User login
Clinical Endocrinology News is an independent news source that provides endocrinologists with timely and relevant news and commentary about clinical developments and the impact of health care policy on the endocrinologist's practice. Specialty topics include Diabetes, Lipid & Metabolic Disorders Menopause, Obesity, Osteoporosis, Pediatric Endocrinology, Pituitary, Thyroid & Adrenal Disorders, and Reproductive Endocrinology. Featured content includes Commentaries, Implementin Health Reform, Law & Medicine, and In the Loop, the blog of Clinical Endocrinology News. Clinical Endocrinology News is owned by Frontline Medical Communications.
addict
addicted
addicting
addiction
adult sites
alcohol
antibody
ass
attorney
audit
auditor
babies
babpa
baby
ban
banned
banning
best
bisexual
bitch
bleach
blog
blow job
bondage
boobs
booty
buy
cannabis
certificate
certification
certified
cheap
cheapest
class action
cocaine
cock
counterfeit drug
crack
crap
crime
criminal
cunt
curable
cure
dangerous
dangers
dead
deadly
death
defend
defended
depedent
dependence
dependent
detergent
dick
die
dildo
drug abuse
drug recall
dying
fag
fake
fatal
fatalities
fatality
free
fuck
gangs
gingivitis
guns
hardcore
herbal
herbs
heroin
herpes
home remedies
homo
horny
hypersensitivity
hypoglycemia treatment
illegal drug use
illegal use of prescription
incest
infant
infants
job
ketoacidosis
kill
killer
killing
kinky
law suit
lawsuit
lawyer
lesbian
marijuana
medicine for hypoglycemia
murder
naked
natural
newborn
nigger
noise
nude
nudity
orgy
over the counter
overdosage
overdose
overdosed
overdosing
penis
pimp
pistol
porn
porno
pornographic
pornography
prison
profanity
purchase
purchasing
pussy
queer
rape
rapist
recall
recreational drug
rob
robberies
sale
sales
sex
sexual
shit
shoot
slut
slutty
stole
stolen
store
sue
suicidal
suicide
supplements
supply company
theft
thief
thieves
tit
toddler
toddlers
toxic
toxin
tragedy
treating dka
treating hypoglycemia
treatment for hypoglycemia
vagina
violence
whore
withdrawal
without prescription
section[contains(@class, 'nav-hidden')]
footer[@id='footer']
div[contains(@class, 'pane-pub-article-imn')]
div[contains(@class, 'pane-pub-home-imn')]
div[contains(@class, 'pane-pub-topic-imn')]
div[contains(@class, 'panel-panel-inner')]
div[contains(@class, 'pane-node-field-article-topics')]
section[contains(@class, 'footer-nav-section-wrapper')]
MASLD often is worse in slim patients
PARIS — Although metabolic liver diseases are mainly seen in patients with obesity or type 2 diabetes, studies have shown that non-alcoholic fatty liver disease, recently renamed metabolic dysfunction-associated steatotic liver disease (MASLD), also affects slim patients. Moreover, the condition could be particularly severe in this population.
A recent study carried out using data from the French Constance cohort showed that of the 25,753 patients with MASLD, 16.3% were lean (BMI of less than 25 kg/m²). In addition, 50% of these patients had no metabolic risk factors.
These slim patients with MASLD were most often young patients, for the most part female, and less likely to present with symptoms of metabolic syndrome. Asian patients were overrepresented in this group.
“These patients probably have genetic and/or environmental risk factors,” commented senior author Lawrence Serfaty, MD, PhD, head of the metabolic liver unit at the new Strasbourg public hospital, during a press conference at the Paris NASH meeting.
The disease was more severe in slim subjects. Overall, 3.6% of the slim subjects had advanced fibrosis (Forns index > 6.9) vs 1.7% of patients with overweight or obesity (P < .001), regardless of demographic variables, metabolic risk factors, and lifestyle. They also had higher alanine aminotransferase levels.
In addition, over the course of a mean follow-up of 3.8 years, liver events (eg, cirrhosis, decompensated cirrhosis, and liver cancer), chronic kidney diseases, and all-cause mortality were much more common in these patients than in patients with overweight or obesity (adjusted hazard ratios of 5.84, 2.49, and 3.01, respectively). It should be noted that these clinical results were linked to fibrosis severity in both slim and overweight subjects with MASLD.
Nonetheless, cardiovascular events remained more common in patients with overweight or obesity, suggesting that obesity itself is a major risk factor for cardiovascular diseases, regardless of MASLD.
“Armed with these results, which confirm those obtained from other studies, we must seek to understand the pathogenesis of the disease in slim patients and study the role of the microbiota, genetics, and diet, as well as determining the effects of alcohol and tobacco, consumption of which was slightly more common in this subpopulation,” said Dr. Serfaty.
According to the study authors, sarcopenia and bile acids could also be involved in the pathogenesis of MASLD in slim patients. The researchers concluded that “due to the relatively low rate of MASLD in slim subjects, screening should target patients presenting with metabolic anomalies and/or unexplained cytolysis.”
This article was translated from the Medscape French edition.
PARIS — Although metabolic liver diseases are mainly seen in patients with obesity or type 2 diabetes, studies have shown that non-alcoholic fatty liver disease, recently renamed metabolic dysfunction-associated steatotic liver disease (MASLD), also affects slim patients. Moreover, the condition could be particularly severe in this population.
A recent study carried out using data from the French Constance cohort showed that of the 25,753 patients with MASLD, 16.3% were lean (BMI of less than 25 kg/m²). In addition, 50% of these patients had no metabolic risk factors.
These slim patients with MASLD were most often young patients, for the most part female, and less likely to present with symptoms of metabolic syndrome. Asian patients were overrepresented in this group.
“These patients probably have genetic and/or environmental risk factors,” commented senior author Lawrence Serfaty, MD, PhD, head of the metabolic liver unit at the new Strasbourg public hospital, during a press conference at the Paris NASH meeting.
The disease was more severe in slim subjects. Overall, 3.6% of the slim subjects had advanced fibrosis (Forns index > 6.9) vs 1.7% of patients with overweight or obesity (P < .001), regardless of demographic variables, metabolic risk factors, and lifestyle. They also had higher alanine aminotransferase levels.
In addition, over the course of a mean follow-up of 3.8 years, liver events (eg, cirrhosis, decompensated cirrhosis, and liver cancer), chronic kidney diseases, and all-cause mortality were much more common in these patients than in patients with overweight or obesity (adjusted hazard ratios of 5.84, 2.49, and 3.01, respectively). It should be noted that these clinical results were linked to fibrosis severity in both slim and overweight subjects with MASLD.
Nonetheless, cardiovascular events remained more common in patients with overweight or obesity, suggesting that obesity itself is a major risk factor for cardiovascular diseases, regardless of MASLD.
“Armed with these results, which confirm those obtained from other studies, we must seek to understand the pathogenesis of the disease in slim patients and study the role of the microbiota, genetics, and diet, as well as determining the effects of alcohol and tobacco, consumption of which was slightly more common in this subpopulation,” said Dr. Serfaty.
According to the study authors, sarcopenia and bile acids could also be involved in the pathogenesis of MASLD in slim patients. The researchers concluded that “due to the relatively low rate of MASLD in slim subjects, screening should target patients presenting with metabolic anomalies and/or unexplained cytolysis.”
This article was translated from the Medscape French edition.
PARIS — Although metabolic liver diseases are mainly seen in patients with obesity or type 2 diabetes, studies have shown that non-alcoholic fatty liver disease, recently renamed metabolic dysfunction-associated steatotic liver disease (MASLD), also affects slim patients. Moreover, the condition could be particularly severe in this population.
A recent study carried out using data from the French Constance cohort showed that of the 25,753 patients with MASLD, 16.3% were lean (BMI of less than 25 kg/m²). In addition, 50% of these patients had no metabolic risk factors.
These slim patients with MASLD were most often young patients, for the most part female, and less likely to present with symptoms of metabolic syndrome. Asian patients were overrepresented in this group.
“These patients probably have genetic and/or environmental risk factors,” commented senior author Lawrence Serfaty, MD, PhD, head of the metabolic liver unit at the new Strasbourg public hospital, during a press conference at the Paris NASH meeting.
The disease was more severe in slim subjects. Overall, 3.6% of the slim subjects had advanced fibrosis (Forns index > 6.9) vs 1.7% of patients with overweight or obesity (P < .001), regardless of demographic variables, metabolic risk factors, and lifestyle. They also had higher alanine aminotransferase levels.
In addition, over the course of a mean follow-up of 3.8 years, liver events (eg, cirrhosis, decompensated cirrhosis, and liver cancer), chronic kidney diseases, and all-cause mortality were much more common in these patients than in patients with overweight or obesity (adjusted hazard ratios of 5.84, 2.49, and 3.01, respectively). It should be noted that these clinical results were linked to fibrosis severity in both slim and overweight subjects with MASLD.
Nonetheless, cardiovascular events remained more common in patients with overweight or obesity, suggesting that obesity itself is a major risk factor for cardiovascular diseases, regardless of MASLD.
“Armed with these results, which confirm those obtained from other studies, we must seek to understand the pathogenesis of the disease in slim patients and study the role of the microbiota, genetics, and diet, as well as determining the effects of alcohol and tobacco, consumption of which was slightly more common in this subpopulation,” said Dr. Serfaty.
According to the study authors, sarcopenia and bile acids could also be involved in the pathogenesis of MASLD in slim patients. The researchers concluded that “due to the relatively low rate of MASLD in slim subjects, screening should target patients presenting with metabolic anomalies and/or unexplained cytolysis.”
This article was translated from the Medscape French edition.
Personalized nutrition therapy promotes diabetes remission
LEIPZIG, GERMANY — For patients newly diagnosed with type 2 diabetes, nutrition therapy is highly effective at achieving remission. “The greater the reduction in body weight, the higher the chances that blood sugar levels will normalize,” Diana Rubin, MD, said at the fall press conference of the German Diabetes Society (DDG). Dr. Rubin is conference president and chief physician of the Center for Nutritional Medicine and Diabetology at Vivantes Humboldt Hospital and the Spandau Hospital, Berlin, Germany.
Because of the development of modern medicines, nutrition therapy has increasingly been pushed into the background over the past 50 years. However, nutrition therapy and weight reduction can effectively delay diabetes for years, said Dr. Rubin. The patients are healthy, without being healed.
Nevertheless, the remission is rarely permanent. Most of the patients develop type 2 diabetes again after 5 years.
Personalized Nutrition Therapy
It is not just developments in medicine that have pushed nutrition therapy into the background. Another contributing factor is that statutory health insurance companies do not cover personalized nutrition counseling as standard, said Dr. Rubin.
Modern research in nutrition therapy has shown that patients with diabetes should receive personalized treatment. However, this idea is not taken into consideration in current diabetes training programs, which are the only forms of nutrition therapy covered by statutory health insurance companies.
Instead, nutrition information is mostly conveyed through group training sessions. Individuals do not necessarily find each other again. What’s more, these sessions are seldom led by nutrition experts. “It is rarely helpful to use a ‘one size fits all’ approach, as is often the case with these group training sessions,” said Dr. Rubin.
The DiRECT study, in which patients reduced their weight by 15 kg and achieved remission rates of almost 90%, is an example of how nutrition therapy can be highly effective. This is especially true if the aims and methods are determined on an individual basis and if there is frequent contact with a therapist. German and international guidelines, including the DDG’s best practice guides from 2022, highlight the importance of personalized nutrition therapy.
Telemedicine Encourages Adherence
“It is very important to consider the current living situation of the person concerned,” said Dr. Rubin. “It is important to set small objectives that can also be implemented in everyday life.” This can only succeed with a professional face-to-face consultation. “Achieving this objective then also becomes realistic — i.e., losing 10% to 15% body weight and maintaining this loss,” she said. “Long-term monitoring is needed to maintain this weight.”
Weight reduction methods should generally be determined according to the preferences of the person concerned, since dietary habits and environments are personal. For example, reducing the intake of carbohydrates and fats, intermittent fasting, or using meal replacement drinks can all be considered.
New data also show that digital apps available on prescription (DiGA) can be helpful for support; this idea is reflected in the DDG’s nutrition best practice guides for patients with type 2 diabetes.
“Studies show that adherence is highly dependent on the amount of contact with therapists and the long-term nature of the treatment,” said Dr. Rubin. She referred to the need for long-term monitoring, during which the patient can be repeatedly reminded of the therapeutic objective. “In this respect, I see a lot of potential in digital apps, and also in telemedicine, to cater to the short-term contact with the person concerned.”
A 2015 meta-analysis of 92 studies revealed a significant reduction in A1c for patients with type 1 or type 2 diabetes when using telemedicine nutrition therapy. Dr. Rubin frequently prescribes DiGAs, which are approved for obesity, “simply because I can recognize it makes it easier for many patients to stick to their goals.”
Dr. Rubin also recommends connecting with sport groups and self-help groups. “Maintaining the weight is a long-term project.”
Abdominal Fat Decisive
Prediabetes is a precursor to type 2 diabetes and entails an increased risk of heart attack, kidney and eye diseases, and various kinds of cancer. To date, physicians have tried to delay the onset of type 2 diabetes by aiming to reduce the weight of patients with prediabetes. However, scientists at the German Center for Diabetes Research showed with the Prediabetes Lifestyle Intervention Study that abdominal fat plays an important role in the remission of prediabetes.
The 1-year program with a healthy diet and increased physical activity was followed by 1105 patients with prediabetes. When every subject lost at least 5% of their weight, it turned out that some achieved remission, and others did not.
People who achieved remission exhibited better insulin sensitivity and had lost more visceral abdominal fat. Visceral abdominal fat can influence insulin sensitivity, not least by an inflammatory reaction in the fatty tissue.
Reducing visceral abdominal fat is clearly crucially important in achieving prediabetes remission. Subjects who achieved remission in the study had a strongly reduced risk for type 2 diabetes for up to 2 years after the end of the program. They had improved kidney function, and their blood vessels were in better condition.
Waist Circumference
According to the new results, the chances of remission increase if body weight is reduced by 5% and waist circumference is reduced by around 4 cm in women and 7 cm in men.
“Based on the new data, remission should be the new therapeutic objective in people with prediabetes. This could potentially change clinical practice and minimize the complication rate for our patients, both male and female,” said author Reiner Jumpertz-von Schwartzenberg, MD, a researcher at the Tübingen University Hospital in Germany.
Prediabetes remission can be assumed if the fasting blood glucose falls below 100 mg/dL (5.6 mmol/L), the 2-hour glucose below 140 mg/dL (7.8 mmol/L), and the A1c value below 5.7%. From the new findings, it can be seen that the chances of remission increase the more the body weight decreases.
Dr. Jumpertz-von Schwartzenberg and his colleagues want to investigate whether this strategy is cost-effective so that the support of payers can also be ensured.
This article was translated from the Medscape German edition.
A version of this article appeared on Medscape.com.
LEIPZIG, GERMANY — For patients newly diagnosed with type 2 diabetes, nutrition therapy is highly effective at achieving remission. “The greater the reduction in body weight, the higher the chances that blood sugar levels will normalize,” Diana Rubin, MD, said at the fall press conference of the German Diabetes Society (DDG). Dr. Rubin is conference president and chief physician of the Center for Nutritional Medicine and Diabetology at Vivantes Humboldt Hospital and the Spandau Hospital, Berlin, Germany.
Because of the development of modern medicines, nutrition therapy has increasingly been pushed into the background over the past 50 years. However, nutrition therapy and weight reduction can effectively delay diabetes for years, said Dr. Rubin. The patients are healthy, without being healed.
Nevertheless, the remission is rarely permanent. Most of the patients develop type 2 diabetes again after 5 years.
Personalized Nutrition Therapy
It is not just developments in medicine that have pushed nutrition therapy into the background. Another contributing factor is that statutory health insurance companies do not cover personalized nutrition counseling as standard, said Dr. Rubin.
Modern research in nutrition therapy has shown that patients with diabetes should receive personalized treatment. However, this idea is not taken into consideration in current diabetes training programs, which are the only forms of nutrition therapy covered by statutory health insurance companies.
Instead, nutrition information is mostly conveyed through group training sessions. Individuals do not necessarily find each other again. What’s more, these sessions are seldom led by nutrition experts. “It is rarely helpful to use a ‘one size fits all’ approach, as is often the case with these group training sessions,” said Dr. Rubin.
