User login
Diabetes Hub contains news and clinical review articles for physicians seeking the most up-to-date information on the rapidly evolving options for treating and preventing Type 2 Diabetes in at-risk patients. The Diabetes Hub is powered by Frontline Medical Communications.
A low-fat vegan diet may lessen diabetic neuropathy pain
ORLANDO – A low-fat vegan diet reduced symptoms of peripheral neuropathy among patients with type 2 diabetes in the randomized, controlled Dietary Intervention for Chronic Diabetic Neuropathy Pain (DINE) study.
After 20 weeks, 17 patients who were assigned to the vegan diet group were more likely than were 18 control patients to have lost weight, to have reductions in pain scores, and to have neurologic improvements in their foot neuropathy.
The findings demonstrate "the potential of a low-fat vegan diet as a treatment for diabetic neuropathy pain," Anne E. Bunner, Ph.D., reported at the annual meeting of the American Association of Diabetes Educators. Other treatment options for diabetic neuropathy offer pain relief, but do not address the underlying nerve damage.
Support measures are needed to ensure the success of major dietary changes, said Dr. Bunner, associate director for clinical research at the Physicians Committee for Responsible Medicine, Washington, D.C.
The findings confirm those of a prior uncontrolled study (J. Nutr. Med. 1994;4:431-9) in which 81% of patients had pain relief with a low-fat, high-fiber vegan diet, Dr. Bunner said. A review of five studies involving more than 16,000 patients with type 2 diabetes showed that tight blood glucose control reduces the severity of diabetic neuropathy but does not eliminate the associated pain.
Dr. Bunner reported that the mean change scores in the diet group vs. the control group were –7.0 vs. –0.7 for body weight, –2.4 vs. –0.2 for body mass index, –9.1 vs. –0.9 for McGill Pain Questionnaire results, and 0.7 vs. –11.7 for foot conductance.
The diet group also experienced improvements in mean change scores for hemoglobin A1c (–0.8), Quality of Life score (–8.4), and Neuropathy Total Symptoms Score (–3.9), but the changes in these scores were not significantly better than those of the control group (–0.1, –4.7, –2.7, respectively).
The control group experienced greater improvements in pain as measured by a visual analogue scale (mean change scores of –1.2 and –2.1* for the diet and control groups, respectively). The change in the diet group was not statistically significant.
Patients in both groups used vitamin B12 supplements during the course of the study, which could explain the improvements in the control group, Dr. Bunner said. B12 deficiency is associated with diabetic neuropathy, but none of the patients had a B12 deficiency at baseline. It is possible that B12 may have been an active treatment or that the motivation associated with being a study participant was associated with the improvements.
Of note, 4 of 17 patients in the diet group were able to reduce the dosages of lipid-lowering medications; 1 increased the dosage. No one in the control group was able to reduce the dosages of lipid-lowering medications; 3 of 18 increased dosages. Ten of 17 diet group patients reduced the dosages of diabetes medications, and 2 of 18 controls reduced the dosages of diabetes medications.
Mean age of the study subjects was 57 years. Those assigned to the diet group were instructed to consume only plant foods, and to limit intake of oils, nuts, and fatty foods. Fat was limited to 3 g per serving or 20-30 g per day. Patients in the diet group also were advised to include 40 g/day of high-fiber foods, and to consume low–glycemic index foods. No limit was placed on portions.
The diet group participated in weekly classes involving nutrition education, social support, cooking demonstrations, and food product sampling.
Both groups used B12 supplements, and the control group was instructed to make no major dietary changes during the 20-week study.
Thirteen of 17 diet group patients were fully compliant with the vegan diet; 8 of the 13 were compliant with the low-fat instructions at both the 10- and 20-week assessment, and 3 of the 13 were compliant with the low-fat instructions at one of the two assessments. Two were fully compliant with the low-fat guidelines, but not the vegan guidelines, and two were noncompliant with both. One patient did not complete the study.
Dr. Bunner reported having no disclosures.
CORRECTED Aug 8: Improvement in pain in the control group, as measured by a visual analogue scale, was misstated in the original story. That value was –2.1.
ORLANDO – A low-fat vegan diet reduced symptoms of peripheral neuropathy among patients with type 2 diabetes in the randomized, controlled Dietary Intervention for Chronic Diabetic Neuropathy Pain (DINE) study.
After 20 weeks, 17 patients who were assigned to the vegan diet group were more likely than were 18 control patients to have lost weight, to have reductions in pain scores, and to have neurologic improvements in their foot neuropathy.
The findings demonstrate "the potential of a low-fat vegan diet as a treatment for diabetic neuropathy pain," Anne E. Bunner, Ph.D., reported at the annual meeting of the American Association of Diabetes Educators. Other treatment options for diabetic neuropathy offer pain relief, but do not address the underlying nerve damage.
Support measures are needed to ensure the success of major dietary changes, said Dr. Bunner, associate director for clinical research at the Physicians Committee for Responsible Medicine, Washington, D.C.
The findings confirm those of a prior uncontrolled study (J. Nutr. Med. 1994;4:431-9) in which 81% of patients had pain relief with a low-fat, high-fiber vegan diet, Dr. Bunner said. A review of five studies involving more than 16,000 patients with type 2 diabetes showed that tight blood glucose control reduces the severity of diabetic neuropathy but does not eliminate the associated pain.
Dr. Bunner reported that the mean change scores in the diet group vs. the control group were –7.0 vs. –0.7 for body weight, –2.4 vs. –0.2 for body mass index, –9.1 vs. –0.9 for McGill Pain Questionnaire results, and 0.7 vs. –11.7 for foot conductance.
The diet group also experienced improvements in mean change scores for hemoglobin A1c (–0.8), Quality of Life score (–8.4), and Neuropathy Total Symptoms Score (–3.9), but the changes in these scores were not significantly better than those of the control group (–0.1, –4.7, –2.7, respectively).
The control group experienced greater improvements in pain as measured by a visual analogue scale (mean change scores of –1.2 and –2.1* for the diet and control groups, respectively). The change in the diet group was not statistically significant.
Patients in both groups used vitamin B12 supplements during the course of the study, which could explain the improvements in the control group, Dr. Bunner said. B12 deficiency is associated with diabetic neuropathy, but none of the patients had a B12 deficiency at baseline. It is possible that B12 may have been an active treatment or that the motivation associated with being a study participant was associated with the improvements.
Of note, 4 of 17 patients in the diet group were able to reduce the dosages of lipid-lowering medications; 1 increased the dosage. No one in the control group was able to reduce the dosages of lipid-lowering medications; 3 of 18 increased dosages. Ten of 17 diet group patients reduced the dosages of diabetes medications, and 2 of 18 controls reduced the dosages of diabetes medications.
Mean age of the study subjects was 57 years. Those assigned to the diet group were instructed to consume only plant foods, and to limit intake of oils, nuts, and fatty foods. Fat was limited to 3 g per serving or 20-30 g per day. Patients in the diet group also were advised to include 40 g/day of high-fiber foods, and to consume low–glycemic index foods. No limit was placed on portions.
The diet group participated in weekly classes involving nutrition education, social support, cooking demonstrations, and food product sampling.
Both groups used B12 supplements, and the control group was instructed to make no major dietary changes during the 20-week study.
Thirteen of 17 diet group patients were fully compliant with the vegan diet; 8 of the 13 were compliant with the low-fat instructions at both the 10- and 20-week assessment, and 3 of the 13 were compliant with the low-fat instructions at one of the two assessments. Two were fully compliant with the low-fat guidelines, but not the vegan guidelines, and two were noncompliant with both. One patient did not complete the study.
Dr. Bunner reported having no disclosures.
CORRECTED Aug 8: Improvement in pain in the control group, as measured by a visual analogue scale, was misstated in the original story. That value was –2.1.
ORLANDO – A low-fat vegan diet reduced symptoms of peripheral neuropathy among patients with type 2 diabetes in the randomized, controlled Dietary Intervention for Chronic Diabetic Neuropathy Pain (DINE) study.
After 20 weeks, 17 patients who were assigned to the vegan diet group were more likely than were 18 control patients to have lost weight, to have reductions in pain scores, and to have neurologic improvements in their foot neuropathy.
The findings demonstrate "the potential of a low-fat vegan diet as a treatment for diabetic neuropathy pain," Anne E. Bunner, Ph.D., reported at the annual meeting of the American Association of Diabetes Educators. Other treatment options for diabetic neuropathy offer pain relief, but do not address the underlying nerve damage.
Support measures are needed to ensure the success of major dietary changes, said Dr. Bunner, associate director for clinical research at the Physicians Committee for Responsible Medicine, Washington, D.C.
The findings confirm those of a prior uncontrolled study (J. Nutr. Med. 1994;4:431-9) in which 81% of patients had pain relief with a low-fat, high-fiber vegan diet, Dr. Bunner said. A review of five studies involving more than 16,000 patients with type 2 diabetes showed that tight blood glucose control reduces the severity of diabetic neuropathy but does not eliminate the associated pain.
Dr. Bunner reported that the mean change scores in the diet group vs. the control group were –7.0 vs. –0.7 for body weight, –2.4 vs. –0.2 for body mass index, –9.1 vs. –0.9 for McGill Pain Questionnaire results, and 0.7 vs. –11.7 for foot conductance.
The diet group also experienced improvements in mean change scores for hemoglobin A1c (–0.8), Quality of Life score (–8.4), and Neuropathy Total Symptoms Score (–3.9), but the changes in these scores were not significantly better than those of the control group (–0.1, –4.7, –2.7, respectively).
The control group experienced greater improvements in pain as measured by a visual analogue scale (mean change scores of –1.2 and –2.1* for the diet and control groups, respectively). The change in the diet group was not statistically significant.
Patients in both groups used vitamin B12 supplements during the course of the study, which could explain the improvements in the control group, Dr. Bunner said. B12 deficiency is associated with diabetic neuropathy, but none of the patients had a B12 deficiency at baseline. It is possible that B12 may have been an active treatment or that the motivation associated with being a study participant was associated with the improvements.
Of note, 4 of 17 patients in the diet group were able to reduce the dosages of lipid-lowering medications; 1 increased the dosage. No one in the control group was able to reduce the dosages of lipid-lowering medications; 3 of 18 increased dosages. Ten of 17 diet group patients reduced the dosages of diabetes medications, and 2 of 18 controls reduced the dosages of diabetes medications.
Mean age of the study subjects was 57 years. Those assigned to the diet group were instructed to consume only plant foods, and to limit intake of oils, nuts, and fatty foods. Fat was limited to 3 g per serving or 20-30 g per day. Patients in the diet group also were advised to include 40 g/day of high-fiber foods, and to consume low–glycemic index foods. No limit was placed on portions.
The diet group participated in weekly classes involving nutrition education, social support, cooking demonstrations, and food product sampling.
Both groups used B12 supplements, and the control group was instructed to make no major dietary changes during the 20-week study.
Thirteen of 17 diet group patients were fully compliant with the vegan diet; 8 of the 13 were compliant with the low-fat instructions at both the 10- and 20-week assessment, and 3 of the 13 were compliant with the low-fat instructions at one of the two assessments. Two were fully compliant with the low-fat guidelines, but not the vegan guidelines, and two were noncompliant with both. One patient did not complete the study.
Dr. Bunner reported having no disclosures.
