User login
In Case You Missed It: COVID
COVID-19 case fatality doubled in heart transplant patients
Heart transplant recipients infected with SARS-CoV-2 are about twice as likely to die from COVID-19 and should be immediately referred to a transplant center for care, according to transplant experts from Northern Italy.
In a COVID Rapid Report published Dec. 9 in JACC Heart Failure, a group led by Tomaso Bottio, MD, PhD, from the University of Padua, Italy, presented findings on 47 heart transplant recipients who tested positive for SARS-Cov-2 between Feb. 21 and June 30.
The investigators found a case fatality rate of 29.7%, compared with 15.4% in the general population. Prevalence of infection was also much higher at 18 cases (vs. 7) per 1,000 population.
“In our opinion, prompt referral to a heart transplant center is crucial for immunosuppressive therapy optimization and cardiologic follow-up,” Dr. Bottio said in an interview.
Beyond the need for careful adjustment of immunosuppression, graft function should be assessed to “avoid acute rejection or decompensation,” he added.
Dr. Bottio and colleagues tracked COVID-19 cases from among the 2,676 heart transplant recipients alive before the onset of the pandemic at seven heart transplant centers in Northern Italy.
Of the 47 recipients who contracted SARS-CoV-2, 38 required hospitalization while 9 remained at home and 14 died. Mean length of stay in hospital was 17.8 days, much longer in survivors than nonsurvivors (23.2 days vs. 8.5 days; P < .001).
Nonsurvivors were significantly older than survivors (72 vs. 58 years; P = .002). Nonsurvivors were also more likely to present with diabetes (P = .04), extra-cardiac arteriopathy (P = .04), previous percutaneous coronary intervention (P = .04), more allograft vasculopathy (P = .04), and more symptoms of heart failure (P = .02).
Although the authors said the high case fatality rate was, unfortunately, expected, they did not expect so many patients to do well at home.
“What most surprised us was the proportion of a- or pauci-symptomatic heart transplanted patients who did well being treated at home without any therapy modifications,” Dr. Bottio shared. They were also surprised to see there were no cases of graft failure caused by infection-related myocarditis.
These findings from Northern Italy are not dissimilar from the 25% case fatality rate seen in a cohort of heart transplant recipients who caught COVID-19 in New York City early in the pandemic.
In another study, this time looking at a wider group of solid organ transplant recipients with SARS-CoV-2 infection at two centers during the first 3 weeks of the outbreak in New York City, 16 of 90 patients (18%) died.
Treatment recommendations?
Recognizing that there is no randomized trial data informing the treatment of this vulnerable patient population, Dr. Bottio and colleagues suggested that, based on their experience, no change in immunosuppression is needed in those who are “pauci-symptomatic” (mildly symptomatic).
“On the other hand, in hospitalized patients a partial reduction in immunosuppressive therapy avoiding full discontinuation and risk of graft rejection seems to be a common strategy in facing the viral infection,” he said. “In addition, the introduction of corticosteroids could help to suspend the onset of the inflammatory cascade responsible for severe forms of the disease.”
Antibiotic prophylaxis appears to be “fundamental,” he added, particularly in hospitalized patients, but “the role of specific antiviral therapies is still not fully understood in our population.”
Since July 1, they’ve seen an additional six patients with a positive test for SARS-CoV-2. Five were asymptomatic and quarantined at home without changing their immunosuppressive therapy. One patient was hospitalized for pneumonia and had immunosuppressive therapy reduced.
Dr. Bottio and the study coauthors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Heart transplant recipients infected with SARS-CoV-2 are about twice as likely to die from COVID-19 and should be immediately referred to a transplant center for care, according to transplant experts from Northern Italy.
In a COVID Rapid Report published Dec. 9 in JACC Heart Failure, a group led by Tomaso Bottio, MD, PhD, from the University of Padua, Italy, presented findings on 47 heart transplant recipients who tested positive for SARS-Cov-2 between Feb. 21 and June 30.
The investigators found a case fatality rate of 29.7%, compared with 15.4% in the general population. Prevalence of infection was also much higher at 18 cases (vs. 7) per 1,000 population.
“In our opinion, prompt referral to a heart transplant center is crucial for immunosuppressive therapy optimization and cardiologic follow-up,” Dr. Bottio said in an interview.
Beyond the need for careful adjustment of immunosuppression, graft function should be assessed to “avoid acute rejection or decompensation,” he added.
Dr. Bottio and colleagues tracked COVID-19 cases from among the 2,676 heart transplant recipients alive before the onset of the pandemic at seven heart transplant centers in Northern Italy.
Of the 47 recipients who contracted SARS-CoV-2, 38 required hospitalization while 9 remained at home and 14 died. Mean length of stay in hospital was 17.8 days, much longer in survivors than nonsurvivors (23.2 days vs. 8.5 days; P < .001).
Nonsurvivors were significantly older than survivors (72 vs. 58 years; P = .002). Nonsurvivors were also more likely to present with diabetes (P = .04), extra-cardiac arteriopathy (P = .04), previous percutaneous coronary intervention (P = .04), more allograft vasculopathy (P = .04), and more symptoms of heart failure (P = .02).
Although the authors said the high case fatality rate was, unfortunately, expected, they did not expect so many patients to do well at home.
“What most surprised us was the proportion of a- or pauci-symptomatic heart transplanted patients who did well being treated at home without any therapy modifications,” Dr. Bottio shared. They were also surprised to see there were no cases of graft failure caused by infection-related myocarditis.
These findings from Northern Italy are not dissimilar from the 25% case fatality rate seen in a cohort of heart transplant recipients who caught COVID-19 in New York City early in the pandemic.
In another study, this time looking at a wider group of solid organ transplant recipients with SARS-CoV-2 infection at two centers during the first 3 weeks of the outbreak in New York City, 16 of 90 patients (18%) died.
Treatment recommendations?
Recognizing that there is no randomized trial data informing the treatment of this vulnerable patient population, Dr. Bottio and colleagues suggested that, based on their experience, no change in immunosuppression is needed in those who are “pauci-symptomatic” (mildly symptomatic).
“On the other hand, in hospitalized patients a partial reduction in immunosuppressive therapy avoiding full discontinuation and risk of graft rejection seems to be a common strategy in facing the viral infection,” he said. “In addition, the introduction of corticosteroids could help to suspend the onset of the inflammatory cascade responsible for severe forms of the disease.”
Antibiotic prophylaxis appears to be “fundamental,” he added, particularly in hospitalized patients, but “the role of specific antiviral therapies is still not fully understood in our population.”
Since July 1, they’ve seen an additional six patients with a positive test for SARS-CoV-2. Five were asymptomatic and quarantined at home without changing their immunosuppressive therapy. One patient was hospitalized for pneumonia and had immunosuppressive therapy reduced.
Dr. Bottio and the study coauthors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Heart transplant recipients infected with SARS-CoV-2 are about twice as likely to die from COVID-19 and should be immediately referred to a transplant center for care, according to transplant experts from Northern Italy.
In a COVID Rapid Report published Dec. 9 in JACC Heart Failure, a group led by Tomaso Bottio, MD, PhD, from the University of Padua, Italy, presented findings on 47 heart transplant recipients who tested positive for SARS-Cov-2 between Feb. 21 and June 30.
The investigators found a case fatality rate of 29.7%, compared with 15.4% in the general population. Prevalence of infection was also much higher at 18 cases (vs. 7) per 1,000 population.
“In our opinion, prompt referral to a heart transplant center is crucial for immunosuppressive therapy optimization and cardiologic follow-up,” Dr. Bottio said in an interview.
Beyond the need for careful adjustment of immunosuppression, graft function should be assessed to “avoid acute rejection or decompensation,” he added.
Dr. Bottio and colleagues tracked COVID-19 cases from among the 2,676 heart transplant recipients alive before the onset of the pandemic at seven heart transplant centers in Northern Italy.
Of the 47 recipients who contracted SARS-CoV-2, 38 required hospitalization while 9 remained at home and 14 died. Mean length of stay in hospital was 17.8 days, much longer in survivors than nonsurvivors (23.2 days vs. 8.5 days; P < .001).
Nonsurvivors were significantly older than survivors (72 vs. 58 years; P = .002). Nonsurvivors were also more likely to present with diabetes (P = .04), extra-cardiac arteriopathy (P = .04), previous percutaneous coronary intervention (P = .04), more allograft vasculopathy (P = .04), and more symptoms of heart failure (P = .02).
Although the authors said the high case fatality rate was, unfortunately, expected, they did not expect so many patients to do well at home.
“What most surprised us was the proportion of a- or pauci-symptomatic heart transplanted patients who did well being treated at home without any therapy modifications,” Dr. Bottio shared. They were also surprised to see there were no cases of graft failure caused by infection-related myocarditis.
These findings from Northern Italy are not dissimilar from the 25% case fatality rate seen in a cohort of heart transplant recipients who caught COVID-19 in New York City early in the pandemic.
In another study, this time looking at a wider group of solid organ transplant recipients with SARS-CoV-2 infection at two centers during the first 3 weeks of the outbreak in New York City, 16 of 90 patients (18%) died.
Treatment recommendations?
Recognizing that there is no randomized trial data informing the treatment of this vulnerable patient population, Dr. Bottio and colleagues suggested that, based on their experience, no change in immunosuppression is needed in those who are “pauci-symptomatic” (mildly symptomatic).
“On the other hand, in hospitalized patients a partial reduction in immunosuppressive therapy avoiding full discontinuation and risk of graft rejection seems to be a common strategy in facing the viral infection,” he said. “In addition, the introduction of corticosteroids could help to suspend the onset of the inflammatory cascade responsible for severe forms of the disease.”
Antibiotic prophylaxis appears to be “fundamental,” he added, particularly in hospitalized patients, but “the role of specific antiviral therapies is still not fully understood in our population.”
Since July 1, they’ve seen an additional six patients with a positive test for SARS-CoV-2. Five were asymptomatic and quarantined at home without changing their immunosuppressive therapy. One patient was hospitalized for pneumonia and had immunosuppressive therapy reduced.
Dr. Bottio and the study coauthors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
COVID-19 mortality rates declined, but vary by hospital
Mortality rates for inpatients with COVID-19 dropped significantly during the first 6 months of the pandemic, but outcomes depend on the hospital where patients receive care, new data show.
“[T]he characteristic that is most associated with poor or worsening hospital outcomes is high or increasing community case rates,” write David A. Asch, MD, MBA, executive director of the Center for Health Care Innovation at the University of Pennsylvania in Philadelphia, and colleagues.
The relationship between COVID-19 mortality rates and local disease prevalence suggests that “hospitals do worse when they are burdened with cases and is consistent with imperatives to flatten the curve,” the authors continue. “As case rates of COVID-19 increase across the nation, hospital mortality outcomes may worsen.”
The researchers published their study online December 22 in JAMA Internal Medicine.
The quick and substantial improvement in survival “is a tribute in part to new science — for example, the science that revealed the benefits of dexamethasone,” Asch told Medscape Medical News. “But it’s also a tribute to the doctors and nurses in the hospitals who developed experience. It’s a cliché to refer to them as heroes, but that is what they are. The science and the heroic experience continues on, and so I’m optimistic that we’ll see even more improvement over time.”
However, the data also indicate that “with lots of disease in the community, hospitals may have a harder time keeping patients alive,” Asch said. “And of course the reason this is bad news is that community level case rates are rising all over, and in some cases at rapid rates. With that rise, we might be giving back some of our past gains in survival — just as the vaccine is beginning to be distributed.”
Examining mortality trends
The researchers analyzed administrative claims data from a large national health insurer. They included data from 38,517 adults who were admitted with COVID-19 to 955 US hospitals between January 1 and June 30 of this year. The investigators estimated hospitals’ risk-standardized rate of 30-day in-hospital mortality or referral to hospice, adjusted for patient-level characteristics.
Overall, 3179 patients (8.25%) died, and 1433 patients (3.7%) were referred to hospice. Risk-standardized mortality or hospice referral rates for individual hospitals ranged from 5.7% to 24.7%. The average rate was 9.1% in the best-performing quintile, compared with 15.7% in the worst-performing quintile.
In a subset of 398 hospitals that had at least 10 patients admitted for COVID-19 during early (January 1 through April 30) and later periods (between May 1 and June 30), rates in all but one hospital improved, and 94% improved by at least 25%. The average risk-standardized event rate declined from 16.6% to 9.3%.
“That rate of relative improvement is striking and encouraging, but perhaps not surprising,” Asch and coauthors write. “Early efforts at treating patients with COVID-19 were based on experience with previously known causes of severe respiratory illness. Later efforts could draw on experiences specific to SARS-CoV-2 infection.”
For instance, doctors tried different inpatient management approaches, such as early vs late assisted ventilation, differences in oxygen flow, prone or supine positioning, and anticoagulation. “Those efforts varied in how systematically they were evaluated, but our results suggest that valuable experience was gained,” the authors note.
In addition, variation between hospitals could reflect differences in quality or different admission thresholds, they continue.
The study provides “a reason for optimism that our healthcare system has improved in our ability to care for persons with COVID-19,” write Leon Boudourakis, MD, MHS, and Amit Uppal, MD, in a related commentary. Boudourakis and Uppal are both affiliated with NYC Health + Hospitals in New York City and with SUNY Downstate and New York University School of Medicine, respectively.
Similar improvements in mortality rates have been reported in the United Kingdom and in a New York City hospital system, the editorialists note. The lower mortality rates may represent clinical, healthcare system, and epidemiologic trends.
“Since the first wave of serious COVID-19 cases, physicians have learned a great deal about the best ways to treat this serious infection,” they say. “Steroids may decrease mortality in patients with respiratory failure. Remdesivir may shorten hospitalizations of patients with serious illness. Anticoagulation and prone positioning may help certain patients. Using noninvasive ventilation and high-flow oxygen therapy may spare subsets of patients from the harms of intubation, such as ventilator-induced lung injury.»
Overwhelmed hospitals
“Hospitals do not perform as well when they are overwhelmed,” which may be a reason for the correlation between community prevalence and mortality rates, Boudourakis and Uppal suggested. “In particular, patients with a precarious respiratory status require expert, meticulous therapy to avoid intubation; those who undergo intubation or have kidney failure require nuanced and timely expert care with ventilatory adjustments and kidney replacement therapy, which are difficult to perform optimally when hospital capacity is strained.”
Although the death rate has fallen to about 9% for hospitalized patients, “9% is still high,” Asch said.
“Our results show that hospitals can’t do it on their own,” Asch said. “They need all of us to keep the community spread of the disease down. The right answer now is the right answer since the beginning of the pandemic: Keep your distance, wash your hands, and wear a mask.”
Asch, Boudourakis, and Uppal have disclosed no relevant financial relationships. A study coauthor reported personal fees and grants from pharmaceutical companies outside the submitted work.
A version of this article first appeared on Medscape.com.
Mortality rates for inpatients with COVID-19 dropped significantly during the first 6 months of the pandemic, but outcomes depend on the hospital where patients receive care, new data show.
“[T]he characteristic that is most associated with poor or worsening hospital outcomes is high or increasing community case rates,” write David A. Asch, MD, MBA, executive director of the Center for Health Care Innovation at the University of Pennsylvania in Philadelphia, and colleagues.
The relationship between COVID-19 mortality rates and local disease prevalence suggests that “hospitals do worse when they are burdened with cases and is consistent with imperatives to flatten the curve,” the authors continue. “As case rates of COVID-19 increase across the nation, hospital mortality outcomes may worsen.”
The researchers published their study online December 22 in JAMA Internal Medicine.
The quick and substantial improvement in survival “is a tribute in part to new science — for example, the science that revealed the benefits of dexamethasone,” Asch told Medscape Medical News. “But it’s also a tribute to the doctors and nurses in the hospitals who developed experience. It’s a cliché to refer to them as heroes, but that is what they are. The science and the heroic experience continues on, and so I’m optimistic that we’ll see even more improvement over time.”
