User login
Clinical Psychiatry News is the online destination and multimedia properties of Clinica Psychiatry News, the independent news publication for psychiatrists. Since 1971, Clinical Psychiatry News has been the leading source of news and commentary about clinical developments in psychiatry as well as health care policy and regulations that affect the physician's practice.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
ketamine
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
suicide
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-cpn')]
div[contains(@class, 'pane-pub-home-cpn')]
div[contains(@class, 'pane-pub-topic-cpn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Today’s top news highlights: COVID-19 could worsen gambling problems, food allergies less common than thought
Here are the stories our MDedge editors across specialties think you need to know about today:
Could COVID-19 worsen gambling problems?
Take isolation, add excess available time and anxiety about illness or finances and you get the potential to increase problem gambling behaviors during the COVID-19 pandemic. A call to action, recently published in the Journal of Addiction Medicine, says it’s essential to gather data and supply guidance on this issue. “People are likely to be experiencing stress at levels they haven’t experienced previously,” said coauthor Marc N. Potenza, MD, PhD, of Yale University, New Haven, Conn. While multiple factors can contribute to addictive behaviors, “with respect to the pandemic, one concern is that so-called negative reinforcement motivations – engaging in an addictive behavior to escape from depressed or negative mood states – may be a driving motivation for a significant number of people during this time,” he said. Read more.
Food allergies in children are less frequent than expected
Food allergies appear to be less common than previously reported among 6- to 10-year-olds in Europe, according to a recent study. Prevalance ranged from a low of 1.4% to a high of 3.8%, both of which are “considerably lower” than the 16% rate based on parental reports of symptoms such as rash, itching, or diarrhea, Linus Grabenhenrich, MD, MPH, and colleagues reported in Allergy. The most commonly reported allergies were to peanuts and hazelnuts, with a prevalence of just over 5% for both. Previous research on pediatric food allergy prevalence has largely consisted of single-center studies with heterogeneous designs, the researchers noted. Read more.
The grocery store hug
William G. Wilkoff, MD, grew up in a family that didn’t embrace hugging, but as a small-town pediatrician he warmed up to the concept so much that he would frequently hug a passing acquaintance at the grocery store. That’s something he misses in the current environment and that he doesn’t expect will return. “[N]early every week I encounter one or two people with whom I have a long and sometimes emotionally charged relationship,” Dr. Wilkoff wrote in a column on MDedge. “Nurses with whom I sweated over difficult delivery room resuscitations. Parents for whom their anxiety was getting in the way of their ability to parent. Parents and caregivers of complex multiply disabled children who are now adults. Peers who have lost a spouse or a child. I’m sure you have your own list of people who send off that we-need-to-hug spark.” Read more.
Identifying structural lesions of axial spondyloarthritis
What constitutes a structural lesion of the sacroiliac joints on MRI that’s indicative of axial spondyloarthritis (axSpA) has long been a matter of conjecture, but the Assessment of SpondyloArthritis International Society (ASAS) MRI Working Group has developed new definitions that show a high degree of specificity in identifying such lesions in the disease. “Previous studies have described structural lesions in different ways, precluding meaningful comparisons between studies,” Walter P. Maksymowych, MD, said at the annual European Congress of Rheumatology, held online this year due to COVID-19. “The ASAS MRI group has generated updated consensus lesion definitions that describe each of the MRI lesions in the sacroiliac joint. These definitions have been validated by seven expert readers from the ASAS MRI group on MRI images from the ASAS classification cohort.” Read more.
Making the world’s skin crawl
Clinicians should be aware of the skin manifestations of COVID-19, especially when triaging patients. In a commentary published on MDedge, Kathleen M. Coerdt and Amor Khachemoune, MD, describe the dermatologic implications of COVID-19, including the clinical manifestations of the disease, risk reduction techniques for patients and providers, personal protective equipment-associated adverse reactions, and the financial impact on dermatologists. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Could COVID-19 worsen gambling problems?
Take isolation, add excess available time and anxiety about illness or finances and you get the potential to increase problem gambling behaviors during the COVID-19 pandemic. A call to action, recently published in the Journal of Addiction Medicine, says it’s essential to gather data and supply guidance on this issue. “People are likely to be experiencing stress at levels they haven’t experienced previously,” said coauthor Marc N. Potenza, MD, PhD, of Yale University, New Haven, Conn. While multiple factors can contribute to addictive behaviors, “with respect to the pandemic, one concern is that so-called negative reinforcement motivations – engaging in an addictive behavior to escape from depressed or negative mood states – may be a driving motivation for a significant number of people during this time,” he said. Read more.
Food allergies in children are less frequent than expected
Food allergies appear to be less common than previously reported among 6- to 10-year-olds in Europe, according to a recent study. Prevalance ranged from a low of 1.4% to a high of 3.8%, both of which are “considerably lower” than the 16% rate based on parental reports of symptoms such as rash, itching, or diarrhea, Linus Grabenhenrich, MD, MPH, and colleagues reported in Allergy. The most commonly reported allergies were to peanuts and hazelnuts, with a prevalence of just over 5% for both. Previous research on pediatric food allergy prevalence has largely consisted of single-center studies with heterogeneous designs, the researchers noted. Read more.
The grocery store hug
William G. Wilkoff, MD, grew up in a family that didn’t embrace hugging, but as a small-town pediatrician he warmed up to the concept so much that he would frequently hug a passing acquaintance at the grocery store. That’s something he misses in the current environment and that he doesn’t expect will return. “[N]early every week I encounter one or two people with whom I have a long and sometimes emotionally charged relationship,” Dr. Wilkoff wrote in a column on MDedge. “Nurses with whom I sweated over difficult delivery room resuscitations. Parents for whom their anxiety was getting in the way of their ability to parent. Parents and caregivers of complex multiply disabled children who are now adults. Peers who have lost a spouse or a child. I’m sure you have your own list of people who send off that we-need-to-hug spark.” Read more.
Identifying structural lesions of axial spondyloarthritis
What constitutes a structural lesion of the sacroiliac joints on MRI that’s indicative of axial spondyloarthritis (axSpA) has long been a matter of conjecture, but the Assessment of SpondyloArthritis International Society (ASAS) MRI Working Group has developed new definitions that show a high degree of specificity in identifying such lesions in the disease. “Previous studies have described structural lesions in different ways, precluding meaningful comparisons between studies,” Walter P. Maksymowych, MD, said at the annual European Congress of Rheumatology, held online this year due to COVID-19. “The ASAS MRI group has generated updated consensus lesion definitions that describe each of the MRI lesions in the sacroiliac joint. These definitions have been validated by seven expert readers from the ASAS MRI group on MRI images from the ASAS classification cohort.” Read more.
Making the world’s skin crawl
Clinicians should be aware of the skin manifestations of COVID-19, especially when triaging patients. In a commentary published on MDedge, Kathleen M. Coerdt and Amor Khachemoune, MD, describe the dermatologic implications of COVID-19, including the clinical manifestations of the disease, risk reduction techniques for patients and providers, personal protective equipment-associated adverse reactions, and the financial impact on dermatologists. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Could COVID-19 worsen gambling problems?
Take isolation, add excess available time and anxiety about illness or finances and you get the potential to increase problem gambling behaviors during the COVID-19 pandemic. A call to action, recently published in the Journal of Addiction Medicine, says it’s essential to gather data and supply guidance on this issue. “People are likely to be experiencing stress at levels they haven’t experienced previously,” said coauthor Marc N. Potenza, MD, PhD, of Yale University, New Haven, Conn. While multiple factors can contribute to addictive behaviors, “with respect to the pandemic, one concern is that so-called negative reinforcement motivations – engaging in an addictive behavior to escape from depressed or negative mood states – may be a driving motivation for a significant number of people during this time,” he said. Read more.
Food allergies in children are less frequent than expected
Food allergies appear to be less common than previously reported among 6- to 10-year-olds in Europe, according to a recent study. Prevalance ranged from a low of 1.4% to a high of 3.8%, both of which are “considerably lower” than the 16% rate based on parental reports of symptoms such as rash, itching, or diarrhea, Linus Grabenhenrich, MD, MPH, and colleagues reported in Allergy. The most commonly reported allergies were to peanuts and hazelnuts, with a prevalence of just over 5% for both. Previous research on pediatric food allergy prevalence has largely consisted of single-center studies with heterogeneous designs, the researchers noted. Read more.
The grocery store hug
William G. Wilkoff, MD, grew up in a family that didn’t embrace hugging, but as a small-town pediatrician he warmed up to the concept so much that he would frequently hug a passing acquaintance at the grocery store. That’s something he misses in the current environment and that he doesn’t expect will return. “[N]early every week I encounter one or two people with whom I have a long and sometimes emotionally charged relationship,” Dr. Wilkoff wrote in a column on MDedge. “Nurses with whom I sweated over difficult delivery room resuscitations. Parents for whom their anxiety was getting in the way of their ability to parent. Parents and caregivers of complex multiply disabled children who are now adults. Peers who have lost a spouse or a child. I’m sure you have your own list of people who send off that we-need-to-hug spark.” Read more.
Identifying structural lesions of axial spondyloarthritis
What constitutes a structural lesion of the sacroiliac joints on MRI that’s indicative of axial spondyloarthritis (axSpA) has long been a matter of conjecture, but the Assessment of SpondyloArthritis International Society (ASAS) MRI Working Group has developed new definitions that show a high degree of specificity in identifying such lesions in the disease. “Previous studies have described structural lesions in different ways, precluding meaningful comparisons between studies,” Walter P. Maksymowych, MD, said at the annual European Congress of Rheumatology, held online this year due to COVID-19. “The ASAS MRI group has generated updated consensus lesion definitions that describe each of the MRI lesions in the sacroiliac joint. These definitions have been validated by seven expert readers from the ASAS MRI group on MRI images from the ASAS classification cohort.” Read more.
Making the world’s skin crawl
Clinicians should be aware of the skin manifestations of COVID-19, especially when triaging patients. In a commentary published on MDedge, Kathleen M. Coerdt and Amor Khachemoune, MD, describe the dermatologic implications of COVID-19, including the clinical manifestations of the disease, risk reduction techniques for patients and providers, personal protective equipment-associated adverse reactions, and the financial impact on dermatologists. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Americans avoided emergency departments early in the pandemic
compared with the corresponding period in 2019, according to a report from the Centers for Disease Control and Prevention.
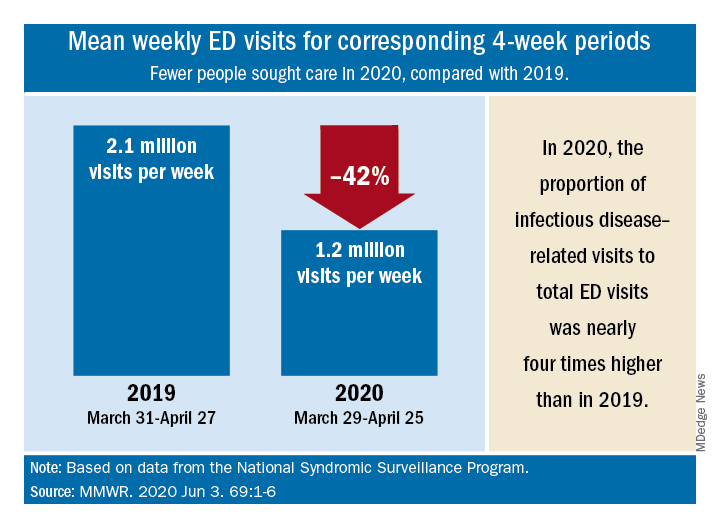
“The striking decline in ED visits nationwide … suggests that the pandemic has altered the use of the ED by the public,” Kathleen P. Hartnett, PhD, and associates at the CDC said June 3 in the Mortality and Morbidity Weekly Report.
The weekly mean was just over 1.2 million ED visits for the 4 weeks from March 29 to April 25, 2020, compared with the nearly 2.2 million visits per week recorded from March 31 to April 27, 2019 – a drop of 42%, based on an analysis of data from the National Syndromic Surveillance Program.
Despite that drop, ED visits for infectious disease–related reasons, taken as a proportion of all 1.2 ED visits during the early pandemic period, were 3.8 times higher than the comparison period in 2019, the investigators reported.
ED visits also were higher in 2020 for specified and unspecified lower respiratory disease not including influenza, pneumonia, asthma, or bronchitis (prevalence ratio of 1.99, compared with 2019), cardiac arrest and ventricular fibrillation (PR, 1.98), and pneumonia not caused by tuberculosis (PR, 1.91), Dr. Hartnett and associates said.
Prevalence ratios for the early pandemic period were down for most other conditions, with some of the largest decreases seen for influenza (PR, 0.16), otitis media (PR, 0.35), and neoplasm-related encounters (PR, 0.40), they said.
Visits have increased each week since reaching their lowest point during April 12-18, but the number for the most recent full week, May 24-30, which was not included in the analysis, was still 26% lower than the corresponding week in 2019, the CDC team pointed out.
“Some persons could be delaying care for conditions that might result in additional mortality if left untreated,” the investigators noted, and those “who use the ED as a safety net because they lack access to primary care and telemedicine might be disproportionately affected if they avoid seeking care because of concerns about the infection risk in the ED.”
SOURCE: Hartnett KP et al. MMWR. 2020 Jun 3. 69:1-6.
compared with the corresponding period in 2019, according to a report from the Centers for Disease Control and Prevention.
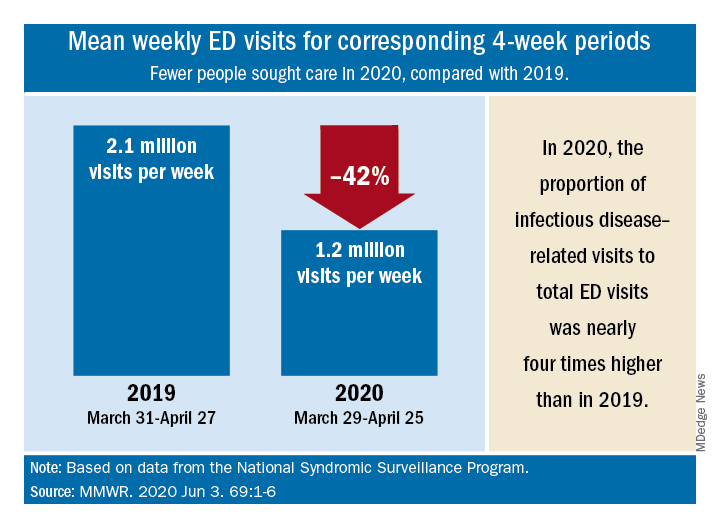
“The striking decline in ED visits nationwide … suggests that the pandemic has altered the use of the ED by the public,” Kathleen P. Hartnett, PhD, and associates at the CDC said June 3 in the Mortality and Morbidity Weekly Report.
The weekly mean was just over 1.2 million ED visits for the 4 weeks from March 29 to April 25, 2020, compared with the nearly 2.2 million visits per week recorded from March 31 to April 27, 2019 – a drop of 42%, based on an analysis of data from the National Syndromic Surveillance Program.
Despite that drop, ED visits for infectious disease–related reasons, taken as a proportion of all 1.2 ED visits during the early pandemic period, were 3.8 times higher than the comparison period in 2019, the investigators reported.
ED visits also were higher in 2020 for specified and unspecified lower respiratory disease not including influenza, pneumonia, asthma, or bronchitis (prevalence ratio of 1.99, compared with 2019), cardiac arrest and ventricular fibrillation (PR, 1.98), and pneumonia not caused by tuberculosis (PR, 1.91), Dr. Hartnett and associates said.
Prevalence ratios for the early pandemic period were down for most other conditions, with some of the largest decreases seen for influenza (PR, 0.16), otitis media (PR, 0.35), and neoplasm-related encounters (PR, 0.40), they said.
Visits have increased each week since reaching their lowest point during April 12-18, but the number for the most recent full week, May 24-30, which was not included in the analysis, was still 26% lower than the corresponding week in 2019, the CDC team pointed out.
“Some persons could be delaying care for conditions that might result in additional mortality if left untreated,” the investigators noted, and those “who use the ED as a safety net because they lack access to primary care and telemedicine might be disproportionately affected if they avoid seeking care because of concerns about the infection risk in the ED.”
SOURCE: Hartnett KP et al. MMWR. 2020 Jun 3. 69:1-6.
compared with the corresponding period in 2019, according to a report from the Centers for Disease Control and Prevention.
