User login
Clinical Psychiatry News is the online destination and multimedia properties of Clinica Psychiatry News, the independent news publication for psychiatrists. Since 1971, Clinical Psychiatry News has been the leading source of news and commentary about clinical developments in psychiatry as well as health care policy and regulations that affect the physician's practice.
Dear Drupal User: You're seeing this because you're logged in to Drupal, and not redirected to MDedge.com/psychiatry.
Depression
adolescent depression
adolescent major depressive disorder
adolescent schizophrenia
adolescent with major depressive disorder
animals
autism
baby
brexpiprazole
child
child bipolar
child depression
child schizophrenia
children with bipolar disorder
children with depression
children with major depressive disorder
compulsive behaviors
cure
elderly bipolar
elderly depression
elderly major depressive disorder
elderly schizophrenia
elderly with dementia
first break
first episode
gambling
gaming
geriatric depression
geriatric major depressive disorder
geriatric schizophrenia
infant
ketamine
kid
major depressive disorder
major depressive disorder in adolescents
major depressive disorder in children
parenting
pediatric
pediatric bipolar
pediatric depression
pediatric major depressive disorder
pediatric schizophrenia
pregnancy
pregnant
rexulti
skin care
suicide
teen
wine
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-cpn')]
div[contains(@class, 'pane-pub-home-cpn')]
div[contains(@class, 'pane-pub-topic-cpn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
Antidepressants may scupper efficacy of MDMA for PTSD
Pooled data from four phase 2 trials reveal that patients with recent SSRI exposure were significantly more likely to continue to meet PTSD diagnostic criteria after methylenedioxymethamphetamine (MDMA)-assisted psychotherapy than their peers who had not recently taken SSRIs.
Although preliminary, the findings have implications for clinical practice if MDMA-assisted psychotherapy is approved by the Food and Drug Administration, Allison Feduccia, PhD, study coauthor and founder of the education platform Psychedelic.Support, said in an interview.
“As psychedelic medicines become available, it’s going to be important that we try to understand what factors impact the response rate and if there are ways that we can improve the treatment outcomes. Allowing for a longer period for tapering completely off SSRIs before initiating MDMA sessions might increase the effectiveness of MDMA,” Dr. Feduccia said.
The study was published online Nov. 20, 2020, in Psychopharmacology (doi: 10.1007/s00213-020-05710-w).
Reduced response
The primary mechanism of action of MDMA involves the same reuptake transporters that are targeted by antidepressant medications commonly prescribed for PTSD. These medications include SSRIs, serotonin-norepinephrine reuptake inhibitors (SNRIs), NRIs, and norepinephrine-dopamine reuptake inhibitors (NDRIs).
Prior research shows that, when MDMA is coadministered with a reuptake inhibitor, subjective and psychological effects of the therapy are attenuated.
The researchers sought to determine whether or not recent tapering off of an antidepressant that targets the same primary binding sites as MDMA would affect treatment response. They analyzed data on 50 adults who underwent two sessions of MDMA-assisted psychotherapy in phase 2 clinical trials.
For 16 of these patients, SSRI therapy was tapered off prior to the MDMA sessions. For 34 patients, SSRI therapy was not tapered off, because the patients had not been taking the medication at the time of initial study screening (nontaper group).
The taper protocols specified that medications be tapered gradually over a period of weeks to minimize withdrawal symptoms and for them to be discontinued at least five half-lives of each drug prior to MDMA administration.
Demographics, baseline PTSD, and depression severity were similar between the taper and the nontaper groups. Participants in the studies had chronic PTSD (symptoms lasting >6 months). Severity scores on the Clinician-Administered PTSD Scale for DSM IV (CAPS-IV) were at least 50.
After MDMA-assisted psychotherapy, the nontaper group had significantly lower (better) CAPS-IV total scores, compared with the taper group (mean, 45.7 vs. 70.3; P = .009).
About two-thirds (63.6%) of the nontaper group no longer met PTSD criteria after MDMA-assisted therapy, compared with only 25% of those in the taper group.
The nontaper group also had lower depression symptom severity scores on the Beck Depression Inventory–II, compared with the taper group (mean, 12.7 vs. 22.6; P = .010).
“Another really interesting” observation, said Dr. Feduccia, is that the expected increases in systolic and diastolic blood pressure following MDMA administration were reduced in the taper group, compared with the nontaper group.
“This suggests that MDMA didn’t have the same physiological response in individuals who tapered SSRIs. This should be followed up,” she said.
The investigators offerred several potential mechanisms for the negative effect of recent SSRI use on MDMA-assisted psychotherapy for PTSD.
These include the down-regulation of binding sites (serotonin, dopamine, and/or norepinephrine) related to SSRI use, reduced MDMA treatment-relevant increases in blood pressure in patients with recent SSRI use, and the possibility that withdrawal symptoms from SSRIs may reduce the effectiveness of MDMA psychotherapy.
Important clinical implications
In a comment, Steven R. Thorp, PhD, professor at Alliant International University, San Diego, said the findings are “very interesting” and likely “not well known.”
“There has been great interest in MDMA-assisted psychotherapy in recent years, and if this finding is replicated, it will have important implications for that research,” Dr. Thorp said.
“Although psychotherapy is often preferred by clients with PTSD, compared to medications, and typically shows efficacy that is as strong or stronger (and longer lasting) than medications, many individuals with PTSD are provided with medication only,” Dr. Thorp noted.
“This study suggests that, in addition to the other potential disadvantages of medications (e.g., cost, side effects, potential for addiction), those who take SSRIs, SNRIs, NRIs, and NDRIs for PTSD may also benefit less from MDMA-assisted psychotherapy,” Dr. Thorp added.
The four phase 2 studies used in the analysis were sponsored by the Multidisciplinary Association for Psychedelic Studies, a nonprofit organization. Dr. Feduccia received salary support for full-time employment with MAPS Public Benefit Corporation. Dr. Thorp disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pooled data from four phase 2 trials reveal that patients with recent SSRI exposure were significantly more likely to continue to meet PTSD diagnostic criteria after methylenedioxymethamphetamine (MDMA)-assisted psychotherapy than their peers who had not recently taken SSRIs.
Although preliminary, the findings have implications for clinical practice if MDMA-assisted psychotherapy is approved by the Food and Drug Administration, Allison Feduccia, PhD, study coauthor and founder of the education platform Psychedelic.Support, said in an interview.
“As psychedelic medicines become available, it’s going to be important that we try to understand what factors impact the response rate and if there are ways that we can improve the treatment outcomes. Allowing for a longer period for tapering completely off SSRIs before initiating MDMA sessions might increase the effectiveness of MDMA,” Dr. Feduccia said.
The study was published online Nov. 20, 2020, in Psychopharmacology (doi: 10.1007/s00213-020-05710-w).
Reduced response
The primary mechanism of action of MDMA involves the same reuptake transporters that are targeted by antidepressant medications commonly prescribed for PTSD. These medications include SSRIs, serotonin-norepinephrine reuptake inhibitors (SNRIs), NRIs, and norepinephrine-dopamine reuptake inhibitors (NDRIs).
Prior research shows that, when MDMA is coadministered with a reuptake inhibitor, subjective and psychological effects of the therapy are attenuated.
The researchers sought to determine whether or not recent tapering off of an antidepressant that targets the same primary binding sites as MDMA would affect treatment response. They analyzed data on 50 adults who underwent two sessions of MDMA-assisted psychotherapy in phase 2 clinical trials.
For 16 of these patients, SSRI therapy was tapered off prior to the MDMA sessions. For 34 patients, SSRI therapy was not tapered off, because the patients had not been taking the medication at the time of initial study screening (nontaper group).
The taper protocols specified that medications be tapered gradually over a period of weeks to minimize withdrawal symptoms and for them to be discontinued at least five half-lives of each drug prior to MDMA administration.
Demographics, baseline PTSD, and depression severity were similar between the taper and the nontaper groups. Participants in the studies had chronic PTSD (symptoms lasting >6 months). Severity scores on the Clinician-Administered PTSD Scale for DSM IV (CAPS-IV) were at least 50.
After MDMA-assisted psychotherapy, the nontaper group had significantly lower (better) CAPS-IV total scores, compared with the taper group (mean, 45.7 vs. 70.3; P = .009).
About two-thirds (63.6%) of the nontaper group no longer met PTSD criteria after MDMA-assisted therapy, compared with only 25% of those in the taper group.
The nontaper group also had lower depression symptom severity scores on the Beck Depression Inventory–II, compared with the taper group (mean, 12.7 vs. 22.6; P = .010).
“Another really interesting” observation, said Dr. Feduccia, is that the expected increases in systolic and diastolic blood pressure following MDMA administration were reduced in the taper group, compared with the nontaper group.
“This suggests that MDMA didn’t have the same physiological response in individuals who tapered SSRIs. This should be followed up,” she said.
The investigators offerred several potential mechanisms for the negative effect of recent SSRI use on MDMA-assisted psychotherapy for PTSD.
These include the down-regulation of binding sites (serotonin, dopamine, and/or norepinephrine) related to SSRI use, reduced MDMA treatment-relevant increases in blood pressure in patients with recent SSRI use, and the possibility that withdrawal symptoms from SSRIs may reduce the effectiveness of MDMA psychotherapy.
Important clinical implications
In a comment, Steven R. Thorp, PhD, professor at Alliant International University, San Diego, said the findings are “very interesting” and likely “not well known.”
“There has been great interest in MDMA-assisted psychotherapy in recent years, and if this finding is replicated, it will have important implications for that research,” Dr. Thorp said.
“Although psychotherapy is often preferred by clients with PTSD, compared to medications, and typically shows efficacy that is as strong or stronger (and longer lasting) than medications, many individuals with PTSD are provided with medication only,” Dr. Thorp noted.
“This study suggests that, in addition to the other potential disadvantages of medications (e.g., cost, side effects, potential for addiction), those who take SSRIs, SNRIs, NRIs, and NDRIs for PTSD may also benefit less from MDMA-assisted psychotherapy,” Dr. Thorp added.
The four phase 2 studies used in the analysis were sponsored by the Multidisciplinary Association for Psychedelic Studies, a nonprofit organization. Dr. Feduccia received salary support for full-time employment with MAPS Public Benefit Corporation. Dr. Thorp disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Pooled data from four phase 2 trials reveal that patients with recent SSRI exposure were significantly more likely to continue to meet PTSD diagnostic criteria after methylenedioxymethamphetamine (MDMA)-assisted psychotherapy than their peers who had not recently taken SSRIs.
Although preliminary, the findings have implications for clinical practice if MDMA-assisted psychotherapy is approved by the Food and Drug Administration, Allison Feduccia, PhD, study coauthor and founder of the education platform Psychedelic.Support, said in an interview.
“As psychedelic medicines become available, it’s going to be important that we try to understand what factors impact the response rate and if there are ways that we can improve the treatment outcomes. Allowing for a longer period for tapering completely off SSRIs before initiating MDMA sessions might increase the effectiveness of MDMA,” Dr. Feduccia said.
The study was published online Nov. 20, 2020, in Psychopharmacology (doi: 10.1007/s00213-020-05710-w).
Reduced response
The primary mechanism of action of MDMA involves the same reuptake transporters that are targeted by antidepressant medications commonly prescribed for PTSD. These medications include SSRIs, serotonin-norepinephrine reuptake inhibitors (SNRIs), NRIs, and norepinephrine-dopamine reuptake inhibitors (NDRIs).
Prior research shows that, when MDMA is coadministered with a reuptake inhibitor, subjective and psychological effects of the therapy are attenuated.
The researchers sought to determine whether or not recent tapering off of an antidepressant that targets the same primary binding sites as MDMA would affect treatment response. They analyzed data on 50 adults who underwent two sessions of MDMA-assisted psychotherapy in phase 2 clinical trials.
For 16 of these patients, SSRI therapy was tapered off prior to the MDMA sessions. For 34 patients, SSRI therapy was not tapered off, because the patients had not been taking the medication at the time of initial study screening (nontaper group).
The taper protocols specified that medications be tapered gradually over a period of weeks to minimize withdrawal symptoms and for them to be discontinued at least five half-lives of each drug prior to MDMA administration.
Demographics, baseline PTSD, and depression severity were similar between the taper and the nontaper groups. Participants in the studies had chronic PTSD (symptoms lasting >6 months). Severity scores on the Clinician-Administered PTSD Scale for DSM IV (CAPS-IV) were at least 50.
After MDMA-assisted psychotherapy, the nontaper group had significantly lower (better) CAPS-IV total scores, compared with the taper group (mean, 45.7 vs. 70.3; P = .009).
About two-thirds (63.6%) of the nontaper group no longer met PTSD criteria after MDMA-assisted therapy, compared with only 25% of those in the taper group.
The nontaper group also had lower depression symptom severity scores on the Beck Depression Inventory–II, compared with the taper group (mean, 12.7 vs. 22.6; P = .010).
“Another really interesting” observation, said Dr. Feduccia, is that the expected increases in systolic and diastolic blood pressure following MDMA administration were reduced in the taper group, compared with the nontaper group.
“This suggests that MDMA didn’t have the same physiological response in individuals who tapered SSRIs. This should be followed up,” she said.
The investigators offerred several potential mechanisms for the negative effect of recent SSRI use on MDMA-assisted psychotherapy for PTSD.
These include the down-regulation of binding sites (serotonin, dopamine, and/or norepinephrine) related to SSRI use, reduced MDMA treatment-relevant increases in blood pressure in patients with recent SSRI use, and the possibility that withdrawal symptoms from SSRIs may reduce the effectiveness of MDMA psychotherapy.
Important clinical implications
In a comment, Steven R. Thorp, PhD, professor at Alliant International University, San Diego, said the findings are “very interesting” and likely “not well known.”
“There has been great interest in MDMA-assisted psychotherapy in recent years, and if this finding is replicated, it will have important implications for that research,” Dr. Thorp said.
“Although psychotherapy is often preferred by clients with PTSD, compared to medications, and typically shows efficacy that is as strong or stronger (and longer lasting) than medications, many individuals with PTSD are provided with medication only,” Dr. Thorp noted.
“This study suggests that, in addition to the other potential disadvantages of medications (e.g., cost, side effects, potential for addiction), those who take SSRIs, SNRIs, NRIs, and NDRIs for PTSD may also benefit less from MDMA-assisted psychotherapy,” Dr. Thorp added.
The four phase 2 studies used in the analysis were sponsored by the Multidisciplinary Association for Psychedelic Studies, a nonprofit organization. Dr. Feduccia received salary support for full-time employment with MAPS Public Benefit Corporation. Dr. Thorp disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Clozapine still underused in refractory schizophrenia
With the exception of clozapine, the selection of an antipsychotic medication for acute treatment is driven by side effects.
That’s a key pearl of wisdom that Stephen R. Marder, MD, shared during a discussion of key criteria for choosing an antipsychotic for patients with schizophrenia.
“It’s a decision that can have huge consequences, both to an individual’s mental health and their physical health,” Dr. Marder said during an annual psychopharmacology update held by the Nevada Psychiatric Association. “If a patient did well and liked a prior antipsychotic, that’s usually evidence that they’ll respond again. That’s been shown numerous times. Aside from that, the largest consideration is usually adverse effects.”
In a multiple-treatments meta-analysis that compared the efficacy and tolerability of 15 antipsychotic drugs in schizophrenia, researchers found that an overall positive change in symptoms occurred with clozapine, compared with any other drug.
“Clozapine is not just the most effective antipsychotic for patients who are treatment resistant; it’s also the most effective antipsychotic in general populations,” said Dr. Marder, the Daniel X. Freedman Professor of Psychiatry at the Semel Institute for Neuroscience and Human Behavior at the University of California, Los Angeles. “The next most effective antipsychotic is amisulpride, which is not available in the U.S., although there’s a company that’s developing a formulation of amisulpride. After that, the 95% confidence intervals overlap, and the differences are probably related not to their true effectiveness but to other circumstances.”
For example, he continued, risperidone and olanzapine were developed in the 1990s. They were always compared with haloperidol and they tended to work a little bit better. “The drugs developed later on in clinical trials tended to be used in patients who were more treatment resistant,” he said. “Aside from clozapine, the differences in effectiveness are relatively small. But the differences in side effects are large.”
The meta-analysis found that haloperidol stood out as the antipsychotic most likely to cause extrapyramidal side effects. Olanzapine and clozapine stood out as causing the most weight gain, while ziprasidone and lurasidone were less likely to cause weight gain. In addition, risperidone, paliperidone, and haloperidol tended to cause the greatest elevation of prolactin levels, while aripiprazole was found to reduce prolactin levels.
“This becomes an important issue, particularly in young people when one is worried about galactorrhea in women or gynecomastia in men, which sometimes happens with risperidone or haloperidol, and to a lesser extent, sexual dysfunction,” said Dr. Marder, who is also director of the VISN 22 Mental Illness Research, Education, and Clinical Center for the Department of Veterans Affairs. “Sedation is a major consideration for clozapine and chlorpromazine, but less for other antipsychotics.”
When do you know if you’ve selected the right medication for your patient? According to a meta-analysis of 42 studies involving 7,450 patients, improvement tends to occur within the first 2 weeks of treatment. “Which means Dr. Marder said. “This has been consequential because it provides guidance for clinicians to make decisions.”
Symptoms that are likely to improve in the first couple of days include agitation and psychomotor excitement. Improvement in psychotic symptoms typically occurs in the following order: those with thought disorder symptoms tend to develop more organized thinking, those with hallucinations tend to experience a decrease the intensity and frequency of their episodes, and those with well-ingrained delusions “tend to experience fewer misinterpretations,” Dr. Marder said. “They may feel less suspicious and they may talk less about delusions.”
Dr. Marder makes it a point to evaluate the antipsychotic response of patients in 2-3 weeks. “If it’s a partial response, continue a bit longer,” he advised. “It it’s no response, switch. And, of course, if the drug isn’t tolerated well, switch.”
He advised against thinking that patients can easily be categorized as being strong responders or nonresponders. Instead, he favors viewing responsiveness to an antipsychotic along a continuum. “Ten to fifteen percent of patients will fail to remit even at first exposure to an antipsychotic medication, but it’s more common that patients will be partial responders,” Dr. Marder said. “One will have to determine whether that response is adequate or not. There’s also the idea that patients sometimes respond vigorously to an antipsychotic early on. For example, first-episode patients tend to respond very well, and they respond at substantially lower doses. But I set a high criteria that we really want patients on an antipsychotic to respond well, to being in a remission that they can live with, not just to be partially remitted.”
In an analysis of response rates, 244 patients with first-episode schizophrenia moved through two antipsychotic trials, followed by a trial with clozapine. For the first two trials, treatment consisted of risperidone followed by olanzapine, or vice versa. About 75% of patients on either drug showed an initial response. “Among those who did not respond in the first trial but were switched to either drug, the response rate was very low, averaging about 16%,” Dr. Marder said. “In other words, if somebody responds poorly to risperidone, they’re not likely to respond to olanzapine, or vice versa. I think this is true among nearly all of the antipsychotic drugs that are available. Patients tend to have sort of an idiosyncratic ability to respond to a nonclozapine antipsychotic. They may respond to one better than the other, but oftentimes they won’t respond well.” When patients in the trial were switched to clozapine, 75% showed an adequate response.
Based on the study findings and on his own clinical practice, Dr. Marder recommends trying one or two antipsychotics before prescribing clozapine. “If they haven’t responded in a couple of weeks, it’s probably good to change them to another antipsychotic,” he said. “If the patient is responding poorly they should go on to clozapine, which I think is very underutilized.”
