User login
EMERGENCY MEDICINE is a practical, peer-reviewed monthly publication and Web site that meets the educational needs of emergency clinicians and urgent care clinicians for their practice.
Ultrasound, cardiac CT valuable in COVID-19 assessment
As if the management of patients with severe COVID-19 infections is not complicated enough, an estimated 50%-60% of patients admitted to an ICU with the disease will have some form of cardiovascular involvement, which further increases their already high risk for morbidity and mortality.
Multimodality cardiovascular imaging, chosen wisely, can both help to direct management of cardiovascular complications associated with COVID-19 and lessen risk of exposure of health care workers to SARS-CoV-2, said members of an expert panel from the American College of Cardiology Cardiovascular Imaging Leadership Council.
“When we face a patient with known or suspected COVID-19, it’s not like any other disease because we face potential exposure risk to personnel doing imaging studies and also to other patients,” corresponding author Marcelo F. Di Carli, MD, of Brigham and Women’s Hospital Boston said in an interview.
“Any imaging study that is being considered should be performed only if we think it will help us make a change in the way that we’re going to treat that particular patient. This is true for imaging in any disease – why would you do an imaging study that will make no difference in treatment? – but the stakes are even higher in COVID-19,” he said.
The panel’s recommendations for cardiovascular imaging in patients with COVID-19 are outlined in a guidance document published online in the Journal of the American College of Cardiology.
Testing and biomarkers
The guidance begins by highlighting the importance of diagnostic testing for COVID-19 infection and the use of universal precautions for health care personnel performing imaging studies, as well as disinfection of imaging equipment and rooms after each use.
Circulating biomarkers that measure end-organ stress or injury, inflammation, hypoperfusion, and activation of thrombosis/hemostasis pathways may be prognostically useful, but “almost none of the widely measured biomarkers represent a specific trigger for imaging outside of that supported by clinical judgment,” the guidance states.
In contrast, low to moderate, nonrising concentrations of markers for myocardial stress, such as B-type natriuretic peptide (BNP) and N-terminal pro-BNP (NT-proBNP), or of myocardial injury, such as cardiac troponins (cTn), may be helpful for excluding the need for imaging.
“Importantly, clinicians should be aware that most patients with abnormal BNP/NT-proBNP or cTn do not have acute heart failure or myocardial infarction; and rise in concentration of either class of biomarker presumably reflects complex processes including direct myocardial stress/injury related to systemic illness,” the panel members wrote.
Oldies but goodies
“One thing that we found out in our review of the literature and in our experiences in our own work settings is that cardiac ultrasound plays a huge role in this disease – like in any disease – but this one in particular,” Dr. Di Carli said. “One of the most feared complications in COVID-19 leads to inflammation of the heart muscle, which then leads to heart dysfunction. And of course cardiac ultrasound, because of its portability, can be performed at bedside to help clinicians ascertain an abnormality in the heart.”
Cardiac CT is also extremely helpful for determining whether patients with ECG findings suggestive of infarction have suffered an actual thrombotic event.
“These patients may best be served by a noninvasive study as compared to an invasive coronary angiogram,” he said.
Clinical scenarios
Cardiologists may be called in to consult on the evaluation of possible cardiogenic components of pulmonary abnormalities in patients who present with dyspnea and chest x-rays showing airspace or interstitial infiltrates suggestive of pneumonia, the authors noted.
“Clinicians will rely on history, physical exam, ECG [electrocardiogram] and biomarkers, and recent cardiac imaging tests if available. Underlying cardiac history including [coronary artery disease], cardiomyopathy, heart failure, and arrhythmia should be sought, and frequent contributors to decompensation should be eliminated,” they wrote.
For patients with suspected cardiac injury, either point-of-care ultrasound or limited echocardiography can be used for the initial evaluation, with additional, more advanced technologies called into play for specific clinical scenarios outlined in the guidance.
For example, the guidance recommends that patients with chest pain and abnormal ECG readings with clinical concern for ST-elevation acute coronary syndrome or high clinical risk for in-hospital mortality from conditions such as cardiogenic shock, dynamic ST-segment changes, or left ventricular ejection fraction less than 40% thought to be caused by non–ST-elevation myocardial infarction be referred for emergent coronary angiography and reperfusion.
In contrast, in patients with chest pain and abnormal ECG but equivocal symptoms, atypical or equivocal ECG abnormalities, or late presentations, point-of-care ultrasound or limited echocardiogram could be used to look for regional wall motion abnormalities and left ventricular ejection fraction, whereas in patients with chest pain and ST-elevation without clear evidence of ST-elevation myocardial infarction, coronary CT angiography can help to rule out ACS and point to alternate diagnoses, the authors said.
The guidance also offers recommendations for imaging in patients with hemodynamic instability (shock or hypotension), patients with new left ventricular dysfunction in the absence of shock or hypotension, and patients with subacute and chronic-phase disease.
Development of the guidance document was supported by the ACC. Dr. Di Carli disclosed institutional grant support from Gilead Sciences and Spectrum Dynamics, and consulting income from Janssen and Bayer.
SOURCE: Rudski L et al. J Am Coll Cardiol. 2020 Jul 22. doi: 10.1016/j.jacc.2020.06.080.
As if the management of patients with severe COVID-19 infections is not complicated enough, an estimated 50%-60% of patients admitted to an ICU with the disease will have some form of cardiovascular involvement, which further increases their already high risk for morbidity and mortality.
Multimodality cardiovascular imaging, chosen wisely, can both help to direct management of cardiovascular complications associated with COVID-19 and lessen risk of exposure of health care workers to SARS-CoV-2, said members of an expert panel from the American College of Cardiology Cardiovascular Imaging Leadership Council.
“When we face a patient with known or suspected COVID-19, it’s not like any other disease because we face potential exposure risk to personnel doing imaging studies and also to other patients,” corresponding author Marcelo F. Di Carli, MD, of Brigham and Women’s Hospital Boston said in an interview.
“Any imaging study that is being considered should be performed only if we think it will help us make a change in the way that we’re going to treat that particular patient. This is true for imaging in any disease – why would you do an imaging study that will make no difference in treatment? – but the stakes are even higher in COVID-19,” he said.
The panel’s recommendations for cardiovascular imaging in patients with COVID-19 are outlined in a guidance document published online in the Journal of the American College of Cardiology.
Testing and biomarkers
The guidance begins by highlighting the importance of diagnostic testing for COVID-19 infection and the use of universal precautions for health care personnel performing imaging studies, as well as disinfection of imaging equipment and rooms after each use.
Circulating biomarkers that measure end-organ stress or injury, inflammation, hypoperfusion, and activation of thrombosis/hemostasis pathways may be prognostically useful, but “almost none of the widely measured biomarkers represent a specific trigger for imaging outside of that supported by clinical judgment,” the guidance states.
In contrast, low to moderate, nonrising concentrations of markers for myocardial stress, such as B-type natriuretic peptide (BNP) and N-terminal pro-BNP (NT-proBNP), or of myocardial injury, such as cardiac troponins (cTn), may be helpful for excluding the need for imaging.
“Importantly, clinicians should be aware that most patients with abnormal BNP/NT-proBNP or cTn do not have acute heart failure or myocardial infarction; and rise in concentration of either class of biomarker presumably reflects complex processes including direct myocardial stress/injury related to systemic illness,” the panel members wrote.
Oldies but goodies
“One thing that we found out in our review of the literature and in our experiences in our own work settings is that cardiac ultrasound plays a huge role in this disease – like in any disease – but this one in particular,” Dr. Di Carli said. “One of the most feared complications in COVID-19 leads to inflammation of the heart muscle, which then leads to heart dysfunction. And of course cardiac ultrasound, because of its portability, can be performed at bedside to help clinicians ascertain an abnormality in the heart.”
Cardiac CT is also extremely helpful for determining whether patients with ECG findings suggestive of infarction have suffered an actual thrombotic event.
“These patients may best be served by a noninvasive study as compared to an invasive coronary angiogram,” he said.
Clinical scenarios
Cardiologists may be called in to consult on the evaluation of possible cardiogenic components of pulmonary abnormalities in patients who present with dyspnea and chest x-rays showing airspace or interstitial infiltrates suggestive of pneumonia, the authors noted.
“Clinicians will rely on history, physical exam, ECG [electrocardiogram] and biomarkers, and recent cardiac imaging tests if available. Underlying cardiac history including [coronary artery disease], cardiomyopathy, heart failure, and arrhythmia should be sought, and frequent contributors to decompensation should be eliminated,” they wrote.
For patients with suspected cardiac injury, either point-of-care ultrasound or limited echocardiography can be used for the initial evaluation, with additional, more advanced technologies called into play for specific clinical scenarios outlined in the guidance.
For example, the guidance recommends that patients with chest pain and abnormal ECG readings with clinical concern for ST-elevation acute coronary syndrome or high clinical risk for in-hospital mortality from conditions such as cardiogenic shock, dynamic ST-segment changes, or left ventricular ejection fraction less than 40% thought to be caused by non–ST-elevation myocardial infarction be referred for emergent coronary angiography and reperfusion.
In contrast, in patients with chest pain and abnormal ECG but equivocal symptoms, atypical or equivocal ECG abnormalities, or late presentations, point-of-care ultrasound or limited echocardiogram could be used to look for regional wall motion abnormalities and left ventricular ejection fraction, whereas in patients with chest pain and ST-elevation without clear evidence of ST-elevation myocardial infarction, coronary CT angiography can help to rule out ACS and point to alternate diagnoses, the authors said.
The guidance also offers recommendations for imaging in patients with hemodynamic instability (shock or hypotension), patients with new left ventricular dysfunction in the absence of shock or hypotension, and patients with subacute and chronic-phase disease.
Development of the guidance document was supported by the ACC. Dr. Di Carli disclosed institutional grant support from Gilead Sciences and Spectrum Dynamics, and consulting income from Janssen and Bayer.
SOURCE: Rudski L et al. J Am Coll Cardiol. 2020 Jul 22. doi: 10.1016/j.jacc.2020.06.080.
As if the management of patients with severe COVID-19 infections is not complicated enough, an estimated 50%-60% of patients admitted to an ICU with the disease will have some form of cardiovascular involvement, which further increases their already high risk for morbidity and mortality.
Multimodality cardiovascular imaging, chosen wisely, can both help to direct management of cardiovascular complications associated with COVID-19 and lessen risk of exposure of health care workers to SARS-CoV-2, said members of an expert panel from the American College of Cardiology Cardiovascular Imaging Leadership Council.
“When we face a patient with known or suspected COVID-19, it’s not like any other disease because we face potential exposure risk to personnel doing imaging studies and also to other patients,” corresponding author Marcelo F. Di Carli, MD, of Brigham and Women’s Hospital Boston said in an interview.
“Any imaging study that is being considered should be performed only if we think it will help us make a change in the way that we’re going to treat that particular patient. This is true for imaging in any disease – why would you do an imaging study that will make no difference in treatment? – but the stakes are even higher in COVID-19,” he said.
The panel’s recommendations for cardiovascular imaging in patients with COVID-19 are outlined in a guidance document published online in the Journal of the American College of Cardiology.
Testing and biomarkers
The guidance begins by highlighting the importance of diagnostic testing for COVID-19 infection and the use of universal precautions for health care personnel performing imaging studies, as well as disinfection of imaging equipment and rooms after each use.
Circulating biomarkers that measure end-organ stress or injury, inflammation, hypoperfusion, and activation of thrombosis/hemostasis pathways may be prognostically useful, but “almost none of the widely measured biomarkers represent a specific trigger for imaging outside of that supported by clinical judgment,” the guidance states.
In contrast, low to moderate, nonrising concentrations of markers for myocardial stress, such as B-type natriuretic peptide (BNP) and N-terminal pro-BNP (NT-proBNP), or of myocardial injury, such as cardiac troponins (cTn), may be helpful for excluding the need for imaging.
“Importantly, clinicians should be aware that most patients with abnormal BNP/NT-proBNP or cTn do not have acute heart failure or myocardial infarction; and rise in concentration of either class of biomarker presumably reflects complex processes including direct myocardial stress/injury related to systemic illness,” the panel members wrote.
Oldies but goodies
“One thing that we found out in our review of the literature and in our experiences in our own work settings is that cardiac ultrasound plays a huge role in this disease – like in any disease – but this one in particular,” Dr. Di Carli said. “One of the most feared complications in COVID-19 leads to inflammation of the heart muscle, which then leads to heart dysfunction. And of course cardiac ultrasound, because of its portability, can be performed at bedside to help clinicians ascertain an abnormality in the heart.”
Cardiac CT is also extremely helpful for determining whether patients with ECG findings suggestive of infarction have suffered an actual thrombotic event.
“These patients may best be served by a noninvasive study as compared to an invasive coronary angiogram,” he said.
Clinical scenarios
Cardiologists may be called in to consult on the evaluation of possible cardiogenic components of pulmonary abnormalities in patients who present with dyspnea and chest x-rays showing airspace or interstitial infiltrates suggestive of pneumonia, the authors noted.
“Clinicians will rely on history, physical exam, ECG [electrocardiogram] and biomarkers, and recent cardiac imaging tests if available. Underlying cardiac history including [coronary artery disease], cardiomyopathy, heart failure, and arrhythmia should be sought, and frequent contributors to decompensation should be eliminated,” they wrote.
For patients with suspected cardiac injury, either point-of-care ultrasound or limited echocardiography can be used for the initial evaluation, with additional, more advanced technologies called into play for specific clinical scenarios outlined in the guidance.
For example, the guidance recommends that patients with chest pain and abnormal ECG readings with clinical concern for ST-elevation acute coronary syndrome or high clinical risk for in-hospital mortality from conditions such as cardiogenic shock, dynamic ST-segment changes, or left ventricular ejection fraction less than 40% thought to be caused by non–ST-elevation myocardial infarction be referred for emergent coronary angiography and reperfusion.
In contrast, in patients with chest pain and abnormal ECG but equivocal symptoms, atypical or equivocal ECG abnormalities, or late presentations, point-of-care ultrasound or limited echocardiogram could be used to look for regional wall motion abnormalities and left ventricular ejection fraction, whereas in patients with chest pain and ST-elevation without clear evidence of ST-elevation myocardial infarction, coronary CT angiography can help to rule out ACS and point to alternate diagnoses, the authors said.
The guidance also offers recommendations for imaging in patients with hemodynamic instability (shock or hypotension), patients with new left ventricular dysfunction in the absence of shock or hypotension, and patients with subacute and chronic-phase disease.
Development of the guidance document was supported by the ACC. Dr. Di Carli disclosed institutional grant support from Gilead Sciences and Spectrum Dynamics, and consulting income from Janssen and Bayer.
SOURCE: Rudski L et al. J Am Coll Cardiol. 2020 Jul 22. doi: 10.1016/j.jacc.2020.06.080.
FROM THE JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Low-dose prasugrel preserves efficacy but lowers bleeding in elderly
In elderly or low-weight patients with acute coronary syndrome (ACS), a reduced dose of prasugrel relative to a full-dose of ticagrelor is associated with lower numerical rates of ischemic events and bleeding events, according to a prespecified substudy of the ISAR-REACT 5 trial.
“The present study provides the strongest support for reduced-dose prasugrel as the standard for elderly and low-weight patients with ACS undergoing an invasive treatment strategy,” according to the senior author, Adnan Kastrati, MD, professor of cardiology and head of the Catheterization Laboratory at Deutsches Herzzentrum, Technical University of Munich.
