User login
The Official Newspaper of the American Association for Thoracic Surgery
Different approaches can combat negative online reviews
Like most physicians, Dr. Susan Hardwick-Smith was used to receiving the occasional negative online review about her practice. But a biting post from several years ago was so wrenching that it nearly drove the Houston ob.gyn. out of medicine for good.
The patient blasted Dr. Hardwick-Smith on a popular review site about her care during a delivery and accused the doctor of attempting to force an unnecessary C-section. The account was inaccurate, but privacy laws prevented Dr. Hardwick-Smith from defending herself online or sharing details of the actual encounter, she said.
“She wrote this very detailed account of what a terrible doctor I was, and in my version of reality, I had saved her baby’s life,” said Dr. Hardwick-Smith. “I felt extremely powerless. I lost a lot of sleep over it, and I was considering giving up delivering babies. It was a real turning point for me.”
Rather than hanging up her white coat, Dr. Hardwick-Smith began working with an online reputation company – eMerit – that works to dilute negative reviews by soliciting a greater number of reviews from patients. The offensive post is now buried under hundreds of other reviews that are primarily positive, she said.
Hiring a reputation management company is one strategy for coping with negative online reviews. But cyberlaw experts stress that removing negative posts altogether is no easy feat. The best move to take often depends on the post, the patient, and the circumstance.
By now, it’s no secret that negative online reviews can significantly impact a medical practice, from influencing patient recruitment to affecting practice revenue to ruining a reputation. A 2015 survey of 2,354 consumers by search marketing firm BrightLocal found that 92% of consumers read online reviews – up from 67% in 2010 – and 40% of consumers had formed an opinion by reading just one to three reviews. Of 2,137 patients who viewed online reviews, 35% selected a physician based on positive reviews, while 37% avoided doctors with negative reviews, according to a 2014 study in JAMA (doi:10.1001/jama.2013.283194).
Reviews have become a strong force in the health care industry, said Peter Yelkovac, an online defamation attorney in Northern Indiana.
“Online reviews have really replaced the common ‘word of mouth’ that used to be the primary source for doctors referrals,” Mr. Yelkovac said in an interview. “Now, [patients] go online. Anyone can type anything they want, whether it’s truthful, untruthful, positive, indifferent, or negative.”
Doctor vs. website
In some cases, contacting a website administrator and requesting a review be removed can end the dilemma, said Michael J. Sacopulos, a medical malpractice defense attorney based in Terre Haute, Ind.
Rating sites generally have “terms of use,” and posts that violate the terms usually will be taken down by site administrators with some nudging, Mr. Sacopulos said in an interview. Other sites have “strike policies,” where a reviewee can request that one or two negative reviews be removed.
Still other sites are not as accommodating. Amazon, for instance, has immunity against content posted on the site, Mr. Sacopulos said. Under the Communications Decency Act, interactive computer services, such as a consumer review website, cannot be liable for content independently created or developed by third-party users. Such sites are hardly motivated to remove negative comments when racy posts can drive traffic to the site, he said.
Eric M. Joseph, MD, a facial plastic surgeon in West Orange, N.J., learned this lesson firsthand when he attempted to have a video removed from YouTube. A poster had uploaded copyright-protected before and after photos from Dr. Joseph’s practice onto YouTube and made disparaging comments about the patients in a video that went viral. Dr. Joseph and the patient both flagged the video for removal, but to no avail.
“It was impossible to [talk to] a human being at Google,” Dr, Joseph said. “It almost didn’t come down, and we were in conversations about suing Google. It took months and a cyberattorney who specializes in copyright infringement.”
The video finally was removed, but not before Dr. Joseph spent $6,000 in legal fees and experienced significant distress from the incident. Although most reviews about his practice are positive, he said, it’s difficult not to be affected by negative posts.
“From a psychological standpoint, it stings,” he said. “The burn of a negative review outweighs the sweetness of a positive review 100 times.”
Reputation companies to the rescue?
Like Dr. Hardwick-Smith, Dr. Joseph has utilized the online reputation management company eMerit to improve his online presence. The company gathers reviews from patients at the point of service and posts them to dominate review sites.
The solution to pollution is dilution, which means counterbalancing negative reviews with more representative reviews,” said Jeffrey Segal, MD, a neurosurgeon and attorney, and the founder of eMerit. “The next step is to deescalate conflict if you know who the patient is – to see if the patient problem can be resolved. Typically a patient is pleasantly surprised that you took the effort to call. Because the bar is so low, it’s very easy to exceed it.”
Physicians subscribe to eMerit on a month-to-month basis, paying $100-$600 a month, depending on the practice’s needs, Dr. Segal said. He touted a greater than 90% renewal rate, and said eMerit has captured and uploaded more than 150,000 patient reviews since its inception.
For the online reputation management company Reputation.com, health care providers have become one of the its most frequent clients, said Michael Fertik, company founder. Reputation.com solicits reviews from patients after appointments and ensures their visibility on top review sites. The platform also integrates reviews from general and health care review sites to help providers address patient feedback and receive alerts when negative reviews are posted. Rates start at $50 a month.
Mr. Fertik noted that more reviews not only overtake negative posts, but they make physicians easier to find by patients.
“If you have more than 10-15 reviews, you have a higher chance of getting a new patient because the search engine is going to favor doctors that have more reviews,” he said. “Doctors that have a small number of reviews don’t exist as far as search engines are concerned.”
However, all online reputation management firms are not equal, Mr. Sacopulos warned. Some are unfamiliar with the health care space, while others are unclear on health care privacy regulations. Mr. Sacopulos learned of a company that was sending patients texts to request reviews, which was likely a privacy violation and a violation of the Telecommunications Act, he said.
““Some [companies] are much more credible, and they understand health care law more than others,” he said. “Some have the technological capabilities to do things, but don’t understand the legal environment, so you need to be very careful [about whom] you pick.”
Time to sue?
Litigation is generally the last resort to fighting unfavorable online reviews. If a doctor believes a review is unfair or defamatory, and all other efforts have been exhausted, a lawyer may be able to help, Mr. Yelkovac said.
“When someone says, ‘I want to sue,’ that’s a possibility, but that’s typically far down the road,” he said. “Lawsuits are expensive. Lawsuits have an unknown outcome, and I would say, many times when you do sue for defamation, [the poster] may or may not have a lot of money, so you may end up spending a lot of money and you don’t recover anything from the patient.”
The majority of the lawsuits Mr. Yelkovac handles related to online reviews seek to unmask the poster with the aid of subpoenas and at times computer forensics, he said. From there, doctors can decide which action to take, such as contacting the poster and asking to have the comment removed.
“Sometimes it’s a surprise,” he said. “Sometimes it’s an ex-employee. Sometimes it’s a family member, or it could potentially be a competitor. Many times it’s not even a patient, and sometimes it’s a patient [who] the doctor never thought would post a review.”
Reviews and malpractice risk
Remember that not all unfavorable reviews are necessarily negative for physicians, said Brant Avondet, founder of Searchlight Enterprises, a malpractice risk prediction and online physician ratings research company.
A pattern of reviews that express the same concerns or frustrations by patients can be used to address and change internal policies and problems, such as multiple complaints about long wait times or a crowded parking lot, he said. Perhaps the front desk staff is repeatedly unfriendly to patients. Taking steps to correct these concerns could help in the long run, Mr. Avondet said.
Searchlight Enterprises recently presented study findings about a suggested link between online ratings and legal risk for physicians at a national medical insurance conference. Mr. Avondet and his colleagues evaluated claims data for 4,000 Florida physicians from the Florida Healthcare Practitioner Data Portal from 2000 to 2016 and studied online physician reviews from top rating sites. Doctors were grouped into three categories: surgical, ob.gyn., and “other” specialties. Findings showed the bottom 10% of surgeons studied (those with the worst online reviews) had 150% as many claims as the average for all surgeons. Surgeons in the top 20% (doctors with the best online reviews) had roughly half of the risk of a claim, compared with the average surgeon. Similar results were found for ob.gyns. and other specialties.
“Low and behold, there’s a huge correlation,” Mr. Avondet said. “There’s no shadow of a doubt that there’s something there that predicts your malpractice risk based on how nice or mean you are in the eyes of the patient.”
Mr. Avondet said he encourages physicians to use online reviews to make improvements, thus lowering their liability.
“Look at these reviews as a lens into your practice and things you might need to correct,” he said. “Use it as [insight] for how you can improve your practice and decrease the risk of getting sued.”
On Twitter @legal_med
Like most physicians, Dr. Susan Hardwick-Smith was used to receiving the occasional negative online review about her practice. But a biting post from several years ago was so wrenching that it nearly drove the Houston ob.gyn. out of medicine for good.
The patient blasted Dr. Hardwick-Smith on a popular review site about her care during a delivery and accused the doctor of attempting to force an unnecessary C-section. The account was inaccurate, but privacy laws prevented Dr. Hardwick-Smith from defending herself online or sharing details of the actual encounter, she said.
“She wrote this very detailed account of what a terrible doctor I was, and in my version of reality, I had saved her baby’s life,” said Dr. Hardwick-Smith. “I felt extremely powerless. I lost a lot of sleep over it, and I was considering giving up delivering babies. It was a real turning point for me.”
Rather than hanging up her white coat, Dr. Hardwick-Smith began working with an online reputation company – eMerit – that works to dilute negative reviews by soliciting a greater number of reviews from patients. The offensive post is now buried under hundreds of other reviews that are primarily positive, she said.
Hiring a reputation management company is one strategy for coping with negative online reviews. But cyberlaw experts stress that removing negative posts altogether is no easy feat. The best move to take often depends on the post, the patient, and the circumstance.
By now, it’s no secret that negative online reviews can significantly impact a medical practice, from influencing patient recruitment to affecting practice revenue to ruining a reputation. A 2015 survey of 2,354 consumers by search marketing firm BrightLocal found that 92% of consumers read online reviews – up from 67% in 2010 – and 40% of consumers had formed an opinion by reading just one to three reviews. Of 2,137 patients who viewed online reviews, 35% selected a physician based on positive reviews, while 37% avoided doctors with negative reviews, according to a 2014 study in JAMA (doi:10.1001/jama.2013.283194).
Reviews have become a strong force in the health care industry, said Peter Yelkovac, an online defamation attorney in Northern Indiana.
“Online reviews have really replaced the common ‘word of mouth’ that used to be the primary source for doctors referrals,” Mr. Yelkovac said in an interview. “Now, [patients] go online. Anyone can type anything they want, whether it’s truthful, untruthful, positive, indifferent, or negative.”
Doctor vs. website
In some cases, contacting a website administrator and requesting a review be removed can end the dilemma, said Michael J. Sacopulos, a medical malpractice defense attorney based in Terre Haute, Ind.
Rating sites generally have “terms of use,” and posts that violate the terms usually will be taken down by site administrators with some nudging, Mr. Sacopulos said in an interview. Other sites have “strike policies,” where a reviewee can request that one or two negative reviews be removed.
Still other sites are not as accommodating. Amazon, for instance, has immunity against content posted on the site, Mr. Sacopulos said. Under the Communications Decency Act, interactive computer services, such as a consumer review website, cannot be liable for content independently created or developed by third-party users. Such sites are hardly motivated to remove negative comments when racy posts can drive traffic to the site, he said.
Eric M. Joseph, MD, a facial plastic surgeon in West Orange, N.J., learned this lesson firsthand when he attempted to have a video removed from YouTube. A poster had uploaded copyright-protected before and after photos from Dr. Joseph’s practice onto YouTube and made disparaging comments about the patients in a video that went viral. Dr. Joseph and the patient both flagged the video for removal, but to no avail.
“It was impossible to [talk to] a human being at Google,” Dr, Joseph said. “It almost didn’t come down, and we were in conversations about suing Google. It took months and a cyberattorney who specializes in copyright infringement.”
The video finally was removed, but not before Dr. Joseph spent $6,000 in legal fees and experienced significant distress from the incident. Although most reviews about his practice are positive, he said, it’s difficult not to be affected by negative posts.
“From a psychological standpoint, it stings,” he said. “The burn of a negative review outweighs the sweetness of a positive review 100 times.”
Reputation companies to the rescue?
Like Dr. Hardwick-Smith, Dr. Joseph has utilized the online reputation management company eMerit to improve his online presence. The company gathers reviews from patients at the point of service and posts them to dominate review sites.
The solution to pollution is dilution, which means counterbalancing negative reviews with more representative reviews,” said Jeffrey Segal, MD, a neurosurgeon and attorney, and the founder of eMerit. “The next step is to deescalate conflict if you know who the patient is – to see if the patient problem can be resolved. Typically a patient is pleasantly surprised that you took the effort to call. Because the bar is so low, it’s very easy to exceed it.”
Physicians subscribe to eMerit on a month-to-month basis, paying $100-$600 a month, depending on the practice’s needs, Dr. Segal said. He touted a greater than 90% renewal rate, and said eMerit has captured and uploaded more than 150,000 patient reviews since its inception.
For the online reputation management company Reputation.com, health care providers have become one of the its most frequent clients, said Michael Fertik, company founder. Reputation.com solicits reviews from patients after appointments and ensures their visibility on top review sites. The platform also integrates reviews from general and health care review sites to help providers address patient feedback and receive alerts when negative reviews are posted. Rates start at $50 a month.
Mr. Fertik noted that more reviews not only overtake negative posts, but they make physicians easier to find by patients.
“If you have more than 10-15 reviews, you have a higher chance of getting a new patient because the search engine is going to favor doctors that have more reviews,” he said. “Doctors that have a small number of reviews don’t exist as far as search engines are concerned.”
