User login
-
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]


Are patient portals living up to the hype? Ask your mother-in-law!
While preparing to write this technology column, I received a great deal of insight from the unlikeliest of sources: my mother-in-law.
Now don’t get me wrong – she’s a truly lovely, intelligent, and capable woman. I have sought her advice often on many things and have always been impressed by her wisdom and pragmatism, but I’ve just never thought of asking her for her opinion on medicine or technology, as I considered her knowledge of both subjects to be limited.
This occasion changed my opinion. In fact, I believe that, as health care IT becomes more complex, people like my mother-in-law may be exactly who we should be looking to for answers.
A few weeks ago, my mother-in-law and I were discussing her recent trip to the doctor. When she mentioned some lab tests, I suggested that we log in to her patient portal to view the results. This elicited several questions and a declaration of frustration.
“Which portal?” she asked. “I have so many and can’t keep all of the websites and passwords straight! Why can’t all of my doctors use the same portal, and why do they all have different password requirements?”
As she spoke these words, I was immediately struck with an unfortunate reality of EHRs: We have done a brilliant job creating state-of-the-art digital castles and have filled them with the data needed to revolutionize care and improve population health – but we haven’t given our patients the keys to get inside.
We must ask ourselves if, in trying to construct fortresses of information around our patients, we have lost sight of the individuals in the center. I believe that we can answer this question and improve the benefits of patient portals, but we all must agree to a few simple steps to streamline the experience for everyone.
Make it easy
A study recently published in the Journal of General Internal Medicine surveyed several hospitals on their usage of patient portals. After determining whether or not the institutions had such portals, the authors then investigated to find out what, if any, guidance was provided to patients about how to use them.
Their findings are frustrating, though not surprising. While 89% of hospitals had some form of patient portal, only 65% of those “had links that were easily found, defined as links accessible within two clicks from the home page.”
Furthermore, even in cases where portals were easily found, good instructions on how to use them were missing. Those instructions that did exist centered on rules and restrictions and laying out “terms and conditions” and informing patients on “what not to do,” rather than explaining how to make the most of the experience.
According to the authors, “this focus on curtailing behavior, and the hurdles placed on finding and understanding guidance, suggest that some hospitals may be prioritizing reducing liability over improving the patient experience with portals.”
If we want our patients to use them, portals must be easy to access and intuitive to use. They also must provide value.
Make it meaningful
Patient portals have proliferated exponentially over the last 10 years, thanks to government incentive programs. One such program, known as “meaningful use,” is primarily responsible for this, as it made implementation of a patient portal one of its core requirements.
Sadly, in spite of its oft-reviled name, the meaningful use program never defined patient-friendly standards of usability for patient portals. As a result, current portals just aren’t very good. Patients like my mother-in-law find them to be too numerous, too unfriendly to use, and too limited, so they are not being used to their full potential.
In fact, many institutions may choose not to enable all of the available features in order to limit technical issues and reduce the burden on providers. In the study referenced above, only 63% of portals offered the ability for patients to communicate directly with their physicians, and only 43% offered the ability to refill prescriptions.
When enabled, these functions improve patient engagement and efficiency. Without them, patients are less likely to log on, and physicians are forced to rely on less-efficient telephone calls or traditional letters to communicate results to their patients.
Put the patient, not the portal, at the center
History has all but forgotten the attempts by tech giants such as Google and Microsoft to create personal health records. While these initially seemed like a wonderful concept, they sadly proved to be a total flop. Some patients embraced the idea, but security concerns and the lack of buy-in from EHR vendors significantly limited their uptake.
They may simply have been ahead of their time.
A decade later, wearable technology and telemedicine are ushering in a new era of patient-centric care. Individuals have been embracing a greater share of the responsibility for their own personal health information, yet most EHRs lack the ability to easily incorporate data acquired outside physicians’ offices.
It’s time for EHR vendors to go all in and change that. Instead of enslaving patients to the tyranny of fragmented health records, they should prioritize the creation of a robust, standardized, and portable health record that travels with the patient, not the other way around.
Have any other ideas on how to improve patient engagement? We’d love to hear about them and share them in a future column.
If you want to contribute but don’t have any ideas, we have a suggestion: Ask your mother-in-law. You may be surprised at what you learn!
Dr. Notte is a family physician and associate chief medical information officer for Abington (Pa.) Hospital–Jefferson Health. Follow him on twitter (@doctornotte). Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health.
Reference
Lee JL et al. J Gen Intern Med. 2019 Nov 12. doi: 10.1007/s11606-019-05528-z.
While preparing to write this technology column, I received a great deal of insight from the unlikeliest of sources: my mother-in-law.
Now don’t get me wrong – she’s a truly lovely, intelligent, and capable woman. I have sought her advice often on many things and have always been impressed by her wisdom and pragmatism, but I’ve just never thought of asking her for her opinion on medicine or technology, as I considered her knowledge of both subjects to be limited.
This occasion changed my opinion. In fact, I believe that, as health care IT becomes more complex, people like my mother-in-law may be exactly who we should be looking to for answers.
A few weeks ago, my mother-in-law and I were discussing her recent trip to the doctor. When she mentioned some lab tests, I suggested that we log in to her patient portal to view the results. This elicited several questions and a declaration of frustration.
“Which portal?” she asked. “I have so many and can’t keep all of the websites and passwords straight! Why can’t all of my doctors use the same portal, and why do they all have different password requirements?”
As she spoke these words, I was immediately struck with an unfortunate reality of EHRs: We have done a brilliant job creating state-of-the-art digital castles and have filled them with the data needed to revolutionize care and improve population health – but we haven’t given our patients the keys to get inside.
We must ask ourselves if, in trying to construct fortresses of information around our patients, we have lost sight of the individuals in the center. I believe that we can answer this question and improve the benefits of patient portals, but we all must agree to a few simple steps to streamline the experience for everyone.
Make it easy
A study recently published in the Journal of General Internal Medicine surveyed several hospitals on their usage of patient portals. After determining whether or not the institutions had such portals, the authors then investigated to find out what, if any, guidance was provided to patients about how to use them.
Their findings are frustrating, though not surprising. While 89% of hospitals had some form of patient portal, only 65% of those “had links that were easily found, defined as links accessible within two clicks from the home page.”
Furthermore, even in cases where portals were easily found, good instructions on how to use them were missing. Those instructions that did exist centered on rules and restrictions and laying out “terms and conditions” and informing patients on “what not to do,” rather than explaining how to make the most of the experience.
According to the authors, “this focus on curtailing behavior, and the hurdles placed on finding and understanding guidance, suggest that some hospitals may be prioritizing reducing liability over improving the patient experience with portals.”
If we want our patients to use them, portals must be easy to access and intuitive to use. They also must provide value.
Make it meaningful
Patient portals have proliferated exponentially over the last 10 years, thanks to government incentive programs. One such program, known as “meaningful use,” is primarily responsible for this, as it made implementation of a patient portal one of its core requirements.
Sadly, in spite of its oft-reviled name, the meaningful use program never defined patient-friendly standards of usability for patient portals. As a result, current portals just aren’t very good. Patients like my mother-in-law find them to be too numerous, too unfriendly to use, and too limited, so they are not being used to their full potential.
In fact, many institutions may choose not to enable all of the available features in order to limit technical issues and reduce the burden on providers. In the study referenced above, only 63% of portals offered the ability for patients to communicate directly with their physicians, and only 43% offered the ability to refill prescriptions.
When enabled, these functions improve patient engagement and efficiency. Without them, patients are less likely to log on, and physicians are forced to rely on less-efficient telephone calls or traditional letters to communicate results to their patients.
Put the patient, not the portal, at the center
History has all but forgotten the attempts by tech giants such as Google and Microsoft to create personal health records. While these initially seemed like a wonderful concept, they sadly proved to be a total flop. Some patients embraced the idea, but security concerns and the lack of buy-in from EHR vendors significantly limited their uptake.
They may simply have been ahead of their time.
A decade later, wearable technology and telemedicine are ushering in a new era of patient-centric care. Individuals have been embracing a greater share of the responsibility for their own personal health information, yet most EHRs lack the ability to easily incorporate data acquired outside physicians’ offices.
It’s time for EHR vendors to go all in and change that. Instead of enslaving patients to the tyranny of fragmented health records, they should prioritize the creation of a robust, standardized, and portable health record that travels with the patient, not the other way around.
Have any other ideas on how to improve patient engagement? We’d love to hear about them and share them in a future column.
If you want to contribute but don’t have any ideas, we have a suggestion: Ask your mother-in-law. You may be surprised at what you learn!
Dr. Notte is a family physician and associate chief medical information officer for Abington (Pa.) Hospital–Jefferson Health. Follow him on twitter (@doctornotte). Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health.
Reference
Lee JL et al. J Gen Intern Med. 2019 Nov 12. doi: 10.1007/s11606-019-05528-z.
While preparing to write this technology column, I received a great deal of insight from the unlikeliest of sources: my mother-in-law.
Now don’t get me wrong – she’s a truly lovely, intelligent, and capable woman. I have sought her advice often on many things and have always been impressed by her wisdom and pragmatism, but I’ve just never thought of asking her for her opinion on medicine or technology, as I considered her knowledge of both subjects to be limited.
This occasion changed my opinion. In fact, I believe that, as health care IT becomes more complex, people like my mother-in-law may be exactly who we should be looking to for answers.
