User login
The Official Newspaper of the American Association for Thoracic Surgery
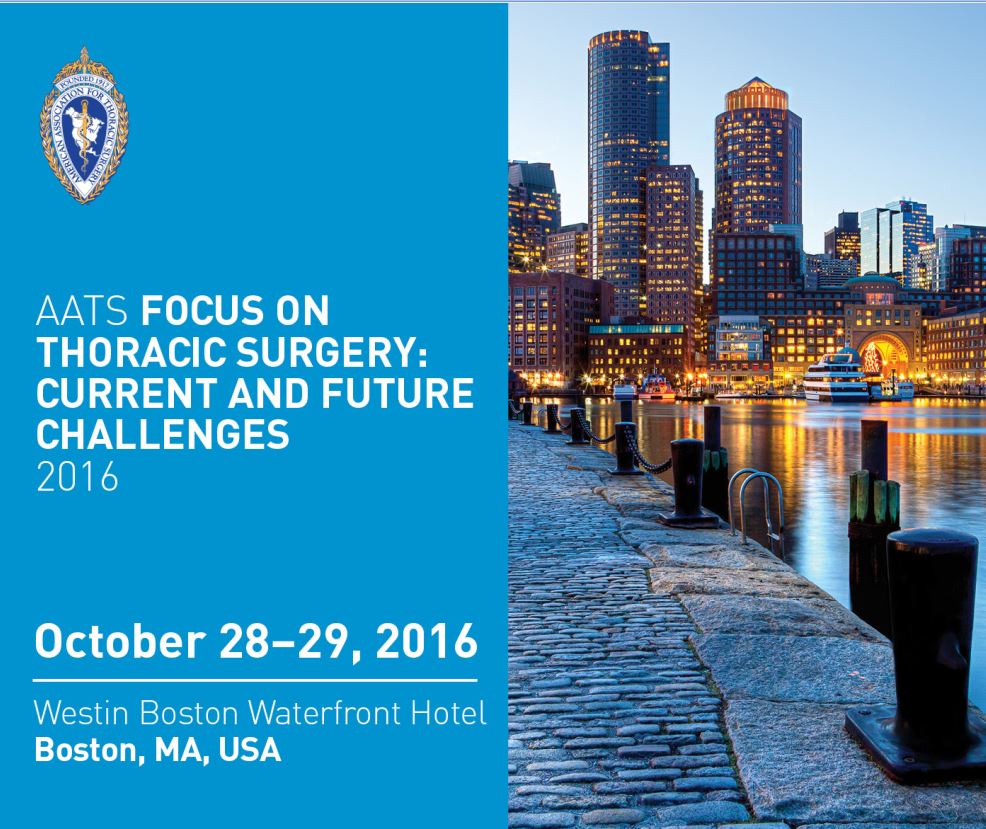
AATS Focus on Thoracic Surgery: Current and Future Challenges
The preliminary program and registration information is now available for AATS Focus on Thoracic Surgery: Current and Future Challenges.
October 28-29, 2016
Westin Boston Waterfront Hotel, Boston, MA
Program Directors
G. Alexander Patterson
David J. Sugarbaker
Program Committee
Thomas A. D’Amico
Shaf Keshavjee
James D. Luketich
Bryan F. Meyers
Scott J. Swanson
Overview
Currently practicing surgeons will be able to improve patient outcomes by enriching their knowledge and technical skills in the definition, diagnosis and resolution of thoracic surgical difficulties and post-operative complications. Expert faculty will provide state-of-the-art solutions to challenges in the field. Attendees will augment their overall understanding of thoracic diseases, upgrade their competency and ability to formulate new clinical strategies, and enhance their diagnosis and surgical treatment of thoracic diseases.
More information: http://aats.org/focus/
The preliminary program and registration information is now available for AATS Focus on Thoracic Surgery: Current and Future Challenges.
October 28-29, 2016
Westin Boston Waterfront Hotel, Boston, MA
Program Directors
G. Alexander Patterson
David J. Sugarbaker
Program Committee
Thomas A. D’Amico
Shaf Keshavjee
James D. Luketich
Bryan F. Meyers
Scott J. Swanson
Overview
Currently practicing surgeons will be able to improve patient outcomes by enriching their knowledge and technical skills in the definition, diagnosis and resolution of thoracic surgical difficulties and post-operative complications. Expert faculty will provide state-of-the-art solutions to challenges in the field. Attendees will augment their overall understanding of thoracic diseases, upgrade their competency and ability to formulate new clinical strategies, and enhance their diagnosis and surgical treatment of thoracic diseases.
More information: http://aats.org/focus/
The preliminary program and registration information is now available for AATS Focus on Thoracic Surgery: Current and Future Challenges.
October 28-29, 2016
Westin Boston Waterfront Hotel, Boston, MA
Program Directors
G. Alexander Patterson
David J. Sugarbaker
Program Committee
Thomas A. D’Amico
Shaf Keshavjee
James D. Luketich
Bryan F. Meyers
Scott J. Swanson
Overview
Currently practicing surgeons will be able to improve patient outcomes by enriching their knowledge and technical skills in the definition, diagnosis and resolution of thoracic surgical difficulties and post-operative complications. Expert faculty will provide state-of-the-art solutions to challenges in the field. Attendees will augment their overall understanding of thoracic diseases, upgrade their competency and ability to formulate new clinical strategies, and enhance their diagnosis and surgical treatment of thoracic diseases.
More information: http://aats.org/focus/
AATS Focus on Thoracic Surgery: Current and Future Challenges
The preliminary program and registration information is now available for AATS Focus on Thoracic Surgery: Current and Future Challenges.
October 28-29, 2016
Westin Boston Waterfront Hotel
Boston, MA
Program Directors
G. Alexander Patterson
David J. Sugarbaker
Program Committee
Thomas A. D’Amico
Shaf Keshavjee
James D. Luketich
Bryan F. Meyers
Scott J. Swanson
Overview
Currently practicing surgeons will be able to improve patient outcomes by enriching their knowledge and technical skills in the definition, diagnosis and resolution of thoracic surgical difficulties and post-operative complications. Expert faculty will provide state-of-the-art solutions to challenges in the field. Attendees will augment their overall understanding of thoracic diseases, upgrade their competency and ability to formulate new clinical strategies, and enhance their diagnosis and surgical treatment of thoracic diseases.
The preliminary program and registration information is now available for AATS Focus on Thoracic Surgery: Current and Future Challenges.
October 28-29, 2016
Westin Boston Waterfront Hotel
Boston, MA
Program Directors
G. Alexander Patterson
David J. Sugarbaker
Program Committee
Thomas A. D’Amico
Shaf Keshavjee
James D. Luketich
Bryan F. Meyers
Scott J. Swanson
Overview
Currently practicing surgeons will be able to improve patient outcomes by enriching their knowledge and technical skills in the definition, diagnosis and resolution of thoracic surgical difficulties and post-operative complications. Expert faculty will provide state-of-the-art solutions to challenges in the field. Attendees will augment their overall understanding of thoracic diseases, upgrade their competency and ability to formulate new clinical strategies, and enhance their diagnosis and surgical treatment of thoracic diseases.
The preliminary program and registration information is now available for AATS Focus on Thoracic Surgery: Current and Future Challenges.
October 28-29, 2016
Westin Boston Waterfront Hotel
Boston, MA
Program Directors
G. Alexander Patterson
David J. Sugarbaker
Program Committee
Thomas A. D’Amico
Shaf Keshavjee
James D. Luketich
Bryan F. Meyers
Scott J. Swanson
Overview
Currently practicing surgeons will be able to improve patient outcomes by enriching their knowledge and technical skills in the definition, diagnosis and resolution of thoracic surgical difficulties and post-operative complications. Expert faculty will provide state-of-the-art solutions to challenges in the field. Attendees will augment their overall understanding of thoracic diseases, upgrade their competency and ability to formulate new clinical strategies, and enhance their diagnosis and surgical treatment of thoracic diseases.
Elusive evidence pervades ESC’s 2016 heart failure guidelines
FLORENCE, ITALY – The 2016 revision of the European Society of Cardiology’s guidelines for diagnosing and treating acute and chronic heart failure highlights the extent to which thinking in the field has changed during the past 4 years, since the prior edition in 2012.
The new European guidelines, unveiled by the ESC’s Heart Failure Association during the group’s annual meeting, also underscore the great dependence that many new approaches have on expert opinion rather than what’s become the keystone of guidelines writing, evidence-based medicine. Frequent reliance on consensus decisions rather than indisputable proof from controlled trials defines what some U.S. specialists see as a divide as wide as the Atlantic between the European and U.S. approaches to guideline writing.
“The guidelines from the ESC are articulated very well; they made their recommendations very clear. But a lot is consensus driven, without new data,” said Dr. Mariell L. Jessup, who serves as both vice chair of the panel currently revising the U.S. heart failure guidelines – expected out later in 2016 – and was also the sole American representative on the panel that produced the ESC guidelines. “The ESC guidelines make clear all the things that need to happen to patients. I hope it will result in better patient care. We are clearly not doing a good job in heart failure. We not only don’t have evidence-based treatments, but people often don’t do a good job [caring for heart failure patients] and they die in the hospital all the time.”
Dr. Javed Butler, another member of the U.S. guidelines panel and professor and chief of cardiology at Stony Brook (N.Y.) University, called the U.S. and European divide a “philosophical perspective of evidence-based medicine.
“U.S. physicians should read the ESC guidelines and make up their own minds. The ESC guidelines are excellent and give you perspective. But U.S. regulatory and payment issues will be driven by U.S. guidelines,” Dr. Butler said in an interview.
But despite their limitations and the limited weight that the ESC guidelines carry for U.S. practice, they have many redeeming features, noted Dr. Mandeep R. Mehra, medical director of the Heart and Vascular Center at Brigham and Women’s Hospital in Boston. The 2016 ESC guidelines “are extraordinarily clear, very practical, and very concise. They are very usable, and provide a fantastic algorithm for managing patients with heart failure with reduced ejection fraction [HFrEF],” he said while discussing the guidelines during the meeting.
U.S. and Europe largely agree on sacubitril/valsartan and ivabradine
Clearly the greatest area of U.S. and European agreement was in the adoption by both guidelines groups of sacubitril/valsartan (Entresto) and ivabradine (Corlanor) as important new components of the basic drug formula for treating patients with HFrEF. In fact, the U.S. guideline writers saw these two additions as so important and timely that they issued a “focused update” in May to the existing, 2013 U.S. heart failure guidelines, and timed release of this update to occur on May 20, 2016, a day before release of the ESC guidelines. But as Dr. Butler noted, this was more of a temporal harmonization than a substantive one, because even here, in a very evidence-based change, the U.S. guidelines for using sacubitril/valsartan differed subtly but importantly from the ESC version.
The U.S. focused update says that treatment of patients with stage C (symptomatic heart failure with structural heart disease) HFrEF should receive treatment with sacubitril/valsartan (also know as an angiotensin receptor neprilysin inhibitor, or ARNI), an ACE inhibitor, or an angiotensin receptor blocker (ARB), as well as evidence-based treatment with a beta-blocker and with a mineralocorticoid receptor antagonist (MRA). A subsequent recommendation in the U.S. focused update said that HFrEF patients with chronic symptoms and New York Heart Association class II or III disease should switch from a stable, tolerated regimen with either an ACE inhibitor or ARB to treatment with sacubitril/valsartan.
In contrast, the new European guideline for sacubitril/valsartan recommends starting patients on this combination formulation only after first demonstrating that patients tolerated treatment with an ACE inhibitor or ARB for at least 30 days and determining that patients remained symptomatic while on one of these treatments. In short, the U.S. guideline gives a green light to starting patients with newly diagnosed, symptomatic HFrEF on sacubitril/valsartan immediately, while the European guideline only sanctions sacubitril/valsartan to start after a patient has spent at least 30 days settling into a multidrug regimen featuring an ACE inhibitor or an ARB when an ACE inhibitor isn’t well tolerated.
“The European guidelines are closely related to the study population enrolled in the PARADIGM-HF trial,” the pivotal trial that showed superiority of sacubitril/valsartan to an ACE inhibitor (N Engl J Med. 2014;371:993-1004), noted Dr. Butler in an interview. “The U.S. guidelines interpreted [the PARADIGM-HF] results in the best interests of a larger patient population. The European guidelines are far more proscriptive in replicating the clinical criteria of the trial. In some patients the sequence of starting a MRA and sacubitril/valsartan matters, but in other patients it is less important.”
Dr. Frank Ruschitzka, a coauthor of the ESC guidelines, said that the reason for the more cautious ESC approach was lack of widespread familiarity with sacubitril/valsartan treatment among cardiologists.
The ESC guidelines on using sacubitril/valsartan “replicated the PARADIGM-HF trial. We have no data right now that it is justifiable to put a [treatment-naive] patient on sacubitril/valsartan to begin with. Another difference between the U.S. and ESC guidelines is when to start a MRA,” said Dr. Ruschitzka, professor and head of cardiology at the Heart Center of the University Hospital in Zurich. “It makes a lot of sense to me to start sacubitril/valsartan early. The PARADIGM trial was positive, but no one has a feel for how to use sacubitril/valsartan. Should we give it to everyone? We said replicate the trial, and gain experience using the drug. We want to bring a life-saving drug to patients, but this is the approach we took. We need more data.”
Dr. Jessup noted that a lot of uncertainty also exists among U.S. clinicians about when to start sacubitril/valsartan. “It’s not been clear which patients to put on sacubitril/valsartan. No guidelines had been out on using it” until mid-May, and “the cost of sacubitril/valsartan is daunting. I have received calls from many people who ask whom am I supposed to use sacubitril/valsartan on? It took years and years to get people to [routinely] start patients on an ACE inhibitor and a beta-blocker, and now we’re telling them to do something else. In my practice it’s a 30-minute conversation with each patient that you need to first stop your ACE inhibitor, and then they often get denied coverage by their insurer,” said Dr. Jessup, professor of medicine at the University of Pennsylvania in Philadelphia. She expressed hope that coverage issues will diminish now that clear guidelines are out endorsing a key role for sacubitril/valsartan.
“We now all have started sacubitril/valsartan on patients” without first starting them on an ACE inhibitor, “but we all need to get a sense of what we can get away with” when using this drug, noted Dr. JoAnn Lindenfeld, professor and director of heart failure and transplant at Vanderbilt University in Nashville.
At least one European cardiologist was skeptical of just how proscriptive the ESC guideline for sacubitril/valsartan will be in actual practice.
“The best treatment [for symptomatic HFrEF] is sacubitril/valsartan, a beta-blocker, and a MRA,” said Dr. John J.V. McMurray, professor of cardiology at Glasgow University and lead investigator for the PARADIGM-HF pivotal trial for sacubitril/valsartan. “The treatment sequence advocated in the guidelines – treat with an ACE inhibitor first and if patients remain symptomatic change to sacubitril/valsartan – is evidence-based medicine. As a guidelines writer and as a promoter of evidence-based medicine, this is absolutely the correct approach. But as a practicing physician I’d go straight for sacubitril/valsartan. Otherwise you’re wasting everybody’s time starting with an ACE inhibitor and then waiting a month to switch,” Dr. McMurray said in an interview.
“It’s pointless to wait. We saw results within 30 days of starting sacubitril/valsartan, so it’s a theoretical risk to wait. Very few patients will become completely asymptomatic on an ACE inhibitor. Everyone who entered PARADIGM-HF was at New York Heart Association class II or higher, and at the time of randomization only a handful of patients were in New York Heart Association class I. Very few patients get to class I. That tells you it’s pretty uncommon for a heart failure patient to become truly asymptomatic with ACE inhibitor treatment. The main problem is that you are inconveniencing everybody with more blood tests and more clinic visits by waiting to start sacubitril/valsartan, said Dr. McMurray, who was not a member of the panel that wrote the new ESC guidelines.
Even less separates the new U.S. focused update and the ESC guidelines for using ivabradine. Both agree on starting the drug on HFrEF patients who remain symptomatic and with a left ventricular ejection fraction of 35% or less despite being on guideline-directed therapy including titration to a maximum beta-blocker dosage and with a persistent heart rate of at least 70 beats/min. The goal of ivabradine treatment is to further reduce heart rate beyond what’s achieved by a maximal beta-blocker dosage.
Perhaps the biggest questions about ivabradine have been why it took so long to enter the U.S. guidelines, and why it is listed in both the U.S. and ESC guidelines as a level II recommendation. Results from the pivotal trial that supported ivabradine’s use in HFrEF patients, SHIFT, first appeared in 2010 (Lancet. 2010 Sep 11;376[9744]:875-95).
Dr. Butler chalked up the drug’s slow entry into U.S. guidelines as the result of a lack of initiative by ivabradine’s initial developer, Servier. “SHIFT did not have any U.S. sites, and Servier never sought Food and Drug Administration approval,” he noted. “Amgen acquired the U.S. rights to ivabradine in 2013,” and the drug received FDA approval in April 2015, Dr. Butler noted, in explaining the drug’s U.S. timeline. As to why its use is a level II recommendation, he noted that the evidence for efficacy came only from the SHIFT trial, questions exist whether the beta-blocker dosages were fully optimized in all patients in this trial, and the benefit was limited to a reduction in heart failure hospitalizations but not in mortality. “I think that patients with persistent heart failure symptoms [and a persistently elevated heart rate] should get ivabradine,” but these caveats limit it to a class II level recommendation, Dr. Butler said.
“There were questions about ivabradine’s benefit in reducing heart failure hospitalization but not mortality, and questions about whether it would benefit patients if their beta-blocker dosage was adequately up titrated. There were also questions about which heart failure patients to use it on,” noted Dr. Lindenfeld, a member of the panel that wrote the U.S. focused update. These concerns in part help explain the delay to integrating ivabradine into U.S. practice guidelines, she said in an interview, but added that additional data and analysis published during the past 3 or so years have clarified ivabradine’s potentially useful role in treating selected HFrEF patients.
New ESC guidelines based on expert opinion
The sections on sacubitril/valsartan and ivabradine occupy a mere 2 pages among more than 55 pages of text and charts that spell out the ESC’s current vision of how physicians should diagnose and manage heart failure patients. While much of what carried over from prior editions of the guidelines is rooted in evidence, many of the new approaches advocated rely on expert opinion or new interpretations of existing data. Here are some of the notable changes and highlights of the 2016 ESC recommendations:
• Heart failure diagnosis. The new ESC guidelines streamline the diagnostic process, which now focuses on five key elements: The patient’s history, physical examination, ECG, serum level of either brain natriuretic peptide (BNP) or N-terminal(NT)-proBNP, and echocardiography. The guidelines specify threshold levels of BNP and NT-proBNP that can effectively rule out heart failure, a BNP level of at least 35 pg/mL or a NT-proBNP level of at least 125 pg/mL.
“The diagnostic minimum levels of BNP and NT-proBNP were designed to rule out heart failure. They both have a high negative predictive value, but at these levels their positive predictive value is low,” explained Dr. Adriaan A. Voors, cochair of the ESC’s guideline-writing panel and professor of cardiology at the University of Groningen, the Netherlands.
But while these levels might be effective for reliable rule out of heart failure, they could mean a large number of patients would qualify for an echocardiographic assessment.
“If we used the ESC’s natriuretic peptide cutoffs, there would be a clear concern about overuse of echo. It’s a cost-effectiveness issue. You wind up doing a lot of echos that will be normal. Echocardiography is very safe, but each echo costs about $400-$500,” commented Dr. Butler.
“The results from the STOP-HF and PONTIAC studies showed that BNP levels can identify people at increased risk for developing heart failure who need more intensive assessment and could also potentially benefit from more attention to heart failure prevention. I suspect the full U.S. guideline update will address this issue, but we have not yet finalized our decisions,” he added.
