User login
The Official Newspaper of the American Association for Thoracic Surgery
Rotor ablation for atrial fibrillation strikes out in first randomized trial
SAN FRANCISCO – Focal impulse and rotor modulation-guided ablation for persistent atrial fibrillation – either alone or in conjunction with other procedures – increased procedural times without improving outcomes, according to the first randomized trial to assess its utility.
In fact, enrollment in the rotor ablation-only (RA) arm was halted early for futility. “There was 100% recurrence” of atrial fibrillation (AF), said senior investigator Dr. Andrea Natale, executive medical director of the Texas Cardiac Arrhythmia Institute, Austin.
“I’m surprised it took this long for a randomized study, because this system has been around for 5 or 6 years,” noted Dr. Natale. “Our community should demand these sorts of studies earlier, because it’s not fair for patients to go on with a procedure for years that has not been proven to be effective.
“For us, unless there is a new version of rotor mapping that I feel is significantly different, this will be the end of rotor ablation in my lab with this system [the Topera Physiologic Rotor Mapping Solution],” Dr. Natale said at the annual scientific sessions of the Heart Rhythm Society.
In the study, his team randomized 29 patients to RA only, 42 to RA plus pulmonary vein antral isolation (PVAI), and 42 to PVAI plus posterior wall and nonpulmonary vein trigger ablation.
At about 1 year, four RA-only patients (14%), 22 RA plus PVAI patients (52%), and 32 patients in the PVAI plus trigger group (76%) were free of AF and atrial tachycardias without antiarrhythmic drugs (P < .0001).
Meanwhile, RA alone and RA plus PVAI cases took about 230 minutes, while the more effective PVAI plus trigger approach took about 130 minutes (P < .001).
There was “a very poor outcome with rotor-only ablation,” Dr. Natale said. “There isn’t a benefit either alone or as an add-on strategy, at least with this mapping software.”
Perhaps “people who think rotors don’t exist are right,” he added. On the other hand, maybe the basket mapping catheter doesn’t touch enough of the left atrium, or the software that makes sense of what the catheter detects needs to be improved, Dr. Natale noted.
All the patients were undergoing their first ablation. They were in their early 60s, on average, and most were men. The mean left atrium diameter was about 47 mm, and mean left ventricle ejection fraction about 55%. There were no statistically significant differences between the study arms, and no significant differences in outcomes between the 70% of patients with persistent AF and the 30% with long-standing persistent AF.
There was no industry funding for the work. Dr. Natale disclosed relationships with Biosense Webster, Boston Scientific, Janssen, Medtronic, and St. Jude Medical.
My gut sense is that there’s something to rotor mapping, but we are not there yet. There are a lot of investment dollars and a lot of bright people working on this. It really is the Holy Grail to find the source of AF.
Dr. John Day is the director of Intermountain Heart Rhythm Specialists in Murray, Utah, and the current president of the Hearth Rhythm Society. He had no disclosures.
My gut sense is that there’s something to rotor mapping, but we are not there yet. There are a lot of investment dollars and a lot of bright people working on this. It really is the Holy Grail to find the source of AF.
Dr. John Day is the director of Intermountain Heart Rhythm Specialists in Murray, Utah, and the current president of the Hearth Rhythm Society. He had no disclosures.
My gut sense is that there’s something to rotor mapping, but we are not there yet. There are a lot of investment dollars and a lot of bright people working on this. It really is the Holy Grail to find the source of AF.
Dr. John Day is the director of Intermountain Heart Rhythm Specialists in Murray, Utah, and the current president of the Hearth Rhythm Society. He had no disclosures.
SAN FRANCISCO – Focal impulse and rotor modulation-guided ablation for persistent atrial fibrillation – either alone or in conjunction with other procedures – increased procedural times without improving outcomes, according to the first randomized trial to assess its utility.
In fact, enrollment in the rotor ablation-only (RA) arm was halted early for futility. “There was 100% recurrence” of atrial fibrillation (AF), said senior investigator Dr. Andrea Natale, executive medical director of the Texas Cardiac Arrhythmia Institute, Austin.
“I’m surprised it took this long for a randomized study, because this system has been around for 5 or 6 years,” noted Dr. Natale. “Our community should demand these sorts of studies earlier, because it’s not fair for patients to go on with a procedure for years that has not been proven to be effective.
“For us, unless there is a new version of rotor mapping that I feel is significantly different, this will be the end of rotor ablation in my lab with this system [the Topera Physiologic Rotor Mapping Solution],” Dr. Natale said at the annual scientific sessions of the Heart Rhythm Society.
In the study, his team randomized 29 patients to RA only, 42 to RA plus pulmonary vein antral isolation (PVAI), and 42 to PVAI plus posterior wall and nonpulmonary vein trigger ablation.
At about 1 year, four RA-only patients (14%), 22 RA plus PVAI patients (52%), and 32 patients in the PVAI plus trigger group (76%) were free of AF and atrial tachycardias without antiarrhythmic drugs (P < .0001).
Meanwhile, RA alone and RA plus PVAI cases took about 230 minutes, while the more effective PVAI plus trigger approach took about 130 minutes (P < .001).
There was “a very poor outcome with rotor-only ablation,” Dr. Natale said. “There isn’t a benefit either alone or as an add-on strategy, at least with this mapping software.”
Perhaps “people who think rotors don’t exist are right,” he added. On the other hand, maybe the basket mapping catheter doesn’t touch enough of the left atrium, or the software that makes sense of what the catheter detects needs to be improved, Dr. Natale noted.
All the patients were undergoing their first ablation. They were in their early 60s, on average, and most were men. The mean left atrium diameter was about 47 mm, and mean left ventricle ejection fraction about 55%. There were no statistically significant differences between the study arms, and no significant differences in outcomes between the 70% of patients with persistent AF and the 30% with long-standing persistent AF.
There was no industry funding for the work. Dr. Natale disclosed relationships with Biosense Webster, Boston Scientific, Janssen, Medtronic, and St. Jude Medical.
SAN FRANCISCO – Focal impulse and rotor modulation-guided ablation for persistent atrial fibrillation – either alone or in conjunction with other procedures – increased procedural times without improving outcomes, according to the first randomized trial to assess its utility.
In fact, enrollment in the rotor ablation-only (RA) arm was halted early for futility. “There was 100% recurrence” of atrial fibrillation (AF), said senior investigator Dr. Andrea Natale, executive medical director of the Texas Cardiac Arrhythmia Institute, Austin.
“I’m surprised it took this long for a randomized study, because this system has been around for 5 or 6 years,” noted Dr. Natale. “Our community should demand these sorts of studies earlier, because it’s not fair for patients to go on with a procedure for years that has not been proven to be effective.
“For us, unless there is a new version of rotor mapping that I feel is significantly different, this will be the end of rotor ablation in my lab with this system [the Topera Physiologic Rotor Mapping Solution],” Dr. Natale said at the annual scientific sessions of the Heart Rhythm Society.
In the study, his team randomized 29 patients to RA only, 42 to RA plus pulmonary vein antral isolation (PVAI), and 42 to PVAI plus posterior wall and nonpulmonary vein trigger ablation.
At about 1 year, four RA-only patients (14%), 22 RA plus PVAI patients (52%), and 32 patients in the PVAI plus trigger group (76%) were free of AF and atrial tachycardias without antiarrhythmic drugs (P < .0001).
Meanwhile, RA alone and RA plus PVAI cases took about 230 minutes, while the more effective PVAI plus trigger approach took about 130 minutes (P < .001).
There was “a very poor outcome with rotor-only ablation,” Dr. Natale said. “There isn’t a benefit either alone or as an add-on strategy, at least with this mapping software.”
Perhaps “people who think rotors don’t exist are right,” he added. On the other hand, maybe the basket mapping catheter doesn’t touch enough of the left atrium, or the software that makes sense of what the catheter detects needs to be improved, Dr. Natale noted.
All the patients were undergoing their first ablation. They were in their early 60s, on average, and most were men. The mean left atrium diameter was about 47 mm, and mean left ventricle ejection fraction about 55%. There were no statistically significant differences between the study arms, and no significant differences in outcomes between the 70% of patients with persistent AF and the 30% with long-standing persistent AF.
There was no industry funding for the work. Dr. Natale disclosed relationships with Biosense Webster, Boston Scientific, Janssen, Medtronic, and St. Jude Medical.
AT HEART RHYTHM 2016
Key clinical point: Focal impulse and rotor modulation-guided ablation for persistent atrial fibrillation – either alone or in conjunction with other procedures – increased procedural times without improving outcomes.
Major finding: At about 1 year, four rotor ablation-only patients (14%), 22 RA plus pulmonary vein antral isolation patients (52.4%), and 32 patients in the PVAI plus trigger group (76%) were free of atrial fibrillation and atrial tachycardias without antiarrhythmic drugs (P < .0001).
Data source: A randomized trial in 113 persistent AF patients.
Disclosures: There was no industry funding for the work. The senior investigator disclosed relationships with Biosense Webster, Boston Scientific, Janssen, Medtronic, and St. Jude Medical.
VIDEO: Cardiothoracic surgeon shortage requires action
BALTIMORE – By 2035, U.S. cardiothoracic surgeons will see a 61% increase in the national caseload, and potentially a 121% increase in cases for each surgeon, according to a data analysis presented at the annual meeting of the American Association for Thoracic Surgery.
Using data from the American Board of Thoracic Surgery, a research team at Ohio State University performed case load calculations for 2035 based on cases per surgeon per year in 2010. The researchers estimated that the average caseload per surgeon in 2035 will be 299 cases, compared with a 2010 caseload of 135 per surgeon. This increase is not matched by the number of surgeons currently trained and certified annually.
Dr. John Ikonomidis, chief of the division of cardiothoracic surgery at the Medical University of South Carolina in Charleston, and a discussant on the presentation, said surgeon retirements and an increase in the population needing treatment have put the specialty in a bind.
“We have a bit of a crisis now, honestly, but this particular paper puts it in even further perspective,” Dr. Ikonomidis said in a video interview. “By 2035 we’re looking at a 3,000-surgeon shortage, relative to what would be available.” He noted that approximately 90 medical residents per year are certified as cardiothoracic surgeons, a rate which will not produce enough CT surgeons to meet the projected shortage.
“We need to continue to have this conversation,” he concluded. “It is a reminder that the predictions we made 15 years ago appear to be true, and we probably need to do something about it, at least in the short term.”
Dr. Ikonomidis reported no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
BALTIMORE – By 2035, U.S. cardiothoracic surgeons will see a 61% increase in the national caseload, and potentially a 121% increase in cases for each surgeon, according to a data analysis presented at the annual meeting of the American Association for Thoracic Surgery.
Using data from the American Board of Thoracic Surgery, a research team at Ohio State University performed case load calculations for 2035 based on cases per surgeon per year in 2010. The researchers estimated that the average caseload per surgeon in 2035 will be 299 cases, compared with a 2010 caseload of 135 per surgeon. This increase is not matched by the number of surgeons currently trained and certified annually.
Dr. John Ikonomidis, chief of the division of cardiothoracic surgery at the Medical University of South Carolina in Charleston, and a discussant on the presentation, said surgeon retirements and an increase in the population needing treatment have put the specialty in a bind.
