User login
Cardiology News is an independent news source that provides cardiologists with timely and relevant news and commentary about clinical developments and the impact of health care policy on cardiology and the cardiologist's practice. Cardiology News Digital Network is the online destination and multimedia properties of Cardiology News, the independent news publication for cardiologists. Cardiology news is the leading source of news and commentary about clinical developments in cardiology as well as health care policy and regulations that affect the cardiologist's practice. Cardiology News Digital Network is owned by Frontline Medical Communications.
Common drug with lots of surprising side effects
A 55-year-old woman comes to clinic for follow-up. She reports her family is worried that she isn’t getting enough sleep and is more tired than usual. The patient reports she is sleeping 8 hours a night and wakes up feeling rested, but she has noticed she has been yawning much more frequently than she remembers in the past.
Past medical history: gastroesophageal reflux disease, hypertension, generalized anxiety disorder, hypothyroidism, and osteoporosis. Medications: amlodipine, lansoprazole, irbesartan, escitalopram, levothyroxine, and alendronate. Physical examination: blood pressure 110/70 mm Hg, pulse 60 bpm. Lower extremities: 1+ edema.
What is the likely cause of her increased yawning?
A. Amlodipine.
B. Alendronate.
C. Irbesartan.
D. Escitalopram.
E. Lansoprazole.
The correct answer here is escitalopram. Selective serotonin reuptake inhibitors in general are well tolerated. Given how commonly these drugs are used, however, there are a number of lesser-known side effects that you are likely to see.
In the above case, this patient has yawning caused by her SSRI. Roncero et al. described a case of yawning in a patient on escitalopram that resolved when the dose of escitalopram was reduced.1 Paroxetine has been reported to cause yawning at both low and high doses.2
In a review of drug-induced yawning, SSRIs as a class were most frequently involved, and sertraline and fluoxetine were implicated in addition to paroxetine.3 The serotonin-norepinephrine reuptake inhibitors duloxetine and venlafaxine have also been associated with yawning.4,5
Hyperhydrosis has also been linked to SSRIs and SNRIs, and both yawning and hyperhidrosis may occur because of an underlying thermoregulatory dysfunction.6
SSRIs have been linked to increased bleeding risk, especially increased risk of upper gastrointestinal hemorrhage. Laporte and colleagues showed an association of SSRI use and risk of bleeding in a meta-analysis of 42 observational studies, with an odds ratio of 1.41 (95% confidence interval, 1.27-1.57; P less than .0001).7 The risk of upper gastrointestinal (UGI) bleeding is further increased if patients are also taking NSAIDs.
Anglin et al. looked at 15 case-control studies and 4 cohort studies and found an OR of 1.66 for UGI bleeding with SSRI use, and an OR of 4.25 for UGI bleeding if SSRI use was combined with NSAID use.8 The number needed to harm is 3,177 for NSAID use in populations at low risk for GI bleeding, but it is much lower (881) in higher-risk populations.8 Make sure to think about patients’ bleeding risks when starting SSRIs.
An issue that comes up frequently is: What is the risk of bleeding in patients on SSRIs who are also on anticoagulants? Dr. Quinn and colleagues looked at the bleeding risk of anticoagulated patients also taking SSRIs in the ROCKET AF trial.9 They found 737 patients who received SSRIs and matched them with other patients not on SSRIs in the trial. All patients in the trial were either receiving rivaroxaban or warfarin for stroke prophylaxis. They found no significant increase risk in bleeding in the patients on SSRIs and anticoagulants.
Take-home points:
- Yawning and hyperhidrosis are interesting side effects of SSRIs.
- Bleeding risk is increased in patients on SSRIs, especially when combined with NSAIDs.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
References
1. Neurologia. 2013 Nov-Dec;28(9):589-90.
2. Psychiatry Clin Neurosci. 2006 Apr;60(2):260.
3. Presse Med. 2014 Oct;43(10 Pt 1):1135-6.
4. Prog Neuropsychopharmacol Biol Psychiatry. 2009 Jun 15;33(4):747.
5. Ann Pharmacother. 2011 Oct;45(10):1297-301.
6. Depress Anxiety. 2017 Dec;34(12):1134-46.
7. Pharmacol Res. 2017 Apr;118:19-32.
8. Am J Gastroenterol. 2014 Jun;109(6):811-9.
9. J Am Heart Assoc. 2018 Aug 7;7(15):e008755.
A 55-year-old woman comes to clinic for follow-up. She reports her family is worried that she isn’t getting enough sleep and is more tired than usual. The patient reports she is sleeping 8 hours a night and wakes up feeling rested, but she has noticed she has been yawning much more frequently than she remembers in the past.
Past medical history: gastroesophageal reflux disease, hypertension, generalized anxiety disorder, hypothyroidism, and osteoporosis. Medications: amlodipine, lansoprazole, irbesartan, escitalopram, levothyroxine, and alendronate. Physical examination: blood pressure 110/70 mm Hg, pulse 60 bpm. Lower extremities: 1+ edema.
What is the likely cause of her increased yawning?
A. Amlodipine.
B. Alendronate.
C. Irbesartan.
D. Escitalopram.
E. Lansoprazole.
The correct answer here is escitalopram. Selective serotonin reuptake inhibitors in general are well tolerated. Given how commonly these drugs are used, however, there are a number of lesser-known side effects that you are likely to see.
In the above case, this patient has yawning caused by her SSRI. Roncero et al. described a case of yawning in a patient on escitalopram that resolved when the dose of escitalopram was reduced.1 Paroxetine has been reported to cause yawning at both low and high doses.2
In a review of drug-induced yawning, SSRIs as a class were most frequently involved, and sertraline and fluoxetine were implicated in addition to paroxetine.3 The serotonin-norepinephrine reuptake inhibitors duloxetine and venlafaxine have also been associated with yawning.4,5
Hyperhydrosis has also been linked to SSRIs and SNRIs, and both yawning and hyperhidrosis may occur because of an underlying thermoregulatory dysfunction.6
SSRIs have been linked to increased bleeding risk, especially increased risk of upper gastrointestinal hemorrhage. Laporte and colleagues showed an association of SSRI use and risk of bleeding in a meta-analysis of 42 observational studies, with an odds ratio of 1.41 (95% confidence interval, 1.27-1.57; P less than .0001).7 The risk of upper gastrointestinal (UGI) bleeding is further increased if patients are also taking NSAIDs.
Anglin et al. looked at 15 case-control studies and 4 cohort studies and found an OR of 1.66 for UGI bleeding with SSRI use, and an OR of 4.25 for UGI bleeding if SSRI use was combined with NSAID use.8 The number needed to harm is 3,177 for NSAID use in populations at low risk for GI bleeding, but it is much lower (881) in higher-risk populations.8 Make sure to think about patients’ bleeding risks when starting SSRIs.
An issue that comes up frequently is: What is the risk of bleeding in patients on SSRIs who are also on anticoagulants? Dr. Quinn and colleagues looked at the bleeding risk of anticoagulated patients also taking SSRIs in the ROCKET AF trial.9 They found 737 patients who received SSRIs and matched them with other patients not on SSRIs in the trial. All patients in the trial were either receiving rivaroxaban or warfarin for stroke prophylaxis. They found no significant increase risk in bleeding in the patients on SSRIs and anticoagulants.
Take-home points:
- Yawning and hyperhidrosis are interesting side effects of SSRIs.
- Bleeding risk is increased in patients on SSRIs, especially when combined with NSAIDs.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
References
1. Neurologia. 2013 Nov-Dec;28(9):589-90.
2. Psychiatry Clin Neurosci. 2006 Apr;60(2):260.
3. Presse Med. 2014 Oct;43(10 Pt 1):1135-6.
4. Prog Neuropsychopharmacol Biol Psychiatry. 2009 Jun 15;33(4):747.
5. Ann Pharmacother. 2011 Oct;45(10):1297-301.
6. Depress Anxiety. 2017 Dec;34(12):1134-46.
7. Pharmacol Res. 2017 Apr;118:19-32.
8. Am J Gastroenterol. 2014 Jun;109(6):811-9.
9. J Am Heart Assoc. 2018 Aug 7;7(15):e008755.
A 55-year-old woman comes to clinic for follow-up. She reports her family is worried that she isn’t getting enough sleep and is more tired than usual. The patient reports she is sleeping 8 hours a night and wakes up feeling rested, but she has noticed she has been yawning much more frequently than she remembers in the past.
Past medical history: gastroesophageal reflux disease, hypertension, generalized anxiety disorder, hypothyroidism, and osteoporosis. Medications: amlodipine, lansoprazole, irbesartan, escitalopram, levothyroxine, and alendronate. Physical examination: blood pressure 110/70 mm Hg, pulse 60 bpm. Lower extremities: 1+ edema.
What is the likely cause of her increased yawning?
A. Amlodipine.
B. Alendronate.
C. Irbesartan.
D. Escitalopram.
E. Lansoprazole.
The correct answer here is escitalopram. Selective serotonin reuptake inhibitors in general are well tolerated. Given how commonly these drugs are used, however, there are a number of lesser-known side effects that you are likely to see.
In the above case, this patient has yawning caused by her SSRI. Roncero et al. described a case of yawning in a patient on escitalopram that resolved when the dose of escitalopram was reduced.1 Paroxetine has been reported to cause yawning at both low and high doses.2
In a review of drug-induced yawning, SSRIs as a class were most frequently involved, and sertraline and fluoxetine were implicated in addition to paroxetine.3 The serotonin-norepinephrine reuptake inhibitors duloxetine and venlafaxine have also been associated with yawning.4,5
Hyperhydrosis has also been linked to SSRIs and SNRIs, and both yawning and hyperhidrosis may occur because of an underlying thermoregulatory dysfunction.6
SSRIs have been linked to increased bleeding risk, especially increased risk of upper gastrointestinal hemorrhage. Laporte and colleagues showed an association of SSRI use and risk of bleeding in a meta-analysis of 42 observational studies, with an odds ratio of 1.41 (95% confidence interval, 1.27-1.57; P less than .0001).7 The risk of upper gastrointestinal (UGI) bleeding is further increased if patients are also taking NSAIDs.
Anglin et al. looked at 15 case-control studies and 4 cohort studies and found an OR of 1.66 for UGI bleeding with SSRI use, and an OR of 4.25 for UGI bleeding if SSRI use was combined with NSAID use.8 The number needed to harm is 3,177 for NSAID use in populations at low risk for GI bleeding, but it is much lower (881) in higher-risk populations.8 Make sure to think about patients’ bleeding risks when starting SSRIs.
An issue that comes up frequently is: What is the risk of bleeding in patients on SSRIs who are also on anticoagulants? Dr. Quinn and colleagues looked at the bleeding risk of anticoagulated patients also taking SSRIs in the ROCKET AF trial.9 They found 737 patients who received SSRIs and matched them with other patients not on SSRIs in the trial. All patients in the trial were either receiving rivaroxaban or warfarin for stroke prophylaxis. They found no significant increase risk in bleeding in the patients on SSRIs and anticoagulants.
Take-home points:
- Yawning and hyperhidrosis are interesting side effects of SSRIs.
- Bleeding risk is increased in patients on SSRIs, especially when combined with NSAIDs.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. Contact Dr. Paauw at [email protected].
References
1. Neurologia. 2013 Nov-Dec;28(9):589-90.
2. Psychiatry Clin Neurosci. 2006 Apr;60(2):260.
3. Presse Med. 2014 Oct;43(10 Pt 1):1135-6.
4. Prog Neuropsychopharmacol Biol Psychiatry. 2009 Jun 15;33(4):747.
5. Ann Pharmacother. 2011 Oct;45(10):1297-301.
6. Depress Anxiety. 2017 Dec;34(12):1134-46.
7. Pharmacol Res. 2017 Apr;118:19-32.
8. Am J Gastroenterol. 2014 Jun;109(6):811-9.
9. J Am Heart Assoc. 2018 Aug 7;7(15):e008755.
ACP maps two potential paths to universal health care
The American College of Physicians is recommending either a single-payer system or a public option within a regulated private insurance system to help deliver universal and affordable access to health care for all Americans.
“We came to the conclusion that two directions or approaches could get us to where we need to be,” ACP President Robert McLean, MD, said in an interview. “We need ... a system that provides universal, affordable access to care.”
After examining the evidence, ACP discarded one option: a direct market-based approach.
“Direct market-based approaches won’t work,” Dr. McLean explained. “If you look at where direct marketplace approaches ... have been implemented, they just will not get you to a place where you are going to get universal coverage, portability, essential benefits, and preexisting condition protection and administrative simplification.”
Dr. McLean highlighted two paths that could achieve universal coverage and better access to health care: a single-payer–financed system, or a publicly financed coverage option within a system of regulated private insurance.
It’s the first time ACP has endorsed a single-payer approach. The college supported the public option that wasn’t included as part of the Affordable Care Act. But ACP’s latest publicly financed proposal offers a deeper level of detail on how to make that option work in the context of a private insurance system.
While the health reform conversation may be a political, ACP doesn’t want to make it a partisan one. ACP’s policy recommendations represent a carefully researched series of ideas backed by evidence-based research, Dr. McLean said.
“There is a lot of nuance behind” the two recommendations, he noted, and those nuances are explored in a series of articles and editorials published Jan. 21 in Annals of Internal Medicine.
Sizing up single payer
The ACP acknowledges that for its single-payer system, the transition could be “politically difficult and strain the federal budget,” according to Ryan A. Crowley, senior analyst at ACP, and colleagues in an article outlining the organization’s vision. “Taxes would probably replace premiums, and private insurance would have a reduced role or be eliminated altogether.”
However, the authors note that a single-payer system could be designed to address concerns from a generally skeptical public, such as providing bulk funding or setting minimum standards to guide state operations. It also could include private insurance to provide supplemental coverage.
Even so, “adopting a single-payer system would be highly disruptive and could lead to price controls that would perpetuate flaws in the current Medicare payment system, including the undervaluation of primary care,” Mr. Crowley and colleagues wrote. “If prices are set too low, it could lead to shortages and longer wait times for services. Without sufficient cost controls, however, the cost of a single-payer system could be too high to be feasible.”
Pondering the public option
Given a single-payer plan’s potential challenges, ACP also is endorsing a public option model, which provides the choice of a government-sponsored health insurance plan to compete with existing private insurance options.
“Depending on its structure and implementation, a public choice (or public option) model available to all could help to achieve universal coverage, better access, and improved outcomes without the disruption of a single-payer approach,” the ACP authors noted.
The public option has its own drawbacks, they acknowledge. Those include an inability to achieve better savings on prescription drugs, compared with a single-payer system. The public option approach also doesn’t do away with the current administrative burden, and access issues related to narrow provider networks would persist.
Dr. McLean noted that a more highly regulated insurance market would be needed to help make the public option model work.
“Insurance companies don’t have regulation in a lot of things that they do,” Dr. McLean said. “We see that as quite problematic. They are kind of running amok at this point.”
Expanding the role of primary care
In either reform scenario, primary care would play a much greater role.
“We need to promote primary care,” Dr. McLean said. That includes better incentives to draw physicians to it. “We have to pay them enough,” he added.
The health care models will need to move away from higher pay to specialties for high-cost, high-volume procedural reimbursement. And they’ll need to recognize the need for placing a higher value on the cognitive services provided at the primary care level.
Also in need of change: physicians’ administrative burdens. Reforms need to address the burden created by value-based care and the poor application and misapplication of quality measures.
Migration to a single-payer environment could would make reducing the administrative burden a lot easier, Dr. McLean said. But it also could be done with a public option approach.
That’s where regulators can play a big role in working with insurers to help address administrative burden – streamlining prior authorization of procedures, the types of forms used, and other policies, Dr. McLean explained.
“The number of insurers and their ability to have their own rules and regulations [make it] incredibly complex for patients as well as physicians trying to figure out how to deliver the care that they need,” he noted.
Dr. McLean hopes that the ACP’s papers will spark conversation, particularly among legislators and regulators.
“The bottom line is we cannot afford to not do something bold,” he cautioned. “It is just not working. Our patients deserve better, and we can do better.”
The American College of Physicians is recommending either a single-payer system or a public option within a regulated private insurance system to help deliver universal and affordable access to health care for all Americans.
“We came to the conclusion that two directions or approaches could get us to where we need to be,” ACP President Robert McLean, MD, said in an interview. “We need ... a system that provides universal, affordable access to care.”
After examining the evidence, ACP discarded one option: a direct market-based approach.
“Direct market-based approaches won’t work,” Dr. McLean explained. “If you look at where direct marketplace approaches ... have been implemented, they just will not get you to a place where you are going to get universal coverage, portability, essential benefits, and preexisting condition protection and administrative simplification.”
Dr. McLean highlighted two paths that could achieve universal coverage and better access to health care: a single-payer–financed system, or a publicly financed coverage option within a system of regulated private insurance.
It’s the first time ACP has endorsed a single-payer approach. The college supported the public option that wasn’t included as part of the Affordable Care Act. But ACP’s latest publicly financed proposal offers a deeper level of detail on how to make that option work in the context of a private insurance system.
While the health reform conversation may be a political, ACP doesn’t want to make it a partisan one. ACP’s policy recommendations represent a carefully researched series of ideas backed by evidence-based research, Dr. McLean said.
“There is a lot of nuance behind” the two recommendations, he noted, and those nuances are explored in a series of articles and editorials published Jan. 21 in Annals of Internal Medicine.
