User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Will your smartphone be the next doctor’s office?
A fingertip pressed against a phone’s camera lens can measure a heart rate. The microphone, kept by the bedside, can screen for sleep apnea. Even the speaker is being tapped, to monitor breathing using sonar technology.
In the best of this new world, the data is conveyed remotely to a medical professional for the convenience and comfort of the patient or, in some cases, to support a clinician without the need for costly hardware.
But using smartphones as diagnostic tools is a work in progress, experts say. Although doctors and their patients have found some real-world success in deploying the phone as a medical device, the overall potential remains unfulfilled and uncertain.
Smartphones come packed with sensors capable of monitoring a patient’s vital signs. They can help assess people for concussions, watch for atrial fibrillation, and conduct mental health wellness checks, to name the uses of a few nascent applications.
Companies and researchers eager to find medical applications for smartphone technology are tapping into modern phones’ built-in cameras and light sensors; microphones; accelerometers, which detect body movements; gyroscopes; and even speakers. The apps then use artificial intelligence software to analyze the collected sights and sounds to create an easy connection between patients and physicians. Earning potential and marketability are evidenced by the more than 350,000 digital health products available in app stores, according to a Grand View Research report.
“It’s very hard to put devices into the patient home or in the hospital, but everybody is just walking around with a cellphone that has a network connection,” said Dr. Andrew Gostine, CEO of the sensor network company Artisight. Most Americans own a smartphone, including more than 60% of people 65 and over, an increase from just 13% a decade ago, according the Pew Research Center. The COVID-19 pandemic has also pushed people to become more comfortable with virtual care.
Some of these products have sought FDA clearance to be marketed as a medical device. That way, if patients must pay to use the software, health insurers are more likely to cover at least part of the cost. Other products are designated as exempt from this regulatory process, placed in the same clinical classification as a Band-Aid. But how the agency handles AI and machine learning–based medical devices is still being adjusted to reflect software’s adaptive nature.
Ensuring accuracy and clinical validation is crucial to securing buy-in from health care providers. And many tools still need fine-tuning, said Eugene Yang, MD, a professor of medicine at the University of Washington, Seattle. Currently, Dr. Yang is testing contactless measurement of blood pressure, heart rate, and oxygen saturation gleaned remotely via Zoom camera footage of a patient’s face.
Judging these new technologies is difficult because they rely on algorithms built by machine learning and artificial intelligence to collect data, rather than the physical tools typically used in hospitals. So researchers cannot “compare apples to apples” with medical industry standards, Dr. Yang said. Failure to build in such assurances undermines the technology’s ultimate goals of easing costs and access because a doctor still must verify results.
“False positives and false negatives lead to more testing and more cost to the health care system,” he said.
Big tech companies like Google have heavily invested in researching this kind of technology, catering to clinicians and in-home caregivers, as well as consumers. Currently, in the Google Fit app, users can check their heart rate by placing their finger on the rear-facing camera lens or track their breathing rate using the front-facing camera.
“If you took the sensor out of the phone and out of a clinical device, they are probably the same thing,” said Shwetak Patel, director of health technologies at Google and a professor of electrical and computer engineering at the University of Washington.
Google’s research uses machine learning and computer vision, a field within AI based on information from visual inputs like videos or images. So instead of using a blood pressure cuff, for example, the algorithm can interpret slight visual changes to the body that serve as proxies and biosignals for a patient’s blood pressure, Mr. Patel said.
Google is also investigating the effectiveness of the built-in microphone for detecting heartbeats and murmurs and using the camera to preserve eyesight by screening for diabetic eye disease, according to information the company published last year.
The tech giant recently purchased Sound Life Sciences, a Seattle startup with an FDA-cleared sonar technology app. It uses a smart device’s speaker to bounce inaudible pulses off a patient’s body to identify movement and monitor breathing.
Binah.ai, based in Israel, is another company using the smartphone camera to calculate vital signs. Its software looks at the region around the eyes, where the skin is a bit thinner, and analyzes the light reflecting off blood vessels back to the lens. The company is wrapping up a U.S. clinical trial and marketing its wellness app directly to insurers and other health companies, said company spokesperson Mona Popilian-Yona.
The applications even reach into disciplines such as optometry and mental health:
- With the microphone, Canary Speech uses the same underlying technology as Amazon’s Alexa to analyze patients’ voices for mental health conditions. The software can integrate with telemedicine appointments and allow clinicians to screen for anxiety and depression using a library of vocal biomarkers and predictive analytics, said Henry O’Connell, the company’s CEO.
- Australia-based ResApp Health last year for its iPhone app that screens for moderate to severe obstructive sleep apnea by listening to breathing and snoring. SleepCheckRx, which will require a prescription, is minimally invasive compared with sleep studies currently used to diagnose sleep apnea. Those can cost thousands of dollars and require an array of tests.
- Brightlamp’s Reflex app is a clinical decision support tool for helping manage concussions and vision rehabilitation, among other things. Using an iPad’s or iPhone’s camera, the mobile app measures how a person’s pupils react to changes in light. Through machine learning analysis, the imagery gives practitioners data points for evaluating patients. Brightlamp sells directly to health care providers and is being used in more than 230 clinics. Clinicians pay a $400 standard annual fee per account, which is currently not covered by insurance. The Department of Defense has an ongoing clinical trial using Reflex.
In some cases, such as with the Reflex app, the data is processed directly on the phone – rather than in the cloud, Brightlamp CEO Kurtis Sluss said. By processing everything on the device, the app avoids running into privacy issues, as streaming data elsewhere requires patient consent.
But algorithms need to be trained and tested by collecting reams of data, and that is an ongoing process.
Researchers, for example, have found that some computer vision applications, like heart rate or blood pressure monitoring, can be less accurate for darker skin. Studies are underway to find better solutions.
Small algorithm glitches can also produce false alarms and frighten patients enough to keep widespread adoption out of reach. For example, Apple’s new car-crash detection feature, available on both the latest iPhone and Apple Watch, was set off when people were riding roller coasters and automatically dialed 911.
“We’re not there yet,” Dr. Yang said. “That’s the bottom line.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
A fingertip pressed against a phone’s camera lens can measure a heart rate. The microphone, kept by the bedside, can screen for sleep apnea. Even the speaker is being tapped, to monitor breathing using sonar technology.
In the best of this new world, the data is conveyed remotely to a medical professional for the convenience and comfort of the patient or, in some cases, to support a clinician without the need for costly hardware.
But using smartphones as diagnostic tools is a work in progress, experts say. Although doctors and their patients have found some real-world success in deploying the phone as a medical device, the overall potential remains unfulfilled and uncertain.
Smartphones come packed with sensors capable of monitoring a patient’s vital signs. They can help assess people for concussions, watch for atrial fibrillation, and conduct mental health wellness checks, to name the uses of a few nascent applications.
Companies and researchers eager to find medical applications for smartphone technology are tapping into modern phones’ built-in cameras and light sensors; microphones; accelerometers, which detect body movements; gyroscopes; and even speakers. The apps then use artificial intelligence software to analyze the collected sights and sounds to create an easy connection between patients and physicians. Earning potential and marketability are evidenced by the more than 350,000 digital health products available in app stores, according to a Grand View Research report.
“It’s very hard to put devices into the patient home or in the hospital, but everybody is just walking around with a cellphone that has a network connection,” said Dr. Andrew Gostine, CEO of the sensor network company Artisight. Most Americans own a smartphone, including more than 60% of people 65 and over, an increase from just 13% a decade ago, according the Pew Research Center. The COVID-19 pandemic has also pushed people to become more comfortable with virtual care.
Some of these products have sought FDA clearance to be marketed as a medical device. That way, if patients must pay to use the software, health insurers are more likely to cover at least part of the cost. Other products are designated as exempt from this regulatory process, placed in the same clinical classification as a Band-Aid. But how the agency handles AI and machine learning–based medical devices is still being adjusted to reflect software’s adaptive nature.
Ensuring accuracy and clinical validation is crucial to securing buy-in from health care providers. And many tools still need fine-tuning, said Eugene Yang, MD, a professor of medicine at the University of Washington, Seattle. Currently, Dr. Yang is testing contactless measurement of blood pressure, heart rate, and oxygen saturation gleaned remotely via Zoom camera footage of a patient’s face.
Judging these new technologies is difficult because they rely on algorithms built by machine learning and artificial intelligence to collect data, rather than the physical tools typically used in hospitals. So researchers cannot “compare apples to apples” with medical industry standards, Dr. Yang said. Failure to build in such assurances undermines the technology’s ultimate goals of easing costs and access because a doctor still must verify results.
“False positives and false negatives lead to more testing and more cost to the health care system,” he said.
Big tech companies like Google have heavily invested in researching this kind of technology, catering to clinicians and in-home caregivers, as well as consumers. Currently, in the Google Fit app, users can check their heart rate by placing their finger on the rear-facing camera lens or track their breathing rate using the front-facing camera.
“If you took the sensor out of the phone and out of a clinical device, they are probably the same thing,” said Shwetak Patel, director of health technologies at Google and a professor of electrical and computer engineering at the University of Washington.
Google’s research uses machine learning and computer vision, a field within AI based on information from visual inputs like videos or images. So instead of using a blood pressure cuff, for example, the algorithm can interpret slight visual changes to the body that serve as proxies and biosignals for a patient’s blood pressure, Mr. Patel said.
Google is also investigating the effectiveness of the built-in microphone for detecting heartbeats and murmurs and using the camera to preserve eyesight by screening for diabetic eye disease, according to information the company published last year.
The tech giant recently purchased Sound Life Sciences, a Seattle startup with an FDA-cleared sonar technology app. It uses a smart device’s speaker to bounce inaudible pulses off a patient’s body to identify movement and monitor breathing.
Binah.ai, based in Israel, is another company using the smartphone camera to calculate vital signs. Its software looks at the region around the eyes, where the skin is a bit thinner, and analyzes the light reflecting off blood vessels back to the lens. The company is wrapping up a U.S. clinical trial and marketing its wellness app directly to insurers and other health companies, said company spokesperson Mona Popilian-Yona.
The applications even reach into disciplines such as optometry and mental health:
- With the microphone, Canary Speech uses the same underlying technology as Amazon’s Alexa to analyze patients’ voices for mental health conditions. The software can integrate with telemedicine appointments and allow clinicians to screen for anxiety and depression using a library of vocal biomarkers and predictive analytics, said Henry O’Connell, the company’s CEO.
- Australia-based ResApp Health last year for its iPhone app that screens for moderate to severe obstructive sleep apnea by listening to breathing and snoring. SleepCheckRx, which will require a prescription, is minimally invasive compared with sleep studies currently used to diagnose sleep apnea. Those can cost thousands of dollars and require an array of tests.
- Brightlamp’s Reflex app is a clinical decision support tool for helping manage concussions and vision rehabilitation, among other things. Using an iPad’s or iPhone’s camera, the mobile app measures how a person’s pupils react to changes in light. Through machine learning analysis, the imagery gives practitioners data points for evaluating patients. Brightlamp sells directly to health care providers and is being used in more than 230 clinics. Clinicians pay a $400 standard annual fee per account, which is currently not covered by insurance. The Department of Defense has an ongoing clinical trial using Reflex.
In some cases, such as with the Reflex app, the data is processed directly on the phone – rather than in the cloud, Brightlamp CEO Kurtis Sluss said. By processing everything on the device, the app avoids running into privacy issues, as streaming data elsewhere requires patient consent.
But algorithms need to be trained and tested by collecting reams of data, and that is an ongoing process.
Researchers, for example, have found that some computer vision applications, like heart rate or blood pressure monitoring, can be less accurate for darker skin. Studies are underway to find better solutions.
Small algorithm glitches can also produce false alarms and frighten patients enough to keep widespread adoption out of reach. For example, Apple’s new car-crash detection feature, available on both the latest iPhone and Apple Watch, was set off when people were riding roller coasters and automatically dialed 911.
“We’re not there yet,” Dr. Yang said. “That’s the bottom line.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
A fingertip pressed against a phone’s camera lens can measure a heart rate. The microphone, kept by the bedside, can screen for sleep apnea. Even the speaker is being tapped, to monitor breathing using sonar technology.
In the best of this new world, the data is conveyed remotely to a medical professional for the convenience and comfort of the patient or, in some cases, to support a clinician without the need for costly hardware.
But using smartphones as diagnostic tools is a work in progress, experts say. Although doctors and their patients have found some real-world success in deploying the phone as a medical device, the overall potential remains unfulfilled and uncertain.
Smartphones come packed with sensors capable of monitoring a patient’s vital signs. They can help assess people for concussions, watch for atrial fibrillation, and conduct mental health wellness checks, to name the uses of a few nascent applications.
Companies and researchers eager to find medical applications for smartphone technology are tapping into modern phones’ built-in cameras and light sensors; microphones; accelerometers, which detect body movements; gyroscopes; and even speakers. The apps then use artificial intelligence software to analyze the collected sights and sounds to create an easy connection between patients and physicians. Earning potential and marketability are evidenced by the more than 350,000 digital health products available in app stores, according to a Grand View Research report.
