User login
Cardiology News is an independent news source that provides cardiologists with timely and relevant news and commentary about clinical developments and the impact of health care policy on cardiology and the cardiologist's practice. Cardiology News Digital Network is the online destination and multimedia properties of Cardiology News, the independent news publication for cardiologists. Cardiology news is the leading source of news and commentary about clinical developments in cardiology as well as health care policy and regulations that affect the cardiologist's practice. Cardiology News Digital Network is owned by Frontline Medical Communications.
Oral danicamtiv improves left atrial contractility in HFrEF
Danicamtiv, a novel oral selective cardiac myosin activator, demonstrated promising beneficial effects on left ventricular systolic function coupled with marked improvements in left atrial volume and function in patients with heart failure with reduced ejection fraction in a phase 2a clinical trial, Adriaan A. Voors, MD, PhD, said at the European Society of Cardiology Heart Failure Discoveries virtual meeting.
Importantly, these improvements weren’t accompanied by any unwelcome significant increase in diastolic stiffness, added Dr. Voors, a cardiologist at the University of Groningen (the Netherlands).
This is a drug whose novel mechanism of action could make it a good fit in combination with existing guideline-recommended therapies known to improve morbidity and mortality in patients with heart failure with reduced ejection fraction (HFrEF), none of which do what danicamtiv does: namely, activates cardiac myosin by enhancing myofibrillar adenosine triphosphatase activity, thereby boosting intrinsic myocardial contractility without any impact upon calcium homeostasis, he explained.
Dr. Voors reported on 40 patients with stable HFrEF and a left ventricular ejection fraction of 35% or less, all on background guideline-directed medical therapy. They were randomized double blind to 7 days of danicamtiv at 50, 75, or 100 mg twice daily, or placebo. A total of 489 ECGs were performed in conjunction with blood draws to measure plasma drug concentrations during the study.
Danicamtiv significantly improved left ventricular stroke volume and global longitudinal and circumferential strain in plasma drug concentration–dependent fashion, while simultaneously decreasing left ventricular end-systolic and end-diastolic diameters. Danicamtiv increased systolic ejection time from 286 milliseconds at baseline by an additional placebo-corrected 15, 36, and 48 milliseconds in patients with low, mid-range, and high drug concentrations.
The cardiac myosin activator’s concentration-dependent salutary effects on left atrial (LA) parameters in this brief study were intriguing, since LA function is often compromised in patients with heart failure and has been shown in prior observational studies to independently predict cardiovascular outcomes, the cardiologist noted. The favorable changes in response to danicamtiv included a reduction in LA minimal volume index and an increase in LA emptying fraction. Also, there were marked improvements in LA function index, by 6.1 and 5.8 points, respectively, in patients with mid- and high drug concentrations, from a baseline of 26 points.
Holter monitoring revealed no increased risk of atrial or ventricular arrhythmias in study participants.
Treatment-emergent adverse events were mild and/or unrelated to treatment and showed no particular pattern. The one serious adverse event in the study was a case of hyperkalemia deemed by investigators to be unrelated to treatment.
Seven of 30 danicamtiv-treated patients developed mild, transient, asymptomatic increases in serum cardiac troponin I and/or high-sensitivity troponin T. Dr. Voors said the significance of this must await further examination in larger clinical trials. A phase 2 clinical trial in patients with HFrEF and paroxysmal or persistent atrial fibrillation is planned in order to learn if chronic therapy with danicamtiv results in sustained LA remodeling and clinical benefits. Another planned phase 2 study will be conducted in patients with selected forms of genetic dilated cardiomyopathy.
Because danicamtiv appears to have no effects on blood pressure, renal function, or electrolytes, Dr. Voors speculated that the drug might prove to be an attractive therapeutic option in patients with advanced refractory heart failure, who often have low blood pressure, poor renal function, and a very low left ventricular ejection fraction.
Discussant Thomas Thum, MD, PhD, commented that danicamtiv has definitely earned an opportunity to show what it can do in larger, long-term clinical trials. He was impressed by the significant increase in systolic ejection time, a good marker for cardiac contractility. But he added that the troponin signal warrants careful scrutiny.
“The slight increase over baseline in the phase 2a study was not correlated with any ECG changes or clinical symptoms. However, whether this is a detrimental biomarker sign of a silent harm to the heart remains to be investigated,” said Dr. Thum, a cardiologist at the Institute of Molecular and Translational Therapeutic Strategies at Hannover (Germany) Medical School.
The phase 2a study finding of a plasma drug concentration–dependent prolongation in isovolumetric relaxation time “warrants some caution in future clinical development in patients with impaired diastolic function,” he added.
Simultaneous with Dr. Voors’ presentation, the study results were published online (Eur J Heart Fail. 2020 Jun 19. doi: 10.1002/ejhf.1933).
The danicamtiv study was sponsored by MyoKardia. Dr. Voors reported receiving research funding from and serving as a consultant to MyoKardia and numerous other companies.
Danicamtiv, a novel oral selective cardiac myosin activator, demonstrated promising beneficial effects on left ventricular systolic function coupled with marked improvements in left atrial volume and function in patients with heart failure with reduced ejection fraction in a phase 2a clinical trial, Adriaan A. Voors, MD, PhD, said at the European Society of Cardiology Heart Failure Discoveries virtual meeting.
Importantly, these improvements weren’t accompanied by any unwelcome significant increase in diastolic stiffness, added Dr. Voors, a cardiologist at the University of Groningen (the Netherlands).
This is a drug whose novel mechanism of action could make it a good fit in combination with existing guideline-recommended therapies known to improve morbidity and mortality in patients with heart failure with reduced ejection fraction (HFrEF), none of which do what danicamtiv does: namely, activates cardiac myosin by enhancing myofibrillar adenosine triphosphatase activity, thereby boosting intrinsic myocardial contractility without any impact upon calcium homeostasis, he explained.
Dr. Voors reported on 40 patients with stable HFrEF and a left ventricular ejection fraction of 35% or less, all on background guideline-directed medical therapy. They were randomized double blind to 7 days of danicamtiv at 50, 75, or 100 mg twice daily, or placebo. A total of 489 ECGs were performed in conjunction with blood draws to measure plasma drug concentrations during the study.
Danicamtiv significantly improved left ventricular stroke volume and global longitudinal and circumferential strain in plasma drug concentration–dependent fashion, while simultaneously decreasing left ventricular end-systolic and end-diastolic diameters. Danicamtiv increased systolic ejection time from 286 milliseconds at baseline by an additional placebo-corrected 15, 36, and 48 milliseconds in patients with low, mid-range, and high drug concentrations.
The cardiac myosin activator’s concentration-dependent salutary effects on left atrial (LA) parameters in this brief study were intriguing, since LA function is often compromised in patients with heart failure and has been shown in prior observational studies to independently predict cardiovascular outcomes, the cardiologist noted. The favorable changes in response to danicamtiv included a reduction in LA minimal volume index and an increase in LA emptying fraction. Also, there were marked improvements in LA function index, by 6.1 and 5.8 points, respectively, in patients with mid- and high drug concentrations, from a baseline of 26 points.
Holter monitoring revealed no increased risk of atrial or ventricular arrhythmias in study participants.
Treatment-emergent adverse events were mild and/or unrelated to treatment and showed no particular pattern. The one serious adverse event in the study was a case of hyperkalemia deemed by investigators to be unrelated to treatment.
Seven of 30 danicamtiv-treated patients developed mild, transient, asymptomatic increases in serum cardiac troponin I and/or high-sensitivity troponin T. Dr. Voors said the significance of this must await further examination in larger clinical trials. A phase 2 clinical trial in patients with HFrEF and paroxysmal or persistent atrial fibrillation is planned in order to learn if chronic therapy with danicamtiv results in sustained LA remodeling and clinical benefits. Another planned phase 2 study will be conducted in patients with selected forms of genetic dilated cardiomyopathy.
Because danicamtiv appears to have no effects on blood pressure, renal function, or electrolytes, Dr. Voors speculated that the drug might prove to be an attractive therapeutic option in patients with advanced refractory heart failure, who often have low blood pressure, poor renal function, and a very low left ventricular ejection fraction.
Discussant Thomas Thum, MD, PhD, commented that danicamtiv has definitely earned an opportunity to show what it can do in larger, long-term clinical trials. He was impressed by the significant increase in systolic ejection time, a good marker for cardiac contractility. But he added that the troponin signal warrants careful scrutiny.
“The slight increase over baseline in the phase 2a study was not correlated with any ECG changes or clinical symptoms. However, whether this is a detrimental biomarker sign of a silent harm to the heart remains to be investigated,” said Dr. Thum, a cardiologist at the Institute of Molecular and Translational Therapeutic Strategies at Hannover (Germany) Medical School.
The phase 2a study finding of a plasma drug concentration–dependent prolongation in isovolumetric relaxation time “warrants some caution in future clinical development in patients with impaired diastolic function,” he added.
Simultaneous with Dr. Voors’ presentation, the study results were published online (Eur J Heart Fail. 2020 Jun 19. doi: 10.1002/ejhf.1933).
The danicamtiv study was sponsored by MyoKardia. Dr. Voors reported receiving research funding from and serving as a consultant to MyoKardia and numerous other companies.
Danicamtiv, a novel oral selective cardiac myosin activator, demonstrated promising beneficial effects on left ventricular systolic function coupled with marked improvements in left atrial volume and function in patients with heart failure with reduced ejection fraction in a phase 2a clinical trial, Adriaan A. Voors, MD, PhD, said at the European Society of Cardiology Heart Failure Discoveries virtual meeting.
Importantly, these improvements weren’t accompanied by any unwelcome significant increase in diastolic stiffness, added Dr. Voors, a cardiologist at the University of Groningen (the Netherlands).
This is a drug whose novel mechanism of action could make it a good fit in combination with existing guideline-recommended therapies known to improve morbidity and mortality in patients with heart failure with reduced ejection fraction (HFrEF), none of which do what danicamtiv does: namely, activates cardiac myosin by enhancing myofibrillar adenosine triphosphatase activity, thereby boosting intrinsic myocardial contractility without any impact upon calcium homeostasis, he explained.
Dr. Voors reported on 40 patients with stable HFrEF and a left ventricular ejection fraction of 35% or less, all on background guideline-directed medical therapy. They were randomized double blind to 7 days of danicamtiv at 50, 75, or 100 mg twice daily, or placebo. A total of 489 ECGs were performed in conjunction with blood draws to measure plasma drug concentrations during the study.
Danicamtiv significantly improved left ventricular stroke volume and global longitudinal and circumferential strain in plasma drug concentration–dependent fashion, while simultaneously decreasing left ventricular end-systolic and end-diastolic diameters. Danicamtiv increased systolic ejection time from 286 milliseconds at baseline by an additional placebo-corrected 15, 36, and 48 milliseconds in patients with low, mid-range, and high drug concentrations.
The cardiac myosin activator’s concentration-dependent salutary effects on left atrial (LA) parameters in this brief study were intriguing, since LA function is often compromised in patients with heart failure and has been shown in prior observational studies to independently predict cardiovascular outcomes, the cardiologist noted. The favorable changes in response to danicamtiv included a reduction in LA minimal volume index and an increase in LA emptying fraction. Also, there were marked improvements in LA function index, by 6.1 and 5.8 points, respectively, in patients with mid- and high drug concentrations, from a baseline of 26 points.
Holter monitoring revealed no increased risk of atrial or ventricular arrhythmias in study participants.
Treatment-emergent adverse events were mild and/or unrelated to treatment and showed no particular pattern. The one serious adverse event in the study was a case of hyperkalemia deemed by investigators to be unrelated to treatment.
Seven of 30 danicamtiv-treated patients developed mild, transient, asymptomatic increases in serum cardiac troponin I and/or high-sensitivity troponin T. Dr. Voors said the significance of this must await further examination in larger clinical trials. A phase 2 clinical trial in patients with HFrEF and paroxysmal or persistent atrial fibrillation is planned in order to learn if chronic therapy with danicamtiv results in sustained LA remodeling and clinical benefits. Another planned phase 2 study will be conducted in patients with selected forms of genetic dilated cardiomyopathy.
Because danicamtiv appears to have no effects on blood pressure, renal function, or electrolytes, Dr. Voors speculated that the drug might prove to be an attractive therapeutic option in patients with advanced refractory heart failure, who often have low blood pressure, poor renal function, and a very low left ventricular ejection fraction.
Discussant Thomas Thum, MD, PhD, commented that danicamtiv has definitely earned an opportunity to show what it can do in larger, long-term clinical trials. He was impressed by the significant increase in systolic ejection time, a good marker for cardiac contractility. But he added that the troponin signal warrants careful scrutiny.
“The slight increase over baseline in the phase 2a study was not correlated with any ECG changes or clinical symptoms. However, whether this is a detrimental biomarker sign of a silent harm to the heart remains to be investigated,” said Dr. Thum, a cardiologist at the Institute of Molecular and Translational Therapeutic Strategies at Hannover (Germany) Medical School.
The phase 2a study finding of a plasma drug concentration–dependent prolongation in isovolumetric relaxation time “warrants some caution in future clinical development in patients with impaired diastolic function,” he added.
Simultaneous with Dr. Voors’ presentation, the study results were published online (Eur J Heart Fail. 2020 Jun 19. doi: 10.1002/ejhf.1933).
The danicamtiv study was sponsored by MyoKardia. Dr. Voors reported receiving research funding from and serving as a consultant to MyoKardia and numerous other companies.
FROM ESC HEART FAILURE 2020
Tendyne device shows promise for mitral annular calcification
Transcatheter implantation of the Tendyne mitral valve replacement device for treatment of mitral regurgitation in patients at prohibitive surgical risk because of severe mitral annular calcification showed considerable promise in a small feasibility study, Paul Sorajja, MD, reported at the virtual annual meeting of the European Association of Percutaneous Cardiovascular Interventions.
There is a huge unmet need for safe and effective therapies for severe mitral annular calcification (MAC).
“Severe MAC often precludes surgical treatment, and there’s a poor prognosis in patients with MAC and mitral regurgitation when untreated, with 2-year survival of about 60% in some studies,” noted Dr. Sorajja, a cardiologist at the Minneapolis Heart Institute Foundation.
Attempts at repurposing transcatheter aortic valves for use in the mitral location have been largely unsatisfactory, he added.
The 6-month outcomes in the 11 patients who received the Tendyne device in the multicenter U.S. feasibility study featured low rates of mortality and nonfatal adverse events, elimination of mitral regurgitation, marked improvement on quality of life measures, and a mean gradient of 4.1 mm Hg. The acute procedural outcomes were encouraging as well.
“We had technical success in 11 of 11 patients, no procedural mortality or left ventricular outflow tract obstruction, no valve embolization or malposition, and no conversion to open heart surgery,” he said.
There was one death caused by mesenteric ischemia 16 days post Tendyne implantation. One patient experienced a nondisabling stroke at day 4. Two patients developed new-onset atrial fibrillation, one of whom cardioverted to sinus rhythm. And one patient had a moderate paravalvular leak that resolved with placement of a plug at 3 months. There were no MIs.
At baseline, 9 of 11 patients were New York Heart Association functional class III and the others were class II. At 6 months, six patients were class I, four were class II, and one was class III. The average score on the Kansas City Cardiomyopathy Questionnaire improved from 45.9 at baseline to 65.5 at 1 month, 77.4 at 3 months, and 70.3 at 6 months.
This was a highly selected study population with a Society of Thoracic Surgery Predicted Risk of Mortality score of 9.03%. Part of the screening process for study participation involved preprocedural CT imaging with simulated device overlay in order to identify candidates who were likely to have an optimal device fit.
Discussant Francesco Maisano, MD, was impressed by how well this simulation resembled the actual results as depicted in side-by-side pre- and postprocedural CT images presented by Dr. Sorajja.
“What really surprised me was the correlation between preprocedural simulation data and the actual CT scan after the procedure. This trial shows that the simulation works, and also that Tendyne is a great alternative to aortic valve-in-MAC for these very-high-risk patients,” said Dr. Maisano, professor of cardiac surgery at the University of Zürich and a pioneer of catheter-based mitral and tricuspid interventions.