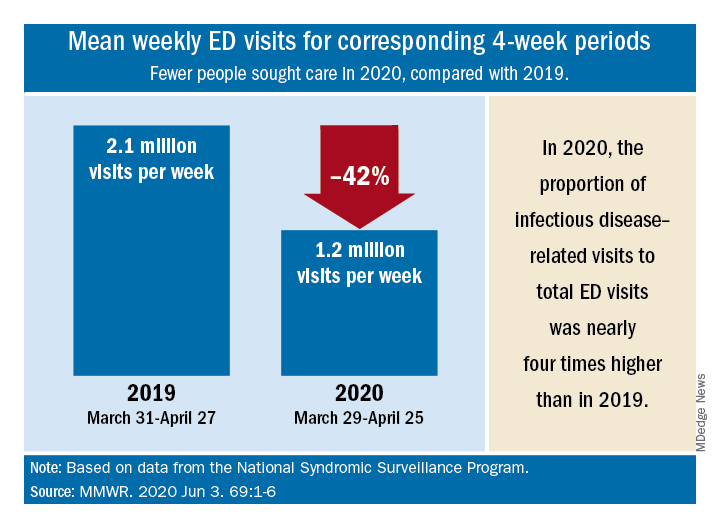
“The striking decline in ED visits nationwide … suggests that the pandemic has altered the use of the ED by the public,” Kathleen P. Hartnett, PhD, and associates at the CDC said June 3 in the Mortality and Morbidity Weekly Report.
The weekly mean was just over 1.2 million ED visits for the 4 weeks from March 29 to April 25, 2020, compared with the nearly 2.2 million visits per week recorded from March 31 to April 27, 2019 – a drop of 42%, based on an analysis of data from the National Syndromic Surveillance Program.
Despite that drop, ED visits for infectious disease–related reasons, taken as a proportion of all 1.2 ED visits during the early pandemic period, were 3.8 times higher than the comparison period in 2019, the investigators reported.
ED visits also were higher in 2020 for specified and unspecified lower respiratory disease not including influenza, pneumonia, asthma, or bronchitis (prevalence ratio of 1.99, compared with 2019), cardiac arrest and ventricular fibrillation (PR, 1.98), and pneumonia not caused by tuberculosis (PR, 1.91), Dr. Hartnett and associates said.
Prevalence ratios for the early pandemic period were down for most other conditions, with some of the largest decreases seen for influenza (PR, 0.16), otitis media (PR, 0.35), and neoplasm-related encounters (PR, 0.40), they said.
Visits have increased each week since reaching their lowest point during April 12-18, but the number for the most recent full week, May 24-30, which was not included in the analysis, was still 26% lower than the corresponding week in 2019, the CDC team pointed out.
“Some persons could be delaying care for conditions that might result in additional mortality if left untreated,” the investigators noted, and those “who use the ED as a safety net because they lack access to primary care and telemedicine might be disproportionately affected if they avoid seeking care because of concerns about the infection risk in the ED.”
SOURCE: Hartnett KP et al. MMWR. 2020 Jun 3. 69:1-6.
FROM MMWR
Is cannabis gaining acceptance as a treatment for neuropathic pain?
, a recent debate on the topic suggests. During the debate, one expert argued for, and another against, there being sufficient evidence for the use of cannabis to treat neuropathic pain, but in the end, they agreed that some patients do benefit.
The discussion took place at the Congress of the European Academy of Neurology (EAN) 2020, which transitioned to a virtual online meeting because of the COVID-19 pandemic.
The cannabis plant has 460 constituents. The two main components are tetrahydrocannabinol (THC) and cannabidiol (CBD). It can be consumed by swallowing oil extracts, by the sublingual route, or by smoking or eating the plant. Cannabis medications already in use include oral THC (nabilone, dronabinol) and an oral mucosal spray, nabiximols (Sativex).
Arguing that therapeutic cannabis is helpful for neuropathic pain, Elon Eisenberg, MD, professor of neurology and pain medicine, Israel Institute of Technology, Haifa, cited a number of encouraging randomized, controlled trials and meta-analyses of studies on the subject.
Opioid substitute
Dr. Eisenberg discussed three relevant articles. One was a 2016 viewpoint article published in JAMA that concluded that “cannabis seems to be a substitute, a rather good one, for opioids,” said Dr. Eisenberg.
A “comprehensive” 440-page review, published by the National Academies Press in 2017, evaluated the evidence to that point and “came to the conclusion there is substantial evidence that cannabis is an effective treatment for chronic pain in adults,” said Dr. Eisenberg.
And a 2018 position paper from the European Pain Federation determined that “the quantity and quality of evidence is such that cannabis-based medicines may be reasonably considered for chronic neuropathic pain,” he said.
He noted that the most recent results from an Israeli prospective cohort registry study that is following more than 851 patients who are taking cannabis over 1 year are positive. Analyses show a steady reduction in pain intensity and improvements in catastrophizing and disability. Importantly, he said, participants are using fewer opioids. However, about 40% of patients in that registry study experienced some adverse event, although most were not serious, said Dr. Eisenberg.
Not convinced
Arguing on the other side – that therapeutic cannabis is not helpful for neuropathic pain – was Nadine Attal, MD, PhD, professor of therapeutics and pain at the University Versailles Saint Quentin, France. She questioned the quality of some of the research to date and stressed that studies should consider neuropathic pain as a primary outcome – not spasticity or pain in general. They should also be double-blind, randomized, and placebo controlled, she said.
In addition, she said these studies should enroll at least 10 patients per group and should continue for 3 weeks or longer.
Dr. Attal wondered which of the many plant derivatives (phytocannabinoids) are used in cannabis studies.
She discussed four meta-analyses or reviews on the topic, some of which she said are “heterogeneous” and don’t provide convincing evidence for cannabis use in neuropathic pain.
For example, one review examined only marijuana, and all studies in it were short term. One of the studies in this review was of spasticity. Another review included two studies of cancer pain, and the most positive study in NP used short-term inhaled THC.
“There is no evidence to date that cannabinoids, including nabiximols or oral THC, administered for at least 3 weeks are more effective than placebo in neuropathic pain,” she concluded.
Some responders
However, Dr. Attal acknowledged that cannabis might be effective for some patients. In her experience, which has been borne out by some observational studies, patients with paroxysmal pain, or sudden stabbing pain, seem to get more relief from cannabis. “It’s absolutely possible that there’s a subgroup of symptoms or a subgroup of patients with specific symptoms who are much better responders to cannabis than others,” she said.
Asked if patients experience increased pain after withdrawing from cannabis, Dr. Eisenberg said he has observed that many patients stop taking cannabis when they start feeling better, but he hasn’t seen severe withdrawal symptoms.
However, there are other concerns related to cannabis use, said Dr. Eisenberg. A major concern regards driving a vehicle. In Israel, getting behind the wheel is prohibited within 6 hours of using cannabis.
But Dr. Eisenberg pointed out that published data on the safety of cannabis and driving were based on recreational users. “We need to keep in mind that recreational users typically use other substances, so we’re not sure the data is accurate,” he said.
There are increasing reports of stroke, transient ischemic attack, and MI among cannabis users. This is especially concerning because many of these cases involve young male adults who have no risk factors, said Dr. Eisenberg.
One conference delegate asked whether legal issues make it difficult to properly investigate cannabis in large studies. Dr. Eisenberg noted that legal concerns may help explain why there have not been any new randomized, controlled trials for about 2 years. “In the U.S., you can’t do clinical trials; cannabis is still regarded as schedule I substance,” he said.
Some physicians “are reluctant to deal with cannabis unless they get better data,” he said. “Doing research on cannabis seems to be somehow out of the mainstream.” Moreover, the research is difficult to carry out, owing to the complexity of the cannabis plant, which has many constituents. Perhaps it’s a matter of identifying and adding particular components to better demonstrate reduced pain, said Dr. Eisenberg.
Another complicating factor is that bioavailability differs considerably from one patient to another, “sometimes even by 10-fold,” he said.
Dr. Attal’s group will be starting a study next January that will enroll a large sample of patients with neuropathic pain or spasticity. In that study, cannabis will be dispensed through pharmacies and primary care. The aim of the study is “to see how it works in a real-life setting,” she said
Those participating in the virtual session were asked to vote on which side they agreed with. About 57% voted in favor of cannabis use, 14% voted against, and 28% had no opinion.
Dr. Eisenberg has received research grants from Rafa Laboratories, Saga Medical Ltd., Israel Pain Association, and Teva Israel. Dr. Attal has received support from Merck Sharp & Dohme, Sanofi, Ipsen, Novartis, Aptinyx, Air Liquide, Lilly, and Grunenthal.
A version of this article originally appeared on Medscape.com.
, a recent debate on the topic suggests. During the debate, one expert argued for, and another against, there being sufficient evidence for the use of cannabis to treat neuropathic pain, but in the end, they agreed that some patients do benefit.
The discussion took place at the Congress of the European Academy of Neurology (EAN) 2020, which transitioned to a virtual online meeting because of the COVID-19 pandemic.
The cannabis plant has 460 constituents. The two main components are tetrahydrocannabinol (THC) and cannabidiol (CBD). It can be consumed by swallowing oil extracts, by the sublingual route, or by smoking or eating the plant. Cannabis medications already in use include oral THC (nabilone, dronabinol) and an oral mucosal spray, nabiximols (Sativex).
Arguing that therapeutic cannabis is helpful for neuropathic pain, Elon Eisenberg, MD, professor of neurology and pain medicine, Israel Institute of Technology, Haifa, cited a number of encouraging randomized, controlled trials and meta-analyses of studies on the subject.
Opioid substitute
Dr. Eisenberg discussed three relevant articles. One was a 2016 viewpoint article published in JAMA that concluded that “cannabis seems to be a substitute, a rather good one, for opioids,” said Dr. Eisenberg.
A “comprehensive” 440-page review, published by the National Academies Press in 2017, evaluated the evidence to that point and “came to the conclusion there is substantial evidence that cannabis is an effective treatment for chronic pain in adults,” said Dr. Eisenberg.
And a 2018 position paper from the European Pain Federation determined that “the quantity and quality of evidence is such that cannabis-based medicines may be reasonably considered for chronic neuropathic pain,” he said.
He noted that the most recent results from an Israeli prospective cohort registry study that is following more than 851 patients who are taking cannabis over 1 year are positive. Analyses show a steady reduction in pain intensity and improvements in catastrophizing and disability. Importantly, he said, participants are using fewer opioids. However, about 40% of patients in that registry study experienced some adverse event, although most were not serious, said Dr. Eisenberg.
Not convinced
Arguing on the other side – that therapeutic cannabis is not helpful for neuropathic pain – was Nadine Attal, MD, PhD, professor of therapeutics and pain at the University Versailles Saint Quentin, France. She questioned the quality of some of the research to date and stressed that studies should consider neuropathic pain as a primary outcome – not spasticity or pain in general. They should also be double-blind, randomized, and placebo controlled, she said.
In addition, she said these studies should enroll at least 10 patients per group and should continue for 3 weeks or longer.
Dr. Attal wondered which of the many plant derivatives (phytocannabinoids) are used in cannabis studies.
She discussed four meta-analyses or reviews on the topic, some of which she said are “heterogeneous” and don’t provide convincing evidence for cannabis use in neuropathic pain.
For example, one review examined only marijuana, and all studies in it were short term. One of the studies in this review was of spasticity. Another review included two studies of cancer pain, and the most positive study in NP used short-term inhaled THC.
“There is no evidence to date that cannabinoids, including nabiximols or oral THC, administered for at least 3 weeks are more effective than placebo in neuropathic pain,” she concluded.
Some responders
However, Dr. Attal acknowledged that cannabis might be effective for some patients. In her experience, which has been borne out by some observational studies, patients with paroxysmal pain, or sudden stabbing pain, seem to get more relief from cannabis. “It’s absolutely possible that there’s a subgroup of symptoms or a subgroup of patients with specific symptoms who are much better responders to cannabis than others,” she said.
Asked if patients experience increased pain after withdrawing from cannabis, Dr. Eisenberg said he has observed that many patients stop taking cannabis when they start feeling better, but he hasn’t seen severe withdrawal symptoms.
However, there are other concerns related to cannabis use, said Dr. Eisenberg. A major concern regards driving a vehicle. In Israel, getting behind the wheel is prohibited within 6 hours of using cannabis.
But Dr. Eisenberg pointed out that published data on the safety of cannabis and driving were based on recreational users. “We need to keep in mind that recreational users typically use other substances, so we’re not sure the data is accurate,” he said.
There are increasing reports of stroke, transient ischemic attack, and MI among cannabis users. This is especially concerning because many of these cases involve young male adults who have no risk factors, said Dr. Eisenberg.
One conference delegate asked whether legal issues make it difficult to properly investigate cannabis in large studies. Dr. Eisenberg noted that legal concerns may help explain why there have not been any new randomized, controlled trials for about 2 years. “In the U.S., you can’t do clinical trials; cannabis is still regarded as schedule I substance,” he said.
Some physicians “are reluctant to deal with cannabis unless they get better data,” he said. “Doing research on cannabis seems to be somehow out of the mainstream.” Moreover, the research is difficult to carry out, owing to the complexity of the cannabis plant, which has many constituents. Perhaps it’s a matter of identifying and adding particular components to better demonstrate reduced pain, said Dr. Eisenberg.
Another complicating factor is that bioavailability differs considerably from one patient to another, “sometimes even by 10-fold,” he said.
Dr. Attal’s group will be starting a study next January that will enroll a large sample of patients with neuropathic pain or spasticity. In that study, cannabis will be dispensed through pharmacies and primary care. The aim of the study is “to see how it works in a real-life setting,” she said
Those participating in the virtual session were asked to vote on which side they agreed with. About 57% voted in favor of cannabis use, 14% voted against, and 28% had no opinion.
Dr. Eisenberg has received research grants from Rafa Laboratories, Saga Medical Ltd., Israel Pain Association, and Teva Israel. Dr. Attal has received support from Merck Sharp & Dohme, Sanofi, Ipsen, Novartis, Aptinyx, Air Liquide, Lilly, and Grunenthal.
A version of this article originally appeared on Medscape.com.
, a recent debate on the topic suggests. During the debate, one expert argued for, and another against, there being sufficient evidence for the use of cannabis to treat neuropathic pain, but in the end, they agreed that some patients do benefit.
The discussion took place at the Congress of the European Academy of Neurology (EAN) 2020, which transitioned to a virtual online meeting because of the COVID-19 pandemic.
The cannabis plant has 460 constituents. The two main components are tetrahydrocannabinol (THC) and cannabidiol (CBD). It can be consumed by swallowing oil extracts, by the sublingual route, or by smoking or eating the plant. Cannabis medications already in use include oral THC (nabilone, dronabinol) and an oral mucosal spray, nabiximols (Sativex).
Arguing that therapeutic cannabis is helpful for neuropathic pain, Elon Eisenberg, MD, professor of neurology and pain medicine, Israel Institute of Technology, Haifa, cited a number of encouraging randomized, controlled trials and meta-analyses of studies on the subject.
Opioid substitute
Dr. Eisenberg discussed three relevant articles. One was a 2016 viewpoint article published in JAMA that concluded that “cannabis seems to be a substitute, a rather good one, for opioids,” said Dr. Eisenberg.
A “comprehensive” 440-page review, published by the National Academies Press in 2017, evaluated the evidence to that point and “came to the conclusion there is substantial evidence that cannabis is an effective treatment for chronic pain in adults,” said Dr. Eisenberg.
And a 2018 position paper from the European Pain Federation determined that “the quantity and quality of evidence is such that cannabis-based medicines may be reasonably considered for chronic neuropathic pain,” he said.
He noted that the most recent results from an Israeli prospective cohort registry study that is following more than 851 patients who are taking cannabis over 1 year are positive. Analyses show a steady reduction in pain intensity and improvements in catastrophizing and disability. Importantly, he said, participants are using fewer opioids. However, about 40% of patients in that registry study experienced some adverse event, although most were not serious, said Dr. Eisenberg.
Not convinced
Arguing on the other side – that therapeutic cannabis is not helpful for neuropathic pain – was Nadine Attal, MD, PhD, professor of therapeutics and pain at the University Versailles Saint Quentin, France. She questioned the quality of some of the research to date and stressed that studies should consider neuropathic pain as a primary outcome – not spasticity or pain in general. They should also be double-blind, randomized, and placebo controlled, she said.
In addition, she said these studies should enroll at least 10 patients per group and should continue for 3 weeks or longer.
Dr. Attal wondered which of the many plant derivatives (phytocannabinoids) are used in cannabis studies.
She discussed four meta-analyses or reviews on the topic, some of which she said are “heterogeneous” and don’t provide convincing evidence for cannabis use in neuropathic pain.
For example, one review examined only marijuana, and all studies in it were short term. One of the studies in this review was of spasticity. Another review included two studies of cancer pain, and the most positive study in NP used short-term inhaled THC.
“There is no evidence to date that cannabinoids, including nabiximols or oral THC, administered for at least 3 weeks are more effective than placebo in neuropathic pain,” she concluded.
Some responders
However, Dr. Attal acknowledged that cannabis might be effective for some patients. In her experience, which has been borne out by some observational studies, patients with paroxysmal pain, or sudden stabbing pain, seem to get more relief from cannabis. “It’s absolutely possible that there’s a subgroup of symptoms or a subgroup of patients with specific symptoms who are much better responders to cannabis than others,” she said.
Asked if patients experience increased pain after withdrawing from cannabis, Dr. Eisenberg said he has observed that many patients stop taking cannabis when they start feeling better, but he hasn’t seen severe withdrawal symptoms.