Sizing up single payer
The ACP acknowledges that for its single-payer system, the transition could be “politically difficult and strain the federal budget,” according to Ryan A. Crowley, senior analyst at ACP, and colleagues in an article outlining the organization’s vision. “Taxes would probably replace premiums, and private insurance would have a reduced role or be eliminated altogether.”
However, the authors note that a single-payer system could be designed to address concerns from a generally skeptical public, such as providing bulk funding or setting minimum standards to guide state operations. It also could include private insurance to provide supplemental coverage.
Even so, “adopting a single-payer system would be highly disruptive and could lead to price controls that would perpetuate flaws in the current Medicare payment system, including the undervaluation of primary care,” Mr. Crowley and colleagues wrote. “If prices are set too low, it could lead to shortages and longer wait times for services. Without sufficient cost controls, however, the cost of a single-payer system could be too high to be feasible.”
Pondering the public option
Given a single-payer plan’s potential challenges, ACP also is endorsing a public option model, which provides the choice of a government-sponsored health insurance plan to compete with existing private insurance options.
“Depending on its structure and implementation, a public choice (or public option) model available to all could help to achieve universal coverage, better access, and improved outcomes without the disruption of a single-payer approach,” the ACP authors noted.
The public option has its own drawbacks, they acknowledge. Those include an inability to achieve better savings on prescription drugs, compared with a single-payer system. The public option approach also doesn’t do away with the current administrative burden, and access issues related to narrow provider networks would persist.
Dr. McLean noted that a more highly regulated insurance market would be needed to help make the public option model work.
“Insurance companies don’t have regulation in a lot of things that they do,” Dr. McLean said. “We see that as quite problematic. They are kind of running amok at this point.”
Expanding the role of primary care
In either reform scenario, primary care would play a much greater role.
“We need to promote primary care,” Dr. McLean said. That includes better incentives to draw physicians to it. “We have to pay them enough,” he added.
The health care models will need to move away from higher pay to specialties for high-cost, high-volume procedural reimbursement. And they’ll need to recognize the need for placing a higher value on the cognitive services provided at the primary care level.
Also in need of change: physicians’ administrative burdens. Reforms need to address the burden created by value-based care and the poor application and misapplication of quality measures.
Migration to a single-payer environment could would make reducing the administrative burden a lot easier, Dr. McLean said. But it also could be done with a public option approach.
That’s where regulators can play a big role in working with insurers to help address administrative burden – streamlining prior authorization of procedures, the types of forms used, and other policies, Dr. McLean explained.
“The number of insurers and their ability to have their own rules and regulations [make it] incredibly complex for patients as well as physicians trying to figure out how to deliver the care that they need,” he noted.
Dr. McLean hopes that the ACP’s papers will spark conversation, particularly among legislators and regulators.
“The bottom line is we cannot afford to not do something bold,” he cautioned. “It is just not working. Our patients deserve better, and we can do better.”
The American College of Physicians is recommending either a single-payer system or a public option within a regulated private insurance system to help deliver universal and affordable access to health care for all Americans.
“We came to the conclusion that two directions or approaches could get us to where we need to be,” ACP President Robert McLean, MD, said in an interview. “We need ... a system that provides universal, affordable access to care.”
After examining the evidence, ACP discarded one option: a direct market-based approach.
“Direct market-based approaches won’t work,” Dr. McLean explained. “If you look at where direct marketplace approaches ... have been implemented, they just will not get you to a place where you are going to get universal coverage, portability, essential benefits, and preexisting condition protection and administrative simplification.”
Dr. McLean highlighted two paths that could achieve universal coverage and better access to health care: a single-payer–financed system, or a publicly financed coverage option within a system of regulated private insurance.
It’s the first time ACP has endorsed a single-payer approach. The college supported the public option that wasn’t included as part of the Affordable Care Act. But ACP’s latest publicly financed proposal offers a deeper level of detail on how to make that option work in the context of a private insurance system.
While the health reform conversation may be a political, ACP doesn’t want to make it a partisan one. ACP’s policy recommendations represent a carefully researched series of ideas backed by evidence-based research, Dr. McLean said.
“There is a lot of nuance behind” the two recommendations, he noted, and those nuances are explored in a series of articles and editorials published Jan. 21 in Annals of Internal Medicine.
Sizing up single payer
The ACP acknowledges that for its single-payer system, the transition could be “politically difficult and strain the federal budget,” according to Ryan A. Crowley, senior analyst at ACP, and colleagues in an article outlining the organization’s vision. “Taxes would probably replace premiums, and private insurance would have a reduced role or be eliminated altogether.”
However, the authors note that a single-payer system could be designed to address concerns from a generally skeptical public, such as providing bulk funding or setting minimum standards to guide state operations. It also could include private insurance to provide supplemental coverage.
Even so, “adopting a single-payer system would be highly disruptive and could lead to price controls that would perpetuate flaws in the current Medicare payment system, including the undervaluation of primary care,” Mr. Crowley and colleagues wrote. “If prices are set too low, it could lead to shortages and longer wait times for services. Without sufficient cost controls, however, the cost of a single-payer system could be too high to be feasible.”
Pondering the public option
Given a single-payer plan’s potential challenges, ACP also is endorsing a public option model, which provides the choice of a government-sponsored health insurance plan to compete with existing private insurance options.
“Depending on its structure and implementation, a public choice (or public option) model available to all could help to achieve universal coverage, better access, and improved outcomes without the disruption of a single-payer approach,” the ACP authors noted.
The public option has its own drawbacks, they acknowledge. Those include an inability to achieve better savings on prescription drugs, compared with a single-payer system. The public option approach also doesn’t do away with the current administrative burden, and access issues related to narrow provider networks would persist.
Dr. McLean noted that a more highly regulated insurance market would be needed to help make the public option model work.
“Insurance companies don’t have regulation in a lot of things that they do,” Dr. McLean said. “We see that as quite problematic. They are kind of running amok at this point.”
Expanding the role of primary care
In either reform scenario, primary care would play a much greater role.
“We need to promote primary care,” Dr. McLean said. That includes better incentives to draw physicians to it. “We have to pay them enough,” he added.
The health care models will need to move away from higher pay to specialties for high-cost, high-volume procedural reimbursement. And they’ll need to recognize the need for placing a higher value on the cognitive services provided at the primary care level.
Also in need of change: physicians’ administrative burdens. Reforms need to address the burden created by value-based care and the poor application and misapplication of quality measures.
Migration to a single-payer environment could would make reducing the administrative burden a lot easier, Dr. McLean said. But it also could be done with a public option approach.
That’s where regulators can play a big role in working with insurers to help address administrative burden – streamlining prior authorization of procedures, the types of forms used, and other policies, Dr. McLean explained.
“The number of insurers and their ability to have their own rules and regulations [make it] incredibly complex for patients as well as physicians trying to figure out how to deliver the care that they need,” he noted.
Dr. McLean hopes that the ACP’s papers will spark conversation, particularly among legislators and regulators.
“The bottom line is we cannot afford to not do something bold,” he cautioned. “It is just not working. Our patients deserve better, and we can do better.”
FROM ANNALS OF INTERNAL MEDICINE
Medscape survey points to generational differences in physician burnout
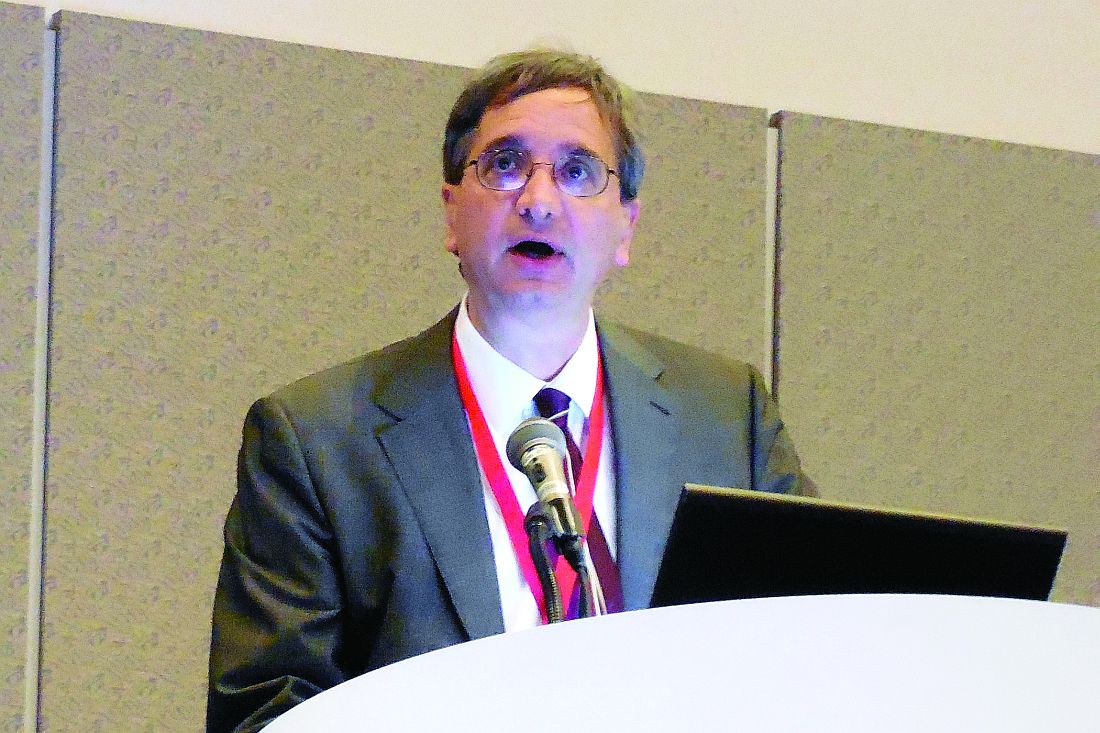
Burnout among physicians appears to have decreased slightly in the past few years, but remains a significant problem for the medical profession, according to the Medscape National Physician Burnout & Suicide Report 2020: The Generational Divide.
A survey of more than 15,000 physicians revealed that 42% reported being burned out, down from 46% who responded to the survey 5 years ago. However, there are variations in the rates based on certain demographic factors such as specialty, age, and gender.
Urology sits at the top of the list as the specialty that is experiencing the highest rate of burnout, with 54% of urologists responding to the survey reporting burnout. Neurology and nephrology followed with rates of burnout at 50% and 49%, respectively. The next five specialties on the list all reported burnout rates of 46%: diabetes and endocrinology, family medicine, radiology, ob.gyn., and rheumatology. Pulmonology specialists reported a burnout rate of 41%. Gastroenterologists reported burnout rates of 37%.
The survey divided participants into three age categories – Millennial (ages 25-39 years), Generation X (ages 40-54 years), and Baby Boomer (ages 55-73 years). Both Millennials and Baby Boomers reported similar rates of burnout (38% and 39%, respectively) and those in Generation X reported a higher rate of burnout (48%).
This higher rate is not unexpected. The survey results cite Carol Bernstein, MD, of the Albert Einstein College of Medicine, New York, as noting that midcareer “is typically the time of highest burnout, which is where Gen Xers are in their career trajectory, suggesting a number of factors outside of work such as caring for children and elderly parents, planning for retirement, can play a role in contributing to burnout.”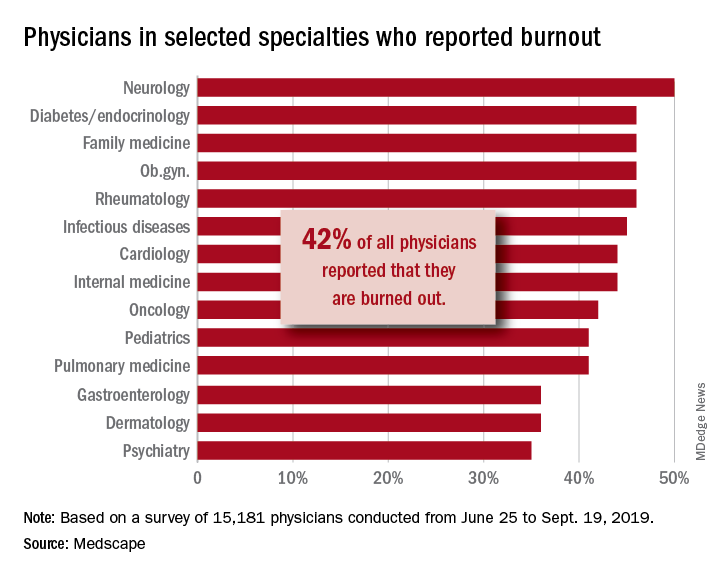
Women also reported a higher rate of burnout, although the rate has dropped from the survey conducted 5 years ago. The rate of burnout among women reported for the 2020 survey was 48%, down from 51% reported 5 years ago. By comparison, the rate of burnout for men was 37% in 2020, down from 43% in 2015.
In terms of what is causing burnout, the biggest contributor is the bureaucratic tasks (charting and paperwork, for example) that physicians must complete, which 55% of respondents to the survey said was the leading cause of burnout. Next was spending too many hours at work (33%); lack of respect from administrators, employers, colleagues, and staff (32%); and the increased computerization of the practice, including the use of electronic health records (30%).
When broken down by age category, the bureaucratic tasks was tops in all three groups (57% for Millennials, 56% for Generation X, and 54% for Baby Boomers), but what ranks next differs slightly by age group. For Millennials, the next two factors were too many hours at work (38%) and lack of respect (35%). Generation X respondents cited the same two factors, both at 33%. Baby Boomers cited computerization as their second-highest factor (41%) and spending too many hours at work as the third-highest factor (31%).
The generations had different approaches to coping with burnout. Millennials (56%) reported sleep as their top-ranked coping strategy, while Gen Xers and Baby Boomers ranked exercise and personal isolation as their top choice. For these two older groups, sleep was ranked last, after other activities such as talking with family and friends.
The survey also asked about depression, and respondents reported a similar rate across all age groups (15%, 18%, and 16%, respectively). Among those who said they were depressed, the three age groups had similar rates of suicidal thoughts (21%, 24%, and 22%).
Perhaps the most striking finding of the survey is the number of physicians who would take a pay cut to achieve a better work-life balance. Among Millennials, 52% would accept a pay cut, compared with 48% of Generation X and 49% of Baby Boomers. A surprising number (36%, 34%, and 31%, respectively, reported that they would accept a $10,000-$20,000 pay cut to have a 20% reduction in work hours. [email protected]
*This story was updated on 1/22/2020.
SOURCE: Kane L et al. Medscape National Physician Burnout & Suicide Report 2020: The Generational Divide. Medscape. 2020 Jan 15.
Burnout among physicians appears to have decreased slightly in the past few years, but remains a significant problem for the medical profession, according to the Medscape National Physician Burnout & Suicide Report 2020: The Generational Divide.
A survey of more than 15,000 physicians revealed that 42% reported being burned out, down from 46% who responded to the survey 5 years ago. However, there are variations in the rates based on certain demographic factors such as specialty, age, and gender.
Urology sits at the top of the list as the specialty that is experiencing the highest rate of burnout, with 54% of urologists responding to the survey reporting burnout. Neurology and nephrology followed with rates of burnout at 50% and 49%, respectively. The next five specialties on the list all reported burnout rates of 46%: diabetes and endocrinology, family medicine, radiology, ob.gyn., and rheumatology. Pulmonology specialists reported a burnout rate of 41%. Gastroenterologists reported burnout rates of 37%.
The survey divided participants into three age categories – Millennial (ages 25-39 years), Generation X (ages 40-54 years), and Baby Boomer (ages 55-73 years). Both Millennials and Baby Boomers reported similar rates of burnout (38% and 39%, respectively) and those in Generation X reported a higher rate of burnout (48%).
This higher rate is not unexpected. The survey results cite Carol Bernstein, MD, of the Albert Einstein College of Medicine, New York, as noting that midcareer “is typically the time of highest burnout, which is where Gen Xers are in their career trajectory, suggesting a number of factors outside of work such as caring for children and elderly parents, planning for retirement, can play a role in contributing to burnout.”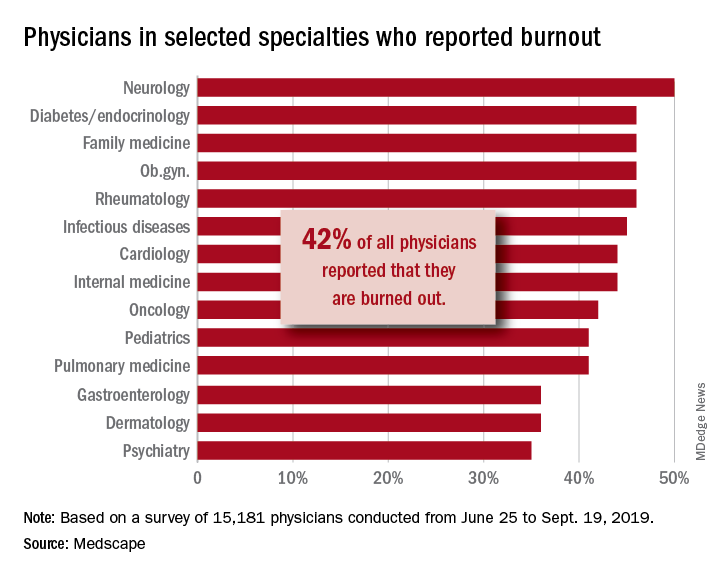
Women also reported a higher rate of burnout, although the rate has dropped from the survey conducted 5 years ago. The rate of burnout among women reported for the 2020 survey was 48%, down from 51% reported 5 years ago. By comparison, the rate of burnout for men was 37% in 2020, down from 43% in 2015.
