User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
div[contains(@class, 'main-prefix')]
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
Spell it out: Writing out common medical terms boosts patient understanding, says study
MI. HTN. hx. Although these abbreviations might make it easier for physicians and other health care professionals to create and consume clinical documentation, the shorthand confuses patients, according to a study published in JAMA Network Open.
Researchers, who conducted clinical trials at three hospitals, found that expansion of 10 common medical abbreviations and acronyms in patient health records significantly increased overall comprehension.
Corresponding author Lisa Grossman Liu, PhD, MD, of Columbia University, New York, told this news organization that “comprehension of abbreviations was much lower than we expected and much lower than the clinicians who participated in this study expected.”
This discovery is particularly relevant in this era of digital care, where providers are now communicating with patients electronically more than ever before – and are required by rules emanating from the 21st Century Cures Act to provide online access to electronic health records.
Using elongated terms
Although the study found that expansion of medical abbreviations and acronyms can improve patient understanding, identifying all of the medical abbreviations that exist is difficult because the terms vary by specialty and geography. The fact that many abbreviations and acronyms have multiple meanings complicates matters even more. For example, the abbreviation PA has 128 possible meanings, Dr. Grossman Liu pointed out.
Technology, fortunately, has advanced in the last few years and is on the cusp of providing a solution. Artificial intelligence systems could help to develop large compendiums of abbreviations and acronyms and then machine learning could elongate the words.
“We’re almost to the point where we have these automated systems that can actually expand abbreviations pretty well and with a great degree of accuracy and ... where those can actually be used in medicine to help with patient communication,” Dr. Grossman Liu said.
Such intervention, however, is not a cure-all.
“There are abbreviations that are really hard to understand even after you expand them, such as MI for myocardial infarction, which is really a tough term all around. It means heart attack. So even if you tell patients, MI means myocardial infarction, they’re still not going to understand it,” Dr. Grossman Liu said.
On the flip side, patients are likely to understand some abbreviations such as hrs, which stands for hours, without elongating the words.
Moving from in-person to online communication
A look at the evolution of clinical documentation explains how this abbreviation problem came to fruition. Prior to this digital age where providers communicate with patients through portals, secure messaging, and other electronic methods, patients and providers would talk face to face. Now, however, electronic written communication is becoming the norm.
“We are not only seeing direct written communication through things like messaging systems or email, but also patients are now reading their medical records online and you can consider that as a form of communication,” Dr. Grossman Liu said. “It’s really interesting that the electronic health record itself has essentially become a medium for communication between patients and providers when previously it was only a way for providers to communicate with themselves and document patient care. So, clinicians use abbreviations because they aren’t intending for patients to see the records.”
Requiring physicians to use complete words in clinical documentation now that electronic records are relied on for patient communication, however, is not a practical solution.
“Abbreviations are so commonly used because they are more efficient to read and more efficient to write. We really shouldn’t be putting the onus on providers to spell out all the abbreviations in their notes. That’s realistically not going to work, because it compromises clinical efficiency,” Dr. Grossman Liu said.
While physicians should not be forced to use complete words in documentation, they should be wary of patients’ unfamiliarity with abbreviations as they communicate in person.
“I use terms like ED constantly when I talk to patients, and it turns out that only 67% of patients understand what you’re talking about when you say ED in reference to the emergency department. So it’s important to be mindful of that,” Dr. Grossman Liu concluded.
A version of this article first appeared on Medscape.com.
MI. HTN. hx. Although these abbreviations might make it easier for physicians and other health care professionals to create and consume clinical documentation, the shorthand confuses patients, according to a study published in JAMA Network Open.
Researchers, who conducted clinical trials at three hospitals, found that expansion of 10 common medical abbreviations and acronyms in patient health records significantly increased overall comprehension.
Corresponding author Lisa Grossman Liu, PhD, MD, of Columbia University, New York, told this news organization that “comprehension of abbreviations was much lower than we expected and much lower than the clinicians who participated in this study expected.”
This discovery is particularly relevant in this era of digital care, where providers are now communicating with patients electronically more than ever before – and are required by rules emanating from the 21st Century Cures Act to provide online access to electronic health records.
Using elongated terms
Although the study found that expansion of medical abbreviations and acronyms can improve patient understanding, identifying all of the medical abbreviations that exist is difficult because the terms vary by specialty and geography. The fact that many abbreviations and acronyms have multiple meanings complicates matters even more. For example, the abbreviation PA has 128 possible meanings, Dr. Grossman Liu pointed out.
Technology, fortunately, has advanced in the last few years and is on the cusp of providing a solution. Artificial intelligence systems could help to develop large compendiums of abbreviations and acronyms and then machine learning could elongate the words.
“We’re almost to the point where we have these automated systems that can actually expand abbreviations pretty well and with a great degree of accuracy and ... where those can actually be used in medicine to help with patient communication,” Dr. Grossman Liu said.
Such intervention, however, is not a cure-all.
“There are abbreviations that are really hard to understand even after you expand them, such as MI for myocardial infarction, which is really a tough term all around. It means heart attack. So even if you tell patients, MI means myocardial infarction, they’re still not going to understand it,” Dr. Grossman Liu said.
On the flip side, patients are likely to understand some abbreviations such as hrs, which stands for hours, without elongating the words.
Moving from in-person to online communication
A look at the evolution of clinical documentation explains how this abbreviation problem came to fruition. Prior to this digital age where providers communicate with patients through portals, secure messaging, and other electronic methods, patients and providers would talk face to face. Now, however, electronic written communication is becoming the norm.
“We are not only seeing direct written communication through things like messaging systems or email, but also patients are now reading their medical records online and you can consider that as a form of communication,” Dr. Grossman Liu said. “It’s really interesting that the electronic health record itself has essentially become a medium for communication between patients and providers when previously it was only a way for providers to communicate with themselves and document patient care. So, clinicians use abbreviations because they aren’t intending for patients to see the records.”
Requiring physicians to use complete words in clinical documentation now that electronic records are relied on for patient communication, however, is not a practical solution.
“Abbreviations are so commonly used because they are more efficient to read and more efficient to write. We really shouldn’t be putting the onus on providers to spell out all the abbreviations in their notes. That’s realistically not going to work, because it compromises clinical efficiency,” Dr. Grossman Liu said.
While physicians should not be forced to use complete words in documentation, they should be wary of patients’ unfamiliarity with abbreviations as they communicate in person.
“I use terms like ED constantly when I talk to patients, and it turns out that only 67% of patients understand what you’re talking about when you say ED in reference to the emergency department. So it’s important to be mindful of that,” Dr. Grossman Liu concluded.
A version of this article first appeared on Medscape.com.
MI. HTN. hx. Although these abbreviations might make it easier for physicians and other health care professionals to create and consume clinical documentation, the shorthand confuses patients, according to a study published in JAMA Network Open.
Researchers, who conducted clinical trials at three hospitals, found that expansion of 10 common medical abbreviations and acronyms in patient health records significantly increased overall comprehension.
Corresponding author Lisa Grossman Liu, PhD, MD, of Columbia University, New York, told this news organization that “comprehension of abbreviations was much lower than we expected and much lower than the clinicians who participated in this study expected.”
This discovery is particularly relevant in this era of digital care, where providers are now communicating with patients electronically more than ever before – and are required by rules emanating from the 21st Century Cures Act to provide online access to electronic health records.
Using elongated terms
Although the study found that expansion of medical abbreviations and acronyms can improve patient understanding, identifying all of the medical abbreviations that exist is difficult because the terms vary by specialty and geography. The fact that many abbreviations and acronyms have multiple meanings complicates matters even more. For example, the abbreviation PA has 128 possible meanings, Dr. Grossman Liu pointed out.
Technology, fortunately, has advanced in the last few years and is on the cusp of providing a solution. Artificial intelligence systems could help to develop large compendiums of abbreviations and acronyms and then machine learning could elongate the words.
“We’re almost to the point where we have these automated systems that can actually expand abbreviations pretty well and with a great degree of accuracy and ... where those can actually be used in medicine to help with patient communication,” Dr. Grossman Liu said.
Such intervention, however, is not a cure-all.
“There are abbreviations that are really hard to understand even after you expand them, such as MI for myocardial infarction, which is really a tough term all around. It means heart attack. So even if you tell patients, MI means myocardial infarction, they’re still not going to understand it,” Dr. Grossman Liu said.
On the flip side, patients are likely to understand some abbreviations such as hrs, which stands for hours, without elongating the words.
Moving from in-person to online communication
A look at the evolution of clinical documentation explains how this abbreviation problem came to fruition. Prior to this digital age where providers communicate with patients through portals, secure messaging, and other electronic methods, patients and providers would talk face to face. Now, however, electronic written communication is becoming the norm.
“We are not only seeing direct written communication through things like messaging systems or email, but also patients are now reading their medical records online and you can consider that as a form of communication,” Dr. Grossman Liu said. “It’s really interesting that the electronic health record itself has essentially become a medium for communication between patients and providers when previously it was only a way for providers to communicate with themselves and document patient care. So, clinicians use abbreviations because they aren’t intending for patients to see the records.”
Requiring physicians to use complete words in clinical documentation now that electronic records are relied on for patient communication, however, is not a practical solution.
“Abbreviations are so commonly used because they are more efficient to read and more efficient to write. We really shouldn’t be putting the onus on providers to spell out all the abbreviations in their notes. That’s realistically not going to work, because it compromises clinical efficiency,” Dr. Grossman Liu said.
While physicians should not be forced to use complete words in documentation, they should be wary of patients’ unfamiliarity with abbreviations as they communicate in person.
“I use terms like ED constantly when I talk to patients, and it turns out that only 67% of patients understand what you’re talking about when you say ED in reference to the emergency department. So it’s important to be mindful of that,” Dr. Grossman Liu concluded.
A version of this article first appeared on Medscape.com.
FROM JAMA NETWORK OPEN
Children and COVID: New cases up by 50%
The latest increase in new child COVID-19 cases seems to be picking up steam, rising by 50% in the last week, according to the American Academy of Pediatrics and the Children’s Hospital Association.
That 50% week-to-week change follows increases of 17%, 44%, 12%, and 28% since the nationwide weekly total fell to its low point for the year (25,915) in the beginning of April, the AAP and CHA said in their weekly COVID report.
Regionally, the distribution of those 93,000 COVID cases was fairly even. The Northeast, which saw the biggest jump for the week, and the Midwest were both around 25,000 new cases, while the South had about 20,000 and the West was lowest with 18,000 or so. At the state/territory level, the largest percent increases over the last 2 weeks were found in Maine and Puerto Rico, with Massachusetts and Vermont just a step behind, the AAP/CHA data show.
In cumulative terms, there have been over 13.1 million cases of COVID-19 among children in the United States, with pediatric cases representing 19.0% of all cases since the pandemic began, the two organizations reported. They also noted a number of important limitations: New York state has never reported cases by age, several states have stopped updating their online dashboards, and states apply a variety of age ranges to define children (Alabama has the smallest range, 0-14 years; South Carolina, Tennessee, and West Virginia the largest, 0-20).
By comparison, the Centers for Disease Control and Prevention put the total number of cases in children aged 0-17 at 12.7 million, although that figure is based on a cumulative number of 73.4 million cases among all ages, which is well short of the reported total of almost 82.4 million as of May 16. COVID cases in children have led to 1,536 deaths so far, the CDC said.
The recent upward trend in new cases also can be seen in the CDC’s data, which show the weekly rate rising from 35 per 100,000 population on March 26 to 102 per 100,000 on May 7 in children aged 0-14 years, with commensurate increases seen among older children over the same period. In turn, the rate of new admissions for children aged 0-17 has gone from a low of 0.13 per 100,000 as late as April 10 up to 0.23 on May 13, the CDC said on its COVID Data Tracker.
One thing not going up these days is vaccinations among the youngest eligible children. The number of 5- to 11-year-olds receiving their initial dose was down to 40,000 for the week of May 5-11, the fewest since the vaccine was approved for that age group. For a change of pace, the number increased among children aged 12-17, as 37,000 got initial vaccinations that week, compared with 29,000 a week earlier, the AAP said in its weekly vaccination report.
The latest increase in new child COVID-19 cases seems to be picking up steam, rising by 50% in the last week, according to the American Academy of Pediatrics and the Children’s Hospital Association.
That 50% week-to-week change follows increases of 17%, 44%, 12%, and 28% since the nationwide weekly total fell to its low point for the year (25,915) in the beginning of April, the AAP and CHA said in their weekly COVID report.
Regionally, the distribution of those 93,000 COVID cases was fairly even. The Northeast, which saw the biggest jump for the week, and the Midwest were both around 25,000 new cases, while the South had about 20,000 and the West was lowest with 18,000 or so. At the state/territory level, the largest percent increases over the last 2 weeks were found in Maine and Puerto Rico, with Massachusetts and Vermont just a step behind, the AAP/CHA data show.
In cumulative terms, there have been over 13.1 million cases of COVID-19 among children in the United States, with pediatric cases representing 19.0% of all cases since the pandemic began, the two organizations reported. They also noted a number of important limitations: New York state has never reported cases by age, several states have stopped updating their online dashboards, and states apply a variety of age ranges to define children (Alabama has the smallest range, 0-14 years; South Carolina, Tennessee, and West Virginia the largest, 0-20).
By comparison, the Centers for Disease Control and Prevention put the total number of cases in children aged 0-17 at 12.7 million, although that figure is based on a cumulative number of 73.4 million cases among all ages, which is well short of the reported total of almost 82.4 million as of May 16. COVID cases in children have led to 1,536 deaths so far, the CDC said.
The recent upward trend in new cases also can be seen in the CDC’s data, which show the weekly rate rising from 35 per 100,000 population on March 26 to 102 per 100,000 on May 7 in children aged 0-14 years, with commensurate increases seen among older children over the same period. In turn, the rate of new admissions for children aged 0-17 has gone from a low of 0.13 per 100,000 as late as April 10 up to 0.23 on May 13, the CDC said on its COVID Data Tracker.
One thing not going up these days is vaccinations among the youngest eligible children. The number of 5- to 11-year-olds receiving their initial dose was down to 40,000 for the week of May 5-11, the fewest since the vaccine was approved for that age group. For a change of pace, the number increased among children aged 12-17, as 37,000 got initial vaccinations that week, compared with 29,000 a week earlier, the AAP said in its weekly vaccination report.
The latest increase in new child COVID-19 cases seems to be picking up steam, rising by 50% in the last week, according to the American Academy of Pediatrics and the Children’s Hospital Association.
That 50% week-to-week change follows increases of 17%, 44%, 12%, and 28% since the nationwide weekly total fell to its low point for the year (25,915) in the beginning of April, the AAP and CHA said in their weekly COVID report.
Regionally, the distribution of those 93,000 COVID cases was fairly even. The Northeast, which saw the biggest jump for the week, and the Midwest were both around 25,000 new cases, while the South had about 20,000 and the West was lowest with 18,000 or so. At the state/territory level, the largest percent increases over the last 2 weeks were found in Maine and Puerto Rico, with Massachusetts and Vermont just a step behind, the AAP/CHA data show.
In cumulative terms, there have been over 13.1 million cases of COVID-19 among children in the United States, with pediatric cases representing 19.0% of all cases since the pandemic began, the two organizations reported. They also noted a number of important limitations: New York state has never reported cases by age, several states have stopped updating their online dashboards, and states apply a variety of age ranges to define children (Alabama has the smallest range, 0-14 years; South Carolina, Tennessee, and West Virginia the largest, 0-20).
By comparison, the Centers for Disease Control and Prevention put the total number of cases in children aged 0-17 at 12.7 million, although that figure is based on a cumulative number of 73.4 million cases among all ages, which is well short of the reported total of almost 82.4 million as of May 16. COVID cases in children have led to 1,536 deaths so far, the CDC said.
The recent upward trend in new cases also can be seen in the CDC’s data, which show the weekly rate rising from 35 per 100,000 population on March 26 to 102 per 100,000 on May 7 in children aged 0-14 years, with commensurate increases seen among older children over the same period. In turn, the rate of new admissions for children aged 0-17 has gone from a low of 0.13 per 100,000 as late as April 10 up to 0.23 on May 13, the CDC said on its COVID Data Tracker.
One thing not going up these days is vaccinations among the youngest eligible children. The number of 5- to 11-year-olds receiving their initial dose was down to 40,000 for the week of May 5-11, the fewest since the vaccine was approved for that age group. For a change of pace, the number increased among children aged 12-17, as 37,000 got initial vaccinations that week, compared with 29,000 a week earlier, the AAP said in its weekly vaccination report.
COVID drove telehealth forward in high gear: Now what?
Before the pandemic hit in 2019, Pooja Aysola, MD, considered herself lucky because she could tap into telehealth for neurology consults in her work as an emergency department physician.
“We would wheel in a computer screen with a neurologist on board every time we had a suspected stroke patient. And I was able to talk directly to the neurologist about my patient’s symptoms. And it was great,” Dr. Aysola said.
The pandemic, however, prompted the need for telehealth in many situations beyond specialty care. As such, investment exploded over the past few years.
“We’re seeing telehealth across all specialties ... more than half of clinicians are now saying that they do believe that virtual visits will surpass in-person visits for primary care needs,” said Dr. Aysola, who also serves as senior director, clinical operations at Wheel, a Texas-based telehealth company.
