User login
-
Vaccine rollout on track, expect 300 million doses through March: Feds
If the initial success of the Pfizer-BioNTech rollout continues, and emergency use authorization (EAU) is granted to Moderna and Johnson & Johnson vaccines in development, Operation Warp Speed officials expect to have 300 million doses of COVID-19 vaccines to distribute across the United States between now and March 31.
The initial rollout remains on track, said Alex Azar, US Department of Health and Human Services (HHS) secretary, during a media briefing today. “We continue to have good news to report. As of today, shipments of vaccine will have been delivered to every delivery site identified by public health jurisdictions for our first wave of shipments.”
Anomalies in shipments to California and Alabama arose when temperature monitors showed the Pfizer vaccine dropped lower than the recommended -80 ºC (-112 °F). These vaccine trays remained on delivery trucks and were returned to Pfizer for prompt replacement, said Operation Warp Speed Chief Operating Officer Gen. Gustave F. Perna.
Azar estimated another 2 million doses of the Pfizer vaccine will be available next week. “And if the Moderna vaccine is authorized by the FDA in the coming days, we have allocated nearly 5.9 million doses of that product.”
The Moderna vaccine data released this week look promising, said Moncef Slaoui, PhD, Operation Warp Speed chief scientific adviser. “In the short term, I expect the protection to be quite significant.”
The findings in the first 2 weeks after the first dose show up to 65% protection, he said, and predicted the second-dose efficacy data will be coming in the next few weeks.
Enrollment in the phase 3 Johnson & Johnson trial with nearly 44,000 participants is expected to end December 17. Initial efficacy results are anticipated by early January, with more complete efficacy numbers by late January, Slaoui said.
The AstraZeneca COVID-19 vaccine trial also is underway with enrollment continuing. “We expect accruement to end in late December or early next year, with first results expected probably in February,” Slaoui said.
Antibody treatments underutilized
The media briefing also addressed COVID-19 therapeutics. Azar reported low uptake of available antibody therapies. “I want to remind Americans that there are two authorized antibody treatments that Operation Warp Speed has supported. They can help prevent hospitalization in those patients with the highest risk for severe disease.”
The higher-risk group includes those who are 65 and older and people with comorbid conditions that put them at increased risk for COVID-19 hospitalization.
The federal government allocated more than 330,000 doses of these treatments and many states have product available, Azar said.
Slaoui agreed, saying there is a “disappointing level of usage of monoclonal antibody therapy in hospitals. We look forward to that improving.”
Up to 3 billion vaccine doses possible
“We now have more than 900 million doses of the vaccine we have contracted delivery for,” Azar said. The government has options to increase that to a total of 3 billion doses.
In addition to the 100 million Pfizer vaccine doses and 100 million Moderna doses already ordered, the government just took an option for another 100 million Moderna doses for the second quarter of 2021. Operation Warp Speed officials are negotiating with Pfizer for additional product as well.
Azar added that there are 100 million doses of the Johnson & Johnson vaccine in active production and expects AstraZeneca can provide 300 million doses of their product.
With the possibility of three or more vaccine products and with 330 million Americans, minus the 70 million or so children under age 16, “we believe we will actually have surplus supplies,” Azar said. Plans are to take the US surplus vaccine and surplus manufacturing capacity “and use that for the benefit of the world community.”
This article first appeared on Medscape.com.
If the initial success of the Pfizer-BioNTech rollout continues, and emergency use authorization (EAU) is granted to Moderna and Johnson & Johnson vaccines in development, Operation Warp Speed officials expect to have 300 million doses of COVID-19 vaccines to distribute across the United States between now and March 31.
The initial rollout remains on track, said Alex Azar, US Department of Health and Human Services (HHS) secretary, during a media briefing today. “We continue to have good news to report. As of today, shipments of vaccine will have been delivered to every delivery site identified by public health jurisdictions for our first wave of shipments.”
Anomalies in shipments to California and Alabama arose when temperature monitors showed the Pfizer vaccine dropped lower than the recommended -80 ºC (-112 °F). These vaccine trays remained on delivery trucks and were returned to Pfizer for prompt replacement, said Operation Warp Speed Chief Operating Officer Gen. Gustave F. Perna.
Azar estimated another 2 million doses of the Pfizer vaccine will be available next week. “And if the Moderna vaccine is authorized by the FDA in the coming days, we have allocated nearly 5.9 million doses of that product.”
The Moderna vaccine data released this week look promising, said Moncef Slaoui, PhD, Operation Warp Speed chief scientific adviser. “In the short term, I expect the protection to be quite significant.”
The findings in the first 2 weeks after the first dose show up to 65% protection, he said, and predicted the second-dose efficacy data will be coming in the next few weeks.
Enrollment in the phase 3 Johnson & Johnson trial with nearly 44,000 participants is expected to end December 17. Initial efficacy results are anticipated by early January, with more complete efficacy numbers by late January, Slaoui said.
The AstraZeneca COVID-19 vaccine trial also is underway with enrollment continuing. “We expect accruement to end in late December or early next year, with first results expected probably in February,” Slaoui said.
Antibody treatments underutilized
The media briefing also addressed COVID-19 therapeutics. Azar reported low uptake of available antibody therapies. “I want to remind Americans that there are two authorized antibody treatments that Operation Warp Speed has supported. They can help prevent hospitalization in those patients with the highest risk for severe disease.”
The higher-risk group includes those who are 65 and older and people with comorbid conditions that put them at increased risk for COVID-19 hospitalization.
The federal government allocated more than 330,000 doses of these treatments and many states have product available, Azar said.
Slaoui agreed, saying there is a “disappointing level of usage of monoclonal antibody therapy in hospitals. We look forward to that improving.”
Up to 3 billion vaccine doses possible
“We now have more than 900 million doses of the vaccine we have contracted delivery for,” Azar said. The government has options to increase that to a total of 3 billion doses.
In addition to the 100 million Pfizer vaccine doses and 100 million Moderna doses already ordered, the government just took an option for another 100 million Moderna doses for the second quarter of 2021. Operation Warp Speed officials are negotiating with Pfizer for additional product as well.
Azar added that there are 100 million doses of the Johnson & Johnson vaccine in active production and expects AstraZeneca can provide 300 million doses of their product.
With the possibility of three or more vaccine products and with 330 million Americans, minus the 70 million or so children under age 16, “we believe we will actually have surplus supplies,” Azar said. Plans are to take the US surplus vaccine and surplus manufacturing capacity “and use that for the benefit of the world community.”
This article first appeared on Medscape.com.
If the initial success of the Pfizer-BioNTech rollout continues, and emergency use authorization (EAU) is granted to Moderna and Johnson & Johnson vaccines in development, Operation Warp Speed officials expect to have 300 million doses of COVID-19 vaccines to distribute across the United States between now and March 31.
The initial rollout remains on track, said Alex Azar, US Department of Health and Human Services (HHS) secretary, during a media briefing today. “We continue to have good news to report. As of today, shipments of vaccine will have been delivered to every delivery site identified by public health jurisdictions for our first wave of shipments.”
Anomalies in shipments to California and Alabama arose when temperature monitors showed the Pfizer vaccine dropped lower than the recommended -80 ºC (-112 °F). These vaccine trays remained on delivery trucks and were returned to Pfizer for prompt replacement, said Operation Warp Speed Chief Operating Officer Gen. Gustave F. Perna.
Azar estimated another 2 million doses of the Pfizer vaccine will be available next week. “And if the Moderna vaccine is authorized by the FDA in the coming days, we have allocated nearly 5.9 million doses of that product.”
The Moderna vaccine data released this week look promising, said Moncef Slaoui, PhD, Operation Warp Speed chief scientific adviser. “In the short term, I expect the protection to be quite significant.”
The findings in the first 2 weeks after the first dose show up to 65% protection, he said, and predicted the second-dose efficacy data will be coming in the next few weeks.
Enrollment in the phase 3 Johnson & Johnson trial with nearly 44,000 participants is expected to end December 17. Initial efficacy results are anticipated by early January, with more complete efficacy numbers by late January, Slaoui said.
The AstraZeneca COVID-19 vaccine trial also is underway with enrollment continuing. “We expect accruement to end in late December or early next year, with first results expected probably in February,” Slaoui said.
Antibody treatments underutilized
The media briefing also addressed COVID-19 therapeutics. Azar reported low uptake of available antibody therapies. “I want to remind Americans that there are two authorized antibody treatments that Operation Warp Speed has supported. They can help prevent hospitalization in those patients with the highest risk for severe disease.”
The higher-risk group includes those who are 65 and older and people with comorbid conditions that put them at increased risk for COVID-19 hospitalization.
The federal government allocated more than 330,000 doses of these treatments and many states have product available, Azar said.
Slaoui agreed, saying there is a “disappointing level of usage of monoclonal antibody therapy in hospitals. We look forward to that improving.”
Up to 3 billion vaccine doses possible
“We now have more than 900 million doses of the vaccine we have contracted delivery for,” Azar said. The government has options to increase that to a total of 3 billion doses.
In addition to the 100 million Pfizer vaccine doses and 100 million Moderna doses already ordered, the government just took an option for another 100 million Moderna doses for the second quarter of 2021. Operation Warp Speed officials are negotiating with Pfizer for additional product as well.
Azar added that there are 100 million doses of the Johnson & Johnson vaccine in active production and expects AstraZeneca can provide 300 million doses of their product.
With the possibility of three or more vaccine products and with 330 million Americans, minus the 70 million or so children under age 16, “we believe we will actually have surplus supplies,” Azar said. Plans are to take the US surplus vaccine and surplus manufacturing capacity “and use that for the benefit of the world community.”
This article first appeared on Medscape.com.
COVID-19 ranks as a leading cause of death in United States
Adults over age 45 were more likely to die from COVID-19 than car crashes, respiratory diseases, drug overdoses, and suicide. And those over age 55 faced even higher rates of dying because of the coronavirus.
“The current exponential increase in COVID-19 is reaching a calamitous scale in the U.S.,” the authors wrote. “Putting these numbers in perspective may be difficult.”
Population health researchers at Virginia Commonwealth University put COVID-19 deaths into context by comparing this year’s numbers to the leading causes of death for March through October 2018, sorting by age.
By October 2020, COVID-19 had become the third leading cause of death overall for those between the ages of 45 and 84 years, following after heart disease and cancer. For those over age 85, COVID-19 was the second leading cause of death, surpassing cancer and following behind heart disease.
For people aged 35-44 years, COVID-19 surpassed car crashes and respiratory diseases and was slightly lower than suicide, heart disease, and cancer. For those under age 35, drug overdoses, suicide, and car crashes remained the leading causes of death.
Importantly, the authors wrote, death rates for the two leading causes – heart disease and cancer – are about 1,700 and 1,600 per day, respectively. COVID-19 deaths have surpassed these numbers individually throughout December and, on Wednesday, beat them combined. More than 3,400 deaths were reported, according to the COVID Tracking Project, marking an all-time high that continues to increase. Hospitalizations were also at a new high, with more than 113,000 COVID-19 patients in hospitals across the country, and another 232,000 new cases were reported.
“With COVID-19 mortality rates now exceeding these thresholds, this infectious disease has become deadlier than heart disease and cancer,” the authors wrote. “Its lethality may increase further as transmission increases with holiday travel and gatherings and with the intensified indoor exposure that winter brings.”
The reported number of COVID-19 deaths is likely a 20% underestimate, they wrote, attributable to delays in reporting and an increase in non–COVID-19 deaths that were undetected and untreated because of pandemic-related disruptions. Since the coronavirus is communicable and spreads easily, COVID-19 deaths are particularly unique and worrying, they said.
“Individuals who die from homicide or cancer do not transmit the risk of morbidity and mortality to those nearby,” they wrote. “Every COVID-19 death signals the possibility of more deaths among close contacts.”
The fall surge in cases and deaths is widespread nationally, as compared to the spring, with hot spots on both coasts and in rural areas, according to an accompanying editorial in JAMA from public health researchers at the Harvard T.H. Chan School of Public Health, Boston. People of color have faced twice the death rate as well, with one in 875 Black people and one in 925 Indigenous people dying from COVID-19, as compared with one in 1,625 White people.
“The year 2020 ends with COVID-19 massively surging, as it was in the spring, to be the leading cause of death,” they wrote. “The accelerating numbers of deaths fall far short of fully capturing each devastating human story: Every death represents untold loss for countless families.”
Vaccines offer hope, they said, but won’t prevent the upcoming increase in COVID-19 hospitalizations and deaths this winter. In 2021, containing the pandemic will require national coordination, resources to help overwhelmed health care workers, new support for state and local public health officials, a stimulus package for schools and businesses, and financial aid for people on the brink of eviction. The country needs federal coordination of testing, contact tracing, personal protective equipment, travel precautions, and a face mask mandate, they wrote.
“Ending this crisis will require not only further advances in treatment but also unprecedented commitment to all aspects of prevention, vaccination, and public health,” they wrote. “Only by doing so can future years see this illness revert back to the unfamiliar and unknown condition it once was.”
This article first appeared on WebMD.com.
Adults over age 45 were more likely to die from COVID-19 than car crashes, respiratory diseases, drug overdoses, and suicide. And those over age 55 faced even higher rates of dying because of the coronavirus.
“The current exponential increase in COVID-19 is reaching a calamitous scale in the U.S.,” the authors wrote. “Putting these numbers in perspective may be difficult.”
Population health researchers at Virginia Commonwealth University put COVID-19 deaths into context by comparing this year’s numbers to the leading causes of death for March through October 2018, sorting by age.
By October 2020, COVID-19 had become the third leading cause of death overall for those between the ages of 45 and 84 years, following after heart disease and cancer. For those over age 85, COVID-19 was the second leading cause of death, surpassing cancer and following behind heart disease.
For people aged 35-44 years, COVID-19 surpassed car crashes and respiratory diseases and was slightly lower than suicide, heart disease, and cancer. For those under age 35, drug overdoses, suicide, and car crashes remained the leading causes of death.
Importantly, the authors wrote, death rates for the two leading causes – heart disease and cancer – are about 1,700 and 1,600 per day, respectively. COVID-19 deaths have surpassed these numbers individually throughout December and, on Wednesday, beat them combined. More than 3,400 deaths were reported, according to the COVID Tracking Project, marking an all-time high that continues to increase. Hospitalizations were also at a new high, with more than 113,000 COVID-19 patients in hospitals across the country, and another 232,000 new cases were reported.
“With COVID-19 mortality rates now exceeding these thresholds, this infectious disease has become deadlier than heart disease and cancer,” the authors wrote. “Its lethality may increase further as transmission increases with holiday travel and gatherings and with the intensified indoor exposure that winter brings.”
The reported number of COVID-19 deaths is likely a 20% underestimate, they wrote, attributable to delays in reporting and an increase in non–COVID-19 deaths that were undetected and untreated because of pandemic-related disruptions. Since the coronavirus is communicable and spreads easily, COVID-19 deaths are particularly unique and worrying, they said.
“Individuals who die from homicide or cancer do not transmit the risk of morbidity and mortality to those nearby,” they wrote. “Every COVID-19 death signals the possibility of more deaths among close contacts.”
The fall surge in cases and deaths is widespread nationally, as compared to the spring, with hot spots on both coasts and in rural areas, according to an accompanying editorial in JAMA from public health researchers at the Harvard T.H. Chan School of Public Health, Boston. People of color have faced twice the death rate as well, with one in 875 Black people and one in 925 Indigenous people dying from COVID-19, as compared with one in 1,625 White people.
“The year 2020 ends with COVID-19 massively surging, as it was in the spring, to be the leading cause of death,” they wrote. “The accelerating numbers of deaths fall far short of fully capturing each devastating human story: Every death represents untold loss for countless families.”
Vaccines offer hope, they said, but won’t prevent the upcoming increase in COVID-19 hospitalizations and deaths this winter. In 2021, containing the pandemic will require national coordination, resources to help overwhelmed health care workers, new support for state and local public health officials, a stimulus package for schools and businesses, and financial aid for people on the brink of eviction. The country needs federal coordination of testing, contact tracing, personal protective equipment, travel precautions, and a face mask mandate, they wrote.
“Ending this crisis will require not only further advances in treatment but also unprecedented commitment to all aspects of prevention, vaccination, and public health,” they wrote. “Only by doing so can future years see this illness revert back to the unfamiliar and unknown condition it once was.”
This article first appeared on WebMD.com.
Adults over age 45 were more likely to die from COVID-19 than car crashes, respiratory diseases, drug overdoses, and suicide. And those over age 55 faced even higher rates of dying because of the coronavirus.
“The current exponential increase in COVID-19 is reaching a calamitous scale in the U.S.,” the authors wrote. “Putting these numbers in perspective may be difficult.”
Population health researchers at Virginia Commonwealth University put COVID-19 deaths into context by comparing this year’s numbers to the leading causes of death for March through October 2018, sorting by age.
By October 2020, COVID-19 had become the third leading cause of death overall for those between the ages of 45 and 84 years, following after heart disease and cancer. For those over age 85, COVID-19 was the second leading cause of death, surpassing cancer and following behind heart disease.
For people aged 35-44 years, COVID-19 surpassed car crashes and respiratory diseases and was slightly lower than suicide, heart disease, and cancer. For those under age 35, drug overdoses, suicide, and car crashes remained the leading causes of death.
Importantly, the authors wrote, death rates for the two leading causes – heart disease and cancer – are about 1,700 and 1,600 per day, respectively. COVID-19 deaths have surpassed these numbers individually throughout December and, on Wednesday, beat them combined. More than 3,400 deaths were reported, according to the COVID Tracking Project, marking an all-time high that continues to increase. Hospitalizations were also at a new high, with more than 113,000 COVID-19 patients in hospitals across the country, and another 232,000 new cases were reported.
“With COVID-19 mortality rates now exceeding these thresholds, this infectious disease has become deadlier than heart disease and cancer,” the authors wrote. “Its lethality may increase further as transmission increases with holiday travel and gatherings and with the intensified indoor exposure that winter brings.”
The reported number of COVID-19 deaths is likely a 20% underestimate, they wrote, attributable to delays in reporting and an increase in non–COVID-19 deaths that were undetected and untreated because of pandemic-related disruptions. Since the coronavirus is communicable and spreads easily, COVID-19 deaths are particularly unique and worrying, they said.
“Individuals who die from homicide or cancer do not transmit the risk of morbidity and mortality to those nearby,” they wrote. “Every COVID-19 death signals the possibility of more deaths among close contacts.”
The fall surge in cases and deaths is widespread nationally, as compared to the spring, with hot spots on both coasts and in rural areas, according to an accompanying editorial in JAMA from public health researchers at the Harvard T.H. Chan School of Public Health, Boston. People of color have faced twice the death rate as well, with one in 875 Black people and one in 925 Indigenous people dying from COVID-19, as compared with one in 1,625 White people.
“The year 2020 ends with COVID-19 massively surging, as it was in the spring, to be the leading cause of death,” they wrote. “The accelerating numbers of deaths fall far short of fully capturing each devastating human story: Every death represents untold loss for countless families.”
Vaccines offer hope, they said, but won’t prevent the upcoming increase in COVID-19 hospitalizations and deaths this winter. In 2021, containing the pandemic will require national coordination, resources to help overwhelmed health care workers, new support for state and local public health officials, a stimulus package for schools and businesses, and financial aid for people on the brink of eviction. The country needs federal coordination of testing, contact tracing, personal protective equipment, travel precautions, and a face mask mandate, they wrote.
“Ending this crisis will require not only further advances in treatment but also unprecedented commitment to all aspects of prevention, vaccination, and public health,” they wrote. “Only by doing so can future years see this illness revert back to the unfamiliar and unknown condition it once was.”
This article first appeared on WebMD.com.
Prospects dim for Medicare drug reimbursement cuts
A proposal to lower Medicare Part B reimbursements for 50 physician-administered drugs and biologics to what drug manufacturers receive for them in other wealthy nations seems unlikely to take effect as planned on January 1, 2021. The proposal has been strongly opposed by the pharmaceutical industry as well as oncologists and other physicians who use the products most often.
At least four lawsuits have been filed in US district courts to block the move, including from Regeneron, manufacturer of the ophthalmic biologic aflibercept, the first agent on the list; the Community Oncology Alliance; the Biotechnology Innovation Organization, California Life Sciences Association, and Biocom; and Pharmaceutical Research and Manufacturers of America, the Association of Community Cancer Centers, the Global Colon Cancer Association, and National Infusion Center Association.
The proposal could hit oncologists/hematologists particularly hard because they are the primary prescribers of about 30 of the 50 agents on the list, including mainstay breast, lung, and prostate cancer treatments and newer immunotherapies. In its filing for injunctive relieve, the Community Oncology Alliance, a trade group for community oncologists, said the proposal exposes “the health and safety of cancer patients and other patients with potentially life-threatening diseases to real danger.”
Hearings are imminent
Hearings on the proposal, which was published by the Centers for Medicare & Medicaid Services (CMS) on November 27 following an executive order September 13, are scheduled for coming days. The first hearing is scheduled for December 18.
Given the looming implementation date, judges are likely to rule quickly on the motions for injunctive relief, said attorney Rachel Sachs, a health law expert and associate professor at the Washington University School of Law, St. Louis, Missouri. The odds are in plaintiffs’ favor based on procedural and Constitutional grounds. “It’s extremely unlikely to survive” the legal onslaught, she told Medscape Medical News.
Among the many issues raised in court filings, the proposal was released as an interim final rule (IFR), meaning it would take effect outside of the usual process of proposed rule, comment period, revision, then implementation. The law allows for bypassing normal rule-making requirements with an IFR, but they are meant for emergency situations — several have been issued in response to the COVID-19 pandemic — and the government must be able to show that delay would be “impracticable, unnecessary, or contrary to the public interest,” Sachs explained.
In contrast, some form of CMS’s new proposal, dubbed the “Most Favored Nation” (MFN) model for drug reimbursements, has been under consideration by the Trump administration since 2018.
