User login
Four-branched arch replacement gets acceptable results
NEW YORK – A total aortic arch replacement approach that uses a four-branched graft with antegrade cerebral perfusion can be done with low rates of in-hospital death and complications, a large series from two institutions in Japan showed.
Kenji Minatoya, MD, of the National Cerebral and Cardiovascular Center in Osaka, Japan, reported that his institution’s approach for total arch replacement (TAR) had an in-hospital death rate of 5.2%.
Dr. Minatoya and his colleagues started using four-branch TAR in the 1980s, switching from retrograde to antegrade cerebral perfusion to protect the brain later on. “The study purpose was to investigate the results of total arch replacement using the four-branch graft as a benchmark in the endovascular era,” he said at the meeting, sponsored by the American Association for Thoracic Surgery.
The study involved 1,005 cases of total arch replacement performed at Dr. Minatoya’s center and at Tokyo Medical University from 2001 to 2016.
The study population included a cohort of 152 people in their 80s. The in-hospital death rate in this group was 11.8%, Dr. Minatoya said. The over-80 group mostly underwent thoracic endovascular aortic repair (TEVAR) beginning in 2008, he said, but in recent years some had open total arch replacement operations.
The univariate analysis showed that chronic kidney disease, long operation times, long durations for coronary bypass and circulatory arrest, and extended time on mechanical ventilation were risk factors for in-hospital death in octogenarians, Dr. Minatoya said. The multivariate analysis showed that male gender along with extended mechanical ventilation were risk factors for in-hospital death in this group, he said.
The overall population included 252 emergent operations, 224 of which were for acute aortic dissections, Dr. Minatoya said. The in-hospital death rate was 4.5% for elective operations and 7.1% for emergent cases, he said. The death rate for isolated, elective total arch replacement was 3.4%.
Focusing on acute aortic dissections, Dr. Minatoya said, “We have adopted an aggressive strategy for entry-site resection, including total arch replacement, in patients with arch tears.” Almost 50% of patients with acute aortic dissection had total arch replacement, he said, with identical 4.9% rates for in-hospital mortality rate and permanent neurological deficit in this group.
The leading overall causes of in-hospital death were low-output syndrome (38.5%), sepsis (25%), respiratory failure (21%) and rupture of the residual aneurysm (9%), Dr. Minatoya said.
Fifteen patients (1.5%) underwent second operations for arch grafts, he said: 11 for pseudoaneurysm; three for hemolysis and one for infection. Other overall measures in the analysis were a permanent neurological dysfunction rate of 3.6%, a temporary neurological dysfunction rate of 6.4%, and no spinal cord complications. Overall 5-year survival was 80.7% and 10-year survival was 63.1%, Dr. Minatoya said.
A total of 311 patients had concomitant procedures. They included aortic valve operations (64); aortic root replacement (38); mitral valve replacement (13); and coronary artery bypass grafting (196).
The typical operation in the study population took about 8 hours, Dr. Minatoya said (482 minutes). Timing of key operative steps were cardiopulmonary time of 254 minutes, cardiac arrest time of 146 minutes, antegrade cerebral perfusion time of 160 minutes and lower-body circulatory arrest time of 62 minutes.
“Since the mean age was 70 years old, we think the survival rate was acceptable,” Dr. Minatoya said, regarding overall study results. Overall risk factors for in-hospital death were short stature, long pump time, chronic kidney disease, and age of 80 and up, he said. Short stature was a risk factor for permanent neurological deficit, and males over age 80 had a higher risk for total arch replacement.
“Total arch replacement using the four-branched graft with antegrade cerebral perfusion could be accomplished with acceptable early and late results,” Dr. Minatoya said. “The branched-arch TEVAR may be a good option for octogenarians and patients with chronic kidney disease.”
Dr. Minatoya had no financial relationships to disclose.
NEW YORK – A total aortic arch replacement approach that uses a four-branched graft with antegrade cerebral perfusion can be done with low rates of in-hospital death and complications, a large series from two institutions in Japan showed.
Kenji Minatoya, MD, of the National Cerebral and Cardiovascular Center in Osaka, Japan, reported that his institution’s approach for total arch replacement (TAR) had an in-hospital death rate of 5.2%.
Dr. Minatoya and his colleagues started using four-branch TAR in the 1980s, switching from retrograde to antegrade cerebral perfusion to protect the brain later on. “The study purpose was to investigate the results of total arch replacement using the four-branch graft as a benchmark in the endovascular era,” he said at the meeting, sponsored by the American Association for Thoracic Surgery.
The study involved 1,005 cases of total arch replacement performed at Dr. Minatoya’s center and at Tokyo Medical University from 2001 to 2016.
The study population included a cohort of 152 people in their 80s. The in-hospital death rate in this group was 11.8%, Dr. Minatoya said. The over-80 group mostly underwent thoracic endovascular aortic repair (TEVAR) beginning in 2008, he said, but in recent years some had open total arch replacement operations.
The univariate analysis showed that chronic kidney disease, long operation times, long durations for coronary bypass and circulatory arrest, and extended time on mechanical ventilation were risk factors for in-hospital death in octogenarians, Dr. Minatoya said. The multivariate analysis showed that male gender along with extended mechanical ventilation were risk factors for in-hospital death in this group, he said.
The overall population included 252 emergent operations, 224 of which were for acute aortic dissections, Dr. Minatoya said. The in-hospital death rate was 4.5% for elective operations and 7.1% for emergent cases, he said. The death rate for isolated, elective total arch replacement was 3.4%.
Focusing on acute aortic dissections, Dr. Minatoya said, “We have adopted an aggressive strategy for entry-site resection, including total arch replacement, in patients with arch tears.” Almost 50% of patients with acute aortic dissection had total arch replacement, he said, with identical 4.9% rates for in-hospital mortality rate and permanent neurological deficit in this group.
The leading overall causes of in-hospital death were low-output syndrome (38.5%), sepsis (25%), respiratory failure (21%) and rupture of the residual aneurysm (9%), Dr. Minatoya said.
Fifteen patients (1.5%) underwent second operations for arch grafts, he said: 11 for pseudoaneurysm; three for hemolysis and one for infection. Other overall measures in the analysis were a permanent neurological dysfunction rate of 3.6%, a temporary neurological dysfunction rate of 6.4%, and no spinal cord complications. Overall 5-year survival was 80.7% and 10-year survival was 63.1%, Dr. Minatoya said.
A total of 311 patients had concomitant procedures. They included aortic valve operations (64); aortic root replacement (38); mitral valve replacement (13); and coronary artery bypass grafting (196).
The typical operation in the study population took about 8 hours, Dr. Minatoya said (482 minutes). Timing of key operative steps were cardiopulmonary time of 254 minutes, cardiac arrest time of 146 minutes, antegrade cerebral perfusion time of 160 minutes and lower-body circulatory arrest time of 62 minutes.
“Since the mean age was 70 years old, we think the survival rate was acceptable,” Dr. Minatoya said, regarding overall study results. Overall risk factors for in-hospital death were short stature, long pump time, chronic kidney disease, and age of 80 and up, he said. Short stature was a risk factor for permanent neurological deficit, and males over age 80 had a higher risk for total arch replacement.
“Total arch replacement using the four-branched graft with antegrade cerebral perfusion could be accomplished with acceptable early and late results,” Dr. Minatoya said. “The branched-arch TEVAR may be a good option for octogenarians and patients with chronic kidney disease.”
Dr. Minatoya had no financial relationships to disclose.
NEW YORK – A total aortic arch replacement approach that uses a four-branched graft with antegrade cerebral perfusion can be done with low rates of in-hospital death and complications, a large series from two institutions in Japan showed.
Kenji Minatoya, MD, of the National Cerebral and Cardiovascular Center in Osaka, Japan, reported that his institution’s approach for total arch replacement (TAR) had an in-hospital death rate of 5.2%.
Dr. Minatoya and his colleagues started using four-branch TAR in the 1980s, switching from retrograde to antegrade cerebral perfusion to protect the brain later on. “The study purpose was to investigate the results of total arch replacement using the four-branch graft as a benchmark in the endovascular era,” he said at the meeting, sponsored by the American Association for Thoracic Surgery.
The study involved 1,005 cases of total arch replacement performed at Dr. Minatoya’s center and at Tokyo Medical University from 2001 to 2016.
The study population included a cohort of 152 people in their 80s. The in-hospital death rate in this group was 11.8%, Dr. Minatoya said. The over-80 group mostly underwent thoracic endovascular aortic repair (TEVAR) beginning in 2008, he said, but in recent years some had open total arch replacement operations.
The univariate analysis showed that chronic kidney disease, long operation times, long durations for coronary bypass and circulatory arrest, and extended time on mechanical ventilation were risk factors for in-hospital death in octogenarians, Dr. Minatoya said. The multivariate analysis showed that male gender along with extended mechanical ventilation were risk factors for in-hospital death in this group, he said.
The overall population included 252 emergent operations, 224 of which were for acute aortic dissections, Dr. Minatoya said. The in-hospital death rate was 4.5% for elective operations and 7.1% for emergent cases, he said. The death rate for isolated, elective total arch replacement was 3.4%.
Focusing on acute aortic dissections, Dr. Minatoya said, “We have adopted an aggressive strategy for entry-site resection, including total arch replacement, in patients with arch tears.” Almost 50% of patients with acute aortic dissection had total arch replacement, he said, with identical 4.9% rates for in-hospital mortality rate and permanent neurological deficit in this group.
The leading overall causes of in-hospital death were low-output syndrome (38.5%), sepsis (25%), respiratory failure (21%) and rupture of the residual aneurysm (9%), Dr. Minatoya said.
Fifteen patients (1.5%) underwent second operations for arch grafts, he said: 11 for pseudoaneurysm; three for hemolysis and one for infection. Other overall measures in the analysis were a permanent neurological dysfunction rate of 3.6%, a temporary neurological dysfunction rate of 6.4%, and no spinal cord complications. Overall 5-year survival was 80.7% and 10-year survival was 63.1%, Dr. Minatoya said.
A total of 311 patients had concomitant procedures. They included aortic valve operations (64); aortic root replacement (38); mitral valve replacement (13); and coronary artery bypass grafting (196).
The typical operation in the study population took about 8 hours, Dr. Minatoya said (482 minutes). Timing of key operative steps were cardiopulmonary time of 254 minutes, cardiac arrest time of 146 minutes, antegrade cerebral perfusion time of 160 minutes and lower-body circulatory arrest time of 62 minutes.
“Since the mean age was 70 years old, we think the survival rate was acceptable,” Dr. Minatoya said, regarding overall study results. Overall risk factors for in-hospital death were short stature, long pump time, chronic kidney disease, and age of 80 and up, he said. Short stature was a risk factor for permanent neurological deficit, and males over age 80 had a higher risk for total arch replacement.
“Total arch replacement using the four-branched graft with antegrade cerebral perfusion could be accomplished with acceptable early and late results,” Dr. Minatoya said. “The branched-arch TEVAR may be a good option for octogenarians and patients with chronic kidney disease.”
Dr. Minatoya had no financial relationships to disclose.
AT THE AATS AORTIC SYMPOSIUM 2016
Key clinical point: Four-branched total aortic arch replacement can achieve acceptable early and late results.
Major finding: Overall in-hospital mortality was 5.2% and 5-year survival was 80.7%.
Data source: Consecutive series of 1,005 patients who had total arch replacement between 2001 and 2016 at two centers in Japan.
Disclosures: Dr. Minatoya reported having no financial disclosures.
Pediatric autologous aortic repair built to last
NEW YORK – With more than 1 million adults living today with congenital aortic disease, cardiovascular surgeons must think of outcomes in terms of decades, not years, when performing aortic arch repair in newborns, infants, and children, according to Charles D. Fraser Jr., M.D.
To that end, an all-autologous approach to aortic arch repair is key in preserving problem-free aortic function in adulthood, said Dr. Fraser, surgeon-in-chief at Texas Children’s Hospital in Houston.
Dr. Fraser reported on his center’s experience with all-autologous aortic arch repair techniques. He reviewed the following five principles that guide aortic arch repair in newborns, infants, and children at Texas Children’s Hospital:
• Use of autologous tissue reconstruction and avoidance of prosthetic material.
• Concomitant intracardiac repair.
• Use of anatomic reconstruction.
• Optimization of ventriculoarterial coupling.
• Preservation of laryngeal nerve function.
“The principles we developed at Texas Children’s Hospital we hope will translate into fewer of these patients that surgeons caring for adults with aortic disease will have to take care of later in life,” Dr. Fraser said at the meeting sponsored by the American Association for Thoracic Surgery. He reviewed cases in which he explained techniques he and his colleagues developed to address long-term outcomes.
The first challenge is to determine when to perform aortic repair in pediatric patients. “A question often asked is how small is too small when assessing the aortic arch in association with significant periductal coarctation?” he said. “Our rule of thumb has been that the arch diameter measured in millimeters should be at least the patient’s weight in kilograms plus one.” In other words, a 3-kg baby should have an aortic arch of at least 4 mm in diameter, he said.
He described the case of a 3.8-kg male baby on prostaglandin E1 who had aortic arch advancement repair and closure of atrial and ventricular septal defects at 8 days of age. The patient had an early origin of the left common carotid artery and a small proximal aortic arch. “This is the kind of patient in which we would do a complete aortic arch reconstruction, again with the autologous technique,” Dr. Fraser said.
In such a patient, Dr. Fraser and his colleagues at Texas Children’s Hospital support the circulation to the brain with antegrade cerebral perfusion, using transcranial Doppler and near-infrared spectroscopy to guide their profusion strategy, before putting the child on cardiac bypass and “profound” hypothermia. Careful planning before cannulation is important to perform the aortic transection at the correct level, he said
He also explained the ascending sliding arch aortoplasty, also known as the “Texas slide,” first described by E. Dean McKenzie, M.D., at Texas Children’s Hospital in 2011 (Ann. Thorac. Surg. 2011;91:805-10) This technique involves sliding a tongue-shaped piece of the ascending aorta underneath the aortic arch to construct an all-autologous repair.
