User login
Clinical Psychiatry News is the online destination and multimedia properties of Clinica Psychiatry News, the independent news publication for psychiatrists. Since 1971, Clinical Psychiatry News has been the leading source of news and commentary about clinical developments in psychiatry as well as health care policy and regulations that affect the physician's practice.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
ketamine
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
suicide
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-cpn')]
div[contains(@class, 'pane-pub-home-cpn')]
div[contains(@class, 'pane-pub-topic-cpn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Family environment important in early psychosis outcomes
Family environment may influence subsequent functional outcomes in patients with first-episode psychosis, new research suggests.
A study of more than 300 patients with first-episode psychosis (FEP) showed that although family environment was not associated with functioning at initial presentation, an interaction developed over time that could have “important implications for early interventions for both patients and caregivers,” investigators reported.
study coinvestigator Norma Verdolini, MD, PhD, bipolar and depressive disorders unit, hospital Clinic Barcelona, University of Barcelona, said in an interview.
The findings were scheduled to be presented at the Congress of the Schizophrenia International Research Society 2020, but the meeting was canceled because of the coronavirus pandemic.
FAST measures
Previous research has shown that family environment influences the development of psychotic symptoms, with negative family environmental factors associated with poor prognoses.
Conversely, one study indicated that a positive family environment is linked to greater improvement in negative and disorganized symptoms in adolescents at imminent risk for psychosis onset.
However, the current investigators noted that the impact of family environment on longitudinal functioning in individuals presenting with FEP is unclear.
To investigate further, they conducted an analysis as part of the PEPs study, which included 335 patients with FEP and 253 healthy controls. Functioning was measured using the Functional Assessment Short Test (FAST), and family environmental styles were evaluated using the Family Environment Scale (FES), which assesses “emotional climate” of a family across 10 domains.
At baseline, the mean total FAST score was 27.8 in patients with FEP versus 3.5 in the healthy controls, indicating substantially worse functioning among the patients. Linear regression analysis indicated that at baseline there was no significant association between aspects of family environment on the FES and functional scores.
Patients were assessed again at 2 years, by which point 283 had been diagnosed with psychotic disorders and 52 with bipolar disorder. The mean total FAST scores were 20.98 among patients with psychotic disorders and 13.8 in those with bipolar disorder.
Family conflict
Results showed that, among those with bipolar disorder, worse functioning on FAST at 2 years was significantly associated with higher rates of open expression of conflict in the family (P = .004).
In patients with psychotic disorders, worse functioning was significantly associated with lower rates of participation in social activities (P = .006) and an achievement-oriented family environment (P = .039). Worse functioning in patients with psychotic disorders was also significantly associated with higher rates of religious practice and values (P = .003).
Dr. Verdolini noted the reason family environment does not appear to have an impact at initial FEP presentation may be that the “first kick” is given by an individual’s genetic liability for psychiatric disorders in combination with the family environment. In reality, the two are intertwined, especially when considering what it means to a family to have one member with a psychiatric disorder, which “will have an impact on the family environment.”
Dr. Verdolini added: “This is not actually the objective family environment,” but the perceived family environment.
“So maybe in the following 2 years the patient who experiences a first episode of psychosis may change their idea of the family environment itself,” she noted. She added that at her institution psychoeducation is offered to FEP patients’ families.
‘Interesting’ findings
Commenting on the study, Nicole Kozloff, MD, from the child, youth, and emerging adult program at the Centre for Addiction and Mental Health in Toronto, said one limitation of the study is that it’s not clear what care patients received – or who in the family completed the FES.
It is also important to note that “measures of association do not necessarily imply that one factor caused the other factor,” said Dr. Kozloff, who was not involved in the research. “For example, it may be that, among people with bipolar disorder, open expression of conflict in the family can lead to worse functioning, or that worse functioning can lead to more conflict in the family.”
Nevertheless, Dr. Kozloff described the finding of an emerging association between the family environment and functioning over time as “interesting.”
When young people with FEP enter treatment, “they have reached a crisis point and are functioning poorly,” she noted.
“It could be that there is less to differentiate among levels of functioning at treatment entry but, after 2 years, the individuals have separated into those who have been responsive to treatment and are functioning well, and those who continue to have functional challenges. And this is where we start to see a relationship with family environment emerge,” Dr. Kozloff said.
She also agreed with Dr. Verdolini’s take on the findings, and that family psychoeducation “can reduce relapse rates in schizophrenia and the emotional burden on the family.”
“We also know that having family involvement in care is one of the most robust predictors that young people with psychosis will remain engaged in mental health services,” she said.
Teaching families about psychosis and its treatment, about problem-solving and communication skills, and providing support to ensure that family members know how to get help in a crisis, “is a key part of comprehensive early psychosis intervention,” Dr. Kozloff said. “It is good for the patient and good for the family, and allows the clinicians to provide better care.”
Articulates clinical practice findings
Also commenting on the results, Brian O’Donoghue, MD, PhD, senior clinical research fellow at Orygen, the National Centre of Excellence in Youth Mental Health in Melbourne, described the research as important, adding that the study highlights the need for sufficient follow-up.
“It makes sense that the involvement of family over time has a strong impact upon outcome and functioning,” he said in an interview.
“These research findings articulate what we see in clinical practice, so it is good to see that it is captured,” added Dr. O’Donoghue, who was not associated with the study.
He noted that it is common for family involvement to influence outcome, especially if the family is positively involved. “It is invaluable toward their recovery. However, conversely, if there are ongoing family stressors, then this can be a trigger for relapse or lack of improvement.”
Overall, the results “really emphasize that the family needs to be involved in care.”
The Early Psychosis Prevention and Intervention Centre where Dr. O’Donoghue is a consultant psychiatrist offers a psychoeducational course “to inform families about psychosis, treatment, and how they can support their family members.”
“We also have family peer support workers and family therapists, which are essential to the service and for the young person’s recovery,” Dr. O’Donoghue said.
The investigators and Dr. O’Donoghue disclosed no relevant financial relationships. Dr. Kozloff reported receiving research funding from the CAMH Foundation, Brain & Behavior Research Foundation, Canadian Institutes of Health Research, and AFP Innovation Fund; honoraria from Humber River Hospital, the University of Calgary (Alta.), and the Canadian Consortium for Early Intervention in Psychosis; and salary support from Inner City Health Associates.
A version of this article originally appeared on Medscape.com.
Family environment may influence subsequent functional outcomes in patients with first-episode psychosis, new research suggests.
A study of more than 300 patients with first-episode psychosis (FEP) showed that although family environment was not associated with functioning at initial presentation, an interaction developed over time that could have “important implications for early interventions for both patients and caregivers,” investigators reported.
study coinvestigator Norma Verdolini, MD, PhD, bipolar and depressive disorders unit, hospital Clinic Barcelona, University of Barcelona, said in an interview.
The findings were scheduled to be presented at the Congress of the Schizophrenia International Research Society 2020, but the meeting was canceled because of the coronavirus pandemic.
FAST measures
Previous research has shown that family environment influences the development of psychotic symptoms, with negative family environmental factors associated with poor prognoses.
Conversely, one study indicated that a positive family environment is linked to greater improvement in negative and disorganized symptoms in adolescents at imminent risk for psychosis onset.
However, the current investigators noted that the impact of family environment on longitudinal functioning in individuals presenting with FEP is unclear.
To investigate further, they conducted an analysis as part of the PEPs study, which included 335 patients with FEP and 253 healthy controls. Functioning was measured using the Functional Assessment Short Test (FAST), and family environmental styles were evaluated using the Family Environment Scale (FES), which assesses “emotional climate” of a family across 10 domains.
At baseline, the mean total FAST score was 27.8 in patients with FEP versus 3.5 in the healthy controls, indicating substantially worse functioning among the patients. Linear regression analysis indicated that at baseline there was no significant association between aspects of family environment on the FES and functional scores.
Patients were assessed again at 2 years, by which point 283 had been diagnosed with psychotic disorders and 52 with bipolar disorder. The mean total FAST scores were 20.98 among patients with psychotic disorders and 13.8 in those with bipolar disorder.
Family conflict
Results showed that, among those with bipolar disorder, worse functioning on FAST at 2 years was significantly associated with higher rates of open expression of conflict in the family (P = .004).
In patients with psychotic disorders, worse functioning was significantly associated with lower rates of participation in social activities (P = .006) and an achievement-oriented family environment (P = .039). Worse functioning in patients with psychotic disorders was also significantly associated with higher rates of religious practice and values (P = .003).
Dr. Verdolini noted the reason family environment does not appear to have an impact at initial FEP presentation may be that the “first kick” is given by an individual’s genetic liability for psychiatric disorders in combination with the family environment. In reality, the two are intertwined, especially when considering what it means to a family to have one member with a psychiatric disorder, which “will have an impact on the family environment.”
Dr. Verdolini added: “This is not actually the objective family environment,” but the perceived family environment.
“So maybe in the following 2 years the patient who experiences a first episode of psychosis may change their idea of the family environment itself,” she noted. She added that at her institution psychoeducation is offered to FEP patients’ families.
‘Interesting’ findings
Commenting on the study, Nicole Kozloff, MD, from the child, youth, and emerging adult program at the Centre for Addiction and Mental Health in Toronto, said one limitation of the study is that it’s not clear what care patients received – or who in the family completed the FES.
It is also important to note that “measures of association do not necessarily imply that one factor caused the other factor,” said Dr. Kozloff, who was not involved in the research. “For example, it may be that, among people with bipolar disorder, open expression of conflict in the family can lead to worse functioning, or that worse functioning can lead to more conflict in the family.”
Nevertheless, Dr. Kozloff described the finding of an emerging association between the family environment and functioning over time as “interesting.”
When young people with FEP enter treatment, “they have reached a crisis point and are functioning poorly,” she noted.
“It could be that there is less to differentiate among levels of functioning at treatment entry but, after 2 years, the individuals have separated into those who have been responsive to treatment and are functioning well, and those who continue to have functional challenges. And this is where we start to see a relationship with family environment emerge,” Dr. Kozloff said.
She also agreed with Dr. Verdolini’s take on the findings, and that family psychoeducation “can reduce relapse rates in schizophrenia and the emotional burden on the family.”
“We also know that having family involvement in care is one of the most robust predictors that young people with psychosis will remain engaged in mental health services,” she said.
Teaching families about psychosis and its treatment, about problem-solving and communication skills, and providing support to ensure that family members know how to get help in a crisis, “is a key part of comprehensive early psychosis intervention,” Dr. Kozloff said. “It is good for the patient and good for the family, and allows the clinicians to provide better care.”
Articulates clinical practice findings
Also commenting on the results, Brian O’Donoghue, MD, PhD, senior clinical research fellow at Orygen, the National Centre of Excellence in Youth Mental Health in Melbourne, described the research as important, adding that the study highlights the need for sufficient follow-up.
“It makes sense that the involvement of family over time has a strong impact upon outcome and functioning,” he said in an interview.
“These research findings articulate what we see in clinical practice, so it is good to see that it is captured,” added Dr. O’Donoghue, who was not associated with the study.
He noted that it is common for family involvement to influence outcome, especially if the family is positively involved. “It is invaluable toward their recovery. However, conversely, if there are ongoing family stressors, then this can be a trigger for relapse or lack of improvement.”
Overall, the results “really emphasize that the family needs to be involved in care.”
The Early Psychosis Prevention and Intervention Centre where Dr. O’Donoghue is a consultant psychiatrist offers a psychoeducational course “to inform families about psychosis, treatment, and how they can support their family members.”
“We also have family peer support workers and family therapists, which are essential to the service and for the young person’s recovery,” Dr. O’Donoghue said.
The investigators and Dr. O’Donoghue disclosed no relevant financial relationships. Dr. Kozloff reported receiving research funding from the CAMH Foundation, Brain & Behavior Research Foundation, Canadian Institutes of Health Research, and AFP Innovation Fund; honoraria from Humber River Hospital, the University of Calgary (Alta.), and the Canadian Consortium for Early Intervention in Psychosis; and salary support from Inner City Health Associates.
A version of this article originally appeared on Medscape.com.
Family environment may influence subsequent functional outcomes in patients with first-episode psychosis, new research suggests.
A study of more than 300 patients with first-episode psychosis (FEP) showed that although family environment was not associated with functioning at initial presentation, an interaction developed over time that could have “important implications for early interventions for both patients and caregivers,” investigators reported.
study coinvestigator Norma Verdolini, MD, PhD, bipolar and depressive disorders unit, hospital Clinic Barcelona, University of Barcelona, said in an interview.
The findings were scheduled to be presented at the Congress of the Schizophrenia International Research Society 2020, but the meeting was canceled because of the coronavirus pandemic.
FAST measures
Previous research has shown that family environment influences the development of psychotic symptoms, with negative family environmental factors associated with poor prognoses.
Conversely, one study indicated that a positive family environment is linked to greater improvement in negative and disorganized symptoms in adolescents at imminent risk for psychosis onset.
However, the current investigators noted that the impact of family environment on longitudinal functioning in individuals presenting with FEP is unclear.
To investigate further, they conducted an analysis as part of the PEPs study, which included 335 patients with FEP and 253 healthy controls. Functioning was measured using the Functional Assessment Short Test (FAST), and family environmental styles were evaluated using the Family Environment Scale (FES), which assesses “emotional climate” of a family across 10 domains.
At baseline, the mean total FAST score was 27.8 in patients with FEP versus 3.5 in the healthy controls, indicating substantially worse functioning among the patients. Linear regression analysis indicated that at baseline there was no significant association between aspects of family environment on the FES and functional scores.
Patients were assessed again at 2 years, by which point 283 had been diagnosed with psychotic disorders and 52 with bipolar disorder. The mean total FAST scores were 20.98 among patients with psychotic disorders and 13.8 in those with bipolar disorder.
Family conflict
Results showed that, among those with bipolar disorder, worse functioning on FAST at 2 years was significantly associated with higher rates of open expression of conflict in the family (P = .004).
In patients with psychotic disorders, worse functioning was significantly associated with lower rates of participation in social activities (P = .006) and an achievement-oriented family environment (P = .039). Worse functioning in patients with psychotic disorders was also significantly associated with higher rates of religious practice and values (P = .003).
Dr. Verdolini noted the reason family environment does not appear to have an impact at initial FEP presentation may be that the “first kick” is given by an individual’s genetic liability for psychiatric disorders in combination with the family environment. In reality, the two are intertwined, especially when considering what it means to a family to have one member with a psychiatric disorder, which “will have an impact on the family environment.”
Dr. Verdolini added: “This is not actually the objective family environment,” but the perceived family environment.
“So maybe in the following 2 years the patient who experiences a first episode of psychosis may change their idea of the family environment itself,” she noted. She added that at her institution psychoeducation is offered to FEP patients’ families.
‘Interesting’ findings
Commenting on the study, Nicole Kozloff, MD, from the child, youth, and emerging adult program at the Centre for Addiction and Mental Health in Toronto, said one limitation of the study is that it’s not clear what care patients received – or who in the family completed the FES.
It is also important to note that “measures of association do not necessarily imply that one factor caused the other factor,” said Dr. Kozloff, who was not involved in the research. “For example, it may be that, among people with bipolar disorder, open expression of conflict in the family can lead to worse functioning, or that worse functioning can lead to more conflict in the family.”
Nevertheless, Dr. Kozloff described the finding of an emerging association between the family environment and functioning over time as “interesting.”
When young people with FEP enter treatment, “they have reached a crisis point and are functioning poorly,” she noted.
“It could be that there is less to differentiate among levels of functioning at treatment entry but, after 2 years, the individuals have separated into those who have been responsive to treatment and are functioning well, and those who continue to have functional challenges. And this is where we start to see a relationship with family environment emerge,” Dr. Kozloff said.
She also agreed with Dr. Verdolini’s take on the findings, and that family psychoeducation “can reduce relapse rates in schizophrenia and the emotional burden on the family.”
“We also know that having family involvement in care is one of the most robust predictors that young people with psychosis will remain engaged in mental health services,” she said.
Teaching families about psychosis and its treatment, about problem-solving and communication skills, and providing support to ensure that family members know how to get help in a crisis, “is a key part of comprehensive early psychosis intervention,” Dr. Kozloff said. “It is good for the patient and good for the family, and allows the clinicians to provide better care.”
Articulates clinical practice findings
Also commenting on the results, Brian O’Donoghue, MD, PhD, senior clinical research fellow at Orygen, the National Centre of Excellence in Youth Mental Health in Melbourne, described the research as important, adding that the study highlights the need for sufficient follow-up.
“It makes sense that the involvement of family over time has a strong impact upon outcome and functioning,” he said in an interview.
“These research findings articulate what we see in clinical practice, so it is good to see that it is captured,” added Dr. O’Donoghue, who was not associated with the study.
He noted that it is common for family involvement to influence outcome, especially if the family is positively involved. “It is invaluable toward their recovery. However, conversely, if there are ongoing family stressors, then this can be a trigger for relapse or lack of improvement.”
Overall, the results “really emphasize that the family needs to be involved in care.”
The Early Psychosis Prevention and Intervention Centre where Dr. O’Donoghue is a consultant psychiatrist offers a psychoeducational course “to inform families about psychosis, treatment, and how they can support their family members.”
“We also have family peer support workers and family therapists, which are essential to the service and for the young person’s recovery,” Dr. O’Donoghue said.
The investigators and Dr. O’Donoghue disclosed no relevant financial relationships. Dr. Kozloff reported receiving research funding from the CAMH Foundation, Brain & Behavior Research Foundation, Canadian Institutes of Health Research, and AFP Innovation Fund; honoraria from Humber River Hospital, the University of Calgary (Alta.), and the Canadian Consortium for Early Intervention in Psychosis; and salary support from Inner City Health Associates.
A version of this article originally appeared on Medscape.com.
FROM SIRS 2020
Myocarditis in COVID-19: An elusive cardiac complication
The COVID-19 literature has been peppered with reports about myocarditis accompanying the disease. If true, this could, in part, explain some of the observed cardiac injury and arrhythmias in seriously ill patients, but also have implications for prognosis.
But endomyocardial biopsies and autopsies, the gold-standard confirmation tests, have been few and far between.
Predictors of death in COVID-19 are older age, cardiovascular comorbidities, and elevated troponin or NT-proBNP – none of which actually fit well with the epidemiology of myocarditis due to other causes, Alida L.P. Caforio, MD, of Padua (Italy) University said in an interview. Myocarditis is traditionally a disease of the young, and most cases are immune-mediated and do not release troponin.
Moreover, myocarditis is a diagnosis of exclusion. For it to be made with any certainty requires proof, by biopsy or autopsy, of inflammatory infiltrates within the myocardium with myocyte necrosis not typical of myocardial infarction, said Dr. Caforio, who chaired the European Society of Cardiology’s writing committee for its 2013 position statement on myocardial and pericardial diseases.
“We have one biopsy-proven case, and in this case there were no viruses in the myocardium, including COVID-19,” she said. “There’s no proof that we have COVID-19 causing myocarditis because it has not been found in the cardiomyocytes.”
Emerging evidence
The virus-negative case from Lombardy, Italy, followed an early case series suggesting fulminant myocarditis was involved in 7% of COVID-related deaths in Wuhan, China.
Other case reports include cardiac magnetic resonance (CMR) findings typical of acute myocarditis in a man with no lung involvement or fever but a massive troponin spike, and myocarditis presenting as reverse takotsubo syndrome in a woman undergoing CMR and endomyocardial biopsy.
A CMR analysis in May said acute myocarditis, by 2018 Lake Louise Criteria, was present in eight of 10 patients with “myocarditis-like syndrome,” and a study just out June 30 said the coronavirus can infect heart cells in a lab dish.
Among the few autopsy series, a preprint on 12 patients with COVID-19 in the Seattle area showed coronavirus in the heart tissue of 1 patient.
“It was a low level, so there’s the possibility that it could be viremia, but the fact we do see actual cardiomyocyte injury associated with inflammation, that’s a myocarditis pattern. So it could be related to the SARS-CoV-2 virus,” said Desiree Marshall, MD, director of autopsy and after-death services, University of Washington Medical Center, Seattle.
The “waters are a little bit muddy,” however, because the patient had a coinfection clinically with influenza and methicillin-susceptible Staphylococcus aureus, which raises the specter that influenza could also have contributed, she said.
Data pending publication from two additional patients show no coronavirus in the heart. Acute respiratory distress syndrome pathology was common in all patients, but there was no evidence of vascular inflammation, such as endotheliitis, Dr. Marshall said.
SARS-CoV-2 cell entry depends on the angiotensin-converting enzyme 2 (ACE2) receptor, which is widely expressed in the heart and on endothelial cells and is linked to inflammatory activation. Autopsy data from three COVID-19 patients showed endothelial cell infection in the heart and diffuse endothelial inflammation, but no sign of lymphocytic myocarditis.
Defining myocarditis
“There are some experts who believe we’re likely still dealing with myocarditis but with atypical features, while others suggest there is no myocarditis by strict classic criteria,” said Peter Liu, MD, chief scientific officer/vice president of research, University of Ottawa Heart Institute.
“I don’t think either extreme is accurate,” he said. “The truth is likely somewhere in between, with evidence of both cardiac injury and inflammation. But nothing in COVID-19, as we know today, is classic; it’s a new disease, so we need to be more open minded as new data emerge.”
Part of the divide may indeed stem from the way myocarditis is defined. “Based on traditional Dallas criteria, classic myocarditis requires evidence of myocyte necrosis, which we have, but also inflammatory cell infiltrate, which we don’t consistently have,” he said. “But on the other hand, there is evidence of inflammation-induced cardiac damage, often aggregated around blood vessels.”
The situation is evolving in recent days, and new data under review demonstrated inflammatory infiltrates, which fits the traditional myocarditis criteria, Dr. Liu noted. Yet the viral etiology for the inflammation is still elusive in definitive proof.
In traditional myocarditis, there is an abundance of lymphocytes and foci of inflammation in the myocardium, but COVID-19 is very unusual, in that these lymphocytes are not as exuberant, he said. Lymphopenia or low lymphocyte counts occur in up to 80% of patients. Also, older patients, who initially made up the bulk of the severe COVID-19 cases, are less T-lymphocyte responsive.
“So the lower your lymphocyte count, the worse your outcome is going to be and the more likely you’re going to get cytokine storm,” Dr. Liu said. “And that may be the reason the suspected myocarditis in COVID-19 is atypical because the lymphocytes, in fact, are being suppressed and there is instead more vasculitis.”
Recent data from myocardial gene expression analysis showed that the viral receptor ACE2 is present in the myocardium, and can be upregulated in conditions such as heart failure, he said. However, the highest ACE2 expression is found in pericytes around blood vessels, not myocytes. “This may explain the preferential vascular involvement often observed.”
Cardiac damage in the young
Evidence started evolving in early April that young COVID-19 patients without lung disease, generally in their 20s and 30s, can have very high troponin peaks and a form of cardiac damage that does not appear to be related to sepsis, systemic shock, or cytokine storm.
“That’s the group that I do think has some myocarditis, but it’s different. It’s not lymphocytic myocarditis, like enteroviral myocarditis,” Leslie T. Cooper Jr., MD, a myocarditis expert at Mayo Clinic, Jacksonville, Florida, said in an interview.
“The data to date suggest that most SARS cardiac injury is related to stress or high circulating cytokine levels. However, myocarditis probably does affect some patients, he added. “The few published cases suggest a role for macrophages or endothelial cells, which could affect cardiac myocyte function. This type of injury could cause the ST-segment elevation MI-like patterns we have seen in young people with normal epicardial coronary arteries.”
Dr. Cooper, who coauthored a report on the management of COVID-19 cardiovascular syndrome, pointed out that it’s been hard for researchers to isolate genome from autopsy samples because of RNA degradation prior to autopsy and the use of formalin fixation for tissues prior to RNA extraction.
“Most labs are not doing next-generation sequencing, and even with that, RNA protection and fresh tissue may be required to detect viral genome,” he said.
No proven therapy
Although up to 50% of acute myocarditis cases undergo spontaneous healing, recognition and multidisciplinary management of clinically suspected myocarditis is important. The optimal treatment remains unclear.
An early case report suggested use of methylprednisolone and intravenous immunoglobulin helped spare the life of a 37-year-old with clinically suspected fulminant myocarditis with cardiogenic shock.
In a related commentary, Dr. Caforio and colleagues pointed out that the World Health Organization considers the use of IV corticosteroids controversial, even in pneumonia due to COVID-19, because it may reduce viral clearance and increase sepsis risk. Intravenous immunoglobulin is also questionable because there is no IgG response to COVID-19 in the plasma donors’ pool.
“Immunosuppression should be reserved for only virus-negative non-COVID myocarditis,” Dr. Caforio said in an interview. “There is no appropriate treatment nowadays for clinically suspected COVID-19 myocarditis. There is no proven therapy for COVID-19, even less for COVID-19 myocarditis.”
Although definitive publication of the RECOVERY trial is still pending, the benefits of dexamethasone – a steroid that works predominantly through its anti-inflammatory effects – appear to be in the sickest patients, such as those requiring ICU admission or respiratory support.
