User login
The Official Newspaper of the American Association for Thoracic Surgery
Study aims to better understand readmissions in pediatric surgery
SAN DIEGO – Readmission rates and the underlying reasons for them vary between medical specialties following surgery in children, a study of national data suggests.
“Hospital readmission is a very hot topic, particularly in light of the Affordable Care Act,” Afif N. Kulaylat, MD, said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference. “Beyond economic costs there are very tangible costs to patients that we must consider. Readmissions have been associated with significant morbidity for patients. They often herald or implicate a postoperative complication. There are also indirect costs to patients and families such as time off from school or work.”
Dr. Kulaylat, of the division of pediatric surgery at Penn State Children’s Hospital, Hershey, Penn., presented findings from a retrospective analysis of NSQIP Pediatric (NSQIP-P), an ongoing collaboration between the ACS and the American Pediatric Surgical Association to improve the care of young patients. The researchers evaluated NSQIP-P data from 2013 and 2014 and focused on unplanned readmission within 30 days, including reasons for readmission based on NSQIP-P readmission categories and ICD-9 readmission codes as categorized by the AHRQ Clinical Classification Software. Multivariate logistic regression was used to evaluate factors associated with unplanned readmission.
Dr. Kulaylat reported results from a cohort of 129,849 patients cared for by 64 NSQIP-P participating hospitals. Among these, the all-cause readmission rate was 4.7%. After excluding patients with planned readmissions, the unplanned readmission rate was found to be 3.9%. From this cohort, 28% required reoperation within 30 days, and the median time from discharge to unplanned readmission was 8 days, with an interquartile range between 3 and 14 days.
Among the procedures captured in NSQIP-P, neurosurgery accounted for the highest readmission rate (10.8%), followed by general/thoracic surgery (5.2%), urology (2.6%), ENT (2%), orthopedic (1.9%), and plastic and reconstructive surgery (1.3%). The most common reason for readmission was surgical site infection at 23%, followed by GI complications such as ileus, obstruction, and constipation (17%); pulmonary-related complications (9%); device-related complications including shunt malfunction (8%); neurologic (7%); pain (6%); other medical diseases (6%); sepsis (5%); electrolytes/dehydration (5%); and urinary tract infection (UTI, 3%). It is estimated that at least two-thirds of unplanned readmissions (63%) were directly related to surgery. “These reasons for readmission and their frequency closely parallel what is seen in adults, with the exception of bleeding complications, which were rare in children compared to adults,” Dr. Kulaylat said.
The top five CPT codes associated with readmissions were laparoscopic appendectomy, laparoscopic gastrostomy tube placement, and three additional codes related to placement and replacement/revision of ventricular shunts/catheters.
Reasons for readmission varied among specialties. For example, among general and thoracic surgery, surgical-site infections (SSI) and GI-related issues dominated, while in neurosurgery SSI and device issues dominated. In urology, UTIs were the most frequent, while ENT had a greater proportion of pulmonary complications. Certain patient variables were also associated with an increased risk of hospital readmission, including comorbidities related to GI, CNS, renal, and immunosuppression and nutrition (P less than .001 for all). The strongest association was the occurrence of a postoperative complication, namely a post-discharge complication.
“The granularity of NSQIP-P can continue to be refined to help predict who is likely to get readmitted or if specific follow-up strategies might identify those headed to readmission,” remarked Robert E. Cilley, MD, a senior author and surgeon-in-chief at Penn State Children’s Hospital. Dr. Kulaylat acknowledged certain limitations of the study, including its retrospective design, the potential for data entry/data interpretation error, and that the researchers were unable to adjust for clustering at the hospital level. Directions of future research include a plan to study readmissions and predictive factors at the procedural level, establish risk-adjusted specialty/procedural-specific benchmarks for readmission rates, and refine the accuracy and reliability of the readmission data. “With these NSQIP-P data there is substantial opportunity for quality improvement as we strive to improve the care of children everywhere,” Dr. Kulaylat said. He reported having no relevant disclosures.
SAN DIEGO – Readmission rates and the underlying reasons for them vary between medical specialties following surgery in children, a study of national data suggests.
“Hospital readmission is a very hot topic, particularly in light of the Affordable Care Act,” Afif N. Kulaylat, MD, said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference. “Beyond economic costs there are very tangible costs to patients that we must consider. Readmissions have been associated with significant morbidity for patients. They often herald or implicate a postoperative complication. There are also indirect costs to patients and families such as time off from school or work.”
Dr. Kulaylat, of the division of pediatric surgery at Penn State Children’s Hospital, Hershey, Penn., presented findings from a retrospective analysis of NSQIP Pediatric (NSQIP-P), an ongoing collaboration between the ACS and the American Pediatric Surgical Association to improve the care of young patients. The researchers evaluated NSQIP-P data from 2013 and 2014 and focused on unplanned readmission within 30 days, including reasons for readmission based on NSQIP-P readmission categories and ICD-9 readmission codes as categorized by the AHRQ Clinical Classification Software. Multivariate logistic regression was used to evaluate factors associated with unplanned readmission.
Dr. Kulaylat reported results from a cohort of 129,849 patients cared for by 64 NSQIP-P participating hospitals. Among these, the all-cause readmission rate was 4.7%. After excluding patients with planned readmissions, the unplanned readmission rate was found to be 3.9%. From this cohort, 28% required reoperation within 30 days, and the median time from discharge to unplanned readmission was 8 days, with an interquartile range between 3 and 14 days.
Among the procedures captured in NSQIP-P, neurosurgery accounted for the highest readmission rate (10.8%), followed by general/thoracic surgery (5.2%), urology (2.6%), ENT (2%), orthopedic (1.9%), and plastic and reconstructive surgery (1.3%). The most common reason for readmission was surgical site infection at 23%, followed by GI complications such as ileus, obstruction, and constipation (17%); pulmonary-related complications (9%); device-related complications including shunt malfunction (8%); neurologic (7%); pain (6%); other medical diseases (6%); sepsis (5%); electrolytes/dehydration (5%); and urinary tract infection (UTI, 3%). It is estimated that at least two-thirds of unplanned readmissions (63%) were directly related to surgery. “These reasons for readmission and their frequency closely parallel what is seen in adults, with the exception of bleeding complications, which were rare in children compared to adults,” Dr. Kulaylat said.
The top five CPT codes associated with readmissions were laparoscopic appendectomy, laparoscopic gastrostomy tube placement, and three additional codes related to placement and replacement/revision of ventricular shunts/catheters.
Reasons for readmission varied among specialties. For example, among general and thoracic surgery, surgical-site infections (SSI) and GI-related issues dominated, while in neurosurgery SSI and device issues dominated. In urology, UTIs were the most frequent, while ENT had a greater proportion of pulmonary complications. Certain patient variables were also associated with an increased risk of hospital readmission, including comorbidities related to GI, CNS, renal, and immunosuppression and nutrition (P less than .001 for all). The strongest association was the occurrence of a postoperative complication, namely a post-discharge complication.
“The granularity of NSQIP-P can continue to be refined to help predict who is likely to get readmitted or if specific follow-up strategies might identify those headed to readmission,” remarked Robert E. Cilley, MD, a senior author and surgeon-in-chief at Penn State Children’s Hospital. Dr. Kulaylat acknowledged certain limitations of the study, including its retrospective design, the potential for data entry/data interpretation error, and that the researchers were unable to adjust for clustering at the hospital level. Directions of future research include a plan to study readmissions and predictive factors at the procedural level, establish risk-adjusted specialty/procedural-specific benchmarks for readmission rates, and refine the accuracy and reliability of the readmission data. “With these NSQIP-P data there is substantial opportunity for quality improvement as we strive to improve the care of children everywhere,” Dr. Kulaylat said. He reported having no relevant disclosures.
SAN DIEGO – Readmission rates and the underlying reasons for them vary between medical specialties following surgery in children, a study of national data suggests.
“Hospital readmission is a very hot topic, particularly in light of the Affordable Care Act,” Afif N. Kulaylat, MD, said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference. “Beyond economic costs there are very tangible costs to patients that we must consider. Readmissions have been associated with significant morbidity for patients. They often herald or implicate a postoperative complication. There are also indirect costs to patients and families such as time off from school or work.”
Dr. Kulaylat, of the division of pediatric surgery at Penn State Children’s Hospital, Hershey, Penn., presented findings from a retrospective analysis of NSQIP Pediatric (NSQIP-P), an ongoing collaboration between the ACS and the American Pediatric Surgical Association to improve the care of young patients. The researchers evaluated NSQIP-P data from 2013 and 2014 and focused on unplanned readmission within 30 days, including reasons for readmission based on NSQIP-P readmission categories and ICD-9 readmission codes as categorized by the AHRQ Clinical Classification Software. Multivariate logistic regression was used to evaluate factors associated with unplanned readmission.
Dr. Kulaylat reported results from a cohort of 129,849 patients cared for by 64 NSQIP-P participating hospitals. Among these, the all-cause readmission rate was 4.7%. After excluding patients with planned readmissions, the unplanned readmission rate was found to be 3.9%. From this cohort, 28% required reoperation within 30 days, and the median time from discharge to unplanned readmission was 8 days, with an interquartile range between 3 and 14 days.
Among the procedures captured in NSQIP-P, neurosurgery accounted for the highest readmission rate (10.8%), followed by general/thoracic surgery (5.2%), urology (2.6%), ENT (2%), orthopedic (1.9%), and plastic and reconstructive surgery (1.3%). The most common reason for readmission was surgical site infection at 23%, followed by GI complications such as ileus, obstruction, and constipation (17%); pulmonary-related complications (9%); device-related complications including shunt malfunction (8%); neurologic (7%); pain (6%); other medical diseases (6%); sepsis (5%); electrolytes/dehydration (5%); and urinary tract infection (UTI, 3%). It is estimated that at least two-thirds of unplanned readmissions (63%) were directly related to surgery. “These reasons for readmission and their frequency closely parallel what is seen in adults, with the exception of bleeding complications, which were rare in children compared to adults,” Dr. Kulaylat said.
The top five CPT codes associated with readmissions were laparoscopic appendectomy, laparoscopic gastrostomy tube placement, and three additional codes related to placement and replacement/revision of ventricular shunts/catheters.
Reasons for readmission varied among specialties. For example, among general and thoracic surgery, surgical-site infections (SSI) and GI-related issues dominated, while in neurosurgery SSI and device issues dominated. In urology, UTIs were the most frequent, while ENT had a greater proportion of pulmonary complications. Certain patient variables were also associated with an increased risk of hospital readmission, including comorbidities related to GI, CNS, renal, and immunosuppression and nutrition (P less than .001 for all). The strongest association was the occurrence of a postoperative complication, namely a post-discharge complication.
“The granularity of NSQIP-P can continue to be refined to help predict who is likely to get readmitted or if specific follow-up strategies might identify those headed to readmission,” remarked Robert E. Cilley, MD, a senior author and surgeon-in-chief at Penn State Children’s Hospital. Dr. Kulaylat acknowledged certain limitations of the study, including its retrospective design, the potential for data entry/data interpretation error, and that the researchers were unable to adjust for clustering at the hospital level. Directions of future research include a plan to study readmissions and predictive factors at the procedural level, establish risk-adjusted specialty/procedural-specific benchmarks for readmission rates, and refine the accuracy and reliability of the readmission data. “With these NSQIP-P data there is substantial opportunity for quality improvement as we strive to improve the care of children everywhere,” Dr. Kulaylat said. He reported having no relevant disclosures.
AT THE ACS NSQIP NATIONAL CONFERENCE
Key clinical point: Readmission rates following pediatric surgery vary between medical specialties.
Major finding: Among the procedures captured in ACS NSQIP Pediatric (NSQIP-P), neurosurgery accounted for the highest readmission rate (10.8%), followed by general/thoracic surgery (5.2%), urology (2.6%), ENT (2%), orthopedic (1.9%), and plastic and reconstructive surgery (1.3%).
Data source: An analysis of 129,849 pediatric patients cared for by 64 NSQIP-P participating hospitals.
Disclosures: Dr. Kulaylat reported having no financial disclosures.
Blood viral RNA may indicate severity of MERS coronavirus clinical course
The presence of blood viral RNA in patients presenting with possible Middle East respiratory syndrome coronavirus (MERS-CoV) may be a very reliable indicator of the severity of the infection’s clinical course, according to a new study published in Emerging Infectious Diseases.
“Our study aimed to evaluate the diagnostic utility of blood specimens for MERS-CoV infection by using large numbers of patients with a single viral origin and to determine the relationship between blood viral detection and clinical characteristics,” wrote the authors, led by So Yeon Kim, MD, of the National Medical Center in Seoul, South Korea.
The investigators recruited 21 MERS-CoV patients within South Korea, all of whom had been previously diagnosed by the Korea Centers for Disease Control and Prevention via respiratory samples and were of “a single viral origin.” All subjects contributed ethylenediaminetetraacetic acid (EDTA)-treated whole blood and serum specimens, from which viral RNA was extracted (Emerg Infect Dis. 2016 Oct 15;22[10]. doi: 10.3201/eid2210.160218).
Viral RNA was detected in 6 of 21 whole blood samples and 6 of 21 serum samples at hospital admission. However, because two patients were viral positive in either specimen subtype of EDTA-treated whole blood or serum, the overall detection rate for the population was 7 of 21 (33%). Being positive for blood viral RNA at admission was found to be associated with a fever of higher than 37.5 °C (99.5 °F) on the date of sample collection (P = .007), being placed on mechanical ventilation at some point during the clinical course (P = .003), extracorporeal membrane oxygenation (P = .025), and death (P = .025).
However, “between the blood viral RNA-positive and -negative groups, we found no differences in age, duration from symptom onset to diagnosis of MERS-CoV infection, or an invasive procedure before the specimens were obtained,” the investigators noted.
The takeaway, the authors underscore, is that although early blood viral RNA presence may not be a useful diagnostic tool, it “might be a good prognostic indicator of severe outcome” due to its high association with worse clinical course.
The research was funded by the National Medical Center Research Institute.
The presence of blood viral RNA in patients presenting with possible Middle East respiratory syndrome coronavirus (MERS-CoV) may be a very reliable indicator of the severity of the infection’s clinical course, according to a new study published in Emerging Infectious Diseases.
“Our study aimed to evaluate the diagnostic utility of blood specimens for MERS-CoV infection by using large numbers of patients with a single viral origin and to determine the relationship between blood viral detection and clinical characteristics,” wrote the authors, led by So Yeon Kim, MD, of the National Medical Center in Seoul, South Korea.
The investigators recruited 21 MERS-CoV patients within South Korea, all of whom had been previously diagnosed by the Korea Centers for Disease Control and Prevention via respiratory samples and were of “a single viral origin.” All subjects contributed ethylenediaminetetraacetic acid (EDTA)-treated whole blood and serum specimens, from which viral RNA was extracted (Emerg Infect Dis. 2016 Oct 15;22[10]. doi: 10.3201/eid2210.160218).