Earlier this year the Tendyne device was approved in Europe for patients with mitral regurgitation who aren’t candidates for surgical valve replacement or transcatheter mitral valve repair. The approval does not, however, extend to MAC. The Abbott device remains investigational in the United States, where the pivotal SUMMIT trial is underway. In one arm of the trial, patients with mitral regurgitation are being randomized to the investigational Tendyne device or to Abbott’s MitraClip, which is approved for that indication. In the other arm, patients with severe MAC at prohibitive surgical risk will get the Tendyne device. Results are expected in 2020.
Dr. Sorajja reported receiving research grants from and serving as a consultant to Abbott, the feasibility study sponsor, as well as to several other medical device companies, as did Dr. Maisano.
Transcatheter implantation of the Tendyne mitral valve replacement device for treatment of mitral regurgitation in patients at prohibitive surgical risk because of severe mitral annular calcification showed considerable promise in a small feasibility study, Paul Sorajja, MD, reported at the virtual annual meeting of the European Association of Percutaneous Cardiovascular Interventions.
There is a huge unmet need for safe and effective therapies for severe mitral annular calcification (MAC).
“Severe MAC often precludes surgical treatment, and there’s a poor prognosis in patients with MAC and mitral regurgitation when untreated, with 2-year survival of about 60% in some studies,” noted Dr. Sorajja, a cardiologist at the Minneapolis Heart Institute Foundation.
Attempts at repurposing transcatheter aortic valves for use in the mitral location have been largely unsatisfactory, he added.
The 6-month outcomes in the 11 patients who received the Tendyne device in the multicenter U.S. feasibility study featured low rates of mortality and nonfatal adverse events, elimination of mitral regurgitation, marked improvement on quality of life measures, and a mean gradient of 4.1 mm Hg. The acute procedural outcomes were encouraging as well.
“We had technical success in 11 of 11 patients, no procedural mortality or left ventricular outflow tract obstruction, no valve embolization or malposition, and no conversion to open heart surgery,” he said.
There was one death caused by mesenteric ischemia 16 days post Tendyne implantation. One patient experienced a nondisabling stroke at day 4. Two patients developed new-onset atrial fibrillation, one of whom cardioverted to sinus rhythm. And one patient had a moderate paravalvular leak that resolved with placement of a plug at 3 months. There were no MIs.
At baseline, 9 of 11 patients were New York Heart Association functional class III and the others were class II. At 6 months, six patients were class I, four were class II, and one was class III. The average score on the Kansas City Cardiomyopathy Questionnaire improved from 45.9 at baseline to 65.5 at 1 month, 77.4 at 3 months, and 70.3 at 6 months.
This was a highly selected study population with a Society of Thoracic Surgery Predicted Risk of Mortality score of 9.03%. Part of the screening process for study participation involved preprocedural CT imaging with simulated device overlay in order to identify candidates who were likely to have an optimal device fit.
Discussant Francesco Maisano, MD, was impressed by how well this simulation resembled the actual results as depicted in side-by-side pre- and postprocedural CT images presented by Dr. Sorajja.
“What really surprised me was the correlation between preprocedural simulation data and the actual CT scan after the procedure. This trial shows that the simulation works, and also that Tendyne is a great alternative to aortic valve-in-MAC for these very-high-risk patients,” said Dr. Maisano, professor of cardiac surgery at the University of Zürich and a pioneer of catheter-based mitral and tricuspid interventions.
Earlier this year the Tendyne device was approved in Europe for patients with mitral regurgitation who aren’t candidates for surgical valve replacement or transcatheter mitral valve repair. The approval does not, however, extend to MAC. The Abbott device remains investigational in the United States, where the pivotal SUMMIT trial is underway. In one arm of the trial, patients with mitral regurgitation are being randomized to the investigational Tendyne device or to Abbott’s MitraClip, which is approved for that indication. In the other arm, patients with severe MAC at prohibitive surgical risk will get the Tendyne device. Results are expected in 2020.
Dr. Sorajja reported receiving research grants from and serving as a consultant to Abbott, the feasibility study sponsor, as well as to several other medical device companies, as did Dr. Maisano.
Transcatheter implantation of the Tendyne mitral valve replacement device for treatment of mitral regurgitation in patients at prohibitive surgical risk because of severe mitral annular calcification showed considerable promise in a small feasibility study, Paul Sorajja, MD, reported at the virtual annual meeting of the European Association of Percutaneous Cardiovascular Interventions.
There is a huge unmet need for safe and effective therapies for severe mitral annular calcification (MAC).
“Severe MAC often precludes surgical treatment, and there’s a poor prognosis in patients with MAC and mitral regurgitation when untreated, with 2-year survival of about 60% in some studies,” noted Dr. Sorajja, a cardiologist at the Minneapolis Heart Institute Foundation.
Attempts at repurposing transcatheter aortic valves for use in the mitral location have been largely unsatisfactory, he added.
The 6-month outcomes in the 11 patients who received the Tendyne device in the multicenter U.S. feasibility study featured low rates of mortality and nonfatal adverse events, elimination of mitral regurgitation, marked improvement on quality of life measures, and a mean gradient of 4.1 mm Hg. The acute procedural outcomes were encouraging as well.
“We had technical success in 11 of 11 patients, no procedural mortality or left ventricular outflow tract obstruction, no valve embolization or malposition, and no conversion to open heart surgery,” he said.
There was one death caused by mesenteric ischemia 16 days post Tendyne implantation. One patient experienced a nondisabling stroke at day 4. Two patients developed new-onset atrial fibrillation, one of whom cardioverted to sinus rhythm. And one patient had a moderate paravalvular leak that resolved with placement of a plug at 3 months. There were no MIs.
At baseline, 9 of 11 patients were New York Heart Association functional class III and the others were class II. At 6 months, six patients were class I, four were class II, and one was class III. The average score on the Kansas City Cardiomyopathy Questionnaire improved from 45.9 at baseline to 65.5 at 1 month, 77.4 at 3 months, and 70.3 at 6 months.
This was a highly selected study population with a Society of Thoracic Surgery Predicted Risk of Mortality score of 9.03%. Part of the screening process for study participation involved preprocedural CT imaging with simulated device overlay in order to identify candidates who were likely to have an optimal device fit.
Discussant Francesco Maisano, MD, was impressed by how well this simulation resembled the actual results as depicted in side-by-side pre- and postprocedural CT images presented by Dr. Sorajja.
“What really surprised me was the correlation between preprocedural simulation data and the actual CT scan after the procedure. This trial shows that the simulation works, and also that Tendyne is a great alternative to aortic valve-in-MAC for these very-high-risk patients,” said Dr. Maisano, professor of cardiac surgery at the University of Zürich and a pioneer of catheter-based mitral and tricuspid interventions.
Earlier this year the Tendyne device was approved in Europe for patients with mitral regurgitation who aren’t candidates for surgical valve replacement or transcatheter mitral valve repair. The approval does not, however, extend to MAC. The Abbott device remains investigational in the United States, where the pivotal SUMMIT trial is underway. In one arm of the trial, patients with mitral regurgitation are being randomized to the investigational Tendyne device or to Abbott’s MitraClip, which is approved for that indication. In the other arm, patients with severe MAC at prohibitive surgical risk will get the Tendyne device. Results are expected in 2020.
Dr. Sorajja reported receiving research grants from and serving as a consultant to Abbott, the feasibility study sponsor, as well as to several other medical device companies, as did Dr. Maisano.
REPORTING FROM EUROPCR 2020
Big pharma sues to block Minnesota insulin affordability law
PhRMA filed the complaint in the U.S. District Court in Minnesota on July 1, the day the Alec Smith Insulin Affordability Act went into effect. The law created the Minnesota Insulin Safety Net Program, which is continuing to operate in the meantime.
Advocates said they were appalled by the PhRMA action.
PhRMA says law is unconstitutional
In the filing, PhRMA’s attorneys said the law is unconstitutional. It “order[s] pharmaceutical manufacturers to give insulin to state residents, on the state’s prescribed terms, at no charge to the recipients and without compensating the manufacturers in any way.”
“A state cannot simply commandeer private property to achieve its public policy goals,” the PhRMA lawyers argued.
The suit said the three leading insulin makers already provide discounts, copayment assistance, and free insulin to “a great number of patients.”
The state has estimated that as many as 30,000 Minnesotans would be eligible for free insulin in the first year of the program. The drugmakers strenuously objected, noting that would mean they would “be compelled to provide 173,800 monthly supplies of free insulin” just in the first year.
“No one living with diabetes should be forced to ration or go without their life-saving insulin because they can’t afford it,” said PhRMA executive vice president and general counsel James C. Stansel in a statement.
The law, said Mr. Stansel, “overlooks common sense solutions to help patients afford their insulin and, despite its claims, still allows for patients to be charged at the pharmacy for the insulin that manufacturers are required to provide for free.”
Advocates decry suit
Advocates had worked for several years to secure passage of the legislation, named in honor of a young man who died in 2017 after rationing his insulin. Minnesota Gov. Tim Walz of the Democratic-Farmer-Labor Party signed the bill into law on April 15.
It requires manufacturers to make at least a 30-day supply of insulin available to those who are in urgent need and cannot afford the medication. Manufacturers can be fined $200,000 per month for not complying.
Mayo Clinic hematologist S. Vincent Rajkumar, MD, who called for action on the cost of insulin in an article published in the January 2020 issue of the Mayo Clinic Proceedings, as reported by Medscape Medical News, said the lawsuit was a “bad move.”
Dr. Rajkumar, the Edward W. and Betty Knight Scripps professor of medicine at the Mayo Clinic, noted that it has strict limits and is aimed to help patients in emergent need.
“There is nothing in the US constitution that prevents states from saving the lives of its citizens who are in imminent danger,” Dr. Rajkumar said. “The only motives for this lawsuit in my opinion are greed and the worry that other states may also choose to put lives of patients ahead of pharma profits.”
Alec Smith’s mother, Nicole Smith-Holt, who is active with T1International’s #insulin4all campaign, took to Twitter to express her anger.
“Throwing up road blocks to securing affordable insulin for the people of MN, haven’t they taken enough innocent lives? How many more bodies are they looking for?” she tweeted. “When are they going to realize we are not going to stop fighting?”
T1International said in a statement: “It is clear that the pharmaceutical industry can see only one thing – their bottom line,” and promised that patients would not give up.
“We will not stop showing them the real price we pay for their greed,” said the organization.
Abigail Hansmeyer, a Minnesota-based #insulin4all advocate, also talked about her frustration at what appeared to be disingenuous behavior by the insulin makers.
“I guess the endless opportunities insulin manufacturer reps had as stakeholders during numerous discussions and negotiations in the making of this law, wasn’t what they wanted,” she tweeted. “They were buying time to protect their profits. Yeah, we’re not done here.”
A version of this article originally appeared on Medscape.com.
PhRMA filed the complaint in the U.S. District Court in Minnesota on July 1, the day the Alec Smith Insulin Affordability Act went into effect. The law created the Minnesota Insulin Safety Net Program, which is continuing to operate in the meantime.
Advocates said they were appalled by the PhRMA action.
PhRMA says law is unconstitutional
In the filing, PhRMA’s attorneys said the law is unconstitutional. It “order[s] pharmaceutical manufacturers to give insulin to state residents, on the state’s prescribed terms, at no charge to the recipients and without compensating the manufacturers in any way.”
“A state cannot simply commandeer private property to achieve its public policy goals,” the PhRMA lawyers argued.
The suit said the three leading insulin makers already provide discounts, copayment assistance, and free insulin to “a great number of patients.”
The state has estimated that as many as 30,000 Minnesotans would be eligible for free insulin in the first year of the program. The drugmakers strenuously objected, noting that would mean they would “be compelled to provide 173,800 monthly supplies of free insulin” just in the first year.
“No one living with diabetes should be forced to ration or go without their life-saving insulin because they can’t afford it,” said PhRMA executive vice president and general counsel James C. Stansel in a statement.
The law, said Mr. Stansel, “overlooks common sense solutions to help patients afford their insulin and, despite its claims, still allows for patients to be charged at the pharmacy for the insulin that manufacturers are required to provide for free.”
Advocates decry suit
Advocates had worked for several years to secure passage of the legislation, named in honor of a young man who died in 2017 after rationing his insulin. Minnesota Gov. Tim Walz of the Democratic-Farmer-Labor Party signed the bill into law on April 15.
It requires manufacturers to make at least a 30-day supply of insulin available to those who are in urgent need and cannot afford the medication. Manufacturers can be fined $200,000 per month for not complying.
Mayo Clinic hematologist S. Vincent Rajkumar, MD, who called for action on the cost of insulin in an article published in the January 2020 issue of the Mayo Clinic Proceedings, as reported by Medscape Medical News, said the lawsuit was a “bad move.”
Dr. Rajkumar, the Edward W. and Betty Knight Scripps professor of medicine at the Mayo Clinic, noted that it has strict limits and is aimed to help patients in emergent need.
“There is nothing in the US constitution that prevents states from saving the lives of its citizens who are in imminent danger,” Dr. Rajkumar said. “The only motives for this lawsuit in my opinion are greed and the worry that other states may also choose to put lives of patients ahead of pharma profits.”
Alec Smith’s mother, Nicole Smith-Holt, who is active with T1International’s #insulin4all campaign, took to Twitter to express her anger.
“Throwing up road blocks to securing affordable insulin for the people of MN, haven’t they taken enough innocent lives? How many more bodies are they looking for?” she tweeted. “When are they going to realize we are not going to stop fighting?”
T1International said in a statement: “It is clear that the pharmaceutical industry can see only one thing – their bottom line,” and promised that patients would not give up.
“We will not stop showing them the real price we pay for their greed,” said the organization.
Abigail Hansmeyer, a Minnesota-based #insulin4all advocate, also talked about her frustration at what appeared to be disingenuous behavior by the insulin makers.
“I guess the endless opportunities insulin manufacturer reps had as stakeholders during numerous discussions and negotiations in the making of this law, wasn’t what they wanted,” she tweeted. “They were buying time to protect their profits. Yeah, we’re not done here.”
A version of this article originally appeared on Medscape.com.
PhRMA filed the complaint in the U.S. District Court in Minnesota on July 1, the day the Alec Smith Insulin Affordability Act went into effect. The law created the Minnesota Insulin Safety Net Program, which is continuing to operate in the meantime.
Advocates said they were appalled by the PhRMA action.
PhRMA says law is unconstitutional
In the filing, PhRMA’s attorneys said the law is unconstitutional. It “order[s] pharmaceutical manufacturers to give insulin to state residents, on the state’s prescribed terms, at no charge to the recipients and without compensating the manufacturers in any way.”
“A state cannot simply commandeer private property to achieve its public policy goals,” the PhRMA lawyers argued.
The suit said the three leading insulin makers already provide discounts, copayment assistance, and free insulin to “a great number of patients.”
The state has estimated that as many as 30,000 Minnesotans would be eligible for free insulin in the first year of the program. The drugmakers strenuously objected, noting that would mean they would “be compelled to provide 173,800 monthly supplies of free insulin” just in the first year.
“No one living with diabetes should be forced to ration or go without their life-saving insulin because they can’t afford it,” said PhRMA executive vice president and general counsel James C. Stansel in a statement.
The law, said Mr. Stansel, “overlooks common sense solutions to help patients afford their insulin and, despite its claims, still allows for patients to be charged at the pharmacy for the insulin that manufacturers are required to provide for free.”
Advocates decry suit
Advocates had worked for several years to secure passage of the legislation, named in honor of a young man who died in 2017 after rationing his insulin. Minnesota Gov. Tim Walz of the Democratic-Farmer-Labor Party signed the bill into law on April 15.
It requires manufacturers to make at least a 30-day supply of insulin available to those who are in urgent need and cannot afford the medication. Manufacturers can be fined $200,000 per month for not complying.
Mayo Clinic hematologist S. Vincent Rajkumar, MD, who called for action on the cost of insulin in an article published in the January 2020 issue of the Mayo Clinic Proceedings, as reported by Medscape Medical News, said the lawsuit was a “bad move.”
Dr. Rajkumar, the Edward W. and Betty Knight Scripps professor of medicine at the Mayo Clinic, noted that it has strict limits and is aimed to help patients in emergent need.
“There is nothing in the US constitution that prevents states from saving the lives of its citizens who are in imminent danger,” Dr. Rajkumar said. “The only motives for this lawsuit in my opinion are greed and the worry that other states may also choose to put lives of patients ahead of pharma profits.”
Alec Smith’s mother, Nicole Smith-Holt, who is active with T1International’s #insulin4all campaign, took to Twitter to express her anger.