• Heart failure classification. The new ESC guidelines created a new heart failure category, midrange ejection fraction, that the writing panel positioned squarely between the two more classic heart failure subgroups, HFrEF and heart failure with preserved ejection fraction (HFpEF). The definition of each of the three subgroups depends on left ventricular ejection fraction as determined by echocardiography: A LVEF of less than 40% defined HFrEF, a LVEF of 40%-49% defined heart failure with midrange ejection fraction (HFmrEF), and a LVEF of 50% or higher defined HFpEF. Diagnostic confirmation of both HFmrEF and HFpEF also requires that patients fulfill certain criteria of structural or functional heart abnormalities.
The category of HFmrEF was created “to stimulate research into how to best manage these patients,” explained Dr. Piotr Ponikowski, chair of the ESC guidelines writing panel. For the time being, it remains a category with only theoretical importance as nothing is known to suggest that management of patients with HFmrEF should in any way differ from patients with HFpEF.
• Acute heart failure. Perhaps the most revolutionary element of the new guidelines is the detailed map they provide to managing patients who present with acute decompensated heart failure and the underlying principles cited to justify this radically different approach.
“The acute heart failure section was completely rewritten,” noted Dr. Ponikowski, professor of heart diseases at the Medical University in Wroclaw, Poland. “We don’t yet have evidence-based treatments” to apply to acute heart failure patients, he admitted, “however we strongly recommend the concept that the shorter the better. Shorten the time of diagnosis and for therapeutic decisions. We have borrowed from acute coronary syndrome. Don’t keep patients in the emergency department for another couple of hours just to see if they will respond. We must be aware that we need to do our best to shorten diagnosis and treatment decisions. Time is an issue. Manage a patient’s congestion and impaired peripheral perfusion within a time frame of 1-2 hours.”
The concept that acute heart failure must be quickly managed as an emergency condition similar to acute coronary syndrome first appeared as a European practice recommendation in 2015, a consensus statement from the European Heart Failure Association and two other collaborating organizations (Eur Heart J. 2015 Aug 7;36[30]:1958-66).
“In 2015, the consensus paper talked about how to handle acute heart failure patients in the emergency department. Now, we have focused on defining the patients’ phenotype and how to categorize their treatment options. We built on the 2015 statement, but the algorithms we now have are original to 2016; they were not in the 2015 paper,” said Dr. Veli-Pekka Harjola, a member of the 2015 consensus group and 2016 guidelines panel who spearheaded writing the acute heart failure section of the new ESC guidelines.
An additional new and notable feature of this section in the 2016 guidelines is its creation of an acronym, CHAMP, designed to guide the management of patients with acute heart failure. CHAMP stands for acute Coronary syndrome, Hypertension emergency, Arrhythmia, acute Mechanical cause, and Pulmonary embolism. The CHAMP acronym’s purpose is to “focus attention on these five specific, potential causes of acute heart failure, life-threatening conditions that need immediate treatment,” explained Dr. Ponikowski.
“CHAMP emphasizes the most critical causes of acute heart failure,” added Dr. Harjola, a cardiologist at Helsinki University Central Hospital. “We created this new acronym” to help clinicians keep in mind what to look for in a patient presenting with acute heart failure.
U.S. cardiologists find things to like in what the Europeans say about managing acute heart failure, as well as aspects to question.
“It makes no sense not to aggressively treat a patient who arrives at an emergency department with acute heart failure. But there is a difference between acute MI or stroke and acute heart failure,” said Dr. Butler. “In acute MI there is the ruptured plaque and thrombus that blocks a coronary artery. In stroke there is a thrombus. These are diseases with a specific onset and treatment target. But with acute heart failure we don’t have a thrombus to treat; we don’t have a specific target. What we’ve learned from studying implanted devices [such as CardioMems] is that the congestion that causes acute heart failure can start 2-3 weeks before a patient develops acute decompensated heart failure and goes to the hospital. We have not found a specific pathophysiologic abnormality in the patient with acute heart failure that is any different from chronic heart failure. This begs the question: If a patient who presents with acute heart failure has a congestion process that’s been going on for 2 or 3 weeks what difference will another 3 hours make? Do we need to replicate the concept of an acute stroke team or acute MI response for acute heart failure?”
Dr. Butler stressed that additional data are expected soon that may help clarify this issue.
“Some large outcome trials in patients with acute heart failure are now underway, one testing serelaxin treatment, another testing ularitide treatment, that are also testing the hypothesis that rapid treatment with these drugs can produce more end-organ protection, stop damage to the heart, kidney and liver, and lead to better long-term outcomes. Until we have those data, the jury is still out” on the benefit patients gain from rapid treatment of acute heart failure. “Until then, it’s not that the data say don’t treat acute heart failure patients aggressively. But we have not yet proven it is similar to treating an acute MI or stroke,” said Dr. Butler.
“U.S. guidelines have tended to stay away from areas where there are no evidence-based data. To their credit, the Europeans will take on something like acute heart failure where we don’t have an adequate evidence base. Despite that, they provide guidelines, which is important because clinicians need guidance even when the evidence is not very good, when the guideline is based mostly on experience and expert consensus.” commented Dr. William T. Abraham, professor and director of cardiovascular medicine at the Ohio State University Wexner Medical Center in Columbus.
“It’s absolutely appropriate to think of acute heart failure as an emergency situation. We know from high-sensitivity troponin assays that troponin levels are increased in 90% of patients who present with acute decompensated heart failure. So most acute heart failure patients are losing heart muscle cells and we should treat them like we treat acute coronary syndrome. Time matters in acute heart failure; time is heart muscle. Treatment needs to break the hemodynamic and neurohormonal storm of acute decompensated heart failure; get the patient stabilized; improve vital organ perfusion, including within the heart; and shift the myocardial oxygen supply and demand equation so myocardial necrosis stops. All of this is important, and study results suggest it’s the correct approach. I’m not sure study results prove it, but studies that have looked at the time course of treatment for acute heart failure showed that early initiation of treatment – within the first 6 hours of onset – compared with 12-24 hours of onset makes a difference in outcomes,” Dr. Abraham said in an interview.
But a major limitation to the potential efficacy of a rapidly initiated management strategy is that few interventions currently exist with proven benefits for acute heart failure patients.
For the time being, rapid intervention means using diuretics relatively quickly and, if there is an indication for treating with a vasoactive medication, using that quickly too. “The rapid approach is really more relevant to the future; it’s relevant to the design of future acute heart failure treatment trials. That is where this early treatment paradigm is important,” as it could potentially apply to new, more effective treatments of the future rather than to the marginally effective treatments now available, Dr. Abraham said.
“For a long we time haven’t pushed how quickly we should act when implementing guideline-directed treatment” for patients with acute heart failure, noted Dr. Mehra. “The CHAMP approach is interesting, and the ESC guidelines are a very interesting move in the direction” of faster action. “They speak to the period of time during which one should act. Hopefully this will help the science of acute decompensated heart failure move forward.”
But for other U.S. experts the issue again pivots on the lack of evidence.
“There is nothing new” about managing acute heart failure, said Dr. Jessup. “The ESC guideline was articulated very well; they made their recommendations very clear. But a lot is consensus driven. There are no new data. The problem with acute heart failure is that the recommendations are what we think clinicians should do. CHAMP is a nice acronym; it’s packaged better, but there are not any new data.”
Comorbidities
A dramatic contrast distinguishes the extent to which the ESC guidelines highlight comorbidities, compared with prevailing U.S. guidelines. The new ESC guidelines highlight and discuss with some detail 16 distinct comorbidities for clinicians to keep in mind when managing heart failure patients, compared with three comorbidities (atrial fibrillation, anemia, and depression) discussed with similar detail in the 2013 U.S. guidelines.
“We are targeting comorbidities to personalize medicine, by subgrouping [heart failure] patients into groups that need to receive special attention,” explained Dr. Stefan D. Anker, a coauthor on the ESC guidelines. “We care about comorbidities because they make the diagnosis of heart failure difficult. They aggravate symptoms and contribute to additional hospitalizations. They interfere with [heart failure] treatment, and because comorbidities have led to exclusions of heart failure patients from trials, we lack evidence of treatment efficacy in patients with certain comorbidities,” said Dr. Anker, a professor of innovative clinical trials at the Medical University in Göttingen, Germany.
“The comorbidity discussion in the ESC guidelines is extremely important,” commented Dr. Abraham. “It supports the need for a multidimensional approach to heart failure patients. A cardiologist may not have all the resources to manage all the comorbidities [a heart failure patient might have]. This is why having a sleep medicine specialist, a diabetes specialist, a nephrologist, etc., involved as part of a heart failure management team can be very valuable. We need to involve subspecialists in managing the comorbidities of heart failure because they clearly have an impact on patient outcome.”
But Dr. Butler had a somewhat different take on how comorbidity management fits into the broader picture of heart failure management.
“There is no doubt that heart failure worsens other comorbidities and other comorbidities worsen heart failure. The relationship is bidirectional between heart failure and chronic obstructive pulmonary disease, liver disease, depression, sleep apnea, renal disease, lung disease, diabetes, etc. The problem is that treating a comorbidity does not necessarily translate into improved heart failure outcomes. Comorbidities are important for heart failure patients and worsen their heart failure outcomes. However, management of a comorbidity should be done primarily for the sake of improving the comorbidity. If you treat depression, for example, and it does not improve a patient’s heart failure, that doesn’t mean you shouldn’t have treated the depression. It just means that we don’t have good data that it will improve heart failure.”
Another limitation from a U.S. perspective is what role treatment of various comorbidities can play in benefiting heart failure patients and how compelling the evidence is for this. Dr. Butler gave as an example the problem with treating iron deficiency in heart failure patients who do not have anemia, a strategy endorsed in the ESC guidelines as a level IIa recommendation.
“The data regarding improved exercise capacity from treatment with intravenous ferric carboxymaltose is pretty convincing,” he said. But patients have benefited from this treatment only with improved function and quality of life, and not with improved survival or fewer hospitalizations.
“Is treating patients to improve their function and help them feel better enough?” Dr. Butler asked. “In other diseases it is. In gastrointestinal disease, if a drug helps patients feel better you approve the drug. We value improved functional capacity for patients with pulmonary hypertension, angina, and peripheral vascular disease. All these indications have drugs approved for improving functional capacity and quality of life. But for heart failure the bar has been set higher. There is a lot of interest in changing this” for heart failure.
“There is interest in running a study of ferric carboxymaltose for heart failure with a mortality endpoint. In the meantime, the impact on improving functional capacity is compelling, and it will be interesting to see what happens in the U.S. guidelines. Currently, in U.S. practice if a heart failure patient has iron-deficiency anemia you treat with intravenous iron replacement and the treatment gets reimbursed without a problem. But if the heart failure patient has iron deficiency without anemia then reimbursement for the cost of iron supplementation can be a problem,” Dr. Butler noted. This may change only if the experts who write the next U.S. heart failure guidelines decide to change the rules of what constitutes a useful heart failure treatment, he said.
Dr. Butler has been a consultant to Novartis and Amgen and several other companies. Dr. Jessup had no disclosures. Dr. Mehra has been a consultant to Teva, Johnson & Johnson, Boston Scientific, and St. Jude. Dr. Ruschitzka has been a consultant to Novartis, Servier, Sanofi, Cardiorentis, Heartware, and St. Jude. Dr. McMurray has received research support from Novartis and Amgen. Dr. Lindenfeld has been a consultant to Novartis, Abbott, Janssen, Relypsa, and Resmed. Dr. Voors has been a consultant to Novartis, Amgen, Servier, and several other drug companies. Dr. Ponikowski has been a consultant to Amgen, Novartis, Servier, and several other drug companies. Dr. Harjola has been a consultant to Novartis, Servier, Bayer, Boehringer Ingelheim, Pfizer, and Resmed. Dr. Abraham has been a consultant to Amgen, Novartis, and several device companies. Dr. Anker has been a consultant to Novartis, Servier, and several other companies.
On Twitter @mitchelzoler
FLORENCE, ITALY – The 2016 revision of the European Society of Cardiology’s guidelines for diagnosing and treating acute and chronic heart failure highlights the extent to which thinking in the field has changed during the past 4 years, since the prior edition in 2012.
The new European guidelines, unveiled by the ESC’s Heart Failure Association during the group’s annual meeting, also underscore the great dependence that many new approaches have on expert opinion rather than what’s become the keystone of guidelines writing, evidence-based medicine. Frequent reliance on consensus decisions rather than indisputable proof from controlled trials defines what some U.S. specialists see as a divide as wide as the Atlantic between the European and U.S. approaches to guideline writing.
“The guidelines from the ESC are articulated very well; they made their recommendations very clear. But a lot is consensus driven, without new data,” said Dr. Mariell L. Jessup, who serves as both vice chair of the panel currently revising the U.S. heart failure guidelines – expected out later in 2016 – and was also the sole American representative on the panel that produced the ESC guidelines. “The ESC guidelines make clear all the things that need to happen to patients. I hope it will result in better patient care. We are clearly not doing a good job in heart failure. We not only don’t have evidence-based treatments, but people often don’t do a good job [caring for heart failure patients] and they die in the hospital all the time.”
Dr. Javed Butler, another member of the U.S. guidelines panel and professor and chief of cardiology at Stony Brook (N.Y.) University, called the U.S. and European divide a “philosophical perspective of evidence-based medicine.
“U.S. physicians should read the ESC guidelines and make up their own minds. The ESC guidelines are excellent and give you perspective. But U.S. regulatory and payment issues will be driven by U.S. guidelines,” Dr. Butler said in an interview.
But despite their limitations and the limited weight that the ESC guidelines carry for U.S. practice, they have many redeeming features, noted Dr. Mandeep R. Mehra, medical director of the Heart and Vascular Center at Brigham and Women’s Hospital in Boston. The 2016 ESC guidelines “are extraordinarily clear, very practical, and very concise. They are very usable, and provide a fantastic algorithm for managing patients with heart failure with reduced ejection fraction [HFrEF],” he said while discussing the guidelines during the meeting.
U.S. and Europe largely agree on sacubitril/valsartan and ivabradine
Clearly the greatest area of U.S. and European agreement was in the adoption by both guidelines groups of sacubitril/valsartan (Entresto) and ivabradine (Corlanor) as important new components of the basic drug formula for treating patients with HFrEF. In fact, the U.S. guideline writers saw these two additions as so important and timely that they issued a “focused update” in May to the existing, 2013 U.S. heart failure guidelines, and timed release of this update to occur on May 20, 2016, a day before release of the ESC guidelines. But as Dr. Butler noted, this was more of a temporal harmonization than a substantive one, because even here, in a very evidence-based change, the U.S. guidelines for using sacubitril/valsartan differed subtly but importantly from the ESC version.
The U.S. focused update says that treatment of patients with stage C (symptomatic heart failure with structural heart disease) HFrEF should receive treatment with sacubitril/valsartan (also know as an angiotensin receptor neprilysin inhibitor, or ARNI), an ACE inhibitor, or an angiotensin receptor blocker (ARB), as well as evidence-based treatment with a beta-blocker and with a mineralocorticoid receptor antagonist (MRA). A subsequent recommendation in the U.S. focused update said that HFrEF patients with chronic symptoms and New York Heart Association class II or III disease should switch from a stable, tolerated regimen with either an ACE inhibitor or ARB to treatment with sacubitril/valsartan.
In contrast, the new European guideline for sacubitril/valsartan recommends starting patients on this combination formulation only after first demonstrating that patients tolerated treatment with an ACE inhibitor or ARB for at least 30 days and determining that patients remained symptomatic while on one of these treatments. In short, the U.S. guideline gives a green light to starting patients with newly diagnosed, symptomatic HFrEF on sacubitril/valsartan immediately, while the European guideline only sanctions sacubitril/valsartan to start after a patient has spent at least 30 days settling into a multidrug regimen featuring an ACE inhibitor or an ARB when an ACE inhibitor isn’t well tolerated.
“The European guidelines are closely related to the study population enrolled in the PARADIGM-HF trial,” the pivotal trial that showed superiority of sacubitril/valsartan to an ACE inhibitor (N Engl J Med. 2014;371:993-1004), noted Dr. Butler in an interview. “The U.S. guidelines interpreted [the PARADIGM-HF] results in the best interests of a larger patient population. The European guidelines are far more proscriptive in replicating the clinical criteria of the trial. In some patients the sequence of starting a MRA and sacubitril/valsartan matters, but in other patients it is less important.”
Dr. Frank Ruschitzka, a coauthor of the ESC guidelines, said that the reason for the more cautious ESC approach was lack of widespread familiarity with sacubitril/valsartan treatment among cardiologists.
The ESC guidelines on using sacubitril/valsartan “replicated the PARADIGM-HF trial. We have no data right now that it is justifiable to put a [treatment-naive] patient on sacubitril/valsartan to begin with. Another difference between the U.S. and ESC guidelines is when to start a MRA,” said Dr. Ruschitzka, professor and head of cardiology at the Heart Center of the University Hospital in Zurich. “It makes a lot of sense to me to start sacubitril/valsartan early. The PARADIGM trial was positive, but no one has a feel for how to use sacubitril/valsartan. Should we give it to everyone? We said replicate the trial, and gain experience using the drug. We want to bring a life-saving drug to patients, but this is the approach we took. We need more data.”
Dr. Jessup noted that a lot of uncertainty also exists among U.S. clinicians about when to start sacubitril/valsartan. “It’s not been clear which patients to put on sacubitril/valsartan. No guidelines had been out on using it” until mid-May, and “the cost of sacubitril/valsartan is daunting. I have received calls from many people who ask whom am I supposed to use sacubitril/valsartan on? It took years and years to get people to [routinely] start patients on an ACE inhibitor and a beta-blocker, and now we’re telling them to do something else. In my practice it’s a 30-minute conversation with each patient that you need to first stop your ACE inhibitor, and then they often get denied coverage by their insurer,” said Dr. Jessup, professor of medicine at the University of Pennsylvania in Philadelphia. She expressed hope that coverage issues will diminish now that clear guidelines are out endorsing a key role for sacubitril/valsartan.
“We now all have started sacubitril/valsartan on patients” without first starting them on an ACE inhibitor, “but we all need to get a sense of what we can get away with” when using this drug, noted Dr. JoAnn Lindenfeld, professor and director of heart failure and transplant at Vanderbilt University in Nashville.
At least one European cardiologist was skeptical of just how proscriptive the ESC guideline for sacubitril/valsartan will be in actual practice.
“The best treatment [for symptomatic HFrEF] is sacubitril/valsartan, a beta-blocker, and a MRA,” said Dr. John J.V. McMurray, professor of cardiology at Glasgow University and lead investigator for the PARADIGM-HF pivotal trial for sacubitril/valsartan. “The treatment sequence advocated in the guidelines – treat with an ACE inhibitor first and if patients remain symptomatic change to sacubitril/valsartan – is evidence-based medicine. As a guidelines writer and as a promoter of evidence-based medicine, this is absolutely the correct approach. But as a practicing physician I’d go straight for sacubitril/valsartan. Otherwise you’re wasting everybody’s time starting with an ACE inhibitor and then waiting a month to switch,” Dr. McMurray said in an interview.
“It’s pointless to wait. We saw results within 30 days of starting sacubitril/valsartan, so it’s a theoretical risk to wait. Very few patients will become completely asymptomatic on an ACE inhibitor. Everyone who entered PARADIGM-HF was at New York Heart Association class II or higher, and at the time of randomization only a handful of patients were in New York Heart Association class I. Very few patients get to class I. That tells you it’s pretty uncommon for a heart failure patient to become truly asymptomatic with ACE inhibitor treatment. The main problem is that you are inconveniencing everybody with more blood tests and more clinic visits by waiting to start sacubitril/valsartan, said Dr. McMurray, who was not a member of the panel that wrote the new ESC guidelines.
Even less separates the new U.S. focused update and the ESC guidelines for using ivabradine. Both agree on starting the drug on HFrEF patients who remain symptomatic and with a left ventricular ejection fraction of 35% or less despite being on guideline-directed therapy including titration to a maximum beta-blocker dosage and with a persistent heart rate of at least 70 beats/min. The goal of ivabradine treatment is to further reduce heart rate beyond what’s achieved by a maximal beta-blocker dosage.