The DiRECT study, in which patients reduced their weight by 15 kg and achieved remission rates of almost 90%, is an example of how nutrition therapy can be highly effective. This is especially true if the aims and methods are determined on an individual basis and if there is frequent contact with a therapist. German and international guidelines, including the DDG’s best practice guides from 2022, highlight the importance of personalized nutrition therapy.
Telemedicine Encourages Adherence
“It is very important to consider the current living situation of the person concerned,” said Dr. Rubin. “It is important to set small objectives that can also be implemented in everyday life.” This can only succeed with a professional face-to-face consultation. “Achieving this objective then also becomes realistic — i.e., losing 10% to 15% body weight and maintaining this loss,” she said. “Long-term monitoring is needed to maintain this weight.”
Weight reduction methods should generally be determined according to the preferences of the person concerned, since dietary habits and environments are personal. For example, reducing the intake of carbohydrates and fats, intermittent fasting, or using meal replacement drinks can all be considered.
New data also show that digital apps available on prescription (DiGA) can be helpful for support; this idea is reflected in the DDG’s nutrition best practice guides for patients with type 2 diabetes.
“Studies show that adherence is highly dependent on the amount of contact with therapists and the long-term nature of the treatment,” said Dr. Rubin. She referred to the need for long-term monitoring, during which the patient can be repeatedly reminded of the therapeutic objective. “In this respect, I see a lot of potential in digital apps, and also in telemedicine, to cater to the short-term contact with the person concerned.”
A 2015 meta-analysis of 92 studies revealed a significant reduction in A1c for patients with type 1 or type 2 diabetes when using telemedicine nutrition therapy. Dr. Rubin frequently prescribes DiGAs, which are approved for obesity, “simply because I can recognize it makes it easier for many patients to stick to their goals.”
Dr. Rubin also recommends connecting with sport groups and self-help groups. “Maintaining the weight is a long-term project.”
Abdominal Fat Decisive
Prediabetes is a precursor to type 2 diabetes and entails an increased risk of heart attack, kidney and eye diseases, and various kinds of cancer. To date, physicians have tried to delay the onset of type 2 diabetes by aiming to reduce the weight of patients with prediabetes. However, scientists at the German Center for Diabetes Research showed with the Prediabetes Lifestyle Intervention Study that abdominal fat plays an important role in the remission of prediabetes.
The 1-year program with a healthy diet and increased physical activity was followed by 1105 patients with prediabetes. When every subject lost at least 5% of their weight, it turned out that some achieved remission, and others did not.
People who achieved remission exhibited better insulin sensitivity and had lost more visceral abdominal fat. Visceral abdominal fat can influence insulin sensitivity, not least by an inflammatory reaction in the fatty tissue.
Reducing visceral abdominal fat is clearly crucially important in achieving prediabetes remission. Subjects who achieved remission in the study had a strongly reduced risk for type 2 diabetes for up to 2 years after the end of the program. They had improved kidney function, and their blood vessels were in better condition.
Waist Circumference
According to the new results, the chances of remission increase if body weight is reduced by 5% and waist circumference is reduced by around 4 cm in women and 7 cm in men.
“Based on the new data, remission should be the new therapeutic objective in people with prediabetes. This could potentially change clinical practice and minimize the complication rate for our patients, both male and female,” said author Reiner Jumpertz-von Schwartzenberg, MD, a researcher at the Tübingen University Hospital in Germany.
Prediabetes remission can be assumed if the fasting blood glucose falls below 100 mg/dL (5.6 mmol/L), the 2-hour glucose below 140 mg/dL (7.8 mmol/L), and the A1c value below 5.7%. From the new findings, it can be seen that the chances of remission increase the more the body weight decreases.
Dr. Jumpertz-von Schwartzenberg and his colleagues want to investigate whether this strategy is cost-effective so that the support of payers can also be ensured.
This article was translated from the Medscape German edition.
A version of this article appeared on Medscape.com.
LEIPZIG, GERMANY — For patients newly diagnosed with type 2 diabetes, nutrition therapy is highly effective at achieving remission. “The greater the reduction in body weight, the higher the chances that blood sugar levels will normalize,” Diana Rubin, MD, said at the fall press conference of the German Diabetes Society (DDG). Dr. Rubin is conference president and chief physician of the Center for Nutritional Medicine and Diabetology at Vivantes Humboldt Hospital and the Spandau Hospital, Berlin, Germany.
Because of the development of modern medicines, nutrition therapy has increasingly been pushed into the background over the past 50 years. However, nutrition therapy and weight reduction can effectively delay diabetes for years, said Dr. Rubin. The patients are healthy, without being healed.
Nevertheless, the remission is rarely permanent. Most of the patients develop type 2 diabetes again after 5 years.
Personalized Nutrition Therapy
It is not just developments in medicine that have pushed nutrition therapy into the background. Another contributing factor is that statutory health insurance companies do not cover personalized nutrition counseling as standard, said Dr. Rubin.
Modern research in nutrition therapy has shown that patients with diabetes should receive personalized treatment. However, this idea is not taken into consideration in current diabetes training programs, which are the only forms of nutrition therapy covered by statutory health insurance companies.
Instead, nutrition information is mostly conveyed through group training sessions. Individuals do not necessarily find each other again. What’s more, these sessions are seldom led by nutrition experts. “It is rarely helpful to use a ‘one size fits all’ approach, as is often the case with these group training sessions,” said Dr. Rubin.
The DiRECT study, in which patients reduced their weight by 15 kg and achieved remission rates of almost 90%, is an example of how nutrition therapy can be highly effective. This is especially true if the aims and methods are determined on an individual basis and if there is frequent contact with a therapist. German and international guidelines, including the DDG’s best practice guides from 2022, highlight the importance of personalized nutrition therapy.
Telemedicine Encourages Adherence
“It is very important to consider the current living situation of the person concerned,” said Dr. Rubin. “It is important to set small objectives that can also be implemented in everyday life.” This can only succeed with a professional face-to-face consultation. “Achieving this objective then also becomes realistic — i.e., losing 10% to 15% body weight and maintaining this loss,” she said. “Long-term monitoring is needed to maintain this weight.”
Weight reduction methods should generally be determined according to the preferences of the person concerned, since dietary habits and environments are personal. For example, reducing the intake of carbohydrates and fats, intermittent fasting, or using meal replacement drinks can all be considered.
New data also show that digital apps available on prescription (DiGA) can be helpful for support; this idea is reflected in the DDG’s nutrition best practice guides for patients with type 2 diabetes.
“Studies show that adherence is highly dependent on the amount of contact with therapists and the long-term nature of the treatment,” said Dr. Rubin. She referred to the need for long-term monitoring, during which the patient can be repeatedly reminded of the therapeutic objective. “In this respect, I see a lot of potential in digital apps, and also in telemedicine, to cater to the short-term contact with the person concerned.”
A 2015 meta-analysis of 92 studies revealed a significant reduction in A1c for patients with type 1 or type 2 diabetes when using telemedicine nutrition therapy. Dr. Rubin frequently prescribes DiGAs, which are approved for obesity, “simply because I can recognize it makes it easier for many patients to stick to their goals.”
Dr. Rubin also recommends connecting with sport groups and self-help groups. “Maintaining the weight is a long-term project.”
Abdominal Fat Decisive
Prediabetes is a precursor to type 2 diabetes and entails an increased risk of heart attack, kidney and eye diseases, and various kinds of cancer. To date, physicians have tried to delay the onset of type 2 diabetes by aiming to reduce the weight of patients with prediabetes. However, scientists at the German Center for Diabetes Research showed with the Prediabetes Lifestyle Intervention Study that abdominal fat plays an important role in the remission of prediabetes.
The 1-year program with a healthy diet and increased physical activity was followed by 1105 patients with prediabetes. When every subject lost at least 5% of their weight, it turned out that some achieved remission, and others did not.
People who achieved remission exhibited better insulin sensitivity and had lost more visceral abdominal fat. Visceral abdominal fat can influence insulin sensitivity, not least by an inflammatory reaction in the fatty tissue.
Reducing visceral abdominal fat is clearly crucially important in achieving prediabetes remission. Subjects who achieved remission in the study had a strongly reduced risk for type 2 diabetes for up to 2 years after the end of the program. They had improved kidney function, and their blood vessels were in better condition.
Waist Circumference
According to the new results, the chances of remission increase if body weight is reduced by 5% and waist circumference is reduced by around 4 cm in women and 7 cm in men.
“Based on the new data, remission should be the new therapeutic objective in people with prediabetes. This could potentially change clinical practice and minimize the complication rate for our patients, both male and female,” said author Reiner Jumpertz-von Schwartzenberg, MD, a researcher at the Tübingen University Hospital in Germany.
Prediabetes remission can be assumed if the fasting blood glucose falls below 100 mg/dL (5.6 mmol/L), the 2-hour glucose below 140 mg/dL (7.8 mmol/L), and the A1c value below 5.7%. From the new findings, it can be seen that the chances of remission increase the more the body weight decreases.
Dr. Jumpertz-von Schwartzenberg and his colleagues want to investigate whether this strategy is cost-effective so that the support of payers can also be ensured.
This article was translated from the Medscape German edition.
A version of this article appeared on Medscape.com.
Link between vitamin D deficiency and obesity unclear
MADRID — The role of vitamin D in the risk for overweight and obesity has been the subject of multiple studies. Though there’s still not enough evidence to reach a decisive conclusion, several ongoing debates are setting the stage for future research.
Irene Bretón, MD, PhD, discussed these debates in a presentation titled “Vitamin D Deficiency and Obesity: Cause or Consequence?” delivered at the 64th Congress of the Spanish Society of Endocrinology and Nutrition (SEEN). Dr. Bretón is president of the Foundation of the Spanish Society of Endocrinology and Nutrition.
“Vitamin D deficiency can arise from different causes. The percentage that can be attributed to solar radiation is extremely variable. Some studies put it at 80%, while others suggest lower figures. Many diseases have also been associated with vitamin D deficiency or with low vitamin D levels (which are not always at the level of deficiency). Nonetheless, we still have a lot to learn about these associations,” she said.
Dr. Bretón pointed out that many of these studies overlook parathyroid hormone testing. “I also think it’s more appropriate to discuss nutritional status of vitamin D as opposed to serum levels, because these data can be misleading. It would be interesting to focus more on vitamin D metabolism and not just plasma levels.”
Vitamin Deficiency
To answer whether obesity and its complications could be related to low vitamin D levels, Dr. Bretón pointed to this vitamin’s profile in various regions of the world and called attention to the fact that none of the studies on this topic include populations with roughly adequate levels of this vitamin.
“This highlights the prevalence of vitamin D deficiency worldwide. It affects approximately 50% of the population, has been described in all age groups, and affects both men and women — particularly pregnant women and those in menopause — and older adults,” said Dr. Bretón.
She also cited the figures backing this fact: 88% have 25-hydroxyvitamin D levels < 30 ng/mL, 37% have levels < 20 ng/mL, and 7% have levels < 10 ng/mL.
“These percentages have brought us to consider their potential link to the current obesity epidemic. Studies in humans have observed a relationship between low plasma levels and markers for obesity and adiposity. Free 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D are known to be reduced in obesity, and treatments to correct vitamin D deficiency are less effective in people with the disease,” she noted.
Regarding the impact in “the opposite direction,” that is, whether obesity affects the nutritional status of vitamin D, Bretón explained that observational studies have generally found a relationship between overweight and obesity and lower plasma levels of vitamin D. “Data from these studies show that each kg/m2 increase in [body mass index (BMI)] is associated with a 1.15% decrease in 25-hydroxyvitamin D. These studies also show that the prevalence of vitamin D deficiency is 35% higher in patients with obesity and 24% higher in those that are overweight compared with individuals of normal weight. A relationship has been observed between vitamin D deficiency and body fat percentage in men and women and in all age groups,” explained Dr. Bretón.
Dr. Bretón noted that the diseases most closely associated with obesity are type 2 diabetes, hypertension, ischemic heart disease, cancer (colon, breast, prostate, and ovarian), inflammatory liver disease, asthma, and inflammatory diseases.
Mechanisms Involved
“People with obesity may experience less solar exposure (more of their body is covered, or they spend more time indoors), but reduced exposure to the sun is known to have less of an influence on vitamin D levels. Studies where people were given radiation to test how their plasma levels of vitamin D respond have found that there is a smaller effect in people with obesity, and that the effect is inversely correlated with BMI: the higher the BMI, the less vitamin D levels increase under exposure to solar radiation.”
Another mechanism is sequestration in adipose tissue, which is the largest reservoir of vitamin D in the body. Nevertheless, factors such as vitamin D concentration in this tissue, regulation of local metabolism, and vitamin uptake and release are less understood. It is therefore unclear whether this mechanism acts to regulate plasma levels.
“This is why severe vitamin D deficiencies (and deficiencies of other fat-soluble vitamins) that occur after bariatric surgery are often not seen in the first year after surgery but develop much later, when the vitamin that has accumulated in adipose tissue is released as weight is lost,” said Dr. Bretón.
“On the other hand, the volumetric dilution in blood that occurs in relation to total body fat content may explain the variability of plasma levels and the response to treatment. Predictive equations have been described,” she explained.
The Prenatal Stage
Dr. Bretón mentioned that the best setting for studying the impact of vitamin D and preventing future obesity is during the initial stages of life, when adipogenesis and fetal programming are occurring.
“Studies in animals have shown how maternal vitamin D deficiency (due to nongenetic or nonepigenetic mechanisms) leads to changes in adipogenesis and programming of adipose reserves. A fetal or perinatal environment with low vitamin D levels programs all these mechanisms differently, and not just adipogenesis and adipocyte differentiation in utero,” she added.
Various mechanisms involved in vitamin D deficiency as a cause of obesity are currently being studied in the prenatal setting. One such mechanism is the interaction between the vitamin D receptor and 1 alpha–hydroxylase, which are present in the adipose tissue and help modulate lipid metabolism.
“The vitamin D receptor is particularly expressed in the early stages of adipocyte differentiation, but its expression drops off as the differentiation process continues. Vitamin D receptor knockout mice have a slender phenotype and are resistant to diet-induced obesity. They also accumulate less fat with age and a high-fat diet,” explained Dr. Bretón.
“However, vitamin D also influences the production of inflammatory adipokines in these early stages of life. It specifically plays a central role in modulating the inflammatory response in adipose tissue. These anti-inflammatory effects appear to be mediated by inhibition of [NF–kappa B] and MAPK signaling pathways. All of this suggests that vitamin D influences both adipogenesis and how the adipose tissue functions,” she added.
Weight Loss
When considering the link between vitamin D and obesity in the context of weight loss, Dr. Bretón explained that studies in this area suggest that weight loss per se is not sufficient to increase serum 25-hydroxyvitamin D. Rather, increased synthesis by the skin or increased dietary intake are the most relevant factors for the nutritional status of this vitamin.
“A recent systematic review looking at the relationship between vitamin D levels and weight loss via caloric restriction and exercise showed a small but significant effect in the sense that weight loss increases vitamin D levels. However, other meta-analyses have not found significant results in this area,” she said.
“In my opinion, these results depend on how long the intervention is performed. If a lot of weight is lost in a short time frame, vitamin D is released into the adipose tissue, a process that doesn’t have any significant impact on the nutritional status of this vitamin. Generally, the effect of this relationship is small (1.5 ng/mL) and of little clinical relevance. Moreover, many systematic reviews have analyzed this relationship following bariatric surgery and have also come up with inconclusive results,” Dr. Bretón added.
What role do treatments play in correcting vitamin D deficiency? Dr. Bretón explained that studies that have examined how fortified foods affect obesity show that though these foods don’t cause significant weight changes, they do affect fat mass and waist circumference. This finding suggests that fortified foods have some impact, not necessarily on weight but perhaps on adiposity.
“To rightly value all this data, one has to pay special attention to the environment and the context where the research took place (children or adults, baseline vitamin D levels, and so on). If fortified foods are directly supplemented with cholecalciferol, the results are very inconsistent. We therefore cannot say that treatment with vitamin D can reduce body weight and adiposity,” she said.
When it comes to the complications from obesity, studies of vitamin D supplementation, cancer, and cardiovascular disease did not find any beneficial effect on preventing these pathologies.