Dr. Aysola spoke during an American Telemedicine Association conference panel addressing how COVID prompted an uptick in telehealth investment and utilization and how such virtual care is likely to evolve moving forward.
Nathaniel Lacktman, a partner at law firm Foley & Lardner, agreed with Dr. Aysola’s assessment of the market.
“The appetite for virtual care has become voracious,” said Mr. Lacktman, who chairs the firm’s telemedicine and digital health team. “It reminds me in some ways of taking my kids out to dinner and saying, ‘Try this new food.’ They’re like, ‘No, I won’t like it.’ They finally get a little taste and they’re like, ‘This is amazing.’”
While there is no doubt that stakeholders – from innovators to investors to providers to patients – will want more than just a taste of telehealth in the future, panelists addressed if this undeniable demand for virtual care was simply a short-term response to the pandemic or if there is a long-term desire to fundamentally change how care is delivered.
Expanding on the pandemic-driven ‘sandbox’
While the uptick in telehealth investment and utilization is not expected to continue at such jarring rates in the future, the panelists pointed out that innovation will proceed but perhaps at a different pace.
“The last 3 years have been a sandbox during which the industry was able to experiment,” said Mr. Lacktman. “What we’re going to see more of even post pandemic is building upon that experimental sandbox and creating models that aren’t just high growth and really quick but that are sustainable and meaningful.”
As such, patients and providers won’t be looking for telehealth to simply provide access to care but to provide a full scope of services while also improving quality.
Rachel Stillman, vice president of 7wireVentures, a Chicago-based venture capital firm, also expects interest in telehealth to continue but at a less frenetic pace. In 2021, the industry witnessed nearly $31 billion of venture financing directed towards digital health companies, she said.
“Now, Q1 2022 has had a little bit of a slower start. But with that said, we still have invested $6 billion in early stage companies. So ... we’re seeing some initial signs perhaps of – I don’t want to call it a slowdown – but increased discipline,” Ms. Stillman said.
Start-up companies will need to carefully position themselves for success in this post pandemic environment. “Ultimately, it really goes down to making sure your fundamentals are strong ... and having a really compelling [return on investment] case for your health plan, your self-insured employer, your health system, or your ultimate buyer,” Ms. Stillman said.
Two models are coming into play as innovation continues, she added. One is a traditional care delivery model whereby a start-up organization is building their own provider network specialized for the conditions or patient populations they are serving.
“Conversely, there are new entrants that are thinking about how they can leverage their insightful and strong technology foundations and platforms for existing provider networks that could benefit from a telemedicine partner,” Ms. Stillman pointed out.
Dr. Aysola added that companies are moving forward strategically to achieve post pandemic success. Some telehealth start-ups, for instance, are “capturing some of the low-hanging fruit, the simple UTIs, the really easy things to treat,” Dr. Aysola said.
Others are addressing the clinician’s experience. “Over 50% of clinicians have thought about leaving their jobs at some point during the pandemic. And so it’s becoming really clear that focusing on the clinician and the clinician’s needs are just imperative to [creating a] winning model post-pandemic,” Dr. Aysola said.
Adapting to the new normal
Health care provider organizations also need to adjust to post pandemic realities. “We work with a number of hospital systems, and it’s astounding how slow they are compared to the start-ups because there’s a lot more constituents; there’s bureaucracy,” Mr. Lacktman said. As a result, “the hospitals are in a more uncomfortable position post pandemic than the start-ups.”
To move forward successfully, these organizations, which are typically risk averse, need to create alignment among legal, compliance, and clinical leaders, Mr. Lacktman advised.
One of the first decisions that these teams need to make is whether they should proceed on their own or enter into a partnership with a start-up or pursue a merger and acquisition. In addition, some health systems, hospitals, and health plans are even opting to establish their own venture funds.
“Building your own venture fund or even investing ... in companies directly or in other venture funds [are strategies] that health systems might be able to leverage both to accelerate partnerships and also really be on top of key trends,” Ms. Stillman said.
No matter how health care systems invest in and implement telemedicine technologies, though, the need to move quickly is paramount.
Traditional health care systems “don’t always have the luxury of time. Things have to be done pretty quickly in order to remain competitive,” Dr. Aysola concluded. “We’ve found that companies can launch a virtual care offering in a matter of weeks. When in reality, if a traditional health care system were to try to launch it on their own, it could take upwards of 15 months.”
A version of this article first appeared on Medscape.com.
Before the pandemic hit in 2019, Pooja Aysola, MD, considered herself lucky because she could tap into telehealth for neurology consults in her work as an emergency department physician.
“We would wheel in a computer screen with a neurologist on board every time we had a suspected stroke patient. And I was able to talk directly to the neurologist about my patient’s symptoms. And it was great,” Dr. Aysola said.
The pandemic, however, prompted the need for telehealth in many situations beyond specialty care. As such, investment exploded over the past few years.
“We’re seeing telehealth across all specialties ... more than half of clinicians are now saying that they do believe that virtual visits will surpass in-person visits for primary care needs,” said Dr. Aysola, who also serves as senior director, clinical operations at Wheel, a Texas-based telehealth company.
Dr. Aysola spoke during an American Telemedicine Association conference panel addressing how COVID prompted an uptick in telehealth investment and utilization and how such virtual care is likely to evolve moving forward.
Nathaniel Lacktman, a partner at law firm Foley & Lardner, agreed with Dr. Aysola’s assessment of the market.
“The appetite for virtual care has become voracious,” said Mr. Lacktman, who chairs the firm’s telemedicine and digital health team. “It reminds me in some ways of taking my kids out to dinner and saying, ‘Try this new food.’ They’re like, ‘No, I won’t like it.’ They finally get a little taste and they’re like, ‘This is amazing.’”
While there is no doubt that stakeholders – from innovators to investors to providers to patients – will want more than just a taste of telehealth in the future, panelists addressed if this undeniable demand for virtual care was simply a short-term response to the pandemic or if there is a long-term desire to fundamentally change how care is delivered.
Expanding on the pandemic-driven ‘sandbox’
While the uptick in telehealth investment and utilization is not expected to continue at such jarring rates in the future, the panelists pointed out that innovation will proceed but perhaps at a different pace.
“The last 3 years have been a sandbox during which the industry was able to experiment,” said Mr. Lacktman. “What we’re going to see more of even post pandemic is building upon that experimental sandbox and creating models that aren’t just high growth and really quick but that are sustainable and meaningful.”
As such, patients and providers won’t be looking for telehealth to simply provide access to care but to provide a full scope of services while also improving quality.
Rachel Stillman, vice president of 7wireVentures, a Chicago-based venture capital firm, also expects interest in telehealth to continue but at a less frenetic pace. In 2021, the industry witnessed nearly $31 billion of venture financing directed towards digital health companies, she said.
“Now, Q1 2022 has had a little bit of a slower start. But with that said, we still have invested $6 billion in early stage companies. So ... we’re seeing some initial signs perhaps of – I don’t want to call it a slowdown – but increased discipline,” Ms. Stillman said.
Start-up companies will need to carefully position themselves for success in this post pandemic environment. “Ultimately, it really goes down to making sure your fundamentals are strong ... and having a really compelling [return on investment] case for your health plan, your self-insured employer, your health system, or your ultimate buyer,” Ms. Stillman said.
Two models are coming into play as innovation continues, she added. One is a traditional care delivery model whereby a start-up organization is building their own provider network specialized for the conditions or patient populations they are serving.
“Conversely, there are new entrants that are thinking about how they can leverage their insightful and strong technology foundations and platforms for existing provider networks that could benefit from a telemedicine partner,” Ms. Stillman pointed out.
Dr. Aysola added that companies are moving forward strategically to achieve post pandemic success. Some telehealth start-ups, for instance, are “capturing some of the low-hanging fruit, the simple UTIs, the really easy things to treat,” Dr. Aysola said.
Others are addressing the clinician’s experience. “Over 50% of clinicians have thought about leaving their jobs at some point during the pandemic. And so it’s becoming really clear that focusing on the clinician and the clinician’s needs are just imperative to [creating a] winning model post-pandemic,” Dr. Aysola said.
Adapting to the new normal
Health care provider organizations also need to adjust to post pandemic realities. “We work with a number of hospital systems, and it’s astounding how slow they are compared to the start-ups because there’s a lot more constituents; there’s bureaucracy,” Mr. Lacktman said. As a result, “the hospitals are in a more uncomfortable position post pandemic than the start-ups.”
To move forward successfully, these organizations, which are typically risk averse, need to create alignment among legal, compliance, and clinical leaders, Mr. Lacktman advised.
One of the first decisions that these teams need to make is whether they should proceed on their own or enter into a partnership with a start-up or pursue a merger and acquisition. In addition, some health systems, hospitals, and health plans are even opting to establish their own venture funds.
“Building your own venture fund or even investing ... in companies directly or in other venture funds [are strategies] that health systems might be able to leverage both to accelerate partnerships and also really be on top of key trends,” Ms. Stillman said.
No matter how health care systems invest in and implement telemedicine technologies, though, the need to move quickly is paramount.
Traditional health care systems “don’t always have the luxury of time. Things have to be done pretty quickly in order to remain competitive,” Dr. Aysola concluded. “We’ve found that companies can launch a virtual care offering in a matter of weeks. When in reality, if a traditional health care system were to try to launch it on their own, it could take upwards of 15 months.”
A version of this article first appeared on Medscape.com.
Before the pandemic hit in 2019, Pooja Aysola, MD, considered herself lucky because she could tap into telehealth for neurology consults in her work as an emergency department physician.
“We would wheel in a computer screen with a neurologist on board every time we had a suspected stroke patient. And I was able to talk directly to the neurologist about my patient’s symptoms. And it was great,” Dr. Aysola said.
The pandemic, however, prompted the need for telehealth in many situations beyond specialty care. As such, investment exploded over the past few years.
“We’re seeing telehealth across all specialties ... more than half of clinicians are now saying that they do believe that virtual visits will surpass in-person visits for primary care needs,” said Dr. Aysola, who also serves as senior director, clinical operations at Wheel, a Texas-based telehealth company.
Dr. Aysola spoke during an American Telemedicine Association conference panel addressing how COVID prompted an uptick in telehealth investment and utilization and how such virtual care is likely to evolve moving forward.
Nathaniel Lacktman, a partner at law firm Foley & Lardner, agreed with Dr. Aysola’s assessment of the market.
“The appetite for virtual care has become voracious,” said Mr. Lacktman, who chairs the firm’s telemedicine and digital health team. “It reminds me in some ways of taking my kids out to dinner and saying, ‘Try this new food.’ They’re like, ‘No, I won’t like it.’ They finally get a little taste and they’re like, ‘This is amazing.’”
While there is no doubt that stakeholders – from innovators to investors to providers to patients – will want more than just a taste of telehealth in the future, panelists addressed if this undeniable demand for virtual care was simply a short-term response to the pandemic or if there is a long-term desire to fundamentally change how care is delivered.
Expanding on the pandemic-driven ‘sandbox’
While the uptick in telehealth investment and utilization is not expected to continue at such jarring rates in the future, the panelists pointed out that innovation will proceed but perhaps at a different pace.
“The last 3 years have been a sandbox during which the industry was able to experiment,” said Mr. Lacktman. “What we’re going to see more of even post pandemic is building upon that experimental sandbox and creating models that aren’t just high growth and really quick but that are sustainable and meaningful.”
As such, patients and providers won’t be looking for telehealth to simply provide access to care but to provide a full scope of services while also improving quality.
Rachel Stillman, vice president of 7wireVentures, a Chicago-based venture capital firm, also expects interest in telehealth to continue but at a less frenetic pace. In 2021, the industry witnessed nearly $31 billion of venture financing directed towards digital health companies, she said.
“Now, Q1 2022 has had a little bit of a slower start. But with that said, we still have invested $6 billion in early stage companies. So ... we’re seeing some initial signs perhaps of – I don’t want to call it a slowdown – but increased discipline,” Ms. Stillman said.
Start-up companies will need to carefully position themselves for success in this post pandemic environment. “Ultimately, it really goes down to making sure your fundamentals are strong ... and having a really compelling [return on investment] case for your health plan, your self-insured employer, your health system, or your ultimate buyer,” Ms. Stillman said.
Two models are coming into play as innovation continues, she added. One is a traditional care delivery model whereby a start-up organization is building their own provider network specialized for the conditions or patient populations they are serving.
“Conversely, there are new entrants that are thinking about how they can leverage their insightful and strong technology foundations and platforms for existing provider networks that could benefit from a telemedicine partner,” Ms. Stillman pointed out.
Dr. Aysola added that companies are moving forward strategically to achieve post pandemic success. Some telehealth start-ups, for instance, are “capturing some of the low-hanging fruit, the simple UTIs, the really easy things to treat,” Dr. Aysola said.
Others are addressing the clinician’s experience. “Over 50% of clinicians have thought about leaving their jobs at some point during the pandemic. And so it’s becoming really clear that focusing on the clinician and the clinician’s needs are just imperative to [creating a] winning model post-pandemic,” Dr. Aysola said.
Adapting to the new normal
Health care provider organizations also need to adjust to post pandemic realities. “We work with a number of hospital systems, and it’s astounding how slow they are compared to the start-ups because there’s a lot more constituents; there’s bureaucracy,” Mr. Lacktman said. As a result, “the hospitals are in a more uncomfortable position post pandemic than the start-ups.”
To move forward successfully, these organizations, which are typically risk averse, need to create alignment among legal, compliance, and clinical leaders, Mr. Lacktman advised.
One of the first decisions that these teams need to make is whether they should proceed on their own or enter into a partnership with a start-up or pursue a merger and acquisition. In addition, some health systems, hospitals, and health plans are even opting to establish their own venture funds.
“Building your own venture fund or even investing ... in companies directly or in other venture funds [are strategies] that health systems might be able to leverage both to accelerate partnerships and also really be on top of key trends,” Ms. Stillman said.
No matter how health care systems invest in and implement telemedicine technologies, though, the need to move quickly is paramount.
Traditional health care systems “don’t always have the luxury of time. Things have to be done pretty quickly in order to remain competitive,” Dr. Aysola concluded. “We’ve found that companies can launch a virtual care offering in a matter of weeks. When in reality, if a traditional health care system were to try to launch it on their own, it could take upwards of 15 months.”
A version of this article first appeared on Medscape.com.
Stroke in the young: Cancer in disguise?
The data were presented by Jamie Verhoeven, MD, Radboud University Medical Centre, the Netherlands, at the recent European Stroke Organisation Conference 2022.
Dr. Verhoeven noted that 10% of all stroke cases occur in individuals younger than 50 years. During the past few decades, the incidence of stroke in the young has steadily increased, whereas the incidence of stroke in older adults has stabilized or decreased.
“Stroke in the young differs from stroke in older patients, and one of the major differences is that stroke in the young has a higher proportion of cryptogenic stroke, with no clear cause found in over one-third of patients,” she said.
Also, having an active cancer is known to be a risk factor for thrombosis. This association is strongest in venous thrombosis and has been less well investigated in arterial thrombosis, Dr. Verhoeven reported.
Her group aimed to investigate whether in some patients with cryptogenic stroke, this may be the first manifestation of an underlying cancer. “If this hypothesis is true, then it would be more obvious in young patients who have a higher incidence of cryptogenic stroke,” she said.
They performed a population-based observational cohort study using diagnostic ICD codes from the national Hospital Discharge Registry in the Netherlands and the Dutch Population Registry from 1998 to 2019.
Patients with a history of cancer before their first stroke and those with central nervous system cancers at the time of stroke or nonmelanoma skin cancers (which have been shown to have no systemic effects) were excluded.
Reference data came from the Netherlands Comprehensive Cancer Organisation, which collects data on all cancer diagnoses in the country.
The researchers identified 27,616 young stroke patients (age range, 15-49 years; median age, 45 years) and 362,782 older stroke patients (age range, 50 years and older; median age, 76 years).
The cumulative incidence of any cancer at 10 years was 3.7% in the younger group and 8.5% in the older group.
The data were compared with matched peers from the general population. The main outcome measures were cumulative incidence of first-ever cancer after stroke (stratified by stroke subtype, age and sex) and standardized incidence rates.
Results showed that the risk for cancer was higher in the younger age group than in the matched general population.
In this age group, the 1-year risk of any new cancer was 2.6 times higher (95% confidence interval, 2.2-3.1) after ischemic stroke and 5.4 times (95% CI, 3.8-7.3) after intracerebral hemorrhage than in matched peers from the general population.
In contrast, in stroke patients older than 50 years, the 1-year risk for any new cancer was 1.2 times higher than the general population after either ischemic or hemorrhagic stroke.
“The younger patients have a higher risk increase of cancer than older patients, and this risk increase is most evident in the first 1 to 2 years after stroke but remains statistically significant for up to 5 to 8 years later,” Dr. Verhoeven said.
The cancers that were most involved in this risk increase were those of the lower respiratory tract, hematologic cancers, and gastrointestinal cancers.
The main strength of this study was the use of national databases that allowed for a very large sample size, but this brings with it the danger of misclassification of events and the lack of clinical data, Dr. Verhoeven noted.