“The way the [Trump] administration rolled this rule out at pretty much the last minute opens them up to greater legal challenges than if they pursued more normal regulatory pathways, which they had the opportunity to do. They are attempting to implement this on a time frame that is unprecedented for as large a change as this is,” said Juliette Cubanski, PhD, deputy director of Medicare policy at the Kaiser Family Foundation, San Francisco, California.
Reimbursement less than acquisition costs
In the proposal, CMS sought to offset the higher prices that pharmaceutical companies charge in the United States when compared with other developed nations — the prices are about double on average.
“One of the largest drivers of increasing Medicare spending is the growing prices for physician-administered separately payable Medicare Part B drugs, which have risen an average of 11.5% annually since 2015, with total spending of approximately $30 billion in 2019,” the agency said in a fact sheet. This is due in large part to “lack of competitive market forces on Medicare Part B drug costs,” it added.
The 50 agents covered by the new proposal are the ones Part B spends the most on, almost $3 billion in 2019 for aflibercept alone, followed closely by pembrolizumab, an immunotherapy used in many different cancer types.
A full list of the drugs and biologicals included in the proposal is on page 50 of the IFR.
CMS estimated that its move would cut reimbursements by approximately 65% once fully implemented in 4 years and save $87.8 billion over the 7 years of the proposed model, as well as reduce cost sharing for beneficiaries.
This model puts the onus on providers to negotiate down drug prices with companies to meet proposed reimbursement limits. However, if companies do not lower their prices, acquisition costs could be substantially lower than reimbursements.
Prescribers and their practices would either have to take the financial hit or stop offering the pharmaceuticals, in which case patients would have to do without, try a different option, or seek care elsewhere, including facilities excluded from the proposal: children’s hospitals, critical access hospitals, cancer hospitals, federally qualified health centers, rural health clinics, and extended neoplastic disease care hospitals.
CMS estimates that in the first year of MFN reimbursements, 9% of beneficiaries would forgo MFN therapies, growing to 19% by year 3, figures that were included in cost savings estimates.
The reimbursement cuts are meant to motivate manufactures to lower prices, but “we have not seen this occur with similar efforts in the past, and drug prices have continued to rise,” said American College of Rheumatology President David Karp, MD, PhD, in a press release. Many of the agents on the list are used by rheumatologists.
Under current policy, Medicare Part B prescribers are reimbursed manufactures’ average sales price plus a 6% add-on. Under the new proposal, reimbursements would be pegged to the lowest price charged among nations of the Organization for Economic Co-operation and Development with a gross domestic product per capita of at least 60% of the US price. In addition to the United States, there are 36 other member countries, including Canada, the United Kingdom, Japan, and Germany.
To remove incentives to prescribe more expensive drugs, the 6% add-on would be replaced with a flat add-on payment per dose, pegged at $148.73 for the first quarter of 2021. There is a hardship exemption for providers if the reimbursement cuts are too drastic, but that involves a lot of paperwork.
This article first appeared on Medscape.com.
A proposal to lower Medicare Part B reimbursements for 50 physician-administered drugs and biologics to what drug manufacturers receive for them in other wealthy nations seems unlikely to take effect as planned on January 1, 2021. The proposal has been strongly opposed by the pharmaceutical industry as well as oncologists and other physicians who use the products most often.
At least four lawsuits have been filed in US district courts to block the move, including from Regeneron, manufacturer of the ophthalmic biologic aflibercept, the first agent on the list; the Community Oncology Alliance; the Biotechnology Innovation Organization, California Life Sciences Association, and Biocom; and Pharmaceutical Research and Manufacturers of America, the Association of Community Cancer Centers, the Global Colon Cancer Association, and National Infusion Center Association.
The proposal could hit oncologists/hematologists particularly hard because they are the primary prescribers of about 30 of the 50 agents on the list, including mainstay breast, lung, and prostate cancer treatments and newer immunotherapies. In its filing for injunctive relieve, the Community Oncology Alliance, a trade group for community oncologists, said the proposal exposes “the health and safety of cancer patients and other patients with potentially life-threatening diseases to real danger.”
Hearings are imminent
Hearings on the proposal, which was published by the Centers for Medicare & Medicaid Services (CMS) on November 27 following an executive order September 13, are scheduled for coming days. The first hearing is scheduled for December 18.
Given the looming implementation date, judges are likely to rule quickly on the motions for injunctive relief, said attorney Rachel Sachs, a health law expert and associate professor at the Washington University School of Law, St. Louis, Missouri. The odds are in plaintiffs’ favor based on procedural and Constitutional grounds. “It’s extremely unlikely to survive” the legal onslaught, she told Medscape Medical News.
Among the many issues raised in court filings, the proposal was released as an interim final rule (IFR), meaning it would take effect outside of the usual process of proposed rule, comment period, revision, then implementation. The law allows for bypassing normal rule-making requirements with an IFR, but they are meant for emergency situations — several have been issued in response to the COVID-19 pandemic — and the government must be able to show that delay would be “impracticable, unnecessary, or contrary to the public interest,” Sachs explained.
In contrast, some form of CMS’s new proposal, dubbed the “Most Favored Nation” (MFN) model for drug reimbursements, has been under consideration by the Trump administration since 2018.
“The way the [Trump] administration rolled this rule out at pretty much the last minute opens them up to greater legal challenges than if they pursued more normal regulatory pathways, which they had the opportunity to do. They are attempting to implement this on a time frame that is unprecedented for as large a change as this is,” said Juliette Cubanski, PhD, deputy director of Medicare policy at the Kaiser Family Foundation, San Francisco, California.
Reimbursement less than acquisition costs
In the proposal, CMS sought to offset the higher prices that pharmaceutical companies charge in the United States when compared with other developed nations — the prices are about double on average.
“One of the largest drivers of increasing Medicare spending is the growing prices for physician-administered separately payable Medicare Part B drugs, which have risen an average of 11.5% annually since 2015, with total spending of approximately $30 billion in 2019,” the agency said in a fact sheet. This is due in large part to “lack of competitive market forces on Medicare Part B drug costs,” it added.
The 50 agents covered by the new proposal are the ones Part B spends the most on, almost $3 billion in 2019 for aflibercept alone, followed closely by pembrolizumab, an immunotherapy used in many different cancer types.
A full list of the drugs and biologicals included in the proposal is on page 50 of the IFR.
CMS estimated that its move would cut reimbursements by approximately 65% once fully implemented in 4 years and save $87.8 billion over the 7 years of the proposed model, as well as reduce cost sharing for beneficiaries.
This model puts the onus on providers to negotiate down drug prices with companies to meet proposed reimbursement limits. However, if companies do not lower their prices, acquisition costs could be substantially lower than reimbursements.
Prescribers and their practices would either have to take the financial hit or stop offering the pharmaceuticals, in which case patients would have to do without, try a different option, or seek care elsewhere, including facilities excluded from the proposal: children’s hospitals, critical access hospitals, cancer hospitals, federally qualified health centers, rural health clinics, and extended neoplastic disease care hospitals.
CMS estimates that in the first year of MFN reimbursements, 9% of beneficiaries would forgo MFN therapies, growing to 19% by year 3, figures that were included in cost savings estimates.
The reimbursement cuts are meant to motivate manufactures to lower prices, but “we have not seen this occur with similar efforts in the past, and drug prices have continued to rise,” said American College of Rheumatology President David Karp, MD, PhD, in a press release. Many of the agents on the list are used by rheumatologists.
Under current policy, Medicare Part B prescribers are reimbursed manufactures’ average sales price plus a 6% add-on. Under the new proposal, reimbursements would be pegged to the lowest price charged among nations of the Organization for Economic Co-operation and Development with a gross domestic product per capita of at least 60% of the US price. In addition to the United States, there are 36 other member countries, including Canada, the United Kingdom, Japan, and Germany.
To remove incentives to prescribe more expensive drugs, the 6% add-on would be replaced with a flat add-on payment per dose, pegged at $148.73 for the first quarter of 2021. There is a hardship exemption for providers if the reimbursement cuts are too drastic, but that involves a lot of paperwork.
This article first appeared on Medscape.com.
A proposal to lower Medicare Part B reimbursements for 50 physician-administered drugs and biologics to what drug manufacturers receive for them in other wealthy nations seems unlikely to take effect as planned on January 1, 2021. The proposal has been strongly opposed by the pharmaceutical industry as well as oncologists and other physicians who use the products most often.
At least four lawsuits have been filed in US district courts to block the move, including from Regeneron, manufacturer of the ophthalmic biologic aflibercept, the first agent on the list; the Community Oncology Alliance; the Biotechnology Innovation Organization, California Life Sciences Association, and Biocom; and Pharmaceutical Research and Manufacturers of America, the Association of Community Cancer Centers, the Global Colon Cancer Association, and National Infusion Center Association.
The proposal could hit oncologists/hematologists particularly hard because they are the primary prescribers of about 30 of the 50 agents on the list, including mainstay breast, lung, and prostate cancer treatments and newer immunotherapies. In its filing for injunctive relieve, the Community Oncology Alliance, a trade group for community oncologists, said the proposal exposes “the health and safety of cancer patients and other patients with potentially life-threatening diseases to real danger.”
Hearings are imminent
Hearings on the proposal, which was published by the Centers for Medicare & Medicaid Services (CMS) on November 27 following an executive order September 13, are scheduled for coming days. The first hearing is scheduled for December 18.
Given the looming implementation date, judges are likely to rule quickly on the motions for injunctive relief, said attorney Rachel Sachs, a health law expert and associate professor at the Washington University School of Law, St. Louis, Missouri. The odds are in plaintiffs’ favor based on procedural and Constitutional grounds. “It’s extremely unlikely to survive” the legal onslaught, she told Medscape Medical News.
Among the many issues raised in court filings, the proposal was released as an interim final rule (IFR), meaning it would take effect outside of the usual process of proposed rule, comment period, revision, then implementation. The law allows for bypassing normal rule-making requirements with an IFR, but they are meant for emergency situations — several have been issued in response to the COVID-19 pandemic — and the government must be able to show that delay would be “impracticable, unnecessary, or contrary to the public interest,” Sachs explained.
In contrast, some form of CMS’s new proposal, dubbed the “Most Favored Nation” (MFN) model for drug reimbursements, has been under consideration by the Trump administration since 2018.
“The way the [Trump] administration rolled this rule out at pretty much the last minute opens them up to greater legal challenges than if they pursued more normal regulatory pathways, which they had the opportunity to do. They are attempting to implement this on a time frame that is unprecedented for as large a change as this is,” said Juliette Cubanski, PhD, deputy director of Medicare policy at the Kaiser Family Foundation, San Francisco, California.
Reimbursement less than acquisition costs
In the proposal, CMS sought to offset the higher prices that pharmaceutical companies charge in the United States when compared with other developed nations — the prices are about double on average.
“One of the largest drivers of increasing Medicare spending is the growing prices for physician-administered separately payable Medicare Part B drugs, which have risen an average of 11.5% annually since 2015, with total spending of approximately $30 billion in 2019,” the agency said in a fact sheet. This is due in large part to “lack of competitive market forces on Medicare Part B drug costs,” it added.
The 50 agents covered by the new proposal are the ones Part B spends the most on, almost $3 billion in 2019 for aflibercept alone, followed closely by pembrolizumab, an immunotherapy used in many different cancer types.
A full list of the drugs and biologicals included in the proposal is on page 50 of the IFR.
CMS estimated that its move would cut reimbursements by approximately 65% once fully implemented in 4 years and save $87.8 billion over the 7 years of the proposed model, as well as reduce cost sharing for beneficiaries.
This model puts the onus on providers to negotiate down drug prices with companies to meet proposed reimbursement limits. However, if companies do not lower their prices, acquisition costs could be substantially lower than reimbursements.
Prescribers and their practices would either have to take the financial hit or stop offering the pharmaceuticals, in which case patients would have to do without, try a different option, or seek care elsewhere, including facilities excluded from the proposal: children’s hospitals, critical access hospitals, cancer hospitals, federally qualified health centers, rural health clinics, and extended neoplastic disease care hospitals.
CMS estimates that in the first year of MFN reimbursements, 9% of beneficiaries would forgo MFN therapies, growing to 19% by year 3, figures that were included in cost savings estimates.
The reimbursement cuts are meant to motivate manufactures to lower prices, but “we have not seen this occur with similar efforts in the past, and drug prices have continued to rise,” said American College of Rheumatology President David Karp, MD, PhD, in a press release. Many of the agents on the list are used by rheumatologists.
Under current policy, Medicare Part B prescribers are reimbursed manufactures’ average sales price plus a 6% add-on. Under the new proposal, reimbursements would be pegged to the lowest price charged among nations of the Organization for Economic Co-operation and Development with a gross domestic product per capita of at least 60% of the US price. In addition to the United States, there are 36 other member countries, including Canada, the United Kingdom, Japan, and Germany.
To remove incentives to prescribe more expensive drugs, the 6% add-on would be replaced with a flat add-on payment per dose, pegged at $148.73 for the first quarter of 2021. There is a hardship exemption for providers if the reimbursement cuts are too drastic, but that involves a lot of paperwork.
This article first appeared on Medscape.com.
COVID-19 vaccines: Safe for immunocompromised patients?
Coronavirus vaccines have become a reality, as they are now being approved and authorized for use in a growing number of countries including the United States. The U.S. Food and Drug Administration has just issued emergency authorization for the use of the COVID-19 vaccine produced by Pfizer and BioNTech. Close behind is the vaccine developed by Moderna, which has also applied to the FDA for emergency authorization.
The efficacy of a two-dose administration of the vaccine has been pegged at 95.0%, and the FDA has said that the 95% credible interval for the vaccine efficacy was 90.3%-97.6%. But as with many initial clinical trials, whether for drugs or vaccines, not all populations were represented in the trial cohort, including individuals who are immunocompromised. At the current time, it is largely unknown how safe or effective the vaccine may be in this large population, many of whom are at high risk for serious COVID-19 complications.
At a special session held during the recent annual meeting of the American Society of Hematology, Anthony Fauci, MD, the nation’s leading infectious disease expert, said that individuals with compromised immune systems, whether because of chemotherapy or a bone marrow transplant, should plan to be vaccinated when the opportunity arises.
In response to a question from ASH President Stephanie J. Lee, MD, of the Fred Hutchinson Cancer Center, Seattle, Dr. Fauci emphasized that, despite being excluded from clinical trials, this population should get vaccinated. “I think we should recommend that they get vaccinated,” he said. “I mean, it is clear that, if you are on immunosuppressive agents, history tells us that you’re not going to have as robust a response as if you had an intact immune system that was not being compromised. But some degree of immunity is better than no degree of immunity.”
That does seem to be the consensus among experts who spoke in interviews: that as long as these are not live attenuated vaccines, they hold no specific risk to an immunocompromised patient, other than any factors specific to the individual that could be a contraindication.
“Patients, family members, friends, and work contacts should be encouraged to receive the vaccine,” said William Stohl, MD, PhD, chief of the division of rheumatology at the University of Southern California, Los Angeles. “Clinicians should advise patients to obtain the vaccine sooner rather than later.”
Kevin C. Wang, MD, PhD, of the department of dermatology at Stanford (Calif.) University, agreed. “I am 100% with Dr. Fauci. Everyone should get the vaccine, even if it may not be as effective,” he said. “I would treat it exactly like the flu vaccines that we recommend folks get every year.”
Dr. Wang noted that he couldn’t think of any contraindications unless the immunosuppressed patients have a history of severe allergic reactions to prior vaccinations. “But I would even say patients with history of cancer, upon recommendation of their oncologists, are likely to be suitable candidates for the vaccine,” he added. “I would say clinicians should approach counseling the same way they counsel patients for the flu vaccine, and as far as I know, there are no concerns for systemic drugs commonly used in dermatology patients.”
However, guidance has not yet been issued from either the FDA or the Centers for Disease Control and Prevention regarding the use of the vaccine in immunocompromised individuals. Given the lack of data, the FDA has said that “it will be something that providers will need to consider on an individual basis,” and that individuals should consult with physicians to weigh the potential benefits and potential risks.
The CDC’s Advisory Committee on Immunization Practices has said that clinicians need more guidance on whether to use the vaccine in pregnant or breastfeeding women, the immunocompromised, or those who have a history of allergies. The CDC itself has not yet released its formal guidance on vaccine use.
COVID-19 vaccines
Vaccines typically require years of research and testing before reaching the clinic, but this year researchers embarked on a global effort to develop safe and effective coronavirus vaccines in record time. Both the Pfizer/BioNTech and Moderna vaccines have only a few months of phase 3 clinical trial data, so much remains unknown about them, including their duration of effect and any long-term safety signals. In addition to excluding immunocompromised individuals, the clinical trials did not include children or pregnant women, so data are lacking for several population subgroups.
But these will not be the only vaccines available, as the pipeline is already becoming crowded. U.S. clinical trial data from a vaccine jointly being developed by Oxford-AstraZeneca, could potentially be ready, along with a request for FDA emergency use authorization, by late January 2021.
In addition, China and Russia have released vaccines, and there are currently 61 vaccines being investigated in clinical trials and at least 85 preclinical products under active investigation.
The vaccine candidates are using both conventional and novel mechanisms of action to elicit an immune response in patients. Conventional methods include attenuated inactivated (killed) virus and recombinant viral protein vaccines to develop immunity. Novel approaches include replication-deficient, adenovirus vector-based vaccines that contain the viral protein, and mRNA-based vaccines, such as the Pfizer and Moderna vaccines, that encode for a SARS-CoV-2 spike protein.
“The special vaccine concern for immunocompromised individuals is introduction of a live virus,” Dr. Stohl said. “Neither the Moderna nor Pfizer vaccines are live viruses, so there should be no special contraindication for such individuals.”
Live vaccine should be avoided in immunocompromised patients, and currently, live SARS-CoV-2 vaccines are only being developed in India and Turkey.
It is not unusual for vaccine trials to begin with cohorts that exclude participants with various health conditions, including those who are immunocompromised. These groups are generally then evaluated in phase 4 trials, or postmarketing surveillance. While the precise number of immunosuppressed adults in the United States is not known, the numbers are believed to be rising because of increased life expectancy among immunosuppressed adults as a result of advances in treatment and new and wider indications for therapies that can affect the immune system.
According to data from the 2013 National Health Interview Survey, an estimated 2.7% of U.S. adults are immunosuppressed. This population covers a broad array of health conditions and medical specialties; people living with inflammatory or autoimmune conditions, such as inflammatory rheumatic diseases (rheumatoid arthritis, axial spondyloarthritis, lupus); inflammatory bowel disease (Crohn’s disease and ulcerative colitis); psoriasis; multiple sclerosis; organ transplant recipients; patients undergoing chemotherapy; and life-long immunosuppression attributable to HIV infection.
As the vaccines begin to roll out and become available, how should clinicians advise their patients, in the absence of any clinical trial data?
Risk vs. benefit
Gilaad Kaplan, MD, MPH, a gastroenterologist and professor of medicine at the University of Calgary (Alta.), noted that the inflammatory bowel disease (IBD) community has dealt with tremendous anxiety during the pandemic because many are immunocompromised because of the medications they use to treat their disease.
“For example, many patients with IBD are on biologics like anti-TNF [tumor necrosis factor] therapies, which are also used in other immune-mediated inflammatory diseases such as rheumatoid arthritis,” he said. “Understandably, individuals with IBD on immunosuppressive medications are concerned about the risk of severe complications due to COVID-19.”
The entire IBD community, along with the world, celebrated the announcement that multiple vaccines are protective against SARS-CoV-2, he noted. “Vaccines offer the potential to reduce the spread of COVID-19, allowing society to revert back to normalcy,” Dr. Kaplan said. “Moreover, for vulnerable populations, including those who are immunocompromised, vaccines offer the potential to directly protect them from the morbidity and mortality associated with COVID-19.”
That said, even though the news of vaccines are extremely promising, some cautions must be raised regarding their use in immunocompromised populations, such as persons with IBD. “The current trials, to my knowledge, did not include immunocompromised individuals and thus, we can only extrapolate from what we know from other trials of different vaccines,” he explained. “We know from prior vaccines studies that the immune response following vaccination is less robust in those who are immunocompromised as compared to a healthy control population.”
Dr. Kaplan also pointed to recent reports of allergic reactions that have been reported in healthy individuals. “We don’t know whether side effects, like allergic reactions, may be different in unstudied populations,” he said. “Thus, the medical and scientific community should prioritize clinical studies of safety and effectiveness of COVID-19 vaccines in immunocompromised populations.”
So, what does this mean for an individual with an immune-mediated inflammatory disease like Crohn’s disease or ulcerative colitis who is immunocompromised? Dr. Kaplan explained that it is a balance between the potential harm of being infected with COVID-19 and the uncertainty of receiving a vaccine in an understudied population. For those who are highly susceptible to dying from COVID-19, such as an older adult with IBD, or someone who faces high exposure, such as a health care worker, the potential protection of the vaccine greatly outweighs the uncertainty.
“However, for individuals who are at otherwise lower risk – for example, young and able to work from home – then waiting a few extra months for postmarketing surveillance studies in immunocompromised populations may be a reasonable approach, as long as these individuals are taking great care to avoid infection,” he said.
No waiting needed
Joel M. Gelfand, MD, MSCE, professor of dermatology and epidemiology at the University of Pennsylvania, Philadelphia, feels that the newly approved vaccine should be safe for most of his patients.
“Patients with psoriatic disease should get the mRNA-based COVID-19 vaccine as soon as possible based on eligibility as determined by the CDC and local public health officials,” he said. “It is not a live vaccine, and therefore patients on biologics or other immune-modulating or immune-suppressing treatment can receive it.”
However, the impact of psoriasis treatment on immune response to the mRNA-based vaccines is not known. Dr. Gelfand noted that, extrapolating from the vaccine literature, there is some evidence that methotrexate reduces response to the influenza vaccine. “However, the clinical significance of this finding is not clear,” he said. “Since the mRNA vaccine needs to be taken twice, a few weeks apart, I do not recommend interrupting or delaying treatment for psoriatic disease while undergoing vaccination for COVID-19.”
