User login
The Official Newspaper of the American Association for Thoracic Surgery
Can anesthesia in infants affect IQ scores?
About 10,000 newborns receive general anesthesia for congenital heart defects every year, and the more exposure they have to inhaled anesthetic agents, the greater effect it may have on their neurologic development, investigators at Children’s Hospital of Philadelphia reported in a study of newborns with hypoplastic left heart syndrome.
While previous studies have linked worse neurodevelopment to patient factors like prematurity and genetics, this is the first study to show a consistent relationship between neurodevelopment outcomes and modifiable factors during cardiac surgery in infants, Laura K. Diaz, MD, and her colleagues reported in the August issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg. 2016;152:482-9).
They studied 96 patients with hypoplastic left heart syndrome (HLHS) or similar syndromes who received volatile anesthetic agents (VAA) at their institution from 1998 to 2003. The patients underwent a battery of neurodevelopmental tests between the ages of 4 and 5 years that included full-scale IQ (FSIQ), verbal IQ (VIQ), performance IQ (PIQ), and processing speed.
“This study provides evidence that in children undergoing staged reconstructive surgery for HLHS, increasing cumulative exposure to VAAs beginning in infancy is associated with worse performance for FSIQ and VIQ, suggesting that VAA exposure may be a modifiable risk factor for adverse neurodevelopment outcomes,” Dr. Diaz and her colleagues wrote.
While survival has improved significantly in recent years for infants with hypoplastic left heart syndrome, physicians have harbored concerns that these children encounter neurodevelopmental issues later on. Dr. Diaz and her colleagues acknowledged that previous studies have shown factors, such as the use of cardiopulmonary bypass (CPB) and hospital length of stay, that could affect neurodevelopment in these children, but the findings have been inconsistent. Instead, those studies have shown such patient-specific factors as birth weight, ethnicity, and hereditary disorders were strong determinants of neurodevelopment in infants who have cardiac surgery, Dr. Diaz and her coauthors pointed out.
Their own previous study of patients with single-ventricle congenital heart disease concurred with the findings of those other studies, but it did not evaluate exposure to anesthesia (J. Thorac. Cardiovasc. Surg. 2014;147:1276-82). That was the focus of their current study.
Among the study group, 94 patients had an initial operation with CPB in their first 30 days of life. All 96 infants in the study group had additional operations, whether cardiac or noncardiac. The study tracked all anesthetic exposures up until the neurodevelopment evaluation in February 2008. All but 2 patients had initial VAA exposure at less than 1 year of age, and 45 at less than 1 month of age. Deep hypothermic circulatory arrest was used uniformly for aortic arch reconstruction.
The study used four different generalized linear models to evaluate anesthesia exposure and neurodevelopment.
For both FSIQ and PIQ, total minimum alveolar concentration hours were deemed to be statistically significant factors for lower scores. For PIQ, birth weight and length of postoperative hospital stay were statistically significant. For processing speed, gestational age and length of hospital stay were statistically significant.
Dr. Diaz and her colleagues said their findings are preliminary and do not justify a change in practice. “Prospective randomized, controlled multicenter clinical trials are indicated to continue to clarify the effects of early and repetitive exposure to VAA in this and other pediatric populations,” the study authors concluded.
Dr. Diaz and the study authors had no financial relationships to disclose.
The study by Dr. Diaz and her colleagues makes all the more clear the need for a prospective randomized trial on the effect inhaled anesthetic agents in infants can have on their neurologic development, Richard A. Jonas, MD, of Children’s National Heart Institute, Children’s National Medical Center, Washington, said in his invited commentary (J. Thorac. Cardiovasc. Surg. 2016;152:490).

|
Dr. Richard A. Jonas |
However, besides the study limitations that Dr. Diaz and her colleagues pointed out in their study, another “problem” Dr. Jonas noted with the study subjects was that they had staged reconstruction for hypoplastic left heart syndrome. “Not only is this group of patients at risk for prenatal effects of their abnormal in utero circulation, but in addition, they all underwent additional cardiac or noncardiac procedures after their initial cardiac surgery,” he said. These factors, along with some degree of cyanosis in their formative years, may help explain why this study is an outlier in that it did not implicate nonoperative factors that other studies implicated, Dr. Jonas said.
Nonetheless, the study is “an important contribution that adds further evidence to the observation that volatile agents can affect neurodevelopmental outcome,” Dr. Jonas said. Hence the need for a prospective randomized trial.
Dr. Jonas had no financial relationships to disclose.
The study by Dr. Diaz and her colleagues makes all the more clear the need for a prospective randomized trial on the effect inhaled anesthetic agents in infants can have on their neurologic development, Richard A. Jonas, MD, of Children’s National Heart Institute, Children’s National Medical Center, Washington, said in his invited commentary (J. Thorac. Cardiovasc. Surg. 2016;152:490).

|
Dr. Richard A. Jonas |
However, besides the study limitations that Dr. Diaz and her colleagues pointed out in their study, another “problem” Dr. Jonas noted with the study subjects was that they had staged reconstruction for hypoplastic left heart syndrome. “Not only is this group of patients at risk for prenatal effects of their abnormal in utero circulation, but in addition, they all underwent additional cardiac or noncardiac procedures after their initial cardiac surgery,” he said. These factors, along with some degree of cyanosis in their formative years, may help explain why this study is an outlier in that it did not implicate nonoperative factors that other studies implicated, Dr. Jonas said.
Nonetheless, the study is “an important contribution that adds further evidence to the observation that volatile agents can affect neurodevelopmental outcome,” Dr. Jonas said. Hence the need for a prospective randomized trial.
Dr. Jonas had no financial relationships to disclose.
The study by Dr. Diaz and her colleagues makes all the more clear the need for a prospective randomized trial on the effect inhaled anesthetic agents in infants can have on their neurologic development, Richard A. Jonas, MD, of Children’s National Heart Institute, Children’s National Medical Center, Washington, said in his invited commentary (J. Thorac. Cardiovasc. Surg. 2016;152:490).

|
Dr. Richard A. Jonas |
However, besides the study limitations that Dr. Diaz and her colleagues pointed out in their study, another “problem” Dr. Jonas noted with the study subjects was that they had staged reconstruction for hypoplastic left heart syndrome. “Not only is this group of patients at risk for prenatal effects of their abnormal in utero circulation, but in addition, they all underwent additional cardiac or noncardiac procedures after their initial cardiac surgery,” he said. These factors, along with some degree of cyanosis in their formative years, may help explain why this study is an outlier in that it did not implicate nonoperative factors that other studies implicated, Dr. Jonas said.
Nonetheless, the study is “an important contribution that adds further evidence to the observation that volatile agents can affect neurodevelopmental outcome,” Dr. Jonas said. Hence the need for a prospective randomized trial.
Dr. Jonas had no financial relationships to disclose.
About 10,000 newborns receive general anesthesia for congenital heart defects every year, and the more exposure they have to inhaled anesthetic agents, the greater effect it may have on their neurologic development, investigators at Children’s Hospital of Philadelphia reported in a study of newborns with hypoplastic left heart syndrome.
While previous studies have linked worse neurodevelopment to patient factors like prematurity and genetics, this is the first study to show a consistent relationship between neurodevelopment outcomes and modifiable factors during cardiac surgery in infants, Laura K. Diaz, MD, and her colleagues reported in the August issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg. 2016;152:482-9).
They studied 96 patients with hypoplastic left heart syndrome (HLHS) or similar syndromes who received volatile anesthetic agents (VAA) at their institution from 1998 to 2003. The patients underwent a battery of neurodevelopmental tests between the ages of 4 and 5 years that included full-scale IQ (FSIQ), verbal IQ (VIQ), performance IQ (PIQ), and processing speed.
“This study provides evidence that in children undergoing staged reconstructive surgery for HLHS, increasing cumulative exposure to VAAs beginning in infancy is associated with worse performance for FSIQ and VIQ, suggesting that VAA exposure may be a modifiable risk factor for adverse neurodevelopment outcomes,” Dr. Diaz and her colleagues wrote.
While survival has improved significantly in recent years for infants with hypoplastic left heart syndrome, physicians have harbored concerns that these children encounter neurodevelopmental issues later on. Dr. Diaz and her colleagues acknowledged that previous studies have shown factors, such as the use of cardiopulmonary bypass (CPB) and hospital length of stay, that could affect neurodevelopment in these children, but the findings have been inconsistent. Instead, those studies have shown such patient-specific factors as birth weight, ethnicity, and hereditary disorders were strong determinants of neurodevelopment in infants who have cardiac surgery, Dr. Diaz and her coauthors pointed out.
Their own previous study of patients with single-ventricle congenital heart disease concurred with the findings of those other studies, but it did not evaluate exposure to anesthesia (J. Thorac. Cardiovasc. Surg. 2014;147:1276-82). That was the focus of their current study.
Among the study group, 94 patients had an initial operation with CPB in their first 30 days of life. All 96 infants in the study group had additional operations, whether cardiac or noncardiac. The study tracked all anesthetic exposures up until the neurodevelopment evaluation in February 2008. All but 2 patients had initial VAA exposure at less than 1 year of age, and 45 at less than 1 month of age. Deep hypothermic circulatory arrest was used uniformly for aortic arch reconstruction.
The study used four different generalized linear models to evaluate anesthesia exposure and neurodevelopment.
For both FSIQ and PIQ, total minimum alveolar concentration hours were deemed to be statistically significant factors for lower scores. For PIQ, birth weight and length of postoperative hospital stay were statistically significant. For processing speed, gestational age and length of hospital stay were statistically significant.
Dr. Diaz and her colleagues said their findings are preliminary and do not justify a change in practice. “Prospective randomized, controlled multicenter clinical trials are indicated to continue to clarify the effects of early and repetitive exposure to VAA in this and other pediatric populations,” the study authors concluded.
Dr. Diaz and the study authors had no financial relationships to disclose.
About 10,000 newborns receive general anesthesia for congenital heart defects every year, and the more exposure they have to inhaled anesthetic agents, the greater effect it may have on their neurologic development, investigators at Children’s Hospital of Philadelphia reported in a study of newborns with hypoplastic left heart syndrome.
While previous studies have linked worse neurodevelopment to patient factors like prematurity and genetics, this is the first study to show a consistent relationship between neurodevelopment outcomes and modifiable factors during cardiac surgery in infants, Laura K. Diaz, MD, and her colleagues reported in the August issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg. 2016;152:482-9).
They studied 96 patients with hypoplastic left heart syndrome (HLHS) or similar syndromes who received volatile anesthetic agents (VAA) at their institution from 1998 to 2003. The patients underwent a battery of neurodevelopmental tests between the ages of 4 and 5 years that included full-scale IQ (FSIQ), verbal IQ (VIQ), performance IQ (PIQ), and processing speed.
“This study provides evidence that in children undergoing staged reconstructive surgery for HLHS, increasing cumulative exposure to VAAs beginning in infancy is associated with worse performance for FSIQ and VIQ, suggesting that VAA exposure may be a modifiable risk factor for adverse neurodevelopment outcomes,” Dr. Diaz and her colleagues wrote.
While survival has improved significantly in recent years for infants with hypoplastic left heart syndrome, physicians have harbored concerns that these children encounter neurodevelopmental issues later on. Dr. Diaz and her colleagues acknowledged that previous studies have shown factors, such as the use of cardiopulmonary bypass (CPB) and hospital length of stay, that could affect neurodevelopment in these children, but the findings have been inconsistent. Instead, those studies have shown such patient-specific factors as birth weight, ethnicity, and hereditary disorders were strong determinants of neurodevelopment in infants who have cardiac surgery, Dr. Diaz and her coauthors pointed out.
Their own previous study of patients with single-ventricle congenital heart disease concurred with the findings of those other studies, but it did not evaluate exposure to anesthesia (J. Thorac. Cardiovasc. Surg. 2014;147:1276-82). That was the focus of their current study.
Among the study group, 94 patients had an initial operation with CPB in their first 30 days of life. All 96 infants in the study group had additional operations, whether cardiac or noncardiac. The study tracked all anesthetic exposures up until the neurodevelopment evaluation in February 2008. All but 2 patients had initial VAA exposure at less than 1 year of age, and 45 at less than 1 month of age. Deep hypothermic circulatory arrest was used uniformly for aortic arch reconstruction.
The study used four different generalized linear models to evaluate anesthesia exposure and neurodevelopment.
For both FSIQ and PIQ, total minimum alveolar concentration hours were deemed to be statistically significant factors for lower scores. For PIQ, birth weight and length of postoperative hospital stay were statistically significant. For processing speed, gestational age and length of hospital stay were statistically significant.
Dr. Diaz and her colleagues said their findings are preliminary and do not justify a change in practice. “Prospective randomized, controlled multicenter clinical trials are indicated to continue to clarify the effects of early and repetitive exposure to VAA in this and other pediatric populations,” the study authors concluded.
Dr. Diaz and the study authors had no financial relationships to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: Volatile inhaled anesthesia may affect neurodevelopment in infants with hypoplastic left heart syndrome.