“Many of the same patients would have systemic inflammation and would have also shown elevated cardiac biomarkers,” Dr. Liu observed. “Therefore, it is conceivable that a subset who had cardiac inflammation also benefited from the treatment. Further data, possibly through subgroup analysis and eventually meta-analysis, may help us to understand if dexamethasone also benefited patients with dominant cardiac injury.”
Dr. Caforio, Dr. Marshall, Dr. Liu, and Dr. Cooper reported having no relevant conflicts of interest.
A version of this article originally appeared on Medscape.com.
The COVID-19 literature has been peppered with reports about myocarditis accompanying the disease. If true, this could, in part, explain some of the observed cardiac injury and arrhythmias in seriously ill patients, but also have implications for prognosis.
But endomyocardial biopsies and autopsies, the gold-standard confirmation tests, have been few and far between.
Predictors of death in COVID-19 are older age, cardiovascular comorbidities, and elevated troponin or NT-proBNP – none of which actually fit well with the epidemiology of myocarditis due to other causes, Alida L.P. Caforio, MD, of Padua (Italy) University said in an interview. Myocarditis is traditionally a disease of the young, and most cases are immune-mediated and do not release troponin.
Moreover, myocarditis is a diagnosis of exclusion. For it to be made with any certainty requires proof, by biopsy or autopsy, of inflammatory infiltrates within the myocardium with myocyte necrosis not typical of myocardial infarction, said Dr. Caforio, who chaired the European Society of Cardiology’s writing committee for its 2013 position statement on myocardial and pericardial diseases.
“We have one biopsy-proven case, and in this case there were no viruses in the myocardium, including COVID-19,” she said. “There’s no proof that we have COVID-19 causing myocarditis because it has not been found in the cardiomyocytes.”
Emerging evidence
The virus-negative case from Lombardy, Italy, followed an early case series suggesting fulminant myocarditis was involved in 7% of COVID-related deaths in Wuhan, China.
Other case reports include cardiac magnetic resonance (CMR) findings typical of acute myocarditis in a man with no lung involvement or fever but a massive troponin spike, and myocarditis presenting as reverse takotsubo syndrome in a woman undergoing CMR and endomyocardial biopsy.
A CMR analysis in May said acute myocarditis, by 2018 Lake Louise Criteria, was present in eight of 10 patients with “myocarditis-like syndrome,” and a study just out June 30 said the coronavirus can infect heart cells in a lab dish.
Among the few autopsy series, a preprint on 12 patients with COVID-19 in the Seattle area showed coronavirus in the heart tissue of 1 patient.
“It was a low level, so there’s the possibility that it could be viremia, but the fact we do see actual cardiomyocyte injury associated with inflammation, that’s a myocarditis pattern. So it could be related to the SARS-CoV-2 virus,” said Desiree Marshall, MD, director of autopsy and after-death services, University of Washington Medical Center, Seattle.
The “waters are a little bit muddy,” however, because the patient had a coinfection clinically with influenza and methicillin-susceptible Staphylococcus aureus, which raises the specter that influenza could also have contributed, she said.
Data pending publication from two additional patients show no coronavirus in the heart. Acute respiratory distress syndrome pathology was common in all patients, but there was no evidence of vascular inflammation, such as endotheliitis, Dr. Marshall said.
SARS-CoV-2 cell entry depends on the angiotensin-converting enzyme 2 (ACE2) receptor, which is widely expressed in the heart and on endothelial cells and is linked to inflammatory activation. Autopsy data from three COVID-19 patients showed endothelial cell infection in the heart and diffuse endothelial inflammation, but no sign of lymphocytic myocarditis.
Defining myocarditis
“There are some experts who believe we’re likely still dealing with myocarditis but with atypical features, while others suggest there is no myocarditis by strict classic criteria,” said Peter Liu, MD, chief scientific officer/vice president of research, University of Ottawa Heart Institute.
“I don’t think either extreme is accurate,” he said. “The truth is likely somewhere in between, with evidence of both cardiac injury and inflammation. But nothing in COVID-19, as we know today, is classic; it’s a new disease, so we need to be more open minded as new data emerge.”
Part of the divide may indeed stem from the way myocarditis is defined. “Based on traditional Dallas criteria, classic myocarditis requires evidence of myocyte necrosis, which we have, but also inflammatory cell infiltrate, which we don’t consistently have,” he said. “But on the other hand, there is evidence of inflammation-induced cardiac damage, often aggregated around blood vessels.”
The situation is evolving in recent days, and new data under review demonstrated inflammatory infiltrates, which fits the traditional myocarditis criteria, Dr. Liu noted. Yet the viral etiology for the inflammation is still elusive in definitive proof.
In traditional myocarditis, there is an abundance of lymphocytes and foci of inflammation in the myocardium, but COVID-19 is very unusual, in that these lymphocytes are not as exuberant, he said. Lymphopenia or low lymphocyte counts occur in up to 80% of patients. Also, older patients, who initially made up the bulk of the severe COVID-19 cases, are less T-lymphocyte responsive.
“So the lower your lymphocyte count, the worse your outcome is going to be and the more likely you’re going to get cytokine storm,” Dr. Liu said. “And that may be the reason the suspected myocarditis in COVID-19 is atypical because the lymphocytes, in fact, are being suppressed and there is instead more vasculitis.”
Recent data from myocardial gene expression analysis showed that the viral receptor ACE2 is present in the myocardium, and can be upregulated in conditions such as heart failure, he said. However, the highest ACE2 expression is found in pericytes around blood vessels, not myocytes. “This may explain the preferential vascular involvement often observed.”
Cardiac damage in the young
Evidence started evolving in early April that young COVID-19 patients without lung disease, generally in their 20s and 30s, can have very high troponin peaks and a form of cardiac damage that does not appear to be related to sepsis, systemic shock, or cytokine storm.
“That’s the group that I do think has some myocarditis, but it’s different. It’s not lymphocytic myocarditis, like enteroviral myocarditis,” Leslie T. Cooper Jr., MD, a myocarditis expert at Mayo Clinic, Jacksonville, Florida, said in an interview.
“The data to date suggest that most SARS cardiac injury is related to stress or high circulating cytokine levels. However, myocarditis probably does affect some patients, he added. “The few published cases suggest a role for macrophages or endothelial cells, which could affect cardiac myocyte function. This type of injury could cause the ST-segment elevation MI-like patterns we have seen in young people with normal epicardial coronary arteries.”
Dr. Cooper, who coauthored a report on the management of COVID-19 cardiovascular syndrome, pointed out that it’s been hard for researchers to isolate genome from autopsy samples because of RNA degradation prior to autopsy and the use of formalin fixation for tissues prior to RNA extraction.
“Most labs are not doing next-generation sequencing, and even with that, RNA protection and fresh tissue may be required to detect viral genome,” he said.
No proven therapy
Although up to 50% of acute myocarditis cases undergo spontaneous healing, recognition and multidisciplinary management of clinically suspected myocarditis is important. The optimal treatment remains unclear.
An early case report suggested use of methylprednisolone and intravenous immunoglobulin helped spare the life of a 37-year-old with clinically suspected fulminant myocarditis with cardiogenic shock.
In a related commentary, Dr. Caforio and colleagues pointed out that the World Health Organization considers the use of IV corticosteroids controversial, even in pneumonia due to COVID-19, because it may reduce viral clearance and increase sepsis risk. Intravenous immunoglobulin is also questionable because there is no IgG response to COVID-19 in the plasma donors’ pool.
“Immunosuppression should be reserved for only virus-negative non-COVID myocarditis,” Dr. Caforio said in an interview. “There is no appropriate treatment nowadays for clinically suspected COVID-19 myocarditis. There is no proven therapy for COVID-19, even less for COVID-19 myocarditis.”
Although definitive publication of the RECOVERY trial is still pending, the benefits of dexamethasone – a steroid that works predominantly through its anti-inflammatory effects – appear to be in the sickest patients, such as those requiring ICU admission or respiratory support.
“Many of the same patients would have systemic inflammation and would have also shown elevated cardiac biomarkers,” Dr. Liu observed. “Therefore, it is conceivable that a subset who had cardiac inflammation also benefited from the treatment. Further data, possibly through subgroup analysis and eventually meta-analysis, may help us to understand if dexamethasone also benefited patients with dominant cardiac injury.”
Dr. Caforio, Dr. Marshall, Dr. Liu, and Dr. Cooper reported having no relevant conflicts of interest.
A version of this article originally appeared on Medscape.com.
The COVID-19 literature has been peppered with reports about myocarditis accompanying the disease. If true, this could, in part, explain some of the observed cardiac injury and arrhythmias in seriously ill patients, but also have implications for prognosis.
But endomyocardial biopsies and autopsies, the gold-standard confirmation tests, have been few and far between.
Predictors of death in COVID-19 are older age, cardiovascular comorbidities, and elevated troponin or NT-proBNP – none of which actually fit well with the epidemiology of myocarditis due to other causes, Alida L.P. Caforio, MD, of Padua (Italy) University said in an interview. Myocarditis is traditionally a disease of the young, and most cases are immune-mediated and do not release troponin.
Moreover, myocarditis is a diagnosis of exclusion. For it to be made with any certainty requires proof, by biopsy or autopsy, of inflammatory infiltrates within the myocardium with myocyte necrosis not typical of myocardial infarction, said Dr. Caforio, who chaired the European Society of Cardiology’s writing committee for its 2013 position statement on myocardial and pericardial diseases.
“We have one biopsy-proven case, and in this case there were no viruses in the myocardium, including COVID-19,” she said. “There’s no proof that we have COVID-19 causing myocarditis because it has not been found in the cardiomyocytes.”
Emerging evidence
The virus-negative case from Lombardy, Italy, followed an early case series suggesting fulminant myocarditis was involved in 7% of COVID-related deaths in Wuhan, China.
Other case reports include cardiac magnetic resonance (CMR) findings typical of acute myocarditis in a man with no lung involvement or fever but a massive troponin spike, and myocarditis presenting as reverse takotsubo syndrome in a woman undergoing CMR and endomyocardial biopsy.
A CMR analysis in May said acute myocarditis, by 2018 Lake Louise Criteria, was present in eight of 10 patients with “myocarditis-like syndrome,” and a study just out June 30 said the coronavirus can infect heart cells in a lab dish.
Among the few autopsy series, a preprint on 12 patients with COVID-19 in the Seattle area showed coronavirus in the heart tissue of 1 patient.
“It was a low level, so there’s the possibility that it could be viremia, but the fact we do see actual cardiomyocyte injury associated with inflammation, that’s a myocarditis pattern. So it could be related to the SARS-CoV-2 virus,” said Desiree Marshall, MD, director of autopsy and after-death services, University of Washington Medical Center, Seattle.
The “waters are a little bit muddy,” however, because the patient had a coinfection clinically with influenza and methicillin-susceptible Staphylococcus aureus, which raises the specter that influenza could also have contributed, she said.
Data pending publication from two additional patients show no coronavirus in the heart. Acute respiratory distress syndrome pathology was common in all patients, but there was no evidence of vascular inflammation, such as endotheliitis, Dr. Marshall said.
SARS-CoV-2 cell entry depends on the angiotensin-converting enzyme 2 (ACE2) receptor, which is widely expressed in the heart and on endothelial cells and is linked to inflammatory activation. Autopsy data from three COVID-19 patients showed endothelial cell infection in the heart and diffuse endothelial inflammation, but no sign of lymphocytic myocarditis.
Defining myocarditis
“There are some experts who believe we’re likely still dealing with myocarditis but with atypical features, while others suggest there is no myocarditis by strict classic criteria,” said Peter Liu, MD, chief scientific officer/vice president of research, University of Ottawa Heart Institute.
“I don’t think either extreme is accurate,” he said. “The truth is likely somewhere in between, with evidence of both cardiac injury and inflammation. But nothing in COVID-19, as we know today, is classic; it’s a new disease, so we need to be more open minded as new data emerge.”
Part of the divide may indeed stem from the way myocarditis is defined. “Based on traditional Dallas criteria, classic myocarditis requires evidence of myocyte necrosis, which we have, but also inflammatory cell infiltrate, which we don’t consistently have,” he said. “But on the other hand, there is evidence of inflammation-induced cardiac damage, often aggregated around blood vessels.”
The situation is evolving in recent days, and new data under review demonstrated inflammatory infiltrates, which fits the traditional myocarditis criteria, Dr. Liu noted. Yet the viral etiology for the inflammation is still elusive in definitive proof.
In traditional myocarditis, there is an abundance of lymphocytes and foci of inflammation in the myocardium, but COVID-19 is very unusual, in that these lymphocytes are not as exuberant, he said. Lymphopenia or low lymphocyte counts occur in up to 80% of patients. Also, older patients, who initially made up the bulk of the severe COVID-19 cases, are less T-lymphocyte responsive.
“So the lower your lymphocyte count, the worse your outcome is going to be and the more likely you’re going to get cytokine storm,” Dr. Liu said. “And that may be the reason the suspected myocarditis in COVID-19 is atypical because the lymphocytes, in fact, are being suppressed and there is instead more vasculitis.”
Recent data from myocardial gene expression analysis showed that the viral receptor ACE2 is present in the myocardium, and can be upregulated in conditions such as heart failure, he said. However, the highest ACE2 expression is found in pericytes around blood vessels, not myocytes. “This may explain the preferential vascular involvement often observed.”
Cardiac damage in the young
Evidence started evolving in early April that young COVID-19 patients without lung disease, generally in their 20s and 30s, can have very high troponin peaks and a form of cardiac damage that does not appear to be related to sepsis, systemic shock, or cytokine storm.
“That’s the group that I do think has some myocarditis, but it’s different. It’s not lymphocytic myocarditis, like enteroviral myocarditis,” Leslie T. Cooper Jr., MD, a myocarditis expert at Mayo Clinic, Jacksonville, Florida, said in an interview.
“The data to date suggest that most SARS cardiac injury is related to stress or high circulating cytokine levels. However, myocarditis probably does affect some patients, he added. “The few published cases suggest a role for macrophages or endothelial cells, which could affect cardiac myocyte function. This type of injury could cause the ST-segment elevation MI-like patterns we have seen in young people with normal epicardial coronary arteries.”
Dr. Cooper, who coauthored a report on the management of COVID-19 cardiovascular syndrome, pointed out that it’s been hard for researchers to isolate genome from autopsy samples because of RNA degradation prior to autopsy and the use of formalin fixation for tissues prior to RNA extraction.
“Most labs are not doing next-generation sequencing, and even with that, RNA protection and fresh tissue may be required to detect viral genome,” he said.
No proven therapy
Although up to 50% of acute myocarditis cases undergo spontaneous healing, recognition and multidisciplinary management of clinically suspected myocarditis is important. The optimal treatment remains unclear.
An early case report suggested use of methylprednisolone and intravenous immunoglobulin helped spare the life of a 37-year-old with clinically suspected fulminant myocarditis with cardiogenic shock.
In a related commentary, Dr. Caforio and colleagues pointed out that the World Health Organization considers the use of IV corticosteroids controversial, even in pneumonia due to COVID-19, because it may reduce viral clearance and increase sepsis risk. Intravenous immunoglobulin is also questionable because there is no IgG response to COVID-19 in the plasma donors’ pool.
“Immunosuppression should be reserved for only virus-negative non-COVID myocarditis,” Dr. Caforio said in an interview. “There is no appropriate treatment nowadays for clinically suspected COVID-19 myocarditis. There is no proven therapy for COVID-19, even less for COVID-19 myocarditis.”
Although definitive publication of the RECOVERY trial is still pending, the benefits of dexamethasone – a steroid that works predominantly through its anti-inflammatory effects – appear to be in the sickest patients, such as those requiring ICU admission or respiratory support.
“Many of the same patients would have systemic inflammation and would have also shown elevated cardiac biomarkers,” Dr. Liu observed. “Therefore, it is conceivable that a subset who had cardiac inflammation also benefited from the treatment. Further data, possibly through subgroup analysis and eventually meta-analysis, may help us to understand if dexamethasone also benefited patients with dominant cardiac injury.”
Dr. Caforio, Dr. Marshall, Dr. Liu, and Dr. Cooper reported having no relevant conflicts of interest.
A version of this article originally appeared on Medscape.com.
‘Doc, can I get a mask exemption?’
As more jurisdictions mandate facial coverings in public, questions have arisen about whether it’s safe for everyone – including those with lung disease – to wear masks.
To address these issues, Medscape spoke with the chief medical officer of the American Lung Association, Dr. Albert Rizzo.
The CDC recommendations on mask wearing say, “Cloth face coverings should not be placed on young children under age 2, anyone who has trouble breathing, or is unconscious, incapacitated, or otherwise unable to remove the mask without assistance.” Does this language suggest that there indeed is a subset of the adult population with lung disease who shouldn’t wear masks?
It makes sense to say that if it makes you uncomfortable to wear a mask because it affects your breathing, you should think twice about getting in a situation where you would have to wear a mask.
I’ve told many of my high-risk patients, “The best way to avoid getting COVID-19 is to stay home and stay away from sick people, especially if you feel that you are not going to be able to wear a mask or facial covering of some sort.”
The reason that some people have trouble with a mask is that they haven’t tried the right style of mask – by that I mean how tightly it fits and the material it’s made out of. Sometimes it really is just that people with lung disease don’t like to have anything covering their faces. Many of these patients feel better where there is air blowing across their faces – they will have a fan blowing even in the middle of winter because they feel more comfortable.
I won’t say it’s all in their heads, but sometimes it’s a matter of desensitizing themselves to wearing a mask. I liken it to people who have sleep apnea. We often have to desensitize them to wearing a mask for sleeping. We tell them to put it on while they are watching TV — don’t hook it up to anything yet, just get used to having something on your face.
I’ve told my patients the same thing about masks for COVID-19. Put on the mask, see how it feels. If you become uncomfortable breathing with it on, take it off, but maybe you can handle it for a half hour or 45 minutes. Find out how much time you have for a trip to the grocery store based on how comfortable you are wearing it at home.
It’s a matter of training the patient, giving them options of how to get comfortable with it, and then making them realize that they have to weigh the benefits and risks of wearing the mask and feeling out of breath versus going out in public and being potentially exposed to coronavirus. And the bottom line is, anybody who is wearing a mask and starts to feel uncomfortable, they can take the mask off.
You mentioned different types of masks. Is there a type of mask that is typically more breathable that clinicians can recommend to patients with lung disease?
First, I remind patients who think they will have trouble breathing with a mask on that they are choosing a mask not so much to protect themselves – that would take an N95 mask to filter out the virus. The mask is worn so that when they cough or drink or speak, they aren’t sending respiratory droplets out into the environment. Even when we speak, respiratory droplets can easily go out as far as 6 feet, or further with coughing or sneezing. With facial coverings, we try to keep those respiratory droplets from getting out and infecting others.
So when choosing a mask, you don’t have to worry as much about a tight-fitting mask. I recommend a loose-fitting mask that covers the nose and mouth and isn’t going to fall off but isn’t so tight around the ears and neck to make them feel uncomfortable. Even though it doesn’t really protect the wearer, it is cutting down on the ability to breathe in droplets – maybe not microscopic particles, but it’s better than nothing.
Is a face shield a reasonable alternative for someone who feels they can’t breathe with a mask on?
Yes. I’m surprised that face shields don’t get more attention. I’ve tried them out, and they are actually more comfortable than masks. They do impede the spilling out of droplets into the public, but they are not as close fitting to the face as a mask. If you want to protect others, the face shield should be adequate. It is not as good at preventing you from breathing in viral particles.
Some people have claimed that wearing a mask makes them hyperventilate and feel like they are going to pass out, or the mask causes them to become hypoxic. Are these valid concerns?
We get two questions about masks from patients who feel that they are short of breath or are worried about wearing a mask. One is whether their oxygen level is dropping. It’s usually not that. It’s usually because they feel that the mask is an impediment to getting air in. Their oxygen levels are stable.
The other question is whether the mask causes CO2 retention. For the mask to trap enough exhaled CO2 and for us to breathe enough of that CO2 back in to raise our CO2 level, it has to be a pretty tight-fitting mask. With the type of masks we are suggesting that people wear, that’s very unlikely to occur.
What can clinicians do to reassure patients with some type of lung disease that they can safely wear masks?
There are a few things they can do right in the office. Have them put the mask on for a few minutes and make sure they feel comfortable with it. With an oximeter, patients can see that their oxygen levels don’t change when they are breathing through the mask for a period of time.
You can’t really measure CO2 retention that easily, but most patients with chronic obstructive pulmonary disease or pulmonary fibrosis don’t have an elevated CO2 at baseline. A little more education is helpful in those situations. In most cases, they aren’t going to retain enough CO2 to have problems wearing a mask.
Only a small percentage of patients with lung disease are CO2 retainers, and many of those patients are being seen by pulmonary specialists. Those are the patients you might want to be more cautious with, to make sure they aren’t wearing anything that is tight fitting or that makes them work harder to breathe. It’s not that the mask is causing CO2 retention, but the increased work of breathing may make it harder to exhale the CO2.
Does a mask interfere with supplemental oxygen in any way?
Supplemental oxygen is typically supplied through a nasal cannula, so 100% oxygen is still getting to the nasal passages and entrained down into the airway, so it shouldn’t be a problem.
Some of the resistance to wearing masks has come from people with asthma. Is it safe for patients with asthma to wear masks, or should these patients be exempt from wearing masks?
In general, the breathing of people with mild asthma, both young and old, should not be impeded by the wearing of facial coverings. The concerns about oxygen and carbon dioxide among patients with more severe lung disease should not play a role in asthma.
Since younger adults with COVID-19 seem to have fewer or no symptoms and may actually be carrying the virus unknowingly, this should be the main population who should wear masks to prevent transmission to others.
Exemptions for mask wearing for mild asthma should be discouraged and dealt with on a case-by-case basis if there is a particular concern for that individual.
How do you respond if a patient asks you for a formal medical exemption to wearing a mask?
We’ve been asked to do a lot of letter writing for patients around going back to work, as well as the issue of wearing masks. The discussion usually revolves around trying to avoid going somewhere where you would have to wear a mask if it makes you feel uncomfortable.
I do not recommend automatically exempting individuals from wearing masks, even many of my pulmonary patients. There needs to be an understanding by the patient regarding the purpose of the mask and the overall advice to stay out of situations where social distancing is not being practiced. If you can take the time to discuss options as mentioned above – mask styles, desensitization, etc – the patient usually understands and will try wearing a mask.
On a case-by-case basis, some individuals may need to be exempted, but I feel this is a small number. I prefer my high-risk (older, chronic disease, etc) patients do everything they can to avoid infection – handwashing, mask wearing, and socially distancing.
They should also realize that even with a note, it is not going to help if they are in the middle of the grocery store and someone confronts them about not wearing a mask. It may help as they enter a store that says “masks required” and they can show it to someone monitoring the door. But I’m not really sure in what situations having that note is going to be helpful if confrontations occur.
Patients are also asking how safe is it for them to go back to work and be out in public. I tell them, nothing is going to be 100% safe. Until we have an effective vaccine, we are all going to have to weigh the potential risks of going to an area where social distancing isn’t maintained, people aren’t wearing face masks, and you can’t wash your hands as much as you’d like to. That’s going to be a struggle for all of us to get back out into situations where people interact socially.
Albert A. Rizzo, MD, is chief medical officer for the American Lung Association, chief of the Section of Pulmonary and Critical Care Medicine at the Christiana Care Health System in Newark, Delaware, and a member of Christiana Care Pulmonary Associates. He is board certified in internal medicine, pulmonary medicine, critical care medicine, and sleep medicine and is a clinical assistant professor of medicine at Thomas Jefferson University Medical School, Philadelphia.
This article first appeared on Medscape.com.
As more jurisdictions mandate facial coverings in public, questions have arisen about whether it’s safe for everyone – including those with lung disease – to wear masks.
To address these issues, Medscape spoke with the chief medical officer of the American Lung Association, Dr. Albert Rizzo.
The CDC recommendations on mask wearing say, “Cloth face coverings should not be placed on young children under age 2, anyone who has trouble breathing, or is unconscious, incapacitated, or otherwise unable to remove the mask without assistance.” Does this language suggest that there indeed is a subset of the adult population with lung disease who shouldn’t wear masks?
It makes sense to say that if it makes you uncomfortable to wear a mask because it affects your breathing, you should think twice about getting in a situation where you would have to wear a mask.
I’ve told many of my high-risk patients, “The best way to avoid getting COVID-19 is to stay home and stay away from sick people, especially if you feel that you are not going to be able to wear a mask or facial covering of some sort.”
The reason that some people have trouble with a mask is that they haven’t tried the right style of mask – by that I mean how tightly it fits and the material it’s made out of. Sometimes it really is just that people with lung disease don’t like to have anything covering their faces. Many of these patients feel better where there is air blowing across their faces – they will have a fan blowing even in the middle of winter because they feel more comfortable.