Given the reports of allergic reactions, he added that it is advisable for patients with a history of life-threatening allergic reactions such as anaphylaxis or who have been advised to carry an epinephrine autoinjector, to talk with their health care provider to determine if COVID-19 vaccination is medically appropriate.
The National Psoriasis Foundation has issued guidance on COVID-19, explained Steven R. Feldman, MD, PhD, professor of dermatology, pathology, and social sciences & health policy at Wake Forest University, Winston-Salem, N.C., who is also a member of the committee that is working on those guidelines and keeping them up to date. “We are in the process of updating the guidelines with information on COVID vaccines,” he said.
He agreed that there are no contraindications for psoriasis patients to receive the vaccine, regardless of whether they are on immunosuppressive treatment, even though definitive data are lacking. “Fortunately, there’s a lot of good data coming out of Italy that patients with psoriasis on biologics do not appear to be at increased risk of getting COVID or of having worse outcomes from COVID,” he said.
Patients are going to ask about the vaccines, and when counseling them, clinicians should discuss the available data, the residual uncertainty, and patients’ concerns should be considered, Dr. Feldman explained. “There may be some concern that steroids and cyclosporine would reduce the effectiveness of vaccines, but there is no concern that any of the drugs would cause increased risk from nonlive vaccines.”
He added that there is evidence that “patients on biologics who receive nonlive vaccines do develop antibody responses and are immunized.”
Boosting efficacy
Even prior to making their announcement, the American College of Rheumatology had said that they would endorse the vaccine for all patients, explained rheumatologist Brett Smith, DO, from Blount Memorial Physicians Group and East Tennessee Children’s Hospital, Alcoa. “The vaccine is safe for all patients, but the problem may be that it’s not as effective,” he said. “But we don’t know that because it hasn’t been tested.”
With other vaccines, biologic medicines are held for 2 weeks before and afterwards, to get the best response. “But some patients don’t want to stop the medication,” Dr. Smith said. “They are afraid that their symptoms will return.”
As for counseling patients as to whether they should receive this vaccine, he explained that he typically doesn’t try to sway patients one way or another until they are really high risk. “When I counsel, it really depends on the individual situation. And for this vaccine, we have to be open to the fact that many people have already made up their mind.”
There are a lot of questions regarding the vaccine. One is the short time frame of development. “Vaccines typically take 6-10 years to come on the market, and this one is now available after a 3-month study,” Dr. Smith said. “Some have already decided that it’s too new for them.”
The process is also new, and patients need to understand that it doesn’t contain an active virus and “you can’t catch coronavirus from it.”
Dr. Smith also explained that, because the vaccine may be less effective in a person using biologic therapies, there is currently no information available on repeat vaccination. “These are all unanswered questions,” he said. “If the antibodies wane in a short time, can we be revaccinated and in what time frame? We just don’t know that yet.”
Marcelo Bonomi, MD, a medical oncologist from The Ohio State University Comprehensive Cancer Center, Columbus, explained that one way to ensure a more optimal response to the vaccine would be to wait until the patient has finished chemotherapy.* “The vaccine can be offered at that time, and in the meantime, they can take other steps to avoid infection,” he said. “If they are very immunosuppressed, it isn’t worth trying to give the vaccine.”
Cancer patients should be encouraged to stay as healthy as possible, and to wear masks and social distance. “It’s a comprehensive approach. Eat healthy, avoid alcohol and tobacco, and exercise. [These things] will help boost the immune system,” Dr. Bonomi said. “Family members should be encouraged to get vaccinated, which will help them avoid infection and exposing the patient.”
Jim Boonyaratanakornkit, MD, PhD, an infectious disease specialist who cares for cancer patients at the Fred Hutchinson Cancer Research Center, agreed. “Giving a vaccine right after a transplant is a futile endeavor,” he said. “We need to wait 6 months to have an immune response.”
He pointed out there may be a continuing higher number of cases, with high levels peaking in Washington in February and March. “Close friends and family should be vaccinated if possible,” he said, “which will help interrupt transmission.”
The vaccines are using new platforms that are totally different, and there is no clear data as to how long the antibodies will persist. “We know that they last for at least 4 months,” said Dr. Boonyaratanakornkit. “We don’t know what level of antibody will protect them from COVID-19 infection. Current studies are being conducted, but we don’t have that information for anyone yet.”
*Correction, 1/7/21: An earlier version of this article misattributed quotes from Dr. Marcelo Bonomi.
Coronavirus vaccines have become a reality, as they are now being approved and authorized for use in a growing number of countries including the United States. The U.S. Food and Drug Administration has just issued emergency authorization for the use of the COVID-19 vaccine produced by Pfizer and BioNTech. Close behind is the vaccine developed by Moderna, which has also applied to the FDA for emergency authorization.
The efficacy of a two-dose administration of the vaccine has been pegged at 95.0%, and the FDA has said that the 95% credible interval for the vaccine efficacy was 90.3%-97.6%. But as with many initial clinical trials, whether for drugs or vaccines, not all populations were represented in the trial cohort, including individuals who are immunocompromised. At the current time, it is largely unknown how safe or effective the vaccine may be in this large population, many of whom are at high risk for serious COVID-19 complications.
At a special session held during the recent annual meeting of the American Society of Hematology, Anthony Fauci, MD, the nation’s leading infectious disease expert, said that individuals with compromised immune systems, whether because of chemotherapy or a bone marrow transplant, should plan to be vaccinated when the opportunity arises.
In response to a question from ASH President Stephanie J. Lee, MD, of the Fred Hutchinson Cancer Center, Seattle, Dr. Fauci emphasized that, despite being excluded from clinical trials, this population should get vaccinated. “I think we should recommend that they get vaccinated,” he said. “I mean, it is clear that, if you are on immunosuppressive agents, history tells us that you’re not going to have as robust a response as if you had an intact immune system that was not being compromised. But some degree of immunity is better than no degree of immunity.”
That does seem to be the consensus among experts who spoke in interviews: that as long as these are not live attenuated vaccines, they hold no specific risk to an immunocompromised patient, other than any factors specific to the individual that could be a contraindication.
“Patients, family members, friends, and work contacts should be encouraged to receive the vaccine,” said William Stohl, MD, PhD, chief of the division of rheumatology at the University of Southern California, Los Angeles. “Clinicians should advise patients to obtain the vaccine sooner rather than later.”
Kevin C. Wang, MD, PhD, of the department of dermatology at Stanford (Calif.) University, agreed. “I am 100% with Dr. Fauci. Everyone should get the vaccine, even if it may not be as effective,” he said. “I would treat it exactly like the flu vaccines that we recommend folks get every year.”
Dr. Wang noted that he couldn’t think of any contraindications unless the immunosuppressed patients have a history of severe allergic reactions to prior vaccinations. “But I would even say patients with history of cancer, upon recommendation of their oncologists, are likely to be suitable candidates for the vaccine,” he added. “I would say clinicians should approach counseling the same way they counsel patients for the flu vaccine, and as far as I know, there are no concerns for systemic drugs commonly used in dermatology patients.”
However, guidance has not yet been issued from either the FDA or the Centers for Disease Control and Prevention regarding the use of the vaccine in immunocompromised individuals. Given the lack of data, the FDA has said that “it will be something that providers will need to consider on an individual basis,” and that individuals should consult with physicians to weigh the potential benefits and potential risks.
The CDC’s Advisory Committee on Immunization Practices has said that clinicians need more guidance on whether to use the vaccine in pregnant or breastfeeding women, the immunocompromised, or those who have a history of allergies. The CDC itself has not yet released its formal guidance on vaccine use.
COVID-19 vaccines
Vaccines typically require years of research and testing before reaching the clinic, but this year researchers embarked on a global effort to develop safe and effective coronavirus vaccines in record time. Both the Pfizer/BioNTech and Moderna vaccines have only a few months of phase 3 clinical trial data, so much remains unknown about them, including their duration of effect and any long-term safety signals. In addition to excluding immunocompromised individuals, the clinical trials did not include children or pregnant women, so data are lacking for several population subgroups.
But these will not be the only vaccines available, as the pipeline is already becoming crowded. U.S. clinical trial data from a vaccine jointly being developed by Oxford-AstraZeneca, could potentially be ready, along with a request for FDA emergency use authorization, by late January 2021.
In addition, China and Russia have released vaccines, and there are currently 61 vaccines being investigated in clinical trials and at least 85 preclinical products under active investigation.
The vaccine candidates are using both conventional and novel mechanisms of action to elicit an immune response in patients. Conventional methods include attenuated inactivated (killed) virus and recombinant viral protein vaccines to develop immunity. Novel approaches include replication-deficient, adenovirus vector-based vaccines that contain the viral protein, and mRNA-based vaccines, such as the Pfizer and Moderna vaccines, that encode for a SARS-CoV-2 spike protein.
“The special vaccine concern for immunocompromised individuals is introduction of a live virus,” Dr. Stohl said. “Neither the Moderna nor Pfizer vaccines are live viruses, so there should be no special contraindication for such individuals.”
Live vaccine should be avoided in immunocompromised patients, and currently, live SARS-CoV-2 vaccines are only being developed in India and Turkey.
It is not unusual for vaccine trials to begin with cohorts that exclude participants with various health conditions, including those who are immunocompromised. These groups are generally then evaluated in phase 4 trials, or postmarketing surveillance. While the precise number of immunosuppressed adults in the United States is not known, the numbers are believed to be rising because of increased life expectancy among immunosuppressed adults as a result of advances in treatment and new and wider indications for therapies that can affect the immune system.
According to data from the 2013 National Health Interview Survey, an estimated 2.7% of U.S. adults are immunosuppressed. This population covers a broad array of health conditions and medical specialties; people living with inflammatory or autoimmune conditions, such as inflammatory rheumatic diseases (rheumatoid arthritis, axial spondyloarthritis, lupus); inflammatory bowel disease (Crohn’s disease and ulcerative colitis); psoriasis; multiple sclerosis; organ transplant recipients; patients undergoing chemotherapy; and life-long immunosuppression attributable to HIV infection.
As the vaccines begin to roll out and become available, how should clinicians advise their patients, in the absence of any clinical trial data?
Risk vs. benefit
Gilaad Kaplan, MD, MPH, a gastroenterologist and professor of medicine at the University of Calgary (Alta.), noted that the inflammatory bowel disease (IBD) community has dealt with tremendous anxiety during the pandemic because many are immunocompromised because of the medications they use to treat their disease.
“For example, many patients with IBD are on biologics like anti-TNF [tumor necrosis factor] therapies, which are also used in other immune-mediated inflammatory diseases such as rheumatoid arthritis,” he said. “Understandably, individuals with IBD on immunosuppressive medications are concerned about the risk of severe complications due to COVID-19.”
The entire IBD community, along with the world, celebrated the announcement that multiple vaccines are protective against SARS-CoV-2, he noted. “Vaccines offer the potential to reduce the spread of COVID-19, allowing society to revert back to normalcy,” Dr. Kaplan said. “Moreover, for vulnerable populations, including those who are immunocompromised, vaccines offer the potential to directly protect them from the morbidity and mortality associated with COVID-19.”
That said, even though the news of vaccines are extremely promising, some cautions must be raised regarding their use in immunocompromised populations, such as persons with IBD. “The current trials, to my knowledge, did not include immunocompromised individuals and thus, we can only extrapolate from what we know from other trials of different vaccines,” he explained. “We know from prior vaccines studies that the immune response following vaccination is less robust in those who are immunocompromised as compared to a healthy control population.”
Dr. Kaplan also pointed to recent reports of allergic reactions that have been reported in healthy individuals. “We don’t know whether side effects, like allergic reactions, may be different in unstudied populations,” he said. “Thus, the medical and scientific community should prioritize clinical studies of safety and effectiveness of COVID-19 vaccines in immunocompromised populations.”
So, what does this mean for an individual with an immune-mediated inflammatory disease like Crohn’s disease or ulcerative colitis who is immunocompromised? Dr. Kaplan explained that it is a balance between the potential harm of being infected with COVID-19 and the uncertainty of receiving a vaccine in an understudied population. For those who are highly susceptible to dying from COVID-19, such as an older adult with IBD, or someone who faces high exposure, such as a health care worker, the potential protection of the vaccine greatly outweighs the uncertainty.
“However, for individuals who are at otherwise lower risk – for example, young and able to work from home – then waiting a few extra months for postmarketing surveillance studies in immunocompromised populations may be a reasonable approach, as long as these individuals are taking great care to avoid infection,” he said.
No waiting needed
Joel M. Gelfand, MD, MSCE, professor of dermatology and epidemiology at the University of Pennsylvania, Philadelphia, feels that the newly approved vaccine should be safe for most of his patients.
“Patients with psoriatic disease should get the mRNA-based COVID-19 vaccine as soon as possible based on eligibility as determined by the CDC and local public health officials,” he said. “It is not a live vaccine, and therefore patients on biologics or other immune-modulating or immune-suppressing treatment can receive it.”
However, the impact of psoriasis treatment on immune response to the mRNA-based vaccines is not known. Dr. Gelfand noted that, extrapolating from the vaccine literature, there is some evidence that methotrexate reduces response to the influenza vaccine. “However, the clinical significance of this finding is not clear,” he said. “Since the mRNA vaccine needs to be taken twice, a few weeks apart, I do not recommend interrupting or delaying treatment for psoriatic disease while undergoing vaccination for COVID-19.”
Given the reports of allergic reactions, he added that it is advisable for patients with a history of life-threatening allergic reactions such as anaphylaxis or who have been advised to carry an epinephrine autoinjector, to talk with their health care provider to determine if COVID-19 vaccination is medically appropriate.
The National Psoriasis Foundation has issued guidance on COVID-19, explained Steven R. Feldman, MD, PhD, professor of dermatology, pathology, and social sciences & health policy at Wake Forest University, Winston-Salem, N.C., who is also a member of the committee that is working on those guidelines and keeping them up to date. “We are in the process of updating the guidelines with information on COVID vaccines,” he said.
He agreed that there are no contraindications for psoriasis patients to receive the vaccine, regardless of whether they are on immunosuppressive treatment, even though definitive data are lacking. “Fortunately, there’s a lot of good data coming out of Italy that patients with psoriasis on biologics do not appear to be at increased risk of getting COVID or of having worse outcomes from COVID,” he said.
Patients are going to ask about the vaccines, and when counseling them, clinicians should discuss the available data, the residual uncertainty, and patients’ concerns should be considered, Dr. Feldman explained. “There may be some concern that steroids and cyclosporine would reduce the effectiveness of vaccines, but there is no concern that any of the drugs would cause increased risk from nonlive vaccines.”
He added that there is evidence that “patients on biologics who receive nonlive vaccines do develop antibody responses and are immunized.”
Boosting efficacy
Even prior to making their announcement, the American College of Rheumatology had said that they would endorse the vaccine for all patients, explained rheumatologist Brett Smith, DO, from Blount Memorial Physicians Group and East Tennessee Children’s Hospital, Alcoa. “The vaccine is safe for all patients, but the problem may be that it’s not as effective,” he said. “But we don’t know that because it hasn’t been tested.”
With other vaccines, biologic medicines are held for 2 weeks before and afterwards, to get the best response. “But some patients don’t want to stop the medication,” Dr. Smith said. “They are afraid that their symptoms will return.”
As for counseling patients as to whether they should receive this vaccine, he explained that he typically doesn’t try to sway patients one way or another until they are really high risk. “When I counsel, it really depends on the individual situation. And for this vaccine, we have to be open to the fact that many people have already made up their mind.”
There are a lot of questions regarding the vaccine. One is the short time frame of development. “Vaccines typically take 6-10 years to come on the market, and this one is now available after a 3-month study,” Dr. Smith said. “Some have already decided that it’s too new for them.”
The process is also new, and patients need to understand that it doesn’t contain an active virus and “you can’t catch coronavirus from it.”
Dr. Smith also explained that, because the vaccine may be less effective in a person using biologic therapies, there is currently no information available on repeat vaccination. “These are all unanswered questions,” he said. “If the antibodies wane in a short time, can we be revaccinated and in what time frame? We just don’t know that yet.”
Marcelo Bonomi, MD, a medical oncologist from The Ohio State University Comprehensive Cancer Center, Columbus, explained that one way to ensure a more optimal response to the vaccine would be to wait until the patient has finished chemotherapy.* “The vaccine can be offered at that time, and in the meantime, they can take other steps to avoid infection,” he said. “If they are very immunosuppressed, it isn’t worth trying to give the vaccine.”
Cancer patients should be encouraged to stay as healthy as possible, and to wear masks and social distance. “It’s a comprehensive approach. Eat healthy, avoid alcohol and tobacco, and exercise. [These things] will help boost the immune system,” Dr. Bonomi said. “Family members should be encouraged to get vaccinated, which will help them avoid infection and exposing the patient.”
Jim Boonyaratanakornkit, MD, PhD, an infectious disease specialist who cares for cancer patients at the Fred Hutchinson Cancer Research Center, agreed. “Giving a vaccine right after a transplant is a futile endeavor,” he said. “We need to wait 6 months to have an immune response.”
He pointed out there may be a continuing higher number of cases, with high levels peaking in Washington in February and March. “Close friends and family should be vaccinated if possible,” he said, “which will help interrupt transmission.”
The vaccines are using new platforms that are totally different, and there is no clear data as to how long the antibodies will persist. “We know that they last for at least 4 months,” said Dr. Boonyaratanakornkit. “We don’t know what level of antibody will protect them from COVID-19 infection. Current studies are being conducted, but we don’t have that information for anyone yet.”
*Correction, 1/7/21: An earlier version of this article misattributed quotes from Dr. Marcelo Bonomi.
Coronavirus vaccines have become a reality, as they are now being approved and authorized for use in a growing number of countries including the United States. The U.S. Food and Drug Administration has just issued emergency authorization for the use of the COVID-19 vaccine produced by Pfizer and BioNTech. Close behind is the vaccine developed by Moderna, which has also applied to the FDA for emergency authorization.
The efficacy of a two-dose administration of the vaccine has been pegged at 95.0%, and the FDA has said that the 95% credible interval for the vaccine efficacy was 90.3%-97.6%. But as with many initial clinical trials, whether for drugs or vaccines, not all populations were represented in the trial cohort, including individuals who are immunocompromised. At the current time, it is largely unknown how safe or effective the vaccine may be in this large population, many of whom are at high risk for serious COVID-19 complications.
At a special session held during the recent annual meeting of the American Society of Hematology, Anthony Fauci, MD, the nation’s leading infectious disease expert, said that individuals with compromised immune systems, whether because of chemotherapy or a bone marrow transplant, should plan to be vaccinated when the opportunity arises.
In response to a question from ASH President Stephanie J. Lee, MD, of the Fred Hutchinson Cancer Center, Seattle, Dr. Fauci emphasized that, despite being excluded from clinical trials, this population should get vaccinated. “I think we should recommend that they get vaccinated,” he said. “I mean, it is clear that, if you are on immunosuppressive agents, history tells us that you’re not going to have as robust a response as if you had an intact immune system that was not being compromised. But some degree of immunity is better than no degree of immunity.”
That does seem to be the consensus among experts who spoke in interviews: that as long as these are not live attenuated vaccines, they hold no specific risk to an immunocompromised patient, other than any factors specific to the individual that could be a contraindication.
“Patients, family members, friends, and work contacts should be encouraged to receive the vaccine,” said William Stohl, MD, PhD, chief of the division of rheumatology at the University of Southern California, Los Angeles. “Clinicians should advise patients to obtain the vaccine sooner rather than later.”
Kevin C. Wang, MD, PhD, of the department of dermatology at Stanford (Calif.) University, agreed. “I am 100% with Dr. Fauci. Everyone should get the vaccine, even if it may not be as effective,” he said. “I would treat it exactly like the flu vaccines that we recommend folks get every year.”
Dr. Wang noted that he couldn’t think of any contraindications unless the immunosuppressed patients have a history of severe allergic reactions to prior vaccinations. “But I would even say patients with history of cancer, upon recommendation of their oncologists, are likely to be suitable candidates for the vaccine,” he added. “I would say clinicians should approach counseling the same way they counsel patients for the flu vaccine, and as far as I know, there are no concerns for systemic drugs commonly used in dermatology patients.”
However, guidance has not yet been issued from either the FDA or the Centers for Disease Control and Prevention regarding the use of the vaccine in immunocompromised individuals. Given the lack of data, the FDA has said that “it will be something that providers will need to consider on an individual basis,” and that individuals should consult with physicians to weigh the potential benefits and potential risks.
The CDC’s Advisory Committee on Immunization Practices has said that clinicians need more guidance on whether to use the vaccine in pregnant or breastfeeding women, the immunocompromised, or those who have a history of allergies. The CDC itself has not yet released its formal guidance on vaccine use.
COVID-19 vaccines
Vaccines typically require years of research and testing before reaching the clinic, but this year researchers embarked on a global effort to develop safe and effective coronavirus vaccines in record time. Both the Pfizer/BioNTech and Moderna vaccines have only a few months of phase 3 clinical trial data, so much remains unknown about them, including their duration of effect and any long-term safety signals. In addition to excluding immunocompromised individuals, the clinical trials did not include children or pregnant women, so data are lacking for several population subgroups.
But these will not be the only vaccines available, as the pipeline is already becoming crowded. U.S. clinical trial data from a vaccine jointly being developed by Oxford-AstraZeneca, could potentially be ready, along with a request for FDA emergency use authorization, by late January 2021.
In addition, China and Russia have released vaccines, and there are currently 61 vaccines being investigated in clinical trials and at least 85 preclinical products under active investigation.
The vaccine candidates are using both conventional and novel mechanisms of action to elicit an immune response in patients. Conventional methods include attenuated inactivated (killed) virus and recombinant viral protein vaccines to develop immunity. Novel approaches include replication-deficient, adenovirus vector-based vaccines that contain the viral protein, and mRNA-based vaccines, such as the Pfizer and Moderna vaccines, that encode for a SARS-CoV-2 spike protein.
“The special vaccine concern for immunocompromised individuals is introduction of a live virus,” Dr. Stohl said. “Neither the Moderna nor Pfizer vaccines are live viruses, so there should be no special contraindication for such individuals.”
