User login
The Journal of Clinical Outcomes Management® is an independent, peer-reviewed journal offering evidence-based, practical information for improving the quality, safety, and value of health care.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Face mask type matters when sterilizing, study finds
according to researchers. The greatest reduction in filtration efficiency after sterilization occurred with surgical face masks.
With plasma vapor hydrogen peroxide (H2O2) sterilization, filtration efficiency of N95 and KN95 masks was maintained at more than 95%, but for surgical face masks, filtration efficiency was reduced to less than 95%. With chlorine dioxide (ClO2) sterilization, on the other hand, filtration efficiency was maintained at above 95% for N95 masks, but for KN95 and surgical face masks, filtration efficiency was reduced to less than 80%.
In a research letter published online June 15 in JAMA Network Open, researchers from the University of Oklahoma Health Sciences Center, Oklahoma City, report the results of a study of the two sterilization techniques on the pressure drop and filtration efficiency of N95, KN95, and surgical face masks.
“The H2O2 treatment showed a small effect on the overall filtration efficiency of the tested masks, but the ClO2 treatment showed marked reduction in the overall filtration efficiency of the KN95s and surgical face masks. All pressure drop changes were within the acceptable range,” the researchers write.
The study did not evaluate the effect of repeated sterilizations on face masks.
Five masks of each type were sterilized with either H2O2 or ClO2. Masks were then placed in a test chamber, and a salt aerosol was nebulized to assess both upstream and downstream filtration as well as pressure drop. The researchers used a mobility particle sizer to measure particle number concentration from 16.8 nm to 514 nm. An acceptable pressure drop was defined as a drop of less than 1.38 inches of water (35 mm) for inhalation.
Although pressure drop changes were within the acceptable range for all three mask types following sterilization with either method, H2O2 sterilization yielded the least reduction in filtration efficacy in all cases. After sterilization with H2O2, filtration efficiencies were 96.6%, 97.1%, and 91.6% for the N95s, KN95s, and the surgical face masks, respectively. In contrast, filtration efficiencies after ClO2 sterilization were 95.1%, 76.2%, and 77.9%, respectively.
The researchers note that, although overall filtration efficiency was maintained with ClO2 sterilization, there was a significant drop in efficiency with respect to particles of approximately 300 nm (0.3 microns) in size. For particles of that size, mean filtration efficiency decreased to 86.2% for N95s, 40.8% for KN95s, and 47.1% for surgical face masks.
The testing described in the report is “quite affordable at $350 per mask type, so it is hard to imagine any health care provider cannot set aside a small budget to conduct such an important test,” author Evan Floyd, PhD, told Medscape Medical News.
Given the high demand for effective face masks and the current risk for counterfeit products, Floyd suggested that individual facilities test all masks intended for use by healthcare workers before and after sterilization procedures.
“However, if for some reason testing is not an option, we would recommend sticking to established brands and suppliers, perhaps reach out to your state health department or a local representative of the strategic stockpile of PPE,” he noted.
The authors acknowledge that further studies using a larger sample size and a greater variety of masks, as well as studies to evaluate different sterilization techniques, are required. Further, “measuring the respirator’s filtration efficiency by aerosol size instead of only measuring the overall filtration efficiency” should also be considered. Such an approach would enable researchers to evaluate the degree to which masks protect against specific infectious agents.
This article first appeared on Medscape.com.
according to researchers. The greatest reduction in filtration efficiency after sterilization occurred with surgical face masks.
With plasma vapor hydrogen peroxide (H2O2) sterilization, filtration efficiency of N95 and KN95 masks was maintained at more than 95%, but for surgical face masks, filtration efficiency was reduced to less than 95%. With chlorine dioxide (ClO2) sterilization, on the other hand, filtration efficiency was maintained at above 95% for N95 masks, but for KN95 and surgical face masks, filtration efficiency was reduced to less than 80%.
In a research letter published online June 15 in JAMA Network Open, researchers from the University of Oklahoma Health Sciences Center, Oklahoma City, report the results of a study of the two sterilization techniques on the pressure drop and filtration efficiency of N95, KN95, and surgical face masks.
“The H2O2 treatment showed a small effect on the overall filtration efficiency of the tested masks, but the ClO2 treatment showed marked reduction in the overall filtration efficiency of the KN95s and surgical face masks. All pressure drop changes were within the acceptable range,” the researchers write.
The study did not evaluate the effect of repeated sterilizations on face masks.
Five masks of each type were sterilized with either H2O2 or ClO2. Masks were then placed in a test chamber, and a salt aerosol was nebulized to assess both upstream and downstream filtration as well as pressure drop. The researchers used a mobility particle sizer to measure particle number concentration from 16.8 nm to 514 nm. An acceptable pressure drop was defined as a drop of less than 1.38 inches of water (35 mm) for inhalation.
Although pressure drop changes were within the acceptable range for all three mask types following sterilization with either method, H2O2 sterilization yielded the least reduction in filtration efficacy in all cases. After sterilization with H2O2, filtration efficiencies were 96.6%, 97.1%, and 91.6% for the N95s, KN95s, and the surgical face masks, respectively. In contrast, filtration efficiencies after ClO2 sterilization were 95.1%, 76.2%, and 77.9%, respectively.
The researchers note that, although overall filtration efficiency was maintained with ClO2 sterilization, there was a significant drop in efficiency with respect to particles of approximately 300 nm (0.3 microns) in size. For particles of that size, mean filtration efficiency decreased to 86.2% for N95s, 40.8% for KN95s, and 47.1% for surgical face masks.
The testing described in the report is “quite affordable at $350 per mask type, so it is hard to imagine any health care provider cannot set aside a small budget to conduct such an important test,” author Evan Floyd, PhD, told Medscape Medical News.
Given the high demand for effective face masks and the current risk for counterfeit products, Floyd suggested that individual facilities test all masks intended for use by healthcare workers before and after sterilization procedures.
“However, if for some reason testing is not an option, we would recommend sticking to established brands and suppliers, perhaps reach out to your state health department or a local representative of the strategic stockpile of PPE,” he noted.
The authors acknowledge that further studies using a larger sample size and a greater variety of masks, as well as studies to evaluate different sterilization techniques, are required. Further, “measuring the respirator’s filtration efficiency by aerosol size instead of only measuring the overall filtration efficiency” should also be considered. Such an approach would enable researchers to evaluate the degree to which masks protect against specific infectious agents.
This article first appeared on Medscape.com.
according to researchers. The greatest reduction in filtration efficiency after sterilization occurred with surgical face masks.
With plasma vapor hydrogen peroxide (H2O2) sterilization, filtration efficiency of N95 and KN95 masks was maintained at more than 95%, but for surgical face masks, filtration efficiency was reduced to less than 95%. With chlorine dioxide (ClO2) sterilization, on the other hand, filtration efficiency was maintained at above 95% for N95 masks, but for KN95 and surgical face masks, filtration efficiency was reduced to less than 80%.
In a research letter published online June 15 in JAMA Network Open, researchers from the University of Oklahoma Health Sciences Center, Oklahoma City, report the results of a study of the two sterilization techniques on the pressure drop and filtration efficiency of N95, KN95, and surgical face masks.
“The H2O2 treatment showed a small effect on the overall filtration efficiency of the tested masks, but the ClO2 treatment showed marked reduction in the overall filtration efficiency of the KN95s and surgical face masks. All pressure drop changes were within the acceptable range,” the researchers write.
The study did not evaluate the effect of repeated sterilizations on face masks.
Five masks of each type were sterilized with either H2O2 or ClO2. Masks were then placed in a test chamber, and a salt aerosol was nebulized to assess both upstream and downstream filtration as well as pressure drop. The researchers used a mobility particle sizer to measure particle number concentration from 16.8 nm to 514 nm. An acceptable pressure drop was defined as a drop of less than 1.38 inches of water (35 mm) for inhalation.
Although pressure drop changes were within the acceptable range for all three mask types following sterilization with either method, H2O2 sterilization yielded the least reduction in filtration efficacy in all cases. After sterilization with H2O2, filtration efficiencies were 96.6%, 97.1%, and 91.6% for the N95s, KN95s, and the surgical face masks, respectively. In contrast, filtration efficiencies after ClO2 sterilization were 95.1%, 76.2%, and 77.9%, respectively.
The researchers note that, although overall filtration efficiency was maintained with ClO2 sterilization, there was a significant drop in efficiency with respect to particles of approximately 300 nm (0.3 microns) in size. For particles of that size, mean filtration efficiency decreased to 86.2% for N95s, 40.8% for KN95s, and 47.1% for surgical face masks.
The testing described in the report is “quite affordable at $350 per mask type, so it is hard to imagine any health care provider cannot set aside a small budget to conduct such an important test,” author Evan Floyd, PhD, told Medscape Medical News.
Given the high demand for effective face masks and the current risk for counterfeit products, Floyd suggested that individual facilities test all masks intended for use by healthcare workers before and after sterilization procedures.
“However, if for some reason testing is not an option, we would recommend sticking to established brands and suppliers, perhaps reach out to your state health department or a local representative of the strategic stockpile of PPE,” he noted.
The authors acknowledge that further studies using a larger sample size and a greater variety of masks, as well as studies to evaluate different sterilization techniques, are required. Further, “measuring the respirator’s filtration efficiency by aerosol size instead of only measuring the overall filtration efficiency” should also be considered. Such an approach would enable researchers to evaluate the degree to which masks protect against specific infectious agents.
This article first appeared on Medscape.com.
Hospitalist well-being during the pandemic
Navigating COVID-19 requires self-care
The global COVID-19 pandemic has escalated everyone’s stress levels, especially clinicians caring for hospitalized patients. New pressures have added to everyday stress, new studies have revised prior patient care recommendations, and the world generally seems upside down. What can a busy hospitalist do to maintain a modicum of sanity in all the craziness?
The stressors facing hospitalists
Uncertainty
Of all the burdens COVID-19 has unleashed, the biggest may be uncertainty. Not only is there unease about the virus itself, there also is legitimate concern about the future of medicine, said Elizabeth Harry, MD, SFHM, a hospitalist and senior director of clinical affairs at the University of Colorado Hospital in Aurora.
“What does it look like after an event like this, particularly in areas like academic medicine and teaching our next generation and getting funding for research? And how do we continue to produce physicians that can provide excellent care?” she asked.
There is also uncertainty in the best way to care for patients, said Eileen Barrett, MD, MPH, SFHM, a hospitalist at the University of New Mexico, Albuquerque.
“There are some models that are emerging to predict who will have a worse outcome, but they’re still not great models, so we have uncertainty for a given patient.” And, she noted, as the science continues to evolve, there exists a constant worry that “you might have inadvertently caused someone harm.”
The financial implications of the pandemic are creating uncertainty too. “When you fund a health care system with elective procedures and you can’t do those, and instead have to shift to the most essential services, a lot of places are seeing a massive deficit, which is going to affect staff morale and some physician offices are going to close,” said Elisabeth Poorman, MD, MPH, a primary care and internal medicine physician and chair of the King County Medical Society Physician Wellness Committee in Seattle.
Fear
When the pandemic began in the United States, “fear of the unknown was perhaps the scariest part, particularly as it pertained to personal protective equipment,” said Mark Rudolph, MD, SFHM, chief experience officer and vice president of patient experience and physician development at Sound Physicians in Tacoma, Wash. “For most clinicians, this is the first time that they are themselves in harm’s way while they do their jobs. And worse, they risk bringing the virus home to their families. That is the concern I hear most.”
Anxiety
Worrying about being able to provide excellent patient care is a big stressor, especially since this is the heart and soul of why most hospitalists have gone into their line of work.
“Part of providing excellent care to your patients is providing excellent supportive care to their families,” Dr. Harry said. “There’s some dissonance there in not being able to allow the family to come visit, but wanting to keep them safe, and it feels really hard to support your patients and support their families in the best way. It can feel like you’re just watching and waiting to see what will happen, and that we don’t have a lot of agency over which direction things take.”
There is concern for health care team members as well, Dr. Harry added. “Physicians care a lot about their teams and how they’re doing. I think there’s a sense of esprit de corps among folks and worry for each other there.”
Guilt
Although you may be at the hospital all day, you may feel guilty when you are not providing direct patient care. Or maybe you or someone on your team has an immunodeficiency and can’t be on the front line. Perhaps one of your team members contracted COVID-19 and you did not. Whatever the case, guilt is another emotion that is rampant among hospitalists right now, Dr. Barrett said.
Burnout
Unfortunately, burnout is a potential reality in times of high stress. “Burnout is dynamic,” said Dr. Poorman. “It’s a process by which your emotional and cognitive reserves are exhausted. The people with the highest burnout are the ones who are still trying to provide the standard of care, or above the standard of care in dysfunctional systems.”
Dr. Harry noted that burnout presents in different ways for different people, but Dr. Rudolph added that it’s crucial for hospitalist team members to watch for signs of burnout so they can intervene and/or get help for their colleagues.
Warning signs in yourself or others that burnout could be on the horizon include:
- Fatigue/exhaustion – Whether emotional or physical (or both), this can become a problem if it “just doesn’t seem to go away despite rest and time away from work,” said Dr. Rudolph.
- Behavioral changes – Any behavior that’s out of the ordinary may be a red flag, like lashing out at someone at work.
- Overwork – Working too much can be caused by an inability to let go of patient care, Dr. Barrett said.
- Not working enough – This may include avoiding tasks and having difficulty meeting deadlines.
- Maladaptive coping behaviors – Excessive consumption of alcohol or drugs is a common coping mechanism. “Even excessive consumption of news is something that people are using to numb out a little bit,” said Dr. Harry.
- Depersonalization – “This is where you start to look at patients, colleagues, or administrators as ‘them’ and you can’t connect as deeply,” Dr. Harry said. “Part of that’s protective and a normal thing to do during a big trauma like this, but it’s also incredibly distancing. Any language that people start using that feels like ‘us’ or ‘them’ is a warning sign.”
- Disengagement – Many people disengage from their work, but Dr. Poorman said physicians tend to disengage from other parts of their lives, such as exercise and family interaction.
Protecting yourself while supporting others
Like the illustration of putting the oxygen mask on yourself first so you can help others, it’s important to protect your own mental and physical health as you support your fellow physicians. Here’s what the experts suggest.
Focus on basic needs
“When you’re in the midst of a trauma, which we are, you don’t want to open all of that up and go to the depths of your thoughts about the grief of all of it because it can actually make the trauma worse,” said Dr. Harry. “There’s a lot of literature that debriefing is really helpful after the event, but if you do it during the event, it can be really dangerous.”
Instead, she said, the goal should be focusing on your basic needs and what you need to do to get through each day, like keeping you and your family in good health. “What is your purpose? Staying connected to why you do this and staying focused on the present is really important,” Dr. Harry noted.
Do your best to get a good night’s sleep, exercise as much as you can, talk to others, and see a mental health provider if your anxiety is too high, advises Dr. Barrett. “Even avoiding blue light from phones and screens within 2 hours of bedtime, parking further away from the hospital and walking, and taking the stairs are things that add up in a big way.”
Keep up your normal routine
“Right now, it’s really critical for clinicians to keep up components of their routine that feel ‘normal,’ ” Dr. Rudolph said. “Whether it’s exercise, playing board games with their kids, or spending time on a hobby, it’s critical to allow yourself these comfortable, predictable, and rewarding detours.”
Set limits
People under stress tend to find unhealthy ways to cope. Instead, try being intentional about what you are consuming by putting limits on things like your news, alcohol consumption, and the number of hours you work, said Dr. Harry.
Implement a culture of wellness
Dr. Barrett believes in creating the work culture we want to be in, one that ensures people have psychological safety, allows them to ask for help, encourages them to disconnect completely from work, and makes them feel valued and listened to. She likes the example of “the pause,” which is called by a team member right after a patient expires.
“It’s a 30-second moment of silence where we reflect on the patient, their loved ones, and every member of the health care team who helped support and treat them,” said Dr. Barrett. “At the conclusion, you say: ‘Thank you. Is there anything you need to be able to go back to the care of other patients?’ Because it’s unnatural to have this terrible thing that happened and then just act like nothing happened.”
Target resources
Be proactive and know where to find resources before you need them, advised Dr. Harry. “Most institutions have free mental health resources, either through their employee assistance programs or HR, plus there’s lots of national organizations that are offering free resources to health care providers.”
Focus on what you can control
Separating what is under your control from what is not is a struggle for everyone, Dr. Poorman said, but it’s helpful to think about the ways you can have an impact and what you’re able to control.
“There was a woman who was diagnosed with early-onset Parkinson’s that I heard giving an interview at the beginning of this pandemic,” she said. “It was the most helpful advice I got, which was: ‘Think of the next good thing you can do.’ You can’t fix everything, so what’s the next good thing you can do?”
Maintain connectivity
Make sure you are utilizing your support circle and staying connected. “That sense of connection is incredibly protective on multiple fronts for depression, for burnout, for suicide ideation, etc.,” Dr. Harry said.
“It doesn’t matter if it’s your teammates at work, your family at home, your best friend from medical school – whomever you can debrief with, vent with, and just share your thoughts and feelings with, these outlets are critical for all of us to process our emotions and diffuse stress and anxiety,” said Dr. Rudolph.
Dr. Poorman is concerned that there could be a spike in physician suicides caused by increased stress, so she also encourages talking openly about what is going on and about getting help when it’s necessary. “Many of us are afraid to seek care because we can actually have our ability to practice medicine questioned, but now is not the time for heroes. Now is the time for people who are willing to recognize their own strengths and limitations to take care of one another.”
Be compassionate toward others
Keep in mind that everyone is stressed out and offer empathy and compassion. “I think everybody’s struggling to try to figure this out and the more that we can give each other the benefit of the doubt and a little grace, the more protective that is,” said Dr. Harry.