Major finding: Different generalized linear models determined an association between minimum alveolar concentration hours and hospital length of stay with lower IQ scores and processing speed.
Data source: Meta-analysis reviewed a subgroup of 96 patients with hypoplastic left heart syndrome who had neurodevelopmental testing at a single center between 1998 and 2003.
Disclosures: The authors have no financial relationships to disclose.
Gallstone disease boosts heart disease risk
Gallstone disease is associated with a 23% higher risk of developing coronary heart disease, according to an analysis published Aug. 18 in Arteriosclerosis, Thrombosis, and Vascular Biology.
“Our results suggest that patients with gallstone disease should be monitored closely based on a careful assessment of both gallstone and heart disease risk factors,” senior author Lu Qi, MD, PhD, said in a statement.
Dr. Qi, professor of epidemiology at Tulane University in New Orleans, and his coinvestigators conducted a meta-analysis of seven distinct studies, which involved a total of 842,553 patients and 51,123 cases of coronary heart disease. Patients with coronary heart disease were investigated further to determine if there was any history of gallstone disease.
Results showed that there was a 23% higher likelihood of coronary heart disease in patients who had gallstone disease, compared with those who did not, with a range of 15%-33% across the studies; the adjusted hazard ratio was 1.23 (95% confidence interval, 1.15-1.33).
Additionally, a separate prospective analysis of three of the included studies was conducted to determine individual risk factors that may contribute to the association between gallstone disease and coronary heart disease. These studies were the Nurses’ Health Study, conducted from 1980 to 2010, the Nurses’ Health Study II, which took place during 1989-2011, and the Health Professionals Follow-up Study, from 1986 through 2010, involving 112,520 women, 112,919 women, and 43,703 men, respectively.
This analysis revealed a 17% increase in coronary heart disease risk (aHR, 1.17; 95% CI, 1.09-1.26). Furthermore, the investigators noted that individuals with a history of gallstone disease who were otherwise healthy – in other words, had no history of obesity, high blood pressure, diabetes, or other disorders commonly associated with coronary heart disease – still stood a higher chance of developing coronary heart disease than individuals with no history of gallstone disease (Arterioscler Thromb Vasc Biol. 2016 Aug 18. doi: 10.1161/atvbaha.116.307507).
“Preventing gallstone disease may also benefit heart health,” Dr. Qi said.
“The potential mechanisms for the association of gallstone diseases with [coronary heart disease] may, at least, include the primary metabolic pathway and the bacterial pathway,” Dr. Qi and his coinvestigators posited, explaining that “among patients with gallstones, especially those with cholesterol gallstones, their bile acid and lecithin secretion rates tend to be depressed and cholesterol secretion rates elevated, which could indicate enhanced cholesterol synthesis and therefore increase cardiovascular disease risk.”
This study was supported by funding from the National Institutes of Health, the Boston Obesity Nutrition Research Center, and the United States–Israel Binational Science Foundation. The authors had no relevant financial disclosures.
Gallstone disease is associated with a 23% higher risk of developing coronary heart disease, according to an analysis published Aug. 18 in Arteriosclerosis, Thrombosis, and Vascular Biology.
“Our results suggest that patients with gallstone disease should be monitored closely based on a careful assessment of both gallstone and heart disease risk factors,” senior author Lu Qi, MD, PhD, said in a statement.
Dr. Qi, professor of epidemiology at Tulane University in New Orleans, and his coinvestigators conducted a meta-analysis of seven distinct studies, which involved a total of 842,553 patients and 51,123 cases of coronary heart disease. Patients with coronary heart disease were investigated further to determine if there was any history of gallstone disease.
Results showed that there was a 23% higher likelihood of coronary heart disease in patients who had gallstone disease, compared with those who did not, with a range of 15%-33% across the studies; the adjusted hazard ratio was 1.23 (95% confidence interval, 1.15-1.33).
Additionally, a separate prospective analysis of three of the included studies was conducted to determine individual risk factors that may contribute to the association between gallstone disease and coronary heart disease. These studies were the Nurses’ Health Study, conducted from 1980 to 2010, the Nurses’ Health Study II, which took place during 1989-2011, and the Health Professionals Follow-up Study, from 1986 through 2010, involving 112,520 women, 112,919 women, and 43,703 men, respectively.
This analysis revealed a 17% increase in coronary heart disease risk (aHR, 1.17; 95% CI, 1.09-1.26). Furthermore, the investigators noted that individuals with a history of gallstone disease who were otherwise healthy – in other words, had no history of obesity, high blood pressure, diabetes, or other disorders commonly associated with coronary heart disease – still stood a higher chance of developing coronary heart disease than individuals with no history of gallstone disease (Arterioscler Thromb Vasc Biol. 2016 Aug 18. doi: 10.1161/atvbaha.116.307507).
“Preventing gallstone disease may also benefit heart health,” Dr. Qi said.
“The potential mechanisms for the association of gallstone diseases with [coronary heart disease] may, at least, include the primary metabolic pathway and the bacterial pathway,” Dr. Qi and his coinvestigators posited, explaining that “among patients with gallstones, especially those with cholesterol gallstones, their bile acid and lecithin secretion rates tend to be depressed and cholesterol secretion rates elevated, which could indicate enhanced cholesterol synthesis and therefore increase cardiovascular disease risk.”
This study was supported by funding from the National Institutes of Health, the Boston Obesity Nutrition Research Center, and the United States–Israel Binational Science Foundation. The authors had no relevant financial disclosures.
Gallstone disease is associated with a 23% higher risk of developing coronary heart disease, according to an analysis published Aug. 18 in Arteriosclerosis, Thrombosis, and Vascular Biology.
“Our results suggest that patients with gallstone disease should be monitored closely based on a careful assessment of both gallstone and heart disease risk factors,” senior author Lu Qi, MD, PhD, said in a statement.
Dr. Qi, professor of epidemiology at Tulane University in New Orleans, and his coinvestigators conducted a meta-analysis of seven distinct studies, which involved a total of 842,553 patients and 51,123 cases of coronary heart disease. Patients with coronary heart disease were investigated further to determine if there was any history of gallstone disease.
Results showed that there was a 23% higher likelihood of coronary heart disease in patients who had gallstone disease, compared with those who did not, with a range of 15%-33% across the studies; the adjusted hazard ratio was 1.23 (95% confidence interval, 1.15-1.33).
Additionally, a separate prospective analysis of three of the included studies was conducted to determine individual risk factors that may contribute to the association between gallstone disease and coronary heart disease. These studies were the Nurses’ Health Study, conducted from 1980 to 2010, the Nurses’ Health Study II, which took place during 1989-2011, and the Health Professionals Follow-up Study, from 1986 through 2010, involving 112,520 women, 112,919 women, and 43,703 men, respectively.
This analysis revealed a 17% increase in coronary heart disease risk (aHR, 1.17; 95% CI, 1.09-1.26). Furthermore, the investigators noted that individuals with a history of gallstone disease who were otherwise healthy – in other words, had no history of obesity, high blood pressure, diabetes, or other disorders commonly associated with coronary heart disease – still stood a higher chance of developing coronary heart disease than individuals with no history of gallstone disease (Arterioscler Thromb Vasc Biol. 2016 Aug 18. doi: 10.1161/atvbaha.116.307507).
“Preventing gallstone disease may also benefit heart health,” Dr. Qi said.
“The potential mechanisms for the association of gallstone diseases with [coronary heart disease] may, at least, include the primary metabolic pathway and the bacterial pathway,” Dr. Qi and his coinvestigators posited, explaining that “among patients with gallstones, especially those with cholesterol gallstones, their bile acid and lecithin secretion rates tend to be depressed and cholesterol secretion rates elevated, which could indicate enhanced cholesterol synthesis and therefore increase cardiovascular disease risk.”
This study was supported by funding from the National Institutes of Health, the Boston Obesity Nutrition Research Center, and the United States–Israel Binational Science Foundation. The authors had no relevant financial disclosures.
FROM ARTERIOSCLEROSIS, THROMBOSIS, AND VASCULAR BIOLOGY
Key clinical point: Gallstone disease is associated with an increased risk for coronary heart disease; preventing the former can help mitigate chances of developing the latter.
Major finding: A meta-analysis revealed a 23% increased chance of CHD in gallstone disease patients.
Data source: A meta-analysis of seven studies involving 842,553 subjects, and a prospective cohort study of 269,142 participants in three separate studies that took place from 1980 to 2011.
Disclosures: Funding provided by NIH, Boston Obesity Nutrition Research Center, and United States–Israel Binational Science Foundation. The authors had no relevant financial disclosures.
Save the Date: AATS Centennial (1917-2017)
April 29 – May 3, 2017
Boston Hynes Convention Center
Boston, MA
President & Annual Meeting Chair
Thoralf M. Sundt, III
Annual Meeting Co-Chairs
Robert D. Jaquiss
Bryan F. Meyers
Reflecting on the Past. Building Our Future. Always Learning.
Please join us in Boston to celebrate the AATS Centennial.
Attendees will commemorate the first 100 years of the AATS and cardiothoracic surgery by enjoying activities and events, as well as viewing historical artifacts and memorabilia.
Celebrate How Far We Have Come: The Centennial officially begins with the Welcome Reception in the Exhibit Hall.
Celebrate Our Leadership: “In the Words of the Presidents” — a commemorative text containing personal reminiscences from most recent AATS past presidents — will be provided to all professional attendees.
Celebrate Our Specialty: The once-in-a-lifetime Centennial Gala will be held at the famed Wang Theatre in the heart of Boston. This black tie affair will include a cocktail reception, sit-down dinner on the stage, and performances from local musicians from prestigious Boston institutes.
Celebrate Our History: “In the Beginning” is a documentary film providing an in-depth look at the formative years of and challenges faced by cardiothoracic surgery. The film includes interviews with past presidents and members of the Centennial Committee.
April 29 – May 3, 2017
Boston Hynes Convention Center
Boston, MA
President & Annual Meeting Chair
Thoralf M. Sundt, III
Annual Meeting Co-Chairs
Robert D. Jaquiss
Bryan F. Meyers
Reflecting on the Past. Building Our Future. Always Learning.
Please join us in Boston to celebrate the AATS Centennial.
Attendees will commemorate the first 100 years of the AATS and cardiothoracic surgery by enjoying activities and events, as well as viewing historical artifacts and memorabilia.
Celebrate How Far We Have Come: The Centennial officially begins with the Welcome Reception in the Exhibit Hall.
Celebrate Our Leadership: “In the Words of the Presidents” — a commemorative text containing personal reminiscences from most recent AATS past presidents — will be provided to all professional attendees.
Celebrate Our Specialty: The once-in-a-lifetime Centennial Gala will be held at the famed Wang Theatre in the heart of Boston. This black tie affair will include a cocktail reception, sit-down dinner on the stage, and performances from local musicians from prestigious Boston institutes.
Celebrate Our History: “In the Beginning” is a documentary film providing an in-depth look at the formative years of and challenges faced by cardiothoracic surgery. The film includes interviews with past presidents and members of the Centennial Committee.
April 29 – May 3, 2017
Boston Hynes Convention Center
Boston, MA
President & Annual Meeting Chair
Thoralf M. Sundt, III
Annual Meeting Co-Chairs
Robert D. Jaquiss
Bryan F. Meyers
Reflecting on the Past. Building Our Future. Always Learning.
Please join us in Boston to celebrate the AATS Centennial.
Attendees will commemorate the first 100 years of the AATS and cardiothoracic surgery by enjoying activities and events, as well as viewing historical artifacts and memorabilia.
Celebrate How Far We Have Come: The Centennial officially begins with the Welcome Reception in the Exhibit Hall.
Celebrate Our Leadership: “In the Words of the Presidents” — a commemorative text containing personal reminiscences from most recent AATS past presidents — will be provided to all professional attendees.
Celebrate Our Specialty: The once-in-a-lifetime Centennial Gala will be held at the famed Wang Theatre in the heart of Boston. This black tie affair will include a cocktail reception, sit-down dinner on the stage, and performances from local musicians from prestigious Boston institutes.
Celebrate Our History: “In the Beginning” is a documentary film providing an in-depth look at the formative years of and challenges faced by cardiothoracic surgery. The film includes interviews with past presidents and members of the Centennial Committee.
A dual Y-shaped stent can improve QOL with airway fistulas
Airway fistula is a rare but life-threatening complication of esophageal surgery, but an innovative technique using two custom-made, Y-shaped metallic stents can preserve airway patency, researchers at Zhengzhou University in China reported in the August issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg. 2016;152:557-63).
The study involved 10 patients who received Y-shaped stents to treat gastrotracheal or gastrobronchial fistulas (GTFs and GBFs, respectively) after esophageal surgery from 2010 through 2014. “Our patients tolerated the stents well and had good palliation of their symptoms,” wrote Teng-Fei Li, MD, and colleagues.
