services, but they had more contact than the other age groups with primary care for mental health problems. Older adults were prescribed antidepressants at the time of the suicide attempt at a lower rate, compared with the middle-aged and younger groups (50% vs. 73% and 66%).
Slightly less than half (44%) of the older adults had a previous history of a suicide attempt – a proportion considerably lower than was reported by patients in the middle-aged and young adult groups (63% and 75%, respectively). Few older adults had a history of a previous NNSI (6% vs. 23% and 63%).
Three-quarters of older adults employed poisoning as the single method of suicide attempt at their index episode, compared with 67% and 59% of the middle-aged and younger groups.
Notably, only half of older adults (52%) met criteria for major depression, determined on the basis of the MINI, compared with three quarters of participants in the other groups (73% and 76%, respectively). Fewer members of the older group met criteria for other psychiatric conditions.
Clouded judgment
The mean total SUAS score was “considerably lower” in the older-adult group than in the other groups. This was also the case for the SUAS subscales for affect, bodily states, control, coping, and emotional reactivity.
Importantly, however, older adults scored higher than younger adults on the SIS total score and the subjective subscale, indicating a higher level of suicidal intent.
The mean SIS total score was 17.8 in the older group, 17.4 in the middle-aged group, and 15.9 in the younger group. The SIS subjective suicide intent score was 10.9 versus 10.6 and 9.4.
“While subjective suicidal intent was higher, compared to the young group, older adults were less likely to fulfill criteria for major depression and several other mental disorders and lower scores were observed on all symptom rating scales, compared to both middle-aged and younger adults,” the investigators wrote.
“Low levels of psychopathology may cloud the clinician’s assessment of the serious nature of suicide attempts in older patients,” they added.
‘Silent generation’
Commenting on the findings, Marnin Heisel, PhD, CPsych, associate professor, departments of psychiatry and of epidemiology and biostatistics, University of Western Ontario, London, said an important takeaway from the study is that, if health care professionals look only for depression or only consider suicide risk in individuals who present with depression, “they might miss older adults who are contemplating suicide or engaging in suicidal behavior.”
Dr. Heisel, who was not involved with the study, observed that older adults are sometimes called the “silent generation” because they often tend to downplay or underreport depressive symptoms, partially because of having been socialized to “keep things to themselves and not to air emotional laundry.”
He recommended that, when assessing potentially suicidal older adults, clinicians select tools specifically designed for use in this age group, particularly the Geriatric Suicide Ideation Scale and the Geriatric Depression Scale. Dr. Heisel also recommended the Center for Epidemiological Studies Depression Scale–Revised Version.
“Beyond a specific scale, the question is to walk into a clinical encounter with a much broader viewpoint, understand who the client is, where they come from, their attitudes, life experience, and what in their experience is going on, their reason for coming to see someone and what they’re struggling with,” he said.
“What we’re seeing with this study is that standard clinical tools don’t necessarily identify some of these richer issues that might contribute to emotional pain, so sometimes the best way to go is a broader clinical interview with a humanistic perspective,” Dr. Heisel concluded.
The study was funded by the Swedish Research Council, the Swedish Research Council for Health, Working Life and Welfare, and the Swedish state, Stockholm County Council and Västerbotten County Council. The investigators and Dr. Heisel have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Older adults may have a high degree of suicidal intent yet still have low scores on scales measuring psychiatric symptoms, such as depression, new research suggests.
In a cross-sectional cohort study of more than 800 adults who presented with self-harm to psychiatric EDs in Sweden, participants aged 65 years and older scored higher than younger and middle-aged adults on measures of suicidal intent.
However, only half of the older group fulfilled criteria for major depression, compared with three-quarters of both the middle-aged and young adult–aged groups.
“Suicidal older persons show a somewhat different clinical picture with relatively low levels of psychopathology but with high suicide intent compared to younger persons,” lead author Stefan Wiktorsson, PhD, University of Gothenburg (Sweden), said in an interview.
“It is therefore of importance for clinicians to carefully evaluate suicidal thinking in this age group. he said.
The findings were published online Aug. 9, 2021, in the American Journal of Geriatric Psychiatry.
Research by age groups ‘lacking’
“While there are large age differences in the prevalence of suicidal behavior, research studies that compare symptomatology and diagnostics in different age groups are lacking,” Dr. Wiktorsson said.
He and his colleagues “wanted to compare psychopathology in young, middle-aged, and older adults in order to increase knowledge about potential differences in symptomatology related to suicidal behavior over the life span.”
The researchers recruited patients aged 18 years and older who had sought or had been referred to emergency psychiatric services for self-harm at three psychiatric hospitals in Sweden between April 2012 and March 2016.
Among all patients, 821 fit inclusion criteria and agreed to participate. The researchers excluded participants who had engaged in nonsuicidal self-injury (NNSI), as determined on the basis of the Columbia Suicide Severity Rating Scale (C-SSRS). The remaining 683 participants, who had attempted suicide, were included in the analysis.
The participants were then divided into the following three groups: older (n = 96; age, 65-97 years; mean age, 77.2 years; 57% women), middle-aged (n = 164; age, 45-64 years; mean age, 53.4 years; 57% women), and younger (n = 423; age, 18-44 years; mean age, 28.3 years; 64% women)
Mental health staff interviewed participants within 7 days of the index episode. They collected information about sociodemographics, health, and contact with health care professionals. They used the C-SSRS to identify characteristics of the suicide attempts, and they used the Suicide Intent Scale (SIS) to evaluate circumstances surrounding the suicide attempt, such as active preparation.
Investigators also used the Mini International Neuropsychiatric Interview (MINI), the Suicide Assessment Scale (SUAS), and the Karolinska Affective and Borderline Symptoms Scale.
Greater disability, pain
Of the older patients, 75% lived alone; 88% of the middle-aged and 48% of the younger participants lived alone. A higher proportion of older participants had severe physical illness/disability and severe chronic pain compared with younger participants (all comparisons, P < .001).
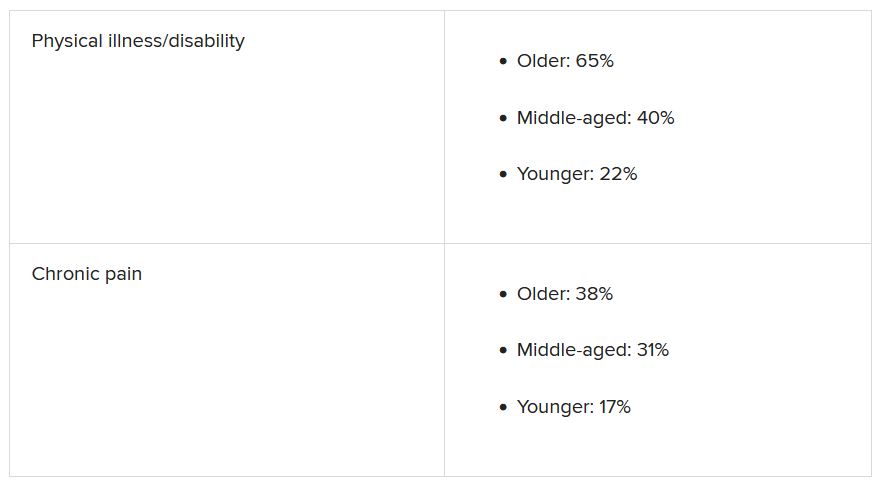
Older adults had less contact with psychiatric services, but they had more contact than the other age groups with primary care for mental health problems. Older adults were prescribed antidepressants at the time of the suicide attempt at a lower rate, compared with the middle-aged and younger groups (50% vs. 73% and 66%).
Slightly less than half (44%) of the older adults had a previous history of a suicide attempt – a proportion considerably lower than was reported by patients in the middle-aged and young adult groups (63% and 75%, respectively). Few older adults had a history of a previous NNSI (6% vs. 23% and 63%).
Three-quarters of older adults employed poisoning as the single method of suicide attempt at their index episode, compared with 67% and 59% of the middle-aged and younger groups.
Notably, only half of older adults (52%) met criteria for major depression, determined on the basis of the MINI, compared with three quarters of participants in the other groups (73% and 76%, respectively). Fewer members of the older group met criteria for other psychiatric conditions.
Clouded judgment
The mean total SUAS score was “considerably lower” in the older-adult group than in the other groups. This was also the case for the SUAS subscales for affect, bodily states, control, coping, and emotional reactivity.
Importantly, however, older adults scored higher than younger adults on the SIS total score and the subjective subscale, indicating a higher level of suicidal intent.
The mean SIS total score was 17.8 in the older group, 17.4 in the middle-aged group, and 15.9 in the younger group. The SIS subjective suicide intent score was 10.9 versus 10.6 and 9.4.
“While subjective suicidal intent was higher, compared to the young group, older adults were less likely to fulfill criteria for major depression and several other mental disorders and lower scores were observed on all symptom rating scales, compared to both middle-aged and younger adults,” the investigators wrote.
“Low levels of psychopathology may cloud the clinician’s assessment of the serious nature of suicide attempts in older patients,” they added.
‘Silent generation’
Commenting on the findings, Marnin Heisel, PhD, CPsych, associate professor, departments of psychiatry and of epidemiology and biostatistics, University of Western Ontario, London, said an important takeaway from the study is that, if health care professionals look only for depression or only consider suicide risk in individuals who present with depression, “they might miss older adults who are contemplating suicide or engaging in suicidal behavior.”