Viral RNA was detected in 6 of 21 whole blood samples and 6 of 21 serum samples at hospital admission. However, because two patients were viral positive in either specimen subtype of EDTA-treated whole blood or serum, the overall detection rate for the population was 7 of 21 (33%). Being positive for blood viral RNA at admission was found to be associated with a fever of higher than 37.5 °C (99.5 °F) on the date of sample collection (P = .007), being placed on mechanical ventilation at some point during the clinical course (P = .003), extracorporeal membrane oxygenation (P = .025), and death (P = .025).
However, “between the blood viral RNA-positive and -negative groups, we found no differences in age, duration from symptom onset to diagnosis of MERS-CoV infection, or an invasive procedure before the specimens were obtained,” the investigators noted.
The takeaway, the authors underscore, is that although early blood viral RNA presence may not be a useful diagnostic tool, it “might be a good prognostic indicator of severe outcome” due to its high association with worse clinical course.
The research was funded by the National Medical Center Research Institute.
The presence of blood viral RNA in patients presenting with possible Middle East respiratory syndrome coronavirus (MERS-CoV) may be a very reliable indicator of the severity of the infection’s clinical course, according to a new study published in Emerging Infectious Diseases.
“Our study aimed to evaluate the diagnostic utility of blood specimens for MERS-CoV infection by using large numbers of patients with a single viral origin and to determine the relationship between blood viral detection and clinical characteristics,” wrote the authors, led by So Yeon Kim, MD, of the National Medical Center in Seoul, South Korea.
The investigators recruited 21 MERS-CoV patients within South Korea, all of whom had been previously diagnosed by the Korea Centers for Disease Control and Prevention via respiratory samples and were of “a single viral origin.” All subjects contributed ethylenediaminetetraacetic acid (EDTA)-treated whole blood and serum specimens, from which viral RNA was extracted (Emerg Infect Dis. 2016 Oct 15;22[10]. doi: 10.3201/eid2210.160218).
Viral RNA was detected in 6 of 21 whole blood samples and 6 of 21 serum samples at hospital admission. However, because two patients were viral positive in either specimen subtype of EDTA-treated whole blood or serum, the overall detection rate for the population was 7 of 21 (33%). Being positive for blood viral RNA at admission was found to be associated with a fever of higher than 37.5 °C (99.5 °F) on the date of sample collection (P = .007), being placed on mechanical ventilation at some point during the clinical course (P = .003), extracorporeal membrane oxygenation (P = .025), and death (P = .025).
However, “between the blood viral RNA-positive and -negative groups, we found no differences in age, duration from symptom onset to diagnosis of MERS-CoV infection, or an invasive procedure before the specimens were obtained,” the investigators noted.
The takeaway, the authors underscore, is that although early blood viral RNA presence may not be a useful diagnostic tool, it “might be a good prognostic indicator of severe outcome” due to its high association with worse clinical course.
The research was funded by the National Medical Center Research Institute.
FROM EMERGING INFECTIOUS DISEASES
Key clinical point: Checking for blood viral RNA at hospital admission may be a reliable indicator of the severity of MERS coronavirus infection clinical course.
Major finding: Blood viral RNA positivity at admission was associated with fever higher than 37.5 °C on the sampling date (P = .007), requirement for mechanical ventilation during the following clinical course (P = .003), extracorporeal membrane oxygenation (P = .025), and patient death (P = .025).
Data source: Prospective analysis of 21 patients with Middle East respiratory syndrome coronavirus (MERS-CoV).
Disclosures: The research was funded by the National Medical Center Research Institute.
Graham Foundation Congratulates Latest 2016 Awardees
Every Heartbeat Valve Matters Fellowship
Sponsored by Edwards Lifesciences
CT surgeons treating patients from underserved populations spend time at an advanced heart valve disease training and educational institution to acquire skills that can be implemented in practice.
Chizoba Efobi, MD
University of Benin Teaching Hospital, Nigeria
Christian Kreutzer, MD
Hospital Nacional Alejandro Posadas, Argentina
Chartarooon Rimsukcharoenchai, MD
Chiang Mai University Hospital, Thailand
René Silva, MD
San Camilo - Holy Family Hospital, Brazil
Fellowship for Advanced Minimally Invasive Thoracic Surgery
Sponsored by Ethicon
Young thoracic or CT surgeons and their surgical teams visit clinical sites for one- and two-day training on VATS Lobectomy.
Mary Carolyn, MD
Saint Joseph’s Hospital
Alexander Kraev, MD
Billings Clinic
Roman Petrov, MD
Marietta Memorial Hospital
Nestor Villamizar Ortiz, MD
University of Miami
Graham Surgical Investigator Program
Supporting the clinical and translational research of young CT surgeons for up to two years.
Isaac George, MD
NewYork-Presbyterian Hospital Columbia University Medical Center
“Cardiac and Skeletal Muscle Metabolic Failure in Diabetic Heart Disease: Role of MSTN/AMPK Signaling”
Alexander Iribarne, MD
Dartmouth Medical School
“Geographic Variation in Screening and Frequency of Re-interventions after Thoracic Aortic Aneurysm Repair Among Medicare Recipients in the United States”
Ethicon Surgical Investigator Award
Ravi Ghanta, MD
University of Virginia
“Improving Stem Cell Engraftment by Optimization of the Mechanical Microenvironment in Ischemic Myocardium”
Intuitive Surgical Investigator Award
Michael Halkos, MD
Emory University
“Hybrid Coronary Revascularization Versus Coronary Artery Bypass Surgery For Patients With Multivessel Coronary Disease”
Oz Lemole Surgical Investigator Award
David Odell, MD
Northwestern University, Feinberg School of Medicine
“Development of a Novel Lung Cancer Quality Improvement Collaborative
North America Clinical Immersion in Advanced Minimally Invasive Thoracic Surgery
Sponsored by Medtronic
Young Chinese thoracic surgeons learn advanced minimally invasive thoracic surgery and comprehensive care screening and diagnosis at North American institutions.
Feng Jiang, MD
Jiangsu Cancer Hospital
Jiageng Li, MD
Cancer Institute and Hospital
Teng Mao, MD
Shanghai Chest Hospital
Hao Wang, MD
Zhongshan Hospital, Fudan University
Ruixiang Zhang, MD
Henan Cancer Hospital
Zhenrong Zhang, MD
China Japan Friendship Hospital
Feng Zhao, MD
Union Hospital, Hubei
Zuli Zhou, MD
Peking University People’s Hospital
Surgical Robotics Fellowship
Sponsored by Intuitive Surgical
North American general thoracic fellows and their attending surgeons spend two days receiving hands-on, advanced training in the Da Vinci robotics system.
Nicholas Baker, MD
University of Pittsburgh Medical Center
Adam Bograd, MD
Memorial Sloan Kettering Cancer Center
Edward Chan, MD
Houston Methodist Hospital
John Cleveland, MD
Keck School of Medicine University of Southern California
Mark Crye, MD
Allegheny Health Network-Allegheny General Hospital
Laura Donahoe, MD
University of Toronto
Crystal Erickson, MD
University of Michigan
Jinny Ha, MD
Johns Hopkins Hospital
Eric Jeng, MD
University of Florida
Peter Kneuertz, MD
New York-Presbyterian Hospital Weill Cornell Medical Center
Moshe Lapidot, MD
Brigham and Women’s Hospital
Antonio Lassaletta, MD
Harvard Medical School, Beth Israel Deaconess Medical Center
Jason Muesse, MD
Emory University
Christian Otero, MD
University of Miami/Jackson Memorial Medical Center
Janani Reisenauer, MD
Mayo Clinic
Smarika Shrestha, MD
Penn State Milton S. Hershey Medical Center
Nicholas Stephens, MD
The University of Texas Medical School at Houston
Huan Huan (Joanne) Sun, MD
NYU Langone Medical Center
John Waters, MD
The University of Texas Medical School at Houston
Brittany Zwischenberger, MD
Duke University
Thoracic Surgery Training Fellowship
Sponsored by Ethicon China
Chinese thoracic training fellows receive advanced training at North American institutions.
Mingsong Wang, MD
Shanghai Xinhua Hospital
Song Xu, MD
Tianjin Medical University General Hospital
Wanpu Yan, MD
Beijing Cancer Hospital
Yong Zhang, MD
First Affiliated Hospital of Xi’an Jiaotong University
Every Heartbeat Valve Matters Fellowship
Sponsored by Edwards Lifesciences
CT surgeons treating patients from underserved populations spend time at an advanced heart valve disease training and educational institution to acquire skills that can be implemented in practice.
Chizoba Efobi, MD
University of Benin Teaching Hospital, Nigeria
Christian Kreutzer, MD
Hospital Nacional Alejandro Posadas, Argentina
Chartarooon Rimsukcharoenchai, MD
Chiang Mai University Hospital, Thailand
René Silva, MD
San Camilo - Holy Family Hospital, Brazil
Fellowship for Advanced Minimally Invasive Thoracic Surgery
Sponsored by Ethicon
Young thoracic or CT surgeons and their surgical teams visit clinical sites for one- and two-day training on VATS Lobectomy.
Mary Carolyn, MD
Saint Joseph’s Hospital
Alexander Kraev, MD
Billings Clinic
Roman Petrov, MD
Marietta Memorial Hospital
Nestor Villamizar Ortiz, MD
University of Miami
Graham Surgical Investigator Program
Supporting the clinical and translational research of young CT surgeons for up to two years.
Isaac George, MD
NewYork-Presbyterian Hospital Columbia University Medical Center
“Cardiac and Skeletal Muscle Metabolic Failure in Diabetic Heart Disease: Role of MSTN/AMPK Signaling”
Alexander Iribarne, MD
Dartmouth Medical School
“Geographic Variation in Screening and Frequency of Re-interventions after Thoracic Aortic Aneurysm Repair Among Medicare Recipients in the United States”
Ethicon Surgical Investigator Award
Ravi Ghanta, MD
University of Virginia
“Improving Stem Cell Engraftment by Optimization of the Mechanical Microenvironment in Ischemic Myocardium”
Intuitive Surgical Investigator Award
Michael Halkos, MD
Emory University
“Hybrid Coronary Revascularization Versus Coronary Artery Bypass Surgery For Patients With Multivessel Coronary Disease”
Oz Lemole Surgical Investigator Award
David Odell, MD
Northwestern University, Feinberg School of Medicine
“Development of a Novel Lung Cancer Quality Improvement Collaborative
North America Clinical Immersion in Advanced Minimally Invasive Thoracic Surgery
Sponsored by Medtronic
Young Chinese thoracic surgeons learn advanced minimally invasive thoracic surgery and comprehensive care screening and diagnosis at North American institutions.
Feng Jiang, MD
Jiangsu Cancer Hospital
Jiageng Li, MD
Cancer Institute and Hospital
Teng Mao, MD
Shanghai Chest Hospital
Hao Wang, MD
Zhongshan Hospital, Fudan University
Ruixiang Zhang, MD
Henan Cancer Hospital
Zhenrong Zhang, MD
China Japan Friendship Hospital
Feng Zhao, MD
Union Hospital, Hubei
Zuli Zhou, MD
Peking University People’s Hospital
Surgical Robotics Fellowship
Sponsored by Intuitive Surgical
North American general thoracic fellows and their attending surgeons spend two days receiving hands-on, advanced training in the Da Vinci robotics system.
Nicholas Baker, MD
University of Pittsburgh Medical Center
Adam Bograd, MD
Memorial Sloan Kettering Cancer Center
Edward Chan, MD
Houston Methodist Hospital
John Cleveland, MD
Keck School of Medicine University of Southern California
Mark Crye, MD
Allegheny Health Network-Allegheny General Hospital
Laura Donahoe, MD
University of Toronto
Crystal Erickson, MD
University of Michigan
Jinny Ha, MD
Johns Hopkins Hospital
Eric Jeng, MD
University of Florida
Peter Kneuertz, MD
New York-Presbyterian Hospital Weill Cornell Medical Center
Moshe Lapidot, MD
Brigham and Women’s Hospital
Antonio Lassaletta, MD
Harvard Medical School, Beth Israel Deaconess Medical Center
Jason Muesse, MD
Emory University
Christian Otero, MD
University of Miami/Jackson Memorial Medical Center
Janani Reisenauer, MD
Mayo Clinic
Smarika Shrestha, MD
Penn State Milton S. Hershey Medical Center
Nicholas Stephens, MD
The University of Texas Medical School at Houston
Huan Huan (Joanne) Sun, MD
NYU Langone Medical Center
John Waters, MD
The University of Texas Medical School at Houston
Brittany Zwischenberger, MD
Duke University
Thoracic Surgery Training Fellowship
Sponsored by Ethicon China
Chinese thoracic training fellows receive advanced training at North American institutions.
Mingsong Wang, MD
Shanghai Xinhua Hospital
Song Xu, MD
Tianjin Medical University General Hospital
Wanpu Yan, MD
Beijing Cancer Hospital
Yong Zhang, MD
First Affiliated Hospital of Xi’an Jiaotong University
Every Heartbeat Valve Matters Fellowship
Sponsored by Edwards Lifesciences
CT surgeons treating patients from underserved populations spend time at an advanced heart valve disease training and educational institution to acquire skills that can be implemented in practice.
Chizoba Efobi, MD
University of Benin Teaching Hospital, Nigeria
Christian Kreutzer, MD
Hospital Nacional Alejandro Posadas, Argentina
Chartarooon Rimsukcharoenchai, MD
Chiang Mai University Hospital, Thailand
René Silva, MD
San Camilo - Holy Family Hospital, Brazil
Fellowship for Advanced Minimally Invasive Thoracic Surgery
Sponsored by Ethicon
Young thoracic or CT surgeons and their surgical teams visit clinical sites for one- and two-day training on VATS Lobectomy.
Mary Carolyn, MD
Saint Joseph’s Hospital
Alexander Kraev, MD
Billings Clinic
Roman Petrov, MD
Marietta Memorial Hospital
Nestor Villamizar Ortiz, MD
University of Miami
Graham Surgical Investigator Program
Supporting the clinical and translational research of young CT surgeons for up to two years.
Isaac George, MD
NewYork-Presbyterian Hospital Columbia University Medical Center
“Cardiac and Skeletal Muscle Metabolic Failure in Diabetic Heart Disease: Role of MSTN/AMPK Signaling”
Alexander Iribarne, MD
Dartmouth Medical School
“Geographic Variation in Screening and Frequency of Re-interventions after Thoracic Aortic Aneurysm Repair Among Medicare Recipients in the United States”
Ethicon Surgical Investigator Award
Ravi Ghanta, MD
University of Virginia
“Improving Stem Cell Engraftment by Optimization of the Mechanical Microenvironment in Ischemic Myocardium”
Intuitive Surgical Investigator Award
Michael Halkos, MD
Emory University
“Hybrid Coronary Revascularization Versus Coronary Artery Bypass Surgery For Patients With Multivessel Coronary Disease”
Oz Lemole Surgical Investigator Award
David Odell, MD
Northwestern University, Feinberg School of Medicine
“Development of a Novel Lung Cancer Quality Improvement Collaborative
North America Clinical Immersion in Advanced Minimally Invasive Thoracic Surgery
Sponsored by Medtronic
Young Chinese thoracic surgeons learn advanced minimally invasive thoracic surgery and comprehensive care screening and diagnosis at North American institutions.
