User login
-
Third-generation Black woman physician makes cancer research history
When Jane Cooke Wright, MD, entered the medical profession in 1945, the notion that toxic drugs could target tumors struck many physicians and patients as outlandish. How could one poison be weaponized against another poison – a cancerous tumor – without creating more havoc? Let alone a combination of two or more chemicals?
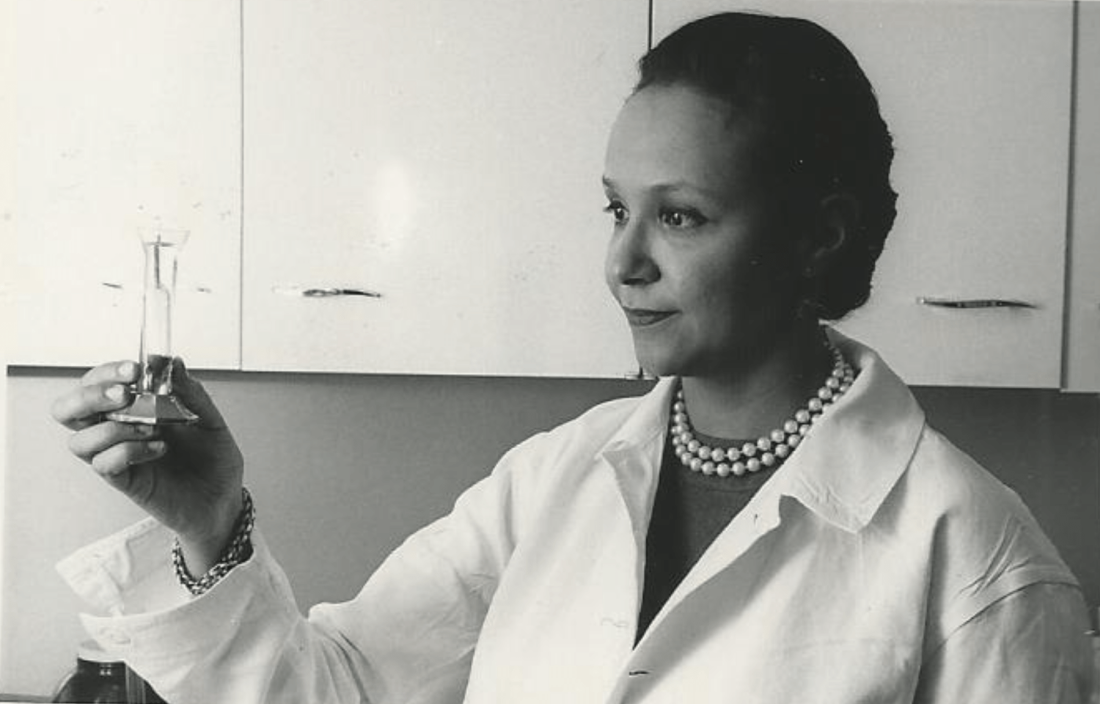
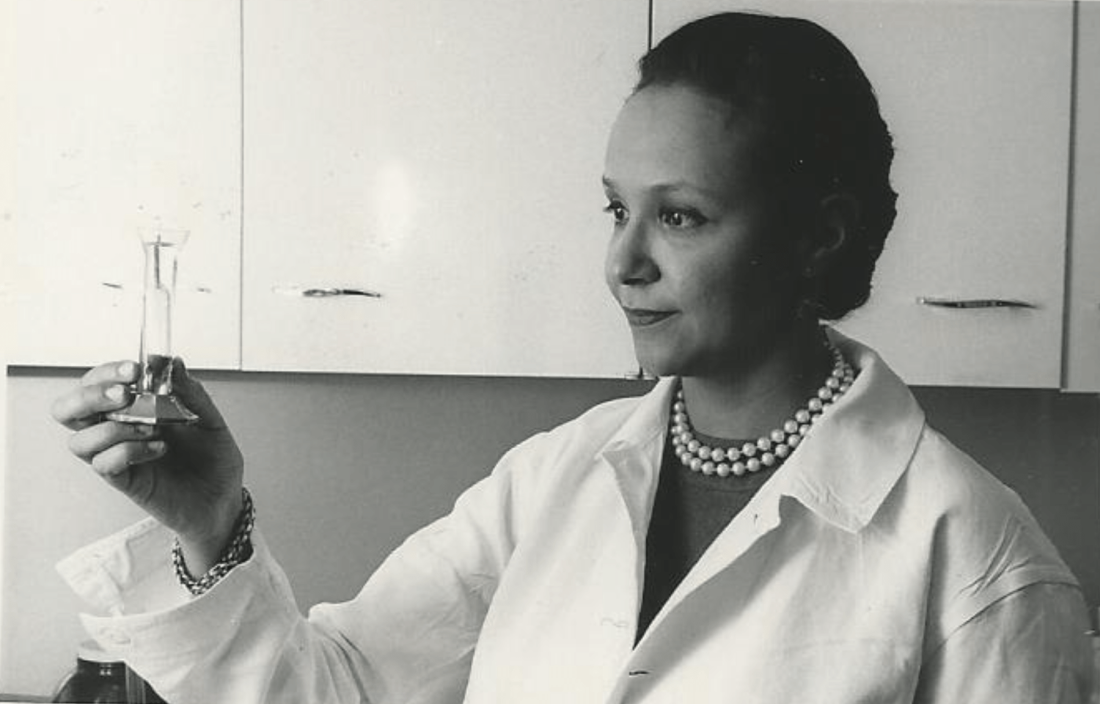
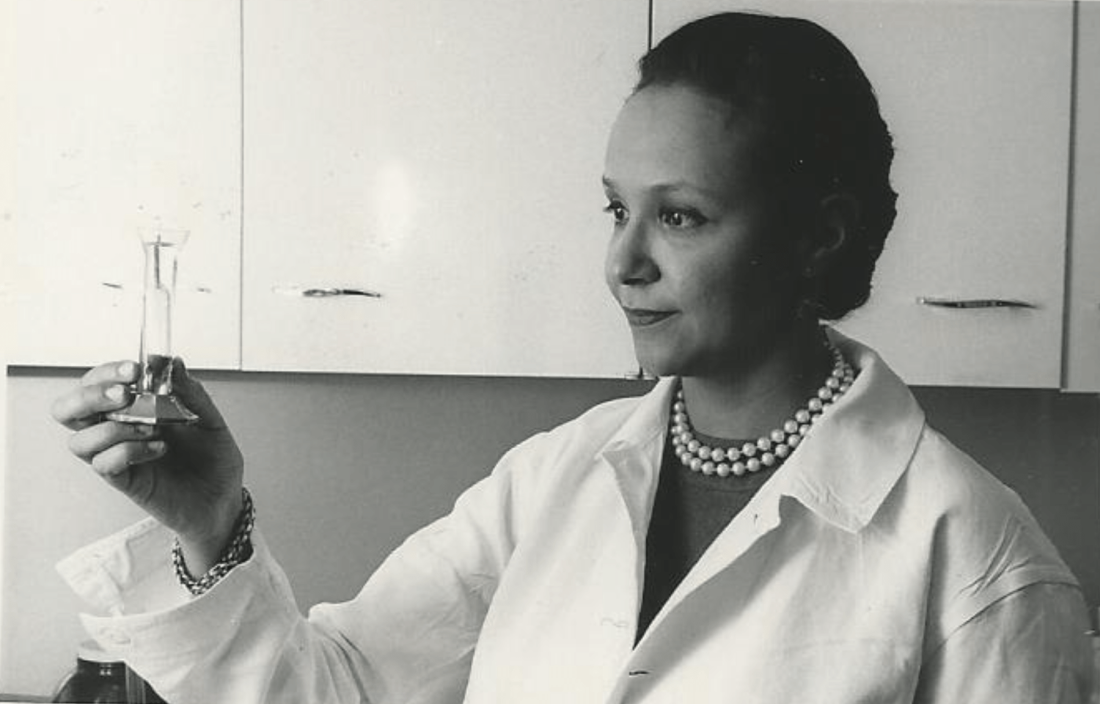
Dr. Wright’s story would be extraordinary enough if she’d looked like most of her colleagues, but this surgeon and researcher stood apart. An African American woman at a time when medicine and science – like politics and law – were almost entirely the domain of White men, Dr. Wright had determination in her blood. Her father, once honored by a crowd of dignitaries that included a First Lady, persevered despite his horrific encounters with racism. She shared her father’s commitment to progress and added her own personal twists. She balanced elegance and beauty with scientific savvy, fierce ambition, and a refusal to be defined by anything other than her accomplishments.
“She didn’t focus on race, not at all,” her daughter Alison Jones, PhD, a psychologist in East Lansing, Mich., said in an interview. “Wherever she was, she wanted to be the best, not the best Black person. It was not about how she performed in a category, and she would get upset if someone said she was good as a Black physician.”
On the road to being the best, Dr. Jones said, her mother set a goal of curing cancer. National Cancer Research Month is a fitting opportunity to look back on a scientist dedicated to bringing humanity closer to that elusive achievement.
Medical legacy blazed in toil and trauma
A strong case could be made that Dr. Jane C. Wright and her father Louis Tompkins Wright, MD, are the most accomplished father-and-daughter team in all of medicine.
The elder Dr. Wright, son of a formerly enslaved man turned physician and a stepson of the first African American to graduate from Yale University, New Haven, Conn., himself graduated from Harvard Medical School in 1915. He earned a Purple Heart while serving in World War I, then went on to become the first Black surgeon to join the staff at Harlem Hospital.
Dr. Wright, who had witnessed mob violence and the aftermath of a lynching as a young man, became a supporter of the Harlem Renaissance and a prominent advocate for civil rights and integration. He served as chairman of the National Association for the Advancement of Colored People and was only the second Black member of the American College of Surgeons.
According to the 2009 book “Black Genius: Inspirational Portraits of African American Leaders,” he successfully treated the rare but devastating venereal disease lymphogranuloma venereum with a new antibiotic developed by his former colleague Yellapragada SubbaRow, MD. Dr. Wright even tried the drug himself, “as a lot of doctors in the olden days did,” according to another of his daughters, the late Barbara Wright Pierce, MD, who was quoted in “Black Genius.” She, too, was a physician.
In 1948, Dr. Jane C. Wright joined her father at Harlem Hospital’s Cancer Research Foundation. There the duo explored the cancer-fighting possibilities of a nitrogen mustard–like chemical agent that had been known since World War I to kill white blood cells. Ironically, Dr. Louis Wright himself suffered lifelong health problems because of an attack from the poisonous gas phosgene during his wartime service.
“Remissions were observed in patients with sarcoma, Hodgkin disease, and chronic myelogenous leukemia, mycosis fungoides, and lymphoma,” reported a 2013 obituary in the journal Oncology of the younger Dr. Wright. “They also performed early research into the clinical efficacy and toxicity of folic acid antagonists, documenting responses in 93 patients with various forms of incurable blood cancers and solid tumors.”
This research appears in a study that was authored by three Dr. Wrights – Dr. Louis T. Wright and his daughters Jane and Barbara.
“The elder Dr. Wright died in 1952, just months after 1,000 people – including Eleanor Roosevelt – honored him at a dinner to dedicate a Harlem Hospital library named after him. He was 61.
Scientific savvy mixed with modesty and elegance
After her father’s death, Dr. Janet C. Wright became director of the hospital’s cancer foundation. From the 1950s to the 1970s, she “worked out ways to use pieces of a patient’s own tumor, removed by surgery and grown in a nutrient culture medium in the laboratory, as a ‘guinea pig for testing drugs,’ ” according to the 1991 book “Black Scientists.” Previously, researchers had focused on mice as test subjects.
This approach also allowed Dr. Wright to determine if specific drugs such as methotrexate, a folic acid antagonist, would help specific patients. “She was looking for predictive activity for chemotherapeutic efficacy in vitro at a time when no one had good predictive tests,” wrote James F. Holland, MD, the late Mount Sinai School of Medicine oncologist, who was quoted in Dr. Wright’s 2013 Oncology obituary.
“Her strict attention to detail and concern for her patients helped determine effective dosing levels and establish treatment guidelines,” the Oncology obituary reported. “She treated patients that other physicians had given up on, and she was among the first small cadre of researchers to carefully test the effects of drugs against cancer in a clinical trial setting.”
Dr. Wright also focused on developing ways to administer chemotherapy, such using a catheter to reach difficult-to-access organs like the spleen without surgery, according to “Black Scientists.”
Along with her work, Dr. Wright’s appearance set her apart. According to “Black Genius,” a newspaper columnist dubbed her one of the 10 most beautiful Back woman in America, and Ebony Magazine in 1966 honored her as one of the best-dressed women in America. It featured a photograph of her in a stunning ivory and yellow brocade gown, noting that she was “in private life Mrs. David J. Jones.” (She’d married the Harvard University Law School graduate in 1946.)
Dr. Wright had a sense of modesty despite her accomplishments, according to her daughter Alison Jones. She even downplayed her own mental powers in a newspaper interview. “I know I’m a member of two minority groups,” she told The New York Post in 1967, “but I don’t think of myself that way. Sure, a woman has to try twice as hard. But – racial prejudice? I’ve met very little of it. It could be I met it – and wasn’t intelligent enough to recognize it.”
Sharp-eyed readers might have glimpsed her modesty nearly 2 decades later. In a 1984 article for the Journal of the National Medical Association, a society of African American physicians, she wrote about the past, present, and future of chemotherapy without noting her own prominent role in its development.
‘Global medical pioneer’ cofounds ASCO – and more
In the 1960s, Dr. Wright joined the influential President’s Commission on Heart Disease, Cancer, and Stroke and was named associate dean at New York Medical College, her alma mater, a first for a black woman at a prominent U.S. medical school. Even more importantly, Dr. Wright was the sole woman among seven physicians who founded the American Society of Clinical Oncology in Chicago in 1964. She served as ASCO’s first Secretary-Treasurer and was honored as its longest surviving founder when she passed away 9 years ago.
“Jane Wright had the vision to see that oncology was an important separate discipline within medicine with far-reaching implications for research and discovery,” Georgetown University Medical Center, Washington, oncologist Sandra M. Swain, MD, a former president of the ASCO and author of the 2013 Oncology obituary of Dr. Wright, said in an interview. “It is truly remarkable that, as a woman and an African American woman, she had a seat at the very small table for the formation of such an important group.”
As her friend and fellow oncologist Edith Mitchell, MD, said in a eulogy, “Dr. Wright led delegations of oncologists to China and the Soviet Union, and countries in Africa and Eastern Europe. She led medical teams providing medical and cancer care and education to other nurses and physicians in Ghana in 1957 and Kenya in 1961. From 1973 to 1984, she served as vice-president of the African Research and Medical foundation.”
Dr. Wright also raised two daughters. A 1968 Ebony article devoted to her career and family declared that neither of her teenagers was interested in medical careers. Their perspectives shifted, however – as had Dr. Wright’s. An undergraduate at Smith College, Dr. Wright majored in art, swam on the varsity team, and had a special affinity for German language studies before she switched to premed.
Like their mother, Dr. Wright’s daughters also changed paths, and they ultimately became the fourth generation of their family to enter the medical field. Dr. Alison Jones, the psychologist, currently works in a prison, while Jane Jones, MD, became a clinical psychiatrist. She’s now retired and lives in Guttenberg, N.J.
Both fondly remember their mother as a supportive force who insisted on excellence. “There couldn’t be any excuses for you not getting where you wanted to go,” Dr. Jane Jones recalled in an interview.
Nevertheless, Dr. Wright was still keenly aware of society’s limits. “She told me I had to be a doctor or lawyer,” Dr. Alison Jones said, “because that’s how you need to survive when you’re Black in America.”
Dr. Wright passed away in 2013 at age 93. “Dr. Jane C. Wright truly has made contributions that have changed the practice of medicine,” noted her friend Dr. Mitchell, an oncologist and a retired brigadier general with the U.S. Air Force who now teaches at Thomas Jefferson University, Philadelphia. “A true pioneer. A concerned mentor. A renowned researcher. A global teacher. A global medical pioneer. A talented researcher, beloved sister, wife, and mother, and a beautiful, kind, and loving human being.”
When Jane Cooke Wright, MD, entered the medical profession in 1945, the notion that toxic drugs could target tumors struck many physicians and patients as outlandish. How could one poison be weaponized against another poison – a cancerous tumor – without creating more havoc? Let alone a combination of two or more chemicals?
Dr. Wright’s story would be extraordinary enough if she’d looked like most of her colleagues, but this surgeon and researcher stood apart. An African American woman at a time when medicine and science – like politics and law – were almost entirely the domain of White men, Dr. Wright had determination in her blood. Her father, once honored by a crowd of dignitaries that included a First Lady, persevered despite his horrific encounters with racism. She shared her father’s commitment to progress and added her own personal twists. She balanced elegance and beauty with scientific savvy, fierce ambition, and a refusal to be defined by anything other than her accomplishments.
“She didn’t focus on race, not at all,” her daughter Alison Jones, PhD, a psychologist in East Lansing, Mich., said in an interview. “Wherever she was, she wanted to be the best, not the best Black person. It was not about how she performed in a category, and she would get upset if someone said she was good as a Black physician.”
On the road to being the best, Dr. Jones said, her mother set a goal of curing cancer. National Cancer Research Month is a fitting opportunity to look back on a scientist dedicated to bringing humanity closer to that elusive achievement.
Medical legacy blazed in toil and trauma
A strong case could be made that Dr. Jane C. Wright and her father Louis Tompkins Wright, MD, are the most accomplished father-and-daughter team in all of medicine.
The elder Dr. Wright, son of a formerly enslaved man turned physician and a stepson of the first African American to graduate from Yale University, New Haven, Conn., himself graduated from Harvard Medical School in 1915. He earned a Purple Heart while serving in World War I, then went on to become the first Black surgeon to join the staff at Harlem Hospital.
Dr. Wright, who had witnessed mob violence and the aftermath of a lynching as a young man, became a supporter of the Harlem Renaissance and a prominent advocate for civil rights and integration. He served as chairman of the National Association for the Advancement of Colored People and was only the second Black member of the American College of Surgeons.
According to the 2009 book “Black Genius: Inspirational Portraits of African American Leaders,” he successfully treated the rare but devastating venereal disease lymphogranuloma venereum with a new antibiotic developed by his former colleague Yellapragada SubbaRow, MD. Dr. Wright even tried the drug himself, “as a lot of doctors in the olden days did,” according to another of his daughters, the late Barbara Wright Pierce, MD, who was quoted in “Black Genius.” She, too, was a physician.
In 1948, Dr. Jane C. Wright joined her father at Harlem Hospital’s Cancer Research Foundation. There the duo explored the cancer-fighting possibilities of a nitrogen mustard–like chemical agent that had been known since World War I to kill white blood cells. Ironically, Dr. Louis Wright himself suffered lifelong health problems because of an attack from the poisonous gas phosgene during his wartime service.
“Remissions were observed in patients with sarcoma, Hodgkin disease, and chronic myelogenous leukemia, mycosis fungoides, and lymphoma,” reported a 2013 obituary in the journal Oncology of the younger Dr. Wright. “They also performed early research into the clinical efficacy and toxicity of folic acid antagonists, documenting responses in 93 patients with various forms of incurable blood cancers and solid tumors.”