However, all online reputation management firms are not equal, Mr. Sacopulos warned. Some are unfamiliar with the health care space, while others are unclear on health care privacy regulations. Mr. Sacopulos learned of a company that was sending patients texts to request reviews, which was likely a privacy violation and a violation of the Telecommunications Act, he said.
““Some [companies] are much more credible, and they understand health care law more than others,” he said. “Some have the technological capabilities to do things, but don’t understand the legal environment, so you need to be very careful [about whom] you pick.”
Time to sue?
Litigation is generally the last resort to fighting unfavorable online reviews. If a doctor believes a review is unfair or defamatory, and all other efforts have been exhausted, a lawyer may be able to help, Mr. Yelkovac said.
“When someone says, ‘I want to sue,’ that’s a possibility, but that’s typically far down the road,” he said. “Lawsuits are expensive. Lawsuits have an unknown outcome, and I would say, many times when you do sue for defamation, [the poster] may or may not have a lot of money, so you may end up spending a lot of money and you don’t recover anything from the patient.”
The majority of the lawsuits Mr. Yelkovac handles related to online reviews seek to unmask the poster with the aid of subpoenas and at times computer forensics, he said. From there, doctors can decide which action to take, such as contacting the poster and asking to have the comment removed.
“Sometimes it’s a surprise,” he said. “Sometimes it’s an ex-employee. Sometimes it’s a family member, or it could potentially be a competitor. Many times it’s not even a patient, and sometimes it’s a patient [who] the doctor never thought would post a review.”
Reviews and malpractice risk
Remember that not all unfavorable reviews are necessarily negative for physicians, said Brant Avondet, founder of Searchlight Enterprises, a malpractice risk prediction and online physician ratings research company.
A pattern of reviews that express the same concerns or frustrations by patients can be used to address and change internal policies and problems, such as multiple complaints about long wait times or a crowded parking lot, he said. Perhaps the front desk staff is repeatedly unfriendly to patients. Taking steps to correct these concerns could help in the long run, Mr. Avondet said.
Searchlight Enterprises recently presented study findings about a suggested link between online ratings and legal risk for physicians at a national medical insurance conference. Mr. Avondet and his colleagues evaluated claims data for 4,000 Florida physicians from the Florida Healthcare Practitioner Data Portal from 2000 to 2016 and studied online physician reviews from top rating sites. Doctors were grouped into three categories: surgical, ob.gyn., and “other” specialties. Findings showed the bottom 10% of surgeons studied (those with the worst online reviews) had 150% as many claims as the average for all surgeons. Surgeons in the top 20% (doctors with the best online reviews) had roughly half of the risk of a claim, compared with the average surgeon. Similar results were found for ob.gyns. and other specialties.
“Low and behold, there’s a huge correlation,” Mr. Avondet said. “There’s no shadow of a doubt that there’s something there that predicts your malpractice risk based on how nice or mean you are in the eyes of the patient.”
Mr. Avondet said he encourages physicians to use online reviews to make improvements, thus lowering their liability.
“Look at these reviews as a lens into your practice and things you might need to correct,” he said. “Use it as [insight] for how you can improve your practice and decrease the risk of getting sued.”
On Twitter @legal_med
Like most physicians, Dr. Susan Hardwick-Smith was used to receiving the occasional negative online review about her practice. But a biting post from several years ago was so wrenching that it nearly drove the Houston ob.gyn. out of medicine for good.
The patient blasted Dr. Hardwick-Smith on a popular review site about her care during a delivery and accused the doctor of attempting to force an unnecessary C-section. The account was inaccurate, but privacy laws prevented Dr. Hardwick-Smith from defending herself online or sharing details of the actual encounter, she said.
“She wrote this very detailed account of what a terrible doctor I was, and in my version of reality, I had saved her baby’s life,” said Dr. Hardwick-Smith. “I felt extremely powerless. I lost a lot of sleep over it, and I was considering giving up delivering babies. It was a real turning point for me.”
Rather than hanging up her white coat, Dr. Hardwick-Smith began working with an online reputation company – eMerit – that works to dilute negative reviews by soliciting a greater number of reviews from patients. The offensive post is now buried under hundreds of other reviews that are primarily positive, she said.
Hiring a reputation management company is one strategy for coping with negative online reviews. But cyberlaw experts stress that removing negative posts altogether is no easy feat. The best move to take often depends on the post, the patient, and the circumstance.
By now, it’s no secret that negative online reviews can significantly impact a medical practice, from influencing patient recruitment to affecting practice revenue to ruining a reputation. A 2015 survey of 2,354 consumers by search marketing firm BrightLocal found that 92% of consumers read online reviews – up from 67% in 2010 – and 40% of consumers had formed an opinion by reading just one to three reviews. Of 2,137 patients who viewed online reviews, 35% selected a physician based on positive reviews, while 37% avoided doctors with negative reviews, according to a 2014 study in JAMA (doi:10.1001/jama.2013.283194).
Reviews have become a strong force in the health care industry, said Peter Yelkovac, an online defamation attorney in Northern Indiana.
“Online reviews have really replaced the common ‘word of mouth’ that used to be the primary source for doctors referrals,” Mr. Yelkovac said in an interview. “Now, [patients] go online. Anyone can type anything they want, whether it’s truthful, untruthful, positive, indifferent, or negative.”
Doctor vs. website
In some cases, contacting a website administrator and requesting a review be removed can end the dilemma, said Michael J. Sacopulos, a medical malpractice defense attorney based in Terre Haute, Ind.
Rating sites generally have “terms of use,” and posts that violate the terms usually will be taken down by site administrators with some nudging, Mr. Sacopulos said in an interview. Other sites have “strike policies,” where a reviewee can request that one or two negative reviews be removed.
Still other sites are not as accommodating. Amazon, for instance, has immunity against content posted on the site, Mr. Sacopulos said. Under the Communications Decency Act, interactive computer services, such as a consumer review website, cannot be liable for content independently created or developed by third-party users. Such sites are hardly motivated to remove negative comments when racy posts can drive traffic to the site, he said.
Eric M. Joseph, MD, a facial plastic surgeon in West Orange, N.J., learned this lesson firsthand when he attempted to have a video removed from YouTube. A poster had uploaded copyright-protected before and after photos from Dr. Joseph’s practice onto YouTube and made disparaging comments about the patients in a video that went viral. Dr. Joseph and the patient both flagged the video for removal, but to no avail.
“It was impossible to [talk to] a human being at Google,” Dr, Joseph said. “It almost didn’t come down, and we were in conversations about suing Google. It took months and a cyberattorney who specializes in copyright infringement.”
The video finally was removed, but not before Dr. Joseph spent $6,000 in legal fees and experienced significant distress from the incident. Although most reviews about his practice are positive, he said, it’s difficult not to be affected by negative posts.
“From a psychological standpoint, it stings,” he said. “The burn of a negative review outweighs the sweetness of a positive review 100 times.”
Reputation companies to the rescue?
Like Dr. Hardwick-Smith, Dr. Joseph has utilized the online reputation management company eMerit to improve his online presence. The company gathers reviews from patients at the point of service and posts them to dominate review sites.
The solution to pollution is dilution, which means counterbalancing negative reviews with more representative reviews,” said Jeffrey Segal, MD, a neurosurgeon and attorney, and the founder of eMerit. “The next step is to deescalate conflict if you know who the patient is – to see if the patient problem can be resolved. Typically a patient is pleasantly surprised that you took the effort to call. Because the bar is so low, it’s very easy to exceed it.”
Physicians subscribe to eMerit on a month-to-month basis, paying $100-$600 a month, depending on the practice’s needs, Dr. Segal said. He touted a greater than 90% renewal rate, and said eMerit has captured and uploaded more than 150,000 patient reviews since its inception.
For the online reputation management company Reputation.com, health care providers have become one of the its most frequent clients, said Michael Fertik, company founder. Reputation.com solicits reviews from patients after appointments and ensures their visibility on top review sites. The platform also integrates reviews from general and health care review sites to help providers address patient feedback and receive alerts when negative reviews are posted. Rates start at $50 a month.
Mr. Fertik noted that more reviews not only overtake negative posts, but they make physicians easier to find by patients.
“If you have more than 10-15 reviews, you have a higher chance of getting a new patient because the search engine is going to favor doctors that have more reviews,” he said. “Doctors that have a small number of reviews don’t exist as far as search engines are concerned.”
However, all online reputation management firms are not equal, Mr. Sacopulos warned. Some are unfamiliar with the health care space, while others are unclear on health care privacy regulations. Mr. Sacopulos learned of a company that was sending patients texts to request reviews, which was likely a privacy violation and a violation of the Telecommunications Act, he said.
““Some [companies] are much more credible, and they understand health care law more than others,” he said. “Some have the technological capabilities to do things, but don’t understand the legal environment, so you need to be very careful [about whom] you pick.”
Time to sue?
Litigation is generally the last resort to fighting unfavorable online reviews. If a doctor believes a review is unfair or defamatory, and all other efforts have been exhausted, a lawyer may be able to help, Mr. Yelkovac said.
“When someone says, ‘I want to sue,’ that’s a possibility, but that’s typically far down the road,” he said. “Lawsuits are expensive. Lawsuits have an unknown outcome, and I would say, many times when you do sue for defamation, [the poster] may or may not have a lot of money, so you may end up spending a lot of money and you don’t recover anything from the patient.”
The majority of the lawsuits Mr. Yelkovac handles related to online reviews seek to unmask the poster with the aid of subpoenas and at times computer forensics, he said. From there, doctors can decide which action to take, such as contacting the poster and asking to have the comment removed.
“Sometimes it’s a surprise,” he said. “Sometimes it’s an ex-employee. Sometimes it’s a family member, or it could potentially be a competitor. Many times it’s not even a patient, and sometimes it’s a patient [who] the doctor never thought would post a review.”
Reviews and malpractice risk
Remember that not all unfavorable reviews are necessarily negative for physicians, said Brant Avondet, founder of Searchlight Enterprises, a malpractice risk prediction and online physician ratings research company.
A pattern of reviews that express the same concerns or frustrations by patients can be used to address and change internal policies and problems, such as multiple complaints about long wait times or a crowded parking lot, he said. Perhaps the front desk staff is repeatedly unfriendly to patients. Taking steps to correct these concerns could help in the long run, Mr. Avondet said.
Searchlight Enterprises recently presented study findings about a suggested link between online ratings and legal risk for physicians at a national medical insurance conference. Mr. Avondet and his colleagues evaluated claims data for 4,000 Florida physicians from the Florida Healthcare Practitioner Data Portal from 2000 to 2016 and studied online physician reviews from top rating sites. Doctors were grouped into three categories: surgical, ob.gyn., and “other” specialties. Findings showed the bottom 10% of surgeons studied (those with the worst online reviews) had 150% as many claims as the average for all surgeons. Surgeons in the top 20% (doctors with the best online reviews) had roughly half of the risk of a claim, compared with the average surgeon. Similar results were found for ob.gyns. and other specialties.
“Low and behold, there’s a huge correlation,” Mr. Avondet said. “There’s no shadow of a doubt that there’s something there that predicts your malpractice risk based on how nice or mean you are in the eyes of the patient.”
Mr. Avondet said he encourages physicians to use online reviews to make improvements, thus lowering their liability.
“Look at these reviews as a lens into your practice and things you might need to correct,” he said. “Use it as [insight] for how you can improve your practice and decrease the risk of getting sued.”
On Twitter @legal_med
Don’t Miss the 2016 Heart Valve Summit: Medical, Surgical & Interventional Decision Making
October 20-22, 2016
Radisson Blu Aqua Hotel
Chicago, IL
Course Directors
David H. Adams
Steven F. Bolling
Robert O. Bonow
Howard C. Herrmann
Nurse Planner
Michele Mistovich
Course Overview
The American College of Cardiology and the American Association for Thoracic Surgery are again partnering to bring together cardiologists and surgeons in a cooperative, case-based course to address the rapid advances in the treatment of valvular heart disease (VHD).
Focusing on interactivity and practical decision-making, this unique conference will engage participants in discussions, debates and potential controversies using real-world cases. Its renowned faculty will include experts on the cutting edge of clinically relevant VHD data.
The interdisciplinary course emphasizes clinical decision-making with medical, surgical and interventional options for patient care, taking into account that constantly changing management tools can impact the surgical team. There will be breakout sessions for cardiologists, cardiac surgeons, nurses and physician assistants designed to help specialists manage their unique challenges from a team perspective.
Target Audience
Cardiologists, interventional cardiologists, cardiothoracic surgeons, internists, nurses, physician assistants and health care professionals involved in VHD evaluation, diagnosis and/or management.
October 20-22, 2016
Radisson Blu Aqua Hotel
Chicago, IL
Course Directors
David H. Adams
Steven F. Bolling
Robert O. Bonow
Howard C. Herrmann
Nurse Planner
Michele Mistovich
Course Overview
The American College of Cardiology and the American Association for Thoracic Surgery are again partnering to bring together cardiologists and surgeons in a cooperative, case-based course to address the rapid advances in the treatment of valvular heart disease (VHD).
Focusing on interactivity and practical decision-making, this unique conference will engage participants in discussions, debates and potential controversies using real-world cases. Its renowned faculty will include experts on the cutting edge of clinically relevant VHD data.
The interdisciplinary course emphasizes clinical decision-making with medical, surgical and interventional options for patient care, taking into account that constantly changing management tools can impact the surgical team. There will be breakout sessions for cardiologists, cardiac surgeons, nurses and physician assistants designed to help specialists manage their unique challenges from a team perspective.