In terms of what is causing burnout, the biggest contributor is the bureaucratic tasks (charting and paperwork, for example) that physicians must complete, which 55% of respondents to the survey said was the leading cause of burnout. Next was spending too many hours at work (33%); lack of respect from administrators, employers, colleagues, and staff (32%); and the increased computerization of the practice, including the use of electronic health records (30%).
When broken down by age category, the bureaucratic tasks was tops in all three groups (57% for Millennials, 56% for Generation X, and 54% for Baby Boomers), but what ranks next differs slightly by age group. For Millennials, the next two factors were too many hours at work (38%) and lack of respect (35%). Generation X respondents cited the same two factors, both at 33%. Baby Boomers cited computerization as their second-highest factor (41%) and spending too many hours at work as the third-highest factor (31%).
The generations had different approaches to coping with burnout. Millennials (56%) reported sleep as their top-ranked coping strategy, while Gen Xers and Baby Boomers ranked exercise and personal isolation as their top choice. For these two older groups, sleep was ranked last, after other activities such as talking with family and friends.
The survey also asked about depression, and respondents reported a similar rate across all age groups (15%, 18%, and 16%, respectively). Among those who said they were depressed, the three age groups had similar rates of suicidal thoughts (21%, 24%, and 22%).
Perhaps the most striking finding of the survey is the number of physicians who would take a pay cut to achieve a better work-life balance. Among Millennials, 52% would accept a pay cut, compared with 48% of Generation X and 49% of Baby Boomers. A surprising number (36%, 34%, and 31%, respectively, reported that they would accept a $10,000-$20,000 pay cut to have a 20% reduction in work hours. [email protected]
*This story was updated on 1/22/2020.
SOURCE: Kane L et al. Medscape National Physician Burnout & Suicide Report 2020: The Generational Divide. Medscape. 2020 Jan 15.
Burnout among physicians appears to have decreased slightly in the past few years, but remains a significant problem for the medical profession, according to the Medscape National Physician Burnout & Suicide Report 2020: The Generational Divide.
A survey of more than 15,000 physicians revealed that 42% reported being burned out, down from 46% who responded to the survey 5 years ago. However, there are variations in the rates based on certain demographic factors such as specialty, age, and gender.
Urology sits at the top of the list as the specialty that is experiencing the highest rate of burnout, with 54% of urologists responding to the survey reporting burnout. Neurology and nephrology followed with rates of burnout at 50% and 49%, respectively. The next five specialties on the list all reported burnout rates of 46%: diabetes and endocrinology, family medicine, radiology, ob.gyn., and rheumatology. Pulmonology specialists reported a burnout rate of 41%. Gastroenterologists reported burnout rates of 37%.
The survey divided participants into three age categories – Millennial (ages 25-39 years), Generation X (ages 40-54 years), and Baby Boomer (ages 55-73 years). Both Millennials and Baby Boomers reported similar rates of burnout (38% and 39%, respectively) and those in Generation X reported a higher rate of burnout (48%).
This higher rate is not unexpected. The survey results cite Carol Bernstein, MD, of the Albert Einstein College of Medicine, New York, as noting that midcareer “is typically the time of highest burnout, which is where Gen Xers are in their career trajectory, suggesting a number of factors outside of work such as caring for children and elderly parents, planning for retirement, can play a role in contributing to burnout.”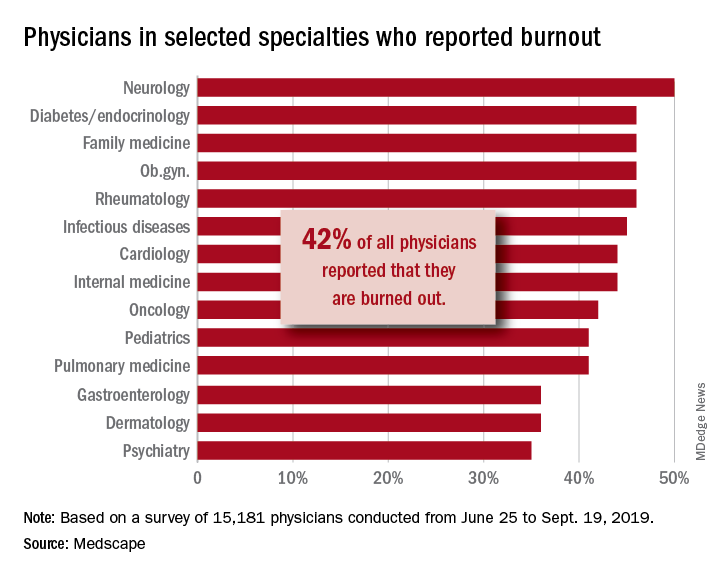
Women also reported a higher rate of burnout, although the rate has dropped from the survey conducted 5 years ago. The rate of burnout among women reported for the 2020 survey was 48%, down from 51% reported 5 years ago. By comparison, the rate of burnout for men was 37% in 2020, down from 43% in 2015.
In terms of what is causing burnout, the biggest contributor is the bureaucratic tasks (charting and paperwork, for example) that physicians must complete, which 55% of respondents to the survey said was the leading cause of burnout. Next was spending too many hours at work (33%); lack of respect from administrators, employers, colleagues, and staff (32%); and the increased computerization of the practice, including the use of electronic health records (30%).
When broken down by age category, the bureaucratic tasks was tops in all three groups (57% for Millennials, 56% for Generation X, and 54% for Baby Boomers), but what ranks next differs slightly by age group. For Millennials, the next two factors were too many hours at work (38%) and lack of respect (35%). Generation X respondents cited the same two factors, both at 33%. Baby Boomers cited computerization as their second-highest factor (41%) and spending too many hours at work as the third-highest factor (31%).
The generations had different approaches to coping with burnout. Millennials (56%) reported sleep as their top-ranked coping strategy, while Gen Xers and Baby Boomers ranked exercise and personal isolation as their top choice. For these two older groups, sleep was ranked last, after other activities such as talking with family and friends.
The survey also asked about depression, and respondents reported a similar rate across all age groups (15%, 18%, and 16%, respectively). Among those who said they were depressed, the three age groups had similar rates of suicidal thoughts (21%, 24%, and 22%).
Perhaps the most striking finding of the survey is the number of physicians who would take a pay cut to achieve a better work-life balance. Among Millennials, 52% would accept a pay cut, compared with 48% of Generation X and 49% of Baby Boomers. A surprising number (36%, 34%, and 31%, respectively, reported that they would accept a $10,000-$20,000 pay cut to have a 20% reduction in work hours. [email protected]
*This story was updated on 1/22/2020.
SOURCE: Kane L et al. Medscape National Physician Burnout & Suicide Report 2020: The Generational Divide. Medscape. 2020 Jan 15.
Adult survivors of childhood cancer are experiencing fewer major cardiac events
Adult survivors of pediatric cancers appear to be experiencing fewer major cardiac events in adulthood partly because of reduced radiotherapy exposure, especially among survivors of Hodgkin lymphoma, recent research published in BMJ has shown.
“Contemporary cancer treatment has focused on advancing cure rates while attempting to minimize long term adverse effects,” Daniel A. Mulrooney, MD, of the Division of Cancer Survivorship, Department of Oncology, at St. Jude Children’s Research Hospital, Arlington, Va., and colleagues wrote. “Patterns of exposure to cardiotoxic treatment have changed over time, with fewer children receiving chest directed radiation, with lower doses and smaller volumes for those who do, and an increased use of anthracyclines, albeit with reduced cumulative doses as the risk for late-onset heart failure became apparent.”
Although research has been published on improved survival rates of children who underwent cancer treatment in the 1990s, compared with those who received treatment in the 1980s and 1970s, Dr. Mulrooney and colleagues set out to determine whether cardiac outcomes were reduced as well. They conducted a retrospective study of 23,462 5-year survivors of pediatric cancer, which consisted of leukemia, brain cancer, Hodgkin lymphoma, non-Hodgkin lymphoma, renal tumors, neuroblastoma, soft-tissue sarcomas, and bone sarcomas diagnosed between January 1970 and December 1999. Researchers compared the cardiac outcomes of the survivors, including heart failure, coronary artery disease, valvular heart disease, pericardial disease, and arrhythmias, with a comparison group of their siblings (n = 5,057) separated by decade. The adult survivors tended to be women (46% vs. 40%) with a median age of 6.1 years at diagnosis and 27.7 years at final follow-up.
Of the 6,193 participants treated for cancer in the 1970s, the 20-year cumulative incidence of heart failure was 0.69%, while the 9,363 participants treated in the 1980s had an incidence of 0.74%, and 7,906 participants in the 1990s had a cumulative incidence of 0.54% over 20 years. The 20-year cumulative incidence for coronary artery disease (CAD) was 0.38% for participants in the 1970s, 0.24% for participants in the 1980s, and 0.19% for participants in the 1990s (P less than .01). Researchers noted the 20-year cumulative incidence of valvular disease, pericardial disease, and arrhythmias did not decrease between the 1970s and the 1990s.
When comparing the rate of major cardiac events of participants in the 1980s and 1990s with those of the 1970s, CAD diagnoses significantly decreased in the 1980s (hazard ratio, 0.65; 95% confidence interval, 0.45-0.92) and 1990s (HR, 0.53; 95% CI, 0.36-0.77), while there was no significant decrease in heart failure or valvular heart disease risk over time. After adjusting for cardiac radiation, overall risk for CAD was attenuated (HR, 0.90; 0.78-1.05), and Hodgkin lymphoma survivors saw the greatest change between unadjusted (HR, 0.77; 95% CI, 0.66-0.89) and adjusted risk (HR, 0.87; 95% CI, 0.69-1.10) when accounting for cardiac radiation.
“While additional longitudinal follow-up is needed to establish whether similar reductions in the cumulative incidence of heart failure can be confirmed in multivariable analysis, these results suggest that efforts to modify cancer therapies in children and promote health surveillance for survivors are beginning to show benefits not only in overall survival but also in late adverse cardiac effects,” the researchers concluded.
In a related editorial, Mike Hawkins, DPhil, of the Centre for Childhood Cancer Survivor Studies, Institute of Applied Health Research at the University of Birmingham (England), and colleagues said that, while measuring cardiotoxicity is important for this patient population, traditional risk factors with independent associations to cardiac outcomes should also be studied. Guidelines on follow-up for these patients are also needed to inform clinical practice, such as those produced by the International Late Effects of Childhood Cancer Guideline Harmonization Group, they added.
“Survivorship issues are extremely important to patients, their families, and their doctors,” they said. “In two research priority setting initiatives in the United Kingdom, detailed consultation with patients with cancer, survivors, families, friends, and healthcare professionals identified further research into the consequences of cancer as a top priority.”
This study was funded by grants from the National Cancer Institute, Cancer Center Support (CORE) to St. Jude Children’s Research Hospital and American Lebanese Syrian Associated Charities. The authors of the study and the editorial reported no relevant conflicts of interest.
SOURCE: Mulrooney A et al. BMJ. 2020. doi: 10.1136/bmj.l6794.
Adult survivors of pediatric cancers appear to be experiencing fewer major cardiac events in adulthood partly because of reduced radiotherapy exposure, especially among survivors of Hodgkin lymphoma, recent research published in BMJ has shown.
“Contemporary cancer treatment has focused on advancing cure rates while attempting to minimize long term adverse effects,” Daniel A. Mulrooney, MD, of the Division of Cancer Survivorship, Department of Oncology, at St. Jude Children’s Research Hospital, Arlington, Va., and colleagues wrote. “Patterns of exposure to cardiotoxic treatment have changed over time, with fewer children receiving chest directed radiation, with lower doses and smaller volumes for those who do, and an increased use of anthracyclines, albeit with reduced cumulative doses as the risk for late-onset heart failure became apparent.”
Although research has been published on improved survival rates of children who underwent cancer treatment in the 1990s, compared with those who received treatment in the 1980s and 1970s, Dr. Mulrooney and colleagues set out to determine whether cardiac outcomes were reduced as well. They conducted a retrospective study of 23,462 5-year survivors of pediatric cancer, which consisted of leukemia, brain cancer, Hodgkin lymphoma, non-Hodgkin lymphoma, renal tumors, neuroblastoma, soft-tissue sarcomas, and bone sarcomas diagnosed between January 1970 and December 1999. Researchers compared the cardiac outcomes of the survivors, including heart failure, coronary artery disease, valvular heart disease, pericardial disease, and arrhythmias, with a comparison group of their siblings (n = 5,057) separated by decade. The adult survivors tended to be women (46% vs. 40%) with a median age of 6.1 years at diagnosis and 27.7 years at final follow-up.
Of the 6,193 participants treated for cancer in the 1970s, the 20-year cumulative incidence of heart failure was 0.69%, while the 9,363 participants treated in the 1980s had an incidence of 0.74%, and 7,906 participants in the 1990s had a cumulative incidence of 0.54% over 20 years. The 20-year cumulative incidence for coronary artery disease (CAD) was 0.38% for participants in the 1970s, 0.24% for participants in the 1980s, and 0.19% for participants in the 1990s (P less than .01). Researchers noted the 20-year cumulative incidence of valvular disease, pericardial disease, and arrhythmias did not decrease between the 1970s and the 1990s.
When comparing the rate of major cardiac events of participants in the 1980s and 1990s with those of the 1970s, CAD diagnoses significantly decreased in the 1980s (hazard ratio, 0.65; 95% confidence interval, 0.45-0.92) and 1990s (HR, 0.53; 95% CI, 0.36-0.77), while there was no significant decrease in heart failure or valvular heart disease risk over time. After adjusting for cardiac radiation, overall risk for CAD was attenuated (HR, 0.90; 0.78-1.05), and Hodgkin lymphoma survivors saw the greatest change between unadjusted (HR, 0.77; 95% CI, 0.66-0.89) and adjusted risk (HR, 0.87; 95% CI, 0.69-1.10) when accounting for cardiac radiation.
“While additional longitudinal follow-up is needed to establish whether similar reductions in the cumulative incidence of heart failure can be confirmed in multivariable analysis, these results suggest that efforts to modify cancer therapies in children and promote health surveillance for survivors are beginning to show benefits not only in overall survival but also in late adverse cardiac effects,” the researchers concluded.
In a related editorial, Mike Hawkins, DPhil, of the Centre for Childhood Cancer Survivor Studies, Institute of Applied Health Research at the University of Birmingham (England), and colleagues said that, while measuring cardiotoxicity is important for this patient population, traditional risk factors with independent associations to cardiac outcomes should also be studied. Guidelines on follow-up for these patients are also needed to inform clinical practice, such as those produced by the International Late Effects of Childhood Cancer Guideline Harmonization Group, they added.
“Survivorship issues are extremely important to patients, their families, and their doctors,” they said. “In two research priority setting initiatives in the United Kingdom, detailed consultation with patients with cancer, survivors, families, friends, and healthcare professionals identified further research into the consequences of cancer as a top priority.”
This study was funded by grants from the National Cancer Institute, Cancer Center Support (CORE) to St. Jude Children’s Research Hospital and American Lebanese Syrian Associated Charities. The authors of the study and the editorial reported no relevant conflicts of interest.
SOURCE: Mulrooney A et al. BMJ. 2020. doi: 10.1136/bmj.l6794.
Adult survivors of pediatric cancers appear to be experiencing fewer major cardiac events in adulthood partly because of reduced radiotherapy exposure, especially among survivors of Hodgkin lymphoma, recent research published in BMJ has shown.
“Contemporary cancer treatment has focused on advancing cure rates while attempting to minimize long term adverse effects,” Daniel A. Mulrooney, MD, of the Division of Cancer Survivorship, Department of Oncology, at St. Jude Children’s Research Hospital, Arlington, Va., and colleagues wrote. “Patterns of exposure to cardiotoxic treatment have changed over time, with fewer children receiving chest directed radiation, with lower doses and smaller volumes for those who do, and an increased use of anthracyclines, albeit with reduced cumulative doses as the risk for late-onset heart failure became apparent.”
Although research has been published on improved survival rates of children who underwent cancer treatment in the 1990s, compared with those who received treatment in the 1980s and 1970s, Dr. Mulrooney and colleagues set out to determine whether cardiac outcomes were reduced as well. They conducted a retrospective study of 23,462 5-year survivors of pediatric cancer, which consisted of leukemia, brain cancer, Hodgkin lymphoma, non-Hodgkin lymphoma, renal tumors, neuroblastoma, soft-tissue sarcomas, and bone sarcomas diagnosed between January 1970 and December 1999. Researchers compared the cardiac outcomes of the survivors, including heart failure, coronary artery disease, valvular heart disease, pericardial disease, and arrhythmias, with a comparison group of their siblings (n = 5,057) separated by decade. The adult survivors tended to be women (46% vs. 40%) with a median age of 6.1 years at diagnosis and 27.7 years at final follow-up.
Of the 6,193 participants treated for cancer in the 1970s, the 20-year cumulative incidence of heart failure was 0.69%, while the 9,363 participants treated in the 1980s had an incidence of 0.74%, and 7,906 participants in the 1990s had a cumulative incidence of 0.54% over 20 years. The 20-year cumulative incidence for coronary artery disease (CAD) was 0.38% for participants in the 1970s, 0.24% for participants in the 1980s, and 0.19% for participants in the 1990s (P less than .01). Researchers noted the 20-year cumulative incidence of valvular disease, pericardial disease, and arrhythmias did not decrease between the 1970s and the 1990s.