Dr. Heisel, who was not involved with the study, observed that older adults are sometimes called the “silent generation” because they often tend to downplay or underreport depressive symptoms, partially because of having been socialized to “keep things to themselves and not to air emotional laundry.”
He recommended that, when assessing potentially suicidal older adults, clinicians select tools specifically designed for use in this age group, particularly the Geriatric Suicide Ideation Scale and the Geriatric Depression Scale. Dr. Heisel also recommended the Center for Epidemiological Studies Depression Scale–Revised Version.
“Beyond a specific scale, the question is to walk into a clinical encounter with a much broader viewpoint, understand who the client is, where they come from, their attitudes, life experience, and what in their experience is going on, their reason for coming to see someone and what they’re struggling with,” he said.
“What we’re seeing with this study is that standard clinical tools don’t necessarily identify some of these richer issues that might contribute to emotional pain, so sometimes the best way to go is a broader clinical interview with a humanistic perspective,” Dr. Heisel concluded.
The study was funded by the Swedish Research Council, the Swedish Research Council for Health, Working Life and Welfare, and the Swedish state, Stockholm County Council and Västerbotten County Council. The investigators and Dr. Heisel have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Older adults may have a high degree of suicidal intent yet still have low scores on scales measuring psychiatric symptoms, such as depression, new research suggests.
In a cross-sectional cohort study of more than 800 adults who presented with self-harm to psychiatric EDs in Sweden, participants aged 65 years and older scored higher than younger and middle-aged adults on measures of suicidal intent.
However, only half of the older group fulfilled criteria for major depression, compared with three-quarters of both the middle-aged and young adult–aged groups.
“Suicidal older persons show a somewhat different clinical picture with relatively low levels of psychopathology but with high suicide intent compared to younger persons,” lead author Stefan Wiktorsson, PhD, University of Gothenburg (Sweden), said in an interview.
“It is therefore of importance for clinicians to carefully evaluate suicidal thinking in this age group. he said.
The findings were published online Aug. 9, 2021, in the American Journal of Geriatric Psychiatry.
Research by age groups ‘lacking’
“While there are large age differences in the prevalence of suicidal behavior, research studies that compare symptomatology and diagnostics in different age groups are lacking,” Dr. Wiktorsson said.
He and his colleagues “wanted to compare psychopathology in young, middle-aged, and older adults in order to increase knowledge about potential differences in symptomatology related to suicidal behavior over the life span.”
The researchers recruited patients aged 18 years and older who had sought or had been referred to emergency psychiatric services for self-harm at three psychiatric hospitals in Sweden between April 2012 and March 2016.
Among all patients, 821 fit inclusion criteria and agreed to participate. The researchers excluded participants who had engaged in nonsuicidal self-injury (NNSI), as determined on the basis of the Columbia Suicide Severity Rating Scale (C-SSRS). The remaining 683 participants, who had attempted suicide, were included in the analysis.
The participants were then divided into the following three groups: older (n = 96; age, 65-97 years; mean age, 77.2 years; 57% women), middle-aged (n = 164; age, 45-64 years; mean age, 53.4 years; 57% women), and younger (n = 423; age, 18-44 years; mean age, 28.3 years; 64% women)
Mental health staff interviewed participants within 7 days of the index episode. They collected information about sociodemographics, health, and contact with health care professionals. They used the C-SSRS to identify characteristics of the suicide attempts, and they used the Suicide Intent Scale (SIS) to evaluate circumstances surrounding the suicide attempt, such as active preparation.
Investigators also used the Mini International Neuropsychiatric Interview (MINI), the Suicide Assessment Scale (SUAS), and the Karolinska Affective and Borderline Symptoms Scale.
Greater disability, pain
Of the older patients, 75% lived alone; 88% of the middle-aged and 48% of the younger participants lived alone. A higher proportion of older participants had severe physical illness/disability and severe chronic pain compared with younger participants (all comparisons, P < .001).
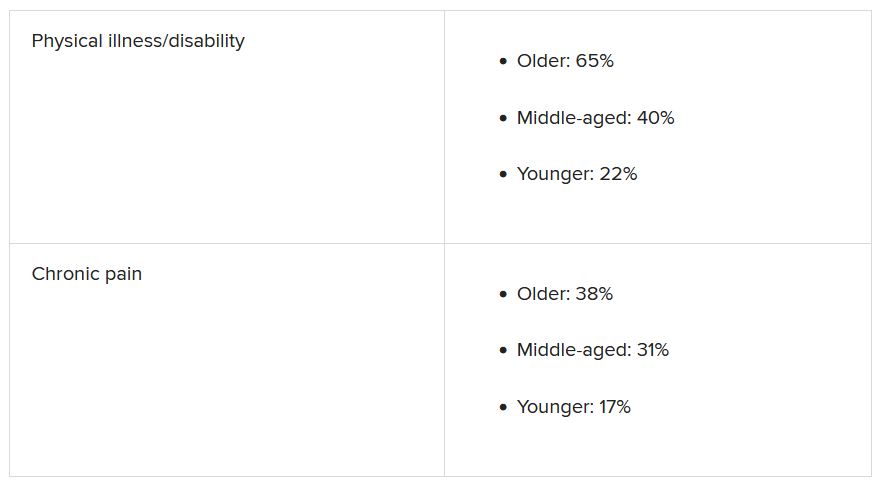
Older adults had less contact with psychiatric services, but they had more contact than the other age groups with primary care for mental health problems. Older adults were prescribed antidepressants at the time of the suicide attempt at a lower rate, compared with the middle-aged and younger groups (50% vs. 73% and 66%).
Slightly less than half (44%) of the older adults had a previous history of a suicide attempt – a proportion considerably lower than was reported by patients in the middle-aged and young adult groups (63% and 75%, respectively). Few older adults had a history of a previous NNSI (6% vs. 23% and 63%).
Three-quarters of older adults employed poisoning as the single method of suicide attempt at their index episode, compared with 67% and 59% of the middle-aged and younger groups.
Notably, only half of older adults (52%) met criteria for major depression, determined on the basis of the MINI, compared with three quarters of participants in the other groups (73% and 76%, respectively). Fewer members of the older group met criteria for other psychiatric conditions.
Clouded judgment
The mean total SUAS score was “considerably lower” in the older-adult group than in the other groups. This was also the case for the SUAS subscales for affect, bodily states, control, coping, and emotional reactivity.
Importantly, however, older adults scored higher than younger adults on the SIS total score and the subjective subscale, indicating a higher level of suicidal intent.
The mean SIS total score was 17.8 in the older group, 17.4 in the middle-aged group, and 15.9 in the younger group. The SIS subjective suicide intent score was 10.9 versus 10.6 and 9.4.
“While subjective suicidal intent was higher, compared to the young group, older adults were less likely to fulfill criteria for major depression and several other mental disorders and lower scores were observed on all symptom rating scales, compared to both middle-aged and younger adults,” the investigators wrote.
“Low levels of psychopathology may cloud the clinician’s assessment of the serious nature of suicide attempts in older patients,” they added.
‘Silent generation’
Commenting on the findings, Marnin Heisel, PhD, CPsych, associate professor, departments of psychiatry and of epidemiology and biostatistics, University of Western Ontario, London, said an important takeaway from the study is that, if health care professionals look only for depression or only consider suicide risk in individuals who present with depression, “they might miss older adults who are contemplating suicide or engaging in suicidal behavior.”
Dr. Heisel, who was not involved with the study, observed that older adults are sometimes called the “silent generation” because they often tend to downplay or underreport depressive symptoms, partially because of having been socialized to “keep things to themselves and not to air emotional laundry.”
He recommended that, when assessing potentially suicidal older adults, clinicians select tools specifically designed for use in this age group, particularly the Geriatric Suicide Ideation Scale and the Geriatric Depression Scale. Dr. Heisel also recommended the Center for Epidemiological Studies Depression Scale–Revised Version.
“Beyond a specific scale, the question is to walk into a clinical encounter with a much broader viewpoint, understand who the client is, where they come from, their attitudes, life experience, and what in their experience is going on, their reason for coming to see someone and what they’re struggling with,” he said.
“What we’re seeing with this study is that standard clinical tools don’t necessarily identify some of these richer issues that might contribute to emotional pain, so sometimes the best way to go is a broader clinical interview with a humanistic perspective,” Dr. Heisel concluded.
The study was funded by the Swedish Research Council, the Swedish Research Council for Health, Working Life and Welfare, and the Swedish state, Stockholm County Council and Västerbotten County Council. The investigators and Dr. Heisel have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Managing sleep in the elderly
Sleep problems are prevalent in older adults, and overmedication is a common cause. Insomnia is a concern, and it might not look the same in older adults as it does in younger populations, especially when neurodegenerative disorders may be present. “There’s often not only the inability to get to sleep and stay asleep in older adults but also changes in their biological rhythms, which is why treatments really need to be focused on both,” Ruth M. Benca, MD, PhD, said in an interview.
Dr. Benca spoke on the topic of insomnia in the elderly at a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists. She is chair of psychiatry at Wake Forest Baptist Health, Winston-Salem, N.C.
Sleep issues strongly affect quality of life and health outcomes in the elderly, and there isn’t a lot of clear guidance for physicians to manage these issues. who spoke at the meeting presented by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
Behavioral approaches are important, because quality of sleep is often affected by daytime activities, such as exercise and light exposure, according to Dr. Benca, who said that those factors can and should be addressed by behavioral interventions. Medications should be used as an adjunct to those treatments. “When we do need to use medications, we need to use ones that have been tested and found to be more helpful than harmful in older adults,” Dr. Benca said.