“It’s very hard to put devices into the patient home or in the hospital, but everybody is just walking around with a cellphone that has a network connection,” said Dr. Andrew Gostine, CEO of the sensor network company Artisight. Most Americans own a smartphone, including more than 60% of people 65 and over, an increase from just 13% a decade ago, according the Pew Research Center. The COVID-19 pandemic has also pushed people to become more comfortable with virtual care.
Some of these products have sought FDA clearance to be marketed as a medical device. That way, if patients must pay to use the software, health insurers are more likely to cover at least part of the cost. Other products are designated as exempt from this regulatory process, placed in the same clinical classification as a Band-Aid. But how the agency handles AI and machine learning–based medical devices is still being adjusted to reflect software’s adaptive nature.
Ensuring accuracy and clinical validation is crucial to securing buy-in from health care providers. And many tools still need fine-tuning, said Eugene Yang, MD, a professor of medicine at the University of Washington, Seattle. Currently, Dr. Yang is testing contactless measurement of blood pressure, heart rate, and oxygen saturation gleaned remotely via Zoom camera footage of a patient’s face.
Judging these new technologies is difficult because they rely on algorithms built by machine learning and artificial intelligence to collect data, rather than the physical tools typically used in hospitals. So researchers cannot “compare apples to apples” with medical industry standards, Dr. Yang said. Failure to build in such assurances undermines the technology’s ultimate goals of easing costs and access because a doctor still must verify results.
“False positives and false negatives lead to more testing and more cost to the health care system,” he said.
Big tech companies like Google have heavily invested in researching this kind of technology, catering to clinicians and in-home caregivers, as well as consumers. Currently, in the Google Fit app, users can check their heart rate by placing their finger on the rear-facing camera lens or track their breathing rate using the front-facing camera.
“If you took the sensor out of the phone and out of a clinical device, they are probably the same thing,” said Shwetak Patel, director of health technologies at Google and a professor of electrical and computer engineering at the University of Washington.
Google’s research uses machine learning and computer vision, a field within AI based on information from visual inputs like videos or images. So instead of using a blood pressure cuff, for example, the algorithm can interpret slight visual changes to the body that serve as proxies and biosignals for a patient’s blood pressure, Mr. Patel said.
Google is also investigating the effectiveness of the built-in microphone for detecting heartbeats and murmurs and using the camera to preserve eyesight by screening for diabetic eye disease, according to information the company published last year.
The tech giant recently purchased Sound Life Sciences, a Seattle startup with an FDA-cleared sonar technology app. It uses a smart device’s speaker to bounce inaudible pulses off a patient’s body to identify movement and monitor breathing.
Binah.ai, based in Israel, is another company using the smartphone camera to calculate vital signs. Its software looks at the region around the eyes, where the skin is a bit thinner, and analyzes the light reflecting off blood vessels back to the lens. The company is wrapping up a U.S. clinical trial and marketing its wellness app directly to insurers and other health companies, said company spokesperson Mona Popilian-Yona.
The applications even reach into disciplines such as optometry and mental health:
- With the microphone, Canary Speech uses the same underlying technology as Amazon’s Alexa to analyze patients’ voices for mental health conditions. The software can integrate with telemedicine appointments and allow clinicians to screen for anxiety and depression using a library of vocal biomarkers and predictive analytics, said Henry O’Connell, the company’s CEO.
- Australia-based ResApp Health last year for its iPhone app that screens for moderate to severe obstructive sleep apnea by listening to breathing and snoring. SleepCheckRx, which will require a prescription, is minimally invasive compared with sleep studies currently used to diagnose sleep apnea. Those can cost thousands of dollars and require an array of tests.
- Brightlamp’s Reflex app is a clinical decision support tool for helping manage concussions and vision rehabilitation, among other things. Using an iPad’s or iPhone’s camera, the mobile app measures how a person’s pupils react to changes in light. Through machine learning analysis, the imagery gives practitioners data points for evaluating patients. Brightlamp sells directly to health care providers and is being used in more than 230 clinics. Clinicians pay a $400 standard annual fee per account, which is currently not covered by insurance. The Department of Defense has an ongoing clinical trial using Reflex.
In some cases, such as with the Reflex app, the data is processed directly on the phone – rather than in the cloud, Brightlamp CEO Kurtis Sluss said. By processing everything on the device, the app avoids running into privacy issues, as streaming data elsewhere requires patient consent.
But algorithms need to be trained and tested by collecting reams of data, and that is an ongoing process.
Researchers, for example, have found that some computer vision applications, like heart rate or blood pressure monitoring, can be less accurate for darker skin. Studies are underway to find better solutions.
Small algorithm glitches can also produce false alarms and frighten patients enough to keep widespread adoption out of reach. For example, Apple’s new car-crash detection feature, available on both the latest iPhone and Apple Watch, was set off when people were riding roller coasters and automatically dialed 911.
“We’re not there yet,” Dr. Yang said. “That’s the bottom line.”
KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
It’s all about the brains: Guilt placebos, transplants, and negative feelings
Guilt reduction, now in deceptive and open-secret forms
Guilt plagues a lot of us, sometimes regularly. Maybe you felt bad about eating the leftovers that your partner was looking forward to eating at the end of the day. Or for not saving a seat for your friend who was running late to the movies. Maybe even hiding a secret that you know would hurt a person’s feelings. We’ve all felt it, and it doesn’t feel good.
But what if there was a pill that would make those feelings seem to hurt less? There’s already a pill for almost everything, right?
Well, researchers from the University of Basel are on the case and have conducted a study suggesting that a placebo might work. They asked participants to write down a time they felt super guilty about something, just to stir up those feelings again, then they were divided into three groups. One group was told they would receive real medication that was actually a placebo, one was told they would get a placebo, and one got nothing. The subjects’ guilty feelings were reduced in both the medication-that-was-really-a-placebo group and placebo-that-was-a-placebo group.
“Our study therefore supports the intriguing finding that placebos work even when they are administered openly, and that explanation of the treatment is key to its effectiveness,” lead author Dilan Sezer said in a written statement.
More research is needed, but the human mind is a very interesting place. It seems like we can convince ourselves of just about anything. Especially to feel less guilty.
It’s a mad, mad, mad, mad scientist’s world
Mad scientists. Life’s just more interesting with a few of them running around, but they’re mostly relegated to works of fiction. Real life is boring; we don’t actually have neurosurgeons going around claiming human brain transplant is technically feasible.
Best of all, this isn’t even Dr. Sergio Canavero’s first rodeo with mad science: In 2015 he claimed human head transplants were technically feasible, and in the past few years has claimed to have rehearsed head transplants on cadavers and successfully repaired spinal cord injuries in animals. Lots of claims in there, but precious little evidence. And contrary to what everyone at the head enhancement clinic says, people will notice if you start going around with a new head.
But let’s get back to brains. Ignoring the fact that brain transplant sounds like a zombie with a PhD nibbling on your skull, the article does appear in a peer-reviewed journal. So surely there’s some level of legitimacy. After all, it’s not like Dr. Canavero is an editor for this journal. [Editor’s note: By that we mean he is an editor for the journal.]
Man, he’s taking all the fun out of this.
Anyway, now that we’ve prefaced this with the mother of all caveats, what exactly is Dr. Canavero proposing with his brain transplant? It’s pretty simple: Just have a robot scoop out the first brain and place it into a fresh body, either a donated but moribund younger body or a cloned body. Reconnect all the nerves and vasculature and you’re good to go. Enjoy your wine and laugh in the face of death.
Naturally, such a … bold proposal is lacking in the details, but who cares about details, anyway? This is mad science, not respectable science. Professionals have standards. And if we hear that a human brain transplant was successfully completed on a non–dark and stormy night and the doctor didn’t cackle madly “It’s alive! It’s alive!” then honestly, what even was the point?
Ambivalence rules!
As the office’s unofficial Sith lord/Star Wars nerd, LOTME takes notice when science extols the benefits of unhappiness: “It’s good to be grumpy: Bad moods make us more detail-oriented, study shows.”
The investigators manipulated the emotions of participants by having them watch a clip from “Sophie’s Choice” or one from “Friends.” Then the subjects listened to short, emotionally neutral stories, some of which contained inconsistencies, with the text displayed on a computer screen. Sorry to say, gang at Central Perk, but round one went to the sad movie.
“When people are in a negative mood, they are more careful and analytical. They scrutinize what’s actually stated in a text, and they don’t just fall back on their default world knowledge,” lead author Vicky Lai, PhD, of the University of Arizona said in a statement from the school.
Negative mood. Careful and analytical. Grumpy is good.
You’ve fallen into Darth Science’s little trap, and we have you now.
A study conducted at the University of Geneva offers a slightly different conclusion. And by slightly different, we mean completely different. People over age 65 who watched a series of short TV clips depicting people in a state of emotional suffering experienced excessive modification of their neuronal connections, compared with those who watched emotionally neutral videos.
The brains of these subjects remained “frozen in a negative state by relating the suffering of others to their own emotional memories,” lead author Sebastian Baez Lugo said in a written release from the university.
Emotional suffering. Frozen brains. Grumpy is … not good?
So there you have it. Darth Science’s lesson for the day: A negative mood makes you careful and analytical, but negative thoughts are bad for your brain.
Guilt reduction, now in deceptive and open-secret forms
Guilt plagues a lot of us, sometimes regularly. Maybe you felt bad about eating the leftovers that your partner was looking forward to eating at the end of the day. Or for not saving a seat for your friend who was running late to the movies. Maybe even hiding a secret that you know would hurt a person’s feelings. We’ve all felt it, and it doesn’t feel good.
But what if there was a pill that would make those feelings seem to hurt less? There’s already a pill for almost everything, right?
Well, researchers from the University of Basel are on the case and have conducted a study suggesting that a placebo might work. They asked participants to write down a time they felt super guilty about something, just to stir up those feelings again, then they were divided into three groups. One group was told they would receive real medication that was actually a placebo, one was told they would get a placebo, and one got nothing. The subjects’ guilty feelings were reduced in both the medication-that-was-really-a-placebo group and placebo-that-was-a-placebo group.
“Our study therefore supports the intriguing finding that placebos work even when they are administered openly, and that explanation of the treatment is key to its effectiveness,” lead author Dilan Sezer said in a written statement.
More research is needed, but the human mind is a very interesting place. It seems like we can convince ourselves of just about anything. Especially to feel less guilty.
It’s a mad, mad, mad, mad scientist’s world
Mad scientists. Life’s just more interesting with a few of them running around, but they’re mostly relegated to works of fiction. Real life is boring; we don’t actually have neurosurgeons going around claiming human brain transplant is technically feasible.
Best of all, this isn’t even Dr. Sergio Canavero’s first rodeo with mad science: In 2015 he claimed human head transplants were technically feasible, and in the past few years has claimed to have rehearsed head transplants on cadavers and successfully repaired spinal cord injuries in animals. Lots of claims in there, but precious little evidence. And contrary to what everyone at the head enhancement clinic says, people will notice if you start going around with a new head.
But let’s get back to brains. Ignoring the fact that brain transplant sounds like a zombie with a PhD nibbling on your skull, the article does appear in a peer-reviewed journal. So surely there’s some level of legitimacy. After all, it’s not like Dr. Canavero is an editor for this journal. [Editor’s note: By that we mean he is an editor for the journal.]
Man, he’s taking all the fun out of this.
Anyway, now that we’ve prefaced this with the mother of all caveats, what exactly is Dr. Canavero proposing with his brain transplant? It’s pretty simple: Just have a robot scoop out the first brain and place it into a fresh body, either a donated but moribund younger body or a cloned body. Reconnect all the nerves and vasculature and you’re good to go. Enjoy your wine and laugh in the face of death.
Naturally, such a … bold proposal is lacking in the details, but who cares about details, anyway? This is mad science, not respectable science. Professionals have standards. And if we hear that a human brain transplant was successfully completed on a non–dark and stormy night and the doctor didn’t cackle madly “It’s alive! It’s alive!” then honestly, what even was the point?
Ambivalence rules!
As the office’s unofficial Sith lord/Star Wars nerd, LOTME takes notice when science extols the benefits of unhappiness: “It’s good to be grumpy: Bad moods make us more detail-oriented, study shows.”
The investigators manipulated the emotions of participants by having them watch a clip from “Sophie’s Choice” or one from “Friends.” Then the subjects listened to short, emotionally neutral stories, some of which contained inconsistencies, with the text displayed on a computer screen. Sorry to say, gang at Central Perk, but round one went to the sad movie.
“When people are in a negative mood, they are more careful and analytical. They scrutinize what’s actually stated in a text, and they don’t just fall back on their default world knowledge,” lead author Vicky Lai, PhD, of the University of Arizona said in a statement from the school.
Negative mood. Careful and analytical. Grumpy is good.
You’ve fallen into Darth Science’s little trap, and we have you now.
