User login
Cardiology News is an independent news source that provides cardiologists with timely and relevant news and commentary about clinical developments and the impact of health care policy on cardiology and the cardiologist's practice. Cardiology News Digital Network is the online destination and multimedia properties of Cardiology News, the independent news publication for cardiologists. Cardiology news is the leading source of news and commentary about clinical developments in cardiology as well as health care policy and regulations that affect the cardiologist's practice. Cardiology News Digital Network is owned by Frontline Medical Communications.
Cardiac symptoms can be first sign of COVID-19
In about 7% of people with confirmed novel coronavirus disease 2019 (COVID-19), and 22% of the critically ill, the virus injures the heart, probably by either attacking it directly or causing a cytokine storm that leads to myocyte apoptosis, according to a report from the Columbia University Division of Cardiology in New York.
Reports from China document patients presenting with palpitations and chest pain without the typical fever and cough.
The exact mechanism of injury is uncertain, but for now, “it appears that the incidence of fulminant myocarditis and profound cardiogenic shock is low; however, the rate of recovery and mode of treatment are yet to be determined,” wrote authors led by Kevin Clerkin, MD, a cardiologist and assistant professor of medicine at Columbia.
High-sensitivity cardiac troponin I (hs-cTnI) might be prognostic. In one Chinese study of hospitalized patients, median hs-cTnI levels were 2.5 pg/mL in survivors on day 4 of symptoms and did not change significantly during follow-up. Among people who died, day 4 hs-cTnI was 8.8 pg/mL and climbed to 290.6 pg/mL by day 22.
“The rise in hs-cTnI tracks with other inflammatory biomarkers ... raising the possibility that this reflects cytokine storm or secondary hemophagocytic lymphohistiocytosis more than isolated myocardial injury,” Dr. Clerkin and colleagues wrote.
But there are also acute heart injury reports out of China, including one man who presented with chest pain and ST-segment elevation, but no coronary obstruction, and another who presented with fulminant myocarditis in addition to severe respiratory manifestations, but with no cardiac history.
Both had depressed left ventricular ejection fractions, enlarged left ventricles, and elevated cardiac biomarkers, and both responded to intravenous immunoglobulin and steroids, among other treatments.
Amid a surge of COVID-19 cases at Columbia, “we have seen both forms of cardiac presentations: those presenting with cardiac predominant symptoms (none have had true [ST-segment elevation myocardial infarctions] yet, but most fall in the myopericarditis group), some of which have required mechanical circulatory support, and those who seem to have secondary myocardial injury with globally elevated inflammatory biomarkers (e.g., ferritin, interleukin-6, lactate dehydrogenase, hs-cTnI, and D-dimer),” Dr. Clerkin said in an interview.
“We are discussing each of these cases in a multidisciplinary fashion with our infectious disease, pulmonary, interventional cardiology, and cardiac surgery colleagues to try to make the best decision based on what we know and as our knowledge evolves,” he said.
The exact cardiac effect of COVID-19 is unknown for now, but it is known already that it rides along with cardiovascular issues. There’s a high prevalence of hypertension, diabetes, and diagnosed cardiovascular disease among patients, but it’s unclear at this point if it’s because the virus favors older people who happen to be more likely to have those problems or if it attacks people with those conditions preferentially.
It might be the latter. The virus that causes COVID-19, severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), invades cells through angiotensin converting enzyme (ACE) 2 receptors, which are highly expressed in the heart.
That raises the question of whether ACE inhibitors or angiotensin receptor blockers might help. However, “at this time, nearly all major societies have recommended against adding or stopping ... antagonists in this setting, unless done on clinical grounds independently of COVID-19, given the lack of evidence,” Dr. Clerkin and his colleagues wrote.
As for heart transplants, the current thinking is to continue them without changes in immunosuppression so long as recipients test negative and haven’t been around anyone who has tested positive for a month. If a donor had COVID-19, they should have been free of the virus by polymerase chain reaction for at least 14 days. The concern is that it might be in the donor heart.
If transplant patients come down with COVID-19, the “data to date [indicate that management] is supportive care and continuation of immunosuppression for mild COVID-19 with reduction of the antimetabolite (mycophenolate or azathioprine), and further treatment based on disease severity and drug availability. Notably, one potential treatment option for COVID-19 is protease inhibitors,” the authors said, but it’s important to remember that they will increase the levels of cyclosporine, tacrolimus, and other calcineurin inhibitor transplant drugs.
At Columbia, “our processes have been adjusted” for heart transplants. “For instance, non-urgent testing (pre- and post-transplant) has been tabled, we have predominantly shifted to noninvasive screening for rejection, and each potential transplant requires more scrutiny for urgency, donor screening/risk for COVID-19, and perioperative management,” Dr. Clerkin said in the interview.
A study out of Wuhan, China, the outbreak epicenter, was reassuring. It found that routine prevention efforts were enough to protect heart transplant patients.
There was no funding, and the authors had no disclosures.
SOURCE: Clerkin KJ et al. Circulation. 2020 Mar 21. doi: 10.1161/CIRCULATIONAHA.120.046941
In about 7% of people with confirmed novel coronavirus disease 2019 (COVID-19), and 22% of the critically ill, the virus injures the heart, probably by either attacking it directly or causing a cytokine storm that leads to myocyte apoptosis, according to a report from the Columbia University Division of Cardiology in New York.
Reports from China document patients presenting with palpitations and chest pain without the typical fever and cough.
The exact mechanism of injury is uncertain, but for now, “it appears that the incidence of fulminant myocarditis and profound cardiogenic shock is low; however, the rate of recovery and mode of treatment are yet to be determined,” wrote authors led by Kevin Clerkin, MD, a cardiologist and assistant professor of medicine at Columbia.
High-sensitivity cardiac troponin I (hs-cTnI) might be prognostic. In one Chinese study of hospitalized patients, median hs-cTnI levels were 2.5 pg/mL in survivors on day 4 of symptoms and did not change significantly during follow-up. Among people who died, day 4 hs-cTnI was 8.8 pg/mL and climbed to 290.6 pg/mL by day 22.
“The rise in hs-cTnI tracks with other inflammatory biomarkers ... raising the possibility that this reflects cytokine storm or secondary hemophagocytic lymphohistiocytosis more than isolated myocardial injury,” Dr. Clerkin and colleagues wrote.
But there are also acute heart injury reports out of China, including one man who presented with chest pain and ST-segment elevation, but no coronary obstruction, and another who presented with fulminant myocarditis in addition to severe respiratory manifestations, but with no cardiac history.
Both had depressed left ventricular ejection fractions, enlarged left ventricles, and elevated cardiac biomarkers, and both responded to intravenous immunoglobulin and steroids, among other treatments.
Amid a surge of COVID-19 cases at Columbia, “we have seen both forms of cardiac presentations: those presenting with cardiac predominant symptoms (none have had true [ST-segment elevation myocardial infarctions] yet, but most fall in the myopericarditis group), some of which have required mechanical circulatory support, and those who seem to have secondary myocardial injury with globally elevated inflammatory biomarkers (e.g., ferritin, interleukin-6, lactate dehydrogenase, hs-cTnI, and D-dimer),” Dr. Clerkin said in an interview.
“We are discussing each of these cases in a multidisciplinary fashion with our infectious disease, pulmonary, interventional cardiology, and cardiac surgery colleagues to try to make the best decision based on what we know and as our knowledge evolves,” he said.
The exact cardiac effect of COVID-19 is unknown for now, but it is known already that it rides along with cardiovascular issues. There’s a high prevalence of hypertension, diabetes, and diagnosed cardiovascular disease among patients, but it’s unclear at this point if it’s because the virus favors older people who happen to be more likely to have those problems or if it attacks people with those conditions preferentially.
It might be the latter. The virus that causes COVID-19, severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), invades cells through angiotensin converting enzyme (ACE) 2 receptors, which are highly expressed in the heart.
That raises the question of whether ACE inhibitors or angiotensin receptor blockers might help. However, “at this time, nearly all major societies have recommended against adding or stopping ... antagonists in this setting, unless done on clinical grounds independently of COVID-19, given the lack of evidence,” Dr. Clerkin and his colleagues wrote.
As for heart transplants, the current thinking is to continue them without changes in immunosuppression so long as recipients test negative and haven’t been around anyone who has tested positive for a month. If a donor had COVID-19, they should have been free of the virus by polymerase chain reaction for at least 14 days. The concern is that it might be in the donor heart.
If transplant patients come down with COVID-19, the “data to date [indicate that management] is supportive care and continuation of immunosuppression for mild COVID-19 with reduction of the antimetabolite (mycophenolate or azathioprine), and further treatment based on disease severity and drug availability. Notably, one potential treatment option for COVID-19 is protease inhibitors,” the authors said, but it’s important to remember that they will increase the levels of cyclosporine, tacrolimus, and other calcineurin inhibitor transplant drugs.
At Columbia, “our processes have been adjusted” for heart transplants. “For instance, non-urgent testing (pre- and post-transplant) has been tabled, we have predominantly shifted to noninvasive screening for rejection, and each potential transplant requires more scrutiny for urgency, donor screening/risk for COVID-19, and perioperative management,” Dr. Clerkin said in the interview.
A study out of Wuhan, China, the outbreak epicenter, was reassuring. It found that routine prevention efforts were enough to protect heart transplant patients.
There was no funding, and the authors had no disclosures.
SOURCE: Clerkin KJ et al. Circulation. 2020 Mar 21. doi: 10.1161/CIRCULATIONAHA.120.046941
In about 7% of people with confirmed novel coronavirus disease 2019 (COVID-19), and 22% of the critically ill, the virus injures the heart, probably by either attacking it directly or causing a cytokine storm that leads to myocyte apoptosis, according to a report from the Columbia University Division of Cardiology in New York.
Reports from China document patients presenting with palpitations and chest pain without the typical fever and cough.
The exact mechanism of injury is uncertain, but for now, “it appears that the incidence of fulminant myocarditis and profound cardiogenic shock is low; however, the rate of recovery and mode of treatment are yet to be determined,” wrote authors led by Kevin Clerkin, MD, a cardiologist and assistant professor of medicine at Columbia.
High-sensitivity cardiac troponin I (hs-cTnI) might be prognostic. In one Chinese study of hospitalized patients, median hs-cTnI levels were 2.5 pg/mL in survivors on day 4 of symptoms and did not change significantly during follow-up. Among people who died, day 4 hs-cTnI was 8.8 pg/mL and climbed to 290.6 pg/mL by day 22.
“The rise in hs-cTnI tracks with other inflammatory biomarkers ... raising the possibility that this reflects cytokine storm or secondary hemophagocytic lymphohistiocytosis more than isolated myocardial injury,” Dr. Clerkin and colleagues wrote.
But there are also acute heart injury reports out of China, including one man who presented with chest pain and ST-segment elevation, but no coronary obstruction, and another who presented with fulminant myocarditis in addition to severe respiratory manifestations, but with no cardiac history.
Both had depressed left ventricular ejection fractions, enlarged left ventricles, and elevated cardiac biomarkers, and both responded to intravenous immunoglobulin and steroids, among other treatments.
Amid a surge of COVID-19 cases at Columbia, “we have seen both forms of cardiac presentations: those presenting with cardiac predominant symptoms (none have had true [ST-segment elevation myocardial infarctions] yet, but most fall in the myopericarditis group), some of which have required mechanical circulatory support, and those who seem to have secondary myocardial injury with globally elevated inflammatory biomarkers (e.g., ferritin, interleukin-6, lactate dehydrogenase, hs-cTnI, and D-dimer),” Dr. Clerkin said in an interview.
“We are discussing each of these cases in a multidisciplinary fashion with our infectious disease, pulmonary, interventional cardiology, and cardiac surgery colleagues to try to make the best decision based on what we know and as our knowledge evolves,” he said.
The exact cardiac effect of COVID-19 is unknown for now, but it is known already that it rides along with cardiovascular issues. There’s a high prevalence of hypertension, diabetes, and diagnosed cardiovascular disease among patients, but it’s unclear at this point if it’s because the virus favors older people who happen to be more likely to have those problems or if it attacks people with those conditions preferentially.
It might be the latter. The virus that causes COVID-19, severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2), invades cells through angiotensin converting enzyme (ACE) 2 receptors, which are highly expressed in the heart.
That raises the question of whether ACE inhibitors or angiotensin receptor blockers might help. However, “at this time, nearly all major societies have recommended against adding or stopping ... antagonists in this setting, unless done on clinical grounds independently of COVID-19, given the lack of evidence,” Dr. Clerkin and his colleagues wrote.
As for heart transplants, the current thinking is to continue them without changes in immunosuppression so long as recipients test negative and haven’t been around anyone who has tested positive for a month. If a donor had COVID-19, they should have been free of the virus by polymerase chain reaction for at least 14 days. The concern is that it might be in the donor heart.
If transplant patients come down with COVID-19, the “data to date [indicate that management] is supportive care and continuation of immunosuppression for mild COVID-19 with reduction of the antimetabolite (mycophenolate or azathioprine), and further treatment based on disease severity and drug availability. Notably, one potential treatment option for COVID-19 is protease inhibitors,” the authors said, but it’s important to remember that they will increase the levels of cyclosporine, tacrolimus, and other calcineurin inhibitor transplant drugs.
At Columbia, “our processes have been adjusted” for heart transplants. “For instance, non-urgent testing (pre- and post-transplant) has been tabled, we have predominantly shifted to noninvasive screening for rejection, and each potential transplant requires more scrutiny for urgency, donor screening/risk for COVID-19, and perioperative management,” Dr. Clerkin said in the interview.
A study out of Wuhan, China, the outbreak epicenter, was reassuring. It found that routine prevention efforts were enough to protect heart transplant patients.
There was no funding, and the authors had no disclosures.
SOURCE: Clerkin KJ et al. Circulation. 2020 Mar 21. doi: 10.1161/CIRCULATIONAHA.120.046941
FROM CIRCULATION
At U.S. Ground Zero for coronavirus, a hospital is transformed
David Baker, MD, a hospitalist at EvergreenHealth in Kirkland, Wash., had just come off a 7-day stretch of work and was early into his usual 7 days off. He’d helped care for some patients from a nearby assisted living facility who had been admitted with puzzlingly severe viral pneumonia that wasn’t influenza.
Though COVID-19, the novel coronavirus that was sickening tens of thousands in the Chinese province of Hubei, was in the back of everyone’s mind in late February, he said he wasn’t really expecting the call notifying him that two of the patients with pneumonia had tested positive for COVID-19.
Michael Chu, MD, was coming onto EvergreenHealth’s hospitalist service at about the time Dr. Baker was rotating off. He recalled learning of the first two positive COVID-19 tests on the evening of Feb. 28 – a Friday. He and his colleagues took in this information, coming to the realization that they were seeing other patients from the same facility who had viral pneumonia and negative influenza tests. “The first cohort of coronavirus patients all came from Life Care,” the Kirkland assisted living facility that was the epicenter of the first identified U.S. outbreak of community-transmitted coronavirus, said Dr. Chu. “They all fit a clinical syndrome” and many of them were critically ill or failing fast, since they were aged and with multiple risk factors, he said during the interviews he and his colleagues participated in.
As he processed the news of the positive tests and his inadvertent exposure to COVID-19, Dr. Baker realized that his duty schedule worked in his favor, since he wasn’t expected back for several more days. When he did come back to work after remaining asymptomatic, he found a much-changed environment as the coronavirus cases poured in and continual adaptations were made to accommodate these patients – and to keep staff and other patients safe.
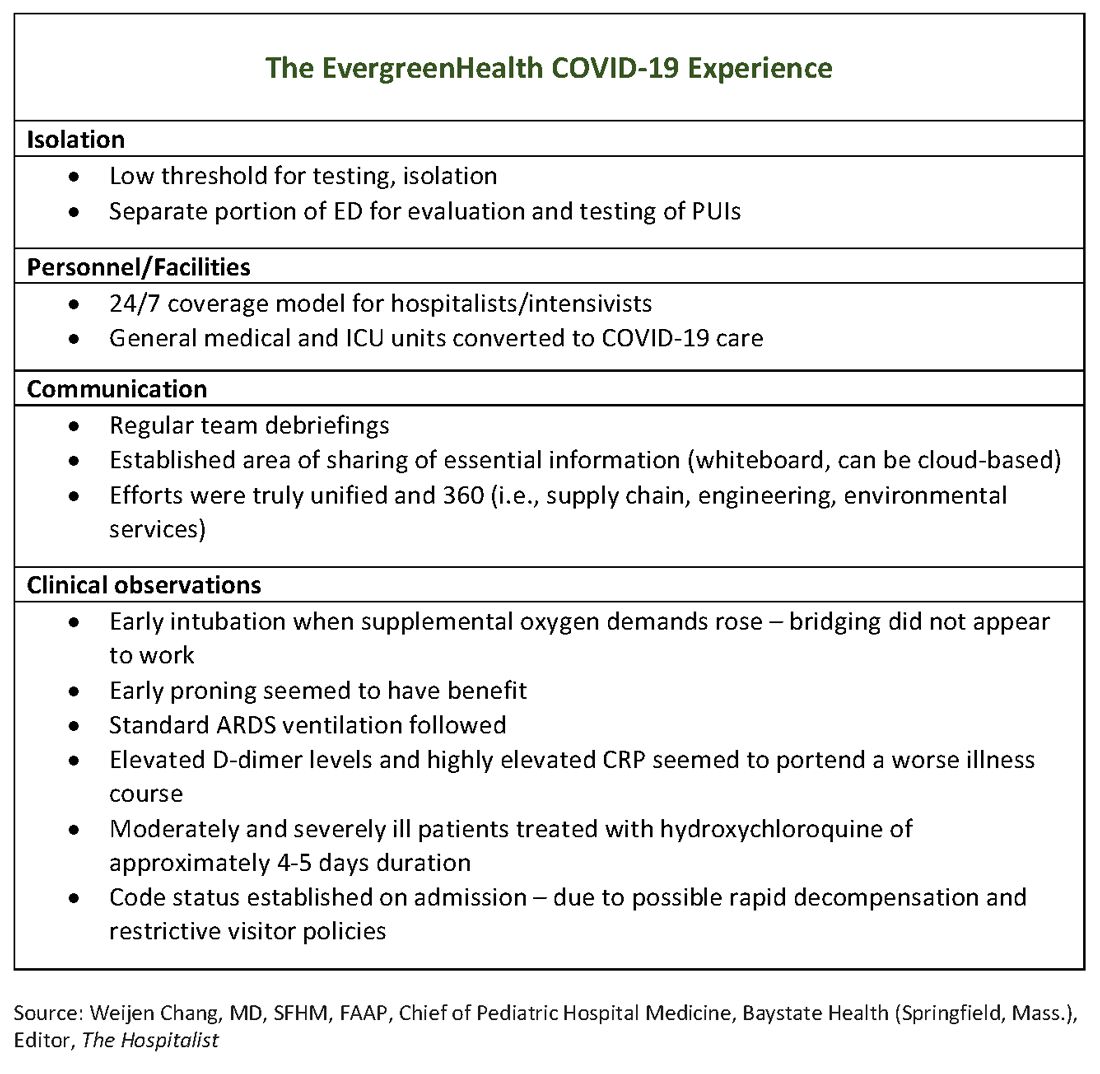
The hospital adapts to a new normal
The usual protocol in EvergreenHealth’s ICU is for the nocturnist hospitalists, such as Dr. Baker, to staff that unit, with intensivists readily available for phone consultation. However, as the numbers of critically ill, ventilated COVID-19 patients climbed, the facility switched to 24/7 staffing with intensivists to augment the hospitalist team, said Nancy Marshall, MD, the director of EvergreenHealth’s hospitalist service.
Dr. Marshall related how the entire hospital rallied to create appropriate – but flexible – staffing and environmental adaptations to the influx of coronavirus patients. “Early on, we established a separate portion of the emergency department to evaluate and test persons under investigation,” for COVID-19, she said. When they realized that they were seeing the nation’s first cluster of community coronavirus transmission, they used “appropriate isolation precautions” when indicated. Triggers for clinical suspicion included not just fever or cough, but also a new requirement for supplemental oxygen and new abnormal findings on chest radiographs.
Patients with confirmed or suspected coronavirus, once admitted, were placed in negative-pressure rooms, and droplet precautions were used with these patients. In the absence of aerosol-generating procedures, those caring for these patients used a standard surgical mask, goggles or face shield, an isolation gown, and gloves. For intubations, bronchoscopies, and other aerosol-generating procedures, N95 masks were used; the facility also has some powered and controlled air-purifying respirators.
In short order, once the size of the outbreak was appreciated, said Dr. Marshall, the entire ICU and half of another general medical floor in the hospital were converted to negative-pressure rooms.
Dr. Marshall said that having daily team debriefings has been essential. The hospitalist team room has a big whiteboard where essential information can be put up and shared. Frequent video conferencing has allowed physicians and advanced practice clinicians on the hospitalist team to ask questions, share concerns, and develop a shared knowledge base and vocabulary as they confronted this novel illness.
The rapid adaptations that EvergreenHealth successfully made depended on a responsive administration, good communication among physician services and with nursing staff, and the active participation of engineering and environmental services teams in adjusting to shifting patient needs, said Dr. Marshall.
“Preparedness is key,” Dr. Chu noted. “Managing this has required a unified effort” that addresses everything from the supply chain for personal protective equipment, to cleaning procedures, to engineering fixes that quickly added negative-pressure rooms.
“I can’t emphasize enough that this is a team sport,” said Dr. Marshall.
The unpredictable clinical course of COVID-19
The chimeric clinical course of COVID-19 means clinicians need to keep an open mind and be ready to act nimbly, said the EvergreenHealth hospitalists. Pattern recognition is a key to competent clinical management of hospitalized patients, but the course of coronavirus thus far defies any convenient application of heuristics.