Listening is meaningful too. “Recognizing opportunities to validate and acknowledge the feelings that are being shared with you by your colleagues is critical,” Dr. Rudolph said. “We all need to know that we’re not alone, that our thoughts and feelings are okay, and when we share a difficult story, the value of someone saying something as simple as, ‘wow, that sounds like it was really hard,’ is immense.”
Be compassionate toward yourself
Try to give yourself a break and be as compassionate with yourself as you would with others. It’s okay that you’re not getting in shape, publishing prolifically, or redesigning your house right now.
“There’s a lot of data linking lack of self-compassion to burnout,” said Dr. Harry. She says there are courses on self-compassion available that help you work on being kinder to yourself.
Get a “battle buddy”
The American Medical Association has a free “buddy system” program called PeerRx to help physicians cope during the pandemic. Dr. Rudolph said that now is a great time to use this military-developed intervention in which each team member checks in with a chosen partner at agreed-upon intervals.
For example, “You can tell that person: ‘If I don’t call my family for a week that’s a red flag for me.’ And then you hold each other accountable to those things,” Dr. Harry said.
The buddy system is another way to harness that sense of connection that is so vital to our health and well-being.
“The simple act of showing that you care … can make all the difference when you’re doing this kind of work that is both challenging and dangerous,” said Dr. Rudolph.
Navigating COVID-19 requires self-care
Navigating COVID-19 requires self-care
The global COVID-19 pandemic has escalated everyone’s stress levels, especially clinicians caring for hospitalized patients. New pressures have added to everyday stress, new studies have revised prior patient care recommendations, and the world generally seems upside down. What can a busy hospitalist do to maintain a modicum of sanity in all the craziness?
The stressors facing hospitalists
Uncertainty
Of all the burdens COVID-19 has unleashed, the biggest may be uncertainty. Not only is there unease about the virus itself, there also is legitimate concern about the future of medicine, said Elizabeth Harry, MD, SFHM, a hospitalist and senior director of clinical affairs at the University of Colorado Hospital in Aurora.
“What does it look like after an event like this, particularly in areas like academic medicine and teaching our next generation and getting funding for research? And how do we continue to produce physicians that can provide excellent care?” she asked.
There is also uncertainty in the best way to care for patients, said Eileen Barrett, MD, MPH, SFHM, a hospitalist at the University of New Mexico, Albuquerque.
“There are some models that are emerging to predict who will have a worse outcome, but they’re still not great models, so we have uncertainty for a given patient.” And, she noted, as the science continues to evolve, there exists a constant worry that “you might have inadvertently caused someone harm.”
The financial implications of the pandemic are creating uncertainty too. “When you fund a health care system with elective procedures and you can’t do those, and instead have to shift to the most essential services, a lot of places are seeing a massive deficit, which is going to affect staff morale and some physician offices are going to close,” said Elisabeth Poorman, MD, MPH, a primary care and internal medicine physician and chair of the King County Medical Society Physician Wellness Committee in Seattle.
Fear
When the pandemic began in the United States, “fear of the unknown was perhaps the scariest part, particularly as it pertained to personal protective equipment,” said Mark Rudolph, MD, SFHM, chief experience officer and vice president of patient experience and physician development at Sound Physicians in Tacoma, Wash. “For most clinicians, this is the first time that they are themselves in harm’s way while they do their jobs. And worse, they risk bringing the virus home to their families. That is the concern I hear most.”
Anxiety
Worrying about being able to provide excellent patient care is a big stressor, especially since this is the heart and soul of why most hospitalists have gone into their line of work.
“Part of providing excellent care to your patients is providing excellent supportive care to their families,” Dr. Harry said. “There’s some dissonance there in not being able to allow the family to come visit, but wanting to keep them safe, and it feels really hard to support your patients and support their families in the best way. It can feel like you’re just watching and waiting to see what will happen, and that we don’t have a lot of agency over which direction things take.”
There is concern for health care team members as well, Dr. Harry added. “Physicians care a lot about their teams and how they’re doing. I think there’s a sense of esprit de corps among folks and worry for each other there.”
Guilt
Although you may be at the hospital all day, you may feel guilty when you are not providing direct patient care. Or maybe you or someone on your team has an immunodeficiency and can’t be on the front line. Perhaps one of your team members contracted COVID-19 and you did not. Whatever the case, guilt is another emotion that is rampant among hospitalists right now, Dr. Barrett said.
Burnout
Unfortunately, burnout is a potential reality in times of high stress. “Burnout is dynamic,” said Dr. Poorman. “It’s a process by which your emotional and cognitive reserves are exhausted. The people with the highest burnout are the ones who are still trying to provide the standard of care, or above the standard of care in dysfunctional systems.”
Dr. Harry noted that burnout presents in different ways for different people, but Dr. Rudolph added that it’s crucial for hospitalist team members to watch for signs of burnout so they can intervene and/or get help for their colleagues.
Warning signs in yourself or others that burnout could be on the horizon include:
- Fatigue/exhaustion – Whether emotional or physical (or both), this can become a problem if it “just doesn’t seem to go away despite rest and time away from work,” said Dr. Rudolph.
- Behavioral changes – Any behavior that’s out of the ordinary may be a red flag, like lashing out at someone at work.
- Overwork – Working too much can be caused by an inability to let go of patient care, Dr. Barrett said.
- Not working enough – This may include avoiding tasks and having difficulty meeting deadlines.
- Maladaptive coping behaviors – Excessive consumption of alcohol or drugs is a common coping mechanism. “Even excessive consumption of news is something that people are using to numb out a little bit,” said Dr. Harry.
- Depersonalization – “This is where you start to look at patients, colleagues, or administrators as ‘them’ and you can’t connect as deeply,” Dr. Harry said. “Part of that’s protective and a normal thing to do during a big trauma like this, but it’s also incredibly distancing. Any language that people start using that feels like ‘us’ or ‘them’ is a warning sign.”
- Disengagement – Many people disengage from their work, but Dr. Poorman said physicians tend to disengage from other parts of their lives, such as exercise and family interaction.
Protecting yourself while supporting others
Like the illustration of putting the oxygen mask on yourself first so you can help others, it’s important to protect your own mental and physical health as you support your fellow physicians. Here’s what the experts suggest.
Focus on basic needs
“When you’re in the midst of a trauma, which we are, you don’t want to open all of that up and go to the depths of your thoughts about the grief of all of it because it can actually make the trauma worse,” said Dr. Harry. “There’s a lot of literature that debriefing is really helpful after the event, but if you do it during the event, it can be really dangerous.”
Instead, she said, the goal should be focusing on your basic needs and what you need to do to get through each day, like keeping you and your family in good health. “What is your purpose? Staying connected to why you do this and staying focused on the present is really important,” Dr. Harry noted.
Do your best to get a good night’s sleep, exercise as much as you can, talk to others, and see a mental health provider if your anxiety is too high, advises Dr. Barrett. “Even avoiding blue light from phones and screens within 2 hours of bedtime, parking further away from the hospital and walking, and taking the stairs are things that add up in a big way.”
Keep up your normal routine
“Right now, it’s really critical for clinicians to keep up components of their routine that feel ‘normal,’ ” Dr. Rudolph said. “Whether it’s exercise, playing board games with their kids, or spending time on a hobby, it’s critical to allow yourself these comfortable, predictable, and rewarding detours.”
Set limits
People under stress tend to find unhealthy ways to cope. Instead, try being intentional about what you are consuming by putting limits on things like your news, alcohol consumption, and the number of hours you work, said Dr. Harry.
Implement a culture of wellness
Dr. Barrett believes in creating the work culture we want to be in, one that ensures people have psychological safety, allows them to ask for help, encourages them to disconnect completely from work, and makes them feel valued and listened to. She likes the example of “the pause,” which is called by a team member right after a patient expires.
“It’s a 30-second moment of silence where we reflect on the patient, their loved ones, and every member of the health care team who helped support and treat them,” said Dr. Barrett. “At the conclusion, you say: ‘Thank you. Is there anything you need to be able to go back to the care of other patients?’ Because it’s unnatural to have this terrible thing that happened and then just act like nothing happened.”
Target resources
Be proactive and know where to find resources before you need them, advised Dr. Harry. “Most institutions have free mental health resources, either through their employee assistance programs or HR, plus there’s lots of national organizations that are offering free resources to health care providers.”
Focus on what you can control
Separating what is under your control from what is not is a struggle for everyone, Dr. Poorman said, but it’s helpful to think about the ways you can have an impact and what you’re able to control.
“There was a woman who was diagnosed with early-onset Parkinson’s that I heard giving an interview at the beginning of this pandemic,” she said. “It was the most helpful advice I got, which was: ‘Think of the next good thing you can do.’ You can’t fix everything, so what’s the next good thing you can do?”
Maintain connectivity
Make sure you are utilizing your support circle and staying connected. “That sense of connection is incredibly protective on multiple fronts for depression, for burnout, for suicide ideation, etc.,” Dr. Harry said.
“It doesn’t matter if it’s your teammates at work, your family at home, your best friend from medical school – whomever you can debrief with, vent with, and just share your thoughts and feelings with, these outlets are critical for all of us to process our emotions and diffuse stress and anxiety,” said Dr. Rudolph.
Dr. Poorman is concerned that there could be a spike in physician suicides caused by increased stress, so she also encourages talking openly about what is going on and about getting help when it’s necessary. “Many of us are afraid to seek care because we can actually have our ability to practice medicine questioned, but now is not the time for heroes. Now is the time for people who are willing to recognize their own strengths and limitations to take care of one another.”
Be compassionate toward others
Keep in mind that everyone is stressed out and offer empathy and compassion. “I think everybody’s struggling to try to figure this out and the more that we can give each other the benefit of the doubt and a little grace, the more protective that is,” said Dr. Harry.
Listening is meaningful too. “Recognizing opportunities to validate and acknowledge the feelings that are being shared with you by your colleagues is critical,” Dr. Rudolph said. “We all need to know that we’re not alone, that our thoughts and feelings are okay, and when we share a difficult story, the value of someone saying something as simple as, ‘wow, that sounds like it was really hard,’ is immense.”
Be compassionate toward yourself
Try to give yourself a break and be as compassionate with yourself as you would with others. It’s okay that you’re not getting in shape, publishing prolifically, or redesigning your house right now.
“There’s a lot of data linking lack of self-compassion to burnout,” said Dr. Harry. She says there are courses on self-compassion available that help you work on being kinder to yourself.
Get a “battle buddy”
The American Medical Association has a free “buddy system” program called PeerRx to help physicians cope during the pandemic. Dr. Rudolph said that now is a great time to use this military-developed intervention in which each team member checks in with a chosen partner at agreed-upon intervals.
For example, “You can tell that person: ‘If I don’t call my family for a week that’s a red flag for me.’ And then you hold each other accountable to those things,” Dr. Harry said.
The buddy system is another way to harness that sense of connection that is so vital to our health and well-being.
“The simple act of showing that you care … can make all the difference when you’re doing this kind of work that is both challenging and dangerous,” said Dr. Rudolph.
The global COVID-19 pandemic has escalated everyone’s stress levels, especially clinicians caring for hospitalized patients. New pressures have added to everyday stress, new studies have revised prior patient care recommendations, and the world generally seems upside down. What can a busy hospitalist do to maintain a modicum of sanity in all the craziness?
The stressors facing hospitalists
Uncertainty
Of all the burdens COVID-19 has unleashed, the biggest may be uncertainty. Not only is there unease about the virus itself, there also is legitimate concern about the future of medicine, said Elizabeth Harry, MD, SFHM, a hospitalist and senior director of clinical affairs at the University of Colorado Hospital in Aurora.
“What does it look like after an event like this, particularly in areas like academic medicine and teaching our next generation and getting funding for research? And how do we continue to produce physicians that can provide excellent care?” she asked.
There is also uncertainty in the best way to care for patients, said Eileen Barrett, MD, MPH, SFHM, a hospitalist at the University of New Mexico, Albuquerque.
“There are some models that are emerging to predict who will have a worse outcome, but they’re still not great models, so we have uncertainty for a given patient.” And, she noted, as the science continues to evolve, there exists a constant worry that “you might have inadvertently caused someone harm.”
The financial implications of the pandemic are creating uncertainty too. “When you fund a health care system with elective procedures and you can’t do those, and instead have to shift to the most essential services, a lot of places are seeing a massive deficit, which is going to affect staff morale and some physician offices are going to close,” said Elisabeth Poorman, MD, MPH, a primary care and internal medicine physician and chair of the King County Medical Society Physician Wellness Committee in Seattle.
Fear
When the pandemic began in the United States, “fear of the unknown was perhaps the scariest part, particularly as it pertained to personal protective equipment,” said Mark Rudolph, MD, SFHM, chief experience officer and vice president of patient experience and physician development at Sound Physicians in Tacoma, Wash. “For most clinicians, this is the first time that they are themselves in harm’s way while they do their jobs. And worse, they risk bringing the virus home to their families. That is the concern I hear most.”
Anxiety
Worrying about being able to provide excellent patient care is a big stressor, especially since this is the heart and soul of why most hospitalists have gone into their line of work.
“Part of providing excellent care to your patients is providing excellent supportive care to their families,” Dr. Harry said. “There’s some dissonance there in not being able to allow the family to come visit, but wanting to keep them safe, and it feels really hard to support your patients and support their families in the best way. It can feel like you’re just watching and waiting to see what will happen, and that we don’t have a lot of agency over which direction things take.”
There is concern for health care team members as well, Dr. Harry added. “Physicians care a lot about their teams and how they’re doing. I think there’s a sense of esprit de corps among folks and worry for each other there.”
Guilt
Although you may be at the hospital all day, you may feel guilty when you are not providing direct patient care. Or maybe you or someone on your team has an immunodeficiency and can’t be on the front line. Perhaps one of your team members contracted COVID-19 and you did not. Whatever the case, guilt is another emotion that is rampant among hospitalists right now, Dr. Barrett said.
Burnout
Unfortunately, burnout is a potential reality in times of high stress. “Burnout is dynamic,” said Dr. Poorman. “It’s a process by which your emotional and cognitive reserves are exhausted. The people with the highest burnout are the ones who are still trying to provide the standard of care, or above the standard of care in dysfunctional systems.”
Dr. Harry noted that burnout presents in different ways for different people, but Dr. Rudolph added that it’s crucial for hospitalist team members to watch for signs of burnout so they can intervene and/or get help for their colleagues.
Warning signs in yourself or others that burnout could be on the horizon include:
- Fatigue/exhaustion – Whether emotional or physical (or both), this can become a problem if it “just doesn’t seem to go away despite rest and time away from work,” said Dr. Rudolph.
- Behavioral changes – Any behavior that’s out of the ordinary may be a red flag, like lashing out at someone at work.
- Overwork – Working too much can be caused by an inability to let go of patient care, Dr. Barrett said.
- Not working enough – This may include avoiding tasks and having difficulty meeting deadlines.
- Maladaptive coping behaviors – Excessive consumption of alcohol or drugs is a common coping mechanism. “Even excessive consumption of news is something that people are using to numb out a little bit,” said Dr. Harry.
- Depersonalization – “This is where you start to look at patients, colleagues, or administrators as ‘them’ and you can’t connect as deeply,” Dr. Harry said. “Part of that’s protective and a normal thing to do during a big trauma like this, but it’s also incredibly distancing. Any language that people start using that feels like ‘us’ or ‘them’ is a warning sign.”
- Disengagement – Many people disengage from their work, but Dr. Poorman said physicians tend to disengage from other parts of their lives, such as exercise and family interaction.
Protecting yourself while supporting others
Like the illustration of putting the oxygen mask on yourself first so you can help others, it’s important to protect your own mental and physical health as you support your fellow physicians. Here’s what the experts suggest.
Focus on basic needs
“When you’re in the midst of a trauma, which we are, you don’t want to open all of that up and go to the depths of your thoughts about the grief of all of it because it can actually make the trauma worse,” said Dr. Harry. “There’s a lot of literature that debriefing is really helpful after the event, but if you do it during the event, it can be really dangerous.”
Instead, she said, the goal should be focusing on your basic needs and what you need to do to get through each day, like keeping you and your family in good health. “What is your purpose? Staying connected to why you do this and staying focused on the present is really important,” Dr. Harry noted.
Do your best to get a good night’s sleep, exercise as much as you can, talk to others, and see a mental health provider if your anxiety is too high, advises Dr. Barrett. “Even avoiding blue light from phones and screens within 2 hours of bedtime, parking further away from the hospital and walking, and taking the stairs are things that add up in a big way.”
Keep up your normal routine
“Right now, it’s really critical for clinicians to keep up components of their routine that feel ‘normal,’ ” Dr. Rudolph said. “Whether it’s exercise, playing board games with their kids, or spending time on a hobby, it’s critical to allow yourself these comfortable, predictable, and rewarding detours.”
Set limits
People under stress tend to find unhealthy ways to cope. Instead, try being intentional about what you are consuming by putting limits on things like your news, alcohol consumption, and the number of hours you work, said Dr. Harry.
Implement a culture of wellness
Dr. Barrett believes in creating the work culture we want to be in, one that ensures people have psychological safety, allows them to ask for help, encourages them to disconnect completely from work, and makes them feel valued and listened to. She likes the example of “the pause,” which is called by a team member right after a patient expires.
“It’s a 30-second moment of silence where we reflect on the patient, their loved ones, and every member of the health care team who helped support and treat them,” said Dr. Barrett. “At the conclusion, you say: ‘Thank you. Is there anything you need to be able to go back to the care of other patients?’ Because it’s unnatural to have this terrible thing that happened and then just act like nothing happened.”