Target Audience
Cardiologists, interventional cardiologists, cardiothoracic surgeons, internists, nurses, physician assistants and health care professionals involved in VHD evaluation, diagnosis and/or management.
October 20-22, 2016
Radisson Blu Aqua Hotel
Chicago, IL
Course Directors
David H. Adams
Steven F. Bolling
Robert O. Bonow
Howard C. Herrmann
Nurse Planner
Michele Mistovich
Course Overview
The American College of Cardiology and the American Association for Thoracic Surgery are again partnering to bring together cardiologists and surgeons in a cooperative, case-based course to address the rapid advances in the treatment of valvular heart disease (VHD).
Focusing on interactivity and practical decision-making, this unique conference will engage participants in discussions, debates and potential controversies using real-world cases. Its renowned faculty will include experts on the cutting edge of clinically relevant VHD data.
The interdisciplinary course emphasizes clinical decision-making with medical, surgical and interventional options for patient care, taking into account that constantly changing management tools can impact the surgical team. There will be breakout sessions for cardiologists, cardiac surgeons, nurses and physician assistants designed to help specialists manage their unique challenges from a team perspective.
Target Audience
Cardiologists, interventional cardiologists, cardiothoracic surgeons, internists, nurses, physician assistants and health care professionals involved in VHD evaluation, diagnosis and/or management.
Registration and Housing Now Open: AATS Clinical Trials Methods Course 2016
October 20-22, 2016
Hyatt Regency O’Hare
Chicago, IL
Program Directors
David H. Harpole, Jr
Marco A. Zenati
This course is an intensive, interactive training program for cardiothoracic surgeons across all subspecialties. It will permit them to acquire the critical skills necessary for effective clinical trial design and implementation. The course is particularly suited for professionals who are planning to apply for clinical trial funding, allowing them to better understand the complex nature of preparing and submitting clinical trial proposals.
Invited faculty includes currently funded clinical trial leading investigators and experts in the field of biostatistics and health sciences research. The program will offer a process in which the clinical trial protocol development can be streamlined. Interactive features will include hands-on focus groups and mock study sessions.
Register Today! Space available for only 40 participants.
October 20-22, 2016
Hyatt Regency O’Hare
Chicago, IL
Program Directors
David H. Harpole, Jr
Marco A. Zenati
This course is an intensive, interactive training program for cardiothoracic surgeons across all subspecialties. It will permit them to acquire the critical skills necessary for effective clinical trial design and implementation. The course is particularly suited for professionals who are planning to apply for clinical trial funding, allowing them to better understand the complex nature of preparing and submitting clinical trial proposals.
Invited faculty includes currently funded clinical trial leading investigators and experts in the field of biostatistics and health sciences research. The program will offer a process in which the clinical trial protocol development can be streamlined. Interactive features will include hands-on focus groups and mock study sessions.
Register Today! Space available for only 40 participants.
October 20-22, 2016
Hyatt Regency O’Hare
Chicago, IL
Program Directors
David H. Harpole, Jr
Marco A. Zenati
This course is an intensive, interactive training program for cardiothoracic surgeons across all subspecialties. It will permit them to acquire the critical skills necessary for effective clinical trial design and implementation. The course is particularly suited for professionals who are planning to apply for clinical trial funding, allowing them to better understand the complex nature of preparing and submitting clinical trial proposals.
Invited faculty includes currently funded clinical trial leading investigators and experts in the field of biostatistics and health sciences research. The program will offer a process in which the clinical trial protocol development can be streamlined. Interactive features will include hands-on focus groups and mock study sessions.
Register Today! Space available for only 40 participants.
Take Advantage of Early Registration for AATS Focus on Thoracic Surgery: Novel Techniques in Lung Cancer — Program Now Online
The preliminary scientific program, along with registration and housing information, is now online for AATS Focus on Thoracic Surgery: Novel Techniques in Lung Cancer.
November 21 – 22, 2014
Renaissance Boston Waterfront Hotel
Boston, MA, USA
Take advantage of early registration rates and register before October 23rd!
Program Directors
G. Alec Patterson, Washington University
David J. Sugarbaker, Baylor College of Medicine
Program Committee Members:
Thomas A. D’Amico, Duke University
Shaf Keshavjee, University of Toronto
James D. Luketich, University of Pittsburgh
Bryan F. Meyers, Washington University
Scott J. Swanson, Brigham and Women’s Hospital
Overview
Lung cancer is the most common cause of cancer-related deaths and second most common malignancy in the Western world. Recent innovations in diagnosis, staging and management of early stage and locally advanced non-small cell lung cancer have changed the paradigm for patient surgical management. There has also been a virtual explosion of technological developments enabling widespread use of minimally invasive techniques, which current and future thoracic surgeons will need to embrace in order to improve patient care.
Join AATS in Boston for the 2014 Focus On Thoracic Surgery whose program will focus on recent developments in Novel Technologies in Lung Cancer. The faculty includes internationally recognized experts in the field, including those knowledgeable about the use of new technology in lung cancer surgical management.
Program Highlights
Imaging and Staging
Surgical Alternatives
Simulation, Education, and Training
Optimal Management of Lung Metastases
Credentialing/ Efficiencies
Intraoperative Management
Video Sessions - Advanced Minimally Invasive Techniques
Honored Guest Speaker
Larry R. KaiserDean, Temple University
The preliminary scientific program, along with registration and housing information, is now online for AATS Focus on Thoracic Surgery: Novel Techniques in Lung Cancer.
November 21 – 22, 2014
Renaissance Boston Waterfront Hotel
Boston, MA, USA
Take advantage of early registration rates and register before October 23rd!
Program Directors
G. Alec Patterson, Washington University
David J. Sugarbaker, Baylor College of Medicine
Program Committee Members:
Thomas A. D’Amico, Duke University
Shaf Keshavjee, University of Toronto
James D. Luketich, University of Pittsburgh
Bryan F. Meyers, Washington University
Scott J. Swanson, Brigham and Women’s Hospital
Overview
Lung cancer is the most common cause of cancer-related deaths and second most common malignancy in the Western world. Recent innovations in diagnosis, staging and management of early stage and locally advanced non-small cell lung cancer have changed the paradigm for patient surgical management. There has also been a virtual explosion of technological developments enabling widespread use of minimally invasive techniques, which current and future thoracic surgeons will need to embrace in order to improve patient care.
Join AATS in Boston for the 2014 Focus On Thoracic Surgery whose program will focus on recent developments in Novel Technologies in Lung Cancer. The faculty includes internationally recognized experts in the field, including those knowledgeable about the use of new technology in lung cancer surgical management.
Program Highlights
Imaging and Staging
Surgical Alternatives
Simulation, Education, and Training
Optimal Management of Lung Metastases
Credentialing/ Efficiencies
Intraoperative Management
Video Sessions - Advanced Minimally Invasive Techniques
Honored Guest Speaker
Larry R. KaiserDean, Temple University
The preliminary scientific program, along with registration and housing information, is now online for AATS Focus on Thoracic Surgery: Novel Techniques in Lung Cancer.
November 21 – 22, 2014
Renaissance Boston Waterfront Hotel
Boston, MA, USA
Take advantage of early registration rates and register before October 23rd!
Program Directors
G. Alec Patterson, Washington University
David J. Sugarbaker, Baylor College of Medicine
Program Committee Members:
Thomas A. D’Amico, Duke University
Shaf Keshavjee, University of Toronto
James D. Luketich, University of Pittsburgh
Bryan F. Meyers, Washington University
Scott J. Swanson, Brigham and Women’s Hospital
Overview
Lung cancer is the most common cause of cancer-related deaths and second most common malignancy in the Western world. Recent innovations in diagnosis, staging and management of early stage and locally advanced non-small cell lung cancer have changed the paradigm for patient surgical management. There has also been a virtual explosion of technological developments enabling widespread use of minimally invasive techniques, which current and future thoracic surgeons will need to embrace in order to improve patient care.
Join AATS in Boston for the 2014 Focus On Thoracic Surgery whose program will focus on recent developments in Novel Technologies in Lung Cancer. The faculty includes internationally recognized experts in the field, including those knowledgeable about the use of new technology in lung cancer surgical management.
Program Highlights
Imaging and Staging
Surgical Alternatives
Simulation, Education, and Training
Optimal Management of Lung Metastases
Credentialing/ Efficiencies
Intraoperative Management
Video Sessions - Advanced Minimally Invasive Techniques
Honored Guest Speaker
Larry R. KaiserDean, Temple University
Anatomic repair of ccTGA did not yield superior survival
BALTIMORE – Anatomic repair did not outperform physiologic repair in patients with congenitally corrected transposition of the great arteries (ccTGA), according to a study presented by Maryam Al-Omair, M.D., of the University of Toronto at the annual meeting of the American Association for Thoracic Surgery.
Dr. Al-Omair and her colleagues hypothesized that patients undergoing anatomic repair for ccTGA would have superior systemic ventricular function and survival. However, their results showed that anatomic repair of ccTGA did not yield superior survival, compared with physiologic repair, and the long-term impact on systemic ventricular function was not certain.
Because of early evidence showing better outcomes of anatomic over physiologic repair for ccTGA, the surgical trend over time greatly favored the use of anatomic repair: At her team’s institution, anatomic repair went from 2.3% in the 1982-1989 period to 92.3% in the 2010-2015 period, Dr. Al-Omair said.
Their study assessed 200 patients (165 with biventricular ccTGA and 35 Fontan patients) who were managed from 1982 to 2015 at the Hospital for Sick Children, Toronto. The patient treatment groups were anatomic repair (38 patients), physiologic repair (89), single-ventricle (Fontan) repair (35), and palliated (no intracardiac repair) patients (38). The median follow-up was 3.4 years for anatomic repair, 13.5 years for physiologic repair, 7.5 years for single-ventricle repair, and 11.8 years with no repair (11.8 years), reflecting their change in practice.
The investigators followed the primary outcome of transplant-free survival and secondary outcomes of late systemic ventricular function and systemic atrioventricular valve function.
They found no significant difference in transplant-free survival at 20 years in the three repair groups assessed from 1892 to 2105: anatomic repair (58%), physiologic repair (71%), and single-ventricle (Fontan) repair (78%). Looking at the latter period of 2000-2015 for 10-year transplant-free survival, they found similar results: anatomic repair (77%), physiologic repair (85%), and single-ventricle (Fontan) repair (100%).
They also found that transplant-free survival in patients who required no intracadiac repair and had no associated lesions such as ventral septal defect or ventral septal defect with pulmonary stenosis was nearly 95% at 25 years.
A multivariate analysis showed no independent predictors of mortality among the three treatments, patient age at index operation, or period of treatment, as well as the need for a permanent pacemaker, or moderately to severely reduced ventricular function or moderate to severe valve regurgitation after the index operation, according to Dr. Al-Omair.
For the secondary outcome of late systemic ventricular function, a multivariate analysis showed that two of the variables were independent predictors: Index operation at or after 2000 was shown to be protective (hazard ratio, 0.152), while a negative association was seen with moderately to severely reduced ventricular function after the index operation (HR, 12.4).
For the secondary outcome of late systemic valve function, a multivariate analysis showed that three of the variables were independent predictors: Fontan operation (HR, 0.124) and index operation at or after 2000 (HR, 0.258) were shown to be protective, while a negative association was seen with moderately to severely reduced valve regurgitation after the index operation (HR, 9.00).
The researchers concluded that midterm Fontan survival was relatively favorable, pushing borderline repair may not be necessary, and “prophylactic banding” and the double-switch procedure should be looked on with caution for lower-risk patients.
“Our study also showed that survival was best in those having no associated lesions requiring operation, indicating that performing an anatomic repair for those not having associated lesions could be counterproductive,” Dr. Al-Omair concluded.
The webcast of the annual meeting presentation is available at www.aats.org.
Dr. Al-Omair reported that she and her colleagues had no relevant financial disclosures.
The choice of anatomic vs. physiologic repair of congenitally corrected transposition of the great arteries is a controversial area, with many well-known surgeons and centers advocating for anatomic repair (a much tougher and more challenging operation) as opposed to physiologic repair. The Toronto group is to be applauded for this honest conclusion, which goes a bit against the currently fashionable “more is better” approach.
Robert Jaquiss, M.D., of Duke University, Durham, N.C., is the congenital heart disease associate medical editor for Thoracic Surgery News.
The choice of anatomic vs. physiologic repair of congenitally corrected transposition of the great arteries is a controversial area, with many well-known surgeons and centers advocating for anatomic repair (a much tougher and more challenging operation) as opposed to physiologic repair. The Toronto group is to be applauded for this honest conclusion, which goes a bit against the currently fashionable “more is better” approach.
Robert Jaquiss, M.D., of Duke University, Durham, N.C., is the congenital heart disease associate medical editor for Thoracic Surgery News.
The choice of anatomic vs. physiologic repair of congenitally corrected transposition of the great arteries is a controversial area, with many well-known surgeons and centers advocating for anatomic repair (a much tougher and more challenging operation) as opposed to physiologic repair. The Toronto group is to be applauded for this honest conclusion, which goes a bit against the currently fashionable “more is better” approach.
Robert Jaquiss, M.D., of Duke University, Durham, N.C., is the congenital heart disease associate medical editor for Thoracic Surgery News.
BALTIMORE – Anatomic repair did not outperform physiologic repair in patients with congenitally corrected transposition of the great arteries (ccTGA), according to a study presented by Maryam Al-Omair, M.D., of the University of Toronto at the annual meeting of the American Association for Thoracic Surgery.
Dr. Al-Omair and her colleagues hypothesized that patients undergoing anatomic repair for ccTGA would have superior systemic ventricular function and survival. However, their results showed that anatomic repair of ccTGA did not yield superior survival, compared with physiologic repair, and the long-term impact on systemic ventricular function was not certain.