“We have a bit of a crisis now, honestly, but this particular paper puts it in even further perspective,” Dr. Ikonomidis said in a video interview. “By 2035 we’re looking at a 3,000-surgeon shortage, relative to what would be available.” He noted that approximately 90 medical residents per year are certified as cardiothoracic surgeons, a rate which will not produce enough CT surgeons to meet the projected shortage.
“We need to continue to have this conversation,” he concluded. “It is a reminder that the predictions we made 15 years ago appear to be true, and we probably need to do something about it, at least in the short term.”
Dr. Ikonomidis reported no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
BALTIMORE – By 2035, U.S. cardiothoracic surgeons will see a 61% increase in the national caseload, and potentially a 121% increase in cases for each surgeon, according to a data analysis presented at the annual meeting of the American Association for Thoracic Surgery.
Using data from the American Board of Thoracic Surgery, a research team at Ohio State University performed case load calculations for 2035 based on cases per surgeon per year in 2010. The researchers estimated that the average caseload per surgeon in 2035 will be 299 cases, compared with a 2010 caseload of 135 per surgeon. This increase is not matched by the number of surgeons currently trained and certified annually.
Dr. John Ikonomidis, chief of the division of cardiothoracic surgery at the Medical University of South Carolina in Charleston, and a discussant on the presentation, said surgeon retirements and an increase in the population needing treatment have put the specialty in a bind.
“We have a bit of a crisis now, honestly, but this particular paper puts it in even further perspective,” Dr. Ikonomidis said in a video interview. “By 2035 we’re looking at a 3,000-surgeon shortage, relative to what would be available.” He noted that approximately 90 medical residents per year are certified as cardiothoracic surgeons, a rate which will not produce enough CT surgeons to meet the projected shortage.
“We need to continue to have this conversation,” he concluded. “It is a reminder that the predictions we made 15 years ago appear to be true, and we probably need to do something about it, at least in the short term.”
Dr. Ikonomidis reported no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
AT THE AATS ANNUAL MEETING
VIDEO: Wedge resection beats SBRT for stage I lung cancer treatment
BALTIMORE – Surgical resection of early-stage non–small cell lung cancer afforded a superior survival advantage for patients than stereotactic body radiation therapy (SBRT), according to a study presented at the 2016 annual meeting of the American Association for Thoracic Surgery.
While an increasing number of non–small cell lung cancer patients have been treated with SBRT, it appears that surgery may still be the better option. Analysis of both matched and unmatched patient groups found that SBRT was associated with significantly lower survival than wedge resection.
“Frankly, I was surprised to see such a big difference between SBRT and wedge resection,” said Dr. Walter Weder, professor of surgery at University Hospital Zürich, in an interview at AATS 2016. Dr Weder served as a discussant on the paper, and said the results confirm that surgeons should be involved in discussions with patients when they are considering treatment options. “Surgery can be done safely... and patients should know this information.”
Dr. Weder reported no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
BALTIMORE – Surgical resection of early-stage non–small cell lung cancer afforded a superior survival advantage for patients than stereotactic body radiation therapy (SBRT), according to a study presented at the 2016 annual meeting of the American Association for Thoracic Surgery.
While an increasing number of non–small cell lung cancer patients have been treated with SBRT, it appears that surgery may still be the better option. Analysis of both matched and unmatched patient groups found that SBRT was associated with significantly lower survival than wedge resection.
“Frankly, I was surprised to see such a big difference between SBRT and wedge resection,” said Dr. Walter Weder, professor of surgery at University Hospital Zürich, in an interview at AATS 2016. Dr Weder served as a discussant on the paper, and said the results confirm that surgeons should be involved in discussions with patients when they are considering treatment options. “Surgery can be done safely... and patients should know this information.”
Dr. Weder reported no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
BALTIMORE – Surgical resection of early-stage non–small cell lung cancer afforded a superior survival advantage for patients than stereotactic body radiation therapy (SBRT), according to a study presented at the 2016 annual meeting of the American Association for Thoracic Surgery.
While an increasing number of non–small cell lung cancer patients have been treated with SBRT, it appears that surgery may still be the better option. Analysis of both matched and unmatched patient groups found that SBRT was associated with significantly lower survival than wedge resection.
“Frankly, I was surprised to see such a big difference between SBRT and wedge resection,” said Dr. Walter Weder, professor of surgery at University Hospital Zürich, in an interview at AATS 2016. Dr Weder served as a discussant on the paper, and said the results confirm that surgeons should be involved in discussions with patients when they are considering treatment options. “Surgery can be done safely... and patients should know this information.”
Dr. Weder reported no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
AT AATS 2016
Surgeons Voice Legislative Priorities at Advocacy Summit 2016
Approximately 300 surgeons and surgical residents participated in the advocacy portion of the 2016 American College of Surgeons (ACS) Leadership & Advocacy Summit. The event provided participants with an opportunity to develop their advocacy skills, learn about legislative and health policy priorities, and advocate in meetings with members of Congress and their staffs.
Surgeons asked lawmakers to use their oversight authority to encourage the Centers for Medicare & Medicaid Services to adopt meaningful quality measures, and physician-developed Alternative Payment Models. ACS members also asked their elected officials to support the Responsible Data Transparency Act, legislation that is being developed by Rep. Bill Flores (R-Tex.). The College is committed to maintaining transparency in the Medicare system to promote high-quality patient care. At issue, however, are third-party groups that are evading established, accurate, valid, and transparent pathways to sensitive Medicare data by using Freedom of Information Act requests to obtain raw physician claims data. This legislation would prevent groups from using questionable, non–risk-adjusted methodologies to conduct performance analyses and publish potentially misleading physician performance ratings on public websites.
Other issues discussed at the Capitol Hill meetings include promotion of the Ensuring Access to General Surgery Act of 2016, legislation being developed that would require that a study be conducted to designate general surgery Health Professional Shortage Areas (HPSAs); cancer-related concerns, including education on the importance of Commission on Cancer accreditation; and improved access to trauma care. Details about the ACS Leadership & Advocacy Summit will be published in the May SurgeonsVoice Monthly and the July issue of the Bulletin at http://bulletin.facs.org/.
Approximately 300 surgeons and surgical residents participated in the advocacy portion of the 2016 American College of Surgeons (ACS) Leadership & Advocacy Summit. The event provided participants with an opportunity to develop their advocacy skills, learn about legislative and health policy priorities, and advocate in meetings with members of Congress and their staffs.
Surgeons asked lawmakers to use their oversight authority to encourage the Centers for Medicare & Medicaid Services to adopt meaningful quality measures, and physician-developed Alternative Payment Models. ACS members also asked their elected officials to support the Responsible Data Transparency Act, legislation that is being developed by Rep. Bill Flores (R-Tex.). The College is committed to maintaining transparency in the Medicare system to promote high-quality patient care. At issue, however, are third-party groups that are evading established, accurate, valid, and transparent pathways to sensitive Medicare data by using Freedom of Information Act requests to obtain raw physician claims data. This legislation would prevent groups from using questionable, non–risk-adjusted methodologies to conduct performance analyses and publish potentially misleading physician performance ratings on public websites.
Other issues discussed at the Capitol Hill meetings include promotion of the Ensuring Access to General Surgery Act of 2016, legislation being developed that would require that a study be conducted to designate general surgery Health Professional Shortage Areas (HPSAs); cancer-related concerns, including education on the importance of Commission on Cancer accreditation; and improved access to trauma care. Details about the ACS Leadership & Advocacy Summit will be published in the May SurgeonsVoice Monthly and the July issue of the Bulletin at http://bulletin.facs.org/.
Approximately 300 surgeons and surgical residents participated in the advocacy portion of the 2016 American College of Surgeons (ACS) Leadership & Advocacy Summit. The event provided participants with an opportunity to develop their advocacy skills, learn about legislative and health policy priorities, and advocate in meetings with members of Congress and their staffs.
Surgeons asked lawmakers to use their oversight authority to encourage the Centers for Medicare & Medicaid Services to adopt meaningful quality measures, and physician-developed Alternative Payment Models. ACS members also asked their elected officials to support the Responsible Data Transparency Act, legislation that is being developed by Rep. Bill Flores (R-Tex.). The College is committed to maintaining transparency in the Medicare system to promote high-quality patient care. At issue, however, are third-party groups that are evading established, accurate, valid, and transparent pathways to sensitive Medicare data by using Freedom of Information Act requests to obtain raw physician claims data. This legislation would prevent groups from using questionable, non–risk-adjusted methodologies to conduct performance analyses and publish potentially misleading physician performance ratings on public websites.
Other issues discussed at the Capitol Hill meetings include promotion of the Ensuring Access to General Surgery Act of 2016, legislation being developed that would require that a study be conducted to designate general surgery Health Professional Shortage Areas (HPSAs); cancer-related concerns, including education on the importance of Commission on Cancer accreditation; and improved access to trauma care. Details about the ACS Leadership & Advocacy Summit will be published in the May SurgeonsVoice Monthly and the July issue of the Bulletin at http://bulletin.facs.org/.
VIDEO: Del Nido cardioplegic solution receives high grade
BALTIMORE – A cardioplegic solution developed by a noted cardiac surgeon has been deemed a “simple and safe” cardio protective strategy in a study presented at the annual meeting of the American Association for Thoracic Surgery.
In an interview at the event, Pedro J. del Nido, MD, chief of cardiac surgery at Boston Children’s Hospital, and inventor of the long-acting Del Nido solution, explained how and why he and his colleagues developed the new cardioplegic solution. He praised the study as uniquely important, given that there have been few prospective, randomized, and controlled comparative studies of cardioplegia targeted at pediatric patients.
“Baby hearts have a slightly different metabolism than adult hearts,” Dr. del Nido said. “Typically in pediatric procedures we not only cool the heart but we lower the whole body temperature... In the adult world we don’t drop the temperature so much.” He also said the method and flow rate of cardioplegia delivery was unique for pediatric patients, given the fragility of the endothelial cells lining their blood vessels.
The study compared the Del Nido solution with the St. Thomas cardioplegia solution. The investigators praised the Del Nido solution’s performance for “better cardiac index profile, lesser troponin-I release, and decreased morbidity.”
Dr. del Nido developed the Del Nido cardioplegic solution, but reported no other relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
BALTIMORE – A cardioplegic solution developed by a noted cardiac surgeon has been deemed a “simple and safe” cardio protective strategy in a study presented at the annual meeting of the American Association for Thoracic Surgery.
In an interview at the event, Pedro J. del Nido, MD, chief of cardiac surgery at Boston Children’s Hospital, and inventor of the long-acting Del Nido solution, explained how and why he and his colleagues developed the new cardioplegic solution. He praised the study as uniquely important, given that there have been few prospective, randomized, and controlled comparative studies of cardioplegia targeted at pediatric patients.
“Baby hearts have a slightly different metabolism than adult hearts,” Dr. del Nido said. “Typically in pediatric procedures we not only cool the heart but we lower the whole body temperature... In the adult world we don’t drop the temperature so much.” He also said the method and flow rate of cardioplegia delivery was unique for pediatric patients, given the fragility of the endothelial cells lining their blood vessels.
The study compared the Del Nido solution with the St. Thomas cardioplegia solution. The investigators praised the Del Nido solution’s performance for “better cardiac index profile, lesser troponin-I release, and decreased morbidity.”