However, there are other concerns related to cannabis use, said Dr. Eisenberg. A major concern regards driving a vehicle. In Israel, getting behind the wheel is prohibited within 6 hours of using cannabis.
But Dr. Eisenberg pointed out that published data on the safety of cannabis and driving were based on recreational users. “We need to keep in mind that recreational users typically use other substances, so we’re not sure the data is accurate,” he said.
There are increasing reports of stroke, transient ischemic attack, and MI among cannabis users. This is especially concerning because many of these cases involve young male adults who have no risk factors, said Dr. Eisenberg.
One conference delegate asked whether legal issues make it difficult to properly investigate cannabis in large studies. Dr. Eisenberg noted that legal concerns may help explain why there have not been any new randomized, controlled trials for about 2 years. “In the U.S., you can’t do clinical trials; cannabis is still regarded as schedule I substance,” he said.
Some physicians “are reluctant to deal with cannabis unless they get better data,” he said. “Doing research on cannabis seems to be somehow out of the mainstream.” Moreover, the research is difficult to carry out, owing to the complexity of the cannabis plant, which has many constituents. Perhaps it’s a matter of identifying and adding particular components to better demonstrate reduced pain, said Dr. Eisenberg.
Another complicating factor is that bioavailability differs considerably from one patient to another, “sometimes even by 10-fold,” he said.
Dr. Attal’s group will be starting a study next January that will enroll a large sample of patients with neuropathic pain or spasticity. In that study, cannabis will be dispensed through pharmacies and primary care. The aim of the study is “to see how it works in a real-life setting,” she said
Those participating in the virtual session were asked to vote on which side they agreed with. About 57% voted in favor of cannabis use, 14% voted against, and 28% had no opinion.
Dr. Eisenberg has received research grants from Rafa Laboratories, Saga Medical Ltd., Israel Pain Association, and Teva Israel. Dr. Attal has received support from Merck Sharp & Dohme, Sanofi, Ipsen, Novartis, Aptinyx, Air Liquide, Lilly, and Grunenthal.
A version of this article originally appeared on Medscape.com.
FROM EAN 2020
Atopic dermatitis in adults, children linked to neuropsychiatric disorders
according to a study presented at the annual meeting of the Society for Investigative Dermatology, held virtually.
“The risk increase ranges from as low as 5% up to 59%, depending on the outcome, with generally greater effects observed among the adults,” Joy Wan, MD, a postdoctoral dermatology fellow at the University of Pennsylvania, Philadelphia, said in her presentation. The risk was independent of other atopic disease, gender, age, and socioeconomic status.
Dr. Wan and colleagues conducted a cohort study of patients with AD in the United Kingdom using data from the Health Improvement Network (THIN) electronic records database, matching AD patients in THIN with up to five patients without AD, similar in age and also registered to general practices. The researchers validated AD disease status using an algorithm that identified patients with a diagnostic code and two therapy codes related to AD. Outcomes of interest included anxiety, depression, bipolar disorder, obsessive-compulsive disorder, ADHD, schizophrenia, and autism. Patients entered into the cohort when they were diagnosed with AD, registered by a practice, or when data from a practice was reported to THIN. The researchers stopped following patients when they developed a neuropsychiatric outcome of interest, left a practice, died, or when the study ended.
“Previous studies have found associations between atopic dermatitis and anxiety, depression, and attention-deficit/hyperactivity disorder. However, many previous studies had been cross-sectional and they were unable to evaluate the directionality of association between atopic dermatitis and neuropsychiatric outcomes, while other previous studies have relied on the self-report of atopic dermatitis and outcomes as well,” Dr. Wan said. “Thus, longitudinal studies, using validated measures of atopic dermatitis, and those that include the entire age span, are really needed.”
Overall, 434,859 children and adolescents under aged 18 with AD in the THIN database were matched to 1,983,589 controls, and 644,802 adults with AD were matched to almost 2,900,000 adults without AD. In the pediatric group, demographics were mostly balanced between children with and without AD: the average age ranged between about 5 and almost 6 years. In pediatric patients with AD, there was a higher rate of allergic rhinitis (6.2% vs. 4%) and asthma (13.5% vs. 9.3%) than in the control group.
For adults, the average age was about 48 years in both groups. Compared with patients who did not have AD, adults with AD also had higher rates of allergic rhinitis (15.2% vs. 9.6%) and asthma (19.9% vs. 12.6%).
After adjusting for age, gender, socioeconomic status, asthma, and allergic rhinitis, Dr. Wan and colleagues found greater rates of bipolar disorder (hazard ratio, 1.34; 95% confidence interval, 1.09-1.65), obsessive-compulsive disorder (HR, 1.30; 95% CI, 1.21-1.41), anxiety (HR, 1.09; 95% CI, 1.07-1.11), and depression (HR, 1.06; 95% CI, 1.04-1.08) among children and adolescents with AD, compared with controls.
In the adult cohort, a diagnosis of AD was associated with an increased risk of autism (HR, 1.53; 95% CI, 1.30-1.80), obsessive-compulsive disorder (HR, 1.49; 95% CI, 1.40-1.59), ADHD (HR, 1.31; 95% CI, 1.13-1.53), anxiety (HR, 1.17; 95% CI, 1.15-1.18), depression (HR, 1.15; 95% CI, 1.14-1.16), and bipolar disorder (HR, 1.12; 95% CI, 1.04-1.21), after adjusting for age, gender, socioeconomic status, asthma, and allergic rhinitis.
One reason for the increased associations among the adults, even for ADHD and autism, which are more characteristically diagnosed in childhood, Dr. Wan said, is that, since they looked at incident outcomes, “many children may already have had these prevalent comorbidities at the time of the entry in the cohort.”
She noted that the study may have observation bias or unknown confounders, but she hopes these results raise awareness of the association between AD and neuropsychiatric disorders, although more research is needed to determine how AD severity affects neuropsychiatric outcomes. “Additional work is needed to really understand the mechanisms that drive these associations, whether it’s mediated through symptoms of atopic dermatitis such as itch and poor sleep, or potentially the stigma of having a chronic skin disease, or perhaps shared pathophysiology between atopic dermatitis and these neuropsychiatric diseases,” she said.
The study was funded by a grant from Pfizer. Dr. Wan reports receiving research funding from Pfizer paid to the University of Pennsylvania.
according to a study presented at the annual meeting of the Society for Investigative Dermatology, held virtually.
“The risk increase ranges from as low as 5% up to 59%, depending on the outcome, with generally greater effects observed among the adults,” Joy Wan, MD, a postdoctoral dermatology fellow at the University of Pennsylvania, Philadelphia, said in her presentation. The risk was independent of other atopic disease, gender, age, and socioeconomic status.
Dr. Wan and colleagues conducted a cohort study of patients with AD in the United Kingdom using data from the Health Improvement Network (THIN) electronic records database, matching AD patients in THIN with up to five patients without AD, similar in age and also registered to general practices. The researchers validated AD disease status using an algorithm that identified patients with a diagnostic code and two therapy codes related to AD. Outcomes of interest included anxiety, depression, bipolar disorder, obsessive-compulsive disorder, ADHD, schizophrenia, and autism. Patients entered into the cohort when they were diagnosed with AD, registered by a practice, or when data from a practice was reported to THIN. The researchers stopped following patients when they developed a neuropsychiatric outcome of interest, left a practice, died, or when the study ended.
“Previous studies have found associations between atopic dermatitis and anxiety, depression, and attention-deficit/hyperactivity disorder. However, many previous studies had been cross-sectional and they were unable to evaluate the directionality of association between atopic dermatitis and neuropsychiatric outcomes, while other previous studies have relied on the self-report of atopic dermatitis and outcomes as well,” Dr. Wan said. “Thus, longitudinal studies, using validated measures of atopic dermatitis, and those that include the entire age span, are really needed.”
Overall, 434,859 children and adolescents under aged 18 with AD in the THIN database were matched to 1,983,589 controls, and 644,802 adults with AD were matched to almost 2,900,000 adults without AD. In the pediatric group, demographics were mostly balanced between children with and without AD: the average age ranged between about 5 and almost 6 years. In pediatric patients with AD, there was a higher rate of allergic rhinitis (6.2% vs. 4%) and asthma (13.5% vs. 9.3%) than in the control group.
For adults, the average age was about 48 years in both groups. Compared with patients who did not have AD, adults with AD also had higher rates of allergic rhinitis (15.2% vs. 9.6%) and asthma (19.9% vs. 12.6%).
After adjusting for age, gender, socioeconomic status, asthma, and allergic rhinitis, Dr. Wan and colleagues found greater rates of bipolar disorder (hazard ratio, 1.34; 95% confidence interval, 1.09-1.65), obsessive-compulsive disorder (HR, 1.30; 95% CI, 1.21-1.41), anxiety (HR, 1.09; 95% CI, 1.07-1.11), and depression (HR, 1.06; 95% CI, 1.04-1.08) among children and adolescents with AD, compared with controls.
In the adult cohort, a diagnosis of AD was associated with an increased risk of autism (HR, 1.53; 95% CI, 1.30-1.80), obsessive-compulsive disorder (HR, 1.49; 95% CI, 1.40-1.59), ADHD (HR, 1.31; 95% CI, 1.13-1.53), anxiety (HR, 1.17; 95% CI, 1.15-1.18), depression (HR, 1.15; 95% CI, 1.14-1.16), and bipolar disorder (HR, 1.12; 95% CI, 1.04-1.21), after adjusting for age, gender, socioeconomic status, asthma, and allergic rhinitis.
One reason for the increased associations among the adults, even for ADHD and autism, which are more characteristically diagnosed in childhood, Dr. Wan said, is that, since they looked at incident outcomes, “many children may already have had these prevalent comorbidities at the time of the entry in the cohort.”
She noted that the study may have observation bias or unknown confounders, but she hopes these results raise awareness of the association between AD and neuropsychiatric disorders, although more research is needed to determine how AD severity affects neuropsychiatric outcomes. “Additional work is needed to really understand the mechanisms that drive these associations, whether it’s mediated through symptoms of atopic dermatitis such as itch and poor sleep, or potentially the stigma of having a chronic skin disease, or perhaps shared pathophysiology between atopic dermatitis and these neuropsychiatric diseases,” she said.
The study was funded by a grant from Pfizer. Dr. Wan reports receiving research funding from Pfizer paid to the University of Pennsylvania.
according to a study presented at the annual meeting of the Society for Investigative Dermatology, held virtually.
“The risk increase ranges from as low as 5% up to 59%, depending on the outcome, with generally greater effects observed among the adults,” Joy Wan, MD, a postdoctoral dermatology fellow at the University of Pennsylvania, Philadelphia, said in her presentation. The risk was independent of other atopic disease, gender, age, and socioeconomic status.
Dr. Wan and colleagues conducted a cohort study of patients with AD in the United Kingdom using data from the Health Improvement Network (THIN) electronic records database, matching AD patients in THIN with up to five patients without AD, similar in age and also registered to general practices. The researchers validated AD disease status using an algorithm that identified patients with a diagnostic code and two therapy codes related to AD. Outcomes of interest included anxiety, depression, bipolar disorder, obsessive-compulsive disorder, ADHD, schizophrenia, and autism. Patients entered into the cohort when they were diagnosed with AD, registered by a practice, or when data from a practice was reported to THIN. The researchers stopped following patients when they developed a neuropsychiatric outcome of interest, left a practice, died, or when the study ended.
“Previous studies have found associations between atopic dermatitis and anxiety, depression, and attention-deficit/hyperactivity disorder. However, many previous studies had been cross-sectional and they were unable to evaluate the directionality of association between atopic dermatitis and neuropsychiatric outcomes, while other previous studies have relied on the self-report of atopic dermatitis and outcomes as well,” Dr. Wan said. “Thus, longitudinal studies, using validated measures of atopic dermatitis, and those that include the entire age span, are really needed.”
Overall, 434,859 children and adolescents under aged 18 with AD in the THIN database were matched to 1,983,589 controls, and 644,802 adults with AD were matched to almost 2,900,000 adults without AD. In the pediatric group, demographics were mostly balanced between children with and without AD: the average age ranged between about 5 and almost 6 years. In pediatric patients with AD, there was a higher rate of allergic rhinitis (6.2% vs. 4%) and asthma (13.5% vs. 9.3%) than in the control group.
For adults, the average age was about 48 years in both groups. Compared with patients who did not have AD, adults with AD also had higher rates of allergic rhinitis (15.2% vs. 9.6%) and asthma (19.9% vs. 12.6%).
After adjusting for age, gender, socioeconomic status, asthma, and allergic rhinitis, Dr. Wan and colleagues found greater rates of bipolar disorder (hazard ratio, 1.34; 95% confidence interval, 1.09-1.65), obsessive-compulsive disorder (HR, 1.30; 95% CI, 1.21-1.41), anxiety (HR, 1.09; 95% CI, 1.07-1.11), and depression (HR, 1.06; 95% CI, 1.04-1.08) among children and adolescents with AD, compared with controls.
In the adult cohort, a diagnosis of AD was associated with an increased risk of autism (HR, 1.53; 95% CI, 1.30-1.80), obsessive-compulsive disorder (HR, 1.49; 95% CI, 1.40-1.59), ADHD (HR, 1.31; 95% CI, 1.13-1.53), anxiety (HR, 1.17; 95% CI, 1.15-1.18), depression (HR, 1.15; 95% CI, 1.14-1.16), and bipolar disorder (HR, 1.12; 95% CI, 1.04-1.21), after adjusting for age, gender, socioeconomic status, asthma, and allergic rhinitis.
One reason for the increased associations among the adults, even for ADHD and autism, which are more characteristically diagnosed in childhood, Dr. Wan said, is that, since they looked at incident outcomes, “many children may already have had these prevalent comorbidities at the time of the entry in the cohort.”
She noted that the study may have observation bias or unknown confounders, but she hopes these results raise awareness of the association between AD and neuropsychiatric disorders, although more research is needed to determine how AD severity affects neuropsychiatric outcomes. “Additional work is needed to really understand the mechanisms that drive these associations, whether it’s mediated through symptoms of atopic dermatitis such as itch and poor sleep, or potentially the stigma of having a chronic skin disease, or perhaps shared pathophysiology between atopic dermatitis and these neuropsychiatric diseases,” she said.
The study was funded by a grant from Pfizer. Dr. Wan reports receiving research funding from Pfizer paid to the University of Pennsylvania.
FROM SID 2020
The grocery store hug
I grew up in a family that was pretty much devoid of physical demonstrations of affection. I certainly felt that my folks loved me, but there was no hugging. I don’t recall ever seeing my parents kiss or touch each other. My dad would occasionally physically tease my mother. For example, I can remember one incident at the dinner table when he was playfully and gently laying a hand on my mother’s arm just as she was raising her fork to her mouth. After about three of these gentle holds, she lifted her water glass and tossed its contents in his face. This was the full extent of physicality in our family.
It wasn’t just my parents. I can’t remember aunts or uncles or cousins ever hugging us when we met. Grandmothers of course would request a hug. I never knew either of my grandfathers, but I suspect they would not have been the hugging kind.
I never felt I was missing out on anything, because in the generally WASPish atmosphere of the community in which I grew up I saw very few public displays of affection. But somewhere over time, hugging crept into the American repertoire of expression. This incursion may have been a ripple effect from the flower power, free love hippiedom of the ‘60s and ‘70s. Or it may have been a symptom of globalization as Americans became more familiar with other cultures in which physical expression was more common.
Whatever the reason for the more widespread adoption of hugging in our social vocabulary with my somewhat physically impoverished upbringing, it took me longer than most folks to comfortably include it in my greeting options. Although I may have come to the dance late, I have fully adopted hugging as a way to greet people with whom I have more than a passing acquaintance.
In fact, the ability to comfortably hug former coworkers, old friends I haven’t seen in years, and parents with whom I had shared a particularly troublesome child is what I miss most about the restrictions that have come with the COVID-19 pandemic. Now when I meet folks in the grocery store with whom I share a special affection that magnetic spark still leaps between our eyes, just visible over our face masks, but mentally and physically we take a step back and say to ourselves that this hug shouldn’t happen and it isn’t going to happen. And that makes me sad.
One of the great perks of practicing pediatrics in a small town and then remaining there in retirement is that nearly every week I encounter one or two people with whom I have a long and sometimes emotionally charged relationship. Nurses with whom I sweated over difficult delivery room resuscitations. Parents for whom their anxiety was getting in the way of their ability to parent. Parents and caregivers of complex multiply disabled children who are now adults. Peers who have lost a spouse or a child.