Because of early evidence showing better outcomes of anatomic over physiologic repair for ccTGA, the surgical trend over time greatly favored the use of anatomic repair: At her team’s institution, anatomic repair went from 2.3% in the 1982-1989 period to 92.3% in the 2010-2015 period, Dr. Al-Omair said.
Their study assessed 200 patients (165 with biventricular ccTGA and 35 Fontan patients) who were managed from 1982 to 2015 at the Hospital for Sick Children, Toronto. The patient treatment groups were anatomic repair (38 patients), physiologic repair (89), single-ventricle (Fontan) repair (35), and palliated (no intracardiac repair) patients (38). The median follow-up was 3.4 years for anatomic repair, 13.5 years for physiologic repair, 7.5 years for single-ventricle repair, and 11.8 years with no repair (11.8 years), reflecting their change in practice.
The investigators followed the primary outcome of transplant-free survival and secondary outcomes of late systemic ventricular function and systemic atrioventricular valve function.
They found no significant difference in transplant-free survival at 20 years in the three repair groups assessed from 1892 to 2105: anatomic repair (58%), physiologic repair (71%), and single-ventricle (Fontan) repair (78%). Looking at the latter period of 2000-2015 for 10-year transplant-free survival, they found similar results: anatomic repair (77%), physiologic repair (85%), and single-ventricle (Fontan) repair (100%).
They also found that transplant-free survival in patients who required no intracadiac repair and had no associated lesions such as ventral septal defect or ventral septal defect with pulmonary stenosis was nearly 95% at 25 years.
A multivariate analysis showed no independent predictors of mortality among the three treatments, patient age at index operation, or period of treatment, as well as the need for a permanent pacemaker, or moderately to severely reduced ventricular function or moderate to severe valve regurgitation after the index operation, according to Dr. Al-Omair.
For the secondary outcome of late systemic ventricular function, a multivariate analysis showed that two of the variables were independent predictors: Index operation at or after 2000 was shown to be protective (hazard ratio, 0.152), while a negative association was seen with moderately to severely reduced ventricular function after the index operation (HR, 12.4).
For the secondary outcome of late systemic valve function, a multivariate analysis showed that three of the variables were independent predictors: Fontan operation (HR, 0.124) and index operation at or after 2000 (HR, 0.258) were shown to be protective, while a negative association was seen with moderately to severely reduced valve regurgitation after the index operation (HR, 9.00).
The researchers concluded that midterm Fontan survival was relatively favorable, pushing borderline repair may not be necessary, and “prophylactic banding” and the double-switch procedure should be looked on with caution for lower-risk patients.
“Our study also showed that survival was best in those having no associated lesions requiring operation, indicating that performing an anatomic repair for those not having associated lesions could be counterproductive,” Dr. Al-Omair concluded.
The webcast of the annual meeting presentation is available at www.aats.org.
Dr. Al-Omair reported that she and her colleagues had no relevant financial disclosures.
BALTIMORE – Anatomic repair did not outperform physiologic repair in patients with congenitally corrected transposition of the great arteries (ccTGA), according to a study presented by Maryam Al-Omair, M.D., of the University of Toronto at the annual meeting of the American Association for Thoracic Surgery.
Dr. Al-Omair and her colleagues hypothesized that patients undergoing anatomic repair for ccTGA would have superior systemic ventricular function and survival. However, their results showed that anatomic repair of ccTGA did not yield superior survival, compared with physiologic repair, and the long-term impact on systemic ventricular function was not certain.
Because of early evidence showing better outcomes of anatomic over physiologic repair for ccTGA, the surgical trend over time greatly favored the use of anatomic repair: At her team’s institution, anatomic repair went from 2.3% in the 1982-1989 period to 92.3% in the 2010-2015 period, Dr. Al-Omair said.
Their study assessed 200 patients (165 with biventricular ccTGA and 35 Fontan patients) who were managed from 1982 to 2015 at the Hospital for Sick Children, Toronto. The patient treatment groups were anatomic repair (38 patients), physiologic repair (89), single-ventricle (Fontan) repair (35), and palliated (no intracardiac repair) patients (38). The median follow-up was 3.4 years for anatomic repair, 13.5 years for physiologic repair, 7.5 years for single-ventricle repair, and 11.8 years with no repair (11.8 years), reflecting their change in practice.
The investigators followed the primary outcome of transplant-free survival and secondary outcomes of late systemic ventricular function and systemic atrioventricular valve function.
They found no significant difference in transplant-free survival at 20 years in the three repair groups assessed from 1892 to 2105: anatomic repair (58%), physiologic repair (71%), and single-ventricle (Fontan) repair (78%). Looking at the latter period of 2000-2015 for 10-year transplant-free survival, they found similar results: anatomic repair (77%), physiologic repair (85%), and single-ventricle (Fontan) repair (100%).
They also found that transplant-free survival in patients who required no intracadiac repair and had no associated lesions such as ventral septal defect or ventral septal defect with pulmonary stenosis was nearly 95% at 25 years.
A multivariate analysis showed no independent predictors of mortality among the three treatments, patient age at index operation, or period of treatment, as well as the need for a permanent pacemaker, or moderately to severely reduced ventricular function or moderate to severe valve regurgitation after the index operation, according to Dr. Al-Omair.
For the secondary outcome of late systemic ventricular function, a multivariate analysis showed that two of the variables were independent predictors: Index operation at or after 2000 was shown to be protective (hazard ratio, 0.152), while a negative association was seen with moderately to severely reduced ventricular function after the index operation (HR, 12.4).
For the secondary outcome of late systemic valve function, a multivariate analysis showed that three of the variables were independent predictors: Fontan operation (HR, 0.124) and index operation at or after 2000 (HR, 0.258) were shown to be protective, while a negative association was seen with moderately to severely reduced valve regurgitation after the index operation (HR, 9.00).
The researchers concluded that midterm Fontan survival was relatively favorable, pushing borderline repair may not be necessary, and “prophylactic banding” and the double-switch procedure should be looked on with caution for lower-risk patients.
“Our study also showed that survival was best in those having no associated lesions requiring operation, indicating that performing an anatomic repair for those not having associated lesions could be counterproductive,” Dr. Al-Omair concluded.
The webcast of the annual meeting presentation is available at www.aats.org.
Dr. Al-Omair reported that she and her colleagues had no relevant financial disclosures.
AT THE AATS ANNUAL MEETING
Key clinical point: Performing an anatomic repair for ccTGA in patients without associated lesions could be counterproductive.
Major finding: There was no significant difference in transplant-free survival at 20 years among anatomic repair (58%), physiologic repair (71%), and single-ventricle repair (78%).
Data source: A single-institution study assessing 200 patients with ccGTA/Fontan who were managed from 1982 to 2015.
Disclosures: Dr. Al-Omair reported that she and her colleagues had no relevant financial disclosures.
Feds plan to raise penalties for false claims
Penalties for health providers under the federal False Claims Act (FCA) are set to double under a proposed rule by the U.S. Department of Justice.
The interim final rule would increase minimum per-claim FCA fines from $5,500 to $10,781 and maximum per-claim penalties would rise from $11,000 to $21,563.
The adjusted civil penalty amounts would apply to civil penalties assessed after Aug. 1, 2016, whose associated violations occurred after Nov. 2, 2015. Violations on or before Nov. 2, 2015, and assessments made prior to Aug. 1, 2016, would continue to be subject to the lower penalties. The rise stems from the federal Civil Monetary Penalties Inflation Adjustment Act, which provides for the regular evaluation and adjustment for inflation of civil monetary penalties to ensure they maintain a deterrent effect, according to a summary of the rule.
The FCA penalizes any person who knowingly submits a false claim to the government or causes another to submit a false claim to the government or who knowingly makes a false record or statement to get a false claim paid by the government. In 2015, the DOJ recovered more than $3.5 billion in FCA settlements and judgments.
Health law experts say the higher penalties may encourage more whistleblowers to file FCA claims against doctors since the potential recoveries would be higher.
“The new maximums may make things still more enticing for relators with visions of increasingly large relators’ shares on the table,” said William W. Horton, a Birmingham, Ala.-based health law attorney and chair of the American Bar Association Health Law Section.
However, Mr. Horton does not believe the rates will have much practical effect in terms of strategy or settlement rates. Right now, the hypothetical penalties in such cases are so enormous they are almost not meaningful, he said in an interview.
“In reality, cases settle based on the amount of actual damages – overpayments, etc. – and not on the penalties, because the penalties are so high,” he said. “I don’t think making them higher is going to change that, because it doesn’t increase the amount of money available for defendants to settle with.”
The ultimate question is whether the higher penalties will help deter health fraud, adds Houston health law attorney Michael E. Clark.
“I don’t see it making a difference,” he said in an interview. “The FCA penalties are particularly ruinous in the health care field since so many claims get made and courts have accepted broad theories of liability.”
The DOJ is accepting comments on the interim final rule until Aug. 29.
On Twitter @legal_med
Penalties for health providers under the federal False Claims Act (FCA) are set to double under a proposed rule by the U.S. Department of Justice.
The interim final rule would increase minimum per-claim FCA fines from $5,500 to $10,781 and maximum per-claim penalties would rise from $11,000 to $21,563.
The adjusted civil penalty amounts would apply to civil penalties assessed after Aug. 1, 2016, whose associated violations occurred after Nov. 2, 2015. Violations on or before Nov. 2, 2015, and assessments made prior to Aug. 1, 2016, would continue to be subject to the lower penalties. The rise stems from the federal Civil Monetary Penalties Inflation Adjustment Act, which provides for the regular evaluation and adjustment for inflation of civil monetary penalties to ensure they maintain a deterrent effect, according to a summary of the rule.
The FCA penalizes any person who knowingly submits a false claim to the government or causes another to submit a false claim to the government or who knowingly makes a false record or statement to get a false claim paid by the government. In 2015, the DOJ recovered more than $3.5 billion in FCA settlements and judgments.
Health law experts say the higher penalties may encourage more whistleblowers to file FCA claims against doctors since the potential recoveries would be higher.
“The new maximums may make things still more enticing for relators with visions of increasingly large relators’ shares on the table,” said William W. Horton, a Birmingham, Ala.-based health law attorney and chair of the American Bar Association Health Law Section.
However, Mr. Horton does not believe the rates will have much practical effect in terms of strategy or settlement rates. Right now, the hypothetical penalties in such cases are so enormous they are almost not meaningful, he said in an interview.
“In reality, cases settle based on the amount of actual damages – overpayments, etc. – and not on the penalties, because the penalties are so high,” he said. “I don’t think making them higher is going to change that, because it doesn’t increase the amount of money available for defendants to settle with.”
The ultimate question is whether the higher penalties will help deter health fraud, adds Houston health law attorney Michael E. Clark.
“I don’t see it making a difference,” he said in an interview. “The FCA penalties are particularly ruinous in the health care field since so many claims get made and courts have accepted broad theories of liability.”
The DOJ is accepting comments on the interim final rule until Aug. 29.
On Twitter @legal_med
Penalties for health providers under the federal False Claims Act (FCA) are set to double under a proposed rule by the U.S. Department of Justice.
The interim final rule would increase minimum per-claim FCA fines from $5,500 to $10,781 and maximum per-claim penalties would rise from $11,000 to $21,563.
The adjusted civil penalty amounts would apply to civil penalties assessed after Aug. 1, 2016, whose associated violations occurred after Nov. 2, 2015. Violations on or before Nov. 2, 2015, and assessments made prior to Aug. 1, 2016, would continue to be subject to the lower penalties. The rise stems from the federal Civil Monetary Penalties Inflation Adjustment Act, which provides for the regular evaluation and adjustment for inflation of civil monetary penalties to ensure they maintain a deterrent effect, according to a summary of the rule.
The FCA penalizes any person who knowingly submits a false claim to the government or causes another to submit a false claim to the government or who knowingly makes a false record or statement to get a false claim paid by the government. In 2015, the DOJ recovered more than $3.5 billion in FCA settlements and judgments.
Health law experts say the higher penalties may encourage more whistleblowers to file FCA claims against doctors since the potential recoveries would be higher.
“The new maximums may make things still more enticing for relators with visions of increasingly large relators’ shares on the table,” said William W. Horton, a Birmingham, Ala.-based health law attorney and chair of the American Bar Association Health Law Section.
However, Mr. Horton does not believe the rates will have much practical effect in terms of strategy or settlement rates. Right now, the hypothetical penalties in such cases are so enormous they are almost not meaningful, he said in an interview.
“In reality, cases settle based on the amount of actual damages – overpayments, etc. – and not on the penalties, because the penalties are so high,” he said. “I don’t think making them higher is going to change that, because it doesn’t increase the amount of money available for defendants to settle with.”
The ultimate question is whether the higher penalties will help deter health fraud, adds Houston health law attorney Michael E. Clark.
“I don’t see it making a difference,” he said in an interview. “The FCA penalties are particularly ruinous in the health care field since so many claims get made and courts have accepted broad theories of liability.”
The DOJ is accepting comments on the interim final rule until Aug. 29.