For obesity’s impact on vitamin D supplementation, it is known that the levels achieved are lower in patients with obesity compared with patients of normal weight. “Compared with other interventions, however, these levels (15.27 ng/mL) are clinically relevant,” she noted.
Future Directions
Dr. Bretón explained that all this evidence has revealed many debates regarding the association of vitamin D levels with obesity. “For example, it appears that obesity could predict low vitamin D levels (not necessarily a deficiency). In turn, these low levels could cause obesity, especially during embryonic development, when programming of adipocyte physiology is taking place.”
Dr. Bretón sees many confounding factors that will need to be elucidated in the future. “One factor is that we aren’t sure whether the patient we’re seeing has vitamin D deficiency or if other factors are in play, like time since weight loss, laboratory technique used to measure vitamin D, nutritional status, geographic location, time of year when the test is performed, et cetera. You also have to assess other factors having to do with obesity, like how adiposity is being measured and whether BMI reflects that adiposity.”
Last, the expert reviewed the major research efforts underway that are based on evidence that vitamin D is associated with insulin resistance. Studies are being performed on pancreatic function, the role of vitamin D levels in ovarian physiology related to insulin resistance (specifically, the role of hyperandrogenism), adipose tissue (vitamin D receptor expression, volumetric dilution), and other components of metabolic syndrome to determine how this vitamin’s status influences the renin-angiotensin system, apoptosis, and cardiovascular risk.
“There is also plenty of research going on surrounding metabolic liver disease, which has a lot to do with the microbiota. So, they’re studying the relationship between vitamin D and dysbiosis, especially regarding local immunomodulation in the gut in relation to the microbiota,” she added.
Another area of research is cancer, focusing primarily on analyzing the nutritional status of vitamin D in relation to the microbiome and how this status may affect the therapeutic effect of chemotherapy and radiation therapy. “It would be interesting to find out whether the effect of immunotherapy varies depending on the patient’s vitamin D status,” concluded Dr. Bretón.
Dr. Bretón’s lecture at the 64th Congress of the SEEN was sponsored by the Foundation for Analysis and Social Studies (FAES).
This article was translated from the Medscape Spanish edition. A version of this article appeared on Medscape.com.
MADRID — The role of vitamin D in the risk for overweight and obesity has been the subject of multiple studies. Though there’s still not enough evidence to reach a decisive conclusion, several ongoing debates are setting the stage for future research.
Irene Bretón, MD, PhD, discussed these debates in a presentation titled “Vitamin D Deficiency and Obesity: Cause or Consequence?” delivered at the 64th Congress of the Spanish Society of Endocrinology and Nutrition (SEEN). Dr. Bretón is president of the Foundation of the Spanish Society of Endocrinology and Nutrition.
“Vitamin D deficiency can arise from different causes. The percentage that can be attributed to solar radiation is extremely variable. Some studies put it at 80%, while others suggest lower figures. Many diseases have also been associated with vitamin D deficiency or with low vitamin D levels (which are not always at the level of deficiency). Nonetheless, we still have a lot to learn about these associations,” she said.
Dr. Bretón pointed out that many of these studies overlook parathyroid hormone testing. “I also think it’s more appropriate to discuss nutritional status of vitamin D as opposed to serum levels, because these data can be misleading. It would be interesting to focus more on vitamin D metabolism and not just plasma levels.”
Vitamin Deficiency
To answer whether obesity and its complications could be related to low vitamin D levels, Dr. Bretón pointed to this vitamin’s profile in various regions of the world and called attention to the fact that none of the studies on this topic include populations with roughly adequate levels of this vitamin.
“This highlights the prevalence of vitamin D deficiency worldwide. It affects approximately 50% of the population, has been described in all age groups, and affects both men and women — particularly pregnant women and those in menopause — and older adults,” said Dr. Bretón.
She also cited the figures backing this fact: 88% have 25-hydroxyvitamin D levels < 30 ng/mL, 37% have levels < 20 ng/mL, and 7% have levels < 10 ng/mL.
“These percentages have brought us to consider their potential link to the current obesity epidemic. Studies in humans have observed a relationship between low plasma levels and markers for obesity and adiposity. Free 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D are known to be reduced in obesity, and treatments to correct vitamin D deficiency are less effective in people with the disease,” she noted.
Regarding the impact in “the opposite direction,” that is, whether obesity affects the nutritional status of vitamin D, Bretón explained that observational studies have generally found a relationship between overweight and obesity and lower plasma levels of vitamin D. “Data from these studies show that each kg/m2 increase in [body mass index (BMI)] is associated with a 1.15% decrease in 25-hydroxyvitamin D. These studies also show that the prevalence of vitamin D deficiency is 35% higher in patients with obesity and 24% higher in those that are overweight compared with individuals of normal weight. A relationship has been observed between vitamin D deficiency and body fat percentage in men and women and in all age groups,” explained Dr. Bretón.
Dr. Bretón noted that the diseases most closely associated with obesity are type 2 diabetes, hypertension, ischemic heart disease, cancer (colon, breast, prostate, and ovarian), inflammatory liver disease, asthma, and inflammatory diseases.
Mechanisms Involved
“People with obesity may experience less solar exposure (more of their body is covered, or they spend more time indoors), but reduced exposure to the sun is known to have less of an influence on vitamin D levels. Studies where people were given radiation to test how their plasma levels of vitamin D respond have found that there is a smaller effect in people with obesity, and that the effect is inversely correlated with BMI: the higher the BMI, the less vitamin D levels increase under exposure to solar radiation.”
Another mechanism is sequestration in adipose tissue, which is the largest reservoir of vitamin D in the body. Nevertheless, factors such as vitamin D concentration in this tissue, regulation of local metabolism, and vitamin uptake and release are less understood. It is therefore unclear whether this mechanism acts to regulate plasma levels.
“This is why severe vitamin D deficiencies (and deficiencies of other fat-soluble vitamins) that occur after bariatric surgery are often not seen in the first year after surgery but develop much later, when the vitamin that has accumulated in adipose tissue is released as weight is lost,” said Dr. Bretón.
“On the other hand, the volumetric dilution in blood that occurs in relation to total body fat content may explain the variability of plasma levels and the response to treatment. Predictive equations have been described,” she explained.
The Prenatal Stage
Dr. Bretón mentioned that the best setting for studying the impact of vitamin D and preventing future obesity is during the initial stages of life, when adipogenesis and fetal programming are occurring.
“Studies in animals have shown how maternal vitamin D deficiency (due to nongenetic or nonepigenetic mechanisms) leads to changes in adipogenesis and programming of adipose reserves. A fetal or perinatal environment with low vitamin D levels programs all these mechanisms differently, and not just adipogenesis and adipocyte differentiation in utero,” she added.
Various mechanisms involved in vitamin D deficiency as a cause of obesity are currently being studied in the prenatal setting. One such mechanism is the interaction between the vitamin D receptor and 1 alpha–hydroxylase, which are present in the adipose tissue and help modulate lipid metabolism.
“The vitamin D receptor is particularly expressed in the early stages of adipocyte differentiation, but its expression drops off as the differentiation process continues. Vitamin D receptor knockout mice have a slender phenotype and are resistant to diet-induced obesity. They also accumulate less fat with age and a high-fat diet,” explained Dr. Bretón.
“However, vitamin D also influences the production of inflammatory adipokines in these early stages of life. It specifically plays a central role in modulating the inflammatory response in adipose tissue. These anti-inflammatory effects appear to be mediated by inhibition of [NF–kappa B] and MAPK signaling pathways. All of this suggests that vitamin D influences both adipogenesis and how the adipose tissue functions,” she added.
Weight Loss
When considering the link between vitamin D and obesity in the context of weight loss, Dr. Bretón explained that studies in this area suggest that weight loss per se is not sufficient to increase serum 25-hydroxyvitamin D. Rather, increased synthesis by the skin or increased dietary intake are the most relevant factors for the nutritional status of this vitamin.
“A recent systematic review looking at the relationship between vitamin D levels and weight loss via caloric restriction and exercise showed a small but significant effect in the sense that weight loss increases vitamin D levels. However, other meta-analyses have not found significant results in this area,” she said.
“In my opinion, these results depend on how long the intervention is performed. If a lot of weight is lost in a short time frame, vitamin D is released into the adipose tissue, a process that doesn’t have any significant impact on the nutritional status of this vitamin. Generally, the effect of this relationship is small (1.5 ng/mL) and of little clinical relevance. Moreover, many systematic reviews have analyzed this relationship following bariatric surgery and have also come up with inconclusive results,” Dr. Bretón added.
What role do treatments play in correcting vitamin D deficiency? Dr. Bretón explained that studies that have examined how fortified foods affect obesity show that though these foods don’t cause significant weight changes, they do affect fat mass and waist circumference. This finding suggests that fortified foods have some impact, not necessarily on weight but perhaps on adiposity.
“To rightly value all this data, one has to pay special attention to the environment and the context where the research took place (children or adults, baseline vitamin D levels, and so on). If fortified foods are directly supplemented with cholecalciferol, the results are very inconsistent. We therefore cannot say that treatment with vitamin D can reduce body weight and adiposity,” she said.
When it comes to the complications from obesity, studies of vitamin D supplementation, cancer, and cardiovascular disease did not find any beneficial effect on preventing these pathologies.
For obesity’s impact on vitamin D supplementation, it is known that the levels achieved are lower in patients with obesity compared with patients of normal weight. “Compared with other interventions, however, these levels (15.27 ng/mL) are clinically relevant,” she noted.
Future Directions
Dr. Bretón explained that all this evidence has revealed many debates regarding the association of vitamin D levels with obesity. “For example, it appears that obesity could predict low vitamin D levels (not necessarily a deficiency). In turn, these low levels could cause obesity, especially during embryonic development, when programming of adipocyte physiology is taking place.”
Dr. Bretón sees many confounding factors that will need to be elucidated in the future. “One factor is that we aren’t sure whether the patient we’re seeing has vitamin D deficiency or if other factors are in play, like time since weight loss, laboratory technique used to measure vitamin D, nutritional status, geographic location, time of year when the test is performed, et cetera. You also have to assess other factors having to do with obesity, like how adiposity is being measured and whether BMI reflects that adiposity.”
Last, the expert reviewed the major research efforts underway that are based on evidence that vitamin D is associated with insulin resistance. Studies are being performed on pancreatic function, the role of vitamin D levels in ovarian physiology related to insulin resistance (specifically, the role of hyperandrogenism), adipose tissue (vitamin D receptor expression, volumetric dilution), and other components of metabolic syndrome to determine how this vitamin’s status influences the renin-angiotensin system, apoptosis, and cardiovascular risk.
“There is also plenty of research going on surrounding metabolic liver disease, which has a lot to do with the microbiota. So, they’re studying the relationship between vitamin D and dysbiosis, especially regarding local immunomodulation in the gut in relation to the microbiota,” she added.
Another area of research is cancer, focusing primarily on analyzing the nutritional status of vitamin D in relation to the microbiome and how this status may affect the therapeutic effect of chemotherapy and radiation therapy. “It would be interesting to find out whether the effect of immunotherapy varies depending on the patient’s vitamin D status,” concluded Dr. Bretón.
Dr. Bretón’s lecture at the 64th Congress of the SEEN was sponsored by the Foundation for Analysis and Social Studies (FAES).
This article was translated from the Medscape Spanish edition. A version of this article appeared on Medscape.com.
MADRID — The role of vitamin D in the risk for overweight and obesity has been the subject of multiple studies. Though there’s still not enough evidence to reach a decisive conclusion, several ongoing debates are setting the stage for future research.
Irene Bretón, MD, PhD, discussed these debates in a presentation titled “Vitamin D Deficiency and Obesity: Cause or Consequence?” delivered at the 64th Congress of the Spanish Society of Endocrinology and Nutrition (SEEN). Dr. Bretón is president of the Foundation of the Spanish Society of Endocrinology and Nutrition.
“Vitamin D deficiency can arise from different causes. The percentage that can be attributed to solar radiation is extremely variable. Some studies put it at 80%, while others suggest lower figures. Many diseases have also been associated with vitamin D deficiency or with low vitamin D levels (which are not always at the level of deficiency). Nonetheless, we still have a lot to learn about these associations,” she said.
Dr. Bretón pointed out that many of these studies overlook parathyroid hormone testing. “I also think it’s more appropriate to discuss nutritional status of vitamin D as opposed to serum levels, because these data can be misleading. It would be interesting to focus more on vitamin D metabolism and not just plasma levels.”
Vitamin Deficiency
To answer whether obesity and its complications could be related to low vitamin D levels, Dr. Bretón pointed to this vitamin’s profile in various regions of the world and called attention to the fact that none of the studies on this topic include populations with roughly adequate levels of this vitamin.
“This highlights the prevalence of vitamin D deficiency worldwide. It affects approximately 50% of the population, has been described in all age groups, and affects both men and women — particularly pregnant women and those in menopause — and older adults,” said Dr. Bretón.
She also cited the figures backing this fact: 88% have 25-hydroxyvitamin D levels < 30 ng/mL, 37% have levels < 20 ng/mL, and 7% have levels < 10 ng/mL.
“These percentages have brought us to consider their potential link to the current obesity epidemic. Studies in humans have observed a relationship between low plasma levels and markers for obesity and adiposity. Free 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D are known to be reduced in obesity, and treatments to correct vitamin D deficiency are less effective in people with the disease,” she noted.
Regarding the impact in “the opposite direction,” that is, whether obesity affects the nutritional status of vitamin D, Bretón explained that observational studies have generally found a relationship between overweight and obesity and lower plasma levels of vitamin D. “Data from these studies show that each kg/m2 increase in [body mass index (BMI)] is associated with a 1.15% decrease in 25-hydroxyvitamin D. These studies also show that the prevalence of vitamin D deficiency is 35% higher in patients with obesity and 24% higher in those that are overweight compared with individuals of normal weight. A relationship has been observed between vitamin D deficiency and body fat percentage in men and women and in all age groups,” explained Dr. Bretón.
Dr. Bretón noted that the diseases most closely associated with obesity are type 2 diabetes, hypertension, ischemic heart disease, cancer (colon, breast, prostate, and ovarian), inflammatory liver disease, asthma, and inflammatory diseases.
Mechanisms Involved
“People with obesity may experience less solar exposure (more of their body is covered, or they spend more time indoors), but reduced exposure to the sun is known to have less of an influence on vitamin D levels. Studies where people were given radiation to test how their plasma levels of vitamin D respond have found that there is a smaller effect in people with obesity, and that the effect is inversely correlated with BMI: the higher the BMI, the less vitamin D levels increase under exposure to solar radiation.”
Another mechanism is sequestration in adipose tissue, which is the largest reservoir of vitamin D in the body. Nevertheless, factors such as vitamin D concentration in this tissue, regulation of local metabolism, and vitamin uptake and release are less understood. It is therefore unclear whether this mechanism acts to regulate plasma levels.
“This is why severe vitamin D deficiencies (and deficiencies of other fat-soluble vitamins) that occur after bariatric surgery are often not seen in the first year after surgery but develop much later, when the vitamin that has accumulated in adipose tissue is released as weight is lost,” said Dr. Bretón.
“On the other hand, the volumetric dilution in blood that occurs in relation to total body fat content may explain the variability of plasma levels and the response to treatment. Predictive equations have been described,” she explained.
The Prenatal Stage
Dr. Bretón mentioned that the best setting for studying the impact of vitamin D and preventing future obesity is during the initial stages of life, when adipogenesis and fetal programming are occurring.
“Studies in animals have shown how maternal vitamin D deficiency (due to nongenetic or nonepigenetic mechanisms) leads to changes in adipogenesis and programming of adipose reserves. A fetal or perinatal environment with low vitamin D levels programs all these mechanisms differently, and not just adipogenesis and adipocyte differentiation in utero,” she added.
Various mechanisms involved in vitamin D deficiency as a cause of obesity are currently being studied in the prenatal setting. One such mechanism is the interaction between the vitamin D receptor and 1 alpha–hydroxylase, which are present in the adipose tissue and help modulate lipid metabolism.
“The vitamin D receptor is particularly expressed in the early stages of adipocyte differentiation, but its expression drops off as the differentiation process continues. Vitamin D receptor knockout mice have a slender phenotype and are resistant to diet-induced obesity. They also accumulate less fat with age and a high-fat diet,” explained Dr. Bretón.