A study conducted at the University of Geneva offers a slightly different conclusion. And by slightly different, we mean completely different. People over age 65 who watched a series of short TV clips depicting people in a state of emotional suffering experienced excessive modification of their neuronal connections, compared with those who watched emotionally neutral videos.
The brains of these subjects remained “frozen in a negative state by relating the suffering of others to their own emotional memories,” lead author Sebastian Baez Lugo said in a written release from the university.
Emotional suffering. Frozen brains. Grumpy is … not good?
So there you have it. Darth Science’s lesson for the day: A negative mood makes you careful and analytical, but negative thoughts are bad for your brain.
Guilt reduction, now in deceptive and open-secret forms
Guilt plagues a lot of us, sometimes regularly. Maybe you felt bad about eating the leftovers that your partner was looking forward to eating at the end of the day. Or for not saving a seat for your friend who was running late to the movies. Maybe even hiding a secret that you know would hurt a person’s feelings. We’ve all felt it, and it doesn’t feel good.
But what if there was a pill that would make those feelings seem to hurt less? There’s already a pill for almost everything, right?
Well, researchers from the University of Basel are on the case and have conducted a study suggesting that a placebo might work. They asked participants to write down a time they felt super guilty about something, just to stir up those feelings again, then they were divided into three groups. One group was told they would receive real medication that was actually a placebo, one was told they would get a placebo, and one got nothing. The subjects’ guilty feelings were reduced in both the medication-that-was-really-a-placebo group and placebo-that-was-a-placebo group.
“Our study therefore supports the intriguing finding that placebos work even when they are administered openly, and that explanation of the treatment is key to its effectiveness,” lead author Dilan Sezer said in a written statement.
More research is needed, but the human mind is a very interesting place. It seems like we can convince ourselves of just about anything. Especially to feel less guilty.
It’s a mad, mad, mad, mad scientist’s world
Mad scientists. Life’s just more interesting with a few of them running around, but they’re mostly relegated to works of fiction. Real life is boring; we don’t actually have neurosurgeons going around claiming human brain transplant is technically feasible.
Best of all, this isn’t even Dr. Sergio Canavero’s first rodeo with mad science: In 2015 he claimed human head transplants were technically feasible, and in the past few years has claimed to have rehearsed head transplants on cadavers and successfully repaired spinal cord injuries in animals. Lots of claims in there, but precious little evidence. And contrary to what everyone at the head enhancement clinic says, people will notice if you start going around with a new head.
But let’s get back to brains. Ignoring the fact that brain transplant sounds like a zombie with a PhD nibbling on your skull, the article does appear in a peer-reviewed journal. So surely there’s some level of legitimacy. After all, it’s not like Dr. Canavero is an editor for this journal. [Editor’s note: By that we mean he is an editor for the journal.]
Man, he’s taking all the fun out of this.
Anyway, now that we’ve prefaced this with the mother of all caveats, what exactly is Dr. Canavero proposing with his brain transplant? It’s pretty simple: Just have a robot scoop out the first brain and place it into a fresh body, either a donated but moribund younger body or a cloned body. Reconnect all the nerves and vasculature and you’re good to go. Enjoy your wine and laugh in the face of death.
Naturally, such a … bold proposal is lacking in the details, but who cares about details, anyway? This is mad science, not respectable science. Professionals have standards. And if we hear that a human brain transplant was successfully completed on a non–dark and stormy night and the doctor didn’t cackle madly “It’s alive! It’s alive!” then honestly, what even was the point?
Ambivalence rules!
As the office’s unofficial Sith lord/Star Wars nerd, LOTME takes notice when science extols the benefits of unhappiness: “It’s good to be grumpy: Bad moods make us more detail-oriented, study shows.”
The investigators manipulated the emotions of participants by having them watch a clip from “Sophie’s Choice” or one from “Friends.” Then the subjects listened to short, emotionally neutral stories, some of which contained inconsistencies, with the text displayed on a computer screen. Sorry to say, gang at Central Perk, but round one went to the sad movie.
“When people are in a negative mood, they are more careful and analytical. They scrutinize what’s actually stated in a text, and they don’t just fall back on their default world knowledge,” lead author Vicky Lai, PhD, of the University of Arizona said in a statement from the school.
Negative mood. Careful and analytical. Grumpy is good.
You’ve fallen into Darth Science’s little trap, and we have you now.
A study conducted at the University of Geneva offers a slightly different conclusion. And by slightly different, we mean completely different. People over age 65 who watched a series of short TV clips depicting people in a state of emotional suffering experienced excessive modification of their neuronal connections, compared with those who watched emotionally neutral videos.
The brains of these subjects remained “frozen in a negative state by relating the suffering of others to their own emotional memories,” lead author Sebastian Baez Lugo said in a written release from the university.
Emotional suffering. Frozen brains. Grumpy is … not good?
So there you have it. Darth Science’s lesson for the day: A negative mood makes you careful and analytical, but negative thoughts are bad for your brain.
Congenital CMV linked to pediatric hyperdiploid ALL
Children with hyperdiploid acute lymphoblastic leukemia (ALL) are much more likely to also have congenital cytomegalovirus (CMV) infection, according to an analysis published in JAMA Network Open.
Although researchers found no association between ALL and congenital CMV infection overall, pediatric patients diagnosed with hyperdiploid ALL had sixfold greater odds of being positive for congenital CMV than cancer-free controls.
“These findings suggest mixed evidence for an association between congenital CMV infection and ALL” and that “a CMV-ALL association may be specific to hyperdiploid ALL,” said investigators, led by Jennifer Geris, PhD, a postdoctoral associate at Baylor College of Medicine, Houston.
A growing body of evidence suggests that CMV, a member of the herpesvirus family, may be a risk factor for ALL. Although the mechanism remains unclear, congenital CMV may encourage proliferation of CD34+ hematopoietic progenitor cells in bone marrow that are vulnerable to oncogenic transformation.
Two prior independent studies have suggested that prenatal CMV infection is associated with an increased risk of childhood ALL. However, given how common CMV infection is (more than 80% seropositivity worldwide) and the relatively rarity of pediatric ALL, Joseph Wiemels, PhD, argued in an accompanying editorial that CMV can’t be a direct cause of leukemia.
“Instead, CMV may play a supportive role” with infection in some infants altering immune function in a way that increases vulnerability to more direct causes of ALL, explained Dr. Wiemels, professor of population and public health sciences at the University of Southern California, Los Angeles. In other words, “exposure to CMV early rather than fulminant infection” at birth “may be the key epidemiologic feature.”
In the current study, Dr. Geris and colleagues tested dried newborn blood spots from 1189 children with ALL and 4,756 controls matched on age, sex, and mother’s race and ethnicity for the presence of cytomegalovirus at birth. Children were born in Michigan on or after Oct. 1, 1987.
Across the entire study population, congenital CMV was detected in 6 ALL cases (0.5%) and 21 controls (0.4%), with no difference in the odds of congenital CMV infection between the two groups. Among subjects positive for congenital CMV, it was not clear who had fulminant, clinically recognized disease and who did not.
Overall, 2 of 74 cases (2.7%) of hyperdiploid ALL were positive for congenital CMV. Compared with all controls in an unmatched analysis, those with hyperdiploid ALL were 6.26 times more likely to be CMV positive.
Overall, the investigators concluded that the current findings, in combination with previous evidence showing a similar connection, “strongly suggest CMV is associated specifically to hyperdiploid ALL.”
Although “the evidence supporting an association between CMV and ALL is tantalizing and mounting rapidly,” Dr. Wiemels noted that “much additional research attention is required to mechanistically describe pathways by which CMV may influence leukemia before the virus could be considered a potential target for prevention or clinical management of ALL.”
“We are still in the early chapters of the book describing the role of CMV and ALL,” but the virus might emerge as a clinical target “with much future promise for the health and well-being of our children,” he said.
The work was funded by the National Institutes of Health, the University of Minnesota, and the Department of Defense. The investigators and editorialist have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Children with hyperdiploid acute lymphoblastic leukemia (ALL) are much more likely to also have congenital cytomegalovirus (CMV) infection, according to an analysis published in JAMA Network Open.
Although researchers found no association between ALL and congenital CMV infection overall, pediatric patients diagnosed with hyperdiploid ALL had sixfold greater odds of being positive for congenital CMV than cancer-free controls.
“These findings suggest mixed evidence for an association between congenital CMV infection and ALL” and that “a CMV-ALL association may be specific to hyperdiploid ALL,” said investigators, led by Jennifer Geris, PhD, a postdoctoral associate at Baylor College of Medicine, Houston.
A growing body of evidence suggests that CMV, a member of the herpesvirus family, may be a risk factor for ALL. Although the mechanism remains unclear, congenital CMV may encourage proliferation of CD34+ hematopoietic progenitor cells in bone marrow that are vulnerable to oncogenic transformation.
Two prior independent studies have suggested that prenatal CMV infection is associated with an increased risk of childhood ALL. However, given how common CMV infection is (more than 80% seropositivity worldwide) and the relatively rarity of pediatric ALL, Joseph Wiemels, PhD, argued in an accompanying editorial that CMV can’t be a direct cause of leukemia.
“Instead, CMV may play a supportive role” with infection in some infants altering immune function in a way that increases vulnerability to more direct causes of ALL, explained Dr. Wiemels, professor of population and public health sciences at the University of Southern California, Los Angeles. In other words, “exposure to CMV early rather than fulminant infection” at birth “may be the key epidemiologic feature.”
In the current study, Dr. Geris and colleagues tested dried newborn blood spots from 1189 children with ALL and 4,756 controls matched on age, sex, and mother’s race and ethnicity for the presence of cytomegalovirus at birth. Children were born in Michigan on or after Oct. 1, 1987.
Across the entire study population, congenital CMV was detected in 6 ALL cases (0.5%) and 21 controls (0.4%), with no difference in the odds of congenital CMV infection between the two groups. Among subjects positive for congenital CMV, it was not clear who had fulminant, clinically recognized disease and who did not.
Overall, 2 of 74 cases (2.7%) of hyperdiploid ALL were positive for congenital CMV. Compared with all controls in an unmatched analysis, those with hyperdiploid ALL were 6.26 times more likely to be CMV positive.
Overall, the investigators concluded that the current findings, in combination with previous evidence showing a similar connection, “strongly suggest CMV is associated specifically to hyperdiploid ALL.”
Although “the evidence supporting an association between CMV and ALL is tantalizing and mounting rapidly,” Dr. Wiemels noted that “much additional research attention is required to mechanistically describe pathways by which CMV may influence leukemia before the virus could be considered a potential target for prevention or clinical management of ALL.”
“We are still in the early chapters of the book describing the role of CMV and ALL,” but the virus might emerge as a clinical target “with much future promise for the health and well-being of our children,” he said.
The work was funded by the National Institutes of Health, the University of Minnesota, and the Department of Defense. The investigators and editorialist have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Children with hyperdiploid acute lymphoblastic leukemia (ALL) are much more likely to also have congenital cytomegalovirus (CMV) infection, according to an analysis published in JAMA Network Open.
Although researchers found no association between ALL and congenital CMV infection overall, pediatric patients diagnosed with hyperdiploid ALL had sixfold greater odds of being positive for congenital CMV than cancer-free controls.
“These findings suggest mixed evidence for an association between congenital CMV infection and ALL” and that “a CMV-ALL association may be specific to hyperdiploid ALL,” said investigators, led by Jennifer Geris, PhD, a postdoctoral associate at Baylor College of Medicine, Houston.
A growing body of evidence suggests that CMV, a member of the herpesvirus family, may be a risk factor for ALL. Although the mechanism remains unclear, congenital CMV may encourage proliferation of CD34+ hematopoietic progenitor cells in bone marrow that are vulnerable to oncogenic transformation.
Two prior independent studies have suggested that prenatal CMV infection is associated with an increased risk of childhood ALL. However, given how common CMV infection is (more than 80% seropositivity worldwide) and the relatively rarity of pediatric ALL, Joseph Wiemels, PhD, argued in an accompanying editorial that CMV can’t be a direct cause of leukemia.
“Instead, CMV may play a supportive role” with infection in some infants altering immune function in a way that increases vulnerability to more direct causes of ALL, explained Dr. Wiemels, professor of population and public health sciences at the University of Southern California, Los Angeles. In other words, “exposure to CMV early rather than fulminant infection” at birth “may be the key epidemiologic feature.”
In the current study, Dr. Geris and colleagues tested dried newborn blood spots from 1189 children with ALL and 4,756 controls matched on age, sex, and mother’s race and ethnicity for the presence of cytomegalovirus at birth. Children were born in Michigan on or after Oct. 1, 1987.
Across the entire study population, congenital CMV was detected in 6 ALL cases (0.5%) and 21 controls (0.4%), with no difference in the odds of congenital CMV infection between the two groups. Among subjects positive for congenital CMV, it was not clear who had fulminant, clinically recognized disease and who did not.
Overall, 2 of 74 cases (2.7%) of hyperdiploid ALL were positive for congenital CMV. Compared with all controls in an unmatched analysis, those with hyperdiploid ALL were 6.26 times more likely to be CMV positive.