I won’t say it’s all in their heads, but sometimes it’s a matter of desensitizing themselves to wearing a mask. I liken it to people who have sleep apnea. We often have to desensitize them to wearing a mask for sleeping. We tell them to put it on while they are watching TV — don’t hook it up to anything yet, just get used to having something on your face.
I’ve told my patients the same thing about masks for COVID-19. Put on the mask, see how it feels. If you become uncomfortable breathing with it on, take it off, but maybe you can handle it for a half hour or 45 minutes. Find out how much time you have for a trip to the grocery store based on how comfortable you are wearing it at home.
It’s a matter of training the patient, giving them options of how to get comfortable with it, and then making them realize that they have to weigh the benefits and risks of wearing the mask and feeling out of breath versus going out in public and being potentially exposed to coronavirus. And the bottom line is, anybody who is wearing a mask and starts to feel uncomfortable, they can take the mask off.
You mentioned different types of masks. Is there a type of mask that is typically more breathable that clinicians can recommend to patients with lung disease?
First, I remind patients who think they will have trouble breathing with a mask on that they are choosing a mask not so much to protect themselves – that would take an N95 mask to filter out the virus. The mask is worn so that when they cough or drink or speak, they aren’t sending respiratory droplets out into the environment. Even when we speak, respiratory droplets can easily go out as far as 6 feet, or further with coughing or sneezing. With facial coverings, we try to keep those respiratory droplets from getting out and infecting others.
So when choosing a mask, you don’t have to worry as much about a tight-fitting mask. I recommend a loose-fitting mask that covers the nose and mouth and isn’t going to fall off but isn’t so tight around the ears and neck to make them feel uncomfortable. Even though it doesn’t really protect the wearer, it is cutting down on the ability to breathe in droplets – maybe not microscopic particles, but it’s better than nothing.
Is a face shield a reasonable alternative for someone who feels they can’t breathe with a mask on?
Yes. I’m surprised that face shields don’t get more attention. I’ve tried them out, and they are actually more comfortable than masks. They do impede the spilling out of droplets into the public, but they are not as close fitting to the face as a mask. If you want to protect others, the face shield should be adequate. It is not as good at preventing you from breathing in viral particles.
Some people have claimed that wearing a mask makes them hyperventilate and feel like they are going to pass out, or the mask causes them to become hypoxic. Are these valid concerns?
We get two questions about masks from patients who feel that they are short of breath or are worried about wearing a mask. One is whether their oxygen level is dropping. It’s usually not that. It’s usually because they feel that the mask is an impediment to getting air in. Their oxygen levels are stable.
The other question is whether the mask causes CO2 retention. For the mask to trap enough exhaled CO2 and for us to breathe enough of that CO2 back in to raise our CO2 level, it has to be a pretty tight-fitting mask. With the type of masks we are suggesting that people wear, that’s very unlikely to occur.
What can clinicians do to reassure patients with some type of lung disease that they can safely wear masks?
There are a few things they can do right in the office. Have them put the mask on for a few minutes and make sure they feel comfortable with it. With an oximeter, patients can see that their oxygen levels don’t change when they are breathing through the mask for a period of time.
You can’t really measure CO2 retention that easily, but most patients with chronic obstructive pulmonary disease or pulmonary fibrosis don’t have an elevated CO2 at baseline. A little more education is helpful in those situations. In most cases, they aren’t going to retain enough CO2 to have problems wearing a mask.
Only a small percentage of patients with lung disease are CO2 retainers, and many of those patients are being seen by pulmonary specialists. Those are the patients you might want to be more cautious with, to make sure they aren’t wearing anything that is tight fitting or that makes them work harder to breathe. It’s not that the mask is causing CO2 retention, but the increased work of breathing may make it harder to exhale the CO2.
Does a mask interfere with supplemental oxygen in any way?
Supplemental oxygen is typically supplied through a nasal cannula, so 100% oxygen is still getting to the nasal passages and entrained down into the airway, so it shouldn’t be a problem.
Some of the resistance to wearing masks has come from people with asthma. Is it safe for patients with asthma to wear masks, or should these patients be exempt from wearing masks?
In general, the breathing of people with mild asthma, both young and old, should not be impeded by the wearing of facial coverings. The concerns about oxygen and carbon dioxide among patients with more severe lung disease should not play a role in asthma.
Since younger adults with COVID-19 seem to have fewer or no symptoms and may actually be carrying the virus unknowingly, this should be the main population who should wear masks to prevent transmission to others.
Exemptions for mask wearing for mild asthma should be discouraged and dealt with on a case-by-case basis if there is a particular concern for that individual.
How do you respond if a patient asks you for a formal medical exemption to wearing a mask?
We’ve been asked to do a lot of letter writing for patients around going back to work, as well as the issue of wearing masks. The discussion usually revolves around trying to avoid going somewhere where you would have to wear a mask if it makes you feel uncomfortable.
I do not recommend automatically exempting individuals from wearing masks, even many of my pulmonary patients. There needs to be an understanding by the patient regarding the purpose of the mask and the overall advice to stay out of situations where social distancing is not being practiced. If you can take the time to discuss options as mentioned above – mask styles, desensitization, etc – the patient usually understands and will try wearing a mask.
On a case-by-case basis, some individuals may need to be exempted, but I feel this is a small number. I prefer my high-risk (older, chronic disease, etc) patients do everything they can to avoid infection – handwashing, mask wearing, and socially distancing.
They should also realize that even with a note, it is not going to help if they are in the middle of the grocery store and someone confronts them about not wearing a mask. It may help as they enter a store that says “masks required” and they can show it to someone monitoring the door. But I’m not really sure in what situations having that note is going to be helpful if confrontations occur.
Patients are also asking how safe is it for them to go back to work and be out in public. I tell them, nothing is going to be 100% safe. Until we have an effective vaccine, we are all going to have to weigh the potential risks of going to an area where social distancing isn’t maintained, people aren’t wearing face masks, and you can’t wash your hands as much as you’d like to. That’s going to be a struggle for all of us to get back out into situations where people interact socially.
Albert A. Rizzo, MD, is chief medical officer for the American Lung Association, chief of the Section of Pulmonary and Critical Care Medicine at the Christiana Care Health System in Newark, Delaware, and a member of Christiana Care Pulmonary Associates. He is board certified in internal medicine, pulmonary medicine, critical care medicine, and sleep medicine and is a clinical assistant professor of medicine at Thomas Jefferson University Medical School, Philadelphia.
This article first appeared on Medscape.com.
As more jurisdictions mandate facial coverings in public, questions have arisen about whether it’s safe for everyone – including those with lung disease – to wear masks.
To address these issues, Medscape spoke with the chief medical officer of the American Lung Association, Dr. Albert Rizzo.
The CDC recommendations on mask wearing say, “Cloth face coverings should not be placed on young children under age 2, anyone who has trouble breathing, or is unconscious, incapacitated, or otherwise unable to remove the mask without assistance.” Does this language suggest that there indeed is a subset of the adult population with lung disease who shouldn’t wear masks?
It makes sense to say that if it makes you uncomfortable to wear a mask because it affects your breathing, you should think twice about getting in a situation where you would have to wear a mask.
I’ve told many of my high-risk patients, “The best way to avoid getting COVID-19 is to stay home and stay away from sick people, especially if you feel that you are not going to be able to wear a mask or facial covering of some sort.”
The reason that some people have trouble with a mask is that they haven’t tried the right style of mask – by that I mean how tightly it fits and the material it’s made out of. Sometimes it really is just that people with lung disease don’t like to have anything covering their faces. Many of these patients feel better where there is air blowing across their faces – they will have a fan blowing even in the middle of winter because they feel more comfortable.
I won’t say it’s all in their heads, but sometimes it’s a matter of desensitizing themselves to wearing a mask. I liken it to people who have sleep apnea. We often have to desensitize them to wearing a mask for sleeping. We tell them to put it on while they are watching TV — don’t hook it up to anything yet, just get used to having something on your face.
I’ve told my patients the same thing about masks for COVID-19. Put on the mask, see how it feels. If you become uncomfortable breathing with it on, take it off, but maybe you can handle it for a half hour or 45 minutes. Find out how much time you have for a trip to the grocery store based on how comfortable you are wearing it at home.
It’s a matter of training the patient, giving them options of how to get comfortable with it, and then making them realize that they have to weigh the benefits and risks of wearing the mask and feeling out of breath versus going out in public and being potentially exposed to coronavirus. And the bottom line is, anybody who is wearing a mask and starts to feel uncomfortable, they can take the mask off.
You mentioned different types of masks. Is there a type of mask that is typically more breathable that clinicians can recommend to patients with lung disease?
First, I remind patients who think they will have trouble breathing with a mask on that they are choosing a mask not so much to protect themselves – that would take an N95 mask to filter out the virus. The mask is worn so that when they cough or drink or speak, they aren’t sending respiratory droplets out into the environment. Even when we speak, respiratory droplets can easily go out as far as 6 feet, or further with coughing or sneezing. With facial coverings, we try to keep those respiratory droplets from getting out and infecting others.
So when choosing a mask, you don’t have to worry as much about a tight-fitting mask. I recommend a loose-fitting mask that covers the nose and mouth and isn’t going to fall off but isn’t so tight around the ears and neck to make them feel uncomfortable. Even though it doesn’t really protect the wearer, it is cutting down on the ability to breathe in droplets – maybe not microscopic particles, but it’s better than nothing.
Is a face shield a reasonable alternative for someone who feels they can’t breathe with a mask on?
Yes. I’m surprised that face shields don’t get more attention. I’ve tried them out, and they are actually more comfortable than masks. They do impede the spilling out of droplets into the public, but they are not as close fitting to the face as a mask. If you want to protect others, the face shield should be adequate. It is not as good at preventing you from breathing in viral particles.
Some people have claimed that wearing a mask makes them hyperventilate and feel like they are going to pass out, or the mask causes them to become hypoxic. Are these valid concerns?
We get two questions about masks from patients who feel that they are short of breath or are worried about wearing a mask. One is whether their oxygen level is dropping. It’s usually not that. It’s usually because they feel that the mask is an impediment to getting air in. Their oxygen levels are stable.
The other question is whether the mask causes CO2 retention. For the mask to trap enough exhaled CO2 and for us to breathe enough of that CO2 back in to raise our CO2 level, it has to be a pretty tight-fitting mask. With the type of masks we are suggesting that people wear, that’s very unlikely to occur.
What can clinicians do to reassure patients with some type of lung disease that they can safely wear masks?
There are a few things they can do right in the office. Have them put the mask on for a few minutes and make sure they feel comfortable with it. With an oximeter, patients can see that their oxygen levels don’t change when they are breathing through the mask for a period of time.
You can’t really measure CO2 retention that easily, but most patients with chronic obstructive pulmonary disease or pulmonary fibrosis don’t have an elevated CO2 at baseline. A little more education is helpful in those situations. In most cases, they aren’t going to retain enough CO2 to have problems wearing a mask.
Only a small percentage of patients with lung disease are CO2 retainers, and many of those patients are being seen by pulmonary specialists. Those are the patients you might want to be more cautious with, to make sure they aren’t wearing anything that is tight fitting or that makes them work harder to breathe. It’s not that the mask is causing CO2 retention, but the increased work of breathing may make it harder to exhale the CO2.
Does a mask interfere with supplemental oxygen in any way?
Supplemental oxygen is typically supplied through a nasal cannula, so 100% oxygen is still getting to the nasal passages and entrained down into the airway, so it shouldn’t be a problem.
Some of the resistance to wearing masks has come from people with asthma. Is it safe for patients with asthma to wear masks, or should these patients be exempt from wearing masks?
In general, the breathing of people with mild asthma, both young and old, should not be impeded by the wearing of facial coverings. The concerns about oxygen and carbon dioxide among patients with more severe lung disease should not play a role in asthma.
Since younger adults with COVID-19 seem to have fewer or no symptoms and may actually be carrying the virus unknowingly, this should be the main population who should wear masks to prevent transmission to others.
Exemptions for mask wearing for mild asthma should be discouraged and dealt with on a case-by-case basis if there is a particular concern for that individual.
How do you respond if a patient asks you for a formal medical exemption to wearing a mask?
We’ve been asked to do a lot of letter writing for patients around going back to work, as well as the issue of wearing masks. The discussion usually revolves around trying to avoid going somewhere where you would have to wear a mask if it makes you feel uncomfortable.
I do not recommend automatically exempting individuals from wearing masks, even many of my pulmonary patients. There needs to be an understanding by the patient regarding the purpose of the mask and the overall advice to stay out of situations where social distancing is not being practiced. If you can take the time to discuss options as mentioned above – mask styles, desensitization, etc – the patient usually understands and will try wearing a mask.
On a case-by-case basis, some individuals may need to be exempted, but I feel this is a small number. I prefer my high-risk (older, chronic disease, etc) patients do everything they can to avoid infection – handwashing, mask wearing, and socially distancing.
They should also realize that even with a note, it is not going to help if they are in the middle of the grocery store and someone confronts them about not wearing a mask. It may help as they enter a store that says “masks required” and they can show it to someone monitoring the door. But I’m not really sure in what situations having that note is going to be helpful if confrontations occur.
Patients are also asking how safe is it for them to go back to work and be out in public. I tell them, nothing is going to be 100% safe. Until we have an effective vaccine, we are all going to have to weigh the potential risks of going to an area where social distancing isn’t maintained, people aren’t wearing face masks, and you can’t wash your hands as much as you’d like to. That’s going to be a struggle for all of us to get back out into situations where people interact socially.
Albert A. Rizzo, MD, is chief medical officer for the American Lung Association, chief of the Section of Pulmonary and Critical Care Medicine at the Christiana Care Health System in Newark, Delaware, and a member of Christiana Care Pulmonary Associates. He is board certified in internal medicine, pulmonary medicine, critical care medicine, and sleep medicine and is a clinical assistant professor of medicine at Thomas Jefferson University Medical School, Philadelphia.
This article first appeared on Medscape.com.
Does moderate drinking slow cognitive decline?
new research suggests. However, at least one expert urges caution in interpreting the findings.
Investigators found that consuming 10-14 alcoholic drinks per week had the strongest cognitive benefit. The findings “add more weight” to the growing body of research identifying beneficial cognitive effects of moderate alcohol consumption, said lead author, Ruiyuan Zhang, MD, of the department of epidemiology and biostatistics at the University of Georgia, Athens. However, Dr. Zhang emphasized that nondrinkers should not take up drinking to protect brain function, as alcohol can have negative effects.
The study was published online in JAMA Network Open.
Slower cognitive decline
The observational study was a secondary analysis of data from the Health and Retirement Study, a nationally representative U.S. survey of middle-aged and older adults. The survey, which began in 1992, is conducted every 2 years and collects health and economic data.
The current analysis used data from 1996 to 2008 and included information from individuals who participated in at least three surveys. The study included 19,887 participants, with a mean age 61.8 years. Most (60.1%) were women and white (85.2%). Mean follow-up was 9.1 years.
Researchers measured cognitive domains of mental status, word recall, and vocabulary. They also calculated a total cognition score, with higher scores indicating better cognitive abilities.
For each cognitive function measure, researchers categorized participants into a consistently low–trajectory group in which cognitive test scores from baseline through follow-up were consistently low or a consistently high–trajectory group, where cognitive test scores from baseline through follow-up were consistently high.
Based on self-reports, the investigators categorized participants as never drinkers (41.8%), former drinkers (39.5%), or current drinkers (18.7%). For current drinkers, researchers determined the number of drinking days per week and number of drinks per day. They further categorized these participants as low to moderate drinkers or heavy drinkers.
One drink was defined as a 12-ounce bottle of beer, a 5-ounce glass of wine, or a 1.5-ounce shot of spirits, said Dr. Zhang.
Women who consumed 8 or more drinks per week and men who drank 15 or more drinks per week were considered heavy drinkers. Other current drinkers were deemed low to moderate drinkers. Most current drinkers (85.2%) were low to moderate drinkers.
Other covariates included age, sex, race/ethnicity, years of education, marital status, tobacco smoking status, and body mass index.
Results showed moderate drinking was associated with relatively high cognitive test scores. After controlling for all covariates, compared with never drinkers, current low to moderate drinkers were significantly less likely to have consistently low trajectories for total cognitive score (odds ratio, 0.66; 95% confidence interval, 0.59-0.74), mental status (OR, 0.71; 95% CI, 0.63-0.81), word recall (OR, 0.74; 95% CI, 0.69-0.80), and vocabulary (OR, 0.64; 95% CI, 0.56-0.74) (all P < .001).
Former drinkers also had better cognitive outcomes for all cognitive domains. Heavy drinkers had lower odds of being in the consistently low trajectory group only for the vocabulary test.
Heavy drinking ‘risky’
Because few participants were deemed to be heavy drinkers, the power to identify an association between heavy drinking and cognitive function was limited. Dr. Zhang acknowledged, though he noted that heavy drinking is “risky.”
“We found that, after the drinking dosage passes the moderate level, the risk of low cognitive function increases very fast, which indicates that heavy drinking may harm cognitive function.” Limiting alcohol consumption “is still very important,” he said.
The associations of alcohol and cognitive functions differed by race/ethnicity. Low to moderate drinking was significantly associated with a lower odds of having a consistently low trajectory for all four cognitive function measures only among white participants.
A possible reason for this is that the study had so few African Americans (who made up only 14.8% of the sample), which limited the ability to identify relationships between alcohol intake and cognitive function, said Dr. Zhang. “Another reason is that the sensitivity to alcohol may be different between white and African American subjects.”
There was a significant U-shaped association between weekly amounts of alcohol and the odds of being in the consistently low–trajectory group for all cognitive functions. Depending on the function tested, the optimal number of weekly drinks ranged from 10-14.
Dr. Zhang noted that, when women were examined separately, alcohol consumption had a significant U-shaped relationship only with word recall, with the optimal dosage being around eight drinks.
U-shaped relationship an ‘important finding’
The U-shaped relationship is “an important finding,” said Dr. Zhang. “It shows that the human body may act differently to low and high doses of alcohol. Knowing why and how this happens is very important as it would help us understand how alcohol affects the function of the human body.”
Sensitivity analyses among participants with no chronic diseases showed the U-shaped association was still significant for scores of total word recall and vocabulary, but not for mental status or total cognition score.
The authors noted that 77.2% of participants had at least one chronic disease. They maintained that the association between alcohol consumption and cognitive function may be applicable both to healthy people and to those with a chronic disease.
The study also found that low to moderate drinkers had slower rates of cognitive decline over time for all cognition domains.
Although the mechanisms underlying the cognitive benefits of alcohol consumption are unclear, the authors believe it may be via cerebrovascular and cardiovascular pathways.
Alcohol may increase levels of brain-derived neurotrophic factor, a key regulator of neuronal plasticity and development in the dorsal striatum, they noted.
Balancing act
However, there’s also evidence that drinking, especially heavy drinking, increases the risk of hypertension, stroke, liver damage, and some cancers. “We think the role of alcohol drinking in cognitive function may be a balance of its beneficial and harmful effects on the cardiovascular system,” said Dr. Zhang.
“For the low to moderate drinker, the beneficial effects may outweigh the harmful effects on the small blood vessels in the brain. In this way, it could preserve cognition,” he added.
Dr. Zhang also noted that the study focused on middle-aged and older adults. “We can’t say whether or not moderate alcohol could benefit younger people” because they may have different characteristics, he said.
The findings of other studies examining the effects of alcohol on cognitive function are mixed. While studies have identified a beneficial effect, others have uncovered no, minimal, or adverse effects. This could be due to the use of different tests of cognitive function or different study populations, said Dr. Zhang.
A limitation of the current study was that assessment of alcohol consumption was based on self-report, which might have introduced recall bias. In addition, because individuals tend to underestimate their alcohol consumption, heavy drinkers could be misclassified as low to moderate drinkers, and low to moderate drinkers as former drinkers.
“This may make our study underestimate the association between low to moderate drinking and cognitive function,” said Dr. Zhang. In addition, alcohol consumption tended to change with time, and this change may be associated with other factors that led to changes in cognitive function, the authors noted.
Interpret with caution
Commenting on the study, Brent P. Forester, MD, chief of the Center of Excellence in Geriatric Psychiatry at McLean Hospital in Belmont, Mass., associate professor of psychiatry at Harvard Medical School, Boston, and a member of the American Psychiatric Association Council on Geriatric Psychiatry, said he views the study with some trepidation.
“As a clinician taking care of older adults, I would be very cautious about overinterpreting the beneficial effects of alcohol before we understand the mechanism better,” he said.
He noted that all of the risk factors associated with heart attack and stroke are also risk factors for Alzheimer’s disease and cognitive decline more broadly. “One of the issues here is how in the world does alcohol reduce cardiovascular and cerebrovascular risks, if you know it increases the risk of hypertension and stroke, regardless of dose.”
With regard to the possible impact of alcohol on brain-derived neurotrophic factor, Dr. Forester said, “it’s an interesting idea” but the actual mechanism is still unclear.
Even with dietary studies, such as those on the Mediterranean diet that include red wine, showing cognitive benefit, Dr. Forester said he’s still concerned about the adverse effects of alcohol on older people. These can include falls and sleep disturbances in addition to cognitive issues, and these effects can increase with age.
He was somewhat surprised at the level of alcohol that the study determined was beneficial. “Essentially, what they’re saying here is that, for men, it’s two drinks a day.” This could be “problematic” as two drinks per day can quickly escalate as individuals build tolerance.
He also pointed out that the study does not determine cause and effect, noting that it’s only an association.
Dr. Forester said the study raises a number of questions, including the type of alcohol study participants consumed and whether this has any impact on cognitive benefit. He also questioned whether the mediating effects of alcohol were associated with something that wasn’t measured, such as socioeconomic status.
Another question, he said, is what factors in individuals’ medical or psychiatric history determine whether they are more or less likely to benefit from low to moderate alcohol intake.
Perhaps alcohol should be recommended only for “select subpopulations” – for example, those who are healthy and have a family history of cognitive decline –but not for those with a history of substance abuse, including alcohol abuse, said Dr. Forester.
“For this population, the last thing you want to do is recommend alcohol to reduce risk of cognitive decline,” he cautioned.
The study was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health. The investigators and Dr. Forester have reported no relevant financial disclosures.
A version of this story originally appeared on Medscape.com.
new research suggests. However, at least one expert urges caution in interpreting the findings.
Investigators found that consuming 10-14 alcoholic drinks per week had the strongest cognitive benefit. The findings “add more weight” to the growing body of research identifying beneficial cognitive effects of moderate alcohol consumption, said lead author, Ruiyuan Zhang, MD, of the department of epidemiology and biostatistics at the University of Georgia, Athens. However, Dr. Zhang emphasized that nondrinkers should not take up drinking to protect brain function, as alcohol can have negative effects.
The study was published online in JAMA Network Open.
Slower cognitive decline
The observational study was a secondary analysis of data from the Health and Retirement Study, a nationally representative U.S. survey of middle-aged and older adults. The survey, which began in 1992, is conducted every 2 years and collects health and economic data.
The current analysis used data from 1996 to 2008 and included information from individuals who participated in at least three surveys. The study included 19,887 participants, with a mean age 61.8 years. Most (60.1%) were women and white (85.2%). Mean follow-up was 9.1 years.
Researchers measured cognitive domains of mental status, word recall, and vocabulary. They also calculated a total cognition score, with higher scores indicating better cognitive abilities.
For each cognitive function measure, researchers categorized participants into a consistently low–trajectory group in which cognitive test scores from baseline through follow-up were consistently low or a consistently high–trajectory group, where cognitive test scores from baseline through follow-up were consistently high.
Based on self-reports, the investigators categorized participants as never drinkers (41.8%), former drinkers (39.5%), or current drinkers (18.7%). For current drinkers, researchers determined the number of drinking days per week and number of drinks per day. They further categorized these participants as low to moderate drinkers or heavy drinkers.
One drink was defined as a 12-ounce bottle of beer, a 5-ounce glass of wine, or a 1.5-ounce shot of spirits, said Dr. Zhang.
Women who consumed 8 or more drinks per week and men who drank 15 or more drinks per week were considered heavy drinkers. Other current drinkers were deemed low to moderate drinkers. Most current drinkers (85.2%) were low to moderate drinkers.
Other covariates included age, sex, race/ethnicity, years of education, marital status, tobacco smoking status, and body mass index.
Results showed moderate drinking was associated with relatively high cognitive test scores. After controlling for all covariates, compared with never drinkers, current low to moderate drinkers were significantly less likely to have consistently low trajectories for total cognitive score (odds ratio, 0.66; 95% confidence interval, 0.59-0.74), mental status (OR, 0.71; 95% CI, 0.63-0.81), word recall (OR, 0.74; 95% CI, 0.69-0.80), and vocabulary (OR, 0.64; 95% CI, 0.56-0.74) (all P < .001).
Former drinkers also had better cognitive outcomes for all cognitive domains. Heavy drinkers had lower odds of being in the consistently low trajectory group only for the vocabulary test.