Perhaps the biggest questions about ivabradine have been why it took so long to enter the U.S. guidelines, and why it is listed in both the U.S. and ESC guidelines as a level II recommendation. Results from the pivotal trial that supported ivabradine’s use in HFrEF patients, SHIFT, first appeared in 2010 (Lancet. 2010 Sep 11;376[9744]:875-95).
Dr. Butler chalked up the drug’s slow entry into U.S. guidelines as the result of a lack of initiative by ivabradine’s initial developer, Servier. “SHIFT did not have any U.S. sites, and Servier never sought Food and Drug Administration approval,” he noted. “Amgen acquired the U.S. rights to ivabradine in 2013,” and the drug received FDA approval in April 2015, Dr. Butler noted, in explaining the drug’s U.S. timeline. As to why its use is a level II recommendation, he noted that the evidence for efficacy came only from the SHIFT trial, questions exist whether the beta-blocker dosages were fully optimized in all patients in this trial, and the benefit was limited to a reduction in heart failure hospitalizations but not in mortality. “I think that patients with persistent heart failure symptoms [and a persistently elevated heart rate] should get ivabradine,” but these caveats limit it to a class II level recommendation, Dr. Butler said.
“There were questions about ivabradine’s benefit in reducing heart failure hospitalization but not mortality, and questions about whether it would benefit patients if their beta-blocker dosage was adequately up titrated. There were also questions about which heart failure patients to use it on,” noted Dr. Lindenfeld, a member of the panel that wrote the U.S. focused update. These concerns in part help explain the delay to integrating ivabradine into U.S. practice guidelines, she said in an interview, but added that additional data and analysis published during the past 3 or so years have clarified ivabradine’s potentially useful role in treating selected HFrEF patients.
New ESC guidelines based on expert opinion
The sections on sacubitril/valsartan and ivabradine occupy a mere 2 pages among more than 55 pages of text and charts that spell out the ESC’s current vision of how physicians should diagnose and manage heart failure patients. While much of what carried over from prior editions of the guidelines is rooted in evidence, many of the new approaches advocated rely on expert opinion or new interpretations of existing data. Here are some of the notable changes and highlights of the 2016 ESC recommendations:
• Heart failure diagnosis. The new ESC guidelines streamline the diagnostic process, which now focuses on five key elements: The patient’s history, physical examination, ECG, serum level of either brain natriuretic peptide (BNP) or N-terminal(NT)-proBNP, and echocardiography. The guidelines specify threshold levels of BNP and NT-proBNP that can effectively rule out heart failure, a BNP level of at least 35 pg/mL or a NT-proBNP level of at least 125 pg/mL.
“The diagnostic minimum levels of BNP and NT-proBNP were designed to rule out heart failure. They both have a high negative predictive value, but at these levels their positive predictive value is low,” explained Dr. Adriaan A. Voors, cochair of the ESC’s guideline-writing panel and professor of cardiology at the University of Groningen, the Netherlands.
But while these levels might be effective for reliable rule out of heart failure, they could mean a large number of patients would qualify for an echocardiographic assessment.
“If we used the ESC’s natriuretic peptide cutoffs, there would be a clear concern about overuse of echo. It’s a cost-effectiveness issue. You wind up doing a lot of echos that will be normal. Echocardiography is very safe, but each echo costs about $400-$500,” commented Dr. Butler.
“The results from the STOP-HF and PONTIAC studies showed that BNP levels can identify people at increased risk for developing heart failure who need more intensive assessment and could also potentially benefit from more attention to heart failure prevention. I suspect the full U.S. guideline update will address this issue, but we have not yet finalized our decisions,” he added.
• Heart failure classification. The new ESC guidelines created a new heart failure category, midrange ejection fraction, that the writing panel positioned squarely between the two more classic heart failure subgroups, HFrEF and heart failure with preserved ejection fraction (HFpEF). The definition of each of the three subgroups depends on left ventricular ejection fraction as determined by echocardiography: A LVEF of less than 40% defined HFrEF, a LVEF of 40%-49% defined heart failure with midrange ejection fraction (HFmrEF), and a LVEF of 50% or higher defined HFpEF. Diagnostic confirmation of both HFmrEF and HFpEF also requires that patients fulfill certain criteria of structural or functional heart abnormalities.
The category of HFmrEF was created “to stimulate research into how to best manage these patients,” explained Dr. Piotr Ponikowski, chair of the ESC guidelines writing panel. For the time being, it remains a category with only theoretical importance as nothing is known to suggest that management of patients with HFmrEF should in any way differ from patients with HFpEF.
• Acute heart failure. Perhaps the most revolutionary element of the new guidelines is the detailed map they provide to managing patients who present with acute decompensated heart failure and the underlying principles cited to justify this radically different approach.
“The acute heart failure section was completely rewritten,” noted Dr. Ponikowski, professor of heart diseases at the Medical University in Wroclaw, Poland. “We don’t yet have evidence-based treatments” to apply to acute heart failure patients, he admitted, “however we strongly recommend the concept that the shorter the better. Shorten the time of diagnosis and for therapeutic decisions. We have borrowed from acute coronary syndrome. Don’t keep patients in the emergency department for another couple of hours just to see if they will respond. We must be aware that we need to do our best to shorten diagnosis and treatment decisions. Time is an issue. Manage a patient’s congestion and impaired peripheral perfusion within a time frame of 1-2 hours.”
The concept that acute heart failure must be quickly managed as an emergency condition similar to acute coronary syndrome first appeared as a European practice recommendation in 2015, a consensus statement from the European Heart Failure Association and two other collaborating organizations (Eur Heart J. 2015 Aug 7;36[30]:1958-66).
“In 2015, the consensus paper talked about how to handle acute heart failure patients in the emergency department. Now, we have focused on defining the patients’ phenotype and how to categorize their treatment options. We built on the 2015 statement, but the algorithms we now have are original to 2016; they were not in the 2015 paper,” said Dr. Veli-Pekka Harjola, a member of the 2015 consensus group and 2016 guidelines panel who spearheaded writing the acute heart failure section of the new ESC guidelines.
An additional new and notable feature of this section in the 2016 guidelines is its creation of an acronym, CHAMP, designed to guide the management of patients with acute heart failure. CHAMP stands for acute Coronary syndrome, Hypertension emergency, Arrhythmia, acute Mechanical cause, and Pulmonary embolism. The CHAMP acronym’s purpose is to “focus attention on these five specific, potential causes of acute heart failure, life-threatening conditions that need immediate treatment,” explained Dr. Ponikowski.
“CHAMP emphasizes the most critical causes of acute heart failure,” added Dr. Harjola, a cardiologist at Helsinki University Central Hospital. “We created this new acronym” to help clinicians keep in mind what to look for in a patient presenting with acute heart failure.
U.S. cardiologists find things to like in what the Europeans say about managing acute heart failure, as well as aspects to question.
“It makes no sense not to aggressively treat a patient who arrives at an emergency department with acute heart failure. But there is a difference between acute MI or stroke and acute heart failure,” said Dr. Butler. “In acute MI there is the ruptured plaque and thrombus that blocks a coronary artery. In stroke there is a thrombus. These are diseases with a specific onset and treatment target. But with acute heart failure we don’t have a thrombus to treat; we don’t have a specific target. What we’ve learned from studying implanted devices [such as CardioMems] is that the congestion that causes acute heart failure can start 2-3 weeks before a patient develops acute decompensated heart failure and goes to the hospital. We have not found a specific pathophysiologic abnormality in the patient with acute heart failure that is any different from chronic heart failure. This begs the question: If a patient who presents with acute heart failure has a congestion process that’s been going on for 2 or 3 weeks what difference will another 3 hours make? Do we need to replicate the concept of an acute stroke team or acute MI response for acute heart failure?”
Dr. Butler stressed that additional data are expected soon that may help clarify this issue.
“Some large outcome trials in patients with acute heart failure are now underway, one testing serelaxin treatment, another testing ularitide treatment, that are also testing the hypothesis that rapid treatment with these drugs can produce more end-organ protection, stop damage to the heart, kidney and liver, and lead to better long-term outcomes. Until we have those data, the jury is still out” on the benefit patients gain from rapid treatment of acute heart failure. “Until then, it’s not that the data say don’t treat acute heart failure patients aggressively. But we have not yet proven it is similar to treating an acute MI or stroke,” said Dr. Butler.
“U.S. guidelines have tended to stay away from areas where there are no evidence-based data. To their credit, the Europeans will take on something like acute heart failure where we don’t have an adequate evidence base. Despite that, they provide guidelines, which is important because clinicians need guidance even when the evidence is not very good, when the guideline is based mostly on experience and expert consensus.” commented Dr. William T. Abraham, professor and director of cardiovascular medicine at the Ohio State University Wexner Medical Center in Columbus.
“It’s absolutely appropriate to think of acute heart failure as an emergency situation. We know from high-sensitivity troponin assays that troponin levels are increased in 90% of patients who present with acute decompensated heart failure. So most acute heart failure patients are losing heart muscle cells and we should treat them like we treat acute coronary syndrome. Time matters in acute heart failure; time is heart muscle. Treatment needs to break the hemodynamic and neurohormonal storm of acute decompensated heart failure; get the patient stabilized; improve vital organ perfusion, including within the heart; and shift the myocardial oxygen supply and demand equation so myocardial necrosis stops. All of this is important, and study results suggest it’s the correct approach. I’m not sure study results prove it, but studies that have looked at the time course of treatment for acute heart failure showed that early initiation of treatment – within the first 6 hours of onset – compared with 12-24 hours of onset makes a difference in outcomes,” Dr. Abraham said in an interview.
But a major limitation to the potential efficacy of a rapidly initiated management strategy is that few interventions currently exist with proven benefits for acute heart failure patients.
For the time being, rapid intervention means using diuretics relatively quickly and, if there is an indication for treating with a vasoactive medication, using that quickly too. “The rapid approach is really more relevant to the future; it’s relevant to the design of future acute heart failure treatment trials. That is where this early treatment paradigm is important,” as it could potentially apply to new, more effective treatments of the future rather than to the marginally effective treatments now available, Dr. Abraham said.
“For a long we time haven’t pushed how quickly we should act when implementing guideline-directed treatment” for patients with acute heart failure, noted Dr. Mehra. “The CHAMP approach is interesting, and the ESC guidelines are a very interesting move in the direction” of faster action. “They speak to the period of time during which one should act. Hopefully this will help the science of acute decompensated heart failure move forward.”
But for other U.S. experts the issue again pivots on the lack of evidence.
“There is nothing new” about managing acute heart failure, said Dr. Jessup. “The ESC guideline was articulated very well; they made their recommendations very clear. But a lot is consensus driven. There are no new data. The problem with acute heart failure is that the recommendations are what we think clinicians should do. CHAMP is a nice acronym; it’s packaged better, but there are not any new data.”
Comorbidities
A dramatic contrast distinguishes the extent to which the ESC guidelines highlight comorbidities, compared with prevailing U.S. guidelines. The new ESC guidelines highlight and discuss with some detail 16 distinct comorbidities for clinicians to keep in mind when managing heart failure patients, compared with three comorbidities (atrial fibrillation, anemia, and depression) discussed with similar detail in the 2013 U.S. guidelines.
“We are targeting comorbidities to personalize medicine, by subgrouping [heart failure] patients into groups that need to receive special attention,” explained Dr. Stefan D. Anker, a coauthor on the ESC guidelines. “We care about comorbidities because they make the diagnosis of heart failure difficult. They aggravate symptoms and contribute to additional hospitalizations. They interfere with [heart failure] treatment, and because comorbidities have led to exclusions of heart failure patients from trials, we lack evidence of treatment efficacy in patients with certain comorbidities,” said Dr. Anker, a professor of innovative clinical trials at the Medical University in Göttingen, Germany.
“The comorbidity discussion in the ESC guidelines is extremely important,” commented Dr. Abraham. “It supports the need for a multidimensional approach to heart failure patients. A cardiologist may not have all the resources to manage all the comorbidities [a heart failure patient might have]. This is why having a sleep medicine specialist, a diabetes specialist, a nephrologist, etc., involved as part of a heart failure management team can be very valuable. We need to involve subspecialists in managing the comorbidities of heart failure because they clearly have an impact on patient outcome.”
But Dr. Butler had a somewhat different take on how comorbidity management fits into the broader picture of heart failure management.
“There is no doubt that heart failure worsens other comorbidities and other comorbidities worsen heart failure. The relationship is bidirectional between heart failure and chronic obstructive pulmonary disease, liver disease, depression, sleep apnea, renal disease, lung disease, diabetes, etc. The problem is that treating a comorbidity does not necessarily translate into improved heart failure outcomes. Comorbidities are important for heart failure patients and worsen their heart failure outcomes. However, management of a comorbidity should be done primarily for the sake of improving the comorbidity. If you treat depression, for example, and it does not improve a patient’s heart failure, that doesn’t mean you shouldn’t have treated the depression. It just means that we don’t have good data that it will improve heart failure.”
Another limitation from a U.S. perspective is what role treatment of various comorbidities can play in benefiting heart failure patients and how compelling the evidence is for this. Dr. Butler gave as an example the problem with treating iron deficiency in heart failure patients who do not have anemia, a strategy endorsed in the ESC guidelines as a level IIa recommendation.
“The data regarding improved exercise capacity from treatment with intravenous ferric carboxymaltose is pretty convincing,” he said. But patients have benefited from this treatment only with improved function and quality of life, and not with improved survival or fewer hospitalizations.
“Is treating patients to improve their function and help them feel better enough?” Dr. Butler asked. “In other diseases it is. In gastrointestinal disease, if a drug helps patients feel better you approve the drug. We value improved functional capacity for patients with pulmonary hypertension, angina, and peripheral vascular disease. All these indications have drugs approved for improving functional capacity and quality of life. But for heart failure the bar has been set higher. There is a lot of interest in changing this” for heart failure.
“There is interest in running a study of ferric carboxymaltose for heart failure with a mortality endpoint. In the meantime, the impact on improving functional capacity is compelling, and it will be interesting to see what happens in the U.S. guidelines. Currently, in U.S. practice if a heart failure patient has iron-deficiency anemia you treat with intravenous iron replacement and the treatment gets reimbursed without a problem. But if the heart failure patient has iron deficiency without anemia then reimbursement for the cost of iron supplementation can be a problem,” Dr. Butler noted. This may change only if the experts who write the next U.S. heart failure guidelines decide to change the rules of what constitutes a useful heart failure treatment, he said.
Dr. Butler has been a consultant to Novartis and Amgen and several other companies. Dr. Jessup had no disclosures. Dr. Mehra has been a consultant to Teva, Johnson & Johnson, Boston Scientific, and St. Jude. Dr. Ruschitzka has been a consultant to Novartis, Servier, Sanofi, Cardiorentis, Heartware, and St. Jude. Dr. McMurray has received research support from Novartis and Amgen. Dr. Lindenfeld has been a consultant to Novartis, Abbott, Janssen, Relypsa, and Resmed. Dr. Voors has been a consultant to Novartis, Amgen, Servier, and several other drug companies. Dr. Ponikowski has been a consultant to Amgen, Novartis, Servier, and several other drug companies. Dr. Harjola has been a consultant to Novartis, Servier, Bayer, Boehringer Ingelheim, Pfizer, and Resmed. Dr. Abraham has been a consultant to Amgen, Novartis, and several device companies. Dr. Anker has been a consultant to Novartis, Servier, and several other companies.
On Twitter @mitchelzoler
FLORENCE, ITALY – The 2016 revision of the European Society of Cardiology’s guidelines for diagnosing and treating acute and chronic heart failure highlights the extent to which thinking in the field has changed during the past 4 years, since the prior edition in 2012.
The new European guidelines, unveiled by the ESC’s Heart Failure Association during the group’s annual meeting, also underscore the great dependence that many new approaches have on expert opinion rather than what’s become the keystone of guidelines writing, evidence-based medicine. Frequent reliance on consensus decisions rather than indisputable proof from controlled trials defines what some U.S. specialists see as a divide as wide as the Atlantic between the European and U.S. approaches to guideline writing.
“The guidelines from the ESC are articulated very well; they made their recommendations very clear. But a lot is consensus driven, without new data,” said Dr. Mariell L. Jessup, who serves as both vice chair of the panel currently revising the U.S. heart failure guidelines – expected out later in 2016 – and was also the sole American representative on the panel that produced the ESC guidelines. “The ESC guidelines make clear all the things that need to happen to patients. I hope it will result in better patient care. We are clearly not doing a good job in heart failure. We not only don’t have evidence-based treatments, but people often don’t do a good job [caring for heart failure patients] and they die in the hospital all the time.”
Dr. Javed Butler, another member of the U.S. guidelines panel and professor and chief of cardiology at Stony Brook (N.Y.) University, called the U.S. and European divide a “philosophical perspective of evidence-based medicine.
“U.S. physicians should read the ESC guidelines and make up their own minds. The ESC guidelines are excellent and give you perspective. But U.S. regulatory and payment issues will be driven by U.S. guidelines,” Dr. Butler said in an interview.
But despite their limitations and the limited weight that the ESC guidelines carry for U.S. practice, they have many redeeming features, noted Dr. Mandeep R. Mehra, medical director of the Heart and Vascular Center at Brigham and Women’s Hospital in Boston. The 2016 ESC guidelines “are extraordinarily clear, very practical, and very concise. They are very usable, and provide a fantastic algorithm for managing patients with heart failure with reduced ejection fraction [HFrEF],” he said while discussing the guidelines during the meeting.
U.S. and Europe largely agree on sacubitril/valsartan and ivabradine
Clearly the greatest area of U.S. and European agreement was in the adoption by both guidelines groups of sacubitril/valsartan (Entresto) and ivabradine (Corlanor) as important new components of the basic drug formula for treating patients with HFrEF. In fact, the U.S. guideline writers saw these two additions as so important and timely that they issued a “focused update” in May to the existing, 2013 U.S. heart failure guidelines, and timed release of this update to occur on May 20, 2016, a day before release of the ESC guidelines. But as Dr. Butler noted, this was more of a temporal harmonization than a substantive one, because even here, in a very evidence-based change, the U.S. guidelines for using sacubitril/valsartan differed subtly but importantly from the ESC version.
The U.S. focused update says that treatment of patients with stage C (symptomatic heart failure with structural heart disease) HFrEF should receive treatment with sacubitril/valsartan (also know as an angiotensin receptor neprilysin inhibitor, or ARNI), an ACE inhibitor, or an angiotensin receptor blocker (ARB), as well as evidence-based treatment with a beta-blocker and with a mineralocorticoid receptor antagonist (MRA). A subsequent recommendation in the U.S. focused update said that HFrEF patients with chronic symptoms and New York Heart Association class II or III disease should switch from a stable, tolerated regimen with either an ACE inhibitor or ARB to treatment with sacubitril/valsartan.
In contrast, the new European guideline for sacubitril/valsartan recommends starting patients on this combination formulation only after first demonstrating that patients tolerated treatment with an ACE inhibitor or ARB for at least 30 days and determining that patients remained symptomatic while on one of these treatments. In short, the U.S. guideline gives a green light to starting patients with newly diagnosed, symptomatic HFrEF on sacubitril/valsartan immediately, while the European guideline only sanctions sacubitril/valsartan to start after a patient has spent at least 30 days settling into a multidrug regimen featuring an ACE inhibitor or an ARB when an ACE inhibitor isn’t well tolerated.
“The European guidelines are closely related to the study population enrolled in the PARADIGM-HF trial,” the pivotal trial that showed superiority of sacubitril/valsartan to an ACE inhibitor (N Engl J Med. 2014;371:993-1004), noted Dr. Butler in an interview. “The U.S. guidelines interpreted [the PARADIGM-HF] results in the best interests of a larger patient population. The European guidelines are far more proscriptive in replicating the clinical criteria of the trial. In some patients the sequence of starting a MRA and sacubitril/valsartan matters, but in other patients it is less important.”
Dr. Frank Ruschitzka, a coauthor of the ESC guidelines, said that the reason for the more cautious ESC approach was lack of widespread familiarity with sacubitril/valsartan treatment among cardiologists.