Those first two patients had some characteristics in common, aside from their arrival from the same long-term care facility They each had unexplained acute respiratory distress syndrome and ground-glass opacities seen on chest CT, said Dr. Marshall. But all agreed it is still not clear who will fare well, and who will do poorly once they are admitted with coronavirus.
“We have noticed that these patients tend to have a rough course,” said Dr. Marshall. The “brisk inflammatory response” seen in some patients manifests in persistent fevers, big C-reactive protein (CRP) elevations, and likely is part of the picture of yet-unknown host factors that contribute to a worse disease course for some, she said. “These patients look toxic for a long time.”
Dr. Chu said that he’s seen even younger, healthier-looking patients admitted from the emergency department who are already quite dyspneic and may be headed for ventilation. These patients may have a low procalcitonin, and will often turn out to have an “impressive-looking” chest x-ray or CT that will show prominent bilateral infiltrates.
On the other hand, said Dr. Marshall, she and her colleagues have admitted frail-appearing nonagenarians who “just kind of sleep it off,” with little more than a cough and intermittent fevers.
Dr. Chu concurred: “So many of these patients had risk factors for severe disease and only had mild illness. Many were really quite stable.”
In terms of managing respiratory status, Dr. Baker said that the time to start planning for intubation is when the supplemental oxygen demands of COVID-19 patients start to go up. Unlike with patients who may be in some respiratory distress from other causes, once these patients have increased Fi02 needs, bridging “doesn’t work. ... They need to be intubated. Early intubation is important.” Clinicians’ level of concern should spike when they see increased work of breathing in a coronavirus patient, regardless of what the numbers are saying, he added.
For coronavirus patients with acute respiratory distress syndrome (ARDS), early proning also seems to provide some benefit, he said. At EvergreenHealth, standard ARDS ventilation protocols are being followed, including low tidal volume ventilation and positive end-expiratory pressure (PEEP) ladders. Coronavirus ventilation management has thus far been “pretty similar to standard practice with ARDS patients,” he said.
The hospitalist team was able to tap into the building knowledge base in China: Two of the EvergreenHealth hospitalists spoke fluent Mandarin, and one had contacts in China that allowed her to connect with Chinese physicians who had been treating COVID-19 patients since that outbreak had started. They established regular communication on WeChat, checking in frequently for updates on therapies and diagnostics being used in China as well.
One benefit of being in communication with colleagues in China, said Dr. Baker, was that they were able to get anecdotal evidence that elevated D-dimer levels and highly elevated CRP levels can portend a worse illness course. These findings seem to have held generally true for EvergreenHealth patients, he said. Dr. Marshall also spoke to the value of early communication with Chinese teams, who confirmed that the picture of a febrile illness with elevated CRP and leukopenia should raise the index of suspicion for coronavirus.
“Patients might improve over a few days, and then in the final 24 hours of their lives, we see changes in hemodynamics,” including reduced ejection fraction consistent with cardiogenic shock, as well as arrhythmias, said Dr. Baker. Some of the early patient deaths at EvergreenHealth followed this pattern, he said, noting that others have called for investigation into whether viral myocarditis is at play in some coronavirus deaths.
Moderately and severely ill coronavirus patients at EvergreenHealth currently receive a course of hydroxychloroquine of approximately 4-5 days’ duration. The hospital obtained remdesivir from Gilead through its compassionate-use program early on, and now is participating in a clinical trial for COVID-19 patients in the ICU.
By March 23, the facility had seen 162 confirmed COVID-19 cases, and 30 patients had died. Twenty-two inpatients had been discharged, and an additional 58 who were seen in the emergency department had been discharged home without admission.
Be suspicious – and prepared
When asked what he’d like his colleagues around the country to know as they diagnose and admit their first patients who are ill with coronavirus, Dr. Baker advised maintaining a high index of suspicion and a low threshold for testing. “I’ve given some thought to this,” he said. “From our reading and what information is out there, we are geared to pick up on the classic symptoms of coronavirus – cough, fever, some gastrointestinal symptoms.” However, many elderly patients “are not good historians. Some may have advanced dementia. ... When patients arrive with no history, we do our best to gather information,” but sometimes a case can still take clinicians by surprise, he said.
Dr. Baker told a cautionary tale of one of his patients, a woman who was admitted for a hip fracture after a fall at an assisted living facility. The patient was mildly hypoxic, but had an unremarkable physical exam, no fever, and a clear chest x-ray. She went to surgery and then to a postoperative floor with no isolation measures. When her respiratory status unexpectedly deteriorated, she was tested for COVID-19 – and was positive.
“When in doubt, isolate,” said Dr. Baker.
Dr. Chu concurred: “As soon as you suspect, move them, rather than testing first.”
Dr. Baker acknowledged, though, that when testing criteria and availability of personal protective equipment and test materials may vary by region, “it’s a challenge, especially with limited resources.”
Dr. Chu said that stringent isolation, though necessary, creates great hardship for patients and families. “It’s really important for us to check in with family members,” he said; patients are alone and afraid, and family members feel cut off – and also afraid on behalf of their ill loved ones. Workflow planning should acknowledge this and allocate extra time for patient connection and a little more time on the phone with families.
Dr. Chu offered a sobering final word. Make sure family members know their ill loved one’s wishes for care, he said: “There’s never been a better time to clarify code status on admission.”
Physicians at EvergreenHealth have created a document that contains consolidated information on what to anticipate and how to prepare for the arrival of COVID-19+ patients, recommendations on maximizing safety in the hospital environment, and key clinical management considerations. The document will be updated as new information arises.
Correction, 3/27/20: An earlier version of this article referenced white blood counts, presence of lymphopenia, and elevated hepatic enzymes for patients at EvergreenHealth when in fact that information pertained to patients in China. That paragraph has been deleted.
David Baker, MD, a hospitalist at EvergreenHealth in Kirkland, Wash., had just come off a 7-day stretch of work and was early into his usual 7 days off. He’d helped care for some patients from a nearby assisted living facility who had been admitted with puzzlingly severe viral pneumonia that wasn’t influenza.
Though COVID-19, the novel coronavirus that was sickening tens of thousands in the Chinese province of Hubei, was in the back of everyone’s mind in late February, he said he wasn’t really expecting the call notifying him that two of the patients with pneumonia had tested positive for COVID-19.
Michael Chu, MD, was coming onto EvergreenHealth’s hospitalist service at about the time Dr. Baker was rotating off. He recalled learning of the first two positive COVID-19 tests on the evening of Feb. 28 – a Friday. He and his colleagues took in this information, coming to the realization that they were seeing other patients from the same facility who had viral pneumonia and negative influenza tests. “The first cohort of coronavirus patients all came from Life Care,” the Kirkland assisted living facility that was the epicenter of the first identified U.S. outbreak of community-transmitted coronavirus, said Dr. Chu. “They all fit a clinical syndrome” and many of them were critically ill or failing fast, since they were aged and with multiple risk factors, he said during the interviews he and his colleagues participated in.
As he processed the news of the positive tests and his inadvertent exposure to COVID-19, Dr. Baker realized that his duty schedule worked in his favor, since he wasn’t expected back for several more days. When he did come back to work after remaining asymptomatic, he found a much-changed environment as the coronavirus cases poured in and continual adaptations were made to accommodate these patients – and to keep staff and other patients safe.
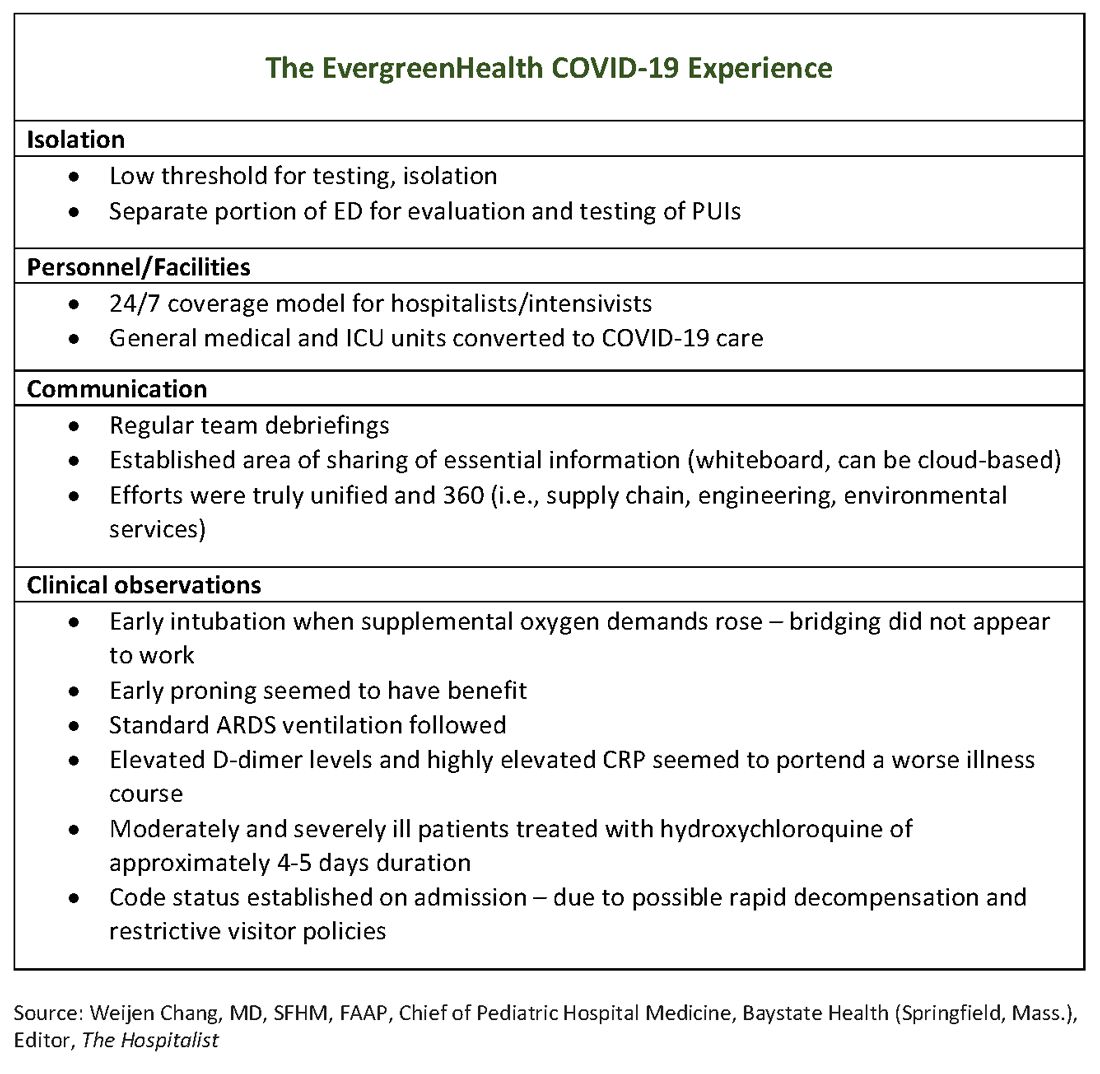
The hospital adapts to a new normal
The usual protocol in EvergreenHealth’s ICU is for the nocturnist hospitalists, such as Dr. Baker, to staff that unit, with intensivists readily available for phone consultation. However, as the numbers of critically ill, ventilated COVID-19 patients climbed, the facility switched to 24/7 staffing with intensivists to augment the hospitalist team, said Nancy Marshall, MD, the director of EvergreenHealth’s hospitalist service.
Dr. Marshall related how the entire hospital rallied to create appropriate – but flexible – staffing and environmental adaptations to the influx of coronavirus patients. “Early on, we established a separate portion of the emergency department to evaluate and test persons under investigation,” for COVID-19, she said. When they realized that they were seeing the nation’s first cluster of community coronavirus transmission, they used “appropriate isolation precautions” when indicated. Triggers for clinical suspicion included not just fever or cough, but also a new requirement for supplemental oxygen and new abnormal findings on chest radiographs.
Patients with confirmed or suspected coronavirus, once admitted, were placed in negative-pressure rooms, and droplet precautions were used with these patients. In the absence of aerosol-generating procedures, those caring for these patients used a standard surgical mask, goggles or face shield, an isolation gown, and gloves. For intubations, bronchoscopies, and other aerosol-generating procedures, N95 masks were used; the facility also has some powered and controlled air-purifying respirators.
In short order, once the size of the outbreak was appreciated, said Dr. Marshall, the entire ICU and half of another general medical floor in the hospital were converted to negative-pressure rooms.
Dr. Marshall said that having daily team debriefings has been essential. The hospitalist team room has a big whiteboard where essential information can be put up and shared. Frequent video conferencing has allowed physicians and advanced practice clinicians on the hospitalist team to ask questions, share concerns, and develop a shared knowledge base and vocabulary as they confronted this novel illness.
The rapid adaptations that EvergreenHealth successfully made depended on a responsive administration, good communication among physician services and with nursing staff, and the active participation of engineering and environmental services teams in adjusting to shifting patient needs, said Dr. Marshall.
“Preparedness is key,” Dr. Chu noted. “Managing this has required a unified effort” that addresses everything from the supply chain for personal protective equipment, to cleaning procedures, to engineering fixes that quickly added negative-pressure rooms.
“I can’t emphasize enough that this is a team sport,” said Dr. Marshall.
The unpredictable clinical course of COVID-19
The chimeric clinical course of COVID-19 means clinicians need to keep an open mind and be ready to act nimbly, said the EvergreenHealth hospitalists. Pattern recognition is a key to competent clinical management of hospitalized patients, but the course of coronavirus thus far defies any convenient application of heuristics.
Those first two patients had some characteristics in common, aside from their arrival from the same long-term care facility They each had unexplained acute respiratory distress syndrome and ground-glass opacities seen on chest CT, said Dr. Marshall. But all agreed it is still not clear who will fare well, and who will do poorly once they are admitted with coronavirus.
“We have noticed that these patients tend to have a rough course,” said Dr. Marshall. The “brisk inflammatory response” seen in some patients manifests in persistent fevers, big C-reactive protein (CRP) elevations, and likely is part of the picture of yet-unknown host factors that contribute to a worse disease course for some, she said. “These patients look toxic for a long time.”
Dr. Chu said that he’s seen even younger, healthier-looking patients admitted from the emergency department who are already quite dyspneic and may be headed for ventilation. These patients may have a low procalcitonin, and will often turn out to have an “impressive-looking” chest x-ray or CT that will show prominent bilateral infiltrates.
On the other hand, said Dr. Marshall, she and her colleagues have admitted frail-appearing nonagenarians who “just kind of sleep it off,” with little more than a cough and intermittent fevers.
Dr. Chu concurred: “So many of these patients had risk factors for severe disease and only had mild illness. Many were really quite stable.”
In terms of managing respiratory status, Dr. Baker said that the time to start planning for intubation is when the supplemental oxygen demands of COVID-19 patients start to go up. Unlike with patients who may be in some respiratory distress from other causes, once these patients have increased Fi02 needs, bridging “doesn’t work. ... They need to be intubated. Early intubation is important.” Clinicians’ level of concern should spike when they see increased work of breathing in a coronavirus patient, regardless of what the numbers are saying, he added.
For coronavirus patients with acute respiratory distress syndrome (ARDS), early proning also seems to provide some benefit, he said. At EvergreenHealth, standard ARDS ventilation protocols are being followed, including low tidal volume ventilation and positive end-expiratory pressure (PEEP) ladders. Coronavirus ventilation management has thus far been “pretty similar to standard practice with ARDS patients,” he said.
The hospitalist team was able to tap into the building knowledge base in China: Two of the EvergreenHealth hospitalists spoke fluent Mandarin, and one had contacts in China that allowed her to connect with Chinese physicians who had been treating COVID-19 patients since that outbreak had started. They established regular communication on WeChat, checking in frequently for updates on therapies and diagnostics being used in China as well.
One benefit of being in communication with colleagues in China, said Dr. Baker, was that they were able to get anecdotal evidence that elevated D-dimer levels and highly elevated CRP levels can portend a worse illness course. These findings seem to have held generally true for EvergreenHealth patients, he said. Dr. Marshall also spoke to the value of early communication with Chinese teams, who confirmed that the picture of a febrile illness with elevated CRP and leukopenia should raise the index of suspicion for coronavirus.
“Patients might improve over a few days, and then in the final 24 hours of their lives, we see changes in hemodynamics,” including reduced ejection fraction consistent with cardiogenic shock, as well as arrhythmias, said Dr. Baker. Some of the early patient deaths at EvergreenHealth followed this pattern, he said, noting that others have called for investigation into whether viral myocarditis is at play in some coronavirus deaths.
Moderately and severely ill coronavirus patients at EvergreenHealth currently receive a course of hydroxychloroquine of approximately 4-5 days’ duration. The hospital obtained remdesivir from Gilead through its compassionate-use program early on, and now is participating in a clinical trial for COVID-19 patients in the ICU.
By March 23, the facility had seen 162 confirmed COVID-19 cases, and 30 patients had died. Twenty-two inpatients had been discharged, and an additional 58 who were seen in the emergency department had been discharged home without admission.
Be suspicious – and prepared
When asked what he’d like his colleagues around the country to know as they diagnose and admit their first patients who are ill with coronavirus, Dr. Baker advised maintaining a high index of suspicion and a low threshold for testing. “I’ve given some thought to this,” he said. “From our reading and what information is out there, we are geared to pick up on the classic symptoms of coronavirus – cough, fever, some gastrointestinal symptoms.” However, many elderly patients “are not good historians. Some may have advanced dementia. ... When patients arrive with no history, we do our best to gather information,” but sometimes a case can still take clinicians by surprise, he said.
Dr. Baker told a cautionary tale of one of his patients, a woman who was admitted for a hip fracture after a fall at an assisted living facility. The patient was mildly hypoxic, but had an unremarkable physical exam, no fever, and a clear chest x-ray. She went to surgery and then to a postoperative floor with no isolation measures. When her respiratory status unexpectedly deteriorated, she was tested for COVID-19 – and was positive.
“When in doubt, isolate,” said Dr. Baker.
Dr. Chu concurred: “As soon as you suspect, move them, rather than testing first.”
Dr. Baker acknowledged, though, that when testing criteria and availability of personal protective equipment and test materials may vary by region, “it’s a challenge, especially with limited resources.”
Dr. Chu said that stringent isolation, though necessary, creates great hardship for patients and families. “It’s really important for us to check in with family members,” he said; patients are alone and afraid, and family members feel cut off – and also afraid on behalf of their ill loved ones. Workflow planning should acknowledge this and allocate extra time for patient connection and a little more time on the phone with families.
Dr. Chu offered a sobering final word. Make sure family members know their ill loved one’s wishes for care, he said: “There’s never been a better time to clarify code status on admission.”
Physicians at EvergreenHealth have created a document that contains consolidated information on what to anticipate and how to prepare for the arrival of COVID-19+ patients, recommendations on maximizing safety in the hospital environment, and key clinical management considerations. The document will be updated as new information arises.
Correction, 3/27/20: An earlier version of this article referenced white blood counts, presence of lymphopenia, and elevated hepatic enzymes for patients at EvergreenHealth when in fact that information pertained to patients in China. That paragraph has been deleted.
David Baker, MD, a hospitalist at EvergreenHealth in Kirkland, Wash., had just come off a 7-day stretch of work and was early into his usual 7 days off. He’d helped care for some patients from a nearby assisted living facility who had been admitted with puzzlingly severe viral pneumonia that wasn’t influenza.
Though COVID-19, the novel coronavirus that was sickening tens of thousands in the Chinese province of Hubei, was in the back of everyone’s mind in late February, he said he wasn’t really expecting the call notifying him that two of the patients with pneumonia had tested positive for COVID-19.
Michael Chu, MD, was coming onto EvergreenHealth’s hospitalist service at about the time Dr. Baker was rotating off. He recalled learning of the first two positive COVID-19 tests on the evening of Feb. 28 – a Friday. He and his colleagues took in this information, coming to the realization that they were seeing other patients from the same facility who had viral pneumonia and negative influenza tests. “The first cohort of coronavirus patients all came from Life Care,” the Kirkland assisted living facility that was the epicenter of the first identified U.S. outbreak of community-transmitted coronavirus, said Dr. Chu. “They all fit a clinical syndrome” and many of them were critically ill or failing fast, since they were aged and with multiple risk factors, he said during the interviews he and his colleagues participated in.
As he processed the news of the positive tests and his inadvertent exposure to COVID-19, Dr. Baker realized that his duty schedule worked in his favor, since he wasn’t expected back for several more days. When he did come back to work after remaining asymptomatic, he found a much-changed environment as the coronavirus cases poured in and continual adaptations were made to accommodate these patients – and to keep staff and other patients safe.