Heavy drinking ‘risky’
Because few participants were deemed to be heavy drinkers, the power to identify an association between heavy drinking and cognitive function was limited. Dr. Zhang acknowledged, though he noted that heavy drinking is “risky.”
“We found that, after the drinking dosage passes the moderate level, the risk of low cognitive function increases very fast, which indicates that heavy drinking may harm cognitive function.” Limiting alcohol consumption “is still very important,” he said.
The associations of alcohol and cognitive functions differed by race/ethnicity. Low to moderate drinking was significantly associated with a lower odds of having a consistently low trajectory for all four cognitive function measures only among white participants.
A possible reason for this is that the study had so few African Americans (who made up only 14.8% of the sample), which limited the ability to identify relationships between alcohol intake and cognitive function, said Dr. Zhang. “Another reason is that the sensitivity to alcohol may be different between white and African American subjects.”
There was a significant U-shaped association between weekly amounts of alcohol and the odds of being in the consistently low–trajectory group for all cognitive functions. Depending on the function tested, the optimal number of weekly drinks ranged from 10-14.
Dr. Zhang noted that, when women were examined separately, alcohol consumption had a significant U-shaped relationship only with word recall, with the optimal dosage being around eight drinks.
U-shaped relationship an ‘important finding’
The U-shaped relationship is “an important finding,” said Dr. Zhang. “It shows that the human body may act differently to low and high doses of alcohol. Knowing why and how this happens is very important as it would help us understand how alcohol affects the function of the human body.”
Sensitivity analyses among participants with no chronic diseases showed the U-shaped association was still significant for scores of total word recall and vocabulary, but not for mental status or total cognition score.
The authors noted that 77.2% of participants had at least one chronic disease. They maintained that the association between alcohol consumption and cognitive function may be applicable both to healthy people and to those with a chronic disease.
The study also found that low to moderate drinkers had slower rates of cognitive decline over time for all cognition domains.
Although the mechanisms underlying the cognitive benefits of alcohol consumption are unclear, the authors believe it may be via cerebrovascular and cardiovascular pathways.
Alcohol may increase levels of brain-derived neurotrophic factor, a key regulator of neuronal plasticity and development in the dorsal striatum, they noted.
Balancing act
However, there’s also evidence that drinking, especially heavy drinking, increases the risk of hypertension, stroke, liver damage, and some cancers. “We think the role of alcohol drinking in cognitive function may be a balance of its beneficial and harmful effects on the cardiovascular system,” said Dr. Zhang.
“For the low to moderate drinker, the beneficial effects may outweigh the harmful effects on the small blood vessels in the brain. In this way, it could preserve cognition,” he added.
Dr. Zhang also noted that the study focused on middle-aged and older adults. “We can’t say whether or not moderate alcohol could benefit younger people” because they may have different characteristics, he said.
The findings of other studies examining the effects of alcohol on cognitive function are mixed. While studies have identified a beneficial effect, others have uncovered no, minimal, or adverse effects. This could be due to the use of different tests of cognitive function or different study populations, said Dr. Zhang.
A limitation of the current study was that assessment of alcohol consumption was based on self-report, which might have introduced recall bias. In addition, because individuals tend to underestimate their alcohol consumption, heavy drinkers could be misclassified as low to moderate drinkers, and low to moderate drinkers as former drinkers.
“This may make our study underestimate the association between low to moderate drinking and cognitive function,” said Dr. Zhang. In addition, alcohol consumption tended to change with time, and this change may be associated with other factors that led to changes in cognitive function, the authors noted.
Interpret with caution
Commenting on the study, Brent P. Forester, MD, chief of the Center of Excellence in Geriatric Psychiatry at McLean Hospital in Belmont, Mass., associate professor of psychiatry at Harvard Medical School, Boston, and a member of the American Psychiatric Association Council on Geriatric Psychiatry, said he views the study with some trepidation.
“As a clinician taking care of older adults, I would be very cautious about overinterpreting the beneficial effects of alcohol before we understand the mechanism better,” he said.
He noted that all of the risk factors associated with heart attack and stroke are also risk factors for Alzheimer’s disease and cognitive decline more broadly. “One of the issues here is how in the world does alcohol reduce cardiovascular and cerebrovascular risks, if you know it increases the risk of hypertension and stroke, regardless of dose.”
With regard to the possible impact of alcohol on brain-derived neurotrophic factor, Dr. Forester said, “it’s an interesting idea” but the actual mechanism is still unclear.
Even with dietary studies, such as those on the Mediterranean diet that include red wine, showing cognitive benefit, Dr. Forester said he’s still concerned about the adverse effects of alcohol on older people. These can include falls and sleep disturbances in addition to cognitive issues, and these effects can increase with age.
He was somewhat surprised at the level of alcohol that the study determined was beneficial. “Essentially, what they’re saying here is that, for men, it’s two drinks a day.” This could be “problematic” as two drinks per day can quickly escalate as individuals build tolerance.
He also pointed out that the study does not determine cause and effect, noting that it’s only an association.
Dr. Forester said the study raises a number of questions, including the type of alcohol study participants consumed and whether this has any impact on cognitive benefit. He also questioned whether the mediating effects of alcohol were associated with something that wasn’t measured, such as socioeconomic status.
Another question, he said, is what factors in individuals’ medical or psychiatric history determine whether they are more or less likely to benefit from low to moderate alcohol intake.
Perhaps alcohol should be recommended only for “select subpopulations” – for example, those who are healthy and have a family history of cognitive decline –but not for those with a history of substance abuse, including alcohol abuse, said Dr. Forester.
“For this population, the last thing you want to do is recommend alcohol to reduce risk of cognitive decline,” he cautioned.
The study was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health. The investigators and Dr. Forester have reported no relevant financial disclosures.
A version of this story originally appeared on Medscape.com.
new research suggests. However, at least one expert urges caution in interpreting the findings.
Investigators found that consuming 10-14 alcoholic drinks per week had the strongest cognitive benefit. The findings “add more weight” to the growing body of research identifying beneficial cognitive effects of moderate alcohol consumption, said lead author, Ruiyuan Zhang, MD, of the department of epidemiology and biostatistics at the University of Georgia, Athens. However, Dr. Zhang emphasized that nondrinkers should not take up drinking to protect brain function, as alcohol can have negative effects.
The study was published online in JAMA Network Open.
Slower cognitive decline
The observational study was a secondary analysis of data from the Health and Retirement Study, a nationally representative U.S. survey of middle-aged and older adults. The survey, which began in 1992, is conducted every 2 years and collects health and economic data.
The current analysis used data from 1996 to 2008 and included information from individuals who participated in at least three surveys. The study included 19,887 participants, with a mean age 61.8 years. Most (60.1%) were women and white (85.2%). Mean follow-up was 9.1 years.
Researchers measured cognitive domains of mental status, word recall, and vocabulary. They also calculated a total cognition score, with higher scores indicating better cognitive abilities.
For each cognitive function measure, researchers categorized participants into a consistently low–trajectory group in which cognitive test scores from baseline through follow-up were consistently low or a consistently high–trajectory group, where cognitive test scores from baseline through follow-up were consistently high.
Based on self-reports, the investigators categorized participants as never drinkers (41.8%), former drinkers (39.5%), or current drinkers (18.7%). For current drinkers, researchers determined the number of drinking days per week and number of drinks per day. They further categorized these participants as low to moderate drinkers or heavy drinkers.
One drink was defined as a 12-ounce bottle of beer, a 5-ounce glass of wine, or a 1.5-ounce shot of spirits, said Dr. Zhang.
Women who consumed 8 or more drinks per week and men who drank 15 or more drinks per week were considered heavy drinkers. Other current drinkers were deemed low to moderate drinkers. Most current drinkers (85.2%) were low to moderate drinkers.
Other covariates included age, sex, race/ethnicity, years of education, marital status, tobacco smoking status, and body mass index.
Results showed moderate drinking was associated with relatively high cognitive test scores. After controlling for all covariates, compared with never drinkers, current low to moderate drinkers were significantly less likely to have consistently low trajectories for total cognitive score (odds ratio, 0.66; 95% confidence interval, 0.59-0.74), mental status (OR, 0.71; 95% CI, 0.63-0.81), word recall (OR, 0.74; 95% CI, 0.69-0.80), and vocabulary (OR, 0.64; 95% CI, 0.56-0.74) (all P < .001).
Former drinkers also had better cognitive outcomes for all cognitive domains. Heavy drinkers had lower odds of being in the consistently low trajectory group only for the vocabulary test.
Heavy drinking ‘risky’
Because few participants were deemed to be heavy drinkers, the power to identify an association between heavy drinking and cognitive function was limited. Dr. Zhang acknowledged, though he noted that heavy drinking is “risky.”
“We found that, after the drinking dosage passes the moderate level, the risk of low cognitive function increases very fast, which indicates that heavy drinking may harm cognitive function.” Limiting alcohol consumption “is still very important,” he said.
The associations of alcohol and cognitive functions differed by race/ethnicity. Low to moderate drinking was significantly associated with a lower odds of having a consistently low trajectory for all four cognitive function measures only among white participants.
A possible reason for this is that the study had so few African Americans (who made up only 14.8% of the sample), which limited the ability to identify relationships between alcohol intake and cognitive function, said Dr. Zhang. “Another reason is that the sensitivity to alcohol may be different between white and African American subjects.”
There was a significant U-shaped association between weekly amounts of alcohol and the odds of being in the consistently low–trajectory group for all cognitive functions. Depending on the function tested, the optimal number of weekly drinks ranged from 10-14.
Dr. Zhang noted that, when women were examined separately, alcohol consumption had a significant U-shaped relationship only with word recall, with the optimal dosage being around eight drinks.
U-shaped relationship an ‘important finding’
The U-shaped relationship is “an important finding,” said Dr. Zhang. “It shows that the human body may act differently to low and high doses of alcohol. Knowing why and how this happens is very important as it would help us understand how alcohol affects the function of the human body.”
Sensitivity analyses among participants with no chronic diseases showed the U-shaped association was still significant for scores of total word recall and vocabulary, but not for mental status or total cognition score.
The authors noted that 77.2% of participants had at least one chronic disease. They maintained that the association between alcohol consumption and cognitive function may be applicable both to healthy people and to those with a chronic disease.
The study also found that low to moderate drinkers had slower rates of cognitive decline over time for all cognition domains.
Although the mechanisms underlying the cognitive benefits of alcohol consumption are unclear, the authors believe it may be via cerebrovascular and cardiovascular pathways.
Alcohol may increase levels of brain-derived neurotrophic factor, a key regulator of neuronal plasticity and development in the dorsal striatum, they noted.
Balancing act
However, there’s also evidence that drinking, especially heavy drinking, increases the risk of hypertension, stroke, liver damage, and some cancers. “We think the role of alcohol drinking in cognitive function may be a balance of its beneficial and harmful effects on the cardiovascular system,” said Dr. Zhang.
“For the low to moderate drinker, the beneficial effects may outweigh the harmful effects on the small blood vessels in the brain. In this way, it could preserve cognition,” he added.
Dr. Zhang also noted that the study focused on middle-aged and older adults. “We can’t say whether or not moderate alcohol could benefit younger people” because they may have different characteristics, he said.
The findings of other studies examining the effects of alcohol on cognitive function are mixed. While studies have identified a beneficial effect, others have uncovered no, minimal, or adverse effects. This could be due to the use of different tests of cognitive function or different study populations, said Dr. Zhang.
A limitation of the current study was that assessment of alcohol consumption was based on self-report, which might have introduced recall bias. In addition, because individuals tend to underestimate their alcohol consumption, heavy drinkers could be misclassified as low to moderate drinkers, and low to moderate drinkers as former drinkers.
“This may make our study underestimate the association between low to moderate drinking and cognitive function,” said Dr. Zhang. In addition, alcohol consumption tended to change with time, and this change may be associated with other factors that led to changes in cognitive function, the authors noted.
Interpret with caution
Commenting on the study, Brent P. Forester, MD, chief of the Center of Excellence in Geriatric Psychiatry at McLean Hospital in Belmont, Mass., associate professor of psychiatry at Harvard Medical School, Boston, and a member of the American Psychiatric Association Council on Geriatric Psychiatry, said he views the study with some trepidation.
“As a clinician taking care of older adults, I would be very cautious about overinterpreting the beneficial effects of alcohol before we understand the mechanism better,” he said.
He noted that all of the risk factors associated with heart attack and stroke are also risk factors for Alzheimer’s disease and cognitive decline more broadly. “One of the issues here is how in the world does alcohol reduce cardiovascular and cerebrovascular risks, if you know it increases the risk of hypertension and stroke, regardless of dose.”
With regard to the possible impact of alcohol on brain-derived neurotrophic factor, Dr. Forester said, “it’s an interesting idea” but the actual mechanism is still unclear.
Even with dietary studies, such as those on the Mediterranean diet that include red wine, showing cognitive benefit, Dr. Forester said he’s still concerned about the adverse effects of alcohol on older people. These can include falls and sleep disturbances in addition to cognitive issues, and these effects can increase with age.
He was somewhat surprised at the level of alcohol that the study determined was beneficial. “Essentially, what they’re saying here is that, for men, it’s two drinks a day.” This could be “problematic” as two drinks per day can quickly escalate as individuals build tolerance.
He also pointed out that the study does not determine cause and effect, noting that it’s only an association.
Dr. Forester said the study raises a number of questions, including the type of alcohol study participants consumed and whether this has any impact on cognitive benefit. He also questioned whether the mediating effects of alcohol were associated with something that wasn’t measured, such as socioeconomic status.
Another question, he said, is what factors in individuals’ medical or psychiatric history determine whether they are more or less likely to benefit from low to moderate alcohol intake.
Perhaps alcohol should be recommended only for “select subpopulations” – for example, those who are healthy and have a family history of cognitive decline –but not for those with a history of substance abuse, including alcohol abuse, said Dr. Forester.
“For this population, the last thing you want to do is recommend alcohol to reduce risk of cognitive decline,” he cautioned.
The study was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health. The investigators and Dr. Forester have reported no relevant financial disclosures.
A version of this story originally appeared on Medscape.com.
How well trained is the class of COVID-19?
During a family medicine rotation at Oregon Health & Sciences University, Portland, third-year medical students are preparing for a patient visit. Only, instead of entering a clinic room, students sit down at a computer. The patient they’re virtually examining – a 42-year-old male cattle rancher with knee problems – is an actor.
He asks for an MRI. A student explains that kneecap pain calls for rehab rather than a scan. The patient pushes back. “It would ease my mind,” he says. “I really need to make sure I can keep the ranch running.” The student must now try to digitally maintain rapport while explaining why imaging isn’t necessary.
When COVID-19 hit, telehealth training and remote learning became major parts of medical education, seemingly overnight. Since the start of the pandemic, students have contended with canceled classes, missed rotations, and revised training timelines, even as the demand for new doctors grows ever more pressing.
Institutions have been forced to rethink how to best establish solid, long-term foundations to ensure that young doctors are adequately trained. “They may find themselves the only doctors to be practicing in a small town,” said Stephen G. Post, PhD, bioethicist and professor at Stony Brook (N.Y.) University. “They have to be ready.”
With limited hands-on access to patients, students must learn in ways most never have before. Medical schools are now test-driving a mix of new and reimagined teaching strategies that aim to produce doctors who will enter medicine just as prepared as their more seasoned peers.
Hands-off education
Soon after starting her pediatrics rotation in March, recent Stanford (Calif.) University graduate Paloma Marin-Nevarez, MD, heard that children were being admitted to her hospital for evaluation to rule out COVID-19. Dr. Marin-Nevarez was assigned to help care for them but never physically met any – an approach called “virtual rounding.”
In virtual rounding, a provider typically goes in, examines a patient, and uses a portable device such as an iPad to send video or take notes about the encounter. Students or others in another room then give input on the patient’s care. “It was bizarre doing rounds on patients I had not met yet, discussing their treatment plans in one of the team rooms,” Dr. Marin-Nevarez said. “There was something very eerie about passing that particular unit that said: ‘Do not enter,’ and never being able to go inside.”
Within weeks, the Association of American Medical Colleges advised medical schools to suspend any activities – including clinical rotations – that involved direct student contact with patients, even those who weren’t COVID-19 positive.
Many schools hope to have students back and participating in some degree of patient care at non–COVID-19 hospital wards as early as July 1, said Michael Gisondi, MD, vice chair of education at Stanford’s department of emergency medicine. Returning students must now adapt to a restricted training environment, often while scrambling to make up training time. “This is uncharted territory for medical schools. Elective cases are down, surgical cases are down. That’s potentially going to decrease exposure to training opportunities.”
When students come back, lectures are still likely to remain on hold at most schools, replaced by Zoom conferences and virtual presentations. That’s not completely new: A trend away from large, traditional classes predated the pandemic. In a 2017-2018 AAMC survey, one in four second-year medical students said they almost never went to in-person lectures. COVID-19 has accelerated this shift.
For faculty who have long emphasized hands-on, in-person learning, the shift presents “a whole pedagogical issue – you don’t necessarily know how to adjust your practices to an online format,” Dr. Gisondi said. Instructors have to be even more flexible in order to engage students. “Every week I ask the students: ‘What’s working? What’s not working?’ ” Dr. Gisondi said about his online classes. “We have to solicit feedback.”
Changes to lectures are the easy part, says Elisabeth Fassas, a second-year student at the University of Maryland, Baltimore County. Before the pandemic, she was taking a clinical medicine course that involved time in the hospital, something that helped link the academic with the practical. “You really get to see the stuff you’re learning being relevant: ‘Here’s a patient who has a cardiology problem,’ ” she said. “[Capturing] that piece of connection to what you’re working toward is going to be tricky, I think.”
Some students who graduated this past spring worry about that clinical time they lost. Many remain acutely conscious of specific knowledge gaps. “I did not get a ton of experience examining crying children or holding babies,” said Dr. Marin-Nevarez, who starts an emergency medicine residency this year. “I am going to have to be transparent with my future instructors and let them know I missed out because of the pandemic.”
Such knowledge gaps mean new doctors will have to make up ground, said Jeremiah Tao, MD, who trains ophthalmology residents at the University of California, Irvine. But Dr. Tao doesn’t see these setbacks as a major long-term problem. His residents are already starting to make up the patient hours they missed in the spring and are refining the skills that got short shrift earlier on. For eligibility, “most boards require a certain number of days of experience. But most of the message from our board is [that] they’re understanding, and they’re going to leave it to the program directors to declare someone competent.”
Robert Johnson, MD, dean of New Jersey Medical School, Newark, said short-term setbacks in training likely won’t translate into longer-term skill deficits. “What most schools have done is overprepare students. We’re sure they have acquired all the skills they need to practice.”
Closing the gaps
To fill existing knowledge gaps and prevent future deficits, institutions hope to strike a balance between keeping trainees safe and providing necessary on-site learning. In line with ongoing AAMC recommendations, which suggest schools curtail student involvement in direct patient care in areas with significant COVID-19 spread, virtual rounding will likely continue.
Many schools may use a hybrid approach, in which students take turns entering patient rooms to perform checkups or observations while other students and instructors watch a video broadcast. “It’s not that different from when I go into the room and supervise a trainee,” Dr. Gisondi said.
Some schools are going even further, transforming education in ways that reflect the demands of a COVID-19–era medical marketplace. Institutions such as Weill Cornell Medicine, New York, and OHSU have invested in telemedicine training for years, but COVID-19 has given telehealth education an additional boost. These types of visits have surged dramatically, underscoring the importance of preparing new doctors to practice in a virtual setting – something that wasn’t common previously. In a 2019 survey, only about a quarter of sampled medical schools offered a telemedicine curriculum.
Simulated telehealth consults such as OHSU’s knee-pain scenario serve several purposes, says Ryan Palmer, EdD, associate dean of education at Northeast Ohio Universities, Rootstown. They virtually teach skills that students need – such as clearly explaining to patients why a care plan is called for – while allowing the trainees to practice forging an emotional connection with patients they are treating remotely.
“It’s less about how you use a specific system,” said Dr. Palmer, who developed OHSU’s TeleOSCE, a telehealth training system that has interested other schools. He sees this as an opportunity, inasmuch as telemedicine is likely to remain an important part of practice for the foreseeable future.
To that end, the AAMC recently hosted an online seminar to help faculty with telehealth instruction. But training such as this can only go so far, said Dr. Johnson. “There are techniques you do have to learn at the patient’s side.”
Dr. Johnson says that a traditional part of medical school at Rutgers has been having students spend time in general practitioners’ offices early on to see what the experience is like. “That’s going to be a problem – I expect many primary care practices will go out of business. Those types of shadowing experiences will probably go away. They may be replaced by experiences at larger clinics.”
Some learning in clinics may soon resume. Although fears about COVID-19 still loom large, Dr. Tao’s ophthalmology residents have started taking on something closer to a normal workload, thanks to patients returning for regular office visits. As people return to medical facilities in larger numbers, hospitals around the country have started separating patients with COVID-19 from others. Dr. Gisondi suggested that this means medical students may be able to circulate in non–COVID-19 wards, provided the institution has enough personal protective equipment. “The inpatient wards are really safe – there’s a low risk of transmission. That’s where core rotations occur.”
The road ahead
In settings where patients’ viral status remains uncertain, such as emergency wards and off-site clinics without rapid testing, in-person learning may be slower to resume. That’s where longer-term changes may come into play. Some schools are preparing digital learning platforms that have the potential to transform medical education.
For example, Haru Okuda, MD, an emergency medicine doctor and director of the Center for Advanced Medical Learning and Simulation at the University of South Florida, Tampa, is testing a new virtual-reality platform called Immertec. Dr. Okuda said that, unlike older teaching tools, the system is not a stale, static virtual environment that will become obsolete. Instead, it uses a live camera to visually teleport students into the space of a real clinic or operating room.
“Let’s say you have students learning gross anatomy, how to dissect the chest. You’d have a cadaver on the table, demonstrating anatomy. The student has a headset – you can see like you’re in the room.” The wraparound visual device allows students to watch surgical maneuvers close up or view additional input from devices such as laparoscopes.
Dr. Okuda acknowledges that educators don’t yet know whether this works as well as older, hands-on methods. As yet, no virtual reality system has touch-based sensors sophisticated enough to simulate even skills such as tying a basic surgical knot, Dr. Gisondi said. And immersive platforms are expensive, which means a gap may occur between schools that can afford them and those that can’t.
The long-term consequences of COVID-19 go beyond costs that institutions may have to bear. Some students are concerned that the pandemic is affecting their mental well-being in ways that may make training a tougher slog. A few students graduated early to serve on the COVID-19 front lines. Others, rather than planning trips to celebrate the gap between medical school and residency, watched from home as young doctors they knew worked under abusive and unsafe conditions.
“Many of us felt powerless, given what we saw happening around us,” said recent University of Michigan, Ann Arbor, graduate Marina Haque, MD. She thinks those feelings, along with the rigors of practicing medicine during a pandemic, may leave her and her colleagues more prone to burnout.
The pandemic has also had a galvanizing effect on students – some excited new doctors are eager to line up for duty on COVID-19 wards. But supervisors say they must weigh young doctors’ desire to serve against the possible risks. “You don’t want people who have a big future ahead of them rushing into these situations and getting severely ill,” said Dr. Post. “There is a balance.”
All these changes, temporary or lasting, have led many to question whether doctors who complete their training under the cloud of the pandemic will be more – or less – prepared than those who came before them. But it’s not really a question of better or worse, says Dr. Johnson, who stresses that medical education has always required flexibility.
“You come into medicine with a plan in mind, but things happen,” he said. He reflected on the HIV pandemic of the late 1980s and early 1990s that influenced his medical career. He hopes young doctors come through the COVID-19 crucible more seasoned, resilient, and confident in crisis situations. “This is a pivotal event in their lives, and it will shape many careers.”
A version of this article originally appeared on Medscape.com.
During a family medicine rotation at Oregon Health & Sciences University, Portland, third-year medical students are preparing for a patient visit. Only, instead of entering a clinic room, students sit down at a computer. The patient they’re virtually examining – a 42-year-old male cattle rancher with knee problems – is an actor.
He asks for an MRI. A student explains that kneecap pain calls for rehab rather than a scan. The patient pushes back. “It would ease my mind,” he says. “I really need to make sure I can keep the ranch running.” The student must now try to digitally maintain rapport while explaining why imaging isn’t necessary.
When COVID-19 hit, telehealth training and remote learning became major parts of medical education, seemingly overnight. Since the start of the pandemic, students have contended with canceled classes, missed rotations, and revised training timelines, even as the demand for new doctors grows ever more pressing.
Institutions have been forced to rethink how to best establish solid, long-term foundations to ensure that young doctors are adequately trained. “They may find themselves the only doctors to be practicing in a small town,” said Stephen G. Post, PhD, bioethicist and professor at Stony Brook (N.Y.) University. “They have to be ready.”
With limited hands-on access to patients, students must learn in ways most never have before. Medical schools are now test-driving a mix of new and reimagined teaching strategies that aim to produce doctors who will enter medicine just as prepared as their more seasoned peers.