CORRECTED Aug 8: Improvement in pain in the control group, as measured by a visual analogue scale, was misstated in the original story. That value was –2.1.
AT AADE 14
Key clinical point: Following a vegan diet might relieve neuropathy pain in patients with type 2 diabetes.
Major finding: After 20 weeks, mean change scores on the McGill Pain Questionnaire were –9.1 for the vegan diet group vs. –0.9 for the control group.
Data source: The randomized, controlled DINE study of 35 patients.
Disclosures: Dr. Bunner reported having no disclosures.
Long-term benefits shown after gastric banding
SAN FRANCISCO – The greater benefits of laparoscopic gastric banding surgery compared with medical treatment for obese patients were maintained for up to 17 years in a study of data on 1,490 patients.
The 527 obese patients (with or without diabetes) who underwent laparoscopic banding were significantly less likely to die of cardiovascular or noncardiovascular causes and were less likely to develop new cases of type 2 diabetes or cardiovascular disease, compared with the 963 nonsurgery patients, Dr. Antonio E. Pontiroli and his associates reported at the annual scientific sessions of the American Diabetes Association.
Patients underwent laparoscopic banding surgery or were seen for a first visit for medical therapy in 1995-2001, and were followed for 11-17 years, through September 2012.
Three percent of the surgery group and 10% of the nonsurgery group died during follow-up, reported Dr. Pontiroli, chair of internal medicine at Università Degli Studi de Milano and San Paolo Hospital, Milan.
To track morbidity, the investigators analyzed records to see which patients got "exemptions" for specific diseases, an Italian government system in which development of a chronic disease exempts someone from having to pay for exams or treatments for that disease. Any exemption obtained after the first surgical or medical visit was considered a proxy of new disease.
New exemptions were granted to 25% in the surgery group and 42% in the nonsurgery group.
Subset analyses divided 385 surgery patients based on the presence or absence of diabetes, and matched the subgroups separately with 681 nonsurgery patients by sex, age, blood pressure, and body mass index.
In the matched comparisons, 3% of the surgery group and 10% of the nonsurgery group died, and exemptions were granted to 22% of the surgery group and 28% of the nonsurgery group, which were statistically significant differences in the intention-to-treat analyses.
Patients in the surgery group were 66% less likely to die than the nonsurgery patients. Patients without diabetes at the first visit were 67% less likely to die than matched nonsurgery patients, and those with diabetes at the first visit were 56% less likely to die compared with matched nonsurgery patients.
Cardiovascular disease, noncardiovascular disease, or neoplasia were significantly less likely to be the causes of death in the surgery group compared with the nonsurgery group. The surgery group recorded significantly fewer hospitalizations during follow-up (120) than the nonsurgery group (273).
New cases of cardiovascular disease (defined by exemptions) appeared in 13% of the surgery group and 22% of the nonsurgery group. In the matched subgroups, 13% who underwent surgery and 18% in the nonsurgery group developed cardiovascular disease.
Among patients without diabetes at baseline, 5% of 454 in the surgery group and 10% of 724 in the nonsurgery group developed diabetes during follow-up. In the subset analysis of matched patients without diabetes at baseline, 4% of 333 in the surgery group and 9% in the nonsurgery group developed diabetes.
The investigators plan another data assessment in 2017 to confirm these long-term findings. Similar studies are needed for other bariatric surgery techniques, he suggested.
Dr. Pontiroli reported financial associations with Sanofi, Eli Lilly, and other companies.
On Twitter @sherryboschert
This is a very interesting study. It was a long-term study, over 17 years, of patients who’d had gastric banding in Milan, looking at development of cardiovascular disease, type 2 diabetes, and death. It is reassuring that there did appear to be favorable outcomes.
There clearly are limitations to the study. The researchers only looked at banding; they didn’t look at sleeve gastrectomies or gastric bypass. The study is specifically related to banding. The comparisons with medical therapies didn’t really define the medical therapies. We’d obviously need details on what they were comparing and whether there are subgroup analyses that could be done.
Nonetheless, they did show that there’s a significant improvement in death rates, cardiovascular death, all-cause death, development of type 2 diabetes, and new cases of cardiovascular disease both in the whole population and in the matched groups. I think these are useful data that are kind of reassuring.
The other thing I would mention: Although bariatric surgery has been done for many years now, it’s really only over the last 10-15 years that the numbers of surgeries have increased hugely. It will be interesting to see the outcomes of the most current cohort over the next 10-15 years.
Dr. Thomas Barber is an associate professor and honorary consultant endocrinologist at the Warwick Medical School, Coventry, England. He gave these comments in an interview at the meeting. Dr. Barber reported having no financial disclosures.
This is a very interesting study. It was a long-term study, over 17 years, of patients who’d had gastric banding in Milan, looking at development of cardiovascular disease, type 2 diabetes, and death. It is reassuring that there did appear to be favorable outcomes.
There clearly are limitations to the study. The researchers only looked at banding; they didn’t look at sleeve gastrectomies or gastric bypass. The study is specifically related to banding. The comparisons with medical therapies didn’t really define the medical therapies. We’d obviously need details on what they were comparing and whether there are subgroup analyses that could be done.
Nonetheless, they did show that there’s a significant improvement in death rates, cardiovascular death, all-cause death, development of type 2 diabetes, and new cases of cardiovascular disease both in the whole population and in the matched groups. I think these are useful data that are kind of reassuring.
The other thing I would mention: Although bariatric surgery has been done for many years now, it’s really only over the last 10-15 years that the numbers of surgeries have increased hugely. It will be interesting to see the outcomes of the most current cohort over the next 10-15 years.
Dr. Thomas Barber is an associate professor and honorary consultant endocrinologist at the Warwick Medical School, Coventry, England. He gave these comments in an interview at the meeting. Dr. Barber reported having no financial disclosures.
This is a very interesting study. It was a long-term study, over 17 years, of patients who’d had gastric banding in Milan, looking at development of cardiovascular disease, type 2 diabetes, and death. It is reassuring that there did appear to be favorable outcomes.
There clearly are limitations to the study. The researchers only looked at banding; they didn’t look at sleeve gastrectomies or gastric bypass. The study is specifically related to banding. The comparisons with medical therapies didn’t really define the medical therapies. We’d obviously need details on what they were comparing and whether there are subgroup analyses that could be done.
Nonetheless, they did show that there’s a significant improvement in death rates, cardiovascular death, all-cause death, development of type 2 diabetes, and new cases of cardiovascular disease both in the whole population and in the matched groups. I think these are useful data that are kind of reassuring.
The other thing I would mention: Although bariatric surgery has been done for many years now, it’s really only over the last 10-15 years that the numbers of surgeries have increased hugely. It will be interesting to see the outcomes of the most current cohort over the next 10-15 years.
Dr. Thomas Barber is an associate professor and honorary consultant endocrinologist at the Warwick Medical School, Coventry, England. He gave these comments in an interview at the meeting. Dr. Barber reported having no financial disclosures.
SAN FRANCISCO – The greater benefits of laparoscopic gastric banding surgery compared with medical treatment for obese patients were maintained for up to 17 years in a study of data on 1,490 patients.
The 527 obese patients (with or without diabetes) who underwent laparoscopic banding were significantly less likely to die of cardiovascular or noncardiovascular causes and were less likely to develop new cases of type 2 diabetes or cardiovascular disease, compared with the 963 nonsurgery patients, Dr. Antonio E. Pontiroli and his associates reported at the annual scientific sessions of the American Diabetes Association.
Patients underwent laparoscopic banding surgery or were seen for a first visit for medical therapy in 1995-2001, and were followed for 11-17 years, through September 2012.
Three percent of the surgery group and 10% of the nonsurgery group died during follow-up, reported Dr. Pontiroli, chair of internal medicine at Università Degli Studi de Milano and San Paolo Hospital, Milan.
To track morbidity, the investigators analyzed records to see which patients got "exemptions" for specific diseases, an Italian government system in which development of a chronic disease exempts someone from having to pay for exams or treatments for that disease. Any exemption obtained after the first surgical or medical visit was considered a proxy of new disease.
New exemptions were granted to 25% in the surgery group and 42% in the nonsurgery group.
Subset analyses divided 385 surgery patients based on the presence or absence of diabetes, and matched the subgroups separately with 681 nonsurgery patients by sex, age, blood pressure, and body mass index.
In the matched comparisons, 3% of the surgery group and 10% of the nonsurgery group died, and exemptions were granted to 22% of the surgery group and 28% of the nonsurgery group, which were statistically significant differences in the intention-to-treat analyses.
Patients in the surgery group were 66% less likely to die than the nonsurgery patients. Patients without diabetes at the first visit were 67% less likely to die than matched nonsurgery patients, and those with diabetes at the first visit were 56% less likely to die compared with matched nonsurgery patients.
Cardiovascular disease, noncardiovascular disease, or neoplasia were significantly less likely to be the causes of death in the surgery group compared with the nonsurgery group. The surgery group recorded significantly fewer hospitalizations during follow-up (120) than the nonsurgery group (273).
New cases of cardiovascular disease (defined by exemptions) appeared in 13% of the surgery group and 22% of the nonsurgery group. In the matched subgroups, 13% who underwent surgery and 18% in the nonsurgery group developed cardiovascular disease.
Among patients without diabetes at baseline, 5% of 454 in the surgery group and 10% of 724 in the nonsurgery group developed diabetes during follow-up. In the subset analysis of matched patients without diabetes at baseline, 4% of 333 in the surgery group and 9% in the nonsurgery group developed diabetes.
The investigators plan another data assessment in 2017 to confirm these long-term findings. Similar studies are needed for other bariatric surgery techniques, he suggested.
Dr. Pontiroli reported financial associations with Sanofi, Eli Lilly, and other companies.
On Twitter @sherryboschert
SAN FRANCISCO – The greater benefits of laparoscopic gastric banding surgery compared with medical treatment for obese patients were maintained for up to 17 years in a study of data on 1,490 patients.
The 527 obese patients (with or without diabetes) who underwent laparoscopic banding were significantly less likely to die of cardiovascular or noncardiovascular causes and were less likely to develop new cases of type 2 diabetes or cardiovascular disease, compared with the 963 nonsurgery patients, Dr. Antonio E. Pontiroli and his associates reported at the annual scientific sessions of the American Diabetes Association.
Patients underwent laparoscopic banding surgery or were seen for a first visit for medical therapy in 1995-2001, and were followed for 11-17 years, through September 2012.
Three percent of the surgery group and 10% of the nonsurgery group died during follow-up, reported Dr. Pontiroli, chair of internal medicine at Università Degli Studi de Milano and San Paolo Hospital, Milan.
To track morbidity, the investigators analyzed records to see which patients got "exemptions" for specific diseases, an Italian government system in which development of a chronic disease exempts someone from having to pay for exams or treatments for that disease. Any exemption obtained after the first surgical or medical visit was considered a proxy of new disease.
New exemptions were granted to 25% in the surgery group and 42% in the nonsurgery group.
Subset analyses divided 385 surgery patients based on the presence or absence of diabetes, and matched the subgroups separately with 681 nonsurgery patients by sex, age, blood pressure, and body mass index.
In the matched comparisons, 3% of the surgery group and 10% of the nonsurgery group died, and exemptions were granted to 22% of the surgery group and 28% of the nonsurgery group, which were statistically significant differences in the intention-to-treat analyses.
