User login
The Official Newspaper of the American Association for Thoracic Surgery
Hospital-acquired respiratory viruses cause significant morbidity, mortality
BOSTON – Hospital-acquired respiratory viral infections may be a significant and underappreciated cause of morbidity and mortality among hospitalized patients.
According to a multisite, retrospective chart review of 44 patients with hospital-acquired respiratory viral illnesses (HA-RVIs), 17 patients (39%) died in-hospital. Further, of the 27 who survived, 18 (66.6%) were discharged to an advanced care setting rather than to home, though just 11/44 (25%) had been living in an advanced care setting before admission.
For the hospitalizations complicated by HA-RVI, the average length of stay was 30.4 days, with a positive respiratory virus panel (RVP) result occurring at a mean 18 days after admission.
“HA-RVIs are an underappreciated event and appear to target the sickest patients in the hospital,” said coauthor Dr. Matthew Sims, director of infectious diseases research at Beaumont Hospital, Rochester, Mich., at a poster session of the annual meeting of the American Society of Microbiology.
First author Dr. Adam K. Skrzynski, also of Beaumont Health, and his coauthors performed the analysis of 4,065 patients with a positive RVP result during hospitalization at a regional hospital system in the September 2011-May 2015 study period; the 1.1% of patients with positive results who formed the study cohort had to have symptoms of a respiratory infection occurring after more than 5 days of hospitalization. Mortality data were collected for the first 33 days of hospitalization.
Positive RVP results for those included in the study came primarily from nasopharyngeal swab (n = 32), with the remainder from bronchoalveolar lavage (n = 11) and sputum (n = 1). Most patients were female (29/44, 66%), and elderly, with an average age of 73.8 years. In an interview, Dr. Sims said that many patients were smokers, and that chronic obstructive pulmonary disease and obesity were common comorbidities.
The prognosis was particularly grim for the 12 patients (27.3%) who were admitted to the ICU: 10 (83.3%) died after an average 9.6 days in the ICU. Advanced interventions did not seem to make a difference, either. “Intubation didn’t help these patients,” said Dr. Sims. Nine patients (20.5%) were intubated within 7 days of their positive RVP results. Intubation lasted an average 7.6 days, and all nine of these patients died.
The RVP came into use in 2011 and made it possible to identify whether a respiratory virus was causing symptoms – and which virus was the culprit – said Dr. Sims. For the studied population, 13 of 44 patients had influenza; 11 of those had influenza A and 2 had influenza B. The next most common pathogen was parainfluenza, with 10 positive RVP results.
Dr. Sims said he and his coinvestigators were surprised to find that, although influenza A was the most common pathogen, only 18.8% of the patients with influenza A died during the study period. “While it is possible that the high frequency of influenza infection in our study may be due to poor vaccine-strain matching for the years in question, the lower mortality rate seen in influenza A infection may be due to our hospital’s mandatory influenza vaccination policy and subsequent protection against mortality,” Dr. Skrzynski and his coauthors wrote.
There were seasonal trends in mortality, with 70.6% of mortality occurring in the spring (April-June) and an additional 23.3% happening in the winter (January-March). Parainfluenza infection peaked in the spring, and influenza peaked in the winter months.
Dr. Sims said the study underlines the importance of encouraging ill hospital staff members to stay home, and family members with respiratory symptoms should not be visiting fragile patients. Dr. Skrzynski and his coauthors also wrote that “immunization of healthcare personnel against influenza should be mandatory.”
Still to be answered, said Dr. Sims, is the association between comorbidities and the potentially lethal effects of HA-RVIs. They are currently performing a matched case-control study to tease out these relationships.
Dr. Skrzynski reported no outside funding source, and the study authors had no financial disclosures.
On Twitter @karioakes
BOSTON – Hospital-acquired respiratory viral infections may be a significant and underappreciated cause of morbidity and mortality among hospitalized patients.
According to a multisite, retrospective chart review of 44 patients with hospital-acquired respiratory viral illnesses (HA-RVIs), 17 patients (39%) died in-hospital. Further, of the 27 who survived, 18 (66.6%) were discharged to an advanced care setting rather than to home, though just 11/44 (25%) had been living in an advanced care setting before admission.
For the hospitalizations complicated by HA-RVI, the average length of stay was 30.4 days, with a positive respiratory virus panel (RVP) result occurring at a mean 18 days after admission.
“HA-RVIs are an underappreciated event and appear to target the sickest patients in the hospital,” said coauthor Dr. Matthew Sims, director of infectious diseases research at Beaumont Hospital, Rochester, Mich., at a poster session of the annual meeting of the American Society of Microbiology.
First author Dr. Adam K. Skrzynski, also of Beaumont Health, and his coauthors performed the analysis of 4,065 patients with a positive RVP result during hospitalization at a regional hospital system in the September 2011-May 2015 study period; the 1.1% of patients with positive results who formed the study cohort had to have symptoms of a respiratory infection occurring after more than 5 days of hospitalization. Mortality data were collected for the first 33 days of hospitalization.
Positive RVP results for those included in the study came primarily from nasopharyngeal swab (n = 32), with the remainder from bronchoalveolar lavage (n = 11) and sputum (n = 1). Most patients were female (29/44, 66%), and elderly, with an average age of 73.8 years. In an interview, Dr. Sims said that many patients were smokers, and that chronic obstructive pulmonary disease and obesity were common comorbidities.
The prognosis was particularly grim for the 12 patients (27.3%) who were admitted to the ICU: 10 (83.3%) died after an average 9.6 days in the ICU. Advanced interventions did not seem to make a difference, either. “Intubation didn’t help these patients,” said Dr. Sims. Nine patients (20.5%) were intubated within 7 days of their positive RVP results. Intubation lasted an average 7.6 days, and all nine of these patients died.
The RVP came into use in 2011 and made it possible to identify whether a respiratory virus was causing symptoms – and which virus was the culprit – said Dr. Sims. For the studied population, 13 of 44 patients had influenza; 11 of those had influenza A and 2 had influenza B. The next most common pathogen was parainfluenza, with 10 positive RVP results.
Dr. Sims said he and his coinvestigators were surprised to find that, although influenza A was the most common pathogen, only 18.8% of the patients with influenza A died during the study period. “While it is possible that the high frequency of influenza infection in our study may be due to poor vaccine-strain matching for the years in question, the lower mortality rate seen in influenza A infection may be due to our hospital’s mandatory influenza vaccination policy and subsequent protection against mortality,” Dr. Skrzynski and his coauthors wrote.
There were seasonal trends in mortality, with 70.6% of mortality occurring in the spring (April-June) and an additional 23.3% happening in the winter (January-March). Parainfluenza infection peaked in the spring, and influenza peaked in the winter months.
Dr. Sims said the study underlines the importance of encouraging ill hospital staff members to stay home, and family members with respiratory symptoms should not be visiting fragile patients. Dr. Skrzynski and his coauthors also wrote that “immunization of healthcare personnel against influenza should be mandatory.”
Still to be answered, said Dr. Sims, is the association between comorbidities and the potentially lethal effects of HA-RVIs. They are currently performing a matched case-control study to tease out these relationships.
Dr. Skrzynski reported no outside funding source, and the study authors had no financial disclosures.
On Twitter @karioakes
BOSTON – Hospital-acquired respiratory viral infections may be a significant and underappreciated cause of morbidity and mortality among hospitalized patients.
According to a multisite, retrospective chart review of 44 patients with hospital-acquired respiratory viral illnesses (HA-RVIs), 17 patients (39%) died in-hospital. Further, of the 27 who survived, 18 (66.6%) were discharged to an advanced care setting rather than to home, though just 11/44 (25%) had been living in an advanced care setting before admission.
For the hospitalizations complicated by HA-RVI, the average length of stay was 30.4 days, with a positive respiratory virus panel (RVP) result occurring at a mean 18 days after admission.
“HA-RVIs are an underappreciated event and appear to target the sickest patients in the hospital,” said coauthor Dr. Matthew Sims, director of infectious diseases research at Beaumont Hospital, Rochester, Mich., at a poster session of the annual meeting of the American Society of Microbiology.
First author Dr. Adam K. Skrzynski, also of Beaumont Health, and his coauthors performed the analysis of 4,065 patients with a positive RVP result during hospitalization at a regional hospital system in the September 2011-May 2015 study period; the 1.1% of patients with positive results who formed the study cohort had to have symptoms of a respiratory infection occurring after more than 5 days of hospitalization. Mortality data were collected for the first 33 days of hospitalization.
Positive RVP results for those included in the study came primarily from nasopharyngeal swab (n = 32), with the remainder from bronchoalveolar lavage (n = 11) and sputum (n = 1). Most patients were female (29/44, 66%), and elderly, with an average age of 73.8 years. In an interview, Dr. Sims said that many patients were smokers, and that chronic obstructive pulmonary disease and obesity were common comorbidities.
The prognosis was particularly grim for the 12 patients (27.3%) who were admitted to the ICU: 10 (83.3%) died after an average 9.6 days in the ICU. Advanced interventions did not seem to make a difference, either. “Intubation didn’t help these patients,” said Dr. Sims. Nine patients (20.5%) were intubated within 7 days of their positive RVP results. Intubation lasted an average 7.6 days, and all nine of these patients died.
The RVP came into use in 2011 and made it possible to identify whether a respiratory virus was causing symptoms – and which virus was the culprit – said Dr. Sims. For the studied population, 13 of 44 patients had influenza; 11 of those had influenza A and 2 had influenza B. The next most common pathogen was parainfluenza, with 10 positive RVP results.
Dr. Sims said he and his coinvestigators were surprised to find that, although influenza A was the most common pathogen, only 18.8% of the patients with influenza A died during the study period. “While it is possible that the high frequency of influenza infection in our study may be due to poor vaccine-strain matching for the years in question, the lower mortality rate seen in influenza A infection may be due to our hospital’s mandatory influenza vaccination policy and subsequent protection against mortality,” Dr. Skrzynski and his coauthors wrote.
There were seasonal trends in mortality, with 70.6% of mortality occurring in the spring (April-June) and an additional 23.3% happening in the winter (January-March). Parainfluenza infection peaked in the spring, and influenza peaked in the winter months.
Dr. Sims said the study underlines the importance of encouraging ill hospital staff members to stay home, and family members with respiratory symptoms should not be visiting fragile patients. Dr. Skrzynski and his coauthors also wrote that “immunization of healthcare personnel against influenza should be mandatory.”
Still to be answered, said Dr. Sims, is the association between comorbidities and the potentially lethal effects of HA-RVIs. They are currently performing a matched case-control study to tease out these relationships.
Dr. Skrzynski reported no outside funding source, and the study authors had no financial disclosures.
On Twitter @karioakes
AT ASM MICROBE 2016
Key clinical point: Hospital-acquired respiratory viral illnesses had a 39% mortality rate.
Major finding: Of 44 symptomatic patients with positive respiratory virus panel screens, 17 died and 2/3 of the survivors went to advanced care settings on discharge.
Data source: Retrospective multisite chart review of 44 patients with HA-RVIs and positive RVP screens.
Disclosures: No external funding source was reported, and the study authors had no disclosures.
IASLC lung cancer staging project proposes changes for new TNM classification
The International Association for the Study of Lung Cancer (IASLC) Staging and Prognostic Factors Committee has developed proposals for revision of the T, N, and M categories of the 8th edition of the TNM Classification for lung cancer due to be published in late 2016. The new classification will be enacted in January 2017.
The changes proposed were based on the results of an analysis of a new database of 94,708 cases donated from 35 sources in 16 countries around the world.
The methods used and the proposals made were published in the Journal of Thoracic Oncology (2016;11:39-51).
Candidate proposals for the TNM stage groups were developed in conjunction with proposed changes to the T and M categories, which were previously published (J Thorac Oncol 2015;10:990-1003, and 2015;10:1515-22). There were no proposed changes to the N.
Changes to some T and M descriptors will result in these cases being assigned to a different stage than that to which they would have been assigned in the 7th edition. In addition, some TNM subsets have been moved to a new stage grouping, according to Dr. Peter Goldstraw of Imperial College, London, and his colleagues on behalf of the IASLC Staging and Prognostic Factors Committee.
Major new proposals
T1 changes: Size cut points have further proliferated in the proposals for the 8th edition, and outgrowth of the emphasis on tumor size in the 7th edition, such that size will now be a descriptor in all T categories, according to the authors. New stage groupings proposed divide stage T1 into T1a, T1b, and T1c, based on the new size cut points of 1 cm and 2 cm. This results in these cases (when associated with the categories N0 and M0) being assigned to stages 1A1, 1A2, and 1A3, respectively, which reflects the statistically different prognosis of these cases.
T3, T4 changes: A new group has been created for the most advanced local disease categories, T3 and T4 associated with N3 disease, but category M0. Such cases will now be classified as stage IIIC, reflecting their worse outcomes than seen in cases involving tumors that remain in stage IIIB. The prognosis for stage IIIC cases is similar to that of stage IVA cases, however the researchers justified the separation, based upon the different treatment approaches used for such cases.
M changes: Although cases with intrathoracic metastatic disease to the contralateral lung or with pleural/pericardial dissemination remain classified as M1a disease, the category M1b will now be assigned to cases with a single metastatic deposit (in one organ) and M1a and M1b cases will be moored to a new stage grouping called IVA. The more common situation of multiple metastatic deposits, usually in more than one organ, will be classified as M1c and staged as IVB. Separation of the M1a and M1b categories was maintained both for further data analysis and because some patients with oligometastatic disease are now receiving more aggressive local therapy in addition to systemic treatment, according to the authors.
Other proposals
A variety of more minor changes to stage groupings has also been proposed, some of which will result in a T descriptor being allocated to a higher stage. In some cases, tumors may be allocated to a different T category entirely, leading to a reclassification of stage. Among the examples given were tumors associated with diaphragmatic invasion to TV, which, when associated with N0 disease, will move from stage IIB to IIA.
Impact on treatment
The relationship of the proposed classification changes to treatment decisions is not direct, the authors stated in their discussion. “Although such changes might raise the issue of whether consequent changes to treatment algorithms are needed, it is important to remind ourselves that stage does not dictate treatment. Stage is one, and perhaps the most important, of several prognostic factors that guide the appropriate treatment option[s] to offer the patient. Any change to established treatment algorithms should be based on clinical judgment informed by prospective trials,” they emphasized.