On Twitter @legal_med
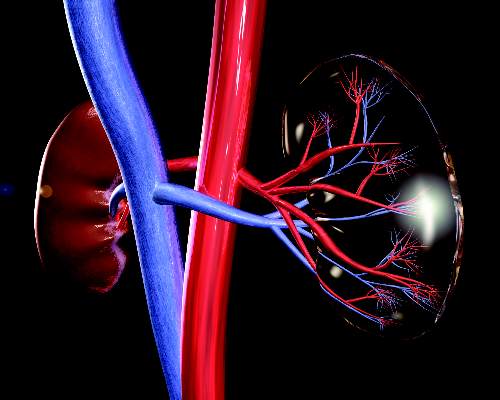
MRI-VA improves view of anomalous coronary arteries
Failure to achieve a rounded and unobstructed ostia in children who have surgery to repair anomalous coronary arteries can put these children at continued risk for sudden death, but cardiac MRI with virtual angioscopy (VA) before and after the operation can give cardiologists a clear picture of a patient’s risk for sudden death and help direct ongoing management, according to a study in the July issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152:205-10).
“Cardiac MRI with virtual angioscopy is an important tool for evaluating anomalous coronary anatomy, myocardial function, and ischemia and should be considered for initial and postoperative assessment of children with anomalous coronary arteries,” lead author Julie A. Brothers, MD, and her coauthors said in reporting their findings.
Anomalous coronary artery is a rare congenital condition in which the left coronary artery (LCA) originates from the right sinus or the right coronary artery (RCA) originates from the left coronary sinus. Dr. Brothers, a pediatric cardiologist, and her colleagues from the Children’s Hospital of Philadelphia and the University of Pennsylvania, also in Philadelphia, studied nine male patients who had operations for anomalous coronary arteries during Feb. 2009-May 2015 in what they said is the first study to document anomalous coronary artery anatomy both before and after surgery. The patients’ average age was 14.1 years; seven had right anomalous coronary arteries and two had left anomalous arteries. After the operations, MRI-VA revealed that two patients still had narrowing in the neo-orifices.
Previous reports recommend surgical repair for all patients with anomalous LCA and for symptomatic patients with anomalous RCA anatomy (Ann Thorac Surg. 2011;92:691-7; Ann Thorac Surg. 2014;98:941-5). MRI-VA allows the surgical team to survey the ostial stenosis before the operation “as if standing within the vessel itself,” Dr. Brothers and her coauthors wrote. Afterward, MRI-VA lets the surgeon and team see if the operation succeeded in repairing the orifices.
In the study population, VA before surgery confirmed elliptical, slit-like orifices in all patients. The operations involved unroofing procedures; two patients also had detachment and resuspension procedures during surgery. After surgery, VA showed that seven patients had round, patent, unobstructed repaired orifices; but two had orifices that were still narrow and somewhat stenotic, Dr. Brothers and her coauthors said. The study group had postoperative MRI-VA an average of 8.6 months after surgery.
“The significance of these findings is unknown; however, if the proposed mechanism of ischemia is due to a slit-like orifice, a continued stenotic orifice may place subjects at risk for sudden death,” the researchers said. The two study patients with the narrowed, stenotic orifices have remained symptom free, with no evidence of ischemia on exercise stress test or cardiac MRI. “These subjects will need to be followed up in the future to monitor for progression or resolution,” the study authors wrote.
Sudden cardiac death (SCD) is more common in anomalous aortic origin of the LCA than the RCA, Dr. Brothers and her colleagues said. Thus, an elliptical, slit-like neo-orifice is a concern because it can become blocked during exercise, possibly leading to lethal ventricular arrhythmia, they said. Ischemia in patients with anomalous coronary artery seems to result from a cumulative effect of exercise.
Patients who undergo the modified unroofing procedure typically have electrocardiography and echocardiography afterward and then get cleared to return to competitive sports in about 3 months if their stress test indicates it. Dr. Brothers and her colleagues said this activity recommendation may need alteration for those patients who have had a heart attack or sudden cardiac arrest, because they may remain at increased risk of SCD after surgery. “At the very least, additional imaging, such as with MRI-VA, should be used in this population,” the study authors said.
While Dr. Brothers and her colleagues acknowledged the small sample size is a limitation of the study, they also pointed out that anomalous coronary artery is a rare disease. They also noted that high-quality VA images can be difficult to obtain in noncompliant patients or those have arrhythmia or irregular breathing. “The images obtained in this study were acquired at an institution very familiar with pediatric cardiac coronary MRI and would be appropriate for assessing the coronary ostia with VA,” they said.
Dr. Brothers and her coauthors had no financial disclosures.
The MRI technique that Dr. Brothers and her colleagues reported on can provide important details of the anomalous coronary anatomy and about myocardial function, Philip S. Naimo, MD, Edward Buratto, MBBS, and Igor Konstantinov, MD, PhD, FRACS, of the Royal Children’s Hospital, University of Melbourne, wrote in their invited commentary. But, the ability to evaluate the neo-ostium after surgery had “particular value,” the commentators said (J. Thorac. Cardiovasc. Surg. 2016 Jul;152:211-12).
MRI with virtual angioscopy can fill help fill in the gaps where the significance of a narrowed neo-ostium is unknown, the commentators said. “The combination of anatomic information on the ostium size, shape, and location, as well as functional information on wall motion and myocardial perfusion, which can be provided by MRI-VA, would be particularly valuable in these patients,” they said.
They also pointed out that MRI-VA could be used in patients who have ongoing but otherwise undetected narrowing of the ostia after the unroofing procedure. At the same time, the technique will also require sufficient caseloads to maintain expertise. “It is safe to say that MRI-VA is here to stay,” Dr. Naimo, Dr. Buratto, and Dr. Konstantinov wrote. “The actual application of this virtual modality will need further refinement to be used routinely.”
The commentary authors had no financial relationships to disclose.
The MRI technique that Dr. Brothers and her colleagues reported on can provide important details of the anomalous coronary anatomy and about myocardial function, Philip S. Naimo, MD, Edward Buratto, MBBS, and Igor Konstantinov, MD, PhD, FRACS, of the Royal Children’s Hospital, University of Melbourne, wrote in their invited commentary. But, the ability to evaluate the neo-ostium after surgery had “particular value,” the commentators said (J. Thorac. Cardiovasc. Surg. 2016 Jul;152:211-12).
MRI with virtual angioscopy can fill help fill in the gaps where the significance of a narrowed neo-ostium is unknown, the commentators said. “The combination of anatomic information on the ostium size, shape, and location, as well as functional information on wall motion and myocardial perfusion, which can be provided by MRI-VA, would be particularly valuable in these patients,” they said.
They also pointed out that MRI-VA could be used in patients who have ongoing but otherwise undetected narrowing of the ostia after the unroofing procedure. At the same time, the technique will also require sufficient caseloads to maintain expertise. “It is safe to say that MRI-VA is here to stay,” Dr. Naimo, Dr. Buratto, and Dr. Konstantinov wrote. “The actual application of this virtual modality will need further refinement to be used routinely.”
The commentary authors had no financial relationships to disclose.
The MRI technique that Dr. Brothers and her colleagues reported on can provide important details of the anomalous coronary anatomy and about myocardial function, Philip S. Naimo, MD, Edward Buratto, MBBS, and Igor Konstantinov, MD, PhD, FRACS, of the Royal Children’s Hospital, University of Melbourne, wrote in their invited commentary. But, the ability to evaluate the neo-ostium after surgery had “particular value,” the commentators said (J. Thorac. Cardiovasc. Surg. 2016 Jul;152:211-12).
MRI with virtual angioscopy can fill help fill in the gaps where the significance of a narrowed neo-ostium is unknown, the commentators said. “The combination of anatomic information on the ostium size, shape, and location, as well as functional information on wall motion and myocardial perfusion, which can be provided by MRI-VA, would be particularly valuable in these patients,” they said.
They also pointed out that MRI-VA could be used in patients who have ongoing but otherwise undetected narrowing of the ostia after the unroofing procedure. At the same time, the technique will also require sufficient caseloads to maintain expertise. “It is safe to say that MRI-VA is here to stay,” Dr. Naimo, Dr. Buratto, and Dr. Konstantinov wrote. “The actual application of this virtual modality will need further refinement to be used routinely.”
The commentary authors had no financial relationships to disclose.
Failure to achieve a rounded and unobstructed ostia in children who have surgery to repair anomalous coronary arteries can put these children at continued risk for sudden death, but cardiac MRI with virtual angioscopy (VA) before and after the operation can give cardiologists a clear picture of a patient’s risk for sudden death and help direct ongoing management, according to a study in the July issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152:205-10).
“Cardiac MRI with virtual angioscopy is an important tool for evaluating anomalous coronary anatomy, myocardial function, and ischemia and should be considered for initial and postoperative assessment of children with anomalous coronary arteries,” lead author Julie A. Brothers, MD, and her coauthors said in reporting their findings.
Anomalous coronary artery is a rare congenital condition in which the left coronary artery (LCA) originates from the right sinus or the right coronary artery (RCA) originates from the left coronary sinus. Dr. Brothers, a pediatric cardiologist, and her colleagues from the Children’s Hospital of Philadelphia and the University of Pennsylvania, also in Philadelphia, studied nine male patients who had operations for anomalous coronary arteries during Feb. 2009-May 2015 in what they said is the first study to document anomalous coronary artery anatomy both before and after surgery. The patients’ average age was 14.1 years; seven had right anomalous coronary arteries and two had left anomalous arteries. After the operations, MRI-VA revealed that two patients still had narrowing in the neo-orifices.
Previous reports recommend surgical repair for all patients with anomalous LCA and for symptomatic patients with anomalous RCA anatomy (Ann Thorac Surg. 2011;92:691-7; Ann Thorac Surg. 2014;98:941-5). MRI-VA allows the surgical team to survey the ostial stenosis before the operation “as if standing within the vessel itself,” Dr. Brothers and her coauthors wrote. Afterward, MRI-VA lets the surgeon and team see if the operation succeeded in repairing the orifices.
In the study population, VA before surgery confirmed elliptical, slit-like orifices in all patients. The operations involved unroofing procedures; two patients also had detachment and resuspension procedures during surgery. After surgery, VA showed that seven patients had round, patent, unobstructed repaired orifices; but two had orifices that were still narrow and somewhat stenotic, Dr. Brothers and her coauthors said. The study group had postoperative MRI-VA an average of 8.6 months after surgery.
“The significance of these findings is unknown; however, if the proposed mechanism of ischemia is due to a slit-like orifice, a continued stenotic orifice may place subjects at risk for sudden death,” the researchers said. The two study patients with the narrowed, stenotic orifices have remained symptom free, with no evidence of ischemia on exercise stress test or cardiac MRI. “These subjects will need to be followed up in the future to monitor for progression or resolution,” the study authors wrote.
Sudden cardiac death (SCD) is more common in anomalous aortic origin of the LCA than the RCA, Dr. Brothers and her colleagues said. Thus, an elliptical, slit-like neo-orifice is a concern because it can become blocked during exercise, possibly leading to lethal ventricular arrhythmia, they said. Ischemia in patients with anomalous coronary artery seems to result from a cumulative effect of exercise.
Patients who undergo the modified unroofing procedure typically have electrocardiography and echocardiography afterward and then get cleared to return to competitive sports in about 3 months if their stress test indicates it. Dr. Brothers and her colleagues said this activity recommendation may need alteration for those patients who have had a heart attack or sudden cardiac arrest, because they may remain at increased risk of SCD after surgery. “At the very least, additional imaging, such as with MRI-VA, should be used in this population,” the study authors said.
While Dr. Brothers and her colleagues acknowledged the small sample size is a limitation of the study, they also pointed out that anomalous coronary artery is a rare disease. They also noted that high-quality VA images can be difficult to obtain in noncompliant patients or those have arrhythmia or irregular breathing. “The images obtained in this study were acquired at an institution very familiar with pediatric cardiac coronary MRI and would be appropriate for assessing the coronary ostia with VA,” they said.
Dr. Brothers and her coauthors had no financial disclosures.
Failure to achieve a rounded and unobstructed ostia in children who have surgery to repair anomalous coronary arteries can put these children at continued risk for sudden death, but cardiac MRI with virtual angioscopy (VA) before and after the operation can give cardiologists a clear picture of a patient’s risk for sudden death and help direct ongoing management, according to a study in the July issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152:205-10).
“Cardiac MRI with virtual angioscopy is an important tool for evaluating anomalous coronary anatomy, myocardial function, and ischemia and should be considered for initial and postoperative assessment of children with anomalous coronary arteries,” lead author Julie A. Brothers, MD, and her coauthors said in reporting their findings.
Anomalous coronary artery is a rare congenital condition in which the left coronary artery (LCA) originates from the right sinus or the right coronary artery (RCA) originates from the left coronary sinus. Dr. Brothers, a pediatric cardiologist, and her colleagues from the Children’s Hospital of Philadelphia and the University of Pennsylvania, also in Philadelphia, studied nine male patients who had operations for anomalous coronary arteries during Feb. 2009-May 2015 in what they said is the first study to document anomalous coronary artery anatomy both before and after surgery. The patients’ average age was 14.1 years; seven had right anomalous coronary arteries and two had left anomalous arteries. After the operations, MRI-VA revealed that two patients still had narrowing in the neo-orifices.
Previous reports recommend surgical repair for all patients with anomalous LCA and for symptomatic patients with anomalous RCA anatomy (Ann Thorac Surg. 2011;92:691-7; Ann Thorac Surg. 2014;98:941-5). MRI-VA allows the surgical team to survey the ostial stenosis before the operation “as if standing within the vessel itself,” Dr. Brothers and her coauthors wrote. Afterward, MRI-VA lets the surgeon and team see if the operation succeeded in repairing the orifices.
In the study population, VA before surgery confirmed elliptical, slit-like orifices in all patients. The operations involved unroofing procedures; two patients also had detachment and resuspension procedures during surgery. After surgery, VA showed that seven patients had round, patent, unobstructed repaired orifices; but two had orifices that were still narrow and somewhat stenotic, Dr. Brothers and her coauthors said. The study group had postoperative MRI-VA an average of 8.6 months after surgery.