Patients in the surgery group were 66% less likely to die than the nonsurgery patients. Patients without diabetes at the first visit were 67% less likely to die than matched nonsurgery patients, and those with diabetes at the first visit were 56% less likely to die compared with matched nonsurgery patients.
Cardiovascular disease, noncardiovascular disease, or neoplasia were significantly less likely to be the causes of death in the surgery group compared with the nonsurgery group. The surgery group recorded significantly fewer hospitalizations during follow-up (120) than the nonsurgery group (273).
New cases of cardiovascular disease (defined by exemptions) appeared in 13% of the surgery group and 22% of the nonsurgery group. In the matched subgroups, 13% who underwent surgery and 18% in the nonsurgery group developed cardiovascular disease.
Among patients without diabetes at baseline, 5% of 454 in the surgery group and 10% of 724 in the nonsurgery group developed diabetes during follow-up. In the subset analysis of matched patients without diabetes at baseline, 4% of 333 in the surgery group and 9% in the nonsurgery group developed diabetes.
The investigators plan another data assessment in 2017 to confirm these long-term findings. Similar studies are needed for other bariatric surgery techniques, he suggested.
Dr. Pontiroli reported financial associations with Sanofi, Eli Lilly, and other companies.
On Twitter @sherryboschert
AT THE ADA ANNUAL SCIENTIFIC SESSIONS
Key clinical point: Gastric banding produced significant benefits in 17 years of follow-up.
Major finding: Obese patients treated with gastric banding were 66% less likely to die, compared with those who received medical therapy.
Data source: An intent-to-treat analysis of data on 1,490 obese patients treated at four Italian centers.
Disclosures: Dr. Pontiroli reported financial associations with Sanofi, Eli Lilly, and other companies.
Intensive blood glucose control: No effect in hyperglycemic patients having CABG
SAN FRANCISCO – Intensive glucose control targeting a blood glucose of 100-140 mg/dL did not significantly reduce perioperative complications or mortality, compared with a less strict glucose target of 141-180 mg/dL in hyperglycemic patients undergoing coronary artery bypass graft surgery, a randomized trial showed.
"Inpatient hyperglycemia is associated with increased hospital complications and mortality," Dr. Guillermo E. Umpierrez said at the annual scientific sessions of the American Diabetes Association. "There have been a lot of controversies regarding what is the best target for glucose targeting in these patients in the perioperative period. There are studies suggesting that improved glycemic control improves outcomes, but others have failed to reproduce this data."
In an effort to address this question, Dr. Umpierrez and his associates at three hospitals in Atlanta conducted the open-label, randomized GLUCO-CABG trial to determine whether intensive glucose control (defined as a blood glucose target of 100-140 mg/dL) reduces perioperative complications, compared with conservative glucose control (defined as a glucose target of 141-180 mg/dL) in hyperglycemic patients undergoing CABG. Their hypothesis was that intensive therapy in the ICU would reduce perioperative complications, compared with a conservative insulin therapy, said Dr. Umpierrez, professor of medicine at Emory University in Atlanta.
The study population included 302 men and women aged 18-80 years with and without a history of diabetes who underwent CABG with or without valve surgery, and who had perioperative hyperglycemia greater than 140 mg/dL during their surgery or ICU stay. Half received intensive insulin therapy, and the other half received conservative insulin therapy. A computerized insulin infusion algorithm (Glytec’s Glucommander) was used to guide continuous IV infusion, which was given in the ICU until the patients were able to eat and/or be transferred to non-ICU services.
The mean age of the patients was 64 years, 72% were male, and their mean body mass index was 30.5 kg/m2. The mean ICU daily blood glucose levels were similar, at 132 mg/dL in the intensive group, compared with 154 mg/dL in the conservative group, and the hospital length of stay was similar between the two groups (11.4 vs. 9.5 days, respectively). In the ICU, a blood glucose level of less than 70 mg/dL occurred in 8% and 2% of the intensive and conservative groups, respectively, a significant difference, while no levels reached less than 40 mg/dL.
After ICU care, there were no differences between the intensive and conservative groups in mean daily blood glucose levels (143 vs. 141 mg/dL, respectively), percentage of patients with hypoglycemia (1% vs. 3%), or hospital readmissions (18% vs. 20%). There were also no differences between groups in rates of mortality, pneumonia, acute kidney injury, respiratory failure, or wound infection.
"The results of this study have significant clinical implications in the management of patients with hyperglycemia and diabetes in critical care units," Dr. Umpierrez said. "This study indicates that a target glucose of 141-180 mg/dL is as safe and effective and results in a lower rate of hypoglycemic events compared to a more intensive target of 100-140 mg/dL."
The study was funded by the National Institutes of Health and by a clinical research award from the American Diabetes Association. Glytec provided the Glucommander and Sanofi provided medications. Dr. Umpierrez has received research funding from and/or has served as an adviser to several pharmaceutical companies.
On Twitter @dougbrunk
SAN FRANCISCO – Intensive glucose control targeting a blood glucose of 100-140 mg/dL did not significantly reduce perioperative complications or mortality, compared with a less strict glucose target of 141-180 mg/dL in hyperglycemic patients undergoing coronary artery bypass graft surgery, a randomized trial showed.
"Inpatient hyperglycemia is associated with increased hospital complications and mortality," Dr. Guillermo E. Umpierrez said at the annual scientific sessions of the American Diabetes Association. "There have been a lot of controversies regarding what is the best target for glucose targeting in these patients in the perioperative period. There are studies suggesting that improved glycemic control improves outcomes, but others have failed to reproduce this data."
In an effort to address this question, Dr. Umpierrez and his associates at three hospitals in Atlanta conducted the open-label, randomized GLUCO-CABG trial to determine whether intensive glucose control (defined as a blood glucose target of 100-140 mg/dL) reduces perioperative complications, compared with conservative glucose control (defined as a glucose target of 141-180 mg/dL) in hyperglycemic patients undergoing CABG. Their hypothesis was that intensive therapy in the ICU would reduce perioperative complications, compared with a conservative insulin therapy, said Dr. Umpierrez, professor of medicine at Emory University in Atlanta.
The study population included 302 men and women aged 18-80 years with and without a history of diabetes who underwent CABG with or without valve surgery, and who had perioperative hyperglycemia greater than 140 mg/dL during their surgery or ICU stay. Half received intensive insulin therapy, and the other half received conservative insulin therapy. A computerized insulin infusion algorithm (Glytec’s Glucommander) was used to guide continuous IV infusion, which was given in the ICU until the patients were able to eat and/or be transferred to non-ICU services.
The mean age of the patients was 64 years, 72% were male, and their mean body mass index was 30.5 kg/m2. The mean ICU daily blood glucose levels were similar, at 132 mg/dL in the intensive group, compared with 154 mg/dL in the conservative group, and the hospital length of stay was similar between the two groups (11.4 vs. 9.5 days, respectively). In the ICU, a blood glucose level of less than 70 mg/dL occurred in 8% and 2% of the intensive and conservative groups, respectively, a significant difference, while no levels reached less than 40 mg/dL.
After ICU care, there were no differences between the intensive and conservative groups in mean daily blood glucose levels (143 vs. 141 mg/dL, respectively), percentage of patients with hypoglycemia (1% vs. 3%), or hospital readmissions (18% vs. 20%). There were also no differences between groups in rates of mortality, pneumonia, acute kidney injury, respiratory failure, or wound infection.
"The results of this study have significant clinical implications in the management of patients with hyperglycemia and diabetes in critical care units," Dr. Umpierrez said. "This study indicates that a target glucose of 141-180 mg/dL is as safe and effective and results in a lower rate of hypoglycemic events compared to a more intensive target of 100-140 mg/dL."
The study was funded by the National Institutes of Health and by a clinical research award from the American Diabetes Association. Glytec provided the Glucommander and Sanofi provided medications. Dr. Umpierrez has received research funding from and/or has served as an adviser to several pharmaceutical companies.
On Twitter @dougbrunk
SAN FRANCISCO – Intensive glucose control targeting a blood glucose of 100-140 mg/dL did not significantly reduce perioperative complications or mortality, compared with a less strict glucose target of 141-180 mg/dL in hyperglycemic patients undergoing coronary artery bypass graft surgery, a randomized trial showed.
"Inpatient hyperglycemia is associated with increased hospital complications and mortality," Dr. Guillermo E. Umpierrez said at the annual scientific sessions of the American Diabetes Association. "There have been a lot of controversies regarding what is the best target for glucose targeting in these patients in the perioperative period. There are studies suggesting that improved glycemic control improves outcomes, but others have failed to reproduce this data."
In an effort to address this question, Dr. Umpierrez and his associates at three hospitals in Atlanta conducted the open-label, randomized GLUCO-CABG trial to determine whether intensive glucose control (defined as a blood glucose target of 100-140 mg/dL) reduces perioperative complications, compared with conservative glucose control (defined as a glucose target of 141-180 mg/dL) in hyperglycemic patients undergoing CABG. Their hypothesis was that intensive therapy in the ICU would reduce perioperative complications, compared with a conservative insulin therapy, said Dr. Umpierrez, professor of medicine at Emory University in Atlanta.
The study population included 302 men and women aged 18-80 years with and without a history of diabetes who underwent CABG with or without valve surgery, and who had perioperative hyperglycemia greater than 140 mg/dL during their surgery or ICU stay. Half received intensive insulin therapy, and the other half received conservative insulin therapy. A computerized insulin infusion algorithm (Glytec’s Glucommander) was used to guide continuous IV infusion, which was given in the ICU until the patients were able to eat and/or be transferred to non-ICU services.
The mean age of the patients was 64 years, 72% were male, and their mean body mass index was 30.5 kg/m2. The mean ICU daily blood glucose levels were similar, at 132 mg/dL in the intensive group, compared with 154 mg/dL in the conservative group, and the hospital length of stay was similar between the two groups (11.4 vs. 9.5 days, respectively). In the ICU, a blood glucose level of less than 70 mg/dL occurred in 8% and 2% of the intensive and conservative groups, respectively, a significant difference, while no levels reached less than 40 mg/dL.
After ICU care, there were no differences between the intensive and conservative groups in mean daily blood glucose levels (143 vs. 141 mg/dL, respectively), percentage of patients with hypoglycemia (1% vs. 3%), or hospital readmissions (18% vs. 20%). There were also no differences between groups in rates of mortality, pneumonia, acute kidney injury, respiratory failure, or wound infection.
"The results of this study have significant clinical implications in the management of patients with hyperglycemia and diabetes in critical care units," Dr. Umpierrez said. "This study indicates that a target glucose of 141-180 mg/dL is as safe and effective and results in a lower rate of hypoglycemic events compared to a more intensive target of 100-140 mg/dL."
The study was funded by the National Institutes of Health and by a clinical research award from the American Diabetes Association. Glytec provided the Glucommander and Sanofi provided medications. Dr. Umpierrez has received research funding from and/or has served as an adviser to several pharmaceutical companies.
On Twitter @dougbrunk
AT THE ADA ANNUAL SCIENTIFIC SESSIONS
Key clinical point: A conservative target glucose of 141-180 mg/dL is as safe and effective as a more intensive target of 100-140 mg/dL, and results in a lower rate of hypoglycemic events.
Major finding: After ICU care, there were no differences between the intensive and conservative groups in mean daily blood glucose levels (143 vs. 141 mg/dL, respectively) or in the percentage of patients with hypoglycemia (1% vs. 3%; P = .68).