A few weeks ago, my mother-in-law and I were discussing her recent trip to the doctor. When she mentioned some lab tests, I suggested that we log in to her patient portal to view the results. This elicited several questions and a declaration of frustration.
“Which portal?” she asked. “I have so many and can’t keep all of the websites and passwords straight! Why can’t all of my doctors use the same portal, and why do they all have different password requirements?”
As she spoke these words, I was immediately struck with an unfortunate reality of EHRs: We have done a brilliant job creating state-of-the-art digital castles and have filled them with the data needed to revolutionize care and improve population health – but we haven’t given our patients the keys to get inside.
We must ask ourselves if, in trying to construct fortresses of information around our patients, we have lost sight of the individuals in the center. I believe that we can answer this question and improve the benefits of patient portals, but we all must agree to a few simple steps to streamline the experience for everyone.
Make it easy
A study recently published in the Journal of General Internal Medicine surveyed several hospitals on their usage of patient portals. After determining whether or not the institutions had such portals, the authors then investigated to find out what, if any, guidance was provided to patients about how to use them.
Their findings are frustrating, though not surprising. While 89% of hospitals had some form of patient portal, only 65% of those “had links that were easily found, defined as links accessible within two clicks from the home page.”
Furthermore, even in cases where portals were easily found, good instructions on how to use them were missing. Those instructions that did exist centered on rules and restrictions and laying out “terms and conditions” and informing patients on “what not to do,” rather than explaining how to make the most of the experience.
According to the authors, “this focus on curtailing behavior, and the hurdles placed on finding and understanding guidance, suggest that some hospitals may be prioritizing reducing liability over improving the patient experience with portals.”
If we want our patients to use them, portals must be easy to access and intuitive to use. They also must provide value.
Make it meaningful
Patient portals have proliferated exponentially over the last 10 years, thanks to government incentive programs. One such program, known as “meaningful use,” is primarily responsible for this, as it made implementation of a patient portal one of its core requirements.
Sadly, in spite of its oft-reviled name, the meaningful use program never defined patient-friendly standards of usability for patient portals. As a result, current portals just aren’t very good. Patients like my mother-in-law find them to be too numerous, too unfriendly to use, and too limited, so they are not being used to their full potential.
In fact, many institutions may choose not to enable all of the available features in order to limit technical issues and reduce the burden on providers. In the study referenced above, only 63% of portals offered the ability for patients to communicate directly with their physicians, and only 43% offered the ability to refill prescriptions.
When enabled, these functions improve patient engagement and efficiency. Without them, patients are less likely to log on, and physicians are forced to rely on less-efficient telephone calls or traditional letters to communicate results to their patients.
Put the patient, not the portal, at the center
History has all but forgotten the attempts by tech giants such as Google and Microsoft to create personal health records. While these initially seemed like a wonderful concept, they sadly proved to be a total flop. Some patients embraced the idea, but security concerns and the lack of buy-in from EHR vendors significantly limited their uptake.
They may simply have been ahead of their time.
A decade later, wearable technology and telemedicine are ushering in a new era of patient-centric care. Individuals have been embracing a greater share of the responsibility for their own personal health information, yet most EHRs lack the ability to easily incorporate data acquired outside physicians’ offices.
It’s time for EHR vendors to go all in and change that. Instead of enslaving patients to the tyranny of fragmented health records, they should prioritize the creation of a robust, standardized, and portable health record that travels with the patient, not the other way around.
Have any other ideas on how to improve patient engagement? We’d love to hear about them and share them in a future column.
If you want to contribute but don’t have any ideas, we have a suggestion: Ask your mother-in-law. You may be surprised at what you learn!
Dr. Notte is a family physician and associate chief medical information officer for Abington (Pa.) Hospital–Jefferson Health. Follow him on twitter (@doctornotte). Dr. Skolnik is professor of family and community medicine at Sidney Kimmel Medical College, Philadelphia, and associate director of the family medicine residency program at Abington Hospital–Jefferson Health.
Reference
Lee JL et al. J Gen Intern Med. 2019 Nov 12. doi: 10.1007/s11606-019-05528-z.
Diagnosing insomnia takes time
Give new patients 1 hour, expert advises
LAS VEGAS – Clinicians should spend 1 hour with patients who present with a chief complaint of insomnia, rather than rushing to a treatment after a 10- to 15-minute office visit, according to John W. Winkelman, MD, PhD.
“Why? Because sleep problems are usually multifactorial, involving psychiatric illness, sleep disorders, medical illness, medication, and poor sleep hygiene/stress,” he said at an annual psychopharmacology update held by the Nevada Psychiatric Association. “There are usually many contributing problems, and sleep quality is only as strong as the weakest link. Maybe you don’t have an hour [to meet with new patients], but you need to give adequate time, otherwise you’re not going to do justice to the problem.”
“Ask, ‘what is it that bothers you most about your insomnia? Is it the time awake at night, your total sleep time, or how you feel during the day?’ Because we’re going to use different approaches based on that chief complaint of the insomnia,” said Dr. Winkelman, chief of the Massachusetts General Sleep Disorders Clinical Research Program in the department of psychiatry at Harvard Medical School, Boston. “Cognitive-behavioral therapy for insomnia [CBT-I], for instance, is very good at reducing time awake at night. It won’t increase total sleep time, but it reduces time awake at night dramatically.”
According to the DSM-5, insomnia disorder is marked by dissatisfaction with sleep quality or quantity associated with at least one of the following: difficulty initiating sleep, difficulty maintaining sleep, and early morning awakening. “Just getting up to pee five times a night is not insomnia,” he said. “Just taking an hour and a half to fall asleep at the beginning of the night is not insomnia. There has to be distress or dysfunction related to the sleep disturbance, for a minimum of three times per week for 3 months.”
Most sleep problems are transient, but 25%-30% last more than 1 year. The differential diagnosis for chronic insomnia includes primary psychiatric disorders, medications, substances, restless legs syndrome, sleep schedule disorders, and obstructive sleep apnea.
“In general, we do not order sleep studies in people with insomnia unless we suspect sleep apnea; it’s just a waste of time,” said Dr. Winkelman, who is also a professor of psychiatry at Harvard Medical School. Indications for polysomnography include loud snoring plus one of the following: daytime sleepiness, witnessed apneas, or refractory hypertension. Other indications include abnormal behaviors or movements during sleep, unexplained excessive daytime sleepiness, and refractory sleep complaints, especially repetitive brief awakenings.
Many common cognitive and behavioral issues can produce or worsen insomnia, including inconsistent bedtimes and wake times. “That irregular schedule wreaks havoc with sleep,” he said. “It messes up the circadian rhythm. Also, homeostatic drive needs to build up: We need to be awake 16 or more hours in order to be sleepy. If people are sleeping until noon on Sundays and then trying to go to bed at their usual time, 10 or 11 at night, they’ve only been awake 10 or 11 hours. That’s why they’re going to have problems falling asleep. Also, a lot of people doze off after dinner in front of the TV. That doesn’t help.”
Spending excessive time in bed can also trigger or worsen insomnia. Dr. Winkelman recommends that people restrict their access to bed to the number of hours it is reasonable to sleep. “I see a lot of people in their 70s and 80s spending 10 hours in bed,” he said. “It doesn’t sound that crazy, but there is no way they’re going to get 10 hours of sleep. It’s physically impossible, so they spend 2 or 3 hours awake at night.” Clock-watching is another no-no. “In the middle of the night you wake up, look at the clock, and say to yourself: ‘Oh my god, I’ve been awake for 3 hours. I have 4 hours left. I need 7 hours. That means I need to go to sleep now!’ ”
An estimated 30%-40% of people with chronic insomnia have a psychiatric disorder. That means “you have to be thorough in your evaluation and act as if you’re doing a structured interview,” Dr. Winkelman said. “Ask about obsessive-compulsive disorder, generalized anxiety disorder, PTSD, et cetera, so that you understand the complete myriad of psychiatric illnesses, because psychiatric illnesses run in gangs. Comorbidity is generally the rule.”
The first-line treatment for chronic insomnia disorder is CBT-I, a multicomponent approach that includes time-in-bed restriction, stimulus control, cognitive therapy, relaxation therapy, and sleep hygiene. According to Dr. Winkelman, the cornerstone of CBT-I is time-in-bed restriction. “Many people with insomnia are spending 8.5 hours in bed to get 6.5 hours of sleep,” he said. “What you do is restrict access to bed to 6.5 hours; you initially sleep deprive them. Over the first few weeks, they hate you. After a few weeks when they start sleeping well, you start gradually increasing time in bed, but they rarely get back to the 8.5 hours in bed they were spending beforehand.”
Online CBT-I programs such as Sleepio can also be effective for improving sleep latency and wake after sleep onset, but not for total sleep time (JAMA Psychiatry. 2017;74[1]:68-75). “Not everybody responds to CBT; 50% don’t respond at a couple of months,” he said. “These are the people you need to think about medication for.”
Medications commonly used for chronic insomnia include benzodiazepine receptor agonists (BzRAs) – temazepam, eszopiclone, triazolam, zolpidem, and zaleplon are Food and Drug Administration approved – melatonin agonists, orexin antagonists, sedating antidepressants, anticonvulsants, and dopaminergic antagonists. “Each of the agents in these categories has somewhat similar mechanisms of action, and similar efficacy and contraindications,” Dr. Winkelman said. “The best way to divide the benzodiazepine receptor agonists is based on half-life. How long do you want drug on receptor in somebody with insomnia? Probably not much longer than 8 hours. Nevertheless, some psychiatrists love clonazepam, which has a 40-hour half-life. The circumstances under which clonazepam should be used for insomnia are small, such as in people with a daytime anxiety disorder.”