This research appears in a study that was authored by three Dr. Wrights – Dr. Louis T. Wright and his daughters Jane and Barbara.
“The elder Dr. Wright died in 1952, just months after 1,000 people – including Eleanor Roosevelt – honored him at a dinner to dedicate a Harlem Hospital library named after him. He was 61.
Scientific savvy mixed with modesty and elegance
After her father’s death, Dr. Janet C. Wright became director of the hospital’s cancer foundation. From the 1950s to the 1970s, she “worked out ways to use pieces of a patient’s own tumor, removed by surgery and grown in a nutrient culture medium in the laboratory, as a ‘guinea pig for testing drugs,’ ” according to the 1991 book “Black Scientists.” Previously, researchers had focused on mice as test subjects.
This approach also allowed Dr. Wright to determine if specific drugs such as methotrexate, a folic acid antagonist, would help specific patients. “She was looking for predictive activity for chemotherapeutic efficacy in vitro at a time when no one had good predictive tests,” wrote James F. Holland, MD, the late Mount Sinai School of Medicine oncologist, who was quoted in Dr. Wright’s 2013 Oncology obituary.
“Her strict attention to detail and concern for her patients helped determine effective dosing levels and establish treatment guidelines,” the Oncology obituary reported. “She treated patients that other physicians had given up on, and she was among the first small cadre of researchers to carefully test the effects of drugs against cancer in a clinical trial setting.”
Dr. Wright also focused on developing ways to administer chemotherapy, such using a catheter to reach difficult-to-access organs like the spleen without surgery, according to “Black Scientists.”
Along with her work, Dr. Wright’s appearance set her apart. According to “Black Genius,” a newspaper columnist dubbed her one of the 10 most beautiful Back woman in America, and Ebony Magazine in 1966 honored her as one of the best-dressed women in America. It featured a photograph of her in a stunning ivory and yellow brocade gown, noting that she was “in private life Mrs. David J. Jones.” (She’d married the Harvard University Law School graduate in 1946.)
Dr. Wright had a sense of modesty despite her accomplishments, according to her daughter Alison Jones. She even downplayed her own mental powers in a newspaper interview. “I know I’m a member of two minority groups,” she told The New York Post in 1967, “but I don’t think of myself that way. Sure, a woman has to try twice as hard. But – racial prejudice? I’ve met very little of it. It could be I met it – and wasn’t intelligent enough to recognize it.”
Sharp-eyed readers might have glimpsed her modesty nearly 2 decades later. In a 1984 article for the Journal of the National Medical Association, a society of African American physicians, she wrote about the past, present, and future of chemotherapy without noting her own prominent role in its development.
‘Global medical pioneer’ cofounds ASCO – and more
In the 1960s, Dr. Wright joined the influential President’s Commission on Heart Disease, Cancer, and Stroke and was named associate dean at New York Medical College, her alma mater, a first for a black woman at a prominent U.S. medical school. Even more importantly, Dr. Wright was the sole woman among seven physicians who founded the American Society of Clinical Oncology in Chicago in 1964. She served as ASCO’s first Secretary-Treasurer and was honored as its longest surviving founder when she passed away 9 years ago.
“Jane Wright had the vision to see that oncology was an important separate discipline within medicine with far-reaching implications for research and discovery,” Georgetown University Medical Center, Washington, oncologist Sandra M. Swain, MD, a former president of the ASCO and author of the 2013 Oncology obituary of Dr. Wright, said in an interview. “It is truly remarkable that, as a woman and an African American woman, she had a seat at the very small table for the formation of such an important group.”
As her friend and fellow oncologist Edith Mitchell, MD, said in a eulogy, “Dr. Wright led delegations of oncologists to China and the Soviet Union, and countries in Africa and Eastern Europe. She led medical teams providing medical and cancer care and education to other nurses and physicians in Ghana in 1957 and Kenya in 1961. From 1973 to 1984, she served as vice-president of the African Research and Medical foundation.”
Dr. Wright also raised two daughters. A 1968 Ebony article devoted to her career and family declared that neither of her teenagers was interested in medical careers. Their perspectives shifted, however – as had Dr. Wright’s. An undergraduate at Smith College, Dr. Wright majored in art, swam on the varsity team, and had a special affinity for German language studies before she switched to premed.
Like their mother, Dr. Wright’s daughters also changed paths, and they ultimately became the fourth generation of their family to enter the medical field. Dr. Alison Jones, the psychologist, currently works in a prison, while Jane Jones, MD, became a clinical psychiatrist. She’s now retired and lives in Guttenberg, N.J.
Both fondly remember their mother as a supportive force who insisted on excellence. “There couldn’t be any excuses for you not getting where you wanted to go,” Dr. Jane Jones recalled in an interview.
Nevertheless, Dr. Wright was still keenly aware of society’s limits. “She told me I had to be a doctor or lawyer,” Dr. Alison Jones said, “because that’s how you need to survive when you’re Black in America.”
Dr. Wright passed away in 2013 at age 93. “Dr. Jane C. Wright truly has made contributions that have changed the practice of medicine,” noted her friend Dr. Mitchell, an oncologist and a retired brigadier general with the U.S. Air Force who now teaches at Thomas Jefferson University, Philadelphia. “A true pioneer. A concerned mentor. A renowned researcher. A global teacher. A global medical pioneer. A talented researcher, beloved sister, wife, and mother, and a beautiful, kind, and loving human being.”
When Jane Cooke Wright, MD, entered the medical profession in 1945, the notion that toxic drugs could target tumors struck many physicians and patients as outlandish. How could one poison be weaponized against another poison – a cancerous tumor – without creating more havoc? Let alone a combination of two or more chemicals?
Dr. Wright’s story would be extraordinary enough if she’d looked like most of her colleagues, but this surgeon and researcher stood apart. An African American woman at a time when medicine and science – like politics and law – were almost entirely the domain of White men, Dr. Wright had determination in her blood. Her father, once honored by a crowd of dignitaries that included a First Lady, persevered despite his horrific encounters with racism. She shared her father’s commitment to progress and added her own personal twists. She balanced elegance and beauty with scientific savvy, fierce ambition, and a refusal to be defined by anything other than her accomplishments.
“She didn’t focus on race, not at all,” her daughter Alison Jones, PhD, a psychologist in East Lansing, Mich., said in an interview. “Wherever she was, she wanted to be the best, not the best Black person. It was not about how she performed in a category, and she would get upset if someone said she was good as a Black physician.”
On the road to being the best, Dr. Jones said, her mother set a goal of curing cancer. National Cancer Research Month is a fitting opportunity to look back on a scientist dedicated to bringing humanity closer to that elusive achievement.
Medical legacy blazed in toil and trauma
A strong case could be made that Dr. Jane C. Wright and her father Louis Tompkins Wright, MD, are the most accomplished father-and-daughter team in all of medicine.
The elder Dr. Wright, son of a formerly enslaved man turned physician and a stepson of the first African American to graduate from Yale University, New Haven, Conn., himself graduated from Harvard Medical School in 1915. He earned a Purple Heart while serving in World War I, then went on to become the first Black surgeon to join the staff at Harlem Hospital.
Dr. Wright, who had witnessed mob violence and the aftermath of a lynching as a young man, became a supporter of the Harlem Renaissance and a prominent advocate for civil rights and integration. He served as chairman of the National Association for the Advancement of Colored People and was only the second Black member of the American College of Surgeons.
According to the 2009 book “Black Genius: Inspirational Portraits of African American Leaders,” he successfully treated the rare but devastating venereal disease lymphogranuloma venereum with a new antibiotic developed by his former colleague Yellapragada SubbaRow, MD. Dr. Wright even tried the drug himself, “as a lot of doctors in the olden days did,” according to another of his daughters, the late Barbara Wright Pierce, MD, who was quoted in “Black Genius.” She, too, was a physician.
In 1948, Dr. Jane C. Wright joined her father at Harlem Hospital’s Cancer Research Foundation. There the duo explored the cancer-fighting possibilities of a nitrogen mustard–like chemical agent that had been known since World War I to kill white blood cells. Ironically, Dr. Louis Wright himself suffered lifelong health problems because of an attack from the poisonous gas phosgene during his wartime service.
“Remissions were observed in patients with sarcoma, Hodgkin disease, and chronic myelogenous leukemia, mycosis fungoides, and lymphoma,” reported a 2013 obituary in the journal Oncology of the younger Dr. Wright. “They also performed early research into the clinical efficacy and toxicity of folic acid antagonists, documenting responses in 93 patients with various forms of incurable blood cancers and solid tumors.”
This research appears in a study that was authored by three Dr. Wrights – Dr. Louis T. Wright and his daughters Jane and Barbara.
“The elder Dr. Wright died in 1952, just months after 1,000 people – including Eleanor Roosevelt – honored him at a dinner to dedicate a Harlem Hospital library named after him. He was 61.
Scientific savvy mixed with modesty and elegance
After her father’s death, Dr. Janet C. Wright became director of the hospital’s cancer foundation. From the 1950s to the 1970s, she “worked out ways to use pieces of a patient’s own tumor, removed by surgery and grown in a nutrient culture medium in the laboratory, as a ‘guinea pig for testing drugs,’ ” according to the 1991 book “Black Scientists.” Previously, researchers had focused on mice as test subjects.
This approach also allowed Dr. Wright to determine if specific drugs such as methotrexate, a folic acid antagonist, would help specific patients. “She was looking for predictive activity for chemotherapeutic efficacy in vitro at a time when no one had good predictive tests,” wrote James F. Holland, MD, the late Mount Sinai School of Medicine oncologist, who was quoted in Dr. Wright’s 2013 Oncology obituary.
“Her strict attention to detail and concern for her patients helped determine effective dosing levels and establish treatment guidelines,” the Oncology obituary reported. “She treated patients that other physicians had given up on, and she was among the first small cadre of researchers to carefully test the effects of drugs against cancer in a clinical trial setting.”
Dr. Wright also focused on developing ways to administer chemotherapy, such using a catheter to reach difficult-to-access organs like the spleen without surgery, according to “Black Scientists.”
Along with her work, Dr. Wright’s appearance set her apart. According to “Black Genius,” a newspaper columnist dubbed her one of the 10 most beautiful Back woman in America, and Ebony Magazine in 1966 honored her as one of the best-dressed women in America. It featured a photograph of her in a stunning ivory and yellow brocade gown, noting that she was “in private life Mrs. David J. Jones.” (She’d married the Harvard University Law School graduate in 1946.)
Dr. Wright had a sense of modesty despite her accomplishments, according to her daughter Alison Jones. She even downplayed her own mental powers in a newspaper interview. “I know I’m a member of two minority groups,” she told The New York Post in 1967, “but I don’t think of myself that way. Sure, a woman has to try twice as hard. But – racial prejudice? I’ve met very little of it. It could be I met it – and wasn’t intelligent enough to recognize it.”
Sharp-eyed readers might have glimpsed her modesty nearly 2 decades later. In a 1984 article for the Journal of the National Medical Association, a society of African American physicians, she wrote about the past, present, and future of chemotherapy without noting her own prominent role in its development.
‘Global medical pioneer’ cofounds ASCO – and more
In the 1960s, Dr. Wright joined the influential President’s Commission on Heart Disease, Cancer, and Stroke and was named associate dean at New York Medical College, her alma mater, a first for a black woman at a prominent U.S. medical school. Even more importantly, Dr. Wright was the sole woman among seven physicians who founded the American Society of Clinical Oncology in Chicago in 1964. She served as ASCO’s first Secretary-Treasurer and was honored as its longest surviving founder when she passed away 9 years ago.
“Jane Wright had the vision to see that oncology was an important separate discipline within medicine with far-reaching implications for research and discovery,” Georgetown University Medical Center, Washington, oncologist Sandra M. Swain, MD, a former president of the ASCO and author of the 2013 Oncology obituary of Dr. Wright, said in an interview. “It is truly remarkable that, as a woman and an African American woman, she had a seat at the very small table for the formation of such an important group.”
As her friend and fellow oncologist Edith Mitchell, MD, said in a eulogy, “Dr. Wright led delegations of oncologists to China and the Soviet Union, and countries in Africa and Eastern Europe. She led medical teams providing medical and cancer care and education to other nurses and physicians in Ghana in 1957 and Kenya in 1961. From 1973 to 1984, she served as vice-president of the African Research and Medical foundation.”
Dr. Wright also raised two daughters. A 1968 Ebony article devoted to her career and family declared that neither of her teenagers was interested in medical careers. Their perspectives shifted, however – as had Dr. Wright’s. An undergraduate at Smith College, Dr. Wright majored in art, swam on the varsity team, and had a special affinity for German language studies before she switched to premed.
Like their mother, Dr. Wright’s daughters also changed paths, and they ultimately became the fourth generation of their family to enter the medical field. Dr. Alison Jones, the psychologist, currently works in a prison, while Jane Jones, MD, became a clinical psychiatrist. She’s now retired and lives in Guttenberg, N.J.
Both fondly remember their mother as a supportive force who insisted on excellence. “There couldn’t be any excuses for you not getting where you wanted to go,” Dr. Jane Jones recalled in an interview.
Nevertheless, Dr. Wright was still keenly aware of society’s limits. “She told me I had to be a doctor or lawyer,” Dr. Alison Jones said, “because that’s how you need to survive when you’re Black in America.”
Dr. Wright passed away in 2013 at age 93. “Dr. Jane C. Wright truly has made contributions that have changed the practice of medicine,” noted her friend Dr. Mitchell, an oncologist and a retired brigadier general with the U.S. Air Force who now teaches at Thomas Jefferson University, Philadelphia. “A true pioneer. A concerned mentor. A renowned researcher. A global teacher. A global medical pioneer. A talented researcher, beloved sister, wife, and mother, and a beautiful, kind, and loving human being.”
How to manage drug interactions with Paxlovid for COVID-19
Misinformation about nirmatrelvir/ritonavir (Paxlovid, Pfizer) for treating mild to moderate COVID-19 in patients at high risk for severe disease is feeding misunderstanding among prescribers and patients, two experts from the Infectious Diseases Society of America (IDSA) have said.
They briefed reporters on potential drug interactions and uncommon cases of a “rebound” effect with the drug, which was granted emergency use authorization by the Food and Drug Administration last December for patients at least 12 years old.
The drug combination works “like a pair of scissors chopping up proteins that are made as the virus replicates inside of cells. Inhibiting that enzyme leads to the cessation of replication,” said Jason C. Gallagher, PharmD, of Temple University School of Pharmacy, Philadelphia.
That’s important because other treatments that target the spike protein, such as monoclonal antibodies, can lose their efficacy as the virus changes. He said that while that’s not impossible for Paxlovid, “we have not seen variants emerging that are resistant to it.”
Potential drug interactions
IDSA recently published updated guidance on potential interactions between Paxlovid and the top 100 drugs, and important considerations for prescribing.
“There is a concern that people have not been prescribing it because of fear of these interactions,” Dr. Gallagher said, explaining that, while in some cases those fears may be valid, in many instances the interaction is manageable.
One example is in two popular statins for heart disease, lovastatin and simvastatin.
“That’s an interaction that can be managed by holding [those drugs] for the 5 days that someone receives Paxlovid,” he said.
Misinformation also is circulating about distribution status of Paxlovid, Dr. Gallagher said.
“We’re in a very different state from that standpoint than we were a month or 2 months ago,” he said, adding that it is widely available in not all but a large number of pharmacies throughout the United States.
He emphasized the importance of drug reconciliation, as many patients will go to a different pharmacy for Paxlovid than they might for their usual prescriptions, so without a full accounting of prescriptions and supplements potential interactions may be missed.
Important interactions to watch
Melanie Thompson, MD, cochair of the HIVMA/IDSA HIV Primary Care Guidance Panel, highlighted some classes of drugs to watch, among them the antiarrhythmics, most of which are contraindicated with Paxlovid.
There are also important interactions with a number of cancer drugs, and consults with oncologists will be critical, she said.
“Likewise, people who have had transplants are likely to be on drugs that have significant ritonavir interactions,” Dr. Thompson said.
People on ergot drugs for migraine cannot take Paxlovid, she said, and “people who take colchicine for gout have to be very careful.”
She said it’s better not to use colchicine while taking Paxlovid, as it is contraindicated, “but it can be managed in certain circumstances with substantial dose reduction.”
A number of mental health drugs can be managed with Paxlovid, Dr. Thompson said. For the antipsychotic drug quetiapine, (Seroquel), a “substantial decrease in dose is required.”
Viagra for ED can be managed
Use of Viagra depends on why it’s being used, Dr. Thompson said. If it’s used for pulmonary hypertension, it is used at a very high dose and that is contraindicated. But if used for erectile dysfunction, the dose needs to be managed when people are on Paxlovid.
She said prescribers must know the kidney function of patients.
“There is a dose reduction that is required if people have impaired kidney function but below a certain level of function, which is 30 mL/min, it’s not recommended to give Paxlovid.”
Dr. Thompson highlighted two other websites for thorough, printable information on drug-drug interactions with Paxlovid: the University of Liverpool’s drug interaction checker and a printable handout from the University of Waterloo in Ontario, Canada.
“We need a 24/7 clinician hotline for Paxlovid to really make it accessible,” she said.
No data yet on ‘rebound’ effect
As to a few recent reports of a “rebound” effect, of people developing COVID-19 symptoms after completing a course of Paxlovid, there are not enough data yet to determine a clear pattern or cause.
“All we have are anecdotal data,” Dr. Thompson said. Current questions for study include whether the 5-day course is not long enough, she said, and whether people more at risk should be given a second course of Paxlovid if they do rebound.
Dr. Gallagher said it’s important to remember that the therapy goal of the drug is to prevent hospitalizations and deaths, and while any rebound is problematic, “it’s possible the use of the medication has already saved a life.”
Dr. Gallagher and Dr. Thompson report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Misinformation about nirmatrelvir/ritonavir (Paxlovid, Pfizer) for treating mild to moderate COVID-19 in patients at high risk for severe disease is feeding misunderstanding among prescribers and patients, two experts from the Infectious Diseases Society of America (IDSA) have said.
They briefed reporters on potential drug interactions and uncommon cases of a “rebound” effect with the drug, which was granted emergency use authorization by the Food and Drug Administration last December for patients at least 12 years old.
The drug combination works “like a pair of scissors chopping up proteins that are made as the virus replicates inside of cells. Inhibiting that enzyme leads to the cessation of replication,” said Jason C. Gallagher, PharmD, of Temple University School of Pharmacy, Philadelphia.
That’s important because other treatments that target the spike protein, such as monoclonal antibodies, can lose their efficacy as the virus changes. He said that while that’s not impossible for Paxlovid, “we have not seen variants emerging that are resistant to it.”
Potential drug interactions
IDSA recently published updated guidance on potential interactions between Paxlovid and the top 100 drugs, and important considerations for prescribing.
“There is a concern that people have not been prescribing it because of fear of these interactions,” Dr. Gallagher said, explaining that, while in some cases those fears may be valid, in many instances the interaction is manageable.
One example is in two popular statins for heart disease, lovastatin and simvastatin.
“That’s an interaction that can be managed by holding [those drugs] for the 5 days that someone receives Paxlovid,” he said.
Misinformation also is circulating about distribution status of Paxlovid, Dr. Gallagher said.
“We’re in a very different state from that standpoint than we were a month or 2 months ago,” he said, adding that it is widely available in not all but a large number of pharmacies throughout the United States.