Dr. del Nido developed the Del Nido cardioplegic solution, but reported no other relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
BALTIMORE – A cardioplegic solution developed by a noted cardiac surgeon has been deemed a “simple and safe” cardio protective strategy in a study presented at the annual meeting of the American Association for Thoracic Surgery.
In an interview at the event, Pedro J. del Nido, MD, chief of cardiac surgery at Boston Children’s Hospital, and inventor of the long-acting Del Nido solution, explained how and why he and his colleagues developed the new cardioplegic solution. He praised the study as uniquely important, given that there have been few prospective, randomized, and controlled comparative studies of cardioplegia targeted at pediatric patients.
“Baby hearts have a slightly different metabolism than adult hearts,” Dr. del Nido said. “Typically in pediatric procedures we not only cool the heart but we lower the whole body temperature... In the adult world we don’t drop the temperature so much.” He also said the method and flow rate of cardioplegia delivery was unique for pediatric patients, given the fragility of the endothelial cells lining their blood vessels.
The study compared the Del Nido solution with the St. Thomas cardioplegia solution. The investigators praised the Del Nido solution’s performance for “better cardiac index profile, lesser troponin-I release, and decreased morbidity.”
Dr. del Nido developed the Del Nido cardioplegic solution, but reported no other relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
AT THE AATS ANNUAL MEETING
VIDEO: Sutureless Heart Valve: A Critical Innovation
BALTIMORE – The sutureless heart valve may now be a “necessity” for contemporary cardiothoracic surgeons, said an expert at the annual meeting of the American Association for Thoracic Surgery.
In an interview at the event, Niv Ad, MD, chief of cardiac surgery at Inova Heart and Vascular Institute, Falls Church, Va., discussed the results of an international trial evaluating clinical outcomes of two patient subgroups implanted with a sutureless valve prosthesis. He was enthusiastic about the trial’s results and the future promise of the sutureless valve.
The study, "Clinical Outcomes in Low and Intermediate-High Risk Groups with a Sutureless Heart Valve," will be presented at 7:30 a.m. on Wednesday.
“This study teaches us that the technology is safe,” he said. “This is really great news for surgeons, cardiologists, and patients. Complications associated with implantation of the valves were fairly low in their incidence, and the survival rates at 1 year were high.”
The study, led by Axel Haverich, MD, of Hannover Medical School in Germany, confirmed the safety and performance of the valve in both patient groups – high and low risk – regardless of the preoperative risk score. Dr. Ad said that sutureless valve technology would likely replace suture technology in all cases, although perhaps not in the near term.
Dr. Ad reported no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
BALTIMORE – The sutureless heart valve may now be a “necessity” for contemporary cardiothoracic surgeons, said an expert at the annual meeting of the American Association for Thoracic Surgery.
In an interview at the event, Niv Ad, MD, chief of cardiac surgery at Inova Heart and Vascular Institute, Falls Church, Va., discussed the results of an international trial evaluating clinical outcomes of two patient subgroups implanted with a sutureless valve prosthesis. He was enthusiastic about the trial’s results and the future promise of the sutureless valve.
The study, "Clinical Outcomes in Low and Intermediate-High Risk Groups with a Sutureless Heart Valve," will be presented at 7:30 a.m. on Wednesday.
“This study teaches us that the technology is safe,” he said. “This is really great news for surgeons, cardiologists, and patients. Complications associated with implantation of the valves were fairly low in their incidence, and the survival rates at 1 year were high.”
The study, led by Axel Haverich, MD, of Hannover Medical School in Germany, confirmed the safety and performance of the valve in both patient groups – high and low risk – regardless of the preoperative risk score. Dr. Ad said that sutureless valve technology would likely replace suture technology in all cases, although perhaps not in the near term.
Dr. Ad reported no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
BALTIMORE – The sutureless heart valve may now be a “necessity” for contemporary cardiothoracic surgeons, said an expert at the annual meeting of the American Association for Thoracic Surgery.
In an interview at the event, Niv Ad, MD, chief of cardiac surgery at Inova Heart and Vascular Institute, Falls Church, Va., discussed the results of an international trial evaluating clinical outcomes of two patient subgroups implanted with a sutureless valve prosthesis. He was enthusiastic about the trial’s results and the future promise of the sutureless valve.
The study, "Clinical Outcomes in Low and Intermediate-High Risk Groups with a Sutureless Heart Valve," will be presented at 7:30 a.m. on Wednesday.
“This study teaches us that the technology is safe,” he said. “This is really great news for surgeons, cardiologists, and patients. Complications associated with implantation of the valves were fairly low in their incidence, and the survival rates at 1 year were high.”
The study, led by Axel Haverich, MD, of Hannover Medical School in Germany, confirmed the safety and performance of the valve in both patient groups – high and low risk – regardless of the preoperative risk score. Dr. Ad said that sutureless valve technology would likely replace suture technology in all cases, although perhaps not in the near term.
Dr. Ad reported no relevant financial disclosures.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
On Twitter @richpizzi
AT THE AATS ANNUAL MEETING
Rhythm control may be best for atrial fib in HFpEF
CHICAGO – Atrial fibrillation with good heart rate control in patients who have heart failure with preserved ejection fraction is independently associated with exercise intolerance, impaired contractile reserve, and a sharply higher mortality rate than in matched HFpEF patients without the arrhythmia, a retrospective analysis showed.
“Our study, the largest of its kind, provides mechanistic evidence from cardiopulmonary testing that a rhythm control strategy may potentially improve peak exercise capacity and survival in this patient population, a finding that of course requires future prospective appraisal in randomized trials comparing rate and rhythm control of atrial fibrillation in HFpEF,” Dr. Mohamed Badreldin Elshazly reported at the annual meeting of the American College of Cardiology.
In the meantime, his study also shows the useful role cardiopulmonary stress testing can play in the setting of atrial fibrillation (AF) in HFpEF, he added.
“Cardiopulmonary stress tests are cheap and easy to do. They’re a big asset for personalized medicine. Using an objective measure like cardiopulmonary stress testing to define the physiologic and hemodynamic consequences of atrial fibrillation in individual patients may help identify those in whom rhythm control may improve exercise tolerance and quality of life, and those who may be okay with rate control,” according to Dr. Elshazly of the Cleveland Clinic.
He noted that while it’s well established that atrial fibrillation is associated with exercise intolerance in patients with heart failure with reduced ejection fraction (HFrEF) and that restoration of sinus rhythm in such patients has a positive impact on exercise hemodynamics, symptom severity, and quality of life, the situation is murkier regarding AF in patients with HFpEF. Prior studies were generally small and unable to establish whether AF was independently associated with exercise intolerance or if HFpEF patients who developed AF were sicker and higher risk.
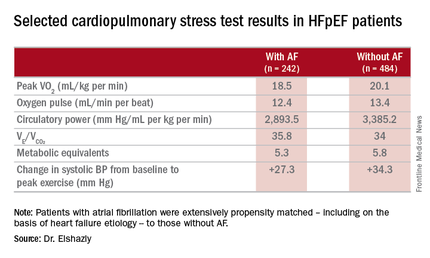
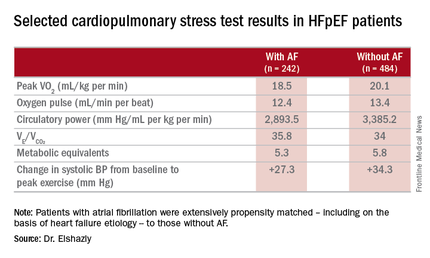
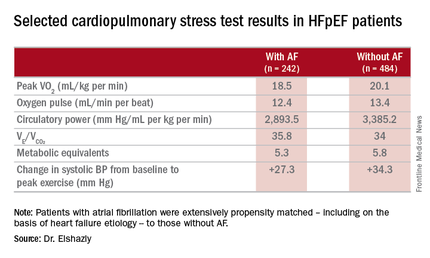
He presented a retrospective, case-control study in a cohort of 1,825 patients with HFpEF referred for maximal, symptom-limited cardiopulmonary stress testing at the Cleveland Clinic. Among these were 242 patients with AF. They were extensively propensity matched – including on the basis of heart failure etiology – to 484 HFpEF patients without AF.
“That’s what makes our study strong. We were the first to be able to do propensity matching and therefore account for other risk factors in our analysis,” Dr. Elshazly explained.
The investigators measured peak oxygen uptake (VO2), the minute ventilation–carbon dioxide production relationship (VE/VCO2) as an indicator of ventilatory efficiency, metabolic equivalents (METS), ventilatory anaerobic threshold, circulatory power as a proxy for cardiac power, peak oxygen pulse as a surrogate for stroke volume, and resting and peak heart rate and systolic blood pressure. The patients with AF were in fibrillation at the time of their cardiopulmonary stress testing.
The HFpEF patients with AF had a mean resting heart rate of 70 beats per minute and a peak rate of 130 bpm. This group showed evidence of impaired peak exercise tolerance as reflected in lower peak VO2, oxygen pulse, and circulatory power at peak exercise. Their VE/VCO2 was higher, indicating impaired ventilatory efficiency. Notably, however, their submaximal exercise capacity was similar to the non-AF controls.
“Atrial fibrillation in these patients is really more of a disease that shows itself in patients when you take them to their peak exercise capacity,” he observed.
All-cause mortality was significantly higher in the AF as compared with no-AF patients with HFpEF. The mortality curves separated early and the divergence grew larger over the course of 8 years of follow-up.
One audience member pointed out that the large mortality difference between the two groups seems disproportionate to the rather modest differences in exercise capacity.
“It brings up an interesting point,” Dr. Elshazly replied. “Maybe the increase in total mortality that we see is being driven by other things besides cardiovascular mortality. Our data doesn’t capture the specific cause of death, be it cancer, for example, but it does raise the idea that this mortality difference is not all driven by cardiovascular mortality, but by atrial fibrillation.”
Dr. Elshazly reported having no financial conflicts of interest regarding his institutionally supported study.
CHICAGO – Atrial fibrillation with good heart rate control in patients who have heart failure with preserved ejection fraction is independently associated with exercise intolerance, impaired contractile reserve, and a sharply higher mortality rate than in matched HFpEF patients without the arrhythmia, a retrospective analysis showed.
“Our study, the largest of its kind, provides mechanistic evidence from cardiopulmonary testing that a rhythm control strategy may potentially improve peak exercise capacity and survival in this patient population, a finding that of course requires future prospective appraisal in randomized trials comparing rate and rhythm control of atrial fibrillation in HFpEF,” Dr. Mohamed Badreldin Elshazly reported at the annual meeting of the American College of Cardiology.
In the meantime, his study also shows the useful role cardiopulmonary stress testing can play in the setting of atrial fibrillation (AF) in HFpEF, he added.
“Cardiopulmonary stress tests are cheap and easy to do. They’re a big asset for personalized medicine. Using an objective measure like cardiopulmonary stress testing to define the physiologic and hemodynamic consequences of atrial fibrillation in individual patients may help identify those in whom rhythm control may improve exercise tolerance and quality of life, and those who may be okay with rate control,” according to Dr. Elshazly of the Cleveland Clinic.
He noted that while it’s well established that atrial fibrillation is associated with exercise intolerance in patients with heart failure with reduced ejection fraction (HFrEF) and that restoration of sinus rhythm in such patients has a positive impact on exercise hemodynamics, symptom severity, and quality of life, the situation is murkier regarding AF in patients with HFpEF. Prior studies were generally small and unable to establish whether AF was independently associated with exercise intolerance or if HFpEF patients who developed AF were sicker and higher risk.