Data source: GLUCO-CABG, a randomized trial of 302 men and women aged 18-80 years who underwent CABG with or without valve surgery and who had perioperative hyperglycemia greater than 140 mg/dL during their surgery or ICU stay.
Disclosures: The study was funded by the National Institutes of Health and by a clinical research award from the American Diabetes Association. Glytec provided the Glucommander and Sanofi provided medications. Dr. Umpierrez has received research funding from and/or has served as an adviser to several pharmaceutical companies.
Data increasingly support plant-based diet for diabetes prevention, care
ORLANDO – Evidence increasingly supports plant-based nutrition for preventing diabetes or improving outcomes in those with diabetes.
The Adventist Health Study-2 (AHS-2), for example, demonstrated that a plant-based eating pattern – defined as ad libitum whole grains, legumes, fruits, and vegetables, and avoidance of all animal products, added oils, and high-fat foods – reduced the incidence of type 2 diabetes. The prospective cohort study involving more than 96,000 adults demonstrated that body mass index and the incidence of diabetes increased in tandem with the amount of animal products in the diet, according to Meghan Jardine, who reviewed the recent literature on plant-based nutrition in a poster presented at the annual meeting of the American Association of Diabetes Educators.
The prevalence of type 2 diabetes among nonvegetarians, semivegetarians, pescovegetarians, lacto-ovovegetarians, and vegans in that study was 7.6%, 6.1%, 4.9%, 3.2%, and 2.9%, respectively, and BMI for each of those groups was 28.8, 27.3, 26.3, 25.7, and 23.6 kg/m2, respectively, said Ms. Jardine, a registered and licensed dietician, certified diabetes educator, and diabetes education coordinator at Parkland Health and Hospital System, Dallas.
AHS-2 also demonstrated increased longevity in those who followed a plant-based eating pattern, with men living 9.5 years longer and women living 6.1 years longer than their meat-eating counterparts (JAMA 2013;173:1230-8).
In addition, a National Institutes of Health study demonstrated that a low-fat vegan diet led to significantly greater improvements in glycemic and lipid control than did a conventional diabetes diet in patients with type 2 diabetes.
Hemoglobin A1c levels in 49 patients on the low-fat vegan diet improved from 8.06 to 7.65 at 74 weeks, but while the levels in 50 patients on the conventional diabetes diet initially improved from 7.93 to about 7.7 at 11 weeks, at 74 weeks they had increased to 7.94 (Diabetes Care 2006;29:1777-83).
Among the other findings that Ms. Jardine mentioned were those from "a remarkable study" in which 17 of 21 patients with sharp, burning pain characteristic of distal polyneuropathy experienced complete pain relief after initiating a low-fat, high-fiber, vegan diet along with a daily 30-minute walk, and findings from several studies that have suggested that plant-based eating preserved renal function.
Moreover, a plant-based eating pattern has been shown to reverse coronary artery disease and improve magnesium intake (which reduces insulin resistance), and the high fiber intake associated with plant-based eating improves glucose control and decreases mortality from circulatory, digestive, and inflammatory disease, she said.
Two recent studies demonstrated that meat consumption substantially increases the risk of type 2 diabetes. Even just a half serving per day increase was associated with a 48% increase over 4 years in one study (JAMA Intern. Med. 2013;173:1328-35).
Ms. Jardine noted that the Academy of Nutrition and Dietetics position is that "appropriately planned vegetarian diets, including total vegetarian or vegan diets, are healthful, nutritionally adequate and may provide health benefits in the prevention and treatment of certain disease," and that such diets have been found to be "highly acceptable in diverse populations with various disease states" (Diabetes Educ. 2010:36:33-48).
She warned that patients with diabetes who are on medications and who begin to follow a plant-based eating pattern should be instructed about how to recognize and treat hypoglycemia, as adjustments to medications that lower glucose, blood pressure, and cholesterol may be needed.
ORLANDO – Evidence increasingly supports plant-based nutrition for preventing diabetes or improving outcomes in those with diabetes.
The Adventist Health Study-2 (AHS-2), for example, demonstrated that a plant-based eating pattern – defined as ad libitum whole grains, legumes, fruits, and vegetables, and avoidance of all animal products, added oils, and high-fat foods – reduced the incidence of type 2 diabetes. The prospective cohort study involving more than 96,000 adults demonstrated that body mass index and the incidence of diabetes increased in tandem with the amount of animal products in the diet, according to Meghan Jardine, who reviewed the recent literature on plant-based nutrition in a poster presented at the annual meeting of the American Association of Diabetes Educators.
The prevalence of type 2 diabetes among nonvegetarians, semivegetarians, pescovegetarians, lacto-ovovegetarians, and vegans in that study was 7.6%, 6.1%, 4.9%, 3.2%, and 2.9%, respectively, and BMI for each of those groups was 28.8, 27.3, 26.3, 25.7, and 23.6 kg/m2, respectively, said Ms. Jardine, a registered and licensed dietician, certified diabetes educator, and diabetes education coordinator at Parkland Health and Hospital System, Dallas.
AHS-2 also demonstrated increased longevity in those who followed a plant-based eating pattern, with men living 9.5 years longer and women living 6.1 years longer than their meat-eating counterparts (JAMA 2013;173:1230-8).
In addition, a National Institutes of Health study demonstrated that a low-fat vegan diet led to significantly greater improvements in glycemic and lipid control than did a conventional diabetes diet in patients with type 2 diabetes.
Hemoglobin A1c levels in 49 patients on the low-fat vegan diet improved from 8.06 to 7.65 at 74 weeks, but while the levels in 50 patients on the conventional diabetes diet initially improved from 7.93 to about 7.7 at 11 weeks, at 74 weeks they had increased to 7.94 (Diabetes Care 2006;29:1777-83).
Among the other findings that Ms. Jardine mentioned were those from "a remarkable study" in which 17 of 21 patients with sharp, burning pain characteristic of distal polyneuropathy experienced complete pain relief after initiating a low-fat, high-fiber, vegan diet along with a daily 30-minute walk, and findings from several studies that have suggested that plant-based eating preserved renal function.
Moreover, a plant-based eating pattern has been shown to reverse coronary artery disease and improve magnesium intake (which reduces insulin resistance), and the high fiber intake associated with plant-based eating improves glucose control and decreases mortality from circulatory, digestive, and inflammatory disease, she said.
Two recent studies demonstrated that meat consumption substantially increases the risk of type 2 diabetes. Even just a half serving per day increase was associated with a 48% increase over 4 years in one study (JAMA Intern. Med. 2013;173:1328-35).
Ms. Jardine noted that the Academy of Nutrition and Dietetics position is that "appropriately planned vegetarian diets, including total vegetarian or vegan diets, are healthful, nutritionally adequate and may provide health benefits in the prevention and treatment of certain disease," and that such diets have been found to be "highly acceptable in diverse populations with various disease states" (Diabetes Educ. 2010:36:33-48).
She warned that patients with diabetes who are on medications and who begin to follow a plant-based eating pattern should be instructed about how to recognize and treat hypoglycemia, as adjustments to medications that lower glucose, blood pressure, and cholesterol may be needed.
ORLANDO – Evidence increasingly supports plant-based nutrition for preventing diabetes or improving outcomes in those with diabetes.
The Adventist Health Study-2 (AHS-2), for example, demonstrated that a plant-based eating pattern – defined as ad libitum whole grains, legumes, fruits, and vegetables, and avoidance of all animal products, added oils, and high-fat foods – reduced the incidence of type 2 diabetes. The prospective cohort study involving more than 96,000 adults demonstrated that body mass index and the incidence of diabetes increased in tandem with the amount of animal products in the diet, according to Meghan Jardine, who reviewed the recent literature on plant-based nutrition in a poster presented at the annual meeting of the American Association of Diabetes Educators.
The prevalence of type 2 diabetes among nonvegetarians, semivegetarians, pescovegetarians, lacto-ovovegetarians, and vegans in that study was 7.6%, 6.1%, 4.9%, 3.2%, and 2.9%, respectively, and BMI for each of those groups was 28.8, 27.3, 26.3, 25.7, and 23.6 kg/m2, respectively, said Ms. Jardine, a registered and licensed dietician, certified diabetes educator, and diabetes education coordinator at Parkland Health and Hospital System, Dallas.
AHS-2 also demonstrated increased longevity in those who followed a plant-based eating pattern, with men living 9.5 years longer and women living 6.1 years longer than their meat-eating counterparts (JAMA 2013;173:1230-8).
In addition, a National Institutes of Health study demonstrated that a low-fat vegan diet led to significantly greater improvements in glycemic and lipid control than did a conventional diabetes diet in patients with type 2 diabetes.
Hemoglobin A1c levels in 49 patients on the low-fat vegan diet improved from 8.06 to 7.65 at 74 weeks, but while the levels in 50 patients on the conventional diabetes diet initially improved from 7.93 to about 7.7 at 11 weeks, at 74 weeks they had increased to 7.94 (Diabetes Care 2006;29:1777-83).
Among the other findings that Ms. Jardine mentioned were those from "a remarkable study" in which 17 of 21 patients with sharp, burning pain characteristic of distal polyneuropathy experienced complete pain relief after initiating a low-fat, high-fiber, vegan diet along with a daily 30-minute walk, and findings from several studies that have suggested that plant-based eating preserved renal function.
Moreover, a plant-based eating pattern has been shown to reverse coronary artery disease and improve magnesium intake (which reduces insulin resistance), and the high fiber intake associated with plant-based eating improves glucose control and decreases mortality from circulatory, digestive, and inflammatory disease, she said.
Two recent studies demonstrated that meat consumption substantially increases the risk of type 2 diabetes. Even just a half serving per day increase was associated with a 48% increase over 4 years in one study (JAMA Intern. Med. 2013;173:1328-35).
Ms. Jardine noted that the Academy of Nutrition and Dietetics position is that "appropriately planned vegetarian diets, including total vegetarian or vegan diets, are healthful, nutritionally adequate and may provide health benefits in the prevention and treatment of certain disease," and that such diets have been found to be "highly acceptable in diverse populations with various disease states" (Diabetes Educ. 2010:36:33-48).
She warned that patients with diabetes who are on medications and who begin to follow a plant-based eating pattern should be instructed about how to recognize and treat hypoglycemia, as adjustments to medications that lower glucose, blood pressure, and cholesterol may be needed.
AT AADE 14
Key clinical point: Vegan diets help.
Major finding: Longevity was increased in men (by 9.5 years) and women (by 6.1 years) with a plant- vs. meat-based diet in one study.
Data source: A review of the literature on plant-based nutrition.
Disclosures: Ms. Jardine reported having no disclosures.
Mindfulness meditation helped veterans with diabetes management
ORLANDO – They weren’t asked to sit in the lotus pose or study with the monks. Rather, a small group of older veterans were introduced to simple mindfulness meditation, and in a short period, they began doing a better job of managing the stress related to their diabetes and lowered their hemoglobin A1c levels.
More importantly, most said they enjoyed meditating, according to Monica DiNardo, Ph.D.
By the end of the 3-month feasibility study, conducted at the Veterans Affairs Pittsburgh Healthcare System, the participants’ diabetes-related stress had dropped by 41% and their HbA1c had dropped by roughly 1%.