Target resources
Be proactive and know where to find resources before you need them, advised Dr. Harry. “Most institutions have free mental health resources, either through their employee assistance programs or HR, plus there’s lots of national organizations that are offering free resources to health care providers.”
Focus on what you can control
Separating what is under your control from what is not is a struggle for everyone, Dr. Poorman said, but it’s helpful to think about the ways you can have an impact and what you’re able to control.
“There was a woman who was diagnosed with early-onset Parkinson’s that I heard giving an interview at the beginning of this pandemic,” she said. “It was the most helpful advice I got, which was: ‘Think of the next good thing you can do.’ You can’t fix everything, so what’s the next good thing you can do?”
Maintain connectivity
Make sure you are utilizing your support circle and staying connected. “That sense of connection is incredibly protective on multiple fronts for depression, for burnout, for suicide ideation, etc.,” Dr. Harry said.
“It doesn’t matter if it’s your teammates at work, your family at home, your best friend from medical school – whomever you can debrief with, vent with, and just share your thoughts and feelings with, these outlets are critical for all of us to process our emotions and diffuse stress and anxiety,” said Dr. Rudolph.
Dr. Poorman is concerned that there could be a spike in physician suicides caused by increased stress, so she also encourages talking openly about what is going on and about getting help when it’s necessary. “Many of us are afraid to seek care because we can actually have our ability to practice medicine questioned, but now is not the time for heroes. Now is the time for people who are willing to recognize their own strengths and limitations to take care of one another.”
Be compassionate toward others
Keep in mind that everyone is stressed out and offer empathy and compassion. “I think everybody’s struggling to try to figure this out and the more that we can give each other the benefit of the doubt and a little grace, the more protective that is,” said Dr. Harry.
Listening is meaningful too. “Recognizing opportunities to validate and acknowledge the feelings that are being shared with you by your colleagues is critical,” Dr. Rudolph said. “We all need to know that we’re not alone, that our thoughts and feelings are okay, and when we share a difficult story, the value of someone saying something as simple as, ‘wow, that sounds like it was really hard,’ is immense.”
Be compassionate toward yourself
Try to give yourself a break and be as compassionate with yourself as you would with others. It’s okay that you’re not getting in shape, publishing prolifically, or redesigning your house right now.
“There’s a lot of data linking lack of self-compassion to burnout,” said Dr. Harry. She says there are courses on self-compassion available that help you work on being kinder to yourself.
Get a “battle buddy”
The American Medical Association has a free “buddy system” program called PeerRx to help physicians cope during the pandemic. Dr. Rudolph said that now is a great time to use this military-developed intervention in which each team member checks in with a chosen partner at agreed-upon intervals.
For example, “You can tell that person: ‘If I don’t call my family for a week that’s a red flag for me.’ And then you hold each other accountable to those things,” Dr. Harry said.
The buddy system is another way to harness that sense of connection that is so vital to our health and well-being.
“The simple act of showing that you care … can make all the difference when you’re doing this kind of work that is both challenging and dangerous,” said Dr. Rudolph.
Few patients with migraine clear barriers to optimal care
, new research shows.
Results from a survey study showed less than 8% of patients with episodic migraine and less than 2% of patients with chronic migraine were able to overcome four key treatment barriers associated with optimal migraine management. These included current medical consultation, appropriate diagnosis, minimally adequate acute and preventive pharmacologic treatment (if indicated), and absence of acute medication overdose.
The researchers also evaluated any potential impact of race, ethnicity, and sociodemographic factors on these barriers.
“While chronic migraine was associated with higher rates of consulting, only 1.8% of respondents with chronic migraine traversed all four barriers compared with 8.5% of those with episodic migraine,” the investigators, led by Dawn C. Buse, PhD, clinical professor of neurology at Albert Einstein College of Medicine of Yeshiva University in New York City, noted.
The study was presented at the virtual annual meeting of the American Headache Society.
Ongoing challenges
Migraineurs’ challenges include receiving an appropriate diagnosis and finding effective acute and preventive treatments, the researchers noted. Many patients do not receive optimal care. Previous research by Dr. Buse and colleagues showed that general clinicians were less likely to provide an appropriate diagnosis of migraine compared with headache specialists.
Among patients with chronic migraine who consulted headache specialists, most did not receive an accurate diagnosis of chronic migraine. Data also indicate that a minority, approximately 34%, of patients with chronic migraine used preventive pharmacologic treatments.
The investigators analyzed data from the Chronic Migraine Epidemiology and Outcomes (CaMEO) study to determine the proportion of patients who overcame four prespecified barriers to good outcomes.
Eligible participants met modified International Classification of Headache Disorders (3rd edition) criteria for migraine, had Migraine Disability Assessment Scores (MIDAS) of grade II or higher, and provided data on health insurance status. In addition, all eligible participants had to be receiving appropriate treatment for either episodic or chronic migraine.
In all, 16,789 participants met criteria for migraine. Of this group, 9,184 patients had a MIDAS score of grade II or higher and reported health insurance status. In this subgroup, 7,930 (86.3%) patients had episodic migraine and 1,254 (13.7%) had chronic migraine.
A total of 2,187 (27.6%) patients with episodic migraine and 512 (40.8%) patients with chronic migraine were under the care of a healthcare professional. Of this group, 1,655 patients with episodic migraine (75.7%) and 168 with chronic migraine (32.8%) reported receiving an appropriate diagnosis.
Of participants who successfully overcame the first two optimal management barriers—a consultation with a healthcare professional and an appropriate diagnosis—1,133 (68.5%) episodic migraineurs and 113 (67.3%) chronic migraineurs reported receiving minimally adequate acute treatment.
Furthermore, 1,430 (86.4%) episodic migraineurs and 127 (75.6%) chronic migraineurs reported receiving minimally adequate preventive medication treatment. In addition, 982 (59.3%) episodic migraineurs and 88 (52.4%) chronic migraineurs received minimally adequate acute and preventive treatment.
Acute medication overuse was relatively common, the investigators reported. A total of 310 (31.6%) patients with episodic migraine and 66 (75%) patients with chronic migraine met criteria for acute medication overuse.
“Overuse of acute medication for migraine in people with chronic migraine is a serious concern and is associated with increased risks of migraine progression, headache-related disability, and anxiety and depression. Active patient management and education is important to reduce the likelihood of medication overuse,” said Dr. Buse.
Among all eligible respondents, only 672 (8.5%) patients with episodic migraine and 22 (1.8%) with chronic migraine overcame all four barriers to optimal care.
The researchers found no significant effect of ethnicity or race on the likelihood of overcoming any barrier, but they acknowledged that participation bias might have contributed to this lack of difference. Higher annual household income was significantly associated with high likelihood of surmounting all four barriers.
“The analysis of sociodemographics revealed that female sex and higher annual household income showed a strong relationship with likelihood of obtaining an accurate episodic migraine or chronic migraine diagnosis,” said Dr. Buse.
“Although the reasons for this are not clear, it may be that women are more likely to convey the full scope of their symptoms during consultation. Additionally, the known prevalence of migraine in women may influence healthcare providers by reducing suspicion of chronic migraine in men,” she added.
The CaMEO Study was funded by Allergan (now AbbVie). Dr. Buse reports receiving grant support and honoraria from Allergan, Amgen, Biohaven, Eli Lilly and Co, and Promius. She also receives compensation for work on the editorial board of Current Pain and Headache Reports.
This article first appeared on Medscape.com.
, new research shows.
Results from a survey study showed less than 8% of patients with episodic migraine and less than 2% of patients with chronic migraine were able to overcome four key treatment barriers associated with optimal migraine management. These included current medical consultation, appropriate diagnosis, minimally adequate acute and preventive pharmacologic treatment (if indicated), and absence of acute medication overdose.
The researchers also evaluated any potential impact of race, ethnicity, and sociodemographic factors on these barriers.
“While chronic migraine was associated with higher rates of consulting, only 1.8% of respondents with chronic migraine traversed all four barriers compared with 8.5% of those with episodic migraine,” the investigators, led by Dawn C. Buse, PhD, clinical professor of neurology at Albert Einstein College of Medicine of Yeshiva University in New York City, noted.
The study was presented at the virtual annual meeting of the American Headache Society.
Ongoing challenges
Migraineurs’ challenges include receiving an appropriate diagnosis and finding effective acute and preventive treatments, the researchers noted. Many patients do not receive optimal care. Previous research by Dr. Buse and colleagues showed that general clinicians were less likely to provide an appropriate diagnosis of migraine compared with headache specialists.
Among patients with chronic migraine who consulted headache specialists, most did not receive an accurate diagnosis of chronic migraine. Data also indicate that a minority, approximately 34%, of patients with chronic migraine used preventive pharmacologic treatments.
The investigators analyzed data from the Chronic Migraine Epidemiology and Outcomes (CaMEO) study to determine the proportion of patients who overcame four prespecified barriers to good outcomes.
Eligible participants met modified International Classification of Headache Disorders (3rd edition) criteria for migraine, had Migraine Disability Assessment Scores (MIDAS) of grade II or higher, and provided data on health insurance status. In addition, all eligible participants had to be receiving appropriate treatment for either episodic or chronic migraine.
In all, 16,789 participants met criteria for migraine. Of this group, 9,184 patients had a MIDAS score of grade II or higher and reported health insurance status. In this subgroup, 7,930 (86.3%) patients had episodic migraine and 1,254 (13.7%) had chronic migraine.
A total of 2,187 (27.6%) patients with episodic migraine and 512 (40.8%) patients with chronic migraine were under the care of a healthcare professional. Of this group, 1,655 patients with episodic migraine (75.7%) and 168 with chronic migraine (32.8%) reported receiving an appropriate diagnosis.
Of participants who successfully overcame the first two optimal management barriers—a consultation with a healthcare professional and an appropriate diagnosis—1,133 (68.5%) episodic migraineurs and 113 (67.3%) chronic migraineurs reported receiving minimally adequate acute treatment.
Furthermore, 1,430 (86.4%) episodic migraineurs and 127 (75.6%) chronic migraineurs reported receiving minimally adequate preventive medication treatment. In addition, 982 (59.3%) episodic migraineurs and 88 (52.4%) chronic migraineurs received minimally adequate acute and preventive treatment.
Acute medication overuse was relatively common, the investigators reported. A total of 310 (31.6%) patients with episodic migraine and 66 (75%) patients with chronic migraine met criteria for acute medication overuse.
“Overuse of acute medication for migraine in people with chronic migraine is a serious concern and is associated with increased risks of migraine progression, headache-related disability, and anxiety and depression. Active patient management and education is important to reduce the likelihood of medication overuse,” said Dr. Buse.
Among all eligible respondents, only 672 (8.5%) patients with episodic migraine and 22 (1.8%) with chronic migraine overcame all four barriers to optimal care.
The researchers found no significant effect of ethnicity or race on the likelihood of overcoming any barrier, but they acknowledged that participation bias might have contributed to this lack of difference. Higher annual household income was significantly associated with high likelihood of surmounting all four barriers.
“The analysis of sociodemographics revealed that female sex and higher annual household income showed a strong relationship with likelihood of obtaining an accurate episodic migraine or chronic migraine diagnosis,” said Dr. Buse.
“Although the reasons for this are not clear, it may be that women are more likely to convey the full scope of their symptoms during consultation. Additionally, the known prevalence of migraine in women may influence healthcare providers by reducing suspicion of chronic migraine in men,” she added.
The CaMEO Study was funded by Allergan (now AbbVie). Dr. Buse reports receiving grant support and honoraria from Allergan, Amgen, Biohaven, Eli Lilly and Co, and Promius. She also receives compensation for work on the editorial board of Current Pain and Headache Reports.
This article first appeared on Medscape.com.
, new research shows.
Results from a survey study showed less than 8% of patients with episodic migraine and less than 2% of patients with chronic migraine were able to overcome four key treatment barriers associated with optimal migraine management. These included current medical consultation, appropriate diagnosis, minimally adequate acute and preventive pharmacologic treatment (if indicated), and absence of acute medication overdose.
The researchers also evaluated any potential impact of race, ethnicity, and sociodemographic factors on these barriers.
“While chronic migraine was associated with higher rates of consulting, only 1.8% of respondents with chronic migraine traversed all four barriers compared with 8.5% of those with episodic migraine,” the investigators, led by Dawn C. Buse, PhD, clinical professor of neurology at Albert Einstein College of Medicine of Yeshiva University in New York City, noted.
The study was presented at the virtual annual meeting of the American Headache Society.
Ongoing challenges
Migraineurs’ challenges include receiving an appropriate diagnosis and finding effective acute and preventive treatments, the researchers noted. Many patients do not receive optimal care. Previous research by Dr. Buse and colleagues showed that general clinicians were less likely to provide an appropriate diagnosis of migraine compared with headache specialists.
Among patients with chronic migraine who consulted headache specialists, most did not receive an accurate diagnosis of chronic migraine. Data also indicate that a minority, approximately 34%, of patients with chronic migraine used preventive pharmacologic treatments.
The investigators analyzed data from the Chronic Migraine Epidemiology and Outcomes (CaMEO) study to determine the proportion of patients who overcame four prespecified barriers to good outcomes.
Eligible participants met modified International Classification of Headache Disorders (3rd edition) criteria for migraine, had Migraine Disability Assessment Scores (MIDAS) of grade II or higher, and provided data on health insurance status. In addition, all eligible participants had to be receiving appropriate treatment for either episodic or chronic migraine.
In all, 16,789 participants met criteria for migraine. Of this group, 9,184 patients had a MIDAS score of grade II or higher and reported health insurance status. In this subgroup, 7,930 (86.3%) patients had episodic migraine and 1,254 (13.7%) had chronic migraine.
A total of 2,187 (27.6%) patients with episodic migraine and 512 (40.8%) patients with chronic migraine were under the care of a healthcare professional. Of this group, 1,655 patients with episodic migraine (75.7%) and 168 with chronic migraine (32.8%) reported receiving an appropriate diagnosis.
Of participants who successfully overcame the first two optimal management barriers—a consultation with a healthcare professional and an appropriate diagnosis—1,133 (68.5%) episodic migraineurs and 113 (67.3%) chronic migraineurs reported receiving minimally adequate acute treatment.
Furthermore, 1,430 (86.4%) episodic migraineurs and 127 (75.6%) chronic migraineurs reported receiving minimally adequate preventive medication treatment. In addition, 982 (59.3%) episodic migraineurs and 88 (52.4%) chronic migraineurs received minimally adequate acute and preventive treatment.
Acute medication overuse was relatively common, the investigators reported. A total of 310 (31.6%) patients with episodic migraine and 66 (75%) patients with chronic migraine met criteria for acute medication overuse.
“Overuse of acute medication for migraine in people with chronic migraine is a serious concern and is associated with increased risks of migraine progression, headache-related disability, and anxiety and depression. Active patient management and education is important to reduce the likelihood of medication overuse,” said Dr. Buse.
Among all eligible respondents, only 672 (8.5%) patients with episodic migraine and 22 (1.8%) with chronic migraine overcame all four barriers to optimal care.
The researchers found no significant effect of ethnicity or race on the likelihood of overcoming any barrier, but they acknowledged that participation bias might have contributed to this lack of difference. Higher annual household income was significantly associated with high likelihood of surmounting all four barriers.
“The analysis of sociodemographics revealed that female sex and higher annual household income showed a strong relationship with likelihood of obtaining an accurate episodic migraine or chronic migraine diagnosis,” said Dr. Buse.
“Although the reasons for this are not clear, it may be that women are more likely to convey the full scope of their symptoms during consultation. Additionally, the known prevalence of migraine in women may influence healthcare providers by reducing suspicion of chronic migraine in men,” she added.
The CaMEO Study was funded by Allergan (now AbbVie). Dr. Buse reports receiving grant support and honoraria from Allergan, Amgen, Biohaven, Eli Lilly and Co, and Promius. She also receives compensation for work on the editorial board of Current Pain and Headache Reports.
This article first appeared on Medscape.com.
From AHS 2020
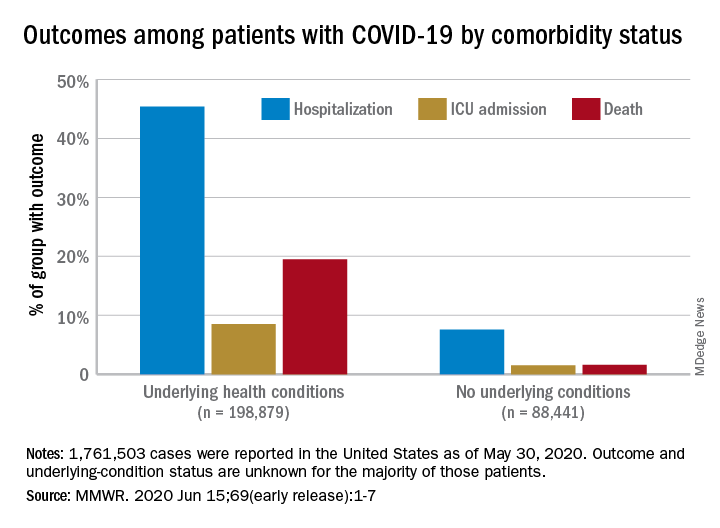
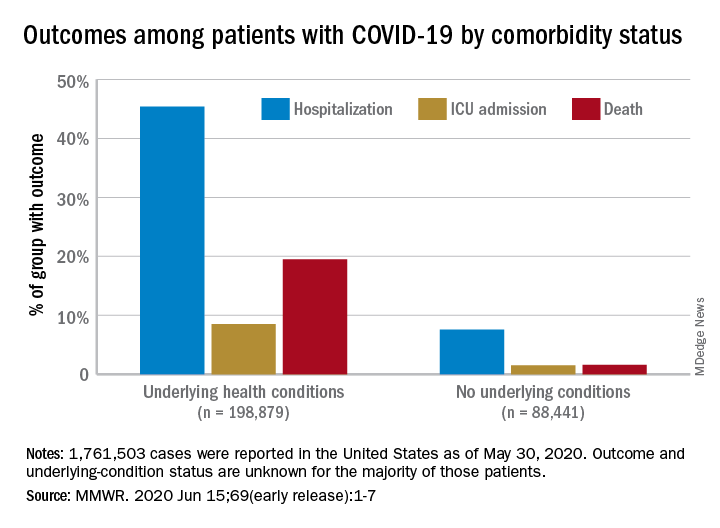
Comorbidities increase COVID-19 deaths by factor of 12
, compared with those who have no such condition, according to the Centers for Disease Control and Prevention.