I can envision a day sometime in the relatively near future that I will be able to hug my two grandchildren whom I haven’t hugged even though they live a short 10-minute walk away. But I have trouble imagining when I will again be able to enjoy and be enriched by those special grocery store hugs that I have grown to savor.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
I grew up in a family that was pretty much devoid of physical demonstrations of affection. I certainly felt that my folks loved me, but there was no hugging. I don’t recall ever seeing my parents kiss or touch each other. My dad would occasionally physically tease my mother. For example, I can remember one incident at the dinner table when he was playfully and gently laying a hand on my mother’s arm just as she was raising her fork to her mouth. After about three of these gentle holds, she lifted her water glass and tossed its contents in his face. This was the full extent of physicality in our family.
It wasn’t just my parents. I can’t remember aunts or uncles or cousins ever hugging us when we met. Grandmothers of course would request a hug. I never knew either of my grandfathers, but I suspect they would not have been the hugging kind.
I never felt I was missing out on anything, because in the generally WASPish atmosphere of the community in which I grew up I saw very few public displays of affection. But somewhere over time, hugging crept into the American repertoire of expression. This incursion may have been a ripple effect from the flower power, free love hippiedom of the ‘60s and ‘70s. Or it may have been a symptom of globalization as Americans became more familiar with other cultures in which physical expression was more common.
Whatever the reason for the more widespread adoption of hugging in our social vocabulary with my somewhat physically impoverished upbringing, it took me longer than most folks to comfortably include it in my greeting options. Although I may have come to the dance late, I have fully adopted hugging as a way to greet people with whom I have more than a passing acquaintance.
In fact, the ability to comfortably hug former coworkers, old friends I haven’t seen in years, and parents with whom I had shared a particularly troublesome child is what I miss most about the restrictions that have come with the COVID-19 pandemic. Now when I meet folks in the grocery store with whom I share a special affection that magnetic spark still leaps between our eyes, just visible over our face masks, but mentally and physically we take a step back and say to ourselves that this hug shouldn’t happen and it isn’t going to happen. And that makes me sad.
One of the great perks of practicing pediatrics in a small town and then remaining there in retirement is that nearly every week I encounter one or two people with whom I have a long and sometimes emotionally charged relationship. Nurses with whom I sweated over difficult delivery room resuscitations. Parents for whom their anxiety was getting in the way of their ability to parent. Parents and caregivers of complex multiply disabled children who are now adults. Peers who have lost a spouse or a child.
I can envision a day sometime in the relatively near future that I will be able to hug my two grandchildren whom I haven’t hugged even though they live a short 10-minute walk away. But I have trouble imagining when I will again be able to enjoy and be enriched by those special grocery store hugs that I have grown to savor.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
I grew up in a family that was pretty much devoid of physical demonstrations of affection. I certainly felt that my folks loved me, but there was no hugging. I don’t recall ever seeing my parents kiss or touch each other. My dad would occasionally physically tease my mother. For example, I can remember one incident at the dinner table when he was playfully and gently laying a hand on my mother’s arm just as she was raising her fork to her mouth. After about three of these gentle holds, she lifted her water glass and tossed its contents in his face. This was the full extent of physicality in our family.
It wasn’t just my parents. I can’t remember aunts or uncles or cousins ever hugging us when we met. Grandmothers of course would request a hug. I never knew either of my grandfathers, but I suspect they would not have been the hugging kind.
I never felt I was missing out on anything, because in the generally WASPish atmosphere of the community in which I grew up I saw very few public displays of affection. But somewhere over time, hugging crept into the American repertoire of expression. This incursion may have been a ripple effect from the flower power, free love hippiedom of the ‘60s and ‘70s. Or it may have been a symptom of globalization as Americans became more familiar with other cultures in which physical expression was more common.
Whatever the reason for the more widespread adoption of hugging in our social vocabulary with my somewhat physically impoverished upbringing, it took me longer than most folks to comfortably include it in my greeting options. Although I may have come to the dance late, I have fully adopted hugging as a way to greet people with whom I have more than a passing acquaintance.
In fact, the ability to comfortably hug former coworkers, old friends I haven’t seen in years, and parents with whom I had shared a particularly troublesome child is what I miss most about the restrictions that have come with the COVID-19 pandemic. Now when I meet folks in the grocery store with whom I share a special affection that magnetic spark still leaps between our eyes, just visible over our face masks, but mentally and physically we take a step back and say to ourselves that this hug shouldn’t happen and it isn’t going to happen. And that makes me sad.
One of the great perks of practicing pediatrics in a small town and then remaining there in retirement is that nearly every week I encounter one or two people with whom I have a long and sometimes emotionally charged relationship. Nurses with whom I sweated over difficult delivery room resuscitations. Parents for whom their anxiety was getting in the way of their ability to parent. Parents and caregivers of complex multiply disabled children who are now adults. Peers who have lost a spouse or a child.
I can envision a day sometime in the relatively near future that I will be able to hug my two grandchildren whom I haven’t hugged even though they live a short 10-minute walk away. But I have trouble imagining when I will again be able to enjoy and be enriched by those special grocery store hugs that I have grown to savor.
Dr. Wilkoff practiced primary care pediatrics in Brunswick, Maine, for nearly 40 years. He has authored several books on behavioral pediatrics, including “How to Say No to Your Toddler.” Email him at [email protected].
Dietary intervention cuts mood swings, other bipolar symptoms
A nutritional intervention with a focus on fatty acids appears to reduce mood swings in patients with bipolar disorder (BD) when used as an adjunct to pharmacotherapy, early research suggests.
In a single-center study, patients with BD who received a diet consisting of high omega-3 plus low omega-6 fatty acids (H3-L6), in addition to usual care, showed significant reductions in mood variability, irritability, and pain, compared with their counterparts who received a diet with usual levels of omega-3 and omega-6 fatty acids commonly consumed in regular U.S. diets.
“Our findings need replication and validation in other studies,” study coinvestigator Erika Saunders, MD, professor and chair of the department of psychiatry and behavioral health at Penn State Health, Hershey, said in an interview.
“While we got really exciting findings, it’s far from confirmatory or the last word on the subject. The fatty acids do two broad things. They incorporate into the membranes of neurons in the brain and they also create signaling molecules throughout the brain and the body that interact with the immune system and the inflammatory system. And we suspect that it is through those mechanisms that this composition of fatty acids is having an effect on mood stability, but lots more work needs to be done to figure that out,” Dr. Saunders added.
The findings were presented at the American Society of Clinical Psychopharmacology 2020 Virtual Conference.
Fewer mood swings
Many patients with bipolar disorder do not achieve complete mood stability with medication, making the need for additional treatments imperative, she added.
“We were interested in looking at treatments that improved mood stability in bipolar disorder that are well tolerated by patients and that can be added to pharmacological treatments. We studied this particular nutritional intervention because biologically it does some of the same things that effective medications for bipolar disorder do and it has been investigated as an effective treatment for conditions like migraine headaches, which has a lot of overlap and comorbidity with bipolar disorder.”
The researchers randomized 41 patients with BD to receive the nutritional intervention of high omega-3 plus low omega-6 (H3-L6) and 41 patients with BD to receive a control diet of usual US levels of omega-3 and omega-6 fatty acids.
The patients were aged 20-75 years (mean age, 43.5 +/– 13.9 years) and 83% were women. They had similar mean levels of mood symptoms and pain.
All patients received group-specific study foods and oils, as well as intensive dietary counseling from a dietitian, access to a website with recipes, and guidance for eating in restaurants. All participants were blinded to the composition of the food that they were eating.
Both the interventional diet and the control diet were tailored for the purposes of the study, noted coinvestigator Sarah Shahriar, a research assistant at Penn State.
“The interventional group had more fatty fish such as salmon and tuna, while the control group had more white fish and fish with less fatty acid content. The interventional group also received a different type of cooking oil, which was a blend of olive and macadamia-nut oil, which was specially formulated by a research nutritional service at the University of North Carolina,” Ms. Shahriar said in an interview.
“They also decreased their red meat consumption and received specially formulated snack foods, which were specifically prepared by [the university’s] research nutritional service. It is important to point out that these diets were for a very specific purpose. We are not saying in any way shape or form that this particular nutritional intervention is good in general,” she added.
After 12 weeks, significant reductions were seen in mood variability, energy, irritability, and pain in the H3-L6 group (P < .001). The only symptom that was significantly lowered in the control group was impulsive thoughts (P = .004).
“The best message for doctors to tell their patients at this point is one of general nutritional health and the importance of nutrition in overall body and brain health, and that [this] can be a very important component of mood,” Dr. Saunders said.
Diet matters
“Highly unsaturated fatty acids are important components of neuronal cell membranes and in cell signaling,” Jessica M. Gannon, MD, University of Pittsburgh, who was not part of the study, said in an interview.
“Omega-6 fatty acids are precursors to proinflammatory compounds. Omega-3 fatty acids eicosapentaenoic acid and docosahexaenoic acid are thought to be competitive inhibitors of omega-6 and thought to have anti-inflammatory effects. Supplementation with omega-3 has been explored in cardiovascular disease, diabetes, and in rheumatologic disorders as well as in a host of psychiatric disorders, including bipolar disorders, where a possible treatment effect has been suggested,” Dr. Gannon said.
Dietary interventions targeting not only increasing omega-3 but also decreasing consumption of omega-6 rich foods could be both effective and attractive to patients invested in a healthy lifestyle for promotion of mental health, especially when they are not optimally controlled by prescribed medications, she added.
“This study suggests that such an intervention could prove beneficial, although significant patient support may be necessary to assure adherence to the diet. I would agree that future studies would be worth pursuing,” Dr. Gannon said.
The investigators and Dr. Gannon have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
A nutritional intervention with a focus on fatty acids appears to reduce mood swings in patients with bipolar disorder (BD) when used as an adjunct to pharmacotherapy, early research suggests.
In a single-center study, patients with BD who received a diet consisting of high omega-3 plus low omega-6 fatty acids (H3-L6), in addition to usual care, showed significant reductions in mood variability, irritability, and pain, compared with their counterparts who received a diet with usual levels of omega-3 and omega-6 fatty acids commonly consumed in regular U.S. diets.
“Our findings need replication and validation in other studies,” study coinvestigator Erika Saunders, MD, professor and chair of the department of psychiatry and behavioral health at Penn State Health, Hershey, said in an interview.
“While we got really exciting findings, it’s far from confirmatory or the last word on the subject. The fatty acids do two broad things. They incorporate into the membranes of neurons in the brain and they also create signaling molecules throughout the brain and the body that interact with the immune system and the inflammatory system. And we suspect that it is through those mechanisms that this composition of fatty acids is having an effect on mood stability, but lots more work needs to be done to figure that out,” Dr. Saunders added.
The findings were presented at the American Society of Clinical Psychopharmacology 2020 Virtual Conference.
Fewer mood swings
Many patients with bipolar disorder do not achieve complete mood stability with medication, making the need for additional treatments imperative, she added.
“We were interested in looking at treatments that improved mood stability in bipolar disorder that are well tolerated by patients and that can be added to pharmacological treatments. We studied this particular nutritional intervention because biologically it does some of the same things that effective medications for bipolar disorder do and it has been investigated as an effective treatment for conditions like migraine headaches, which has a lot of overlap and comorbidity with bipolar disorder.”
The researchers randomized 41 patients with BD to receive the nutritional intervention of high omega-3 plus low omega-6 (H3-L6) and 41 patients with BD to receive a control diet of usual US levels of omega-3 and omega-6 fatty acids.
The patients were aged 20-75 years (mean age, 43.5 +/– 13.9 years) and 83% were women. They had similar mean levels of mood symptoms and pain.
All patients received group-specific study foods and oils, as well as intensive dietary counseling from a dietitian, access to a website with recipes, and guidance for eating in restaurants. All participants were blinded to the composition of the food that they were eating.
Both the interventional diet and the control diet were tailored for the purposes of the study, noted coinvestigator Sarah Shahriar, a research assistant at Penn State.
“The interventional group had more fatty fish such as salmon and tuna, while the control group had more white fish and fish with less fatty acid content. The interventional group also received a different type of cooking oil, which was a blend of olive and macadamia-nut oil, which was specially formulated by a research nutritional service at the University of North Carolina,” Ms. Shahriar said in an interview.
“They also decreased their red meat consumption and received specially formulated snack foods, which were specifically prepared by [the university’s] research nutritional service. It is important to point out that these diets were for a very specific purpose. We are not saying in any way shape or form that this particular nutritional intervention is good in general,” she added.
After 12 weeks, significant reductions were seen in mood variability, energy, irritability, and pain in the H3-L6 group (P < .001). The only symptom that was significantly lowered in the control group was impulsive thoughts (P = .004).
“The best message for doctors to tell their patients at this point is one of general nutritional health and the importance of nutrition in overall body and brain health, and that [this] can be a very important component of mood,” Dr. Saunders said.
Diet matters
“Highly unsaturated fatty acids are important components of neuronal cell membranes and in cell signaling,” Jessica M. Gannon, MD, University of Pittsburgh, who was not part of the study, said in an interview.
“Omega-6 fatty acids are precursors to proinflammatory compounds. Omega-3 fatty acids eicosapentaenoic acid and docosahexaenoic acid are thought to be competitive inhibitors of omega-6 and thought to have anti-inflammatory effects. Supplementation with omega-3 has been explored in cardiovascular disease, diabetes, and in rheumatologic disorders as well as in a host of psychiatric disorders, including bipolar disorders, where a possible treatment effect has been suggested,” Dr. Gannon said.
Dietary interventions targeting not only increasing omega-3 but also decreasing consumption of omega-6 rich foods could be both effective and attractive to patients invested in a healthy lifestyle for promotion of mental health, especially when they are not optimally controlled by prescribed medications, she added.
“This study suggests that such an intervention could prove beneficial, although significant patient support may be necessary to assure adherence to the diet. I would agree that future studies would be worth pursuing,” Dr. Gannon said.
The investigators and Dr. Gannon have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
A nutritional intervention with a focus on fatty acids appears to reduce mood swings in patients with bipolar disorder (BD) when used as an adjunct to pharmacotherapy, early research suggests.
In a single-center study, patients with BD who received a diet consisting of high omega-3 plus low omega-6 fatty acids (H3-L6), in addition to usual care, showed significant reductions in mood variability, irritability, and pain, compared with their counterparts who received a diet with usual levels of omega-3 and omega-6 fatty acids commonly consumed in regular U.S. diets.
“Our findings need replication and validation in other studies,” study coinvestigator Erika Saunders, MD, professor and chair of the department of psychiatry and behavioral health at Penn State Health, Hershey, said in an interview.
“While we got really exciting findings, it’s far from confirmatory or the last word on the subject. The fatty acids do two broad things. They incorporate into the membranes of neurons in the brain and they also create signaling molecules throughout the brain and the body that interact with the immune system and the inflammatory system. And we suspect that it is through those mechanisms that this composition of fatty acids is having an effect on mood stability, but lots more work needs to be done to figure that out,” Dr. Saunders added.
The findings were presented at the American Society of Clinical Psychopharmacology 2020 Virtual Conference.
Fewer mood swings
Many patients with bipolar disorder do not achieve complete mood stability with medication, making the need for additional treatments imperative, she added.
“We were interested in looking at treatments that improved mood stability in bipolar disorder that are well tolerated by patients and that can be added to pharmacological treatments. We studied this particular nutritional intervention because biologically it does some of the same things that effective medications for bipolar disorder do and it has been investigated as an effective treatment for conditions like migraine headaches, which has a lot of overlap and comorbidity with bipolar disorder.”
The researchers randomized 41 patients with BD to receive the nutritional intervention of high omega-3 plus low omega-6 (H3-L6) and 41 patients with BD to receive a control diet of usual US levels of omega-3 and omega-6 fatty acids.
The patients were aged 20-75 years (mean age, 43.5 +/– 13.9 years) and 83% were women. They had similar mean levels of mood symptoms and pain.
All patients received group-specific study foods and oils, as well as intensive dietary counseling from a dietitian, access to a website with recipes, and guidance for eating in restaurants. All participants were blinded to the composition of the food that they were eating.
Both the interventional diet and the control diet were tailored for the purposes of the study, noted coinvestigator Sarah Shahriar, a research assistant at Penn State.
“The interventional group had more fatty fish such as salmon and tuna, while the control group had more white fish and fish with less fatty acid content. The interventional group also received a different type of cooking oil, which was a blend of olive and macadamia-nut oil, which was specially formulated by a research nutritional service at the University of North Carolina,” Ms. Shahriar said in an interview.
“They also decreased their red meat consumption and received specially formulated snack foods, which were specifically prepared by [the university’s] research nutritional service. It is important to point out that these diets were for a very specific purpose. We are not saying in any way shape or form that this particular nutritional intervention is good in general,” she added.
After 12 weeks, significant reductions were seen in mood variability, energy, irritability, and pain in the H3-L6 group (P < .001). The only symptom that was significantly lowered in the control group was impulsive thoughts (P = .004).
“The best message for doctors to tell their patients at this point is one of general nutritional health and the importance of nutrition in overall body and brain health, and that [this] can be a very important component of mood,” Dr. Saunders said.
Diet matters
“Highly unsaturated fatty acids are important components of neuronal cell membranes and in cell signaling,” Jessica M. Gannon, MD, University of Pittsburgh, who was not part of the study, said in an interview.