“Young stroke patients are at increased risk of developing a new cancer in the years following their stroke compared to peers from the general population, but this risk is only marginally increased in the older stroke population,” she concluded.
She pointed out that it is not possible to confirm any causal relation from this study design, but a clear association has been shown.
“We need more studies into this field. We need a large clinical dataset to examine which clinical phenotypes are associated with possible underlying cancers to identify which patients are most at risk. We are already working on this,” she said. “Then it remains to be investigated whether screening for an underlying cancer should be added to the diagnostic workup in young stroke patients.”
Commenting on the study after the presentation, William Whiteley, BM, PhD, a clinical epidemiologist at the University of Edinburgh, Scotland, and a consultant neurologist in NHS Lothian, said it was difficult to know whether the link shown between stroke and cancer was causal, but the effect size in this study was “quite large.”
He pointed out that the associations with bowel and lung cancer could be due to shared risk factors, such as smoking, but he said the finding on a link with hematologic cancers is “interesting.”
Noting that there are links between hematologic cancers and thrombotic events, he said: “People have wondered if that is because of clonal expansion, which has been shown to increase the risk of atherosclerosis, so the question is whether this is some kind of common risk factor here.”
Dr. Verhoeven said she did not believe that shared risk factors fully explained the difference in increased risks between young and older patients.
“It does not fully explain why the risk of cancer is specifically higher in the first 1 to 2 years after the stroke diagnosis. I would think if it was just shared risk factors, the risk increase should remain relatively stable, or even increase due to the build-up of exposure to risk factors over the years,” she said.
Dr. Whiteley said that data like these are “really useful in trying to estimate these associations and it gives us some hypotheses to investigate in smaller mechanistic studies.”
Asked whether these data justify screening younger cryptogenic stroke patients more systematically for cancer, Dr. Whiteley replied: “I think we need some absolute risk estimates for that; for example, what proportion of younger patients would be at risk over the next few years when that screening would make a difference.”
Dr. Verhoeven reports no disclosures.
A version of this article first appeared on Medscape.com.
The data were presented by Jamie Verhoeven, MD, Radboud University Medical Centre, the Netherlands, at the recent European Stroke Organisation Conference 2022.
Dr. Verhoeven noted that 10% of all stroke cases occur in individuals younger than 50 years. During the past few decades, the incidence of stroke in the young has steadily increased, whereas the incidence of stroke in older adults has stabilized or decreased.
“Stroke in the young differs from stroke in older patients, and one of the major differences is that stroke in the young has a higher proportion of cryptogenic stroke, with no clear cause found in over one-third of patients,” she said.
Also, having an active cancer is known to be a risk factor for thrombosis. This association is strongest in venous thrombosis and has been less well investigated in arterial thrombosis, Dr. Verhoeven reported.
Her group aimed to investigate whether in some patients with cryptogenic stroke, this may be the first manifestation of an underlying cancer. “If this hypothesis is true, then it would be more obvious in young patients who have a higher incidence of cryptogenic stroke,” she said.
They performed a population-based observational cohort study using diagnostic ICD codes from the national Hospital Discharge Registry in the Netherlands and the Dutch Population Registry from 1998 to 2019.
Patients with a history of cancer before their first stroke and those with central nervous system cancers at the time of stroke or nonmelanoma skin cancers (which have been shown to have no systemic effects) were excluded.
Reference data came from the Netherlands Comprehensive Cancer Organisation, which collects data on all cancer diagnoses in the country.
The researchers identified 27,616 young stroke patients (age range, 15-49 years; median age, 45 years) and 362,782 older stroke patients (age range, 50 years and older; median age, 76 years).
The cumulative incidence of any cancer at 10 years was 3.7% in the younger group and 8.5% in the older group.
The data were compared with matched peers from the general population. The main outcome measures were cumulative incidence of first-ever cancer after stroke (stratified by stroke subtype, age and sex) and standardized incidence rates.
Results showed that the risk for cancer was higher in the younger age group than in the matched general population.
In this age group, the 1-year risk of any new cancer was 2.6 times higher (95% confidence interval, 2.2-3.1) after ischemic stroke and 5.4 times (95% CI, 3.8-7.3) after intracerebral hemorrhage than in matched peers from the general population.
In contrast, in stroke patients older than 50 years, the 1-year risk for any new cancer was 1.2 times higher than the general population after either ischemic or hemorrhagic stroke.
“The younger patients have a higher risk increase of cancer than older patients, and this risk increase is most evident in the first 1 to 2 years after stroke but remains statistically significant for up to 5 to 8 years later,” Dr. Verhoeven said.
The cancers that were most involved in this risk increase were those of the lower respiratory tract, hematologic cancers, and gastrointestinal cancers.
The main strength of this study was the use of national databases that allowed for a very large sample size, but this brings with it the danger of misclassification of events and the lack of clinical data, Dr. Verhoeven noted.
“Young stroke patients are at increased risk of developing a new cancer in the years following their stroke compared to peers from the general population, but this risk is only marginally increased in the older stroke population,” she concluded.
She pointed out that it is not possible to confirm any causal relation from this study design, but a clear association has been shown.
“We need more studies into this field. We need a large clinical dataset to examine which clinical phenotypes are associated with possible underlying cancers to identify which patients are most at risk. We are already working on this,” she said. “Then it remains to be investigated whether screening for an underlying cancer should be added to the diagnostic workup in young stroke patients.”
Commenting on the study after the presentation, William Whiteley, BM, PhD, a clinical epidemiologist at the University of Edinburgh, Scotland, and a consultant neurologist in NHS Lothian, said it was difficult to know whether the link shown between stroke and cancer was causal, but the effect size in this study was “quite large.”
He pointed out that the associations with bowel and lung cancer could be due to shared risk factors, such as smoking, but he said the finding on a link with hematologic cancers is “interesting.”
Noting that there are links between hematologic cancers and thrombotic events, he said: “People have wondered if that is because of clonal expansion, which has been shown to increase the risk of atherosclerosis, so the question is whether this is some kind of common risk factor here.”
Dr. Verhoeven said she did not believe that shared risk factors fully explained the difference in increased risks between young and older patients.
“It does not fully explain why the risk of cancer is specifically higher in the first 1 to 2 years after the stroke diagnosis. I would think if it was just shared risk factors, the risk increase should remain relatively stable, or even increase due to the build-up of exposure to risk factors over the years,” she said.
Dr. Whiteley said that data like these are “really useful in trying to estimate these associations and it gives us some hypotheses to investigate in smaller mechanistic studies.”
Asked whether these data justify screening younger cryptogenic stroke patients more systematically for cancer, Dr. Whiteley replied: “I think we need some absolute risk estimates for that; for example, what proportion of younger patients would be at risk over the next few years when that screening would make a difference.”
Dr. Verhoeven reports no disclosures.
A version of this article first appeared on Medscape.com.
The data were presented by Jamie Verhoeven, MD, Radboud University Medical Centre, the Netherlands, at the recent European Stroke Organisation Conference 2022.
Dr. Verhoeven noted that 10% of all stroke cases occur in individuals younger than 50 years. During the past few decades, the incidence of stroke in the young has steadily increased, whereas the incidence of stroke in older adults has stabilized or decreased.
“Stroke in the young differs from stroke in older patients, and one of the major differences is that stroke in the young has a higher proportion of cryptogenic stroke, with no clear cause found in over one-third of patients,” she said.
Also, having an active cancer is known to be a risk factor for thrombosis. This association is strongest in venous thrombosis and has been less well investigated in arterial thrombosis, Dr. Verhoeven reported.
Her group aimed to investigate whether in some patients with cryptogenic stroke, this may be the first manifestation of an underlying cancer. “If this hypothesis is true, then it would be more obvious in young patients who have a higher incidence of cryptogenic stroke,” she said.
They performed a population-based observational cohort study using diagnostic ICD codes from the national Hospital Discharge Registry in the Netherlands and the Dutch Population Registry from 1998 to 2019.
Patients with a history of cancer before their first stroke and those with central nervous system cancers at the time of stroke or nonmelanoma skin cancers (which have been shown to have no systemic effects) were excluded.
Reference data came from the Netherlands Comprehensive Cancer Organisation, which collects data on all cancer diagnoses in the country.
The researchers identified 27,616 young stroke patients (age range, 15-49 years; median age, 45 years) and 362,782 older stroke patients (age range, 50 years and older; median age, 76 years).
The cumulative incidence of any cancer at 10 years was 3.7% in the younger group and 8.5% in the older group.
The data were compared with matched peers from the general population. The main outcome measures were cumulative incidence of first-ever cancer after stroke (stratified by stroke subtype, age and sex) and standardized incidence rates.
Results showed that the risk for cancer was higher in the younger age group than in the matched general population.
In this age group, the 1-year risk of any new cancer was 2.6 times higher (95% confidence interval, 2.2-3.1) after ischemic stroke and 5.4 times (95% CI, 3.8-7.3) after intracerebral hemorrhage than in matched peers from the general population.
In contrast, in stroke patients older than 50 years, the 1-year risk for any new cancer was 1.2 times higher than the general population after either ischemic or hemorrhagic stroke.
“The younger patients have a higher risk increase of cancer than older patients, and this risk increase is most evident in the first 1 to 2 years after stroke but remains statistically significant for up to 5 to 8 years later,” Dr. Verhoeven said.
The cancers that were most involved in this risk increase were those of the lower respiratory tract, hematologic cancers, and gastrointestinal cancers.
The main strength of this study was the use of national databases that allowed for a very large sample size, but this brings with it the danger of misclassification of events and the lack of clinical data, Dr. Verhoeven noted.
“Young stroke patients are at increased risk of developing a new cancer in the years following their stroke compared to peers from the general population, but this risk is only marginally increased in the older stroke population,” she concluded.
She pointed out that it is not possible to confirm any causal relation from this study design, but a clear association has been shown.
“We need more studies into this field. We need a large clinical dataset to examine which clinical phenotypes are associated with possible underlying cancers to identify which patients are most at risk. We are already working on this,” she said. “Then it remains to be investigated whether screening for an underlying cancer should be added to the diagnostic workup in young stroke patients.”
Commenting on the study after the presentation, William Whiteley, BM, PhD, a clinical epidemiologist at the University of Edinburgh, Scotland, and a consultant neurologist in NHS Lothian, said it was difficult to know whether the link shown between stroke and cancer was causal, but the effect size in this study was “quite large.”
He pointed out that the associations with bowel and lung cancer could be due to shared risk factors, such as smoking, but he said the finding on a link with hematologic cancers is “interesting.”
Noting that there are links between hematologic cancers and thrombotic events, he said: “People have wondered if that is because of clonal expansion, which has been shown to increase the risk of atherosclerosis, so the question is whether this is some kind of common risk factor here.”
Dr. Verhoeven said she did not believe that shared risk factors fully explained the difference in increased risks between young and older patients.
“It does not fully explain why the risk of cancer is specifically higher in the first 1 to 2 years after the stroke diagnosis. I would think if it was just shared risk factors, the risk increase should remain relatively stable, or even increase due to the build-up of exposure to risk factors over the years,” she said.
Dr. Whiteley said that data like these are “really useful in trying to estimate these associations and it gives us some hypotheses to investigate in smaller mechanistic studies.”
Asked whether these data justify screening younger cryptogenic stroke patients more systematically for cancer, Dr. Whiteley replied: “I think we need some absolute risk estimates for that; for example, what proportion of younger patients would be at risk over the next few years when that screening would make a difference.”
Dr. Verhoeven reports no disclosures.
A version of this article first appeared on Medscape.com.
FROM ESOC 2022
Gallstone disease may be a harbinger of pancreatic cancer
in a SEER-Medicare database analysis. Patients with PDAC were six times more likely to have had gallstone disease in the year prior to diagnosis than noncancer patients, they found.
“We can’t be certain at this time as to whether gallstone disease is a precursor to PDAC or whether it is the end result of PDAC, but we do know there is an association, and we plan to explore it further,” commented study author Teviah Sachs, MD, MPH, Boston Medical Center.
“We don’t want anyone with gallstone disease to think that they have pancreatic cancer because, certainly, the overwhelming majority of patients with gallstone disease do not have pancreatic cancer,” he emphasized.
“But I would say to physicians that if you have a patient who presents with gallstone disease and they have other symptoms, you should not necessarily attribute those symptoms just to their gallstone disease,” Dr. Sachs commented.
“The diagnosis of pancreatic cancer should be on the differential in patients who present with symptoms that might not otherwise correlate with typical gallstones,” he added.
Dr. Sachs was speaking at a press briefing ahead of the annual Digestive Disease Week® (DDW), where the study will be presented.
“PDAC is often fatal because it’s frequently not diagnosed until it is late-stage disease,” Dr. Sachs noted.
Complicating earlier diagnosis is the fact that symptoms of PDAC often mirror those associated with gallstone disease and gallbladder infection, “both of which have been demonstrated to be risk factors for PDAC,” Dr. Sachs added.
Annual incidence
The purpose of the present study was to compare the incidence of cholelithiasis or cholecystitis in the year before a diagnosis of PDAC with the annual incidence in the general population.
A total of 18,700 patients with PDAC, median age 76 years, were identified in the SEER-Medicare database between 2008 and 2015. The incidence of hospital visits for gallstone disease in the year prior to PDAC diagnosis as well as the annual incidence of gallstone disease in the SEER-Medicare noncancer cohort were assessed.
An average of 99,287 patients per year were available from the noncancer cohort, 0.8% of whom had gallstone disease and 0.3% of whom had their gallbladders removed. In contrast, in the year before their diagnosis, 4.7% of PDAC patients had a diagnosis of gallstone disease and 1.6% had their gallbladders removed.
“Gallstone disease does not cause pancreatic cancer,” lead author, Marianna Papageorge, MD, research fellow, also of Boston Medical Center, said in a statement.
“But understanding its association with PDAC can help combat the high mortality rate with pancreatic cancer by providing the opportunity for earlier diagnosis and treatment,” she added.
A version of this article first appeared on Medscape.com.
in a SEER-Medicare database analysis. Patients with PDAC were six times more likely to have had gallstone disease in the year prior to diagnosis than noncancer patients, they found.
“We can’t be certain at this time as to whether gallstone disease is a precursor to PDAC or whether it is the end result of PDAC, but we do know there is an association, and we plan to explore it further,” commented study author Teviah Sachs, MD, MPH, Boston Medical Center.
“We don’t want anyone with gallstone disease to think that they have pancreatic cancer because, certainly, the overwhelming majority of patients with gallstone disease do not have pancreatic cancer,” he emphasized.
“But I would say to physicians that if you have a patient who presents with gallstone disease and they have other symptoms, you should not necessarily attribute those symptoms just to their gallstone disease,” Dr. Sachs commented.
“The diagnosis of pancreatic cancer should be on the differential in patients who present with symptoms that might not otherwise correlate with typical gallstones,” he added.
Dr. Sachs was speaking at a press briefing ahead of the annual Digestive Disease Week® (DDW), where the study will be presented.
“PDAC is often fatal because it’s frequently not diagnosed until it is late-stage disease,” Dr. Sachs noted.
Complicating earlier diagnosis is the fact that symptoms of PDAC often mirror those associated with gallstone disease and gallbladder infection, “both of which have been demonstrated to be risk factors for PDAC,” Dr. Sachs added.
Annual incidence
The purpose of the present study was to compare the incidence of cholelithiasis or cholecystitis in the year before a diagnosis of PDAC with the annual incidence in the general population.
A total of 18,700 patients with PDAC, median age 76 years, were identified in the SEER-Medicare database between 2008 and 2015. The incidence of hospital visits for gallstone disease in the year prior to PDAC diagnosis as well as the annual incidence of gallstone disease in the SEER-Medicare noncancer cohort were assessed.
An average of 99,287 patients per year were available from the noncancer cohort, 0.8% of whom had gallstone disease and 0.3% of whom had their gallbladders removed. In contrast, in the year before their diagnosis, 4.7% of PDAC patients had a diagnosis of gallstone disease and 1.6% had their gallbladders removed.
“Gallstone disease does not cause pancreatic cancer,” lead author, Marianna Papageorge, MD, research fellow, also of Boston Medical Center, said in a statement.
“But understanding its association with PDAC can help combat the high mortality rate with pancreatic cancer by providing the opportunity for earlier diagnosis and treatment,” she added.
A version of this article first appeared on Medscape.com.
in a SEER-Medicare database analysis. Patients with PDAC were six times more likely to have had gallstone disease in the year prior to diagnosis than noncancer patients, they found.
“We can’t be certain at this time as to whether gallstone disease is a precursor to PDAC or whether it is the end result of PDAC, but we do know there is an association, and we plan to explore it further,” commented study author Teviah Sachs, MD, MPH, Boston Medical Center.
“We don’t want anyone with gallstone disease to think that they have pancreatic cancer because, certainly, the overwhelming majority of patients with gallstone disease do not have pancreatic cancer,” he emphasized.
“But I would say to physicians that if you have a patient who presents with gallstone disease and they have other symptoms, you should not necessarily attribute those symptoms just to their gallstone disease,” Dr. Sachs commented.
“The diagnosis of pancreatic cancer should be on the differential in patients who present with symptoms that might not otherwise correlate with typical gallstones,” he added.