Many Food and Drug Administration–approved drugs should be used with caution or avoided in the elderly. The Beers criteria provide a useful list of potentially problematic drugs, and removing those drugs from consideration leaves just a few options, including the melatonin receptor agonist ramelteon, low doses of the tricyclic antidepressant doxepin, and dual orexin receptor antagonists, which are being tested in older adults, including some with dementia, Dr. Benca said.
Other drugs like benzodiazepines and related “Z” drugs can cause problems like amnesia, confusion, and psychomotor issues. “They’re advised against because there are some concerns about those side effects,” Dr. Benca said.
Sleep disturbance itself can be the result of polypharmacy. Even something as simple as a diuretic can interrupt slumber because of nocturnal bathroom visits. Antihypertensives and drugs that affect the central nervous system, including antidepressants, can affect sleep. “I’ve had patients get horrible dreams and nightmares from antihypertensive drugs. So there’s a very long laundry list of drugs that can affect sleep in a negative way,” said Dr. Benca.
Physicians have a tendency to prescribe more drugs to a patient without eliminating any, which can result in complex situations. “We see this sort of chasing the tail: You give a drug, it may have a positive effect on the primary thing you want to treat, but it has a side effect. When you give another drug to treat that side effect, it in turn has its own side effect. We keep piling on drugs,” Dr. Benca said.
“So if [a patient is] on medications for an indication, and particularly for sleep or other things, and the patient isn’t getting better, what we might want to do is slowly to withdraw things. Even for older adults who are on sleeping medications and maybe are doing better, sometimes we can decrease the dose [of the other drugs], or get them off those drugs or put them on something that might be less likely to have side effects,” Dr. Benca said.
To do that, she suggests taking a history to determine when the sleep problem began, and whether it coincided with adding or changing a medication. Another approach is to look at the list of current medications, and look for drugs that are prescribed for a problem and where the problem still persists. “You might want to take that away first, before you start adding something else,” said Dr. Benca.
Another challenge is that physicians are often unwilling to investigate sleep disorders, which are more common in older adults. Physicians can be reluctant to prescribe sleep medications, and may also be unfamiliar with behavioral interventions. “For a lot of providers, getting into sleep issues is like opening a Pandora’s Box. I think mostly physicians are taught: Don’t do this, and don’t do that. They’re not as well versed in the things that they can and should do,” said Dr. Benca.
If attempts to treat insomnia don’t succeed, or if the physician suspects a movement disorder or primary sleep disorder like sleep apnea, then the patients should be referred to a sleep specialist, according to Dr. Benca.
During the question-and-answer period following her talk, a questioner brought up the increasingly common use of cannabis to improve sleep. That can be tricky because it can be difficult to stop cannabis use, because of the rebound insomnia that may persist. She noted that there are ongoing studies on the potential impact of cannabidiol oil.
Dr. Benca was also asked about patients who take sedatives chronically and seem to be doing well. She emphasized the need for finding the lowest effective dose of a short-acting medication. “Patients should be monitored frequently, at least every 6 months. Just monitor your patient carefully.”
Dr. Benca is a consultant for Eisai, Genomind, Idorsia, Jazz, Merck, Sage, and Sunovion.
Sleep problems are prevalent in older adults, and overmedication is a common cause. Insomnia is a concern, and it might not look the same in older adults as it does in younger populations, especially when neurodegenerative disorders may be present. “There’s often not only the inability to get to sleep and stay asleep in older adults but also changes in their biological rhythms, which is why treatments really need to be focused on both,” Ruth M. Benca, MD, PhD, said in an interview.
Dr. Benca spoke on the topic of insomnia in the elderly at a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists. She is chair of psychiatry at Wake Forest Baptist Health, Winston-Salem, N.C.
Sleep issues strongly affect quality of life and health outcomes in the elderly, and there isn’t a lot of clear guidance for physicians to manage these issues. who spoke at the meeting presented by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
Behavioral approaches are important, because quality of sleep is often affected by daytime activities, such as exercise and light exposure, according to Dr. Benca, who said that those factors can and should be addressed by behavioral interventions. Medications should be used as an adjunct to those treatments. “When we do need to use medications, we need to use ones that have been tested and found to be more helpful than harmful in older adults,” Dr. Benca said.
Many Food and Drug Administration–approved drugs should be used with caution or avoided in the elderly. The Beers criteria provide a useful list of potentially problematic drugs, and removing those drugs from consideration leaves just a few options, including the melatonin receptor agonist ramelteon, low doses of the tricyclic antidepressant doxepin, and dual orexin receptor antagonists, which are being tested in older adults, including some with dementia, Dr. Benca said.
Other drugs like benzodiazepines and related “Z” drugs can cause problems like amnesia, confusion, and psychomotor issues. “They’re advised against because there are some concerns about those side effects,” Dr. Benca said.
Sleep disturbance itself can be the result of polypharmacy. Even something as simple as a diuretic can interrupt slumber because of nocturnal bathroom visits. Antihypertensives and drugs that affect the central nervous system, including antidepressants, can affect sleep. “I’ve had patients get horrible dreams and nightmares from antihypertensive drugs. So there’s a very long laundry list of drugs that can affect sleep in a negative way,” said Dr. Benca.
Physicians have a tendency to prescribe more drugs to a patient without eliminating any, which can result in complex situations. “We see this sort of chasing the tail: You give a drug, it may have a positive effect on the primary thing you want to treat, but it has a side effect. When you give another drug to treat that side effect, it in turn has its own side effect. We keep piling on drugs,” Dr. Benca said.
“So if [a patient is] on medications for an indication, and particularly for sleep or other things, and the patient isn’t getting better, what we might want to do is slowly to withdraw things. Even for older adults who are on sleeping medications and maybe are doing better, sometimes we can decrease the dose [of the other drugs], or get them off those drugs or put them on something that might be less likely to have side effects,” Dr. Benca said.
To do that, she suggests taking a history to determine when the sleep problem began, and whether it coincided with adding or changing a medication. Another approach is to look at the list of current medications, and look for drugs that are prescribed for a problem and where the problem still persists. “You might want to take that away first, before you start adding something else,” said Dr. Benca.
Another challenge is that physicians are often unwilling to investigate sleep disorders, which are more common in older adults. Physicians can be reluctant to prescribe sleep medications, and may also be unfamiliar with behavioral interventions. “For a lot of providers, getting into sleep issues is like opening a Pandora’s Box. I think mostly physicians are taught: Don’t do this, and don’t do that. They’re not as well versed in the things that they can and should do,” said Dr. Benca.
If attempts to treat insomnia don’t succeed, or if the physician suspects a movement disorder or primary sleep disorder like sleep apnea, then the patients should be referred to a sleep specialist, according to Dr. Benca.
During the question-and-answer period following her talk, a questioner brought up the increasingly common use of cannabis to improve sleep. That can be tricky because it can be difficult to stop cannabis use, because of the rebound insomnia that may persist. She noted that there are ongoing studies on the potential impact of cannabidiol oil.
Dr. Benca was also asked about patients who take sedatives chronically and seem to be doing well. She emphasized the need for finding the lowest effective dose of a short-acting medication. “Patients should be monitored frequently, at least every 6 months. Just monitor your patient carefully.”
Dr. Benca is a consultant for Eisai, Genomind, Idorsia, Jazz, Merck, Sage, and Sunovion.
Sleep problems are prevalent in older adults, and overmedication is a common cause. Insomnia is a concern, and it might not look the same in older adults as it does in younger populations, especially when neurodegenerative disorders may be present. “There’s often not only the inability to get to sleep and stay asleep in older adults but also changes in their biological rhythms, which is why treatments really need to be focused on both,” Ruth M. Benca, MD, PhD, said in an interview.
Dr. Benca spoke on the topic of insomnia in the elderly at a virtual meeting presented by Current Psychiatry and the American Academy of Clinical Psychiatrists. She is chair of psychiatry at Wake Forest Baptist Health, Winston-Salem, N.C.
Sleep issues strongly affect quality of life and health outcomes in the elderly, and there isn’t a lot of clear guidance for physicians to manage these issues. who spoke at the meeting presented by MedscapeLive. MedscapeLive and this news organization are owned by the same parent company.
Behavioral approaches are important, because quality of sleep is often affected by daytime activities, such as exercise and light exposure, according to Dr. Benca, who said that those factors can and should be addressed by behavioral interventions. Medications should be used as an adjunct to those treatments. “When we do need to use medications, we need to use ones that have been tested and found to be more helpful than harmful in older adults,” Dr. Benca said.
Many Food and Drug Administration–approved drugs should be used with caution or avoided in the elderly. The Beers criteria provide a useful list of potentially problematic drugs, and removing those drugs from consideration leaves just a few options, including the melatonin receptor agonist ramelteon, low doses of the tricyclic antidepressant doxepin, and dual orexin receptor antagonists, which are being tested in older adults, including some with dementia, Dr. Benca said.
Other drugs like benzodiazepines and related “Z” drugs can cause problems like amnesia, confusion, and psychomotor issues. “They’re advised against because there are some concerns about those side effects,” Dr. Benca said.
Sleep disturbance itself can be the result of polypharmacy. Even something as simple as a diuretic can interrupt slumber because of nocturnal bathroom visits. Antihypertensives and drugs that affect the central nervous system, including antidepressants, can affect sleep. “I’ve had patients get horrible dreams and nightmares from antihypertensive drugs. So there’s a very long laundry list of drugs that can affect sleep in a negative way,” said Dr. Benca.