Consider trying triazolam, zolpidem, and zaleplon for patients who have problems falling asleep, he said, while oxazepam and eszopiclone are sensible options for people who have difficulty falling and staying asleep. Clinical response to BzRAs is common, yet only about half of people who have insomnia remit with one of these agents.
Dr. Winkelman said that patients and physicians often ask him whether BzRAs and other agents used as sleep aids are addictive. Abuse is identified when recurrent use causes clinically and functionally significant impairment, such as health problems; disability; and failure to meet major responsibilities at work, home, or school. “These are concerns with BzRAs. Misuse and abuse generally occur in younger people. Once you get to 35 years old, misuse rates get very low. In older people, rates of side effects go up.
“Tolerance, physiological and psychological dependence, and nonmedical diversion are also of concern,” he said. However, for the majority of people, BzRA hypnotics are effective and safe.
As for other agents, meta-analyses have demonstrated that melatonin 1-3 mg can help people fall asleep when it’s not being endogenously released. “That’s during the day,” he said. “That might be most relevant for jet lag and for people doing shift work.” Two orexin antagonists on the market for insomnia include suvorexant and lemborexant 10-20 mg. Advantages of these include little abuse liability and few side effects. “In one head-to-head polysomnography study in the elderly, lemborexant was superior to zolpidem 6.25 mg CR on both objective and subjective ability to fall asleep and stay asleep,” Dr. Winkelman said. (JAMA Netw Open. 2019;2[12]:e1918254).
Antidepressants are another treatment option, including mirtazapine 15-30 mg, trazodone 25-100 mg, and amitriptyline and doxepin (10-50 mg). Advantages include little abuse liability, while potential drawbacks include daytime sedation, weight gain, and anticholinergic side effects. Meanwhile, atypical antipsychotics such as quetiapine 25-100 mg have long been known to be helpful for sleep. “Advantages are that they’re anxiolytic, they’re mood stabilizing, and there is little abuse liability,” Dr. Winkelman said. “Drawbacks are that they’re probably less effective than BzRAs, they cause daytime sedation, weight gain, risks of extrapyramidal symptoms and glucose and lipid abnormalities.”
Dr. Winkelman said that he uses “a fair amount” of the anticonvulsant gabapentin as a second- or third-line hypnotic agent. “I usually start with 300 mg [at bedtime],” he added. “Drawbacks are that it’s probably less effective than BzRAs; it affects cognition; and can cause daytime sedation, dizziness, and weight gain. There are also concerns about abuse.”
Dr. Winkelman reported that he has received grant/research support from Merck, the RLS Foundation, and Luitpold Pharmaceuticals. He is also a consultant for Advance Medical, Avadel Pharmaceuticals, and UpToDate and is a member of the speakers’ bureau for Luitpold.
Give new patients 1 hour, expert advises
Give new patients 1 hour, expert advises
LAS VEGAS – Clinicians should spend 1 hour with patients who present with a chief complaint of insomnia, rather than rushing to a treatment after a 10- to 15-minute office visit, according to John W. Winkelman, MD, PhD.
“Why? Because sleep problems are usually multifactorial, involving psychiatric illness, sleep disorders, medical illness, medication, and poor sleep hygiene/stress,” he said at an annual psychopharmacology update held by the Nevada Psychiatric Association. “There are usually many contributing problems, and sleep quality is only as strong as the weakest link. Maybe you don’t have an hour [to meet with new patients], but you need to give adequate time, otherwise you’re not going to do justice to the problem.”
“Ask, ‘what is it that bothers you most about your insomnia? Is it the time awake at night, your total sleep time, or how you feel during the day?’ Because we’re going to use different approaches based on that chief complaint of the insomnia,” said Dr. Winkelman, chief of the Massachusetts General Sleep Disorders Clinical Research Program in the department of psychiatry at Harvard Medical School, Boston. “Cognitive-behavioral therapy for insomnia [CBT-I], for instance, is very good at reducing time awake at night. It won’t increase total sleep time, but it reduces time awake at night dramatically.”
According to the DSM-5, insomnia disorder is marked by dissatisfaction with sleep quality or quantity associated with at least one of the following: difficulty initiating sleep, difficulty maintaining sleep, and early morning awakening. “Just getting up to pee five times a night is not insomnia,” he said. “Just taking an hour and a half to fall asleep at the beginning of the night is not insomnia. There has to be distress or dysfunction related to the sleep disturbance, for a minimum of three times per week for 3 months.”
Most sleep problems are transient, but 25%-30% last more than 1 year. The differential diagnosis for chronic insomnia includes primary psychiatric disorders, medications, substances, restless legs syndrome, sleep schedule disorders, and obstructive sleep apnea.
“In general, we do not order sleep studies in people with insomnia unless we suspect sleep apnea; it’s just a waste of time,” said Dr. Winkelman, who is also a professor of psychiatry at Harvard Medical School. Indications for polysomnography include loud snoring plus one of the following: daytime sleepiness, witnessed apneas, or refractory hypertension. Other indications include abnormal behaviors or movements during sleep, unexplained excessive daytime sleepiness, and refractory sleep complaints, especially repetitive brief awakenings.
Many common cognitive and behavioral issues can produce or worsen insomnia, including inconsistent bedtimes and wake times. “That irregular schedule wreaks havoc with sleep,” he said. “It messes up the circadian rhythm. Also, homeostatic drive needs to build up: We need to be awake 16 or more hours in order to be sleepy. If people are sleeping until noon on Sundays and then trying to go to bed at their usual time, 10 or 11 at night, they’ve only been awake 10 or 11 hours. That’s why they’re going to have problems falling asleep. Also, a lot of people doze off after dinner in front of the TV. That doesn’t help.”
Spending excessive time in bed can also trigger or worsen insomnia. Dr. Winkelman recommends that people restrict their access to bed to the number of hours it is reasonable to sleep. “I see a lot of people in their 70s and 80s spending 10 hours in bed,” he said. “It doesn’t sound that crazy, but there is no way they’re going to get 10 hours of sleep. It’s physically impossible, so they spend 2 or 3 hours awake at night.” Clock-watching is another no-no. “In the middle of the night you wake up, look at the clock, and say to yourself: ‘Oh my god, I’ve been awake for 3 hours. I have 4 hours left. I need 7 hours. That means I need to go to sleep now!’ ”
An estimated 30%-40% of people with chronic insomnia have a psychiatric disorder. That means “you have to be thorough in your evaluation and act as if you’re doing a structured interview,” Dr. Winkelman said. “Ask about obsessive-compulsive disorder, generalized anxiety disorder, PTSD, et cetera, so that you understand the complete myriad of psychiatric illnesses, because psychiatric illnesses run in gangs. Comorbidity is generally the rule.”
The first-line treatment for chronic insomnia disorder is CBT-I, a multicomponent approach that includes time-in-bed restriction, stimulus control, cognitive therapy, relaxation therapy, and sleep hygiene. According to Dr. Winkelman, the cornerstone of CBT-I is time-in-bed restriction. “Many people with insomnia are spending 8.5 hours in bed to get 6.5 hours of sleep,” he said. “What you do is restrict access to bed to 6.5 hours; you initially sleep deprive them. Over the first few weeks, they hate you. After a few weeks when they start sleeping well, you start gradually increasing time in bed, but they rarely get back to the 8.5 hours in bed they were spending beforehand.”
Online CBT-I programs such as Sleepio can also be effective for improving sleep latency and wake after sleep onset, but not for total sleep time (JAMA Psychiatry. 2017;74[1]:68-75). “Not everybody responds to CBT; 50% don’t respond at a couple of months,” he said. “These are the people you need to think about medication for.”
Medications commonly used for chronic insomnia include benzodiazepine receptor agonists (BzRAs) – temazepam, eszopiclone, triazolam, zolpidem, and zaleplon are Food and Drug Administration approved – melatonin agonists, orexin antagonists, sedating antidepressants, anticonvulsants, and dopaminergic antagonists. “Each of the agents in these categories has somewhat similar mechanisms of action, and similar efficacy and contraindications,” Dr. Winkelman said. “The best way to divide the benzodiazepine receptor agonists is based on half-life. How long do you want drug on receptor in somebody with insomnia? Probably not much longer than 8 hours. Nevertheless, some psychiatrists love clonazepam, which has a 40-hour half-life. The circumstances under which clonazepam should be used for insomnia are small, such as in people with a daytime anxiety disorder.”
Consider trying triazolam, zolpidem, and zaleplon for patients who have problems falling asleep, he said, while oxazepam and eszopiclone are sensible options for people who have difficulty falling and staying asleep. Clinical response to BzRAs is common, yet only about half of people who have insomnia remit with one of these agents.
Dr. Winkelman said that patients and physicians often ask him whether BzRAs and other agents used as sleep aids are addictive. Abuse is identified when recurrent use causes clinically and functionally significant impairment, such as health problems; disability; and failure to meet major responsibilities at work, home, or school. “These are concerns with BzRAs. Misuse and abuse generally occur in younger people. Once you get to 35 years old, misuse rates get very low. In older people, rates of side effects go up.
“Tolerance, physiological and psychological dependence, and nonmedical diversion are also of concern,” he said. However, for the majority of people, BzRA hypnotics are effective and safe.