He presented a retrospective, case-control study in a cohort of 1,825 patients with HFpEF referred for maximal, symptom-limited cardiopulmonary stress testing at the Cleveland Clinic. Among these were 242 patients with AF. They were extensively propensity matched – including on the basis of heart failure etiology – to 484 HFpEF patients without AF.
“That’s what makes our study strong. We were the first to be able to do propensity matching and therefore account for other risk factors in our analysis,” Dr. Elshazly explained.
The investigators measured peak oxygen uptake (VO2), the minute ventilation–carbon dioxide production relationship (VE/VCO2) as an indicator of ventilatory efficiency, metabolic equivalents (METS), ventilatory anaerobic threshold, circulatory power as a proxy for cardiac power, peak oxygen pulse as a surrogate for stroke volume, and resting and peak heart rate and systolic blood pressure. The patients with AF were in fibrillation at the time of their cardiopulmonary stress testing.
The HFpEF patients with AF had a mean resting heart rate of 70 beats per minute and a peak rate of 130 bpm. This group showed evidence of impaired peak exercise tolerance as reflected in lower peak VO2, oxygen pulse, and circulatory power at peak exercise. Their VE/VCO2 was higher, indicating impaired ventilatory efficiency. Notably, however, their submaximal exercise capacity was similar to the non-AF controls.
“Atrial fibrillation in these patients is really more of a disease that shows itself in patients when you take them to their peak exercise capacity,” he observed.
All-cause mortality was significantly higher in the AF as compared with no-AF patients with HFpEF. The mortality curves separated early and the divergence grew larger over the course of 8 years of follow-up.
One audience member pointed out that the large mortality difference between the two groups seems disproportionate to the rather modest differences in exercise capacity.
“It brings up an interesting point,” Dr. Elshazly replied. “Maybe the increase in total mortality that we see is being driven by other things besides cardiovascular mortality. Our data doesn’t capture the specific cause of death, be it cancer, for example, but it does raise the idea that this mortality difference is not all driven by cardiovascular mortality, but by atrial fibrillation.”
Dr. Elshazly reported having no financial conflicts of interest regarding his institutionally supported study.
CHICAGO – Atrial fibrillation with good heart rate control in patients who have heart failure with preserved ejection fraction is independently associated with exercise intolerance, impaired contractile reserve, and a sharply higher mortality rate than in matched HFpEF patients without the arrhythmia, a retrospective analysis showed.
“Our study, the largest of its kind, provides mechanistic evidence from cardiopulmonary testing that a rhythm control strategy may potentially improve peak exercise capacity and survival in this patient population, a finding that of course requires future prospective appraisal in randomized trials comparing rate and rhythm control of atrial fibrillation in HFpEF,” Dr. Mohamed Badreldin Elshazly reported at the annual meeting of the American College of Cardiology.
In the meantime, his study also shows the useful role cardiopulmonary stress testing can play in the setting of atrial fibrillation (AF) in HFpEF, he added.
“Cardiopulmonary stress tests are cheap and easy to do. They’re a big asset for personalized medicine. Using an objective measure like cardiopulmonary stress testing to define the physiologic and hemodynamic consequences of atrial fibrillation in individual patients may help identify those in whom rhythm control may improve exercise tolerance and quality of life, and those who may be okay with rate control,” according to Dr. Elshazly of the Cleveland Clinic.
He noted that while it’s well established that atrial fibrillation is associated with exercise intolerance in patients with heart failure with reduced ejection fraction (HFrEF) and that restoration of sinus rhythm in such patients has a positive impact on exercise hemodynamics, symptom severity, and quality of life, the situation is murkier regarding AF in patients with HFpEF. Prior studies were generally small and unable to establish whether AF was independently associated with exercise intolerance or if HFpEF patients who developed AF were sicker and higher risk.
He presented a retrospective, case-control study in a cohort of 1,825 patients with HFpEF referred for maximal, symptom-limited cardiopulmonary stress testing at the Cleveland Clinic. Among these were 242 patients with AF. They were extensively propensity matched – including on the basis of heart failure etiology – to 484 HFpEF patients without AF.
“That’s what makes our study strong. We were the first to be able to do propensity matching and therefore account for other risk factors in our analysis,” Dr. Elshazly explained.
The investigators measured peak oxygen uptake (VO2), the minute ventilation–carbon dioxide production relationship (VE/VCO2) as an indicator of ventilatory efficiency, metabolic equivalents (METS), ventilatory anaerobic threshold, circulatory power as a proxy for cardiac power, peak oxygen pulse as a surrogate for stroke volume, and resting and peak heart rate and systolic blood pressure. The patients with AF were in fibrillation at the time of their cardiopulmonary stress testing.
The HFpEF patients with AF had a mean resting heart rate of 70 beats per minute and a peak rate of 130 bpm. This group showed evidence of impaired peak exercise tolerance as reflected in lower peak VO2, oxygen pulse, and circulatory power at peak exercise. Their VE/VCO2 was higher, indicating impaired ventilatory efficiency. Notably, however, their submaximal exercise capacity was similar to the non-AF controls.
“Atrial fibrillation in these patients is really more of a disease that shows itself in patients when you take them to their peak exercise capacity,” he observed.
All-cause mortality was significantly higher in the AF as compared with no-AF patients with HFpEF. The mortality curves separated early and the divergence grew larger over the course of 8 years of follow-up.
One audience member pointed out that the large mortality difference between the two groups seems disproportionate to the rather modest differences in exercise capacity.
“It brings up an interesting point,” Dr. Elshazly replied. “Maybe the increase in total mortality that we see is being driven by other things besides cardiovascular mortality. Our data doesn’t capture the specific cause of death, be it cancer, for example, but it does raise the idea that this mortality difference is not all driven by cardiovascular mortality, but by atrial fibrillation.”
Dr. Elshazly reported having no financial conflicts of interest regarding his institutionally supported study.
AT ACC 16
Key clinical point: Atrial fibrillation in patients with heart failure with preserved ejection fraction is associated with exercise intolerance and increased mortality.
Major finding: Mean peak VO2 was 18.5 mL/kg per minute in patients with HFpEF and atrial fibrillation, significantly less than the 20.1 mL/kg per minute in controls.
Data source: A retrospective, single-institution study of cardiopulmonary stress test findings and 8-year mortality in 242 patients with HFpEF and atrial fibrillation and 484 propensity-matched controls with HFpEF and no arrhythmia.
Disclosures: The presenter reported having no financial conflicts of interest regarding his institutionally supported study.
Daptomycin beats infective endocarditis caused by several pathogens
AT ECCMID 2016
AMSTERDAM – Daptomycin successfully treated infective endocarditis in 90% of patients who developed it after undergoing heart valve replacement, according to a report presented at the annual congress of the European Society of Clinical Microbiology and Infectious Diseases.
Dr. Achyut Guleri, clinical director of laboratory medicine at Blackpool Victoria Hospital, Lancashire, England, said the lipopeptide antibiotic was equally effective against methicillin- and penicillin-resistant Staphylococcus aureus, coagulase-negative staphylococcus, and enterococci.
“This is particularly good to know because sometimes in real life, on the shop floor, you don’t always have a very clear insight into what you’re trying to treat,” said Dr. Guleri. “It’s reassuring to see that the success rate is similar in all these infections.”
He presented a subgroup analysis of patients enrolled in European Cubicin Outcomes Registry and Experience (EUCORE), a retrospective, noninterventional, postmarketing registry. The 4-year study reported real-world clinical experience of daptomycin use for the treatment of Gram-positive infections in patients with infective endocarditis who had undergone heart valve replacement.
Typically, Dr. Guleri said, vancomycin, either alone or with rifampicin, is recommended for the infection. “However, with increasing antibiotic resistance, vancomycin doesn’t inspire much confidence, especially for MRSA infections,” he noted.
Daptomycin is increasingly employed as an alternative treatment. It exhibits rapid bactericidal activity against a wide range of Gram-positive pathogens, including MRSA. It’s approved for the treatment of right-sided infective endocarditis due to S. aureus, at a dose of 6 mg/kg per day. However, higher doses are now recommended by several international guidelines and are often used for hard-to-treat infections, Dr. Guleri said.
EUCORE comprised 6,075 patients from 18 countries who were enrolled from 2006 to 2012. Patients were followed until 2014. Of this group, 610 had infective endocarditis and 198 underwent valve replacement. Most were male (70%); mean age was 58 years. Medical comorbidities were common and included renal disease, sepsis, diabetes, pulmonary disease, gastrointestinal disease, cerebrovascular disease and inflammatory diseases.
Culture results were available for 87%. Of these, 68% were positive. The most common pathogen was S. aureus (37%). Half of these isolates were penicillin resistant and 35% were methicillin resistant. Enterococci were responsible for 14% of the infections, and coagulase-negative staph for 32%. The rest were caused by other pathogens.
Before trying daptomycin, most patients (83%) had already been treated with an antibiotic, which was employed in conjunction with another antibiotic in 77% of cases. The concomitant medications included rifampicin (31%), aminoglycosides (29%) and carbapenems (18%).
The overall clinical cure rate at 2 years was 90%. Daptomycin was equally effective in left- and right-sided disease, and was more effective in penicillin-resistant staph (95%) than methicillin-resistant staph (80%). The cure rate was also good in coagulase-negative staph (81%) and enterococci (75%).
High doses were more effective than low doses. At 4 mg/kg per day, the cure rate was 61%. At 6 mg/kg per day, it was 86%, and at more than 6 mg/kg per day, it was 90%.
Adverse events were rare (3%). Three patients developed increased creatine phosphokinase levels; one patient developed rhabdomyolysis and one developed cholestasis. Agranulocytosis developed in three patients and eosinophilic pneumonia in three. One patient developed a rash. No one discontinued the drug due to a side effect.
Dr. Guleri had no financial disclosures.
On Twitter @Alz_Gal
AT ECCMID 2016
AMSTERDAM – Daptomycin successfully treated infective endocarditis in 90% of patients who developed it after undergoing heart valve replacement, according to a report presented at the annual congress of the European Society of Clinical Microbiology and Infectious Diseases.
Dr. Achyut Guleri, clinical director of laboratory medicine at Blackpool Victoria Hospital, Lancashire, England, said the lipopeptide antibiotic was equally effective against methicillin- and penicillin-resistant Staphylococcus aureus, coagulase-negative staphylococcus, and enterococci.
“This is particularly good to know because sometimes in real life, on the shop floor, you don’t always have a very clear insight into what you’re trying to treat,” said Dr. Guleri. “It’s reassuring to see that the success rate is similar in all these infections.”
He presented a subgroup analysis of patients enrolled in European Cubicin Outcomes Registry and Experience (EUCORE), a retrospective, noninterventional, postmarketing registry. The 4-year study reported real-world clinical experience of daptomycin use for the treatment of Gram-positive infections in patients with infective endocarditis who had undergone heart valve replacement.
Typically, Dr. Guleri said, vancomycin, either alone or with rifampicin, is recommended for the infection. “However, with increasing antibiotic resistance, vancomycin doesn’t inspire much confidence, especially for MRSA infections,” he noted.