Six patients died within 8 months for unrelated reasons – either tumors (four patients), or hemoptysis or pulmonary infection (one each). In one patient, the carinal fistula enlarged 4 months after stenting, but the researchers successfully placed an additional small Y-shaped stent. At the publication of the paper, this patient and three others had survived, Dr. Li and colleagues said.
After esophagectomy, fistulas can form between the tracheobronchial tree and stomach for a variety of reasons. A metallic stent would seem the logical choice after fistula formation, but it can be problematic, Dr. Li and colleagues pointed out. “Most often the clinician faces a situation in which the esophageal stent should have a larger diameter on the gastric side, making stenting the alimentary side of the fistula insufficient,” they said. The risk of stent migration is high, and the bifurcated structure of the trachea and main bronchi can cause leakage and stent displacement.
The researchers noted that Y-shaped self-expanding stents have been used for sealing airway fistulas, but they don’t always fully seal large GTFs and GBFs. Their primary objective in studying the combined-type Y-shaped covered metallic stent was to determine the safety and feasibility of the technique; the secondary aim was to evaluate long-term patency and complication rates.
They designed a Y-shaped stent delivery system (Micro-Tech) and used a combined bundle-and-push to insert the main body of the stent. In all, they inserted 20 Y-shaped stents in the 10 patients, although two stents did not fully expand and were dilated with a balloon. The researchers reported resolution of coughing during eating, toleration of liquid or semiliquid diet, and no complications after insertion.
Dr. Li and colleagues also developed strategies to avoid complications of Y-shaped stents, which have been known to retain secretions because they hinder cilia function. “To avoid this, we provided sputum suction and administered continuous high-concentration oxygen during the procedure,” they noted. Also, speed and agility in placement are important. “The operation should be performed as rapidly and gently as possible to avoid irritation to the airway,” Dr. Li and colleagues wrote. The postoperative course involved IV expectorants and antiasthma agents and aerosol inhalation of terbutaline. Surveillance bronchoscopes and debridement of granulation tissue helped avoid stent obstruction.
Nonetheless, the researches acknowledged limitations of the retrospective study, namely its small sample size and lack of a control group.
Dr. Li and colleagues had no financial relationships to disclose.
The Zhengzhou University investigators provide an opportunity to “think outside the box” when managing complex airway fistulas, Waël C. Hanna, MDCM, of McMaster University and St. Joseph’s Healthcare in Hamilton, Ontario, said in his invited commentary (J Thorac Cardiovasc Surg. 2016;152:564).

|
Dr. Waël Hanna |
Dr. Hanna credited a couple of innovations in their technique to overcome the challenge of Y stents that “remain notoriously difficult to position”: eliminating rigid bronchoscopy and using angiography-guided oral delivery; and developing the hybrid deployment mechanism.
Dr. Hanna also noted two “important nuances” of the technique: The stents are custom-made based on the length and location of the fistula; and the routine placement of two stents, with a limb of the smaller Y stent projecting through a limb of the larger Y stent to seal the entire airway. “This Y-en-Y technique using perfectly fitted stents is likely what caused the excellent outcomes that are reported in this series,” Dr. Hanna said.
But their approach may not be a practical solution to complex airway fistulas soon, he said. “Most of us who see the occasional case are unlikely to be able to commission custom-made Y stents,” he said. What’s more, the deployment mechanism is complicated, and the effect on patient quality of life is unclear.
Dr. Hanna had no financial relationships to disclose.
The Zhengzhou University investigators provide an opportunity to “think outside the box” when managing complex airway fistulas, Waël C. Hanna, MDCM, of McMaster University and St. Joseph’s Healthcare in Hamilton, Ontario, said in his invited commentary (J Thorac Cardiovasc Surg. 2016;152:564).

|
Dr. Waël Hanna |
Dr. Hanna credited a couple of innovations in their technique to overcome the challenge of Y stents that “remain notoriously difficult to position”: eliminating rigid bronchoscopy and using angiography-guided oral delivery; and developing the hybrid deployment mechanism.
Dr. Hanna also noted two “important nuances” of the technique: The stents are custom-made based on the length and location of the fistula; and the routine placement of two stents, with a limb of the smaller Y stent projecting through a limb of the larger Y stent to seal the entire airway. “This Y-en-Y technique using perfectly fitted stents is likely what caused the excellent outcomes that are reported in this series,” Dr. Hanna said.
But their approach may not be a practical solution to complex airway fistulas soon, he said. “Most of us who see the occasional case are unlikely to be able to commission custom-made Y stents,” he said. What’s more, the deployment mechanism is complicated, and the effect on patient quality of life is unclear.
Dr. Hanna had no financial relationships to disclose.
The Zhengzhou University investigators provide an opportunity to “think outside the box” when managing complex airway fistulas, Waël C. Hanna, MDCM, of McMaster University and St. Joseph’s Healthcare in Hamilton, Ontario, said in his invited commentary (J Thorac Cardiovasc Surg. 2016;152:564).

|
Dr. Waël Hanna |
Dr. Hanna credited a couple of innovations in their technique to overcome the challenge of Y stents that “remain notoriously difficult to position”: eliminating rigid bronchoscopy and using angiography-guided oral delivery; and developing the hybrid deployment mechanism.
Dr. Hanna also noted two “important nuances” of the technique: The stents are custom-made based on the length and location of the fistula; and the routine placement of two stents, with a limb of the smaller Y stent projecting through a limb of the larger Y stent to seal the entire airway. “This Y-en-Y technique using perfectly fitted stents is likely what caused the excellent outcomes that are reported in this series,” Dr. Hanna said.
But their approach may not be a practical solution to complex airway fistulas soon, he said. “Most of us who see the occasional case are unlikely to be able to commission custom-made Y stents,” he said. What’s more, the deployment mechanism is complicated, and the effect on patient quality of life is unclear.
Dr. Hanna had no financial relationships to disclose.
Airway fistula is a rare but life-threatening complication of esophageal surgery, but an innovative technique using two custom-made, Y-shaped metallic stents can preserve airway patency, researchers at Zhengzhou University in China reported in the August issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg. 2016;152:557-63).
The study involved 10 patients who received Y-shaped stents to treat gastrotracheal or gastrobronchial fistulas (GTFs and GBFs, respectively) after esophageal surgery from 2010 through 2014. “Our patients tolerated the stents well and had good palliation of their symptoms,” wrote Teng-Fei Li, MD, and colleagues.
Six patients died within 8 months for unrelated reasons – either tumors (four patients), or hemoptysis or pulmonary infection (one each). In one patient, the carinal fistula enlarged 4 months after stenting, but the researchers successfully placed an additional small Y-shaped stent. At the publication of the paper, this patient and three others had survived, Dr. Li and colleagues said.
After esophagectomy, fistulas can form between the tracheobronchial tree and stomach for a variety of reasons. A metallic stent would seem the logical choice after fistula formation, but it can be problematic, Dr. Li and colleagues pointed out. “Most often the clinician faces a situation in which the esophageal stent should have a larger diameter on the gastric side, making stenting the alimentary side of the fistula insufficient,” they said. The risk of stent migration is high, and the bifurcated structure of the trachea and main bronchi can cause leakage and stent displacement.
The researchers noted that Y-shaped self-expanding stents have been used for sealing airway fistulas, but they don’t always fully seal large GTFs and GBFs. Their primary objective in studying the combined-type Y-shaped covered metallic stent was to determine the safety and feasibility of the technique; the secondary aim was to evaluate long-term patency and complication rates.
They designed a Y-shaped stent delivery system (Micro-Tech) and used a combined bundle-and-push to insert the main body of the stent. In all, they inserted 20 Y-shaped stents in the 10 patients, although two stents did not fully expand and were dilated with a balloon. The researchers reported resolution of coughing during eating, toleration of liquid or semiliquid diet, and no complications after insertion.
Dr. Li and colleagues also developed strategies to avoid complications of Y-shaped stents, which have been known to retain secretions because they hinder cilia function. “To avoid this, we provided sputum suction and administered continuous high-concentration oxygen during the procedure,” they noted. Also, speed and agility in placement are important. “The operation should be performed as rapidly and gently as possible to avoid irritation to the airway,” Dr. Li and colleagues wrote. The postoperative course involved IV expectorants and antiasthma agents and aerosol inhalation of terbutaline. Surveillance bronchoscopes and debridement of granulation tissue helped avoid stent obstruction.
Nonetheless, the researches acknowledged limitations of the retrospective study, namely its small sample size and lack of a control group.
Dr. Li and colleagues had no financial relationships to disclose.
Airway fistula is a rare but life-threatening complication of esophageal surgery, but an innovative technique using two custom-made, Y-shaped metallic stents can preserve airway patency, researchers at Zhengzhou University in China reported in the August issue of the Journal of Thoracic and Cardiovascular Surgery (J Thorac Cardiovasc Surg. 2016;152:557-63).
The study involved 10 patients who received Y-shaped stents to treat gastrotracheal or gastrobronchial fistulas (GTFs and GBFs, respectively) after esophageal surgery from 2010 through 2014. “Our patients tolerated the stents well and had good palliation of their symptoms,” wrote Teng-Fei Li, MD, and colleagues.
Six patients died within 8 months for unrelated reasons – either tumors (four patients), or hemoptysis or pulmonary infection (one each). In one patient, the carinal fistula enlarged 4 months after stenting, but the researchers successfully placed an additional small Y-shaped stent. At the publication of the paper, this patient and three others had survived, Dr. Li and colleagues said.
After esophagectomy, fistulas can form between the tracheobronchial tree and stomach for a variety of reasons. A metallic stent would seem the logical choice after fistula formation, but it can be problematic, Dr. Li and colleagues pointed out. “Most often the clinician faces a situation in which the esophageal stent should have a larger diameter on the gastric side, making stenting the alimentary side of the fistula insufficient,” they said. The risk of stent migration is high, and the bifurcated structure of the trachea and main bronchi can cause leakage and stent displacement.
The researchers noted that Y-shaped self-expanding stents have been used for sealing airway fistulas, but they don’t always fully seal large GTFs and GBFs. Their primary objective in studying the combined-type Y-shaped covered metallic stent was to determine the safety and feasibility of the technique; the secondary aim was to evaluate long-term patency and complication rates.
They designed a Y-shaped stent delivery system (Micro-Tech) and used a combined bundle-and-push to insert the main body of the stent. In all, they inserted 20 Y-shaped stents in the 10 patients, although two stents did not fully expand and were dilated with a balloon. The researchers reported resolution of coughing during eating, toleration of liquid or semiliquid diet, and no complications after insertion.
Dr. Li and colleagues also developed strategies to avoid complications of Y-shaped stents, which have been known to retain secretions because they hinder cilia function. “To avoid this, we provided sputum suction and administered continuous high-concentration oxygen during the procedure,” they noted. Also, speed and agility in placement are important. “The operation should be performed as rapidly and gently as possible to avoid irritation to the airway,” Dr. Li and colleagues wrote. The postoperative course involved IV expectorants and antiasthma agents and aerosol inhalation of terbutaline. Surveillance bronchoscopes and debridement of granulation tissue helped avoid stent obstruction.
Nonetheless, the researches acknowledged limitations of the retrospective study, namely its small sample size and lack of a control group.
Dr. Li and colleagues had no financial relationships to disclose.
FROM THE JOURNAL OF THORACIC AND CARDIOVASCULAR SURGERY
Key clinical point: A combined type Y-shaped self-expandable coated metallic stent is a new approach for treatment of airway fistulas.
Major finding: Ten patients received the stents; all of them reported improved quality of life. Six died within 8 months because of unrelated factors.
Data source: Single-institution retrospective review of 10 patients with gastrotracheal or gastrobronchial fistulas who received the stent to reopen the airway.
Disclosures: Dr. Li and coauthors had no financial relationships to disclose. The study received support from the National High-Tech R&D Program of China.
Model estimates risk of pneumonia after CABG
A model incorporating 17 easily obtainable preoperative variables may help clinicians estimate patients’ risk of developing pneumonia after undergoing coronary artery bypass graft surgery, according to a report published in Annals of Thoracic Surgery.
“This model may be used to inform clinician-patient decision making and to identify opportunities for mitigating a patient’s risk,” said Raymond J. Strobel, a medical student at the University of Michigan, Ann Arbor, and his associates.
Postoperative pneumonia is the most common hospital-acquired infection following CABG, and it raises mortality risk fourfold and increases length of stay threefold. But reliable estimation of patient risk of post-CABG pneumonia has been difficult because of its low relative incidence – roughly 3% – and because most studies of the disorder are nearly a decade out of date.
To devise a predictive model using current data, Mr. Strobel and his associates assessed numerous potential risk factors and outcomes for 16,084 consecutive patients undergoing CABG at all 33 cardiac centers across Michigan during a 3-year period. They identified 531 cases of post-CABG pneumonia (3.3%) in this cohort.
The investigators performed a univariate analysis to test the associations between pneumonia and numerous factors related to patient demographics, medical history, comorbid diseases, laboratory values, cardiac anatomy, cardiac function, pulmonary function, the CABG procedure, and the institution where the procedure was performed. Variables that were found to be significantly associated with pneumonia (though usually with small absolute magnitudes) were then assessed in a multivariate analysis, which was further refined to create the final model.