“In patients with bicuspid aortic valves, we often observe that the ascending aorta is extremely elongated,” he said. “The idea is to take advantage of that and slide the ascending aorta completely up underneath the aortic arch and construct an all-autologous arch advancement type of repair.”
He presented the case of a 4-year-old boy with coarctation of the aorta in whom the Texas slide was indicated. “If this patient were treated with a simple coarctectomy, the patient would be subject to a life with a moderately hypoplastic aortic arch, and over the course of time, this could be problematic,” Dr. Fraser said. “The sliding reconstruction has relevance not only to the status of the aortic arch over the long term but it also has a profound effect on ventricular function.”
He noted a single-center, retrospective study from the United Kingdom that demonstrated that the quality of the aortic arch reconstruction, and the related opportunity for ventricular arterial coupling, directly correlate with long-term performance of the aortic arch in patients with hypoplastic left heart syndrome (J Thorac Cardiovasc Surg. 2014;148:1526-33).
“This is very important as part of the growing population of these patients who need long-term management, most of whom we’re anticipating managing not just for years, but for decades,” Dr. Fraser said.
He said he had no relevant financial disclosures.
NEW YORK – With more than 1 million adults living today with congenital aortic disease, cardiovascular surgeons must think of outcomes in terms of decades, not years, when performing aortic arch repair in newborns, infants, and children, according to Charles D. Fraser Jr., M.D.
To that end, an all-autologous approach to aortic arch repair is key in preserving problem-free aortic function in adulthood, said Dr. Fraser, surgeon-in-chief at Texas Children’s Hospital in Houston.
Dr. Fraser reported on his center’s experience with all-autologous aortic arch repair techniques. He reviewed the following five principles that guide aortic arch repair in newborns, infants, and children at Texas Children’s Hospital:
• Use of autologous tissue reconstruction and avoidance of prosthetic material.
• Concomitant intracardiac repair.
• Use of anatomic reconstruction.
• Optimization of ventriculoarterial coupling.
• Preservation of laryngeal nerve function.
“The principles we developed at Texas Children’s Hospital we hope will translate into fewer of these patients that surgeons caring for adults with aortic disease will have to take care of later in life,” Dr. Fraser said at the meeting sponsored by the American Association for Thoracic Surgery. He reviewed cases in which he explained techniques he and his colleagues developed to address long-term outcomes.
The first challenge is to determine when to perform aortic repair in pediatric patients. “A question often asked is how small is too small when assessing the aortic arch in association with significant periductal coarctation?” he said. “Our rule of thumb has been that the arch diameter measured in millimeters should be at least the patient’s weight in kilograms plus one.” In other words, a 3-kg baby should have an aortic arch of at least 4 mm in diameter, he said.
He described the case of a 3.8-kg male baby on prostaglandin E1 who had aortic arch advancement repair and closure of atrial and ventricular septal defects at 8 days of age. The patient had an early origin of the left common carotid artery and a small proximal aortic arch. “This is the kind of patient in which we would do a complete aortic arch reconstruction, again with the autologous technique,” Dr. Fraser said.
In such a patient, Dr. Fraser and his colleagues at Texas Children’s Hospital support the circulation to the brain with antegrade cerebral perfusion, using transcranial Doppler and near-infrared spectroscopy to guide their profusion strategy, before putting the child on cardiac bypass and “profound” hypothermia. Careful planning before cannulation is important to perform the aortic transection at the correct level, he said
He also explained the ascending sliding arch aortoplasty, also known as the “Texas slide,” first described by E. Dean McKenzie, M.D., at Texas Children’s Hospital in 2011 (Ann. Thorac. Surg. 2011;91:805-10) This technique involves sliding a tongue-shaped piece of the ascending aorta underneath the aortic arch to construct an all-autologous repair.
“In patients with bicuspid aortic valves, we often observe that the ascending aorta is extremely elongated,” he said. “The idea is to take advantage of that and slide the ascending aorta completely up underneath the aortic arch and construct an all-autologous arch advancement type of repair.”
He presented the case of a 4-year-old boy with coarctation of the aorta in whom the Texas slide was indicated. “If this patient were treated with a simple coarctectomy, the patient would be subject to a life with a moderately hypoplastic aortic arch, and over the course of time, this could be problematic,” Dr. Fraser said. “The sliding reconstruction has relevance not only to the status of the aortic arch over the long term but it also has a profound effect on ventricular function.”
He noted a single-center, retrospective study from the United Kingdom that demonstrated that the quality of the aortic arch reconstruction, and the related opportunity for ventricular arterial coupling, directly correlate with long-term performance of the aortic arch in patients with hypoplastic left heart syndrome (J Thorac Cardiovasc Surg. 2014;148:1526-33).
“This is very important as part of the growing population of these patients who need long-term management, most of whom we’re anticipating managing not just for years, but for decades,” Dr. Fraser said.
He said he had no relevant financial disclosures.
NEW YORK – With more than 1 million adults living today with congenital aortic disease, cardiovascular surgeons must think of outcomes in terms of decades, not years, when performing aortic arch repair in newborns, infants, and children, according to Charles D. Fraser Jr., M.D.
To that end, an all-autologous approach to aortic arch repair is key in preserving problem-free aortic function in adulthood, said Dr. Fraser, surgeon-in-chief at Texas Children’s Hospital in Houston.
Dr. Fraser reported on his center’s experience with all-autologous aortic arch repair techniques. He reviewed the following five principles that guide aortic arch repair in newborns, infants, and children at Texas Children’s Hospital:
• Use of autologous tissue reconstruction and avoidance of prosthetic material.
• Concomitant intracardiac repair.
• Use of anatomic reconstruction.
• Optimization of ventriculoarterial coupling.
• Preservation of laryngeal nerve function.
“The principles we developed at Texas Children’s Hospital we hope will translate into fewer of these patients that surgeons caring for adults with aortic disease will have to take care of later in life,” Dr. Fraser said at the meeting sponsored by the American Association for Thoracic Surgery. He reviewed cases in which he explained techniques he and his colleagues developed to address long-term outcomes.
The first challenge is to determine when to perform aortic repair in pediatric patients. “A question often asked is how small is too small when assessing the aortic arch in association with significant periductal coarctation?” he said. “Our rule of thumb has been that the arch diameter measured in millimeters should be at least the patient’s weight in kilograms plus one.” In other words, a 3-kg baby should have an aortic arch of at least 4 mm in diameter, he said.
He described the case of a 3.8-kg male baby on prostaglandin E1 who had aortic arch advancement repair and closure of atrial and ventricular septal defects at 8 days of age. The patient had an early origin of the left common carotid artery and a small proximal aortic arch. “This is the kind of patient in which we would do a complete aortic arch reconstruction, again with the autologous technique,” Dr. Fraser said.
In such a patient, Dr. Fraser and his colleagues at Texas Children’s Hospital support the circulation to the brain with antegrade cerebral perfusion, using transcranial Doppler and near-infrared spectroscopy to guide their profusion strategy, before putting the child on cardiac bypass and “profound” hypothermia. Careful planning before cannulation is important to perform the aortic transection at the correct level, he said
He also explained the ascending sliding arch aortoplasty, also known as the “Texas slide,” first described by E. Dean McKenzie, M.D., at Texas Children’s Hospital in 2011 (Ann. Thorac. Surg. 2011;91:805-10) This technique involves sliding a tongue-shaped piece of the ascending aorta underneath the aortic arch to construct an all-autologous repair.
“In patients with bicuspid aortic valves, we often observe that the ascending aorta is extremely elongated,” he said. “The idea is to take advantage of that and slide the ascending aorta completely up underneath the aortic arch and construct an all-autologous arch advancement type of repair.”
He presented the case of a 4-year-old boy with coarctation of the aorta in whom the Texas slide was indicated. “If this patient were treated with a simple coarctectomy, the patient would be subject to a life with a moderately hypoplastic aortic arch, and over the course of time, this could be problematic,” Dr. Fraser said. “The sliding reconstruction has relevance not only to the status of the aortic arch over the long term but it also has a profound effect on ventricular function.”
He noted a single-center, retrospective study from the United Kingdom that demonstrated that the quality of the aortic arch reconstruction, and the related opportunity for ventricular arterial coupling, directly correlate with long-term performance of the aortic arch in patients with hypoplastic left heart syndrome (J Thorac Cardiovasc Surg. 2014;148:1526-33).
“This is very important as part of the growing population of these patients who need long-term management, most of whom we’re anticipating managing not just for years, but for decades,” Dr. Fraser said.
He said he had no relevant financial disclosures.
AT AATS AORTIC SYMPOSIUM 2016
Key clinical point: Surgeons must think of outcomes for operations to correct aortic arch disease in children in the context of decades, not years.
Major finding: Five principles should guide autologous aortic arch repair in newborns, infants, and children.
Data source: Case studies from Texas Children’s Hospital.
Disclosures: Dr. Fraser reported having no relevant financial disclosures.
Protective hypothermia during arch surgery lacked benefit, study shows
NEW YORK – Deep hypothermia may affect long-term survival in individuals who have aortic arch surgery with antegrade cerebral perfusion (ACP), but not short-term outcomes in terms of death and major morbidities, according to a Baylor College of Medicine study.
The study evaluated outcomes of 544 consecutive patients who had proximal and total aortic arch surgery and received ACP for more than 30 minutes over a 10-year period, said lead investigator Ourania Preventza, MD, of the division of cardiothoracic surgery at the college in Houston. The researchers compared results of three different hypothermia levels: deep hypothermia at 14.1°-20° C; low-moderate at 20.1°-23.9° C; and high-moderate at 24°-28° C. The study also classified ACP time in two levels: 31-45 minutes for 238 patients (43.8%); and 45 minutes or more in 306 patients (56.3%).
“The different temperature levels did not significantly affect the short-term mortality and major morbidity rates,” Dr. Preventza said. “Reoperation for bleeding was associated with lower temperature (14.1°-20° C). The long-term survival rate in patients who underwent proximal arch surgery involving ACP for more than 30 minutes and use of moderate hypothermia (20.1°-28° C) were actually improved.”
While the outcomes showed small variations between the three groups, with deep hypothermia being associated with a higher percentage of adverse outcomes, Dr. Preventza said the differences were not statistically significant. The overall operative mortality rate was 12.5% (68 patients): 15.5% (18 patients) in the deep-hypothermia group; 11.8% (31 patients) in the low-moderate group; and 11.5% (19 patients) in the high-moderate group (P = 0.54).
The patients who underwent deep hypothermia were more likely to receive unilateral ACP, and those who underwent moderate hypothermia were more likely to have bilateral ACP, Dr. Preventza said at the meeting sponsored by the American Association for Thoracic Surgery. The deep-hypothermia group had higher transfusion rates, but, again, the researchers did not consider this variation to be statistically significant.
In the deep-hypothermia group, 20.9% of patients had a reoperation for bleeding, compared with 11.3% in the overall group and 7.7% and 10.2% in the low- and high-moderate groups, respectively, Dr. Preventza reported. Multivariate analysis revealed that higher temperature was associated with less bleeding, with an odds ratio of 0.61 (P = 0.015).
Deep hypothermia was related to statistically significant differences in the rates of permanent stroke and permanent neurologic events in the univariate analysis only, Dr. Preventza said: 6.3% and 7.2%, respectively, in the overall analysis vs. 12.2% for both events in the deep-hypothermia group. In the propensity score analysis, the rates of permanent stroke and permanent neurologic events in the moderate-hypothermia group were 7.6% and 8.5%, respectively, vs. 11.3% for both events in the deep-hypothermia group, a nonsignificant difference.
“With regard to permanent stoke and permanent neurological events, the multivariate analysis showed that preoperatively a neurologic deficit as well as acute type I aortic dissection were associated with adverse neurological events,” she said.
“However,” Dr. Preventza added, “the surprising thing is that when we looked at long-term survival for the entire cohort, we saw that the patients with moderate hypothermia did better.”
Kaplan-Meier analysis for the propensity pairs showed that the probability of survival at 8 years was 55.3% for the deep-hypothermia group vs. 68.5% for the moderate-hypothermia group.
The approach the Baylor researchers used involved cannulating the axillary or innominate artery in most patients before administering ACP, although a few patients had femoral or direct aortic cannulation, Dr. Preventza said. For bilateral ACP, the researchers delivered cerebral perfusion via a 9-French Pruitt balloon-tip catheter (LeMaitre Vascular) in the left common carotid artery. To protect the brain, they administered perfusion at 8-12 cc/kg per min and maintained a perfusion pressure of 50-70 mm Hg, as measured via the radial arterial line and guided by near-infrared spectroscopy.
Dr. Preventza had no relevant disclosures.
NEW YORK – Deep hypothermia may affect long-term survival in individuals who have aortic arch surgery with antegrade cerebral perfusion (ACP), but not short-term outcomes in terms of death and major morbidities, according to a Baylor College of Medicine study.
The study evaluated outcomes of 544 consecutive patients who had proximal and total aortic arch surgery and received ACP for more than 30 minutes over a 10-year period, said lead investigator Ourania Preventza, MD, of the division of cardiothoracic surgery at the college in Houston. The researchers compared results of three different hypothermia levels: deep hypothermia at 14.1°-20° C; low-moderate at 20.1°-23.9° C; and high-moderate at 24°-28° C. The study also classified ACP time in two levels: 31-45 minutes for 238 patients (43.8%); and 45 minutes or more in 306 patients (56.3%).
“The different temperature levels did not significantly affect the short-term mortality and major morbidity rates,” Dr. Preventza said. “Reoperation for bleeding was associated with lower temperature (14.1°-20° C). The long-term survival rate in patients who underwent proximal arch surgery involving ACP for more than 30 minutes and use of moderate hypothermia (20.1°-28° C) were actually improved.”
While the outcomes showed small variations between the three groups, with deep hypothermia being associated with a higher percentage of adverse outcomes, Dr. Preventza said the differences were not statistically significant. The overall operative mortality rate was 12.5% (68 patients): 15.5% (18 patients) in the deep-hypothermia group; 11.8% (31 patients) in the low-moderate group; and 11.5% (19 patients) in the high-moderate group (P = 0.54).