Feng Jiang, MD
Jiangsu Cancer Hospital
Jiageng Li, MD
Cancer Institute and Hospital
Teng Mao, MD
Shanghai Chest Hospital
Hao Wang, MD
Zhongshan Hospital, Fudan University
Ruixiang Zhang, MD
Henan Cancer Hospital
Zhenrong Zhang, MD
China Japan Friendship Hospital
Feng Zhao, MD
Union Hospital, Hubei
Zuli Zhou, MD
Peking University People’s Hospital
Surgical Robotics Fellowship
Sponsored by Intuitive Surgical
North American general thoracic fellows and their attending surgeons spend two days receiving hands-on, advanced training in the Da Vinci robotics system.
Nicholas Baker, MD
University of Pittsburgh Medical Center
Adam Bograd, MD
Memorial Sloan Kettering Cancer Center
Edward Chan, MD
Houston Methodist Hospital
John Cleveland, MD
Keck School of Medicine University of Southern California
Mark Crye, MD
Allegheny Health Network-Allegheny General Hospital
Laura Donahoe, MD
University of Toronto
Crystal Erickson, MD
University of Michigan
Jinny Ha, MD
Johns Hopkins Hospital
Eric Jeng, MD
University of Florida
Peter Kneuertz, MD
New York-Presbyterian Hospital Weill Cornell Medical Center
Moshe Lapidot, MD
Brigham and Women’s Hospital
Antonio Lassaletta, MD
Harvard Medical School, Beth Israel Deaconess Medical Center
Jason Muesse, MD
Emory University
Christian Otero, MD
University of Miami/Jackson Memorial Medical Center
Janani Reisenauer, MD
Mayo Clinic
Smarika Shrestha, MD
Penn State Milton S. Hershey Medical Center
Nicholas Stephens, MD
The University of Texas Medical School at Houston
Huan Huan (Joanne) Sun, MD
NYU Langone Medical Center
John Waters, MD
The University of Texas Medical School at Houston
Brittany Zwischenberger, MD
Duke University
Thoracic Surgery Training Fellowship
Sponsored by Ethicon China
Chinese thoracic training fellows receive advanced training at North American institutions.
Mingsong Wang, MD
Shanghai Xinhua Hospital
Song Xu, MD
Tianjin Medical University General Hospital
Wanpu Yan, MD
Beijing Cancer Hospital
Yong Zhang, MD
First Affiliated Hospital of Xi’an Jiaotong University
Using transcatheter aortic valves for severe mitral annular calcification
PARIS – Transcatheter mitral valve replacement using a repurposed transcatheter aortic valve in patients with severe symptomatic native mitral valve disease and severe mitral annular calcification is feasible and may be an option in carefully selected patients who aren’t candidates for surgery, Mayra Guerrero, MD, said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
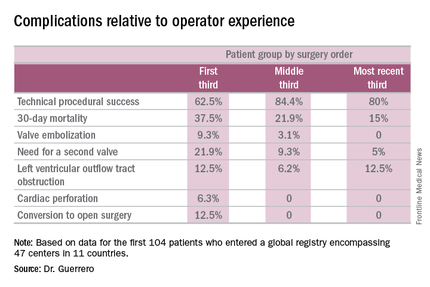
However, at this early point in development, the procedure is associated with an exceptionally steep learning curve, said Dr. Guerrero, director of cardiac structural interventions at the NorthShore University Health System in Evanston, Ill.
She presented the procedural and 30-day outcomes for the first 104 patients entered into a global registry encompassing 47 centers in 11 countries. Nearly 90% of patients received an Edwards SAPIEN XT or SAPIEN 3 valve. The EuroPCR results update an earlier report on the first 64 patients in the registry (JACC Cardiovasc Interv. 2016 Jul 11;9[13]:1361-71).
The results, she said, are reminiscent of the early days in transcatheter aortic valve replacement, which were marked by an initial very high early mortality rate that fell dramatically as technology and techniques improved.
“We know that there are important things we need to improve. Left ventricular outflow tract obstruction is the Achilles heel of this procedure; we need to work on its prevention and management. We need better annulus sizing methods. We need to find the best delivery method and improve our patient selection in order to avoid taking on patients who are too sick. Still, even during this early experience, the technical success rate has improved, and 30-day mortality continues to drop,” Dr. Guerrero said.
Indeed, the 30-day all-cause mortality rate of 25% in the first 104 patients doesn’t tell the whole story. The rate was 37.5% in the first third of patients, fell to 21.9% in the second tertile, and then to 15% in the most recent tertile.
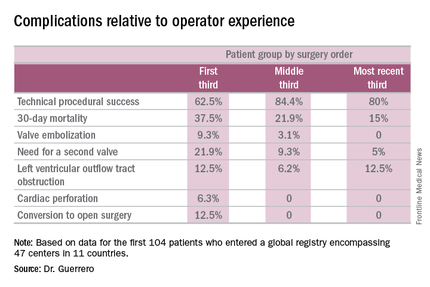
Similarly, the technical success rate of the procedure according to Mitral Valve Academic Research Consortium criteria improved from 62.5% in the first tertile of patients to 84.4% and 80% in the second and third, respectively, she continued.
The rates of almost all complications went down with greater operator experience, too. The notable exception was left ventricular outflow tract obstruction (LVOTO). It occurred in 12.5% of patients in the first tertile and remained unchanged in the third.
It’s noteworthy that the majority of deaths were noncardiac in nature. Patients with mitral annular calcification are a high-risk group even before they develop valvular dysfunction. They are typically older and have multiple comorbidities. Participants in the global registry had a mean Society of Thoracic Surgeons score of 14.4; 38% had diabetes, 45% had chronic obstructive pulmonary disease, 35% had heart failure, 34% had previously undergone coronary artery bypass surgery, and roughly half of patients had a prior aortic valve replacement.
Causes of noncardiac mortality within 30 days included multiorgan failure in 8.6% of subjects, pneumonia in 2.9%, infection in 1.9%, and one fatal thoracentesis-related bleeding complication.
Cardiovascular deaths included two cases due to left ventricular perforation, two fatal strokes, an MI due to air emboli, a lethal complete atrioventricular block, and three deaths owing to LVOTO.
Alcohol ablation met with some success as a bailout treatment in cases of LVOTO with hemodynamic compromise after transmitral valve replacement in the global registry. All six treated patients had significant improvement initially, although the LVOTO recurred the next day in one instance. Four of the six patients were discharged from the hospital. One patient died because of atrioventricular block, and another from multiorgan failure 3 weeks after alcohol ablation of the LVOTO.
Dr. Guerrero has been a leader in this new field. She reported the first percutaneous implantation of a balloon expandable transcatheter valve in a native mitral valve without a surgical incision (Catheter Cardiovasc Interv. 2014 Jun 1;83[7]:E287-91), and more recently, together with coworkers developed a percutaneous alcohol ablation technique for acute reduction of LVOTO due to transcatheter mitral valve replacement (Catheter Cardiovasc Interv. 2016 Jul 5. doi:10.1002/ccd.26649).
She is now the principal investigator in the ongoing Mitral Implantation of Transcatheter Valves (MITRAL) trial, a physician-sponsored, 90-patient pilot study underway at six U.S. sites. MITRAL is recruiting three patient populations for transcatheter mitral valve replacement: patients like those in the global registry, with native mitral valve disease and severe mitral annular calcification; those with a symptomatic failing surgical ring with severe mitral regurgitation or stenosis; and patients with a symptomatic failing surgical bioprosthesis with severe mitral regurgitation or stenosis.
Discussant Nicolo Piazza, MD, of McGill University, Montreal, said transcatheter mitral valve replacement in mitral valve disease with severe mitral annular calcification in patients unsuitable for surgery “definitely represents an unmet clinical need in our practice today.” But he urged caution in interpreting the global registry data.
“This is a real world registry study with inherent selection bias and physician reporting bias,” the cardiologist said.
“We are leveraging a therapy from the aortic field into the mitral field. Of course, we do not have dedicated devices yet to treat these patients. The main finding of this study is that the procedure is actually feasible,” Dr. Piazza said.
Still, it’s sobering that at least 1 in 10 treated patients experiences LVOTO, 1 in 10 requires a second valve, and technical success is achieved in 3 out of 4 patients, he added.
Dr. Piazza predicted that multislice CT scans will be “extremely important” in refining patient selection criteria for the procedure, and echocardiography will be helpful in understanding the optimal procedural techniques and viewing angles. Work also needs to be done on developing optimal anticoagulation protocols in order to avoid valve thrombosis.
Dr. Guerrero reported serving as a consultant to Edwards Lifesciences. Dr. Piazza is a consultant to Medtronic and MicroPort.
PARIS – Transcatheter mitral valve replacement using a repurposed transcatheter aortic valve in patients with severe symptomatic native mitral valve disease and severe mitral annular calcification is feasible and may be an option in carefully selected patients who aren’t candidates for surgery, Mayra Guerrero, MD, said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
However, at this early point in development, the procedure is associated with an exceptionally steep learning curve, said Dr. Guerrero, director of cardiac structural interventions at the NorthShore University Health System in Evanston, Ill.
She presented the procedural and 30-day outcomes for the first 104 patients entered into a global registry encompassing 47 centers in 11 countries. Nearly 90% of patients received an Edwards SAPIEN XT or SAPIEN 3 valve. The EuroPCR results update an earlier report on the first 64 patients in the registry (JACC Cardiovasc Interv. 2016 Jul 11;9[13]:1361-71).
The results, she said, are reminiscent of the early days in transcatheter aortic valve replacement, which were marked by an initial very high early mortality rate that fell dramatically as technology and techniques improved.
“We know that there are important things we need to improve. Left ventricular outflow tract obstruction is the Achilles heel of this procedure; we need to work on its prevention and management. We need better annulus sizing methods. We need to find the best delivery method and improve our patient selection in order to avoid taking on patients who are too sick. Still, even during this early experience, the technical success rate has improved, and 30-day mortality continues to drop,” Dr. Guerrero said.
Indeed, the 30-day all-cause mortality rate of 25% in the first 104 patients doesn’t tell the whole story. The rate was 37.5% in the first third of patients, fell to 21.9% in the second tertile, and then to 15% in the most recent tertile.
Similarly, the technical success rate of the procedure according to Mitral Valve Academic Research Consortium criteria improved from 62.5% in the first tertile of patients to 84.4% and 80% in the second and third, respectively, she continued.
The rates of almost all complications went down with greater operator experience, too. The notable exception was left ventricular outflow tract obstruction (LVOTO). It occurred in 12.5% of patients in the first tertile and remained unchanged in the third.
It’s noteworthy that the majority of deaths were noncardiac in nature. Patients with mitral annular calcification are a high-risk group even before they develop valvular dysfunction. They are typically older and have multiple comorbidities. Participants in the global registry had a mean Society of Thoracic Surgeons score of 14.4; 38% had diabetes, 45% had chronic obstructive pulmonary disease, 35% had heart failure, 34% had previously undergone coronary artery bypass surgery, and roughly half of patients had a prior aortic valve replacement.
Causes of noncardiac mortality within 30 days included multiorgan failure in 8.6% of subjects, pneumonia in 2.9%, infection in 1.9%, and one fatal thoracentesis-related bleeding complication.
Cardiovascular deaths included two cases due to left ventricular perforation, two fatal strokes, an MI due to air emboli, a lethal complete atrioventricular block, and three deaths owing to LVOTO.
Alcohol ablation met with some success as a bailout treatment in cases of LVOTO with hemodynamic compromise after transmitral valve replacement in the global registry. All six treated patients had significant improvement initially, although the LVOTO recurred the next day in one instance. Four of the six patients were discharged from the hospital. One patient died because of atrioventricular block, and another from multiorgan failure 3 weeks after alcohol ablation of the LVOTO.
Dr. Guerrero has been a leader in this new field. She reported the first percutaneous implantation of a balloon expandable transcatheter valve in a native mitral valve without a surgical incision (Catheter Cardiovasc Interv. 2014 Jun 1;83[7]:E287-91), and more recently, together with coworkers developed a percutaneous alcohol ablation technique for acute reduction of LVOTO due to transcatheter mitral valve replacement (Catheter Cardiovasc Interv. 2016 Jul 5. doi:10.1002/ccd.26649).
She is now the principal investigator in the ongoing Mitral Implantation of Transcatheter Valves (MITRAL) trial, a physician-sponsored, 90-patient pilot study underway at six U.S. sites. MITRAL is recruiting three patient populations for transcatheter mitral valve replacement: patients like those in the global registry, with native mitral valve disease and severe mitral annular calcification; those with a symptomatic failing surgical ring with severe mitral regurgitation or stenosis; and patients with a symptomatic failing surgical bioprosthesis with severe mitral regurgitation or stenosis.
Discussant Nicolo Piazza, MD, of McGill University, Montreal, said transcatheter mitral valve replacement in mitral valve disease with severe mitral annular calcification in patients unsuitable for surgery “definitely represents an unmet clinical need in our practice today.” But he urged caution in interpreting the global registry data.
“This is a real world registry study with inherent selection bias and physician reporting bias,” the cardiologist said.
“We are leveraging a therapy from the aortic field into the mitral field. Of course, we do not have dedicated devices yet to treat these patients. The main finding of this study is that the procedure is actually feasible,” Dr. Piazza said.
Still, it’s sobering that at least 1 in 10 treated patients experiences LVOTO, 1 in 10 requires a second valve, and technical success is achieved in 3 out of 4 patients, he added.
Dr. Piazza predicted that multislice CT scans will be “extremely important” in refining patient selection criteria for the procedure, and echocardiography will be helpful in understanding the optimal procedural techniques and viewing angles. Work also needs to be done on developing optimal anticoagulation protocols in order to avoid valve thrombosis.
Dr. Guerrero reported serving as a consultant to Edwards Lifesciences. Dr. Piazza is a consultant to Medtronic and MicroPort.
PARIS – Transcatheter mitral valve replacement using a repurposed transcatheter aortic valve in patients with severe symptomatic native mitral valve disease and severe mitral annular calcification is feasible and may be an option in carefully selected patients who aren’t candidates for surgery, Mayra Guerrero, MD, said at the annual congress of the European Association of Percutaneous Cardiovascular Interventions.
However, at this early point in development, the procedure is associated with an exceptionally steep learning curve, said Dr. Guerrero, director of cardiac structural interventions at the NorthShore University Health System in Evanston, Ill.