Dr. Sachs was speaking at a press briefing ahead of the annual Digestive Disease Week® (DDW), where the study will be presented.
“PDAC is often fatal because it’s frequently not diagnosed until it is late-stage disease,” Dr. Sachs noted.
Complicating earlier diagnosis is the fact that symptoms of PDAC often mirror those associated with gallstone disease and gallbladder infection, “both of which have been demonstrated to be risk factors for PDAC,” Dr. Sachs added.
Annual incidence
The purpose of the present study was to compare the incidence of cholelithiasis or cholecystitis in the year before a diagnosis of PDAC with the annual incidence in the general population.
A total of 18,700 patients with PDAC, median age 76 years, were identified in the SEER-Medicare database between 2008 and 2015. The incidence of hospital visits for gallstone disease in the year prior to PDAC diagnosis as well as the annual incidence of gallstone disease in the SEER-Medicare noncancer cohort were assessed.
An average of 99,287 patients per year were available from the noncancer cohort, 0.8% of whom had gallstone disease and 0.3% of whom had their gallbladders removed. In contrast, in the year before their diagnosis, 4.7% of PDAC patients had a diagnosis of gallstone disease and 1.6% had their gallbladders removed.
“Gallstone disease does not cause pancreatic cancer,” lead author, Marianna Papageorge, MD, research fellow, also of Boston Medical Center, said in a statement.
“But understanding its association with PDAC can help combat the high mortality rate with pancreatic cancer by providing the opportunity for earlier diagnosis and treatment,” she added.
A version of this article first appeared on Medscape.com.
FROM DDW 2022
Ondansetron use for acute gastroenteritis in children accelerates
Use of oral ondansetron for acute gastroenteritis in children in an emergency setting increased significantly between 2006 and 2018, but use of intravenous fluids remained consistent, based on data from a cross-sectional analysis.
Recommendations for managing acute gastroenteritis in children include oral rehydration therapy for mild to moderate cases and intravenous rehydration for severe cases, Brett Burstein, MDCM, of McGill University, Montreal, and colleagues wrote.
Oral ondansetron has been shown to reduce vomiting and the need for intravenous rehydration, as well as reduce the need for hospitalization in children with evidence of dehydration, but has no significant benefits for children who are not dehydrated, the researchers noted.
“Given the high prevalence and costs associated with acute gastroenteritis treatment for children, understanding national trends in management in a broad, generalizable sample is important,” they wrote.
In a study published in JAMA Network Open, the researchers identified data from the National Hospital Ambulatory Medical Care Survey from Jan. 1, 2006, to Dec. 31, 2018. They analyzed ED visits by individuals younger than 18 years with either a primary discharge diagnosis of acute gastroenteritis or a primary diagnosis of nausea, vomiting, diarrhea, or dehydration with a secondary diagnosis of acute gastroenteritis. The study population included 4,122 patients with a mean age of 4.8 years. Approximately 85% of the visits were to nonacademic EDs, and 80% were to nonpediatric EDs.
Overall, ED visits for acute gastroenteritis increased over time, from 1.23 million in 2006 to 1.87 million in 2018 (P = .03 for trend). ED visits for acute gastroenteritis also increased significantly as a proportion of all ED pediatric visits, from 4.7% in 2006 to 5.6% in 2018 (P = .02 for trend).
Notably, the use of ondansetron increased from 10.6% in 2006 to 59.2% in 2018; however, intravenous rehydration and hospitalizations remained consistent over the study period, the researchers wrote. Approximately half of children who received intravenous fluids (53.9%) and those hospitalized (49.1%) also received ondansetron.
“Approximately half of children administered intravenous fluids or hospitalized did not receive ondansetron, suggesting that many children without dehydration receive ondansetron with limited benefit, whereas those most likely to benefit receive intravenous fluids without an adequate trial of ondansetron and oral rehydration therapy,” the researchers wrote in their discussion of the findings.
The study findings were limited by several factors including the lack of data on detailed patient-level information such as severity of dehydration, the researchers noted. Other limitations include lack of data on return visits and lack of data on the route of medication administration, which means that the perceived lack of benefit from ondansetron may be the result of children treated with both intravenous ondansetron and fluids, they said.
“Ondansetron-supported oral rehydration therapy for appropriately selected children can achieve intravenous rehydration rates of 9%, more than threefold lower than 2018 national estimates,” and more initiatives are needed to optimize ondansetron and reduce the excessive use of intravenous fluids, the researchers concluded.
Emergency care setting may promote IV fluid use
“Acute gastroenteritis has remained a major cause of pediatric morbidity and mortality worldwide with significant costs for the health care system,” Tim Joos, MD, a Seattle-based clinician with a combination internal medicine/pediatrics practice who was not involved in the current study, said in an interview. “The authors highlight that although ondansetron use for acute gastroenteritis in the ED has increased substantially, there are still a number of children who receive intravenous fluids in the ED without a trial of ondansetron and [oral rehydration therapy] first. For the individual patient, it is not surprising that the fast-paced culture of the ED doesn’t cater to a watchful waiting approach. This highlights the need for a more protocol-based algorithm for care of these patients upon check-in.
“Often the practice in the ED is a single dose of ondansetron, followed by attempts at oral rehydration 30 minutes later,” said Dr. Joos. “It would be interesting to know the extent that outpatient clinics are practicing this model prior to sending the patient on to the ED. Despite it becoming a common practice, there is still ongoing research into the efficacy and safety of multidose oral ondansetron at home in reducing ED visits/hospitalizations.”
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Joos had no financial conflicts to disclose. Lead author Dr. Burstein received a career award from the Quebec Health Research Fund.
Use of oral ondansetron for acute gastroenteritis in children in an emergency setting increased significantly between 2006 and 2018, but use of intravenous fluids remained consistent, based on data from a cross-sectional analysis.
Recommendations for managing acute gastroenteritis in children include oral rehydration therapy for mild to moderate cases and intravenous rehydration for severe cases, Brett Burstein, MDCM, of McGill University, Montreal, and colleagues wrote.
Oral ondansetron has been shown to reduce vomiting and the need for intravenous rehydration, as well as reduce the need for hospitalization in children with evidence of dehydration, but has no significant benefits for children who are not dehydrated, the researchers noted.
“Given the high prevalence and costs associated with acute gastroenteritis treatment for children, understanding national trends in management in a broad, generalizable sample is important,” they wrote.
In a study published in JAMA Network Open, the researchers identified data from the National Hospital Ambulatory Medical Care Survey from Jan. 1, 2006, to Dec. 31, 2018. They analyzed ED visits by individuals younger than 18 years with either a primary discharge diagnosis of acute gastroenteritis or a primary diagnosis of nausea, vomiting, diarrhea, or dehydration with a secondary diagnosis of acute gastroenteritis. The study population included 4,122 patients with a mean age of 4.8 years. Approximately 85% of the visits were to nonacademic EDs, and 80% were to nonpediatric EDs.
Overall, ED visits for acute gastroenteritis increased over time, from 1.23 million in 2006 to 1.87 million in 2018 (P = .03 for trend). ED visits for acute gastroenteritis also increased significantly as a proportion of all ED pediatric visits, from 4.7% in 2006 to 5.6% in 2018 (P = .02 for trend).
Notably, the use of ondansetron increased from 10.6% in 2006 to 59.2% in 2018; however, intravenous rehydration and hospitalizations remained consistent over the study period, the researchers wrote. Approximately half of children who received intravenous fluids (53.9%) and those hospitalized (49.1%) also received ondansetron.
“Approximately half of children administered intravenous fluids or hospitalized did not receive ondansetron, suggesting that many children without dehydration receive ondansetron with limited benefit, whereas those most likely to benefit receive intravenous fluids without an adequate trial of ondansetron and oral rehydration therapy,” the researchers wrote in their discussion of the findings.
The study findings were limited by several factors including the lack of data on detailed patient-level information such as severity of dehydration, the researchers noted. Other limitations include lack of data on return visits and lack of data on the route of medication administration, which means that the perceived lack of benefit from ondansetron may be the result of children treated with both intravenous ondansetron and fluids, they said.
“Ondansetron-supported oral rehydration therapy for appropriately selected children can achieve intravenous rehydration rates of 9%, more than threefold lower than 2018 national estimates,” and more initiatives are needed to optimize ondansetron and reduce the excessive use of intravenous fluids, the researchers concluded.
Emergency care setting may promote IV fluid use
“Acute gastroenteritis has remained a major cause of pediatric morbidity and mortality worldwide with significant costs for the health care system,” Tim Joos, MD, a Seattle-based clinician with a combination internal medicine/pediatrics practice who was not involved in the current study, said in an interview. “The authors highlight that although ondansetron use for acute gastroenteritis in the ED has increased substantially, there are still a number of children who receive intravenous fluids in the ED without a trial of ondansetron and [oral rehydration therapy] first. For the individual patient, it is not surprising that the fast-paced culture of the ED doesn’t cater to a watchful waiting approach. This highlights the need for a more protocol-based algorithm for care of these patients upon check-in.
“Often the practice in the ED is a single dose of ondansetron, followed by attempts at oral rehydration 30 minutes later,” said Dr. Joos. “It would be interesting to know the extent that outpatient clinics are practicing this model prior to sending the patient on to the ED. Despite it becoming a common practice, there is still ongoing research into the efficacy and safety of multidose oral ondansetron at home in reducing ED visits/hospitalizations.”
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Joos had no financial conflicts to disclose. Lead author Dr. Burstein received a career award from the Quebec Health Research Fund.
Use of oral ondansetron for acute gastroenteritis in children in an emergency setting increased significantly between 2006 and 2018, but use of intravenous fluids remained consistent, based on data from a cross-sectional analysis.
Recommendations for managing acute gastroenteritis in children include oral rehydration therapy for mild to moderate cases and intravenous rehydration for severe cases, Brett Burstein, MDCM, of McGill University, Montreal, and colleagues wrote.
Oral ondansetron has been shown to reduce vomiting and the need for intravenous rehydration, as well as reduce the need for hospitalization in children with evidence of dehydration, but has no significant benefits for children who are not dehydrated, the researchers noted.
“Given the high prevalence and costs associated with acute gastroenteritis treatment for children, understanding national trends in management in a broad, generalizable sample is important,” they wrote.
In a study published in JAMA Network Open, the researchers identified data from the National Hospital Ambulatory Medical Care Survey from Jan. 1, 2006, to Dec. 31, 2018. They analyzed ED visits by individuals younger than 18 years with either a primary discharge diagnosis of acute gastroenteritis or a primary diagnosis of nausea, vomiting, diarrhea, or dehydration with a secondary diagnosis of acute gastroenteritis. The study population included 4,122 patients with a mean age of 4.8 years. Approximately 85% of the visits were to nonacademic EDs, and 80% were to nonpediatric EDs.
Overall, ED visits for acute gastroenteritis increased over time, from 1.23 million in 2006 to 1.87 million in 2018 (P = .03 for trend). ED visits for acute gastroenteritis also increased significantly as a proportion of all ED pediatric visits, from 4.7% in 2006 to 5.6% in 2018 (P = .02 for trend).
Notably, the use of ondansetron increased from 10.6% in 2006 to 59.2% in 2018; however, intravenous rehydration and hospitalizations remained consistent over the study period, the researchers wrote. Approximately half of children who received intravenous fluids (53.9%) and those hospitalized (49.1%) also received ondansetron.
“Approximately half of children administered intravenous fluids or hospitalized did not receive ondansetron, suggesting that many children without dehydration receive ondansetron with limited benefit, whereas those most likely to benefit receive intravenous fluids without an adequate trial of ondansetron and oral rehydration therapy,” the researchers wrote in their discussion of the findings.
The study findings were limited by several factors including the lack of data on detailed patient-level information such as severity of dehydration, the researchers noted. Other limitations include lack of data on return visits and lack of data on the route of medication administration, which means that the perceived lack of benefit from ondansetron may be the result of children treated with both intravenous ondansetron and fluids, they said.
“Ondansetron-supported oral rehydration therapy for appropriately selected children can achieve intravenous rehydration rates of 9%, more than threefold lower than 2018 national estimates,” and more initiatives are needed to optimize ondansetron and reduce the excessive use of intravenous fluids, the researchers concluded.
Emergency care setting may promote IV fluid use
“Acute gastroenteritis has remained a major cause of pediatric morbidity and mortality worldwide with significant costs for the health care system,” Tim Joos, MD, a Seattle-based clinician with a combination internal medicine/pediatrics practice who was not involved in the current study, said in an interview. “The authors highlight that although ondansetron use for acute gastroenteritis in the ED has increased substantially, there are still a number of children who receive intravenous fluids in the ED without a trial of ondansetron and [oral rehydration therapy] first. For the individual patient, it is not surprising that the fast-paced culture of the ED doesn’t cater to a watchful waiting approach. This highlights the need for a more protocol-based algorithm for care of these patients upon check-in.
“Often the practice in the ED is a single dose of ondansetron, followed by attempts at oral rehydration 30 minutes later,” said Dr. Joos. “It would be interesting to know the extent that outpatient clinics are practicing this model prior to sending the patient on to the ED. Despite it becoming a common practice, there is still ongoing research into the efficacy and safety of multidose oral ondansetron at home in reducing ED visits/hospitalizations.”
The study received no outside funding. The researchers had no financial conflicts to disclose. Dr. Joos had no financial conflicts to disclose. Lead author Dr. Burstein received a career award from the Quebec Health Research Fund.
FROM JAMA NETWORK OPEN
IBD after age 60: More evidence antibiotics play a role
Most studies to date have assessed a link between antibiotics and IBD in younger patients, lead researcher Adam S. Faye, MD, said during a media briefing that previewed select research for the annual Digestive Disease Week® (DDW).
The impact of antibiotic use on the incidence of IBD in older adults is really unknown, he added.
In contrast to younger people with IBD, who tend to have a strong family history or genetic predisposition to developing Crohn’s disease or ulcerative colitis, the cause is likely different in older populations.
“There’s clearly something in the environment that’s driving this new older-onset IBD,” said Dr. Faye, who is an assistant professor of medicine and population health at New York University.
Antibiotics as a contributing link
Dr. Faye and colleagues took a closer look at antibiotics as contributing to this link. They studied 2.3 million patient records in Denmark’s national medical registry from 2000 to 2018. They identified people aged 60 years and older who were newly diagnosed with IBD, and they then assessed the number, frequency, and timing of any antibiotic prescriptions.
They found that IBD was 27% more likely in this age group if the patients had received any antibiotic prescription.
They also found that the chance of developing IBD was higher as the number of antibiotic prescriptions increased. For example, IBD was 55% more likely if a person had received two prescriptions, and it was 96% more likely with four prescriptions. The risk really jumped with five or more antibiotic prescriptions – a person with this many prescriptions was more than 2.3 times (236%) more likely to be diagnosed with IBD than those who had not been prescribed antibiotics in the prior 5 years.
Not all antibiotics were equal, however. For example, the investigators found no link with nitrofurantoin, an antibiotic commonly prescribed for urinary tract infections. In contrast, all other antibiotic agents that were evaluated, and especially fluoroquinolones, nitroimidazoles, and macrolides, were associated with IBD.
Timing made some difference.
“The risk was highest if antibiotics were prescribed within the 1- to 2-year period before diagnosis, and it declined as you go farther out. But the risks persist,” Dr. Faye said. He noted that they even found that risk was elevated 10 years out.
The investigators also considered whether the antibiotic agent or infection was behind the association.
Dr. Faye cited previous research, again in younger people with IBD, that revealed that “infections plus antibiotics substantially increase the odds or risk of developing IBD more than the infection alone.
“So there really does seem to be something that the antibiotics are doing here,” Dr. Faye said.
A leading theory is that antibiotics disrupt the gut microbiota and increase the risk for developing IBD. “But, obviously, it’s quite complicated,” he said.
Clinical implications
The findings suggest that older people who may have IBD should be screened for prior antibiotic use, Dr. Faye said.
“This is a result that really has important implications for diagnosing older adults with new gastrointestinal symptoms,” he said. “Inflammatory bowel disease often can be overlooked in older adults because there’s a lot of different diagnoses you’re thinking of.”
IBD “should be considered, especially if you have a patient who’s reporting multiple courses of antibiotics in the last few years,” he added.
The results suggest another reason that antimicrobial stewardship programs should promote judicial use of these agents beyond concerns about resistance.
“We think of antibiotic stewardship to prevent the development of multidrug-resistant organisms, but we should be thinking about it to also prevent the development of inflammatory bowel disease,” Dr. Faye said.
Although this study adds to the evidence implicating antibiotics and expands the concept to an older population, “we really don’t have a great handle on what all of the environmental and other factors are,” he said.
Some researchers point to smoking and diet, among other factors, but the interplay remains unknown, Dr. Faye added.
The study is important because the incidence of IBD is increasing within the older population, “and this is one of the first studies to look at it,” he said.
Dr. Faye and colleagues plan to start a new study to evaluate other environmental factors.
“Hopefully, we’ll have more within the next few years to report,” he said.
Shedding more light on older-onset IBD worldwide
“It’s a well-done study,” Aline Charabaty, MD, said in a comment. “We are seeing that there’s an increase of incidence of IBD in the entire population, but even more so in the elderly.”