In late 2019, the Food and Drug Administration approved lumateperone, a presynaptic D2 partial agonist and a postsynaptic D2 antagonist, for the treatment of schizophrenia in adults. “Its dopamine blockage doesn’t lead to increased dopamine, so it seems to work differently than other antipsychotics,” Dr. Marder said. “It’s effective at lower D2 affinity, which is similar to drugs like clozapine, and it has greater 5 HT2A:D2 antagonism.” It appears to have a relatively benign safety profile, including minimal weight gain, minimal metabolic adverse effects, and minimal extrapyramidal effects. “However, I think the jury’s out,” he added. “There is very little information about head-to-head comparisons between lumateperone and other antipsychotics.”
The new kid on the block is the Alkermes agent AKLS 3831, a combination drug of olanzapine-samidorphan, for the treatment of adults with schizophrenia and adults with bipolar I disorder. In December 2020, the FDA accepted the company’s New Drug Application and set the Prescription Drug User Fee Act target action date of June 1, 2021. Results from a phase 2 trial demonstrated mitigation of olanzapine-induced weight gain with the opioid antagonist samidorphan. “This is not a weight-loss drug,” Dr. Marder said. “It’s just a formulation that causes less weight gain. For patients who do well on olanzapine, putting them on this combination may be helpful in preventing weight gain.”
Dr. Marder disclosed that he has served as a consultant for AbbVie, Allergan, Boehringer Ingelheim, Forum, Genentech, Lundbeck, Neurocrine, Otsuka, Roche, Sunovion, Takeda, Targacept, and Teva. He has also received research support from Boehringer Ingelheim, Neurocrine, and Takeda, and is a section editor for UpToDate.
With the exception of clozapine, the selection of an antipsychotic medication for acute treatment is driven by side effects.
That’s a key pearl of wisdom that Stephen R. Marder, MD, shared during a discussion of key criteria for choosing an antipsychotic for patients with schizophrenia.
“It’s a decision that can have huge consequences, both to an individual’s mental health and their physical health,” Dr. Marder said during an annual psychopharmacology update held by the Nevada Psychiatric Association. “If a patient did well and liked a prior antipsychotic, that’s usually evidence that they’ll respond again. That’s been shown numerous times. Aside from that, the largest consideration is usually adverse effects.”
In a multiple-treatments meta-analysis that compared the efficacy and tolerability of 15 antipsychotic drugs in schizophrenia, researchers found that an overall positive change in symptoms occurred with clozapine, compared with any other drug.
“Clozapine is not just the most effective antipsychotic for patients who are treatment resistant; it’s also the most effective antipsychotic in general populations,” said Dr. Marder, the Daniel X. Freedman Professor of Psychiatry at the Semel Institute for Neuroscience and Human Behavior at the University of California, Los Angeles. “The next most effective antipsychotic is amisulpride, which is not available in the U.S., although there’s a company that’s developing a formulation of amisulpride. After that, the 95% confidence intervals overlap, and the differences are probably related not to their true effectiveness but to other circumstances.”
For example, he continued, risperidone and olanzapine were developed in the 1990s. They were always compared with haloperidol and they tended to work a little bit better. “The drugs developed later on in clinical trials tended to be used in patients who were more treatment resistant,” he said. “Aside from clozapine, the differences in effectiveness are relatively small. But the differences in side effects are large.”
The meta-analysis found that haloperidol stood out as the antipsychotic most likely to cause extrapyramidal side effects. Olanzapine and clozapine stood out as causing the most weight gain, while ziprasidone and lurasidone were less likely to cause weight gain. In addition, risperidone, paliperidone, and haloperidol tended to cause the greatest elevation of prolactin levels, while aripiprazole was found to reduce prolactin levels.
“This becomes an important issue, particularly in young people when one is worried about galactorrhea in women or gynecomastia in men, which sometimes happens with risperidone or haloperidol, and to a lesser extent, sexual dysfunction,” said Dr. Marder, who is also director of the VISN 22 Mental Illness Research, Education, and Clinical Center for the Department of Veterans Affairs. “Sedation is a major consideration for clozapine and chlorpromazine, but less for other antipsychotics.”
When do you know if you’ve selected the right medication for your patient? According to a meta-analysis of 42 studies involving 7,450 patients, improvement tends to occur within the first 2 weeks of treatment. “Which means Dr. Marder said. “This has been consequential because it provides guidance for clinicians to make decisions.”
Symptoms that are likely to improve in the first couple of days include agitation and psychomotor excitement. Improvement in psychotic symptoms typically occurs in the following order: those with thought disorder symptoms tend to develop more organized thinking, those with hallucinations tend to experience a decrease the intensity and frequency of their episodes, and those with well-ingrained delusions “tend to experience fewer misinterpretations,” Dr. Marder said. “They may feel less suspicious and they may talk less about delusions.”
Dr. Marder makes it a point to evaluate the antipsychotic response of patients in 2-3 weeks. “If it’s a partial response, continue a bit longer,” he advised. “It it’s no response, switch. And, of course, if the drug isn’t tolerated well, switch.”
He advised against thinking that patients can easily be categorized as being strong responders or nonresponders. Instead, he favors viewing responsiveness to an antipsychotic along a continuum. “Ten to fifteen percent of patients will fail to remit even at first exposure to an antipsychotic medication, but it’s more common that patients will be partial responders,” Dr. Marder said. “One will have to determine whether that response is adequate or not. There’s also the idea that patients sometimes respond vigorously to an antipsychotic early on. For example, first-episode patients tend to respond very well, and they respond at substantially lower doses. But I set a high criteria that we really want patients on an antipsychotic to respond well, to being in a remission that they can live with, not just to be partially remitted.”
In an analysis of response rates, 244 patients with first-episode schizophrenia moved through two antipsychotic trials, followed by a trial with clozapine. For the first two trials, treatment consisted of risperidone followed by olanzapine, or vice versa. About 75% of patients on either drug showed an initial response. “Among those who did not respond in the first trial but were switched to either drug, the response rate was very low, averaging about 16%,” Dr. Marder said. “In other words, if somebody responds poorly to risperidone, they’re not likely to respond to olanzapine, or vice versa. I think this is true among nearly all of the antipsychotic drugs that are available. Patients tend to have sort of an idiosyncratic ability to respond to a nonclozapine antipsychotic. They may respond to one better than the other, but oftentimes they won’t respond well.” When patients in the trial were switched to clozapine, 75% showed an adequate response.
Based on the study findings and on his own clinical practice, Dr. Marder recommends trying one or two antipsychotics before prescribing clozapine. “If they haven’t responded in a couple of weeks, it’s probably good to change them to another antipsychotic,” he said. “If the patient is responding poorly they should go on to clozapine, which I think is very underutilized.”
In late 2019, the Food and Drug Administration approved lumateperone, a presynaptic D2 partial agonist and a postsynaptic D2 antagonist, for the treatment of schizophrenia in adults. “Its dopamine blockage doesn’t lead to increased dopamine, so it seems to work differently than other antipsychotics,” Dr. Marder said. “It’s effective at lower D2 affinity, which is similar to drugs like clozapine, and it has greater 5 HT2A:D2 antagonism.” It appears to have a relatively benign safety profile, including minimal weight gain, minimal metabolic adverse effects, and minimal extrapyramidal effects. “However, I think the jury’s out,” he added. “There is very little information about head-to-head comparisons between lumateperone and other antipsychotics.”
The new kid on the block is the Alkermes agent AKLS 3831, a combination drug of olanzapine-samidorphan, for the treatment of adults with schizophrenia and adults with bipolar I disorder. In December 2020, the FDA accepted the company’s New Drug Application and set the Prescription Drug User Fee Act target action date of June 1, 2021. Results from a phase 2 trial demonstrated mitigation of olanzapine-induced weight gain with the opioid antagonist samidorphan. “This is not a weight-loss drug,” Dr. Marder said. “It’s just a formulation that causes less weight gain. For patients who do well on olanzapine, putting them on this combination may be helpful in preventing weight gain.”
Dr. Marder disclosed that he has served as a consultant for AbbVie, Allergan, Boehringer Ingelheim, Forum, Genentech, Lundbeck, Neurocrine, Otsuka, Roche, Sunovion, Takeda, Targacept, and Teva. He has also received research support from Boehringer Ingelheim, Neurocrine, and Takeda, and is a section editor for UpToDate.
With the exception of clozapine, the selection of an antipsychotic medication for acute treatment is driven by side effects.
That’s a key pearl of wisdom that Stephen R. Marder, MD, shared during a discussion of key criteria for choosing an antipsychotic for patients with schizophrenia.
“It’s a decision that can have huge consequences, both to an individual’s mental health and their physical health,” Dr. Marder said during an annual psychopharmacology update held by the Nevada Psychiatric Association. “If a patient did well and liked a prior antipsychotic, that’s usually evidence that they’ll respond again. That’s been shown numerous times. Aside from that, the largest consideration is usually adverse effects.”
In a multiple-treatments meta-analysis that compared the efficacy and tolerability of 15 antipsychotic drugs in schizophrenia, researchers found that an overall positive change in symptoms occurred with clozapine, compared with any other drug.
“Clozapine is not just the most effective antipsychotic for patients who are treatment resistant; it’s also the most effective antipsychotic in general populations,” said Dr. Marder, the Daniel X. Freedman Professor of Psychiatry at the Semel Institute for Neuroscience and Human Behavior at the University of California, Los Angeles. “The next most effective antipsychotic is amisulpride, which is not available in the U.S., although there’s a company that’s developing a formulation of amisulpride. After that, the 95% confidence intervals overlap, and the differences are probably related not to their true effectiveness but to other circumstances.”
For example, he continued, risperidone and olanzapine were developed in the 1990s. They were always compared with haloperidol and they tended to work a little bit better. “The drugs developed later on in clinical trials tended to be used in patients who were more treatment resistant,” he said. “Aside from clozapine, the differences in effectiveness are relatively small. But the differences in side effects are large.”
The meta-analysis found that haloperidol stood out as the antipsychotic most likely to cause extrapyramidal side effects. Olanzapine and clozapine stood out as causing the most weight gain, while ziprasidone and lurasidone were less likely to cause weight gain. In addition, risperidone, paliperidone, and haloperidol tended to cause the greatest elevation of prolactin levels, while aripiprazole was found to reduce prolactin levels.
“This becomes an important issue, particularly in young people when one is worried about galactorrhea in women or gynecomastia in men, which sometimes happens with risperidone or haloperidol, and to a lesser extent, sexual dysfunction,” said Dr. Marder, who is also director of the VISN 22 Mental Illness Research, Education, and Clinical Center for the Department of Veterans Affairs. “Sedation is a major consideration for clozapine and chlorpromazine, but less for other antipsychotics.”
When do you know if you’ve selected the right medication for your patient? According to a meta-analysis of 42 studies involving 7,450 patients, improvement tends to occur within the first 2 weeks of treatment. “Which means Dr. Marder said. “This has been consequential because it provides guidance for clinicians to make decisions.”
Symptoms that are likely to improve in the first couple of days include agitation and psychomotor excitement. Improvement in psychotic symptoms typically occurs in the following order: those with thought disorder symptoms tend to develop more organized thinking, those with hallucinations tend to experience a decrease the intensity and frequency of their episodes, and those with well-ingrained delusions “tend to experience fewer misinterpretations,” Dr. Marder said. “They may feel less suspicious and they may talk less about delusions.”
Dr. Marder makes it a point to evaluate the antipsychotic response of patients in 2-3 weeks. “If it’s a partial response, continue a bit longer,” he advised. “It it’s no response, switch. And, of course, if the drug isn’t tolerated well, switch.”
He advised against thinking that patients can easily be categorized as being strong responders or nonresponders. Instead, he favors viewing responsiveness to an antipsychotic along a continuum. “Ten to fifteen percent of patients will fail to remit even at first exposure to an antipsychotic medication, but it’s more common that patients will be partial responders,” Dr. Marder said. “One will have to determine whether that response is adequate or not. There’s also the idea that patients sometimes respond vigorously to an antipsychotic early on. For example, first-episode patients tend to respond very well, and they respond at substantially lower doses. But I set a high criteria that we really want patients on an antipsychotic to respond well, to being in a remission that they can live with, not just to be partially remitted.”
In an analysis of response rates, 244 patients with first-episode schizophrenia moved through two antipsychotic trials, followed by a trial with clozapine. For the first two trials, treatment consisted of risperidone followed by olanzapine, or vice versa. About 75% of patients on either drug showed an initial response. “Among those who did not respond in the first trial but were switched to either drug, the response rate was very low, averaging about 16%,” Dr. Marder said. “In other words, if somebody responds poorly to risperidone, they’re not likely to respond to olanzapine, or vice versa. I think this is true among nearly all of the antipsychotic drugs that are available. Patients tend to have sort of an idiosyncratic ability to respond to a nonclozapine antipsychotic. They may respond to one better than the other, but oftentimes they won’t respond well.” When patients in the trial were switched to clozapine, 75% showed an adequate response.
Based on the study findings and on his own clinical practice, Dr. Marder recommends trying one or two antipsychotics before prescribing clozapine. “If they haven’t responded in a couple of weeks, it’s probably good to change them to another antipsychotic,” he said. “If the patient is responding poorly they should go on to clozapine, which I think is very underutilized.”
In late 2019, the Food and Drug Administration approved lumateperone, a presynaptic D2 partial agonist and a postsynaptic D2 antagonist, for the treatment of schizophrenia in adults. “Its dopamine blockage doesn’t lead to increased dopamine, so it seems to work differently than other antipsychotics,” Dr. Marder said. “It’s effective at lower D2 affinity, which is similar to drugs like clozapine, and it has greater 5 HT2A:D2 antagonism.” It appears to have a relatively benign safety profile, including minimal weight gain, minimal metabolic adverse effects, and minimal extrapyramidal effects. “However, I think the jury’s out,” he added. “There is very little information about head-to-head comparisons between lumateperone and other antipsychotics.”
The new kid on the block is the Alkermes agent AKLS 3831, a combination drug of olanzapine-samidorphan, for the treatment of adults with schizophrenia and adults with bipolar I disorder. In December 2020, the FDA accepted the company’s New Drug Application and set the Prescription Drug User Fee Act target action date of June 1, 2021. Results from a phase 2 trial demonstrated mitigation of olanzapine-induced weight gain with the opioid antagonist samidorphan. “This is not a weight-loss drug,” Dr. Marder said. “It’s just a formulation that causes less weight gain. For patients who do well on olanzapine, putting them on this combination may be helpful in preventing weight gain.”
Dr. Marder disclosed that he has served as a consultant for AbbVie, Allergan, Boehringer Ingelheim, Forum, Genentech, Lundbeck, Neurocrine, Otsuka, Roche, Sunovion, Takeda, Targacept, and Teva. He has also received research support from Boehringer Ingelheim, Neurocrine, and Takeda, and is a section editor for UpToDate.
FROM NPA 2021
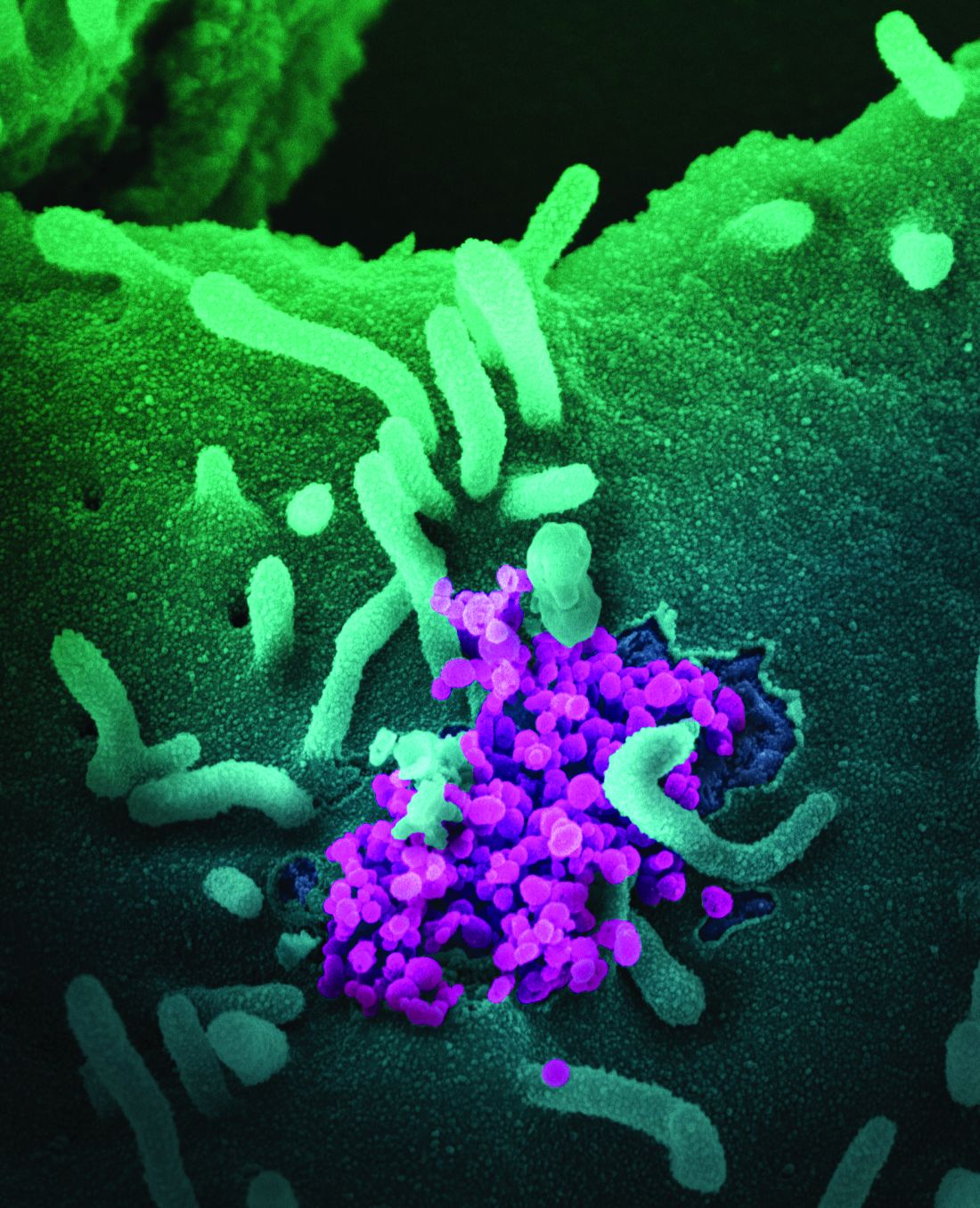
PPE protected critical care staff from COVID-19 transmission
, a new study has found.
“Other staff, other areas of the hospital, and the wider community are more likely sources of infection,” said lead author Kate El Bouzidi, MRCP, South London Specialist Virology Centre, King’s College Hospital NHS Foundation Trust, London.
She noted that 60% of critical care staff were symptomatic during the first wave of the coronavirus pandemic and 20% were antibody positive, with 10% asymptomatic. “Staff acquisition peaked 3 weeks before the peak of COVID-19 ICU admission, and personal protective equipment (PPE) was effective at preventing transmission from patients.” Working in other areas of the hospital was associated with higher seroprevalence, Dr. El Bouzidi noted.
The findings were presented at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
The novel coronavirus was spreading around the world, and when it reached northern Italy, medical authorities began to think in terms of how it might overwhelm the health care system in the United Kingdom, explained Dr. El Bouzidi.