“However, vitamin D also influences the production of inflammatory adipokines in these early stages of life. It specifically plays a central role in modulating the inflammatory response in adipose tissue. These anti-inflammatory effects appear to be mediated by inhibition of [NF–kappa B] and MAPK signaling pathways. All of this suggests that vitamin D influences both adipogenesis and how the adipose tissue functions,” she added.
Weight Loss
When considering the link between vitamin D and obesity in the context of weight loss, Dr. Bretón explained that studies in this area suggest that weight loss per se is not sufficient to increase serum 25-hydroxyvitamin D. Rather, increased synthesis by the skin or increased dietary intake are the most relevant factors for the nutritional status of this vitamin.
“A recent systematic review looking at the relationship between vitamin D levels and weight loss via caloric restriction and exercise showed a small but significant effect in the sense that weight loss increases vitamin D levels. However, other meta-analyses have not found significant results in this area,” she said.
“In my opinion, these results depend on how long the intervention is performed. If a lot of weight is lost in a short time frame, vitamin D is released into the adipose tissue, a process that doesn’t have any significant impact on the nutritional status of this vitamin. Generally, the effect of this relationship is small (1.5 ng/mL) and of little clinical relevance. Moreover, many systematic reviews have analyzed this relationship following bariatric surgery and have also come up with inconclusive results,” Dr. Bretón added.
What role do treatments play in correcting vitamin D deficiency? Dr. Bretón explained that studies that have examined how fortified foods affect obesity show that though these foods don’t cause significant weight changes, they do affect fat mass and waist circumference. This finding suggests that fortified foods have some impact, not necessarily on weight but perhaps on adiposity.
“To rightly value all this data, one has to pay special attention to the environment and the context where the research took place (children or adults, baseline vitamin D levels, and so on). If fortified foods are directly supplemented with cholecalciferol, the results are very inconsistent. We therefore cannot say that treatment with vitamin D can reduce body weight and adiposity,” she said.
When it comes to the complications from obesity, studies of vitamin D supplementation, cancer, and cardiovascular disease did not find any beneficial effect on preventing these pathologies.
For obesity’s impact on vitamin D supplementation, it is known that the levels achieved are lower in patients with obesity compared with patients of normal weight. “Compared with other interventions, however, these levels (15.27 ng/mL) are clinically relevant,” she noted.
Future Directions
Dr. Bretón explained that all this evidence has revealed many debates regarding the association of vitamin D levels with obesity. “For example, it appears that obesity could predict low vitamin D levels (not necessarily a deficiency). In turn, these low levels could cause obesity, especially during embryonic development, when programming of adipocyte physiology is taking place.”
Dr. Bretón sees many confounding factors that will need to be elucidated in the future. “One factor is that we aren’t sure whether the patient we’re seeing has vitamin D deficiency or if other factors are in play, like time since weight loss, laboratory technique used to measure vitamin D, nutritional status, geographic location, time of year when the test is performed, et cetera. You also have to assess other factors having to do with obesity, like how adiposity is being measured and whether BMI reflects that adiposity.”
Last, the expert reviewed the major research efforts underway that are based on evidence that vitamin D is associated with insulin resistance. Studies are being performed on pancreatic function, the role of vitamin D levels in ovarian physiology related to insulin resistance (specifically, the role of hyperandrogenism), adipose tissue (vitamin D receptor expression, volumetric dilution), and other components of metabolic syndrome to determine how this vitamin’s status influences the renin-angiotensin system, apoptosis, and cardiovascular risk.
“There is also plenty of research going on surrounding metabolic liver disease, which has a lot to do with the microbiota. So, they’re studying the relationship between vitamin D and dysbiosis, especially regarding local immunomodulation in the gut in relation to the microbiota,” she added.
Another area of research is cancer, focusing primarily on analyzing the nutritional status of vitamin D in relation to the microbiome and how this status may affect the therapeutic effect of chemotherapy and radiation therapy. “It would be interesting to find out whether the effect of immunotherapy varies depending on the patient’s vitamin D status,” concluded Dr. Bretón.
Dr. Bretón’s lecture at the 64th Congress of the SEEN was sponsored by the Foundation for Analysis and Social Studies (FAES).
This article was translated from the Medscape Spanish edition. A version of this article appeared on Medscape.com.
Most stop taking weight loss drugs within 1 year
Patients receiving semaglutide for weight loss show a significantly higher rate of continuing the medication at 1 year compared with less effective anti-obesity drugs. However, even among those patients, continuation declines to fewer than half of patients.
“We now have effective US Food and Drug Administration–approved anti-obesity medications; [however], this study shows that in a real-world setting, the vast majority of patients discontinued their prescription fills within the first year,” said first author Hamlet Gasoyan, PhD, lead author of the study and a researcher with Cleveland Clinic’s Center for Value-Based Care Research, said in a press statement.
The study was published online in the journal Obesity.
While breakthrough drugs such as glucagon-like peptide-1 (GLP-1) receptor agonists have shown high efficacy in achieving weight loss while providing a host of other health benefits, their discontinuation has been shown to potentially result in a rapid regaining of weight that was lost, as well as a reversal of the other health benefits, such as cardiometabolic improvements, the study authors wrote.
To evaluate rates of persistence with those along with other weight loss medications and factors associated with discontinuation, Dr. Gasoyan and colleagues conducted a retrospective cohort study, identifying 1911 patients with obesity, who had an initial anti-obesity medication prescription filled between 2015 and 2022 at Cleveland Clinic centers in Ohio and Florida.
Over the study period, 25% of patients filled a prescription for semaglutide, 34% for naltrexone-bupropion, 26% for phentermine-topiramate, 14% for liraglutide, and 0.9% for orlistat.
The patients had a median baseline BMI of 38, with obesity defined as a BMI of 30 or higher.
Medication Continuation Drops After 3 Months
With a median follow-up time of 2.4 years, the rate of persistence to the medications overall dropped from 44% at 3 months to 33% at 6 months and just 19% at 12 months.
In a multivariate analysis, semaglutide was associated with the highest odds of 1-year persistence (adjusted odds ratio [AOR], 4.26), while naltrexone-bupropion had the lowest odds (AOR, 0.68), compared with phentermine-topiramate. The other agents did not have significantly different odds of persistence.
Semaglutide and liraglutide also had the highest persistence rates overall, including at 3 months (63% and 52%, respectively) and 6 months (56% and 37%, respectively).
Those with higher weight loss at 6 months had a higher likelihood of remaining on the weight loss medication at 1 year, with a 1% increase in weight loss at 6 months associated with 6% increased odds of still being persistent at year 1 (adjusted odds ratio, 1.06).
Those who did continue medications at 1 year had a mean of 10% weight loss at 12 months compared with just 2% among individuals who were not persistent (P <.001).
Most patients (84%) in the study were privately insured, and weight loss drug adherence varied significantly based on the insurance carrier.
Studies demonstrating the effects of discontinuing treatment with semaglutide include the STEP 1 trial extension, which showed that 1 year after discontinuation of treatment and lifestyle intervention, participants regained two thirds of their lost weight on average, and the cardiometabolic improvements with the weight loss were reversed.
In light of those findings, “the current scientific knowledge favors using anti-obesity medications longer term for weight loss maintenance if they are well-tolerated and have resulted in clinically meaningful weight loss,” Dr. Gasoyan told this news organization.
Paradoxically, the possible regaining of weight could be a factor in some insurers denying longer-term coverage, he noted.
Discontinuing Medications Means Regaining Appetite
Anne Peters, MD, a professor of medicine at USC’s Keck School of Medicine in Los Angeles and director of the USC Clinical Diabetes Programs, underscored that the possibility of regaining weight with discontinuation of GLP-1 receptor agonists is indeed “a big concern because your appetite comes back in spades when you take away the effect of these hormones,” she told this news organization. “For that reason, I don’t ever tell people to stop cold turkey.”
Regarding the question of how long patients should remain on the medications, Peters said the scenario might be compared to the need for patients with type 1 diabetes to be on insulin, which is a gut hormone.
“These medications are also gut hormones, and some patients may need to also be on them for life to maintain the benefits,” she said.
“If a patient for some reason wishes to come off of the medication, for instance in order to be on less medicine, I have them titrate down and usually there will be a dose where they actually need only a small dose.
“I even have some patients who just take semaglutide once a month who are able to manage to maintain their weight loss,” Dr. Peters noted.
“But the whole goal in people who are overweight or obese is to establish a new set point and maintain whatever that new target weight is.”
Dr. Peters agreed that the loss of insurance coverage for the medications can throw a big wrench into that maintenance, presenting adverse effects of its own by causing a lack of treatment continuity.
“When you lose weight, you lose lean body mass and fat mass, but when you regain, it’s primary fat mass, so if you go on and off these drugs, it can contribute to a loss of lean mass. Therefore, these drugs should not be taken if someone is going to go on and off them repeatedly.”
The study received funding from the National Cancer Institute. Dr. Peters has consulted for Eli Lilly in the past.
A version of this article appeared on Medscape.com.
Patients receiving semaglutide for weight loss show a significantly higher rate of continuing the medication at 1 year compared with less effective anti-obesity drugs. However, even among those patients, continuation declines to fewer than half of patients.
“We now have effective US Food and Drug Administration–approved anti-obesity medications; [however], this study shows that in a real-world setting, the vast majority of patients discontinued their prescription fills within the first year,” said first author Hamlet Gasoyan, PhD, lead author of the study and a researcher with Cleveland Clinic’s Center for Value-Based Care Research, said in a press statement.
The study was published online in the journal Obesity.
While breakthrough drugs such as glucagon-like peptide-1 (GLP-1) receptor agonists have shown high efficacy in achieving weight loss while providing a host of other health benefits, their discontinuation has been shown to potentially result in a rapid regaining of weight that was lost, as well as a reversal of the other health benefits, such as cardiometabolic improvements, the study authors wrote.
To evaluate rates of persistence with those along with other weight loss medications and factors associated with discontinuation, Dr. Gasoyan and colleagues conducted a retrospective cohort study, identifying 1911 patients with obesity, who had an initial anti-obesity medication prescription filled between 2015 and 2022 at Cleveland Clinic centers in Ohio and Florida.
Over the study period, 25% of patients filled a prescription for semaglutide, 34% for naltrexone-bupropion, 26% for phentermine-topiramate, 14% for liraglutide, and 0.9% for orlistat.
The patients had a median baseline BMI of 38, with obesity defined as a BMI of 30 or higher.
Medication Continuation Drops After 3 Months
With a median follow-up time of 2.4 years, the rate of persistence to the medications overall dropped from 44% at 3 months to 33% at 6 months and just 19% at 12 months.
In a multivariate analysis, semaglutide was associated with the highest odds of 1-year persistence (adjusted odds ratio [AOR], 4.26), while naltrexone-bupropion had the lowest odds (AOR, 0.68), compared with phentermine-topiramate. The other agents did not have significantly different odds of persistence.
Semaglutide and liraglutide also had the highest persistence rates overall, including at 3 months (63% and 52%, respectively) and 6 months (56% and 37%, respectively).
Those with higher weight loss at 6 months had a higher likelihood of remaining on the weight loss medication at 1 year, with a 1% increase in weight loss at 6 months associated with 6% increased odds of still being persistent at year 1 (adjusted odds ratio, 1.06).
Those who did continue medications at 1 year had a mean of 10% weight loss at 12 months compared with just 2% among individuals who were not persistent (P <.001).
Most patients (84%) in the study were privately insured, and weight loss drug adherence varied significantly based on the insurance carrier.
Studies demonstrating the effects of discontinuing treatment with semaglutide include the STEP 1 trial extension, which showed that 1 year after discontinuation of treatment and lifestyle intervention, participants regained two thirds of their lost weight on average, and the cardiometabolic improvements with the weight loss were reversed.
In light of those findings, “the current scientific knowledge favors using anti-obesity medications longer term for weight loss maintenance if they are well-tolerated and have resulted in clinically meaningful weight loss,” Dr. Gasoyan told this news organization.
Paradoxically, the possible regaining of weight could be a factor in some insurers denying longer-term coverage, he noted.
Discontinuing Medications Means Regaining Appetite
Anne Peters, MD, a professor of medicine at USC’s Keck School of Medicine in Los Angeles and director of the USC Clinical Diabetes Programs, underscored that the possibility of regaining weight with discontinuation of GLP-1 receptor agonists is indeed “a big concern because your appetite comes back in spades when you take away the effect of these hormones,” she told this news organization. “For that reason, I don’t ever tell people to stop cold turkey.”
Regarding the question of how long patients should remain on the medications, Peters said the scenario might be compared to the need for patients with type 1 diabetes to be on insulin, which is a gut hormone.
“These medications are also gut hormones, and some patients may need to also be on them for life to maintain the benefits,” she said.
“If a patient for some reason wishes to come off of the medication, for instance in order to be on less medicine, I have them titrate down and usually there will be a dose where they actually need only a small dose.
“I even have some patients who just take semaglutide once a month who are able to manage to maintain their weight loss,” Dr. Peters noted.
“But the whole goal in people who are overweight or obese is to establish a new set point and maintain whatever that new target weight is.”
Dr. Peters agreed that the loss of insurance coverage for the medications can throw a big wrench into that maintenance, presenting adverse effects of its own by causing a lack of treatment continuity.
“When you lose weight, you lose lean body mass and fat mass, but when you regain, it’s primary fat mass, so if you go on and off these drugs, it can contribute to a loss of lean mass. Therefore, these drugs should not be taken if someone is going to go on and off them repeatedly.”
The study received funding from the National Cancer Institute. Dr. Peters has consulted for Eli Lilly in the past.
A version of this article appeared on Medscape.com.
Patients receiving semaglutide for weight loss show a significantly higher rate of continuing the medication at 1 year compared with less effective anti-obesity drugs. However, even among those patients, continuation declines to fewer than half of patients.
“We now have effective US Food and Drug Administration–approved anti-obesity medications; [however], this study shows that in a real-world setting, the vast majority of patients discontinued their prescription fills within the first year,” said first author Hamlet Gasoyan, PhD, lead author of the study and a researcher with Cleveland Clinic’s Center for Value-Based Care Research, said in a press statement.
The study was published online in the journal Obesity.
While breakthrough drugs such as glucagon-like peptide-1 (GLP-1) receptor agonists have shown high efficacy in achieving weight loss while providing a host of other health benefits, their discontinuation has been shown to potentially result in a rapid regaining of weight that was lost, as well as a reversal of the other health benefits, such as cardiometabolic improvements, the study authors wrote.
To evaluate rates of persistence with those along with other weight loss medications and factors associated with discontinuation, Dr. Gasoyan and colleagues conducted a retrospective cohort study, identifying 1911 patients with obesity, who had an initial anti-obesity medication prescription filled between 2015 and 2022 at Cleveland Clinic centers in Ohio and Florida.
Over the study period, 25% of patients filled a prescription for semaglutide, 34% for naltrexone-bupropion, 26% for phentermine-topiramate, 14% for liraglutide, and 0.9% for orlistat.
The patients had a median baseline BMI of 38, with obesity defined as a BMI of 30 or higher.
Medication Continuation Drops After 3 Months
With a median follow-up time of 2.4 years, the rate of persistence to the medications overall dropped from 44% at 3 months to 33% at 6 months and just 19% at 12 months.
In a multivariate analysis, semaglutide was associated with the highest odds of 1-year persistence (adjusted odds ratio [AOR], 4.26), while naltrexone-bupropion had the lowest odds (AOR, 0.68), compared with phentermine-topiramate. The other agents did not have significantly different odds of persistence.
Semaglutide and liraglutide also had the highest persistence rates overall, including at 3 months (63% and 52%, respectively) and 6 months (56% and 37%, respectively).
Those with higher weight loss at 6 months had a higher likelihood of remaining on the weight loss medication at 1 year, with a 1% increase in weight loss at 6 months associated with 6% increased odds of still being persistent at year 1 (adjusted odds ratio, 1.06).
Those who did continue medications at 1 year had a mean of 10% weight loss at 12 months compared with just 2% among individuals who were not persistent (P <.001).
Most patients (84%) in the study were privately insured, and weight loss drug adherence varied significantly based on the insurance carrier.