He emphasized the importance of drug reconciliation, as many patients will go to a different pharmacy for Paxlovid than they might for their usual prescriptions, so without a full accounting of prescriptions and supplements potential interactions may be missed.
Important interactions to watch
Melanie Thompson, MD, cochair of the HIVMA/IDSA HIV Primary Care Guidance Panel, highlighted some classes of drugs to watch, among them the antiarrhythmics, most of which are contraindicated with Paxlovid.
There are also important interactions with a number of cancer drugs, and consults with oncologists will be critical, she said.
“Likewise, people who have had transplants are likely to be on drugs that have significant ritonavir interactions,” Dr. Thompson said.
People on ergot drugs for migraine cannot take Paxlovid, she said, and “people who take colchicine for gout have to be very careful.”
She said it’s better not to use colchicine while taking Paxlovid, as it is contraindicated, “but it can be managed in certain circumstances with substantial dose reduction.”
A number of mental health drugs can be managed with Paxlovid, Dr. Thompson said. For the antipsychotic drug quetiapine, (Seroquel), a “substantial decrease in dose is required.”
Viagra for ED can be managed
Use of Viagra depends on why it’s being used, Dr. Thompson said. If it’s used for pulmonary hypertension, it is used at a very high dose and that is contraindicated. But if used for erectile dysfunction, the dose needs to be managed when people are on Paxlovid.
She said prescribers must know the kidney function of patients.
“There is a dose reduction that is required if people have impaired kidney function but below a certain level of function, which is 30 mL/min, it’s not recommended to give Paxlovid.”
Dr. Thompson highlighted two other websites for thorough, printable information on drug-drug interactions with Paxlovid: the University of Liverpool’s drug interaction checker and a printable handout from the University of Waterloo in Ontario, Canada.
“We need a 24/7 clinician hotline for Paxlovid to really make it accessible,” she said.
No data yet on ‘rebound’ effect
As to a few recent reports of a “rebound” effect, of people developing COVID-19 symptoms after completing a course of Paxlovid, there are not enough data yet to determine a clear pattern or cause.
“All we have are anecdotal data,” Dr. Thompson said. Current questions for study include whether the 5-day course is not long enough, she said, and whether people more at risk should be given a second course of Paxlovid if they do rebound.
Dr. Gallagher said it’s important to remember that the therapy goal of the drug is to prevent hospitalizations and deaths, and while any rebound is problematic, “it’s possible the use of the medication has already saved a life.”
Dr. Gallagher and Dr. Thompson report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Misinformation about nirmatrelvir/ritonavir (Paxlovid, Pfizer) for treating mild to moderate COVID-19 in patients at high risk for severe disease is feeding misunderstanding among prescribers and patients, two experts from the Infectious Diseases Society of America (IDSA) have said.
They briefed reporters on potential drug interactions and uncommon cases of a “rebound” effect with the drug, which was granted emergency use authorization by the Food and Drug Administration last December for patients at least 12 years old.
The drug combination works “like a pair of scissors chopping up proteins that are made as the virus replicates inside of cells. Inhibiting that enzyme leads to the cessation of replication,” said Jason C. Gallagher, PharmD, of Temple University School of Pharmacy, Philadelphia.
That’s important because other treatments that target the spike protein, such as monoclonal antibodies, can lose their efficacy as the virus changes. He said that while that’s not impossible for Paxlovid, “we have not seen variants emerging that are resistant to it.”
Potential drug interactions
IDSA recently published updated guidance on potential interactions between Paxlovid and the top 100 drugs, and important considerations for prescribing.
“There is a concern that people have not been prescribing it because of fear of these interactions,” Dr. Gallagher said, explaining that, while in some cases those fears may be valid, in many instances the interaction is manageable.
One example is in two popular statins for heart disease, lovastatin and simvastatin.
“That’s an interaction that can be managed by holding [those drugs] for the 5 days that someone receives Paxlovid,” he said.
Misinformation also is circulating about distribution status of Paxlovid, Dr. Gallagher said.
“We’re in a very different state from that standpoint than we were a month or 2 months ago,” he said, adding that it is widely available in not all but a large number of pharmacies throughout the United States.
He emphasized the importance of drug reconciliation, as many patients will go to a different pharmacy for Paxlovid than they might for their usual prescriptions, so without a full accounting of prescriptions and supplements potential interactions may be missed.
Important interactions to watch
Melanie Thompson, MD, cochair of the HIVMA/IDSA HIV Primary Care Guidance Panel, highlighted some classes of drugs to watch, among them the antiarrhythmics, most of which are contraindicated with Paxlovid.
There are also important interactions with a number of cancer drugs, and consults with oncologists will be critical, she said.
“Likewise, people who have had transplants are likely to be on drugs that have significant ritonavir interactions,” Dr. Thompson said.
People on ergot drugs for migraine cannot take Paxlovid, she said, and “people who take colchicine for gout have to be very careful.”
She said it’s better not to use colchicine while taking Paxlovid, as it is contraindicated, “but it can be managed in certain circumstances with substantial dose reduction.”
A number of mental health drugs can be managed with Paxlovid, Dr. Thompson said. For the antipsychotic drug quetiapine, (Seroquel), a “substantial decrease in dose is required.”
Viagra for ED can be managed
Use of Viagra depends on why it’s being used, Dr. Thompson said. If it’s used for pulmonary hypertension, it is used at a very high dose and that is contraindicated. But if used for erectile dysfunction, the dose needs to be managed when people are on Paxlovid.
She said prescribers must know the kidney function of patients.
“There is a dose reduction that is required if people have impaired kidney function but below a certain level of function, which is 30 mL/min, it’s not recommended to give Paxlovid.”
Dr. Thompson highlighted two other websites for thorough, printable information on drug-drug interactions with Paxlovid: the University of Liverpool’s drug interaction checker and a printable handout from the University of Waterloo in Ontario, Canada.
“We need a 24/7 clinician hotline for Paxlovid to really make it accessible,” she said.
No data yet on ‘rebound’ effect
As to a few recent reports of a “rebound” effect, of people developing COVID-19 symptoms after completing a course of Paxlovid, there are not enough data yet to determine a clear pattern or cause.
“All we have are anecdotal data,” Dr. Thompson said. Current questions for study include whether the 5-day course is not long enough, she said, and whether people more at risk should be given a second course of Paxlovid if they do rebound.
Dr. Gallagher said it’s important to remember that the therapy goal of the drug is to prevent hospitalizations and deaths, and while any rebound is problematic, “it’s possible the use of the medication has already saved a life.”
Dr. Gallagher and Dr. Thompson report no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Young leukemia survivors still dying early, study shows
Although adolescents and young adults (AYAs) who survive leukemia are living much longer than ever before, their life spans are still shorter than those of the general population, a new study concludes.
The study found that the 10-year survival of AYA leukemia survivors was approximately 10% lower than that of the age-adjusted U.S. general population at large.
These differences persisted for up to 30 years of follow-up.
“We need to think about the long-term life span and the quality of life for our patients. Cure is not enough for our AYA cancer survivors,” said senior author Michael Roth, MD, associate professor of pediatric patient care and director of the Childhood Cancer Survivorship Clinic at the University of Texas MD Anderson Cancer Center, Houston.
“Once these patients reach the survivorship stage of their journey, they may encounter additional side effects as a result of intensive treatment, lack of access to quality health care, and other issues that may negatively impact their health and overall survival,” he said in a statement.
The study was published in Cancer Epidemiology, Biomarkers and Prevention.
Demographics play role in survival
AYAs were defined as those persons aged 15-39 years. For their study, Dr. Roth and colleagues used the Surveillance, Epidemiology, and End Results (SEER) registry to identify 1,938 AYA survivors of acute lymphoblastic leukemia (ALL) and 2,350 AYA survivors of acute myeloid leukemia (AML) who were diagnosed from 1980 to 2009. They were followed for a median of 12 years.
The median age at diagnosis was 23 years for ALL and 28 years for AML.
Among ALL survivors, 6% were Black, 7% were Asian or Pacific Islander, 29% were Hispanic, and 58% were White. Among AML survivors, 9% were Black, 10% were Asian or Pacific Islander, 22% were Hispanic, and 59% were White. Ten-year survival for ALL and AML survivors was 87% and 89%, respectively. For the general population, it was 99%.
For ALL survivors, the 10-year survival was 83% for those diagnosed in the 1980s; it was 88% for those diagnosed in the 1990s and in the 2000s. The pattern was similar for AML survivors: 82%, 90%, and 90%.
The most common cause of death during early survivorship was acute leukemia. Deaths plateaued approximately 10 years after the initial diagnosis.
“Some of these patients aren’t being fully cured of their initial cancer, so between 5 and 10 years post initial diagnosis, most of the deaths are due to disease progression or relapse, whereas after that, most of the deaths result from late side effects from treatment, including cardiovascular disease and secondary cancers,” Dr. Roth said. Mortality from other causes continued to rise during the survivorship period. Subsequent malignancies and cardiac disease were the most common causes of death for both ALL and AML survivors.
A recent study found that AYA cancer survivors face nearly a twofold higher risk of dying from a new primary cancer, compared with peers in the general population.
When looking at key demographics, the authors found that older age at diagnosis was significantly associated with differential long-term survival (P < .0001 for both ALL and AML). Each additional year older at diagnosis was associated with a 6% and 5% decrease in long-term survival for both types of leukemia.
The decade in which the diagnosis was made had a significant difference in long-term survival both for patients with ALL and those with AML. Long-term survival times for those diagnosed in the 1990s were more than twice those of patients diagnosed in the 1980s for ALL (unadjusted P = .008) and AML (unadjusted P = .0002). Survival times were also more than twice those of patients diagnosed in the 2000s versus the 1980s for ALL (unadjusted P = .009) and AML (unadjusted P = .0003).
No significant long-term survival differences were observed for those diagnosed in the 2000s, compared with the 1990s, for either leukemia.
“The data from the national registry used for this study gave us insights into some possible challenges AML and ALL patients may encounter throughout survivorship, but we need to more thoroughly survey their journey,” Dr. Roth said. “An examination of their socioeconomic status, comorbidities, access to quality health care, and other risk factors that may impact their survivorship is warranted.”
The research was supported by the National Cancer Institute at the National Institutes of Health, the Archer Charitable Foundation, and LyondellBasell. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Although adolescents and young adults (AYAs) who survive leukemia are living much longer than ever before, their life spans are still shorter than those of the general population, a new study concludes.
The study found that the 10-year survival of AYA leukemia survivors was approximately 10% lower than that of the age-adjusted U.S. general population at large.
These differences persisted for up to 30 years of follow-up.
“We need to think about the long-term life span and the quality of life for our patients. Cure is not enough for our AYA cancer survivors,” said senior author Michael Roth, MD, associate professor of pediatric patient care and director of the Childhood Cancer Survivorship Clinic at the University of Texas MD Anderson Cancer Center, Houston.
“Once these patients reach the survivorship stage of their journey, they may encounter additional side effects as a result of intensive treatment, lack of access to quality health care, and other issues that may negatively impact their health and overall survival,” he said in a statement.
The study was published in Cancer Epidemiology, Biomarkers and Prevention.
Demographics play role in survival
AYAs were defined as those persons aged 15-39 years. For their study, Dr. Roth and colleagues used the Surveillance, Epidemiology, and End Results (SEER) registry to identify 1,938 AYA survivors of acute lymphoblastic leukemia (ALL) and 2,350 AYA survivors of acute myeloid leukemia (AML) who were diagnosed from 1980 to 2009. They were followed for a median of 12 years.
The median age at diagnosis was 23 years for ALL and 28 years for AML.
Among ALL survivors, 6% were Black, 7% were Asian or Pacific Islander, 29% were Hispanic, and 58% were White. Among AML survivors, 9% were Black, 10% were Asian or Pacific Islander, 22% were Hispanic, and 59% were White. Ten-year survival for ALL and AML survivors was 87% and 89%, respectively. For the general population, it was 99%.
For ALL survivors, the 10-year survival was 83% for those diagnosed in the 1980s; it was 88% for those diagnosed in the 1990s and in the 2000s. The pattern was similar for AML survivors: 82%, 90%, and 90%.
The most common cause of death during early survivorship was acute leukemia. Deaths plateaued approximately 10 years after the initial diagnosis.
“Some of these patients aren’t being fully cured of their initial cancer, so between 5 and 10 years post initial diagnosis, most of the deaths are due to disease progression or relapse, whereas after that, most of the deaths result from late side effects from treatment, including cardiovascular disease and secondary cancers,” Dr. Roth said. Mortality from other causes continued to rise during the survivorship period. Subsequent malignancies and cardiac disease were the most common causes of death for both ALL and AML survivors.
A recent study found that AYA cancer survivors face nearly a twofold higher risk of dying from a new primary cancer, compared with peers in the general population.
When looking at key demographics, the authors found that older age at diagnosis was significantly associated with differential long-term survival (P < .0001 for both ALL and AML). Each additional year older at diagnosis was associated with a 6% and 5% decrease in long-term survival for both types of leukemia.
The decade in which the diagnosis was made had a significant difference in long-term survival both for patients with ALL and those with AML. Long-term survival times for those diagnosed in the 1990s were more than twice those of patients diagnosed in the 1980s for ALL (unadjusted P = .008) and AML (unadjusted P = .0002). Survival times were also more than twice those of patients diagnosed in the 2000s versus the 1980s for ALL (unadjusted P = .009) and AML (unadjusted P = .0003).
No significant long-term survival differences were observed for those diagnosed in the 2000s, compared with the 1990s, for either leukemia.
“The data from the national registry used for this study gave us insights into some possible challenges AML and ALL patients may encounter throughout survivorship, but we need to more thoroughly survey their journey,” Dr. Roth said. “An examination of their socioeconomic status, comorbidities, access to quality health care, and other risk factors that may impact their survivorship is warranted.”
The research was supported by the National Cancer Institute at the National Institutes of Health, the Archer Charitable Foundation, and LyondellBasell. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Although adolescents and young adults (AYAs) who survive leukemia are living much longer than ever before, their life spans are still shorter than those of the general population, a new study concludes.
The study found that the 10-year survival of AYA leukemia survivors was approximately 10% lower than that of the age-adjusted U.S. general population at large.
These differences persisted for up to 30 years of follow-up.
“We need to think about the long-term life span and the quality of life for our patients. Cure is not enough for our AYA cancer survivors,” said senior author Michael Roth, MD, associate professor of pediatric patient care and director of the Childhood Cancer Survivorship Clinic at the University of Texas MD Anderson Cancer Center, Houston.
“Once these patients reach the survivorship stage of their journey, they may encounter additional side effects as a result of intensive treatment, lack of access to quality health care, and other issues that may negatively impact their health and overall survival,” he said in a statement.
The study was published in Cancer Epidemiology, Biomarkers and Prevention.
Demographics play role in survival
AYAs were defined as those persons aged 15-39 years. For their study, Dr. Roth and colleagues used the Surveillance, Epidemiology, and End Results (SEER) registry to identify 1,938 AYA survivors of acute lymphoblastic leukemia (ALL) and 2,350 AYA survivors of acute myeloid leukemia (AML) who were diagnosed from 1980 to 2009. They were followed for a median of 12 years.
The median age at diagnosis was 23 years for ALL and 28 years for AML.
Among ALL survivors, 6% were Black, 7% were Asian or Pacific Islander, 29% were Hispanic, and 58% were White. Among AML survivors, 9% were Black, 10% were Asian or Pacific Islander, 22% were Hispanic, and 59% were White. Ten-year survival for ALL and AML survivors was 87% and 89%, respectively. For the general population, it was 99%.
For ALL survivors, the 10-year survival was 83% for those diagnosed in the 1980s; it was 88% for those diagnosed in the 1990s and in the 2000s. The pattern was similar for AML survivors: 82%, 90%, and 90%.
The most common cause of death during early survivorship was acute leukemia. Deaths plateaued approximately 10 years after the initial diagnosis.
“Some of these patients aren’t being fully cured of their initial cancer, so between 5 and 10 years post initial diagnosis, most of the deaths are due to disease progression or relapse, whereas after that, most of the deaths result from late side effects from treatment, including cardiovascular disease and secondary cancers,” Dr. Roth said. Mortality from other causes continued to rise during the survivorship period. Subsequent malignancies and cardiac disease were the most common causes of death for both ALL and AML survivors.
A recent study found that AYA cancer survivors face nearly a twofold higher risk of dying from a new primary cancer, compared with peers in the general population.
When looking at key demographics, the authors found that older age at diagnosis was significantly associated with differential long-term survival (P < .0001 for both ALL and AML). Each additional year older at diagnosis was associated with a 6% and 5% decrease in long-term survival for both types of leukemia.
The decade in which the diagnosis was made had a significant difference in long-term survival both for patients with ALL and those with AML. Long-term survival times for those diagnosed in the 1990s were more than twice those of patients diagnosed in the 1980s for ALL (unadjusted P = .008) and AML (unadjusted P = .0002). Survival times were also more than twice those of patients diagnosed in the 2000s versus the 1980s for ALL (unadjusted P = .009) and AML (unadjusted P = .0003).
No significant long-term survival differences were observed for those diagnosed in the 2000s, compared with the 1990s, for either leukemia.
“The data from the national registry used for this study gave us insights into some possible challenges AML and ALL patients may encounter throughout survivorship, but we need to more thoroughly survey their journey,” Dr. Roth said. “An examination of their socioeconomic status, comorbidities, access to quality health care, and other risk factors that may impact their survivorship is warranted.”
The research was supported by the National Cancer Institute at the National Institutes of Health, the Archer Charitable Foundation, and LyondellBasell. The authors disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM CANCER EPIDEMIOLOGY, BIOMARKERS AND PREVENTION
SCAI issues guidelines for PFO management, makes case for expansion
The first-ever guidelines for interventional cardiologists using percutaneous patent foramen ovale closure recommend expanding the use of the procedure beyond the Food and Drug Administration–approved indication following PFO-associated ischemic stroke, adding clarification about the use of PFO with anticoagulation and hedging against abuse and overuse of the procedure, said the chair of the guideline writing committee.
“The most important things surrounding these guidelines are to help clinicians and policymakers – third-party payers – to address PFO in patient subsets that were not included in the large randomized clinical trials that led to FDA approval,” said writing group chair Clifford J. Kavinsky, MD, PhD, chief of structural and interventional cardiology at Rush University Medical Center, Chicago.
The Society for Cardiovascular Angiography & Interventions issued the guidelines at its annual scientific sessions meeting in Atlanta and published them simultaneously in the society’s journal.
The guidelines issue strong and conditional recommendations. The former means clinicians should order the intervention for most patients; the latter means decisionmaking is more nuanced and should consider contributing factors.
The guidelines clarify patient selection for PFO closure outside the “pretty narrow” indication the FDA approved, Dr. Kavinsky said, which is for PFO-associated ischemic stroke in patients aged 18-60 years.
“So what about patients who are older than 60? What about patients who had their stroke 10 years ago?” Dr. Kavinsky asked. “Those are issues that were unanswered in the randomized clinical trials.”
The guidelines also refine recommendations about anticoagulation in these patients, including its use after PFO closure in selected patients, Dr. Kavinsky noted. “It’s the opinion of the panel that although anticoagulants may be effective, because of issues of noncompliance, because of issues of interruption of therapy by physicians for a variety of reasons, including surgery or noncompliance, that it is preferable to do a PFO device closure to giving anticoagulant therapy.”