Physicians have a tendency to prescribe more drugs to a patient without eliminating any, which can result in complex situations. “We see this sort of chasing the tail: You give a drug, it may have a positive effect on the primary thing you want to treat, but it has a side effect. When you give another drug to treat that side effect, it in turn has its own side effect. We keep piling on drugs,” Dr. Benca said.
“So if [a patient is] on medications for an indication, and particularly for sleep or other things, and the patient isn’t getting better, what we might want to do is slowly to withdraw things. Even for older adults who are on sleeping medications and maybe are doing better, sometimes we can decrease the dose [of the other drugs], or get them off those drugs or put them on something that might be less likely to have side effects,” Dr. Benca said.
To do that, she suggests taking a history to determine when the sleep problem began, and whether it coincided with adding or changing a medication. Another approach is to look at the list of current medications, and look for drugs that are prescribed for a problem and where the problem still persists. “You might want to take that away first, before you start adding something else,” said Dr. Benca.
Another challenge is that physicians are often unwilling to investigate sleep disorders, which are more common in older adults. Physicians can be reluctant to prescribe sleep medications, and may also be unfamiliar with behavioral interventions. “For a lot of providers, getting into sleep issues is like opening a Pandora’s Box. I think mostly physicians are taught: Don’t do this, and don’t do that. They’re not as well versed in the things that they can and should do,” said Dr. Benca.
If attempts to treat insomnia don’t succeed, or if the physician suspects a movement disorder or primary sleep disorder like sleep apnea, then the patients should be referred to a sleep specialist, according to Dr. Benca.
During the question-and-answer period following her talk, a questioner brought up the increasingly common use of cannabis to improve sleep. That can be tricky because it can be difficult to stop cannabis use, because of the rebound insomnia that may persist. She noted that there are ongoing studies on the potential impact of cannabidiol oil.
Dr. Benca was also asked about patients who take sedatives chronically and seem to be doing well. She emphasized the need for finding the lowest effective dose of a short-acting medication. “Patients should be monitored frequently, at least every 6 months. Just monitor your patient carefully.”
Dr. Benca is a consultant for Eisai, Genomind, Idorsia, Jazz, Merck, Sage, and Sunovion.
FROM FOCUS ON NEUROPSYCHIATRY 2021
Inflation will be the end of medicine
Inflation is the senility of democracies.
–Sylvia Townsend Warner
Electronic medical records? No, all of these are minor annoyances in the face of the practice killer, inflation.
Physicians live in a closed box where medical reimbursements are fixed, directly or by contract proxy to the government (Medicare) pay rate. Inflation is projected to be between 5% and 10% this year. We cannot increase our rates to increase the salaries of our employees, cover our increased medical disposable costs, and pay more for our state licensures and DEA registrations. No, we must try to find savings in our budget, which we have been squeezing for years.
Currently, medicine is facing a 9.75% cut in Medicare reimbursements, which will reset most private insurance rates, based on a percentage of Medicare. The temporary 3.75% conversion factor (CF) increase for all services is expiring. Also expiring is the 2% sequester from the Budget Control Act of 2011 (BCA), signed into law in August 2011. This was originally scheduled to sunset in 2021, but is going to continue to 2030.
A 4% statutory pay-as-you-go (PAYGO) sequester resulting from passage of the American Rescue Plan Act is being imposed. Statutory PAYGO is a policy written into law (it can be changed only through new legislation) that requires deficit neutrality overall in the laws (other than annual appropriations) enacted by Congress and imposes automatic spending reductions at the end of the year if such laws increase the deficit when they are added together.
There is a statutory freeze on Medicare Physician Fee Schedule (PFS) updates until 2026, at which time an annual increase of 0.25%, which is lower than inflation, will be enacted. This adds up to a 9.75% cut in Medicare pay until at least 2026. Recall that almost all of your private insurance contracts are tied to Medicare (some more, some less) and that this cut to the physician is doubled if your overhead is fixed at the typical 50% for most practices. This means an almost 20% cut in take-home pay for most physicians.
Now, when considering the most recent inflation number, which projects 5%-10% inflation for this year and at least 2% annually in the future, which compounds yearly (the Fed target), you are looking at catastrophic numbers.
The conversion factor – the pool of money doled out to physicians – has failed to keep pace with inflation – even at 2%-3% a year – and reimbursement is only 50% of what it was when created in 1998, despite small increases by Congress along the way. A recent Wall Street Journal guest editorial claimed that Medicare payments benefited from cost of living adjustments, same as Social Security. I do not agree, hence the 50% pay gap since 1998.
In addition, the costs of running a practice have increased by 37% between 2001 and 2020, 1.7% per year, according to the Medicare Economic Index.
Some of this may include general inflation, but certainly new OSHA rules, electronic medical records, Medicare quality improvement measures, and assorted other costs do not. So based on my own conservative estimate, on top of the 50% decline in the payment pool, physicians’ noninflationary operating costs increased by at least another 10% over the last 20 odd years. This is a 60% decline in reimbursements!
Medicare payments have been under pressure from the Centers for Medicare & Medicaid Services (CMS) anti-inflationary payment policies for more than 20 years. While physician services represent a very modest portion of the overall growth in health care costs, they are an easy target for cuts when policymakers seek to limit spending. Although we avoided direct cuts to reimbursements caused by the Medicare sustainable growth rate formula (SGR) – which was enacted in 1997 and repealed in 2015 – Medicare provider payments have remained constrained by a budget-neutral financing system.
There used to be ways out of the box. Physicians could go to work for hospitals or have their practices acquired by them, resulting in much better hospital-based reimbursement. This has been eliminated by site-neutral payments, which while instituted by President Trump, are unopposed by President Biden. You could also join larger groups with some loss of autonomy, which could presumably negotiate better rates with private insurers as another way out, but these rates are almost always based on a percentage of Medicare as noted above.
There may be a bit of good news, with price transparency being instituted, which again is unopposed by the Biden administration. At least private practice physicians may be able to show their services are a bargain compared to hospitals.
One could also take the low road, and sell out to private equity, but I suspect these deals will become much less attractive since some of these entities are going broke and all will feel the bite of lower reimbursements.
Physicians and patients should rise up and demand better reimbursements for physicians, or there will be no physicians to see. This is not greed, a bigger house, or a newer car, this is becoming a matter of practice survival. And seniors are not greedy, they have paid hundreds of thousands of dollars into Medicare in taxes for health insurance in retirement.
Physicians and retirees should contact their federal legislators and let them know a 9.75% cut is untenable and ask for Medicare rates to be fixed to the cost of living, just as Social Security is. Before we fund trillions of dollars in new government programs, perhaps we should look to the solvency of the existing ones we have.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
Inflation is the senility of democracies.
–Sylvia Townsend Warner
Electronic medical records? No, all of these are minor annoyances in the face of the practice killer, inflation.
Physicians live in a closed box where medical reimbursements are fixed, directly or by contract proxy to the government (Medicare) pay rate. Inflation is projected to be between 5% and 10% this year. We cannot increase our rates to increase the salaries of our employees, cover our increased medical disposable costs, and pay more for our state licensures and DEA registrations. No, we must try to find savings in our budget, which we have been squeezing for years.
Currently, medicine is facing a 9.75% cut in Medicare reimbursements, which will reset most private insurance rates, based on a percentage of Medicare. The temporary 3.75% conversion factor (CF) increase for all services is expiring. Also expiring is the 2% sequester from the Budget Control Act of 2011 (BCA), signed into law in August 2011. This was originally scheduled to sunset in 2021, but is going to continue to 2030.
A 4% statutory pay-as-you-go (PAYGO) sequester resulting from passage of the American Rescue Plan Act is being imposed. Statutory PAYGO is a policy written into law (it can be changed only through new legislation) that requires deficit neutrality overall in the laws (other than annual appropriations) enacted by Congress and imposes automatic spending reductions at the end of the year if such laws increase the deficit when they are added together.
There is a statutory freeze on Medicare Physician Fee Schedule (PFS) updates until 2026, at which time an annual increase of 0.25%, which is lower than inflation, will be enacted. This adds up to a 9.75% cut in Medicare pay until at least 2026. Recall that almost all of your private insurance contracts are tied to Medicare (some more, some less) and that this cut to the physician is doubled if your overhead is fixed at the typical 50% for most practices. This means an almost 20% cut in take-home pay for most physicians.
Now, when considering the most recent inflation number, which projects 5%-10% inflation for this year and at least 2% annually in the future, which compounds yearly (the Fed target), you are looking at catastrophic numbers.
The conversion factor – the pool of money doled out to physicians – has failed to keep pace with inflation – even at 2%-3% a year – and reimbursement is only 50% of what it was when created in 1998, despite small increases by Congress along the way. A recent Wall Street Journal guest editorial claimed that Medicare payments benefited from cost of living adjustments, same as Social Security. I do not agree, hence the 50% pay gap since 1998.
In addition, the costs of running a practice have increased by 37% between 2001 and 2020, 1.7% per year, according to the Medicare Economic Index.
Some of this may include general inflation, but certainly new OSHA rules, electronic medical records, Medicare quality improvement measures, and assorted other costs do not. So based on my own conservative estimate, on top of the 50% decline in the payment pool, physicians’ noninflationary operating costs increased by at least another 10% over the last 20 odd years. This is a 60% decline in reimbursements!