Studies demonstrating the effects of discontinuing treatment with semaglutide include the STEP 1 trial extension, which showed that 1 year after discontinuation of treatment and lifestyle intervention, participants regained two thirds of their lost weight on average, and the cardiometabolic improvements with the weight loss were reversed.
In light of those findings, “the current scientific knowledge favors using anti-obesity medications longer term for weight loss maintenance if they are well-tolerated and have resulted in clinically meaningful weight loss,” Dr. Gasoyan told this news organization.
Paradoxically, the possible regaining of weight could be a factor in some insurers denying longer-term coverage, he noted.
Discontinuing Medications Means Regaining Appetite
Anne Peters, MD, a professor of medicine at USC’s Keck School of Medicine in Los Angeles and director of the USC Clinical Diabetes Programs, underscored that the possibility of regaining weight with discontinuation of GLP-1 receptor agonists is indeed “a big concern because your appetite comes back in spades when you take away the effect of these hormones,” she told this news organization. “For that reason, I don’t ever tell people to stop cold turkey.”
Regarding the question of how long patients should remain on the medications, Peters said the scenario might be compared to the need for patients with type 1 diabetes to be on insulin, which is a gut hormone.
“These medications are also gut hormones, and some patients may need to also be on them for life to maintain the benefits,” she said.
“If a patient for some reason wishes to come off of the medication, for instance in order to be on less medicine, I have them titrate down and usually there will be a dose where they actually need only a small dose.
“I even have some patients who just take semaglutide once a month who are able to manage to maintain their weight loss,” Dr. Peters noted.
“But the whole goal in people who are overweight or obese is to establish a new set point and maintain whatever that new target weight is.”
Dr. Peters agreed that the loss of insurance coverage for the medications can throw a big wrench into that maintenance, presenting adverse effects of its own by causing a lack of treatment continuity.
“When you lose weight, you lose lean body mass and fat mass, but when you regain, it’s primary fat mass, so if you go on and off these drugs, it can contribute to a loss of lean mass. Therefore, these drugs should not be taken if someone is going to go on and off them repeatedly.”
The study received funding from the National Cancer Institute. Dr. Peters has consulted for Eli Lilly in the past.
A version of this article appeared on Medscape.com.
FROM OBESITY
Vegan diet may curb hot flashes by altering the gut microbiome
TOPLINE:
METHODOLOGY:
- For this exploratory analysis, postmenopausal women with two or more moderate to severe hot flashes daily were randomly assigned in two successive cohorts to consume a low-fat vegan diet with cooked soybeans or their usual diet.
- Over a 12-week period, frequency and severity of hot flashes were recorded on a mobile application.
- Researchers used deep shotgun metagenomic sequencing to analyze the gut microbiome at baseline and 12 weeks in a subset of 11 women in the dietary intervention group.
TAKEAWAY:
- In the subset receiving microbiome analysis, total hot flashes decreased by 95%, moderate to severe hot flashes decreased by 96%, and severe hot flashes disappeared during the dietary intervention.
- The relative abundance of Porphyromonas and Prevotella corporis decreased in participants on the diet intervention, and this correlated with a reduction in severe daytime hot flashes.
- The relative abundance of Clostridium asparagiforme also decreased in participants on the low-fat vegan diet, and this change correlated with a reduction in total severe and severe nighttime hot flashes.
- However, after correction for multiple comparisons, these associations were no longer significant.
IN PRACTICE:
“The targeted and untargeted gut microbiome analysis was robust and revealed important changes in the gut microbiome composition in response to a low-fat vegan diet and large correlations with symptomatic changes,” the authors write. “Larger randomized clinical trials are needed to further investigate these findings.”
SOURCE:
The study, with first author Hana Kahleova, MD, PhD, with the Physicians Committee for Responsible Medicine, in Washington, DC, was published online November 8 in Complementary Therapies in Medicine.
LIMITATIONS:
The gut microbiome analysis was only performed in a small subset of women on the diet intervention, with no control group. Although strong associations were noted between several gut bacteria and changes in hot flash frequency, and nominally statistically significant relative abundance changes were observed, robust statistical significance cannot be concluded for any of the reported gut microbiome assessments when the modestly large number of total comparisons is taken into account.
DISCLOSURES:
The study was funded by the Physicians Committee for Responsible Medicine. The authors report no conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- For this exploratory analysis, postmenopausal women with two or more moderate to severe hot flashes daily were randomly assigned in two successive cohorts to consume a low-fat vegan diet with cooked soybeans or their usual diet.
- Over a 12-week period, frequency and severity of hot flashes were recorded on a mobile application.
- Researchers used deep shotgun metagenomic sequencing to analyze the gut microbiome at baseline and 12 weeks in a subset of 11 women in the dietary intervention group.
TAKEAWAY:
- In the subset receiving microbiome analysis, total hot flashes decreased by 95%, moderate to severe hot flashes decreased by 96%, and severe hot flashes disappeared during the dietary intervention.
- The relative abundance of Porphyromonas and Prevotella corporis decreased in participants on the diet intervention, and this correlated with a reduction in severe daytime hot flashes.
- The relative abundance of Clostridium asparagiforme also decreased in participants on the low-fat vegan diet, and this change correlated with a reduction in total severe and severe nighttime hot flashes.
- However, after correction for multiple comparisons, these associations were no longer significant.
IN PRACTICE:
“The targeted and untargeted gut microbiome analysis was robust and revealed important changes in the gut microbiome composition in response to a low-fat vegan diet and large correlations with symptomatic changes,” the authors write. “Larger randomized clinical trials are needed to further investigate these findings.”
SOURCE:
The study, with first author Hana Kahleova, MD, PhD, with the Physicians Committee for Responsible Medicine, in Washington, DC, was published online November 8 in Complementary Therapies in Medicine.
LIMITATIONS:
The gut microbiome analysis was only performed in a small subset of women on the diet intervention, with no control group. Although strong associations were noted between several gut bacteria and changes in hot flash frequency, and nominally statistically significant relative abundance changes were observed, robust statistical significance cannot be concluded for any of the reported gut microbiome assessments when the modestly large number of total comparisons is taken into account.
DISCLOSURES:
The study was funded by the Physicians Committee for Responsible Medicine. The authors report no conflicts of interest.
A version of this article appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- For this exploratory analysis, postmenopausal women with two or more moderate to severe hot flashes daily were randomly assigned in two successive cohorts to consume a low-fat vegan diet with cooked soybeans or their usual diet.
- Over a 12-week period, frequency and severity of hot flashes were recorded on a mobile application.
- Researchers used deep shotgun metagenomic sequencing to analyze the gut microbiome at baseline and 12 weeks in a subset of 11 women in the dietary intervention group.
TAKEAWAY:
- In the subset receiving microbiome analysis, total hot flashes decreased by 95%, moderate to severe hot flashes decreased by 96%, and severe hot flashes disappeared during the dietary intervention.
- The relative abundance of Porphyromonas and Prevotella corporis decreased in participants on the diet intervention, and this correlated with a reduction in severe daytime hot flashes.
- The relative abundance of Clostridium asparagiforme also decreased in participants on the low-fat vegan diet, and this change correlated with a reduction in total severe and severe nighttime hot flashes.
- However, after correction for multiple comparisons, these associations were no longer significant.
IN PRACTICE:
“The targeted and untargeted gut microbiome analysis was robust and revealed important changes in the gut microbiome composition in response to a low-fat vegan diet and large correlations with symptomatic changes,” the authors write. “Larger randomized clinical trials are needed to further investigate these findings.”
SOURCE:
The study, with first author Hana Kahleova, MD, PhD, with the Physicians Committee for Responsible Medicine, in Washington, DC, was published online November 8 in Complementary Therapies in Medicine.
LIMITATIONS:
The gut microbiome analysis was only performed in a small subset of women on the diet intervention, with no control group. Although strong associations were noted between several gut bacteria and changes in hot flash frequency, and nominally statistically significant relative abundance changes were observed, robust statistical significance cannot be concluded for any of the reported gut microbiome assessments when the modestly large number of total comparisons is taken into account.
DISCLOSURES:
The study was funded by the Physicians Committee for Responsible Medicine. The authors report no conflicts of interest.
A version of this article appeared on Medscape.com.
Vegan diet confers cardiometabolic benefits
TOPLINE:
Compared with a healthy omnivore diet, low-density lipoprotein cholesterol (LDL-C) as well as fasting insulin and weight loss in a randomized controlled trial of identical twins.
METHODOLOGY:
- Researchers randomly assigned 22 pairs of healthy adult identical twins (34 women, mean age 39 years, mean body mass index 25.9) to a healthy vegan or omnivore diet (1 twin per pair) for 8 weeks.
- For the first 4 weeks, diet-specific meals were provided via a meal delivery service. For the final 4 weeks, participants prepared their own diet-appropriate meals/snacks.
- The primary outcome was change in LDL-C; secondary outcomes included changes in body weight and fasting insulin.
TAKEAWAY:
- After 8 weeks, twins eating a vegan diet showed a significant mean decrease of 13.9 mg/dL in LDL-C compared with twins eating an omnivorous diet.
- The vegan diet also led to a significant mean decrease of 2.9 Times New RomanμIU/mL in fasting insulin and 1.9 kg in body weight after 8 weeks compared with the omnivore diet, although weight loss was observed in both diet groups.
- The vegan diet group also had a larger but nonsignificant absolute median decrease in fasting HDL-C triglycerides, vitamin B12, glucose, and trimethylamine N-oxide levels at 8 weeks.
IN PRACTICE:
“Our results corroborate a previous finding showing that eating a vegan diet can improve cardiovascular health. Clinicians may consider recommending plant-based diets to reduce cardiometabolic risk factors, as well as aligning with environmental benefits,” the researchers concluded.
SOURCE:
The study, with first author Matthew J. Landry, PhD, RDN, Stanford Prevention Research Center, Stanford University School of Medicine, California, was published online November 30 in JAMA Network Open.
LIMITATIONS:
The adult twin population was generally healthy and findings may not be generalizable to other populations. The sample size was small, and the duration of intervention was short and there was no follow-up period, which limits insights on stability and sustainability of the diets.
DISCLOSURES:
Funding was provided by the Vogt Foundation, and grants from Stanford University and the National Heart, Lung, and Blood Institute. Dr. Landry has no relevant disclosures. One author reported receiving funding from Beyond Meat outside of this study.
A version of this article appeared on Medscape.com.
TOPLINE:
Compared with a healthy omnivore diet, low-density lipoprotein cholesterol (LDL-C) as well as fasting insulin and weight loss in a randomized controlled trial of identical twins.
METHODOLOGY:
- Researchers randomly assigned 22 pairs of healthy adult identical twins (34 women, mean age 39 years, mean body mass index 25.9) to a healthy vegan or omnivore diet (1 twin per pair) for 8 weeks.
- For the first 4 weeks, diet-specific meals were provided via a meal delivery service. For the final 4 weeks, participants prepared their own diet-appropriate meals/snacks.
- The primary outcome was change in LDL-C; secondary outcomes included changes in body weight and fasting insulin.
TAKEAWAY:
- After 8 weeks, twins eating a vegan diet showed a significant mean decrease of 13.9 mg/dL in LDL-C compared with twins eating an omnivorous diet.
- The vegan diet also led to a significant mean decrease of 2.9 Times New RomanμIU/mL in fasting insulin and 1.9 kg in body weight after 8 weeks compared with the omnivore diet, although weight loss was observed in both diet groups.
- The vegan diet group also had a larger but nonsignificant absolute median decrease in fasting HDL-C triglycerides, vitamin B12, glucose, and trimethylamine N-oxide levels at 8 weeks.
IN PRACTICE:
“Our results corroborate a previous finding showing that eating a vegan diet can improve cardiovascular health. Clinicians may consider recommending plant-based diets to reduce cardiometabolic risk factors, as well as aligning with environmental benefits,” the researchers concluded.
SOURCE:
The study, with first author Matthew J. Landry, PhD, RDN, Stanford Prevention Research Center, Stanford University School of Medicine, California, was published online November 30 in JAMA Network Open.
LIMITATIONS:
The adult twin population was generally healthy and findings may not be generalizable to other populations. The sample size was small, and the duration of intervention was short and there was no follow-up period, which limits insights on stability and sustainability of the diets.
DISCLOSURES:
Funding was provided by the Vogt Foundation, and grants from Stanford University and the National Heart, Lung, and Blood Institute. Dr. Landry has no relevant disclosures. One author reported receiving funding from Beyond Meat outside of this study.
A version of this article appeared on Medscape.com.
TOPLINE:
Compared with a healthy omnivore diet, low-density lipoprotein cholesterol (LDL-C) as well as fasting insulin and weight loss in a randomized controlled trial of identical twins.
METHODOLOGY:
- Researchers randomly assigned 22 pairs of healthy adult identical twins (34 women, mean age 39 years, mean body mass index 25.9) to a healthy vegan or omnivore diet (1 twin per pair) for 8 weeks.
- For the first 4 weeks, diet-specific meals were provided via a meal delivery service. For the final 4 weeks, participants prepared their own diet-appropriate meals/snacks.
- The primary outcome was change in LDL-C; secondary outcomes included changes in body weight and fasting insulin.
TAKEAWAY:
- After 8 weeks, twins eating a vegan diet showed a significant mean decrease of 13.9 mg/dL in LDL-C compared with twins eating an omnivorous diet.
- The vegan diet also led to a significant mean decrease of 2.9 Times New RomanμIU/mL in fasting insulin and 1.9 kg in body weight after 8 weeks compared with the omnivore diet, although weight loss was observed in both diet groups.
- The vegan diet group also had a larger but nonsignificant absolute median decrease in fasting HDL-C triglycerides, vitamin B12, glucose, and trimethylamine N-oxide levels at 8 weeks.
IN PRACTICE:
“Our results corroborate a previous finding showing that eating a vegan diet can improve cardiovascular health. Clinicians may consider recommending plant-based diets to reduce cardiometabolic risk factors, as well as aligning with environmental benefits,” the researchers concluded.
SOURCE:
The study, with first author Matthew J. Landry, PhD, RDN, Stanford Prevention Research Center, Stanford University School of Medicine, California, was published online November 30 in JAMA Network Open.
LIMITATIONS:
The adult twin population was generally healthy and findings may not be generalizable to other populations. The sample size was small, and the duration of intervention was short and there was no follow-up period, which limits insights on stability and sustainability of the diets.
DISCLOSURES:
Funding was provided by the Vogt Foundation, and grants from Stanford University and the National Heart, Lung, and Blood Institute. Dr. Landry has no relevant disclosures. One author reported receiving funding from Beyond Meat outside of this study.
A version of this article appeared on Medscape.com.
Are you sure your patient is alive?
This transcript has been edited for clarity.
Much of my research focuses on what is known as clinical decision support — prompts and messages to providers to help them make good decisions for their patients. I know that these things can be annoying, which is exactly why I study them — to figure out which ones actually help.
When I got started on this about 10 years ago, we were learning a lot about how best to message providers about their patients. My team had developed a simple alert for acute kidney injury (AKI). We knew that providers often missed the diagnosis, so maybe letting them know would improve patient outcomes.
As we tested the alert, we got feedback, and I have kept an email from an ICU doctor from those early days. It read:
Dear Dr. Wilson: Thank you for the automated alert informing me that my patient had AKI. Regrettably, the alert fired about an hour after the patient had died. I feel that the information is less than actionable at this time.
Our early system had neglected to add a conditional flag ensuring that the patient was still alive at the time it sent the alert message. A small oversight, but one that had very large implications. Future studies would show that “false positive” alerts like this seriously degrade physician confidence in the system. And why wouldn’t they?
Not knowing the vital status of a patient can have major consequences.
Health systems send messages to their patients all the time: reminders of appointments, reminders for preventive care, reminders for vaccinations, and so on.
But what if the patient being reminded has died? It’s a waste of resources, of course, but more than that, it can be painful for their families and reflects poorly on the health care system. Of all the people who should know whether someone is alive or dead, shouldn’t their doctor be at the top of the list?
A new study in JAMA Internal Medicine quantifies this very phenomenon.