New stage groupings should be used in any trials of novel therapies, they added.
“We hope that the thoracic oncology community finds the proposals of value and that, when accepted, will have a positive impact on the effectiveness of treatment for lung cancer, which will benefit patients around the globe,” the researchers concluded.
The research to develop the new proposals was funded by the IASLC, including funds obtained through unrestricted grants obtained from the pharmaceutical industry. The authors reported no other disclosures.
The 8th edition of the TNM staging is upon us. It is the summary of analysis of 90,000 cases and data collected over 11 years. It behooves every thoracic surgeon taking care of patients with lung cancer to familiarize themselves with the new version. The staging proposal is available as an open access article on the Journal of Thoracic Oncology website.
From a statistical viewpoint, this edition fits the data better than previous editions did. However, from a practical application, it is more cumbersome to use routinely in a busy clinic. One hopes that we can soon say, “There’s an app for that!” Such interfacing will enhance the application of this edition significantly.

|
Dr. Sai Yendamuri |
The new edition of the staging system is particularly important for surgeons for two reasons. The first is the formal recognition that patients with oligometastatic disease have a better prognosis than other stage IV disease and may be amenable to multimodality therapies with curative intent, as is currently performed by select clinical teams. The second is the further refinement of stage I disease with respect to tumor size. Combined with the new histologic classification of adenocarcinoma and its proposed integration with the TNM classification, the debate of sublobar vs. lobar resection for stage I NSCLC will become more nuanced. These implications for the practicing thoracic surgeon make the manuscript mandatory reading.
Dr. Sai Yendamuri is chair, department of thoracic surgery, and director, thoracic surgery research laboratory, and a professor of oncology at Roswell Park Cancer Institute, Buffalo, N.Y. He is also the general thoracic editor for Thoracic Surgery News.
The 8th edition of the TNM staging is upon us. It is the summary of analysis of 90,000 cases and data collected over 11 years. It behooves every thoracic surgeon taking care of patients with lung cancer to familiarize themselves with the new version. The staging proposal is available as an open access article on the Journal of Thoracic Oncology website.
From a statistical viewpoint, this edition fits the data better than previous editions did. However, from a practical application, it is more cumbersome to use routinely in a busy clinic. One hopes that we can soon say, “There’s an app for that!” Such interfacing will enhance the application of this edition significantly.

|
Dr. Sai Yendamuri |
The new edition of the staging system is particularly important for surgeons for two reasons. The first is the formal recognition that patients with oligometastatic disease have a better prognosis than other stage IV disease and may be amenable to multimodality therapies with curative intent, as is currently performed by select clinical teams. The second is the further refinement of stage I disease with respect to tumor size. Combined with the new histologic classification of adenocarcinoma and its proposed integration with the TNM classification, the debate of sublobar vs. lobar resection for stage I NSCLC will become more nuanced. These implications for the practicing thoracic surgeon make the manuscript mandatory reading.
Dr. Sai Yendamuri is chair, department of thoracic surgery, and director, thoracic surgery research laboratory, and a professor of oncology at Roswell Park Cancer Institute, Buffalo, N.Y. He is also the general thoracic editor for Thoracic Surgery News.
The 8th edition of the TNM staging is upon us. It is the summary of analysis of 90,000 cases and data collected over 11 years. It behooves every thoracic surgeon taking care of patients with lung cancer to familiarize themselves with the new version. The staging proposal is available as an open access article on the Journal of Thoracic Oncology website.
From a statistical viewpoint, this edition fits the data better than previous editions did. However, from a practical application, it is more cumbersome to use routinely in a busy clinic. One hopes that we can soon say, “There’s an app for that!” Such interfacing will enhance the application of this edition significantly.

|
Dr. Sai Yendamuri |
The new edition of the staging system is particularly important for surgeons for two reasons. The first is the formal recognition that patients with oligometastatic disease have a better prognosis than other stage IV disease and may be amenable to multimodality therapies with curative intent, as is currently performed by select clinical teams. The second is the further refinement of stage I disease with respect to tumor size. Combined with the new histologic classification of adenocarcinoma and its proposed integration with the TNM classification, the debate of sublobar vs. lobar resection for stage I NSCLC will become more nuanced. These implications for the practicing thoracic surgeon make the manuscript mandatory reading.
Dr. Sai Yendamuri is chair, department of thoracic surgery, and director, thoracic surgery research laboratory, and a professor of oncology at Roswell Park Cancer Institute, Buffalo, N.Y. He is also the general thoracic editor for Thoracic Surgery News.
The International Association for the Study of Lung Cancer (IASLC) Staging and Prognostic Factors Committee has developed proposals for revision of the T, N, and M categories of the 8th edition of the TNM Classification for lung cancer due to be published in late 2016. The new classification will be enacted in January 2017.
The changes proposed were based on the results of an analysis of a new database of 94,708 cases donated from 35 sources in 16 countries around the world.
The methods used and the proposals made were published in the Journal of Thoracic Oncology (2016;11:39-51).
Candidate proposals for the TNM stage groups were developed in conjunction with proposed changes to the T and M categories, which were previously published (J Thorac Oncol 2015;10:990-1003, and 2015;10:1515-22). There were no proposed changes to the N.
Changes to some T and M descriptors will result in these cases being assigned to a different stage than that to which they would have been assigned in the 7th edition. In addition, some TNM subsets have been moved to a new stage grouping, according to Dr. Peter Goldstraw of Imperial College, London, and his colleagues on behalf of the IASLC Staging and Prognostic Factors Committee.
Major new proposals
T1 changes: Size cut points have further proliferated in the proposals for the 8th edition, and outgrowth of the emphasis on tumor size in the 7th edition, such that size will now be a descriptor in all T categories, according to the authors. New stage groupings proposed divide stage T1 into T1a, T1b, and T1c, based on the new size cut points of 1 cm and 2 cm. This results in these cases (when associated with the categories N0 and M0) being assigned to stages 1A1, 1A2, and 1A3, respectively, which reflects the statistically different prognosis of these cases.
T3, T4 changes: A new group has been created for the most advanced local disease categories, T3 and T4 associated with N3 disease, but category M0. Such cases will now be classified as stage IIIC, reflecting their worse outcomes than seen in cases involving tumors that remain in stage IIIB. The prognosis for stage IIIC cases is similar to that of stage IVA cases, however the researchers justified the separation, based upon the different treatment approaches used for such cases.
M changes: Although cases with intrathoracic metastatic disease to the contralateral lung or with pleural/pericardial dissemination remain classified as M1a disease, the category M1b will now be assigned to cases with a single metastatic deposit (in one organ) and M1a and M1b cases will be moored to a new stage grouping called IVA. The more common situation of multiple metastatic deposits, usually in more than one organ, will be classified as M1c and staged as IVB. Separation of the M1a and M1b categories was maintained both for further data analysis and because some patients with oligometastatic disease are now receiving more aggressive local therapy in addition to systemic treatment, according to the authors.
Other proposals
A variety of more minor changes to stage groupings has also been proposed, some of which will result in a T descriptor being allocated to a higher stage. In some cases, tumors may be allocated to a different T category entirely, leading to a reclassification of stage. Among the examples given were tumors associated with diaphragmatic invasion to TV, which, when associated with N0 disease, will move from stage IIB to IIA.
Impact on treatment
The relationship of the proposed classification changes to treatment decisions is not direct, the authors stated in their discussion. “Although such changes might raise the issue of whether consequent changes to treatment algorithms are needed, it is important to remind ourselves that stage does not dictate treatment. Stage is one, and perhaps the most important, of several prognostic factors that guide the appropriate treatment option[s] to offer the patient. Any change to established treatment algorithms should be based on clinical judgment informed by prospective trials,” they emphasized.
New stage groupings should be used in any trials of novel therapies, they added.
“We hope that the thoracic oncology community finds the proposals of value and that, when accepted, will have a positive impact on the effectiveness of treatment for lung cancer, which will benefit patients around the globe,” the researchers concluded.
The research to develop the new proposals was funded by the IASLC, including funds obtained through unrestricted grants obtained from the pharmaceutical industry. The authors reported no other disclosures.
The International Association for the Study of Lung Cancer (IASLC) Staging and Prognostic Factors Committee has developed proposals for revision of the T, N, and M categories of the 8th edition of the TNM Classification for lung cancer due to be published in late 2016. The new classification will be enacted in January 2017.
The changes proposed were based on the results of an analysis of a new database of 94,708 cases donated from 35 sources in 16 countries around the world.
The methods used and the proposals made were published in the Journal of Thoracic Oncology (2016;11:39-51).
Candidate proposals for the TNM stage groups were developed in conjunction with proposed changes to the T and M categories, which were previously published (J Thorac Oncol 2015;10:990-1003, and 2015;10:1515-22). There were no proposed changes to the N.
Changes to some T and M descriptors will result in these cases being assigned to a different stage than that to which they would have been assigned in the 7th edition. In addition, some TNM subsets have been moved to a new stage grouping, according to Dr. Peter Goldstraw of Imperial College, London, and his colleagues on behalf of the IASLC Staging and Prognostic Factors Committee.
Major new proposals
T1 changes: Size cut points have further proliferated in the proposals for the 8th edition, and outgrowth of the emphasis on tumor size in the 7th edition, such that size will now be a descriptor in all T categories, according to the authors. New stage groupings proposed divide stage T1 into T1a, T1b, and T1c, based on the new size cut points of 1 cm and 2 cm. This results in these cases (when associated with the categories N0 and M0) being assigned to stages 1A1, 1A2, and 1A3, respectively, which reflects the statistically different prognosis of these cases.
T3, T4 changes: A new group has been created for the most advanced local disease categories, T3 and T4 associated with N3 disease, but category M0. Such cases will now be classified as stage IIIC, reflecting their worse outcomes than seen in cases involving tumors that remain in stage IIIB. The prognosis for stage IIIC cases is similar to that of stage IVA cases, however the researchers justified the separation, based upon the different treatment approaches used for such cases.
M changes: Although cases with intrathoracic metastatic disease to the contralateral lung or with pleural/pericardial dissemination remain classified as M1a disease, the category M1b will now be assigned to cases with a single metastatic deposit (in one organ) and M1a and M1b cases will be moored to a new stage grouping called IVA. The more common situation of multiple metastatic deposits, usually in more than one organ, will be classified as M1c and staged as IVB. Separation of the M1a and M1b categories was maintained both for further data analysis and because some patients with oligometastatic disease are now receiving more aggressive local therapy in addition to systemic treatment, according to the authors.
Other proposals
A variety of more minor changes to stage groupings has also been proposed, some of which will result in a T descriptor being allocated to a higher stage. In some cases, tumors may be allocated to a different T category entirely, leading to a reclassification of stage. Among the examples given were tumors associated with diaphragmatic invasion to TV, which, when associated with N0 disease, will move from stage IIB to IIA.
Impact on treatment
The relationship of the proposed classification changes to treatment decisions is not direct, the authors stated in their discussion. “Although such changes might raise the issue of whether consequent changes to treatment algorithms are needed, it is important to remind ourselves that stage does not dictate treatment. Stage is one, and perhaps the most important, of several prognostic factors that guide the appropriate treatment option[s] to offer the patient. Any change to established treatment algorithms should be based on clinical judgment informed by prospective trials,” they emphasized.
New stage groupings should be used in any trials of novel therapies, they added.
“We hope that the thoracic oncology community finds the proposals of value and that, when accepted, will have a positive impact on the effectiveness of treatment for lung cancer, which will benefit patients around the globe,” the researchers concluded.
The research to develop the new proposals was funded by the IASLC, including funds obtained through unrestricted grants obtained from the pharmaceutical industry. The authors reported no other disclosures.
FROM THE JOURNAL OF THORACIC ONCOLOGY
Key clinical point: New lung cancer classification to become effective January 2017.
Major finding: Size will now be a descriptor in all T categories, according to the authors. New stage groupings proposed dividing stage T1 into T1a, T1b, and T1c, based on the new size cut points of 1 cm and 2 cm.
Data source: The International Association for the Study of Lung Cancer (IASLC) Staging and Prognostic Factors Committee has developed proposals for revision of the T, N, and M categories of the 8th edition of the TNM Classification for lung cancer.
Disclosures: The research to develop the new proposals was funded by the IASLC, including funds obtained through unrestricted grants obtained from the pharmaceutical industry. The authors reported no other disclosures.
Web app boosts lung cancer survival
CHICAGO – A simple Web-based mobile application (web-app) improved survival time and quality of life of patients with advanced lung cancer, according to a randomized study presented at the annual meeting of the American Society of Clinical Oncology.
The study was stopped at the planned interim survival analysis that occurred after 121 evaluable patients because of survival benefit favoring the web-app arm. The application, called Moovcare, allowed patients to report symptoms over time and stay in close touch with their care providers after their initial surgery, chemotherapy, or radiation therapy.
“The 1-year survival was 75% in the Moovcare vs. 49% in the control arm,” said lead author Dr. Fabrice Denis of the Institut Inter-régional de Cancérologie Jean Bernard in LeMans, France, in a press conference.
Dr. Denis identified several reasons why a web-app could be useful in treating patients with lung cancer. Even with more than 1 million lung cancer deaths a year worldwide, there is no standard follow-up, and relapses do not occur on a 3 or 6-month schedule of planned visits. So patients often wait several weeks until their next visit to report symptoms indicative of a relapse. They may also be reluctant to report symptoms because of shame over how they contracted the disease, for example, from smoking. And patients are often hesitant to “bother” the doctor with symptoms between visits. All these reasons can contribute to suboptimal therapy and worse outcomes.
Investigators designed Moovcare to allow patients to report symptoms weekly, facilitating early detection of relapse or dangerous medical conditions and triggering early supportive care. They compared the web-app to a control of usual, nonpersonalized follow-up in a French multicenter prospective, randomized trial.