“There was a lot of interest at this time about health care workers who were particularly vulnerable and also about the allocation of resources and rationing of care, particularly in intensive care,” she said. “And this only intensified when our prime minister was admitted to intensive care. About this time, antibody testing also became available.”
The goal of their study was to determine the SARS-CoV-2 seroprevalence in critical care staff, as well as look at the correlation between antibody status, prior swab testing, and COVID-19 symptoms.
The survey was conducted at Kings College Hospital in London, which is a tertiary-care teaching center. The critical care department is one of the largest in the United Kingdom. The authors estimate that more than 800 people worked in the critical care units, and between March and April 2020, more than 2,000 patients with COVID-19 were admitted, of whom 180 required care in the ICU.
“There was good PPE available in the ICU units right from the start,” she said, “and staff testing was available.”
All staff working in the critical care department participated in the study, which required serum samples and completion of a questionnaire. The samples were tested via six different assays to measure receptor-binding domain, nucleoprotein, and tri-spike, with one antibody result determined for each sample.
Of the 625 staff members, 384 (61.4%) had previously reported experiencing symptoms and 124 (19.8%) had sent a swab for testing. COVID-19 infection had been confirmed in 37 of those health care workers (29.8%).
Overall, 21% were positive for SARS-CoV-2 antibodies, of whom 9.9% had been asymptomatic.
“We were surprised to find that 61% of staff reported symptoms they felt could be consistent with COVID-19,” she said, noting that fatigue, headache, and cough were the most common symptoms reported. “Seroprevalence was reported in 31% of symptomatic staff and in 5% of those without symptoms.”
Seroprevalence differed by role in a critical care unit, although it did not significantly differ by factors such as age, sex, ethnicity, or underlying conditions. Consultants, who are senior physicians, were twice as likely to test positive, compared with junior doctors. The reason for this finding is not clear, but it may lie in the nature of their work responsibilities, such as performing more aerosol-generating procedures in the ICU or in other departments.
The investigators looked at the timing of infections and found that they preceded peak of patient admissions by 3 weeks, with peak onset of staff symptoms in early March. At this time, Dr. El Bouzidi noted, there were very few patients with COVID-19 in the hospital, and good PPE was available throughout this time period.
“Staff were unlikely to be infected by ICU patients, and therefore PPE was largely effective,” she said. “Other sources of infection were more likely to be the cause, such as interactions with other staff, meetings, or contact in break rooms. Routine mask-wearing throughout the hospital was only encouraged as of June 15.”
There were several limitations to the study, such as the cross-sectional design, reliance on response/recall, the fact that antibody tests are unlikely to detect all previous infections, and no genomic data were available to confirm infections. Even though the study had limitations, Dr. El Bouzidi concluded that ICU staff are unlikely to contract COVID-19 from patients but that other staff, other areas of the hospital, and the wider community are more likely sources of infection.
These findings, she added, demonstrate that PPE was effective at preventing transmission from patients and that protective measures need to be maintained when staff is away from the bedside.
In commenting on the study, Greg S. Martin, MD, professor of medicine in the division of pulmonary, allergy, critical care and sleep medicine, Emory University, Atlanta, noted that, even though the study was conducted almost a year ago, the results are still relevant with regard to the effectiveness of PPE.
“There was a huge amount of uncertainty about PPE – what was most effective, could we reuse it, how to sterilize it, what about surfaces, and so on,” he said. “Even for people who work in ICU and who are familiar with the environment and familiar with the patients, there was 1,000 times more uncertainty about everything they were doing.”
Dr. Martin believes that the situation has improved. “It’s not that we take COVID more lightly, but I think the staff is more comfortable dealing with it,” he said. “They now know what they need to do on an hourly and daily basis to stay safe. The PPE had become second nature to them now, with all the other precautions.”
, a new study has found.
“Other staff, other areas of the hospital, and the wider community are more likely sources of infection,” said lead author Kate El Bouzidi, MRCP, South London Specialist Virology Centre, King’s College Hospital NHS Foundation Trust, London.
She noted that 60% of critical care staff were symptomatic during the first wave of the coronavirus pandemic and 20% were antibody positive, with 10% asymptomatic. “Staff acquisition peaked 3 weeks before the peak of COVID-19 ICU admission, and personal protective equipment (PPE) was effective at preventing transmission from patients.” Working in other areas of the hospital was associated with higher seroprevalence, Dr. El Bouzidi noted.
The findings were presented at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
The novel coronavirus was spreading around the world, and when it reached northern Italy, medical authorities began to think in terms of how it might overwhelm the health care system in the United Kingdom, explained Dr. El Bouzidi.
“There was a lot of interest at this time about health care workers who were particularly vulnerable and also about the allocation of resources and rationing of care, particularly in intensive care,” she said. “And this only intensified when our prime minister was admitted to intensive care. About this time, antibody testing also became available.”
The goal of their study was to determine the SARS-CoV-2 seroprevalence in critical care staff, as well as look at the correlation between antibody status, prior swab testing, and COVID-19 symptoms.
The survey was conducted at Kings College Hospital in London, which is a tertiary-care teaching center. The critical care department is one of the largest in the United Kingdom. The authors estimate that more than 800 people worked in the critical care units, and between March and April 2020, more than 2,000 patients with COVID-19 were admitted, of whom 180 required care in the ICU.
“There was good PPE available in the ICU units right from the start,” she said, “and staff testing was available.”
All staff working in the critical care department participated in the study, which required serum samples and completion of a questionnaire. The samples were tested via six different assays to measure receptor-binding domain, nucleoprotein, and tri-spike, with one antibody result determined for each sample.
Of the 625 staff members, 384 (61.4%) had previously reported experiencing symptoms and 124 (19.8%) had sent a swab for testing. COVID-19 infection had been confirmed in 37 of those health care workers (29.8%).
Overall, 21% were positive for SARS-CoV-2 antibodies, of whom 9.9% had been asymptomatic.
“We were surprised to find that 61% of staff reported symptoms they felt could be consistent with COVID-19,” she said, noting that fatigue, headache, and cough were the most common symptoms reported. “Seroprevalence was reported in 31% of symptomatic staff and in 5% of those without symptoms.”
Seroprevalence differed by role in a critical care unit, although it did not significantly differ by factors such as age, sex, ethnicity, or underlying conditions. Consultants, who are senior physicians, were twice as likely to test positive, compared with junior doctors. The reason for this finding is not clear, but it may lie in the nature of their work responsibilities, such as performing more aerosol-generating procedures in the ICU or in other departments.
The investigators looked at the timing of infections and found that they preceded peak of patient admissions by 3 weeks, with peak onset of staff symptoms in early March. At this time, Dr. El Bouzidi noted, there were very few patients with COVID-19 in the hospital, and good PPE was available throughout this time period.
“Staff were unlikely to be infected by ICU patients, and therefore PPE was largely effective,” she said. “Other sources of infection were more likely to be the cause, such as interactions with other staff, meetings, or contact in break rooms. Routine mask-wearing throughout the hospital was only encouraged as of June 15.”
There were several limitations to the study, such as the cross-sectional design, reliance on response/recall, the fact that antibody tests are unlikely to detect all previous infections, and no genomic data were available to confirm infections. Even though the study had limitations, Dr. El Bouzidi concluded that ICU staff are unlikely to contract COVID-19 from patients but that other staff, other areas of the hospital, and the wider community are more likely sources of infection.
These findings, she added, demonstrate that PPE was effective at preventing transmission from patients and that protective measures need to be maintained when staff is away from the bedside.
In commenting on the study, Greg S. Martin, MD, professor of medicine in the division of pulmonary, allergy, critical care and sleep medicine, Emory University, Atlanta, noted that, even though the study was conducted almost a year ago, the results are still relevant with regard to the effectiveness of PPE.
“There was a huge amount of uncertainty about PPE – what was most effective, could we reuse it, how to sterilize it, what about surfaces, and so on,” he said. “Even for people who work in ICU and who are familiar with the environment and familiar with the patients, there was 1,000 times more uncertainty about everything they were doing.”
Dr. Martin believes that the situation has improved. “It’s not that we take COVID more lightly, but I think the staff is more comfortable dealing with it,” he said. “They now know what they need to do on an hourly and daily basis to stay safe. The PPE had become second nature to them now, with all the other precautions.”
, a new study has found.
“Other staff, other areas of the hospital, and the wider community are more likely sources of infection,” said lead author Kate El Bouzidi, MRCP, South London Specialist Virology Centre, King’s College Hospital NHS Foundation Trust, London.
She noted that 60% of critical care staff were symptomatic during the first wave of the coronavirus pandemic and 20% were antibody positive, with 10% asymptomatic. “Staff acquisition peaked 3 weeks before the peak of COVID-19 ICU admission, and personal protective equipment (PPE) was effective at preventing transmission from patients.” Working in other areas of the hospital was associated with higher seroprevalence, Dr. El Bouzidi noted.
The findings were presented at the Critical Care Congress sponsored by the Society of Critical Care Medicine.
The novel coronavirus was spreading around the world, and when it reached northern Italy, medical authorities began to think in terms of how it might overwhelm the health care system in the United Kingdom, explained Dr. El Bouzidi.
“There was a lot of interest at this time about health care workers who were particularly vulnerable and also about the allocation of resources and rationing of care, particularly in intensive care,” she said. “And this only intensified when our prime minister was admitted to intensive care. About this time, antibody testing also became available.”
The goal of their study was to determine the SARS-CoV-2 seroprevalence in critical care staff, as well as look at the correlation between antibody status, prior swab testing, and COVID-19 symptoms.
The survey was conducted at Kings College Hospital in London, which is a tertiary-care teaching center. The critical care department is one of the largest in the United Kingdom. The authors estimate that more than 800 people worked in the critical care units, and between March and April 2020, more than 2,000 patients with COVID-19 were admitted, of whom 180 required care in the ICU.
“There was good PPE available in the ICU units right from the start,” she said, “and staff testing was available.”
All staff working in the critical care department participated in the study, which required serum samples and completion of a questionnaire. The samples were tested via six different assays to measure receptor-binding domain, nucleoprotein, and tri-spike, with one antibody result determined for each sample.
Of the 625 staff members, 384 (61.4%) had previously reported experiencing symptoms and 124 (19.8%) had sent a swab for testing. COVID-19 infection had been confirmed in 37 of those health care workers (29.8%).
Overall, 21% were positive for SARS-CoV-2 antibodies, of whom 9.9% had been asymptomatic.
“We were surprised to find that 61% of staff reported symptoms they felt could be consistent with COVID-19,” she said, noting that fatigue, headache, and cough were the most common symptoms reported. “Seroprevalence was reported in 31% of symptomatic staff and in 5% of those without symptoms.”
Seroprevalence differed by role in a critical care unit, although it did not significantly differ by factors such as age, sex, ethnicity, or underlying conditions. Consultants, who are senior physicians, were twice as likely to test positive, compared with junior doctors. The reason for this finding is not clear, but it may lie in the nature of their work responsibilities, such as performing more aerosol-generating procedures in the ICU or in other departments.
The investigators looked at the timing of infections and found that they preceded peak of patient admissions by 3 weeks, with peak onset of staff symptoms in early March. At this time, Dr. El Bouzidi noted, there were very few patients with COVID-19 in the hospital, and good PPE was available throughout this time period.
“Staff were unlikely to be infected by ICU patients, and therefore PPE was largely effective,” she said. “Other sources of infection were more likely to be the cause, such as interactions with other staff, meetings, or contact in break rooms. Routine mask-wearing throughout the hospital was only encouraged as of June 15.”
There were several limitations to the study, such as the cross-sectional design, reliance on response/recall, the fact that antibody tests are unlikely to detect all previous infections, and no genomic data were available to confirm infections. Even though the study had limitations, Dr. El Bouzidi concluded that ICU staff are unlikely to contract COVID-19 from patients but that other staff, other areas of the hospital, and the wider community are more likely sources of infection.
These findings, she added, demonstrate that PPE was effective at preventing transmission from patients and that protective measures need to be maintained when staff is away from the bedside.
In commenting on the study, Greg S. Martin, MD, professor of medicine in the division of pulmonary, allergy, critical care and sleep medicine, Emory University, Atlanta, noted that, even though the study was conducted almost a year ago, the results are still relevant with regard to the effectiveness of PPE.
“There was a huge amount of uncertainty about PPE – what was most effective, could we reuse it, how to sterilize it, what about surfaces, and so on,” he said. “Even for people who work in ICU and who are familiar with the environment and familiar with the patients, there was 1,000 times more uncertainty about everything they were doing.”
Dr. Martin believes that the situation has improved. “It’s not that we take COVID more lightly, but I think the staff is more comfortable dealing with it,” he said. “They now know what they need to do on an hourly and daily basis to stay safe. The PPE had become second nature to them now, with all the other precautions.”
FROM CCC50
Inpatient psychiatrist? Maybe I’ll be a vaccinator instead
Now that completion of residency is fast approaching, I am asked regularly what I plan to do when I become a Real Doctor on July 1. It feels like it wasn’t so long ago I was trying to decide if I should even go to medical school, then later, if I should go into psychiatry, family medicine, or emergency medicine. And here I am at another decision point, another of the regular, 4-year milestones in my journey to full physicianhood.
A surprising thing happened to me during my psychiatry training: I fell in love with acute care. Instead of outpatient care, I preferred the longer hours with patients who insist they are Jesus Christ, believe deeply they are being actively pursued by the FBI, and sometimes eat their own feces. I was in awe of the remarkable capacity of the human brain to convince a graduate-school educated man with bipolar disorder that it is acceptable to call in bomb threats to a hospital. To lead a patient on a conservatorship to believe that I am not a doctor but, instead, a seamstress or leave socks full of feces as presents for Santa Claus (lots of feces in inpatient psychiatry). To believe their spouses are not humans or hear voices telling them they should jump off a bridge, sustaining near-lethal injuries. I was hooked.
Psychiatry as a field is not for those requiring instant gratification. Other than Ativan challenges and the remarkably quick response some patients have to ECT, outcomes of our treatments are usually modest, and they take time. We often delude ourselves into thinking that bumping a patient’s fluoxetine from 10 mg to 20 mg will be The Thing that changes a patient’s life. We address our own sense of helplessness as much as that of our patients, who are desperate for something, for someone, to do something that will alter the course of their lives.
Of course, what I can offer my patients usually falls short of their lofty expectations of my prowess. I offer them compassion, validation, empathy. I offer them medications for which we usually have meager data and meager results. I cannot find them shelter but for a few nights, perhaps a week. I rarely, in settings in which primary diagnoses of substance use and personality disorders are forbidden by insurance companies, can help them with their addiction to methamphetamine. I cannot cure their maladaptive characterological pathology stemming from childhood attachment trauma. To address my own sense of failure as a healer, I resort to the bottom of Maslow’s hierarchy of needs, providing their choice of juice box, more blankets. I slow-roll their discharges overnight so that they can stay in the ER hallway instead of spending the night outside in the rare Southern California rain.
In my 3rd year of residency, we were thrown into a pandemic. I felt both terrified of getting COVID-19 in the hospital and inadequate as a physician. I did not want to be intubating patients, but even more, I dreaded the potential “psychiatry-friendly” assignment of calling the family members of those who had perished from the disease. Rumors circulated that certain versions of surge planning had the inpatient psychiatry unit transitioned to a COVID unit and psychiatry residents “redeployed” to cover medicine floors. Fortunately, we did not have to (or have not yet had to) endure this apocalyptic episode of worst-case scenario. I remained a psychiatrist-in-training, seeing occasional COVID patients but with full personal protective equipment and the ability to maintain some physical distance to complete my examinations. Coming home to my apartment building in scrubs, now acceptable attire on inpatient units – it always should have been since, as we have established, our units are filled with feces – I early on felt like a leper. Later on, I was treated with dignity and respect, like a hero.
My position as a non–frontline-physician was personally challenging. I wanted to help, felt like I should and could help. I am a helper-in-recovery who has spent years learning to achieve a balance of service and loyalty to others and my own desires. The initial guilt I felt at feeling appreciated during the nightly celebration of health care workers downtown ultimately dissipated. I was no hero, nor did I claim to be one. I made peace with my pandemic hobbies of sourdough bread-baking, Moscow mule-making, jigsaw-puzzling, and, briefly, running (before a calcaneal stress fracture reminded me that I am not built for land exercise). I went to work; I came home. My cat was happy.
Then, in rapid succession, vaccines were approved and distributed. My hospital had partnered with the county to administer them at a new superstation, and they were in desperate need of licensed humans to be vaccinators. They cared not that I had given very few (n = 3) injections and only during medical school. I watched the YouTube videos on the Z-track technique for IMs, learned about needle gauges, and went off to the baseball stadium.
I loved this new gig, disproportionately. The 8+ hours flew by, 100 vaccines given to occupants of cars who had eagerly waited hours for the privilege of being vaccinated by an almost-psychiatrist. It was not the technical expertise of sticking a needle into someone’s arm that gave me a dopamine rush, nor the microstress of preparing the syringes with a flimsy needle and a slight caffeine-induced tremor while trying to flick air bubbles out of the syringe without dropping the precious vaccine vial. It was not the travel nurse asking me why anyone – especially an overworked resident – would volunteer to do this for free, while she and others were making “stupid amounts of money” to do the same job.
What drove me to keep volunteering for no pay, only Cheez-Its available as sustenance, minimal gratitude from my employer, long hours on my feet doing a task that was rote and at which I probably would never completely excel? On my second shift, I realized why I found it so gratifying to be a vaccinator: There was a perfect 1:1 correspondence in what patients wanted at that moment and in what I had to offer them. They did not want me to fix their lives, secure them housing, or go back in time and remove them from abusive homes so they could grow up to be more functional, happier adults. They merely wanted a shot. They were profusely grateful, hopeful that this was the Beginning of the End. Nobody spat on me; nobody called me obscene names. Nobody was upset with me for involuntarily holding them against their will. My services were welcome, appreciated. I had lovely, superficial conversations with dozens of people. I felt connected to strangers in a way that has been sorely lacking since March 2020. Understandably mistaken for a nurse throughout the day, I felt more like a bona fide physician than I had in over a year.
I know the adrenaline rush will fade, that volunteer-vaccinating in my free time will eventually become less exciting to me. I know I won’t be able to convince my colleagues indefinitely that volunteering together is a great, institution-sanctioned bonding opportunity. I know the initial enthusiasm over vaccine distribution will fade as the pandemic continues to transform our everyday lives and threaten the health of millions, the economy, and the sanctity of normal human interactions. The gratitude and hopefulness may well be replaced with frustration over waiting hours in a car to get an injection from a psychiatrist, with fear that this promised panacea may not restore normalcy anytime soon. But right now, 11 months into a pandemic that has left our profession exhausted and jaded, the coprophilia and catatonia have temporarily lost their allure. So, I’m adding “vaccinator” to my list of pandemic hobbies.
Dr. Stone is a chief resident in psychiatry at the University of California, San Diego. Before deciding to become a physician, she obtained a master’s degree in public health and worked in health policy research studying empathy and patient-doctor interactions. She has a passion for public psychiatry and acute care, and she dabbles in physician wellness, medical education, and the interface of psychiatry and primary care. Dr. Stone has no disclosures.
Now that completion of residency is fast approaching, I am asked regularly what I plan to do when I become a Real Doctor on July 1. It feels like it wasn’t so long ago I was trying to decide if I should even go to medical school, then later, if I should go into psychiatry, family medicine, or emergency medicine. And here I am at another decision point, another of the regular, 4-year milestones in my journey to full physicianhood.