The study was small – 28 patients – and it was not controlled, "so we really can’t draw generalizations from this," said Dr. DiNardo, who presented the study at the annual meeting of the American Association of Diabetes Educators. What it does show, she said, is that introducing the program wasn’t a distraction to the diabetes education process.
Helping patients manage diabetes-related stress is important, especially in the veteran population, where a quarter, or nearly a 1 million individuals, have diabetes.
And while healthy coping is one of seven self-care behaviors recommended by the AADE7 framework, many persons with diabetes don’t receive training for healthy coping strategies to deal with the stress that usually comes along with having diabetes.
"There’s a need to incorporate practical, evidence-based programs into diabetes self-management education (DSME) to fill this gap," said Dr. DiNardo, a diabetes nurse practitioner and an educator at the VA Pittsburgh.
To assess the feasibility of implementing a brief mindfulness intervention within diabetes self-management education, Dr. DiNardo and her colleagues created an intervention called Mind-STRIDE (Mindfulness Stress Reduction in Diabetes Education).
The research team used several assessment tools, including the Five Facet Mindfulness Questionnaire, Perceived Stress Scale, and Problem Areas in Diabetes Scale (to measure diabetes-related stress) to measure the changes over time.
The 28 veterans, who were on average 60 years old, were enrolled in DSME. The majority had type 2 diabetes and their HbA1c levels were higher than 7%. Also, half of the group was college educated, nearly 70% were married, and 60% were retired or disabled.
The group received a 90-minute training in mindfulness following their DSME session. Participants were given a CD, recorded by Dr. DiNardo, to practice with at home. They were also given practice diaries. They received a 30-minute booster session 1 month later.
Twenty of the 28 individuals stayed in the study; 11 completed their practice diaries. All said they found the intervention interesting and easy to understand, and almost all said that they learned something new and planned to continue practicing mindfulness.
Results after 3 months showed that there was a significant negative correlation between awareness and nonjudgment – two elements of the five-facet mindfulness – and diabetes-related stress. In contrast, the two facets showed a significant positive correlation with coping abilities. There were also significant positive correlations between the two facets and diabetes self management and the total AADE7 score.
Dr. DiNardo speculated that the meditation helped participants remove the self-judgment attached to having the disease and gain the ability to be aware of the disease and how to cope with it.
When assessing baseline to 3-month gain and effect size for various assessments, all showed changes in a "hopeful" direction, said Dr. DiNardo.
The most significant trend over the 3-month period was the 40% drop in diabetes-related stress (difference in raw scores), measured by the Problem Areas in Diabetes Scale. Meanwhile, awareness and coping ability increased slightly during the study period.
Dr. DiNardo said that the cost associated with implementing the program was minimal, and the only requirement was access to someone who knew mindfulness meditation.
"We need innovative therapy to promote healthy behaviors for patients with diabetes," she said. Mind-body therapies have the potential to serve as a bridge between the clinic and home and give patients yet another tool to manage their diabetes.
Dr. DiNardo had no financial disclosures. The study was supported by a grant from AADE.
On Twitter @naseemmiller
ORLANDO – They weren’t asked to sit in the lotus pose or study with the monks. Rather, a small group of older veterans were introduced to simple mindfulness meditation, and in a short period, they began doing a better job of managing the stress related to their diabetes and lowered their hemoglobin A1c levels.
More importantly, most said they enjoyed meditating, according to Monica DiNardo, Ph.D.
By the end of the 3-month feasibility study, conducted at the Veterans Affairs Pittsburgh Healthcare System, the participants’ diabetes-related stress had dropped by 41% and their HbA1c had dropped by roughly 1%.
The study was small – 28 patients – and it was not controlled, "so we really can’t draw generalizations from this," said Dr. DiNardo, who presented the study at the annual meeting of the American Association of Diabetes Educators. What it does show, she said, is that introducing the program wasn’t a distraction to the diabetes education process.
Helping patients manage diabetes-related stress is important, especially in the veteran population, where a quarter, or nearly a 1 million individuals, have diabetes.
And while healthy coping is one of seven self-care behaviors recommended by the AADE7 framework, many persons with diabetes don’t receive training for healthy coping strategies to deal with the stress that usually comes along with having diabetes.
"There’s a need to incorporate practical, evidence-based programs into diabetes self-management education (DSME) to fill this gap," said Dr. DiNardo, a diabetes nurse practitioner and an educator at the VA Pittsburgh.
To assess the feasibility of implementing a brief mindfulness intervention within diabetes self-management education, Dr. DiNardo and her colleagues created an intervention called Mind-STRIDE (Mindfulness Stress Reduction in Diabetes Education).
The research team used several assessment tools, including the Five Facet Mindfulness Questionnaire, Perceived Stress Scale, and Problem Areas in Diabetes Scale (to measure diabetes-related stress) to measure the changes over time.
The 28 veterans, who were on average 60 years old, were enrolled in DSME. The majority had type 2 diabetes and their HbA1c levels were higher than 7%. Also, half of the group was college educated, nearly 70% were married, and 60% were retired or disabled.
The group received a 90-minute training in mindfulness following their DSME session. Participants were given a CD, recorded by Dr. DiNardo, to practice with at home. They were also given practice diaries. They received a 30-minute booster session 1 month later.
Twenty of the 28 individuals stayed in the study; 11 completed their practice diaries. All said they found the intervention interesting and easy to understand, and almost all said that they learned something new and planned to continue practicing mindfulness.
Results after 3 months showed that there was a significant negative correlation between awareness and nonjudgment – two elements of the five-facet mindfulness – and diabetes-related stress. In contrast, the two facets showed a significant positive correlation with coping abilities. There were also significant positive correlations between the two facets and diabetes self management and the total AADE7 score.
Dr. DiNardo speculated that the meditation helped participants remove the self-judgment attached to having the disease and gain the ability to be aware of the disease and how to cope with it.
When assessing baseline to 3-month gain and effect size for various assessments, all showed changes in a "hopeful" direction, said Dr. DiNardo.
The most significant trend over the 3-month period was the 40% drop in diabetes-related stress (difference in raw scores), measured by the Problem Areas in Diabetes Scale. Meanwhile, awareness and coping ability increased slightly during the study period.
Dr. DiNardo said that the cost associated with implementing the program was minimal, and the only requirement was access to someone who knew mindfulness meditation.
"We need innovative therapy to promote healthy behaviors for patients with diabetes," she said. Mind-body therapies have the potential to serve as a bridge between the clinic and home and give patients yet another tool to manage their diabetes.
Dr. DiNardo had no financial disclosures. The study was supported by a grant from AADE.
On Twitter @naseemmiller
ORLANDO – They weren’t asked to sit in the lotus pose or study with the monks. Rather, a small group of older veterans were introduced to simple mindfulness meditation, and in a short period, they began doing a better job of managing the stress related to their diabetes and lowered their hemoglobin A1c levels.
More importantly, most said they enjoyed meditating, according to Monica DiNardo, Ph.D.
By the end of the 3-month feasibility study, conducted at the Veterans Affairs Pittsburgh Healthcare System, the participants’ diabetes-related stress had dropped by 41% and their HbA1c had dropped by roughly 1%.
The study was small – 28 patients – and it was not controlled, "so we really can’t draw generalizations from this," said Dr. DiNardo, who presented the study at the annual meeting of the American Association of Diabetes Educators. What it does show, she said, is that introducing the program wasn’t a distraction to the diabetes education process.
Helping patients manage diabetes-related stress is important, especially in the veteran population, where a quarter, or nearly a 1 million individuals, have diabetes.
And while healthy coping is one of seven self-care behaviors recommended by the AADE7 framework, many persons with diabetes don’t receive training for healthy coping strategies to deal with the stress that usually comes along with having diabetes.
"There’s a need to incorporate practical, evidence-based programs into diabetes self-management education (DSME) to fill this gap," said Dr. DiNardo, a diabetes nurse practitioner and an educator at the VA Pittsburgh.
To assess the feasibility of implementing a brief mindfulness intervention within diabetes self-management education, Dr. DiNardo and her colleagues created an intervention called Mind-STRIDE (Mindfulness Stress Reduction in Diabetes Education).
The research team used several assessment tools, including the Five Facet Mindfulness Questionnaire, Perceived Stress Scale, and Problem Areas in Diabetes Scale (to measure diabetes-related stress) to measure the changes over time.
The 28 veterans, who were on average 60 years old, were enrolled in DSME. The majority had type 2 diabetes and their HbA1c levels were higher than 7%. Also, half of the group was college educated, nearly 70% were married, and 60% were retired or disabled.
The group received a 90-minute training in mindfulness following their DSME session. Participants were given a CD, recorded by Dr. DiNardo, to practice with at home. They were also given practice diaries. They received a 30-minute booster session 1 month later.
Twenty of the 28 individuals stayed in the study; 11 completed their practice diaries. All said they found the intervention interesting and easy to understand, and almost all said that they learned something new and planned to continue practicing mindfulness.
Results after 3 months showed that there was a significant negative correlation between awareness and nonjudgment – two elements of the five-facet mindfulness – and diabetes-related stress. In contrast, the two facets showed a significant positive correlation with coping abilities. There were also significant positive correlations between the two facets and diabetes self management and the total AADE7 score.
Dr. DiNardo speculated that the meditation helped participants remove the self-judgment attached to having the disease and gain the ability to be aware of the disease and how to cope with it.
When assessing baseline to 3-month gain and effect size for various assessments, all showed changes in a "hopeful" direction, said Dr. DiNardo.
The most significant trend over the 3-month period was the 40% drop in diabetes-related stress (difference in raw scores), measured by the Problem Areas in Diabetes Scale. Meanwhile, awareness and coping ability increased slightly during the study period.
Dr. DiNardo said that the cost associated with implementing the program was minimal, and the only requirement was access to someone who knew mindfulness meditation.
"We need innovative therapy to promote healthy behaviors for patients with diabetes," she said. Mind-body therapies have the potential to serve as a bridge between the clinic and home and give patients yet another tool to manage their diabetes.
Dr. DiNardo had no financial disclosures. The study was supported by a grant from AADE.
On Twitter @naseemmiller
AT AADE 2014
Key clinical point: Mindfulness meditation can be incorporated to diabetes education at minimal cost.
Major finding: By the end of the 3-month feasibility study, the participants’ diabetes-related stress had dropped by 41% and their HbA1c had dropped by roughly 1%.
Data source: 28 patients with diabetes enrolled in DSME.
Disclosures: Dr. DiNardo had no disclosures.
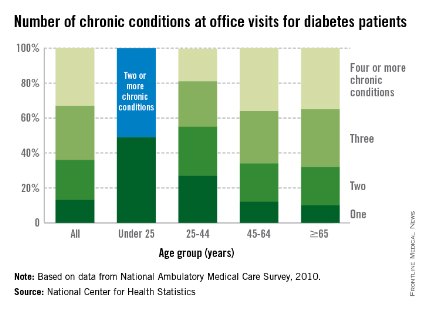
Additional chronic conditions seen in 87% of diabetes patients
In 2010, 87% of diabetes patients who visited an office-based physician had at least one additional chronic condition, the National Center for Health Statistics reported.
For diabetes patients under the age of 25 years, just over half (51%) of their visits involved patients who had two or more additional chronic conditions, and the number of conditions increased with age. Among those aged 25-44 years, 72% of visits in 2010 involved patients with two or more chronic conditions, according to the NCHS.
