User login
-
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]


Asthma Across a Woman’s Lifespan
1. Chowdhury NU et al. Eur Respir Rev. 2021;30(162):210067. doi:10.1183/16000617.0067-2021
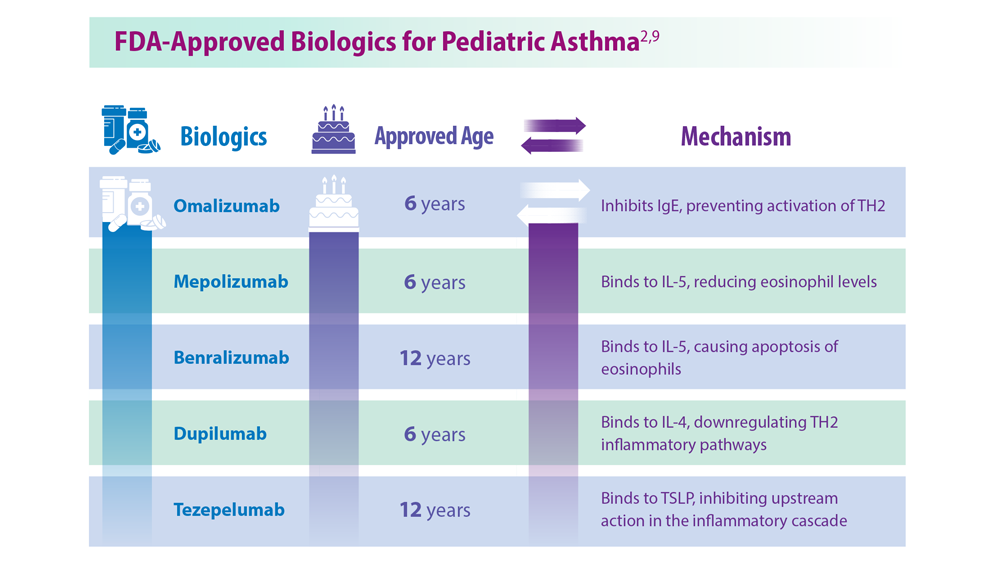
2. Perikleous EP et al. J Pers Med. 2022;12(6):999. doi:10.3390/jpm12060999
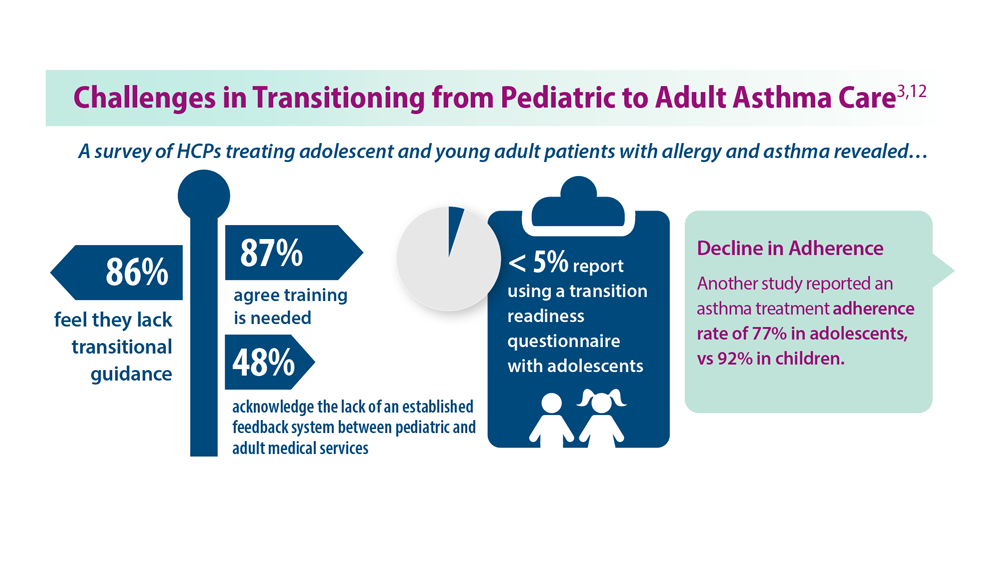
3. Khaleva E et al. Clin Transl Allergy. 2020;10:40. doi:10.1186/s13601-020-00340-z
4. Robijn AL et al. Curr Opin Pulm Med. 2019;25(1):11-17. doi:10.1097/MCP.0000000000000538
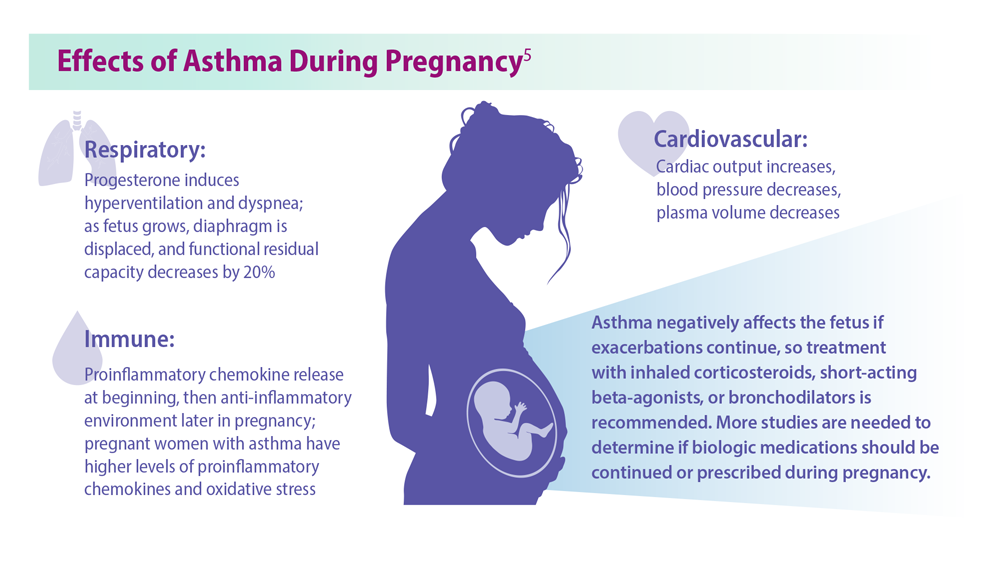
5. Bravo-Solarte DC et al. Allergy Asthma Proc. 2023;44(1):24-34. doi:10.2500/aap.2023.44.220077
6. Wang G et al. J Matern Fetal Neonatal Med. 2014;27(9):934-942. doi:10.3109/14767058.2013.847080
7. Hough KP et al. Front Med (Lausanne). 2020;7:191. doi:10.3389/fmed.2020.00191
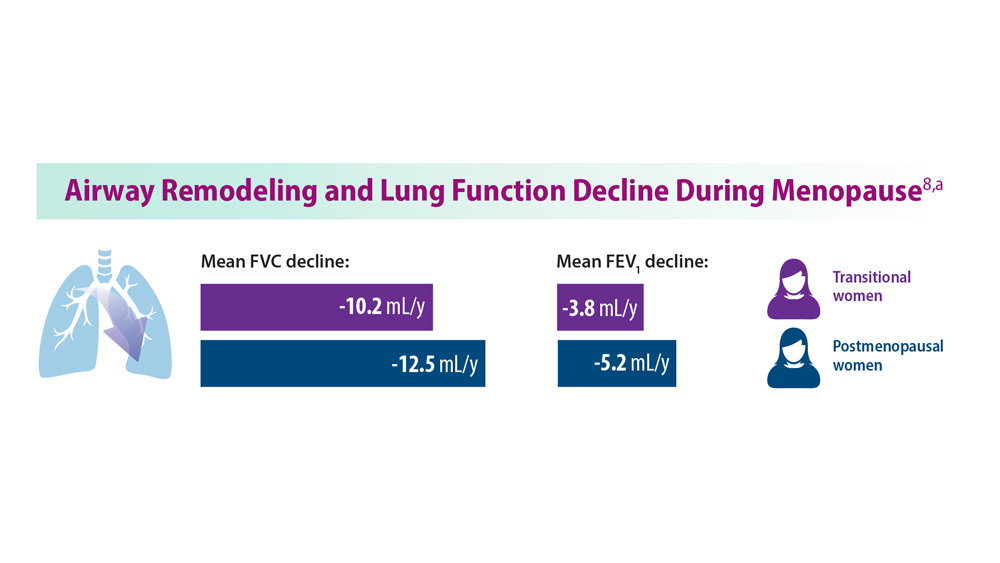
8. Triebner K et al. Am J Respir Crit Care Med. 2017;195(8):1058-1065. doi:10.1164/rccm.201605-0968OC
9. Bacharier LB, Jackson DJ. J Allergy Clin Immunol. 2023;151(3):581-589. doi:10.1016/j.jaci.2023.01.002
10. An amazing journey: how young lungs develop. American Lung Association. Published May 11, 2018. Accessed June 28, 2023. https://www.lung.org/blog/how-young-lungs-develop
11. Strunk RC et al. J Allergy Clin Immunol. 2006;118(5):1040-1047. doi:10.1016/j.jaci.2006.07.053
12. Kaplan A, Price D. J Asthma Allergy. 2020;13:39-49. doi:10.2147/JAA.S233268
1. Chowdhury NU et al. Eur Respir Rev. 2021;30(162):210067. doi:10.1183/16000617.0067-2021
2. Perikleous EP et al. J Pers Med. 2022;12(6):999. doi:10.3390/jpm12060999
3. Khaleva E et al. Clin Transl Allergy. 2020;10:40. doi:10.1186/s13601-020-00340-z
4. Robijn AL et al. Curr Opin Pulm Med. 2019;25(1):11-17. doi:10.1097/MCP.0000000000000538
5. Bravo-Solarte DC et al. Allergy Asthma Proc. 2023;44(1):24-34. doi:10.2500/aap.2023.44.220077
6. Wang G et al. J Matern Fetal Neonatal Med. 2014;27(9):934-942. doi:10.3109/14767058.2013.847080
7. Hough KP et al. Front Med (Lausanne). 2020;7:191. doi:10.3389/fmed.2020.00191
8. Triebner K et al. Am J Respir Crit Care Med. 2017;195(8):1058-1065. doi:10.1164/rccm.201605-0968OC
9. Bacharier LB, Jackson DJ. J Allergy Clin Immunol. 2023;151(3):581-589. doi:10.1016/j.jaci.2023.01.002
10. An amazing journey: how young lungs develop. American Lung Association. Published May 11, 2018. Accessed June 28, 2023. https://www.lung.org/blog/how-young-lungs-develop
11. Strunk RC et al. J Allergy Clin Immunol. 2006;118(5):1040-1047. doi:10.1016/j.jaci.2006.07.053
12. Kaplan A, Price D. J Asthma Allergy. 2020;13:39-49. doi:10.2147/JAA.S233268
1. Chowdhury NU et al. Eur Respir Rev. 2021;30(162):210067. doi:10.1183/16000617.0067-2021
2. Perikleous EP et al. J Pers Med. 2022;12(6):999. doi:10.3390/jpm12060999
3. Khaleva E et al. Clin Transl Allergy. 2020;10:40. doi:10.1186/s13601-020-00340-z
4. Robijn AL et al. Curr Opin Pulm Med. 2019;25(1):11-17. doi:10.1097/MCP.0000000000000538
5. Bravo-Solarte DC et al. Allergy Asthma Proc. 2023;44(1):24-34. doi:10.2500/aap.2023.44.220077
6. Wang G et al. J Matern Fetal Neonatal Med. 2014;27(9):934-942. doi:10.3109/14767058.2013.847080
7. Hough KP et al. Front Med (Lausanne). 2020;7:191. doi:10.3389/fmed.2020.00191
8. Triebner K et al. Am J Respir Crit Care Med. 2017;195(8):1058-1065. doi:10.1164/rccm.201605-0968OC
9. Bacharier LB, Jackson DJ. J Allergy Clin Immunol. 2023;151(3):581-589. doi:10.1016/j.jaci.2023.01.002
10. An amazing journey: how young lungs develop. American Lung Association. Published May 11, 2018. Accessed June 28, 2023. https://www.lung.org/blog/how-young-lungs-develop
11. Strunk RC et al. J Allergy Clin Immunol. 2006;118(5):1040-1047. doi:10.1016/j.jaci.2006.07.053
12. Kaplan A, Price D. J Asthma Allergy. 2020;13:39-49. doi:10.2147/JAA.S233268
Pulmonology Data Trends 2023 (Slideshow)
CHEST Physician presents the 2023 edition of Pulmonology Data Trends (click to read). This special issue provides updates on hot topics in pulmonology through original infographics and visual storytelling.