The ESC guidelines on using sacubitril/valsartan “replicated the PARADIGM-HF trial. We have no data right now that it is justifiable to put a [treatment-naive] patient on sacubitril/valsartan to begin with. Another difference between the U.S. and ESC guidelines is when to start a MRA,” said Dr. Ruschitzka, professor and head of cardiology at the Heart Center of the University Hospital in Zurich. “It makes a lot of sense to me to start sacubitril/valsartan early. The PARADIGM trial was positive, but no one has a feel for how to use sacubitril/valsartan. Should we give it to everyone? We said replicate the trial, and gain experience using the drug. We want to bring a life-saving drug to patients, but this is the approach we took. We need more data.”
Dr. Jessup noted that a lot of uncertainty also exists among U.S. clinicians about when to start sacubitril/valsartan. “It’s not been clear which patients to put on sacubitril/valsartan. No guidelines had been out on using it” until mid-May, and “the cost of sacubitril/valsartan is daunting. I have received calls from many people who ask whom am I supposed to use sacubitril/valsartan on? It took years and years to get people to [routinely] start patients on an ACE inhibitor and a beta-blocker, and now we’re telling them to do something else. In my practice it’s a 30-minute conversation with each patient that you need to first stop your ACE inhibitor, and then they often get denied coverage by their insurer,” said Dr. Jessup, professor of medicine at the University of Pennsylvania in Philadelphia. She expressed hope that coverage issues will diminish now that clear guidelines are out endorsing a key role for sacubitril/valsartan.
“We now all have started sacubitril/valsartan on patients” without first starting them on an ACE inhibitor, “but we all need to get a sense of what we can get away with” when using this drug, noted Dr. JoAnn Lindenfeld, professor and director of heart failure and transplant at Vanderbilt University in Nashville.
At least one European cardiologist was skeptical of just how proscriptive the ESC guideline for sacubitril/valsartan will be in actual practice.
“The best treatment [for symptomatic HFrEF] is sacubitril/valsartan, a beta-blocker, and a MRA,” said Dr. John J.V. McMurray, professor of cardiology at Glasgow University and lead investigator for the PARADIGM-HF pivotal trial for sacubitril/valsartan. “The treatment sequence advocated in the guidelines – treat with an ACE inhibitor first and if patients remain symptomatic change to sacubitril/valsartan – is evidence-based medicine. As a guidelines writer and as a promoter of evidence-based medicine, this is absolutely the correct approach. But as a practicing physician I’d go straight for sacubitril/valsartan. Otherwise you’re wasting everybody’s time starting with an ACE inhibitor and then waiting a month to switch,” Dr. McMurray said in an interview.
“It’s pointless to wait. We saw results within 30 days of starting sacubitril/valsartan, so it’s a theoretical risk to wait. Very few patients will become completely asymptomatic on an ACE inhibitor. Everyone who entered PARADIGM-HF was at New York Heart Association class II or higher, and at the time of randomization only a handful of patients were in New York Heart Association class I. Very few patients get to class I. That tells you it’s pretty uncommon for a heart failure patient to become truly asymptomatic with ACE inhibitor treatment. The main problem is that you are inconveniencing everybody with more blood tests and more clinic visits by waiting to start sacubitril/valsartan, said Dr. McMurray, who was not a member of the panel that wrote the new ESC guidelines.
Even less separates the new U.S. focused update and the ESC guidelines for using ivabradine. Both agree on starting the drug on HFrEF patients who remain symptomatic and with a left ventricular ejection fraction of 35% or less despite being on guideline-directed therapy including titration to a maximum beta-blocker dosage and with a persistent heart rate of at least 70 beats/min. The goal of ivabradine treatment is to further reduce heart rate beyond what’s achieved by a maximal beta-blocker dosage.
Perhaps the biggest questions about ivabradine have been why it took so long to enter the U.S. guidelines, and why it is listed in both the U.S. and ESC guidelines as a level II recommendation. Results from the pivotal trial that supported ivabradine’s use in HFrEF patients, SHIFT, first appeared in 2010 (Lancet. 2010 Sep 11;376[9744]:875-95).
Dr. Butler chalked up the drug’s slow entry into U.S. guidelines as the result of a lack of initiative by ivabradine’s initial developer, Servier. “SHIFT did not have any U.S. sites, and Servier never sought Food and Drug Administration approval,” he noted. “Amgen acquired the U.S. rights to ivabradine in 2013,” and the drug received FDA approval in April 2015, Dr. Butler noted, in explaining the drug’s U.S. timeline. As to why its use is a level II recommendation, he noted that the evidence for efficacy came only from the SHIFT trial, questions exist whether the beta-blocker dosages were fully optimized in all patients in this trial, and the benefit was limited to a reduction in heart failure hospitalizations but not in mortality. “I think that patients with persistent heart failure symptoms [and a persistently elevated heart rate] should get ivabradine,” but these caveats limit it to a class II level recommendation, Dr. Butler said.
“There were questions about ivabradine’s benefit in reducing heart failure hospitalization but not mortality, and questions about whether it would benefit patients if their beta-blocker dosage was adequately up titrated. There were also questions about which heart failure patients to use it on,” noted Dr. Lindenfeld, a member of the panel that wrote the U.S. focused update. These concerns in part help explain the delay to integrating ivabradine into U.S. practice guidelines, she said in an interview, but added that additional data and analysis published during the past 3 or so years have clarified ivabradine’s potentially useful role in treating selected HFrEF patients.
New ESC guidelines based on expert opinion
The sections on sacubitril/valsartan and ivabradine occupy a mere 2 pages among more than 55 pages of text and charts that spell out the ESC’s current vision of how physicians should diagnose and manage heart failure patients. While much of what carried over from prior editions of the guidelines is rooted in evidence, many of the new approaches advocated rely on expert opinion or new interpretations of existing data. Here are some of the notable changes and highlights of the 2016 ESC recommendations:
• Heart failure diagnosis. The new ESC guidelines streamline the diagnostic process, which now focuses on five key elements: The patient’s history, physical examination, ECG, serum level of either brain natriuretic peptide (BNP) or N-terminal(NT)-proBNP, and echocardiography. The guidelines specify threshold levels of BNP and NT-proBNP that can effectively rule out heart failure, a BNP level of at least 35 pg/mL or a NT-proBNP level of at least 125 pg/mL.
“The diagnostic minimum levels of BNP and NT-proBNP were designed to rule out heart failure. They both have a high negative predictive value, but at these levels their positive predictive value is low,” explained Dr. Adriaan A. Voors, cochair of the ESC’s guideline-writing panel and professor of cardiology at the University of Groningen, the Netherlands.
But while these levels might be effective for reliable rule out of heart failure, they could mean a large number of patients would qualify for an echocardiographic assessment.
“If we used the ESC’s natriuretic peptide cutoffs, there would be a clear concern about overuse of echo. It’s a cost-effectiveness issue. You wind up doing a lot of echos that will be normal. Echocardiography is very safe, but each echo costs about $400-$500,” commented Dr. Butler.
“The results from the STOP-HF and PONTIAC studies showed that BNP levels can identify people at increased risk for developing heart failure who need more intensive assessment and could also potentially benefit from more attention to heart failure prevention. I suspect the full U.S. guideline update will address this issue, but we have not yet finalized our decisions,” he added.
• Heart failure classification. The new ESC guidelines created a new heart failure category, midrange ejection fraction, that the writing panel positioned squarely between the two more classic heart failure subgroups, HFrEF and heart failure with preserved ejection fraction (HFpEF). The definition of each of the three subgroups depends on left ventricular ejection fraction as determined by echocardiography: A LVEF of less than 40% defined HFrEF, a LVEF of 40%-49% defined heart failure with midrange ejection fraction (HFmrEF), and a LVEF of 50% or higher defined HFpEF. Diagnostic confirmation of both HFmrEF and HFpEF also requires that patients fulfill certain criteria of structural or functional heart abnormalities.
The category of HFmrEF was created “to stimulate research into how to best manage these patients,” explained Dr. Piotr Ponikowski, chair of the ESC guidelines writing panel. For the time being, it remains a category with only theoretical importance as nothing is known to suggest that management of patients with HFmrEF should in any way differ from patients with HFpEF.
• Acute heart failure. Perhaps the most revolutionary element of the new guidelines is the detailed map they provide to managing patients who present with acute decompensated heart failure and the underlying principles cited to justify this radically different approach.
“The acute heart failure section was completely rewritten,” noted Dr. Ponikowski, professor of heart diseases at the Medical University in Wroclaw, Poland. “We don’t yet have evidence-based treatments” to apply to acute heart failure patients, he admitted, “however we strongly recommend the concept that the shorter the better. Shorten the time of diagnosis and for therapeutic decisions. We have borrowed from acute coronary syndrome. Don’t keep patients in the emergency department for another couple of hours just to see if they will respond. We must be aware that we need to do our best to shorten diagnosis and treatment decisions. Time is an issue. Manage a patient’s congestion and impaired peripheral perfusion within a time frame of 1-2 hours.”
The concept that acute heart failure must be quickly managed as an emergency condition similar to acute coronary syndrome first appeared as a European practice recommendation in 2015, a consensus statement from the European Heart Failure Association and two other collaborating organizations (Eur Heart J. 2015 Aug 7;36[30]:1958-66).
“In 2015, the consensus paper talked about how to handle acute heart failure patients in the emergency department. Now, we have focused on defining the patients’ phenotype and how to categorize their treatment options. We built on the 2015 statement, but the algorithms we now have are original to 2016; they were not in the 2015 paper,” said Dr. Veli-Pekka Harjola, a member of the 2015 consensus group and 2016 guidelines panel who spearheaded writing the acute heart failure section of the new ESC guidelines.
An additional new and notable feature of this section in the 2016 guidelines is its creation of an acronym, CHAMP, designed to guide the management of patients with acute heart failure. CHAMP stands for acute Coronary syndrome, Hypertension emergency, Arrhythmia, acute Mechanical cause, and Pulmonary embolism. The CHAMP acronym’s purpose is to “focus attention on these five specific, potential causes of acute heart failure, life-threatening conditions that need immediate treatment,” explained Dr. Ponikowski.
“CHAMP emphasizes the most critical causes of acute heart failure,” added Dr. Harjola, a cardiologist at Helsinki University Central Hospital. “We created this new acronym” to help clinicians keep in mind what to look for in a patient presenting with acute heart failure.
U.S. cardiologists find things to like in what the Europeans say about managing acute heart failure, as well as aspects to question.
“It makes no sense not to aggressively treat a patient who arrives at an emergency department with acute heart failure. But there is a difference between acute MI or stroke and acute heart failure,” said Dr. Butler. “In acute MI there is the ruptured plaque and thrombus that blocks a coronary artery. In stroke there is a thrombus. These are diseases with a specific onset and treatment target. But with acute heart failure we don’t have a thrombus to treat; we don’t have a specific target. What we’ve learned from studying implanted devices [such as CardioMems] is that the congestion that causes acute heart failure can start 2-3 weeks before a patient develops acute decompensated heart failure and goes to the hospital. We have not found a specific pathophysiologic abnormality in the patient with acute heart failure that is any different from chronic heart failure. This begs the question: If a patient who presents with acute heart failure has a congestion process that’s been going on for 2 or 3 weeks what difference will another 3 hours make? Do we need to replicate the concept of an acute stroke team or acute MI response for acute heart failure?”
Dr. Butler stressed that additional data are expected soon that may help clarify this issue.
“Some large outcome trials in patients with acute heart failure are now underway, one testing serelaxin treatment, another testing ularitide treatment, that are also testing the hypothesis that rapid treatment with these drugs can produce more end-organ protection, stop damage to the heart, kidney and liver, and lead to better long-term outcomes. Until we have those data, the jury is still out” on the benefit patients gain from rapid treatment of acute heart failure. “Until then, it’s not that the data say don’t treat acute heart failure patients aggressively. But we have not yet proven it is similar to treating an acute MI or stroke,” said Dr. Butler.
“U.S. guidelines have tended to stay away from areas where there are no evidence-based data. To their credit, the Europeans will take on something like acute heart failure where we don’t have an adequate evidence base. Despite that, they provide guidelines, which is important because clinicians need guidance even when the evidence is not very good, when the guideline is based mostly on experience and expert consensus.” commented Dr. William T. Abraham, professor and director of cardiovascular medicine at the Ohio State University Wexner Medical Center in Columbus.
“It’s absolutely appropriate to think of acute heart failure as an emergency situation. We know from high-sensitivity troponin assays that troponin levels are increased in 90% of patients who present with acute decompensated heart failure. So most acute heart failure patients are losing heart muscle cells and we should treat them like we treat acute coronary syndrome. Time matters in acute heart failure; time is heart muscle. Treatment needs to break the hemodynamic and neurohormonal storm of acute decompensated heart failure; get the patient stabilized; improve vital organ perfusion, including within the heart; and shift the myocardial oxygen supply and demand equation so myocardial necrosis stops. All of this is important, and study results suggest it’s the correct approach. I’m not sure study results prove it, but studies that have looked at the time course of treatment for acute heart failure showed that early initiation of treatment – within the first 6 hours of onset – compared with 12-24 hours of onset makes a difference in outcomes,” Dr. Abraham said in an interview.
But a major limitation to the potential efficacy of a rapidly initiated management strategy is that few interventions currently exist with proven benefits for acute heart failure patients.
For the time being, rapid intervention means using diuretics relatively quickly and, if there is an indication for treating with a vasoactive medication, using that quickly too. “The rapid approach is really more relevant to the future; it’s relevant to the design of future acute heart failure treatment trials. That is where this early treatment paradigm is important,” as it could potentially apply to new, more effective treatments of the future rather than to the marginally effective treatments now available, Dr. Abraham said.
“For a long we time haven’t pushed how quickly we should act when implementing guideline-directed treatment” for patients with acute heart failure, noted Dr. Mehra. “The CHAMP approach is interesting, and the ESC guidelines are a very interesting move in the direction” of faster action. “They speak to the period of time during which one should act. Hopefully this will help the science of acute decompensated heart failure move forward.”
But for other U.S. experts the issue again pivots on the lack of evidence.
“There is nothing new” about managing acute heart failure, said Dr. Jessup. “The ESC guideline was articulated very well; they made their recommendations very clear. But a lot is consensus driven. There are no new data. The problem with acute heart failure is that the recommendations are what we think clinicians should do. CHAMP is a nice acronym; it’s packaged better, but there are not any new data.”
Comorbidities
A dramatic contrast distinguishes the extent to which the ESC guidelines highlight comorbidities, compared with prevailing U.S. guidelines. The new ESC guidelines highlight and discuss with some detail 16 distinct comorbidities for clinicians to keep in mind when managing heart failure patients, compared with three comorbidities (atrial fibrillation, anemia, and depression) discussed with similar detail in the 2013 U.S. guidelines.
“We are targeting comorbidities to personalize medicine, by subgrouping [heart failure] patients into groups that need to receive special attention,” explained Dr. Stefan D. Anker, a coauthor on the ESC guidelines. “We care about comorbidities because they make the diagnosis of heart failure difficult. They aggravate symptoms and contribute to additional hospitalizations. They interfere with [heart failure] treatment, and because comorbidities have led to exclusions of heart failure patients from trials, we lack evidence of treatment efficacy in patients with certain comorbidities,” said Dr. Anker, a professor of innovative clinical trials at the Medical University in Göttingen, Germany.
“The comorbidity discussion in the ESC guidelines is extremely important,” commented Dr. Abraham. “It supports the need for a multidimensional approach to heart failure patients. A cardiologist may not have all the resources to manage all the comorbidities [a heart failure patient might have]. This is why having a sleep medicine specialist, a diabetes specialist, a nephrologist, etc., involved as part of a heart failure management team can be very valuable. We need to involve subspecialists in managing the comorbidities of heart failure because they clearly have an impact on patient outcome.”
But Dr. Butler had a somewhat different take on how comorbidity management fits into the broader picture of heart failure management.
“There is no doubt that heart failure worsens other comorbidities and other comorbidities worsen heart failure. The relationship is bidirectional between heart failure and chronic obstructive pulmonary disease, liver disease, depression, sleep apnea, renal disease, lung disease, diabetes, etc. The problem is that treating a comorbidity does not necessarily translate into improved heart failure outcomes. Comorbidities are important for heart failure patients and worsen their heart failure outcomes. However, management of a comorbidity should be done primarily for the sake of improving the comorbidity. If you treat depression, for example, and it does not improve a patient’s heart failure, that doesn’t mean you shouldn’t have treated the depression. It just means that we don’t have good data that it will improve heart failure.”
Another limitation from a U.S. perspective is what role treatment of various comorbidities can play in benefiting heart failure patients and how compelling the evidence is for this. Dr. Butler gave as an example the problem with treating iron deficiency in heart failure patients who do not have anemia, a strategy endorsed in the ESC guidelines as a level IIa recommendation.
“The data regarding improved exercise capacity from treatment with intravenous ferric carboxymaltose is pretty convincing,” he said. But patients have benefited from this treatment only with improved function and quality of life, and not with improved survival or fewer hospitalizations.
“Is treating patients to improve their function and help them feel better enough?” Dr. Butler asked. “In other diseases it is. In gastrointestinal disease, if a drug helps patients feel better you approve the drug. We value improved functional capacity for patients with pulmonary hypertension, angina, and peripheral vascular disease. All these indications have drugs approved for improving functional capacity and quality of life. But for heart failure the bar has been set higher. There is a lot of interest in changing this” for heart failure.
“There is interest in running a study of ferric carboxymaltose for heart failure with a mortality endpoint. In the meantime, the impact on improving functional capacity is compelling, and it will be interesting to see what happens in the U.S. guidelines. Currently, in U.S. practice if a heart failure patient has iron-deficiency anemia you treat with intravenous iron replacement and the treatment gets reimbursed without a problem. But if the heart failure patient has iron deficiency without anemia then reimbursement for the cost of iron supplementation can be a problem,” Dr. Butler noted. This may change only if the experts who write the next U.S. heart failure guidelines decide to change the rules of what constitutes a useful heart failure treatment, he said.
Dr. Butler has been a consultant to Novartis and Amgen and several other companies. Dr. Jessup had no disclosures. Dr. Mehra has been a consultant to Teva, Johnson & Johnson, Boston Scientific, and St. Jude. Dr. Ruschitzka has been a consultant to Novartis, Servier, Sanofi, Cardiorentis, Heartware, and St. Jude. Dr. McMurray has received research support from Novartis and Amgen. Dr. Lindenfeld has been a consultant to Novartis, Abbott, Janssen, Relypsa, and Resmed. Dr. Voors has been a consultant to Novartis, Amgen, Servier, and several other drug companies. Dr. Ponikowski has been a consultant to Amgen, Novartis, Servier, and several other drug companies. Dr. Harjola has been a consultant to Novartis, Servier, Bayer, Boehringer Ingelheim, Pfizer, and Resmed. Dr. Abraham has been a consultant to Amgen, Novartis, and several device companies. Dr. Anker has been a consultant to Novartis, Servier, and several other companies.
On Twitter @mitchelzoler
EXPERT ANALYSIS FROM HEART FAILURE 2016
Medicare Trust Fund projected to run dry in 2028
The Medicare Trust Fund is projected to become insolvent in 2028, 2 years earlier than projected this time last year.
The change is based on two key factors: an expected reduction in payroll taxes and a slowdown in declining rate of inpatient utilization, Andy Slavitt, acting administrator of the Centers for Medicare & Medicaid Services said at a June 22 press conference to review the annual Medicare Trustees report.
“The good news is inpatient utilization is still declining, it’s just declining at a slightly lower rate,” Mr. Slavitt said.
He also highlighted the continuing rising cost of prescription medications, which he called “a major driver” in Medicare spending growth.
“For the second year in a row, we saw spending growth for prescription drugs dramatically outpace cost growth for other Medicare services,” Mr. Slavitt said. “Through 2025, Medicare Part D expenditures per enrollee are estimated to increase nearly 50% higher than the estimated increase in GDP per capita and higher than the combined per enrollee growth rate of Medicare Part A and Medicare Part B combined.”