Researchers examined 11,658 primary care patients in their health system who met the criteria of being “seriously ill” and followed them for 2 years. During that period of time, 25% were recorded as deceased in the electronic health record. But 30.8% had died. That left 676 patients who had died, but were not known to have died, left in the system.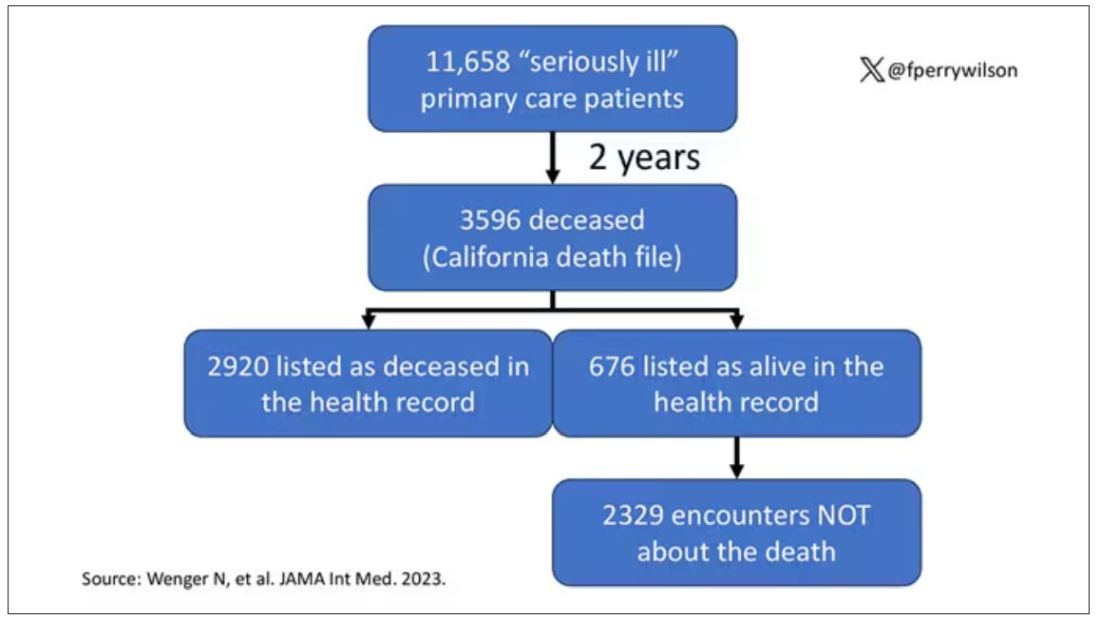
And those 676 were not left to rest in peace. They received 221 telephone and 338 health portal messages not related to death, and 920 letters reminding them about unmet primary care metrics like flu shots and cancer screening. Orders were entered into the health record for things like vaccines and routine screenings for 158 patients, and 310 future appointments — destined to be no-shows — were still on the books. One can only imagine the frustration of families checking their mail and finding yet another letter reminding their deceased loved one to get a mammogram.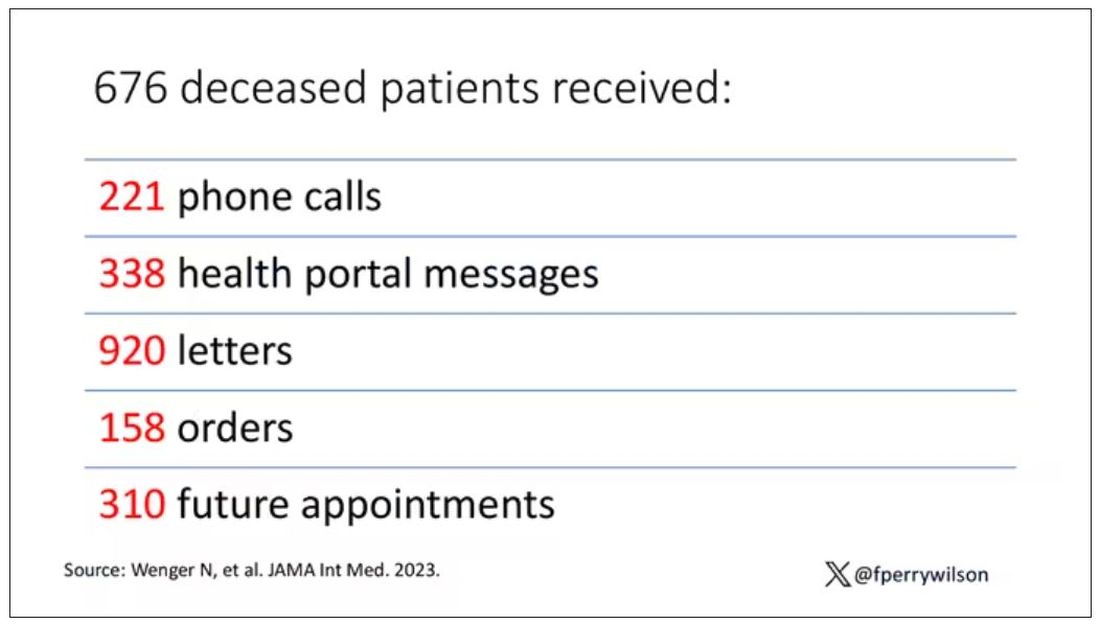
How did the researchers figure out who had died? It turns out it’s not that hard. California keeps a record of all deaths in the state; they simply had to search it. Like all state death records, they tend to lag a bit so it’s not clinically terribly useful, but it works. California and most other states also have a very accurate and up-to-date death file which can only be used by law enforcement to investigate criminal activity and fraud; health care is left in the lurch.
Nationwide, there is the real-time fact of death service, supported by the National Association for Public Health Statistics and Information Systems. This allows employers to verify, in real time, whether the person applying for a job is alive. Healthcare systems are not allowed to use it.
Let’s also remember that very few people die in this country without some health care agency knowing about it and recording it. But sharing of medical information is so poor in the United States that your patient could die in a hospital one city away from you and you might not find out until you’re calling them to see why they missed a scheduled follow-up appointment.
These events — the embarrassing lack of knowledge about the very vital status of our patients — highlight a huge problem with health care in our country. The fragmented health care system is terrible at data sharing, in part because of poor protocols, in part because of unfounded concerns about patient privacy, and in part because of a tendency to hoard data that might be valuable in the future. It has to stop. We need to know how our patients are doing even when they are not sitting in front of us. When it comes to life and death, the knowledge is out there; we just can’t access it. Seems like a pretty easy fix.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com .
This transcript has been edited for clarity.
Much of my research focuses on what is known as clinical decision support — prompts and messages to providers to help them make good decisions for their patients. I know that these things can be annoying, which is exactly why I study them — to figure out which ones actually help.
When I got started on this about 10 years ago, we were learning a lot about how best to message providers about their patients. My team had developed a simple alert for acute kidney injury (AKI). We knew that providers often missed the diagnosis, so maybe letting them know would improve patient outcomes.
As we tested the alert, we got feedback, and I have kept an email from an ICU doctor from those early days. It read:
Dear Dr. Wilson: Thank you for the automated alert informing me that my patient had AKI. Regrettably, the alert fired about an hour after the patient had died. I feel that the information is less than actionable at this time.
Our early system had neglected to add a conditional flag ensuring that the patient was still alive at the time it sent the alert message. A small oversight, but one that had very large implications. Future studies would show that “false positive” alerts like this seriously degrade physician confidence in the system. And why wouldn’t they?
Not knowing the vital status of a patient can have major consequences.
Health systems send messages to their patients all the time: reminders of appointments, reminders for preventive care, reminders for vaccinations, and so on.
But what if the patient being reminded has died? It’s a waste of resources, of course, but more than that, it can be painful for their families and reflects poorly on the health care system. Of all the people who should know whether someone is alive or dead, shouldn’t their doctor be at the top of the list?
A new study in JAMA Internal Medicine quantifies this very phenomenon.
Researchers examined 11,658 primary care patients in their health system who met the criteria of being “seriously ill” and followed them for 2 years. During that period of time, 25% were recorded as deceased in the electronic health record. But 30.8% had died. That left 676 patients who had died, but were not known to have died, left in the system.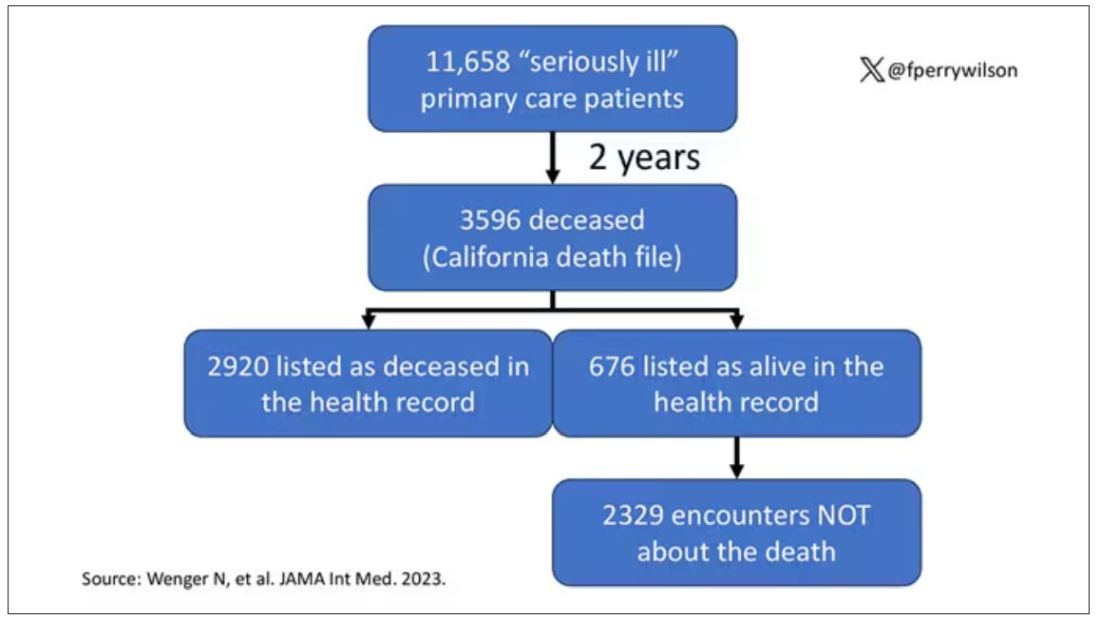
And those 676 were not left to rest in peace. They received 221 telephone and 338 health portal messages not related to death, and 920 letters reminding them about unmet primary care metrics like flu shots and cancer screening. Orders were entered into the health record for things like vaccines and routine screenings for 158 patients, and 310 future appointments — destined to be no-shows — were still on the books. One can only imagine the frustration of families checking their mail and finding yet another letter reminding their deceased loved one to get a mammogram.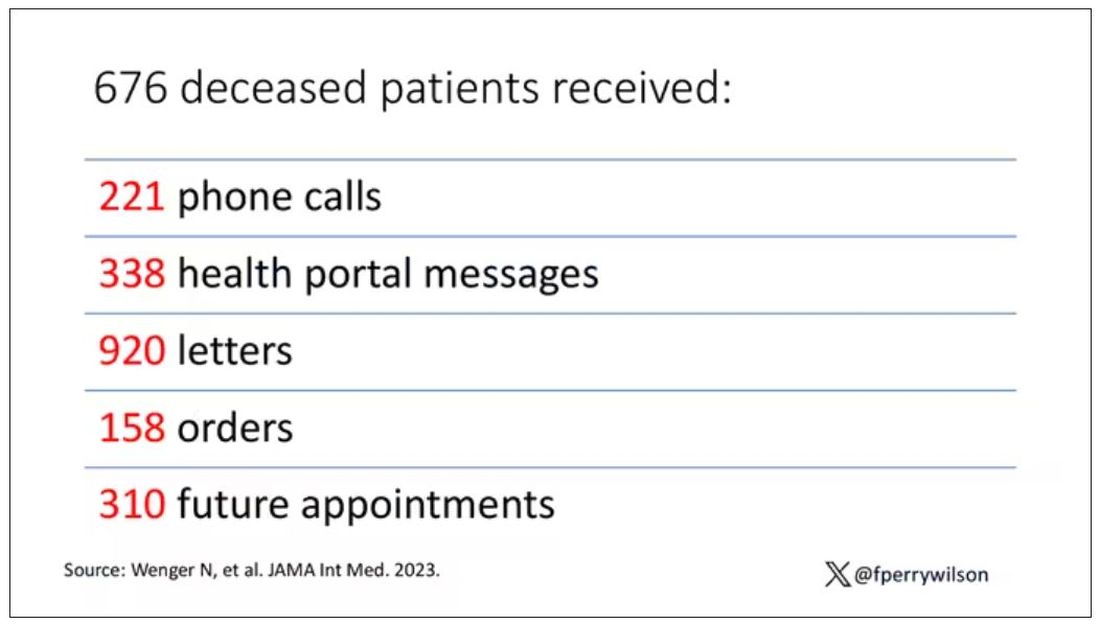
How did the researchers figure out who had died? It turns out it’s not that hard. California keeps a record of all deaths in the state; they simply had to search it. Like all state death records, they tend to lag a bit so it’s not clinically terribly useful, but it works. California and most other states also have a very accurate and up-to-date death file which can only be used by law enforcement to investigate criminal activity and fraud; health care is left in the lurch.
Nationwide, there is the real-time fact of death service, supported by the National Association for Public Health Statistics and Information Systems. This allows employers to verify, in real time, whether the person applying for a job is alive. Healthcare systems are not allowed to use it.
Let’s also remember that very few people die in this country without some health care agency knowing about it and recording it. But sharing of medical information is so poor in the United States that your patient could die in a hospital one city away from you and you might not find out until you’re calling them to see why they missed a scheduled follow-up appointment.
These events — the embarrassing lack of knowledge about the very vital status of our patients — highlight a huge problem with health care in our country. The fragmented health care system is terrible at data sharing, in part because of poor protocols, in part because of unfounded concerns about patient privacy, and in part because of a tendency to hoard data that might be valuable in the future. It has to stop. We need to know how our patients are doing even when they are not sitting in front of us. When it comes to life and death, the knowledge is out there; we just can’t access it. Seems like a pretty easy fix.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com .
This transcript has been edited for clarity.
Much of my research focuses on what is known as clinical decision support — prompts and messages to providers to help them make good decisions for their patients. I know that these things can be annoying, which is exactly why I study them — to figure out which ones actually help.
When I got started on this about 10 years ago, we were learning a lot about how best to message providers about their patients. My team had developed a simple alert for acute kidney injury (AKI). We knew that providers often missed the diagnosis, so maybe letting them know would improve patient outcomes.
As we tested the alert, we got feedback, and I have kept an email from an ICU doctor from those early days. It read:
Dear Dr. Wilson: Thank you for the automated alert informing me that my patient had AKI. Regrettably, the alert fired about an hour after the patient had died. I feel that the information is less than actionable at this time.
Our early system had neglected to add a conditional flag ensuring that the patient was still alive at the time it sent the alert message. A small oversight, but one that had very large implications. Future studies would show that “false positive” alerts like this seriously degrade physician confidence in the system. And why wouldn’t they?
Not knowing the vital status of a patient can have major consequences.
Health systems send messages to their patients all the time: reminders of appointments, reminders for preventive care, reminders for vaccinations, and so on.
But what if the patient being reminded has died? It’s a waste of resources, of course, but more than that, it can be painful for their families and reflects poorly on the health care system. Of all the people who should know whether someone is alive or dead, shouldn’t their doctor be at the top of the list?
A new study in JAMA Internal Medicine quantifies this very phenomenon.