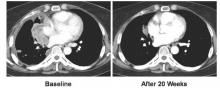
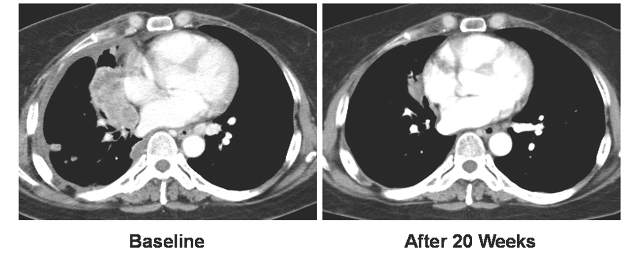
Patients (n = 121) with stage II/node-positive to stage IV (90% stage III/IV) nonprogressive small cell or non–small cell lung cancer were randomly assigned 1:1 to the two arms of the trial. They had to have Internet access, prior experience with email, performance status of 0-2, and an initial symptom score less than 7. Patients could be taking tyrosine kinase inhibitors or on maintenance therapy. Monitoring visits were the same for both groups every 3 months or more frequently. Patients in the control arm received more frequent computed tomographic (CT) imaging than did ones in the web-app arm, and CT scans could be performed at any time in either group based on the investigator’s clinical judgment, or in the case of the web-app, as suggested by patient report in the algorithm.
The median follow up was 9 months. Relapse rates were close to 50% for both groups. The 1-year survival of 75% in the Moovcare to 49% in the control arm gave a 1-year absolute survival increase of 26%. Median survival was 19 months vs. 12 months, a 7-month improvement in median survival for the Moovcare arm. The hazard ratio for death in the web-app arm, compared with the control arm was 0.325 (95% confidence interval, 0.157-0.672; P = .0025).
When they relapsed, 77% of patients in the web-app arm had a good performance status, compared with 33% in the control arm. “This led to 74% of patients receiving optimal therapy in the Moovcare arm vs. 33% in the control arm,” Dr. Denis said. “And the number of imaging [procedures] was reduced by 50% per patient per year.”
Overall quality of life was better in the web-app arm, as assessed using standard quality of life questionnaires.
Moovcare works by having patients or their relatives report 12 symptoms weekly (for example, asthenia, cough, dyspnea, anorexia, etc.) using a smartphone, tablet, or computer. An algorithm analyzes an association of symptoms and triggers email alerts to health care providers if relapse or dangerous medical conditions may be occurring. Providers follow up alerts by phone and schedule visits and imaging. “The sensitivity of the algorithm was high and was validated in two prospective studies,” Dr. Denis said. Sensitivity was 86%-100%.
Moovcare allowed earlier detection of relapse and improved overall survival for three reasons. “It allowed higher performance status at relapse, leading to more optimal therapy for relapsing patients. Dangerous medical conditions were detected earlier and treated earlier. It favored earlier supportive care, which improved quality of life. Less imaging was needed and performed at the right time,” Dr. Denis said.
Patients were monitored on a weekly basis, allowing more personalized care. The Moovcare web-app has been evaluated prospectively in about 300 patients, providing a high level of evidence of its utility in improving outcomes for patients with advanced lung cancer.
Press conference moderator Dr. Patricia Ganz commented that Moovcare is an example of a new way to improve the delivery of high-quality care to patients. “If we had a drug or some new intervention that caused this level of survival benefit, wouldn’t we want to go out and use it?” she asked. “This is a tremendous advance. This is personalized medicine. This is really tailoring it to the patient, and you can see how simple it is to collect this kind of data from the patient and then bring them in in between what would have been a scheduled visit.” She said the app overcomes the barrier of patients putting off reporting symptoms until their next visit or their reluctance to “bother the doctor.”
She said the app alerts the health care team to potential problems and prompts them to “use tests when appropriate, not on a schedule, [which] leads to avoidance of waste in the follow-up of care of our patients.”
CHICAGO – A simple Web-based mobile application (web-app) improved survival time and quality of life of patients with advanced lung cancer, according to a randomized study presented at the annual meeting of the American Society of Clinical Oncology.
The study was stopped at the planned interim survival analysis that occurred after 121 evaluable patients because of survival benefit favoring the web-app arm. The application, called Moovcare, allowed patients to report symptoms over time and stay in close touch with their care providers after their initial surgery, chemotherapy, or radiation therapy.
“The 1-year survival was 75% in the Moovcare vs. 49% in the control arm,” said lead author Dr. Fabrice Denis of the Institut Inter-régional de Cancérologie Jean Bernard in LeMans, France, in a press conference.
Dr. Denis identified several reasons why a web-app could be useful in treating patients with lung cancer. Even with more than 1 million lung cancer deaths a year worldwide, there is no standard follow-up, and relapses do not occur on a 3 or 6-month schedule of planned visits. So patients often wait several weeks until their next visit to report symptoms indicative of a relapse. They may also be reluctant to report symptoms because of shame over how they contracted the disease, for example, from smoking. And patients are often hesitant to “bother” the doctor with symptoms between visits. All these reasons can contribute to suboptimal therapy and worse outcomes.
Investigators designed Moovcare to allow patients to report symptoms weekly, facilitating early detection of relapse or dangerous medical conditions and triggering early supportive care. They compared the web-app to a control of usual, nonpersonalized follow-up in a French multicenter prospective, randomized trial.
Patients (n = 121) with stage II/node-positive to stage IV (90% stage III/IV) nonprogressive small cell or non–small cell lung cancer were randomly assigned 1:1 to the two arms of the trial. They had to have Internet access, prior experience with email, performance status of 0-2, and an initial symptom score less than 7. Patients could be taking tyrosine kinase inhibitors or on maintenance therapy. Monitoring visits were the same for both groups every 3 months or more frequently. Patients in the control arm received more frequent computed tomographic (CT) imaging than did ones in the web-app arm, and CT scans could be performed at any time in either group based on the investigator’s clinical judgment, or in the case of the web-app, as suggested by patient report in the algorithm.
The median follow up was 9 months. Relapse rates were close to 50% for both groups. The 1-year survival of 75% in the Moovcare to 49% in the control arm gave a 1-year absolute survival increase of 26%. Median survival was 19 months vs. 12 months, a 7-month improvement in median survival for the Moovcare arm. The hazard ratio for death in the web-app arm, compared with the control arm was 0.325 (95% confidence interval, 0.157-0.672; P = .0025).
When they relapsed, 77% of patients in the web-app arm had a good performance status, compared with 33% in the control arm. “This led to 74% of patients receiving optimal therapy in the Moovcare arm vs. 33% in the control arm,” Dr. Denis said. “And the number of imaging [procedures] was reduced by 50% per patient per year.”
Overall quality of life was better in the web-app arm, as assessed using standard quality of life questionnaires.
Moovcare works by having patients or their relatives report 12 symptoms weekly (for example, asthenia, cough, dyspnea, anorexia, etc.) using a smartphone, tablet, or computer. An algorithm analyzes an association of symptoms and triggers email alerts to health care providers if relapse or dangerous medical conditions may be occurring. Providers follow up alerts by phone and schedule visits and imaging. “The sensitivity of the algorithm was high and was validated in two prospective studies,” Dr. Denis said. Sensitivity was 86%-100%.
Moovcare allowed earlier detection of relapse and improved overall survival for three reasons. “It allowed higher performance status at relapse, leading to more optimal therapy for relapsing patients. Dangerous medical conditions were detected earlier and treated earlier. It favored earlier supportive care, which improved quality of life. Less imaging was needed and performed at the right time,” Dr. Denis said.
Patients were monitored on a weekly basis, allowing more personalized care. The Moovcare web-app has been evaluated prospectively in about 300 patients, providing a high level of evidence of its utility in improving outcomes for patients with advanced lung cancer.
Press conference moderator Dr. Patricia Ganz commented that Moovcare is an example of a new way to improve the delivery of high-quality care to patients. “If we had a drug or some new intervention that caused this level of survival benefit, wouldn’t we want to go out and use it?” she asked. “This is a tremendous advance. This is personalized medicine. This is really tailoring it to the patient, and you can see how simple it is to collect this kind of data from the patient and then bring them in in between what would have been a scheduled visit.” She said the app overcomes the barrier of patients putting off reporting symptoms until their next visit or their reluctance to “bother the doctor.”
She said the app alerts the health care team to potential problems and prompts them to “use tests when appropriate, not on a schedule, [which] leads to avoidance of waste in the follow-up of care of our patients.”
CHICAGO – A simple Web-based mobile application (web-app) improved survival time and quality of life of patients with advanced lung cancer, according to a randomized study presented at the annual meeting of the American Society of Clinical Oncology.
The study was stopped at the planned interim survival analysis that occurred after 121 evaluable patients because of survival benefit favoring the web-app arm. The application, called Moovcare, allowed patients to report symptoms over time and stay in close touch with their care providers after their initial surgery, chemotherapy, or radiation therapy.
“The 1-year survival was 75% in the Moovcare vs. 49% in the control arm,” said lead author Dr. Fabrice Denis of the Institut Inter-régional de Cancérologie Jean Bernard in LeMans, France, in a press conference.
Dr. Denis identified several reasons why a web-app could be useful in treating patients with lung cancer. Even with more than 1 million lung cancer deaths a year worldwide, there is no standard follow-up, and relapses do not occur on a 3 or 6-month schedule of planned visits. So patients often wait several weeks until their next visit to report symptoms indicative of a relapse. They may also be reluctant to report symptoms because of shame over how they contracted the disease, for example, from smoking. And patients are often hesitant to “bother” the doctor with symptoms between visits. All these reasons can contribute to suboptimal therapy and worse outcomes.
Investigators designed Moovcare to allow patients to report symptoms weekly, facilitating early detection of relapse or dangerous medical conditions and triggering early supportive care. They compared the web-app to a control of usual, nonpersonalized follow-up in a French multicenter prospective, randomized trial.
Patients (n = 121) with stage II/node-positive to stage IV (90% stage III/IV) nonprogressive small cell or non–small cell lung cancer were randomly assigned 1:1 to the two arms of the trial. They had to have Internet access, prior experience with email, performance status of 0-2, and an initial symptom score less than 7. Patients could be taking tyrosine kinase inhibitors or on maintenance therapy. Monitoring visits were the same for both groups every 3 months or more frequently. Patients in the control arm received more frequent computed tomographic (CT) imaging than did ones in the web-app arm, and CT scans could be performed at any time in either group based on the investigator’s clinical judgment, or in the case of the web-app, as suggested by patient report in the algorithm.
The median follow up was 9 months. Relapse rates were close to 50% for both groups. The 1-year survival of 75% in the Moovcare to 49% in the control arm gave a 1-year absolute survival increase of 26%. Median survival was 19 months vs. 12 months, a 7-month improvement in median survival for the Moovcare arm. The hazard ratio for death in the web-app arm, compared with the control arm was 0.325 (95% confidence interval, 0.157-0.672; P = .0025).
When they relapsed, 77% of patients in the web-app arm had a good performance status, compared with 33% in the control arm. “This led to 74% of patients receiving optimal therapy in the Moovcare arm vs. 33% in the control arm,” Dr. Denis said. “And the number of imaging [procedures] was reduced by 50% per patient per year.”
Overall quality of life was better in the web-app arm, as assessed using standard quality of life questionnaires.
Moovcare works by having patients or their relatives report 12 symptoms weekly (for example, asthenia, cough, dyspnea, anorexia, etc.) using a smartphone, tablet, or computer. An algorithm analyzes an association of symptoms and triggers email alerts to health care providers if relapse or dangerous medical conditions may be occurring. Providers follow up alerts by phone and schedule visits and imaging. “The sensitivity of the algorithm was high and was validated in two prospective studies,” Dr. Denis said. Sensitivity was 86%-100%.
Moovcare allowed earlier detection of relapse and improved overall survival for three reasons. “It allowed higher performance status at relapse, leading to more optimal therapy for relapsing patients. Dangerous medical conditions were detected earlier and treated earlier. It favored earlier supportive care, which improved quality of life. Less imaging was needed and performed at the right time,” Dr. Denis said.
Patients were monitored on a weekly basis, allowing more personalized care. The Moovcare web-app has been evaluated prospectively in about 300 patients, providing a high level of evidence of its utility in improving outcomes for patients with advanced lung cancer.
Press conference moderator Dr. Patricia Ganz commented that Moovcare is an example of a new way to improve the delivery of high-quality care to patients. “If we had a drug or some new intervention that caused this level of survival benefit, wouldn’t we want to go out and use it?” she asked. “This is a tremendous advance. This is personalized medicine. This is really tailoring it to the patient, and you can see how simple it is to collect this kind of data from the patient and then bring them in in between what would have been a scheduled visit.” She said the app overcomes the barrier of patients putting off reporting symptoms until their next visit or their reluctance to “bother the doctor.”
She said the app alerts the health care team to potential problems and prompts them to “use tests when appropriate, not on a schedule, [which] leads to avoidance of waste in the follow-up of care of our patients.”
AT THE 2016 ASCO ANNUAL MEETING
Key clinical point: A Web-based app improves survival for advanced lung cancer patients.
Major finding: Survival improved by 26% for web-app patients vs. controls.
Data source: Multicenter, prospective, phase III, randomized trial of 121 patients.
Disclosures: Dr. Denis has received honoraria and expenses from several pharmaceutical companies and has received institutional research funding from Sivan. Dr. Patricia Ganz reported stock and other ownership interest in Abbott Laboratories, GlaxoSmithKline, Johnson & Johnson, Merck, Novartis, Pfizer, and Teva.
Three AATS Graham Foundation Programs are Now Open for Application
Advanced Valve Disease Educational Fellowship
Sponsored by Medtronic
Offers surgeons the opportunity to interactively observe valvular heart disease specialists and connect with them about treatment, technical skills, and management of perioperative patients for a minimum of one month and three months.
Deadline: July 1, 2016
Evarts A. Graham Memorial Traveling Fellowship
Enhances the training of international academic CT surgeons and increases their international contacts by underwriting one-year of study at North American institutions. Includes a $75,000 stipend and round-trip airfare. Since 1951, fellows have included 64 individuals from 32 countries.
Deadline: July 1, 2016
Third John Alexander Research Scholarship
Supports North American surgeons with a two-year $160,000 grant to pursue research, training and clinical experience. Scholarships are named after past presidents of the Association. To date, 34 awardees have received over $4 million in grants.
Deadline: July 1, 2016
Advanced Valve Disease Educational Fellowship
Sponsored by Medtronic
Offers surgeons the opportunity to interactively observe valvular heart disease specialists and connect with them about treatment, technical skills, and management of perioperative patients for a minimum of one month and three months.
Deadline: July 1, 2016
Evarts A. Graham Memorial Traveling Fellowship
Enhances the training of international academic CT surgeons and increases their international contacts by underwriting one-year of study at North American institutions. Includes a $75,000 stipend and round-trip airfare. Since 1951, fellows have included 64 individuals from 32 countries.