Many of the recommendations cover PFO closure alongside antiplatelet or anticoagulation therapy. Key conditional recommendations for patients who haven’t had a PFO-related stroke are:
- Avoiding its routine use in patients with chronic migraines, prior decompression illness (DCI), thrombophilia, atrial septal aneurysm, transient ischemic attack (TIA), or deep vein thrombosis (DVT).
- Considering PFO closure in patients with platypnea-orthodeoxia syndrome (POS) with no other discernible cause of hypoxia or systemic embolism in whom other embolic causes have been ruled out.
In patients who’ve had a PFO-related stroke, the guidelines strongly recommend PFO closure versus antiplatelet therapy alone, but conditionally, not in patients with atrial fibrillation who’ve had an ischemic stroke. They also conditionally suggest PFO closure rather than long-term antiplatelet therapy alone in PFO stroke patients aged 60 and older, as well as those with thrombophilia already on antiplatelet therapy but not anticoagulation. However, the guidelines make no recommendation on PFO closure based on how much time has passed since the previous stroke.
“Furthermore,” Dr. Kavinsky said, “in patients who require lifelong anticoagulation because of recurrent DVT or recurrent pulmonary emboli or thrombopenia, if they’ve had a PFO-mediated stroke, then it’s our opinion that they should have their PFO closed in addition to taking lifelong anticoagulation because of the same issues of noncompliance and interruption of therapy.” Those are conditional recommendations.
The guideline also checks a box in the FDA labeling that mandated agreement between cardiology and neurology in patient selection. The American Academy of Neurology (AAN) issued its own guideline in 2020 for patients with stroke and PFO. In Europe, the European Society of Cardiology issued two position papers on expanded applications of PFO closure.
The recommendations on when PFO closure shouldn’t be done are noteworthy, Dr. Kavinsky said. “PFOs are present in 25% of the adult population, so the number of patients with PFO is huge and the indication for the FDA is really narrow: to reduce the risk of recurrent stroke in patients with PFO-mediated stroke. So, there’s the tremendous potential for abuse out there, of excessive procedures, of doing unnecessary procedures.”
The guidelines are a follow-up to the operator institutional requirements document SCAI issued in 2019 that set requirements for hospital offering and physicians performing PFO closure, Dr. Kavinsky added.
In an editorial accompanying the published guideline, Robert J. Sommer, MD, and Jamil A. Aboulhosn, MD, wrote that they support the recommendations “which help spotlight and clarify the growing list of potential indications for PFO closure.” They noted that the guidelines panel’s “strong” recommendations were for indications validated by randomized trials and that “conditional” recommendations were based on panelists’ experience and observational data.
“It is critical to recognize that most of these guidelines represent consensus opinion only,” wrote Dr. Sommer, who specializes in adult congenital and pediatric cardiology at Columbia University Irving Medical Center, New York, and Dr. Aboulhosn, an interventional cardiologist at Ronald Reagan University of California, Los Angeles, Medical Center. They emphasized the guidelines’ “heavy emphasis” on shared decisionmaking with patients.
Dr. Kavinsky is a principal investigator for Edwards Lifesciences, W.L. Gore and Associates, Medtronic, and Abbott. Dr. Sommer is a principal investigator and investigator in studies sponsored by W.L. Gore & Associates. Dr. Aboulhosn is a consultant to Abbott Medical.
The first-ever guidelines for interventional cardiologists using percutaneous patent foramen ovale closure recommend expanding the use of the procedure beyond the Food and Drug Administration–approved indication following PFO-associated ischemic stroke, adding clarification about the use of PFO with anticoagulation and hedging against abuse and overuse of the procedure, said the chair of the guideline writing committee.
“The most important things surrounding these guidelines are to help clinicians and policymakers – third-party payers – to address PFO in patient subsets that were not included in the large randomized clinical trials that led to FDA approval,” said writing group chair Clifford J. Kavinsky, MD, PhD, chief of structural and interventional cardiology at Rush University Medical Center, Chicago.
The Society for Cardiovascular Angiography & Interventions issued the guidelines at its annual scientific sessions meeting in Atlanta and published them simultaneously in the society’s journal.
The guidelines issue strong and conditional recommendations. The former means clinicians should order the intervention for most patients; the latter means decisionmaking is more nuanced and should consider contributing factors.
The guidelines clarify patient selection for PFO closure outside the “pretty narrow” indication the FDA approved, Dr. Kavinsky said, which is for PFO-associated ischemic stroke in patients aged 18-60 years.
“So what about patients who are older than 60? What about patients who had their stroke 10 years ago?” Dr. Kavinsky asked. “Those are issues that were unanswered in the randomized clinical trials.”
The guidelines also refine recommendations about anticoagulation in these patients, including its use after PFO closure in selected patients, Dr. Kavinsky noted. “It’s the opinion of the panel that although anticoagulants may be effective, because of issues of noncompliance, because of issues of interruption of therapy by physicians for a variety of reasons, including surgery or noncompliance, that it is preferable to do a PFO device closure to giving anticoagulant therapy.”
Many of the recommendations cover PFO closure alongside antiplatelet or anticoagulation therapy. Key conditional recommendations for patients who haven’t had a PFO-related stroke are:
- Avoiding its routine use in patients with chronic migraines, prior decompression illness (DCI), thrombophilia, atrial septal aneurysm, transient ischemic attack (TIA), or deep vein thrombosis (DVT).
- Considering PFO closure in patients with platypnea-orthodeoxia syndrome (POS) with no other discernible cause of hypoxia or systemic embolism in whom other embolic causes have been ruled out.
In patients who’ve had a PFO-related stroke, the guidelines strongly recommend PFO closure versus antiplatelet therapy alone, but conditionally, not in patients with atrial fibrillation who’ve had an ischemic stroke. They also conditionally suggest PFO closure rather than long-term antiplatelet therapy alone in PFO stroke patients aged 60 and older, as well as those with thrombophilia already on antiplatelet therapy but not anticoagulation. However, the guidelines make no recommendation on PFO closure based on how much time has passed since the previous stroke.
“Furthermore,” Dr. Kavinsky said, “in patients who require lifelong anticoagulation because of recurrent DVT or recurrent pulmonary emboli or thrombopenia, if they’ve had a PFO-mediated stroke, then it’s our opinion that they should have their PFO closed in addition to taking lifelong anticoagulation because of the same issues of noncompliance and interruption of therapy.” Those are conditional recommendations.
The guideline also checks a box in the FDA labeling that mandated agreement between cardiology and neurology in patient selection. The American Academy of Neurology (AAN) issued its own guideline in 2020 for patients with stroke and PFO. In Europe, the European Society of Cardiology issued two position papers on expanded applications of PFO closure.
The recommendations on when PFO closure shouldn’t be done are noteworthy, Dr. Kavinsky said. “PFOs are present in 25% of the adult population, so the number of patients with PFO is huge and the indication for the FDA is really narrow: to reduce the risk of recurrent stroke in patients with PFO-mediated stroke. So, there’s the tremendous potential for abuse out there, of excessive procedures, of doing unnecessary procedures.”
The guidelines are a follow-up to the operator institutional requirements document SCAI issued in 2019 that set requirements for hospital offering and physicians performing PFO closure, Dr. Kavinsky added.
In an editorial accompanying the published guideline, Robert J. Sommer, MD, and Jamil A. Aboulhosn, MD, wrote that they support the recommendations “which help spotlight and clarify the growing list of potential indications for PFO closure.” They noted that the guidelines panel’s “strong” recommendations were for indications validated by randomized trials and that “conditional” recommendations were based on panelists’ experience and observational data.
“It is critical to recognize that most of these guidelines represent consensus opinion only,” wrote Dr. Sommer, who specializes in adult congenital and pediatric cardiology at Columbia University Irving Medical Center, New York, and Dr. Aboulhosn, an interventional cardiologist at Ronald Reagan University of California, Los Angeles, Medical Center. They emphasized the guidelines’ “heavy emphasis” on shared decisionmaking with patients.
Dr. Kavinsky is a principal investigator for Edwards Lifesciences, W.L. Gore and Associates, Medtronic, and Abbott. Dr. Sommer is a principal investigator and investigator in studies sponsored by W.L. Gore & Associates. Dr. Aboulhosn is a consultant to Abbott Medical.
The first-ever guidelines for interventional cardiologists using percutaneous patent foramen ovale closure recommend expanding the use of the procedure beyond the Food and Drug Administration–approved indication following PFO-associated ischemic stroke, adding clarification about the use of PFO with anticoagulation and hedging against abuse and overuse of the procedure, said the chair of the guideline writing committee.
“The most important things surrounding these guidelines are to help clinicians and policymakers – third-party payers – to address PFO in patient subsets that were not included in the large randomized clinical trials that led to FDA approval,” said writing group chair Clifford J. Kavinsky, MD, PhD, chief of structural and interventional cardiology at Rush University Medical Center, Chicago.
The Society for Cardiovascular Angiography & Interventions issued the guidelines at its annual scientific sessions meeting in Atlanta and published them simultaneously in the society’s journal.
The guidelines issue strong and conditional recommendations. The former means clinicians should order the intervention for most patients; the latter means decisionmaking is more nuanced and should consider contributing factors.
The guidelines clarify patient selection for PFO closure outside the “pretty narrow” indication the FDA approved, Dr. Kavinsky said, which is for PFO-associated ischemic stroke in patients aged 18-60 years.
“So what about patients who are older than 60? What about patients who had their stroke 10 years ago?” Dr. Kavinsky asked. “Those are issues that were unanswered in the randomized clinical trials.”
The guidelines also refine recommendations about anticoagulation in these patients, including its use after PFO closure in selected patients, Dr. Kavinsky noted. “It’s the opinion of the panel that although anticoagulants may be effective, because of issues of noncompliance, because of issues of interruption of therapy by physicians for a variety of reasons, including surgery or noncompliance, that it is preferable to do a PFO device closure to giving anticoagulant therapy.”
Many of the recommendations cover PFO closure alongside antiplatelet or anticoagulation therapy. Key conditional recommendations for patients who haven’t had a PFO-related stroke are:
- Avoiding its routine use in patients with chronic migraines, prior decompression illness (DCI), thrombophilia, atrial septal aneurysm, transient ischemic attack (TIA), or deep vein thrombosis (DVT).
- Considering PFO closure in patients with platypnea-orthodeoxia syndrome (POS) with no other discernible cause of hypoxia or systemic embolism in whom other embolic causes have been ruled out.
In patients who’ve had a PFO-related stroke, the guidelines strongly recommend PFO closure versus antiplatelet therapy alone, but conditionally, not in patients with atrial fibrillation who’ve had an ischemic stroke. They also conditionally suggest PFO closure rather than long-term antiplatelet therapy alone in PFO stroke patients aged 60 and older, as well as those with thrombophilia already on antiplatelet therapy but not anticoagulation. However, the guidelines make no recommendation on PFO closure based on how much time has passed since the previous stroke.
“Furthermore,” Dr. Kavinsky said, “in patients who require lifelong anticoagulation because of recurrent DVT or recurrent pulmonary emboli or thrombopenia, if they’ve had a PFO-mediated stroke, then it’s our opinion that they should have their PFO closed in addition to taking lifelong anticoagulation because of the same issues of noncompliance and interruption of therapy.” Those are conditional recommendations.
The guideline also checks a box in the FDA labeling that mandated agreement between cardiology and neurology in patient selection. The American Academy of Neurology (AAN) issued its own guideline in 2020 for patients with stroke and PFO. In Europe, the European Society of Cardiology issued two position papers on expanded applications of PFO closure.
The recommendations on when PFO closure shouldn’t be done are noteworthy, Dr. Kavinsky said. “PFOs are present in 25% of the adult population, so the number of patients with PFO is huge and the indication for the FDA is really narrow: to reduce the risk of recurrent stroke in patients with PFO-mediated stroke. So, there’s the tremendous potential for abuse out there, of excessive procedures, of doing unnecessary procedures.”
The guidelines are a follow-up to the operator institutional requirements document SCAI issued in 2019 that set requirements for hospital offering and physicians performing PFO closure, Dr. Kavinsky added.
In an editorial accompanying the published guideline, Robert J. Sommer, MD, and Jamil A. Aboulhosn, MD, wrote that they support the recommendations “which help spotlight and clarify the growing list of potential indications for PFO closure.” They noted that the guidelines panel’s “strong” recommendations were for indications validated by randomized trials and that “conditional” recommendations were based on panelists’ experience and observational data.
“It is critical to recognize that most of these guidelines represent consensus opinion only,” wrote Dr. Sommer, who specializes in adult congenital and pediatric cardiology at Columbia University Irving Medical Center, New York, and Dr. Aboulhosn, an interventional cardiologist at Ronald Reagan University of California, Los Angeles, Medical Center. They emphasized the guidelines’ “heavy emphasis” on shared decisionmaking with patients.
Dr. Kavinsky is a principal investigator for Edwards Lifesciences, W.L. Gore and Associates, Medtronic, and Abbott. Dr. Sommer is a principal investigator and investigator in studies sponsored by W.L. Gore & Associates. Dr. Aboulhosn is a consultant to Abbott Medical.
FROM SCAI 2022
Updated AHA/ASA guideline changes care for spontaneous intracerebral hemorrhage
Many strategies widely considered “standard care” for managing spontaneous intracerebral hemorrhage (ICH) are not as effective as previously thought and are no longer recommended in updated guidelines from the American Heart Association/American Stroke Association (ASA).
Compression stockings, antiseizure medication, and steroid treatment are among the treatments with uncertain effectiveness, the writing group says.
The 2022 Guideline for the Management of Patients With Spontaneous ICH was published online in Stroke. The 80-page document contains major changes and refinements to the 2015 guideline on ICH management.
“Advances have been made in an array of fields related to ICH, including the organization of regional health care systems, reversal of the negative effects of blood thinners, minimally invasive surgical procedures, and the underlying disease in small blood vessels,” Steven M. Greenberg, MD, PhD, chair of the guideline writing group with Harvard Medical School and Massachusetts General Hospital, both in Boston, said in a news release.
“We’ve updated sections across the board. There’s probably no area that went untouched with some tweaking and new evidence added that led to some changes in level of evidence or strength of a recommendation,” Dr. Greenberg added in an interview with this news organization.
“Each section comes with knowledge gaps, and it wasn’t hard to come up with knowledge gaps in every section,” Dr. Greenberg acknowledged.
Time-honored treatments no more?
Among the key updates are changes to some “time-honored” treatments that continue to be used with some “regularity” for patients with ICH, yet appear to confer either no benefit or harm, Dr. Greenberg said.
For example, for emergency or critical care treatment of ICH, prophylactic corticosteroids or continuous hyperosmolar therapy is not recommended, because it appears to have no benefit for outcome, while use of platelet transfusions outside the setting of emergency surgery or severe thrombocytopenia appears to worsen outcome, the authors say.
Use of graduated knee- or thigh-high compression stockings alone is not an effective prophylactic therapy for prevention of deep vein thrombosis (DVT). Instead, intermittent pneumatic compression (IPC) starting on the day of diagnosis is now recommended for DVT prophylaxis.
“This is an area where we still have a lot of exploration to do. It is unclear whether even specialized compression devices reduce the risks of deep vein thrombosis or improve the overall health of people with a brain bleed,” Dr. Greenberg said in the release.
The new guidance advises against use of antiseizure or antidepressant medications for ICH patients in whom there is no evidence of seizures or depression.
In clinical trials, antiseizure medication did not contribute to improvements in functionality or long-term seizure control, and the use of antidepressants increased the chance of bone fractures, the authors say.
The guideline also provides updated recommendations for acute reversal of anticoagulation after ICH. It highlights the use of protein complex concentrate for reversal of vitamin K antagonists, such as warfarin; idarucizumab for reversal of the thrombin inhibitor dabigatran; and andexanet alfa for reversal of factor Xa inhibitors, such as rivaroxaban, apixaban, and edoxaban.
For acute blood pressure lowering after mild to moderate ICH, treatment regimens that limit blood pressure variability and achieve smooth, sustained blood pressure control appear to reduce hematoma expansion and yield better functional outcome, the guideline says.
It also notes that minimally invasive approaches for hematoma evacuation, compared with medical management alone‚ have been shown to reduce mortality.
For patients with cerebellar hemorrhage, indications for immediate surgical evacuation with or without an external ventricular drain to reduce mortality now include larger volume (> 15 mL) in addition to previously recommended indications of neurologic deterioration, brainstem compression, and hydrocephalus, the authors note.
However, a “major knowledge gap is whether we can improve functional outcome with hematoma evacuation,” Dr. Greenberg said.
Multidisciplinary care
For rehabilitation after ICH, the guideline reinforces the importance of having a multidisciplinary team to develop a comprehensive plan for recovery.
Starting rehabilitation activities such as stretching and functional task training may be considered 24 to 48 hours following mild or moderate ICH. However, early aggressive mobilization within the first 24 hours has been linked to an increased risk of death within 14 days after an ICH, the guideline says.
Knowledge gaps include how soon it’s safe to return to work, drive, and participate in other social engagements. Recommendations on sexual activity and exercise levels that are safe after a stroke are also needed.
“People need additional help with these lifestyle changes, whether it’s moving around more, curbing their alcohol use, or eating healthier foods. This all happens after they leave the hospital, and we need to be sure we are empowering families with the information they may need to be properly supportive,” Dr. Greenberg says in the release.
The guideline points to the patient’s home caregiver as a “key and sometimes overlooked” member of the care team. It recommends psychosocial education, practical support, and training for the caregiver to improve the patient’s balance, activity level, and overall quality of life.
Opportunity for prevention?
The guideline also suggests there may be an opportunity to prevent ICH in some people through neuroimaging markers.
While neuroimaging is not routinely performed as a part of risk stratification for primary ICH risk, damage to small blood vessels that is associated with ICH may be evident on MRI that could signal future ICH risk, the guideline says.
“We added to the guidelines for the first time a section on mostly imaging markers of risk for having a first-ever hemorrhage,” Dr. Greenberg said in an interview.
“We don’t make any recommendations as to how to act on these markers because there is a knowledge gap. The hope is that we’ll see growth in our ability to predict first-ever hemorrhage and be able to do things to prevent first-ever hemorrhage,” he said.
“We believe the wide range of knowledge set forth in the new guideline will translate into meaningful improvements in ICH care,” Dr. Greenberg adds in the release.
The updated guideline has been endorsed by the American Association of Neurological Surgeons and Congress of Neurological Surgeons, the Society of Vascular and Interventional Neurology, and the Neurocritical Care Society. The American Academy of Neurology has affirmed the value of this statement as an educational tool for neurologists.
This research had no commercial funding. Dr. Greenberg has disclosed no relevant financial relationships. A complete list of disclosures for the guideline group is available with the original article.
A version of this article first appeared on Medscape.com.
Many strategies widely considered “standard care” for managing spontaneous intracerebral hemorrhage (ICH) are not as effective as previously thought and are no longer recommended in updated guidelines from the American Heart Association/American Stroke Association (ASA).
Compression stockings, antiseizure medication, and steroid treatment are among the treatments with uncertain effectiveness, the writing group says.
The 2022 Guideline for the Management of Patients With Spontaneous ICH was published online in Stroke. The 80-page document contains major changes and refinements to the 2015 guideline on ICH management.