Overall, the investigators concluded that the current findings, in combination with previous evidence showing a similar connection, “strongly suggest CMV is associated specifically to hyperdiploid ALL.”
Although “the evidence supporting an association between CMV and ALL is tantalizing and mounting rapidly,” Dr. Wiemels noted that “much additional research attention is required to mechanistically describe pathways by which CMV may influence leukemia before the virus could be considered a potential target for prevention or clinical management of ALL.”
“We are still in the early chapters of the book describing the role of CMV and ALL,” but the virus might emerge as a clinical target “with much future promise for the health and well-being of our children,” he said.
The work was funded by the National Institutes of Health, the University of Minnesota, and the Department of Defense. The investigators and editorialist have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
How to talk with patients in ways that help them feel heard and understood
How do we become those professionals and make sure that we are doing a good job connecting and communicating with our patients?
Here are a few suggestions on how to do this.
Practice intent listening
When a patient shares their symptoms with you, show genuine curiosity and concern. Ask clarifying questions. Ask how the symptom or problem is affecting their day-to-day life. Avoid quick, rapid-fire questions back at the patient. Do not accept a patient self-diagnosis.
When a patient with a first-time headache says they are having a migraine headache, for example, ask many clarifying questions to make sure you can make a diagnosis of headache type, then use all the information you have gathered to educate the patient on what you believe they have.
It is easy to jump to treatment, but we always want to make sure we have the diagnosis correct first. By intently listening, it also makes it much easier to tell a patient you do not know what is causing their symptoms, but that you and the patient will be vigilant for any future clues that may lead to a diagnosis.
Use terminology that patients understand
Rachael Gotlieb, MD, and colleagues published an excellent study with eye-opening results on common phrases we use as health care providers and how often patients do not understand them.
Only 9% of patients understood what was meant when they were asked if they have been febrile. Only 2% understood what was meant by “I am concerned the patient has an occult infection.” Only 21% understood that “your xray findings were quite impressive” was bad news.
It is easy to avoid these medical language traps, we just have to check our doctor speak. Ask, “Do you have a fever?” Say, “I am concerned you may have an infection that is hard to find.”
Several other terms we use all the time in explaining things to patients that I have found most patients do not understand are the terms bilateral, systemic, and significant. Think carefully as you explain things to patients and check back to have them repeat to you what they think you said.
Be comfortable saying you don’t know
Many symptoms in medicine end up not being diagnosable. When a patient shares symptoms that do not fit a pattern of a disease, it is important to share with them why you think it is okay to wait and watch, even if you do not have a diagnosis.
Patients find it comforting that you are so honest with them. Doing this also has the benefit of gaining patients’ trust when you are sure about something, because it tells them you don’t have an answer for everything.
Ask your patients what they think is causing their symptoms
This way, you know what their big fear is. You can address what they are worried about, even if it isn’t something you are considering.
Patients are often fearful of a disease a close friend or relative has, so when they get new symptoms, they fear diseases that we might not think of. By knowing what they are fearful of, you can reassure when appropriate.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
How do we become those professionals and make sure that we are doing a good job connecting and communicating with our patients?
Here are a few suggestions on how to do this.
Practice intent listening
When a patient shares their symptoms with you, show genuine curiosity and concern. Ask clarifying questions. Ask how the symptom or problem is affecting their day-to-day life. Avoid quick, rapid-fire questions back at the patient. Do not accept a patient self-diagnosis.
When a patient with a first-time headache says they are having a migraine headache, for example, ask many clarifying questions to make sure you can make a diagnosis of headache type, then use all the information you have gathered to educate the patient on what you believe they have.
It is easy to jump to treatment, but we always want to make sure we have the diagnosis correct first. By intently listening, it also makes it much easier to tell a patient you do not know what is causing their symptoms, but that you and the patient will be vigilant for any future clues that may lead to a diagnosis.
Use terminology that patients understand
Rachael Gotlieb, MD, and colleagues published an excellent study with eye-opening results on common phrases we use as health care providers and how often patients do not understand them.
Only 9% of patients understood what was meant when they were asked if they have been febrile. Only 2% understood what was meant by “I am concerned the patient has an occult infection.” Only 21% understood that “your xray findings were quite impressive” was bad news.
It is easy to avoid these medical language traps, we just have to check our doctor speak. Ask, “Do you have a fever?” Say, “I am concerned you may have an infection that is hard to find.”
Several other terms we use all the time in explaining things to patients that I have found most patients do not understand are the terms bilateral, systemic, and significant. Think carefully as you explain things to patients and check back to have them repeat to you what they think you said.
Be comfortable saying you don’t know
Many symptoms in medicine end up not being diagnosable. When a patient shares symptoms that do not fit a pattern of a disease, it is important to share with them why you think it is okay to wait and watch, even if you do not have a diagnosis.
Patients find it comforting that you are so honest with them. Doing this also has the benefit of gaining patients’ trust when you are sure about something, because it tells them you don’t have an answer for everything.
Ask your patients what they think is causing their symptoms
This way, you know what their big fear is. You can address what they are worried about, even if it isn’t something you are considering.
Patients are often fearful of a disease a close friend or relative has, so when they get new symptoms, they fear diseases that we might not think of. By knowing what they are fearful of, you can reassure when appropriate.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
How do we become those professionals and make sure that we are doing a good job connecting and communicating with our patients?
Here are a few suggestions on how to do this.
Practice intent listening
When a patient shares their symptoms with you, show genuine curiosity and concern. Ask clarifying questions. Ask how the symptom or problem is affecting their day-to-day life. Avoid quick, rapid-fire questions back at the patient. Do not accept a patient self-diagnosis.
When a patient with a first-time headache says they are having a migraine headache, for example, ask many clarifying questions to make sure you can make a diagnosis of headache type, then use all the information you have gathered to educate the patient on what you believe they have.
It is easy to jump to treatment, but we always want to make sure we have the diagnosis correct first. By intently listening, it also makes it much easier to tell a patient you do not know what is causing their symptoms, but that you and the patient will be vigilant for any future clues that may lead to a diagnosis.
Use terminology that patients understand
Rachael Gotlieb, MD, and colleagues published an excellent study with eye-opening results on common phrases we use as health care providers and how often patients do not understand them.
Only 9% of patients understood what was meant when they were asked if they have been febrile. Only 2% understood what was meant by “I am concerned the patient has an occult infection.” Only 21% understood that “your xray findings were quite impressive” was bad news.
It is easy to avoid these medical language traps, we just have to check our doctor speak. Ask, “Do you have a fever?” Say, “I am concerned you may have an infection that is hard to find.”
Several other terms we use all the time in explaining things to patients that I have found most patients do not understand are the terms bilateral, systemic, and significant. Think carefully as you explain things to patients and check back to have them repeat to you what they think you said.
Be comfortable saying you don’t know
Many symptoms in medicine end up not being diagnosable. When a patient shares symptoms that do not fit a pattern of a disease, it is important to share with them why you think it is okay to wait and watch, even if you do not have a diagnosis.
Patients find it comforting that you are so honest with them. Doing this also has the benefit of gaining patients’ trust when you are sure about something, because it tells them you don’t have an answer for everything.
Ask your patients what they think is causing their symptoms
This way, you know what their big fear is. You can address what they are worried about, even if it isn’t something you are considering.
Patients are often fearful of a disease a close friend or relative has, so when they get new symptoms, they fear diseases that we might not think of. By knowing what they are fearful of, you can reassure when appropriate.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
Possible bivalent vaccine link to strokes in people over 65
who got the shot, the Centers for Disease Control and Prevention and the Food and Drug Administration said in a joint news release.
The release did not recommend people change their vaccine practices, saying the database finding probably did not represent a “true clinical risk.” The CDC said everybody, including people over 65, should stay up to date on their COVID vaccines, including the bivalent booster.
The news release said the Vaccine Safety Datalink (VSD), “a near real-time surveillance system,” raised a safety concern about the Pfizer/BioNTech booster.
“Rapid-response investigation of the signal in the VSD raised a question of whether people 65 and older who have received the Pfizer-BioNTech COVID-19 Vaccine, Bivalent were more likely to have an ischemic stroke in the 21 days following vaccination compared with days 22-44 following vaccination,” the news release said.
Ischemic strokes are blockages of blood to the brain, often caused by blood clots.
“Although the totality of the data currently suggests that it is very unlikely that the signal in VSD (Vaccine Safety Datalink) represents a true clinical risk, we believe it is important to share this information with the public, as we have in the past, when one of our safety monitoring systems detects a signal,” the release said.
No higher likelihood of strokes linked to the Pfizer bivalent vaccine had been found by Pfizer/BioNTech, the Department of Veterans Affairs, the Vaccine Adverse Event Reporting System maintained by the CDC and the FDA, or other agencies that monitor reactions of vaccines, the news release said. No safety issues about strokes have been identified with the Moderna bivalent vaccine.
CNN, citing a CDC official, reported that about 550,000 seniors who got Pfizer bivalent boosters were tracked by the VSD, and 130 of them had strokes within 3 weeks of getting the shot. None of those 130 people died, CNN said. The official spoke on the condition of anonymity because they weren’t authorized to share the data.
The issue will be discussed at the January meeting of the FDA’s Vaccines and Related Biological Products Advisory Committee.
In a joint statement, Pfizer and BioNTech said: “Neither Pfizer and BioNTech nor the CDC or FDA have observed similar findings across numerous other monitoring systems in the U.S. and globally and there is no evidence to conclude that ischemic stroke is associated with the use of the companies’ COVID-19 vaccines.”
Bivalent boosters contain two strains of vaccine – one to protect against the original COVID-19 virus and another targeting Omicron subvariants.
A version of this article first appeared on WebMD.com.
who got the shot, the Centers for Disease Control and Prevention and the Food and Drug Administration said in a joint news release.
The release did not recommend people change their vaccine practices, saying the database finding probably did not represent a “true clinical risk.” The CDC said everybody, including people over 65, should stay up to date on their COVID vaccines, including the bivalent booster.
The news release said the Vaccine Safety Datalink (VSD), “a near real-time surveillance system,” raised a safety concern about the Pfizer/BioNTech booster.
“Rapid-response investigation of the signal in the VSD raised a question of whether people 65 and older who have received the Pfizer-BioNTech COVID-19 Vaccine, Bivalent were more likely to have an ischemic stroke in the 21 days following vaccination compared with days 22-44 following vaccination,” the news release said.
Ischemic strokes are blockages of blood to the brain, often caused by blood clots.
“Although the totality of the data currently suggests that it is very unlikely that the signal in VSD (Vaccine Safety Datalink) represents a true clinical risk, we believe it is important to share this information with the public, as we have in the past, when one of our safety monitoring systems detects a signal,” the release said.
No higher likelihood of strokes linked to the Pfizer bivalent vaccine had been found by Pfizer/BioNTech, the Department of Veterans Affairs, the Vaccine Adverse Event Reporting System maintained by the CDC and the FDA, or other agencies that monitor reactions of vaccines, the news release said. No safety issues about strokes have been identified with the Moderna bivalent vaccine.
CNN, citing a CDC official, reported that about 550,000 seniors who got Pfizer bivalent boosters were tracked by the VSD, and 130 of them had strokes within 3 weeks of getting the shot. None of those 130 people died, CNN said. The official spoke on the condition of anonymity because they weren’t authorized to share the data.
The issue will be discussed at the January meeting of the FDA’s Vaccines and Related Biological Products Advisory Committee.
In a joint statement, Pfizer and BioNTech said: “Neither Pfizer and BioNTech nor the CDC or FDA have observed similar findings across numerous other monitoring systems in the U.S. and globally and there is no evidence to conclude that ischemic stroke is associated with the use of the companies’ COVID-19 vaccines.”
Bivalent boosters contain two strains of vaccine – one to protect against the original COVID-19 virus and another targeting Omicron subvariants.
A version of this article first appeared on WebMD.com.
who got the shot, the Centers for Disease Control and Prevention and the Food and Drug Administration said in a joint news release.
The release did not recommend people change their vaccine practices, saying the database finding probably did not represent a “true clinical risk.” The CDC said everybody, including people over 65, should stay up to date on their COVID vaccines, including the bivalent booster.
The news release said the Vaccine Safety Datalink (VSD), “a near real-time surveillance system,” raised a safety concern about the Pfizer/BioNTech booster.
“Rapid-response investigation of the signal in the VSD raised a question of whether people 65 and older who have received the Pfizer-BioNTech COVID-19 Vaccine, Bivalent were more likely to have an ischemic stroke in the 21 days following vaccination compared with days 22-44 following vaccination,” the news release said.
Ischemic strokes are blockages of blood to the brain, often caused by blood clots.
“Although the totality of the data currently suggests that it is very unlikely that the signal in VSD (Vaccine Safety Datalink) represents a true clinical risk, we believe it is important to share this information with the public, as we have in the past, when one of our safety monitoring systems detects a signal,” the release said.