Medicare payments have been under pressure from the Centers for Medicare & Medicaid Services (CMS) anti-inflationary payment policies for more than 20 years. While physician services represent a very modest portion of the overall growth in health care costs, they are an easy target for cuts when policymakers seek to limit spending. Although we avoided direct cuts to reimbursements caused by the Medicare sustainable growth rate formula (SGR) – which was enacted in 1997 and repealed in 2015 – Medicare provider payments have remained constrained by a budget-neutral financing system.
There used to be ways out of the box. Physicians could go to work for hospitals or have their practices acquired by them, resulting in much better hospital-based reimbursement. This has been eliminated by site-neutral payments, which while instituted by President Trump, are unopposed by President Biden. You could also join larger groups with some loss of autonomy, which could presumably negotiate better rates with private insurers as another way out, but these rates are almost always based on a percentage of Medicare as noted above.
There may be a bit of good news, with price transparency being instituted, which again is unopposed by the Biden administration. At least private practice physicians may be able to show their services are a bargain compared to hospitals.
One could also take the low road, and sell out to private equity, but I suspect these deals will become much less attractive since some of these entities are going broke and all will feel the bite of lower reimbursements.
Physicians and patients should rise up and demand better reimbursements for physicians, or there will be no physicians to see. This is not greed, a bigger house, or a newer car, this is becoming a matter of practice survival. And seniors are not greedy, they have paid hundreds of thousands of dollars into Medicare in taxes for health insurance in retirement.
Physicians and retirees should contact their federal legislators and let them know a 9.75% cut is untenable and ask for Medicare rates to be fixed to the cost of living, just as Social Security is. Before we fund trillions of dollars in new government programs, perhaps we should look to the solvency of the existing ones we have.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
Inflation is the senility of democracies.
–Sylvia Townsend Warner
Electronic medical records? No, all of these are minor annoyances in the face of the practice killer, inflation.
Physicians live in a closed box where medical reimbursements are fixed, directly or by contract proxy to the government (Medicare) pay rate. Inflation is projected to be between 5% and 10% this year. We cannot increase our rates to increase the salaries of our employees, cover our increased medical disposable costs, and pay more for our state licensures and DEA registrations. No, we must try to find savings in our budget, which we have been squeezing for years.
Currently, medicine is facing a 9.75% cut in Medicare reimbursements, which will reset most private insurance rates, based on a percentage of Medicare. The temporary 3.75% conversion factor (CF) increase for all services is expiring. Also expiring is the 2% sequester from the Budget Control Act of 2011 (BCA), signed into law in August 2011. This was originally scheduled to sunset in 2021, but is going to continue to 2030.
A 4% statutory pay-as-you-go (PAYGO) sequester resulting from passage of the American Rescue Plan Act is being imposed. Statutory PAYGO is a policy written into law (it can be changed only through new legislation) that requires deficit neutrality overall in the laws (other than annual appropriations) enacted by Congress and imposes automatic spending reductions at the end of the year if such laws increase the deficit when they are added together.
There is a statutory freeze on Medicare Physician Fee Schedule (PFS) updates until 2026, at which time an annual increase of 0.25%, which is lower than inflation, will be enacted. This adds up to a 9.75% cut in Medicare pay until at least 2026. Recall that almost all of your private insurance contracts are tied to Medicare (some more, some less) and that this cut to the physician is doubled if your overhead is fixed at the typical 50% for most practices. This means an almost 20% cut in take-home pay for most physicians.
Now, when considering the most recent inflation number, which projects 5%-10% inflation for this year and at least 2% annually in the future, which compounds yearly (the Fed target), you are looking at catastrophic numbers.
The conversion factor – the pool of money doled out to physicians – has failed to keep pace with inflation – even at 2%-3% a year – and reimbursement is only 50% of what it was when created in 1998, despite small increases by Congress along the way. A recent Wall Street Journal guest editorial claimed that Medicare payments benefited from cost of living adjustments, same as Social Security. I do not agree, hence the 50% pay gap since 1998.
In addition, the costs of running a practice have increased by 37% between 2001 and 2020, 1.7% per year, according to the Medicare Economic Index.
Some of this may include general inflation, but certainly new OSHA rules, electronic medical records, Medicare quality improvement measures, and assorted other costs do not. So based on my own conservative estimate, on top of the 50% decline in the payment pool, physicians’ noninflationary operating costs increased by at least another 10% over the last 20 odd years. This is a 60% decline in reimbursements!
Medicare payments have been under pressure from the Centers for Medicare & Medicaid Services (CMS) anti-inflationary payment policies for more than 20 years. While physician services represent a very modest portion of the overall growth in health care costs, they are an easy target for cuts when policymakers seek to limit spending. Although we avoided direct cuts to reimbursements caused by the Medicare sustainable growth rate formula (SGR) – which was enacted in 1997 and repealed in 2015 – Medicare provider payments have remained constrained by a budget-neutral financing system.
There used to be ways out of the box. Physicians could go to work for hospitals or have their practices acquired by them, resulting in much better hospital-based reimbursement. This has been eliminated by site-neutral payments, which while instituted by President Trump, are unopposed by President Biden. You could also join larger groups with some loss of autonomy, which could presumably negotiate better rates with private insurers as another way out, but these rates are almost always based on a percentage of Medicare as noted above.
There may be a bit of good news, with price transparency being instituted, which again is unopposed by the Biden administration. At least private practice physicians may be able to show their services are a bargain compared to hospitals.
One could also take the low road, and sell out to private equity, but I suspect these deals will become much less attractive since some of these entities are going broke and all will feel the bite of lower reimbursements.
Physicians and patients should rise up and demand better reimbursements for physicians, or there will be no physicians to see. This is not greed, a bigger house, or a newer car, this is becoming a matter of practice survival. And seniors are not greedy, they have paid hundreds of thousands of dollars into Medicare in taxes for health insurance in retirement.
Physicians and retirees should contact their federal legislators and let them know a 9.75% cut is untenable and ask for Medicare rates to be fixed to the cost of living, just as Social Security is. Before we fund trillions of dollars in new government programs, perhaps we should look to the solvency of the existing ones we have.
Dr. Coldiron is in private practice but maintains a clinical assistant professorship at the University of Cincinnati. He cares for patients, teaches medical students and residents, and has several active clinical research projects. Dr. Coldiron is the author of more than 80 scientific letters, papers, and several book chapters, and he speaks frequently on a variety of topics. He is a past president of the American Academy of Dermatology. Write to him at [email protected].
Connecticut chapter of ACC at center of Twitter dustup
Tweets from a black female medical student about the perils of being on call after lengthy hospital shifts was met with a stinging rebuke from the Twitter account of the Connecticut chapter of the American College of Cardiology – prompting an apology and some high-octane exchanges on medical Twitter.
In a series of Tweets, “queen of anonymous medicine” @QueenMD202X describes one friend “working 87 hours this week and 13 days straight” and a second, a third-year medical student working a 15-hour surgical shift. “That is cruel,” she writes, “15-hour shift? For what?????”
In response to a Tweet suggesting that being on call can be a valuable experience for students to know what they’re facing once they get to residency, @QueenMD202X pointed out the 15-hour shifts aren’t just a one-off.
In a now-deleted Tweet that nevertheless appears in several additional tweets as a screenshot, @ConnecticutACC replied: “You might be in the wrong field. You sound very angry probably unsuitable for patient care when your mental state is as you describe it. Emotions are contagious.”
The response from the medical and broader Twitter community was swift, with several tweets calling the chapter’s reply insensitive and racist.
In another Tweet, @BrittGratreak responded by stating: “I think institutions need to be more transparent how they basically weigh the costs & benefits of writing a memorial statement for students who die by suicide rather than investing in changing the toxic culture of medical education to prevent deaths & producing harmed physicians.”
Within hours, Connecticut-ACC issued an apology from their now-deleted account and questioned the origins of the Tweet. “We sincerely apologize for the earlier post as the views do not represent the values or beliefs of the Chapter or broader ACC. We are working to ID its origins. Burnout & well-being are critical issues [that] ACC/CCACC is working to address on behalf of members at all career stages.”
Speaking to this news organization, Connecticut-ACC president and governor Craig McPherson, MD, Yale University, New Haven, Conn., said the chapter believes its account was hacked.
“We provide limited password access to our Twitter account, and we assume, since we’ve contacted most of the individuals who had access to the current password and all of the them deny any knowledge, the account got hacked … it’s just one of those unfortunate aspects of social media,” he said.
The password was quickly changed after the chapter learned of the Tweet on Wednesday and the account has since been closed, at Dr. McPherson’s request.
“We don’t condone that kind of language, that kind of remark. It’s highly inappropriate, and I certainly agree with anyone that voiced that opinion in the Twitterstorm that followed,” he said. “But as I said at the outset, I have no control over what people say on social media once it’s out there. All we can do is apologize for the fact our Twitter feed was used as a vehicle for those comments, which we consider inappropriate.”
Asked whether he considered the remarks racist, Dr. McPherson replied: “That’s not for me to judge.”
ACC president Dipti Itchhaporia, MD, however, weighed in this afternoon with a Tweet citing the need to address clinician well-being and an inclusive workplace.
Some on Twitter recalled their own long hours as a medical student or defended the need to inculcate students in the long hours they’ll face as physicians. Others observed that neither ACC nor its Connecticut chapter addressed the issue of medical student hours in their response. Although fellow and resident hours are regulated, Dr. McPherson pointed out that it’s up to each individual medical school to set the hours for their students.