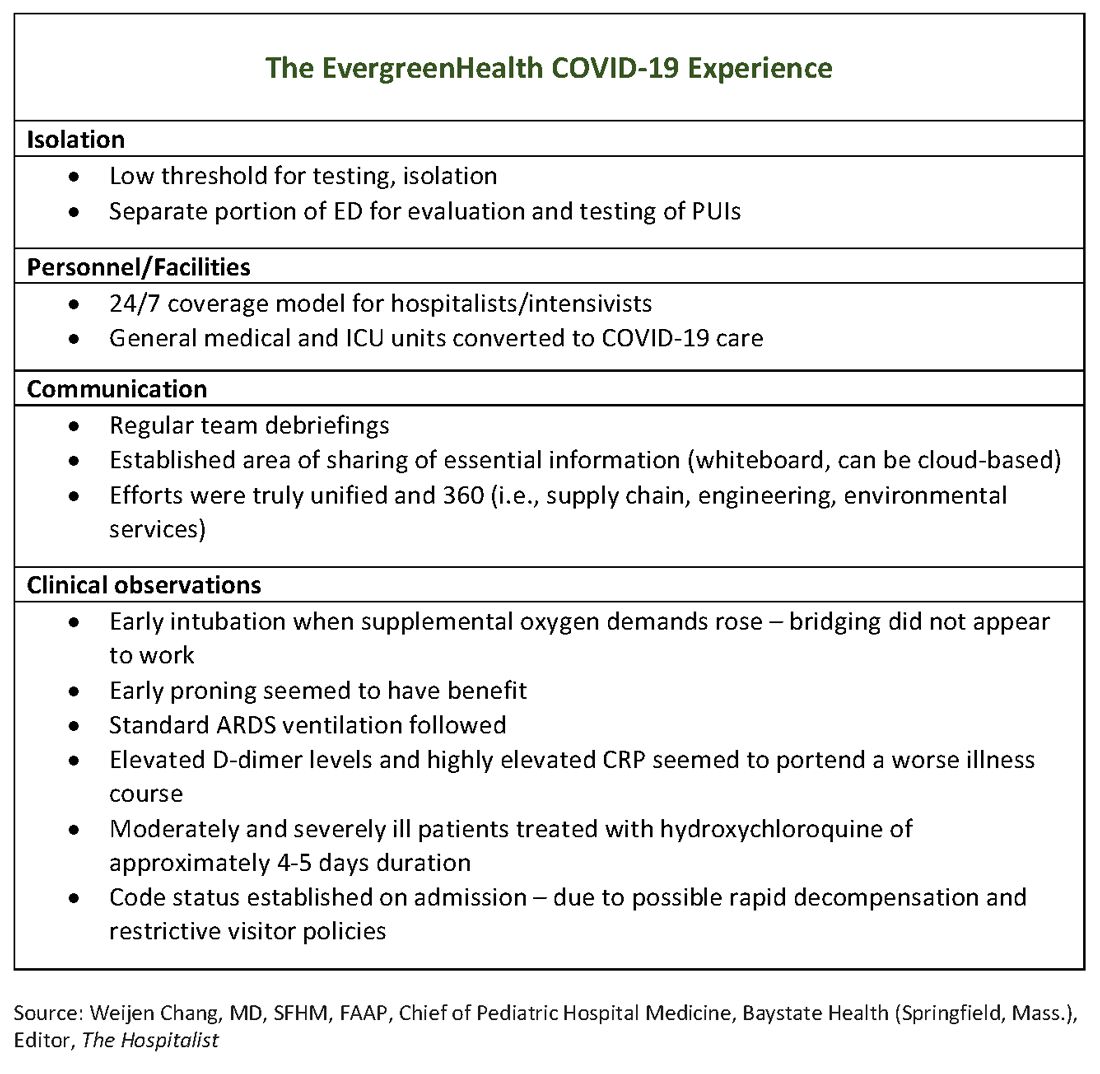
The hospital adapts to a new normal
The usual protocol in EvergreenHealth’s ICU is for the nocturnist hospitalists, such as Dr. Baker, to staff that unit, with intensivists readily available for phone consultation. However, as the numbers of critically ill, ventilated COVID-19 patients climbed, the facility switched to 24/7 staffing with intensivists to augment the hospitalist team, said Nancy Marshall, MD, the director of EvergreenHealth’s hospitalist service.
Dr. Marshall related how the entire hospital rallied to create appropriate – but flexible – staffing and environmental adaptations to the influx of coronavirus patients. “Early on, we established a separate portion of the emergency department to evaluate and test persons under investigation,” for COVID-19, she said. When they realized that they were seeing the nation’s first cluster of community coronavirus transmission, they used “appropriate isolation precautions” when indicated. Triggers for clinical suspicion included not just fever or cough, but also a new requirement for supplemental oxygen and new abnormal findings on chest radiographs.
Patients with confirmed or suspected coronavirus, once admitted, were placed in negative-pressure rooms, and droplet precautions were used with these patients. In the absence of aerosol-generating procedures, those caring for these patients used a standard surgical mask, goggles or face shield, an isolation gown, and gloves. For intubations, bronchoscopies, and other aerosol-generating procedures, N95 masks were used; the facility also has some powered and controlled air-purifying respirators.
In short order, once the size of the outbreak was appreciated, said Dr. Marshall, the entire ICU and half of another general medical floor in the hospital were converted to negative-pressure rooms.
Dr. Marshall said that having daily team debriefings has been essential. The hospitalist team room has a big whiteboard where essential information can be put up and shared. Frequent video conferencing has allowed physicians and advanced practice clinicians on the hospitalist team to ask questions, share concerns, and develop a shared knowledge base and vocabulary as they confronted this novel illness.
The rapid adaptations that EvergreenHealth successfully made depended on a responsive administration, good communication among physician services and with nursing staff, and the active participation of engineering and environmental services teams in adjusting to shifting patient needs, said Dr. Marshall.
“Preparedness is key,” Dr. Chu noted. “Managing this has required a unified effort” that addresses everything from the supply chain for personal protective equipment, to cleaning procedures, to engineering fixes that quickly added negative-pressure rooms.
“I can’t emphasize enough that this is a team sport,” said Dr. Marshall.
The unpredictable clinical course of COVID-19
The chimeric clinical course of COVID-19 means clinicians need to keep an open mind and be ready to act nimbly, said the EvergreenHealth hospitalists. Pattern recognition is a key to competent clinical management of hospitalized patients, but the course of coronavirus thus far defies any convenient application of heuristics.
Those first two patients had some characteristics in common, aside from their arrival from the same long-term care facility They each had unexplained acute respiratory distress syndrome and ground-glass opacities seen on chest CT, said Dr. Marshall. But all agreed it is still not clear who will fare well, and who will do poorly once they are admitted with coronavirus.
“We have noticed that these patients tend to have a rough course,” said Dr. Marshall. The “brisk inflammatory response” seen in some patients manifests in persistent fevers, big C-reactive protein (CRP) elevations, and likely is part of the picture of yet-unknown host factors that contribute to a worse disease course for some, she said. “These patients look toxic for a long time.”
Dr. Chu said that he’s seen even younger, healthier-looking patients admitted from the emergency department who are already quite dyspneic and may be headed for ventilation. These patients may have a low procalcitonin, and will often turn out to have an “impressive-looking” chest x-ray or CT that will show prominent bilateral infiltrates.
On the other hand, said Dr. Marshall, she and her colleagues have admitted frail-appearing nonagenarians who “just kind of sleep it off,” with little more than a cough and intermittent fevers.
Dr. Chu concurred: “So many of these patients had risk factors for severe disease and only had mild illness. Many were really quite stable.”
In terms of managing respiratory status, Dr. Baker said that the time to start planning for intubation is when the supplemental oxygen demands of COVID-19 patients start to go up. Unlike with patients who may be in some respiratory distress from other causes, once these patients have increased Fi02 needs, bridging “doesn’t work. ... They need to be intubated. Early intubation is important.” Clinicians’ level of concern should spike when they see increased work of breathing in a coronavirus patient, regardless of what the numbers are saying, he added.
For coronavirus patients with acute respiratory distress syndrome (ARDS), early proning also seems to provide some benefit, he said. At EvergreenHealth, standard ARDS ventilation protocols are being followed, including low tidal volume ventilation and positive end-expiratory pressure (PEEP) ladders. Coronavirus ventilation management has thus far been “pretty similar to standard practice with ARDS patients,” he said.
The hospitalist team was able to tap into the building knowledge base in China: Two of the EvergreenHealth hospitalists spoke fluent Mandarin, and one had contacts in China that allowed her to connect with Chinese physicians who had been treating COVID-19 patients since that outbreak had started. They established regular communication on WeChat, checking in frequently for updates on therapies and diagnostics being used in China as well.
One benefit of being in communication with colleagues in China, said Dr. Baker, was that they were able to get anecdotal evidence that elevated D-dimer levels and highly elevated CRP levels can portend a worse illness course. These findings seem to have held generally true for EvergreenHealth patients, he said. Dr. Marshall also spoke to the value of early communication with Chinese teams, who confirmed that the picture of a febrile illness with elevated CRP and leukopenia should raise the index of suspicion for coronavirus.
“Patients might improve over a few days, and then in the final 24 hours of their lives, we see changes in hemodynamics,” including reduced ejection fraction consistent with cardiogenic shock, as well as arrhythmias, said Dr. Baker. Some of the early patient deaths at EvergreenHealth followed this pattern, he said, noting that others have called for investigation into whether viral myocarditis is at play in some coronavirus deaths.
Moderately and severely ill coronavirus patients at EvergreenHealth currently receive a course of hydroxychloroquine of approximately 4-5 days’ duration. The hospital obtained remdesivir from Gilead through its compassionate-use program early on, and now is participating in a clinical trial for COVID-19 patients in the ICU.
By March 23, the facility had seen 162 confirmed COVID-19 cases, and 30 patients had died. Twenty-two inpatients had been discharged, and an additional 58 who were seen in the emergency department had been discharged home without admission.
Be suspicious – and prepared
When asked what he’d like his colleagues around the country to know as they diagnose and admit their first patients who are ill with coronavirus, Dr. Baker advised maintaining a high index of suspicion and a low threshold for testing. “I’ve given some thought to this,” he said. “From our reading and what information is out there, we are geared to pick up on the classic symptoms of coronavirus – cough, fever, some gastrointestinal symptoms.” However, many elderly patients “are not good historians. Some may have advanced dementia. ... When patients arrive with no history, we do our best to gather information,” but sometimes a case can still take clinicians by surprise, he said.
Dr. Baker told a cautionary tale of one of his patients, a woman who was admitted for a hip fracture after a fall at an assisted living facility. The patient was mildly hypoxic, but had an unremarkable physical exam, no fever, and a clear chest x-ray. She went to surgery and then to a postoperative floor with no isolation measures. When her respiratory status unexpectedly deteriorated, she was tested for COVID-19 – and was positive.
“When in doubt, isolate,” said Dr. Baker.
Dr. Chu concurred: “As soon as you suspect, move them, rather than testing first.”
Dr. Baker acknowledged, though, that when testing criteria and availability of personal protective equipment and test materials may vary by region, “it’s a challenge, especially with limited resources.”
Dr. Chu said that stringent isolation, though necessary, creates great hardship for patients and families. “It’s really important for us to check in with family members,” he said; patients are alone and afraid, and family members feel cut off – and also afraid on behalf of their ill loved ones. Workflow planning should acknowledge this and allocate extra time for patient connection and a little more time on the phone with families.
Dr. Chu offered a sobering final word. Make sure family members know their ill loved one’s wishes for care, he said: “There’s never been a better time to clarify code status on admission.”
Physicians at EvergreenHealth have created a document that contains consolidated information on what to anticipate and how to prepare for the arrival of COVID-19+ patients, recommendations on maximizing safety in the hospital environment, and key clinical management considerations. The document will be updated as new information arises.
Correction, 3/27/20: An earlier version of this article referenced white blood counts, presence of lymphopenia, and elevated hepatic enzymes for patients at EvergreenHealth when in fact that information pertained to patients in China. That paragraph has been deleted.
Perspective from the heartland: Cancer care and research during a public health crisis
I have no knowledge of, or experience with, managing a cancer patient during a pandemic. However, from the published and otherwise shared experience of others, we should not allow ourselves to underestimate the voracity of the coronavirus pandemic on our patients, communities, and health care systems.
Data from China suggest cancer patients infected with SARS-CoV-2 face a 3.5 times higher risk of mechanical ventilation, intensive care unit admission, or death, compared with infected patients without cancer (Lancet Oncol 2020;21:335-7).
Health care workers in Seattle have also shared their experiences battling coronavirus infections in cancer patients (J Natl Compr Canc Netw. 2020 Mar 20. doi: 10.6004/jnccn.2020.7560). Masumi Ueda, MD, of Seattle Cancer Care Alliance, and colleagues reviewed their decisions in multiple domains over a 7-week period, during which the state of Washington went from a single case of SARS-CoV-2 infection to nearly 650 cases and 40 deaths.
Making tough treatment decisions
Dr. Ueda and colleagues contrasted their customary resource-rich, innovation-oriented, cancer-combatting environment with their current circumstance, in which they must prioritize treatment for patients for whom the risk-reward balance has tilted substantially toward “risk.”
The authors noted that their most difficult decisions were those regarding delay of cancer treatment. They suggested that plans for potentially curative adjuvant therapy should likely proceed, but, for patients with metastatic disease, the equation is more nuanced.
In some cases, treatment should be delayed or interrupted with recognition of how that could result in worsening performance status and admission for symptom palliation, further stressing inpatient resources.
The authors suggested scenarios for prioritizing cancer surgery. For example, several months of systemic therapy (ideally, low-risk systemic therapy such as hormone therapy for breast or prostate cancer) and surgical delay may be worthwhile, without compromising patient care.
Patients with aggressive hematologic malignancy requiring urgent systemic treatment (potentially stem cell transplantation and cellular immunotherapies) should be treated promptly. However, even in those cases, opportunities should be sought to lessen immunosuppression and transition care as quickly as possible to the outpatient clinic, according to guidelines from the American Society of Transplantation and Cellular Therapy.
See one, do one, teach one
Rendering patient care during a pandemic would be unique for me. However, I, like all physicians, am familiar with feelings of inadequacy at times of professional challenge. On countless occasions, I have started my day or walked into a patient’s room wondering whether I will have the fortitude, knowledge, creativity, or help I need to get through that day or make that patient “better” by any definition of that word.
We all know the formula: “Work hard. Make evidence-based, personalized decisions for those who have entrusted their care to us. Learn from those encounters. Teach from our knowledge and experience – that is, ‘See one, do one, teach one.’ ”
The Seattle oncologists are living the lives of first responders and deserve our admiration for putting pen to paper so we can learn from their considerable, relevant experience.
Similar admiration is due to Giuseppe Curigliano, MD, of the European Institute of Oncology in Milan. In the ASCO Daily News, Dr. Curigliano described an epidemic that, within 3 weeks, overloaded the health care system across northern Italy.
Hospitalization was needed for over 60% of infected patients, and nearly 15% of those patients needed intensive care unit services for respiratory distress. The Italians centralized oncology care in specialized hubs, with spokes of institutions working in parallel to provide cancer-specific care in a COVID-free environment.
To build upon cancer-specific information from Italy and other areas hard-hit by COVID-19, more than 30 cancer centers have joined together to form the COVID-19 and Cancer Consortium. The consortium’s website hosts a survey designed to “capture details related to cancer patients presumed to have COVID-19.”
Calculating deaths and long-term consequences for cancer care delivery
It is proper that the authors from China, Italy, and Seattle did not focus attention on the case fatality rate from the COVID-19 pandemic among cancer patients. To say the least, it would be complicated to tally the direct mortality – either overall or in clinically important subsets of patients, including country-specific cohorts.
What we know from published reports is that, in Italy, cancer patients account for about 20% of deaths from coronavirus. In China, the case-fatality rate for patients with cancer was 5.6% (JAMA. 2020 Feb 24. doi: 10.1001/jama.2020.2648).
However, we know nothing about the indirect death toll from malignancy (without coronavirus infection) that was untreated or managed less than optimally because of personnel and physical resources that were diverted to COVID-19–associated cases.
Similarly, we cannot begin to estimate indirect consequences of the pandemic to oncology practices, such as accelerated burnout and posttraumatic stress disorder, as well as the long-range effects of economic turmoil on patients, health care workers, and provider organizations.
What happens to cancer trials?
From China, Italy, and Seattle, thus far, there is little information about how the pandemic will affect the vital clinical research endeavor. The Seattle physicians did say they plan to enroll patients on clinical trials only when the trial offers a high chance of benefiting the patient over standard therapy alone.
Fortunately, the National Institutes of Health and Food and Drug Administration have released guidance documents related to clinical trials.
The National Cancer Institute (NCI) has also released guidance documents (March 13 guidance; March 23 guidance) for patients on clinical trials supported by the NCI Cancer Therapy Evaluation Program (CTEP) and the NCI Community Oncology Research Program (NCORP).
CTEP and NCORP are making reasonable accommodations to suspend monitoring visits and audits, allow tele–follow-up visits for patients, and permit local physicians to provide care for patients on study. In addition, with appropriate procedural adherence and documentation, CTEP and NCORP will allow oral investigational medicines to be mailed directly to patients’ homes.
Planned NCI National Clinical Trials Network meetings will be conducted via remote access webinars, conference calls, and similar technology. These adjustments – and probably many more to come – are geared toward facilitating ongoing care to proceed safely and with minimal risk for patients currently receiving investigational therapies and for the sites and investigators engaged in those studies.
Each of us has probably faced a personal “defining professional moment,” when we had to utilize every skill in our arsenal and examine the motivations that led us to a career in oncology. However, it is clear from the forgoing clinical and research processes and guidelines that the COVID-19 pandemic is such a defining professional moment for each of us, in every community we serve.
Critical junctures like this cause more rapid behavior change and innovation than the slow-moving pace that characterizes our idealized preferences. As oncologists who embrace new data and behavioral change, we stand to learn processes that will facilitate more perfected systems of care than the one that preceded this unprecedented crisis, promote more efficient sharing of high-quality information, and improve the outcome for our future patients.
Dr. Lyss was an oncologist and researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
I have no knowledge of, or experience with, managing a cancer patient during a pandemic. However, from the published and otherwise shared experience of others, we should not allow ourselves to underestimate the voracity of the coronavirus pandemic on our patients, communities, and health care systems.
Data from China suggest cancer patients infected with SARS-CoV-2 face a 3.5 times higher risk of mechanical ventilation, intensive care unit admission, or death, compared with infected patients without cancer (Lancet Oncol 2020;21:335-7).
Health care workers in Seattle have also shared their experiences battling coronavirus infections in cancer patients (J Natl Compr Canc Netw. 2020 Mar 20. doi: 10.6004/jnccn.2020.7560). Masumi Ueda, MD, of Seattle Cancer Care Alliance, and colleagues reviewed their decisions in multiple domains over a 7-week period, during which the state of Washington went from a single case of SARS-CoV-2 infection to nearly 650 cases and 40 deaths.
Making tough treatment decisions
Dr. Ueda and colleagues contrasted their customary resource-rich, innovation-oriented, cancer-combatting environment with their current circumstance, in which they must prioritize treatment for patients for whom the risk-reward balance has tilted substantially toward “risk.”
The authors noted that their most difficult decisions were those regarding delay of cancer treatment. They suggested that plans for potentially curative adjuvant therapy should likely proceed, but, for patients with metastatic disease, the equation is more nuanced.
In some cases, treatment should be delayed or interrupted with recognition of how that could result in worsening performance status and admission for symptom palliation, further stressing inpatient resources.
The authors suggested scenarios for prioritizing cancer surgery. For example, several months of systemic therapy (ideally, low-risk systemic therapy such as hormone therapy for breast or prostate cancer) and surgical delay may be worthwhile, without compromising patient care.
Patients with aggressive hematologic malignancy requiring urgent systemic treatment (potentially stem cell transplantation and cellular immunotherapies) should be treated promptly. However, even in those cases, opportunities should be sought to lessen immunosuppression and transition care as quickly as possible to the outpatient clinic, according to guidelines from the American Society of Transplantation and Cellular Therapy.
See one, do one, teach one
Rendering patient care during a pandemic would be unique for me. However, I, like all physicians, am familiar with feelings of inadequacy at times of professional challenge. On countless occasions, I have started my day or walked into a patient’s room wondering whether I will have the fortitude, knowledge, creativity, or help I need to get through that day or make that patient “better” by any definition of that word.
We all know the formula: “Work hard. Make evidence-based, personalized decisions for those who have entrusted their care to us. Learn from those encounters. Teach from our knowledge and experience – that is, ‘See one, do one, teach one.’ ”
The Seattle oncologists are living the lives of first responders and deserve our admiration for putting pen to paper so we can learn from their considerable, relevant experience.
Similar admiration is due to Giuseppe Curigliano, MD, of the European Institute of Oncology in Milan. In the ASCO Daily News, Dr. Curigliano described an epidemic that, within 3 weeks, overloaded the health care system across northern Italy.
Hospitalization was needed for over 60% of infected patients, and nearly 15% of those patients needed intensive care unit services for respiratory distress. The Italians centralized oncology care in specialized hubs, with spokes of institutions working in parallel to provide cancer-specific care in a COVID-free environment.
To build upon cancer-specific information from Italy and other areas hard-hit by COVID-19, more than 30 cancer centers have joined together to form the COVID-19 and Cancer Consortium. The consortium’s website hosts a survey designed to “capture details related to cancer patients presumed to have COVID-19.”
Calculating deaths and long-term consequences for cancer care delivery
It is proper that the authors from China, Italy, and Seattle did not focus attention on the case fatality rate from the COVID-19 pandemic among cancer patients. To say the least, it would be complicated to tally the direct mortality – either overall or in clinically important subsets of patients, including country-specific cohorts.
What we know from published reports is that, in Italy, cancer patients account for about 20% of deaths from coronavirus. In China, the case-fatality rate for patients with cancer was 5.6% (JAMA. 2020 Feb 24. doi: 10.1001/jama.2020.2648).
However, we know nothing about the indirect death toll from malignancy (without coronavirus infection) that was untreated or managed less than optimally because of personnel and physical resources that were diverted to COVID-19–associated cases.
Similarly, we cannot begin to estimate indirect consequences of the pandemic to oncology practices, such as accelerated burnout and posttraumatic stress disorder, as well as the long-range effects of economic turmoil on patients, health care workers, and provider organizations.
What happens to cancer trials?
From China, Italy, and Seattle, thus far, there is little information about how the pandemic will affect the vital clinical research endeavor. The Seattle physicians did say they plan to enroll patients on clinical trials only when the trial offers a high chance of benefiting the patient over standard therapy alone.