Daptomycin is increasingly employed as an alternative treatment. It exhibits rapid bactericidal activity against a wide range of Gram-positive pathogens, including MRSA. It’s approved for the treatment of right-sided infective endocarditis due to S. aureus, at a dose of 6 mg/kg per day. However, higher doses are now recommended by several international guidelines and are often used for hard-to-treat infections, Dr. Guleri said.
EUCORE comprised 6,075 patients from 18 countries who were enrolled from 2006 to 2012. Patients were followed until 2014. Of this group, 610 had infective endocarditis and 198 underwent valve replacement. Most were male (70%); mean age was 58 years. Medical comorbidities were common and included renal disease, sepsis, diabetes, pulmonary disease, gastrointestinal disease, cerebrovascular disease and inflammatory diseases.
Culture results were available for 87%. Of these, 68% were positive. The most common pathogen was S. aureus (37%). Half of these isolates were penicillin resistant and 35% were methicillin resistant. Enterococci were responsible for 14% of the infections, and coagulase-negative staph for 32%. The rest were caused by other pathogens.
Before trying daptomycin, most patients (83%) had already been treated with an antibiotic, which was employed in conjunction with another antibiotic in 77% of cases. The concomitant medications included rifampicin (31%), aminoglycosides (29%) and carbapenems (18%).
The overall clinical cure rate at 2 years was 90%. Daptomycin was equally effective in left- and right-sided disease, and was more effective in penicillin-resistant staph (95%) than methicillin-resistant staph (80%). The cure rate was also good in coagulase-negative staph (81%) and enterococci (75%).
High doses were more effective than low doses. At 4 mg/kg per day, the cure rate was 61%. At 6 mg/kg per day, it was 86%, and at more than 6 mg/kg per day, it was 90%.
Adverse events were rare (3%). Three patients developed increased creatine phosphokinase levels; one patient developed rhabdomyolysis and one developed cholestasis. Agranulocytosis developed in three patients and eosinophilic pneumonia in three. One patient developed a rash. No one discontinued the drug due to a side effect.
Dr. Guleri had no financial disclosures.
On Twitter @Alz_Gal
AT ECCMID 2016
AMSTERDAM – Daptomycin successfully treated infective endocarditis in 90% of patients who developed it after undergoing heart valve replacement, according to a report presented at the annual congress of the European Society of Clinical Microbiology and Infectious Diseases.
Dr. Achyut Guleri, clinical director of laboratory medicine at Blackpool Victoria Hospital, Lancashire, England, said the lipopeptide antibiotic was equally effective against methicillin- and penicillin-resistant Staphylococcus aureus, coagulase-negative staphylococcus, and enterococci.
“This is particularly good to know because sometimes in real life, on the shop floor, you don’t always have a very clear insight into what you’re trying to treat,” said Dr. Guleri. “It’s reassuring to see that the success rate is similar in all these infections.”
He presented a subgroup analysis of patients enrolled in European Cubicin Outcomes Registry and Experience (EUCORE), a retrospective, noninterventional, postmarketing registry. The 4-year study reported real-world clinical experience of daptomycin use for the treatment of Gram-positive infections in patients with infective endocarditis who had undergone heart valve replacement.
Typically, Dr. Guleri said, vancomycin, either alone or with rifampicin, is recommended for the infection. “However, with increasing antibiotic resistance, vancomycin doesn’t inspire much confidence, especially for MRSA infections,” he noted.
Daptomycin is increasingly employed as an alternative treatment. It exhibits rapid bactericidal activity against a wide range of Gram-positive pathogens, including MRSA. It’s approved for the treatment of right-sided infective endocarditis due to S. aureus, at a dose of 6 mg/kg per day. However, higher doses are now recommended by several international guidelines and are often used for hard-to-treat infections, Dr. Guleri said.
EUCORE comprised 6,075 patients from 18 countries who were enrolled from 2006 to 2012. Patients were followed until 2014. Of this group, 610 had infective endocarditis and 198 underwent valve replacement. Most were male (70%); mean age was 58 years. Medical comorbidities were common and included renal disease, sepsis, diabetes, pulmonary disease, gastrointestinal disease, cerebrovascular disease and inflammatory diseases.
Culture results were available for 87%. Of these, 68% were positive. The most common pathogen was S. aureus (37%). Half of these isolates were penicillin resistant and 35% were methicillin resistant. Enterococci were responsible for 14% of the infections, and coagulase-negative staph for 32%. The rest were caused by other pathogens.
Before trying daptomycin, most patients (83%) had already been treated with an antibiotic, which was employed in conjunction with another antibiotic in 77% of cases. The concomitant medications included rifampicin (31%), aminoglycosides (29%) and carbapenems (18%).
The overall clinical cure rate at 2 years was 90%. Daptomycin was equally effective in left- and right-sided disease, and was more effective in penicillin-resistant staph (95%) than methicillin-resistant staph (80%). The cure rate was also good in coagulase-negative staph (81%) and enterococci (75%).
High doses were more effective than low doses. At 4 mg/kg per day, the cure rate was 61%. At 6 mg/kg per day, it was 86%, and at more than 6 mg/kg per day, it was 90%.
Adverse events were rare (3%). Three patients developed increased creatine phosphokinase levels; one patient developed rhabdomyolysis and one developed cholestasis. Agranulocytosis developed in three patients and eosinophilic pneumonia in three. One patient developed a rash. No one discontinued the drug due to a side effect.
Dr. Guleri had no financial disclosures.
On Twitter @Alz_Gal
Key clinical point: Daptomycin had a high cure rate for infective endocarditis caused by MRSA, MSSA, coagulase-negative staph, and enterococci.
Major finding: The 2-year clinical cure rate was 90% for S. aureus infections.
Data source: Retrospective analysis of EUCORE, which comprised 198 patients.
Disclosures: Dr. Guleri had no financial disclosures.
FIRST reflections: Impact of ACGME duty hours on CT practitioners
Several months ago, Dr. Bilimoria and his colleagues published the long awaited study in NEJM essentially contradicting adverse effects of strict duty hours on patient outcomes (N Engl J Med. 2016 374:713-2). The study, known as the FIRST trial, was published in the March issue of Thoracic Surgery News. Although the study enrolled general surgery residents, its conclusion impacts no specialty more than cardiothoracic surgery, where frequent handoffs complicate tedious perioperative care of sick patients stall learning opportunities for young trainees.
As Dr. Shari Meyerson eloquently noted in her perspective piece for Thoracic Surgery News (March 2016, page 4), surgery training needs to adapt to meet the modern day needs of trainees to rest and spend time with family and friends, with those of exposure to complex clinical scenarios in a short residency period. Arguably, CT surgery trainees are some of the most motivated and driven; to limit their experience on a national level may be shortsighted. On the other hand, appropriate incorporation of advanced practice providers (APPs) may help allay some patient care challenges, free valuable family time, and allow thoracic residents to function well in a more flexible ACGME duty-hour paradigm. To add thoracic relevance to the findings of Dr. Bilimoria and his colleagues, the debate is brought to Thoracic Surgery News by our colleagues from different training pathways below:
Dr. Antonoff: “Due to the timing of my medical school matriculation, I completed my surgical clerkships in the preregulated duty-hour era. I had expectations of what my life would be like as a surgeon when I applied for the general surgery match, and frankly, my expectations prepared me for a life that would revolve around my education, my technical training, and my commitment to patient care. During my years as a junior resident, my surgical training program gradually adapted in recognition of the new guidelines, but it took time. I spent 3 years in the research lab, and, after I came out as a senior resident, I discovered that the rules of the game had totally changed. While duty hours for me, as a senior trainee, were still fairly open, I found that my interns and junior residents had to play by completely new rules. In some ways, on rare occasions, I felt frustrated and resentful of the fact that my duties as a chief resident and thoracic fellow included many of the tasks that I’d done as an intern, because my interns would ‘expire’ after 16 hours. However, much more often, I felt bad for those who came after me.
They seemed desperate to operate, eager to see their patients’ problems through to resolution, and embarrassed to have to end their days earlier than the more senior members of the team. I feel fortunate that I had years of frequent in-house call after long days in the operating room and followed by post-call days of more operating. I finished my junior years without fear of any sick patient in the hospital, I finished my general surgery training without fear of any emergent operation, and I finished my fellowship with confidence that I could get a patient through just about anything if I had access to a cannula.
My early experiences as an attending have certainly kept me humble, and I’ve spent many a night worried about my patients, rethinking choices that I’ve made and stitches that I’ve thrown. But I thank my lucky stars that I was exposed to phenomenal training, and that I had the privilege and opportunity to work the hours needed to reach a reasonable level of safety! I can only imagine that if I’d have spent fewer nights in the hospital, that I’d feel even more anxiety and nausea at this early stage of my surgical career.
As elaborated in the editorial by Dr. Birkmeyer (N Engl J Med. 2016;374:783-4), it is not surprising that patient outcomes did not immediately depend on whether the programs had adhered strictly to the ACGME duty-hour rules. Limited numbers of patients experience critical events during shift change, and hospitals are evolving to function with greater reliance on midlevel practitioners and attending physicians. I would not expect the short-term results of duty-hour flexibility to demonstrate any impact on patient care. However, I do fear that there will be a mid-term impact on trainee accountability and autonomy, which will ultimately impact the competence of the attending surgeons of the future, and downstream potential long-term impact on day-to-day patient outcomes.
As a wife and mother of 3, I recognize that we, as a specialty, need to find ways to support our trainees and their families and to help them live happy lives conducive to functioning outside the hospital. I believe that we can do this with support, mentorship, and advocacy; I do not believe that it requires cutting back on the training that we are all, in the end, so incredibly grateful to receive.”
Dr. Mara Antonoff is an assistant professor of thoracic and cardiovascular surgery at UT MD Anderson Cancer Center. She performed her General Surgery training at the University of Minnesota, 2004-2012, and her Thoracic Surgery Training at Washington University, as a traditional 2-year resident, 2012-2014.
Dr. Stephens: “There is nothing that replaces being bedside. Whether it be a postoperative patient struggling with low cardiac output syndrome overnight, or a patient with a high pressor requirement the etiology of which you are trying to uncover, or a patient you have been following who suddenly arrests, the value of seeing a patient’s trajectory longitudinally is critical to developing clinical acumen. When as an attending I will get called in the middle of the night about a postoperative patient not “doing well,” I will be drawing on my years of being on call and being bedside with my patients.
Patient care is the ultimate goal, and it is clear that overworked residents are at higher risk for making mistakes that jeopardize patient care, which nobody wants. However, the restrictions that duty hours place don’t allow the flexibility necessary for a specialty such as ours, and in fact strict adherence to such regulations inhibits opportunities for our learning. Also concerning is the “shift-work” mentality that seems to be increasingly pervasive with the implementation of duty hours. As has been well documented, and as I have seen personally, the constant patient handoffs that are requisite to implementation of duty hours pose their own perils in terms of patient safety.
Ultimately, these are our patients and we are responsible. Once we are attendings, those responsibilities will not be turned off after we have reached some prespecified hour limit.
The question then remains how best to implement a system across a wide variety of programs that ensures both patient safety and adequate clinical experience in the context of a culture of patient responsibility for the residents. As the NEJM study (N Engl J Med. 2016 374:713-2) shows, flexibility in implementation of duty hours did not result in increased complications, but resulted in improved resident satisfaction in continuity of care and handoffs. In my opinion, this study then encourages specialties such as ours to be more flexible in work hours, to encourage residents when there is a learning opportunity that previously they would be prohibited from taking part in to take hold of that opportunity, and to use this flexibility in implementation of duty hours to combat the invading “shift-work” mentality that will only jeopardize patient care.”