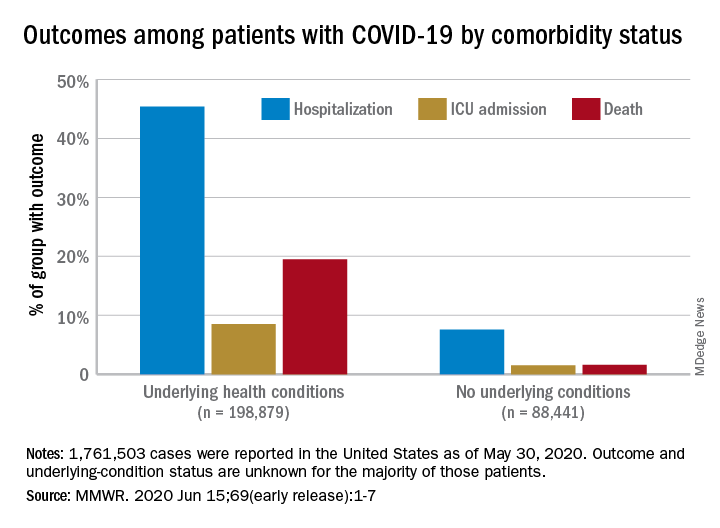
Among those with underlying conditions such as cardiovascular disease or diabetes, 45.4% of patients with COVID-19 were hospitalized, versus 7.6% of patients without an underlying condition, said Erin K. Stokes, MPH, and associates of the CDC COVID-19 Emergency Response team.
The difference in deaths was even greater over the study period of Jan. 22–May 30, 2020: 19.5% of COVID-19 patients with underlying conditions died, compared with 1.6% of those with no underlying condition. The gap narrowed, however, for ICU admissions, with corresponding rates of 8.5% and 1.5%, the investigators reported June 15 in the Morbidity and Mortality Weekly Report.
“The COVID-19 pandemic continues to be severe, particularly in certain population groups,” they said.
The cumulative incidence of laboratory-confirmed cases up to May 30, for instance, was nearly twice as high for those aged 80 years and over (902 per 100,000 population) than for those aged 70-79 years (464.2 per 100,000). Those aged 50-59 years had the second-highest incidence, 550.5 per 100,000, Ms. Stokes and associates said.
“Among cases with known race and ethnicity, 33% of persons were Hispanic, 22% were black, and 1.3% were [American Indian/Alaska Native]. These findings suggest that persons in these groups, who account for 18%, 13%, and 0.7% of the U.S. population, respectively, are disproportionately affected by the COVID-19 pandemic,” they wrote.
Another source of disparity: “Incidence among males and females was similar overall, [but] severe outcomes were more commonly reported among males,” the investigators noted. Cumulative incidence was 401.1 per 100,000 for males and 406.0 for females, but 6.0% of male patients died, compared with 4.8% of females.
As of May 30, a total of 1,761,503 cases and 103,700 deaths had been reported to the CDC. Of those cases, approximately 1.3 million were included in the analysis, with data on individual underlying health conditions available for 287,320 (22%). The split on those cases was 198,879 with health conditions and 88,411 without, the CDC data show.
The most frequently reported underlying conditions were cardiovascular disease (32%), diabetes (30%), chronic lung disease (18%), and renal disease (7.6%), and there were no significant differences between males and females, Ms. Stokes and associates said.
The pandemic “is an ongoing public health crisis in the United States that continues to affect all populations and result in severe outcomes including death,” they said, emphasizing “the continued need for community mitigation strategies, especially for vulnerable populations, to slow COVID-19 transmission.”
SOURCE: Stokes EK et al. MMWR. 2020 Jun 15;69(early release):1-7.
, compared with those who have no such condition, according to the Centers for Disease Control and Prevention.
Among those with underlying conditions such as cardiovascular disease or diabetes, 45.4% of patients with COVID-19 were hospitalized, versus 7.6% of patients without an underlying condition, said Erin K. Stokes, MPH, and associates of the CDC COVID-19 Emergency Response team.
The difference in deaths was even greater over the study period of Jan. 22–May 30, 2020: 19.5% of COVID-19 patients with underlying conditions died, compared with 1.6% of those with no underlying condition. The gap narrowed, however, for ICU admissions, with corresponding rates of 8.5% and 1.5%, the investigators reported June 15 in the Morbidity and Mortality Weekly Report.
“The COVID-19 pandemic continues to be severe, particularly in certain population groups,” they said.
The cumulative incidence of laboratory-confirmed cases up to May 30, for instance, was nearly twice as high for those aged 80 years and over (902 per 100,000 population) than for those aged 70-79 years (464.2 per 100,000). Those aged 50-59 years had the second-highest incidence, 550.5 per 100,000, Ms. Stokes and associates said.
“Among cases with known race and ethnicity, 33% of persons were Hispanic, 22% were black, and 1.3% were [American Indian/Alaska Native]. These findings suggest that persons in these groups, who account for 18%, 13%, and 0.7% of the U.S. population, respectively, are disproportionately affected by the COVID-19 pandemic,” they wrote.
Another source of disparity: “Incidence among males and females was similar overall, [but] severe outcomes were more commonly reported among males,” the investigators noted. Cumulative incidence was 401.1 per 100,000 for males and 406.0 for females, but 6.0% of male patients died, compared with 4.8% of females.
As of May 30, a total of 1,761,503 cases and 103,700 deaths had been reported to the CDC. Of those cases, approximately 1.3 million were included in the analysis, with data on individual underlying health conditions available for 287,320 (22%). The split on those cases was 198,879 with health conditions and 88,411 without, the CDC data show.
The most frequently reported underlying conditions were cardiovascular disease (32%), diabetes (30%), chronic lung disease (18%), and renal disease (7.6%), and there were no significant differences between males and females, Ms. Stokes and associates said.
The pandemic “is an ongoing public health crisis in the United States that continues to affect all populations and result in severe outcomes including death,” they said, emphasizing “the continued need for community mitigation strategies, especially for vulnerable populations, to slow COVID-19 transmission.”
SOURCE: Stokes EK et al. MMWR. 2020 Jun 15;69(early release):1-7.
, compared with those who have no such condition, according to the Centers for Disease Control and Prevention.
Among those with underlying conditions such as cardiovascular disease or diabetes, 45.4% of patients with COVID-19 were hospitalized, versus 7.6% of patients without an underlying condition, said Erin K. Stokes, MPH, and associates of the CDC COVID-19 Emergency Response team.
The difference in deaths was even greater over the study period of Jan. 22–May 30, 2020: 19.5% of COVID-19 patients with underlying conditions died, compared with 1.6% of those with no underlying condition. The gap narrowed, however, for ICU admissions, with corresponding rates of 8.5% and 1.5%, the investigators reported June 15 in the Morbidity and Mortality Weekly Report.
“The COVID-19 pandemic continues to be severe, particularly in certain population groups,” they said.
The cumulative incidence of laboratory-confirmed cases up to May 30, for instance, was nearly twice as high for those aged 80 years and over (902 per 100,000 population) than for those aged 70-79 years (464.2 per 100,000). Those aged 50-59 years had the second-highest incidence, 550.5 per 100,000, Ms. Stokes and associates said.
“Among cases with known race and ethnicity, 33% of persons were Hispanic, 22% were black, and 1.3% were [American Indian/Alaska Native]. These findings suggest that persons in these groups, who account for 18%, 13%, and 0.7% of the U.S. population, respectively, are disproportionately affected by the COVID-19 pandemic,” they wrote.
Another source of disparity: “Incidence among males and females was similar overall, [but] severe outcomes were more commonly reported among males,” the investigators noted. Cumulative incidence was 401.1 per 100,000 for males and 406.0 for females, but 6.0% of male patients died, compared with 4.8% of females.
As of May 30, a total of 1,761,503 cases and 103,700 deaths had been reported to the CDC. Of those cases, approximately 1.3 million were included in the analysis, with data on individual underlying health conditions available for 287,320 (22%). The split on those cases was 198,879 with health conditions and 88,411 without, the CDC data show.
The most frequently reported underlying conditions were cardiovascular disease (32%), diabetes (30%), chronic lung disease (18%), and renal disease (7.6%), and there were no significant differences between males and females, Ms. Stokes and associates said.
The pandemic “is an ongoing public health crisis in the United States that continues to affect all populations and result in severe outcomes including death,” they said, emphasizing “the continued need for community mitigation strategies, especially for vulnerable populations, to slow COVID-19 transmission.”
SOURCE: Stokes EK et al. MMWR. 2020 Jun 15;69(early release):1-7.
FROM MMWR
Weight loss stays consistent in one- and two-step in gastric band conversion
with either a one- or two-step procedure, a study of 78 patients showed.
“Laparoscopic adjustable gastric banding (LAGB) has largely fallen out of favor, likely related to variable efficacy in weight reduction coupled with poor effectiveness in reducing obesity related comorbidities like type 2 diabetes and hypercholesterolemia,” Vasu Chirumamilla, MD, of Westchester Medical Center, Valhalla, N.Y., and colleagues wrote in a poster presented at the virtual Annual Minimally Invasive Surgery Symposium sponsored by Global Academy for Medical Education.
LAGB also can cause complications including, slippage, erosion, and gastric pouch dilation; subsequently many patients undergo conversion to laparoscopic sleeve gastrectomy (LSG). However, the impact of a one-step vs. two-step conversion procedure on patient weight loss remains unclear, the researchers said.
To compare weight loss after the two types of procedures, the researchers reviewed data from 78 patients (71 women) aged 15-74 years treated between 2013 and 2018 at a multi-surgeon, private practice bariatric surgery center. All patients had a history of LAGB; 31 underwent conversion to LSG in one stage, and 47 underwent conversion in two stages. Weight loss, defined as the percentage excess weight loss, was the primary endpoint.
The average excess weight loss was 44% for patients in both the one-stage and two-stage groups, and body mass index decreased by 8.9 points and 8.8 points, respectively, in the two groups, the researchers wrote.
Patients in the two-stage group experienced a significant increase in body mass index (P = .008) during the time between band removal to sleeve gastrectomy, which was an average of 207 days, they said.
The findings were limited in part by the small sample size and retrospective design, and more data are needed to compare complication rates in one-stage and two-stage procedures, the researchers noted. However, the results showed “no difference in excess weight loss in patients converted from laparoscopic adjustable gastric band to sleeve gastrectomy in one-stage versus a two-stage procedure,” they concluded.
“LAGB used to be a very popular weight loss procedure – bands were placed in a great deal of patients,” Dr. Chirumamilla said in an interview. “Now those patients are presenting with increasing frequency to bariatric surgeons with band complications or weight regain. The volume for LSG is increasing and results in percentage excess weight loss of approximately 65% versus approximately 42% for LAGB,” he said. A goal of the study was to provide patients and the surgeons with a more informed approach to performing and consenting to the particular operation, he added.
“The results have not surprised us, because as long as done by experienced surgeons on compliant patients the weight loss outcomes from the day of surgery onward should be equivalent,” Dr. Chirumamilla explained. “We were also not surprised to find that patients undergoing a two-stage conversion gained weight before their second-stage sleeve gastrectomy.”
The bottom line for clinicians is that “patients getting a conversion from band to sleeve in one-stage versus two-stages experience the same percentage excess body weight loss from time of surgery,” although two-stage patients do gain weight while awaiting their second-stage sleeve gastrectomy, Dr. Chirumamilla said.
“More research is needed to compare short- and long-term complications rates between one-stage and two-stage conversions. The ideal research situation would be a randomized, multicenter, large volume study to reduce bias,” he noted.
Dr. Chirumamilla’s collaborators included Akia Caine MD, Zachary Ballinger, Rebecca Castro, Thomas Cerabona MD, and Ashutosh Kaul MD, of the surgical group Advanced Surgeons at nygetfit.com.
Global Academy for Medical Education and this news organization are owned by the same parent company. The study received no outside funding. The researchers had no financial conflicts to disclose.
SOURCE: Chirumamilla V et al. MISS 2020. Poster PA-14.
with either a one- or two-step procedure, a study of 78 patients showed.
“Laparoscopic adjustable gastric banding (LAGB) has largely fallen out of favor, likely related to variable efficacy in weight reduction coupled with poor effectiveness in reducing obesity related comorbidities like type 2 diabetes and hypercholesterolemia,” Vasu Chirumamilla, MD, of Westchester Medical Center, Valhalla, N.Y., and colleagues wrote in a poster presented at the virtual Annual Minimally Invasive Surgery Symposium sponsored by Global Academy for Medical Education.
LAGB also can cause complications including, slippage, erosion, and gastric pouch dilation; subsequently many patients undergo conversion to laparoscopic sleeve gastrectomy (LSG). However, the impact of a one-step vs. two-step conversion procedure on patient weight loss remains unclear, the researchers said.
To compare weight loss after the two types of procedures, the researchers reviewed data from 78 patients (71 women) aged 15-74 years treated between 2013 and 2018 at a multi-surgeon, private practice bariatric surgery center. All patients had a history of LAGB; 31 underwent conversion to LSG in one stage, and 47 underwent conversion in two stages. Weight loss, defined as the percentage excess weight loss, was the primary endpoint.
The average excess weight loss was 44% for patients in both the one-stage and two-stage groups, and body mass index decreased by 8.9 points and 8.8 points, respectively, in the two groups, the researchers wrote.
Patients in the two-stage group experienced a significant increase in body mass index (P = .008) during the time between band removal to sleeve gastrectomy, which was an average of 207 days, they said.
The findings were limited in part by the small sample size and retrospective design, and more data are needed to compare complication rates in one-stage and two-stage procedures, the researchers noted. However, the results showed “no difference in excess weight loss in patients converted from laparoscopic adjustable gastric band to sleeve gastrectomy in one-stage versus a two-stage procedure,” they concluded.
“LAGB used to be a very popular weight loss procedure – bands were placed in a great deal of patients,” Dr. Chirumamilla said in an interview. “Now those patients are presenting with increasing frequency to bariatric surgeons with band complications or weight regain. The volume for LSG is increasing and results in percentage excess weight loss of approximately 65% versus approximately 42% for LAGB,” he said. A goal of the study was to provide patients and the surgeons with a more informed approach to performing and consenting to the particular operation, he added.
“The results have not surprised us, because as long as done by experienced surgeons on compliant patients the weight loss outcomes from the day of surgery onward should be equivalent,” Dr. Chirumamilla explained. “We were also not surprised to find that patients undergoing a two-stage conversion gained weight before their second-stage sleeve gastrectomy.”
The bottom line for clinicians is that “patients getting a conversion from band to sleeve in one-stage versus two-stages experience the same percentage excess body weight loss from time of surgery,” although two-stage patients do gain weight while awaiting their second-stage sleeve gastrectomy, Dr. Chirumamilla said.
“More research is needed to compare short- and long-term complications rates between one-stage and two-stage conversions. The ideal research situation would be a randomized, multicenter, large volume study to reduce bias,” he noted.
Dr. Chirumamilla’s collaborators included Akia Caine MD, Zachary Ballinger, Rebecca Castro, Thomas Cerabona MD, and Ashutosh Kaul MD, of the surgical group Advanced Surgeons at nygetfit.com.
Global Academy for Medical Education and this news organization are owned by the same parent company. The study received no outside funding. The researchers had no financial conflicts to disclose.
SOURCE: Chirumamilla V et al. MISS 2020. Poster PA-14.
with either a one- or two-step procedure, a study of 78 patients showed.
“Laparoscopic adjustable gastric banding (LAGB) has largely fallen out of favor, likely related to variable efficacy in weight reduction coupled with poor effectiveness in reducing obesity related comorbidities like type 2 diabetes and hypercholesterolemia,” Vasu Chirumamilla, MD, of Westchester Medical Center, Valhalla, N.Y., and colleagues wrote in a poster presented at the virtual Annual Minimally Invasive Surgery Symposium sponsored by Global Academy for Medical Education.
LAGB also can cause complications including, slippage, erosion, and gastric pouch dilation; subsequently many patients undergo conversion to laparoscopic sleeve gastrectomy (LSG). However, the impact of a one-step vs. two-step conversion procedure on patient weight loss remains unclear, the researchers said.
To compare weight loss after the two types of procedures, the researchers reviewed data from 78 patients (71 women) aged 15-74 years treated between 2013 and 2018 at a multi-surgeon, private practice bariatric surgery center. All patients had a history of LAGB; 31 underwent conversion to LSG in one stage, and 47 underwent conversion in two stages. Weight loss, defined as the percentage excess weight loss, was the primary endpoint.
The average excess weight loss was 44% for patients in both the one-stage and two-stage groups, and body mass index decreased by 8.9 points and 8.8 points, respectively, in the two groups, the researchers wrote.
Patients in the two-stage group experienced a significant increase in body mass index (P = .008) during the time between band removal to sleeve gastrectomy, which was an average of 207 days, they said.