In the 45- to 64-year age group, 88% of visits were made by patients with two or more chronic conditions, with 36% involving patients who had four or more such conditions. Among those aged 65 years and over, 90% of visits by patients with diabetes were made by those with two or more additional chronic conditions, the NCHS report said.
The analysis was based on data from the National Ambulatory Medical Care Survey. Information was collected on 13 other chronic conditions besides diabetes: arthritis, asthma, cancer, chronic kidney disease, chronic obstructive pulmonary disease, heart failure, coronary heart disease, depression, hyperlipidemia, hypertension, obesity, osteoporosis, and stroke.
In 2010, 87% of diabetes patients who visited an office-based physician had at least one additional chronic condition, the National Center for Health Statistics reported.
For diabetes patients under the age of 25 years, just over half (51%) of their visits involved patients who had two or more additional chronic conditions, and the number of conditions increased with age. Among those aged 25-44 years, 72% of visits in 2010 involved patients with two or more chronic conditions, according to the NCHS.
In the 45- to 64-year age group, 88% of visits were made by patients with two or more chronic conditions, with 36% involving patients who had four or more such conditions. Among those aged 65 years and over, 90% of visits by patients with diabetes were made by those with two or more additional chronic conditions, the NCHS report said.
The analysis was based on data from the National Ambulatory Medical Care Survey. Information was collected on 13 other chronic conditions besides diabetes: arthritis, asthma, cancer, chronic kidney disease, chronic obstructive pulmonary disease, heart failure, coronary heart disease, depression, hyperlipidemia, hypertension, obesity, osteoporosis, and stroke.
In 2010, 87% of diabetes patients who visited an office-based physician had at least one additional chronic condition, the National Center for Health Statistics reported.
For diabetes patients under the age of 25 years, just over half (51%) of their visits involved patients who had two or more additional chronic conditions, and the number of conditions increased with age. Among those aged 25-44 years, 72% of visits in 2010 involved patients with two or more chronic conditions, according to the NCHS.
In the 45- to 64-year age group, 88% of visits were made by patients with two or more chronic conditions, with 36% involving patients who had four or more such conditions. Among those aged 65 years and over, 90% of visits by patients with diabetes were made by those with two or more additional chronic conditions, the NCHS report said.
The analysis was based on data from the National Ambulatory Medical Care Survey. Information was collected on 13 other chronic conditions besides diabetes: arthritis, asthma, cancer, chronic kidney disease, chronic obstructive pulmonary disease, heart failure, coronary heart disease, depression, hyperlipidemia, hypertension, obesity, osteoporosis, and stroke.
Pharmacist-led clinic helps improve diabetes outcomes
SAN FRANCISCO – Hemoglobin A1c levels fell by 2.4% in veterans with diabetes whose primary care physicians referred them to a 6-month pharmacist-led intense management clinic, compared with a 0.2% drop in similar patients who did not attend the clinic.
That translates to a $9,104 reduction in estimated 3-year medical costs for each patient seen in the clinic and a $1,803 drop in costs in the comparison group, reported Candis M. Morello, Pharm.D. The changes in HbA1c and costs in the intervention group were significant, compared with the nonclinic group.
After factoring in the $61,992 cost of the pharmacist over 3 years, $7.81 would be saved for every $1 spent on the program, said Dr. Morello of the University of California, San Diego, and director of the diabetes intense medical management clinic in the Veterans Affairs San Diego Healthcare System.
The clinic is a collaborative practice between an endocrinologist and a doctor of pharmacy who also is a certified diabetes educator and has full prescribing privileges. The pharmacist spends 4 hours/week in the clinic and 3 hours/week on phone follow-up calls to manage 60 patients per year who have HbA1c levels of at least 8%, high comorbidity, and complex medication regimens.
Patients are referred by primary care providers for the 6-month "tune-up" clinic involving three to five hour-long, one-on-one visits between the patient and the pharmacist. After that, patients return to their primary care providers but can make follow-up phone calls to the clinic.
The tune-up focuses on finding the best combination of medications for the individual patient, education on medication adherence, simplifying the drug regimen to fit around the patient’s schedule, and setting personalized goals.
The study compared clinic patients with a random sample of patients treated by primary care providers in the same time period. Initial HbA1c levels were 10.5% in the clinic group and 9.3% in the comparison group, Dr. Morello and her associates reported at the annual scientific session of the American Diabetes Association.
They used a published regression model applied to retrospective chart data to estimate the 3-year costs of medical care (Diabetes Care 1997;20:1847-53). Based on baseline health status (largely driven by HbA1c levels), estimated costs per patient were $42,032 in the clinic group and $37,065 in the comparison group. Assuming that HbA1c changes were maintained 3 years later, estimated costs of care were $32,928 in the clinic group and $35,262 in the comparison group.
For 60 patients seen per year in the clinic, that amounts to a cumulative potential $546,240 savings from reduced costs, for a benefit-to-cost ratio of $8.81 and a return on investment of $7.81, she said.
If mean HbA1c levels rise by 1% over 3 years, the estimated medical cost avoided would be $6,412 per patient in the clinic group, still better than results in the comparison group, a secondary analysis found. That adds up to $384,720 in costs avoided over 3 years, for a benefit-to-cost ratio of $6.21 and a $5.21 return on investment after factoring in the cost of the pharmacist.
"I’m pretty sure that spending a little bit of money on the front end saves money on the back end," Dr. Morello said.
She reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Hemoglobin A1c levels fell by 2.4% in veterans with diabetes whose primary care physicians referred them to a 6-month pharmacist-led intense management clinic, compared with a 0.2% drop in similar patients who did not attend the clinic.
That translates to a $9,104 reduction in estimated 3-year medical costs for each patient seen in the clinic and a $1,803 drop in costs in the comparison group, reported Candis M. Morello, Pharm.D. The changes in HbA1c and costs in the intervention group were significant, compared with the nonclinic group.
After factoring in the $61,992 cost of the pharmacist over 3 years, $7.81 would be saved for every $1 spent on the program, said Dr. Morello of the University of California, San Diego, and director of the diabetes intense medical management clinic in the Veterans Affairs San Diego Healthcare System.
The clinic is a collaborative practice between an endocrinologist and a doctor of pharmacy who also is a certified diabetes educator and has full prescribing privileges. The pharmacist spends 4 hours/week in the clinic and 3 hours/week on phone follow-up calls to manage 60 patients per year who have HbA1c levels of at least 8%, high comorbidity, and complex medication regimens.
Patients are referred by primary care providers for the 6-month "tune-up" clinic involving three to five hour-long, one-on-one visits between the patient and the pharmacist. After that, patients return to their primary care providers but can make follow-up phone calls to the clinic.
The tune-up focuses on finding the best combination of medications for the individual patient, education on medication adherence, simplifying the drug regimen to fit around the patient’s schedule, and setting personalized goals.
The study compared clinic patients with a random sample of patients treated by primary care providers in the same time period. Initial HbA1c levels were 10.5% in the clinic group and 9.3% in the comparison group, Dr. Morello and her associates reported at the annual scientific session of the American Diabetes Association.
They used a published regression model applied to retrospective chart data to estimate the 3-year costs of medical care (Diabetes Care 1997;20:1847-53). Based on baseline health status (largely driven by HbA1c levels), estimated costs per patient were $42,032 in the clinic group and $37,065 in the comparison group. Assuming that HbA1c changes were maintained 3 years later, estimated costs of care were $32,928 in the clinic group and $35,262 in the comparison group.
For 60 patients seen per year in the clinic, that amounts to a cumulative potential $546,240 savings from reduced costs, for a benefit-to-cost ratio of $8.81 and a return on investment of $7.81, she said.
If mean HbA1c levels rise by 1% over 3 years, the estimated medical cost avoided would be $6,412 per patient in the clinic group, still better than results in the comparison group, a secondary analysis found. That adds up to $384,720 in costs avoided over 3 years, for a benefit-to-cost ratio of $6.21 and a $5.21 return on investment after factoring in the cost of the pharmacist.
"I’m pretty sure that spending a little bit of money on the front end saves money on the back end," Dr. Morello said.
She reported having no financial disclosures.
On Twitter @sherryboschert
SAN FRANCISCO – Hemoglobin A1c levels fell by 2.4% in veterans with diabetes whose primary care physicians referred them to a 6-month pharmacist-led intense management clinic, compared with a 0.2% drop in similar patients who did not attend the clinic.
That translates to a $9,104 reduction in estimated 3-year medical costs for each patient seen in the clinic and a $1,803 drop in costs in the comparison group, reported Candis M. Morello, Pharm.D. The changes in HbA1c and costs in the intervention group were significant, compared with the nonclinic group.
After factoring in the $61,992 cost of the pharmacist over 3 years, $7.81 would be saved for every $1 spent on the program, said Dr. Morello of the University of California, San Diego, and director of the diabetes intense medical management clinic in the Veterans Affairs San Diego Healthcare System.
The clinic is a collaborative practice between an endocrinologist and a doctor of pharmacy who also is a certified diabetes educator and has full prescribing privileges. The pharmacist spends 4 hours/week in the clinic and 3 hours/week on phone follow-up calls to manage 60 patients per year who have HbA1c levels of at least 8%, high comorbidity, and complex medication regimens.
Patients are referred by primary care providers for the 6-month "tune-up" clinic involving three to five hour-long, one-on-one visits between the patient and the pharmacist. After that, patients return to their primary care providers but can make follow-up phone calls to the clinic.
The tune-up focuses on finding the best combination of medications for the individual patient, education on medication adherence, simplifying the drug regimen to fit around the patient’s schedule, and setting personalized goals.
The study compared clinic patients with a random sample of patients treated by primary care providers in the same time period. Initial HbA1c levels were 10.5% in the clinic group and 9.3% in the comparison group, Dr. Morello and her associates reported at the annual scientific session of the American Diabetes Association.
They used a published regression model applied to retrospective chart data to estimate the 3-year costs of medical care (Diabetes Care 1997;20:1847-53). Based on baseline health status (largely driven by HbA1c levels), estimated costs per patient were $42,032 in the clinic group and $37,065 in the comparison group. Assuming that HbA1c changes were maintained 3 years later, estimated costs of care were $32,928 in the clinic group and $35,262 in the comparison group.
For 60 patients seen per year in the clinic, that amounts to a cumulative potential $546,240 savings from reduced costs, for a benefit-to-cost ratio of $8.81 and a return on investment of $7.81, she said.
If mean HbA1c levels rise by 1% over 3 years, the estimated medical cost avoided would be $6,412 per patient in the clinic group, still better than results in the comparison group, a secondary analysis found. That adds up to $384,720 in costs avoided over 3 years, for a benefit-to-cost ratio of $6.21 and a $5.21 return on investment after factoring in the cost of the pharmacist.
"I’m pretty sure that spending a little bit of money on the front end saves money on the back end," Dr. Morello said.
She reported having no financial disclosures.
On Twitter @sherryboschert
AT THE ADA ANNUAL SCIENTIFIC SESSION
Key clinical point: A 6-month pharmacist-led diabetes clinic lowered HbA1c levels and reduced estimated costs.
Major finding: HbA1c levels fell by 2.4% in the intervention group and 0.2% in the comparison group.
Data source: A retrospective comparison of data on 85 patients in the intervention group and 51 patients seen in primary care clinics.