As for other agents, meta-analyses have demonstrated that melatonin 1-3 mg can help people fall asleep when it’s not being endogenously released. “That’s during the day,” he said. “That might be most relevant for jet lag and for people doing shift work.” Two orexin antagonists on the market for insomnia include suvorexant and lemborexant 10-20 mg. Advantages of these include little abuse liability and few side effects. “In one head-to-head polysomnography study in the elderly, lemborexant was superior to zolpidem 6.25 mg CR on both objective and subjective ability to fall asleep and stay asleep,” Dr. Winkelman said. (JAMA Netw Open. 2019;2[12]:e1918254).
Antidepressants are another treatment option, including mirtazapine 15-30 mg, trazodone 25-100 mg, and amitriptyline and doxepin (10-50 mg). Advantages include little abuse liability, while potential drawbacks include daytime sedation, weight gain, and anticholinergic side effects. Meanwhile, atypical antipsychotics such as quetiapine 25-100 mg have long been known to be helpful for sleep. “Advantages are that they’re anxiolytic, they’re mood stabilizing, and there is little abuse liability,” Dr. Winkelman said. “Drawbacks are that they’re probably less effective than BzRAs, they cause daytime sedation, weight gain, risks of extrapyramidal symptoms and glucose and lipid abnormalities.”
Dr. Winkelman said that he uses “a fair amount” of the anticonvulsant gabapentin as a second- or third-line hypnotic agent. “I usually start with 300 mg [at bedtime],” he added. “Drawbacks are that it’s probably less effective than BzRAs; it affects cognition; and can cause daytime sedation, dizziness, and weight gain. There are also concerns about abuse.”
Dr. Winkelman reported that he has received grant/research support from Merck, the RLS Foundation, and Luitpold Pharmaceuticals. He is also a consultant for Advance Medical, Avadel Pharmaceuticals, and UpToDate and is a member of the speakers’ bureau for Luitpold.
LAS VEGAS – Clinicians should spend 1 hour with patients who present with a chief complaint of insomnia, rather than rushing to a treatment after a 10- to 15-minute office visit, according to John W. Winkelman, MD, PhD.
“Why? Because sleep problems are usually multifactorial, involving psychiatric illness, sleep disorders, medical illness, medication, and poor sleep hygiene/stress,” he said at an annual psychopharmacology update held by the Nevada Psychiatric Association. “There are usually many contributing problems, and sleep quality is only as strong as the weakest link. Maybe you don’t have an hour [to meet with new patients], but you need to give adequate time, otherwise you’re not going to do justice to the problem.”
“Ask, ‘what is it that bothers you most about your insomnia? Is it the time awake at night, your total sleep time, or how you feel during the day?’ Because we’re going to use different approaches based on that chief complaint of the insomnia,” said Dr. Winkelman, chief of the Massachusetts General Sleep Disorders Clinical Research Program in the department of psychiatry at Harvard Medical School, Boston. “Cognitive-behavioral therapy for insomnia [CBT-I], for instance, is very good at reducing time awake at night. It won’t increase total sleep time, but it reduces time awake at night dramatically.”
According to the DSM-5, insomnia disorder is marked by dissatisfaction with sleep quality or quantity associated with at least one of the following: difficulty initiating sleep, difficulty maintaining sleep, and early morning awakening. “Just getting up to pee five times a night is not insomnia,” he said. “Just taking an hour and a half to fall asleep at the beginning of the night is not insomnia. There has to be distress or dysfunction related to the sleep disturbance, for a minimum of three times per week for 3 months.”
Most sleep problems are transient, but 25%-30% last more than 1 year. The differential diagnosis for chronic insomnia includes primary psychiatric disorders, medications, substances, restless legs syndrome, sleep schedule disorders, and obstructive sleep apnea.
“In general, we do not order sleep studies in people with insomnia unless we suspect sleep apnea; it’s just a waste of time,” said Dr. Winkelman, who is also a professor of psychiatry at Harvard Medical School. Indications for polysomnography include loud snoring plus one of the following: daytime sleepiness, witnessed apneas, or refractory hypertension. Other indications include abnormal behaviors or movements during sleep, unexplained excessive daytime sleepiness, and refractory sleep complaints, especially repetitive brief awakenings.
Many common cognitive and behavioral issues can produce or worsen insomnia, including inconsistent bedtimes and wake times. “That irregular schedule wreaks havoc with sleep,” he said. “It messes up the circadian rhythm. Also, homeostatic drive needs to build up: We need to be awake 16 or more hours in order to be sleepy. If people are sleeping until noon on Sundays and then trying to go to bed at their usual time, 10 or 11 at night, they’ve only been awake 10 or 11 hours. That’s why they’re going to have problems falling asleep. Also, a lot of people doze off after dinner in front of the TV. That doesn’t help.”
Spending excessive time in bed can also trigger or worsen insomnia. Dr. Winkelman recommends that people restrict their access to bed to the number of hours it is reasonable to sleep. “I see a lot of people in their 70s and 80s spending 10 hours in bed,” he said. “It doesn’t sound that crazy, but there is no way they’re going to get 10 hours of sleep. It’s physically impossible, so they spend 2 or 3 hours awake at night.” Clock-watching is another no-no. “In the middle of the night you wake up, look at the clock, and say to yourself: ‘Oh my god, I’ve been awake for 3 hours. I have 4 hours left. I need 7 hours. That means I need to go to sleep now!’ ”
An estimated 30%-40% of people with chronic insomnia have a psychiatric disorder. That means “you have to be thorough in your evaluation and act as if you’re doing a structured interview,” Dr. Winkelman said. “Ask about obsessive-compulsive disorder, generalized anxiety disorder, PTSD, et cetera, so that you understand the complete myriad of psychiatric illnesses, because psychiatric illnesses run in gangs. Comorbidity is generally the rule.”
The first-line treatment for chronic insomnia disorder is CBT-I, a multicomponent approach that includes time-in-bed restriction, stimulus control, cognitive therapy, relaxation therapy, and sleep hygiene. According to Dr. Winkelman, the cornerstone of CBT-I is time-in-bed restriction. “Many people with insomnia are spending 8.5 hours in bed to get 6.5 hours of sleep,” he said. “What you do is restrict access to bed to 6.5 hours; you initially sleep deprive them. Over the first few weeks, they hate you. After a few weeks when they start sleeping well, you start gradually increasing time in bed, but they rarely get back to the 8.5 hours in bed they were spending beforehand.”
Online CBT-I programs such as Sleepio can also be effective for improving sleep latency and wake after sleep onset, but not for total sleep time (JAMA Psychiatry. 2017;74[1]:68-75). “Not everybody responds to CBT; 50% don’t respond at a couple of months,” he said. “These are the people you need to think about medication for.”
Medications commonly used for chronic insomnia include benzodiazepine receptor agonists (BzRAs) – temazepam, eszopiclone, triazolam, zolpidem, and zaleplon are Food and Drug Administration approved – melatonin agonists, orexin antagonists, sedating antidepressants, anticonvulsants, and dopaminergic antagonists. “Each of the agents in these categories has somewhat similar mechanisms of action, and similar efficacy and contraindications,” Dr. Winkelman said. “The best way to divide the benzodiazepine receptor agonists is based on half-life. How long do you want drug on receptor in somebody with insomnia? Probably not much longer than 8 hours. Nevertheless, some psychiatrists love clonazepam, which has a 40-hour half-life. The circumstances under which clonazepam should be used for insomnia are small, such as in people with a daytime anxiety disorder.”
Consider trying triazolam, zolpidem, and zaleplon for patients who have problems falling asleep, he said, while oxazepam and eszopiclone are sensible options for people who have difficulty falling and staying asleep. Clinical response to BzRAs is common, yet only about half of people who have insomnia remit with one of these agents.
Dr. Winkelman said that patients and physicians often ask him whether BzRAs and other agents used as sleep aids are addictive. Abuse is identified when recurrent use causes clinically and functionally significant impairment, such as health problems; disability; and failure to meet major responsibilities at work, home, or school. “These are concerns with BzRAs. Misuse and abuse generally occur in younger people. Once you get to 35 years old, misuse rates get very low. In older people, rates of side effects go up.
“Tolerance, physiological and psychological dependence, and nonmedical diversion are also of concern,” he said. However, for the majority of people, BzRA hypnotics are effective and safe.
As for other agents, meta-analyses have demonstrated that melatonin 1-3 mg can help people fall asleep when it’s not being endogenously released. “That’s during the day,” he said. “That might be most relevant for jet lag and for people doing shift work.” Two orexin antagonists on the market for insomnia include suvorexant and lemborexant 10-20 mg. Advantages of these include little abuse liability and few side effects. “In one head-to-head polysomnography study in the elderly, lemborexant was superior to zolpidem 6.25 mg CR on both objective and subjective ability to fall asleep and stay asleep,” Dr. Winkelman said. (JAMA Netw Open. 2019;2[12]:e1918254).
Antidepressants are another treatment option, including mirtazapine 15-30 mg, trazodone 25-100 mg, and amitriptyline and doxepin (10-50 mg). Advantages include little abuse liability, while potential drawbacks include daytime sedation, weight gain, and anticholinergic side effects. Meanwhile, atypical antipsychotics such as quetiapine 25-100 mg have long been known to be helpful for sleep. “Advantages are that they’re anxiolytic, they’re mood stabilizing, and there is little abuse liability,” Dr. Winkelman said. “Drawbacks are that they’re probably less effective than BzRAs, they cause daytime sedation, weight gain, risks of extrapyramidal symptoms and glucose and lipid abnormalities.”