The patients who underwent deep hypothermia were more likely to receive unilateral ACP, and those who underwent moderate hypothermia were more likely to have bilateral ACP, Dr. Preventza said at the meeting sponsored by the American Association for Thoracic Surgery. The deep-hypothermia group had higher transfusion rates, but, again, the researchers did not consider this variation to be statistically significant.
In the deep-hypothermia group, 20.9% of patients had a reoperation for bleeding, compared with 11.3% in the overall group and 7.7% and 10.2% in the low- and high-moderate groups, respectively, Dr. Preventza reported. Multivariate analysis revealed that higher temperature was associated with less bleeding, with an odds ratio of 0.61 (P = 0.015).
Deep hypothermia was related to statistically significant differences in the rates of permanent stroke and permanent neurologic events in the univariate analysis only, Dr. Preventza said: 6.3% and 7.2%, respectively, in the overall analysis vs. 12.2% for both events in the deep-hypothermia group. In the propensity score analysis, the rates of permanent stroke and permanent neurologic events in the moderate-hypothermia group were 7.6% and 8.5%, respectively, vs. 11.3% for both events in the deep-hypothermia group, a nonsignificant difference.
“With regard to permanent stoke and permanent neurological events, the multivariate analysis showed that preoperatively a neurologic deficit as well as acute type I aortic dissection were associated with adverse neurological events,” she said.
“However,” Dr. Preventza added, “the surprising thing is that when we looked at long-term survival for the entire cohort, we saw that the patients with moderate hypothermia did better.”
Kaplan-Meier analysis for the propensity pairs showed that the probability of survival at 8 years was 55.3% for the deep-hypothermia group vs. 68.5% for the moderate-hypothermia group.
The approach the Baylor researchers used involved cannulating the axillary or innominate artery in most patients before administering ACP, although a few patients had femoral or direct aortic cannulation, Dr. Preventza said. For bilateral ACP, the researchers delivered cerebral perfusion via a 9-French Pruitt balloon-tip catheter (LeMaitre Vascular) in the left common carotid artery. To protect the brain, they administered perfusion at 8-12 cc/kg per min and maintained a perfusion pressure of 50-70 mm Hg, as measured via the radial arterial line and guided by near-infrared spectroscopy.
Dr. Preventza had no relevant disclosures.
NEW YORK – Deep hypothermia may affect long-term survival in individuals who have aortic arch surgery with antegrade cerebral perfusion (ACP), but not short-term outcomes in terms of death and major morbidities, according to a Baylor College of Medicine study.
The study evaluated outcomes of 544 consecutive patients who had proximal and total aortic arch surgery and received ACP for more than 30 minutes over a 10-year period, said lead investigator Ourania Preventza, MD, of the division of cardiothoracic surgery at the college in Houston. The researchers compared results of three different hypothermia levels: deep hypothermia at 14.1°-20° C; low-moderate at 20.1°-23.9° C; and high-moderate at 24°-28° C. The study also classified ACP time in two levels: 31-45 minutes for 238 patients (43.8%); and 45 minutes or more in 306 patients (56.3%).
“The different temperature levels did not significantly affect the short-term mortality and major morbidity rates,” Dr. Preventza said. “Reoperation for bleeding was associated with lower temperature (14.1°-20° C). The long-term survival rate in patients who underwent proximal arch surgery involving ACP for more than 30 minutes and use of moderate hypothermia (20.1°-28° C) were actually improved.”
While the outcomes showed small variations between the three groups, with deep hypothermia being associated with a higher percentage of adverse outcomes, Dr. Preventza said the differences were not statistically significant. The overall operative mortality rate was 12.5% (68 patients): 15.5% (18 patients) in the deep-hypothermia group; 11.8% (31 patients) in the low-moderate group; and 11.5% (19 patients) in the high-moderate group (P = 0.54).
The patients who underwent deep hypothermia were more likely to receive unilateral ACP, and those who underwent moderate hypothermia were more likely to have bilateral ACP, Dr. Preventza said at the meeting sponsored by the American Association for Thoracic Surgery. The deep-hypothermia group had higher transfusion rates, but, again, the researchers did not consider this variation to be statistically significant.
In the deep-hypothermia group, 20.9% of patients had a reoperation for bleeding, compared with 11.3% in the overall group and 7.7% and 10.2% in the low- and high-moderate groups, respectively, Dr. Preventza reported. Multivariate analysis revealed that higher temperature was associated with less bleeding, with an odds ratio of 0.61 (P = 0.015).
Deep hypothermia was related to statistically significant differences in the rates of permanent stroke and permanent neurologic events in the univariate analysis only, Dr. Preventza said: 6.3% and 7.2%, respectively, in the overall analysis vs. 12.2% for both events in the deep-hypothermia group. In the propensity score analysis, the rates of permanent stroke and permanent neurologic events in the moderate-hypothermia group were 7.6% and 8.5%, respectively, vs. 11.3% for both events in the deep-hypothermia group, a nonsignificant difference.
“With regard to permanent stoke and permanent neurological events, the multivariate analysis showed that preoperatively a neurologic deficit as well as acute type I aortic dissection were associated with adverse neurological events,” she said.
“However,” Dr. Preventza added, “the surprising thing is that when we looked at long-term survival for the entire cohort, we saw that the patients with moderate hypothermia did better.”
Kaplan-Meier analysis for the propensity pairs showed that the probability of survival at 8 years was 55.3% for the deep-hypothermia group vs. 68.5% for the moderate-hypothermia group.
The approach the Baylor researchers used involved cannulating the axillary or innominate artery in most patients before administering ACP, although a few patients had femoral or direct aortic cannulation, Dr. Preventza said. For bilateral ACP, the researchers delivered cerebral perfusion via a 9-French Pruitt balloon-tip catheter (LeMaitre Vascular) in the left common carotid artery. To protect the brain, they administered perfusion at 8-12 cc/kg per min and maintained a perfusion pressure of 50-70 mm Hg, as measured via the radial arterial line and guided by near-infrared spectroscopy.
Dr. Preventza had no relevant disclosures.
AT AATS AORTIC SYMPOSIUM 2016
Key clinical point: Differing temperatures of hypothermia did not affect death or morbidity in patients who had aortic arch surgery with more than 30 minutes of antegrade cerebral perfusion.
Major finding: The overall operative death rate in the study was 12.4% with no statistically significant differences between three different hypothermia groups.
Data source: Series of 510 consecutive patients who had proximal and total arch surgery and received antegrade cerebral perfusion for more than 30 minutes over a 10-year period.
Disclosures: Dr. Preventza reported having no financial disclosures.
Surgery for acute type A dissection shows 20-year shift to valve sparing, biological valves
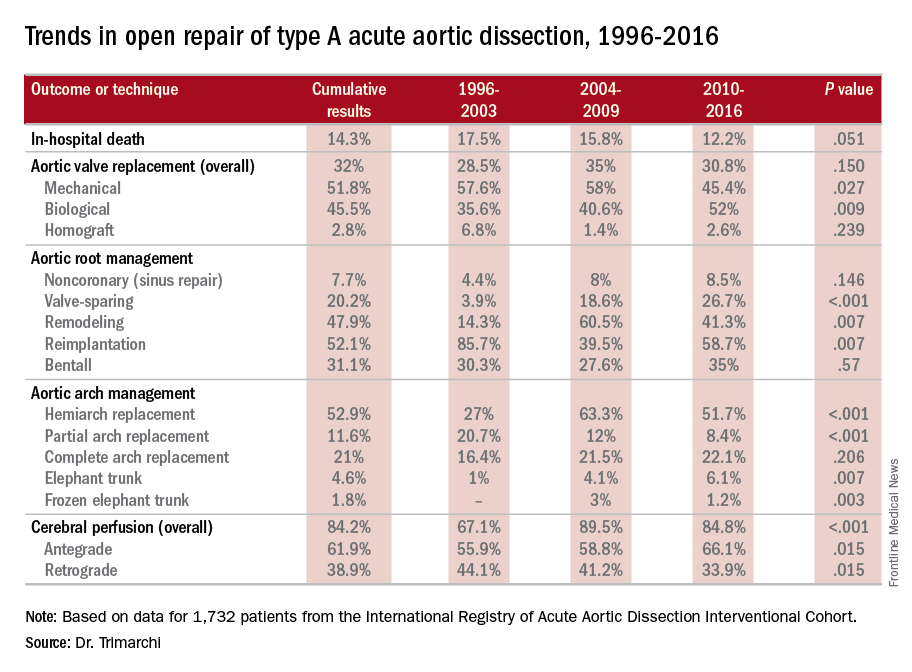
NEW YORK – A study of an international database of individuals who have had open repair for acute type A aortic dissection (ATAAD) has revealed that in the past 20 years, cardiovascular surgeons have widely embraced valve-sparing procedures, bioprosthetic valves, and cerebral profusion strategies, according to a report here on the latest analysis of the database.
The most telling result is the decline in overall mortality, Santi Trimarchi, MD, PhD, of the University of Milan IRCCS Policlinico San Donato in Italy reported on behalf of the International Registry of Acute Aortic Dissection (IRAD) Interventional Cohort (IVC). The cohort analyzed surgery techniques and outcomes of 1,732 patients who had open repair from 1996 to 2016, clustering results in three time intervals: 1996-2003; 2004-2009; and 2010-2015.
“We noted in the registry that the overall in-hospital mortality rate was 14.3%, and this mortality decreased over time from 17.5% in the first six-year time span to 12.2% in the last six years,” Dr. Trimarchi said.

Among other trends the study identified are greater reliance on biological vs. mechanical valves, an increase in valve-sparing procedures, and steady use of Bentall procedures throughout the study period. “Operative techniques for redo aortic valve repair have been improving over the time, and that’s why we see more frequent use of biologic valves,” he said at the meeting, sponsored by the American Association for Thoracic Surgery.
“Cerebral profusion management has been widely adopted,” Dr. Trimarchi said. “Also there is an important trend showing an increasing utilization of antegrade cerebral profusion while we see a negative trend of the utilization of retrograde brain protection.”
Dr. Trimarchi attributed the detail the study generated to the survey form sent to the 26 IRAD-IVC sites around the world. The form measures 131 different variables, he said.
“Using this new specific surgical data form, we think we can address some surgical issues and report better data from the IRAD registry results on acute dissection,” he said. “These analyses have shown there have been significant changes in operative strategy over time in terms of managing such patients, and more importantly, a significant decrease in in-hospital mortality was observed in a 20-year time period.”
Dr. Trimarchi disclosed that he has received speaking and consulting fees and research support from W.L. Gore & Associates and Medtronic. IRAD is supported by W.L. Gore, Active Sites, Medtronic, Varbedian Aortic Research Fund, the Hewlett Foundation, the Mardigian Foundation, UM Faculty Group Practice, Terumo, and Ann and Bob Aikens.
NEW YORK – A study of an international database of individuals who have had open repair for acute type A aortic dissection (ATAAD) has revealed that in the past 20 years, cardiovascular surgeons have widely embraced valve-sparing procedures, bioprosthetic valves, and cerebral profusion strategies, according to a report here on the latest analysis of the database.
The most telling result is the decline in overall mortality, Santi Trimarchi, MD, PhD, of the University of Milan IRCCS Policlinico San Donato in Italy reported on behalf of the International Registry of Acute Aortic Dissection (IRAD) Interventional Cohort (IVC). The cohort analyzed surgery techniques and outcomes of 1,732 patients who had open repair from 1996 to 2016, clustering results in three time intervals: 1996-2003; 2004-2009; and 2010-2015.
“We noted in the registry that the overall in-hospital mortality rate was 14.3%, and this mortality decreased over time from 17.5% in the first six-year time span to 12.2% in the last six years,” Dr. Trimarchi said.

Among other trends the study identified are greater reliance on biological vs. mechanical valves, an increase in valve-sparing procedures, and steady use of Bentall procedures throughout the study period. “Operative techniques for redo aortic valve repair have been improving over the time, and that’s why we see more frequent use of biologic valves,” he said at the meeting, sponsored by the American Association for Thoracic Surgery.
“Cerebral profusion management has been widely adopted,” Dr. Trimarchi said. “Also there is an important trend showing an increasing utilization of antegrade cerebral profusion while we see a negative trend of the utilization of retrograde brain protection.”
Dr. Trimarchi attributed the detail the study generated to the survey form sent to the 26 IRAD-IVC sites around the world. The form measures 131 different variables, he said.
“Using this new specific surgical data form, we think we can address some surgical issues and report better data from the IRAD registry results on acute dissection,” he said. “These analyses have shown there have been significant changes in operative strategy over time in terms of managing such patients, and more importantly, a significant decrease in in-hospital mortality was observed in a 20-year time period.”
Dr. Trimarchi disclosed that he has received speaking and consulting fees and research support from W.L. Gore & Associates and Medtronic. IRAD is supported by W.L. Gore, Active Sites, Medtronic, Varbedian Aortic Research Fund, the Hewlett Foundation, the Mardigian Foundation, UM Faculty Group Practice, Terumo, and Ann and Bob Aikens.
NEW YORK – A study of an international database of individuals who have had open repair for acute type A aortic dissection (ATAAD) has revealed that in the past 20 years, cardiovascular surgeons have widely embraced valve-sparing procedures, bioprosthetic valves, and cerebral profusion strategies, according to a report here on the latest analysis of the database.
The most telling result is the decline in overall mortality, Santi Trimarchi, MD, PhD, of the University of Milan IRCCS Policlinico San Donato in Italy reported on behalf of the International Registry of Acute Aortic Dissection (IRAD) Interventional Cohort (IVC). The cohort analyzed surgery techniques and outcomes of 1,732 patients who had open repair from 1996 to 2016, clustering results in three time intervals: 1996-2003; 2004-2009; and 2010-2015.
“We noted in the registry that the overall in-hospital mortality rate was 14.3%, and this mortality decreased over time from 17.5% in the first six-year time span to 12.2% in the last six years,” Dr. Trimarchi said.