Deadline: July 1, 2016
Third John Alexander Research Scholarship
Supports North American surgeons with a two-year $160,000 grant to pursue research, training and clinical experience. Scholarships are named after past presidents of the Association. To date, 34 awardees have received over $4 million in grants.
Deadline: July 1, 2016
Advanced Valve Disease Educational Fellowship
Sponsored by Medtronic
Offers surgeons the opportunity to interactively observe valvular heart disease specialists and connect with them about treatment, technical skills, and management of perioperative patients for a minimum of one month and three months.
Deadline: July 1, 2016
Evarts A. Graham Memorial Traveling Fellowship
Enhances the training of international academic CT surgeons and increases their international contacts by underwriting one-year of study at North American institutions. Includes a $75,000 stipend and round-trip airfare. Since 1951, fellows have included 64 individuals from 32 countries.
Deadline: July 1, 2016
Third John Alexander Research Scholarship
Supports North American surgeons with a two-year $160,000 grant to pursue research, training and clinical experience. Scholarships are named after past presidents of the Association. To date, 34 awardees have received over $4 million in grants.
Deadline: July 1, 2016
Vandetanib shows variable response, toxicity in RET-positive NSCLC
CHICAGO – The RET tyrosine kinase inhibitor vandetanib shows marked yet variable antitumor activity and toxicity in patients whose RET-positive non–small cell lung cancer (NSCLC) was unsuccessfully treated with chemotherapy, according to results of two small phase II trials presented at the annual meeting of the American Society of Clinical Oncology.
The overall response rates were 53% and 61% in two independent trials conducted by Dr. Takashi Seto of the National Kyushu Cancer Center, Japan, and by Dr. Se-Hoon Lee of Sungkyunkwan University, South Korea, respectively.
Compared to previous studies with other RET inhibitors, though all had small cohorts, there were many similarities in response rates. Progression-free survival was the most variable, but was much higher in the cabozantinib data reported at the 2015 ASCO annual meeting, according to moderator Dr. Karen Reckamp of the City of Hope Comprehensive Cancer Center, Duarte, Calif. “Vandetanib may have lower response rates than some of the others,” she said.
RET is a tyrosine kinase domain that fuses to and undergoes rearrangements with KIF5B and CCDC6 genes. This fusion and subsequent rearrangement results in ligand-dependent dimerization, which causes tumor growth. RET rearrangements were first identified in thyroid cancers.
“RET fusions were identified as new driver oncogenes of NSCLC in 2012 and observed in 1%-2% of all NSCLC,” Dr. Seto said. “Non–small cell lung cancer with RET rearrangement is regarded as a unique entity in terms of pathogenesis,” said Dr. Lee. There are currently multiple RET inhibitors in various stages of development.
In the trial headed by Dr. Seto, the Japanese genetic screening network was utilized to identify 34 NSCLC patients with RET rearrangements. Among the 34 patients, 17 met the eligibility requirements of having failed at least one prior chemotherapy treatment. Of those 17 patients, the median age was 59 years, 74% were female, all had adenocarcinomas, and 68% were nonsmokers.
All 17 patients received vandetanib at a dose of 300 mg once daily. The overall response rate was 53% (90% confidence interval, 31-74), and the disease control rate was 88%. The median progression-free survival was 4.7 months (90% CI, 2.8-8.3).
There was a marked difference in overall response rate and progression-free survival among RET fusion subtypes. For CCDC6-RET, the overall response was 83% and the progression-free survival was 8.3 months. For KIF5B-RET, the overall response was 20% with a median progression-free survival of 2.9 months.
Dr. Seto noted that there was no known biological explanation for the observed discrepancy in response rate or survival.
Dr. Seto reported that the safety profile was similar to previous reports. Four patients ended treatment due to adverse events while 16 experienced dose interruptions due to treatment-related toxicities. The most common grade three and four toxicities were hypertension (58%), rash (16%), and diarrhea (11%).
In the trial headed by Dr. Lee, 18 patients with RET rearrangements (confirmed by fluorescent in situ hybridization) met the eligibility requirement of having failed platinum-based chemotherapy. The median age of the cohort was 55 years, and 33% were female.
Similar to Dr. Seto’s study, all 18 patients received vandetanib at 300 mg once daily. Of the 18 patient cohort, 17% achieved partial remission and 44% achieved stable disease. Seven patients had no remission or stabilization. There were no treatment-related mortalities or grade 4 adverse events. Two grade 3 adverse events were reported.
“Looking at these two studies together, I think the important thing about the characteristics you see [is] that the age range is very similar [with a] median in the 50’s,” commented Dr. Reckamp. “The male to female ratio is actually opposite in both so [this] can occur in both men and women. The smoking status, interestingly is similar in both, where about a third of patients were former smokers. Most of the patients had adenocarcinoma. Many of these patients were highly previously treated. Only the Seto group looked at RET fusion partner, which may be important in looking at efficacy for these agents.” Vandetanib is a “challenging drug to tolerate,” Dr. Reckamp also noted.
“Is there a preferred RET inhibitor in small cell lung cancer?” Dr. Reckamp asked. “There are many RET inhibitors approved for other cancer types at this point, and they are multitargeted tyrosine kinases. In small studies they have similar efficacy. Toxicities vary because of the off-target effects, and most of the [treatment] decisions were made based on potential toxicities rather than differing efficacy. So none is really differentiated as the best choice, and it is unlikely that we are going to have the trials to evaluate them head to head.”
Dr. Reckamp suggested that “most patients with adenocarcinoma” should be tested for RET rearrangements. “Both men and women, both smokers and nonsmokers. And if you don’t test, you won’t find it. And if you don’t find it, you won’t be able to treat.” Dr. Reckamp also noted that next generation sequencing (NGS) should be the preferred method of identifying RET status because NGS uses less tissue, provides genetic sequencing, and allows for the identification of binding partners.
“Does targeting RET improve patient outcomes?” she continued. “Because that is really the question we need to answer if we need to move forward with RET inhibition for lung cancer. So there are variable response rates, less than other inhibitors of other oncogenic-driven tumors, that’s for sure... But if you look at the data, and these are [for] heavily pretreated patients for the most part, the response rates are better than second-line cytotoxic chemotherapy that we have had in the past and similar to unselected checkpoint inhibition. So there is potential for improving outcomes, and again if we don’t know someone is RET, we potentially are not going to offer a treatment that could help them live longer or better.”
When asked how she would treat a newly-diagnosed patient with RET-positive NSCLC, Dr. Reckamp said she would treat with first-line chemotherapy rather than a tyrosine kinase inhibitor (TKI) but would enroll the patient in whatever TKI trial was ongoing at that point in time.
“There are multiple trials that are ongoing,” Dr. Reckamp said. “It is unlikely that a comparison trial will be completed and so we are going to have to look at these trials next to each other and differentiate based on toxicity [and] perceived efficacy.”
Specifically, Dr. Reckamp believes the medical community needs to move toward “universal testing” for RET status in lung cancer patients. Resistance and combination therapies will also need to be assessed in future studies.
“RET is important in lung cancer, and should be targeted. We now need to find the best way to do that,” Dr. Reckamp concluded.
The trial headed by Dr. Seto was funded by the Japan Agency for Medical Research and Development, AMED, and AstraZeneca. Dr. Seto reported receiving honoraria and research funding from multiple companies including AstraZeneca. The trial headed by Dr. Lee was funded by AstraZeneca Korea. Dr. Lee reported having a consulting or advisory role and receiving honoraria and research funding from AstraZeneca, Pfizer, and Roche/Genentech.
CHICAGO – The RET tyrosine kinase inhibitor vandetanib shows marked yet variable antitumor activity and toxicity in patients whose RET-positive non–small cell lung cancer (NSCLC) was unsuccessfully treated with chemotherapy, according to results of two small phase II trials presented at the annual meeting of the American Society of Clinical Oncology.
The overall response rates were 53% and 61% in two independent trials conducted by Dr. Takashi Seto of the National Kyushu Cancer Center, Japan, and by Dr. Se-Hoon Lee of Sungkyunkwan University, South Korea, respectively.
Compared to previous studies with other RET inhibitors, though all had small cohorts, there were many similarities in response rates. Progression-free survival was the most variable, but was much higher in the cabozantinib data reported at the 2015 ASCO annual meeting, according to moderator Dr. Karen Reckamp of the City of Hope Comprehensive Cancer Center, Duarte, Calif. “Vandetanib may have lower response rates than some of the others,” she said.
RET is a tyrosine kinase domain that fuses to and undergoes rearrangements with KIF5B and CCDC6 genes. This fusion and subsequent rearrangement results in ligand-dependent dimerization, which causes tumor growth. RET rearrangements were first identified in thyroid cancers.
“RET fusions were identified as new driver oncogenes of NSCLC in 2012 and observed in 1%-2% of all NSCLC,” Dr. Seto said. “Non–small cell lung cancer with RET rearrangement is regarded as a unique entity in terms of pathogenesis,” said Dr. Lee. There are currently multiple RET inhibitors in various stages of development.
In the trial headed by Dr. Seto, the Japanese genetic screening network was utilized to identify 34 NSCLC patients with RET rearrangements. Among the 34 patients, 17 met the eligibility requirements of having failed at least one prior chemotherapy treatment. Of those 17 patients, the median age was 59 years, 74% were female, all had adenocarcinomas, and 68% were nonsmokers.
All 17 patients received vandetanib at a dose of 300 mg once daily. The overall response rate was 53% (90% confidence interval, 31-74), and the disease control rate was 88%. The median progression-free survival was 4.7 months (90% CI, 2.8-8.3).
There was a marked difference in overall response rate and progression-free survival among RET fusion subtypes. For CCDC6-RET, the overall response was 83% and the progression-free survival was 8.3 months. For KIF5B-RET, the overall response was 20% with a median progression-free survival of 2.9 months.
Dr. Seto noted that there was no known biological explanation for the observed discrepancy in response rate or survival.
Dr. Seto reported that the safety profile was similar to previous reports. Four patients ended treatment due to adverse events while 16 experienced dose interruptions due to treatment-related toxicities. The most common grade three and four toxicities were hypertension (58%), rash (16%), and diarrhea (11%).
In the trial headed by Dr. Lee, 18 patients with RET rearrangements (confirmed by fluorescent in situ hybridization) met the eligibility requirement of having failed platinum-based chemotherapy. The median age of the cohort was 55 years, and 33% were female.
Similar to Dr. Seto’s study, all 18 patients received vandetanib at 300 mg once daily. Of the 18 patient cohort, 17% achieved partial remission and 44% achieved stable disease. Seven patients had no remission or stabilization. There were no treatment-related mortalities or grade 4 adverse events. Two grade 3 adverse events were reported.
“Looking at these two studies together, I think the important thing about the characteristics you see [is] that the age range is very similar [with a] median in the 50’s,” commented Dr. Reckamp. “The male to female ratio is actually opposite in both so [this] can occur in both men and women. The smoking status, interestingly is similar in both, where about a third of patients were former smokers. Most of the patients had adenocarcinoma. Many of these patients were highly previously treated. Only the Seto group looked at RET fusion partner, which may be important in looking at efficacy for these agents.” Vandetanib is a “challenging drug to tolerate,” Dr. Reckamp also noted.
“Is there a preferred RET inhibitor in small cell lung cancer?” Dr. Reckamp asked. “There are many RET inhibitors approved for other cancer types at this point, and they are multitargeted tyrosine kinases. In small studies they have similar efficacy. Toxicities vary because of the off-target effects, and most of the [treatment] decisions were made based on potential toxicities rather than differing efficacy. So none is really differentiated as the best choice, and it is unlikely that we are going to have the trials to evaluate them head to head.”
Dr. Reckamp suggested that “most patients with adenocarcinoma” should be tested for RET rearrangements. “Both men and women, both smokers and nonsmokers. And if you don’t test, you won’t find it. And if you don’t find it, you won’t be able to treat.” Dr. Reckamp also noted that next generation sequencing (NGS) should be the preferred method of identifying RET status because NGS uses less tissue, provides genetic sequencing, and allows for the identification of binding partners.
“Does targeting RET improve patient outcomes?” she continued. “Because that is really the question we need to answer if we need to move forward with RET inhibition for lung cancer. So there are variable response rates, less than other inhibitors of other oncogenic-driven tumors, that’s for sure... But if you look at the data, and these are [for] heavily pretreated patients for the most part, the response rates are better than second-line cytotoxic chemotherapy that we have had in the past and similar to unselected checkpoint inhibition. So there is potential for improving outcomes, and again if we don’t know someone is RET, we potentially are not going to offer a treatment that could help them live longer or better.”
When asked how she would treat a newly-diagnosed patient with RET-positive NSCLC, Dr. Reckamp said she would treat with first-line chemotherapy rather than a tyrosine kinase inhibitor (TKI) but would enroll the patient in whatever TKI trial was ongoing at that point in time.
“There are multiple trials that are ongoing,” Dr. Reckamp said. “It is unlikely that a comparison trial will be completed and so we are going to have to look at these trials next to each other and differentiate based on toxicity [and] perceived efficacy.”
Specifically, Dr. Reckamp believes the medical community needs to move toward “universal testing” for RET status in lung cancer patients. Resistance and combination therapies will also need to be assessed in future studies.
“RET is important in lung cancer, and should be targeted. We now need to find the best way to do that,” Dr. Reckamp concluded.
The trial headed by Dr. Seto was funded by the Japan Agency for Medical Research and Development, AMED, and AstraZeneca. Dr. Seto reported receiving honoraria and research funding from multiple companies including AstraZeneca. The trial headed by Dr. Lee was funded by AstraZeneca Korea. Dr. Lee reported having a consulting or advisory role and receiving honoraria and research funding from AstraZeneca, Pfizer, and Roche/Genentech.
CHICAGO – The RET tyrosine kinase inhibitor vandetanib shows marked yet variable antitumor activity and toxicity in patients whose RET-positive non–small cell lung cancer (NSCLC) was unsuccessfully treated with chemotherapy, according to results of two small phase II trials presented at the annual meeting of the American Society of Clinical Oncology.
The overall response rates were 53% and 61% in two independent trials conducted by Dr. Takashi Seto of the National Kyushu Cancer Center, Japan, and by Dr. Se-Hoon Lee of Sungkyunkwan University, South Korea, respectively.