In this issue:
Long-Awaited RSV Vaccines Now Available for Older Adults and Pediatric Patients
Burton L. Lesnick, MD, FCCP
Decreasing Pulmonary Embolism-Related Mortality
Parth Rali, MD
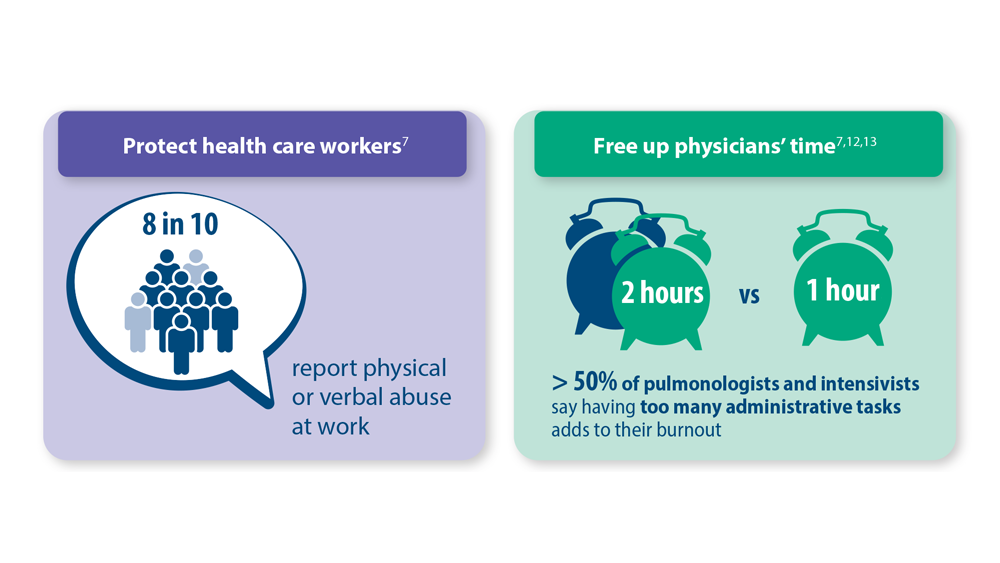
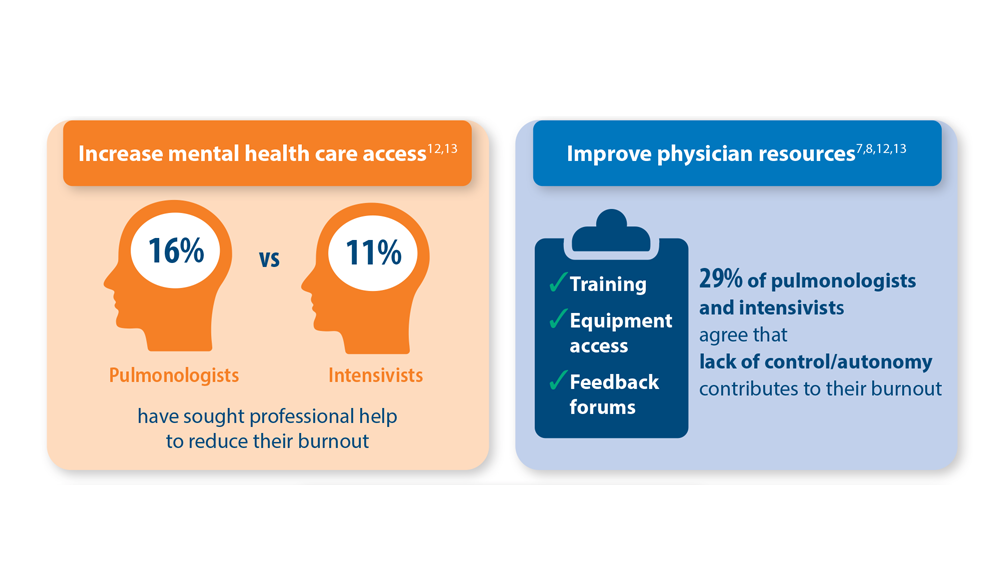
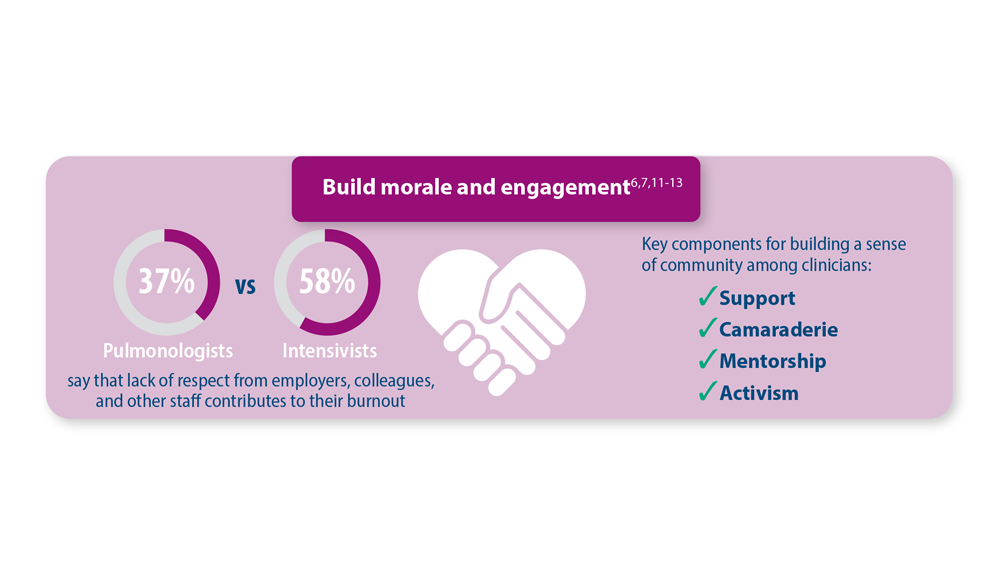
Addressing Physician Burnout in Pulmonology and Critical Care
Kelly Vranas, MD, MCR
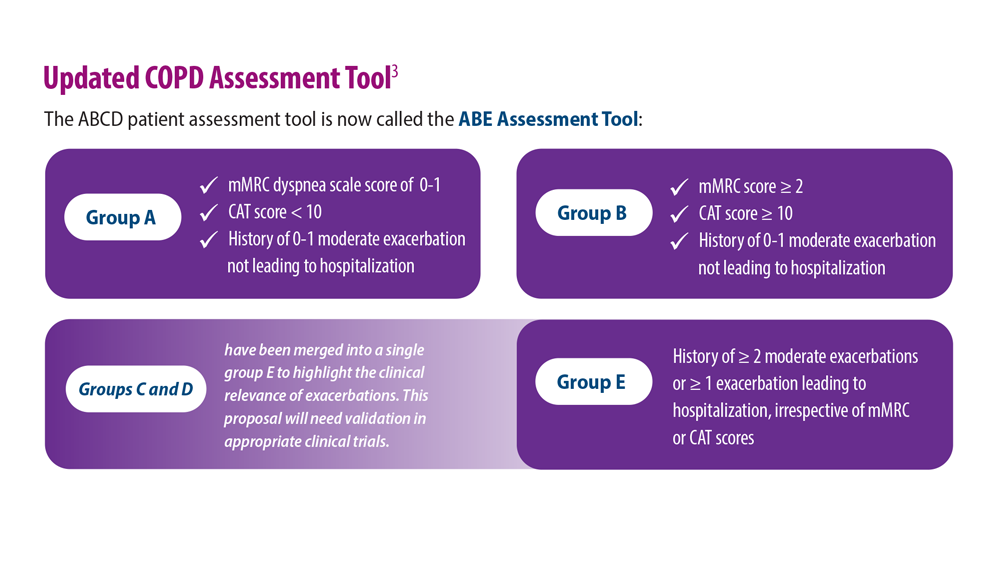
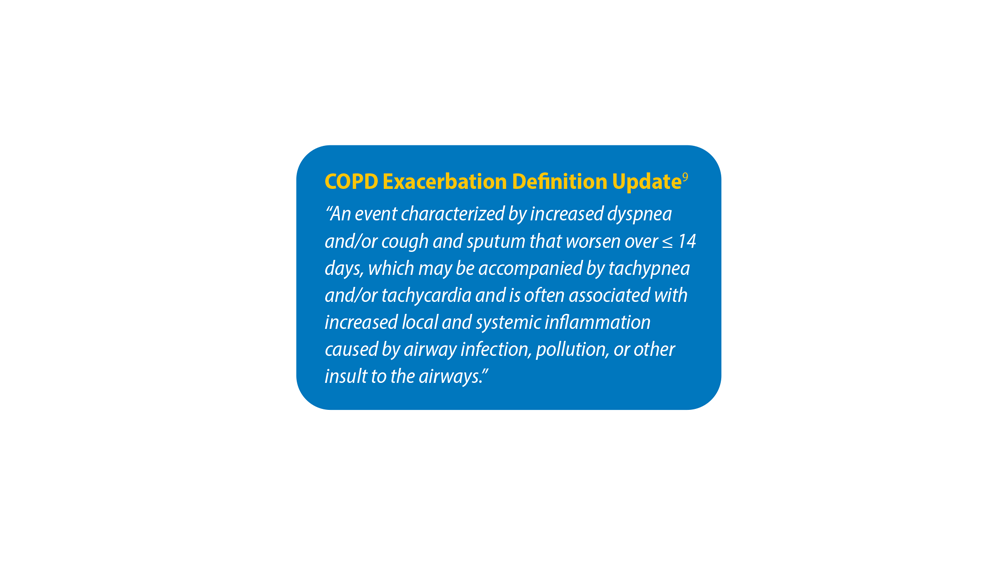
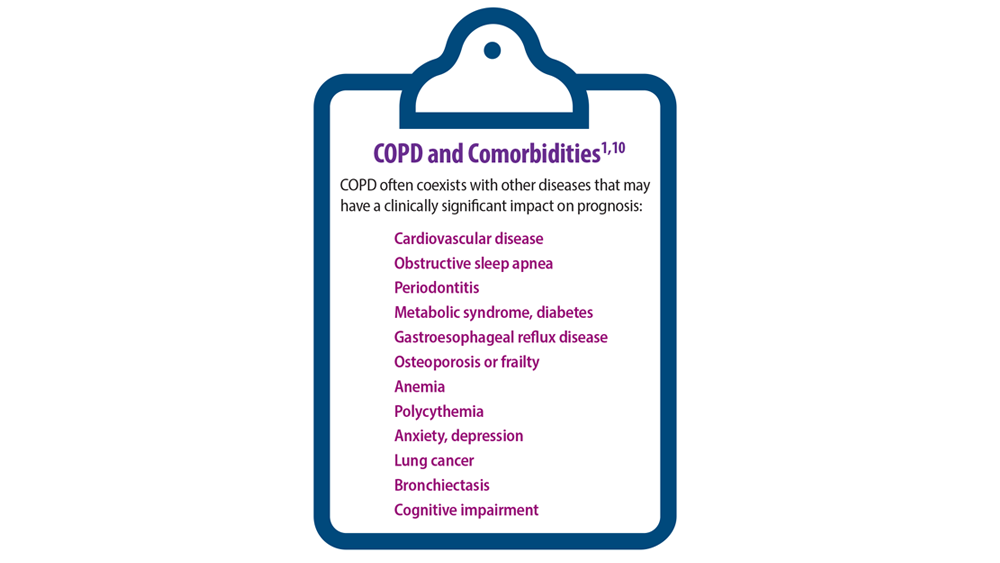
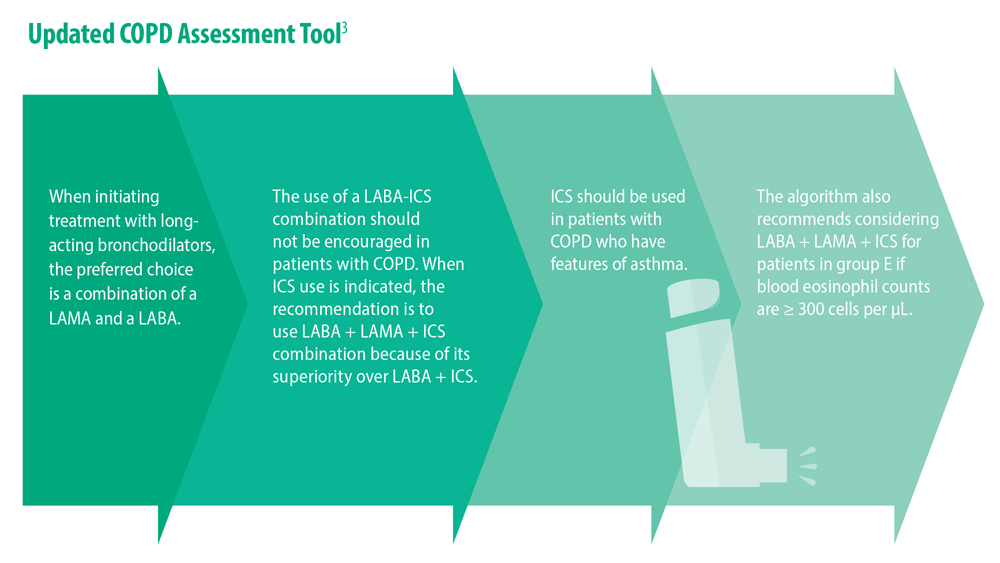
Updated Guidelines for COPD Management: 2023 GOLD Strategy Report
Muhammad Adrish, MD, MBA, FCCP, FCCM
Progressive Pulmonary Fibrosis: Understanding Its Many Forms
Tejaswini Kulkarni, MD, MPH, FCCP
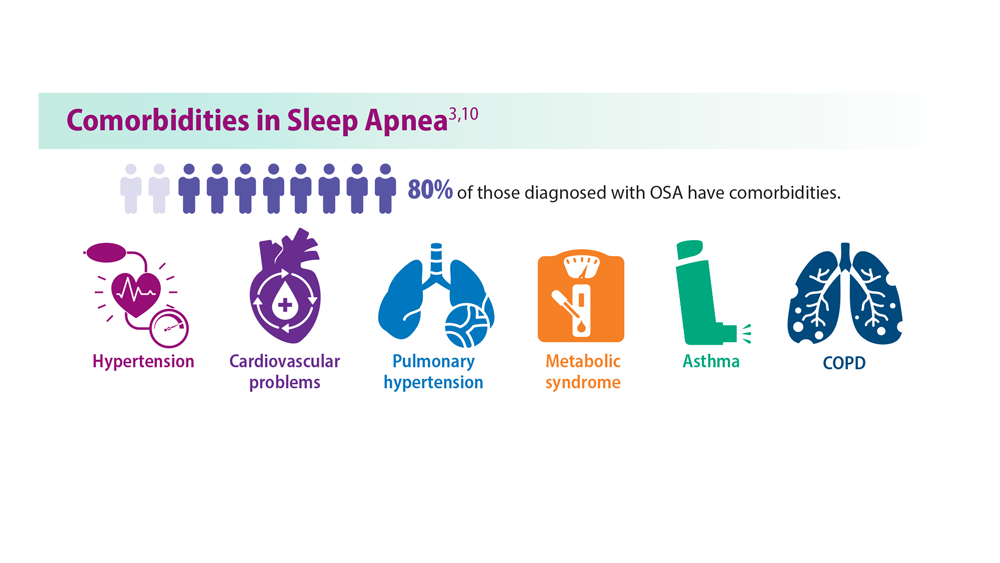
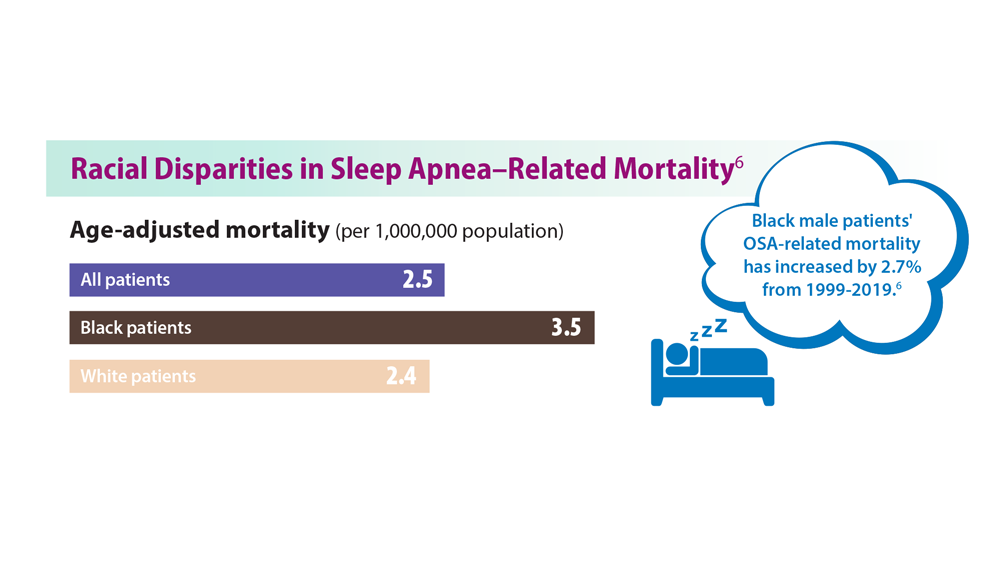
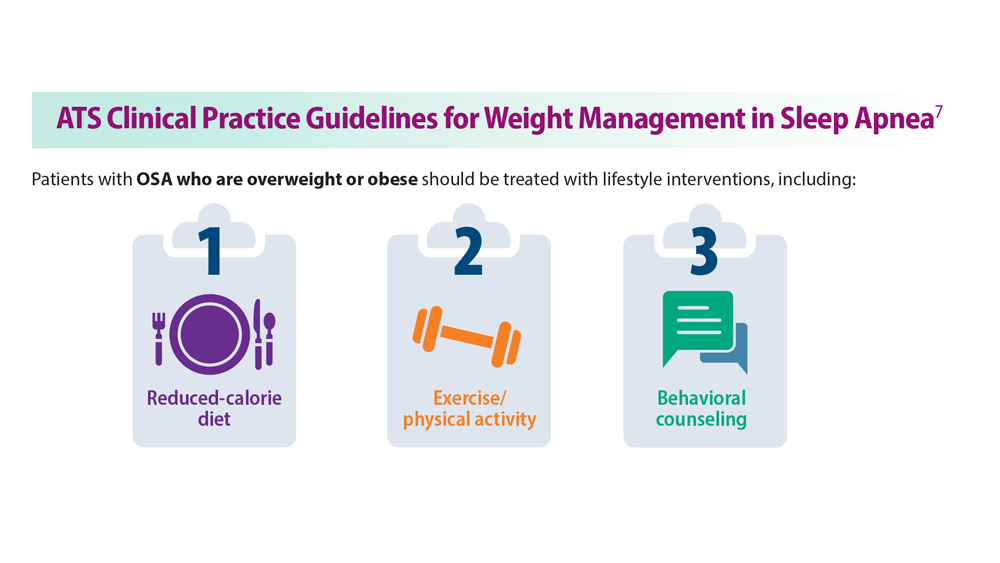
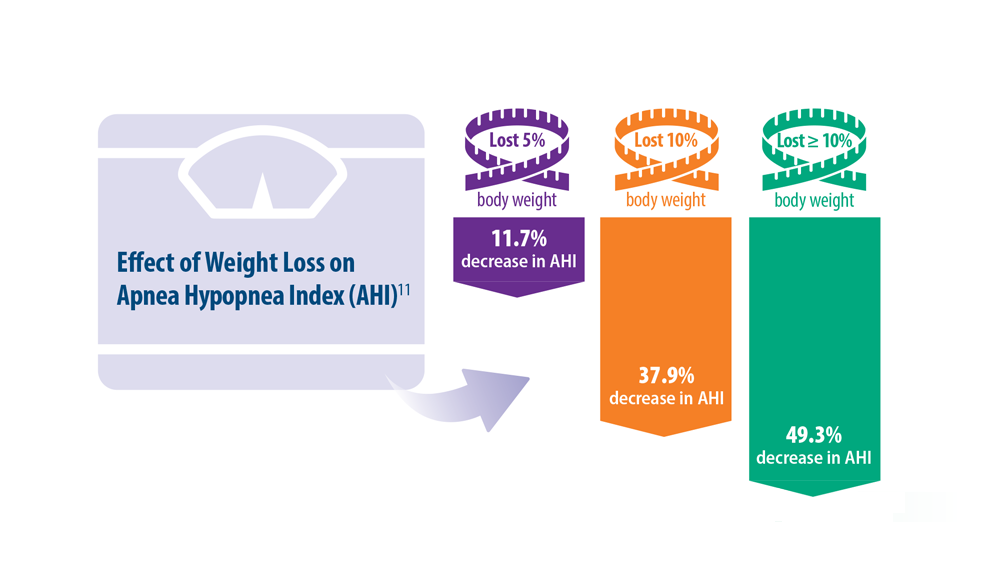
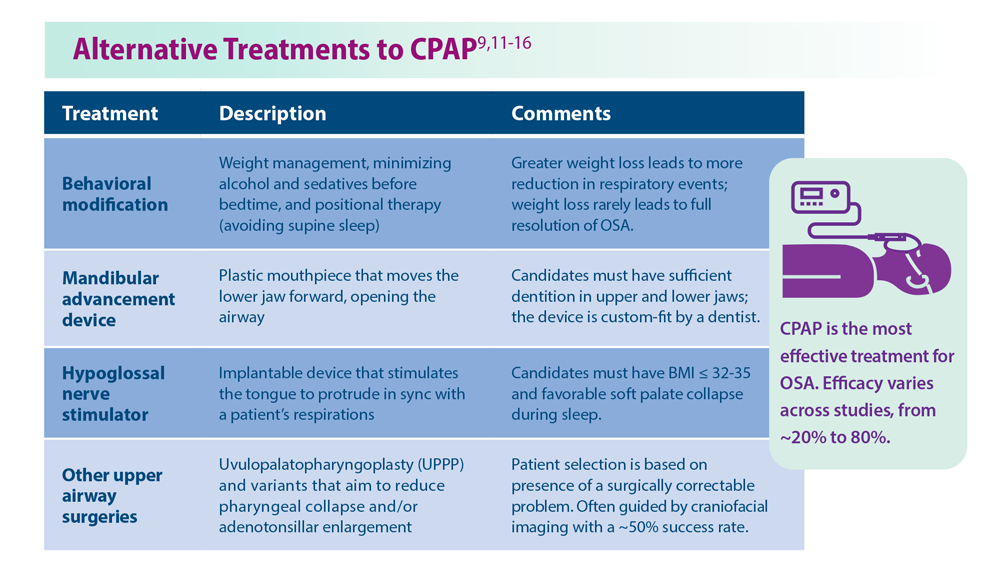
Sleep Apnea: Comorbidities, Racial Disparities, Weight Guidelines, and Alternatives to CPAP
Lauren Tobias, MD, FCCP
Lung Cancer Screening: A Need for Adjunctive Testing
Eric S. Edell, MD, FCCP
Asthma Across a Woman’s Lifespan
Navitha Ramesh, MD, FCCP
Tuberculosis Management: Returning to Pre-Pandemic Priorities
Patricio Escalante, MD, MSc, FCCP, and Paige K. Marty, MD
Long COVID: Advocating for Patients and Implementing Effective Techniques
Kyle B. Enfield, MD, MS, FSHEA, FCCM
CHEST Physician presents the 2023 edition of Pulmonology Data Trends (click to read). This special issue provides updates on hot topics in pulmonology through original infographics and visual storytelling.