However, the data also indicate that “with lots of disease in the community, hospitals may have a harder time keeping patients alive,” Asch said. “And of course the reason this is bad news is that community level case rates are rising all over, and in some cases at rapid rates. With that rise, we might be giving back some of our past gains in survival — just as the vaccine is beginning to be distributed.”
Examining mortality trends
The researchers analyzed administrative claims data from a large national health insurer. They included data from 38,517 adults who were admitted with COVID-19 to 955 US hospitals between January 1 and June 30 of this year. The investigators estimated hospitals’ risk-standardized rate of 30-day in-hospital mortality or referral to hospice, adjusted for patient-level characteristics.
Overall, 3179 patients (8.25%) died, and 1433 patients (3.7%) were referred to hospice. Risk-standardized mortality or hospice referral rates for individual hospitals ranged from 5.7% to 24.7%. The average rate was 9.1% in the best-performing quintile, compared with 15.7% in the worst-performing quintile.
In a subset of 398 hospitals that had at least 10 patients admitted for COVID-19 during early (January 1 through April 30) and later periods (between May 1 and June 30), rates in all but one hospital improved, and 94% improved by at least 25%. The average risk-standardized event rate declined from 16.6% to 9.3%.
“That rate of relative improvement is striking and encouraging, but perhaps not surprising,” Asch and coauthors write. “Early efforts at treating patients with COVID-19 were based on experience with previously known causes of severe respiratory illness. Later efforts could draw on experiences specific to SARS-CoV-2 infection.”
For instance, doctors tried different inpatient management approaches, such as early vs late assisted ventilation, differences in oxygen flow, prone or supine positioning, and anticoagulation. “Those efforts varied in how systematically they were evaluated, but our results suggest that valuable experience was gained,” the authors note.
In addition, variation between hospitals could reflect differences in quality or different admission thresholds, they continue.
The study provides “a reason for optimism that our healthcare system has improved in our ability to care for persons with COVID-19,” write Leon Boudourakis, MD, MHS, and Amit Uppal, MD, in a related commentary. Boudourakis and Uppal are both affiliated with NYC Health + Hospitals in New York City and with SUNY Downstate and New York University School of Medicine, respectively.
Similar improvements in mortality rates have been reported in the United Kingdom and in a New York City hospital system, the editorialists note. The lower mortality rates may represent clinical, healthcare system, and epidemiologic trends.
“Since the first wave of serious COVID-19 cases, physicians have learned a great deal about the best ways to treat this serious infection,” they say. “Steroids may decrease mortality in patients with respiratory failure. Remdesivir may shorten hospitalizations of patients with serious illness. Anticoagulation and prone positioning may help certain patients. Using noninvasive ventilation and high-flow oxygen therapy may spare subsets of patients from the harms of intubation, such as ventilator-induced lung injury.»
Overwhelmed hospitals
“Hospitals do not perform as well when they are overwhelmed,” which may be a reason for the correlation between community prevalence and mortality rates, Boudourakis and Uppal suggested. “In particular, patients with a precarious respiratory status require expert, meticulous therapy to avoid intubation; those who undergo intubation or have kidney failure require nuanced and timely expert care with ventilatory adjustments and kidney replacement therapy, which are difficult to perform optimally when hospital capacity is strained.”
Although the death rate has fallen to about 9% for hospitalized patients, “9% is still high,” Asch said.
“Our results show that hospitals can’t do it on their own,” Asch said. “They need all of us to keep the community spread of the disease down. The right answer now is the right answer since the beginning of the pandemic: Keep your distance, wash your hands, and wear a mask.”
Asch, Boudourakis, and Uppal have disclosed no relevant financial relationships. A study coauthor reported personal fees and grants from pharmaceutical companies outside the submitted work.
A version of this article first appeared on Medscape.com.
Mortality rates for inpatients with COVID-19 dropped significantly during the first 6 months of the pandemic, but outcomes depend on the hospital where patients receive care, new data show.
“[T]he characteristic that is most associated with poor or worsening hospital outcomes is high or increasing community case rates,” write David A. Asch, MD, MBA, executive director of the Center for Health Care Innovation at the University of Pennsylvania in Philadelphia, and colleagues.
The relationship between COVID-19 mortality rates and local disease prevalence suggests that “hospitals do worse when they are burdened with cases and is consistent with imperatives to flatten the curve,” the authors continue. “As case rates of COVID-19 increase across the nation, hospital mortality outcomes may worsen.”
The researchers published their study online December 22 in JAMA Internal Medicine.
The quick and substantial improvement in survival “is a tribute in part to new science — for example, the science that revealed the benefits of dexamethasone,” Asch told Medscape Medical News. “But it’s also a tribute to the doctors and nurses in the hospitals who developed experience. It’s a cliché to refer to them as heroes, but that is what they are. The science and the heroic experience continues on, and so I’m optimistic that we’ll see even more improvement over time.”
However, the data also indicate that “with lots of disease in the community, hospitals may have a harder time keeping patients alive,” Asch said. “And of course the reason this is bad news is that community level case rates are rising all over, and in some cases at rapid rates. With that rise, we might be giving back some of our past gains in survival — just as the vaccine is beginning to be distributed.”
Examining mortality trends
The researchers analyzed administrative claims data from a large national health insurer. They included data from 38,517 adults who were admitted with COVID-19 to 955 US hospitals between January 1 and June 30 of this year. The investigators estimated hospitals’ risk-standardized rate of 30-day in-hospital mortality or referral to hospice, adjusted for patient-level characteristics.
Overall, 3179 patients (8.25%) died, and 1433 patients (3.7%) were referred to hospice. Risk-standardized mortality or hospice referral rates for individual hospitals ranged from 5.7% to 24.7%. The average rate was 9.1% in the best-performing quintile, compared with 15.7% in the worst-performing quintile.
In a subset of 398 hospitals that had at least 10 patients admitted for COVID-19 during early (January 1 through April 30) and later periods (between May 1 and June 30), rates in all but one hospital improved, and 94% improved by at least 25%. The average risk-standardized event rate declined from 16.6% to 9.3%.
“That rate of relative improvement is striking and encouraging, but perhaps not surprising,” Asch and coauthors write. “Early efforts at treating patients with COVID-19 were based on experience with previously known causes of severe respiratory illness. Later efforts could draw on experiences specific to SARS-CoV-2 infection.”
For instance, doctors tried different inpatient management approaches, such as early vs late assisted ventilation, differences in oxygen flow, prone or supine positioning, and anticoagulation. “Those efforts varied in how systematically they were evaluated, but our results suggest that valuable experience was gained,” the authors note.
In addition, variation between hospitals could reflect differences in quality or different admission thresholds, they continue.
The study provides “a reason for optimism that our healthcare system has improved in our ability to care for persons with COVID-19,” write Leon Boudourakis, MD, MHS, and Amit Uppal, MD, in a related commentary. Boudourakis and Uppal are both affiliated with NYC Health + Hospitals in New York City and with SUNY Downstate and New York University School of Medicine, respectively.
Similar improvements in mortality rates have been reported in the United Kingdom and in a New York City hospital system, the editorialists note. The lower mortality rates may represent clinical, healthcare system, and epidemiologic trends.
“Since the first wave of serious COVID-19 cases, physicians have learned a great deal about the best ways to treat this serious infection,” they say. “Steroids may decrease mortality in patients with respiratory failure. Remdesivir may shorten hospitalizations of patients with serious illness. Anticoagulation and prone positioning may help certain patients. Using noninvasive ventilation and high-flow oxygen therapy may spare subsets of patients from the harms of intubation, such as ventilator-induced lung injury.»
Overwhelmed hospitals
“Hospitals do not perform as well when they are overwhelmed,” which may be a reason for the correlation between community prevalence and mortality rates, Boudourakis and Uppal suggested. “In particular, patients with a precarious respiratory status require expert, meticulous therapy to avoid intubation; those who undergo intubation or have kidney failure require nuanced and timely expert care with ventilatory adjustments and kidney replacement therapy, which are difficult to perform optimally when hospital capacity is strained.”
Although the death rate has fallen to about 9% for hospitalized patients, “9% is still high,” Asch said.
“Our results show that hospitals can’t do it on their own,” Asch said. “They need all of us to keep the community spread of the disease down. The right answer now is the right answer since the beginning of the pandemic: Keep your distance, wash your hands, and wear a mask.”
Asch, Boudourakis, and Uppal have disclosed no relevant financial relationships. A study coauthor reported personal fees and grants from pharmaceutical companies outside the submitted work.
A version of this article first appeared on Medscape.com.
After COVID-19 infection, antibodies highly protective for months, prospective study shows
results of the first prospective study of the subject revealed.
The main message for health care workers is, “if you’ve had COVID, at least in the short term, you are unlikely to get it again,” David Eyre, DPhil, senior author, associate professor at the Big Data Institute and infectious diseases clinician at the University of Oxford (England), said in an interview.
Dr. Eyre and colleagues assessed for the presence of two antibodies to SARS-CoV-2 among 12,541 health care workers in the United Kingdom, including about 10% who had a history of polymerase chain reaction (PCR)–confirmed infection. Of those, 223 who did not have antibodies tested positive on PCR for the virus during 31 weeks of follow-up; two participants who did not have antibodies at baseline tested positive.
The study was published online Dec. 23 in The New England Journal of Medicine.
“It’s great news because there have been so many questions regarding whether or not you can be protected against reinfection, and this health care worker study is really an elegant way to address that question,” Mark Slifka, PhD, said in an interview when asked to comment on the findings.
Although “there are millions of people in the U.S. who have been infected with COVID, we don’t know how common reinfection is,” said Dr. Slifka, a researcher at the Oregon National Primate Research Center and professor at Oregon Health & Science University, Portland.
The likelihood of a subsequent positive PCR test result was 1.09 per 10,000 days at risk among those without antibodies, compared with 0.13 per 10,000 days among those with anti-spike antibodies.
The investigators also assessed for the presence of anti–nucleocapsid IgG antibody titers. They found a significant trend for increasing PCR-positive test results with increasing antibody levels. As with the anti-spike antibody findings, 226 of 11,543 health care providers who did not have anti–nucleocapsid IgG antibodies subsequently tested positive on PCR; by contrast, two of 1,172 participants who did not have antibodies tested positive. Adjusted for age, sex, and calendar time, this finding translates to a 0.11 incidence rate ratio (0.13 per 10,000 days at risk; 95% confidence interval, 0.03-0.45; P = .002).
“This is a study a number of us have been trying to do,” said Christopher L. King, MD, PhD, professor of pathology and associate professor of medicine at Case Western Reserve University, Cleveland.
“To really follow a group like this longitudinally like they’ve done, with a large population, and to see such a big difference – it really confirms our suspicion that those who do become infected and develop an antibody response are significantly protected from reinfection.
“What’s great about this study is it’s nearly a 10-fold reduction in risk if you’ve recovered from COVID and have antibodies,” said Dr. King, who was not involved with the research. “That’s what a lot of us have been wanting to know.”
Unanswered questions remain
“How long this immunity lasts, we don’t know,” Dr. King said. He predicted that antibody protection could last a year to a year and a half. The duration of protection could vary. “We know some people lose their antibodies pretty quickly, and other people don’t,” he said.
Dr. Slifka said the suggestion of “a substantially reduced risk for at least 6 months ... is great news, and the timing couldn’t be better, because we’re rolling out the vaccines.”
Not all antibody responses are alike. For example, data indicate that antibody levels following immunization with the Pfizer/BioNTech or Moderna vaccines are higher on average than those of people who’ve had a natural infection, Dr. King said. He added that initial data on the AstraZeneca COVID-19 vaccine in development showed lower antibody levels compared with natural immunity.
The Centers for Disease Control and Prevention recommends immunization for those with a history of infection. “People who have gotten sick with COVID-19 may still benefit from getting vaccinated,” the CDC notes on its Facts About COVID-19 Vaccines website. “Due to the severe health risks associated with COVID-19 and the fact that re-infection with COVID-19 is possible, people may be advised to get a COVID-19 vaccine even if they have been sick with COVID-19 before,” the CDC stated.
The agency also notes that people appear to become susceptible to reinfection approximately 90 days after onset of infection. However, the new evidence from the UK study that persons have up to 6 months of immune protection might lead to a modification of recommendations, especially at a time when vaccine supplies are limited, Dr. Slifka said.
Another unanswered question is why the two study participants with antibodies subsequently tested positive for reinfection. “There are a lot of things that could have made these people more susceptible,” Dr. King said. For example, they could have been heavily exposed to SARS-CoV-2 or been immunocompromised for another reason.
Furthermore, the immune response involves more than antibody levels, Dr. King noted. Research in rhesus monkeys suggests that T cells play a role, but not as prominent a part as antibodies. “What I think is protecting us from infection is primarily the antibodies, although the T cells are probably important. Once you get infected, the T cells are probably playing a more important role in terms of whether you get very sick or not,” he said.
Multiplication + addition = more protected?
The 90% natural immunity protection in the study approaches the 95% efficacy associated with the Pfizer and Moderna vaccines, Dr. Slifka noted. Even without immunization, this could mean a portion of the U.S. population is already protected against future infection.
Furthermore, the CDC estimates that there are about 7.7 cases of COVID-19 for every case reported.
As of Sept. 30, the CDC reported that there were 6,891,764 confirmed cases. The agency estimated that overall, approximately 53 million people in the United States have been infected. More recent numbers from Johns Hopkins University’s Coronavirus Resource Center indicate that there were 18.2 million cases in the United States as of Dec. 22. If that tally is multiplied by 7.7, the total number protected could approach 140 million, Dr. Slifka said.
“That could really be a boost in terms of knocking this pandemic down in the next couple of months,” Dr. Slifka said.
“Now, if we were to modify the current recommendations and briefly defer vaccination of people with confirmed cases of COVID-19 until later on, we could start reaching herd immunity pretty quickly,” he added.
Real-life implications
“There is no such thing as 100% protection, even from the infection itself. So when you’re dealing with someone with possible exposure to COVID-19, you still need to follow the proper precautions,” Dr. Slifka said.
Nonetheless, he said, “This is great news for those on the front lines who are wondering whether or not they would have any protection if they had COVID-19 before. And the answer is yes – there is a very good chance they will have protection, based on this quite large study.”
One limitation of the study is that the population consisted predominantly of healthy adult health care workers aged 65 years or younger. “Further studies are needed to assess postinfection immunity in other populations, including children, older adults, and persons with coexisting conditions, including immunosuppression,” the researchers noted.
Dr. Eyre plans to continue following the health care workers in the study, some of whom have been vaccinated for COVID-19. This ongoing research will allow him and coinvestigators to “confirm the protection offered by vaccination and investigate how postvaccine antibody responses vary by whether you have had COVID-19 before or not. We also want to understand more about how long postinfection immunity lasts.”
Dr. Eyre has received grants as a Robinson Foundation Fellow and NIHR Oxford BRC senior fellow during the conduct of the study. Dr. Slifka and Dr. King report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
results of the first prospective study of the subject revealed.
The main message for health care workers is, “if you’ve had COVID, at least in the short term, you are unlikely to get it again,” David Eyre, DPhil, senior author, associate professor at the Big Data Institute and infectious diseases clinician at the University of Oxford (England), said in an interview.
Dr. Eyre and colleagues assessed for the presence of two antibodies to SARS-CoV-2 among 12,541 health care workers in the United Kingdom, including about 10% who had a history of polymerase chain reaction (PCR)–confirmed infection. Of those, 223 who did not have antibodies tested positive on PCR for the virus during 31 weeks of follow-up; two participants who did not have antibodies at baseline tested positive.
The study was published online Dec. 23 in The New England Journal of Medicine.
“It’s great news because there have been so many questions regarding whether or not you can be protected against reinfection, and this health care worker study is really an elegant way to address that question,” Mark Slifka, PhD, said in an interview when asked to comment on the findings.