The main results of ISAR-REACT 5, an open-label, head-to-head comparison of prasugrel and ticagrelor in patients with ACS, showed that the risk of the composite primary endpoint of death, myocardial infarction, or stroke 1 year after randomization was significantly higher for those on ticagrelor than prasugrel (hazard ratio, 1.39; P = .006). The bleeding risk on ticagrelor was also higher but not significantly different (5.4% vs. 4.8%; P = .46) (Schüpke S et al. N Engl J Med. 2019 Oct;381:1524-34).
In this substudy newly published in Annals of Internal Medicine, outcomes were compared in the 1,099 patients who were 75 years or older or weighed less than 60 kg. In this group, unlike those younger or weighing more, patients were randomized to receive a reduced maintenance dose of 5 mg of once-daily prasugrel (rather than 10 mg) or full dose ticagrelor (90 mg twice daily).
At 1 year, the low-dose prasugrel strategy relative to ticagrelor was associated with a lower rate of events (12.7% vs. 14.6%) and a lower rate of bleeding (8.1% vs. 10.6%), defined as Bleeding Academic Research Consortium (BARC) type 3-5 events.
Neither the 18% reduction for the efficacy endpoint (HR, 0.82; 95% CI 0.60-1.14) nor the 28% reduction in the bleeding endpoint (HR, 0.72; 95% CI 0.46-1.12) reached significance, but Dr. Kastrati reported that there was a significant “treatment effect-by-study-group interaction” for BARC 1-5 bleeding (P = .004) favoring prasugrel. This supports low-dose prasugrel as a strategy to prevent the excess bleeding risk previously observed with the standard 10-mg dose of prasugrel.
In other words, a reduced dose of prasugrel, compared with the standard dose of ticagrelor, in low-weight and elderly patients “is associated with maintained anti-ischemic efficacy while protecting these patients against the excess risk of bleeding,” he and his coinvestigators concluded.
Low-weight and older patients represented 27% of those enrolled in ISAR-REACT 5. When compared to the study population as a whole, the risk for both ischemic and bleeding events was at least twice as high, the authors of an accompanying editorial observed. They praised this effort to refine the optimal antiplatelet regimen in a very-high-risk ACS population.
“The current analysis suggests that the prasugrel dose reduction regimen for elderly or underweight patients with ACS is effective and safe,” according to the editorial coauthors, David Conen, MD, and P.J. Devereaux, MD, PhD, who are affiliated with the Population Health Research Institute, Hamilton, Ontario.
This substudy was underpowered to show superiority for the efficacy and safety outcomes in elderly and low-weight ACS patients, which makes these results “hypothesis generating,” but the authors believe that they provide the best available evidence for selecting antiplatelet therapy in this challenging subgroup. Although the exclusion of patients at very high risk of bleeding from ISAR-REACT 5 suggest findings might not be relevant to all elderly and low-weight individuals, the investigators believe the data do inform clinical practice.
“Our study is the first head-to-head randomized comparison of the reduced dose of prasugrel against standard dose of ticagrelor in elderly and low-weight patients,” said Dr. Kastrati in an interview. “Specifically designed studies for this subset of patients are very unlikely to be conducted in the future.”
Dr. Kastrati reported no potential conflicts of interest relevant to this study.
SOURCE: Menichelli M et al. Ann Intern Med. 2020 Jul 21. doi: 10.7326/M20-1806.
In elderly or low-weight patients with acute coronary syndrome (ACS), a reduced dose of prasugrel relative to a full-dose of ticagrelor is associated with lower numerical rates of ischemic events and bleeding events, according to a prespecified substudy of the ISAR-REACT 5 trial.
“The present study provides the strongest support for reduced-dose prasugrel as the standard for elderly and low-weight patients with ACS undergoing an invasive treatment strategy,” according to the senior author, Adnan Kastrati, MD, professor of cardiology and head of the Catheterization Laboratory at Deutsches Herzzentrum, Technical University of Munich.
The main results of ISAR-REACT 5, an open-label, head-to-head comparison of prasugrel and ticagrelor in patients with ACS, showed that the risk of the composite primary endpoint of death, myocardial infarction, or stroke 1 year after randomization was significantly higher for those on ticagrelor than prasugrel (hazard ratio, 1.39; P = .006). The bleeding risk on ticagrelor was also higher but not significantly different (5.4% vs. 4.8%; P = .46) (Schüpke S et al. N Engl J Med. 2019 Oct;381:1524-34).
In this substudy newly published in Annals of Internal Medicine, outcomes were compared in the 1,099 patients who were 75 years or older or weighed less than 60 kg. In this group, unlike those younger or weighing more, patients were randomized to receive a reduced maintenance dose of 5 mg of once-daily prasugrel (rather than 10 mg) or full dose ticagrelor (90 mg twice daily).
At 1 year, the low-dose prasugrel strategy relative to ticagrelor was associated with a lower rate of events (12.7% vs. 14.6%) and a lower rate of bleeding (8.1% vs. 10.6%), defined as Bleeding Academic Research Consortium (BARC) type 3-5 events.
Neither the 18% reduction for the efficacy endpoint (HR, 0.82; 95% CI 0.60-1.14) nor the 28% reduction in the bleeding endpoint (HR, 0.72; 95% CI 0.46-1.12) reached significance, but Dr. Kastrati reported that there was a significant “treatment effect-by-study-group interaction” for BARC 1-5 bleeding (P = .004) favoring prasugrel. This supports low-dose prasugrel as a strategy to prevent the excess bleeding risk previously observed with the standard 10-mg dose of prasugrel.
In other words, a reduced dose of prasugrel, compared with the standard dose of ticagrelor, in low-weight and elderly patients “is associated with maintained anti-ischemic efficacy while protecting these patients against the excess risk of bleeding,” he and his coinvestigators concluded.
Low-weight and older patients represented 27% of those enrolled in ISAR-REACT 5. When compared to the study population as a whole, the risk for both ischemic and bleeding events was at least twice as high, the authors of an accompanying editorial observed. They praised this effort to refine the optimal antiplatelet regimen in a very-high-risk ACS population.
“The current analysis suggests that the prasugrel dose reduction regimen for elderly or underweight patients with ACS is effective and safe,” according to the editorial coauthors, David Conen, MD, and P.J. Devereaux, MD, PhD, who are affiliated with the Population Health Research Institute, Hamilton, Ontario.
This substudy was underpowered to show superiority for the efficacy and safety outcomes in elderly and low-weight ACS patients, which makes these results “hypothesis generating,” but the authors believe that they provide the best available evidence for selecting antiplatelet therapy in this challenging subgroup. Although the exclusion of patients at very high risk of bleeding from ISAR-REACT 5 suggest findings might not be relevant to all elderly and low-weight individuals, the investigators believe the data do inform clinical practice.
“Our study is the first head-to-head randomized comparison of the reduced dose of prasugrel against standard dose of ticagrelor in elderly and low-weight patients,” said Dr. Kastrati in an interview. “Specifically designed studies for this subset of patients are very unlikely to be conducted in the future.”
Dr. Kastrati reported no potential conflicts of interest relevant to this study.
SOURCE: Menichelli M et al. Ann Intern Med. 2020 Jul 21. doi: 10.7326/M20-1806.
In elderly or low-weight patients with acute coronary syndrome (ACS), a reduced dose of prasugrel relative to a full-dose of ticagrelor is associated with lower numerical rates of ischemic events and bleeding events, according to a prespecified substudy of the ISAR-REACT 5 trial.
“The present study provides the strongest support for reduced-dose prasugrel as the standard for elderly and low-weight patients with ACS undergoing an invasive treatment strategy,” according to the senior author, Adnan Kastrati, MD, professor of cardiology and head of the Catheterization Laboratory at Deutsches Herzzentrum, Technical University of Munich.
The main results of ISAR-REACT 5, an open-label, head-to-head comparison of prasugrel and ticagrelor in patients with ACS, showed that the risk of the composite primary endpoint of death, myocardial infarction, or stroke 1 year after randomization was significantly higher for those on ticagrelor than prasugrel (hazard ratio, 1.39; P = .006). The bleeding risk on ticagrelor was also higher but not significantly different (5.4% vs. 4.8%; P = .46) (Schüpke S et al. N Engl J Med. 2019 Oct;381:1524-34).
In this substudy newly published in Annals of Internal Medicine, outcomes were compared in the 1,099 patients who were 75 years or older or weighed less than 60 kg. In this group, unlike those younger or weighing more, patients were randomized to receive a reduced maintenance dose of 5 mg of once-daily prasugrel (rather than 10 mg) or full dose ticagrelor (90 mg twice daily).
At 1 year, the low-dose prasugrel strategy relative to ticagrelor was associated with a lower rate of events (12.7% vs. 14.6%) and a lower rate of bleeding (8.1% vs. 10.6%), defined as Bleeding Academic Research Consortium (BARC) type 3-5 events.
Neither the 18% reduction for the efficacy endpoint (HR, 0.82; 95% CI 0.60-1.14) nor the 28% reduction in the bleeding endpoint (HR, 0.72; 95% CI 0.46-1.12) reached significance, but Dr. Kastrati reported that there was a significant “treatment effect-by-study-group interaction” for BARC 1-5 bleeding (P = .004) favoring prasugrel. This supports low-dose prasugrel as a strategy to prevent the excess bleeding risk previously observed with the standard 10-mg dose of prasugrel.
In other words, a reduced dose of prasugrel, compared with the standard dose of ticagrelor, in low-weight and elderly patients “is associated with maintained anti-ischemic efficacy while protecting these patients against the excess risk of bleeding,” he and his coinvestigators concluded.
Low-weight and older patients represented 27% of those enrolled in ISAR-REACT 5. When compared to the study population as a whole, the risk for both ischemic and bleeding events was at least twice as high, the authors of an accompanying editorial observed. They praised this effort to refine the optimal antiplatelet regimen in a very-high-risk ACS population.
“The current analysis suggests that the prasugrel dose reduction regimen for elderly or underweight patients with ACS is effective and safe,” according to the editorial coauthors, David Conen, MD, and P.J. Devereaux, MD, PhD, who are affiliated with the Population Health Research Institute, Hamilton, Ontario.
This substudy was underpowered to show superiority for the efficacy and safety outcomes in elderly and low-weight ACS patients, which makes these results “hypothesis generating,” but the authors believe that they provide the best available evidence for selecting antiplatelet therapy in this challenging subgroup. Although the exclusion of patients at very high risk of bleeding from ISAR-REACT 5 suggest findings might not be relevant to all elderly and low-weight individuals, the investigators believe the data do inform clinical practice.
“Our study is the first head-to-head randomized comparison of the reduced dose of prasugrel against standard dose of ticagrelor in elderly and low-weight patients,” said Dr. Kastrati in an interview. “Specifically designed studies for this subset of patients are very unlikely to be conducted in the future.”
Dr. Kastrati reported no potential conflicts of interest relevant to this study.
SOURCE: Menichelli M et al. Ann Intern Med. 2020 Jul 21. doi: 10.7326/M20-1806.
FROM ANNALS OF INTERNAL MEDICINE
Quitting smoking after MI has huge benefits in young adults
Young adult smokers who stop smoking in the first year after an initial myocardial infarction are far less likely to die over the next 10 years than their peers who continue to smoke. Yet nearly two-thirds keep smoking after the event, according to new data from the Partners YOUNG-MI Registry.
“Smoking is one of the most common risk factors for developing an MI at a young age. ... This reinforces the need to have more young individuals avoid, or quit, the use of tobacco,” Ron Blankstein, MD, Brigham and Women’s Hospital and Harvard Medical School, Boston, said in an interview.
Yet, the finding that 62% of young adults continue to smoke 1 year after MI points to an “enormous need for better smoking cessation efforts following a heart attack,” he said.
“Powerful” message for clinicians
“This study joins an incredibly powerful body of evidence that says if you quit smoking, you’re going to live longer,” said Michael Fiore, MD, MPH, MBA, director of the University of Wisconsin Center for Tobacco Research and Intervention, Madison, who wasn’t involved in the study.
“As physicians, there is nothing we can do that will have a greater impact for our patients than quitting smoking. The study is a powerful call for clinicians to intervene with their patients that smoke – both if you have an MI or if you don’t,” Dr. Fiore told this news organization.
The study involved 2,072 individuals 50 years or younger (median age, 45 years; 81% male) who were hospitalized for an initial MI at two large academic medical centers in Boston. Of these, 33.9% were never-smokers, 13.6% were former smokers, and 52.5% were smokers at the time of their MI.
During a median follow-up of 10.2 years, those who quit smoking had a significantly lower rate of death from any cause (unadjusted hazard ratio, 0.35; 95% confidence interval, 0.19-0.63; P < .001) and a cardiovascular cause (HR, 0.29; 95% CI, 0.11-0.79; P = .02), relative to those who continued to smoke.
The results remained statistically significant in a propensity-matched analysis for both all-cause (HR, 0.30; 95% CI, 0.16-0.56; P < .001) and CV mortality (HR, 0.19; 95% CI, 0.06-0.56; P = .003).
“Although patients who quit smoking were similar to those who continued to smoke with respect to their baseline characteristics, smoking cessation was associated with an approximate 70%-80% reduction in all-cause and CV mortality,” the authors note in their article, published online July 8 in JAMA Network Open.
They say it’s also noteworthy that long-term death rates of never-smokers and former smokers who quit before the MI were nearly identical.
‘A failure of our health care system’
The bottom line, said Dr. Blankstein, is that it is “never too late to quit, and those who experience an MI should do so right away. Our health care system must help promote such efforts, as there is immense room for improvement.”
Dr. Fiore said: “When I see an article like this, it just reminds me that, if you’re really thinking about staying healthy, there is nothing better you can do to improve the quality and longevity of your life than quitting smoking.”
The observation that many patients continue to smoke after MI is a “failure of our health care system, and it’s an individual failure in that these individuals are not able to overcome their powerful nicotine dependence. It’s an unfortunate occurrence that’s resulting in unnecessary deaths,” said Dr. Fiore.
There is no “magic bullet” to overcome nicotine addiction, but there are approved treatments that can “substantially boost quit rates,” he noted.
The two most effective smoking-cessation treatments are varenicline (Chantix) and combination nicotine replacement therapy, a patch combined ideally with nicotine mini lozenges, particularly when combined with some brief counseling, said Fiore.
He encourages cardiologists to get their patients to commit to quitting and then link them to resources such as 1-800-QUIT-NOW or SmokeFree.gov.
Funding for the study was provided by grants from the National Heart, Lung, and Blood Institute. Dr. Blankstein reported receiving research support from Amgen and Astellas. Dr. Fiore had no relevant disclosures.
A version of this article originally appeared on Medscape.com.
Young adult smokers who stop smoking in the first year after an initial myocardial infarction are far less likely to die over the next 10 years than their peers who continue to smoke. Yet nearly two-thirds keep smoking after the event, according to new data from the Partners YOUNG-MI Registry.
“Smoking is one of the most common risk factors for developing an MI at a young age. ... This reinforces the need to have more young individuals avoid, or quit, the use of tobacco,” Ron Blankstein, MD, Brigham and Women’s Hospital and Harvard Medical School, Boston, said in an interview.
Yet, the finding that 62% of young adults continue to smoke 1 year after MI points to an “enormous need for better smoking cessation efforts following a heart attack,” he said.
“Powerful” message for clinicians
“This study joins an incredibly powerful body of evidence that says if you quit smoking, you’re going to live longer,” said Michael Fiore, MD, MPH, MBA, director of the University of Wisconsin Center for Tobacco Research and Intervention, Madison, who wasn’t involved in the study.
“As physicians, there is nothing we can do that will have a greater impact for our patients than quitting smoking. The study is a powerful call for clinicians to intervene with their patients that smoke – both if you have an MI or if you don’t,” Dr. Fiore told this news organization.