No higher likelihood of strokes linked to the Pfizer bivalent vaccine had been found by Pfizer/BioNTech, the Department of Veterans Affairs, the Vaccine Adverse Event Reporting System maintained by the CDC and the FDA, or other agencies that monitor reactions of vaccines, the news release said. No safety issues about strokes have been identified with the Moderna bivalent vaccine.
CNN, citing a CDC official, reported that about 550,000 seniors who got Pfizer bivalent boosters were tracked by the VSD, and 130 of them had strokes within 3 weeks of getting the shot. None of those 130 people died, CNN said. The official spoke on the condition of anonymity because they weren’t authorized to share the data.
The issue will be discussed at the January meeting of the FDA’s Vaccines and Related Biological Products Advisory Committee.
In a joint statement, Pfizer and BioNTech said: “Neither Pfizer and BioNTech nor the CDC or FDA have observed similar findings across numerous other monitoring systems in the U.S. and globally and there is no evidence to conclude that ischemic stroke is associated with the use of the companies’ COVID-19 vaccines.”
Bivalent boosters contain two strains of vaccine – one to protect against the original COVID-19 virus and another targeting Omicron subvariants.
A version of this article first appeared on WebMD.com.
CDC frets over further dip in kindergarten vaccination rates
The percentage of kindergarteners in the United States who have received routine vaccines to protect against illnesses such as measles, whooping cough, and polio has declined for 2 straight years, a new study has found.
Drops in vaccine coverage leave communities more susceptible to outbreaks of vaccine-preventable diseases, such as those that occurred in 2022, public health officials said.
Coverage for four vaccines – against measles, mumps, and rubella (MMR); diphtheria, tetanus, and acellular pertussis (DTaP); poliovirus; and varicella – among kindergarten students was about 95% in 2019-2020.
The rate fell to 94% the following year.
For the 2021-2022 school year, coverage dropped another point, to 93%, according to the report, published online in Morbidity and Mortality Weekly Report.
The rate of vaccination overall remains high, but about 250,000 kindergarten students may not be protected against measles, the researchers estimate. Measles, which is highly infectious, can lead to serious illness and even death in children who have not been vaccinated against the virus.
“In 2022, two communities in the United States responded to outbreaks of measles where children have been hospitalized,” Georgina Peacock, MD, MPH, director of the immunization services division of the Centers for Disease Control and Prevention, said in a media briefing about the report. “One community reported a case of paralytic polio in an unvaccinated person. These outbreaks were preventable. The best way to prevent these diseases and their devastating impact on children is through vaccination.”
Exemptions steady
For the new study, Ranee Seither, MPH, with the CDC’s National Center for Immunization and Respiratory Diseases and her colleagues analyzed data reported by states to estimate nationwide coverage for the four routine vaccines.
The number of students with exemptions remained low, at 2.6%, but another 3.9% who were without exemptions were not up to date with the MMR vaccine, the investigators report.
In a separate study, researchers found that vaccination coverage for 2-year-olds has increased. Approximately 70% of children were up to date with a seven-vaccine series by age 24 months. The coverage rate was higher for children born during 2018-2019 than for those born during 2016-2017.
Although the COVID-19 pandemic was not associated with decreased vaccination rates in this younger age group overall, coverage fell by 4-5 percentage points for children living below the poverty level or in rural areas, according to the study.
In addition, uninsured children were eight times more likely than those with private insurance to not be vaccinated by their second birthday, the researchers found.
Strategies to increase vaccination coverage include enforcing school vaccination requirements and holding vaccination clinics at schools, the CDC said.
“Providers should review children’s histories and recommend needed vaccinations during every clinical encounter and address parental hesitancy to help reduce disparities and ensure that all children are protected from vaccine-preventable diseases,” the agency said.
To that end, the agency launched an initiative this week called Let’s RISE (Routine Immunizations on Schedule for Everyone) to provide clinicians with resources to help patients get on track with their immunizations.
Hundreds of thousands unprotected
MMR vaccination coverage for kindergartners is the lowest it has been in over a decade, Dr. Peacock noted. Decreased coverage for kindergarten students might be tied to pandemic-related disruptions in health care systems and schools, she said. School administrators and parents may have been less focused on routine vaccination paperwork amid the return to in-person learning, for instance.
Hesitancy about COVID vaccines could be affecting routine vaccinations. “That’s something that we are watching very closely,” Dr. Peacock said.
The 2-point decrease in vaccination coverage “translates to hundreds of thousands of children starting school without being fully protected” against preventable diseases that can spread easily in classrooms, Sean O’Leary, MD, chair of the American Academy of Pediatrics’ Committee on Infectious Diseases, said.
Despite the drop in coverage, Dr. O’Leary said he saw some encouraging signs in the data: Nonmedical exemptions for kindergarten students have not increased. And the vast majority of parents are still having their children vaccinated. At the same time, the reports highlight a need to address child poverty and improve vaccine access in rural areas, he said.
A version of this article first appeared on Medscape.com.
The percentage of kindergarteners in the United States who have received routine vaccines to protect against illnesses such as measles, whooping cough, and polio has declined for 2 straight years, a new study has found.
Drops in vaccine coverage leave communities more susceptible to outbreaks of vaccine-preventable diseases, such as those that occurred in 2022, public health officials said.
Coverage for four vaccines – against measles, mumps, and rubella (MMR); diphtheria, tetanus, and acellular pertussis (DTaP); poliovirus; and varicella – among kindergarten students was about 95% in 2019-2020.
The rate fell to 94% the following year.
For the 2021-2022 school year, coverage dropped another point, to 93%, according to the report, published online in Morbidity and Mortality Weekly Report.
The rate of vaccination overall remains high, but about 250,000 kindergarten students may not be protected against measles, the researchers estimate. Measles, which is highly infectious, can lead to serious illness and even death in children who have not been vaccinated against the virus.
“In 2022, two communities in the United States responded to outbreaks of measles where children have been hospitalized,” Georgina Peacock, MD, MPH, director of the immunization services division of the Centers for Disease Control and Prevention, said in a media briefing about the report. “One community reported a case of paralytic polio in an unvaccinated person. These outbreaks were preventable. The best way to prevent these diseases and their devastating impact on children is through vaccination.”
Exemptions steady
For the new study, Ranee Seither, MPH, with the CDC’s National Center for Immunization and Respiratory Diseases and her colleagues analyzed data reported by states to estimate nationwide coverage for the four routine vaccines.
The number of students with exemptions remained low, at 2.6%, but another 3.9% who were without exemptions were not up to date with the MMR vaccine, the investigators report.
In a separate study, researchers found that vaccination coverage for 2-year-olds has increased. Approximately 70% of children were up to date with a seven-vaccine series by age 24 months. The coverage rate was higher for children born during 2018-2019 than for those born during 2016-2017.
Although the COVID-19 pandemic was not associated with decreased vaccination rates in this younger age group overall, coverage fell by 4-5 percentage points for children living below the poverty level or in rural areas, according to the study.
In addition, uninsured children were eight times more likely than those with private insurance to not be vaccinated by their second birthday, the researchers found.
Strategies to increase vaccination coverage include enforcing school vaccination requirements and holding vaccination clinics at schools, the CDC said.
“Providers should review children’s histories and recommend needed vaccinations during every clinical encounter and address parental hesitancy to help reduce disparities and ensure that all children are protected from vaccine-preventable diseases,” the agency said.
To that end, the agency launched an initiative this week called Let’s RISE (Routine Immunizations on Schedule for Everyone) to provide clinicians with resources to help patients get on track with their immunizations.
Hundreds of thousands unprotected
MMR vaccination coverage for kindergartners is the lowest it has been in over a decade, Dr. Peacock noted. Decreased coverage for kindergarten students might be tied to pandemic-related disruptions in health care systems and schools, she said. School administrators and parents may have been less focused on routine vaccination paperwork amid the return to in-person learning, for instance.
Hesitancy about COVID vaccines could be affecting routine vaccinations. “That’s something that we are watching very closely,” Dr. Peacock said.
The 2-point decrease in vaccination coverage “translates to hundreds of thousands of children starting school without being fully protected” against preventable diseases that can spread easily in classrooms, Sean O’Leary, MD, chair of the American Academy of Pediatrics’ Committee on Infectious Diseases, said.
Despite the drop in coverage, Dr. O’Leary said he saw some encouraging signs in the data: Nonmedical exemptions for kindergarten students have not increased. And the vast majority of parents are still having their children vaccinated. At the same time, the reports highlight a need to address child poverty and improve vaccine access in rural areas, he said.
A version of this article first appeared on Medscape.com.
The percentage of kindergarteners in the United States who have received routine vaccines to protect against illnesses such as measles, whooping cough, and polio has declined for 2 straight years, a new study has found.
Drops in vaccine coverage leave communities more susceptible to outbreaks of vaccine-preventable diseases, such as those that occurred in 2022, public health officials said.
Coverage for four vaccines – against measles, mumps, and rubella (MMR); diphtheria, tetanus, and acellular pertussis (DTaP); poliovirus; and varicella – among kindergarten students was about 95% in 2019-2020.
The rate fell to 94% the following year.
For the 2021-2022 school year, coverage dropped another point, to 93%, according to the report, published online in Morbidity and Mortality Weekly Report.
The rate of vaccination overall remains high, but about 250,000 kindergarten students may not be protected against measles, the researchers estimate. Measles, which is highly infectious, can lead to serious illness and even death in children who have not been vaccinated against the virus.
“In 2022, two communities in the United States responded to outbreaks of measles where children have been hospitalized,” Georgina Peacock, MD, MPH, director of the immunization services division of the Centers for Disease Control and Prevention, said in a media briefing about the report. “One community reported a case of paralytic polio in an unvaccinated person. These outbreaks were preventable. The best way to prevent these diseases and their devastating impact on children is through vaccination.”
Exemptions steady
For the new study, Ranee Seither, MPH, with the CDC’s National Center for Immunization and Respiratory Diseases and her colleagues analyzed data reported by states to estimate nationwide coverage for the four routine vaccines.
The number of students with exemptions remained low, at 2.6%, but another 3.9% who were without exemptions were not up to date with the MMR vaccine, the investigators report.
In a separate study, researchers found that vaccination coverage for 2-year-olds has increased. Approximately 70% of children were up to date with a seven-vaccine series by age 24 months. The coverage rate was higher for children born during 2018-2019 than for those born during 2016-2017.
Although the COVID-19 pandemic was not associated with decreased vaccination rates in this younger age group overall, coverage fell by 4-5 percentage points for children living below the poverty level or in rural areas, according to the study.
In addition, uninsured children were eight times more likely than those with private insurance to not be vaccinated by their second birthday, the researchers found.
Strategies to increase vaccination coverage include enforcing school vaccination requirements and holding vaccination clinics at schools, the CDC said.
“Providers should review children’s histories and recommend needed vaccinations during every clinical encounter and address parental hesitancy to help reduce disparities and ensure that all children are protected from vaccine-preventable diseases,” the agency said.
To that end, the agency launched an initiative this week called Let’s RISE (Routine Immunizations on Schedule for Everyone) to provide clinicians with resources to help patients get on track with their immunizations.
Hundreds of thousands unprotected
MMR vaccination coverage for kindergartners is the lowest it has been in over a decade, Dr. Peacock noted. Decreased coverage for kindergarten students might be tied to pandemic-related disruptions in health care systems and schools, she said. School administrators and parents may have been less focused on routine vaccination paperwork amid the return to in-person learning, for instance.
Hesitancy about COVID vaccines could be affecting routine vaccinations. “That’s something that we are watching very closely,” Dr. Peacock said.
The 2-point decrease in vaccination coverage “translates to hundreds of thousands of children starting school without being fully protected” against preventable diseases that can spread easily in classrooms, Sean O’Leary, MD, chair of the American Academy of Pediatrics’ Committee on Infectious Diseases, said.
Despite the drop in coverage, Dr. O’Leary said he saw some encouraging signs in the data: Nonmedical exemptions for kindergarten students have not increased. And the vast majority of parents are still having their children vaccinated. At the same time, the reports highlight a need to address child poverty and improve vaccine access in rural areas, he said.
A version of this article first appeared on Medscape.com.
FROM THE MMWR
Children and COVID: ED visits and hospitalizations start to fall again
Emergency department visits and hospitalizations for COVID-19 in children appear to be following the declining trend set by weekly cases since early December, based on data from the Centers for Disease Control and Prevention.