IBD is likely caused by a combination of factors, including genetics, environmental influences, and dysfunction of the gut immune system, agreed Dr. Charabaty, who is an assistant clinical professor in the division of gastroenterology at Johns Hopkins University, Baltimore.
The research “goes along with other studies that we’ve done in the pediatric and adult populations that show antibiotics exposure increases the risk of developing inflammatory bowel disease,” she said.
For a broader perspective of the study’s findings, Dr. Faye was asked during the media briefing if the results of this Danish registry study would be generalizable to the U.S. population.
“The simplest answer is we’ll need to redo this study within the U.S. to make absolutely sure,” Dr. Faye said. She noted that prior studies in the United States and elsewhere have found a risk associated with antibiotics, although again these studies focused on younger patients.
Dr. Charabaty was more certain that the findings were meaningful outside of Denmark.
“I definitely think this will apply to our U.S. population,” added Dr. Charabaty, who is also the clinical director of the IBD Center at Johns Hopkins–Sibley Memorial Hospital, Washington. “We have very similar practices in terms of how we approach antibiotic use.
“This could be one of the risk factors that’s promoting an increase in IBD everywhere,” she added.
The study was conducted in partnership with the Danish National Center of Excellence PREDICT Program. Dr. Faye and Dr. Charabaty did not report any conflicts of interest related to this study.
A version of this article first appeared on Medscape.com.
Most studies to date have assessed a link between antibiotics and IBD in younger patients, lead researcher Adam S. Faye, MD, said during a media briefing that previewed select research for the annual Digestive Disease Week® (DDW).
The impact of antibiotic use on the incidence of IBD in older adults is really unknown, he added.
In contrast to younger people with IBD, who tend to have a strong family history or genetic predisposition to developing Crohn’s disease or ulcerative colitis, the cause is likely different in older populations.
“There’s clearly something in the environment that’s driving this new older-onset IBD,” said Dr. Faye, who is an assistant professor of medicine and population health at New York University.
Antibiotics as a contributing link
Dr. Faye and colleagues took a closer look at antibiotics as contributing to this link. They studied 2.3 million patient records in Denmark’s national medical registry from 2000 to 2018. They identified people aged 60 years and older who were newly diagnosed with IBD, and they then assessed the number, frequency, and timing of any antibiotic prescriptions.
They found that IBD was 27% more likely in this age group if the patients had received any antibiotic prescription.
They also found that the chance of developing IBD was higher as the number of antibiotic prescriptions increased. For example, IBD was 55% more likely if a person had received two prescriptions, and it was 96% more likely with four prescriptions. The risk really jumped with five or more antibiotic prescriptions – a person with this many prescriptions was more than 2.3 times (236%) more likely to be diagnosed with IBD than those who had not been prescribed antibiotics in the prior 5 years.
Not all antibiotics were equal, however. For example, the investigators found no link with nitrofurantoin, an antibiotic commonly prescribed for urinary tract infections. In contrast, all other antibiotic agents that were evaluated, and especially fluoroquinolones, nitroimidazoles, and macrolides, were associated with IBD.
Timing made some difference.
“The risk was highest if antibiotics were prescribed within the 1- to 2-year period before diagnosis, and it declined as you go farther out. But the risks persist,” Dr. Faye said. He noted that they even found that risk was elevated 10 years out.
The investigators also considered whether the antibiotic agent or infection was behind the association.
Dr. Faye cited previous research, again in younger people with IBD, that revealed that “infections plus antibiotics substantially increase the odds or risk of developing IBD more than the infection alone.
“So there really does seem to be something that the antibiotics are doing here,” Dr. Faye said.
A leading theory is that antibiotics disrupt the gut microbiota and increase the risk for developing IBD. “But, obviously, it’s quite complicated,” he said.
Clinical implications
The findings suggest that older people who may have IBD should be screened for prior antibiotic use, Dr. Faye said.
“This is a result that really has important implications for diagnosing older adults with new gastrointestinal symptoms,” he said. “Inflammatory bowel disease often can be overlooked in older adults because there’s a lot of different diagnoses you’re thinking of.”
IBD “should be considered, especially if you have a patient who’s reporting multiple courses of antibiotics in the last few years,” he added.
The results suggest another reason that antimicrobial stewardship programs should promote judicial use of these agents beyond concerns about resistance.
“We think of antibiotic stewardship to prevent the development of multidrug-resistant organisms, but we should be thinking about it to also prevent the development of inflammatory bowel disease,” Dr. Faye said.
Although this study adds to the evidence implicating antibiotics and expands the concept to an older population, “we really don’t have a great handle on what all of the environmental and other factors are,” he said.
Some researchers point to smoking and diet, among other factors, but the interplay remains unknown, Dr. Faye added.
The study is important because the incidence of IBD is increasing within the older population, “and this is one of the first studies to look at it,” he said.
Dr. Faye and colleagues plan to start a new study to evaluate other environmental factors.
“Hopefully, we’ll have more within the next few years to report,” he said.
Shedding more light on older-onset IBD worldwide
“It’s a well-done study,” Aline Charabaty, MD, said in a comment. “We are seeing that there’s an increase of incidence of IBD in the entire population, but even more so in the elderly.”
IBD is likely caused by a combination of factors, including genetics, environmental influences, and dysfunction of the gut immune system, agreed Dr. Charabaty, who is an assistant clinical professor in the division of gastroenterology at Johns Hopkins University, Baltimore.
The research “goes along with other studies that we’ve done in the pediatric and adult populations that show antibiotics exposure increases the risk of developing inflammatory bowel disease,” she said.
For a broader perspective of the study’s findings, Dr. Faye was asked during the media briefing if the results of this Danish registry study would be generalizable to the U.S. population.
“The simplest answer is we’ll need to redo this study within the U.S. to make absolutely sure,” Dr. Faye said. She noted that prior studies in the United States and elsewhere have found a risk associated with antibiotics, although again these studies focused on younger patients.
Dr. Charabaty was more certain that the findings were meaningful outside of Denmark.
“I definitely think this will apply to our U.S. population,” added Dr. Charabaty, who is also the clinical director of the IBD Center at Johns Hopkins–Sibley Memorial Hospital, Washington. “We have very similar practices in terms of how we approach antibiotic use.
“This could be one of the risk factors that’s promoting an increase in IBD everywhere,” she added.
The study was conducted in partnership with the Danish National Center of Excellence PREDICT Program. Dr. Faye and Dr. Charabaty did not report any conflicts of interest related to this study.
A version of this article first appeared on Medscape.com.
Most studies to date have assessed a link between antibiotics and IBD in younger patients, lead researcher Adam S. Faye, MD, said during a media briefing that previewed select research for the annual Digestive Disease Week® (DDW).
The impact of antibiotic use on the incidence of IBD in older adults is really unknown, he added.
In contrast to younger people with IBD, who tend to have a strong family history or genetic predisposition to developing Crohn’s disease or ulcerative colitis, the cause is likely different in older populations.
“There’s clearly something in the environment that’s driving this new older-onset IBD,” said Dr. Faye, who is an assistant professor of medicine and population health at New York University.
Antibiotics as a contributing link
Dr. Faye and colleagues took a closer look at antibiotics as contributing to this link. They studied 2.3 million patient records in Denmark’s national medical registry from 2000 to 2018. They identified people aged 60 years and older who were newly diagnosed with IBD, and they then assessed the number, frequency, and timing of any antibiotic prescriptions.
They found that IBD was 27% more likely in this age group if the patients had received any antibiotic prescription.
They also found that the chance of developing IBD was higher as the number of antibiotic prescriptions increased. For example, IBD was 55% more likely if a person had received two prescriptions, and it was 96% more likely with four prescriptions. The risk really jumped with five or more antibiotic prescriptions – a person with this many prescriptions was more than 2.3 times (236%) more likely to be diagnosed with IBD than those who had not been prescribed antibiotics in the prior 5 years.
Not all antibiotics were equal, however. For example, the investigators found no link with nitrofurantoin, an antibiotic commonly prescribed for urinary tract infections. In contrast, all other antibiotic agents that were evaluated, and especially fluoroquinolones, nitroimidazoles, and macrolides, were associated with IBD.
Timing made some difference.
“The risk was highest if antibiotics were prescribed within the 1- to 2-year period before diagnosis, and it declined as you go farther out. But the risks persist,” Dr. Faye said. He noted that they even found that risk was elevated 10 years out.
The investigators also considered whether the antibiotic agent or infection was behind the association.
Dr. Faye cited previous research, again in younger people with IBD, that revealed that “infections plus antibiotics substantially increase the odds or risk of developing IBD more than the infection alone.
“So there really does seem to be something that the antibiotics are doing here,” Dr. Faye said.
A leading theory is that antibiotics disrupt the gut microbiota and increase the risk for developing IBD. “But, obviously, it’s quite complicated,” he said.
Clinical implications
The findings suggest that older people who may have IBD should be screened for prior antibiotic use, Dr. Faye said.
“This is a result that really has important implications for diagnosing older adults with new gastrointestinal symptoms,” he said. “Inflammatory bowel disease often can be overlooked in older adults because there’s a lot of different diagnoses you’re thinking of.”
IBD “should be considered, especially if you have a patient who’s reporting multiple courses of antibiotics in the last few years,” he added.
The results suggest another reason that antimicrobial stewardship programs should promote judicial use of these agents beyond concerns about resistance.
“We think of antibiotic stewardship to prevent the development of multidrug-resistant organisms, but we should be thinking about it to also prevent the development of inflammatory bowel disease,” Dr. Faye said.
Although this study adds to the evidence implicating antibiotics and expands the concept to an older population, “we really don’t have a great handle on what all of the environmental and other factors are,” he said.
Some researchers point to smoking and diet, among other factors, but the interplay remains unknown, Dr. Faye added.
The study is important because the incidence of IBD is increasing within the older population, “and this is one of the first studies to look at it,” he said.
Dr. Faye and colleagues plan to start a new study to evaluate other environmental factors.
“Hopefully, we’ll have more within the next few years to report,” he said.
Shedding more light on older-onset IBD worldwide
“It’s a well-done study,” Aline Charabaty, MD, said in a comment. “We are seeing that there’s an increase of incidence of IBD in the entire population, but even more so in the elderly.”
IBD is likely caused by a combination of factors, including genetics, environmental influences, and dysfunction of the gut immune system, agreed Dr. Charabaty, who is an assistant clinical professor in the division of gastroenterology at Johns Hopkins University, Baltimore.
The research “goes along with other studies that we’ve done in the pediatric and adult populations that show antibiotics exposure increases the risk of developing inflammatory bowel disease,” she said.
For a broader perspective of the study’s findings, Dr. Faye was asked during the media briefing if the results of this Danish registry study would be generalizable to the U.S. population.
“The simplest answer is we’ll need to redo this study within the U.S. to make absolutely sure,” Dr. Faye said. She noted that prior studies in the United States and elsewhere have found a risk associated with antibiotics, although again these studies focused on younger patients.
Dr. Charabaty was more certain that the findings were meaningful outside of Denmark.
“I definitely think this will apply to our U.S. population,” added Dr. Charabaty, who is also the clinical director of the IBD Center at Johns Hopkins–Sibley Memorial Hospital, Washington. “We have very similar practices in terms of how we approach antibiotic use.
“This could be one of the risk factors that’s promoting an increase in IBD everywhere,” she added.
The study was conducted in partnership with the Danish National Center of Excellence PREDICT Program. Dr. Faye and Dr. Charabaty did not report any conflicts of interest related to this study.
A version of this article first appeared on Medscape.com.
FROM DDW 2022
Neuropsychiatric risks of COVID-19: New data
The neuropsychiatric ramifications of severe COVID-19 infection appear to be no different than for other severe acute respiratory infections (SARI).
This suggests that disease severity, rather than pathogen, is the most relevant factor in new-onset neuropsychiatric illness, the investigators note.
The risk of new-onset neuropsychological illness after severe COVID-19 infection are “substantial, but similar to those after other severe respiratory infections,” study investigator Peter Watkinson, MD, Nuffield Department of Clinical Neurosciences, University of Oxford, and John Radcliffe Hospital, Oxford, England, told this news organization.
The study was published online in JAMA Psychiatry.
Significant mental health burden
Research has shown a significant burden of neuropsychological illness after severe COVID-19 infection. However, it’s unclear how this risk compares to SARI.
To investigate, Dr. Watkinson and colleagues evaluated electronic health record data on more than 8.3 million adults, including 16,679 (0.02%) who survived a hospital admission for SARI and 32,525 (0.03%) who survived a hospital stay for COVID-19.
Compared with the remaining population, risks of new anxiety disorder, dementia, psychotic disorder, depression, and bipolar disorder diagnoses were significantly and similarly increased in adults surviving hospitalization for either COVID-19 or SARI.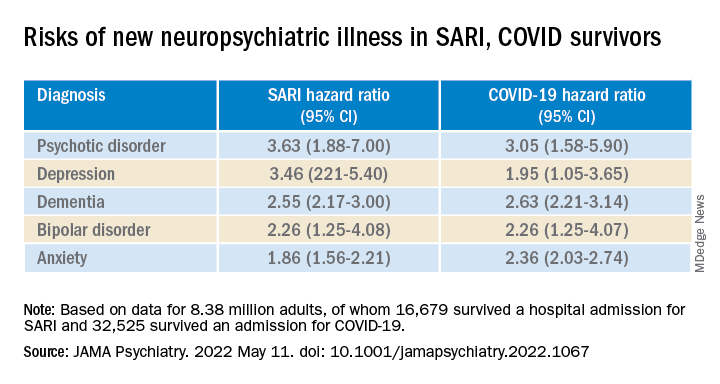
Compared with the wider population, survivors of severe SARI or COVID-19 were also at increased risk of starting treatment with antidepressants, hypnotics/anxiolytics, or antipsychotics.
When comparing survivors of SARI hospitalization to survivors of COVID-19 hospitalization, no significant differences were observed in the postdischarge rates of new-onset anxiety disorder, dementia, depression, or bipolar affective disorder.
The SARI and COVID groups also did not differ in terms of their postdischarge risks of antidepressant or hypnotic/anxiolytic use, but the COVID survivors had a 20% lower risk of starting an antipsychotic.
“In this cohort study, SARI were found to be associated with significant postacute neuropsychiatric morbidity, for which COVID-19 is not distinctly different,” Dr. Watkinson and colleagues write.
“These results may help refine our understanding of the post–severe COVID-19 phenotype and may inform post-discharge support for patients requiring hospital-based and intensive care for SARI regardless of causative pathogen,” they write.
Caveats, cautionary notes
Kevin McConway, PhD, emeritus professor of applied statistics at the Open University in Milton Keynes, England, described the study as “impressive.” However, he pointed out that the study’s observational design is a limitation.
“One can never be absolutely certain about the interpretation of findings of an observational study. What the research can’t tell us is what caused the increased psychiatric risks for people hospitalized with COVID-19 or some other serious respiratory disease,” Dr. McConway said.
“It can’t tell us what might happen in the future, when, we all hope, many fewer are being hospitalized with COVID-19 than was the case in those first two waves, and the current backlog of provision of some health services has decreased,” he added.
“So we can’t just say that, in general, serious COVID-19 has much the same neuropsychiatric consequences as other very serious respiratory illness. Maybe it does, maybe it doesn’t,” Dr. McConway cautioned.
Max Taquet, PhD, with the University of Oxford, noted that the study is limited to hospitalized adult patients, leaving open the question of risk in nonhospitalized individuals – which is the overwhelming majority of patients with COVID-19 – or in children.
Whether the neuropsychiatric risks have remained the same since the emergence of the Omicron variant also remains “an open question since all patients in this study were diagnosed before July 2021,” Dr. Taquet said in statement.
The study was funded by the Wellcome Trust, the John Fell Oxford University Press Research Fund, the Oxford Wellcome Institutional Strategic Support Fund and Cancer Research UK, through the Cancer Research UK Oxford Centre. Dr. Watkinson disclosed grants from the National Institute for Health Research and Sensyne Health outside the submitted work; and serving as chief medical officer for Sensyne Health prior to this work, as well as holding shares in the company. Dr. McConway is a trustee of the UK Science Media Centre and a member of its advisory committee. His comments were provided in his capacity as an independent professional statistician. Dr. Taquet has worked on similar studies trying to identify, quantify, and specify the neurological and psychiatric consequences of COVID-19.
A version of this article first appeared on Medscape.com.
The neuropsychiatric ramifications of severe COVID-19 infection appear to be no different than for other severe acute respiratory infections (SARI).
This suggests that disease severity, rather than pathogen, is the most relevant factor in new-onset neuropsychiatric illness, the investigators note.
The risk of new-onset neuropsychological illness after severe COVID-19 infection are “substantial, but similar to those after other severe respiratory infections,” study investigator Peter Watkinson, MD, Nuffield Department of Clinical Neurosciences, University of Oxford, and John Radcliffe Hospital, Oxford, England, told this news organization.
The study was published online in JAMA Psychiatry.
Significant mental health burden
Research has shown a significant burden of neuropsychological illness after severe COVID-19 infection. However, it’s unclear how this risk compares to SARI.
To investigate, Dr. Watkinson and colleagues evaluated electronic health record data on more than 8.3 million adults, including 16,679 (0.02%) who survived a hospital admission for SARI and 32,525 (0.03%) who survived a hospital stay for COVID-19.