Overall, total Medicare expenditures “are slightly lower than estimated last year,” Mr. Slavitt said, adding that over the next decade, “Medicare per-enrollee spending is projected to continue to grow slower than historical rates, at 4.3%, lower than the growth in overall per capita national health expenditures.”
The growth rate is not projected to trigger the activation of the Independent Payment Advisory Board, according to the report.
In 2015, Medicare covered 55.3 million people, including 46.3 million aged 65 and older, and 9 million disabled individuals.
The Medicare Trust Fund is projected to become insolvent in 2028, 2 years earlier than projected this time last year.
The change is based on two key factors: an expected reduction in payroll taxes and a slowdown in declining rate of inpatient utilization, Andy Slavitt, acting administrator of the Centers for Medicare & Medicaid Services said at a June 22 press conference to review the annual Medicare Trustees report.
“The good news is inpatient utilization is still declining, it’s just declining at a slightly lower rate,” Mr. Slavitt said.
He also highlighted the continuing rising cost of prescription medications, which he called “a major driver” in Medicare spending growth.
“For the second year in a row, we saw spending growth for prescription drugs dramatically outpace cost growth for other Medicare services,” Mr. Slavitt said. “Through 2025, Medicare Part D expenditures per enrollee are estimated to increase nearly 50% higher than the estimated increase in GDP per capita and higher than the combined per enrollee growth rate of Medicare Part A and Medicare Part B combined.”
Overall, total Medicare expenditures “are slightly lower than estimated last year,” Mr. Slavitt said, adding that over the next decade, “Medicare per-enrollee spending is projected to continue to grow slower than historical rates, at 4.3%, lower than the growth in overall per capita national health expenditures.”
The growth rate is not projected to trigger the activation of the Independent Payment Advisory Board, according to the report.
In 2015, Medicare covered 55.3 million people, including 46.3 million aged 65 and older, and 9 million disabled individuals.
The Medicare Trust Fund is projected to become insolvent in 2028, 2 years earlier than projected this time last year.
The change is based on two key factors: an expected reduction in payroll taxes and a slowdown in declining rate of inpatient utilization, Andy Slavitt, acting administrator of the Centers for Medicare & Medicaid Services said at a June 22 press conference to review the annual Medicare Trustees report.
“The good news is inpatient utilization is still declining, it’s just declining at a slightly lower rate,” Mr. Slavitt said.
He also highlighted the continuing rising cost of prescription medications, which he called “a major driver” in Medicare spending growth.
“For the second year in a row, we saw spending growth for prescription drugs dramatically outpace cost growth for other Medicare services,” Mr. Slavitt said. “Through 2025, Medicare Part D expenditures per enrollee are estimated to increase nearly 50% higher than the estimated increase in GDP per capita and higher than the combined per enrollee growth rate of Medicare Part A and Medicare Part B combined.”
Overall, total Medicare expenditures “are slightly lower than estimated last year,” Mr. Slavitt said, adding that over the next decade, “Medicare per-enrollee spending is projected to continue to grow slower than historical rates, at 4.3%, lower than the growth in overall per capita national health expenditures.”
The growth rate is not projected to trigger the activation of the Independent Payment Advisory Board, according to the report.
In 2015, Medicare covered 55.3 million people, including 46.3 million aged 65 and older, and 9 million disabled individuals.
Wedge resection showed improved survival over SBRT for early-stage NSCLC
BALTIMORE – Wedge resection was associated with significantly improved overall 5-year survival, compared with stereotactic body radiation therapy (SBRT) in patients with operable clinical Stage IA non–small cell lung cancer, according to a study of more than 8,000 patients.
Despite the fact that surgical resection has been the standard of care for early-stage non–small cell lung cancer (NSCLC), an increasing number of patients with potentially operable early-stage NSCLC are now being treated with SBRT, study investigator Dr. Babatunde A. Yerokun said at the annual meeting of the American Association for Thoracic Surgery.
“Our data show that thoracic surgeons should be included in the evaluation of these patients, and operative candidates with ct1A NO MO NSCLC should continue to receive a wedge resection vs. SBRT when technically feasible,” said Dr. Yerokun of Duke University, Durham, N.C. “Prospective studies are needed to determine the appropriate role of SBRT in management of these patients,” he concluded.
Dr. Yerokun and his colleagues examined overall survival of patients with cT1N0 lung cancer who underwent SBRT or wedge resection as reported in the National Cancer Data Base from 2003 to 2011. Survival was assessed using Kaplan-Meier and propensity-score matched analysis. The researchers matched groups according to common prognostic covariates, including age, sex, race, education, insurance status, facility type, and Charlson/Deyo comorbidity score, as well as tumor histology, size, and location.
Patients identified as having cT1N0 NSCLC with a tumor less than 2 cm underwent SBRT (1,514 patients) or wedge resection (6,923). Compared with the wedge resection cohort, the SBRT patients were significantly older (74 vs. 69 years) and significantly more likely to be treated at an academic comprehensive cancer program (47% vs. 37%). The median Charlson/Deyo score was lower in the SBRT patients (0 vs. 1).
In unmatched analysis, SBRT was associated with significantly lower survival than wedge resection (5-year overall survival: 32% vs. 55%). In the propensity matching, all baseline covariates, including co-morbidity scores, facility type, and tumor size, were well balanced between the SBRT and wedge groups, with 1,398 patients in each group.
However, even in the matched groups, SBRT was associated with significantly lower 5-year overall survival than wedge (33% vs. 52%). When the investigators performed a propensity matched subgroup analysis in younger patients (age less than 60 years) who had a Charlson/Deyo score of 0, SBRT was associated with worse survival with a 5-year overall survival of 59% vs. 82% for SBRT and wedge resection, respectively.
Additionally, Dr. Yerokun and his colleagues conducted a sensitivity analysis comparing centers that performed predominately wedge resection with centers that performed predominately SBRT. After the exclusion of centers with low-volume and centers that conducted either 100% wedge resection or 100% SBRT only, centers that performed predominately wedge resection were more likely to have significantly better 3-year survival.
A video of the original presentation from the AATS Annual Meeting is available online.
Dr. Yerokun reported that he had no disclosures related to this presentation.
On Twitter @ThoracicTweets
BALTIMORE – Wedge resection was associated with significantly improved overall 5-year survival, compared with stereotactic body radiation therapy (SBRT) in patients with operable clinical Stage IA non–small cell lung cancer, according to a study of more than 8,000 patients.
Despite the fact that surgical resection has been the standard of care for early-stage non–small cell lung cancer (NSCLC), an increasing number of patients with potentially operable early-stage NSCLC are now being treated with SBRT, study investigator Dr. Babatunde A. Yerokun said at the annual meeting of the American Association for Thoracic Surgery.
“Our data show that thoracic surgeons should be included in the evaluation of these patients, and operative candidates with ct1A NO MO NSCLC should continue to receive a wedge resection vs. SBRT when technically feasible,” said Dr. Yerokun of Duke University, Durham, N.C. “Prospective studies are needed to determine the appropriate role of SBRT in management of these patients,” he concluded.
Dr. Yerokun and his colleagues examined overall survival of patients with cT1N0 lung cancer who underwent SBRT or wedge resection as reported in the National Cancer Data Base from 2003 to 2011. Survival was assessed using Kaplan-Meier and propensity-score matched analysis. The researchers matched groups according to common prognostic covariates, including age, sex, race, education, insurance status, facility type, and Charlson/Deyo comorbidity score, as well as tumor histology, size, and location.
Patients identified as having cT1N0 NSCLC with a tumor less than 2 cm underwent SBRT (1,514 patients) or wedge resection (6,923). Compared with the wedge resection cohort, the SBRT patients were significantly older (74 vs. 69 years) and significantly more likely to be treated at an academic comprehensive cancer program (47% vs. 37%). The median Charlson/Deyo score was lower in the SBRT patients (0 vs. 1).
In unmatched analysis, SBRT was associated with significantly lower survival than wedge resection (5-year overall survival: 32% vs. 55%). In the propensity matching, all baseline covariates, including co-morbidity scores, facility type, and tumor size, were well balanced between the SBRT and wedge groups, with 1,398 patients in each group.
However, even in the matched groups, SBRT was associated with significantly lower 5-year overall survival than wedge (33% vs. 52%). When the investigators performed a propensity matched subgroup analysis in younger patients (age less than 60 years) who had a Charlson/Deyo score of 0, SBRT was associated with worse survival with a 5-year overall survival of 59% vs. 82% for SBRT and wedge resection, respectively.
Additionally, Dr. Yerokun and his colleagues conducted a sensitivity analysis comparing centers that performed predominately wedge resection with centers that performed predominately SBRT. After the exclusion of centers with low-volume and centers that conducted either 100% wedge resection or 100% SBRT only, centers that performed predominately wedge resection were more likely to have significantly better 3-year survival.
A video of the original presentation from the AATS Annual Meeting is available online.
Dr. Yerokun reported that he had no disclosures related to this presentation.
On Twitter @ThoracicTweets
BALTIMORE – Wedge resection was associated with significantly improved overall 5-year survival, compared with stereotactic body radiation therapy (SBRT) in patients with operable clinical Stage IA non–small cell lung cancer, according to a study of more than 8,000 patients.
Despite the fact that surgical resection has been the standard of care for early-stage non–small cell lung cancer (NSCLC), an increasing number of patients with potentially operable early-stage NSCLC are now being treated with SBRT, study investigator Dr. Babatunde A. Yerokun said at the annual meeting of the American Association for Thoracic Surgery.
“Our data show that thoracic surgeons should be included in the evaluation of these patients, and operative candidates with ct1A NO MO NSCLC should continue to receive a wedge resection vs. SBRT when technically feasible,” said Dr. Yerokun of Duke University, Durham, N.C. “Prospective studies are needed to determine the appropriate role of SBRT in management of these patients,” he concluded.
Dr. Yerokun and his colleagues examined overall survival of patients with cT1N0 lung cancer who underwent SBRT or wedge resection as reported in the National Cancer Data Base from 2003 to 2011. Survival was assessed using Kaplan-Meier and propensity-score matched analysis. The researchers matched groups according to common prognostic covariates, including age, sex, race, education, insurance status, facility type, and Charlson/Deyo comorbidity score, as well as tumor histology, size, and location.
Patients identified as having cT1N0 NSCLC with a tumor less than 2 cm underwent SBRT (1,514 patients) or wedge resection (6,923). Compared with the wedge resection cohort, the SBRT patients were significantly older (74 vs. 69 years) and significantly more likely to be treated at an academic comprehensive cancer program (47% vs. 37%). The median Charlson/Deyo score was lower in the SBRT patients (0 vs. 1).
In unmatched analysis, SBRT was associated with significantly lower survival than wedge resection (5-year overall survival: 32% vs. 55%). In the propensity matching, all baseline covariates, including co-morbidity scores, facility type, and tumor size, were well balanced between the SBRT and wedge groups, with 1,398 patients in each group.
However, even in the matched groups, SBRT was associated with significantly lower 5-year overall survival than wedge (33% vs. 52%). When the investigators performed a propensity matched subgroup analysis in younger patients (age less than 60 years) who had a Charlson/Deyo score of 0, SBRT was associated with worse survival with a 5-year overall survival of 59% vs. 82% for SBRT and wedge resection, respectively.
Additionally, Dr. Yerokun and his colleagues conducted a sensitivity analysis comparing centers that performed predominately wedge resection with centers that performed predominately SBRT. After the exclusion of centers with low-volume and centers that conducted either 100% wedge resection or 100% SBRT only, centers that performed predominately wedge resection were more likely to have significantly better 3-year survival.
A video of the original presentation from the AATS Annual Meeting is available online.
Dr. Yerokun reported that he had no disclosures related to this presentation.
On Twitter @ThoracicTweets
AT THE AATS ANNUAL MEETING
Key clinical point: Wedge resection outperformed SBRT in terms of mortality for early-stage NSCLC.
Major finding: In matched groups, SBRT was associated with significantly lower 5-year overall survival than was wedge resection (32% vs. 50%).
Data source: The study assessed more than 8.000 patients with early stage NSCLC who had either wedge resection or SBRT from the National Cancer Database from 2003 to 2011.
Disclosures: Dr. Yerokun had no relevant disclosures.
Esophagectomy 30-day readmission rate pegged at 19%
BALTIMORE – Approximately one in five patients is readmitted after esophagectomy, and leading risk factors for readmission are longer operative time, post-surgical ICU admission, and preoperative blood transfusions, according to a single-center study of 86 patients.
As one of the first reports on readmissions following esophagectomy with complete follow-up, this study, conducted at the Mayo Clinic in Rochester, Minn., demonstrates that even in a high volume center with specialization in esophageal and foregut surgery, readmission after esophagectomy is not uncommon, researchers reported at the annual meeting of the American Association for Thoracic Surgery.
“In the context of increasing pressures to reduce length of stay, we must also put in the effort to better understand our readmission rates and the important factors that affect them,” said study investigator Dr. Stephen Cassivi. “Reporting on ‘improved’ lengths of stay without accompanying data on readmission rates is not telling the whole story.”
According to the Mayo Clinic research team, identifying risk factors that predict readmissions might permit improved patient management and outcomes.
“Careful collection of data regarding patient outcomes, including unplanned hospital readmissions is essential to improve the quality of patient care since national databases can leave gaps in data regarding follow-up of these patients by failing to identify all readmissions after their surgery,” said Dr. Karen J. Dickinson, who presented the study at the meeting.
The study was designed such that all patients undergoing an elective esophagectomy between August 2013 and July 2014 were contacted directly to follow up on whether they had been readmitted to any medical institution within 30 days of dismissal from the Mayo Clinic. Among all patients who underwent esophagectomy during the one-year study period, 86 patients met the study inclusion criteria. Follow-up was complete in 100% of patients, according to Dr. Dickinson.
Median age of the patients at the time of surgery was 63 years, and the majority of patients were men (70 patients). The most common operative approach was transthoracic (Ivor Lewis) esophagectomy (72%); 7% of cases were performed using a minimally invasive approach. Overall 30-day mortality was 2% (2/86), and anastomotic leak occurred in 8% of the patients.
Median length of stay was 9 days, and the rate of unplanned 30-day readmission was 19% (16 patients). Of these patients, 88% were readmitted to the Mayo Clinic and 12% were readmitted to other medical institutions.
The most common reasons for readmission were due to respiratory causes such as dyspnea, pleural effusions or pneumonia and gastrointestinal causes, including bowel obstruction and anastomotic complications.
Using multivariable analysis, the researchers found that the factors significantly associated with unplanned readmission were postoperative ICU admission (13% in non-readmitted, 38% in admitted), perioperative blood transfusion (12% vs. 38%), and operative length (368 vs. 460 minutes). Importantly, initial hospital length of stay was not associated with the need for readmission. Furthermore, ASA score, sex, BMI, neoadjuvant therapy, and postoperative pain scores also were not associated with unplanned readmission.
“Identifying these risk factors in the perioperative and postoperative setting may provide opportunities for decreasing morbidity, improving readmission rates, and enhancing overall patient outcomes,” Dr. Dickinson concluded.
A video of this presentation at the AATS Annual Meeting is available online.
Dr. Dickinson and her colleagues reported having no relevant disclosures.
On Twitter @ThoracicTweets
BALTIMORE – Approximately one in five patients is readmitted after esophagectomy, and leading risk factors for readmission are longer operative time, post-surgical ICU admission, and preoperative blood transfusions, according to a single-center study of 86 patients.
As one of the first reports on readmissions following esophagectomy with complete follow-up, this study, conducted at the Mayo Clinic in Rochester, Minn., demonstrates that even in a high volume center with specialization in esophageal and foregut surgery, readmission after esophagectomy is not uncommon, researchers reported at the annual meeting of the American Association for Thoracic Surgery.
“In the context of increasing pressures to reduce length of stay, we must also put in the effort to better understand our readmission rates and the important factors that affect them,” said study investigator Dr. Stephen Cassivi. “Reporting on ‘improved’ lengths of stay without accompanying data on readmission rates is not telling the whole story.”
According to the Mayo Clinic research team, identifying risk factors that predict readmissions might permit improved patient management and outcomes.
“Careful collection of data regarding patient outcomes, including unplanned hospital readmissions is essential to improve the quality of patient care since national databases can leave gaps in data regarding follow-up of these patients by failing to identify all readmissions after their surgery,” said Dr. Karen J. Dickinson, who presented the study at the meeting.
The study was designed such that all patients undergoing an elective esophagectomy between August 2013 and July 2014 were contacted directly to follow up on whether they had been readmitted to any medical institution within 30 days of dismissal from the Mayo Clinic. Among all patients who underwent esophagectomy during the one-year study period, 86 patients met the study inclusion criteria. Follow-up was complete in 100% of patients, according to Dr. Dickinson.
Median age of the patients at the time of surgery was 63 years, and the majority of patients were men (70 patients). The most common operative approach was transthoracic (Ivor Lewis) esophagectomy (72%); 7% of cases were performed using a minimally invasive approach. Overall 30-day mortality was 2% (2/86), and anastomotic leak occurred in 8% of the patients.
Median length of stay was 9 days, and the rate of unplanned 30-day readmission was 19% (16 patients). Of these patients, 88% were readmitted to the Mayo Clinic and 12% were readmitted to other medical institutions.
The most common reasons for readmission were due to respiratory causes such as dyspnea, pleural effusions or pneumonia and gastrointestinal causes, including bowel obstruction and anastomotic complications.
Using multivariable analysis, the researchers found that the factors significantly associated with unplanned readmission were postoperative ICU admission (13% in non-readmitted, 38% in admitted), perioperative blood transfusion (12% vs. 38%), and operative length (368 vs. 460 minutes). Importantly, initial hospital length of stay was not associated with the need for readmission. Furthermore, ASA score, sex, BMI, neoadjuvant therapy, and postoperative pain scores also were not associated with unplanned readmission.
“Identifying these risk factors in the perioperative and postoperative setting may provide opportunities for decreasing morbidity, improving readmission rates, and enhancing overall patient outcomes,” Dr. Dickinson concluded.
A video of this presentation at the AATS Annual Meeting is available online.
Dr. Dickinson and her colleagues reported having no relevant disclosures.
On Twitter @ThoracicTweets
BALTIMORE – Approximately one in five patients is readmitted after esophagectomy, and leading risk factors for readmission are longer operative time, post-surgical ICU admission, and preoperative blood transfusions, according to a single-center study of 86 patients.
As one of the first reports on readmissions following esophagectomy with complete follow-up, this study, conducted at the Mayo Clinic in Rochester, Minn., demonstrates that even in a high volume center with specialization in esophageal and foregut surgery, readmission after esophagectomy is not uncommon, researchers reported at the annual meeting of the American Association for Thoracic Surgery.
“In the context of increasing pressures to reduce length of stay, we must also put in the effort to better understand our readmission rates and the important factors that affect them,” said study investigator Dr. Stephen Cassivi. “Reporting on ‘improved’ lengths of stay without accompanying data on readmission rates is not telling the whole story.”
According to the Mayo Clinic research team, identifying risk factors that predict readmissions might permit improved patient management and outcomes.
“Careful collection of data regarding patient outcomes, including unplanned hospital readmissions is essential to improve the quality of patient care since national databases can leave gaps in data regarding follow-up of these patients by failing to identify all readmissions after their surgery,” said Dr. Karen J. Dickinson, who presented the study at the meeting.
The study was designed such that all patients undergoing an elective esophagectomy between August 2013 and July 2014 were contacted directly to follow up on whether they had been readmitted to any medical institution within 30 days of dismissal from the Mayo Clinic. Among all patients who underwent esophagectomy during the one-year study period, 86 patients met the study inclusion criteria. Follow-up was complete in 100% of patients, according to Dr. Dickinson.