Researchers examined 11,658 primary care patients in their health system who met the criteria of being “seriously ill” and followed them for 2 years. During that period of time, 25% were recorded as deceased in the electronic health record. But 30.8% had died. That left 676 patients who had died, but were not known to have died, left in the system.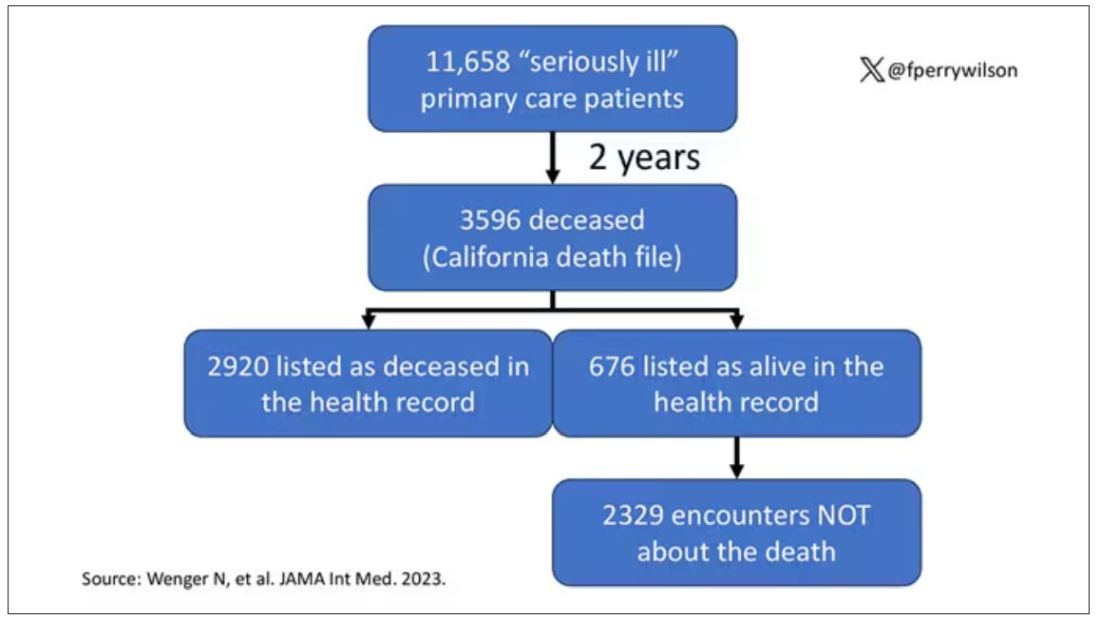
And those 676 were not left to rest in peace. They received 221 telephone and 338 health portal messages not related to death, and 920 letters reminding them about unmet primary care metrics like flu shots and cancer screening. Orders were entered into the health record for things like vaccines and routine screenings for 158 patients, and 310 future appointments — destined to be no-shows — were still on the books. One can only imagine the frustration of families checking their mail and finding yet another letter reminding their deceased loved one to get a mammogram.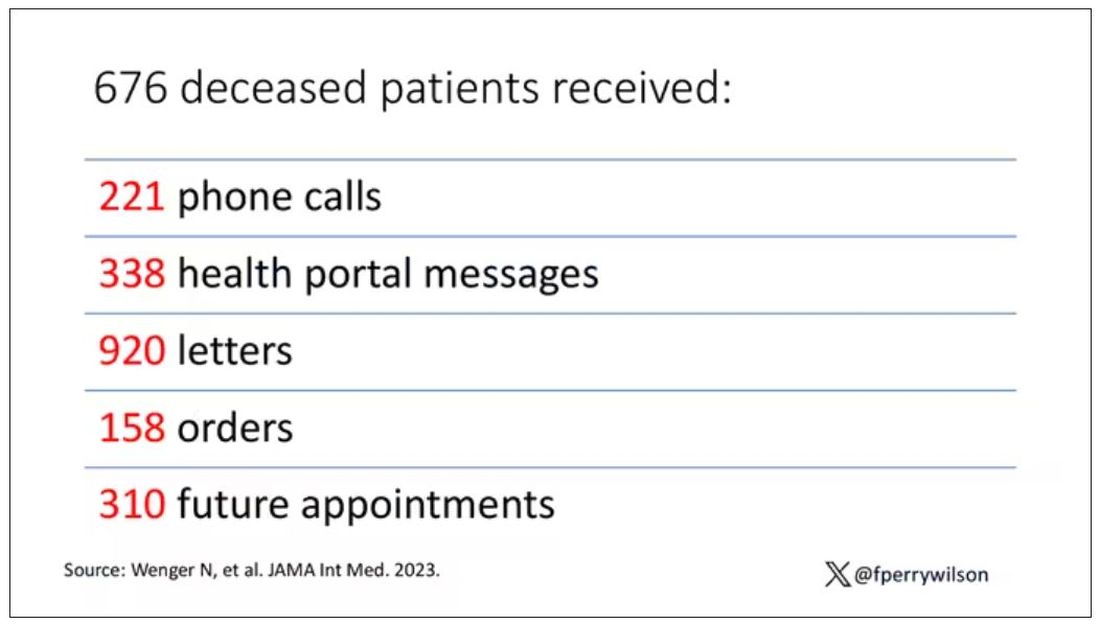
How did the researchers figure out who had died? It turns out it’s not that hard. California keeps a record of all deaths in the state; they simply had to search it. Like all state death records, they tend to lag a bit so it’s not clinically terribly useful, but it works. California and most other states also have a very accurate and up-to-date death file which can only be used by law enforcement to investigate criminal activity and fraud; health care is left in the lurch.
Nationwide, there is the real-time fact of death service, supported by the National Association for Public Health Statistics and Information Systems. This allows employers to verify, in real time, whether the person applying for a job is alive. Healthcare systems are not allowed to use it.
Let’s also remember that very few people die in this country without some health care agency knowing about it and recording it. But sharing of medical information is so poor in the United States that your patient could die in a hospital one city away from you and you might not find out until you’re calling them to see why they missed a scheduled follow-up appointment.
These events — the embarrassing lack of knowledge about the very vital status of our patients — highlight a huge problem with health care in our country. The fragmented health care system is terrible at data sharing, in part because of poor protocols, in part because of unfounded concerns about patient privacy, and in part because of a tendency to hoard data that might be valuable in the future. It has to stop. We need to know how our patients are doing even when they are not sitting in front of us. When it comes to life and death, the knowledge is out there; we just can’t access it. Seems like a pretty easy fix.
Dr. Wilson is associate professor of medicine and public health and director of the Clinical and Translational Research Accelerator at Yale University, New Haven, Connecticut. He has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com .
Meet the newest acronym in primary care: CKM
The advisory, published recently in Circulation introduces the concept of CKM health and reevaluates the relationships between obesity, diabetes, kidney disease, and cardiovascular disease (CVD).
“This approach not only raises awareness, it also empowers PCPs to diagnose and treat these conditions more holistically,” Salim Hayek, MD, associate professor of cardiovascular disease and internal medicine, and medical director of the Frankel Cardiovascular Center Clinics at the University of Michigan in Ann Arbor, said in an interview.
New CKM Staging, Testing, and Care Strategies
The advisory introduces a new scoring system that ranges from stage 0 (patients with no risk factors for CKM) through stage 4 (patients with clinical CVD in CKM syndrome). Each stage requires specific management strategies and may include screening starting at age 30 years for diabetes, hypertension, and heart failure.
“Stage 0 CKM is usually found in young people, and CKM risk factors and scores typically increase as people age,” said Sean M. Drake, MD, a primary care physician at Henry Ford Health in Sterling Heights, Michigan.
Dr. Drake advised PCPs to encourage patients who are at stage 0 to maintain ideal cardiovascular health and to monitor those at risk of progressing through the stages.
While PCPs already perform many of the tests the advisory recommends, the conditions overlap and an abnormality in one system should prompt more testing for other conditions. Additional tests, such as urine albumin-creatinine ratio, and more frequent glomerular filtration rate and lipid profile are advised, according to Dr. Drake.
“There also appears to be a role for additional cardiac testing, including echocardiograms and coronary CT scans, and for liver fibrosis screening,” Dr. Drake said. “Medications such as SGLT2 inhibitors, GLP-1 receptor agonists, and ACE inhibitors, beyond current routine use, are emphasized.”
To better characterize body composition and help diagnose metabolic syndrome, the advisory also recommends measuring waist circumference, which is not routine practice, noted Joshua J. Joseph, MD, MPH, an associate professor of endocrinology, diabetes, and metabolism at The Ohio State University Wexner Medical Center in Columbus, and a co-author of the advisory.
Recognizing the interconnected nature of cardiac, kidney, and metabolic diseases encourages a shift in mindset for clinicians, according to Neha Pagidipati, MD, MPH, a cardiologist at Duke Health in Durham, North Carolina.
“We have often been trained to focus on the specific problem in front of us,” Dr. Pagidipati said. “We need to be hyper-aware that many patients we see are at risk for multiple CKM entities. We need to be proactive about screening for and treating these when appropriate.”
The advisory emphasizes the need for CKM coordinators to support teams of clinicians from primary care, cardiology, endocrinology, nephrology, nursing, and pharmacy, as well as social workers, care navigators, or community health workers, Dr. Joseph said.
“The advisory repositions the PCP at the forefront of CKM care coordination, marking a departure from the traditional model where subspecialists primarily manage complications,” Dr. Hayek added.
Changes to Payment
The new recommendations are consistent with current management guidelines for obesity, hypertriglyceridemia, hypertension, type 2 diabetes, and chronic kidney disease.
“The advisory provides integrated algorithms for cardiovascular prevention and management, with specific therapeutic guidance tied to CKM stages, bringing together the current evidence for best practices from the various guidelines and filling gaps in a unified approach,” Dr. Joseph said.
In addition, the advisory draws attention to the care of younger patients, who may be at increased risk for cardiovascular disease due to lifestyle factors, according to Nishant Shah, MD, assistant professor of medicine at Duke.
“It considers barriers to care that prevent people from optimizing their cardiovascular health,” Dr. Shah said.
Although the advisory does not specify proposed payment changes to support the new care model, the move towards value-based care may require billing practices that accommodate integrated care as well as more frequent and more specialized testing, Dr. Hayek said.
“The advisory is an empowering tool for PCPs, underscoring their critical role in healthcare,” Dr. Hayek said. “It encourages PCPs to advocate for integrated care within their practices and to consider workflow adjustments that enhance the identification and initiation of preventive care for at-risk patients.”
Funding information was not provided.
Dr. Joseph reports no relevant financial involvements; several advisory co-authors report financial involvements with pharmaceutical companies. Dr. Pagidipati reports relevant financial involvement with pharmaceutical companies. Dr. Hayek, Dr. Drake, and Dr. Shah report no relevant financial involvements. Dr. Joseph is an author of the advisory. Dr. Pagidipati, Dr. Hayek, Dr. Drake, and Dr. Shah were not involved in the writing of the advisory.
A version of this article appeared on Medscape.com.
The advisory, published recently in Circulation introduces the concept of CKM health and reevaluates the relationships between obesity, diabetes, kidney disease, and cardiovascular disease (CVD).
“This approach not only raises awareness, it also empowers PCPs to diagnose and treat these conditions more holistically,” Salim Hayek, MD, associate professor of cardiovascular disease and internal medicine, and medical director of the Frankel Cardiovascular Center Clinics at the University of Michigan in Ann Arbor, said in an interview.
New CKM Staging, Testing, and Care Strategies
The advisory introduces a new scoring system that ranges from stage 0 (patients with no risk factors for CKM) through stage 4 (patients with clinical CVD in CKM syndrome). Each stage requires specific management strategies and may include screening starting at age 30 years for diabetes, hypertension, and heart failure.
“Stage 0 CKM is usually found in young people, and CKM risk factors and scores typically increase as people age,” said Sean M. Drake, MD, a primary care physician at Henry Ford Health in Sterling Heights, Michigan.
Dr. Drake advised PCPs to encourage patients who are at stage 0 to maintain ideal cardiovascular health and to monitor those at risk of progressing through the stages.
While PCPs already perform many of the tests the advisory recommends, the conditions overlap and an abnormality in one system should prompt more testing for other conditions. Additional tests, such as urine albumin-creatinine ratio, and more frequent glomerular filtration rate and lipid profile are advised, according to Dr. Drake.
“There also appears to be a role for additional cardiac testing, including echocardiograms and coronary CT scans, and for liver fibrosis screening,” Dr. Drake said. “Medications such as SGLT2 inhibitors, GLP-1 receptor agonists, and ACE inhibitors, beyond current routine use, are emphasized.”
To better characterize body composition and help diagnose metabolic syndrome, the advisory also recommends measuring waist circumference, which is not routine practice, noted Joshua J. Joseph, MD, MPH, an associate professor of endocrinology, diabetes, and metabolism at The Ohio State University Wexner Medical Center in Columbus, and a co-author of the advisory.
Recognizing the interconnected nature of cardiac, kidney, and metabolic diseases encourages a shift in mindset for clinicians, according to Neha Pagidipati, MD, MPH, a cardiologist at Duke Health in Durham, North Carolina.
“We have often been trained to focus on the specific problem in front of us,” Dr. Pagidipati said. “We need to be hyper-aware that many patients we see are at risk for multiple CKM entities. We need to be proactive about screening for and treating these when appropriate.”
The advisory emphasizes the need for CKM coordinators to support teams of clinicians from primary care, cardiology, endocrinology, nephrology, nursing, and pharmacy, as well as social workers, care navigators, or community health workers, Dr. Joseph said.
“The advisory repositions the PCP at the forefront of CKM care coordination, marking a departure from the traditional model where subspecialists primarily manage complications,” Dr. Hayek added.
Changes to Payment
The new recommendations are consistent with current management guidelines for obesity, hypertriglyceridemia, hypertension, type 2 diabetes, and chronic kidney disease.
“The advisory provides integrated algorithms for cardiovascular prevention and management, with specific therapeutic guidance tied to CKM stages, bringing together the current evidence for best practices from the various guidelines and filling gaps in a unified approach,” Dr. Joseph said.
In addition, the advisory draws attention to the care of younger patients, who may be at increased risk for cardiovascular disease due to lifestyle factors, according to Nishant Shah, MD, assistant professor of medicine at Duke.
“It considers barriers to care that prevent people from optimizing their cardiovascular health,” Dr. Shah said.
Although the advisory does not specify proposed payment changes to support the new care model, the move towards value-based care may require billing practices that accommodate integrated care as well as more frequent and more specialized testing, Dr. Hayek said.
“The advisory is an empowering tool for PCPs, underscoring their critical role in healthcare,” Dr. Hayek said. “It encourages PCPs to advocate for integrated care within their practices and to consider workflow adjustments that enhance the identification and initiation of preventive care for at-risk patients.”
Funding information was not provided.
Dr. Joseph reports no relevant financial involvements; several advisory co-authors report financial involvements with pharmaceutical companies. Dr. Pagidipati reports relevant financial involvement with pharmaceutical companies. Dr. Hayek, Dr. Drake, and Dr. Shah report no relevant financial involvements. Dr. Joseph is an author of the advisory. Dr. Pagidipati, Dr. Hayek, Dr. Drake, and Dr. Shah were not involved in the writing of the advisory.
A version of this article appeared on Medscape.com.
The advisory, published recently in Circulation introduces the concept of CKM health and reevaluates the relationships between obesity, diabetes, kidney disease, and cardiovascular disease (CVD).
“This approach not only raises awareness, it also empowers PCPs to diagnose and treat these conditions more holistically,” Salim Hayek, MD, associate professor of cardiovascular disease and internal medicine, and medical director of the Frankel Cardiovascular Center Clinics at the University of Michigan in Ann Arbor, said in an interview.
New CKM Staging, Testing, and Care Strategies
The advisory introduces a new scoring system that ranges from stage 0 (patients with no risk factors for CKM) through stage 4 (patients with clinical CVD in CKM syndrome). Each stage requires specific management strategies and may include screening starting at age 30 years for diabetes, hypertension, and heart failure.
“Stage 0 CKM is usually found in young people, and CKM risk factors and scores typically increase as people age,” said Sean M. Drake, MD, a primary care physician at Henry Ford Health in Sterling Heights, Michigan.
Dr. Drake advised PCPs to encourage patients who are at stage 0 to maintain ideal cardiovascular health and to monitor those at risk of progressing through the stages.
While PCPs already perform many of the tests the advisory recommends, the conditions overlap and an abnormality in one system should prompt more testing for other conditions. Additional tests, such as urine albumin-creatinine ratio, and more frequent glomerular filtration rate and lipid profile are advised, according to Dr. Drake.
“There also appears to be a role for additional cardiac testing, including echocardiograms and coronary CT scans, and for liver fibrosis screening,” Dr. Drake said. “Medications such as SGLT2 inhibitors, GLP-1 receptor agonists, and ACE inhibitors, beyond current routine use, are emphasized.”
To better characterize body composition and help diagnose metabolic syndrome, the advisory also recommends measuring waist circumference, which is not routine practice, noted Joshua J. Joseph, MD, MPH, an associate professor of endocrinology, diabetes, and metabolism at The Ohio State University Wexner Medical Center in Columbus, and a co-author of the advisory.