“Advances have been made in an array of fields related to ICH, including the organization of regional health care systems, reversal of the negative effects of blood thinners, minimally invasive surgical procedures, and the underlying disease in small blood vessels,” Steven M. Greenberg, MD, PhD, chair of the guideline writing group with Harvard Medical School and Massachusetts General Hospital, both in Boston, said in a news release.
“We’ve updated sections across the board. There’s probably no area that went untouched with some tweaking and new evidence added that led to some changes in level of evidence or strength of a recommendation,” Dr. Greenberg added in an interview with this news organization.
“Each section comes with knowledge gaps, and it wasn’t hard to come up with knowledge gaps in every section,” Dr. Greenberg acknowledged.
Time-honored treatments no more?
Among the key updates are changes to some “time-honored” treatments that continue to be used with some “regularity” for patients with ICH, yet appear to confer either no benefit or harm, Dr. Greenberg said.
For example, for emergency or critical care treatment of ICH, prophylactic corticosteroids or continuous hyperosmolar therapy is not recommended, because it appears to have no benefit for outcome, while use of platelet transfusions outside the setting of emergency surgery or severe thrombocytopenia appears to worsen outcome, the authors say.
Use of graduated knee- or thigh-high compression stockings alone is not an effective prophylactic therapy for prevention of deep vein thrombosis (DVT). Instead, intermittent pneumatic compression (IPC) starting on the day of diagnosis is now recommended for DVT prophylaxis.
“This is an area where we still have a lot of exploration to do. It is unclear whether even specialized compression devices reduce the risks of deep vein thrombosis or improve the overall health of people with a brain bleed,” Dr. Greenberg said in the release.
The new guidance advises against use of antiseizure or antidepressant medications for ICH patients in whom there is no evidence of seizures or depression.
In clinical trials, antiseizure medication did not contribute to improvements in functionality or long-term seizure control, and the use of antidepressants increased the chance of bone fractures, the authors say.
The guideline also provides updated recommendations for acute reversal of anticoagulation after ICH. It highlights the use of protein complex concentrate for reversal of vitamin K antagonists, such as warfarin; idarucizumab for reversal of the thrombin inhibitor dabigatran; and andexanet alfa for reversal of factor Xa inhibitors, such as rivaroxaban, apixaban, and edoxaban.
For acute blood pressure lowering after mild to moderate ICH, treatment regimens that limit blood pressure variability and achieve smooth, sustained blood pressure control appear to reduce hematoma expansion and yield better functional outcome, the guideline says.
It also notes that minimally invasive approaches for hematoma evacuation, compared with medical management alone‚ have been shown to reduce mortality.
For patients with cerebellar hemorrhage, indications for immediate surgical evacuation with or without an external ventricular drain to reduce mortality now include larger volume (> 15 mL) in addition to previously recommended indications of neurologic deterioration, brainstem compression, and hydrocephalus, the authors note.
However, a “major knowledge gap is whether we can improve functional outcome with hematoma evacuation,” Dr. Greenberg said.
Multidisciplinary care
For rehabilitation after ICH, the guideline reinforces the importance of having a multidisciplinary team to develop a comprehensive plan for recovery.
Starting rehabilitation activities such as stretching and functional task training may be considered 24 to 48 hours following mild or moderate ICH. However, early aggressive mobilization within the first 24 hours has been linked to an increased risk of death within 14 days after an ICH, the guideline says.
Knowledge gaps include how soon it’s safe to return to work, drive, and participate in other social engagements. Recommendations on sexual activity and exercise levels that are safe after a stroke are also needed.
“People need additional help with these lifestyle changes, whether it’s moving around more, curbing their alcohol use, or eating healthier foods. This all happens after they leave the hospital, and we need to be sure we are empowering families with the information they may need to be properly supportive,” Dr. Greenberg says in the release.
The guideline points to the patient’s home caregiver as a “key and sometimes overlooked” member of the care team. It recommends psychosocial education, practical support, and training for the caregiver to improve the patient’s balance, activity level, and overall quality of life.
Opportunity for prevention?
The guideline also suggests there may be an opportunity to prevent ICH in some people through neuroimaging markers.
While neuroimaging is not routinely performed as a part of risk stratification for primary ICH risk, damage to small blood vessels that is associated with ICH may be evident on MRI that could signal future ICH risk, the guideline says.
“We added to the guidelines for the first time a section on mostly imaging markers of risk for having a first-ever hemorrhage,” Dr. Greenberg said in an interview.
“We don’t make any recommendations as to how to act on these markers because there is a knowledge gap. The hope is that we’ll see growth in our ability to predict first-ever hemorrhage and be able to do things to prevent first-ever hemorrhage,” he said.
“We believe the wide range of knowledge set forth in the new guideline will translate into meaningful improvements in ICH care,” Dr. Greenberg adds in the release.
The updated guideline has been endorsed by the American Association of Neurological Surgeons and Congress of Neurological Surgeons, the Society of Vascular and Interventional Neurology, and the Neurocritical Care Society. The American Academy of Neurology has affirmed the value of this statement as an educational tool for neurologists.
This research had no commercial funding. Dr. Greenberg has disclosed no relevant financial relationships. A complete list of disclosures for the guideline group is available with the original article.
A version of this article first appeared on Medscape.com.
Many strategies widely considered “standard care” for managing spontaneous intracerebral hemorrhage (ICH) are not as effective as previously thought and are no longer recommended in updated guidelines from the American Heart Association/American Stroke Association (ASA).
Compression stockings, antiseizure medication, and steroid treatment are among the treatments with uncertain effectiveness, the writing group says.
The 2022 Guideline for the Management of Patients With Spontaneous ICH was published online in Stroke. The 80-page document contains major changes and refinements to the 2015 guideline on ICH management.
“Advances have been made in an array of fields related to ICH, including the organization of regional health care systems, reversal of the negative effects of blood thinners, minimally invasive surgical procedures, and the underlying disease in small blood vessels,” Steven M. Greenberg, MD, PhD, chair of the guideline writing group with Harvard Medical School and Massachusetts General Hospital, both in Boston, said in a news release.
“We’ve updated sections across the board. There’s probably no area that went untouched with some tweaking and new evidence added that led to some changes in level of evidence or strength of a recommendation,” Dr. Greenberg added in an interview with this news organization.
“Each section comes with knowledge gaps, and it wasn’t hard to come up with knowledge gaps in every section,” Dr. Greenberg acknowledged.
Time-honored treatments no more?
Among the key updates are changes to some “time-honored” treatments that continue to be used with some “regularity” for patients with ICH, yet appear to confer either no benefit or harm, Dr. Greenberg said.
For example, for emergency or critical care treatment of ICH, prophylactic corticosteroids or continuous hyperosmolar therapy is not recommended, because it appears to have no benefit for outcome, while use of platelet transfusions outside the setting of emergency surgery or severe thrombocytopenia appears to worsen outcome, the authors say.
Use of graduated knee- or thigh-high compression stockings alone is not an effective prophylactic therapy for prevention of deep vein thrombosis (DVT). Instead, intermittent pneumatic compression (IPC) starting on the day of diagnosis is now recommended for DVT prophylaxis.
“This is an area where we still have a lot of exploration to do. It is unclear whether even specialized compression devices reduce the risks of deep vein thrombosis or improve the overall health of people with a brain bleed,” Dr. Greenberg said in the release.
The new guidance advises against use of antiseizure or antidepressant medications for ICH patients in whom there is no evidence of seizures or depression.
In clinical trials, antiseizure medication did not contribute to improvements in functionality or long-term seizure control, and the use of antidepressants increased the chance of bone fractures, the authors say.
The guideline also provides updated recommendations for acute reversal of anticoagulation after ICH. It highlights the use of protein complex concentrate for reversal of vitamin K antagonists, such as warfarin; idarucizumab for reversal of the thrombin inhibitor dabigatran; and andexanet alfa for reversal of factor Xa inhibitors, such as rivaroxaban, apixaban, and edoxaban.
For acute blood pressure lowering after mild to moderate ICH, treatment regimens that limit blood pressure variability and achieve smooth, sustained blood pressure control appear to reduce hematoma expansion and yield better functional outcome, the guideline says.
It also notes that minimally invasive approaches for hematoma evacuation, compared with medical management alone‚ have been shown to reduce mortality.
For patients with cerebellar hemorrhage, indications for immediate surgical evacuation with or without an external ventricular drain to reduce mortality now include larger volume (> 15 mL) in addition to previously recommended indications of neurologic deterioration, brainstem compression, and hydrocephalus, the authors note.
However, a “major knowledge gap is whether we can improve functional outcome with hematoma evacuation,” Dr. Greenberg said.
Multidisciplinary care
For rehabilitation after ICH, the guideline reinforces the importance of having a multidisciplinary team to develop a comprehensive plan for recovery.
Starting rehabilitation activities such as stretching and functional task training may be considered 24 to 48 hours following mild or moderate ICH. However, early aggressive mobilization within the first 24 hours has been linked to an increased risk of death within 14 days after an ICH, the guideline says.
Knowledge gaps include how soon it’s safe to return to work, drive, and participate in other social engagements. Recommendations on sexual activity and exercise levels that are safe after a stroke are also needed.
“People need additional help with these lifestyle changes, whether it’s moving around more, curbing their alcohol use, or eating healthier foods. This all happens after they leave the hospital, and we need to be sure we are empowering families with the information they may need to be properly supportive,” Dr. Greenberg says in the release.
The guideline points to the patient’s home caregiver as a “key and sometimes overlooked” member of the care team. It recommends psychosocial education, practical support, and training for the caregiver to improve the patient’s balance, activity level, and overall quality of life.
Opportunity for prevention?
The guideline also suggests there may be an opportunity to prevent ICH in some people through neuroimaging markers.
While neuroimaging is not routinely performed as a part of risk stratification for primary ICH risk, damage to small blood vessels that is associated with ICH may be evident on MRI that could signal future ICH risk, the guideline says.
“We added to the guidelines for the first time a section on mostly imaging markers of risk for having a first-ever hemorrhage,” Dr. Greenberg said in an interview.
“We don’t make any recommendations as to how to act on these markers because there is a knowledge gap. The hope is that we’ll see growth in our ability to predict first-ever hemorrhage and be able to do things to prevent first-ever hemorrhage,” he said.
“We believe the wide range of knowledge set forth in the new guideline will translate into meaningful improvements in ICH care,” Dr. Greenberg adds in the release.
The updated guideline has been endorsed by the American Association of Neurological Surgeons and Congress of Neurological Surgeons, the Society of Vascular and Interventional Neurology, and the Neurocritical Care Society. The American Academy of Neurology has affirmed the value of this statement as an educational tool for neurologists.
This research had no commercial funding. Dr. Greenberg has disclosed no relevant financial relationships. A complete list of disclosures for the guideline group is available with the original article.
A version of this article first appeared on Medscape.com.
Improved cancer survival in states with ACA Medicaid expansion
compared with patients in states that did not adopt the expansion.
The finding comes from an American Cancer Society study of more than 2 million patients with newly diagnosed cancer, published online in the Journal of the National Cancer Institute.
The analysis also showed that the evidence was strongest for malignancies with poor prognosis such as lung, pancreatic, and liver cancer, and also for colorectal cancer.
Importantly, improvements in survival were larger in non-Hispanic Black patients and individuals residing in rural areas, suggesting there was a narrowing of disparities in cancer survival by race and rurality.
“Our findings provide further evidence of the importance of expanding Medicaid eligibility in all states, particularly considering the economic crisis and health care disruptions caused by the COVID-19 pandemic,” said lead author Xuesong Han, PhD, scientific director of health services research at the American Cancer Society, in a statement. “What’s encouraging is the American Rescue Plan Act of 2021 provides new incentives for Medicaid expansion in states that have yet to increase eligibility.”
The ACA provided states with incentives to expand Medicaid eligibility to all low-income adults under 138% federal poverty level, regardless of parental status.
As of last month, just 12 states have not yet opted for Medicaid expansion, even though the American Rescue Plan Act of 2021 provides new incentives for those remaining jurisdictions. But to date, none of the remaining states have taken advantage of these new incentives.
An interactive map showing the status of Medicare expansion by state is available here. The 12 states that have not adopted Medicare expansion (as of April) are Alabama, Florida, Georgia, Kansas, Mississippi, North Carolina, South Carolina, South Dakota, Tennessee, Texas, Wisconsin, and Wyoming.
The benefit of Medicaid expansion on cancer outcomes has already been observed in other studies. The first study to show a survival benefit was presented at the 2020 American Society of Clinical Oncology annual meeting. That analysis showed that cancer mortality declined by 29% in states that expanded Medicaid and by 25% in those that did not. The authors also noted that the greatest mortality benefit was observed in Hispanic patients.
Improved survival with expansion
In the current paper, Dr. Han and colleagues used population-based cancer registries from 42 states and compared data on patients aged 18-62 years who were diagnosed with cancer in a period of 2 years before (2010-2012) and after (2014-2016) ACA Medicaid expansion. They were followed through Sept. 30, 2013, and Dec. 31, 2017, respectively.
The analysis involved a total of 2.5 million patients, of whom 1.52 million lived in states that adopted Medicaid expansion and compared with 1 million patients were in states that did not.
Patients with grouped by sex, race and ethnicity, census tract-level poverty, and rurality. The authors note that non-Hispanic Black patients and those from high poverty areas and nonmetropolitan areas were disproportionately represented in nonexpansion states.
During the 2-year follow-up period, a total of 453,487 deaths occurred (257,950 in expansion states and 195,537 in nonexpansion states).
Overall, patients in expansion states generally had better survival versus those in nonexpansion states, the authors comment. However, for most cancer types, overall survival improved after the ACA for both groups of states.
The 2-year overall survival increased from 80.6% before the ACA to 82.2% post ACA in expansion states and from 78.7% to 80% in nonexpansion states.
This extrapolated to net increase of 0.44 percentage points in expansion states after adjusting for sociodemographic factors. By cancer site, the net increase was greater for colorectal cancer, lung cancer, non-Hodgkin’s lymphoma, pancreatic cancer, and liver cancer.
For Hispanic patients, 2-year survival also increased but was similar in expansion and nonexpansion states, and little net change was associated with Medicaid expansion.
“Our study shows that the increase was largely driven by improvements in survival for cancer types with poor prognosis, suggesting improved access to timely and effective treatments,” said Dr. Han. “It adds to accumulating evidence of the multiple benefits of Medicaid expansion.”
A version of this article first appeared on Medscape.com.
compared with patients in states that did not adopt the expansion.
The finding comes from an American Cancer Society study of more than 2 million patients with newly diagnosed cancer, published online in the Journal of the National Cancer Institute.
The analysis also showed that the evidence was strongest for malignancies with poor prognosis such as lung, pancreatic, and liver cancer, and also for colorectal cancer.
Importantly, improvements in survival were larger in non-Hispanic Black patients and individuals residing in rural areas, suggesting there was a narrowing of disparities in cancer survival by race and rurality.
“Our findings provide further evidence of the importance of expanding Medicaid eligibility in all states, particularly considering the economic crisis and health care disruptions caused by the COVID-19 pandemic,” said lead author Xuesong Han, PhD, scientific director of health services research at the American Cancer Society, in a statement. “What’s encouraging is the American Rescue Plan Act of 2021 provides new incentives for Medicaid expansion in states that have yet to increase eligibility.”
The ACA provided states with incentives to expand Medicaid eligibility to all low-income adults under 138% federal poverty level, regardless of parental status.
As of last month, just 12 states have not yet opted for Medicaid expansion, even though the American Rescue Plan Act of 2021 provides new incentives for those remaining jurisdictions. But to date, none of the remaining states have taken advantage of these new incentives.
An interactive map showing the status of Medicare expansion by state is available here. The 12 states that have not adopted Medicare expansion (as of April) are Alabama, Florida, Georgia, Kansas, Mississippi, North Carolina, South Carolina, South Dakota, Tennessee, Texas, Wisconsin, and Wyoming.
The benefit of Medicaid expansion on cancer outcomes has already been observed in other studies. The first study to show a survival benefit was presented at the 2020 American Society of Clinical Oncology annual meeting. That analysis showed that cancer mortality declined by 29% in states that expanded Medicaid and by 25% in those that did not. The authors also noted that the greatest mortality benefit was observed in Hispanic patients.
Improved survival with expansion
In the current paper, Dr. Han and colleagues used population-based cancer registries from 42 states and compared data on patients aged 18-62 years who were diagnosed with cancer in a period of 2 years before (2010-2012) and after (2014-2016) ACA Medicaid expansion. They were followed through Sept. 30, 2013, and Dec. 31, 2017, respectively.
The analysis involved a total of 2.5 million patients, of whom 1.52 million lived in states that adopted Medicaid expansion and compared with 1 million patients were in states that did not.
Patients with grouped by sex, race and ethnicity, census tract-level poverty, and rurality. The authors note that non-Hispanic Black patients and those from high poverty areas and nonmetropolitan areas were disproportionately represented in nonexpansion states.
During the 2-year follow-up period, a total of 453,487 deaths occurred (257,950 in expansion states and 195,537 in nonexpansion states).
Overall, patients in expansion states generally had better survival versus those in nonexpansion states, the authors comment. However, for most cancer types, overall survival improved after the ACA for both groups of states.
The 2-year overall survival increased from 80.6% before the ACA to 82.2% post ACA in expansion states and from 78.7% to 80% in nonexpansion states.
This extrapolated to net increase of 0.44 percentage points in expansion states after adjusting for sociodemographic factors. By cancer site, the net increase was greater for colorectal cancer, lung cancer, non-Hodgkin’s lymphoma, pancreatic cancer, and liver cancer.
For Hispanic patients, 2-year survival also increased but was similar in expansion and nonexpansion states, and little net change was associated with Medicaid expansion.
“Our study shows that the increase was largely driven by improvements in survival for cancer types with poor prognosis, suggesting improved access to timely and effective treatments,” said Dr. Han. “It adds to accumulating evidence of the multiple benefits of Medicaid expansion.”
A version of this article first appeared on Medscape.com.
compared with patients in states that did not adopt the expansion.
The finding comes from an American Cancer Society study of more than 2 million patients with newly diagnosed cancer, published online in the Journal of the National Cancer Institute.
The analysis also showed that the evidence was strongest for malignancies with poor prognosis such as lung, pancreatic, and liver cancer, and also for colorectal cancer.
Importantly, improvements in survival were larger in non-Hispanic Black patients and individuals residing in rural areas, suggesting there was a narrowing of disparities in cancer survival by race and rurality.
“Our findings provide further evidence of the importance of expanding Medicaid eligibility in all states, particularly considering the economic crisis and health care disruptions caused by the COVID-19 pandemic,” said lead author Xuesong Han, PhD, scientific director of health services research at the American Cancer Society, in a statement. “What’s encouraging is the American Rescue Plan Act of 2021 provides new incentives for Medicaid expansion in states that have yet to increase eligibility.”
The ACA provided states with incentives to expand Medicaid eligibility to all low-income adults under 138% federal poverty level, regardless of parental status.
As of last month, just 12 states have not yet opted for Medicaid expansion, even though the American Rescue Plan Act of 2021 provides new incentives for those remaining jurisdictions. But to date, none of the remaining states have taken advantage of these new incentives.