. New cases took a different path that had the weekly total falling through November before taking a big jump during the week of Nov. 27 to Dec. 3 – the count doubled from 30,000 the previous week to 63,000 – and then decreased again, the CDC reported.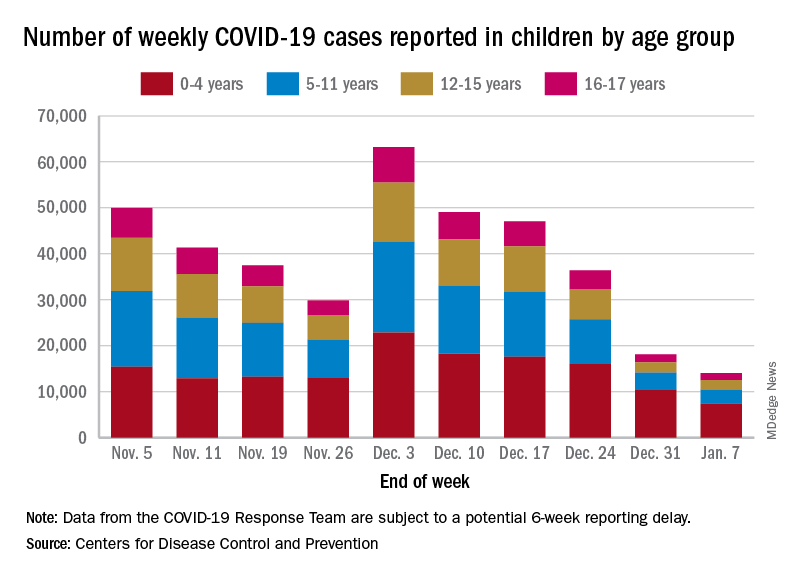
The proportion of ED visits with COVID, which was down to 1.0% of all ED visits (7-day average) for children aged 0-4 years on Nov. 4, was up to 3.2% on Jan. 3 but slipped to 2.5% as of Jan. 10. The patterns for older children are similar, with some differences in timing and lower peaks (1.7% for 12- to 15-year-olds and 1.9% for those aged 16-17), according to the CDC’s COVID Data Tracker.
The trend for new hospital admissions of children with confirmed COVID showed a similar rise through December, and the latest data for the very beginning of January suggest an even faster drop, although there is more of a reporting lag with hospitalization data, compared with ED visits, the CDC noted.
The most current data (Dec. 30 to Jan. 5) available from the American Academy of Pediatrics and the Children’s Hospital Association show less volatility in the number of weekly cases through November and December, with the peak being about 48,000 in mid-December. The AAP/CHA totals for the last 2 weeks, however, were both higher than the CDC’s corresponding counts, which are more preliminary and subject to revision.
The CDC puts the total number of COVID cases in children at 16.7 million – about 17.2% of all cases – as of Jan. 11, with 1,981 deaths reported so far. The AAP and CHA are not tracking deaths, but their case total as of Jan. 5 was 15.2 million, which represents 18.1% of cases in all ages. The AAP/CHA report is based on data reported publicly by an ever-decreasing number of states and territories.
Emergency department visits and hospitalizations for COVID-19 in children appear to be following the declining trend set by weekly cases since early December, based on data from the Centers for Disease Control and Prevention.
. New cases took a different path that had the weekly total falling through November before taking a big jump during the week of Nov. 27 to Dec. 3 – the count doubled from 30,000 the previous week to 63,000 – and then decreased again, the CDC reported.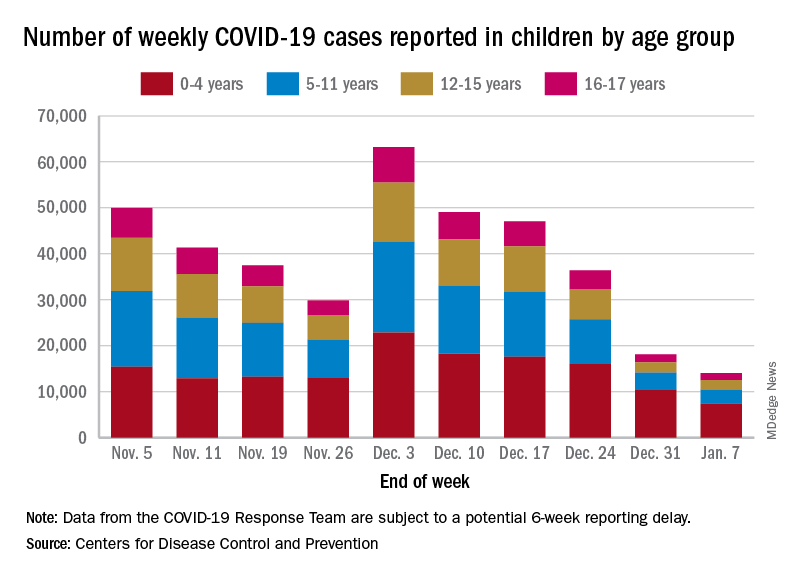
The proportion of ED visits with COVID, which was down to 1.0% of all ED visits (7-day average) for children aged 0-4 years on Nov. 4, was up to 3.2% on Jan. 3 but slipped to 2.5% as of Jan. 10. The patterns for older children are similar, with some differences in timing and lower peaks (1.7% for 12- to 15-year-olds and 1.9% for those aged 16-17), according to the CDC’s COVID Data Tracker.
The trend for new hospital admissions of children with confirmed COVID showed a similar rise through December, and the latest data for the very beginning of January suggest an even faster drop, although there is more of a reporting lag with hospitalization data, compared with ED visits, the CDC noted.
The most current data (Dec. 30 to Jan. 5) available from the American Academy of Pediatrics and the Children’s Hospital Association show less volatility in the number of weekly cases through November and December, with the peak being about 48,000 in mid-December. The AAP/CHA totals for the last 2 weeks, however, were both higher than the CDC’s corresponding counts, which are more preliminary and subject to revision.
The CDC puts the total number of COVID cases in children at 16.7 million – about 17.2% of all cases – as of Jan. 11, with 1,981 deaths reported so far. The AAP and CHA are not tracking deaths, but their case total as of Jan. 5 was 15.2 million, which represents 18.1% of cases in all ages. The AAP/CHA report is based on data reported publicly by an ever-decreasing number of states and territories.
Emergency department visits and hospitalizations for COVID-19 in children appear to be following the declining trend set by weekly cases since early December, based on data from the Centers for Disease Control and Prevention.
. New cases took a different path that had the weekly total falling through November before taking a big jump during the week of Nov. 27 to Dec. 3 – the count doubled from 30,000 the previous week to 63,000 – and then decreased again, the CDC reported.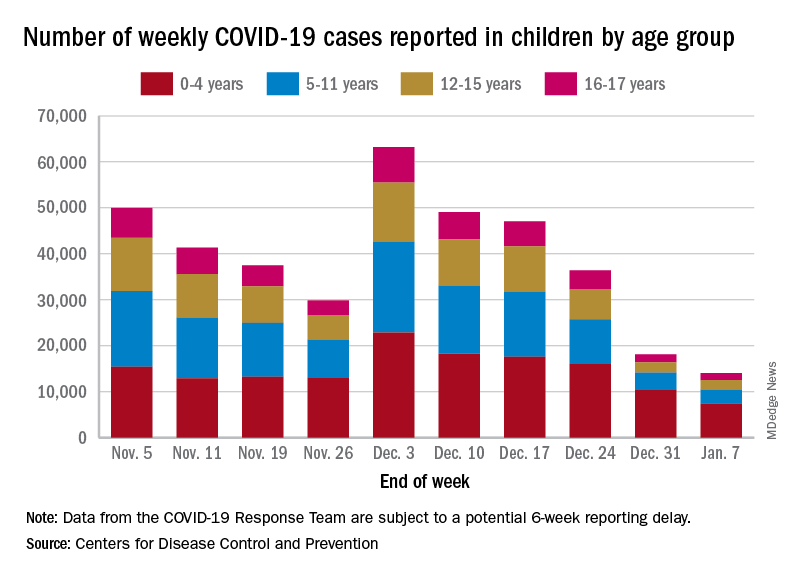
The proportion of ED visits with COVID, which was down to 1.0% of all ED visits (7-day average) for children aged 0-4 years on Nov. 4, was up to 3.2% on Jan. 3 but slipped to 2.5% as of Jan. 10. The patterns for older children are similar, with some differences in timing and lower peaks (1.7% for 12- to 15-year-olds and 1.9% for those aged 16-17), according to the CDC’s COVID Data Tracker.
The trend for new hospital admissions of children with confirmed COVID showed a similar rise through December, and the latest data for the very beginning of January suggest an even faster drop, although there is more of a reporting lag with hospitalization data, compared with ED visits, the CDC noted.
The most current data (Dec. 30 to Jan. 5) available from the American Academy of Pediatrics and the Children’s Hospital Association show less volatility in the number of weekly cases through November and December, with the peak being about 48,000 in mid-December. The AAP/CHA totals for the last 2 weeks, however, were both higher than the CDC’s corresponding counts, which are more preliminary and subject to revision.
The CDC puts the total number of COVID cases in children at 16.7 million – about 17.2% of all cases – as of Jan. 11, with 1,981 deaths reported so far. The AAP and CHA are not tracking deaths, but their case total as of Jan. 5 was 15.2 million, which represents 18.1% of cases in all ages. The AAP/CHA report is based on data reported publicly by an ever-decreasing number of states and territories.
Add this to the list of long COVID symptoms: Stigma
Most people with long COVID find they’re facing stigma due to their condition, according to a new report from researchers in the United Kingdom. In short: Relatives and friends may not believe they’re truly sick.
The U.K. team found that more than three-quarters of people studied had experienced stigma often or always.
In fact, 95% of people with long COVID faced at least one type of stigma at least sometimes, according to the study, published in November in the journal PLOS One.
Those conclusions had surprised the study’s lead researcher, Marija Pantelic, PhD, a public health lecturer at Brighton and Sussex Medical School, England.
“After years of working on HIV-related stigma, I was shocked to see how many people were turning a blind eye to and dismissing the difficulties experienced by people with long COVID,” Dr. Pantelic says. “It has also been clear to me from the start that this stigma is detrimental not just for people’s dignity, but also public health.”
Even some doctors argue that the growing attention paid to long COVID is excessive.
“It’s often normal to experience mild fatigue or weaknesses for weeks after being sick and inactive and not eating well. Calling these cases long COVID is the medicalization of modern life,” Marty Makary, MD, a surgeon and public policy researcher at Johns Hopkins University, Baltimore, wrote in a commentary in the Wall Street Journal.
Other doctors strongly disagree, including Alba Azola, MD, codirector of the Johns Hopkins Post-Acute COVID-19 Team and an expert in the stigma surrounding long COVID.
“Putting that spin on things, it’s just hurting people,” she says.
One example is people who cannot return to work.
“A lot of their family members tell me that they’re being lazy,” Dr. Azola says. “That’s part of the public stigma, that these are people just trying to get out of work.”
Some experts say the U.K. study represents a landmark.
“When you have data like this on long COVID stigma, it becomes more difficult to deny its existence or address it,” says Naomi Torres-Mackie, PhD, a clinical psychologist at Lenox Hill Hospital in New York. She also is head of research at the New York–based Mental Health Coalition, a group of experts working to end the stigma surrounding mental health.
She recalls her first patient with long COVID.
“She experienced the discomfort and pain itself, and then she had this crushing feeling that it wasn’t valid, or real. She felt very alone in it,” Dr. Torres-Mackie says.
Another one of her patients is working at her job from home but facing doubt about her condition from her employers.
“Every month, her medical doctor has to produce a letter confirming her medical condition,” Dr. Torres-Mackie says.
Taking part in the British stigma survey were 1,166 people, including 966 residents of the United Kingdom, with the average age of 48. Nearly 85% were female, and more than three-quarters were educated at the university level or higher.
Half of them said they had a clinical diagnosis of long COVID.
More than 60% of them said that at least some of the time, they were cautious about who they talked to about their condition. And fully 34% of those who did disclose their diagnosis said that they regretted having done so.
That’s a difficult experience for those with long COVID, says Leonard Jason, PhD, a professor of psychology at DePaul University in Chicago.
“It’s like they’re traumatized by the initial experience of being sick, and retraumatized by the response of others to them,” he says.
Unexplained illnesses are not well-regarded by the general public, Dr. Jason says.
He gave the example of multiple sclerosis. Before the 1980s, those with MS were considered to have a psychological illness, he says. “Then, in the 1980s, there were biomarkers that said, ‘Here’s the evidence.’ ”
The British study described three types of stigma stemming from the long COVID diagnosis of those questioned:
- Enacted stigma: People were directly treated unfairly because of their condition.
- Internalized stigma: People felt embarrassed by that condition.
- Anticipated stigma: People expected they would be treated poorly because of their diagnosis.
Dr. Azola calls the medical community a major problem when it comes to dealing with long COVID.
“What I see with my patients is medical trauma,” she says. They may have symptoms that send them to the emergency room, and then the tests come back negative. “Instead of tracking the patients’ symptoms, patients get told, ‘Everything looks good, you can go home, this is a panic attack,’ ” she says.
Some people go online to search for treatments, sometimes launching GoFundMe campaigns to raise money for unreliable treatments.
Long COVID patients may have gone through 5 to 10 doctors before they arrive for treatment with the Johns Hopkins Post-Acute COVID-19 Team. The clinic began in April 2020 remotely and in August of that year in person.
Today, the clinic staff spends an hour with a first-time long COVID patient, hearing their stories and helping relieve anxiety, Dr. Azola says.
The phenomenon of long COVID is similar to what patients have had with chronic fatigue syndrome, lupus, or fibromyalgia, where people have symptoms that are hard to explain, says Jennifer Chevinsky, MD, deputy public health officer for Riverside County, Calif.