Compared with the remaining population, risks of new anxiety disorder, dementia, psychotic disorder, depression, and bipolar disorder diagnoses were significantly and similarly increased in adults surviving hospitalization for either COVID-19 or SARI.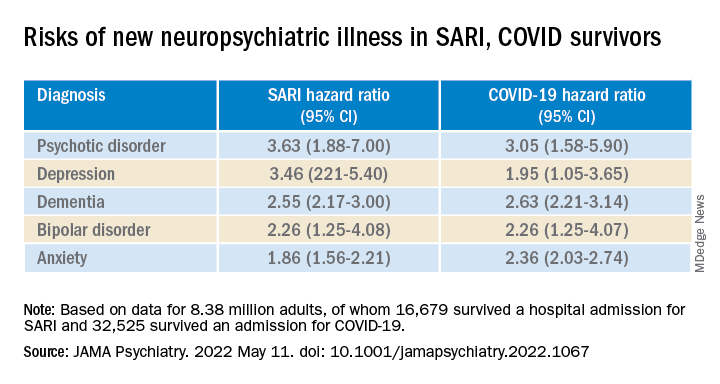
Compared with the wider population, survivors of severe SARI or COVID-19 were also at increased risk of starting treatment with antidepressants, hypnotics/anxiolytics, or antipsychotics.
When comparing survivors of SARI hospitalization to survivors of COVID-19 hospitalization, no significant differences were observed in the postdischarge rates of new-onset anxiety disorder, dementia, depression, or bipolar affective disorder.
The SARI and COVID groups also did not differ in terms of their postdischarge risks of antidepressant or hypnotic/anxiolytic use, but the COVID survivors had a 20% lower risk of starting an antipsychotic.
“In this cohort study, SARI were found to be associated with significant postacute neuropsychiatric morbidity, for which COVID-19 is not distinctly different,” Dr. Watkinson and colleagues write.
“These results may help refine our understanding of the post–severe COVID-19 phenotype and may inform post-discharge support for patients requiring hospital-based and intensive care for SARI regardless of causative pathogen,” they write.
Caveats, cautionary notes
Kevin McConway, PhD, emeritus professor of applied statistics at the Open University in Milton Keynes, England, described the study as “impressive.” However, he pointed out that the study’s observational design is a limitation.
“One can never be absolutely certain about the interpretation of findings of an observational study. What the research can’t tell us is what caused the increased psychiatric risks for people hospitalized with COVID-19 or some other serious respiratory disease,” Dr. McConway said.
“It can’t tell us what might happen in the future, when, we all hope, many fewer are being hospitalized with COVID-19 than was the case in those first two waves, and the current backlog of provision of some health services has decreased,” he added.
“So we can’t just say that, in general, serious COVID-19 has much the same neuropsychiatric consequences as other very serious respiratory illness. Maybe it does, maybe it doesn’t,” Dr. McConway cautioned.
Max Taquet, PhD, with the University of Oxford, noted that the study is limited to hospitalized adult patients, leaving open the question of risk in nonhospitalized individuals – which is the overwhelming majority of patients with COVID-19 – or in children.
Whether the neuropsychiatric risks have remained the same since the emergence of the Omicron variant also remains “an open question since all patients in this study were diagnosed before July 2021,” Dr. Taquet said in statement.
The study was funded by the Wellcome Trust, the John Fell Oxford University Press Research Fund, the Oxford Wellcome Institutional Strategic Support Fund and Cancer Research UK, through the Cancer Research UK Oxford Centre. Dr. Watkinson disclosed grants from the National Institute for Health Research and Sensyne Health outside the submitted work; and serving as chief medical officer for Sensyne Health prior to this work, as well as holding shares in the company. Dr. McConway is a trustee of the UK Science Media Centre and a member of its advisory committee. His comments were provided in his capacity as an independent professional statistician. Dr. Taquet has worked on similar studies trying to identify, quantify, and specify the neurological and psychiatric consequences of COVID-19.
A version of this article first appeared on Medscape.com.
The neuropsychiatric ramifications of severe COVID-19 infection appear to be no different than for other severe acute respiratory infections (SARI).
This suggests that disease severity, rather than pathogen, is the most relevant factor in new-onset neuropsychiatric illness, the investigators note.
The risk of new-onset neuropsychological illness after severe COVID-19 infection are “substantial, but similar to those after other severe respiratory infections,” study investigator Peter Watkinson, MD, Nuffield Department of Clinical Neurosciences, University of Oxford, and John Radcliffe Hospital, Oxford, England, told this news organization.
The study was published online in JAMA Psychiatry.
Significant mental health burden
Research has shown a significant burden of neuropsychological illness after severe COVID-19 infection. However, it’s unclear how this risk compares to SARI.
To investigate, Dr. Watkinson and colleagues evaluated electronic health record data on more than 8.3 million adults, including 16,679 (0.02%) who survived a hospital admission for SARI and 32,525 (0.03%) who survived a hospital stay for COVID-19.
Compared with the remaining population, risks of new anxiety disorder, dementia, psychotic disorder, depression, and bipolar disorder diagnoses were significantly and similarly increased in adults surviving hospitalization for either COVID-19 or SARI.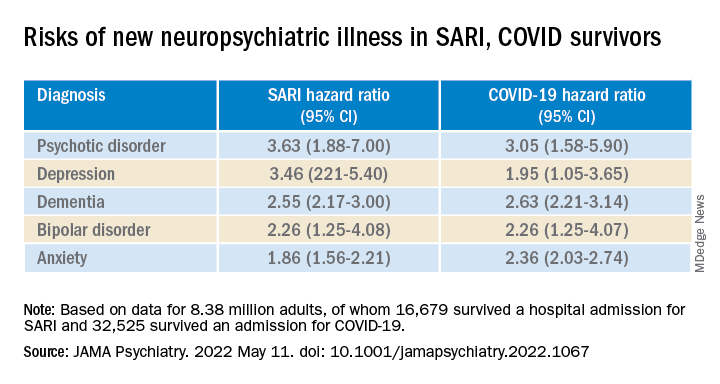
Compared with the wider population, survivors of severe SARI or COVID-19 were also at increased risk of starting treatment with antidepressants, hypnotics/anxiolytics, or antipsychotics.
When comparing survivors of SARI hospitalization to survivors of COVID-19 hospitalization, no significant differences were observed in the postdischarge rates of new-onset anxiety disorder, dementia, depression, or bipolar affective disorder.
The SARI and COVID groups also did not differ in terms of their postdischarge risks of antidepressant or hypnotic/anxiolytic use, but the COVID survivors had a 20% lower risk of starting an antipsychotic.
“In this cohort study, SARI were found to be associated with significant postacute neuropsychiatric morbidity, for which COVID-19 is not distinctly different,” Dr. Watkinson and colleagues write.
“These results may help refine our understanding of the post–severe COVID-19 phenotype and may inform post-discharge support for patients requiring hospital-based and intensive care for SARI regardless of causative pathogen,” they write.
Caveats, cautionary notes
Kevin McConway, PhD, emeritus professor of applied statistics at the Open University in Milton Keynes, England, described the study as “impressive.” However, he pointed out that the study’s observational design is a limitation.
“One can never be absolutely certain about the interpretation of findings of an observational study. What the research can’t tell us is what caused the increased psychiatric risks for people hospitalized with COVID-19 or some other serious respiratory disease,” Dr. McConway said.
“It can’t tell us what might happen in the future, when, we all hope, many fewer are being hospitalized with COVID-19 than was the case in those first two waves, and the current backlog of provision of some health services has decreased,” he added.
“So we can’t just say that, in general, serious COVID-19 has much the same neuropsychiatric consequences as other very serious respiratory illness. Maybe it does, maybe it doesn’t,” Dr. McConway cautioned.
Max Taquet, PhD, with the University of Oxford, noted that the study is limited to hospitalized adult patients, leaving open the question of risk in nonhospitalized individuals – which is the overwhelming majority of patients with COVID-19 – or in children.
Whether the neuropsychiatric risks have remained the same since the emergence of the Omicron variant also remains “an open question since all patients in this study were diagnosed before July 2021,” Dr. Taquet said in statement.
The study was funded by the Wellcome Trust, the John Fell Oxford University Press Research Fund, the Oxford Wellcome Institutional Strategic Support Fund and Cancer Research UK, through the Cancer Research UK Oxford Centre. Dr. Watkinson disclosed grants from the National Institute for Health Research and Sensyne Health outside the submitted work; and serving as chief medical officer for Sensyne Health prior to this work, as well as holding shares in the company. Dr. McConway is a trustee of the UK Science Media Centre and a member of its advisory committee. His comments were provided in his capacity as an independent professional statistician. Dr. Taquet has worked on similar studies trying to identify, quantify, and specify the neurological and psychiatric consequences of COVID-19.
A version of this article first appeared on Medscape.com.
Are physician white coats becoming obsolete? How docs dress for work now
Early in the COVID-19 pandemic, Trisha Pasricha, MD, a gastroenterologist and research fellow at Massachusetts General Hospital in Boston, was talking to a patient who had been hospitalized for a peptic ulcer.
Like other physicians in her institution, Dr. Pasricha was wearing scrubs instead of a white coat, out of concern that the white coat might be more prone to accumulating or transmitting COVID-19 pathogens. Her badge identified her as a physician, and she introduced herself clearly as “Dr. Pasricha.”
The patient “required an emergent procedure, which I discussed with him,” Dr. Pasricha told this news organization. “I went over what the procedure entailed, the risks and benefits, and the need for informed consent. The patient nodded and seemed to understand, but at the end of the discussion he said: ‘That all sounds fine, but I need to speak to the doctor first.’ ”
Dr. Pasricha was taken aback. She wondered: “Who did he think I was the whole time that I was reviewing medical concerns, explaining medical concepts, and describing a procedure in a way that a physician would describe it?”
She realized the reason he didn’t correctly identify her was that, clad only in scrubs, she was less easily recognizable as a physician. And to be misidentified as technicians, nurses, physician assistants, or other health care professionals, according to Dr. Pasricha.
Dr. Pasricha said she has been the recipient of this “implicit bias” not only from patients but also from members of the health care team, and added that other female colleagues have told her that they’ve had similar experiences, especially when they’re not wearing a white coat.
Changing times, changing trends
When COVID-19 began to spread, “there was an initial concern that COVID-19 was passed through surfaces, and concerns about whether white coats could carry viral particles,” according to Jordan Steinberg, MD, PhD, surgical director of the craniofacial program at Nicklaus Children’s Pediatric Specialists/Nicklaus Children’s Health System, Miami. “Hospitals didn’t want to launder the white coats as frequently as scrubs, due to cost concerns. There was also a concern raised that a necktie might dangle in patients’ faces, coming in closer contact with pathogens, so more physicians were wearing scrubs.”
Yet even before the pandemic, physician attire in hospital and outpatient settings had started to change. Dr. Steinberg, who is also a clinical associate professor at Florida International University, Miami, told this news organization that, in his previous appointment at Johns Hopkins University, Baltimore, he and his colleagues “had noticed in our institution, as well as other facilities, an increasing trend that moved from white coats worn over professional attire toward more casual dress among medical staff – increased wearing of casual fleece or softshell jackets with the institutional logo.”
This was especially true with trainees and the “younger generation,” who were preferring “what I would almost call ‘warm-up clothes,’ gym clothes, and less shirt-tie-white-coat attire for men or white-coats-and-business attire for women.” Dr. Steinberg thinks that some physicians prefer the fleece with the institutional logo “because it’s like wearing your favorite sports team jersey. It gives a sense of belonging.”
Todd Shaffer, MD, MBA, a family physician at University Physicians Associates, Truman Medical Centers and the Lakewood Medical Pavilion, Kansas City, Mo., has been at his institution for 30 years and has seen a similar trend. “At one point, things were very formal,” he told this news organization. But attire was already becoming less formal before the pandemic, and new changes took place during the pandemic, as physicians began wearing scrubs instead of white coats because of fears of viral contamination.
Now, there is less concern about potential viral contamination with the white coat. Yet many physicians continue to wear scrubs – especially those who interact with patients with COVID – and it has become more acceptable to do so, or to wear personal protective equipment (PPE) over ordinary clothing, but it is less common in routine clinical practice, said Dr. Shaffer, a member of the board of directors of the American Academy of Family Physicians.
“The world has changed since COVID. People feel more comfortable dressing more casually during professional Zoom calls, when they have the convenience of working from home,” said Dr. Shaffer, who is also a professor of family medicine at University of Missouri–Kansas City.
Dr. Shaffer himself hasn’t worn a white coat for years. “I’m more likely to wear medium casual pants. I’ve bought some nicer shirts, so I still look professional and upbeat. I don’t always tuck in my shirt, and I don’t dress as formally.” He wears PPE and a mask and/or face shield when treating patients with COVID-19. And he wears a white coat “when someone wants a photograph taken with the doctors – with the stethoscope draped around my neck.”
Traditional symbol of medicine
Because of the changing mores, Dr. Steinberg and colleagues at Johns Hopkins wondered if there might still be a role for professional attire and white coats and what patients prefer. To investigate the question, they surveyed 487 U.S. adults in the spring of 2020.
Respondents were asked where and how frequently they see health care professionals wearing white coats, scrubs, and fleece or softshell jackets. They were also shown photographs depicting models wearing various types of attire commonly seen in health care settings and were asked to rank the “health care provider’s” level of experience, professionalism, and friendliness.
The majority of participants said they had seen health care practitioners in white coats “most of the time,” in scrubs “sometimes,” and in fleece or softshell jackets “rarely.” Models in white coats were regarded by respondents as more experienced and professional, although those in softshell jackets were perceived as friendlier.
There were age as well as regional differences in the responses, Dr. Steinberg said. Older respondents were significantly more likely than their younger counterparts to perceive a model wearing a white coat over business attire as being more experienced, and – in all regions of the United States except the West coast – respondents gave lower professionalism scores to providers wearing fleece jackets with scrubs underneath.
Respondents tended to prefer surgeons wearing a white coat with scrubs underneath, while a white coat over business attire was the preferred dress code for family physicians and dermatologists.
“People tended to respond as if there was a more professional element in the white coat. The age-old symbol of the white coat still marked something important,” Dr. Steinberg said. “Our data suggest that the white coat isn’t ready to die just yet. People still see an air of authority and a traditional symbol of medicine. Nevertheless, I do think it will become less common than it used to be, especially in certain regions of the country.”
Organic, subtle changes
Christopher Petrilli, MD, assistant professor at New York University, conducted research in 2018 regarding physician attire by surveying over 4,000 patients in 10 U.S. academic hospitals. His team found that most patients continued to prefer physicians to wear formal attire under a white coat, especially older respondents.
Dr. Petrilli and colleagues have been studying the issue of physician attire since 2015. “The big issue when we did our initial study – which might not be accurate anymore – is that few hospitals actually had a uniform dress code,” said Dr. Petrilli, the medical director of clinical documentation improvement and the clinical lead of value-based medicine at NYU Langone Hospitals. “When we looked at ‘honor roll hospitals’ during our study, we cold-called these hospitals and also looked online for their dress code policies. Except for the Mayo Clinic, hospitals that had dress code policies were more generic.”
For example, the American Medical Association guidance merely states that attire should be “clean, unsoiled, and appropriate to the setting of care” and recommends weighing research findings regarding textile transmission of health care–associated infections when individual institutions determine their dress code policies. The AMA’s last policy discussion took place in 2015 and its guidance has not changed since the pandemic.
Regardless of what institutions and patients prefer, some research suggests that many physicians would prefer to stay with wearing scrubs rather than reverting to the white coat. One study of 151 hospitalists, conducted in Ireland, found that three-quarters wanted scrubs to remain standard attire, despite the fact that close to half had experienced changes in patients› perception in the absence of their white coat and “professional attire.”
Jennifer Workman, MD, assistant professor of pediatrics, division of pediatric critical care, University of Utah, Salt Lake City, said in an interview that, as the pandemic has “waxed and waned, some trends have reverted to what they were prepandemic, but other physicians have stayed with wearing scrubs.”
Much depends on practice setting, said Dr. Workman, who is also the medical director of pediatric sepsis at Intermountain Care. In pediatrics, for example, many physicians prefer not to wear white coats when they are interacting with young children or adolescents.
Like Dr. Shaffer, Dr. Workman has seen changes in physicians’ attire during video meetings, where they often dress more casually, perhaps wearing sweatshirts. And in the hospital, more are continuing to wear scrubs. “But I don’t see it as people trying to consciously experiment or push boundaries,” she said. “I see it as a more organic, subtle shift.”
Dr. Petrilli thinks that, at this juncture, it’s “pretty heterogeneous as to who is going to return to formal attire and a white coat and who won’t.” Further research needs to be done into currently evolving trends. “We need a more thorough survey looking at changes. We need to ask [physician respondents]: ‘What is your current attire, and how has it changed?’ ”
Navigating the gender divide
In their study, Dr. Steinberg and colleagues found that respondents perceived a male model wearing business attire underneath any type of outerwear (white coat or fleece) to be significantly more professional than a female model wearing the same attire. Respondents also perceived males wearing scrubs to be more professional than females wearing scrubs.