Hands-off education
Soon after starting her pediatrics rotation in March, recent Stanford (Calif.) University graduate Paloma Marin-Nevarez, MD, heard that children were being admitted to her hospital for evaluation to rule out COVID-19. Dr. Marin-Nevarez was assigned to help care for them but never physically met any – an approach called “virtual rounding.”
In virtual rounding, a provider typically goes in, examines a patient, and uses a portable device such as an iPad to send video or take notes about the encounter. Students or others in another room then give input on the patient’s care. “It was bizarre doing rounds on patients I had not met yet, discussing their treatment plans in one of the team rooms,” Dr. Marin-Nevarez said. “There was something very eerie about passing that particular unit that said: ‘Do not enter,’ and never being able to go inside.”
Within weeks, the Association of American Medical Colleges advised medical schools to suspend any activities – including clinical rotations – that involved direct student contact with patients, even those who weren’t COVID-19 positive.
Many schools hope to have students back and participating in some degree of patient care at non–COVID-19 hospital wards as early as July 1, said Michael Gisondi, MD, vice chair of education at Stanford’s department of emergency medicine. Returning students must now adapt to a restricted training environment, often while scrambling to make up training time. “This is uncharted territory for medical schools. Elective cases are down, surgical cases are down. That’s potentially going to decrease exposure to training opportunities.”
When students come back, lectures are still likely to remain on hold at most schools, replaced by Zoom conferences and virtual presentations. That’s not completely new: A trend away from large, traditional classes predated the pandemic. In a 2017-2018 AAMC survey, one in four second-year medical students said they almost never went to in-person lectures. COVID-19 has accelerated this shift.
For faculty who have long emphasized hands-on, in-person learning, the shift presents “a whole pedagogical issue – you don’t necessarily know how to adjust your practices to an online format,” Dr. Gisondi said. Instructors have to be even more flexible in order to engage students. “Every week I ask the students: ‘What’s working? What’s not working?’ ” Dr. Gisondi said about his online classes. “We have to solicit feedback.”
Changes to lectures are the easy part, says Elisabeth Fassas, a second-year student at the University of Maryland, Baltimore County. Before the pandemic, she was taking a clinical medicine course that involved time in the hospital, something that helped link the academic with the practical. “You really get to see the stuff you’re learning being relevant: ‘Here’s a patient who has a cardiology problem,’ ” she said. “[Capturing] that piece of connection to what you’re working toward is going to be tricky, I think.”
Some students who graduated this past spring worry about that clinical time they lost. Many remain acutely conscious of specific knowledge gaps. “I did not get a ton of experience examining crying children or holding babies,” said Dr. Marin-Nevarez, who starts an emergency medicine residency this year. “I am going to have to be transparent with my future instructors and let them know I missed out because of the pandemic.”
Such knowledge gaps mean new doctors will have to make up ground, said Jeremiah Tao, MD, who trains ophthalmology residents at the University of California, Irvine. But Dr. Tao doesn’t see these setbacks as a major long-term problem. His residents are already starting to make up the patient hours they missed in the spring and are refining the skills that got short shrift earlier on. For eligibility, “most boards require a certain number of days of experience. But most of the message from our board is [that] they’re understanding, and they’re going to leave it to the program directors to declare someone competent.”
Robert Johnson, MD, dean of New Jersey Medical School, Newark, said short-term setbacks in training likely won’t translate into longer-term skill deficits. “What most schools have done is overprepare students. We’re sure they have acquired all the skills they need to practice.”
Closing the gaps
To fill existing knowledge gaps and prevent future deficits, institutions hope to strike a balance between keeping trainees safe and providing necessary on-site learning. In line with ongoing AAMC recommendations, which suggest schools curtail student involvement in direct patient care in areas with significant COVID-19 spread, virtual rounding will likely continue.
Many schools may use a hybrid approach, in which students take turns entering patient rooms to perform checkups or observations while other students and instructors watch a video broadcast. “It’s not that different from when I go into the room and supervise a trainee,” Dr. Gisondi said.
Some schools are going even further, transforming education in ways that reflect the demands of a COVID-19–era medical marketplace. Institutions such as Weill Cornell Medicine, New York, and OHSU have invested in telemedicine training for years, but COVID-19 has given telehealth education an additional boost. These types of visits have surged dramatically, underscoring the importance of preparing new doctors to practice in a virtual setting – something that wasn’t common previously. In a 2019 survey, only about a quarter of sampled medical schools offered a telemedicine curriculum.
Simulated telehealth consults such as OHSU’s knee-pain scenario serve several purposes, says Ryan Palmer, EdD, associate dean of education at Northeast Ohio Universities, Rootstown. They virtually teach skills that students need – such as clearly explaining to patients why a care plan is called for – while allowing the trainees to practice forging an emotional connection with patients they are treating remotely.
“It’s less about how you use a specific system,” said Dr. Palmer, who developed OHSU’s TeleOSCE, a telehealth training system that has interested other schools. He sees this as an opportunity, inasmuch as telemedicine is likely to remain an important part of practice for the foreseeable future.
To that end, the AAMC recently hosted an online seminar to help faculty with telehealth instruction. But training such as this can only go so far, said Dr. Johnson. “There are techniques you do have to learn at the patient’s side.”
Dr. Johnson says that a traditional part of medical school at Rutgers has been having students spend time in general practitioners’ offices early on to see what the experience is like. “That’s going to be a problem – I expect many primary care practices will go out of business. Those types of shadowing experiences will probably go away. They may be replaced by experiences at larger clinics.”
Some learning in clinics may soon resume. Although fears about COVID-19 still loom large, Dr. Tao’s ophthalmology residents have started taking on something closer to a normal workload, thanks to patients returning for regular office visits. As people return to medical facilities in larger numbers, hospitals around the country have started separating patients with COVID-19 from others. Dr. Gisondi suggested that this means medical students may be able to circulate in non–COVID-19 wards, provided the institution has enough personal protective equipment. “The inpatient wards are really safe – there’s a low risk of transmission. That’s where core rotations occur.”
The road ahead
In settings where patients’ viral status remains uncertain, such as emergency wards and off-site clinics without rapid testing, in-person learning may be slower to resume. That’s where longer-term changes may come into play. Some schools are preparing digital learning platforms that have the potential to transform medical education.
For example, Haru Okuda, MD, an emergency medicine doctor and director of the Center for Advanced Medical Learning and Simulation at the University of South Florida, Tampa, is testing a new virtual-reality platform called Immertec. Dr. Okuda said that, unlike older teaching tools, the system is not a stale, static virtual environment that will become obsolete. Instead, it uses a live camera to visually teleport students into the space of a real clinic or operating room.
“Let’s say you have students learning gross anatomy, how to dissect the chest. You’d have a cadaver on the table, demonstrating anatomy. The student has a headset – you can see like you’re in the room.” The wraparound visual device allows students to watch surgical maneuvers close up or view additional input from devices such as laparoscopes.
Dr. Okuda acknowledges that educators don’t yet know whether this works as well as older, hands-on methods. As yet, no virtual reality system has touch-based sensors sophisticated enough to simulate even skills such as tying a basic surgical knot, Dr. Gisondi said. And immersive platforms are expensive, which means a gap may occur between schools that can afford them and those that can’t.
The long-term consequences of COVID-19 go beyond costs that institutions may have to bear. Some students are concerned that the pandemic is affecting their mental well-being in ways that may make training a tougher slog. A few students graduated early to serve on the COVID-19 front lines. Others, rather than planning trips to celebrate the gap between medical school and residency, watched from home as young doctors they knew worked under abusive and unsafe conditions.
“Many of us felt powerless, given what we saw happening around us,” said recent University of Michigan, Ann Arbor, graduate Marina Haque, MD. She thinks those feelings, along with the rigors of practicing medicine during a pandemic, may leave her and her colleagues more prone to burnout.
The pandemic has also had a galvanizing effect on students – some excited new doctors are eager to line up for duty on COVID-19 wards. But supervisors say they must weigh young doctors’ desire to serve against the possible risks. “You don’t want people who have a big future ahead of them rushing into these situations and getting severely ill,” said Dr. Post. “There is a balance.”
All these changes, temporary or lasting, have led many to question whether doctors who complete their training under the cloud of the pandemic will be more – or less – prepared than those who came before them. But it’s not really a question of better or worse, says Dr. Johnson, who stresses that medical education has always required flexibility.
“You come into medicine with a plan in mind, but things happen,” he said. He reflected on the HIV pandemic of the late 1980s and early 1990s that influenced his medical career. He hopes young doctors come through the COVID-19 crucible more seasoned, resilient, and confident in crisis situations. “This is a pivotal event in their lives, and it will shape many careers.”
A version of this article originally appeared on Medscape.com.
During a family medicine rotation at Oregon Health & Sciences University, Portland, third-year medical students are preparing for a patient visit. Only, instead of entering a clinic room, students sit down at a computer. The patient they’re virtually examining – a 42-year-old male cattle rancher with knee problems – is an actor.
He asks for an MRI. A student explains that kneecap pain calls for rehab rather than a scan. The patient pushes back. “It would ease my mind,” he says. “I really need to make sure I can keep the ranch running.” The student must now try to digitally maintain rapport while explaining why imaging isn’t necessary.
When COVID-19 hit, telehealth training and remote learning became major parts of medical education, seemingly overnight. Since the start of the pandemic, students have contended with canceled classes, missed rotations, and revised training timelines, even as the demand for new doctors grows ever more pressing.
Institutions have been forced to rethink how to best establish solid, long-term foundations to ensure that young doctors are adequately trained. “They may find themselves the only doctors to be practicing in a small town,” said Stephen G. Post, PhD, bioethicist and professor at Stony Brook (N.Y.) University. “They have to be ready.”
With limited hands-on access to patients, students must learn in ways most never have before. Medical schools are now test-driving a mix of new and reimagined teaching strategies that aim to produce doctors who will enter medicine just as prepared as their more seasoned peers.
Hands-off education
Soon after starting her pediatrics rotation in March, recent Stanford (Calif.) University graduate Paloma Marin-Nevarez, MD, heard that children were being admitted to her hospital for evaluation to rule out COVID-19. Dr. Marin-Nevarez was assigned to help care for them but never physically met any – an approach called “virtual rounding.”
In virtual rounding, a provider typically goes in, examines a patient, and uses a portable device such as an iPad to send video or take notes about the encounter. Students or others in another room then give input on the patient’s care. “It was bizarre doing rounds on patients I had not met yet, discussing their treatment plans in one of the team rooms,” Dr. Marin-Nevarez said. “There was something very eerie about passing that particular unit that said: ‘Do not enter,’ and never being able to go inside.”
Within weeks, the Association of American Medical Colleges advised medical schools to suspend any activities – including clinical rotations – that involved direct student contact with patients, even those who weren’t COVID-19 positive.
Many schools hope to have students back and participating in some degree of patient care at non–COVID-19 hospital wards as early as July 1, said Michael Gisondi, MD, vice chair of education at Stanford’s department of emergency medicine. Returning students must now adapt to a restricted training environment, often while scrambling to make up training time. “This is uncharted territory for medical schools. Elective cases are down, surgical cases are down. That’s potentially going to decrease exposure to training opportunities.”
When students come back, lectures are still likely to remain on hold at most schools, replaced by Zoom conferences and virtual presentations. That’s not completely new: A trend away from large, traditional classes predated the pandemic. In a 2017-2018 AAMC survey, one in four second-year medical students said they almost never went to in-person lectures. COVID-19 has accelerated this shift.
For faculty who have long emphasized hands-on, in-person learning, the shift presents “a whole pedagogical issue – you don’t necessarily know how to adjust your practices to an online format,” Dr. Gisondi said. Instructors have to be even more flexible in order to engage students. “Every week I ask the students: ‘What’s working? What’s not working?’ ” Dr. Gisondi said about his online classes. “We have to solicit feedback.”
Changes to lectures are the easy part, says Elisabeth Fassas, a second-year student at the University of Maryland, Baltimore County. Before the pandemic, she was taking a clinical medicine course that involved time in the hospital, something that helped link the academic with the practical. “You really get to see the stuff you’re learning being relevant: ‘Here’s a patient who has a cardiology problem,’ ” she said. “[Capturing] that piece of connection to what you’re working toward is going to be tricky, I think.”
Some students who graduated this past spring worry about that clinical time they lost. Many remain acutely conscious of specific knowledge gaps. “I did not get a ton of experience examining crying children or holding babies,” said Dr. Marin-Nevarez, who starts an emergency medicine residency this year. “I am going to have to be transparent with my future instructors and let them know I missed out because of the pandemic.”
Such knowledge gaps mean new doctors will have to make up ground, said Jeremiah Tao, MD, who trains ophthalmology residents at the University of California, Irvine. But Dr. Tao doesn’t see these setbacks as a major long-term problem. His residents are already starting to make up the patient hours they missed in the spring and are refining the skills that got short shrift earlier on. For eligibility, “most boards require a certain number of days of experience. But most of the message from our board is [that] they’re understanding, and they’re going to leave it to the program directors to declare someone competent.”
Robert Johnson, MD, dean of New Jersey Medical School, Newark, said short-term setbacks in training likely won’t translate into longer-term skill deficits. “What most schools have done is overprepare students. We’re sure they have acquired all the skills they need to practice.”
Closing the gaps
To fill existing knowledge gaps and prevent future deficits, institutions hope to strike a balance between keeping trainees safe and providing necessary on-site learning. In line with ongoing AAMC recommendations, which suggest schools curtail student involvement in direct patient care in areas with significant COVID-19 spread, virtual rounding will likely continue.
Many schools may use a hybrid approach, in which students take turns entering patient rooms to perform checkups or observations while other students and instructors watch a video broadcast. “It’s not that different from when I go into the room and supervise a trainee,” Dr. Gisondi said.
Some schools are going even further, transforming education in ways that reflect the demands of a COVID-19–era medical marketplace. Institutions such as Weill Cornell Medicine, New York, and OHSU have invested in telemedicine training for years, but COVID-19 has given telehealth education an additional boost. These types of visits have surged dramatically, underscoring the importance of preparing new doctors to practice in a virtual setting – something that wasn’t common previously. In a 2019 survey, only about a quarter of sampled medical schools offered a telemedicine curriculum.
Simulated telehealth consults such as OHSU’s knee-pain scenario serve several purposes, says Ryan Palmer, EdD, associate dean of education at Northeast Ohio Universities, Rootstown. They virtually teach skills that students need – such as clearly explaining to patients why a care plan is called for – while allowing the trainees to practice forging an emotional connection with patients they are treating remotely.
“It’s less about how you use a specific system,” said Dr. Palmer, who developed OHSU’s TeleOSCE, a telehealth training system that has interested other schools. He sees this as an opportunity, inasmuch as telemedicine is likely to remain an important part of practice for the foreseeable future.
To that end, the AAMC recently hosted an online seminar to help faculty with telehealth instruction. But training such as this can only go so far, said Dr. Johnson. “There are techniques you do have to learn at the patient’s side.”
Dr. Johnson says that a traditional part of medical school at Rutgers has been having students spend time in general practitioners’ offices early on to see what the experience is like. “That’s going to be a problem – I expect many primary care practices will go out of business. Those types of shadowing experiences will probably go away. They may be replaced by experiences at larger clinics.”
Some learning in clinics may soon resume. Although fears about COVID-19 still loom large, Dr. Tao’s ophthalmology residents have started taking on something closer to a normal workload, thanks to patients returning for regular office visits. As people return to medical facilities in larger numbers, hospitals around the country have started separating patients with COVID-19 from others. Dr. Gisondi suggested that this means medical students may be able to circulate in non–COVID-19 wards, provided the institution has enough personal protective equipment. “The inpatient wards are really safe – there’s a low risk of transmission. That’s where core rotations occur.”
The road ahead
In settings where patients’ viral status remains uncertain, such as emergency wards and off-site clinics without rapid testing, in-person learning may be slower to resume. That’s where longer-term changes may come into play. Some schools are preparing digital learning platforms that have the potential to transform medical education.
For example, Haru Okuda, MD, an emergency medicine doctor and director of the Center for Advanced Medical Learning and Simulation at the University of South Florida, Tampa, is testing a new virtual-reality platform called Immertec. Dr. Okuda said that, unlike older teaching tools, the system is not a stale, static virtual environment that will become obsolete. Instead, it uses a live camera to visually teleport students into the space of a real clinic or operating room.
“Let’s say you have students learning gross anatomy, how to dissect the chest. You’d have a cadaver on the table, demonstrating anatomy. The student has a headset – you can see like you’re in the room.” The wraparound visual device allows students to watch surgical maneuvers close up or view additional input from devices such as laparoscopes.
Dr. Okuda acknowledges that educators don’t yet know whether this works as well as older, hands-on methods. As yet, no virtual reality system has touch-based sensors sophisticated enough to simulate even skills such as tying a basic surgical knot, Dr. Gisondi said. And immersive platforms are expensive, which means a gap may occur between schools that can afford them and those that can’t.
The long-term consequences of COVID-19 go beyond costs that institutions may have to bear. Some students are concerned that the pandemic is affecting their mental well-being in ways that may make training a tougher slog. A few students graduated early to serve on the COVID-19 front lines. Others, rather than planning trips to celebrate the gap between medical school and residency, watched from home as young doctors they knew worked under abusive and unsafe conditions.
“Many of us felt powerless, given what we saw happening around us,” said recent University of Michigan, Ann Arbor, graduate Marina Haque, MD. She thinks those feelings, along with the rigors of practicing medicine during a pandemic, may leave her and her colleagues more prone to burnout.
The pandemic has also had a galvanizing effect on students – some excited new doctors are eager to line up for duty on COVID-19 wards. But supervisors say they must weigh young doctors’ desire to serve against the possible risks. “You don’t want people who have a big future ahead of them rushing into these situations and getting severely ill,” said Dr. Post. “There is a balance.”
All these changes, temporary or lasting, have led many to question whether doctors who complete their training under the cloud of the pandemic will be more – or less – prepared than those who came before them. But it’s not really a question of better or worse, says Dr. Johnson, who stresses that medical education has always required flexibility.
“You come into medicine with a plan in mind, but things happen,” he said. He reflected on the HIV pandemic of the late 1980s and early 1990s that influenced his medical career. He hopes young doctors come through the COVID-19 crucible more seasoned, resilient, and confident in crisis situations. “This is a pivotal event in their lives, and it will shape many careers.”
A version of this article originally appeared on Medscape.com.
WHO plans to address airborne COVID-19 transmission
WHO will likely address airborne transmission of the virus after a commentary from almost 240 multidisciplinary scientists raised the alarm that virus particles could remain airborne longer that previously appreciated, particularly in poorly ventilated indoor spaces.
“Airborne route of infection transmission is significant, but so far completely undermined, and not recognized by the decision makers and bodies responsible for infection control,” lead commentary author Lidia Morawska, PhD, told Medscape Medical News.
“This means that no control measures are taken to mitigate airborne transmission and, as a consequence, people are infected and can die,” said Morawska, director of the International Laboratory for Air Quality and Health at Queensland University of Technology in Brisbane, Australia. “We wanted to bring this to the attention of the world to prevent this from happening.”
The commentary was published July 6 in Clinical Infectious Diseases.
WHO leaders defended their progress in announcing any changes regarding how COVID-19 can be transmitted during a virtual press briefing today. They have collaborated since April with some of the scientists who coauthored the commentary, for example, said Maria Van Kerkhove, PhD, WHO technical lead on COVID-19.
“We have been working on a scientific brief ... to consolidate knowledge around transmission,” she added.
One focus will be on how masks protect healthcare workers. “We are also looking at the possible role of airborne transmission in other settings,” Van Kerkhove said. “We will be releasing our brief in the coming days.”
“We acknowledge there is emerging evidence in this field,” Benedetta Allegranzi, MD, WHO technical lead on COVID-19, said during the briefing from Geneva. “Therefore, we believe we have to be open to this evidence and its implications.”
WHO participated in an international research meeting last week that addressed means for controlling modes of COVID-19 transmission, Allegranzi said. “Our group and others really highlighted importance of research on different modes of transmission, including droplets of different sizes and their relative importance,” she said. Another aim was determining the dose of the virus required for airborne transmission.
“These fields of research are really growing but not definitive. More evidence needs to be gathered and evaluated,” she explained.
In the meantime, Allegranzi said, “the possibility of airborne transmission in public settings – especially closed, poorly ventilated settings – cannot be ruled out.”
Morawska said the evidence already exists. “A continuous surprise is that it takes the world such a long time to accept this, while this has such solid scientific foundation.” As an example, she cited an April report she coauthored in the journal Environment International. She and colleagues call for “national authorities to acknowledge the reality that the virus spreads through air and recommend that adequate control measures be implemented to prevent further spread of the SARS-CoV-2 virus, in particularly removal of the virus-laden droplets from indoor air by ventilation.”
The take-home message from the commentary, Morawska said, is a call to action. The authors state there is a need “to provide sufficient and effective ventilation (supply clean outdoor air, minimize recirculating air) particularly in public buildings, workplace environments, schools, hospitals, and aged care homes.”
WHO Chief Scientist Soumya Swaminathan, MD, explained why the organization remains cautious about making premature pronouncements regarding airborne transmission. “Any guidance we put out has implications for billions of people around the world, so we want to be as careful as possible,” she said during the press briefing. “We have to consider the weight of the evidence.”
“We are constantly looking for information on how we can do better,” Swaminathan added. WHO officials are reviewing hundreds of scientific reports every day, she said, and not all are of good quality. For this reason, she and other scientists at WHO perform a “living systematic review” – updating the consensus of evidence on a weekly basis.
“This process on COVID-19 will, I am sure, continue for the weeks and months to come,” she added.
This article first appeared on Medscape.com.
WHO will likely address airborne transmission of the virus after a commentary from almost 240 multidisciplinary scientists raised the alarm that virus particles could remain airborne longer that previously appreciated, particularly in poorly ventilated indoor spaces.
“Airborne route of infection transmission is significant, but so far completely undermined, and not recognized by the decision makers and bodies responsible for infection control,” lead commentary author Lidia Morawska, PhD, told Medscape Medical News.
“This means that no control measures are taken to mitigate airborne transmission and, as a consequence, people are infected and can die,” said Morawska, director of the International Laboratory for Air Quality and Health at Queensland University of Technology in Brisbane, Australia. “We wanted to bring this to the attention of the world to prevent this from happening.”
The commentary was published July 6 in Clinical Infectious Diseases.
WHO leaders defended their progress in announcing any changes regarding how COVID-19 can be transmitted during a virtual press briefing today. They have collaborated since April with some of the scientists who coauthored the commentary, for example, said Maria Van Kerkhove, PhD, WHO technical lead on COVID-19.
“We have been working on a scientific brief ... to consolidate knowledge around transmission,” she added.
One focus will be on how masks protect healthcare workers. “We are also looking at the possible role of airborne transmission in other settings,” Van Kerkhove said. “We will be releasing our brief in the coming days.”
“We acknowledge there is emerging evidence in this field,” Benedetta Allegranzi, MD, WHO technical lead on COVID-19, said during the briefing from Geneva. “Therefore, we believe we have to be open to this evidence and its implications.”
WHO participated in an international research meeting last week that addressed means for controlling modes of COVID-19 transmission, Allegranzi said. “Our group and others really highlighted importance of research on different modes of transmission, including droplets of different sizes and their relative importance,” she said. Another aim was determining the dose of the virus required for airborne transmission.
“These fields of research are really growing but not definitive. More evidence needs to be gathered and evaluated,” she explained.
In the meantime, Allegranzi said, “the possibility of airborne transmission in public settings – especially closed, poorly ventilated settings – cannot be ruled out.”
Morawska said the evidence already exists. “A continuous surprise is that it takes the world such a long time to accept this, while this has such solid scientific foundation.” As an example, she cited an April report she coauthored in the journal Environment International. She and colleagues call for “national authorities to acknowledge the reality that the virus spreads through air and recommend that adequate control measures be implemented to prevent further spread of the SARS-CoV-2 virus, in particularly removal of the virus-laden droplets from indoor air by ventilation.”
The take-home message from the commentary, Morawska said, is a call to action. The authors state there is a need “to provide sufficient and effective ventilation (supply clean outdoor air, minimize recirculating air) particularly in public buildings, workplace environments, schools, hospitals, and aged care homes.”
WHO Chief Scientist Soumya Swaminathan, MD, explained why the organization remains cautious about making premature pronouncements regarding airborne transmission. “Any guidance we put out has implications for billions of people around the world, so we want to be as careful as possible,” she said during the press briefing. “We have to consider the weight of the evidence.”
“We are constantly looking for information on how we can do better,” Swaminathan added. WHO officials are reviewing hundreds of scientific reports every day, she said, and not all are of good quality. For this reason, she and other scientists at WHO perform a “living systematic review” – updating the consensus of evidence on a weekly basis.
“This process on COVID-19 will, I am sure, continue for the weeks and months to come,” she added.
This article first appeared on Medscape.com.