“Throwing up road blocks to securing affordable insulin for the people of MN, haven’t they taken enough innocent lives? How many more bodies are they looking for?” she tweeted. “When are they going to realize we are not going to stop fighting?”
T1International said in a statement: “It is clear that the pharmaceutical industry can see only one thing – their bottom line,” and promised that patients would not give up.
“We will not stop showing them the real price we pay for their greed,” said the organization.
Abigail Hansmeyer, a Minnesota-based #insulin4all advocate, also talked about her frustration at what appeared to be disingenuous behavior by the insulin makers.
“I guess the endless opportunities insulin manufacturer reps had as stakeholders during numerous discussions and negotiations in the making of this law, wasn’t what they wanted,” she tweeted. “They were buying time to protect their profits. Yeah, we’re not done here.”
A version of this article originally appeared on Medscape.com.
Bariatric embolotherapy helps shed pounds in obese patients
Transcatheter bariatric embolotherapy (TBE) provides sustained weight loss without serious adverse effects among obese patients, results of a pilot sham-controlled study suggest.
At 6-month follow-up, the patients receiving the intervention had lost 7.4 kg (16.3 lbs), compared with 3.0 kg (6.6 lbs) in those randomized to a sham procedure in an intention-to-treat analysis (P = .034).
Results were similar in a per-protocol analysis (9.4 kg/20.7 lbs vs. 1.9 kg/4.1 lbs; P = .0002).
Weight loss after embolotherapy was sustained over 12 months, falling 7.8 kg (17.1 lbs) from baseline in the intention-to-treat population (P = .0011) and 9.3 kg (20.5 lbs) in the per-protocol population (P = .0005).
Safety events after TBE were mild nausea or vomiting, reported Vivek Reddy, MD, Mount Sinai Hospital, New York City. Five participants had minor, asymptomatic ulcers that required no additional treatment.
“In this randomized pilot trial, we established the proof of principle that transcatheter bariatric embolotherapy of the left gastric artery is safe and it promotes clinically significant weight loss,” he concluded at PCR e-Course, the virtual meeting of the Congress of European Association of Percutaneous Cardiovascular Interventions 2020.
Although bariatric surgery is highly effective, he noted that the associated morbidity and mortality limit its use to the severely obese with a body mass index (BMI) typically over 40 kg/m2.
TBE is a minimally invasive approach that uses a custom occlusion balloon microcatheter and robotic manifold to inject 300- to 500-mcm beads to the left gastric artery. Preclinical and case studies suggest it promotes weight loss by reducing ghrelin, an appetite-stimulating hormone secreted from the gastric fundus, Dr. Reddy said.
The study enrolled 44 patients (aged 21-60 years) with a BMI of 35-55, excluding those with prior bariatric surgery and a history of ulcers, type 2 diabetes, chronic aspirin or nonsteroidal inflammatory use, and active Helicobacter pylori infection.
A total of 40 patients were randomly assigned to TBE or a sham procedure, in which lidocaine was applied to the femoral area and propofol infused for 1 hour. The two groups were well matched, with a mean age of 45 vs. 46 years, weight of 110 kg vs. 119 kg, and BMI of 39 vs. 40, Dr. Reddy noted.
Embolotherapy was performed at a single center in Prague, and, on average, took 82.3 minutes and used 127 mL of contrast, 163 Gy/cm2 radiation, and 4.2 mL of microspheres. A single vessel was injected in 80% of cases.
The intention-to-treat population comprised 19 TBE and 18 control subjects, and the per-protocol population comprised 15 TBE and 16 control subjects, after the exclusion of patients in whom embolotherapy was unsuccessful or incomplete or who withdrew consent.
All patients received endoscopy at baseline and 1 week, as well as an intensive 19-session lifestyle and dietary education intervention out to 6 months.
Patients who underwent TBE had significant improvement in hunger scores at 6 and 12 months, compared with baseline. Similarly, quality of life improved across all six domains, including significant gains in physical function, self-esteem, and overall quality of life at both time points, Dr. Reddy reported.
Dr. Reddy disclosed receiving research support from Endobar Solutions.
This article first appeared on Medscape.com.
Transcatheter bariatric embolotherapy (TBE) provides sustained weight loss without serious adverse effects among obese patients, results of a pilot sham-controlled study suggest.
At 6-month follow-up, the patients receiving the intervention had lost 7.4 kg (16.3 lbs), compared with 3.0 kg (6.6 lbs) in those randomized to a sham procedure in an intention-to-treat analysis (P = .034).
Results were similar in a per-protocol analysis (9.4 kg/20.7 lbs vs. 1.9 kg/4.1 lbs; P = .0002).
Weight loss after embolotherapy was sustained over 12 months, falling 7.8 kg (17.1 lbs) from baseline in the intention-to-treat population (P = .0011) and 9.3 kg (20.5 lbs) in the per-protocol population (P = .0005).
Safety events after TBE were mild nausea or vomiting, reported Vivek Reddy, MD, Mount Sinai Hospital, New York City. Five participants had minor, asymptomatic ulcers that required no additional treatment.
“In this randomized pilot trial, we established the proof of principle that transcatheter bariatric embolotherapy of the left gastric artery is safe and it promotes clinically significant weight loss,” he concluded at PCR e-Course, the virtual meeting of the Congress of European Association of Percutaneous Cardiovascular Interventions 2020.
Although bariatric surgery is highly effective, he noted that the associated morbidity and mortality limit its use to the severely obese with a body mass index (BMI) typically over 40 kg/m2.
TBE is a minimally invasive approach that uses a custom occlusion balloon microcatheter and robotic manifold to inject 300- to 500-mcm beads to the left gastric artery. Preclinical and case studies suggest it promotes weight loss by reducing ghrelin, an appetite-stimulating hormone secreted from the gastric fundus, Dr. Reddy said.
The study enrolled 44 patients (aged 21-60 years) with a BMI of 35-55, excluding those with prior bariatric surgery and a history of ulcers, type 2 diabetes, chronic aspirin or nonsteroidal inflammatory use, and active Helicobacter pylori infection.
A total of 40 patients were randomly assigned to TBE or a sham procedure, in which lidocaine was applied to the femoral area and propofol infused for 1 hour. The two groups were well matched, with a mean age of 45 vs. 46 years, weight of 110 kg vs. 119 kg, and BMI of 39 vs. 40, Dr. Reddy noted.
Embolotherapy was performed at a single center in Prague, and, on average, took 82.3 minutes and used 127 mL of contrast, 163 Gy/cm2 radiation, and 4.2 mL of microspheres. A single vessel was injected in 80% of cases.
The intention-to-treat population comprised 19 TBE and 18 control subjects, and the per-protocol population comprised 15 TBE and 16 control subjects, after the exclusion of patients in whom embolotherapy was unsuccessful or incomplete or who withdrew consent.
All patients received endoscopy at baseline and 1 week, as well as an intensive 19-session lifestyle and dietary education intervention out to 6 months.
Patients who underwent TBE had significant improvement in hunger scores at 6 and 12 months, compared with baseline. Similarly, quality of life improved across all six domains, including significant gains in physical function, self-esteem, and overall quality of life at both time points, Dr. Reddy reported.
Dr. Reddy disclosed receiving research support from Endobar Solutions.
This article first appeared on Medscape.com.
Transcatheter bariatric embolotherapy (TBE) provides sustained weight loss without serious adverse effects among obese patients, results of a pilot sham-controlled study suggest.
At 6-month follow-up, the patients receiving the intervention had lost 7.4 kg (16.3 lbs), compared with 3.0 kg (6.6 lbs) in those randomized to a sham procedure in an intention-to-treat analysis (P = .034).
Results were similar in a per-protocol analysis (9.4 kg/20.7 lbs vs. 1.9 kg/4.1 lbs; P = .0002).
Weight loss after embolotherapy was sustained over 12 months, falling 7.8 kg (17.1 lbs) from baseline in the intention-to-treat population (P = .0011) and 9.3 kg (20.5 lbs) in the per-protocol population (P = .0005).
Safety events after TBE were mild nausea or vomiting, reported Vivek Reddy, MD, Mount Sinai Hospital, New York City. Five participants had minor, asymptomatic ulcers that required no additional treatment.
“In this randomized pilot trial, we established the proof of principle that transcatheter bariatric embolotherapy of the left gastric artery is safe and it promotes clinically significant weight loss,” he concluded at PCR e-Course, the virtual meeting of the Congress of European Association of Percutaneous Cardiovascular Interventions 2020.
Although bariatric surgery is highly effective, he noted that the associated morbidity and mortality limit its use to the severely obese with a body mass index (BMI) typically over 40 kg/m2.
TBE is a minimally invasive approach that uses a custom occlusion balloon microcatheter and robotic manifold to inject 300- to 500-mcm beads to the left gastric artery. Preclinical and case studies suggest it promotes weight loss by reducing ghrelin, an appetite-stimulating hormone secreted from the gastric fundus, Dr. Reddy said.
The study enrolled 44 patients (aged 21-60 years) with a BMI of 35-55, excluding those with prior bariatric surgery and a history of ulcers, type 2 diabetes, chronic aspirin or nonsteroidal inflammatory use, and active Helicobacter pylori infection.
A total of 40 patients were randomly assigned to TBE or a sham procedure, in which lidocaine was applied to the femoral area and propofol infused for 1 hour. The two groups were well matched, with a mean age of 45 vs. 46 years, weight of 110 kg vs. 119 kg, and BMI of 39 vs. 40, Dr. Reddy noted.
Embolotherapy was performed at a single center in Prague, and, on average, took 82.3 minutes and used 127 mL of contrast, 163 Gy/cm2 radiation, and 4.2 mL of microspheres. A single vessel was injected in 80% of cases.
The intention-to-treat population comprised 19 TBE and 18 control subjects, and the per-protocol population comprised 15 TBE and 16 control subjects, after the exclusion of patients in whom embolotherapy was unsuccessful or incomplete or who withdrew consent.
All patients received endoscopy at baseline and 1 week, as well as an intensive 19-session lifestyle and dietary education intervention out to 6 months.
Patients who underwent TBE had significant improvement in hunger scores at 6 and 12 months, compared with baseline. Similarly, quality of life improved across all six domains, including significant gains in physical function, self-esteem, and overall quality of life at both time points, Dr. Reddy reported.
Dr. Reddy disclosed receiving research support from Endobar Solutions.
This article first appeared on Medscape.com.
Physician shortage grows in latest projections
Fifteen-year projections for the shortage of primary care and specialty physicians in the United States grew to between 54,000 and 139,000 in the latest annual report by the Association of American Medical Colleges.
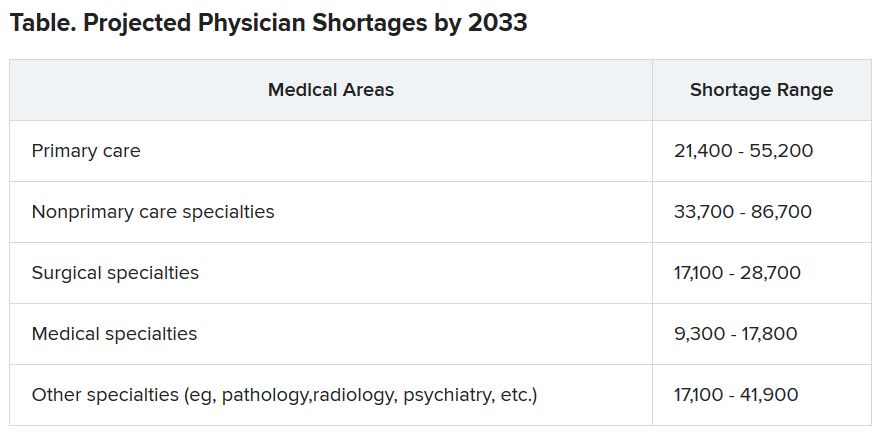
Those estimates are up from last year’s projections of a shortfall of 46,900-121,900 by 2032.
The Complexities of Physician Supply and Demand: Projections from 2018 to 2033, was the sixth annual study conducted for the AAMC by the Life Science division of global analytics firm IHS Markit.
This analysis, conducted in 2019, includes supply and demand scenarios but predates the COVID-19 pandemic.
In a telephone press briefing this morning, David J. Skorton, MD, AAMC’s president and CEO, told reporters that the pandemic has highlighted the acute effects of physician shortages.
“We’ve seen in stark detail how fragile and quickly overwhelmed America’s health care system truly is, and we’re nowhere near out of the woods with this public health emergency yet,” he said.
The persistent shortages mean people “will have ongoing difficulty accessing the care that they need, especially as we all age.”
Some of the biggest shortages will be seen in non–primary care specialists. Dr. Skorton notes that, during the pandemic, shortages of specialists in hospital settings, including critical care, emergency medicine, pulmonology, and infectious disease, are an urgent concern.
Population trends continue to be the biggest drivers of the shortage. Report authors found that by 2033, the U.S. population is expected to grow by 10.4% from 327 million to 361 million, with wide differences by age.
The under-18 population is expected to grow by 3.9%, whereas the numbers of those aged 65 and older is expected to balloon by 45.1% in that time, thus stoking demand for specialties focused on care for older Americans.
Physician age is also a large factor in the projections. More than two in five currently active physicians will be 65 or older in the next 10 years, according to the report. A wave of retirements will have a large impact on the supply of physicians.
The report explains that the projected shortages remain under predictable scenarios: an increase in the use of advanced practice nurses (APRNs) and physician assistants (PAs), more care in alternate settings such as retail clinics, and changes in payment and delivery.
According to the report, the supply of APRNs and PAs is on track to double over the next 15 years (with growth rates varying by APRN and PA specialty).
“At current rates of production, by 2033 APRN supply will grow by 276,000 [full-time equivalents (FTEs)] and PA supply by nearly 138,000 FTEs,” the report states.
However, authors acknowledge there is scant evidence on what effect these numbers will have on demand for physicians.
The report points out that if underserved communities were able to access health care in numbers similar to those without barriers imposed by where they live or what insurance they have, demand could rise beyond the projections in this report by an additional 74,000 to 145,000 physicians.
Stemming the shortages
The first step in addressing the shortage, Dr. Skorton said, is assuring a healthy physician pipeline to meet the demand for generations.
“One essential step that we believe Congress must take is to end the freeze that has been in place since 1997 that limits federal support for residency training of new physicians,” Skorton said.
He noted that AAMC supports the bipartisan Resident Physician Shortage Reduction Act, introduced to Congress in 2019, which calls for an increase in Medicare support for 3000 new residency positions each year over the next 5 years.
However, additional steps are needed, including enabling advanced practice providers to play a greater role in increasing the health care workforce, Dr. Skorton said.
Pointing out some of the effects of physician shortages, Janis M. Orlowski, MD, chief health care officer for the AAMC, noted that high rates of maternal morbidity are partially linked to lack of adequate numbers of physicians in the United States, and a lack of behavioral health specialists has exacerbated effects of the opioid epidemic.
Shortages are already evident in the current pandemic, she added, saying, “Today we see governors calling for retired physicians or physicians from other states to come and help battle the pandemic within their states.”
The report explains that long-term effects on physician numbers from the pandemic likely will include workforce exits because of COVID-19 deaths, early retirements from burnout, or a shift in interest in certain specialties.
Karen Fisher, JD, chief public policy officer for AAMC, said telehealth will also play an important role in bridging gaps in access to care, and its importance has already been seen in this first wave of the pandemic.
She noted that temporary federal waivers have made it easier for those enrolled in Medicare, Medicaid, and the Children’s Health Insurance Program to receive telehealth services during the pandemic.
Expanding the access to telehealth permanently will be important in helping to fill gaps, Ms. Fisher said.
Dr. Skorton, Dr. Orlowski, and Ms. Fisher have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Fifteen-year projections for the shortage of primary care and specialty physicians in the United States grew to between 54,000 and 139,000 in the latest annual report by the Association of American Medical Colleges.