Among other trends the study identified are greater reliance on biological vs. mechanical valves, an increase in valve-sparing procedures, and steady use of Bentall procedures throughout the study period. “Operative techniques for redo aortic valve repair have been improving over the time, and that’s why we see more frequent use of biologic valves,” he said at the meeting, sponsored by the American Association for Thoracic Surgery.
“Cerebral profusion management has been widely adopted,” Dr. Trimarchi said. “Also there is an important trend showing an increasing utilization of antegrade cerebral profusion while we see a negative trend of the utilization of retrograde brain protection.”
Dr. Trimarchi attributed the detail the study generated to the survey form sent to the 26 IRAD-IVC sites around the world. The form measures 131 different variables, he said.
“Using this new specific surgical data form, we think we can address some surgical issues and report better data from the IRAD registry results on acute dissection,” he said. “These analyses have shown there have been significant changes in operative strategy over time in terms of managing such patients, and more importantly, a significant decrease in in-hospital mortality was observed in a 20-year time period.”
Dr. Trimarchi disclosed that he has received speaking and consulting fees and research support from W.L. Gore & Associates and Medtronic. IRAD is supported by W.L. Gore, Active Sites, Medtronic, Varbedian Aortic Research Fund, the Hewlett Foundation, the Mardigian Foundation, UM Faculty Group Practice, Terumo, and Ann and Bob Aikens.
AT AATS AORTIC SYMPOSIUM 2016
Key clinical point: Operations for acute type A aortic dissection (ATAAD) have seen significant changes in technique over the past 20 years.
Major finding: Use of biological valves increased from 35.6% of procedures to 52% over the study period while reliance of mechanical valves declined from 57.6% to 45.4%.
Data source: Interventional Cohort database of 1,732 patients enrolled in the International Registry of Acute Aortic Dissection database who had open surgery for ATAAD from February 1996 to March 2015.
Disclosures: Dr. Trimarchi disclosed having receive speaking and consulting fees from W.L. Gore & Associates and Medtronic as well as research support from the two companies. IRAD is supported by W.L. Gore, Active Sites, Medtronic, Varbedian Aortic Research Fund, the Hewlett Foundation, the Mardigian Foundation, UM Faculty Group Practice, Terumo, and Ann and Bob Aikens.
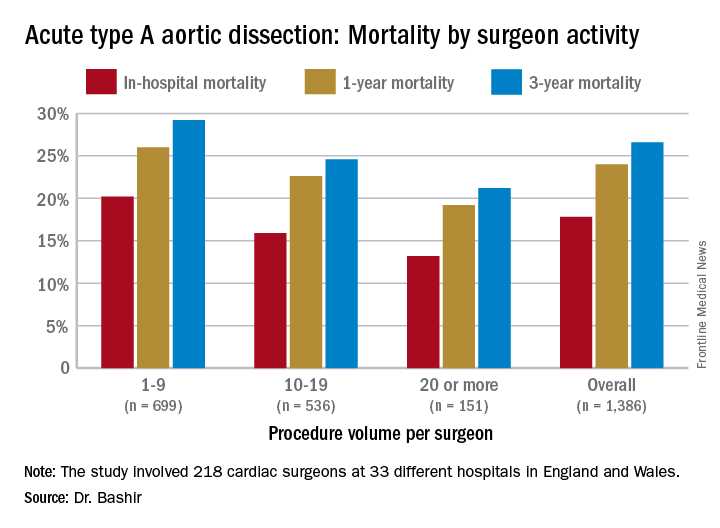
Study quantifies volume disparities for ATAD repair in the U.K.
NEW YORK – Mastery is the product of repetition, and it has long been taken for granted that surgeons and centers that perform a high volume of an operation will have better results than those who don’t do the operation as often, but a study out of the United Kingdom has determined just how much better high-volume centers are when it comes to repair of acute type A aortic dissection (ATAD) – and what the in-hospital mortality odds ratio is for lower-volume surgeons.
Specifically, that odds ratio is 1.64 (P = .030), Mohamad Bashir, MD, PhD, MRCS, a research fellow at Liverpool Heart and Chest Hospital, said in reporting early results of the study here. Lower-volume surgeons had worse outcomes in 12 of 14 different operative metrics the study evaluated, most notably in-hospital mortality: 20.2% for lower-volume surgeons vs. 15.2% for higher-volume surgeons. “There is an initiative in the U.K. to change the trend,” Dr. Bashir said. Full study results will be published in an upcoming issue of BMJ, he said.
“In-hospital mortality for surgeons who operate on 20 or more procedures is very good at 13.2%, and the same follows for 90-day mortality, one-year mortality and three-year mortality,” Dr. Bashir said.
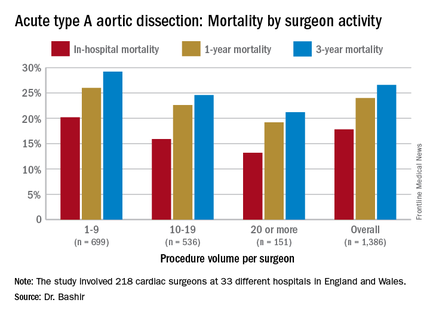
The study evaluated 1,386 ATAD procedures in the National Institute for Cardiovascular Outcomes Research database by 218 different cardiac surgeons at 33 different hospitals in England and Wales from April 2007 to March 2013. That would make the average number of procedures per surgeon 6.4, Dr. Bashir said, but a closer look at each surgeon’s case load reveals some disconcerting trends: almost 80% of the surgeons performed fewer than 10 ATAD repairs in the 6-year span of the study, and 34 surgeons, or about 15%, just did a single procedure in that time. The highest-volume surgeon did 32 procedures. The minimum hospital volume was 8 ATAD operations and the maximum was 103.
The study stratified lower- and higher-volume surgeon groups by characteristics of the patients they operated on. “The differences between these two groups are pretty interesting because we noticed that the lower-volume surgeons are actually operating on patients who are diabetic, who are smokers, who use inotropic support prior to anesthesia and who also have an injection fraction that is significant,” Dr. Bashir said.
In drilling down into those characteristics, people with diabetes made up 6% of the lower-volume surgeons’ cases vs. 3.1% of the higher-volume surgeons’ cases, despite an almost 50-50 split in share of procedures between the two surgeon groups. Current smokers comprised 20.5% of the lower-volume surgeons’ patients vs. 15.5% of their high-volume counterparts’ patients. Operative characteristics in terms of urgency of surgery were similar between the two groups. However Dr. Bashir noted, lower-volume surgeons had longer times for cardiopulmonary bypass, aortic cross-clamping, and circulatory arrest.
The study investigators applied a multivariable logistic regression model to determine predictors of in-hospital mortality for ATAD. “The odds ratio (OR) of mortality for lower-volume surgeons is 1.64, which is statistically significant,” Dr. Bashir said. Odds ratios for other predictors are: previous cardiac surgery, 2.51; peripheral vascular disease, 2.15; preoperative cardiogenic shock, 2.05; salvage operation, 5.57; and concomitant coronary artery bypass procedure, 2.98. For 5-year mortality, the odds ratio was 1.37 for the lower-volume surgeons.
Dr. Bashir laid out how the National Health Service can use the study results. “Concentration of expertise and volume to the appropriate surgeons and centers who perform increasingly more work and more complex aortic cases would be required to change the paradigm of acute type A aortic dissection outcomes in the U.K.,” he said. “It is reasonable to suggest that there should be a national standardization mandate and a quality-improvement framework of acute aortic dissection treatment.”
Dr. Bashir had no financial relationships to disclose.
NEW YORK – Mastery is the product of repetition, and it has long been taken for granted that surgeons and centers that perform a high volume of an operation will have better results than those who don’t do the operation as often, but a study out of the United Kingdom has determined just how much better high-volume centers are when it comes to repair of acute type A aortic dissection (ATAD) – and what the in-hospital mortality odds ratio is for lower-volume surgeons.
Specifically, that odds ratio is 1.64 (P = .030), Mohamad Bashir, MD, PhD, MRCS, a research fellow at Liverpool Heart and Chest Hospital, said in reporting early results of the study here. Lower-volume surgeons had worse outcomes in 12 of 14 different operative metrics the study evaluated, most notably in-hospital mortality: 20.2% for lower-volume surgeons vs. 15.2% for higher-volume surgeons. “There is an initiative in the U.K. to change the trend,” Dr. Bashir said. Full study results will be published in an upcoming issue of BMJ, he said.
“In-hospital mortality for surgeons who operate on 20 or more procedures is very good at 13.2%, and the same follows for 90-day mortality, one-year mortality and three-year mortality,” Dr. Bashir said.
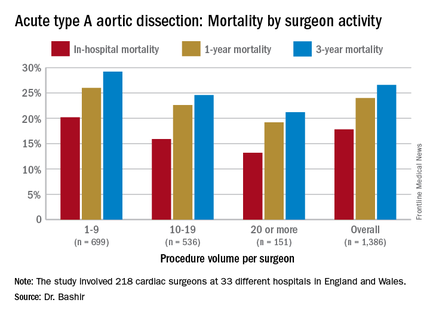
The study evaluated 1,386 ATAD procedures in the National Institute for Cardiovascular Outcomes Research database by 218 different cardiac surgeons at 33 different hospitals in England and Wales from April 2007 to March 2013. That would make the average number of procedures per surgeon 6.4, Dr. Bashir said, but a closer look at each surgeon’s case load reveals some disconcerting trends: almost 80% of the surgeons performed fewer than 10 ATAD repairs in the 6-year span of the study, and 34 surgeons, or about 15%, just did a single procedure in that time. The highest-volume surgeon did 32 procedures. The minimum hospital volume was 8 ATAD operations and the maximum was 103.
The study stratified lower- and higher-volume surgeon groups by characteristics of the patients they operated on. “The differences between these two groups are pretty interesting because we noticed that the lower-volume surgeons are actually operating on patients who are diabetic, who are smokers, who use inotropic support prior to anesthesia and who also have an injection fraction that is significant,” Dr. Bashir said.
In drilling down into those characteristics, people with diabetes made up 6% of the lower-volume surgeons’ cases vs. 3.1% of the higher-volume surgeons’ cases, despite an almost 50-50 split in share of procedures between the two surgeon groups. Current smokers comprised 20.5% of the lower-volume surgeons’ patients vs. 15.5% of their high-volume counterparts’ patients. Operative characteristics in terms of urgency of surgery were similar between the two groups. However Dr. Bashir noted, lower-volume surgeons had longer times for cardiopulmonary bypass, aortic cross-clamping, and circulatory arrest.
The study investigators applied a multivariable logistic regression model to determine predictors of in-hospital mortality for ATAD. “The odds ratio (OR) of mortality for lower-volume surgeons is 1.64, which is statistically significant,” Dr. Bashir said. Odds ratios for other predictors are: previous cardiac surgery, 2.51; peripheral vascular disease, 2.15; preoperative cardiogenic shock, 2.05; salvage operation, 5.57; and concomitant coronary artery bypass procedure, 2.98. For 5-year mortality, the odds ratio was 1.37 for the lower-volume surgeons.
Dr. Bashir laid out how the National Health Service can use the study results. “Concentration of expertise and volume to the appropriate surgeons and centers who perform increasingly more work and more complex aortic cases would be required to change the paradigm of acute type A aortic dissection outcomes in the U.K.,” he said. “It is reasonable to suggest that there should be a national standardization mandate and a quality-improvement framework of acute aortic dissection treatment.”
Dr. Bashir had no financial relationships to disclose.
NEW YORK – Mastery is the product of repetition, and it has long been taken for granted that surgeons and centers that perform a high volume of an operation will have better results than those who don’t do the operation as often, but a study out of the United Kingdom has determined just how much better high-volume centers are when it comes to repair of acute type A aortic dissection (ATAD) – and what the in-hospital mortality odds ratio is for lower-volume surgeons.
Specifically, that odds ratio is 1.64 (P = .030), Mohamad Bashir, MD, PhD, MRCS, a research fellow at Liverpool Heart and Chest Hospital, said in reporting early results of the study here. Lower-volume surgeons had worse outcomes in 12 of 14 different operative metrics the study evaluated, most notably in-hospital mortality: 20.2% for lower-volume surgeons vs. 15.2% for higher-volume surgeons. “There is an initiative in the U.K. to change the trend,” Dr. Bashir said. Full study results will be published in an upcoming issue of BMJ, he said.
“In-hospital mortality for surgeons who operate on 20 or more procedures is very good at 13.2%, and the same follows for 90-day mortality, one-year mortality and three-year mortality,” Dr. Bashir said.
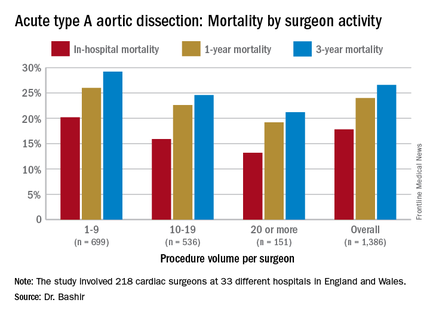
The study evaluated 1,386 ATAD procedures in the National Institute for Cardiovascular Outcomes Research database by 218 different cardiac surgeons at 33 different hospitals in England and Wales from April 2007 to March 2013. That would make the average number of procedures per surgeon 6.4, Dr. Bashir said, but a closer look at each surgeon’s case load reveals some disconcerting trends: almost 80% of the surgeons performed fewer than 10 ATAD repairs in the 6-year span of the study, and 34 surgeons, or about 15%, just did a single procedure in that time. The highest-volume surgeon did 32 procedures. The minimum hospital volume was 8 ATAD operations and the maximum was 103.
The study stratified lower- and higher-volume surgeon groups by characteristics of the patients they operated on. “The differences between these two groups are pretty interesting because we noticed that the lower-volume surgeons are actually operating on patients who are diabetic, who are smokers, who use inotropic support prior to anesthesia and who also have an injection fraction that is significant,” Dr. Bashir said.