“The significance of these findings is unknown; however, if the proposed mechanism of ischemia is due to a slit-like orifice, a continued stenotic orifice may place subjects at risk for sudden death,” the researchers said. The two study patients with the narrowed, stenotic orifices have remained symptom free, with no evidence of ischemia on exercise stress test or cardiac MRI. “These subjects will need to be followed up in the future to monitor for progression or resolution,” the study authors wrote.
Sudden cardiac death (SCD) is more common in anomalous aortic origin of the LCA than the RCA, Dr. Brothers and her colleagues said. Thus, an elliptical, slit-like neo-orifice is a concern because it can become blocked during exercise, possibly leading to lethal ventricular arrhythmia, they said. Ischemia in patients with anomalous coronary artery seems to result from a cumulative effect of exercise.
Patients who undergo the modified unroofing procedure typically have electrocardiography and echocardiography afterward and then get cleared to return to competitive sports in about 3 months if their stress test indicates it. Dr. Brothers and her colleagues said this activity recommendation may need alteration for those patients who have had a heart attack or sudden cardiac arrest, because they may remain at increased risk of SCD after surgery. “At the very least, additional imaging, such as with MRI-VA, should be used in this population,” the study authors said.
While Dr. Brothers and her colleagues acknowledged the small sample size is a limitation of the study, they also pointed out that anomalous coronary artery is a rare disease. They also noted that high-quality VA images can be difficult to obtain in noncompliant patients or those have arrhythmia or irregular breathing. “The images obtained in this study were acquired at an institution very familiar with pediatric cardiac coronary MRI and would be appropriate for assessing the coronary ostia with VA,” they said.
Dr. Brothers and her coauthors had no financial disclosures.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Cardiac MRI with virtual angioscopy (VA) can perform pre- and postoperative assessment in pediatric patients with anomalous coronary arteries.
Major finding: MRI-VA showed that neo-ostium in seven patients were round and unobstructed after surgery, but remained elliptical and somewhat stenotic in two patients.
Data source: Nine male patients aged 5-19 years who had modified unroofing procedure for anomalous coronary artery anatomy at a single institution between February 2009 and May 2015.
Disclosures: Dr. Brothers and coauthors had no financial relationships to disclose.
Syndecan-1 may predict kidney injury after ped heart surgery
Acute kidney injury is a common complication after pediatric cardiac surgery, but measuring for a specific genetic protein immediately after cardiac surgery may improve cardiac surgeons’ ability to predict patients at higher risk of AKI, according to researchers from Brazil. The study results are in the July issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152-178-86).
“Plasma syndecan-1 levels measured early in the postoperative period were independently associated with severe acute kidney injury,” wrote Candice Torres de Melo Bezerra Cavalcante, MD, of Heart Hospital of Messejana and Federal University of Ceará.
Their prospective cohort study involved 289 pediatric patients who had cardiac surgery at their institution between September 2013 and December 2014.
Dr. Cavalcante and colleagues acknowledged that the traditional biomarker for renal function, serum creatinine, only increases appreciably after the glomerular filtration rate declines 50%, impairing physicians’ ability to detect AKI early enough to treat it. “This delay can explain, in part the, negative results in AKI therapeutic clinical trials,” they wrote.
They evaluated two different endothelial biomarkers in addition to syndecan-1 with regard to their capacity for predicting severe AKI: plasma ICAM-1, a marker of endothelial cell activation; and E-selectin, an endothelial cell adhesion molecule. Syndecan-1 works as a biomarker of injury to the glycocalyx protein that surrounds endothelial cell membranes that acts as a permeability barrier and prevents the cells from adhering to blood. They found that median syndecan-1 levels soon after surgery were higher in patients with severe AKI, 103.6 vs. 42.3 ng/mL.
“Although syndecan-1 is not a renal-specific biomarker, there has been recent increasing evidence that endothelial injury has an important role in AKI pathophysiology,” the researchers noted.
Study results showed the higher the level of syndecan-1, the greater the adjusted odds ratio (OR) for severe AKI. Levels of less than 17 ng/mL were considered normal; 17.1-46.7 ng/mL carried an adjusted OR of 1.42; 47.4-93.1 ng/mL had an adjusted OR of 2.05; and levels 96.3 or greater had an OR of 8.87.
“Maintenance of endothelial glycocalyx integrity can be a therapeutic target to reduce AKI in this setting,” the researchers wrote.
The authors acknowledged that the study was done at a single center that had dialysis and death rates three and five times higher, respectively, than those of developed countries; and it measured syndecan-1 at only one time point almost immediately after the operation.
“Adding postoperative syndecan-1, even when using a clinical model that already incorporates variables from renal angina index, results in significant improvement in the capacity to predict severe AKI,” Dr. Cavalcante and colleagues concluded.
They had no financial relationships to disclose.
Results of AKI in heart surgery patients have been “sobering,” with up to 56% of these patients being diagnosed with AKI, but research such as that by Dr. Cavalcante and colleagues represents a new approach to improving outcomes by combining clinical risk factors with specific biomarkers to identify patients at risk, Petros V. Anagnostopoulos, MD, of American Family Children’s Hospital, University of Wisconsin, said in his invited commentary (J Thorac Cardiovasc Surg. 2016;152[1]:187-8).
Dr. Anagnostopoulos acknowledged problems with traditional markers for renal function. “An ideal biomarker should be sensitive, easy to measure, reproducible, and inexpensive,” he said. “Finally, when combined with clinical prediction models, it should potentiate the discrimination of these models.”
Syndecan-1 answers that call, he said. “It peaks early and is cheap, fast, and easy to measure with readily available methods, which makes it an ideal early biomarker of AKI,” Dr. Anagnostopoulos said. Even so, he pointed out potential shortcomings of syndecan-1: It is not renal specific and it does not increase before the operation.
But he applauded Dr. Cavalcante and colleagues for pursuing research to combine clinical risk factors with specific biomarkers. “It is very likely that this type of clinical research will become prevalent in the near future and will hopefully produce results that will allow better individual patient-specific risk stratification,” Dr. Anagnostopoulos said.
He had no financial relationships to disclose.
Results of AKI in heart surgery patients have been “sobering,” with up to 56% of these patients being diagnosed with AKI, but research such as that by Dr. Cavalcante and colleagues represents a new approach to improving outcomes by combining clinical risk factors with specific biomarkers to identify patients at risk, Petros V. Anagnostopoulos, MD, of American Family Children’s Hospital, University of Wisconsin, said in his invited commentary (J Thorac Cardiovasc Surg. 2016;152[1]:187-8).
Dr. Anagnostopoulos acknowledged problems with traditional markers for renal function. “An ideal biomarker should be sensitive, easy to measure, reproducible, and inexpensive,” he said. “Finally, when combined with clinical prediction models, it should potentiate the discrimination of these models.”
Syndecan-1 answers that call, he said. “It peaks early and is cheap, fast, and easy to measure with readily available methods, which makes it an ideal early biomarker of AKI,” Dr. Anagnostopoulos said. Even so, he pointed out potential shortcomings of syndecan-1: It is not renal specific and it does not increase before the operation.
But he applauded Dr. Cavalcante and colleagues for pursuing research to combine clinical risk factors with specific biomarkers. “It is very likely that this type of clinical research will become prevalent in the near future and will hopefully produce results that will allow better individual patient-specific risk stratification,” Dr. Anagnostopoulos said.
He had no financial relationships to disclose.
Results of AKI in heart surgery patients have been “sobering,” with up to 56% of these patients being diagnosed with AKI, but research such as that by Dr. Cavalcante and colleagues represents a new approach to improving outcomes by combining clinical risk factors with specific biomarkers to identify patients at risk, Petros V. Anagnostopoulos, MD, of American Family Children’s Hospital, University of Wisconsin, said in his invited commentary (J Thorac Cardiovasc Surg. 2016;152[1]:187-8).
Dr. Anagnostopoulos acknowledged problems with traditional markers for renal function. “An ideal biomarker should be sensitive, easy to measure, reproducible, and inexpensive,” he said. “Finally, when combined with clinical prediction models, it should potentiate the discrimination of these models.”
Syndecan-1 answers that call, he said. “It peaks early and is cheap, fast, and easy to measure with readily available methods, which makes it an ideal early biomarker of AKI,” Dr. Anagnostopoulos said. Even so, he pointed out potential shortcomings of syndecan-1: It is not renal specific and it does not increase before the operation.
But he applauded Dr. Cavalcante and colleagues for pursuing research to combine clinical risk factors with specific biomarkers. “It is very likely that this type of clinical research will become prevalent in the near future and will hopefully produce results that will allow better individual patient-specific risk stratification,” Dr. Anagnostopoulos said.
He had no financial relationships to disclose.
Acute kidney injury is a common complication after pediatric cardiac surgery, but measuring for a specific genetic protein immediately after cardiac surgery may improve cardiac surgeons’ ability to predict patients at higher risk of AKI, according to researchers from Brazil. The study results are in the July issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152-178-86).
“Plasma syndecan-1 levels measured early in the postoperative period were independently associated with severe acute kidney injury,” wrote Candice Torres de Melo Bezerra Cavalcante, MD, of Heart Hospital of Messejana and Federal University of Ceará.
Their prospective cohort study involved 289 pediatric patients who had cardiac surgery at their institution between September 2013 and December 2014.
Dr. Cavalcante and colleagues acknowledged that the traditional biomarker for renal function, serum creatinine, only increases appreciably after the glomerular filtration rate declines 50%, impairing physicians’ ability to detect AKI early enough to treat it. “This delay can explain, in part the, negative results in AKI therapeutic clinical trials,” they wrote.
They evaluated two different endothelial biomarkers in addition to syndecan-1 with regard to their capacity for predicting severe AKI: plasma ICAM-1, a marker of endothelial cell activation; and E-selectin, an endothelial cell adhesion molecule. Syndecan-1 works as a biomarker of injury to the glycocalyx protein that surrounds endothelial cell membranes that acts as a permeability barrier and prevents the cells from adhering to blood. They found that median syndecan-1 levels soon after surgery were higher in patients with severe AKI, 103.6 vs. 42.3 ng/mL.
“Although syndecan-1 is not a renal-specific biomarker, there has been recent increasing evidence that endothelial injury has an important role in AKI pathophysiology,” the researchers noted.
Study results showed the higher the level of syndecan-1, the greater the adjusted odds ratio (OR) for severe AKI. Levels of less than 17 ng/mL were considered normal; 17.1-46.7 ng/mL carried an adjusted OR of 1.42; 47.4-93.1 ng/mL had an adjusted OR of 2.05; and levels 96.3 or greater had an OR of 8.87.
“Maintenance of endothelial glycocalyx integrity can be a therapeutic target to reduce AKI in this setting,” the researchers wrote.
The authors acknowledged that the study was done at a single center that had dialysis and death rates three and five times higher, respectively, than those of developed countries; and it measured syndecan-1 at only one time point almost immediately after the operation.
“Adding postoperative syndecan-1, even when using a clinical model that already incorporates variables from renal angina index, results in significant improvement in the capacity to predict severe AKI,” Dr. Cavalcante and colleagues concluded.
They had no financial relationships to disclose.
Acute kidney injury is a common complication after pediatric cardiac surgery, but measuring for a specific genetic protein immediately after cardiac surgery may improve cardiac surgeons’ ability to predict patients at higher risk of AKI, according to researchers from Brazil. The study results are in the July issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152-178-86).
“Plasma syndecan-1 levels measured early in the postoperative period were independently associated with severe acute kidney injury,” wrote Candice Torres de Melo Bezerra Cavalcante, MD, of Heart Hospital of Messejana and Federal University of Ceará.
Their prospective cohort study involved 289 pediatric patients who had cardiac surgery at their institution between September 2013 and December 2014.
Dr. Cavalcante and colleagues acknowledged that the traditional biomarker for renal function, serum creatinine, only increases appreciably after the glomerular filtration rate declines 50%, impairing physicians’ ability to detect AKI early enough to treat it. “This delay can explain, in part the, negative results in AKI therapeutic clinical trials,” they wrote.
They evaluated two different endothelial biomarkers in addition to syndecan-1 with regard to their capacity for predicting severe AKI: plasma ICAM-1, a marker of endothelial cell activation; and E-selectin, an endothelial cell adhesion molecule. Syndecan-1 works as a biomarker of injury to the glycocalyx protein that surrounds endothelial cell membranes that acts as a permeability barrier and prevents the cells from adhering to blood. They found that median syndecan-1 levels soon after surgery were higher in patients with severe AKI, 103.6 vs. 42.3 ng/mL.
“Although syndecan-1 is not a renal-specific biomarker, there has been recent increasing evidence that endothelial injury has an important role in AKI pathophysiology,” the researchers noted.
Study results showed the higher the level of syndecan-1, the greater the adjusted odds ratio (OR) for severe AKI. Levels of less than 17 ng/mL were considered normal; 17.1-46.7 ng/mL carried an adjusted OR of 1.42; 47.4-93.1 ng/mL had an adjusted OR of 2.05; and levels 96.3 or greater had an OR of 8.87.
“Maintenance of endothelial glycocalyx integrity can be a therapeutic target to reduce AKI in this setting,” the researchers wrote.
The authors acknowledged that the study was done at a single center that had dialysis and death rates three and five times higher, respectively, than those of developed countries; and it measured syndecan-1 at only one time point almost immediately after the operation.
“Adding postoperative syndecan-1, even when using a clinical model that already incorporates variables from renal angina index, results in significant improvement in the capacity to predict severe AKI,” Dr. Cavalcante and colleagues concluded.