The final model includes 17 factors that clearly raise the risk of post-CABG pneumonia. These include an elevated leukocyte count; a decreased hematocrit; older patient age; comorbidities such as peripheral vascular disease, diabetes, and liver disease; markers of pulmonary impairment such as cigarette smoking, the need for home oxygen therapy, and chronic lung disease; markers of cardiac dysfunction such as a recent history of arrhythmia and decreased ejection fraction; and emergency or urgent rather than elective operative status.
“This model performs well and demonstrates robustness across important clinical subgroups and centers,” the investigators said (Ann Thorac Surg. 2016 Jun 1; doi: 10.1016/j.athoracsur.2016.03.074).
In particular, this study identified preoperative leukocytosis to be a significant predictor of post-CABG pneumonia across several subgroups of patients. “We speculate that patients presenting with an elevated white blood cell count before surgery may be mounting an immune response against a pathogen and that the insult of CABG significantly increases their odds of postoperative pneumonia. ... It may be prudent to delay surgery until the source of leukocytosis is satisfactorily investigated, if not identified and treated, or the leukocytosis has otherwise resolved,” Mr. Strobel and his associates noted.
A model incorporating 17 easily obtainable preoperative variables may help clinicians estimate patients’ risk of developing pneumonia after undergoing coronary artery bypass graft surgery, according to a report published in Annals of Thoracic Surgery.
“This model may be used to inform clinician-patient decision making and to identify opportunities for mitigating a patient’s risk,” said Raymond J. Strobel, a medical student at the University of Michigan, Ann Arbor, and his associates.
Postoperative pneumonia is the most common hospital-acquired infection following CABG, and it raises mortality risk fourfold and increases length of stay threefold. But reliable estimation of patient risk of post-CABG pneumonia has been difficult because of its low relative incidence – roughly 3% – and because most studies of the disorder are nearly a decade out of date.
To devise a predictive model using current data, Mr. Strobel and his associates assessed numerous potential risk factors and outcomes for 16,084 consecutive patients undergoing CABG at all 33 cardiac centers across Michigan during a 3-year period. They identified 531 cases of post-CABG pneumonia (3.3%) in this cohort.
The investigators performed a univariate analysis to test the associations between pneumonia and numerous factors related to patient demographics, medical history, comorbid diseases, laboratory values, cardiac anatomy, cardiac function, pulmonary function, the CABG procedure, and the institution where the procedure was performed. Variables that were found to be significantly associated with pneumonia (though usually with small absolute magnitudes) were then assessed in a multivariate analysis, which was further refined to create the final model.
The final model includes 17 factors that clearly raise the risk of post-CABG pneumonia. These include an elevated leukocyte count; a decreased hematocrit; older patient age; comorbidities such as peripheral vascular disease, diabetes, and liver disease; markers of pulmonary impairment such as cigarette smoking, the need for home oxygen therapy, and chronic lung disease; markers of cardiac dysfunction such as a recent history of arrhythmia and decreased ejection fraction; and emergency or urgent rather than elective operative status.
“This model performs well and demonstrates robustness across important clinical subgroups and centers,” the investigators said (Ann Thorac Surg. 2016 Jun 1; doi: 10.1016/j.athoracsur.2016.03.074).
In particular, this study identified preoperative leukocytosis to be a significant predictor of post-CABG pneumonia across several subgroups of patients. “We speculate that patients presenting with an elevated white blood cell count before surgery may be mounting an immune response against a pathogen and that the insult of CABG significantly increases their odds of postoperative pneumonia. ... It may be prudent to delay surgery until the source of leukocytosis is satisfactorily investigated, if not identified and treated, or the leukocytosis has otherwise resolved,” Mr. Strobel and his associates noted.
A model incorporating 17 easily obtainable preoperative variables may help clinicians estimate patients’ risk of developing pneumonia after undergoing coronary artery bypass graft surgery, according to a report published in Annals of Thoracic Surgery.
“This model may be used to inform clinician-patient decision making and to identify opportunities for mitigating a patient’s risk,” said Raymond J. Strobel, a medical student at the University of Michigan, Ann Arbor, and his associates.
Postoperative pneumonia is the most common hospital-acquired infection following CABG, and it raises mortality risk fourfold and increases length of stay threefold. But reliable estimation of patient risk of post-CABG pneumonia has been difficult because of its low relative incidence – roughly 3% – and because most studies of the disorder are nearly a decade out of date.
To devise a predictive model using current data, Mr. Strobel and his associates assessed numerous potential risk factors and outcomes for 16,084 consecutive patients undergoing CABG at all 33 cardiac centers across Michigan during a 3-year period. They identified 531 cases of post-CABG pneumonia (3.3%) in this cohort.
The investigators performed a univariate analysis to test the associations between pneumonia and numerous factors related to patient demographics, medical history, comorbid diseases, laboratory values, cardiac anatomy, cardiac function, pulmonary function, the CABG procedure, and the institution where the procedure was performed. Variables that were found to be significantly associated with pneumonia (though usually with small absolute magnitudes) were then assessed in a multivariate analysis, which was further refined to create the final model.
The final model includes 17 factors that clearly raise the risk of post-CABG pneumonia. These include an elevated leukocyte count; a decreased hematocrit; older patient age; comorbidities such as peripheral vascular disease, diabetes, and liver disease; markers of pulmonary impairment such as cigarette smoking, the need for home oxygen therapy, and chronic lung disease; markers of cardiac dysfunction such as a recent history of arrhythmia and decreased ejection fraction; and emergency or urgent rather than elective operative status.
“This model performs well and demonstrates robustness across important clinical subgroups and centers,” the investigators said (Ann Thorac Surg. 2016 Jun 1; doi: 10.1016/j.athoracsur.2016.03.074).
In particular, this study identified preoperative leukocytosis to be a significant predictor of post-CABG pneumonia across several subgroups of patients. “We speculate that patients presenting with an elevated white blood cell count before surgery may be mounting an immune response against a pathogen and that the insult of CABG significantly increases their odds of postoperative pneumonia. ... It may be prudent to delay surgery until the source of leukocytosis is satisfactorily investigated, if not identified and treated, or the leukocytosis has otherwise resolved,” Mr. Strobel and his associates noted.
FROM ANNALS OF THORACIC SURGERY
Key clinical point: A model incorporating 17 easily obtainable preoperative variables helps estimate patients’ risk of developing pneumonia after coronary artery bypass surgery.
Major finding: Seventeen factors clearly raise the risk of post-CABG pneumonia, including an elevated leukocyte count, a decreased hematocrit, cigarette smoking, and the need for home oxygen therapy.
Data source: A prospective observational cohort study assessing numerous risk factors in 16,084 CABG patients.
Disclosures: This study was funded in part by the U.S. Agency for Healthcare Research and Quality, Blue Cross and Blue Shield of Michigan, and Blue Care Network. The authors’ financial disclosures were not provided.
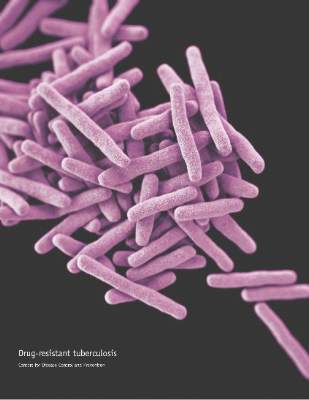
Don’t delay treatment for patients with TB and HIV
Clinicians should treat patients diagnosed with HIV and tuberculosis for both conditions immediately, according to new guidelines on the treatment of drug-susceptible tuberculosis.
The clinical practice guidelines were issued collectively by three organizations: the American Thoracic Society (ATS), the U.S. Centers for Disease Control and Prevention (CDC), and the Infectious Diseases Society of America (IDSA), and published online in Clinical Infectious Diseases.
The guidelines recommend starting TB treatment for all patients as soon as an infection is suspected, rather than waiting for test results, and focusing on daily therapy to reduce the risk of relapse. In addition, all TB patients should receive comprehensive care, including direct observed therapy (DOT) when appropriate (Clin Infect Dis. 2016 Aug 10. doi: 10.1093/cid/ciw376).
“Treatment of tuberculosis is focused on both curing the individual patient and minimizing the transmission,” wrote Payam Nahid, MD, professor of medicine at the University of California, San Francisco, and his colleagues on the guidelines committee.
The guidelines’ section on treatment of tuberculosis in special situations addresses management of TB in patients with conditions including HIV, extrapulmonary TB, culture-negative pulmonary TB, pregnancy, renal disease, and hepatic disease, as well as treatment of children and the elderly.
With regard to HIV, the guidelines recommend the standard 6-month daily TB treatment for HIV patients on antiretroviral therapy. This treatment includes 2 months of isoniazid (INH), rifampin (RIF), pyrazinamide (PZA), and ethambutol (EMB), followed by a continuation phase of 4 months of INH and RIF.
“Patients with HIV infection and tuberculosis are at an increased risk of developing paradoxical worsening of symptoms, signs, or clinical manifestations of tuberculosis after beginning antituberculosis and antiretroviral treatments,” according to the guidelines. These responses are defined as Immune Reconstitution Inflammatory Syndrome (IRIS). However, IRIS does not appear to impact the simultaneous treatment of TB and HIV, and the condition can be managed symptomatically if it occurs, the researchers noted.
The guidelines identified several areas in need of further study, including new TB drugs and treatment plans; the effects of biomarkers to help design individual therapy; TB in special populations including HIV patients, pregnant women, and children; and treatment delivery strategies.
The guidelines also are endorsed by the European Respiratory Society (ERS) and the U.S. National Tuberculosis Controllers Association (NCTA).
The American Thoracic Society, the Infections Diseases Society of America, and the Centers for Disease Control and Prevention provided financial support. Lead author Dr. Nahid had no financial conflicts to disclose.
Clinicians should treat patients diagnosed with HIV and tuberculosis for both conditions immediately, according to new guidelines on the treatment of drug-susceptible tuberculosis.
The clinical practice guidelines were issued collectively by three organizations: the American Thoracic Society (ATS), the U.S. Centers for Disease Control and Prevention (CDC), and the Infectious Diseases Society of America (IDSA), and published online in Clinical Infectious Diseases.
The guidelines recommend starting TB treatment for all patients as soon as an infection is suspected, rather than waiting for test results, and focusing on daily therapy to reduce the risk of relapse. In addition, all TB patients should receive comprehensive care, including direct observed therapy (DOT) when appropriate (Clin Infect Dis. 2016 Aug 10. doi: 10.1093/cid/ciw376).
“Treatment of tuberculosis is focused on both curing the individual patient and minimizing the transmission,” wrote Payam Nahid, MD, professor of medicine at the University of California, San Francisco, and his colleagues on the guidelines committee.
The guidelines’ section on treatment of tuberculosis in special situations addresses management of TB in patients with conditions including HIV, extrapulmonary TB, culture-negative pulmonary TB, pregnancy, renal disease, and hepatic disease, as well as treatment of children and the elderly.
With regard to HIV, the guidelines recommend the standard 6-month daily TB treatment for HIV patients on antiretroviral therapy. This treatment includes 2 months of isoniazid (INH), rifampin (RIF), pyrazinamide (PZA), and ethambutol (EMB), followed by a continuation phase of 4 months of INH and RIF.
“Patients with HIV infection and tuberculosis are at an increased risk of developing paradoxical worsening of symptoms, signs, or clinical manifestations of tuberculosis after beginning antituberculosis and antiretroviral treatments,” according to the guidelines. These responses are defined as Immune Reconstitution Inflammatory Syndrome (IRIS). However, IRIS does not appear to impact the simultaneous treatment of TB and HIV, and the condition can be managed symptomatically if it occurs, the researchers noted.
The guidelines identified several areas in need of further study, including new TB drugs and treatment plans; the effects of biomarkers to help design individual therapy; TB in special populations including HIV patients, pregnant women, and children; and treatment delivery strategies.
The guidelines also are endorsed by the European Respiratory Society (ERS) and the U.S. National Tuberculosis Controllers Association (NCTA).
The American Thoracic Society, the Infections Diseases Society of America, and the Centers for Disease Control and Prevention provided financial support. Lead author Dr. Nahid had no financial conflicts to disclose.
Clinicians should treat patients diagnosed with HIV and tuberculosis for both conditions immediately, according to new guidelines on the treatment of drug-susceptible tuberculosis.
The clinical practice guidelines were issued collectively by three organizations: the American Thoracic Society (ATS), the U.S. Centers for Disease Control and Prevention (CDC), and the Infectious Diseases Society of America (IDSA), and published online in Clinical Infectious Diseases.
The guidelines recommend starting TB treatment for all patients as soon as an infection is suspected, rather than waiting for test results, and focusing on daily therapy to reduce the risk of relapse. In addition, all TB patients should receive comprehensive care, including direct observed therapy (DOT) when appropriate (Clin Infect Dis. 2016 Aug 10. doi: 10.1093/cid/ciw376).