Live vaccine should be avoided in immunocompromised patients, and currently, live SARS-CoV-2 vaccines are only being developed in India and Turkey.
It is not unusual for vaccine trials to begin with cohorts that exclude participants with various health conditions, including those who are immunocompromised. These groups are generally then evaluated in phase 4 trials, or postmarketing surveillance. While the precise number of immunosuppressed adults in the United States is not known, the numbers are believed to be rising because of increased life expectancy among immunosuppressed adults as a result of advances in treatment and new and wider indications for therapies that can affect the immune system.
According to data from the 2013 National Health Interview Survey, an estimated 2.7% of U.S. adults are immunosuppressed. This population covers a broad array of health conditions and medical specialties; people living with inflammatory or autoimmune conditions, such as inflammatory rheumatic diseases (rheumatoid arthritis, axial spondyloarthritis, lupus); inflammatory bowel disease (Crohn’s disease and ulcerative colitis); psoriasis; multiple sclerosis; organ transplant recipients; patients undergoing chemotherapy; and life-long immunosuppression attributable to HIV infection.
As the vaccines begin to roll out and become available, how should clinicians advise their patients, in the absence of any clinical trial data?
Risk vs. benefit
Gilaad Kaplan, MD, MPH, a gastroenterologist and professor of medicine at the University of Calgary (Alta.), noted that the inflammatory bowel disease (IBD) community has dealt with tremendous anxiety during the pandemic because many are immunocompromised because of the medications they use to treat their disease.
“For example, many patients with IBD are on biologics like anti-TNF [tumor necrosis factor] therapies, which are also used in other immune-mediated inflammatory diseases such as rheumatoid arthritis,” he said. “Understandably, individuals with IBD on immunosuppressive medications are concerned about the risk of severe complications due to COVID-19.”
The entire IBD community, along with the world, celebrated the announcement that multiple vaccines are protective against SARS-CoV-2, he noted. “Vaccines offer the potential to reduce the spread of COVID-19, allowing society to revert back to normalcy,” Dr. Kaplan said. “Moreover, for vulnerable populations, including those who are immunocompromised, vaccines offer the potential to directly protect them from the morbidity and mortality associated with COVID-19.”
That said, even though the news of vaccines are extremely promising, some cautions must be raised regarding their use in immunocompromised populations, such as persons with IBD. “The current trials, to my knowledge, did not include immunocompromised individuals and thus, we can only extrapolate from what we know from other trials of different vaccines,” he explained. “We know from prior vaccines studies that the immune response following vaccination is less robust in those who are immunocompromised as compared to a healthy control population.”
Dr. Kaplan also pointed to recent reports of allergic reactions that have been reported in healthy individuals. “We don’t know whether side effects, like allergic reactions, may be different in unstudied populations,” he said. “Thus, the medical and scientific community should prioritize clinical studies of safety and effectiveness of COVID-19 vaccines in immunocompromised populations.”
So, what does this mean for an individual with an immune-mediated inflammatory disease like Crohn’s disease or ulcerative colitis who is immunocompromised? Dr. Kaplan explained that it is a balance between the potential harm of being infected with COVID-19 and the uncertainty of receiving a vaccine in an understudied population. For those who are highly susceptible to dying from COVID-19, such as an older adult with IBD, or someone who faces high exposure, such as a health care worker, the potential protection of the vaccine greatly outweighs the uncertainty.
“However, for individuals who are at otherwise lower risk – for example, young and able to work from home – then waiting a few extra months for postmarketing surveillance studies in immunocompromised populations may be a reasonable approach, as long as these individuals are taking great care to avoid infection,” he said.
No waiting needed
Joel M. Gelfand, MD, MSCE, professor of dermatology and epidemiology at the University of Pennsylvania, Philadelphia, feels that the newly approved vaccine should be safe for most of his patients.
“Patients with psoriatic disease should get the mRNA-based COVID-19 vaccine as soon as possible based on eligibility as determined by the CDC and local public health officials,” he said. “It is not a live vaccine, and therefore patients on biologics or other immune-modulating or immune-suppressing treatment can receive it.”
However, the impact of psoriasis treatment on immune response to the mRNA-based vaccines is not known. Dr. Gelfand noted that, extrapolating from the vaccine literature, there is some evidence that methotrexate reduces response to the influenza vaccine. “However, the clinical significance of this finding is not clear,” he said. “Since the mRNA vaccine needs to be taken twice, a few weeks apart, I do not recommend interrupting or delaying treatment for psoriatic disease while undergoing vaccination for COVID-19.”
Given the reports of allergic reactions, he added that it is advisable for patients with a history of life-threatening allergic reactions such as anaphylaxis or who have been advised to carry an epinephrine autoinjector, to talk with their health care provider to determine if COVID-19 vaccination is medically appropriate.
The National Psoriasis Foundation has issued guidance on COVID-19, explained Steven R. Feldman, MD, PhD, professor of dermatology, pathology, and social sciences & health policy at Wake Forest University, Winston-Salem, N.C., who is also a member of the committee that is working on those guidelines and keeping them up to date. “We are in the process of updating the guidelines with information on COVID vaccines,” he said.
He agreed that there are no contraindications for psoriasis patients to receive the vaccine, regardless of whether they are on immunosuppressive treatment, even though definitive data are lacking. “Fortunately, there’s a lot of good data coming out of Italy that patients with psoriasis on biologics do not appear to be at increased risk of getting COVID or of having worse outcomes from COVID,” he said.
Patients are going to ask about the vaccines, and when counseling them, clinicians should discuss the available data, the residual uncertainty, and patients’ concerns should be considered, Dr. Feldman explained. “There may be some concern that steroids and cyclosporine would reduce the effectiveness of vaccines, but there is no concern that any of the drugs would cause increased risk from nonlive vaccines.”
He added that there is evidence that “patients on biologics who receive nonlive vaccines do develop antibody responses and are immunized.”
Boosting efficacy
Even prior to making their announcement, the American College of Rheumatology had said that they would endorse the vaccine for all patients, explained rheumatologist Brett Smith, DO, from Blount Memorial Physicians Group and East Tennessee Children’s Hospital, Alcoa. “The vaccine is safe for all patients, but the problem may be that it’s not as effective,” he said. “But we don’t know that because it hasn’t been tested.”
With other vaccines, biologic medicines are held for 2 weeks before and afterwards, to get the best response. “But some patients don’t want to stop the medication,” Dr. Smith said. “They are afraid that their symptoms will return.”
As for counseling patients as to whether they should receive this vaccine, he explained that he typically doesn’t try to sway patients one way or another until they are really high risk. “When I counsel, it really depends on the individual situation. And for this vaccine, we have to be open to the fact that many people have already made up their mind.”
There are a lot of questions regarding the vaccine. One is the short time frame of development. “Vaccines typically take 6-10 years to come on the market, and this one is now available after a 3-month study,” Dr. Smith said. “Some have already decided that it’s too new for them.”
The process is also new, and patients need to understand that it doesn’t contain an active virus and “you can’t catch coronavirus from it.”
Dr. Smith also explained that, because the vaccine may be less effective in a person using biologic therapies, there is currently no information available on repeat vaccination. “These are all unanswered questions,” he said. “If the antibodies wane in a short time, can we be revaccinated and in what time frame? We just don’t know that yet.”
Marcelo Bonomi, MD, a medical oncologist from The Ohio State University Comprehensive Cancer Center, Columbus, explained that one way to ensure a more optimal response to the vaccine would be to wait until the patient has finished chemotherapy.* “The vaccine can be offered at that time, and in the meantime, they can take other steps to avoid infection,” he said. “If they are very immunosuppressed, it isn’t worth trying to give the vaccine.”
Cancer patients should be encouraged to stay as healthy as possible, and to wear masks and social distance. “It’s a comprehensive approach. Eat healthy, avoid alcohol and tobacco, and exercise. [These things] will help boost the immune system,” Dr. Bonomi said. “Family members should be encouraged to get vaccinated, which will help them avoid infection and exposing the patient.”
Jim Boonyaratanakornkit, MD, PhD, an infectious disease specialist who cares for cancer patients at the Fred Hutchinson Cancer Research Center, agreed. “Giving a vaccine right after a transplant is a futile endeavor,” he said. “We need to wait 6 months to have an immune response.”
He pointed out there may be a continuing higher number of cases, with high levels peaking in Washington in February and March. “Close friends and family should be vaccinated if possible,” he said, “which will help interrupt transmission.”
The vaccines are using new platforms that are totally different, and there is no clear data as to how long the antibodies will persist. “We know that they last for at least 4 months,” said Dr. Boonyaratanakornkit. “We don’t know what level of antibody will protect them from COVID-19 infection. Current studies are being conducted, but we don’t have that information for anyone yet.”
*Correction, 1/7/21: An earlier version of this article misattributed quotes from Dr. Marcelo Bonomi.
On the horizon: Asciminib, a new drug for treating r/r CML
The investigational drug asciminib (being developed by Novartis) may become the new kid on the block for the treatment of chronic phase chronic myeloid leukemia (CMP-CP) for patients who have relapsed on or are refractory to at least two prior tyrosine kinase inhibitors (TKIs).
New results from the ASCEMBL study (NCT03106779) show that patients who received asciminib, which works differently from currently approved therapies for CML-CP, achieved better responses, compared with bosutinib (Bosulif) as third-line therapy.
“The ASCEMBL study opens a new chapter for CML, proving comparatively superior efficacy and excellent safety for a new class of ABL inhibitors,” coinvestigator Michael J. Mauro, MD, from Memorial Sloan Kettering Cancer Center, New York, said in an interview.
The trial was presented as a late-breaking abstract at the annual meeting of the American Society of Hematology.
Asciminib is a first-of-a-kind STAMP (Specifically Targeting the ABL Myristoyl Pocket) inhibitor that works differently from currently approved TKIs, which are adenosine triphosphate (ATP)-–competitive ABL inhibitors.
Five TKIs have been approved by the Food and Drug Administration to treat CML: imatinib (Gleevec; generics), nilotinib (Tasigna), dasatinib (Sprycel), bosutinib, and ponatinib (Iclusig).
All of them inhibit BCR/ABL tyrosine kinase by binding to the ATP-binding pocket.
Most patients with TKI resistant disease develop mutations in the ATP-binding pocket, explained Michael Jay Styler, MD, associate professor at Fox Chase–Temple University Hospital bone marrow transplant program, Fox Chase Cancer Center, Philadelphia.
By inactivating the protein through binding outside the ATP site, asciminib is a novel BCR-ABL inhibitor and may be a superior alternative to further traditional TKIs. “This agent promises to be an important addition to our treatment armamentarium for CML,” Dr. Styler said in an interview.
Another expert agreed. “Although we have many excellent therapies for CML, having a new medication that targets BCR-ABL in a novel way is still welcome to help us better care for CML patients,” Gabriela S. Hobbs, MD, said in an interview. Dr. Hobbs is the clinical director of leukemia services at Boston’s Mass General Cancer Center.
Patients in this study had previously been receiving at least two different types of TKIs. “The responses looked very encouraging for this group of heavily pretreated patients. Although CML patients do very well on current therapies, those that don’t get a response with TKI remain a difficult clinical challenge,” Dr. Hobbs said.
“This is the first study comparing asciminib to a TKI directly (in this case bosutinib) and it showed safety as well as preliminary evidence of efficacy. I look forward to seeing additional studies with this promising drug and to have a new drug to add to the CML arsenal,” she added.
Identifying patients who will benefit from asciminib
Patients with CML are currently sequenced through more than one second-generation TKI, Dr. Mauro commented. “If imatinib and a second-generation TKI have not served a patient well, only bosutinib has been studied in the third line and comparatively in the ASCEMBL study.” Asciminib was shown to be superior and could offer a clear alternative to ponatinib, which would be the other choice and is typically given even later after sequencing all other available options.
Dr. Hobbs agreed. “This is a challenging group of patients to manage as their options are limited. Ponatinib is often the drug of choice in these scenarios, as well as bone marrow transplant.”
They also agreed that it may be effective (alone or in combination) in treating patients with T315I-mutation CML, which is a particularly challenging disease.
Senior study author Andreas Hochhaus, MD, of the Klinik für Innere Medizin II in Jena, Germany, who presented the data at the meeting, noted new trials to test the efficacy of asciminib alone or in combination in earlier lines of therapy are ongoing and include the investigator-initiated FASCINATION study (first-line asciminib in combination) in Germany (NCT03906292).
ASCEMBL study details
ASCEMBL is a phase 3 study in which patients with CML who had received at least two previous TKIs were randomized to asciminib (n = 157) 40 mg twice daily or bosutinib (n = 76) 500 mg once daily. In a protocol amendment, patients with documented failure on bosutinib were allowed to switch to asciminib.
The main reason for discontinuing the last TKI therapy was lack of efficacy in approximately two-thirds of patients. More patients in the asciminib than the bosutinib group received two prior lines of therapy (52% vs. 40%); the others had received three or more prior lines of therapy.
Median follow-up for the data cutoff was 14.9 months.
Dr. Hochhaus reported that treatment discontinuation was lower in patients receiving asciminib than bosutinib (38% vs. 70%) and was mostly due to lack of efficacy (21% vs. 32%) or adverse events (5% vs. 21%).
The study met its primary endpoint: major molecular response (MMR) was approximately twice as high with asciminib than bosutinib at 24 weeks (25.5% vs. 13.2%; P = .029). Treatment effect for MMR was 12.2%. Median duration of exposure to asciminib was 43.4 weeks for asciminib and 29.2 weeks for bosutinib.
“Consistent treatment effect was seen across all subgroups of patients, and MMR rates were consistently high for patients on asciminib across all prior lines of therapy,” Dr. Hochhaus reported.
The probability of achieving MMR at 24 weeks was higher for patients receiving asciminib (25% vs. 11.9%) and started at week 12, he noted. Complete cytogenetic response was also higher for patients receiving asciminib (40.8% vs. 24.2%).
The occurrence of grade 3 or higher adverse events was lower with asciminib than bosutinib (51% vs. 61%). Thrombocytopenia and neutropenia were more common with asciminib and gastrointestinal events were more common with bosutinib. Arterial occlusion events were reported in five patients receiving asciminib and one patient receiving bosutinib. Most of these patients had prior exposure to imatinib, nilotinib, and/or dasatinib.
Dr. Mauro, a coinvestigator of the phase 3 study, also treated patients with the drug in the phase 1 study. “I feel asciminib has proven to be very well tolerated, with rare to absent cases of intolerance,” he said. Cardiovascular and cardiopulmonary adverse events are exceedingly rare as well.
Longer follow-up of the ASCEMBL study and continued follow-up of the myriad of groups from the phase 1 trial (T315I-positive patients treated with higher-dose asciminib, combination therapy with imatinib/nilotinib/dasatinib plus asciminib, and others) will be essential to settle any questions regarding selective adverse events of interest such as vascular occlusion, Dr. Mauro noted.
Dr. Hochhaus has reported receiving research funding from Novartis, Incyte, Pfizer, and Bristol-Myers Squibb. Dr. Hobbs has reported serving on advisory boards for Novartis. Dr. Mauro has reported financial relationships with Bristol-Myers Squibb, Novartis, Takeda, Pfizer, and Sun Pharma/SPARC.
A version of this article first appeared on Medscape.com.
The investigational drug asciminib (being developed by Novartis) may become the new kid on the block for the treatment of chronic phase chronic myeloid leukemia (CMP-CP) for patients who have relapsed on or are refractory to at least two prior tyrosine kinase inhibitors (TKIs).
New results from the ASCEMBL study (NCT03106779) show that patients who received asciminib, which works differently from currently approved therapies for CML-CP, achieved better responses, compared with bosutinib (Bosulif) as third-line therapy.
“The ASCEMBL study opens a new chapter for CML, proving comparatively superior efficacy and excellent safety for a new class of ABL inhibitors,” coinvestigator Michael J. Mauro, MD, from Memorial Sloan Kettering Cancer Center, New York, said in an interview.
The trial was presented as a late-breaking abstract at the annual meeting of the American Society of Hematology.
Asciminib is a first-of-a-kind STAMP (Specifically Targeting the ABL Myristoyl Pocket) inhibitor that works differently from currently approved TKIs, which are adenosine triphosphate (ATP)-–competitive ABL inhibitors.
Five TKIs have been approved by the Food and Drug Administration to treat CML: imatinib (Gleevec; generics), nilotinib (Tasigna), dasatinib (Sprycel), bosutinib, and ponatinib (Iclusig).
All of them inhibit BCR/ABL tyrosine kinase by binding to the ATP-binding pocket.
Most patients with TKI resistant disease develop mutations in the ATP-binding pocket, explained Michael Jay Styler, MD, associate professor at Fox Chase–Temple University Hospital bone marrow transplant program, Fox Chase Cancer Center, Philadelphia.
By inactivating the protein through binding outside the ATP site, asciminib is a novel BCR-ABL inhibitor and may be a superior alternative to further traditional TKIs. “This agent promises to be an important addition to our treatment armamentarium for CML,” Dr. Styler said in an interview.
Another expert agreed. “Although we have many excellent therapies for CML, having a new medication that targets BCR-ABL in a novel way is still welcome to help us better care for CML patients,” Gabriela S. Hobbs, MD, said in an interview. Dr. Hobbs is the clinical director of leukemia services at Boston’s Mass General Cancer Center.
Patients in this study had previously been receiving at least two different types of TKIs. “The responses looked very encouraging for this group of heavily pretreated patients. Although CML patients do very well on current therapies, those that don’t get a response with TKI remain a difficult clinical challenge,” Dr. Hobbs said.
“This is the first study comparing asciminib to a TKI directly (in this case bosutinib) and it showed safety as well as preliminary evidence of efficacy. I look forward to seeing additional studies with this promising drug and to have a new drug to add to the CML arsenal,” she added.
Identifying patients who will benefit from asciminib
Patients with CML are currently sequenced through more than one second-generation TKI, Dr. Mauro commented. “If imatinib and a second-generation TKI have not served a patient well, only bosutinib has been studied in the third line and comparatively in the ASCEMBL study.” Asciminib was shown to be superior and could offer a clear alternative to ponatinib, which would be the other choice and is typically given even later after sequencing all other available options.
Dr. Hobbs agreed. “This is a challenging group of patients to manage as their options are limited. Ponatinib is often the drug of choice in these scenarios, as well as bone marrow transplant.”
They also agreed that it may be effective (alone or in combination) in treating patients with T315I-mutation CML, which is a particularly challenging disease.
Senior study author Andreas Hochhaus, MD, of the Klinik für Innere Medizin II in Jena, Germany, who presented the data at the meeting, noted new trials to test the efficacy of asciminib alone or in combination in earlier lines of therapy are ongoing and include the investigator-initiated FASCINATION study (first-line asciminib in combination) in Germany (NCT03906292).
ASCEMBL study details
ASCEMBL is a phase 3 study in which patients with CML who had received at least two previous TKIs were randomized to asciminib (n = 157) 40 mg twice daily or bosutinib (n = 76) 500 mg once daily. In a protocol amendment, patients with documented failure on bosutinib were allowed to switch to asciminib.
The main reason for discontinuing the last TKI therapy was lack of efficacy in approximately two-thirds of patients. More patients in the asciminib than the bosutinib group received two prior lines of therapy (52% vs. 40%); the others had received three or more prior lines of therapy.
Median follow-up for the data cutoff was 14.9 months.
Dr. Hochhaus reported that treatment discontinuation was lower in patients receiving asciminib than bosutinib (38% vs. 70%) and was mostly due to lack of efficacy (21% vs. 32%) or adverse events (5% vs. 21%).
The study met its primary endpoint: major molecular response (MMR) was approximately twice as high with asciminib than bosutinib at 24 weeks (25.5% vs. 13.2%; P = .029). Treatment effect for MMR was 12.2%. Median duration of exposure to asciminib was 43.4 weeks for asciminib and 29.2 weeks for bosutinib.
“Consistent treatment effect was seen across all subgroups of patients, and MMR rates were consistently high for patients on asciminib across all prior lines of therapy,” Dr. Hochhaus reported.
The probability of achieving MMR at 24 weeks was higher for patients receiving asciminib (25% vs. 11.9%) and started at week 12, he noted. Complete cytogenetic response was also higher for patients receiving asciminib (40.8% vs. 24.2%).
The occurrence of grade 3 or higher adverse events was lower with asciminib than bosutinib (51% vs. 61%). Thrombocytopenia and neutropenia were more common with asciminib and gastrointestinal events were more common with bosutinib. Arterial occlusion events were reported in five patients receiving asciminib and one patient receiving bosutinib. Most of these patients had prior exposure to imatinib, nilotinib, and/or dasatinib.
Dr. Mauro, a coinvestigator of the phase 3 study, also treated patients with the drug in the phase 1 study. “I feel asciminib has proven to be very well tolerated, with rare to absent cases of intolerance,” he said. Cardiovascular and cardiopulmonary adverse events are exceedingly rare as well.
Longer follow-up of the ASCEMBL study and continued follow-up of the myriad of groups from the phase 1 trial (T315I-positive patients treated with higher-dose asciminib, combination therapy with imatinib/nilotinib/dasatinib plus asciminib, and others) will be essential to settle any questions regarding selective adverse events of interest such as vascular occlusion, Dr. Mauro noted.
Dr. Hochhaus has reported receiving research funding from Novartis, Incyte, Pfizer, and Bristol-Myers Squibb. Dr. Hobbs has reported serving on advisory boards for Novartis. Dr. Mauro has reported financial relationships with Bristol-Myers Squibb, Novartis, Takeda, Pfizer, and Sun Pharma/SPARC.
A version of this article first appeared on Medscape.com.
The investigational drug asciminib (being developed by Novartis) may become the new kid on the block for the treatment of chronic phase chronic myeloid leukemia (CMP-CP) for patients who have relapsed on or are refractory to at least two prior tyrosine kinase inhibitors (TKIs).