She presented the procedural and 30-day outcomes for the first 104 patients entered into a global registry encompassing 47 centers in 11 countries. Nearly 90% of patients received an Edwards SAPIEN XT or SAPIEN 3 valve. The EuroPCR results update an earlier report on the first 64 patients in the registry (JACC Cardiovasc Interv. 2016 Jul 11;9[13]:1361-71).
The results, she said, are reminiscent of the early days in transcatheter aortic valve replacement, which were marked by an initial very high early mortality rate that fell dramatically as technology and techniques improved.
“We know that there are important things we need to improve. Left ventricular outflow tract obstruction is the Achilles heel of this procedure; we need to work on its prevention and management. We need better annulus sizing methods. We need to find the best delivery method and improve our patient selection in order to avoid taking on patients who are too sick. Still, even during this early experience, the technical success rate has improved, and 30-day mortality continues to drop,” Dr. Guerrero said.
Indeed, the 30-day all-cause mortality rate of 25% in the first 104 patients doesn’t tell the whole story. The rate was 37.5% in the first third of patients, fell to 21.9% in the second tertile, and then to 15% in the most recent tertile.
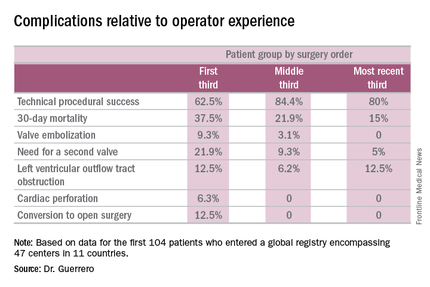
Similarly, the technical success rate of the procedure according to Mitral Valve Academic Research Consortium criteria improved from 62.5% in the first tertile of patients to 84.4% and 80% in the second and third, respectively, she continued.
The rates of almost all complications went down with greater operator experience, too. The notable exception was left ventricular outflow tract obstruction (LVOTO). It occurred in 12.5% of patients in the first tertile and remained unchanged in the third.
It’s noteworthy that the majority of deaths were noncardiac in nature. Patients with mitral annular calcification are a high-risk group even before they develop valvular dysfunction. They are typically older and have multiple comorbidities. Participants in the global registry had a mean Society of Thoracic Surgeons score of 14.4; 38% had diabetes, 45% had chronic obstructive pulmonary disease, 35% had heart failure, 34% had previously undergone coronary artery bypass surgery, and roughly half of patients had a prior aortic valve replacement.
Causes of noncardiac mortality within 30 days included multiorgan failure in 8.6% of subjects, pneumonia in 2.9%, infection in 1.9%, and one fatal thoracentesis-related bleeding complication.
Cardiovascular deaths included two cases due to left ventricular perforation, two fatal strokes, an MI due to air emboli, a lethal complete atrioventricular block, and three deaths owing to LVOTO.
Alcohol ablation met with some success as a bailout treatment in cases of LVOTO with hemodynamic compromise after transmitral valve replacement in the global registry. All six treated patients had significant improvement initially, although the LVOTO recurred the next day in one instance. Four of the six patients were discharged from the hospital. One patient died because of atrioventricular block, and another from multiorgan failure 3 weeks after alcohol ablation of the LVOTO.
Dr. Guerrero has been a leader in this new field. She reported the first percutaneous implantation of a balloon expandable transcatheter valve in a native mitral valve without a surgical incision (Catheter Cardiovasc Interv. 2014 Jun 1;83[7]:E287-91), and more recently, together with coworkers developed a percutaneous alcohol ablation technique for acute reduction of LVOTO due to transcatheter mitral valve replacement (Catheter Cardiovasc Interv. 2016 Jul 5. doi:10.1002/ccd.26649).
She is now the principal investigator in the ongoing Mitral Implantation of Transcatheter Valves (MITRAL) trial, a physician-sponsored, 90-patient pilot study underway at six U.S. sites. MITRAL is recruiting three patient populations for transcatheter mitral valve replacement: patients like those in the global registry, with native mitral valve disease and severe mitral annular calcification; those with a symptomatic failing surgical ring with severe mitral regurgitation or stenosis; and patients with a symptomatic failing surgical bioprosthesis with severe mitral regurgitation or stenosis.
Discussant Nicolo Piazza, MD, of McGill University, Montreal, said transcatheter mitral valve replacement in mitral valve disease with severe mitral annular calcification in patients unsuitable for surgery “definitely represents an unmet clinical need in our practice today.” But he urged caution in interpreting the global registry data.
“This is a real world registry study with inherent selection bias and physician reporting bias,” the cardiologist said.
“We are leveraging a therapy from the aortic field into the mitral field. Of course, we do not have dedicated devices yet to treat these patients. The main finding of this study is that the procedure is actually feasible,” Dr. Piazza said.
Still, it’s sobering that at least 1 in 10 treated patients experiences LVOTO, 1 in 10 requires a second valve, and technical success is achieved in 3 out of 4 patients, he added.
Dr. Piazza predicted that multislice CT scans will be “extremely important” in refining patient selection criteria for the procedure, and echocardiography will be helpful in understanding the optimal procedural techniques and viewing angles. Work also needs to be done on developing optimal anticoagulation protocols in order to avoid valve thrombosis.
Dr. Guerrero reported serving as a consultant to Edwards Lifesciences. Dr. Piazza is a consultant to Medtronic and MicroPort.
AT EUROPCR 2016
Key clinical point: A report from a global registry of transcatheter aortic valve implantation in the mitral position shows the procedure is feasible.
Major finding: Thirty-day mortality fell from 37.5% in the first third of treated patients to 15% in the most recent tertile.
Data source: A real world registry that includes 104 patients at 47 centers in 11 countries to date.
Disclosures: The study presenter reported serving as a consultant to Edwards Lifesciences.
MCR-1 gene a growing concern for antibiotic resistance
The MCR-1 gene is quickly emerging as a powerful roadblock in the fight against antibiotic-resistant bacteria, according to experts from the Centers for Disease Control and Prevention.
Alex J. Kallen, MD, of the CDC in Atlanta, said in an Aug. 2 webinar – cohosted by CDC and the Partnership for Quality Care – that the CDC is closely monitoring the emergence of antibiotic resistant bacteria in the United States. The prevailing message of Dr. Kallen and his CDC colleague Arjun Srinivasan, MD was that the importance of the MCR-1 gene should not be underestimated.
First discovered in a human patient last year, the presence of the MCR-1 gene makes bacteria resistant to colistin, an antibiotic used often as a last resort to “treat patients with multidrug-resistant infections,” according to the CDC. Because the MCR-1 gene exists on a plasmid, or a small piece of DNA, it is easily transferable among bacteria, making it a problem for health care providers treating a patient infected with bacteria that has the gene.
“As of this year, all state and some local health departments will be funded to respond to [antibiotic resistance] threats, including emerging threats like [MCR-1], within their jurisdiction,” Dr. Kallen said. This funding could be used to support technical assistance, contact investigations, and laboratory testing, among other things.
In order to help prevent the spread of MCR-1 and mitigate cases of novel antimicrobial resistance, health care providers and facilities should institute recommended intensive care precautions as soon as resistance is identified, along with alerting their local public health office. Isolates should be saved, and prospective and retrospective surveillance should be implemented to “identify isolates with similar phenotypes.” If an infected patient is being transferred to another facility, that facility should be notified ahead of time about the patient and what protocols to follow.
Because antibiotic-resistant organisms do not spread through the air like influenza, the risk that these organisms pose to health care workers is relatively low, Dr. Srinivasan explained. However, he stressed that a multifaceted, team-based approach to antibiotic stewardship and decontamination of health care facilities is absolutely necessary to achieve the best results for both patients and staff.
“We are now beginning to recognize that the contamination of surfaces and items in our health care environment is increasingly a problem in the transmission of these drug-resistant organisms,” Dr. Srinivasan explained. He said that, given the complexity of a typical health care environment, such as a hospital room or operating theater, it’s perhaps not so surprising that keeping everything clean is not the top priority.
In addition to making sure hospital rooms and other areas are properly cleaned, simple things like washing hands and keeping surfaces clean are just as important. Dr. Srinivasan pointed to a 2006 study by Philip C. Carling, MD, and his associates which showed that educational interventions can lead to substantial increases in hygiene and cleanliness, and that training of new staff is also important. Furthermore, giving staff enough time to properly clean rooms could significantly contribute to curtailing MCR-1 bacteria from spreading, he said.
“The other thing to keep in mind is that if we lose effective therapy, if we lose antibiotic therapy, the infections that are currently very treatable and are seldom deadly could again become very, very serious threats to life,” Dr. Srinivasan warned, specifically citing Escherichia coli, which is the leading cause of urinary tract infections. If community strains of E.coli become resistant to typical antibiotic treatment, these cases could become “difficult, if not impossible to treat.”
According to data shared by Dr. Srinivasan, in 2013 there were 2,049,422 illnesses in the United States attributed to antibiotic resistance and 23,000 fatalities.
The MCR-1 gene is quickly emerging as a powerful roadblock in the fight against antibiotic-resistant bacteria, according to experts from the Centers for Disease Control and Prevention.
Alex J. Kallen, MD, of the CDC in Atlanta, said in an Aug. 2 webinar – cohosted by CDC and the Partnership for Quality Care – that the CDC is closely monitoring the emergence of antibiotic resistant bacteria in the United States. The prevailing message of Dr. Kallen and his CDC colleague Arjun Srinivasan, MD was that the importance of the MCR-1 gene should not be underestimated.
First discovered in a human patient last year, the presence of the MCR-1 gene makes bacteria resistant to colistin, an antibiotic used often as a last resort to “treat patients with multidrug-resistant infections,” according to the CDC. Because the MCR-1 gene exists on a plasmid, or a small piece of DNA, it is easily transferable among bacteria, making it a problem for health care providers treating a patient infected with bacteria that has the gene.
“As of this year, all state and some local health departments will be funded to respond to [antibiotic resistance] threats, including emerging threats like [MCR-1], within their jurisdiction,” Dr. Kallen said. This funding could be used to support technical assistance, contact investigations, and laboratory testing, among other things.
In order to help prevent the spread of MCR-1 and mitigate cases of novel antimicrobial resistance, health care providers and facilities should institute recommended intensive care precautions as soon as resistance is identified, along with alerting their local public health office. Isolates should be saved, and prospective and retrospective surveillance should be implemented to “identify isolates with similar phenotypes.” If an infected patient is being transferred to another facility, that facility should be notified ahead of time about the patient and what protocols to follow.
Because antibiotic-resistant organisms do not spread through the air like influenza, the risk that these organisms pose to health care workers is relatively low, Dr. Srinivasan explained. However, he stressed that a multifaceted, team-based approach to antibiotic stewardship and decontamination of health care facilities is absolutely necessary to achieve the best results for both patients and staff.
“We are now beginning to recognize that the contamination of surfaces and items in our health care environment is increasingly a problem in the transmission of these drug-resistant organisms,” Dr. Srinivasan explained. He said that, given the complexity of a typical health care environment, such as a hospital room or operating theater, it’s perhaps not so surprising that keeping everything clean is not the top priority.
In addition to making sure hospital rooms and other areas are properly cleaned, simple things like washing hands and keeping surfaces clean are just as important. Dr. Srinivasan pointed to a 2006 study by Philip C. Carling, MD, and his associates which showed that educational interventions can lead to substantial increases in hygiene and cleanliness, and that training of new staff is also important. Furthermore, giving staff enough time to properly clean rooms could significantly contribute to curtailing MCR-1 bacteria from spreading, he said.
“The other thing to keep in mind is that if we lose effective therapy, if we lose antibiotic therapy, the infections that are currently very treatable and are seldom deadly could again become very, very serious threats to life,” Dr. Srinivasan warned, specifically citing Escherichia coli, which is the leading cause of urinary tract infections. If community strains of E.coli become resistant to typical antibiotic treatment, these cases could become “difficult, if not impossible to treat.”
According to data shared by Dr. Srinivasan, in 2013 there were 2,049,422 illnesses in the United States attributed to antibiotic resistance and 23,000 fatalities.
The MCR-1 gene is quickly emerging as a powerful roadblock in the fight against antibiotic-resistant bacteria, according to experts from the Centers for Disease Control and Prevention.
Alex J. Kallen, MD, of the CDC in Atlanta, said in an Aug. 2 webinar – cohosted by CDC and the Partnership for Quality Care – that the CDC is closely monitoring the emergence of antibiotic resistant bacteria in the United States. The prevailing message of Dr. Kallen and his CDC colleague Arjun Srinivasan, MD was that the importance of the MCR-1 gene should not be underestimated.
First discovered in a human patient last year, the presence of the MCR-1 gene makes bacteria resistant to colistin, an antibiotic used often as a last resort to “treat patients with multidrug-resistant infections,” according to the CDC. Because the MCR-1 gene exists on a plasmid, or a small piece of DNA, it is easily transferable among bacteria, making it a problem for health care providers treating a patient infected with bacteria that has the gene.
“As of this year, all state and some local health departments will be funded to respond to [antibiotic resistance] threats, including emerging threats like [MCR-1], within their jurisdiction,” Dr. Kallen said. This funding could be used to support technical assistance, contact investigations, and laboratory testing, among other things.
In order to help prevent the spread of MCR-1 and mitigate cases of novel antimicrobial resistance, health care providers and facilities should institute recommended intensive care precautions as soon as resistance is identified, along with alerting their local public health office. Isolates should be saved, and prospective and retrospective surveillance should be implemented to “identify isolates with similar phenotypes.” If an infected patient is being transferred to another facility, that facility should be notified ahead of time about the patient and what protocols to follow.
Because antibiotic-resistant organisms do not spread through the air like influenza, the risk that these organisms pose to health care workers is relatively low, Dr. Srinivasan explained. However, he stressed that a multifaceted, team-based approach to antibiotic stewardship and decontamination of health care facilities is absolutely necessary to achieve the best results for both patients and staff.
“We are now beginning to recognize that the contamination of surfaces and items in our health care environment is increasingly a problem in the transmission of these drug-resistant organisms,” Dr. Srinivasan explained. He said that, given the complexity of a typical health care environment, such as a hospital room or operating theater, it’s perhaps not so surprising that keeping everything clean is not the top priority.
In addition to making sure hospital rooms and other areas are properly cleaned, simple things like washing hands and keeping surfaces clean are just as important. Dr. Srinivasan pointed to a 2006 study by Philip C. Carling, MD, and his associates which showed that educational interventions can lead to substantial increases in hygiene and cleanliness, and that training of new staff is also important. Furthermore, giving staff enough time to properly clean rooms could significantly contribute to curtailing MCR-1 bacteria from spreading, he said.
“The other thing to keep in mind is that if we lose effective therapy, if we lose antibiotic therapy, the infections that are currently very treatable and are seldom deadly could again become very, very serious threats to life,” Dr. Srinivasan warned, specifically citing Escherichia coli, which is the leading cause of urinary tract infections. If community strains of E.coli become resistant to typical antibiotic treatment, these cases could become “difficult, if not impossible to treat.”