“Treatment of tuberculosis is focused on both curing the individual patient and minimizing the transmission,” wrote Payam Nahid, MD, professor of medicine at the University of California, San Francisco, and his colleagues on the guidelines committee.
The guidelines’ section on treatment of tuberculosis in special situations addresses management of TB in patients with conditions including HIV, extrapulmonary TB, culture-negative pulmonary TB, pregnancy, renal disease, and hepatic disease, as well as treatment of children and the elderly.
With regard to HIV, the guidelines recommend the standard 6-month daily TB treatment for HIV patients on antiretroviral therapy. This treatment includes 2 months of isoniazid (INH), rifampin (RIF), pyrazinamide (PZA), and ethambutol (EMB), followed by a continuation phase of 4 months of INH and RIF.
“Patients with HIV infection and tuberculosis are at an increased risk of developing paradoxical worsening of symptoms, signs, or clinical manifestations of tuberculosis after beginning antituberculosis and antiretroviral treatments,” according to the guidelines. These responses are defined as Immune Reconstitution Inflammatory Syndrome (IRIS). However, IRIS does not appear to impact the simultaneous treatment of TB and HIV, and the condition can be managed symptomatically if it occurs, the researchers noted.
The guidelines identified several areas in need of further study, including new TB drugs and treatment plans; the effects of biomarkers to help design individual therapy; TB in special populations including HIV patients, pregnant women, and children; and treatment delivery strategies.
The guidelines also are endorsed by the European Respiratory Society (ERS) and the U.S. National Tuberculosis Controllers Association (NCTA).
The American Thoracic Society, the Infections Diseases Society of America, and the Centers for Disease Control and Prevention provided financial support. Lead author Dr. Nahid had no financial conflicts to disclose.
FROM CLINICAL INFECTIOUS DISEASES
Key clinical point: Clinicians should treat patients diagnosed with HIV and tuberculosis for both conditions immediately.
Major finding: A four-drug regimen of INH, RIF, PZA, and EMB remains the preferred initial treatment for drug-susceptible pulmonary tuberculosis. Treatment should be initiated promptly even before diagnostic test results are known in patients with high likelihood of having tuberculosis.
Data source: Nine PICO (population, intervention, comparators, outcomes) questions and associated recommendations for the treatment of patients diagnosed with both HIV and TB, developed based on the evidence appraised using GRADE (Grading of Recommendations Assessment, Development, and Evaluation) methodology.
Disclosures: The American Thoracic Society, the Infections Diseases Society of America, and the Centers for Disease Control and Prevention provided financial support. Lead author Dr. Nahid had no financial conflicts to disclose.
CMV viremia not culprit in high mortality of TB/HIV coinfection
DURBAN, SOUTH AFRICA – Cytomegalovirus viremia is common among patients hospitalized for HIV-associated tuberculosis, but it appears to be a bystander rather than a contributor to the high mortality seen in this population, Amy Ward, MD, said at the 21st International AIDS Conference.
“CMV [cytomegalovirus] viremia is likely a marker of more severe immunodeficiency rather than a direct contributor to mortality,” she concluded based upon the findings of her prospective cohort study. The finding means therapies for CMV viremia will not open up a new avenue of potentially life-saving treatments for these patients.
In other severe immunodeficiency conditions, such as after organ transplant, CMV viremia is directly related to increased mortality, and ganciclovir therapy can prevent progression to clinical disease and death, explained Dr. Ward of the University of Cape Town, South Africa.
She presented a prospective cohort study of 256 HIV-infected South African adults, median age 36 years, who were hospitalized with a new diagnosis of TB. At enrollment, their median CD4 count was 64 cells/mm3. Only 35% were on antiretroviral therapy (ART); 44% had previously been on ART, 21% were ART-naive, and 41% had a positive TB blood culture.
CMV viremia was present in 31%, and CMV viral load was 1,000 copies/mL or more in half of them. None had CMV retinitis, based on panoptic fundoscopy at enrollment. HIV-related retinal pathologies at enrollment included disseminated cryptococcal disease, ocular TB granules, and HIV retinitis.
The primary endpoint of the study was mortality at 12 weeks on anti-TB therapy. The mortality rate was 38% in the CMV viremic group, significantly higher than the 17.8% mortality rate seen in the CMV-negative patients.
In a univariate Cox proportional hazards regression analysis, CMV viremia was associated with a 2.1-fold increased risk for 12-week mortality. But advancing age, a low CD4 count, and decreasing serum albumin were also risk factors.
When these variables were incorporated in a multivariate regression analysis along with HIV viral load, tuberculosis blood culture results, and gender, CMV viremia was no longer a significant risk factor for 12-week mortality. Age was the sole significant predictor of death. Patients who were at least 36 years old had a 32.8% mortality rate, compared with a 14.1% rate in those who were younger. The CD4 count didn’t differ significantly by age; however, the prevalence of CMV viremia was 38% in the older group and 26.3% in patients under age 36.
“Those patients who were 36 years old and above had a higher mortality and were more likely to have CMV viremia, both findings perhaps reflecting premature aging of the immune system,” Dr. Ward said.
Also, no dose-response was seen between CMV viral load and mortality risk. The 12-week mortality rate was 33.3% in patients with a CMV viral load below 1,000 copies/mL and similar at 34.1% in those with a viral load above that cutpoint, she noted.
The study was funded by the Wellcome Trust and the South African Medical Research Council. Dr. Ward reported having no financial conflicts of interest.
DURBAN, SOUTH AFRICA – Cytomegalovirus viremia is common among patients hospitalized for HIV-associated tuberculosis, but it appears to be a bystander rather than a contributor to the high mortality seen in this population, Amy Ward, MD, said at the 21st International AIDS Conference.
“CMV [cytomegalovirus] viremia is likely a marker of more severe immunodeficiency rather than a direct contributor to mortality,” she concluded based upon the findings of her prospective cohort study. The finding means therapies for CMV viremia will not open up a new avenue of potentially life-saving treatments for these patients.
In other severe immunodeficiency conditions, such as after organ transplant, CMV viremia is directly related to increased mortality, and ganciclovir therapy can prevent progression to clinical disease and death, explained Dr. Ward of the University of Cape Town, South Africa.
She presented a prospective cohort study of 256 HIV-infected South African adults, median age 36 years, who were hospitalized with a new diagnosis of TB. At enrollment, their median CD4 count was 64 cells/mm3. Only 35% were on antiretroviral therapy (ART); 44% had previously been on ART, 21% were ART-naive, and 41% had a positive TB blood culture.
CMV viremia was present in 31%, and CMV viral load was 1,000 copies/mL or more in half of them. None had CMV retinitis, based on panoptic fundoscopy at enrollment. HIV-related retinal pathologies at enrollment included disseminated cryptococcal disease, ocular TB granules, and HIV retinitis.
The primary endpoint of the study was mortality at 12 weeks on anti-TB therapy. The mortality rate was 38% in the CMV viremic group, significantly higher than the 17.8% mortality rate seen in the CMV-negative patients.
In a univariate Cox proportional hazards regression analysis, CMV viremia was associated with a 2.1-fold increased risk for 12-week mortality. But advancing age, a low CD4 count, and decreasing serum albumin were also risk factors.
When these variables were incorporated in a multivariate regression analysis along with HIV viral load, tuberculosis blood culture results, and gender, CMV viremia was no longer a significant risk factor for 12-week mortality. Age was the sole significant predictor of death. Patients who were at least 36 years old had a 32.8% mortality rate, compared with a 14.1% rate in those who were younger. The CD4 count didn’t differ significantly by age; however, the prevalence of CMV viremia was 38% in the older group and 26.3% in patients under age 36.
“Those patients who were 36 years old and above had a higher mortality and were more likely to have CMV viremia, both findings perhaps reflecting premature aging of the immune system,” Dr. Ward said.
Also, no dose-response was seen between CMV viral load and mortality risk. The 12-week mortality rate was 33.3% in patients with a CMV viral load below 1,000 copies/mL and similar at 34.1% in those with a viral load above that cutpoint, she noted.
The study was funded by the Wellcome Trust and the South African Medical Research Council. Dr. Ward reported having no financial conflicts of interest.
DURBAN, SOUTH AFRICA – Cytomegalovirus viremia is common among patients hospitalized for HIV-associated tuberculosis, but it appears to be a bystander rather than a contributor to the high mortality seen in this population, Amy Ward, MD, said at the 21st International AIDS Conference.
“CMV [cytomegalovirus] viremia is likely a marker of more severe immunodeficiency rather than a direct contributor to mortality,” she concluded based upon the findings of her prospective cohort study. The finding means therapies for CMV viremia will not open up a new avenue of potentially life-saving treatments for these patients.
In other severe immunodeficiency conditions, such as after organ transplant, CMV viremia is directly related to increased mortality, and ganciclovir therapy can prevent progression to clinical disease and death, explained Dr. Ward of the University of Cape Town, South Africa.
She presented a prospective cohort study of 256 HIV-infected South African adults, median age 36 years, who were hospitalized with a new diagnosis of TB. At enrollment, their median CD4 count was 64 cells/mm3. Only 35% were on antiretroviral therapy (ART); 44% had previously been on ART, 21% were ART-naive, and 41% had a positive TB blood culture.
CMV viremia was present in 31%, and CMV viral load was 1,000 copies/mL or more in half of them. None had CMV retinitis, based on panoptic fundoscopy at enrollment. HIV-related retinal pathologies at enrollment included disseminated cryptococcal disease, ocular TB granules, and HIV retinitis.
The primary endpoint of the study was mortality at 12 weeks on anti-TB therapy. The mortality rate was 38% in the CMV viremic group, significantly higher than the 17.8% mortality rate seen in the CMV-negative patients.
In a univariate Cox proportional hazards regression analysis, CMV viremia was associated with a 2.1-fold increased risk for 12-week mortality. But advancing age, a low CD4 count, and decreasing serum albumin were also risk factors.
When these variables were incorporated in a multivariate regression analysis along with HIV viral load, tuberculosis blood culture results, and gender, CMV viremia was no longer a significant risk factor for 12-week mortality. Age was the sole significant predictor of death. Patients who were at least 36 years old had a 32.8% mortality rate, compared with a 14.1% rate in those who were younger. The CD4 count didn’t differ significantly by age; however, the prevalence of CMV viremia was 38% in the older group and 26.3% in patients under age 36.
“Those patients who were 36 years old and above had a higher mortality and were more likely to have CMV viremia, both findings perhaps reflecting premature aging of the immune system,” Dr. Ward said.
Also, no dose-response was seen between CMV viral load and mortality risk. The 12-week mortality rate was 33.3% in patients with a CMV viral load below 1,000 copies/mL and similar at 34.1% in those with a viral load above that cutpoint, she noted.
The study was funded by the Wellcome Trust and the South African Medical Research Council. Dr. Ward reported having no financial conflicts of interest.
AT AIDS 2016
Key clinical point: Cytomegalovirus viremia is common in patients hospitalized for HIV-associated tuberculosis, but treating the CMV infection is unlikely to reduce the coinfected group’s high mortality rate.
Major finding: Cytomegalovirus viremia was present in nearly one-third of a group of hospitalized patients with HIV infection and tuberculosis, but was not an independent risk factor for their 23% mortality rate at 12 weeks.
Data source: This was a prospective cohort study including 256 hospitalized patients coinfected with HIV and newly diagnosed tuberculosis.
Disclosures: The study was funded by the Wellcome Trust and the South African Medical Research Council. The presenter reported having no financial conflicts of interest.
Thymectomy improves clinical outcomes for myasthenia gravis
Thymectomy improved 3-year clinical outcomes and proved superior to medical therapy for mild to severe nonthymomatous myasthenia gravis, according to a report published online Aug. 11 in the New England Journal of Medicine.
Compared with standard prednisone therapy, thymectomy plus prednisone decreased the number and severity of symptoms, allowed the lowering of steroid doses, decreased the number and length of hospitalizations for disease exacerbations, reduced the need for immunosuppressive agents, and improved health-related quality of life in an international, randomized clinical trial, said Gil I. Wolfe, MD, of the department of neurology, State University of New York at Buffalo and his associates.
Until now, thymectomy was known to be beneficial in some cases of myasthenia gravis “but with widely varying rates of clinical improvement or remission.” And the success of immunotherapy has raised the question of whether an invasive surgery is necessary. Data from randomized, controlled studies have been sparse.
Moreover, thymectomy rarely causes adverse effects, but “the procedure can cost up to $80,000 and can be associated with operative complications that need to be weighed against benefits.” In comparison, medical therapy with glucocorticoids and other immunosuppressive agents is less invasive but is definitely associated with adverse events, including some that are life threatening, and negatively impacts quality of life, the investigators said.
To address the lack of randomized controlled trial data, they assessed 3-year outcomes in 126 patients treated at 67 medical centers in 18 countries during a 6-year period. The study participants were aged 18-65 years, had a disease duration of less than 5 years at enrollment (median duration, 1 year), and had class II (mild generalized disease) to class IV (severe generalized disease) myasthenia gravis. These patients were randomly assigned to undergo thymectomy and receive standard prednisone therapy (66 participants) or to receive standard prednisone alone (60 participants).