They had no financial relationships to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: The biomarker syndecan-1 may aid in determining acute kidney injury risk for children having cardiac surgery.
Major finding: Children with elevated levels of syndecan-1 had a two- to ninefold greater risk of acute kidney injury.
Data source: Single-institution, prospective cohort study of 289 pediatric patients who had cardiac surgery from September 2013 to December 2014.
Disclosures: Dr. Cavalcante and coauthors had no financial relationships to disclose.
Making the case for CABG using bilateral thoracic arteries
Cardiac surgeons have been slow to embrace bilateral internal thoracic arteries (ITAs) for coronary artery bypass grafting (CABG) despite accumulating evidence that this technique achieves better long-term survival than the single-artery technique, perhaps because they think the bilateral technique is more difficult. However, investigators from Johns Hopkins University have found no difference in results between four different bilateral ITAs techniques regardless of complexity.
Their single-center study analyzed outcomes from 762 patients at Johns Hopkins who had CABG by way of one of four different bilateral ITA (BITA) techniques between 1997 and 2014. The results are in the July issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152:120-7).
“We found no significant difference in terms of long-term survival or freedom from repeat revascularization between different configurations of BITA use,” wrote J. Trent Magruder, MD, and his colleagues.
Dr. Magruder and his coauthors cited 13 reports that found BITA achieved better graft patency and long-term survival than did single internal thoracic arteries, but they noted the lack of reports comparing different BITA techniques. “Given the paucity of comparative data on long-term outcomes of various BITA configurations, we sought to study differences in mortality and the need for repeat revascularization among patients receiving varying BITA graft configurations at our institution,” they said.
The four groups and types of BITA procedures they analyzed were:
LL/RL group, in situ left ITA (LITA) anastomosed to the left anterior descending artery (LAD) with in situ right ITA (RITA) anastomosed to the left coronary circulation (n = 239).
LL/RR group, in situ LITA-LAD and in situ RITA-right coronary circulation (n = 239 patients).
RL/LL group, in situ RITA-LAD with in situ LITA-left coronary circulation (n = 185 patients).
Y group, in situ LITA-LAD with a free RITA as a composite graft with inflow from the LITA or a saphenous vein graft (n = 99 patients).
BITA cases comprised 5.7% of all 14,502 CABG procedures Johns Hopkins cardiac surgeons performed through the study period (60 BITA cases were dropped from the analysis because of incomplete data). That rate is about in line with a previously reported use rate of 4% of CABG procedures in the United States (Circulation. 2009;120:935-40).
Among the reasons Dr. Magruder and his coauthors cited for the lack of uptake of BITA among cardiac surgeons are discrepancies in survival data, a perceived high risk of complications such as sternal surgical site infections in patients with diabetes or chronic obstructive pulmonary disease or in those who are obese, and increased operative time and risk of bleeding.
With regard to the operation itself, the mean cross-clamp and coronary bypass times and number of bypass grafts were similar among all four groups, the latter ranging from 3.0 for the RL/LL group to 3.4 for the Y group. However, the researchers did find appreciable differences in rates of transfusions during the operation and skeletonization of the RITA at harvest. The Y group had the highest rates for both – 57.6% had transfusions and 72.7% had skeletonized RITA at harvest – followed by the RL/LL with rates of 43.2% for transfusions and 31.4% with skeletonized RITA. Rates for both intraoperative transfusion and RITA skeletonization were 24.7% and 8%, respectively, in the LL/RL group; and 37.7% and 18%, respectively, in the LL/RR group.
In-hospital complications, including reintervention for bleeding, heart attack, stroke, inflammation of the mediastinum, and death, were similar among all four groups. There were no in-hospital heart attacks. The only statistically significant difference was in hospital stay, ranging from an average of 6.1 days for the LL/RL group to 7.4 for both the LL/RR and RL/LL groups.
Through the duration of follow-up, the overall rate for repeat percutaneous coronary intervention was 7.6% – highest among the RL/LL (9.2%) and Y groups (9%). Those in the LL/RR group had the highest rates of repeat CABG: 1.7% vs. 0.8% for LL/RL group, 0.5% for the RL/LL group and 0% for group Y. Rates of late cardiac death were around 5% for the first three groups, but none were reported in group Y.
Dr. Magruder and colleagues acknowledged their study used a limited sample size for each procedure, but that their findings show that cardiac surgeons should choose their BITA configuration based on individual patient factors. “In general, the technically simplest operations should be selected because more complex procedures offer no additional benefit,” they said.
Dr. Magruder and his coauthors had no financial disclosures.
The take-home message of the study by Dr. Magruder and colleagues is that using bilateral internal thoracic arteries (BITA) is more important than the specific configuration, Saswata Deb, MD, BSc, and Stephen E. Fremes, MD, MSc, BSc, of the University of Toronto wrote in their invited commentary (J Thorac Cardiovasc Surg. 2016;152:128-30). “In other words: BITA – just do it!” they wrote.
Because the survival advantage of BITA in CABG typically becomes apparent 10 years or more after the operation, the Johns Hopkins study, along with the Arterial Revascularization Trial that compares BITA with single ITA (Semin Thorac Cardiovasc Surg. 2014;26:76-94), can help redefine how cardiac surgeons select conduits for CABG, the commentators said.
“What does this particular study add?” they asked. “Point estimates for the adjusted hazard ratio of death or repeat revascularization were close to unity for each of the primary grafting hypothesis comparisons.”
Dr. Deb and Dr. Fremes had no financial relationships to disclose.
The take-home message of the study by Dr. Magruder and colleagues is that using bilateral internal thoracic arteries (BITA) is more important than the specific configuration, Saswata Deb, MD, BSc, and Stephen E. Fremes, MD, MSc, BSc, of the University of Toronto wrote in their invited commentary (J Thorac Cardiovasc Surg. 2016;152:128-30). “In other words: BITA – just do it!” they wrote.
Because the survival advantage of BITA in CABG typically becomes apparent 10 years or more after the operation, the Johns Hopkins study, along with the Arterial Revascularization Trial that compares BITA with single ITA (Semin Thorac Cardiovasc Surg. 2014;26:76-94), can help redefine how cardiac surgeons select conduits for CABG, the commentators said.
“What does this particular study add?” they asked. “Point estimates for the adjusted hazard ratio of death or repeat revascularization were close to unity for each of the primary grafting hypothesis comparisons.”
Dr. Deb and Dr. Fremes had no financial relationships to disclose.
The take-home message of the study by Dr. Magruder and colleagues is that using bilateral internal thoracic arteries (BITA) is more important than the specific configuration, Saswata Deb, MD, BSc, and Stephen E. Fremes, MD, MSc, BSc, of the University of Toronto wrote in their invited commentary (J Thorac Cardiovasc Surg. 2016;152:128-30). “In other words: BITA – just do it!” they wrote.
Because the survival advantage of BITA in CABG typically becomes apparent 10 years or more after the operation, the Johns Hopkins study, along with the Arterial Revascularization Trial that compares BITA with single ITA (Semin Thorac Cardiovasc Surg. 2014;26:76-94), can help redefine how cardiac surgeons select conduits for CABG, the commentators said.
“What does this particular study add?” they asked. “Point estimates for the adjusted hazard ratio of death or repeat revascularization were close to unity for each of the primary grafting hypothesis comparisons.”
Dr. Deb and Dr. Fremes had no financial relationships to disclose.
Cardiac surgeons have been slow to embrace bilateral internal thoracic arteries (ITAs) for coronary artery bypass grafting (CABG) despite accumulating evidence that this technique achieves better long-term survival than the single-artery technique, perhaps because they think the bilateral technique is more difficult. However, investigators from Johns Hopkins University have found no difference in results between four different bilateral ITAs techniques regardless of complexity.
Their single-center study analyzed outcomes from 762 patients at Johns Hopkins who had CABG by way of one of four different bilateral ITA (BITA) techniques between 1997 and 2014. The results are in the July issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152:120-7).
“We found no significant difference in terms of long-term survival or freedom from repeat revascularization between different configurations of BITA use,” wrote J. Trent Magruder, MD, and his colleagues.
Dr. Magruder and his coauthors cited 13 reports that found BITA achieved better graft patency and long-term survival than did single internal thoracic arteries, but they noted the lack of reports comparing different BITA techniques. “Given the paucity of comparative data on long-term outcomes of various BITA configurations, we sought to study differences in mortality and the need for repeat revascularization among patients receiving varying BITA graft configurations at our institution,” they said.
The four groups and types of BITA procedures they analyzed were:
LL/RL group, in situ left ITA (LITA) anastomosed to the left anterior descending artery (LAD) with in situ right ITA (RITA) anastomosed to the left coronary circulation (n = 239).
LL/RR group, in situ LITA-LAD and in situ RITA-right coronary circulation (n = 239 patients).
RL/LL group, in situ RITA-LAD with in situ LITA-left coronary circulation (n = 185 patients).
Y group, in situ LITA-LAD with a free RITA as a composite graft with inflow from the LITA or a saphenous vein graft (n = 99 patients).
BITA cases comprised 5.7% of all 14,502 CABG procedures Johns Hopkins cardiac surgeons performed through the study period (60 BITA cases were dropped from the analysis because of incomplete data). That rate is about in line with a previously reported use rate of 4% of CABG procedures in the United States (Circulation. 2009;120:935-40).
Among the reasons Dr. Magruder and his coauthors cited for the lack of uptake of BITA among cardiac surgeons are discrepancies in survival data, a perceived high risk of complications such as sternal surgical site infections in patients with diabetes or chronic obstructive pulmonary disease or in those who are obese, and increased operative time and risk of bleeding.
With regard to the operation itself, the mean cross-clamp and coronary bypass times and number of bypass grafts were similar among all four groups, the latter ranging from 3.0 for the RL/LL group to 3.4 for the Y group. However, the researchers did find appreciable differences in rates of transfusions during the operation and skeletonization of the RITA at harvest. The Y group had the highest rates for both – 57.6% had transfusions and 72.7% had skeletonized RITA at harvest – followed by the RL/LL with rates of 43.2% for transfusions and 31.4% with skeletonized RITA. Rates for both intraoperative transfusion and RITA skeletonization were 24.7% and 8%, respectively, in the LL/RL group; and 37.7% and 18%, respectively, in the LL/RR group.
In-hospital complications, including reintervention for bleeding, heart attack, stroke, inflammation of the mediastinum, and death, were similar among all four groups. There were no in-hospital heart attacks. The only statistically significant difference was in hospital stay, ranging from an average of 6.1 days for the LL/RL group to 7.4 for both the LL/RR and RL/LL groups.
Through the duration of follow-up, the overall rate for repeat percutaneous coronary intervention was 7.6% – highest among the RL/LL (9.2%) and Y groups (9%). Those in the LL/RR group had the highest rates of repeat CABG: 1.7% vs. 0.8% for LL/RL group, 0.5% for the RL/LL group and 0% for group Y. Rates of late cardiac death were around 5% for the first three groups, but none were reported in group Y.
Dr. Magruder and colleagues acknowledged their study used a limited sample size for each procedure, but that their findings show that cardiac surgeons should choose their BITA configuration based on individual patient factors. “In general, the technically simplest operations should be selected because more complex procedures offer no additional benefit,” they said.
Dr. Magruder and his coauthors had no financial disclosures.
Cardiac surgeons have been slow to embrace bilateral internal thoracic arteries (ITAs) for coronary artery bypass grafting (CABG) despite accumulating evidence that this technique achieves better long-term survival than the single-artery technique, perhaps because they think the bilateral technique is more difficult. However, investigators from Johns Hopkins University have found no difference in results between four different bilateral ITAs techniques regardless of complexity.
Their single-center study analyzed outcomes from 762 patients at Johns Hopkins who had CABG by way of one of four different bilateral ITA (BITA) techniques between 1997 and 2014. The results are in the July issue of the Journal of Thoracic and Cardiovascular Surgery (2016;152:120-7).
“We found no significant difference in terms of long-term survival or freedom from repeat revascularization between different configurations of BITA use,” wrote J. Trent Magruder, MD, and his colleagues.
Dr. Magruder and his coauthors cited 13 reports that found BITA achieved better graft patency and long-term survival than did single internal thoracic arteries, but they noted the lack of reports comparing different BITA techniques. “Given the paucity of comparative data on long-term outcomes of various BITA configurations, we sought to study differences in mortality and the need for repeat revascularization among patients receiving varying BITA graft configurations at our institution,” they said.
The four groups and types of BITA procedures they analyzed were:
LL/RL group, in situ left ITA (LITA) anastomosed to the left anterior descending artery (LAD) with in situ right ITA (RITA) anastomosed to the left coronary circulation (n = 239).
LL/RR group, in situ LITA-LAD and in situ RITA-right coronary circulation (n = 239 patients).
RL/LL group, in situ RITA-LAD with in situ LITA-left coronary circulation (n = 185 patients).
Y group, in situ LITA-LAD with a free RITA as a composite graft with inflow from the LITA or a saphenous vein graft (n = 99 patients).
BITA cases comprised 5.7% of all 14,502 CABG procedures Johns Hopkins cardiac surgeons performed through the study period (60 BITA cases were dropped from the analysis because of incomplete data). That rate is about in line with a previously reported use rate of 4% of CABG procedures in the United States (Circulation. 2009;120:935-40).
Among the reasons Dr. Magruder and his coauthors cited for the lack of uptake of BITA among cardiac surgeons are discrepancies in survival data, a perceived high risk of complications such as sternal surgical site infections in patients with diabetes or chronic obstructive pulmonary disease or in those who are obese, and increased operative time and risk of bleeding.