“Omega-6 fatty acids are precursors to proinflammatory compounds. Omega-3 fatty acids eicosapentaenoic acid and docosahexaenoic acid are thought to be competitive inhibitors of omega-6 and thought to have anti-inflammatory effects. Supplementation with omega-3 has been explored in cardiovascular disease, diabetes, and in rheumatologic disorders as well as in a host of psychiatric disorders, including bipolar disorders, where a possible treatment effect has been suggested,” Dr. Gannon said.
Dietary interventions targeting not only increasing omega-3 but also decreasing consumption of omega-6 rich foods could be both effective and attractive to patients invested in a healthy lifestyle for promotion of mental health, especially when they are not optimally controlled by prescribed medications, she added.
“This study suggests that such an intervention could prove beneficial, although significant patient support may be necessary to assure adherence to the diet. I would agree that future studies would be worth pursuing,” Dr. Gannon said.
The investigators and Dr. Gannon have reported no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
COVID-19: Problematic gambling could worsen
The confluence of isolation, excess available time, and anxiety about illness or finances as a result of the COVID-19 pandemic have the potential to increase problem gambling behaviors during this public health emergency, so it’s essential to gather data and supply guidance on this issue, according to a call to action published May 18 in the Journal of Addiction Medicine.
“When facing an unforeseen situation with confinement, fear of disease, and financial uncertainty for the future, problem gambling may be an important health hazard to monitor and prevent during and following the COVID-19 crisis, especially given current online gambling availability,” wrote Anders Håkansson, PhD, of Lund University in Sweden and coauthors.
Both stress and trauma have been linked to gambling problems, and both are occurring during the pandemic, said coauthor Marc N. Potenza, MD, PhD, of Yale University, New Haven, Conn., in an interview.
“People are likely to be experiencing stress at levels they haven’t experienced previously,” Dr. Potenza said. While multiple factors can contribute to addictive behaviors, “with respect to the pandemic, one concern is that so-called negative reinforcement motivations – engaging in an addictive behavior to escape from depressed or negative mood states – may be a driving motivation for a significant number of people during this time,” he said.
David Hodgins, PhD, CPsych, a professor of psychology at the University of Calgary in Alberta, who was not involved with the commentary, noted that gambling relapse is triggered by “negative emotional states, interpersonal stress, and financial stress” – all three of which the pandemic contributes to.
Financial stress can especially “inflame erroneous gambling-related cognitions,” he said in an interview, including “beliefs such as the idea that gambling can solve financial problems, even when this is statistically almost impossible as debt increases, and that debt has been caused by gambling.”
Increased social isolation also is particularly problematic, pointed out Shane W. Kraus, PhD, from the University of Nevada, Las Vegas. Dr. Kraus also was not involved with the paper.
“If someone is already struggling with already negative emotions, negative feelings, thoughts, and depression, and you’re now isolating them quite a bit, that’s not going to be a recipe for success,” Dr. Kraus said in an interview.
Dr. Potenza said.
“We should be mindful of ways in which people develop addictions in these settings,” he said. “One of the aspects of the pandemic is that many people are at home for longer periods of time, and they use digital technologies more frequently.”
The use of digital technologies can include interaction on social media platforms and on meeting applications such as Zoom, but such use also offers opportunities for problematic gambling, gaming, and pornography use. The World Health Organization recognizes addiction disorders for gambling and for gaming, and online gaming platforms and pornography sites have reported substantial increases in their traffic during the pandemic, Dr. Potenza said.
The increase in frequency is unsurprising and not necessarily a concern by itself, Dr. Kraus said.
“It’s all about loss of control or difficulty engaging or disengaging,” Dr. Kraus said. “When you can’t stop doing something even if you like it or love it, when it interferes with your day-to-day activities and relationships, that’s when it’s a problem.”
Gambling online: Easy, available
The authors note that past research has identified increased gambling problems during economic crises in other countries.
“While currently speculative, financial hardships may promote gambling as individuals may be motivated to gamble to try to win money,” the authors suggested. “Although presently limited, existing data suggest that COVID-19–related financial concerns may increase gambling-related harms, and this possibility merits systematic research.”
But trends and characteristics of the gambling market, including direct effects from the pandemic, can potentially influence behaviors, too. Most casinos have closed during the pandemic, and most of the sports that people bet on have been canceled or postponed.
“Fewer people are gambling on sports, but they turn then to other areas,” Dr. Potenza said. “If they can’t bet on major league type sports, they might gamble on more local sporting events, or they may bet on other activities going on in society during the pandemic.”
But online gambling poses greater risk.
“Properties of online gambling may constitute a particular health hazard when many people are confined to their homes and have had rapid changes in working conditions, psychosocial stress, anxiety, and depression, as has been described in China,” the paper’s authors wrote. “Online gambling may be particularly concerning due to its availability and velocity” and association with higher debt levels.
In addition to online gaming’s ease and availability, past research has found patients report boredom and escapism as reasons they turned to it.
Again, boredom on its own is not necessarily a problem, but for those who already struggle with addictive behaviors, it can be a trigger, Dr. Kraus said.
“Boredom is very tough for them because it’s often associated with negative emotions,” such as dwelling on things not going well in their lives, he said. “In a pandemic, people are by themselves quite a bit, socially isolated, so for those who are struggling already with some depression or anxiety, it’s only going to be increased.”
Online gaming trends may vary with demographics, however. Dr. Kraus noted that his former clinic at the Veterans Administration has been seeing lower gambling in patients with addictive disorders, but those patients are also older and primarily frequented casinos.
“It’s going to depend on age and familiarity with technology,” he said, but even if older problem gamblers are not going to the Internet now, “let’s wait and see what happens in the next 2 or 3 months.”
The authors noted results from a small survey of patients in treatment for gambling addiction at the Bellvitge University Hospital in Barcelona, Spain, where two of the coauthors work. They conducted telephone surveys with 26 patients about the first 4 weeks of sheltering in place because of the coronavirus. All but four of the patients were male, and their average age was 45 years.
“Most presented worries about increased uncertainties, such as the negative impact on their work, risk of COVID-19 infection of themselves or their loved ones and their treatment,” the authors reported.
Although 19% were completely abstinent, an additional 12% (n = 3) reported worsened gambling. In addition, almost half (46%) reported anxiety symptoms and more than a quarter (27%) had depressive symptoms.
Appropriate care
A particularly complicating factor of the pandemic is how it has disrupted traditional ways of seeking health care, particularly with how much mental health and other medical care has shifted to telehealth and online delivery, Dr. Potenza pointed out.
“This is a change for many people, and it’s important for both caretakers and people in treatment to be mindful of this and to try to ensure that appropriate services are maintained for people during this time,” he said.
For example, 12-step programs traditionally meet in person, which is largely impossible during the pandemic. Some have moved meetings online, and other programs have turned to apps, such as the Addiction Policy Forum’s app Connections, an empirically validated digital therapy platform that lets patients and clinicians remain connected with remote check-ins.
The move to more telehealth may actually increase access, suggested Dr. Hodgins.
“There is no evidence that this is less effective, and in fact, its convenience might be an advantage in reaching more people,” he said. “More challenging is offering group therapies remotely, but this is also feasible.”
The treatment with the strongest evidence remains cognitive-behavioral therapy (CBT), Dr. Hodgins said.
“This therapy, in part, helps people become aware of their erroneous cognitions and to challenge them, but also helps people restructure their activities to change their habits,” he said. He also noted the rise of online therapy, whether supported by a therapist or entirely self-directed, such as Gambling Self-help.
“These programs typically provide cognitive behavior content but also content that comes from studying how people recover from gambling problems,” he said. “The challenge of completely self-directed approaches is follow-through. Like most online content, people tend to flit around more than they might in therapy.” Still, he added, research has shown good outcomes from these programs.
Dr. Potenza also noted that several organizations, including the International Society of Addiction Medicine and Children and Screens, have been hosting webinars related to COVID-19 coping and/or addiction that clinicians and patients might find helpful.
Identification of problematic behaviors
One challenge in watching for problematic gambling behaviors during the pandemic is the set of unusual living circumstances for most people right now. At almost no other time in history have people been primarily confined to their homes, many unable to go to work or working from home, with extra leisure time and nowhere to go.
“With the COVID-19 pandemic, a lot of daily life has changed,” Dr. Potenza said. “It’s unclear whether certain behaviors that have become habitual during the pandemic, such as gaming or online gambling, will then interfere with daily life when the pandemic subsides.”
“The problem is, a small proportion of people who are very vulnerable will develop a disorder and might maintain it,” Dr. Kraus said. Those who already struggle with mental health and may be out of work have greater potential for problematic behaviors.
Dr. Potenza collaborated with other psychiatrists in drafting consensus guidelines on maintaining healthy use of the Internet specifically during the pandemic (Compr Psychiatry. 2020 Jul. doi: 10.10161/comppsych.2020.152180).
“It’s important to think about where one draws the line between normative everyday behaviors – behaviors that are not interfering with life functioning – and those that do interfere with life functioning,” Dr. Potenza said. “If someone is having difficulty making work or family or school obligations, these are important signs that the behavior may be problematic.”
He offered suggestions for things people can do to promote their health during the pandemic, such as having regular routines that include getting physical exercise and social interaction, dining with family if isolating together, and making time for self-care. He also recommended setting limits on the use of digital devices and aiming for a healthy balance in keeping up with the news. The idea is to stay aware of what’s happening without getting burned out or traumatized by news coverage.
Guidance for clinicians
An urgent need for research and guidelines related to gambling and the pandemic exists, the authors argued.
In the meantime, aside from various validated screeners available, Dr. Kraus offered some practical advice for clinicians checking in with their patients: “Ask your patients what they have been doing to cope with this difficult time.”
Some might mention their faith, family, or friends, and others might not have an answer or mention drinking, gaming, or engaging in other activities. “We all do things to cope. Sometimes you use healthy coping and sometimes you use unhealthy coping,” Dr. Kraus said. “I would have a dialogue with my patients around, ‘How are you getting through? What’s helping you? What are some things you’ve tried that are tripping you up?’ ”
If gambling in particular is a possible concern, he encouraged clinicians to ask their patients whether they have tried to quit or what would happen if they stopped gambling.
“What we’d expect is the problem gamblers will have more irritability, crankiness, difficulty with quitting,” he said.
Dr. Hodgins agreed that checking in on how patients’ lives and activities have changed, and their emotion reactions to those changes, is prudent.
“The change in activities might be healthy or might include increased addictive behaviors, including increased use of substances, gaming, pornography, food, and gambling,” he said.
In addition, the paper authors list several examples of guidelines that might be considered in drafting guidance for clinicians, including the following:
- Limiting the extent of gambling
- Not gambling to regulate negative emotions
- Not gambling in order to try to solve financial problems or financial concerns
- Not gambling under the influence of alcohol or drugs
- Carefully monitoring gambling-related time and financial expenditures
- Maintaining and establishing daily routines involving activities other than gambling
- Minding gambling-related attitudes and behaviors in the presence of minors
- Not starting to gamble because of stressors
The research did not receive external funding. Dr. Håkansson has received research funding from the Swedish Sport Foundation, the Swedish alcohol monopoly Systembolaget, and the Swedish state-owned gambling operator AB Svenska Spel. He is working with the company Kontigo Care on devices for gambling addiction follow-up care. Dr. Potenza has received consulting or advisory compensation from several entities, including the Addiction Policy Forum, AXA Gaming, Idorsia, Opiant, and RiverMend Health. Dr. Potenza has received research funding from Mohegan Sun casino and the National Center for Responsible Gaming. No other authors or outside sources had industry-related disclosures.
SOURCE: Håkansson A et al. J Addict Med. 2020 May 18. doi: 10.1097/ADM.0000000000000690.
The confluence of isolation, excess available time, and anxiety about illness or finances as a result of the COVID-19 pandemic have the potential to increase problem gambling behaviors during this public health emergency, so it’s essential to gather data and supply guidance on this issue, according to a call to action published May 18 in the Journal of Addiction Medicine.
“When facing an unforeseen situation with confinement, fear of disease, and financial uncertainty for the future, problem gambling may be an important health hazard to monitor and prevent during and following the COVID-19 crisis, especially given current online gambling availability,” wrote Anders Håkansson, PhD, of Lund University in Sweden and coauthors.
Both stress and trauma have been linked to gambling problems, and both are occurring during the pandemic, said coauthor Marc N. Potenza, MD, PhD, of Yale University, New Haven, Conn., in an interview.
“People are likely to be experiencing stress at levels they haven’t experienced previously,” Dr. Potenza said. While multiple factors can contribute to addictive behaviors, “with respect to the pandemic, one concern is that so-called negative reinforcement motivations – engaging in an addictive behavior to escape from depressed or negative mood states – may be a driving motivation for a significant number of people during this time,” he said.
David Hodgins, PhD, CPsych, a professor of psychology at the University of Calgary in Alberta, who was not involved with the commentary, noted that gambling relapse is triggered by “negative emotional states, interpersonal stress, and financial stress” – all three of which the pandemic contributes to.
Financial stress can especially “inflame erroneous gambling-related cognitions,” he said in an interview, including “beliefs such as the idea that gambling can solve financial problems, even when this is statistically almost impossible as debt increases, and that debt has been caused by gambling.”
Increased social isolation also is particularly problematic, pointed out Shane W. Kraus, PhD, from the University of Nevada, Las Vegas. Dr. Kraus also was not involved with the paper.
“If someone is already struggling with already negative emotions, negative feelings, thoughts, and depression, and you’re now isolating them quite a bit, that’s not going to be a recipe for success,” Dr. Kraus said in an interview.
Dr. Potenza said.
“We should be mindful of ways in which people develop addictions in these settings,” he said. “One of the aspects of the pandemic is that many people are at home for longer periods of time, and they use digital technologies more frequently.”
The use of digital technologies can include interaction on social media platforms and on meeting applications such as Zoom, but such use also offers opportunities for problematic gambling, gaming, and pornography use. The World Health Organization recognizes addiction disorders for gambling and for gaming, and online gaming platforms and pornography sites have reported substantial increases in their traffic during the pandemic, Dr. Potenza said.
The increase in frequency is unsurprising and not necessarily a concern by itself, Dr. Kraus said.
“It’s all about loss of control or difficulty engaging or disengaging,” Dr. Kraus said. “When you can’t stop doing something even if you like it or love it, when it interferes with your day-to-day activities and relationships, that’s when it’s a problem.”
Gambling online: Easy, available
The authors note that past research has identified increased gambling problems during economic crises in other countries.
“While currently speculative, financial hardships may promote gambling as individuals may be motivated to gamble to try to win money,” the authors suggested. “Although presently limited, existing data suggest that COVID-19–related financial concerns may increase gambling-related harms, and this possibility merits systematic research.”
But trends and characteristics of the gambling market, including direct effects from the pandemic, can potentially influence behaviors, too. Most casinos have closed during the pandemic, and most of the sports that people bet on have been canceled or postponed.
“Fewer people are gambling on sports, but they turn then to other areas,” Dr. Potenza said. “If they can’t bet on major league type sports, they might gamble on more local sporting events, or they may bet on other activities going on in society during the pandemic.”
But online gambling poses greater risk.
“Properties of online gambling may constitute a particular health hazard when many people are confined to their homes and have had rapid changes in working conditions, psychosocial stress, anxiety, and depression, as has been described in China,” the paper’s authors wrote. “Online gambling may be particularly concerning due to its availability and velocity” and association with higher debt levels.
In addition to online gaming’s ease and availability, past research has found patients report boredom and escapism as reasons they turned to it.
Again, boredom on its own is not necessarily a problem, but for those who already struggle with addictive behaviors, it can be a trigger, Dr. Kraus said.
“Boredom is very tough for them because it’s often associated with negative emotions,” such as dwelling on things not going well in their lives, he said. “In a pandemic, people are by themselves quite a bit, socially isolated, so for those who are struggling already with some depression or anxiety, it’s only going to be increased.”
Online gaming trends may vary with demographics, however. Dr. Kraus noted that his former clinic at the Veterans Administration has been seeing lower gambling in patients with addictive disorders, but those patients are also older and primarily frequented casinos.
“It’s going to depend on age and familiarity with technology,” he said, but even if older problem gamblers are not going to the Internet now, “let’s wait and see what happens in the next 2 or 3 months.”
The authors noted results from a small survey of patients in treatment for gambling addiction at the Bellvitge University Hospital in Barcelona, Spain, where two of the coauthors work. They conducted telephone surveys with 26 patients about the first 4 weeks of sheltering in place because of the coronavirus. All but four of the patients were male, and their average age was 45 years.
“Most presented worries about increased uncertainties, such as the negative impact on their work, risk of COVID-19 infection of themselves or their loved ones and their treatment,” the authors reported.
Although 19% were completely abstinent, an additional 12% (n = 3) reported worsened gambling. In addition, almost half (46%) reported anxiety symptoms and more than a quarter (27%) had depressive symptoms.