New results from the ASCEMBL study (NCT03106779) show that patients who received asciminib, which works differently from currently approved therapies for CML-CP, achieved better responses, compared with bosutinib (Bosulif) as third-line therapy.
“The ASCEMBL study opens a new chapter for CML, proving comparatively superior efficacy and excellent safety for a new class of ABL inhibitors,” coinvestigator Michael J. Mauro, MD, from Memorial Sloan Kettering Cancer Center, New York, said in an interview.
The trial was presented as a late-breaking abstract at the annual meeting of the American Society of Hematology.
Asciminib is a first-of-a-kind STAMP (Specifically Targeting the ABL Myristoyl Pocket) inhibitor that works differently from currently approved TKIs, which are adenosine triphosphate (ATP)-–competitive ABL inhibitors.
Five TKIs have been approved by the Food and Drug Administration to treat CML: imatinib (Gleevec; generics), nilotinib (Tasigna), dasatinib (Sprycel), bosutinib, and ponatinib (Iclusig).
All of them inhibit BCR/ABL tyrosine kinase by binding to the ATP-binding pocket.
Most patients with TKI resistant disease develop mutations in the ATP-binding pocket, explained Michael Jay Styler, MD, associate professor at Fox Chase–Temple University Hospital bone marrow transplant program, Fox Chase Cancer Center, Philadelphia.
By inactivating the protein through binding outside the ATP site, asciminib is a novel BCR-ABL inhibitor and may be a superior alternative to further traditional TKIs. “This agent promises to be an important addition to our treatment armamentarium for CML,” Dr. Styler said in an interview.
Another expert agreed. “Although we have many excellent therapies for CML, having a new medication that targets BCR-ABL in a novel way is still welcome to help us better care for CML patients,” Gabriela S. Hobbs, MD, said in an interview. Dr. Hobbs is the clinical director of leukemia services at Boston’s Mass General Cancer Center.
Patients in this study had previously been receiving at least two different types of TKIs. “The responses looked very encouraging for this group of heavily pretreated patients. Although CML patients do very well on current therapies, those that don’t get a response with TKI remain a difficult clinical challenge,” Dr. Hobbs said.
“This is the first study comparing asciminib to a TKI directly (in this case bosutinib) and it showed safety as well as preliminary evidence of efficacy. I look forward to seeing additional studies with this promising drug and to have a new drug to add to the CML arsenal,” she added.
Identifying patients who will benefit from asciminib
Patients with CML are currently sequenced through more than one second-generation TKI, Dr. Mauro commented. “If imatinib and a second-generation TKI have not served a patient well, only bosutinib has been studied in the third line and comparatively in the ASCEMBL study.” Asciminib was shown to be superior and could offer a clear alternative to ponatinib, which would be the other choice and is typically given even later after sequencing all other available options.
Dr. Hobbs agreed. “This is a challenging group of patients to manage as their options are limited. Ponatinib is often the drug of choice in these scenarios, as well as bone marrow transplant.”
They also agreed that it may be effective (alone or in combination) in treating patients with T315I-mutation CML, which is a particularly challenging disease.
Senior study author Andreas Hochhaus, MD, of the Klinik für Innere Medizin II in Jena, Germany, who presented the data at the meeting, noted new trials to test the efficacy of asciminib alone or in combination in earlier lines of therapy are ongoing and include the investigator-initiated FASCINATION study (first-line asciminib in combination) in Germany (NCT03906292).
ASCEMBL study details
ASCEMBL is a phase 3 study in which patients with CML who had received at least two previous TKIs were randomized to asciminib (n = 157) 40 mg twice daily or bosutinib (n = 76) 500 mg once daily. In a protocol amendment, patients with documented failure on bosutinib were allowed to switch to asciminib.
The main reason for discontinuing the last TKI therapy was lack of efficacy in approximately two-thirds of patients. More patients in the asciminib than the bosutinib group received two prior lines of therapy (52% vs. 40%); the others had received three or more prior lines of therapy.
Median follow-up for the data cutoff was 14.9 months.
Dr. Hochhaus reported that treatment discontinuation was lower in patients receiving asciminib than bosutinib (38% vs. 70%) and was mostly due to lack of efficacy (21% vs. 32%) or adverse events (5% vs. 21%).
The study met its primary endpoint: major molecular response (MMR) was approximately twice as high with asciminib than bosutinib at 24 weeks (25.5% vs. 13.2%; P = .029). Treatment effect for MMR was 12.2%. Median duration of exposure to asciminib was 43.4 weeks for asciminib and 29.2 weeks for bosutinib.
“Consistent treatment effect was seen across all subgroups of patients, and MMR rates were consistently high for patients on asciminib across all prior lines of therapy,” Dr. Hochhaus reported.
The probability of achieving MMR at 24 weeks was higher for patients receiving asciminib (25% vs. 11.9%) and started at week 12, he noted. Complete cytogenetic response was also higher for patients receiving asciminib (40.8% vs. 24.2%).
The occurrence of grade 3 or higher adverse events was lower with asciminib than bosutinib (51% vs. 61%). Thrombocytopenia and neutropenia were more common with asciminib and gastrointestinal events were more common with bosutinib. Arterial occlusion events were reported in five patients receiving asciminib and one patient receiving bosutinib. Most of these patients had prior exposure to imatinib, nilotinib, and/or dasatinib.
Dr. Mauro, a coinvestigator of the phase 3 study, also treated patients with the drug in the phase 1 study. “I feel asciminib has proven to be very well tolerated, with rare to absent cases of intolerance,” he said. Cardiovascular and cardiopulmonary adverse events are exceedingly rare as well.
Longer follow-up of the ASCEMBL study and continued follow-up of the myriad of groups from the phase 1 trial (T315I-positive patients treated with higher-dose asciminib, combination therapy with imatinib/nilotinib/dasatinib plus asciminib, and others) will be essential to settle any questions regarding selective adverse events of interest such as vascular occlusion, Dr. Mauro noted.
Dr. Hochhaus has reported receiving research funding from Novartis, Incyte, Pfizer, and Bristol-Myers Squibb. Dr. Hobbs has reported serving on advisory boards for Novartis. Dr. Mauro has reported financial relationships with Bristol-Myers Squibb, Novartis, Takeda, Pfizer, and Sun Pharma/SPARC.
A version of this article first appeared on Medscape.com.
Four-item prognostic index predicts survival in adult Burkitt lymphoma
A newly devised, validated prognostic tool – the Burkitt Lymphoma International Prognostic Index – can consistently identify low-risk patients who might benefit from treatment de-escalation, and high-risk patients who are unlikely to be cured with current therapies and may require novel approaches, investigators said.
In a cohort of patients treated at international sites, patients with a low-risk score on the BL-IPI had a 3-year progression-free survival (PFS) rate of 96%, and 3-year overall survival rate (OS) of 99%. In contrast, the 3-year PFS rate for patients in the high-risk category was 63%, and the 3-year OS rate was 64%, reported Adam J Olszewski, MD, from the Lifespan Cancer Institute at Rhode Island Hospital and The Miriam Hospital, both in Providence.
“The Burkitt Lymphoma International Prognostic Index – or the ‘BLI-PI’ [‘blippy’] as it was inevitably called – is a novel prognostic index that is specific to Burkitt lymphoma. It has been validated with sufficient calibration and discrimination in external data sets to allow for simple stratification and comparison of risk distribution in geographically diverse cohorts,” he said in an oral abstract presented virtually during the annual meeting of the American Society of Hematology.
Inconsistent criteria
There is a need for a Burkitt-specific index, he said, because of significant differences in age, stage at presentation, and abnormal lactate dehydrogenase (LDH) levels between patients with Burkitt and those with diffuse large B-cell lymphoma (DLBCL), and because historical definitions of “low-risk” Burkitt lymphoma have been inconsistent, with less than 10% of patients falling into this group, leaving the remainder in a undifferentiated “high-risk” category.
“Burkitt lymphoma is considered highly curable, but current therapy requires administration of dose-intense chemoimmunotherapy for which there are many chemotherapy backbone regimens developed across the world, and used mostly locally. These are often studied in phase 2 studies with limited sample sizes, which makes it difficult to compare populations across trials,” Dr. Olszewski said.
A validated prognostic index can help clinicians and researchers compare cohorts and can be used to help design future trials, he added.
To devise the BL-IPI, the investigators first selected a retrospective cohort of 570 adults with Burkitt lymphoma treated at 30 U.S. centers for whom data on outcomes were available.
They determined the best prognostic cutoffs for age, LDH, hemoglobin and albumin levels, and identified independent risk factors using stepwise selection in Cox regression and lasso regression analysis, a machine learning approach. The variables included age; sex; HIV-positivity status; loss of MYC rearrangement; performance status; stage; nodal involvement; marrow involvement; central nervous system involvement; and LDH, hemoglobin, and albumin levels.
For validation, they pooled data from European, Canadian, Australian, and U.K. studies to identify 457 patients for whom retrospective treatment and outcomes data were available.
The derivation and validation cohorts were similar in most respects, expect for a higher proportion of patients with Eastern Cooperative Oncology Group performance status scores of 2 or higher in the validation cohort (22% vs. 35%), and a higher proportion of patients with CNS involvement in the U.S.-based derivation cohort (19% vs. 10%, respectively).
Therapy also differed markedly between the U.S. and international cohorts, with about 30% each of U.S. patients receiving either the CODOX-M/IVAC (cyclophosphamide, vincristine, doxorubicin, high-dose methotrexate/ifosfamide, etoposide, and high-dose cytarabine) regimen, DA-EPOCH-R (dose-adjusted etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin, and rituximab) regimen, or hCVAD/MA (fractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone alternating with high-dose methotrexate and cytarabine) regimen, and the remaining 10% receiving other, unspecified therapy.
In contrast, 65% of the patients in the international (validation) cohort received CODOX-M/IVAC, 10% and 9%, respectively, received DA-EPOCH-R and hCVAD/MA, and 16% receiving other regimens.
Rituximab was administered to 91% of U.S. and 95% of international patients.
Higher survival rates outside US
Both PFS and OS were higher in the international versus U.S. cohort. At a median follow-up of 45 months, the PFS rate in the United States was 65%, and the OS rate was 70%.
In the international cohort, after a median follow-up of 52 months, the PFS rate was 75%, and the OS rate was 76%, the investigators found.
Reasons for the differences may be because of differences in treatment regimens, socioeconomic and racial disparities in the United States versus other countries, or to decentralized Burkitt lymphoma therapy in the United States, Dr. Olszewski said.
In univariate analysis, factors significantly predictive of worse PFS included age 40 years or older, ECOG performance status 2 or greater, stage 3 or 4 disease, marrow involvement, CNS involvement, LDH more than three times the upper limit of normal, and hemoglobin <11.5 g/dL (P < .001 for all preceding), as well as albumin <3.5 g/dL (P = .001).
“However, the multivariable analysis was more complicated, because many of these factors were overlapping, and most patients with high LDH also had advanced disease, and this group also encompassed patients who had bone marrow and CNS involvement,” he said.
Using the two types of regression analysis mentioned before, investigators identified ECOG performance status 2 or greater (P = .001), age 40 and older (P = .005), LDH greater than three times the upper limit of normal (P < .001) and CNS involvement (P = .002) as significant predictors for worse outcomes in multivariable analysis, and were included in the final model.
“We initially had five groups according to the number of these factors, but we observed that the survival curves for patients with two, three, or four factors were overlapping, and not significantly different, so ultimately we had three risk groups. In the derivation (U.S.) cohort, patients in the low-risk group, with no risk factors, a 3-year PFS of 92%, compared with 72% for patients with one risk factor (intermediate risk), and 53% for patients with two to four risk factors (high risk).
Respective hazard ratios for worse PFS in the low-, intermediate-, and high-risk groups were 1 (reference), 4.15 (95% confidence interval, 1.99-8.68), and 8.83 (95% CI, 4.32-18.03).
Respective HR for worse OS was 1, 7.06 (95% CI, 2.55-19.53), and 15.12 (95% CI, 5.58-40.99).
There were no significant differences in either PFS or OS when either LDH or stage was added into the model.
The BL-IPI was prognostic for PFS and OS in all subgroups, including HIV-positive or -negative patients, those with MYC rearrangements, stage 1 or 2 versus stage 3 or 4, or those treated with rituximab versus those who were not.
As noted before, 3-year PFS rates in the validation cohort for low, intermediate, high-risk groups were 96%, 82%, and 63% respectively, and 3-year OS rates were 99%, 85%, and 64%.
Why the CNS discrepancy?
In the question and answer session following the presentation, comoderator Christopher J. Melani, MD, from the Lymphoid Malignancies Branch at the National Cancer Institute in Bethesda, Md., said that “it was interesting to see the difference between CNS involvement in both the U.S. and the international cohort,” and asked whether Dr. Olszweski could elaborate on whether baseline CNS involvement was assessed by contrast-enhanced MRI of flow cytometry studies of cerebrospinal fluid.
“Could some of these differences between the U.S. and the international cohort be from the baseline assessment differing between the two?” he asked.
Dr. Olszewski replied that the retrospective nature of the data precluded capturing those data, but added that “I do suspect there may be some differences in the way that central nervous system is staged in different countries. In the United States the use of flow cytometry is more commonly employed, but we don’t know how it is used internationally. We do not know how often this is staged radiographically.”
Asked by others who viewed the presentation whether extranodal disease or peripheral blood involvement were prognostic in the final model, Dr. Olszewski replied that “one has to understand that, when one constructs a prognostic index, there is a balance between trying to input as much information as possible and to create something that is useful, clinically meaningful, and accurate.”
He said that, despite trying different models with different factors, “we couldn’t get the discrimination to be much better than the basic model that we ultimately created, so we favored using a more parsimonious model.”
No study funding source was reported. Dr. Olszewski reported research funding from Spectrum Pharmaceuticals, Genentech, TG Therapeutics, and Adaptive Biotechnologies. Dr. Melani reported having no relevant conflicts of interest.
SOURCE: Olszewski AJ et al. ASH 2020, Abstract 705.
A newly devised, validated prognostic tool – the Burkitt Lymphoma International Prognostic Index – can consistently identify low-risk patients who might benefit from treatment de-escalation, and high-risk patients who are unlikely to be cured with current therapies and may require novel approaches, investigators said.
In a cohort of patients treated at international sites, patients with a low-risk score on the BL-IPI had a 3-year progression-free survival (PFS) rate of 96%, and 3-year overall survival rate (OS) of 99%. In contrast, the 3-year PFS rate for patients in the high-risk category was 63%, and the 3-year OS rate was 64%, reported Adam J Olszewski, MD, from the Lifespan Cancer Institute at Rhode Island Hospital and The Miriam Hospital, both in Providence.
“The Burkitt Lymphoma International Prognostic Index – or the ‘BLI-PI’ [‘blippy’] as it was inevitably called – is a novel prognostic index that is specific to Burkitt lymphoma. It has been validated with sufficient calibration and discrimination in external data sets to allow for simple stratification and comparison of risk distribution in geographically diverse cohorts,” he said in an oral abstract presented virtually during the annual meeting of the American Society of Hematology.
Inconsistent criteria
There is a need for a Burkitt-specific index, he said, because of significant differences in age, stage at presentation, and abnormal lactate dehydrogenase (LDH) levels between patients with Burkitt and those with diffuse large B-cell lymphoma (DLBCL), and because historical definitions of “low-risk” Burkitt lymphoma have been inconsistent, with less than 10% of patients falling into this group, leaving the remainder in a undifferentiated “high-risk” category.
“Burkitt lymphoma is considered highly curable, but current therapy requires administration of dose-intense chemoimmunotherapy for which there are many chemotherapy backbone regimens developed across the world, and used mostly locally. These are often studied in phase 2 studies with limited sample sizes, which makes it difficult to compare populations across trials,” Dr. Olszewski said.
A validated prognostic index can help clinicians and researchers compare cohorts and can be used to help design future trials, he added.
To devise the BL-IPI, the investigators first selected a retrospective cohort of 570 adults with Burkitt lymphoma treated at 30 U.S. centers for whom data on outcomes were available.
They determined the best prognostic cutoffs for age, LDH, hemoglobin and albumin levels, and identified independent risk factors using stepwise selection in Cox regression and lasso regression analysis, a machine learning approach. The variables included age; sex; HIV-positivity status; loss of MYC rearrangement; performance status; stage; nodal involvement; marrow involvement; central nervous system involvement; and LDH, hemoglobin, and albumin levels.
For validation, they pooled data from European, Canadian, Australian, and U.K. studies to identify 457 patients for whom retrospective treatment and outcomes data were available.
The derivation and validation cohorts were similar in most respects, expect for a higher proportion of patients with Eastern Cooperative Oncology Group performance status scores of 2 or higher in the validation cohort (22% vs. 35%), and a higher proportion of patients with CNS involvement in the U.S.-based derivation cohort (19% vs. 10%, respectively).
Therapy also differed markedly between the U.S. and international cohorts, with about 30% each of U.S. patients receiving either the CODOX-M/IVAC (cyclophosphamide, vincristine, doxorubicin, high-dose methotrexate/ifosfamide, etoposide, and high-dose cytarabine) regimen, DA-EPOCH-R (dose-adjusted etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin, and rituximab) regimen, or hCVAD/MA (fractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone alternating with high-dose methotrexate and cytarabine) regimen, and the remaining 10% receiving other, unspecified therapy.
In contrast, 65% of the patients in the international (validation) cohort received CODOX-M/IVAC, 10% and 9%, respectively, received DA-EPOCH-R and hCVAD/MA, and 16% receiving other regimens.
Rituximab was administered to 91% of U.S. and 95% of international patients.
Higher survival rates outside US
Both PFS and OS were higher in the international versus U.S. cohort. At a median follow-up of 45 months, the PFS rate in the United States was 65%, and the OS rate was 70%.
In the international cohort, after a median follow-up of 52 months, the PFS rate was 75%, and the OS rate was 76%, the investigators found.
Reasons for the differences may be because of differences in treatment regimens, socioeconomic and racial disparities in the United States versus other countries, or to decentralized Burkitt lymphoma therapy in the United States, Dr. Olszewski said.
In univariate analysis, factors significantly predictive of worse PFS included age 40 years or older, ECOG performance status 2 or greater, stage 3 or 4 disease, marrow involvement, CNS involvement, LDH more than three times the upper limit of normal, and hemoglobin <11.5 g/dL (P < .001 for all preceding), as well as albumin <3.5 g/dL (P = .001).
“However, the multivariable analysis was more complicated, because many of these factors were overlapping, and most patients with high LDH also had advanced disease, and this group also encompassed patients who had bone marrow and CNS involvement,” he said.
Using the two types of regression analysis mentioned before, investigators identified ECOG performance status 2 or greater (P = .001), age 40 and older (P = .005), LDH greater than three times the upper limit of normal (P < .001) and CNS involvement (P = .002) as significant predictors for worse outcomes in multivariable analysis, and were included in the final model.
“We initially had five groups according to the number of these factors, but we observed that the survival curves for patients with two, three, or four factors were overlapping, and not significantly different, so ultimately we had three risk groups. In the derivation (U.S.) cohort, patients in the low-risk group, with no risk factors, a 3-year PFS of 92%, compared with 72% for patients with one risk factor (intermediate risk), and 53% for patients with two to four risk factors (high risk).
Respective hazard ratios for worse PFS in the low-, intermediate-, and high-risk groups were 1 (reference), 4.15 (95% confidence interval, 1.99-8.68), and 8.83 (95% CI, 4.32-18.03).
Respective HR for worse OS was 1, 7.06 (95% CI, 2.55-19.53), and 15.12 (95% CI, 5.58-40.99).
There were no significant differences in either PFS or OS when either LDH or stage was added into the model.
The BL-IPI was prognostic for PFS and OS in all subgroups, including HIV-positive or -negative patients, those with MYC rearrangements, stage 1 or 2 versus stage 3 or 4, or those treated with rituximab versus those who were not.
As noted before, 3-year PFS rates in the validation cohort for low, intermediate, high-risk groups were 96%, 82%, and 63% respectively, and 3-year OS rates were 99%, 85%, and 64%.
Why the CNS discrepancy?
In the question and answer session following the presentation, comoderator Christopher J. Melani, MD, from the Lymphoid Malignancies Branch at the National Cancer Institute in Bethesda, Md., said that “it was interesting to see the difference between CNS involvement in both the U.S. and the international cohort,” and asked whether Dr. Olszweski could elaborate on whether baseline CNS involvement was assessed by contrast-enhanced MRI of flow cytometry studies of cerebrospinal fluid.
“Could some of these differences between the U.S. and the international cohort be from the baseline assessment differing between the two?” he asked.
Dr. Olszewski replied that the retrospective nature of the data precluded capturing those data, but added that “I do suspect there may be some differences in the way that central nervous system is staged in different countries. In the United States the use of flow cytometry is more commonly employed, but we don’t know how it is used internationally. We do not know how often this is staged radiographically.”
Asked by others who viewed the presentation whether extranodal disease or peripheral blood involvement were prognostic in the final model, Dr. Olszewski replied that “one has to understand that, when one constructs a prognostic index, there is a balance between trying to input as much information as possible and to create something that is useful, clinically meaningful, and accurate.”
He said that, despite trying different models with different factors, “we couldn’t get the discrimination to be much better than the basic model that we ultimately created, so we favored using a more parsimonious model.”
No study funding source was reported. Dr. Olszewski reported research funding from Spectrum Pharmaceuticals, Genentech, TG Therapeutics, and Adaptive Biotechnologies. Dr. Melani reported having no relevant conflicts of interest.
SOURCE: Olszewski AJ et al. ASH 2020, Abstract 705.
A newly devised, validated prognostic tool – the Burkitt Lymphoma International Prognostic Index – can consistently identify low-risk patients who might benefit from treatment de-escalation, and high-risk patients who are unlikely to be cured with current therapies and may require novel approaches, investigators said.