Disclosures: Dr. Morello reported having no financial disclosures.
High sodium intake increases heart disease risk in type 2 diabetics
High sodium intake can double the risk of cardiovascular disease in type 2 diabetes patients – and increase it nearly 10-fold if the diabetes is poorly controlled, according to a recent study.
"It was suggested that dietary salt restriction as medical nutritional treatment would be useful to prevent complications of diabetes in patients with type 2 diabetes," Chika Horikawa of the University of Niigata, Japan, and her colleagues reported online (J. Clin. Endocrinol. Metab. 2014 July 22 [doi:10.1210/jc.2013-4315]).
The researchers assessed mean daily sodium intake from a baseline dietary survey of 1,588 participants, aged 40-70 years, with type 2 diabetes and hemoglobin A1c levels of at least 6.5%. The participants were recruited from 59 university and general hospitals in Japan and then tracked from intake, from January 1995 to March 1996, until March 2003 for cardiovascular disease, overt nephropathy, diabetic retinopathy, and all-cause mortality.
Over the 8 years of follow-up, cardiovascular disease occurred at a rate of 13.61 incidents/1,000 patient-years. Participants consuming the highest quartile of sodium – a mean 5.9 g/day – were twice as likely (hazard ratio, 2.07) as those consuming the lowest quartile – a mean 2.8 g/day – to develop cardiovascular disease, a significant difference. A sodium intake in the second and third quartiles increased cardiovascular disease risk 1.70 and 1.47 times, respectively, compared to the first quartile.
Patients with HbA1c greater than 9% and consuming sodium in the highest quartile were 9.91 times more likely to develop cardiovascular disease than were those in the first quartile with HbA1c less than 9%. The researchers found no association between sodium intake and risk of overt nephropathy, diabetic retinopathy, or all-cause mortality.
The research was funded by Honjo International Scholarship Foundation, the University of Tsukuba Research Infrastructure Support Program, the Japan Society for the Promotion of Science and the Japanese Ministry of Health, Labor and Welfare. The authors had no disclosures.
High sodium intake can double the risk of cardiovascular disease in type 2 diabetes patients – and increase it nearly 10-fold if the diabetes is poorly controlled, according to a recent study.
"It was suggested that dietary salt restriction as medical nutritional treatment would be useful to prevent complications of diabetes in patients with type 2 diabetes," Chika Horikawa of the University of Niigata, Japan, and her colleagues reported online (J. Clin. Endocrinol. Metab. 2014 July 22 [doi:10.1210/jc.2013-4315]).
The researchers assessed mean daily sodium intake from a baseline dietary survey of 1,588 participants, aged 40-70 years, with type 2 diabetes and hemoglobin A1c levels of at least 6.5%. The participants were recruited from 59 university and general hospitals in Japan and then tracked from intake, from January 1995 to March 1996, until March 2003 for cardiovascular disease, overt nephropathy, diabetic retinopathy, and all-cause mortality.
Over the 8 years of follow-up, cardiovascular disease occurred at a rate of 13.61 incidents/1,000 patient-years. Participants consuming the highest quartile of sodium – a mean 5.9 g/day – were twice as likely (hazard ratio, 2.07) as those consuming the lowest quartile – a mean 2.8 g/day – to develop cardiovascular disease, a significant difference. A sodium intake in the second and third quartiles increased cardiovascular disease risk 1.70 and 1.47 times, respectively, compared to the first quartile.
Patients with HbA1c greater than 9% and consuming sodium in the highest quartile were 9.91 times more likely to develop cardiovascular disease than were those in the first quartile with HbA1c less than 9%. The researchers found no association between sodium intake and risk of overt nephropathy, diabetic retinopathy, or all-cause mortality.
The research was funded by Honjo International Scholarship Foundation, the University of Tsukuba Research Infrastructure Support Program, the Japan Society for the Promotion of Science and the Japanese Ministry of Health, Labor and Welfare. The authors had no disclosures.
High sodium intake can double the risk of cardiovascular disease in type 2 diabetes patients – and increase it nearly 10-fold if the diabetes is poorly controlled, according to a recent study.
"It was suggested that dietary salt restriction as medical nutritional treatment would be useful to prevent complications of diabetes in patients with type 2 diabetes," Chika Horikawa of the University of Niigata, Japan, and her colleagues reported online (J. Clin. Endocrinol. Metab. 2014 July 22 [doi:10.1210/jc.2013-4315]).
The researchers assessed mean daily sodium intake from a baseline dietary survey of 1,588 participants, aged 40-70 years, with type 2 diabetes and hemoglobin A1c levels of at least 6.5%. The participants were recruited from 59 university and general hospitals in Japan and then tracked from intake, from January 1995 to March 1996, until March 2003 for cardiovascular disease, overt nephropathy, diabetic retinopathy, and all-cause mortality.
Over the 8 years of follow-up, cardiovascular disease occurred at a rate of 13.61 incidents/1,000 patient-years. Participants consuming the highest quartile of sodium – a mean 5.9 g/day – were twice as likely (hazard ratio, 2.07) as those consuming the lowest quartile – a mean 2.8 g/day – to develop cardiovascular disease, a significant difference. A sodium intake in the second and third quartiles increased cardiovascular disease risk 1.70 and 1.47 times, respectively, compared to the first quartile.
Patients with HbA1c greater than 9% and consuming sodium in the highest quartile were 9.91 times more likely to develop cardiovascular disease than were those in the first quartile with HbA1c less than 9%. The researchers found no association between sodium intake and risk of overt nephropathy, diabetic retinopathy, or all-cause mortality.
The research was funded by Honjo International Scholarship Foundation, the University of Tsukuba Research Infrastructure Support Program, the Japan Society for the Promotion of Science and the Japanese Ministry of Health, Labor and Welfare. The authors had no disclosures.
FROM THE JOURNAL OF CLINICAL ENDOCRINOLOGY & METABOLISM
Key clinical point: People with diabetes who consumed the highest rates of sodium were twice as likely to develop cardiovascular disease.
Major finding: Patients with type 2 diabetes with a mean daily sodium intake of 5.9 g are twice as likely (HR, 2.07) to develop cardiovascular disease than patients with diabetes who consume a mean daily 2.8 g of sodium (P less than.01).
Data source: A Japanese nationwide cohort study in 1,588 participants with type 2 diabetes and HbA1c of at least 6.5%.
Disclosures: The research was funded by Honjo International Scholarship Foundation, the University of Tsukuba Research Infrastructure Support Program, the Japan Society for the Promotion of Science and the Japanese Ministry of Health, Labor and Welfare. The authors had no disclosures.
FDA approves empagliflozin for adults with type 2 diabetes
The Food and Drug Administration has approved once-daily oral empagliflozin for adults with type 2 diabetes, based on seven studies with nearly 4,500 patients.
Empagliflozin is a sodium glucose cotransporter 2 (SGLT2) inhibitor that blocks the reabsorption of glucose by the kidney, increases glucose excretion, and lowers blood glucose levels. It has been studied "as a stand-alone therapy and in combination with other type 2 diabetes therapies including metformin, sulfonylureas, pioglitazone, and insulin," according to an Aug. 1 FDA statement announcing the approval.
Boehringer Ingelheim Pharmaceuticals will market empagliflozin as Jardiance.
This is the third SGLT2 inhibitor approved by the FDA, following the approval of dapagliflozin (Farxiga) in January 2014 and canagliflozin (Invokana) in March 2013.
The most common side effects of treatment are genital infections in women and urinary tract infections, according to the FDA. Treatment can also cause dehydration resulting in hypotension, with dizziness and/or fainting, as well as reduced renal function. "The elderly, patients with impaired renal function, and patients on diuretics to treat other conditions appeared to be more susceptible to this risk," the FDA noted.
Empagliflozin should not be used to treat patients with severe renal impairment or end-stage renal disease, or who are on dialysis. The drug also should not be used in patients with diabetic ketoacidosis and those with type 1 diabetes.
Boehringer Ingelheim must conduct four postmarketing studies of empagliflozin: a cardiovascular outcomes trial, which is already underway; a pediatric pharmacokinetic/pharmacodynamic study; a pediatric safety and efficacy study (which will include evaluations of bone health and development); and a juvenile animal toxicity study. The animal study will have "a particular focus on renal development, bone development, and growth," the FDA statement said.
In May, the European Commission approved empagliflozin for treating adults with type 2 diabetes.
The Food and Drug Administration has approved once-daily oral empagliflozin for adults with type 2 diabetes, based on seven studies with nearly 4,500 patients.
Empagliflozin is a sodium glucose cotransporter 2 (SGLT2) inhibitor that blocks the reabsorption of glucose by the kidney, increases glucose excretion, and lowers blood glucose levels. It has been studied "as a stand-alone therapy and in combination with other type 2 diabetes therapies including metformin, sulfonylureas, pioglitazone, and insulin," according to an Aug. 1 FDA statement announcing the approval.
Boehringer Ingelheim Pharmaceuticals will market empagliflozin as Jardiance.
This is the third SGLT2 inhibitor approved by the FDA, following the approval of dapagliflozin (Farxiga) in January 2014 and canagliflozin (Invokana) in March 2013.
The most common side effects of treatment are genital infections in women and urinary tract infections, according to the FDA. Treatment can also cause dehydration resulting in hypotension, with dizziness and/or fainting, as well as reduced renal function. "The elderly, patients with impaired renal function, and patients on diuretics to treat other conditions appeared to be more susceptible to this risk," the FDA noted.
Empagliflozin should not be used to treat patients with severe renal impairment or end-stage renal disease, or who are on dialysis. The drug also should not be used in patients with diabetic ketoacidosis and those with type 1 diabetes.
Boehringer Ingelheim must conduct four postmarketing studies of empagliflozin: a cardiovascular outcomes trial, which is already underway; a pediatric pharmacokinetic/pharmacodynamic study; a pediatric safety and efficacy study (which will include evaluations of bone health and development); and a juvenile animal toxicity study. The animal study will have "a particular focus on renal development, bone development, and growth," the FDA statement said.
In May, the European Commission approved empagliflozin for treating adults with type 2 diabetes.
The Food and Drug Administration has approved once-daily oral empagliflozin for adults with type 2 diabetes, based on seven studies with nearly 4,500 patients.
Empagliflozin is a sodium glucose cotransporter 2 (SGLT2) inhibitor that blocks the reabsorption of glucose by the kidney, increases glucose excretion, and lowers blood glucose levels. It has been studied "as a stand-alone therapy and in combination with other type 2 diabetes therapies including metformin, sulfonylureas, pioglitazone, and insulin," according to an Aug. 1 FDA statement announcing the approval.
Boehringer Ingelheim Pharmaceuticals will market empagliflozin as Jardiance.
This is the third SGLT2 inhibitor approved by the FDA, following the approval of dapagliflozin (Farxiga) in January 2014 and canagliflozin (Invokana) in March 2013.
The most common side effects of treatment are genital infections in women and urinary tract infections, according to the FDA. Treatment can also cause dehydration resulting in hypotension, with dizziness and/or fainting, as well as reduced renal function. "The elderly, patients with impaired renal function, and patients on diuretics to treat other conditions appeared to be more susceptible to this risk," the FDA noted.
Empagliflozin should not be used to treat patients with severe renal impairment or end-stage renal disease, or who are on dialysis. The drug also should not be used in patients with diabetic ketoacidosis and those with type 1 diabetes.