Appropriate care
A particularly complicating factor of the pandemic is how it has disrupted traditional ways of seeking health care, particularly with how much mental health and other medical care has shifted to telehealth and online delivery, Dr. Potenza pointed out.
“This is a change for many people, and it’s important for both caretakers and people in treatment to be mindful of this and to try to ensure that appropriate services are maintained for people during this time,” he said.
For example, 12-step programs traditionally meet in person, which is largely impossible during the pandemic. Some have moved meetings online, and other programs have turned to apps, such as the Addiction Policy Forum’s app Connections, an empirically validated digital therapy platform that lets patients and clinicians remain connected with remote check-ins.
The move to more telehealth may actually increase access, suggested Dr. Hodgins.
“There is no evidence that this is less effective, and in fact, its convenience might be an advantage in reaching more people,” he said. “More challenging is offering group therapies remotely, but this is also feasible.”
The treatment with the strongest evidence remains cognitive-behavioral therapy (CBT), Dr. Hodgins said.
“This therapy, in part, helps people become aware of their erroneous cognitions and to challenge them, but also helps people restructure their activities to change their habits,” he said. He also noted the rise of online therapy, whether supported by a therapist or entirely self-directed, such as Gambling Self-help.
“These programs typically provide cognitive behavior content but also content that comes from studying how people recover from gambling problems,” he said. “The challenge of completely self-directed approaches is follow-through. Like most online content, people tend to flit around more than they might in therapy.” Still, he added, research has shown good outcomes from these programs.
Dr. Potenza also noted that several organizations, including the International Society of Addiction Medicine and Children and Screens, have been hosting webinars related to COVID-19 coping and/or addiction that clinicians and patients might find helpful.
Identification of problematic behaviors
One challenge in watching for problematic gambling behaviors during the pandemic is the set of unusual living circumstances for most people right now. At almost no other time in history have people been primarily confined to their homes, many unable to go to work or working from home, with extra leisure time and nowhere to go.
“With the COVID-19 pandemic, a lot of daily life has changed,” Dr. Potenza said. “It’s unclear whether certain behaviors that have become habitual during the pandemic, such as gaming or online gambling, will then interfere with daily life when the pandemic subsides.”
“The problem is, a small proportion of people who are very vulnerable will develop a disorder and might maintain it,” Dr. Kraus said. Those who already struggle with mental health and may be out of work have greater potential for problematic behaviors.
Dr. Potenza collaborated with other psychiatrists in drafting consensus guidelines on maintaining healthy use of the Internet specifically during the pandemic (Compr Psychiatry. 2020 Jul. doi: 10.10161/comppsych.2020.152180).
“It’s important to think about where one draws the line between normative everyday behaviors – behaviors that are not interfering with life functioning – and those that do interfere with life functioning,” Dr. Potenza said. “If someone is having difficulty making work or family or school obligations, these are important signs that the behavior may be problematic.”
He offered suggestions for things people can do to promote their health during the pandemic, such as having regular routines that include getting physical exercise and social interaction, dining with family if isolating together, and making time for self-care. He also recommended setting limits on the use of digital devices and aiming for a healthy balance in keeping up with the news. The idea is to stay aware of what’s happening without getting burned out or traumatized by news coverage.
Guidance for clinicians
An urgent need for research and guidelines related to gambling and the pandemic exists, the authors argued.
In the meantime, aside from various validated screeners available, Dr. Kraus offered some practical advice for clinicians checking in with their patients: “Ask your patients what they have been doing to cope with this difficult time.”
Some might mention their faith, family, or friends, and others might not have an answer or mention drinking, gaming, or engaging in other activities. “We all do things to cope. Sometimes you use healthy coping and sometimes you use unhealthy coping,” Dr. Kraus said. “I would have a dialogue with my patients around, ‘How are you getting through? What’s helping you? What are some things you’ve tried that are tripping you up?’ ”
If gambling in particular is a possible concern, he encouraged clinicians to ask their patients whether they have tried to quit or what would happen if they stopped gambling.
“What we’d expect is the problem gamblers will have more irritability, crankiness, difficulty with quitting,” he said.
Dr. Hodgins agreed that checking in on how patients’ lives and activities have changed, and their emotion reactions to those changes, is prudent.
“The change in activities might be healthy or might include increased addictive behaviors, including increased use of substances, gaming, pornography, food, and gambling,” he said.
In addition, the paper authors list several examples of guidelines that might be considered in drafting guidance for clinicians, including the following:
- Limiting the extent of gambling
- Not gambling to regulate negative emotions
- Not gambling in order to try to solve financial problems or financial concerns
- Not gambling under the influence of alcohol or drugs
- Carefully monitoring gambling-related time and financial expenditures
- Maintaining and establishing daily routines involving activities other than gambling
- Minding gambling-related attitudes and behaviors in the presence of minors
- Not starting to gamble because of stressors
The research did not receive external funding. Dr. Håkansson has received research funding from the Swedish Sport Foundation, the Swedish alcohol monopoly Systembolaget, and the Swedish state-owned gambling operator AB Svenska Spel. He is working with the company Kontigo Care on devices for gambling addiction follow-up care. Dr. Potenza has received consulting or advisory compensation from several entities, including the Addiction Policy Forum, AXA Gaming, Idorsia, Opiant, and RiverMend Health. Dr. Potenza has received research funding from Mohegan Sun casino and the National Center for Responsible Gaming. No other authors or outside sources had industry-related disclosures.
SOURCE: Håkansson A et al. J Addict Med. 2020 May 18. doi: 10.1097/ADM.0000000000000690.
The confluence of isolation, excess available time, and anxiety about illness or finances as a result of the COVID-19 pandemic have the potential to increase problem gambling behaviors during this public health emergency, so it’s essential to gather data and supply guidance on this issue, according to a call to action published May 18 in the Journal of Addiction Medicine.
“When facing an unforeseen situation with confinement, fear of disease, and financial uncertainty for the future, problem gambling may be an important health hazard to monitor and prevent during and following the COVID-19 crisis, especially given current online gambling availability,” wrote Anders Håkansson, PhD, of Lund University in Sweden and coauthors.
Both stress and trauma have been linked to gambling problems, and both are occurring during the pandemic, said coauthor Marc N. Potenza, MD, PhD, of Yale University, New Haven, Conn., in an interview.
“People are likely to be experiencing stress at levels they haven’t experienced previously,” Dr. Potenza said. While multiple factors can contribute to addictive behaviors, “with respect to the pandemic, one concern is that so-called negative reinforcement motivations – engaging in an addictive behavior to escape from depressed or negative mood states – may be a driving motivation for a significant number of people during this time,” he said.
David Hodgins, PhD, CPsych, a professor of psychology at the University of Calgary in Alberta, who was not involved with the commentary, noted that gambling relapse is triggered by “negative emotional states, interpersonal stress, and financial stress” – all three of which the pandemic contributes to.
Financial stress can especially “inflame erroneous gambling-related cognitions,” he said in an interview, including “beliefs such as the idea that gambling can solve financial problems, even when this is statistically almost impossible as debt increases, and that debt has been caused by gambling.”
Increased social isolation also is particularly problematic, pointed out Shane W. Kraus, PhD, from the University of Nevada, Las Vegas. Dr. Kraus also was not involved with the paper.
“If someone is already struggling with already negative emotions, negative feelings, thoughts, and depression, and you’re now isolating them quite a bit, that’s not going to be a recipe for success,” Dr. Kraus said in an interview.
Dr. Potenza said.
“We should be mindful of ways in which people develop addictions in these settings,” he said. “One of the aspects of the pandemic is that many people are at home for longer periods of time, and they use digital technologies more frequently.”
The use of digital technologies can include interaction on social media platforms and on meeting applications such as Zoom, but such use also offers opportunities for problematic gambling, gaming, and pornography use. The World Health Organization recognizes addiction disorders for gambling and for gaming, and online gaming platforms and pornography sites have reported substantial increases in their traffic during the pandemic, Dr. Potenza said.
The increase in frequency is unsurprising and not necessarily a concern by itself, Dr. Kraus said.
“It’s all about loss of control or difficulty engaging or disengaging,” Dr. Kraus said. “When you can’t stop doing something even if you like it or love it, when it interferes with your day-to-day activities and relationships, that’s when it’s a problem.”
Gambling online: Easy, available
The authors note that past research has identified increased gambling problems during economic crises in other countries.
“While currently speculative, financial hardships may promote gambling as individuals may be motivated to gamble to try to win money,” the authors suggested. “Although presently limited, existing data suggest that COVID-19–related financial concerns may increase gambling-related harms, and this possibility merits systematic research.”
But trends and characteristics of the gambling market, including direct effects from the pandemic, can potentially influence behaviors, too. Most casinos have closed during the pandemic, and most of the sports that people bet on have been canceled or postponed.
“Fewer people are gambling on sports, but they turn then to other areas,” Dr. Potenza said. “If they can’t bet on major league type sports, they might gamble on more local sporting events, or they may bet on other activities going on in society during the pandemic.”
But online gambling poses greater risk.
“Properties of online gambling may constitute a particular health hazard when many people are confined to their homes and have had rapid changes in working conditions, psychosocial stress, anxiety, and depression, as has been described in China,” the paper’s authors wrote. “Online gambling may be particularly concerning due to its availability and velocity” and association with higher debt levels.
In addition to online gaming’s ease and availability, past research has found patients report boredom and escapism as reasons they turned to it.
Again, boredom on its own is not necessarily a problem, but for those who already struggle with addictive behaviors, it can be a trigger, Dr. Kraus said.
“Boredom is very tough for them because it’s often associated with negative emotions,” such as dwelling on things not going well in their lives, he said. “In a pandemic, people are by themselves quite a bit, socially isolated, so for those who are struggling already with some depression or anxiety, it’s only going to be increased.”
Online gaming trends may vary with demographics, however. Dr. Kraus noted that his former clinic at the Veterans Administration has been seeing lower gambling in patients with addictive disorders, but those patients are also older and primarily frequented casinos.
“It’s going to depend on age and familiarity with technology,” he said, but even if older problem gamblers are not going to the Internet now, “let’s wait and see what happens in the next 2 or 3 months.”
The authors noted results from a small survey of patients in treatment for gambling addiction at the Bellvitge University Hospital in Barcelona, Spain, where two of the coauthors work. They conducted telephone surveys with 26 patients about the first 4 weeks of sheltering in place because of the coronavirus. All but four of the patients were male, and their average age was 45 years.
“Most presented worries about increased uncertainties, such as the negative impact on their work, risk of COVID-19 infection of themselves or their loved ones and their treatment,” the authors reported.
Although 19% were completely abstinent, an additional 12% (n = 3) reported worsened gambling. In addition, almost half (46%) reported anxiety symptoms and more than a quarter (27%) had depressive symptoms.
Appropriate care
A particularly complicating factor of the pandemic is how it has disrupted traditional ways of seeking health care, particularly with how much mental health and other medical care has shifted to telehealth and online delivery, Dr. Potenza pointed out.
“This is a change for many people, and it’s important for both caretakers and people in treatment to be mindful of this and to try to ensure that appropriate services are maintained for people during this time,” he said.
For example, 12-step programs traditionally meet in person, which is largely impossible during the pandemic. Some have moved meetings online, and other programs have turned to apps, such as the Addiction Policy Forum’s app Connections, an empirically validated digital therapy platform that lets patients and clinicians remain connected with remote check-ins.
The move to more telehealth may actually increase access, suggested Dr. Hodgins.
“There is no evidence that this is less effective, and in fact, its convenience might be an advantage in reaching more people,” he said. “More challenging is offering group therapies remotely, but this is also feasible.”
The treatment with the strongest evidence remains cognitive-behavioral therapy (CBT), Dr. Hodgins said.
“This therapy, in part, helps people become aware of their erroneous cognitions and to challenge them, but also helps people restructure their activities to change their habits,” he said. He also noted the rise of online therapy, whether supported by a therapist or entirely self-directed, such as Gambling Self-help.
“These programs typically provide cognitive behavior content but also content that comes from studying how people recover from gambling problems,” he said. “The challenge of completely self-directed approaches is follow-through. Like most online content, people tend to flit around more than they might in therapy.” Still, he added, research has shown good outcomes from these programs.
Dr. Potenza also noted that several organizations, including the International Society of Addiction Medicine and Children and Screens, have been hosting webinars related to COVID-19 coping and/or addiction that clinicians and patients might find helpful.
Identification of problematic behaviors
One challenge in watching for problematic gambling behaviors during the pandemic is the set of unusual living circumstances for most people right now. At almost no other time in history have people been primarily confined to their homes, many unable to go to work or working from home, with extra leisure time and nowhere to go.
“With the COVID-19 pandemic, a lot of daily life has changed,” Dr. Potenza said. “It’s unclear whether certain behaviors that have become habitual during the pandemic, such as gaming or online gambling, will then interfere with daily life when the pandemic subsides.”
“The problem is, a small proportion of people who are very vulnerable will develop a disorder and might maintain it,” Dr. Kraus said. Those who already struggle with mental health and may be out of work have greater potential for problematic behaviors.
Dr. Potenza collaborated with other psychiatrists in drafting consensus guidelines on maintaining healthy use of the Internet specifically during the pandemic (Compr Psychiatry. 2020 Jul. doi: 10.10161/comppsych.2020.152180).
“It’s important to think about where one draws the line between normative everyday behaviors – behaviors that are not interfering with life functioning – and those that do interfere with life functioning,” Dr. Potenza said. “If someone is having difficulty making work or family or school obligations, these are important signs that the behavior may be problematic.”
He offered suggestions for things people can do to promote their health during the pandemic, such as having regular routines that include getting physical exercise and social interaction, dining with family if isolating together, and making time for self-care. He also recommended setting limits on the use of digital devices and aiming for a healthy balance in keeping up with the news. The idea is to stay aware of what’s happening without getting burned out or traumatized by news coverage.
Guidance for clinicians
An urgent need for research and guidelines related to gambling and the pandemic exists, the authors argued.
In the meantime, aside from various validated screeners available, Dr. Kraus offered some practical advice for clinicians checking in with their patients: “Ask your patients what they have been doing to cope with this difficult time.”
Some might mention their faith, family, or friends, and others might not have an answer or mention drinking, gaming, or engaging in other activities. “We all do things to cope. Sometimes you use healthy coping and sometimes you use unhealthy coping,” Dr. Kraus said. “I would have a dialogue with my patients around, ‘How are you getting through? What’s helping you? What are some things you’ve tried that are tripping you up?’ ”
If gambling in particular is a possible concern, he encouraged clinicians to ask their patients whether they have tried to quit or what would happen if they stopped gambling.
“What we’d expect is the problem gamblers will have more irritability, crankiness, difficulty with quitting,” he said.
Dr. Hodgins agreed that checking in on how patients’ lives and activities have changed, and their emotion reactions to those changes, is prudent.
“The change in activities might be healthy or might include increased addictive behaviors, including increased use of substances, gaming, pornography, food, and gambling,” he said.
In addition, the paper authors list several examples of guidelines that might be considered in drafting guidance for clinicians, including the following:
- Limiting the extent of gambling
- Not gambling to regulate negative emotions
- Not gambling in order to try to solve financial problems or financial concerns
- Not gambling under the influence of alcohol or drugs
- Carefully monitoring gambling-related time and financial expenditures
- Maintaining and establishing daily routines involving activities other than gambling
- Minding gambling-related attitudes and behaviors in the presence of minors
- Not starting to gamble because of stressors
The research did not receive external funding. Dr. Håkansson has received research funding from the Swedish Sport Foundation, the Swedish alcohol monopoly Systembolaget, and the Swedish state-owned gambling operator AB Svenska Spel. He is working with the company Kontigo Care on devices for gambling addiction follow-up care. Dr. Potenza has received consulting or advisory compensation from several entities, including the Addiction Policy Forum, AXA Gaming, Idorsia, Opiant, and RiverMend Health. Dr. Potenza has received research funding from Mohegan Sun casino and the National Center for Responsible Gaming. No other authors or outside sources had industry-related disclosures.
SOURCE: Håkansson A et al. J Addict Med. 2020 May 18. doi: 10.1097/ADM.0000000000000690.
FROM THE JOURNAL OF ADDICTION MEDICINE
Today’s top news highlights: Addressing racism in maternity care, group forms to protect health professionals from retaliation
Here are the stories our MDedge editors across specialties think you need to know about today:
Addressing racism in the maternal mortality crisis
The emerging racial disparities in COVID-19 incidence and outcomes in the United States are on a collision course with long-standing racial disparities in U.S. maternal care and mortality. “The saying is that ‘the virus doesn’t discriminate,’ but it understands our biases, right? So, the virus takes advantage of the weaknesses in our system,” said Joia A. Crear-Perry, MD, an ob.gyn. and founder and president of the National Birth Equity Collaborative, a New Orleans–based research, training, and advocacy organization working to optimize black maternal and infant health. This article is part of an ongoing feature series on the crisis in maternal mortality in the United States. Here we explore potential solutions for addressing the inequities as proposed by thought leaders and key stakeholders. Read more.