Fortunately, the National Institutes of Health and Food and Drug Administration have released guidance documents related to clinical trials.
The National Cancer Institute (NCI) has also released guidance documents (March 13 guidance; March 23 guidance) for patients on clinical trials supported by the NCI Cancer Therapy Evaluation Program (CTEP) and the NCI Community Oncology Research Program (NCORP).
CTEP and NCORP are making reasonable accommodations to suspend monitoring visits and audits, allow tele–follow-up visits for patients, and permit local physicians to provide care for patients on study. In addition, with appropriate procedural adherence and documentation, CTEP and NCORP will allow oral investigational medicines to be mailed directly to patients’ homes.
Planned NCI National Clinical Trials Network meetings will be conducted via remote access webinars, conference calls, and similar technology. These adjustments – and probably many more to come – are geared toward facilitating ongoing care to proceed safely and with minimal risk for patients currently receiving investigational therapies and for the sites and investigators engaged in those studies.
Each of us has probably faced a personal “defining professional moment,” when we had to utilize every skill in our arsenal and examine the motivations that led us to a career in oncology. However, it is clear from the forgoing clinical and research processes and guidelines that the COVID-19 pandemic is such a defining professional moment for each of us, in every community we serve.
Critical junctures like this cause more rapid behavior change and innovation than the slow-moving pace that characterizes our idealized preferences. As oncologists who embrace new data and behavioral change, we stand to learn processes that will facilitate more perfected systems of care than the one that preceded this unprecedented crisis, promote more efficient sharing of high-quality information, and improve the outcome for our future patients.
Dr. Lyss was an oncologist and researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
I have no knowledge of, or experience with, managing a cancer patient during a pandemic. However, from the published and otherwise shared experience of others, we should not allow ourselves to underestimate the voracity of the coronavirus pandemic on our patients, communities, and health care systems.
Data from China suggest cancer patients infected with SARS-CoV-2 face a 3.5 times higher risk of mechanical ventilation, intensive care unit admission, or death, compared with infected patients without cancer (Lancet Oncol 2020;21:335-7).
Health care workers in Seattle have also shared their experiences battling coronavirus infections in cancer patients (J Natl Compr Canc Netw. 2020 Mar 20. doi: 10.6004/jnccn.2020.7560). Masumi Ueda, MD, of Seattle Cancer Care Alliance, and colleagues reviewed their decisions in multiple domains over a 7-week period, during which the state of Washington went from a single case of SARS-CoV-2 infection to nearly 650 cases and 40 deaths.
Making tough treatment decisions
Dr. Ueda and colleagues contrasted their customary resource-rich, innovation-oriented, cancer-combatting environment with their current circumstance, in which they must prioritize treatment for patients for whom the risk-reward balance has tilted substantially toward “risk.”
The authors noted that their most difficult decisions were those regarding delay of cancer treatment. They suggested that plans for potentially curative adjuvant therapy should likely proceed, but, for patients with metastatic disease, the equation is more nuanced.
In some cases, treatment should be delayed or interrupted with recognition of how that could result in worsening performance status and admission for symptom palliation, further stressing inpatient resources.
The authors suggested scenarios for prioritizing cancer surgery. For example, several months of systemic therapy (ideally, low-risk systemic therapy such as hormone therapy for breast or prostate cancer) and surgical delay may be worthwhile, without compromising patient care.
Patients with aggressive hematologic malignancy requiring urgent systemic treatment (potentially stem cell transplantation and cellular immunotherapies) should be treated promptly. However, even in those cases, opportunities should be sought to lessen immunosuppression and transition care as quickly as possible to the outpatient clinic, according to guidelines from the American Society of Transplantation and Cellular Therapy.
See one, do one, teach one
Rendering patient care during a pandemic would be unique for me. However, I, like all physicians, am familiar with feelings of inadequacy at times of professional challenge. On countless occasions, I have started my day or walked into a patient’s room wondering whether I will have the fortitude, knowledge, creativity, or help I need to get through that day or make that patient “better” by any definition of that word.
We all know the formula: “Work hard. Make evidence-based, personalized decisions for those who have entrusted their care to us. Learn from those encounters. Teach from our knowledge and experience – that is, ‘See one, do one, teach one.’ ”
The Seattle oncologists are living the lives of first responders and deserve our admiration for putting pen to paper so we can learn from their considerable, relevant experience.
Similar admiration is due to Giuseppe Curigliano, MD, of the European Institute of Oncology in Milan. In the ASCO Daily News, Dr. Curigliano described an epidemic that, within 3 weeks, overloaded the health care system across northern Italy.
Hospitalization was needed for over 60% of infected patients, and nearly 15% of those patients needed intensive care unit services for respiratory distress. The Italians centralized oncology care in specialized hubs, with spokes of institutions working in parallel to provide cancer-specific care in a COVID-free environment.
To build upon cancer-specific information from Italy and other areas hard-hit by COVID-19, more than 30 cancer centers have joined together to form the COVID-19 and Cancer Consortium. The consortium’s website hosts a survey designed to “capture details related to cancer patients presumed to have COVID-19.”
Calculating deaths and long-term consequences for cancer care delivery
It is proper that the authors from China, Italy, and Seattle did not focus attention on the case fatality rate from the COVID-19 pandemic among cancer patients. To say the least, it would be complicated to tally the direct mortality – either overall or in clinically important subsets of patients, including country-specific cohorts.
What we know from published reports is that, in Italy, cancer patients account for about 20% of deaths from coronavirus. In China, the case-fatality rate for patients with cancer was 5.6% (JAMA. 2020 Feb 24. doi: 10.1001/jama.2020.2648).
However, we know nothing about the indirect death toll from malignancy (without coronavirus infection) that was untreated or managed less than optimally because of personnel and physical resources that were diverted to COVID-19–associated cases.
Similarly, we cannot begin to estimate indirect consequences of the pandemic to oncology practices, such as accelerated burnout and posttraumatic stress disorder, as well as the long-range effects of economic turmoil on patients, health care workers, and provider organizations.
What happens to cancer trials?
From China, Italy, and Seattle, thus far, there is little information about how the pandemic will affect the vital clinical research endeavor. The Seattle physicians did say they plan to enroll patients on clinical trials only when the trial offers a high chance of benefiting the patient over standard therapy alone.
Fortunately, the National Institutes of Health and Food and Drug Administration have released guidance documents related to clinical trials.
The National Cancer Institute (NCI) has also released guidance documents (March 13 guidance; March 23 guidance) for patients on clinical trials supported by the NCI Cancer Therapy Evaluation Program (CTEP) and the NCI Community Oncology Research Program (NCORP).
CTEP and NCORP are making reasonable accommodations to suspend monitoring visits and audits, allow tele–follow-up visits for patients, and permit local physicians to provide care for patients on study. In addition, with appropriate procedural adherence and documentation, CTEP and NCORP will allow oral investigational medicines to be mailed directly to patients’ homes.
Planned NCI National Clinical Trials Network meetings will be conducted via remote access webinars, conference calls, and similar technology. These adjustments – and probably many more to come – are geared toward facilitating ongoing care to proceed safely and with minimal risk for patients currently receiving investigational therapies and for the sites and investigators engaged in those studies.
Each of us has probably faced a personal “defining professional moment,” when we had to utilize every skill in our arsenal and examine the motivations that led us to a career in oncology. However, it is clear from the forgoing clinical and research processes and guidelines that the COVID-19 pandemic is such a defining professional moment for each of us, in every community we serve.
Critical junctures like this cause more rapid behavior change and innovation than the slow-moving pace that characterizes our idealized preferences. As oncologists who embrace new data and behavioral change, we stand to learn processes that will facilitate more perfected systems of care than the one that preceded this unprecedented crisis, promote more efficient sharing of high-quality information, and improve the outcome for our future patients.
Dr. Lyss was an oncologist and researcher for more than 35 years before his recent retirement. His clinical and research interests were focused on breast and lung cancers, as well as expanding clinical trial access to medically underserved populations. He is based in St. Louis. He has no conflicts of interest.
Psychiatrists deemed ‘essential’ in time of COVID-19
New American Psychiatric Association poll shows depth of anxiety
The coronavirus pandemic weighs heavily on psychiatric patients with conditions such as anxiety, depression and PTSD. Meanwhile, a national poll released March 25 by the American Psychiatric Association shows that almost half of all Americans are anxious about contracting COVID-19 and 40% are anxious about becoming seriously ill or dying from the virus. In light of stressors on patients and nonpatients alike, mental health professionals have a key role in helping to alleviate suffering tied to the public health crisis, according to psychiatrists from across the country.
“There’s so much we can do to help people put order on this chaos,” said Shaili Jain, MD, section chief of outpatient mental health with the Veterans Affairs Palo Alto (Calif.) Health Care System, in an interview. “We are essential workers in this time.”
Dr. Jain, who specializes in treating PTSD, said those patients are especially vulnerable to the stress and disruptions spawned by the pandemic. “When you go to the grocery store and there’s no food, that can be triggering for people who survived situations with a feeling of calamity or panic,” she said. “People are reporting worsening of nightmares and spontaneous panic attacks after having been stable with symptoms for many months. These are the kinds of stories that are starting to filter through.”
To make things even more difficult, she said, shelter-in-place orders are preventing patients from taking advantage of healthy coping strategies, such as working out at the gym or going to support groups. “We have an invaluable role to play in trying to prevent long-term consequences by going into problem-solving modes with patients.” Dr. Jain offered several tips that might help patients who are suffering:
- Use technology to stay in touch with support communities and boost self-care. “How can you be flexible with FaceTime, Skype, or phone even if you might not be able to have that face-to-face time? What are you doing to double down on your efforts at self-care – listening to music, reading, daily meditation, or walks? Double down on what you can do to prevent anxiety and stress levels from building up.”
- Take breaks from the news, which can contribute to hypervigilance and disrupted sleep. “I’m seeing that people are going down these rabbit holes of having the news or social media on 24/7,” Dr. Jain said. “You have to stay informed. But you need to pick trusted news sources and have chunks of time that are free of coronavirus coverage.” Understand that life is going to be difficult for a while. “We’re doing a lot of reassurance and education,” she said, “helping people to know and accept that the next few days, weeks, and months are going to be stressful.”
Dr. Jain cautioned colleagues, however, that “there will be a tsunami” of mental illness when the coronavirus crisis lifts. She is especially concerned about patient populations that are socioeconomically disadvantaged already and how their lives with be affected by lost wages, unemployment, and business failures. “Medical professionals will see the consequences of this in the days and weeks and months after the pandemic has settled,” she predicted.
The APA poll shows that, early in the crisis, more than 60% of people are anxious about family and loved ones contracting COVID-19.
Maintaining ‘reflective space’ essential
At the Austen Riggs Center, a psychiatric residential treatment facility in Stockbridge, Mass., staff and patients are adjusting to new rules that aim to prevent transmission of the novel coronavirus. “Social distancing requirements are having a huge impact,” said Eric M. Plakun, MD, medical director and CEO of Austen Riggs, in an interview. “You can’t have groups in the same way; you can’t have families come in for a family meeting; you can’t have quite the same the freedom to come and go. A lot of management issues are being addressed, but it is crucial also to maintain the ‘reflective space’ essential to do the kind of clinical work we do.” One approach, he said, is virtual meetings with colleagues that address on-the-job management issues, but also leave a space for how staff members are feeling.
“It’s easy to get into crisis-response mode,” he said, “where you’re always managing but never leave a space to talk about vulnerability, helplessness, and fear.”
As the facility’s staff adjusts by embracing teleconference technology and adapting group meetings to the 6-feet-apart rule,
Dr. Plakun said he said, noting that patients have approached staff members to say they want to collaborate about changes. “That’s a credible offer we intend to accept.”
Still, communicating with patients as a whole about the coronavirus can be difficult. As Dr. Plakun noted, it’s now impossible to bring 75 people together into one room for a meeting. “If you have four to five smaller meetings, how do you maintain some congruence in the information that’s presented?”
Dr. Plakun suggested that colleagues find time to engage in the familiar, such as face-to-face clinical work. “That’s been the most reassuring and rewarding part of my day since it feels almost like normal,” he said.
Stocking up on medications
Jessica “Jessi” Gold, MD, MS, an assistant professor at Washington University in St. Louis, often treats college students. Asian students started to worry early in the pandemic, she said in an interview.
“At the beginning, there were a lot of concerns about the public’s view: ‘Did this come from China? Is it China’s fault?’ A lot of our students felt that if they coughed, and they were a white person, they’d be OK. But if they were Asian, everyone would wonder why they were in class and not at home. That got worse over time: the fear about – and anxiety from – stoking racism.”
Later, as classes began to be canceled, Dr. Gold started to see the psychological effects of disruption and uncertainty about the future. “This can lead people to feel like what they knew before is just not there anymore. This can obviously cause anxiety but also has the potential to cause depression.” Patients also might slip into overuse of alcohol and drugs, or they might engage in other kinds of harmful behavior. Eating disorders, for example, “are ways to have control when other things aren’t in control,” she said.
Dr. Gold pointed to research into the mental health after effects of quarantines, such as those imposed during the SARS outbreak. A review of 24 studies published this year found that most “reported negative psychological effects, including post-traumatic stress symptoms, confusion, and anger. Stressors included longer quarantine duration, infection fears, frustration, boredom, inadequate supplies, inadequate information, financial loss, and stigma. Some researchers have suggested long-lasting effects” (Lancet. 2020;395:912-20).
Dr. Gold is urging patients to recall the warning signs that alerted them to psychological downturns in the past: “Try to remember what those warning signs are and pay attention to whether you see them.” And, Dr. Gold said, she asks patients to think about what has helped them get better.
In some cases, she said, patients are already preparing themselves for experiencing mental distress by stocking up on medications. “Some people have a bottle of 10-20 pills that they only use in emergencies and keep as a kind of security blanket,” she said, and she’s seen some of them ask for refills. It seems they’ve either taken the pills recently or want to stash them just in case. This makes sense, since their anxiety is higher, she said.
Dr. Gold cautioned that psychiatrists need to be careful to not overextend themselves when they’re not treating patients. “It is easy to be therapist to friends, family, and colleagues,” she said, “but we need to take care of ourselves, too.”
Dr. Jain is author of “The Unspeakable Mind: Stories of Trauma and Healing From the Frontlines of PTSD Science” (New York: Harper, 2019). She has no other disclosures. Dr. Plakun and Dr. Gold reported no relevant disclosures.
New American Psychiatric Association poll shows depth of anxiety
New American Psychiatric Association poll shows depth of anxiety
The coronavirus pandemic weighs heavily on psychiatric patients with conditions such as anxiety, depression and PTSD. Meanwhile, a national poll released March 25 by the American Psychiatric Association shows that almost half of all Americans are anxious about contracting COVID-19 and 40% are anxious about becoming seriously ill or dying from the virus. In light of stressors on patients and nonpatients alike, mental health professionals have a key role in helping to alleviate suffering tied to the public health crisis, according to psychiatrists from across the country.
“There’s so much we can do to help people put order on this chaos,” said Shaili Jain, MD, section chief of outpatient mental health with the Veterans Affairs Palo Alto (Calif.) Health Care System, in an interview. “We are essential workers in this time.”
Dr. Jain, who specializes in treating PTSD, said those patients are especially vulnerable to the stress and disruptions spawned by the pandemic. “When you go to the grocery store and there’s no food, that can be triggering for people who survived situations with a feeling of calamity or panic,” she said. “People are reporting worsening of nightmares and spontaneous panic attacks after having been stable with symptoms for many months. These are the kinds of stories that are starting to filter through.”
To make things even more difficult, she said, shelter-in-place orders are preventing patients from taking advantage of healthy coping strategies, such as working out at the gym or going to support groups. “We have an invaluable role to play in trying to prevent long-term consequences by going into problem-solving modes with patients.” Dr. Jain offered several tips that might help patients who are suffering:
- Use technology to stay in touch with support communities and boost self-care. “How can you be flexible with FaceTime, Skype, or phone even if you might not be able to have that face-to-face time? What are you doing to double down on your efforts at self-care – listening to music, reading, daily meditation, or walks? Double down on what you can do to prevent anxiety and stress levels from building up.”
- Take breaks from the news, which can contribute to hypervigilance and disrupted sleep. “I’m seeing that people are going down these rabbit holes of having the news or social media on 24/7,” Dr. Jain said. “You have to stay informed. But you need to pick trusted news sources and have chunks of time that are free of coronavirus coverage.” Understand that life is going to be difficult for a while. “We’re doing a lot of reassurance and education,” she said, “helping people to know and accept that the next few days, weeks, and months are going to be stressful.”
Dr. Jain cautioned colleagues, however, that “there will be a tsunami” of mental illness when the coronavirus crisis lifts. She is especially concerned about patient populations that are socioeconomically disadvantaged already and how their lives with be affected by lost wages, unemployment, and business failures. “Medical professionals will see the consequences of this in the days and weeks and months after the pandemic has settled,” she predicted.
The APA poll shows that, early in the crisis, more than 60% of people are anxious about family and loved ones contracting COVID-19.
Maintaining ‘reflective space’ essential
At the Austen Riggs Center, a psychiatric residential treatment facility in Stockbridge, Mass., staff and patients are adjusting to new rules that aim to prevent transmission of the novel coronavirus. “Social distancing requirements are having a huge impact,” said Eric M. Plakun, MD, medical director and CEO of Austen Riggs, in an interview. “You can’t have groups in the same way; you can’t have families come in for a family meeting; you can’t have quite the same the freedom to come and go. A lot of management issues are being addressed, but it is crucial also to maintain the ‘reflective space’ essential to do the kind of clinical work we do.” One approach, he said, is virtual meetings with colleagues that address on-the-job management issues, but also leave a space for how staff members are feeling.
“It’s easy to get into crisis-response mode,” he said, “where you’re always managing but never leave a space to talk about vulnerability, helplessness, and fear.”
As the facility’s staff adjusts by embracing teleconference technology and adapting group meetings to the 6-feet-apart rule,
Dr. Plakun said he said, noting that patients have approached staff members to say they want to collaborate about changes. “That’s a credible offer we intend to accept.”
Still, communicating with patients as a whole about the coronavirus can be difficult. As Dr. Plakun noted, it’s now impossible to bring 75 people together into one room for a meeting. “If you have four to five smaller meetings, how do you maintain some congruence in the information that’s presented?”
Dr. Plakun suggested that colleagues find time to engage in the familiar, such as face-to-face clinical work. “That’s been the most reassuring and rewarding part of my day since it feels almost like normal,” he said.
Stocking up on medications
Jessica “Jessi” Gold, MD, MS, an assistant professor at Washington University in St. Louis, often treats college students. Asian students started to worry early in the pandemic, she said in an interview.
“At the beginning, there were a lot of concerns about the public’s view: ‘Did this come from China? Is it China’s fault?’ A lot of our students felt that if they coughed, and they were a white person, they’d be OK. But if they were Asian, everyone would wonder why they were in class and not at home. That got worse over time: the fear about – and anxiety from – stoking racism.”
Later, as classes began to be canceled, Dr. Gold started to see the psychological effects of disruption and uncertainty about the future. “This can lead people to feel like what they knew before is just not there anymore. This can obviously cause anxiety but also has the potential to cause depression.” Patients also might slip into overuse of alcohol and drugs, or they might engage in other kinds of harmful behavior. Eating disorders, for example, “are ways to have control when other things aren’t in control,” she said.
Dr. Gold pointed to research into the mental health after effects of quarantines, such as those imposed during the SARS outbreak. A review of 24 studies published this year found that most “reported negative psychological effects, including post-traumatic stress symptoms, confusion, and anger. Stressors included longer quarantine duration, infection fears, frustration, boredom, inadequate supplies, inadequate information, financial loss, and stigma. Some researchers have suggested long-lasting effects” (Lancet. 2020;395:912-20).
Dr. Gold is urging patients to recall the warning signs that alerted them to psychological downturns in the past: “Try to remember what those warning signs are and pay attention to whether you see them.” And, Dr. Gold said, she asks patients to think about what has helped them get better.
In some cases, she said, patients are already preparing themselves for experiencing mental distress by stocking up on medications. “Some people have a bottle of 10-20 pills that they only use in emergencies and keep as a kind of security blanket,” she said, and she’s seen some of them ask for refills. It seems they’ve either taken the pills recently or want to stash them just in case. This makes sense, since their anxiety is higher, she said.
Dr. Gold cautioned that psychiatrists need to be careful to not overextend themselves when they’re not treating patients. “It is easy to be therapist to friends, family, and colleagues,” she said, “but we need to take care of ourselves, too.”
Dr. Jain is author of “The Unspeakable Mind: Stories of Trauma and Healing From the Frontlines of PTSD Science” (New York: Harper, 2019). She has no other disclosures. Dr. Plakun and Dr. Gold reported no relevant disclosures.
The coronavirus pandemic weighs heavily on psychiatric patients with conditions such as anxiety, depression and PTSD. Meanwhile, a national poll released March 25 by the American Psychiatric Association shows that almost half of all Americans are anxious about contracting COVID-19 and 40% are anxious about becoming seriously ill or dying from the virus. In light of stressors on patients and nonpatients alike, mental health professionals have a key role in helping to alleviate suffering tied to the public health crisis, according to psychiatrists from across the country.
“There’s so much we can do to help people put order on this chaos,” said Shaili Jain, MD, section chief of outpatient mental health with the Veterans Affairs Palo Alto (Calif.) Health Care System, in an interview. “We are essential workers in this time.”