Boehringer Ingelheim must conduct four postmarketing studies of empagliflozin: a cardiovascular outcomes trial, which is already underway; a pediatric pharmacokinetic/pharmacodynamic study; a pediatric safety and efficacy study (which will include evaluations of bone health and development); and a juvenile animal toxicity study. The animal study will have "a particular focus on renal development, bone development, and growth," the FDA statement said.
In May, the European Commission approved empagliflozin for treating adults with type 2 diabetes.
Donated IVF eggs linked to gestational hypertension
MUNICH – Women pregnant with an embryo produced by in vitro fertilization of a donated egg developed gestational hypertension at nearly four times the rate of matched women who were pregnant following IVF with a self egg, in a multicenter, case-control study with 580 participants.
In addition, preeclampsia was more than four times higher in the women who had received a donor egg as part of an IVF procedure, compared with women who used a self egg for their IVF, Dr. Hélène Letur-Könirsch reported at the annual meeting of the European Society of Human Reproduction and Embryology.
Although the mechanism underlying this association is not known, one possible explanation is that when a woman carries an embryo that is completely allogenic, it triggers modified immune tolerance that leads to impaired trophoblast implantation. Other candidate hypotheses are that defective genes in the mother trigger abnormal metabolic pathways that cause hypertension and preeclampsia, and that ovarian insufficiency features reduced ovarian steroid production, causing vascular and immunologic changes that lead to pregnancy-induced hypertension.
Results from several prior studies also had shown a link between use of a donor egg for IVF and an increased rate of gestational hypertension and preeclampsia, but most prior studies had been smaller and failed to adequately control for possible confounders, said Dr. Letur-Könirsch, an endocrinologist at the Fertility Center of the Institut Mutualiste Montsouris in Paris.
She and her associates from seven IVF centers in France pooled data from their entire series of IVF cases that involved donated eggs during the period from February 2005 to September 2012, a total of 217 pregnant women. The analysis matched these cases with 363 control women who had IVF pregnancies during the study period using self eggs by parameters such as age, parity, time of pregnancy, and whether the IVF procedure involved transfer of a fresh or frozen embryo.
Women in the study averaged 35 years of age, with 82% aged 39 years or younger. Average body mass index was virtually identical in both groups, about 24 kg/m2, and the live-birth rate was 79% in both groups. All women in both groups were normotensive prior to their IVF procedure.
The incidence of pregnancy-induced hypertension, defined as blood pressure that reached at least 140/90 mm Hg when measured in office on both arms with two separate measurements, was about 29% in the women who received a donated egg and 14% in those who used a self egg. Development of preeclampsia, defined as persistent gestational hypertension plus proteinuria of at least 0.3 g/day, occurred in about 18% of women who received a donated egg and 7% in those who used a self egg.
In a multivariate analysis that controlled for age, pregnancy history, and use of a fresh or frozen embryo, women who used a donated egg had a 3.9-fold increased rate of pregnancy-induced hypertension and a 4.6-fold increased rate of preeclampsia, compared with women who used a self egg – both statistically significant differences.
The findings suggested that before a woman embarks on pregnancy using a donated egg, she should undergo thorough evaluation for preexisting risk factors for gestational hypertension, including hypertension, obesity, diabetes, renal disease, chronic infection, autoimmune diseases such as systemic lupus erythematosus, a family history of preeclampsia, and living at a high altitude. If these risk factors are present, they should be controlled if possible. Women who have one or more of these risk factors may also be candidates for prophylactic treatment with aspirin to prevent development of preeclampsia, especially if they develop pregnancy-induced hypertension.
During pregnancy, women who received a donor egg should undergo regular and frequent blood pressure measurement, as well as assessment for other possible abnormalities such as Doppler ultrasound examination of uterine arteries and measuring serum and urine markers.
"Physicians and patients must be aware of the risk [from donor eggs] to assure that these women get adequate monitoring and management during pregnancy," Dr. Letur-Könirsch said.
Dr. Letur-Könirsch had no disclosures.
On Twitter @mitchelzoler
MUNICH – Women pregnant with an embryo produced by in vitro fertilization of a donated egg developed gestational hypertension at nearly four times the rate of matched women who were pregnant following IVF with a self egg, in a multicenter, case-control study with 580 participants.
In addition, preeclampsia was more than four times higher in the women who had received a donor egg as part of an IVF procedure, compared with women who used a self egg for their IVF, Dr. Hélène Letur-Könirsch reported at the annual meeting of the European Society of Human Reproduction and Embryology.
Although the mechanism underlying this association is not known, one possible explanation is that when a woman carries an embryo that is completely allogenic, it triggers modified immune tolerance that leads to impaired trophoblast implantation. Other candidate hypotheses are that defective genes in the mother trigger abnormal metabolic pathways that cause hypertension and preeclampsia, and that ovarian insufficiency features reduced ovarian steroid production, causing vascular and immunologic changes that lead to pregnancy-induced hypertension.
Results from several prior studies also had shown a link between use of a donor egg for IVF and an increased rate of gestational hypertension and preeclampsia, but most prior studies had been smaller and failed to adequately control for possible confounders, said Dr. Letur-Könirsch, an endocrinologist at the Fertility Center of the Institut Mutualiste Montsouris in Paris.
She and her associates from seven IVF centers in France pooled data from their entire series of IVF cases that involved donated eggs during the period from February 2005 to September 2012, a total of 217 pregnant women. The analysis matched these cases with 363 control women who had IVF pregnancies during the study period using self eggs by parameters such as age, parity, time of pregnancy, and whether the IVF procedure involved transfer of a fresh or frozen embryo.
Women in the study averaged 35 years of age, with 82% aged 39 years or younger. Average body mass index was virtually identical in both groups, about 24 kg/m2, and the live-birth rate was 79% in both groups. All women in both groups were normotensive prior to their IVF procedure.
The incidence of pregnancy-induced hypertension, defined as blood pressure that reached at least 140/90 mm Hg when measured in office on both arms with two separate measurements, was about 29% in the women who received a donated egg and 14% in those who used a self egg. Development of preeclampsia, defined as persistent gestational hypertension plus proteinuria of at least 0.3 g/day, occurred in about 18% of women who received a donated egg and 7% in those who used a self egg.
In a multivariate analysis that controlled for age, pregnancy history, and use of a fresh or frozen embryo, women who used a donated egg had a 3.9-fold increased rate of pregnancy-induced hypertension and a 4.6-fold increased rate of preeclampsia, compared with women who used a self egg – both statistically significant differences.
The findings suggested that before a woman embarks on pregnancy using a donated egg, she should undergo thorough evaluation for preexisting risk factors for gestational hypertension, including hypertension, obesity, diabetes, renal disease, chronic infection, autoimmune diseases such as systemic lupus erythematosus, a family history of preeclampsia, and living at a high altitude. If these risk factors are present, they should be controlled if possible. Women who have one or more of these risk factors may also be candidates for prophylactic treatment with aspirin to prevent development of preeclampsia, especially if they develop pregnancy-induced hypertension.
During pregnancy, women who received a donor egg should undergo regular and frequent blood pressure measurement, as well as assessment for other possible abnormalities such as Doppler ultrasound examination of uterine arteries and measuring serum and urine markers.
"Physicians and patients must be aware of the risk [from donor eggs] to assure that these women get adequate monitoring and management during pregnancy," Dr. Letur-Könirsch said.
Dr. Letur-Könirsch had no disclosures.
On Twitter @mitchelzoler
MUNICH – Women pregnant with an embryo produced by in vitro fertilization of a donated egg developed gestational hypertension at nearly four times the rate of matched women who were pregnant following IVF with a self egg, in a multicenter, case-control study with 580 participants.
In addition, preeclampsia was more than four times higher in the women who had received a donor egg as part of an IVF procedure, compared with women who used a self egg for their IVF, Dr. Hélène Letur-Könirsch reported at the annual meeting of the European Society of Human Reproduction and Embryology.
Although the mechanism underlying this association is not known, one possible explanation is that when a woman carries an embryo that is completely allogenic, it triggers modified immune tolerance that leads to impaired trophoblast implantation. Other candidate hypotheses are that defective genes in the mother trigger abnormal metabolic pathways that cause hypertension and preeclampsia, and that ovarian insufficiency features reduced ovarian steroid production, causing vascular and immunologic changes that lead to pregnancy-induced hypertension.
Results from several prior studies also had shown a link between use of a donor egg for IVF and an increased rate of gestational hypertension and preeclampsia, but most prior studies had been smaller and failed to adequately control for possible confounders, said Dr. Letur-Könirsch, an endocrinologist at the Fertility Center of the Institut Mutualiste Montsouris in Paris.
She and her associates from seven IVF centers in France pooled data from their entire series of IVF cases that involved donated eggs during the period from February 2005 to September 2012, a total of 217 pregnant women. The analysis matched these cases with 363 control women who had IVF pregnancies during the study period using self eggs by parameters such as age, parity, time of pregnancy, and whether the IVF procedure involved transfer of a fresh or frozen embryo.
Women in the study averaged 35 years of age, with 82% aged 39 years or younger. Average body mass index was virtually identical in both groups, about 24 kg/m2, and the live-birth rate was 79% in both groups. All women in both groups were normotensive prior to their IVF procedure.
The incidence of pregnancy-induced hypertension, defined as blood pressure that reached at least 140/90 mm Hg when measured in office on both arms with two separate measurements, was about 29% in the women who received a donated egg and 14% in those who used a self egg. Development of preeclampsia, defined as persistent gestational hypertension plus proteinuria of at least 0.3 g/day, occurred in about 18% of women who received a donated egg and 7% in those who used a self egg.
In a multivariate analysis that controlled for age, pregnancy history, and use of a fresh or frozen embryo, women who used a donated egg had a 3.9-fold increased rate of pregnancy-induced hypertension and a 4.6-fold increased rate of preeclampsia, compared with women who used a self egg – both statistically significant differences.
The findings suggested that before a woman embarks on pregnancy using a donated egg, she should undergo thorough evaluation for preexisting risk factors for gestational hypertension, including hypertension, obesity, diabetes, renal disease, chronic infection, autoimmune diseases such as systemic lupus erythematosus, a family history of preeclampsia, and living at a high altitude. If these risk factors are present, they should be controlled if possible. Women who have one or more of these risk factors may also be candidates for prophylactic treatment with aspirin to prevent development of preeclampsia, especially if they develop pregnancy-induced hypertension.
During pregnancy, women who received a donor egg should undergo regular and frequent blood pressure measurement, as well as assessment for other possible abnormalities such as Doppler ultrasound examination of uterine arteries and measuring serum and urine markers.
"Physicians and patients must be aware of the risk [from donor eggs] to assure that these women get adequate monitoring and management during pregnancy," Dr. Letur-Könirsch said.
Dr. Letur-Könirsch had no disclosures.
On Twitter @mitchelzoler
AT ESHRE 2014
Key clinical point: Women who became pregnant by in vitro fertilization with a donated egg had a substantially increased risk of pregnancy-induced hypertension and preeclampsia.
Major finding: Women with IVF pregnancy using donated eggs had a 3.9-fold increased rate of gestational hypertension, compared with women using self eggs.
Data source: A case-control study with 580 women who underwent IVF at any of seven French fertility clinics.
Disclosures: Dr. Letur-Könirsch had no disclosures.