Although “there are millions of people in the U.S. who have been infected with COVID, we don’t know how common reinfection is,” said Dr. Slifka, a researcher at the Oregon National Primate Research Center and professor at Oregon Health & Science University, Portland.
The likelihood of a subsequent positive PCR test result was 1.09 per 10,000 days at risk among those without antibodies, compared with 0.13 per 10,000 days among those with anti-spike antibodies.
The investigators also assessed for the presence of anti–nucleocapsid IgG antibody titers. They found a significant trend for increasing PCR-positive test results with increasing antibody levels. As with the anti-spike antibody findings, 226 of 11,543 health care providers who did not have anti–nucleocapsid IgG antibodies subsequently tested positive on PCR; by contrast, two of 1,172 participants who did not have antibodies tested positive. Adjusted for age, sex, and calendar time, this finding translates to a 0.11 incidence rate ratio (0.13 per 10,000 days at risk; 95% confidence interval, 0.03-0.45; P = .002).
“This is a study a number of us have been trying to do,” said Christopher L. King, MD, PhD, professor of pathology and associate professor of medicine at Case Western Reserve University, Cleveland.
“To really follow a group like this longitudinally like they’ve done, with a large population, and to see such a big difference – it really confirms our suspicion that those who do become infected and develop an antibody response are significantly protected from reinfection.
“What’s great about this study is it’s nearly a 10-fold reduction in risk if you’ve recovered from COVID and have antibodies,” said Dr. King, who was not involved with the research. “That’s what a lot of us have been wanting to know.”
Unanswered questions remain
“How long this immunity lasts, we don’t know,” Dr. King said. He predicted that antibody protection could last a year to a year and a half. The duration of protection could vary. “We know some people lose their antibodies pretty quickly, and other people don’t,” he said.
Dr. Slifka said the suggestion of “a substantially reduced risk for at least 6 months ... is great news, and the timing couldn’t be better, because we’re rolling out the vaccines.”
Not all antibody responses are alike. For example, data indicate that antibody levels following immunization with the Pfizer/BioNTech or Moderna vaccines are higher on average than those of people who’ve had a natural infection, Dr. King said. He added that initial data on the AstraZeneca COVID-19 vaccine in development showed lower antibody levels compared with natural immunity.
The Centers for Disease Control and Prevention recommends immunization for those with a history of infection. “People who have gotten sick with COVID-19 may still benefit from getting vaccinated,” the CDC notes on its Facts About COVID-19 Vaccines website. “Due to the severe health risks associated with COVID-19 and the fact that re-infection with COVID-19 is possible, people may be advised to get a COVID-19 vaccine even if they have been sick with COVID-19 before,” the CDC stated.
The agency also notes that people appear to become susceptible to reinfection approximately 90 days after onset of infection. However, the new evidence from the UK study that persons have up to 6 months of immune protection might lead to a modification of recommendations, especially at a time when vaccine supplies are limited, Dr. Slifka said.
Another unanswered question is why the two study participants with antibodies subsequently tested positive for reinfection. “There are a lot of things that could have made these people more susceptible,” Dr. King said. For example, they could have been heavily exposed to SARS-CoV-2 or been immunocompromised for another reason.
Furthermore, the immune response involves more than antibody levels, Dr. King noted. Research in rhesus monkeys suggests that T cells play a role, but not as prominent a part as antibodies. “What I think is protecting us from infection is primarily the antibodies, although the T cells are probably important. Once you get infected, the T cells are probably playing a more important role in terms of whether you get very sick or not,” he said.
Multiplication + addition = more protected?
The 90% natural immunity protection in the study approaches the 95% efficacy associated with the Pfizer and Moderna vaccines, Dr. Slifka noted. Even without immunization, this could mean a portion of the U.S. population is already protected against future infection.
Furthermore, the CDC estimates that there are about 7.7 cases of COVID-19 for every case reported.
As of Sept. 30, the CDC reported that there were 6,891,764 confirmed cases. The agency estimated that overall, approximately 53 million people in the United States have been infected. More recent numbers from Johns Hopkins University’s Coronavirus Resource Center indicate that there were 18.2 million cases in the United States as of Dec. 22. If that tally is multiplied by 7.7, the total number protected could approach 140 million, Dr. Slifka said.
“That could really be a boost in terms of knocking this pandemic down in the next couple of months,” Dr. Slifka said.
“Now, if we were to modify the current recommendations and briefly defer vaccination of people with confirmed cases of COVID-19 until later on, we could start reaching herd immunity pretty quickly,” he added.
Real-life implications
“There is no such thing as 100% protection, even from the infection itself. So when you’re dealing with someone with possible exposure to COVID-19, you still need to follow the proper precautions,” Dr. Slifka said.
Nonetheless, he said, “This is great news for those on the front lines who are wondering whether or not they would have any protection if they had COVID-19 before. And the answer is yes – there is a very good chance they will have protection, based on this quite large study.”
One limitation of the study is that the population consisted predominantly of healthy adult health care workers aged 65 years or younger. “Further studies are needed to assess postinfection immunity in other populations, including children, older adults, and persons with coexisting conditions, including immunosuppression,” the researchers noted.
Dr. Eyre plans to continue following the health care workers in the study, some of whom have been vaccinated for COVID-19. This ongoing research will allow him and coinvestigators to “confirm the protection offered by vaccination and investigate how postvaccine antibody responses vary by whether you have had COVID-19 before or not. We also want to understand more about how long postinfection immunity lasts.”
Dr. Eyre has received grants as a Robinson Foundation Fellow and NIHR Oxford BRC senior fellow during the conduct of the study. Dr. Slifka and Dr. King report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
results of the first prospective study of the subject revealed.
The main message for health care workers is, “if you’ve had COVID, at least in the short term, you are unlikely to get it again,” David Eyre, DPhil, senior author, associate professor at the Big Data Institute and infectious diseases clinician at the University of Oxford (England), said in an interview.
Dr. Eyre and colleagues assessed for the presence of two antibodies to SARS-CoV-2 among 12,541 health care workers in the United Kingdom, including about 10% who had a history of polymerase chain reaction (PCR)–confirmed infection. Of those, 223 who did not have antibodies tested positive on PCR for the virus during 31 weeks of follow-up; two participants who did not have antibodies at baseline tested positive.
The study was published online Dec. 23 in The New England Journal of Medicine.
“It’s great news because there have been so many questions regarding whether or not you can be protected against reinfection, and this health care worker study is really an elegant way to address that question,” Mark Slifka, PhD, said in an interview when asked to comment on the findings.
Although “there are millions of people in the U.S. who have been infected with COVID, we don’t know how common reinfection is,” said Dr. Slifka, a researcher at the Oregon National Primate Research Center and professor at Oregon Health & Science University, Portland.
The likelihood of a subsequent positive PCR test result was 1.09 per 10,000 days at risk among those without antibodies, compared with 0.13 per 10,000 days among those with anti-spike antibodies.
The investigators also assessed for the presence of anti–nucleocapsid IgG antibody titers. They found a significant trend for increasing PCR-positive test results with increasing antibody levels. As with the anti-spike antibody findings, 226 of 11,543 health care providers who did not have anti–nucleocapsid IgG antibodies subsequently tested positive on PCR; by contrast, two of 1,172 participants who did not have antibodies tested positive. Adjusted for age, sex, and calendar time, this finding translates to a 0.11 incidence rate ratio (0.13 per 10,000 days at risk; 95% confidence interval, 0.03-0.45; P = .002).
“This is a study a number of us have been trying to do,” said Christopher L. King, MD, PhD, professor of pathology and associate professor of medicine at Case Western Reserve University, Cleveland.
“To really follow a group like this longitudinally like they’ve done, with a large population, and to see such a big difference – it really confirms our suspicion that those who do become infected and develop an antibody response are significantly protected from reinfection.
“What’s great about this study is it’s nearly a 10-fold reduction in risk if you’ve recovered from COVID and have antibodies,” said Dr. King, who was not involved with the research. “That’s what a lot of us have been wanting to know.”
Unanswered questions remain
“How long this immunity lasts, we don’t know,” Dr. King said. He predicted that antibody protection could last a year to a year and a half. The duration of protection could vary. “We know some people lose their antibodies pretty quickly, and other people don’t,” he said.
Dr. Slifka said the suggestion of “a substantially reduced risk for at least 6 months ... is great news, and the timing couldn’t be better, because we’re rolling out the vaccines.”
Not all antibody responses are alike. For example, data indicate that antibody levels following immunization with the Pfizer/BioNTech or Moderna vaccines are higher on average than those of people who’ve had a natural infection, Dr. King said. He added that initial data on the AstraZeneca COVID-19 vaccine in development showed lower antibody levels compared with natural immunity.
The Centers for Disease Control and Prevention recommends immunization for those with a history of infection. “People who have gotten sick with COVID-19 may still benefit from getting vaccinated,” the CDC notes on its Facts About COVID-19 Vaccines website. “Due to the severe health risks associated with COVID-19 and the fact that re-infection with COVID-19 is possible, people may be advised to get a COVID-19 vaccine even if they have been sick with COVID-19 before,” the CDC stated.
The agency also notes that people appear to become susceptible to reinfection approximately 90 days after onset of infection. However, the new evidence from the UK study that persons have up to 6 months of immune protection might lead to a modification of recommendations, especially at a time when vaccine supplies are limited, Dr. Slifka said.
Another unanswered question is why the two study participants with antibodies subsequently tested positive for reinfection. “There are a lot of things that could have made these people more susceptible,” Dr. King said. For example, they could have been heavily exposed to SARS-CoV-2 or been immunocompromised for another reason.
Furthermore, the immune response involves more than antibody levels, Dr. King noted. Research in rhesus monkeys suggests that T cells play a role, but not as prominent a part as antibodies. “What I think is protecting us from infection is primarily the antibodies, although the T cells are probably important. Once you get infected, the T cells are probably playing a more important role in terms of whether you get very sick or not,” he said.
Multiplication + addition = more protected?
The 90% natural immunity protection in the study approaches the 95% efficacy associated with the Pfizer and Moderna vaccines, Dr. Slifka noted. Even without immunization, this could mean a portion of the U.S. population is already protected against future infection.
Furthermore, the CDC estimates that there are about 7.7 cases of COVID-19 for every case reported.
As of Sept. 30, the CDC reported that there were 6,891,764 confirmed cases. The agency estimated that overall, approximately 53 million people in the United States have been infected. More recent numbers from Johns Hopkins University’s Coronavirus Resource Center indicate that there were 18.2 million cases in the United States as of Dec. 22. If that tally is multiplied by 7.7, the total number protected could approach 140 million, Dr. Slifka said.
“That could really be a boost in terms of knocking this pandemic down in the next couple of months,” Dr. Slifka said.
“Now, if we were to modify the current recommendations and briefly defer vaccination of people with confirmed cases of COVID-19 until later on, we could start reaching herd immunity pretty quickly,” he added.
Real-life implications
“There is no such thing as 100% protection, even from the infection itself. So when you’re dealing with someone with possible exposure to COVID-19, you still need to follow the proper precautions,” Dr. Slifka said.
Nonetheless, he said, “This is great news for those on the front lines who are wondering whether or not they would have any protection if they had COVID-19 before. And the answer is yes – there is a very good chance they will have protection, based on this quite large study.”
One limitation of the study is that the population consisted predominantly of healthy adult health care workers aged 65 years or younger. “Further studies are needed to assess postinfection immunity in other populations, including children, older adults, and persons with coexisting conditions, including immunosuppression,” the researchers noted.
Dr. Eyre plans to continue following the health care workers in the study, some of whom have been vaccinated for COVID-19. This ongoing research will allow him and coinvestigators to “confirm the protection offered by vaccination and investigate how postvaccine antibody responses vary by whether you have had COVID-19 before or not. We also want to understand more about how long postinfection immunity lasts.”
Dr. Eyre has received grants as a Robinson Foundation Fellow and NIHR Oxford BRC senior fellow during the conduct of the study. Dr. Slifka and Dr. King report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Hospital volumes start to fall again, even as COVID-19 soars
Hospital volumes, which had largely recovered in September after crashing last spring, are dropping again, according to new data from Strata Decision Technologies, a Chicago-based analytics firm.
For the 2 weeks that ended Nov. 28, inpatient admissions were 6.2% below what they’d been on Nov. 14 and 2.1% below what they’d been on Oct. 28. Compared with the same intervals in 2019, admissions were off 4.4% for the 14-day period and 3.7% for the 30-day period.
Although those aren’t large percentages, Strata’s report, based on data from about 275 client hospitals, notes that what kept the volumes up was the increasing number of COVID-19 cases. If COVID-19 cases are not considered, admissions would have been down “double digits,” said Steve Lefar, executive director of StrataDataScience, a division of Strata Decision Technologies, in an interview with this news organization.
“Hip and knee replacements, cardiac procedures, and other procedures are significantly down year over year. Infectious disease cases, in contrast, have skyrocketed,” Mr. Lefar said. “Many things went way down that hadn’t fully recovered. It’s COVID-19 that really brought the volume back up.”
Observation and emergency department visits also dropped from already low levels. For the 2 weeks that ended Nov. 28, observation visits were off 8.4%; for the previous month, 10.1%. Compared with 2019, they were down 22.3% and 18.6%, respectively.
ED visits fell 3.7% for the 2-week period, 0.6% for the month. They dropped 21% and 18.7%, respectively, compared with those periods from the previous year.
What these data reflect, Mr. Lefar said, is that people have avoided EDs and are staying away from them more than ever because of COVID-19 fears. This behavior could be problematic for people who have concerning symptoms, such as chest pains, that should be evaluated by an ED physician, he noted.
Daily outpatient visits were down 18.4% for the 14-day period and 9.3% for the 30-day period. But, compared with 2019, ambulatory visits increased 5.8% for the 2-week period and 4.7% for the previous month.
Long-term trends
The outpatient visit data should be viewed in the context of the overall trend since the pandemic began. Strata broke down service lines for the period between March 20 and Nov. 7. The analysis shows that evaluation and management (E/M) encounters, the largest outpatient visit category, fell 58% during this period, compared with the same interval in 2019. Visits for diabetes, hypertension, and minor acute infections and injuries were also way down.
Mr. Lefar observed that the E/M visit category was only for in-person visits, which many patients have ditched in favor of telehealth encounters. At the same time, he noted, “people are going in less for chronic disease visits. So there’s an interplay between less in-person visits, more telehealth, and maybe people going to other sites that aren’t on the hospital campus. But people are going less [to outpatient clinics].”
In the year-to-year comparison, volume was down substantially in other service lines, including cancer (–9.2%), cardiology (–20%), dermatology (–31%), endocrine (–18.8%), ENT (–42.5%), gastroenterology (–24.3%), nephrology (–15%), obstetrics (–15.6%), orthopedics (–28.2%), and general surgery (–22.2%). Major procedures decreased by 21.8%.
In contrast, the infectious disease category jumped 86% over 2019, and “other infectious and parasitic diseases” – i.e., COVID-19 – soared 222%.
There was a much bigger crash in admissions, observation visits, and ED visits last spring than in November, the report shows. “What happened nationally last spring is that everyone shut down,” Mr. Lefar explained. “All the electives were canceled. Even cancer surgery was shut down, along with many other procedures. That’s what drove that crash. But the provider community quickly learned that this is going to be a long haul, and we’re going to have to reopen. We’re going to do it safely, but we’re going to make sure people get the necessary care. We can’t put off cancer care or colonoscopies and other screenings that save lives.”
System starts to break down
The current wave of COVID-19, however, is beginning to change the definition of necessary care, he said. “Hospitals are reaching the breaking point between staff exhaustion and hospital capacity reaching its limit. In Texas, hospitals are starting to shut down certain essential non-COVID care. They’re turning away some nonurgent cases – the electives that were starting to come back.”