An interactive map showing the status of Medicare expansion by state is available here. The 12 states that have not adopted Medicare expansion (as of April) are Alabama, Florida, Georgia, Kansas, Mississippi, North Carolina, South Carolina, South Dakota, Tennessee, Texas, Wisconsin, and Wyoming.
The benefit of Medicaid expansion on cancer outcomes has already been observed in other studies. The first study to show a survival benefit was presented at the 2020 American Society of Clinical Oncology annual meeting. That analysis showed that cancer mortality declined by 29% in states that expanded Medicaid and by 25% in those that did not. The authors also noted that the greatest mortality benefit was observed in Hispanic patients.
Improved survival with expansion
In the current paper, Dr. Han and colleagues used population-based cancer registries from 42 states and compared data on patients aged 18-62 years who were diagnosed with cancer in a period of 2 years before (2010-2012) and after (2014-2016) ACA Medicaid expansion. They were followed through Sept. 30, 2013, and Dec. 31, 2017, respectively.
The analysis involved a total of 2.5 million patients, of whom 1.52 million lived in states that adopted Medicaid expansion and compared with 1 million patients were in states that did not.
Patients with grouped by sex, race and ethnicity, census tract-level poverty, and rurality. The authors note that non-Hispanic Black patients and those from high poverty areas and nonmetropolitan areas were disproportionately represented in nonexpansion states.
During the 2-year follow-up period, a total of 453,487 deaths occurred (257,950 in expansion states and 195,537 in nonexpansion states).
Overall, patients in expansion states generally had better survival versus those in nonexpansion states, the authors comment. However, for most cancer types, overall survival improved after the ACA for both groups of states.
The 2-year overall survival increased from 80.6% before the ACA to 82.2% post ACA in expansion states and from 78.7% to 80% in nonexpansion states.
This extrapolated to net increase of 0.44 percentage points in expansion states after adjusting for sociodemographic factors. By cancer site, the net increase was greater for colorectal cancer, lung cancer, non-Hodgkin’s lymphoma, pancreatic cancer, and liver cancer.
For Hispanic patients, 2-year survival also increased but was similar in expansion and nonexpansion states, and little net change was associated with Medicaid expansion.
“Our study shows that the increase was largely driven by improvements in survival for cancer types with poor prognosis, suggesting improved access to timely and effective treatments,” said Dr. Han. “It adds to accumulating evidence of the multiple benefits of Medicaid expansion.”
A version of this article first appeared on Medscape.com.
Cancer patients unaware of their increased thrombosis risk
It is up to their physician to discuss this with them.
This link is explained by the authors of an article in Cancer Treatment and Research Communications that reports results of a survey carried out by the European Cancer Patient Coalition (ECPC). “The aim of this pan-European patient survey was to assess patient awareness and knowledge about cancer-associated thrombosis (CAT), including risk factors, signs and symptoms, and interventions, to better prevent and treat CAT,” write the authors. “The idea was to create a sort of starting point for subsequent communication and information strategies and for comparing the results of any action taken in this area,” they add.
A roundtable discussion that included oncology healthcare professionals, policymakers, and patient advocates was convened to discuss and review the evidence regarding their ongoing concerns of excessive CAT-associated morbidity and mortality, as well as patients’ desire for greater CAT awareness.
“These discussions demonstrated that very little change had occurred over the years and that greater knowledge about CAT was still needed across the spectrum of healthcare practitioners and patients, particularly regarding primary and secondary prevention of thrombosis,” the authors write.
It was from this starting point that the idea for the pan-European survey was born. The ECPC, widely viewed as the “unified voice of cancer patients across Europe,” led the survey. This survey spanned six countries (France, Germany, Greece, Italy, United Kingdom, and Spain) and involved 1,365 patients and caregivers. The ECPC survey result was originally released at World Thrombosis Day in late 2018.
In an interview, Anna Falanga, MD, the main author of the article and professor of hematology at the University of Milan-Bicocca, Italy, reviewed the results and explained how to improve knowledge of CAT among patients with cancer.
“Data support that up to 20% of patients with cancer will experience venous thromboembolism (VTE), which is approximately 4–5 times higher than the general population,” said Dr. Falanga, who is also chief of the department of immunohematology and transfusion medicine and the Thrombosis and Hemostasis Center at the Hospital Papa Giovanni XXIII, in Bergamo, Italy.
“We have known about the link between thrombosis and cancer since the 19th century, but it has taken until midway through the last century for our level of understanding and awareness of the problem to reach its current level. Initially, this was limited to fundamental research, with large advances in our understanding of the mechanisms of the link between the two; it has only been more recently that we have had clinical studies that have piqued the interest of healthcare professionals, who were previously uninterested in the topic,” she said.
Poor understanding
One piece of data stands out from the European survey: Nearly three quarters of respondents (72%) said that before taking part in the survey, they were not aware that people with cancer have a higher-than-normal risk of developing thrombosis. “We asked participants to rate their overall understanding of CAT on a scale of 1 (low) to 10 (high), with the average (mean) score obtained being 4.1. Only 21% of patients gave a rating of 7 or above (high understanding). The average rating was very similar in the different countries surveyed,” write the authors. They note that the survey also assessed how much participants had learned about the topic from their physicians.
Approximately 35% of patients were made aware of CAT either immediately before or at the time of their cancer diagnosis. Of particular concern, one quarter (26%) of respondents (the largest proportion) noted that they first became aware of CAT when they suffered a blood clot. The average rating was very similar in the different countries surveyed. “Let us not forget that cancer and cancer treatments themselves cause a number of side effects, some of which can be very serious, so in some ways, a clot might be seen as a minor problem. Yet, in reality, it isn’t. It is a significant cause of death and disease in cancer patients,” said Dr. Falanga.
When discussing prevention, most respondents (87%) said they were aware that taking a walk could reduce their risk. Slightly fewer were aware that stopping smoking could reduce their risk (75%), and even fewer were aware that keeping hydrated (63%) and stretching their legs (55%) could reduce their risk.
Symptoms of CAT appeared to be relatively well known; 73% of survey participants indicated that they were aware that swelling in the foot, ankle, or leg could be a sign of DVT, and 71% indicated that shortness of breath could be a sign of pulmonary embolism (PE). “Other symptoms, however, were less well known, with just over half (57%) of participants being aware that pain, cramping, and tenderness could be a sign of DVT. About one third (33%) knew that irregular heartbeat could be a sign of PE. These results varied between countries,” according to the authors.
The survey highlighted that just over a third of respondents said that they were currently using anticoagulants, although almost all (96%) knew that anticoagulants could be used to effectively treat thrombosis. Only 41% of those using anticoagulants said they had been told about any possible side effects.
The Italian situation
The report containing the full results of the European survey goes even further, since, in addition to its overall results, it also gives information about individual countries.
The data from Italy, which are based on 246 persons, show that only 27% of patients and caregivers were aware of the increased risk of thrombosis after a cancer diagnosis. This figure is in line with the overall results of the survey, although the average score of the 10-point scale was lower for the Italy cohort (3.3/10 vs 4.1/10).
The results are more variable in terms of knowledge of risk factors. Most respondents (89%) said that they were aware of the risks related to inactivity. Just over half (52%), however, said that they were aware of the risks related to radiotherapy. Nevertheless, 75% of participants knew about the risks relating to cancer surgery and chemotherapy. “To all intents and purposes, all types of cancer drug can significantly affect the risk of developing a clot. And this is also the case for more modern types of treatment, such as immunotherapy,” said Dr. Falanga.
Most respondents reported that they got information about cancer-associated thrombosis verbally, usually from their hospital doctor (11%). Some respondents (6%) said that they found out about it from their own research, usually online. Almost 1 in 4 patients (24%) in Italy said that they first became aware of CAT when they suffered a blood clot. Answers to questions about knowledge of symptoms show that 58% of Italian patients and caregivers know that swelling of the lower limbs can be a symptom of DVT, and the same percentage knows that shortness of breath might indicate PE.
In terms of preventive action, the picture in Italy is somewhat variable: 74% of participants were aware of the importance of walking, but far fewer knew about the need to stop smoking (57%) and stretch the legs (35%). Of the 41% of Italians who were also taking an anticoagulant drug, 53% said that they knew about the possible side effects of such medication.
Which way forward?
“The high rate of CAT suggests that, despite the clinical evidence and clear guideline recommendations for patients with cancer, CAT prevention and recognition remain low among healthcare professionals,” the authors write.
The results of the ECPC survey further confirm those of previous studies, highlighting patients’ lack of knowledge about CAT and the need for more in-depth discussions between physician and patient.
So, what can be done? As highlighted by previous studies, “patients’ experiences are an education in themselves, particularly for the oncology care team,” the authors write. “Once the patient has a thrombosis, the opportunity for thrombosis prevention, which should be the most crucial focus of the care clinics (surgical, oncology, and palliative care), is gone,” they add.
“Oncology professionals, as well as other members of the patient’s care team (eg, internists, surgeons, nurses), need to perform better, at every stage of the patient’s cancer pathway, to ensure patients are aware of CAT and their individual risk to develop a blood clot,” said Dr. Falanga. She explained that in this group, it is the general practitioner who is the first contact. “These professionals are on the front line of the battle; they are among the first healthcare workers given the chance to suspect a clot and should, therefore, be fully aware of the increased risk in oncology patients,” she reiterated.
Experts agree on the fact that a multidisciplinary approach is of utmost importance in this context: the different roles in the team must be clear. “It is also fundamental to establish who does what in terms of educating and informing the patient,” said Dr. Falanga.
The researchers also put forward an example of a successful initiative: the Venous Thromboembolism Prevention in the Ambulatory Cancer Clinic (VTE-PACC) program. The initiative was developed by experts from the University of Vermont and was described in a recent article in JCO Oncology Practice.
Numerous resources are available online to help physicians talk to their patients and explain the risks linked to CAT along the continuum of cancer care. Among them is a resource titled, “Cancer Associated Thrombosis (CAT): Be Clot Conscious,” which can be found on the ECPC’s website.
“We have a collective responsibility using the ECPC patient survey as a baseline to inform patients with cancer on how to identify signs and symptoms of CAT to enable faster diagnosis and treatment,” the authors conclude.
This article was translated from Univadis Italy.
It is up to their physician to discuss this with them.
This link is explained by the authors of an article in Cancer Treatment and Research Communications that reports results of a survey carried out by the European Cancer Patient Coalition (ECPC). “The aim of this pan-European patient survey was to assess patient awareness and knowledge about cancer-associated thrombosis (CAT), including risk factors, signs and symptoms, and interventions, to better prevent and treat CAT,” write the authors. “The idea was to create a sort of starting point for subsequent communication and information strategies and for comparing the results of any action taken in this area,” they add.
A roundtable discussion that included oncology healthcare professionals, policymakers, and patient advocates was convened to discuss and review the evidence regarding their ongoing concerns of excessive CAT-associated morbidity and mortality, as well as patients’ desire for greater CAT awareness.
“These discussions demonstrated that very little change had occurred over the years and that greater knowledge about CAT was still needed across the spectrum of healthcare practitioners and patients, particularly regarding primary and secondary prevention of thrombosis,” the authors write.
It was from this starting point that the idea for the pan-European survey was born. The ECPC, widely viewed as the “unified voice of cancer patients across Europe,” led the survey. This survey spanned six countries (France, Germany, Greece, Italy, United Kingdom, and Spain) and involved 1,365 patients and caregivers. The ECPC survey result was originally released at World Thrombosis Day in late 2018.
In an interview, Anna Falanga, MD, the main author of the article and professor of hematology at the University of Milan-Bicocca, Italy, reviewed the results and explained how to improve knowledge of CAT among patients with cancer.
“Data support that up to 20% of patients with cancer will experience venous thromboembolism (VTE), which is approximately 4–5 times higher than the general population,” said Dr. Falanga, who is also chief of the department of immunohematology and transfusion medicine and the Thrombosis and Hemostasis Center at the Hospital Papa Giovanni XXIII, in Bergamo, Italy.
“We have known about the link between thrombosis and cancer since the 19th century, but it has taken until midway through the last century for our level of understanding and awareness of the problem to reach its current level. Initially, this was limited to fundamental research, with large advances in our understanding of the mechanisms of the link between the two; it has only been more recently that we have had clinical studies that have piqued the interest of healthcare professionals, who were previously uninterested in the topic,” she said.
Poor understanding
One piece of data stands out from the European survey: Nearly three quarters of respondents (72%) said that before taking part in the survey, they were not aware that people with cancer have a higher-than-normal risk of developing thrombosis. “We asked participants to rate their overall understanding of CAT on a scale of 1 (low) to 10 (high), with the average (mean) score obtained being 4.1. Only 21% of patients gave a rating of 7 or above (high understanding). The average rating was very similar in the different countries surveyed,” write the authors. They note that the survey also assessed how much participants had learned about the topic from their physicians.
Approximately 35% of patients were made aware of CAT either immediately before or at the time of their cancer diagnosis. Of particular concern, one quarter (26%) of respondents (the largest proportion) noted that they first became aware of CAT when they suffered a blood clot. The average rating was very similar in the different countries surveyed. “Let us not forget that cancer and cancer treatments themselves cause a number of side effects, some of which can be very serious, so in some ways, a clot might be seen as a minor problem. Yet, in reality, it isn’t. It is a significant cause of death and disease in cancer patients,” said Dr. Falanga.
When discussing prevention, most respondents (87%) said they were aware that taking a walk could reduce their risk. Slightly fewer were aware that stopping smoking could reduce their risk (75%), and even fewer were aware that keeping hydrated (63%) and stretching their legs (55%) could reduce their risk.
Symptoms of CAT appeared to be relatively well known; 73% of survey participants indicated that they were aware that swelling in the foot, ankle, or leg could be a sign of DVT, and 71% indicated that shortness of breath could be a sign of pulmonary embolism (PE). “Other symptoms, however, were less well known, with just over half (57%) of participants being aware that pain, cramping, and tenderness could be a sign of DVT. About one third (33%) knew that irregular heartbeat could be a sign of PE. These results varied between countries,” according to the authors.
The survey highlighted that just over a third of respondents said that they were currently using anticoagulants, although almost all (96%) knew that anticoagulants could be used to effectively treat thrombosis. Only 41% of those using anticoagulants said they had been told about any possible side effects.
The Italian situation
The report containing the full results of the European survey goes even further, since, in addition to its overall results, it also gives information about individual countries.
The data from Italy, which are based on 246 persons, show that only 27% of patients and caregivers were aware of the increased risk of thrombosis after a cancer diagnosis. This figure is in line with the overall results of the survey, although the average score of the 10-point scale was lower for the Italy cohort (3.3/10 vs 4.1/10).
The results are more variable in terms of knowledge of risk factors. Most respondents (89%) said that they were aware of the risks related to inactivity. Just over half (52%), however, said that they were aware of the risks related to radiotherapy. Nevertheless, 75% of participants knew about the risks relating to cancer surgery and chemotherapy. “To all intents and purposes, all types of cancer drug can significantly affect the risk of developing a clot. And this is also the case for more modern types of treatment, such as immunotherapy,” said Dr. Falanga.
Most respondents reported that they got information about cancer-associated thrombosis verbally, usually from their hospital doctor (11%). Some respondents (6%) said that they found out about it from their own research, usually online. Almost 1 in 4 patients (24%) in Italy said that they first became aware of CAT when they suffered a blood clot. Answers to questions about knowledge of symptoms show that 58% of Italian patients and caregivers know that swelling of the lower limbs can be a symptom of DVT, and the same percentage knows that shortness of breath might indicate PE.
In terms of preventive action, the picture in Italy is somewhat variable: 74% of participants were aware of the importance of walking, but far fewer knew about the need to stop smoking (57%) and stretch the legs (35%). Of the 41% of Italians who were also taking an anticoagulant drug, 53% said that they knew about the possible side effects of such medication.
Which way forward?
“The high rate of CAT suggests that, despite the clinical evidence and clear guideline recommendations for patients with cancer, CAT prevention and recognition remain low among healthcare professionals,” the authors write.
The results of the ECPC survey further confirm those of previous studies, highlighting patients’ lack of knowledge about CAT and the need for more in-depth discussions between physician and patient.
So, what can be done? As highlighted by previous studies, “patients’ experiences are an education in themselves, particularly for the oncology care team,” the authors write. “Once the patient has a thrombosis, the opportunity for thrombosis prevention, which should be the most crucial focus of the care clinics (surgical, oncology, and palliative care), is gone,” they add.
“Oncology professionals, as well as other members of the patient’s care team (eg, internists, surgeons, nurses), need to perform better, at every stage of the patient’s cancer pathway, to ensure patients are aware of CAT and their individual risk to develop a blood clot,” said Dr. Falanga. She explained that in this group, it is the general practitioner who is the first contact. “These professionals are on the front line of the battle; they are among the first healthcare workers given the chance to suspect a clot and should, therefore, be fully aware of the increased risk in oncology patients,” she reiterated.
Experts agree on the fact that a multidisciplinary approach is of utmost importance in this context: the different roles in the team must be clear. “It is also fundamental to establish who does what in terms of educating and informing the patient,” said Dr. Falanga.
The researchers also put forward an example of a successful initiative: the Venous Thromboembolism Prevention in the Ambulatory Cancer Clinic (VTE-PACC) program. The initiative was developed by experts from the University of Vermont and was described in a recent article in JCO Oncology Practice.
Numerous resources are available online to help physicians talk to their patients and explain the risks linked to CAT along the continuum of cancer care. Among them is a resource titled, “Cancer Associated Thrombosis (CAT): Be Clot Conscious,” which can be found on the ECPC’s website.
“We have a collective responsibility using the ECPC patient survey as a baseline to inform patients with cancer on how to identify signs and symptoms of CAT to enable faster diagnosis and treatment,” the authors conclude.
This article was translated from Univadis Italy.
It is up to their physician to discuss this with them.
This link is explained by the authors of an article in Cancer Treatment and Research Communications that reports results of a survey carried out by the European Cancer Patient Coalition (ECPC). “The aim of this pan-European patient survey was to assess patient awareness and knowledge about cancer-associated thrombosis (CAT), including risk factors, signs and symptoms, and interventions, to better prevent and treat CAT,” write the authors. “The idea was to create a sort of starting point for subsequent communication and information strategies and for comparing the results of any action taken in this area,” they add.
A roundtable discussion that included oncology healthcare professionals, policymakers, and patient advocates was convened to discuss and review the evidence regarding their ongoing concerns of excessive CAT-associated morbidity and mortality, as well as patients’ desire for greater CAT awareness.
“These discussions demonstrated that very little change had occurred over the years and that greater knowledge about CAT was still needed across the spectrum of healthcare practitioners and patients, particularly regarding primary and secondary prevention of thrombosis,” the authors write.
It was from this starting point that the idea for the pan-European survey was born. The ECPC, widely viewed as the “unified voice of cancer patients across Europe,” led the survey. This survey spanned six countries (France, Germany, Greece, Italy, United Kingdom, and Spain) and involved 1,365 patients and caregivers. The ECPC survey result was originally released at World Thrombosis Day in late 2018.
In an interview, Anna Falanga, MD, the main author of the article and professor of hematology at the University of Milan-Bicocca, Italy, reviewed the results and explained how to improve knowledge of CAT among patients with cancer.