The findings were limited in part by the small sample size and retrospective design, and more data are needed to compare complication rates in one-stage and two-stage procedures, the researchers noted. However, the results showed “no difference in excess weight loss in patients converted from laparoscopic adjustable gastric band to sleeve gastrectomy in one-stage versus a two-stage procedure,” they concluded.
“LAGB used to be a very popular weight loss procedure – bands were placed in a great deal of patients,” Dr. Chirumamilla said in an interview. “Now those patients are presenting with increasing frequency to bariatric surgeons with band complications or weight regain. The volume for LSG is increasing and results in percentage excess weight loss of approximately 65% versus approximately 42% for LAGB,” he said. A goal of the study was to provide patients and the surgeons with a more informed approach to performing and consenting to the particular operation, he added.
“The results have not surprised us, because as long as done by experienced surgeons on compliant patients the weight loss outcomes from the day of surgery onward should be equivalent,” Dr. Chirumamilla explained. “We were also not surprised to find that patients undergoing a two-stage conversion gained weight before their second-stage sleeve gastrectomy.”
The bottom line for clinicians is that “patients getting a conversion from band to sleeve in one-stage versus two-stages experience the same percentage excess body weight loss from time of surgery,” although two-stage patients do gain weight while awaiting their second-stage sleeve gastrectomy, Dr. Chirumamilla said.
“More research is needed to compare short- and long-term complications rates between one-stage and two-stage conversions. The ideal research situation would be a randomized, multicenter, large volume study to reduce bias,” he noted.
Dr. Chirumamilla’s collaborators included Akia Caine MD, Zachary Ballinger, Rebecca Castro, Thomas Cerabona MD, and Ashutosh Kaul MD, of the surgical group Advanced Surgeons at nygetfit.com.
Global Academy for Medical Education and this news organization are owned by the same parent company. The study received no outside funding. The researchers had no financial conflicts to disclose.
SOURCE: Chirumamilla V et al. MISS 2020. Poster PA-14.
FROM MISS
Key clinical point: Weight loss was the same for patients after conversions from LAGB to LSG in both one-step and two-step procedures.
Major finding: The average excess weight loss was 44% for patients in both one-step and two-step conversion groups, and body mass index decreased by approximately 9 points in both groups.
Study details: The data come from a retrospective study of 78 adults who underwent conversion from LABG to LSG.
Disclosures: The study received no outside funding. The researchers had no financial conflicts to disclose.
Source: Chirumamilla V et al. MISS 2020. Poster PA-14.
Omitting whole body irradiation before HSCT: Trial stopped early
Hematopoietic stem cell transplantation (HSCT) may offer the chance of a cure for patients with leukemia and other blood cancers, but the process of preparing the body to receive such a transplant can be brutal, involving whole body irradiation as well as chemotherapy conditioning. New results show that both steps are needed: a trial that omitted whole body irradiation in young patients with acute lymphoblastic leukemia (ALL) was stopped early because of significantly poorer outcomes.
The multicenter, global FORUM (For Omitting Radiation Under Majority Age) trial involved 75 centers in 17 countries between 2013 and 2018.
“Our study shows significantly better outcomes for total body irradiation compared to myeloablative chemo-conditioning arms, with no differences between the [two] chemo-conditioning groups,” concluded Christina Peters, MD, professor of pediatrics in the department of stem cell transplantation at St Anna Children’s Hospital in Vienna.
, she added.
Dr. Peters presented the findings as part of the virtual annual congress of the European Hematology Association.
Describing the results as “sobering,” session comoderator Shai Izraeli, MD, director of the department of hematology-oncology at Schneider Children’s Medical Center, in Petah Tikva, Israel, said an online comment from the virtual meeting audience reflected the reaction to these unwelcome results: “So we are still stuck with total body irradiation?”
Dr. Peters said the good news is that the number of patients needing to undergo stem cell transplants is low, and with research advances, may hopefully drop even further.
“Only 10% of patients under the age of 18 nowadays undergo allogeneic HSCT, and perhaps in the future that will become even less if we are able to rescue some of the groups with other immunological measures such as CAR-T cells and antibodies,” she said.
“I think it is very important to better identify those who really need total body irradiation in the future,” she added.
In an interview, Dr. Izraeli agreed.
“The prognosis of children after bone marrow transplantation is excellent – the majority are cured from their leukemia,” he said. “And we have to remember that those who undergo bone marrow transplant have the worst leukemias.”
He pointed out that, in fact, contemporary chemotherapy alone is effective in the treatment of more than 90% of patients with ALL younger than aged 18.
For the 10% of patients who do not respond to chemotherapy alone and undergo allogeneic HSCT, about 50%-80% of pediatric patients who have resistant leukemia are cured. However, the total body irradiation used to prepare the body to receive the transplant is linked to potentially serious consequences later in life, including sterility, lung problems, growth retardation, and secondary cancer.
To determine if the irradiation component could be safely replaced with a chemotherapy-based conditioning approach, Dr. Peters and colleagues conducted the FORUM trial.
In total 413 patients undergoing HSCT were enrolled and randomized to pretransplant conditioning with total body irradiation and etoposide (n = 202) or a chemotherapy-only approach with fludarabine/thiotepa/busulfan (flu/thio/bu; n = 99) or fludarabine/thiotepa/treosulfan (treo; n = 93).
Most patients (72%) had B-cell precursor ALL and 23% had T-cell ALL. Just over half (54%) were transplanted in first complete remission (CR1), 40% in CR2, and 4% in CR3.
The source of stem cells was bone marrow for most patients (82%); peripheral blood stem cell for 12%, and cord blood for 4%.
Study stopped early
The aim of the study was to demonstrate noninferiority with the chemotherapy approach.
However, the significantly inferior outcome observed in the chemotherapy-only group led to randomization being halted in March 2019.
The 2-year overall survival in the intent-to-treat (ITT) analysis, with a mean observation time of 2.1 years, was 0.75 ± 0.04 for chemo-conditioning versus 0.91 ± 0.02 for total body irradiation/etoposide (ITT P < .001).
The ITT analysis showed relapses were significantly higher in the chemo-conditioning group (2-year cumulative incidence of relapse [CIR], 0.33) compared with the total body irradiation group (CIR, 0.12; P < .001).
The 2-year event-free survival (EFS) rate was also significantly higher in the total body irradiation group (0.86 vs 0.58; P < .001), and transplant-related mortality over 2 years was lower with total body irradiation (0.02 vs 0.09; P = .02).
A per-protocol analysis showed the 2-year overall survival to be the same in the two chemotherapy groups (both 0.77 ± 0.05) compared with 0.91 ± 0.02 in the total body irradiation group (P = .003).
“In this cohort [the 91% overall survival rate] may even be lower than contemporary intensive frontline therapy results that are achieved nowadays,” Dr. Peters said.
In looking at subgroups, there were no significant differences according to age group or cancer phenotype, while MLL rearrangement was associated with higher relapse incidence.
Remission status was found to notably influence EFS, dropping from 0.91 in CR1 patients with total body irradiation to 0.76 in CR2 patients. However, total body irradiation remained significantly higher compared with the chemo-conditioning groups in CR1 (P = .004) and CR2 (P < .001).
Transplant-related mortality was not significantly different between the total body irradiation and chemo-conditioning groups in the CR1 or CR2 groups (P = .09 and P = .18, respectively), despite the significant difference when remission status was not included.
Overall, “we tried to identify subgroups in which total body irradiation might be eliminated, however in all analyses, total body irradiation was better than chemo-conditioning in all arms,” Dr. Peters said.
Meanwhile, the findings underscore that even when patients cannot receive total body irradiation, the alternative chemo-conditioning therapy in fact shows favorable efficacy on its own, Dr. Izraeli said.
“The prognosis of the chemotherapy group is also quite remarkably good, although less than the total body irradiation arm. This means that if for some reason total body irradiation cannot be given, the chemotherapy is a very reasonable alternative.”
Dr. Peters has reported relationships with Amgen, Novartis, Pfizer, Medac, Jazz, and Neovii. Dr. Izraeli has reported no relevant financial relationships.
SOURCE: EHA Congress. Abstract S102.
A version of this article originally appeared on Medscape.com.
Hematopoietic stem cell transplantation (HSCT) may offer the chance of a cure for patients with leukemia and other blood cancers, but the process of preparing the body to receive such a transplant can be brutal, involving whole body irradiation as well as chemotherapy conditioning. New results show that both steps are needed: a trial that omitted whole body irradiation in young patients with acute lymphoblastic leukemia (ALL) was stopped early because of significantly poorer outcomes.
The multicenter, global FORUM (For Omitting Radiation Under Majority Age) trial involved 75 centers in 17 countries between 2013 and 2018.
“Our study shows significantly better outcomes for total body irradiation compared to myeloablative chemo-conditioning arms, with no differences between the [two] chemo-conditioning groups,” concluded Christina Peters, MD, professor of pediatrics in the department of stem cell transplantation at St Anna Children’s Hospital in Vienna.
, she added.
Dr. Peters presented the findings as part of the virtual annual congress of the European Hematology Association.
Describing the results as “sobering,” session comoderator Shai Izraeli, MD, director of the department of hematology-oncology at Schneider Children’s Medical Center, in Petah Tikva, Israel, said an online comment from the virtual meeting audience reflected the reaction to these unwelcome results: “So we are still stuck with total body irradiation?”
Dr. Peters said the good news is that the number of patients needing to undergo stem cell transplants is low, and with research advances, may hopefully drop even further.
“Only 10% of patients under the age of 18 nowadays undergo allogeneic HSCT, and perhaps in the future that will become even less if we are able to rescue some of the groups with other immunological measures such as CAR-T cells and antibodies,” she said.
“I think it is very important to better identify those who really need total body irradiation in the future,” she added.
In an interview, Dr. Izraeli agreed.
“The prognosis of children after bone marrow transplantation is excellent – the majority are cured from their leukemia,” he said. “And we have to remember that those who undergo bone marrow transplant have the worst leukemias.”
He pointed out that, in fact, contemporary chemotherapy alone is effective in the treatment of more than 90% of patients with ALL younger than aged 18.
For the 10% of patients who do not respond to chemotherapy alone and undergo allogeneic HSCT, about 50%-80% of pediatric patients who have resistant leukemia are cured. However, the total body irradiation used to prepare the body to receive the transplant is linked to potentially serious consequences later in life, including sterility, lung problems, growth retardation, and secondary cancer.
To determine if the irradiation component could be safely replaced with a chemotherapy-based conditioning approach, Dr. Peters and colleagues conducted the FORUM trial.
In total 413 patients undergoing HSCT were enrolled and randomized to pretransplant conditioning with total body irradiation and etoposide (n = 202) or a chemotherapy-only approach with fludarabine/thiotepa/busulfan (flu/thio/bu; n = 99) or fludarabine/thiotepa/treosulfan (treo; n = 93).
Most patients (72%) had B-cell precursor ALL and 23% had T-cell ALL. Just over half (54%) were transplanted in first complete remission (CR1), 40% in CR2, and 4% in CR3.
The source of stem cells was bone marrow for most patients (82%); peripheral blood stem cell for 12%, and cord blood for 4%.
Study stopped early
The aim of the study was to demonstrate noninferiority with the chemotherapy approach.
However, the significantly inferior outcome observed in the chemotherapy-only group led to randomization being halted in March 2019.
The 2-year overall survival in the intent-to-treat (ITT) analysis, with a mean observation time of 2.1 years, was 0.75 ± 0.04 for chemo-conditioning versus 0.91 ± 0.02 for total body irradiation/etoposide (ITT P < .001).
The ITT analysis showed relapses were significantly higher in the chemo-conditioning group (2-year cumulative incidence of relapse [CIR], 0.33) compared with the total body irradiation group (CIR, 0.12; P < .001).
The 2-year event-free survival (EFS) rate was also significantly higher in the total body irradiation group (0.86 vs 0.58; P < .001), and transplant-related mortality over 2 years was lower with total body irradiation (0.02 vs 0.09; P = .02).
A per-protocol analysis showed the 2-year overall survival to be the same in the two chemotherapy groups (both 0.77 ± 0.05) compared with 0.91 ± 0.02 in the total body irradiation group (P = .003).
“In this cohort [the 91% overall survival rate] may even be lower than contemporary intensive frontline therapy results that are achieved nowadays,” Dr. Peters said.
In looking at subgroups, there were no significant differences according to age group or cancer phenotype, while MLL rearrangement was associated with higher relapse incidence.
Remission status was found to notably influence EFS, dropping from 0.91 in CR1 patients with total body irradiation to 0.76 in CR2 patients. However, total body irradiation remained significantly higher compared with the chemo-conditioning groups in CR1 (P = .004) and CR2 (P < .001).
Transplant-related mortality was not significantly different between the total body irradiation and chemo-conditioning groups in the CR1 or CR2 groups (P = .09 and P = .18, respectively), despite the significant difference when remission status was not included.
Overall, “we tried to identify subgroups in which total body irradiation might be eliminated, however in all analyses, total body irradiation was better than chemo-conditioning in all arms,” Dr. Peters said.
Meanwhile, the findings underscore that even when patients cannot receive total body irradiation, the alternative chemo-conditioning therapy in fact shows favorable efficacy on its own, Dr. Izraeli said.
“The prognosis of the chemotherapy group is also quite remarkably good, although less than the total body irradiation arm. This means that if for some reason total body irradiation cannot be given, the chemotherapy is a very reasonable alternative.”
Dr. Peters has reported relationships with Amgen, Novartis, Pfizer, Medac, Jazz, and Neovii. Dr. Izraeli has reported no relevant financial relationships.
SOURCE: EHA Congress. Abstract S102.
A version of this article originally appeared on Medscape.com.
Hematopoietic stem cell transplantation (HSCT) may offer the chance of a cure for patients with leukemia and other blood cancers, but the process of preparing the body to receive such a transplant can be brutal, involving whole body irradiation as well as chemotherapy conditioning. New results show that both steps are needed: a trial that omitted whole body irradiation in young patients with acute lymphoblastic leukemia (ALL) was stopped early because of significantly poorer outcomes.
The multicenter, global FORUM (For Omitting Radiation Under Majority Age) trial involved 75 centers in 17 countries between 2013 and 2018.
“Our study shows significantly better outcomes for total body irradiation compared to myeloablative chemo-conditioning arms, with no differences between the [two] chemo-conditioning groups,” concluded Christina Peters, MD, professor of pediatrics in the department of stem cell transplantation at St Anna Children’s Hospital in Vienna.
, she added.
Dr. Peters presented the findings as part of the virtual annual congress of the European Hematology Association.
Describing the results as “sobering,” session comoderator Shai Izraeli, MD, director of the department of hematology-oncology at Schneider Children’s Medical Center, in Petah Tikva, Israel, said an online comment from the virtual meeting audience reflected the reaction to these unwelcome results: “So we are still stuck with total body irradiation?”
Dr. Peters said the good news is that the number of patients needing to undergo stem cell transplants is low, and with research advances, may hopefully drop even further.
“Only 10% of patients under the age of 18 nowadays undergo allogeneic HSCT, and perhaps in the future that will become even less if we are able to rescue some of the groups with other immunological measures such as CAR-T cells and antibodies,” she said.
“I think it is very important to better identify those who really need total body irradiation in the future,” she added.
In an interview, Dr. Izraeli agreed.
“The prognosis of children after bone marrow transplantation is excellent – the majority are cured from their leukemia,” he said. “And we have to remember that those who undergo bone marrow transplant have the worst leukemias.”
He pointed out that, in fact, contemporary chemotherapy alone is effective in the treatment of more than 90% of patients with ALL younger than aged 18.
For the 10% of patients who do not respond to chemotherapy alone and undergo allogeneic HSCT, about 50%-80% of pediatric patients who have resistant leukemia are cured. However, the total body irradiation used to prepare the body to receive the transplant is linked to potentially serious consequences later in life, including sterility, lung problems, growth retardation, and secondary cancer.
To determine if the irradiation component could be safely replaced with a chemotherapy-based conditioning approach, Dr. Peters and colleagues conducted the FORUM trial.
In total 413 patients undergoing HSCT were enrolled and randomized to pretransplant conditioning with total body irradiation and etoposide (n = 202) or a chemotherapy-only approach with fludarabine/thiotepa/busulfan (flu/thio/bu; n = 99) or fludarabine/thiotepa/treosulfan (treo; n = 93).
Most patients (72%) had B-cell precursor ALL and 23% had T-cell ALL. Just over half (54%) were transplanted in first complete remission (CR1), 40% in CR2, and 4% in CR3.
The source of stem cells was bone marrow for most patients (82%); peripheral blood stem cell for 12%, and cord blood for 4%.
Study stopped early
The aim of the study was to demonstrate noninferiority with the chemotherapy approach.
However, the significantly inferior outcome observed in the chemotherapy-only group led to randomization being halted in March 2019.
The 2-year overall survival in the intent-to-treat (ITT) analysis, with a mean observation time of 2.1 years, was 0.75 ± 0.04 for chemo-conditioning versus 0.91 ± 0.02 for total body irradiation/etoposide (ITT P < .001).
The ITT analysis showed relapses were significantly higher in the chemo-conditioning group (2-year cumulative incidence of relapse [CIR], 0.33) compared with the total body irradiation group (CIR, 0.12; P < .001).
The 2-year event-free survival (EFS) rate was also significantly higher in the total body irradiation group (0.86 vs 0.58; P < .001), and transplant-related mortality over 2 years was lower with total body irradiation (0.02 vs 0.09; P = .02).
A per-protocol analysis showed the 2-year overall survival to be the same in the two chemotherapy groups (both 0.77 ± 0.05) compared with 0.91 ± 0.02 in the total body irradiation group (P = .003).