Recognizing the interconnected nature of cardiac, kidney, and metabolic diseases encourages a shift in mindset for clinicians, according to Neha Pagidipati, MD, MPH, a cardiologist at Duke Health in Durham, North Carolina.
“We have often been trained to focus on the specific problem in front of us,” Dr. Pagidipati said. “We need to be hyper-aware that many patients we see are at risk for multiple CKM entities. We need to be proactive about screening for and treating these when appropriate.”
The advisory emphasizes the need for CKM coordinators to support teams of clinicians from primary care, cardiology, endocrinology, nephrology, nursing, and pharmacy, as well as social workers, care navigators, or community health workers, Dr. Joseph said.
“The advisory repositions the PCP at the forefront of CKM care coordination, marking a departure from the traditional model where subspecialists primarily manage complications,” Dr. Hayek added.
Changes to Payment
The new recommendations are consistent with current management guidelines for obesity, hypertriglyceridemia, hypertension, type 2 diabetes, and chronic kidney disease.
“The advisory provides integrated algorithms for cardiovascular prevention and management, with specific therapeutic guidance tied to CKM stages, bringing together the current evidence for best practices from the various guidelines and filling gaps in a unified approach,” Dr. Joseph said.
In addition, the advisory draws attention to the care of younger patients, who may be at increased risk for cardiovascular disease due to lifestyle factors, according to Nishant Shah, MD, assistant professor of medicine at Duke.
“It considers barriers to care that prevent people from optimizing their cardiovascular health,” Dr. Shah said.
Although the advisory does not specify proposed payment changes to support the new care model, the move towards value-based care may require billing practices that accommodate integrated care as well as more frequent and more specialized testing, Dr. Hayek said.
“The advisory is an empowering tool for PCPs, underscoring their critical role in healthcare,” Dr. Hayek said. “It encourages PCPs to advocate for integrated care within their practices and to consider workflow adjustments that enhance the identification and initiation of preventive care for at-risk patients.”
Funding information was not provided.
Dr. Joseph reports no relevant financial involvements; several advisory co-authors report financial involvements with pharmaceutical companies. Dr. Pagidipati reports relevant financial involvement with pharmaceutical companies. Dr. Hayek, Dr. Drake, and Dr. Shah report no relevant financial involvements. Dr. Joseph is an author of the advisory. Dr. Pagidipati, Dr. Hayek, Dr. Drake, and Dr. Shah were not involved in the writing of the advisory.
A version of this article appeared on Medscape.com.
FROM CIRCULATION
Early age at first period raises type 2 diabetes risk
TOPLINE:
, a retrospective study of US women under age 65 found.
METHODOLOGY:
- Researchers analyzed data from 17,377 women who were aged 20-65 years when they participated in a National Health and Nutrition Examination Survey (NHANES) from 1999 to 2018 and reported their age at first menstruation, which was classified as ≤ 10, 11, 12, 13, 14, or ≥ 15 years of age.
- In total, 0.2% of the women (1773) had type 2 diabetes; of these, 11.5% (205) had cardiovascular disease (CVD), defined as coronary heart disease (CHD), myocardial infarction, or stroke.
- Compared with women who had their first menstrual period at age 13 (the mean age in this population), those who had their period at age ≤ 10 had a significantly greater risk of having type 2 diabetes, after adjustment for age, race/ethnicity, education, parity, menopause status, family history of diabetes, smoking status, physical activity, alcohol consumption, and body mass index (odds ratio, 1.32; 95% CI, 1.03-1.69; P trend = .03).
- Among the women with diabetes, compared with those who had their first menstrual period at age 13, those who had it at age ≤ 10 had a significantly greater risk of having stroke (OR, 2.66; 95% CI, 1.07-6.64; P trend = .02), but not CVD or CHD, after adjustment for these multiple variables.
TAKEAWAY:
- In a racially and ethnically diverse national sample of US women younger than 65, “extremely early” age at first menstrual period was associated with significantly increased risk for type 2 diabetes; among the women with type 2 diabetes, it was associated with significantly increased risk for stroke but not CVD or CHD, after adjustment for multiple variables.
- Early age at menarche may be an early indicator of the cardiometabolic disease trajectory in women.
IN PRACTICE:
“Women with early-life exposures such as early age at menarche need to be further examined for diabetes and prevention research and strategies for progression of diabetes complications,” the study authors write.
SOURCE:
The authors, mainly from Tulane University School of Public Health and Tropical Medicine, New Orleans, Louisiana, and also from Harvard Medical School, Boston, Massachusetts, published their findings in BMJ Nutrition, Prevention & Health.
LIMITATIONS:
- The women who participated in NHANES may not be representative of all women in the United States (selection bias).
- The study only included women who reported the age when they had their first menstrual period (selection bias).
- This was a cross-sectional, observational study, so it cannot show causality.
- The women may have reported the wrong age at which they had their first period (recall bias and social desirability bias).
- The women may have inaccurately reported CVD and type 2 diabetes (recall bias and social desirability bias).
DISCLOSURES:
The researchers were supported by grants from the National Heart, Lung, and Blood Institute and from the National Institute of General Medical Sciences of the National Institutes of Health.
A version of this article first appeared on Medscape.com.
TOPLINE:
, a retrospective study of US women under age 65 found.
METHODOLOGY:
- Researchers analyzed data from 17,377 women who were aged 20-65 years when they participated in a National Health and Nutrition Examination Survey (NHANES) from 1999 to 2018 and reported their age at first menstruation, which was classified as ≤ 10, 11, 12, 13, 14, or ≥ 15 years of age.
- In total, 0.2% of the women (1773) had type 2 diabetes; of these, 11.5% (205) had cardiovascular disease (CVD), defined as coronary heart disease (CHD), myocardial infarction, or stroke.
- Compared with women who had their first menstrual period at age 13 (the mean age in this population), those who had their period at age ≤ 10 had a significantly greater risk of having type 2 diabetes, after adjustment for age, race/ethnicity, education, parity, menopause status, family history of diabetes, smoking status, physical activity, alcohol consumption, and body mass index (odds ratio, 1.32; 95% CI, 1.03-1.69; P trend = .03).
- Among the women with diabetes, compared with those who had their first menstrual period at age 13, those who had it at age ≤ 10 had a significantly greater risk of having stroke (OR, 2.66; 95% CI, 1.07-6.64; P trend = .02), but not CVD or CHD, after adjustment for these multiple variables.
TAKEAWAY:
- In a racially and ethnically diverse national sample of US women younger than 65, “extremely early” age at first menstrual period was associated with significantly increased risk for type 2 diabetes; among the women with type 2 diabetes, it was associated with significantly increased risk for stroke but not CVD or CHD, after adjustment for multiple variables.
- Early age at menarche may be an early indicator of the cardiometabolic disease trajectory in women.
IN PRACTICE:
“Women with early-life exposures such as early age at menarche need to be further examined for diabetes and prevention research and strategies for progression of diabetes complications,” the study authors write.
SOURCE:
The authors, mainly from Tulane University School of Public Health and Tropical Medicine, New Orleans, Louisiana, and also from Harvard Medical School, Boston, Massachusetts, published their findings in BMJ Nutrition, Prevention & Health.
LIMITATIONS:
- The women who participated in NHANES may not be representative of all women in the United States (selection bias).
- The study only included women who reported the age when they had their first menstrual period (selection bias).
- This was a cross-sectional, observational study, so it cannot show causality.
- The women may have reported the wrong age at which they had their first period (recall bias and social desirability bias).
- The women may have inaccurately reported CVD and type 2 diabetes (recall bias and social desirability bias).
DISCLOSURES:
The researchers were supported by grants from the National Heart, Lung, and Blood Institute and from the National Institute of General Medical Sciences of the National Institutes of Health.
A version of this article first appeared on Medscape.com.
TOPLINE:
, a retrospective study of US women under age 65 found.
METHODOLOGY:
- Researchers analyzed data from 17,377 women who were aged 20-65 years when they participated in a National Health and Nutrition Examination Survey (NHANES) from 1999 to 2018 and reported their age at first menstruation, which was classified as ≤ 10, 11, 12, 13, 14, or ≥ 15 years of age.
- In total, 0.2% of the women (1773) had type 2 diabetes; of these, 11.5% (205) had cardiovascular disease (CVD), defined as coronary heart disease (CHD), myocardial infarction, or stroke.
- Compared with women who had their first menstrual period at age 13 (the mean age in this population), those who had their period at age ≤ 10 had a significantly greater risk of having type 2 diabetes, after adjustment for age, race/ethnicity, education, parity, menopause status, family history of diabetes, smoking status, physical activity, alcohol consumption, and body mass index (odds ratio, 1.32; 95% CI, 1.03-1.69; P trend = .03).
- Among the women with diabetes, compared with those who had their first menstrual period at age 13, those who had it at age ≤ 10 had a significantly greater risk of having stroke (OR, 2.66; 95% CI, 1.07-6.64; P trend = .02), but not CVD or CHD, after adjustment for these multiple variables.
TAKEAWAY:
- In a racially and ethnically diverse national sample of US women younger than 65, “extremely early” age at first menstrual period was associated with significantly increased risk for type 2 diabetes; among the women with type 2 diabetes, it was associated with significantly increased risk for stroke but not CVD or CHD, after adjustment for multiple variables.
- Early age at menarche may be an early indicator of the cardiometabolic disease trajectory in women.
IN PRACTICE:
“Women with early-life exposures such as early age at menarche need to be further examined for diabetes and prevention research and strategies for progression of diabetes complications,” the study authors write.
SOURCE:
The authors, mainly from Tulane University School of Public Health and Tropical Medicine, New Orleans, Louisiana, and also from Harvard Medical School, Boston, Massachusetts, published their findings in BMJ Nutrition, Prevention & Health.
LIMITATIONS:
- The women who participated in NHANES may not be representative of all women in the United States (selection bias).
- The study only included women who reported the age when they had their first menstrual period (selection bias).
- This was a cross-sectional, observational study, so it cannot show causality.
- The women may have reported the wrong age at which they had their first period (recall bias and social desirability bias).
- The women may have inaccurately reported CVD and type 2 diabetes (recall bias and social desirability bias).
DISCLOSURES:
The researchers were supported by grants from the National Heart, Lung, and Blood Institute and from the National Institute of General Medical Sciences of the National Institutes of Health.
A version of this article first appeared on Medscape.com.
Reducing albumin improves kidney and heart function in people with type 2 diabetes
TOPLINE:
Reducing the urine albumin-to-creatinine ratio (UACR) significantly reduces kidney risk in people with type 2 diabetes, per new research in the Annals of Internal Medicine.
METHODOLOGY:
- Post hoc retrospective analysis of two phase 3 double-blind trials of finerenone in people with type 2 diabetes and chronic kidney disease
- Quantify the long-term health effects of reducing UACR within 4 months of taking finerenone by examining the records of 12,512 participants with an equal chance of receiving finerenone or placebo
- Isolate the impact of UACR reduction on kidney function and cardiovascular function by tracking health indicators related to the kidneys and the heart in participants for up to 4 years
TAKEAWAY:
- Over half of participants who received finerenone had reduced UACR by at least 30% from the baseline of 514 mg/g at the 4-month point after starting treatment, and the median UACR reduction in this group was 33%.
- By 4 months, a little over a quarter of participants who received the placebo had reduced their UACR levels by at least 30%, and the median UACR reduction in this group was 2.6%.
- A UACR reduction of at least 30% reduced kidney risk by 64%, as measured by reductions in kidney failure, sufficient glomerular filtration, and death from kidney disease.
- A UACR reduction of at least 30% reduced cardiovascular risk by 26%, as measured by fewer incidences of cardiovascular death, nonfatal infarction or stroke, and hospitalization for heart failure.
IN PRACTICE:
“Achieving early UACR reduction can lead to tangible benefits for kidney and cardiovascular health,” the authors note.
SOURCE:
The study was published in the Annals of Internal Medicine; the lead author is Rajiv Agarwal, MD, MS.
LIMITATIONS:
The study pertains only to finerenone, so the findings cannot be extrapolated to other drugs with different mechanisms of action.
DISCLOSURES:
Bayer AG Pharmaceuticals, which manufactures finerenone, was the primary funder of the study. The US National Institutes of Health and Veterans Administration also provided funding. Some study authors are full-time employees of Bayer AG. Many authors report consulting relationships with various pharmaceutical companies.
A version of this article appeared on Medscape.com.
TOPLINE:
Reducing the urine albumin-to-creatinine ratio (UACR) significantly reduces kidney risk in people with type 2 diabetes, per new research in the Annals of Internal Medicine.
METHODOLOGY:
- Post hoc retrospective analysis of two phase 3 double-blind trials of finerenone in people with type 2 diabetes and chronic kidney disease
- Quantify the long-term health effects of reducing UACR within 4 months of taking finerenone by examining the records of 12,512 participants with an equal chance of receiving finerenone or placebo
- Isolate the impact of UACR reduction on kidney function and cardiovascular function by tracking health indicators related to the kidneys and the heart in participants for up to 4 years
TAKEAWAY:
- Over half of participants who received finerenone had reduced UACR by at least 30% from the baseline of 514 mg/g at the 4-month point after starting treatment, and the median UACR reduction in this group was 33%.
- By 4 months, a little over a quarter of participants who received the placebo had reduced their UACR levels by at least 30%, and the median UACR reduction in this group was 2.6%.
- A UACR reduction of at least 30% reduced kidney risk by 64%, as measured by reductions in kidney failure, sufficient glomerular filtration, and death from kidney disease.
- A UACR reduction of at least 30% reduced cardiovascular risk by 26%, as measured by fewer incidences of cardiovascular death, nonfatal infarction or stroke, and hospitalization for heart failure.
IN PRACTICE:
“Achieving early UACR reduction can lead to tangible benefits for kidney and cardiovascular health,” the authors note.
SOURCE:
The study was published in the Annals of Internal Medicine; the lead author is Rajiv Agarwal, MD, MS.
LIMITATIONS:
The study pertains only to finerenone, so the findings cannot be extrapolated to other drugs with different mechanisms of action.
DISCLOSURES:
Bayer AG Pharmaceuticals, which manufactures finerenone, was the primary funder of the study. The US National Institutes of Health and Veterans Administration also provided funding. Some study authors are full-time employees of Bayer AG. Many authors report consulting relationships with various pharmaceutical companies.
A version of this article appeared on Medscape.com.
TOPLINE:
Reducing the urine albumin-to-creatinine ratio (UACR) significantly reduces kidney risk in people with type 2 diabetes, per new research in the Annals of Internal Medicine.
METHODOLOGY:
- Post hoc retrospective analysis of two phase 3 double-blind trials of finerenone in people with type 2 diabetes and chronic kidney disease
- Quantify the long-term health effects of reducing UACR within 4 months of taking finerenone by examining the records of 12,512 participants with an equal chance of receiving finerenone or placebo
- Isolate the impact of UACR reduction on kidney function and cardiovascular function by tracking health indicators related to the kidneys and the heart in participants for up to 4 years
TAKEAWAY:
- Over half of participants who received finerenone had reduced UACR by at least 30% from the baseline of 514 mg/g at the 4-month point after starting treatment, and the median UACR reduction in this group was 33%.
- By 4 months, a little over a quarter of participants who received the placebo had reduced their UACR levels by at least 30%, and the median UACR reduction in this group was 2.6%.
- A UACR reduction of at least 30% reduced kidney risk by 64%, as measured by reductions in kidney failure, sufficient glomerular filtration, and death from kidney disease.
- A UACR reduction of at least 30% reduced cardiovascular risk by 26%, as measured by fewer incidences of cardiovascular death, nonfatal infarction or stroke, and hospitalization for heart failure.
IN PRACTICE:
“Achieving early UACR reduction can lead to tangible benefits for kidney and cardiovascular health,” the authors note.
SOURCE:
The study was published in the Annals of Internal Medicine; the lead author is Rajiv Agarwal, MD, MS.
LIMITATIONS:
The study pertains only to finerenone, so the findings cannot be extrapolated to other drugs with different mechanisms of action.
DISCLOSURES:
Bayer AG Pharmaceuticals, which manufactures finerenone, was the primary funder of the study. The US National Institutes of Health and Veterans Administration also provided funding. Some study authors are full-time employees of Bayer AG. Many authors report consulting relationships with various pharmaceutical companies.
A version of this article appeared on Medscape.com.