Dr. Elizabeth H. Stephens, MD, PhD is a Cardiothoracic Surgery, resident, PGY4, at Columbia University, New York, as an Integrated I-6 Resident.
Dr. Brown: “I took the traditional 5-year of General Surgery + 2 years of Cardiothoracic Surgery training route to becoming a General Thoracic Surgeon. My General Surgery experience was invaluable to my development as a surgeon. However, after all of those years of General Surgery cases and minimal exposure to Cardiothoracic Surgery cases, coupled with minimal overlap between the two specialties with regard to patient care, I found the learning curve in fellowship to be very steep. I was fortunate to train in a program with phenomenal physician extender support [APPs] in addition to top-notch colleagues in other specialties and excellent nursing, which allowed me to spend the majority of those 2 years in the operating room and completely focused on patient care. During that final phase of training, I welcomed flexibility with regard to the work-hour restrictions to ensure that I was acquiring the experience I needed prior to starting my own practice.”
Lisa M. Brown, MD, MAS, Assistant Professor of Thoracic Surgery, UC Davis Health System, Calif.; Training Institution: Washington University
Dr. Lee: “I started my surgical training in 2005, 2 years after the implementation of the 80-hour workweek restriction. Fortunately for my personal life, my training program took the restriction very seriously and strictly enforced it. As a result, I had scheduled periods off from work, and rarely worked more than 80 hours per week over the course of general surgery. On those occasions that I did, the next weeks, or preceding weeks would be shorter, to compensate. As a product of a 4+3 Thoracic Surgery residency in this environment, the 80-hour workweek extended to my subspecialty training. Our cardiac surgery time strictly enforced the go-home post-call policy. As a result, I believe my duty hours during Thoracic Surgery are likely shorter overall than many other programs.
Everyone hears the rumors of other programs lying about their duty hours. Fortunately, mine was not one of these. Despite this, or because of this, I received top-notch training. At the same time and more importantly, I started a family. I married my wife a week before my internship started, and am still married to the same person. We had two precious daughters during my Thoracic Surgery years. I don’t believe this would have been possible without duty-hours restrictions.
To create an environment where such a task was possible, my program hired an army of mid-level practitioners to deal with the day-to-day tasks of providing cardiothoracic surgical care to the patients, both in the intensive care unit and on the ward.
I rarely had to write a history and physical during Thoracic Surgery training. I consented fewer patients than I have fingers on my hands. I pulled even fewer chest tubes. I can now no longer remember having pulled a central line. I learned these tasks when I was a junior resident. What I did instead as a senior resident was perform over 900 cardiothoracic procedures as the primary surgeon. Now, as an attending surgeon, I still don’t write full histories and physicals by myself. I certainly don’t pull chest tubes and central lines. I consent patients by having a conversation with them, which I did as a resident, but I don’t bring a piece of paper with me in to the clinic room. I have a physician assistant who helps me fill in the gaps.
In 8 months of practice, I have performed over 15 thoracic organ transplants, repaired over 15 aortic dissections, half of whom required root replacements, performed more double-valve surgeries than straightforward single-valve replacements, started a minimally invasive atrial fibrillation surgical program, and applied almost every shred of knowledge and experience gained in 3 years of Thoracic Surgery Residency to a busy clinical practice. Most importantly, I continue to come home and watch my two daughters grow up.
With that perspective, I don’t believe the question should be whether or not programs should have the flexibility to enforce or not enforce duty-hours restrictions. It should be, how could every program find a way to effectively train residents to be good physicians and still allow them a personal life?”
Dr. Anson Lee is an Assistant Professor of Cardiac Surgery, Stanford University, Calif.; Training: 4+3 CT Residency, at Washington University, St. Louis.
Ms. Bohlman: “As a physician assistant in cardiac surgery, I represent the reality that physicians with a critical patient population appreciate consistency in their patient management. However, working in a university hospital setting also requires that surgical residents receive appropriate training. With the recently implemented duty restriction hours on resident training programs, advanced practice providers (APPs) have been utilized as an excellent solution for scheduling conflicts without compromising patient care. An example to this point is evident in my own place of work.
Approximately 1 year ago, our surgical intensive care unit transitioned from resident care to a combination of residents and APPs. At that time, the APPs were tasked with the complete care of all cardiac surgery patients. This change reduced the quantity and acuity of patients for which the residents were responsible and therefore allowed for more flexible hours along with a more manageable patient load. These changes, among others, have contributed to improved patient outcomes in the cardiac surgery patient population within our institution. With the increase in APPs that have training in various specialties, there comes an increasing ability to not only fill the gaps in scheduling but to do so with an extension of the providing physician. Although the NEJM article demonstrated no difference in patient outcomes between resident programs with restricted duty hours versus more flexible duty-hour policies, I foresee the future of medicine focusing on trained APPs as a complement to the care that the residents provide.”
Allison Bohlman is a Physician Assistant at Rush University Medical Center in the Integrated cardiovascular thoracic intensive care unit.
Several months ago, Dr. Bilimoria and his colleagues published the long awaited study in NEJM essentially contradicting adverse effects of strict duty hours on patient outcomes (N Engl J Med. 2016 374:713-2). The study, known as the FIRST trial, was published in the March issue of Thoracic Surgery News. Although the study enrolled general surgery residents, its conclusion impacts no specialty more than cardiothoracic surgery, where frequent handoffs complicate tedious perioperative care of sick patients stall learning opportunities for young trainees.
As Dr. Shari Meyerson eloquently noted in her perspective piece for Thoracic Surgery News (March 2016, page 4), surgery training needs to adapt to meet the modern day needs of trainees to rest and spend time with family and friends, with those of exposure to complex clinical scenarios in a short residency period. Arguably, CT surgery trainees are some of the most motivated and driven; to limit their experience on a national level may be shortsighted. On the other hand, appropriate incorporation of advanced practice providers (APPs) may help allay some patient care challenges, free valuable family time, and allow thoracic residents to function well in a more flexible ACGME duty-hour paradigm. To add thoracic relevance to the findings of Dr. Bilimoria and his colleagues, the debate is brought to Thoracic Surgery News by our colleagues from different training pathways below:
Dr. Antonoff: “Due to the timing of my medical school matriculation, I completed my surgical clerkships in the preregulated duty-hour era. I had expectations of what my life would be like as a surgeon when I applied for the general surgery match, and frankly, my expectations prepared me for a life that would revolve around my education, my technical training, and my commitment to patient care. During my years as a junior resident, my surgical training program gradually adapted in recognition of the new guidelines, but it took time. I spent 3 years in the research lab, and, after I came out as a senior resident, I discovered that the rules of the game had totally changed. While duty hours for me, as a senior trainee, were still fairly open, I found that my interns and junior residents had to play by completely new rules. In some ways, on rare occasions, I felt frustrated and resentful of the fact that my duties as a chief resident and thoracic fellow included many of the tasks that I’d done as an intern, because my interns would ‘expire’ after 16 hours. However, much more often, I felt bad for those who came after me.
They seemed desperate to operate, eager to see their patients’ problems through to resolution, and embarrassed to have to end their days earlier than the more senior members of the team. I feel fortunate that I had years of frequent in-house call after long days in the operating room and followed by post-call days of more operating. I finished my junior years without fear of any sick patient in the hospital, I finished my general surgery training without fear of any emergent operation, and I finished my fellowship with confidence that I could get a patient through just about anything if I had access to a cannula.
My early experiences as an attending have certainly kept me humble, and I’ve spent many a night worried about my patients, rethinking choices that I’ve made and stitches that I’ve thrown. But I thank my lucky stars that I was exposed to phenomenal training, and that I had the privilege and opportunity to work the hours needed to reach a reasonable level of safety! I can only imagine that if I’d have spent fewer nights in the hospital, that I’d feel even more anxiety and nausea at this early stage of my surgical career.
As elaborated in the editorial by Dr. Birkmeyer (N Engl J Med. 2016;374:783-4), it is not surprising that patient outcomes did not immediately depend on whether the programs had adhered strictly to the ACGME duty-hour rules. Limited numbers of patients experience critical events during shift change, and hospitals are evolving to function with greater reliance on midlevel practitioners and attending physicians. I would not expect the short-term results of duty-hour flexibility to demonstrate any impact on patient care. However, I do fear that there will be a mid-term impact on trainee accountability and autonomy, which will ultimately impact the competence of the attending surgeons of the future, and downstream potential long-term impact on day-to-day patient outcomes.
As a wife and mother of 3, I recognize that we, as a specialty, need to find ways to support our trainees and their families and to help them live happy lives conducive to functioning outside the hospital. I believe that we can do this with support, mentorship, and advocacy; I do not believe that it requires cutting back on the training that we are all, in the end, so incredibly grateful to receive.”
Dr. Mara Antonoff is an assistant professor of thoracic and cardiovascular surgery at UT MD Anderson Cancer Center. She performed her General Surgery training at the University of Minnesota, 2004-2012, and her Thoracic Surgery Training at Washington University, as a traditional 2-year resident, 2012-2014.
Dr. Stephens: “There is nothing that replaces being bedside. Whether it be a postoperative patient struggling with low cardiac output syndrome overnight, or a patient with a high pressor requirement the etiology of which you are trying to uncover, or a patient you have been following who suddenly arrests, the value of seeing a patient’s trajectory longitudinally is critical to developing clinical acumen. When as an attending I will get called in the middle of the night about a postoperative patient not “doing well,” I will be drawing on my years of being on call and being bedside with my patients.
Patient care is the ultimate goal, and it is clear that overworked residents are at higher risk for making mistakes that jeopardize patient care, which nobody wants. However, the restrictions that duty hours place don’t allow the flexibility necessary for a specialty such as ours, and in fact strict adherence to such regulations inhibits opportunities for our learning. Also concerning is the “shift-work” mentality that seems to be increasingly pervasive with the implementation of duty hours. As has been well documented, and as I have seen personally, the constant patient handoffs that are requisite to implementation of duty hours pose their own perils in terms of patient safety.
Ultimately, these are our patients and we are responsible. Once we are attendings, those responsibilities will not be turned off after we have reached some prespecified hour limit.
The question then remains how best to implement a system across a wide variety of programs that ensures both patient safety and adequate clinical experience in the context of a culture of patient responsibility for the residents. As the NEJM study (N Engl J Med. 2016 374:713-2) shows, flexibility in implementation of duty hours did not result in increased complications, but resulted in improved resident satisfaction in continuity of care and handoffs. In my opinion, this study then encourages specialties such as ours to be more flexible in work hours, to encourage residents when there is a learning opportunity that previously they would be prohibited from taking part in to take hold of that opportunity, and to use this flexibility in implementation of duty hours to combat the invading “shift-work” mentality that will only jeopardize patient care.”
Dr. Elizabeth H. Stephens, MD, PhD is a Cardiothoracic Surgery, resident, PGY4, at Columbia University, New York, as an Integrated I-6 Resident.