The study involved 2,072 individuals 50 years or younger (median age, 45 years; 81% male) who were hospitalized for an initial MI at two large academic medical centers in Boston. Of these, 33.9% were never-smokers, 13.6% were former smokers, and 52.5% were smokers at the time of their MI.
During a median follow-up of 10.2 years, those who quit smoking had a significantly lower rate of death from any cause (unadjusted hazard ratio, 0.35; 95% confidence interval, 0.19-0.63; P < .001) and a cardiovascular cause (HR, 0.29; 95% CI, 0.11-0.79; P = .02), relative to those who continued to smoke.
The results remained statistically significant in a propensity-matched analysis for both all-cause (HR, 0.30; 95% CI, 0.16-0.56; P < .001) and CV mortality (HR, 0.19; 95% CI, 0.06-0.56; P = .003).
“Although patients who quit smoking were similar to those who continued to smoke with respect to their baseline characteristics, smoking cessation was associated with an approximate 70%-80% reduction in all-cause and CV mortality,” the authors note in their article, published online July 8 in JAMA Network Open.
They say it’s also noteworthy that long-term death rates of never-smokers and former smokers who quit before the MI were nearly identical.
‘A failure of our health care system’
The bottom line, said Dr. Blankstein, is that it is “never too late to quit, and those who experience an MI should do so right away. Our health care system must help promote such efforts, as there is immense room for improvement.”
Dr. Fiore said: “When I see an article like this, it just reminds me that, if you’re really thinking about staying healthy, there is nothing better you can do to improve the quality and longevity of your life than quitting smoking.”
The observation that many patients continue to smoke after MI is a “failure of our health care system, and it’s an individual failure in that these individuals are not able to overcome their powerful nicotine dependence. It’s an unfortunate occurrence that’s resulting in unnecessary deaths,” said Dr. Fiore.
There is no “magic bullet” to overcome nicotine addiction, but there are approved treatments that can “substantially boost quit rates,” he noted.
The two most effective smoking-cessation treatments are varenicline (Chantix) and combination nicotine replacement therapy, a patch combined ideally with nicotine mini lozenges, particularly when combined with some brief counseling, said Fiore.
He encourages cardiologists to get their patients to commit to quitting and then link them to resources such as 1-800-QUIT-NOW or SmokeFree.gov.
Funding for the study was provided by grants from the National Heart, Lung, and Blood Institute. Dr. Blankstein reported receiving research support from Amgen and Astellas. Dr. Fiore had no relevant disclosures.
A version of this article originally appeared on Medscape.com.
Young adult smokers who stop smoking in the first year after an initial myocardial infarction are far less likely to die over the next 10 years than their peers who continue to smoke. Yet nearly two-thirds keep smoking after the event, according to new data from the Partners YOUNG-MI Registry.
“Smoking is one of the most common risk factors for developing an MI at a young age. ... This reinforces the need to have more young individuals avoid, or quit, the use of tobacco,” Ron Blankstein, MD, Brigham and Women’s Hospital and Harvard Medical School, Boston, said in an interview.
Yet, the finding that 62% of young adults continue to smoke 1 year after MI points to an “enormous need for better smoking cessation efforts following a heart attack,” he said.
“Powerful” message for clinicians
“This study joins an incredibly powerful body of evidence that says if you quit smoking, you’re going to live longer,” said Michael Fiore, MD, MPH, MBA, director of the University of Wisconsin Center for Tobacco Research and Intervention, Madison, who wasn’t involved in the study.
“As physicians, there is nothing we can do that will have a greater impact for our patients than quitting smoking. The study is a powerful call for clinicians to intervene with their patients that smoke – both if you have an MI or if you don’t,” Dr. Fiore told this news organization.
The study involved 2,072 individuals 50 years or younger (median age, 45 years; 81% male) who were hospitalized for an initial MI at two large academic medical centers in Boston. Of these, 33.9% were never-smokers, 13.6% were former smokers, and 52.5% were smokers at the time of their MI.
During a median follow-up of 10.2 years, those who quit smoking had a significantly lower rate of death from any cause (unadjusted hazard ratio, 0.35; 95% confidence interval, 0.19-0.63; P < .001) and a cardiovascular cause (HR, 0.29; 95% CI, 0.11-0.79; P = .02), relative to those who continued to smoke.
The results remained statistically significant in a propensity-matched analysis for both all-cause (HR, 0.30; 95% CI, 0.16-0.56; P < .001) and CV mortality (HR, 0.19; 95% CI, 0.06-0.56; P = .003).
“Although patients who quit smoking were similar to those who continued to smoke with respect to their baseline characteristics, smoking cessation was associated with an approximate 70%-80% reduction in all-cause and CV mortality,” the authors note in their article, published online July 8 in JAMA Network Open.
They say it’s also noteworthy that long-term death rates of never-smokers and former smokers who quit before the MI were nearly identical.
‘A failure of our health care system’
The bottom line, said Dr. Blankstein, is that it is “never too late to quit, and those who experience an MI should do so right away. Our health care system must help promote such efforts, as there is immense room for improvement.”
Dr. Fiore said: “When I see an article like this, it just reminds me that, if you’re really thinking about staying healthy, there is nothing better you can do to improve the quality and longevity of your life than quitting smoking.”
The observation that many patients continue to smoke after MI is a “failure of our health care system, and it’s an individual failure in that these individuals are not able to overcome their powerful nicotine dependence. It’s an unfortunate occurrence that’s resulting in unnecessary deaths,” said Dr. Fiore.
There is no “magic bullet” to overcome nicotine addiction, but there are approved treatments that can “substantially boost quit rates,” he noted.
The two most effective smoking-cessation treatments are varenicline (Chantix) and combination nicotine replacement therapy, a patch combined ideally with nicotine mini lozenges, particularly when combined with some brief counseling, said Fiore.
He encourages cardiologists to get their patients to commit to quitting and then link them to resources such as 1-800-QUIT-NOW or SmokeFree.gov.
Funding for the study was provided by grants from the National Heart, Lung, and Blood Institute. Dr. Blankstein reported receiving research support from Amgen and Astellas. Dr. Fiore had no relevant disclosures.
A version of this article originally appeared on Medscape.com.
CMS to broaden transcatheter mitral valve repair coverage, and change its name
The first order of business in the long-awaited, recently released Centers for Medicare & Medicaid Services (CMS) proposed national coverage decision (NCD) for transcatheter mitral valve repair (TMVR) was to get rid of its familiar moniker.
The document tosses the term TMVR in favor of transcatheter edge-to-edge repair (TEER) “to more precisely define the treatment addressed in this NCD” and differentiate it from other therapies that repair or replace the mitral valve.
(In an off-the-cuff Twitter poll launched right after the CMS document’s release, 80.3% of respondents answered that they “hate” the new acronym and the remainder said they “love” it; those two were the poll’s only choices.)
The NCD proposal goes on to say that CMS coverage of TEER would expand to include treatment of symptomatic moderate-to-severe or severe functional mitral regurgitation (MR) when used with maximally tolerated guideline-directed medical therapy.
The proposed NCD has been expected since March 2019 when the US Food and Drug Administration (FDA) approved the MitraClip (Abbott Vascular) for secondary functional MR. Medicare has covered MitraClip for primary degenerative MR since 2014.
Abbott announced in October 2019 that it would ramp up production of the MitraClip, which is currently the only FDA-approved TEER device.
Further specifications
Even as the new proposed NCD would add CMS coverage for functional MR, it would also decline a coverage statement for degenerative MR. Instead, it proposes to leave such coverage decisions to local Medical Administrative Contractors (MACs), given a relatively low incidence of clip intervention for degenerative MR. Less than 1% of the Medicare population undergo TEER of the mitral valve for that indication, the document says.
“The MACs are structured to be able to take into account local patient, physician, and institutional factors, which are especially important when overall prevalence is very low.”
The proposal also emphasizes that patients undergoing such covered TEER procedures be “under the care of a heart failure physician specialist experienced in the care and treatment of mitral valve disease,» with additional care provided by a heart team that includes a cardiac surgeon, interventional cardiologist, interventional echocardiographer.
The new document is generally consistent with a Consensus Statement from the American Association for Thoracic Surgery, the American College of Cardiology (ACC), the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons published in December 2019 and covered then by theheart.org / Medscape Cardiology.
In anticipation the CMS coverage proposal, the ACC earlier this year published a Focused Update of the 2017 Expert Consensus Decision Pathway on the Management of Mitral Regurgitation to reflect new evidence in the field, mainly the recent clinical trial data on functional MR from the MITRA-FR and COAPT trials.
“The proposed criteria are nicely guided by the multisociety consensus document, which sought to foster optimal patient outcomes while also maintaining access to TEER,” Sammy Elmariah, MD, MPH, from Massachusetts General Hospital in Boston, commented by email.
“These criteria, in conjunction with results of the COAPT trial, establish TEER as the standard of care for patients with symptomatic functional MR despite guideline-directed medical therapy who do not possess an alternative indication for cardiac surgery,” said Elmariah, a coauthor on both the Consensus Statement and the Focused Update.
The proposed NCD seems “reasonable,” cardiothoracic surgeon Michael J. Reardon, MD, Houston Methodist Hospital, said by email. But he thought there might be some objections to the requirement for TEER centers to have a surgery program with a minimum annual volume for mitral-valve surgeries.
The proposed NCD says a hospital must have “a surgical program that performs ≥25 total mitral valve surgical procedures for severe MR per year, of which at least 10 must be mitral valve repairs.”
“There is a very definite relationship between mitral valve surgery volume and surgical outcomes and between TEER volume and TEER outcomes, but no real relationship between mitral valve surgery volumes and TEER outcomes,” Reardon said. “A mitral valve surgery program is important, but how many cases do you need to be able to start and run a TEER program?”
Edwards Lifesciences is currently testing its own device for TEER: the PASCAL transcatheter mitral valve repair system. Early findings from the company’s ongoing CLASP IID trial, a head-to-head comparison of Pascal and MitraClip, are expected in December 2023.
CMS is seeking comments on the proposed national coverage determination, and will render a final decision within 60 days of the end of the 30-day public comment period.
Elmariah discloses receiving research grants from the American Heart Association, the National Institutes of Health, Edwards Lifesciences, Svelte Medical, and Medtronic, and consulting fees from AstraZeneca. Reardon recently reported no relevant conflicts of interest.
This article first appeared on Medscape.com.
The first order of business in the long-awaited, recently released Centers for Medicare & Medicaid Services (CMS) proposed national coverage decision (NCD) for transcatheter mitral valve repair (TMVR) was to get rid of its familiar moniker.
The document tosses the term TMVR in favor of transcatheter edge-to-edge repair (TEER) “to more precisely define the treatment addressed in this NCD” and differentiate it from other therapies that repair or replace the mitral valve.
(In an off-the-cuff Twitter poll launched right after the CMS document’s release, 80.3% of respondents answered that they “hate” the new acronym and the remainder said they “love” it; those two were the poll’s only choices.)
The NCD proposal goes on to say that CMS coverage of TEER would expand to include treatment of symptomatic moderate-to-severe or severe functional mitral regurgitation (MR) when used with maximally tolerated guideline-directed medical therapy.
The proposed NCD has been expected since March 2019 when the US Food and Drug Administration (FDA) approved the MitraClip (Abbott Vascular) for secondary functional MR. Medicare has covered MitraClip for primary degenerative MR since 2014.
Abbott announced in October 2019 that it would ramp up production of the MitraClip, which is currently the only FDA-approved TEER device.
Further specifications
Even as the new proposed NCD would add CMS coverage for functional MR, it would also decline a coverage statement for degenerative MR. Instead, it proposes to leave such coverage decisions to local Medical Administrative Contractors (MACs), given a relatively low incidence of clip intervention for degenerative MR. Less than 1% of the Medicare population undergo TEER of the mitral valve for that indication, the document says.
“The MACs are structured to be able to take into account local patient, physician, and institutional factors, which are especially important when overall prevalence is very low.”
The proposal also emphasizes that patients undergoing such covered TEER procedures be “under the care of a heart failure physician specialist experienced in the care and treatment of mitral valve disease,» with additional care provided by a heart team that includes a cardiac surgeon, interventional cardiologist, interventional echocardiographer.
The new document is generally consistent with a Consensus Statement from the American Association for Thoracic Surgery, the American College of Cardiology (ACC), the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons published in December 2019 and covered then by theheart.org / Medscape Cardiology.
In anticipation the CMS coverage proposal, the ACC earlier this year published a Focused Update of the 2017 Expert Consensus Decision Pathway on the Management of Mitral Regurgitation to reflect new evidence in the field, mainly the recent clinical trial data on functional MR from the MITRA-FR and COAPT trials.
“The proposed criteria are nicely guided by the multisociety consensus document, which sought to foster optimal patient outcomes while also maintaining access to TEER,” Sammy Elmariah, MD, MPH, from Massachusetts General Hospital in Boston, commented by email.
“These criteria, in conjunction with results of the COAPT trial, establish TEER as the standard of care for patients with symptomatic functional MR despite guideline-directed medical therapy who do not possess an alternative indication for cardiac surgery,” said Elmariah, a coauthor on both the Consensus Statement and the Focused Update.
The proposed NCD seems “reasonable,” cardiothoracic surgeon Michael J. Reardon, MD, Houston Methodist Hospital, said by email. But he thought there might be some objections to the requirement for TEER centers to have a surgery program with a minimum annual volume for mitral-valve surgeries.
The proposed NCD says a hospital must have “a surgical program that performs ≥25 total mitral valve surgical procedures for severe MR per year, of which at least 10 must be mitral valve repairs.”
“There is a very definite relationship between mitral valve surgery volume and surgical outcomes and between TEER volume and TEER outcomes, but no real relationship between mitral valve surgery volumes and TEER outcomes,” Reardon said. “A mitral valve surgery program is important, but how many cases do you need to be able to start and run a TEER program?”
Edwards Lifesciences is currently testing its own device for TEER: the PASCAL transcatheter mitral valve repair system. Early findings from the company’s ongoing CLASP IID trial, a head-to-head comparison of Pascal and MitraClip, are expected in December 2023.
CMS is seeking comments on the proposed national coverage determination, and will render a final decision within 60 days of the end of the 30-day public comment period.
Elmariah discloses receiving research grants from the American Heart Association, the National Institutes of Health, Edwards Lifesciences, Svelte Medical, and Medtronic, and consulting fees from AstraZeneca. Reardon recently reported no relevant conflicts of interest.
This article first appeared on Medscape.com.
The first order of business in the long-awaited, recently released Centers for Medicare & Medicaid Services (CMS) proposed national coverage decision (NCD) for transcatheter mitral valve repair (TMVR) was to get rid of its familiar moniker.
The document tosses the term TMVR in favor of transcatheter edge-to-edge repair (TEER) “to more precisely define the treatment addressed in this NCD” and differentiate it from other therapies that repair or replace the mitral valve.
(In an off-the-cuff Twitter poll launched right after the CMS document’s release, 80.3% of respondents answered that they “hate” the new acronym and the remainder said they “love” it; those two were the poll’s only choices.)
The NCD proposal goes on to say that CMS coverage of TEER would expand to include treatment of symptomatic moderate-to-severe or severe functional mitral regurgitation (MR) when used with maximally tolerated guideline-directed medical therapy.
The proposed NCD has been expected since March 2019 when the US Food and Drug Administration (FDA) approved the MitraClip (Abbott Vascular) for secondary functional MR. Medicare has covered MitraClip for primary degenerative MR since 2014.