According to data shared by Dr. Srinivasan, in 2013 there were 2,049,422 illnesses in the United States attributed to antibiotic resistance and 23,000 fatalities.
Biomarker-driven targeted therapy feasible for NSCLC
Biomarker-driven targeted therapy was found feasible for heavily pretreated, metastatic non–small-cell lung cancer in a phase II trial reported online Aug. 1 in the Journal of Clinical Oncology.
The open-label multicenter umbrella study under the Biomarker-Integrated Approaches of Targeted Therapy for Lung Cancer Elimination (BATTLE) trial, called the BATTLE-2, involved 200 patients with advanced NSCLC refractory to platinum-based chemotherapy and multiple other treatments. All patients underwent tumor tissue biopsies for biomarker and gene expression analyses.
The results of those assessments were then used to perform “adaptive randomization” in which the patients were assigned to one of four treatment arms deemed most likely to control their particular malignancy, said Vassiliki Papadimitrakopoulou, MD, professor of medicine in the department of thoracic/head and neck medical oncology at the University of Texas MD Anderson Cancer Center, Houston, and her associates.
One group of 22 patients received 150 mg erlotinib once daily; the second group (42 patients) received 150 mg erlotinib daily plus 135 mg of the AKT inhibitor MK-2206 once weekly; the third group (75 patients) received 100 mg per week of MK-2206 plus 100 mg of the MEK inhibitor AZD6244 once daily; and the fourth group (61 patients) received 400 mg of sorafenib twice daily. A total of 186 patients were evaluable at 8 weeks, and the overall rate of disease control was 48% at that time. After a median follow-up of 20 months, the median progression-free survival was 2.0 months, median overall survival was 6.5 months, and the 1-year survival was 28%.
The primary endpoint of the study – disease control rate at 8 weeks – was not significantly different among the four treatment groups. It was 32% in group 1, 50% in group 2, 53% in group 3, and 46% in group 4. There were no complete responses and only 6 partial responses: 3 patients in group 3 and 3 patients in group 4. However, the study demonstrated “the utility of real-time biopsies for broad profiling of tumors that serve as a discovery vehicle for better target selection,” the investigators said (J Clin Oncol. 2016 Aug 1. doi:10.1200/JCO.2015.66.0084).
“We are currently pursuing alternative strategies in targeting KRAS mut+ tumors by incorporating knowledge derived from BATTLE 2,” they added.
This study was supported by Merck, Bayer Healthcare Pharmaceuticals, and the National Cancer Institute. Dr. Papadimitrakopoulou and her associates reported ties to numerous industry sources.
“Notwithstanding the low bar of the relatively unconventional endpoint of 8-week [disease control rate], BATTLE-2 should be recognized as a valuable contribution to the field, despite it failing to demonstrate encouraging efficacy in any of the treatment arms or patient subsets,” Howard (Jack) West, MD, wrote in an accompanying editorial (J Clin Oncol. 2016 Aug 1. doi: 10.1200/JCO.2016.68.8226).
But the main result of this study was that all treatment arms produced a disappointing 8-week disease control rate averaging 48%, with no treatment proving to be more promising than the others, with no complete responses and only rare partial responses, and with a progression-free survival of only 2 months in every group, he wrote. However, molecular targeting sometimes benefits small subgroups of patients, such as when advanced squamous NSCLC responds to afatinib. In this study, a subgroup of 52 patients whose tumors showed KRAS mut+ mutations had a significantly longer progression-free survival if they did not receive erlotinib.
Dr. West is affiliated with the Swedish Cancer Institute, Seattle. He reported ties to numerous industry sources.
“Notwithstanding the low bar of the relatively unconventional endpoint of 8-week [disease control rate], BATTLE-2 should be recognized as a valuable contribution to the field, despite it failing to demonstrate encouraging efficacy in any of the treatment arms or patient subsets,” Howard (Jack) West, MD, wrote in an accompanying editorial (J Clin Oncol. 2016 Aug 1. doi: 10.1200/JCO.2016.68.8226).
But the main result of this study was that all treatment arms produced a disappointing 8-week disease control rate averaging 48%, with no treatment proving to be more promising than the others, with no complete responses and only rare partial responses, and with a progression-free survival of only 2 months in every group, he wrote. However, molecular targeting sometimes benefits small subgroups of patients, such as when advanced squamous NSCLC responds to afatinib. In this study, a subgroup of 52 patients whose tumors showed KRAS mut+ mutations had a significantly longer progression-free survival if they did not receive erlotinib.
Dr. West is affiliated with the Swedish Cancer Institute, Seattle. He reported ties to numerous industry sources.
“Notwithstanding the low bar of the relatively unconventional endpoint of 8-week [disease control rate], BATTLE-2 should be recognized as a valuable contribution to the field, despite it failing to demonstrate encouraging efficacy in any of the treatment arms or patient subsets,” Howard (Jack) West, MD, wrote in an accompanying editorial (J Clin Oncol. 2016 Aug 1. doi: 10.1200/JCO.2016.68.8226).
But the main result of this study was that all treatment arms produced a disappointing 8-week disease control rate averaging 48%, with no treatment proving to be more promising than the others, with no complete responses and only rare partial responses, and with a progression-free survival of only 2 months in every group, he wrote. However, molecular targeting sometimes benefits small subgroups of patients, such as when advanced squamous NSCLC responds to afatinib. In this study, a subgroup of 52 patients whose tumors showed KRAS mut+ mutations had a significantly longer progression-free survival if they did not receive erlotinib.
Dr. West is affiliated with the Swedish Cancer Institute, Seattle. He reported ties to numerous industry sources.
Biomarker-driven targeted therapy was found feasible for heavily pretreated, metastatic non–small-cell lung cancer in a phase II trial reported online Aug. 1 in the Journal of Clinical Oncology.
The open-label multicenter umbrella study under the Biomarker-Integrated Approaches of Targeted Therapy for Lung Cancer Elimination (BATTLE) trial, called the BATTLE-2, involved 200 patients with advanced NSCLC refractory to platinum-based chemotherapy and multiple other treatments. All patients underwent tumor tissue biopsies for biomarker and gene expression analyses.
The results of those assessments were then used to perform “adaptive randomization” in which the patients were assigned to one of four treatment arms deemed most likely to control their particular malignancy, said Vassiliki Papadimitrakopoulou, MD, professor of medicine in the department of thoracic/head and neck medical oncology at the University of Texas MD Anderson Cancer Center, Houston, and her associates.
One group of 22 patients received 150 mg erlotinib once daily; the second group (42 patients) received 150 mg erlotinib daily plus 135 mg of the AKT inhibitor MK-2206 once weekly; the third group (75 patients) received 100 mg per week of MK-2206 plus 100 mg of the MEK inhibitor AZD6244 once daily; and the fourth group (61 patients) received 400 mg of sorafenib twice daily. A total of 186 patients were evaluable at 8 weeks, and the overall rate of disease control was 48% at that time. After a median follow-up of 20 months, the median progression-free survival was 2.0 months, median overall survival was 6.5 months, and the 1-year survival was 28%.
The primary endpoint of the study – disease control rate at 8 weeks – was not significantly different among the four treatment groups. It was 32% in group 1, 50% in group 2, 53% in group 3, and 46% in group 4. There were no complete responses and only 6 partial responses: 3 patients in group 3 and 3 patients in group 4. However, the study demonstrated “the utility of real-time biopsies for broad profiling of tumors that serve as a discovery vehicle for better target selection,” the investigators said (J Clin Oncol. 2016 Aug 1. doi:10.1200/JCO.2015.66.0084).
“We are currently pursuing alternative strategies in targeting KRAS mut+ tumors by incorporating knowledge derived from BATTLE 2,” they added.
This study was supported by Merck, Bayer Healthcare Pharmaceuticals, and the National Cancer Institute. Dr. Papadimitrakopoulou and her associates reported ties to numerous industry sources.
Biomarker-driven targeted therapy was found feasible for heavily pretreated, metastatic non–small-cell lung cancer in a phase II trial reported online Aug. 1 in the Journal of Clinical Oncology.
The open-label multicenter umbrella study under the Biomarker-Integrated Approaches of Targeted Therapy for Lung Cancer Elimination (BATTLE) trial, called the BATTLE-2, involved 200 patients with advanced NSCLC refractory to platinum-based chemotherapy and multiple other treatments. All patients underwent tumor tissue biopsies for biomarker and gene expression analyses.
The results of those assessments were then used to perform “adaptive randomization” in which the patients were assigned to one of four treatment arms deemed most likely to control their particular malignancy, said Vassiliki Papadimitrakopoulou, MD, professor of medicine in the department of thoracic/head and neck medical oncology at the University of Texas MD Anderson Cancer Center, Houston, and her associates.
One group of 22 patients received 150 mg erlotinib once daily; the second group (42 patients) received 150 mg erlotinib daily plus 135 mg of the AKT inhibitor MK-2206 once weekly; the third group (75 patients) received 100 mg per week of MK-2206 plus 100 mg of the MEK inhibitor AZD6244 once daily; and the fourth group (61 patients) received 400 mg of sorafenib twice daily. A total of 186 patients were evaluable at 8 weeks, and the overall rate of disease control was 48% at that time. After a median follow-up of 20 months, the median progression-free survival was 2.0 months, median overall survival was 6.5 months, and the 1-year survival was 28%.
The primary endpoint of the study – disease control rate at 8 weeks – was not significantly different among the four treatment groups. It was 32% in group 1, 50% in group 2, 53% in group 3, and 46% in group 4. There were no complete responses and only 6 partial responses: 3 patients in group 3 and 3 patients in group 4. However, the study demonstrated “the utility of real-time biopsies for broad profiling of tumors that serve as a discovery vehicle for better target selection,” the investigators said (J Clin Oncol. 2016 Aug 1. doi:10.1200/JCO.2015.66.0084).
“We are currently pursuing alternative strategies in targeting KRAS mut+ tumors by incorporating knowledge derived from BATTLE 2,” they added.
This study was supported by Merck, Bayer Healthcare Pharmaceuticals, and the National Cancer Institute. Dr. Papadimitrakopoulou and her associates reported ties to numerous industry sources.
FROM THE JOURNAL OF CLINICAL ONCOLOGY
Key clinical point: Biomarker-driven targeted therapy was found feasible for heavily pretreated, metastatic NSCLC.
Major finding: The primary endpoint – disease control rate at 8 weeks – was 32% in group 1, 50% in group 2, 53% in group 3, and 46% in group 4.
Data source: A randomized open-label phase II study involving 200 patients with heavily pretreated, metastatic NSCLC.
Disclosures: This study was supported by Merck, Bayer Healthcare Pharmaceuticals, and the National Cancer Institute. Dr. Papadimitrakopoulou and her associates reported ties to numerous industry sources.
Post-AMI death risk model has high predictive accuracy
An updated risk model based on data from patients presenting after acute myocardial infarction to a broad spectrum of U.S. hospitals appears to predict with a high degree of accuracy which patients are at the greatest risk for in-hospital mortality, investigators say.
Created from data on more than 240,000 patients presenting to one of 655 U.S. hospitals in 2012 and 2013 following ST-segment elevation myocardial infarction (STEMI) or non–ST-segment elevation MI (NSTEMI), the model identified the following independent risk factors for in-hospital mortality: age, heart rate, systolic blood pressure, presentation to the hospital after cardiac arrest, presentation in cardiogenic shock, presentation in heart failure, presentation with STEMI, creatinine clearance, and troponin ratio, reported Robert L. McNamara, MD, of Yale University, New Haven, Conn.
The investigators are participants in the ACTION (Acute Coronary Treatment and Intervention Outcomes Network) Registry–GWTG (Get With the Guidelines).
“The new ACTION Registry–GWTG in-hospital mortality risk model and risk score represent robust, parsimonious, and contemporary risk adjustment methodology for use in routine clinical care and hospital quality assessment. The addition of risk adjustment for patients presenting after cardiac arrest is critically important and enables a fairer assessment across hospitals with varied case mix,” they wrote (J Am Coll Cardiol. 2016 Aug 1;68[6]:626-35).
The revised risk model has the potential to facilitate hospital quality assessments and help investigators to identify specific factors that could help clinicians even further lower death rates, the investigators write.
Further mortality reductions?
Although improvements in care of patients with acute MI over the last several decades have driven the in-hospital death rate from 29% in 1969 down to less than 7% today, there are still more than 100,000 AMI-related in-hospital deaths in the United States annually, with wide variations across hospitals, Dr. McNamara and colleagues noted.
A previous risk model published by ACTION Registry–GWTG members included data on patients treated at 306 U.S. hospitals and provided a simple, validated in-hospital mortality and risk score.
Since that model was published, however, the dataset was expanded to include patients presenting after cardiac arrest at the time of AMI presentation.
“Being able to adjust for cardiac arrest is critical because it is a well-documented predictor of mortality. Moreover, continued improvement in AMI care mandates periodic updates to the risk models so that hospitals can assess their quality as contemporary care continues to evolve,” the authors wrote.
To see whether they could develop a new and improved model and risk score, they analyzed data on 243,440 patients treated at one of 655 hospitals in the voluntary network. Data on 145,952 patients (60% of the total), 57,039 of whom presented with STEMI, and 88,913 of whom presented with NSTEMI, were used to for the derivation sample.
Data on the remaining 97,488 (38,060 with STEMI and 59,428 with NSTEMI) were used to create the validation sample.
The authors found that for the total cohort, the in-hospital mortality rate was 4.6%. In multivariate models controlled for demographic and clinical factors, independent risk factors significantly associated with in-hospital mortality (validation cohort) were:
• Presentation after cardiac arrest (odds ratio, 5.15).
• Presentation in cardiogenic shock (OR, 4.22).
• Presentation in heart failure (OR, 1.83).
• STEMI on electrocardiography (OR, 1.81).
• Age, per 5 years (OR, 1.24).
• Systolic BP, per 10 mm Hg decrease (OR, 1.19).
• Creatinine clearance per 5/mL/min/1.73 m2 decrease (OR, 1.11).
• Heart rate per 10 beats/min (OR, 1.09).
• Troponin ratio, per 5 units (OR, 1.05).
The 95% confidence intervals for all of the above factors were significant.
The C-statistic, a standard measure of the predictive accuracy of a logistic regression model, was 0.88, indicating that the final ACTION Registry–GWTG in-hospital mortality model had a high level of discrimination in both the derivation and validation populations, the authors state.
The ACTION Registry–GWTG is a Program of the American College of Cardiology and the American Heart Association, with funding from Schering-Plough and the Bristol-Myers Squibb/Sanofi Pharmaceutical Partnership. Dr. McNamara serves on a clinical trials endpoint adjudication committee for Pfizer. Other coauthors reported multiple financial relationships with pharmaceutical and medical device companies.