“Data support that up to 20% of patients with cancer will experience venous thromboembolism (VTE), which is approximately 4–5 times higher than the general population,” said Dr. Falanga, who is also chief of the department of immunohematology and transfusion medicine and the Thrombosis and Hemostasis Center at the Hospital Papa Giovanni XXIII, in Bergamo, Italy.
“We have known about the link between thrombosis and cancer since the 19th century, but it has taken until midway through the last century for our level of understanding and awareness of the problem to reach its current level. Initially, this was limited to fundamental research, with large advances in our understanding of the mechanisms of the link between the two; it has only been more recently that we have had clinical studies that have piqued the interest of healthcare professionals, who were previously uninterested in the topic,” she said.
Poor understanding
One piece of data stands out from the European survey: Nearly three quarters of respondents (72%) said that before taking part in the survey, they were not aware that people with cancer have a higher-than-normal risk of developing thrombosis. “We asked participants to rate their overall understanding of CAT on a scale of 1 (low) to 10 (high), with the average (mean) score obtained being 4.1. Only 21% of patients gave a rating of 7 or above (high understanding). The average rating was very similar in the different countries surveyed,” write the authors. They note that the survey also assessed how much participants had learned about the topic from their physicians.
Approximately 35% of patients were made aware of CAT either immediately before or at the time of their cancer diagnosis. Of particular concern, one quarter (26%) of respondents (the largest proportion) noted that they first became aware of CAT when they suffered a blood clot. The average rating was very similar in the different countries surveyed. “Let us not forget that cancer and cancer treatments themselves cause a number of side effects, some of which can be very serious, so in some ways, a clot might be seen as a minor problem. Yet, in reality, it isn’t. It is a significant cause of death and disease in cancer patients,” said Dr. Falanga.
When discussing prevention, most respondents (87%) said they were aware that taking a walk could reduce their risk. Slightly fewer were aware that stopping smoking could reduce their risk (75%), and even fewer were aware that keeping hydrated (63%) and stretching their legs (55%) could reduce their risk.
Symptoms of CAT appeared to be relatively well known; 73% of survey participants indicated that they were aware that swelling in the foot, ankle, or leg could be a sign of DVT, and 71% indicated that shortness of breath could be a sign of pulmonary embolism (PE). “Other symptoms, however, were less well known, with just over half (57%) of participants being aware that pain, cramping, and tenderness could be a sign of DVT. About one third (33%) knew that irregular heartbeat could be a sign of PE. These results varied between countries,” according to the authors.
The survey highlighted that just over a third of respondents said that they were currently using anticoagulants, although almost all (96%) knew that anticoagulants could be used to effectively treat thrombosis. Only 41% of those using anticoagulants said they had been told about any possible side effects.
The Italian situation
The report containing the full results of the European survey goes even further, since, in addition to its overall results, it also gives information about individual countries.
The data from Italy, which are based on 246 persons, show that only 27% of patients and caregivers were aware of the increased risk of thrombosis after a cancer diagnosis. This figure is in line with the overall results of the survey, although the average score of the 10-point scale was lower for the Italy cohort (3.3/10 vs 4.1/10).
The results are more variable in terms of knowledge of risk factors. Most respondents (89%) said that they were aware of the risks related to inactivity. Just over half (52%), however, said that they were aware of the risks related to radiotherapy. Nevertheless, 75% of participants knew about the risks relating to cancer surgery and chemotherapy. “To all intents and purposes, all types of cancer drug can significantly affect the risk of developing a clot. And this is also the case for more modern types of treatment, such as immunotherapy,” said Dr. Falanga.
Most respondents reported that they got information about cancer-associated thrombosis verbally, usually from their hospital doctor (11%). Some respondents (6%) said that they found out about it from their own research, usually online. Almost 1 in 4 patients (24%) in Italy said that they first became aware of CAT when they suffered a blood clot. Answers to questions about knowledge of symptoms show that 58% of Italian patients and caregivers know that swelling of the lower limbs can be a symptom of DVT, and the same percentage knows that shortness of breath might indicate PE.
In terms of preventive action, the picture in Italy is somewhat variable: 74% of participants were aware of the importance of walking, but far fewer knew about the need to stop smoking (57%) and stretch the legs (35%). Of the 41% of Italians who were also taking an anticoagulant drug, 53% said that they knew about the possible side effects of such medication.
Which way forward?
“The high rate of CAT suggests that, despite the clinical evidence and clear guideline recommendations for patients with cancer, CAT prevention and recognition remain low among healthcare professionals,” the authors write.
The results of the ECPC survey further confirm those of previous studies, highlighting patients’ lack of knowledge about CAT and the need for more in-depth discussions between physician and patient.
So, what can be done? As highlighted by previous studies, “patients’ experiences are an education in themselves, particularly for the oncology care team,” the authors write. “Once the patient has a thrombosis, the opportunity for thrombosis prevention, which should be the most crucial focus of the care clinics (surgical, oncology, and palliative care), is gone,” they add.
“Oncology professionals, as well as other members of the patient’s care team (eg, internists, surgeons, nurses), need to perform better, at every stage of the patient’s cancer pathway, to ensure patients are aware of CAT and their individual risk to develop a blood clot,” said Dr. Falanga. She explained that in this group, it is the general practitioner who is the first contact. “These professionals are on the front line of the battle; they are among the first healthcare workers given the chance to suspect a clot and should, therefore, be fully aware of the increased risk in oncology patients,” she reiterated.
Experts agree on the fact that a multidisciplinary approach is of utmost importance in this context: the different roles in the team must be clear. “It is also fundamental to establish who does what in terms of educating and informing the patient,” said Dr. Falanga.
The researchers also put forward an example of a successful initiative: the Venous Thromboembolism Prevention in the Ambulatory Cancer Clinic (VTE-PACC) program. The initiative was developed by experts from the University of Vermont and was described in a recent article in JCO Oncology Practice.
Numerous resources are available online to help physicians talk to their patients and explain the risks linked to CAT along the continuum of cancer care. Among them is a resource titled, “Cancer Associated Thrombosis (CAT): Be Clot Conscious,” which can be found on the ECPC’s website.
“We have a collective responsibility using the ECPC patient survey as a baseline to inform patients with cancer on how to identify signs and symptoms of CAT to enable faster diagnosis and treatment,” the authors conclude.
This article was translated from Univadis Italy.
FROM CANCER TREATMENT AND RESEARCH COMMUNICATIONS
Common brain parasite linked to attractiveness, new study
That Toxoplasma gondii looks good on you
Parasite and attractiveness don’t usually go together, but it appears that nobody told Toxoplasma gondii. The world’s most successful parasite affects 30%-50% of the world’s population, and it’s mainly thought to go after the brain in humans, possibly changing behavior and leading to neurological disorders and mental illness.
Now, are you ready to be super confused? According to a recent study, those affected with T. gondii were seen as more attractive and healthy looking, compared with noninfected people. It doesn’t make much sense to us, but it could be an evolutionary thing: The more attractive the parasite makes a person or animal, the more likely it is to spread.
“Some sexually transmitted parasites, such as T. gondii, may produce changes in the appearance and behavior of the human host, either as a by-product of the infection or as the result of the manipulation of the parasite to increase its spread to new hosts,” Javier Borráz-León, PhD, of the University of Turku (Finland), and associates wrote in PeerJ.
Previous research has suggested that men with more testosterone are more likely to become infected because of their behavior with the extra hormones. It’s also been noted that the parasite may manipulate hormones for its own gain, but that’s not proven. Infected women were found to have a lower BMI, more confidence in their appearance, and more partners. Dr. Borráz-León and associates also found that “Toxoplasma-infected subjects had significantly lower facial fluctuating asymmetry than the noninfected people,” ScienceAlert said.
We usually perceive parasites as a bad thing, but honestly this one isn’t sounding too bad. It seems to help with some confidence boosters, and who doesn’t want that? We’re thinking that T. gondii could be the Next Big Thing. All it needs is some marketing and … what if it was covered with nonpareils?
Give it to me straight, Doc. Don’t sugar coat it.
Okay, so he’s not a doctor – not a medical doctor, anyway – but that’s exactly what he did. William H. Grover, PhD, has sugar coated drugs in the name of fraud prevention. We will explain.
The sugar coating comes in the form of nonpareils, the tiny and colorful round sprinkles often found covering small discs of chocolate. Dr. Grover, a bioengineering professor at the University of California, Riverside, who has been working on ways to ensure the authenticity of pharmaceuticals, “started wondering how many different patterns of colored nonpareils were possible on these candies,” he said in a statement from the university.
With just eight colors and an average of 92 individual nonpareils on each candy, the combinations, he found out, are almost endless. Could the same thing be done with a pill? Could the nonpareils be applied as a coating to a pill, giving it a unique pattern that could be stored by the manufacturer and used later as identification?
After much time and effort involving edible cake-decorating glue, Tylenol capsules, smartphones, and computer simulations, he produced CandyCode, an algorithm that converts a photo of a nonpareil-covered pill “into a set of text strings suitable for storing in a computer database and querying by consumers,” the statement explained.
Dr. Grover also mentioned a side benefit: “Anecdotally, I found that CandyCoded caplets were more pleasant to swallow than plain caplets, confirming Mary Poppins’ classic observation about the relationship between sugar and medicine.”
First of all, we can’t believe we just used a Mary Poppins reference. Not exactly what you’d call MDedgey, is it? Second of all, what about the children? We’re talking about drugs that, literally, have been turned into candy. Are the kids going to love them, too? Sounds more like a job for Mr. Yuk.
So you want to be a superhero?
Be honest, who didn’t want to be a superhero when they were a kid? There’s a reason every other movie released in the past decade has been a superhero movie. That’s how we’ve ended up with the millionth Batman reboot and Marvel scraping the bottom of the C-list hero barrel. (Seriously, who’d actually heard of Moon Knight before now?)
Point is, we all like to fantasize, and now a meta-analysis from researchers in Germany and the United States has given us all a reason to strike those dashing superhero poses. Through evaluation of 130 studies and over 10,000 people, the researchers found that power posing (and perfect posture) was strongly associated with increased confidence and self-worth. It was also associated with improved behavior, though the connection was less strong.
Sadly though, the research found no connection with power posing and changes in testosterone or cortisol levels. Standing like a superhero may make you feel good, but it won’t give your body any cool powers or superhuman abilities. But don’t despair, because we’re not finished yet. In fact, it may be the biggest news we’ve ever reported for LOTME: A group of scientists from the University of Kentucky has assembled the full genome of a salamander.
Wait, we have more! Beyond having a genome ten times bigger than a human, this salamander, the axolotl from Mexico, is the model of natural regeneration. Name a body part, and the axolotl can grow it back. It can even regenerate portions of its brain. And now that we have access to the complete genome, it’s possible that one day we could use the axolotl’s regeneration for ourselves. Growing back limbs, regenerating spinal cords, the sky’s the limit. And if Wolverine and Deadpool are anything to go by, it’s all you need to get that superhero career off the ground. Salamander powers may not have the cachet of a radioactive spider, but we’ll take what we can get.
Post your way to financial hardship
After you pump your gas at the gas station, how do you pay? At the pump or inside? How frequently do you post to your social media pages? What kind of content are you posting?
That kind of nontraditional credit data hasn’t been considered by lenders and credit agencies, but that is changing. The reasoning? It’s opening more opportunities for those without much credit history. But according to a paper published by Janine S. Hiller of Virginia Tech and Lindsay Sain Jones, a financial regulation researcher at the University of Georgia, this just opens a can of worms.
Why is this so dangerous? Well, alternative credit scoring isn’t covered by the Fair Credit Reporting Act or Equal Opportunity Act, so the consumer doesn’t have the ability to dispute any data the credit agencies or lenders receive. Then there’s the “credit boost,” which some companies offer to gain access to the consumer’s data. Often there are no limitations on how long it’s kept. That purchase you made 2 years ago can come back to haunt you.
It also creates a cause for the possibility of discrimination based on “lifestyle-related data points,” which some lenders use to determine creditworthiness: zip code, age, gender, race, socioeconomic status. Even where the consumer went to college is a factor taken under consideration.
“There are all kinds of factors that can be correlated with creditworthiness, but that doesn’t mean they should be used,” Ms. Jones said in the EurekAlert statement.
Let’s say someone applies for a loan needed for a medical procedure. They could be denied because the lender or a credit-reporting agency didn’t like the data they received (most times without the consumer’s consent). Talk about a broken system.
That Toxoplasma gondii looks good on you
Parasite and attractiveness don’t usually go together, but it appears that nobody told Toxoplasma gondii. The world’s most successful parasite affects 30%-50% of the world’s population, and it’s mainly thought to go after the brain in humans, possibly changing behavior and leading to neurological disorders and mental illness.
Now, are you ready to be super confused? According to a recent study, those affected with T. gondii were seen as more attractive and healthy looking, compared with noninfected people. It doesn’t make much sense to us, but it could be an evolutionary thing: The more attractive the parasite makes a person or animal, the more likely it is to spread.
“Some sexually transmitted parasites, such as T. gondii, may produce changes in the appearance and behavior of the human host, either as a by-product of the infection or as the result of the manipulation of the parasite to increase its spread to new hosts,” Javier Borráz-León, PhD, of the University of Turku (Finland), and associates wrote in PeerJ.
Previous research has suggested that men with more testosterone are more likely to become infected because of their behavior with the extra hormones. It’s also been noted that the parasite may manipulate hormones for its own gain, but that’s not proven. Infected women were found to have a lower BMI, more confidence in their appearance, and more partners. Dr. Borráz-León and associates also found that “Toxoplasma-infected subjects had significantly lower facial fluctuating asymmetry than the noninfected people,” ScienceAlert said.
We usually perceive parasites as a bad thing, but honestly this one isn’t sounding too bad. It seems to help with some confidence boosters, and who doesn’t want that? We’re thinking that T. gondii could be the Next Big Thing. All it needs is some marketing and … what if it was covered with nonpareils?
Give it to me straight, Doc. Don’t sugar coat it.
Okay, so he’s not a doctor – not a medical doctor, anyway – but that’s exactly what he did. William H. Grover, PhD, has sugar coated drugs in the name of fraud prevention. We will explain.
The sugar coating comes in the form of nonpareils, the tiny and colorful round sprinkles often found covering small discs of chocolate. Dr. Grover, a bioengineering professor at the University of California, Riverside, who has been working on ways to ensure the authenticity of pharmaceuticals, “started wondering how many different patterns of colored nonpareils were possible on these candies,” he said in a statement from the university.
With just eight colors and an average of 92 individual nonpareils on each candy, the combinations, he found out, are almost endless. Could the same thing be done with a pill? Could the nonpareils be applied as a coating to a pill, giving it a unique pattern that could be stored by the manufacturer and used later as identification?
After much time and effort involving edible cake-decorating glue, Tylenol capsules, smartphones, and computer simulations, he produced CandyCode, an algorithm that converts a photo of a nonpareil-covered pill “into a set of text strings suitable for storing in a computer database and querying by consumers,” the statement explained.
Dr. Grover also mentioned a side benefit: “Anecdotally, I found that CandyCoded caplets were more pleasant to swallow than plain caplets, confirming Mary Poppins’ classic observation about the relationship between sugar and medicine.”
First of all, we can’t believe we just used a Mary Poppins reference. Not exactly what you’d call MDedgey, is it? Second of all, what about the children? We’re talking about drugs that, literally, have been turned into candy. Are the kids going to love them, too? Sounds more like a job for Mr. Yuk.
So you want to be a superhero?
Be honest, who didn’t want to be a superhero when they were a kid? There’s a reason every other movie released in the past decade has been a superhero movie. That’s how we’ve ended up with the millionth Batman reboot and Marvel scraping the bottom of the C-list hero barrel. (Seriously, who’d actually heard of Moon Knight before now?)
Point is, we all like to fantasize, and now a meta-analysis from researchers in Germany and the United States has given us all a reason to strike those dashing superhero poses. Through evaluation of 130 studies and over 10,000 people, the researchers found that power posing (and perfect posture) was strongly associated with increased confidence and self-worth. It was also associated with improved behavior, though the connection was less strong.
Sadly though, the research found no connection with power posing and changes in testosterone or cortisol levels. Standing like a superhero may make you feel good, but it won’t give your body any cool powers or superhuman abilities. But don’t despair, because we’re not finished yet. In fact, it may be the biggest news we’ve ever reported for LOTME: A group of scientists from the University of Kentucky has assembled the full genome of a salamander.
Wait, we have more! Beyond having a genome ten times bigger than a human, this salamander, the axolotl from Mexico, is the model of natural regeneration. Name a body part, and the axolotl can grow it back. It can even regenerate portions of its brain. And now that we have access to the complete genome, it’s possible that one day we could use the axolotl’s regeneration for ourselves. Growing back limbs, regenerating spinal cords, the sky’s the limit. And if Wolverine and Deadpool are anything to go by, it’s all you need to get that superhero career off the ground. Salamander powers may not have the cachet of a radioactive spider, but we’ll take what we can get.
Post your way to financial hardship
After you pump your gas at the gas station, how do you pay? At the pump or inside? How frequently do you post to your social media pages? What kind of content are you posting?
That kind of nontraditional credit data hasn’t been considered by lenders and credit agencies, but that is changing. The reasoning? It’s opening more opportunities for those without much credit history. But according to a paper published by Janine S. Hiller of Virginia Tech and Lindsay Sain Jones, a financial regulation researcher at the University of Georgia, this just opens a can of worms.
Why is this so dangerous? Well, alternative credit scoring isn’t covered by the Fair Credit Reporting Act or Equal Opportunity Act, so the consumer doesn’t have the ability to dispute any data the credit agencies or lenders receive. Then there’s the “credit boost,” which some companies offer to gain access to the consumer’s data. Often there are no limitations on how long it’s kept. That purchase you made 2 years ago can come back to haunt you.
It also creates a cause for the possibility of discrimination based on “lifestyle-related data points,” which some lenders use to determine creditworthiness: zip code, age, gender, race, socioeconomic status. Even where the consumer went to college is a factor taken under consideration.
“There are all kinds of factors that can be correlated with creditworthiness, but that doesn’t mean they should be used,” Ms. Jones said in the EurekAlert statement.
Let’s say someone applies for a loan needed for a medical procedure. They could be denied because the lender or a credit-reporting agency didn’t like the data they received (most times without the consumer’s consent). Talk about a broken system.
That Toxoplasma gondii looks good on you
Parasite and attractiveness don’t usually go together, but it appears that nobody told Toxoplasma gondii. The world’s most successful parasite affects 30%-50% of the world’s population, and it’s mainly thought to go after the brain in humans, possibly changing behavior and leading to neurological disorders and mental illness.
Now, are you ready to be super confused? According to a recent study, those affected with T. gondii were seen as more attractive and healthy looking, compared with noninfected people. It doesn’t make much sense to us, but it could be an evolutionary thing: The more attractive the parasite makes a person or animal, the more likely it is to spread.
“Some sexually transmitted parasites, such as T. gondii, may produce changes in the appearance and behavior of the human host, either as a by-product of the infection or as the result of the manipulation of the parasite to increase its spread to new hosts,” Javier Borráz-León, PhD, of the University of Turku (Finland), and associates wrote in PeerJ.