Abbott announced in October 2019 that it would ramp up production of the MitraClip, which is currently the only FDA-approved TEER device.
Further specifications
Even as the new proposed NCD would add CMS coverage for functional MR, it would also decline a coverage statement for degenerative MR. Instead, it proposes to leave such coverage decisions to local Medical Administrative Contractors (MACs), given a relatively low incidence of clip intervention for degenerative MR. Less than 1% of the Medicare population undergo TEER of the mitral valve for that indication, the document says.
“The MACs are structured to be able to take into account local patient, physician, and institutional factors, which are especially important when overall prevalence is very low.”
The proposal also emphasizes that patients undergoing such covered TEER procedures be “under the care of a heart failure physician specialist experienced in the care and treatment of mitral valve disease,» with additional care provided by a heart team that includes a cardiac surgeon, interventional cardiologist, interventional echocardiographer.
The new document is generally consistent with a Consensus Statement from the American Association for Thoracic Surgery, the American College of Cardiology (ACC), the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons published in December 2019 and covered then by theheart.org / Medscape Cardiology.
In anticipation the CMS coverage proposal, the ACC earlier this year published a Focused Update of the 2017 Expert Consensus Decision Pathway on the Management of Mitral Regurgitation to reflect new evidence in the field, mainly the recent clinical trial data on functional MR from the MITRA-FR and COAPT trials.
“The proposed criteria are nicely guided by the multisociety consensus document, which sought to foster optimal patient outcomes while also maintaining access to TEER,” Sammy Elmariah, MD, MPH, from Massachusetts General Hospital in Boston, commented by email.
“These criteria, in conjunction with results of the COAPT trial, establish TEER as the standard of care for patients with symptomatic functional MR despite guideline-directed medical therapy who do not possess an alternative indication for cardiac surgery,” said Elmariah, a coauthor on both the Consensus Statement and the Focused Update.
The proposed NCD seems “reasonable,” cardiothoracic surgeon Michael J. Reardon, MD, Houston Methodist Hospital, said by email. But he thought there might be some objections to the requirement for TEER centers to have a surgery program with a minimum annual volume for mitral-valve surgeries.
The proposed NCD says a hospital must have “a surgical program that performs ≥25 total mitral valve surgical procedures for severe MR per year, of which at least 10 must be mitral valve repairs.”
“There is a very definite relationship between mitral valve surgery volume and surgical outcomes and between TEER volume and TEER outcomes, but no real relationship between mitral valve surgery volumes and TEER outcomes,” Reardon said. “A mitral valve surgery program is important, but how many cases do you need to be able to start and run a TEER program?”
Edwards Lifesciences is currently testing its own device for TEER: the PASCAL transcatheter mitral valve repair system. Early findings from the company’s ongoing CLASP IID trial, a head-to-head comparison of Pascal and MitraClip, are expected in December 2023.
CMS is seeking comments on the proposed national coverage determination, and will render a final decision within 60 days of the end of the 30-day public comment period.
Elmariah discloses receiving research grants from the American Heart Association, the National Institutes of Health, Edwards Lifesciences, Svelte Medical, and Medtronic, and consulting fees from AstraZeneca. Reardon recently reported no relevant conflicts of interest.
This article first appeared on Medscape.com.
Even mild obesity raises severe COVID-19 risks
People with a body mass index of 30 kg/m2 or above are at significantly increased risk for severe COVID-19, while a BMI of 35 and higher dramatically increases the risk for death, new research suggests.
The data, from nearly 500 patients hospitalized with COVID-19 in March and April 2020, were published in the European Journal of Endocrinology by Matteo Rottoli, MD, of the Alma Mater Studiorum, University of Bologna (Italy), and colleagues.
The data support the recent change by the Centers for Disease Control and Prevention to lower the cutoff for categorizing a person at increased risk from COVID-19 from a BMI of 40 down to 30. However, in the United Kingdom, the National Health Service still lists only a BMI of 40 or above as placing a person at “moderate risk (clinically vulnerable).”
“This finding calls for prevention and treatment strategies to reduce the risk of infection and hospitalization in patients with relevant degrees of obesity, supporting a revision of the BMI cutoff of 40 kg/m2, which was proposed as an independent risk factor for an adverse outcome of COVID-19 in the ... guidelines for social distancing in the United Kingdom: It may be appropriate to include patients with BMI >30 among those at higher risk for COVID-19 severe progression,” the authors wrote.
The study included 482 adults admitted with confirmed COVID-19 to a single Italian hospital between March 1 and April 20, 2020. Of those, 41.9% had a BMI of less than 25 (normal weight), 36.5% had a BMI of 25-29.9 (overweight), and 21.6% had BMI of at least 30 (obese). Of the obese group, 20 (4.1%) had BMIs of at least 35, while 18 patients (3.7%) had BMIs of less than 20 (underweight).
Among those with obesity, 51.9% experienced respiratory failure, 36.4% were admitted to the ICU, 25% required mechanical ventilation, and 29.8% died within 30 days of symptom onset.
Patients with BMIs of at least 30 had significantly increased risks for respiratory failure (odds ratio, 2.48; P = .001), ICU admission (OR, 5.28; P < .001), and death (2.35, P = .017), compared with those with lower BMIs. Within the group classified as obese, the risks of respiratory failure and ICU admission were higher, with BMIs of 30-34.9 (OR, 2.32; P = .004 and OR, 4.96; P < .001, respectively) and for BMIs of at least 35 (OR, 3.24; P = .019 and OR, 6.58; P < .001, respectively).
The risk of death was significantly higher among patients with a BMI of at least 35 (OR, 12.1; P < .001).
Every 1-unit increase in BMI was significantly associated with all outcomes, but there was no significant difference in any outcome between the 25-29.9 BMI category and normal weight. In all models, the BMI cutoff for increased risk was 30.
The authors reported no disclosures.
SOURCE: Rottoli M et al. Eur J Endocrinol. 2020 Jul 1. doi: 10.1530/EJE-20-054.
People with a body mass index of 30 kg/m2 or above are at significantly increased risk for severe COVID-19, while a BMI of 35 and higher dramatically increases the risk for death, new research suggests.
The data, from nearly 500 patients hospitalized with COVID-19 in March and April 2020, were published in the European Journal of Endocrinology by Matteo Rottoli, MD, of the Alma Mater Studiorum, University of Bologna (Italy), and colleagues.
The data support the recent change by the Centers for Disease Control and Prevention to lower the cutoff for categorizing a person at increased risk from COVID-19 from a BMI of 40 down to 30. However, in the United Kingdom, the National Health Service still lists only a BMI of 40 or above as placing a person at “moderate risk (clinically vulnerable).”
“This finding calls for prevention and treatment strategies to reduce the risk of infection and hospitalization in patients with relevant degrees of obesity, supporting a revision of the BMI cutoff of 40 kg/m2, which was proposed as an independent risk factor for an adverse outcome of COVID-19 in the ... guidelines for social distancing in the United Kingdom: It may be appropriate to include patients with BMI >30 among those at higher risk for COVID-19 severe progression,” the authors wrote.
The study included 482 adults admitted with confirmed COVID-19 to a single Italian hospital between March 1 and April 20, 2020. Of those, 41.9% had a BMI of less than 25 (normal weight), 36.5% had a BMI of 25-29.9 (overweight), and 21.6% had BMI of at least 30 (obese). Of the obese group, 20 (4.1%) had BMIs of at least 35, while 18 patients (3.7%) had BMIs of less than 20 (underweight).
Among those with obesity, 51.9% experienced respiratory failure, 36.4% were admitted to the ICU, 25% required mechanical ventilation, and 29.8% died within 30 days of symptom onset.
Patients with BMIs of at least 30 had significantly increased risks for respiratory failure (odds ratio, 2.48; P = .001), ICU admission (OR, 5.28; P < .001), and death (2.35, P = .017), compared with those with lower BMIs. Within the group classified as obese, the risks of respiratory failure and ICU admission were higher, with BMIs of 30-34.9 (OR, 2.32; P = .004 and OR, 4.96; P < .001, respectively) and for BMIs of at least 35 (OR, 3.24; P = .019 and OR, 6.58; P < .001, respectively).
The risk of death was significantly higher among patients with a BMI of at least 35 (OR, 12.1; P < .001).
Every 1-unit increase in BMI was significantly associated with all outcomes, but there was no significant difference in any outcome between the 25-29.9 BMI category and normal weight. In all models, the BMI cutoff for increased risk was 30.
The authors reported no disclosures.
SOURCE: Rottoli M et al. Eur J Endocrinol. 2020 Jul 1. doi: 10.1530/EJE-20-054.
People with a body mass index of 30 kg/m2 or above are at significantly increased risk for severe COVID-19, while a BMI of 35 and higher dramatically increases the risk for death, new research suggests.
The data, from nearly 500 patients hospitalized with COVID-19 in March and April 2020, were published in the European Journal of Endocrinology by Matteo Rottoli, MD, of the Alma Mater Studiorum, University of Bologna (Italy), and colleagues.
The data support the recent change by the Centers for Disease Control and Prevention to lower the cutoff for categorizing a person at increased risk from COVID-19 from a BMI of 40 down to 30. However, in the United Kingdom, the National Health Service still lists only a BMI of 40 or above as placing a person at “moderate risk (clinically vulnerable).”
“This finding calls for prevention and treatment strategies to reduce the risk of infection and hospitalization in patients with relevant degrees of obesity, supporting a revision of the BMI cutoff of 40 kg/m2, which was proposed as an independent risk factor for an adverse outcome of COVID-19 in the ... guidelines for social distancing in the United Kingdom: It may be appropriate to include patients with BMI >30 among those at higher risk for COVID-19 severe progression,” the authors wrote.
The study included 482 adults admitted with confirmed COVID-19 to a single Italian hospital between March 1 and April 20, 2020. Of those, 41.9% had a BMI of less than 25 (normal weight), 36.5% had a BMI of 25-29.9 (overweight), and 21.6% had BMI of at least 30 (obese). Of the obese group, 20 (4.1%) had BMIs of at least 35, while 18 patients (3.7%) had BMIs of less than 20 (underweight).
Among those with obesity, 51.9% experienced respiratory failure, 36.4% were admitted to the ICU, 25% required mechanical ventilation, and 29.8% died within 30 days of symptom onset.
Patients with BMIs of at least 30 had significantly increased risks for respiratory failure (odds ratio, 2.48; P = .001), ICU admission (OR, 5.28; P < .001), and death (2.35, P = .017), compared with those with lower BMIs. Within the group classified as obese, the risks of respiratory failure and ICU admission were higher, with BMIs of 30-34.9 (OR, 2.32; P = .004 and OR, 4.96; P < .001, respectively) and for BMIs of at least 35 (OR, 3.24; P = .019 and OR, 6.58; P < .001, respectively).
The risk of death was significantly higher among patients with a BMI of at least 35 (OR, 12.1; P < .001).
Every 1-unit increase in BMI was significantly associated with all outcomes, but there was no significant difference in any outcome between the 25-29.9 BMI category and normal weight. In all models, the BMI cutoff for increased risk was 30.
The authors reported no disclosures.
SOURCE: Rottoli M et al. Eur J Endocrinol. 2020 Jul 1. doi: 10.1530/EJE-20-054.
FROM THE EUROPEAN JOURNAL OF ENDOCRINOLOGY
Used together, troponin and coronary calcium improve CV risk assessment
If either high sensitivity cardiac troponin (hs-cTnT) or coronary artery calcium (CAC) are elevated, the 10-year risk of atherosclerotic cardiovascular disease (ASCVD) climbs substantially, which suggests these biomarkers yield more prognostic information when they are used together, according to a cohort study with a median 15 years of follow-up.
Among those with a double negative result, meaning hs-cTnT was less than the limit of detection (<3 ng/L) and the CAC score was zero, only 2.8% developed ASCVD within 10 years, but the rates climbed to 4.6% if hs-cTnT was detectable and to 9.8% if the CAC score exceeded zero even when the other biomarker was negative.
“The increased risk for ASCVD among those with discordant results indicate that their prognostic information is complementary, favoring their conjoined use for risk prediction,” reported a multicenter team of investigators led by Allan S. Jaffe, MD, professor of laboratory medicine and pathology, Mayo Clinic, Rochester, Minn.
The study was performed with data from 6,749 participants in the Multi-Ethnic Study of Atherosclerosis (MESA), which is a longitudinal, community-based study funded by the National Heart, Lung, and Blood Institute. Over the course of long-term follow-up in a patient population that was about half female, 39% non-Hispanic white, 28% Black, 22% Hispanic American, and 12% Asian, ASCVD events were evaluated in relation to both biomarkers measured at baseline.
At baseline, both biomarkers were negative in 22%, both positive in 40%, and discordant in 38%.
After a median follow-up of 15 years, when 1,002 ASCVD events had occurred, the crude rate of ASCVD was 2.8 per 1,000 person-years in the double-negative group. When compared with this, the adjusted hazard ratio for ASCVD among those with double positive biomarkers was 3.5 (P < .00001). Increased risk was also highly significant if just hs-cTnT was positive (HR, 1.59; P = .003) or if just CAC was positive (HR, 2.74; P < .00001).
The added value of using both biomarkers to identify individuals at very low risk of ASCVD makes sense, according to the authors of an accompanying editorial. Written by a team led by John W. McEvoy, MB, BCh, National University of Ireland, Galway, the editorial explained why the information is complementary.
“CAC indicates subclinical atherosclerosis, whereas hs-cTnT indicates myocardial ischemia or damage, not just from coronary stenosis but also due to other conditions like hypertensive heart and left ventricular hypertrophy,” the authors stated.
Although they maintained that adding N-terminal pro-brain natriuretic peptide, which could be drawn from the same blood sample as hs-cTnT, might prove to be an even better but still simple strategy to identify low-risk patients, they praised the concept of combining biomarkers.
“If one’s wish is to identify truly low-risk individuals, then it appears that it takes two negative ASCVD biomarkers to make that wish come true,” the authors of the editorial concluded.
Relative to alternative methods of ASCVD risk assessment, measurement of these biomarkers might be useful for sparing patients from interventions, such as lipid lowering with statin therapy, being considered on the basis of conventional risk factors alone.
Dr. Jaffe said in an interview that he considers the two-biomarker assessment to be a useful tool in the low-risk population that he studied, but he does not consider this strategy as a substitute for other methods, such as those outline in the 2019 ACC/AHA guidelines that address the entire spectrum of risk, although work is planned to see if this approach can be extended to this broader group.*
“The data we have presented now is a good start and suggests that these two objective measures can identify those who are at very low risk and avoid adding individuals who may not be at as low risk if only one of the two tests is used,” Dr. Jaffe explained.
“Given there are now techniques to measure coronary calcium from any chest CT study, and that high sensitivity cardiac troponin is a relatively inexpensive test, putting them together should really help risk stratify patients,” he added.
When asked whether this approach will eventually replace conventional methods of ASCVD risk assessment, such as those proposed in the 2019 American College of Cardiology/American Heart Association guidelines for the primary prevention of cardiovascular disease (Circulation. 2019;140:e596-e646), he said maybe.
“The answer is that we will probe that question in our ongoing studies using continuous data in an attempt to evaluate how to use this approach to risk stratify larger numbers of individuals,” Dr. Jaffe replied.
The senior investigator, Dr. Jaffe, has consulting relationships with many pharmaceutical companies. The editorial authors had no relevant disclosures.
SOURCE: Sandoval Y et al. J Am Coll Cardiol. 2020;76:357-370.
*Correction, 7/27/20: An earlier version of this article mischaracterized Dr. Jaffe's statement.