A version of this article first appeared on Medscape.com.
Tweets from a black female medical student about the perils of being on call after lengthy hospital shifts was met with a stinging rebuke from the Twitter account of the Connecticut chapter of the American College of Cardiology – prompting an apology and some high-octane exchanges on medical Twitter.
In a series of Tweets, “queen of anonymous medicine” @QueenMD202X describes one friend “working 87 hours this week and 13 days straight” and a second, a third-year medical student working a 15-hour surgical shift. “That is cruel,” she writes, “15-hour shift? For what?????”
In response to a Tweet suggesting that being on call can be a valuable experience for students to know what they’re facing once they get to residency, @QueenMD202X pointed out the 15-hour shifts aren’t just a one-off.
In a now-deleted Tweet that nevertheless appears in several additional tweets as a screenshot, @ConnecticutACC replied: “You might be in the wrong field. You sound very angry probably unsuitable for patient care when your mental state is as you describe it. Emotions are contagious.”
The response from the medical and broader Twitter community was swift, with several tweets calling the chapter’s reply insensitive and racist.
In another Tweet, @BrittGratreak responded by stating: “I think institutions need to be more transparent how they basically weigh the costs & benefits of writing a memorial statement for students who die by suicide rather than investing in changing the toxic culture of medical education to prevent deaths & producing harmed physicians.”
Within hours, Connecticut-ACC issued an apology from their now-deleted account and questioned the origins of the Tweet. “We sincerely apologize for the earlier post as the views do not represent the values or beliefs of the Chapter or broader ACC. We are working to ID its origins. Burnout & well-being are critical issues [that] ACC/CCACC is working to address on behalf of members at all career stages.”
Speaking to this news organization, Connecticut-ACC president and governor Craig McPherson, MD, Yale University, New Haven, Conn., said the chapter believes its account was hacked.
“We provide limited password access to our Twitter account, and we assume, since we’ve contacted most of the individuals who had access to the current password and all of the them deny any knowledge, the account got hacked … it’s just one of those unfortunate aspects of social media,” he said.
The password was quickly changed after the chapter learned of the Tweet on Wednesday and the account has since been closed, at Dr. McPherson’s request.
“We don’t condone that kind of language, that kind of remark. It’s highly inappropriate, and I certainly agree with anyone that voiced that opinion in the Twitterstorm that followed,” he said. “But as I said at the outset, I have no control over what people say on social media once it’s out there. All we can do is apologize for the fact our Twitter feed was used as a vehicle for those comments, which we consider inappropriate.”
Asked whether he considered the remarks racist, Dr. McPherson replied: “That’s not for me to judge.”
ACC president Dipti Itchhaporia, MD, however, weighed in this afternoon with a Tweet citing the need to address clinician well-being and an inclusive workplace.
Some on Twitter recalled their own long hours as a medical student or defended the need to inculcate students in the long hours they’ll face as physicians. Others observed that neither ACC nor its Connecticut chapter addressed the issue of medical student hours in their response. Although fellow and resident hours are regulated, Dr. McPherson pointed out that it’s up to each individual medical school to set the hours for their students.
A version of this article first appeared on Medscape.com.
Tweets from a black female medical student about the perils of being on call after lengthy hospital shifts was met with a stinging rebuke from the Twitter account of the Connecticut chapter of the American College of Cardiology – prompting an apology and some high-octane exchanges on medical Twitter.
In a series of Tweets, “queen of anonymous medicine” @QueenMD202X describes one friend “working 87 hours this week and 13 days straight” and a second, a third-year medical student working a 15-hour surgical shift. “That is cruel,” she writes, “15-hour shift? For what?????”
In response to a Tweet suggesting that being on call can be a valuable experience for students to know what they’re facing once they get to residency, @QueenMD202X pointed out the 15-hour shifts aren’t just a one-off.
In a now-deleted Tweet that nevertheless appears in several additional tweets as a screenshot, @ConnecticutACC replied: “You might be in the wrong field. You sound very angry probably unsuitable for patient care when your mental state is as you describe it. Emotions are contagious.”
The response from the medical and broader Twitter community was swift, with several tweets calling the chapter’s reply insensitive and racist.
In another Tweet, @BrittGratreak responded by stating: “I think institutions need to be more transparent how they basically weigh the costs & benefits of writing a memorial statement for students who die by suicide rather than investing in changing the toxic culture of medical education to prevent deaths & producing harmed physicians.”
Within hours, Connecticut-ACC issued an apology from their now-deleted account and questioned the origins of the Tweet. “We sincerely apologize for the earlier post as the views do not represent the values or beliefs of the Chapter or broader ACC. We are working to ID its origins. Burnout & well-being are critical issues [that] ACC/CCACC is working to address on behalf of members at all career stages.”
Speaking to this news organization, Connecticut-ACC president and governor Craig McPherson, MD, Yale University, New Haven, Conn., said the chapter believes its account was hacked.
“We provide limited password access to our Twitter account, and we assume, since we’ve contacted most of the individuals who had access to the current password and all of the them deny any knowledge, the account got hacked … it’s just one of those unfortunate aspects of social media,” he said.
The password was quickly changed after the chapter learned of the Tweet on Wednesday and the account has since been closed, at Dr. McPherson’s request.
“We don’t condone that kind of language, that kind of remark. It’s highly inappropriate, and I certainly agree with anyone that voiced that opinion in the Twitterstorm that followed,” he said. “But as I said at the outset, I have no control over what people say on social media once it’s out there. All we can do is apologize for the fact our Twitter feed was used as a vehicle for those comments, which we consider inappropriate.”
Asked whether he considered the remarks racist, Dr. McPherson replied: “That’s not for me to judge.”
ACC president Dipti Itchhaporia, MD, however, weighed in this afternoon with a Tweet citing the need to address clinician well-being and an inclusive workplace.
Some on Twitter recalled their own long hours as a medical student or defended the need to inculcate students in the long hours they’ll face as physicians. Others observed that neither ACC nor its Connecticut chapter addressed the issue of medical student hours in their response. Although fellow and resident hours are regulated, Dr. McPherson pointed out that it’s up to each individual medical school to set the hours for their students.
A version of this article first appeared on Medscape.com.
Doctor wins restraining order against CVS after prescription ban
In an Aug. 11 decision, District Court Judge William Bertelsman ordered CVS to stop refusing prescriptions written by Kendall E. Hansen, MD. Judge Bertelsman ruled that Dr. Hansen is likely to succeed in his claim that CVS barred his prescriptions without evidence that he violated any law or professional protocol. The restraining order will remain in place while Dr. Hansen’s lawsuit against CVS Pharmacy proceeds.
Ronald W. Chapman II, an attorney representing Dr. Hansen, said the order is groundbreaking and that, to his knowledge, it’s the first time a federal court has overturned a pharmacy’s decision to block a prescriber.
“We believe that CVS’ decision was based solely on algorithms they use to analyze prescriber practices and not an any individual review of patient records,” Mr. Chapman said. “In fact, we invited CVS to come out to Dr. Hansen’s practice and look at how he was treating patients and ensure things were compliant, but they refused. Instead, they had a phone call with him then cut his patients off.”
Michael DeAngelis, a spokesman for CVS, said the court’s order illustrates the proverbial rock and hard place that pharmacies are placed between in the country’s fight against the misuse of prescription opioids.
“It is alleged in many lawsuits that pharmacies fill too many opioid prescriptions and should operate programs that use data to block prescriptions written by some doctors,” Mr. DeAngelis told this news organization. “And yet other lawsuits, including this one, argue that we should not operate programs that may block prescriptions. Such contradictions are grossly unfair to the pharmacy profession.”
Mr. DeAngelis declined to comment about Dr. Hansen’s claims or specify what led CVS to refuse his prescriptions.
Dr. Hansen declined to comment for this story through his attorney.
Dr. Hansen is no stranger to the spotlight. The Northern Kentucky pain doctor made headlines in 2012 when two of his horses, Fast and Accurate, and Hansen, ran in the Kentucky Derby. In February 2019, he drew media attention when his practice, Interventional Pain Specialists in Crestview Hills, Ky., was raided by federal agents. Dr. Hansen owns and operates the facility, which serves patients in Kentucky, Ohio, and Indiana.
The search yielded no findings, and no charges were filed, according to Mr. Chapman. Scott Hardcorn, director of the Northern Kentucky Drug Strike Force, confirmed that his agency assisted in the operation but said he was unaware of the outcome and that his officers generated no reports from the investigation. A spokesperson for the Drug Enforcement Administration would not comment about the investigation and directed a reporter for this news organization to the DEA website where enforcement actions are listed. No records or actions against Dr. Hansen can be found.
The CVS complaint stems from actions taken by the pharmacy against Dr. Hansen earlier this year. In June, a pharmacy representative allegedly contacted Dr. Hansen by phone and asked him questions about his practice and his prescribing practices, according to his lawsuit filed in U.S. District Court for the Eastern District of Kentucky. During the call, the representative did not inform Dr. Hansen that any of his prescriptions were in question or were suspected of being medically unnecessary, the complaint alleges.
On July 28, 2021, CVS sent Dr. Hansen a letter announcing that its pharmacies would no longer be honoring his prescriptions. The letter, entered as an exhibit in the lawsuit, states that CVS contacted Dr. Hansen twice in 2021 about his prescribing practices, once in May and again in June.