Dr. Jain, who specializes in treating PTSD, said those patients are especially vulnerable to the stress and disruptions spawned by the pandemic. “When you go to the grocery store and there’s no food, that can be triggering for people who survived situations with a feeling of calamity or panic,” she said. “People are reporting worsening of nightmares and spontaneous panic attacks after having been stable with symptoms for many months. These are the kinds of stories that are starting to filter through.”
To make things even more difficult, she said, shelter-in-place orders are preventing patients from taking advantage of healthy coping strategies, such as working out at the gym or going to support groups. “We have an invaluable role to play in trying to prevent long-term consequences by going into problem-solving modes with patients.” Dr. Jain offered several tips that might help patients who are suffering:
- Use technology to stay in touch with support communities and boost self-care. “How can you be flexible with FaceTime, Skype, or phone even if you might not be able to have that face-to-face time? What are you doing to double down on your efforts at self-care – listening to music, reading, daily meditation, or walks? Double down on what you can do to prevent anxiety and stress levels from building up.”
- Take breaks from the news, which can contribute to hypervigilance and disrupted sleep. “I’m seeing that people are going down these rabbit holes of having the news or social media on 24/7,” Dr. Jain said. “You have to stay informed. But you need to pick trusted news sources and have chunks of time that are free of coronavirus coverage.” Understand that life is going to be difficult for a while. “We’re doing a lot of reassurance and education,” she said, “helping people to know and accept that the next few days, weeks, and months are going to be stressful.”
Dr. Jain cautioned colleagues, however, that “there will be a tsunami” of mental illness when the coronavirus crisis lifts. She is especially concerned about patient populations that are socioeconomically disadvantaged already and how their lives with be affected by lost wages, unemployment, and business failures. “Medical professionals will see the consequences of this in the days and weeks and months after the pandemic has settled,” she predicted.
The APA poll shows that, early in the crisis, more than 60% of people are anxious about family and loved ones contracting COVID-19.
Maintaining ‘reflective space’ essential
At the Austen Riggs Center, a psychiatric residential treatment facility in Stockbridge, Mass., staff and patients are adjusting to new rules that aim to prevent transmission of the novel coronavirus. “Social distancing requirements are having a huge impact,” said Eric M. Plakun, MD, medical director and CEO of Austen Riggs, in an interview. “You can’t have groups in the same way; you can’t have families come in for a family meeting; you can’t have quite the same the freedom to come and go. A lot of management issues are being addressed, but it is crucial also to maintain the ‘reflective space’ essential to do the kind of clinical work we do.” One approach, he said, is virtual meetings with colleagues that address on-the-job management issues, but also leave a space for how staff members are feeling.
“It’s easy to get into crisis-response mode,” he said, “where you’re always managing but never leave a space to talk about vulnerability, helplessness, and fear.”
As the facility’s staff adjusts by embracing teleconference technology and adapting group meetings to the 6-feet-apart rule,
Dr. Plakun said he said, noting that patients have approached staff members to say they want to collaborate about changes. “That’s a credible offer we intend to accept.”
Still, communicating with patients as a whole about the coronavirus can be difficult. As Dr. Plakun noted, it’s now impossible to bring 75 people together into one room for a meeting. “If you have four to five smaller meetings, how do you maintain some congruence in the information that’s presented?”
Dr. Plakun suggested that colleagues find time to engage in the familiar, such as face-to-face clinical work. “That’s been the most reassuring and rewarding part of my day since it feels almost like normal,” he said.
Stocking up on medications
Jessica “Jessi” Gold, MD, MS, an assistant professor at Washington University in St. Louis, often treats college students. Asian students started to worry early in the pandemic, she said in an interview.
“At the beginning, there were a lot of concerns about the public’s view: ‘Did this come from China? Is it China’s fault?’ A lot of our students felt that if they coughed, and they were a white person, they’d be OK. But if they were Asian, everyone would wonder why they were in class and not at home. That got worse over time: the fear about – and anxiety from – stoking racism.”
Later, as classes began to be canceled, Dr. Gold started to see the psychological effects of disruption and uncertainty about the future. “This can lead people to feel like what they knew before is just not there anymore. This can obviously cause anxiety but also has the potential to cause depression.” Patients also might slip into overuse of alcohol and drugs, or they might engage in other kinds of harmful behavior. Eating disorders, for example, “are ways to have control when other things aren’t in control,” she said.
Dr. Gold pointed to research into the mental health after effects of quarantines, such as those imposed during the SARS outbreak. A review of 24 studies published this year found that most “reported negative psychological effects, including post-traumatic stress symptoms, confusion, and anger. Stressors included longer quarantine duration, infection fears, frustration, boredom, inadequate supplies, inadequate information, financial loss, and stigma. Some researchers have suggested long-lasting effects” (Lancet. 2020;395:912-20).
Dr. Gold is urging patients to recall the warning signs that alerted them to psychological downturns in the past: “Try to remember what those warning signs are and pay attention to whether you see them.” And, Dr. Gold said, she asks patients to think about what has helped them get better.
In some cases, she said, patients are already preparing themselves for experiencing mental distress by stocking up on medications. “Some people have a bottle of 10-20 pills that they only use in emergencies and keep as a kind of security blanket,” she said, and she’s seen some of them ask for refills. It seems they’ve either taken the pills recently or want to stash them just in case. This makes sense, since their anxiety is higher, she said.
Dr. Gold cautioned that psychiatrists need to be careful to not overextend themselves when they’re not treating patients. “It is easy to be therapist to friends, family, and colleagues,” she said, “but we need to take care of ourselves, too.”
Dr. Jain is author of “The Unspeakable Mind: Stories of Trauma and Healing From the Frontlines of PTSD Science” (New York: Harper, 2019). She has no other disclosures. Dr. Plakun and Dr. Gold reported no relevant disclosures.
Hospitals muzzle doctors and nurses on PPE, COVID-19 cases
Over the past month, an orthopedic surgeon has watched as the crowd of sick patients at his hospital has grown, while the supply of personal protective equipment (PPE) for staff has diminished. As he prepares for another day of staffing testing tents and places his one and only mask across his face, he also receives a daily reminder from hospital management: Don’t talk about it.
The surgeon, who works in a COVID-19 hot spot in the Northeast, spoke on the condition of anonymity for fear of employer retribution.
“It’s very clear; no one is allowed to speak for the institution or of the institution,” he said in an interview. “We get a daily warning about being very prudent about posts on personal accounts. They’ve talked about this with respect to various issues: case numbers, case severity, testing availability, [and] PPEs.”
The warnings mean staff at the hospital suffer in silence, unable to share the troubling situation with the public or request assistance with supplies.
“I have one mask. We’re expected to reuse them, unless you were exposed or worked with a known COVID victim,” the surgeon said. “However, with the numbers in our region rapidly increasing, you can’t assume that people don’t have it or that you don’t have particles on your mask, even if you’re not in a known quarantine zone within the institution.”
As the COVID-19 health crisis rages on, online platforms have become a common place for health professionals to lament short supplies, share concerns, tell stories, and plead for help. But at the same time, other physicians, nurses, and health care workers are being muzzled by hospital administrators and threatened with discipline for speaking out about coronavirus caseloads and dwindling supplies. Some worry the gag orders are muddying the picture of how hospitals are faring in the pandemic, while placing the safety of frontline workers at risk.
The silencing of physicians by hospitals about PPE shortages and other COVID-19 issues has become widespread, said Nisha Mehta, MD, a physician advocate and community leader who writes about PPE on social media. Physicians are being warned not to speak or post publicly about their COVID-19 experiences, including PPE shortages, case specifics, and the percentage of full hospital beds, Dr. Mehta said in an interview. In some cases, physicians who have posted have been forced to take down the posts or have faced retribution for speaking out, she said.
“There’s definitely a big fear among physicians, particularly employed physicians, in terms of what the consequences may be for telling their stories,” Dr. Mehta said. “I find that counterproductive. I understand not inducing panic, but these are real stories that are important for people to understand so they do stay home and increase the systemic pressure to get sufficient PPE, so that we can preserve our health care workforce for a problem that is going to get worse before it gets better.”
Meanwhile, an Indiana hospitalist who took to social media to ask for masks for hospitals in his area says he was immediately reprimanded by his management after the posts came to light. The hospitalist posted on a social media platform to request donations of N95 masks after hearing members of the public had purchased such masks. He hoped his plea would aid preparation for the pandemic at local hospitals, explained the physician, who spoke on the condition of anonymity.
Shortly afterward, administrators from his hospital contacted the online forum’s moderator and the posts were removed, he said. During a subsequent conversation, administrators warned the doctor not to make such posts about PPE because it made the hospital appear incompetent.
“I was told, ‘we can handle this, we don’t need the public’s help,’” the physician said. “I was hurt and upset. I was trying to help protect my peers.”
After landing on the management’s radar, the hospitalist said he was reprimanded a second time about posts on a separate personal social media account. The second time, the private posts to friends and family were related to COVID-19 and PPE, but did not include any protected health information, he said. However, administrators did not like the content of the posts, and he was told management was monitoring his activity on social media, he said.
“The larger message is that patients are money,” the hospitalist said. “The corporate side of medicine rules out over the medicine side. Image and making sure there is a consistent cash flow trumps all else.”
Another frontline physician who works at a large New York hospital, said staff have been cautioned not to talk with the media and to be careful what they post on social media regarding COVID-19. The general rule is that only information approved by administrators can be shared, said the physician, who spoke on the condition of anonymity.
“[The health system] is very protective of their public image,” he said. “In the past, people that have posted things that they don’t like get spoken to quickly and/or fired depending on what was written. I could only imagine that would be the situation regarding COVID-19. They are very strict.”
The frontline physician, who has close contact with COVID-19 patients, said he has access to N95 masks at the moment, but when he requested higher-level protective gear, hospital management refused the request and denied that such supplies were needed.
“Safety of frontline workers appears to not be taken seriously,” he said of his hospital. “Everyone is stressed, but at the end of the day, the administration is sitting there, while the rest of us are putting ourselves at risk.”
We reached out to one hospital for comment, but messages were not returned. Other hospitals were not contacted because physicians feared they would face retribution. We also contacted the American Hospital Association but they did not immediately respond.
In Chicago, an email by a nurse to her coworkers about the safety of masks has resulted in a lawsuit after the nurse says she was fired for sharing her concerns with staff. The nurse, Lauri Mazurkiewicz, sent an email to staffers at Northwestern Memorial Hospital stating the surgical masks provided by the hospital were less effective against airborne particles than were N95 masks, according to a lawsuit filed March 23 in Cook County Circuit Court. Ms. Mazurkiewicz was terminated the next day in retaliation for her email, the lawsuit alleges.
Ms. Mazurkiewicz could not be reached for comment by press time.
Christopher King, a spokesman for Northwestern Medicine, said the hospital is reviewing the lawsuit.
“As Northwestern Medicine continues to respond to this unprecedented health care pandemic, the health and well-being of our patients, our staff and our employees is our highest priority,” he said in a statement. “We take these matters seriously and we are currently reviewing the complaint. At this time, we will not be commenting further.”
John Mandrola, MD, a Louisville, Ky.–based cardiologist who has written about the recent muzzling of frontline physicians with respect to the coronavirus, said he is not surprised that some hospitals are preventing physicians from sharing their experiences.
“Before C19, in many hospital systems, there was a culture of fear amongst employed clinicians,” he said. “Employed clinicians see other employed physicians being terminated for speaking frankly about problems. It takes scant few of these cases to create a culture of silence.”
Dr. Mandrola, who is a regular Medscape contributor, said that a number of doctors have reached out to him privately about PPE scarcity and shared that they were explicitly warned by administrators not to talk about the shortfalls. Leadership at Dr. Mandrola’s hospital has not issued the same warnings, he said.
“From the hat of total transparency, I think the public is not getting a full view of the impending potential problems that are going to come by doctors not speaking publicly,” he said. “On the other hand, hospital leadership is doing the best they can. It’s not the hospitals’ fault. Hospital administrators can’t manufacture masks.”
From a public health standpoint, Dr. Mehta said that not allowing health professionals to speak publicly about the situations at their hospitals is “irresponsible.” The public deserves to know what is happening, she said, and the health care workforce needs to prepare for what is to come.
“It’s so important that we hear from our colleagues,” she said. “It’s important to hear those accounts so we can prepare for what we’re about to face. Data is crucial. The more you learn from each other, the better shot we have at successfully treating cases and ultimately beating this.”
With the critical shortage of PPE at his hospital and the inability to speak out about the problem, the orthopedic surgeon foresees the dilemma continuing to worsen.
“It’s not only the lives of front-line health care workers that are at risk, but it’s those that they’re going to spread it to and those that are going to be coming to the hospital requiring our care,” he said. “If we don’t have a fully functioning health care force, our capacity is going to be diminished that much further.”
Over the past month, an orthopedic surgeon has watched as the crowd of sick patients at his hospital has grown, while the supply of personal protective equipment (PPE) for staff has diminished. As he prepares for another day of staffing testing tents and places his one and only mask across his face, he also receives a daily reminder from hospital management: Don’t talk about it.
The surgeon, who works in a COVID-19 hot spot in the Northeast, spoke on the condition of anonymity for fear of employer retribution.
“It’s very clear; no one is allowed to speak for the institution or of the institution,” he said in an interview. “We get a daily warning about being very prudent about posts on personal accounts. They’ve talked about this with respect to various issues: case numbers, case severity, testing availability, [and] PPEs.”
The warnings mean staff at the hospital suffer in silence, unable to share the troubling situation with the public or request assistance with supplies.
“I have one mask. We’re expected to reuse them, unless you were exposed or worked with a known COVID victim,” the surgeon said. “However, with the numbers in our region rapidly increasing, you can’t assume that people don’t have it or that you don’t have particles on your mask, even if you’re not in a known quarantine zone within the institution.”
As the COVID-19 health crisis rages on, online platforms have become a common place for health professionals to lament short supplies, share concerns, tell stories, and plead for help. But at the same time, other physicians, nurses, and health care workers are being muzzled by hospital administrators and threatened with discipline for speaking out about coronavirus caseloads and dwindling supplies. Some worry the gag orders are muddying the picture of how hospitals are faring in the pandemic, while placing the safety of frontline workers at risk.
The silencing of physicians by hospitals about PPE shortages and other COVID-19 issues has become widespread, said Nisha Mehta, MD, a physician advocate and community leader who writes about PPE on social media. Physicians are being warned not to speak or post publicly about their COVID-19 experiences, including PPE shortages, case specifics, and the percentage of full hospital beds, Dr. Mehta said in an interview. In some cases, physicians who have posted have been forced to take down the posts or have faced retribution for speaking out, she said.
“There’s definitely a big fear among physicians, particularly employed physicians, in terms of what the consequences may be for telling their stories,” Dr. Mehta said. “I find that counterproductive. I understand not inducing panic, but these are real stories that are important for people to understand so they do stay home and increase the systemic pressure to get sufficient PPE, so that we can preserve our health care workforce for a problem that is going to get worse before it gets better.”
Meanwhile, an Indiana hospitalist who took to social media to ask for masks for hospitals in his area says he was immediately reprimanded by his management after the posts came to light. The hospitalist posted on a social media platform to request donations of N95 masks after hearing members of the public had purchased such masks. He hoped his plea would aid preparation for the pandemic at local hospitals, explained the physician, who spoke on the condition of anonymity.
Shortly afterward, administrators from his hospital contacted the online forum’s moderator and the posts were removed, he said. During a subsequent conversation, administrators warned the doctor not to make such posts about PPE because it made the hospital appear incompetent.
“I was told, ‘we can handle this, we don’t need the public’s help,’” the physician said. “I was hurt and upset. I was trying to help protect my peers.”
After landing on the management’s radar, the hospitalist said he was reprimanded a second time about posts on a separate personal social media account. The second time, the private posts to friends and family were related to COVID-19 and PPE, but did not include any protected health information, he said. However, administrators did not like the content of the posts, and he was told management was monitoring his activity on social media, he said.
“The larger message is that patients are money,” the hospitalist said. “The corporate side of medicine rules out over the medicine side. Image and making sure there is a consistent cash flow trumps all else.”
Another frontline physician who works at a large New York hospital, said staff have been cautioned not to talk with the media and to be careful what they post on social media regarding COVID-19. The general rule is that only information approved by administrators can be shared, said the physician, who spoke on the condition of anonymity.
“[The health system] is very protective of their public image,” he said. “In the past, people that have posted things that they don’t like get spoken to quickly and/or fired depending on what was written. I could only imagine that would be the situation regarding COVID-19. They are very strict.”
The frontline physician, who has close contact with COVID-19 patients, said he has access to N95 masks at the moment, but when he requested higher-level protective gear, hospital management refused the request and denied that such supplies were needed.
“Safety of frontline workers appears to not be taken seriously,” he said of his hospital. “Everyone is stressed, but at the end of the day, the administration is sitting there, while the rest of us are putting ourselves at risk.”
We reached out to one hospital for comment, but messages were not returned. Other hospitals were not contacted because physicians feared they would face retribution. We also contacted the American Hospital Association but they did not immediately respond.
In Chicago, an email by a nurse to her coworkers about the safety of masks has resulted in a lawsuit after the nurse says she was fired for sharing her concerns with staff. The nurse, Lauri Mazurkiewicz, sent an email to staffers at Northwestern Memorial Hospital stating the surgical masks provided by the hospital were less effective against airborne particles than were N95 masks, according to a lawsuit filed March 23 in Cook County Circuit Court. Ms. Mazurkiewicz was terminated the next day in retaliation for her email, the lawsuit alleges.
Ms. Mazurkiewicz could not be reached for comment by press time.
Christopher King, a spokesman for Northwestern Medicine, said the hospital is reviewing the lawsuit.
“As Northwestern Medicine continues to respond to this unprecedented health care pandemic, the health and well-being of our patients, our staff and our employees is our highest priority,” he said in a statement. “We take these matters seriously and we are currently reviewing the complaint. At this time, we will not be commenting further.”
John Mandrola, MD, a Louisville, Ky.–based cardiologist who has written about the recent muzzling of frontline physicians with respect to the coronavirus, said he is not surprised that some hospitals are preventing physicians from sharing their experiences.
“Before C19, in many hospital systems, there was a culture of fear amongst employed clinicians,” he said. “Employed clinicians see other employed physicians being terminated for speaking frankly about problems. It takes scant few of these cases to create a culture of silence.”
Dr. Mandrola, who is a regular Medscape contributor, said that a number of doctors have reached out to him privately about PPE scarcity and shared that they were explicitly warned by administrators not to talk about the shortfalls. Leadership at Dr. Mandrola’s hospital has not issued the same warnings, he said.
“From the hat of total transparency, I think the public is not getting a full view of the impending potential problems that are going to come by doctors not speaking publicly,” he said. “On the other hand, hospital leadership is doing the best they can. It’s not the hospitals’ fault. Hospital administrators can’t manufacture masks.”
From a public health standpoint, Dr. Mehta said that not allowing health professionals to speak publicly about the situations at their hospitals is “irresponsible.” The public deserves to know what is happening, she said, and the health care workforce needs to prepare for what is to come.
“It’s so important that we hear from our colleagues,” she said. “It’s important to hear those accounts so we can prepare for what we’re about to face. Data is crucial. The more you learn from each other, the better shot we have at successfully treating cases and ultimately beating this.”
With the critical shortage of PPE at his hospital and the inability to speak out about the problem, the orthopedic surgeon foresees the dilemma continuing to worsen.
“It’s not only the lives of front-line health care workers that are at risk, but it’s those that they’re going to spread it to and those that are going to be coming to the hospital requiring our care,” he said. “If we don’t have a fully functioning health care force, our capacity is going to be diminished that much further.”
Over the past month, an orthopedic surgeon has watched as the crowd of sick patients at his hospital has grown, while the supply of personal protective equipment (PPE) for staff has diminished. As he prepares for another day of staffing testing tents and places his one and only mask across his face, he also receives a daily reminder from hospital management: Don’t talk about it.
The surgeon, who works in a COVID-19 hot spot in the Northeast, spoke on the condition of anonymity for fear of employer retribution.
“It’s very clear; no one is allowed to speak for the institution or of the institution,” he said in an interview. “We get a daily warning about being very prudent about posts on personal accounts. They’ve talked about this with respect to various issues: case numbers, case severity, testing availability, [and] PPEs.”
The warnings mean staff at the hospital suffer in silence, unable to share the troubling situation with the public or request assistance with supplies.
“I have one mask. We’re expected to reuse them, unless you were exposed or worked with a known COVID victim,” the surgeon said. “However, with the numbers in our region rapidly increasing, you can’t assume that people don’t have it or that you don’t have particles on your mask, even if you’re not in a known quarantine zone within the institution.”
As the COVID-19 health crisis rages on, online platforms have become a common place for health professionals to lament short supplies, share concerns, tell stories, and plead for help. But at the same time, other physicians, nurses, and health care workers are being muzzled by hospital administrators and threatened with discipline for speaking out about coronavirus caseloads and dwindling supplies. Some worry the gag orders are muddying the picture of how hospitals are faring in the pandemic, while placing the safety of frontline workers at risk.
The silencing of physicians by hospitals about PPE shortages and other COVID-19 issues has become widespread, said Nisha Mehta, MD, a physician advocate and community leader who writes about PPE on social media. Physicians are being warned not to speak or post publicly about their COVID-19 experiences, including PPE shortages, case specifics, and the percentage of full hospital beds, Dr. Mehta said in an interview. In some cases, physicians who have posted have been forced to take down the posts or have faced retribution for speaking out, she said.
“There’s definitely a big fear among physicians, particularly employed physicians, in terms of what the consequences may be for telling their stories,” Dr. Mehta said. “I find that counterproductive. I understand not inducing panic, but these are real stories that are important for people to understand so they do stay home and increase the systemic pressure to get sufficient PPE, so that we can preserve our health care workforce for a problem that is going to get worse before it gets better.”