Previous research has suggested that men with more testosterone are more likely to become infected because of their behavior with the extra hormones. It’s also been noted that the parasite may manipulate hormones for its own gain, but that’s not proven. Infected women were found to have a lower BMI, more confidence in their appearance, and more partners. Dr. Borráz-León and associates also found that “Toxoplasma-infected subjects had significantly lower facial fluctuating asymmetry than the noninfected people,” ScienceAlert said.
We usually perceive parasites as a bad thing, but honestly this one isn’t sounding too bad. It seems to help with some confidence boosters, and who doesn’t want that? We’re thinking that T. gondii could be the Next Big Thing. All it needs is some marketing and … what if it was covered with nonpareils?
Give it to me straight, Doc. Don’t sugar coat it.
Okay, so he’s not a doctor – not a medical doctor, anyway – but that’s exactly what he did. William H. Grover, PhD, has sugar coated drugs in the name of fraud prevention. We will explain.
The sugar coating comes in the form of nonpareils, the tiny and colorful round sprinkles often found covering small discs of chocolate. Dr. Grover, a bioengineering professor at the University of California, Riverside, who has been working on ways to ensure the authenticity of pharmaceuticals, “started wondering how many different patterns of colored nonpareils were possible on these candies,” he said in a statement from the university.
With just eight colors and an average of 92 individual nonpareils on each candy, the combinations, he found out, are almost endless. Could the same thing be done with a pill? Could the nonpareils be applied as a coating to a pill, giving it a unique pattern that could be stored by the manufacturer and used later as identification?
After much time and effort involving edible cake-decorating glue, Tylenol capsules, smartphones, and computer simulations, he produced CandyCode, an algorithm that converts a photo of a nonpareil-covered pill “into a set of text strings suitable for storing in a computer database and querying by consumers,” the statement explained.
Dr. Grover also mentioned a side benefit: “Anecdotally, I found that CandyCoded caplets were more pleasant to swallow than plain caplets, confirming Mary Poppins’ classic observation about the relationship between sugar and medicine.”
First of all, we can’t believe we just used a Mary Poppins reference. Not exactly what you’d call MDedgey, is it? Second of all, what about the children? We’re talking about drugs that, literally, have been turned into candy. Are the kids going to love them, too? Sounds more like a job for Mr. Yuk.
So you want to be a superhero?
Be honest, who didn’t want to be a superhero when they were a kid? There’s a reason every other movie released in the past decade has been a superhero movie. That’s how we’ve ended up with the millionth Batman reboot and Marvel scraping the bottom of the C-list hero barrel. (Seriously, who’d actually heard of Moon Knight before now?)
Point is, we all like to fantasize, and now a meta-analysis from researchers in Germany and the United States has given us all a reason to strike those dashing superhero poses. Through evaluation of 130 studies and over 10,000 people, the researchers found that power posing (and perfect posture) was strongly associated with increased confidence and self-worth. It was also associated with improved behavior, though the connection was less strong.
Sadly though, the research found no connection with power posing and changes in testosterone or cortisol levels. Standing like a superhero may make you feel good, but it won’t give your body any cool powers or superhuman abilities. But don’t despair, because we’re not finished yet. In fact, it may be the biggest news we’ve ever reported for LOTME: A group of scientists from the University of Kentucky has assembled the full genome of a salamander.
Wait, we have more! Beyond having a genome ten times bigger than a human, this salamander, the axolotl from Mexico, is the model of natural regeneration. Name a body part, and the axolotl can grow it back. It can even regenerate portions of its brain. And now that we have access to the complete genome, it’s possible that one day we could use the axolotl’s regeneration for ourselves. Growing back limbs, regenerating spinal cords, the sky’s the limit. And if Wolverine and Deadpool are anything to go by, it’s all you need to get that superhero career off the ground. Salamander powers may not have the cachet of a radioactive spider, but we’ll take what we can get.
Post your way to financial hardship
After you pump your gas at the gas station, how do you pay? At the pump or inside? How frequently do you post to your social media pages? What kind of content are you posting?
That kind of nontraditional credit data hasn’t been considered by lenders and credit agencies, but that is changing. The reasoning? It’s opening more opportunities for those without much credit history. But according to a paper published by Janine S. Hiller of Virginia Tech and Lindsay Sain Jones, a financial regulation researcher at the University of Georgia, this just opens a can of worms.
Why is this so dangerous? Well, alternative credit scoring isn’t covered by the Fair Credit Reporting Act or Equal Opportunity Act, so the consumer doesn’t have the ability to dispute any data the credit agencies or lenders receive. Then there’s the “credit boost,” which some companies offer to gain access to the consumer’s data. Often there are no limitations on how long it’s kept. That purchase you made 2 years ago can come back to haunt you.
It also creates a cause for the possibility of discrimination based on “lifestyle-related data points,” which some lenders use to determine creditworthiness: zip code, age, gender, race, socioeconomic status. Even where the consumer went to college is a factor taken under consideration.
“There are all kinds of factors that can be correlated with creditworthiness, but that doesn’t mean they should be used,” Ms. Jones said in the EurekAlert statement.
Let’s say someone applies for a loan needed for a medical procedure. They could be denied because the lender or a credit-reporting agency didn’t like the data they received (most times without the consumer’s consent). Talk about a broken system.
Omicron breakthrough cases boost protection, studies say
two preprint studies show.
The University of Washington, Seattle, working with Vir Biotechnology of San Francisco, looked at blood samples of vaccinated people who had breakthrough cases of Delta or Omicron and compared the samples with three other groups: people who caught COVID and were later vaccinated, vaccinated people who were never infected, and people who were infected and never vaccinated.
The vaccinated people who had a breakthrough case of Omicron produced antibodies that helped protect against coronavirus variants, whereas unvaccinated people who caught Omicron didn’t produce as many antibodies, the study showed.
BioNTech, the German biotechnology company, found that people who’d been double and triple vaccinated and then became infected with Omicron had a better B-cell response than people who’d gotten a booster shot but had not been infected.
The University of Washington research team also came up with similar findings about B cells.
The findings don’t mean people should deliberately try to become infected with COVID, said Alexandra Walls, PhD, one of the University of Washington scientists, according to Business Standard.
But the study does indicate “that we are at the point where we may want to consider having a different vaccine to boost people,” said David Veesler, PhD, of the University of Washington team.
“We should think about breakthrough infections as essentially equivalent to another dose of vaccine,” John Wherry, PhD, a professor and director of the Institute for Immunology at the University of Pennsylvania, Philadelphia, told Business Standard. Dr. Wherry was not involved in the studies but reviewed the BioNTech study.
A version of this article first appeared on WebMD.com.
two preprint studies show.
The University of Washington, Seattle, working with Vir Biotechnology of San Francisco, looked at blood samples of vaccinated people who had breakthrough cases of Delta or Omicron and compared the samples with three other groups: people who caught COVID and were later vaccinated, vaccinated people who were never infected, and people who were infected and never vaccinated.
The vaccinated people who had a breakthrough case of Omicron produced antibodies that helped protect against coronavirus variants, whereas unvaccinated people who caught Omicron didn’t produce as many antibodies, the study showed.
BioNTech, the German biotechnology company, found that people who’d been double and triple vaccinated and then became infected with Omicron had a better B-cell response than people who’d gotten a booster shot but had not been infected.
The University of Washington research team also came up with similar findings about B cells.
The findings don’t mean people should deliberately try to become infected with COVID, said Alexandra Walls, PhD, one of the University of Washington scientists, according to Business Standard.
But the study does indicate “that we are at the point where we may want to consider having a different vaccine to boost people,” said David Veesler, PhD, of the University of Washington team.
“We should think about breakthrough infections as essentially equivalent to another dose of vaccine,” John Wherry, PhD, a professor and director of the Institute for Immunology at the University of Pennsylvania, Philadelphia, told Business Standard. Dr. Wherry was not involved in the studies but reviewed the BioNTech study.
A version of this article first appeared on WebMD.com.
two preprint studies show.
The University of Washington, Seattle, working with Vir Biotechnology of San Francisco, looked at blood samples of vaccinated people who had breakthrough cases of Delta or Omicron and compared the samples with three other groups: people who caught COVID and were later vaccinated, vaccinated people who were never infected, and people who were infected and never vaccinated.
The vaccinated people who had a breakthrough case of Omicron produced antibodies that helped protect against coronavirus variants, whereas unvaccinated people who caught Omicron didn’t produce as many antibodies, the study showed.
BioNTech, the German biotechnology company, found that people who’d been double and triple vaccinated and then became infected with Omicron had a better B-cell response than people who’d gotten a booster shot but had not been infected.
The University of Washington research team also came up with similar findings about B cells.
The findings don’t mean people should deliberately try to become infected with COVID, said Alexandra Walls, PhD, one of the University of Washington scientists, according to Business Standard.
But the study does indicate “that we are at the point where we may want to consider having a different vaccine to boost people,” said David Veesler, PhD, of the University of Washington team.
“We should think about breakthrough infections as essentially equivalent to another dose of vaccine,” John Wherry, PhD, a professor and director of the Institute for Immunology at the University of Pennsylvania, Philadelphia, told Business Standard. Dr. Wherry was not involved in the studies but reviewed the BioNTech study.
A version of this article first appeared on WebMD.com.
Student loan forgiveness plans exclude physicians
In the run up to the midterm elections in November, President Biden has warmed to student loan forgiveness. However, before even being proposed,
What was the plan?
During the 2020 election, student loan forgiveness was a hot topic as the COVID epidemic raged. The CARES Act has placed all federal student loans in forbearance, with no payments made and the interest rate set to 0% to prevent further accrual. While this was tremendously useful to 45 million borrowers around the country (including the author), nothing material was done to deal with the loans.
The Biden Administration’s approach at that time was multi-tiered and chaotic. Plans were put forward that either expanded Public Service Loan Forgiveness (PSLF) or capped it. Plans were put forward that either extended free undergraduate or severely limited it through Pell Grants. Unfortunately, that duality continues today, with current plans not having a clear goal or a target group of beneficiaries.
Necessary CARES Act extensions
The Biden Administration has attempted repeatedly to turn the student loan apparatus back on, restarting payments en masse. However, each time, they are beset by challenges, ranging from repeat COVID spikes to servicer withdrawals or macroeconomic indicators of a recession.
At each step, the administration has had little choice but to extend the CARES Act forbearance, lest they suffer retribution for hastily resuming payments for 45 million borrowers without the apparatus to do so. Two years ago, the major federal servicers laid off hundreds, if not thousands, of staffers responsible for payment processing, accounting, customer care, and taxation. Hiring, training, and staffing these positions is nontrivial.
The administration has been out of step with servicers such that three of the largest have chosen not to renew their contracts: Navient, MyFedLoan, and Granite State Management and Resources. This has left 15 million borrowers in the lurch, not knowing who their servicer is – and, even worse, losing track of qualifying payments toward programs like PSLF.
Avenues of forgiveness
There are two major pathways to forgiveness. It is widely believed that the executive branch has the authority to broadly forgive student loans under executive order and managed through the U.S. Department of Education.
The alternative is through congressional action, voting on forgiveness as an economic stimulus plan. There is little appetite in Congress for forgiveness, and prominent congresspeople like Senator Warren and Senator Schumer have both pushed the executive branch for forgiveness in recognition of this.
What has been proposed?
First, it’s important to state that as headline-grabbing as it is to see that $50,000 of forgiveness has been proposed, the reality is that President Biden has repeatedly stated that he will not be in favor of that level of forgiveness. Instead, the number most commonly being discussed is $10,000. This would represent an unprecedented amount of support, alleviating 35% of borrowers of all student debt.
The impact of proposed forgiveness plans for physicians
For the medical community, sadly, this doesn’t represent a significant amount of forgiveness. At graduation, the average MD has $203,000 in debt, and the average DO has $258,000 in debt. These numbers grow during residency for years before any meaningful payments are made.
Further weakening forgiveness plans for physicians has been two caps proposed by the administration in recent days. The first is an income cap of $125,000. While this would maintain forgiveness for nearly all residents and fellows, this would exclude nearly every practicing physician. The alternative to an income cap is specific exclusion of certain careers seen to be high-earning: doctors and lawyers.
The bottom line
Physicians are unlikely to be included in any forgiveness plans being proposed recently by the Biden Administration. If they are considered, it will be for exclusion from any forgiveness offered.
For physicians no longer eligible for PSLF, this exclusion needs to be considered in managing the student loan debt associated with becoming a doctor.
Dr. Palmer is a part-time instructor, department of pediatrics, Harvard Medical School, Boston, and staff physician, department of medical critical care, Boston Children’s Hospital. He disclosed that he serves as director for Panacea Financial.
A version of this article first appeared on Medscape.com.
In the run up to the midterm elections in November, President Biden has warmed to student loan forgiveness. However, before even being proposed,
What was the plan?
During the 2020 election, student loan forgiveness was a hot topic as the COVID epidemic raged. The CARES Act has placed all federal student loans in forbearance, with no payments made and the interest rate set to 0% to prevent further accrual. While this was tremendously useful to 45 million borrowers around the country (including the author), nothing material was done to deal with the loans.
The Biden Administration’s approach at that time was multi-tiered and chaotic. Plans were put forward that either expanded Public Service Loan Forgiveness (PSLF) or capped it. Plans were put forward that either extended free undergraduate or severely limited it through Pell Grants. Unfortunately, that duality continues today, with current plans not having a clear goal or a target group of beneficiaries.
Necessary CARES Act extensions
The Biden Administration has attempted repeatedly to turn the student loan apparatus back on, restarting payments en masse. However, each time, they are beset by challenges, ranging from repeat COVID spikes to servicer withdrawals or macroeconomic indicators of a recession.
At each step, the administration has had little choice but to extend the CARES Act forbearance, lest they suffer retribution for hastily resuming payments for 45 million borrowers without the apparatus to do so. Two years ago, the major federal servicers laid off hundreds, if not thousands, of staffers responsible for payment processing, accounting, customer care, and taxation. Hiring, training, and staffing these positions is nontrivial.
The administration has been out of step with servicers such that three of the largest have chosen not to renew their contracts: Navient, MyFedLoan, and Granite State Management and Resources. This has left 15 million borrowers in the lurch, not knowing who their servicer is – and, even worse, losing track of qualifying payments toward programs like PSLF.
Avenues of forgiveness
There are two major pathways to forgiveness. It is widely believed that the executive branch has the authority to broadly forgive student loans under executive order and managed through the U.S. Department of Education.
The alternative is through congressional action, voting on forgiveness as an economic stimulus plan. There is little appetite in Congress for forgiveness, and prominent congresspeople like Senator Warren and Senator Schumer have both pushed the executive branch for forgiveness in recognition of this.
What has been proposed?
First, it’s important to state that as headline-grabbing as it is to see that $50,000 of forgiveness has been proposed, the reality is that President Biden has repeatedly stated that he will not be in favor of that level of forgiveness. Instead, the number most commonly being discussed is $10,000. This would represent an unprecedented amount of support, alleviating 35% of borrowers of all student debt.
The impact of proposed forgiveness plans for physicians
For the medical community, sadly, this doesn’t represent a significant amount of forgiveness. At graduation, the average MD has $203,000 in debt, and the average DO has $258,000 in debt. These numbers grow during residency for years before any meaningful payments are made.
Further weakening forgiveness plans for physicians has been two caps proposed by the administration in recent days. The first is an income cap of $125,000. While this would maintain forgiveness for nearly all residents and fellows, this would exclude nearly every practicing physician. The alternative to an income cap is specific exclusion of certain careers seen to be high-earning: doctors and lawyers.
The bottom line
Physicians are unlikely to be included in any forgiveness plans being proposed recently by the Biden Administration. If they are considered, it will be for exclusion from any forgiveness offered.
For physicians no longer eligible for PSLF, this exclusion needs to be considered in managing the student loan debt associated with becoming a doctor.
Dr. Palmer is a part-time instructor, department of pediatrics, Harvard Medical School, Boston, and staff physician, department of medical critical care, Boston Children’s Hospital. He disclosed that he serves as director for Panacea Financial.
A version of this article first appeared on Medscape.com.
In the run up to the midterm elections in November, President Biden has warmed to student loan forgiveness. However, before even being proposed,
What was the plan?
During the 2020 election, student loan forgiveness was a hot topic as the COVID epidemic raged. The CARES Act has placed all federal student loans in forbearance, with no payments made and the interest rate set to 0% to prevent further accrual. While this was tremendously useful to 45 million borrowers around the country (including the author), nothing material was done to deal with the loans.
The Biden Administration’s approach at that time was multi-tiered and chaotic. Plans were put forward that either expanded Public Service Loan Forgiveness (PSLF) or capped it. Plans were put forward that either extended free undergraduate or severely limited it through Pell Grants. Unfortunately, that duality continues today, with current plans not having a clear goal or a target group of beneficiaries.
Necessary CARES Act extensions
The Biden Administration has attempted repeatedly to turn the student loan apparatus back on, restarting payments en masse. However, each time, they are beset by challenges, ranging from repeat COVID spikes to servicer withdrawals or macroeconomic indicators of a recession.
At each step, the administration has had little choice but to extend the CARES Act forbearance, lest they suffer retribution for hastily resuming payments for 45 million borrowers without the apparatus to do so. Two years ago, the major federal servicers laid off hundreds, if not thousands, of staffers responsible for payment processing, accounting, customer care, and taxation. Hiring, training, and staffing these positions is nontrivial.
The administration has been out of step with servicers such that three of the largest have chosen not to renew their contracts: Navient, MyFedLoan, and Granite State Management and Resources. This has left 15 million borrowers in the lurch, not knowing who their servicer is – and, even worse, losing track of qualifying payments toward programs like PSLF.
Avenues of forgiveness
There are two major pathways to forgiveness. It is widely believed that the executive branch has the authority to broadly forgive student loans under executive order and managed through the U.S. Department of Education.
The alternative is through congressional action, voting on forgiveness as an economic stimulus plan. There is little appetite in Congress for forgiveness, and prominent congresspeople like Senator Warren and Senator Schumer have both pushed the executive branch for forgiveness in recognition of this.
What has been proposed?
First, it’s important to state that as headline-grabbing as it is to see that $50,000 of forgiveness has been proposed, the reality is that President Biden has repeatedly stated that he will not be in favor of that level of forgiveness. Instead, the number most commonly being discussed is $10,000. This would represent an unprecedented amount of support, alleviating 35% of borrowers of all student debt.
The impact of proposed forgiveness plans for physicians
For the medical community, sadly, this doesn’t represent a significant amount of forgiveness. At graduation, the average MD has $203,000 in debt, and the average DO has $258,000 in debt. These numbers grow during residency for years before any meaningful payments are made.
Further weakening forgiveness plans for physicians has been two caps proposed by the administration in recent days. The first is an income cap of $125,000. While this would maintain forgiveness for nearly all residents and fellows, this would exclude nearly every practicing physician. The alternative to an income cap is specific exclusion of certain careers seen to be high-earning: doctors and lawyers.
The bottom line
Physicians are unlikely to be included in any forgiveness plans being proposed recently by the Biden Administration. If they are considered, it will be for exclusion from any forgiveness offered.
For physicians no longer eligible for PSLF, this exclusion needs to be considered in managing the student loan debt associated with becoming a doctor.
Dr. Palmer is a part-time instructor, department of pediatrics, Harvard Medical School, Boston, and staff physician, department of medical critical care, Boston Children’s Hospital. He disclosed that he serves as director for Panacea Financial.
A version of this article first appeared on Medscape.com.