“Despite our attempts to resolve the concerns with your controlled substance prescribing patterns, these concerns persist,” Kahra Lutkiewicz, director of CVS’ retail pharmacy professional practice, wrote in the letter. “Thus, we are writing to inform you that effective Aug. 5, 2021, CVS/pharmacy stores will no longer be able to fill prescriptions that you write for controlled substances. We take our compliance obligations very seriously, and after careful consideration, find it necessary to take this action.”
The letter does not explain the details behind CVS’ concerns.
Dr. Hansen sued CVS on Aug. 4 for tortious interference with a business relationship and defamation, among other claims. His complaint alleges that Dr. Hansen and his patients will suffer irreparable injury if the prescription decision stands. More than 250 of Dr. Hansen’s patients use CVS pharmacies for their prescriptions, and some are locked into using the pharmacy because of insurance contracts, Mr. Chapman said.
“There really is nowhere else for these patients to go,” Mr. Chapman said. “They would have to go to a new doctor and establish a new relationship, and obviously that has devastating consequences when we’re talking about people who need their medication.”
CVS has not yet issued a written response to the lawsuit. In his order, Judge Bertelsman stated that a preliminary conference was held in which all parties were represented and stated their positions to the judge.
“Plaintiffs are likely to succeed on the merits of their claims that defendant has interfered with plaintiffs’ relationships with their patients by refusing to fill prescriptions written by plaintiffs, and defendant has done so without evidence that plaintiffs have violated any law or professional protocol related to such prescriptions,” Judge Bertelsman wrote. “The balance of the hardships between the parties weighs in favor of issuing a temporary restraining order inasmuch as defendant’s actions pose a threat to plaintiffs’ professional reputation and livelihood and ... because plaintiffs’ patients’ medical care is implicated by defendant’s actions, the public interest weighs in favor of issuance of the temporary restraining order.”
Dr. Hansen is currently embroiled in several other legal battles as both a plaintiff and a defendant.
In 2019, a patient sued him for negligence and fraud for allegedly performing medically unnecessary and excessive injection therapy. The suit claims the patient was required to undergo injection therapy on a continuing basis in order to receive her narcotic pain medication, according to the lawsuit filed in Kenton Circuit Court. The complaint alleges that Dr. Hansen made false representations to the patient and to her insurers that the injections were necessary for the treatment of the patient’s chronic pain.
The federal government is not involved in the case.
The negligence lawsuit is in the discovery stage, and attorneys plan to collect Dr. Hansen’s deposition soon, said Eric Deters, a spokesman for Deters Law, a law firm based in Independence, Ky., that is representing the patient.
“The crux is that he performs unnecessary pain procedures and forces you to get an unnecessary procedure before giving you your medication,” Mr. Deters said.
However, Dr. Hansen’s and Mr. Deters’ history together includes a recent riff, according to an August 2021 lawsuit filed by Dr. Hansen against the law firm. Dr. Hansen was a former medical expert in cases for Deters and Associates, but the relationship turned sour when attorneys believed Dr. Hansen was retained as an expert in a case against their clients, according to Dr. Hansen’s suit. Dr. Hansen claims that as retribution, Deters and Associates issued a medical malpractice lawsuit against him in 2020, even though attorneys allegedly knew the statute of limitations had run out. A trial court dismissed the 2020 lawsuit against Dr. Hansen as being untimely filed. Dr. Hansen’s lawsuit alleges wrongful use of civil proceedings and requests compensatory, punitive damages and court costs from the law firm.
The law firm has faced trouble in the past. In August 2021, the Ohio Supreme Court ordered that Mr. Deters pay a $6,500 fine for engaging in the unauthorized practice of law. Mr. Deters’ Kentucky law license has been suspended since 2013 for ethics infractions, according to court records. He retired from law in 2014 and now acts as a spokesperson and office manager for the law firm. The fine resulted from legal advice given by Mr. Deters to two clients at the law firm, according to the Ohio Supreme Court decision.
As for the CVS lawsuit, an upcoming hearing will determine whether the federal court issues a permanent injunction against CVS’s actions. CVS officials have not said whether they will fight the temporary restraining order or the withdrawal of their prescription ban against Dr. Hansen.
A version of this article first appeared on Medscape.com.
In an Aug. 11 decision, District Court Judge William Bertelsman ordered CVS to stop refusing prescriptions written by Kendall E. Hansen, MD. Judge Bertelsman ruled that Dr. Hansen is likely to succeed in his claim that CVS barred his prescriptions without evidence that he violated any law or professional protocol. The restraining order will remain in place while Dr. Hansen’s lawsuit against CVS Pharmacy proceeds.
Ronald W. Chapman II, an attorney representing Dr. Hansen, said the order is groundbreaking and that, to his knowledge, it’s the first time a federal court has overturned a pharmacy’s decision to block a prescriber.
“We believe that CVS’ decision was based solely on algorithms they use to analyze prescriber practices and not an any individual review of patient records,” Mr. Chapman said. “In fact, we invited CVS to come out to Dr. Hansen’s practice and look at how he was treating patients and ensure things were compliant, but they refused. Instead, they had a phone call with him then cut his patients off.”
Michael DeAngelis, a spokesman for CVS, said the court’s order illustrates the proverbial rock and hard place that pharmacies are placed between in the country’s fight against the misuse of prescription opioids.
“It is alleged in many lawsuits that pharmacies fill too many opioid prescriptions and should operate programs that use data to block prescriptions written by some doctors,” Mr. DeAngelis told this news organization. “And yet other lawsuits, including this one, argue that we should not operate programs that may block prescriptions. Such contradictions are grossly unfair to the pharmacy profession.”
Mr. DeAngelis declined to comment about Dr. Hansen’s claims or specify what led CVS to refuse his prescriptions.
Dr. Hansen declined to comment for this story through his attorney.
Dr. Hansen is no stranger to the spotlight. The Northern Kentucky pain doctor made headlines in 2012 when two of his horses, Fast and Accurate, and Hansen, ran in the Kentucky Derby. In February 2019, he drew media attention when his practice, Interventional Pain Specialists in Crestview Hills, Ky., was raided by federal agents. Dr. Hansen owns and operates the facility, which serves patients in Kentucky, Ohio, and Indiana.
The search yielded no findings, and no charges were filed, according to Mr. Chapman. Scott Hardcorn, director of the Northern Kentucky Drug Strike Force, confirmed that his agency assisted in the operation but said he was unaware of the outcome and that his officers generated no reports from the investigation. A spokesperson for the Drug Enforcement Administration would not comment about the investigation and directed a reporter for this news organization to the DEA website where enforcement actions are listed. No records or actions against Dr. Hansen can be found.
The CVS complaint stems from actions taken by the pharmacy against Dr. Hansen earlier this year. In June, a pharmacy representative allegedly contacted Dr. Hansen by phone and asked him questions about his practice and his prescribing practices, according to his lawsuit filed in U.S. District Court for the Eastern District of Kentucky. During the call, the representative did not inform Dr. Hansen that any of his prescriptions were in question or were suspected of being medically unnecessary, the complaint alleges.
On July 28, 2021, CVS sent Dr. Hansen a letter announcing that its pharmacies would no longer be honoring his prescriptions. The letter, entered as an exhibit in the lawsuit, states that CVS contacted Dr. Hansen twice in 2021 about his prescribing practices, once in May and again in June.
“Despite our attempts to resolve the concerns with your controlled substance prescribing patterns, these concerns persist,” Kahra Lutkiewicz, director of CVS’ retail pharmacy professional practice, wrote in the letter. “Thus, we are writing to inform you that effective Aug. 5, 2021, CVS/pharmacy stores will no longer be able to fill prescriptions that you write for controlled substances. We take our compliance obligations very seriously, and after careful consideration, find it necessary to take this action.”
The letter does not explain the details behind CVS’ concerns.
Dr. Hansen sued CVS on Aug. 4 for tortious interference with a business relationship and defamation, among other claims. His complaint alleges that Dr. Hansen and his patients will suffer irreparable injury if the prescription decision stands. More than 250 of Dr. Hansen’s patients use CVS pharmacies for their prescriptions, and some are locked into using the pharmacy because of insurance contracts, Mr. Chapman said.
“There really is nowhere else for these patients to go,” Mr. Chapman said. “They would have to go to a new doctor and establish a new relationship, and obviously that has devastating consequences when we’re talking about people who need their medication.”
CVS has not yet issued a written response to the lawsuit. In his order, Judge Bertelsman stated that a preliminary conference was held in which all parties were represented and stated their positions to the judge.
“Plaintiffs are likely to succeed on the merits of their claims that defendant has interfered with plaintiffs’ relationships with their patients by refusing to fill prescriptions written by plaintiffs, and defendant has done so without evidence that plaintiffs have violated any law or professional protocol related to such prescriptions,” Judge Bertelsman wrote. “The balance of the hardships between the parties weighs in favor of issuing a temporary restraining order inasmuch as defendant’s actions pose a threat to plaintiffs’ professional reputation and livelihood and ... because plaintiffs’ patients’ medical care is implicated by defendant’s actions, the public interest weighs in favor of issuance of the temporary restraining order.”
Dr. Hansen is currently embroiled in several other legal battles as both a plaintiff and a defendant.