Male models in white coats over business attire were also more likely to be identified as physicians, compared with female models in the same attire. Females were also more likely to be misidentified as nonphysician health care professionals.
Shikha Jain, MD, assistant professor of medicine at the University of Illinois Cancer Center in Chicago, said that Dr. Steinberg’s study confirmed experiences that she and other female physicians have had. Wearing a white coat makes it more likely that a patient will identify you as a physician, but women are less likely to be identified as physicians, regardless of what they wear.
“I think that individuals of color and especially people with intersectional identities – such as women of color – are even more frequently targeted and stereotyped. Numerous studies have shown that a person of color is less likely to be seen as an authority figure, and studies have shown that physicians of color are less likely to be identified as ‘physicians,’ compared to a Caucasian individual,” she said.
Does that mean that female physicians should revert back to prepandemic white coats rather than scrubs or more casual attire? Not necessarily, according to Dr. Jain.
“The typical dress code guidance is that physicians should dress ‘professionally,’ but what that means is a question that needs to be addressed,” Dr. Jain said. “Medicine has evolved from the days of house calls, in which one’s patient population is a very small, intimate group of people in the physician’s community. Yet now, we’ve given rebirth to the ‘house call’ when we do telemedicine with a patient in his or her home. And in the old days, doctors often had offices their homes and now, with telemedicine, patients often see the interior of their physician’s home.” As the delivery of medicine evolves, concepts of “professionalism” – what is defined as “casual” and what is defined as “formal” – is also evolving.
The more important issue, according to Dr. Jain, is to “continue the conversation” about the discrepancies between how men and women are treated in medicine. Attire is one arena in which this issue plays out, and it’s a “bigger picture” that goes beyond the white coat.
Dr. Jain has been “told by patients that a particular outfit doesn’t make me look like a doctor or that scrubs make me look younger. I don’t think my male colleagues have been subjected to these types of remarks, but my female colleagues have heard them as well.”
Even fellow health care providers have commented on Dr. Jain’s clothing. She was presenting at a major medical conference via video and was wearing a similar outfit to the one she wore for her headshot. “Thirty seconds before beginning my talk, one of the male physicians said: ‘Are you wearing the same outfit you wore for your headshot?’ I can’t imagine a man commenting that another man was wearing the same jacket or tie that he wore in the photograph. I found it odd that this was something that someone felt the need to comment on right before I was about to address a large group of people in a professional capacity.”
Addressing these systemic issues “needs to be done and amplified not only by women but also by men in medicine,” said Dr. Jain, founder and director of Women in Medicine, an organization consisting of women physicians whose goal is to “find and implement solutions to gender inequity.”
Dr. Jain said the organization offers an Inclusive Leadership Development Lab – a course specifically for men in health care leadership positions to learn how to be more equitable, inclusive leaders.
A personal decision
Dr. Pasricha hopes she “handled the patient’s misidentification graciously.” She explained to him that she would be the physician conducting the procedure. The patient was initially “a little embarrassed” that he had misidentified her, but she put him at ease and “we moved forward quickly.”
At this point, although some of her colleagues have continued to wear scrubs or have returned to wearing fleeces with hospital logos, Dr. Pasricha prefers to wear a white coat in both inpatient and outpatient settings because it reduces the likelihood of misidentification.
And white coats can be more convenient – for example, Dr. Jain likes the fact that the white coat has pockets where she can put her stethoscope and other items, while some of her professional clothes don’t always have pockets.
Dr. Jain noted that there are some institutions where everyone seems to wear white coats, not only the physician – “from the chaplain to the phlebotomist to the social worker.” In those settings, the white coat no longer distinguishes physicians from nonphysicians, and so wearing a white coat may not confer additional credibility as a physician.
Nevertheless, “if you want to wear a white coat, if you feel it gives you that added level of authority, if you feel it tells people more clearly that you’re a physician, by all means go ahead and do so,” she said. “There’s no ‘one-size-fits-all’ strategy or solution. What’s more important than your clothing is your professionalism.”
A version of this article first appeared on Medscape.com.
Early in the COVID-19 pandemic, Trisha Pasricha, MD, a gastroenterologist and research fellow at Massachusetts General Hospital in Boston, was talking to a patient who had been hospitalized for a peptic ulcer.
Like other physicians in her institution, Dr. Pasricha was wearing scrubs instead of a white coat, out of concern that the white coat might be more prone to accumulating or transmitting COVID-19 pathogens. Her badge identified her as a physician, and she introduced herself clearly as “Dr. Pasricha.”
The patient “required an emergent procedure, which I discussed with him,” Dr. Pasricha told this news organization. “I went over what the procedure entailed, the risks and benefits, and the need for informed consent. The patient nodded and seemed to understand, but at the end of the discussion he said: ‘That all sounds fine, but I need to speak to the doctor first.’ ”
Dr. Pasricha was taken aback. She wondered: “Who did he think I was the whole time that I was reviewing medical concerns, explaining medical concepts, and describing a procedure in a way that a physician would describe it?”
She realized the reason he didn’t correctly identify her was that, clad only in scrubs, she was less easily recognizable as a physician. And to be misidentified as technicians, nurses, physician assistants, or other health care professionals, according to Dr. Pasricha.
Dr. Pasricha said she has been the recipient of this “implicit bias” not only from patients but also from members of the health care team, and added that other female colleagues have told her that they’ve had similar experiences, especially when they’re not wearing a white coat.
Changing times, changing trends
When COVID-19 began to spread, “there was an initial concern that COVID-19 was passed through surfaces, and concerns about whether white coats could carry viral particles,” according to Jordan Steinberg, MD, PhD, surgical director of the craniofacial program at Nicklaus Children’s Pediatric Specialists/Nicklaus Children’s Health System, Miami. “Hospitals didn’t want to launder the white coats as frequently as scrubs, due to cost concerns. There was also a concern raised that a necktie might dangle in patients’ faces, coming in closer contact with pathogens, so more physicians were wearing scrubs.”
Yet even before the pandemic, physician attire in hospital and outpatient settings had started to change. Dr. Steinberg, who is also a clinical associate professor at Florida International University, Miami, told this news organization that, in his previous appointment at Johns Hopkins University, Baltimore, he and his colleagues “had noticed in our institution, as well as other facilities, an increasing trend that moved from white coats worn over professional attire toward more casual dress among medical staff – increased wearing of casual fleece or softshell jackets with the institutional logo.”
This was especially true with trainees and the “younger generation,” who were preferring “what I would almost call ‘warm-up clothes,’ gym clothes, and less shirt-tie-white-coat attire for men or white-coats-and-business attire for women.” Dr. Steinberg thinks that some physicians prefer the fleece with the institutional logo “because it’s like wearing your favorite sports team jersey. It gives a sense of belonging.”
Todd Shaffer, MD, MBA, a family physician at University Physicians Associates, Truman Medical Centers and the Lakewood Medical Pavilion, Kansas City, Mo., has been at his institution for 30 years and has seen a similar trend. “At one point, things were very formal,” he told this news organization. But attire was already becoming less formal before the pandemic, and new changes took place during the pandemic, as physicians began wearing scrubs instead of white coats because of fears of viral contamination.
Now, there is less concern about potential viral contamination with the white coat. Yet many physicians continue to wear scrubs – especially those who interact with patients with COVID – and it has become more acceptable to do so, or to wear personal protective equipment (PPE) over ordinary clothing, but it is less common in routine clinical practice, said Dr. Shaffer, a member of the board of directors of the American Academy of Family Physicians.
“The world has changed since COVID. People feel more comfortable dressing more casually during professional Zoom calls, when they have the convenience of working from home,” said Dr. Shaffer, who is also a professor of family medicine at University of Missouri–Kansas City.
Dr. Shaffer himself hasn’t worn a white coat for years. “I’m more likely to wear medium casual pants. I’ve bought some nicer shirts, so I still look professional and upbeat. I don’t always tuck in my shirt, and I don’t dress as formally.” He wears PPE and a mask and/or face shield when treating patients with COVID-19. And he wears a white coat “when someone wants a photograph taken with the doctors – with the stethoscope draped around my neck.”
Traditional symbol of medicine
Because of the changing mores, Dr. Steinberg and colleagues at Johns Hopkins wondered if there might still be a role for professional attire and white coats and what patients prefer. To investigate the question, they surveyed 487 U.S. adults in the spring of 2020.
Respondents were asked where and how frequently they see health care professionals wearing white coats, scrubs, and fleece or softshell jackets. They were also shown photographs depicting models wearing various types of attire commonly seen in health care settings and were asked to rank the “health care provider’s” level of experience, professionalism, and friendliness.
The majority of participants said they had seen health care practitioners in white coats “most of the time,” in scrubs “sometimes,” and in fleece or softshell jackets “rarely.” Models in white coats were regarded by respondents as more experienced and professional, although those in softshell jackets were perceived as friendlier.
There were age as well as regional differences in the responses, Dr. Steinberg said. Older respondents were significantly more likely than their younger counterparts to perceive a model wearing a white coat over business attire as being more experienced, and – in all regions of the United States except the West coast – respondents gave lower professionalism scores to providers wearing fleece jackets with scrubs underneath.
Respondents tended to prefer surgeons wearing a white coat with scrubs underneath, while a white coat over business attire was the preferred dress code for family physicians and dermatologists.
“People tended to respond as if there was a more professional element in the white coat. The age-old symbol of the white coat still marked something important,” Dr. Steinberg said. “Our data suggest that the white coat isn’t ready to die just yet. People still see an air of authority and a traditional symbol of medicine. Nevertheless, I do think it will become less common than it used to be, especially in certain regions of the country.”
Organic, subtle changes
Christopher Petrilli, MD, assistant professor at New York University, conducted research in 2018 regarding physician attire by surveying over 4,000 patients in 10 U.S. academic hospitals. His team found that most patients continued to prefer physicians to wear formal attire under a white coat, especially older respondents.
Dr. Petrilli and colleagues have been studying the issue of physician attire since 2015. “The big issue when we did our initial study – which might not be accurate anymore – is that few hospitals actually had a uniform dress code,” said Dr. Petrilli, the medical director of clinical documentation improvement and the clinical lead of value-based medicine at NYU Langone Hospitals. “When we looked at ‘honor roll hospitals’ during our study, we cold-called these hospitals and also looked online for their dress code policies. Except for the Mayo Clinic, hospitals that had dress code policies were more generic.”
For example, the American Medical Association guidance merely states that attire should be “clean, unsoiled, and appropriate to the setting of care” and recommends weighing research findings regarding textile transmission of health care–associated infections when individual institutions determine their dress code policies. The AMA’s last policy discussion took place in 2015 and its guidance has not changed since the pandemic.
Regardless of what institutions and patients prefer, some research suggests that many physicians would prefer to stay with wearing scrubs rather than reverting to the white coat. One study of 151 hospitalists, conducted in Ireland, found that three-quarters wanted scrubs to remain standard attire, despite the fact that close to half had experienced changes in patients› perception in the absence of their white coat and “professional attire.”
Jennifer Workman, MD, assistant professor of pediatrics, division of pediatric critical care, University of Utah, Salt Lake City, said in an interview that, as the pandemic has “waxed and waned, some trends have reverted to what they were prepandemic, but other physicians have stayed with wearing scrubs.”
Much depends on practice setting, said Dr. Workman, who is also the medical director of pediatric sepsis at Intermountain Care. In pediatrics, for example, many physicians prefer not to wear white coats when they are interacting with young children or adolescents.
Like Dr. Shaffer, Dr. Workman has seen changes in physicians’ attire during video meetings, where they often dress more casually, perhaps wearing sweatshirts. And in the hospital, more are continuing to wear scrubs. “But I don’t see it as people trying to consciously experiment or push boundaries,” she said. “I see it as a more organic, subtle shift.”
Dr. Petrilli thinks that, at this juncture, it’s “pretty heterogeneous as to who is going to return to formal attire and a white coat and who won’t.” Further research needs to be done into currently evolving trends. “We need a more thorough survey looking at changes. We need to ask [physician respondents]: ‘What is your current attire, and how has it changed?’ ”
Navigating the gender divide
In their study, Dr. Steinberg and colleagues found that respondents perceived a male model wearing business attire underneath any type of outerwear (white coat or fleece) to be significantly more professional than a female model wearing the same attire. Respondents also perceived males wearing scrubs to be more professional than females wearing scrubs.
Male models in white coats over business attire were also more likely to be identified as physicians, compared with female models in the same attire. Females were also more likely to be misidentified as nonphysician health care professionals.
Shikha Jain, MD, assistant professor of medicine at the University of Illinois Cancer Center in Chicago, said that Dr. Steinberg’s study confirmed experiences that she and other female physicians have had. Wearing a white coat makes it more likely that a patient will identify you as a physician, but women are less likely to be identified as physicians, regardless of what they wear.
“I think that individuals of color and especially people with intersectional identities – such as women of color – are even more frequently targeted and stereotyped. Numerous studies have shown that a person of color is less likely to be seen as an authority figure, and studies have shown that physicians of color are less likely to be identified as ‘physicians,’ compared to a Caucasian individual,” she said.
Does that mean that female physicians should revert back to prepandemic white coats rather than scrubs or more casual attire? Not necessarily, according to Dr. Jain.
“The typical dress code guidance is that physicians should dress ‘professionally,’ but what that means is a question that needs to be addressed,” Dr. Jain said. “Medicine has evolved from the days of house calls, in which one’s patient population is a very small, intimate group of people in the physician’s community. Yet now, we’ve given rebirth to the ‘house call’ when we do telemedicine with a patient in his or her home. And in the old days, doctors often had offices their homes and now, with telemedicine, patients often see the interior of their physician’s home.” As the delivery of medicine evolves, concepts of “professionalism” – what is defined as “casual” and what is defined as “formal” – is also evolving.
The more important issue, according to Dr. Jain, is to “continue the conversation” about the discrepancies between how men and women are treated in medicine. Attire is one arena in which this issue plays out, and it’s a “bigger picture” that goes beyond the white coat.
Dr. Jain has been “told by patients that a particular outfit doesn’t make me look like a doctor or that scrubs make me look younger. I don’t think my male colleagues have been subjected to these types of remarks, but my female colleagues have heard them as well.”
Even fellow health care providers have commented on Dr. Jain’s clothing. She was presenting at a major medical conference via video and was wearing a similar outfit to the one she wore for her headshot. “Thirty seconds before beginning my talk, one of the male physicians said: ‘Are you wearing the same outfit you wore for your headshot?’ I can’t imagine a man commenting that another man was wearing the same jacket or tie that he wore in the photograph. I found it odd that this was something that someone felt the need to comment on right before I was about to address a large group of people in a professional capacity.”
Addressing these systemic issues “needs to be done and amplified not only by women but also by men in medicine,” said Dr. Jain, founder and director of Women in Medicine, an organization consisting of women physicians whose goal is to “find and implement solutions to gender inequity.”
Dr. Jain said the organization offers an Inclusive Leadership Development Lab – a course specifically for men in health care leadership positions to learn how to be more equitable, inclusive leaders.
A personal decision
Dr. Pasricha hopes she “handled the patient’s misidentification graciously.” She explained to him that she would be the physician conducting the procedure. The patient was initially “a little embarrassed” that he had misidentified her, but she put him at ease and “we moved forward quickly.”
At this point, although some of her colleagues have continued to wear scrubs or have returned to wearing fleeces with hospital logos, Dr. Pasricha prefers to wear a white coat in both inpatient and outpatient settings because it reduces the likelihood of misidentification.
And white coats can be more convenient – for example, Dr. Jain likes the fact that the white coat has pockets where she can put her stethoscope and other items, while some of her professional clothes don’t always have pockets.
Dr. Jain noted that there are some institutions where everyone seems to wear white coats, not only the physician – “from the chaplain to the phlebotomist to the social worker.” In those settings, the white coat no longer distinguishes physicians from nonphysicians, and so wearing a white coat may not confer additional credibility as a physician.
Nevertheless, “if you want to wear a white coat, if you feel it gives you that added level of authority, if you feel it tells people more clearly that you’re a physician, by all means go ahead and do so,” she said. “There’s no ‘one-size-fits-all’ strategy or solution. What’s more important than your clothing is your professionalism.”
A version of this article first appeared on Medscape.com.
Early in the COVID-19 pandemic, Trisha Pasricha, MD, a gastroenterologist and research fellow at Massachusetts General Hospital in Boston, was talking to a patient who had been hospitalized for a peptic ulcer.
Like other physicians in her institution, Dr. Pasricha was wearing scrubs instead of a white coat, out of concern that the white coat might be more prone to accumulating or transmitting COVID-19 pathogens. Her badge identified her as a physician, and she introduced herself clearly as “Dr. Pasricha.”
The patient “required an emergent procedure, which I discussed with him,” Dr. Pasricha told this news organization. “I went over what the procedure entailed, the risks and benefits, and the need for informed consent. The patient nodded and seemed to understand, but at the end of the discussion he said: ‘That all sounds fine, but I need to speak to the doctor first.’ ”
Dr. Pasricha was taken aback. She wondered: “Who did he think I was the whole time that I was reviewing medical concerns, explaining medical concepts, and describing a procedure in a way that a physician would describe it?”