In this issue:
Long-Awaited RSV Vaccines Now Available for Older Adults and Pediatric Patients
Burton L. Lesnick, MD, FCCP
Decreasing Pulmonary Embolism-Related Mortality
Parth Rali, MD
Addressing Physician Burnout in Pulmonology and Critical Care
Kelly Vranas, MD, MCR
Updated Guidelines for COPD Management: 2023 GOLD Strategy Report
Muhammad Adrish, MD, MBA, FCCP, FCCM
Progressive Pulmonary Fibrosis: Understanding Its Many Forms
Tejaswini Kulkarni, MD, MPH, FCCP
Sleep Apnea: Comorbidities, Racial Disparities, Weight Guidelines, and Alternatives to CPAP
Lauren Tobias, MD, FCCP
Lung Cancer Screening: A Need for Adjunctive Testing
Eric S. Edell, MD, FCCP
Asthma Across a Woman’s Lifespan
Navitha Ramesh, MD, FCCP
Tuberculosis Management: Returning to Pre-Pandemic Priorities
Patricio Escalante, MD, MSc, FCCP, and Paige K. Marty, MD
Long COVID: Advocating for Patients and Implementing Effective Techniques
Kyle B. Enfield, MD, MS, FSHEA, FCCM
CHEST Physician presents the 2023 edition of Pulmonology Data Trends (click to read). This special issue provides updates on hot topics in pulmonology through original infographics and visual storytelling.
In this issue:
Long-Awaited RSV Vaccines Now Available for Older Adults and Pediatric Patients
Burton L. Lesnick, MD, FCCP
Decreasing Pulmonary Embolism-Related Mortality
Parth Rali, MD
Addressing Physician Burnout in Pulmonology and Critical Care
Kelly Vranas, MD, MCR
Updated Guidelines for COPD Management: 2023 GOLD Strategy Report
Muhammad Adrish, MD, MBA, FCCP, FCCM
Progressive Pulmonary Fibrosis: Understanding Its Many Forms
Tejaswini Kulkarni, MD, MPH, FCCP
Sleep Apnea: Comorbidities, Racial Disparities, Weight Guidelines, and Alternatives to CPAP
Lauren Tobias, MD, FCCP
Lung Cancer Screening: A Need for Adjunctive Testing
Eric S. Edell, MD, FCCP
Asthma Across a Woman’s Lifespan
Navitha Ramesh, MD, FCCP
Tuberculosis Management: Returning to Pre-Pandemic Priorities
Patricio Escalante, MD, MSc, FCCP, and Paige K. Marty, MD
Long COVID: Advocating for Patients and Implementing Effective Techniques
Kyle B. Enfield, MD, MS, FSHEA, FCCM
Sleep Apnea: Comorbidities, Racial Disparities, Weight Guidelines, and Alternatives to CPAP
1. Gottlieb DJ, Punjabi NM. JAMA. 2020;323(14):1389-1400. doi:10.1001/jama.2020.3514
2. Slowik JM et al. Obstructive Sleep Apnea. In: StatPearls. Treasure Island (FL): StatPearls Publishing; December 11, 2022.
3. Bonsignore MR et al. Multidiscip Respir Med. 2019;14:8. doi:10.1186/s40248-019-0172-9
4. Schwartz SW et al. Sleep Breath. 2016;20(3):947-955. doi:10.1007/s11325-016-1316-1
5. Grandner MA et al. Sleep Med. 2016;18:7-18. doi:10.1016/j.sleep.2015.01.020
6. Lee YC et al. Sleep Med. 2022;90:204-213. doi:10.1016/j.sleep.2021.11.014
7. Hudgel DW et al. Am J Respir Crit Care Med. 2018;198(6):e70-e87. doi:10.1164/rccm.201807-1326ST
8. Lloyd R et al. J Clin Sleep Med. 2022;18(11):2673-2680. doi:10.5664/jcsm.10244
9. Nokes B et al. Expert Rev Respir Med. 2022;16(8):917-929. doi:10.1080/17476348.2022.2112669
10. Pinto JA et al. Int Arch Otorhinolaryngol. 2016;20(2):145-150.doi:10.1055/s-0036-1579546
11. Georgoulis M et al. J Clin Sleep Med. 2022;18(5):1251-1261. doi:10.5664/jcsm.9834
12. Askland K et al. Cochrane Database Syst Rev. 2020;4(4):CD007736. doi:10.1002/14651858.CD007736.pub3
13. Jugé L et al. Sleep. 2022;45(6):zsac044. doi:10.1093/sleep/zsac044
14. Strollo PJ Jr et al. N Engl J Med. 2014;370(2):139-149. doi:10.1056/NEJMoa1308659
15. Fattal D et al. J Clin Sleep Med. 2022;18(12):2723-2729. doi:10.5664/jcsm.10190
16. He M et al. Otolaryngol Head Neck Surg. 2019;161(3):401-411. doi:10.1177/0194599819840356
1. Gottlieb DJ, Punjabi NM. JAMA. 2020;323(14):1389-1400. doi:10.1001/jama.2020.3514
2. Slowik JM et al. Obstructive Sleep Apnea. In: StatPearls. Treasure Island (FL): StatPearls Publishing; December 11, 2022.
3. Bonsignore MR et al. Multidiscip Respir Med. 2019;14:8. doi:10.1186/s40248-019-0172-9
4. Schwartz SW et al. Sleep Breath. 2016;20(3):947-955. doi:10.1007/s11325-016-1316-1
5. Grandner MA et al. Sleep Med. 2016;18:7-18. doi:10.1016/j.sleep.2015.01.020
6. Lee YC et al. Sleep Med. 2022;90:204-213. doi:10.1016/j.sleep.2021.11.014
7. Hudgel DW et al. Am J Respir Crit Care Med. 2018;198(6):e70-e87. doi:10.1164/rccm.201807-1326ST
8. Lloyd R et al. J Clin Sleep Med. 2022;18(11):2673-2680. doi:10.5664/jcsm.10244
9. Nokes B et al. Expert Rev Respir Med. 2022;16(8):917-929. doi:10.1080/17476348.2022.2112669
10. Pinto JA et al. Int Arch Otorhinolaryngol. 2016;20(2):145-150.doi:10.1055/s-0036-1579546
11. Georgoulis M et al. J Clin Sleep Med. 2022;18(5):1251-1261. doi:10.5664/jcsm.9834
12. Askland K et al. Cochrane Database Syst Rev. 2020;4(4):CD007736. doi:10.1002/14651858.CD007736.pub3
13. Jugé L et al. Sleep. 2022;45(6):zsac044. doi:10.1093/sleep/zsac044
14. Strollo PJ Jr et al. N Engl J Med. 2014;370(2):139-149. doi:10.1056/NEJMoa1308659
15. Fattal D et al. J Clin Sleep Med. 2022;18(12):2723-2729. doi:10.5664/jcsm.10190
16. He M et al. Otolaryngol Head Neck Surg. 2019;161(3):401-411. doi:10.1177/0194599819840356
1. Gottlieb DJ, Punjabi NM. JAMA. 2020;323(14):1389-1400. doi:10.1001/jama.2020.3514
2. Slowik JM et al. Obstructive Sleep Apnea. In: StatPearls. Treasure Island (FL): StatPearls Publishing; December 11, 2022.
3. Bonsignore MR et al. Multidiscip Respir Med. 2019;14:8. doi:10.1186/s40248-019-0172-9
4. Schwartz SW et al. Sleep Breath. 2016;20(3):947-955. doi:10.1007/s11325-016-1316-1
5. Grandner MA et al. Sleep Med. 2016;18:7-18. doi:10.1016/j.sleep.2015.01.020
6. Lee YC et al. Sleep Med. 2022;90:204-213. doi:10.1016/j.sleep.2021.11.014
7. Hudgel DW et al. Am J Respir Crit Care Med. 2018;198(6):e70-e87. doi:10.1164/rccm.201807-1326ST
8. Lloyd R et al. J Clin Sleep Med. 2022;18(11):2673-2680. doi:10.5664/jcsm.10244
9. Nokes B et al. Expert Rev Respir Med. 2022;16(8):917-929. doi:10.1080/17476348.2022.2112669
10. Pinto JA et al. Int Arch Otorhinolaryngol. 2016;20(2):145-150.doi:10.1055/s-0036-1579546
11. Georgoulis M et al. J Clin Sleep Med. 2022;18(5):1251-1261. doi:10.5664/jcsm.9834
12. Askland K et al. Cochrane Database Syst Rev. 2020;4(4):CD007736. doi:10.1002/14651858.CD007736.pub3
13. Jugé L et al. Sleep. 2022;45(6):zsac044. doi:10.1093/sleep/zsac044
14. Strollo PJ Jr et al. N Engl J Med. 2014;370(2):139-149. doi:10.1056/NEJMoa1308659
15. Fattal D et al. J Clin Sleep Med. 2022;18(12):2723-2729. doi:10.5664/jcsm.10190
16. He M et al. Otolaryngol Head Neck Surg. 2019;161(3):401-411. doi:10.1177/0194599819840356
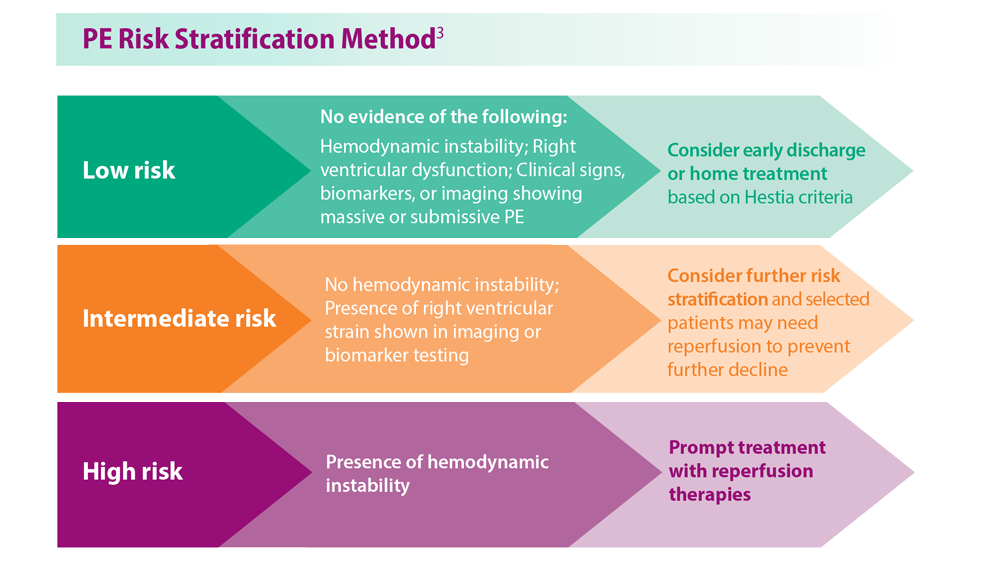
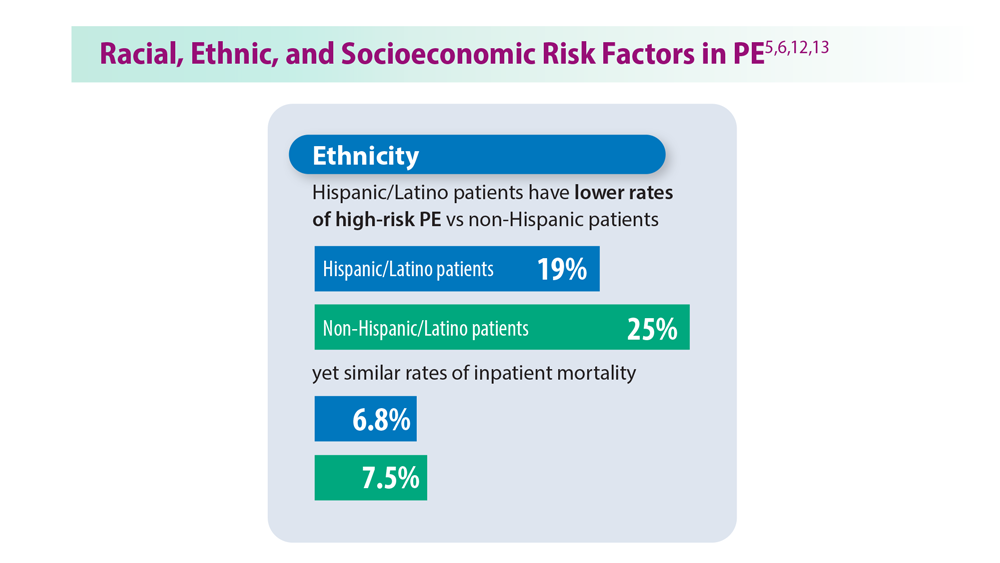
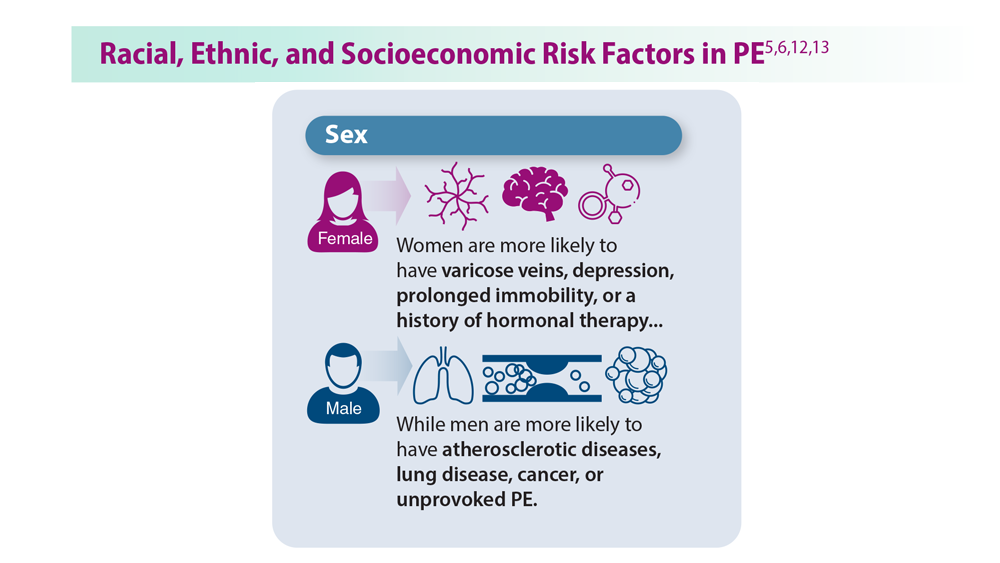
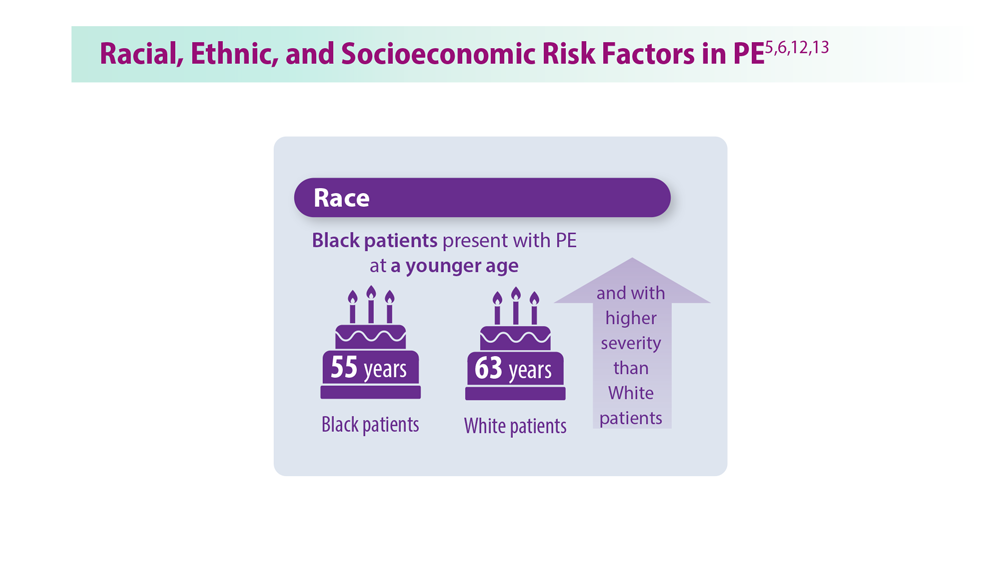
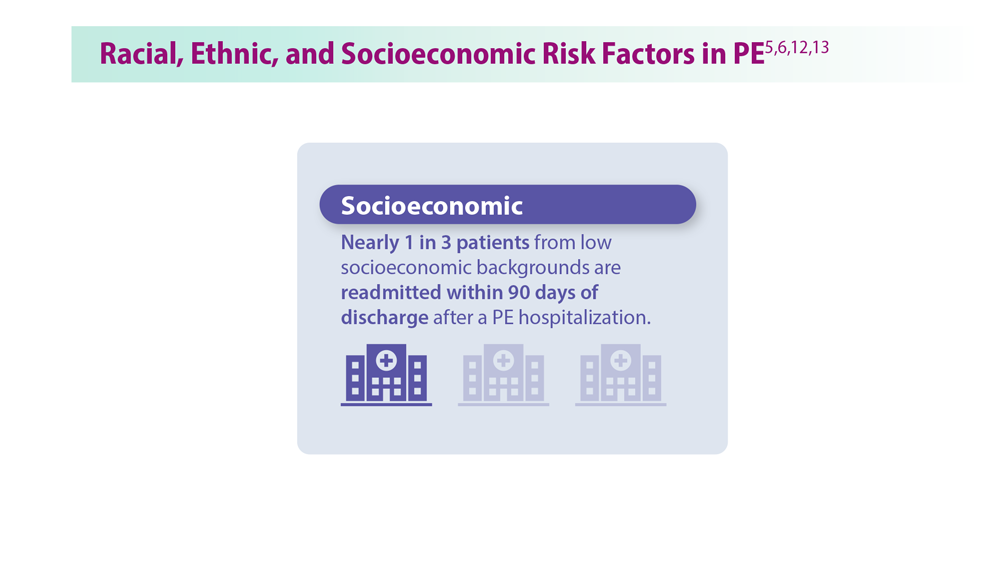
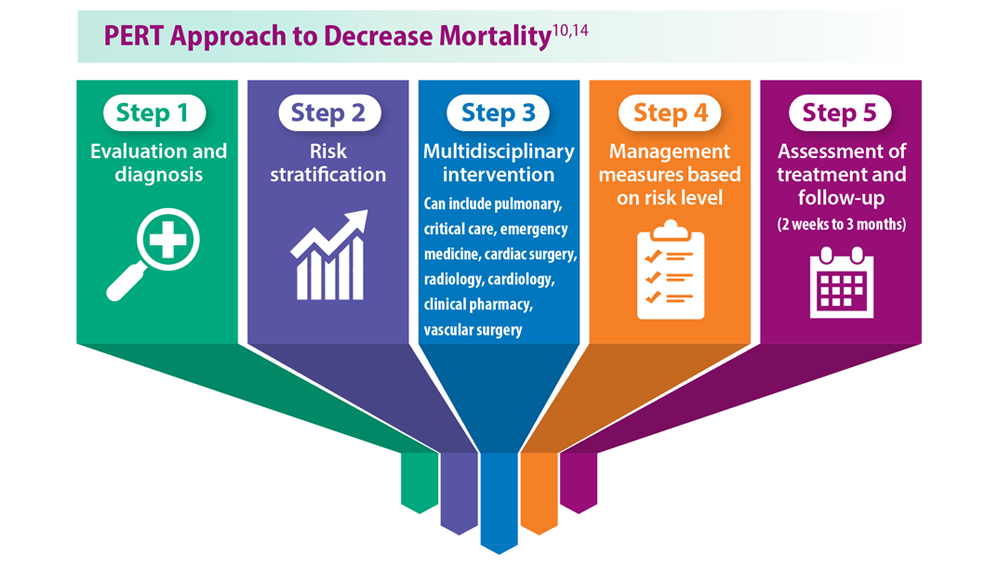
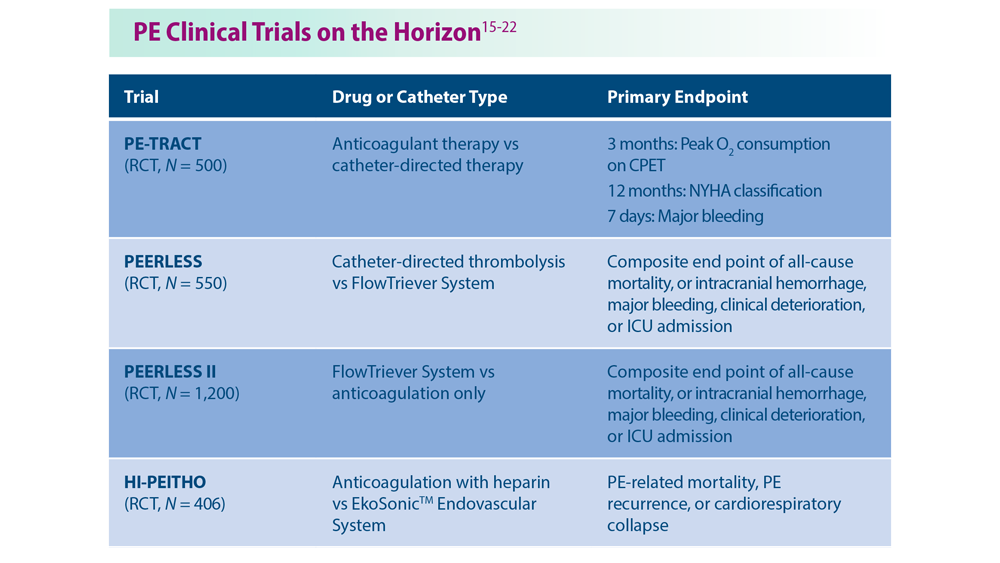
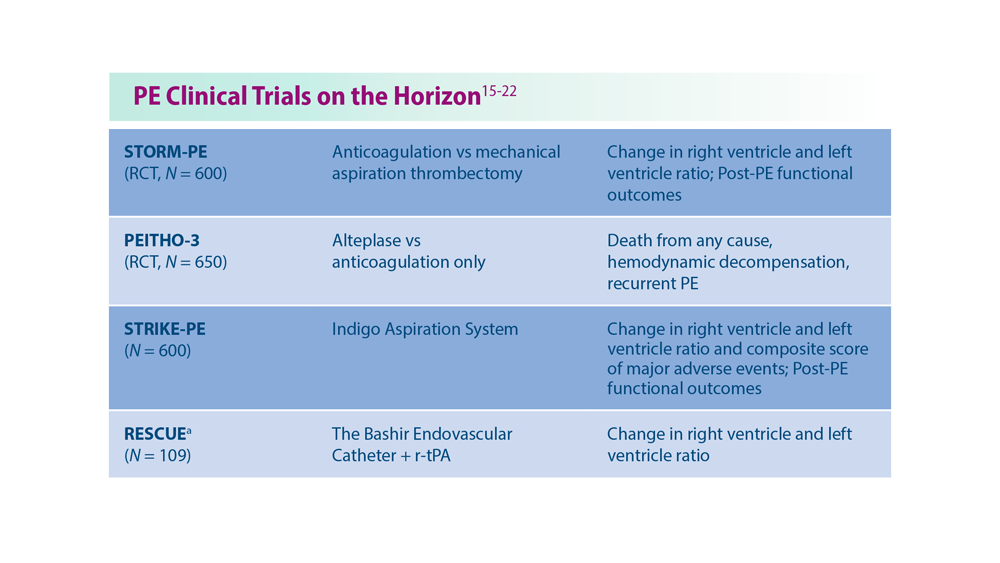
Decreasing Pulmonary Embolism-Related Mortality
- Centers for Disease Control and Prevention. Data and statistics on venous thromboembolism. Last reviewed June 28, 2023. Accessed July 18, 2023. https://www.cdc.gov/ncbddd/dvt/data.html
- Becattini C et al. Chest. 2016;149(1):192-200. doi:10.1378/chest.15-0808
- Triantafyllou GA et al. Semin Respir Crit Care Med. 2021;42(2):183-198.doi:10.1055/s-0041-1722898