If either high sensitivity cardiac troponin (hs-cTnT) or coronary artery calcium (CAC) are elevated, the 10-year risk of atherosclerotic cardiovascular disease (ASCVD) climbs substantially, which suggests these biomarkers yield more prognostic information when they are used together, according to a cohort study with a median 15 years of follow-up.
Among those with a double negative result, meaning hs-cTnT was less than the limit of detection (<3 ng/L) and the CAC score was zero, only 2.8% developed ASCVD within 10 years, but the rates climbed to 4.6% if hs-cTnT was detectable and to 9.8% if the CAC score exceeded zero even when the other biomarker was negative.
“The increased risk for ASCVD among those with discordant results indicate that their prognostic information is complementary, favoring their conjoined use for risk prediction,” reported a multicenter team of investigators led by Allan S. Jaffe, MD, professor of laboratory medicine and pathology, Mayo Clinic, Rochester, Minn.
The study was performed with data from 6,749 participants in the Multi-Ethnic Study of Atherosclerosis (MESA), which is a longitudinal, community-based study funded by the National Heart, Lung, and Blood Institute. Over the course of long-term follow-up in a patient population that was about half female, 39% non-Hispanic white, 28% Black, 22% Hispanic American, and 12% Asian, ASCVD events were evaluated in relation to both biomarkers measured at baseline.
At baseline, both biomarkers were negative in 22%, both positive in 40%, and discordant in 38%.
After a median follow-up of 15 years, when 1,002 ASCVD events had occurred, the crude rate of ASCVD was 2.8 per 1,000 person-years in the double-negative group. When compared with this, the adjusted hazard ratio for ASCVD among those with double positive biomarkers was 3.5 (P < .00001). Increased risk was also highly significant if just hs-cTnT was positive (HR, 1.59; P = .003) or if just CAC was positive (HR, 2.74; P < .00001).
The added value of using both biomarkers to identify individuals at very low risk of ASCVD makes sense, according to the authors of an accompanying editorial. Written by a team led by John W. McEvoy, MB, BCh, National University of Ireland, Galway, the editorial explained why the information is complementary.
“CAC indicates subclinical atherosclerosis, whereas hs-cTnT indicates myocardial ischemia or damage, not just from coronary stenosis but also due to other conditions like hypertensive heart and left ventricular hypertrophy,” the authors stated.
Although they maintained that adding N-terminal pro-brain natriuretic peptide, which could be drawn from the same blood sample as hs-cTnT, might prove to be an even better but still simple strategy to identify low-risk patients, they praised the concept of combining biomarkers.
“If one’s wish is to identify truly low-risk individuals, then it appears that it takes two negative ASCVD biomarkers to make that wish come true,” the authors of the editorial concluded.
Relative to alternative methods of ASCVD risk assessment, measurement of these biomarkers might be useful for sparing patients from interventions, such as lipid lowering with statin therapy, being considered on the basis of conventional risk factors alone.
Dr. Jaffe said in an interview that he considers the two-biomarker assessment to be a useful tool in the low-risk population that he studied, but he does not consider this strategy as a substitute for other methods, such as those outline in the 2019 ACC/AHA guidelines that address the entire spectrum of risk, although work is planned to see if this approach can be extended to this broader group.*
“The data we have presented now is a good start and suggests that these two objective measures can identify those who are at very low risk and avoid adding individuals who may not be at as low risk if only one of the two tests is used,” Dr. Jaffe explained.
“Given there are now techniques to measure coronary calcium from any chest CT study, and that high sensitivity cardiac troponin is a relatively inexpensive test, putting them together should really help risk stratify patients,” he added.
When asked whether this approach will eventually replace conventional methods of ASCVD risk assessment, such as those proposed in the 2019 American College of Cardiology/American Heart Association guidelines for the primary prevention of cardiovascular disease (Circulation. 2019;140:e596-e646), he said maybe.
“The answer is that we will probe that question in our ongoing studies using continuous data in an attempt to evaluate how to use this approach to risk stratify larger numbers of individuals,” Dr. Jaffe replied.
The senior investigator, Dr. Jaffe, has consulting relationships with many pharmaceutical companies. The editorial authors had no relevant disclosures.
SOURCE: Sandoval Y et al. J Am Coll Cardiol. 2020;76:357-370.
*Correction, 7/27/20: An earlier version of this article mischaracterized Dr. Jaffe's statement.
If either high sensitivity cardiac troponin (hs-cTnT) or coronary artery calcium (CAC) are elevated, the 10-year risk of atherosclerotic cardiovascular disease (ASCVD) climbs substantially, which suggests these biomarkers yield more prognostic information when they are used together, according to a cohort study with a median 15 years of follow-up.
Among those with a double negative result, meaning hs-cTnT was less than the limit of detection (<3 ng/L) and the CAC score was zero, only 2.8% developed ASCVD within 10 years, but the rates climbed to 4.6% if hs-cTnT was detectable and to 9.8% if the CAC score exceeded zero even when the other biomarker was negative.
“The increased risk for ASCVD among those with discordant results indicate that their prognostic information is complementary, favoring their conjoined use for risk prediction,” reported a multicenter team of investigators led by Allan S. Jaffe, MD, professor of laboratory medicine and pathology, Mayo Clinic, Rochester, Minn.
The study was performed with data from 6,749 participants in the Multi-Ethnic Study of Atherosclerosis (MESA), which is a longitudinal, community-based study funded by the National Heart, Lung, and Blood Institute. Over the course of long-term follow-up in a patient population that was about half female, 39% non-Hispanic white, 28% Black, 22% Hispanic American, and 12% Asian, ASCVD events were evaluated in relation to both biomarkers measured at baseline.
At baseline, both biomarkers were negative in 22%, both positive in 40%, and discordant in 38%.
After a median follow-up of 15 years, when 1,002 ASCVD events had occurred, the crude rate of ASCVD was 2.8 per 1,000 person-years in the double-negative group. When compared with this, the adjusted hazard ratio for ASCVD among those with double positive biomarkers was 3.5 (P < .00001). Increased risk was also highly significant if just hs-cTnT was positive (HR, 1.59; P = .003) or if just CAC was positive (HR, 2.74; P < .00001).
The added value of using both biomarkers to identify individuals at very low risk of ASCVD makes sense, according to the authors of an accompanying editorial. Written by a team led by John W. McEvoy, MB, BCh, National University of Ireland, Galway, the editorial explained why the information is complementary.
“CAC indicates subclinical atherosclerosis, whereas hs-cTnT indicates myocardial ischemia or damage, not just from coronary stenosis but also due to other conditions like hypertensive heart and left ventricular hypertrophy,” the authors stated.
Although they maintained that adding N-terminal pro-brain natriuretic peptide, which could be drawn from the same blood sample as hs-cTnT, might prove to be an even better but still simple strategy to identify low-risk patients, they praised the concept of combining biomarkers.
“If one’s wish is to identify truly low-risk individuals, then it appears that it takes two negative ASCVD biomarkers to make that wish come true,” the authors of the editorial concluded.
Relative to alternative methods of ASCVD risk assessment, measurement of these biomarkers might be useful for sparing patients from interventions, such as lipid lowering with statin therapy, being considered on the basis of conventional risk factors alone.
Dr. Jaffe said in an interview that he considers the two-biomarker assessment to be a useful tool in the low-risk population that he studied, but he does not consider this strategy as a substitute for other methods, such as those outline in the 2019 ACC/AHA guidelines that address the entire spectrum of risk, although work is planned to see if this approach can be extended to this broader group.*
“The data we have presented now is a good start and suggests that these two objective measures can identify those who are at very low risk and avoid adding individuals who may not be at as low risk if only one of the two tests is used,” Dr. Jaffe explained.
“Given there are now techniques to measure coronary calcium from any chest CT study, and that high sensitivity cardiac troponin is a relatively inexpensive test, putting them together should really help risk stratify patients,” he added.
When asked whether this approach will eventually replace conventional methods of ASCVD risk assessment, such as those proposed in the 2019 American College of Cardiology/American Heart Association guidelines for the primary prevention of cardiovascular disease (Circulation. 2019;140:e596-e646), he said maybe.
“The answer is that we will probe that question in our ongoing studies using continuous data in an attempt to evaluate how to use this approach to risk stratify larger numbers of individuals,” Dr. Jaffe replied.
The senior investigator, Dr. Jaffe, has consulting relationships with many pharmaceutical companies. The editorial authors had no relevant disclosures.
SOURCE: Sandoval Y et al. J Am Coll Cardiol. 2020;76:357-370.
*Correction, 7/27/20: An earlier version of this article mischaracterized Dr. Jaffe's statement.
FROM JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Ex-nursing assistant pleads guilty in West Virginia insulin deaths
A former nursing assistant and Army veteran pleaded guilty to federal murder charges this week in connection with the 2017-2018 deaths of seven patients in a West Virginia veteran’s hospital, according to news reports.
Prosecutors said in court documents filed on July 13 that Reta Mays, 46, injected lethal doses of insulin into seven veterans at the Louis A. Johnson VA Medical Center (VAMC) in rural Clarksburg, W.Va.
Their blood glucose levels plummeted, and each died shortly after their injections, according to the Tennessean.
An eighth patient, a 92-year-old man whom Mays is accused of assaulting with an insulin injection, initially survived after staff were able to stabilize him but died 2 weeks later at a nursing home, NPR reports.
According to NPR, US Attorney Jarod Douglas told the court Tuesday that the medical investigator could not determine whether the insulin contributed to the man’s death but that it was Mays’ intention to kill him.
“No one watched while she injected them with lethal doses of insulin during an 11-month killing rampage,” the Washington Post reported.
No motive offered
The Post article said no motive has been established, but after a 2-year investigation into a pattern of suspicious deaths that took the hospital almost a year to detect, Mays, who had denied any wrongdoing in multiple interviews with investigators, told a federal judge she preyed on some of the country›s most vulnerable service members.
An attorney for Mays, Brian Kornbrath, contacted by Medscape Medical News, said: “The defense team decided that we would have no public comment at this time.”
According to court documents from the Northern District of West Virginia, Mays was charged with seven counts of second-degree murder and one count of assault with intent to commit murder in connection with the patient who died later.
Mays was hired at the VAMC in Clarksburg in June 2015. She worked from 7:30 PM to 8:00 AM in the medical surgical unit, court documents say.
According to the documents, “VAMC Clarksburg did not require a nursing assistant to have a certification or licensure for initial appointment or as a condition of continuing employment.”
The documents indicate that in June 2018, a hospitalist employed by VAMC Clarksburg reported concern about several deaths from unexplained hypoglycemic events in the same ward and noted that many of the affected patients did not have diabetes.
By that time, according to the Tennessean, “at least eight patients had died under suspicious circumstances. Several had been embalmed and buried, destroying potential evidence. One veteran had been cremated.”
An internal investigation began, followed by a criminal investigation, and in July 2018, Mays was removed from patient care.
Mays fired in 2019 because of lies on resume; claims suffers from PTSD
The Post reports that Mays was fired from the hospital in 2019, 7 months after she was banned from patient care, «after it was discovered she had lied about her qualifications on her resume.»
Court documents indicate that her duties included acting as a sitter for patients, checking vital signs, intake and output, and testing blood glucose levels, but she was not qualified to administer medications, including insulin.
Similarities in the deaths were evident, the Post reported. Citing sources familiar with the case, the report said, “elderly patients in private rooms were injected in their abdomen and limbs with insulin the hospital had not ordered.”
The Post reported that Mays sobbed by the end of the hearing on Tuesday.
The article notes that Mays has three sons and served in the Army National Guard from November 2000 to April 2001 and again from February 2003 to May 2004, when she was deployed to Iraq and Kuwait. She told the judge she was taking medication for posttraumatic stress disorder.
By pleading guilty, she waived her right to have the case presented to a grand jury. A sentencing hearing has not been scheduled, the Post reports.
NPR notes that prosecutors have requested that Mays serve seven consecutive life sentences and an additional 20 years in prison.
“Our hearts go out to those affected by these tragic deaths”
A spokesman for VAMC Clarksburg said in a statement to Medscape Medical News: “Our hearts go out to those affected by these tragic deaths. Clarksburg VA Medical Center discovered these allegations and reported them to VA›s independent inspector general more than 2 years ago. Clarksburg VA Medical Center also fired the individual at the center of the allegations.
“We’re glad the Department of Justice stepped in to push this investigation across the finish line and hopeful our court system will deliver the justice Clarksburg-area Veterans and families deserve.”
According to the Tennessean, Michael Missal, inspector general for the Department of Veteran Affairs, said the agency is investigating the hospital’s practices, “including medication management and communications among staffers.”
This article first appeared on Medscape.com.
A former nursing assistant and Army veteran pleaded guilty to federal murder charges this week in connection with the 2017-2018 deaths of seven patients in a West Virginia veteran’s hospital, according to news reports.
Prosecutors said in court documents filed on July 13 that Reta Mays, 46, injected lethal doses of insulin into seven veterans at the Louis A. Johnson VA Medical Center (VAMC) in rural Clarksburg, W.Va.
Their blood glucose levels plummeted, and each died shortly after their injections, according to the Tennessean.
An eighth patient, a 92-year-old man whom Mays is accused of assaulting with an insulin injection, initially survived after staff were able to stabilize him but died 2 weeks later at a nursing home, NPR reports.
According to NPR, US Attorney Jarod Douglas told the court Tuesday that the medical investigator could not determine whether the insulin contributed to the man’s death but that it was Mays’ intention to kill him.
“No one watched while she injected them with lethal doses of insulin during an 11-month killing rampage,” the Washington Post reported.
No motive offered
The Post article said no motive has been established, but after a 2-year investigation into a pattern of suspicious deaths that took the hospital almost a year to detect, Mays, who had denied any wrongdoing in multiple interviews with investigators, told a federal judge she preyed on some of the country›s most vulnerable service members.
An attorney for Mays, Brian Kornbrath, contacted by Medscape Medical News, said: “The defense team decided that we would have no public comment at this time.”
According to court documents from the Northern District of West Virginia, Mays was charged with seven counts of second-degree murder and one count of assault with intent to commit murder in connection with the patient who died later.
Mays was hired at the VAMC in Clarksburg in June 2015. She worked from 7:30 PM to 8:00 AM in the medical surgical unit, court documents say.
According to the documents, “VAMC Clarksburg did not require a nursing assistant to have a certification or licensure for initial appointment or as a condition of continuing employment.”
The documents indicate that in June 2018, a hospitalist employed by VAMC Clarksburg reported concern about several deaths from unexplained hypoglycemic events in the same ward and noted that many of the affected patients did not have diabetes.
By that time, according to the Tennessean, “at least eight patients had died under suspicious circumstances. Several had been embalmed and buried, destroying potential evidence. One veteran had been cremated.”
An internal investigation began, followed by a criminal investigation, and in July 2018, Mays was removed from patient care.
Mays fired in 2019 because of lies on resume; claims suffers from PTSD
The Post reports that Mays was fired from the hospital in 2019, 7 months after she was banned from patient care, «after it was discovered she had lied about her qualifications on her resume.»
Court documents indicate that her duties included acting as a sitter for patients, checking vital signs, intake and output, and testing blood glucose levels, but she was not qualified to administer medications, including insulin.
Similarities in the deaths were evident, the Post reported. Citing sources familiar with the case, the report said, “elderly patients in private rooms were injected in their abdomen and limbs with insulin the hospital had not ordered.”
The Post reported that Mays sobbed by the end of the hearing on Tuesday.
The article notes that Mays has three sons and served in the Army National Guard from November 2000 to April 2001 and again from February 2003 to May 2004, when she was deployed to Iraq and Kuwait. She told the judge she was taking medication for posttraumatic stress disorder.