In 2019, a patient sued him for negligence and fraud for allegedly performing medically unnecessary and excessive injection therapy. The suit claims the patient was required to undergo injection therapy on a continuing basis in order to receive her narcotic pain medication, according to the lawsuit filed in Kenton Circuit Court. The complaint alleges that Dr. Hansen made false representations to the patient and to her insurers that the injections were necessary for the treatment of the patient’s chronic pain.
The federal government is not involved in the case.
The negligence lawsuit is in the discovery stage, and attorneys plan to collect Dr. Hansen’s deposition soon, said Eric Deters, a spokesman for Deters Law, a law firm based in Independence, Ky., that is representing the patient.
“The crux is that he performs unnecessary pain procedures and forces you to get an unnecessary procedure before giving you your medication,” Mr. Deters said.
However, Dr. Hansen’s and Mr. Deters’ history together includes a recent riff, according to an August 2021 lawsuit filed by Dr. Hansen against the law firm. Dr. Hansen was a former medical expert in cases for Deters and Associates, but the relationship turned sour when attorneys believed Dr. Hansen was retained as an expert in a case against their clients, according to Dr. Hansen’s suit. Dr. Hansen claims that as retribution, Deters and Associates issued a medical malpractice lawsuit against him in 2020, even though attorneys allegedly knew the statute of limitations had run out. A trial court dismissed the 2020 lawsuit against Dr. Hansen as being untimely filed. Dr. Hansen’s lawsuit alleges wrongful use of civil proceedings and requests compensatory, punitive damages and court costs from the law firm.
The law firm has faced trouble in the past. In August 2021, the Ohio Supreme Court ordered that Mr. Deters pay a $6,500 fine for engaging in the unauthorized practice of law. Mr. Deters’ Kentucky law license has been suspended since 2013 for ethics infractions, according to court records. He retired from law in 2014 and now acts as a spokesperson and office manager for the law firm. The fine resulted from legal advice given by Mr. Deters to two clients at the law firm, according to the Ohio Supreme Court decision.
As for the CVS lawsuit, an upcoming hearing will determine whether the federal court issues a permanent injunction against CVS’s actions. CVS officials have not said whether they will fight the temporary restraining order or the withdrawal of their prescription ban against Dr. Hansen.
A version of this article first appeared on Medscape.com.
In an Aug. 11 decision, District Court Judge William Bertelsman ordered CVS to stop refusing prescriptions written by Kendall E. Hansen, MD. Judge Bertelsman ruled that Dr. Hansen is likely to succeed in his claim that CVS barred his prescriptions without evidence that he violated any law or professional protocol. The restraining order will remain in place while Dr. Hansen’s lawsuit against CVS Pharmacy proceeds.
Ronald W. Chapman II, an attorney representing Dr. Hansen, said the order is groundbreaking and that, to his knowledge, it’s the first time a federal court has overturned a pharmacy’s decision to block a prescriber.
“We believe that CVS’ decision was based solely on algorithms they use to analyze prescriber practices and not an any individual review of patient records,” Mr. Chapman said. “In fact, we invited CVS to come out to Dr. Hansen’s practice and look at how he was treating patients and ensure things were compliant, but they refused. Instead, they had a phone call with him then cut his patients off.”
Michael DeAngelis, a spokesman for CVS, said the court’s order illustrates the proverbial rock and hard place that pharmacies are placed between in the country’s fight against the misuse of prescription opioids.
“It is alleged in many lawsuits that pharmacies fill too many opioid prescriptions and should operate programs that use data to block prescriptions written by some doctors,” Mr. DeAngelis told this news organization. “And yet other lawsuits, including this one, argue that we should not operate programs that may block prescriptions. Such contradictions are grossly unfair to the pharmacy profession.”
Mr. DeAngelis declined to comment about Dr. Hansen’s claims or specify what led CVS to refuse his prescriptions.
Dr. Hansen declined to comment for this story through his attorney.
Dr. Hansen is no stranger to the spotlight. The Northern Kentucky pain doctor made headlines in 2012 when two of his horses, Fast and Accurate, and Hansen, ran in the Kentucky Derby. In February 2019, he drew media attention when his practice, Interventional Pain Specialists in Crestview Hills, Ky., was raided by federal agents. Dr. Hansen owns and operates the facility, which serves patients in Kentucky, Ohio, and Indiana.
The search yielded no findings, and no charges were filed, according to Mr. Chapman. Scott Hardcorn, director of the Northern Kentucky Drug Strike Force, confirmed that his agency assisted in the operation but said he was unaware of the outcome and that his officers generated no reports from the investigation. A spokesperson for the Drug Enforcement Administration would not comment about the investigation and directed a reporter for this news organization to the DEA website where enforcement actions are listed. No records or actions against Dr. Hansen can be found.
The CVS complaint stems from actions taken by the pharmacy against Dr. Hansen earlier this year. In June, a pharmacy representative allegedly contacted Dr. Hansen by phone and asked him questions about his practice and his prescribing practices, according to his lawsuit filed in U.S. District Court for the Eastern District of Kentucky. During the call, the representative did not inform Dr. Hansen that any of his prescriptions were in question or were suspected of being medically unnecessary, the complaint alleges.
On July 28, 2021, CVS sent Dr. Hansen a letter announcing that its pharmacies would no longer be honoring his prescriptions. The letter, entered as an exhibit in the lawsuit, states that CVS contacted Dr. Hansen twice in 2021 about his prescribing practices, once in May and again in June.
“Despite our attempts to resolve the concerns with your controlled substance prescribing patterns, these concerns persist,” Kahra Lutkiewicz, director of CVS’ retail pharmacy professional practice, wrote in the letter. “Thus, we are writing to inform you that effective Aug. 5, 2021, CVS/pharmacy stores will no longer be able to fill prescriptions that you write for controlled substances. We take our compliance obligations very seriously, and after careful consideration, find it necessary to take this action.”
The letter does not explain the details behind CVS’ concerns.
Dr. Hansen sued CVS on Aug. 4 for tortious interference with a business relationship and defamation, among other claims. His complaint alleges that Dr. Hansen and his patients will suffer irreparable injury if the prescription decision stands. More than 250 of Dr. Hansen’s patients use CVS pharmacies for their prescriptions, and some are locked into using the pharmacy because of insurance contracts, Mr. Chapman said.
“There really is nowhere else for these patients to go,” Mr. Chapman said. “They would have to go to a new doctor and establish a new relationship, and obviously that has devastating consequences when we’re talking about people who need their medication.”
CVS has not yet issued a written response to the lawsuit. In his order, Judge Bertelsman stated that a preliminary conference was held in which all parties were represented and stated their positions to the judge.
“Plaintiffs are likely to succeed on the merits of their claims that defendant has interfered with plaintiffs’ relationships with their patients by refusing to fill prescriptions written by plaintiffs, and defendant has done so without evidence that plaintiffs have violated any law or professional protocol related to such prescriptions,” Judge Bertelsman wrote. “The balance of the hardships between the parties weighs in favor of issuing a temporary restraining order inasmuch as defendant’s actions pose a threat to plaintiffs’ professional reputation and livelihood and ... because plaintiffs’ patients’ medical care is implicated by defendant’s actions, the public interest weighs in favor of issuance of the temporary restraining order.”
Dr. Hansen is currently embroiled in several other legal battles as both a plaintiff and a defendant.
In 2019, a patient sued him for negligence and fraud for allegedly performing medically unnecessary and excessive injection therapy. The suit claims the patient was required to undergo injection therapy on a continuing basis in order to receive her narcotic pain medication, according to the lawsuit filed in Kenton Circuit Court. The complaint alleges that Dr. Hansen made false representations to the patient and to her insurers that the injections were necessary for the treatment of the patient’s chronic pain.
The federal government is not involved in the case.
The negligence lawsuit is in the discovery stage, and attorneys plan to collect Dr. Hansen’s deposition soon, said Eric Deters, a spokesman for Deters Law, a law firm based in Independence, Ky., that is representing the patient.
“The crux is that he performs unnecessary pain procedures and forces you to get an unnecessary procedure before giving you your medication,” Mr. Deters said.
However, Dr. Hansen’s and Mr. Deters’ history together includes a recent riff, according to an August 2021 lawsuit filed by Dr. Hansen against the law firm. Dr. Hansen was a former medical expert in cases for Deters and Associates, but the relationship turned sour when attorneys believed Dr. Hansen was retained as an expert in a case against their clients, according to Dr. Hansen’s suit. Dr. Hansen claims that as retribution, Deters and Associates issued a medical malpractice lawsuit against him in 2020, even though attorneys allegedly knew the statute of limitations had run out. A trial court dismissed the 2020 lawsuit against Dr. Hansen as being untimely filed. Dr. Hansen’s lawsuit alleges wrongful use of civil proceedings and requests compensatory, punitive damages and court costs from the law firm.
The law firm has faced trouble in the past. In August 2021, the Ohio Supreme Court ordered that Mr. Deters pay a $6,500 fine for engaging in the unauthorized practice of law. Mr. Deters’ Kentucky law license has been suspended since 2013 for ethics infractions, according to court records. He retired from law in 2014 and now acts as a spokesperson and office manager for the law firm. The fine resulted from legal advice given by Mr. Deters to two clients at the law firm, according to the Ohio Supreme Court decision.
As for the CVS lawsuit, an upcoming hearing will determine whether the federal court issues a permanent injunction against CVS’s actions. CVS officials have not said whether they will fight the temporary restraining order or the withdrawal of their prescription ban against Dr. Hansen.
A version of this article first appeared on Medscape.com.