- Ng ACC et al. Respiration. 2013;85(5):408-416. doi:10.1159/000342024
- Phillips AR et al. J Am Heart Assoc. 2021;10(17):e021818. doi:10.1161/JAHA.121.021818
- Wadhera RK et al. J Am Heart Assoc. 2021;10(13):e021117. doi:10.1161/JAHA.121.021117
- Bashir R et al. JACC Cardiovasc Interv. 2022;15(23):2427-2436. doi:10.1016/j.jcin.2022.09.011
- Patel NJ et al. Int J Cardiol. 2019;287:116-117. doi:10.1016/j.ijcard.2019.04.029
- Li X et al. Ann Transl Med. 2021;9(10):838. doi:10.21037/atm-21-975
- Rivera-Lebron BN et al. Chest. 2021;159(1):347-355. doi:10.1016/j.chest.2020.07.065
- Noto JG, Rali P. Pulm Circ. 2022;12(1):e12021. doi:10.1002/pul2.12021
- Snyder DJ et al. Vasc Med. 2023;28(3):222-232. doi:10.1177/1358863X231157441
- Bikdeli B et al. Semin Thromb Hemost. 2023. doi:10.1055/s-0043-1764231
- Fleitas Sosa D et al. Eur Respir Rev. 2022;31(165):220023. doi:10.1183/16000617.0023-2022
- Pulmonary embolism - thrombus removal with catheter-directed therapy (PE-TRACT). ClinicalTrials.gov. Updated July 17, 2023. Accessed July 18, 2023. https://clinicaltrials.gov/ct2/show/NCT05591118
- The PEERLESS study (PEERLESS). ClinicalTrials.gov. Updated Jun 23, 2023. Accessed July 18, 2023. https://clinicaltrials.gov/ct2/show/NCT05111613
- Inari Medical, Inc. Inari Medical announces Peerless II, a randomized controlled trial evaluating clinical outcomes of the FlowTriever® system vs. anticoagulation in pulmonary embolism patients [press release]. Published May 22,2023. Accessed July 18, 2023. https://ir.inarimedical.com/news-releases/news-release-details/inari-medical-announces-peerless-ii-randomized-controlled-trial
- Ultrasound-facilitated, catheter-directed, thrombolysis in intermediate-high risk pulmonary embolism (HI-PEITHO). ClinicalTrials.gov. Updated July 17, 2023. Accessed July 18, 2023. https://clinicaltrials.gov/ct2/show/NCT04790370
- Comparison of two pulmonary embolism treatments. ClinicalTrials.gov. Updated May 31, 2023. Accessed July 18, 2023. https://clinicaltrials.gov/ct2/show/NCT05684796
- Pulmonary Embolism International THrOmbolysis Study-3 (PEITHO-3).ClinicalTrials.gov. Updated June 8, 2023. Accessed July 18, 2023. https://clinicaltrials.gov/ct2/show/NCT04430569
- Study of the long-term safety and outcomes of treating pulmonary embolism with the Indigo Aspiration System. ClinicalTrials.gov. Updated May 11, 2023. Accessed July 18, 2023. https://clinicaltrials.gov/ct2/show/NCT04798261
- Bashir R et al. J Am Coll Cardiol Intv. 2022;15(23):2427-2436. doi:10.1016/j.jcin.2022.09.011
- Centers for Disease Control and Prevention. Data and statistics on venous thromboembolism. Last reviewed June 28, 2023. Accessed July 18, 2023. https://www.cdc.gov/ncbddd/dvt/data.html
- Becattini C et al. Chest. 2016;149(1):192-200. doi:10.1378/chest.15-0808
- Triantafyllou GA et al. Semin Respir Crit Care Med. 2021;42(2):183-198.doi:10.1055/s-0041-1722898
- Ng ACC et al. Respiration. 2013;85(5):408-416. doi:10.1159/000342024
- Phillips AR et al. J Am Heart Assoc. 2021;10(17):e021818. doi:10.1161/JAHA.121.021818
- Wadhera RK et al. J Am Heart Assoc. 2021;10(13):e021117. doi:10.1161/JAHA.121.021117
- Bashir R et al. JACC Cardiovasc Interv. 2022;15(23):2427-2436. doi:10.1016/j.jcin.2022.09.011
- Patel NJ et al. Int J Cardiol. 2019;287:116-117. doi:10.1016/j.ijcard.2019.04.029
- Li X et al. Ann Transl Med. 2021;9(10):838. doi:10.21037/atm-21-975
- Rivera-Lebron BN et al. Chest. 2021;159(1):347-355. doi:10.1016/j.chest.2020.07.065
- Noto JG, Rali P. Pulm Circ. 2022;12(1):e12021. doi:10.1002/pul2.12021
- Snyder DJ et al. Vasc Med. 2023;28(3):222-232. doi:10.1177/1358863X231157441
- Bikdeli B et al. Semin Thromb Hemost. 2023. doi:10.1055/s-0043-1764231
- Fleitas Sosa D et al. Eur Respir Rev. 2022;31(165):220023. doi:10.1183/16000617.0023-2022
- Pulmonary embolism - thrombus removal with catheter-directed therapy (PE-TRACT). ClinicalTrials.gov. Updated July 17, 2023. Accessed July 18, 2023. https://clinicaltrials.gov/ct2/show/NCT05591118
- The PEERLESS study (PEERLESS). ClinicalTrials.gov. Updated Jun 23, 2023. Accessed July 18, 2023. https://clinicaltrials.gov/ct2/show/NCT05111613
- Inari Medical, Inc. Inari Medical announces Peerless II, a randomized controlled trial evaluating clinical outcomes of the FlowTriever® system vs. anticoagulation in pulmonary embolism patients [press release]. Published May 22,2023. Accessed July 18, 2023. https://ir.inarimedical.com/news-releases/news-release-details/inari-medical-announces-peerless-ii-randomized-controlled-trial
- Ultrasound-facilitated, catheter-directed, thrombolysis in intermediate-high risk pulmonary embolism (HI-PEITHO). ClinicalTrials.gov. Updated July 17, 2023. Accessed July 18, 2023. https://clinicaltrials.gov/ct2/show/NCT04790370
- Comparison of two pulmonary embolism treatments. ClinicalTrials.gov. Updated May 31, 2023. Accessed July 18, 2023. https://clinicaltrials.gov/ct2/show/NCT05684796
- Pulmonary Embolism International THrOmbolysis Study-3 (PEITHO-3).ClinicalTrials.gov. Updated June 8, 2023. Accessed July 18, 2023. https://clinicaltrials.gov/ct2/show/NCT04430569
- Study of the long-term safety and outcomes of treating pulmonary embolism with the Indigo Aspiration System. ClinicalTrials.gov. Updated May 11, 2023. Accessed July 18, 2023. https://clinicaltrials.gov/ct2/show/NCT04798261
- Bashir R et al. J Am Coll Cardiol Intv. 2022;15(23):2427-2436. doi:10.1016/j.jcin.2022.09.011
- Centers for Disease Control and Prevention. Data and statistics on venous thromboembolism. Last reviewed June 28, 2023. Accessed July 18, 2023. https://www.cdc.gov/ncbddd/dvt/data.html
- Becattini C et al. Chest. 2016;149(1):192-200. doi:10.1378/chest.15-0808
- Triantafyllou GA et al. Semin Respir Crit Care Med. 2021;42(2):183-198.doi:10.1055/s-0041-1722898
- Ng ACC et al. Respiration. 2013;85(5):408-416. doi:10.1159/000342024
- Phillips AR et al. J Am Heart Assoc. 2021;10(17):e021818. doi:10.1161/JAHA.121.021818
- Wadhera RK et al. J Am Heart Assoc. 2021;10(13):e021117. doi:10.1161/JAHA.121.021117
- Bashir R et al. JACC Cardiovasc Interv. 2022;15(23):2427-2436. doi:10.1016/j.jcin.2022.09.011
- Patel NJ et al. Int J Cardiol. 2019;287:116-117. doi:10.1016/j.ijcard.2019.04.029
- Li X et al. Ann Transl Med. 2021;9(10):838. doi:10.21037/atm-21-975
- Rivera-Lebron BN et al. Chest. 2021;159(1):347-355. doi:10.1016/j.chest.2020.07.065
- Noto JG, Rali P. Pulm Circ. 2022;12(1):e12021. doi:10.1002/pul2.12021
- Snyder DJ et al. Vasc Med. 2023;28(3):222-232. doi:10.1177/1358863X231157441
- Bikdeli B et al. Semin Thromb Hemost. 2023. doi:10.1055/s-0043-1764231
- Fleitas Sosa D et al. Eur Respir Rev. 2022;31(165):220023. doi:10.1183/16000617.0023-2022
- Pulmonary embolism - thrombus removal with catheter-directed therapy (PE-TRACT). ClinicalTrials.gov. Updated July 17, 2023. Accessed July 18, 2023. https://clinicaltrials.gov/ct2/show/NCT05591118
- The PEERLESS study (PEERLESS). ClinicalTrials.gov. Updated Jun 23, 2023. Accessed July 18, 2023. https://clinicaltrials.gov/ct2/show/NCT05111613
- Inari Medical, Inc. Inari Medical announces Peerless II, a randomized controlled trial evaluating clinical outcomes of the FlowTriever® system vs. anticoagulation in pulmonary embolism patients [press release]. Published May 22,2023. Accessed July 18, 2023. https://ir.inarimedical.com/news-releases/news-release-details/inari-medical-announces-peerless-ii-randomized-controlled-trial