By pleading guilty, she waived her right to have the case presented to a grand jury. A sentencing hearing has not been scheduled, the Post reports.
NPR notes that prosecutors have requested that Mays serve seven consecutive life sentences and an additional 20 years in prison.
“Our hearts go out to those affected by these tragic deaths”
A spokesman for VAMC Clarksburg said in a statement to Medscape Medical News: “Our hearts go out to those affected by these tragic deaths. Clarksburg VA Medical Center discovered these allegations and reported them to VA›s independent inspector general more than 2 years ago. Clarksburg VA Medical Center also fired the individual at the center of the allegations.
“We’re glad the Department of Justice stepped in to push this investigation across the finish line and hopeful our court system will deliver the justice Clarksburg-area Veterans and families deserve.”
According to the Tennessean, Michael Missal, inspector general for the Department of Veteran Affairs, said the agency is investigating the hospital’s practices, “including medication management and communications among staffers.”
This article first appeared on Medscape.com.
A former nursing assistant and Army veteran pleaded guilty to federal murder charges this week in connection with the 2017-2018 deaths of seven patients in a West Virginia veteran’s hospital, according to news reports.
Prosecutors said in court documents filed on July 13 that Reta Mays, 46, injected lethal doses of insulin into seven veterans at the Louis A. Johnson VA Medical Center (VAMC) in rural Clarksburg, W.Va.
Their blood glucose levels plummeted, and each died shortly after their injections, according to the Tennessean.
An eighth patient, a 92-year-old man whom Mays is accused of assaulting with an insulin injection, initially survived after staff were able to stabilize him but died 2 weeks later at a nursing home, NPR reports.
According to NPR, US Attorney Jarod Douglas told the court Tuesday that the medical investigator could not determine whether the insulin contributed to the man’s death but that it was Mays’ intention to kill him.
“No one watched while she injected them with lethal doses of insulin during an 11-month killing rampage,” the Washington Post reported.
No motive offered
The Post article said no motive has been established, but after a 2-year investigation into a pattern of suspicious deaths that took the hospital almost a year to detect, Mays, who had denied any wrongdoing in multiple interviews with investigators, told a federal judge she preyed on some of the country›s most vulnerable service members.
An attorney for Mays, Brian Kornbrath, contacted by Medscape Medical News, said: “The defense team decided that we would have no public comment at this time.”
According to court documents from the Northern District of West Virginia, Mays was charged with seven counts of second-degree murder and one count of assault with intent to commit murder in connection with the patient who died later.
Mays was hired at the VAMC in Clarksburg in June 2015. She worked from 7:30 PM to 8:00 AM in the medical surgical unit, court documents say.
According to the documents, “VAMC Clarksburg did not require a nursing assistant to have a certification or licensure for initial appointment or as a condition of continuing employment.”
The documents indicate that in June 2018, a hospitalist employed by VAMC Clarksburg reported concern about several deaths from unexplained hypoglycemic events in the same ward and noted that many of the affected patients did not have diabetes.
By that time, according to the Tennessean, “at least eight patients had died under suspicious circumstances. Several had been embalmed and buried, destroying potential evidence. One veteran had been cremated.”
An internal investigation began, followed by a criminal investigation, and in July 2018, Mays was removed from patient care.
Mays fired in 2019 because of lies on resume; claims suffers from PTSD
The Post reports that Mays was fired from the hospital in 2019, 7 months after she was banned from patient care, «after it was discovered she had lied about her qualifications on her resume.»
Court documents indicate that her duties included acting as a sitter for patients, checking vital signs, intake and output, and testing blood glucose levels, but she was not qualified to administer medications, including insulin.
Similarities in the deaths were evident, the Post reported. Citing sources familiar with the case, the report said, “elderly patients in private rooms were injected in their abdomen and limbs with insulin the hospital had not ordered.”
The Post reported that Mays sobbed by the end of the hearing on Tuesday.
The article notes that Mays has three sons and served in the Army National Guard from November 2000 to April 2001 and again from February 2003 to May 2004, when she was deployed to Iraq and Kuwait. She told the judge she was taking medication for posttraumatic stress disorder.
By pleading guilty, she waived her right to have the case presented to a grand jury. A sentencing hearing has not been scheduled, the Post reports.
NPR notes that prosecutors have requested that Mays serve seven consecutive life sentences and an additional 20 years in prison.
“Our hearts go out to those affected by these tragic deaths”
A spokesman for VAMC Clarksburg said in a statement to Medscape Medical News: “Our hearts go out to those affected by these tragic deaths. Clarksburg VA Medical Center discovered these allegations and reported them to VA›s independent inspector general more than 2 years ago. Clarksburg VA Medical Center also fired the individual at the center of the allegations.
“We’re glad the Department of Justice stepped in to push this investigation across the finish line and hopeful our court system will deliver the justice Clarksburg-area Veterans and families deserve.”
According to the Tennessean, Michael Missal, inspector general for the Department of Veteran Affairs, said the agency is investigating the hospital’s practices, “including medication management and communications among staffers.”
This article first appeared on Medscape.com.
PCI or not, mortality climbs with post-ACS bleeding complications
Patients with acute coronary syndromes (ACS) with later bleeding complications that were at least moderate in severity showed a 15-fold increased risk of dying within 30 days, compared with those without such bleeding, in a pooled analysis of four randomized antithrombotic-therapy trials.
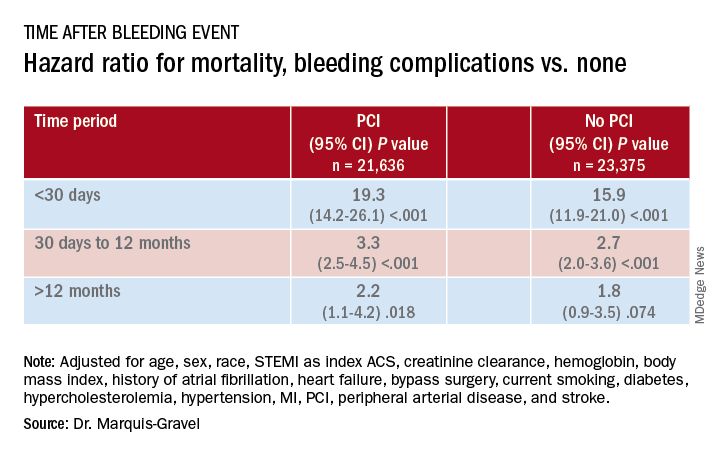
Mortality 1 month to 1 year after a bleeding event was not as sharply increased, but there was still almost triple the risk seen in patients without bleeding complications.
In both cases, the risk increase was independent of whether percutaneous coronary intervention (PCI) had been part of the management of ACS, concludes the study, published in the July 14 issue of the Journal of the American College of Cardiology.
“We showed that postdischarge bleeding was associated with a pretty bad prognosis, in terms of all-cause mortality, regardless of the index treatment – PCI or medical therapy,” lead author Guillaume Marquis-Gravel, MD, MSc, Duke Clinical Research Institute, Durham, N.C., said in an interview.
“Our data suggest that we should care about bleeding prevention in patients who had a previous ACS, regardless of the treatment strategy, as much as we care for prevention of future ischemic events,” said Dr. Marquis-Gravel, who is also an interventional cardiologist at the Montreal Heart Institute.
“This large-scale analysis clearly demonstrates that bleeding events occurring among ACS patients with coronary stents carry the same prognostic significance in magnitude and time course as among patients who do not undergo PCI,” observed Derek Chew, MBBS, MPH, PhD, of Flinders University, Adelaide, Australia, and Jack Wei Chieh Tan, MBBS, MBA, of National Heart Centre, Singapore, in an accompanying editorial.
“Therefore, at least in the later phases of planning antithrombotic therapy, when weighting bleeding risk in these conditions, these estimates should not be ‘discounted’ for the absence or presence of PCI during the initial ACS management,” they wrote.
A “proven assumption”
“A great deal of research has previously been conducted to tailor DAPT [dual-antiplatelet therapy] and to minimize bleeding risk following PCI based on the proven assumption that bleeding is associated with adverse clinical outcomes,” Dr. Marques-Gravel explained.
“The prognostic impact of postdischarge bleeding has not been studied thoroughly in patients with ACS who were only treated medically with DAPT without PCI.” Yet this population makes up a large proportion of the ACS population, and patients are “generally older and sicker” and therefore at increased risk for both ischemic and bleeding events, he said.
The researchers explored those issues in a post hoc pooled analysis of four randomized comparisons of antithrombotic strategies in patients with ACS: APPRAISE-2, PLATO, TRACER, and TRILOGY ACS. The analyses tracked bleeding events that took place from a landmark time of 7 days after presentation with ACS over a median follow-up of 1 year in 45,011 patients (31.3% female), 48% of whom were managed with PCI.
Those treated with PCI, compared with those medically managed only, tended to be younger, more often male, more likely to have ST-segment elevation myocardial infarction (STEMI) as their ACS, and less likely to have cardiovascular comorbidities.
During the total follow-up of 48,717 person-years, the postdischarge rate of moderate, severe, or life-threatening bleeding defined by GUSTO criteria reached 2.6 events per 100 patient-years. A total of 2,149 patients died, and mortality was consistently higher in patients who had such bleeding complications. They showed an adjusted hazard ratio of 15.7 (95% confidence interval, 12.3-20.0) for mortality within 30 days, compared with patients without bleeds. Their HR for mortality at 30 days to 1 year was 2.7 (95% CI, 2.1-3.4).
The association between bleeding complications and mortality remained consistent, regardless of whether patients had undergone PCI for their ACS (interaction P = .240).
A pragmatic interpretation
Although an observational study can’t show causality between bleeding and mortality, Dr. Marquis-Gravel cautioned, “the fact that the majority of deaths occurred early after the bleeding event, within 30 days, is strongly suggestive of a causal relationship.”
He recommended a “pragmatic interpretation” of the study: “Bleeding avoidance strategies tested in PCI populations, including short-term DAPT or aspirin-free strategies, should also be considered in medically treated patients with ACS deemed at higher risk of bleeding.”
“It is clear that bleeding events after successful PCI for an ACS are independently associated with increased mortality and morbidity,” Debabrata Mukherjee, MD, of Texas Tech University, El Paso, said in an interview.
“Every effort should be made to minimize bleeding events with the use of appropriate access site for PCI, dosing, selection, and duration of antiplatelet and antithrombotic agents, and use of proton pump inhibitors when appropriate,” he said.
The clinical decision-making involved in this individualized approach “is often not easy,” said Dr. Mukherjee, who was not involved in the current study. “Integrating patients and clinical pharmacists in choosing optimal antithrombotic therapies post-MI is likely to be helpful” in the process.
Although “major bleeding following ACS increases the risk of mortality for both medically managed and PCI-managed patients with ACS, the vast majority of deaths, 90%, occur in those that have not had a bleed,” Mamas A. Mamas, DPhil, Keele University, Staffordshire, England, said in an interview.
“It is important to understand the causes of death in this population and think about how interventions may impact on this,” agreed Dr. Mamas, who was not involved in the study.
Dr. Marquis-Gravel reported receiving speaking fees and honoraria from Servier and Novartis; disclosures for the other authors are in the report. Dr. Chew reported receiving speaking fees and institutional grants in aid from Roche Diagnostics, AstraZeneca, and Edwards Lifesciences. Dr. Tan discloses receiving speaking fees and educational grants from Amgen, Roche Diagnostics, AstraZeneca, Bayer, and Abbott Vascular. Dr. Mukherjee and Dr. Mamas report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Patients with acute coronary syndromes (ACS) with later bleeding complications that were at least moderate in severity showed a 15-fold increased risk of dying within 30 days, compared with those without such bleeding, in a pooled analysis of four randomized antithrombotic-therapy trials.
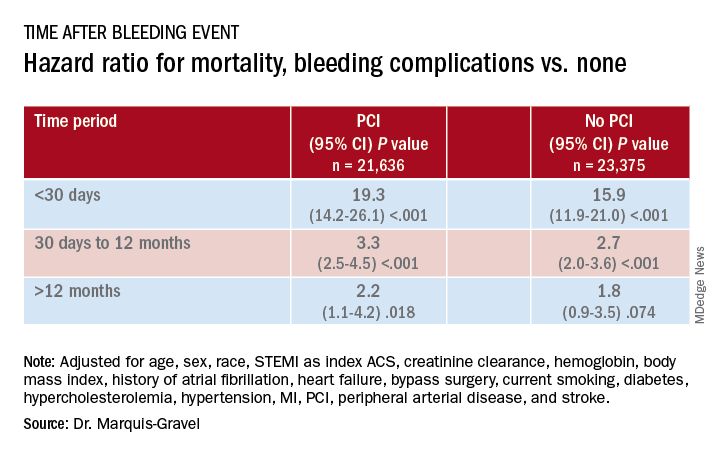
Mortality 1 month to 1 year after a bleeding event was not as sharply increased, but there was still almost triple the risk seen in patients without bleeding complications.
In both cases, the risk increase was independent of whether percutaneous coronary intervention (PCI) had been part of the management of ACS, concludes the study, published in the July 14 issue of the Journal of the American College of Cardiology.
“We showed that postdischarge bleeding was associated with a pretty bad prognosis, in terms of all-cause mortality, regardless of the index treatment – PCI or medical therapy,” lead author Guillaume Marquis-Gravel, MD, MSc, Duke Clinical Research Institute, Durham, N.C., said in an interview.
“Our data suggest that we should care about bleeding prevention in patients who had a previous ACS, regardless of the treatment strategy, as much as we care for prevention of future ischemic events,” said Dr. Marquis-Gravel, who is also an interventional cardiologist at the Montreal Heart Institute.
“This large-scale analysis clearly demonstrates that bleeding events occurring among ACS patients with coronary stents carry the same prognostic significance in magnitude and time course as among patients who do not undergo PCI,” observed Derek Chew, MBBS, MPH, PhD, of Flinders University, Adelaide, Australia, and Jack Wei Chieh Tan, MBBS, MBA, of National Heart Centre, Singapore, in an accompanying editorial.
“Therefore, at least in the later phases of planning antithrombotic therapy, when weighting bleeding risk in these conditions, these estimates should not be ‘discounted’ for the absence or presence of PCI during the initial ACS management,” they wrote.
A “proven assumption”
“A great deal of research has previously been conducted to tailor DAPT [dual-antiplatelet therapy] and to minimize bleeding risk following PCI based on the proven assumption that bleeding is associated with adverse clinical outcomes,” Dr. Marques-Gravel explained.
“The prognostic impact of postdischarge bleeding has not been studied thoroughly in patients with ACS who were only treated medically with DAPT without PCI.” Yet this population makes up a large proportion of the ACS population, and patients are “generally older and sicker” and therefore at increased risk for both ischemic and bleeding events, he said.
The researchers explored those issues in a post hoc pooled analysis of four randomized comparisons of antithrombotic strategies in patients with ACS: APPRAISE-2, PLATO, TRACER, and TRILOGY ACS. The analyses tracked bleeding events that took place from a landmark time of 7 days after presentation with ACS over a median follow-up of 1 year in 45,011 patients (31.3% female), 48% of whom were managed with PCI.
Those treated with PCI, compared with those medically managed only, tended to be younger, more often male, more likely to have ST-segment elevation myocardial infarction (STEMI) as their ACS, and less likely to have cardiovascular comorbidities.