Data analyses for the risk models developed by the ACTION Registry generally showed good accuracy and precision. The calibration information showed that patients with a cardiac arrest experienced much greater risk for mortality than did the other major groups (STEMI, NSTEMI, or no cardiac arrest). Until now, clinicians and researchers have generally used either the TIMI [Thrombolysis in Myocardial Infarction] or GRACE [Global Registry of Acute Coronary Events] score to guide therapeutic decisions. With the advent of the ACTION score, which appears to be most helpful for patients with moderate to severe disease, and the HEART [history, ECG, age, risk factor, troponin] score, which targets care for patients with minimal to mild disease, there are other options. Recently, the DAPT (Dual Antiplatelet Therapy) investigators published a prediction algorithm that provides yet another prognostic score to assess risk of ischemic events and risk of bleeding in patients who have undergone percutaneous coronary intervention. The key variables in the DAPT score are age, cigarette smoking, diabetes, MI at presentation, previous percutaneous coronary intervention or previous MI, use of a paclitaxel-eluting stent, stent diameter of less than 3 mm, heart failure or reduced ejection fraction, and use of a vein graft stent.
A comprehensive cross validation and comparison across at least some of the algorithms – TIMI, GRACE, HEART, DAPT, and ACTION – would help at this point. Interventions and decision points have evolved over the past 15 years, and evaluation of relatively contemporary data would be especially helpful. For example, the HEART score is likely to be used in situations in which the negative predictive capabilities are most important. The ACTION score is likely to be most useful in severely ill patients and to provide guidance for newer interventions. If detailed information concerning stents is available, then the DAPT score should prove helpful.
It is likely that one score does not fit all. Each algorithm provides a useful summary of risk to help guide decision making for patients with ischemic symptoms, depending on the severity of the signs and symptoms at presentation and the duration of the follow-up interval. Consensus building would help to move this field forward for hospital-based management of patients evaluated for cardiac ischemia.
Peter W.F. Wilson, MD, of the Atlanta VAMC and Emory Clinical Cardiovascular Research
Institute, Atlanta; and Ralph B. D’Agostino Sr., PhD, of the department of mathematics and statistics, Boston University, made these comments in an accompanying editorial (J Am Coll Cardiol. 2016 Aug 1;68[6]:636-8). They reported no relevant disclosures.
Data analyses for the risk models developed by the ACTION Registry generally showed good accuracy and precision. The calibration information showed that patients with a cardiac arrest experienced much greater risk for mortality than did the other major groups (STEMI, NSTEMI, or no cardiac arrest). Until now, clinicians and researchers have generally used either the TIMI [Thrombolysis in Myocardial Infarction] or GRACE [Global Registry of Acute Coronary Events] score to guide therapeutic decisions. With the advent of the ACTION score, which appears to be most helpful for patients with moderate to severe disease, and the HEART [history, ECG, age, risk factor, troponin] score, which targets care for patients with minimal to mild disease, there are other options. Recently, the DAPT (Dual Antiplatelet Therapy) investigators published a prediction algorithm that provides yet another prognostic score to assess risk of ischemic events and risk of bleeding in patients who have undergone percutaneous coronary intervention. The key variables in the DAPT score are age, cigarette smoking, diabetes, MI at presentation, previous percutaneous coronary intervention or previous MI, use of a paclitaxel-eluting stent, stent diameter of less than 3 mm, heart failure or reduced ejection fraction, and use of a vein graft stent.
A comprehensive cross validation and comparison across at least some of the algorithms – TIMI, GRACE, HEART, DAPT, and ACTION – would help at this point. Interventions and decision points have evolved over the past 15 years, and evaluation of relatively contemporary data would be especially helpful. For example, the HEART score is likely to be used in situations in which the negative predictive capabilities are most important. The ACTION score is likely to be most useful in severely ill patients and to provide guidance for newer interventions. If detailed information concerning stents is available, then the DAPT score should prove helpful.
It is likely that one score does not fit all. Each algorithm provides a useful summary of risk to help guide decision making for patients with ischemic symptoms, depending on the severity of the signs and symptoms at presentation and the duration of the follow-up interval. Consensus building would help to move this field forward for hospital-based management of patients evaluated for cardiac ischemia.
Peter W.F. Wilson, MD, of the Atlanta VAMC and Emory Clinical Cardiovascular Research
Institute, Atlanta; and Ralph B. D’Agostino Sr., PhD, of the department of mathematics and statistics, Boston University, made these comments in an accompanying editorial (J Am Coll Cardiol. 2016 Aug 1;68[6]:636-8). They reported no relevant disclosures.
Data analyses for the risk models developed by the ACTION Registry generally showed good accuracy and precision. The calibration information showed that patients with a cardiac arrest experienced much greater risk for mortality than did the other major groups (STEMI, NSTEMI, or no cardiac arrest). Until now, clinicians and researchers have generally used either the TIMI [Thrombolysis in Myocardial Infarction] or GRACE [Global Registry of Acute Coronary Events] score to guide therapeutic decisions. With the advent of the ACTION score, which appears to be most helpful for patients with moderate to severe disease, and the HEART [history, ECG, age, risk factor, troponin] score, which targets care for patients with minimal to mild disease, there are other options. Recently, the DAPT (Dual Antiplatelet Therapy) investigators published a prediction algorithm that provides yet another prognostic score to assess risk of ischemic events and risk of bleeding in patients who have undergone percutaneous coronary intervention. The key variables in the DAPT score are age, cigarette smoking, diabetes, MI at presentation, previous percutaneous coronary intervention or previous MI, use of a paclitaxel-eluting stent, stent diameter of less than 3 mm, heart failure or reduced ejection fraction, and use of a vein graft stent.
A comprehensive cross validation and comparison across at least some of the algorithms – TIMI, GRACE, HEART, DAPT, and ACTION – would help at this point. Interventions and decision points have evolved over the past 15 years, and evaluation of relatively contemporary data would be especially helpful. For example, the HEART score is likely to be used in situations in which the negative predictive capabilities are most important. The ACTION score is likely to be most useful in severely ill patients and to provide guidance for newer interventions. If detailed information concerning stents is available, then the DAPT score should prove helpful.
It is likely that one score does not fit all. Each algorithm provides a useful summary of risk to help guide decision making for patients with ischemic symptoms, depending on the severity of the signs and symptoms at presentation and the duration of the follow-up interval. Consensus building would help to move this field forward for hospital-based management of patients evaluated for cardiac ischemia.
Peter W.F. Wilson, MD, of the Atlanta VAMC and Emory Clinical Cardiovascular Research
Institute, Atlanta; and Ralph B. D’Agostino Sr., PhD, of the department of mathematics and statistics, Boston University, made these comments in an accompanying editorial (J Am Coll Cardiol. 2016 Aug 1;68[6]:636-8). They reported no relevant disclosures.
An updated risk model based on data from patients presenting after acute myocardial infarction to a broad spectrum of U.S. hospitals appears to predict with a high degree of accuracy which patients are at the greatest risk for in-hospital mortality, investigators say.
Created from data on more than 240,000 patients presenting to one of 655 U.S. hospitals in 2012 and 2013 following ST-segment elevation myocardial infarction (STEMI) or non–ST-segment elevation MI (NSTEMI), the model identified the following independent risk factors for in-hospital mortality: age, heart rate, systolic blood pressure, presentation to the hospital after cardiac arrest, presentation in cardiogenic shock, presentation in heart failure, presentation with STEMI, creatinine clearance, and troponin ratio, reported Robert L. McNamara, MD, of Yale University, New Haven, Conn.
The investigators are participants in the ACTION (Acute Coronary Treatment and Intervention Outcomes Network) Registry–GWTG (Get With the Guidelines).
“The new ACTION Registry–GWTG in-hospital mortality risk model and risk score represent robust, parsimonious, and contemporary risk adjustment methodology for use in routine clinical care and hospital quality assessment. The addition of risk adjustment for patients presenting after cardiac arrest is critically important and enables a fairer assessment across hospitals with varied case mix,” they wrote (J Am Coll Cardiol. 2016 Aug 1;68[6]:626-35).
The revised risk model has the potential to facilitate hospital quality assessments and help investigators to identify specific factors that could help clinicians even further lower death rates, the investigators write.
Further mortality reductions?
Although improvements in care of patients with acute MI over the last several decades have driven the in-hospital death rate from 29% in 1969 down to less than 7% today, there are still more than 100,000 AMI-related in-hospital deaths in the United States annually, with wide variations across hospitals, Dr. McNamara and colleagues noted.
A previous risk model published by ACTION Registry–GWTG members included data on patients treated at 306 U.S. hospitals and provided a simple, validated in-hospital mortality and risk score.
Since that model was published, however, the dataset was expanded to include patients presenting after cardiac arrest at the time of AMI presentation.
“Being able to adjust for cardiac arrest is critical because it is a well-documented predictor of mortality. Moreover, continued improvement in AMI care mandates periodic updates to the risk models so that hospitals can assess their quality as contemporary care continues to evolve,” the authors wrote.
To see whether they could develop a new and improved model and risk score, they analyzed data on 243,440 patients treated at one of 655 hospitals in the voluntary network. Data on 145,952 patients (60% of the total), 57,039 of whom presented with STEMI, and 88,913 of whom presented with NSTEMI, were used to for the derivation sample.
Data on the remaining 97,488 (38,060 with STEMI and 59,428 with NSTEMI) were used to create the validation sample.
The authors found that for the total cohort, the in-hospital mortality rate was 4.6%. In multivariate models controlled for demographic and clinical factors, independent risk factors significantly associated with in-hospital mortality (validation cohort) were:
• Presentation after cardiac arrest (odds ratio, 5.15).
• Presentation in cardiogenic shock (OR, 4.22).
• Presentation in heart failure (OR, 1.83).
• STEMI on electrocardiography (OR, 1.81).
• Age, per 5 years (OR, 1.24).
• Systolic BP, per 10 mm Hg decrease (OR, 1.19).
• Creatinine clearance per 5/mL/min/1.73 m2 decrease (OR, 1.11).
• Heart rate per 10 beats/min (OR, 1.09).
• Troponin ratio, per 5 units (OR, 1.05).
The 95% confidence intervals for all of the above factors were significant.
The C-statistic, a standard measure of the predictive accuracy of a logistic regression model, was 0.88, indicating that the final ACTION Registry–GWTG in-hospital mortality model had a high level of discrimination in both the derivation and validation populations, the authors state.
The ACTION Registry–GWTG is a Program of the American College of Cardiology and the American Heart Association, with funding from Schering-Plough and the Bristol-Myers Squibb/Sanofi Pharmaceutical Partnership. Dr. McNamara serves on a clinical trials endpoint adjudication committee for Pfizer. Other coauthors reported multiple financial relationships with pharmaceutical and medical device companies.
An updated risk model based on data from patients presenting after acute myocardial infarction to a broad spectrum of U.S. hospitals appears to predict with a high degree of accuracy which patients are at the greatest risk for in-hospital mortality, investigators say.
Created from data on more than 240,000 patients presenting to one of 655 U.S. hospitals in 2012 and 2013 following ST-segment elevation myocardial infarction (STEMI) or non–ST-segment elevation MI (NSTEMI), the model identified the following independent risk factors for in-hospital mortality: age, heart rate, systolic blood pressure, presentation to the hospital after cardiac arrest, presentation in cardiogenic shock, presentation in heart failure, presentation with STEMI, creatinine clearance, and troponin ratio, reported Robert L. McNamara, MD, of Yale University, New Haven, Conn.
The investigators are participants in the ACTION (Acute Coronary Treatment and Intervention Outcomes Network) Registry–GWTG (Get With the Guidelines).
“The new ACTION Registry–GWTG in-hospital mortality risk model and risk score represent robust, parsimonious, and contemporary risk adjustment methodology for use in routine clinical care and hospital quality assessment. The addition of risk adjustment for patients presenting after cardiac arrest is critically important and enables a fairer assessment across hospitals with varied case mix,” they wrote (J Am Coll Cardiol. 2016 Aug 1;68[6]:626-35).
The revised risk model has the potential to facilitate hospital quality assessments and help investigators to identify specific factors that could help clinicians even further lower death rates, the investigators write.
Further mortality reductions?
Although improvements in care of patients with acute MI over the last several decades have driven the in-hospital death rate from 29% in 1969 down to less than 7% today, there are still more than 100,000 AMI-related in-hospital deaths in the United States annually, with wide variations across hospitals, Dr. McNamara and colleagues noted.
A previous risk model published by ACTION Registry–GWTG members included data on patients treated at 306 U.S. hospitals and provided a simple, validated in-hospital mortality and risk score.
Since that model was published, however, the dataset was expanded to include patients presenting after cardiac arrest at the time of AMI presentation.
“Being able to adjust for cardiac arrest is critical because it is a well-documented predictor of mortality. Moreover, continued improvement in AMI care mandates periodic updates to the risk models so that hospitals can assess their quality as contemporary care continues to evolve,” the authors wrote.
To see whether they could develop a new and improved model and risk score, they analyzed data on 243,440 patients treated at one of 655 hospitals in the voluntary network. Data on 145,952 patients (60% of the total), 57,039 of whom presented with STEMI, and 88,913 of whom presented with NSTEMI, were used to for the derivation sample.
Data on the remaining 97,488 (38,060 with STEMI and 59,428 with NSTEMI) were used to create the validation sample.
The authors found that for the total cohort, the in-hospital mortality rate was 4.6%. In multivariate models controlled for demographic and clinical factors, independent risk factors significantly associated with in-hospital mortality (validation cohort) were:
• Presentation after cardiac arrest (odds ratio, 5.15).
• Presentation in cardiogenic shock (OR, 4.22).
• Presentation in heart failure (OR, 1.83).
• STEMI on electrocardiography (OR, 1.81).
• Age, per 5 years (OR, 1.24).
• Systolic BP, per 10 mm Hg decrease (OR, 1.19).
• Creatinine clearance per 5/mL/min/1.73 m2 decrease (OR, 1.11).
• Heart rate per 10 beats/min (OR, 1.09).
• Troponin ratio, per 5 units (OR, 1.05).
The 95% confidence intervals for all of the above factors were significant.
The C-statistic, a standard measure of the predictive accuracy of a logistic regression model, was 0.88, indicating that the final ACTION Registry–GWTG in-hospital mortality model had a high level of discrimination in both the derivation and validation populations, the authors state.
The ACTION Registry–GWTG is a Program of the American College of Cardiology and the American Heart Association, with funding from Schering-Plough and the Bristol-Myers Squibb/Sanofi Pharmaceutical Partnership. Dr. McNamara serves on a clinical trials endpoint adjudication committee for Pfizer. Other coauthors reported multiple financial relationships with pharmaceutical and medical device companies.
FROM JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Key clinical point: An updated cardiac mortality risk model may help to further reduce in-hospital deaths following acute myocardial infarction.