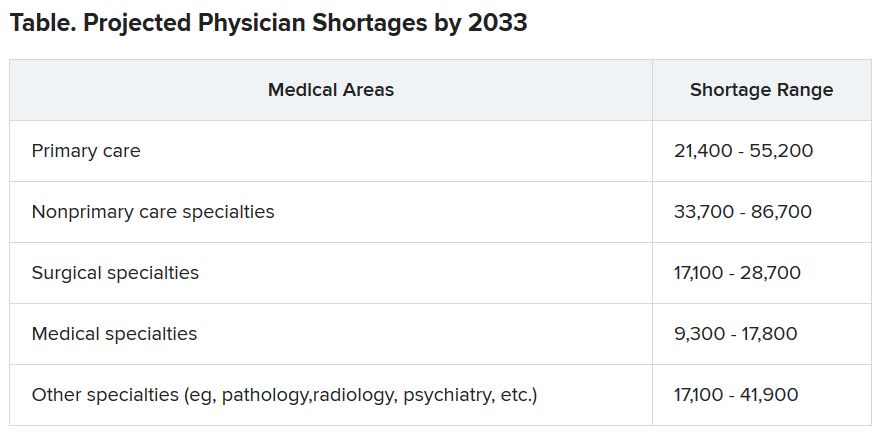
Those estimates are up from last year’s projections of a shortfall of 46,900-121,900 by 2032.
The Complexities of Physician Supply and Demand: Projections from 2018 to 2033, was the sixth annual study conducted for the AAMC by the Life Science division of global analytics firm IHS Markit.
This analysis, conducted in 2019, includes supply and demand scenarios but predates the COVID-19 pandemic.
In a telephone press briefing this morning, David J. Skorton, MD, AAMC’s president and CEO, told reporters that the pandemic has highlighted the acute effects of physician shortages.
“We’ve seen in stark detail how fragile and quickly overwhelmed America’s health care system truly is, and we’re nowhere near out of the woods with this public health emergency yet,” he said.
The persistent shortages mean people “will have ongoing difficulty accessing the care that they need, especially as we all age.”
Some of the biggest shortages will be seen in non–primary care specialists. Dr. Skorton notes that, during the pandemic, shortages of specialists in hospital settings, including critical care, emergency medicine, pulmonology, and infectious disease, are an urgent concern.
Population trends continue to be the biggest drivers of the shortage. Report authors found that by 2033, the U.S. population is expected to grow by 10.4% from 327 million to 361 million, with wide differences by age.
The under-18 population is expected to grow by 3.9%, whereas the numbers of those aged 65 and older is expected to balloon by 45.1% in that time, thus stoking demand for specialties focused on care for older Americans.
Physician age is also a large factor in the projections. More than two in five currently active physicians will be 65 or older in the next 10 years, according to the report. A wave of retirements will have a large impact on the supply of physicians.
The report explains that the projected shortages remain under predictable scenarios: an increase in the use of advanced practice nurses (APRNs) and physician assistants (PAs), more care in alternate settings such as retail clinics, and changes in payment and delivery.
According to the report, the supply of APRNs and PAs is on track to double over the next 15 years (with growth rates varying by APRN and PA specialty).
“At current rates of production, by 2033 APRN supply will grow by 276,000 [full-time equivalents (FTEs)] and PA supply by nearly 138,000 FTEs,” the report states.
However, authors acknowledge there is scant evidence on what effect these numbers will have on demand for physicians.
The report points out that if underserved communities were able to access health care in numbers similar to those without barriers imposed by where they live or what insurance they have, demand could rise beyond the projections in this report by an additional 74,000 to 145,000 physicians.
Stemming the shortages
The first step in addressing the shortage, Dr. Skorton said, is assuring a healthy physician pipeline to meet the demand for generations.
“One essential step that we believe Congress must take is to end the freeze that has been in place since 1997 that limits federal support for residency training of new physicians,” Skorton said.
He noted that AAMC supports the bipartisan Resident Physician Shortage Reduction Act, introduced to Congress in 2019, which calls for an increase in Medicare support for 3000 new residency positions each year over the next 5 years.
However, additional steps are needed, including enabling advanced practice providers to play a greater role in increasing the health care workforce, Dr. Skorton said.
Pointing out some of the effects of physician shortages, Janis M. Orlowski, MD, chief health care officer for the AAMC, noted that high rates of maternal morbidity are partially linked to lack of adequate numbers of physicians in the United States, and a lack of behavioral health specialists has exacerbated effects of the opioid epidemic.
Shortages are already evident in the current pandemic, she added, saying, “Today we see governors calling for retired physicians or physicians from other states to come and help battle the pandemic within their states.”
The report explains that long-term effects on physician numbers from the pandemic likely will include workforce exits because of COVID-19 deaths, early retirements from burnout, or a shift in interest in certain specialties.
Karen Fisher, JD, chief public policy officer for AAMC, said telehealth will also play an important role in bridging gaps in access to care, and its importance has already been seen in this first wave of the pandemic.
She noted that temporary federal waivers have made it easier for those enrolled in Medicare, Medicaid, and the Children’s Health Insurance Program to receive telehealth services during the pandemic.
Expanding the access to telehealth permanently will be important in helping to fill gaps, Ms. Fisher said.
Dr. Skorton, Dr. Orlowski, and Ms. Fisher have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Fifteen-year projections for the shortage of primary care and specialty physicians in the United States grew to between 54,000 and 139,000 in the latest annual report by the Association of American Medical Colleges.
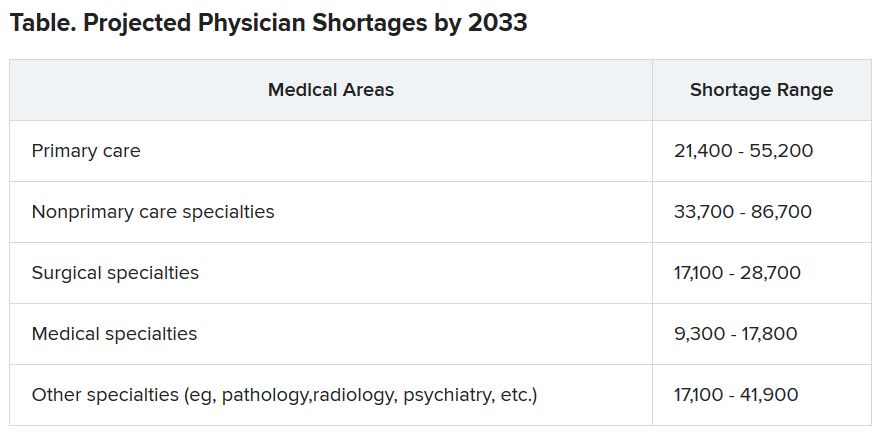
Those estimates are up from last year’s projections of a shortfall of 46,900-121,900 by 2032.
The Complexities of Physician Supply and Demand: Projections from 2018 to 2033, was the sixth annual study conducted for the AAMC by the Life Science division of global analytics firm IHS Markit.
This analysis, conducted in 2019, includes supply and demand scenarios but predates the COVID-19 pandemic.
In a telephone press briefing this morning, David J. Skorton, MD, AAMC’s president and CEO, told reporters that the pandemic has highlighted the acute effects of physician shortages.
“We’ve seen in stark detail how fragile and quickly overwhelmed America’s health care system truly is, and we’re nowhere near out of the woods with this public health emergency yet,” he said.
The persistent shortages mean people “will have ongoing difficulty accessing the care that they need, especially as we all age.”
Some of the biggest shortages will be seen in non–primary care specialists. Dr. Skorton notes that, during the pandemic, shortages of specialists in hospital settings, including critical care, emergency medicine, pulmonology, and infectious disease, are an urgent concern.
Population trends continue to be the biggest drivers of the shortage. Report authors found that by 2033, the U.S. population is expected to grow by 10.4% from 327 million to 361 million, with wide differences by age.
The under-18 population is expected to grow by 3.9%, whereas the numbers of those aged 65 and older is expected to balloon by 45.1% in that time, thus stoking demand for specialties focused on care for older Americans.
Physician age is also a large factor in the projections. More than two in five currently active physicians will be 65 or older in the next 10 years, according to the report. A wave of retirements will have a large impact on the supply of physicians.
The report explains that the projected shortages remain under predictable scenarios: an increase in the use of advanced practice nurses (APRNs) and physician assistants (PAs), more care in alternate settings such as retail clinics, and changes in payment and delivery.
According to the report, the supply of APRNs and PAs is on track to double over the next 15 years (with growth rates varying by APRN and PA specialty).
“At current rates of production, by 2033 APRN supply will grow by 276,000 [full-time equivalents (FTEs)] and PA supply by nearly 138,000 FTEs,” the report states.
However, authors acknowledge there is scant evidence on what effect these numbers will have on demand for physicians.
The report points out that if underserved communities were able to access health care in numbers similar to those without barriers imposed by where they live or what insurance they have, demand could rise beyond the projections in this report by an additional 74,000 to 145,000 physicians.
Stemming the shortages
The first step in addressing the shortage, Dr. Skorton said, is assuring a healthy physician pipeline to meet the demand for generations.
“One essential step that we believe Congress must take is to end the freeze that has been in place since 1997 that limits federal support for residency training of new physicians,” Skorton said.
He noted that AAMC supports the bipartisan Resident Physician Shortage Reduction Act, introduced to Congress in 2019, which calls for an increase in Medicare support for 3000 new residency positions each year over the next 5 years.
However, additional steps are needed, including enabling advanced practice providers to play a greater role in increasing the health care workforce, Dr. Skorton said.
Pointing out some of the effects of physician shortages, Janis M. Orlowski, MD, chief health care officer for the AAMC, noted that high rates of maternal morbidity are partially linked to lack of adequate numbers of physicians in the United States, and a lack of behavioral health specialists has exacerbated effects of the opioid epidemic.
Shortages are already evident in the current pandemic, she added, saying, “Today we see governors calling for retired physicians or physicians from other states to come and help battle the pandemic within their states.”
The report explains that long-term effects on physician numbers from the pandemic likely will include workforce exits because of COVID-19 deaths, early retirements from burnout, or a shift in interest in certain specialties.
Karen Fisher, JD, chief public policy officer for AAMC, said telehealth will also play an important role in bridging gaps in access to care, and its importance has already been seen in this first wave of the pandemic.
She noted that temporary federal waivers have made it easier for those enrolled in Medicare, Medicaid, and the Children’s Health Insurance Program to receive telehealth services during the pandemic.
Expanding the access to telehealth permanently will be important in helping to fill gaps, Ms. Fisher said.
Dr. Skorton, Dr. Orlowski, and Ms. Fisher have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Diagnostic criteria may miss some MIS-C cases, experts say
New data from active surveillance of the severe inflammatory condition associated with COVID-19 in previously healthy children provide further insight into the prevalence and course of the rare syndrome, but experts are concerned that current diagnostic criteria may not capture the true scope of the problem.
In separate reports published online June 29 in the New England Journal of Medicine, researchers from the New York State Department of Health and the Centers for Disease Control and Prevention (CDC) describe the epidemiology and clinical features of multisystem inflammatory syndrome in children (MIS-C) on the basis of information derived from targeted surveillance programs in New York State and across the country.
For the New York study, Elizabeth M. Dufort, MD, from the New York Department of Health in Albany and colleagues analyzed MIS-C surveillance data from 106 hospitals across the state. Of 191 suspected MIS-C cases reported to the Department of Health from March 1 through May 10, 99 met the state’s interim case definition of the condition and were included in the analysis.
The incidence rate for MIS-C was two cases per 100,000 individuals younger than 21 years, whereas the incidence rate of confirmed COVID-19 cases in this age group was 322 per 100,000. Most cases occurred approximately 1 month after the state’s COVID-19 peak.
“Among our patients, predominantly from the New York Metropolitan Region, 40% were black and 36% were Hispanic. This may be a reflection of the well-documented elevated incidence of SARS-CoV-2 infection among black and Hispanic communities,” the authors report.
All children presented with fever or chills, and most had tachycardia (97%) and gastrointestinal symptoms (80%). Rash (60%), conjunctival infection (56%), hypotension (32%), and mucosal changes (27%) were reported. Among all of the children, levels of inflammatory markers were elevated, including levels of C-reactive protein (100%), D-dimer (91%), and troponin (71%). More than one third of the patients (36%) were diagnosed with myocarditis, and an additional 16% had clinical myocarditis.
Of the full cohort, 80% of the children required intensive care, 62% received vasopressor support, and two children died.
The high prevalence of cardiac dysfunction or depression, coagulopathy, gastrointestinal symptoms, mild respiratory symptoms, and indications for supplemental oxygen in patients with MIS-C stands in contrast to the clinical picture observed in most acute cases of COVID-19 in hospitalized children, the authors write.
“Although most children have mild or no illness from SARS-CoV-2 infection, MIS-C may follow Covid-19 or asymptomatic SARS-CoV-2 infection. Recognition of the syndrome and early identification of children with MIS-C, including early monitoring of blood pressure and electrocardiographic and echocardiographic evaluation, could inform appropriate supportive care and other potential therapeutic options,” they continue.
The incidence of MIS-C among children infected with SARS-CoV-2 is unclear because children with COVID-19 often have mild or no symptoms and because children are not tested as frequently, the authors state. For this reason, “[i]t is crucial to establish surveillance for MIS-C cases, particularly in communities with higher levels of SARS-CoV-2 transmission.”
Important Differences From Kawasaki Disease
In a separate study, Leora R. Feldstein, MD, of the CDC, and colleagues report 186 cases of MIS-C collected through targeted surveillance of pediatric health centers in 26 US states from March 15 to May 20, 2020. As with the New York cohort, a disproportionate number of children in this cohort were black (25%) and Hispanic or Latino (31%).
Similar to the New York cohort, 80% of the children in this group required intensive care, 48% received vasoactive support, 20% required invasive mechanical ventilation, and four children died. Skin rashes, gastrointestinal symptoms, cardiovascular and hematologic effects, mucous changes, and elevations of inflammatory biomarkers were also similarly observed.
The researchers note that, although many of the features of MIS-C overlap with Kawasaki disease, there are some important differences, particularly with respect to the nature of cardiovascular involvement. “Approximately 5% of children with Kawasaki’s disease in the United States present with cardiovascular shock leading to vasopressor or inotropic support, as compared with 50% of the patients in our series,” the authors write.
In addition, coronary-artery aneurysms affect approximately one quarter of Kawasaki disease patients within 21 days of disease onset. “In our series, a maximum z score of 2.5 or higher in the left anterior descending or right coronary artery was reported in 8% of the patients overall and in 9% of patients with echocardiograms,” they report.
Additional differentiating features include patient age and race/ethnicity. Kawasaki disease occurs most commonly in children younger than 5 years. The median age in the multistate study was 8.3 years, and nearly half of the children in the New York cohort were in the 6- to 12-year age group. Further, Kawasaki disease is disproportionately prevalent in children of Asian descent.
Despite the differences, “until more is known about long-term cardiac sequelae of MIS-C, providers could consider following Kawasaki’s disease guidelines for follow-up, which recommend repeat echocardiographic imaging at 1 to 2 weeks.”
As was the case in the New York series, treatment in the multistate cohort most commonly included intravenous immunoglobulin and systemic glucocorticoids. Optimal management, however, will require a better understanding of the pathogenesis of MIS-C, Feldstein and colleagues write.
Questions Remain
With the accumulating data on this syndrome, the MIS-C picture seems to be getting incrementally clearer, but there is still much uncertainty, according to Michael Levin, FMedSci, PhD, from the Department of Infectious Disease, Imperial College London, United Kingdom.
“The recognition and description of new diseases often resemble the parable of the blind men and the elephant, with each declaring that the part of the beast they have touched fully defines it,” he writes in an accompanying editorial.
“As the coronavirus disease 2019 (Covid-19) pandemic has evolved, case reports have appeared describing children with unusual febrile illnesses that have features of Kawasaki’s disease, toxic shock syndrome, acute abdominal conditions, and encephalopathy, along with other reports of children with fever, elevated inflammatory markers, and multisystem involvement. It is now apparent that these reports were describing different clinical presentations of a new childhood inflammatory disorder.”
Although a consistent clinical picture is emerging, “[t]he published reports have used a variety of hastily developed case definitions based on the most severe cases, possibly missing less serious cases,” Levin writes. In particular, both the CDC and World Health Organization definitions require evidence of SARS-CoV-2 infection or exposure, which might contribute to underrecognition and underreporting because asymptomatic infections are common and antibody testing is not universally available.
“There is concern that children meeting current diagnostic criteria for MIS-C are the ‘tip of the iceberg,’ and a bigger problem may be lurking below the waterline,” Levin states. With approximately 1000 cases of the syndrome reported worldwide, “do we now have a clear picture of the new disorder, or as in the story of the blind men and the elephant, has only part of the beast been described?”