“In this cohort [the 91% overall survival rate] may even be lower than contemporary intensive frontline therapy results that are achieved nowadays,” Dr. Peters said.
In looking at subgroups, there were no significant differences according to age group or cancer phenotype, while MLL rearrangement was associated with higher relapse incidence.
Remission status was found to notably influence EFS, dropping from 0.91 in CR1 patients with total body irradiation to 0.76 in CR2 patients. However, total body irradiation remained significantly higher compared with the chemo-conditioning groups in CR1 (P = .004) and CR2 (P < .001).
Transplant-related mortality was not significantly different between the total body irradiation and chemo-conditioning groups in the CR1 or CR2 groups (P = .09 and P = .18, respectively), despite the significant difference when remission status was not included.
Overall, “we tried to identify subgroups in which total body irradiation might be eliminated, however in all analyses, total body irradiation was better than chemo-conditioning in all arms,” Dr. Peters said.
Meanwhile, the findings underscore that even when patients cannot receive total body irradiation, the alternative chemo-conditioning therapy in fact shows favorable efficacy on its own, Dr. Izraeli said.
“The prognosis of the chemotherapy group is also quite remarkably good, although less than the total body irradiation arm. This means that if for some reason total body irradiation cannot be given, the chemotherapy is a very reasonable alternative.”
Dr. Peters has reported relationships with Amgen, Novartis, Pfizer, Medac, Jazz, and Neovii. Dr. Izraeli has reported no relevant financial relationships.
SOURCE: EHA Congress. Abstract S102.
A version of this article originally appeared on Medscape.com.
FROM EHA CONGRESS
Lurbinectedin approved for metastatic SCLC
Patients with metastatic small-cell lung cancer (SCLC) whose disease has progressed after or during treatment with platinum-based chemotherapy now have a new option to try — lurbinectedin (Zepzelca, Jazz Pharma/PharmaMar).
The drug was granted accelerated approval by the US Food and Drug Administration (FDA) based on response data. Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trial, the FDA notes.
“Small-cell lung cancer is a disease with limited treatment options,” said Bruce Cozadd, chairman and CEO of Jazz Pharmaceuticals. “While patients may initially respond to traditional chemotherapy, they often experience an aggressive recurrence that is historically resistant to treatment.”
“Seeing first-hand the aggressive nature of SCLC and knowing that the large majority of those diagnosed will experience relapse, I am excited to see an effective new treatment demonstrating durable responses,” Jeff Petty, MD, oncology specialist, Wake Forest Baptist Health, Winston-Salem, North Carolina, commented in the company press release. This new drug “is an important and much-needed addition to the treatment landscape for relapsing SCLC,” he added.
Approval based on monotherapy trial
The approval is based on a monotherapy clinical trial in 105 patients, which was published in May in Lancet Oncology, with first author José Trigo, MD, from the Hospital Universitario Virgen de la Victoria in Malaga, Spain.
These were adult patients with both platinum-sensitive and platinum-resistant SCLC who had disease progression after treatment with platinum-based chemotherapy. They were treated at 26 hospitals across six European countries and the US. All patients received lurbinectedin at 3.2 mg/m2 by intravenous infusion over 1 hour. Median follow-up was 17.1 months.
Overall response by investigator assessment was seen in 37 (35.2%) of the 105 patients. The response was greater (at 45%) among the patients with platinum-sensitive disease and smaller (22.2%) among those with platinum-resistant disease.
Lurbinectedin demonstrated a median duration of response of 5.3 months as measured by investigator assessment.
In a post-hoc analysis, among the 37 patients who had an initial objective response, the median overall survival was just over 1 year (12.6 months). It was even longer among patients who had platinum-sensitive disease (15.8 months), although it was shorter in patients with resistant disease (10.9 months).
These data are “particularly encouraging,” comment the authors of an accompanying editorial, led by Oscar Arrieta, MD, from the Thoracic Oncology Unit at the Instituto Nacional de Cancerología in Mexico City, Mexico. These response rates “outperform all previous results achieved with topotecan and other less established treatment schemes including cyclophosphamide, doxorubicin, and vincristine, or platinum re-challenge, in this setting.”
“Lurbinectedin represents an innovative approach to conventional anti-cancer drugs, with an elegant mechanism of action based on the inhibition of transcription-dependent replication stress and genome instability of tumor cells,” the editorialists comment. “The drug binds to specific DNA triplets commonly found in transcription sites and triggers cellular apoptosis.”
“At present, the only evidence-based second-line treatment approved for SCLC is topotecan, a topoisomerase 1 inhibitor with moderate activity in patients with sensitive disease, although its effect is much less evident in patients with resistant SCLC,” they continue.
“Overall, the study by Trigo and colleagues presents novel data for a very challenging disease for which few treatment options exist, and the data on response and survival do seem to outperform data from historical controls,” Arrieta and colleagues write.
The editorialists also note that, in this trial, a few patients had received immunotherapy as part of their first-line treatment, and some of these patients (5 of 8 patients, 68%) had “an outstanding rate of durable response to lurbinectedin.” This raises the possibility of a synergistic effect between immunotherapy and lurbinectedin, as the combination seems to enhance immune memory and impair subsequent tumor growth, they add. Further trials will need to explore sequencing of therapy, they suggest.
A large phase 3 study known as ATLANTIS is currently underway.
The most common grade 3-4 adverse events in the present trial were hematologic abnormalities: anemia (9% of patients), leukopenia (29%), neutropenia (46%), and thrombocytopenia (7%). Serious treatment-related adverse events occurred in 10% of patients, of which neutropenia and febrile neutropenia were the most common (5% each). No treatment-related deaths were reported.
The study was funded by PharmaMar. Trigo and coauthors, and Arrieta and fellow editorialists, all report relationships with pharmaceutical companies, as detailed in the published articles.
This article first appeared on Medscape.com.
Patients with metastatic small-cell lung cancer (SCLC) whose disease has progressed after or during treatment with platinum-based chemotherapy now have a new option to try — lurbinectedin (Zepzelca, Jazz Pharma/PharmaMar).
The drug was granted accelerated approval by the US Food and Drug Administration (FDA) based on response data. Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trial, the FDA notes.
“Small-cell lung cancer is a disease with limited treatment options,” said Bruce Cozadd, chairman and CEO of Jazz Pharmaceuticals. “While patients may initially respond to traditional chemotherapy, they often experience an aggressive recurrence that is historically resistant to treatment.”
“Seeing first-hand the aggressive nature of SCLC and knowing that the large majority of those diagnosed will experience relapse, I am excited to see an effective new treatment demonstrating durable responses,” Jeff Petty, MD, oncology specialist, Wake Forest Baptist Health, Winston-Salem, North Carolina, commented in the company press release. This new drug “is an important and much-needed addition to the treatment landscape for relapsing SCLC,” he added.
Approval based on monotherapy trial
The approval is based on a monotherapy clinical trial in 105 patients, which was published in May in Lancet Oncology, with first author José Trigo, MD, from the Hospital Universitario Virgen de la Victoria in Malaga, Spain.
These were adult patients with both platinum-sensitive and platinum-resistant SCLC who had disease progression after treatment with platinum-based chemotherapy. They were treated at 26 hospitals across six European countries and the US. All patients received lurbinectedin at 3.2 mg/m2 by intravenous infusion over 1 hour. Median follow-up was 17.1 months.
Overall response by investigator assessment was seen in 37 (35.2%) of the 105 patients. The response was greater (at 45%) among the patients with platinum-sensitive disease and smaller (22.2%) among those with platinum-resistant disease.
Lurbinectedin demonstrated a median duration of response of 5.3 months as measured by investigator assessment.
In a post-hoc analysis, among the 37 patients who had an initial objective response, the median overall survival was just over 1 year (12.6 months). It was even longer among patients who had platinum-sensitive disease (15.8 months), although it was shorter in patients with resistant disease (10.9 months).
These data are “particularly encouraging,” comment the authors of an accompanying editorial, led by Oscar Arrieta, MD, from the Thoracic Oncology Unit at the Instituto Nacional de Cancerología in Mexico City, Mexico. These response rates “outperform all previous results achieved with topotecan and other less established treatment schemes including cyclophosphamide, doxorubicin, and vincristine, or platinum re-challenge, in this setting.”
“Lurbinectedin represents an innovative approach to conventional anti-cancer drugs, with an elegant mechanism of action based on the inhibition of transcription-dependent replication stress and genome instability of tumor cells,” the editorialists comment. “The drug binds to specific DNA triplets commonly found in transcription sites and triggers cellular apoptosis.”
“At present, the only evidence-based second-line treatment approved for SCLC is topotecan, a topoisomerase 1 inhibitor with moderate activity in patients with sensitive disease, although its effect is much less evident in patients with resistant SCLC,” they continue.
“Overall, the study by Trigo and colleagues presents novel data for a very challenging disease for which few treatment options exist, and the data on response and survival do seem to outperform data from historical controls,” Arrieta and colleagues write.
The editorialists also note that, in this trial, a few patients had received immunotherapy as part of their first-line treatment, and some of these patients (5 of 8 patients, 68%) had “an outstanding rate of durable response to lurbinectedin.” This raises the possibility of a synergistic effect between immunotherapy and lurbinectedin, as the combination seems to enhance immune memory and impair subsequent tumor growth, they add. Further trials will need to explore sequencing of therapy, they suggest.
A large phase 3 study known as ATLANTIS is currently underway.
The most common grade 3-4 adverse events in the present trial were hematologic abnormalities: anemia (9% of patients), leukopenia (29%), neutropenia (46%), and thrombocytopenia (7%). Serious treatment-related adverse events occurred in 10% of patients, of which neutropenia and febrile neutropenia were the most common (5% each). No treatment-related deaths were reported.
The study was funded by PharmaMar. Trigo and coauthors, and Arrieta and fellow editorialists, all report relationships with pharmaceutical companies, as detailed in the published articles.
This article first appeared on Medscape.com.
Patients with metastatic small-cell lung cancer (SCLC) whose disease has progressed after or during treatment with platinum-based chemotherapy now have a new option to try — lurbinectedin (Zepzelca, Jazz Pharma/PharmaMar).
The drug was granted accelerated approval by the US Food and Drug Administration (FDA) based on response data. Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory trial, the FDA notes.
“Small-cell lung cancer is a disease with limited treatment options,” said Bruce Cozadd, chairman and CEO of Jazz Pharmaceuticals. “While patients may initially respond to traditional chemotherapy, they often experience an aggressive recurrence that is historically resistant to treatment.”
“Seeing first-hand the aggressive nature of SCLC and knowing that the large majority of those diagnosed will experience relapse, I am excited to see an effective new treatment demonstrating durable responses,” Jeff Petty, MD, oncology specialist, Wake Forest Baptist Health, Winston-Salem, North Carolina, commented in the company press release. This new drug “is an important and much-needed addition to the treatment landscape for relapsing SCLC,” he added.
Approval based on monotherapy trial
The approval is based on a monotherapy clinical trial in 105 patients, which was published in May in Lancet Oncology, with first author José Trigo, MD, from the Hospital Universitario Virgen de la Victoria in Malaga, Spain.
These were adult patients with both platinum-sensitive and platinum-resistant SCLC who had disease progression after treatment with platinum-based chemotherapy. They were treated at 26 hospitals across six European countries and the US. All patients received lurbinectedin at 3.2 mg/m2 by intravenous infusion over 1 hour. Median follow-up was 17.1 months.
Overall response by investigator assessment was seen in 37 (35.2%) of the 105 patients. The response was greater (at 45%) among the patients with platinum-sensitive disease and smaller (22.2%) among those with platinum-resistant disease.
Lurbinectedin demonstrated a median duration of response of 5.3 months as measured by investigator assessment.
In a post-hoc analysis, among the 37 patients who had an initial objective response, the median overall survival was just over 1 year (12.6 months). It was even longer among patients who had platinum-sensitive disease (15.8 months), although it was shorter in patients with resistant disease (10.9 months).
These data are “particularly encouraging,” comment the authors of an accompanying editorial, led by Oscar Arrieta, MD, from the Thoracic Oncology Unit at the Instituto Nacional de Cancerología in Mexico City, Mexico. These response rates “outperform all previous results achieved with topotecan and other less established treatment schemes including cyclophosphamide, doxorubicin, and vincristine, or platinum re-challenge, in this setting.”
“Lurbinectedin represents an innovative approach to conventional anti-cancer drugs, with an elegant mechanism of action based on the inhibition of transcription-dependent replication stress and genome instability of tumor cells,” the editorialists comment. “The drug binds to specific DNA triplets commonly found in transcription sites and triggers cellular apoptosis.”
“At present, the only evidence-based second-line treatment approved for SCLC is topotecan, a topoisomerase 1 inhibitor with moderate activity in patients with sensitive disease, although its effect is much less evident in patients with resistant SCLC,” they continue.
“Overall, the study by Trigo and colleagues presents novel data for a very challenging disease for which few treatment options exist, and the data on response and survival do seem to outperform data from historical controls,” Arrieta and colleagues write.
The editorialists also note that, in this trial, a few patients had received immunotherapy as part of their first-line treatment, and some of these patients (5 of 8 patients, 68%) had “an outstanding rate of durable response to lurbinectedin.” This raises the possibility of a synergistic effect between immunotherapy and lurbinectedin, as the combination seems to enhance immune memory and impair subsequent tumor growth, they add. Further trials will need to explore sequencing of therapy, they suggest.
A large phase 3 study known as ATLANTIS is currently underway.
The most common grade 3-4 adverse events in the present trial were hematologic abnormalities: anemia (9% of patients), leukopenia (29%), neutropenia (46%), and thrombocytopenia (7%). Serious treatment-related adverse events occurred in 10% of patients, of which neutropenia and febrile neutropenia were the most common (5% each). No treatment-related deaths were reported.
The study was funded by PharmaMar. Trigo and coauthors, and Arrieta and fellow editorialists, all report relationships with pharmaceutical companies, as detailed in the published articles.
This article first appeared on Medscape.com.
Health experts link rise in Arizona COVID cases to end of stay-at-home order
With new daily coronavirus cases rising in at least two dozen states,
Arizona has emerged as one of the country’s newest coronavirus hot spots, with the weekly average of daily cases more than doubling from 2 weeks ago. The total number of people hospitalized is climbing, too.
Over the past week, Arizona has seen an average of more than 1,300 new COVID-19 cases each day.
After the state’s largest hospital system warned about a shortage of ICU beds, Arizona Gov. Doug Ducey, a Republican, pushed back on claims that the health care system could soon be overwhelmed.
“The entire time we’ve been focused on a possible worst-case scenario with surge capacity for hospital beds, ICU beds and ventilators,” Ducey told reporters on Thursday. “Those are not needed or necessary right now.”
While he acknowledged a spike in positive cases, Ducey said a second stay-at-home order was “not under discussion.”
“We put the stay-at-home order there so we could prepare for what we are going through,” he said.
Some states have reopened more slowly with a set of specific benchmarks for different regions, but Arizona took a more aggressive approach.
The state began easing restrictions on businesses in early May and lifted its statewide lockdown order after May 15. Under Arizona’s reopening plan, businesses are advised to follow federal guidance on social distancing.
There is also no requirement for everyone to wear masks in public.
Public health experts agree: The timing of this spike reflects the state’s reopening.
“Perhaps, Arizona will be a warning sign to other areas,” said Katherine Ellingson, an epidemiologist at the University of Arizona. “We never had that consistent downward trend that would signal it’s time to reopen and we have everything in place to do it safely.”
Before Arizona lifted its stay-at-home order, only about 5% of COVID-19 tests registered as positive. On Monday, that number was around 16%.
A slower reopening gives public health agencies time to identify whether cases are rising and then respond with contact tracing and isolating those who are infected.
“With a fast, rapid reopening, we don’t have the time to mobilize those resources,” said Ellingson.
Maricopa County, home to about 60% of the state’s population, has ramped up contact tracing in recent weeks, but it may not have enough capacity if the surge in cases continues.
Dr. Peter Hotez said the spike in Arizona, as well as in parts of Texas such as Houston, Dallas and Austin, is the consequence of removing restrictions too quickly and without a public health system that can keep pace.
“It was just ‘open it up’ and then more or less business as usual, with a little bit of window dressing,” said Hotez, the dean for the National School of Tropical Medicine at Baylor College of Medicine in Houston. “This is not an abstract number of cases. We’re seeing people pile into intensive care units.”
Arizona’s governor has also faced criticism from the mayors of Arizona’s two biggest cities for not putting in place more stringent requirements.
“There is a pandemic and it’s spreading uncontrollably,” said Tucson Mayor Regina Romero, a Democrat. Ducey, she said, “is just putting up his hands and saying ‘the spread is happening and we just have to go about our business.’”
And the governor’s executive order forbids local governments from implementing their own extra measures, which adds to Romero’s frustration. Texas has a similar measure.
“What he did was pretty much tie the hands of mayors and public health officials,” Romero said.
Arizona’s hospital industry has tried to tamp down fears that it’s on the verge of a crisis. Hospitals are still performing elective surgeries.
“It’s very unfortunate because hospitals right now in Arizona are quite busy with elective procedures,” said Saskia Popescu, a Phoenix-based epidemiologist with George Mason University. “You throw in increasing cases of COVID, and that’s going to very much stress your hospital systems.”
Phoenix’s triple-digit summer temperatures actually may fuel the spread of the virus. People forgo outdoor activities and retreat to air-conditioned indoor spaces, where the risk of transmitting the virus goes up significantly.
“My concern is we’re going to see a lot more people in close quarters for prolonged periods of time,” Popescu said.
Since the stay-at-home order was lifted, Popescu and others say they’ve seen people returning to a pre-pandemic mindset, neglecting to wear masks or maintain social distance. Videos of crowded bars have only propelled these fears.