“Stigma within medicine or health care is nothing new,” she says.
In Chicago, Dr. Jason notes that the federal government’s decision to invest hundreds of millions of dollars in long COVID research “shows the government is helping destigmatize it.”
Dr. Pantelic says she and her colleagues are continuing their research.
“We are interested in understanding the impacts of this stigma, and how to mitigate any adverse outcomes for patients and services,” she says.
A version of this article first appeared on WebMD.com.
Most people with long COVID find they’re facing stigma due to their condition, according to a new report from researchers in the United Kingdom. In short: Relatives and friends may not believe they’re truly sick.
The U.K. team found that more than three-quarters of people studied had experienced stigma often or always.
In fact, 95% of people with long COVID faced at least one type of stigma at least sometimes, according to the study, published in November in the journal PLOS One.
Those conclusions had surprised the study’s lead researcher, Marija Pantelic, PhD, a public health lecturer at Brighton and Sussex Medical School, England.
“After years of working on HIV-related stigma, I was shocked to see how many people were turning a blind eye to and dismissing the difficulties experienced by people with long COVID,” Dr. Pantelic says. “It has also been clear to me from the start that this stigma is detrimental not just for people’s dignity, but also public health.”
Even some doctors argue that the growing attention paid to long COVID is excessive.
“It’s often normal to experience mild fatigue or weaknesses for weeks after being sick and inactive and not eating well. Calling these cases long COVID is the medicalization of modern life,” Marty Makary, MD, a surgeon and public policy researcher at Johns Hopkins University, Baltimore, wrote in a commentary in the Wall Street Journal.
Other doctors strongly disagree, including Alba Azola, MD, codirector of the Johns Hopkins Post-Acute COVID-19 Team and an expert in the stigma surrounding long COVID.
“Putting that spin on things, it’s just hurting people,” she says.
One example is people who cannot return to work.
“A lot of their family members tell me that they’re being lazy,” Dr. Azola says. “That’s part of the public stigma, that these are people just trying to get out of work.”
Some experts say the U.K. study represents a landmark.
“When you have data like this on long COVID stigma, it becomes more difficult to deny its existence or address it,” says Naomi Torres-Mackie, PhD, a clinical psychologist at Lenox Hill Hospital in New York. She also is head of research at the New York–based Mental Health Coalition, a group of experts working to end the stigma surrounding mental health.
She recalls her first patient with long COVID.
“She experienced the discomfort and pain itself, and then she had this crushing feeling that it wasn’t valid, or real. She felt very alone in it,” Dr. Torres-Mackie says.
Another one of her patients is working at her job from home but facing doubt about her condition from her employers.
“Every month, her medical doctor has to produce a letter confirming her medical condition,” Dr. Torres-Mackie says.
Taking part in the British stigma survey were 1,166 people, including 966 residents of the United Kingdom, with the average age of 48. Nearly 85% were female, and more than three-quarters were educated at the university level or higher.
Half of them said they had a clinical diagnosis of long COVID.
More than 60% of them said that at least some of the time, they were cautious about who they talked to about their condition. And fully 34% of those who did disclose their diagnosis said that they regretted having done so.
That’s a difficult experience for those with long COVID, says Leonard Jason, PhD, a professor of psychology at DePaul University in Chicago.
“It’s like they’re traumatized by the initial experience of being sick, and retraumatized by the response of others to them,” he says.
Unexplained illnesses are not well-regarded by the general public, Dr. Jason says.
He gave the example of multiple sclerosis. Before the 1980s, those with MS were considered to have a psychological illness, he says. “Then, in the 1980s, there were biomarkers that said, ‘Here’s the evidence.’ ”
The British study described three types of stigma stemming from the long COVID diagnosis of those questioned:
- Enacted stigma: People were directly treated unfairly because of their condition.
- Internalized stigma: People felt embarrassed by that condition.
- Anticipated stigma: People expected they would be treated poorly because of their diagnosis.
Dr. Azola calls the medical community a major problem when it comes to dealing with long COVID.
“What I see with my patients is medical trauma,” she says. They may have symptoms that send them to the emergency room, and then the tests come back negative. “Instead of tracking the patients’ symptoms, patients get told, ‘Everything looks good, you can go home, this is a panic attack,’ ” she says.
Some people go online to search for treatments, sometimes launching GoFundMe campaigns to raise money for unreliable treatments.
Long COVID patients may have gone through 5 to 10 doctors before they arrive for treatment with the Johns Hopkins Post-Acute COVID-19 Team. The clinic began in April 2020 remotely and in August of that year in person.
Today, the clinic staff spends an hour with a first-time long COVID patient, hearing their stories and helping relieve anxiety, Dr. Azola says.
The phenomenon of long COVID is similar to what patients have had with chronic fatigue syndrome, lupus, or fibromyalgia, where people have symptoms that are hard to explain, says Jennifer Chevinsky, MD, deputy public health officer for Riverside County, Calif.
“Stigma within medicine or health care is nothing new,” she says.
In Chicago, Dr. Jason notes that the federal government’s decision to invest hundreds of millions of dollars in long COVID research “shows the government is helping destigmatize it.”
Dr. Pantelic says she and her colleagues are continuing their research.
“We are interested in understanding the impacts of this stigma, and how to mitigate any adverse outcomes for patients and services,” she says.
A version of this article first appeared on WebMD.com.
Most people with long COVID find they’re facing stigma due to their condition, according to a new report from researchers in the United Kingdom. In short: Relatives and friends may not believe they’re truly sick.
The U.K. team found that more than three-quarters of people studied had experienced stigma often or always.
In fact, 95% of people with long COVID faced at least one type of stigma at least sometimes, according to the study, published in November in the journal PLOS One.
Those conclusions had surprised the study’s lead researcher, Marija Pantelic, PhD, a public health lecturer at Brighton and Sussex Medical School, England.
“After years of working on HIV-related stigma, I was shocked to see how many people were turning a blind eye to and dismissing the difficulties experienced by people with long COVID,” Dr. Pantelic says. “It has also been clear to me from the start that this stigma is detrimental not just for people’s dignity, but also public health.”
Even some doctors argue that the growing attention paid to long COVID is excessive.
“It’s often normal to experience mild fatigue or weaknesses for weeks after being sick and inactive and not eating well. Calling these cases long COVID is the medicalization of modern life,” Marty Makary, MD, a surgeon and public policy researcher at Johns Hopkins University, Baltimore, wrote in a commentary in the Wall Street Journal.
Other doctors strongly disagree, including Alba Azola, MD, codirector of the Johns Hopkins Post-Acute COVID-19 Team and an expert in the stigma surrounding long COVID.
“Putting that spin on things, it’s just hurting people,” she says.
One example is people who cannot return to work.
“A lot of their family members tell me that they’re being lazy,” Dr. Azola says. “That’s part of the public stigma, that these are people just trying to get out of work.”
Some experts say the U.K. study represents a landmark.
“When you have data like this on long COVID stigma, it becomes more difficult to deny its existence or address it,” says Naomi Torres-Mackie, PhD, a clinical psychologist at Lenox Hill Hospital in New York. She also is head of research at the New York–based Mental Health Coalition, a group of experts working to end the stigma surrounding mental health.
She recalls her first patient with long COVID.
“She experienced the discomfort and pain itself, and then she had this crushing feeling that it wasn’t valid, or real. She felt very alone in it,” Dr. Torres-Mackie says.
Another one of her patients is working at her job from home but facing doubt about her condition from her employers.
“Every month, her medical doctor has to produce a letter confirming her medical condition,” Dr. Torres-Mackie says.
Taking part in the British stigma survey were 1,166 people, including 966 residents of the United Kingdom, with the average age of 48. Nearly 85% were female, and more than three-quarters were educated at the university level or higher.
Half of them said they had a clinical diagnosis of long COVID.
More than 60% of them said that at least some of the time, they were cautious about who they talked to about their condition. And fully 34% of those who did disclose their diagnosis said that they regretted having done so.
That’s a difficult experience for those with long COVID, says Leonard Jason, PhD, a professor of psychology at DePaul University in Chicago.
“It’s like they’re traumatized by the initial experience of being sick, and retraumatized by the response of others to them,” he says.
Unexplained illnesses are not well-regarded by the general public, Dr. Jason says.
He gave the example of multiple sclerosis. Before the 1980s, those with MS were considered to have a psychological illness, he says. “Then, in the 1980s, there were biomarkers that said, ‘Here’s the evidence.’ ”
The British study described three types of stigma stemming from the long COVID diagnosis of those questioned:
- Enacted stigma: People were directly treated unfairly because of their condition.
- Internalized stigma: People felt embarrassed by that condition.
- Anticipated stigma: People expected they would be treated poorly because of their diagnosis.
Dr. Azola calls the medical community a major problem when it comes to dealing with long COVID.
“What I see with my patients is medical trauma,” she says. They may have symptoms that send them to the emergency room, and then the tests come back negative. “Instead of tracking the patients’ symptoms, patients get told, ‘Everything looks good, you can go home, this is a panic attack,’ ” she says.
Some people go online to search for treatments, sometimes launching GoFundMe campaigns to raise money for unreliable treatments.
Long COVID patients may have gone through 5 to 10 doctors before they arrive for treatment with the Johns Hopkins Post-Acute COVID-19 Team. The clinic began in April 2020 remotely and in August of that year in person.
Today, the clinic staff spends an hour with a first-time long COVID patient, hearing their stories and helping relieve anxiety, Dr. Azola says.
The phenomenon of long COVID is similar to what patients have had with chronic fatigue syndrome, lupus, or fibromyalgia, where people have symptoms that are hard to explain, says Jennifer Chevinsky, MD, deputy public health officer for Riverside County, Calif.
“Stigma within medicine or health care is nothing new,” she says.
In Chicago, Dr. Jason notes that the federal government’s decision to invest hundreds of millions of dollars in long COVID research “shows the government is helping destigmatize it.”
Dr. Pantelic says she and her colleagues are continuing their research.
“We are interested in understanding the impacts of this stigma, and how to mitigate any adverse outcomes for patients and services,” she says.
A version of this article first appeared on WebMD.com.
PLOS ONE
What the FTC’s proposed ban on noncompete agreements could mean for physicians, other clinicians
The proposed rule seeks to ban companies from enforcing noncompete clauses in employment contracts, a practice that represents an “unfair method of competition” with “exploitative and widespread” impacts, including suppression of wages, innovation, and entrepreneurial spirit, the FTC said. The public has 60 days to submit comments on the proposal before the FTC issues the final rule.
Employers often include noncompete clauses in physician contracts because they want to avoid having patients leave their health care system and follow a doctor to a competitor. A 2018 survey of primary care physicians found that about half of office-based physicians and 37% of physicians employed at hospitals or freestanding care centers were bound by restrictive covenants.
“A federal ban on noncompete agreements will ensure that physicians nationwide can finally change jobs without fear of being sued,” Erik B. Smith, MD, JD, clinical assistant professor of anesthesiology at the University of Southern California, Los Angeles, said in an interview.
Many doctors would like to see noncompete agreements vanish, but some physicians still favor them.
“As a small-practice owner, I am personally against this. The noncompete helps me take a risk and hire a physician. It typically takes 2-3 years for me to break even. I think this will further consolidate employment with large hospital systems unfortunately,” Texas cardiologist Rishin Shah, MD, recently tweeted in response to the FTC announcement.
Dr. Smith, who has advocated for noncompete reform, said about half of states currently allow the controversial clauses.
However, several states have recently passed laws restricting their use. California, North Dakota, and Oklahoma ban noncompetes, although some narrowly defined exceptions, such as the sale of a business, remain.
Other states, like Colorado, Illinois, and Oregon, broadly ban noncompete clauses, except for workers earning above a certain threshold. For example, in Colorado, noncompete agreements are permitted for highly compensated employees earning more than $101,250.
Despite additional restrictions on noncompete agreements for workers in the District of Columbia, the new legislation does not apply to physicians earning total compensation of $250,000 or more. However, their employers must define the geographic parameters of the noncompete and limit postemployment restrictions to 2 years.
Restrictive covenants are “uniquely challenging to family medicine’s emphasis on longitudinal care and the patient-physician relationship,” said Tochi Iroku-Malize, MD, MPH, president of the American Academy of Family Physicians. The limitations imposed by noncompete agreements “potentially reduce patient choice, lower the quality of care for patients, and ultimately harm the foundation of family medicine – our relationships with our patients.”
Although the proposed rule aligns with President Biden’s executive order promoting economic competition, Dr. Smith said a national ban on noncompete agreements may push the limits of FTC authority.
“This new rule will certainly result in a ‘major questions doctrine’ Supreme Court challenge,” said Dr. Smith, and possibly be struck down if the court determines an administrative overstep into areas of “vast economic or political significance.”
A controversial policy
The American Medical Association’s code of ethics discourages covenants that “unreasonably restrict” the ability of physicians to practice following contract termination. And in 2022, the AMA cited “overly broad” noncompete language as a red flag young physicians should watch out for during contract negotiations.