Dr. Winkelman said that he uses “a fair amount” of the anticonvulsant gabapentin as a second- or third-line hypnotic agent. “I usually start with 300 mg [at bedtime],” he added. “Drawbacks are that it’s probably less effective than BzRAs; it affects cognition; and can cause daytime sedation, dizziness, and weight gain. There are also concerns about abuse.”
Dr. Winkelman reported that he has received grant/research support from Merck, the RLS Foundation, and Luitpold Pharmaceuticals. He is also a consultant for Advance Medical, Avadel Pharmaceuticals, and UpToDate and is a member of the speakers’ bureau for Luitpold.
EXPERT ANALYSIS FROM NPA 2020
Supreme Court roundup: Latest health care decisions
The Trump administration can move forward with expanding a rule that makes it more difficult for immigrants to remain in the United States if they receive health care assistance, the U.S. Supreme Court ruled in a 5-4 vote.
The Feb. 21 order allows the administration to broaden the so-called “public charge rule” while legal challenges against the expanded regulation continue in the lower courts. The Supreme Court’s decision, which lifts a preliminary injunction against the expansion, applies to enforcement only in Illinois, where a district court blocked the revised rule from moving forward in October 2019. The Supreme Court’s measure follows another 5-4 order in January, in which justices lifted a nationwide injunction against the revised rule.
Under the long-standing public charge rule, immigration officials can refuse to admit immigrants into the United States or can deny them permanent legal status if they are deemed likely to become a public charge. Previously, immigration officers considered cash aid, such as Temporary Assistance for Needy Families or long-term institutionalized care, as potential public charge reasons for denial.
The revised regulation allows officials to consider previously excluded programs in their determination, including nonemergency Medicaid, the Supplemental Nutrition Assistance Program, and several housing programs. Use of these programs for more than 12 months in the aggregate during a 36-month period may result in a “public charge” designation and lead to green card denial.
Eight legal challenges were immediately filed against the rule changes, including a complaint issued by 14 states. At least five trial courts have since blocked the measure, while appeals courts have lifted some of the injunctions and upheld enforcement.
In its Jan. 27 order lifting the nationwide injunction, Associate Justice Neil M. Gorsuch wrote that nationwide injunctions are being overused by trial courts with negative consequences.
“The real problem here is the increasingly common practice of trial courts ordering relief that transcends the cases before them. Whether framed as injunctions of ‘nationwide,’ ‘universal,’ or ‘cosmic’ scope, these orders share the same basic flaw – they direct how the defendant must act toward persons who are not parties to the case,” he wrote. “It has become increasingly apparent that this court must, at some point, confront these important objections to this increasingly widespread practice. As the brief and furious history of the regulation before us illustrates, the routine issuance of universal injunctions is patently unworkable, sowing chaos for litigants, the government, courts, and all those affected by these conflicting decisions.”
In the court’s Feb. 21 order lifting the injunction in Illinois, justices gave no explanation for overturning the lower court’s injunction. However, Associate Justice Sonia Sotomayor issued a sharply-worded dissent, criticizing her fellow justices for allowing the rule to proceed.
“In sum, the government’s only claimed hardship is that it must enforce an existing interpretation of an immigration rule in one state – just as it has done for the past 20 years – while an updated version of the rule takes effect in the remaining 49,” she wrote. “The government has not quantified or explained any burdens that would arise from this state of the world.”
ACA cases still in limbo
Meanwhile, the Supreme Court still has not decided whether it will hear Texas v. United States, a case that could effectively dismantle the Affordable Care Act.
The high court was expected to announce whether it would take the high-profile case at a private Feb. 21 conference, but the justices have released no update. The case was relisted for consideration at the court’s Feb. 28 conference.
Texas v. United States stems from a lawsuit by 20 Republican state attorneys general and governors that was filed after Congress zeroed out the ACA’s individual mandate penalty in 2017. The plaintiffs contend the now-valueless mandate is no longer constitutional and thus, the entire ACA should be struck down. Because the Trump administration declined to defend the law, a coalition of Democratic attorneys general and governors intervened in the case as defendants.
In 2018, a Texas district court ruled in favor of the plaintiffs and declared the entire health care law invalid. The 5th U.S. Circuit Court of Appeals partially affirmed the district court’s decision, ruling that the mandate was unconstitutional, but sending the case back to the lower court for more analysis on severability. The Democratic attorneys general and governors appealed the decision to the U.S. Supreme Court.
If the Supreme Court agrees to hear the challenge, the court could fast-track the case and schedule arguments for the current term or wait until its next term, which starts in October 2020. If justices decline to hear the case, the challenge will remain with the district court for more analysis about the law’s severability.
Another ACA-related case – Maine Community Health Options v. U.S. – also remains in limbo. Justices heard the case, which was consolidated with two similar challenges, on Dec. 10, 2019, but still have not issued a decision.
The consolidated challenges center on whether the federal government owes insurers billions based on an Affordable Care Act provision intended to help health plans mitigate risk under the law. The ACA’s risk corridor program required the U.S. Department of Health & Human Services to collect funds from profitable insurers that offered qualified health plans under the exchanges and distribute the funds to insurers with excessive losses. Collections from profitable insurers under the program fell short in 2014, 2015, and 2016, while losses steadily grew, resulting in the HHS paying about 12 cents on the dollar in payments to insurers. More than 150 insurers now allege they were shortchanged and they want the Supreme Court to force the government to reimburse them to the tune of $12 billion.
The Department of Justice counters that the government is not required to pay the insurers because of appropriations measures passed by Congress in 2014 and in later years that limited the funding available to compensate insurers for their losses.
The federal government and insurers have each experienced wins and losses at the lower court level. Most recently, the U.S. Court of Appeals for the Federal Circuit decided in favor of the government, ruling that while the ACA required the government to compensate the insurers for their losses, the appropriations measures repealed or suspended that requirement.
A Supreme Court decision in the case could come as soon as Feb. 26.
Court to hear women’s health cases
Two closely watched reproductive health cases will go before the court this spring.
On March 4, justices will hear oral arguments in June Medical Services v. Russo, regarding the constitutionality of a Louisiana law that requires physicians performing abortions to have admitting privileges at a nearby hospital. Doctors who perform abortions without admitting privileges at a hospital within 30 miles face fines and imprisonment, according to the state law, originally passed in 2014. Clinics that employ such doctors can also have their licenses revoked.
June Medical Services LLC, a women’s health clinic, sued over the law. A district court ruled in favor of the plaintiff, but the 5th U.S. Circuit Court of Appeals reversed and upheld Louisiana’s law. The clinic appealed to the U.S. Supreme Court. Louisiana officials argue the challenge should be dismissed, and the law allowed to proceed, because the plaintiffs lack standing.
The Supreme Court in 2016 heard a similar case – Whole Woman’s Health v. Hellerstedt – concerning a comparable law in Texas. In that case, justices struck down the measure as unconstitutional.
And on April 29, justices will hear arguments in Little Sisters of the Poor v. Pennsylvania, a consolidated case about whether the Trump administration acted properly when it expanded exemptions under the Affordable Care Act’s contraceptive mandate. Entities that object to providing contraception on the basis of religious beliefs can opt out of complying with the mandate, according to the 2018 regulations. Additionally, nonprofit organizations and small businesses that have nonreligious moral convictions against the mandate can skip compliance. A number of states and entities sued over the new rules.
A federal appeals court temporarily barred the regulations from moving forward, ruling the plaintiffs were likely to succeed in proving the Trump administration did not follow appropriate procedures when it promulgated the new rules and that the regulations were not authorized under the ACA.
Justices will decide whether the parties have standing in the case, whether the Trump administration followed correct rule-making procedures, and if the regulations can stand.
The Trump administration can move forward with expanding a rule that makes it more difficult for immigrants to remain in the United States if they receive health care assistance, the U.S. Supreme Court ruled in a 5-4 vote.
The Feb. 21 order allows the administration to broaden the so-called “public charge rule” while legal challenges against the expanded regulation continue in the lower courts. The Supreme Court’s decision, which lifts a preliminary injunction against the expansion, applies to enforcement only in Illinois, where a district court blocked the revised rule from moving forward in October 2019. The Supreme Court’s measure follows another 5-4 order in January, in which justices lifted a nationwide injunction against the revised rule.
Under the long-standing public charge rule, immigration officials can refuse to admit immigrants into the United States or can deny them permanent legal status if they are deemed likely to become a public charge. Previously, immigration officers considered cash aid, such as Temporary Assistance for Needy Families or long-term institutionalized care, as potential public charge reasons for denial.
The revised regulation allows officials to consider previously excluded programs in their determination, including nonemergency Medicaid, the Supplemental Nutrition Assistance Program, and several housing programs. Use of these programs for more than 12 months in the aggregate during a 36-month period may result in a “public charge” designation and lead to green card denial.
Eight legal challenges were immediately filed against the rule changes, including a complaint issued by 14 states. At least five trial courts have since blocked the measure, while appeals courts have lifted some of the injunctions and upheld enforcement.
In its Jan. 27 order lifting the nationwide injunction, Associate Justice Neil M. Gorsuch wrote that nationwide injunctions are being overused by trial courts with negative consequences.