In drilling down into those characteristics, people with diabetes made up 6% of the lower-volume surgeons’ cases vs. 3.1% of the higher-volume surgeons’ cases, despite an almost 50-50 split in share of procedures between the two surgeon groups. Current smokers comprised 20.5% of the lower-volume surgeons’ patients vs. 15.5% of their high-volume counterparts’ patients. Operative characteristics in terms of urgency of surgery were similar between the two groups. However Dr. Bashir noted, lower-volume surgeons had longer times for cardiopulmonary bypass, aortic cross-clamping, and circulatory arrest.
The study investigators applied a multivariable logistic regression model to determine predictors of in-hospital mortality for ATAD. “The odds ratio (OR) of mortality for lower-volume surgeons is 1.64, which is statistically significant,” Dr. Bashir said. Odds ratios for other predictors are: previous cardiac surgery, 2.51; peripheral vascular disease, 2.15; preoperative cardiogenic shock, 2.05; salvage operation, 5.57; and concomitant coronary artery bypass procedure, 2.98. For 5-year mortality, the odds ratio was 1.37 for the lower-volume surgeons.
Dr. Bashir laid out how the National Health Service can use the study results. “Concentration of expertise and volume to the appropriate surgeons and centers who perform increasingly more work and more complex aortic cases would be required to change the paradigm of acute type A aortic dissection outcomes in the U.K.,” he said. “It is reasonable to suggest that there should be a national standardization mandate and a quality-improvement framework of acute aortic dissection treatment.”
Dr. Bashir had no financial relationships to disclose.
AT THE AMERICAN ASSOCIATION FOR THORACIC SURGERY AORTIC SYMPOSIUM
Key clinical point: Patients undergoing repair of acute type A aortic dissection (ATAD) by lower-volume surgeons have high mortality in comparison with those undergoing repair by the highest-volume surgeons.
Major finding: In-hospital mortality for ATAD repair was 20.2% for lower-volume surgeons and 15.3% for higher-volume surgeons.
Data source: Analysis of 1,386 ATAD procedures from April 2007 to March 2013 in the National Institute for Cardiovascular Outcomes Research data.
Disclosures: Dr. Bashir reported having no financial disclosures.
Guideline tweak addresses conflicting recommendations on BAV
NEW YORK – While overall guidelines for aortic repair surgery have not changed significantly in the past 5 years, guidelines for the timing of surgery in patients with bicuspid aortic valves and enlarged aortas have undergone some updating in an attempt to clear up disparities in different guidelines on when to operate on those patients.
Lars G. Svensson, MD, PhD, chairman of the Cleveland Clinic Heart and Vascular Institute, coauthor of the clarification statement by the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines (J Thorac Cardiovasc Surg. 2016;151:959-66), reported on the guidelines clarification at the meeting sponsored by the American Association for Thoracic Surgery. He noted that five different clinical guidelines between 2010 and 2014 recommended five different size thresholds for prophylactic aortic root or ascending aortic surgery in the setting of bicuspid aortic valve (BAV), ranging from 4 cm to greater than 5.5 cm. “This created a bit of a quandary and controversy between different guidelines and time periods,” he said.
Dr. Svensson and Loren Hiratzka, MD, medical director of cardiac surgery for TriHealth in Cincinnati, and their colleagues drafted the guideline clarification that makes the following recommendations for aortic root and ascending aorta repair or replacement when patients have BAV (strength of recommendation):
• Surgery is indicated to replace the aortic root or ascending aorta in asymptomatic patients with BAV if the diameter of the aortic root or ascending aorta is 5.5 cm or greater (Class 1).
• Surgical repair is indicated for asymptomatic patients with BAV if the root or ascending aorta diameter is 5 cm or greater in two scenarios: if the patient has an additional risk factor for dissection, such as family history or excessive aortic growth rate; or if the patient is a low surgical risk and has access to an experienced surgeon at a high-volume center (Class IIa).
The guideline update also addresses BAV in patients with Turner syndrome. The 2010 joint guidelines of 10 societies left some questions with regard to surgery in these patients, Dr. Svensson said. The established guidelines included a Class IIb recommendation for imaging of the heart and aorta to help determine the aorta risk in patients with Turner syndrome who had additional risk factors, including BAV, aortic coarctation and/or hypertension, or were planning a pregnancy.
The updated guideline includes Class IIa recommendation that in short-statured patients with Turner syndrome and BAV, measurement of the aortic root or ascending aorta diameter may not predict the dissection risk as well as aortic diameter index greater than 2.5 cm/m2. The updated recommendations also draw on one study that reported that in patients with BAV, a maximum aortic cross-sectional area-to-height ratio of 10 cm2/m or greater was also predictive of aortic dissection. (Ann Thorac Surg. 2015;100:1666-73)
The updated recommendations for open surgery for ascending aortic aneurysm include separate valve and ascending aortic replacement in patients without significant aortic root dilatation or in elderly patients, or in younger patients with minimal dilatation who have aortic valve disease; and excision of the sinuses of Valsalva with a modified David reimplantation when technically feasible in patients with connective tissue disease and others with dilatation of the aortic root and sinuses. For patients in whom the latter procedure is not feasible, root replacement with valved graft conduit would be indicated, Dr. Svensson said.
Dr. Svensson also reported on recent studies that validated recommendations in established guidelines.
Studies of circulatory arrest practices in aortic arch surgery as prescribed by established guidelines showed confirmatory results, he said. “The one point I would make about circulatory arrest is that we found in a fairly large study of 1,352 circulatory arrest patients that we reduced the risk of stroke by 40% when we used the axillary artery with a side a graft,” he said (Ann Thorac Surg. 2004;78:1274-84). His own institution’s clinical trial of 121 patients who received antegrade or retrograde brain perfusion showed rates of 0.8% for each stroke and operative death, he said (J Thorac Cardiovasc Surg. 2015;150:1140-7).
“What was also of interest there was no difference in outcomes with antegrade vs. retrograde brain profusion,” he said. “I think protection of the brain is pretty good if you follow the fundamental principles of brain protection.”
He also reported on a recent study at his institution that documented the benefits of intrathecal papaverine (IP) for spinal cord protection during descending open and endovascular aortic repairs. In 398 aortic repairs from 2001-2009, the rates of spinal cord injury were 23% in the non-IP group vs. 7% in the IP group (P = .07) in a matched cohort.
He noted that the clinical guidelines of the American Association for Thoracic Surgery as well as AATS/Society of Thoracic Surgeons joint guidelines are open to input. “If you have areas where you think guideline should be written about, please let me or other members of the committee know,” he said.
Dr. Svensson had no disclosures relevant to his presentation.
NEW YORK – While overall guidelines for aortic repair surgery have not changed significantly in the past 5 years, guidelines for the timing of surgery in patients with bicuspid aortic valves and enlarged aortas have undergone some updating in an attempt to clear up disparities in different guidelines on when to operate on those patients.
Lars G. Svensson, MD, PhD, chairman of the Cleveland Clinic Heart and Vascular Institute, coauthor of the clarification statement by the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines (J Thorac Cardiovasc Surg. 2016;151:959-66), reported on the guidelines clarification at the meeting sponsored by the American Association for Thoracic Surgery. He noted that five different clinical guidelines between 2010 and 2014 recommended five different size thresholds for prophylactic aortic root or ascending aortic surgery in the setting of bicuspid aortic valve (BAV), ranging from 4 cm to greater than 5.5 cm. “This created a bit of a quandary and controversy between different guidelines and time periods,” he said.
Dr. Svensson and Loren Hiratzka, MD, medical director of cardiac surgery for TriHealth in Cincinnati, and their colleagues drafted the guideline clarification that makes the following recommendations for aortic root and ascending aorta repair or replacement when patients have BAV (strength of recommendation):
• Surgery is indicated to replace the aortic root or ascending aorta in asymptomatic patients with BAV if the diameter of the aortic root or ascending aorta is 5.5 cm or greater (Class 1).
• Surgical repair is indicated for asymptomatic patients with BAV if the root or ascending aorta diameter is 5 cm or greater in two scenarios: if the patient has an additional risk factor for dissection, such as family history or excessive aortic growth rate; or if the patient is a low surgical risk and has access to an experienced surgeon at a high-volume center (Class IIa).
The guideline update also addresses BAV in patients with Turner syndrome. The 2010 joint guidelines of 10 societies left some questions with regard to surgery in these patients, Dr. Svensson said. The established guidelines included a Class IIb recommendation for imaging of the heart and aorta to help determine the aorta risk in patients with Turner syndrome who had additional risk factors, including BAV, aortic coarctation and/or hypertension, or were planning a pregnancy.
The updated guideline includes Class IIa recommendation that in short-statured patients with Turner syndrome and BAV, measurement of the aortic root or ascending aorta diameter may not predict the dissection risk as well as aortic diameter index greater than 2.5 cm/m2. The updated recommendations also draw on one study that reported that in patients with BAV, a maximum aortic cross-sectional area-to-height ratio of 10 cm2/m or greater was also predictive of aortic dissection. (Ann Thorac Surg. 2015;100:1666-73)
The updated recommendations for open surgery for ascending aortic aneurysm include separate valve and ascending aortic replacement in patients without significant aortic root dilatation or in elderly patients, or in younger patients with minimal dilatation who have aortic valve disease; and excision of the sinuses of Valsalva with a modified David reimplantation when technically feasible in patients with connective tissue disease and others with dilatation of the aortic root and sinuses. For patients in whom the latter procedure is not feasible, root replacement with valved graft conduit would be indicated, Dr. Svensson said.
Dr. Svensson also reported on recent studies that validated recommendations in established guidelines.
Studies of circulatory arrest practices in aortic arch surgery as prescribed by established guidelines showed confirmatory results, he said. “The one point I would make about circulatory arrest is that we found in a fairly large study of 1,352 circulatory arrest patients that we reduced the risk of stroke by 40% when we used the axillary artery with a side a graft,” he said (Ann Thorac Surg. 2004;78:1274-84). His own institution’s clinical trial of 121 patients who received antegrade or retrograde brain perfusion showed rates of 0.8% for each stroke and operative death, he said (J Thorac Cardiovasc Surg. 2015;150:1140-7).
“What was also of interest there was no difference in outcomes with antegrade vs. retrograde brain profusion,” he said. “I think protection of the brain is pretty good if you follow the fundamental principles of brain protection.”
He also reported on a recent study at his institution that documented the benefits of intrathecal papaverine (IP) for spinal cord protection during descending open and endovascular aortic repairs. In 398 aortic repairs from 2001-2009, the rates of spinal cord injury were 23% in the non-IP group vs. 7% in the IP group (P = .07) in a matched cohort.
He noted that the clinical guidelines of the American Association for Thoracic Surgery as well as AATS/Society of Thoracic Surgeons joint guidelines are open to input. “If you have areas where you think guideline should be written about, please let me or other members of the committee know,” he said.
Dr. Svensson had no disclosures relevant to his presentation.
NEW YORK – While overall guidelines for aortic repair surgery have not changed significantly in the past 5 years, guidelines for the timing of surgery in patients with bicuspid aortic valves and enlarged aortas have undergone some updating in an attempt to clear up disparities in different guidelines on when to operate on those patients.
Lars G. Svensson, MD, PhD, chairman of the Cleveland Clinic Heart and Vascular Institute, coauthor of the clarification statement by the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines (J Thorac Cardiovasc Surg. 2016;151:959-66), reported on the guidelines clarification at the meeting sponsored by the American Association for Thoracic Surgery. He noted that five different clinical guidelines between 2010 and 2014 recommended five different size thresholds for prophylactic aortic root or ascending aortic surgery in the setting of bicuspid aortic valve (BAV), ranging from 4 cm to greater than 5.5 cm. “This created a bit of a quandary and controversy between different guidelines and time periods,” he said.
Dr. Svensson and Loren Hiratzka, MD, medical director of cardiac surgery for TriHealth in Cincinnati, and their colleagues drafted the guideline clarification that makes the following recommendations for aortic root and ascending aorta repair or replacement when patients have BAV (strength of recommendation):
• Surgery is indicated to replace the aortic root or ascending aorta in asymptomatic patients with BAV if the diameter of the aortic root or ascending aorta is 5.5 cm or greater (Class 1).
• Surgical repair is indicated for asymptomatic patients with BAV if the root or ascending aorta diameter is 5 cm or greater in two scenarios: if the patient has an additional risk factor for dissection, such as family history or excessive aortic growth rate; or if the patient is a low surgical risk and has access to an experienced surgeon at a high-volume center (Class IIa).
The guideline update also addresses BAV in patients with Turner syndrome. The 2010 joint guidelines of 10 societies left some questions with regard to surgery in these patients, Dr. Svensson said. The established guidelines included a Class IIb recommendation for imaging of the heart and aorta to help determine the aorta risk in patients with Turner syndrome who had additional risk factors, including BAV, aortic coarctation and/or hypertension, or were planning a pregnancy.
The updated guideline includes Class IIa recommendation that in short-statured patients with Turner syndrome and BAV, measurement of the aortic root or ascending aorta diameter may not predict the dissection risk as well as aortic diameter index greater than 2.5 cm/m2. The updated recommendations also draw on one study that reported that in patients with BAV, a maximum aortic cross-sectional area-to-height ratio of 10 cm2/m or greater was also predictive of aortic dissection. (Ann Thorac Surg. 2015;100:1666-73)
The updated recommendations for open surgery for ascending aortic aneurysm include separate valve and ascending aortic replacement in patients without significant aortic root dilatation or in elderly patients, or in younger patients with minimal dilatation who have aortic valve disease; and excision of the sinuses of Valsalva with a modified David reimplantation when technically feasible in patients with connective tissue disease and others with dilatation of the aortic root and sinuses. For patients in whom the latter procedure is not feasible, root replacement with valved graft conduit would be indicated, Dr. Svensson said.
Dr. Svensson also reported on recent studies that validated recommendations in established guidelines.
Studies of circulatory arrest practices in aortic arch surgery as prescribed by established guidelines showed confirmatory results, he said. “The one point I would make about circulatory arrest is that we found in a fairly large study of 1,352 circulatory arrest patients that we reduced the risk of stroke by 40% when we used the axillary artery with a side a graft,” he said (Ann Thorac Surg. 2004;78:1274-84). His own institution’s clinical trial of 121 patients who received antegrade or retrograde brain perfusion showed rates of 0.8% for each stroke and operative death, he said (J Thorac Cardiovasc Surg. 2015;150:1140-7).