With regard to the operation itself, the mean cross-clamp and coronary bypass times and number of bypass grafts were similar among all four groups, the latter ranging from 3.0 for the RL/LL group to 3.4 for the Y group. However, the researchers did find appreciable differences in rates of transfusions during the operation and skeletonization of the RITA at harvest. The Y group had the highest rates for both – 57.6% had transfusions and 72.7% had skeletonized RITA at harvest – followed by the RL/LL with rates of 43.2% for transfusions and 31.4% with skeletonized RITA. Rates for both intraoperative transfusion and RITA skeletonization were 24.7% and 8%, respectively, in the LL/RL group; and 37.7% and 18%, respectively, in the LL/RR group.
In-hospital complications, including reintervention for bleeding, heart attack, stroke, inflammation of the mediastinum, and death, were similar among all four groups. There were no in-hospital heart attacks. The only statistically significant difference was in hospital stay, ranging from an average of 6.1 days for the LL/RL group to 7.4 for both the LL/RR and RL/LL groups.
Through the duration of follow-up, the overall rate for repeat percutaneous coronary intervention was 7.6% – highest among the RL/LL (9.2%) and Y groups (9%). Those in the LL/RR group had the highest rates of repeat CABG: 1.7% vs. 0.8% for LL/RL group, 0.5% for the RL/LL group and 0% for group Y. Rates of late cardiac death were around 5% for the first three groups, but none were reported in group Y.
Dr. Magruder and colleagues acknowledged their study used a limited sample size for each procedure, but that their findings show that cardiac surgeons should choose their BITA configuration based on individual patient factors. “In general, the technically simplest operations should be selected because more complex procedures offer no additional benefit,” they said.
Dr. Magruder and his coauthors had no financial disclosures.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: No specific technique for bilateral internal thoracic artery (BITA) graft in coronary artery bypass grafting (CABG) has an advantage over other techniques.
Major finding: Among four different BITA configurations, no in-hospital deaths occurred and the late cardiac death rate was around 5% for three of the four groups and 0% for the fourth group.
Data source: Single-center, retrospective study of 762 patients who had CABG with use of BITA from 1997 to 2014.
Disclosures: Dr. Magruder and colleagues reported having no financial disclosures.
Four-branched arch replacement gets acceptable results
NEW YORK – A total aortic arch replacement approach that uses a four-branched graft with antegrade cerebral perfusion can be done with low rates of in-hospital death and complications, a large series from two institutions in Japan showed.
Kenji Minatoya, MD, of the National Cerebral and Cardiovascular Center in Osaka, Japan, reported that his institution’s approach for total arch replacement (TAR) had an in-hospital death rate of 5.2%.
Dr. Minatoya and his colleagues started using four-branch TAR in the 1980s, switching from retrograde to antegrade cerebral perfusion to protect the brain later on. “The study purpose was to investigate the results of total arch replacement using the four-branch graft as a benchmark in the endovascular era,” he said at the meeting, sponsored by the American Association for Thoracic Surgery.
The study involved 1,005 cases of total arch replacement performed at Dr. Minatoya’s center and at Tokyo Medical University from 2001 to 2016.
The study population included a cohort of 152 people in their 80s. The in-hospital death rate in this group was 11.8%, Dr. Minatoya said. The over-80 group mostly underwent thoracic endovascular aortic repair (TEVAR) beginning in 2008, he said, but in recent years some had open total arch replacement operations.
The univariate analysis showed that chronic kidney disease, long operation times, long durations for coronary bypass and circulatory arrest, and extended time on mechanical ventilation were risk factors for in-hospital death in octogenarians, Dr. Minatoya said. The multivariate analysis showed that male gender along with extended mechanical ventilation were risk factors for in-hospital death in this group, he said.
The overall population included 252 emergent operations, 224 of which were for acute aortic dissections, Dr. Minatoya said. The in-hospital death rate was 4.5% for elective operations and 7.1% for emergent cases, he said. The death rate for isolated, elective total arch replacement was 3.4%.
Focusing on acute aortic dissections, Dr. Minatoya said, “We have adopted an aggressive strategy for entry-site resection, including total arch replacement, in patients with arch tears.” Almost 50% of patients with acute aortic dissection had total arch replacement, he said, with identical 4.9% rates for in-hospital mortality rate and permanent neurological deficit in this group.
The leading overall causes of in-hospital death were low-output syndrome (38.5%), sepsis (25%), respiratory failure (21%) and rupture of the residual aneurysm (9%), Dr. Minatoya said.
Fifteen patients (1.5%) underwent second operations for arch grafts, he said: 11 for pseudoaneurysm; three for hemolysis and one for infection. Other overall measures in the analysis were a permanent neurological dysfunction rate of 3.6%, a temporary neurological dysfunction rate of 6.4%, and no spinal cord complications. Overall 5-year survival was 80.7% and 10-year survival was 63.1%, Dr. Minatoya said.
A total of 311 patients had concomitant procedures. They included aortic valve operations (64); aortic root replacement (38); mitral valve replacement (13); and coronary artery bypass grafting (196).
The typical operation in the study population took about 8 hours, Dr. Minatoya said (482 minutes). Timing of key operative steps were cardiopulmonary time of 254 minutes, cardiac arrest time of 146 minutes, antegrade cerebral perfusion time of 160 minutes and lower-body circulatory arrest time of 62 minutes.
“Since the mean age was 70 years old, we think the survival rate was acceptable,” Dr. Minatoya said, regarding overall study results. Overall risk factors for in-hospital death were short stature, long pump time, chronic kidney disease, and age of 80 and up, he said. Short stature was a risk factor for permanent neurological deficit, and males over age 80 had a higher risk for total arch replacement.
“Total arch replacement using the four-branched graft with antegrade cerebral perfusion could be accomplished with acceptable early and late results,” Dr. Minatoya said. “The branched-arch TEVAR may be a good option for octogenarians and patients with chronic kidney disease.”
Dr. Minatoya had no financial relationships to disclose.
NEW YORK – A total aortic arch replacement approach that uses a four-branched graft with antegrade cerebral perfusion can be done with low rates of in-hospital death and complications, a large series from two institutions in Japan showed.
Kenji Minatoya, MD, of the National Cerebral and Cardiovascular Center in Osaka, Japan, reported that his institution’s approach for total arch replacement (TAR) had an in-hospital death rate of 5.2%.
Dr. Minatoya and his colleagues started using four-branch TAR in the 1980s, switching from retrograde to antegrade cerebral perfusion to protect the brain later on. “The study purpose was to investigate the results of total arch replacement using the four-branch graft as a benchmark in the endovascular era,” he said at the meeting, sponsored by the American Association for Thoracic Surgery.
The study involved 1,005 cases of total arch replacement performed at Dr. Minatoya’s center and at Tokyo Medical University from 2001 to 2016.
The study population included a cohort of 152 people in their 80s. The in-hospital death rate in this group was 11.8%, Dr. Minatoya said. The over-80 group mostly underwent thoracic endovascular aortic repair (TEVAR) beginning in 2008, he said, but in recent years some had open total arch replacement operations.
The univariate analysis showed that chronic kidney disease, long operation times, long durations for coronary bypass and circulatory arrest, and extended time on mechanical ventilation were risk factors for in-hospital death in octogenarians, Dr. Minatoya said. The multivariate analysis showed that male gender along with extended mechanical ventilation were risk factors for in-hospital death in this group, he said.
The overall population included 252 emergent operations, 224 of which were for acute aortic dissections, Dr. Minatoya said. The in-hospital death rate was 4.5% for elective operations and 7.1% for emergent cases, he said. The death rate for isolated, elective total arch replacement was 3.4%.
Focusing on acute aortic dissections, Dr. Minatoya said, “We have adopted an aggressive strategy for entry-site resection, including total arch replacement, in patients with arch tears.” Almost 50% of patients with acute aortic dissection had total arch replacement, he said, with identical 4.9% rates for in-hospital mortality rate and permanent neurological deficit in this group.
The leading overall causes of in-hospital death were low-output syndrome (38.5%), sepsis (25%), respiratory failure (21%) and rupture of the residual aneurysm (9%), Dr. Minatoya said.
Fifteen patients (1.5%) underwent second operations for arch grafts, he said: 11 for pseudoaneurysm; three for hemolysis and one for infection. Other overall measures in the analysis were a permanent neurological dysfunction rate of 3.6%, a temporary neurological dysfunction rate of 6.4%, and no spinal cord complications. Overall 5-year survival was 80.7% and 10-year survival was 63.1%, Dr. Minatoya said.
A total of 311 patients had concomitant procedures. They included aortic valve operations (64); aortic root replacement (38); mitral valve replacement (13); and coronary artery bypass grafting (196).
The typical operation in the study population took about 8 hours, Dr. Minatoya said (482 minutes). Timing of key operative steps were cardiopulmonary time of 254 minutes, cardiac arrest time of 146 minutes, antegrade cerebral perfusion time of 160 minutes and lower-body circulatory arrest time of 62 minutes.
“Since the mean age was 70 years old, we think the survival rate was acceptable,” Dr. Minatoya said, regarding overall study results. Overall risk factors for in-hospital death were short stature, long pump time, chronic kidney disease, and age of 80 and up, he said. Short stature was a risk factor for permanent neurological deficit, and males over age 80 had a higher risk for total arch replacement.
“Total arch replacement using the four-branched graft with antegrade cerebral perfusion could be accomplished with acceptable early and late results,” Dr. Minatoya said. “The branched-arch TEVAR may be a good option for octogenarians and patients with chronic kidney disease.”
Dr. Minatoya had no financial relationships to disclose.
NEW YORK – A total aortic arch replacement approach that uses a four-branched graft with antegrade cerebral perfusion can be done with low rates of in-hospital death and complications, a large series from two institutions in Japan showed.
Kenji Minatoya, MD, of the National Cerebral and Cardiovascular Center in Osaka, Japan, reported that his institution’s approach for total arch replacement (TAR) had an in-hospital death rate of 5.2%.
Dr. Minatoya and his colleagues started using four-branch TAR in the 1980s, switching from retrograde to antegrade cerebral perfusion to protect the brain later on. “The study purpose was to investigate the results of total arch replacement using the four-branch graft as a benchmark in the endovascular era,” he said at the meeting, sponsored by the American Association for Thoracic Surgery.
The study involved 1,005 cases of total arch replacement performed at Dr. Minatoya’s center and at Tokyo Medical University from 2001 to 2016.
The study population included a cohort of 152 people in their 80s. The in-hospital death rate in this group was 11.8%, Dr. Minatoya said. The over-80 group mostly underwent thoracic endovascular aortic repair (TEVAR) beginning in 2008, he said, but in recent years some had open total arch replacement operations.
The univariate analysis showed that chronic kidney disease, long operation times, long durations for coronary bypass and circulatory arrest, and extended time on mechanical ventilation were risk factors for in-hospital death in octogenarians, Dr. Minatoya said. The multivariate analysis showed that male gender along with extended mechanical ventilation were risk factors for in-hospital death in this group, he said.
The overall population included 252 emergent operations, 224 of which were for acute aortic dissections, Dr. Minatoya said. The in-hospital death rate was 4.5% for elective operations and 7.1% for emergent cases, he said. The death rate for isolated, elective total arch replacement was 3.4%.
Focusing on acute aortic dissections, Dr. Minatoya said, “We have adopted an aggressive strategy for entry-site resection, including total arch replacement, in patients with arch tears.” Almost 50% of patients with acute aortic dissection had total arch replacement, he said, with identical 4.9% rates for in-hospital mortality rate and permanent neurological deficit in this group.
The leading overall causes of in-hospital death were low-output syndrome (38.5%), sepsis (25%), respiratory failure (21%) and rupture of the residual aneurysm (9%), Dr. Minatoya said.
Fifteen patients (1.5%) underwent second operations for arch grafts, he said: 11 for pseudoaneurysm; three for hemolysis and one for infection. Other overall measures in the analysis were a permanent neurological dysfunction rate of 3.6%, a temporary neurological dysfunction rate of 6.4%, and no spinal cord complications. Overall 5-year survival was 80.7% and 10-year survival was 63.1%, Dr. Minatoya said.
A total of 311 patients had concomitant procedures. They included aortic valve operations (64); aortic root replacement (38); mitral valve replacement (13); and coronary artery bypass grafting (196).
The typical operation in the study population took about 8 hours, Dr. Minatoya said (482 minutes). Timing of key operative steps were cardiopulmonary time of 254 minutes, cardiac arrest time of 146 minutes, antegrade cerebral perfusion time of 160 minutes and lower-body circulatory arrest time of 62 minutes.
“Since the mean age was 70 years old, we think the survival rate was acceptable,” Dr. Minatoya said, regarding overall study results. Overall risk factors for in-hospital death were short stature, long pump time, chronic kidney disease, and age of 80 and up, he said. Short stature was a risk factor for permanent neurological deficit, and males over age 80 had a higher risk for total arch replacement.
“Total arch replacement using the four-branched graft with antegrade cerebral perfusion could be accomplished with acceptable early and late results,” Dr. Minatoya said. “The branched-arch TEVAR may be a good option for octogenarians and patients with chronic kidney disease.”
Dr. Minatoya had no financial relationships to disclose.
AT THE AATS AORTIC SYMPOSIUM 2016
Key clinical point: Four-branched total aortic arch replacement can achieve acceptable early and late results.
Major finding: Overall in-hospital mortality was 5.2% and 5-year survival was 80.7%.
Data source: Consecutive series of 1,005 patients who had total arch replacement between 2001 and 2016 at two centers in Japan.
Disclosures: Dr. Minatoya reported having no financial disclosures.