During the total follow-up of 48,717 person-years, the postdischarge rate of moderate, severe, or life-threatening bleeding defined by GUSTO criteria reached 2.6 events per 100 patient-years. A total of 2,149 patients died, and mortality was consistently higher in patients who had such bleeding complications. They showed an adjusted hazard ratio of 15.7 (95% confidence interval, 12.3-20.0) for mortality within 30 days, compared with patients without bleeds. Their HR for mortality at 30 days to 1 year was 2.7 (95% CI, 2.1-3.4).
The association between bleeding complications and mortality remained consistent, regardless of whether patients had undergone PCI for their ACS (interaction P = .240).
A pragmatic interpretation
Although an observational study can’t show causality between bleeding and mortality, Dr. Marquis-Gravel cautioned, “the fact that the majority of deaths occurred early after the bleeding event, within 30 days, is strongly suggestive of a causal relationship.”
He recommended a “pragmatic interpretation” of the study: “Bleeding avoidance strategies tested in PCI populations, including short-term DAPT or aspirin-free strategies, should also be considered in medically treated patients with ACS deemed at higher risk of bleeding.”
“It is clear that bleeding events after successful PCI for an ACS are independently associated with increased mortality and morbidity,” Debabrata Mukherjee, MD, of Texas Tech University, El Paso, said in an interview.
“Every effort should be made to minimize bleeding events with the use of appropriate access site for PCI, dosing, selection, and duration of antiplatelet and antithrombotic agents, and use of proton pump inhibitors when appropriate,” he said.
The clinical decision-making involved in this individualized approach “is often not easy,” said Dr. Mukherjee, who was not involved in the current study. “Integrating patients and clinical pharmacists in choosing optimal antithrombotic therapies post-MI is likely to be helpful” in the process.
Although “major bleeding following ACS increases the risk of mortality for both medically managed and PCI-managed patients with ACS, the vast majority of deaths, 90%, occur in those that have not had a bleed,” Mamas A. Mamas, DPhil, Keele University, Staffordshire, England, said in an interview.
“It is important to understand the causes of death in this population and think about how interventions may impact on this,” agreed Dr. Mamas, who was not involved in the study.
Dr. Marquis-Gravel reported receiving speaking fees and honoraria from Servier and Novartis; disclosures for the other authors are in the report. Dr. Chew reported receiving speaking fees and institutional grants in aid from Roche Diagnostics, AstraZeneca, and Edwards Lifesciences. Dr. Tan discloses receiving speaking fees and educational grants from Amgen, Roche Diagnostics, AstraZeneca, Bayer, and Abbott Vascular. Dr. Mukherjee and Dr. Mamas report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Patients with acute coronary syndromes (ACS) with later bleeding complications that were at least moderate in severity showed a 15-fold increased risk of dying within 30 days, compared with those without such bleeding, in a pooled analysis of four randomized antithrombotic-therapy trials.
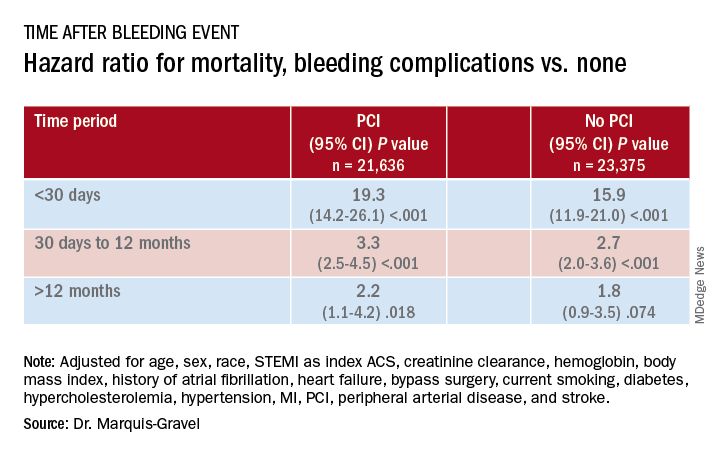
Mortality 1 month to 1 year after a bleeding event was not as sharply increased, but there was still almost triple the risk seen in patients without bleeding complications.
In both cases, the risk increase was independent of whether percutaneous coronary intervention (PCI) had been part of the management of ACS, concludes the study, published in the July 14 issue of the Journal of the American College of Cardiology.
“We showed that postdischarge bleeding was associated with a pretty bad prognosis, in terms of all-cause mortality, regardless of the index treatment – PCI or medical therapy,” lead author Guillaume Marquis-Gravel, MD, MSc, Duke Clinical Research Institute, Durham, N.C., said in an interview.
“Our data suggest that we should care about bleeding prevention in patients who had a previous ACS, regardless of the treatment strategy, as much as we care for prevention of future ischemic events,” said Dr. Marquis-Gravel, who is also an interventional cardiologist at the Montreal Heart Institute.
“This large-scale analysis clearly demonstrates that bleeding events occurring among ACS patients with coronary stents carry the same prognostic significance in magnitude and time course as among patients who do not undergo PCI,” observed Derek Chew, MBBS, MPH, PhD, of Flinders University, Adelaide, Australia, and Jack Wei Chieh Tan, MBBS, MBA, of National Heart Centre, Singapore, in an accompanying editorial.
“Therefore, at least in the later phases of planning antithrombotic therapy, when weighting bleeding risk in these conditions, these estimates should not be ‘discounted’ for the absence or presence of PCI during the initial ACS management,” they wrote.
A “proven assumption”
“A great deal of research has previously been conducted to tailor DAPT [dual-antiplatelet therapy] and to minimize bleeding risk following PCI based on the proven assumption that bleeding is associated with adverse clinical outcomes,” Dr. Marques-Gravel explained.
“The prognostic impact of postdischarge bleeding has not been studied thoroughly in patients with ACS who were only treated medically with DAPT without PCI.” Yet this population makes up a large proportion of the ACS population, and patients are “generally older and sicker” and therefore at increased risk for both ischemic and bleeding events, he said.
The researchers explored those issues in a post hoc pooled analysis of four randomized comparisons of antithrombotic strategies in patients with ACS: APPRAISE-2, PLATO, TRACER, and TRILOGY ACS. The analyses tracked bleeding events that took place from a landmark time of 7 days after presentation with ACS over a median follow-up of 1 year in 45,011 patients (31.3% female), 48% of whom were managed with PCI.
Those treated with PCI, compared with those medically managed only, tended to be younger, more often male, more likely to have ST-segment elevation myocardial infarction (STEMI) as their ACS, and less likely to have cardiovascular comorbidities.
During the total follow-up of 48,717 person-years, the postdischarge rate of moderate, severe, or life-threatening bleeding defined by GUSTO criteria reached 2.6 events per 100 patient-years. A total of 2,149 patients died, and mortality was consistently higher in patients who had such bleeding complications. They showed an adjusted hazard ratio of 15.7 (95% confidence interval, 12.3-20.0) for mortality within 30 days, compared with patients without bleeds. Their HR for mortality at 30 days to 1 year was 2.7 (95% CI, 2.1-3.4).
The association between bleeding complications and mortality remained consistent, regardless of whether patients had undergone PCI for their ACS (interaction P = .240).
A pragmatic interpretation
Although an observational study can’t show causality between bleeding and mortality, Dr. Marquis-Gravel cautioned, “the fact that the majority of deaths occurred early after the bleeding event, within 30 days, is strongly suggestive of a causal relationship.”
He recommended a “pragmatic interpretation” of the study: “Bleeding avoidance strategies tested in PCI populations, including short-term DAPT or aspirin-free strategies, should also be considered in medically treated patients with ACS deemed at higher risk of bleeding.”
“It is clear that bleeding events after successful PCI for an ACS are independently associated with increased mortality and morbidity,” Debabrata Mukherjee, MD, of Texas Tech University, El Paso, said in an interview.
“Every effort should be made to minimize bleeding events with the use of appropriate access site for PCI, dosing, selection, and duration of antiplatelet and antithrombotic agents, and use of proton pump inhibitors when appropriate,” he said.
The clinical decision-making involved in this individualized approach “is often not easy,” said Dr. Mukherjee, who was not involved in the current study. “Integrating patients and clinical pharmacists in choosing optimal antithrombotic therapies post-MI is likely to be helpful” in the process.
Although “major bleeding following ACS increases the risk of mortality for both medically managed and PCI-managed patients with ACS, the vast majority of deaths, 90%, occur in those that have not had a bleed,” Mamas A. Mamas, DPhil, Keele University, Staffordshire, England, said in an interview.
“It is important to understand the causes of death in this population and think about how interventions may impact on this,” agreed Dr. Mamas, who was not involved in the study.
Dr. Marquis-Gravel reported receiving speaking fees and honoraria from Servier and Novartis; disclosures for the other authors are in the report. Dr. Chew reported receiving speaking fees and institutional grants in aid from Roche Diagnostics, AstraZeneca, and Edwards Lifesciences. Dr. Tan discloses receiving speaking fees and educational grants from Amgen, Roche Diagnostics, AstraZeneca, Bayer, and Abbott Vascular. Dr. Mukherjee and Dr. Mamas report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
SGLT2 inhibitors, developed for T2D, now ‘belong to cardiologists and nephrologists’
It’s passé to think of the sodium-glucose cotransporter 2 (SGLT2) inhibitor drugs as agents that primarily treat hyperglycemia because their major clinical role has rapidly morphed into treating or preventing heart failure and chronic kidney disease.
This change suddenly thrust primary responsibility for prescribing these drug into the hands of cardiologists and nephrologists, though endocrinologists, diabetologists, and primary care physicians remain in the prescribing mix, experts agreed at the virtual annual scientific sessions of the American Diabetes Association.
“Glucose lowering plays little or no role in the cardiorenal protection from drugs in the sodium-glucose cotransporter 2 inhibitor class,” said David Z. Cherney, MD, a nephrologist and professor of medicine at the University of Toronto.
The SGLT2 inhibitor drugs “belong to cardiologists and nephrologists,” declared endocrinologist Yehuda Handelsman, MD, an endocrinologist and diabetes specialist who is medical director of The Metabolic Institute of America in Tarzana, Calif.
But therein lies a problem. “Cardiologists and nephrologists often say that they don’t want to start SGLT2 inhibitors because they do not want to interfere with the glucose reducing medications a patient takes,” Dr. Cherney added.
“Cardiologists are absolutely afraid to prescribe SGLT2 inhibitors,” claimed John J.V. McMurray MD, a professor of medical cardiology at the University of Glasgow. “Cardiologists need to talk with diabetologists about the importance of treating heart failure” in patients with type 2 diabetes (T2D), and diabetologists “need to help cardiologists understand how to use these and other effective glucose-lowering drugs that reduce cardiovascular disease risk,” said Dr. McMurray during the ADA sessions.
“I don’t think any medical specialty owns this drug class,” said Silvio E. Inzucchi, MD, professor of medicine at Yale University, New Haven, Conn., and director of the Yale Medicine Diabetes Center. “No permission is needed” from an endocrinologist for another specialist to prescribe an SGLT2 inhibitor to patients with T2D or to appropriate patients without diabetes, he maintained.
The need for greater involvement by cardiologists in prescribing SGLT2 inhibitors to patients with T2D was underscored in findings recently reported by Dr. Inzucchi and associates. They analyzed the physician encounters that patients with T2D had with cardiologists and endocrinologists during 2017 at two U.S. health systems: one centered around clinicians affiliated with Yale Medicine and Yale University, and a second with clinicians drawn from the staffs of the Saint Luke’s Health System, including Saint Luke’s Mid America Heart Institute in Kansas City, Mo.
During 2017, the two systems has outpatient encounters with 109,747 patients with T2D, who averaged 67 years of age and were roughly evenly split between women and men: 43% had prevalent cardiovascular disease, including 30% with coronary artery disease and 15% with heart failure. These patients had more than 110,000 physician visits, and the number of these consultations with a cardiologist was double the number with an endocrinologist, Dr. Inzucchi and associates recently reported (Cardiovasc Endocrinol Metab. 2020 Jun;9[2]:56-9).
Among the 30% of T2D patients with prevalent cardiovascular disease, the consultation rate with a cardiologist was four times greater than with an endocrinologist; among the 15% with heart failure, a visit with a cardiologist was nearly seven times more common that with an endocrinologist.
“Based on these data, cardiovascular specialists encouraging the use of these medications, or, if comfortable, actually prescribing these medications, would likely significantly hasten the adoption of evidence-based glucose-lowering therapies in those patients most apt to benefit from them,” concluded the study’s authors.
Dr. Cherney has been a consultant to or has received honoraria from AstraZeneca, Boehringer Ingelheim, Janssen, Lilly, Merck, Mitsubishi Tanabe Pharma, and Sanofi. Dr. Handelsman has been a consultant to or speaker on behalf of Amarin, Amgen, Applied Therapeutic, AstraZeneca, Boehringer Ingelheim, Esperion, Gilead, Janssen, Merck, Merck-Pfizer, Novo Nordisk, Regeneron, and Sanofi. Dr. McMurray’s employer, the University of Glasgow, received payments from AstraZeneca for his involvement in trials involving dapagliflozin. Dr. Inzucchi has been a consultant to or helped run trials for Abbott, AstraZeneca, Boehringer Ingelheim, Merck, Novo Nordisk, Sanofi/Lexicon, and vTv Therapeutics.
It’s passé to think of the sodium-glucose cotransporter 2 (SGLT2) inhibitor drugs as agents that primarily treat hyperglycemia because their major clinical role has rapidly morphed into treating or preventing heart failure and chronic kidney disease.
This change suddenly thrust primary responsibility for prescribing these drug into the hands of cardiologists and nephrologists, though endocrinologists, diabetologists, and primary care physicians remain in the prescribing mix, experts agreed at the virtual annual scientific sessions of the American Diabetes Association.
“Glucose lowering plays little or no role in the cardiorenal protection from drugs in the sodium-glucose cotransporter 2 inhibitor class,” said David Z. Cherney, MD, a nephrologist and professor of medicine at the University of Toronto.
The SGLT2 inhibitor drugs “belong to cardiologists and nephrologists,” declared endocrinologist Yehuda Handelsman, MD, an endocrinologist and diabetes specialist who is medical director of The Metabolic Institute of America in Tarzana, Calif.
But therein lies a problem. “Cardiologists and nephrologists often say that they don’t want to start SGLT2 inhibitors because they do not want to interfere with the glucose reducing medications a patient takes,” Dr. Cherney added.
“Cardiologists are absolutely afraid to prescribe SGLT2 inhibitors,” claimed John J.V. McMurray MD, a professor of medical cardiology at the University of Glasgow. “Cardiologists need to talk with diabetologists about the importance of treating heart failure” in patients with type 2 diabetes (T2D), and diabetologists “need to help cardiologists understand how to use these and other effective glucose-lowering drugs that reduce cardiovascular disease risk,” said Dr. McMurray during the ADA sessions.
“I don’t think any medical specialty owns this drug class,” said Silvio E. Inzucchi, MD, professor of medicine at Yale University, New Haven, Conn., and director of the Yale Medicine Diabetes Center. “No permission is needed” from an endocrinologist for another specialist to prescribe an SGLT2 inhibitor to patients with T2D or to appropriate patients without diabetes, he maintained.
The need for greater involvement by cardiologists in prescribing SGLT2 inhibitors to patients with T2D was underscored in findings recently reported by Dr. Inzucchi and associates. They analyzed the physician encounters that patients with T2D had with cardiologists and endocrinologists during 2017 at two U.S. health systems: one centered around clinicians affiliated with Yale Medicine and Yale University, and a second with clinicians drawn from the staffs of the Saint Luke’s Health System, including Saint Luke’s Mid America Heart Institute in Kansas City, Mo.