WHO will likely address airborne transmission of the virus after a commentary from almost 240 multidisciplinary scientists raised the alarm that virus particles could remain airborne longer that previously appreciated, particularly in poorly ventilated indoor spaces.
“Airborne route of infection transmission is significant, but so far completely undermined, and not recognized by the decision makers and bodies responsible for infection control,” lead commentary author Lidia Morawska, PhD, told Medscape Medical News.
“This means that no control measures are taken to mitigate airborne transmission and, as a consequence, people are infected and can die,” said Morawska, director of the International Laboratory for Air Quality and Health at Queensland University of Technology in Brisbane, Australia. “We wanted to bring this to the attention of the world to prevent this from happening.”
The commentary was published July 6 in Clinical Infectious Diseases.
WHO leaders defended their progress in announcing any changes regarding how COVID-19 can be transmitted during a virtual press briefing today. They have collaborated since April with some of the scientists who coauthored the commentary, for example, said Maria Van Kerkhove, PhD, WHO technical lead on COVID-19.
“We have been working on a scientific brief ... to consolidate knowledge around transmission,” she added.
One focus will be on how masks protect healthcare workers. “We are also looking at the possible role of airborne transmission in other settings,” Van Kerkhove said. “We will be releasing our brief in the coming days.”
“We acknowledge there is emerging evidence in this field,” Benedetta Allegranzi, MD, WHO technical lead on COVID-19, said during the briefing from Geneva. “Therefore, we believe we have to be open to this evidence and its implications.”
WHO participated in an international research meeting last week that addressed means for controlling modes of COVID-19 transmission, Allegranzi said. “Our group and others really highlighted importance of research on different modes of transmission, including droplets of different sizes and their relative importance,” she said. Another aim was determining the dose of the virus required for airborne transmission.
“These fields of research are really growing but not definitive. More evidence needs to be gathered and evaluated,” she explained.
In the meantime, Allegranzi said, “the possibility of airborne transmission in public settings – especially closed, poorly ventilated settings – cannot be ruled out.”
Morawska said the evidence already exists. “A continuous surprise is that it takes the world such a long time to accept this, while this has such solid scientific foundation.” As an example, she cited an April report she coauthored in the journal Environment International. She and colleagues call for “national authorities to acknowledge the reality that the virus spreads through air and recommend that adequate control measures be implemented to prevent further spread of the SARS-CoV-2 virus, in particularly removal of the virus-laden droplets from indoor air by ventilation.”
The take-home message from the commentary, Morawska said, is a call to action. The authors state there is a need “to provide sufficient and effective ventilation (supply clean outdoor air, minimize recirculating air) particularly in public buildings, workplace environments, schools, hospitals, and aged care homes.”
WHO Chief Scientist Soumya Swaminathan, MD, explained why the organization remains cautious about making premature pronouncements regarding airborne transmission. “Any guidance we put out has implications for billions of people around the world, so we want to be as careful as possible,” she said during the press briefing. “We have to consider the weight of the evidence.”
“We are constantly looking for information on how we can do better,” Swaminathan added. WHO officials are reviewing hundreds of scientific reports every day, she said, and not all are of good quality. For this reason, she and other scientists at WHO perform a “living systematic review” – updating the consensus of evidence on a weekly basis.
“This process on COVID-19 will, I am sure, continue for the weeks and months to come,” she added.
This article first appeared on Medscape.com.
Meditations in an emergency: Talking through pandemic anxiety with a pioneer of mind-body medicine
Andrew N. Wilner, MD: Welcome to Medscape. I’m Dr Andrew Wilner. Today I have a special guest, Dr James Gordon, founder and executive director of the Center for Mind-Body Medicine. Welcome, Dr Gordon.
James S. Gordon, MD: Thank you very much. It’s good to be with you.
Dr. Wilner: Thanks for joining us. We are recording this in late May 2020, in the midst of the coronavirus pandemic. Millions of people have been infected. Hundreds of thousands have died. Millions have lost their jobs. I think it’s fair to say that people are under a greater degree of stress than they’re normally accustomed to. Would you agree with that?
Dr. Gordon: I think it’s more than fair to say that everybody in the United States, and actually pretty much everyone in the world, is under extreme stress. And that compounds any stresses that they’ve experienced before in their lives. Everyone is affected.
Dr. Wilner: The mind-body medicine concept is one that you’ve pursued for decades. Tell us a little bit about the Center for Mind-Body Medicine and how that’s led to the program that you have to help us deal with the coronavirus.
Dr. Gordon: I started the Center for Mind-Body Medicine about 30 years ago. I’d been a researcher at the National Institute of Mental Health for a number of years, in private practice, and a professor at Georgetown Medical School. But I wanted to really focus on how to change and enrich medicine by making self-care, self-awareness, and group support central to all healthcare.
Western medicine is enormously powerful in certain situations, such as physical trauma, high levels of infection, congenital anomalies. But we’re not so good at working with chronic physical or psychological problems. Those are much more complex.
We’ve been discovering that what is going to make the long-term difference in conditions like type 2 diabetes, pain syndromes, hypertension, depression, and anxiety are those approaches that we can learn to do for ourselves. These are changes we can make in how we deal with stress, eat, exercise, relate to other people, and whether we find meaning and purpose in our lives.
by wars, climate-related disasters, the opioid epidemic, chronic poverty, historical trauma. We do a lot of work with indigenous people here in North America. We’ve worked in a number of communities where school shootings have traumatized everyone.
What we’ve learned over these past 25 years, and what interested me professionally as well as personally over the past 50 years, is what we’re now bringing out on an even larger scale. The kind of approaches that we’ve developed, studied, and published research on are exactly what everyone needs to include and incorporate in their daily life, as well as in their medical and health care, from now on.
Dr. Wilner: Do you have a program that’s specifically for health care providers?
Dr. Gordon: Yes. The Center for Mind-Body Medicine is primarily an educational organization rather than a service organization. Since the beginning, I’ve been focused on training health professionals. My first passion was for training physicians – I’m a physician, so there’s a feeling of fellowship there – but also health care workers and mental health professionals of every kind.
We teach health professionals a whole system, a comprehensive program of techniques of self-awareness and self-care. We teach them so that they can practice on themselves and study the underlying science, so they can then teach what they’ve learned to the patients or clients they work with. They integrate it into what they’re already doing, regardless of their specialty. At times we also offer some of the same kinds of mind-body skills groups that are the fundamental part of our training as a stand-alone intervention. You can’t really teach other people how to take care of themselves unless you’re also doing it yourself. Otherwise, it’s just a theory.
Dr. Wilner: As a neurologist, I’m interested in the mind-body system. You are a psychiatrist and understand that it’s a lot more difficult to objectify certain things. What is stress? What is happiness? What is sadness? It’s very hard to measure. You can have scales, but it requires insight on the part of the individual. So I think it’s certainly an ambitious project.
Dr. Gordon: You’re absolutely right. It requires insight. And one of the shortcomings of our medical education is that it doesn’t encourage us to look inside ourselves enough. There’s so much focus on objectivity and on data, that we’ve lost some of the subjective art of medicine.
My experience with myself, as well as with the thousands of people we’ve trained here in the United States and around the world and the many hundreds of thousands with whom they’ve worked, is that all of us have a greater capacity to understand and help ourselves than we ordinarily think or than most of us learn about in our medical education.
This work is saying to people to take a little bit of time and relax a little in order to allow yourself to come into a meditative state. And I don’t mean anything fancy by that. Meditation is just being relaxed. Moment-to-moment awareness doesn’t have to do with any particular religion or spiritual practice. It’s part of all of them. If you can get into that state, then you can begin to say, “Oh, that’s what’s going on with me. That’s why my pain is worse.”
For example, you often wonder in people with peripheral neuropathy why it becomes worse or better at certain points. I would encourage neurologists and other physicians to ask your patients, “Why do you think it’s worse?” They may say, “I don’t know, doc; that’s why I’m here.” But I would ask them to take a couple of minutes to let me know. They could think it has something to do with the fact that they had a big fight with their wife that morning, they don’t want to go to work, or whatever it is. This is part of the lost art that we need to bring back into medicine for ourselves and especially for our patients.
Dr. Wilner: Can you give me an example of some of the exercises you’d do in a class?
Dr. Gordon: All of the exercises and our entire program that we teach at the Center for Mind-Body Medicine is in this new book of mine, “The Transformation: Discovering Wholeness and Healing After Trauma.” It’s really the distillation of not just the past 25 or 30 years, but really 50 years of work.
The techniques are all pretty simple and, as we say, evidence based. There is evidence that shows how they work on us physiologically, as well as psychologically. And they’re all pretty easy to teach to anyone.
Myself and about 60 or 70 of our faculty at the Center for Mind-Body Medicine are currently leading online groups. Then several hundred of the other people we’ve trained are also leading these groups. We’re still counting it up, but we probably have between 700 and 1,000 groups going around the world, led by our faculty and by people we’ve trained.
We teach a different technique every week in these online groups. Last week, after getting people energized and focused, we did a written dialogue with an emotion. You put down the initial of your name – in my case, “J” for Jim – and create a dialogue with an emotion, such as sadness. I would write it as fast as I can.
I would say, “OK, Sadness. Why are you here? What are you doing? I don’t enjoy having you around.” And Sadness writes back to me, “But you need me.” And J says, “What do you mean I need you?” And Sadness says, “Well, your brother died 7 weeks ago, didn’t he?” And I say, “Yes, he did.” And Sadness says, “Aren’t you sad?” I say, “Yes. I’m terribly sad and grieving all the time. But I wasn’t thinking about him at this moment.” And Sadness says, “But he’s there with you all the time and that sadness is in you.” And I say, “You mean it’s in me even here, now, as I’m talking with Andrew in this interview?” And Sadness says, “Yes. You can talk about your work. But in between the words, as you take a breath, don’t you feel it in your chest?” That’s the way the dialogue goes.
Dr. Wilner: What about specifically with the coronavirus? Fear is certainly an emotion. Nobody wants to get sick and die. Nobody wants to bring this disease home to their family. People are reluctant to even go outside and you can’t shake someone’s hand. Are there precedents for this?
Dr. Gordon: There are precedents, but only relatively small groups were affected before by, for example, severe acute respiratory syndrome or H1N1, at least in the United States. But we haven’t seen a global pandemic like this since 1918. None of us was around then – or I certainly wasn’t around. So for most everyone, not only has it not happened before, but we’ve never been so globally aware of everything that’s going on and how different groups are reacting.
I’ve been reading Daniel Defoe’s book, “A Journal of the Plague Year.” It’s really very interesting. It’s about the bubonic plague in 1665 London, although he wrote it in the 1720s. Some of the same things were going on then: the enormous fear, the isolation; rich people being able to escape, poor people having nowhere to go; conspiracy theories of one kind or another, about where the plague came from or blaming a group of people for it; magical thinking that it’s just going to go away. All of those things that happened several hundred years ago are going on now.
And we’re all simultaneously aware of all those things. There’s not only the fear, which should be universal because it’s a reasonable response to this situation, but also the terrible confusion about what to do. The President is saying one thing, governors something else; Anthony Fauci is saying something else, and Deborah Birx is saying something a little bit different. There’s this tremendous confusion that overlays the fear, and I think everybody is more or less feeling these things.
So yes, a dialogue with fear is a good thing to do because it can be clarifying. What we need here is a sense of, what is it that makes sense for me to do? What precautions should I take? What precautions shouldn’t I take?
I have a 17-year-old son who lives with his mom in California. He and I were on the phone the other day. He’s a basketball player and very serious about it. He said, “I don’t want to put my life on hold.” And my response was, “If you go outside too soon, your life may be on hold for a hell of a lot longer than if you stay inside because, if you get sick, it’s serious. But you also need to start looking at the evidence and asking yourself the right questions because I can’t be there all the time and neither can your mom.”
Everybody really needs to use these kinds of tools to help themselves. The tools we teach are extremely good at bringing us back into a state of psychological and physiological balance — slow, deep breathing being a very basic one. Because it’s only in that state that we’re going to be able to make the most intelligent decisions about what to do. It’s only in that state that we’re going to be able to really look our fear in the face and find out what we should be afraid of and what we shouldn’t be afraid of.
It’s a process that’s very much integrated. We’re talking now about how to deal with the emotions. But the first part of what we do in our groups and our online trainings and webinars is teach people to just take a few deep breaths. Just take a few deep breaths in through the nose, out through the mouth, with your belly soft and relaxed. You can keep breathing this way while talking. That’s the antidote to the fight-or-flight response. We all learn about fight-or-flight in first-year physiology. We need to deal with it. We need to bring ourselves into balance. That’s the way we’re going to make the wisest decisions for ourselves and be best able to help our patients.
Dr. Wilner: As you mentioned, part of modern culture is that we now have access to all of this information worldwide. There’s a continual stream of newsfeeds, people flipping on their phones, receiving constant updates, 24/7. That’s a new phenomenon. Does that steal from us the time we had before for just breathing and synthesizing data as opposed to just acquiring it all the time?
Dr. Gordon: You’re absolutely right. It does and it’s a challenge. It can’t steal from us unless we’re letting our emotional, psychological, and physiological pockets be picked!
What we need to do is to make it our priority to come into balance. I don’t watch news all day long – a little tiny bit in the morning and in the evening, just to get a sense of what’s happening. That’s enough. And I think everybody needs to take a step back, ask if this is really what they want to be doing, and to come into balance.
The other thing that’s really important is physical activity, especially during this time. In addition to using slow, deep breathing to come into balance, physical exercise and movement of any kind is extremely good as an antidote to fight-or-flight and that shut-down, freeze-up response that we get into when we feel completely overwhelmed.
We’ve got to take it into our own hands. The media just want to sell us things. Let’s face it: They’re not here for our good. Our job as physicians and health care professionals is to really reinforce for people not only what we can do for them but what they can do for themselves.
Dr. Wilner: I’m certainly interested in learning more about mind-body medicine. For those who feel the same, where do you recommend they go to learn more?
Dr. Gordon: We have a website, cmbm.org, which features a number of webinars. I do a free webinar there every week. We have mind-body skills groups that meet once a week for 8 weeks. There are six physicians in my group and all kinds of health professionals in other groups. We have a training program that we’re bringing online. We’ve trained well over 6,000 people around the world and would love to train more. You can read about that on the website.
We’re starting to do more and more consulting with health care organizations. We’re working with the largest division of Veterans Affairs, which is in Florida, as well as in south Georgia and the Caribbean. We’re working with a large health system in Indiana and others elsewhere. In addition, we’re working with groups of physicians and mental health professionals, helping them to integrate what we have to offer into what they’re already doing.
That’s our job – to help you do your job.
Dr. Wilner: Dr Gordon, I feel more relaxed just speaking with you. Thank you for talking with me and sharing your experiences with Medscape. I look forward to learning more.
Dr. Gordon: Thank you. My pleasure.
A version of this article originally appeared on Medscape.com.
Andrew N. Wilner, MD: Welcome to Medscape. I’m Dr Andrew Wilner. Today I have a special guest, Dr James Gordon, founder and executive director of the Center for Mind-Body Medicine. Welcome, Dr Gordon.
James S. Gordon, MD: Thank you very much. It’s good to be with you.
Dr. Wilner: Thanks for joining us. We are recording this in late May 2020, in the midst of the coronavirus pandemic. Millions of people have been infected. Hundreds of thousands have died. Millions have lost their jobs. I think it’s fair to say that people are under a greater degree of stress than they’re normally accustomed to. Would you agree with that?
Dr. Gordon: I think it’s more than fair to say that everybody in the United States, and actually pretty much everyone in the world, is under extreme stress. And that compounds any stresses that they’ve experienced before in their lives. Everyone is affected.
Dr. Wilner: The mind-body medicine concept is one that you’ve pursued for decades. Tell us a little bit about the Center for Mind-Body Medicine and how that’s led to the program that you have to help us deal with the coronavirus.
Dr. Gordon: I started the Center for Mind-Body Medicine about 30 years ago. I’d been a researcher at the National Institute of Mental Health for a number of years, in private practice, and a professor at Georgetown Medical School. But I wanted to really focus on how to change and enrich medicine by making self-care, self-awareness, and group support central to all healthcare.
Western medicine is enormously powerful in certain situations, such as physical trauma, high levels of infection, congenital anomalies. But we’re not so good at working with chronic physical or psychological problems. Those are much more complex.
We’ve been discovering that what is going to make the long-term difference in conditions like type 2 diabetes, pain syndromes, hypertension, depression, and anxiety are those approaches that we can learn to do for ourselves. These are changes we can make in how we deal with stress, eat, exercise, relate to other people, and whether we find meaning and purpose in our lives.
by wars, climate-related disasters, the opioid epidemic, chronic poverty, historical trauma. We do a lot of work with indigenous people here in North America. We’ve worked in a number of communities where school shootings have traumatized everyone.
What we’ve learned over these past 25 years, and what interested me professionally as well as personally over the past 50 years, is what we’re now bringing out on an even larger scale. The kind of approaches that we’ve developed, studied, and published research on are exactly what everyone needs to include and incorporate in their daily life, as well as in their medical and health care, from now on.
Dr. Wilner: Do you have a program that’s specifically for health care providers?
Dr. Gordon: Yes. The Center for Mind-Body Medicine is primarily an educational organization rather than a service organization. Since the beginning, I’ve been focused on training health professionals. My first passion was for training physicians – I’m a physician, so there’s a feeling of fellowship there – but also health care workers and mental health professionals of every kind.
We teach health professionals a whole system, a comprehensive program of techniques of self-awareness and self-care. We teach them so that they can practice on themselves and study the underlying science, so they can then teach what they’ve learned to the patients or clients they work with. They integrate it into what they’re already doing, regardless of their specialty. At times we also offer some of the same kinds of mind-body skills groups that are the fundamental part of our training as a stand-alone intervention. You can’t really teach other people how to take care of themselves unless you’re also doing it yourself. Otherwise, it’s just a theory.
Dr. Wilner: As a neurologist, I’m interested in the mind-body system. You are a psychiatrist and understand that it’s a lot more difficult to objectify certain things. What is stress? What is happiness? What is sadness? It’s very hard to measure. You can have scales, but it requires insight on the part of the individual. So I think it’s certainly an ambitious project.
Dr. Gordon: You’re absolutely right. It requires insight. And one of the shortcomings of our medical education is that it doesn’t encourage us to look inside ourselves enough. There’s so much focus on objectivity and on data, that we’ve lost some of the subjective art of medicine.
My experience with myself, as well as with the thousands of people we’ve trained here in the United States and around the world and the many hundreds of thousands with whom they’ve worked, is that all of us have a greater capacity to understand and help ourselves than we ordinarily think or than most of us learn about in our medical education.
This work is saying to people to take a little bit of time and relax a little in order to allow yourself to come into a meditative state. And I don’t mean anything fancy by that. Meditation is just being relaxed. Moment-to-moment awareness doesn’t have to do with any particular religion or spiritual practice. It’s part of all of them. If you can get into that state, then you can begin to say, “Oh, that’s what’s going on with me. That’s why my pain is worse.”
For example, you often wonder in people with peripheral neuropathy why it becomes worse or better at certain points. I would encourage neurologists and other physicians to ask your patients, “Why do you think it’s worse?” They may say, “I don’t know, doc; that’s why I’m here.” But I would ask them to take a couple of minutes to let me know. They could think it has something to do with the fact that they had a big fight with their wife that morning, they don’t want to go to work, or whatever it is. This is part of the lost art that we need to bring back into medicine for ourselves and especially for our patients.
Dr. Wilner: Can you give me an example of some of the exercises you’d do in a class?
Dr. Gordon: All of the exercises and our entire program that we teach at the Center for Mind-Body Medicine is in this new book of mine, “The Transformation: Discovering Wholeness and Healing After Trauma.” It’s really the distillation of not just the past 25 or 30 years, but really 50 years of work.
The techniques are all pretty simple and, as we say, evidence based. There is evidence that shows how they work on us physiologically, as well as psychologically. And they’re all pretty easy to teach to anyone.
Myself and about 60 or 70 of our faculty at the Center for Mind-Body Medicine are currently leading online groups. Then several hundred of the other people we’ve trained are also leading these groups. We’re still counting it up, but we probably have between 700 and 1,000 groups going around the world, led by our faculty and by people we’ve trained.
We teach a different technique every week in these online groups. Last week, after getting people energized and focused, we did a written dialogue with an emotion. You put down the initial of your name – in my case, “J” for Jim – and create a dialogue with an emotion, such as sadness. I would write it as fast as I can.
I would say, “OK, Sadness. Why are you here? What are you doing? I don’t enjoy having you around.” And Sadness writes back to me, “But you need me.” And J says, “What do you mean I need you?” And Sadness says, “Well, your brother died 7 weeks ago, didn’t he?” And I say, “Yes, he did.” And Sadness says, “Aren’t you sad?” I say, “Yes. I’m terribly sad and grieving all the time. But I wasn’t thinking about him at this moment.” And Sadness says, “But he’s there with you all the time and that sadness is in you.” And I say, “You mean it’s in me even here, now, as I’m talking with Andrew in this interview?” And Sadness says, “Yes. You can talk about your work. But in between the words, as you take a breath, don’t you feel it in your chest?” That’s the way the dialogue goes.
Dr. Wilner: What about specifically with the coronavirus? Fear is certainly an emotion. Nobody wants to get sick and die. Nobody wants to bring this disease home to their family. People are reluctant to even go outside and you can’t shake someone’s hand. Are there precedents for this?
Dr. Gordon: There are precedents, but only relatively small groups were affected before by, for example, severe acute respiratory syndrome or H1N1, at least in the United States. But we haven’t seen a global pandemic like this since 1918. None of us was around then – or I certainly wasn’t around. So for most everyone, not only has it not happened before, but we’ve never been so globally aware of everything that’s going on and how different groups are reacting.
I’ve been reading Daniel Defoe’s book, “A Journal of the Plague Year.” It’s really very interesting. It’s about the bubonic plague in 1665 London, although he wrote it in the 1720s. Some of the same things were going on then: the enormous fear, the isolation; rich people being able to escape, poor people having nowhere to go; conspiracy theories of one kind or another, about where the plague came from or blaming a group of people for it; magical thinking that it’s just going to go away. All of those things that happened several hundred years ago are going on now.
And we’re all simultaneously aware of all those things. There’s not only the fear, which should be universal because it’s a reasonable response to this situation, but also the terrible confusion about what to do. The President is saying one thing, governors something else; Anthony Fauci is saying something else, and Deborah Birx is saying something a little bit different. There’s this tremendous confusion that overlays the fear, and I think everybody is more or less feeling these things.
So yes, a dialogue with fear is a good thing to do because it can be clarifying. What we need here is a sense of, what is it that makes sense for me to do? What precautions should I take? What precautions shouldn’t I take?
I have a 17-year-old son who lives with his mom in California. He and I were on the phone the other day. He’s a basketball player and very serious about it. He said, “I don’t want to put my life on hold.” And my response was, “If you go outside too soon, your life may be on hold for a hell of a lot longer than if you stay inside because, if you get sick, it’s serious. But you also need to start looking at the evidence and asking yourself the right questions because I can’t be there all the time and neither can your mom.”
Everybody really needs to use these kinds of tools to help themselves. The tools we teach are extremely good at bringing us back into a state of psychological and physiological balance — slow, deep breathing being a very basic one. Because it’s only in that state that we’re going to be able to make the most intelligent decisions about what to do. It’s only in that state that we’re going to be able to really look our fear in the face and find out what we should be afraid of and what we shouldn’t be afraid of.
It’s a process that’s very much integrated. We’re talking now about how to deal with the emotions. But the first part of what we do in our groups and our online trainings and webinars is teach people to just take a few deep breaths. Just take a few deep breaths in through the nose, out through the mouth, with your belly soft and relaxed. You can keep breathing this way while talking. That’s the antidote to the fight-or-flight response. We all learn about fight-or-flight in first-year physiology. We need to deal with it. We need to bring ourselves into balance. That’s the way we’re going to make the wisest decisions for ourselves and be best able to help our patients.
Dr. Wilner: As you mentioned, part of modern culture is that we now have access to all of this information worldwide. There’s a continual stream of newsfeeds, people flipping on their phones, receiving constant updates, 24/7. That’s a new phenomenon. Does that steal from us the time we had before for just breathing and synthesizing data as opposed to just acquiring it all the time?
Dr. Gordon: You’re absolutely right. It does and it’s a challenge. It can’t steal from us unless we’re letting our emotional, psychological, and physiological pockets be picked!
What we need to do is to make it our priority to come into balance. I don’t watch news all day long – a little tiny bit in the morning and in the evening, just to get a sense of what’s happening. That’s enough. And I think everybody needs to take a step back, ask if this is really what they want to be doing, and to come into balance.
The other thing that’s really important is physical activity, especially during this time. In addition to using slow, deep breathing to come into balance, physical exercise and movement of any kind is extremely good as an antidote to fight-or-flight and that shut-down, freeze-up response that we get into when we feel completely overwhelmed.