How about nonurgent COVID cases? Mr. Lefar said there’s evidence that some of those patients are also being diverted. “Some experts speculate that the turn-away rate of people with confirmed COVID is starting to go up, and hospitals are sending them home with oxygen or an oxygen meter and saying, ‘If it gets worse, come back.’ They just don’t have the critical care capacity – and that should scare the heck out of everybody.”
Strata doesn’t yet have the data to confirm this, he said, “but it appears that some people are being sent home. This may be partly because providers are better at telling which patients are acute, and there are better things they can send them home with. It’s not necessarily worse care, but we don’t know. But we’re definitely seeing a higher send-home rate of patients showing up with COVID.”
Hospital profit margins are cratering again, because the COVID-19 cases aren’t generating nearly as much profit as the lucrative procedures that, in many cases, have been put off, Mr. Lefar said. “Even though CMS is paying 20% more for verified COVID-19 patients, we know that the costs on these patients are much higher than expected, so they’re not making much money on these cases.”
For about a third of hospitals, margins are currently negative, he said. That is about the same percentage as in September. In April, 60% of health systems were losing money, he added. “The CARES Act saved some of them,” he noted.
A version of this article first appeared on Medscape.com.
Hospital volumes, which had largely recovered in September after crashing last spring, are dropping again, according to new data from Strata Decision Technologies, a Chicago-based analytics firm.
For the 2 weeks that ended Nov. 28, inpatient admissions were 6.2% below what they’d been on Nov. 14 and 2.1% below what they’d been on Oct. 28. Compared with the same intervals in 2019, admissions were off 4.4% for the 14-day period and 3.7% for the 30-day period.
Although those aren’t large percentages, Strata’s report, based on data from about 275 client hospitals, notes that what kept the volumes up was the increasing number of COVID-19 cases. If COVID-19 cases are not considered, admissions would have been down “double digits,” said Steve Lefar, executive director of StrataDataScience, a division of Strata Decision Technologies, in an interview with this news organization.
“Hip and knee replacements, cardiac procedures, and other procedures are significantly down year over year. Infectious disease cases, in contrast, have skyrocketed,” Mr. Lefar said. “Many things went way down that hadn’t fully recovered. It’s COVID-19 that really brought the volume back up.”
Observation and emergency department visits also dropped from already low levels. For the 2 weeks that ended Nov. 28, observation visits were off 8.4%; for the previous month, 10.1%. Compared with 2019, they were down 22.3% and 18.6%, respectively.
ED visits fell 3.7% for the 2-week period, 0.6% for the month. They dropped 21% and 18.7%, respectively, compared with those periods from the previous year.
What these data reflect, Mr. Lefar said, is that people have avoided EDs and are staying away from them more than ever because of COVID-19 fears. This behavior could be problematic for people who have concerning symptoms, such as chest pains, that should be evaluated by an ED physician, he noted.
Daily outpatient visits were down 18.4% for the 14-day period and 9.3% for the 30-day period. But, compared with 2019, ambulatory visits increased 5.8% for the 2-week period and 4.7% for the previous month.
Long-term trends
The outpatient visit data should be viewed in the context of the overall trend since the pandemic began. Strata broke down service lines for the period between March 20 and Nov. 7. The analysis shows that evaluation and management (E/M) encounters, the largest outpatient visit category, fell 58% during this period, compared with the same interval in 2019. Visits for diabetes, hypertension, and minor acute infections and injuries were also way down.
Mr. Lefar observed that the E/M visit category was only for in-person visits, which many patients have ditched in favor of telehealth encounters. At the same time, he noted, “people are going in less for chronic disease visits. So there’s an interplay between less in-person visits, more telehealth, and maybe people going to other sites that aren’t on the hospital campus. But people are going less [to outpatient clinics].”
In the year-to-year comparison, volume was down substantially in other service lines, including cancer (–9.2%), cardiology (–20%), dermatology (–31%), endocrine (–18.8%), ENT (–42.5%), gastroenterology (–24.3%), nephrology (–15%), obstetrics (–15.6%), orthopedics (–28.2%), and general surgery (–22.2%). Major procedures decreased by 21.8%.
In contrast, the infectious disease category jumped 86% over 2019, and “other infectious and parasitic diseases” – i.e., COVID-19 – soared 222%.
There was a much bigger crash in admissions, observation visits, and ED visits last spring than in November, the report shows. “What happened nationally last spring is that everyone shut down,” Mr. Lefar explained. “All the electives were canceled. Even cancer surgery was shut down, along with many other procedures. That’s what drove that crash. But the provider community quickly learned that this is going to be a long haul, and we’re going to have to reopen. We’re going to do it safely, but we’re going to make sure people get the necessary care. We can’t put off cancer care or colonoscopies and other screenings that save lives.”
System starts to break down
The current wave of COVID-19, however, is beginning to change the definition of necessary care, he said. “Hospitals are reaching the breaking point between staff exhaustion and hospital capacity reaching its limit. In Texas, hospitals are starting to shut down certain essential non-COVID care. They’re turning away some nonurgent cases – the electives that were starting to come back.”
How about nonurgent COVID cases? Mr. Lefar said there’s evidence that some of those patients are also being diverted. “Some experts speculate that the turn-away rate of people with confirmed COVID is starting to go up, and hospitals are sending them home with oxygen or an oxygen meter and saying, ‘If it gets worse, come back.’ They just don’t have the critical care capacity – and that should scare the heck out of everybody.”
Strata doesn’t yet have the data to confirm this, he said, “but it appears that some people are being sent home. This may be partly because providers are better at telling which patients are acute, and there are better things they can send them home with. It’s not necessarily worse care, but we don’t know. But we’re definitely seeing a higher send-home rate of patients showing up with COVID.”
Hospital profit margins are cratering again, because the COVID-19 cases aren’t generating nearly as much profit as the lucrative procedures that, in many cases, have been put off, Mr. Lefar said. “Even though CMS is paying 20% more for verified COVID-19 patients, we know that the costs on these patients are much higher than expected, so they’re not making much money on these cases.”
For about a third of hospitals, margins are currently negative, he said. That is about the same percentage as in September. In April, 60% of health systems were losing money, he added. “The CARES Act saved some of them,” he noted.
A version of this article first appeared on Medscape.com.
Hospital volumes, which had largely recovered in September after crashing last spring, are dropping again, according to new data from Strata Decision Technologies, a Chicago-based analytics firm.
For the 2 weeks that ended Nov. 28, inpatient admissions were 6.2% below what they’d been on Nov. 14 and 2.1% below what they’d been on Oct. 28. Compared with the same intervals in 2019, admissions were off 4.4% for the 14-day period and 3.7% for the 30-day period.
Although those aren’t large percentages, Strata’s report, based on data from about 275 client hospitals, notes that what kept the volumes up was the increasing number of COVID-19 cases. If COVID-19 cases are not considered, admissions would have been down “double digits,” said Steve Lefar, executive director of StrataDataScience, a division of Strata Decision Technologies, in an interview with this news organization.
“Hip and knee replacements, cardiac procedures, and other procedures are significantly down year over year. Infectious disease cases, in contrast, have skyrocketed,” Mr. Lefar said. “Many things went way down that hadn’t fully recovered. It’s COVID-19 that really brought the volume back up.”
Observation and emergency department visits also dropped from already low levels. For the 2 weeks that ended Nov. 28, observation visits were off 8.4%; for the previous month, 10.1%. Compared with 2019, they were down 22.3% and 18.6%, respectively.
ED visits fell 3.7% for the 2-week period, 0.6% for the month. They dropped 21% and 18.7%, respectively, compared with those periods from the previous year.
What these data reflect, Mr. Lefar said, is that people have avoided EDs and are staying away from them more than ever because of COVID-19 fears. This behavior could be problematic for people who have concerning symptoms, such as chest pains, that should be evaluated by an ED physician, he noted.
Daily outpatient visits were down 18.4% for the 14-day period and 9.3% for the 30-day period. But, compared with 2019, ambulatory visits increased 5.8% for the 2-week period and 4.7% for the previous month.
Long-term trends
The outpatient visit data should be viewed in the context of the overall trend since the pandemic began. Strata broke down service lines for the period between March 20 and Nov. 7. The analysis shows that evaluation and management (E/M) encounters, the largest outpatient visit category, fell 58% during this period, compared with the same interval in 2019. Visits for diabetes, hypertension, and minor acute infections and injuries were also way down.
Mr. Lefar observed that the E/M visit category was only for in-person visits, which many patients have ditched in favor of telehealth encounters. At the same time, he noted, “people are going in less for chronic disease visits. So there’s an interplay between less in-person visits, more telehealth, and maybe people going to other sites that aren’t on the hospital campus. But people are going less [to outpatient clinics].”
In the year-to-year comparison, volume was down substantially in other service lines, including cancer (–9.2%), cardiology (–20%), dermatology (–31%), endocrine (–18.8%), ENT (–42.5%), gastroenterology (–24.3%), nephrology (–15%), obstetrics (–15.6%), orthopedics (–28.2%), and general surgery (–22.2%). Major procedures decreased by 21.8%.
In contrast, the infectious disease category jumped 86% over 2019, and “other infectious and parasitic diseases” – i.e., COVID-19 – soared 222%.
There was a much bigger crash in admissions, observation visits, and ED visits last spring than in November, the report shows. “What happened nationally last spring is that everyone shut down,” Mr. Lefar explained. “All the electives were canceled. Even cancer surgery was shut down, along with many other procedures. That’s what drove that crash. But the provider community quickly learned that this is going to be a long haul, and we’re going to have to reopen. We’re going to do it safely, but we’re going to make sure people get the necessary care. We can’t put off cancer care or colonoscopies and other screenings that save lives.”
System starts to break down
The current wave of COVID-19, however, is beginning to change the definition of necessary care, he said. “Hospitals are reaching the breaking point between staff exhaustion and hospital capacity reaching its limit. In Texas, hospitals are starting to shut down certain essential non-COVID care. They’re turning away some nonurgent cases – the electives that were starting to come back.”
How about nonurgent COVID cases? Mr. Lefar said there’s evidence that some of those patients are also being diverted. “Some experts speculate that the turn-away rate of people with confirmed COVID is starting to go up, and hospitals are sending them home with oxygen or an oxygen meter and saying, ‘If it gets worse, come back.’ They just don’t have the critical care capacity – and that should scare the heck out of everybody.”
Strata doesn’t yet have the data to confirm this, he said, “but it appears that some people are being sent home. This may be partly because providers are better at telling which patients are acute, and there are better things they can send them home with. It’s not necessarily worse care, but we don’t know. But we’re definitely seeing a higher send-home rate of patients showing up with COVID.”
Hospital profit margins are cratering again, because the COVID-19 cases aren’t generating nearly as much profit as the lucrative procedures that, in many cases, have been put off, Mr. Lefar said. “Even though CMS is paying 20% more for verified COVID-19 patients, we know that the costs on these patients are much higher than expected, so they’re not making much money on these cases.”
For about a third of hospitals, margins are currently negative, he said. That is about the same percentage as in September. In April, 60% of health systems were losing money, he added. “The CARES Act saved some of them,” he noted.
A version of this article first appeared on Medscape.com.
Pregnant women should be offered COVID-19 vaccine, experts agree
according to guidance from the Centers for Disease Control and Prevention, the American College of Obstetricians and Gynecologists, and the Society for Maternal-Fetal Medicine.
Pregnant women who opt not to receive the vaccine should be supported in that decision as well, a practice advisory from ACOG recommends.
“Pregnant women who experience fever following vaccination should be counseled to take acetaminophen,” the advisory notes.
In addition, women do not need to avoid pregnancy after receiving the Pfizer-BioNTech COVID-19 vaccine, according to the CDC’s interim clinical considerations for its use. The U.S. Food and Drug Administration issued an emergency use authorization for the vaccine on Dec. 11.
Although investigators excluded pregnant women from clinical trials, experts believe that mRNA vaccines, which are not live vaccines, “are unlikely to pose a risk for people who are pregnant” and “are not thought to be a risk to the breastfeeding infant,” the CDC notes.
Meanwhile, women who are pregnant may be at greater risk of severe COVID-19, even though the absolute risk of severe illness is low. COVID-19 also may increase the risk of adverse pregnancy outcomes, such as preterm birth, although the data have been mixed with some studies finding an association and others not.
“If pregnant people are part of a group that is recommended to receive a COVID-19 vaccine (e.g., health care personnel), they may choose to be vaccinated,” the CDC advises. “A conversation between the patient and their clinical team may assist with decisions regarding the use of vaccines approved under EUA for the prevention of COVID-19. While a conversation with a health care provider may be helpful, it is not required prior to vaccination.”
Acknowledging side effects and uncertainty
ACOG’s advisory reiterates that approach. The group notes that, based on the mRNA vaccine’s mechanism of action and its safety and efficacy in clinical trials, “it is expected that the safety and efficacy profile of the vaccine for pregnant individuals would be similar to that observed in nonpregnant individuals ... That said, there are no safety data specific to mRNA vaccine use in pregnant or lactating individuals and the potential risks to a pregnant individual and the fetus are unknown.”
In clinical trials, most participants experienced mild influenza-like symptoms following vaccination, including injection site reactions, fatigue, chills, muscle and joint pain, and headache. Among participants aged 18-55 years, fever greater than 38°C occurred in 3.7% of participants after the first dose and in 15.8% after the second dose. Most symptoms resolved within a few days.
Women who are pregnant should treat fever with acetaminophen because “fever has been associated with adverse pregnancy outcomes,” according to the ACOG guidance. “Acetaminophen has been proven to be safe for use in pregnancy and does not appear to impact antibody response to COVID-19 vaccines.” Patients may treat other vaccine side effects, such as injection-site soreness with acetaminophen as well.
When counseling patients, clinicians should explain that side effects are a normal part of developing antibodies to protect against COVID-19. “Regardless of their decision,” the group says, “these conversations provide an opportunity to remind patients about the importance of other prevention measures such as hand washing, physical distancing, and wearing a mask.”
More data expected
Data from developmental and reproductive toxicity studies in animals are expected soon, the CDC said. In addition, the manufacturer is following clinical trial participants who became pregnant during the study.
Women who are pregnant and their physicians should weigh factors such as the extent of COVID-19 transmission in the community, the patient’s risk of contracting COVID-19, risks of COVID-19 to the patient and fetus, vaccine efficacy and side effects, and the lack of data about COVID-19 vaccination during pregnancy.
The Society for Maternal-Fetal Medicine recommends that pregnant and lactating women have access to COVID-19 vaccines in general and has advocated for the inclusion of women who are pregnant or lactating in vaccine trials. The society has suggested that health care professionals “counsel their patients that the theoretical risk of fetal harm from mRNA vaccines is very low.” It published resources this week for physicians and patients focused on COVID-19 vaccination and pregnancy.
In a review published online Dec. 10 in the American Journal of Obstetrics & Gynecology MFM, Amanda M. Craig, MD, of Duke University Health System in Durham, N.C., and coauthors note that there “is a theoretical risk for fetal harm from any untested medical intervention and this is no different for COVID-19 vaccines.”
“Pregnant individuals should be given the opportunity, along with their obstetric provider, to weigh the potential risk of severe maternal disease against the unknown risk of fetal exposure, and make an autonomous decision about whether or not to accept vaccine until pregnancy safety data are available,” they write.
A version of this article first appeared on Medscape.com.
according to guidance from the Centers for Disease Control and Prevention, the American College of Obstetricians and Gynecologists, and the Society for Maternal-Fetal Medicine.
Pregnant women who opt not to receive the vaccine should be supported in that decision as well, a practice advisory from ACOG recommends.
“Pregnant women who experience fever following vaccination should be counseled to take acetaminophen,” the advisory notes.