Median age of the patients at the time of surgery was 63 years, and the majority of patients were men (70 patients). The most common operative approach was transthoracic (Ivor Lewis) esophagectomy (72%); 7% of cases were performed using a minimally invasive approach. Overall 30-day mortality was 2% (2/86), and anastomotic leak occurred in 8% of the patients.
Median length of stay was 9 days, and the rate of unplanned 30-day readmission was 19% (16 patients). Of these patients, 88% were readmitted to the Mayo Clinic and 12% were readmitted to other medical institutions.
The most common reasons for readmission were due to respiratory causes such as dyspnea, pleural effusions or pneumonia and gastrointestinal causes, including bowel obstruction and anastomotic complications.
Using multivariable analysis, the researchers found that the factors significantly associated with unplanned readmission were postoperative ICU admission (13% in non-readmitted, 38% in admitted), perioperative blood transfusion (12% vs. 38%), and operative length (368 vs. 460 minutes). Importantly, initial hospital length of stay was not associated with the need for readmission. Furthermore, ASA score, sex, BMI, neoadjuvant therapy, and postoperative pain scores also were not associated with unplanned readmission.
“Identifying these risk factors in the perioperative and postoperative setting may provide opportunities for decreasing morbidity, improving readmission rates, and enhancing overall patient outcomes,” Dr. Dickinson concluded.
A video of this presentation at the AATS Annual Meeting is available online.
Dr. Dickinson and her colleagues reported having no relevant disclosures.
On Twitter @ThoracicTweets
AT THE AATS ANNUAL MEETING
Key clinical point: Operative length, perioperative blood transfusions, and postoperative ICU admission were significant risk factors for readmission after esophagectomy.
Major finding: The rate of unplanned 30-day readmission was 19%.
Data source: The study assessed 86 patients who underwent esophagectomy at the Mayo Clinic between August 2012 and July 2014.
Disclosures: Dr. Dickinson and her colleagues reported having no relevant disclosures.
Low paravalvular leak shown in real-world registry of Sapien 3 recipients
PARIS – The initial report from a large, prospective registry documenting outcomes in recipients of the Edwards Sapien 3 transcatheter aortic valve in real-world clinical practice confirm that the excellent results seen earlier in the rarified, randomized clinical trial setting are routinely reproducible in everyday practice, Dr. Olaf Wendler said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
“The big thing with the Sapien 3 is the reduction in paravalvular leakage. Our rate of moderate or severe paravalvular leakage in the registry at 30 days is only 3.1%, with 73.6% of patients having no or only trace paravalvular leakage,” reported Dr. Wendler, professor of cardiothoracic surgery at King’s College Hospital, London.
The mean gradient improved from 43.8 mm Hg at baseline to 11.7 mm Hg at discharge, while the effective orifice area climbed from 0.72 to 1.67 cm2.
He presented 30-day outcomes from the SOURCE 3 registry for 1,947 recipients of the Edwards Sapien 3 valve during transcatheter aortic valve replacement at 80 European centers in 10 countries. Their average age was 81.6 years. Updates will continue during a planned 5 years of prospective follow-up.
“This will be a very rich dataset for subgroup analyses. We now have a number of procedural variables we can analyze over time. We will have good data to get to better outcomes in terms of how best to perform the procedure if you do it with a Sapien valve,” he explained.
Among the key findings: The lower profile of the Sapien 3 delivery system, compared with earlier iterations of the Sapien valve, enabled 87% of patients in the registry to undergo TAVR via transfemoral access. And, in these 1,695 patients, whose mean logistic EuroSCORE was 17.8, the 30-day rates of all-cause mortality and disabling stroke were just 1.9% and 0.5%, respectively.
“I think there are not many series that have shown better results than these,” Dr. Wendler commented.
The non–transfemoral-access group is a very different, higher surgical risk cohort with lots more comorbid conditions. Their mean logistic EuroSCORE was 21.8. Yet in this group, the 30-day all-cause mortality and disabling stroke rates were still only 4% and 0.8%.
The transfemoral access group had markedly lower rates of life-threatening bleeding (4%), new-onset atrial fibrillation (4.8%), extended ventilation (3.5%), stage 2-3 acute kidney injury (0.8%), plus a 2-day shorter mean hospital length of stay.
Sixty percent of transfemoral access patients had their TAVR done under conscious sedation. These 1,018 patients constitute the largest dataset ever treated using conscious sedation with one valve system. The conscious sedation group had significantly lower baseline rates of carotid artery disease, prior coronary artery bypass graft surgery, and heart failure than did patients who received general anesthesia. At 30 days post-TAVR, the conscious sedation group had significantly lower rates of extended ventilation and postdilatation, and they received less contrast volume than did the general anesthesia group. However, they had a significantly higher incidence of stroke: 1.7%, compared with 0.6% for the general anesthesia group.
“Why that is the case we don’t know at the moment. We need to look into this more in the future,” the surgeon said.
A particularly impressive finding was how well Sapien 3 valve recipients with a low left ventricular ejection fraction have done. For example, 30-day all-cause mortality in the 100 patients with a baseline LVEF below 30% was 3%, not significantly different from the 1.8% rate in the 1,198 subjects with an LVEF greater than 50% or the 2.6% in patients with an LVEF of 30%-50%.
“Three percent all-cause mortality with an ejection fraction below 30% is just remarkable from my point of view,” Dr. Wendler said.
The 778 who didn’t undergo balloon aortic valvuloplasty prior to Sapien 3 implantation did not fare any worse than did those who did in terms of 30-day all-cause mortality or all strokes, but they did have significantly higher rates of life-threatening bleeding and major vascular complications.
The SOURCE 3 registry is sponsored by Edwards Lifesciences. Dr. Wendler serves as a consultant to the company.
PARIS – The initial report from a large, prospective registry documenting outcomes in recipients of the Edwards Sapien 3 transcatheter aortic valve in real-world clinical practice confirm that the excellent results seen earlier in the rarified, randomized clinical trial setting are routinely reproducible in everyday practice, Dr. Olaf Wendler said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
“The big thing with the Sapien 3 is the reduction in paravalvular leakage. Our rate of moderate or severe paravalvular leakage in the registry at 30 days is only 3.1%, with 73.6% of patients having no or only trace paravalvular leakage,” reported Dr. Wendler, professor of cardiothoracic surgery at King’s College Hospital, London.
The mean gradient improved from 43.8 mm Hg at baseline to 11.7 mm Hg at discharge, while the effective orifice area climbed from 0.72 to 1.67 cm2.
He presented 30-day outcomes from the SOURCE 3 registry for 1,947 recipients of the Edwards Sapien 3 valve during transcatheter aortic valve replacement at 80 European centers in 10 countries. Their average age was 81.6 years. Updates will continue during a planned 5 years of prospective follow-up.
“This will be a very rich dataset for subgroup analyses. We now have a number of procedural variables we can analyze over time. We will have good data to get to better outcomes in terms of how best to perform the procedure if you do it with a Sapien valve,” he explained.
Among the key findings: The lower profile of the Sapien 3 delivery system, compared with earlier iterations of the Sapien valve, enabled 87% of patients in the registry to undergo TAVR via transfemoral access. And, in these 1,695 patients, whose mean logistic EuroSCORE was 17.8, the 30-day rates of all-cause mortality and disabling stroke were just 1.9% and 0.5%, respectively.
“I think there are not many series that have shown better results than these,” Dr. Wendler commented.
The non–transfemoral-access group is a very different, higher surgical risk cohort with lots more comorbid conditions. Their mean logistic EuroSCORE was 21.8. Yet in this group, the 30-day all-cause mortality and disabling stroke rates were still only 4% and 0.8%.
The transfemoral access group had markedly lower rates of life-threatening bleeding (4%), new-onset atrial fibrillation (4.8%), extended ventilation (3.5%), stage 2-3 acute kidney injury (0.8%), plus a 2-day shorter mean hospital length of stay.
Sixty percent of transfemoral access patients had their TAVR done under conscious sedation. These 1,018 patients constitute the largest dataset ever treated using conscious sedation with one valve system. The conscious sedation group had significantly lower baseline rates of carotid artery disease, prior coronary artery bypass graft surgery, and heart failure than did patients who received general anesthesia. At 30 days post-TAVR, the conscious sedation group had significantly lower rates of extended ventilation and postdilatation, and they received less contrast volume than did the general anesthesia group. However, they had a significantly higher incidence of stroke: 1.7%, compared with 0.6% for the general anesthesia group.
“Why that is the case we don’t know at the moment. We need to look into this more in the future,” the surgeon said.
A particularly impressive finding was how well Sapien 3 valve recipients with a low left ventricular ejection fraction have done. For example, 30-day all-cause mortality in the 100 patients with a baseline LVEF below 30% was 3%, not significantly different from the 1.8% rate in the 1,198 subjects with an LVEF greater than 50% or the 2.6% in patients with an LVEF of 30%-50%.
“Three percent all-cause mortality with an ejection fraction below 30% is just remarkable from my point of view,” Dr. Wendler said.
The 778 who didn’t undergo balloon aortic valvuloplasty prior to Sapien 3 implantation did not fare any worse than did those who did in terms of 30-day all-cause mortality or all strokes, but they did have significantly higher rates of life-threatening bleeding and major vascular complications.
The SOURCE 3 registry is sponsored by Edwards Lifesciences. Dr. Wendler serves as a consultant to the company.
PARIS – The initial report from a large, prospective registry documenting outcomes in recipients of the Edwards Sapien 3 transcatheter aortic valve in real-world clinical practice confirm that the excellent results seen earlier in the rarified, randomized clinical trial setting are routinely reproducible in everyday practice, Dr. Olaf Wendler said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
“The big thing with the Sapien 3 is the reduction in paravalvular leakage. Our rate of moderate or severe paravalvular leakage in the registry at 30 days is only 3.1%, with 73.6% of patients having no or only trace paravalvular leakage,” reported Dr. Wendler, professor of cardiothoracic surgery at King’s College Hospital, London.
The mean gradient improved from 43.8 mm Hg at baseline to 11.7 mm Hg at discharge, while the effective orifice area climbed from 0.72 to 1.67 cm2.
He presented 30-day outcomes from the SOURCE 3 registry for 1,947 recipients of the Edwards Sapien 3 valve during transcatheter aortic valve replacement at 80 European centers in 10 countries. Their average age was 81.6 years. Updates will continue during a planned 5 years of prospective follow-up.
“This will be a very rich dataset for subgroup analyses. We now have a number of procedural variables we can analyze over time. We will have good data to get to better outcomes in terms of how best to perform the procedure if you do it with a Sapien valve,” he explained.
Among the key findings: The lower profile of the Sapien 3 delivery system, compared with earlier iterations of the Sapien valve, enabled 87% of patients in the registry to undergo TAVR via transfemoral access. And, in these 1,695 patients, whose mean logistic EuroSCORE was 17.8, the 30-day rates of all-cause mortality and disabling stroke were just 1.9% and 0.5%, respectively.
“I think there are not many series that have shown better results than these,” Dr. Wendler commented.
The non–transfemoral-access group is a very different, higher surgical risk cohort with lots more comorbid conditions. Their mean logistic EuroSCORE was 21.8. Yet in this group, the 30-day all-cause mortality and disabling stroke rates were still only 4% and 0.8%.
The transfemoral access group had markedly lower rates of life-threatening bleeding (4%), new-onset atrial fibrillation (4.8%), extended ventilation (3.5%), stage 2-3 acute kidney injury (0.8%), plus a 2-day shorter mean hospital length of stay.
Sixty percent of transfemoral access patients had their TAVR done under conscious sedation. These 1,018 patients constitute the largest dataset ever treated using conscious sedation with one valve system. The conscious sedation group had significantly lower baseline rates of carotid artery disease, prior coronary artery bypass graft surgery, and heart failure than did patients who received general anesthesia. At 30 days post-TAVR, the conscious sedation group had significantly lower rates of extended ventilation and postdilatation, and they received less contrast volume than did the general anesthesia group. However, they had a significantly higher incidence of stroke: 1.7%, compared with 0.6% for the general anesthesia group.
“Why that is the case we don’t know at the moment. We need to look into this more in the future,” the surgeon said.
A particularly impressive finding was how well Sapien 3 valve recipients with a low left ventricular ejection fraction have done. For example, 30-day all-cause mortality in the 100 patients with a baseline LVEF below 30% was 3%, not significantly different from the 1.8% rate in the 1,198 subjects with an LVEF greater than 50% or the 2.6% in patients with an LVEF of 30%-50%.
“Three percent all-cause mortality with an ejection fraction below 30% is just remarkable from my point of view,” Dr. Wendler said.
The 778 who didn’t undergo balloon aortic valvuloplasty prior to Sapien 3 implantation did not fare any worse than did those who did in terms of 30-day all-cause mortality or all strokes, but they did have significantly higher rates of life-threatening bleeding and major vascular complications.
The SOURCE 3 registry is sponsored by Edwards Lifesciences. Dr. Wendler serves as a consultant to the company.
AT EUROPCR 2016
Key clinical point: Only 3.1% of patients had moderate or severe paravalvular leak at 30 days after TAVR with the Sapien 3.
Major finding: The 30-day, all-cause mortality and disabling stroke rates were 1.9% and 0.5% in Sapien 3 valve recipients whose transcatheter aortic valve replacement was done by the transfemoral route.
Data source: A prospective multicenter European registry which includes 1,947 patients who underwent transcatheter aortic valve replacement with the Edwards Sapien 3 valve in real-world commercial settings.
Disclosures: The SOURCE 3 registry is sponsored by Edwards Lifesciences. Dr. Wendler serves as a consultant to the company.
Challenging ‘dogma’ of allografts in infectious endocarditis
When a patient undergoes aortic valve replacement for infective endocarditis, conventional thinking holds that cardiac surgeons should use homografts because they have greater resistance to infection, but a recent study of more than 300 cases at two academic medical centers concluded that homografts may not necessarily offer such a benefit.
The study, published in the June issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:1239-48), involved 304 consecutive adult patients on whom 30-40 different surgeons performed operations for active infective endocarditis (IE) in the aortic valve from 2002 to 2014.
“Our findings suggest that patient-specific factors, such as age and implant preference, as well as technical reconstructive considerations, should drive prosthetic choice, rather than surgical dogma,” said Joon Bum Kim, Ph.D., of Massachusetts General Hospital, Harvard Medical School, both in Boston, and Asan Medical Center in Seoul, Korea, and his colleagues.
The study found that cardiac surgeons favored homografts over conventional prostheses when the patient had prosthetic valve endocarditis (58.1% vs. 28.8%) and methicillin-resistant Staphylococcus aureus (25.6% vs. 12.1%), both significant differences.
“No significant benefit to the use of homografts was demonstrable with regard to resistance to reinfection in the setting of IE,” Dr. Kim and his colleagues said.
Because reinfection after valve replacement for IE is such a strong concern, the debate over which prosthesis is best has ensued for decades. The researchers pointed out that the evidence favoring autologous or allogeneic tissue over synthetic material in the infective field is weak, mostly built on single-armed observational studies without comparison to conventional prosthesis.
With that in mind, the researchers pooled data from two institutions to compare short- and long-term results for homograft vs. conventional prosthetic valves in patients with IE. In this study group, 86 (28.3%) had homografts, 139 (45.7%) had xenograft prostheses, and 79 (26%) mechanical prostheses. The homograft group had more than twice the rate of early death than did the conventional group – 19.8% vs. 9.2%, a significant difference (P = .019).
During follow-up, which ranged from 4.7 to 72.6 months, 60 patients (19.7%) of the total group died and 23 (7.7%) experienced reinfection, but rates did not vary between the homograft and conventional prosthesis groups, Dr. Kim and his colleagues reported.
Demographics were similar between the three groups with a few exceptions Those who received the mechanical prostheses were younger (mean age, 47.2 years vs. 55.6 and 59.8 for the homograft and xenograft groups, respectively), had lower rates of diabetes (5.1% vs. 10.5% and 12.2%) and had less-severe disease based on New York Heart Association functional class III or IV scores (34.2% vs. 54.7% and 53.2%). The types of IE pathogens also differed among the three groups; methicillin-resistant staphylococci was most common in the homograft group (25.6%), whereas the viridans group streptococci was the leading cause of IE in the mechanical (38% ) and xenograft groups (25.2% ).
The use of homografts involves a highly complex operation, typically requiring a complete aortic root replacement, which “may be the major drawback in recommending it to patients already at high risk of operative mortality,” the investigators wrote. The durability of homografts makes their use limited for younger patients, and such grafts are somewhat scarce and require cryopreservation. “Therefore, the notion that homografts are required may in practice present an obstacle to appropriate surgical management of patients who have IE,” Dr. Kim and his coauthors wrote. All patients but one in the homograft group received aortic arch replacement (98.8%) whereas 30 of the patients in the conventional group did so (13.8%).
The study findings are consistent with an earlier comparative study (Ann. Thorac. Surg. 2012;93:480-07), according to Dr. Kim and his colleagues. “These findings suggest that patient-specific factors, such as patient preferences and technical considerations, should be the principal drivers of choices of valve prostheses,” they said. “Furthermore, lack of access to homografts should not be considered an obstacle to surgical therapy for this serious condition.”
Coauthor Dr. Sundt disclosed that he is a consultant for Thrasos Therapeutics. Dr. Kim and the other coauthors had no financial disclosures.
The study by Dr. Kim and his colleagues joins a series of reports questioning conventional thinking on the use of homografts to prevent recurrent infective endocarditis (IE), but their propensity matching does not account for surgeon bias in selecting a prosthesis, Dr. James K. Kirklin of the University of Alabama at Birmingham said in his invited commentary (J Thorac. Cardiovasc Surg. 2016 May;151:1230-1).
For example, surgeon preference may account for the wide disparity in full root replacements, depending on the type of prosthesis, Dr. Kirklin said. “Some experienced homograft surgeons have preferred the intra-aortic cylinder technique or infracoronary implantation, which avoids the short-term and longer-term complexities of full root replacement and has demonstrated long-term structural durability equivalent to that of the full root replacement,” he said.
Also, experienced homograft surgeons may prefer the homograft for its resistance to infection and adaptability to severe root infection in individual patients, particularly in those with severe infection with an abscess. And he cautioned against the study’s implication that conventional prostheses are equivocal in the setting of IE.
“Of considerable importance, however, is the evidence-based conclusion that surgical referral of routine surgical aortic valve endocarditis to a center experienced with aortic homograft surgery is not necessary, and a justifiable expectation is that aortic valve endocarditis requiring operation can be safely and appropriately managed in centers with standard aortic valve surgery experience who do not have access to or experience with aortic valve homografts,” Dr. Kirklin concluded.
Dr. Kirklin had no financial relationships to disclose.

|
Dr. Christopher M. Feindel |
The series by Dr. Kim and his colleagues, one of the largest of acute infective endocarditis to date, provides further evidence that the type of prosthesis used in surgery for IE involving the aortic valve probably does not affect long-term outcomes or reinfection rates, Dr. Christopher M. Feindel of the University of Toronto said in his invited commentary (J Thorac Cardiovasc Surg. 2016 May;151:1249-50).
However, Dr. Feindel said, “numerous confounding factors” inherent in any observational study could raise questions about the conclusion.
“This article delivers an important message, although not all surgeons will agree with the statistical approach taken by Dr. Kim and his colleagues,” Dr. Feindel said. The propensity scoring method the study used lacked all baseline variables that affect treatment choice and outcomes, “a crucial assumption for effective use of the propensity score,” he said. However, given the multitude of variables in patients with acute and complex IE, he said most surgeons would be hard pressed to accept that’s even possible in the model the study used.
Dr. Feindel also said a close examination of the 115 patients who underwent root replacement would have been “very instructional,” and the lack of follow-up on valve-related complications in almost 25% of the patients is another limitation of the study.
Nonetheless, the conclusions of Dr. Kim and his colleagues are “reasonable,” Dr. Feindel said. “Clearly, this article contributes important additional information to the surgical management of IE that will help guide surgeons, especially when it comes to prosthesis of choice,” he concluded. “It is up to the reader to decide whether this report finally puts to rest the “dogma” that homografts should preferentially be used in the setting of IE.”