“The real problem here is the increasingly common practice of trial courts ordering relief that transcends the cases before them. Whether framed as injunctions of ‘nationwide,’ ‘universal,’ or ‘cosmic’ scope, these orders share the same basic flaw – they direct how the defendant must act toward persons who are not parties to the case,” he wrote. “It has become increasingly apparent that this court must, at some point, confront these important objections to this increasingly widespread practice. As the brief and furious history of the regulation before us illustrates, the routine issuance of universal injunctions is patently unworkable, sowing chaos for litigants, the government, courts, and all those affected by these conflicting decisions.”
In the court’s Feb. 21 order lifting the injunction in Illinois, justices gave no explanation for overturning the lower court’s injunction. However, Associate Justice Sonia Sotomayor issued a sharply-worded dissent, criticizing her fellow justices for allowing the rule to proceed.
“In sum, the government’s only claimed hardship is that it must enforce an existing interpretation of an immigration rule in one state – just as it has done for the past 20 years – while an updated version of the rule takes effect in the remaining 49,” she wrote. “The government has not quantified or explained any burdens that would arise from this state of the world.”
ACA cases still in limbo
Meanwhile, the Supreme Court still has not decided whether it will hear Texas v. United States, a case that could effectively dismantle the Affordable Care Act.
The high court was expected to announce whether it would take the high-profile case at a private Feb. 21 conference, but the justices have released no update. The case was relisted for consideration at the court’s Feb. 28 conference.
Texas v. United States stems from a lawsuit by 20 Republican state attorneys general and governors that was filed after Congress zeroed out the ACA’s individual mandate penalty in 2017. The plaintiffs contend the now-valueless mandate is no longer constitutional and thus, the entire ACA should be struck down. Because the Trump administration declined to defend the law, a coalition of Democratic attorneys general and governors intervened in the case as defendants.
In 2018, a Texas district court ruled in favor of the plaintiffs and declared the entire health care law invalid. The 5th U.S. Circuit Court of Appeals partially affirmed the district court’s decision, ruling that the mandate was unconstitutional, but sending the case back to the lower court for more analysis on severability. The Democratic attorneys general and governors appealed the decision to the U.S. Supreme Court.
If the Supreme Court agrees to hear the challenge, the court could fast-track the case and schedule arguments for the current term or wait until its next term, which starts in October 2020. If justices decline to hear the case, the challenge will remain with the district court for more analysis about the law’s severability.
Another ACA-related case – Maine Community Health Options v. U.S. – also remains in limbo. Justices heard the case, which was consolidated with two similar challenges, on Dec. 10, 2019, but still have not issued a decision.
The consolidated challenges center on whether the federal government owes insurers billions based on an Affordable Care Act provision intended to help health plans mitigate risk under the law. The ACA’s risk corridor program required the U.S. Department of Health & Human Services to collect funds from profitable insurers that offered qualified health plans under the exchanges and distribute the funds to insurers with excessive losses. Collections from profitable insurers under the program fell short in 2014, 2015, and 2016, while losses steadily grew, resulting in the HHS paying about 12 cents on the dollar in payments to insurers. More than 150 insurers now allege they were shortchanged and they want the Supreme Court to force the government to reimburse them to the tune of $12 billion.
The Department of Justice counters that the government is not required to pay the insurers because of appropriations measures passed by Congress in 2014 and in later years that limited the funding available to compensate insurers for their losses.
The federal government and insurers have each experienced wins and losses at the lower court level. Most recently, the U.S. Court of Appeals for the Federal Circuit decided in favor of the government, ruling that while the ACA required the government to compensate the insurers for their losses, the appropriations measures repealed or suspended that requirement.
A Supreme Court decision in the case could come as soon as Feb. 26.
Court to hear women’s health cases
Two closely watched reproductive health cases will go before the court this spring.
On March 4, justices will hear oral arguments in June Medical Services v. Russo, regarding the constitutionality of a Louisiana law that requires physicians performing abortions to have admitting privileges at a nearby hospital. Doctors who perform abortions without admitting privileges at a hospital within 30 miles face fines and imprisonment, according to the state law, originally passed in 2014. Clinics that employ such doctors can also have their licenses revoked.
June Medical Services LLC, a women’s health clinic, sued over the law. A district court ruled in favor of the plaintiff, but the 5th U.S. Circuit Court of Appeals reversed and upheld Louisiana’s law. The clinic appealed to the U.S. Supreme Court. Louisiana officials argue the challenge should be dismissed, and the law allowed to proceed, because the plaintiffs lack standing.
The Supreme Court in 2016 heard a similar case – Whole Woman’s Health v. Hellerstedt – concerning a comparable law in Texas. In that case, justices struck down the measure as unconstitutional.
And on April 29, justices will hear arguments in Little Sisters of the Poor v. Pennsylvania, a consolidated case about whether the Trump administration acted properly when it expanded exemptions under the Affordable Care Act’s contraceptive mandate. Entities that object to providing contraception on the basis of religious beliefs can opt out of complying with the mandate, according to the 2018 regulations. Additionally, nonprofit organizations and small businesses that have nonreligious moral convictions against the mandate can skip compliance. A number of states and entities sued over the new rules.
A federal appeals court temporarily barred the regulations from moving forward, ruling the plaintiffs were likely to succeed in proving the Trump administration did not follow appropriate procedures when it promulgated the new rules and that the regulations were not authorized under the ACA.
Justices will decide whether the parties have standing in the case, whether the Trump administration followed correct rule-making procedures, and if the regulations can stand.
The Trump administration can move forward with expanding a rule that makes it more difficult for immigrants to remain in the United States if they receive health care assistance, the U.S. Supreme Court ruled in a 5-4 vote.
The Feb. 21 order allows the administration to broaden the so-called “public charge rule” while legal challenges against the expanded regulation continue in the lower courts. The Supreme Court’s decision, which lifts a preliminary injunction against the expansion, applies to enforcement only in Illinois, where a district court blocked the revised rule from moving forward in October 2019. The Supreme Court’s measure follows another 5-4 order in January, in which justices lifted a nationwide injunction against the revised rule.
Under the long-standing public charge rule, immigration officials can refuse to admit immigrants into the United States or can deny them permanent legal status if they are deemed likely to become a public charge. Previously, immigration officers considered cash aid, such as Temporary Assistance for Needy Families or long-term institutionalized care, as potential public charge reasons for denial.
The revised regulation allows officials to consider previously excluded programs in their determination, including nonemergency Medicaid, the Supplemental Nutrition Assistance Program, and several housing programs. Use of these programs for more than 12 months in the aggregate during a 36-month period may result in a “public charge” designation and lead to green card denial.
Eight legal challenges were immediately filed against the rule changes, including a complaint issued by 14 states. At least five trial courts have since blocked the measure, while appeals courts have lifted some of the injunctions and upheld enforcement.
In its Jan. 27 order lifting the nationwide injunction, Associate Justice Neil M. Gorsuch wrote that nationwide injunctions are being overused by trial courts with negative consequences.
“The real problem here is the increasingly common practice of trial courts ordering relief that transcends the cases before them. Whether framed as injunctions of ‘nationwide,’ ‘universal,’ or ‘cosmic’ scope, these orders share the same basic flaw – they direct how the defendant must act toward persons who are not parties to the case,” he wrote. “It has become increasingly apparent that this court must, at some point, confront these important objections to this increasingly widespread practice. As the brief and furious history of the regulation before us illustrates, the routine issuance of universal injunctions is patently unworkable, sowing chaos for litigants, the government, courts, and all those affected by these conflicting decisions.”
In the court’s Feb. 21 order lifting the injunction in Illinois, justices gave no explanation for overturning the lower court’s injunction. However, Associate Justice Sonia Sotomayor issued a sharply-worded dissent, criticizing her fellow justices for allowing the rule to proceed.
“In sum, the government’s only claimed hardship is that it must enforce an existing interpretation of an immigration rule in one state – just as it has done for the past 20 years – while an updated version of the rule takes effect in the remaining 49,” she wrote. “The government has not quantified or explained any burdens that would arise from this state of the world.”
ACA cases still in limbo
Meanwhile, the Supreme Court still has not decided whether it will hear Texas v. United States, a case that could effectively dismantle the Affordable Care Act.
The high court was expected to announce whether it would take the high-profile case at a private Feb. 21 conference, but the justices have released no update. The case was relisted for consideration at the court’s Feb. 28 conference.
Texas v. United States stems from a lawsuit by 20 Republican state attorneys general and governors that was filed after Congress zeroed out the ACA’s individual mandate penalty in 2017. The plaintiffs contend the now-valueless mandate is no longer constitutional and thus, the entire ACA should be struck down. Because the Trump administration declined to defend the law, a coalition of Democratic attorneys general and governors intervened in the case as defendants.
In 2018, a Texas district court ruled in favor of the plaintiffs and declared the entire health care law invalid. The 5th U.S. Circuit Court of Appeals partially affirmed the district court’s decision, ruling that the mandate was unconstitutional, but sending the case back to the lower court for more analysis on severability. The Democratic attorneys general and governors appealed the decision to the U.S. Supreme Court.
If the Supreme Court agrees to hear the challenge, the court could fast-track the case and schedule arguments for the current term or wait until its next term, which starts in October 2020. If justices decline to hear the case, the challenge will remain with the district court for more analysis about the law’s severability.
Another ACA-related case – Maine Community Health Options v. U.S. – also remains in limbo. Justices heard the case, which was consolidated with two similar challenges, on Dec. 10, 2019, but still have not issued a decision.