- Ultrasound-facilitated, catheter-directed, thrombolysis in intermediate-high risk pulmonary embolism (HI-PEITHO). ClinicalTrials.gov. Updated July 17, 2023. Accessed July 18, 2023. https://clinicaltrials.gov/ct2/show/NCT04790370
- Comparison of two pulmonary embolism treatments. ClinicalTrials.gov. Updated May 31, 2023. Accessed July 18, 2023. https://clinicaltrials.gov/ct2/show/NCT05684796
- Pulmonary Embolism International THrOmbolysis Study-3 (PEITHO-3).ClinicalTrials.gov. Updated June 8, 2023. Accessed July 18, 2023. https://clinicaltrials.gov/ct2/show/NCT04430569
- Study of the long-term safety and outcomes of treating pulmonary embolism with the Indigo Aspiration System. ClinicalTrials.gov. Updated May 11, 2023. Accessed July 18, 2023. https://clinicaltrials.gov/ct2/show/NCT04798261
- Bashir R et al. J Am Coll Cardiol Intv. 2022;15(23):2427-2436. doi:10.1016/j.jcin.2022.09.011
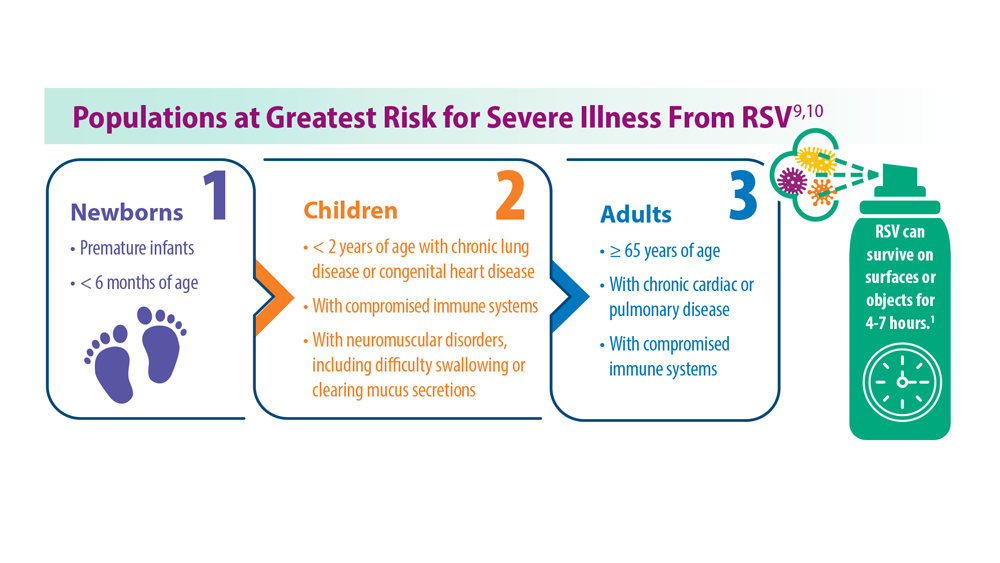
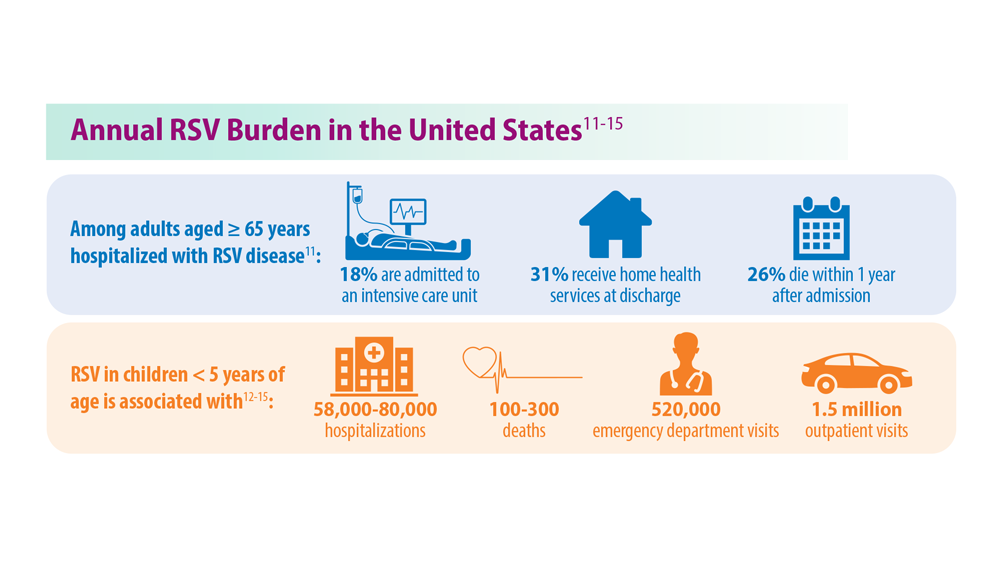
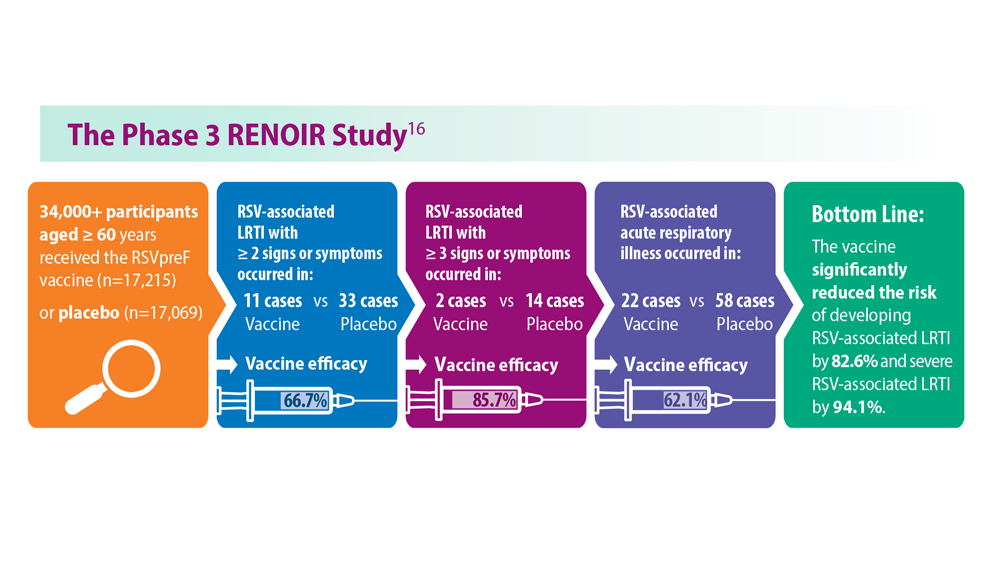
Long-Awaited RSV Vaccines Now Available for Older Adults and Pediatric Patients
- Jha A et al. Respiratory syncytial virus. In: Hui DS, Rossi GA, Johnston SL, eds. Respiratory Syncytial Virus. SARS, MERS and Other Viral Lung Infections. European Respiratory Society; 2016:chap 5. Accessed May 17, 2023.
- Ginsburg SA, Srikantiah P. Lancet Glob Health. 2021;9(12):e1644-e6145. doi:10.1016/S2214-109X(21)00455-1
- US Food and Drug Administration. FDA approves first respiratory syncytial virus (RSV) vaccine [press release]. Published May 3, 2023. Accessed May 17, 2023. https://www.fda.gov/news-events/press-announcements/fda-approves-first-respiratory-syncytial-virus-rsv-vaccine
- US Food and Drug Administration. FDA Approves New Drug to Prevent RSV in Babies and Toddlers [press release]. Published July 17, 2023. Accessed August 11, 2023. https://www.fda.gov/news-events/press-announcements/fda-approves-new-drug-prevent-rsv-babies-and-toddlers
- US Food and Drug Administration. FDA Approves First Vaccine for Pregnant Individuals to Prevent RSV in Infants. Published August 21, 2023. Accessed August 22, 2023. https://www.fda.gov/news-events/press-announcements/fda-approves-first-vaccine-pregnant-individuals-prevent-rsv-infants
- Madhi SA et al. N Engl J Med. 2020;383(5):426-439. doi:10.1056/ NEJMoa1908380
- Centers for Disease Control. Advisory Committee on Immunization Practices (ACIP) Meeting recommendations, August 2023. https://www.cdc.gov/vaccines/acip/recommendations.html
- Hammit LL et al. N Engl J Med. 2022;386(9):837-846. doi:10.1056/ NEJMoa2110275
- Centers for Disease Control and Prevention. RSV in infants and young children. Updated October 28, 2022. Accessed May 30, 2023. https://www.cdc.gov/rsv/ high-risk/infants-young-children.html
- Centers for Disease Control and Prevention. RSV in older adults and adults with chronic medical conditions. Updated October 28, 2022. Accessed May 30, 2023. https://www.cdc.gov/rsv/high-risk/older-adults.html
- Widmer K et al. J Infect Dis. 2012;206(1):56-62. doi:10.1093/infdis/jis309
- Hall CB et al. N Engl J Med. 2009;360(6):588-598. doi:10.1056/NEJMoa0804877
- McLaughlin JM et al. Open Forum Infect Dis. 2022;9(7):ofac300. doi:10.1093/ofid/ofac300
- Thompson et al. JAMA. 2003;289(2):179-186. doi:10.1001/jama.289.2.179
- Hansen CL et al. JAMA Netw Open. 2022;5(2):e220527. doi:10.1001/jamanetworkopen.2022.0527
- Walsh EE et al; RENOIR Clinical Trial Group. N Engl J Med. 2023;388(16):1465-1477. doi:10.1056/NEJMoa2213836
- Martin JA et al. Natl Vital Stat Rep. 2019;68(13):1-47. PMID:32501202
- Townsi N et al. Eur Clin Respir J. 2018;5(1):1487214. doi:10.1080/20018525.20 18.1487214
- Malek A et al. Am J Reprod Immunol. 1994;32(1):8-14. doi:10.1111/j.1600-0897.1994.tb00873.x
- Kampmann B et al; MATISSE Study Group. N Engl J Med. 2023;388(16):1451- 1464. doi:10.1056/NEJMoa2216480
- Synagis (palivizumab) injection prescribing information. Published June 2023. Accessed August 2023. https://www.synagis.com/synagis.pdf
- Jha A et al. Respiratory syncytial virus. In: Hui DS, Rossi GA, Johnston SL, eds. Respiratory Syncytial Virus. SARS, MERS and Other Viral Lung Infections. European Respiratory Society; 2016:chap 5. Accessed May 17, 2023.
- Ginsburg SA, Srikantiah P. Lancet Glob Health. 2021;9(12):e1644-e6145. doi:10.1016/S2214-109X(21)00455-1
- US Food and Drug Administration. FDA approves first respiratory syncytial virus (RSV) vaccine [press release]. Published May 3, 2023. Accessed May 17, 2023. https://www.fda.gov/news-events/press-announcements/fda-approves-first-respiratory-syncytial-virus-rsv-vaccine
- US Food and Drug Administration. FDA Approves New Drug to Prevent RSV in Babies and Toddlers [press release]. Published July 17, 2023. Accessed August 11, 2023. https://www.fda.gov/news-events/press-announcements/fda-approves-new-drug-prevent-rsv-babies-and-toddlers
- US Food and Drug Administration. FDA Approves First Vaccine for Pregnant Individuals to Prevent RSV in Infants. Published August 21, 2023. Accessed August 22, 2023. https://www.fda.gov/news-events/press-announcements/fda-approves-first-vaccine-pregnant-individuals-prevent-rsv-infants
- Madhi SA et al. N Engl J Med. 2020;383(5):426-439. doi:10.1056/ NEJMoa1908380
- Centers for Disease Control. Advisory Committee on Immunization Practices (ACIP) Meeting recommendations, August 2023. https://www.cdc.gov/vaccines/acip/recommendations.html
- Hammit LL et al. N Engl J Med. 2022;386(9):837-846. doi:10.1056/ NEJMoa2110275
- Centers for Disease Control and Prevention. RSV in infants and young children. Updated October 28, 2022. Accessed May 30, 2023. https://www.cdc.gov/rsv/ high-risk/infants-young-children.html
- Centers for Disease Control and Prevention. RSV in older adults and adults with chronic medical conditions. Updated October 28, 2022. Accessed May 30, 2023. https://www.cdc.gov/rsv/high-risk/older-adults.html
- Widmer K et al. J Infect Dis. 2012;206(1):56-62. doi:10.1093/infdis/jis309
- Hall CB et al. N Engl J Med. 2009;360(6):588-598. doi:10.1056/NEJMoa0804877
- McLaughlin JM et al. Open Forum Infect Dis. 2022;9(7):ofac300. doi:10.1093/ofid/ofac300
- Thompson et al. JAMA. 2003;289(2):179-186. doi:10.1001/jama.289.2.179
- Hansen CL et al. JAMA Netw Open. 2022;5(2):e220527. doi:10.1001/jamanetworkopen.2022.0527
- Walsh EE et al; RENOIR Clinical Trial Group. N Engl J Med. 2023;388(16):1465-1477. doi:10.1056/NEJMoa2213836
- Martin JA et al. Natl Vital Stat Rep. 2019;68(13):1-47. PMID:32501202
- Townsi N et al. Eur Clin Respir J. 2018;5(1):1487214. doi:10.1080/20018525.20 18.1487214
- Malek A et al. Am J Reprod Immunol. 1994;32(1):8-14. doi:10.1111/j.1600-0897.1994.tb00873.x
- Kampmann B et al; MATISSE Study Group. N Engl J Med. 2023;388(16):1451- 1464. doi:10.1056/NEJMoa2216480
- Synagis (palivizumab) injection prescribing information. Published June 2023. Accessed August 2023. https://www.synagis.com/synagis.pdf
- Jha A et al. Respiratory syncytial virus. In: Hui DS, Rossi GA, Johnston SL, eds. Respiratory Syncytial Virus. SARS, MERS and Other Viral Lung Infections. European Respiratory Society; 2016:chap 5. Accessed May 17, 2023.