Dr. Feindel had no relationships to disclose.
The study by Dr. Kim and his colleagues joins a series of reports questioning conventional thinking on the use of homografts to prevent recurrent infective endocarditis (IE), but their propensity matching does not account for surgeon bias in selecting a prosthesis, Dr. James K. Kirklin of the University of Alabama at Birmingham said in his invited commentary (J Thorac. Cardiovasc Surg. 2016 May;151:1230-1).
For example, surgeon preference may account for the wide disparity in full root replacements, depending on the type of prosthesis, Dr. Kirklin said. “Some experienced homograft surgeons have preferred the intra-aortic cylinder technique or infracoronary implantation, which avoids the short-term and longer-term complexities of full root replacement and has demonstrated long-term structural durability equivalent to that of the full root replacement,” he said.
Also, experienced homograft surgeons may prefer the homograft for its resistance to infection and adaptability to severe root infection in individual patients, particularly in those with severe infection with an abscess. And he cautioned against the study’s implication that conventional prostheses are equivocal in the setting of IE.
“Of considerable importance, however, is the evidence-based conclusion that surgical referral of routine surgical aortic valve endocarditis to a center experienced with aortic homograft surgery is not necessary, and a justifiable expectation is that aortic valve endocarditis requiring operation can be safely and appropriately managed in centers with standard aortic valve surgery experience who do not have access to or experience with aortic valve homografts,” Dr. Kirklin concluded.
Dr. Kirklin had no financial relationships to disclose.

|
Dr. Christopher M. Feindel |
The series by Dr. Kim and his colleagues, one of the largest of acute infective endocarditis to date, provides further evidence that the type of prosthesis used in surgery for IE involving the aortic valve probably does not affect long-term outcomes or reinfection rates, Dr. Christopher M. Feindel of the University of Toronto said in his invited commentary (J Thorac Cardiovasc Surg. 2016 May;151:1249-50).
However, Dr. Feindel said, “numerous confounding factors” inherent in any observational study could raise questions about the conclusion.
“This article delivers an important message, although not all surgeons will agree with the statistical approach taken by Dr. Kim and his colleagues,” Dr. Feindel said. The propensity scoring method the study used lacked all baseline variables that affect treatment choice and outcomes, “a crucial assumption for effective use of the propensity score,” he said. However, given the multitude of variables in patients with acute and complex IE, he said most surgeons would be hard pressed to accept that’s even possible in the model the study used.
Dr. Feindel also said a close examination of the 115 patients who underwent root replacement would have been “very instructional,” and the lack of follow-up on valve-related complications in almost 25% of the patients is another limitation of the study.
Nonetheless, the conclusions of Dr. Kim and his colleagues are “reasonable,” Dr. Feindel said. “Clearly, this article contributes important additional information to the surgical management of IE that will help guide surgeons, especially when it comes to prosthesis of choice,” he concluded. “It is up to the reader to decide whether this report finally puts to rest the “dogma” that homografts should preferentially be used in the setting of IE.”
Dr. Feindel had no relationships to disclose.
The study by Dr. Kim and his colleagues joins a series of reports questioning conventional thinking on the use of homografts to prevent recurrent infective endocarditis (IE), but their propensity matching does not account for surgeon bias in selecting a prosthesis, Dr. James K. Kirklin of the University of Alabama at Birmingham said in his invited commentary (J Thorac. Cardiovasc Surg. 2016 May;151:1230-1).
For example, surgeon preference may account for the wide disparity in full root replacements, depending on the type of prosthesis, Dr. Kirklin said. “Some experienced homograft surgeons have preferred the intra-aortic cylinder technique or infracoronary implantation, which avoids the short-term and longer-term complexities of full root replacement and has demonstrated long-term structural durability equivalent to that of the full root replacement,” he said.
Also, experienced homograft surgeons may prefer the homograft for its resistance to infection and adaptability to severe root infection in individual patients, particularly in those with severe infection with an abscess. And he cautioned against the study’s implication that conventional prostheses are equivocal in the setting of IE.
“Of considerable importance, however, is the evidence-based conclusion that surgical referral of routine surgical aortic valve endocarditis to a center experienced with aortic homograft surgery is not necessary, and a justifiable expectation is that aortic valve endocarditis requiring operation can be safely and appropriately managed in centers with standard aortic valve surgery experience who do not have access to or experience with aortic valve homografts,” Dr. Kirklin concluded.
Dr. Kirklin had no financial relationships to disclose.

|
Dr. Christopher M. Feindel |
The series by Dr. Kim and his colleagues, one of the largest of acute infective endocarditis to date, provides further evidence that the type of prosthesis used in surgery for IE involving the aortic valve probably does not affect long-term outcomes or reinfection rates, Dr. Christopher M. Feindel of the University of Toronto said in his invited commentary (J Thorac Cardiovasc Surg. 2016 May;151:1249-50).
However, Dr. Feindel said, “numerous confounding factors” inherent in any observational study could raise questions about the conclusion.
“This article delivers an important message, although not all surgeons will agree with the statistical approach taken by Dr. Kim and his colleagues,” Dr. Feindel said. The propensity scoring method the study used lacked all baseline variables that affect treatment choice and outcomes, “a crucial assumption for effective use of the propensity score,” he said. However, given the multitude of variables in patients with acute and complex IE, he said most surgeons would be hard pressed to accept that’s even possible in the model the study used.
Dr. Feindel also said a close examination of the 115 patients who underwent root replacement would have been “very instructional,” and the lack of follow-up on valve-related complications in almost 25% of the patients is another limitation of the study.
Nonetheless, the conclusions of Dr. Kim and his colleagues are “reasonable,” Dr. Feindel said. “Clearly, this article contributes important additional information to the surgical management of IE that will help guide surgeons, especially when it comes to prosthesis of choice,” he concluded. “It is up to the reader to decide whether this report finally puts to rest the “dogma” that homografts should preferentially be used in the setting of IE.”
Dr. Feindel had no relationships to disclose.
When a patient undergoes aortic valve replacement for infective endocarditis, conventional thinking holds that cardiac surgeons should use homografts because they have greater resistance to infection, but a recent study of more than 300 cases at two academic medical centers concluded that homografts may not necessarily offer such a benefit.
The study, published in the June issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:1239-48), involved 304 consecutive adult patients on whom 30-40 different surgeons performed operations for active infective endocarditis (IE) in the aortic valve from 2002 to 2014.
“Our findings suggest that patient-specific factors, such as age and implant preference, as well as technical reconstructive considerations, should drive prosthetic choice, rather than surgical dogma,” said Joon Bum Kim, Ph.D., of Massachusetts General Hospital, Harvard Medical School, both in Boston, and Asan Medical Center in Seoul, Korea, and his colleagues.
The study found that cardiac surgeons favored homografts over conventional prostheses when the patient had prosthetic valve endocarditis (58.1% vs. 28.8%) and methicillin-resistant Staphylococcus aureus (25.6% vs. 12.1%), both significant differences.
“No significant benefit to the use of homografts was demonstrable with regard to resistance to reinfection in the setting of IE,” Dr. Kim and his colleagues said.
Because reinfection after valve replacement for IE is such a strong concern, the debate over which prosthesis is best has ensued for decades. The researchers pointed out that the evidence favoring autologous or allogeneic tissue over synthetic material in the infective field is weak, mostly built on single-armed observational studies without comparison to conventional prosthesis.
With that in mind, the researchers pooled data from two institutions to compare short- and long-term results for homograft vs. conventional prosthetic valves in patients with IE. In this study group, 86 (28.3%) had homografts, 139 (45.7%) had xenograft prostheses, and 79 (26%) mechanical prostheses. The homograft group had more than twice the rate of early death than did the conventional group – 19.8% vs. 9.2%, a significant difference (P = .019).
During follow-up, which ranged from 4.7 to 72.6 months, 60 patients (19.7%) of the total group died and 23 (7.7%) experienced reinfection, but rates did not vary between the homograft and conventional prosthesis groups, Dr. Kim and his colleagues reported.
Demographics were similar between the three groups with a few exceptions Those who received the mechanical prostheses were younger (mean age, 47.2 years vs. 55.6 and 59.8 for the homograft and xenograft groups, respectively), had lower rates of diabetes (5.1% vs. 10.5% and 12.2%) and had less-severe disease based on New York Heart Association functional class III or IV scores (34.2% vs. 54.7% and 53.2%). The types of IE pathogens also differed among the three groups; methicillin-resistant staphylococci was most common in the homograft group (25.6%), whereas the viridans group streptococci was the leading cause of IE in the mechanical (38% ) and xenograft groups (25.2% ).
The use of homografts involves a highly complex operation, typically requiring a complete aortic root replacement, which “may be the major drawback in recommending it to patients already at high risk of operative mortality,” the investigators wrote. The durability of homografts makes their use limited for younger patients, and such grafts are somewhat scarce and require cryopreservation. “Therefore, the notion that homografts are required may in practice present an obstacle to appropriate surgical management of patients who have IE,” Dr. Kim and his coauthors wrote. All patients but one in the homograft group received aortic arch replacement (98.8%) whereas 30 of the patients in the conventional group did so (13.8%).
The study findings are consistent with an earlier comparative study (Ann. Thorac. Surg. 2012;93:480-07), according to Dr. Kim and his colleagues. “These findings suggest that patient-specific factors, such as patient preferences and technical considerations, should be the principal drivers of choices of valve prostheses,” they said. “Furthermore, lack of access to homografts should not be considered an obstacle to surgical therapy for this serious condition.”
Coauthor Dr. Sundt disclosed that he is a consultant for Thrasos Therapeutics. Dr. Kim and the other coauthors had no financial disclosures.
When a patient undergoes aortic valve replacement for infective endocarditis, conventional thinking holds that cardiac surgeons should use homografts because they have greater resistance to infection, but a recent study of more than 300 cases at two academic medical centers concluded that homografts may not necessarily offer such a benefit.
The study, published in the June issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:1239-48), involved 304 consecutive adult patients on whom 30-40 different surgeons performed operations for active infective endocarditis (IE) in the aortic valve from 2002 to 2014.
“Our findings suggest that patient-specific factors, such as age and implant preference, as well as technical reconstructive considerations, should drive prosthetic choice, rather than surgical dogma,” said Joon Bum Kim, Ph.D., of Massachusetts General Hospital, Harvard Medical School, both in Boston, and Asan Medical Center in Seoul, Korea, and his colleagues.
The study found that cardiac surgeons favored homografts over conventional prostheses when the patient had prosthetic valve endocarditis (58.1% vs. 28.8%) and methicillin-resistant Staphylococcus aureus (25.6% vs. 12.1%), both significant differences.
“No significant benefit to the use of homografts was demonstrable with regard to resistance to reinfection in the setting of IE,” Dr. Kim and his colleagues said.
Because reinfection after valve replacement for IE is such a strong concern, the debate over which prosthesis is best has ensued for decades. The researchers pointed out that the evidence favoring autologous or allogeneic tissue over synthetic material in the infective field is weak, mostly built on single-armed observational studies without comparison to conventional prosthesis.
With that in mind, the researchers pooled data from two institutions to compare short- and long-term results for homograft vs. conventional prosthetic valves in patients with IE. In this study group, 86 (28.3%) had homografts, 139 (45.7%) had xenograft prostheses, and 79 (26%) mechanical prostheses. The homograft group had more than twice the rate of early death than did the conventional group – 19.8% vs. 9.2%, a significant difference (P = .019).
During follow-up, which ranged from 4.7 to 72.6 months, 60 patients (19.7%) of the total group died and 23 (7.7%) experienced reinfection, but rates did not vary between the homograft and conventional prosthesis groups, Dr. Kim and his colleagues reported.
Demographics were similar between the three groups with a few exceptions Those who received the mechanical prostheses were younger (mean age, 47.2 years vs. 55.6 and 59.8 for the homograft and xenograft groups, respectively), had lower rates of diabetes (5.1% vs. 10.5% and 12.2%) and had less-severe disease based on New York Heart Association functional class III or IV scores (34.2% vs. 54.7% and 53.2%). The types of IE pathogens also differed among the three groups; methicillin-resistant staphylococci was most common in the homograft group (25.6%), whereas the viridans group streptococci was the leading cause of IE in the mechanical (38% ) and xenograft groups (25.2% ).
The use of homografts involves a highly complex operation, typically requiring a complete aortic root replacement, which “may be the major drawback in recommending it to patients already at high risk of operative mortality,” the investigators wrote. The durability of homografts makes their use limited for younger patients, and such grafts are somewhat scarce and require cryopreservation. “Therefore, the notion that homografts are required may in practice present an obstacle to appropriate surgical management of patients who have IE,” Dr. Kim and his coauthors wrote. All patients but one in the homograft group received aortic arch replacement (98.8%) whereas 30 of the patients in the conventional group did so (13.8%).
The study findings are consistent with an earlier comparative study (Ann. Thorac. Surg. 2012;93:480-07), according to Dr. Kim and his colleagues. “These findings suggest that patient-specific factors, such as patient preferences and technical considerations, should be the principal drivers of choices of valve prostheses,” they said. “Furthermore, lack of access to homografts should not be considered an obstacle to surgical therapy for this serious condition.”
Coauthor Dr. Sundt disclosed that he is a consultant for Thrasos Therapeutics. Dr. Kim and the other coauthors had no financial disclosures.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Use of homografts showed no significant benefit, compared with conventional prosthetic valves when the patient has infective endocarditis involving the aortic valve.
Major finding: The homograft group had more than twice the rate of early death than the conventional group, 19.8% vs. 9.2%, but in longer-term follow-up, the survival rates did not differ between groups.
Data source: 304 consecutive adult patients from the perspective database of two tertiary academic centers who had surgery for active infective endocarditis involving the aortic valve from 2002 to 2014.
Disclosures: Coauthor Dr. Sundt, disclosed he is a consultant for Thrasos Therapeutics. Dr. Kim and the other coauthors had no financial disclosures.
Additional antibiotics needed when implanting cryopreserved human aortic grafts
Infections of aortic prosthetic grafts can be a devastating complication, and while cryopreserved human allografts (CHA) can continue to possess antibacterial activity even after 5 years or more in storage, cardiac surgeons may want to apply additional antibiotic agents during implantation to boost bacterial resistance, investigators from Germany reported in the May issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:1251-9).
The researchers compared three different antibiotic regimens used in processing CHA aortic tissue and valves to determine the impact each can have on long-term bacterial resistance.
“Antibiotic combinations applied during CHA processing have a significant influence on their infection resistance,” said Dr. Viola Steffen of Hannover (Germany) Medical School and her colleagues. The average storage time of CHAs was 8.5 years, with the longest having been stored for 10 years.
The study involved microbiologic tests in vitro of three different antibiotic regimens used in processing CHA: gentamicin-piperacillin-vancomycin-metronidazole-amphotericin B (group A); gentamicin-piperacillin-flucloxacillin-metronidazole-amphotericin B (group B); and meropenem-vancomycin-tobramycin-colistin-amphotericin B (group C). The combinations are used to counteract Staphylococcus epidermidis and Staphylococcus aureus.
The study exposed pieces of 10 CHAs to different microbes and determined that regimen groups B and C were more effective than group A in eradicating gram-positive organisms. Specifically, group C was most resistant to Escherichia coli, whereas group B was most effective against Pseudomonas aeruginosa. Aortic tissue showed significantly less contamination with staphylococcal bacteria than valve grafts, the study reported.
Dr. Steffen and her colleagues said that tissue banks use antibiotic protocols during CHA processing, but they differ substantially. “Our results support the hypothesis that infection resistance of CHAs depends on the antibiotic pretreatment during processing and their residual activity,” they said.
The study had four key findings:
• The infection resistance of aortic wall and valve tissue differed significantly.
• In aortic wall specimens, group A specimens exhibited increased adherence of S. epidermidis, with vancomycin in group A and flucloxacillin in group B being the only differentiating agents between the two.
• Cryopreserved aortic vessels had a propensity toward reduced infection resistance against P. aeruginosa.
• Morphologic changes occurred in the microorganisms, especially rod-shaped E. coli, indicating that regional antibiotic release alters bacterial growth without eliminating all adherent bacteria.
Dr. Steffen and her colleagues noted that while previous studies determined that residual concentrations of antibiotics used in processing CHA heart valves and blood vessels are still present after they are prepared for implantation, they neither measured the antibacterial affect, clarified the period of cryopreservation nor differentiated between valve and vessel tissue (PLoS One. 2014;9:e112679; Transfus Med Hemother. 2011;38:379-86).
The Hannover researchers found that only a few gram-positive microorganisms adhered to aortic wall specimens, although they found “extensive adherence” of S. epidermidis in group A specimens. Valves, however, “were completely colonized” with both strains of staphylococcal bacteria, although the severity of contamination varied depending on the regimen used.
The findings raise some questions about the antibiotic properties of CHAs. “Because their infection resistance depends on the antibiotic combination selected during processing, further investigations concerning this treatment are necessary to improve the antimicrobial activity against frequent and highly virulent infection-causing bacteria,” Dr. Steffen and her colleagues said.
Dr. Steffen and her coauthors had no financial relationships to disclose.
Infections of aortic prosthetic grafts can be a devastating complication, and while cryopreserved human allografts (CHA) can continue to possess antibacterial activity even after 5 years or more in storage, cardiac surgeons may want to apply additional antibiotic agents during implantation to boost bacterial resistance, investigators from Germany reported in the May issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:1251-9).
The researchers compared three different antibiotic regimens used in processing CHA aortic tissue and valves to determine the impact each can have on long-term bacterial resistance.
“Antibiotic combinations applied during CHA processing have a significant influence on their infection resistance,” said Dr. Viola Steffen of Hannover (Germany) Medical School and her colleagues. The average storage time of CHAs was 8.5 years, with the longest having been stored for 10 years.
The study involved microbiologic tests in vitro of three different antibiotic regimens used in processing CHA: gentamicin-piperacillin-vancomycin-metronidazole-amphotericin B (group A); gentamicin-piperacillin-flucloxacillin-metronidazole-amphotericin B (group B); and meropenem-vancomycin-tobramycin-colistin-amphotericin B (group C). The combinations are used to counteract Staphylococcus epidermidis and Staphylococcus aureus.
The study exposed pieces of 10 CHAs to different microbes and determined that regimen groups B and C were more effective than group A in eradicating gram-positive organisms. Specifically, group C was most resistant to Escherichia coli, whereas group B was most effective against Pseudomonas aeruginosa. Aortic tissue showed significantly less contamination with staphylococcal bacteria than valve grafts, the study reported.
Dr. Steffen and her colleagues said that tissue banks use antibiotic protocols during CHA processing, but they differ substantially. “Our results support the hypothesis that infection resistance of CHAs depends on the antibiotic pretreatment during processing and their residual activity,” they said.
The study had four key findings:
• The infection resistance of aortic wall and valve tissue differed significantly.
• In aortic wall specimens, group A specimens exhibited increased adherence of S. epidermidis, with vancomycin in group A and flucloxacillin in group B being the only differentiating agents between the two.
• Cryopreserved aortic vessels had a propensity toward reduced infection resistance against P. aeruginosa.
• Morphologic changes occurred in the microorganisms, especially rod-shaped E. coli, indicating that regional antibiotic release alters bacterial growth without eliminating all adherent bacteria.
Dr. Steffen and her colleagues noted that while previous studies determined that residual concentrations of antibiotics used in processing CHA heart valves and blood vessels are still present after they are prepared for implantation, they neither measured the antibacterial affect, clarified the period of cryopreservation nor differentiated between valve and vessel tissue (PLoS One. 2014;9:e112679; Transfus Med Hemother. 2011;38:379-86).
The Hannover researchers found that only a few gram-positive microorganisms adhered to aortic wall specimens, although they found “extensive adherence” of S. epidermidis in group A specimens. Valves, however, “were completely colonized” with both strains of staphylococcal bacteria, although the severity of contamination varied depending on the regimen used.