A ‘Beacon’ for physicians, nurses facing retaliation
Sejal Hathi, MD, and two colleagues had long kicked around the idea of starting a nonprofit group that would center on civic and legal advocacy. Once the COVID-19 pandemic hit, the three friends – who have a mix of legal, medical, and advocacy backgrounds – began chatting by email and through Zoom video meetings about how to make the plan a reality. The new organization – named Beacon – quickly mobilized, assembled their team, and launched a website. Beacon’s first project now aims to highlight and protect the legal rights of medical professionals who speak out about personal protection equipment supply and other matters of public concern related to coronavirus. “There are a flurry of reports coming our way about physicians and nurses, as well as other health care workers, who are for whatever reason being disciplined or retaliated against for simply seeking appropriate safety policies at their workplaces,” Dr. Hathi said. “What we’ve found is that many of them don’t even know what their options look like. Doctors, nurses, health care workers are not the typical type to engage politically, to speak out, [or to] advocate for themselves.” Read more.
COVID-19 ravages the Navajo Nation
The Navajo Nation has the most cases of the COVID-19 virus of any tribe in the United States, and numbers as of May 31, 2020, are 5,348, with 246 confirmed deaths. These devastating numbers, which might be leveling off, are associated with Navajo people having higher-than-average rates of diabetes, heart disease, and cancer. This is compounded with 30%-40% of homes having no electricity or running water, and a poverty rate of about 38%. “We endured and learned from each Naayee, hunger, and death to name a few adversities. The COVID-19 pandemic, or “Big Cough” (Dikos Nitsaa’igii -19 in Navajo language), is a monster confronting the Navajo today. It has had significant impact on our nation and people,” Mary Hasbah Roessel, MD, a Navajo board-certified psychiatrist practicing in Santa Fe, N.M., wrote in a commentary on MDedge. Read more.
Heart pump system authorized for COVID-19 patients
The Food and Drug Administration issued an emergency use authorization (EUA) for use of the Impella RP heart pump system in COVID-19 patients with right heart failure or decompensation. The EUA indication for the Impella RP system is to provide temporary right ventricular support for up to 14 days in critical care patients with a body surface area of at least 1.5 m2 for the treatment of acute right heart failure or decompensation caused by complications related to COVID-19, including pulmonary embolism. Read more.
Deprescribing hypertension meds looks safe for older adults
Some patients aged 80 years or older can potentially cut back on their number of antihypertensive meds, under physician guidance, without an important loss of blood pressure control, researchers concluded based on findings from a randomized multicenter trial. The study, called Optimising Treatment for Mild Systolic Hypertension in the Elderly (OPTIMISE), entered “patients in whom the benefits of taking blood pressure-lowering treatments might start to be outweighed by the potential harms,” said James P. Sheppard, PhD, of University of Oxford (England). The report was published in JAMA. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Addressing racism in the maternal mortality crisis
The emerging racial disparities in COVID-19 incidence and outcomes in the United States are on a collision course with long-standing racial disparities in U.S. maternal care and mortality. “The saying is that ‘the virus doesn’t discriminate,’ but it understands our biases, right? So, the virus takes advantage of the weaknesses in our system,” said Joia A. Crear-Perry, MD, an ob.gyn. and founder and president of the National Birth Equity Collaborative, a New Orleans–based research, training, and advocacy organization working to optimize black maternal and infant health. This article is part of an ongoing feature series on the crisis in maternal mortality in the United States. Here we explore potential solutions for addressing the inequities as proposed by thought leaders and key stakeholders. Read more.
A ‘Beacon’ for physicians, nurses facing retaliation
Sejal Hathi, MD, and two colleagues had long kicked around the idea of starting a nonprofit group that would center on civic and legal advocacy. Once the COVID-19 pandemic hit, the three friends – who have a mix of legal, medical, and advocacy backgrounds – began chatting by email and through Zoom video meetings about how to make the plan a reality. The new organization – named Beacon – quickly mobilized, assembled their team, and launched a website. Beacon’s first project now aims to highlight and protect the legal rights of medical professionals who speak out about personal protection equipment supply and other matters of public concern related to coronavirus. “There are a flurry of reports coming our way about physicians and nurses, as well as other health care workers, who are for whatever reason being disciplined or retaliated against for simply seeking appropriate safety policies at their workplaces,” Dr. Hathi said. “What we’ve found is that many of them don’t even know what their options look like. Doctors, nurses, health care workers are not the typical type to engage politically, to speak out, [or to] advocate for themselves.” Read more.
COVID-19 ravages the Navajo Nation
The Navajo Nation has the most cases of the COVID-19 virus of any tribe in the United States, and numbers as of May 31, 2020, are 5,348, with 246 confirmed deaths. These devastating numbers, which might be leveling off, are associated with Navajo people having higher-than-average rates of diabetes, heart disease, and cancer. This is compounded with 30%-40% of homes having no electricity or running water, and a poverty rate of about 38%. “We endured and learned from each Naayee, hunger, and death to name a few adversities. The COVID-19 pandemic, or “Big Cough” (Dikos Nitsaa’igii -19 in Navajo language), is a monster confronting the Navajo today. It has had significant impact on our nation and people,” Mary Hasbah Roessel, MD, a Navajo board-certified psychiatrist practicing in Santa Fe, N.M., wrote in a commentary on MDedge. Read more.
Heart pump system authorized for COVID-19 patients
The Food and Drug Administration issued an emergency use authorization (EUA) for use of the Impella RP heart pump system in COVID-19 patients with right heart failure or decompensation. The EUA indication for the Impella RP system is to provide temporary right ventricular support for up to 14 days in critical care patients with a body surface area of at least 1.5 m2 for the treatment of acute right heart failure or decompensation caused by complications related to COVID-19, including pulmonary embolism. Read more.
Deprescribing hypertension meds looks safe for older adults
Some patients aged 80 years or older can potentially cut back on their number of antihypertensive meds, under physician guidance, without an important loss of blood pressure control, researchers concluded based on findings from a randomized multicenter trial. The study, called Optimising Treatment for Mild Systolic Hypertension in the Elderly (OPTIMISE), entered “patients in whom the benefits of taking blood pressure-lowering treatments might start to be outweighed by the potential harms,” said James P. Sheppard, PhD, of University of Oxford (England). The report was published in JAMA. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
Here are the stories our MDedge editors across specialties think you need to know about today:
Addressing racism in the maternal mortality crisis
The emerging racial disparities in COVID-19 incidence and outcomes in the United States are on a collision course with long-standing racial disparities in U.S. maternal care and mortality. “The saying is that ‘the virus doesn’t discriminate,’ but it understands our biases, right? So, the virus takes advantage of the weaknesses in our system,” said Joia A. Crear-Perry, MD, an ob.gyn. and founder and president of the National Birth Equity Collaborative, a New Orleans–based research, training, and advocacy organization working to optimize black maternal and infant health. This article is part of an ongoing feature series on the crisis in maternal mortality in the United States. Here we explore potential solutions for addressing the inequities as proposed by thought leaders and key stakeholders. Read more.
A ‘Beacon’ for physicians, nurses facing retaliation
Sejal Hathi, MD, and two colleagues had long kicked around the idea of starting a nonprofit group that would center on civic and legal advocacy. Once the COVID-19 pandemic hit, the three friends – who have a mix of legal, medical, and advocacy backgrounds – began chatting by email and through Zoom video meetings about how to make the plan a reality. The new organization – named Beacon – quickly mobilized, assembled their team, and launched a website. Beacon’s first project now aims to highlight and protect the legal rights of medical professionals who speak out about personal protection equipment supply and other matters of public concern related to coronavirus. “There are a flurry of reports coming our way about physicians and nurses, as well as other health care workers, who are for whatever reason being disciplined or retaliated against for simply seeking appropriate safety policies at their workplaces,” Dr. Hathi said. “What we’ve found is that many of them don’t even know what their options look like. Doctors, nurses, health care workers are not the typical type to engage politically, to speak out, [or to] advocate for themselves.” Read more.
COVID-19 ravages the Navajo Nation
The Navajo Nation has the most cases of the COVID-19 virus of any tribe in the United States, and numbers as of May 31, 2020, are 5,348, with 246 confirmed deaths. These devastating numbers, which might be leveling off, are associated with Navajo people having higher-than-average rates of diabetes, heart disease, and cancer. This is compounded with 30%-40% of homes having no electricity or running water, and a poverty rate of about 38%. “We endured and learned from each Naayee, hunger, and death to name a few adversities. The COVID-19 pandemic, or “Big Cough” (Dikos Nitsaa’igii -19 in Navajo language), is a monster confronting the Navajo today. It has had significant impact on our nation and people,” Mary Hasbah Roessel, MD, a Navajo board-certified psychiatrist practicing in Santa Fe, N.M., wrote in a commentary on MDedge. Read more.
Heart pump system authorized for COVID-19 patients
The Food and Drug Administration issued an emergency use authorization (EUA) for use of the Impella RP heart pump system in COVID-19 patients with right heart failure or decompensation. The EUA indication for the Impella RP system is to provide temporary right ventricular support for up to 14 days in critical care patients with a body surface area of at least 1.5 m2 for the treatment of acute right heart failure or decompensation caused by complications related to COVID-19, including pulmonary embolism. Read more.
Deprescribing hypertension meds looks safe for older adults
Some patients aged 80 years or older can potentially cut back on their number of antihypertensive meds, under physician guidance, without an important loss of blood pressure control, researchers concluded based on findings from a randomized multicenter trial. The study, called Optimising Treatment for Mild Systolic Hypertension in the Elderly (OPTIMISE), entered “patients in whom the benefits of taking blood pressure-lowering treatments might start to be outweighed by the potential harms,” said James P. Sheppard, PhD, of University of Oxford (England). The report was published in JAMA. Read more.
For more on COVID-19, visit our Resource Center. All of our latest news is available on MDedge.com.
COVID-19: New group stands up for health professionals facing retaliation
Sejal Hathi, MD, and two colleagues had long kicked around the idea of starting a nonprofit group that would center on civic and legal advocacy.
Once the COVID-19 pandemic hit, the three friends – who have a mix of legal, medical, and advocacy backgrounds – began chatting by email and through Zoom video meetings about how to make the plan a reality.
“When COVID came around, we began talking about where we could make a difference and help people where help was needed most,” said Dr. Hathi, an internal medicine resident at Massachusetts General Hospital in Boston. “We decided the PPE issue makes a good first focus.”
The new organization – named Beacon – quickly mobilized, assembled their team, and launched a website. Beacon’s first project now aims to highlight and protect the legal rights of medical professionals who speak out about personal protection equipment (PPE) supply and other matters of public concern related to coronavirus.
In recent months, health care professionals have reported being reprimanded or even terminated for publicly discussing PPE shortages or sharing safety concerns. Other clinicians say they can’t share their experiences for fear of reprisal by their hospitals.
“The centrality of adequate PPE is pretty undeniable at this point,” said John Paul Schnapper-Casteras, JD, an attorney and cofounder of the organization. “In terms of speaking up about matters of workplace safety and public concern, when health care workers share knowledge, correct problems – and in some cases, blow the whistle – it affirmatively benefits medical science, disease control, and the public interest,” he said in an interview. “We have seen in other countries, the disastrous consequences that can stem from silencing medical professionals who try to speak out.”
Letter highlights hospitals’ obligations
As part of their efforts, Beacon leaders drafted a strongly worded letter on behalf of health care workers outlining the legal obligations of hospitals to ensure workplace safety, underscoring the federal protections that bar retaliation against employees who exercise their workplace rights. Whistleblower protections under the Occupational Safety and Health Act, the False Claims Act, and the National Labor Relations Act, for instance, prohibit retaliation against employees for blowing the whistle on unsafe or unlawful conditions.
Beacon’s letter urges hospitals to adopt a uniform policy that recognizes “the importance and legitimacy of doctors, nurses, and medical professionals who research, write, and speak about the use and supply of PPE in addressing coronavirus.”
“We are deeply troubled by reports that medical professionals are being fired, retaliated against, disciplined, or threatened for speaking (or potentially speaking) about PPE shortages and related safety conditions that directly place their and their patients’ lives in danger,” the letter states. “As a matter of law, medical personnel have a wide range of rights that protect their employment status and ability to comment on matters of public concern (and provide a cause of action in court if these rights are violated).”
Dr. Hathi, who over the last decade has founded two social enterprises advancing women’s rights, said organizers have sent the letter to hospitals and health systems that were publicly reported or otherwise known to have threatened, terminated, or retaliated against employees for protesting PPE shortages or speaking up about unsafe working conditions during this crisis. The letter is available on the Beacon website.
“Many letters have been written [recently] criticizing hospitals for retaliating against their workers,” Dr. Hathi said. “Ours amplifies this voice. But it also serves as a tool for self-empowerment, a stark warning to health systems that their actions bear consequences, and an assurance to health workers across the country that we’re listening and we’re here to help them safeguard their rights and their dignity at work.”
Dr. Hathi and her colleagues have also circulated the letter on social media and other platforms as a petition that health care professionals and others can sign in support of fair and safe treatment of employees with respect to PPE. So far, the group has collected signatures from individuals, communities, and organizations representing about 35,000 people, Dr. Hathi said.
Workplace rights, legal options
Beacon leaders have also begun counseling and advising health care workers who have experienced retaliation or discipline associated with PPE issues. Educating medical professionals about their workplace rights and legal options is another key focus of the group, according to its founders.
“There are a flurry of reports coming our way about physicians and nurses, as well as other health care workers, who are for whatever reason being disciplined or retaliated against for simply seeking appropriate safety policies at their workplaces,” Dr. Hathi said. “What we’ve found is that many of them don’t even know what their options look like. Doctors, nurses, health care workers are not the typical type to engage politically, to speak out, [or to] advocate for themselves.”
In one instance, they heard from a physician who wanted to protect nurses at his hospital because they did not have masks and were being coughed on by COVID-19 patients. The doctor requested that his hospital supply masks to the nurses. After making the request, the physician was disciplined by hospital leadership, Dr. Hathi said. In another case, a physician assistant told the group she was terminated because she wanted to wear her own mask in a hospital that was treating COVID patients.
“She was not allowed to, and she was fired for even bringing it up,” said Sheel Tyle, JD, an attorney and Beacon cofounder.
Beacon intends to assist health care workers who face such retaliation and discipline in a number of ways, Mr. Tyle said. For instance, by helping an individual get compensation for what happened, aiding the professional in getting their job back, or helping the worker retain a severance package of some kind, he said.
“And then there is the larger public policy issue of preventing the hospital from being a bad actor,” Mr. Tyle said. “That can be done through state or federal complaints, largely under different statutes related to workplace protection or OSHA. Our group [has] lawyers that could represent clients individually as well as a number of friends who are attorneys in various states who we could partner with, depending on the situation.”
While the organization is positioned to represent health professionals in lawsuits if necessary, Mr. Tyle emphasized that litigation is not the intended goal of the group. Rather, they are seeking to deter hospitals and others from being “bad actors,” through any number of methods, including communication, advocacy, or complaints.
Ultimately, Dr. Hathi said she hopes the organization’s efforts activate health care workers as an organizing body and in the process, spark policy change at the federal level to better protect health care workers.
“The challenges we’re facing now – protecting workplace safety, employee voice, a living wage, adequate sick and family leave – long predate this pandemic,” Dr. Hathi said. “But they’ve deepened and acquired existential significance as, battered by policy failures and the unsparing virus itself, physicians shed their political indifference and join a growing nationwide chorus to restore workers’ rights and to fundamentally reimagine our broken healthcare system. Now, more than ever before, organizations like Beacon are vital for arming health workers in this fight.”
Sejal Hathi, MD, and two colleagues had long kicked around the idea of starting a nonprofit group that would center on civic and legal advocacy.
Once the COVID-19 pandemic hit, the three friends – who have a mix of legal, medical, and advocacy backgrounds – began chatting by email and through Zoom video meetings about how to make the plan a reality.
“When COVID came around, we began talking about where we could make a difference and help people where help was needed most,” said Dr. Hathi, an internal medicine resident at Massachusetts General Hospital in Boston. “We decided the PPE issue makes a good first focus.”
The new organization – named Beacon – quickly mobilized, assembled their team, and launched a website. Beacon’s first project now aims to highlight and protect the legal rights of medical professionals who speak out about personal protection equipment (PPE) supply and other matters of public concern related to coronavirus.
In recent months, health care professionals have reported being reprimanded or even terminated for publicly discussing PPE shortages or sharing safety concerns. Other clinicians say they can’t share their experiences for fear of reprisal by their hospitals.
“The centrality of adequate PPE is pretty undeniable at this point,” said John Paul Schnapper-Casteras, JD, an attorney and cofounder of the organization. “In terms of speaking up about matters of workplace safety and public concern, when health care workers share knowledge, correct problems – and in some cases, blow the whistle – it affirmatively benefits medical science, disease control, and the public interest,” he said in an interview. “We have seen in other countries, the disastrous consequences that can stem from silencing medical professionals who try to speak out.”
