User login
To the Editor:
A 38-year-old microbiologist presented to a primary care physician with fevers, night sweats, myalgia, and headaches of 2 weeks’ duration. She was treated for a presumed viral illness with antipyretics and fluids. The patient subsequently developed a persistent nonproductive cough and chest pain as well as painful nodules of the lower legs and a vesicular rash over the trunk and arms. The patient worked closely with Yersinia pestis and Francisella tularensis and because of the occupational exposure had a thorough evaluation. An increased bacterial agglutinin titer for F tularensis from 1:40 to 1:1280 was noted during repeat testing over a 1-week period and a polymerase chain reaction test of sputum was positive for F tularensis. Chest radiography revealed right lower lobe pneumonia and adenopathy. The patient was admitted to the hospital for pneumonic tularemia and was treated with streptomycin with rapid improvement; however, after development of tinnitus and vertigo she was switched to ciprofloxacin.


|
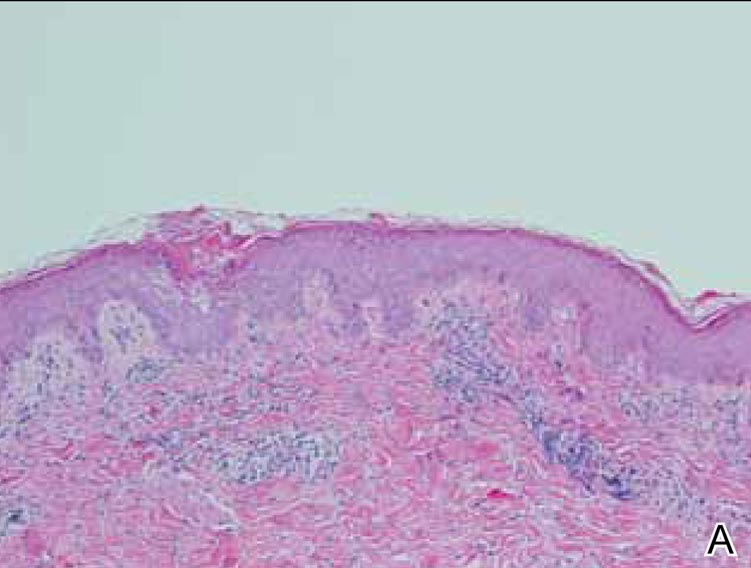
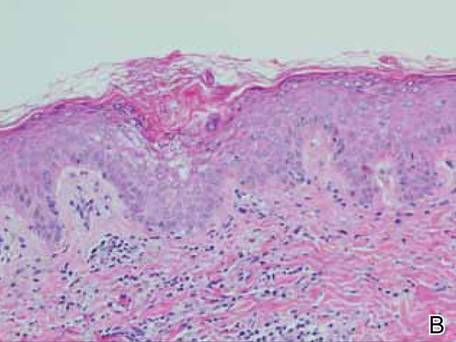
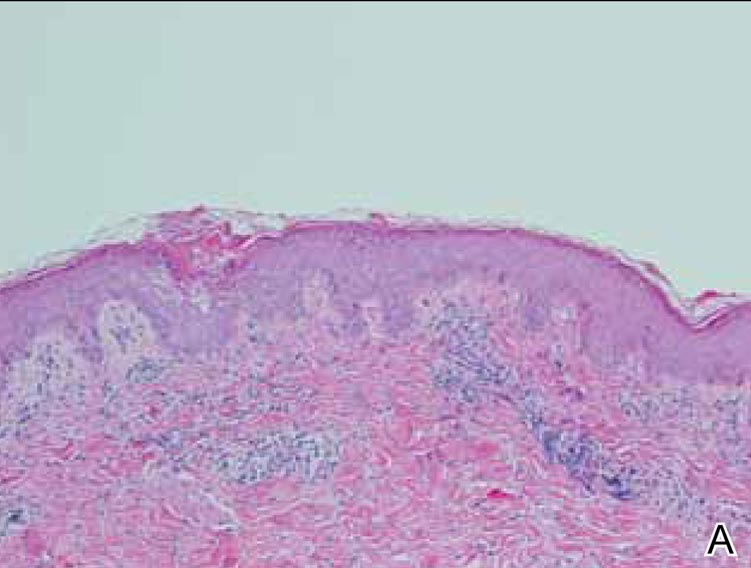
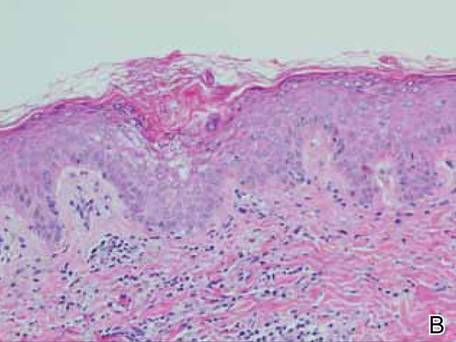
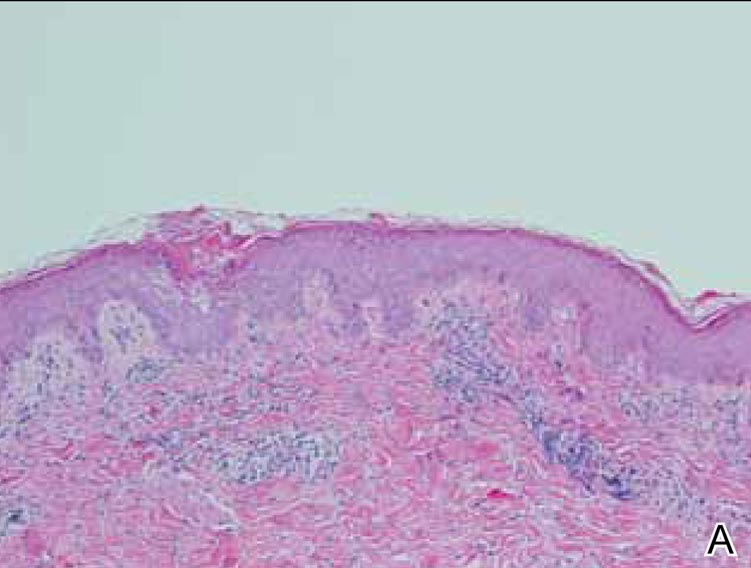
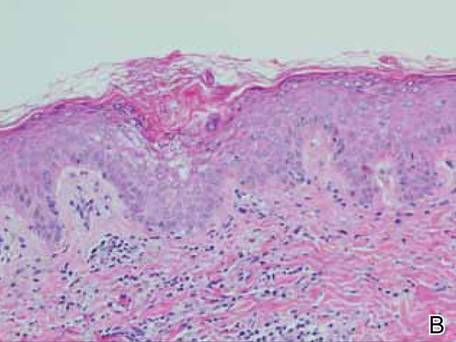
Dermatology was consulted to evaluate the patient’s nonpruritic vesicular rash that had been present for 6 days. Examination revealed multiple erythematous papules and plaques with vesicles rimming the periphery or studded throughout the lesions (Figures 1 and 2). Tender ecchymotic subcutaneous nodules of the lower extremities consistent with erythema nodosum also were present. Punch biopsies taken from vesicular papules of the back showed superficial perivascular inflammation and vesiculation within the epidermis (Figure 3). Polymerase chain reaction analysis revealed F tularensis. The patient was discharged with continued improvement after completion of the 1-month antibiotic regimen.