Meanwhile, an Indiana hospitalist who took to social media to ask for masks for hospitals in his area says he was immediately reprimanded by his management after the posts came to light. The hospitalist posted on a social media platform to request donations of N95 masks after hearing members of the public had purchased such masks. He hoped his plea would aid preparation for the pandemic at local hospitals, explained the physician, who spoke on the condition of anonymity.
Shortly afterward, administrators from his hospital contacted the online forum’s moderator and the posts were removed, he said. During a subsequent conversation, administrators warned the doctor not to make such posts about PPE because it made the hospital appear incompetent.
“I was told, ‘we can handle this, we don’t need the public’s help,’” the physician said. “I was hurt and upset. I was trying to help protect my peers.”
After landing on the management’s radar, the hospitalist said he was reprimanded a second time about posts on a separate personal social media account. The second time, the private posts to friends and family were related to COVID-19 and PPE, but did not include any protected health information, he said. However, administrators did not like the content of the posts, and he was told management was monitoring his activity on social media, he said.
“The larger message is that patients are money,” the hospitalist said. “The corporate side of medicine rules out over the medicine side. Image and making sure there is a consistent cash flow trumps all else.”
Another frontline physician who works at a large New York hospital, said staff have been cautioned not to talk with the media and to be careful what they post on social media regarding COVID-19. The general rule is that only information approved by administrators can be shared, said the physician, who spoke on the condition of anonymity.
“[The health system] is very protective of their public image,” he said. “In the past, people that have posted things that they don’t like get spoken to quickly and/or fired depending on what was written. I could only imagine that would be the situation regarding COVID-19. They are very strict.”
The frontline physician, who has close contact with COVID-19 patients, said he has access to N95 masks at the moment, but when he requested higher-level protective gear, hospital management refused the request and denied that such supplies were needed.
“Safety of frontline workers appears to not be taken seriously,” he said of his hospital. “Everyone is stressed, but at the end of the day, the administration is sitting there, while the rest of us are putting ourselves at risk.”
We reached out to one hospital for comment, but messages were not returned. Other hospitals were not contacted because physicians feared they would face retribution. We also contacted the American Hospital Association but they did not immediately respond.
In Chicago, an email by a nurse to her coworkers about the safety of masks has resulted in a lawsuit after the nurse says she was fired for sharing her concerns with staff. The nurse, Lauri Mazurkiewicz, sent an email to staffers at Northwestern Memorial Hospital stating the surgical masks provided by the hospital were less effective against airborne particles than were N95 masks, according to a lawsuit filed March 23 in Cook County Circuit Court. Ms. Mazurkiewicz was terminated the next day in retaliation for her email, the lawsuit alleges.
Ms. Mazurkiewicz could not be reached for comment by press time.
Christopher King, a spokesman for Northwestern Medicine, said the hospital is reviewing the lawsuit.
“As Northwestern Medicine continues to respond to this unprecedented health care pandemic, the health and well-being of our patients, our staff and our employees is our highest priority,” he said in a statement. “We take these matters seriously and we are currently reviewing the complaint. At this time, we will not be commenting further.”
John Mandrola, MD, a Louisville, Ky.–based cardiologist who has written about the recent muzzling of frontline physicians with respect to the coronavirus, said he is not surprised that some hospitals are preventing physicians from sharing their experiences.
“Before C19, in many hospital systems, there was a culture of fear amongst employed clinicians,” he said. “Employed clinicians see other employed physicians being terminated for speaking frankly about problems. It takes scant few of these cases to create a culture of silence.”
Dr. Mandrola, who is a regular Medscape contributor, said that a number of doctors have reached out to him privately about PPE scarcity and shared that they were explicitly warned by administrators not to talk about the shortfalls. Leadership at Dr. Mandrola’s hospital has not issued the same warnings, he said.
“From the hat of total transparency, I think the public is not getting a full view of the impending potential problems that are going to come by doctors not speaking publicly,” he said. “On the other hand, hospital leadership is doing the best they can. It’s not the hospitals’ fault. Hospital administrators can’t manufacture masks.”
From a public health standpoint, Dr. Mehta said that not allowing health professionals to speak publicly about the situations at their hospitals is “irresponsible.” The public deserves to know what is happening, she said, and the health care workforce needs to prepare for what is to come.
“It’s so important that we hear from our colleagues,” she said. “It’s important to hear those accounts so we can prepare for what we’re about to face. Data is crucial. The more you learn from each other, the better shot we have at successfully treating cases and ultimately beating this.”
With the critical shortage of PPE at his hospital and the inability to speak out about the problem, the orthopedic surgeon foresees the dilemma continuing to worsen.
“It’s not only the lives of front-line health care workers that are at risk, but it’s those that they’re going to spread it to and those that are going to be coming to the hospital requiring our care,” he said. “If we don’t have a fully functioning health care force, our capacity is going to be diminished that much further.”
COVID-19 shifts telehealth to the center of cardiology
during the COVID-19 pandemic.
During a recent telehealth webinar, Ami Bhatt, MD, director of the adult congenital heart disease program, Massachusetts General Hospital, Boston, said they’ve gone from seeing 400 patients a day in their clinic to fewer than 40 and are trying to push that number even lower and use virtual care as much as possible.
“The reason is we are having to send home physicians who are exposed and it’s cutting into our workforce very quickly. So the more people you could have at home doing work virtually is important because you’re going to need to call them in [during] the next couple of weeks,” she said. “And our PPE [personal protective equipment] is running low. So if we can afford to not have someone come in the office and not wear a mask because they had a cough, that’s a mask that can be used by someone performing CPR in an ICU.”
The hospital also adopted a train-the-trainer method to bring its existing telehealth program to cardiology, said Dr. Bhatt, who coauthored the American College of Cardiology’s recent guidance on establishing telehealth in the cardiology clinic.
“We find that sending people tip sheets and PowerPoints in addition to everything that is happening ... is too much,” Dr. Bhatt observed. “So actually holding your friend’s hand and walking them through it once you’ve learned how to do it has been really great in terms of adoption. Otherwise, everyone would fall back on phone, which is OK for now, but we need to establish a long-term plan.”
During the same March 20 webinar, David Konur, CEO of the Cardiovascular Institute of the South, Houma, La., said they began doing telecardiology more than 5 years ago and now do about 30,000 “patient touches” a month with 24/7 access.
“This is certainly an unprecedented time,” he said. “COVID-19 is shining a very bright light on the barriers that exist in health care, as well as the friction that exists to accessing care for all of our patients.”
New mandates
A new Food and Drug Administration policy, temporarily relaxing prior guidance on certain connected remote monitoring devices such as ECGs and cardiac monitors, is part of a shifting landscape to reduce barriers to telehealth during the ongoing pandemic. The increased flexibility may increase access to important patient physiological data, while eliminating unnecessary patient contact and easing the burden on healthcare facilities and providers, the agency said in the new guidance, issued March 20.
As such, the FDA “does not intend to object to limited modifications to the indications, claims, functionality, or hardware or software of FDA-cleared noninvasive remote monitoring devices that are used to support patient monitoring.”
Modifications could include the addition of monitoring statements for patients with COVID-19 or coexisting conditions such as hypertension and heart failure; a change to the indications or claims related to home use of devices previously cleared for use only in health care settings; and changes to hardware or software to increase remote monitoring capability. The approved devices listed in the guidance are clinical electronic thermometers, ECGs, cardiac monitors, ECG software for over-the-counter use, pulse oximetry, noninvasive blood pressure monitors, respiratory rate/breathing frequency monitors, and electronic stethoscopes.
The FDA policy comes just days after the Centers for Medicare & Medicaid Services expanded telehealth coverage to Medicare beneficiaries and the Office for Civil Rights at the U.S. Department of Health & Human Services said it would not penalize health care providers for using such non–HIPAA compliant third-party apps as Skype or Google Hangouts video. The HHS also signaled that physicians would be allowed to practice across state lines during the COVID-19 crisis.
“All these mandates have come in a time of desperation where we’re doing the best that we can to provide for patients and keep them safe,” Eugenia Gianos, MD, system director of cardiovascular prevention at Northwell Health and director of the Women’s Cardiovascular Center, Lenox Hill Hospital, New York, said in an interview. “Realistically, the whole digital realm has a lot of promise for our patients.” She noted that telehealth programs are still being developed for the department, but that office visits have been purposely scaled back by more than 75% to protect patients as well as health care providers. “In times of need, the most promising technologies we have, have to come to the forefront,” Dr. Gianos said. “So using the data from the home – whether they have a blood pressure cuff or something that tracks their heart rate or their weight – when we don’t otherwise have data, is of great value.”
Andrew M. Freeman, MD, director of clinical cardiology and operations at National Jewish Hospital in Denver, said “in the current situation, telehealth is the most viable option because it keeps patients safe and physicians safe. So it wouldn’t surprise me if every institution in the country, if not worldwide, is very rapidly pursuing this kind of approach.”
Exactly how many programs or cardiologists were already using telehealth is impossible to say, although the ACC is planning to survey its members on their practices during the COVID-19 pandemic, he noted.
The situation is so fluid that ACC is already revising its March 13 telehealth guidance to reflect the recent policy changes. Another document is being prepared to provide physicians with a template for the telehealth space, said Dr. Freeman, who coauthored the telehealth guidance and also serves on the ACC’s Innovation Leadership Council.
The new FDA policy allowing greater flexibility on remote monitoring devices is somewhat “vaguely worded,” Dr. Freeman noted, but highlights the ability of existing technology to provide essential patient data from home. “I think as we add adjuncts to the things we’re used to in the normal face-to-face visit, it’s going to make the face-to-face visit less required,” he said.
Questions remain, however, on implementing telehealth for new patients and whether payers will follow HHS’s decision not to conduct audits to ensure a prior relationship existed. The potential for telehealth to reach across state lines also is being viewed cautiously until tested legally, Dr. Freeman observed.
“If there’s one blessing in this awful disease that we have received, is that it may really give the power to clinicians, hospital systems, and payers to make telehealth a true viable, sustainable solution for good care that’s readily available to folks,” he said.
Fast-tracked research
On March 24, the American Heart Association announced it is committing $2.5 million for fast-tracked research grants for projects than can turn around results within 9-12 months and focus on how this novel coronavirus affects heart and brain health.
Additional funding also will be made available to the AHA’s new Center for Health Technology & Innovation’s Strategically Focused Research Networks to develop rapid technology solutions to aid in dealing with the pandemic.
The rapid response grant is an “unprecedented but logical move for the organization in these extraordinary times,” AHA President Bob Harrington, MD, chair of medicine at Stanford (Calif.) University, said in a statement. “We are committed to quickly bringing together and supporting some of the brightest minds in research science and clinical care who are shovel ready with the laboratories, tools, and data resources to immediately begin work on addressing this emergent issue.”
Dr. Freeman and Dr. Bhatt have disclosed no relevant financial relationships. Dr. Harrington is on the editorial board for Medscape Cardiology.
A version of this article originally appeared on Medscape.com
during the COVID-19 pandemic.
During a recent telehealth webinar, Ami Bhatt, MD, director of the adult congenital heart disease program, Massachusetts General Hospital, Boston, said they’ve gone from seeing 400 patients a day in their clinic to fewer than 40 and are trying to push that number even lower and use virtual care as much as possible.
“The reason is we are having to send home physicians who are exposed and it’s cutting into our workforce very quickly. So the more people you could have at home doing work virtually is important because you’re going to need to call them in [during] the next couple of weeks,” she said. “And our PPE [personal protective equipment] is running low. So if we can afford to not have someone come in the office and not wear a mask because they had a cough, that’s a mask that can be used by someone performing CPR in an ICU.”
The hospital also adopted a train-the-trainer method to bring its existing telehealth program to cardiology, said Dr. Bhatt, who coauthored the American College of Cardiology’s recent guidance on establishing telehealth in the cardiology clinic.
“We find that sending people tip sheets and PowerPoints in addition to everything that is happening ... is too much,” Dr. Bhatt observed. “So actually holding your friend’s hand and walking them through it once you’ve learned how to do it has been really great in terms of adoption. Otherwise, everyone would fall back on phone, which is OK for now, but we need to establish a long-term plan.”
During the same March 20 webinar, David Konur, CEO of the Cardiovascular Institute of the South, Houma, La., said they began doing telecardiology more than 5 years ago and now do about 30,000 “patient touches” a month with 24/7 access.
“This is certainly an unprecedented time,” he said. “COVID-19 is shining a very bright light on the barriers that exist in health care, as well as the friction that exists to accessing care for all of our patients.”
New mandates
A new Food and Drug Administration policy, temporarily relaxing prior guidance on certain connected remote monitoring devices such as ECGs and cardiac monitors, is part of a shifting landscape to reduce barriers to telehealth during the ongoing pandemic. The increased flexibility may increase access to important patient physiological data, while eliminating unnecessary patient contact and easing the burden on healthcare facilities and providers, the agency said in the new guidance, issued March 20.
As such, the FDA “does not intend to object to limited modifications to the indications, claims, functionality, or hardware or software of FDA-cleared noninvasive remote monitoring devices that are used to support patient monitoring.”
Modifications could include the addition of monitoring statements for patients with COVID-19 or coexisting conditions such as hypertension and heart failure; a change to the indications or claims related to home use of devices previously cleared for use only in health care settings; and changes to hardware or software to increase remote monitoring capability. The approved devices listed in the guidance are clinical electronic thermometers, ECGs, cardiac monitors, ECG software for over-the-counter use, pulse oximetry, noninvasive blood pressure monitors, respiratory rate/breathing frequency monitors, and electronic stethoscopes.
The FDA policy comes just days after the Centers for Medicare & Medicaid Services expanded telehealth coverage to Medicare beneficiaries and the Office for Civil Rights at the U.S. Department of Health & Human Services said it would not penalize health care providers for using such non–HIPAA compliant third-party apps as Skype or Google Hangouts video. The HHS also signaled that physicians would be allowed to practice across state lines during the COVID-19 crisis.
“All these mandates have come in a time of desperation where we’re doing the best that we can to provide for patients and keep them safe,” Eugenia Gianos, MD, system director of cardiovascular prevention at Northwell Health and director of the Women’s Cardiovascular Center, Lenox Hill Hospital, New York, said in an interview. “Realistically, the whole digital realm has a lot of promise for our patients.” She noted that telehealth programs are still being developed for the department, but that office visits have been purposely scaled back by more than 75% to protect patients as well as health care providers. “In times of need, the most promising technologies we have, have to come to the forefront,” Dr. Gianos said. “So using the data from the home – whether they have a blood pressure cuff or something that tracks their heart rate or their weight – when we don’t otherwise have data, is of great value.”
Andrew M. Freeman, MD, director of clinical cardiology and operations at National Jewish Hospital in Denver, said “in the current situation, telehealth is the most viable option because it keeps patients safe and physicians safe. So it wouldn’t surprise me if every institution in the country, if not worldwide, is very rapidly pursuing this kind of approach.”
Exactly how many programs or cardiologists were already using telehealth is impossible to say, although the ACC is planning to survey its members on their practices during the COVID-19 pandemic, he noted.
The situation is so fluid that ACC is already revising its March 13 telehealth guidance to reflect the recent policy changes. Another document is being prepared to provide physicians with a template for the telehealth space, said Dr. Freeman, who coauthored the telehealth guidance and also serves on the ACC’s Innovation Leadership Council.
The new FDA policy allowing greater flexibility on remote monitoring devices is somewhat “vaguely worded,” Dr. Freeman noted, but highlights the ability of existing technology to provide essential patient data from home. “I think as we add adjuncts to the things we’re used to in the normal face-to-face visit, it’s going to make the face-to-face visit less required,” he said.
Questions remain, however, on implementing telehealth for new patients and whether payers will follow HHS’s decision not to conduct audits to ensure a prior relationship existed. The potential for telehealth to reach across state lines also is being viewed cautiously until tested legally, Dr. Freeman observed.
“If there’s one blessing in this awful disease that we have received, is that it may really give the power to clinicians, hospital systems, and payers to make telehealth a true viable, sustainable solution for good care that’s readily available to folks,” he said.
Fast-tracked research
On March 24, the American Heart Association announced it is committing $2.5 million for fast-tracked research grants for projects than can turn around results within 9-12 months and focus on how this novel coronavirus affects heart and brain health.
Additional funding also will be made available to the AHA’s new Center for Health Technology & Innovation’s Strategically Focused Research Networks to develop rapid technology solutions to aid in dealing with the pandemic.
The rapid response grant is an “unprecedented but logical move for the organization in these extraordinary times,” AHA President Bob Harrington, MD, chair of medicine at Stanford (Calif.) University, said in a statement. “We are committed to quickly bringing together and supporting some of the brightest minds in research science and clinical care who are shovel ready with the laboratories, tools, and data resources to immediately begin work on addressing this emergent issue.”
Dr. Freeman and Dr. Bhatt have disclosed no relevant financial relationships. Dr. Harrington is on the editorial board for Medscape Cardiology.
A version of this article originally appeared on Medscape.com
during the COVID-19 pandemic.
During a recent telehealth webinar, Ami Bhatt, MD, director of the adult congenital heart disease program, Massachusetts General Hospital, Boston, said they’ve gone from seeing 400 patients a day in their clinic to fewer than 40 and are trying to push that number even lower and use virtual care as much as possible.
“The reason is we are having to send home physicians who are exposed and it’s cutting into our workforce very quickly. So the more people you could have at home doing work virtually is important because you’re going to need to call them in [during] the next couple of weeks,” she said. “And our PPE [personal protective equipment] is running low. So if we can afford to not have someone come in the office and not wear a mask because they had a cough, that’s a mask that can be used by someone performing CPR in an ICU.”
The hospital also adopted a train-the-trainer method to bring its existing telehealth program to cardiology, said Dr. Bhatt, who coauthored the American College of Cardiology’s recent guidance on establishing telehealth in the cardiology clinic.
“We find that sending people tip sheets and PowerPoints in addition to everything that is happening ... is too much,” Dr. Bhatt observed. “So actually holding your friend’s hand and walking them through it once you’ve learned how to do it has been really great in terms of adoption. Otherwise, everyone would fall back on phone, which is OK for now, but we need to establish a long-term plan.”
During the same March 20 webinar, David Konur, CEO of the Cardiovascular Institute of the South, Houma, La., said they began doing telecardiology more than 5 years ago and now do about 30,000 “patient touches” a month with 24/7 access.
“This is certainly an unprecedented time,” he said. “COVID-19 is shining a very bright light on the barriers that exist in health care, as well as the friction that exists to accessing care for all of our patients.”
New mandates
A new Food and Drug Administration policy, temporarily relaxing prior guidance on certain connected remote monitoring devices such as ECGs and cardiac monitors, is part of a shifting landscape to reduce barriers to telehealth during the ongoing pandemic. The increased flexibility may increase access to important patient physiological data, while eliminating unnecessary patient contact and easing the burden on healthcare facilities and providers, the agency said in the new guidance, issued March 20.
As such, the FDA “does not intend to object to limited modifications to the indications, claims, functionality, or hardware or software of FDA-cleared noninvasive remote monitoring devices that are used to support patient monitoring.”
Modifications could include the addition of monitoring statements for patients with COVID-19 or coexisting conditions such as hypertension and heart failure; a change to the indications or claims related to home use of devices previously cleared for use only in health care settings; and changes to hardware or software to increase remote monitoring capability. The approved devices listed in the guidance are clinical electronic thermometers, ECGs, cardiac monitors, ECG software for over-the-counter use, pulse oximetry, noninvasive blood pressure monitors, respiratory rate/breathing frequency monitors, and electronic stethoscopes.
The FDA policy comes just days after the Centers for Medicare & Medicaid Services expanded telehealth coverage to Medicare beneficiaries and the Office for Civil Rights at the U.S. Department of Health & Human Services said it would not penalize health care providers for using such non–HIPAA compliant third-party apps as Skype or Google Hangouts video. The HHS also signaled that physicians would be allowed to practice across state lines during the COVID-19 crisis.
“All these mandates have come in a time of desperation where we’re doing the best that we can to provide for patients and keep them safe,” Eugenia Gianos, MD, system director of cardiovascular prevention at Northwell Health and director of the Women’s Cardiovascular Center, Lenox Hill Hospital, New York, said in an interview. “Realistically, the whole digital realm has a lot of promise for our patients.” She noted that telehealth programs are still being developed for the department, but that office visits have been purposely scaled back by more than 75% to protect patients as well as health care providers. “In times of need, the most promising technologies we have, have to come to the forefront,” Dr. Gianos said. “So using the data from the home – whether they have a blood pressure cuff or something that tracks their heart rate or their weight – when we don’t otherwise have data, is of great value.”
Andrew M. Freeman, MD, director of clinical cardiology and operations at National Jewish Hospital in Denver, said “in the current situation, telehealth is the most viable option because it keeps patients safe and physicians safe. So it wouldn’t surprise me if every institution in the country, if not worldwide, is very rapidly pursuing this kind of approach.”
Exactly how many programs or cardiologists were already using telehealth is impossible to say, although the ACC is planning to survey its members on their practices during the COVID-19 pandemic, he noted.
The situation is so fluid that ACC is already revising its March 13 telehealth guidance to reflect the recent policy changes. Another document is being prepared to provide physicians with a template for the telehealth space, said Dr. Freeman, who coauthored the telehealth guidance and also serves on the ACC’s Innovation Leadership Council.
The new FDA policy allowing greater flexibility on remote monitoring devices is somewhat “vaguely worded,” Dr. Freeman noted, but highlights the ability of existing technology to provide essential patient data from home. “I think as we add adjuncts to the things we’re used to in the normal face-to-face visit, it’s going to make the face-to-face visit less required,” he said.