Adrienne Randolph, MD, of Boston Children’s Hospital, who is a coauthor of the multistate report, agrees that there is still much to learn about MIS-C before the whole beast can be understood. In an interview with Medscape Medical News, she listed the following key questions that have yet to be answered:
- Why do some children get MIS-C and not others?
- What is the long-term outcome of children with MIS-C?
- How can we differentiate MIS-C from acute COVID-19 infection in children with respiratory failure?
- Does MIS-C occur in young adults?
Randolph said her team is taking the best path forward toward answering these questions, including conducting a second study to identify risk factors for MIS-C and longer-term follow-up studies with the National Institutes of Health. “We are also getting consent to collect blood samples and look at other tests to help distinguish MIS-C from acute COVID-19 infection,” she said. She encouraged heightened awareness among physicians who care for young adults to consider MIS-C in patients aged 21 years and older who present with similar signs and symptoms.
On the basis of the answers to these and additional questions, the case definitions for MIS-C may need refinement to capture the wider spectrum of illness, Levin writes in his editorial. “The challenges of this new condition will now be to understand its pathophysiological mechanisms, to develop diagnostics, and to define the best treatment.”
Kleinman has received grants from the Health Services Resources Administration outside the submitted work. Maddux has received grants from the NIH/NICHD and the Francis Family Foundation outside the submitted work. Randolph has received grants from Genentech and personal fees from La Jolla Pharma outside the submitted work and others from the CDC during the conduct of the study.
This article first appeared on Medscape.com.
New data from active surveillance of the severe inflammatory condition associated with COVID-19 in previously healthy children provide further insight into the prevalence and course of the rare syndrome, but experts are concerned that current diagnostic criteria may not capture the true scope of the problem.
In separate reports published online June 29 in the New England Journal of Medicine, researchers from the New York State Department of Health and the Centers for Disease Control and Prevention (CDC) describe the epidemiology and clinical features of multisystem inflammatory syndrome in children (MIS-C) on the basis of information derived from targeted surveillance programs in New York State and across the country.
For the New York study, Elizabeth M. Dufort, MD, from the New York Department of Health in Albany and colleagues analyzed MIS-C surveillance data from 106 hospitals across the state. Of 191 suspected MIS-C cases reported to the Department of Health from March 1 through May 10, 99 met the state’s interim case definition of the condition and were included in the analysis.
The incidence rate for MIS-C was two cases per 100,000 individuals younger than 21 years, whereas the incidence rate of confirmed COVID-19 cases in this age group was 322 per 100,000. Most cases occurred approximately 1 month after the state’s COVID-19 peak.
“Among our patients, predominantly from the New York Metropolitan Region, 40% were black and 36% were Hispanic. This may be a reflection of the well-documented elevated incidence of SARS-CoV-2 infection among black and Hispanic communities,” the authors report.
All children presented with fever or chills, and most had tachycardia (97%) and gastrointestinal symptoms (80%). Rash (60%), conjunctival infection (56%), hypotension (32%), and mucosal changes (27%) were reported. Among all of the children, levels of inflammatory markers were elevated, including levels of C-reactive protein (100%), D-dimer (91%), and troponin (71%). More than one third of the patients (36%) were diagnosed with myocarditis, and an additional 16% had clinical myocarditis.
Of the full cohort, 80% of the children required intensive care, 62% received vasopressor support, and two children died.
The high prevalence of cardiac dysfunction or depression, coagulopathy, gastrointestinal symptoms, mild respiratory symptoms, and indications for supplemental oxygen in patients with MIS-C stands in contrast to the clinical picture observed in most acute cases of COVID-19 in hospitalized children, the authors write.
“Although most children have mild or no illness from SARS-CoV-2 infection, MIS-C may follow Covid-19 or asymptomatic SARS-CoV-2 infection. Recognition of the syndrome and early identification of children with MIS-C, including early monitoring of blood pressure and electrocardiographic and echocardiographic evaluation, could inform appropriate supportive care and other potential therapeutic options,” they continue.
The incidence of MIS-C among children infected with SARS-CoV-2 is unclear because children with COVID-19 often have mild or no symptoms and because children are not tested as frequently, the authors state. For this reason, “[i]t is crucial to establish surveillance for MIS-C cases, particularly in communities with higher levels of SARS-CoV-2 transmission.”
Important Differences From Kawasaki Disease
In a separate study, Leora R. Feldstein, MD, of the CDC, and colleagues report 186 cases of MIS-C collected through targeted surveillance of pediatric health centers in 26 US states from March 15 to May 20, 2020. As with the New York cohort, a disproportionate number of children in this cohort were black (25%) and Hispanic or Latino (31%).
Similar to the New York cohort, 80% of the children in this group required intensive care, 48% received vasoactive support, 20% required invasive mechanical ventilation, and four children died. Skin rashes, gastrointestinal symptoms, cardiovascular and hematologic effects, mucous changes, and elevations of inflammatory biomarkers were also similarly observed.
The researchers note that, although many of the features of MIS-C overlap with Kawasaki disease, there are some important differences, particularly with respect to the nature of cardiovascular involvement. “Approximately 5% of children with Kawasaki’s disease in the United States present with cardiovascular shock leading to vasopressor or inotropic support, as compared with 50% of the patients in our series,” the authors write.
In addition, coronary-artery aneurysms affect approximately one quarter of Kawasaki disease patients within 21 days of disease onset. “In our series, a maximum z score of 2.5 or higher in the left anterior descending or right coronary artery was reported in 8% of the patients overall and in 9% of patients with echocardiograms,” they report.
Additional differentiating features include patient age and race/ethnicity. Kawasaki disease occurs most commonly in children younger than 5 years. The median age in the multistate study was 8.3 years, and nearly half of the children in the New York cohort were in the 6- to 12-year age group. Further, Kawasaki disease is disproportionately prevalent in children of Asian descent.
Despite the differences, “until more is known about long-term cardiac sequelae of MIS-C, providers could consider following Kawasaki’s disease guidelines for follow-up, which recommend repeat echocardiographic imaging at 1 to 2 weeks.”
As was the case in the New York series, treatment in the multistate cohort most commonly included intravenous immunoglobulin and systemic glucocorticoids. Optimal management, however, will require a better understanding of the pathogenesis of MIS-C, Feldstein and colleagues write.
Questions Remain
With the accumulating data on this syndrome, the MIS-C picture seems to be getting incrementally clearer, but there is still much uncertainty, according to Michael Levin, FMedSci, PhD, from the Department of Infectious Disease, Imperial College London, United Kingdom.
“The recognition and description of new diseases often resemble the parable of the blind men and the elephant, with each declaring that the part of the beast they have touched fully defines it,” he writes in an accompanying editorial.
“As the coronavirus disease 2019 (Covid-19) pandemic has evolved, case reports have appeared describing children with unusual febrile illnesses that have features of Kawasaki’s disease, toxic shock syndrome, acute abdominal conditions, and encephalopathy, along with other reports of children with fever, elevated inflammatory markers, and multisystem involvement. It is now apparent that these reports were describing different clinical presentations of a new childhood inflammatory disorder.”
Although a consistent clinical picture is emerging, “[t]he published reports have used a variety of hastily developed case definitions based on the most severe cases, possibly missing less serious cases,” Levin writes. In particular, both the CDC and World Health Organization definitions require evidence of SARS-CoV-2 infection or exposure, which might contribute to underrecognition and underreporting because asymptomatic infections are common and antibody testing is not universally available.
“There is concern that children meeting current diagnostic criteria for MIS-C are the ‘tip of the iceberg,’ and a bigger problem may be lurking below the waterline,” Levin states. With approximately 1000 cases of the syndrome reported worldwide, “do we now have a clear picture of the new disorder, or as in the story of the blind men and the elephant, has only part of the beast been described?”
Adrienne Randolph, MD, of Boston Children’s Hospital, who is a coauthor of the multistate report, agrees that there is still much to learn about MIS-C before the whole beast can be understood. In an interview with Medscape Medical News, she listed the following key questions that have yet to be answered:
- Why do some children get MIS-C and not others?
- What is the long-term outcome of children with MIS-C?
- How can we differentiate MIS-C from acute COVID-19 infection in children with respiratory failure?
- Does MIS-C occur in young adults?
Randolph said her team is taking the best path forward toward answering these questions, including conducting a second study to identify risk factors for MIS-C and longer-term follow-up studies with the National Institutes of Health. “We are also getting consent to collect blood samples and look at other tests to help distinguish MIS-C from acute COVID-19 infection,” she said. She encouraged heightened awareness among physicians who care for young adults to consider MIS-C in patients aged 21 years and older who present with similar signs and symptoms.
On the basis of the answers to these and additional questions, the case definitions for MIS-C may need refinement to capture the wider spectrum of illness, Levin writes in his editorial. “The challenges of this new condition will now be to understand its pathophysiological mechanisms, to develop diagnostics, and to define the best treatment.”
Kleinman has received grants from the Health Services Resources Administration outside the submitted work. Maddux has received grants from the NIH/NICHD and the Francis Family Foundation outside the submitted work. Randolph has received grants from Genentech and personal fees from La Jolla Pharma outside the submitted work and others from the CDC during the conduct of the study.
This article first appeared on Medscape.com.
New data from active surveillance of the severe inflammatory condition associated with COVID-19 in previously healthy children provide further insight into the prevalence and course of the rare syndrome, but experts are concerned that current diagnostic criteria may not capture the true scope of the problem.
In separate reports published online June 29 in the New England Journal of Medicine, researchers from the New York State Department of Health and the Centers for Disease Control and Prevention (CDC) describe the epidemiology and clinical features of multisystem inflammatory syndrome in children (MIS-C) on the basis of information derived from targeted surveillance programs in New York State and across the country.
For the New York study, Elizabeth M. Dufort, MD, from the New York Department of Health in Albany and colleagues analyzed MIS-C surveillance data from 106 hospitals across the state. Of 191 suspected MIS-C cases reported to the Department of Health from March 1 through May 10, 99 met the state’s interim case definition of the condition and were included in the analysis.
The incidence rate for MIS-C was two cases per 100,000 individuals younger than 21 years, whereas the incidence rate of confirmed COVID-19 cases in this age group was 322 per 100,000. Most cases occurred approximately 1 month after the state’s COVID-19 peak.
“Among our patients, predominantly from the New York Metropolitan Region, 40% were black and 36% were Hispanic. This may be a reflection of the well-documented elevated incidence of SARS-CoV-2 infection among black and Hispanic communities,” the authors report.
All children presented with fever or chills, and most had tachycardia (97%) and gastrointestinal symptoms (80%). Rash (60%), conjunctival infection (56%), hypotension (32%), and mucosal changes (27%) were reported. Among all of the children, levels of inflammatory markers were elevated, including levels of C-reactive protein (100%), D-dimer (91%), and troponin (71%). More than one third of the patients (36%) were diagnosed with myocarditis, and an additional 16% had clinical myocarditis.
Of the full cohort, 80% of the children required intensive care, 62% received vasopressor support, and two children died.
The high prevalence of cardiac dysfunction or depression, coagulopathy, gastrointestinal symptoms, mild respiratory symptoms, and indications for supplemental oxygen in patients with MIS-C stands in contrast to the clinical picture observed in most acute cases of COVID-19 in hospitalized children, the authors write.
“Although most children have mild or no illness from SARS-CoV-2 infection, MIS-C may follow Covid-19 or asymptomatic SARS-CoV-2 infection. Recognition of the syndrome and early identification of children with MIS-C, including early monitoring of blood pressure and electrocardiographic and echocardiographic evaluation, could inform appropriate supportive care and other potential therapeutic options,” they continue.
The incidence of MIS-C among children infected with SARS-CoV-2 is unclear because children with COVID-19 often have mild or no symptoms and because children are not tested as frequently, the authors state. For this reason, “[i]t is crucial to establish surveillance for MIS-C cases, particularly in communities with higher levels of SARS-CoV-2 transmission.”
Important Differences From Kawasaki Disease
In a separate study, Leora R. Feldstein, MD, of the CDC, and colleagues report 186 cases of MIS-C collected through targeted surveillance of pediatric health centers in 26 US states from March 15 to May 20, 2020. As with the New York cohort, a disproportionate number of children in this cohort were black (25%) and Hispanic or Latino (31%).
Similar to the New York cohort, 80% of the children in this group required intensive care, 48% received vasoactive support, 20% required invasive mechanical ventilation, and four children died. Skin rashes, gastrointestinal symptoms, cardiovascular and hematologic effects, mucous changes, and elevations of inflammatory biomarkers were also similarly observed.
The researchers note that, although many of the features of MIS-C overlap with Kawasaki disease, there are some important differences, particularly with respect to the nature of cardiovascular involvement. “Approximately 5% of children with Kawasaki’s disease in the United States present with cardiovascular shock leading to vasopressor or inotropic support, as compared with 50% of the patients in our series,” the authors write.
In addition, coronary-artery aneurysms affect approximately one quarter of Kawasaki disease patients within 21 days of disease onset. “In our series, a maximum z score of 2.5 or higher in the left anterior descending or right coronary artery was reported in 8% of the patients overall and in 9% of patients with echocardiograms,” they report.
Additional differentiating features include patient age and race/ethnicity. Kawasaki disease occurs most commonly in children younger than 5 years. The median age in the multistate study was 8.3 years, and nearly half of the children in the New York cohort were in the 6- to 12-year age group. Further, Kawasaki disease is disproportionately prevalent in children of Asian descent.
Despite the differences, “until more is known about long-term cardiac sequelae of MIS-C, providers could consider following Kawasaki’s disease guidelines for follow-up, which recommend repeat echocardiographic imaging at 1 to 2 weeks.”
As was the case in the New York series, treatment in the multistate cohort most commonly included intravenous immunoglobulin and systemic glucocorticoids. Optimal management, however, will require a better understanding of the pathogenesis of MIS-C, Feldstein and colleagues write.
Questions Remain
With the accumulating data on this syndrome, the MIS-C picture seems to be getting incrementally clearer, but there is still much uncertainty, according to Michael Levin, FMedSci, PhD, from the Department of Infectious Disease, Imperial College London, United Kingdom.
“The recognition and description of new diseases often resemble the parable of the blind men and the elephant, with each declaring that the part of the beast they have touched fully defines it,” he writes in an accompanying editorial.
“As the coronavirus disease 2019 (Covid-19) pandemic has evolved, case reports have appeared describing children with unusual febrile illnesses that have features of Kawasaki’s disease, toxic shock syndrome, acute abdominal conditions, and encephalopathy, along with other reports of children with fever, elevated inflammatory markers, and multisystem involvement. It is now apparent that these reports were describing different clinical presentations of a new childhood inflammatory disorder.”
Although a consistent clinical picture is emerging, “[t]he published reports have used a variety of hastily developed case definitions based on the most severe cases, possibly missing less serious cases,” Levin writes. In particular, both the CDC and World Health Organization definitions require evidence of SARS-CoV-2 infection or exposure, which might contribute to underrecognition and underreporting because asymptomatic infections are common and antibody testing is not universally available.
“There is concern that children meeting current diagnostic criteria for MIS-C are the ‘tip of the iceberg,’ and a bigger problem may be lurking below the waterline,” Levin states. With approximately 1000 cases of the syndrome reported worldwide, “do we now have a clear picture of the new disorder, or as in the story of the blind men and the elephant, has only part of the beast been described?”
Adrienne Randolph, MD, of Boston Children’s Hospital, who is a coauthor of the multistate report, agrees that there is still much to learn about MIS-C before the whole beast can be understood. In an interview with Medscape Medical News, she listed the following key questions that have yet to be answered:
- Why do some children get MIS-C and not others?
- What is the long-term outcome of children with MIS-C?
- How can we differentiate MIS-C from acute COVID-19 infection in children with respiratory failure?
- Does MIS-C occur in young adults?
Randolph said her team is taking the best path forward toward answering these questions, including conducting a second study to identify risk factors for MIS-C and longer-term follow-up studies with the National Institutes of Health. “We are also getting consent to collect blood samples and look at other tests to help distinguish MIS-C from acute COVID-19 infection,” she said. She encouraged heightened awareness among physicians who care for young adults to consider MIS-C in patients aged 21 years and older who present with similar signs and symptoms.