Vesicular papules and plaques are uncommon cutaneous manifestations of tularemia with few reports since the first documented cases of vesicular tularemia.1,2 A summary of 654 cases of tularemia in 1928 revealed 1 case with a vesicular rash.3 A retrospective review of 234 cases in Sweden in 2007 noted a vesicular rash in 7 patients (3.0%),4 and 2 subsequent cases of vesicular skin lesions in children with culture-positive tularemia initially were misdiagnosed as herpes simplex virus or varicella-zoster virus.5
Fewer than 200 cases of tularemia are reported to the Centers for Disease Control and Prevention annually, yet outbreaks do occur.5 Tularemia is primarily contracted through contact with infected animals (eg, rabbits) or vector insects (eg, deer flies, Dermacentor ticks). However, the disease remains a concern as a potential bioweapon via inhalation of aerosolized particles. A victim of bioterrorism may present in a manner similar to our patient. Although the threat of bioterrorism and incidence of tularemia in the United States is low, vesicular papules may be a presentation of tularemia and should be considered in the evaluation of a vesicular rash.
|
1. Pearse R. Insect bites. Northwest Med. 1911;3:81-82.
2. Francis E. The occurrence of tularemia in nature as a disease of man. Pub Health Rep. 1921;36:1731-1746.
3. Francis E. A summary of present knowledge of tularemia. Medicine. 1928;7:411-432.
4. Eliasson H, Bäck E. Tularaemia in an emergent area in Sweden: an analysis of 234 cases in five years. Scand J Infect Dis. 2007;39:880-889.
5. Byington C, Bender J, Ampofo K, et al. Tularemia with vesicular skin lesions may be mistaken for infection with herpes viruses. Clin Infect Dis. 2008;47:e4-e6.
To the Editor:
A 38-year-old microbiologist presented to a primary care physician with fevers, night sweats, myalgia, and headaches of 2 weeks’ duration. She was treated for a presumed viral illness with antipyretics and fluids. The patient subsequently developed a persistent nonproductive cough and chest pain as well as painful nodules of the lower legs and a vesicular rash over the trunk and arms. The patient worked closely with Yersinia pestis and Francisella tularensis and because of the occupational exposure had a thorough evaluation. An increased bacterial agglutinin titer for F tularensis from 1:40 to 1:1280 was noted during repeat testing over a 1-week period and a polymerase chain reaction test of sputum was positive for F tularensis. Chest radiography revealed right lower lobe pneumonia and adenopathy. The patient was admitted to the hospital for pneumonic tularemia and was treated with streptomycin with rapid improvement; however, after development of tinnitus and vertigo she was switched to ciprofloxacin.


|
Dermatology was consulted to evaluate the patient’s nonpruritic vesicular rash that had been present for 6 days. Examination revealed multiple erythematous papules and plaques with vesicles rimming the periphery or studded throughout the lesions (Figures 1 and 2). Tender ecchymotic subcutaneous nodules of the lower extremities consistent with erythema nodosum also were present. Punch biopsies taken from vesicular papules of the back showed superficial perivascular inflammation and vesiculation within the epidermis (Figure 3). Polymerase chain reaction analysis revealed F tularensis. The patient was discharged with continued improvement after completion of the 1-month antibiotic regimen.
Vesicular papules and plaques are uncommon cutaneous manifestations of tularemia with few reports since the first documented cases of vesicular tularemia.1,2 A summary of 654 cases of tularemia in 1928 revealed 1 case with a vesicular rash.3 A retrospective review of 234 cases in Sweden in 2007 noted a vesicular rash in 7 patients (3.0%),4 and 2 subsequent cases of vesicular skin lesions in children with culture-positive tularemia initially were misdiagnosed as herpes simplex virus or varicella-zoster virus.5
Fewer than 200 cases of tularemia are reported to the Centers for Disease Control and Prevention annually, yet outbreaks do occur.5 Tularemia is primarily contracted through contact with infected animals (eg, rabbits) or vector insects (eg, deer flies, Dermacentor ticks). However, the disease remains a concern as a potential bioweapon via inhalation of aerosolized particles. A victim of bioterrorism may present in a manner similar to our patient. Although the threat of bioterrorism and incidence of tularemia in the United States is low, vesicular papules may be a presentation of tularemia and should be considered in the evaluation of a vesicular rash.