In a cohort of patients treated at international sites, patients with a low-risk score on the BL-IPI had a 3-year progression-free survival (PFS) rate of 96%, and 3-year overall survival rate (OS) of 99%. In contrast, the 3-year PFS rate for patients in the high-risk category was 63%, and the 3-year OS rate was 64%, reported Adam J Olszewski, MD, from the Lifespan Cancer Institute at Rhode Island Hospital and The Miriam Hospital, both in Providence.
“The Burkitt Lymphoma International Prognostic Index – or the ‘BLI-PI’ [‘blippy’] as it was inevitably called – is a novel prognostic index that is specific to Burkitt lymphoma. It has been validated with sufficient calibration and discrimination in external data sets to allow for simple stratification and comparison of risk distribution in geographically diverse cohorts,” he said in an oral abstract presented virtually during the annual meeting of the American Society of Hematology.
Inconsistent criteria
There is a need for a Burkitt-specific index, he said, because of significant differences in age, stage at presentation, and abnormal lactate dehydrogenase (LDH) levels between patients with Burkitt and those with diffuse large B-cell lymphoma (DLBCL), and because historical definitions of “low-risk” Burkitt lymphoma have been inconsistent, with less than 10% of patients falling into this group, leaving the remainder in a undifferentiated “high-risk” category.
“Burkitt lymphoma is considered highly curable, but current therapy requires administration of dose-intense chemoimmunotherapy for which there are many chemotherapy backbone regimens developed across the world, and used mostly locally. These are often studied in phase 2 studies with limited sample sizes, which makes it difficult to compare populations across trials,” Dr. Olszewski said.
A validated prognostic index can help clinicians and researchers compare cohorts and can be used to help design future trials, he added.
To devise the BL-IPI, the investigators first selected a retrospective cohort of 570 adults with Burkitt lymphoma treated at 30 U.S. centers for whom data on outcomes were available.
They determined the best prognostic cutoffs for age, LDH, hemoglobin and albumin levels, and identified independent risk factors using stepwise selection in Cox regression and lasso regression analysis, a machine learning approach. The variables included age; sex; HIV-positivity status; loss of MYC rearrangement; performance status; stage; nodal involvement; marrow involvement; central nervous system involvement; and LDH, hemoglobin, and albumin levels.
For validation, they pooled data from European, Canadian, Australian, and U.K. studies to identify 457 patients for whom retrospective treatment and outcomes data were available.
The derivation and validation cohorts were similar in most respects, expect for a higher proportion of patients with Eastern Cooperative Oncology Group performance status scores of 2 or higher in the validation cohort (22% vs. 35%), and a higher proportion of patients with CNS involvement in the U.S.-based derivation cohort (19% vs. 10%, respectively).
Therapy also differed markedly between the U.S. and international cohorts, with about 30% each of U.S. patients receiving either the CODOX-M/IVAC (cyclophosphamide, vincristine, doxorubicin, high-dose methotrexate/ifosfamide, etoposide, and high-dose cytarabine) regimen, DA-EPOCH-R (dose-adjusted etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin, and rituximab) regimen, or hCVAD/MA (fractionated cyclophosphamide, vincristine, doxorubicin, and dexamethasone alternating with high-dose methotrexate and cytarabine) regimen, and the remaining 10% receiving other, unspecified therapy.
In contrast, 65% of the patients in the international (validation) cohort received CODOX-M/IVAC, 10% and 9%, respectively, received DA-EPOCH-R and hCVAD/MA, and 16% receiving other regimens.
Rituximab was administered to 91% of U.S. and 95% of international patients.
Higher survival rates outside US
Both PFS and OS were higher in the international versus U.S. cohort. At a median follow-up of 45 months, the PFS rate in the United States was 65%, and the OS rate was 70%.
In the international cohort, after a median follow-up of 52 months, the PFS rate was 75%, and the OS rate was 76%, the investigators found.
Reasons for the differences may be because of differences in treatment regimens, socioeconomic and racial disparities in the United States versus other countries, or to decentralized Burkitt lymphoma therapy in the United States, Dr. Olszewski said.
In univariate analysis, factors significantly predictive of worse PFS included age 40 years or older, ECOG performance status 2 or greater, stage 3 or 4 disease, marrow involvement, CNS involvement, LDH more than three times the upper limit of normal, and hemoglobin <11.5 g/dL (P < .001 for all preceding), as well as albumin <3.5 g/dL (P = .001).
“However, the multivariable analysis was more complicated, because many of these factors were overlapping, and most patients with high LDH also had advanced disease, and this group also encompassed patients who had bone marrow and CNS involvement,” he said.
Using the two types of regression analysis mentioned before, investigators identified ECOG performance status 2 or greater (P = .001), age 40 and older (P = .005), LDH greater than three times the upper limit of normal (P < .001) and CNS involvement (P = .002) as significant predictors for worse outcomes in multivariable analysis, and were included in the final model.
“We initially had five groups according to the number of these factors, but we observed that the survival curves for patients with two, three, or four factors were overlapping, and not significantly different, so ultimately we had three risk groups. In the derivation (U.S.) cohort, patients in the low-risk group, with no risk factors, a 3-year PFS of 92%, compared with 72% for patients with one risk factor (intermediate risk), and 53% for patients with two to four risk factors (high risk).
Respective hazard ratios for worse PFS in the low-, intermediate-, and high-risk groups were 1 (reference), 4.15 (95% confidence interval, 1.99-8.68), and 8.83 (95% CI, 4.32-18.03).
Respective HR for worse OS was 1, 7.06 (95% CI, 2.55-19.53), and 15.12 (95% CI, 5.58-40.99).
There were no significant differences in either PFS or OS when either LDH or stage was added into the model.
The BL-IPI was prognostic for PFS and OS in all subgroups, including HIV-positive or -negative patients, those with MYC rearrangements, stage 1 or 2 versus stage 3 or 4, or those treated with rituximab versus those who were not.
As noted before, 3-year PFS rates in the validation cohort for low, intermediate, high-risk groups were 96%, 82%, and 63% respectively, and 3-year OS rates were 99%, 85%, and 64%.
Why the CNS discrepancy?
In the question and answer session following the presentation, comoderator Christopher J. Melani, MD, from the Lymphoid Malignancies Branch at the National Cancer Institute in Bethesda, Md., said that “it was interesting to see the difference between CNS involvement in both the U.S. and the international cohort,” and asked whether Dr. Olszweski could elaborate on whether baseline CNS involvement was assessed by contrast-enhanced MRI of flow cytometry studies of cerebrospinal fluid.
“Could some of these differences between the U.S. and the international cohort be from the baseline assessment differing between the two?” he asked.
Dr. Olszewski replied that the retrospective nature of the data precluded capturing those data, but added that “I do suspect there may be some differences in the way that central nervous system is staged in different countries. In the United States the use of flow cytometry is more commonly employed, but we don’t know how it is used internationally. We do not know how often this is staged radiographically.”
Asked by others who viewed the presentation whether extranodal disease or peripheral blood involvement were prognostic in the final model, Dr. Olszewski replied that “one has to understand that, when one constructs a prognostic index, there is a balance between trying to input as much information as possible and to create something that is useful, clinically meaningful, and accurate.”
He said that, despite trying different models with different factors, “we couldn’t get the discrimination to be much better than the basic model that we ultimately created, so we favored using a more parsimonious model.”
No study funding source was reported. Dr. Olszewski reported research funding from Spectrum Pharmaceuticals, Genentech, TG Therapeutics, and Adaptive Biotechnologies. Dr. Melani reported having no relevant conflicts of interest.
SOURCE: Olszewski AJ et al. ASH 2020, Abstract 705.
FROM ASH 2020
Well tolerated with promising responses in ALL/LL: Venetoclax plus navitoclax plus chemotherapy
In heavily pretreated pediatric patients with relapsed or refractory acute lymphoblastic leukemia (ALL) or lymphoblastic lymphoma (LL), venetoclax plus navitoclax with chemotherapy was well tolerated with promising responses, according to results of a phase 1 trial. Delayed count recovery, however, stated lead author Jeffrey E. Rubnitz, MD, PhD, St. Jude’s Children’s Research Hospital, Memphis, remained a key safety concern.
Unmet medical need
Despite intensive chemotherapy and novel therapeutics, Dr. Rubnitz said in a virtual oral presentation at the annual meeting of the American Society of Hematology, patients with relapsed or refractory ALL and LL have a poor prognosis and represent an unmet medical need. Venetoclax, a potent, highly selective oral B-cell lymphoma 2 inhibitor, and navitoclax, an oral BCL-2, BCL-XL, and BCL-W inhibitor, directly bind their BCL-2 family member targets to promote apoptosis. In ALL preclinical models, venetoclax and navitoclax have demonstrated antileukemic effects, which suggests dependence on BCL-2 family members. Venetoclax efficacy associated with BCL-2 family inhibition may be potentiated and dose-limiting thrombocytopenia associated with standard-dose navitoclax monotherapy may be avoided by adding venetoclax to low-dose navitoclax. Previous reports of an ongoing phase 1, multicenter, open-label, dose-escalation study in an adult and pediatric population (NCT03181126), Dr. Rubnitz noted, showed the venetoclax/navitoclax/chemotherapy combination to be well tolerated with promising response rates. In the current report, Dr. Rubnitz presented data on the safety, tolerability, pharmacokinetics, and antitumor activity of the triplet regimen in the subgroup of pediatric patients.
The study included pediatric patients (ages, 4-18 years and weight ≥20 kg) receiving venetoclax (weight-adjusted equivalent of 400 mg daily) and navitoclax at three dose levels (25, 50, 100 mg) for patients weighing ≥45 kg and two dose levels (25, 50 mg) for patients weighing <45 kg. At investigator’s discretion, patients could receive chemotherapy (polyethylene glycosylated–asparaginase, vincristine, and dexamethasone). The primary outcomes were safety (including incidence of dose-limiting toxicities and adverse events) and pharmacokinetics. A safety expansion cohort assessed a 21-day dosing schedule of venetoclax at 400 mg followed by 7 days off plus navitoclax at 50 mg (patients ≥45 kg) or 25 mg (patients <45 kg).
Investigators enrolled 18 patients <18 years (median age, 10 years; range, 6-16; 56% male), with 12 in the dose-escalation cohort and 6 in the safety-expansion cohort. Three patients had prior chimeric antigen receptor (CAR) T treatment and four had received prior stem cell transplantation. In the overall cohort, B-cell ALL was most common (n = 13, 72%), with T-cell ALL (n = 3, 17%) and LL (n = 2, 11%) following. The median number of prior therapies was 2 (range 1-6). All patients received chemotherapy.
Grade 3-4 adverse events
Venetoclax-related grade 3-4 adverse events occurred in 56% of patients. Similarly, navitoclax-related grade 3-4 events were reported in 56% of patients. Navitoclax dose-limiting toxicities occurred in two patients (11%), delayed count recovery on 25 mg and sepsis on 50 mg. No grade 5 adverse events and tumor lysis syndrome were reported.
Among secondary endpoint efficacy parameters, complete responses, CRs with incomplete marrow recovery (CRi) and CRs without platelet recovery (CRp) combined occurred in 62% of B-ALL patients (8/13), 33% of T-cell ALL patients (1/3) and in 50% of LL patients (1/2). Separately, CRs/CRis/CRps occurred in 33%/22%/0% of all patients, respectively.
Subsequently, 5 of 18 (28%) of patients proceeded to stem cell transplantation and 3 (17%) to CAR T. Eight patients (44%) died from disease progression.
BH3 profiling
BH3 profiling revealed that at baseline, patients with B-cell ALL had more diversity in BCL-2 and BCL-XL dependency than did patients with T-cell ALL or early T-cell precursor ALL. The fact that responses were observed in patients who were BCL-2 or BCL-XL dependent, Dr. Rubnitz said, supports the use of venetoclax plus navitoclax in these patients. Analysis of these results led to a recommended phase 2 dose for pediatric patients of 400 mg venetoclax with 25 mg navitoclax (for patients weighing <45 kg) or 50 mg navitoclax (for patients weighing 45 kg or more).
Dr. Rubnitz concluded: “Venetoclax plus navitoclax plus chemotherapy was well tolerated in pediatric patients with relapsed/refractory ALL or LL, with promising response rates observed in a heavily pretreated pediatric population.”
Asked whether the combination might be used also before the refractory setting, in a minimal residual disease (MRD) setting, Dr. Rubnitz replied: “We have a lot of safety data on venetoclax but very little on navitoclax. The next trial, being developed by Seth Karol, MD, will include relapsed patients. MRD-positive patients will also be eligible for enrollment.” To a further question as to whether guiding titration via BH3 profiling would lead to improved outcomes, Dr. Rubnitz said, “I think BH3 profiling can be used to identify which patients will respond to these drugs, but we are still a long way from using it for titrating the doses and dose ratios for the two drugs.”
Dr. Rubnitz disclosed research funding from AbbVie.
SOURCE: Rubnitz JE et al. ASH 2020, Abstract 466.
In heavily pretreated pediatric patients with relapsed or refractory acute lymphoblastic leukemia (ALL) or lymphoblastic lymphoma (LL), venetoclax plus navitoclax with chemotherapy was well tolerated with promising responses, according to results of a phase 1 trial. Delayed count recovery, however, stated lead author Jeffrey E. Rubnitz, MD, PhD, St. Jude’s Children’s Research Hospital, Memphis, remained a key safety concern.
Unmet medical need
Despite intensive chemotherapy and novel therapeutics, Dr. Rubnitz said in a virtual oral presentation at the annual meeting of the American Society of Hematology, patients with relapsed or refractory ALL and LL have a poor prognosis and represent an unmet medical need. Venetoclax, a potent, highly selective oral B-cell lymphoma 2 inhibitor, and navitoclax, an oral BCL-2, BCL-XL, and BCL-W inhibitor, directly bind their BCL-2 family member targets to promote apoptosis. In ALL preclinical models, venetoclax and navitoclax have demonstrated antileukemic effects, which suggests dependence on BCL-2 family members. Venetoclax efficacy associated with BCL-2 family inhibition may be potentiated and dose-limiting thrombocytopenia associated with standard-dose navitoclax monotherapy may be avoided by adding venetoclax to low-dose navitoclax. Previous reports of an ongoing phase 1, multicenter, open-label, dose-escalation study in an adult and pediatric population (NCT03181126), Dr. Rubnitz noted, showed the venetoclax/navitoclax/chemotherapy combination to be well tolerated with promising response rates. In the current report, Dr. Rubnitz presented data on the safety, tolerability, pharmacokinetics, and antitumor activity of the triplet regimen in the subgroup of pediatric patients.
The study included pediatric patients (ages, 4-18 years and weight ≥20 kg) receiving venetoclax (weight-adjusted equivalent of 400 mg daily) and navitoclax at three dose levels (25, 50, 100 mg) for patients weighing ≥45 kg and two dose levels (25, 50 mg) for patients weighing <45 kg. At investigator’s discretion, patients could receive chemotherapy (polyethylene glycosylated–asparaginase, vincristine, and dexamethasone). The primary outcomes were safety (including incidence of dose-limiting toxicities and adverse events) and pharmacokinetics. A safety expansion cohort assessed a 21-day dosing schedule of venetoclax at 400 mg followed by 7 days off plus navitoclax at 50 mg (patients ≥45 kg) or 25 mg (patients <45 kg).
Investigators enrolled 18 patients <18 years (median age, 10 years; range, 6-16; 56% male), with 12 in the dose-escalation cohort and 6 in the safety-expansion cohort. Three patients had prior chimeric antigen receptor (CAR) T treatment and four had received prior stem cell transplantation. In the overall cohort, B-cell ALL was most common (n = 13, 72%), with T-cell ALL (n = 3, 17%) and LL (n = 2, 11%) following. The median number of prior therapies was 2 (range 1-6). All patients received chemotherapy.
Grade 3-4 adverse events
Venetoclax-related grade 3-4 adverse events occurred in 56% of patients. Similarly, navitoclax-related grade 3-4 events were reported in 56% of patients. Navitoclax dose-limiting toxicities occurred in two patients (11%), delayed count recovery on 25 mg and sepsis on 50 mg. No grade 5 adverse events and tumor lysis syndrome were reported.
Among secondary endpoint efficacy parameters, complete responses, CRs with incomplete marrow recovery (CRi) and CRs without platelet recovery (CRp) combined occurred in 62% of B-ALL patients (8/13), 33% of T-cell ALL patients (1/3) and in 50% of LL patients (1/2). Separately, CRs/CRis/CRps occurred in 33%/22%/0% of all patients, respectively.
Subsequently, 5 of 18 (28%) of patients proceeded to stem cell transplantation and 3 (17%) to CAR T. Eight patients (44%) died from disease progression.
BH3 profiling
BH3 profiling revealed that at baseline, patients with B-cell ALL had more diversity in BCL-2 and BCL-XL dependency than did patients with T-cell ALL or early T-cell precursor ALL. The fact that responses were observed in patients who were BCL-2 or BCL-XL dependent, Dr. Rubnitz said, supports the use of venetoclax plus navitoclax in these patients. Analysis of these results led to a recommended phase 2 dose for pediatric patients of 400 mg venetoclax with 25 mg navitoclax (for patients weighing <45 kg) or 50 mg navitoclax (for patients weighing 45 kg or more).
Dr. Rubnitz concluded: “Venetoclax plus navitoclax plus chemotherapy was well tolerated in pediatric patients with relapsed/refractory ALL or LL, with promising response rates observed in a heavily pretreated pediatric population.”
Asked whether the combination might be used also before the refractory setting, in a minimal residual disease (MRD) setting, Dr. Rubnitz replied: “We have a lot of safety data on venetoclax but very little on navitoclax. The next trial, being developed by Seth Karol, MD, will include relapsed patients. MRD-positive patients will also be eligible for enrollment.” To a further question as to whether guiding titration via BH3 profiling would lead to improved outcomes, Dr. Rubnitz said, “I think BH3 profiling can be used to identify which patients will respond to these drugs, but we are still a long way from using it for titrating the doses and dose ratios for the two drugs.”
Dr. Rubnitz disclosed research funding from AbbVie.
SOURCE: Rubnitz JE et al. ASH 2020, Abstract 466.
In heavily pretreated pediatric patients with relapsed or refractory acute lymphoblastic leukemia (ALL) or lymphoblastic lymphoma (LL), venetoclax plus navitoclax with chemotherapy was well tolerated with promising responses, according to results of a phase 1 trial. Delayed count recovery, however, stated lead author Jeffrey E. Rubnitz, MD, PhD, St. Jude’s Children’s Research Hospital, Memphis, remained a key safety concern.
Unmet medical need
Despite intensive chemotherapy and novel therapeutics, Dr. Rubnitz said in a virtual oral presentation at the annual meeting of the American Society of Hematology, patients with relapsed or refractory ALL and LL have a poor prognosis and represent an unmet medical need. Venetoclax, a potent, highly selective oral B-cell lymphoma 2 inhibitor, and navitoclax, an oral BCL-2, BCL-XL, and BCL-W inhibitor, directly bind their BCL-2 family member targets to promote apoptosis. In ALL preclinical models, venetoclax and navitoclax have demonstrated antileukemic effects, which suggests dependence on BCL-2 family members. Venetoclax efficacy associated with BCL-2 family inhibition may be potentiated and dose-limiting thrombocytopenia associated with standard-dose navitoclax monotherapy may be avoided by adding venetoclax to low-dose navitoclax. Previous reports of an ongoing phase 1, multicenter, open-label, dose-escalation study in an adult and pediatric population (NCT03181126), Dr. Rubnitz noted, showed the venetoclax/navitoclax/chemotherapy combination to be well tolerated with promising response rates. In the current report, Dr. Rubnitz presented data on the safety, tolerability, pharmacokinetics, and antitumor activity of the triplet regimen in the subgroup of pediatric patients.
The study included pediatric patients (ages, 4-18 years and weight ≥20 kg) receiving venetoclax (weight-adjusted equivalent of 400 mg daily) and navitoclax at three dose levels (25, 50, 100 mg) for patients weighing ≥45 kg and two dose levels (25, 50 mg) for patients weighing <45 kg. At investigator’s discretion, patients could receive chemotherapy (polyethylene glycosylated–asparaginase, vincristine, and dexamethasone). The primary outcomes were safety (including incidence of dose-limiting toxicities and adverse events) and pharmacokinetics. A safety expansion cohort assessed a 21-day dosing schedule of venetoclax at 400 mg followed by 7 days off plus navitoclax at 50 mg (patients ≥45 kg) or 25 mg (patients <45 kg).
Investigators enrolled 18 patients <18 years (median age, 10 years; range, 6-16; 56% male), with 12 in the dose-escalation cohort and 6 in the safety-expansion cohort. Three patients had prior chimeric antigen receptor (CAR) T treatment and four had received prior stem cell transplantation. In the overall cohort, B-cell ALL was most common (n = 13, 72%), with T-cell ALL (n = 3, 17%) and LL (n = 2, 11%) following. The median number of prior therapies was 2 (range 1-6). All patients received chemotherapy.
Grade 3-4 adverse events
Venetoclax-related grade 3-4 adverse events occurred in 56% of patients. Similarly, navitoclax-related grade 3-4 events were reported in 56% of patients. Navitoclax dose-limiting toxicities occurred in two patients (11%), delayed count recovery on 25 mg and sepsis on 50 mg. No grade 5 adverse events and tumor lysis syndrome were reported.
Among secondary endpoint efficacy parameters, complete responses, CRs with incomplete marrow recovery (CRi) and CRs without platelet recovery (CRp) combined occurred in 62% of B-ALL patients (8/13), 33% of T-cell ALL patients (1/3) and in 50% of LL patients (1/2). Separately, CRs/CRis/CRps occurred in 33%/22%/0% of all patients, respectively.
Subsequently, 5 of 18 (28%) of patients proceeded to stem cell transplantation and 3 (17%) to CAR T. Eight patients (44%) died from disease progression.
BH3 profiling
BH3 profiling revealed that at baseline, patients with B-cell ALL had more diversity in BCL-2 and BCL-XL dependency than did patients with T-cell ALL or early T-cell precursor ALL. The fact that responses were observed in patients who were BCL-2 or BCL-XL dependent, Dr. Rubnitz said, supports the use of venetoclax plus navitoclax in these patients. Analysis of these results led to a recommended phase 2 dose for pediatric patients of 400 mg venetoclax with 25 mg navitoclax (for patients weighing <45 kg) or 50 mg navitoclax (for patients weighing 45 kg or more).