A surprising thing happened to me during my psychiatry training: I fell in love with acute care. Instead of outpatient care, I preferred the longer hours with patients who insist they are Jesus Christ, believe deeply they are being actively pursued by the FBI, and sometimes eat their own feces. I was in awe of the remarkable capacity of the human brain to convince a graduate-school educated man with bipolar disorder that it is acceptable to call in bomb threats to a hospital. To lead a patient on a conservatorship to believe that I am not a doctor but, instead, a seamstress or leave socks full of feces as presents for Santa Claus (lots of feces in inpatient psychiatry). To believe their spouses are not humans or hear voices telling them they should jump off a bridge, sustaining near-lethal injuries. I was hooked.
Psychiatry as a field is not for those requiring instant gratification. Other than Ativan challenges and the remarkably quick response some patients have to ECT, outcomes of our treatments are usually modest, and they take time. We often delude ourselves into thinking that bumping a patient’s fluoxetine from 10 mg to 20 mg will be The Thing that changes a patient’s life. We address our own sense of helplessness as much as that of our patients, who are desperate for something, for someone, to do something that will alter the course of their lives.
Of course, what I can offer my patients usually falls short of their lofty expectations of my prowess. I offer them compassion, validation, empathy. I offer them medications for which we usually have meager data and meager results. I cannot find them shelter but for a few nights, perhaps a week. I rarely, in settings in which primary diagnoses of substance use and personality disorders are forbidden by insurance companies, can help them with their addiction to methamphetamine. I cannot cure their maladaptive characterological pathology stemming from childhood attachment trauma. To address my own sense of failure as a healer, I resort to the bottom of Maslow’s hierarchy of needs, providing their choice of juice box, more blankets. I slow-roll their discharges overnight so that they can stay in the ER hallway instead of spending the night outside in the rare Southern California rain.
In my 3rd year of residency, we were thrown into a pandemic. I felt both terrified of getting COVID-19 in the hospital and inadequate as a physician. I did not want to be intubating patients, but even more, I dreaded the potential “psychiatry-friendly” assignment of calling the family members of those who had perished from the disease. Rumors circulated that certain versions of surge planning had the inpatient psychiatry unit transitioned to a COVID unit and psychiatry residents “redeployed” to cover medicine floors. Fortunately, we did not have to (or have not yet had to) endure this apocalyptic episode of worst-case scenario. I remained a psychiatrist-in-training, seeing occasional COVID patients but with full personal protective equipment and the ability to maintain some physical distance to complete my examinations. Coming home to my apartment building in scrubs, now acceptable attire on inpatient units – it always should have been since, as we have established, our units are filled with feces – I early on felt like a leper. Later on, I was treated with dignity and respect, like a hero.
My position as a non–frontline-physician was personally challenging. I wanted to help, felt like I should and could help. I am a helper-in-recovery who has spent years learning to achieve a balance of service and loyalty to others and my own desires. The initial guilt I felt at feeling appreciated during the nightly celebration of health care workers downtown ultimately dissipated. I was no hero, nor did I claim to be one. I made peace with my pandemic hobbies of sourdough bread-baking, Moscow mule-making, jigsaw-puzzling, and, briefly, running (before a calcaneal stress fracture reminded me that I am not built for land exercise). I went to work; I came home. My cat was happy.
Then, in rapid succession, vaccines were approved and distributed. My hospital had partnered with the county to administer them at a new superstation, and they were in desperate need of licensed humans to be vaccinators. They cared not that I had given very few (n = 3) injections and only during medical school. I watched the YouTube videos on the Z-track technique for IMs, learned about needle gauges, and went off to the baseball stadium.
I loved this new gig, disproportionately. The 8+ hours flew by, 100 vaccines given to occupants of cars who had eagerly waited hours for the privilege of being vaccinated by an almost-psychiatrist. It was not the technical expertise of sticking a needle into someone’s arm that gave me a dopamine rush, nor the microstress of preparing the syringes with a flimsy needle and a slight caffeine-induced tremor while trying to flick air bubbles out of the syringe without dropping the precious vaccine vial. It was not the travel nurse asking me why anyone – especially an overworked resident – would volunteer to do this for free, while she and others were making “stupid amounts of money” to do the same job.
What drove me to keep volunteering for no pay, only Cheez-Its available as sustenance, minimal gratitude from my employer, long hours on my feet doing a task that was rote and at which I probably would never completely excel? On my second shift, I realized why I found it so gratifying to be a vaccinator: There was a perfect 1:1 correspondence in what patients wanted at that moment and in what I had to offer them. They did not want me to fix their lives, secure them housing, or go back in time and remove them from abusive homes so they could grow up to be more functional, happier adults. They merely wanted a shot. They were profusely grateful, hopeful that this was the Beginning of the End. Nobody spat on me; nobody called me obscene names. Nobody was upset with me for involuntarily holding them against their will. My services were welcome, appreciated. I had lovely, superficial conversations with dozens of people. I felt connected to strangers in a way that has been sorely lacking since March 2020. Understandably mistaken for a nurse throughout the day, I felt more like a bona fide physician than I had in over a year.
I know the adrenaline rush will fade, that volunteer-vaccinating in my free time will eventually become less exciting to me. I know I won’t be able to convince my colleagues indefinitely that volunteering together is a great, institution-sanctioned bonding opportunity. I know the initial enthusiasm over vaccine distribution will fade as the pandemic continues to transform our everyday lives and threaten the health of millions, the economy, and the sanctity of normal human interactions. The gratitude and hopefulness may well be replaced with frustration over waiting hours in a car to get an injection from a psychiatrist, with fear that this promised panacea may not restore normalcy anytime soon. But right now, 11 months into a pandemic that has left our profession exhausted and jaded, the coprophilia and catatonia have temporarily lost their allure. So, I’m adding “vaccinator” to my list of pandemic hobbies.
Dr. Stone is a chief resident in psychiatry at the University of California, San Diego. Before deciding to become a physician, she obtained a master’s degree in public health and worked in health policy research studying empathy and patient-doctor interactions. She has a passion for public psychiatry and acute care, and she dabbles in physician wellness, medical education, and the interface of psychiatry and primary care. Dr. Stone has no disclosures.
Now that completion of residency is fast approaching, I am asked regularly what I plan to do when I become a Real Doctor on July 1. It feels like it wasn’t so long ago I was trying to decide if I should even go to medical school, then later, if I should go into psychiatry, family medicine, or emergency medicine. And here I am at another decision point, another of the regular, 4-year milestones in my journey to full physicianhood.
A surprising thing happened to me during my psychiatry training: I fell in love with acute care. Instead of outpatient care, I preferred the longer hours with patients who insist they are Jesus Christ, believe deeply they are being actively pursued by the FBI, and sometimes eat their own feces. I was in awe of the remarkable capacity of the human brain to convince a graduate-school educated man with bipolar disorder that it is acceptable to call in bomb threats to a hospital. To lead a patient on a conservatorship to believe that I am not a doctor but, instead, a seamstress or leave socks full of feces as presents for Santa Claus (lots of feces in inpatient psychiatry). To believe their spouses are not humans or hear voices telling them they should jump off a bridge, sustaining near-lethal injuries. I was hooked.
Psychiatry as a field is not for those requiring instant gratification. Other than Ativan challenges and the remarkably quick response some patients have to ECT, outcomes of our treatments are usually modest, and they take time. We often delude ourselves into thinking that bumping a patient’s fluoxetine from 10 mg to 20 mg will be The Thing that changes a patient’s life. We address our own sense of helplessness as much as that of our patients, who are desperate for something, for someone, to do something that will alter the course of their lives.
Of course, what I can offer my patients usually falls short of their lofty expectations of my prowess. I offer them compassion, validation, empathy. I offer them medications for which we usually have meager data and meager results. I cannot find them shelter but for a few nights, perhaps a week. I rarely, in settings in which primary diagnoses of substance use and personality disorders are forbidden by insurance companies, can help them with their addiction to methamphetamine. I cannot cure their maladaptive characterological pathology stemming from childhood attachment trauma. To address my own sense of failure as a healer, I resort to the bottom of Maslow’s hierarchy of needs, providing their choice of juice box, more blankets. I slow-roll their discharges overnight so that they can stay in the ER hallway instead of spending the night outside in the rare Southern California rain.
In my 3rd year of residency, we were thrown into a pandemic. I felt both terrified of getting COVID-19 in the hospital and inadequate as a physician. I did not want to be intubating patients, but even more, I dreaded the potential “psychiatry-friendly” assignment of calling the family members of those who had perished from the disease. Rumors circulated that certain versions of surge planning had the inpatient psychiatry unit transitioned to a COVID unit and psychiatry residents “redeployed” to cover medicine floors. Fortunately, we did not have to (or have not yet had to) endure this apocalyptic episode of worst-case scenario. I remained a psychiatrist-in-training, seeing occasional COVID patients but with full personal protective equipment and the ability to maintain some physical distance to complete my examinations. Coming home to my apartment building in scrubs, now acceptable attire on inpatient units – it always should have been since, as we have established, our units are filled with feces – I early on felt like a leper. Later on, I was treated with dignity and respect, like a hero.
My position as a non–frontline-physician was personally challenging. I wanted to help, felt like I should and could help. I am a helper-in-recovery who has spent years learning to achieve a balance of service and loyalty to others and my own desires. The initial guilt I felt at feeling appreciated during the nightly celebration of health care workers downtown ultimately dissipated. I was no hero, nor did I claim to be one. I made peace with my pandemic hobbies of sourdough bread-baking, Moscow mule-making, jigsaw-puzzling, and, briefly, running (before a calcaneal stress fracture reminded me that I am not built for land exercise). I went to work; I came home. My cat was happy.
Then, in rapid succession, vaccines were approved and distributed. My hospital had partnered with the county to administer them at a new superstation, and they were in desperate need of licensed humans to be vaccinators. They cared not that I had given very few (n = 3) injections and only during medical school. I watched the YouTube videos on the Z-track technique for IMs, learned about needle gauges, and went off to the baseball stadium.
I loved this new gig, disproportionately. The 8+ hours flew by, 100 vaccines given to occupants of cars who had eagerly waited hours for the privilege of being vaccinated by an almost-psychiatrist. It was not the technical expertise of sticking a needle into someone’s arm that gave me a dopamine rush, nor the microstress of preparing the syringes with a flimsy needle and a slight caffeine-induced tremor while trying to flick air bubbles out of the syringe without dropping the precious vaccine vial. It was not the travel nurse asking me why anyone – especially an overworked resident – would volunteer to do this for free, while she and others were making “stupid amounts of money” to do the same job.
What drove me to keep volunteering for no pay, only Cheez-Its available as sustenance, minimal gratitude from my employer, long hours on my feet doing a task that was rote and at which I probably would never completely excel? On my second shift, I realized why I found it so gratifying to be a vaccinator: There was a perfect 1:1 correspondence in what patients wanted at that moment and in what I had to offer them. They did not want me to fix their lives, secure them housing, or go back in time and remove them from abusive homes so they could grow up to be more functional, happier adults. They merely wanted a shot. They were profusely grateful, hopeful that this was the Beginning of the End. Nobody spat on me; nobody called me obscene names. Nobody was upset with me for involuntarily holding them against their will. My services were welcome, appreciated. I had lovely, superficial conversations with dozens of people. I felt connected to strangers in a way that has been sorely lacking since March 2020. Understandably mistaken for a nurse throughout the day, I felt more like a bona fide physician than I had in over a year.
I know the adrenaline rush will fade, that volunteer-vaccinating in my free time will eventually become less exciting to me. I know I won’t be able to convince my colleagues indefinitely that volunteering together is a great, institution-sanctioned bonding opportunity. I know the initial enthusiasm over vaccine distribution will fade as the pandemic continues to transform our everyday lives and threaten the health of millions, the economy, and the sanctity of normal human interactions. The gratitude and hopefulness may well be replaced with frustration over waiting hours in a car to get an injection from a psychiatrist, with fear that this promised panacea may not restore normalcy anytime soon. But right now, 11 months into a pandemic that has left our profession exhausted and jaded, the coprophilia and catatonia have temporarily lost their allure. So, I’m adding “vaccinator” to my list of pandemic hobbies.
Dr. Stone is a chief resident in psychiatry at the University of California, San Diego. Before deciding to become a physician, she obtained a master’s degree in public health and worked in health policy research studying empathy and patient-doctor interactions. She has a passion for public psychiatry and acute care, and she dabbles in physician wellness, medical education, and the interface of psychiatry and primary care. Dr. Stone has no disclosures.
Psychiatrist recounts haunting ordeal with an anonymous stalker
Looking back on his experience of being stalked by a former patient for nearly 1 year, William J. Newman, MD, regrets not reaching out to colleagues about the patient boundary violations earlier than he did.
“My mindset was: ‘Maybe I did something wrong that created this,’ ” Dr. Newman, professor and interim chair of psychiatry at Saint Louis University, said during an annual psychopharmacology update held by the Nevada Psychiatric Association. “That’s a common theme among victims of stalking, being kind of embarrassed and not wanting to share it with other people.”
Dr. Newman’s ordeal began in August 2014, when the first of several threatening emails messages were sent to his account at the University of California, Davis, where he held a faculty post and worked on the teaching service at the Sacramento Mental Health Treatment Center, a county hospital that serves mainly uninsured or underinsured populations. The messages always contained a nonspecific email recipient name and the first wasn’t terribly worrisome, Dr. Newman said. It basically read (profanities excluded): “What is wrong with you? Leave me alone. All I want is some privacy.”
About 3 months later, he received another message in a similar writing pattern, but the name of the sender was “god devil,” which raised a red flag to him. “Once you start to get religious concepts, people are compelled to commit acts when they believe they’re doing so beyond the laws of the land and are doing so for a religious purpose,” said Dr. Newman, who is immediate past president of the American Academy of Psychiatry and the Law.
The content of the message contained the first name of a coworker and phrasing inferring suicide, which gave Dr. Newman a hint that it was someone he had cared for at the mental health treatment center, “but as anybody who has worked on a busy inpatient service can tell you, you encounter several suicidal patients, and this didn’t really narrow it down,” he said. “This told me the person had presented after a suicide attempt. In some ways, that made me a little more concerned, because because they don’t really worry about the consequences of being shot by law enforcement or dying in an attack.”
Dr. Newman contacted the university’s information technology team, which was able to trace all messages to an IP address from a computer located at a downtown branch of the public library, which had surveillance video. Armed with this information, he contacted the Sacramento Police Department to see if they would help. He had “what I can only describe as an unsatisfying and somewhat condescending conversation with an officer, who said: ‘Sir, we can’t just go around asking people questions without knowing they did something wrong. There’s nothing we’re going to do.’ ”
Between November 2014 and May 2015, Dr. Newman continued to receive periodic messages from the individual of varied length and intensity.
“Some messages were more disorganized and difficult to follow, while others were very intense and pointed about my imminent death,” he recalled. “I started to ignore these messages as much as possible, tried to put my head in the sand and move forward.”
However, one phrase contained in a message read “you won’t even recognize me,” which gave Dr. Newman pause. “It highlighted the idea that because I don’t know who this is, they could walk up to me on the sidewalk, and I would have no idea, which in its own right is somewhat terrorizing.”
At this point, he contacted the police again, telling them he was fearful for his imminent safety. He also met with his department chair and administrators, who helped Dr. Newman develop a plan to enter and exit the hospital at different times. Then, in May 2015, the stalker sent Dr. Newman another email message threatening not only his life, but the lives of his colleagues at the hospital.
“This was viewed as a terroristic threat, because [it inferred that] other people were going to be shot other than just me,” he said.
After this, Dr. Newman’s administrators contacted the police about the threat, who identified the individual through video surveillance footage at the public library and began to search for him. It was a patient who had been on testosterone and previously had sent similar messages to another mental health provider in town and wound up showing up at that person’s office with a loaded firearm.
“At that point, the police were called to the scene, picked the individual up, and took him to a local emergency room where he was placed on an involuntary 5150 psychiatric hold,” he said. “It was frustrating to me that this was very much minimized and kind of put to the side.”
Once he learned the stalker’s name, Dr. Newman had no recollection of the individual. “The patient had presented after a carbon monoxide overdose, had been sent to a local emergency room and came to my service,” he said. “It was a very nonconfrontational hospitalization, nothing out of the ordinary.”
At this point, the stalker was still at large, so Dr. Newman wrote farewell notes to his wife, children, and loved ones, “just in case,” he said. “I had those tucked away. That wasn’t an overly pleasant experience.” He also lived away from his family outside of Sacramento while police searched for his stalker.
In late May 2015, police located and arrested the individual, and Dr. Newman began a series of conversations with the District Attorney’s office. “They told me there were seven terroristic threat charges that had been levied. They said they were taking this very seriously and [that the case] would be going to trial.” About 1 year later, after Dr. Newman’s move to Missouri, the District Attorney indicated that there would be a court trial and that Dr. Newman would be asked to serve as a fact witness. “I gave them all the information I had, talked to investigators, and the process was moving along for about a year to the point that they had an anticipated trial date,” he said. About 1 year later, he received an automated phone message which stated that the individual had been released from jail. He called the District Attorney to ask what happened.
“He said the judge didn’t really want to deal with this [case] anymore, and accepted a plea with time served and released him,” Dr. Newman said. “That was the outcome of the situation.”
According to a 1997 study of 100 stalking victims, 94% made major lifestyle changes after their ordeal, 82% modified usual activities, 73% increased security measures, 70% curtailed social outings, 53% decreased/stopped work or school, and 39% relocated. “You do change a lot of what you do and how you do it in your life when you’ve had this experience, especially when it’s been a chronic experience for months or years,” said Dr. Newman, who is also medical director of adult psychiatric inpatient services for Saint Louis University. “To this day I get antsy any time I think about the story or prepare to talk about it. It remains uncomfortable even 6 years later, even without an ongoing direct threat at this point.”
The physiological impact of chronic stalking also takes its toll. The body releases adrenaline and cortisol as part of the fight or flight response, while chronic stress “is when you feel an increased stress response and have adrenaline and cortisol elevated for an extended period of time,” he said. “There are negative impacts in terms of increased inflammation in the body and in the brain. I have spoken to several professionals who have been stalked by former patients. Commonly, they have been diagnosed in the period after that with an autoimmune illness or a cancer. Less than a year after my stalking situation ended, I was diagnosed with a metastatic cancer and had to start chemotherapy. I would not at all be surprised that those things are highly related to one another.”
When patient boundary violations start to become problematic or worrisome, Dr. Newman advised reaching out to colleagues and law enforcement for help. “Don’t let it go on insidiously for an extended period of time,” he said. “I think that was the biggest lesson I learned.”
He reported having no financial disclosures.
Looking back on his experience of being stalked by a former patient for nearly 1 year, William J. Newman, MD, regrets not reaching out to colleagues about the patient boundary violations earlier than he did.
“My mindset was: ‘Maybe I did something wrong that created this,’ ” Dr. Newman, professor and interim chair of psychiatry at Saint Louis University, said during an annual psychopharmacology update held by the Nevada Psychiatric Association. “That’s a common theme among victims of stalking, being kind of embarrassed and not wanting to share it with other people.”
Dr. Newman’s ordeal began in August 2014, when the first of several threatening emails messages were sent to his account at the University of California, Davis, where he held a faculty post and worked on the teaching service at the Sacramento Mental Health Treatment Center, a county hospital that serves mainly uninsured or underinsured populations. The messages always contained a nonspecific email recipient name and the first wasn’t terribly worrisome, Dr. Newman said. It basically read (profanities excluded): “What is wrong with you? Leave me alone. All I want is some privacy.”