Major finding: The C-statistic for the model, a measure of predictive accuracy, was 0.88.
Data source: Updated risk model and in-hospital mortality score based on data from 243,440 patients following an AMI in 655 U.S. hospitals.
Disclosures: The ACTION Registry-GWTG is a Program of the American College of Cardiology and the American Heart Association, with funding from Schering-Plough and the Bristol-Myers Squibb/Sanofi Pharmaceutical Partnership. Dr. McNamara serves on a clinical trials endpoint adjudication committee for Pfizer. Other coauthors reported multiple financial relationships with pharmaceutical and medical device companies.
Study highlights cardiovascular benefits, lower GI risks of low-dose aspirin
Resuming low-dose aspirin after an initial lower gastrointestinal bleed significantly increased the chances of recurrence but protected against serious cardiovascular events, based on a single-center retrospective study published in the August issue of Gastroenterology.
In contrast, “we did not find concomitant use of anticoagulants, antiplatelets, and steroids as a predictor of recurrent lower GI bleeding,” said Dr. Francis Chan of the Prince of Wales Hospital in Hong Kong and his associates. “This may be due to the low percentage of concomitant drug use in both groups. Multicenter studies with a large number of patients will be required to identify additional risk factors for recurrent lower GI bleeding with aspirin use.”
Low-dose aspirin has long been known to help prevent coronary artery and cerebrovascular disease, and more recently has been found to potentially reduce the risk of several types of cancer, the researchers noted. Aspirin is well known to increase the risk of upper GI bleeding, but some studies have also linked it to lower GI bleeding. However, “patients with underlying cardiovascular diseases often require lifelong aspirin,” they added. The risks and benefits of stopping or remaining on aspirin after an initial lower GI bleed are unclear (Gastroenterology 2016 Apr 26. doi: 10.1053/j.gastro.2016.04.013).
Accordingly, the researchers retrospectively studied 295 patients who had an initial aspirin-associated lower GI bleed, defined as 325 mg aspirin a day within a week of bleeding onset. All patients had melena or hematochezia documented by an attending physician and had no endoscopic evidence of upper GI bleeding.
For patients who continued using aspirin at least half the time, the 5-year cumulative incidence of recurrent lower GI bleeding was 19% (95% confidence interval [CI], 13%-25%) – more than double the rate among patients who used aspirin 20% or less of the time (5-year cumulative incidence, 7%; 95% CI, 3%-13%; P = .01). However, the 5-year cumulative incidence of serious cardiovascular events among nonusers was 37% (95% CI, 27%-46%), while the rate among aspirin users was 23% (95% CI, 17%-30%; P = .02). Mortality from noncardiovascular causes was also higher among nonusers (27%) than users (8%; P less than .001), probably because nonusers of aspirin tended to be older than users, but perhaps also because aspirin had a “nonvascular protective effect,” the researchers said.
A multivariate analysis confirmed these findings, linking lower GI bleeding to aspirin but not to use of steroids, anticoagulants, or antiplatelet drugs, or to age, sex, alcohol consumption, smoking, comorbidities, or cardiovascular risks. Indeed, continued aspirin use nearly tripled the chances of a recurrent lower GI bleed (hazard ratio, 2.76; 95% CI, 1.3-6.0; P = .01), but cut the risk of serious cardiovascular events by about 40% (HR, 0.59; 95% CI, 0.4-0.9; P = .02).
Deciding whether to resume aspirin after a severe lower GI bleed “presents a management dilemma for physicians, patients, and their families, particularly in the absence of risk-mitigating therapies and a lack of data on the risks and benefits of resuming aspirin,” the investigators emphasized. Their findings highlight the importance of weighing the cardiovascular benefits of aspirin against GI toxicity, they said. “Since there is substantial risk of recurrent bleeding, physicians should critically evaluate individual patients’ cardiovascular risk before resuming aspirin therapy. Our findings also suggest a need for a composite endpoint to evaluate clinically significant events throughout the GI tract in patients receiving antiplatelet drugs.”
The Chinese University of Hong Kong funded the study. Dr. Chan reported financial ties to Pfizer, Eisai, Takeda, Otsuka, and Astrazeneca.
Resuming low-dose aspirin after an initial lower gastrointestinal bleed significantly increased the chances of recurrence but protected against serious cardiovascular events, based on a single-center retrospective study published in the August issue of Gastroenterology.
In contrast, “we did not find concomitant use of anticoagulants, antiplatelets, and steroids as a predictor of recurrent lower GI bleeding,” said Dr. Francis Chan of the Prince of Wales Hospital in Hong Kong and his associates. “This may be due to the low percentage of concomitant drug use in both groups. Multicenter studies with a large number of patients will be required to identify additional risk factors for recurrent lower GI bleeding with aspirin use.”
Low-dose aspirin has long been known to help prevent coronary artery and cerebrovascular disease, and more recently has been found to potentially reduce the risk of several types of cancer, the researchers noted. Aspirin is well known to increase the risk of upper GI bleeding, but some studies have also linked it to lower GI bleeding. However, “patients with underlying cardiovascular diseases often require lifelong aspirin,” they added. The risks and benefits of stopping or remaining on aspirin after an initial lower GI bleed are unclear (Gastroenterology 2016 Apr 26. doi: 10.1053/j.gastro.2016.04.013).
Accordingly, the researchers retrospectively studied 295 patients who had an initial aspirin-associated lower GI bleed, defined as 325 mg aspirin a day within a week of bleeding onset. All patients had melena or hematochezia documented by an attending physician and had no endoscopic evidence of upper GI bleeding.
For patients who continued using aspirin at least half the time, the 5-year cumulative incidence of recurrent lower GI bleeding was 19% (95% confidence interval [CI], 13%-25%) – more than double the rate among patients who used aspirin 20% or less of the time (5-year cumulative incidence, 7%; 95% CI, 3%-13%; P = .01). However, the 5-year cumulative incidence of serious cardiovascular events among nonusers was 37% (95% CI, 27%-46%), while the rate among aspirin users was 23% (95% CI, 17%-30%; P = .02). Mortality from noncardiovascular causes was also higher among nonusers (27%) than users (8%; P less than .001), probably because nonusers of aspirin tended to be older than users, but perhaps also because aspirin had a “nonvascular protective effect,” the researchers said.
A multivariate analysis confirmed these findings, linking lower GI bleeding to aspirin but not to use of steroids, anticoagulants, or antiplatelet drugs, or to age, sex, alcohol consumption, smoking, comorbidities, or cardiovascular risks. Indeed, continued aspirin use nearly tripled the chances of a recurrent lower GI bleed (hazard ratio, 2.76; 95% CI, 1.3-6.0; P = .01), but cut the risk of serious cardiovascular events by about 40% (HR, 0.59; 95% CI, 0.4-0.9; P = .02).
Deciding whether to resume aspirin after a severe lower GI bleed “presents a management dilemma for physicians, patients, and their families, particularly in the absence of risk-mitigating therapies and a lack of data on the risks and benefits of resuming aspirin,” the investigators emphasized. Their findings highlight the importance of weighing the cardiovascular benefits of aspirin against GI toxicity, they said. “Since there is substantial risk of recurrent bleeding, physicians should critically evaluate individual patients’ cardiovascular risk before resuming aspirin therapy. Our findings also suggest a need for a composite endpoint to evaluate clinically significant events throughout the GI tract in patients receiving antiplatelet drugs.”
The Chinese University of Hong Kong funded the study. Dr. Chan reported financial ties to Pfizer, Eisai, Takeda, Otsuka, and Astrazeneca.
Resuming low-dose aspirin after an initial lower gastrointestinal bleed significantly increased the chances of recurrence but protected against serious cardiovascular events, based on a single-center retrospective study published in the August issue of Gastroenterology.
In contrast, “we did not find concomitant use of anticoagulants, antiplatelets, and steroids as a predictor of recurrent lower GI bleeding,” said Dr. Francis Chan of the Prince of Wales Hospital in Hong Kong and his associates. “This may be due to the low percentage of concomitant drug use in both groups. Multicenter studies with a large number of patients will be required to identify additional risk factors for recurrent lower GI bleeding with aspirin use.”
Low-dose aspirin has long been known to help prevent coronary artery and cerebrovascular disease, and more recently has been found to potentially reduce the risk of several types of cancer, the researchers noted. Aspirin is well known to increase the risk of upper GI bleeding, but some studies have also linked it to lower GI bleeding. However, “patients with underlying cardiovascular diseases often require lifelong aspirin,” they added. The risks and benefits of stopping or remaining on aspirin after an initial lower GI bleed are unclear (Gastroenterology 2016 Apr 26. doi: 10.1053/j.gastro.2016.04.013).
Accordingly, the researchers retrospectively studied 295 patients who had an initial aspirin-associated lower GI bleed, defined as 325 mg aspirin a day within a week of bleeding onset. All patients had melena or hematochezia documented by an attending physician and had no endoscopic evidence of upper GI bleeding.
For patients who continued using aspirin at least half the time, the 5-year cumulative incidence of recurrent lower GI bleeding was 19% (95% confidence interval [CI], 13%-25%) – more than double the rate among patients who used aspirin 20% or less of the time (5-year cumulative incidence, 7%; 95% CI, 3%-13%; P = .01). However, the 5-year cumulative incidence of serious cardiovascular events among nonusers was 37% (95% CI, 27%-46%), while the rate among aspirin users was 23% (95% CI, 17%-30%; P = .02). Mortality from noncardiovascular causes was also higher among nonusers (27%) than users (8%; P less than .001), probably because nonusers of aspirin tended to be older than users, but perhaps also because aspirin had a “nonvascular protective effect,” the researchers said.
A multivariate analysis confirmed these findings, linking lower GI bleeding to aspirin but not to use of steroids, anticoagulants, or antiplatelet drugs, or to age, sex, alcohol consumption, smoking, comorbidities, or cardiovascular risks. Indeed, continued aspirin use nearly tripled the chances of a recurrent lower GI bleed (hazard ratio, 2.76; 95% CI, 1.3-6.0; P = .01), but cut the risk of serious cardiovascular events by about 40% (HR, 0.59; 95% CI, 0.4-0.9; P = .02).
Deciding whether to resume aspirin after a severe lower GI bleed “presents a management dilemma for physicians, patients, and their families, particularly in the absence of risk-mitigating therapies and a lack of data on the risks and benefits of resuming aspirin,” the investigators emphasized. Their findings highlight the importance of weighing the cardiovascular benefits of aspirin against GI toxicity, they said. “Since there is substantial risk of recurrent bleeding, physicians should critically evaluate individual patients’ cardiovascular risk before resuming aspirin therapy. Our findings also suggest a need for a composite endpoint to evaluate clinically significant events throughout the GI tract in patients receiving antiplatelet drugs.”
The Chinese University of Hong Kong funded the study. Dr. Chan reported financial ties to Pfizer, Eisai, Takeda, Otsuka, and Astrazeneca.
FROM GASTROENTEROLOGY
Key clinical point: Resuming low-dose aspirin after a lower gastrointestinal bleed increased the risk of recurrence but protected against cardiovascular events.
Major finding: At 5 years, the cumulative incidence of recurrent lower GI bleeding was 19% for patients who stayed on aspirin and 7% for patients who largely stopped it (P = .01). The cumulative incidence of serious cardiovascular events was 25% for users and 37% for nonusers (P = .02).
Data source: A single-center 5-year retrospective cohort study of 295 patients with aspirin-associated melena or hematochezia and no upper gastrointestinal bleeding.
Disclosures: The Chinese University of Hong Kong funded the study. Dr. Chan reported financial ties to Pfizer, Eisai, Takeda, Otsuka, and Astrazeneca.
Surgeons raise red flag on proposed 2017 physician fee schedule
The physician fee schedule for 2017 proposed by the Centers for Medicare & Medicaid Services has raised a red flag for the American College of Surgeons (ACS).
A proposal related to data collection on the transition of all 10- and 90- day global codes to 0-day codes in the proposed physician fee schedule 2017 is the area of greatest concern to the ACS. The provision would require all surgeons and other physicians who receive payment from these codes to devote many hours to collecting and reporting these data.
Two years ago, the CMS had pushed this exact transition through in regulation. However, Congress halted that transition in the Medicare Access and CHIP Reauthorization Act (MACRA), instead directing the CMS to study the effects of the transition by collecting data from a “representative sample” of physicians who receive payment from these codes.
For most surgical procedures, Medicare pays surgeons for either 10 or 90 days of care that include the procedure itself and postoperative care. Most global codes are 90-day codes. The CMS would have debundled the global payments 2 years ago had Congress not intervened.
However, in the proposed physician fee schedule update for 2017, the CMS would require all physicians to report data on these codes, something the ACS believes is overly burdensome.
“ACS believes that this proposal does not align with the MACRA requirement that CMS only collect data from a representative sample of physicians performing 10- or 90-day global codes,” ACS Regulatory Affairs Manager Vinita Ollapally told ACS Surgery News. “ACS is currently pursuing a legislative strategy that urges CMS to not finalize the proposal to collect data from all practitioners who perform 10- and 90-day global services, and instead revise the policy to collect data on 10- and 90-day global services from a ‘representative sample’ of practitioners.”
The college is developing a definition for what it believes that representative sample should include and expects to have that ready when the ACS files its comments on the physician fee schedule update proposal. Comments on the proposal are due Sept. 6.
The proposed update, published July 15 in the Federal Register, brings in several new policies aimed at improving physician payment for caring for patients with multiple chronic conditions; mental and behavioral health issues; and cognitive impairment or mobility-related issues.
Among the provisions in the 800+ page proposal are revised billing codes that would more accurately recognize the work of primary care and other cognitive specialties. The changes, according to the CMS, will help “better identify and value primary care, care management, and cognitive services.”
The agency is proposing several coding changes that “could improve health care delivery for all types of services holding the most promise for healthier people and smarter spending, and advance our health equity goals,” according to a CMS fact sheet.
The proposed fee schedule also would update how quality is measured and reported by accountable care organizations in the Medicare Shared Savings Program, align Accountable Care Organization reporting with the Physician Quality Reporting System, and change how beneficiaries are assigned to an ACO. Potentially misvalued services also would continue to be reviewed under the proposal.
The agency is also proposing a code to allow for the payment of advanced care planning services furnished via telehealth.
The physician fee schedule for 2017 proposed by the Centers for Medicare & Medicaid Services has raised a red flag for the American College of Surgeons (ACS).
A proposal related to data collection on the transition of all 10- and 90- day global codes to 0-day codes in the proposed physician fee schedule 2017 is the area of greatest concern to the ACS. The provision would require all surgeons and other physicians who receive payment from these codes to devote many hours to collecting and reporting these data.
Two years ago, the CMS had pushed this exact transition through in regulation. However, Congress halted that transition in the Medicare Access and CHIP Reauthorization Act (MACRA), instead directing the CMS to study the effects of the transition by collecting data from a “representative sample” of physicians who receive payment from these codes.