When comparing the rate of major cardiac events of participants in the 1980s and 1990s with those of the 1970s, CAD diagnoses significantly decreased in the 1980s (hazard ratio, 0.65; 95% confidence interval, 0.45-0.92) and 1990s (HR, 0.53; 95% CI, 0.36-0.77), while there was no significant decrease in heart failure or valvular heart disease risk over time. After adjusting for cardiac radiation, overall risk for CAD was attenuated (HR, 0.90; 0.78-1.05), and Hodgkin lymphoma survivors saw the greatest change between unadjusted (HR, 0.77; 95% CI, 0.66-0.89) and adjusted risk (HR, 0.87; 95% CI, 0.69-1.10) when accounting for cardiac radiation.
“While additional longitudinal follow-up is needed to establish whether similar reductions in the cumulative incidence of heart failure can be confirmed in multivariable analysis, these results suggest that efforts to modify cancer therapies in children and promote health surveillance for survivors are beginning to show benefits not only in overall survival but also in late adverse cardiac effects,” the researchers concluded.
In a related editorial, Mike Hawkins, DPhil, of the Centre for Childhood Cancer Survivor Studies, Institute of Applied Health Research at the University of Birmingham (England), and colleagues said that, while measuring cardiotoxicity is important for this patient population, traditional risk factors with independent associations to cardiac outcomes should also be studied. Guidelines on follow-up for these patients are also needed to inform clinical practice, such as those produced by the International Late Effects of Childhood Cancer Guideline Harmonization Group, they added.
“Survivorship issues are extremely important to patients, their families, and their doctors,” they said. “In two research priority setting initiatives in the United Kingdom, detailed consultation with patients with cancer, survivors, families, friends, and healthcare professionals identified further research into the consequences of cancer as a top priority.”
This study was funded by grants from the National Cancer Institute, Cancer Center Support (CORE) to St. Jude Children’s Research Hospital and American Lebanese Syrian Associated Charities. The authors of the study and the editorial reported no relevant conflicts of interest.
SOURCE: Mulrooney A et al. BMJ. 2020. doi: 10.1136/bmj.l6794.
FROM BMJ
Alan Alda, Scripps Research join forces to improve science communication
LA JOLLA, CALIF. – The first time that legendary actor Alan Alda conducted an interview for “Scientific American Frontiers” on PBS, an award-winning series that ran for more than a decade, he remembers learning a lesson in humility.
“I wasn’t as smart as I thought I was,” he told a crowd of largely scientists and medical professionals who gathered in a small auditorium on the campus of Scripps Research on Jan. 16, 2020. “I didn’t realize the value of ignorance. I have a natural supply of it. I began to use it and say [to interviewees]: ‘I don’t understand what that means.’ Sometimes it would be basic physics and they’d look at me like I was a school child. I am a very curious person. What I discovered was, I was bringing out their humanity by my own curiosity, by the way I related to them, which I developed through studying improvisation as an actor, and relating as an actor to other actors.”
Mr. Alda, 83, appeared on the research campus to announce that Scripps Research is the new West Coast home of Alda Communication Training, which will work in tandem with the Alan Alda Center for Communicating Science at the State University of New York at Stony Brook, a nonprofit organization that Mr. Alda helped found in 2009.
Immersive training experience
“This will be a center where people can come to get training in effective communication,” said Mr. Alda, who is the winner of six Emmy Awards and six Golden Globe awards. “It’s an experiential kind of training. We don’t give tips. We don’t give lectures. We put you through exercises that are fun and actually make you laugh, but turn you into a better communicator, so you’re better able to connect to the people you’re talking to.”
To date, the Alan Alda Center for Communicating Science has trained more than 15,000 scientific leaders in the United States and other countries. The location at Scripps Research makes it more convenient for West Coast–based researchers and industry leaders to participate. “One of the things we wished, for years, we had was a place where we could train scientists and researchers and medical professionals all up and down the West Coast,” he said.
Recently, more than 30 of Scripps Research scientists participated in Mr. Alda’s training program, an immersive and engaging experience that helps participants learn to empathize with an audience and present their work in a way that connects with different stakeholders. The skills and strategies can help participants relate to prospective investors and philanthropists, government officials, members of the media, peers across scientific disciplines, and the general public.
Earlier in the day that he spoke on the Scripps campus, Mr. Alda encountered some of the Scripps researchers who had participated in that training. “One group of scientists came in and we shook hands,” he said. “They introduced themselves and said: ‘We’re working on infectious diseases.’ I said: ‘Oh my God; I just shook hands with you!’ No matter what I asked them, they had a clear way to express what they did. Then I realized they had studied with Alda Communications.”
Why communication matters
During the early stages of forming what became the Alan Alda Center for Communicating Science, one Nobel Prize winner at a major university dismissed the importance of improving the communication skills of young scientists. “He said to me: ‘We don’t have time for that; we have too much science to teach,’ ” said Mr. Alda, who played Army surgeon “Hawkeye” Pierce on the TV series “M*A*S*H”. “But communication is the essence of science. How can you do science unless you communicate with other scientists? There’s a stereotype that scientists are not as good at communicating as other people are. It’s true that they often speak a language that a lot of us don’t understand, but we all speak a language that is hard for other people to understand if we know something in great depth. We want to tell all the details; we want to speak in our special language because it makes us feel good.”
He underscored the importance of scientists being able to effectively communicate with the general public, “because the public needs to understand how important science is to their lives. It matters because at a place like [Scripps Research], understanding how nature works is put to work to keep our health secure.” Members of the public, he continued, “are busy living their lives; they’re busy working and bringing up their children. They haven’t spent 20, 30, 40 years devoted to a single aspect of nature the way scientists have. We can’t expect them to know as much as professional scientists, so we have to help them understand it. I hope we find ways to increase curiosity. I don’t know how to do that. I wish somebody would do a study on it, how you can take someone with a modicum of curiosity and help them enlarge it so it gives them the pleasure of discovering things about nature or understanding things about nature that other people don’t discover. Curiosity is the key to staying alive. That would bring us to a point of more people understanding science.”
Cultivating a sense of responsibility is another key to effective communication. “It’s the job of the person leading the discussion to make clear to the person listening,” Mr. Alda said. “You get the impression that ‘this person is my responsibility. I have to take care of them, so they understand what’s going on.’ ”
Parkinson’s disease diagnosis
During a question-and-answer session, Mr. Alda opened up about his Parkinson’s disease, which he said was diagnosed about 5 years ago. In 2018, he decided to speak publicly about his diagnosis for the first time.
“The reason was that I wanted to communicate to people who had recently been diagnosed not to believe or give into the stereotype that when you get a diagnosis, your life is over,” said Mr. Alda, who received the Public Welfare Medal from the National Academy of Sciences in 2016. “Under the burden of that belief, some people won’t tell their family or workplace colleagues. There are exercises you can do and medications you can take to prolong the time it takes before Parkinson’s gets much more serious. It’s not to diminish the fact that it can get really bad; but to think that your life is over as soon as you get a diagnosis is wrong.”
He added: “I’ve gone 5 years and I’m almost busier than I’ve ever been. I’m getting a lot accomplished and I look forward to I don’t know how many years. As long as I have them, I’m going to be grateful. It’s amazing how great it feels not to keep the diagnosis a secret.”
The first 2-day training session at Scripps Research will be held in June 2020. Additional sessions are scheduled to take place in October and December. Registration is available at aldacommunicationtraining.com/workshops.
LA JOLLA, CALIF. – The first time that legendary actor Alan Alda conducted an interview for “Scientific American Frontiers” on PBS, an award-winning series that ran for more than a decade, he remembers learning a lesson in humility.
“I wasn’t as smart as I thought I was,” he told a crowd of largely scientists and medical professionals who gathered in a small auditorium on the campus of Scripps Research on Jan. 16, 2020. “I didn’t realize the value of ignorance. I have a natural supply of it. I began to use it and say [to interviewees]: ‘I don’t understand what that means.’ Sometimes it would be basic physics and they’d look at me like I was a school child. I am a very curious person. What I discovered was, I was bringing out their humanity by my own curiosity, by the way I related to them, which I developed through studying improvisation as an actor, and relating as an actor to other actors.”
Mr. Alda, 83, appeared on the research campus to announce that Scripps Research is the new West Coast home of Alda Communication Training, which will work in tandem with the Alan Alda Center for Communicating Science at the State University of New York at Stony Brook, a nonprofit organization that Mr. Alda helped found in 2009.
Immersive training experience
“This will be a center where people can come to get training in effective communication,” said Mr. Alda, who is the winner of six Emmy Awards and six Golden Globe awards. “It’s an experiential kind of training. We don’t give tips. We don’t give lectures. We put you through exercises that are fun and actually make you laugh, but turn you into a better communicator, so you’re better able to connect to the people you’re talking to.”
To date, the Alan Alda Center for Communicating Science has trained more than 15,000 scientific leaders in the United States and other countries. The location at Scripps Research makes it more convenient for West Coast–based researchers and industry leaders to participate. “One of the things we wished, for years, we had was a place where we could train scientists and researchers and medical professionals all up and down the West Coast,” he said.
Recently, more than 30 of Scripps Research scientists participated in Mr. Alda’s training program, an immersive and engaging experience that helps participants learn to empathize with an audience and present their work in a way that connects with different stakeholders. The skills and strategies can help participants relate to prospective investors and philanthropists, government officials, members of the media, peers across scientific disciplines, and the general public.
Earlier in the day that he spoke on the Scripps campus, Mr. Alda encountered some of the Scripps researchers who had participated in that training. “One group of scientists came in and we shook hands,” he said. “They introduced themselves and said: ‘We’re working on infectious diseases.’ I said: ‘Oh my God; I just shook hands with you!’ No matter what I asked them, they had a clear way to express what they did. Then I realized they had studied with Alda Communications.”
Why communication matters
During the early stages of forming what became the Alan Alda Center for Communicating Science, one Nobel Prize winner at a major university dismissed the importance of improving the communication skills of young scientists. “He said to me: ‘We don’t have time for that; we have too much science to teach,’ ” said Mr. Alda, who played Army surgeon “Hawkeye” Pierce on the TV series “M*A*S*H”. “But communication is the essence of science. How can you do science unless you communicate with other scientists? There’s a stereotype that scientists are not as good at communicating as other people are. It’s true that they often speak a language that a lot of us don’t understand, but we all speak a language that is hard for other people to understand if we know something in great depth. We want to tell all the details; we want to speak in our special language because it makes us feel good.”
He underscored the importance of scientists being able to effectively communicate with the general public, “because the public needs to understand how important science is to their lives. It matters because at a place like [Scripps Research], understanding how nature works is put to work to keep our health secure.” Members of the public, he continued, “are busy living their lives; they’re busy working and bringing up their children. They haven’t spent 20, 30, 40 years devoted to a single aspect of nature the way scientists have. We can’t expect them to know as much as professional scientists, so we have to help them understand it. I hope we find ways to increase curiosity. I don’t know how to do that. I wish somebody would do a study on it, how you can take someone with a modicum of curiosity and help them enlarge it so it gives them the pleasure of discovering things about nature or understanding things about nature that other people don’t discover. Curiosity is the key to staying alive. That would bring us to a point of more people understanding science.”
Cultivating a sense of responsibility is another key to effective communication. “It’s the job of the person leading the discussion to make clear to the person listening,” Mr. Alda said. “You get the impression that ‘this person is my responsibility. I have to take care of them, so they understand what’s going on.’ ”
Parkinson’s disease diagnosis
During a question-and-answer session, Mr. Alda opened up about his Parkinson’s disease, which he said was diagnosed about 5 years ago. In 2018, he decided to speak publicly about his diagnosis for the first time.
“The reason was that I wanted to communicate to people who had recently been diagnosed not to believe or give into the stereotype that when you get a diagnosis, your life is over,” said Mr. Alda, who received the Public Welfare Medal from the National Academy of Sciences in 2016. “Under the burden of that belief, some people won’t tell their family or workplace colleagues. There are exercises you can do and medications you can take to prolong the time it takes before Parkinson’s gets much more serious. It’s not to diminish the fact that it can get really bad; but to think that your life is over as soon as you get a diagnosis is wrong.”
He added: “I’ve gone 5 years and I’m almost busier than I’ve ever been. I’m getting a lot accomplished and I look forward to I don’t know how many years. As long as I have them, I’m going to be grateful. It’s amazing how great it feels not to keep the diagnosis a secret.”
The first 2-day training session at Scripps Research will be held in June 2020. Additional sessions are scheduled to take place in October and December. Registration is available at aldacommunicationtraining.com/workshops.
LA JOLLA, CALIF. – The first time that legendary actor Alan Alda conducted an interview for “Scientific American Frontiers” on PBS, an award-winning series that ran for more than a decade, he remembers learning a lesson in humility.
“I wasn’t as smart as I thought I was,” he told a crowd of largely scientists and medical professionals who gathered in a small auditorium on the campus of Scripps Research on Jan. 16, 2020. “I didn’t realize the value of ignorance. I have a natural supply of it. I began to use it and say [to interviewees]: ‘I don’t understand what that means.’ Sometimes it would be basic physics and they’d look at me like I was a school child. I am a very curious person. What I discovered was, I was bringing out their humanity by my own curiosity, by the way I related to them, which I developed through studying improvisation as an actor, and relating as an actor to other actors.”
Mr. Alda, 83, appeared on the research campus to announce that Scripps Research is the new West Coast home of Alda Communication Training, which will work in tandem with the Alan Alda Center for Communicating Science at the State University of New York at Stony Brook, a nonprofit organization that Mr. Alda helped found in 2009.
Immersive training experience
“This will be a center where people can come to get training in effective communication,” said Mr. Alda, who is the winner of six Emmy Awards and six Golden Globe awards. “It’s an experiential kind of training. We don’t give tips. We don’t give lectures. We put you through exercises that are fun and actually make you laugh, but turn you into a better communicator, so you’re better able to connect to the people you’re talking to.”
To date, the Alan Alda Center for Communicating Science has trained more than 15,000 scientific leaders in the United States and other countries. The location at Scripps Research makes it more convenient for West Coast–based researchers and industry leaders to participate. “One of the things we wished, for years, we had was a place where we could train scientists and researchers and medical professionals all up and down the West Coast,” he said.
Recently, more than 30 of Scripps Research scientists participated in Mr. Alda’s training program, an immersive and engaging experience that helps participants learn to empathize with an audience and present their work in a way that connects with different stakeholders. The skills and strategies can help participants relate to prospective investors and philanthropists, government officials, members of the media, peers across scientific disciplines, and the general public.
Earlier in the day that he spoke on the Scripps campus, Mr. Alda encountered some of the Scripps researchers who had participated in that training. “One group of scientists came in and we shook hands,” he said. “They introduced themselves and said: ‘We’re working on infectious diseases.’ I said: ‘Oh my God; I just shook hands with you!’ No matter what I asked them, they had a clear way to express what they did. Then I realized they had studied with Alda Communications.”
Why communication matters
During the early stages of forming what became the Alan Alda Center for Communicating Science, one Nobel Prize winner at a major university dismissed the importance of improving the communication skills of young scientists. “He said to me: ‘We don’t have time for that; we have too much science to teach,’ ” said Mr. Alda, who played Army surgeon “Hawkeye” Pierce on the TV series “M*A*S*H”. “But communication is the essence of science. How can you do science unless you communicate with other scientists? There’s a stereotype that scientists are not as good at communicating as other people are. It’s true that they often speak a language that a lot of us don’t understand, but we all speak a language that is hard for other people to understand if we know something in great depth. We want to tell all the details; we want to speak in our special language because it makes us feel good.”
He underscored the importance of scientists being able to effectively communicate with the general public, “because the public needs to understand how important science is to their lives. It matters because at a place like [Scripps Research], understanding how nature works is put to work to keep our health secure.” Members of the public, he continued, “are busy living their lives; they’re busy working and bringing up their children. They haven’t spent 20, 30, 40 years devoted to a single aspect of nature the way scientists have. We can’t expect them to know as much as professional scientists, so we have to help them understand it. I hope we find ways to increase curiosity. I don’t know how to do that. I wish somebody would do a study on it, how you can take someone with a modicum of curiosity and help them enlarge it so it gives them the pleasure of discovering things about nature or understanding things about nature that other people don’t discover. Curiosity is the key to staying alive. That would bring us to a point of more people understanding science.”
Cultivating a sense of responsibility is another key to effective communication. “It’s the job of the person leading the discussion to make clear to the person listening,” Mr. Alda said. “You get the impression that ‘this person is my responsibility. I have to take care of them, so they understand what’s going on.’ ”
Parkinson’s disease diagnosis
During a question-and-answer session, Mr. Alda opened up about his Parkinson’s disease, which he said was diagnosed about 5 years ago. In 2018, he decided to speak publicly about his diagnosis for the first time.
“The reason was that I wanted to communicate to people who had recently been diagnosed not to believe or give into the stereotype that when you get a diagnosis, your life is over,” said Mr. Alda, who received the Public Welfare Medal from the National Academy of Sciences in 2016. “Under the burden of that belief, some people won’t tell their family or workplace colleagues. There are exercises you can do and medications you can take to prolong the time it takes before Parkinson’s gets much more serious. It’s not to diminish the fact that it can get really bad; but to think that your life is over as soon as you get a diagnosis is wrong.”
He added: “I’ve gone 5 years and I’m almost busier than I’ve ever been. I’m getting a lot accomplished and I look forward to I don’t know how many years. As long as I have them, I’m going to be grateful. It’s amazing how great it feels not to keep the diagnosis a secret.”
The first 2-day training session at Scripps Research will be held in June 2020. Additional sessions are scheduled to take place in October and December. Registration is available at aldacommunicationtraining.com/workshops.