“What was also of interest there was no difference in outcomes with antegrade vs. retrograde brain profusion,” he said. “I think protection of the brain is pretty good if you follow the fundamental principles of brain protection.”
He also reported on a recent study at his institution that documented the benefits of intrathecal papaverine (IP) for spinal cord protection during descending open and endovascular aortic repairs. In 398 aortic repairs from 2001-2009, the rates of spinal cord injury were 23% in the non-IP group vs. 7% in the IP group (P = .07) in a matched cohort.
He noted that the clinical guidelines of the American Association for Thoracic Surgery as well as AATS/Society of Thoracic Surgeons joint guidelines are open to input. “If you have areas where you think guideline should be written about, please let me or other members of the committee know,” he said.
Dr. Svensson had no disclosures relevant to his presentation.
AT THE AATS AORTIC SYMPOSIUM 2016
Key clinical point: Various clinical guidelines provided five different recommendations for the timing of aortic repair surgery in patients with bicuspid aortic valves.
Major finding: Recent updates in guidelines provide clarity on when an aortic repair is needed in the setting of aortic bicuspid valve.
Data source: American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines.
Disclosures: Dr. Svensson had no relevant financial relationships to disclose.
The ‘guilty’ associates of silent thoracic aneurysm fingered
NEW YORK – Aortic aneurysm ranks as one of the top 20 causes of death in the United States. Most of these aneurysms are clinically silent until they rupture, but Yale cardiovascular surgeon John A. Elefteriades, MD, has developed a clinical paradigm that identifies eight markers that physicians can use to detect the disease before it strikes.
Dr. Elefteriades calls his paradigm “Guilt by Association.” It is based on an article he published online last year in the journal Open Heart (2015;2:e000169).
“What we need is for our colleagues in affiliated disciplines to recognize the importance of these offenders in indicating the presence of thoracic aortic aneurysm,” he said, reporting on the paradigm at the meeting sponsored by the American Association for Thoracic Surgery. He noted that studies from Japan of people who had died from out-of-hospital cardiac arrest found that 8% of them had a type A aortic dissection (Am J Cardiol 2016;117:1826-30).
He outlined eight “associates” of thoracic aortic aneurysm (TAA): intracranial aneurysm; bovine aortic arch; abdominal aortic aneurysm; simple renal cysts; bicuspid aortic valve; family history; positive thumb-palm test; and temporal arteritis and other autoimmune disorders.
A patient with TAA has a 10% likelihood of harboring an intracranial aneurysm (Am J Cardiol 2010;105:417-20). “It’s even more common in the descending, compared to the ascending group in examples that we’ve identified,” Dr. Elefteriades said. Particularly vulnerable are patients over age 70 and those with an intracranial aneurysm larger than 4 mm: the former has a 9% chance of harboring a TAA, the latter a 6% chance, he said.
The bovine arch had been thought to be benign, but, Dr. Elefteriades said, “We don’t think it is.”
Bovine arch refers to a group of congenital aortic arch vessels with an aberrant origin of the left common carotid artery. “We recently looked at this as a marker for thoracic aortic disease, and please note that 20% of our TAA patients have a bovine arch,” he said. “This is much higher than in the general population.”
Abdominal aortic aneurysm has long been associated with TAA, he said. “When these aneurysms are identified by ultrasound, it’s important that the thoracic aorta be checked as well,” he said.
“This is a message for internists and our vascular colleagues.”
Simple renal cysts have been found in patients with TAA at a “much higher” rate than the general population, as high as 57% of those with descending aortic aneurysms vs. 11%-13.7% of the general population, Dr. Elefteriades said (J. Am. Heart Assoc. 2016;5:e002248). Simple renal cysts are detected by abdominal CT scan. “It’s just a matter of a few more slices with the CT scan to get the entirety of the thoracic aorta evaluated,” he said.
“We encourage our radiology colleagues to do this when a renal cyst is detected.”
Bicuspid aortic valve mandates “support from our cardiac colleagues when they find one of these to let the patient know he has to be monitored lifelong for later development of this aneurysm,” Dr. Elefteriades said.
Family history of TAA has been known as a strong predictor, but genetic studies have provided clarity on the association (Arch Surg. 1999;134:361‐7). “If the proband has a thoracic aortic aneurysm, there’s 21% likelihood there’s a family member who is affected with an aneurysm somewhere in the body,” he said.
Location of aneurysms in family members is also important, Dr. Elefteriades said. “If the proband has a ascending aortic aneurysm, the kindred also have an ascending aortic aneurysm; but if the proband has a descending aneurysm, the likelihood is that the kindred will have an abdominal aortic aneurysm,” he said. “To identify silent disease, it’s very important we check siblings and children, and now, of course, we’re using whole-exome sequencing.” So far, Dr. Elefteriades has obtained whole-exome sequencing in 200 patients.
The thumb-palm test involves the patient touching the thumb to the palm; the thumb crossing the edge of the flat palm is an indicator of connective tissue disease. “It doesn’t cost anything,” Dr. Elefteriades said. “It is a very simple thing for internists to do to identify those connective tissue diseases.”
Temporal arteritis has become increasingly common in elderly women. “They have a markedly increased likelihood of having a thoracic aortic aneurysm – about 8% in some studies,’ Dr. Elefteriades said. “So we want our neurology colleagues to be aware of this and to look for thoracic aortic aneurysm.”
Dr. Elefteriades disclosed he has received consulting fees from Baxter, Covidien, Datascope, and CryoLife, and a research grant from Medtronic.
NEW YORK – Aortic aneurysm ranks as one of the top 20 causes of death in the United States. Most of these aneurysms are clinically silent until they rupture, but Yale cardiovascular surgeon John A. Elefteriades, MD, has developed a clinical paradigm that identifies eight markers that physicians can use to detect the disease before it strikes.
Dr. Elefteriades calls his paradigm “Guilt by Association.” It is based on an article he published online last year in the journal Open Heart (2015;2:e000169).
“What we need is for our colleagues in affiliated disciplines to recognize the importance of these offenders in indicating the presence of thoracic aortic aneurysm,” he said, reporting on the paradigm at the meeting sponsored by the American Association for Thoracic Surgery. He noted that studies from Japan of people who had died from out-of-hospital cardiac arrest found that 8% of them had a type A aortic dissection (Am J Cardiol 2016;117:1826-30).
He outlined eight “associates” of thoracic aortic aneurysm (TAA): intracranial aneurysm; bovine aortic arch; abdominal aortic aneurysm; simple renal cysts; bicuspid aortic valve; family history; positive thumb-palm test; and temporal arteritis and other autoimmune disorders.
A patient with TAA has a 10% likelihood of harboring an intracranial aneurysm (Am J Cardiol 2010;105:417-20). “It’s even more common in the descending, compared to the ascending group in examples that we’ve identified,” Dr. Elefteriades said. Particularly vulnerable are patients over age 70 and those with an intracranial aneurysm larger than 4 mm: the former has a 9% chance of harboring a TAA, the latter a 6% chance, he said.
The bovine arch had been thought to be benign, but, Dr. Elefteriades said, “We don’t think it is.”
Bovine arch refers to a group of congenital aortic arch vessels with an aberrant origin of the left common carotid artery. “We recently looked at this as a marker for thoracic aortic disease, and please note that 20% of our TAA patients have a bovine arch,” he said. “This is much higher than in the general population.”
Abdominal aortic aneurysm has long been associated with TAA, he said. “When these aneurysms are identified by ultrasound, it’s important that the thoracic aorta be checked as well,” he said.
“This is a message for internists and our vascular colleagues.”
Simple renal cysts have been found in patients with TAA at a “much higher” rate than the general population, as high as 57% of those with descending aortic aneurysms vs. 11%-13.7% of the general population, Dr. Elefteriades said (J. Am. Heart Assoc. 2016;5:e002248). Simple renal cysts are detected by abdominal CT scan. “It’s just a matter of a few more slices with the CT scan to get the entirety of the thoracic aorta evaluated,” he said.
“We encourage our radiology colleagues to do this when a renal cyst is detected.”
Bicuspid aortic valve mandates “support from our cardiac colleagues when they find one of these to let the patient know he has to be monitored lifelong for later development of this aneurysm,” Dr. Elefteriades said.
Family history of TAA has been known as a strong predictor, but genetic studies have provided clarity on the association (Arch Surg. 1999;134:361‐7). “If the proband has a thoracic aortic aneurysm, there’s 21% likelihood there’s a family member who is affected with an aneurysm somewhere in the body,” he said.
Location of aneurysms in family members is also important, Dr. Elefteriades said. “If the proband has a ascending aortic aneurysm, the kindred also have an ascending aortic aneurysm; but if the proband has a descending aneurysm, the likelihood is that the kindred will have an abdominal aortic aneurysm,” he said. “To identify silent disease, it’s very important we check siblings and children, and now, of course, we’re using whole-exome sequencing.” So far, Dr. Elefteriades has obtained whole-exome sequencing in 200 patients.
The thumb-palm test involves the patient touching the thumb to the palm; the thumb crossing the edge of the flat palm is an indicator of connective tissue disease. “It doesn’t cost anything,” Dr. Elefteriades said. “It is a very simple thing for internists to do to identify those connective tissue diseases.”
Temporal arteritis has become increasingly common in elderly women. “They have a markedly increased likelihood of having a thoracic aortic aneurysm – about 8% in some studies,’ Dr. Elefteriades said. “So we want our neurology colleagues to be aware of this and to look for thoracic aortic aneurysm.”
Dr. Elefteriades disclosed he has received consulting fees from Baxter, Covidien, Datascope, and CryoLife, and a research grant from Medtronic.
NEW YORK – Aortic aneurysm ranks as one of the top 20 causes of death in the United States. Most of these aneurysms are clinically silent until they rupture, but Yale cardiovascular surgeon John A. Elefteriades, MD, has developed a clinical paradigm that identifies eight markers that physicians can use to detect the disease before it strikes.
Dr. Elefteriades calls his paradigm “Guilt by Association.” It is based on an article he published online last year in the journal Open Heart (2015;2:e000169).
“What we need is for our colleagues in affiliated disciplines to recognize the importance of these offenders in indicating the presence of thoracic aortic aneurysm,” he said, reporting on the paradigm at the meeting sponsored by the American Association for Thoracic Surgery. He noted that studies from Japan of people who had died from out-of-hospital cardiac arrest found that 8% of them had a type A aortic dissection (Am J Cardiol 2016;117:1826-30).
He outlined eight “associates” of thoracic aortic aneurysm (TAA): intracranial aneurysm; bovine aortic arch; abdominal aortic aneurysm; simple renal cysts; bicuspid aortic valve; family history; positive thumb-palm test; and temporal arteritis and other autoimmune disorders.
A patient with TAA has a 10% likelihood of harboring an intracranial aneurysm (Am J Cardiol 2010;105:417-20). “It’s even more common in the descending, compared to the ascending group in examples that we’ve identified,” Dr. Elefteriades said. Particularly vulnerable are patients over age 70 and those with an intracranial aneurysm larger than 4 mm: the former has a 9% chance of harboring a TAA, the latter a 6% chance, he said.
The bovine arch had been thought to be benign, but, Dr. Elefteriades said, “We don’t think it is.”
Bovine arch refers to a group of congenital aortic arch vessels with an aberrant origin of the left common carotid artery. “We recently looked at this as a marker for thoracic aortic disease, and please note that 20% of our TAA patients have a bovine arch,” he said. “This is much higher than in the general population.”
Abdominal aortic aneurysm has long been associated with TAA, he said. “When these aneurysms are identified by ultrasound, it’s important that the thoracic aorta be checked as well,” he said.
“This is a message for internists and our vascular colleagues.”
Simple renal cysts have been found in patients with TAA at a “much higher” rate than the general population, as high as 57% of those with descending aortic aneurysms vs. 11%-13.7% of the general population, Dr. Elefteriades said (J. Am. Heart Assoc. 2016;5:e002248). Simple renal cysts are detected by abdominal CT scan. “It’s just a matter of a few more slices with the CT scan to get the entirety of the thoracic aorta evaluated,” he said.
“We encourage our radiology colleagues to do this when a renal cyst is detected.”
Bicuspid aortic valve mandates “support from our cardiac colleagues when they find one of these to let the patient know he has to be monitored lifelong for later development of this aneurysm,” Dr. Elefteriades said.
Family history of TAA has been known as a strong predictor, but genetic studies have provided clarity on the association (Arch Surg. 1999;134:361‐7). “If the proband has a thoracic aortic aneurysm, there’s 21% likelihood there’s a family member who is affected with an aneurysm somewhere in the body,” he said.
Location of aneurysms in family members is also important, Dr. Elefteriades said. “If the proband has a ascending aortic aneurysm, the kindred also have an ascending aortic aneurysm; but if the proband has a descending aneurysm, the likelihood is that the kindred will have an abdominal aortic aneurysm,” he said. “To identify silent disease, it’s very important we check siblings and children, and now, of course, we’re using whole-exome sequencing.” So far, Dr. Elefteriades has obtained whole-exome sequencing in 200 patients.
The thumb-palm test involves the patient touching the thumb to the palm; the thumb crossing the edge of the flat palm is an indicator of connective tissue disease. “It doesn’t cost anything,” Dr. Elefteriades said. “It is a very simple thing for internists to do to identify those connective tissue diseases.”
Temporal arteritis has become increasingly common in elderly women. “They have a markedly increased likelihood of having a thoracic aortic aneurysm – about 8% in some studies,’ Dr. Elefteriades said. “So we want our neurology colleagues to be aware of this and to look for thoracic aortic aneurysm.”
Dr. Elefteriades disclosed he has received consulting fees from Baxter, Covidien, Datascope, and CryoLife, and a research grant from Medtronic.
EXPERT ANALYSIS FROM AATS AORTIC SYMPOSIUM 2016
Key clinical point: Eight markers may detect silent thoracic aneurysms before rupture.