For most surgical procedures, Medicare pays surgeons for either 10 or 90 days of care that include the procedure itself and postoperative care. Most global codes are 90-day codes. The CMS would have debundled the global payments 2 years ago had Congress not intervened.
However, in the proposed physician fee schedule update for 2017, the CMS would require all physicians to report data on these codes, something the ACS believes is overly burdensome.
“ACS believes that this proposal does not align with the MACRA requirement that CMS only collect data from a representative sample of physicians performing 10- or 90-day global codes,” ACS Regulatory Affairs Manager Vinita Ollapally told ACS Surgery News. “ACS is currently pursuing a legislative strategy that urges CMS to not finalize the proposal to collect data from all practitioners who perform 10- and 90-day global services, and instead revise the policy to collect data on 10- and 90-day global services from a ‘representative sample’ of practitioners.”
The college is developing a definition for what it believes that representative sample should include and expects to have that ready when the ACS files its comments on the physician fee schedule update proposal. Comments on the proposal are due Sept. 6.
The proposed update, published July 15 in the Federal Register, brings in several new policies aimed at improving physician payment for caring for patients with multiple chronic conditions; mental and behavioral health issues; and cognitive impairment or mobility-related issues.
Among the provisions in the 800+ page proposal are revised billing codes that would more accurately recognize the work of primary care and other cognitive specialties. The changes, according to the CMS, will help “better identify and value primary care, care management, and cognitive services.”
The agency is proposing several coding changes that “could improve health care delivery for all types of services holding the most promise for healthier people and smarter spending, and advance our health equity goals,” according to a CMS fact sheet.
The proposed fee schedule also would update how quality is measured and reported by accountable care organizations in the Medicare Shared Savings Program, align Accountable Care Organization reporting with the Physician Quality Reporting System, and change how beneficiaries are assigned to an ACO. Potentially misvalued services also would continue to be reviewed under the proposal.
The agency is also proposing a code to allow for the payment of advanced care planning services furnished via telehealth.
The physician fee schedule for 2017 proposed by the Centers for Medicare & Medicaid Services has raised a red flag for the American College of Surgeons (ACS).
A proposal related to data collection on the transition of all 10- and 90- day global codes to 0-day codes in the proposed physician fee schedule 2017 is the area of greatest concern to the ACS. The provision would require all surgeons and other physicians who receive payment from these codes to devote many hours to collecting and reporting these data.
Two years ago, the CMS had pushed this exact transition through in regulation. However, Congress halted that transition in the Medicare Access and CHIP Reauthorization Act (MACRA), instead directing the CMS to study the effects of the transition by collecting data from a “representative sample” of physicians who receive payment from these codes.
For most surgical procedures, Medicare pays surgeons for either 10 or 90 days of care that include the procedure itself and postoperative care. Most global codes are 90-day codes. The CMS would have debundled the global payments 2 years ago had Congress not intervened.
However, in the proposed physician fee schedule update for 2017, the CMS would require all physicians to report data on these codes, something the ACS believes is overly burdensome.
“ACS believes that this proposal does not align with the MACRA requirement that CMS only collect data from a representative sample of physicians performing 10- or 90-day global codes,” ACS Regulatory Affairs Manager Vinita Ollapally told ACS Surgery News. “ACS is currently pursuing a legislative strategy that urges CMS to not finalize the proposal to collect data from all practitioners who perform 10- and 90-day global services, and instead revise the policy to collect data on 10- and 90-day global services from a ‘representative sample’ of practitioners.”
The college is developing a definition for what it believes that representative sample should include and expects to have that ready when the ACS files its comments on the physician fee schedule update proposal. Comments on the proposal are due Sept. 6.
The proposed update, published July 15 in the Federal Register, brings in several new policies aimed at improving physician payment for caring for patients with multiple chronic conditions; mental and behavioral health issues; and cognitive impairment or mobility-related issues.
Among the provisions in the 800+ page proposal are revised billing codes that would more accurately recognize the work of primary care and other cognitive specialties. The changes, according to the CMS, will help “better identify and value primary care, care management, and cognitive services.”
The agency is proposing several coding changes that “could improve health care delivery for all types of services holding the most promise for healthier people and smarter spending, and advance our health equity goals,” according to a CMS fact sheet.
The proposed fee schedule also would update how quality is measured and reported by accountable care organizations in the Medicare Shared Savings Program, align Accountable Care Organization reporting with the Physician Quality Reporting System, and change how beneficiaries are assigned to an ACO. Potentially misvalued services also would continue to be reviewed under the proposal.
The agency is also proposing a code to allow for the payment of advanced care planning services furnished via telehealth.
Transfers to tertiary acute care surgery service point to shortage of rural general surgeons
Nearly half of all transfer patients admitted to a tertiary facility’s acute care surgery service over a 12-month period underwent only basic surgical procedures or required no intervention after the transfer, according to a retrospective chart review.
The 161 patients transferred through the acute care surgery system during the 2014 study period were in need of the services for which they were transferred; thus, the findings highlight a “concerning lack of general surgery resources” in the community, Brittany Misercola, MD, and her colleagues at Maine Medical Center, Portland, reported in the Journal of Surgical Research.
Acute care surgery (ACS) is a relatively new paradigm – borne in part out of a heavy call burden for trauma and general surgeons – for managing patients in need of non–trauma-related emergency surgery, the investigators explained.
“At the same time as the ACS paradigm has developed, rural areas are suffering worsening shortages of physicians, especially specialists like surgeons. Another change has been regionalization of sick, complex, and resource-intensive patients to larger hospitals with more specialized care.
However, no one has yet examined the effect of an ACS service in a predominantly rural area, given these changes in health care,” they wrote (J Surg Res. 2016. [doi:10.106/j.jss.2016.06.090]).
Patients included all adults aged 18 and older admitted between Jan. 1 and Dec. 31, 2014, excluding elective surgical and trauma patients. Transfer patients were admitted from 29 different institutions. The hospital is the largest in Maine, with a wide and rural catchment area. Transfer patients came from every county in the state, with a few from outside the state; 18% were transferred from a Maine Critical Access Hospital.
Compared with 611 local patients admitted through the emergency department or from local long-term care facilities, the transfer patients were older (61.2 years vs. 54.7 years), had more comorbidities (Charlson Comorbidity Index, or CCI, of 4 vs. 3.1), and required more resources (length of stay, 8.2 vs. 3.4 days; intensive care unit admission, 24% vs. 6%), the investigators reported.
Stratification by CCI showed that the difference in length of stay between transfer and local patients was largest in those with a low CCI (0-3), compared with those with a higher CCI.
The admission diagnosis was similar in the transferred and local patients, with pancreaticobiliary and small bowel complaints being the most common (29% and 30%, and 25% and 23%, respectively, for the two diagnoses). The most common interventions were laparoscopic cholecystectomy in both groups (29% and 25%, respectively). Subspecialty interventions were also similar in the groups, and were performed in 10% and 8%, respectively.
However, the transfer patients were more likely than the local patients to not require any intervention, including subspecialty care (32% vs. 23%), they said, noting that the most common reason for admission without operative intervention was “small bowel obstruction, followed by diverticulitis without drainable abscess and mesenteric ischemia.”
The transfer patients also were more likely to have Medicare (55% vs. 24%) and less likely to be privately insured (26% vs. 45%).
The discharge destination differed significantly between the groups, with local patients being more likely to be discharged directly to home (76% vs. 46%), and transfer patients more often discharged home with services (46% vs. 12%) or to acute rehabilitation or skilled nursing facilities (12% vs. 9%). In-hospital mortality and discharge to hospice care also were more likely among transfer patients (6% vs. 2%).
“If changes are not made to support rural hospitals in caring for these patients, tertiary centers in larger cities will see increasing volume of basic surgical emergencies. As such, investing in community hospitals is important to improve patient outcomes not only locally but also after transfer to tertiary referral centers,” they wrote, adding that additional research on the populations most affected is needed.
The authors reported having no relevant financial disclosures.
Nearly half of all transfer patients admitted to a tertiary facility’s acute care surgery service over a 12-month period underwent only basic surgical procedures or required no intervention after the transfer, according to a retrospective chart review.
The 161 patients transferred through the acute care surgery system during the 2014 study period were in need of the services for which they were transferred; thus, the findings highlight a “concerning lack of general surgery resources” in the community, Brittany Misercola, MD, and her colleagues at Maine Medical Center, Portland, reported in the Journal of Surgical Research.
Acute care surgery (ACS) is a relatively new paradigm – borne in part out of a heavy call burden for trauma and general surgeons – for managing patients in need of non–trauma-related emergency surgery, the investigators explained.
“At the same time as the ACS paradigm has developed, rural areas are suffering worsening shortages of physicians, especially specialists like surgeons. Another change has been regionalization of sick, complex, and resource-intensive patients to larger hospitals with more specialized care.
However, no one has yet examined the effect of an ACS service in a predominantly rural area, given these changes in health care,” they wrote (J Surg Res. 2016. [doi:10.106/j.jss.2016.06.090]).
Patients included all adults aged 18 and older admitted between Jan. 1 and Dec. 31, 2014, excluding elective surgical and trauma patients. Transfer patients were admitted from 29 different institutions. The hospital is the largest in Maine, with a wide and rural catchment area. Transfer patients came from every county in the state, with a few from outside the state; 18% were transferred from a Maine Critical Access Hospital.
Compared with 611 local patients admitted through the emergency department or from local long-term care facilities, the transfer patients were older (61.2 years vs. 54.7 years), had more comorbidities (Charlson Comorbidity Index, or CCI, of 4 vs. 3.1), and required more resources (length of stay, 8.2 vs. 3.4 days; intensive care unit admission, 24% vs. 6%), the investigators reported.
Stratification by CCI showed that the difference in length of stay between transfer and local patients was largest in those with a low CCI (0-3), compared with those with a higher CCI.
The admission diagnosis was similar in the transferred and local patients, with pancreaticobiliary and small bowel complaints being the most common (29% and 30%, and 25% and 23%, respectively, for the two diagnoses). The most common interventions were laparoscopic cholecystectomy in both groups (29% and 25%, respectively). Subspecialty interventions were also similar in the groups, and were performed in 10% and 8%, respectively.
However, the transfer patients were more likely than the local patients to not require any intervention, including subspecialty care (32% vs. 23%), they said, noting that the most common reason for admission without operative intervention was “small bowel obstruction, followed by diverticulitis without drainable abscess and mesenteric ischemia.”
The transfer patients also were more likely to have Medicare (55% vs. 24%) and less likely to be privately insured (26% vs. 45%).
The discharge destination differed significantly between the groups, with local patients being more likely to be discharged directly to home (76% vs. 46%), and transfer patients more often discharged home with services (46% vs. 12%) or to acute rehabilitation or skilled nursing facilities (12% vs. 9%). In-hospital mortality and discharge to hospice care also were more likely among transfer patients (6% vs. 2%).
“If changes are not made to support rural hospitals in caring for these patients, tertiary centers in larger cities will see increasing volume of basic surgical emergencies. As such, investing in community hospitals is important to improve patient outcomes not only locally but also after transfer to tertiary referral centers,” they wrote, adding that additional research on the populations most affected is needed.
The authors reported having no relevant financial disclosures.
Nearly half of all transfer patients admitted to a tertiary facility’s acute care surgery service over a 12-month period underwent only basic surgical procedures or required no intervention after the transfer, according to a retrospective chart review.
The 161 patients transferred through the acute care surgery system during the 2014 study period were in need of the services for which they were transferred; thus, the findings highlight a “concerning lack of general surgery resources” in the community, Brittany Misercola, MD, and her colleagues at Maine Medical Center, Portland, reported in the Journal of Surgical Research.
Acute care surgery (ACS) is a relatively new paradigm – borne in part out of a heavy call burden for trauma and general surgeons – for managing patients in need of non–trauma-related emergency surgery, the investigators explained.
“At the same time as the ACS paradigm has developed, rural areas are suffering worsening shortages of physicians, especially specialists like surgeons. Another change has been regionalization of sick, complex, and resource-intensive patients to larger hospitals with more specialized care.
However, no one has yet examined the effect of an ACS service in a predominantly rural area, given these changes in health care,” they wrote (J Surg Res. 2016. [doi:10.106/j.jss.2016.06.090]).
Patients included all adults aged 18 and older admitted between Jan. 1 and Dec. 31, 2014, excluding elective surgical and trauma patients. Transfer patients were admitted from 29 different institutions. The hospital is the largest in Maine, with a wide and rural catchment area. Transfer patients came from every county in the state, with a few from outside the state; 18% were transferred from a Maine Critical Access Hospital.
Compared with 611 local patients admitted through the emergency department or from local long-term care facilities, the transfer patients were older (61.2 years vs. 54.7 years), had more comorbidities (Charlson Comorbidity Index, or CCI, of 4 vs. 3.1), and required more resources (length of stay, 8.2 vs. 3.4 days; intensive care unit admission, 24% vs. 6%), the investigators reported.
Stratification by CCI showed that the difference in length of stay between transfer and local patients was largest in those with a low CCI (0-3), compared with those with a higher CCI.
The admission diagnosis was similar in the transferred and local patients, with pancreaticobiliary and small bowel complaints being the most common (29% and 30%, and 25% and 23%, respectively, for the two diagnoses). The most common interventions were laparoscopic cholecystectomy in both groups (29% and 25%, respectively). Subspecialty interventions were also similar in the groups, and were performed in 10% and 8%, respectively.
However, the transfer patients were more likely than the local patients to not require any intervention, including subspecialty care (32% vs. 23%), they said, noting that the most common reason for admission without operative intervention was “small bowel obstruction, followed by diverticulitis without drainable abscess and mesenteric ischemia.”
The transfer patients also were more likely to have Medicare (55% vs. 24%) and less likely to be privately insured (26% vs. 45%).
The discharge destination differed significantly between the groups, with local patients being more likely to be discharged directly to home (76% vs. 46%), and transfer patients more often discharged home with services (46% vs. 12%) or to acute rehabilitation or skilled nursing facilities (12% vs. 9%). In-hospital mortality and discharge to hospice care also were more likely among transfer patients (6% vs. 2%).
“If changes are not made to support rural hospitals in caring for these patients, tertiary centers in larger cities will see increasing volume of basic surgical emergencies. As such, investing in community hospitals is important to improve patient outcomes not only locally but also after transfer to tertiary referral centers,” they wrote, adding that additional research on the populations most affected is needed.
The authors reported having no relevant financial disclosures.
FROM THE JOURNAL OF SURGICAL RESEARCH
Key clinical point: Transfer of patients to a tertiary facility and acute care surgery service who require basic surgical procedures or no intervention points to a shortage of general surgery capability in the rural areas.
Major finding: Transfer patients were more likely than local patients to not require any intervention, including subspecialty care (32% vs. 23%).
Data source: A retrospective review of 772 patient charts.
Disclosures: The authors reported having no relevant financial disclosures.