Cardiovascular risks associated with cannabis use
Researchers are recommending routine screening of marijuana use in cardiovascular care settings.
A review of current evidence suggests an association between marijuana use and adverse cardiovascular effects, as well as interactions between marijuana and cardiovascular medications.
Although more research is needed, the review authors suggested patients may benefit from marijuana screening and testing as well as discussions about the potential risks of marijuana use in the setting of cardiovascular disease.
Ersilia M. DeFilippis, MD, of Columbia University Irving Medical Center in New York and colleagues conducted this review, which was published in the Journal of the American College of Cardiology.
The authors noted that research on marijuana use and cardiovascular disease is limited. The different forms of cannabis and various routes of administration have made it difficult to draw concrete conclusions about marijuana products. Additionally, there have been no randomized, controlled trials of marijuana products in the United States because such trials are illegal; however, there are observational studies linking marijuana use and adverse cardiovascular effects.
Snapshot of available evidence
One study showed that smoking marijuana produces many of the same cardiotoxic chemicals produced by smoking tobacco (BMJ. 2003 May 3;326[7396]:942-3). Another study suggested marijuana smokers may have greater exposure to harmful chemicals (J Psychoactive Drugs. 1988 Jan-Mar;20[1]:43-6).
More specifically, a meta-analysis suggested that smoking marijuana was one of the top three triggers of myocardial infarction (Lancet. 2011 Feb 26;377[9767]:732-40). And in a systematic analysis, 28 of 33 studies linked marijuana use to an increased risk of acute coronary syndromes (Clin Toxicol [Phila]. 2019 Oct;57[10]:831-41).
Furthermore, a study of 2.5 million marijuana users showed that 3% experienced arrhythmias (Int J Cardiol. 2018 Aug 1;264:91-2). A population survey showed that people who smoked marijuana in the past year experienced a 3.3-fold higher rate of cerebrovascular events (Aust N Z J Public Health. 2016 Jun;40[3]:226-30).
Studies have also indicated that cannabinoids can affect cardiovascular medications, including antiarrhythmics, calcium-channel blockers, isosorbide dinitrate/mononitrate, statins, beta-blockers, warfarin, theophylline, and nonsteroidal anti-inflammatory drugs (Medicines [Basel]. 2018 Dec 23;6[1] pii: E3; Curr Top Behav Neurosci. 2017;32:249-62; Pharmacogenet Genomics. 2009 Jul;19[7]:559-62; Ann Pharmacother. 2009 Jul;43[7]:1347-53; Pharmacol Ther. 2019 Sep;201:25-38).
Reviewer recommendations
Cardiovascular specialists should be informed about regulations governing marijuana products, as well as “potential health consequences of marijuana and its derivatives,” according to Dr. DeFilippis and colleagues.
The authors recommend routinely screening patients for marijuana use, perhaps using the Daily Sessions, Frequency, Age of Onset, and Quantity of Cannabis Use Inventory (PLoS One. 2017 May 26;12[5]:e0178194) or the Cannabis Abuse Screening Test (Int J Methods Psychiatr Res. 2018 Jun;27[2]:e1597).
The authors say urine toxicology “may be reasonable” for patients with myocardial infarction or new-onset heart failure. Such testing is required for patients undergoing a heart transplant because marijuana use may affect their candidacy.
Dr. DeFilippis and colleagues say cardiovascular specialists should inform patients about the risks associated with marijuana use. The authors recommend shared decision making for patients who use marijuana for symptom management or palliative purposes.
Three review authors disclosed relationships with many different pharmaceutical companies. One author disclosed relationships with Medscape Cardiology and WebMD, which are owned by the same parent company as MDedge.
SOURCE: J Am Coll Cardiol. 2020 Jan 20. doi: 10.1016/j.jacc.2019.11.025.
Researchers are recommending routine screening of marijuana use in cardiovascular care settings.
A review of current evidence suggests an association between marijuana use and adverse cardiovascular effects, as well as interactions between marijuana and cardiovascular medications.
Although more research is needed, the review authors suggested patients may benefit from marijuana screening and testing as well as discussions about the potential risks of marijuana use in the setting of cardiovascular disease.
Ersilia M. DeFilippis, MD, of Columbia University Irving Medical Center in New York and colleagues conducted this review, which was published in the Journal of the American College of Cardiology.
The authors noted that research on marijuana use and cardiovascular disease is limited. The different forms of cannabis and various routes of administration have made it difficult to draw concrete conclusions about marijuana products. Additionally, there have been no randomized, controlled trials of marijuana products in the United States because such trials are illegal; however, there are observational studies linking marijuana use and adverse cardiovascular effects.
Snapshot of available evidence
One study showed that smoking marijuana produces many of the same cardiotoxic chemicals produced by smoking tobacco (BMJ. 2003 May 3;326[7396]:942-3). Another study suggested marijuana smokers may have greater exposure to harmful chemicals (J Psychoactive Drugs. 1988 Jan-Mar;20[1]:43-6).
More specifically, a meta-analysis suggested that smoking marijuana was one of the top three triggers of myocardial infarction (Lancet. 2011 Feb 26;377[9767]:732-40). And in a systematic analysis, 28 of 33 studies linked marijuana use to an increased risk of acute coronary syndromes (Clin Toxicol [Phila]. 2019 Oct;57[10]:831-41).
Furthermore, a study of 2.5 million marijuana users showed that 3% experienced arrhythmias (Int J Cardiol. 2018 Aug 1;264:91-2). A population survey showed that people who smoked marijuana in the past year experienced a 3.3-fold higher rate of cerebrovascular events (Aust N Z J Public Health. 2016 Jun;40[3]:226-30).
Studies have also indicated that cannabinoids can affect cardiovascular medications, including antiarrhythmics, calcium-channel blockers, isosorbide dinitrate/mononitrate, statins, beta-blockers, warfarin, theophylline, and nonsteroidal anti-inflammatory drugs (Medicines [Basel]. 2018 Dec 23;6[1] pii: E3; Curr Top Behav Neurosci. 2017;32:249-62; Pharmacogenet Genomics. 2009 Jul;19[7]:559-62; Ann Pharmacother. 2009 Jul;43[7]:1347-53; Pharmacol Ther. 2019 Sep;201:25-38).
Reviewer recommendations
Cardiovascular specialists should be informed about regulations governing marijuana products, as well as “potential health consequences of marijuana and its derivatives,” according to Dr. DeFilippis and colleagues.
The authors recommend routinely screening patients for marijuana use, perhaps using the Daily Sessions, Frequency, Age of Onset, and Quantity of Cannabis Use Inventory (PLoS One. 2017 May 26;12[5]:e0178194) or the Cannabis Abuse Screening Test (Int J Methods Psychiatr Res. 2018 Jun;27[2]:e1597).
The authors say urine toxicology “may be reasonable” for patients with myocardial infarction or new-onset heart failure. Such testing is required for patients undergoing a heart transplant because marijuana use may affect their candidacy.
Dr. DeFilippis and colleagues say cardiovascular specialists should inform patients about the risks associated with marijuana use. The authors recommend shared decision making for patients who use marijuana for symptom management or palliative purposes.
Three review authors disclosed relationships with many different pharmaceutical companies. One author disclosed relationships with Medscape Cardiology and WebMD, which are owned by the same parent company as MDedge.
SOURCE: J Am Coll Cardiol. 2020 Jan 20. doi: 10.1016/j.jacc.2019.11.025.
Researchers are recommending routine screening of marijuana use in cardiovascular care settings.
A review of current evidence suggests an association between marijuana use and adverse cardiovascular effects, as well as interactions between marijuana and cardiovascular medications.
Although more research is needed, the review authors suggested patients may benefit from marijuana screening and testing as well as discussions about the potential risks of marijuana use in the setting of cardiovascular disease.
Ersilia M. DeFilippis, MD, of Columbia University Irving Medical Center in New York and colleagues conducted this review, which was published in the Journal of the American College of Cardiology.
The authors noted that research on marijuana use and cardiovascular disease is limited. The different forms of cannabis and various routes of administration have made it difficult to draw concrete conclusions about marijuana products. Additionally, there have been no randomized, controlled trials of marijuana products in the United States because such trials are illegal; however, there are observational studies linking marijuana use and adverse cardiovascular effects.
Snapshot of available evidence
One study showed that smoking marijuana produces many of the same cardiotoxic chemicals produced by smoking tobacco (BMJ. 2003 May 3;326[7396]:942-3). Another study suggested marijuana smokers may have greater exposure to harmful chemicals (J Psychoactive Drugs. 1988 Jan-Mar;20[1]:43-6).
More specifically, a meta-analysis suggested that smoking marijuana was one of the top three triggers of myocardial infarction (Lancet. 2011 Feb 26;377[9767]:732-40). And in a systematic analysis, 28 of 33 studies linked marijuana use to an increased risk of acute coronary syndromes (Clin Toxicol [Phila]. 2019 Oct;57[10]:831-41).
Furthermore, a study of 2.5 million marijuana users showed that 3% experienced arrhythmias (Int J Cardiol. 2018 Aug 1;264:91-2). A population survey showed that people who smoked marijuana in the past year experienced a 3.3-fold higher rate of cerebrovascular events (Aust N Z J Public Health. 2016 Jun;40[3]:226-30).
Studies have also indicated that cannabinoids can affect cardiovascular medications, including antiarrhythmics, calcium-channel blockers, isosorbide dinitrate/mononitrate, statins, beta-blockers, warfarin, theophylline, and nonsteroidal anti-inflammatory drugs (Medicines [Basel]. 2018 Dec 23;6[1] pii: E3; Curr Top Behav Neurosci. 2017;32:249-62; Pharmacogenet Genomics. 2009 Jul;19[7]:559-62; Ann Pharmacother. 2009 Jul;43[7]:1347-53; Pharmacol Ther. 2019 Sep;201:25-38).
Reviewer recommendations
Cardiovascular specialists should be informed about regulations governing marijuana products, as well as “potential health consequences of marijuana and its derivatives,” according to Dr. DeFilippis and colleagues.
The authors recommend routinely screening patients for marijuana use, perhaps using the Daily Sessions, Frequency, Age of Onset, and Quantity of Cannabis Use Inventory (PLoS One. 2017 May 26;12[5]:e0178194) or the Cannabis Abuse Screening Test (Int J Methods Psychiatr Res. 2018 Jun;27[2]:e1597).
The authors say urine toxicology “may be reasonable” for patients with myocardial infarction or new-onset heart failure. Such testing is required for patients undergoing a heart transplant because marijuana use may affect their candidacy.
Dr. DeFilippis and colleagues say cardiovascular specialists should inform patients about the risks associated with marijuana use. The authors recommend shared decision making for patients who use marijuana for symptom management or palliative purposes.
Three review authors disclosed relationships with many different pharmaceutical companies. One author disclosed relationships with Medscape Cardiology and WebMD, which are owned by the same parent company as MDedge.
SOURCE: J Am Coll Cardiol. 2020 Jan 20. doi: 10.1016/j.jacc.2019.11.025.
FROM JOURNAL OF THE AMERICAN COLLEGE OF CARDIOLOGY
Cognitive screening of older physicians: What’s fair?
Cognitive screening of 141 clinicians 70 years or older at Yale New Haven (Conn.) Hospital identified 18 with cognitive deficits likely to impair their ability to practice medicine. Six retired and 12 agreed to limit their practice to closely proctored environments, according to a report in JAMA.
It was part of a program to screen all practitioners 70 years or older who apply for reappointment to the medical staff, and every 2 years thereafter, due to “concerns about the potentially compromised ability of older clinicians,” said the authors, Yale rheumatologist and geriatrician Leo M. Cooney Jr., MD, and Thomas Balcezak, MD, Yale New Haven’s chief medical officer.
Yale is not alone. Intermountain Healthcare, Stanford Hospitals and Clinics, Scripps Health Care, Penn Medicine, and the University of California, San Diego, are among the institutions with similar programs.
The move is being driven by the aging of the medical community. About 15% of U.S. physicians are over 65 years old, a tripling from 23,000 in 1980 to 73,000 in 2012-2016, and the number is growing, according to an editorial by Jeffrey L. Saver, MD, professor of neurology and senior associate vice president of neurology at the University of California, Los Angeles.
Given the trend, “it is not surprising that the issue of screening aging physicians for cognitive deficits has gained attention over the last decade,” Katrina Armstrong, MD, chair of the department of medicine at Massachusetts General Hospital, Boston, and Eileen E. Reynolds, MD, associate professor of medicine at Beth Israel Deaconess Medical Center, Boston, noted in a second editorial.
“Cognitive decline often accompanies aging, and the prevalence of dementia increases rapidly after age 70 years,” they said.
The data on whether older clinicians pose a risk to patients is limited and somewhat mixed. An analysis of 736,537 Medicare hospitalizations found no association between physician age and 30-day patient mortality among physicians 60 years or older with more than 201 admissions per year, but higher mortality among older physicians with lower volumes.
A meta-analysis of 62 studies showed that “older physicians have less factual knowledge, are less likely to adhere to appropriate standards of care, and may also have poorer patient outcomes.”
The new Yale data, meanwhile, suggests that “approximately 13% [18 of 141] of physicians and other clinicians older than 70 years should not be practicing independently,” Dr. Armstrong and Dr. Reynolds said in their editorial.
There is support for screening efforts. “As a profession that deals with human life, medical practitioners must obviously have the cognitive capacity to safely practice medicine. I applaud the approach taken by Yale New Haven Hospital in that cognitive abilities themselves, and not simply funds of knowledge, are assessed,” said Richard J. Caselli, MD, professor of neurology at the Mayo Clinic Arizona, Scottsdale, and a leader of the Alzheimer’s disease program there.
However, it’s not hard to imagine highly competent but older physicians taking umbrage at cognitive screening, and there’s been pushback. Stanford was considering a Yale-like approach but opted instead for peer review after opposition. Objections from the Utah Medical Association led Utah to enact a law banning age-based physician screening. In 2015, the American Medical Association issued a report calling for the development of guidelines and standards for assessing competency in aging physicians, but the AMA House of Delegates shelved it pending further study.
There are concerns about age discrimination, discounting the accumulated wisdom of long-practicing physicians, and misclassifying competent physicians, particularly those who provide quality care in rural and other underserved areas. Indeed, 8 of 14 clinicians who screened positive at Yale and underwent more extensive testing were allowed to recredential, “suggesting that the false-positive screening rate could be as high as 57%,” Dr. Armstrong and Dr. Reynolds noted.
The consensus seems to be that there probably is a need for some sort of screening, but it must be both sound and fair. Rather than a piecemeal institutional approach, perhaps there is “an important opportunity for other groups, including specialty boards and state licensing boards” to standardize the process, they said.
Among other things, assessments could focus less on test scores and more on the practice of medicine. For instance, fine motor skill/motor planning assessments for surgeons, and intermediate results could trigger a more extensive assessment of actual clinical performance, perhaps even direct observation, Dr. Saver said in his editorial.
As far as clinical performance goes, none of the 18 clinicians at Yale had previous performance problems. “Was this a failure of the system to report impaired physicians or were these physicians compensating sufficiently to avoid detection?” In either case, “cognitive testing should be a red flag that triggers other clinical assessments,” said Carl I. Cohen, MD, professor and director of the division of geriatric psychiatry at the State University of New York, Brooklyn.
The original plan at Yale was for neurologic and ophthalmologic examinations beginning at age 70, but ultimately it was decided to go with a battery of 16 tests to assess visual scanning and psychomotor efficiency, processing speed under pressure, concentration, and working memory, among other things. Testing takes about 50-90 minutes, and is graded by single neuropsychologist to ensure consistency. Results were compared with normative scores from both older and younger clinicians.
To prevent clinicians from preparing for it, Yale isn’t releasing its test battery.
Suboptimal performance triggered additional evaluations, including in-depth assessment of intellectual, memory, and executive function. Final reviews and recommendations were made by a committee that included a geriatrician, the clinician’s section or department chair, and current and past chief medical officers.
Among the 18 providers who demonstrated deficits impairing their ability to practice medicine, 5 were 70-74 years old; 4 were 75-79; and 9 were 80 years or older. Minor abnormalities were found in 34 other candidates (24.1%); they were allowed to recredential but were scheduled for rescreening at 1-year intervals, instead of every 2 years.
The mean age among the 141 screened clinicians was 74.3 years and ranged from 69 to 92 years; 86% were men. Applicants included 125 physicians (88.7%) as well as 5 advanced practice registered nurses; 4 dentists; 3 psychologists; 2 podiatrists; 1 physician associate; and 1 midwife.
The authors had no relevant disclosures.
SOURCE: Cooney L et al. JAMA. 2020 Jan 14;323(2):179-80.
Cognitive screening of 141 clinicians 70 years or older at Yale New Haven (Conn.) Hospital identified 18 with cognitive deficits likely to impair their ability to practice medicine. Six retired and 12 agreed to limit their practice to closely proctored environments, according to a report in JAMA.
It was part of a program to screen all practitioners 70 years or older who apply for reappointment to the medical staff, and every 2 years thereafter, due to “concerns about the potentially compromised ability of older clinicians,” said the authors, Yale rheumatologist and geriatrician Leo M. Cooney Jr., MD, and Thomas Balcezak, MD, Yale New Haven’s chief medical officer.
Yale is not alone. Intermountain Healthcare, Stanford Hospitals and Clinics, Scripps Health Care, Penn Medicine, and the University of California, San Diego, are among the institutions with similar programs.