About 3 months later, he received another message in a similar writing pattern, but the name of the sender was “god devil,” which raised a red flag to him. “Once you start to get religious concepts, people are compelled to commit acts when they believe they’re doing so beyond the laws of the land and are doing so for a religious purpose,” said Dr. Newman, who is immediate past president of the American Academy of Psychiatry and the Law.
The content of the message contained the first name of a coworker and phrasing inferring suicide, which gave Dr. Newman a hint that it was someone he had cared for at the mental health treatment center, “but as anybody who has worked on a busy inpatient service can tell you, you encounter several suicidal patients, and this didn’t really narrow it down,” he said. “This told me the person had presented after a suicide attempt. In some ways, that made me a little more concerned, because because they don’t really worry about the consequences of being shot by law enforcement or dying in an attack.”
Dr. Newman contacted the university’s information technology team, which was able to trace all messages to an IP address from a computer located at a downtown branch of the public library, which had surveillance video. Armed with this information, he contacted the Sacramento Police Department to see if they would help. He had “what I can only describe as an unsatisfying and somewhat condescending conversation with an officer, who said: ‘Sir, we can’t just go around asking people questions without knowing they did something wrong. There’s nothing we’re going to do.’ ”
Between November 2014 and May 2015, Dr. Newman continued to receive periodic messages from the individual of varied length and intensity.
“Some messages were more disorganized and difficult to follow, while others were very intense and pointed about my imminent death,” he recalled. “I started to ignore these messages as much as possible, tried to put my head in the sand and move forward.”
However, one phrase contained in a message read “you won’t even recognize me,” which gave Dr. Newman pause. “It highlighted the idea that because I don’t know who this is, they could walk up to me on the sidewalk, and I would have no idea, which in its own right is somewhat terrorizing.”
At this point, he contacted the police again, telling them he was fearful for his imminent safety. He also met with his department chair and administrators, who helped Dr. Newman develop a plan to enter and exit the hospital at different times. Then, in May 2015, the stalker sent Dr. Newman another email message threatening not only his life, but the lives of his colleagues at the hospital.
“This was viewed as a terroristic threat, because [it inferred that] other people were going to be shot other than just me,” he said.
After this, Dr. Newman’s administrators contacted the police about the threat, who identified the individual through video surveillance footage at the public library and began to search for him. It was a patient who had been on testosterone and previously had sent similar messages to another mental health provider in town and wound up showing up at that person’s office with a loaded firearm.
“At that point, the police were called to the scene, picked the individual up, and took him to a local emergency room where he was placed on an involuntary 5150 psychiatric hold,” he said. “It was frustrating to me that this was very much minimized and kind of put to the side.”
Once he learned the stalker’s name, Dr. Newman had no recollection of the individual. “The patient had presented after a carbon monoxide overdose, had been sent to a local emergency room and came to my service,” he said. “It was a very nonconfrontational hospitalization, nothing out of the ordinary.”
At this point, the stalker was still at large, so Dr. Newman wrote farewell notes to his wife, children, and loved ones, “just in case,” he said. “I had those tucked away. That wasn’t an overly pleasant experience.” He also lived away from his family outside of Sacramento while police searched for his stalker.
In late May 2015, police located and arrested the individual, and Dr. Newman began a series of conversations with the District Attorney’s office. “They told me there were seven terroristic threat charges that had been levied. They said they were taking this very seriously and [that the case] would be going to trial.” About 1 year later, after Dr. Newman’s move to Missouri, the District Attorney indicated that there would be a court trial and that Dr. Newman would be asked to serve as a fact witness. “I gave them all the information I had, talked to investigators, and the process was moving along for about a year to the point that they had an anticipated trial date,” he said. About 1 year later, he received an automated phone message which stated that the individual had been released from jail. He called the District Attorney to ask what happened.
“He said the judge didn’t really want to deal with this [case] anymore, and accepted a plea with time served and released him,” Dr. Newman said. “That was the outcome of the situation.”
According to a 1997 study of 100 stalking victims, 94% made major lifestyle changes after their ordeal, 82% modified usual activities, 73% increased security measures, 70% curtailed social outings, 53% decreased/stopped work or school, and 39% relocated. “You do change a lot of what you do and how you do it in your life when you’ve had this experience, especially when it’s been a chronic experience for months or years,” said Dr. Newman, who is also medical director of adult psychiatric inpatient services for Saint Louis University. “To this day I get antsy any time I think about the story or prepare to talk about it. It remains uncomfortable even 6 years later, even without an ongoing direct threat at this point.”
The physiological impact of chronic stalking also takes its toll. The body releases adrenaline and cortisol as part of the fight or flight response, while chronic stress “is when you feel an increased stress response and have adrenaline and cortisol elevated for an extended period of time,” he said. “There are negative impacts in terms of increased inflammation in the body and in the brain. I have spoken to several professionals who have been stalked by former patients. Commonly, they have been diagnosed in the period after that with an autoimmune illness or a cancer. Less than a year after my stalking situation ended, I was diagnosed with a metastatic cancer and had to start chemotherapy. I would not at all be surprised that those things are highly related to one another.”
When patient boundary violations start to become problematic or worrisome, Dr. Newman advised reaching out to colleagues and law enforcement for help. “Don’t let it go on insidiously for an extended period of time,” he said. “I think that was the biggest lesson I learned.”
He reported having no financial disclosures.
Looking back on his experience of being stalked by a former patient for nearly 1 year, William J. Newman, MD, regrets not reaching out to colleagues about the patient boundary violations earlier than he did.
“My mindset was: ‘Maybe I did something wrong that created this,’ ” Dr. Newman, professor and interim chair of psychiatry at Saint Louis University, said during an annual psychopharmacology update held by the Nevada Psychiatric Association. “That’s a common theme among victims of stalking, being kind of embarrassed and not wanting to share it with other people.”
Dr. Newman’s ordeal began in August 2014, when the first of several threatening emails messages were sent to his account at the University of California, Davis, where he held a faculty post and worked on the teaching service at the Sacramento Mental Health Treatment Center, a county hospital that serves mainly uninsured or underinsured populations. The messages always contained a nonspecific email recipient name and the first wasn’t terribly worrisome, Dr. Newman said. It basically read (profanities excluded): “What is wrong with you? Leave me alone. All I want is some privacy.”
About 3 months later, he received another message in a similar writing pattern, but the name of the sender was “god devil,” which raised a red flag to him. “Once you start to get religious concepts, people are compelled to commit acts when they believe they’re doing so beyond the laws of the land and are doing so for a religious purpose,” said Dr. Newman, who is immediate past president of the American Academy of Psychiatry and the Law.
The content of the message contained the first name of a coworker and phrasing inferring suicide, which gave Dr. Newman a hint that it was someone he had cared for at the mental health treatment center, “but as anybody who has worked on a busy inpatient service can tell you, you encounter several suicidal patients, and this didn’t really narrow it down,” he said. “This told me the person had presented after a suicide attempt. In some ways, that made me a little more concerned, because because they don’t really worry about the consequences of being shot by law enforcement or dying in an attack.”
Dr. Newman contacted the university’s information technology team, which was able to trace all messages to an IP address from a computer located at a downtown branch of the public library, which had surveillance video. Armed with this information, he contacted the Sacramento Police Department to see if they would help. He had “what I can only describe as an unsatisfying and somewhat condescending conversation with an officer, who said: ‘Sir, we can’t just go around asking people questions without knowing they did something wrong. There’s nothing we’re going to do.’ ”
Between November 2014 and May 2015, Dr. Newman continued to receive periodic messages from the individual of varied length and intensity.
“Some messages were more disorganized and difficult to follow, while others were very intense and pointed about my imminent death,” he recalled. “I started to ignore these messages as much as possible, tried to put my head in the sand and move forward.”
However, one phrase contained in a message read “you won’t even recognize me,” which gave Dr. Newman pause. “It highlighted the idea that because I don’t know who this is, they could walk up to me on the sidewalk, and I would have no idea, which in its own right is somewhat terrorizing.”
At this point, he contacted the police again, telling them he was fearful for his imminent safety. He also met with his department chair and administrators, who helped Dr. Newman develop a plan to enter and exit the hospital at different times. Then, in May 2015, the stalker sent Dr. Newman another email message threatening not only his life, but the lives of his colleagues at the hospital.
“This was viewed as a terroristic threat, because [it inferred that] other people were going to be shot other than just me,” he said.
After this, Dr. Newman’s administrators contacted the police about the threat, who identified the individual through video surveillance footage at the public library and began to search for him. It was a patient who had been on testosterone and previously had sent similar messages to another mental health provider in town and wound up showing up at that person’s office with a loaded firearm.
“At that point, the police were called to the scene, picked the individual up, and took him to a local emergency room where he was placed on an involuntary 5150 psychiatric hold,” he said. “It was frustrating to me that this was very much minimized and kind of put to the side.”
Once he learned the stalker’s name, Dr. Newman had no recollection of the individual. “The patient had presented after a carbon monoxide overdose, had been sent to a local emergency room and came to my service,” he said. “It was a very nonconfrontational hospitalization, nothing out of the ordinary.”
At this point, the stalker was still at large, so Dr. Newman wrote farewell notes to his wife, children, and loved ones, “just in case,” he said. “I had those tucked away. That wasn’t an overly pleasant experience.” He also lived away from his family outside of Sacramento while police searched for his stalker.
In late May 2015, police located and arrested the individual, and Dr. Newman began a series of conversations with the District Attorney’s office. “They told me there were seven terroristic threat charges that had been levied. They said they were taking this very seriously and [that the case] would be going to trial.” About 1 year later, after Dr. Newman’s move to Missouri, the District Attorney indicated that there would be a court trial and that Dr. Newman would be asked to serve as a fact witness. “I gave them all the information I had, talked to investigators, and the process was moving along for about a year to the point that they had an anticipated trial date,” he said. About 1 year later, he received an automated phone message which stated that the individual had been released from jail. He called the District Attorney to ask what happened.
“He said the judge didn’t really want to deal with this [case] anymore, and accepted a plea with time served and released him,” Dr. Newman said. “That was the outcome of the situation.”
According to a 1997 study of 100 stalking victims, 94% made major lifestyle changes after their ordeal, 82% modified usual activities, 73% increased security measures, 70% curtailed social outings, 53% decreased/stopped work or school, and 39% relocated. “You do change a lot of what you do and how you do it in your life when you’ve had this experience, especially when it’s been a chronic experience for months or years,” said Dr. Newman, who is also medical director of adult psychiatric inpatient services for Saint Louis University. “To this day I get antsy any time I think about the story or prepare to talk about it. It remains uncomfortable even 6 years later, even without an ongoing direct threat at this point.”
The physiological impact of chronic stalking also takes its toll. The body releases adrenaline and cortisol as part of the fight or flight response, while chronic stress “is when you feel an increased stress response and have adrenaline and cortisol elevated for an extended period of time,” he said. “There are negative impacts in terms of increased inflammation in the body and in the brain. I have spoken to several professionals who have been stalked by former patients. Commonly, they have been diagnosed in the period after that with an autoimmune illness or a cancer. Less than a year after my stalking situation ended, I was diagnosed with a metastatic cancer and had to start chemotherapy. I would not at all be surprised that those things are highly related to one another.”
When patient boundary violations start to become problematic or worrisome, Dr. Newman advised reaching out to colleagues and law enforcement for help. “Don’t let it go on insidiously for an extended period of time,” he said. “I think that was the biggest lesson I learned.”
He reported having no financial disclosures.
FROM NPA 2021
ColCORONA: More questions than answers for colchicine in COVID-19
Science by press release and preprint has cooled clinician enthusiasm for the use of colchicine in nonhospitalized patients with COVID-19, despite a pressing need for early treatments.
As previously reported by this news organization, a Jan. 22 press release announced that the massive ColCORONA study missed its primary endpoint of hospitalization or death among 4,488 newly diagnosed patients at increased risk for hospitalization.
But it also touted that use of the anti-inflammatory drug significantly reduced the primary endpoint in 4,159 of those patients with polymerase chain reaction–confirmed COVID and led to reductions of 25%, 50%, and 44%, respectively, for hospitalizations, ventilations, and death.
Lead investigator Jean-Claude Tardif, MD, director of the Montreal Heart Institute Research Centre, deemed the findings a “medical breakthrough.”
When the preprint released a few days later, however, newly revealed confidence intervals showed colchicine did not meaningfully reduce the need for mechanical ventilation (odds ratio, 0.50; 95% confidence interval, 0.23-1.07) or death alone (OR, 0.56; 95% CI, 0.19-1.66).
Further, the significant benefit on the primary outcome came at the cost of a fivefold increase in pulmonary embolism (11 vs. 2; P = .01), which was not mentioned in the press release.
“Whether this represents a real phenomenon or simply the play of chance is not known,” Dr. Tardif and colleagues noted later in the preprint.
“I read the preprint on colchicine and I have so many questions,” Aaron E. Glatt, MD, spokesperson for the Infectious Diseases Society of America and chief of infectious diseases, Mount Sinai South Nassau, Hewlett, N.Y., said in an interview. “I’ve been burned too many times with COVID and prefer to see better data.
“People sometimes say if you wait for perfect data, people are going to die,” he said. “Yeah, but we have no idea if people are going to die from getting this drug more than not getting it. That’s what concerns me. How many pulmonary emboli are going to be fatal versus the slight benefit that the study showed?”
The pushback to the non–peer-reviewed data on social media and via emails was so strong that Dr. Tardif posted a nearly 2,000-word letter responding to the many questions at play.
Chief among them was why the trial, originally planned for 6,000 patients, was stopped early by the investigators without consultation with the data safety monitoring board (DSMB).
The explanation in the letter that logistical issues like running the study call center, budget constraints, and a perceived need to quickly communicate the results left some calling foul that the study wasn’t allowed to finish and come to a more definitive conclusion.
“I can be a little bit sympathetic to their cause but at the same time the DSMB should have said no,” said David Boulware, MD, MPH, who led a recent hydroxychloroquine trial in COVID-19. “The problem is we’re sort of left in limbo, where some people kind of believe it and some say it’s not really a thing. So it’s not really moving the needle, as far as guidelines go.”
Indeed, a Twitter poll by cardiologist James Januzzi Jr., MD, captured the uncertainty, with 28% of respondents saying the trial was “neutral,” 58% saying “maybe but meh,” and 14% saying “colchicine for all.”
Another poll cheekily asked whether ColCORONA was the Gamestop/Reddit equivalent of COVID.
“The press release really didn’t help things because it very much oversold the effect. That, I think, poisoned the well,” said Dr. Boulware, professor of medicine in infectious diseases at the University of Minnesota, Minneapolis.
“The question I’m left with is not whether colchicine works, but who does it work in,” he said. “That’s really the fundamental question because it does seem that there are probably high-risk groups in their trial and others where they benefit, whereas other groups don’t benefit. In the subgroup analysis, there was absolutely no beneficial effect in women.”
According to the authors, the number needed to treat to prevent one death or hospitalization was 71 overall, but 29 for patients with diabetes, 31 for those aged 70 years and older, 53 for patients with respiratory disease, and 25 for those with coronary disease or heart failure.
Men are at higher risk overall for poor outcomes. But “the authors didn’t present a multivariable analysis, so it is unclear if another factor, such as a differential prevalence of smoking or cardiovascular risk factors, contributed to the differential benefit,” Rachel Bender Ignacio, MD, MPH, infectious disease specialist, University of Washington, Seattle, said in an interview.
Importantly, in this pragmatic study, duration and severity of symptoms were not reported, observed Dr. Bender Ignacio, who is also a STOP-COVID-2 investigator. “We don’t yet have data as to whether colchicine shortens duration or severity of symptoms or prevents long COVID, so we need more data on that.”
The overall risk for serious adverse events was lower in the colchicine group, but the difference in pulmonary embolism (PE) was striking, she said. This could be caused by a real biologic effect, or it’s possible that persons with shortness of breath and hypoxia, without evident viral pneumonia on chest x-ray after a positive COVID-19 test, were more likely to receive a CT-PE study.
The press release also failed to include information, later noted in the preprint, that the MHI has submitted two patents related to colchicine: “Methods of treating a coronavirus infection using colchicine” and “Early administration of low-dose colchicine after myocardial infarction.”
Reached for clarification, MHI communications adviser Camille Turbide said in an interview that the first patent “simply refers to the novel concept of preventing complications of COVID-19, such as admission to the hospital, with colchicine as tested in the ColCORONA study.”
The second patent, she said, refers to the “novel concept that administering colchicine early after a major adverse cardiovascular event is better than waiting several days,” as supported by the COLCOT study, which Dr. Tardif also led.
The patents are being reviewed by authorities and “Dr. Tardif has waived his rights in these patents and does not stand to benefit financially at all if colchicine becomes used as a treatment for COVID-19,” Ms. Turbide said.
Dr. Tardif did not respond to interview requests for this story. Dr. Glatt said conflicts of interest must be assessed and are “something that is of great concern in any scientific study.”
Cardiologist Steve Nissen, MD, of the Cleveland Clinic said in an interview that, “despite the negative results, the study does suggest that colchicine might have a benefit and should be studied in future trials. These findings are not sufficient evidence to suggest use of the drug in patients infected with COVID-19.”
He noted that adverse effects like diarrhea were expected but that the excess PE was unexpected and needs greater clarification.
“Stopping the trial for administrative reasons is puzzling and undermined the ability of the trial to give a reliable answer,” Dr. Nissen said. “This is a reasonable pilot study that should be viewed as hypothesis generating but inconclusive.”
Several sources said a new trial is unlikely, particularly given the cost and 28 trials already evaluating colchicine. Among these are RECOVERY and COLCOVID, testing whether colchicine can reduce the duration of hospitalization or death in hospitalized patients with COVID-19.
Because there are so many trials ongoing right now, including for antivirals and other immunomodulators, it’s important that, if colchicine comes to routine clinical use, it provides access to treatment for those not able or willing to access clinical trials, rather than impeding clinical trial enrollment, Dr. Bender Ignacio suggested.
“We have already learned the lesson in the pandemic that early adoption of potentially promising therapies can negatively impact our ability to study and develop other promising treatments,” she said.
The trial was coordinated by the Montreal Heart Institute and funded by the government of Quebec; the National Heart, Lung, and Blood Institute of the National Institutes of Health; Montreal philanthropist Sophie Desmarais, and the COVID-19 Therapeutics Accelerator launched by the Bill & Melinda Gates Foundation, Wellcome, and Mastercard. CGI, Dacima, and Pharmascience of Montreal were also collaborators. Dr. Glatt reported no conflicts of interest. Dr. Boulware reported receiving $18 in food and beverages from Gilead Sciences in 2018.
A version of this article first appeared on Medscape.com.
Science by press release and preprint has cooled clinician enthusiasm for the use of colchicine in nonhospitalized patients with COVID-19, despite a pressing need for early treatments.
As previously reported by this news organization, a Jan. 22 press release announced that the massive ColCORONA study missed its primary endpoint of hospitalization or death among 4,488 newly diagnosed patients at increased risk for hospitalization.
But it also touted that use of the anti-inflammatory drug significantly reduced the primary endpoint in 4,159 of those patients with polymerase chain reaction–confirmed COVID and led to reductions of 25%, 50%, and 44%, respectively, for hospitalizations, ventilations, and death.