We’ve got to take it into our own hands. The media just want to sell us things. Let’s face it: They’re not here for our good. Our job as physicians and health care professionals is to really reinforce for people not only what we can do for them but what they can do for themselves.
Dr. Wilner: I’m certainly interested in learning more about mind-body medicine. For those who feel the same, where do you recommend they go to learn more?
Dr. Gordon: We have a website, cmbm.org, which features a number of webinars. I do a free webinar there every week. We have mind-body skills groups that meet once a week for 8 weeks. There are six physicians in my group and all kinds of health professionals in other groups. We have a training program that we’re bringing online. We’ve trained well over 6,000 people around the world and would love to train more. You can read about that on the website.
We’re starting to do more and more consulting with health care organizations. We’re working with the largest division of Veterans Affairs, which is in Florida, as well as in south Georgia and the Caribbean. We’re working with a large health system in Indiana and others elsewhere. In addition, we’re working with groups of physicians and mental health professionals, helping them to integrate what we have to offer into what they’re already doing.
That’s our job – to help you do your job.
Dr. Wilner: Dr Gordon, I feel more relaxed just speaking with you. Thank you for talking with me and sharing your experiences with Medscape. I look forward to learning more.
Dr. Gordon: Thank you. My pleasure.
A version of this article originally appeared on Medscape.com.
Andrew N. Wilner, MD: Welcome to Medscape. I’m Dr Andrew Wilner. Today I have a special guest, Dr James Gordon, founder and executive director of the Center for Mind-Body Medicine. Welcome, Dr Gordon.
James S. Gordon, MD: Thank you very much. It’s good to be with you.
Dr. Wilner: Thanks for joining us. We are recording this in late May 2020, in the midst of the coronavirus pandemic. Millions of people have been infected. Hundreds of thousands have died. Millions have lost their jobs. I think it’s fair to say that people are under a greater degree of stress than they’re normally accustomed to. Would you agree with that?
Dr. Gordon: I think it’s more than fair to say that everybody in the United States, and actually pretty much everyone in the world, is under extreme stress. And that compounds any stresses that they’ve experienced before in their lives. Everyone is affected.
Dr. Wilner: The mind-body medicine concept is one that you’ve pursued for decades. Tell us a little bit about the Center for Mind-Body Medicine and how that’s led to the program that you have to help us deal with the coronavirus.
Dr. Gordon: I started the Center for Mind-Body Medicine about 30 years ago. I’d been a researcher at the National Institute of Mental Health for a number of years, in private practice, and a professor at Georgetown Medical School. But I wanted to really focus on how to change and enrich medicine by making self-care, self-awareness, and group support central to all healthcare.
Western medicine is enormously powerful in certain situations, such as physical trauma, high levels of infection, congenital anomalies. But we’re not so good at working with chronic physical or psychological problems. Those are much more complex.
We’ve been discovering that what is going to make the long-term difference in conditions like type 2 diabetes, pain syndromes, hypertension, depression, and anxiety are those approaches that we can learn to do for ourselves. These are changes we can make in how we deal with stress, eat, exercise, relate to other people, and whether we find meaning and purpose in our lives.
by wars, climate-related disasters, the opioid epidemic, chronic poverty, historical trauma. We do a lot of work with indigenous people here in North America. We’ve worked in a number of communities where school shootings have traumatized everyone.
What we’ve learned over these past 25 years, and what interested me professionally as well as personally over the past 50 years, is what we’re now bringing out on an even larger scale. The kind of approaches that we’ve developed, studied, and published research on are exactly what everyone needs to include and incorporate in their daily life, as well as in their medical and health care, from now on.
Dr. Wilner: Do you have a program that’s specifically for health care providers?
Dr. Gordon: Yes. The Center for Mind-Body Medicine is primarily an educational organization rather than a service organization. Since the beginning, I’ve been focused on training health professionals. My first passion was for training physicians – I’m a physician, so there’s a feeling of fellowship there – but also health care workers and mental health professionals of every kind.
We teach health professionals a whole system, a comprehensive program of techniques of self-awareness and self-care. We teach them so that they can practice on themselves and study the underlying science, so they can then teach what they’ve learned to the patients or clients they work with. They integrate it into what they’re already doing, regardless of their specialty. At times we also offer some of the same kinds of mind-body skills groups that are the fundamental part of our training as a stand-alone intervention. You can’t really teach other people how to take care of themselves unless you’re also doing it yourself. Otherwise, it’s just a theory.
Dr. Wilner: As a neurologist, I’m interested in the mind-body system. You are a psychiatrist and understand that it’s a lot more difficult to objectify certain things. What is stress? What is happiness? What is sadness? It’s very hard to measure. You can have scales, but it requires insight on the part of the individual. So I think it’s certainly an ambitious project.
Dr. Gordon: You’re absolutely right. It requires insight. And one of the shortcomings of our medical education is that it doesn’t encourage us to look inside ourselves enough. There’s so much focus on objectivity and on data, that we’ve lost some of the subjective art of medicine.
My experience with myself, as well as with the thousands of people we’ve trained here in the United States and around the world and the many hundreds of thousands with whom they’ve worked, is that all of us have a greater capacity to understand and help ourselves than we ordinarily think or than most of us learn about in our medical education.
This work is saying to people to take a little bit of time and relax a little in order to allow yourself to come into a meditative state. And I don’t mean anything fancy by that. Meditation is just being relaxed. Moment-to-moment awareness doesn’t have to do with any particular religion or spiritual practice. It’s part of all of them. If you can get into that state, then you can begin to say, “Oh, that’s what’s going on with me. That’s why my pain is worse.”
For example, you often wonder in people with peripheral neuropathy why it becomes worse or better at certain points. I would encourage neurologists and other physicians to ask your patients, “Why do you think it’s worse?” They may say, “I don’t know, doc; that’s why I’m here.” But I would ask them to take a couple of minutes to let me know. They could think it has something to do with the fact that they had a big fight with their wife that morning, they don’t want to go to work, or whatever it is. This is part of the lost art that we need to bring back into medicine for ourselves and especially for our patients.
Dr. Wilner: Can you give me an example of some of the exercises you’d do in a class?
Dr. Gordon: All of the exercises and our entire program that we teach at the Center for Mind-Body Medicine is in this new book of mine, “The Transformation: Discovering Wholeness and Healing After Trauma.” It’s really the distillation of not just the past 25 or 30 years, but really 50 years of work.
The techniques are all pretty simple and, as we say, evidence based. There is evidence that shows how they work on us physiologically, as well as psychologically. And they’re all pretty easy to teach to anyone.
Myself and about 60 or 70 of our faculty at the Center for Mind-Body Medicine are currently leading online groups. Then several hundred of the other people we’ve trained are also leading these groups. We’re still counting it up, but we probably have between 700 and 1,000 groups going around the world, led by our faculty and by people we’ve trained.
We teach a different technique every week in these online groups. Last week, after getting people energized and focused, we did a written dialogue with an emotion. You put down the initial of your name – in my case, “J” for Jim – and create a dialogue with an emotion, such as sadness. I would write it as fast as I can.
I would say, “OK, Sadness. Why are you here? What are you doing? I don’t enjoy having you around.” And Sadness writes back to me, “But you need me.” And J says, “What do you mean I need you?” And Sadness says, “Well, your brother died 7 weeks ago, didn’t he?” And I say, “Yes, he did.” And Sadness says, “Aren’t you sad?” I say, “Yes. I’m terribly sad and grieving all the time. But I wasn’t thinking about him at this moment.” And Sadness says, “But he’s there with you all the time and that sadness is in you.” And I say, “You mean it’s in me even here, now, as I’m talking with Andrew in this interview?” And Sadness says, “Yes. You can talk about your work. But in between the words, as you take a breath, don’t you feel it in your chest?” That’s the way the dialogue goes.
Dr. Wilner: What about specifically with the coronavirus? Fear is certainly an emotion. Nobody wants to get sick and die. Nobody wants to bring this disease home to their family. People are reluctant to even go outside and you can’t shake someone’s hand. Are there precedents for this?
Dr. Gordon: There are precedents, but only relatively small groups were affected before by, for example, severe acute respiratory syndrome or H1N1, at least in the United States. But we haven’t seen a global pandemic like this since 1918. None of us was around then – or I certainly wasn’t around. So for most everyone, not only has it not happened before, but we’ve never been so globally aware of everything that’s going on and how different groups are reacting.
I’ve been reading Daniel Defoe’s book, “A Journal of the Plague Year.” It’s really very interesting. It’s about the bubonic plague in 1665 London, although he wrote it in the 1720s. Some of the same things were going on then: the enormous fear, the isolation; rich people being able to escape, poor people having nowhere to go; conspiracy theories of one kind or another, about where the plague came from or blaming a group of people for it; magical thinking that it’s just going to go away. All of those things that happened several hundred years ago are going on now.
And we’re all simultaneously aware of all those things. There’s not only the fear, which should be universal because it’s a reasonable response to this situation, but also the terrible confusion about what to do. The President is saying one thing, governors something else; Anthony Fauci is saying something else, and Deborah Birx is saying something a little bit different. There’s this tremendous confusion that overlays the fear, and I think everybody is more or less feeling these things.
So yes, a dialogue with fear is a good thing to do because it can be clarifying. What we need here is a sense of, what is it that makes sense for me to do? What precautions should I take? What precautions shouldn’t I take?
I have a 17-year-old son who lives with his mom in California. He and I were on the phone the other day. He’s a basketball player and very serious about it. He said, “I don’t want to put my life on hold.” And my response was, “If you go outside too soon, your life may be on hold for a hell of a lot longer than if you stay inside because, if you get sick, it’s serious. But you also need to start looking at the evidence and asking yourself the right questions because I can’t be there all the time and neither can your mom.”
Everybody really needs to use these kinds of tools to help themselves. The tools we teach are extremely good at bringing us back into a state of psychological and physiological balance — slow, deep breathing being a very basic one. Because it’s only in that state that we’re going to be able to make the most intelligent decisions about what to do. It’s only in that state that we’re going to be able to really look our fear in the face and find out what we should be afraid of and what we shouldn’t be afraid of.
It’s a process that’s very much integrated. We’re talking now about how to deal with the emotions. But the first part of what we do in our groups and our online trainings and webinars is teach people to just take a few deep breaths. Just take a few deep breaths in through the nose, out through the mouth, with your belly soft and relaxed. You can keep breathing this way while talking. That’s the antidote to the fight-or-flight response. We all learn about fight-or-flight in first-year physiology. We need to deal with it. We need to bring ourselves into balance. That’s the way we’re going to make the wisest decisions for ourselves and be best able to help our patients.
Dr. Wilner: As you mentioned, part of modern culture is that we now have access to all of this information worldwide. There’s a continual stream of newsfeeds, people flipping on their phones, receiving constant updates, 24/7. That’s a new phenomenon. Does that steal from us the time we had before for just breathing and synthesizing data as opposed to just acquiring it all the time?
Dr. Gordon: You’re absolutely right. It does and it’s a challenge. It can’t steal from us unless we’re letting our emotional, psychological, and physiological pockets be picked!
What we need to do is to make it our priority to come into balance. I don’t watch news all day long – a little tiny bit in the morning and in the evening, just to get a sense of what’s happening. That’s enough. And I think everybody needs to take a step back, ask if this is really what they want to be doing, and to come into balance.
The other thing that’s really important is physical activity, especially during this time. In addition to using slow, deep breathing to come into balance, physical exercise and movement of any kind is extremely good as an antidote to fight-or-flight and that shut-down, freeze-up response that we get into when we feel completely overwhelmed.
We’ve got to take it into our own hands. The media just want to sell us things. Let’s face it: They’re not here for our good. Our job as physicians and health care professionals is to really reinforce for people not only what we can do for them but what they can do for themselves.
Dr. Wilner: I’m certainly interested in learning more about mind-body medicine. For those who feel the same, where do you recommend they go to learn more?
Dr. Gordon: We have a website, cmbm.org, which features a number of webinars. I do a free webinar there every week. We have mind-body skills groups that meet once a week for 8 weeks. There are six physicians in my group and all kinds of health professionals in other groups. We have a training program that we’re bringing online. We’ve trained well over 6,000 people around the world and would love to train more. You can read about that on the website.
We’re starting to do more and more consulting with health care organizations. We’re working with the largest division of Veterans Affairs, which is in Florida, as well as in south Georgia and the Caribbean. We’re working with a large health system in Indiana and others elsewhere. In addition, we’re working with groups of physicians and mental health professionals, helping them to integrate what we have to offer into what they’re already doing.
That’s our job – to help you do your job.
Dr. Wilner: Dr Gordon, I feel more relaxed just speaking with you. Thank you for talking with me and sharing your experiences with Medscape. I look forward to learning more.
Dr. Gordon: Thank you. My pleasure.
A version of this article originally appeared on Medscape.com.
Beefed up inpatient/outpatient care transition is key to suicide prevention
The care transition period between inpatient psychiatric hospitalization and initiation of outpatient mental health services is a time of extraordinarily heightened suicide risk that has been woefully neglected, according to speakers from the National Action Alliance for Suicide Prevention at the virtual annual meeting of the American Association of Suicidology.
This transition period traditionally has been a time when nobody really takes responsibility for patient care. In an effort to close this potentially deadly gap in services, the alliance recently has issued a report entitled, “Best Practices in Care Transitions for Individuals with Suicide Risk: Inpatient Care to Outpatient Care.” The recommendations focus on specific, innovative, evidence-based strategies that health care systems can use to prevent patients from falling through the cracks in care, mainly by implementing protocols aimed at fostering interorganizational teamwork between inpatient and outpatient behavioral health services.
“I believe that improving care transitions in the United States is the area where we can likely save the most lives. It’s within our grasp if we can just do this better,” declared Richard McKeon, PhD, MPH, chief of the Suicide Prevention Branch at the Center for Mental Health Services within SAMHSA, the Substance Abuse and Mental Health Services Administration.
He cited a recent meta-analysis that concluded that the risk of suicide during the first week post discharge after psychiatric hospitalization is a staggering 300 times greater than in the general population, while in the first month, the risk is increased 200-fold. The meta-analysis included 29 studies encompassing 3,551 suicides during the first month and 24 studies reporting 1,928 suicides during the first week post discharge (BMJ Open. 2019 Mar 23;9[3]:e023883. doi: 10.1136/bmjopen-2018-023883).
Everyone in the mental health field as well as patients and their families should know those statistics, but they don’t.
“I think it’s natural for people to think someone who’s been discharged from an inpatient unit or the emergency department is not at risk, when in reality it’s still a high-risk time. Suicide risk is not like a light switch that you can just switch off,” the clinical psychologist observed.
He cited other harrowing statistics that underscore the vast problem of poor care transitions. Nationally, fully one-third of patients don’t complete a single outpatient visit within the first 30 days after discharge from inpatient behavioral health care. And one in seven people who die by suicide have had contact with inpatient mental health services in the year before they died.
“That doesn’t mean that inpatient care did not do everything that they could do. What it does reflect is the need to make sure that there’s follow-up care after inpatient discharge. Too often, people don’t get the follow-up care that they need. And the research literature is clear that intervention can save lives,” Dr. McKeon said.
Panelist Becky Stoll, LCSW, vice president for crisis and disaster management at Centerstone Health in Nashville, Tenn., noted, “We see a lot of no-shows on the outpatient side, because nobody ever asked the patients if they can actually get to the outpatient appointment that’s been made.
“We have got to figure out this care transition and do better. The road to mental health is paved with Swiss cheese. There are so many holes to fall into, even if you know how to navigate the system – and most of the people we’re serving don’t know how,” observed Ms. Stoll, who, like Dr. McKeon, was among the coauthors of the alliance’s guidelines on best practices in care transitions. Ms. Stoll also serves on the AAS board as crisis services division chair.*
The National Action Alliance for Suicide Prevention is a public/private partnership whose goal is to advance the National Strategy for Suicide Prevention, which was developed by the alliance and the U.S. Surgeon General. The alliance includes mental health professionals as well as influential leaders from the military, journalism, entertainment, railroad, health insurance, law enforcement, defense, education, technology, and other industries.
Dr. McKeon and Ms. Stall were joined by Karen Johnson, MSW, another coauthor of the guidelines. They shared highlights of the report.
Inpatient provider strategies
Discharge and crisis safety planning should begin upon admission, according to Ms. Johnson, senior vice president for clinical services and division compliance at Universal Health Services, which owns and operates more than 200 behavioral health facilities across the United States.
Inpatient and outpatient care providers need to sit down and develop collaborative protocols and negotiate a memorandum of understanding regarding expectations, which absolutely must include procedures to ensure timely electronic delivery of medical records and other key documents to the outpatient care providers. The inpatient providers need to work collaboratively with the patient, family, and community support resources to develop a safety plan – including reduced access to lethal mean – as part of predischarge planning.
Among the strategies routinely employed on the inpatient side at Universal Health Services are advance scheduling of an initial outpatient appointment within 24-72 hours post discharge. Also, someone on the inpatient team is tasked with connecting with the outpatient provider prior to discharge to develop rapport.
“If our outpatient providers are located in our facility, as many of them are, we ask them to come in and attend inpatient team meetings to identify and meet with patients who are appropriate for continuing care in outpatient settings,” she explained. “A soft, warm handoff is critical.”
At these team meetings, the appropriateness of step-down care in the form of partial hospitalization or intensive outpatient care is weighed. Someone from the inpatient side is charged with maintaining contact with the patient until after the first outpatient appointment. Ongoing caring contact in the form of brief, encouraging postcards, emails, or texts that do not require a response from the patient should be maintained for several months.
Strategies for outpatient providers
Ms. Stoll is a big believer in the guideline-recommended practice of notifying the inpatient provider that the patient kept the outpatient appointment, along with having a system for red-flagging no-shows for prompt follow-up by a crisis management team.
She and her colleagues at Centerstone Health have conducted two studies of an intensive patient outreach program designed for the first 30 days of the care transition. The program included many elements of the alliance’s best practices guidelines. The yearlong first study, funded by Blue Cross/Blue Shield of Tennessee, documented zero suicides and 92% freedom from emergency department visits during the care transition period, along with greater than $400,000 savings in health care costs, compared with usual care. The second study, funded by SAMHSA, showed much the same over a 2-year period.
She emphasized that this was not a high-tech, intensive intervention. She characterized it, instead as “high-touch follow-up.
“It’s some staff and a phone and a laptop, nothing fancy, just a person who’s competent and confident and skilled with a laptop. With that, you can do some pretty amazing stuff: Get people what they need, keep them alive, and oh, guess what? You can also save a lot of health care dollars that can be put back into the system,” Ms. Stoll said.
She recognizes that it’s a lot to ask busy outpatient providers to leave their practice during the workday to participate in inpatient team meetings addressing discharge planning, as recommended in the alliance guidelines. But in this regard, she sees a silver lining to the COVID-19 pandemic, in that it forces health professionals to rely upon newly opened channels of telemedicine.
“COVID-19 is giving us an opportunity to do things in a different way. Things don’t just have to be done in person. , where we can do things in a more innovative way,” she said.
Dr. McKeon agreed that reimbursement issues have long impeded efforts to improve the inpatient to outpatient care transition. He added that it will be really important that adequate reimbursement of remote forms of care remain in place after COVID-19 fades.
“This is exactly the kind of thing that’s needed to improve care transitions,” according to Dr. McKeon.
*This story was updated 7/9/2020.
The care transition period between inpatient psychiatric hospitalization and initiation of outpatient mental health services is a time of extraordinarily heightened suicide risk that has been woefully neglected, according to speakers from the National Action Alliance for Suicide Prevention at the virtual annual meeting of the American Association of Suicidology.
This transition period traditionally has been a time when nobody really takes responsibility for patient care. In an effort to close this potentially deadly gap in services, the alliance recently has issued a report entitled, “Best Practices in Care Transitions for Individuals with Suicide Risk: Inpatient Care to Outpatient Care.” The recommendations focus on specific, innovative, evidence-based strategies that health care systems can use to prevent patients from falling through the cracks in care, mainly by implementing protocols aimed at fostering interorganizational teamwork between inpatient and outpatient behavioral health services.
“I believe that improving care transitions in the United States is the area where we can likely save the most lives. It’s within our grasp if we can just do this better,” declared Richard McKeon, PhD, MPH, chief of the Suicide Prevention Branch at the Center for Mental Health Services within SAMHSA, the Substance Abuse and Mental Health Services Administration.
He cited a recent meta-analysis that concluded that the risk of suicide during the first week post discharge after psychiatric hospitalization is a staggering 300 times greater than in the general population, while in the first month, the risk is increased 200-fold. The meta-analysis included 29 studies encompassing 3,551 suicides during the first month and 24 studies reporting 1,928 suicides during the first week post discharge (BMJ Open. 2019 Mar 23;9[3]:e023883. doi: 10.1136/bmjopen-2018-023883).
Everyone in the mental health field as well as patients and their families should know those statistics, but they don’t.
“I think it’s natural for people to think someone who’s been discharged from an inpatient unit or the emergency department is not at risk, when in reality it’s still a high-risk time. Suicide risk is not like a light switch that you can just switch off,” the clinical psychologist observed.
He cited other harrowing statistics that underscore the vast problem of poor care transitions. Nationally, fully one-third of patients don’t complete a single outpatient visit within the first 30 days after discharge from inpatient behavioral health care. And one in seven people who die by suicide have had contact with inpatient mental health services in the year before they died.
“That doesn’t mean that inpatient care did not do everything that they could do. What it does reflect is the need to make sure that there’s follow-up care after inpatient discharge. Too often, people don’t get the follow-up care that they need. And the research literature is clear that intervention can save lives,” Dr. McKeon said.
Panelist Becky Stoll, LCSW, vice president for crisis and disaster management at Centerstone Health in Nashville, Tenn., noted, “We see a lot of no-shows on the outpatient side, because nobody ever asked the patients if they can actually get to the outpatient appointment that’s been made.
“We have got to figure out this care transition and do better. The road to mental health is paved with Swiss cheese. There are so many holes to fall into, even if you know how to navigate the system – and most of the people we’re serving don’t know how,” observed Ms. Stoll, who, like Dr. McKeon, was among the coauthors of the alliance’s guidelines on best practices in care transitions. Ms. Stoll also serves on the AAS board as crisis services division chair.*
The National Action Alliance for Suicide Prevention is a public/private partnership whose goal is to advance the National Strategy for Suicide Prevention, which was developed by the alliance and the U.S. Surgeon General. The alliance includes mental health professionals as well as influential leaders from the military, journalism, entertainment, railroad, health insurance, law enforcement, defense, education, technology, and other industries.
Dr. McKeon and Ms. Stall were joined by Karen Johnson, MSW, another coauthor of the guidelines. They shared highlights of the report.
Inpatient provider strategies
Discharge and crisis safety planning should begin upon admission, according to Ms. Johnson, senior vice president for clinical services and division compliance at Universal Health Services, which owns and operates more than 200 behavioral health facilities across the United States.
Inpatient and outpatient care providers need to sit down and develop collaborative protocols and negotiate a memorandum of understanding regarding expectations, which absolutely must include procedures to ensure timely electronic delivery of medical records and other key documents to the outpatient care providers. The inpatient providers need to work collaboratively with the patient, family, and community support resources to develop a safety plan – including reduced access to lethal mean – as part of predischarge planning.
Among the strategies routinely employed on the inpatient side at Universal Health Services are advance scheduling of an initial outpatient appointment within 24-72 hours post discharge. Also, someone on the inpatient team is tasked with connecting with the outpatient provider prior to discharge to develop rapport.
“If our outpatient providers are located in our facility, as many of them are, we ask them to come in and attend inpatient team meetings to identify and meet with patients who are appropriate for continuing care in outpatient settings,” she explained. “A soft, warm handoff is critical.”
At these team meetings, the appropriateness of step-down care in the form of partial hospitalization or intensive outpatient care is weighed. Someone from the inpatient side is charged with maintaining contact with the patient until after the first outpatient appointment. Ongoing caring contact in the form of brief, encouraging postcards, emails, or texts that do not require a response from the patient should be maintained for several months.
Strategies for outpatient providers
Ms. Stoll is a big believer in the guideline-recommended practice of notifying the inpatient provider that the patient kept the outpatient appointment, along with having a system for red-flagging no-shows for prompt follow-up by a crisis management team.
She and her colleagues at Centerstone Health have conducted two studies of an intensive patient outreach program designed for the first 30 days of the care transition. The program included many elements of the alliance’s best practices guidelines. The yearlong first study, funded by Blue Cross/Blue Shield of Tennessee, documented zero suicides and 92% freedom from emergency department visits during the care transition period, along with greater than $400,000 savings in health care costs, compared with usual care. The second study, funded by SAMHSA, showed much the same over a 2-year period.
She emphasized that this was not a high-tech, intensive intervention. She characterized it, instead as “high-touch follow-up.
“It’s some staff and a phone and a laptop, nothing fancy, just a person who’s competent and confident and skilled with a laptop. With that, you can do some pretty amazing stuff: Get people what they need, keep them alive, and oh, guess what? You can also save a lot of health care dollars that can be put back into the system,” Ms. Stoll said.