She realized the reason he didn’t correctly identify her was that, clad only in scrubs, she was less easily recognizable as a physician. And to be misidentified as technicians, nurses, physician assistants, or other health care professionals, according to Dr. Pasricha.
Dr. Pasricha said she has been the recipient of this “implicit bias” not only from patients but also from members of the health care team, and added that other female colleagues have told her that they’ve had similar experiences, especially when they’re not wearing a white coat.
Changing times, changing trends
When COVID-19 began to spread, “there was an initial concern that COVID-19 was passed through surfaces, and concerns about whether white coats could carry viral particles,” according to Jordan Steinberg, MD, PhD, surgical director of the craniofacial program at Nicklaus Children’s Pediatric Specialists/Nicklaus Children’s Health System, Miami. “Hospitals didn’t want to launder the white coats as frequently as scrubs, due to cost concerns. There was also a concern raised that a necktie might dangle in patients’ faces, coming in closer contact with pathogens, so more physicians were wearing scrubs.”
Yet even before the pandemic, physician attire in hospital and outpatient settings had started to change. Dr. Steinberg, who is also a clinical associate professor at Florida International University, Miami, told this news organization that, in his previous appointment at Johns Hopkins University, Baltimore, he and his colleagues “had noticed in our institution, as well as other facilities, an increasing trend that moved from white coats worn over professional attire toward more casual dress among medical staff – increased wearing of casual fleece or softshell jackets with the institutional logo.”
This was especially true with trainees and the “younger generation,” who were preferring “what I would almost call ‘warm-up clothes,’ gym clothes, and less shirt-tie-white-coat attire for men or white-coats-and-business attire for women.” Dr. Steinberg thinks that some physicians prefer the fleece with the institutional logo “because it’s like wearing your favorite sports team jersey. It gives a sense of belonging.”
Todd Shaffer, MD, MBA, a family physician at University Physicians Associates, Truman Medical Centers and the Lakewood Medical Pavilion, Kansas City, Mo., has been at his institution for 30 years and has seen a similar trend. “At one point, things were very formal,” he told this news organization. But attire was already becoming less formal before the pandemic, and new changes took place during the pandemic, as physicians began wearing scrubs instead of white coats because of fears of viral contamination.
Now, there is less concern about potential viral contamination with the white coat. Yet many physicians continue to wear scrubs – especially those who interact with patients with COVID – and it has become more acceptable to do so, or to wear personal protective equipment (PPE) over ordinary clothing, but it is less common in routine clinical practice, said Dr. Shaffer, a member of the board of directors of the American Academy of Family Physicians.
“The world has changed since COVID. People feel more comfortable dressing more casually during professional Zoom calls, when they have the convenience of working from home,” said Dr. Shaffer, who is also a professor of family medicine at University of Missouri–Kansas City.
Dr. Shaffer himself hasn’t worn a white coat for years. “I’m more likely to wear medium casual pants. I’ve bought some nicer shirts, so I still look professional and upbeat. I don’t always tuck in my shirt, and I don’t dress as formally.” He wears PPE and a mask and/or face shield when treating patients with COVID-19. And he wears a white coat “when someone wants a photograph taken with the doctors – with the stethoscope draped around my neck.”
Traditional symbol of medicine
Because of the changing mores, Dr. Steinberg and colleagues at Johns Hopkins wondered if there might still be a role for professional attire and white coats and what patients prefer. To investigate the question, they surveyed 487 U.S. adults in the spring of 2020.
Respondents were asked where and how frequently they see health care professionals wearing white coats, scrubs, and fleece or softshell jackets. They were also shown photographs depicting models wearing various types of attire commonly seen in health care settings and were asked to rank the “health care provider’s” level of experience, professionalism, and friendliness.
The majority of participants said they had seen health care practitioners in white coats “most of the time,” in scrubs “sometimes,” and in fleece or softshell jackets “rarely.” Models in white coats were regarded by respondents as more experienced and professional, although those in softshell jackets were perceived as friendlier.
There were age as well as regional differences in the responses, Dr. Steinberg said. Older respondents were significantly more likely than their younger counterparts to perceive a model wearing a white coat over business attire as being more experienced, and – in all regions of the United States except the West coast – respondents gave lower professionalism scores to providers wearing fleece jackets with scrubs underneath.
Respondents tended to prefer surgeons wearing a white coat with scrubs underneath, while a white coat over business attire was the preferred dress code for family physicians and dermatologists.
“People tended to respond as if there was a more professional element in the white coat. The age-old symbol of the white coat still marked something important,” Dr. Steinberg said. “Our data suggest that the white coat isn’t ready to die just yet. People still see an air of authority and a traditional symbol of medicine. Nevertheless, I do think it will become less common than it used to be, especially in certain regions of the country.”
Organic, subtle changes
Christopher Petrilli, MD, assistant professor at New York University, conducted research in 2018 regarding physician attire by surveying over 4,000 patients in 10 U.S. academic hospitals. His team found that most patients continued to prefer physicians to wear formal attire under a white coat, especially older respondents.
Dr. Petrilli and colleagues have been studying the issue of physician attire since 2015. “The big issue when we did our initial study – which might not be accurate anymore – is that few hospitals actually had a uniform dress code,” said Dr. Petrilli, the medical director of clinical documentation improvement and the clinical lead of value-based medicine at NYU Langone Hospitals. “When we looked at ‘honor roll hospitals’ during our study, we cold-called these hospitals and also looked online for their dress code policies. Except for the Mayo Clinic, hospitals that had dress code policies were more generic.”
For example, the American Medical Association guidance merely states that attire should be “clean, unsoiled, and appropriate to the setting of care” and recommends weighing research findings regarding textile transmission of health care–associated infections when individual institutions determine their dress code policies. The AMA’s last policy discussion took place in 2015 and its guidance has not changed since the pandemic.
Regardless of what institutions and patients prefer, some research suggests that many physicians would prefer to stay with wearing scrubs rather than reverting to the white coat. One study of 151 hospitalists, conducted in Ireland, found that three-quarters wanted scrubs to remain standard attire, despite the fact that close to half had experienced changes in patients› perception in the absence of their white coat and “professional attire.”
Jennifer Workman, MD, assistant professor of pediatrics, division of pediatric critical care, University of Utah, Salt Lake City, said in an interview that, as the pandemic has “waxed and waned, some trends have reverted to what they were prepandemic, but other physicians have stayed with wearing scrubs.”
Much depends on practice setting, said Dr. Workman, who is also the medical director of pediatric sepsis at Intermountain Care. In pediatrics, for example, many physicians prefer not to wear white coats when they are interacting with young children or adolescents.
Like Dr. Shaffer, Dr. Workman has seen changes in physicians’ attire during video meetings, where they often dress more casually, perhaps wearing sweatshirts. And in the hospital, more are continuing to wear scrubs. “But I don’t see it as people trying to consciously experiment or push boundaries,” she said. “I see it as a more organic, subtle shift.”
Dr. Petrilli thinks that, at this juncture, it’s “pretty heterogeneous as to who is going to return to formal attire and a white coat and who won’t.” Further research needs to be done into currently evolving trends. “We need a more thorough survey looking at changes. We need to ask [physician respondents]: ‘What is your current attire, and how has it changed?’ ”
Navigating the gender divide
In their study, Dr. Steinberg and colleagues found that respondents perceived a male model wearing business attire underneath any type of outerwear (white coat or fleece) to be significantly more professional than a female model wearing the same attire. Respondents also perceived males wearing scrubs to be more professional than females wearing scrubs.
Male models in white coats over business attire were also more likely to be identified as physicians, compared with female models in the same attire. Females were also more likely to be misidentified as nonphysician health care professionals.
Shikha Jain, MD, assistant professor of medicine at the University of Illinois Cancer Center in Chicago, said that Dr. Steinberg’s study confirmed experiences that she and other female physicians have had. Wearing a white coat makes it more likely that a patient will identify you as a physician, but women are less likely to be identified as physicians, regardless of what they wear.
“I think that individuals of color and especially people with intersectional identities – such as women of color – are even more frequently targeted and stereotyped. Numerous studies have shown that a person of color is less likely to be seen as an authority figure, and studies have shown that physicians of color are less likely to be identified as ‘physicians,’ compared to a Caucasian individual,” she said.
Does that mean that female physicians should revert back to prepandemic white coats rather than scrubs or more casual attire? Not necessarily, according to Dr. Jain.
“The typical dress code guidance is that physicians should dress ‘professionally,’ but what that means is a question that needs to be addressed,” Dr. Jain said. “Medicine has evolved from the days of house calls, in which one’s patient population is a very small, intimate group of people in the physician’s community. Yet now, we’ve given rebirth to the ‘house call’ when we do telemedicine with a patient in his or her home. And in the old days, doctors often had offices their homes and now, with telemedicine, patients often see the interior of their physician’s home.” As the delivery of medicine evolves, concepts of “professionalism” – what is defined as “casual” and what is defined as “formal” – is also evolving.
The more important issue, according to Dr. Jain, is to “continue the conversation” about the discrepancies between how men and women are treated in medicine. Attire is one arena in which this issue plays out, and it’s a “bigger picture” that goes beyond the white coat.
Dr. Jain has been “told by patients that a particular outfit doesn’t make me look like a doctor or that scrubs make me look younger. I don’t think my male colleagues have been subjected to these types of remarks, but my female colleagues have heard them as well.”
Even fellow health care providers have commented on Dr. Jain’s clothing. She was presenting at a major medical conference via video and was wearing a similar outfit to the one she wore for her headshot. “Thirty seconds before beginning my talk, one of the male physicians said: ‘Are you wearing the same outfit you wore for your headshot?’ I can’t imagine a man commenting that another man was wearing the same jacket or tie that he wore in the photograph. I found it odd that this was something that someone felt the need to comment on right before I was about to address a large group of people in a professional capacity.”
Addressing these systemic issues “needs to be done and amplified not only by women but also by men in medicine,” said Dr. Jain, founder and director of Women in Medicine, an organization consisting of women physicians whose goal is to “find and implement solutions to gender inequity.”
Dr. Jain said the organization offers an Inclusive Leadership Development Lab – a course specifically for men in health care leadership positions to learn how to be more equitable, inclusive leaders.
A personal decision
Dr. Pasricha hopes she “handled the patient’s misidentification graciously.” She explained to him that she would be the physician conducting the procedure. The patient was initially “a little embarrassed” that he had misidentified her, but she put him at ease and “we moved forward quickly.”
At this point, although some of her colleagues have continued to wear scrubs or have returned to wearing fleeces with hospital logos, Dr. Pasricha prefers to wear a white coat in both inpatient and outpatient settings because it reduces the likelihood of misidentification.
And white coats can be more convenient – for example, Dr. Jain likes the fact that the white coat has pockets where she can put her stethoscope and other items, while some of her professional clothes don’t always have pockets.
Dr. Jain noted that there are some institutions where everyone seems to wear white coats, not only the physician – “from the chaplain to the phlebotomist to the social worker.” In those settings, the white coat no longer distinguishes physicians from nonphysicians, and so wearing a white coat may not confer additional credibility as a physician.
Nevertheless, “if you want to wear a white coat, if you feel it gives you that added level of authority, if you feel it tells people more clearly that you’re a physician, by all means go ahead and do so,” she said. “There’s no ‘one-size-fits-all’ strategy or solution. What’s more important than your clothing is your professionalism.”
A version of this article first appeared on Medscape.com.
Using anti-inflammatory drugs may prolong back pain
A new study questions the conventional wisdom of using steroids and anti-inflammatory drugs like ibuprofen to treat low back pain if exercise and other nondrug therapies don’t work right away.
Those medications offer relief from acute pain but may actually increase a person’s chances of developing chronic pain, said the investigators for a study published in Science Translational Medicine. The study results indicate that
“For many decades it’s been standard medical practice to treat pain with anti-inflammatory drugs,” Jeffrey Mogil, PhD, a psychology professor at McGill University, Montreal, said in a school news release. “But we found that this short-term fix could lead to longer-term problems.”
Researchers looked at low back pain because it’s so common, with 25% of U.S. adults saying they had low back pain in the previous 3 months, according to the Centers for Disease Control and Prevention. Acute back pain is defined as lasting less than 4 weeks while chronic back pain lasts more than 12 weeks.
By examining blood samples, researchers discovered that people whose low back pain was resolved had high inflammation driven by neutrophils, a type of white blood cell that helps the body fight infection, the study said.
“Neutrophils dominate the early stages of inflammation and set the stage for repair of tissue damage. Inflammation occurs for a reason, and it looks like it’s dangerous to interfere with it,” Dr. Mogil said in the news release.
The research team found that blocking neutrophils in mice prolonged pain in the animals up to 10-fold. Pain also was prolonged when the mice were given anti-inflammatory drugs and steroids, the news release says.
McGill University said other studies support the findings. The school cited an analysis of 500,000 people in the United Kingdom. The analysis found that those taking anti-inflammatory drugs for pain were more likely to have pain 2 to 10 years later.
While saying the study suggests it’s time to reconsider how pain is treated, the researchers called for clinical trials on humans, not just observations of people with low back pain.
Experts warned about accepting the results without further investigation.
“It’s intriguing but requires further study,” Steven J. Atlas, MD, director of the Primary Care Research & Quality Improvement Network at Massachusetts General Hospital, Boston, told The New York Times.
A version of this article first appeared on WebMD.com.
A new study questions the conventional wisdom of using steroids and anti-inflammatory drugs like ibuprofen to treat low back pain if exercise and other nondrug therapies don’t work right away.
Those medications offer relief from acute pain but may actually increase a person’s chances of developing chronic pain, said the investigators for a study published in Science Translational Medicine. The study results indicate that
“For many decades it’s been standard medical practice to treat pain with anti-inflammatory drugs,” Jeffrey Mogil, PhD, a psychology professor at McGill University, Montreal, said in a school news release. “But we found that this short-term fix could lead to longer-term problems.”
Researchers looked at low back pain because it’s so common, with 25% of U.S. adults saying they had low back pain in the previous 3 months, according to the Centers for Disease Control and Prevention. Acute back pain is defined as lasting less than 4 weeks while chronic back pain lasts more than 12 weeks.
By examining blood samples, researchers discovered that people whose low back pain was resolved had high inflammation driven by neutrophils, a type of white blood cell that helps the body fight infection, the study said.
“Neutrophils dominate the early stages of inflammation and set the stage for repair of tissue damage. Inflammation occurs for a reason, and it looks like it’s dangerous to interfere with it,” Dr. Mogil said in the news release.
The research team found that blocking neutrophils in mice prolonged pain in the animals up to 10-fold. Pain also was prolonged when the mice were given anti-inflammatory drugs and steroids, the news release says.
McGill University said other studies support the findings. The school cited an analysis of 500,000 people in the United Kingdom. The analysis found that those taking anti-inflammatory drugs for pain were more likely to have pain 2 to 10 years later.
While saying the study suggests it’s time to reconsider how pain is treated, the researchers called for clinical trials on humans, not just observations of people with low back pain.
Experts warned about accepting the results without further investigation.
“It’s intriguing but requires further study,” Steven J. Atlas, MD, director of the Primary Care Research & Quality Improvement Network at Massachusetts General Hospital, Boston, told The New York Times.
A version of this article first appeared on WebMD.com.
A new study questions the conventional wisdom of using steroids and anti-inflammatory drugs like ibuprofen to treat low back pain if exercise and other nondrug therapies don’t work right away.
Those medications offer relief from acute pain but may actually increase a person’s chances of developing chronic pain, said the investigators for a study published in Science Translational Medicine. The study results indicate that
“For many decades it’s been standard medical practice to treat pain with anti-inflammatory drugs,” Jeffrey Mogil, PhD, a psychology professor at McGill University, Montreal, said in a school news release. “But we found that this short-term fix could lead to longer-term problems.”
Researchers looked at low back pain because it’s so common, with 25% of U.S. adults saying they had low back pain in the previous 3 months, according to the Centers for Disease Control and Prevention. Acute back pain is defined as lasting less than 4 weeks while chronic back pain lasts more than 12 weeks.
By examining blood samples, researchers discovered that people whose low back pain was resolved had high inflammation driven by neutrophils, a type of white blood cell that helps the body fight infection, the study said.
“Neutrophils dominate the early stages of inflammation and set the stage for repair of tissue damage. Inflammation occurs for a reason, and it looks like it’s dangerous to interfere with it,” Dr. Mogil said in the news release.
The research team found that blocking neutrophils in mice prolonged pain in the animals up to 10-fold. Pain also was prolonged when the mice were given anti-inflammatory drugs and steroids, the news release says.
McGill University said other studies support the findings. The school cited an analysis of 500,000 people in the United Kingdom. The analysis found that those taking anti-inflammatory drugs for pain were more likely to have pain 2 to 10 years later.
While saying the study suggests it’s time to reconsider how pain is treated, the researchers called for clinical trials on humans, not just observations of people with low back pain.
Experts warned about accepting the results without further investigation.
“It’s intriguing but requires further study,” Steven J. Atlas, MD, director of the Primary Care Research & Quality Improvement Network at Massachusetts General Hospital, Boston, told The New York Times.
A version of this article first appeared on WebMD.com.
FROM SCIENCE TRANSLATIONAL MEDICINE