Questions remain, however, on implementing telehealth for new patients and whether payers will follow HHS’s decision not to conduct audits to ensure a prior relationship existed. The potential for telehealth to reach across state lines also is being viewed cautiously until tested legally, Dr. Freeman observed.
“If there’s one blessing in this awful disease that we have received, is that it may really give the power to clinicians, hospital systems, and payers to make telehealth a true viable, sustainable solution for good care that’s readily available to folks,” he said.
Fast-tracked research
On March 24, the American Heart Association announced it is committing $2.5 million for fast-tracked research grants for projects than can turn around results within 9-12 months and focus on how this novel coronavirus affects heart and brain health.
Additional funding also will be made available to the AHA’s new Center for Health Technology & Innovation’s Strategically Focused Research Networks to develop rapid technology solutions to aid in dealing with the pandemic.
The rapid response grant is an “unprecedented but logical move for the organization in these extraordinary times,” AHA President Bob Harrington, MD, chair of medicine at Stanford (Calif.) University, said in a statement. “We are committed to quickly bringing together and supporting some of the brightest minds in research science and clinical care who are shovel ready with the laboratories, tools, and data resources to immediately begin work on addressing this emergent issue.”
Dr. Freeman and Dr. Bhatt have disclosed no relevant financial relationships. Dr. Harrington is on the editorial board for Medscape Cardiology.
A version of this article originally appeared on Medscape.com
Is COVID-19 leading to a mental illness pandemic?
People living through this crisis are experiencing trauma
We are in the midst of an epidemic and possibly pandemic of anxiety and distress. The worry that folks have about themselves, families, finances, and work is overwhelming for millions.
I speak with people who report periods of racing thoughts jumping back in time and thinking of roads not taken. They also talk about their thoughts jumping forward with life plans of what they’ll do to change their lives in the future – if they survive COVID-19.
that is well-controlled with care (and even without care). Those people are suffering even more. Meanwhile, people with obsessive-compulsive disorder that had been under control appear to have worsened with the added stress.
Social distancing has disrupted our everyday routines. For many, there is no work, no spending time with people we care about, no going to movies or shows, no doing discretionary shopping, no going to school. Parents with children at home report frustration about balancing working from home with completing home-schooling packets. Physicians on the front lines of this unprecedented time report not having the proper protective equipment and worrying about the possibility of exposing their families to SARS-CoV-2.
We hear stories about the illness and even deaths of some young and middle-aged people with no underlying conditions, not to mention the loss of older adults. People are bursting into tears, and becoming easily frustrated and angry. Add in nightmares, ongoing anxiety states, insomnia, and decreased concentration.
We are seeing news reports of people stocking up on guns and ammunition and a case of one taking – and dying from – nonpharmaceutical grade chloroquine in an effort to prevent COVID-19.
I spoke with Juliana Tseng, PsyD, a clinical psychologist based in New York, and she said that the hype, half-truths, and false information from some outlets in the popular media are making things worse. Dr. Tseng added that the lack of coordination among local, state, and federal governments also is increasing fear and alienation.
As I see this period in time, my first thoughts are that we are witnessing a national epidemic of trauma. Specifically, what we have here is a clinical picture of PTSD.
PTSD is defined clearly as a traumatic disorder with a real or perceived fracture with life. Isolation (which we are creating as a way to “flatten the curve” or slow the spread of COVID-19), although that strategy is in our best personal and public health interests, is both painful and stressful. Frustration, flashbacks of past life experiences plus flashbacks of being ill are reported in people I’ve spoken with. Avoidance, even though it is planned in this instance, is part of the PTSD complex.
What can we as mental health professionals do to help alleviate this suffering?
First, of course, we must listen to the scientific experts and the data – and tell people to do the same. Most experts will say that COVID-19 is a mild or moderate illness for the vast majority of people. We also must encourage people to observe precautions outlined by the Centers for Disease Control and Prevention, such as distancing from people, hand washing, and avoiding those who are ill. Explain to people that, currently, there is no vaccine to prevent COVID-19. Treatment is mainly supportive, and some medication trials are being explored. However, we can empower people by helping them to develop skills aimed at increasing the ability to relax and focus on more positive aspects of life to break the chain of the stress and tension of anxiety as well as control the PTSD.
For more than 40 years, I have helped people master relaxation techniques and guided imagery. When taught properly, people are able to use these techniques on their own.
To begin, I teach people how to relax, using a simple three-point method:
- Get comfortable in a nice chair, and slowly count from one to three. At the count of one, do one thing: “roll your eyes up to the top of your head.”
- At the count of two, do two things, “close your lids on your eyes and take a deep breath.”
- At three, exhale slowly, relax your eyes, and concentrate on a restful feeling of floating.
- Do this for about 30 seconds to a minute.
- Count backward, from three to two to one and open your eyes.
The person will notice how nice and restful they will feel.
After that exercise, get the person to move to the graduate level and go beyond just relaxation. In the following exercise, people can go into a relaxed state by imagining a movie screen. Tell the person to do two things:
1. Look at the imagined movie screen and project on it any pleasant scene you wish; this is your screen. You will feel yourself becoming more and more relaxed. The person can do this one, two, three or whatever times a day. The exercise can last 1 minute or 5.
2. Incorporate the 1, 2, 3 relaxation described earlier, allowing yourself to float into this restful state and go to your movie screen. Now, on the screen, imagine a thick line down the center, and on the left side, project your worries and anxieties and fears. The idea is to see but not experience them. Then shift to the ride side of the screen, and again, visualize any pleasant scene you wish. Again, do this for 1 minute or 5 minutes, whatever works.
You will notice that the pleasant scene on the right will overcome the anxiety scene on the left, in that pleasantness, in most instances, overcomes anxiety. For many, these techniques have proved very useful – whether the problem is anxiety or fear – or both. In my experience, these techniques are a good beginning for controlling PTSD and successfully treating it.
We are in the midst of what could be the biggest public health crisis that America has faced since the 1918 pandemic, also known as the Spanish flu. The lockdowns, quarantines, and the myriad of other disruptions can lead to alienation. In fact, it would be strange for us not to experience strong emotions under these extreme conditions. Life will get better! In the meantime, let’s encourage people to hope, pray, and use relaxation techniques and guided imagery approaches to help control anxiety, worry, stress, and issues related to PTSD. These approaches can give our minds and bodies periods of relaxation and recovery, and ultimately, they can calm our minds.
Dr. London is a practicing psychiatrist and has been a newspaper columnist for 35 years, specializing in and writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019). He has no conflicts of interest.
People living through this crisis are experiencing trauma
People living through this crisis are experiencing trauma
We are in the midst of an epidemic and possibly pandemic of anxiety and distress. The worry that folks have about themselves, families, finances, and work is overwhelming for millions.
I speak with people who report periods of racing thoughts jumping back in time and thinking of roads not taken. They also talk about their thoughts jumping forward with life plans of what they’ll do to change their lives in the future – if they survive COVID-19.
that is well-controlled with care (and even without care). Those people are suffering even more. Meanwhile, people with obsessive-compulsive disorder that had been under control appear to have worsened with the added stress.
Social distancing has disrupted our everyday routines. For many, there is no work, no spending time with people we care about, no going to movies or shows, no doing discretionary shopping, no going to school. Parents with children at home report frustration about balancing working from home with completing home-schooling packets. Physicians on the front lines of this unprecedented time report not having the proper protective equipment and worrying about the possibility of exposing their families to SARS-CoV-2.
We hear stories about the illness and even deaths of some young and middle-aged people with no underlying conditions, not to mention the loss of older adults. People are bursting into tears, and becoming easily frustrated and angry. Add in nightmares, ongoing anxiety states, insomnia, and decreased concentration.
We are seeing news reports of people stocking up on guns and ammunition and a case of one taking – and dying from – nonpharmaceutical grade chloroquine in an effort to prevent COVID-19.
I spoke with Juliana Tseng, PsyD, a clinical psychologist based in New York, and she said that the hype, half-truths, and false information from some outlets in the popular media are making things worse. Dr. Tseng added that the lack of coordination among local, state, and federal governments also is increasing fear and alienation.
As I see this period in time, my first thoughts are that we are witnessing a national epidemic of trauma. Specifically, what we have here is a clinical picture of PTSD.
PTSD is defined clearly as a traumatic disorder with a real or perceived fracture with life. Isolation (which we are creating as a way to “flatten the curve” or slow the spread of COVID-19), although that strategy is in our best personal and public health interests, is both painful and stressful. Frustration, flashbacks of past life experiences plus flashbacks of being ill are reported in people I’ve spoken with. Avoidance, even though it is planned in this instance, is part of the PTSD complex.
What can we as mental health professionals do to help alleviate this suffering?
First, of course, we must listen to the scientific experts and the data – and tell people to do the same. Most experts will say that COVID-19 is a mild or moderate illness for the vast majority of people. We also must encourage people to observe precautions outlined by the Centers for Disease Control and Prevention, such as distancing from people, hand washing, and avoiding those who are ill. Explain to people that, currently, there is no vaccine to prevent COVID-19. Treatment is mainly supportive, and some medication trials are being explored. However, we can empower people by helping them to develop skills aimed at increasing the ability to relax and focus on more positive aspects of life to break the chain of the stress and tension of anxiety as well as control the PTSD.
For more than 40 years, I have helped people master relaxation techniques and guided imagery. When taught properly, people are able to use these techniques on their own.
To begin, I teach people how to relax, using a simple three-point method:
- Get comfortable in a nice chair, and slowly count from one to three. At the count of one, do one thing: “roll your eyes up to the top of your head.”
- At the count of two, do two things, “close your lids on your eyes and take a deep breath.”
- At three, exhale slowly, relax your eyes, and concentrate on a restful feeling of floating.
- Do this for about 30 seconds to a minute.
- Count backward, from three to two to one and open your eyes.
The person will notice how nice and restful they will feel.
After that exercise, get the person to move to the graduate level and go beyond just relaxation. In the following exercise, people can go into a relaxed state by imagining a movie screen. Tell the person to do two things:
1. Look at the imagined movie screen and project on it any pleasant scene you wish; this is your screen. You will feel yourself becoming more and more relaxed. The person can do this one, two, three or whatever times a day. The exercise can last 1 minute or 5.
2. Incorporate the 1, 2, 3 relaxation described earlier, allowing yourself to float into this restful state and go to your movie screen. Now, on the screen, imagine a thick line down the center, and on the left side, project your worries and anxieties and fears. The idea is to see but not experience them. Then shift to the ride side of the screen, and again, visualize any pleasant scene you wish. Again, do this for 1 minute or 5 minutes, whatever works.
You will notice that the pleasant scene on the right will overcome the anxiety scene on the left, in that pleasantness, in most instances, overcomes anxiety. For many, these techniques have proved very useful – whether the problem is anxiety or fear – or both. In my experience, these techniques are a good beginning for controlling PTSD and successfully treating it.
We are in the midst of what could be the biggest public health crisis that America has faced since the 1918 pandemic, also known as the Spanish flu. The lockdowns, quarantines, and the myriad of other disruptions can lead to alienation. In fact, it would be strange for us not to experience strong emotions under these extreme conditions. Life will get better! In the meantime, let’s encourage people to hope, pray, and use relaxation techniques and guided imagery approaches to help control anxiety, worry, stress, and issues related to PTSD. These approaches can give our minds and bodies periods of relaxation and recovery, and ultimately, they can calm our minds.
Dr. London is a practicing psychiatrist and has been a newspaper columnist for 35 years, specializing in and writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019). He has no conflicts of interest.
We are in the midst of an epidemic and possibly pandemic of anxiety and distress. The worry that folks have about themselves, families, finances, and work is overwhelming for millions.
I speak with people who report periods of racing thoughts jumping back in time and thinking of roads not taken. They also talk about their thoughts jumping forward with life plans of what they’ll do to change their lives in the future – if they survive COVID-19.
that is well-controlled with care (and even without care). Those people are suffering even more. Meanwhile, people with obsessive-compulsive disorder that had been under control appear to have worsened with the added stress.
Social distancing has disrupted our everyday routines. For many, there is no work, no spending time with people we care about, no going to movies or shows, no doing discretionary shopping, no going to school. Parents with children at home report frustration about balancing working from home with completing home-schooling packets. Physicians on the front lines of this unprecedented time report not having the proper protective equipment and worrying about the possibility of exposing their families to SARS-CoV-2.
We hear stories about the illness and even deaths of some young and middle-aged people with no underlying conditions, not to mention the loss of older adults. People are bursting into tears, and becoming easily frustrated and angry. Add in nightmares, ongoing anxiety states, insomnia, and decreased concentration.
We are seeing news reports of people stocking up on guns and ammunition and a case of one taking – and dying from – nonpharmaceutical grade chloroquine in an effort to prevent COVID-19.
I spoke with Juliana Tseng, PsyD, a clinical psychologist based in New York, and she said that the hype, half-truths, and false information from some outlets in the popular media are making things worse. Dr. Tseng added that the lack of coordination among local, state, and federal governments also is increasing fear and alienation.
As I see this period in time, my first thoughts are that we are witnessing a national epidemic of trauma. Specifically, what we have here is a clinical picture of PTSD.
PTSD is defined clearly as a traumatic disorder with a real or perceived fracture with life. Isolation (which we are creating as a way to “flatten the curve” or slow the spread of COVID-19), although that strategy is in our best personal and public health interests, is both painful and stressful. Frustration, flashbacks of past life experiences plus flashbacks of being ill are reported in people I’ve spoken with. Avoidance, even though it is planned in this instance, is part of the PTSD complex.
What can we as mental health professionals do to help alleviate this suffering?
First, of course, we must listen to the scientific experts and the data – and tell people to do the same. Most experts will say that COVID-19 is a mild or moderate illness for the vast majority of people. We also must encourage people to observe precautions outlined by the Centers for Disease Control and Prevention, such as distancing from people, hand washing, and avoiding those who are ill. Explain to people that, currently, there is no vaccine to prevent COVID-19. Treatment is mainly supportive, and some medication trials are being explored. However, we can empower people by helping them to develop skills aimed at increasing the ability to relax and focus on more positive aspects of life to break the chain of the stress and tension of anxiety as well as control the PTSD.
For more than 40 years, I have helped people master relaxation techniques and guided imagery. When taught properly, people are able to use these techniques on their own.
To begin, I teach people how to relax, using a simple three-point method:
- Get comfortable in a nice chair, and slowly count from one to three. At the count of one, do one thing: “roll your eyes up to the top of your head.”
- At the count of two, do two things, “close your lids on your eyes and take a deep breath.”
- At three, exhale slowly, relax your eyes, and concentrate on a restful feeling of floating.
- Do this for about 30 seconds to a minute.
- Count backward, from three to two to one and open your eyes.
The person will notice how nice and restful they will feel.
After that exercise, get the person to move to the graduate level and go beyond just relaxation. In the following exercise, people can go into a relaxed state by imagining a movie screen. Tell the person to do two things:
1. Look at the imagined movie screen and project on it any pleasant scene you wish; this is your screen. You will feel yourself becoming more and more relaxed. The person can do this one, two, three or whatever times a day. The exercise can last 1 minute or 5.
2. Incorporate the 1, 2, 3 relaxation described earlier, allowing yourself to float into this restful state and go to your movie screen. Now, on the screen, imagine a thick line down the center, and on the left side, project your worries and anxieties and fears. The idea is to see but not experience them. Then shift to the ride side of the screen, and again, visualize any pleasant scene you wish. Again, do this for 1 minute or 5 minutes, whatever works.
You will notice that the pleasant scene on the right will overcome the anxiety scene on the left, in that pleasantness, in most instances, overcomes anxiety. For many, these techniques have proved very useful – whether the problem is anxiety or fear – or both. In my experience, these techniques are a good beginning for controlling PTSD and successfully treating it.
We are in the midst of what could be the biggest public health crisis that America has faced since the 1918 pandemic, also known as the Spanish flu. The lockdowns, quarantines, and the myriad of other disruptions can lead to alienation. In fact, it would be strange for us not to experience strong emotions under these extreme conditions. Life will get better! In the meantime, let’s encourage people to hope, pray, and use relaxation techniques and guided imagery approaches to help control anxiety, worry, stress, and issues related to PTSD. These approaches can give our minds and bodies periods of relaxation and recovery, and ultimately, they can calm our minds.
Dr. London is a practicing psychiatrist and has been a newspaper columnist for 35 years, specializing in and writing about short-term therapy, including cognitive-behavioral therapy and guided imagery. He is author of “Find Freedom Fast” (New York: Kettlehole Publishing, 2019). He has no conflicts of interest.
Dr. Douglas Paauw reflects on practicing in the COVID-19 world
As we are all facing uncertainties in caring for our patients amid the COVID-19 pandemic, I practice at the University of Washington, Seattle, in an area that initially had the highest prevalence of COVID-19 cases in the United States.
I have never felt better about being a part of the medical profession because of the altruism, compassion, and deep caring I have seen displayed by my colleagues, our nurses, our staff, and our students. I am proud to have worked with all of them while trying to figure out how to practice in this environment.
These times are really difficult and challenging as we face new problems every day. Last week, we had to send our students home, and we switched to phone and telehealth visits to keep our patients and staff safer.
I have had some unanticipated electronic messages from patients during this time. Two of my patients with major medical problems and very dependent on their medications were stranded internationally and running out of medications. I had the family of an incarcerated patient contact me for a letter because that patient was moved to a part of a jail where all patients with upper respiratory infection symptoms were being housed. My patient has severe immunosuppression, and they were requesting an exception for him.
Another of my patients, who has sarcoidosis and is immunosuppressed, informed me that her daughter who lives with her was diagnosed with COVID-19. After 3 days, this patient told me she had become febrile and short of breath. I instructed her patient to go to a hospital, where she was also diagnosed with COVID-19 and was admitted. This patient was discharged within 24 hours, because the utilization review department did not feel she should be in the hospital.
The lack of beds is forcing physicians to frequently make tough decisions like the one made for this patient. This unfortunate reality raises the question of: “How do you manage a patient you are worried about from his or her home?”
In this particular case, I sent my patient an oxygen saturation monitor. We touched base frequently, and I felt okay as long as her saturations on room air were above 90%. So far, she has done okay.
More recently, I received a message from a patient recently diagnosed with Mycobacterium avium complex. I learned that this patient and her disabled husband’s caregiver refused to continue to provide care to them, because my patient had a cough, which began 2 months prior. In this case, a COVID-19 test was done for the explicit purpose of getting the caregiver to return to work.
So how do we face this?
Burnout had been high before this difficult time. But now physicians are being called to care for more and sicker patients without the necessary personal protective gear. Our physicians have demonstrated strength and commitment to patients in their response to this challenge, but they need help from others, including regulators.
I think a first step that needs to be taken is to decrease the volume of documentation physicians are required to make in this time where we are forced to triage to what is most important and drop what isn’t. How is spending so much time documenting instead of seeing the high volumes of patients who need to be seen a good thing? Documentation to the level that Medicare has required isn’t going to work. In fact, it has never been a good thing and is a big driver of burnout.
Our health care system was broken and badly injured before this crisis, and I think now might be a time when positive changes for the future occur. In fact, COVID-19 has resulted in some temporary changes in medicine that I would like to see outlast this outbreak. The telehealth option is now available, for example, and this kind of care is covered much more broadly by Medicare under the 1135 waiver – this has been needed for years. Being able to conduct regular clinic visits via telehealth without the marked restrictions that were previously in place is a big advance. It is currently in place for this emergency only, but this is the time to start pushing hard to make sure this option will be permanent.
I invite you to help me fight for long-term change. Write a letter to the editor of your local newspaper or blog, share your thoughts on social media, and tweet. (I suggest using #documentationordoctors or, although a bit long, #excessivedocumentationcostslives.) This is an unprecedented time in modern medicine. Traumatic times are when the greatest changes occur. Let’s hope for the better.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. He frequently contributes Pearl of the Month and Myth of the Month columns to MDedge, and he serves on the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact Dr. Paauw at [email protected].
As we are all facing uncertainties in caring for our patients amid the COVID-19 pandemic, I practice at the University of Washington, Seattle, in an area that initially had the highest prevalence of COVID-19 cases in the United States.
I have never felt better about being a part of the medical profession because of the altruism, compassion, and deep caring I have seen displayed by my colleagues, our nurses, our staff, and our students. I am proud to have worked with all of them while trying to figure out how to practice in this environment.
These times are really difficult and challenging as we face new problems every day. Last week, we had to send our students home, and we switched to phone and telehealth visits to keep our patients and staff safer.
I have had some unanticipated electronic messages from patients during this time. Two of my patients with major medical problems and very dependent on their medications were stranded internationally and running out of medications. I had the family of an incarcerated patient contact me for a letter because that patient was moved to a part of a jail where all patients with upper respiratory infection symptoms were being housed. My patient has severe immunosuppression, and they were requesting an exception for him.
Another of my patients, who has sarcoidosis and is immunosuppressed, informed me that her daughter who lives with her was diagnosed with COVID-19. After 3 days, this patient told me she had become febrile and short of breath. I instructed her patient to go to a hospital, where she was also diagnosed with COVID-19 and was admitted. This patient was discharged within 24 hours, because the utilization review department did not feel she should be in the hospital.
The lack of beds is forcing physicians to frequently make tough decisions like the one made for this patient. This unfortunate reality raises the question of: “How do you manage a patient you are worried about from his or her home?”
In this particular case, I sent my patient an oxygen saturation monitor. We touched base frequently, and I felt okay as long as her saturations on room air were above 90%. So far, she has done okay.
More recently, I received a message from a patient recently diagnosed with Mycobacterium avium complex. I learned that this patient and her disabled husband’s caregiver refused to continue to provide care to them, because my patient had a cough, which began 2 months prior. In this case, a COVID-19 test was done for the explicit purpose of getting the caregiver to return to work.
So how do we face this?