Thymectomy was performed using a median sternotomy “with the goal of an en bloc resection of all mediastinal tissue that could anatomically contain gross or microscopic thymus.”
At follow-up, time-weighted average scores on the Quantitative Myasthenia Gravis scale were significantly lower by 2.85 points, indicating improved clinical status, in the thymectomy group than in the control group. Time-weighted average prednisone dose also was significantly lower, at an average alternate-day dose of 44 mg in the thymectomy group and 60 mg in the control group, Dr. Wolfe and his associates said (N Engl J Med. 2016 Aug 11. doi: 10.1056/NEJMoa1602489).
On a measure of treatment-related complications, scores favored thymectomy with regard to the number of patients with symptoms, the total number of symptoms, and the distress level related to symptoms throughout the study period. Fewer patients in the thymectomy group required hospitalization for exacerbations of myasthenia gravis (9% vs. 37%), and the mean cumulative number of hospital days was lower with thymectomy (8.4 vs. 19.2).
In addition, scores on the Myasthenia Gravis Activities of Daily Living scale favored thymectomy (2.24 vs. 3.41). Fewer patients in the thymectomy group required azathioprine (17% vs. 0.48%). And the percentage of patients who reported having minimal manifestations of the disease at 3 years was significantly higher with thymectomy (67%) than with prednisone alone (47%).
This study was supported by the National Institute of Neurological Disorders and Stroke, the Muscular Dystrophy Association, and the Myasthenia Gravis Foundation of America and received no commercial support. Dr. Wolfe reported ties to Alexion Pharmaceuticals, Alpha Cancer Technologies, Argenx, Baxalta, CSL Behring, Grifols, and UCB, and his associates reported ties to numerous industry sources.
Landmark trial establishes effectiveness of thymectomy in myasthenia gravis
One of the many challenges of treating patients with myasthenia gravis (MG) is the fluctuating nature of symptoms and deficits. The neurologist or neuromuscular specialist must decide whether the disease is truly worsening, whether the patient is experiencing more pronounced symptoms from intercurrent illness or the effects of a medication known to affect the neuromuscular junction adversely, or whether the patient is concerned that there might be worsening disease when all objective measures indicate stability. These factors make treatment decisions more difficult in MG than for many other neuromuscular disorders.
Similarly, researchers considering a trial investigating treatment efficacy in MG face the complex issues of disease fluctuation in cohorts of individuals with the disease, varying levels of corticosteroid and immunosuppressant doses in different MG patients, and thorny ethical dilemmas in providing accepted therapies but not withholding effective treatments from those in need.
Dr. Wolfe and his colleagues demonstrate that they have navigated these treacherous waters. They have succeeded in completing a landmark controlled clinical trial which establishes the effectiveness of transsternal thymectomy with adjuvant corticosteroid therapy in nonthymomatous MG vs. oral prednisone without surgery. While this international 36-center trial managed to recruit 126 subjects over a 6-year period, using sound inclusion and exclusion criteria and a meticulous trial design, the number of patients is not sufficient to allow for as robust a subgroup analysis for age, gender, and a variety of clinical variables reflecting severity of disease as would have been hoped for by the MG community.
Nonetheless, this paper sets the use of thymectomy in nonthymomatous MG on firmer ground going forward. The investigators will doubtless be presenting further data from the trial, including clinical-pathologic correlates and other relevant novel observations. In addition, Wolfe et al. have opened the door for future trials of thymectomy in MG to address such issues as the benefits vs. risks of performing the operation via the traditional transsternal vs. alternative non–sternal splitting approaches.
Benn E. Smith, MD, is an associate professor of neurology at the Mayo Clinic in Scottsdale, Ariz. and is the director of the sensory laboratory there. Dr. Smith is on the Editorial Advisory Board of Clinical Neurology News.
End to an 80-year controversy
These findings from Wolfe et al. end an 80-year controversy over the effectiveness of thymectomy for patients with myasthenia gravis.
Perhaps the most important benefit for patients is that even when they require prednisone following the surgery, they can take lower doses, endure fewer glucocorticoid-related symptoms, and experience less distress from those symptoms than patients who don’t undergo thymectomy.
Unfortunately, the study results cannot offer further clarity regarding patient selection for thymectomy. The patient population in this trial was so small that subgroup analyses couldn’t allow conclusions regarding the relative effectiveness of thymectomy in men vs. women or younger vs. older patients.
Allan H. Ropper, MD, is in the department of neurology at Brigham and Women’s Hospital and Harvard Medical School, both in Boston. His financial disclosures are available at NEJM.org. Dr. Ropper made these remarks in an editorial accompanying Dr. Wolfe’s report (N Engl J Med. 2016 Aug 11. doi: 10.1056/NEJMe1607953).
Landmark trial establishes effectiveness of thymectomy in myasthenia gravis
One of the many challenges of treating patients with myasthenia gravis (MG) is the fluctuating nature of symptoms and deficits. The neurologist or neuromuscular specialist must decide whether the disease is truly worsening, whether the patient is experiencing more pronounced symptoms from intercurrent illness or the effects of a medication known to affect the neuromuscular junction adversely, or whether the patient is concerned that there might be worsening disease when all objective measures indicate stability. These factors make treatment decisions more difficult in MG than for many other neuromuscular disorders.
Similarly, researchers considering a trial investigating treatment efficacy in MG face the complex issues of disease fluctuation in cohorts of individuals with the disease, varying levels of corticosteroid and immunosuppressant doses in different MG patients, and thorny ethical dilemmas in providing accepted therapies but not withholding effective treatments from those in need.
Dr. Wolfe and his colleagues demonstrate that they have navigated these treacherous waters. They have succeeded in completing a landmark controlled clinical trial which establishes the effectiveness of transsternal thymectomy with adjuvant corticosteroid therapy in nonthymomatous MG vs. oral prednisone without surgery. While this international 36-center trial managed to recruit 126 subjects over a 6-year period, using sound inclusion and exclusion criteria and a meticulous trial design, the number of patients is not sufficient to allow for as robust a subgroup analysis for age, gender, and a variety of clinical variables reflecting severity of disease as would have been hoped for by the MG community.
Nonetheless, this paper sets the use of thymectomy in nonthymomatous MG on firmer ground going forward. The investigators will doubtless be presenting further data from the trial, including clinical-pathologic correlates and other relevant novel observations. In addition, Wolfe et al. have opened the door for future trials of thymectomy in MG to address such issues as the benefits vs. risks of performing the operation via the traditional transsternal vs. alternative non–sternal splitting approaches.
Benn E. Smith, MD, is an associate professor of neurology at the Mayo Clinic in Scottsdale, Ariz. and is the director of the sensory laboratory there. Dr. Smith is on the Editorial Advisory Board of Clinical Neurology News.
End to an 80-year controversy
These findings from Wolfe et al. end an 80-year controversy over the effectiveness of thymectomy for patients with myasthenia gravis.
Perhaps the most important benefit for patients is that even when they require prednisone following the surgery, they can take lower doses, endure fewer glucocorticoid-related symptoms, and experience less distress from those symptoms than patients who don’t undergo thymectomy.
Unfortunately, the study results cannot offer further clarity regarding patient selection for thymectomy. The patient population in this trial was so small that subgroup analyses couldn’t allow conclusions regarding the relative effectiveness of thymectomy in men vs. women or younger vs. older patients.
Allan H. Ropper, MD, is in the department of neurology at Brigham and Women’s Hospital and Harvard Medical School, both in Boston. His financial disclosures are available at NEJM.org. Dr. Ropper made these remarks in an editorial accompanying Dr. Wolfe’s report (N Engl J Med. 2016 Aug 11. doi: 10.1056/NEJMe1607953).
Landmark trial establishes effectiveness of thymectomy in myasthenia gravis
One of the many challenges of treating patients with myasthenia gravis (MG) is the fluctuating nature of symptoms and deficits. The neurologist or neuromuscular specialist must decide whether the disease is truly worsening, whether the patient is experiencing more pronounced symptoms from intercurrent illness or the effects of a medication known to affect the neuromuscular junction adversely, or whether the patient is concerned that there might be worsening disease when all objective measures indicate stability. These factors make treatment decisions more difficult in MG than for many other neuromuscular disorders.
Similarly, researchers considering a trial investigating treatment efficacy in MG face the complex issues of disease fluctuation in cohorts of individuals with the disease, varying levels of corticosteroid and immunosuppressant doses in different MG patients, and thorny ethical dilemmas in providing accepted therapies but not withholding effective treatments from those in need.
Dr. Wolfe and his colleagues demonstrate that they have navigated these treacherous waters. They have succeeded in completing a landmark controlled clinical trial which establishes the effectiveness of transsternal thymectomy with adjuvant corticosteroid therapy in nonthymomatous MG vs. oral prednisone without surgery. While this international 36-center trial managed to recruit 126 subjects over a 6-year period, using sound inclusion and exclusion criteria and a meticulous trial design, the number of patients is not sufficient to allow for as robust a subgroup analysis for age, gender, and a variety of clinical variables reflecting severity of disease as would have been hoped for by the MG community.
Nonetheless, this paper sets the use of thymectomy in nonthymomatous MG on firmer ground going forward. The investigators will doubtless be presenting further data from the trial, including clinical-pathologic correlates and other relevant novel observations. In addition, Wolfe et al. have opened the door for future trials of thymectomy in MG to address such issues as the benefits vs. risks of performing the operation via the traditional transsternal vs. alternative non–sternal splitting approaches.
Benn E. Smith, MD, is an associate professor of neurology at the Mayo Clinic in Scottsdale, Ariz. and is the director of the sensory laboratory there. Dr. Smith is on the Editorial Advisory Board of Clinical Neurology News.
End to an 80-year controversy
These findings from Wolfe et al. end an 80-year controversy over the effectiveness of thymectomy for patients with myasthenia gravis.
Perhaps the most important benefit for patients is that even when they require prednisone following the surgery, they can take lower doses, endure fewer glucocorticoid-related symptoms, and experience less distress from those symptoms than patients who don’t undergo thymectomy.
Unfortunately, the study results cannot offer further clarity regarding patient selection for thymectomy. The patient population in this trial was so small that subgroup analyses couldn’t allow conclusions regarding the relative effectiveness of thymectomy in men vs. women or younger vs. older patients.
Allan H. Ropper, MD, is in the department of neurology at Brigham and Women’s Hospital and Harvard Medical School, both in Boston. His financial disclosures are available at NEJM.org. Dr. Ropper made these remarks in an editorial accompanying Dr. Wolfe’s report (N Engl J Med. 2016 Aug 11. doi: 10.1056/NEJMe1607953).
Thymectomy improved 3-year clinical outcomes and proved superior to medical therapy for mild to severe nonthymomatous myasthenia gravis, according to a report published online Aug. 11 in the New England Journal of Medicine.
Compared with standard prednisone therapy, thymectomy plus prednisone decreased the number and severity of symptoms, allowed the lowering of steroid doses, decreased the number and length of hospitalizations for disease exacerbations, reduced the need for immunosuppressive agents, and improved health-related quality of life in an international, randomized clinical trial, said Gil I. Wolfe, MD, of the department of neurology, State University of New York at Buffalo and his associates.
Until now, thymectomy was known to be beneficial in some cases of myasthenia gravis “but with widely varying rates of clinical improvement or remission.” And the success of immunotherapy has raised the question of whether an invasive surgery is necessary. Data from randomized, controlled studies have been sparse.
Moreover, thymectomy rarely causes adverse effects, but “the procedure can cost up to $80,000 and can be associated with operative complications that need to be weighed against benefits.” In comparison, medical therapy with glucocorticoids and other immunosuppressive agents is less invasive but is definitely associated with adverse events, including some that are life threatening, and negatively impacts quality of life, the investigators said.
To address the lack of randomized controlled trial data, they assessed 3-year outcomes in 126 patients treated at 67 medical centers in 18 countries during a 6-year period. The study participants were aged 18-65 years, had a disease duration of less than 5 years at enrollment (median duration, 1 year), and had class II (mild generalized disease) to class IV (severe generalized disease) myasthenia gravis. These patients were randomly assigned to undergo thymectomy and receive standard prednisone therapy (66 participants) or to receive standard prednisone alone (60 participants).
Thymectomy was performed using a median sternotomy “with the goal of an en bloc resection of all mediastinal tissue that could anatomically contain gross or microscopic thymus.”
At follow-up, time-weighted average scores on the Quantitative Myasthenia Gravis scale were significantly lower by 2.85 points, indicating improved clinical status, in the thymectomy group than in the control group. Time-weighted average prednisone dose also was significantly lower, at an average alternate-day dose of 44 mg in the thymectomy group and 60 mg in the control group, Dr. Wolfe and his associates said (N Engl J Med. 2016 Aug 11. doi: 10.1056/NEJMoa1602489).