The move is being driven by the aging of the medical community. About 15% of U.S. physicians are over 65 years old, a tripling from 23,000 in 1980 to 73,000 in 2012-2016, and the number is growing, according to an editorial by Jeffrey L. Saver, MD, professor of neurology and senior associate vice president of neurology at the University of California, Los Angeles.
Given the trend, “it is not surprising that the issue of screening aging physicians for cognitive deficits has gained attention over the last decade,” Katrina Armstrong, MD, chair of the department of medicine at Massachusetts General Hospital, Boston, and Eileen E. Reynolds, MD, associate professor of medicine at Beth Israel Deaconess Medical Center, Boston, noted in a second editorial.
“Cognitive decline often accompanies aging, and the prevalence of dementia increases rapidly after age 70 years,” they said.
The data on whether older clinicians pose a risk to patients is limited and somewhat mixed. An analysis of 736,537 Medicare hospitalizations found no association between physician age and 30-day patient mortality among physicians 60 years or older with more than 201 admissions per year, but higher mortality among older physicians with lower volumes.
A meta-analysis of 62 studies showed that “older physicians have less factual knowledge, are less likely to adhere to appropriate standards of care, and may also have poorer patient outcomes.”
The new Yale data, meanwhile, suggests that “approximately 13% [18 of 141] of physicians and other clinicians older than 70 years should not be practicing independently,” Dr. Armstrong and Dr. Reynolds said in their editorial.
There is support for screening efforts. “As a profession that deals with human life, medical practitioners must obviously have the cognitive capacity to safely practice medicine. I applaud the approach taken by Yale New Haven Hospital in that cognitive abilities themselves, and not simply funds of knowledge, are assessed,” said Richard J. Caselli, MD, professor of neurology at the Mayo Clinic Arizona, Scottsdale, and a leader of the Alzheimer’s disease program there.
However, it’s not hard to imagine highly competent but older physicians taking umbrage at cognitive screening, and there’s been pushback. Stanford was considering a Yale-like approach but opted instead for peer review after opposition. Objections from the Utah Medical Association led Utah to enact a law banning age-based physician screening. In 2015, the American Medical Association issued a report calling for the development of guidelines and standards for assessing competency in aging physicians, but the AMA House of Delegates shelved it pending further study.
There are concerns about age discrimination, discounting the accumulated wisdom of long-practicing physicians, and misclassifying competent physicians, particularly those who provide quality care in rural and other underserved areas. Indeed, 8 of 14 clinicians who screened positive at Yale and underwent more extensive testing were allowed to recredential, “suggesting that the false-positive screening rate could be as high as 57%,” Dr. Armstrong and Dr. Reynolds noted.
The consensus seems to be that there probably is a need for some sort of screening, but it must be both sound and fair. Rather than a piecemeal institutional approach, perhaps there is “an important opportunity for other groups, including specialty boards and state licensing boards” to standardize the process, they said.
Among other things, assessments could focus less on test scores and more on the practice of medicine. For instance, fine motor skill/motor planning assessments for surgeons, and intermediate results could trigger a more extensive assessment of actual clinical performance, perhaps even direct observation, Dr. Saver said in his editorial.
As far as clinical performance goes, none of the 18 clinicians at Yale had previous performance problems. “Was this a failure of the system to report impaired physicians or were these physicians compensating sufficiently to avoid detection?” In either case, “cognitive testing should be a red flag that triggers other clinical assessments,” said Carl I. Cohen, MD, professor and director of the division of geriatric psychiatry at the State University of New York, Brooklyn.
The original plan at Yale was for neurologic and ophthalmologic examinations beginning at age 70, but ultimately it was decided to go with a battery of 16 tests to assess visual scanning and psychomotor efficiency, processing speed under pressure, concentration, and working memory, among other things. Testing takes about 50-90 minutes, and is graded by single neuropsychologist to ensure consistency. Results were compared with normative scores from both older and younger clinicians.
To prevent clinicians from preparing for it, Yale isn’t releasing its test battery.
Suboptimal performance triggered additional evaluations, including in-depth assessment of intellectual, memory, and executive function. Final reviews and recommendations were made by a committee that included a geriatrician, the clinician’s section or department chair, and current and past chief medical officers.
Among the 18 providers who demonstrated deficits impairing their ability to practice medicine, 5 were 70-74 years old; 4 were 75-79; and 9 were 80 years or older. Minor abnormalities were found in 34 other candidates (24.1%); they were allowed to recredential but were scheduled for rescreening at 1-year intervals, instead of every 2 years.
The mean age among the 141 screened clinicians was 74.3 years and ranged from 69 to 92 years; 86% were men. Applicants included 125 physicians (88.7%) as well as 5 advanced practice registered nurses; 4 dentists; 3 psychologists; 2 podiatrists; 1 physician associate; and 1 midwife.
The authors had no relevant disclosures.
SOURCE: Cooney L et al. JAMA. 2020 Jan 14;323(2):179-80.
Cognitive screening of 141 clinicians 70 years or older at Yale New Haven (Conn.) Hospital identified 18 with cognitive deficits likely to impair their ability to practice medicine. Six retired and 12 agreed to limit their practice to closely proctored environments, according to a report in JAMA.
It was part of a program to screen all practitioners 70 years or older who apply for reappointment to the medical staff, and every 2 years thereafter, due to “concerns about the potentially compromised ability of older clinicians,” said the authors, Yale rheumatologist and geriatrician Leo M. Cooney Jr., MD, and Thomas Balcezak, MD, Yale New Haven’s chief medical officer.
Yale is not alone. Intermountain Healthcare, Stanford Hospitals and Clinics, Scripps Health Care, Penn Medicine, and the University of California, San Diego, are among the institutions with similar programs.
The move is being driven by the aging of the medical community. About 15% of U.S. physicians are over 65 years old, a tripling from 23,000 in 1980 to 73,000 in 2012-2016, and the number is growing, according to an editorial by Jeffrey L. Saver, MD, professor of neurology and senior associate vice president of neurology at the University of California, Los Angeles.
Given the trend, “it is not surprising that the issue of screening aging physicians for cognitive deficits has gained attention over the last decade,” Katrina Armstrong, MD, chair of the department of medicine at Massachusetts General Hospital, Boston, and Eileen E. Reynolds, MD, associate professor of medicine at Beth Israel Deaconess Medical Center, Boston, noted in a second editorial.
“Cognitive decline often accompanies aging, and the prevalence of dementia increases rapidly after age 70 years,” they said.
The data on whether older clinicians pose a risk to patients is limited and somewhat mixed. An analysis of 736,537 Medicare hospitalizations found no association between physician age and 30-day patient mortality among physicians 60 years or older with more than 201 admissions per year, but higher mortality among older physicians with lower volumes.
A meta-analysis of 62 studies showed that “older physicians have less factual knowledge, are less likely to adhere to appropriate standards of care, and may also have poorer patient outcomes.”
The new Yale data, meanwhile, suggests that “approximately 13% [18 of 141] of physicians and other clinicians older than 70 years should not be practicing independently,” Dr. Armstrong and Dr. Reynolds said in their editorial.
There is support for screening efforts. “As a profession that deals with human life, medical practitioners must obviously have the cognitive capacity to safely practice medicine. I applaud the approach taken by Yale New Haven Hospital in that cognitive abilities themselves, and not simply funds of knowledge, are assessed,” said Richard J. Caselli, MD, professor of neurology at the Mayo Clinic Arizona, Scottsdale, and a leader of the Alzheimer’s disease program there.
However, it’s not hard to imagine highly competent but older physicians taking umbrage at cognitive screening, and there’s been pushback. Stanford was considering a Yale-like approach but opted instead for peer review after opposition. Objections from the Utah Medical Association led Utah to enact a law banning age-based physician screening. In 2015, the American Medical Association issued a report calling for the development of guidelines and standards for assessing competency in aging physicians, but the AMA House of Delegates shelved it pending further study.
There are concerns about age discrimination, discounting the accumulated wisdom of long-practicing physicians, and misclassifying competent physicians, particularly those who provide quality care in rural and other underserved areas. Indeed, 8 of 14 clinicians who screened positive at Yale and underwent more extensive testing were allowed to recredential, “suggesting that the false-positive screening rate could be as high as 57%,” Dr. Armstrong and Dr. Reynolds noted.
The consensus seems to be that there probably is a need for some sort of screening, but it must be both sound and fair. Rather than a piecemeal institutional approach, perhaps there is “an important opportunity for other groups, including specialty boards and state licensing boards” to standardize the process, they said.
Among other things, assessments could focus less on test scores and more on the practice of medicine. For instance, fine motor skill/motor planning assessments for surgeons, and intermediate results could trigger a more extensive assessment of actual clinical performance, perhaps even direct observation, Dr. Saver said in his editorial.
As far as clinical performance goes, none of the 18 clinicians at Yale had previous performance problems. “Was this a failure of the system to report impaired physicians or were these physicians compensating sufficiently to avoid detection?” In either case, “cognitive testing should be a red flag that triggers other clinical assessments,” said Carl I. Cohen, MD, professor and director of the division of geriatric psychiatry at the State University of New York, Brooklyn.
The original plan at Yale was for neurologic and ophthalmologic examinations beginning at age 70, but ultimately it was decided to go with a battery of 16 tests to assess visual scanning and psychomotor efficiency, processing speed under pressure, concentration, and working memory, among other things. Testing takes about 50-90 minutes, and is graded by single neuropsychologist to ensure consistency. Results were compared with normative scores from both older and younger clinicians.
To prevent clinicians from preparing for it, Yale isn’t releasing its test battery.
Suboptimal performance triggered additional evaluations, including in-depth assessment of intellectual, memory, and executive function. Final reviews and recommendations were made by a committee that included a geriatrician, the clinician’s section or department chair, and current and past chief medical officers.
Among the 18 providers who demonstrated deficits impairing their ability to practice medicine, 5 were 70-74 years old; 4 were 75-79; and 9 were 80 years or older. Minor abnormalities were found in 34 other candidates (24.1%); they were allowed to recredential but were scheduled for rescreening at 1-year intervals, instead of every 2 years.
The mean age among the 141 screened clinicians was 74.3 years and ranged from 69 to 92 years; 86% were men. Applicants included 125 physicians (88.7%) as well as 5 advanced practice registered nurses; 4 dentists; 3 psychologists; 2 podiatrists; 1 physician associate; and 1 midwife.
The authors had no relevant disclosures.
SOURCE: Cooney L et al. JAMA. 2020 Jan 14;323(2):179-80.
FROM JAMA
FDA approves CV disease benefit for once-weekly semaglutide
(Ozempic, Novo Nordisk) in the treatment of type 2 diabetes and has added new trial data information to the label of the oral version (Rybelsus, Novo Nordisk) pertaining to CV safety.
The agency expanded the once-weekly injectable semaglutide’s label to include an indication for reducing the risk for major adverse cardiovascular events (MACE), including CV death, nonfatal myocardial infarction (MI), or nonfatal stroke, in adults with type 2 diabetes who have established CV disease.
Initially approved for the treatment of type 2 diabetes in adults in December 2017, once-weekly subcutaneously injectable semaglutide comes in 0.5-mg and 1.0-mg doses in a dedicated prefilled pen device.
The approval for the new indication was based on data from the 2-year randomized Trial to Evaluate Cardiovascular and Other Long-term Outcomes With Semaglutide in Subjects With Type 2 Diabetes (SUSTAIN 6), in which injectable semaglutide or placebo was added to standard of care in 3,297 adults with type 2 diabetes and established CV disease.
As reported by Medscape Medical News in September 2016, patients who underwent treatment with one of the two doses of semaglutide had a significant 26% lower risk for the primary composite outcome of first occurrence of CV death, nonfatal MI, or nonfatal stroke, compared with those who received placebo.
The reduced CV risk was driven primarily by significant reductions in nonfatal stroke and nonfatal MI (39% and 26%, respectively). There was no difference in CV death between drug and placebo groups. Gastrointestinal adverse events were more frequent with semaglutide than placebo, with the majority occurring during the first 30 weeks.
The oral semaglutide formulation, taken daily in 7-mg or 14-mg doses, was approved for the treatment of type 2 diabetes in September 2019, the first orally available GLP-1 agonist.
Now, the FDA has updated the prescribing information in the clinical studies section (section 14) to include results from the randomized, placebo-controlled, 3,183-subject Trial Investigating the Cardiovascular Safety of Oral Semaglutide in Subjects With Type 2 Diabetes (PIONEER 6), reported in June 2019, which found a nonsignificant 21% reduction in three-component MACE with oral semaglutide. The addition to the label for Rybelsus is with regard to CV safety, not benefit.
SOUL: Large ongoing CV outcomes trial for oral semaglutide
In June 2019, Novo Nordisk initiated a larger CV outcomes trial of oral semaglutide, A Heart Disease Study of Semaglutide in Patients With Type 2 Diabetes (SOUL). The trial, which includes 9,642 adults with type 2 diabetes and established CV disease, is further investigating the drug’s effects on the incidence of MACE. The estimated completion date is July 2024.
Semaglutide joins a growing list of drugs approved for treating type 2 diabetes that have been granted additional label indications for benefits beyond the lowering of glucose.
These include Novo Nordisk’s other injectable GLP-1 agonist, liraglutide (Victoza), additionally approved for reducing CV events in high-risk patients with type 2 diabetes, and the sodium-glucose transport 2 inhibitors empagliflozin (Jardiance, Boehringer Ingelheim/Lilly), for reducing CV death; canagliflozin (Invokana, Janssen), for reducing major adverse CV events,; kidney disease, CV death, and heart failure hospitalization; and dapagliflozin (Farxiga, AstraZeneca), for reducing heart failure hospitalization.
Recently, in an exclusive Medscape Medical News article, some experts questioned the design of these CV outcomes trials, suggesting that imbalances in glycemic control, blood pressure, and diuretic use between treatment and placebo arms could have biased the CV and renal outcomes of the trials in favor of the study drugs
A version of this story originally appeared on Medscape.com.
(Ozempic, Novo Nordisk) in the treatment of type 2 diabetes and has added new trial data information to the label of the oral version (Rybelsus, Novo Nordisk) pertaining to CV safety.
The agency expanded the once-weekly injectable semaglutide’s label to include an indication for reducing the risk for major adverse cardiovascular events (MACE), including CV death, nonfatal myocardial infarction (MI), or nonfatal stroke, in adults with type 2 diabetes who have established CV disease.
Initially approved for the treatment of type 2 diabetes in adults in December 2017, once-weekly subcutaneously injectable semaglutide comes in 0.5-mg and 1.0-mg doses in a dedicated prefilled pen device.
The approval for the new indication was based on data from the 2-year randomized Trial to Evaluate Cardiovascular and Other Long-term Outcomes With Semaglutide in Subjects With Type 2 Diabetes (SUSTAIN 6), in which injectable semaglutide or placebo was added to standard of care in 3,297 adults with type 2 diabetes and established CV disease.
As reported by Medscape Medical News in September 2016, patients who underwent treatment with one of the two doses of semaglutide had a significant 26% lower risk for the primary composite outcome of first occurrence of CV death, nonfatal MI, or nonfatal stroke, compared with those who received placebo.
The reduced CV risk was driven primarily by significant reductions in nonfatal stroke and nonfatal MI (39% and 26%, respectively). There was no difference in CV death between drug and placebo groups. Gastrointestinal adverse events were more frequent with semaglutide than placebo, with the majority occurring during the first 30 weeks.
The oral semaglutide formulation, taken daily in 7-mg or 14-mg doses, was approved for the treatment of type 2 diabetes in September 2019, the first orally available GLP-1 agonist.
Now, the FDA has updated the prescribing information in the clinical studies section (section 14) to include results from the randomized, placebo-controlled, 3,183-subject Trial Investigating the Cardiovascular Safety of Oral Semaglutide in Subjects With Type 2 Diabetes (PIONEER 6), reported in June 2019, which found a nonsignificant 21% reduction in three-component MACE with oral semaglutide. The addition to the label for Rybelsus is with regard to CV safety, not benefit.
SOUL: Large ongoing CV outcomes trial for oral semaglutide
In June 2019, Novo Nordisk initiated a larger CV outcomes trial of oral semaglutide, A Heart Disease Study of Semaglutide in Patients With Type 2 Diabetes (SOUL). The trial, which includes 9,642 adults with type 2 diabetes and established CV disease, is further investigating the drug’s effects on the incidence of MACE. The estimated completion date is July 2024.
Semaglutide joins a growing list of drugs approved for treating type 2 diabetes that have been granted additional label indications for benefits beyond the lowering of glucose.
These include Novo Nordisk’s other injectable GLP-1 agonist, liraglutide (Victoza), additionally approved for reducing CV events in high-risk patients with type 2 diabetes, and the sodium-glucose transport 2 inhibitors empagliflozin (Jardiance, Boehringer Ingelheim/Lilly), for reducing CV death; canagliflozin (Invokana, Janssen), for reducing major adverse CV events,; kidney disease, CV death, and heart failure hospitalization; and dapagliflozin (Farxiga, AstraZeneca), for reducing heart failure hospitalization.
Recently, in an exclusive Medscape Medical News article, some experts questioned the design of these CV outcomes trials, suggesting that imbalances in glycemic control, blood pressure, and diuretic use between treatment and placebo arms could have biased the CV and renal outcomes of the trials in favor of the study drugs
A version of this story originally appeared on Medscape.com.
(Ozempic, Novo Nordisk) in the treatment of type 2 diabetes and has added new trial data information to the label of the oral version (Rybelsus, Novo Nordisk) pertaining to CV safety.