She recognizes that it’s a lot to ask busy outpatient providers to leave their practice during the workday to participate in inpatient team meetings addressing discharge planning, as recommended in the alliance guidelines. But in this regard, she sees a silver lining to the COVID-19 pandemic, in that it forces health professionals to rely upon newly opened channels of telemedicine.
“COVID-19 is giving us an opportunity to do things in a different way. Things don’t just have to be done in person. , where we can do things in a more innovative way,” she said.
Dr. McKeon agreed that reimbursement issues have long impeded efforts to improve the inpatient to outpatient care transition. He added that it will be really important that adequate reimbursement of remote forms of care remain in place after COVID-19 fades.
“This is exactly the kind of thing that’s needed to improve care transitions,” according to Dr. McKeon.
*This story was updated 7/9/2020.
The care transition period between inpatient psychiatric hospitalization and initiation of outpatient mental health services is a time of extraordinarily heightened suicide risk that has been woefully neglected, according to speakers from the National Action Alliance for Suicide Prevention at the virtual annual meeting of the American Association of Suicidology.
This transition period traditionally has been a time when nobody really takes responsibility for patient care. In an effort to close this potentially deadly gap in services, the alliance recently has issued a report entitled, “Best Practices in Care Transitions for Individuals with Suicide Risk: Inpatient Care to Outpatient Care.” The recommendations focus on specific, innovative, evidence-based strategies that health care systems can use to prevent patients from falling through the cracks in care, mainly by implementing protocols aimed at fostering interorganizational teamwork between inpatient and outpatient behavioral health services.
“I believe that improving care transitions in the United States is the area where we can likely save the most lives. It’s within our grasp if we can just do this better,” declared Richard McKeon, PhD, MPH, chief of the Suicide Prevention Branch at the Center for Mental Health Services within SAMHSA, the Substance Abuse and Mental Health Services Administration.
He cited a recent meta-analysis that concluded that the risk of suicide during the first week post discharge after psychiatric hospitalization is a staggering 300 times greater than in the general population, while in the first month, the risk is increased 200-fold. The meta-analysis included 29 studies encompassing 3,551 suicides during the first month and 24 studies reporting 1,928 suicides during the first week post discharge (BMJ Open. 2019 Mar 23;9[3]:e023883. doi: 10.1136/bmjopen-2018-023883).
Everyone in the mental health field as well as patients and their families should know those statistics, but they don’t.
“I think it’s natural for people to think someone who’s been discharged from an inpatient unit or the emergency department is not at risk, when in reality it’s still a high-risk time. Suicide risk is not like a light switch that you can just switch off,” the clinical psychologist observed.
He cited other harrowing statistics that underscore the vast problem of poor care transitions. Nationally, fully one-third of patients don’t complete a single outpatient visit within the first 30 days after discharge from inpatient behavioral health care. And one in seven people who die by suicide have had contact with inpatient mental health services in the year before they died.
“That doesn’t mean that inpatient care did not do everything that they could do. What it does reflect is the need to make sure that there’s follow-up care after inpatient discharge. Too often, people don’t get the follow-up care that they need. And the research literature is clear that intervention can save lives,” Dr. McKeon said.
Panelist Becky Stoll, LCSW, vice president for crisis and disaster management at Centerstone Health in Nashville, Tenn., noted, “We see a lot of no-shows on the outpatient side, because nobody ever asked the patients if they can actually get to the outpatient appointment that’s been made.
“We have got to figure out this care transition and do better. The road to mental health is paved with Swiss cheese. There are so many holes to fall into, even if you know how to navigate the system – and most of the people we’re serving don’t know how,” observed Ms. Stoll, who, like Dr. McKeon, was among the coauthors of the alliance’s guidelines on best practices in care transitions. Ms. Stoll also serves on the AAS board as crisis services division chair.*
The National Action Alliance for Suicide Prevention is a public/private partnership whose goal is to advance the National Strategy for Suicide Prevention, which was developed by the alliance and the U.S. Surgeon General. The alliance includes mental health professionals as well as influential leaders from the military, journalism, entertainment, railroad, health insurance, law enforcement, defense, education, technology, and other industries.
Dr. McKeon and Ms. Stall were joined by Karen Johnson, MSW, another coauthor of the guidelines. They shared highlights of the report.
Inpatient provider strategies
Discharge and crisis safety planning should begin upon admission, according to Ms. Johnson, senior vice president for clinical services and division compliance at Universal Health Services, which owns and operates more than 200 behavioral health facilities across the United States.
Inpatient and outpatient care providers need to sit down and develop collaborative protocols and negotiate a memorandum of understanding regarding expectations, which absolutely must include procedures to ensure timely electronic delivery of medical records and other key documents to the outpatient care providers. The inpatient providers need to work collaboratively with the patient, family, and community support resources to develop a safety plan – including reduced access to lethal mean – as part of predischarge planning.
Among the strategies routinely employed on the inpatient side at Universal Health Services are advance scheduling of an initial outpatient appointment within 24-72 hours post discharge. Also, someone on the inpatient team is tasked with connecting with the outpatient provider prior to discharge to develop rapport.
“If our outpatient providers are located in our facility, as many of them are, we ask them to come in and attend inpatient team meetings to identify and meet with patients who are appropriate for continuing care in outpatient settings,” she explained. “A soft, warm handoff is critical.”
At these team meetings, the appropriateness of step-down care in the form of partial hospitalization or intensive outpatient care is weighed. Someone from the inpatient side is charged with maintaining contact with the patient until after the first outpatient appointment. Ongoing caring contact in the form of brief, encouraging postcards, emails, or texts that do not require a response from the patient should be maintained for several months.
Strategies for outpatient providers
Ms. Stoll is a big believer in the guideline-recommended practice of notifying the inpatient provider that the patient kept the outpatient appointment, along with having a system for red-flagging no-shows for prompt follow-up by a crisis management team.
She and her colleagues at Centerstone Health have conducted two studies of an intensive patient outreach program designed for the first 30 days of the care transition. The program included many elements of the alliance’s best practices guidelines. The yearlong first study, funded by Blue Cross/Blue Shield of Tennessee, documented zero suicides and 92% freedom from emergency department visits during the care transition period, along with greater than $400,000 savings in health care costs, compared with usual care. The second study, funded by SAMHSA, showed much the same over a 2-year period.
She emphasized that this was not a high-tech, intensive intervention. She characterized it, instead as “high-touch follow-up.
“It’s some staff and a phone and a laptop, nothing fancy, just a person who’s competent and confident and skilled with a laptop. With that, you can do some pretty amazing stuff: Get people what they need, keep them alive, and oh, guess what? You can also save a lot of health care dollars that can be put back into the system,” Ms. Stoll said.
She recognizes that it’s a lot to ask busy outpatient providers to leave their practice during the workday to participate in inpatient team meetings addressing discharge planning, as recommended in the alliance guidelines. But in this regard, she sees a silver lining to the COVID-19 pandemic, in that it forces health professionals to rely upon newly opened channels of telemedicine.
“COVID-19 is giving us an opportunity to do things in a different way. Things don’t just have to be done in person. , where we can do things in a more innovative way,” she said.
Dr. McKeon agreed that reimbursement issues have long impeded efforts to improve the inpatient to outpatient care transition. He added that it will be really important that adequate reimbursement of remote forms of care remain in place after COVID-19 fades.
“This is exactly the kind of thing that’s needed to improve care transitions,” according to Dr. McKeon.
*This story was updated 7/9/2020.
FROM AAS20
Amid pandemic, Virginia hospital’s opioid overdoses up nearly 10-fold
Opioid overdoses have shot up by almost 10-fold at a Virginia ED since March, a new report finds. The report provides more evidence that the coronavirus pandemic is sparking a severe medical crisis among illicit drug users.
“Health care providers should closely monitor the number of overdoses coming into their hospitals and in the surrounding community during this time,” study lead author and postdoctoral research fellow Taylor Ochalek, PhD, said in an interview. “If they do notice an increasing trend of overdoses, they should spread awareness in the community to the general public, and offer resources and information for those that may be seeking help and/or may be at a high risk of overdosing.”
Dr. Ochalek presented the study findings at the virtual annual meeting of the College on Problems of Drug Dependence.
According to the report, opioid overdoses at the VCU Medical Center in Richmond, Va., grew from an average of six a month from February to December 2019 to 50, 57, and 63 in March, April, and May 2020. Of the 171 cases in the later time frame, the average age was 44 years, 72% were male, and 82% were African American.
“The steep increase in overdoses began primarily in March,” said Dr. Ochalek, of Virginia Commonwealth University in Richmond. “This timing coincides with the Virginia governor’s state of emergency declaration, stay-at-home order, and closure of nonessential businesses order.”
The researchers did not provide details about the types of opioids used, the patient outcomes, or whether the patients tested positive for COVID-19. It’s unclear whether the pandemic directly spawned a higher number of overdoses, but there are growing signs of a stark nationwide trend.
“Nationwide, federal and local officials are reporting alarming spikes in drug overdoses – a hidden epidemic within the coronavirus pandemic,” the Washington Post reported on July 1, pointing to increases in Kentucky, Virginia, and the Chicago area.
Meanwhile, the federal Overdose Detection Mapping Application Program, which tracks overdoses nationwide, issued 191% more “spike alerts” in January to April 2020 than in the same time period in 2019. However, the spike alerts began to increase in January, weeks before the pandemic began to take hold.
The findings are consistent with trends in Houston, where overdose calls were up 31% in the first 3 months of 2020, compared with 2019, said psychologist James Bray, PhD, of the University of Texas, San Antonio, in an interview. More recent data suggest that the numbers are rising even higher, said Dr. Bray, who works with Houston first responders and has analyzed data.
Dr. Bray said.
Another potential factor is the disruption in the illicit drug supply chain because of limits on crossings at the southern border, said ED physician Scott Weiner, MD, MPH, of Brigham and Women’s Hospital and Harvard Medical School, both in Boston. “As a result, opioids of extremely variable potency have infiltrated markets, and people using drugs may not be used to the new doses, especially if they are high-potency fentanyl analogues.”
Moving forward, Dr. Bray said, “people need continued access to treatment. Telehealth and other virtual services need to be provided so that people can continue to have access to treatment even during the pandemic.”
Dr. Weiner also emphasized the importance of treatment for patients who overdose on opioids. “In my previous work, we discovered that about 1 in 20 patients who are treated in an emergency department and survive would die within 1 year. That number will likely increase drastically during COVID,” he said. “When a patient presents after overdose, we must intervene aggressively with buprenorphine and other harm-reduction techniques to save these lives.”
The study was funded by the National Institutes of Health. Dr. Ochalek, Dr. Weiner, and Dr. Bray reported no relevant disclosures.
Opioid overdoses have shot up by almost 10-fold at a Virginia ED since March, a new report finds. The report provides more evidence that the coronavirus pandemic is sparking a severe medical crisis among illicit drug users.
“Health care providers should closely monitor the number of overdoses coming into their hospitals and in the surrounding community during this time,” study lead author and postdoctoral research fellow Taylor Ochalek, PhD, said in an interview. “If they do notice an increasing trend of overdoses, they should spread awareness in the community to the general public, and offer resources and information for those that may be seeking help and/or may be at a high risk of overdosing.”
Dr. Ochalek presented the study findings at the virtual annual meeting of the College on Problems of Drug Dependence.
According to the report, opioid overdoses at the VCU Medical Center in Richmond, Va., grew from an average of six a month from February to December 2019 to 50, 57, and 63 in March, April, and May 2020. Of the 171 cases in the later time frame, the average age was 44 years, 72% were male, and 82% were African American.
“The steep increase in overdoses began primarily in March,” said Dr. Ochalek, of Virginia Commonwealth University in Richmond. “This timing coincides with the Virginia governor’s state of emergency declaration, stay-at-home order, and closure of nonessential businesses order.”
The researchers did not provide details about the types of opioids used, the patient outcomes, or whether the patients tested positive for COVID-19. It’s unclear whether the pandemic directly spawned a higher number of overdoses, but there are growing signs of a stark nationwide trend.
“Nationwide, federal and local officials are reporting alarming spikes in drug overdoses – a hidden epidemic within the coronavirus pandemic,” the Washington Post reported on July 1, pointing to increases in Kentucky, Virginia, and the Chicago area.
Meanwhile, the federal Overdose Detection Mapping Application Program, which tracks overdoses nationwide, issued 191% more “spike alerts” in January to April 2020 than in the same time period in 2019. However, the spike alerts began to increase in January, weeks before the pandemic began to take hold.
The findings are consistent with trends in Houston, where overdose calls were up 31% in the first 3 months of 2020, compared with 2019, said psychologist James Bray, PhD, of the University of Texas, San Antonio, in an interview. More recent data suggest that the numbers are rising even higher, said Dr. Bray, who works with Houston first responders and has analyzed data.
Dr. Bray said.
Another potential factor is the disruption in the illicit drug supply chain because of limits on crossings at the southern border, said ED physician Scott Weiner, MD, MPH, of Brigham and Women’s Hospital and Harvard Medical School, both in Boston. “As a result, opioids of extremely variable potency have infiltrated markets, and people using drugs may not be used to the new doses, especially if they are high-potency fentanyl analogues.”
Moving forward, Dr. Bray said, “people need continued access to treatment. Telehealth and other virtual services need to be provided so that people can continue to have access to treatment even during the pandemic.”
Dr. Weiner also emphasized the importance of treatment for patients who overdose on opioids. “In my previous work, we discovered that about 1 in 20 patients who are treated in an emergency department and survive would die within 1 year. That number will likely increase drastically during COVID,” he said. “When a patient presents after overdose, we must intervene aggressively with buprenorphine and other harm-reduction techniques to save these lives.”
The study was funded by the National Institutes of Health. Dr. Ochalek, Dr. Weiner, and Dr. Bray reported no relevant disclosures.
Opioid overdoses have shot up by almost 10-fold at a Virginia ED since March, a new report finds. The report provides more evidence that the coronavirus pandemic is sparking a severe medical crisis among illicit drug users.
“Health care providers should closely monitor the number of overdoses coming into their hospitals and in the surrounding community during this time,” study lead author and postdoctoral research fellow Taylor Ochalek, PhD, said in an interview. “If they do notice an increasing trend of overdoses, they should spread awareness in the community to the general public, and offer resources and information for those that may be seeking help and/or may be at a high risk of overdosing.”
Dr. Ochalek presented the study findings at the virtual annual meeting of the College on Problems of Drug Dependence.
According to the report, opioid overdoses at the VCU Medical Center in Richmond, Va., grew from an average of six a month from February to December 2019 to 50, 57, and 63 in March, April, and May 2020. Of the 171 cases in the later time frame, the average age was 44 years, 72% were male, and 82% were African American.
“The steep increase in overdoses began primarily in March,” said Dr. Ochalek, of Virginia Commonwealth University in Richmond. “This timing coincides with the Virginia governor’s state of emergency declaration, stay-at-home order, and closure of nonessential businesses order.”
The researchers did not provide details about the types of opioids used, the patient outcomes, or whether the patients tested positive for COVID-19. It’s unclear whether the pandemic directly spawned a higher number of overdoses, but there are growing signs of a stark nationwide trend.
“Nationwide, federal and local officials are reporting alarming spikes in drug overdoses – a hidden epidemic within the coronavirus pandemic,” the Washington Post reported on July 1, pointing to increases in Kentucky, Virginia, and the Chicago area.
Meanwhile, the federal Overdose Detection Mapping Application Program, which tracks overdoses nationwide, issued 191% more “spike alerts” in January to April 2020 than in the same time period in 2019. However, the spike alerts began to increase in January, weeks before the pandemic began to take hold.
The findings are consistent with trends in Houston, where overdose calls were up 31% in the first 3 months of 2020, compared with 2019, said psychologist James Bray, PhD, of the University of Texas, San Antonio, in an interview. More recent data suggest that the numbers are rising even higher, said Dr. Bray, who works with Houston first responders and has analyzed data.
Dr. Bray said.
Another potential factor is the disruption in the illicit drug supply chain because of limits on crossings at the southern border, said ED physician Scott Weiner, MD, MPH, of Brigham and Women’s Hospital and Harvard Medical School, both in Boston. “As a result, opioids of extremely variable potency have infiltrated markets, and people using drugs may not be used to the new doses, especially if they are high-potency fentanyl analogues.”
Moving forward, Dr. Bray said, “people need continued access to treatment. Telehealth and other virtual services need to be provided so that people can continue to have access to treatment even during the pandemic.”
Dr. Weiner also emphasized the importance of treatment for patients who overdose on opioids. “In my previous work, we discovered that about 1 in 20 patients who are treated in an emergency department and survive would die within 1 year. That number will likely increase drastically during COVID,” he said. “When a patient presents after overdose, we must intervene aggressively with buprenorphine and other harm-reduction techniques to save these lives.”
The study was funded by the National Institutes of Health. Dr. Ochalek, Dr. Weiner, and Dr. Bray reported no relevant disclosures.
FROM CPDD 2020
Use of nonopioid pain meds is on the rise
Opioid and nonopioid prescription pain medications have taken different journeys since 2009, but they ended up in the same place in 2018, according to a recent report from the National Center for Health Statistics.
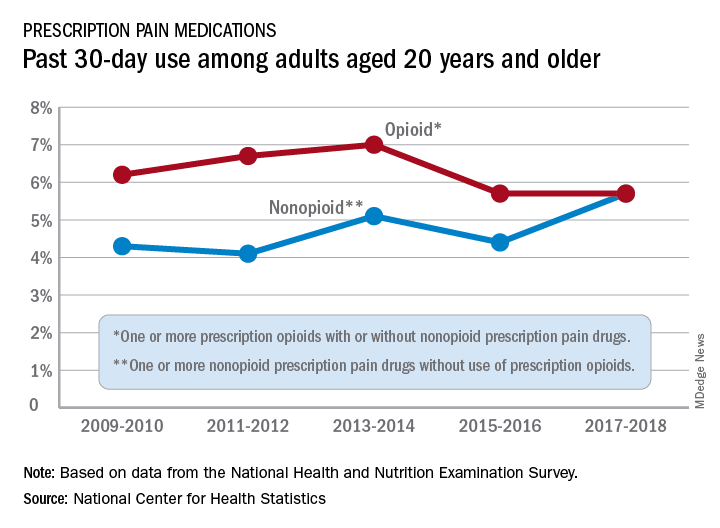
At least by one measure, anyway. Survey data from 2009 to 2010 show that 6.2% of adults aged 20 years and older had taken at least one prescription opioid in the last 30 days and 4.3% had used a prescription nonopioid without an opioid. By 2017-2018, past 30-day use of both drug groups was 5.7%, Craig M. Hales, MD, and associates said in an NCHS data brief.
“Opioids may be prescribed together with nonopioid pain medications, [but] nonpharmacologic and nonopioid-containing pharmacologic therapies are preferred for management of chronic pain,” the NCHS researchers noted.
as did the short-term increase in nonopioids from 2015-2016 to 2017-2018, but the 10-year trend for opioids was not significant, based on data from the National Health and Nutrition Examination Survey.
Much of the analysis focused on 2015-2018, when 30-day use of any prescription pain medication was reported by 10.7% of adults aged 20 years and older, with use of opioids at 5.7% and nonopioids at 5.0%. For women, use of any pain drug was 12.6% (6.4% opioid, 6.2% nonopioid) from 2015 to 2018, compared with 8.7% for men (4.9%, 3.8%), Dr. Hales and associates reported.
Past 30-day use of both opioids and nonopioids over those 4 years was highest for non-Hispanic whites and lowest, by a significant margin for both drug groups, among non-Hispanic Asian adults, a pattern that held for both men and women, they said.
Opioid and nonopioid prescription pain medications have taken different journeys since 2009, but they ended up in the same place in 2018, according to a recent report from the National Center for Health Statistics.
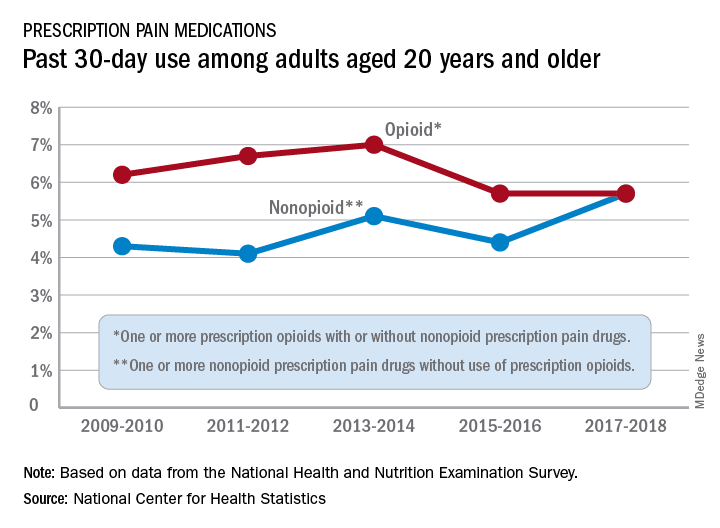
At least by one measure, anyway. Survey data from 2009 to 2010 show that 6.2% of adults aged 20 years and older had taken at least one prescription opioid in the last 30 days and 4.3% had used a prescription nonopioid without an opioid. By 2017-2018, past 30-day use of both drug groups was 5.7%, Craig M. Hales, MD, and associates said in an NCHS data brief.
“Opioids may be prescribed together with nonopioid pain medications, [but] nonpharmacologic and nonopioid-containing pharmacologic therapies are preferred for management of chronic pain,” the NCHS researchers noted.
as did the short-term increase in nonopioids from 2015-2016 to 2017-2018, but the 10-year trend for opioids was not significant, based on data from the National Health and Nutrition Examination Survey.
Much of the analysis focused on 2015-2018, when 30-day use of any prescription pain medication was reported by 10.7% of adults aged 20 years and older, with use of opioids at 5.7% and nonopioids at 5.0%. For women, use of any pain drug was 12.6% (6.4% opioid, 6.2% nonopioid) from 2015 to 2018, compared with 8.7% for men (4.9%, 3.8%), Dr. Hales and associates reported.
Past 30-day use of both opioids and nonopioids over those 4 years was highest for non-Hispanic whites and lowest, by a significant margin for both drug groups, among non-Hispanic Asian adults, a pattern that held for both men and women, they said.
Opioid and nonopioid prescription pain medications have taken different journeys since 2009, but they ended up in the same place in 2018, according to a recent report from the National Center for Health Statistics.
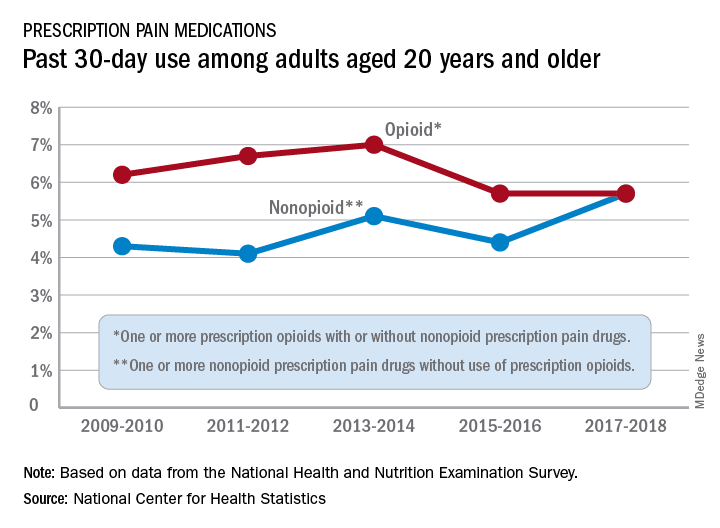
At least by one measure, anyway. Survey data from 2009 to 2010 show that 6.2% of adults aged 20 years and older had taken at least one prescription opioid in the last 30 days and 4.3% had used a prescription nonopioid without an opioid. By 2017-2018, past 30-day use of both drug groups was 5.7%, Craig M. Hales, MD, and associates said in an NCHS data brief.
“Opioids may be prescribed together with nonopioid pain medications, [but] nonpharmacologic and nonopioid-containing pharmacologic therapies are preferred for management of chronic pain,” the NCHS researchers noted.
as did the short-term increase in nonopioids from 2015-2016 to 2017-2018, but the 10-year trend for opioids was not significant, based on data from the National Health and Nutrition Examination Survey.
Much of the analysis focused on 2015-2018, when 30-day use of any prescription pain medication was reported by 10.7% of adults aged 20 years and older, with use of opioids at 5.7% and nonopioids at 5.0%. For women, use of any pain drug was 12.6% (6.4% opioid, 6.2% nonopioid) from 2015 to 2018, compared with 8.7% for men (4.9%, 3.8%), Dr. Hales and associates reported.
Past 30-day use of both opioids and nonopioids over those 4 years was highest for non-Hispanic whites and lowest, by a significant margin for both drug groups, among non-Hispanic Asian adults, a pattern that held for both men and women, they said.