On Thursday, however, Arizona’s top doctor stressed there were also dangers to keeping the state on lockdown, including the mental health effects of loneliness and isolation.
“We know that it’s in the community. We are not going to be able to stop the spread. And so we can’t stop living as well,” said Dr. Cara Christ, health director for the Arizona Department of Health Services.
But Dr. Quinn Snyder, an emergency medicine physician in Mesa, Arizona, said there needs to be more consistent messaging on public health measures like wearing masks.
“Frankly, I just think a wholesale reevaluation of where we’re at is critical right now, but I can tell you that we’re not doing nearly enough,” said Snyder, who has seen the uptick in seriously ill COVID-19 patients firsthand.
“If we continue to head down this path, the virus will press our health care facilities beyond capacity, where we’re going to have to be making tough decisions like who gets a ventilator and who doesn’t.”
A version of this article originally appeared on Kaiser Health News, which is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
With new daily coronavirus cases rising in at least two dozen states,
Arizona has emerged as one of the country’s newest coronavirus hot spots, with the weekly average of daily cases more than doubling from 2 weeks ago. The total number of people hospitalized is climbing, too.
Over the past week, Arizona has seen an average of more than 1,300 new COVID-19 cases each day.
After the state’s largest hospital system warned about a shortage of ICU beds, Arizona Gov. Doug Ducey, a Republican, pushed back on claims that the health care system could soon be overwhelmed.
“The entire time we’ve been focused on a possible worst-case scenario with surge capacity for hospital beds, ICU beds and ventilators,” Ducey told reporters on Thursday. “Those are not needed or necessary right now.”
While he acknowledged a spike in positive cases, Ducey said a second stay-at-home order was “not under discussion.”
“We put the stay-at-home order there so we could prepare for what we are going through,” he said.
Some states have reopened more slowly with a set of specific benchmarks for different regions, but Arizona took a more aggressive approach.
The state began easing restrictions on businesses in early May and lifted its statewide lockdown order after May 15. Under Arizona’s reopening plan, businesses are advised to follow federal guidance on social distancing.
There is also no requirement for everyone to wear masks in public.
Public health experts agree: The timing of this spike reflects the state’s reopening.
“Perhaps, Arizona will be a warning sign to other areas,” said Katherine Ellingson, an epidemiologist at the University of Arizona. “We never had that consistent downward trend that would signal it’s time to reopen and we have everything in place to do it safely.”
Before Arizona lifted its stay-at-home order, only about 5% of COVID-19 tests registered as positive. On Monday, that number was around 16%.
A slower reopening gives public health agencies time to identify whether cases are rising and then respond with contact tracing and isolating those who are infected.
“With a fast, rapid reopening, we don’t have the time to mobilize those resources,” said Ellingson.
Maricopa County, home to about 60% of the state’s population, has ramped up contact tracing in recent weeks, but it may not have enough capacity if the surge in cases continues.
Dr. Peter Hotez said the spike in Arizona, as well as in parts of Texas such as Houston, Dallas and Austin, is the consequence of removing restrictions too quickly and without a public health system that can keep pace.
“It was just ‘open it up’ and then more or less business as usual, with a little bit of window dressing,” said Hotez, the dean for the National School of Tropical Medicine at Baylor College of Medicine in Houston. “This is not an abstract number of cases. We’re seeing people pile into intensive care units.”
Arizona’s governor has also faced criticism from the mayors of Arizona’s two biggest cities for not putting in place more stringent requirements.
“There is a pandemic and it’s spreading uncontrollably,” said Tucson Mayor Regina Romero, a Democrat. Ducey, she said, “is just putting up his hands and saying ‘the spread is happening and we just have to go about our business.’”
And the governor’s executive order forbids local governments from implementing their own extra measures, which adds to Romero’s frustration. Texas has a similar measure.
“What he did was pretty much tie the hands of mayors and public health officials,” Romero said.
Arizona’s hospital industry has tried to tamp down fears that it’s on the verge of a crisis. Hospitals are still performing elective surgeries.
“It’s very unfortunate because hospitals right now in Arizona are quite busy with elective procedures,” said Saskia Popescu, a Phoenix-based epidemiologist with George Mason University. “You throw in increasing cases of COVID, and that’s going to very much stress your hospital systems.”
Phoenix’s triple-digit summer temperatures actually may fuel the spread of the virus. People forgo outdoor activities and retreat to air-conditioned indoor spaces, where the risk of transmitting the virus goes up significantly.
“My concern is we’re going to see a lot more people in close quarters for prolonged periods of time,” Popescu said.
Since the stay-at-home order was lifted, Popescu and others say they’ve seen people returning to a pre-pandemic mindset, neglecting to wear masks or maintain social distance. Videos of crowded bars have only propelled these fears.
On Thursday, however, Arizona’s top doctor stressed there were also dangers to keeping the state on lockdown, including the mental health effects of loneliness and isolation.
“We know that it’s in the community. We are not going to be able to stop the spread. And so we can’t stop living as well,” said Dr. Cara Christ, health director for the Arizona Department of Health Services.
But Dr. Quinn Snyder, an emergency medicine physician in Mesa, Arizona, said there needs to be more consistent messaging on public health measures like wearing masks.
“Frankly, I just think a wholesale reevaluation of where we’re at is critical right now, but I can tell you that we’re not doing nearly enough,” said Snyder, who has seen the uptick in seriously ill COVID-19 patients firsthand.
“If we continue to head down this path, the virus will press our health care facilities beyond capacity, where we’re going to have to be making tough decisions like who gets a ventilator and who doesn’t.”
A version of this article originally appeared on Kaiser Health News, which is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
With new daily coronavirus cases rising in at least two dozen states,
Arizona has emerged as one of the country’s newest coronavirus hot spots, with the weekly average of daily cases more than doubling from 2 weeks ago. The total number of people hospitalized is climbing, too.
Over the past week, Arizona has seen an average of more than 1,300 new COVID-19 cases each day.
After the state’s largest hospital system warned about a shortage of ICU beds, Arizona Gov. Doug Ducey, a Republican, pushed back on claims that the health care system could soon be overwhelmed.
“The entire time we’ve been focused on a possible worst-case scenario with surge capacity for hospital beds, ICU beds and ventilators,” Ducey told reporters on Thursday. “Those are not needed or necessary right now.”
While he acknowledged a spike in positive cases, Ducey said a second stay-at-home order was “not under discussion.”
“We put the stay-at-home order there so we could prepare for what we are going through,” he said.
Some states have reopened more slowly with a set of specific benchmarks for different regions, but Arizona took a more aggressive approach.
The state began easing restrictions on businesses in early May and lifted its statewide lockdown order after May 15. Under Arizona’s reopening plan, businesses are advised to follow federal guidance on social distancing.
There is also no requirement for everyone to wear masks in public.
Public health experts agree: The timing of this spike reflects the state’s reopening.
“Perhaps, Arizona will be a warning sign to other areas,” said Katherine Ellingson, an epidemiologist at the University of Arizona. “We never had that consistent downward trend that would signal it’s time to reopen and we have everything in place to do it safely.”
Before Arizona lifted its stay-at-home order, only about 5% of COVID-19 tests registered as positive. On Monday, that number was around 16%.
A slower reopening gives public health agencies time to identify whether cases are rising and then respond with contact tracing and isolating those who are infected.
“With a fast, rapid reopening, we don’t have the time to mobilize those resources,” said Ellingson.
Maricopa County, home to about 60% of the state’s population, has ramped up contact tracing in recent weeks, but it may not have enough capacity if the surge in cases continues.
Dr. Peter Hotez said the spike in Arizona, as well as in parts of Texas such as Houston, Dallas and Austin, is the consequence of removing restrictions too quickly and without a public health system that can keep pace.
“It was just ‘open it up’ and then more or less business as usual, with a little bit of window dressing,” said Hotez, the dean for the National School of Tropical Medicine at Baylor College of Medicine in Houston. “This is not an abstract number of cases. We’re seeing people pile into intensive care units.”
Arizona’s governor has also faced criticism from the mayors of Arizona’s two biggest cities for not putting in place more stringent requirements.
“There is a pandemic and it’s spreading uncontrollably,” said Tucson Mayor Regina Romero, a Democrat. Ducey, she said, “is just putting up his hands and saying ‘the spread is happening and we just have to go about our business.’”
And the governor’s executive order forbids local governments from implementing their own extra measures, which adds to Romero’s frustration. Texas has a similar measure.
“What he did was pretty much tie the hands of mayors and public health officials,” Romero said.
Arizona’s hospital industry has tried to tamp down fears that it’s on the verge of a crisis. Hospitals are still performing elective surgeries.
“It’s very unfortunate because hospitals right now in Arizona are quite busy with elective procedures,” said Saskia Popescu, a Phoenix-based epidemiologist with George Mason University. “You throw in increasing cases of COVID, and that’s going to very much stress your hospital systems.”
Phoenix’s triple-digit summer temperatures actually may fuel the spread of the virus. People forgo outdoor activities and retreat to air-conditioned indoor spaces, where the risk of transmitting the virus goes up significantly.
“My concern is we’re going to see a lot more people in close quarters for prolonged periods of time,” Popescu said.
Since the stay-at-home order was lifted, Popescu and others say they’ve seen people returning to a pre-pandemic mindset, neglecting to wear masks or maintain social distance. Videos of crowded bars have only propelled these fears.
On Thursday, however, Arizona’s top doctor stressed there were also dangers to keeping the state on lockdown, including the mental health effects of loneliness and isolation.
“We know that it’s in the community. We are not going to be able to stop the spread. And so we can’t stop living as well,” said Dr. Cara Christ, health director for the Arizona Department of Health Services.
But Dr. Quinn Snyder, an emergency medicine physician in Mesa, Arizona, said there needs to be more consistent messaging on public health measures like wearing masks.
“Frankly, I just think a wholesale reevaluation of where we’re at is critical right now, but I can tell you that we’re not doing nearly enough,” said Snyder, who has seen the uptick in seriously ill COVID-19 patients firsthand.
“If we continue to head down this path, the virus will press our health care facilities beyond capacity, where we’re going to have to be making tough decisions like who gets a ventilator and who doesn’t.”
A version of this article originally appeared on Kaiser Health News, which is a nonprofit national health policy news service. It is an editorially independent program of the Henry J. Kaiser Family Foundation that is not affiliated with Kaiser Permanente.
CAC scoring pinpoints stenoses in asymptomatic diabetes patients
For diabetes patients with no cardiovascular symptoms despite certain risk factors, incorporating coronary calcium scoring into a silent myocardial ischemia screening algorithm may be an effective and cost-conscious strategy that avoids missed coronary stenoses suitable for revascularization, results of a recent study suggest.
Zero patients in need of revascularization were missed in a risk stratification model in which screening for silent myocardial ischemia (SMI) was done only for patients with peripheral artery disease, severe nephropathy, or a high coronary artery calcium (CAC) score, according to investigator Paul Valensi, MD.
In practical terms, that means stress myocardial scintigraphy to detect SMI could be reserved for patients with evidence of target organ damage or a CAC score of 100 or higher, according to Dr. Valensi, head of the department of endocrinology, diabetology, and nutrition at Jean Verdier Hospital in Bondy, France.
“The strategy appears to be a good compromise, and the most cost effective strategy,” Dr. Valensi said in a presentation of the results at the virtual annual scientific sessions of the American Diabetes Association.
Utility of CAC scoring in diabetes
This algorithm proposed by Dr. Valenti and colleagues is a “reasonable” approach to guide risk stratification in asymptomatic diabetes patients, said Matthew J. Budoff, MD, professor of medicine and director of cardiac CT at Harbor-UCLA Medical Center in Torrance, Calif.
“Calcium scoring could certainly help you identify those patients (at increased risk) as a first-line test, because if their calcium score is zero, their chance of having obstructive disease is probably either zero or very close to zero,” Dr. Budoff said in an interview.
Using CAC scores to assess cardiovascular risk in asymptomatic adults with diabetes was supported by 2010 guidelines from the American College of Cardiology and the American Heart Association, Dr. Budoff said, while 2019 guidelines from the European Society of Cardiology (ESC) describe CAC score combined with CT as a potential risk modifier in the evaluation of certain asymptomatic patients with diabetes.
“We are starting to see that we might be able to understand diabetes better and the cardiovascular implications by understanding how much plaque (patients) have at the time that we see them,” Dr. Budoff said in a presentation on use of CAC scans he gave earlier at the virtual ADA meeting.
In the interview, Dr. Budoff also noted that CAC scores may be particularly useful for guiding use of statins, PCSK9 (proprotein convertase subtilisin kexin 9) inhibitors, or other treatments in patients with diabetes: “There are a lot of therapies that we can apply, if we knew somebody was at higher risk, that would potentially help them avoid a heart attack, stroke, or cardiovascular death,” he said.
CAC scoring and coronary artery stenoses
Although about 20% of patients with type 2 diabetes have SMI, screening for it is “debated,” according to Dr. Valensi.
The recent ESC guidelines state that while routine screening for coronary artery disease in asymptomatic diabetics is not recommended, stress testing or coronary angiography “may be indicated” in asymptomatic diabetics in the very-high cardiovascular risk category.
That position is based on a lack of benefit seen with a broad screening strategy, the guidelines say, possibly due in part to low event rates in randomized controlled trials that have studied the approach.
Using CAC scoring could change the equation by helping to identify a greater proportion of type 2 diabetics with SMI, according to Dr. Valensi.
“The role of the CAC score in the strategy of detection of SMI needs to be defined, and this role may depend on the a priori cardiovascular risk,” he said.
Dr. Valensi and colleagues accordingly tested several different approaches to selecting asymptomatic diabetic patients for SMI screening to see how they would perform in finding patients with coronary stenoses eligible for revascularization.
Their study included 416 diabetes patients with diabetes at very high cardiovascular risk but with no cardiac history or symptoms. A total of 40 patients (9.6%) had SMI, including 15 patients in which coronary stenoses were found; of those, 11 (73.5%) underwent a revascularization procedure.
They found that, by performing myocardial scintigraphy only in those patients with peripheral artery disease or severe nephropathy, they would have missed 6 patients with coronary stenosis suitable for revascularization among the 275 patients who did not meet those target organ damage criteria.
By contrast, zero patients would have been missed by performing myocardial scintigraphy in patients who either met those target organ damage criteria, or who had an elevated CAC score.
“We suggest screening for SMI, using stress myocardial CT scanning and coronary stenosis screening, only the patients with peripheral artery disease or severe nephropathy or with a high CAC score over 100 Agatston units,” said Dr. Valensi.
Dr. Valensi reported disclosures related to Merck Sharp Dohme, Novo Nordisk, Pierre Fabre, Eli Lilly, Bristol-Myers Squibb, AstraZeneca, Daiichi-Sankyo, and others. Coauthors provided no disclosures related to the research. Dr. Budoff reported that he has served as a paid consultant to GE.
SOURCE: Berkane N et al. ADA 2020. Abstract 8-OR.
For diabetes patients with no cardiovascular symptoms despite certain risk factors, incorporating coronary calcium scoring into a silent myocardial ischemia screening algorithm may be an effective and cost-conscious strategy that avoids missed coronary stenoses suitable for revascularization, results of a recent study suggest.
Zero patients in need of revascularization were missed in a risk stratification model in which screening for silent myocardial ischemia (SMI) was done only for patients with peripheral artery disease, severe nephropathy, or a high coronary artery calcium (CAC) score, according to investigator Paul Valensi, MD.
In practical terms, that means stress myocardial scintigraphy to detect SMI could be reserved for patients with evidence of target organ damage or a CAC score of 100 or higher, according to Dr. Valensi, head of the department of endocrinology, diabetology, and nutrition at Jean Verdier Hospital in Bondy, France.
“The strategy appears to be a good compromise, and the most cost effective strategy,” Dr. Valensi said in a presentation of the results at the virtual annual scientific sessions of the American Diabetes Association.
Utility of CAC scoring in diabetes
This algorithm proposed by Dr. Valenti and colleagues is a “reasonable” approach to guide risk stratification in asymptomatic diabetes patients, said Matthew J. Budoff, MD, professor of medicine and director of cardiac CT at Harbor-UCLA Medical Center in Torrance, Calif.
“Calcium scoring could certainly help you identify those patients (at increased risk) as a first-line test, because if their calcium score is zero, their chance of having obstructive disease is probably either zero or very close to zero,” Dr. Budoff said in an interview.
Using CAC scores to assess cardiovascular risk in asymptomatic adults with diabetes was supported by 2010 guidelines from the American College of Cardiology and the American Heart Association, Dr. Budoff said, while 2019 guidelines from the European Society of Cardiology (ESC) describe CAC score combined with CT as a potential risk modifier in the evaluation of certain asymptomatic patients with diabetes.
“We are starting to see that we might be able to understand diabetes better and the cardiovascular implications by understanding how much plaque (patients) have at the time that we see them,” Dr. Budoff said in a presentation on use of CAC scans he gave earlier at the virtual ADA meeting.
In the interview, Dr. Budoff also noted that CAC scores may be particularly useful for guiding use of statins, PCSK9 (proprotein convertase subtilisin kexin 9) inhibitors, or other treatments in patients with diabetes: “There are a lot of therapies that we can apply, if we knew somebody was at higher risk, that would potentially help them avoid a heart attack, stroke, or cardiovascular death,” he said.
CAC scoring and coronary artery stenoses
Although about 20% of patients with type 2 diabetes have SMI, screening for it is “debated,” according to Dr. Valensi.
The recent ESC guidelines state that while routine screening for coronary artery disease in asymptomatic diabetics is not recommended, stress testing or coronary angiography “may be indicated” in asymptomatic diabetics in the very-high cardiovascular risk category.