Lead investigator Jean-Claude Tardif, MD, director of the Montreal Heart Institute Research Centre, deemed the findings a “medical breakthrough.”
When the preprint released a few days later, however, newly revealed confidence intervals showed colchicine did not meaningfully reduce the need for mechanical ventilation (odds ratio, 0.50; 95% confidence interval, 0.23-1.07) or death alone (OR, 0.56; 95% CI, 0.19-1.66).
Further, the significant benefit on the primary outcome came at the cost of a fivefold increase in pulmonary embolism (11 vs. 2; P = .01), which was not mentioned in the press release.
“Whether this represents a real phenomenon or simply the play of chance is not known,” Dr. Tardif and colleagues noted later in the preprint.
“I read the preprint on colchicine and I have so many questions,” Aaron E. Glatt, MD, spokesperson for the Infectious Diseases Society of America and chief of infectious diseases, Mount Sinai South Nassau, Hewlett, N.Y., said in an interview. “I’ve been burned too many times with COVID and prefer to see better data.
“People sometimes say if you wait for perfect data, people are going to die,” he said. “Yeah, but we have no idea if people are going to die from getting this drug more than not getting it. That’s what concerns me. How many pulmonary emboli are going to be fatal versus the slight benefit that the study showed?”
The pushback to the non–peer-reviewed data on social media and via emails was so strong that Dr. Tardif posted a nearly 2,000-word letter responding to the many questions at play.
Chief among them was why the trial, originally planned for 6,000 patients, was stopped early by the investigators without consultation with the data safety monitoring board (DSMB).
The explanation in the letter that logistical issues like running the study call center, budget constraints, and a perceived need to quickly communicate the results left some calling foul that the study wasn’t allowed to finish and come to a more definitive conclusion.
“I can be a little bit sympathetic to their cause but at the same time the DSMB should have said no,” said David Boulware, MD, MPH, who led a recent hydroxychloroquine trial in COVID-19. “The problem is we’re sort of left in limbo, where some people kind of believe it and some say it’s not really a thing. So it’s not really moving the needle, as far as guidelines go.”
Indeed, a Twitter poll by cardiologist James Januzzi Jr., MD, captured the uncertainty, with 28% of respondents saying the trial was “neutral,” 58% saying “maybe but meh,” and 14% saying “colchicine for all.”
Another poll cheekily asked whether ColCORONA was the Gamestop/Reddit equivalent of COVID.
“The press release really didn’t help things because it very much oversold the effect. That, I think, poisoned the well,” said Dr. Boulware, professor of medicine in infectious diseases at the University of Minnesota, Minneapolis.
“The question I’m left with is not whether colchicine works, but who does it work in,” he said. “That’s really the fundamental question because it does seem that there are probably high-risk groups in their trial and others where they benefit, whereas other groups don’t benefit. In the subgroup analysis, there was absolutely no beneficial effect in women.”
According to the authors, the number needed to treat to prevent one death or hospitalization was 71 overall, but 29 for patients with diabetes, 31 for those aged 70 years and older, 53 for patients with respiratory disease, and 25 for those with coronary disease or heart failure.
Men are at higher risk overall for poor outcomes. But “the authors didn’t present a multivariable analysis, so it is unclear if another factor, such as a differential prevalence of smoking or cardiovascular risk factors, contributed to the differential benefit,” Rachel Bender Ignacio, MD, MPH, infectious disease specialist, University of Washington, Seattle, said in an interview.
Importantly, in this pragmatic study, duration and severity of symptoms were not reported, observed Dr. Bender Ignacio, who is also a STOP-COVID-2 investigator. “We don’t yet have data as to whether colchicine shortens duration or severity of symptoms or prevents long COVID, so we need more data on that.”
The overall risk for serious adverse events was lower in the colchicine group, but the difference in pulmonary embolism (PE) was striking, she said. This could be caused by a real biologic effect, or it’s possible that persons with shortness of breath and hypoxia, without evident viral pneumonia on chest x-ray after a positive COVID-19 test, were more likely to receive a CT-PE study.
The press release also failed to include information, later noted in the preprint, that the MHI has submitted two patents related to colchicine: “Methods of treating a coronavirus infection using colchicine” and “Early administration of low-dose colchicine after myocardial infarction.”
Reached for clarification, MHI communications adviser Camille Turbide said in an interview that the first patent “simply refers to the novel concept of preventing complications of COVID-19, such as admission to the hospital, with colchicine as tested in the ColCORONA study.”
The second patent, she said, refers to the “novel concept that administering colchicine early after a major adverse cardiovascular event is better than waiting several days,” as supported by the COLCOT study, which Dr. Tardif also led.
The patents are being reviewed by authorities and “Dr. Tardif has waived his rights in these patents and does not stand to benefit financially at all if colchicine becomes used as a treatment for COVID-19,” Ms. Turbide said.
Dr. Tardif did not respond to interview requests for this story. Dr. Glatt said conflicts of interest must be assessed and are “something that is of great concern in any scientific study.”
Cardiologist Steve Nissen, MD, of the Cleveland Clinic said in an interview that, “despite the negative results, the study does suggest that colchicine might have a benefit and should be studied in future trials. These findings are not sufficient evidence to suggest use of the drug in patients infected with COVID-19.”
He noted that adverse effects like diarrhea were expected but that the excess PE was unexpected and needs greater clarification.
“Stopping the trial for administrative reasons is puzzling and undermined the ability of the trial to give a reliable answer,” Dr. Nissen said. “This is a reasonable pilot study that should be viewed as hypothesis generating but inconclusive.”
Several sources said a new trial is unlikely, particularly given the cost and 28 trials already evaluating colchicine. Among these are RECOVERY and COLCOVID, testing whether colchicine can reduce the duration of hospitalization or death in hospitalized patients with COVID-19.
Because there are so many trials ongoing right now, including for antivirals and other immunomodulators, it’s important that, if colchicine comes to routine clinical use, it provides access to treatment for those not able or willing to access clinical trials, rather than impeding clinical trial enrollment, Dr. Bender Ignacio suggested.
“We have already learned the lesson in the pandemic that early adoption of potentially promising therapies can negatively impact our ability to study and develop other promising treatments,” she said.
The trial was coordinated by the Montreal Heart Institute and funded by the government of Quebec; the National Heart, Lung, and Blood Institute of the National Institutes of Health; Montreal philanthropist Sophie Desmarais, and the COVID-19 Therapeutics Accelerator launched by the Bill & Melinda Gates Foundation, Wellcome, and Mastercard. CGI, Dacima, and Pharmascience of Montreal were also collaborators. Dr. Glatt reported no conflicts of interest. Dr. Boulware reported receiving $18 in food and beverages from Gilead Sciences in 2018.
A version of this article first appeared on Medscape.com.
Science by press release and preprint has cooled clinician enthusiasm for the use of colchicine in nonhospitalized patients with COVID-19, despite a pressing need for early treatments.
As previously reported by this news organization, a Jan. 22 press release announced that the massive ColCORONA study missed its primary endpoint of hospitalization or death among 4,488 newly diagnosed patients at increased risk for hospitalization.
But it also touted that use of the anti-inflammatory drug significantly reduced the primary endpoint in 4,159 of those patients with polymerase chain reaction–confirmed COVID and led to reductions of 25%, 50%, and 44%, respectively, for hospitalizations, ventilations, and death.
Lead investigator Jean-Claude Tardif, MD, director of the Montreal Heart Institute Research Centre, deemed the findings a “medical breakthrough.”
When the preprint released a few days later, however, newly revealed confidence intervals showed colchicine did not meaningfully reduce the need for mechanical ventilation (odds ratio, 0.50; 95% confidence interval, 0.23-1.07) or death alone (OR, 0.56; 95% CI, 0.19-1.66).
Further, the significant benefit on the primary outcome came at the cost of a fivefold increase in pulmonary embolism (11 vs. 2; P = .01), which was not mentioned in the press release.
“Whether this represents a real phenomenon or simply the play of chance is not known,” Dr. Tardif and colleagues noted later in the preprint.
“I read the preprint on colchicine and I have so many questions,” Aaron E. Glatt, MD, spokesperson for the Infectious Diseases Society of America and chief of infectious diseases, Mount Sinai South Nassau, Hewlett, N.Y., said in an interview. “I’ve been burned too many times with COVID and prefer to see better data.
“People sometimes say if you wait for perfect data, people are going to die,” he said. “Yeah, but we have no idea if people are going to die from getting this drug more than not getting it. That’s what concerns me. How many pulmonary emboli are going to be fatal versus the slight benefit that the study showed?”
The pushback to the non–peer-reviewed data on social media and via emails was so strong that Dr. Tardif posted a nearly 2,000-word letter responding to the many questions at play.
Chief among them was why the trial, originally planned for 6,000 patients, was stopped early by the investigators without consultation with the data safety monitoring board (DSMB).
The explanation in the letter that logistical issues like running the study call center, budget constraints, and a perceived need to quickly communicate the results left some calling foul that the study wasn’t allowed to finish and come to a more definitive conclusion.
“I can be a little bit sympathetic to their cause but at the same time the DSMB should have said no,” said David Boulware, MD, MPH, who led a recent hydroxychloroquine trial in COVID-19. “The problem is we’re sort of left in limbo, where some people kind of believe it and some say it’s not really a thing. So it’s not really moving the needle, as far as guidelines go.”
Indeed, a Twitter poll by cardiologist James Januzzi Jr., MD, captured the uncertainty, with 28% of respondents saying the trial was “neutral,” 58% saying “maybe but meh,” and 14% saying “colchicine for all.”
Another poll cheekily asked whether ColCORONA was the Gamestop/Reddit equivalent of COVID.
“The press release really didn’t help things because it very much oversold the effect. That, I think, poisoned the well,” said Dr. Boulware, professor of medicine in infectious diseases at the University of Minnesota, Minneapolis.
“The question I’m left with is not whether colchicine works, but who does it work in,” he said. “That’s really the fundamental question because it does seem that there are probably high-risk groups in their trial and others where they benefit, whereas other groups don’t benefit. In the subgroup analysis, there was absolutely no beneficial effect in women.”
According to the authors, the number needed to treat to prevent one death or hospitalization was 71 overall, but 29 for patients with diabetes, 31 for those aged 70 years and older, 53 for patients with respiratory disease, and 25 for those with coronary disease or heart failure.
Men are at higher risk overall for poor outcomes. But “the authors didn’t present a multivariable analysis, so it is unclear if another factor, such as a differential prevalence of smoking or cardiovascular risk factors, contributed to the differential benefit,” Rachel Bender Ignacio, MD, MPH, infectious disease specialist, University of Washington, Seattle, said in an interview.
Importantly, in this pragmatic study, duration and severity of symptoms were not reported, observed Dr. Bender Ignacio, who is also a STOP-COVID-2 investigator. “We don’t yet have data as to whether colchicine shortens duration or severity of symptoms or prevents long COVID, so we need more data on that.”
The overall risk for serious adverse events was lower in the colchicine group, but the difference in pulmonary embolism (PE) was striking, she said. This could be caused by a real biologic effect, or it’s possible that persons with shortness of breath and hypoxia, without evident viral pneumonia on chest x-ray after a positive COVID-19 test, were more likely to receive a CT-PE study.
The press release also failed to include information, later noted in the preprint, that the MHI has submitted two patents related to colchicine: “Methods of treating a coronavirus infection using colchicine” and “Early administration of low-dose colchicine after myocardial infarction.”
Reached for clarification, MHI communications adviser Camille Turbide said in an interview that the first patent “simply refers to the novel concept of preventing complications of COVID-19, such as admission to the hospital, with colchicine as tested in the ColCORONA study.”
The second patent, she said, refers to the “novel concept that administering colchicine early after a major adverse cardiovascular event is better than waiting several days,” as supported by the COLCOT study, which Dr. Tardif also led.
The patents are being reviewed by authorities and “Dr. Tardif has waived his rights in these patents and does not stand to benefit financially at all if colchicine becomes used as a treatment for COVID-19,” Ms. Turbide said.
Dr. Tardif did not respond to interview requests for this story. Dr. Glatt said conflicts of interest must be assessed and are “something that is of great concern in any scientific study.”
Cardiologist Steve Nissen, MD, of the Cleveland Clinic said in an interview that, “despite the negative results, the study does suggest that colchicine might have a benefit and should be studied in future trials. These findings are not sufficient evidence to suggest use of the drug in patients infected with COVID-19.”
He noted that adverse effects like diarrhea were expected but that the excess PE was unexpected and needs greater clarification.
“Stopping the trial for administrative reasons is puzzling and undermined the ability of the trial to give a reliable answer,” Dr. Nissen said. “This is a reasonable pilot study that should be viewed as hypothesis generating but inconclusive.”
Several sources said a new trial is unlikely, particularly given the cost and 28 trials already evaluating colchicine. Among these are RECOVERY and COLCOVID, testing whether colchicine can reduce the duration of hospitalization or death in hospitalized patients with COVID-19.
Because there are so many trials ongoing right now, including for antivirals and other immunomodulators, it’s important that, if colchicine comes to routine clinical use, it provides access to treatment for those not able or willing to access clinical trials, rather than impeding clinical trial enrollment, Dr. Bender Ignacio suggested.
“We have already learned the lesson in the pandemic that early adoption of potentially promising therapies can negatively impact our ability to study and develop other promising treatments,” she said.
The trial was coordinated by the Montreal Heart Institute and funded by the government of Quebec; the National Heart, Lung, and Blood Institute of the National Institutes of Health; Montreal philanthropist Sophie Desmarais, and the COVID-19 Therapeutics Accelerator launched by the Bill & Melinda Gates Foundation, Wellcome, and Mastercard. CGI, Dacima, and Pharmascience of Montreal were also collaborators. Dr. Glatt reported no conflicts of interest. Dr. Boulware reported receiving $18 in food and beverages from Gilead Sciences in 2018.
A version of this article first appeared on Medscape.com.
Brain connectivity patterns reliably identify ADHD
Functional brain connectivity patterns are a stable biomarker of attention-deficit/hyperactivity disorder, new research suggests.
By applying a machine-learning approach to brain-imaging data, investigators were able to identify with 99% accuracy the adult study participants who had been diagnosed with ADHD in childhood.
“Even though the symptoms of ADHD may be less apparent in adulthood, the brain-wiring signature seems to be persistent,” study investigator Christopher McNorgan, PhD, of the department of psychology, State University of New York at Buffalo told this news organization.
The findings were published online Dec. 17, 2020, in Frontiers of Psychology.
Deep-learning neural networks
The researchers analyzed archived functional magnetic resonance imaging (fMRI) and behavioral data for 80 adults (mean age, 24 years; 64 male). Of these participants, 55 were diagnosed with ADHD in childhood and 25 were not.
The fMRI data were obtained during a response inhibition task that tested the individual’s ability to not respond automatically; for example, not saying “Simon Says” after someone else makes the comment.
The behavioral data included scores on the Iowa Gambling Task (IGT), which is used to measure impulsivity and risk taking.
“Usually, but not always, people with ADHD make riskier choices on this task,” Dr. McNorgan noted.
The investigators measured the amount of interconnectedness among different brain regions during the response inhibition task, which was repeated four times.
Patterns of interconnectivity were then fed into a deep-learning neural network that learned which patterns belonged to the ADHD group vs. those without ADHD (control group) and which patterns belonged to the high vs. low scorers on the IGT.
Caveats, cautionary notes
“The trained models are then tested on brain patterns they had never seen before, and we found the models would make the correct ADHD diagnosis and could tell apart the high and low scorers on the IGT 99% of the time,” Dr. McNorgan reported.
“The trained classifiers make predictions by calculating probabilities, and the neural networks learned how each of the brain connections contributes towards the final classification probability. We identified the set of brain connections that had the greatest influence on these probability calculations,” he noted.
Because the network classified both ADHD diagnosis and gambling task performance, the researchers were able to distinguish between connections that predicted ADHD when gambling performance was poor, as is typical for patients with ADHD, and those predicting ADHD when gambling performance was uncharacteristically good.
While more work is needed, the findings have potential clinical relevance, Dr. McNorgan said.
“ADHD can be difficult to diagnose reliably. If expense wasn’t an issue, fMRI may be able to help make diagnosis more reliable and objective,” he added.
However, because individuals with ADHD have different behavioral profiles, such as scoring atypically well on the IGT, additional studies using this approach may help identify brain networks “that are more or less active in those with ADHD that show a particular diagnostic trait,” he said.
“This could help inform what treatments might be more effective for those individuals,” Dr. McNorgan said.
Of course, he added, “clinicians’ diagnostic expertise is still required, as I would not base an ADHD diagnosis solely on the results of a single brain scan.”
No cross-validation
Commenting on the findings for this news organization, Vince Calhoun, PhD, neuroscientist and founding director of the Center for Translational Research in Neuroimaging and Data Science, Atlanta, a joint effort between Georgia State, Georgia Tech, and Emory University, noted some study limitations.
One cautionary note is that the investigators “appear to select relevant regions to include in the model based on activation to the task, then computed the predictions using the subset of regions that showed strong activation. The issue is this was done on the same data, so there was no cross-validation of this ‘feature selection’ step,” said Dr. Calhoun, who was not involved with the research. “This is a type of circularity which can lead to inflated accuracies,” he added.
Dr. Calhoun also noted that “multiple ADHD classification studies” have reported accuracies above 90%. In addition, there were only 80 participants in the current dataset.
“That’s relatively small for making strong claims about high accuracies as has been reported elsewhere,” he said.
Dr. McNorgan and Dr. Calhoun have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Functional brain connectivity patterns are a stable biomarker of attention-deficit/hyperactivity disorder, new research suggests.
By applying a machine-learning approach to brain-imaging data, investigators were able to identify with 99% accuracy the adult study participants who had been diagnosed with ADHD in childhood.
“Even though the symptoms of ADHD may be less apparent in adulthood, the brain-wiring signature seems to be persistent,” study investigator Christopher McNorgan, PhD, of the department of psychology, State University of New York at Buffalo told this news organization.
The findings were published online Dec. 17, 2020, in Frontiers of Psychology.
Deep-learning neural networks
The researchers analyzed archived functional magnetic resonance imaging (fMRI) and behavioral data for 80 adults (mean age, 24 years; 64 male). Of these participants, 55 were diagnosed with ADHD in childhood and 25 were not.
The fMRI data were obtained during a response inhibition task that tested the individual’s ability to not respond automatically; for example, not saying “Simon Says” after someone else makes the comment.
The behavioral data included scores on the Iowa Gambling Task (IGT), which is used to measure impulsivity and risk taking.
“Usually, but not always, people with ADHD make riskier choices on this task,” Dr. McNorgan noted.
The investigators measured the amount of interconnectedness among different brain regions during the response inhibition task, which was repeated four times.
Patterns of interconnectivity were then fed into a deep-learning neural network that learned which patterns belonged to the ADHD group vs. those without ADHD (control group) and which patterns belonged to the high vs. low scorers on the IGT.
Caveats, cautionary notes
“The trained models are then tested on brain patterns they had never seen before, and we found the models would make the correct ADHD diagnosis and could tell apart the high and low scorers on the IGT 99% of the time,” Dr. McNorgan reported.
“The trained classifiers make predictions by calculating probabilities, and the neural networks learned how each of the brain connections contributes towards the final classification probability. We identified the set of brain connections that had the greatest influence on these probability calculations,” he noted.
Because the network classified both ADHD diagnosis and gambling task performance, the researchers were able to distinguish between connections that predicted ADHD when gambling performance was poor, as is typical for patients with ADHD, and those predicting ADHD when gambling performance was uncharacteristically good.