In addition, women do not need to avoid pregnancy after receiving the Pfizer-BioNTech COVID-19 vaccine, according to the CDC’s interim clinical considerations for its use. The U.S. Food and Drug Administration issued an emergency use authorization for the vaccine on Dec. 11.
Although investigators excluded pregnant women from clinical trials, experts believe that mRNA vaccines, which are not live vaccines, “are unlikely to pose a risk for people who are pregnant” and “are not thought to be a risk to the breastfeeding infant,” the CDC notes.
Meanwhile, women who are pregnant may be at greater risk of severe COVID-19, even though the absolute risk of severe illness is low. COVID-19 also may increase the risk of adverse pregnancy outcomes, such as preterm birth, although the data have been mixed with some studies finding an association and others not.
“If pregnant people are part of a group that is recommended to receive a COVID-19 vaccine (e.g., health care personnel), they may choose to be vaccinated,” the CDC advises. “A conversation between the patient and their clinical team may assist with decisions regarding the use of vaccines approved under EUA for the prevention of COVID-19. While a conversation with a health care provider may be helpful, it is not required prior to vaccination.”
Acknowledging side effects and uncertainty
ACOG’s advisory reiterates that approach. The group notes that, based on the mRNA vaccine’s mechanism of action and its safety and efficacy in clinical trials, “it is expected that the safety and efficacy profile of the vaccine for pregnant individuals would be similar to that observed in nonpregnant individuals ... That said, there are no safety data specific to mRNA vaccine use in pregnant or lactating individuals and the potential risks to a pregnant individual and the fetus are unknown.”
In clinical trials, most participants experienced mild influenza-like symptoms following vaccination, including injection site reactions, fatigue, chills, muscle and joint pain, and headache. Among participants aged 18-55 years, fever greater than 38°C occurred in 3.7% of participants after the first dose and in 15.8% after the second dose. Most symptoms resolved within a few days.
Women who are pregnant should treat fever with acetaminophen because “fever has been associated with adverse pregnancy outcomes,” according to the ACOG guidance. “Acetaminophen has been proven to be safe for use in pregnancy and does not appear to impact antibody response to COVID-19 vaccines.” Patients may treat other vaccine side effects, such as injection-site soreness with acetaminophen as well.
When counseling patients, clinicians should explain that side effects are a normal part of developing antibodies to protect against COVID-19. “Regardless of their decision,” the group says, “these conversations provide an opportunity to remind patients about the importance of other prevention measures such as hand washing, physical distancing, and wearing a mask.”
More data expected
Data from developmental and reproductive toxicity studies in animals are expected soon, the CDC said. In addition, the manufacturer is following clinical trial participants who became pregnant during the study.
Women who are pregnant and their physicians should weigh factors such as the extent of COVID-19 transmission in the community, the patient’s risk of contracting COVID-19, risks of COVID-19 to the patient and fetus, vaccine efficacy and side effects, and the lack of data about COVID-19 vaccination during pregnancy.
The Society for Maternal-Fetal Medicine recommends that pregnant and lactating women have access to COVID-19 vaccines in general and has advocated for the inclusion of women who are pregnant or lactating in vaccine trials. The society has suggested that health care professionals “counsel their patients that the theoretical risk of fetal harm from mRNA vaccines is very low.” It published resources this week for physicians and patients focused on COVID-19 vaccination and pregnancy.
In a review published online Dec. 10 in the American Journal of Obstetrics & Gynecology MFM, Amanda M. Craig, MD, of Duke University Health System in Durham, N.C., and coauthors note that there “is a theoretical risk for fetal harm from any untested medical intervention and this is no different for COVID-19 vaccines.”
“Pregnant individuals should be given the opportunity, along with their obstetric provider, to weigh the potential risk of severe maternal disease against the unknown risk of fetal exposure, and make an autonomous decision about whether or not to accept vaccine until pregnancy safety data are available,” they write.
A version of this article first appeared on Medscape.com.
according to guidance from the Centers for Disease Control and Prevention, the American College of Obstetricians and Gynecologists, and the Society for Maternal-Fetal Medicine.
Pregnant women who opt not to receive the vaccine should be supported in that decision as well, a practice advisory from ACOG recommends.
“Pregnant women who experience fever following vaccination should be counseled to take acetaminophen,” the advisory notes.
In addition, women do not need to avoid pregnancy after receiving the Pfizer-BioNTech COVID-19 vaccine, according to the CDC’s interim clinical considerations for its use. The U.S. Food and Drug Administration issued an emergency use authorization for the vaccine on Dec. 11.
Although investigators excluded pregnant women from clinical trials, experts believe that mRNA vaccines, which are not live vaccines, “are unlikely to pose a risk for people who are pregnant” and “are not thought to be a risk to the breastfeeding infant,” the CDC notes.
Meanwhile, women who are pregnant may be at greater risk of severe COVID-19, even though the absolute risk of severe illness is low. COVID-19 also may increase the risk of adverse pregnancy outcomes, such as preterm birth, although the data have been mixed with some studies finding an association and others not.
“If pregnant people are part of a group that is recommended to receive a COVID-19 vaccine (e.g., health care personnel), they may choose to be vaccinated,” the CDC advises. “A conversation between the patient and their clinical team may assist with decisions regarding the use of vaccines approved under EUA for the prevention of COVID-19. While a conversation with a health care provider may be helpful, it is not required prior to vaccination.”
Acknowledging side effects and uncertainty
ACOG’s advisory reiterates that approach. The group notes that, based on the mRNA vaccine’s mechanism of action and its safety and efficacy in clinical trials, “it is expected that the safety and efficacy profile of the vaccine for pregnant individuals would be similar to that observed in nonpregnant individuals ... That said, there are no safety data specific to mRNA vaccine use in pregnant or lactating individuals and the potential risks to a pregnant individual and the fetus are unknown.”
In clinical trials, most participants experienced mild influenza-like symptoms following vaccination, including injection site reactions, fatigue, chills, muscle and joint pain, and headache. Among participants aged 18-55 years, fever greater than 38°C occurred in 3.7% of participants after the first dose and in 15.8% after the second dose. Most symptoms resolved within a few days.
Women who are pregnant should treat fever with acetaminophen because “fever has been associated with adverse pregnancy outcomes,” according to the ACOG guidance. “Acetaminophen has been proven to be safe for use in pregnancy and does not appear to impact antibody response to COVID-19 vaccines.” Patients may treat other vaccine side effects, such as injection-site soreness with acetaminophen as well.
When counseling patients, clinicians should explain that side effects are a normal part of developing antibodies to protect against COVID-19. “Regardless of their decision,” the group says, “these conversations provide an opportunity to remind patients about the importance of other prevention measures such as hand washing, physical distancing, and wearing a mask.”
More data expected
Data from developmental and reproductive toxicity studies in animals are expected soon, the CDC said. In addition, the manufacturer is following clinical trial participants who became pregnant during the study.
Women who are pregnant and their physicians should weigh factors such as the extent of COVID-19 transmission in the community, the patient’s risk of contracting COVID-19, risks of COVID-19 to the patient and fetus, vaccine efficacy and side effects, and the lack of data about COVID-19 vaccination during pregnancy.
The Society for Maternal-Fetal Medicine recommends that pregnant and lactating women have access to COVID-19 vaccines in general and has advocated for the inclusion of women who are pregnant or lactating in vaccine trials. The society has suggested that health care professionals “counsel their patients that the theoretical risk of fetal harm from mRNA vaccines is very low.” It published resources this week for physicians and patients focused on COVID-19 vaccination and pregnancy.
In a review published online Dec. 10 in the American Journal of Obstetrics & Gynecology MFM, Amanda M. Craig, MD, of Duke University Health System in Durham, N.C., and coauthors note that there “is a theoretical risk for fetal harm from any untested medical intervention and this is no different for COVID-19 vaccines.”
“Pregnant individuals should be given the opportunity, along with their obstetric provider, to weigh the potential risk of severe maternal disease against the unknown risk of fetal exposure, and make an autonomous decision about whether or not to accept vaccine until pregnancy safety data are available,” they write.
A version of this article first appeared on Medscape.com.
Moderna’s COVID-19 vaccine deemed ‘highly effective,’ but further studies needed
The Food and Drug Administration’s Vaccines and Related Biological Products Advisory Committee (VRBPAC) evaluated
The panel acknowledged that further studies will be required post issuance of an Emergency Use Authorization (EUA) to collect additional data on the safety and effectiveness of the vaccine. A briefing document released by the FDA on Dec. 17, 2020, summarized interim results and included recommendations from VRBPAC on use of Moderna’s mRNA-1273 COVID-19 vaccine.
“On November 30, 2020, ModernaTX (the Sponsor) submitted an EUA request to FDA for an investigational COVID-19 vaccine (mRNA-1273) intended to prevent COVID-19,” the committee wrote.
The mRNA-1273 vaccine trial
Among 30,351 individuals aged 18 years and older, the efficacy, safety, and immunogenicity of the mRNA-1273 vaccine candidate was evaluated in a randomized, stratified, observer-blind, placebo-controlled phase 3 study. Participants were randomly assigned (1:1) to receive two injections of either 100 mcg of mRNA-1273 (n = 15,181) or saline placebo (n = 15,170) administered intramuscularly on day 1 and day 29.
The primary efficacy endpoint was efficacy of mRNA-1273 against PCR-confirmed COVID-19 with onset at least 14 days following the second dose. The primary safety endpoint was to characterize the safety of the vaccine following one or two doses.
Efficacy
Among 27,817 subjects included in the first interim analysis (data cutoff: Nov. 7, 2020), 5 cases of COVID-19 with onset at least 14 days after the second dose occurred among vaccine recipients and 90 case occurred among placebo recipients, corresponding to 94.5% vaccine efficacy (95% confidence interval, 86.5%-97.8%).
“Subgroup analyses of the primary efficacy endpoint showed similar efficacy point estimates across age groups, genders, racial and ethnic groups, and participants with medical comorbidities associated with high risk of severe COVID-19,” they reported.
Data from the final scheduled analysis of the primary efficacy endpoint (data cutoff: Nov. 21, 2020; median follow-up of >2 months after dose 2), demonstrated 94.1% vaccine efficacy (95% confidence interval, 89.3%-96.8%), corresponding to 11 cases of COVID-19 in the vaccine group and 185 cases in the placebo group.
When stratified by age, the vaccine efficacy was 95.6% (95% CI, 90.6%-97.9%) for individuals 18-64 years of age and 86.4% (95% CI, 61.4%-95.5%) for those 65 years of age or older.
In addition, results from secondary analyses indicated benefit for mRNA-1273 in preventing severe COVID-19 cases, COVID-19 in those with prior SARS-CoV-2 infection, and infection after the first dose, but these data were not conclusive.
Safety
Among 30,350 subjects included in the first interim analysis (data cutoff: Nov. 11, 2020; median follow-up of 7 weeks post second dose), no specific safety concerns were observed that would prevent issuance of an EUA.
Additional safety data (data cutoff: Nov. 25, 2020; median follow-up of 9 weeks post second dose) were provided on Dec. 7, 2020, but did not change the conclusions from the first interim analysis.
The most common vaccine-related adverse reactions were injection site pain (91.6%), fatigue (68.5%), headache (63.0%), muscle pain (59.6%), joint pain (44.8%), and chills (43.4%).
“The frequency of serious adverse events (SAEs) was low (1.0% in the mRNA-1273 arm and 1.0% in the placebo arm), without meaningful imbalances between study arms,” they reported.
Myocardial infarction (0.03%), nephrolithiasis (0.02%), and cholecystitis (0.02%) were the most common SAEs that were numerically greater in the vaccine arm than the placebo arm; however, the small number of cases does not infer a casual relationship.
“The 2-dose vaccination regimen was highly effective in preventing PCR-confirmed COVID-19 occurring at least 14 days after receipt of the second dose,” the committee wrote. “[However], it is critical to continue to gather data about the vaccine even after it is made available under EUA.”
The associated phase 3 study was sponsored by ModernaTX.
SOURCE: FDA Briefing Document: Moderna COVID-19 Vaccine. FDA Vaccines and Related Biological Products Advisory Committee. Published Dec. 17, 2020.
The Food and Drug Administration’s Vaccines and Related Biological Products Advisory Committee (VRBPAC) evaluated
The panel acknowledged that further studies will be required post issuance of an Emergency Use Authorization (EUA) to collect additional data on the safety and effectiveness of the vaccine. A briefing document released by the FDA on Dec. 17, 2020, summarized interim results and included recommendations from VRBPAC on use of Moderna’s mRNA-1273 COVID-19 vaccine.
“On November 30, 2020, ModernaTX (the Sponsor) submitted an EUA request to FDA for an investigational COVID-19 vaccine (mRNA-1273) intended to prevent COVID-19,” the committee wrote.
The mRNA-1273 vaccine trial
Among 30,351 individuals aged 18 years and older, the efficacy, safety, and immunogenicity of the mRNA-1273 vaccine candidate was evaluated in a randomized, stratified, observer-blind, placebo-controlled phase 3 study. Participants were randomly assigned (1:1) to receive two injections of either 100 mcg of mRNA-1273 (n = 15,181) or saline placebo (n = 15,170) administered intramuscularly on day 1 and day 29.
The primary efficacy endpoint was efficacy of mRNA-1273 against PCR-confirmed COVID-19 with onset at least 14 days following the second dose. The primary safety endpoint was to characterize the safety of the vaccine following one or two doses.
Efficacy
Among 27,817 subjects included in the first interim analysis (data cutoff: Nov. 7, 2020), 5 cases of COVID-19 with onset at least 14 days after the second dose occurred among vaccine recipients and 90 case occurred among placebo recipients, corresponding to 94.5% vaccine efficacy (95% confidence interval, 86.5%-97.8%).
“Subgroup analyses of the primary efficacy endpoint showed similar efficacy point estimates across age groups, genders, racial and ethnic groups, and participants with medical comorbidities associated with high risk of severe COVID-19,” they reported.
Data from the final scheduled analysis of the primary efficacy endpoint (data cutoff: Nov. 21, 2020; median follow-up of >2 months after dose 2), demonstrated 94.1% vaccine efficacy (95% confidence interval, 89.3%-96.8%), corresponding to 11 cases of COVID-19 in the vaccine group and 185 cases in the placebo group.
When stratified by age, the vaccine efficacy was 95.6% (95% CI, 90.6%-97.9%) for individuals 18-64 years of age and 86.4% (95% CI, 61.4%-95.5%) for those 65 years of age or older.
In addition, results from secondary analyses indicated benefit for mRNA-1273 in preventing severe COVID-19 cases, COVID-19 in those with prior SARS-CoV-2 infection, and infection after the first dose, but these data were not conclusive.
Safety
Among 30,350 subjects included in the first interim analysis (data cutoff: Nov. 11, 2020; median follow-up of 7 weeks post second dose), no specific safety concerns were observed that would prevent issuance of an EUA.
Additional safety data (data cutoff: Nov. 25, 2020; median follow-up of 9 weeks post second dose) were provided on Dec. 7, 2020, but did not change the conclusions from the first interim analysis.
The most common vaccine-related adverse reactions were injection site pain (91.6%), fatigue (68.5%), headache (63.0%), muscle pain (59.6%), joint pain (44.8%), and chills (43.4%).
“The frequency of serious adverse events (SAEs) was low (1.0% in the mRNA-1273 arm and 1.0% in the placebo arm), without meaningful imbalances between study arms,” they reported.
Myocardial infarction (0.03%), nephrolithiasis (0.02%), and cholecystitis (0.02%) were the most common SAEs that were numerically greater in the vaccine arm than the placebo arm; however, the small number of cases does not infer a casual relationship.
“The 2-dose vaccination regimen was highly effective in preventing PCR-confirmed COVID-19 occurring at least 14 days after receipt of the second dose,” the committee wrote. “[However], it is critical to continue to gather data about the vaccine even after it is made available under EUA.”
The associated phase 3 study was sponsored by ModernaTX.