Dr. Brown: “I took the traditional 5-year of General Surgery + 2 years of Cardiothoracic Surgery training route to becoming a General Thoracic Surgeon. My General Surgery experience was invaluable to my development as a surgeon. However, after all of those years of General Surgery cases and minimal exposure to Cardiothoracic Surgery cases, coupled with minimal overlap between the two specialties with regard to patient care, I found the learning curve in fellowship to be very steep. I was fortunate to train in a program with phenomenal physician extender support [APPs] in addition to top-notch colleagues in other specialties and excellent nursing, which allowed me to spend the majority of those 2 years in the operating room and completely focused on patient care. During that final phase of training, I welcomed flexibility with regard to the work-hour restrictions to ensure that I was acquiring the experience I needed prior to starting my own practice.”
Lisa M. Brown, MD, MAS, Assistant Professor of Thoracic Surgery, UC Davis Health System, Calif.; Training Institution: Washington University
Dr. Lee: “I started my surgical training in 2005, 2 years after the implementation of the 80-hour workweek restriction. Fortunately for my personal life, my training program took the restriction very seriously and strictly enforced it. As a result, I had scheduled periods off from work, and rarely worked more than 80 hours per week over the course of general surgery. On those occasions that I did, the next weeks, or preceding weeks would be shorter, to compensate. As a product of a 4+3 Thoracic Surgery residency in this environment, the 80-hour workweek extended to my subspecialty training. Our cardiac surgery time strictly enforced the go-home post-call policy. As a result, I believe my duty hours during Thoracic Surgery are likely shorter overall than many other programs.
Everyone hears the rumors of other programs lying about their duty hours. Fortunately, mine was not one of these. Despite this, or because of this, I received top-notch training. At the same time and more importantly, I started a family. I married my wife a week before my internship started, and am still married to the same person. We had two precious daughters during my Thoracic Surgery years. I don’t believe this would have been possible without duty-hours restrictions.
To create an environment where such a task was possible, my program hired an army of mid-level practitioners to deal with the day-to-day tasks of providing cardiothoracic surgical care to the patients, both in the intensive care unit and on the ward.
I rarely had to write a history and physical during Thoracic Surgery training. I consented fewer patients than I have fingers on my hands. I pulled even fewer chest tubes. I can now no longer remember having pulled a central line. I learned these tasks when I was a junior resident. What I did instead as a senior resident was perform over 900 cardiothoracic procedures as the primary surgeon. Now, as an attending surgeon, I still don’t write full histories and physicals by myself. I certainly don’t pull chest tubes and central lines. I consent patients by having a conversation with them, which I did as a resident, but I don’t bring a piece of paper with me in to the clinic room. I have a physician assistant who helps me fill in the gaps.
In 8 months of practice, I have performed over 15 thoracic organ transplants, repaired over 15 aortic dissections, half of whom required root replacements, performed more double-valve surgeries than straightforward single-valve replacements, started a minimally invasive atrial fibrillation surgical program, and applied almost every shred of knowledge and experience gained in 3 years of Thoracic Surgery Residency to a busy clinical practice. Most importantly, I continue to come home and watch my two daughters grow up.
With that perspective, I don’t believe the question should be whether or not programs should have the flexibility to enforce or not enforce duty-hours restrictions. It should be, how could every program find a way to effectively train residents to be good physicians and still allow them a personal life?”
Dr. Anson Lee is an Assistant Professor of Cardiac Surgery, Stanford University, Calif.; Training: 4+3 CT Residency, at Washington University, St. Louis.
Ms. Bohlman: “As a physician assistant in cardiac surgery, I represent the reality that physicians with a critical patient population appreciate consistency in their patient management. However, working in a university hospital setting also requires that surgical residents receive appropriate training. With the recently implemented duty restriction hours on resident training programs, advanced practice providers (APPs) have been utilized as an excellent solution for scheduling conflicts without compromising patient care. An example to this point is evident in my own place of work.
Approximately 1 year ago, our surgical intensive care unit transitioned from resident care to a combination of residents and APPs. At that time, the APPs were tasked with the complete care of all cardiac surgery patients. This change reduced the quantity and acuity of patients for which the residents were responsible and therefore allowed for more flexible hours along with a more manageable patient load. These changes, among others, have contributed to improved patient outcomes in the cardiac surgery patient population within our institution. With the increase in APPs that have training in various specialties, there comes an increasing ability to not only fill the gaps in scheduling but to do so with an extension of the providing physician. Although the NEJM article demonstrated no difference in patient outcomes between resident programs with restricted duty hours versus more flexible duty-hour policies, I foresee the future of medicine focusing on trained APPs as a complement to the care that the residents provide.”
Allison Bohlman is a Physician Assistant at Rush University Medical Center in the Integrated cardiovascular thoracic intensive care unit.
Several months ago, Dr. Bilimoria and his colleagues published the long awaited study in NEJM essentially contradicting adverse effects of strict duty hours on patient outcomes (N Engl J Med. 2016 374:713-2). The study, known as the FIRST trial, was published in the March issue of Thoracic Surgery News. Although the study enrolled general surgery residents, its conclusion impacts no specialty more than cardiothoracic surgery, where frequent handoffs complicate tedious perioperative care of sick patients stall learning opportunities for young trainees.
As Dr. Shari Meyerson eloquently noted in her perspective piece for Thoracic Surgery News (March 2016, page 4), surgery training needs to adapt to meet the modern day needs of trainees to rest and spend time with family and friends, with those of exposure to complex clinical scenarios in a short residency period. Arguably, CT surgery trainees are some of the most motivated and driven; to limit their experience on a national level may be shortsighted. On the other hand, appropriate incorporation of advanced practice providers (APPs) may help allay some patient care challenges, free valuable family time, and allow thoracic residents to function well in a more flexible ACGME duty-hour paradigm. To add thoracic relevance to the findings of Dr. Bilimoria and his colleagues, the debate is brought to Thoracic Surgery News by our colleagues from different training pathways below:
Dr. Antonoff: “Due to the timing of my medical school matriculation, I completed my surgical clerkships in the preregulated duty-hour era. I had expectations of what my life would be like as a surgeon when I applied for the general surgery match, and frankly, my expectations prepared me for a life that would revolve around my education, my technical training, and my commitment to patient care. During my years as a junior resident, my surgical training program gradually adapted in recognition of the new guidelines, but it took time. I spent 3 years in the research lab, and, after I came out as a senior resident, I discovered that the rules of the game had totally changed. While duty hours for me, as a senior trainee, were still fairly open, I found that my interns and junior residents had to play by completely new rules. In some ways, on rare occasions, I felt frustrated and resentful of the fact that my duties as a chief resident and thoracic fellow included many of the tasks that I’d done as an intern, because my interns would ‘expire’ after 16 hours. However, much more often, I felt bad for those who came after me.
They seemed desperate to operate, eager to see their patients’ problems through to resolution, and embarrassed to have to end their days earlier than the more senior members of the team. I feel fortunate that I had years of frequent in-house call after long days in the operating room and followed by post-call days of more operating. I finished my junior years without fear of any sick patient in the hospital, I finished my general surgery training without fear of any emergent operation, and I finished my fellowship with confidence that I could get a patient through just about anything if I had access to a cannula.
My early experiences as an attending have certainly kept me humble, and I’ve spent many a night worried about my patients, rethinking choices that I’ve made and stitches that I’ve thrown. But I thank my lucky stars that I was exposed to phenomenal training, and that I had the privilege and opportunity to work the hours needed to reach a reasonable level of safety! I can only imagine that if I’d have spent fewer nights in the hospital, that I’d feel even more anxiety and nausea at this early stage of my surgical career.
As elaborated in the editorial by Dr. Birkmeyer (N Engl J Med. 2016;374:783-4), it is not surprising that patient outcomes did not immediately depend on whether the programs had adhered strictly to the ACGME duty-hour rules. Limited numbers of patients experience critical events during shift change, and hospitals are evolving to function with greater reliance on midlevel practitioners and attending physicians. I would not expect the short-term results of duty-hour flexibility to demonstrate any impact on patient care. However, I do fear that there will be a mid-term impact on trainee accountability and autonomy, which will ultimately impact the competence of the attending surgeons of the future, and downstream potential long-term impact on day-to-day patient outcomes.
As a wife and mother of 3, I recognize that we, as a specialty, need to find ways to support our trainees and their families and to help them live happy lives conducive to functioning outside the hospital. I believe that we can do this with support, mentorship, and advocacy; I do not believe that it requires cutting back on the training that we are all, in the end, so incredibly grateful to receive.”
Dr. Mara Antonoff is an assistant professor of thoracic and cardiovascular surgery at UT MD Anderson Cancer Center. She performed her General Surgery training at the University of Minnesota, 2004-2012, and her Thoracic Surgery Training at Washington University, as a traditional 2-year resident, 2012-2014.
Dr. Stephens: “There is nothing that replaces being bedside. Whether it be a postoperative patient struggling with low cardiac output syndrome overnight, or a patient with a high pressor requirement the etiology of which you are trying to uncover, or a patient you have been following who suddenly arrests, the value of seeing a patient’s trajectory longitudinally is critical to developing clinical acumen. When as an attending I will get called in the middle of the night about a postoperative patient not “doing well,” I will be drawing on my years of being on call and being bedside with my patients.
Patient care is the ultimate goal, and it is clear that overworked residents are at higher risk for making mistakes that jeopardize patient care, which nobody wants. However, the restrictions that duty hours place don’t allow the flexibility necessary for a specialty such as ours, and in fact strict adherence to such regulations inhibits opportunities for our learning. Also concerning is the “shift-work” mentality that seems to be increasingly pervasive with the implementation of duty hours. As has been well documented, and as I have seen personally, the constant patient handoffs that are requisite to implementation of duty hours pose their own perils in terms of patient safety.
Ultimately, these are our patients and we are responsible. Once we are attendings, those responsibilities will not be turned off after we have reached some prespecified hour limit.
The question then remains how best to implement a system across a wide variety of programs that ensures both patient safety and adequate clinical experience in the context of a culture of patient responsibility for the residents. As the NEJM study (N Engl J Med. 2016 374:713-2) shows, flexibility in implementation of duty hours did not result in increased complications, but resulted in improved resident satisfaction in continuity of care and handoffs. In my opinion, this study then encourages specialties such as ours to be more flexible in work hours, to encourage residents when there is a learning opportunity that previously they would be prohibited from taking part in to take hold of that opportunity, and to use this flexibility in implementation of duty hours to combat the invading “shift-work” mentality that will only jeopardize patient care.”
Dr. Elizabeth H. Stephens, MD, PhD is a Cardiothoracic Surgery, resident, PGY4, at Columbia University, New York, as an Integrated I-6 Resident.
Dr. Brown: “I took the traditional 5-year of General Surgery + 2 years of Cardiothoracic Surgery training route to becoming a General Thoracic Surgeon. My General Surgery experience was invaluable to my development as a surgeon. However, after all of those years of General Surgery cases and minimal exposure to Cardiothoracic Surgery cases, coupled with minimal overlap between the two specialties with regard to patient care, I found the learning curve in fellowship to be very steep. I was fortunate to train in a program with phenomenal physician extender support [APPs] in addition to top-notch colleagues in other specialties and excellent nursing, which allowed me to spend the majority of those 2 years in the operating room and completely focused on patient care. During that final phase of training, I welcomed flexibility with regard to the work-hour restrictions to ensure that I was acquiring the experience I needed prior to starting my own practice.”