While more work is needed, the findings have potential clinical relevance, Dr. McNorgan said.
“ADHD can be difficult to diagnose reliably. If expense wasn’t an issue, fMRI may be able to help make diagnosis more reliable and objective,” he added.
However, because individuals with ADHD have different behavioral profiles, such as scoring atypically well on the IGT, additional studies using this approach may help identify brain networks “that are more or less active in those with ADHD that show a particular diagnostic trait,” he said.
“This could help inform what treatments might be more effective for those individuals,” Dr. McNorgan said.
Of course, he added, “clinicians’ diagnostic expertise is still required, as I would not base an ADHD diagnosis solely on the results of a single brain scan.”
No cross-validation
Commenting on the findings for this news organization, Vince Calhoun, PhD, neuroscientist and founding director of the Center for Translational Research in Neuroimaging and Data Science, Atlanta, a joint effort between Georgia State, Georgia Tech, and Emory University, noted some study limitations.
One cautionary note is that the investigators “appear to select relevant regions to include in the model based on activation to the task, then computed the predictions using the subset of regions that showed strong activation. The issue is this was done on the same data, so there was no cross-validation of this ‘feature selection’ step,” said Dr. Calhoun, who was not involved with the research. “This is a type of circularity which can lead to inflated accuracies,” he added.
Dr. Calhoun also noted that “multiple ADHD classification studies” have reported accuracies above 90%. In addition, there were only 80 participants in the current dataset.
“That’s relatively small for making strong claims about high accuracies as has been reported elsewhere,” he said.
Dr. McNorgan and Dr. Calhoun have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Functional brain connectivity patterns are a stable biomarker of attention-deficit/hyperactivity disorder, new research suggests.
By applying a machine-learning approach to brain-imaging data, investigators were able to identify with 99% accuracy the adult study participants who had been diagnosed with ADHD in childhood.
“Even though the symptoms of ADHD may be less apparent in adulthood, the brain-wiring signature seems to be persistent,” study investigator Christopher McNorgan, PhD, of the department of psychology, State University of New York at Buffalo told this news organization.
The findings were published online Dec. 17, 2020, in Frontiers of Psychology.
Deep-learning neural networks
The researchers analyzed archived functional magnetic resonance imaging (fMRI) and behavioral data for 80 adults (mean age, 24 years; 64 male). Of these participants, 55 were diagnosed with ADHD in childhood and 25 were not.
The fMRI data were obtained during a response inhibition task that tested the individual’s ability to not respond automatically; for example, not saying “Simon Says” after someone else makes the comment.
The behavioral data included scores on the Iowa Gambling Task (IGT), which is used to measure impulsivity and risk taking.
“Usually, but not always, people with ADHD make riskier choices on this task,” Dr. McNorgan noted.
The investigators measured the amount of interconnectedness among different brain regions during the response inhibition task, which was repeated four times.
Patterns of interconnectivity were then fed into a deep-learning neural network that learned which patterns belonged to the ADHD group vs. those without ADHD (control group) and which patterns belonged to the high vs. low scorers on the IGT.
Caveats, cautionary notes
“The trained models are then tested on brain patterns they had never seen before, and we found the models would make the correct ADHD diagnosis and could tell apart the high and low scorers on the IGT 99% of the time,” Dr. McNorgan reported.
“The trained classifiers make predictions by calculating probabilities, and the neural networks learned how each of the brain connections contributes towards the final classification probability. We identified the set of brain connections that had the greatest influence on these probability calculations,” he noted.
Because the network classified both ADHD diagnosis and gambling task performance, the researchers were able to distinguish between connections that predicted ADHD when gambling performance was poor, as is typical for patients with ADHD, and those predicting ADHD when gambling performance was uncharacteristically good.
While more work is needed, the findings have potential clinical relevance, Dr. McNorgan said.
“ADHD can be difficult to diagnose reliably. If expense wasn’t an issue, fMRI may be able to help make diagnosis more reliable and objective,” he added.
However, because individuals with ADHD have different behavioral profiles, such as scoring atypically well on the IGT, additional studies using this approach may help identify brain networks “that are more or less active in those with ADHD that show a particular diagnostic trait,” he said.
“This could help inform what treatments might be more effective for those individuals,” Dr. McNorgan said.
Of course, he added, “clinicians’ diagnostic expertise is still required, as I would not base an ADHD diagnosis solely on the results of a single brain scan.”
No cross-validation
Commenting on the findings for this news organization, Vince Calhoun, PhD, neuroscientist and founding director of the Center for Translational Research in Neuroimaging and Data Science, Atlanta, a joint effort between Georgia State, Georgia Tech, and Emory University, noted some study limitations.
One cautionary note is that the investigators “appear to select relevant regions to include in the model based on activation to the task, then computed the predictions using the subset of regions that showed strong activation. The issue is this was done on the same data, so there was no cross-validation of this ‘feature selection’ step,” said Dr. Calhoun, who was not involved with the research. “This is a type of circularity which can lead to inflated accuracies,” he added.
Dr. Calhoun also noted that “multiple ADHD classification studies” have reported accuracies above 90%. In addition, there were only 80 participants in the current dataset.
“That’s relatively small for making strong claims about high accuracies as has been reported elsewhere,” he said.
Dr. McNorgan and Dr. Calhoun have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Vaccine may blunt effects of deadly synthetic opioids
New experimental vaccines could stop the worst effects of synthetic fentanyl and carfentanil, two drugs that have been major drivers of the opioid epidemic in the United States, according to a new study published in ACS Chemical Biology on Feb. 3, 2021.
During several experiments in mice, the vaccines prevented respiratory depression, which is the main cause of overdose deaths. The vaccines also reduced the amount of drug that was distributed to the brain. Once in the brain, synthetic opioids prompt the body to slow down breathing, and when too much of the drug is consumed, breathing can stop.
“Synthetic opioids are not only extremely deadly but also addictive and easy to manufacture, making them a formidable public health threat, especially when the coronavirus crisis is negatively impacting mental health,” Kim Janda, PhD, a chemist at Scripps Research Institute in La Jolla, Calif., who developed the vaccines, said in a statement.
Fentanyl is up to 100 times stronger than morphine, and carfentanil, which is often used by veterinarians to sedate large animals such as elephants, is up to 10,000 times stronger than morphine. Carfentanil isn’t as well-known as a street drug, but it’s being used more often as an additive in heroin and cocaine.
“We’ve shown it is possible to prevent these unnecessary deaths by eliciting antibodies that stop the drug from reaching the brain,” he said.
The vaccines could be used in emergency situations to treat overdoses and as a therapy for those with substance abuse disorders, Dr. Janda said. In addition, the vaccines could protect military officers who are exposed to opioids as chemical weapons, and they may also help opioid-sniffing police dogs to train for the job.
The vaccines are still in the early stages of testing, but looking at the latest data “brings us hope that this approach will work to treat a number of opioid-related maladies,” Dr. Janda said.
In December, the CDC reported that more than 81,000 drug overdose deaths happened in the United States between May 2019 and May 2020, which was the highest number ever recorded in a 12-month period. Synthetic opioids, particularly illegally created fentanyl, were to blame.
“Unfortunately, currently battling a pandemic,” Dr. Janda said. “We look forward to continuing our vaccine research and translating it to the clinic, where we can begin to make an impact on the opioid crisis.”
A version of this article first appeared on Medscape.com.
New experimental vaccines could stop the worst effects of synthetic fentanyl and carfentanil, two drugs that have been major drivers of the opioid epidemic in the United States, according to a new study published in ACS Chemical Biology on Feb. 3, 2021.
During several experiments in mice, the vaccines prevented respiratory depression, which is the main cause of overdose deaths. The vaccines also reduced the amount of drug that was distributed to the brain. Once in the brain, synthetic opioids prompt the body to slow down breathing, and when too much of the drug is consumed, breathing can stop.
“Synthetic opioids are not only extremely deadly but also addictive and easy to manufacture, making them a formidable public health threat, especially when the coronavirus crisis is negatively impacting mental health,” Kim Janda, PhD, a chemist at Scripps Research Institute in La Jolla, Calif., who developed the vaccines, said in a statement.
Fentanyl is up to 100 times stronger than morphine, and carfentanil, which is often used by veterinarians to sedate large animals such as elephants, is up to 10,000 times stronger than morphine. Carfentanil isn’t as well-known as a street drug, but it’s being used more often as an additive in heroin and cocaine.
“We’ve shown it is possible to prevent these unnecessary deaths by eliciting antibodies that stop the drug from reaching the brain,” he said.
The vaccines could be used in emergency situations to treat overdoses and as a therapy for those with substance abuse disorders, Dr. Janda said. In addition, the vaccines could protect military officers who are exposed to opioids as chemical weapons, and they may also help opioid-sniffing police dogs to train for the job.
The vaccines are still in the early stages of testing, but looking at the latest data “brings us hope that this approach will work to treat a number of opioid-related maladies,” Dr. Janda said.
In December, the CDC reported that more than 81,000 drug overdose deaths happened in the United States between May 2019 and May 2020, which was the highest number ever recorded in a 12-month period. Synthetic opioids, particularly illegally created fentanyl, were to blame.
“Unfortunately, currently battling a pandemic,” Dr. Janda said. “We look forward to continuing our vaccine research and translating it to the clinic, where we can begin to make an impact on the opioid crisis.”
A version of this article first appeared on Medscape.com.
New experimental vaccines could stop the worst effects of synthetic fentanyl and carfentanil, two drugs that have been major drivers of the opioid epidemic in the United States, according to a new study published in ACS Chemical Biology on Feb. 3, 2021.
During several experiments in mice, the vaccines prevented respiratory depression, which is the main cause of overdose deaths. The vaccines also reduced the amount of drug that was distributed to the brain. Once in the brain, synthetic opioids prompt the body to slow down breathing, and when too much of the drug is consumed, breathing can stop.
“Synthetic opioids are not only extremely deadly but also addictive and easy to manufacture, making them a formidable public health threat, especially when the coronavirus crisis is negatively impacting mental health,” Kim Janda, PhD, a chemist at Scripps Research Institute in La Jolla, Calif., who developed the vaccines, said in a statement.
Fentanyl is up to 100 times stronger than morphine, and carfentanil, which is often used by veterinarians to sedate large animals such as elephants, is up to 10,000 times stronger than morphine. Carfentanil isn’t as well-known as a street drug, but it’s being used more often as an additive in heroin and cocaine.
“We’ve shown it is possible to prevent these unnecessary deaths by eliciting antibodies that stop the drug from reaching the brain,” he said.
The vaccines could be used in emergency situations to treat overdoses and as a therapy for those with substance abuse disorders, Dr. Janda said. In addition, the vaccines could protect military officers who are exposed to opioids as chemical weapons, and they may also help opioid-sniffing police dogs to train for the job.
The vaccines are still in the early stages of testing, but looking at the latest data “brings us hope that this approach will work to treat a number of opioid-related maladies,” Dr. Janda said.
In December, the CDC reported that more than 81,000 drug overdose deaths happened in the United States between May 2019 and May 2020, which was the highest number ever recorded in a 12-month period. Synthetic opioids, particularly illegally created fentanyl, were to blame.
“Unfortunately, currently battling a pandemic,” Dr. Janda said. “We look forward to continuing our vaccine research and translating it to the clinic, where we can begin to make an impact on the opioid crisis.”
A version of this article first appeared on Medscape.com.
Study: COVID cases have been ‘severely undercounted’
Large numbers of COVID-19 cases have been undetected and unreported, which has resulted in severe undercounting of the total number of people who have been infected during the pandemic, according to a new study published Monday in the journal PLOS ONE.
In the United States, the number of COVID-19 cases is likely three times that of reported cases. According to the study, more than 71 million Americans have contracted the virus during the pandemic, and 7 million were infected or potentially contagious last week.
Public health officials rely on case counts to guide decisions, so the undercounting should be considered while trying to end the pandemic.
“The estimates of actual infections reveal for the first time the true severity of COVID-19 across the U.S. and in countries worldwide,” Jungsik Noh, PhD, a bioinformatics professor at the University of Texas Southwestern Medical Center, said in a statement.
Dr. Noh and colleague Gaudenz Danuser created a computational model that uses machine-learning strategies to estimate the actual number of daily cases in the United States and the 50 most-infected countries.
The model pulls data from the Johns Hopkins University database and the COVID Tracking Project, as well as large-scale surveys conducted by the CDC and several states. The algorithm uses the number of reported deaths, which is thought to be more accurate than the number of lab-confirmed cases, as the basis for calculations.
In 25 of the 50 countries, the “actual” cumulative cases were estimated to be 5-20 times greater than the confirmed cases. In the United States, Belgium, and Brazil, about 10% of the population has contracted the coronavirus, according to the model. At the beginning of February, about 11% of the population in Pennsylvania had current infections, which was the highest rate of any state. About 0.15% of residents in Minnesota had infections, and about 2.5% of residents in New York and Texas had infections.
“Knowing the true severity in different regions will help us effectively fight against the virus spreading,” Dr. Noh said. “The currently infected population is the cause of future infections and deaths. Its actual size in a region is a crucial variable required when determining the severity of COVID-19 and building strategies against regional outbreaks.”
A version of this article first appeared on WebMD.com.
Large numbers of COVID-19 cases have been undetected and unreported, which has resulted in severe undercounting of the total number of people who have been infected during the pandemic, according to a new study published Monday in the journal PLOS ONE.
In the United States, the number of COVID-19 cases is likely three times that of reported cases. According to the study, more than 71 million Americans have contracted the virus during the pandemic, and 7 million were infected or potentially contagious last week.
Public health officials rely on case counts to guide decisions, so the undercounting should be considered while trying to end the pandemic.
“The estimates of actual infections reveal for the first time the true severity of COVID-19 across the U.S. and in countries worldwide,” Jungsik Noh, PhD, a bioinformatics professor at the University of Texas Southwestern Medical Center, said in a statement.
Dr. Noh and colleague Gaudenz Danuser created a computational model that uses machine-learning strategies to estimate the actual number of daily cases in the United States and the 50 most-infected countries.
The model pulls data from the Johns Hopkins University database and the COVID Tracking Project, as well as large-scale surveys conducted by the CDC and several states. The algorithm uses the number of reported deaths, which is thought to be more accurate than the number of lab-confirmed cases, as the basis for calculations.
In 25 of the 50 countries, the “actual” cumulative cases were estimated to be 5-20 times greater than the confirmed cases. In the United States, Belgium, and Brazil, about 10% of the population has contracted the coronavirus, according to the model. At the beginning of February, about 11% of the population in Pennsylvania had current infections, which was the highest rate of any state. About 0.15% of residents in Minnesota had infections, and about 2.5% of residents in New York and Texas had infections.
“Knowing the true severity in different regions will help us effectively fight against the virus spreading,” Dr. Noh said. “The currently infected population is the cause of future infections and deaths. Its actual size in a region is a crucial variable required when determining the severity of COVID-19 and building strategies against regional outbreaks.”
A version of this article first appeared on WebMD.com.
Large numbers of COVID-19 cases have been undetected and unreported, which has resulted in severe undercounting of the total number of people who have been infected during the pandemic, according to a new study published Monday in the journal PLOS ONE.
In the United States, the number of COVID-19 cases is likely three times that of reported cases. According to the study, more than 71 million Americans have contracted the virus during the pandemic, and 7 million were infected or potentially contagious last week.
Public health officials rely on case counts to guide decisions, so the undercounting should be considered while trying to end the pandemic.
“The estimates of actual infections reveal for the first time the true severity of COVID-19 across the U.S. and in countries worldwide,” Jungsik Noh, PhD, a bioinformatics professor at the University of Texas Southwestern Medical Center, said in a statement.
Dr. Noh and colleague Gaudenz Danuser created a computational model that uses machine-learning strategies to estimate the actual number of daily cases in the United States and the 50 most-infected countries.
The model pulls data from the Johns Hopkins University database and the COVID Tracking Project, as well as large-scale surveys conducted by the CDC and several states. The algorithm uses the number of reported deaths, which is thought to be more accurate than the number of lab-confirmed cases, as the basis for calculations.
In 25 of the 50 countries, the “actual” cumulative cases were estimated to be 5-20 times greater than the confirmed cases. In the United States, Belgium, and Brazil, about 10% of the population has contracted the coronavirus, according to the model. At the beginning of February, about 11% of the population in Pennsylvania had current infections, which was the highest rate of any state. About 0.15% of residents in Minnesota had infections, and about 2.5% of residents in New York and Texas had infections.
“Knowing the true severity in different regions will help us effectively fight against the virus spreading,” Dr. Noh said. “The currently infected population is the cause of future infections and deaths. Its actual size in a region is a crucial variable required when determining the severity of COVID-19 and building strategies against regional outbreaks.”
A version of this article first appeared on WebMD.com.
Teenagers get in the queue for COVID-19 vaccines
The vaccinations can’t come soon enough for parents like Stacy Hillenburg, a developmental therapist in Aurora, Ill., whose 9-year-old son takes immunosuppressants because he had a heart transplant when he was 7 weeks old. Although school-age children aren’t yet included in clinical trials, if her 12- and 13-year-old daughters could get vaccinated, along with both parents, then the family could relax some of the protocols they currently follow to prevent infection.
Whenever they are around other people, even masked and socially distanced, they come home and immediately shower and change their clothes. So far, no one in the family has been infected with COVID, but the anxiety is ever-present. “I can’t wait for it to come out,” Ms. Hillenburg said of a pediatric COVID vaccine. “It will ease my mind so much.”
She isn’t alone in that anticipation. In the fall, the American Academy of Pediatrics and other pediatric vaccine experts urged faster action on pediatric vaccine trials and worried that children would be left behind as adults gained protection from COVID. But recent developments have eased those concerns.
“Over the next couple of months, we will be doing trials in an age-deescalation manner,” with studies moving gradually to younger children, Anthony S. Fauci, MD, chief medical adviser on COVID-19 to the president, said in a coronavirus response team briefing on Jan. 29. “So that hopefully, as we get to the late spring and summer, we will have children being able to be vaccinated.”
Pfizer completed enrollment of 2,259 teens aged 12-15 years in late January and expects to move forward with a separate pediatric trial of children aged 5-11 years by this spring, Keanna Ghazvini, senior associate for global media relations at Pfizer, said in an interview.
Enrollment in Moderna’s TeenCove study of adolescents ages 12-17 years began slowly in late December, but the pace has since picked up, said company spokesperson Colleen Hussey. “We continue to bring clinical trial sites online, and we are on track to provide updated data around mid-year 2021.” A trial extension in children 11 years and younger is expected to begin later in 2021.
Johnson & Johnson and AstraZeneca said they expect to begin adolescent trials in early 2021, according to data shared by the Advisory Committee on Immunization Practices. An interim analysis of J&J’s Janssen COVID-19 vaccine trial data, released on Jan. 29, showed it was 72% effective in US participants aged 18 years or older. AstraZeneca’s U.S. trial in adults is ongoing.
Easing the burden
Vaccination could lessen children’s risk of severe disease as well as the social and emotional burdens of the pandemic, says James Campbell, MD, a pediatric infectious disease specialist at the University of Maryland’s Center for Vaccine Development in Baltimore, which was involved in the Moderna and early-phase Pfizer trials. He coauthored a September 2020 article in Clinical Infectious Diseases titled: “Warp Speed for COVID-19 vaccines: Why are children stuck in neutral?”