The consolidated challenges center on whether the federal government owes insurers billions based on an Affordable Care Act provision intended to help health plans mitigate risk under the law. The ACA’s risk corridor program required the U.S. Department of Health & Human Services to collect funds from profitable insurers that offered qualified health plans under the exchanges and distribute the funds to insurers with excessive losses. Collections from profitable insurers under the program fell short in 2014, 2015, and 2016, while losses steadily grew, resulting in the HHS paying about 12 cents on the dollar in payments to insurers. More than 150 insurers now allege they were shortchanged and they want the Supreme Court to force the government to reimburse them to the tune of $12 billion.
The Department of Justice counters that the government is not required to pay the insurers because of appropriations measures passed by Congress in 2014 and in later years that limited the funding available to compensate insurers for their losses.
The federal government and insurers have each experienced wins and losses at the lower court level. Most recently, the U.S. Court of Appeals for the Federal Circuit decided in favor of the government, ruling that while the ACA required the government to compensate the insurers for their losses, the appropriations measures repealed or suspended that requirement.
A Supreme Court decision in the case could come as soon as Feb. 26.
Court to hear women’s health cases
Two closely watched reproductive health cases will go before the court this spring.
On March 4, justices will hear oral arguments in June Medical Services v. Russo, regarding the constitutionality of a Louisiana law that requires physicians performing abortions to have admitting privileges at a nearby hospital. Doctors who perform abortions without admitting privileges at a hospital within 30 miles face fines and imprisonment, according to the state law, originally passed in 2014. Clinics that employ such doctors can also have their licenses revoked.
June Medical Services LLC, a women’s health clinic, sued over the law. A district court ruled in favor of the plaintiff, but the 5th U.S. Circuit Court of Appeals reversed and upheld Louisiana’s law. The clinic appealed to the U.S. Supreme Court. Louisiana officials argue the challenge should be dismissed, and the law allowed to proceed, because the plaintiffs lack standing.
The Supreme Court in 2016 heard a similar case – Whole Woman’s Health v. Hellerstedt – concerning a comparable law in Texas. In that case, justices struck down the measure as unconstitutional.
And on April 29, justices will hear arguments in Little Sisters of the Poor v. Pennsylvania, a consolidated case about whether the Trump administration acted properly when it expanded exemptions under the Affordable Care Act’s contraceptive mandate. Entities that object to providing contraception on the basis of religious beliefs can opt out of complying with the mandate, according to the 2018 regulations. Additionally, nonprofit organizations and small businesses that have nonreligious moral convictions against the mandate can skip compliance. A number of states and entities sued over the new rules.
A federal appeals court temporarily barred the regulations from moving forward, ruling the plaintiffs were likely to succeed in proving the Trump administration did not follow appropriate procedures when it promulgated the new rules and that the regulations were not authorized under the ACA.
Justices will decide whether the parties have standing in the case, whether the Trump administration followed correct rule-making procedures, and if the regulations can stand.
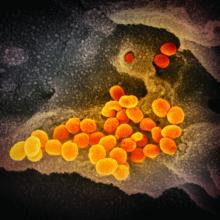
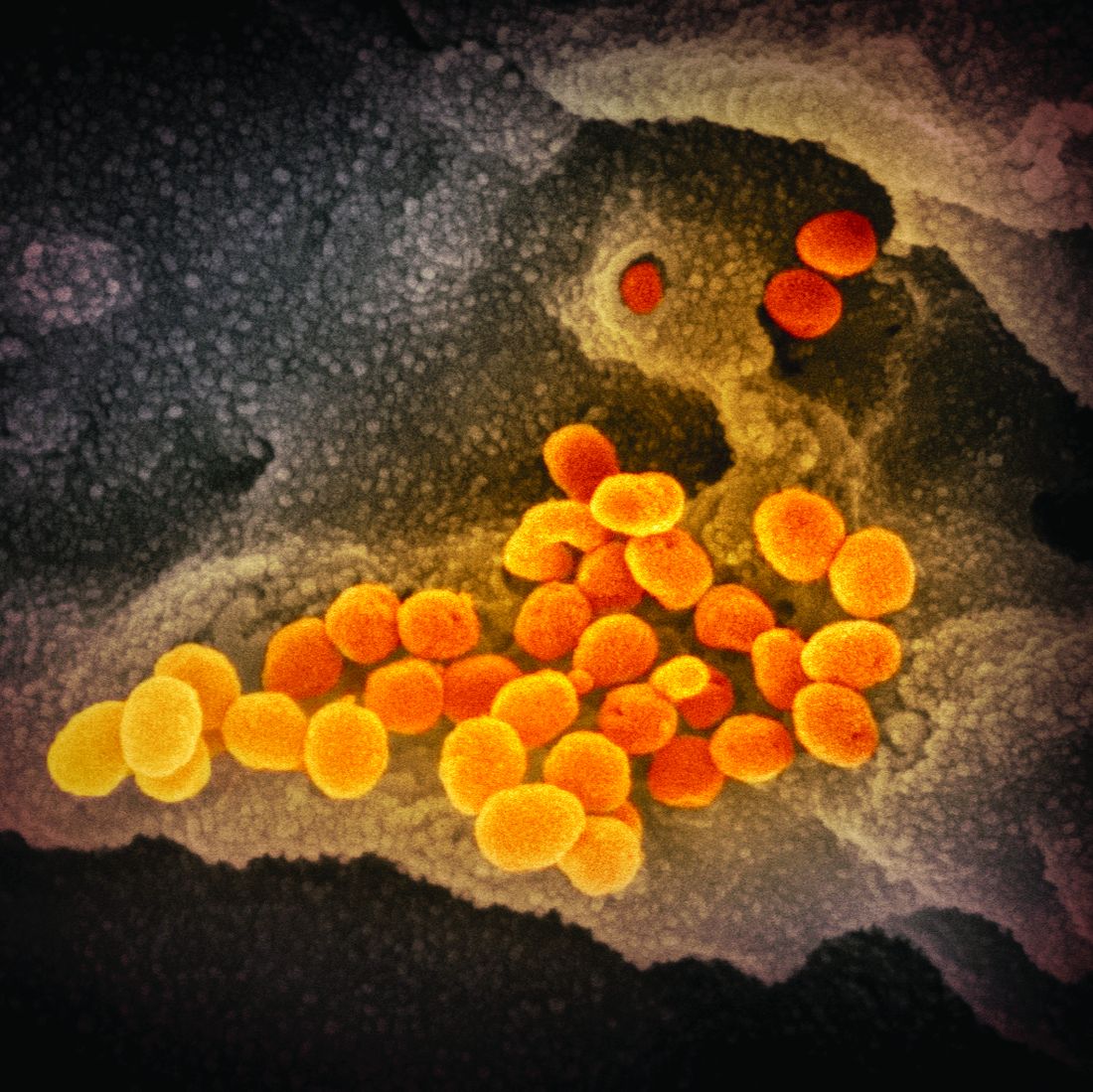
COVID-19: Time to ‘take the risk of scaring people’
It’s past time to call the novel coronavirus, COVID-19, a pandemic and “time to push people to prepare, and guide their prep,” according to risk communication experts.
Medical messaging about containing or stopping the spread of the virus is doing more harm than good, write Peter Sandman, PhD, and Jody Lanard, MD, both based in New York City, in a recent blog post.
“We are near-certain that the desperate-sounding last-ditch containment messaging of recent days is contributing to a massive global misperception,” they warn.
“The most crucial (and overdue) risk communication task … is to help people visualize their communities when ‘keeping it out’ – containment – is no longer relevant.”
That message is embraced by several experts who spoke to Medscape Medical News.
“I’m jealous of what [they] have written: It is so clear, so correct, and so practical,” said David Fisman, MD, MPH, professor of epidemiology at the University of Toronto, Canada. “I think WHO [World Health Organization] is shying away from the P word,” he continued, referring to the organization’s continuing decision not to call the outbreak a pandemic.
“I fully support exactly what [Sandman and Lanard] are saying,” said Michael Osterholm, PhD, MPH, professor of environmental health sciences and director of the Center for Infectious Disease Research and Policy (CIDRAP) at the University of Minnesota in Minneapolis.
Sandman and Lanard write. “Hardly any officials are telling civil society and the general public how to get ready for this pandemic.”
Effective communication should inform people of what to expect now, they continue: “[T]he end of most quarantines, travel restrictions, contact tracing, and other measures designed to keep ‘them’ from infecting ‘us,’ and the switch to measures like canceling mass events designed to keep us from infecting each other.”
Among the new messages that should be delivered are things like:
- Stockpiling nonperishable food and prescription meds.
- Considering care of sick family members.
- Cross-training work personnel so one person’s absence won’t derail an organization’s ability to function.
“We hope that governments and healthcare institutions are using this time wisely,” Sandman and Lanard continue. “We know that ordinary citizens are not being asked to do so. In most countries … ordinary citizens have not been asked to prepare. Instead, they have been led to expect that their governments will keep the virus from their doors.”
This article first appeared on Medscape.com.
It’s past time to call the novel coronavirus, COVID-19, a pandemic and “time to push people to prepare, and guide their prep,” according to risk communication experts.
Medical messaging about containing or stopping the spread of the virus is doing more harm than good, write Peter Sandman, PhD, and Jody Lanard, MD, both based in New York City, in a recent blog post.