Compared to previous studies with other RET inhibitors, though all had small cohorts, there were many similarities in response rates. Progression-free survival was the most variable, but was much higher in the cabozantinib data reported at the 2015 ASCO annual meeting, according to moderator Dr. Karen Reckamp of the City of Hope Comprehensive Cancer Center, Duarte, Calif. “Vandetanib may have lower response rates than some of the others,” she said.
RET is a tyrosine kinase domain that fuses to and undergoes rearrangements with KIF5B and CCDC6 genes. This fusion and subsequent rearrangement results in ligand-dependent dimerization, which causes tumor growth. RET rearrangements were first identified in thyroid cancers.
“RET fusions were identified as new driver oncogenes of NSCLC in 2012 and observed in 1%-2% of all NSCLC,” Dr. Seto said. “Non–small cell lung cancer with RET rearrangement is regarded as a unique entity in terms of pathogenesis,” said Dr. Lee. There are currently multiple RET inhibitors in various stages of development.
In the trial headed by Dr. Seto, the Japanese genetic screening network was utilized to identify 34 NSCLC patients with RET rearrangements. Among the 34 patients, 17 met the eligibility requirements of having failed at least one prior chemotherapy treatment. Of those 17 patients, the median age was 59 years, 74% were female, all had adenocarcinomas, and 68% were nonsmokers.
All 17 patients received vandetanib at a dose of 300 mg once daily. The overall response rate was 53% (90% confidence interval, 31-74), and the disease control rate was 88%. The median progression-free survival was 4.7 months (90% CI, 2.8-8.3).
There was a marked difference in overall response rate and progression-free survival among RET fusion subtypes. For CCDC6-RET, the overall response was 83% and the progression-free survival was 8.3 months. For KIF5B-RET, the overall response was 20% with a median progression-free survival of 2.9 months.
Dr. Seto noted that there was no known biological explanation for the observed discrepancy in response rate or survival.
Dr. Seto reported that the safety profile was similar to previous reports. Four patients ended treatment due to adverse events while 16 experienced dose interruptions due to treatment-related toxicities. The most common grade three and four toxicities were hypertension (58%), rash (16%), and diarrhea (11%).
In the trial headed by Dr. Lee, 18 patients with RET rearrangements (confirmed by fluorescent in situ hybridization) met the eligibility requirement of having failed platinum-based chemotherapy. The median age of the cohort was 55 years, and 33% were female.
Similar to Dr. Seto’s study, all 18 patients received vandetanib at 300 mg once daily. Of the 18 patient cohort, 17% achieved partial remission and 44% achieved stable disease. Seven patients had no remission or stabilization. There were no treatment-related mortalities or grade 4 adverse events. Two grade 3 adverse events were reported.
“Looking at these two studies together, I think the important thing about the characteristics you see [is] that the age range is very similar [with a] median in the 50’s,” commented Dr. Reckamp. “The male to female ratio is actually opposite in both so [this] can occur in both men and women. The smoking status, interestingly is similar in both, where about a third of patients were former smokers. Most of the patients had adenocarcinoma. Many of these patients were highly previously treated. Only the Seto group looked at RET fusion partner, which may be important in looking at efficacy for these agents.” Vandetanib is a “challenging drug to tolerate,” Dr. Reckamp also noted.
“Is there a preferred RET inhibitor in small cell lung cancer?” Dr. Reckamp asked. “There are many RET inhibitors approved for other cancer types at this point, and they are multitargeted tyrosine kinases. In small studies they have similar efficacy. Toxicities vary because of the off-target effects, and most of the [treatment] decisions were made based on potential toxicities rather than differing efficacy. So none is really differentiated as the best choice, and it is unlikely that we are going to have the trials to evaluate them head to head.”
Dr. Reckamp suggested that “most patients with adenocarcinoma” should be tested for RET rearrangements. “Both men and women, both smokers and nonsmokers. And if you don’t test, you won’t find it. And if you don’t find it, you won’t be able to treat.” Dr. Reckamp also noted that next generation sequencing (NGS) should be the preferred method of identifying RET status because NGS uses less tissue, provides genetic sequencing, and allows for the identification of binding partners.
“Does targeting RET improve patient outcomes?” she continued. “Because that is really the question we need to answer if we need to move forward with RET inhibition for lung cancer. So there are variable response rates, less than other inhibitors of other oncogenic-driven tumors, that’s for sure... But if you look at the data, and these are [for] heavily pretreated patients for the most part, the response rates are better than second-line cytotoxic chemotherapy that we have had in the past and similar to unselected checkpoint inhibition. So there is potential for improving outcomes, and again if we don’t know someone is RET, we potentially are not going to offer a treatment that could help them live longer or better.”
When asked how she would treat a newly-diagnosed patient with RET-positive NSCLC, Dr. Reckamp said she would treat with first-line chemotherapy rather than a tyrosine kinase inhibitor (TKI) but would enroll the patient in whatever TKI trial was ongoing at that point in time.
“There are multiple trials that are ongoing,” Dr. Reckamp said. “It is unlikely that a comparison trial will be completed and so we are going to have to look at these trials next to each other and differentiate based on toxicity [and] perceived efficacy.”
Specifically, Dr. Reckamp believes the medical community needs to move toward “universal testing” for RET status in lung cancer patients. Resistance and combination therapies will also need to be assessed in future studies.
“RET is important in lung cancer, and should be targeted. We now need to find the best way to do that,” Dr. Reckamp concluded.
The trial headed by Dr. Seto was funded by the Japan Agency for Medical Research and Development, AMED, and AstraZeneca. Dr. Seto reported receiving honoraria and research funding from multiple companies including AstraZeneca. The trial headed by Dr. Lee was funded by AstraZeneca Korea. Dr. Lee reported having a consulting or advisory role and receiving honoraria and research funding from AstraZeneca, Pfizer, and Roche/Genentech.
AT THE 2016 ASCO ANNUAL MEETING
Key clinical point: Vandetanib shows marked yet variable anti-tumor activity and toxicity in patients with RET-rearranged NSCLC.
Major finding: The overall response rates were 53% and 61% in two independent trials.
Data source: Two independently-conducted multicenter phase II trials of patients with RET-rearranged non-small cell lung cancer.
Disclosures: The trial headed by Dr. Seto was funded by the Japan Agency for Medical Research and Development, AMED, and AstraZeneca. Dr. Seto reported receiving honoraria and research funding from multiple companies including AstraZeneca. The trial headed by Dr. Lee was funded by AstraZeneca Korea Ltd. Dr. Lee reported having a consulting or advisory role and receiving honoraria and research funding from AstraZeneca, Pfizer, and Roche/Genentech.
VIDEO: Lobectomy quality requires linking outcomes to process change
BALTIMORE – An “introspective” analysis connecting patient outcomes with process changes may lead to significant surgical quality improvement, according to a study presented at the 2016 annual meeting of the American Association for Thoracic Surgery.
The case study detailed the University of Alabama at Birmingham School of Medicine’s attempt to identify the metrics used for the Society of Thoracic Surgeons lobectomy ranking, and show how the institution used root cause analysis with “lean” and process improvements to improve outcomes from Jan. 2006 until July 2014 in order to achieve a three star STS ranking.
UAB researchers found that their most common root cause analysis was failure to escalate care. The institution implemented process improvements such as increasing pulmonary rehabilitation prior to surgery, adding a respiratory therapist, eliminating (lean) non-valued steps, favoring stereotactic radiotherapy and segmentectomy instead of lobectomy for marginal patients, and using minimally invasive lobectomy. They ultimately achieved a three-star STS ranking.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Stephen D. Cassivi, professor of surgery at the Mayo Clinic in Rochester, Minn., and a discussant on the paper at AATS 2016, said in an interview that the research was important because it encourages surgeons to discuss and reevaluate quality improvement measures. He noted that early phases of surgical quality improvement was based on process measures, specifically around the idea that if surgeons were attentive to process measures, their outcome measures would improve. But over time, the emphasis on process measures has dissipated in favor of outcomes-focused analysis.
“Now that we have more robust [outcomes] data... we can examine our practices in a more thoughtful, data-driven, evidence-based way,” Dr. Cassivi said. He added that the shift from process measures to outcome measures is important in that surgeons can easily interpret and compare outcomes data across facilities. But he noted that there is a downside: If an institution’s outcome measures are not up to standard, it is sometimes difficult to determine why.
“The current way that the [outcomes] data are reported and processed is not easily interpretable into which processes we need to adapt,” Dr. Cassivi said. “There is still work that needs to be done, but [this paper] is a first step.”
Dr. Cassivi reported no relevant financial disclosures.
On Twitter @richpizzi
BALTIMORE – An “introspective” analysis connecting patient outcomes with process changes may lead to significant surgical quality improvement, according to a study presented at the 2016 annual meeting of the American Association for Thoracic Surgery.
The case study detailed the University of Alabama at Birmingham School of Medicine’s attempt to identify the metrics used for the Society of Thoracic Surgeons lobectomy ranking, and show how the institution used root cause analysis with “lean” and process improvements to improve outcomes from Jan. 2006 until July 2014 in order to achieve a three star STS ranking.
UAB researchers found that their most common root cause analysis was failure to escalate care. The institution implemented process improvements such as increasing pulmonary rehabilitation prior to surgery, adding a respiratory therapist, eliminating (lean) non-valued steps, favoring stereotactic radiotherapy and segmentectomy instead of lobectomy for marginal patients, and using minimally invasive lobectomy. They ultimately achieved a three-star STS ranking.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Stephen D. Cassivi, professor of surgery at the Mayo Clinic in Rochester, Minn., and a discussant on the paper at AATS 2016, said in an interview that the research was important because it encourages surgeons to discuss and reevaluate quality improvement measures. He noted that early phases of surgical quality improvement was based on process measures, specifically around the idea that if surgeons were attentive to process measures, their outcome measures would improve. But over time, the emphasis on process measures has dissipated in favor of outcomes-focused analysis.
“Now that we have more robust [outcomes] data... we can examine our practices in a more thoughtful, data-driven, evidence-based way,” Dr. Cassivi said. He added that the shift from process measures to outcome measures is important in that surgeons can easily interpret and compare outcomes data across facilities. But he noted that there is a downside: If an institution’s outcome measures are not up to standard, it is sometimes difficult to determine why.
“The current way that the [outcomes] data are reported and processed is not easily interpretable into which processes we need to adapt,” Dr. Cassivi said. “There is still work that needs to be done, but [this paper] is a first step.”
Dr. Cassivi reported no relevant financial disclosures.
On Twitter @richpizzi
BALTIMORE – An “introspective” analysis connecting patient outcomes with process changes may lead to significant surgical quality improvement, according to a study presented at the 2016 annual meeting of the American Association for Thoracic Surgery.
The case study detailed the University of Alabama at Birmingham School of Medicine’s attempt to identify the metrics used for the Society of Thoracic Surgeons lobectomy ranking, and show how the institution used root cause analysis with “lean” and process improvements to improve outcomes from Jan. 2006 until July 2014 in order to achieve a three star STS ranking.
UAB researchers found that their most common root cause analysis was failure to escalate care. The institution implemented process improvements such as increasing pulmonary rehabilitation prior to surgery, adding a respiratory therapist, eliminating (lean) non-valued steps, favoring stereotactic radiotherapy and segmentectomy instead of lobectomy for marginal patients, and using minimally invasive lobectomy. They ultimately achieved a three-star STS ranking.
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
Dr. Stephen D. Cassivi, professor of surgery at the Mayo Clinic in Rochester, Minn., and a discussant on the paper at AATS 2016, said in an interview that the research was important because it encourages surgeons to discuss and reevaluate quality improvement measures. He noted that early phases of surgical quality improvement was based on process measures, specifically around the idea that if surgeons were attentive to process measures, their outcome measures would improve. But over time, the emphasis on process measures has dissipated in favor of outcomes-focused analysis.
“Now that we have more robust [outcomes] data... we can examine our practices in a more thoughtful, data-driven, evidence-based way,” Dr. Cassivi said. He added that the shift from process measures to outcome measures is important in that surgeons can easily interpret and compare outcomes data across facilities. But he noted that there is a downside: If an institution’s outcome measures are not up to standard, it is sometimes difficult to determine why.
“The current way that the [outcomes] data are reported and processed is not easily interpretable into which processes we need to adapt,” Dr. Cassivi said. “There is still work that needs to be done, but [this paper] is a first step.”
Dr. Cassivi reported no relevant financial disclosures.
On Twitter @richpizzi
AT THE AATS ANNUAL MEETING
VIDEO: Surgical quality measures boost survival in cancer patients
BALTIMORE – Surgeons’ adherence to select quality measures when treating stage IIIA non–small-cell lung cancer patients led to improved patient survival, according to a study presented at the 2016 annual meeting of the American Association for Thoracic Surgery.
Researchers at Washington University in St. Louis identified 10,323 patients who received surgery for Stage IIIA NSCLC in the National Cancer Data Base from 2006 to 2010, and chose four quality measures that should have been met by surgeons: delivery of neoadjuvant multiagent chemotherapy (with or without radiation therapy); performing a lobectomy or greater resection; obtaining more than 10 lymph nodes, and achieving an R0 resection.
The researchers said 12.8% of patients met all four quality measures. Kaplan-Meier analysis demonstrated improved overall median survival by number of quality measures obtained: 0 quality measures, 12.7 months; 1 quality measure, 25.0 months; 2 quality measures, 31.4 months; 3 quality measures, 36.6 months; and 4 quality measures, 43.5 months.
In an interview, Dr. Mark S. Allen, professor of surgery at the Mayo Clinic in Rochester, Minn., and a discussant on the paper at AATS 2016, said the most striking result of the study was that such a low percentage of patients had all four quality measures performed for stage IIIA cancer. He called that finding “disappointing.”
“In general, [the study] shows there is still some work to be done to improve the quality when we operate on stage IIIA patients,” Dr. Allen said. “I’m not sure we do the greatest job of staging them clinically. When they are staged properly they probably do need preoperative chemotherapy, and I’m not sure we do that all the time.” He added that surgeon education about quality outcomes was critical to process improvement and patient outcomes.
Dr. Allen reported no relevant financial disclosures.
On Twitter @richpizzi
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BALTIMORE – Surgeons’ adherence to select quality measures when treating stage IIIA non–small-cell lung cancer patients led to improved patient survival, according to a study presented at the 2016 annual meeting of the American Association for Thoracic Surgery.