Lisa M. Brown, MD, MAS, Assistant Professor of Thoracic Surgery, UC Davis Health System, Calif.; Training Institution: Washington University
Dr. Lee: “I started my surgical training in 2005, 2 years after the implementation of the 80-hour workweek restriction. Fortunately for my personal life, my training program took the restriction very seriously and strictly enforced it. As a result, I had scheduled periods off from work, and rarely worked more than 80 hours per week over the course of general surgery. On those occasions that I did, the next weeks, or preceding weeks would be shorter, to compensate. As a product of a 4+3 Thoracic Surgery residency in this environment, the 80-hour workweek extended to my subspecialty training. Our cardiac surgery time strictly enforced the go-home post-call policy. As a result, I believe my duty hours during Thoracic Surgery are likely shorter overall than many other programs.
Everyone hears the rumors of other programs lying about their duty hours. Fortunately, mine was not one of these. Despite this, or because of this, I received top-notch training. At the same time and more importantly, I started a family. I married my wife a week before my internship started, and am still married to the same person. We had two precious daughters during my Thoracic Surgery years. I don’t believe this would have been possible without duty-hours restrictions.
To create an environment where such a task was possible, my program hired an army of mid-level practitioners to deal with the day-to-day tasks of providing cardiothoracic surgical care to the patients, both in the intensive care unit and on the ward.
I rarely had to write a history and physical during Thoracic Surgery training. I consented fewer patients than I have fingers on my hands. I pulled even fewer chest tubes. I can now no longer remember having pulled a central line. I learned these tasks when I was a junior resident. What I did instead as a senior resident was perform over 900 cardiothoracic procedures as the primary surgeon. Now, as an attending surgeon, I still don’t write full histories and physicals by myself. I certainly don’t pull chest tubes and central lines. I consent patients by having a conversation with them, which I did as a resident, but I don’t bring a piece of paper with me in to the clinic room. I have a physician assistant who helps me fill in the gaps.
In 8 months of practice, I have performed over 15 thoracic organ transplants, repaired over 15 aortic dissections, half of whom required root replacements, performed more double-valve surgeries than straightforward single-valve replacements, started a minimally invasive atrial fibrillation surgical program, and applied almost every shred of knowledge and experience gained in 3 years of Thoracic Surgery Residency to a busy clinical practice. Most importantly, I continue to come home and watch my two daughters grow up.
With that perspective, I don’t believe the question should be whether or not programs should have the flexibility to enforce or not enforce duty-hours restrictions. It should be, how could every program find a way to effectively train residents to be good physicians and still allow them a personal life?”
Dr. Anson Lee is an Assistant Professor of Cardiac Surgery, Stanford University, Calif.; Training: 4+3 CT Residency, at Washington University, St. Louis.
Ms. Bohlman: “As a physician assistant in cardiac surgery, I represent the reality that physicians with a critical patient population appreciate consistency in their patient management. However, working in a university hospital setting also requires that surgical residents receive appropriate training. With the recently implemented duty restriction hours on resident training programs, advanced practice providers (APPs) have been utilized as an excellent solution for scheduling conflicts without compromising patient care. An example to this point is evident in my own place of work.
Approximately 1 year ago, our surgical intensive care unit transitioned from resident care to a combination of residents and APPs. At that time, the APPs were tasked with the complete care of all cardiac surgery patients. This change reduced the quantity and acuity of patients for which the residents were responsible and therefore allowed for more flexible hours along with a more manageable patient load. These changes, among others, have contributed to improved patient outcomes in the cardiac surgery patient population within our institution. With the increase in APPs that have training in various specialties, there comes an increasing ability to not only fill the gaps in scheduling but to do so with an extension of the providing physician. Although the NEJM article demonstrated no difference in patient outcomes between resident programs with restricted duty hours versus more flexible duty-hour policies, I foresee the future of medicine focusing on trained APPs as a complement to the care that the residents provide.”
Allison Bohlman is a Physician Assistant at Rush University Medical Center in the Integrated cardiovascular thoracic intensive care unit.
CMS promises streamlined, flexible program to replace meaningful use
Meaningful use would get a new name and an emphasis on flexibility under a proposal from the Centers for Medicare & Medicaid Services.
“We’re proposing today to replace meaningful use in the physician office with a new effort that moves the emphasis away from the use of information technology to one that supports patient care, supported by better and more connected technology,” CMS Acting Administrator Andy Slavitt said during an April 27 press teleconference to introduce the changes.
“The program, Advancing Care Information, is designed to be far simpler, less burdensome, and more flexible,” Mr. Slavitt said. “If this proposal is finalized, it will replace the current meaningful use program for physician offices and will be effective January 1, 2017, along with the other components of the MACRA implementations.”
Mr. Slavitt and Dr. Karen DeSalvo, National Coordinator for Health Information Technology, noted in a blog postthat the improvements “should increase providers’ ability to use technology in ways that are more relevant to their needs and the needs of their patients.”
The changes come as part of a larger proposed regulation to implement the Medicare Access and CHIP Reauthorization Act, released online April 27 and scheduled for publication in the Federal Register on May 9.
MACRA will create two systems under which doctors will be paid for the quality of care they provide. The changes to the meaningful use program will affect physicians who choose to participate in the Merit-based Incentive Payment System (MIPS). Under the proposed rule, efforts under the new Advancing Care Information program would account for 25% of the score used to determine pay for office-based physicians under Medicare.
The key difference between the proposed program and meaningful use is that physicians will no longer be faced with an all-or-nothing requirement for meeting criteria to qualify for extra payments under the MIPS program.
Advancing Care Information has been divided into two parts. The first is reporting measures and has been streamlined to 11 measures, down from 18. Reporting on computerized physician order entry and clinical decision support measures have been eliminated.
The second part is based on performance measures, with multiple pathways to achieve those targets, which allow physicians to select the measures that best align with their needs.
There also is an opportunity to earn an extra point if a physician is reporting to more than one public health registry.
“We’ve also taken this opportunity to really focus more on aligning quality, on seeing that we are streamlining workflow and creating opportunities for electronic health record and health IT developers to create products that really meet the needs and expectations of clinicians and providers on the front lines,” Dr. DeSalvo said during the April 27 call.
The proposal also emphasizes interoperability, information exchange, and security measures and requires that patients be able to access their health care information easily through the use of apps and other consumer-friendly technology, according to the blog post.
The proposed rule also emphasizes open data sharing and interoperability, something that has been a continual drag on the current meaningful use program.
Comments on the proposed rule can be made at www.regulations.gov and are due June 26.
Meaningful use would get a new name and an emphasis on flexibility under a proposal from the Centers for Medicare & Medicaid Services.
“We’re proposing today to replace meaningful use in the physician office with a new effort that moves the emphasis away from the use of information technology to one that supports patient care, supported by better and more connected technology,” CMS Acting Administrator Andy Slavitt said during an April 27 press teleconference to introduce the changes.
“The program, Advancing Care Information, is designed to be far simpler, less burdensome, and more flexible,” Mr. Slavitt said. “If this proposal is finalized, it will replace the current meaningful use program for physician offices and will be effective January 1, 2017, along with the other components of the MACRA implementations.”
Mr. Slavitt and Dr. Karen DeSalvo, National Coordinator for Health Information Technology, noted in a blog postthat the improvements “should increase providers’ ability to use technology in ways that are more relevant to their needs and the needs of their patients.”
The changes come as part of a larger proposed regulation to implement the Medicare Access and CHIP Reauthorization Act, released online April 27 and scheduled for publication in the Federal Register on May 9.
MACRA will create two systems under which doctors will be paid for the quality of care they provide. The changes to the meaningful use program will affect physicians who choose to participate in the Merit-based Incentive Payment System (MIPS). Under the proposed rule, efforts under the new Advancing Care Information program would account for 25% of the score used to determine pay for office-based physicians under Medicare.
The key difference between the proposed program and meaningful use is that physicians will no longer be faced with an all-or-nothing requirement for meeting criteria to qualify for extra payments under the MIPS program.
Advancing Care Information has been divided into two parts. The first is reporting measures and has been streamlined to 11 measures, down from 18. Reporting on computerized physician order entry and clinical decision support measures have been eliminated.
The second part is based on performance measures, with multiple pathways to achieve those targets, which allow physicians to select the measures that best align with their needs.
There also is an opportunity to earn an extra point if a physician is reporting to more than one public health registry.
“We’ve also taken this opportunity to really focus more on aligning quality, on seeing that we are streamlining workflow and creating opportunities for electronic health record and health IT developers to create products that really meet the needs and expectations of clinicians and providers on the front lines,” Dr. DeSalvo said during the April 27 call.
The proposal also emphasizes interoperability, information exchange, and security measures and requires that patients be able to access their health care information easily through the use of apps and other consumer-friendly technology, according to the blog post.
The proposed rule also emphasizes open data sharing and interoperability, something that has been a continual drag on the current meaningful use program.
Comments on the proposed rule can be made at www.regulations.gov and are due June 26.
Meaningful use would get a new name and an emphasis on flexibility under a proposal from the Centers for Medicare & Medicaid Services.
“We’re proposing today to replace meaningful use in the physician office with a new effort that moves the emphasis away from the use of information technology to one that supports patient care, supported by better and more connected technology,” CMS Acting Administrator Andy Slavitt said during an April 27 press teleconference to introduce the changes.
“The program, Advancing Care Information, is designed to be far simpler, less burdensome, and more flexible,” Mr. Slavitt said. “If this proposal is finalized, it will replace the current meaningful use program for physician offices and will be effective January 1, 2017, along with the other components of the MACRA implementations.”
Mr. Slavitt and Dr. Karen DeSalvo, National Coordinator for Health Information Technology, noted in a blog postthat the improvements “should increase providers’ ability to use technology in ways that are more relevant to their needs and the needs of their patients.”
The changes come as part of a larger proposed regulation to implement the Medicare Access and CHIP Reauthorization Act, released online April 27 and scheduled for publication in the Federal Register on May 9.
MACRA will create two systems under which doctors will be paid for the quality of care they provide. The changes to the meaningful use program will affect physicians who choose to participate in the Merit-based Incentive Payment System (MIPS). Under the proposed rule, efforts under the new Advancing Care Information program would account for 25% of the score used to determine pay for office-based physicians under Medicare.
The key difference between the proposed program and meaningful use is that physicians will no longer be faced with an all-or-nothing requirement for meeting criteria to qualify for extra payments under the MIPS program.
Advancing Care Information has been divided into two parts. The first is reporting measures and has been streamlined to 11 measures, down from 18. Reporting on computerized physician order entry and clinical decision support measures have been eliminated.
The second part is based on performance measures, with multiple pathways to achieve those targets, which allow physicians to select the measures that best align with their needs.
There also is an opportunity to earn an extra point if a physician is reporting to more than one public health registry.
“We’ve also taken this opportunity to really focus more on aligning quality, on seeing that we are streamlining workflow and creating opportunities for electronic health record and health IT developers to create products that really meet the needs and expectations of clinicians and providers on the front lines,” Dr. DeSalvo said during the April 27 call.
The proposal also emphasizes interoperability, information exchange, and security measures and requires that patients be able to access their health care information easily through the use of apps and other consumer-friendly technology, according to the blog post.
The proposed rule also emphasizes open data sharing and interoperability, something that has been a continual drag on the current meaningful use program.
Comments on the proposed rule can be made at www.regulations.gov and are due June 26.