The agency expanded the once-weekly injectable semaglutide’s label to include an indication for reducing the risk for major adverse cardiovascular events (MACE), including CV death, nonfatal myocardial infarction (MI), or nonfatal stroke, in adults with type 2 diabetes who have established CV disease.
Initially approved for the treatment of type 2 diabetes in adults in December 2017, once-weekly subcutaneously injectable semaglutide comes in 0.5-mg and 1.0-mg doses in a dedicated prefilled pen device.
The approval for the new indication was based on data from the 2-year randomized Trial to Evaluate Cardiovascular and Other Long-term Outcomes With Semaglutide in Subjects With Type 2 Diabetes (SUSTAIN 6), in which injectable semaglutide or placebo was added to standard of care in 3,297 adults with type 2 diabetes and established CV disease.
As reported by Medscape Medical News in September 2016, patients who underwent treatment with one of the two doses of semaglutide had a significant 26% lower risk for the primary composite outcome of first occurrence of CV death, nonfatal MI, or nonfatal stroke, compared with those who received placebo.
The reduced CV risk was driven primarily by significant reductions in nonfatal stroke and nonfatal MI (39% and 26%, respectively). There was no difference in CV death between drug and placebo groups. Gastrointestinal adverse events were more frequent with semaglutide than placebo, with the majority occurring during the first 30 weeks.
The oral semaglutide formulation, taken daily in 7-mg or 14-mg doses, was approved for the treatment of type 2 diabetes in September 2019, the first orally available GLP-1 agonist.
Now, the FDA has updated the prescribing information in the clinical studies section (section 14) to include results from the randomized, placebo-controlled, 3,183-subject Trial Investigating the Cardiovascular Safety of Oral Semaglutide in Subjects With Type 2 Diabetes (PIONEER 6), reported in June 2019, which found a nonsignificant 21% reduction in three-component MACE with oral semaglutide. The addition to the label for Rybelsus is with regard to CV safety, not benefit.
SOUL: Large ongoing CV outcomes trial for oral semaglutide
In June 2019, Novo Nordisk initiated a larger CV outcomes trial of oral semaglutide, A Heart Disease Study of Semaglutide in Patients With Type 2 Diabetes (SOUL). The trial, which includes 9,642 adults with type 2 diabetes and established CV disease, is further investigating the drug’s effects on the incidence of MACE. The estimated completion date is July 2024.
Semaglutide joins a growing list of drugs approved for treating type 2 diabetes that have been granted additional label indications for benefits beyond the lowering of glucose.
These include Novo Nordisk’s other injectable GLP-1 agonist, liraglutide (Victoza), additionally approved for reducing CV events in high-risk patients with type 2 diabetes, and the sodium-glucose transport 2 inhibitors empagliflozin (Jardiance, Boehringer Ingelheim/Lilly), for reducing CV death; canagliflozin (Invokana, Janssen), for reducing major adverse CV events,; kidney disease, CV death, and heart failure hospitalization; and dapagliflozin (Farxiga, AstraZeneca), for reducing heart failure hospitalization.
Recently, in an exclusive Medscape Medical News article, some experts questioned the design of these CV outcomes trials, suggesting that imbalances in glycemic control, blood pressure, and diuretic use between treatment and placebo arms could have biased the CV and renal outcomes of the trials in favor of the study drugs
A version of this story originally appeared on Medscape.com.
Sarcopenia associated with increased cardiometabolic risk
LOS ANGELES –
“Loss of lean body mass and function with aging decreases the amount of metabolically active tissue, which can lead to insulin resistance,” Elena Volpi, MD, said at the World Congress on Insulin Resistance, Diabetes and Cardiovascular Disease. “Insulin resistance reduces muscle protein anabolism and accelerates sarcopenia, perpetuating a vicious cycle.”
Sarcopenia, the involuntary loss of muscle mass and function that occurs with aging, is an ICD-10 codable condition that can be diagnosed by measuring muscle strength and quality, said Dr. Volpi, director of the Sealy Center on Aging at the University of Texas Medical Branch at Galveston. In the Health, Aging and Body Composition Study (Health ABC), researchers followed 2,292 relatively healthy adults aged 70-79 years for an average of 4.9 years (J Gerontol A Biol Sci Med. 2006;61[1]:72-7). The researchers used isokinetic dynamometry to measure knee extension strength, isometric dynamometry to measure grip strength, CT scan to measure thigh muscle area, and dual X-ray absorptiometry to determine leg and arm lean soft-tissue mass. “Those individuals who started with the highest levels of muscle strength had the greatest survival, while those who had the lowest levels of muscle strength died earlier,” said Dr. Volpi, who was not affiliated with the study. “That was true for both men and women.”
More recently, researchers conducted a pooled analysis of nine cohort studies involving 34,485 community-dwelling older individuals who were tested with gait speed and followed for 6-21 years (JAMA. 2011;305[1]:50-8). They found that a higher gait speed was associated with higher survival at 5 and 10 years (P less than .001). “Muscle mass also appears to be associated in part with mortality and survival, although the association is not as strong as measures of strength and gait speed,” Dr. Volpi said.
Data from the 2009 Korea National Health and Nutrition Examination Survey of 1,537 participants, aged 65 years and older, found that sarcopenia is independently associated with cardiovascular disease (PLoS One. 2013 Mar 22. doi: 10.1371/journal.pone.0060119). Most of the risk factors for cardiovascular disease – such as age, waist circumference, body mass index, fasting plasma glucose, and total cholesterol – showed significant negative correlations with the ratio between appendicular skeletal muscle mass and body weight. Multiple logistic regression analysis demonstrated that sarcopenia was associated with cardiovascular disease, independent of other well-documented risk factors, renal function, and medications (odds ratio, 1.77; P = .025).
In addition, data from the British Regional Heart Study, which followed 4,252 older men for a mean of 11.3 years, found an association of sarcopenia and adiposity with cardiovascular mortality and all-cause mortality (J Am Geriatr Soc. 2014;62[2]:253-60). Specifically, all-cause mortality risk was significantly greater in men in the sarcopenic and obese groups (HRs, 1.41 and 1.21, respectively), compared with those in the optimal reference group, with the highest risk in sarcopenic obese individuals (HR, 1.72) after adjustment for lifestyle characteristics.
“Diabetes also accelerates loss of lean body mass in older adults,” added Dr. Volpi. “Data from the Health ABC study showed that individuals who did not have diabetes at the beginning of the 6-year observation period ... lost the least amount of muscle, compared with those who had undiagnosed or already diagnosed diabetes.”
The precise way in which sarcopenia is linked to metabolic disease remains elusive, she continued, but current evidence suggests that sarcopenia is characterized by a reduction in the protein synthetic response to metabolic stimulation by amino acids, exercise, and insulin in skeletal muscle. “This reduction in the anabolic response to protein synthesis is called anabolic resistance of aging, and it is mediated by reduced acute activation of mTORC1 [mTOR complex 1] signaling,” Dr. Volpi said. “There’s another step upstream of the mTORC1, in which the amino acids and insulin have to cross the blood-muscle barrier. Amino acids need to be transported into the muscle actively, like glucose. That is an important unexplored area that may contribute to sarcopenia.”
Dr. Volpi went on to note that endothelial dysfunction underlies muscle anabolic resistance and cardiovascular risk and is likely to be a fundamental cause of both problems. Recent studies have shown that increased levels of physical activity improve endothelial function, enhance insulin sensitivity and anabolic sensitivity to nutrients, and reduce cardiovascular risk.
For example, in a cohort of 45 nonfrail older adults with a mean age of 72 years, Dr. Volpi and colleagues carried out a phase 1, double-blind, placebo-controlled, randomized clinical trial to determine if chronic essential amino acid supplementation, aerobic exercise training, or a combination of the two interventions could improve muscle mass and function by stimulating muscle protein synthesis over the course of 24 weeks (J Gerontol A Biol Sci Med Sci. 2019;74[10]:1598-604). “We found that exercise supervised three times per week on a treadmill for 6 months improved physical function in both groups randomized to exercise,” Dr. Volpi said. “Disappointingly, there was no change in total lean mass with any of the interventions. There was a decrease in fat mass with exercise alone, and no change with exercise and amino acids. [Of note is that] the individuals who were randomized to the amino acids plus exercise group had a significant increase in leg strength, whereas the others did not.”
Preliminary findings from ongoing work by Dr. Volpi and colleagues suggest that, in diabetes, muscle protein synthesis and blood flow really “are not different in response to insulin in healthy older adults and diabetic older adults because they don’t change at all. However, we did find alterations in amino acid trafficking in diabetes. We found that older individuals with type 2 diabetes had a reduction of amino acid transport and a higher intracellular amino acid concentration, compared with age-matched, healthier individuals. The intracellular amino acid clearance improved in the healthy, nondiabetic older adults with hyperinsulinemia, whereas it did not change in diabetic older adults. As a result, the net muscle protein balance improved a little in the nondiabetic patients, but did not change in the diabetic patients.”
The researchers are evaluating older patients with type 2 diabetes to see whether there are alterations in vascular reactivity and protein synthesis and whether those can be overcome by resistance-exercise training. “Preliminary results show that flow-mediated dilation can actually increase in an older diabetic patient with resistance exercise training three times a week for 3 months,” she said. “Exercise can improve both endothelial dysfunction and sarcopenia and therefore improve physical function and reduce cardiovascular risk.”
Dr. Volpi reported having no relevant disclosures.
LOS ANGELES –
“Loss of lean body mass and function with aging decreases the amount of metabolically active tissue, which can lead to insulin resistance,” Elena Volpi, MD, said at the World Congress on Insulin Resistance, Diabetes and Cardiovascular Disease. “Insulin resistance reduces muscle protein anabolism and accelerates sarcopenia, perpetuating a vicious cycle.”
Sarcopenia, the involuntary loss of muscle mass and function that occurs with aging, is an ICD-10 codable condition that can be diagnosed by measuring muscle strength and quality, said Dr. Volpi, director of the Sealy Center on Aging at the University of Texas Medical Branch at Galveston. In the Health, Aging and Body Composition Study (Health ABC), researchers followed 2,292 relatively healthy adults aged 70-79 years for an average of 4.9 years (J Gerontol A Biol Sci Med. 2006;61[1]:72-7). The researchers used isokinetic dynamometry to measure knee extension strength, isometric dynamometry to measure grip strength, CT scan to measure thigh muscle area, and dual X-ray absorptiometry to determine leg and arm lean soft-tissue mass. “Those individuals who started with the highest levels of muscle strength had the greatest survival, while those who had the lowest levels of muscle strength died earlier,” said Dr. Volpi, who was not affiliated with the study. “That was true for both men and women.”
More recently, researchers conducted a pooled analysis of nine cohort studies involving 34,485 community-dwelling older individuals who were tested with gait speed and followed for 6-21 years (JAMA. 2011;305[1]:50-8). They found that a higher gait speed was associated with higher survival at 5 and 10 years (P less than .001). “Muscle mass also appears to be associated in part with mortality and survival, although the association is not as strong as measures of strength and gait speed,” Dr. Volpi said.
Data from the 2009 Korea National Health and Nutrition Examination Survey of 1,537 participants, aged 65 years and older, found that sarcopenia is independently associated with cardiovascular disease (PLoS One. 2013 Mar 22. doi: 10.1371/journal.pone.0060119). Most of the risk factors for cardiovascular disease – such as age, waist circumference, body mass index, fasting plasma glucose, and total cholesterol – showed significant negative correlations with the ratio between appendicular skeletal muscle mass and body weight. Multiple logistic regression analysis demonstrated that sarcopenia was associated with cardiovascular disease, independent of other well-documented risk factors, renal function, and medications (odds ratio, 1.77; P = .025).
In addition, data from the British Regional Heart Study, which followed 4,252 older men for a mean of 11.3 years, found an association of sarcopenia and adiposity with cardiovascular mortality and all-cause mortality (J Am Geriatr Soc. 2014;62[2]:253-60). Specifically, all-cause mortality risk was significantly greater in men in the sarcopenic and obese groups (HRs, 1.41 and 1.21, respectively), compared with those in the optimal reference group, with the highest risk in sarcopenic obese individuals (HR, 1.72) after adjustment for lifestyle characteristics.
“Diabetes also accelerates loss of lean body mass in older adults,” added Dr. Volpi. “Data from the Health ABC study showed that individuals who did not have diabetes at the beginning of the 6-year observation period ... lost the least amount of muscle, compared with those who had undiagnosed or already diagnosed diabetes.”
The precise way in which sarcopenia is linked to metabolic disease remains elusive, she continued, but current evidence suggests that sarcopenia is characterized by a reduction in the protein synthetic response to metabolic stimulation by amino acids, exercise, and insulin in skeletal muscle. “This reduction in the anabolic response to protein synthesis is called anabolic resistance of aging, and it is mediated by reduced acute activation of mTORC1 [mTOR complex 1] signaling,” Dr. Volpi said. “There’s another step upstream of the mTORC1, in which the amino acids and insulin have to cross the blood-muscle barrier. Amino acids need to be transported into the muscle actively, like glucose. That is an important unexplored area that may contribute to sarcopenia.”
Dr. Volpi went on to note that endothelial dysfunction underlies muscle anabolic resistance and cardiovascular risk and is likely to be a fundamental cause of both problems. Recent studies have shown that increased levels of physical activity improve endothelial function, enhance insulin sensitivity and anabolic sensitivity to nutrients, and reduce cardiovascular risk.
For example, in a cohort of 45 nonfrail older adults with a mean age of 72 years, Dr. Volpi and colleagues carried out a phase 1, double-blind, placebo-controlled, randomized clinical trial to determine if chronic essential amino acid supplementation, aerobic exercise training, or a combination of the two interventions could improve muscle mass and function by stimulating muscle protein synthesis over the course of 24 weeks (J Gerontol A Biol Sci Med Sci. 2019;74[10]:1598-604). “We found that exercise supervised three times per week on a treadmill for 6 months improved physical function in both groups randomized to exercise,” Dr. Volpi said. “Disappointingly, there was no change in total lean mass with any of the interventions. There was a decrease in fat mass with exercise alone, and no change with exercise and amino acids. [Of note is that] the individuals who were randomized to the amino acids plus exercise group had a significant increase in leg strength, whereas the others did not.”
Preliminary findings from ongoing work by Dr. Volpi and colleagues suggest that, in diabetes, muscle protein synthesis and blood flow really “are not different in response to insulin in healthy older adults and diabetic older adults because they don’t change at all. However, we did find alterations in amino acid trafficking in diabetes. We found that older individuals with type 2 diabetes had a reduction of amino acid transport and a higher intracellular amino acid concentration, compared with age-matched, healthier individuals. The intracellular amino acid clearance improved in the healthy, nondiabetic older adults with hyperinsulinemia, whereas it did not change in diabetic older adults. As a result, the net muscle protein balance improved a little in the nondiabetic patients, but did not change in the diabetic patients.”
The researchers are evaluating older patients with type 2 diabetes to see whether there are alterations in vascular reactivity and protein synthesis and whether those can be overcome by resistance-exercise training. “Preliminary results show that flow-mediated dilation can actually increase in an older diabetic patient with resistance exercise training three times a week for 3 months,” she said. “Exercise can improve both endothelial dysfunction and sarcopenia and therefore improve physical function and reduce cardiovascular risk.”
Dr. Volpi reported having no relevant disclosures.
LOS ANGELES –
“Loss of lean body mass and function with aging decreases the amount of metabolically active tissue, which can lead to insulin resistance,” Elena Volpi, MD, said at the World Congress on Insulin Resistance, Diabetes and Cardiovascular Disease. “Insulin resistance reduces muscle protein anabolism and accelerates sarcopenia, perpetuating a vicious cycle.”
Sarcopenia, the involuntary loss of muscle mass and function that occurs with aging, is an ICD-10 codable condition that can be diagnosed by measuring muscle strength and quality, said Dr. Volpi, director of the Sealy Center on Aging at the University of Texas Medical Branch at Galveston. In the Health, Aging and Body Composition Study (Health ABC), researchers followed 2,292 relatively healthy adults aged 70-79 years for an average of 4.9 years (J Gerontol A Biol Sci Med. 2006;61[1]:72-7). The researchers used isokinetic dynamometry to measure knee extension strength, isometric dynamometry to measure grip strength, CT scan to measure thigh muscle area, and dual X-ray absorptiometry to determine leg and arm lean soft-tissue mass. “Those individuals who started with the highest levels of muscle strength had the greatest survival, while those who had the lowest levels of muscle strength died earlier,” said Dr. Volpi, who was not affiliated with the study. “That was true for both men and women.”
More recently, researchers conducted a pooled analysis of nine cohort studies involving 34,485 community-dwelling older individuals who were tested with gait speed and followed for 6-21 years (JAMA. 2011;305[1]:50-8). They found that a higher gait speed was associated with higher survival at 5 and 10 years (P less than .001). “Muscle mass also appears to be associated in part with mortality and survival, although the association is not as strong as measures of strength and gait speed,” Dr. Volpi said.
Data from the 2009 Korea National Health and Nutrition Examination Survey of 1,537 participants, aged 65 years and older, found that sarcopenia is independently associated with cardiovascular disease (PLoS One. 2013 Mar 22. doi: 10.1371/journal.pone.0060119). Most of the risk factors for cardiovascular disease – such as age, waist circumference, body mass index, fasting plasma glucose, and total cholesterol – showed significant negative correlations with the ratio between appendicular skeletal muscle mass and body weight. Multiple logistic regression analysis demonstrated that sarcopenia was associated with cardiovascular disease, independent of other well-documented risk factors, renal function, and medications (odds ratio, 1.77; P = .025).