SOURCE: FDA Briefing Document: Moderna COVID-19 Vaccine. FDA Vaccines and Related Biological Products Advisory Committee. Published Dec. 17, 2020.
The Food and Drug Administration’s Vaccines and Related Biological Products Advisory Committee (VRBPAC) evaluated
The panel acknowledged that further studies will be required post issuance of an Emergency Use Authorization (EUA) to collect additional data on the safety and effectiveness of the vaccine. A briefing document released by the FDA on Dec. 17, 2020, summarized interim results and included recommendations from VRBPAC on use of Moderna’s mRNA-1273 COVID-19 vaccine.
“On November 30, 2020, ModernaTX (the Sponsor) submitted an EUA request to FDA for an investigational COVID-19 vaccine (mRNA-1273) intended to prevent COVID-19,” the committee wrote.
The mRNA-1273 vaccine trial
Among 30,351 individuals aged 18 years and older, the efficacy, safety, and immunogenicity of the mRNA-1273 vaccine candidate was evaluated in a randomized, stratified, observer-blind, placebo-controlled phase 3 study. Participants were randomly assigned (1:1) to receive two injections of either 100 mcg of mRNA-1273 (n = 15,181) or saline placebo (n = 15,170) administered intramuscularly on day 1 and day 29.
The primary efficacy endpoint was efficacy of mRNA-1273 against PCR-confirmed COVID-19 with onset at least 14 days following the second dose. The primary safety endpoint was to characterize the safety of the vaccine following one or two doses.
Efficacy
Among 27,817 subjects included in the first interim analysis (data cutoff: Nov. 7, 2020), 5 cases of COVID-19 with onset at least 14 days after the second dose occurred among vaccine recipients and 90 case occurred among placebo recipients, corresponding to 94.5% vaccine efficacy (95% confidence interval, 86.5%-97.8%).
“Subgroup analyses of the primary efficacy endpoint showed similar efficacy point estimates across age groups, genders, racial and ethnic groups, and participants with medical comorbidities associated with high risk of severe COVID-19,” they reported.
Data from the final scheduled analysis of the primary efficacy endpoint (data cutoff: Nov. 21, 2020; median follow-up of >2 months after dose 2), demonstrated 94.1% vaccine efficacy (95% confidence interval, 89.3%-96.8%), corresponding to 11 cases of COVID-19 in the vaccine group and 185 cases in the placebo group.
When stratified by age, the vaccine efficacy was 95.6% (95% CI, 90.6%-97.9%) for individuals 18-64 years of age and 86.4% (95% CI, 61.4%-95.5%) for those 65 years of age or older.
In addition, results from secondary analyses indicated benefit for mRNA-1273 in preventing severe COVID-19 cases, COVID-19 in those with prior SARS-CoV-2 infection, and infection after the first dose, but these data were not conclusive.
Safety
Among 30,350 subjects included in the first interim analysis (data cutoff: Nov. 11, 2020; median follow-up of 7 weeks post second dose), no specific safety concerns were observed that would prevent issuance of an EUA.
Additional safety data (data cutoff: Nov. 25, 2020; median follow-up of 9 weeks post second dose) were provided on Dec. 7, 2020, but did not change the conclusions from the first interim analysis.
The most common vaccine-related adverse reactions were injection site pain (91.6%), fatigue (68.5%), headache (63.0%), muscle pain (59.6%), joint pain (44.8%), and chills (43.4%).
“The frequency of serious adverse events (SAEs) was low (1.0% in the mRNA-1273 arm and 1.0% in the placebo arm), without meaningful imbalances between study arms,” they reported.
Myocardial infarction (0.03%), nephrolithiasis (0.02%), and cholecystitis (0.02%) were the most common SAEs that were numerically greater in the vaccine arm than the placebo arm; however, the small number of cases does not infer a casual relationship.
“The 2-dose vaccination regimen was highly effective in preventing PCR-confirmed COVID-19 occurring at least 14 days after receipt of the second dose,” the committee wrote. “[However], it is critical to continue to gather data about the vaccine even after it is made available under EUA.”
The associated phase 3 study was sponsored by ModernaTX.
SOURCE: FDA Briefing Document: Moderna COVID-19 Vaccine. FDA Vaccines and Related Biological Products Advisory Committee. Published Dec. 17, 2020.
Key clinical point: The FDA’s Vaccines and Related Biological Products Advisory Committee regarded Moderna’s COVID-19 vaccine as highly effective with a favorable safety profile, based on interim phase 3 results.
Major finding: The two-dose vaccine regimen had a low frequency of serious adverse events (1.0% each in the mRNA-1273 and placebo arms, respectively) and demonstrated 94.1% (95% CI, 89.3%-96.8%) vaccine efficacy.
Study details: A briefing document summarized interim data and recommendations from the FDA’s VRBPAC on Moderna’s mRNA-1273 COVID-19 vaccine.
Disclosures: The associated phase 3 study was sponsored by ModernaTX.
Source: FDA Briefing Document: Moderna COVID-19 Vaccine. FDA Vaccines and Related Biological Products Advisory Committee. Published Dec. 17, 2020.
Child abuse visits to EDs declined in 2020, but not admissions
but the visits in 2020 were significantly more likely to result in hospitalization, based on analysis of a national ED database.

The number of ED visits involving child abuse and neglect was down by 53% during the 4-week period from March 29 to April 25, 2020, compared with the 4 weeks from March 31 to April 27, 2019. The proportion of those ED visits that ended in hospitalizations, however, increased from 2.1% in 2019 to 3.2% in 2020, Elizabeth Swedo, MD, and associates at the Centers for Disease Control and Prevention said in the Morbidity and Mortality Weekly Report.
“ED visits related to suspected or confirmed child abuse and neglect decreased beginning the week of March 15, 2020, coinciding with the declaration of a national emergency related to COVID-19 and implementation of community mitigation measures,” they wrote.
An earlier study involving the same database (the National Syndromic Surveillance Program) showed that, over the two same 4-week periods, the volume of all ED visits in 2020 was down 72% for children aged 10 years and younger and 71% for those aged 11-14 years.
In the current study, however, all age subgroups had significant increases in hospital admissions. The proportion of ED visits related to child abuse and neglect that resulted in hospitalization rose from 3.5% in 2019 to 5.3% in 2020 among ages 0-4 years, 0.7% to 1.3% for ages 5-11 years, and 1.6% to 2.2% for adolescents aged 12-17, Dr. Swedo and associates reported.
The absence of a corresponding drop in hospitalizations may be tied to risk factors related to the pandemic, “such as loss of income, increased stress related to parental child care and schooling responsibilities, and increased substance use and mental health conditions among adults,” the investigators added.
The National Syndromic Surveillance Program receives daily data from 3,310 EDs in 47 states, but the number of facilities meeting the investigators’ criteria averaged 2,970 a week for the 8 weeks of the study period.
SOURCE: Swedo E et al. MMWR. 2020 Dec. 11;69(49):1841-7.
but the visits in 2020 were significantly more likely to result in hospitalization, based on analysis of a national ED database.

The number of ED visits involving child abuse and neglect was down by 53% during the 4-week period from March 29 to April 25, 2020, compared with the 4 weeks from March 31 to April 27, 2019. The proportion of those ED visits that ended in hospitalizations, however, increased from 2.1% in 2019 to 3.2% in 2020, Elizabeth Swedo, MD, and associates at the Centers for Disease Control and Prevention said in the Morbidity and Mortality Weekly Report.
“ED visits related to suspected or confirmed child abuse and neglect decreased beginning the week of March 15, 2020, coinciding with the declaration of a national emergency related to COVID-19 and implementation of community mitigation measures,” they wrote.
An earlier study involving the same database (the National Syndromic Surveillance Program) showed that, over the two same 4-week periods, the volume of all ED visits in 2020 was down 72% for children aged 10 years and younger and 71% for those aged 11-14 years.
In the current study, however, all age subgroups had significant increases in hospital admissions. The proportion of ED visits related to child abuse and neglect that resulted in hospitalization rose from 3.5% in 2019 to 5.3% in 2020 among ages 0-4 years, 0.7% to 1.3% for ages 5-11 years, and 1.6% to 2.2% for adolescents aged 12-17, Dr. Swedo and associates reported.
The absence of a corresponding drop in hospitalizations may be tied to risk factors related to the pandemic, “such as loss of income, increased stress related to parental child care and schooling responsibilities, and increased substance use and mental health conditions among adults,” the investigators added.
The National Syndromic Surveillance Program receives daily data from 3,310 EDs in 47 states, but the number of facilities meeting the investigators’ criteria averaged 2,970 a week for the 8 weeks of the study period.
SOURCE: Swedo E et al. MMWR. 2020 Dec. 11;69(49):1841-7.
but the visits in 2020 were significantly more likely to result in hospitalization, based on analysis of a national ED database.

The number of ED visits involving child abuse and neglect was down by 53% during the 4-week period from March 29 to April 25, 2020, compared with the 4 weeks from March 31 to April 27, 2019. The proportion of those ED visits that ended in hospitalizations, however, increased from 2.1% in 2019 to 3.2% in 2020, Elizabeth Swedo, MD, and associates at the Centers for Disease Control and Prevention said in the Morbidity and Mortality Weekly Report.
“ED visits related to suspected or confirmed child abuse and neglect decreased beginning the week of March 15, 2020, coinciding with the declaration of a national emergency related to COVID-19 and implementation of community mitigation measures,” they wrote.
An earlier study involving the same database (the National Syndromic Surveillance Program) showed that, over the two same 4-week periods, the volume of all ED visits in 2020 was down 72% for children aged 10 years and younger and 71% for those aged 11-14 years.
In the current study, however, all age subgroups had significant increases in hospital admissions. The proportion of ED visits related to child abuse and neglect that resulted in hospitalization rose from 3.5% in 2019 to 5.3% in 2020 among ages 0-4 years, 0.7% to 1.3% for ages 5-11 years, and 1.6% to 2.2% for adolescents aged 12-17, Dr. Swedo and associates reported.
The absence of a corresponding drop in hospitalizations may be tied to risk factors related to the pandemic, “such as loss of income, increased stress related to parental child care and schooling responsibilities, and increased substance use and mental health conditions among adults,” the investigators added.
The National Syndromic Surveillance Program receives daily data from 3,310 EDs in 47 states, but the number of facilities meeting the investigators’ criteria averaged 2,970 a week for the 8 weeks of the study period.
SOURCE: Swedo E et al. MMWR. 2020 Dec. 11;69(49):1841-7.
FROM MMWR
Call to arms: vaccinating the health workforce of 21 million strong
As the first American health care workers rolled up their sleeves for a COVID-19 vaccine, the images were instantly frozen in history, marking the triumph of scientific know-how and ingenuity. Cameras captured the first trucks pulling out of a warehouse in Portage, Mich., to the applause of workers and area residents. A day later, Boston Medical Center employees – some dressed in scrubs and wearing masks, face shields, and protective gowns – literally danced on the sidewalk when doses arrived. Some have photographed themselves getting the vaccine and posted it on social media, tagging it #MyCOVIDVax.
But the real story of the debut of COVID-19 vaccination is more methodical than monumental, a celebration of teamwork rather than of conquest. As hospitals waited for their first allotment, they reviewed their carefully drafted plans. They relied on each other, reaching across the usual divisions of competition and working collaboratively to share the limited supply. Their priority lists for the first vaccinations included environmental services workers who clean patient rooms and the critical care physicians who work to save lives.
“Health care workers have pulled together throughout this pandemic,” said Melanie Swift, MD, cochair of the COVID-19 Vaccine Allocation and Distribution Work Group at Mayo Clinic in Rochester, Minn. “We’ve gone through the darkest of years relying so heavily on each other,” she said. “Now we’re pulling together to get out of it.”
Still, a rollout of this magnitude has hitches. Stanford issued an apology Dec. 18 after its medical residents protested a vaccine distribution plan that left out nearly all of its residents and fellows, many of whom regularly treat patients with COVID-19.
There have already been more than 287,000 COVID-19 cases and 953 deaths among health care workers, according to the Centers for Disease Control and Prevention. In its guidance, the agency pointed out that the “continued protection of them at work, at home, and in the community remains a national priority.” That means vaccinating a workforce of about 21 million people, often the largest group of employees in a community.
“It collectively takes all of us to vaccinate our teams to maintain that stability in our health care infrastructure across the metro Atlanta area,” Christy Norman, PharmD, vice president of pharmacy services at Emory Healthcare, told reporters in a briefing as the health system awaited its first delivery.
Don’t waste a dose
One overriding imperative prevails: Hospitals don’t want to waste any doses. The storage requirements of the Pfizer vaccine make that tricky.
Once vials are removed from the pizza-box-shaped containers in ultracold storage and placed in a refrigerator, they must be used within 5 days. Thawed five-dose vials must be brought to room temperature before they are diluted, and they can remain at room temperature for no more than 2 hours. Once they are diluted with 1.8 mL of a 0.9% sodium chloride injection, the vials must be used within 6 hours.
COVID-19 precautions require employees to stay physically distant while they wait their turn for vaccination, which means the process can’t mirror typical large-scale flu immunization programs.
To prioritize groups, the vaccination planners at Mayo conducted a thorough risk stratification, considering each employee’s duties. Do they work in a dedicated COVID-19 unit? Do they handle lab tests or collect swabs? Do they work in the ICU or emergency department?
“We have applied some principles to make sure that as we roll it out, we prioritize people who are at greatest risk of ongoing exposure and who are really critical to maintaining the COVID response and other essential health services,” said Dr. Swift, associate medical director of Mayo’s occupational health service.
Mayo employees who are eligible for the first doses can sign up for appointments through the medical record system. If it seems likely that some doses will be left over at the end of the vaccination period – perhaps because of missed appointments – supervisors in high-risk areas can refer other health care workers. Mayo gave its first vaccines on Dec. 18, but the vaccination program began in earnest the following week. With the pleasant surprise that each five-dose vial actually provides six doses, 474 vials will allow for the vaccination of 2,844 employees in the top-priority group. “It’s going to expand each week or few days as we get more and more vaccine,” Dr. Swift said.
Sharing vials with small rural hospitals
Minnesota is using a hub-and-spoke system to give small rural hospitals access to the Pfizer vaccine, even though they lack ultracold storage and can’t use a minimum order of 975 doses. Large hospitals, acting as hubs, are sharing their orders. (The minimum order for Moderna is 100 doses.)
In south-central Minnesota, for example, two hub hospitals each have six spoke hospitals. Five of the 14 hospitals are independent, and the rest are part of large hospital systems, but affiliation doesn’t matter, said Eric Weller, regional health care preparedness coordinator for the South Central Healthcare Coalition. “We are all working together. It doesn’t matter what system you’re from,” he said. “We’re working for the good of the community.”
Each hospital designed a process to provide vaccine education, prioritize groups, allocate appointments, register people for vaccination, obtain signed consent forms, administer vaccines in a COVID-safe way, and provide follow-up appointments for the second dose. “We’re using some of the lessons we learned during H1N1,” said Mr. Weller, referring to immunization during the 2009 influenza pandemic. “The difference is that during H1N1, you could have lines of people.”
Coordinating the appointments will be more important than ever. “One of the vaccination strategies is to get people in groups of five, so you use one vial on those five people and don’t waste it,” he said.
Logistics are somewhat different for the Moderna vaccine, which will come in 10-dose vials that can be refrigerated for up to 30 days.
Both vaccines may produce mild flulike symptoms, such as fatigue, headache, or muscle pain, particularly after the second dose. That’s a sign that the immune system is reacting to the vaccine, but it’s also another consideration in the vaccination plans, because health care workers might take a day or two off work. “We’re not going to vaccinate a whole department at one time. It will be staggered,” said Kevin Smith, MD, medical director of the occupational medicine program at ProMedica, a health care system based in Toledo, Ohio.