- Ginsburg SA, Srikantiah P. Lancet Glob Health. 2021;9(12):e1644-e6145. doi:10.1016/S2214-109X(21)00455-1
- US Food and Drug Administration. FDA approves first respiratory syncytial virus (RSV) vaccine [press release]. Published May 3, 2023. Accessed May 17, 2023. https://www.fda.gov/news-events/press-announcements/fda-approves-first-respiratory-syncytial-virus-rsv-vaccine
- US Food and Drug Administration. FDA Approves New Drug to Prevent RSV in Babies and Toddlers [press release]. Published July 17, 2023. Accessed August 11, 2023. https://www.fda.gov/news-events/press-announcements/fda-approves-new-drug-prevent-rsv-babies-and-toddlers
- US Food and Drug Administration. FDA Approves First Vaccine for Pregnant Individuals to Prevent RSV in Infants. Published August 21, 2023. Accessed August 22, 2023. https://www.fda.gov/news-events/press-announcements/fda-approves-first-vaccine-pregnant-individuals-prevent-rsv-infants
- Madhi SA et al. N Engl J Med. 2020;383(5):426-439. doi:10.1056/ NEJMoa1908380
- Centers for Disease Control. Advisory Committee on Immunization Practices (ACIP) Meeting recommendations, August 2023. https://www.cdc.gov/vaccines/acip/recommendations.html
- Hammit LL et al. N Engl J Med. 2022;386(9):837-846. doi:10.1056/ NEJMoa2110275
- Centers for Disease Control and Prevention. RSV in infants and young children. Updated October 28, 2022. Accessed May 30, 2023. https://www.cdc.gov/rsv/ high-risk/infants-young-children.html
- Centers for Disease Control and Prevention. RSV in older adults and adults with chronic medical conditions. Updated October 28, 2022. Accessed May 30, 2023. https://www.cdc.gov/rsv/high-risk/older-adults.html
- Widmer K et al. J Infect Dis. 2012;206(1):56-62. doi:10.1093/infdis/jis309
- Hall CB et al. N Engl J Med. 2009;360(6):588-598. doi:10.1056/NEJMoa0804877
- McLaughlin JM et al. Open Forum Infect Dis. 2022;9(7):ofac300. doi:10.1093/ofid/ofac300
- Thompson et al. JAMA. 2003;289(2):179-186. doi:10.1001/jama.289.2.179
- Hansen CL et al. JAMA Netw Open. 2022;5(2):e220527. doi:10.1001/jamanetworkopen.2022.0527
- Walsh EE et al; RENOIR Clinical Trial Group. N Engl J Med. 2023;388(16):1465-1477. doi:10.1056/NEJMoa2213836
- Martin JA et al. Natl Vital Stat Rep. 2019;68(13):1-47. PMID:32501202
- Townsi N et al. Eur Clin Respir J. 2018;5(1):1487214. doi:10.1080/20018525.20 18.1487214
- Malek A et al. Am J Reprod Immunol. 1994;32(1):8-14. doi:10.1111/j.1600-0897.1994.tb00873.x
- Kampmann B et al; MATISSE Study Group. N Engl J Med. 2023;388(16):1451- 1464. doi:10.1056/NEJMoa2216480
- Synagis (palivizumab) injection prescribing information. Published June 2023. Accessed August 2023. https://www.synagis.com/synagis.pdf
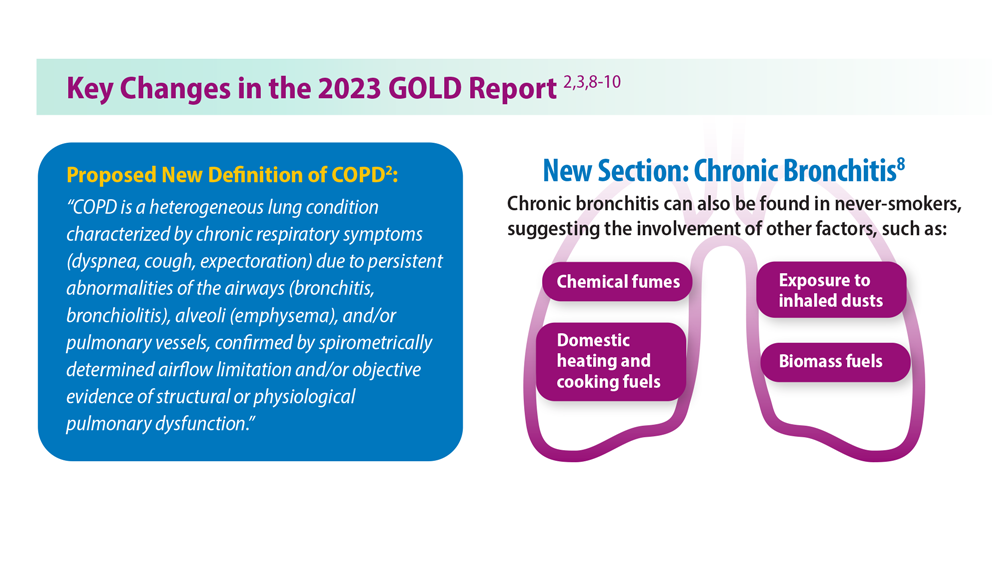
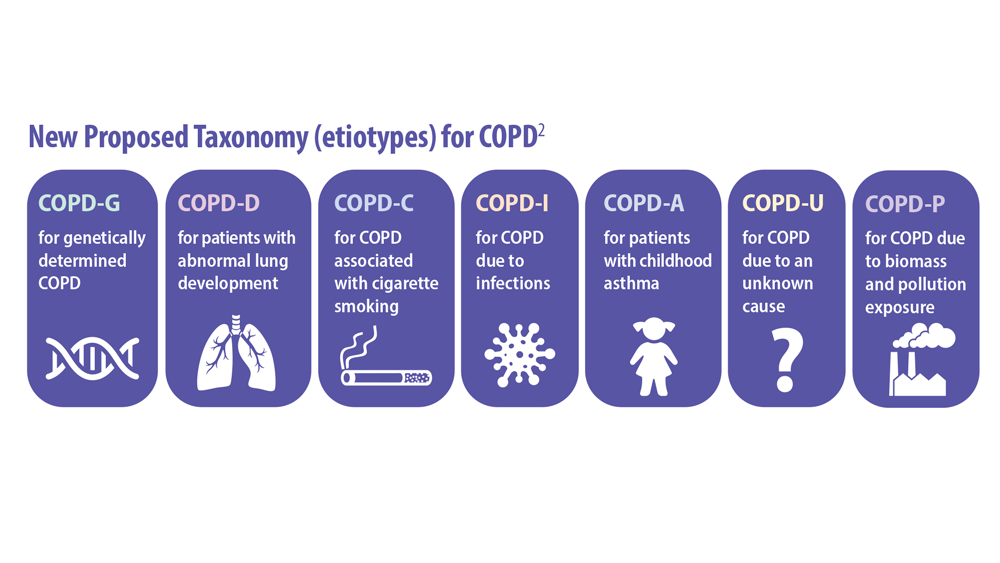
Updated Guidelines for COPD Management: 2023 GOLD Strategy Report
- Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (2023 Report). Published 2023. Accessed June 6, 2023. https://goldcopd.org/2023-gold-report-2/
- Celli B et al. Am J Respir Crit Care Med. 2022;206(11):1317. doi:10.1164/rccm.202204-0671PP
- Han M et al. Lancet Respir Med. 2013;1(1):43-50. doi:10.1016/S2213-2600(12)70044-9
- Klijn SL et al. NPJ Prim Care Respir Med. 2017;27(1):24. doi:10.1038/s41533-017-0022-1
- Chan AH et al. J Allergy Clin Immunol Pract. 2015;3(3):335-349.e1-e5. doi:10.1016/j.jaip.2015.01.024
- Brusselle G et al. Int J Chron Obstruct Pulmon Dis. 2015;10:2207-2217. doi:10.2147/COPD.S91694
- Salvi SS, Barnes PJ. Lancet. 2009;374(9691):733-743. doi:10.1016/S0140-6736(09)61303-9
- Trupin L et al. Eur Respir J. 2003;22(3):462-469. doi:10.1183/09031936.03.00094203
- Celli BR et al. Am J Respir Crit Care Med. 2021;204(11):1251-1258. doi:10.1164/rccm.202108-1819PP
- Barnes PJ, Celli BR. Eur Respir J. 2009;33(5):1165-1185. doi:10.1183/09031936.00128008
- Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (2023 Report). Published 2023. Accessed June 6, 2023. https://goldcopd.org/2023-gold-report-2/
- Celli B et al. Am J Respir Crit Care Med. 2022;206(11):1317. doi:10.1164/rccm.202204-0671PP
- Han M et al. Lancet Respir Med. 2013;1(1):43-50. doi:10.1016/S2213-2600(12)70044-9
- Klijn SL et al. NPJ Prim Care Respir Med. 2017;27(1):24. doi:10.1038/s41533-017-0022-1
- Chan AH et al. J Allergy Clin Immunol Pract. 2015;3(3):335-349.e1-e5. doi:10.1016/j.jaip.2015.01.024
- Brusselle G et al. Int J Chron Obstruct Pulmon Dis. 2015;10:2207-2217. doi:10.2147/COPD.S91694
- Salvi SS, Barnes PJ. Lancet. 2009;374(9691):733-743. doi:10.1016/S0140-6736(09)61303-9
- Trupin L et al. Eur Respir J. 2003;22(3):462-469. doi:10.1183/09031936.03.00094203
- Celli BR et al. Am J Respir Crit Care Med. 2021;204(11):1251-1258. doi:10.1164/rccm.202108-1819PP
- Barnes PJ, Celli BR. Eur Respir J. 2009;33(5):1165-1185. doi:10.1183/09031936.00128008
- Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (2023 Report). Published 2023. Accessed June 6, 2023. https://goldcopd.org/2023-gold-report-2/
- Celli B et al. Am J Respir Crit Care Med. 2022;206(11):1317. doi:10.1164/rccm.202204-0671PP
- Han M et al. Lancet Respir Med. 2013;1(1):43-50. doi:10.1016/S2213-2600(12)70044-9
- Klijn SL et al. NPJ Prim Care Respir Med. 2017;27(1):24. doi:10.1038/s41533-017-0022-1
- Chan AH et al. J Allergy Clin Immunol Pract. 2015;3(3):335-349.e1-e5. doi:10.1016/j.jaip.2015.01.024
- Brusselle G et al. Int J Chron Obstruct Pulmon Dis. 2015;10:2207-2217. doi:10.2147/COPD.S91694
- Salvi SS, Barnes PJ. Lancet. 2009;374(9691):733-743. doi:10.1016/S0140-6736(09)61303-9
- Trupin L et al. Eur Respir J. 2003;22(3):462-469. doi:10.1183/09031936.03.00094203
- Celli BR et al. Am J Respir Crit Care Med. 2021;204(11):1251-1258. doi:10.1164/rccm.202108-1819PP
- Barnes PJ, Celli BR. Eur Respir J. 2009;33(5):1165-1185. doi:10.1183/09031936.00128008
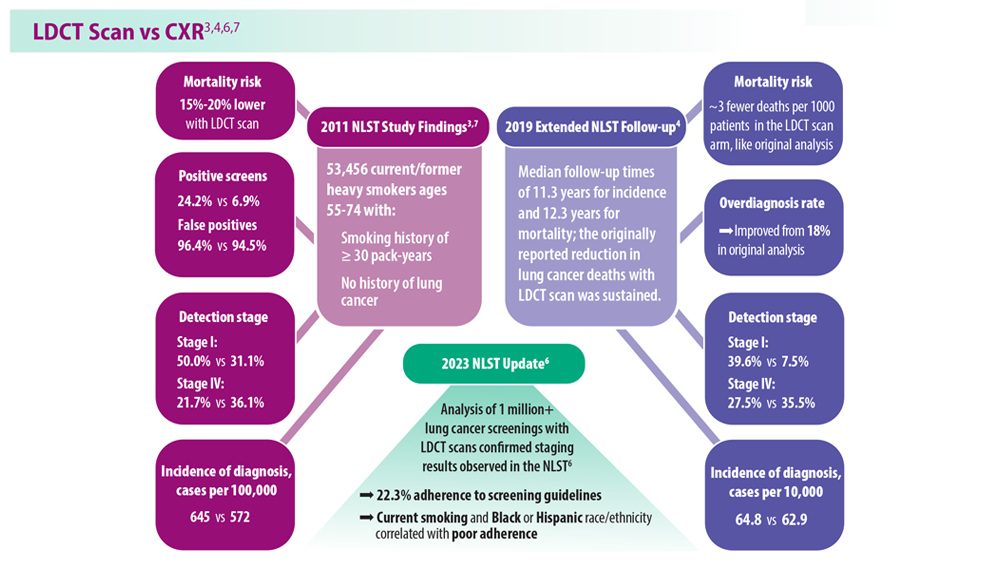
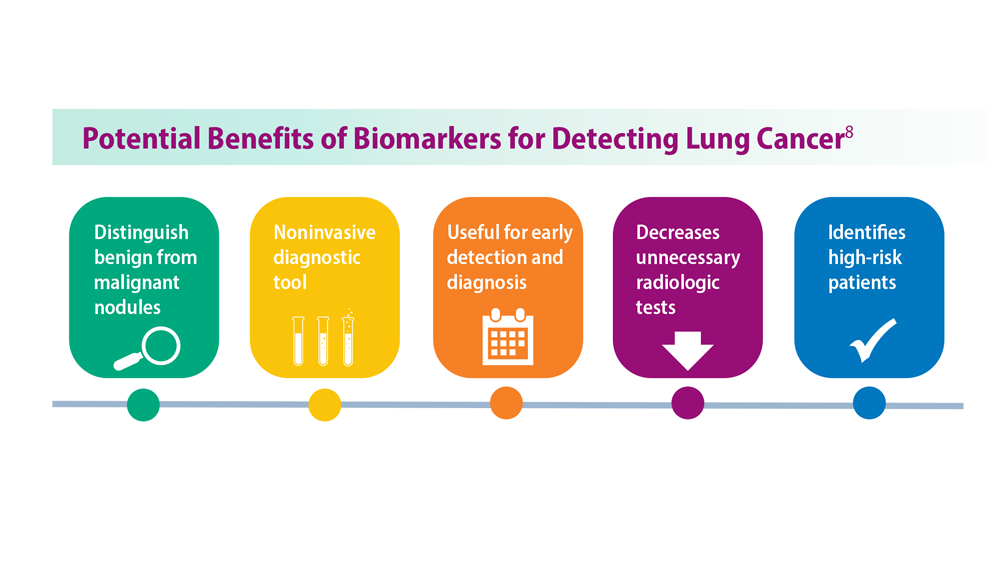
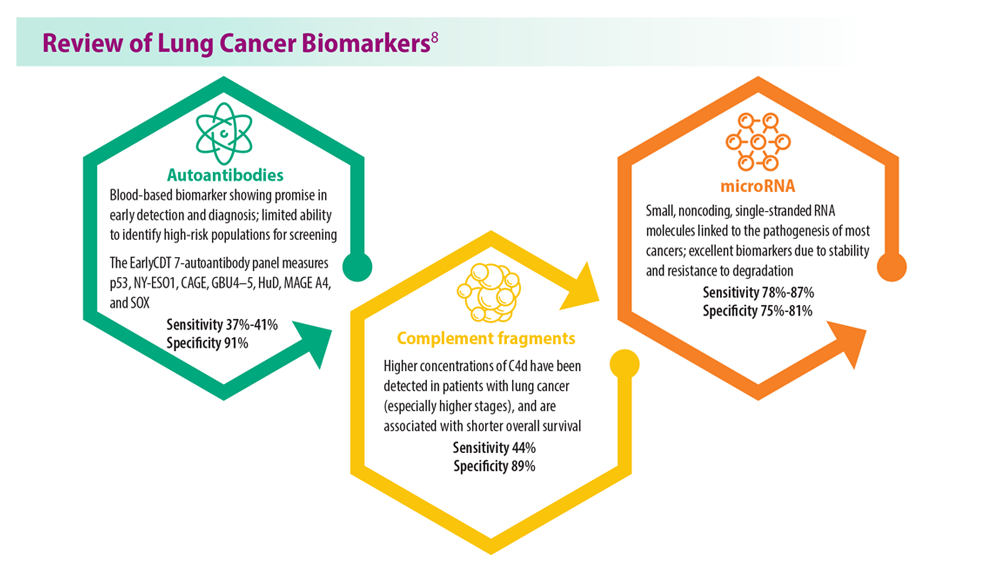
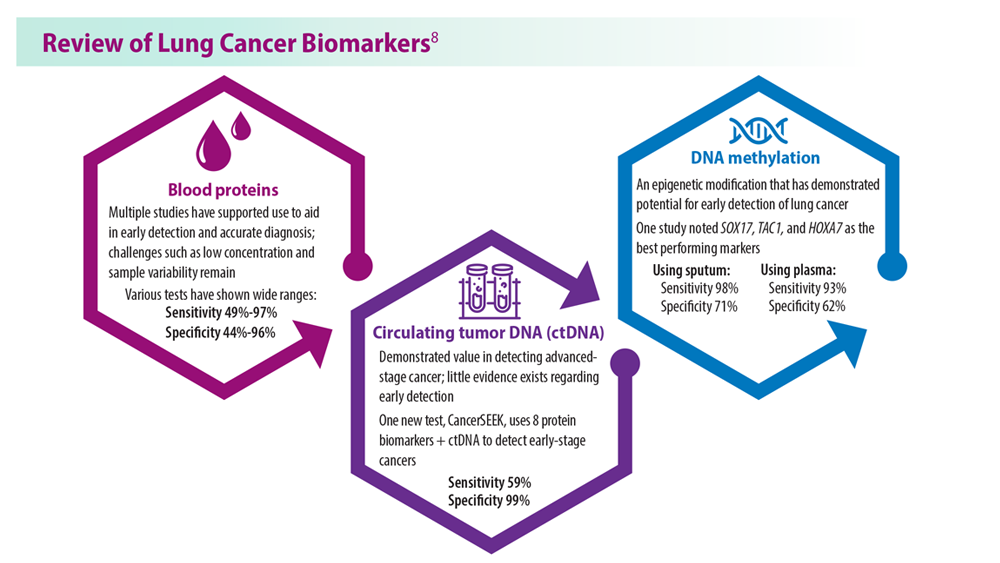
Lung Cancer Screening: A Need for Adjunctive Testing
- Naidch DP et al. Radiology. 1990;175(3):729-731. doi:10.1148/radiology.175.3.2343122
- Kaneko M et al. Radiology. 1996;201(3):798-802. doi:10.1148/radiology.201.3.8939234
- National Lung Screening Trial Research Team. Radiology. 2011;258(1):243-253. doi:10.1148/radiol.10091808
- National Lung Screening Trial Research Team. J Thorac Oncol. 2019;14(10):1732-1742. doi:10.1016/j.jtho.2019.05.044
- Mazzone PJ et al. Chest. 2021;160(5):e427-e494. doi:10.1016/j.chest.2021.06.063
- Tanner NT et al. Chest. 2023;S0012-3692(23)00175-7. doi:10.1016/j.chest.2023.02.003
- National Lung Screening Trial Research Team. N Engl J Med. 2011;365(5):395- 409. doi:10.1056/NEJMoa1102873
- Marmor HN et al. Curr Chall Thorac Surg. 2023;5:5. doi:10.21037/ccts-20-171
- Naidch DP et al. Radiology. 1990;175(3):729-731. doi:10.1148/radiology.175.3.2343122
- Kaneko M et al. Radiology. 1996;201(3):798-802. doi:10.1148/radiology.201.3.8939234
- National Lung Screening Trial Research Team. Radiology. 2011;258(1):243-253. doi:10.1148/radiol.10091808
- National Lung Screening Trial Research Team. J Thorac Oncol. 2019;14(10):1732-1742. doi:10.1016/j.jtho.2019.05.044
- Mazzone PJ et al. Chest. 2021;160(5):e427-e494. doi:10.1016/j.chest.2021.06.063
- Tanner NT et al. Chest. 2023;S0012-3692(23)00175-7. doi:10.1016/j.chest.2023.02.003
- National Lung Screening Trial Research Team. N Engl J Med. 2011;365(5):395- 409. doi:10.1056/NEJMoa1102873
- Marmor HN et al. Curr Chall Thorac Surg. 2023;5:5. doi:10.21037/ccts-20-171
- Naidch DP et al. Radiology. 1990;175(3):729-731. doi:10.1148/radiology.175.3.2343122