Researchers at Washington University in St. Louis identified 10,323 patients who received surgery for Stage IIIA NSCLC in the National Cancer Data Base from 2006 to 2010, and chose four quality measures that should have been met by surgeons: delivery of neoadjuvant multiagent chemotherapy (with or without radiation therapy); performing a lobectomy or greater resection; obtaining more than 10 lymph nodes, and achieving an R0 resection.
The researchers said 12.8% of patients met all four quality measures. Kaplan-Meier analysis demonstrated improved overall median survival by number of quality measures obtained: 0 quality measures, 12.7 months; 1 quality measure, 25.0 months; 2 quality measures, 31.4 months; 3 quality measures, 36.6 months; and 4 quality measures, 43.5 months.
In an interview, Dr. Mark S. Allen, professor of surgery at the Mayo Clinic in Rochester, Minn., and a discussant on the paper at AATS 2016, said the most striking result of the study was that such a low percentage of patients had all four quality measures performed for stage IIIA cancer. He called that finding “disappointing.”
“In general, [the study] shows there is still some work to be done to improve the quality when we operate on stage IIIA patients,” Dr. Allen said. “I’m not sure we do the greatest job of staging them clinically. When they are staged properly they probably do need preoperative chemotherapy, and I’m not sure we do that all the time.” He added that surgeon education about quality outcomes was critical to process improvement and patient outcomes.
Dr. Allen reported no relevant financial disclosures.
On Twitter @richpizzi
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
BALTIMORE – Surgeons’ adherence to select quality measures when treating stage IIIA non–small-cell lung cancer patients led to improved patient survival, according to a study presented at the 2016 annual meeting of the American Association for Thoracic Surgery.
Researchers at Washington University in St. Louis identified 10,323 patients who received surgery for Stage IIIA NSCLC in the National Cancer Data Base from 2006 to 2010, and chose four quality measures that should have been met by surgeons: delivery of neoadjuvant multiagent chemotherapy (with or without radiation therapy); performing a lobectomy or greater resection; obtaining more than 10 lymph nodes, and achieving an R0 resection.
The researchers said 12.8% of patients met all four quality measures. Kaplan-Meier analysis demonstrated improved overall median survival by number of quality measures obtained: 0 quality measures, 12.7 months; 1 quality measure, 25.0 months; 2 quality measures, 31.4 months; 3 quality measures, 36.6 months; and 4 quality measures, 43.5 months.
In an interview, Dr. Mark S. Allen, professor of surgery at the Mayo Clinic in Rochester, Minn., and a discussant on the paper at AATS 2016, said the most striking result of the study was that such a low percentage of patients had all four quality measures performed for stage IIIA cancer. He called that finding “disappointing.”
“In general, [the study] shows there is still some work to be done to improve the quality when we operate on stage IIIA patients,” Dr. Allen said. “I’m not sure we do the greatest job of staging them clinically. When they are staged properly they probably do need preoperative chemotherapy, and I’m not sure we do that all the time.” He added that surgeon education about quality outcomes was critical to process improvement and patient outcomes.
Dr. Allen reported no relevant financial disclosures.
On Twitter @richpizzi
The video associated with this article is no longer available on this site. Please view all of our videos on the MDedge YouTube channel
AT THE AATS ANNUAL MEETING
TAVR cerebral protection device appears safe, effective
PARIS – The TriGuard neuroprotection device for use during transcatheter aortic valve replacement effectively prevented strokes while raising no safety concerns in a pooled analysis of three controlled trials, according to Dr. Alexandra J. Lansky.
The TriGuard, which is investigational in the United States but approved in Europe, also significantly reduced the risk of central nervous system infarction, as assessed by diffusion-weighted MRI. Moreover, when imaging did show CNS infarcts in patients with the TriGuard in place during their TAVR (transcatheter aortic valve replacement), the total brain lesion volume was about 40% less than in controls without the neuroprotection device, according to Dr. Lansky, professor of medicine and director of the cardiovascular clinical research program at Yale University in New Haven, Conn.
“Essentially what’s happening is that we’re reducing with this device the frequency of CNS infarctions, and also reducing the size of the lesions when they are present,” she said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
The TriGuard is designed to fill an unmet need for stroke protection in TAVR patients. The incidence of clinical stroke within 30 days after TAVR in recent randomized controlled trials is 1.5%-6%. But there is clear evidence of underreporting of stroke in these trials. When neurologists examine TAVR patients or the patients are evaluated by serial testing using the NIH Stroke Scale plus brain imaging, the 30-day stroke rates are 15%-28%, according to the cardiologist.
“We know that about 50% of these strokes happen in the periprocedural period, and stroke is one of the strongest predictors of mortality, conferring a three- to ninefold increased risk,” Dr. Lansky emphasized.
She presented a pooled analysis including 59 TriGuard recipients and 83 controls who underwent TAVR in the DEFLECT I and III trials and the NeuroTAVR registry. They were evaluated using the NIH Stroke Scale before TAVR and again at 4 and 30 days post procedure. In addition, they underwent brain imaging via diffusion-weighted MRI 4 days post TAVR.
Stroke as defined by the Valve Academic Research Consortium–2 (VARC2) criteria occurred in none of the TriGuard group but in 6% of controls. And stroke as defined by the American Stroke Association, which requires a worsening score on the serial NIH Stroke Scale measurements plus imaging evidence of CNS infarction, occurred in 0 TriGuard-protected patients and in 19% of controls.
The incidence of CNS infarction on MRI was 92% in controls and 72% in the TriGuard group. Thus, 28% of patients with the TriGuard in place developed no brain infarct lesions at all; that’s a first for any TAVR neuroprotection device, according to Dr. Lansky.
In patients with CNS lesions, the total lesion volume was 101 mm3 in the TriGuard group, compared with 174 mm3 in the controls. The average lesion volume was 25 mm3 in the TriGuard group versus 43 mm3 in the controls.
TriGuard is a relatively simple device consisting of a single-wire nitinol frame and mesh filter with a pore size of 130 mcm. It’s designed to deflect emboli during TAVR while allowing maximal cerebral blood flow. After being delivered by a 9 French sheath from the contralateral femoral artery, the device sits at the roof of the aortic arch. Importantly, it covers all three cerebral arteries, Dr. Lansky said. The device is held in position by a stabilizer in the innominate artery.
Although introducing an additional element into TAVR raises the theoretic possibility of safety concerns, no safety signal was seen in the pooled analysis. In-hospital major adverse event rates were similar in the two groups.
Asked why 72% of patients with the TriGuard in place nonetheless developed CNS infarcts, Dr. Lansky said she believes the device has gaps on the sides that allow smaller emboli to pass through. Future iterations of the TriGuard will address this.
The clinical significance of the CNS infarcts seen on MRI in TAVR patients is a controversial issue among interventional cardiologists. Some cardiologists consider these to be silent lesions of dubious clinical relevance. That’s not Dr. Lansky’s view.
“When you track these MRI lesions out to 30 days, many times they disappear. They don’t disappear because there’s no damage; they disappear because the cells die. When you talk to neurologists about the MRI lesions, they will tell you that they actually represent cell death and correlate with brain infarction,” she said.
Dr. Nicolo Piazza commented that he considered the pooled analysis findings hypothesis generating but not definitive because of baseline imbalances between the two study arms. The control group had numerically higher – albeit not statistically significantly so – rates of atrial fibrillation at hospital admission as well as higher Society of Thoracic Surgeons risk scores, both of which increase stroke risk, noted Dr. Piazza of McGill University in Montreal.
Dr. Lansky replied that the much larger ongoing pivotal randomized, phase III REFLECT trial should provide definitive answers.
She reported receiving institutional research grant support from Keystone Heart, which produces the TriGuard device.
PARIS – The TriGuard neuroprotection device for use during transcatheter aortic valve replacement effectively prevented strokes while raising no safety concerns in a pooled analysis of three controlled trials, according to Dr. Alexandra J. Lansky.
The TriGuard, which is investigational in the United States but approved in Europe, also significantly reduced the risk of central nervous system infarction, as assessed by diffusion-weighted MRI. Moreover, when imaging did show CNS infarcts in patients with the TriGuard in place during their TAVR (transcatheter aortic valve replacement), the total brain lesion volume was about 40% less than in controls without the neuroprotection device, according to Dr. Lansky, professor of medicine and director of the cardiovascular clinical research program at Yale University in New Haven, Conn.
“Essentially what’s happening is that we’re reducing with this device the frequency of CNS infarctions, and also reducing the size of the lesions when they are present,” she said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
The TriGuard is designed to fill an unmet need for stroke protection in TAVR patients. The incidence of clinical stroke within 30 days after TAVR in recent randomized controlled trials is 1.5%-6%. But there is clear evidence of underreporting of stroke in these trials. When neurologists examine TAVR patients or the patients are evaluated by serial testing using the NIH Stroke Scale plus brain imaging, the 30-day stroke rates are 15%-28%, according to the cardiologist.
“We know that about 50% of these strokes happen in the periprocedural period, and stroke is one of the strongest predictors of mortality, conferring a three- to ninefold increased risk,” Dr. Lansky emphasized.
She presented a pooled analysis including 59 TriGuard recipients and 83 controls who underwent TAVR in the DEFLECT I and III trials and the NeuroTAVR registry. They were evaluated using the NIH Stroke Scale before TAVR and again at 4 and 30 days post procedure. In addition, they underwent brain imaging via diffusion-weighted MRI 4 days post TAVR.
Stroke as defined by the Valve Academic Research Consortium–2 (VARC2) criteria occurred in none of the TriGuard group but in 6% of controls. And stroke as defined by the American Stroke Association, which requires a worsening score on the serial NIH Stroke Scale measurements plus imaging evidence of CNS infarction, occurred in 0 TriGuard-protected patients and in 19% of controls.
The incidence of CNS infarction on MRI was 92% in controls and 72% in the TriGuard group. Thus, 28% of patients with the TriGuard in place developed no brain infarct lesions at all; that’s a first for any TAVR neuroprotection device, according to Dr. Lansky.
In patients with CNS lesions, the total lesion volume was 101 mm3 in the TriGuard group, compared with 174 mm3 in the controls. The average lesion volume was 25 mm3 in the TriGuard group versus 43 mm3 in the controls.
TriGuard is a relatively simple device consisting of a single-wire nitinol frame and mesh filter with a pore size of 130 mcm. It’s designed to deflect emboli during TAVR while allowing maximal cerebral blood flow. After being delivered by a 9 French sheath from the contralateral femoral artery, the device sits at the roof of the aortic arch. Importantly, it covers all three cerebral arteries, Dr. Lansky said. The device is held in position by a stabilizer in the innominate artery.
Although introducing an additional element into TAVR raises the theoretic possibility of safety concerns, no safety signal was seen in the pooled analysis. In-hospital major adverse event rates were similar in the two groups.
Asked why 72% of patients with the TriGuard in place nonetheless developed CNS infarcts, Dr. Lansky said she believes the device has gaps on the sides that allow smaller emboli to pass through. Future iterations of the TriGuard will address this.
The clinical significance of the CNS infarcts seen on MRI in TAVR patients is a controversial issue among interventional cardiologists. Some cardiologists consider these to be silent lesions of dubious clinical relevance. That’s not Dr. Lansky’s view.
“When you track these MRI lesions out to 30 days, many times they disappear. They don’t disappear because there’s no damage; they disappear because the cells die. When you talk to neurologists about the MRI lesions, they will tell you that they actually represent cell death and correlate with brain infarction,” she said.
Dr. Nicolo Piazza commented that he considered the pooled analysis findings hypothesis generating but not definitive because of baseline imbalances between the two study arms. The control group had numerically higher – albeit not statistically significantly so – rates of atrial fibrillation at hospital admission as well as higher Society of Thoracic Surgeons risk scores, both of which increase stroke risk, noted Dr. Piazza of McGill University in Montreal.
Dr. Lansky replied that the much larger ongoing pivotal randomized, phase III REFLECT trial should provide definitive answers.
She reported receiving institutional research grant support from Keystone Heart, which produces the TriGuard device.
PARIS – The TriGuard neuroprotection device for use during transcatheter aortic valve replacement effectively prevented strokes while raising no safety concerns in a pooled analysis of three controlled trials, according to Dr. Alexandra J. Lansky.
The TriGuard, which is investigational in the United States but approved in Europe, also significantly reduced the risk of central nervous system infarction, as assessed by diffusion-weighted MRI. Moreover, when imaging did show CNS infarcts in patients with the TriGuard in place during their TAVR (transcatheter aortic valve replacement), the total brain lesion volume was about 40% less than in controls without the neuroprotection device, according to Dr. Lansky, professor of medicine and director of the cardiovascular clinical research program at Yale University in New Haven, Conn.
“Essentially what’s happening is that we’re reducing with this device the frequency of CNS infarctions, and also reducing the size of the lesions when they are present,” she said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
The TriGuard is designed to fill an unmet need for stroke protection in TAVR patients. The incidence of clinical stroke within 30 days after TAVR in recent randomized controlled trials is 1.5%-6%. But there is clear evidence of underreporting of stroke in these trials. When neurologists examine TAVR patients or the patients are evaluated by serial testing using the NIH Stroke Scale plus brain imaging, the 30-day stroke rates are 15%-28%, according to the cardiologist.
“We know that about 50% of these strokes happen in the periprocedural period, and stroke is one of the strongest predictors of mortality, conferring a three- to ninefold increased risk,” Dr. Lansky emphasized.
She presented a pooled analysis including 59 TriGuard recipients and 83 controls who underwent TAVR in the DEFLECT I and III trials and the NeuroTAVR registry. They were evaluated using the NIH Stroke Scale before TAVR and again at 4 and 30 days post procedure. In addition, they underwent brain imaging via diffusion-weighted MRI 4 days post TAVR.
Stroke as defined by the Valve Academic Research Consortium–2 (VARC2) criteria occurred in none of the TriGuard group but in 6% of controls. And stroke as defined by the American Stroke Association, which requires a worsening score on the serial NIH Stroke Scale measurements plus imaging evidence of CNS infarction, occurred in 0 TriGuard-protected patients and in 19% of controls.
The incidence of CNS infarction on MRI was 92% in controls and 72% in the TriGuard group. Thus, 28% of patients with the TriGuard in place developed no brain infarct lesions at all; that’s a first for any TAVR neuroprotection device, according to Dr. Lansky.
In patients with CNS lesions, the total lesion volume was 101 mm3 in the TriGuard group, compared with 174 mm3 in the controls. The average lesion volume was 25 mm3 in the TriGuard group versus 43 mm3 in the controls.