Dr. Smith said he plans to encourage employees to use V-Safe, an app created by the CDC to track adverse effects in people who receive the vaccine. He pointed out that a day or two of achiness will be better than coping with the symptoms of COVID-19. Some employees who recovered from the infection still feel fatigued or haven’t regained their sense of taste and smell. “We are still monitoring quite a few employees to make sure they get back to 100%,” he said.
Hope for ending the pandemic
Public health officials have worried about vaccine hesitancy, even among health care workers, but so far, that concern seems overshadowed by enthusiasm. Dr. Smith said his department has been fielding calls from employees who want to know when they will be able to get the vaccine. “I think everyone feels relief,” he said. “We’re at the beginning of the end.”
At Mayo, Dr. Swift is surveying staff to gauge the willingness to get the vaccine, but she already senses excitement among employees. “No doubt there are still people who are hesitant, but I’m feeling a shift,” she said. “I’m feeling this momentum building of health care workers coming on board and wanting to take this vaccine, which is good, because they will set an example for their patients.”
For Colleen Kelley, MD, an infectious disease physician at Emory University in Atlanta who was principal investigator for an Emory-affiliated Moderna clinical trial site, it has been an emotional time. “Things were looking very bleak and dark for a time, and then we started to get these efficacy results that were greater than anyone imagined,” she said.
Dr. Kelley spends time talking to journalists and educating physician colleagues and hospital employees about how the vaccine was developed so quickly and how it works. “Everyone asks me, ‘Should I get it? Are you going to get it?’ My answer is ‘yes’ and ‘yes,’ “ she said. “I am 1,000% confident that the benefits of widespread vaccination outweigh the risks of continued COVID and a continued pandemic.”
A version of this article first appeared on Medscape.com.
As the first American health care workers rolled up their sleeves for a COVID-19 vaccine, the images were instantly frozen in history, marking the triumph of scientific know-how and ingenuity. Cameras captured the first trucks pulling out of a warehouse in Portage, Mich., to the applause of workers and area residents. A day later, Boston Medical Center employees – some dressed in scrubs and wearing masks, face shields, and protective gowns – literally danced on the sidewalk when doses arrived. Some have photographed themselves getting the vaccine and posted it on social media, tagging it #MyCOVIDVax.
But the real story of the debut of COVID-19 vaccination is more methodical than monumental, a celebration of teamwork rather than of conquest. As hospitals waited for their first allotment, they reviewed their carefully drafted plans. They relied on each other, reaching across the usual divisions of competition and working collaboratively to share the limited supply. Their priority lists for the first vaccinations included environmental services workers who clean patient rooms and the critical care physicians who work to save lives.
“Health care workers have pulled together throughout this pandemic,” said Melanie Swift, MD, cochair of the COVID-19 Vaccine Allocation and Distribution Work Group at Mayo Clinic in Rochester, Minn. “We’ve gone through the darkest of years relying so heavily on each other,” she said. “Now we’re pulling together to get out of it.”
Still, a rollout of this magnitude has hitches. Stanford issued an apology Dec. 18 after its medical residents protested a vaccine distribution plan that left out nearly all of its residents and fellows, many of whom regularly treat patients with COVID-19.
There have already been more than 287,000 COVID-19 cases and 953 deaths among health care workers, according to the Centers for Disease Control and Prevention. In its guidance, the agency pointed out that the “continued protection of them at work, at home, and in the community remains a national priority.” That means vaccinating a workforce of about 21 million people, often the largest group of employees in a community.
“It collectively takes all of us to vaccinate our teams to maintain that stability in our health care infrastructure across the metro Atlanta area,” Christy Norman, PharmD, vice president of pharmacy services at Emory Healthcare, told reporters in a briefing as the health system awaited its first delivery.
Don’t waste a dose
One overriding imperative prevails: Hospitals don’t want to waste any doses. The storage requirements of the Pfizer vaccine make that tricky.
Once vials are removed from the pizza-box-shaped containers in ultracold storage and placed in a refrigerator, they must be used within 5 days. Thawed five-dose vials must be brought to room temperature before they are diluted, and they can remain at room temperature for no more than 2 hours. Once they are diluted with 1.8 mL of a 0.9% sodium chloride injection, the vials must be used within 6 hours.
COVID-19 precautions require employees to stay physically distant while they wait their turn for vaccination, which means the process can’t mirror typical large-scale flu immunization programs.
To prioritize groups, the vaccination planners at Mayo conducted a thorough risk stratification, considering each employee’s duties. Do they work in a dedicated COVID-19 unit? Do they handle lab tests or collect swabs? Do they work in the ICU or emergency department?
“We have applied some principles to make sure that as we roll it out, we prioritize people who are at greatest risk of ongoing exposure and who are really critical to maintaining the COVID response and other essential health services,” said Dr. Swift, associate medical director of Mayo’s occupational health service.
Mayo employees who are eligible for the first doses can sign up for appointments through the medical record system. If it seems likely that some doses will be left over at the end of the vaccination period – perhaps because of missed appointments – supervisors in high-risk areas can refer other health care workers. Mayo gave its first vaccines on Dec. 18, but the vaccination program began in earnest the following week. With the pleasant surprise that each five-dose vial actually provides six doses, 474 vials will allow for the vaccination of 2,844 employees in the top-priority group. “It’s going to expand each week or few days as we get more and more vaccine,” Dr. Swift said.
Sharing vials with small rural hospitals
Minnesota is using a hub-and-spoke system to give small rural hospitals access to the Pfizer vaccine, even though they lack ultracold storage and can’t use a minimum order of 975 doses. Large hospitals, acting as hubs, are sharing their orders. (The minimum order for Moderna is 100 doses.)
In south-central Minnesota, for example, two hub hospitals each have six spoke hospitals. Five of the 14 hospitals are independent, and the rest are part of large hospital systems, but affiliation doesn’t matter, said Eric Weller, regional health care preparedness coordinator for the South Central Healthcare Coalition. “We are all working together. It doesn’t matter what system you’re from,” he said. “We’re working for the good of the community.”
Each hospital designed a process to provide vaccine education, prioritize groups, allocate appointments, register people for vaccination, obtain signed consent forms, administer vaccines in a COVID-safe way, and provide follow-up appointments for the second dose. “We’re using some of the lessons we learned during H1N1,” said Mr. Weller, referring to immunization during the 2009 influenza pandemic. “The difference is that during H1N1, you could have lines of people.”
Coordinating the appointments will be more important than ever. “One of the vaccination strategies is to get people in groups of five, so you use one vial on those five people and don’t waste it,” he said.
Logistics are somewhat different for the Moderna vaccine, which will come in 10-dose vials that can be refrigerated for up to 30 days.
Both vaccines may produce mild flulike symptoms, such as fatigue, headache, or muscle pain, particularly after the second dose. That’s a sign that the immune system is reacting to the vaccine, but it’s also another consideration in the vaccination plans, because health care workers might take a day or two off work. “We’re not going to vaccinate a whole department at one time. It will be staggered,” said Kevin Smith, MD, medical director of the occupational medicine program at ProMedica, a health care system based in Toledo, Ohio.
Dr. Smith said he plans to encourage employees to use V-Safe, an app created by the CDC to track adverse effects in people who receive the vaccine. He pointed out that a day or two of achiness will be better than coping with the symptoms of COVID-19. Some employees who recovered from the infection still feel fatigued or haven’t regained their sense of taste and smell. “We are still monitoring quite a few employees to make sure they get back to 100%,” he said.
Hope for ending the pandemic
Public health officials have worried about vaccine hesitancy, even among health care workers, but so far, that concern seems overshadowed by enthusiasm. Dr. Smith said his department has been fielding calls from employees who want to know when they will be able to get the vaccine. “I think everyone feels relief,” he said. “We’re at the beginning of the end.”
At Mayo, Dr. Swift is surveying staff to gauge the willingness to get the vaccine, but she already senses excitement among employees. “No doubt there are still people who are hesitant, but I’m feeling a shift,” she said. “I’m feeling this momentum building of health care workers coming on board and wanting to take this vaccine, which is good, because they will set an example for their patients.”
For Colleen Kelley, MD, an infectious disease physician at Emory University in Atlanta who was principal investigator for an Emory-affiliated Moderna clinical trial site, it has been an emotional time. “Things were looking very bleak and dark for a time, and then we started to get these efficacy results that were greater than anyone imagined,” she said.
Dr. Kelley spends time talking to journalists and educating physician colleagues and hospital employees about how the vaccine was developed so quickly and how it works. “Everyone asks me, ‘Should I get it? Are you going to get it?’ My answer is ‘yes’ and ‘yes,’ “ she said. “I am 1,000% confident that the benefits of widespread vaccination outweigh the risks of continued COVID and a continued pandemic.”
A version of this article first appeared on Medscape.com.
As the first American health care workers rolled up their sleeves for a COVID-19 vaccine, the images were instantly frozen in history, marking the triumph of scientific know-how and ingenuity. Cameras captured the first trucks pulling out of a warehouse in Portage, Mich., to the applause of workers and area residents. A day later, Boston Medical Center employees – some dressed in scrubs and wearing masks, face shields, and protective gowns – literally danced on the sidewalk when doses arrived. Some have photographed themselves getting the vaccine and posted it on social media, tagging it #MyCOVIDVax.
But the real story of the debut of COVID-19 vaccination is more methodical than monumental, a celebration of teamwork rather than of conquest. As hospitals waited for their first allotment, they reviewed their carefully drafted plans. They relied on each other, reaching across the usual divisions of competition and working collaboratively to share the limited supply. Their priority lists for the first vaccinations included environmental services workers who clean patient rooms and the critical care physicians who work to save lives.
“Health care workers have pulled together throughout this pandemic,” said Melanie Swift, MD, cochair of the COVID-19 Vaccine Allocation and Distribution Work Group at Mayo Clinic in Rochester, Minn. “We’ve gone through the darkest of years relying so heavily on each other,” she said. “Now we’re pulling together to get out of it.”
Still, a rollout of this magnitude has hitches. Stanford issued an apology Dec. 18 after its medical residents protested a vaccine distribution plan that left out nearly all of its residents and fellows, many of whom regularly treat patients with COVID-19.
There have already been more than 287,000 COVID-19 cases and 953 deaths among health care workers, according to the Centers for Disease Control and Prevention. In its guidance, the agency pointed out that the “continued protection of them at work, at home, and in the community remains a national priority.” That means vaccinating a workforce of about 21 million people, often the largest group of employees in a community.
“It collectively takes all of us to vaccinate our teams to maintain that stability in our health care infrastructure across the metro Atlanta area,” Christy Norman, PharmD, vice president of pharmacy services at Emory Healthcare, told reporters in a briefing as the health system awaited its first delivery.
Don’t waste a dose
One overriding imperative prevails: Hospitals don’t want to waste any doses. The storage requirements of the Pfizer vaccine make that tricky.
Once vials are removed from the pizza-box-shaped containers in ultracold storage and placed in a refrigerator, they must be used within 5 days. Thawed five-dose vials must be brought to room temperature before they are diluted, and they can remain at room temperature for no more than 2 hours. Once they are diluted with 1.8 mL of a 0.9% sodium chloride injection, the vials must be used within 6 hours.
COVID-19 precautions require employees to stay physically distant while they wait their turn for vaccination, which means the process can’t mirror typical large-scale flu immunization programs.
To prioritize groups, the vaccination planners at Mayo conducted a thorough risk stratification, considering each employee’s duties. Do they work in a dedicated COVID-19 unit? Do they handle lab tests or collect swabs? Do they work in the ICU or emergency department?
“We have applied some principles to make sure that as we roll it out, we prioritize people who are at greatest risk of ongoing exposure and who are really critical to maintaining the COVID response and other essential health services,” said Dr. Swift, associate medical director of Mayo’s occupational health service.
Mayo employees who are eligible for the first doses can sign up for appointments through the medical record system. If it seems likely that some doses will be left over at the end of the vaccination period – perhaps because of missed appointments – supervisors in high-risk areas can refer other health care workers. Mayo gave its first vaccines on Dec. 18, but the vaccination program began in earnest the following week. With the pleasant surprise that each five-dose vial actually provides six doses, 474 vials will allow for the vaccination of 2,844 employees in the top-priority group. “It’s going to expand each week or few days as we get more and more vaccine,” Dr. Swift said.
Sharing vials with small rural hospitals
Minnesota is using a hub-and-spoke system to give small rural hospitals access to the Pfizer vaccine, even though they lack ultracold storage and can’t use a minimum order of 975 doses. Large hospitals, acting as hubs, are sharing their orders. (The minimum order for Moderna is 100 doses.)
In south-central Minnesota, for example, two hub hospitals each have six spoke hospitals. Five of the 14 hospitals are independent, and the rest are part of large hospital systems, but affiliation doesn’t matter, said Eric Weller, regional health care preparedness coordinator for the South Central Healthcare Coalition. “We are all working together. It doesn’t matter what system you’re from,” he said. “We’re working for the good of the community.”
Each hospital designed a process to provide vaccine education, prioritize groups, allocate appointments, register people for vaccination, obtain signed consent forms, administer vaccines in a COVID-safe way, and provide follow-up appointments for the second dose. “We’re using some of the lessons we learned during H1N1,” said Mr. Weller, referring to immunization during the 2009 influenza pandemic. “The difference is that during H1N1, you could have lines of people.”
Coordinating the appointments will be more important than ever. “One of the vaccination strategies is to get people in groups of five, so you use one vial on those five people and don’t waste it,” he said.
Logistics are somewhat different for the Moderna vaccine, which will come in 10-dose vials that can be refrigerated for up to 30 days.
Both vaccines may produce mild flulike symptoms, such as fatigue, headache, or muscle pain, particularly after the second dose. That’s a sign that the immune system is reacting to the vaccine, but it’s also another consideration in the vaccination plans, because health care workers might take a day or two off work. “We’re not going to vaccinate a whole department at one time. It will be staggered,” said Kevin Smith, MD, medical director of the occupational medicine program at ProMedica, a health care system based in Toledo, Ohio.
Dr. Smith said he plans to encourage employees to use V-Safe, an app created by the CDC to track adverse effects in people who receive the vaccine. He pointed out that a day or two of achiness will be better than coping with the symptoms of COVID-19. Some employees who recovered from the infection still feel fatigued or haven’t regained their sense of taste and smell. “We are still monitoring quite a few employees to make sure they get back to 100%,” he said.
Hope for ending the pandemic
Public health officials have worried about vaccine hesitancy, even among health care workers, but so far, that concern seems overshadowed by enthusiasm. Dr. Smith said his department has been fielding calls from employees who want to know when they will be able to get the vaccine. “I think everyone feels relief,” he said. “We’re at the beginning of the end.”
At Mayo, Dr. Swift is surveying staff to gauge the willingness to get the vaccine, but she already senses excitement among employees. “No doubt there are still people who are hesitant, but I’m feeling a shift,” she said. “I’m feeling this momentum building of health care workers coming on board and wanting to take this vaccine, which is good, because they will set an example for their patients.”
For Colleen Kelley, MD, an infectious disease physician at Emory University in Atlanta who was principal investigator for an Emory-affiliated Moderna clinical trial site, it has been an emotional time. “Things were looking very bleak and dark for a time, and then we started to get these efficacy results that were greater than anyone imagined,” she said.
Dr. Kelley spends time talking to journalists and educating physician colleagues and hospital employees about how the vaccine was developed so quickly and how it works. “Everyone asks me, ‘Should I get it? Are you going to get it?’ My answer is ‘yes’ and ‘yes,’ “ she said. “I am 1,000% confident that the benefits of widespread vaccination outweigh the risks of continued COVID and a continued pandemic.”
A version of this article first appeared on Medscape.com.