On the basis of the answers to these and additional questions, the case definitions for MIS-C may need refinement to capture the wider spectrum of illness, Levin writes in his editorial. “The challenges of this new condition will now be to understand its pathophysiological mechanisms, to develop diagnostics, and to define the best treatment.”
Kleinman has received grants from the Health Services Resources Administration outside the submitted work. Maddux has received grants from the NIH/NICHD and the Francis Family Foundation outside the submitted work. Randolph has received grants from Genentech and personal fees from La Jolla Pharma outside the submitted work and others from the CDC during the conduct of the study.
This article first appeared on Medscape.com.
Captopril questioned for diabetes patients in COVID-19 setting
Captopril appears to be associated with a higher rate of pulmonary adverse reactions in patients with diabetes than that of other ACE inhibitors or angiotensin receptor blockers (ARBs) and therefore may not be the best choice for patients with diabetes and COVID-19, a new study suggests.
The study was published online in the Journal of the American Pharmacists Association.
The authors, led by Emma G. Stafford, PharmD, University of Missouri-Kansas City School of Pharmacy, note that diabetes seems to confer a higher risk of adverse outcomes in COVID-19 infection and there is conflicting data on the contribution of ACE inhibitors and ARBs, commonly used medications in diabetes, on the mortality and morbidity of COVID-19.
“In light of the recent COVID-19 outbreak, more research is needed to understand the effects that diabetes (and its medications) may have on the respiratory system and how that could affect the management of diseases such as COVID-19,” they say.
“Although ACE inhibitors and ARBs are generally considered to have similar adverse event profiles, evaluation of postmarketing adverse events may shed light on minute differences that could have important clinical impacts,” they add.
For the current study, the researchers analyzed data from multiple publicly available data sources on adverse drug reactions in patients with diabetes taking ACE inhibitors or ARBs. The data included all adverse drug events (ADEs) reported nationally to the US Food and Drug Administration and internationally to the Medical Dictionary for Regulatory Activities (MedDRA).
Results showed that captopril, the first ACE inhibitor approved back in 1981, has a higher incidence of pulmonary ADEs in patients with diabetes as compared with other ACE-inhibitor drugs (P = .005) as well as a statistically significant difference in pulmonary events compared with ARBs (P = .012).
“These analyses suggest that pharmacists and clinicians will need to consider the specific medication’s adverse event profile, particularly captopril, on how it may affect infections and other acute disease states that alter pulmonary function, such as COVID-19,” the authors conclude.
They say that the high incidence of pulmonary adverse drug effects with captopril “highlights the fact that the drugs belonging in one class are not identical and that its pharmacokinetics and pharmacodynamics can affect the patients’ health especially during acute processes like COVID-19.”
“This is especially important as current observational studies of COVID-19 patients tend to group drugs within a class and are not analyzing the potential differences within each class,” they add.
They note that ACE inhibitors can be broadly classified into 3 structural classes: sulfhydryl-, dicarboxyl-, and phosphorous- containing molecules. Notably, captopril is the only currently available ACE inhibitor belonging to the sulfhydryl-containing class and may explain the higher incidence of adverse drug effects observed, they comment.
“Health care providers have been left with many questions when treating patients with COVID-19, including how ACE inhibitors or ARBs may affect their clinical course. Results from this study may be helpful when prescribing or continuing ACE inhibitors or ARBs for patients with diabetes and infections or illnesses that may affect pulmonary function, such as COVID-19,” they conclude.
Questioning safety in COVID-19 an “overreach”
Commenting for Medscape Medical News, Michael A. Weber, MD, professor of medicine at State University of New York, said he thought the current article appears to overreach in questioning captopril’s safety in the COVID-19 setting.
“Captopril was the first ACE inhibitor available for clinical use. In early prescribing its dosage was not well understood and it might have been administered in excessive amounts,” Weber notes.
“There were some renal and other adverse effects reported that at first were attributed to the fact that captopril, unlike any other popular ACE inhibitors, contained a sulfhydryl (SH) group in its molecule,” he said. “It is not clear whether this feature could be responsible for the increased pulmonary side effects and potential danger to COVID-19 patients now reported with captopril in this new pharmacy article.”
But he adds: “The article contains no evidence that the effect of captopril or any other ACE inhibitor on the pulmonary ACE-2 enzyme has a deleterious effect on outcomes of COVID-19 disease. In any case, captopril — which should be prescribed in a twice-daily dose — is not frequently prescribed these days since newer ACE inhibitors are effective with just once-daily dosing.”
This article first appeared on Medscape.com.
Captopril appears to be associated with a higher rate of pulmonary adverse reactions in patients with diabetes than that of other ACE inhibitors or angiotensin receptor blockers (ARBs) and therefore may not be the best choice for patients with diabetes and COVID-19, a new study suggests.
The study was published online in the Journal of the American Pharmacists Association.
The authors, led by Emma G. Stafford, PharmD, University of Missouri-Kansas City School of Pharmacy, note that diabetes seems to confer a higher risk of adverse outcomes in COVID-19 infection and there is conflicting data on the contribution of ACE inhibitors and ARBs, commonly used medications in diabetes, on the mortality and morbidity of COVID-19.
“In light of the recent COVID-19 outbreak, more research is needed to understand the effects that diabetes (and its medications) may have on the respiratory system and how that could affect the management of diseases such as COVID-19,” they say.
“Although ACE inhibitors and ARBs are generally considered to have similar adverse event profiles, evaluation of postmarketing adverse events may shed light on minute differences that could have important clinical impacts,” they add.
For the current study, the researchers analyzed data from multiple publicly available data sources on adverse drug reactions in patients with diabetes taking ACE inhibitors or ARBs. The data included all adverse drug events (ADEs) reported nationally to the US Food and Drug Administration and internationally to the Medical Dictionary for Regulatory Activities (MedDRA).
Results showed that captopril, the first ACE inhibitor approved back in 1981, has a higher incidence of pulmonary ADEs in patients with diabetes as compared with other ACE-inhibitor drugs (P = .005) as well as a statistically significant difference in pulmonary events compared with ARBs (P = .012).
“These analyses suggest that pharmacists and clinicians will need to consider the specific medication’s adverse event profile, particularly captopril, on how it may affect infections and other acute disease states that alter pulmonary function, such as COVID-19,” the authors conclude.
They say that the high incidence of pulmonary adverse drug effects with captopril “highlights the fact that the drugs belonging in one class are not identical and that its pharmacokinetics and pharmacodynamics can affect the patients’ health especially during acute processes like COVID-19.”
“This is especially important as current observational studies of COVID-19 patients tend to group drugs within a class and are not analyzing the potential differences within each class,” they add.
They note that ACE inhibitors can be broadly classified into 3 structural classes: sulfhydryl-, dicarboxyl-, and phosphorous- containing molecules. Notably, captopril is the only currently available ACE inhibitor belonging to the sulfhydryl-containing class and may explain the higher incidence of adverse drug effects observed, they comment.
“Health care providers have been left with many questions when treating patients with COVID-19, including how ACE inhibitors or ARBs may affect their clinical course. Results from this study may be helpful when prescribing or continuing ACE inhibitors or ARBs for patients with diabetes and infections or illnesses that may affect pulmonary function, such as COVID-19,” they conclude.
Questioning safety in COVID-19 an “overreach”
Commenting for Medscape Medical News, Michael A. Weber, MD, professor of medicine at State University of New York, said he thought the current article appears to overreach in questioning captopril’s safety in the COVID-19 setting.
“Captopril was the first ACE inhibitor available for clinical use. In early prescribing its dosage was not well understood and it might have been administered in excessive amounts,” Weber notes.
“There were some renal and other adverse effects reported that at first were attributed to the fact that captopril, unlike any other popular ACE inhibitors, contained a sulfhydryl (SH) group in its molecule,” he said. “It is not clear whether this feature could be responsible for the increased pulmonary side effects and potential danger to COVID-19 patients now reported with captopril in this new pharmacy article.”
But he adds: “The article contains no evidence that the effect of captopril or any other ACE inhibitor on the pulmonary ACE-2 enzyme has a deleterious effect on outcomes of COVID-19 disease. In any case, captopril — which should be prescribed in a twice-daily dose — is not frequently prescribed these days since newer ACE inhibitors are effective with just once-daily dosing.”
This article first appeared on Medscape.com.
Captopril appears to be associated with a higher rate of pulmonary adverse reactions in patients with diabetes than that of other ACE inhibitors or angiotensin receptor blockers (ARBs) and therefore may not be the best choice for patients with diabetes and COVID-19, a new study suggests.
The study was published online in the Journal of the American Pharmacists Association.
The authors, led by Emma G. Stafford, PharmD, University of Missouri-Kansas City School of Pharmacy, note that diabetes seems to confer a higher risk of adverse outcomes in COVID-19 infection and there is conflicting data on the contribution of ACE inhibitors and ARBs, commonly used medications in diabetes, on the mortality and morbidity of COVID-19.
“In light of the recent COVID-19 outbreak, more research is needed to understand the effects that diabetes (and its medications) may have on the respiratory system and how that could affect the management of diseases such as COVID-19,” they say.
“Although ACE inhibitors and ARBs are generally considered to have similar adverse event profiles, evaluation of postmarketing adverse events may shed light on minute differences that could have important clinical impacts,” they add.
For the current study, the researchers analyzed data from multiple publicly available data sources on adverse drug reactions in patients with diabetes taking ACE inhibitors or ARBs. The data included all adverse drug events (ADEs) reported nationally to the US Food and Drug Administration and internationally to the Medical Dictionary for Regulatory Activities (MedDRA).
Results showed that captopril, the first ACE inhibitor approved back in 1981, has a higher incidence of pulmonary ADEs in patients with diabetes as compared with other ACE-inhibitor drugs (P = .005) as well as a statistically significant difference in pulmonary events compared with ARBs (P = .012).
“These analyses suggest that pharmacists and clinicians will need to consider the specific medication’s adverse event profile, particularly captopril, on how it may affect infections and other acute disease states that alter pulmonary function, such as COVID-19,” the authors conclude.
They say that the high incidence of pulmonary adverse drug effects with captopril “highlights the fact that the drugs belonging in one class are not identical and that its pharmacokinetics and pharmacodynamics can affect the patients’ health especially during acute processes like COVID-19.”
“This is especially important as current observational studies of COVID-19 patients tend to group drugs within a class and are not analyzing the potential differences within each class,” they add.
They note that ACE inhibitors can be broadly classified into 3 structural classes: sulfhydryl-, dicarboxyl-, and phosphorous- containing molecules. Notably, captopril is the only currently available ACE inhibitor belonging to the sulfhydryl-containing class and may explain the higher incidence of adverse drug effects observed, they comment.
“Health care providers have been left with many questions when treating patients with COVID-19, including how ACE inhibitors or ARBs may affect their clinical course. Results from this study may be helpful when prescribing or continuing ACE inhibitors or ARBs for patients with diabetes and infections or illnesses that may affect pulmonary function, such as COVID-19,” they conclude.
Questioning safety in COVID-19 an “overreach”
Commenting for Medscape Medical News, Michael A. Weber, MD, professor of medicine at State University of New York, said he thought the current article appears to overreach in questioning captopril’s safety in the COVID-19 setting.
“Captopril was the first ACE inhibitor available for clinical use. In early prescribing its dosage was not well understood and it might have been administered in excessive amounts,” Weber notes.
“There were some renal and other adverse effects reported that at first were attributed to the fact that captopril, unlike any other popular ACE inhibitors, contained a sulfhydryl (SH) group in its molecule,” he said. “It is not clear whether this feature could be responsible for the increased pulmonary side effects and potential danger to COVID-19 patients now reported with captopril in this new pharmacy article.”
But he adds: “The article contains no evidence that the effect of captopril or any other ACE inhibitor on the pulmonary ACE-2 enzyme has a deleterious effect on outcomes of COVID-19 disease. In any case, captopril — which should be prescribed in a twice-daily dose — is not frequently prescribed these days since newer ACE inhibitors are effective with just once-daily dosing.”
This article first appeared on Medscape.com.
Self-measured BP monitoring at home ‘more important than ever’
.
“With fewer patients visiting medical offices during the COVID-19 pandemic, SMBP monitoring is more important than ever for people at risk for hypertension and uncontrolled BP,” writing group chair Daichi Shimbo, MD, said in a statement.
“There should be investment in creating and supporting the infrastructure for expanding self-measured BP monitoring, as well as increasing coverage for patient- and provider-related costs,” Dr. Shimbo, director, The Columbia Hypertension Center, Columbia University Irving Medical Center, New York, said in an interview.
The statement, Self-Measured Blood Pressure Monitoring at Home, was published June 22 in Circulation.
It provides “contemporary information” on the use, efficacy, and cost-effectiveness of SMBP at home for the diagnosis and management of hypertension.
The writing group noted that hypertension is one of the most important risk factors for cardiovascular disease. Several American and international guidelines support the use of SMBP.
“Indications include the diagnosis of white-coat hypertension and masked hypertension and the identification of white-coat effect and masked uncontrolled hypertension. Other indications include confirming the diagnosis of resistant hypertension and detecting morning hypertension,” the group pointed out.
Use validated devices
Devices that are validated for clinical accuracy should be used for SMBP monitoring, the writing group advised. Validated devices that use the oscillometric method are preferred, and a standardized BP measurement (with appropriately sized cuffs) and monitoring protocol should be followed.
The group noted that meta-analyses of randomized trials indicate that SMBP monitoring is associated with a reduction in BP and improved BP control, and the benefits are greatest when it is used along with other interventions, such as education and counseling, that can be delivered via phone or telehealth visits by nurses and care coordinators.
There are “sufficient data” to indicate that adding SMBP monitoring to office-based monitoring is cost-effective compared with office BP monitoring alone or usual care in patients with high office BP, the writing group said.
Potential cost savings associated with SMBP monitoring include a reduction in office visit follow-ups as a result of improved BP control, avoidance of possible overtreatment in patients with white-coat hypertension, and improvement in quality of life.
They noted that randomized controlled trials assessing the impact of SMBP monitoring on cardiovascular outcomes are needed.
Barriers to widespread use
The use of SMBP monitoring is “essential” for the self-management of hypertension and has “great appeal” for expanding the benefits of cardiovascular prevention, the writing group said. They acknowledged, however, that transitioning from solely office-based BP management to a strategy that includes SMBP monitoring is not without actual and potential barriers.
The group recommends addressing these barriers by:
- Educating patients and providers about the benefits of SMBP monitoring and the optimal approaches for SMBP monitoring.
- Establishing clinical core competency criteria to ensure high-quality SMBP monitoring is supported in clinical practice.
- Incorporating cointerventions that increase the effectiveness of SMBP monitoring, including behavioral change management and counseling, communication of treatment recommendations back to patients, medication management, and prescription and adherence monitoring.
- Creating systems for SMBP readings to be transferred from devices to electronic health records.
- Improving public and private health insurance coverage of validated SMBP monitoring devices prescribed by a health care provider.
- Reimbursing providers for costs associated with training patients, transmitting BP data, interpreting and reporting BP readings, and delivering cointerventions.
Increasing the use of SMBP monitoring is a major focus area of Target: BP – a national initiative of the AHA and AMA launched in response to the high prevalence of uncontrolled BP.
Target: BP helps health care organizations and care teams improve BP control rates through the evidence-based MAP BP Program.
MAP is an acronym that stands for Measure BP accurately every time it’s measured, Act rapidly to manage uncontrolled BP, and Partner with patients to promote BP self-management.
This research had no commercial funding. Dr. Shimbo has disclosed no relevant conflicts of interest. A complete list of disclosures for the writing group is available with the original article.
A version of this article originally appeared on Medscape.com.
.
“With fewer patients visiting medical offices during the COVID-19 pandemic, SMBP monitoring is more important than ever for people at risk for hypertension and uncontrolled BP,” writing group chair Daichi Shimbo, MD, said in a statement.
“There should be investment in creating and supporting the infrastructure for expanding self-measured BP monitoring, as well as increasing coverage for patient- and provider-related costs,” Dr. Shimbo, director, The Columbia Hypertension Center, Columbia University Irving Medical Center, New York, said in an interview.
The statement, Self-Measured Blood Pressure Monitoring at Home, was published June 22 in Circulation.
It provides “contemporary information” on the use, efficacy, and cost-effectiveness of SMBP at home for the diagnosis and management of hypertension.
The writing group noted that hypertension is one of the most important risk factors for cardiovascular disease. Several American and international guidelines support the use of SMBP.