On a measure of treatment-related complications, scores favored thymectomy with regard to the number of patients with symptoms, the total number of symptoms, and the distress level related to symptoms throughout the study period. Fewer patients in the thymectomy group required hospitalization for exacerbations of myasthenia gravis (9% vs. 37%), and the mean cumulative number of hospital days was lower with thymectomy (8.4 vs. 19.2).
In addition, scores on the Myasthenia Gravis Activities of Daily Living scale favored thymectomy (2.24 vs. 3.41). Fewer patients in the thymectomy group required azathioprine (17% vs. 0.48%). And the percentage of patients who reported having minimal manifestations of the disease at 3 years was significantly higher with thymectomy (67%) than with prednisone alone (47%).
This study was supported by the National Institute of Neurological Disorders and Stroke, the Muscular Dystrophy Association, and the Myasthenia Gravis Foundation of America and received no commercial support. Dr. Wolfe reported ties to Alexion Pharmaceuticals, Alpha Cancer Technologies, Argenx, Baxalta, CSL Behring, Grifols, and UCB, and his associates reported ties to numerous industry sources.
Thymectomy improved 3-year clinical outcomes and proved superior to medical therapy for mild to severe nonthymomatous myasthenia gravis, according to a report published online Aug. 11 in the New England Journal of Medicine.
Compared with standard prednisone therapy, thymectomy plus prednisone decreased the number and severity of symptoms, allowed the lowering of steroid doses, decreased the number and length of hospitalizations for disease exacerbations, reduced the need for immunosuppressive agents, and improved health-related quality of life in an international, randomized clinical trial, said Gil I. Wolfe, MD, of the department of neurology, State University of New York at Buffalo and his associates.
Until now, thymectomy was known to be beneficial in some cases of myasthenia gravis “but with widely varying rates of clinical improvement or remission.” And the success of immunotherapy has raised the question of whether an invasive surgery is necessary. Data from randomized, controlled studies have been sparse.
Moreover, thymectomy rarely causes adverse effects, but “the procedure can cost up to $80,000 and can be associated with operative complications that need to be weighed against benefits.” In comparison, medical therapy with glucocorticoids and other immunosuppressive agents is less invasive but is definitely associated with adverse events, including some that are life threatening, and negatively impacts quality of life, the investigators said.
To address the lack of randomized controlled trial data, they assessed 3-year outcomes in 126 patients treated at 67 medical centers in 18 countries during a 6-year period. The study participants were aged 18-65 years, had a disease duration of less than 5 years at enrollment (median duration, 1 year), and had class II (mild generalized disease) to class IV (severe generalized disease) myasthenia gravis. These patients were randomly assigned to undergo thymectomy and receive standard prednisone therapy (66 participants) or to receive standard prednisone alone (60 participants).
Thymectomy was performed using a median sternotomy “with the goal of an en bloc resection of all mediastinal tissue that could anatomically contain gross or microscopic thymus.”
At follow-up, time-weighted average scores on the Quantitative Myasthenia Gravis scale were significantly lower by 2.85 points, indicating improved clinical status, in the thymectomy group than in the control group. Time-weighted average prednisone dose also was significantly lower, at an average alternate-day dose of 44 mg in the thymectomy group and 60 mg in the control group, Dr. Wolfe and his associates said (N Engl J Med. 2016 Aug 11. doi: 10.1056/NEJMoa1602489).
On a measure of treatment-related complications, scores favored thymectomy with regard to the number of patients with symptoms, the total number of symptoms, and the distress level related to symptoms throughout the study period. Fewer patients in the thymectomy group required hospitalization for exacerbations of myasthenia gravis (9% vs. 37%), and the mean cumulative number of hospital days was lower with thymectomy (8.4 vs. 19.2).
In addition, scores on the Myasthenia Gravis Activities of Daily Living scale favored thymectomy (2.24 vs. 3.41). Fewer patients in the thymectomy group required azathioprine (17% vs. 0.48%). And the percentage of patients who reported having minimal manifestations of the disease at 3 years was significantly higher with thymectomy (67%) than with prednisone alone (47%).
This study was supported by the National Institute of Neurological Disorders and Stroke, the Muscular Dystrophy Association, and the Myasthenia Gravis Foundation of America and received no commercial support. Dr. Wolfe reported ties to Alexion Pharmaceuticals, Alpha Cancer Technologies, Argenx, Baxalta, CSL Behring, Grifols, and UCB, and his associates reported ties to numerous industry sources.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
Key clinical point: Thymectomy improved 3-year clinical outcomes and was superior to medical therapy for mild to severe nonthymomatous myasthenia gravis.
Major finding: Scores on the Quantitative Myasthenia Gravis scale were significantly lower by 2.85 points, indicating improved clinical status, in the thymectomy group than in the control group.
Data source: An international, randomized, medication-controlled trial involving 126 patients at 67 medical centers.
Disclosures: This study was supported by the National Institute of Neurological Disorders and Stroke, the Muscular Dystrophy Association, and the Myasthenia Gravis Foundation of America and received no commercial support. Dr. Wolfe reported ties to Alexion Pharmaceuticals, Alpha Cancer Technologies, Argenx, Baxalta, CSL Behring, Grifols, and UCB, and his associates reported ties to numerous industry sources.
Hospital safety culture may influence surgical outcomes
SAN DIEGO – Hospital safety culture may positively influence certain surgical patient outcomes, results from a study of 56 Illinois hospitals demonstrated.
“Efforts to improve awareness of safety and quality improvement principles should be encouraged at both the surgical system and hospital levels,” David D. Odell, MD, said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference. “Safety culture itself is a concept [that] is increasingly viewed as important in the delivery of high-quality care. Yet in the surgical world, very little is known about how hospital culture actually influences outcomes for our patients.”
Dr. Odell, a thoracic surgeon at Northwestern Memorial Hospital, Chicago, discussed results from a study by the Illinois Surgical Quality Improvement Collaborative, a group of Illinois hospitals working together to improve the quality of surgical care in the state. Participants in the Collaborative include 56 hospitals, including all academic medical centers in the state, as well as 11 rural hospitals. Combined, these facilities perform 60% of general surgery operations in the state and 80% of all complex operations, impacting more than 600,000 patients each year.
In an effort to evaluate the relationship between hospital safety culture and surgical patient outcomes, Dr. Odell and his associates invited staff of Collaborative members to complete the Safety Attitudes Questionnaire (SAQ), a 56-item validated tool for assessment of hospital culture. Domains focused on were teamwork, communication, engagement, and leadership. The SAQ was given to administrators, staff, and front-line providers “to measure safety culture across all levels of the hospital,” Dr. Odell said. Percent positive responses were calculated at the hospital level for each of the eight domains to calculate a composite measure of safety. The researchers measured the impact of safety culture by assessing positive SAQ response rates. Outcome variables of interest were morbidity, mortality, death or serious morbidity, and readmission. Hospital-level risk-adjusted event rates and linear regression models were used to assess the impact of safety culture while controlling for teaching status, rural location, trauma center designation, hospital control (management), and the annual surgical volume.
Of the 49 participating hospitals represented in the survey responses, 49% had an Accreditation Council for Graduate Medical Education (ACGME)-accredited residency program, 12% were rural, 61% provided trauma care, 35% had a religious affiliation, 57% were “other” not-for-profit, and the mean total surgical volume was 11,412 cases.
Dr. Odell reported that by domain, SAQ responses were most positive for operating room safety and lowest for hospital management. “That doesn’t necessarily reflect the management’s outcomes only, but the views of those who took the survey toward management,” he said.
When the researchers evaluated the impact of a more-positive safety culture on the risk-adjusted outcome measures, they observed a statistically significant impact on morbidity following surgery (P = .02). The trend was similar although not statistically significant for death/serious morbidity (P = .08), mortality (P =. 20), or readmission (P = .68).
Dr. Odell acknowledged certain limitations of the study, including its retrospective design and the fact that the SAQ is a subjective assessment tool. “Not all [staff invited] were surveyed,” he added. “We sent out just under 1,400 surveys and we had a response rate of 44%.”
Staff from participating institutions of the Collaborative meet on a semiannual basis to share ideas, celebrate successes and learn from each other’s experiences, Dr. Odell said. Ongoing efforts to improve safety culture include fostering opportunities for mentorship in quality improvement and process improvement endeavors, as well as the provision of educational materials targeted at all levels of hospital staff “so that we can get everyone thinking and speaking the same language when it comes to quality improvement,” he said.
The Collaborative is funded by Blue Cross Blue Shield of Illinois. Dr. Odell reported having no financial disclosures.
SAN DIEGO – Hospital safety culture may positively influence certain surgical patient outcomes, results from a study of 56 Illinois hospitals demonstrated.
“Efforts to improve awareness of safety and quality improvement principles should be encouraged at both the surgical system and hospital levels,” David D. Odell, MD, said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference. “Safety culture itself is a concept [that] is increasingly viewed as important in the delivery of high-quality care. Yet in the surgical world, very little is known about how hospital culture actually influences outcomes for our patients.”
Dr. Odell, a thoracic surgeon at Northwestern Memorial Hospital, Chicago, discussed results from a study by the Illinois Surgical Quality Improvement Collaborative, a group of Illinois hospitals working together to improve the quality of surgical care in the state. Participants in the Collaborative include 56 hospitals, including all academic medical centers in the state, as well as 11 rural hospitals. Combined, these facilities perform 60% of general surgery operations in the state and 80% of all complex operations, impacting more than 600,000 patients each year.
In an effort to evaluate the relationship between hospital safety culture and surgical patient outcomes, Dr. Odell and his associates invited staff of Collaborative members to complete the Safety Attitudes Questionnaire (SAQ), a 56-item validated tool for assessment of hospital culture. Domains focused on were teamwork, communication, engagement, and leadership. The SAQ was given to administrators, staff, and front-line providers “to measure safety culture across all levels of the hospital,” Dr. Odell said. Percent positive responses were calculated at the hospital level for each of the eight domains to calculate a composite measure of safety. The researchers measured the impact of safety culture by assessing positive SAQ response rates. Outcome variables of interest were morbidity, mortality, death or serious morbidity, and readmission. Hospital-level risk-adjusted event rates and linear regression models were used to assess the impact of safety culture while controlling for teaching status, rural location, trauma center designation, hospital control (management), and the annual surgical volume.
Of the 49 participating hospitals represented in the survey responses, 49% had an Accreditation Council for Graduate Medical Education (ACGME)-accredited residency program, 12% were rural, 61% provided trauma care, 35% had a religious affiliation, 57% were “other” not-for-profit, and the mean total surgical volume was 11,412 cases.
Dr. Odell reported that by domain, SAQ responses were most positive for operating room safety and lowest for hospital management. “That doesn’t necessarily reflect the management’s outcomes only, but the views of those who took the survey toward management,” he said.
When the researchers evaluated the impact of a more-positive safety culture on the risk-adjusted outcome measures, they observed a statistically significant impact on morbidity following surgery (P = .02). The trend was similar although not statistically significant for death/serious morbidity (P = .08), mortality (P =. 20), or readmission (P = .68).
Dr. Odell acknowledged certain limitations of the study, including its retrospective design and the fact that the SAQ is a subjective assessment tool. “Not all [staff invited] were surveyed,” he added. “We sent out just under 1,400 surveys and we had a response rate of 44%.”
Staff from participating institutions of the Collaborative meet on a semiannual basis to share ideas, celebrate successes and learn from each other’s experiences, Dr. Odell said. Ongoing efforts to improve safety culture include fostering opportunities for mentorship in quality improvement and process improvement endeavors, as well as the provision of educational materials targeted at all levels of hospital staff “so that we can get everyone thinking and speaking the same language when it comes to quality improvement,” he said.
The Collaborative is funded by Blue Cross Blue Shield of Illinois. Dr. Odell reported having no financial disclosures.
SAN DIEGO – Hospital safety culture may positively influence certain surgical patient outcomes, results from a study of 56 Illinois hospitals demonstrated.
“Efforts to improve awareness of safety and quality improvement principles should be encouraged at both the surgical system and hospital levels,” David D. Odell, MD, said at the American College of Surgeons/National Surgical Quality Improvement Program National Conference. “Safety culture itself is a concept [that] is increasingly viewed as important in the delivery of high-quality care. Yet in the surgical world, very little is known about how hospital culture actually influences outcomes for our patients.”
Dr. Odell, a thoracic surgeon at Northwestern Memorial Hospital, Chicago, discussed results from a study by the Illinois Surgical Quality Improvement Collaborative, a group of Illinois hospitals working together to improve the quality of surgical care in the state. Participants in the Collaborative include 56 hospitals, including all academic medical centers in the state, as well as 11 rural hospitals. Combined, these facilities perform 60% of general surgery operations in the state and 80% of all complex operations, impacting more than 600,000 patients each year.