Dr. Rubnitz concluded: “Venetoclax plus navitoclax plus chemotherapy was well tolerated in pediatric patients with relapsed/refractory ALL or LL, with promising response rates observed in a heavily pretreated pediatric population.”
Asked whether the combination might be used also before the refractory setting, in a minimal residual disease (MRD) setting, Dr. Rubnitz replied: “We have a lot of safety data on venetoclax but very little on navitoclax. The next trial, being developed by Seth Karol, MD, will include relapsed patients. MRD-positive patients will also be eligible for enrollment.” To a further question as to whether guiding titration via BH3 profiling would lead to improved outcomes, Dr. Rubnitz said, “I think BH3 profiling can be used to identify which patients will respond to these drugs, but we are still a long way from using it for titrating the doses and dose ratios for the two drugs.”
Dr. Rubnitz disclosed research funding from AbbVie.
SOURCE: Rubnitz JE et al. ASH 2020, Abstract 466.
FROM ASH 2020
FDA clears first OTC rapid at-home COVID diagnostic test
The Food and Drug Administration has issued an emergency-use authorization (EUA) for the first COVID-19 diagnostic test that can be completed at home without a prescription.
Authorization of the Ellume COVID-19 Home Test is “a major milestone in diagnostic testing for COVID-19,” FDA Commissioner Stephen M. Hahn, MD, said in a news release.
“By authorizing a test for over-the-counter use, the FDA allows it to be sold in places like drug stores, where a patient can buy it, swab their nose, run the test, and find out their results in as little as 20 minutes,” said Dr. Hahn.
The Ellume COVID-19 Home Test is a rapid antigen test that detects fragments of the SARS-CoV-2 virus from a nasal swab sample taken from anyone aged 2 years and older, including those not showing any symptoms.
In testing, the Ellume COVID-19 Home Test correctly identified 96% of positive samples and 100% of negative samples in individuals with symptoms.
In people without symptoms, the test correctly identified 91% of positive samples and 96% of negative samples, the FDA said.
The test includes a sterile nasal swab, a dropper, processing fluid, and a Bluetooth-connected analyzer for use with an app on the user’s smartphone. The sample is analyzed and results are automatically transmitted to the user’s smartphone.
“The Ellume COVID-19 home test’s core technology combines ultra-sensitive optics, electronics, and proprietary software to leverage best-in-class digital immunoassay technology with next-generation multi-quantum dot fluorescence technology,” the company said in a news release.
The mobile app requires individuals to input their ZIP code and date of birth, with optional fields including name and email address. The app automatically reports the results as appropriate to public health authorities to monitor disease prevalence.
Ellume expects to produce more than 3 million tests in January 2021. The company said the test will cost around $30.
FDA authorization of this first fully at-home nonprescription COVID-19 diagnostic test follows last month’s EUA for the first prescription COVID-19 test for home use, as reported this news organization.
Since the start of the pandemic, the FDA has authorized more than 225 diagnostic tests for COVID-19, including more than 25 tests that allow for home collection of samples, which are then sent to a lab for testing.
“As we continue to authorize additional tests for home use, we are helping expand Americans’ access to testing, reducing the burden on laboratories and test supplies, and giving Americans more testing options from the comfort and safety of their own homes,” Dr. Hahn said.
“This test, like other antigen tests, is less sensitive and less specific than typical molecular tests run in a lab,” said Jeffrey Shuren, MD, JD, director of FDA’s Center for Devices and Radiological Health, in the release. “However, the fact that it can be used completely at home and return results quickly means that it can play an important role in response to the pandemic.”
As with other antigen tests, a small percentage of positive and negative results from the Ellume test may be false. In patients without symptoms, positive results should be treated as presumptively positive until confirmed by another test as soon as possible, the FDA advised.
This is especially true if there are fewer infections in a particular community, as false-positive results can be more common when antigen tests are used in populations where there is a low prevalence of COVID-19, the agency said.
Because all tests can give false-negative and false-positive results, individuals with positive results should self-isolate and seek additional care from their health care provider.
Individuals who test negative and have symptoms of COVID-19 should follow up with their health care provider, as negative results don’t preclude an individual from SARS-CoV-2 infection.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has issued an emergency-use authorization (EUA) for the first COVID-19 diagnostic test that can be completed at home without a prescription.
Authorization of the Ellume COVID-19 Home Test is “a major milestone in diagnostic testing for COVID-19,” FDA Commissioner Stephen M. Hahn, MD, said in a news release.
“By authorizing a test for over-the-counter use, the FDA allows it to be sold in places like drug stores, where a patient can buy it, swab their nose, run the test, and find out their results in as little as 20 minutes,” said Dr. Hahn.
The Ellume COVID-19 Home Test is a rapid antigen test that detects fragments of the SARS-CoV-2 virus from a nasal swab sample taken from anyone aged 2 years and older, including those not showing any symptoms.
In testing, the Ellume COVID-19 Home Test correctly identified 96% of positive samples and 100% of negative samples in individuals with symptoms.
In people without symptoms, the test correctly identified 91% of positive samples and 96% of negative samples, the FDA said.
The test includes a sterile nasal swab, a dropper, processing fluid, and a Bluetooth-connected analyzer for use with an app on the user’s smartphone. The sample is analyzed and results are automatically transmitted to the user’s smartphone.
“The Ellume COVID-19 home test’s core technology combines ultra-sensitive optics, electronics, and proprietary software to leverage best-in-class digital immunoassay technology with next-generation multi-quantum dot fluorescence technology,” the company said in a news release.
The mobile app requires individuals to input their ZIP code and date of birth, with optional fields including name and email address. The app automatically reports the results as appropriate to public health authorities to monitor disease prevalence.
Ellume expects to produce more than 3 million tests in January 2021. The company said the test will cost around $30.
FDA authorization of this first fully at-home nonprescription COVID-19 diagnostic test follows last month’s EUA for the first prescription COVID-19 test for home use, as reported this news organization.
Since the start of the pandemic, the FDA has authorized more than 225 diagnostic tests for COVID-19, including more than 25 tests that allow for home collection of samples, which are then sent to a lab for testing.
“As we continue to authorize additional tests for home use, we are helping expand Americans’ access to testing, reducing the burden on laboratories and test supplies, and giving Americans more testing options from the comfort and safety of their own homes,” Dr. Hahn said.
“This test, like other antigen tests, is less sensitive and less specific than typical molecular tests run in a lab,” said Jeffrey Shuren, MD, JD, director of FDA’s Center for Devices and Radiological Health, in the release. “However, the fact that it can be used completely at home and return results quickly means that it can play an important role in response to the pandemic.”
As with other antigen tests, a small percentage of positive and negative results from the Ellume test may be false. In patients without symptoms, positive results should be treated as presumptively positive until confirmed by another test as soon as possible, the FDA advised.
This is especially true if there are fewer infections in a particular community, as false-positive results can be more common when antigen tests are used in populations where there is a low prevalence of COVID-19, the agency said.
Because all tests can give false-negative and false-positive results, individuals with positive results should self-isolate and seek additional care from their health care provider.
Individuals who test negative and have symptoms of COVID-19 should follow up with their health care provider, as negative results don’t preclude an individual from SARS-CoV-2 infection.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has issued an emergency-use authorization (EUA) for the first COVID-19 diagnostic test that can be completed at home without a prescription.
Authorization of the Ellume COVID-19 Home Test is “a major milestone in diagnostic testing for COVID-19,” FDA Commissioner Stephen M. Hahn, MD, said in a news release.
“By authorizing a test for over-the-counter use, the FDA allows it to be sold in places like drug stores, where a patient can buy it, swab their nose, run the test, and find out their results in as little as 20 minutes,” said Dr. Hahn.
The Ellume COVID-19 Home Test is a rapid antigen test that detects fragments of the SARS-CoV-2 virus from a nasal swab sample taken from anyone aged 2 years and older, including those not showing any symptoms.
In testing, the Ellume COVID-19 Home Test correctly identified 96% of positive samples and 100% of negative samples in individuals with symptoms.
In people without symptoms, the test correctly identified 91% of positive samples and 96% of negative samples, the FDA said.
The test includes a sterile nasal swab, a dropper, processing fluid, and a Bluetooth-connected analyzer for use with an app on the user’s smartphone. The sample is analyzed and results are automatically transmitted to the user’s smartphone.
“The Ellume COVID-19 home test’s core technology combines ultra-sensitive optics, electronics, and proprietary software to leverage best-in-class digital immunoassay technology with next-generation multi-quantum dot fluorescence technology,” the company said in a news release.
The mobile app requires individuals to input their ZIP code and date of birth, with optional fields including name and email address. The app automatically reports the results as appropriate to public health authorities to monitor disease prevalence.
Ellume expects to produce more than 3 million tests in January 2021. The company said the test will cost around $30.
FDA authorization of this first fully at-home nonprescription COVID-19 diagnostic test follows last month’s EUA for the first prescription COVID-19 test for home use, as reported this news organization.
Since the start of the pandemic, the FDA has authorized more than 225 diagnostic tests for COVID-19, including more than 25 tests that allow for home collection of samples, which are then sent to a lab for testing.
“As we continue to authorize additional tests for home use, we are helping expand Americans’ access to testing, reducing the burden on laboratories and test supplies, and giving Americans more testing options from the comfort and safety of their own homes,” Dr. Hahn said.
“This test, like other antigen tests, is less sensitive and less specific than typical molecular tests run in a lab,” said Jeffrey Shuren, MD, JD, director of FDA’s Center for Devices and Radiological Health, in the release. “However, the fact that it can be used completely at home and return results quickly means that it can play an important role in response to the pandemic.”
As with other antigen tests, a small percentage of positive and negative results from the Ellume test may be false. In patients without symptoms, positive results should be treated as presumptively positive until confirmed by another test as soon as possible, the FDA advised.
This is especially true if there are fewer infections in a particular community, as false-positive results can be more common when antigen tests are used in populations where there is a low prevalence of COVID-19, the agency said.
Because all tests can give false-negative and false-positive results, individuals with positive results should self-isolate and seek additional care from their health care provider.
Individuals who test negative and have symptoms of COVID-19 should follow up with their health care provider, as negative results don’t preclude an individual from SARS-CoV-2 infection.
A version of this article first appeared on Medscape.com.
Six big changes coming for office-visit coding
Betsy Nicoletti, MS, a nationally recognized coding expert, will take your coding questions via email and provide guidance on how to code properly to maximize reimbursement. Have a question about coding? Send it to [email protected].
thanks to the American Medical Association.
The first major changes to the definitions for E/M services will be in effect as of Jan. 1, 2021, with all payers expected to adopt these new guidelines. In particular, the AMA has revised the definitions for E/M codes 99202-99215 in the Current Procedural Terminology (CPT) 2021 codebook. The existing guidelines were developed in 1995 and 1997 and remain in effect for all other E/M services determined by history, exam, and medical decision-making (MDM).
What do the new changes mean to you? In 2021, for new and established office and other outpatient services reported with codes 99202-99215, a clinician may select the code on the basis of time or MDM.
There are three elements in MDM, and two of three are required. These elements are the number and complexity of problems addressed, amount and/or complexity of data to be reviewed and analyzed, and risk of complications and/or morbidity or mortality of patient management.
Make sure you familiarize yourself with these six big changes. It may take a bit of time to integrate these new processes into your daily routine, but wrapping your head around them as soon as possible can help boost your bottom line:
1. History and exam don’t count toward level of service
Physicians, advanced practice registered nurses, and physician assistants won’t use history or exam to select what level of code to bill for office visits 99202-99215, as they did in the past. They need only document a medically appropriate history and exam. The history may be obtained by staff members and reviewed by the billing practitioner.
While specific history and exam requirements disappear for office visit codes, they remain for all other types of visits, selected on the basis of history, exam, and MDM, such as hospital services, nursing facility services, and home and domiciliary care. So, say goodbye to “all other systems reviewed and negative” in office notes, but keep it handy for those other E/M codes.
2. All time spent caring for the patient on a particular day counts
This includes all time spent on the day of service, including preparing to see the patient, seeing the patient, phone calls or other work done after the visit (if not billed with a care management or other CPT code), and documenting in the medical record. The AMA developed new guidelines for using time for office and other outpatient services. For codes 99202-99215, count all of the face-to-face and non–face-to-face time spent by the billing clinician on the day of the visit. Counseling does not need to be more than 50% of the total time.
Do not include any staff time or time spent on any days before or after the visit. This allows clinicians to capture the work when a significant amount of it takes place before or after the visit with the patient, and to bill for it on the day of the visit.
According to the 2021 CPT codebook, physician or other qualified health care professional time includes the following activities:
- Preparing to see the patient (e.g., review of tests).
- Obtaining and/or reviewing separately obtained history.
- Performing a medically appropriate examination and/or evaluation.
- Counseling and educating the patient/family/caregiver.
- Ordering medications, tests, or procedures.
- Referring and communicating with other health care professionals (when not separately reported).
- Documenting clinical information in the electronic or other health record.
- Independently interpreting results (not separately reported) and communicating results to the patient/family/caregiver.
- Care coordination (not separately reported).
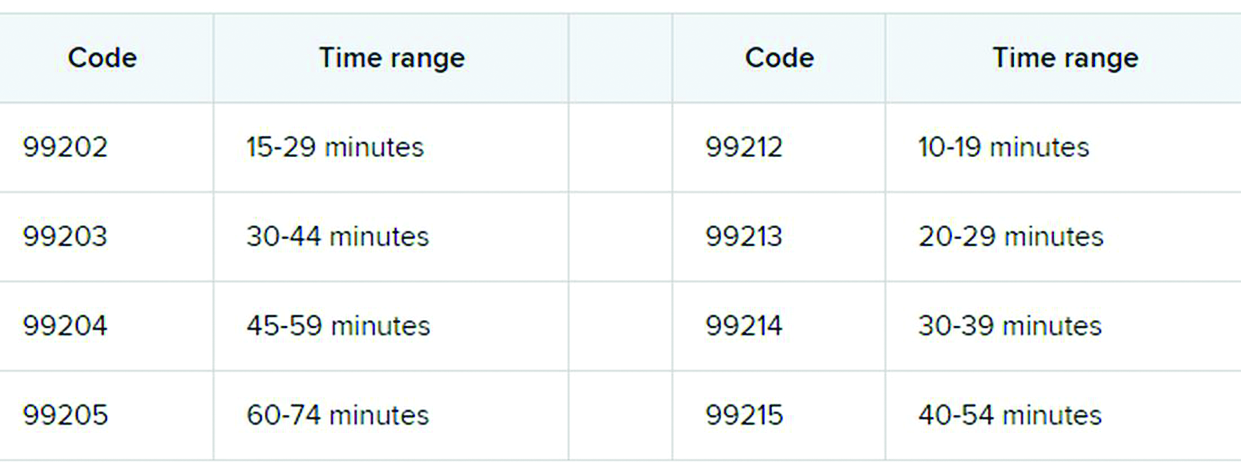
3. Soon to be gone: ‘new to the examiner’ and ‘workup planned’
The current guidelines don’t differentiate between a new problem to the clinician or an established problem to the clinician. So it doesn’t matter whether you’re hearing about a particular problem for the first time or the fifth time. The new office and outpatient services guidelines define problems only as they relate to the patient. For example, when selecting a level of service, a chronic problem with a mild exacerbation is the same level whether it’s the primary care physician seeing the patient for the 10th time to help manage her diabetes or the endocrinologist seeing the patient for the first time.
In the current guidelines (1995 and 1997), additional weight is given in selecting the level of MDM for a problem that’s new to the examiner with a workup planned, yet when the diagnostic test couldn’t be completed at the visit. This concept is gone from element of number and complexity of new problems. Ordering diagnostic tests is part of the second element, the amount and/or complexity of data to be reviewed.
4. Different guidelines if you need a history from a parent or other source
The new guidelines recognize the additional work required by the clinician when the patient is unable to give a history or when the practitioner doesn’t find the history to be reliable.
For example, in the case of a baby or child who is unable to give a history, the parent counts as an “independent historian,” according to the new guidelines. Likewise, for a patient with dementia, the caregiver counts as a historian. Note, however, that the criteria is not met simply because the patient is accompanied by another person. The additional weight in selecting the level of service is based on the patient being unable to give a reliable history.
Bottom line: In cases where patients are unable to communicate clearly, physicians or other providers should document the necessity of getting a complete history and who provided it.
5. A new spin on social determinants of health (SDoH)
In the risk of morbidity and/or mortality element, conditions described as “social determinants of health” are considered moderate complexity. SDoH are social and environmental factors that affect a patient’s health and medical outcomes. These include homelessness, inability to afford medications, food insecurity, and occupational exposure to risk factors. These circumstances are reported with codes in categories Z55-Z65.
In the past, physicians often documented this information in their office notes but rarely added a diagnosis code that described the patient’s situation. The ICD-10-CM code set includes codes that describe these factors. Using them allows the practice to track patients who have increased needs, and it communicates to payers the complexity of caring for these patients.
6. Risks related to surgery are defined
The current guidelines assign different levels of risk to minor and major surgery. They also include differentiation for “minor surgery with no identified risk factors,” “minor surgery with identified risk factors,” “elective major surgery with no identified risk factors,” and “elective major surgery with identified risk factors.” The old guidelines didn’t state whether the risk factors pertained to the patient – such as smoking, heart disease, or high body mass index – or to the procedure itself.
The new guidelines specifically say that it’s both. In the risk column, “decision regarding minor surgery with identified patient or procedure risk factors” and “decision regarding elective major surgery without patient or procedure risk factors” are both considered moderate. “Decision regarding elective major surgery with identified patient or procedure risk factors” and “decision regarding emergency major surgery” are in the high complexity column for risk.
Keep in mind that two of three elements are required: the number and complexity of problems, amount of data, and morbidity/mortality risk. Risk of morbidity/mortality alone doesn’t count as the basis for selecting the code. Of course, when surgeons see this, they ask, “What major procedures don’t have identified risk factors?”
Note, too, that these new CPT guidelines do not define the terms “minor” and “major” surgery. For payment reasons related to the postop period, the Centers for Medicare & Medicaid Services defines minor surgery as a procedure with 0-10 global days and a major surgery as a procedure with 90 global days. However, there are many procedures with 0 global days (endoscopy, cardiac catheterization) that are not minor procedures. Hopefully, the AMA will clarify this in 2021.
What’s the take-away for clinicians?
There are sure to be shifts in coding patterns based on these new guidelines. Some specialties will find that not being able to select a service based on history and exam alone will lower the level of service for which they can bill. Some practices, on the other hand, will be able to code for more high-level visits, without the need for a complete review of systems or a comprehensive exam.
The biggest challenge will be for practices that provide services both in the hospital and in the office, because they’ll have to use both sets of guidelines, depending on which type of service they’re performing.
For more details on what’s coming your way beginning on New Year’s Day, you may want to read the 16-page AMA document .
A version of this article first appeared on Medscape.com.
Betsy Nicoletti, MS, a nationally recognized coding expert, will take your coding questions via email and provide guidance on how to code properly to maximize reimbursement. Have a question about coding? Send it to [email protected].
thanks to the American Medical Association.
The first major changes to the definitions for E/M services will be in effect as of Jan. 1, 2021, with all payers expected to adopt these new guidelines. In particular, the AMA has revised the definitions for E/M codes 99202-99215 in the Current Procedural Terminology (CPT) 2021 codebook. The existing guidelines were developed in 1995 and 1997 and remain in effect for all other E/M services determined by history, exam, and medical decision-making (MDM).
What do the new changes mean to you? In 2021, for new and established office and other outpatient services reported with codes 99202-99215, a clinician may select the code on the basis of time or MDM.
There are three elements in MDM, and two of three are required. These elements are the number and complexity of problems addressed, amount and/or complexity of data to be reviewed and analyzed, and risk of complications and/or morbidity or mortality of patient management.
Make sure you familiarize yourself with these six big changes. It may take a bit of time to integrate these new processes into your daily routine, but wrapping your head around them as soon as possible can help boost your bottom line:
1. History and exam don’t count toward level of service
Physicians, advanced practice registered nurses, and physician assistants won’t use history or exam to select what level of code to bill for office visits 99202-99215, as they did in the past. They need only document a medically appropriate history and exam. The history may be obtained by staff members and reviewed by the billing practitioner.
While specific history and exam requirements disappear for office visit codes, they remain for all other types of visits, selected on the basis of history, exam, and MDM, such as hospital services, nursing facility services, and home and domiciliary care. So, say goodbye to “all other systems reviewed and negative” in office notes, but keep it handy for those other E/M codes.
2. All time spent caring for the patient on a particular day counts
This includes all time spent on the day of service, including preparing to see the patient, seeing the patient, phone calls or other work done after the visit (if not billed with a care management or other CPT code), and documenting in the medical record. The AMA developed new guidelines for using time for office and other outpatient services. For codes 99202-99215, count all of the face-to-face and non–face-to-face time spent by the billing clinician on the day of the visit. Counseling does not need to be more than 50% of the total time.
Do not include any staff time or time spent on any days before or after the visit. This allows clinicians to capture the work when a significant amount of it takes place before or after the visit with the patient, and to bill for it on the day of the visit.
According to the 2021 CPT codebook, physician or other qualified health care professional time includes the following activities:
- Preparing to see the patient (e.g., review of tests).
- Obtaining and/or reviewing separately obtained history.
- Performing a medically appropriate examination and/or evaluation.
- Counseling and educating the patient/family/caregiver.
- Ordering medications, tests, or procedures.
- Referring and communicating with other health care professionals (when not separately reported).
- Documenting clinical information in the electronic or other health record.
- Independently interpreting results (not separately reported) and communicating results to the patient/family/caregiver.
- Care coordination (not separately reported).