The adolescent trials are a vital step to ensure timely vaccine access for teens and younger children. “It is reasonable, when you have limited vaccine, that your rollout goes to the highest priority and then moves to lower and lower priorities. In adults, we’re just saying: ‘Wait your turn,’ ” he said of the current vaccination effort. “If we didn’t have the [vaccine trial] data in children, we’d be saying: ‘You don’t have a turn.’ ”
As the pandemic has worn on, the burden on children has grown. As of Tuesday, 269 children had died of COVID-19. That is well above the highest annual death toll recorded during a regular flu season – 188 flu deaths among children and adolescents under 18 in the 2019-2020 and 2017-2018 flu seasons.
Children are less likely to transmit COVID-19 in their household than adults, according to a meta-analysis of 54 studies published in JAMA Network Open. But that does not necessarily mean children are less infectious, the authors said, noting that unmeasured factors could have affected the spread of infection among adults.
Moreover, children and adolescents need protection from COVID infection – and from the potential for severe disease or lingering effects – and, given that there are 74 million children and teens in the United States, their vaccination is an important part of stopping the pandemic, said Grace Lee, MD, professor of pediatrics at Stanford (Calif.) University, and cochair of ACIP’s COVID-19 Vaccine Safety Technical Subgroup.
“In order to interrupt transmission, I don’t see how we’re going to do that without vaccinating children and adolescents,” she said.
Dr. Lee said her 16-year-old daughter misses the normal teenage social life and is excited about getting the vaccine when she is eligible. (Adolescents without high-risk conditions are in the lowest vaccination tier, according to ACIP recommendations.) “There is truly individual protection to be gained,” Dr. Lee said.
She noted that researchers continue to assess the immune responses to the adult vaccines – even looking at immune characteristics of the small percentage of people who aren’t protected from infection – and that information helps in the evaluation of the pediatric immune responses. As the trials expand to younger children and infants, dosing will be a major focus. “How many doses do they need they need to receive the same immunity? Safety considerations will be critically important,” she said.
Teen trials underway
Pfizer/BioNTech extended its adult trial to 16- and 17-year-olds in October, which enabled older teens to be included in its emergency-use authorization. They and younger teens, ages 12-15, receive the same dose as adults.
The ongoing trials with Pfizer and Moderna vaccines are immunobridging trials, designed to study safety and immunogenicity. Investigators will compare the teens’ immune response with the findings from the larger adult trials. When the trials expand to school-age children (6-12 years), protocols call for testing the safety and immunogenicity of a half-dose vaccine as well as the full dose.
Children ages 2-5 years and infants and toddlers will be enrolled in future trials, studying safety and immunogenicity of full, half, or even quarter dosages. The Pediatric Research Equity Act of 2003 requires licensed vaccines to be tested for safety and efficacy in children, unless they are not appropriate for a pediatric population.
Demand for the teen trials has been strong. At Cincinnati Children’s Hospital Medical Center, 259 teenagers joined the Pfizer/BioNTech trial, but some teenagers were turned away when the trial’s national enrollment closed in late January.
“Many of the children are having no side effects, and if they are, they’re having the same [effects] as the young adults – local redness or pain, fatigue, and headaches,” said Robert Frenck, MD, director of the Cincinnati Children’s Gamble Program for Clinical Studies.
Parents may share some of the vaccine hesitancy that has affected adult vaccination. But that is balanced by the hope that vaccines will end the pandemic and usher in a new normal. “If it looks like [vaccines] will increase the likelihood of children returning to school safely, that may be a motivating factor,” Dr. Frenck said.
Cody Meissner, MD, chief of the pediatric infectious disease service at Tufts Medical Center, Boston, was initially cautious about the extension of vaccination to adolescents. A member of the Vaccine and Related Biological Products Advisory Committee, which evaluates data and makes recommendations to the Food and Drug Administration, Dr. Meissner initially abstained in the vote on the Pfizer/BioNTech emergency-use authorization for people 16 and older.
He noted that, at the time the committee reviewed the Pfizer vaccine, the company had data available for just 134 teenagers, half of whom received a placebo. But the vaccination of 34 million adults has provided robust data about the vaccine’s safety, and the trial expansion into adolescents is important.
“I’m comfortable with the way these trials are going now,” he said. “This is the way I was hoping they would go.”
Ms. Hillenburg is on the parent advisory board of Voices for Vaccines, an organization of parents supporting vaccination that is affiliated with the Task Force for Global Health, an Atlanta-based independent public health organization. Dr. Campbell’s institution has received funds to conduct clinical trials from the National Institutes of Health and several companies, including Merck, GlaxoSmithKline, Sanofi, Pfizer, and Moderna. He has served pro bono on many safety and data monitoring committees. Dr. Frenck’s institution is receiving funds to conduct the Pfizer trial. In the past 5 years, he has also participated in clinical trials for GlaxoSmithKline, Merck, and Meissa vaccines. Dr. Lee and Dr. Meissner disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The vaccinations can’t come soon enough for parents like Stacy Hillenburg, a developmental therapist in Aurora, Ill., whose 9-year-old son takes immunosuppressants because he had a heart transplant when he was 7 weeks old. Although school-age children aren’t yet included in clinical trials, if her 12- and 13-year-old daughters could get vaccinated, along with both parents, then the family could relax some of the protocols they currently follow to prevent infection.
Whenever they are around other people, even masked and socially distanced, they come home and immediately shower and change their clothes. So far, no one in the family has been infected with COVID, but the anxiety is ever-present. “I can’t wait for it to come out,” Ms. Hillenburg said of a pediatric COVID vaccine. “It will ease my mind so much.”
She isn’t alone in that anticipation. In the fall, the American Academy of Pediatrics and other pediatric vaccine experts urged faster action on pediatric vaccine trials and worried that children would be left behind as adults gained protection from COVID. But recent developments have eased those concerns.
“Over the next couple of months, we will be doing trials in an age-deescalation manner,” with studies moving gradually to younger children, Anthony S. Fauci, MD, chief medical adviser on COVID-19 to the president, said in a coronavirus response team briefing on Jan. 29. “So that hopefully, as we get to the late spring and summer, we will have children being able to be vaccinated.”
Pfizer completed enrollment of 2,259 teens aged 12-15 years in late January and expects to move forward with a separate pediatric trial of children aged 5-11 years by this spring, Keanna Ghazvini, senior associate for global media relations at Pfizer, said in an interview.
Enrollment in Moderna’s TeenCove study of adolescents ages 12-17 years began slowly in late December, but the pace has since picked up, said company spokesperson Colleen Hussey. “We continue to bring clinical trial sites online, and we are on track to provide updated data around mid-year 2021.” A trial extension in children 11 years and younger is expected to begin later in 2021.
Johnson & Johnson and AstraZeneca said they expect to begin adolescent trials in early 2021, according to data shared by the Advisory Committee on Immunization Practices. An interim analysis of J&J’s Janssen COVID-19 vaccine trial data, released on Jan. 29, showed it was 72% effective in US participants aged 18 years or older. AstraZeneca’s U.S. trial in adults is ongoing.
Easing the burden
Vaccination could lessen children’s risk of severe disease as well as the social and emotional burdens of the pandemic, says James Campbell, MD, a pediatric infectious disease specialist at the University of Maryland’s Center for Vaccine Development in Baltimore, which was involved in the Moderna and early-phase Pfizer trials. He coauthored a September 2020 article in Clinical Infectious Diseases titled: “Warp Speed for COVID-19 vaccines: Why are children stuck in neutral?”
The adolescent trials are a vital step to ensure timely vaccine access for teens and younger children. “It is reasonable, when you have limited vaccine, that your rollout goes to the highest priority and then moves to lower and lower priorities. In adults, we’re just saying: ‘Wait your turn,’ ” he said of the current vaccination effort. “If we didn’t have the [vaccine trial] data in children, we’d be saying: ‘You don’t have a turn.’ ”
As the pandemic has worn on, the burden on children has grown. As of Tuesday, 269 children had died of COVID-19. That is well above the highest annual death toll recorded during a regular flu season – 188 flu deaths among children and adolescents under 18 in the 2019-2020 and 2017-2018 flu seasons.
Children are less likely to transmit COVID-19 in their household than adults, according to a meta-analysis of 54 studies published in JAMA Network Open. But that does not necessarily mean children are less infectious, the authors said, noting that unmeasured factors could have affected the spread of infection among adults.
Moreover, children and adolescents need protection from COVID infection – and from the potential for severe disease or lingering effects – and, given that there are 74 million children and teens in the United States, their vaccination is an important part of stopping the pandemic, said Grace Lee, MD, professor of pediatrics at Stanford (Calif.) University, and cochair of ACIP’s COVID-19 Vaccine Safety Technical Subgroup.
“In order to interrupt transmission, I don’t see how we’re going to do that without vaccinating children and adolescents,” she said.
Dr. Lee said her 16-year-old daughter misses the normal teenage social life and is excited about getting the vaccine when she is eligible. (Adolescents without high-risk conditions are in the lowest vaccination tier, according to ACIP recommendations.) “There is truly individual protection to be gained,” Dr. Lee said.
She noted that researchers continue to assess the immune responses to the adult vaccines – even looking at immune characteristics of the small percentage of people who aren’t protected from infection – and that information helps in the evaluation of the pediatric immune responses. As the trials expand to younger children and infants, dosing will be a major focus. “How many doses do they need they need to receive the same immunity? Safety considerations will be critically important,” she said.
Teen trials underway
Pfizer/BioNTech extended its adult trial to 16- and 17-year-olds in October, which enabled older teens to be included in its emergency-use authorization. They and younger teens, ages 12-15, receive the same dose as adults.
The ongoing trials with Pfizer and Moderna vaccines are immunobridging trials, designed to study safety and immunogenicity. Investigators will compare the teens’ immune response with the findings from the larger adult trials. When the trials expand to school-age children (6-12 years), protocols call for testing the safety and immunogenicity of a half-dose vaccine as well as the full dose.
Children ages 2-5 years and infants and toddlers will be enrolled in future trials, studying safety and immunogenicity of full, half, or even quarter dosages. The Pediatric Research Equity Act of 2003 requires licensed vaccines to be tested for safety and efficacy in children, unless they are not appropriate for a pediatric population.
Demand for the teen trials has been strong. At Cincinnati Children’s Hospital Medical Center, 259 teenagers joined the Pfizer/BioNTech trial, but some teenagers were turned away when the trial’s national enrollment closed in late January.
“Many of the children are having no side effects, and if they are, they’re having the same [effects] as the young adults – local redness or pain, fatigue, and headaches,” said Robert Frenck, MD, director of the Cincinnati Children’s Gamble Program for Clinical Studies.
Parents may share some of the vaccine hesitancy that has affected adult vaccination. But that is balanced by the hope that vaccines will end the pandemic and usher in a new normal. “If it looks like [vaccines] will increase the likelihood of children returning to school safely, that may be a motivating factor,” Dr. Frenck said.
Cody Meissner, MD, chief of the pediatric infectious disease service at Tufts Medical Center, Boston, was initially cautious about the extension of vaccination to adolescents. A member of the Vaccine and Related Biological Products Advisory Committee, which evaluates data and makes recommendations to the Food and Drug Administration, Dr. Meissner initially abstained in the vote on the Pfizer/BioNTech emergency-use authorization for people 16 and older.
He noted that, at the time the committee reviewed the Pfizer vaccine, the company had data available for just 134 teenagers, half of whom received a placebo. But the vaccination of 34 million adults has provided robust data about the vaccine’s safety, and the trial expansion into adolescents is important.
“I’m comfortable with the way these trials are going now,” he said. “This is the way I was hoping they would go.”
Ms. Hillenburg is on the parent advisory board of Voices for Vaccines, an organization of parents supporting vaccination that is affiliated with the Task Force for Global Health, an Atlanta-based independent public health organization. Dr. Campbell’s institution has received funds to conduct clinical trials from the National Institutes of Health and several companies, including Merck, GlaxoSmithKline, Sanofi, Pfizer, and Moderna. He has served pro bono on many safety and data monitoring committees. Dr. Frenck’s institution is receiving funds to conduct the Pfizer trial. In the past 5 years, he has also participated in clinical trials for GlaxoSmithKline, Merck, and Meissa vaccines. Dr. Lee and Dr. Meissner disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
The vaccinations can’t come soon enough for parents like Stacy Hillenburg, a developmental therapist in Aurora, Ill., whose 9-year-old son takes immunosuppressants because he had a heart transplant when he was 7 weeks old. Although school-age children aren’t yet included in clinical trials, if her 12- and 13-year-old daughters could get vaccinated, along with both parents, then the family could relax some of the protocols they currently follow to prevent infection.
Whenever they are around other people, even masked and socially distanced, they come home and immediately shower and change their clothes. So far, no one in the family has been infected with COVID, but the anxiety is ever-present. “I can’t wait for it to come out,” Ms. Hillenburg said of a pediatric COVID vaccine. “It will ease my mind so much.”
She isn’t alone in that anticipation. In the fall, the American Academy of Pediatrics and other pediatric vaccine experts urged faster action on pediatric vaccine trials and worried that children would be left behind as adults gained protection from COVID. But recent developments have eased those concerns.
“Over the next couple of months, we will be doing trials in an age-deescalation manner,” with studies moving gradually to younger children, Anthony S. Fauci, MD, chief medical adviser on COVID-19 to the president, said in a coronavirus response team briefing on Jan. 29. “So that hopefully, as we get to the late spring and summer, we will have children being able to be vaccinated.”
Pfizer completed enrollment of 2,259 teens aged 12-15 years in late January and expects to move forward with a separate pediatric trial of children aged 5-11 years by this spring, Keanna Ghazvini, senior associate for global media relations at Pfizer, said in an interview.
Enrollment in Moderna’s TeenCove study of adolescents ages 12-17 years began slowly in late December, but the pace has since picked up, said company spokesperson Colleen Hussey. “We continue to bring clinical trial sites online, and we are on track to provide updated data around mid-year 2021.” A trial extension in children 11 years and younger is expected to begin later in 2021.
Johnson & Johnson and AstraZeneca said they expect to begin adolescent trials in early 2021, according to data shared by the Advisory Committee on Immunization Practices. An interim analysis of J&J’s Janssen COVID-19 vaccine trial data, released on Jan. 29, showed it was 72% effective in US participants aged 18 years or older. AstraZeneca’s U.S. trial in adults is ongoing.
Easing the burden
Vaccination could lessen children’s risk of severe disease as well as the social and emotional burdens of the pandemic, says James Campbell, MD, a pediatric infectious disease specialist at the University of Maryland’s Center for Vaccine Development in Baltimore, which was involved in the Moderna and early-phase Pfizer trials. He coauthored a September 2020 article in Clinical Infectious Diseases titled: “Warp Speed for COVID-19 vaccines: Why are children stuck in neutral?”
The adolescent trials are a vital step to ensure timely vaccine access for teens and younger children. “It is reasonable, when you have limited vaccine, that your rollout goes to the highest priority and then moves to lower and lower priorities. In adults, we’re just saying: ‘Wait your turn,’ ” he said of the current vaccination effort. “If we didn’t have the [vaccine trial] data in children, we’d be saying: ‘You don’t have a turn.’ ”
As the pandemic has worn on, the burden on children has grown. As of Tuesday, 269 children had died of COVID-19. That is well above the highest annual death toll recorded during a regular flu season – 188 flu deaths among children and adolescents under 18 in the 2019-2020 and 2017-2018 flu seasons.
Children are less likely to transmit COVID-19 in their household than adults, according to a meta-analysis of 54 studies published in JAMA Network Open. But that does not necessarily mean children are less infectious, the authors said, noting that unmeasured factors could have affected the spread of infection among adults.
Moreover, children and adolescents need protection from COVID infection – and from the potential for severe disease or lingering effects – and, given that there are 74 million children and teens in the United States, their vaccination is an important part of stopping the pandemic, said Grace Lee, MD, professor of pediatrics at Stanford (Calif.) University, and cochair of ACIP’s COVID-19 Vaccine Safety Technical Subgroup.
“In order to interrupt transmission, I don’t see how we’re going to do that without vaccinating children and adolescents,” she said.
Dr. Lee said her 16-year-old daughter misses the normal teenage social life and is excited about getting the vaccine when she is eligible. (Adolescents without high-risk conditions are in the lowest vaccination tier, according to ACIP recommendations.) “There is truly individual protection to be gained,” Dr. Lee said.
She noted that researchers continue to assess the immune responses to the adult vaccines – even looking at immune characteristics of the small percentage of people who aren’t protected from infection – and that information helps in the evaluation of the pediatric immune responses. As the trials expand to younger children and infants, dosing will be a major focus. “How many doses do they need they need to receive the same immunity? Safety considerations will be critically important,” she said.
Teen trials underway
Pfizer/BioNTech extended its adult trial to 16- and 17-year-olds in October, which enabled older teens to be included in its emergency-use authorization. They and younger teens, ages 12-15, receive the same dose as adults.
The ongoing trials with Pfizer and Moderna vaccines are immunobridging trials, designed to study safety and immunogenicity. Investigators will compare the teens’ immune response with the findings from the larger adult trials. When the trials expand to school-age children (6-12 years), protocols call for testing the safety and immunogenicity of a half-dose vaccine as well as the full dose.
Children ages 2-5 years and infants and toddlers will be enrolled in future trials, studying safety and immunogenicity of full, half, or even quarter dosages. The Pediatric Research Equity Act of 2003 requires licensed vaccines to be tested for safety and efficacy in children, unless they are not appropriate for a pediatric population.
Demand for the teen trials has been strong. At Cincinnati Children’s Hospital Medical Center, 259 teenagers joined the Pfizer/BioNTech trial, but some teenagers were turned away when the trial’s national enrollment closed in late January.
“Many of the children are having no side effects, and if they are, they’re having the same [effects] as the young adults – local redness or pain, fatigue, and headaches,” said Robert Frenck, MD, director of the Cincinnati Children’s Gamble Program for Clinical Studies.
Parents may share some of the vaccine hesitancy that has affected adult vaccination. But that is balanced by the hope that vaccines will end the pandemic and usher in a new normal. “If it looks like [vaccines] will increase the likelihood of children returning to school safely, that may be a motivating factor,” Dr. Frenck said.
Cody Meissner, MD, chief of the pediatric infectious disease service at Tufts Medical Center, Boston, was initially cautious about the extension of vaccination to adolescents. A member of the Vaccine and Related Biological Products Advisory Committee, which evaluates data and makes recommendations to the Food and Drug Administration, Dr. Meissner initially abstained in the vote on the Pfizer/BioNTech emergency-use authorization for people 16 and older.
He noted that, at the time the committee reviewed the Pfizer vaccine, the company had data available for just 134 teenagers, half of whom received a placebo. But the vaccination of 34 million adults has provided robust data about the vaccine’s safety, and the trial expansion into adolescents is important.
“I’m comfortable with the way these trials are going now,” he said. “This is the way I was hoping they would go.”
Ms. Hillenburg is on the parent advisory board of Voices for Vaccines, an organization of parents supporting vaccination that is affiliated with the Task Force for Global Health, an Atlanta-based independent public health organization. Dr. Campbell’s institution has received funds to conduct clinical trials from the National Institutes of Health and several companies, including Merck, GlaxoSmithKline, Sanofi, Pfizer, and Moderna. He has served pro bono on many safety and data monitoring committees. Dr. Frenck’s institution is receiving funds to conduct the Pfizer trial. In the past 5 years, he has also participated in clinical trials for GlaxoSmithKline, Merck, and Meissa vaccines. Dr. Lee and Dr. Meissner disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.