In an effort to evaluate the relationship between hospital safety culture and surgical patient outcomes, Dr. Odell and his associates invited staff of Collaborative members to complete the Safety Attitudes Questionnaire (SAQ), a 56-item validated tool for assessment of hospital culture. Domains focused on were teamwork, communication, engagement, and leadership. The SAQ was given to administrators, staff, and front-line providers “to measure safety culture across all levels of the hospital,” Dr. Odell said. Percent positive responses were calculated at the hospital level for each of the eight domains to calculate a composite measure of safety. The researchers measured the impact of safety culture by assessing positive SAQ response rates. Outcome variables of interest were morbidity, mortality, death or serious morbidity, and readmission. Hospital-level risk-adjusted event rates and linear regression models were used to assess the impact of safety culture while controlling for teaching status, rural location, trauma center designation, hospital control (management), and the annual surgical volume.
Of the 49 participating hospitals represented in the survey responses, 49% had an Accreditation Council for Graduate Medical Education (ACGME)-accredited residency program, 12% were rural, 61% provided trauma care, 35% had a religious affiliation, 57% were “other” not-for-profit, and the mean total surgical volume was 11,412 cases.
Dr. Odell reported that by domain, SAQ responses were most positive for operating room safety and lowest for hospital management. “That doesn’t necessarily reflect the management’s outcomes only, but the views of those who took the survey toward management,” he said.
When the researchers evaluated the impact of a more-positive safety culture on the risk-adjusted outcome measures, they observed a statistically significant impact on morbidity following surgery (P = .02). The trend was similar although not statistically significant for death/serious morbidity (P = .08), mortality (P =. 20), or readmission (P = .68).
Dr. Odell acknowledged certain limitations of the study, including its retrospective design and the fact that the SAQ is a subjective assessment tool. “Not all [staff invited] were surveyed,” he added. “We sent out just under 1,400 surveys and we had a response rate of 44%.”
Staff from participating institutions of the Collaborative meet on a semiannual basis to share ideas, celebrate successes and learn from each other’s experiences, Dr. Odell said. Ongoing efforts to improve safety culture include fostering opportunities for mentorship in quality improvement and process improvement endeavors, as well as the provision of educational materials targeted at all levels of hospital staff “so that we can get everyone thinking and speaking the same language when it comes to quality improvement,” he said.
The Collaborative is funded by Blue Cross Blue Shield of Illinois. Dr. Odell reported having no financial disclosures.
EXPERT ANALYSIS AT THE ACS NSQIP NATIONAL CONFERENCE
Key clinical point: A positive hospital safety culture significantly impacted morbidity following surgery.
Major finding: When the researchers evaluated the impact of a positive safety culture on risk-adjusted outcome measures, they observed a statistically significant impact on morbidity following surgery (P = .02).
Data source: A retrospective study by the Illinois Surgical Quality Improvement Collaborative, a group of 56 hospitals in the state.
Disclosures: The Collaborative is funded by Blue Cross Blue Shield of Illinois. Dr. Odell reported having no financial disclosures.
ACS NSQIP Geriatric Surgery Pilot Collaborative: Evaluating variables for inclusion
SAN DIEGO – A project to assess geriatric-specific variables for inclusion in the American College of Surgeons/National Surgical Quality Improvement Program National Conference is underway, according to Thomas N. Robinson, MD.
Dr. Robinson discussed results from the ACS-NSQIP Geriatric Surgery Pilot Collaborative, an effort launched in January 2014 with the ultimate goal of evaluating specific geriatric variables for incorporation into the ACS NSQIP set of essential variables collected by all participating hospitals.
Dr. Robinson, professor of surgery at the University of Colorado, Denver, said that 23 clinical sites in the United States are currently studying the following geriatric-specific variables in surgery patients aged 65 and older:
• Origin from home with support (to determine baseline functional status: lives alone at home, lives with support in home, origin status not from home).
• Discharge functional health status (ability to perform activities of daily living).
• Discharge with/without services (to capture care needs upon discharge).
• Preoperative use of a mobility aid.
• Preoperative history of prior falls.
• Postoperative history of pressure ulcer.
• Fall risk on discharge.
• New mobility aid on discharge.
• History of dementia.
• Competency status on admission.
• Postoperative delirium (yes or no).
• Hospice care on admission (yes or no).
• Do Not Resuscitate (DNR) order in place on admission (yes or no).
• DNR order during hospitalization (yes or no).
• Setting where DNR order was placed.
• Postoperative palliative care consult (yes or no).
• 30-day postoperative outcomes: functional health status (ability to perform activities of daily living), physical function compared with baseline, and living location.
The number of surgery cases in the collaborative grew from 7,235 in the first 6 months of 2014 to 24,835 cases in the last 6 months of 2015. The top 10 operations were total joint arthroplasty (29%), colectomy (12%), spine (8%), hip fracture (7%), carotid endarterectomy (4%), hysterectomy (4%), lung resection (2%), open lower extremity bypass (2%), laparoscopic cholecystectomy (2%), and pancreatectomy (2%).
Dr. Robinson reported that the rate of preoperative dementia among cases studied in the collaborative was 10%. “The incorporation of dementia into a surgical dataset represents an important step forward in providing quality surgical care for the elderly,” he said. “Dementia is a global public health concern.” He went on to note that patients with dementia have a 2.5-fold increased risk of developing postoperative delirium, making it “the perfect place to start a quality project. One in three cases of delirium is preventable. In our data set, delirium is associated with a hospital stay that’s 4 days longer, an increased chance of requiring discharge to an institutional care facility, an increased chance of a serious complication, and a higher 30-day mortality.”
Simple, low-tech bedside interventions such as ambulating in the hall three times a day, orienting the person, having the person sleep at night rather than sleep during the day, and avoiding medications with high risk for adverse events in older adults can prevent postoperative delirium, Dr. Robinson said.
One way that the Geriatric Surgery Pilot Collaborative can improve the surgical care of older adults is by fostering quality programs initiated at the participating local hospitals. “Preserving function after hospital stays is a first major goal,” he said. Another strategy involves creating a multidisciplinary frailty assessment to aid with decision making and risk assessment. “This takes into consideration NSQIP variables such as function, nutrition, comorbidity burden, cognition, social vulnerability, and mobility,” he said. The final and ultimate goal of the geriatric surgery collaborative is to establish a foundation of quality measurement for the Coalition for Quality in Geriatric Surgery, a project initiated by the American College of Surgeons to systematically improve the surgical care of older adults.
Dr. Robinson reported having no relevant financial disclosures.
SAN DIEGO – A project to assess geriatric-specific variables for inclusion in the American College of Surgeons/National Surgical Quality Improvement Program National Conference is underway, according to Thomas N. Robinson, MD.
Dr. Robinson discussed results from the ACS-NSQIP Geriatric Surgery Pilot Collaborative, an effort launched in January 2014 with the ultimate goal of evaluating specific geriatric variables for incorporation into the ACS NSQIP set of essential variables collected by all participating hospitals.
Dr. Robinson, professor of surgery at the University of Colorado, Denver, said that 23 clinical sites in the United States are currently studying the following geriatric-specific variables in surgery patients aged 65 and older:
• Origin from home with support (to determine baseline functional status: lives alone at home, lives with support in home, origin status not from home).
• Discharge functional health status (ability to perform activities of daily living).
• Discharge with/without services (to capture care needs upon discharge).
• Preoperative use of a mobility aid.
• Preoperative history of prior falls.
• Postoperative history of pressure ulcer.
• Fall risk on discharge.
• New mobility aid on discharge.
• History of dementia.
• Competency status on admission.
• Postoperative delirium (yes or no).
• Hospice care on admission (yes or no).
• Do Not Resuscitate (DNR) order in place on admission (yes or no).
• DNR order during hospitalization (yes or no).
• Setting where DNR order was placed.
• Postoperative palliative care consult (yes or no).
• 30-day postoperative outcomes: functional health status (ability to perform activities of daily living), physical function compared with baseline, and living location.
The number of surgery cases in the collaborative grew from 7,235 in the first 6 months of 2014 to 24,835 cases in the last 6 months of 2015. The top 10 operations were total joint arthroplasty (29%), colectomy (12%), spine (8%), hip fracture (7%), carotid endarterectomy (4%), hysterectomy (4%), lung resection (2%), open lower extremity bypass (2%), laparoscopic cholecystectomy (2%), and pancreatectomy (2%).
Dr. Robinson reported that the rate of preoperative dementia among cases studied in the collaborative was 10%. “The incorporation of dementia into a surgical dataset represents an important step forward in providing quality surgical care for the elderly,” he said. “Dementia is a global public health concern.” He went on to note that patients with dementia have a 2.5-fold increased risk of developing postoperative delirium, making it “the perfect place to start a quality project. One in three cases of delirium is preventable. In our data set, delirium is associated with a hospital stay that’s 4 days longer, an increased chance of requiring discharge to an institutional care facility, an increased chance of a serious complication, and a higher 30-day mortality.”
Simple, low-tech bedside interventions such as ambulating in the hall three times a day, orienting the person, having the person sleep at night rather than sleep during the day, and avoiding medications with high risk for adverse events in older adults can prevent postoperative delirium, Dr. Robinson said.
One way that the Geriatric Surgery Pilot Collaborative can improve the surgical care of older adults is by fostering quality programs initiated at the participating local hospitals. “Preserving function after hospital stays is a first major goal,” he said. Another strategy involves creating a multidisciplinary frailty assessment to aid with decision making and risk assessment. “This takes into consideration NSQIP variables such as function, nutrition, comorbidity burden, cognition, social vulnerability, and mobility,” he said. The final and ultimate goal of the geriatric surgery collaborative is to establish a foundation of quality measurement for the Coalition for Quality in Geriatric Surgery, a project initiated by the American College of Surgeons to systematically improve the surgical care of older adults.
Dr. Robinson reported having no relevant financial disclosures.
SAN DIEGO – A project to assess geriatric-specific variables for inclusion in the American College of Surgeons/National Surgical Quality Improvement Program National Conference is underway, according to Thomas N. Robinson, MD.
Dr. Robinson discussed results from the ACS-NSQIP Geriatric Surgery Pilot Collaborative, an effort launched in January 2014 with the ultimate goal of evaluating specific geriatric variables for incorporation into the ACS NSQIP set of essential variables collected by all participating hospitals.
Dr. Robinson, professor of surgery at the University of Colorado, Denver, said that 23 clinical sites in the United States are currently studying the following geriatric-specific variables in surgery patients aged 65 and older:
• Origin from home with support (to determine baseline functional status: lives alone at home, lives with support in home, origin status not from home).
• Discharge functional health status (ability to perform activities of daily living).
• Discharge with/without services (to capture care needs upon discharge).
• Preoperative use of a mobility aid.
• Preoperative history of prior falls.
• Postoperative history of pressure ulcer.
• Fall risk on discharge.
• New mobility aid on discharge.
• History of dementia.
• Competency status on admission.
• Postoperative delirium (yes or no).
• Hospice care on admission (yes or no).
• Do Not Resuscitate (DNR) order in place on admission (yes or no).
• DNR order during hospitalization (yes or no).
• Setting where DNR order was placed.
• Postoperative palliative care consult (yes or no).
• 30-day postoperative outcomes: functional health status (ability to perform activities of daily living), physical function compared with baseline, and living location.
The number of surgery cases in the collaborative grew from 7,235 in the first 6 months of 2014 to 24,835 cases in the last 6 months of 2015. The top 10 operations were total joint arthroplasty (29%), colectomy (12%), spine (8%), hip fracture (7%), carotid endarterectomy (4%), hysterectomy (4%), lung resection (2%), open lower extremity bypass (2%), laparoscopic cholecystectomy (2%), and pancreatectomy (2%).
Dr. Robinson reported that the rate of preoperative dementia among cases studied in the collaborative was 10%. “The incorporation of dementia into a surgical dataset represents an important step forward in providing quality surgical care for the elderly,” he said. “Dementia is a global public health concern.” He went on to note that patients with dementia have a 2.5-fold increased risk of developing postoperative delirium, making it “the perfect place to start a quality project. One in three cases of delirium is preventable. In our data set, delirium is associated with a hospital stay that’s 4 days longer, an increased chance of requiring discharge to an institutional care facility, an increased chance of a serious complication, and a higher 30-day mortality.”
Simple, low-tech bedside interventions such as ambulating in the hall three times a day, orienting the person, having the person sleep at night rather than sleep during the day, and avoiding medications with high risk for adverse events in older adults can prevent postoperative delirium, Dr. Robinson said.
One way that the Geriatric Surgery Pilot Collaborative can improve the surgical care of older adults is by fostering quality programs initiated at the participating local hospitals. “Preserving function after hospital stays is a first major goal,” he said. Another strategy involves creating a multidisciplinary frailty assessment to aid with decision making and risk assessment. “This takes into consideration NSQIP variables such as function, nutrition, comorbidity burden, cognition, social vulnerability, and mobility,” he said. The final and ultimate goal of the geriatric surgery collaborative is to establish a foundation of quality measurement for the Coalition for Quality in Geriatric Surgery, a project initiated by the American College of Surgeons to systematically improve the surgical care of older adults.
Dr. Robinson reported having no relevant financial disclosures.
EXPERT ANALYSIS AT THE ACS NSQIP NATIONAL CONFERENCE