The findings raise some questions about the antibiotic properties of CHAs. “Because their infection resistance depends on the antibiotic combination selected during processing, further investigations concerning this treatment are necessary to improve the antimicrobial activity against frequent and highly virulent infection-causing bacteria,” Dr. Steffen and her colleagues said.
Dr. Steffen and her coauthors had no financial relationships to disclose.
Infections of aortic prosthetic grafts can be a devastating complication, and while cryopreserved human allografts (CHA) can continue to possess antibacterial activity even after 5 years or more in storage, cardiac surgeons may want to apply additional antibiotic agents during implantation to boost bacterial resistance, investigators from Germany reported in the May issue of the Journal of Thoracic and Cardiovascular Surgery (2016;151:1251-9).
The researchers compared three different antibiotic regimens used in processing CHA aortic tissue and valves to determine the impact each can have on long-term bacterial resistance.
“Antibiotic combinations applied during CHA processing have a significant influence on their infection resistance,” said Dr. Viola Steffen of Hannover (Germany) Medical School and her colleagues. The average storage time of CHAs was 8.5 years, with the longest having been stored for 10 years.
The study involved microbiologic tests in vitro of three different antibiotic regimens used in processing CHA: gentamicin-piperacillin-vancomycin-metronidazole-amphotericin B (group A); gentamicin-piperacillin-flucloxacillin-metronidazole-amphotericin B (group B); and meropenem-vancomycin-tobramycin-colistin-amphotericin B (group C). The combinations are used to counteract Staphylococcus epidermidis and Staphylococcus aureus.
The study exposed pieces of 10 CHAs to different microbes and determined that regimen groups B and C were more effective than group A in eradicating gram-positive organisms. Specifically, group C was most resistant to Escherichia coli, whereas group B was most effective against Pseudomonas aeruginosa. Aortic tissue showed significantly less contamination with staphylococcal bacteria than valve grafts, the study reported.
Dr. Steffen and her colleagues said that tissue banks use antibiotic protocols during CHA processing, but they differ substantially. “Our results support the hypothesis that infection resistance of CHAs depends on the antibiotic pretreatment during processing and their residual activity,” they said.
The study had four key findings:
• The infection resistance of aortic wall and valve tissue differed significantly.
• In aortic wall specimens, group A specimens exhibited increased adherence of S. epidermidis, with vancomycin in group A and flucloxacillin in group B being the only differentiating agents between the two.
• Cryopreserved aortic vessels had a propensity toward reduced infection resistance against P. aeruginosa.
• Morphologic changes occurred in the microorganisms, especially rod-shaped E. coli, indicating that regional antibiotic release alters bacterial growth without eliminating all adherent bacteria.
Dr. Steffen and her colleagues noted that while previous studies determined that residual concentrations of antibiotics used in processing CHA heart valves and blood vessels are still present after they are prepared for implantation, they neither measured the antibacterial affect, clarified the period of cryopreservation nor differentiated between valve and vessel tissue (PLoS One. 2014;9:e112679; Transfus Med Hemother. 2011;38:379-86).
The Hannover researchers found that only a few gram-positive microorganisms adhered to aortic wall specimens, although they found “extensive adherence” of S. epidermidis in group A specimens. Valves, however, “were completely colonized” with both strains of staphylococcal bacteria, although the severity of contamination varied depending on the regimen used.
The findings raise some questions about the antibiotic properties of CHAs. “Because their infection resistance depends on the antibiotic combination selected during processing, further investigations concerning this treatment are necessary to improve the antimicrobial activity against frequent and highly virulent infection-causing bacteria,” Dr. Steffen and her colleagues said.
Dr. Steffen and her coauthors had no financial relationships to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: The infection resistance of cryopreserved human allografts (CHAs) depends on antibiotic pretreatment during processing.
Major finding: Cardiac surgeons can recommend CHAs to patients either with active destructive infections or at high risk of reinfection, but they may want to apply additional antibiotic agents during implantation to enhance bacterial resistance.
Data source: Pieces of 10 CHAs were microbiologically tested in vitro and exposed to bacterial contamination and the number of attached bacteria quantified.
Disclosures: Dr. Steffen and her coauthors had no financial relationships to disclose.
Does congenital cardiac surgery training need a makeover?
Trainees in congenital cardiac surgery fellowship programs are doing more operations since the programs became accredited in 2007, but no clear parameters have emerged to determine if certification has improved the quality of training, according to an evaluation of fellowship training programs published in the June issue of the Journal of Thoracic and Cardiovascular Surgery (2016 Jun;151:1488-95).
Overall, the training has become standardized, the fellows’ operative experience is “robust,” and fellows are mostly satisfied since the Accreditation Council of Graduate Medical Education (ACGME) recognized congenital cardiac surgery as a fellowship in 2007, lead study author Dr. Brian Kogon of Emory University, Atlanta, said.
However, Dr. Kogon and his colleagues also found some shortcomings in fellowship training. They received survey responses from 36 of 44 fellows in 12 accredited programs nationwide. To determine if fellows were meeting minimum case requirements, they also reviewed operative logs of 38 of the 44 fellows. They compared their findings to a study of congenital cardiac surgery fellowship programs they did pre-ACGME accreditation (J Thorac Cardiovasc Surg. 2006 Dec;132:1280). “The number of operations performed by the fellows during their training was underwhelming, and most of the fellows were dissatisfied with their operative experience,” Dr. Kogon and his colleagues wrote in the earlier study.
The study found that all fellows achieved the minimum number of 75 total cases the standards require for graduation, with a median of 136; and the minimum standard of 36 specific qualifying cases with a median of 63. However, seven did not meet the minimum of five complex neonate cases. Among other types of operations for which fellows failed to meet the minimum cases were atrioventricular septal defect repair, arch reconstruction including coarctation procedures and systemic-to-pulmonary artery shunt procedures.
The comparative lack of adult cardiac surgery operations was also considered a potential problem, the authors noted, pointing out that “the number of adults who have congenital heart disease now exceeds the number of children who have the disease, and many of these patients will require an operation.”
Another shortcoming the study found was a drop-off in international fellowships since 2007. “This change places us at risk of becoming intellectually isolated and losing international relationships that are critical to the future of our specialty,” Dr. Kogon and his colleagues wrote. Graduated fellows also acknowledged dissatisfaction with their lack of exposure to neonate surgery.
The study also determined the following demographics of the fellows: 83% are men and the median age at graduation was 40 years, with a range of 35-48 years. Only 25% of graduates participated in nonsurgical rotations such as cardiac catheterization and echocardiography.
“Although the operative experience seems to be much more robust, and this finding has been corroborated in other surgical disciplines after the advent of ACGME accreditation, comparing training before and after the accreditation process came into existence is difficult,” Dr. Kogon and his colleagues said.
The study also noted that the Thoracic Surgery Directors Association developed a congenital curriculum for congenital cardiothoracic surgery fellows, but only 28% used that curriculum and only 61% used any formal curriculum. “Unfortunately, regardless of the curriculum, only 50% of the graduates found it helpful,” Dr. Kogon and his colleagues said.
And regardless of the curriculum, only half of the graduates have passed the written qualifying and oral certifying examinations after completing their fellowship. “Although the curriculum is quite robust, the latter statistic suggests that we need either more emphasis on education by the program directors or a better and/or different curriculum,” Dr. Kogon and his colleagues said. However, they added that “after training, former fellows have adequate case volumes and mixes and seem to be thriving in the field.”
Dr. Kogon and his study coauthors had no financial disclosures.
In his invited commentary, Dr. Charles D. Fraser Jr. of Texas Children’s Hospital, Baylor University, Houston, called the study findings that only 50% of congenital cardiac surgery fellowship graduates had passed the congenital examination “quite disturbing” and the demographic data and surgical and nonsurgical experience of the trainees “thought provoking” (J Thorac Cardiovasc Surg. 2016;151:1496-7)
“Is the bar too high or too low?” Dr. Fraser asked. He suggested the fellowship training system for congenital cardiac surgeons may be a work in progress. “For one, having a median age of 40 years for graduates is unacceptable,” he said. For half of trainees to not pass the examination “at this advanced age is tragic.” That 25% of fellows participate in nonsurgical rotations “also is concerning.”
|
Dr. Charles D. Fraser |
A challenge is that after fellows complete their training in general and cardiothoracic surgery, opportunities to operate on newborns in a new fellowship setting are extremely limited, Dr. Fraser said. “To expect someone to be able to perform complex newborn heart surgery with excellent outcomes in a brand-new environment after just learning how to perform adult cardiac surgery is unrealistic,” he said.
Dr. Fraser said 1 formal year of training for congenital cardiac surgery fellows may not be enough. “Our colleagues in general pediatric surgery have a 2-year fellowship, and our specialty is every bit as complex as theirs,” he said. The basic American Board of Thoracic Surgery thoracic fellowship should have more latitude in its congenital heart surgery rotations, including exposure to pediatrics, neonatal/pediatric critical care, and the nonsurgical rotations the study referred to. Congenital heart surgery fellowships should also embrace adult congenital heart surgery with a more formalized experience requirement, he said.
“As a specialty, we owe it to our fine young surgeon candidates to offer the most robust and fair pathway to success while never compromising on the public trust and patient well-being,” Dr. Fraser said.
Dr. Fraser is chief of the division of congenital heart surgery at Baylor and codirector of the Texas Children’s Heart Center. He had no financial relationships to disclose.
In his invited commentary, Dr. Charles D. Fraser Jr. of Texas Children’s Hospital, Baylor University, Houston, called the study findings that only 50% of congenital cardiac surgery fellowship graduates had passed the congenital examination “quite disturbing” and the demographic data and surgical and nonsurgical experience of the trainees “thought provoking” (J Thorac Cardiovasc Surg. 2016;151:1496-7)
“Is the bar too high or too low?” Dr. Fraser asked. He suggested the fellowship training system for congenital cardiac surgeons may be a work in progress. “For one, having a median age of 40 years for graduates is unacceptable,” he said. For half of trainees to not pass the examination “at this advanced age is tragic.” That 25% of fellows participate in nonsurgical rotations “also is concerning.”
|
Dr. Charles D. Fraser |
A challenge is that after fellows complete their training in general and cardiothoracic surgery, opportunities to operate on newborns in a new fellowship setting are extremely limited, Dr. Fraser said. “To expect someone to be able to perform complex newborn heart surgery with excellent outcomes in a brand-new environment after just learning how to perform adult cardiac surgery is unrealistic,” he said.
Dr. Fraser said 1 formal year of training for congenital cardiac surgery fellows may not be enough. “Our colleagues in general pediatric surgery have a 2-year fellowship, and our specialty is every bit as complex as theirs,” he said. The basic American Board of Thoracic Surgery thoracic fellowship should have more latitude in its congenital heart surgery rotations, including exposure to pediatrics, neonatal/pediatric critical care, and the nonsurgical rotations the study referred to. Congenital heart surgery fellowships should also embrace adult congenital heart surgery with a more formalized experience requirement, he said.
“As a specialty, we owe it to our fine young surgeon candidates to offer the most robust and fair pathway to success while never compromising on the public trust and patient well-being,” Dr. Fraser said.
Dr. Fraser is chief of the division of congenital heart surgery at Baylor and codirector of the Texas Children’s Heart Center. He had no financial relationships to disclose.
In his invited commentary, Dr. Charles D. Fraser Jr. of Texas Children’s Hospital, Baylor University, Houston, called the study findings that only 50% of congenital cardiac surgery fellowship graduates had passed the congenital examination “quite disturbing” and the demographic data and surgical and nonsurgical experience of the trainees “thought provoking” (J Thorac Cardiovasc Surg. 2016;151:1496-7)
“Is the bar too high or too low?” Dr. Fraser asked. He suggested the fellowship training system for congenital cardiac surgeons may be a work in progress. “For one, having a median age of 40 years for graduates is unacceptable,” he said. For half of trainees to not pass the examination “at this advanced age is tragic.” That 25% of fellows participate in nonsurgical rotations “also is concerning.”
|
Dr. Charles D. Fraser |
A challenge is that after fellows complete their training in general and cardiothoracic surgery, opportunities to operate on newborns in a new fellowship setting are extremely limited, Dr. Fraser said. “To expect someone to be able to perform complex newborn heart surgery with excellent outcomes in a brand-new environment after just learning how to perform adult cardiac surgery is unrealistic,” he said.
Dr. Fraser said 1 formal year of training for congenital cardiac surgery fellows may not be enough. “Our colleagues in general pediatric surgery have a 2-year fellowship, and our specialty is every bit as complex as theirs,” he said. The basic American Board of Thoracic Surgery thoracic fellowship should have more latitude in its congenital heart surgery rotations, including exposure to pediatrics, neonatal/pediatric critical care, and the nonsurgical rotations the study referred to. Congenital heart surgery fellowships should also embrace adult congenital heart surgery with a more formalized experience requirement, he said.
“As a specialty, we owe it to our fine young surgeon candidates to offer the most robust and fair pathway to success while never compromising on the public trust and patient well-being,” Dr. Fraser said.
Dr. Fraser is chief of the division of congenital heart surgery at Baylor and codirector of the Texas Children’s Heart Center. He had no financial relationships to disclose.
Trainees in congenital cardiac surgery fellowship programs are doing more operations since the programs became accredited in 2007, but no clear parameters have emerged to determine if certification has improved the quality of training, according to an evaluation of fellowship training programs published in the June issue of the Journal of Thoracic and Cardiovascular Surgery (2016 Jun;151:1488-95).
Overall, the training has become standardized, the fellows’ operative experience is “robust,” and fellows are mostly satisfied since the Accreditation Council of Graduate Medical Education (ACGME) recognized congenital cardiac surgery as a fellowship in 2007, lead study author Dr. Brian Kogon of Emory University, Atlanta, said.
However, Dr. Kogon and his colleagues also found some shortcomings in fellowship training. They received survey responses from 36 of 44 fellows in 12 accredited programs nationwide. To determine if fellows were meeting minimum case requirements, they also reviewed operative logs of 38 of the 44 fellows. They compared their findings to a study of congenital cardiac surgery fellowship programs they did pre-ACGME accreditation (J Thorac Cardiovasc Surg. 2006 Dec;132:1280). “The number of operations performed by the fellows during their training was underwhelming, and most of the fellows were dissatisfied with their operative experience,” Dr. Kogon and his colleagues wrote in the earlier study.
The study found that all fellows achieved the minimum number of 75 total cases the standards require for graduation, with a median of 136; and the minimum standard of 36 specific qualifying cases with a median of 63. However, seven did not meet the minimum of five complex neonate cases. Among other types of operations for which fellows failed to meet the minimum cases were atrioventricular septal defect repair, arch reconstruction including coarctation procedures and systemic-to-pulmonary artery shunt procedures.
The comparative lack of adult cardiac surgery operations was also considered a potential problem, the authors noted, pointing out that “the number of adults who have congenital heart disease now exceeds the number of children who have the disease, and many of these patients will require an operation.”
Another shortcoming the study found was a drop-off in international fellowships since 2007. “This change places us at risk of becoming intellectually isolated and losing international relationships that are critical to the future of our specialty,” Dr. Kogon and his colleagues wrote. Graduated fellows also acknowledged dissatisfaction with their lack of exposure to neonate surgery.
The study also determined the following demographics of the fellows: 83% are men and the median age at graduation was 40 years, with a range of 35-48 years. Only 25% of graduates participated in nonsurgical rotations such as cardiac catheterization and echocardiography.
“Although the operative experience seems to be much more robust, and this finding has been corroborated in other surgical disciplines after the advent of ACGME accreditation, comparing training before and after the accreditation process came into existence is difficult,” Dr. Kogon and his colleagues said.
The study also noted that the Thoracic Surgery Directors Association developed a congenital curriculum for congenital cardiothoracic surgery fellows, but only 28% used that curriculum and only 61% used any formal curriculum. “Unfortunately, regardless of the curriculum, only 50% of the graduates found it helpful,” Dr. Kogon and his colleagues said.
And regardless of the curriculum, only half of the graduates have passed the written qualifying and oral certifying examinations after completing their fellowship. “Although the curriculum is quite robust, the latter statistic suggests that we need either more emphasis on education by the program directors or a better and/or different curriculum,” Dr. Kogon and his colleagues said. However, they added that “after training, former fellows have adequate case volumes and mixes and seem to be thriving in the field.”
Dr. Kogon and his study coauthors had no financial disclosures.
Trainees in congenital cardiac surgery fellowship programs are doing more operations since the programs became accredited in 2007, but no clear parameters have emerged to determine if certification has improved the quality of training, according to an evaluation of fellowship training programs published in the June issue of the Journal of Thoracic and Cardiovascular Surgery (2016 Jun;151:1488-95).
Overall, the training has become standardized, the fellows’ operative experience is “robust,” and fellows are mostly satisfied since the Accreditation Council of Graduate Medical Education (ACGME) recognized congenital cardiac surgery as a fellowship in 2007, lead study author Dr. Brian Kogon of Emory University, Atlanta, said.
However, Dr. Kogon and his colleagues also found some shortcomings in fellowship training. They received survey responses from 36 of 44 fellows in 12 accredited programs nationwide. To determine if fellows were meeting minimum case requirements, they also reviewed operative logs of 38 of the 44 fellows. They compared their findings to a study of congenital cardiac surgery fellowship programs they did pre-ACGME accreditation (J Thorac Cardiovasc Surg. 2006 Dec;132:1280). “The number of operations performed by the fellows during their training was underwhelming, and most of the fellows were dissatisfied with their operative experience,” Dr. Kogon and his colleagues wrote in the earlier study.
The study found that all fellows achieved the minimum number of 75 total cases the standards require for graduation, with a median of 136; and the minimum standard of 36 specific qualifying cases with a median of 63. However, seven did not meet the minimum of five complex neonate cases. Among other types of operations for which fellows failed to meet the minimum cases were atrioventricular septal defect repair, arch reconstruction including coarctation procedures and systemic-to-pulmonary artery shunt procedures.
The comparative lack of adult cardiac surgery operations was also considered a potential problem, the authors noted, pointing out that “the number of adults who have congenital heart disease now exceeds the number of children who have the disease, and many of these patients will require an operation.”
Another shortcoming the study found was a drop-off in international fellowships since 2007. “This change places us at risk of becoming intellectually isolated and losing international relationships that are critical to the future of our specialty,” Dr. Kogon and his colleagues wrote. Graduated fellows also acknowledged dissatisfaction with their lack of exposure to neonate surgery.
The study also determined the following demographics of the fellows: 83% are men and the median age at graduation was 40 years, with a range of 35-48 years. Only 25% of graduates participated in nonsurgical rotations such as cardiac catheterization and echocardiography.
“Although the operative experience seems to be much more robust, and this finding has been corroborated in other surgical disciplines after the advent of ACGME accreditation, comparing training before and after the accreditation process came into existence is difficult,” Dr. Kogon and his colleagues said.
The study also noted that the Thoracic Surgery Directors Association developed a congenital curriculum for congenital cardiothoracic surgery fellows, but only 28% used that curriculum and only 61% used any formal curriculum. “Unfortunately, regardless of the curriculum, only 50% of the graduates found it helpful,” Dr. Kogon and his colleagues said.
And regardless of the curriculum, only half of the graduates have passed the written qualifying and oral certifying examinations after completing their fellowship. “Although the curriculum is quite robust, the latter statistic suggests that we need either more emphasis on education by the program directors or a better and/or different curriculum,” Dr. Kogon and his colleagues said. However, they added that “after training, former fellows have adequate case volumes and mixes and seem to be thriving in the field.”
Dr. Kogon and his study coauthors had no financial disclosures.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Since congenital cardiac fellowship programs became accredited in 2007, training requirements have been standardized and the surgical experience robust.
Major finding: Recent graduates of fellowship programs are thriving in practice, but shortcomings with existing fellowship training exist, including only 50% gaining certification by passing the written and oral exams.
Data source: The study drew on survey responses from 36 of 44 fellows in 12 accredited programs and a review of operative logs of 38 of the 44 fellows.
Disclosures: Dr. Kogon and his study coauthors had no financial disclosures.