Major finding: The eight “associates” of TAA include intracranial aneurysm; bovine aortic arch; abdominal aortic aneurysm; simple renal cysts; and bicuspid aortic valve.
Data source: The “Guilt by Association” paradigm was based upon a review of the literature by Dr. Elefteriades and his own published reports.
Disclosures: Dr. Elefteriades disclosed he has received consulting fees from Baxter, Covidien, Datascope, and CryoLife, and a research grant from Medtroni
Point/Counterpoint: What’s best for chronic dissection: TEVAR or open?
TEVAR is the best procedure.
At Cedars-Sinai Medical Center, 70% of the aortic operations are performed in open fashion, but in patients with chronic type B aortic dissection, thoracic endovascular repair (TEVAR) is the preferred option. Goals of TEVAR in the setting of chronic type B dissection are to seal off the intimomedial tears, re-route blood to the true lumen, and induce false lumen thrombosis in the descending thoracic aorta, promoting reverse aortic remodeling and reducing future reinterventions.
TEVAR in patients with chronic type B aortic dissection has the best results if the following five rules apply: the patient should be older than 40 years of age and not have connective tissue disorder; there should be a proper proximal landing zone; the distal landing zone at the celiac artery should be smaller than 4 cm to allow for reverse remodeling; most of the large intimomedial tears should be in the descending aorta; and at least three visceral vessels should come off the true lumen. With this clinical scenario, the majority of centers will have excellent results with TEVAR.
TEVAR for chronic type B aortic dissection comes with three usual concerns: short-term outcomes; reverse aortic remodeling; and long-term outcomes.
In evaluating short-term outcomes of TEVAR in chronic type B aortic dissection, many large, single-center studies, including ours, have documented the superior results.1,2 The VIRTUE study reported an operative mortality and 30-day hospitality mortality of zero and spinal cord ischemia rate of 3.8% in a prospective, multi-center review.3 A meta-analysis of TEVAR for chronic dissection that involved 567 patients reported a 30-day mortality rate of 3.2%, paraplegia rate of 0.45%, a stroke rate of 1.5%, and retrograde type A dissection rate of 0.7%.4
These outcomes are far better than those reported in a meta-analysis of open repair for chronic dissection (771 patients): post-1997 mortality of 8.8% (the overall 30-day mortality rate was 12.5%); paraplegia of 6%; and renal failure with hemodialysis of 4%.5 A statewide analysis of elective open repair for thoracoabdominal aortic aneurysm, including chronic dissections, in California had a 30-day mortality rate of 19.7%.6
With regard to reverse aortic remodeling, acceptable results with TEVAR have been reported. The INSTEAD-XL study reported that at 5 years, 73% of patients had reverse aortic remodeling, with absolute risk reduction of 12.4%, compared with optimal medical therapy.7 A systematic review reported an 85.7% median rate of false lumen thrombosis.4 In the past some surgeons were concerned about a thick septum and whether it would give way and allow reverse remodeling; these studies confirmed that it does. The radial force of a stent graft over time will enlarge to the size that you would expect and it will cause the false lumen thrombosis.
Our group has provided anatomical indicators to achieve reverse remodeling in chronic type B dissection, including the location and size of intimomedial tears above the celiac artery.8 A patient with this anatomy has a great chance of not requiring any future reinterventions if the tears are mostly within the thoracic aorta upper fit.
Large multicenter studies also provide answers to the third concern about TEVAR for chronic aortic dissection – long-term outcomes – and found that they are comparable to open surgery. A study of the Medtronic Thoracic Endovascular Registry (MOTHER) database, a prospective, multicenter, adjudicated registry, looked at three types of aortic pathology: chronic aortic dissection (CAD); acute aortic dissection (AAD); and thoracic aortic aneurysm (TAA). The 195 patients with CAD had the best all-cause mortality outcomes: 3.2 per 100 patient years.9 Aortic-related mortality was also lowest in the CAD group: 0.4 per 100 patient years vs. 0.6 for TAA and 1.2 for AAD.
The reintervention rates for patients with aortic dissection were high, compared with TAA in the MOTHER registry. INSTEAD XL revealed all-cause and aortic-related mortality, respectively, at 11.1% and 6.9% in patients with chronic type B dissection treated with TEVAR at 5 years.
Last but not least, TEVAR is the first choice for many elderly or frail patients with type B aortic dissection. Recovery after the open procedure is much more difficult for this population. Our specialty frequently underappreciates quality of life after an aortic operation.
Overall, TEVAR for chronic type B aortic dissection is feasible, reproducible, and less invasive than open repair. It has acceptable early results, rate of reverse aortic modeling, and late mortality, and although its reintervention rate can be significant, that can be reduced with experience and a careful algorithmic approach.
Dr. Ali Khoynezhad is a professor of cardiovascular surgery, director of aortic surgery, and co-director of the atrial fibrillation program at Cedars-Sinai Heart Institute, Los Angeles. He disclosed receiving research grants from Medtronic, Gore, and Vascutek.
1. J Thorac Cardiovasc Surg. 2008 May;135:1103-9.
2. J Thorac Cardiovasc Surg. 2011 Feb;141:322-7.
3. Eur J Vasc Endovasc Surg. 2011 Feb;41:159-66.
4. Eur J Vasc Endovasc Surg. 2011 Nov;42:632-47.
5. J Vasc Surg. 2010 Oct;52:3S-9S.
6. J Vasc Surg. 2006 Feb;43:217-22.
7. Circ Cardiovasc Interv. 2013 Aug;6:407-16.
8. J Vasc Surg. 2010 Sep;52:562-8.
9. Circulation. 2013 Jan;127:24-32.
Open repair is the better procedure.
It’s my contention that open repair is still the gold standard for chronic thoracoabdominal aortic dissection. It has a record of outstanding results in high-volume centers of excellence with low morbidity and mortality and very good long-term survival. It has no anatomical constraints. It’s a durable repair and there are no device- or procedure-related proximal and/or distal aortic complications. Reintervention on the operated segment is very rare.1-6
Thoracic endovascular repair (TEVAR), despite having very good procedural results, has challenges in the successful treatment of chronic aortic dissection. Morbidity is low, as are rates of spinal cord ischemia, stroke, and renal failure. However, thoracic remodeling at the level of the endograft is in the 70%-88% range, which means that 12%-30% of patients do not have protection in the form of reverse aortic remodeling. In the abdominal aorta, remodeling is uncommon, with 11%-23% thrombosis of the false lumen even with advantageous anatomy. Survival in several series is in the 60%-80% range at 3 and 5 years. TEVAR creates new challenges for chronic thoracoabdominal aortic dissection: retrograde type A dissections have been as high as 2%-7%; 15%-30% of cases require intervention; and stent graft-induced new entry (SINE) has been reported as high as 36%.
Specific anatomical features are not suitable for TEVAR. They include multiple visceral vessels off of the false lumen; multiple fenestrations, especially in the abdominal aorta; dissection within the dissection; and pseudocoarctation. The durability of the endovascular graft for chronic aortic dissection is unknown; it’s a relatively new procedure so the long-term data is lacking.
Success of the endovascular approach depends on aortic remodeling, and it’s my contention that the thoracic devices now available cannot effectively treat a chronic thoracoabdominal aortic dissection. There are steps surgeons can take to improve their success, but procedures specifically addressing the false lumen are not time-tested and thoracoabdominal-specific devices are not widely available in the United States. And of course, morbidity and mortality will increase with the complexity of the endovascular repair.
Our in-hospital outcomes with open repair of chronic thoracoabdominal aortic dissection using deep hypothermia and circulatory arrest have been excellent: mortality rate of 3.6%; a stroke rate of 1%; permanent spinal cord ischemia rate 2.6%; and a 0% rate of patients on permanent hemodialysis. Our hospital length of stay is approximately 12 days. Blood product transfusion is reasonable with a mean blood product transfusion of 9 units for the hospital admission. The reintervention rate is 1% for infected grafts, 3.1% for anastomotic pseudoaneurysm and 3.6% for growth of a distal aneurysm. Long-term survival is very good: 93% at one year; 79% at five years; and 57% at 10 years.
There’s no denying that mortality rates for endovascular repair are excellent. There’s no denying that open repair is much more invasive. And if the patient is of advanced age, is frail and has comorbidities, the endovascular repair can have a certain advantage.
But for false lumen obliteration, the advantage goes to open repair. With regard to reintervention, certainly the advantage is with open repair. For durability, from what we know currently, open repair has the advantage. There are no stent-induced new entries in open repair; and open repair can address any and all anatomy. A successful endograft repair requires fixation and seal in the appropriate aortic anatomy; it demands good proximal and distal landing zones. However, in chronic dissection, there is the added complexity of having to address the false lumen flow from an untreated abdominal aortic segment.
For patients with connective tissue disorders, open repair is still the gold standard. As for long-term survival, the advantage goes to open only because the endovascular approach is relatively new. If it’s done in high-volume centers with great experience, open repair has a mortality advantage as well.
Dr. Joel Corvera is an assistant professor of surgery and director of thoracic and vascular surgery at Indiana University, Indianapolis. He had no relationships to disclose.
1. Eur J Vasc Endovasc Surg. 2011 Feb;41:159-66.
2. J Thorac Cardiovasc Surg. 2011 Feb;141:322-7.
3. Ann Cardiothorac Surg. 2014 May;3:264-74.
4. J Thorac Cardiovasc Surg. 2010 Jun;139:1548-53.
5. Ann Thorac Surg. 2013 Mar;95:914-21.
TEVAR is the best procedure.
At Cedars-Sinai Medical Center, 70% of the aortic operations are performed in open fashion, but in patients with chronic type B aortic dissection, thoracic endovascular repair (TEVAR) is the preferred option. Goals of TEVAR in the setting of chronic type B dissection are to seal off the intimomedial tears, re-route blood to the true lumen, and induce false lumen thrombosis in the descending thoracic aorta, promoting reverse aortic remodeling and reducing future reinterventions.
TEVAR in patients with chronic type B aortic dissection has the best results if the following five rules apply: the patient should be older than 40 years of age and not have connective tissue disorder; there should be a proper proximal landing zone; the distal landing zone at the celiac artery should be smaller than 4 cm to allow for reverse remodeling; most of the large intimomedial tears should be in the descending aorta; and at least three visceral vessels should come off the true lumen. With this clinical scenario, the majority of centers will have excellent results with TEVAR.
TEVAR for chronic type B aortic dissection comes with three usual concerns: short-term outcomes; reverse aortic remodeling; and long-term outcomes.
In evaluating short-term outcomes of TEVAR in chronic type B aortic dissection, many large, single-center studies, including ours, have documented the superior results.1,2 The VIRTUE study reported an operative mortality and 30-day hospitality mortality of zero and spinal cord ischemia rate of 3.8% in a prospective, multi-center review.3 A meta-analysis of TEVAR for chronic dissection that involved 567 patients reported a 30-day mortality rate of 3.2%, paraplegia rate of 0.45%, a stroke rate of 1.5%, and retrograde type A dissection rate of 0.7%.4
These outcomes are far better than those reported in a meta-analysis of open repair for chronic dissection (771 patients): post-1997 mortality of 8.8% (the overall 30-day mortality rate was 12.5%); paraplegia of 6%; and renal failure with hemodialysis of 4%.5 A statewide analysis of elective open repair for thoracoabdominal aortic aneurysm, including chronic dissections, in California had a 30-day mortality rate of 19.7%.6
With regard to reverse aortic remodeling, acceptable results with TEVAR have been reported. The INSTEAD-XL study reported that at 5 years, 73% of patients had reverse aortic remodeling, with absolute risk reduction of 12.4%, compared with optimal medical therapy.7 A systematic review reported an 85.7% median rate of false lumen thrombosis.4 In the past some surgeons were concerned about a thick septum and whether it would give way and allow reverse remodeling; these studies confirmed that it does. The radial force of a stent graft over time will enlarge to the size that you would expect and it will cause the false lumen thrombosis.
Our group has provided anatomical indicators to achieve reverse remodeling in chronic type B dissection, including the location and size of intimomedial tears above the celiac artery.8 A patient with this anatomy has a great chance of not requiring any future reinterventions if the tears are mostly within the thoracic aorta upper fit.
Large multicenter studies also provide answers to the third concern about TEVAR for chronic aortic dissection – long-term outcomes – and found that they are comparable to open surgery. A study of the Medtronic Thoracic Endovascular Registry (MOTHER) database, a prospective, multicenter, adjudicated registry, looked at three types of aortic pathology: chronic aortic dissection (CAD); acute aortic dissection (AAD); and thoracic aortic aneurysm (TAA). The 195 patients with CAD had the best all-cause mortality outcomes: 3.2 per 100 patient years.9 Aortic-related mortality was also lowest in the CAD group: 0.4 per 100 patient years vs. 0.6 for TAA and 1.2 for AAD.
The reintervention rates for patients with aortic dissection were high, compared with TAA in the MOTHER registry. INSTEAD XL revealed all-cause and aortic-related mortality, respectively, at 11.1% and 6.9% in patients with chronic type B dissection treated with TEVAR at 5 years.
Last but not least, TEVAR is the first choice for many elderly or frail patients with type B aortic dissection. Recovery after the open procedure is much more difficult for this population. Our specialty frequently underappreciates quality of life after an aortic operation.
Overall, TEVAR for chronic type B aortic dissection is feasible, reproducible, and less invasive than open repair. It has acceptable early results, rate of reverse aortic modeling, and late mortality, and although its reintervention rate can be significant, that can be reduced with experience and a careful algorithmic approach.
Dr. Ali Khoynezhad is a professor of cardiovascular surgery, director of aortic surgery, and co-director of the atrial fibrillation program at Cedars-Sinai Heart Institute, Los Angeles. He disclosed receiving research grants from Medtronic, Gore, and Vascutek.