That position is based on a lack of benefit seen with a broad screening strategy, the guidelines say, possibly due in part to low event rates in randomized controlled trials that have studied the approach.
Using CAC scoring could change the equation by helping to identify a greater proportion of type 2 diabetics with SMI, according to Dr. Valensi.
“The role of the CAC score in the strategy of detection of SMI needs to be defined, and this role may depend on the a priori cardiovascular risk,” he said.
Dr. Valensi and colleagues accordingly tested several different approaches to selecting asymptomatic diabetic patients for SMI screening to see how they would perform in finding patients with coronary stenoses eligible for revascularization.
Their study included 416 diabetes patients with diabetes at very high cardiovascular risk but with no cardiac history or symptoms. A total of 40 patients (9.6%) had SMI, including 15 patients in which coronary stenoses were found; of those, 11 (73.5%) underwent a revascularization procedure.
They found that, by performing myocardial scintigraphy only in those patients with peripheral artery disease or severe nephropathy, they would have missed 6 patients with coronary stenosis suitable for revascularization among the 275 patients who did not meet those target organ damage criteria.
By contrast, zero patients would have been missed by performing myocardial scintigraphy in patients who either met those target organ damage criteria, or who had an elevated CAC score.
“We suggest screening for SMI, using stress myocardial CT scanning and coronary stenosis screening, only the patients with peripheral artery disease or severe nephropathy or with a high CAC score over 100 Agatston units,” said Dr. Valensi.
Dr. Valensi reported disclosures related to Merck Sharp Dohme, Novo Nordisk, Pierre Fabre, Eli Lilly, Bristol-Myers Squibb, AstraZeneca, Daiichi-Sankyo, and others. Coauthors provided no disclosures related to the research. Dr. Budoff reported that he has served as a paid consultant to GE.
SOURCE: Berkane N et al. ADA 2020. Abstract 8-OR.
For diabetes patients with no cardiovascular symptoms despite certain risk factors, incorporating coronary calcium scoring into a silent myocardial ischemia screening algorithm may be an effective and cost-conscious strategy that avoids missed coronary stenoses suitable for revascularization, results of a recent study suggest.
Zero patients in need of revascularization were missed in a risk stratification model in which screening for silent myocardial ischemia (SMI) was done only for patients with peripheral artery disease, severe nephropathy, or a high coronary artery calcium (CAC) score, according to investigator Paul Valensi, MD.
In practical terms, that means stress myocardial scintigraphy to detect SMI could be reserved for patients with evidence of target organ damage or a CAC score of 100 or higher, according to Dr. Valensi, head of the department of endocrinology, diabetology, and nutrition at Jean Verdier Hospital in Bondy, France.
“The strategy appears to be a good compromise, and the most cost effective strategy,” Dr. Valensi said in a presentation of the results at the virtual annual scientific sessions of the American Diabetes Association.
Utility of CAC scoring in diabetes
This algorithm proposed by Dr. Valenti and colleagues is a “reasonable” approach to guide risk stratification in asymptomatic diabetes patients, said Matthew J. Budoff, MD, professor of medicine and director of cardiac CT at Harbor-UCLA Medical Center in Torrance, Calif.
“Calcium scoring could certainly help you identify those patients (at increased risk) as a first-line test, because if their calcium score is zero, their chance of having obstructive disease is probably either zero or very close to zero,” Dr. Budoff said in an interview.
Using CAC scores to assess cardiovascular risk in asymptomatic adults with diabetes was supported by 2010 guidelines from the American College of Cardiology and the American Heart Association, Dr. Budoff said, while 2019 guidelines from the European Society of Cardiology (ESC) describe CAC score combined with CT as a potential risk modifier in the evaluation of certain asymptomatic patients with diabetes.
“We are starting to see that we might be able to understand diabetes better and the cardiovascular implications by understanding how much plaque (patients) have at the time that we see them,” Dr. Budoff said in a presentation on use of CAC scans he gave earlier at the virtual ADA meeting.
In the interview, Dr. Budoff also noted that CAC scores may be particularly useful for guiding use of statins, PCSK9 (proprotein convertase subtilisin kexin 9) inhibitors, or other treatments in patients with diabetes: “There are a lot of therapies that we can apply, if we knew somebody was at higher risk, that would potentially help them avoid a heart attack, stroke, or cardiovascular death,” he said.
CAC scoring and coronary artery stenoses
Although about 20% of patients with type 2 diabetes have SMI, screening for it is “debated,” according to Dr. Valensi.
The recent ESC guidelines state that while routine screening for coronary artery disease in asymptomatic diabetics is not recommended, stress testing or coronary angiography “may be indicated” in asymptomatic diabetics in the very-high cardiovascular risk category.
That position is based on a lack of benefit seen with a broad screening strategy, the guidelines say, possibly due in part to low event rates in randomized controlled trials that have studied the approach.
Using CAC scoring could change the equation by helping to identify a greater proportion of type 2 diabetics with SMI, according to Dr. Valensi.
“The role of the CAC score in the strategy of detection of SMI needs to be defined, and this role may depend on the a priori cardiovascular risk,” he said.
Dr. Valensi and colleagues accordingly tested several different approaches to selecting asymptomatic diabetic patients for SMI screening to see how they would perform in finding patients with coronary stenoses eligible for revascularization.
Their study included 416 diabetes patients with diabetes at very high cardiovascular risk but with no cardiac history or symptoms. A total of 40 patients (9.6%) had SMI, including 15 patients in which coronary stenoses were found; of those, 11 (73.5%) underwent a revascularization procedure.
They found that, by performing myocardial scintigraphy only in those patients with peripheral artery disease or severe nephropathy, they would have missed 6 patients with coronary stenosis suitable for revascularization among the 275 patients who did not meet those target organ damage criteria.
By contrast, zero patients would have been missed by performing myocardial scintigraphy in patients who either met those target organ damage criteria, or who had an elevated CAC score.
“We suggest screening for SMI, using stress myocardial CT scanning and coronary stenosis screening, only the patients with peripheral artery disease or severe nephropathy or with a high CAC score over 100 Agatston units,” said Dr. Valensi.
Dr. Valensi reported disclosures related to Merck Sharp Dohme, Novo Nordisk, Pierre Fabre, Eli Lilly, Bristol-Myers Squibb, AstraZeneca, Daiichi-Sankyo, and others. Coauthors provided no disclosures related to the research. Dr. Budoff reported that he has served as a paid consultant to GE.
SOURCE: Berkane N et al. ADA 2020. Abstract 8-OR.
FROM ADA 2020
Gardasil-9 approved for prevention of head and neck cancers
The US Food and Drug Administration (FDA) has expanded the indication for the Gardasil-9 (Merck) vaccine to include prevention of oropharyngeal and other head and neck cancers caused by HPV types 16, 18, 31, 33, 45, 52, and 58.
This new indication is approved under the FDA’s accelerated approval program and is based on the vaccine’s effectiveness in preventing HPV-related anogenital disease. Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory clinical trial, which is currently underway.
“At Merck, working to help prevent certain HPV-related cancers has been a priority for more than two decades,” Alain Luxembourg, MD, director, clinical research, Merck Research Laboratories, said in a statement. “Today’s approval for the prevention of HPV-related oropharyngeal and other head and neck cancers represents an important step in Merck’s mission to help reduce the number of men and women affected by certain HPV-related cancers.”
This new indication doesn’t affect the current recommendations that are already in place. In 2018, a supplemental application for Gardasil 9 was approved to include women and men aged 27 through 45 years for preventing a variety of cancers including cervical, vulvar, vaginal, and anal cancer as well as genital warts. But cancers of the head and neck were not included.
The original Gardasil vaccine came on the market in 2006, with an indication to prevent certain cancers and diseases caused by HPV types 6, 11, 16, and 18. It is no longer distributed in the United States.
In 2014, the FDA approved Gardasil 9, which extends the vaccine coverage for the initial four HPV types as five additional types (31, 33, 45, 52, and 58), and its initial indication was for use in both men and women between the ages of 9 through 26 years.
Head and neck cancers surpass cervical cancer
More than 2 decades ago, researchers first found a connection between HPV and a subset of head and neck cancers (Curr Opin Oncol. 1999;11(3):191-199). The cancers associated with HPV also appeared to have a different biology and disease pattern, as well as a better prognosis, compared with those that were unrelated. HPV is now responsible for the majority of oropharyngeal squamous cell cancers diagnosed in the United States.
A study published last year found that oral HPV infections were occurring with significantly less frequency among sexually active female adolescents who had received the quadrivalent vaccine, as compared with those who were unvaccinated.
These findings provided evidence that HPV vaccination was associated with a reduced frequency of HPV infection in the oral cavity, suggesting that vaccination could decrease the future risk of HPV-associated head and neck cancers.
The omission of head and neck cancers from the initial list of indications for the vaccine is notable because, according to data from the Centers for Disease Control and Prevention (CDC), oropharyngeal cancers are now the most common malignancy caused by HPV, surpassing cervical cancer.
Who will benefit?
An estimated 14 million new HPV infections occur every year in the United States, according to the CDC, and about 80% of individuals who are sexually active have been exposed at some point during their lifetime. In most people, however, the virus will clear on its own without causing any illness or symptoms.
In a Medscape videoblog, Sandra Adamson Fryhofer, MD, MACP, FRCP, helped clarify the adult population most likely to benefit from the vaccine. She pointed out that the HPV vaccine doesn’t treat HPV-related disease or help clear infections, and there are currently no clinical antibody tests or titers that can predict immunity.
“Many adults aged 27-45 have already been exposed to HPV early in life,” she said. Those in a long-term mutually monogamous relationship are not likely to get a new HPV infection. Those with multiple prior sex partners are more likely to have already been exposed to vaccine serotypes. For them, the vaccine will be less effective.”
Fryhofer added that individuals who are now at risk for exposure to a new HPV infection from a new sex partner are the ones most likely to benefit from HPV vaccination.
Confirmation needed
The FDA’s accelerated approval is contingent on confirmatory data, and Merck opened a clinical trial this past February to evaluate the efficacy, immunogenicity, and safety of the 9-valent HPV vaccine in men 20 to 45 years of age. The phase 3 multicenter randomized trial will have an estimated enrollment of 6000 men.
This article first appeared on Medscape.com.
The US Food and Drug Administration (FDA) has expanded the indication for the Gardasil-9 (Merck) vaccine to include prevention of oropharyngeal and other head and neck cancers caused by HPV types 16, 18, 31, 33, 45, 52, and 58.
This new indication is approved under the FDA’s accelerated approval program and is based on the vaccine’s effectiveness in preventing HPV-related anogenital disease. Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory clinical trial, which is currently underway.
“At Merck, working to help prevent certain HPV-related cancers has been a priority for more than two decades,” Alain Luxembourg, MD, director, clinical research, Merck Research Laboratories, said in a statement. “Today’s approval for the prevention of HPV-related oropharyngeal and other head and neck cancers represents an important step in Merck’s mission to help reduce the number of men and women affected by certain HPV-related cancers.”
This new indication doesn’t affect the current recommendations that are already in place. In 2018, a supplemental application for Gardasil 9 was approved to include women and men aged 27 through 45 years for preventing a variety of cancers including cervical, vulvar, vaginal, and anal cancer as well as genital warts. But cancers of the head and neck were not included.
The original Gardasil vaccine came on the market in 2006, with an indication to prevent certain cancers and diseases caused by HPV types 6, 11, 16, and 18. It is no longer distributed in the United States.
In 2014, the FDA approved Gardasil 9, which extends the vaccine coverage for the initial four HPV types as five additional types (31, 33, 45, 52, and 58), and its initial indication was for use in both men and women between the ages of 9 through 26 years.
Head and neck cancers surpass cervical cancer
More than 2 decades ago, researchers first found a connection between HPV and a subset of head and neck cancers (Curr Opin Oncol. 1999;11(3):191-199). The cancers associated with HPV also appeared to have a different biology and disease pattern, as well as a better prognosis, compared with those that were unrelated. HPV is now responsible for the majority of oropharyngeal squamous cell cancers diagnosed in the United States.
A study published last year found that oral HPV infections were occurring with significantly less frequency among sexually active female adolescents who had received the quadrivalent vaccine, as compared with those who were unvaccinated.
These findings provided evidence that HPV vaccination was associated with a reduced frequency of HPV infection in the oral cavity, suggesting that vaccination could decrease the future risk of HPV-associated head and neck cancers.
The omission of head and neck cancers from the initial list of indications for the vaccine is notable because, according to data from the Centers for Disease Control and Prevention (CDC), oropharyngeal cancers are now the most common malignancy caused by HPV, surpassing cervical cancer.
Who will benefit?
An estimated 14 million new HPV infections occur every year in the United States, according to the CDC, and about 80% of individuals who are sexually active have been exposed at some point during their lifetime. In most people, however, the virus will clear on its own without causing any illness or symptoms.
In a Medscape videoblog, Sandra Adamson Fryhofer, MD, MACP, FRCP, helped clarify the adult population most likely to benefit from the vaccine. She pointed out that the HPV vaccine doesn’t treat HPV-related disease or help clear infections, and there are currently no clinical antibody tests or titers that can predict immunity.
“Many adults aged 27-45 have already been exposed to HPV early in life,” she said. Those in a long-term mutually monogamous relationship are not likely to get a new HPV infection. Those with multiple prior sex partners are more likely to have already been exposed to vaccine serotypes. For them, the vaccine will be less effective.”
Fryhofer added that individuals who are now at risk for exposure to a new HPV infection from a new sex partner are the ones most likely to benefit from HPV vaccination.
Confirmation needed
The FDA’s accelerated approval is contingent on confirmatory data, and Merck opened a clinical trial this past February to evaluate the efficacy, immunogenicity, and safety of the 9-valent HPV vaccine in men 20 to 45 years of age. The phase 3 multicenter randomized trial will have an estimated enrollment of 6000 men.
This article first appeared on Medscape.com.
The US Food and Drug Administration (FDA) has expanded the indication for the Gardasil-9 (Merck) vaccine to include prevention of oropharyngeal and other head and neck cancers caused by HPV types 16, 18, 31, 33, 45, 52, and 58.
This new indication is approved under the FDA’s accelerated approval program and is based on the vaccine’s effectiveness in preventing HPV-related anogenital disease. Continued approval for this indication may be contingent upon verification and description of clinical benefit in a confirmatory clinical trial, which is currently underway.
“At Merck, working to help prevent certain HPV-related cancers has been a priority for more than two decades,” Alain Luxembourg, MD, director, clinical research, Merck Research Laboratories, said in a statement. “Today’s approval for the prevention of HPV-related oropharyngeal and other head and neck cancers represents an important step in Merck’s mission to help reduce the number of men and women affected by certain HPV-related cancers.”
This new indication doesn’t affect the current recommendations that are already in place. In 2018, a supplemental application for Gardasil 9 was approved to include women and men aged 27 through 45 years for preventing a variety of cancers including cervical, vulvar, vaginal, and anal cancer as well as genital warts. But cancers of the head and neck were not included.
The original Gardasil vaccine came on the market in 2006, with an indication to prevent certain cancers and diseases caused by HPV types 6, 11, 16, and 18. It is no longer distributed in the United States.
In 2014, the FDA approved Gardasil 9, which extends the vaccine coverage for the initial four HPV types as five additional types (31, 33, 45, 52, and 58), and its initial indication was for use in both men and women between the ages of 9 through 26 years.
Head and neck cancers surpass cervical cancer
More than 2 decades ago, researchers first found a connection between HPV and a subset of head and neck cancers (Curr Opin Oncol. 1999;11(3):191-199). The cancers associated with HPV also appeared to have a different biology and disease pattern, as well as a better prognosis, compared with those that were unrelated. HPV is now responsible for the majority of oropharyngeal squamous cell cancers diagnosed in the United States.
A study published last year found that oral HPV infections were occurring with significantly less frequency among sexually active female adolescents who had received the quadrivalent vaccine, as compared with those who were unvaccinated.
These findings provided evidence that HPV vaccination was associated with a reduced frequency of HPV infection in the oral cavity, suggesting that vaccination could decrease the future risk of HPV-associated head and neck cancers.
The omission of head and neck cancers from the initial list of indications for the vaccine is notable because, according to data from the Centers for Disease Control and Prevention (CDC), oropharyngeal cancers are now the most common malignancy caused by HPV, surpassing cervical cancer.
Who will benefit?
An estimated 14 million new HPV infections occur every year in the United States, according to the CDC, and about 80% of individuals who are sexually active have been exposed at some point during their lifetime. In most people, however, the virus will clear on its own without causing any illness or symptoms.
In a Medscape videoblog, Sandra Adamson Fryhofer, MD, MACP, FRCP, helped clarify the adult population most likely to benefit from the vaccine. She pointed out that the HPV vaccine doesn’t treat HPV-related disease or help clear infections, and there are currently no clinical antibody tests or titers that can predict immunity.
“Many adults aged 27-45 have already been exposed to HPV early in life,” she said. Those in a long-term mutually monogamous relationship are not likely to get a new HPV infection. Those with multiple prior sex partners are more likely to have already been exposed to vaccine serotypes. For them, the vaccine will be less effective.”
Fryhofer added that individuals who are now at risk for exposure to a new HPV infection from a new sex partner are the ones most likely to benefit from HPV vaccination.
Confirmation needed
The FDA’s accelerated approval is contingent on confirmatory data, and Merck opened a clinical trial this past February to evaluate the efficacy, immunogenicity, and safety of the 9-valent HPV vaccine in men 20 to 45 years of age. The phase 3 multicenter randomized trial will have an estimated enrollment of 6000 men.
This article first appeared on Medscape.com.