Burnout had been high before this difficult time. But now physicians are being called to care for more and sicker patients without the necessary personal protective gear. Our physicians have demonstrated strength and commitment to patients in their response to this challenge, but they need help from others, including regulators.
I think a first step that needs to be taken is to decrease the volume of documentation physicians are required to make in this time where we are forced to triage to what is most important and drop what isn’t. How is spending so much time documenting instead of seeing the high volumes of patients who need to be seen a good thing? Documentation to the level that Medicare has required isn’t going to work. In fact, it has never been a good thing and is a big driver of burnout.
Our health care system was broken and badly injured before this crisis, and I think now might be a time when positive changes for the future occur. In fact, COVID-19 has resulted in some temporary changes in medicine that I would like to see outlast this outbreak. The telehealth option is now available, for example, and this kind of care is covered much more broadly by Medicare under the 1135 waiver – this has been needed for years. Being able to conduct regular clinic visits via telehealth without the marked restrictions that were previously in place is a big advance. It is currently in place for this emergency only, but this is the time to start pushing hard to make sure this option will be permanent.
I invite you to help me fight for long-term change. Write a letter to the editor of your local newspaper or blog, share your thoughts on social media, and tweet. (I suggest using #documentationordoctors or, although a bit long, #excessivedocumentationcostslives.) This is an unprecedented time in modern medicine. Traumatic times are when the greatest changes occur. Let’s hope for the better.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. He frequently contributes Pearl of the Month and Myth of the Month columns to MDedge, and he serves on the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact Dr. Paauw at [email protected].
As we are all facing uncertainties in caring for our patients amid the COVID-19 pandemic, I practice at the University of Washington, Seattle, in an area that initially had the highest prevalence of COVID-19 cases in the United States.
I have never felt better about being a part of the medical profession because of the altruism, compassion, and deep caring I have seen displayed by my colleagues, our nurses, our staff, and our students. I am proud to have worked with all of them while trying to figure out how to practice in this environment.
These times are really difficult and challenging as we face new problems every day. Last week, we had to send our students home, and we switched to phone and telehealth visits to keep our patients and staff safer.
I have had some unanticipated electronic messages from patients during this time. Two of my patients with major medical problems and very dependent on their medications were stranded internationally and running out of medications. I had the family of an incarcerated patient contact me for a letter because that patient was moved to a part of a jail where all patients with upper respiratory infection symptoms were being housed. My patient has severe immunosuppression, and they were requesting an exception for him.
Another of my patients, who has sarcoidosis and is immunosuppressed, informed me that her daughter who lives with her was diagnosed with COVID-19. After 3 days, this patient told me she had become febrile and short of breath. I instructed her patient to go to a hospital, where she was also diagnosed with COVID-19 and was admitted. This patient was discharged within 24 hours, because the utilization review department did not feel she should be in the hospital.
The lack of beds is forcing physicians to frequently make tough decisions like the one made for this patient. This unfortunate reality raises the question of: “How do you manage a patient you are worried about from his or her home?”
In this particular case, I sent my patient an oxygen saturation monitor. We touched base frequently, and I felt okay as long as her saturations on room air were above 90%. So far, she has done okay.
More recently, I received a message from a patient recently diagnosed with Mycobacterium avium complex. I learned that this patient and her disabled husband’s caregiver refused to continue to provide care to them, because my patient had a cough, which began 2 months prior. In this case, a COVID-19 test was done for the explicit purpose of getting the caregiver to return to work.
So how do we face this?
Burnout had been high before this difficult time. But now physicians are being called to care for more and sicker patients without the necessary personal protective gear. Our physicians have demonstrated strength and commitment to patients in their response to this challenge, but they need help from others, including regulators.
I think a first step that needs to be taken is to decrease the volume of documentation physicians are required to make in this time where we are forced to triage to what is most important and drop what isn’t. How is spending so much time documenting instead of seeing the high volumes of patients who need to be seen a good thing? Documentation to the level that Medicare has required isn’t going to work. In fact, it has never been a good thing and is a big driver of burnout.
Our health care system was broken and badly injured before this crisis, and I think now might be a time when positive changes for the future occur. In fact, COVID-19 has resulted in some temporary changes in medicine that I would like to see outlast this outbreak. The telehealth option is now available, for example, and this kind of care is covered much more broadly by Medicare under the 1135 waiver – this has been needed for years. Being able to conduct regular clinic visits via telehealth without the marked restrictions that were previously in place is a big advance. It is currently in place for this emergency only, but this is the time to start pushing hard to make sure this option will be permanent.
I invite you to help me fight for long-term change. Write a letter to the editor of your local newspaper or blog, share your thoughts on social media, and tweet. (I suggest using #documentationordoctors or, although a bit long, #excessivedocumentationcostslives.) This is an unprecedented time in modern medicine. Traumatic times are when the greatest changes occur. Let’s hope for the better.
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and he serves as third-year medical student clerkship director at the University of Washington. He frequently contributes Pearl of the Month and Myth of the Month columns to MDedge, and he serves on the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact Dr. Paauw at [email protected].
Due to the COVID-19 pandemic, the AAN urges feds to further expand telehealth benefits
On March 17, the Trump administration announced an expansion of telehealth benefits to help stop the spread of COVID-19 and allow more Medicare patients to receive virtual care without having to visit a healthcare center or physician office.
Under the expansion, Medicare will pay for office, hospital, and other visits furnished via telehealth across the country and including in the patient’s home, delivered by a range of providers, such as physicians, nurse practitioners, clinical psychologists, and licensed clinical social workers.
Prior to this waiver, Medicare would only pay for telehealth on a limited basis, such as when the patient receiving the service was in a designated rural area.
However, in a letter to Alex Azar, secretary of the U.S. Department of Health & Human Services (HHS), the AAN says the easing of restrictions on telehealth should be extended beyond Medicare fee-for-service to both Medicare Advantage and Medicaid patients.
Practice changing?
“It is very heartening that the government is stepping up to the plate” and lifting many telemedicine restrictions, Neil Busis, MD, member of the AAN Health Policy Subcommittee, said in an interview.
Dr. Busis, who leads the telemedicine program for the department of neurology at NYU Langone Health in New York, said the global pandemic has “heightened, focused, and sharpened” attention to the need for telehealth services, particularly for neurology.
“By definition, a lot of neurology patients have mobility problems, traveling is a burden, making it difficult to see a neurologist,” he said.
Dr. Busis hopes these waivers in telehealth, made on a temporary and emergency basis, will become permanent once the COVID-19 pandemic has passed.
“What we hope is that the usefulness of various virtual technologies tested in the crucible of this pandemic will stimulate people to think about it once the pandemic is over and not rescind these loosening of restrictions, and that this will be the beginning of a new era for telemedicine,” he said.
The COVID-19 pandemic may be a “catalyst to accelerate the incorporation of non-face-to-face care into our armamentarium,” he added.
“What we have discovered in recent years is non-face-to-face care with enabling communication technologies is as effective in many clinical situations as face-to-face care. Now is the time to really focus on making the virtual experience as good as possible and to make it as available to as many people as possible,” said Dr. Busis.
Reduce regulatory burdens
The AAN also calls on the federal government to urge states to take action to ensure access to telehealth services and allow telehealth companies to provide telehealth technology and education free of charge to providers who don’t currently use telehealth in their practices.
“The AAN notes that doing so may implicate provisions of the Anti-Kickback Statute. We believe during the current emergency that HHS should issue guidance making it clear to providers that accepting free access to telehealth platforms and education does not put them at risk of violating fraud and abuse laws,” the letter, signed by AAN President James Stevens, MD, stated.
The AAN also wants the government to reduce regulatory burdens during this public health emergency to allow physicians more time to focus on patient care. “This is especially true for providers that are self-quarantining or are in a practice that is experiencing staffing shortages due to self-quarantines,” he wrote.
Specifically, the AAN asked the Centers for Medicare & Medicaid Services to extend the March 31 deadline for physicians to submit their data for the Merit-based Incentive Payment System program for calendar year 2019 (and other compliance deadlines) by at least 30 days.
The AAN also calls on the CMS to delay implementation of the Appropriate Use Criteria program by 1 year, saying that many providers will not have the capacity to “meaningfully” participate in the current testing year for the program.
A version of this article originally appeared on Medscape.com.
On March 17, the Trump administration announced an expansion of telehealth benefits to help stop the spread of COVID-19 and allow more Medicare patients to receive virtual care without having to visit a healthcare center or physician office.
Under the expansion, Medicare will pay for office, hospital, and other visits furnished via telehealth across the country and including in the patient’s home, delivered by a range of providers, such as physicians, nurse practitioners, clinical psychologists, and licensed clinical social workers.
Prior to this waiver, Medicare would only pay for telehealth on a limited basis, such as when the patient receiving the service was in a designated rural area.
However, in a letter to Alex Azar, secretary of the U.S. Department of Health & Human Services (HHS), the AAN says the easing of restrictions on telehealth should be extended beyond Medicare fee-for-service to both Medicare Advantage and Medicaid patients.
Practice changing?
“It is very heartening that the government is stepping up to the plate” and lifting many telemedicine restrictions, Neil Busis, MD, member of the AAN Health Policy Subcommittee, said in an interview.
Dr. Busis, who leads the telemedicine program for the department of neurology at NYU Langone Health in New York, said the global pandemic has “heightened, focused, and sharpened” attention to the need for telehealth services, particularly for neurology.
“By definition, a lot of neurology patients have mobility problems, traveling is a burden, making it difficult to see a neurologist,” he said.
Dr. Busis hopes these waivers in telehealth, made on a temporary and emergency basis, will become permanent once the COVID-19 pandemic has passed.
“What we hope is that the usefulness of various virtual technologies tested in the crucible of this pandemic will stimulate people to think about it once the pandemic is over and not rescind these loosening of restrictions, and that this will be the beginning of a new era for telemedicine,” he said.
The COVID-19 pandemic may be a “catalyst to accelerate the incorporation of non-face-to-face care into our armamentarium,” he added.
“What we have discovered in recent years is non-face-to-face care with enabling communication technologies is as effective in many clinical situations as face-to-face care. Now is the time to really focus on making the virtual experience as good as possible and to make it as available to as many people as possible,” said Dr. Busis.
Reduce regulatory burdens
The AAN also calls on the federal government to urge states to take action to ensure access to telehealth services and allow telehealth companies to provide telehealth technology and education free of charge to providers who don’t currently use telehealth in their practices.
“The AAN notes that doing so may implicate provisions of the Anti-Kickback Statute. We believe during the current emergency that HHS should issue guidance making it clear to providers that accepting free access to telehealth platforms and education does not put them at risk of violating fraud and abuse laws,” the letter, signed by AAN President James Stevens, MD, stated.
The AAN also wants the government to reduce regulatory burdens during this public health emergency to allow physicians more time to focus on patient care. “This is especially true for providers that are self-quarantining or are in a practice that is experiencing staffing shortages due to self-quarantines,” he wrote.
Specifically, the AAN asked the Centers for Medicare & Medicaid Services to extend the March 31 deadline for physicians to submit their data for the Merit-based Incentive Payment System program for calendar year 2019 (and other compliance deadlines) by at least 30 days.
The AAN also calls on the CMS to delay implementation of the Appropriate Use Criteria program by 1 year, saying that many providers will not have the capacity to “meaningfully” participate in the current testing year for the program.
A version of this article originally appeared on Medscape.com.
On March 17, the Trump administration announced an expansion of telehealth benefits to help stop the spread of COVID-19 and allow more Medicare patients to receive virtual care without having to visit a healthcare center or physician office.
Under the expansion, Medicare will pay for office, hospital, and other visits furnished via telehealth across the country and including in the patient’s home, delivered by a range of providers, such as physicians, nurse practitioners, clinical psychologists, and licensed clinical social workers.
Prior to this waiver, Medicare would only pay for telehealth on a limited basis, such as when the patient receiving the service was in a designated rural area.
However, in a letter to Alex Azar, secretary of the U.S. Department of Health & Human Services (HHS), the AAN says the easing of restrictions on telehealth should be extended beyond Medicare fee-for-service to both Medicare Advantage and Medicaid patients.
Practice changing?
“It is very heartening that the government is stepping up to the plate” and lifting many telemedicine restrictions, Neil Busis, MD, member of the AAN Health Policy Subcommittee, said in an interview.
Dr. Busis, who leads the telemedicine program for the department of neurology at NYU Langone Health in New York, said the global pandemic has “heightened, focused, and sharpened” attention to the need for telehealth services, particularly for neurology.
“By definition, a lot of neurology patients have mobility problems, traveling is a burden, making it difficult to see a neurologist,” he said.
Dr. Busis hopes these waivers in telehealth, made on a temporary and emergency basis, will become permanent once the COVID-19 pandemic has passed.
“What we hope is that the usefulness of various virtual technologies tested in the crucible of this pandemic will stimulate people to think about it once the pandemic is over and not rescind these loosening of restrictions, and that this will be the beginning of a new era for telemedicine,” he said.
The COVID-19 pandemic may be a “catalyst to accelerate the incorporation of non-face-to-face care into our armamentarium,” he added.
“What we have discovered in recent years is non-face-to-face care with enabling communication technologies is as effective in many clinical situations as face-to-face care. Now is the time to really focus on making the virtual experience as good as possible and to make it as available to as many people as possible,” said Dr. Busis.
Reduce regulatory burdens
The AAN also calls on the federal government to urge states to take action to ensure access to telehealth services and allow telehealth companies to provide telehealth technology and education free of charge to providers who don’t currently use telehealth in their practices.
“The AAN notes that doing so may implicate provisions of the Anti-Kickback Statute. We believe during the current emergency that HHS should issue guidance making it clear to providers that accepting free access to telehealth platforms and education does not put them at risk of violating fraud and abuse laws,” the letter, signed by AAN President James Stevens, MD, stated.
The AAN also wants the government to reduce regulatory burdens during this public health emergency to allow physicians more time to focus on patient care. “This is especially true for providers that are self-quarantining or are in a practice that is experiencing staffing shortages due to self-quarantines,” he wrote.
Specifically, the AAN asked the Centers for Medicare & Medicaid Services to extend the March 31 deadline for physicians to submit their data for the Merit-based Incentive Payment System program for calendar year 2019 (and other compliance deadlines) by at least 30 days.
The AAN also calls on the CMS to delay implementation of the Appropriate Use Criteria program by 1 year, saying that many providers will not have the capacity to “meaningfully” participate in the current testing year for the program.
A version of this article originally appeared on Medscape.com.
‘Larger-than-life’ physician Stephen Schwartz dies of COVID-19 at 78
Stephen M. Schwartz, MD, PhD, a pioneer in the field of vascular biology and a longtime professor of pathology at the University of Washington, Seattle, died March 17, 2020, after being hospitalized with COVID-19. He was 78.
“This has become all too real,” UW president Ana Mari Cauce said on Facebook, where she described Dr. Schwartz as “larger than life,” and superimposed a photo of him in front of Mount Rainier, according to a report in the Seattle Times.
Dr. Schwartz is “rightfully considered a giant among investigators of the biology of smooth muscle cells and the structure of blood vessels,” Paul Ramsey, MD, CEO of UW Medicine, said in a statement. He will be remembered for his “vigorous advocacy for research and for the field of vascular biology as well as for his many trainees who have gone on to great success as independent investigators in the field of vascular pathobiology,” Dr. Ramsey said.
Dr. Schwartz received a BA in biology from Harvard University in 1963 and an MD from Boston University in 1967. Dr. Schwartz started a residency in the UW department of pathology in 1967 and received his PhD from the institution in 1973. From 1974 to 1979, he was an assistant professor of pathology and became a full professor in 1984.
Dr. Schwartz was also an adjunct professor in the UW departments of bioengineering and medicine, “reflective of his many collaborative relationships with faculty in other departments in our medical school and in the world,” Dr. Ramsey said.
“Dr. Schwartz left a lasting imprint on the UW School of Medicine and the broader scientific community. He will be greatly missed,” he added.
‘A great loss’
Dr. Schwartz chaired numerous national and international meetings in the field of vascular biology. He was the founding chair of the Gordon Research Conference on Vascular Biology and a cofounder and second president of the North American Vascular Biology Organization (NAVBO). He created NAVBO’s flagship summer course, Vasculata.
“The NAVBO community has suffered a great loss,” Bernadette Englert, executive officer for the organization, said in a statement. He will be “sorely missed by generations of vascular biologists and pathologists.”
News of Dr. Schwartz’s passing lit up Twitter. Here are just a few comments:
UW lost to COVID-19 “beloved professor Stephen Schwartz, a pioneer in vascular biology and a larger-than-life scientist. Steve, you will be missed!” Rong Tian, MD, PhD, with the bioengineering department, wrote in a tweet.
“Stephen Schwartz was a giant in vascular biology and a mentor to countless faculty and trainees, including myself. He will be deeply missed,” said Kelly Stevens, PhD, also from the bioengineering department.
A version of this article originally appeared on Medscape.com.
Stephen M. Schwartz, MD, PhD, a pioneer in the field of vascular biology and a longtime professor of pathology at the University of Washington, Seattle, died March 17, 2020, after being hospitalized with COVID-19. He was 78.
“This has become all too real,” UW president Ana Mari Cauce said on Facebook, where she described Dr. Schwartz as “larger than life,” and superimposed a photo of him in front of Mount Rainier, according to a report in the Seattle Times.
Dr. Schwartz is “rightfully considered a giant among investigators of the biology of smooth muscle cells and the structure of blood vessels,” Paul Ramsey, MD, CEO of UW Medicine, said in a statement. He will be remembered for his “vigorous advocacy for research and for the field of vascular biology as well as for his many trainees who have gone on to great success as independent investigators in the field of vascular pathobiology,” Dr. Ramsey said.
Dr. Schwartz received a BA in biology from Harvard University in 1963 and an MD from Boston University in 1967. Dr. Schwartz started a residency in the UW department of pathology in 1967 and received his PhD from the institution in 1973. From 1974 to 1979, he was an assistant professor of pathology and became a full professor in 1984.
Dr. Schwartz was also an adjunct professor in the UW departments of bioengineering and medicine, “reflective of his many collaborative relationships with faculty in other departments in our medical school and in the world,” Dr. Ramsey said.
“Dr. Schwartz left a lasting imprint on the UW School of Medicine and the broader scientific community. He will be greatly missed,” he added.
‘A great loss’
Dr. Schwartz chaired numerous national and international meetings in the field of vascular biology. He was the founding chair of the Gordon Research Conference on Vascular Biology and a cofounder and second president of the North American Vascular Biology Organization (NAVBO). He created NAVBO’s flagship summer course, Vasculata.
“The NAVBO community has suffered a great loss,” Bernadette Englert, executive officer for the organization, said in a statement. He will be “sorely missed by generations of vascular biologists and pathologists.”
News of Dr. Schwartz’s passing lit up Twitter. Here are just a few comments:
UW lost to COVID-19 “beloved professor Stephen Schwartz, a pioneer in vascular biology and a larger-than-life scientist. Steve, you will be missed!” Rong Tian, MD, PhD, with the bioengineering department, wrote in a tweet.
“Stephen Schwartz was a giant in vascular biology and a mentor to countless faculty and trainees, including myself. He will be deeply missed,” said Kelly Stevens, PhD, also from the bioengineering department.
A version of this article originally appeared on Medscape.com.
Stephen M. Schwartz, MD, PhD, a pioneer in the field of vascular biology and a longtime professor of pathology at the University of Washington, Seattle, died March 17, 2020, after being hospitalized with COVID-19. He was 78.
“This has become all too real,” UW president Ana Mari Cauce said on Facebook, where she described Dr. Schwartz as “larger than life,” and superimposed a photo of him in front of Mount Rainier, according to a report in the Seattle Times.
Dr. Schwartz is “rightfully considered a giant among investigators of the biology of smooth muscle cells and the structure of blood vessels,” Paul Ramsey, MD, CEO of UW Medicine, said in a statement. He will be remembered for his “vigorous advocacy for research and for the field of vascular biology as well as for his many trainees who have gone on to great success as independent investigators in the field of vascular pathobiology,” Dr. Ramsey said.
Dr. Schwartz received a BA in biology from Harvard University in 1963 and an MD from Boston University in 1967. Dr. Schwartz started a residency in the UW department of pathology in 1967 and received his PhD from the institution in 1973. From 1974 to 1979, he was an assistant professor of pathology and became a full professor in 1984.
Dr. Schwartz was also an adjunct professor in the UW departments of bioengineering and medicine, “reflective of his many collaborative relationships with faculty in other departments in our medical school and in the world,” Dr. Ramsey said.
“Dr. Schwartz left a lasting imprint on the UW School of Medicine and the broader scientific community. He will be greatly missed,” he added.
‘A great loss’
Dr. Schwartz chaired numerous national and international meetings in the field of vascular biology. He was the founding chair of the Gordon Research Conference on Vascular Biology and a cofounder and second president of the North American Vascular Biology Organization (NAVBO). He created NAVBO’s flagship summer course, Vasculata.
“The NAVBO community has suffered a great loss,” Bernadette Englert, executive officer for the organization, said in a statement. He will be “sorely missed by generations of vascular biologists and pathologists.”
News of Dr. Schwartz’s passing lit up Twitter. Here are just a few comments:
UW lost to COVID-19 “beloved professor Stephen Schwartz, a pioneer in vascular biology and a larger-than-life scientist. Steve, you will be missed!” Rong Tian, MD, PhD, with the bioengineering department, wrote in a tweet.
“Stephen Schwartz was a giant in vascular biology and a mentor to countless faculty and trainees, including myself. He will be deeply missed,” said Kelly Stevens, PhD, also from the bioengineering department.
A version of this article originally appeared on Medscape.com.

