But in 2020, the AMA asked the FTC not to use its rulemaking authority to regulate noncompete clauses in physician employment contracts, and instead, relegate enforcement of such agreements to each state. The American Hospital Association expressed similar views.
Still, the FTC said that eliminating noncompete clauses will increase annual wages by $300 billion, allow 30 million Americans to pursue better job opportunities, and encourage hiring competition among employers. It will also save consumers up to $148 billion in health care costs annually.
“Noncompetes block workers from freely switching jobs, depriving them of higher wages and better working conditions, and depriving businesses of a talent pool that they need to build and expand,” Lina M. Khan, FTC chair, said in a press release about the proposal.
A national ban on noncompetes would keep more physicians in the industry and practicing in their communities, a win for patients and providers, said Dr. Smith. It could also compel employers to offer more competitive employment packages, including fair wages, better work conditions, and a culture of well-being and patient safety.
“Whatever the final rule is, I’m certain it will be legally challenged,” said Dr. Smith, adding that the nation’s most prominent business lobbying group, the Chamber of Commerce, has already issued a statement calling the rule “blatantly unlawful."
A version of this article first appeared on Medscape.com.
The proposed rule seeks to ban companies from enforcing noncompete clauses in employment contracts, a practice that represents an “unfair method of competition” with “exploitative and widespread” impacts, including suppression of wages, innovation, and entrepreneurial spirit, the FTC said. The public has 60 days to submit comments on the proposal before the FTC issues the final rule.
Employers often include noncompete clauses in physician contracts because they want to avoid having patients leave their health care system and follow a doctor to a competitor. A 2018 survey of primary care physicians found that about half of office-based physicians and 37% of physicians employed at hospitals or freestanding care centers were bound by restrictive covenants.
“A federal ban on noncompete agreements will ensure that physicians nationwide can finally change jobs without fear of being sued,” Erik B. Smith, MD, JD, clinical assistant professor of anesthesiology at the University of Southern California, Los Angeles, said in an interview.
Many doctors would like to see noncompete agreements vanish, but some physicians still favor them.
“As a small-practice owner, I am personally against this. The noncompete helps me take a risk and hire a physician. It typically takes 2-3 years for me to break even. I think this will further consolidate employment with large hospital systems unfortunately,” Texas cardiologist Rishin Shah, MD, recently tweeted in response to the FTC announcement.
Dr. Smith, who has advocated for noncompete reform, said about half of states currently allow the controversial clauses.
However, several states have recently passed laws restricting their use. California, North Dakota, and Oklahoma ban noncompetes, although some narrowly defined exceptions, such as the sale of a business, remain.
Other states, like Colorado, Illinois, and Oregon, broadly ban noncompete clauses, except for workers earning above a certain threshold. For example, in Colorado, noncompete agreements are permitted for highly compensated employees earning more than $101,250.
Despite additional restrictions on noncompete agreements for workers in the District of Columbia, the new legislation does not apply to physicians earning total compensation of $250,000 or more. However, their employers must define the geographic parameters of the noncompete and limit postemployment restrictions to 2 years.
Restrictive covenants are “uniquely challenging to family medicine’s emphasis on longitudinal care and the patient-physician relationship,” said Tochi Iroku-Malize, MD, MPH, president of the American Academy of Family Physicians. The limitations imposed by noncompete agreements “potentially reduce patient choice, lower the quality of care for patients, and ultimately harm the foundation of family medicine – our relationships with our patients.”
Although the proposed rule aligns with President Biden’s executive order promoting economic competition, Dr. Smith said a national ban on noncompete agreements may push the limits of FTC authority.
“This new rule will certainly result in a ‘major questions doctrine’ Supreme Court challenge,” said Dr. Smith, and possibly be struck down if the court determines an administrative overstep into areas of “vast economic or political significance.”
A controversial policy
The American Medical Association’s code of ethics discourages covenants that “unreasonably restrict” the ability of physicians to practice following contract termination. And in 2022, the AMA cited “overly broad” noncompete language as a red flag young physicians should watch out for during contract negotiations.
But in 2020, the AMA asked the FTC not to use its rulemaking authority to regulate noncompete clauses in physician employment contracts, and instead, relegate enforcement of such agreements to each state. The American Hospital Association expressed similar views.
Still, the FTC said that eliminating noncompete clauses will increase annual wages by $300 billion, allow 30 million Americans to pursue better job opportunities, and encourage hiring competition among employers. It will also save consumers up to $148 billion in health care costs annually.
“Noncompetes block workers from freely switching jobs, depriving them of higher wages and better working conditions, and depriving businesses of a talent pool that they need to build and expand,” Lina M. Khan, FTC chair, said in a press release about the proposal.
A national ban on noncompetes would keep more physicians in the industry and practicing in their communities, a win for patients and providers, said Dr. Smith. It could also compel employers to offer more competitive employment packages, including fair wages, better work conditions, and a culture of well-being and patient safety.
“Whatever the final rule is, I’m certain it will be legally challenged,” said Dr. Smith, adding that the nation’s most prominent business lobbying group, the Chamber of Commerce, has already issued a statement calling the rule “blatantly unlawful."
A version of this article first appeared on Medscape.com.
The proposed rule seeks to ban companies from enforcing noncompete clauses in employment contracts, a practice that represents an “unfair method of competition” with “exploitative and widespread” impacts, including suppression of wages, innovation, and entrepreneurial spirit, the FTC said. The public has 60 days to submit comments on the proposal before the FTC issues the final rule.
Employers often include noncompete clauses in physician contracts because they want to avoid having patients leave their health care system and follow a doctor to a competitor. A 2018 survey of primary care physicians found that about half of office-based physicians and 37% of physicians employed at hospitals or freestanding care centers were bound by restrictive covenants.
“A federal ban on noncompete agreements will ensure that physicians nationwide can finally change jobs without fear of being sued,” Erik B. Smith, MD, JD, clinical assistant professor of anesthesiology at the University of Southern California, Los Angeles, said in an interview.
Many doctors would like to see noncompete agreements vanish, but some physicians still favor them.
“As a small-practice owner, I am personally against this. The noncompete helps me take a risk and hire a physician. It typically takes 2-3 years for me to break even. I think this will further consolidate employment with large hospital systems unfortunately,” Texas cardiologist Rishin Shah, MD, recently tweeted in response to the FTC announcement.
Dr. Smith, who has advocated for noncompete reform, said about half of states currently allow the controversial clauses.
However, several states have recently passed laws restricting their use. California, North Dakota, and Oklahoma ban noncompetes, although some narrowly defined exceptions, such as the sale of a business, remain.
Other states, like Colorado, Illinois, and Oregon, broadly ban noncompete clauses, except for workers earning above a certain threshold. For example, in Colorado, noncompete agreements are permitted for highly compensated employees earning more than $101,250.
Despite additional restrictions on noncompete agreements for workers in the District of Columbia, the new legislation does not apply to physicians earning total compensation of $250,000 or more. However, their employers must define the geographic parameters of the noncompete and limit postemployment restrictions to 2 years.
Restrictive covenants are “uniquely challenging to family medicine’s emphasis on longitudinal care and the patient-physician relationship,” said Tochi Iroku-Malize, MD, MPH, president of the American Academy of Family Physicians. The limitations imposed by noncompete agreements “potentially reduce patient choice, lower the quality of care for patients, and ultimately harm the foundation of family medicine – our relationships with our patients.”
Although the proposed rule aligns with President Biden’s executive order promoting economic competition, Dr. Smith said a national ban on noncompete agreements may push the limits of FTC authority.
“This new rule will certainly result in a ‘major questions doctrine’ Supreme Court challenge,” said Dr. Smith, and possibly be struck down if the court determines an administrative overstep into areas of “vast economic or political significance.”
A controversial policy
The American Medical Association’s code of ethics discourages covenants that “unreasonably restrict” the ability of physicians to practice following contract termination. And in 2022, the AMA cited “overly broad” noncompete language as a red flag young physicians should watch out for during contract negotiations.
But in 2020, the AMA asked the FTC not to use its rulemaking authority to regulate noncompete clauses in physician employment contracts, and instead, relegate enforcement of such agreements to each state. The American Hospital Association expressed similar views.
Still, the FTC said that eliminating noncompete clauses will increase annual wages by $300 billion, allow 30 million Americans to pursue better job opportunities, and encourage hiring competition among employers. It will also save consumers up to $148 billion in health care costs annually.
“Noncompetes block workers from freely switching jobs, depriving them of higher wages and better working conditions, and depriving businesses of a talent pool that they need to build and expand,” Lina M. Khan, FTC chair, said in a press release about the proposal.
A national ban on noncompetes would keep more physicians in the industry and practicing in their communities, a win for patients and providers, said Dr. Smith. It could also compel employers to offer more competitive employment packages, including fair wages, better work conditions, and a culture of well-being and patient safety.
“Whatever the final rule is, I’m certain it will be legally challenged,” said Dr. Smith, adding that the nation’s most prominent business lobbying group, the Chamber of Commerce, has already issued a statement calling the rule “blatantly unlawful."
A version of this article first appeared on Medscape.com.
COVID leading cause of death among law enforcement for third year
A new report says 70 officers died of COVID-related causes after getting the virus while on the job. The number is down dramatically from 2021, when 405 officer deaths were attributed to COVID.
The annual count was published Wednesday by the National Law Enforcement Officers Memorial Fund.
In total, 226 officers died in the line of duty in 2022, which is a decrease of 61% from 2021.
The decrease “is almost entirely related to the significant reduction in COVID-19 deaths,” the report stated. The authors said the decline was likely due to “reduced infection rates and the broad availability and use of vaccinations.”
Reported deaths included federal, state, tribal, and local law enforcement officers.
Firearms-related fatalities were the second-leading cause of death among officers, with 64 in 2022. That count sustains a 21% increase seen in 2021, up from the decade-long average of 53 firearms-related deaths annually from 2010 to 2020.
Traffic-related causes ranked third for cause of death in 2022, accounting for 56 deaths.
“While overall line-of-duty deaths are trending down, the continuing trend of greater-than-average firearms-related deaths continues to be a serious concern,” Marcia Ferranto, the organization’s chief executive officer, said in a news release. “Using and reporting on this data allows us to highlight the continuing cost of maintaining our democracy, regrettably measured in the lives of the many law enforcement professionals who sacrifice everything fulfilling their promise to serve and protect.”
A version of this article first appeared on WebMD.com.
A new report says 70 officers died of COVID-related causes after getting the virus while on the job. The number is down dramatically from 2021, when 405 officer deaths were attributed to COVID.
The annual count was published Wednesday by the National Law Enforcement Officers Memorial Fund.
In total, 226 officers died in the line of duty in 2022, which is a decrease of 61% from 2021.
The decrease “is almost entirely related to the significant reduction in COVID-19 deaths,” the report stated. The authors said the decline was likely due to “reduced infection rates and the broad availability and use of vaccinations.”
Reported deaths included federal, state, tribal, and local law enforcement officers.
Firearms-related fatalities were the second-leading cause of death among officers, with 64 in 2022. That count sustains a 21% increase seen in 2021, up from the decade-long average of 53 firearms-related deaths annually from 2010 to 2020.
Traffic-related causes ranked third for cause of death in 2022, accounting for 56 deaths.
“While overall line-of-duty deaths are trending down, the continuing trend of greater-than-average firearms-related deaths continues to be a serious concern,” Marcia Ferranto, the organization’s chief executive officer, said in a news release. “Using and reporting on this data allows us to highlight the continuing cost of maintaining our democracy, regrettably measured in the lives of the many law enforcement professionals who sacrifice everything fulfilling their promise to serve and protect.”
A version of this article first appeared on WebMD.com.
A new report says 70 officers died of COVID-related causes after getting the virus while on the job. The number is down dramatically from 2021, when 405 officer deaths were attributed to COVID.
The annual count was published Wednesday by the National Law Enforcement Officers Memorial Fund.
In total, 226 officers died in the line of duty in 2022, which is a decrease of 61% from 2021.
The decrease “is almost entirely related to the significant reduction in COVID-19 deaths,” the report stated. The authors said the decline was likely due to “reduced infection rates and the broad availability and use of vaccinations.”
Reported deaths included federal, state, tribal, and local law enforcement officers.
Firearms-related fatalities were the second-leading cause of death among officers, with 64 in 2022. That count sustains a 21% increase seen in 2021, up from the decade-long average of 53 firearms-related deaths annually from 2010 to 2020.
Traffic-related causes ranked third for cause of death in 2022, accounting for 56 deaths.
“While overall line-of-duty deaths are trending down, the continuing trend of greater-than-average firearms-related deaths continues to be a serious concern,” Marcia Ferranto, the organization’s chief executive officer, said in a news release. “Using and reporting on this data allows us to highlight the continuing cost of maintaining our democracy, regrettably measured in the lives of the many law enforcement professionals who sacrifice everything fulfilling their promise to serve and protect.”
A version of this article first appeared on WebMD.com.