“Indications include the diagnosis of white-coat hypertension and masked hypertension and the identification of white-coat effect and masked uncontrolled hypertension. Other indications include confirming the diagnosis of resistant hypertension and detecting morning hypertension,” the group pointed out.
Use validated devices
Devices that are validated for clinical accuracy should be used for SMBP monitoring, the writing group advised. Validated devices that use the oscillometric method are preferred, and a standardized BP measurement (with appropriately sized cuffs) and monitoring protocol should be followed.
The group noted that meta-analyses of randomized trials indicate that SMBP monitoring is associated with a reduction in BP and improved BP control, and the benefits are greatest when it is used along with other interventions, such as education and counseling, that can be delivered via phone or telehealth visits by nurses and care coordinators.
There are “sufficient data” to indicate that adding SMBP monitoring to office-based monitoring is cost-effective compared with office BP monitoring alone or usual care in patients with high office BP, the writing group said.
Potential cost savings associated with SMBP monitoring include a reduction in office visit follow-ups as a result of improved BP control, avoidance of possible overtreatment in patients with white-coat hypertension, and improvement in quality of life.
They noted that randomized controlled trials assessing the impact of SMBP monitoring on cardiovascular outcomes are needed.
Barriers to widespread use
The use of SMBP monitoring is “essential” for the self-management of hypertension and has “great appeal” for expanding the benefits of cardiovascular prevention, the writing group said. They acknowledged, however, that transitioning from solely office-based BP management to a strategy that includes SMBP monitoring is not without actual and potential barriers.
The group recommends addressing these barriers by:
- Educating patients and providers about the benefits of SMBP monitoring and the optimal approaches for SMBP monitoring.
- Establishing clinical core competency criteria to ensure high-quality SMBP monitoring is supported in clinical practice.
- Incorporating cointerventions that increase the effectiveness of SMBP monitoring, including behavioral change management and counseling, communication of treatment recommendations back to patients, medication management, and prescription and adherence monitoring.
- Creating systems for SMBP readings to be transferred from devices to electronic health records.
- Improving public and private health insurance coverage of validated SMBP monitoring devices prescribed by a health care provider.
- Reimbursing providers for costs associated with training patients, transmitting BP data, interpreting and reporting BP readings, and delivering cointerventions.
Increasing the use of SMBP monitoring is a major focus area of Target: BP – a national initiative of the AHA and AMA launched in response to the high prevalence of uncontrolled BP.
Target: BP helps health care organizations and care teams improve BP control rates through the evidence-based MAP BP Program.
MAP is an acronym that stands for Measure BP accurately every time it’s measured, Act rapidly to manage uncontrolled BP, and Partner with patients to promote BP self-management.
This research had no commercial funding. Dr. Shimbo has disclosed no relevant conflicts of interest. A complete list of disclosures for the writing group is available with the original article.
A version of this article originally appeared on Medscape.com.
.
“With fewer patients visiting medical offices during the COVID-19 pandemic, SMBP monitoring is more important than ever for people at risk for hypertension and uncontrolled BP,” writing group chair Daichi Shimbo, MD, said in a statement.
“There should be investment in creating and supporting the infrastructure for expanding self-measured BP monitoring, as well as increasing coverage for patient- and provider-related costs,” Dr. Shimbo, director, The Columbia Hypertension Center, Columbia University Irving Medical Center, New York, said in an interview.
The statement, Self-Measured Blood Pressure Monitoring at Home, was published June 22 in Circulation.
It provides “contemporary information” on the use, efficacy, and cost-effectiveness of SMBP at home for the diagnosis and management of hypertension.
The writing group noted that hypertension is one of the most important risk factors for cardiovascular disease. Several American and international guidelines support the use of SMBP.
“Indications include the diagnosis of white-coat hypertension and masked hypertension and the identification of white-coat effect and masked uncontrolled hypertension. Other indications include confirming the diagnosis of resistant hypertension and detecting morning hypertension,” the group pointed out.
Use validated devices
Devices that are validated for clinical accuracy should be used for SMBP monitoring, the writing group advised. Validated devices that use the oscillometric method are preferred, and a standardized BP measurement (with appropriately sized cuffs) and monitoring protocol should be followed.
The group noted that meta-analyses of randomized trials indicate that SMBP monitoring is associated with a reduction in BP and improved BP control, and the benefits are greatest when it is used along with other interventions, such as education and counseling, that can be delivered via phone or telehealth visits by nurses and care coordinators.
There are “sufficient data” to indicate that adding SMBP monitoring to office-based monitoring is cost-effective compared with office BP monitoring alone or usual care in patients with high office BP, the writing group said.
Potential cost savings associated with SMBP monitoring include a reduction in office visit follow-ups as a result of improved BP control, avoidance of possible overtreatment in patients with white-coat hypertension, and improvement in quality of life.
They noted that randomized controlled trials assessing the impact of SMBP monitoring on cardiovascular outcomes are needed.
Barriers to widespread use
The use of SMBP monitoring is “essential” for the self-management of hypertension and has “great appeal” for expanding the benefits of cardiovascular prevention, the writing group said. They acknowledged, however, that transitioning from solely office-based BP management to a strategy that includes SMBP monitoring is not without actual and potential barriers.
The group recommends addressing these barriers by:
- Educating patients and providers about the benefits of SMBP monitoring and the optimal approaches for SMBP monitoring.
- Establishing clinical core competency criteria to ensure high-quality SMBP monitoring is supported in clinical practice.
- Incorporating cointerventions that increase the effectiveness of SMBP monitoring, including behavioral change management and counseling, communication of treatment recommendations back to patients, medication management, and prescription and adherence monitoring.
- Creating systems for SMBP readings to be transferred from devices to electronic health records.
- Improving public and private health insurance coverage of validated SMBP monitoring devices prescribed by a health care provider.
- Reimbursing providers for costs associated with training patients, transmitting BP data, interpreting and reporting BP readings, and delivering cointerventions.
Increasing the use of SMBP monitoring is a major focus area of Target: BP – a national initiative of the AHA and AMA launched in response to the high prevalence of uncontrolled BP.
Target: BP helps health care organizations and care teams improve BP control rates through the evidence-based MAP BP Program.
MAP is an acronym that stands for Measure BP accurately every time it’s measured, Act rapidly to manage uncontrolled BP, and Partner with patients to promote BP self-management.
This research had no commercial funding. Dr. Shimbo has disclosed no relevant conflicts of interest. A complete list of disclosures for the writing group is available with the original article.
A version of this article originally appeared on Medscape.com.
Lawmakers question mental health disclosure rules
State medical licensing queries criticized
Several federal lawmakers on June 30 questioned state policies that require disclosure of mental health treatment as part of medical licensing applications and renewals, citing concerns about creating barriers to psychiatric care for clinicians.
Mental health–related questions on state medical boards’ licensing applications are especially worrisome with many clinicians, including ED staff, immersed in the physical and emotional challenges involved in treating waves of people with COVID-19, lawmakers said during a hearing of the House Energy and Commerce Committee’s health panel.
“We must consider the mental health of the providers on the front lines of the pandemic,” said Rep. Morgan Griffith, a Virginia Republican.
The issue of state medical boards’ disclosure rules was not on the official agenda for the House Energy and Commerce health subcommittee’s hearing. And there was no discussion of any specific state medical board’s regulations. The Energy and Commerce health subcommittee is working on more than 20 bills related to mental health, including measures intended to aid first responders, such as firemen and emergency medical personnel, and students.
This hearing marked an early stage in the process for a planned package of mental health legislation, said Rep. Michael C. Burgess, MD, of Texas, who is the top Republican on the Energy and Commerce health subcommittee. There may be opportunities as this legislation advances to add provisions intended to aid physicians, said Dr. Burgess, who practiced for many years as an ob.gyn. before being elected to Congress.
“We knew that suicide was a problem among our colleagues prior to the onset of this coronavirus epidemic and I know it is more pronounced now,” he said.
Dr. Burgess then solicited specific recommendations from the hearing’s witnesses on steps needed to help clinicians’ mental health.
The first suggestion offered in reply by Jeffrey L. Geller, MD, MPH, appearing in his role as president of the American Psychiatric Association, was that Congress should look for ways to encourage states to alter their licensing procedures.
The hearing comes on the heels of the APA, the American Academy of Family Physicians, and more than 40 other groups having jointly signed a statement calling for changes to disclosure rules about mental health.
“Licensing and credentialing applications by covered entities should only employ narrowly focused questions that address current functional impairment,” the statement said. “Additionally, we strongly support The Joint Commission (TJC) statement on Removing Barriers to Mental Health Care for Clinicians and Health Care Staff. TJC ‘supports the removal of any barriers that inhibit clinicians and health care staff from accessing mental health care services.’ ”
Physicians and other clinicians must be able to safely secure treatment for mental or other health issues, just as any other individual,” the groups wrote. “A provider’s history of mental illness or substance use disorder should not be used as any indication of their current or future ability to practice competently and without impairment.”
Also among the signers to this statement was the Federation of State Medical Boards, which has been leading an effort for years to change licensing.
In 2018, the FSMB recommended state medical boards reconsider whether it is necessary to include probing questions about a physician applicant’s mental health, addiction, or substance use on applications for medical licensure or their renewal. While the intent of these questions may be to protect patients, these queries can discourage physicians from getting needed help, the FSMB said.
Several states have since revised or considered revising their license applications and renewals. In May 2020, The Joint Commission urged broader adoption of recommendations from the FSMB and the American Medical Association to limit queries about clinicians’ mental health to “conditions that currently impair the clinicians’ ability to perform their job.”
“We strongly encourage organizations to not ask about past history of mental health conditions or treatment,” said The Joint Commission, which accredits hospitals, in a statement. “It is critical that we ensure health care workers can feel free to access mental health resources.”
Rep. Susan Brooks, an Indiana Republican who is an attorney, suggested there may need to be a broader look at how state officials pose questions about past mental health treatment to people in many professions, including her own.
“It does build on the stigma on accessing services” to know a state or licensing authority may question a professional about receiving treatment for mental health, she said.
Also at the hearing, Rep. Nanette Diaz Barragán, a California Democrat, spoke of her own reaction to seeing a question about mental health treatment while applying for a White House internship. During her college years, Rep. Barragán had to cope with her father’s terminal illness.
“I remember thinking to myself: ‘Jeez, if I end up seeing a mental health expert maybe one day I couldn’t work in government,’ ” she said.
State medical licensing queries criticized
State medical licensing queries criticized
Several federal lawmakers on June 30 questioned state policies that require disclosure of mental health treatment as part of medical licensing applications and renewals, citing concerns about creating barriers to psychiatric care for clinicians.
Mental health–related questions on state medical boards’ licensing applications are especially worrisome with many clinicians, including ED staff, immersed in the physical and emotional challenges involved in treating waves of people with COVID-19, lawmakers said during a hearing of the House Energy and Commerce Committee’s health panel.
“We must consider the mental health of the providers on the front lines of the pandemic,” said Rep. Morgan Griffith, a Virginia Republican.
The issue of state medical boards’ disclosure rules was not on the official agenda for the House Energy and Commerce health subcommittee’s hearing. And there was no discussion of any specific state medical board’s regulations. The Energy and Commerce health subcommittee is working on more than 20 bills related to mental health, including measures intended to aid first responders, such as firemen and emergency medical personnel, and students.
This hearing marked an early stage in the process for a planned package of mental health legislation, said Rep. Michael C. Burgess, MD, of Texas, who is the top Republican on the Energy and Commerce health subcommittee. There may be opportunities as this legislation advances to add provisions intended to aid physicians, said Dr. Burgess, who practiced for many years as an ob.gyn. before being elected to Congress.
“We knew that suicide was a problem among our colleagues prior to the onset of this coronavirus epidemic and I know it is more pronounced now,” he said.
Dr. Burgess then solicited specific recommendations from the hearing’s witnesses on steps needed to help clinicians’ mental health.
The first suggestion offered in reply by Jeffrey L. Geller, MD, MPH, appearing in his role as president of the American Psychiatric Association, was that Congress should look for ways to encourage states to alter their licensing procedures.
The hearing comes on the heels of the APA, the American Academy of Family Physicians, and more than 40 other groups having jointly signed a statement calling for changes to disclosure rules about mental health.
“Licensing and credentialing applications by covered entities should only employ narrowly focused questions that address current functional impairment,” the statement said. “Additionally, we strongly support The Joint Commission (TJC) statement on Removing Barriers to Mental Health Care for Clinicians and Health Care Staff. TJC ‘supports the removal of any barriers that inhibit clinicians and health care staff from accessing mental health care services.’ ”
Physicians and other clinicians must be able to safely secure treatment for mental or other health issues, just as any other individual,” the groups wrote. “A provider’s history of mental illness or substance use disorder should not be used as any indication of their current or future ability to practice competently and without impairment.”
Also among the signers to this statement was the Federation of State Medical Boards, which has been leading an effort for years to change licensing.
In 2018, the FSMB recommended state medical boards reconsider whether it is necessary to include probing questions about a physician applicant’s mental health, addiction, or substance use on applications for medical licensure or their renewal. While the intent of these questions may be to protect patients, these queries can discourage physicians from getting needed help, the FSMB said.
Several states have since revised or considered revising their license applications and renewals. In May 2020, The Joint Commission urged broader adoption of recommendations from the FSMB and the American Medical Association to limit queries about clinicians’ mental health to “conditions that currently impair the clinicians’ ability to perform their job.”
“We strongly encourage organizations to not ask about past history of mental health conditions or treatment,” said The Joint Commission, which accredits hospitals, in a statement. “It is critical that we ensure health care workers can feel free to access mental health resources.”
Rep. Susan Brooks, an Indiana Republican who is an attorney, suggested there may need to be a broader look at how state officials pose questions about past mental health treatment to people in many professions, including her own.
“It does build on the stigma on accessing services” to know a state or licensing authority may question a professional about receiving treatment for mental health, she said.
Also at the hearing, Rep. Nanette Diaz Barragán, a California Democrat, spoke of her own reaction to seeing a question about mental health treatment while applying for a White House internship. During her college years, Rep. Barragán had to cope with her father’s terminal illness.
“I remember thinking to myself: ‘Jeez, if I end up seeing a mental health expert maybe one day I couldn’t work in government,’ ” she said.
Several federal lawmakers on June 30 questioned state policies that require disclosure of mental health treatment as part of medical licensing applications and renewals, citing concerns about creating barriers to psychiatric care for clinicians.
Mental health–related questions on state medical boards’ licensing applications are especially worrisome with many clinicians, including ED staff, immersed in the physical and emotional challenges involved in treating waves of people with COVID-19, lawmakers said during a hearing of the House Energy and Commerce Committee’s health panel.
“We must consider the mental health of the providers on the front lines of the pandemic,” said Rep. Morgan Griffith, a Virginia Republican.
The issue of state medical boards’ disclosure rules was not on the official agenda for the House Energy and Commerce health subcommittee’s hearing. And there was no discussion of any specific state medical board’s regulations. The Energy and Commerce health subcommittee is working on more than 20 bills related to mental health, including measures intended to aid first responders, such as firemen and emergency medical personnel, and students.
This hearing marked an early stage in the process for a planned package of mental health legislation, said Rep. Michael C. Burgess, MD, of Texas, who is the top Republican on the Energy and Commerce health subcommittee. There may be opportunities as this legislation advances to add provisions intended to aid physicians, said Dr. Burgess, who practiced for many years as an ob.gyn. before being elected to Congress.
“We knew that suicide was a problem among our colleagues prior to the onset of this coronavirus epidemic and I know it is more pronounced now,” he said.
Dr. Burgess then solicited specific recommendations from the hearing’s witnesses on steps needed to help clinicians’ mental health.
The first suggestion offered in reply by Jeffrey L. Geller, MD, MPH, appearing in his role as president of the American Psychiatric Association, was that Congress should look for ways to encourage states to alter their licensing procedures.
The hearing comes on the heels of the APA, the American Academy of Family Physicians, and more than 40 other groups having jointly signed a statement calling for changes to disclosure rules about mental health.
“Licensing and credentialing applications by covered entities should only employ narrowly focused questions that address current functional impairment,” the statement said. “Additionally, we strongly support The Joint Commission (TJC) statement on Removing Barriers to Mental Health Care for Clinicians and Health Care Staff. TJC ‘supports the removal of any barriers that inhibit clinicians and health care staff from accessing mental health care services.’ ”
Physicians and other clinicians must be able to safely secure treatment for mental or other health issues, just as any other individual,” the groups wrote. “A provider’s history of mental illness or substance use disorder should not be used as any indication of their current or future ability to practice competently and without impairment.”