- Kaneko M et al. Radiology. 1996;201(3):798-802. doi:10.1148/radiology.201.3.8939234
- National Lung Screening Trial Research Team. Radiology. 2011;258(1):243-253. doi:10.1148/radiol.10091808
- National Lung Screening Trial Research Team. J Thorac Oncol. 2019;14(10):1732-1742. doi:10.1016/j.jtho.2019.05.044
- Mazzone PJ et al. Chest. 2021;160(5):e427-e494. doi:10.1016/j.chest.2021.06.063
- Tanner NT et al. Chest. 2023;S0012-3692(23)00175-7. doi:10.1016/j.chest.2023.02.003
- National Lung Screening Trial Research Team. N Engl J Med. 2011;365(5):395- 409. doi:10.1056/NEJMoa1102873
- Marmor HN et al. Curr Chall Thorac Surg. 2023;5:5. doi:10.21037/ccts-20-171
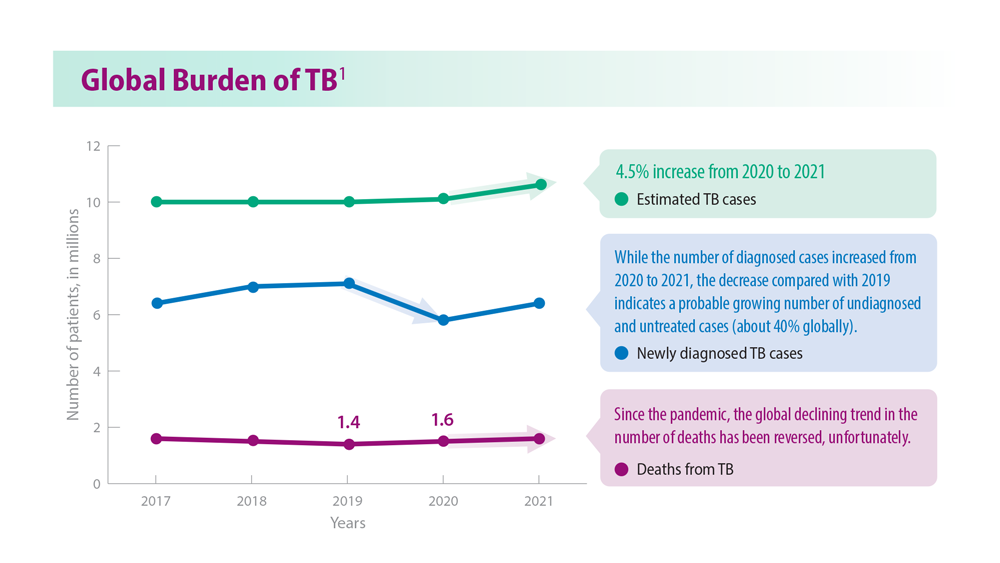
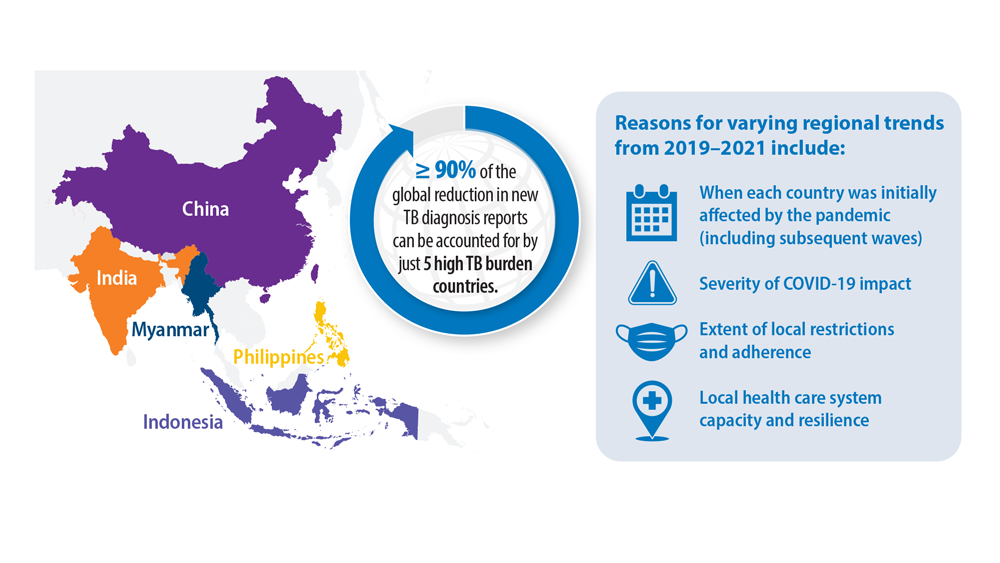
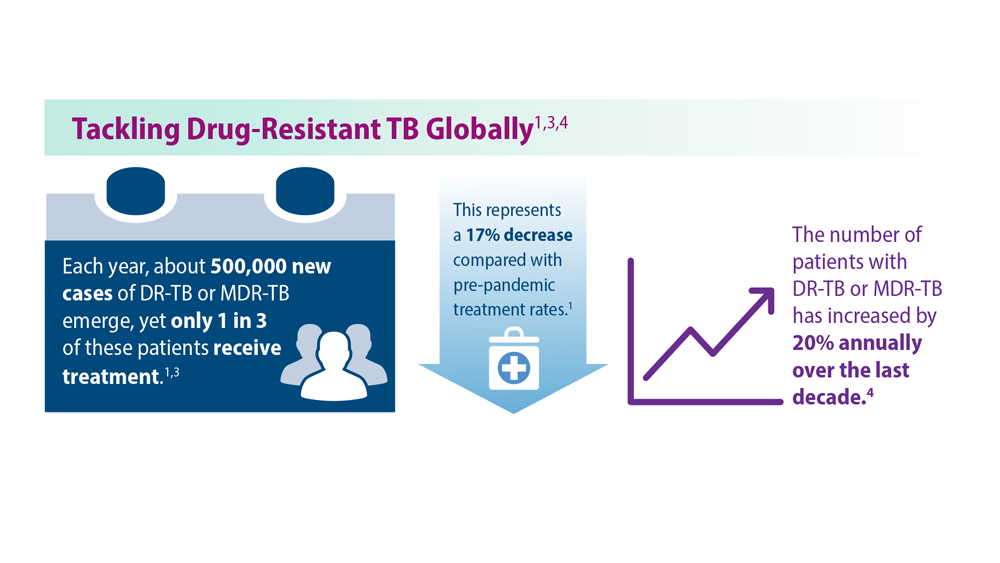
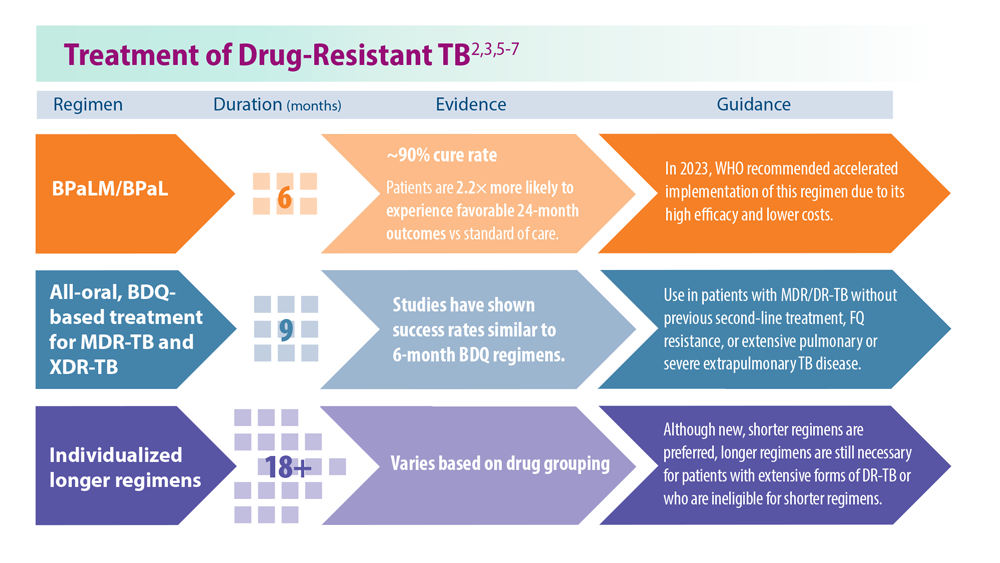
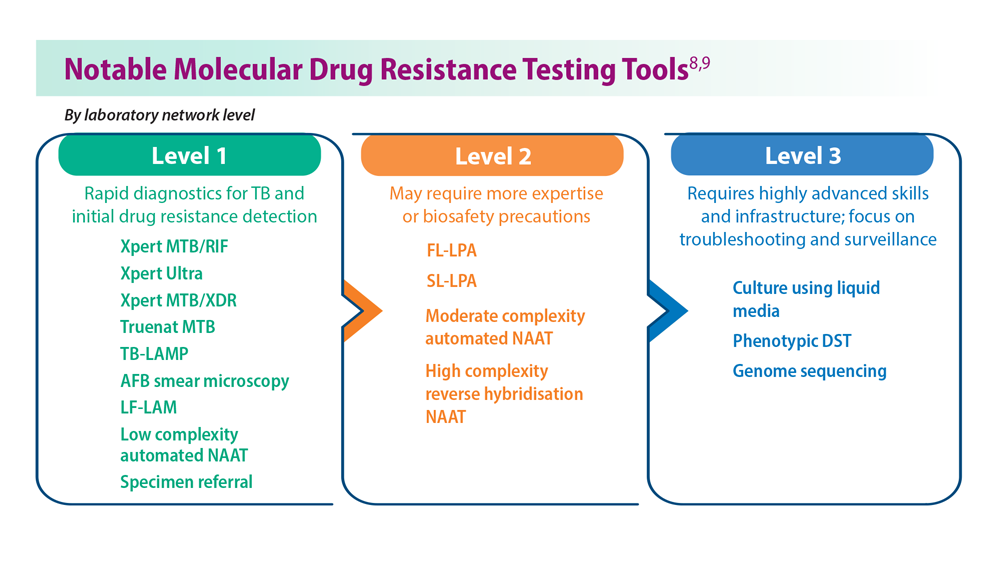
Tuberculosis Management: Returning to Pre-Pandemic Priorities
- Global tuberculosis report 2022. World Health Organization. Published October 27, 2022. Accessed June 26, 2023. https://www.who.int/publications/i/item/9789240061729
- WHO consolidated guidelines on tuberculosis. Module 4: treatment – drug-resistant tuberculosis treatment, 2022 update. World Health Organization. Published December 15, 2022. Accessed June 26, 2023. https://www.who.int/publications/i/item/9789240063129
- Migliori GB, Tiberi S. Int J Tuberc Lung Dis. 2022 ;26(7):590-591. doi:10.5588/ijtld.22.0263.
- Lange C et al. Am J Respir Crit Care Med. 2022;205(10):1142-1144. doi:10.1164/rccm.202202-0393ED
- Esmail A et al. Am J Respir Crit Care Med. 2022;205(10):1214-1227. doi:10.1164/rccm.202107-1779OC
- WHO BPaLM Accelerator Platform: to support the call to action for implementation of the shorter and more effective treatment for all people suffering from drug-resistant TB. World Health Organization. Published May 9, 2023. Accessed June 26, 2023. https://www.who.int/news-room/events/detail/2023/05/09/default-calendar/who-bpalm-accelerator-platform–to-support-the-call-to-action-for-implementation-of-the-shorter-and-moreeffective-
- Trevisi L et al. Am J Respir Crit Care Med. 2023;207(11):1525-1532. doi:10.1164/rccm.202211-2125OC
- Domínguez J et al; TBnet and RESIST-TB networks. Lancet Infect Dis. 2023;23(4):e122-e137. doi:10.1016/S1473-3099(22)00875-1
- WHO operational handbook on tuberculosis: module 3: diagnosis: rapid diagnostics for tuberculosis detection, 2021 update. World Health Organization. Published July 7, 2021. Accessed June 26, 2023. https://www.who.int/publications/i/item/9789240030589treatment-for-all-people-suffering-from-drug-resistant-tb
- Global tuberculosis report 2022. World Health Organization. Published October 27, 2022. Accessed June 26, 2023. https://www.who.int/publications/i/item/9789240061729
- WHO consolidated guidelines on tuberculosis. Module 4: treatment – drug-resistant tuberculosis treatment, 2022 update. World Health Organization. Published December 15, 2022. Accessed June 26, 2023. https://www.who.int/publications/i/item/9789240063129
- Migliori GB, Tiberi S. Int J Tuberc Lung Dis. 2022 ;26(7):590-591. doi:10.5588/ijtld.22.0263.
- Lange C et al. Am J Respir Crit Care Med. 2022;205(10):1142-1144. doi:10.1164/rccm.202202-0393ED
- Esmail A et al. Am J Respir Crit Care Med. 2022;205(10):1214-1227. doi:10.1164/rccm.202107-1779OC
- WHO BPaLM Accelerator Platform: to support the call to action for implementation of the shorter and more effective treatment for all people suffering from drug-resistant TB. World Health Organization. Published May 9, 2023. Accessed June 26, 2023. https://www.who.int/news-room/events/detail/2023/05/09/default-calendar/who-bpalm-accelerator-platform–to-support-the-call-to-action-for-implementation-of-the-shorter-and-moreeffective-
- Trevisi L et al. Am J Respir Crit Care Med. 2023;207(11):1525-1532. doi:10.1164/rccm.202211-2125OC
- Domínguez J et al; TBnet and RESIST-TB networks. Lancet Infect Dis. 2023;23(4):e122-e137. doi:10.1016/S1473-3099(22)00875-1
- WHO operational handbook on tuberculosis: module 3: diagnosis: rapid diagnostics for tuberculosis detection, 2021 update. World Health Organization. Published July 7, 2021. Accessed June 26, 2023. https://www.who.int/publications/i/item/9789240030589treatment-for-all-people-suffering-from-drug-resistant-tb
- Global tuberculosis report 2022. World Health Organization. Published October 27, 2022. Accessed June 26, 2023. https://www.who.int/publications/i/item/9789240061729
- WHO consolidated guidelines on tuberculosis. Module 4: treatment – drug-resistant tuberculosis treatment, 2022 update. World Health Organization. Published December 15, 2022. Accessed June 26, 2023. https://www.who.int/publications/i/item/9789240063129
- Migliori GB, Tiberi S. Int J Tuberc Lung Dis. 2022 ;26(7):590-591. doi:10.5588/ijtld.22.0263.
- Lange C et al. Am J Respir Crit Care Med. 2022;205(10):1142-1144. doi:10.1164/rccm.202202-0393ED
- Esmail A et al. Am J Respir Crit Care Med. 2022;205(10):1214-1227. doi:10.1164/rccm.202107-1779OC
- WHO BPaLM Accelerator Platform: to support the call to action for implementation of the shorter and more effective treatment for all people suffering from drug-resistant TB. World Health Organization. Published May 9, 2023. Accessed June 26, 2023. https://www.who.int/news-room/events/detail/2023/05/09/default-calendar/who-bpalm-accelerator-platform–to-support-the-call-to-action-for-implementation-of-the-shorter-and-moreeffective-
- Trevisi L et al. Am J Respir Crit Care Med. 2023;207(11):1525-1532. doi:10.1164/rccm.202211-2125OC
- Domínguez J et al; TBnet and RESIST-TB networks. Lancet Infect Dis. 2023;23(4):e122-e137. doi:10.1016/S1473-3099(22)00875-1
- WHO operational handbook on tuberculosis: module 3: diagnosis: rapid diagnostics for tuberculosis detection, 2021 update. World Health Organization. Published July 7, 2021. Accessed June 26, 2023. https://www.who.int/publications/i/item/9789240030589treatment-for-all-people-suffering-from-drug-resistant-tb
CPAP adherence curbs severe cardiovascular disease outcomes
, based on data from more than 4,000 individuals.
Obstructive sleep apnea (OSA) is associated with an increased risk of cardiovascular diseases, but the association between management of OSA with a continuous positive-airway pressure device (CPAP) and major adverse cardiac or cerebrovascular events (MACCEs) remains unclear, wrote Manuel Sánchez-de-la-Torre, PhD, of the University of Lleida, Spain, and colleagues.
In a meta-analysis published in JAMA, the researchers reviewed data from 4,186 individuals with a mean age of 61.2 years; 82.1% were men. The study population included 2,097 patients who used CPAP and 2,089 who did not. The mean apnea-hypopnea index (AHI) was 31.2 events per hour, and OSA was defined as an oxygen desaturation index of 12 events or more per hour or an AHI of 15 events or more per hour. The composite primary outcome included the first MACCE, or death from cardiovascular causes, myocardial infarction, stroke, revascularization procedure, hospital admission for heart failure, hospital admission for unstable angina, or hospital admission for transient ischemic attack. Each of these components was a secondary endpoint.
Overall, the primary outcome of MACCE was similar for CPAP and non-CPAP using patients (hazard ratio, 1.01) with a total of 349 MACCE events in the CPAP group and 342 in the non-CPAP group. The mean adherence to CPAP was 3.1 hours per day. A total of 38.5% of patients in the CPAP group met the criteria for good adherence, defined as a mean of 4 or more hours per day.