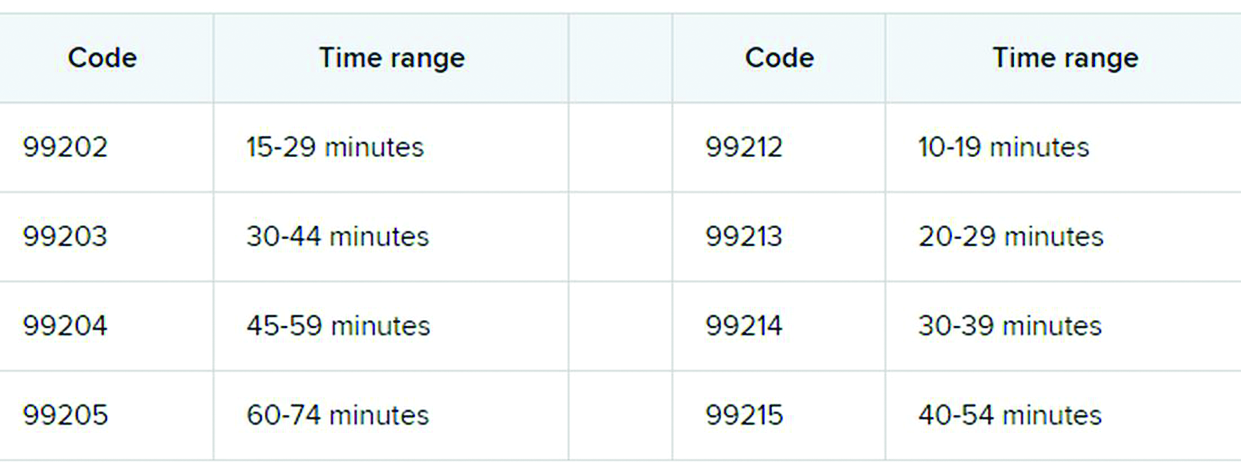
3. Soon to be gone: ‘new to the examiner’ and ‘workup planned’
The current guidelines don’t differentiate between a new problem to the clinician or an established problem to the clinician. So it doesn’t matter whether you’re hearing about a particular problem for the first time or the fifth time. The new office and outpatient services guidelines define problems only as they relate to the patient. For example, when selecting a level of service, a chronic problem with a mild exacerbation is the same level whether it’s the primary care physician seeing the patient for the 10th time to help manage her diabetes or the endocrinologist seeing the patient for the first time.
In the current guidelines (1995 and 1997), additional weight is given in selecting the level of MDM for a problem that’s new to the examiner with a workup planned, yet when the diagnostic test couldn’t be completed at the visit. This concept is gone from element of number and complexity of new problems. Ordering diagnostic tests is part of the second element, the amount and/or complexity of data to be reviewed.
4. Different guidelines if you need a history from a parent or other source
The new guidelines recognize the additional work required by the clinician when the patient is unable to give a history or when the practitioner doesn’t find the history to be reliable.
For example, in the case of a baby or child who is unable to give a history, the parent counts as an “independent historian,” according to the new guidelines. Likewise, for a patient with dementia, the caregiver counts as a historian. Note, however, that the criteria is not met simply because the patient is accompanied by another person. The additional weight in selecting the level of service is based on the patient being unable to give a reliable history.
Bottom line: In cases where patients are unable to communicate clearly, physicians or other providers should document the necessity of getting a complete history and who provided it.
5. A new spin on social determinants of health (SDoH)
In the risk of morbidity and/or mortality element, conditions described as “social determinants of health” are considered moderate complexity. SDoH are social and environmental factors that affect a patient’s health and medical outcomes. These include homelessness, inability to afford medications, food insecurity, and occupational exposure to risk factors. These circumstances are reported with codes in categories Z55-Z65.
In the past, physicians often documented this information in their office notes but rarely added a diagnosis code that described the patient’s situation. The ICD-10-CM code set includes codes that describe these factors. Using them allows the practice to track patients who have increased needs, and it communicates to payers the complexity of caring for these patients.
6. Risks related to surgery are defined
The current guidelines assign different levels of risk to minor and major surgery. They also include differentiation for “minor surgery with no identified risk factors,” “minor surgery with identified risk factors,” “elective major surgery with no identified risk factors,” and “elective major surgery with identified risk factors.” The old guidelines didn’t state whether the risk factors pertained to the patient – such as smoking, heart disease, or high body mass index – or to the procedure itself.
The new guidelines specifically say that it’s both. In the risk column, “decision regarding minor surgery with identified patient or procedure risk factors” and “decision regarding elective major surgery without patient or procedure risk factors” are both considered moderate. “Decision regarding elective major surgery with identified patient or procedure risk factors” and “decision regarding emergency major surgery” are in the high complexity column for risk.
Keep in mind that two of three elements are required: the number and complexity of problems, amount of data, and morbidity/mortality risk. Risk of morbidity/mortality alone doesn’t count as the basis for selecting the code. Of course, when surgeons see this, they ask, “What major procedures don’t have identified risk factors?”
Note, too, that these new CPT guidelines do not define the terms “minor” and “major” surgery. For payment reasons related to the postop period, the Centers for Medicare & Medicaid Services defines minor surgery as a procedure with 0-10 global days and a major surgery as a procedure with 90 global days. However, there are many procedures with 0 global days (endoscopy, cardiac catheterization) that are not minor procedures. Hopefully, the AMA will clarify this in 2021.
What’s the take-away for clinicians?
There are sure to be shifts in coding patterns based on these new guidelines. Some specialties will find that not being able to select a service based on history and exam alone will lower the level of service for which they can bill. Some practices, on the other hand, will be able to code for more high-level visits, without the need for a complete review of systems or a comprehensive exam.
The biggest challenge will be for practices that provide services both in the hospital and in the office, because they’ll have to use both sets of guidelines, depending on which type of service they’re performing.
For more details on what’s coming your way beginning on New Year’s Day, you may want to read the 16-page AMA document .
A version of this article first appeared on Medscape.com.
Betsy Nicoletti, MS, a nationally recognized coding expert, will take your coding questions via email and provide guidance on how to code properly to maximize reimbursement. Have a question about coding? Send it to [email protected].
thanks to the American Medical Association.
The first major changes to the definitions for E/M services will be in effect as of Jan. 1, 2021, with all payers expected to adopt these new guidelines. In particular, the AMA has revised the definitions for E/M codes 99202-99215 in the Current Procedural Terminology (CPT) 2021 codebook. The existing guidelines were developed in 1995 and 1997 and remain in effect for all other E/M services determined by history, exam, and medical decision-making (MDM).
What do the new changes mean to you? In 2021, for new and established office and other outpatient services reported with codes 99202-99215, a clinician may select the code on the basis of time or MDM.
There are three elements in MDM, and two of three are required. These elements are the number and complexity of problems addressed, amount and/or complexity of data to be reviewed and analyzed, and risk of complications and/or morbidity or mortality of patient management.
Make sure you familiarize yourself with these six big changes. It may take a bit of time to integrate these new processes into your daily routine, but wrapping your head around them as soon as possible can help boost your bottom line:
1. History and exam don’t count toward level of service
Physicians, advanced practice registered nurses, and physician assistants won’t use history or exam to select what level of code to bill for office visits 99202-99215, as they did in the past. They need only document a medically appropriate history and exam. The history may be obtained by staff members and reviewed by the billing practitioner.
While specific history and exam requirements disappear for office visit codes, they remain for all other types of visits, selected on the basis of history, exam, and MDM, such as hospital services, nursing facility services, and home and domiciliary care. So, say goodbye to “all other systems reviewed and negative” in office notes, but keep it handy for those other E/M codes.
2. All time spent caring for the patient on a particular day counts
This includes all time spent on the day of service, including preparing to see the patient, seeing the patient, phone calls or other work done after the visit (if not billed with a care management or other CPT code), and documenting in the medical record. The AMA developed new guidelines for using time for office and other outpatient services. For codes 99202-99215, count all of the face-to-face and non–face-to-face time spent by the billing clinician on the day of the visit. Counseling does not need to be more than 50% of the total time.
Do not include any staff time or time spent on any days before or after the visit. This allows clinicians to capture the work when a significant amount of it takes place before or after the visit with the patient, and to bill for it on the day of the visit.
According to the 2021 CPT codebook, physician or other qualified health care professional time includes the following activities:
- Preparing to see the patient (e.g., review of tests).
- Obtaining and/or reviewing separately obtained history.
- Performing a medically appropriate examination and/or evaluation.
- Counseling and educating the patient/family/caregiver.
- Ordering medications, tests, or procedures.
- Referring and communicating with other health care professionals (when not separately reported).
- Documenting clinical information in the electronic or other health record.
- Independently interpreting results (not separately reported) and communicating results to the patient/family/caregiver.
- Care coordination (not separately reported).
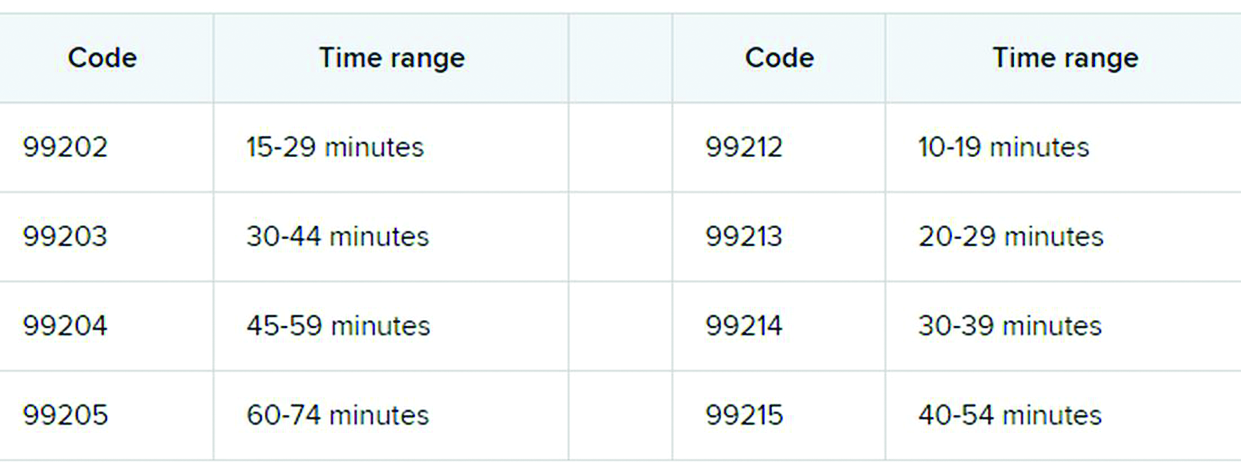
3. Soon to be gone: ‘new to the examiner’ and ‘workup planned’
The current guidelines don’t differentiate between a new problem to the clinician or an established problem to the clinician. So it doesn’t matter whether you’re hearing about a particular problem for the first time or the fifth time. The new office and outpatient services guidelines define problems only as they relate to the patient. For example, when selecting a level of service, a chronic problem with a mild exacerbation is the same level whether it’s the primary care physician seeing the patient for the 10th time to help manage her diabetes or the endocrinologist seeing the patient for the first time.
In the current guidelines (1995 and 1997), additional weight is given in selecting the level of MDM for a problem that’s new to the examiner with a workup planned, yet when the diagnostic test couldn’t be completed at the visit. This concept is gone from element of number and complexity of new problems. Ordering diagnostic tests is part of the second element, the amount and/or complexity of data to be reviewed.
4. Different guidelines if you need a history from a parent or other source
The new guidelines recognize the additional work required by the clinician when the patient is unable to give a history or when the practitioner doesn’t find the history to be reliable.
For example, in the case of a baby or child who is unable to give a history, the parent counts as an “independent historian,” according to the new guidelines. Likewise, for a patient with dementia, the caregiver counts as a historian. Note, however, that the criteria is not met simply because the patient is accompanied by another person. The additional weight in selecting the level of service is based on the patient being unable to give a reliable history.
Bottom line: In cases where patients are unable to communicate clearly, physicians or other providers should document the necessity of getting a complete history and who provided it.
5. A new spin on social determinants of health (SDoH)
In the risk of morbidity and/or mortality element, conditions described as “social determinants of health” are considered moderate complexity. SDoH are social and environmental factors that affect a patient’s health and medical outcomes. These include homelessness, inability to afford medications, food insecurity, and occupational exposure to risk factors. These circumstances are reported with codes in categories Z55-Z65.
In the past, physicians often documented this information in their office notes but rarely added a diagnosis code that described the patient’s situation. The ICD-10-CM code set includes codes that describe these factors. Using them allows the practice to track patients who have increased needs, and it communicates to payers the complexity of caring for these patients.
6. Risks related to surgery are defined
The current guidelines assign different levels of risk to minor and major surgery. They also include differentiation for “minor surgery with no identified risk factors,” “minor surgery with identified risk factors,” “elective major surgery with no identified risk factors,” and “elective major surgery with identified risk factors.” The old guidelines didn’t state whether the risk factors pertained to the patient – such as smoking, heart disease, or high body mass index – or to the procedure itself.
The new guidelines specifically say that it’s both. In the risk column, “decision regarding minor surgery with identified patient or procedure risk factors” and “decision regarding elective major surgery without patient or procedure risk factors” are both considered moderate. “Decision regarding elective major surgery with identified patient or procedure risk factors” and “decision regarding emergency major surgery” are in the high complexity column for risk.
Keep in mind that two of three elements are required: the number and complexity of problems, amount of data, and morbidity/mortality risk. Risk of morbidity/mortality alone doesn’t count as the basis for selecting the code. Of course, when surgeons see this, they ask, “What major procedures don’t have identified risk factors?”
Note, too, that these new CPT guidelines do not define the terms “minor” and “major” surgery. For payment reasons related to the postop period, the Centers for Medicare & Medicaid Services defines minor surgery as a procedure with 0-10 global days and a major surgery as a procedure with 90 global days. However, there are many procedures with 0 global days (endoscopy, cardiac catheterization) that are not minor procedures. Hopefully, the AMA will clarify this in 2021.
What’s the take-away for clinicians?
There are sure to be shifts in coding patterns based on these new guidelines. Some specialties will find that not being able to select a service based on history and exam alone will lower the level of service for which they can bill. Some practices, on the other hand, will be able to code for more high-level visits, without the need for a complete review of systems or a comprehensive exam.
The biggest challenge will be for practices that provide services both in the hospital and in the office, because they’ll have to use both sets of guidelines, depending on which type of service they’re performing.
For more details on what’s coming your way beginning on New Year’s Day, you may want to read the 16-page AMA document .
A version of this article first appeared on Medscape.com.
COVID-related harm to HCWs must be tracked more rigorously: NAS panel
A panel of scientific experts is urging the nation to do more to track morbidity and mortality among health care workers (HCWs), given the large and disproportionate number who have been infected with or died from SARS-CoV-2.
The National Academies of Sciences, Engineering, and Medicine’s Standing Committee on Emerging Infectious Diseases and 21st Century Health Threats issued a 10-page “rapid expert consultation” on what is known about deaths and mental health problems among HCWs associated with the COVID-19 pandemic and how to protect workers.
“The absence of a uniform national framework and inconsistent requirements across states for collecting, recording, and reporting HCW mortality and morbidity data associated with COVID-19 impairs anyone’s ability to make comparisons, do combined analyses, or draw conclusions about the scale of the problem,” says the panel in the report.
Mental health, in particular, needs to be examined, it says. Although the data are still limited, the prevalence of burnout and suicide “points to a serious concern,” according to the report.
“As with mortality due to COVID-19, there are currently no national systems nor reporting standards for morbidity measures related to the pandemic, such as mental health status, provider well-being, and other psychological effects on HCWs,” the report says.
A more robust national system that collected data on circumstances and interventions that may raise or lower risk, as well as on where the infection occurred, “would support the adoption of effective mitigation strategies,” says the report. It would also facilitate epidemiologic studies on risk factors, such as face-to-face contact with COVID-19 patients and the availability and use of personal protective equipment (PPE). Studies could also examine the impact of institutional requirements for masking.
Studies have consistently shown that universal mask wearing and access to appropriate PPE support the physical safety and mental health of HCWs, says the report.
Track scale of crisis
The committee cited many gaps in the current system. The Occupational Safety and Health Administration, for instance, doesn’t count deaths from occupationally acquired infection. Many states don’t report COVID-19 deaths by profession. The Centers for Disease Control and Prevention (CDC) relies on case report forms from local health departments for all COVID-19 cases, which typically are lacking in specifics, such as occupation or job setting, says the committee’s report.
As of Nov. 3, the CDC had reported 786 deaths among HCWs that were attributable to COVID-19 – a far lower number than other sources have reported.
The committee notes that much could be done immediately. A National Academy of Medicine panel on clinician well-being and resilience in August recommended that the CDC establish a national epidemiologic tracking program to measure HCWs’ well-being, assess the acute and long-term effects of COVID-19 on those workers, and report on the outcomes of interventions.
Such a program “is needed to comprehensively acknowledge the scale of the COVID-19 crisis and protect the health care workforce that is already stretched to the breaking point in many locations,” the committee says in its report.
A version of this article originally appeared on Medscape.com.
A panel of scientific experts is urging the nation to do more to track morbidity and mortality among health care workers (HCWs), given the large and disproportionate number who have been infected with or died from SARS-CoV-2.
The National Academies of Sciences, Engineering, and Medicine’s Standing Committee on Emerging Infectious Diseases and 21st Century Health Threats issued a 10-page “rapid expert consultation” on what is known about deaths and mental health problems among HCWs associated with the COVID-19 pandemic and how to protect workers.
“The absence of a uniform national framework and inconsistent requirements across states for collecting, recording, and reporting HCW mortality and morbidity data associated with COVID-19 impairs anyone’s ability to make comparisons, do combined analyses, or draw conclusions about the scale of the problem,” says the panel in the report.
Mental health, in particular, needs to be examined, it says. Although the data are still limited, the prevalence of burnout and suicide “points to a serious concern,” according to the report.
“As with mortality due to COVID-19, there are currently no national systems nor reporting standards for morbidity measures related to the pandemic, such as mental health status, provider well-being, and other psychological effects on HCWs,” the report says.
A more robust national system that collected data on circumstances and interventions that may raise or lower risk, as well as on where the infection occurred, “would support the adoption of effective mitigation strategies,” says the report. It would also facilitate epidemiologic studies on risk factors, such as face-to-face contact with COVID-19 patients and the availability and use of personal protective equipment (PPE). Studies could also examine the impact of institutional requirements for masking.
Studies have consistently shown that universal mask wearing and access to appropriate PPE support the physical safety and mental health of HCWs, says the report.
Track scale of crisis
The committee cited many gaps in the current system. The Occupational Safety and Health Administration, for instance, doesn’t count deaths from occupationally acquired infection. Many states don’t report COVID-19 deaths by profession. The Centers for Disease Control and Prevention (CDC) relies on case report forms from local health departments for all COVID-19 cases, which typically are lacking in specifics, such as occupation or job setting, says the committee’s report.
As of Nov. 3, the CDC had reported 786 deaths among HCWs that were attributable to COVID-19 – a far lower number than other sources have reported.
The committee notes that much could be done immediately. A National Academy of Medicine panel on clinician well-being and resilience in August recommended that the CDC establish a national epidemiologic tracking program to measure HCWs’ well-being, assess the acute and long-term effects of COVID-19 on those workers, and report on the outcomes of interventions.
Such a program “is needed to comprehensively acknowledge the scale of the COVID-19 crisis and protect the health care workforce that is already stretched to the breaking point in many locations,” the committee says in its report.
A version of this article originally appeared on Medscape.com.
A panel of scientific experts is urging the nation to do more to track morbidity and mortality among health care workers (HCWs), given the large and disproportionate number who have been infected with or died from SARS-CoV-2.
The National Academies of Sciences, Engineering, and Medicine’s Standing Committee on Emerging Infectious Diseases and 21st Century Health Threats issued a 10-page “rapid expert consultation” on what is known about deaths and mental health problems among HCWs associated with the COVID-19 pandemic and how to protect workers.
“The absence of a uniform national framework and inconsistent requirements across states for collecting, recording, and reporting HCW mortality and morbidity data associated with COVID-19 impairs anyone’s ability to make comparisons, do combined analyses, or draw conclusions about the scale of the problem,” says the panel in the report.
Mental health, in particular, needs to be examined, it says. Although the data are still limited, the prevalence of burnout and suicide “points to a serious concern,” according to the report.
“As with mortality due to COVID-19, there are currently no national systems nor reporting standards for morbidity measures related to the pandemic, such as mental health status, provider well-being, and other psychological effects on HCWs,” the report says.
A more robust national system that collected data on circumstances and interventions that may raise or lower risk, as well as on where the infection occurred, “would support the adoption of effective mitigation strategies,” says the report. It would also facilitate epidemiologic studies on risk factors, such as face-to-face contact with COVID-19 patients and the availability and use of personal protective equipment (PPE). Studies could also examine the impact of institutional requirements for masking.
Studies have consistently shown that universal mask wearing and access to appropriate PPE support the physical safety and mental health of HCWs, says the report.
Track scale of crisis
The committee cited many gaps in the current system. The Occupational Safety and Health Administration, for instance, doesn’t count deaths from occupationally acquired infection. Many states don’t report COVID-19 deaths by profession. The Centers for Disease Control and Prevention (CDC) relies on case report forms from local health departments for all COVID-19 cases, which typically are lacking in specifics, such as occupation or job setting, says the committee’s report.
As of Nov. 3, the CDC had reported 786 deaths among HCWs that were attributable to COVID-19 – a far lower number than other sources have reported.
The committee notes that much could be done immediately. A National Academy of Medicine panel on clinician well-being and resilience in August recommended that the CDC establish a national epidemiologic tracking program to measure HCWs’ well-being, assess the acute and long-term effects of COVID-19 on those workers, and report on the outcomes of interventions.
Such a program “is needed to comprehensively acknowledge the scale of the COVID-19 crisis and protect the health care workforce that is already stretched to the breaking point in many locations,” the committee says in its report.
A version of this article originally appeared on Medscape.com.