COVID-19 anticoagulation trials ‘paused’ for futility, safety
Parts of three linked studies investigating increased levels of anticoagulation in hospitalized COVID-19 patients have been “paused” because of futility and safety concerns, a statement from the U.S. National Heart, Lung, and Blood Institute (NHLBI) confirms.
The trials involved are the REMAP-CAP, ACTIV-4, and ATTACC studies.
The statement also says that a potential for harm in this subgroup could not be excluded, noting that increased bleeding is a known complication of full-dose anticoagulation. The trials are working urgently to undertake additional analyses, which will be made available as soon as possible.
The three clinical trial platforms are working together to test the effects of full therapeutic doses of anticoagulants vs. lower prophylactic doses in COVID-19 patients.
Informed by the deliberations of the data safety monitoring boards of these trials, all of the trial sites have paused enrollment of the most critically ill hospitalized patients with COVID-19.
Enrollment continues in the trials for moderately ill hospitalized COVID-19 patients, the statement notes.
“Whether the use of full-dose compared to low-dose anticoagulants leads to better outcomes in hospitalized patients with less COVID-19 severe disease remains a very important question,” the NHLBI statement says.
Patients who require full dose anticoagulants for another medical indication are not included in these trials.
The statement explains that COVID-19 is associated with significant inflammation and clinical and pathologic evidence of widespread blood clots. These trials were launched because clinicians have observed that many patients ill with COVID-19, including those who have died from the disease, formed blood clots throughout their bodies, even in their smallest blood vessels. This unusual clotting can cause multiple health complications, including lung failure, myocardial infarction, and stroke.
The three trials are the result of a collaboration between major international partners. The trials include: the Randomized, Embedded, Multi-factorial Adaptive Platform Trial for Community-Acquired Pneumonia (REMAP-CAP) Therapeutic Anticoagulation; Accelerating COVID-19 Therapeutic Interventions and Vaccines-4 (ACTIV-4) Antithrombotics Inpatient; and Antithrombotic Therapy to Ameliorate Complications of COVID-19 (ATTACC).
The trials, which span four continents, have the common goal of assessing the benefit of full doses of anticoagulants to treat moderately ill or critically ill adults hospitalized for COVID-19, compared with a lower dose often used to prevent blood clots in hospitalized patients.
In the United States, the ACTIV-4 trial is being led by a collaborative effort involving a number of universities, including the University of Pittsburgh and New York University.
The trials are supported by multiple international funding organizations including the National Institutes of Health, Canadian Institutes of Health Research, the National Institute for Health Research (UK), the National Health and Medical Research Council (Australia), and the PREPARE and RECOVER consortia (European Union).
A version of this story first appeared on Medscape.com.
Parts of three linked studies investigating increased levels of anticoagulation in hospitalized COVID-19 patients have been “paused” because of futility and safety concerns, a statement from the U.S. National Heart, Lung, and Blood Institute (NHLBI) confirms.
The trials involved are the REMAP-CAP, ACTIV-4, and ATTACC studies.
The statement also says that a potential for harm in this subgroup could not be excluded, noting that increased bleeding is a known complication of full-dose anticoagulation. The trials are working urgently to undertake additional analyses, which will be made available as soon as possible.
The three clinical trial platforms are working together to test the effects of full therapeutic doses of anticoagulants vs. lower prophylactic doses in COVID-19 patients.
Informed by the deliberations of the data safety monitoring boards of these trials, all of the trial sites have paused enrollment of the most critically ill hospitalized patients with COVID-19.
Enrollment continues in the trials for moderately ill hospitalized COVID-19 patients, the statement notes.
“Whether the use of full-dose compared to low-dose anticoagulants leads to better outcomes in hospitalized patients with less COVID-19 severe disease remains a very important question,” the NHLBI statement says.
Patients who require full dose anticoagulants for another medical indication are not included in these trials.
The statement explains that COVID-19 is associated with significant inflammation and clinical and pathologic evidence of widespread blood clots. These trials were launched because clinicians have observed that many patients ill with COVID-19, including those who have died from the disease, formed blood clots throughout their bodies, even in their smallest blood vessels. This unusual clotting can cause multiple health complications, including lung failure, myocardial infarction, and stroke.
The three trials are the result of a collaboration between major international partners. The trials include: the Randomized, Embedded, Multi-factorial Adaptive Platform Trial for Community-Acquired Pneumonia (REMAP-CAP) Therapeutic Anticoagulation; Accelerating COVID-19 Therapeutic Interventions and Vaccines-4 (ACTIV-4) Antithrombotics Inpatient; and Antithrombotic Therapy to Ameliorate Complications of COVID-19 (ATTACC).
The trials, which span four continents, have the common goal of assessing the benefit of full doses of anticoagulants to treat moderately ill or critically ill adults hospitalized for COVID-19, compared with a lower dose often used to prevent blood clots in hospitalized patients.
In the United States, the ACTIV-4 trial is being led by a collaborative effort involving a number of universities, including the University of Pittsburgh and New York University.
The trials are supported by multiple international funding organizations including the National Institutes of Health, Canadian Institutes of Health Research, the National Institute for Health Research (UK), the National Health and Medical Research Council (Australia), and the PREPARE and RECOVER consortia (European Union).
A version of this story first appeared on Medscape.com.
Parts of three linked studies investigating increased levels of anticoagulation in hospitalized COVID-19 patients have been “paused” because of futility and safety concerns, a statement from the U.S. National Heart, Lung, and Blood Institute (NHLBI) confirms.
The trials involved are the REMAP-CAP, ACTIV-4, and ATTACC studies.
The statement also says that a potential for harm in this subgroup could not be excluded, noting that increased bleeding is a known complication of full-dose anticoagulation. The trials are working urgently to undertake additional analyses, which will be made available as soon as possible.
The three clinical trial platforms are working together to test the effects of full therapeutic doses of anticoagulants vs. lower prophylactic doses in COVID-19 patients.
Informed by the deliberations of the data safety monitoring boards of these trials, all of the trial sites have paused enrollment of the most critically ill hospitalized patients with COVID-19.
Enrollment continues in the trials for moderately ill hospitalized COVID-19 patients, the statement notes.
“Whether the use of full-dose compared to low-dose anticoagulants leads to better outcomes in hospitalized patients with less COVID-19 severe disease remains a very important question,” the NHLBI statement says.
Patients who require full dose anticoagulants for another medical indication are not included in these trials.
The statement explains that COVID-19 is associated with significant inflammation and clinical and pathologic evidence of widespread blood clots. These trials were launched because clinicians have observed that many patients ill with COVID-19, including those who have died from the disease, formed blood clots throughout their bodies, even in their smallest blood vessels. This unusual clotting can cause multiple health complications, including lung failure, myocardial infarction, and stroke.
The three trials are the result of a collaboration between major international partners. The trials include: the Randomized, Embedded, Multi-factorial Adaptive Platform Trial for Community-Acquired Pneumonia (REMAP-CAP) Therapeutic Anticoagulation; Accelerating COVID-19 Therapeutic Interventions and Vaccines-4 (ACTIV-4) Antithrombotics Inpatient; and Antithrombotic Therapy to Ameliorate Complications of COVID-19 (ATTACC).
The trials, which span four continents, have the common goal of assessing the benefit of full doses of anticoagulants to treat moderately ill or critically ill adults hospitalized for COVID-19, compared with a lower dose often used to prevent blood clots in hospitalized patients.
In the United States, the ACTIV-4 trial is being led by a collaborative effort involving a number of universities, including the University of Pittsburgh and New York University.
The trials are supported by multiple international funding organizations including the National Institutes of Health, Canadian Institutes of Health Research, the National Institute for Health Research (UK), the National Health and Medical Research Council (Australia), and the PREPARE and RECOVER consortia (European Union).
A version of this story first appeared on Medscape.com.
Latest rise in child COVID-19 cases is relatively small
For the seventh week out of the last eight, more new cases of COVID-19 in children were reported in the United States than any week before, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
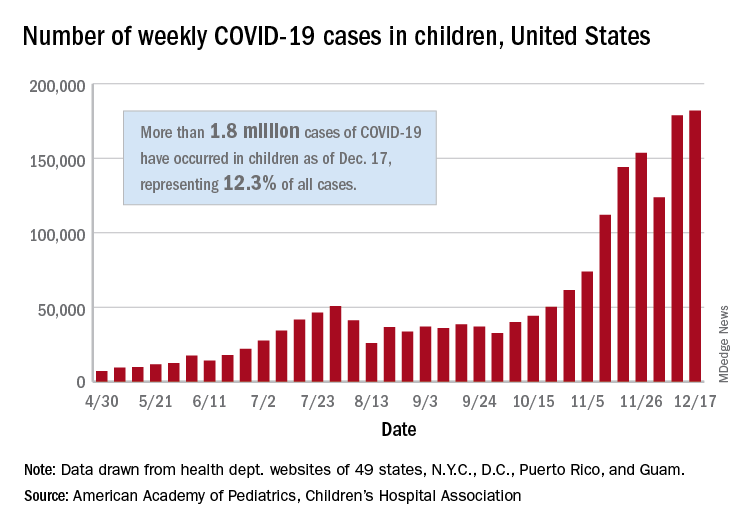
There were just over 182,000 new cases of COVID-19 in children during the week ending Dec. 17, topping the previous high of almost 179,000 set the previous week. – a stretch of 11 weeks that has produced only one decline, based on data from the latest AAP/CHA weekly report.
As of Dec. 17, there had been over 1.8 million cases of COVID-19 in children, which represents 12.3% of all U.S. cases. For the week, 14% of all cases occurred in children, which was up slightly from 13.8% the week before (Dec. 10). The overall rate of coronavirus infection is now 2,420 cases per 100,000 children in the population, the AAP and CHA said.
A total of 30 states are above that national rate, with North Dakota the highest at 7,515 cases per 100,000 children, followed by South Dakota (5,618), Wyoming (5,157), Wisconsin (5,106), and Tennessee (4,994). Wyoming has the highest proportion of cases occurring in children at 20.8%, but that is down from 23.4% in mid-November, based on data collected by the AAP and CHA from the health department websites of 49 states (New York does not provide age distributions), the District of Columbia, New York City, Puerto Rico, and Guam.
In the last 2 weeks, however, the largest percent increases in new cases came in states with low-to-average rates of cumulative child infection. California, Connecticut, Delaware, Maine, Maryland, New Hampshire, and Vermont all saw increases of over 35% from Dec. 3 to Dec. 17, while the smallest increases occurred in Hawaii, North Dakota, and Wyoming, the AAP and CHA reported.
For the seventh week out of the last eight, more new cases of COVID-19 in children were reported in the United States than any week before, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
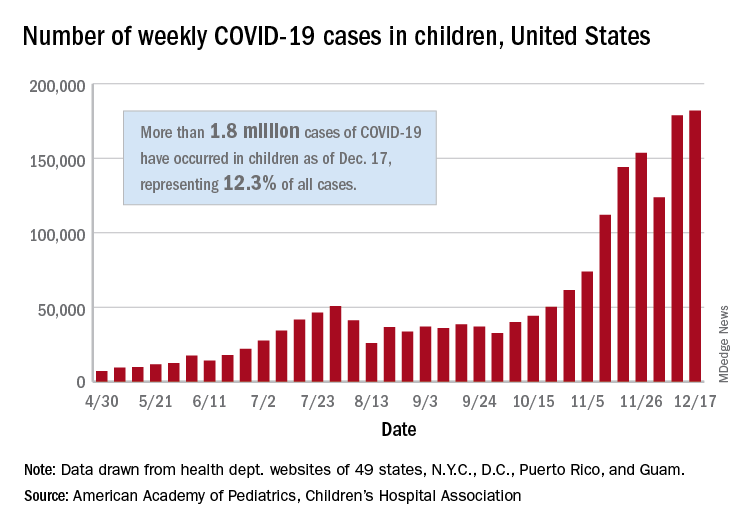
There were just over 182,000 new cases of COVID-19 in children during the week ending Dec. 17, topping the previous high of almost 179,000 set the previous week. – a stretch of 11 weeks that has produced only one decline, based on data from the latest AAP/CHA weekly report.
As of Dec. 17, there had been over 1.8 million cases of COVID-19 in children, which represents 12.3% of all U.S. cases. For the week, 14% of all cases occurred in children, which was up slightly from 13.8% the week before (Dec. 10). The overall rate of coronavirus infection is now 2,420 cases per 100,000 children in the population, the AAP and CHA said.
A total of 30 states are above that national rate, with North Dakota the highest at 7,515 cases per 100,000 children, followed by South Dakota (5,618), Wyoming (5,157), Wisconsin (5,106), and Tennessee (4,994). Wyoming has the highest proportion of cases occurring in children at 20.8%, but that is down from 23.4% in mid-November, based on data collected by the AAP and CHA from the health department websites of 49 states (New York does not provide age distributions), the District of Columbia, New York City, Puerto Rico, and Guam.
In the last 2 weeks, however, the largest percent increases in new cases came in states with low-to-average rates of cumulative child infection. California, Connecticut, Delaware, Maine, Maryland, New Hampshire, and Vermont all saw increases of over 35% from Dec. 3 to Dec. 17, while the smallest increases occurred in Hawaii, North Dakota, and Wyoming, the AAP and CHA reported.
For the seventh week out of the last eight, more new cases of COVID-19 in children were reported in the United States than any week before, according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
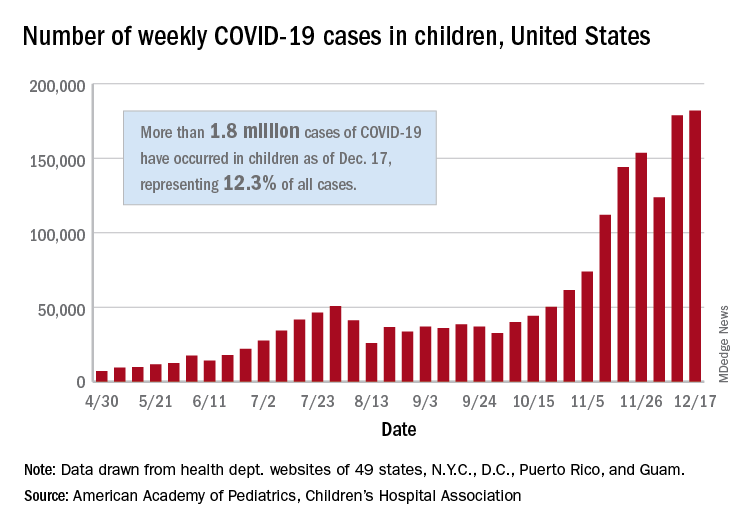
There were just over 182,000 new cases of COVID-19 in children during the week ending Dec. 17, topping the previous high of almost 179,000 set the previous week. – a stretch of 11 weeks that has produced only one decline, based on data from the latest AAP/CHA weekly report.
As of Dec. 17, there had been over 1.8 million cases of COVID-19 in children, which represents 12.3% of all U.S. cases. For the week, 14% of all cases occurred in children, which was up slightly from 13.8% the week before (Dec. 10). The overall rate of coronavirus infection is now 2,420 cases per 100,000 children in the population, the AAP and CHA said.
A total of 30 states are above that national rate, with North Dakota the highest at 7,515 cases per 100,000 children, followed by South Dakota (5,618), Wyoming (5,157), Wisconsin (5,106), and Tennessee (4,994). Wyoming has the highest proportion of cases occurring in children at 20.8%, but that is down from 23.4% in mid-November, based on data collected by the AAP and CHA from the health department websites of 49 states (New York does not provide age distributions), the District of Columbia, New York City, Puerto Rico, and Guam.
In the last 2 weeks, however, the largest percent increases in new cases came in states with low-to-average rates of cumulative child infection. California, Connecticut, Delaware, Maine, Maryland, New Hampshire, and Vermont all saw increases of over 35% from Dec. 3 to Dec. 17, while the smallest increases occurred in Hawaii, North Dakota, and Wyoming, the AAP and CHA reported.