However, as defined, good adherence to CPAP significantly reduced the risk of MACCE, compared with no CPAP use (HR, 0.69), and a sensitivity analysis showed a significant risk reduction, compared with patients who did not meet the criteria for good adherence (HR, 0.55; P = .005).
“Adherence to treatment is complex to determine and there are other potential factors that could affect patient adherence, such as health education, motivation, attitude, self-efficacy, psychosocial factors, and other health care system–related features,” the researchers wrote in their discussion.
The findings were limited by several factors including the evaluation only of CPAP as a treatment for OSA, and the inability to assess separate components of the composite endpoint, the researchers noted. Other limitations included the relatively small number of female patients, reliance mainly on at-home sleep apnea tests, and the potential for selection bias, they said.
However, the results suggest that CPAP adherence is important to prevention of secondary cardiovascular outcomes in OSA patients, and that implementation of specific and personalized strategies to improve adherence to treatment should be a clinical priority, they concluded.
The study was funded by the Instituto de Salud Carlos III, the European Union and FEDER, IRBLleida–Fundació Dr Pifarré, SEPAR, ResMed Ltd. (Australia), Associació Lleidatana de Respiratori, and CIBERES. Dr Sánchez-de-la-Torre also disclosed financial support from a Ramón y Cajal grant.
, based on data from more than 4,000 individuals.
Obstructive sleep apnea (OSA) is associated with an increased risk of cardiovascular diseases, but the association between management of OSA with a continuous positive-airway pressure device (CPAP) and major adverse cardiac or cerebrovascular events (MACCEs) remains unclear, wrote Manuel Sánchez-de-la-Torre, PhD, of the University of Lleida, Spain, and colleagues.
In a meta-analysis published in JAMA, the researchers reviewed data from 4,186 individuals with a mean age of 61.2 years; 82.1% were men. The study population included 2,097 patients who used CPAP and 2,089 who did not. The mean apnea-hypopnea index (AHI) was 31.2 events per hour, and OSA was defined as an oxygen desaturation index of 12 events or more per hour or an AHI of 15 events or more per hour. The composite primary outcome included the first MACCE, or death from cardiovascular causes, myocardial infarction, stroke, revascularization procedure, hospital admission for heart failure, hospital admission for unstable angina, or hospital admission for transient ischemic attack. Each of these components was a secondary endpoint.
Overall, the primary outcome of MACCE was similar for CPAP and non-CPAP using patients (hazard ratio, 1.01) with a total of 349 MACCE events in the CPAP group and 342 in the non-CPAP group. The mean adherence to CPAP was 3.1 hours per day. A total of 38.5% of patients in the CPAP group met the criteria for good adherence, defined as a mean of 4 or more hours per day.
However, as defined, good adherence to CPAP significantly reduced the risk of MACCE, compared with no CPAP use (HR, 0.69), and a sensitivity analysis showed a significant risk reduction, compared with patients who did not meet the criteria for good adherence (HR, 0.55; P = .005).
“Adherence to treatment is complex to determine and there are other potential factors that could affect patient adherence, such as health education, motivation, attitude, self-efficacy, psychosocial factors, and other health care system–related features,” the researchers wrote in their discussion.
The findings were limited by several factors including the evaluation only of CPAP as a treatment for OSA, and the inability to assess separate components of the composite endpoint, the researchers noted. Other limitations included the relatively small number of female patients, reliance mainly on at-home sleep apnea tests, and the potential for selection bias, they said.
However, the results suggest that CPAP adherence is important to prevention of secondary cardiovascular outcomes in OSA patients, and that implementation of specific and personalized strategies to improve adherence to treatment should be a clinical priority, they concluded.
The study was funded by the Instituto de Salud Carlos III, the European Union and FEDER, IRBLleida–Fundació Dr Pifarré, SEPAR, ResMed Ltd. (Australia), Associació Lleidatana de Respiratori, and CIBERES. Dr Sánchez-de-la-Torre also disclosed financial support from a Ramón y Cajal grant.
, based on data from more than 4,000 individuals.
Obstructive sleep apnea (OSA) is associated with an increased risk of cardiovascular diseases, but the association between management of OSA with a continuous positive-airway pressure device (CPAP) and major adverse cardiac or cerebrovascular events (MACCEs) remains unclear, wrote Manuel Sánchez-de-la-Torre, PhD, of the University of Lleida, Spain, and colleagues.
In a meta-analysis published in JAMA, the researchers reviewed data from 4,186 individuals with a mean age of 61.2 years; 82.1% were men. The study population included 2,097 patients who used CPAP and 2,089 who did not. The mean apnea-hypopnea index (AHI) was 31.2 events per hour, and OSA was defined as an oxygen desaturation index of 12 events or more per hour or an AHI of 15 events or more per hour. The composite primary outcome included the first MACCE, or death from cardiovascular causes, myocardial infarction, stroke, revascularization procedure, hospital admission for heart failure, hospital admission for unstable angina, or hospital admission for transient ischemic attack. Each of these components was a secondary endpoint.
Overall, the primary outcome of MACCE was similar for CPAP and non-CPAP using patients (hazard ratio, 1.01) with a total of 349 MACCE events in the CPAP group and 342 in the non-CPAP group. The mean adherence to CPAP was 3.1 hours per day. A total of 38.5% of patients in the CPAP group met the criteria for good adherence, defined as a mean of 4 or more hours per day.
However, as defined, good adherence to CPAP significantly reduced the risk of MACCE, compared with no CPAP use (HR, 0.69), and a sensitivity analysis showed a significant risk reduction, compared with patients who did not meet the criteria for good adherence (HR, 0.55; P = .005).
“Adherence to treatment is complex to determine and there are other potential factors that could affect patient adherence, such as health education, motivation, attitude, self-efficacy, psychosocial factors, and other health care system–related features,” the researchers wrote in their discussion.
The findings were limited by several factors including the evaluation only of CPAP as a treatment for OSA, and the inability to assess separate components of the composite endpoint, the researchers noted. Other limitations included the relatively small number of female patients, reliance mainly on at-home sleep apnea tests, and the potential for selection bias, they said.
However, the results suggest that CPAP adherence is important to prevention of secondary cardiovascular outcomes in OSA patients, and that implementation of specific and personalized strategies to improve adherence to treatment should be a clinical priority, they concluded.
The study was funded by the Instituto de Salud Carlos III, the European Union and FEDER, IRBLleida–Fundació Dr Pifarré, SEPAR, ResMed Ltd. (Australia), Associació Lleidatana de Respiratori, and CIBERES. Dr Sánchez-de-la-Torre also disclosed financial support from a Ramón y Cajal grant.
FROM JAMA
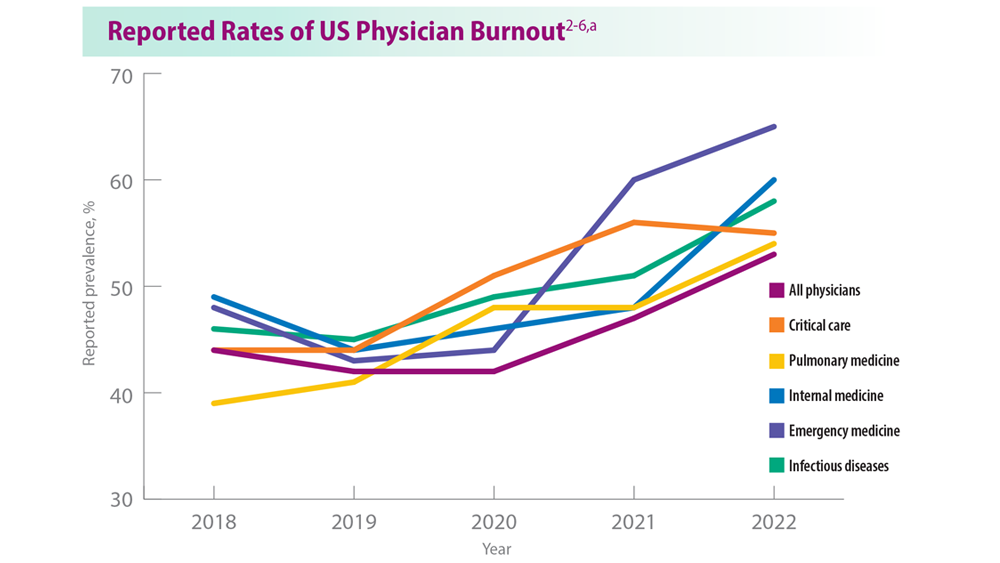
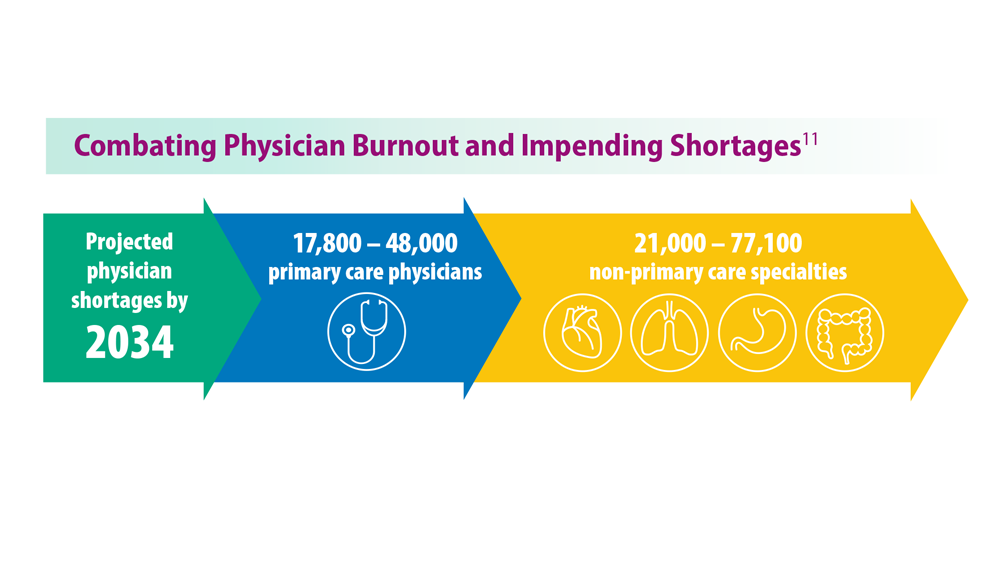
Addressing Physician Burnout in Pulmonology and Critical Care
- Moss M et al. Crit Care Med. 2016;44(7):1414-1421. doi:10.1097/CCM.000000000000188
- Medscape National Physician Burnout, Depression & Suicide Report 2019. Medscape. January 16, 2019. Accessed June 22, 2023. https://www.medscape.com/slideshow/2019-lifestyle-burnout-depression-6011056#1
- Medscape National Physician Burnout & Suicide Report 2020: The Generational Divide. Medscape. January 15, 2020. Accessed June 22, 2023. https://www.medscape.com/slideshow/2020-lifestyle-burnout-6012460#1
- ‘Death by 1000 Cuts’: Medscape National Physician Burnout & Suicide Report 2021. Medscape. January 22, 2021. Accessed June 22, 2023. https://www.medscape.com/slideshow/2021-lifestyle-burnout-6013456#2
- Physician Burnout Report 2022: Stress, Anxiety, and Anger. Medscape. January 21, 2022. Accessed June 22, 2023. https://www.medscape.com/slideshow/2022-lifestyle-burnout-6014664#1
- ‘I Cry but No One Cares’: Physician Burnout & Depression Report 2023. Medscape. January 27, 2023. Accessed June 22, 2023. https://www.medscape.com/slideshow/2023-lifestyle-burnout-6016058#1
- Murthy VH. N Engl J Med. 2022;387(7):577-579. doi:10.1056/NEJMp2207252
- Vranas KC et al. Chest. 2021;160(5):1714-1728. doi:10.1016/j.chest.2021.05.041
- Kerlin MP et al. Ann Am Thorac Soc. 2022;19(2):329-331. doi:10.1513/AnnalsATS.202105-567RL
- Dean W et al. Fed Pract. 2019;36(9):400-402. PMID: 31571807
- Association of American Medical Colleges. The Complexities of Physician Supply and Demand: Projections from 2019 to 2034. June 2021. https://www.aamc.org/media/54681/download?attachment
- Medscape Pulmonologist Lifestyle, Happiness & Burnout Report 2023: Contentment Amid Stress. February 24, 2023. Accessed June 28, 2023. https://www.medscape.com/slideshow/2023-lifestyle-pulmonologist-6016092#1
- Medscape Intensivist Lifestyle, Happiness & Burnout Report 2023: Contentment Amid Stress. February 24, 2023. Accessed June 28, 2023. https://www.medscape.com/slideshow/2023-lifestyle-intensivist-6016072#1
- Moss M et al. Crit Care Med. 2016;44(7):1414-1421. doi:10.1097/CCM.000000000000188
- Medscape National Physician Burnout, Depression & Suicide Report 2019. Medscape. January 16, 2019. Accessed June 22, 2023. https://www.medscape.com/slideshow/2019-lifestyle-burnout-depression-6011056#1
- Medscape National Physician Burnout & Suicide Report 2020: The Generational Divide. Medscape. January 15, 2020. Accessed June 22, 2023. https://www.medscape.com/slideshow/2020-lifestyle-burnout-6012460#1
- ‘Death by 1000 Cuts’: Medscape National Physician Burnout & Suicide Report 2021. Medscape. January 22, 2021. Accessed June 22, 2023. https://www.medscape.com/slideshow/2021-lifestyle-burnout-6013456#2
- Physician Burnout Report 2022: Stress, Anxiety, and Anger. Medscape. January 21, 2022. Accessed June 22, 2023. https://www.medscape.com/slideshow/2022-lifestyle-burnout-6014664#1
- ‘I Cry but No One Cares’: Physician Burnout & Depression Report 2023. Medscape. January 27, 2023. Accessed June 22, 2023. https://www.medscape.com/slideshow/2023-lifestyle-burnout-6016058#1
- Murthy VH. N Engl J Med. 2022;387(7):577-579. doi:10.1056/NEJMp2207252
- Vranas KC et al. Chest. 2021;160(5):1714-1728. doi:10.1016/j.chest.2021.05.041
- Kerlin MP et al. Ann Am Thorac Soc. 2022;19(2):329-331. doi:10.1513/AnnalsATS.202105-567RL
- Dean W et al. Fed Pract. 2019;36(9):400-402. PMID: 31571807
- Association of American Medical Colleges. The Complexities of Physician Supply and Demand: Projections from 2019 to 2034. June 2021. https://www.aamc.org/media/54681/download?attachment
- Medscape Pulmonologist Lifestyle, Happiness & Burnout Report 2023: Contentment Amid Stress. February 24, 2023. Accessed June 28, 2023. https://www.medscape.com/slideshow/2023-lifestyle-pulmonologist-6016092#1
- Medscape Intensivist Lifestyle, Happiness & Burnout Report 2023: Contentment Amid Stress. February 24, 2023. Accessed June 28, 2023. https://www.medscape.com/slideshow/2023-lifestyle-intensivist-6016072#1
- Moss M et al. Crit Care Med. 2016;44(7):1414-1421. doi:10.1097/CCM.000000000000188
- Medscape National Physician Burnout, Depression & Suicide Report 2019. Medscape. January 16, 2019. Accessed June 22, 2023. https://www.medscape.com/slideshow/2019-lifestyle-burnout-depression-6011056#1
- Medscape National Physician Burnout & Suicide Report 2020: The Generational Divide. Medscape. January 15, 2020. Accessed June 22, 2023. https://www.medscape.com/slideshow/2020-lifestyle-burnout-6012460#1
- ‘Death by 1000 Cuts’: Medscape National Physician Burnout & Suicide Report 2021. Medscape. January 22, 2021. Accessed June 22, 2023. https://www.medscape.com/slideshow/2021-lifestyle-burnout-6013456#2
- Physician Burnout Report 2022: Stress, Anxiety, and Anger. Medscape. January 21, 2022. Accessed June 22, 2023. https://www.medscape.com/slideshow/2022-lifestyle-burnout-6014664#1
- ‘I Cry but No One Cares’: Physician Burnout & Depression Report 2023. Medscape. January 27, 2023. Accessed June 22, 2023. https://www.medscape.com/slideshow/2023-lifestyle-burnout-6016058#1
- Murthy VH. N Engl J Med. 2022;387(7):577-579. doi:10.1056/NEJMp2207252
- Vranas KC et al. Chest. 2021;160(5):1714-1728. doi:10.1016/j.chest.2021.05.041
- Kerlin MP et al. Ann Am Thorac Soc. 2022;19(2):329-331. doi:10.1513/AnnalsATS.202105-567RL
- Dean W et al. Fed Pract. 2019;36(9):400-402. PMID: 31571807
- Association of American Medical Colleges. The Complexities of Physician Supply and Demand: Projections from 2019 to 2034. June 2021. https://www.aamc.org/media/54681/download?attachment
- Medscape Pulmonologist Lifestyle, Happiness & Burnout Report 2023: Contentment Amid Stress. February 24, 2023. Accessed June 28, 2023. https://www.medscape.com/slideshow/2023-lifestyle-pulmonologist-6016092#1
- Medscape Intensivist Lifestyle, Happiness & Burnout Report 2023: Contentment Amid Stress. February 24, 2023. Accessed June 28, 2023. https://www.medscape.com/slideshow/2023-lifestyle-intensivist-6016072#1