1. J Thorac Cardiovasc Surg. 2008 May;135:1103-9.
2. J Thorac Cardiovasc Surg. 2011 Feb;141:322-7.
3. Eur J Vasc Endovasc Surg. 2011 Feb;41:159-66.
4. Eur J Vasc Endovasc Surg. 2011 Nov;42:632-47.
5. J Vasc Surg. 2010 Oct;52:3S-9S.
6. J Vasc Surg. 2006 Feb;43:217-22.
7. Circ Cardiovasc Interv. 2013 Aug;6:407-16.
8. J Vasc Surg. 2010 Sep;52:562-8.
9. Circulation. 2013 Jan;127:24-32.
Open repair is the better procedure.
It’s my contention that open repair is still the gold standard for chronic thoracoabdominal aortic dissection. It has a record of outstanding results in high-volume centers of excellence with low morbidity and mortality and very good long-term survival. It has no anatomical constraints. It’s a durable repair and there are no device- or procedure-related proximal and/or distal aortic complications. Reintervention on the operated segment is very rare.1-6
Thoracic endovascular repair (TEVAR), despite having very good procedural results, has challenges in the successful treatment of chronic aortic dissection. Morbidity is low, as are rates of spinal cord ischemia, stroke, and renal failure. However, thoracic remodeling at the level of the endograft is in the 70%-88% range, which means that 12%-30% of patients do not have protection in the form of reverse aortic remodeling. In the abdominal aorta, remodeling is uncommon, with 11%-23% thrombosis of the false lumen even with advantageous anatomy. Survival in several series is in the 60%-80% range at 3 and 5 years. TEVAR creates new challenges for chronic thoracoabdominal aortic dissection: retrograde type A dissections have been as high as 2%-7%; 15%-30% of cases require intervention; and stent graft-induced new entry (SINE) has been reported as high as 36%.
Specific anatomical features are not suitable for TEVAR. They include multiple visceral vessels off of the false lumen; multiple fenestrations, especially in the abdominal aorta; dissection within the dissection; and pseudocoarctation. The durability of the endovascular graft for chronic aortic dissection is unknown; it’s a relatively new procedure so the long-term data is lacking.
Success of the endovascular approach depends on aortic remodeling, and it’s my contention that the thoracic devices now available cannot effectively treat a chronic thoracoabdominal aortic dissection. There are steps surgeons can take to improve their success, but procedures specifically addressing the false lumen are not time-tested and thoracoabdominal-specific devices are not widely available in the United States. And of course, morbidity and mortality will increase with the complexity of the endovascular repair.
Our in-hospital outcomes with open repair of chronic thoracoabdominal aortic dissection using deep hypothermia and circulatory arrest have been excellent: mortality rate of 3.6%; a stroke rate of 1%; permanent spinal cord ischemia rate 2.6%; and a 0% rate of patients on permanent hemodialysis. Our hospital length of stay is approximately 12 days. Blood product transfusion is reasonable with a mean blood product transfusion of 9 units for the hospital admission. The reintervention rate is 1% for infected grafts, 3.1% for anastomotic pseudoaneurysm and 3.6% for growth of a distal aneurysm. Long-term survival is very good: 93% at one year; 79% at five years; and 57% at 10 years.
There’s no denying that mortality rates for endovascular repair are excellent. There’s no denying that open repair is much more invasive. And if the patient is of advanced age, is frail and has comorbidities, the endovascular repair can have a certain advantage.
But for false lumen obliteration, the advantage goes to open repair. With regard to reintervention, certainly the advantage is with open repair. For durability, from what we know currently, open repair has the advantage. There are no stent-induced new entries in open repair; and open repair can address any and all anatomy. A successful endograft repair requires fixation and seal in the appropriate aortic anatomy; it demands good proximal and distal landing zones. However, in chronic dissection, there is the added complexity of having to address the false lumen flow from an untreated abdominal aortic segment.
For patients with connective tissue disorders, open repair is still the gold standard. As for long-term survival, the advantage goes to open only because the endovascular approach is relatively new. If it’s done in high-volume centers with great experience, open repair has a mortality advantage as well.
Dr. Joel Corvera is an assistant professor of surgery and director of thoracic and vascular surgery at Indiana University, Indianapolis. He had no relationships to disclose.
1. Eur J Vasc Endovasc Surg. 2011 Feb;41:159-66.
2. J Thorac Cardiovasc Surg. 2011 Feb;141:322-7.
3. Ann Cardiothorac Surg. 2014 May;3:264-74.
4. J Thorac Cardiovasc Surg. 2010 Jun;139:1548-53.
5. Ann Thorac Surg. 2013 Mar;95:914-21.
TEVAR is the best procedure.
At Cedars-Sinai Medical Center, 70% of the aortic operations are performed in open fashion, but in patients with chronic type B aortic dissection, thoracic endovascular repair (TEVAR) is the preferred option. Goals of TEVAR in the setting of chronic type B dissection are to seal off the intimomedial tears, re-route blood to the true lumen, and induce false lumen thrombosis in the descending thoracic aorta, promoting reverse aortic remodeling and reducing future reinterventions.
TEVAR in patients with chronic type B aortic dissection has the best results if the following five rules apply: the patient should be older than 40 years of age and not have connective tissue disorder; there should be a proper proximal landing zone; the distal landing zone at the celiac artery should be smaller than 4 cm to allow for reverse remodeling; most of the large intimomedial tears should be in the descending aorta; and at least three visceral vessels should come off the true lumen. With this clinical scenario, the majority of centers will have excellent results with TEVAR.
TEVAR for chronic type B aortic dissection comes with three usual concerns: short-term outcomes; reverse aortic remodeling; and long-term outcomes.
In evaluating short-term outcomes of TEVAR in chronic type B aortic dissection, many large, single-center studies, including ours, have documented the superior results.1,2 The VIRTUE study reported an operative mortality and 30-day hospitality mortality of zero and spinal cord ischemia rate of 3.8% in a prospective, multi-center review.3 A meta-analysis of TEVAR for chronic dissection that involved 567 patients reported a 30-day mortality rate of 3.2%, paraplegia rate of 0.45%, a stroke rate of 1.5%, and retrograde type A dissection rate of 0.7%.4
These outcomes are far better than those reported in a meta-analysis of open repair for chronic dissection (771 patients): post-1997 mortality of 8.8% (the overall 30-day mortality rate was 12.5%); paraplegia of 6%; and renal failure with hemodialysis of 4%.5 A statewide analysis of elective open repair for thoracoabdominal aortic aneurysm, including chronic dissections, in California had a 30-day mortality rate of 19.7%.6
With regard to reverse aortic remodeling, acceptable results with TEVAR have been reported. The INSTEAD-XL study reported that at 5 years, 73% of patients had reverse aortic remodeling, with absolute risk reduction of 12.4%, compared with optimal medical therapy.7 A systematic review reported an 85.7% median rate of false lumen thrombosis.4 In the past some surgeons were concerned about a thick septum and whether it would give way and allow reverse remodeling; these studies confirmed that it does. The radial force of a stent graft over time will enlarge to the size that you would expect and it will cause the false lumen thrombosis.
Our group has provided anatomical indicators to achieve reverse remodeling in chronic type B dissection, including the location and size of intimomedial tears above the celiac artery.8 A patient with this anatomy has a great chance of not requiring any future reinterventions if the tears are mostly within the thoracic aorta upper fit.
Large multicenter studies also provide answers to the third concern about TEVAR for chronic aortic dissection – long-term outcomes – and found that they are comparable to open surgery. A study of the Medtronic Thoracic Endovascular Registry (MOTHER) database, a prospective, multicenter, adjudicated registry, looked at three types of aortic pathology: chronic aortic dissection (CAD); acute aortic dissection (AAD); and thoracic aortic aneurysm (TAA). The 195 patients with CAD had the best all-cause mortality outcomes: 3.2 per 100 patient years.9 Aortic-related mortality was also lowest in the CAD group: 0.4 per 100 patient years vs. 0.6 for TAA and 1.2 for AAD.
The reintervention rates for patients with aortic dissection were high, compared with TAA in the MOTHER registry. INSTEAD XL revealed all-cause and aortic-related mortality, respectively, at 11.1% and 6.9% in patients with chronic type B dissection treated with TEVAR at 5 years.
Last but not least, TEVAR is the first choice for many elderly or frail patients with type B aortic dissection. Recovery after the open procedure is much more difficult for this population. Our specialty frequently underappreciates quality of life after an aortic operation.
Overall, TEVAR for chronic type B aortic dissection is feasible, reproducible, and less invasive than open repair. It has acceptable early results, rate of reverse aortic modeling, and late mortality, and although its reintervention rate can be significant, that can be reduced with experience and a careful algorithmic approach.
Dr. Ali Khoynezhad is a professor of cardiovascular surgery, director of aortic surgery, and co-director of the atrial fibrillation program at Cedars-Sinai Heart Institute, Los Angeles. He disclosed receiving research grants from Medtronic, Gore, and Vascutek.
1. J Thorac Cardiovasc Surg. 2008 May;135:1103-9.
2. J Thorac Cardiovasc Surg. 2011 Feb;141:322-7.
3. Eur J Vasc Endovasc Surg. 2011 Feb;41:159-66.
4. Eur J Vasc Endovasc Surg. 2011 Nov;42:632-47.
5. J Vasc Surg. 2010 Oct;52:3S-9S.
6. J Vasc Surg. 2006 Feb;43:217-22.
7. Circ Cardiovasc Interv. 2013 Aug;6:407-16.
8. J Vasc Surg. 2010 Sep;52:562-8.
9. Circulation. 2013 Jan;127:24-32.
Open repair is the better procedure.
It’s my contention that open repair is still the gold standard for chronic thoracoabdominal aortic dissection. It has a record of outstanding results in high-volume centers of excellence with low morbidity and mortality and very good long-term survival. It has no anatomical constraints. It’s a durable repair and there are no device- or procedure-related proximal and/or distal aortic complications. Reintervention on the operated segment is very rare.1-6
Thoracic endovascular repair (TEVAR), despite having very good procedural results, has challenges in the successful treatment of chronic aortic dissection. Morbidity is low, as are rates of spinal cord ischemia, stroke, and renal failure. However, thoracic remodeling at the level of the endograft is in the 70%-88% range, which means that 12%-30% of patients do not have protection in the form of reverse aortic remodeling. In the abdominal aorta, remodeling is uncommon, with 11%-23% thrombosis of the false lumen even with advantageous anatomy. Survival in several series is in the 60%-80% range at 3 and 5 years. TEVAR creates new challenges for chronic thoracoabdominal aortic dissection: retrograde type A dissections have been as high as 2%-7%; 15%-30% of cases require intervention; and stent graft-induced new entry (SINE) has been reported as high as 36%.
Specific anatomical features are not suitable for TEVAR. They include multiple visceral vessels off of the false lumen; multiple fenestrations, especially in the abdominal aorta; dissection within the dissection; and pseudocoarctation. The durability of the endovascular graft for chronic aortic dissection is unknown; it’s a relatively new procedure so the long-term data is lacking.
Success of the endovascular approach depends on aortic remodeling, and it’s my contention that the thoracic devices now available cannot effectively treat a chronic thoracoabdominal aortic dissection. There are steps surgeons can take to improve their success, but procedures specifically addressing the false lumen are not time-tested and thoracoabdominal-specific devices are not widely available in the United States. And of course, morbidity and mortality will increase with the complexity of the endovascular repair.
Our in-hospital outcomes with open repair of chronic thoracoabdominal aortic dissection using deep hypothermia and circulatory arrest have been excellent: mortality rate of 3.6%; a stroke rate of 1%; permanent spinal cord ischemia rate 2.6%; and a 0% rate of patients on permanent hemodialysis. Our hospital length of stay is approximately 12 days. Blood product transfusion is reasonable with a mean blood product transfusion of 9 units for the hospital admission. The reintervention rate is 1% for infected grafts, 3.1% for anastomotic pseudoaneurysm and 3.6% for growth of a distal aneurysm. Long-term survival is very good: 93% at one year; 79% at five years; and 57% at 10 years.
There’s no denying that mortality rates for endovascular repair are excellent. There’s no denying that open repair is much more invasive. And if the patient is of advanced age, is frail and has comorbidities, the endovascular repair can have a certain advantage.
But for false lumen obliteration, the advantage goes to open repair. With regard to reintervention, certainly the advantage is with open repair. For durability, from what we know currently, open repair has the advantage. There are no stent-induced new entries in open repair; and open repair can address any and all anatomy. A successful endograft repair requires fixation and seal in the appropriate aortic anatomy; it demands good proximal and distal landing zones. However, in chronic dissection, there is the added complexity of having to address the false lumen flow from an untreated abdominal aortic segment.
For patients with connective tissue disorders, open repair is still the gold standard. As for long-term survival, the advantage goes to open only because the endovascular approach is relatively new. If it’s done in high-volume centers with great experience, open repair has a mortality advantage as well.
Dr. Joel Corvera is an assistant professor of surgery and director of thoracic and vascular surgery at Indiana University, Indianapolis. He had no relationships to disclose.
1. Eur J Vasc Endovasc Surg. 2011 Feb;41:159-66.
2. J Thorac Cardiovasc Surg. 2011 Feb;141:322-7.
3. Ann Cardiothorac Surg. 2014 May;3:264-74.
4. J Thorac Cardiovasc Surg. 2010 Jun;139:1548-53.
5. Ann Thorac Surg. 2013 Mar;95:914-21.
EXPERT ANALYSIS FROM THE AMERICAN ASSOCIATION FOR THORACIC SURGERY AORTIC SYMPOSIUM 2016
Key clinical point: Open repair for chronic thoracoabdominal aortic dissection has been the “gold standard” with good results, but thoracic endovascular repair (TEVAR) may have even lower mortality and complications in selected patients.
Major finding: Open and endovascular repair for thoracoabdominal aortic dissection have comparable results, but the former is a better choice for younger patients while the latter provides an option for elderly and more frail patients.
Data source: The presenters cited several studies to support their positions, including an analysis of 1,010 patients from the California Office of Statewide Health Planning and Development for 1991-2002 and 196-patient series from Indiana University.
Disclosures: Dr. Khoynezhad disclosed receiving research grants from Medtronic, Gore, and Vascutek. Dr. Corvera had no financial relationships to disclose.