During 2017, the two systems has outpatient encounters with 109,747 patients with T2D, who averaged 67 years of age and were roughly evenly split between women and men: 43% had prevalent cardiovascular disease, including 30% with coronary artery disease and 15% with heart failure. These patients had more than 110,000 physician visits, and the number of these consultations with a cardiologist was double the number with an endocrinologist, Dr. Inzucchi and associates recently reported (Cardiovasc Endocrinol Metab. 2020 Jun;9[2]:56-9).
Among the 30% of T2D patients with prevalent cardiovascular disease, the consultation rate with a cardiologist was four times greater than with an endocrinologist; among the 15% with heart failure, a visit with a cardiologist was nearly seven times more common that with an endocrinologist.
“Based on these data, cardiovascular specialists encouraging the use of these medications, or, if comfortable, actually prescribing these medications, would likely significantly hasten the adoption of evidence-based glucose-lowering therapies in those patients most apt to benefit from them,” concluded the study’s authors.
Dr. Cherney has been a consultant to or has received honoraria from AstraZeneca, Boehringer Ingelheim, Janssen, Lilly, Merck, Mitsubishi Tanabe Pharma, and Sanofi. Dr. Handelsman has been a consultant to or speaker on behalf of Amarin, Amgen, Applied Therapeutic, AstraZeneca, Boehringer Ingelheim, Esperion, Gilead, Janssen, Merck, Merck-Pfizer, Novo Nordisk, Regeneron, and Sanofi. Dr. McMurray’s employer, the University of Glasgow, received payments from AstraZeneca for his involvement in trials involving dapagliflozin. Dr. Inzucchi has been a consultant to or helped run trials for Abbott, AstraZeneca, Boehringer Ingelheim, Merck, Novo Nordisk, Sanofi/Lexicon, and vTv Therapeutics.
It’s passé to think of the sodium-glucose cotransporter 2 (SGLT2) inhibitor drugs as agents that primarily treat hyperglycemia because their major clinical role has rapidly morphed into treating or preventing heart failure and chronic kidney disease.
This change suddenly thrust primary responsibility for prescribing these drug into the hands of cardiologists and nephrologists, though endocrinologists, diabetologists, and primary care physicians remain in the prescribing mix, experts agreed at the virtual annual scientific sessions of the American Diabetes Association.
“Glucose lowering plays little or no role in the cardiorenal protection from drugs in the sodium-glucose cotransporter 2 inhibitor class,” said David Z. Cherney, MD, a nephrologist and professor of medicine at the University of Toronto.
The SGLT2 inhibitor drugs “belong to cardiologists and nephrologists,” declared endocrinologist Yehuda Handelsman, MD, an endocrinologist and diabetes specialist who is medical director of The Metabolic Institute of America in Tarzana, Calif.
But therein lies a problem. “Cardiologists and nephrologists often say that they don’t want to start SGLT2 inhibitors because they do not want to interfere with the glucose reducing medications a patient takes,” Dr. Cherney added.
“Cardiologists are absolutely afraid to prescribe SGLT2 inhibitors,” claimed John J.V. McMurray MD, a professor of medical cardiology at the University of Glasgow. “Cardiologists need to talk with diabetologists about the importance of treating heart failure” in patients with type 2 diabetes (T2D), and diabetologists “need to help cardiologists understand how to use these and other effective glucose-lowering drugs that reduce cardiovascular disease risk,” said Dr. McMurray during the ADA sessions.
“I don’t think any medical specialty owns this drug class,” said Silvio E. Inzucchi, MD, professor of medicine at Yale University, New Haven, Conn., and director of the Yale Medicine Diabetes Center. “No permission is needed” from an endocrinologist for another specialist to prescribe an SGLT2 inhibitor to patients with T2D or to appropriate patients without diabetes, he maintained.
The need for greater involvement by cardiologists in prescribing SGLT2 inhibitors to patients with T2D was underscored in findings recently reported by Dr. Inzucchi and associates. They analyzed the physician encounters that patients with T2D had with cardiologists and endocrinologists during 2017 at two U.S. health systems: one centered around clinicians affiliated with Yale Medicine and Yale University, and a second with clinicians drawn from the staffs of the Saint Luke’s Health System, including Saint Luke’s Mid America Heart Institute in Kansas City, Mo.
During 2017, the two systems has outpatient encounters with 109,747 patients with T2D, who averaged 67 years of age and were roughly evenly split between women and men: 43% had prevalent cardiovascular disease, including 30% with coronary artery disease and 15% with heart failure. These patients had more than 110,000 physician visits, and the number of these consultations with a cardiologist was double the number with an endocrinologist, Dr. Inzucchi and associates recently reported (Cardiovasc Endocrinol Metab. 2020 Jun;9[2]:56-9).
Among the 30% of T2D patients with prevalent cardiovascular disease, the consultation rate with a cardiologist was four times greater than with an endocrinologist; among the 15% with heart failure, a visit with a cardiologist was nearly seven times more common that with an endocrinologist.
“Based on these data, cardiovascular specialists encouraging the use of these medications, or, if comfortable, actually prescribing these medications, would likely significantly hasten the adoption of evidence-based glucose-lowering therapies in those patients most apt to benefit from them,” concluded the study’s authors.
Dr. Cherney has been a consultant to or has received honoraria from AstraZeneca, Boehringer Ingelheim, Janssen, Lilly, Merck, Mitsubishi Tanabe Pharma, and Sanofi. Dr. Handelsman has been a consultant to or speaker on behalf of Amarin, Amgen, Applied Therapeutic, AstraZeneca, Boehringer Ingelheim, Esperion, Gilead, Janssen, Merck, Merck-Pfizer, Novo Nordisk, Regeneron, and Sanofi. Dr. McMurray’s employer, the University of Glasgow, received payments from AstraZeneca for his involvement in trials involving dapagliflozin. Dr. Inzucchi has been a consultant to or helped run trials for Abbott, AstraZeneca, Boehringer Ingelheim, Merck, Novo Nordisk, Sanofi/Lexicon, and vTv Therapeutics.
FROM ADA 2020
Guidance addresses elders with diabetes during COVID-19
Two experts in geriatric diabetes are offering some contemporary practical recommendations for diabetes management in older adults during the COVID-19 pandemic.
The viewpoint, entitled, “Caring for Older Adults With Diabetes During the COVID-19 Pandemic,” was published online in JAMA Internal Medicine by Medha N. Munshi, MD, director of the geriatrics program at the Joslin Diabetes Center, Boston, and Sarah L. Sy, MD, a geriatrician in the same program.
Adults aged 70 years and older with comorbidities such as diabetes are among those at highest risk for adverse outcomes and mortality due to COVID-19.
At the same time, those who don’t have the illness face major challenges in avoiding it, including disruptions in normal activities and barriers to receiving health care.
Although telemedicine has become much more widely adopted in diabetes management since the pandemic began, older adults may not be as tech savvy, may not have computer or Internet access, and/or may have cognitive dysfunction that precludes its use.
“These unprecedented times pose a great challenge to this heterogeneous population with varying levels of complexity, frailty, and multimorbidity,” Munshi and Sy point out, noting that “clinicians can lessen the load by guiding, reassuring, and supporting them through this pandemic time.”
Because the pandemic could last for several months longer, the authors offer the following advice for clinicians who care for older adults with diabetes.
- Accessibility to health care: When possible, use telemedicine, diabetes care apps, or platforms to obtain data from glucose meters, continuous glucose monitors, and/or pumps. When use of technology isn’t possible, schedule telephone appointments and have the patient or caregiver read the glucose values.
- Multicomplexity and geriatric syndromes: Identify high-risk patients, such as those with or recurrent , and prioritize patient goals. If appropriate, simplify the diabetes treatment plan and reinforce with repeated education and instructions. Glucose goals may need to be liberalized. Advise patients to stay hydrated to minimize the risk of dehydration and falls. Take steps to avoid hypoglycemia, reduce polypharmacy, and consolidate medication doses.
- Burden of diabetes self-care: Bloodwork for can be delayed by a few months. Patients with can decrease the frequency of blood glucose checks if their glucose levels are generally within acceptable range. Encourage patients to eat healthily with regular meals rather than optimizing the diet for glucose levels, and adjust medications for any changes in diet. Advise safe options for physical activity such as walking inside the home or walking in place for 10 minutes, three times per day, and incorporating strength training, such as with resistance bands. Online exercise programs are another option.
- Psychological stress: Check in with patients and encourage them to stay as connected as possible using technology (phone, video chat, text message), letters, or cards with family, friends, and/or religious communities. Screen for , using either the Geriatric Depression Scale or Patient Health Questionnaire-2, and refer to mental health colleagues if appropriate. Speak or email with caregivers to assess the patient’s mental health state and offer local support resources, if needed.
- Medication and equipment issues: Refill 90-day prescriptions and equipment, and request mail or home (contactless) delivery. Patients should also have backups in case of equipment failures, such as syringes and long-acting insulin in case of pump failure, and test strips/meter for continuous glucose monitor problems.
Munshi and Sy conclude: “Many of the recommendations presented in this article are practical and will continue to be relevant after COVID-19. When this is all over, patients will remember how we made them feel, and how we kept them safe and healthy at home.”
Munshi is a consultant for Sanofi and Lilly. Sy has reported no relevant financial relationships.
This article first appeared on Medscape.com.
Two experts in geriatric diabetes are offering some contemporary practical recommendations for diabetes management in older adults during the COVID-19 pandemic.
The viewpoint, entitled, “Caring for Older Adults With Diabetes During the COVID-19 Pandemic,” was published online in JAMA Internal Medicine by Medha N. Munshi, MD, director of the geriatrics program at the Joslin Diabetes Center, Boston, and Sarah L. Sy, MD, a geriatrician in the same program.
Adults aged 70 years and older with comorbidities such as diabetes are among those at highest risk for adverse outcomes and mortality due to COVID-19.
At the same time, those who don’t have the illness face major challenges in avoiding it, including disruptions in normal activities and barriers to receiving health care.
Although telemedicine has become much more widely adopted in diabetes management since the pandemic began, older adults may not be as tech savvy, may not have computer or Internet access, and/or may have cognitive dysfunction that precludes its use.
“These unprecedented times pose a great challenge to this heterogeneous population with varying levels of complexity, frailty, and multimorbidity,” Munshi and Sy point out, noting that “clinicians can lessen the load by guiding, reassuring, and supporting them through this pandemic time.”
Because the pandemic could last for several months longer, the authors offer the following advice for clinicians who care for older adults with diabetes.
- Accessibility to health care: When possible, use telemedicine, diabetes care apps, or platforms to obtain data from glucose meters, continuous glucose monitors, and/or pumps. When use of technology isn’t possible, schedule telephone appointments and have the patient or caregiver read the glucose values.
- Multicomplexity and geriatric syndromes: Identify high-risk patients, such as those with or recurrent , and prioritize patient goals. If appropriate, simplify the diabetes treatment plan and reinforce with repeated education and instructions. Glucose goals may need to be liberalized. Advise patients to stay hydrated to minimize the risk of dehydration and falls. Take steps to avoid hypoglycemia, reduce polypharmacy, and consolidate medication doses.
- Burden of diabetes self-care: Bloodwork for can be delayed by a few months. Patients with can decrease the frequency of blood glucose checks if their glucose levels are generally within acceptable range. Encourage patients to eat healthily with regular meals rather than optimizing the diet for glucose levels, and adjust medications for any changes in diet. Advise safe options for physical activity such as walking inside the home or walking in place for 10 minutes, three times per day, and incorporating strength training, such as with resistance bands. Online exercise programs are another option.
- Psychological stress: Check in with patients and encourage them to stay as connected as possible using technology (phone, video chat, text message), letters, or cards with family, friends, and/or religious communities. Screen for , using either the Geriatric Depression Scale or Patient Health Questionnaire-2, and refer to mental health colleagues if appropriate. Speak or email with caregivers to assess the patient’s mental health state and offer local support resources, if needed.
- Medication and equipment issues: Refill 90-day prescriptions and equipment, and request mail or home (contactless) delivery. Patients should also have backups in case of equipment failures, such as syringes and long-acting insulin in case of pump failure, and test strips/meter for continuous glucose monitor problems.
Munshi and Sy conclude: “Many of the recommendations presented in this article are practical and will continue to be relevant after COVID-19. When this is all over, patients will remember how we made them feel, and how we kept them safe and healthy at home.”
Munshi is a consultant for Sanofi and Lilly. Sy has reported no relevant financial relationships.
This article first appeared on Medscape.com.
Two experts in geriatric diabetes are offering some contemporary practical recommendations for diabetes management in older adults during the COVID-19 pandemic.
The viewpoint, entitled, “Caring for Older Adults With Diabetes During the COVID-19 Pandemic,” was published online in JAMA Internal Medicine by Medha N. Munshi, MD, director of the geriatrics program at the Joslin Diabetes Center, Boston, and Sarah L. Sy, MD, a geriatrician in the same program.
Adults aged 70 years and older with comorbidities such as diabetes are among those at highest risk for adverse outcomes and mortality due to COVID-19.
At the same time, those who don’t have the illness face major challenges in avoiding it, including disruptions in normal activities and barriers to receiving health care.
Although telemedicine has become much more widely adopted in diabetes management since the pandemic began, older adults may not be as tech savvy, may not have computer or Internet access, and/or may have cognitive dysfunction that precludes its use.
“These unprecedented times pose a great challenge to this heterogeneous population with varying levels of complexity, frailty, and multimorbidity,” Munshi and Sy point out, noting that “clinicians can lessen the load by guiding, reassuring, and supporting them through this pandemic time.”
Because the pandemic could last for several months longer, the authors offer the following advice for clinicians who care for older adults with diabetes.
- Accessibility to health care: When possible, use telemedicine, diabetes care apps, or platforms to obtain data from glucose meters, continuous glucose monitors, and/or pumps. When use of technology isn’t possible, schedule telephone appointments and have the patient or caregiver read the glucose values.
- Multicomplexity and geriatric syndromes: Identify high-risk patients, such as those with or recurrent , and prioritize patient goals. If appropriate, simplify the diabetes treatment plan and reinforce with repeated education and instructions. Glucose goals may need to be liberalized. Advise patients to stay hydrated to minimize the risk of dehydration and falls. Take steps to avoid hypoglycemia, reduce polypharmacy, and consolidate medication doses.
- Burden of diabetes self-care: Bloodwork for can be delayed by a few months. Patients with can decrease the frequency of blood glucose checks if their glucose levels are generally within acceptable range. Encourage patients to eat healthily with regular meals rather than optimizing the diet for glucose levels, and adjust medications for any changes in diet. Advise safe options for physical activity such as walking inside the home or walking in place for 10 minutes, three times per day, and incorporating strength training, such as with resistance bands. Online exercise programs are another option.
- Psychological stress: Check in with patients and encourage them to stay as connected as possible using technology (phone, video chat, text message), letters, or cards with family, friends, and/or religious communities. Screen for , using either the Geriatric Depression Scale or Patient Health Questionnaire-2, and refer to mental health colleagues if appropriate. Speak or email with caregivers to assess the patient’s mental health state and offer local support resources, if needed.
- Medication and equipment issues: Refill 90-day prescriptions and equipment, and request mail or home (contactless) delivery. Patients should also have backups in case of equipment failures, such as syringes and long-acting insulin in case of pump failure, and test strips/meter for continuous glucose monitor problems.
Munshi and Sy conclude: “Many of the recommendations presented in this article are practical and will continue to be relevant after COVID-19. When this is all over, patients will remember how we made them feel, and how we kept them safe and healthy at home.”
Munshi is a consultant for Sanofi and Lilly. Sy has reported no relevant financial relationships.
This article first appeared on Medscape.com.