Letter highlights hospitals’ obligations
As part of their efforts, Beacon leaders drafted a strongly worded letter on behalf of health care workers outlining the legal obligations of hospitals to ensure workplace safety, underscoring the federal protections that bar retaliation against employees who exercise their workplace rights. Whistleblower protections under the Occupational Safety and Health Act, the False Claims Act, and the National Labor Relations Act, for instance, prohibit retaliation against employees for blowing the whistle on unsafe or unlawful conditions.
Beacon’s letter urges hospitals to adopt a uniform policy that recognizes “the importance and legitimacy of doctors, nurses, and medical professionals who research, write, and speak about the use and supply of PPE in addressing coronavirus.”
“We are deeply troubled by reports that medical professionals are being fired, retaliated against, disciplined, or threatened for speaking (or potentially speaking) about PPE shortages and related safety conditions that directly place their and their patients’ lives in danger,” the letter states. “As a matter of law, medical personnel have a wide range of rights that protect their employment status and ability to comment on matters of public concern (and provide a cause of action in court if these rights are violated).”
Dr. Hathi, who over the last decade has founded two social enterprises advancing women’s rights, said organizers have sent the letter to hospitals and health systems that were publicly reported or otherwise known to have threatened, terminated, or retaliated against employees for protesting PPE shortages or speaking up about unsafe working conditions during this crisis. The letter is available on the Beacon website.
“Many letters have been written [recently] criticizing hospitals for retaliating against their workers,” Dr. Hathi said. “Ours amplifies this voice. But it also serves as a tool for self-empowerment, a stark warning to health systems that their actions bear consequences, and an assurance to health workers across the country that we’re listening and we’re here to help them safeguard their rights and their dignity at work.”
Dr. Hathi and her colleagues have also circulated the letter on social media and other platforms as a petition that health care professionals and others can sign in support of fair and safe treatment of employees with respect to PPE. So far, the group has collected signatures from individuals, communities, and organizations representing about 35,000 people, Dr. Hathi said.
Workplace rights, legal options
Beacon leaders have also begun counseling and advising health care workers who have experienced retaliation or discipline associated with PPE issues. Educating medical professionals about their workplace rights and legal options is another key focus of the group, according to its founders.
“There are a flurry of reports coming our way about physicians and nurses, as well as other health care workers, who are for whatever reason being disciplined or retaliated against for simply seeking appropriate safety policies at their workplaces,” Dr. Hathi said. “What we’ve found is that many of them don’t even know what their options look like. Doctors, nurses, health care workers are not the typical type to engage politically, to speak out, [or to] advocate for themselves.”
In one instance, they heard from a physician who wanted to protect nurses at his hospital because they did not have masks and were being coughed on by COVID-19 patients. The doctor requested that his hospital supply masks to the nurses. After making the request, the physician was disciplined by hospital leadership, Dr. Hathi said. In another case, a physician assistant told the group she was terminated because she wanted to wear her own mask in a hospital that was treating COVID patients.
“She was not allowed to, and she was fired for even bringing it up,” said Sheel Tyle, JD, an attorney and Beacon cofounder.
Beacon intends to assist health care workers who face such retaliation and discipline in a number of ways, Mr. Tyle said. For instance, by helping an individual get compensation for what happened, aiding the professional in getting their job back, or helping the worker retain a severance package of some kind, he said.
“And then there is the larger public policy issue of preventing the hospital from being a bad actor,” Mr. Tyle said. “That can be done through state or federal complaints, largely under different statutes related to workplace protection or OSHA. Our group [has] lawyers that could represent clients individually as well as a number of friends who are attorneys in various states who we could partner with, depending on the situation.”
While the organization is positioned to represent health professionals in lawsuits if necessary, Mr. Tyle emphasized that litigation is not the intended goal of the group. Rather, they are seeking to deter hospitals and others from being “bad actors,” through any number of methods, including communication, advocacy, or complaints.
Ultimately, Dr. Hathi said she hopes the organization’s efforts activate health care workers as an organizing body and in the process, spark policy change at the federal level to better protect health care workers.
“The challenges we’re facing now – protecting workplace safety, employee voice, a living wage, adequate sick and family leave – long predate this pandemic,” Dr. Hathi said. “But they’ve deepened and acquired existential significance as, battered by policy failures and the unsparing virus itself, physicians shed their political indifference and join a growing nationwide chorus to restore workers’ rights and to fundamentally reimagine our broken healthcare system. Now, more than ever before, organizations like Beacon are vital for arming health workers in this fight.”
Sejal Hathi, MD, and two colleagues had long kicked around the idea of starting a nonprofit group that would center on civic and legal advocacy.
Once the COVID-19 pandemic hit, the three friends – who have a mix of legal, medical, and advocacy backgrounds – began chatting by email and through Zoom video meetings about how to make the plan a reality.
“When COVID came around, we began talking about where we could make a difference and help people where help was needed most,” said Dr. Hathi, an internal medicine resident at Massachusetts General Hospital in Boston. “We decided the PPE issue makes a good first focus.”
The new organization – named Beacon – quickly mobilized, assembled their team, and launched a website. Beacon’s first project now aims to highlight and protect the legal rights of medical professionals who speak out about personal protection equipment (PPE) supply and other matters of public concern related to coronavirus.
In recent months, health care professionals have reported being reprimanded or even terminated for publicly discussing PPE shortages or sharing safety concerns. Other clinicians say they can’t share their experiences for fear of reprisal by their hospitals.
“The centrality of adequate PPE is pretty undeniable at this point,” said John Paul Schnapper-Casteras, JD, an attorney and cofounder of the organization. “In terms of speaking up about matters of workplace safety and public concern, when health care workers share knowledge, correct problems – and in some cases, blow the whistle – it affirmatively benefits medical science, disease control, and the public interest,” he said in an interview. “We have seen in other countries, the disastrous consequences that can stem from silencing medical professionals who try to speak out.”
Letter highlights hospitals’ obligations
As part of their efforts, Beacon leaders drafted a strongly worded letter on behalf of health care workers outlining the legal obligations of hospitals to ensure workplace safety, underscoring the federal protections that bar retaliation against employees who exercise their workplace rights. Whistleblower protections under the Occupational Safety and Health Act, the False Claims Act, and the National Labor Relations Act, for instance, prohibit retaliation against employees for blowing the whistle on unsafe or unlawful conditions.
Beacon’s letter urges hospitals to adopt a uniform policy that recognizes “the importance and legitimacy of doctors, nurses, and medical professionals who research, write, and speak about the use and supply of PPE in addressing coronavirus.”
“We are deeply troubled by reports that medical professionals are being fired, retaliated against, disciplined, or threatened for speaking (or potentially speaking) about PPE shortages and related safety conditions that directly place their and their patients’ lives in danger,” the letter states. “As a matter of law, medical personnel have a wide range of rights that protect their employment status and ability to comment on matters of public concern (and provide a cause of action in court if these rights are violated).”
Dr. Hathi, who over the last decade has founded two social enterprises advancing women’s rights, said organizers have sent the letter to hospitals and health systems that were publicly reported or otherwise known to have threatened, terminated, or retaliated against employees for protesting PPE shortages or speaking up about unsafe working conditions during this crisis. The letter is available on the Beacon website.
“Many letters have been written [recently] criticizing hospitals for retaliating against their workers,” Dr. Hathi said. “Ours amplifies this voice. But it also serves as a tool for self-empowerment, a stark warning to health systems that their actions bear consequences, and an assurance to health workers across the country that we’re listening and we’re here to help them safeguard their rights and their dignity at work.”
Dr. Hathi and her colleagues have also circulated the letter on social media and other platforms as a petition that health care professionals and others can sign in support of fair and safe treatment of employees with respect to PPE. So far, the group has collected signatures from individuals, communities, and organizations representing about 35,000 people, Dr. Hathi said.
Workplace rights, legal options
Beacon leaders have also begun counseling and advising health care workers who have experienced retaliation or discipline associated with PPE issues. Educating medical professionals about their workplace rights and legal options is another key focus of the group, according to its founders.
“There are a flurry of reports coming our way about physicians and nurses, as well as other health care workers, who are for whatever reason being disciplined or retaliated against for simply seeking appropriate safety policies at their workplaces,” Dr. Hathi said. “What we’ve found is that many of them don’t even know what their options look like. Doctors, nurses, health care workers are not the typical type to engage politically, to speak out, [or to] advocate for themselves.”
In one instance, they heard from a physician who wanted to protect nurses at his hospital because they did not have masks and were being coughed on by COVID-19 patients. The doctor requested that his hospital supply masks to the nurses. After making the request, the physician was disciplined by hospital leadership, Dr. Hathi said. In another case, a physician assistant told the group she was terminated because she wanted to wear her own mask in a hospital that was treating COVID patients.
“She was not allowed to, and she was fired for even bringing it up,” said Sheel Tyle, JD, an attorney and Beacon cofounder.
Beacon intends to assist health care workers who face such retaliation and discipline in a number of ways, Mr. Tyle said. For instance, by helping an individual get compensation for what happened, aiding the professional in getting their job back, or helping the worker retain a severance package of some kind, he said.
“And then there is the larger public policy issue of preventing the hospital from being a bad actor,” Mr. Tyle said. “That can be done through state or federal complaints, largely under different statutes related to workplace protection or OSHA. Our group [has] lawyers that could represent clients individually as well as a number of friends who are attorneys in various states who we could partner with, depending on the situation.”
While the organization is positioned to represent health professionals in lawsuits if necessary, Mr. Tyle emphasized that litigation is not the intended goal of the group. Rather, they are seeking to deter hospitals and others from being “bad actors,” through any number of methods, including communication, advocacy, or complaints.
Ultimately, Dr. Hathi said she hopes the organization’s efforts activate health care workers as an organizing body and in the process, spark policy change at the federal level to better protect health care workers.
“The challenges we’re facing now – protecting workplace safety, employee voice, a living wage, adequate sick and family leave – long predate this pandemic,” Dr. Hathi said. “But they’ve deepened and acquired existential significance as, battered by policy failures and the unsparing virus itself, physicians shed their political indifference and join a growing nationwide chorus to restore workers’ rights and to fundamentally reimagine our broken healthcare system. Now, more than ever before, organizations like Beacon are vital for arming health workers in this fight.”
FDA okays emergency use for Impella RP in COVID-19 right heart failure
The Food and Drug Administration issued an emergency use authorization for use of the Impella RP heart pump system in COVID-19 patients with right heart failure or decompensation, Abiomed announced June 1.
“Based on extrapolation of data from the approved indication and reported clinical experience, FDA has concluded that the Impella RP may be effective at providing temporary right ventricular support for the treatment of acute right heart failure or decompensation caused by COVID-19 complications, including PE [pulmonary embolism],” the letter noted.
It cited, for example, use of the temporary heart pump in a 59-year-old woman suffering from COVID-19 who went into right ventricular failure and became hypotensive after an acute PE was removed. After placement of the device, the patient experienced a “dramatic and immediate” improvement in arterial pressure and the device was removed on the fifth day, according to Amir Kaki, MD, and Ted Schreiber, MD, of Ascension St. John Hospital, Detroit, whose review of the case has been posted online.
“Acute pulmonary embolism is clearly being recognized as a life-threatening manifestation of COVID-19. Impella RP is an important tool to help cardiologists save lives during this pandemic,” Dr. Kaki said in the letter. “As we have demonstrated in our series of patients, early recognition of right ventricular dysfunction and early placement of the Impella RP for patients who are hypotensive can be lifesaving.”
Other data cited in support of the Impella RP emergency use authorization (EUA) include a 2019 series of hemodynamically unstable patients with PE in Japan and a 2017 case report of a 47-year-old man with right ventricular failure, profound shock, and a massive PE.
The FDA granted premarket approval of the Impella RP system in 2017 to provide temporary right ventricular support for up to 14 days in patients with a body surface area of at least 1.5 m2 who develop acute right heart failure or decompensation following left ventricular assist device implantation, MI, heart transplant, or open-heart surgery.
The EUA indication for the Impella RP system is to provide temporary right ventricular support for up to 14 days in critical care patients with a body surface area of at least 1.5 m2 for the treatment of acute right heart failure or decompensation caused by complications related to COVID-19, including PE.
The Impella RP is authorized only for emergency use under the EUA and only for the duration of the circumstances justifying use of EUAs, the letter noted.
Last year, concerns were raised about off-indication use after interim results from a postapproval study suggested a higher risk for death than seen in premarket studies treated with the temporary heart pump.
A version of this article originally appeared on Medscape.com.
The Food and Drug Administration issued an emergency use authorization for use of the Impella RP heart pump system in COVID-19 patients with right heart failure or decompensation, Abiomed announced June 1.
“Based on extrapolation of data from the approved indication and reported clinical experience, FDA has concluded that the Impella RP may be effective at providing temporary right ventricular support for the treatment of acute right heart failure or decompensation caused by COVID-19 complications, including PE [pulmonary embolism],” the letter noted.
It cited, for example, use of the temporary heart pump in a 59-year-old woman suffering from COVID-19 who went into right ventricular failure and became hypotensive after an acute PE was removed. After placement of the device, the patient experienced a “dramatic and immediate” improvement in arterial pressure and the device was removed on the fifth day, according to Amir Kaki, MD, and Ted Schreiber, MD, of Ascension St. John Hospital, Detroit, whose review of the case has been posted online.
“Acute pulmonary embolism is clearly being recognized as a life-threatening manifestation of COVID-19. Impella RP is an important tool to help cardiologists save lives during this pandemic,” Dr. Kaki said in the letter. “As we have demonstrated in our series of patients, early recognition of right ventricular dysfunction and early placement of the Impella RP for patients who are hypotensive can be lifesaving.”
Other data cited in support of the Impella RP emergency use authorization (EUA) include a 2019 series of hemodynamically unstable patients with PE in Japan and a 2017 case report of a 47-year-old man with right ventricular failure, profound shock, and a massive PE.
The FDA granted premarket approval of the Impella RP system in 2017 to provide temporary right ventricular support for up to 14 days in patients with a body surface area of at least 1.5 m2 who develop acute right heart failure or decompensation following left ventricular assist device implantation, MI, heart transplant, or open-heart surgery.
The EUA indication for the Impella RP system is to provide temporary right ventricular support for up to 14 days in critical care patients with a body surface area of at least 1.5 m2 for the treatment of acute right heart failure or decompensation caused by complications related to COVID-19, including PE.
The Impella RP is authorized only for emergency use under the EUA and only for the duration of the circumstances justifying use of EUAs, the letter noted.
Last year, concerns were raised about off-indication use after interim results from a postapproval study suggested a higher risk for death than seen in premarket studies treated with the temporary heart pump.
A version of this article originally appeared on Medscape.com.
The Food and Drug Administration issued an emergency use authorization for use of the Impella RP heart pump system in COVID-19 patients with right heart failure or decompensation, Abiomed announced June 1.
“Based on extrapolation of data from the approved indication and reported clinical experience, FDA has concluded that the Impella RP may be effective at providing temporary right ventricular support for the treatment of acute right heart failure or decompensation caused by COVID-19 complications, including PE [pulmonary embolism],” the letter noted.
It cited, for example, use of the temporary heart pump in a 59-year-old woman suffering from COVID-19 who went into right ventricular failure and became hypotensive after an acute PE was removed. After placement of the device, the patient experienced a “dramatic and immediate” improvement in arterial pressure and the device was removed on the fifth day, according to Amir Kaki, MD, and Ted Schreiber, MD, of Ascension St. John Hospital, Detroit, whose review of the case has been posted online.
“Acute pulmonary embolism is clearly being recognized as a life-threatening manifestation of COVID-19. Impella RP is an important tool to help cardiologists save lives during this pandemic,” Dr. Kaki said in the letter. “As we have demonstrated in our series of patients, early recognition of right ventricular dysfunction and early placement of the Impella RP for patients who are hypotensive can be lifesaving.”
Other data cited in support of the Impella RP emergency use authorization (EUA) include a 2019 series of hemodynamically unstable patients with PE in Japan and a 2017 case report of a 47-year-old man with right ventricular failure, profound shock, and a massive PE.
The FDA granted premarket approval of the Impella RP system in 2017 to provide temporary right ventricular support for up to 14 days in patients with a body surface area of at least 1.5 m2 who develop acute right heart failure or decompensation following left ventricular assist device implantation, MI, heart transplant, or open-heart surgery.
The EUA indication for the Impella RP system is to provide temporary right ventricular support for up to 14 days in critical care patients with a body surface area of at least 1.5 m2 for the treatment of acute right heart failure or decompensation caused by complications related to COVID-19, including PE.
The Impella RP is authorized only for emergency use under the EUA and only for the duration of the circumstances justifying use of EUAs, the letter noted.
Last year, concerns were raised about off-indication use after interim results from a postapproval study suggested a higher risk for death than seen in premarket studies treated with the temporary heart pump.
A version of this article originally appeared on Medscape.com.