Also among the signers to this statement was the Federation of State Medical Boards, which has been leading an effort for years to change licensing.
In 2018, the FSMB recommended state medical boards reconsider whether it is necessary to include probing questions about a physician applicant’s mental health, addiction, or substance use on applications for medical licensure or their renewal. While the intent of these questions may be to protect patients, these queries can discourage physicians from getting needed help, the FSMB said.
Several states have since revised or considered revising their license applications and renewals. In May 2020, The Joint Commission urged broader adoption of recommendations from the FSMB and the American Medical Association to limit queries about clinicians’ mental health to “conditions that currently impair the clinicians’ ability to perform their job.”
“We strongly encourage organizations to not ask about past history of mental health conditions or treatment,” said The Joint Commission, which accredits hospitals, in a statement. “It is critical that we ensure health care workers can feel free to access mental health resources.”
Rep. Susan Brooks, an Indiana Republican who is an attorney, suggested there may need to be a broader look at how state officials pose questions about past mental health treatment to people in many professions, including her own.
“It does build on the stigma on accessing services” to know a state or licensing authority may question a professional about receiving treatment for mental health, she said.
Also at the hearing, Rep. Nanette Diaz Barragán, a California Democrat, spoke of her own reaction to seeing a question about mental health treatment while applying for a White House internship. During her college years, Rep. Barragán had to cope with her father’s terminal illness.
“I remember thinking to myself: ‘Jeez, if I end up seeing a mental health expert maybe one day I couldn’t work in government,’ ” she said.
FROM A HOUSE ENERGY AND COMMERCE’S HEALTH SUBCOMMITTEE HEARING
Chewed prasugrel for primary PCI? Forget it!
And cangrelor, in turn, is superior to oral prasugrel, according to the randomized FABOLUS FASTER trial, Marco Valgimigli, MD, PhD, reported at the virtual annual meeting of the European Association of Percutaneous Cardiovascular Interventions.
Moreover, contrary to conventional wisdom, chewed prasugrel (Effient) proved no better than swallowing the tablets whole for platelet inhibition, said Dr. Valgimigli, an interventional cardiologist at the University of Bern (Switzerland).
He explained that standard administration of the newer oral P2Y12 inhibitors prasugrel and ticagrelor (Brilinta) in patients undergoing percutaneous coronary intervention (PCI) for ST-elevation MI (STEMI) does not provide optimal early inhibition of platelet aggregation. The parenteral antiplatelet drugs tirofiban and cangrelor have been shown to provide faster and more prolonged inhibition of platelet aggregation than the oral P2Y12 inhibitors.
But there has been no head-to-head comparative data for the glycoprotein IIb/IIIA inhibitor tirofiban (Aggrastat) and the P2Y12 inhibitor cangrelor (Kengreal) in the setting of primary PCI for STEMI. This was the impetus for FABOLUS FASTER, the first study to compare the pharmacodynamic effects of the two parenteral antiplatelet agents. The trial also looked at how these potent parenteral drugs, compared with chewed prasugrel, another previously unexamined yet highly practical issue.
The three-center, multinational, open-label FABOLUS FASTER trial randomized 122 patients undergoing primary PCI for STEMI to one of three arms: a standard intravenous bolus and 2-hour infusion of either the P2Y12 inhibitor cangrelor (Kengreal) or the glycoprotein IIb/IIIA inhibitor tirofiban (Aggrastat), followed in either case by 60 mg of oral prasugrel, or a third arm in which patients didn’t receive either drug but were instead randomized to a 60-mg loading dose of chewed or whole prasugrel tablets.
The primary study endpoint was inhibition of platelet aggregation at 30 minutes as measured by light transmittance aggregometry in response to 20 mcmol/L of adenosine diphosphate (ADP).
Tirofiban was the unequivocal winner with 95% inhibition, as compared with 34.1% with cangrelor, 10.5% with chewed prasugrel, and 6.3% with prasugrel swallowed whole, even though the concentration of prasugrel’s active metabolite was far greater at 62.3 ng/mL after prasugrel was chewed, compared with 17.1 ng/mL when swallowed in integral tablet form.
The rate of nonresponsiveness to tirofiban as defined by greater than 59% platelet aggregation was zero for tirofiban during its 2-hour infusion, then a scant 8% thereafter during repeated testing at 3 and 4-6 hours. In contrast, the cangrelor nonresponsiveness rate was 50%-58% during the 2-hour infusion, rising to 82% at 3 hours.
FABOLUS FASTER, while not powered for clinical endpoints, might nevertheless have important clinical implications, according to Dr. Valgimigli. First, the superiority of the intravenous drugs tirofiban and cangrelor over prasugrel for early, strong platelet inhibition underscores the importance of giving parenteral antiplatelet drugs over oral therapy during the acute phase of STEMI therapy. Moreover, tirofiban’s outstanding performance – and the high residual platelet reactivity associated with cangrelor – makes a strong case for large comparative, randomized trials of the two drugs, with hard clinical endpoints.
Discussant Christoph K. Naber, MD, PhD, opined that he personally doesn’t consider the FABOLUS FASTER results practice changing, for a couple of reasons.
“Platelet inhibition measured by ADP in vitro is not necessarily related to true effects in vivo. We know that platelets are activated by multiple mechanisms, and the ADP pathway is just one of them,” said Dr. Naber, an interventional cardiologist at the Wilhemshaven (Germany) Clinic.
Also, there’s a good reason why no glycoprotein IIb/IIIA inhibitors are approved for treatment of STEMI, and why tirofiban, despite its impressive antiplatelet effects, is currently largely reserved for bailout situations, such as complex lesions with large thrombus burden. It’s because tirofiban’s potent antiplatelet activity is accompanied by a high risk of bleeding, he added.
However, Dr. Valgimigli noted that this conviction about excessive bleeding risk is mainly based on older studies in which glycoprotein IIb/IIIA inhibitors were administered for prolonged duration through femoral access sites. He argued that it’s time for large clinical trials examining the risk/benefit ratio of short infusion of these agents in the contemporary practice of primary PCI for STEMI.
Simultaneously with Dr. Valgimigli’s presentation, the FABOLUS FASTER results were published online (Circulation. 2020 Jun 27; doi: 10.1161/CIRCULATIONAHA.120.046928).
Dr. Valgimigli reported that Medicure, the sponsor of the FABOLUS FASTER trial, provided an institutional research grant to conduct the study. He also disclosed receiving research grants and personal fees outside the scope of this study from a dozen pharmaceutical and medical device companies. Dr. Naber reported having no financial conflicts.
And cangrelor, in turn, is superior to oral prasugrel, according to the randomized FABOLUS FASTER trial, Marco Valgimigli, MD, PhD, reported at the virtual annual meeting of the European Association of Percutaneous Cardiovascular Interventions.
Moreover, contrary to conventional wisdom, chewed prasugrel (Effient) proved no better than swallowing the tablets whole for platelet inhibition, said Dr. Valgimigli, an interventional cardiologist at the University of Bern (Switzerland).
He explained that standard administration of the newer oral P2Y12 inhibitors prasugrel and ticagrelor (Brilinta) in patients undergoing percutaneous coronary intervention (PCI) for ST-elevation MI (STEMI) does not provide optimal early inhibition of platelet aggregation. The parenteral antiplatelet drugs tirofiban and cangrelor have been shown to provide faster and more prolonged inhibition of platelet aggregation than the oral P2Y12 inhibitors.
But there has been no head-to-head comparative data for the glycoprotein IIb/IIIA inhibitor tirofiban (Aggrastat) and the P2Y12 inhibitor cangrelor (Kengreal) in the setting of primary PCI for STEMI. This was the impetus for FABOLUS FASTER, the first study to compare the pharmacodynamic effects of the two parenteral antiplatelet agents. The trial also looked at how these potent parenteral drugs, compared with chewed prasugrel, another previously unexamined yet highly practical issue.
The three-center, multinational, open-label FABOLUS FASTER trial randomized 122 patients undergoing primary PCI for STEMI to one of three arms: a standard intravenous bolus and 2-hour infusion of either the P2Y12 inhibitor cangrelor (Kengreal) or the glycoprotein IIb/IIIA inhibitor tirofiban (Aggrastat), followed in either case by 60 mg of oral prasugrel, or a third arm in which patients didn’t receive either drug but were instead randomized to a 60-mg loading dose of chewed or whole prasugrel tablets.
The primary study endpoint was inhibition of platelet aggregation at 30 minutes as measured by light transmittance aggregometry in response to 20 mcmol/L of adenosine diphosphate (ADP).
Tirofiban was the unequivocal winner with 95% inhibition, as compared with 34.1% with cangrelor, 10.5% with chewed prasugrel, and 6.3% with prasugrel swallowed whole, even though the concentration of prasugrel’s active metabolite was far greater at 62.3 ng/mL after prasugrel was chewed, compared with 17.1 ng/mL when swallowed in integral tablet form.
The rate of nonresponsiveness to tirofiban as defined by greater than 59% platelet aggregation was zero for tirofiban during its 2-hour infusion, then a scant 8% thereafter during repeated testing at 3 and 4-6 hours. In contrast, the cangrelor nonresponsiveness rate was 50%-58% during the 2-hour infusion, rising to 82% at 3 hours.
FABOLUS FASTER, while not powered for clinical endpoints, might nevertheless have important clinical implications, according to Dr. Valgimigli. First, the superiority of the intravenous drugs tirofiban and cangrelor over prasugrel for early, strong platelet inhibition underscores the importance of giving parenteral antiplatelet drugs over oral therapy during the acute phase of STEMI therapy. Moreover, tirofiban’s outstanding performance – and the high residual platelet reactivity associated with cangrelor – makes a strong case for large comparative, randomized trials of the two drugs, with hard clinical endpoints.
Discussant Christoph K. Naber, MD, PhD, opined that he personally doesn’t consider the FABOLUS FASTER results practice changing, for a couple of reasons.
“Platelet inhibition measured by ADP in vitro is not necessarily related to true effects in vivo. We know that platelets are activated by multiple mechanisms, and the ADP pathway is just one of them,” said Dr. Naber, an interventional cardiologist at the Wilhemshaven (Germany) Clinic.
Also, there’s a good reason why no glycoprotein IIb/IIIA inhibitors are approved for treatment of STEMI, and why tirofiban, despite its impressive antiplatelet effects, is currently largely reserved for bailout situations, such as complex lesions with large thrombus burden. It’s because tirofiban’s potent antiplatelet activity is accompanied by a high risk of bleeding, he added.
However, Dr. Valgimigli noted that this conviction about excessive bleeding risk is mainly based on older studies in which glycoprotein IIb/IIIA inhibitors were administered for prolonged duration through femoral access sites. He argued that it’s time for large clinical trials examining the risk/benefit ratio of short infusion of these agents in the contemporary practice of primary PCI for STEMI.
Simultaneously with Dr. Valgimigli’s presentation, the FABOLUS FASTER results were published online (Circulation. 2020 Jun 27; doi: 10.1161/CIRCULATIONAHA.120.046928).
Dr. Valgimigli reported that Medicure, the sponsor of the FABOLUS FASTER trial, provided an institutional research grant to conduct the study. He also disclosed receiving research grants and personal fees outside the scope of this study from a dozen pharmaceutical and medical device companies. Dr. Naber reported having no financial conflicts.
And cangrelor, in turn, is superior to oral prasugrel, according to the randomized FABOLUS FASTER trial, Marco Valgimigli, MD, PhD, reported at the virtual annual meeting of the European Association of Percutaneous Cardiovascular Interventions.
Moreover, contrary to conventional wisdom, chewed prasugrel (Effient) proved no better than swallowing the tablets whole for platelet inhibition, said Dr. Valgimigli, an interventional cardiologist at the University of Bern (Switzerland).
He explained that standard administration of the newer oral P2Y12 inhibitors prasugrel and ticagrelor (Brilinta) in patients undergoing percutaneous coronary intervention (PCI) for ST-elevation MI (STEMI) does not provide optimal early inhibition of platelet aggregation. The parenteral antiplatelet drugs tirofiban and cangrelor have been shown to provide faster and more prolonged inhibition of platelet aggregation than the oral P2Y12 inhibitors.
But there has been no head-to-head comparative data for the glycoprotein IIb/IIIA inhibitor tirofiban (Aggrastat) and the P2Y12 inhibitor cangrelor (Kengreal) in the setting of primary PCI for STEMI. This was the impetus for FABOLUS FASTER, the first study to compare the pharmacodynamic effects of the two parenteral antiplatelet agents. The trial also looked at how these potent parenteral drugs, compared with chewed prasugrel, another previously unexamined yet highly practical issue.
The three-center, multinational, open-label FABOLUS FASTER trial randomized 122 patients undergoing primary PCI for STEMI to one of three arms: a standard intravenous bolus and 2-hour infusion of either the P2Y12 inhibitor cangrelor (Kengreal) or the glycoprotein IIb/IIIA inhibitor tirofiban (Aggrastat), followed in either case by 60 mg of oral prasugrel, or a third arm in which patients didn’t receive either drug but were instead randomized to a 60-mg loading dose of chewed or whole prasugrel tablets.
The primary study endpoint was inhibition of platelet aggregation at 30 minutes as measured by light transmittance aggregometry in response to 20 mcmol/L of adenosine diphosphate (ADP).
Tirofiban was the unequivocal winner with 95% inhibition, as compared with 34.1% with cangrelor, 10.5% with chewed prasugrel, and 6.3% with prasugrel swallowed whole, even though the concentration of prasugrel’s active metabolite was far greater at 62.3 ng/mL after prasugrel was chewed, compared with 17.1 ng/mL when swallowed in integral tablet form.
The rate of nonresponsiveness to tirofiban as defined by greater than 59% platelet aggregation was zero for tirofiban during its 2-hour infusion, then a scant 8% thereafter during repeated testing at 3 and 4-6 hours. In contrast, the cangrelor nonresponsiveness rate was 50%-58% during the 2-hour infusion, rising to 82% at 3 hours.
FABOLUS FASTER, while not powered for clinical endpoints, might nevertheless have important clinical implications, according to Dr. Valgimigli. First, the superiority of the intravenous drugs tirofiban and cangrelor over prasugrel for early, strong platelet inhibition underscores the importance of giving parenteral antiplatelet drugs over oral therapy during the acute phase of STEMI therapy. Moreover, tirofiban’s outstanding performance – and the high residual platelet reactivity associated with cangrelor – makes a strong case for large comparative, randomized trials of the two drugs, with hard clinical endpoints.
Discussant Christoph K. Naber, MD, PhD, opined that he personally doesn’t consider the FABOLUS FASTER results practice changing, for a couple of reasons.
“Platelet inhibition measured by ADP in vitro is not necessarily related to true effects in vivo. We know that platelets are activated by multiple mechanisms, and the ADP pathway is just one of them,” said Dr. Naber, an interventional cardiologist at the Wilhemshaven (Germany) Clinic.
Also, there’s a good reason why no glycoprotein IIb/IIIA inhibitors are approved for treatment of STEMI, and why tirofiban, despite its impressive antiplatelet effects, is currently largely reserved for bailout situations, such as complex lesions with large thrombus burden. It’s because tirofiban’s potent antiplatelet activity is accompanied by a high risk of bleeding, he added.
However, Dr. Valgimigli noted that this conviction about excessive bleeding risk is mainly based on older studies in which glycoprotein IIb/IIIA inhibitors were administered for prolonged duration through femoral access sites. He argued that it’s time for large clinical trials examining the risk/benefit ratio of short infusion of these agents in the contemporary practice of primary PCI for STEMI.
Simultaneously with Dr. Valgimigli’s presentation, the FABOLUS FASTER results were published online (Circulation. 2020 Jun 27; doi: 10.1161/CIRCULATIONAHA.120.046928).
Dr. Valgimigli reported that Medicure, the sponsor of the FABOLUS FASTER trial, provided an institutional research grant to conduct the study. He also disclosed receiving research grants and personal fees outside the scope of this study from a dozen pharmaceutical and medical device companies. Dr. Naber reported having no financial conflicts.
REPORTING FROM EUROPCR 2020