TriGuard is a relatively simple device consisting of a single-wire nitinol frame and mesh filter with a pore size of 130 mcm. It’s designed to deflect emboli during TAVR while allowing maximal cerebral blood flow. After being delivered by a 9 French sheath from the contralateral femoral artery, the device sits at the roof of the aortic arch. Importantly, it covers all three cerebral arteries, Dr. Lansky said. The device is held in position by a stabilizer in the innominate artery.
Although introducing an additional element into TAVR raises the theoretic possibility of safety concerns, no safety signal was seen in the pooled analysis. In-hospital major adverse event rates were similar in the two groups.
Asked why 72% of patients with the TriGuard in place nonetheless developed CNS infarcts, Dr. Lansky said she believes the device has gaps on the sides that allow smaller emboli to pass through. Future iterations of the TriGuard will address this.
The clinical significance of the CNS infarcts seen on MRI in TAVR patients is a controversial issue among interventional cardiologists. Some cardiologists consider these to be silent lesions of dubious clinical relevance. That’s not Dr. Lansky’s view.
“When you track these MRI lesions out to 30 days, many times they disappear. They don’t disappear because there’s no damage; they disappear because the cells die. When you talk to neurologists about the MRI lesions, they will tell you that they actually represent cell death and correlate with brain infarction,” she said.
Dr. Nicolo Piazza commented that he considered the pooled analysis findings hypothesis generating but not definitive because of baseline imbalances between the two study arms. The control group had numerically higher – albeit not statistically significantly so – rates of atrial fibrillation at hospital admission as well as higher Society of Thoracic Surgeons risk scores, both of which increase stroke risk, noted Dr. Piazza of McGill University in Montreal.
Dr. Lansky replied that the much larger ongoing pivotal randomized, phase III REFLECT trial should provide definitive answers.
She reported receiving institutional research grant support from Keystone Heart, which produces the TriGuard device.
AT EUROPCR 2016
Key clinical point: The TriGuard neuroprotection device for use in TAVR effectively prevented strokes.
Major finding: The 30-day incidence of stroke in TAVR patients with the TriGard embolic protection device in place was 0, compared with 6% or 19% in controls, depending upon the stroke definition used.
Data source: A post hoc analysis of pooled data on 59 TriGuard recipients and 83 controls in three trials.
Disclosures: The presenter reported receiving institutional research grant support from Keystone Heart, which produces the TriGuard device.
Esophageal perforation severity scoring system reliably stratifies patients
The Pittsburgh perforation severity score (PSS) can be used to improve decision making in the management of esophageal perforation, findings from a retrospective, multicenter study have shown.
Dr. Michael Schweigert and his colleagues performed a study of 288 patients with esophageal perforation treated at 11 centers between 1990 and 2014, using them as a completely independent population to validate whether the PSS could be used to stratify such patients into discrete subgroups with differential outcomes.
The PSS was analyzed using logistic regression as a continuous variable and stratified into low, intermediate and high score groups, according to their report published in the Journal of Thoracic and Cardiovascular Surgery (2016 Apr;151:1002-11).
Operative management was more frequent than nonoperative management (200 patients, or 69.4% vs. 30.6%), according to Dr. Schweigert of the Städtisches Klinikum Dresden Friedrichstadt, Germany, and his colleagues. Patients with esophageal cancer (34/43; 79%) and stricture (18/23; 78.3%) mainly were treated operatively. The most common type of surgery was primary repair (83 patients), followed by surgical drainage (38 patients).
Perforation-related morbidity was seen in 180 patients (65%), with sepsis (21%) and pneumonia (19%) being most common. Overall in-hospital mortality was 20%, and the median length of stay was 27 days.
Patients with fatal outcomes had a significantly higher median PSS score (11 vs. 1) and the median PSS was significantly higher in operatively managed cases, compared with nonoperative cases (5 vs. 4, P = .0001). The researchers found that the PSS score predicted morbidity well, with an area under the curve (AUC) of 0.77, as well as mortality (AUC = 0.83). However, prediction of the need for operative management was not as good (AUC = 0.65).
Based upon their analysis, the researchers proposed a treatment decision tree in which group I (low PSS patients) should have a focus of nonoperative management. Group 2 patients (medium PSS) with non–contained leak preferably should be managed by surgery.
They found that the high-risk group (PSS greater than 5) had the worst prognosis and highest mortality, with the odds for mortality being 8 times higher than that the intermediate group and 18 times higher than the low-risk group. “Because these patients are most endangered by esophageal perforation, early and aggressive treatment is mandatory to avoid fatal outcomes,” the authors stated.
They found that nonoperative management was not associated with higher mortality or more unfavorable outcome regarding perforation-related morbidity or length of stay, but they pointed out that nonoperative treatment was only successful in 60% of cases, with 36 out of the 88 nonoperative patients eventually undergoing surgery and 8 undergoing esophagectomy. But patients with a high perforation severity score were 3.37 times more likely to have operative management compared to low-scoring patients. “Better selective criteria for nonoperative management are urgently required,” they stated.
“The Pittsburgh PSS is helpful to assess the severity and potential consequences of esophageal injury and stratifies patients into low-, intermediate-, and high-risk groups with differential morbidity and mortality outcomes. Prospective studies are required to analyze the influence of the Pittsburgh scoring system on the treatment of esophageal perforation,” the researchers concluded.
The authors reported having no disclosures.
A webcast of the AATS Annual Meeting presentation of this paper is available.

|
Dr. Mara B. Antonoff |
Schweigert and his colleagues suggest that the Pittsburgh scoring system may identify patients suitable for nonoperative management. The authors retrospectively found less morbidity/mortality and less-frequent operative management among patients in Group 1, and thus, a recommendation was formulated favoring less-invasive management for these individuals.
The additional step of evaluating the success of nonoperative management in each group, either through further analyses of the current study or with future prospective studies is needed in order to make such recommendations.
Further demonstrating the utility of the Pittsburgh esophageal PSS, this study supports the notion that prospective, large-scale studies are in need, and that such scoring systems will be instrumental in standardizing data across centers.
Dr. Mara B. Antonoff is from the department of thoracic and cardiothoracic surgery at the University of Texas MD Anderson Cancer Center, Houston. Her remarks were made as part of an invited commentary on the article (J Thorac Cardiovasc Surg. 2016 Apr;151:1012-3).

|
Dr. Mara B. Antonoff |
Schweigert and his colleagues suggest that the Pittsburgh scoring system may identify patients suitable for nonoperative management. The authors retrospectively found less morbidity/mortality and less-frequent operative management among patients in Group 1, and thus, a recommendation was formulated favoring less-invasive management for these individuals.
The additional step of evaluating the success of nonoperative management in each group, either through further analyses of the current study or with future prospective studies is needed in order to make such recommendations.
Further demonstrating the utility of the Pittsburgh esophageal PSS, this study supports the notion that prospective, large-scale studies are in need, and that such scoring systems will be instrumental in standardizing data across centers.
Dr. Mara B. Antonoff is from the department of thoracic and cardiothoracic surgery at the University of Texas MD Anderson Cancer Center, Houston. Her remarks were made as part of an invited commentary on the article (J Thorac Cardiovasc Surg. 2016 Apr;151:1012-3).

|
Dr. Mara B. Antonoff |
Schweigert and his colleagues suggest that the Pittsburgh scoring system may identify patients suitable for nonoperative management. The authors retrospectively found less morbidity/mortality and less-frequent operative management among patients in Group 1, and thus, a recommendation was formulated favoring less-invasive management for these individuals.
The additional step of evaluating the success of nonoperative management in each group, either through further analyses of the current study or with future prospective studies is needed in order to make such recommendations.
Further demonstrating the utility of the Pittsburgh esophageal PSS, this study supports the notion that prospective, large-scale studies are in need, and that such scoring systems will be instrumental in standardizing data across centers.
Dr. Mara B. Antonoff is from the department of thoracic and cardiothoracic surgery at the University of Texas MD Anderson Cancer Center, Houston. Her remarks were made as part of an invited commentary on the article (J Thorac Cardiovasc Surg. 2016 Apr;151:1012-3).
The Pittsburgh perforation severity score (PSS) can be used to improve decision making in the management of esophageal perforation, findings from a retrospective, multicenter study have shown.
Dr. Michael Schweigert and his colleagues performed a study of 288 patients with esophageal perforation treated at 11 centers between 1990 and 2014, using them as a completely independent population to validate whether the PSS could be used to stratify such patients into discrete subgroups with differential outcomes.
The PSS was analyzed using logistic regression as a continuous variable and stratified into low, intermediate and high score groups, according to their report published in the Journal of Thoracic and Cardiovascular Surgery (2016 Apr;151:1002-11).
Operative management was more frequent than nonoperative management (200 patients, or 69.4% vs. 30.6%), according to Dr. Schweigert of the Städtisches Klinikum Dresden Friedrichstadt, Germany, and his colleagues. Patients with esophageal cancer (34/43; 79%) and stricture (18/23; 78.3%) mainly were treated operatively. The most common type of surgery was primary repair (83 patients), followed by surgical drainage (38 patients).
Perforation-related morbidity was seen in 180 patients (65%), with sepsis (21%) and pneumonia (19%) being most common. Overall in-hospital mortality was 20%, and the median length of stay was 27 days.
Patients with fatal outcomes had a significantly higher median PSS score (11 vs. 1) and the median PSS was significantly higher in operatively managed cases, compared with nonoperative cases (5 vs. 4, P = .0001). The researchers found that the PSS score predicted morbidity well, with an area under the curve (AUC) of 0.77, as well as mortality (AUC = 0.83). However, prediction of the need for operative management was not as good (AUC = 0.65).
Based upon their analysis, the researchers proposed a treatment decision tree in which group I (low PSS patients) should have a focus of nonoperative management. Group 2 patients (medium PSS) with non–contained leak preferably should be managed by surgery.
They found that the high-risk group (PSS greater than 5) had the worst prognosis and highest mortality, with the odds for mortality being 8 times higher than that the intermediate group and 18 times higher than the low-risk group. “Because these patients are most endangered by esophageal perforation, early and aggressive treatment is mandatory to avoid fatal outcomes,” the authors stated.
They found that nonoperative management was not associated with higher mortality or more unfavorable outcome regarding perforation-related morbidity or length of stay, but they pointed out that nonoperative treatment was only successful in 60% of cases, with 36 out of the 88 nonoperative patients eventually undergoing surgery and 8 undergoing esophagectomy. But patients with a high perforation severity score were 3.37 times more likely to have operative management compared to low-scoring patients. “Better selective criteria for nonoperative management are urgently required,” they stated.
“The Pittsburgh PSS is helpful to assess the severity and potential consequences of esophageal injury and stratifies patients into low-, intermediate-, and high-risk groups with differential morbidity and mortality outcomes. Prospective studies are required to analyze the influence of the Pittsburgh scoring system on the treatment of esophageal perforation,” the researchers concluded.
The authors reported having no disclosures.
A webcast of the AATS Annual Meeting presentation of this paper is available.
The Pittsburgh perforation severity score (PSS) can be used to improve decision making in the management of esophageal perforation, findings from a retrospective, multicenter study have shown.
Dr. Michael Schweigert and his colleagues performed a study of 288 patients with esophageal perforation treated at 11 centers between 1990 and 2014, using them as a completely independent population to validate whether the PSS could be used to stratify such patients into discrete subgroups with differential outcomes.
The PSS was analyzed using logistic regression as a continuous variable and stratified into low, intermediate and high score groups, according to their report published in the Journal of Thoracic and Cardiovascular Surgery (2016 Apr;151:1002-11).
Operative management was more frequent than nonoperative management (200 patients, or 69.4% vs. 30.6%), according to Dr. Schweigert of the Städtisches Klinikum Dresden Friedrichstadt, Germany, and his colleagues. Patients with esophageal cancer (34/43; 79%) and stricture (18/23; 78.3%) mainly were treated operatively. The most common type of surgery was primary repair (83 patients), followed by surgical drainage (38 patients).
Perforation-related morbidity was seen in 180 patients (65%), with sepsis (21%) and pneumonia (19%) being most common. Overall in-hospital mortality was 20%, and the median length of stay was 27 days.
Patients with fatal outcomes had a significantly higher median PSS score (11 vs. 1) and the median PSS was significantly higher in operatively managed cases, compared with nonoperative cases (5 vs. 4, P = .0001). The researchers found that the PSS score predicted morbidity well, with an area under the curve (AUC) of 0.77, as well as mortality (AUC = 0.83). However, prediction of the need for operative management was not as good (AUC = 0.65).
Based upon their analysis, the researchers proposed a treatment decision tree in which group I (low PSS patients) should have a focus of nonoperative management. Group 2 patients (medium PSS) with non–contained leak preferably should be managed by surgery.
They found that the high-risk group (PSS greater than 5) had the worst prognosis and highest mortality, with the odds for mortality being 8 times higher than that the intermediate group and 18 times higher than the low-risk group. “Because these patients are most endangered by esophageal perforation, early and aggressive treatment is mandatory to avoid fatal outcomes,” the authors stated.
They found that nonoperative management was not associated with higher mortality or more unfavorable outcome regarding perforation-related morbidity or length of stay, but they pointed out that nonoperative treatment was only successful in 60% of cases, with 36 out of the 88 nonoperative patients eventually undergoing surgery and 8 undergoing esophagectomy. But patients with a high perforation severity score were 3.37 times more likely to have operative management compared to low-scoring patients. “Better selective criteria for nonoperative management are urgently required,” they stated.
“The Pittsburgh PSS is helpful to assess the severity and potential consequences of esophageal injury and stratifies patients into low-, intermediate-, and high-risk groups with differential morbidity and mortality outcomes. Prospective studies are required to analyze the influence of the Pittsburgh scoring system on the treatment of esophageal perforation,” the researchers concluded.
The authors reported having no disclosures.
A webcast of the AATS Annual Meeting presentation of this paper is available.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Scoring system reliably stratifies patients into low-, intermediate-, and high-risk groups.
Major finding: Patients with a high perforation severity score were 3.37 times more likely to have operative management, compared with low-scoring patients.
Data source: A retrospective study was performed on 288 patients with esophageal perforation at 11 centers since 1990.
Disclosures: The authors presented no relevant disclosures.