|
To the Editor:
A 38-year-old microbiologist presented to a primary care physician with fevers, night sweats, myalgia, and headaches of 2 weeks’ duration. She was treated for a presumed viral illness with antipyretics and fluids. The patient subsequently developed a persistent nonproductive cough and chest pain as well as painful nodules of the lower legs and a vesicular rash over the trunk and arms. The patient worked closely with Yersinia pestis and Francisella tularensis and because of the occupational exposure had a thorough evaluation. An increased bacterial agglutinin titer for F tularensis from 1:40 to 1:1280 was noted during repeat testing over a 1-week period and a polymerase chain reaction test of sputum was positive for F tularensis. Chest radiography revealed right lower lobe pneumonia and adenopathy. The patient was admitted to the hospital for pneumonic tularemia and was treated with streptomycin with rapid improvement; however, after development of tinnitus and vertigo she was switched to ciprofloxacin.


|
Dermatology was consulted to evaluate the patient’s nonpruritic vesicular rash that had been present for 6 days. Examination revealed multiple erythematous papules and plaques with vesicles rimming the periphery or studded throughout the lesions (Figures 1 and 2). Tender ecchymotic subcutaneous nodules of the lower extremities consistent with erythema nodosum also were present. Punch biopsies taken from vesicular papules of the back showed superficial perivascular inflammation and vesiculation within the epidermis (Figure 3). Polymerase chain reaction analysis revealed F tularensis. The patient was discharged with continued improvement after completion of the 1-month antibiotic regimen.
Vesicular papules and plaques are uncommon cutaneous manifestations of tularemia with few reports since the first documented cases of vesicular tularemia.1,2 A summary of 654 cases of tularemia in 1928 revealed 1 case with a vesicular rash.3 A retrospective review of 234 cases in Sweden in 2007 noted a vesicular rash in 7 patients (3.0%),4 and 2 subsequent cases of vesicular skin lesions in children with culture-positive tularemia initially were misdiagnosed as herpes simplex virus or varicella-zoster virus.5
Fewer than 200 cases of tularemia are reported to the Centers for Disease Control and Prevention annually, yet outbreaks do occur.5 Tularemia is primarily contracted through contact with infected animals (eg, rabbits) or vector insects (eg, deer flies, Dermacentor ticks). However, the disease remains a concern as a potential bioweapon via inhalation of aerosolized particles. A victim of bioterrorism may present in a manner similar to our patient. Although the threat of bioterrorism and incidence of tularemia in the United States is low, vesicular papules may be a presentation of tularemia and should be considered in the evaluation of a vesicular rash.
|
1. Pearse R. Insect bites. Northwest Med. 1911;3:81-82.
2. Francis E. The occurrence of tularemia in nature as a disease of man. Pub Health Rep. 1921;36:1731-1746.
3. Francis E. A summary of present knowledge of tularemia. Medicine. 1928;7:411-432.
4. Eliasson H, Bäck E. Tularaemia in an emergent area in Sweden: an analysis of 234 cases in five years. Scand J Infect Dis. 2007;39:880-889.
5. Byington C, Bender J, Ampofo K, et al. Tularemia with vesicular skin lesions may be mistaken for infection with herpes viruses. Clin Infect Dis. 2008;47:e4-e6.
1. Pearse R. Insect bites. Northwest Med. 1911;3:81-82.
2. Francis E. The occurrence of tularemia in nature as a disease of man. Pub Health Rep. 1921;36:1731-1746.
3. Francis E. A summary of present knowledge of tularemia. Medicine. 1928;7:411-432.
4. Eliasson H, Bäck E. Tularaemia in an emergent area in Sweden: an analysis of 234 cases in five years. Scand J Infect Dis. 2007;39:880-889.
5. Byington C, Bender J, Ampofo K, et al. Tularemia with vesicular skin lesions may be mistaken for infection with herpes viruses. Clin Infect Dis. 2008;47:e4-e6.