In addition, data from the British Regional Heart Study, which followed 4,252 older men for a mean of 11.3 years, found an association of sarcopenia and adiposity with cardiovascular mortality and all-cause mortality (J Am Geriatr Soc. 2014;62[2]:253-60). Specifically, all-cause mortality risk was significantly greater in men in the sarcopenic and obese groups (HRs, 1.41 and 1.21, respectively), compared with those in the optimal reference group, with the highest risk in sarcopenic obese individuals (HR, 1.72) after adjustment for lifestyle characteristics.
“Diabetes also accelerates loss of lean body mass in older adults,” added Dr. Volpi. “Data from the Health ABC study showed that individuals who did not have diabetes at the beginning of the 6-year observation period ... lost the least amount of muscle, compared with those who had undiagnosed or already diagnosed diabetes.”
The precise way in which sarcopenia is linked to metabolic disease remains elusive, she continued, but current evidence suggests that sarcopenia is characterized by a reduction in the protein synthetic response to metabolic stimulation by amino acids, exercise, and insulin in skeletal muscle. “This reduction in the anabolic response to protein synthesis is called anabolic resistance of aging, and it is mediated by reduced acute activation of mTORC1 [mTOR complex 1] signaling,” Dr. Volpi said. “There’s another step upstream of the mTORC1, in which the amino acids and insulin have to cross the blood-muscle barrier. Amino acids need to be transported into the muscle actively, like glucose. That is an important unexplored area that may contribute to sarcopenia.”
Dr. Volpi went on to note that endothelial dysfunction underlies muscle anabolic resistance and cardiovascular risk and is likely to be a fundamental cause of both problems. Recent studies have shown that increased levels of physical activity improve endothelial function, enhance insulin sensitivity and anabolic sensitivity to nutrients, and reduce cardiovascular risk.
For example, in a cohort of 45 nonfrail older adults with a mean age of 72 years, Dr. Volpi and colleagues carried out a phase 1, double-blind, placebo-controlled, randomized clinical trial to determine if chronic essential amino acid supplementation, aerobic exercise training, or a combination of the two interventions could improve muscle mass and function by stimulating muscle protein synthesis over the course of 24 weeks (J Gerontol A Biol Sci Med Sci. 2019;74[10]:1598-604). “We found that exercise supervised three times per week on a treadmill for 6 months improved physical function in both groups randomized to exercise,” Dr. Volpi said. “Disappointingly, there was no change in total lean mass with any of the interventions. There was a decrease in fat mass with exercise alone, and no change with exercise and amino acids. [Of note is that] the individuals who were randomized to the amino acids plus exercise group had a significant increase in leg strength, whereas the others did not.”
Preliminary findings from ongoing work by Dr. Volpi and colleagues suggest that, in diabetes, muscle protein synthesis and blood flow really “are not different in response to insulin in healthy older adults and diabetic older adults because they don’t change at all. However, we did find alterations in amino acid trafficking in diabetes. We found that older individuals with type 2 diabetes had a reduction of amino acid transport and a higher intracellular amino acid concentration, compared with age-matched, healthier individuals. The intracellular amino acid clearance improved in the healthy, nondiabetic older adults with hyperinsulinemia, whereas it did not change in diabetic older adults. As a result, the net muscle protein balance improved a little in the nondiabetic patients, but did not change in the diabetic patients.”
The researchers are evaluating older patients with type 2 diabetes to see whether there are alterations in vascular reactivity and protein synthesis and whether those can be overcome by resistance-exercise training. “Preliminary results show that flow-mediated dilation can actually increase in an older diabetic patient with resistance exercise training three times a week for 3 months,” she said. “Exercise can improve both endothelial dysfunction and sarcopenia and therefore improve physical function and reduce cardiovascular risk.”
Dr. Volpi reported having no relevant disclosures.
EXPERT ANALYSIS FROM WCIRDC 2019
The power and promise of person-generated health data – part 1
The time shared during clinical encounters provides small peeks into patients’ lives that get documented as episodic snapshots in electronic health records. But there is little information about how patients are doing outside of the office. With increasing emphasis on filling out mandatory parts of the EHR, there is less time available for in-depth, in-office conversations and phone follow-ups.
At the same time, it has become clear that it is not just the medicines we prescribe that affect our patients’ lives. Their behaviors outside of the office – being physically active, eating well, getting a good night’s rest, and adhering to medications – also impact their health outcomes.
The explosion of technology and personal data in our increasingly connected world provides powerful new sources of health and behavior information that generate new understanding of patients’ lives in their everyday settings.
The ubiquity and remarkable technological progress of personal computing devices – including wearables, smartphones, and tablets – along with the multitude of sensor modalities embedded within these devices, has enabled us to establish a continuous connection with people who want to share information about their behavior and daily life.
Such rich, longitudinal information, known as person-generated health data (PGHD), can be searched for physiological and behavioral signatures that can be used in combination with traditional clinical information to predict, diagnose, and treat disease. It can also be used to understand the safety and effectiveness of medical interventions.
PGHD is defined as wellness and/or health-related data created, recorded, or gathered by individuals. It reflects events and interactions that occur during an person’s everyday life. Systematically gathering this information and organizing it to better understand patients’ approach to their health or their unique experience living with disease provides meaningful insights that complement the data traditionally collected as part of clinical trials or periodic office visits.
PGHD can produce a rich picture of a person’s health or symptom burden with disease. It allows the opportunity to measure the real human burden of a patient’s disease and how it changes over time, with an opportunity to detect changes in symptoms in real time.
PGHD can also enable participation in health research.
An example would be the work of Evidation Health in San Mateo, Calif. Evidation provides a platform to run research studies utilizing technology and systems to measure health in everyday life. Its app, Achievement, collects continuous behavior-related data from smartphones, wearables, connected devices, and apps. That provides opportunities for participants to join research studies that develop novel measures designed to quantify health outcomes in a way that more accurately reflects an individual’s day-to-day activities and experience. All data collected are at the direction of and with the permission of the individual.
“Achievers” are given points for taking health-related actions such as tracking steps or their sleep, which convert to cash that can be kept or donated to their favorite charities. Achievement’s 3.5 million diverse participants also receive offers to join research studies. This paradigm shift dramatically expands access to research to increase diversity, shortens the time to first data through rapid recruitment, and enhances retention rates by making it easier to engage. To date, more than 1 million users have chosen to participate in research studies. The technology is bringing new data and insights to health research; it supports important questions about quality of life, medical products’ real-world effectiveness, and the development of hyperpersonalized health care services.
This new type of data is transforming medical research by creating real-world studies of unprecedented size, such as the Apple Heart Study – a virtual study with more than 400,000 enrolled participants – which was designed to test the accuracy of Apple Watches in safely identifying atrial fibrillation. The FDA has cleared two features on the Apple Watch: the device’s ability to detect and notify the user of an irregular heart rhythm, and the ability to take a single-lead EKG feature that can provide a rhythm strip for a clinician to review.
The FDA clearance letters specify that the apps are “not intended to replace traditional methods of diagnosis or treatment.” They provide extra information, and that information might be helpful – but the apps won’t replace a doctor’s visit. It remains to be seen how these data will be used, but they have the potential to identify atrial fibrillation early, leading to treatment that may prevent devastating strokes.
Another example of home-generated health data is a tool that has obtained FDA clearance as a diagnostic device with insurance reimbursement: WatchPAT, a portable sleep apnea diagnostic device. WatchPAT is worn like a simple wristwatch, with no need for belts, wires, or nasal cannulas.
Over time, in-home tests like these that are of minimal inconvenience to the patient and reflect a real-world experience may eclipse traditional sleep studies that require patients to spend the night in a clinic while attached to wires and monitors.
Health data generated by connected populations will yield novel insights that may help us better predict, diagnose, and treat disease. These are examples of innovations that can extend clinicians’ abilities to remotely monitor or diagnose health conditions, and we can expect that more will continue to be integrated into the clinical and research settings in the near future.
In part 2 of this series, we will discuss novel digital measures and studies utilizing PGHD to impact population health.
Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and associate director, family medicine residency program, Abington (Pa.) Jefferson Health. Dr. Foschini is cofounder and chief data scientist at Evidation Health in San Mateo, Calif. Bray Patrick-Lake is a patient thought leader and director, strategic partnerships, at Evidation Health.
References
Determining real-world data’s fitness for use and the role of reliability, September 2019. Duke-Margolis Center for Health Policy.
N Engl J Med. 2019 Nov 14;381(20):1909-17.
The time shared during clinical encounters provides small peeks into patients’ lives that get documented as episodic snapshots in electronic health records. But there is little information about how patients are doing outside of the office. With increasing emphasis on filling out mandatory parts of the EHR, there is less time available for in-depth, in-office conversations and phone follow-ups.
At the same time, it has become clear that it is not just the medicines we prescribe that affect our patients’ lives. Their behaviors outside of the office – being physically active, eating well, getting a good night’s rest, and adhering to medications – also impact their health outcomes.
The explosion of technology and personal data in our increasingly connected world provides powerful new sources of health and behavior information that generate new understanding of patients’ lives in their everyday settings.
The ubiquity and remarkable technological progress of personal computing devices – including wearables, smartphones, and tablets – along with the multitude of sensor modalities embedded within these devices, has enabled us to establish a continuous connection with people who want to share information about their behavior and daily life.
Such rich, longitudinal information, known as person-generated health data (PGHD), can be searched for physiological and behavioral signatures that can be used in combination with traditional clinical information to predict, diagnose, and treat disease. It can also be used to understand the safety and effectiveness of medical interventions.
PGHD is defined as wellness and/or health-related data created, recorded, or gathered by individuals. It reflects events and interactions that occur during an person’s everyday life. Systematically gathering this information and organizing it to better understand patients’ approach to their health or their unique experience living with disease provides meaningful insights that complement the data traditionally collected as part of clinical trials or periodic office visits.
PGHD can produce a rich picture of a person’s health or symptom burden with disease. It allows the opportunity to measure the real human burden of a patient’s disease and how it changes over time, with an opportunity to detect changes in symptoms in real time.
PGHD can also enable participation in health research.
An example would be the work of Evidation Health in San Mateo, Calif. Evidation provides a platform to run research studies utilizing technology and systems to measure health in everyday life. Its app, Achievement, collects continuous behavior-related data from smartphones, wearables, connected devices, and apps. That provides opportunities for participants to join research studies that develop novel measures designed to quantify health outcomes in a way that more accurately reflects an individual’s day-to-day activities and experience. All data collected are at the direction of and with the permission of the individual.
“Achievers” are given points for taking health-related actions such as tracking steps or their sleep, which convert to cash that can be kept or donated to their favorite charities. Achievement’s 3.5 million diverse participants also receive offers to join research studies. This paradigm shift dramatically expands access to research to increase diversity, shortens the time to first data through rapid recruitment, and enhances retention rates by making it easier to engage. To date, more than 1 million users have chosen to participate in research studies. The technology is bringing new data and insights to health research; it supports important questions about quality of life, medical products’ real-world effectiveness, and the development of hyperpersonalized health care services.
This new type of data is transforming medical research by creating real-world studies of unprecedented size, such as the Apple Heart Study – a virtual study with more than 400,000 enrolled participants – which was designed to test the accuracy of Apple Watches in safely identifying atrial fibrillation. The FDA has cleared two features on the Apple Watch: the device’s ability to detect and notify the user of an irregular heart rhythm, and the ability to take a single-lead EKG feature that can provide a rhythm strip for a clinician to review.
The FDA clearance letters specify that the apps are “not intended to replace traditional methods of diagnosis or treatment.” They provide extra information, and that information might be helpful – but the apps won’t replace a doctor’s visit. It remains to be seen how these data will be used, but they have the potential to identify atrial fibrillation early, leading to treatment that may prevent devastating strokes.
Another example of home-generated health data is a tool that has obtained FDA clearance as a diagnostic device with insurance reimbursement: WatchPAT, a portable sleep apnea diagnostic device. WatchPAT is worn like a simple wristwatch, with no need for belts, wires, or nasal cannulas.
Over time, in-home tests like these that are of minimal inconvenience to the patient and reflect a real-world experience may eclipse traditional sleep studies that require patients to spend the night in a clinic while attached to wires and monitors.
Health data generated by connected populations will yield novel insights that may help us better predict, diagnose, and treat disease. These are examples of innovations that can extend clinicians’ abilities to remotely monitor or diagnose health conditions, and we can expect that more will continue to be integrated into the clinical and research settings in the near future.
In part 2 of this series, we will discuss novel digital measures and studies utilizing PGHD to impact population health.
Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and associate director, family medicine residency program, Abington (Pa.) Jefferson Health. Dr. Foschini is cofounder and chief data scientist at Evidation Health in San Mateo, Calif. Bray Patrick-Lake is a patient thought leader and director, strategic partnerships, at Evidation Health.
References
Determining real-world data’s fitness for use and the role of reliability, September 2019. Duke-Margolis Center for Health Policy.
N Engl J Med. 2019 Nov 14;381(20):1909-17.
The time shared during clinical encounters provides small peeks into patients’ lives that get documented as episodic snapshots in electronic health records. But there is little information about how patients are doing outside of the office. With increasing emphasis on filling out mandatory parts of the EHR, there is less time available for in-depth, in-office conversations and phone follow-ups.
At the same time, it has become clear that it is not just the medicines we prescribe that affect our patients’ lives. Their behaviors outside of the office – being physically active, eating well, getting a good night’s rest, and adhering to medications – also impact their health outcomes.
The explosion of technology and personal data in our increasingly connected world provides powerful new sources of health and behavior information that generate new understanding of patients’ lives in their everyday settings.
The ubiquity and remarkable technological progress of personal computing devices – including wearables, smartphones, and tablets – along with the multitude of sensor modalities embedded within these devices, has enabled us to establish a continuous connection with people who want to share information about their behavior and daily life.
Such rich, longitudinal information, known as person-generated health data (PGHD), can be searched for physiological and behavioral signatures that can be used in combination with traditional clinical information to predict, diagnose, and treat disease. It can also be used to understand the safety and effectiveness of medical interventions.
PGHD is defined as wellness and/or health-related data created, recorded, or gathered by individuals. It reflects events and interactions that occur during an person’s everyday life. Systematically gathering this information and organizing it to better understand patients’ approach to their health or their unique experience living with disease provides meaningful insights that complement the data traditionally collected as part of clinical trials or periodic office visits.
PGHD can produce a rich picture of a person’s health or symptom burden with disease. It allows the opportunity to measure the real human burden of a patient’s disease and how it changes over time, with an opportunity to detect changes in symptoms in real time.
PGHD can also enable participation in health research.
An example would be the work of Evidation Health in San Mateo, Calif. Evidation provides a platform to run research studies utilizing technology and systems to measure health in everyday life. Its app, Achievement, collects continuous behavior-related data from smartphones, wearables, connected devices, and apps. That provides opportunities for participants to join research studies that develop novel measures designed to quantify health outcomes in a way that more accurately reflects an individual’s day-to-day activities and experience. All data collected are at the direction of and with the permission of the individual.
“Achievers” are given points for taking health-related actions such as tracking steps or their sleep, which convert to cash that can be kept or donated to their favorite charities. Achievement’s 3.5 million diverse participants also receive offers to join research studies. This paradigm shift dramatically expands access to research to increase diversity, shortens the time to first data through rapid recruitment, and enhances retention rates by making it easier to engage. To date, more than 1 million users have chosen to participate in research studies. The technology is bringing new data and insights to health research; it supports important questions about quality of life, medical products’ real-world effectiveness, and the development of hyperpersonalized health care services.
This new type of data is transforming medical research by creating real-world studies of unprecedented size, such as the Apple Heart Study – a virtual study with more than 400,000 enrolled participants – which was designed to test the accuracy of Apple Watches in safely identifying atrial fibrillation. The FDA has cleared two features on the Apple Watch: the device’s ability to detect and notify the user of an irregular heart rhythm, and the ability to take a single-lead EKG feature that can provide a rhythm strip for a clinician to review.
The FDA clearance letters specify that the apps are “not intended to replace traditional methods of diagnosis or treatment.” They provide extra information, and that information might be helpful – but the apps won’t replace a doctor’s visit. It remains to be seen how these data will be used, but they have the potential to identify atrial fibrillation early, leading to treatment that may prevent devastating strokes.
Another example of home-generated health data is a tool that has obtained FDA clearance as a diagnostic device with insurance reimbursement: WatchPAT, a portable sleep apnea diagnostic device. WatchPAT is worn like a simple wristwatch, with no need for belts, wires, or nasal cannulas.
Over time, in-home tests like these that are of minimal inconvenience to the patient and reflect a real-world experience may eclipse traditional sleep studies that require patients to spend the night in a clinic while attached to wires and monitors.
Health data generated by connected populations will yield novel insights that may help us better predict, diagnose, and treat disease. These are examples of innovations that can extend clinicians’ abilities to remotely monitor or diagnose health conditions, and we can expect that more will continue to be integrated into the clinical and research settings in the near future.
In part 2 of this series, we will discuss novel digital measures and studies utilizing PGHD to impact population health.
Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Thomas Jefferson University, Philadelphia, and associate director, family medicine residency program, Abington (Pa.) Jefferson Health. Dr. Foschini is cofounder and chief data scientist at Evidation Health in San Mateo, Calif. Bray Patrick-Lake is a patient thought leader and director, strategic partnerships, at Evidation Health.
References
Determining real-world data’s fitness for use and the role of reliability, September 2019. Duke-Margolis Center for Health Policy.
N Engl J Med. 2019 Nov 14;381(20):1909-17.