Pulmonary function testing adds little to STS risk scores
Routine preoperative pulmonary function tests appear to have only limited utility in predicting outcomes in patients undergoing cardiothoracic surgery when the Society of Thoracic Surgeons risk score is available, according to the results of a retrospective study.
Dr. Alexander Ivanov of New York Methodist Hospital, Brooklyn, and his colleagues conducted a database analysis of 1,685 patients undergoing index cardiac surgery at New York Methodist Hospital between April 2004 and January 2014. They used the STS risk model version 2.73 to estimate postoperative risk of respiratory failure (defined as the need for mechanical ventilation greater than or equal to 72 hours, or reintubation), prolonged postoperative length of stay (defined as greater than 14 days), and 30-day all cause mortality in these patients, according to their report in The Journal of Thoracic and Cardiovascular Surgery (2016;151:1183-9).
They plotted the receiver operating characteristics curve for the STS score for each of these adverse events and compared the resulting area under the curve (AUC) with the AUC after adding pulmonary function testing parameters and COPD classifications.
A total of 1,412 patients had a calculated STS score, of which 751 underwent pulmonary function testing (53%). In general, patients who had pulmonary function testing were older and had higher rates of comorbidities and more complex cardiothoracic surgery compared with their counterparts, according to Dr. Ivanov. These patients also had significantly elevated STS risk for prolonged ventilation (12.4% vs. 10.3%), prolonged postoperative length of stay (8.9% vs. 7.2%), and 30-day mortality (2.7% vs. 2.2%).
The decision to perform pulmonary testing was left to the treating physician. Of those patients tested, 652 had bedside spirometry and 99 had formal laboratory testing. Forced expiratory volume in 1 second (FEV1) and forced volume vital capacity (FVC) values were determined by taking the best of three trials. COPD was diagnosed in cases of an FEV1/FVC ratio of less than 70%.
Among these patients, 4.5% developed postoperative respiratory failure, and there was no statistically significant difference in the respiratory failure rate between patients with and without pulmonary function testing. In addition, there was no significant difference in 30-day mortality between these patients (1.9% vs. 2.1%). However, a total of 6.9% had a prolonged postoperative length of stay, with a significantly higher rate in the patients with pulmonary function testing than without (8.8% vs. 4.7%).
Dr. Ivanov and his colleagues found that the AUC of the STS score was 0.65 (95% confidence interval [CI], 0.55-0.74)for respiratory failure, 0.67 (95% CI, 0.6-0.74) for prolonged postoperative length of stay, and 0.74 (95% CI, 0.6-0.87) for 30-day mortality. Even though the STS score based upon clinical definitions of lung disease afforded only modest discriminatory ability for the three studied outcomes, they found that there was no significant added benefit to the predictive ability of these STS scores obtained by incorporating any of the pulmonary function testing parameters or COPD classifications studied.
“A possible physiological explanation for these findings may be that the examined pulmonary function testing variables do not depend solely on pulmonary parameters such as airway diameter, degree of obstruction, or lung elasticity, but rather on a patient’s effort and muscle “strength,” characteristics that are already well captured and accounted for in the current STS model,” the researchers stated.
“The STS score calculated with clinical information on lung disease status offers modest discriminatory ability for respiratory failure, prolonged postoperative length of stay, and 30-day mortality after CT surgery, which cannot be improved by adding PFT parameters or PFT-derived COPD categorization,” they wrote. “Therefore, routine preoperative PFTs may have only limited clinical utility in patients undergoing CT surgery when the STS score is readily available. Further prospective studies will be helpful in confirming these conclusions,” Dr. Ivanov and his colleagues noted.
The authors reported that they had nothing to disclose.
Chronic lung disease is one of the risk factors included in the STS model for mortality, renal failure, prolonged ventilation, sternal wound infection, reoperation, and length of hospital stay. Mild, moderate, and severe CLD increases the odds ratio for those complications. A total of 20% of almost 1 million patients used in developing the current STS risk model had CLD.

|
Dr. Juan A. Crestanello |
The authors found that none of the pulmonary function testing parameters added to the predictive ability of the STS risk model for operative mortality, prolonged ventilation, or prolonged length of hospital stay. Because CLD is 1 of 40 preoperative and operative variables used in the STS risk model, an improvement in discrimination of only 1 of 40 variables is very unlikely to improve the overall model.
One may be tempted to conclude that it is not worth performing pulmonary function testing before cardiac surgery. However, remember once again the importance of precise and accurate data to support risk stratification. In science, behind each word resides a precise definition; without a pulmonary function test, we cannot define chronic lung disease severity.
Dr. Juan A. Crestanello is in the division of cardiac surgery, Wexner Medical Center, Ohio State University, Columbus. His remarks are from an invited commentary (J Thorac Cardiovasc Surg. 2016;151:1189-90).
Chronic lung disease is one of the risk factors included in the STS model for mortality, renal failure, prolonged ventilation, sternal wound infection, reoperation, and length of hospital stay. Mild, moderate, and severe CLD increases the odds ratio for those complications. A total of 20% of almost 1 million patients used in developing the current STS risk model had CLD.

|
Dr. Juan A. Crestanello |
The authors found that none of the pulmonary function testing parameters added to the predictive ability of the STS risk model for operative mortality, prolonged ventilation, or prolonged length of hospital stay. Because CLD is 1 of 40 preoperative and operative variables used in the STS risk model, an improvement in discrimination of only 1 of 40 variables is very unlikely to improve the overall model.
One may be tempted to conclude that it is not worth performing pulmonary function testing before cardiac surgery. However, remember once again the importance of precise and accurate data to support risk stratification. In science, behind each word resides a precise definition; without a pulmonary function test, we cannot define chronic lung disease severity.
Dr. Juan A. Crestanello is in the division of cardiac surgery, Wexner Medical Center, Ohio State University, Columbus. His remarks are from an invited commentary (J Thorac Cardiovasc Surg. 2016;151:1189-90).
Chronic lung disease is one of the risk factors included in the STS model for mortality, renal failure, prolonged ventilation, sternal wound infection, reoperation, and length of hospital stay. Mild, moderate, and severe CLD increases the odds ratio for those complications. A total of 20% of almost 1 million patients used in developing the current STS risk model had CLD.

|
Dr. Juan A. Crestanello |
The authors found that none of the pulmonary function testing parameters added to the predictive ability of the STS risk model for operative mortality, prolonged ventilation, or prolonged length of hospital stay. Because CLD is 1 of 40 preoperative and operative variables used in the STS risk model, an improvement in discrimination of only 1 of 40 variables is very unlikely to improve the overall model.
One may be tempted to conclude that it is not worth performing pulmonary function testing before cardiac surgery. However, remember once again the importance of precise and accurate data to support risk stratification. In science, behind each word resides a precise definition; without a pulmonary function test, we cannot define chronic lung disease severity.
Dr. Juan A. Crestanello is in the division of cardiac surgery, Wexner Medical Center, Ohio State University, Columbus. His remarks are from an invited commentary (J Thorac Cardiovasc Surg. 2016;151:1189-90).
Routine preoperative pulmonary function tests appear to have only limited utility in predicting outcomes in patients undergoing cardiothoracic surgery when the Society of Thoracic Surgeons risk score is available, according to the results of a retrospective study.
Dr. Alexander Ivanov of New York Methodist Hospital, Brooklyn, and his colleagues conducted a database analysis of 1,685 patients undergoing index cardiac surgery at New York Methodist Hospital between April 2004 and January 2014. They used the STS risk model version 2.73 to estimate postoperative risk of respiratory failure (defined as the need for mechanical ventilation greater than or equal to 72 hours, or reintubation), prolonged postoperative length of stay (defined as greater than 14 days), and 30-day all cause mortality in these patients, according to their report in The Journal of Thoracic and Cardiovascular Surgery (2016;151:1183-9).
They plotted the receiver operating characteristics curve for the STS score for each of these adverse events and compared the resulting area under the curve (AUC) with the AUC after adding pulmonary function testing parameters and COPD classifications.
A total of 1,412 patients had a calculated STS score, of which 751 underwent pulmonary function testing (53%). In general, patients who had pulmonary function testing were older and had higher rates of comorbidities and more complex cardiothoracic surgery compared with their counterparts, according to Dr. Ivanov. These patients also had significantly elevated STS risk for prolonged ventilation (12.4% vs. 10.3%), prolonged postoperative length of stay (8.9% vs. 7.2%), and 30-day mortality (2.7% vs. 2.2%).
The decision to perform pulmonary testing was left to the treating physician. Of those patients tested, 652 had bedside spirometry and 99 had formal laboratory testing. Forced expiratory volume in 1 second (FEV1) and forced volume vital capacity (FVC) values were determined by taking the best of three trials. COPD was diagnosed in cases of an FEV1/FVC ratio of less than 70%.
Among these patients, 4.5% developed postoperative respiratory failure, and there was no statistically significant difference in the respiratory failure rate between patients with and without pulmonary function testing. In addition, there was no significant difference in 30-day mortality between these patients (1.9% vs. 2.1%). However, a total of 6.9% had a prolonged postoperative length of stay, with a significantly higher rate in the patients with pulmonary function testing than without (8.8% vs. 4.7%).
Dr. Ivanov and his colleagues found that the AUC of the STS score was 0.65 (95% confidence interval [CI], 0.55-0.74)for respiratory failure, 0.67 (95% CI, 0.6-0.74) for prolonged postoperative length of stay, and 0.74 (95% CI, 0.6-0.87) for 30-day mortality. Even though the STS score based upon clinical definitions of lung disease afforded only modest discriminatory ability for the three studied outcomes, they found that there was no significant added benefit to the predictive ability of these STS scores obtained by incorporating any of the pulmonary function testing parameters or COPD classifications studied.
“A possible physiological explanation for these findings may be that the examined pulmonary function testing variables do not depend solely on pulmonary parameters such as airway diameter, degree of obstruction, or lung elasticity, but rather on a patient’s effort and muscle “strength,” characteristics that are already well captured and accounted for in the current STS model,” the researchers stated.
“The STS score calculated with clinical information on lung disease status offers modest discriminatory ability for respiratory failure, prolonged postoperative length of stay, and 30-day mortality after CT surgery, which cannot be improved by adding PFT parameters or PFT-derived COPD categorization,” they wrote. “Therefore, routine preoperative PFTs may have only limited clinical utility in patients undergoing CT surgery when the STS score is readily available. Further prospective studies will be helpful in confirming these conclusions,” Dr. Ivanov and his colleagues noted.
The authors reported that they had nothing to disclose.
Routine preoperative pulmonary function tests appear to have only limited utility in predicting outcomes in patients undergoing cardiothoracic surgery when the Society of Thoracic Surgeons risk score is available, according to the results of a retrospective study.
Dr. Alexander Ivanov of New York Methodist Hospital, Brooklyn, and his colleagues conducted a database analysis of 1,685 patients undergoing index cardiac surgery at New York Methodist Hospital between April 2004 and January 2014. They used the STS risk model version 2.73 to estimate postoperative risk of respiratory failure (defined as the need for mechanical ventilation greater than or equal to 72 hours, or reintubation), prolonged postoperative length of stay (defined as greater than 14 days), and 30-day all cause mortality in these patients, according to their report in The Journal of Thoracic and Cardiovascular Surgery (2016;151:1183-9).
They plotted the receiver operating characteristics curve for the STS score for each of these adverse events and compared the resulting area under the curve (AUC) with the AUC after adding pulmonary function testing parameters and COPD classifications.
A total of 1,412 patients had a calculated STS score, of which 751 underwent pulmonary function testing (53%). In general, patients who had pulmonary function testing were older and had higher rates of comorbidities and more complex cardiothoracic surgery compared with their counterparts, according to Dr. Ivanov. These patients also had significantly elevated STS risk for prolonged ventilation (12.4% vs. 10.3%), prolonged postoperative length of stay (8.9% vs. 7.2%), and 30-day mortality (2.7% vs. 2.2%).
The decision to perform pulmonary testing was left to the treating physician. Of those patients tested, 652 had bedside spirometry and 99 had formal laboratory testing. Forced expiratory volume in 1 second (FEV1) and forced volume vital capacity (FVC) values were determined by taking the best of three trials. COPD was diagnosed in cases of an FEV1/FVC ratio of less than 70%.
Among these patients, 4.5% developed postoperative respiratory failure, and there was no statistically significant difference in the respiratory failure rate between patients with and without pulmonary function testing. In addition, there was no significant difference in 30-day mortality between these patients (1.9% vs. 2.1%). However, a total of 6.9% had a prolonged postoperative length of stay, with a significantly higher rate in the patients with pulmonary function testing than without (8.8% vs. 4.7%).
Dr. Ivanov and his colleagues found that the AUC of the STS score was 0.65 (95% confidence interval [CI], 0.55-0.74)for respiratory failure, 0.67 (95% CI, 0.6-0.74) for prolonged postoperative length of stay, and 0.74 (95% CI, 0.6-0.87) for 30-day mortality. Even though the STS score based upon clinical definitions of lung disease afforded only modest discriminatory ability for the three studied outcomes, they found that there was no significant added benefit to the predictive ability of these STS scores obtained by incorporating any of the pulmonary function testing parameters or COPD classifications studied.
“A possible physiological explanation for these findings may be that the examined pulmonary function testing variables do not depend solely on pulmonary parameters such as airway diameter, degree of obstruction, or lung elasticity, but rather on a patient’s effort and muscle “strength,” characteristics that are already well captured and accounted for in the current STS model,” the researchers stated.
“The STS score calculated with clinical information on lung disease status offers modest discriminatory ability for respiratory failure, prolonged postoperative length of stay, and 30-day mortality after CT surgery, which cannot be improved by adding PFT parameters or PFT-derived COPD categorization,” they wrote. “Therefore, routine preoperative PFTs may have only limited clinical utility in patients undergoing CT surgery when the STS score is readily available. Further prospective studies will be helpful in confirming these conclusions,” Dr. Ivanov and his colleagues noted.
The authors reported that they had nothing to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Additional pulmonary function testing adds little predictive value to STS risk scoring when available.
Major finding: There was no significant added benefit to the predictive ability of STS scores obtained by incorporating any of the pulmonary function testing parameters or COPD classifications studied, as determined by AUC analysis.
Data source: A retrospective, database analysis of 1,685 patients undergoing index cardiac surgery at a single center between April 2004 and January 2014.
Disclosures: The authors reported that they had no disclosures.