“We are near-certain that the desperate-sounding last-ditch containment messaging of recent days is contributing to a massive global misperception,” they warn.
“The most crucial (and overdue) risk communication task … is to help people visualize their communities when ‘keeping it out’ – containment – is no longer relevant.”
That message is embraced by several experts who spoke to Medscape Medical News.
“I’m jealous of what [they] have written: It is so clear, so correct, and so practical,” said David Fisman, MD, MPH, professor of epidemiology at the University of Toronto, Canada. “I think WHO [World Health Organization] is shying away from the P word,” he continued, referring to the organization’s continuing decision not to call the outbreak a pandemic.
“I fully support exactly what [Sandman and Lanard] are saying,” said Michael Osterholm, PhD, MPH, professor of environmental health sciences and director of the Center for Infectious Disease Research and Policy (CIDRAP) at the University of Minnesota in Minneapolis.
Sandman and Lanard write. “Hardly any officials are telling civil society and the general public how to get ready for this pandemic.”
Effective communication should inform people of what to expect now, they continue: “[T]he end of most quarantines, travel restrictions, contact tracing, and other measures designed to keep ‘them’ from infecting ‘us,’ and the switch to measures like canceling mass events designed to keep us from infecting each other.”
Among the new messages that should be delivered are things like:
- Stockpiling nonperishable food and prescription meds.
- Considering care of sick family members.
- Cross-training work personnel so one person’s absence won’t derail an organization’s ability to function.
“We hope that governments and healthcare institutions are using this time wisely,” Sandman and Lanard continue. “We know that ordinary citizens are not being asked to do so. In most countries … ordinary citizens have not been asked to prepare. Instead, they have been led to expect that their governments will keep the virus from their doors.”
This article first appeared on Medscape.com.
It’s past time to call the novel coronavirus, COVID-19, a pandemic and “time to push people to prepare, and guide their prep,” according to risk communication experts.
Medical messaging about containing or stopping the spread of the virus is doing more harm than good, write Peter Sandman, PhD, and Jody Lanard, MD, both based in New York City, in a recent blog post.
“We are near-certain that the desperate-sounding last-ditch containment messaging of recent days is contributing to a massive global misperception,” they warn.
“The most crucial (and overdue) risk communication task … is to help people visualize their communities when ‘keeping it out’ – containment – is no longer relevant.”
That message is embraced by several experts who spoke to Medscape Medical News.
“I’m jealous of what [they] have written: It is so clear, so correct, and so practical,” said David Fisman, MD, MPH, professor of epidemiology at the University of Toronto, Canada. “I think WHO [World Health Organization] is shying away from the P word,” he continued, referring to the organization’s continuing decision not to call the outbreak a pandemic.
“I fully support exactly what [Sandman and Lanard] are saying,” said Michael Osterholm, PhD, MPH, professor of environmental health sciences and director of the Center for Infectious Disease Research and Policy (CIDRAP) at the University of Minnesota in Minneapolis.
Sandman and Lanard write. “Hardly any officials are telling civil society and the general public how to get ready for this pandemic.”
Effective communication should inform people of what to expect now, they continue: “[T]he end of most quarantines, travel restrictions, contact tracing, and other measures designed to keep ‘them’ from infecting ‘us,’ and the switch to measures like canceling mass events designed to keep us from infecting each other.”
Among the new messages that should be delivered are things like:
- Stockpiling nonperishable food and prescription meds.
- Considering care of sick family members.
- Cross-training work personnel so one person’s absence won’t derail an organization’s ability to function.
“We hope that governments and healthcare institutions are using this time wisely,” Sandman and Lanard continue. “We know that ordinary citizens are not being asked to do so. In most countries … ordinary citizens have not been asked to prepare. Instead, they have been led to expect that their governments will keep the virus from their doors.”
This article first appeared on Medscape.com.
FDA okays first generic of ProAir HFA
Generic albuterol sulfate inhalation, from Perrigo Pharmaceutical, is indicated for the treatment or prevention of bronchospasm in people aged 4 years or older who have reversible obstructive airway disease, as well as for the prevention of exercise-induced bronchospasm.
“Approval of the first generic drug product for one of the most commonly used rescue inhalers in the US is part of our long-standing commitment to advance patient access to lower-cost, high-quality generic drug products that are as safe and effective as their brand name counterparts, and to expand opportunities to bring generic copies of complex drugs to the market,” FDA Commissioner Stephen Hahn, MD, said in a news release.
Metered-dose inhalers are hard to duplicate because of the complexities of their formulation or mode of delivery. “As a result, too many complex drugs lack generic competition even after patents and exclusivities no longer block generic approval,” he explained.
“Supporting development and approval of generic copies of these complex medicines so that these products can get to patients has been a major focus of our efforts to improve competition and access and to lower drug prices. Getting more generic copies of complex drugs to the market is a key priority for how we’ll help bring new savings to consumers,” Hahn added.
In the United States, more than 26 million people suffer from asthma; about 7 million of these people are children.
Perrigo said it will immediately launch a limited quantity of generic albuterol sulfate and, in collaboration with its development and manufacturing partner, Catalent Pharma Solutions, is ramping up production to meet future demand.
The company “anticipates that we will be in a position to provide a steady supply of this product by the fourth quarter of 2020,” Perrigo Executive Vice President and Rx Pharmaceuticals President Sharon Kochan said in a statement.
This article originally appeared on Medscape.com.
Generic albuterol sulfate inhalation, from Perrigo Pharmaceutical, is indicated for the treatment or prevention of bronchospasm in people aged 4 years or older who have reversible obstructive airway disease, as well as for the prevention of exercise-induced bronchospasm.
“Approval of the first generic drug product for one of the most commonly used rescue inhalers in the US is part of our long-standing commitment to advance patient access to lower-cost, high-quality generic drug products that are as safe and effective as their brand name counterparts, and to expand opportunities to bring generic copies of complex drugs to the market,” FDA Commissioner Stephen Hahn, MD, said in a news release.
Metered-dose inhalers are hard to duplicate because of the complexities of their formulation or mode of delivery. “As a result, too many complex drugs lack generic competition even after patents and exclusivities no longer block generic approval,” he explained.
“Supporting development and approval of generic copies of these complex medicines so that these products can get to patients has been a major focus of our efforts to improve competition and access and to lower drug prices. Getting more generic copies of complex drugs to the market is a key priority for how we’ll help bring new savings to consumers,” Hahn added.
In the United States, more than 26 million people suffer from asthma; about 7 million of these people are children.
Perrigo said it will immediately launch a limited quantity of generic albuterol sulfate and, in collaboration with its development and manufacturing partner, Catalent Pharma Solutions, is ramping up production to meet future demand.
The company “anticipates that we will be in a position to provide a steady supply of this product by the fourth quarter of 2020,” Perrigo Executive Vice President and Rx Pharmaceuticals President Sharon Kochan said in a statement.
This article originally appeared on Medscape.com.
Generic albuterol sulfate inhalation, from Perrigo Pharmaceutical, is indicated for the treatment or prevention of bronchospasm in people aged 4 years or older who have reversible obstructive airway disease, as well as for the prevention of exercise-induced bronchospasm.
“Approval of the first generic drug product for one of the most commonly used rescue inhalers in the US is part of our long-standing commitment to advance patient access to lower-cost, high-quality generic drug products that are as safe and effective as their brand name counterparts, and to expand opportunities to bring generic copies of complex drugs to the market,” FDA Commissioner Stephen Hahn, MD, said in a news release.
Metered-dose inhalers are hard to duplicate because of the complexities of their formulation or mode of delivery. “As a result, too many complex drugs lack generic competition even after patents and exclusivities no longer block generic approval,” he explained.
“Supporting development and approval of generic copies of these complex medicines so that these products can get to patients has been a major focus of our efforts to improve competition and access and to lower drug prices. Getting more generic copies of complex drugs to the market is a key priority for how we’ll help bring new savings to consumers,” Hahn added.
In the United States, more than 26 million people suffer from asthma; about 7 million of these people are children.
Perrigo said it will immediately launch a limited quantity of generic albuterol sulfate and, in collaboration with its development and manufacturing partner, Catalent Pharma Solutions, is ramping up production to meet future demand.
The company “anticipates that we will be in a position to provide a steady supply of this product by the fourth quarter of 2020,” Perrigo Executive Vice President and Rx Pharmaceuticals President Sharon Kochan said in a statement.
This article originally appeared on Medscape.com.
CDC expects eventual community spread of coronavirus in U.S.
“We have for many weeks been saying that, while we hope this is not going to be severe, we are planning as if it is,” Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the CDC, said during a Feb. 25, 2020, telebriefing with reporters. “The data over the last week and the spread in other countries has certainly raised our level of concern and raised our level expectation that we are going to have community spread here.”
Dr. Messonnier noted that the coronavirus is now showing signs of community spread without a known source of exposure in a number of countries, including in Hong Kong, Iran, Italy, Japan, Singapore, South Korea, Taiwan, and Thailand. This has now raised the belief that there will be more widespread outbreaks in the United States.
“What we still don’t know is what that will look like,” she said. “As many of you know, we can have community spread in the United States and have it be reasonably mild. We can have community spread in the U.S. and have it be very severe. That is what we don’t completely know yet and we certainly also don’t exactly know when it is going to happen.”
She reiterated the number of actions being taken to slow the potential spread in the United States, including detecting, tracking, and isolating all cases, as well as restricting travel into the United States and issuing travel advisories for countries where coronavirus outbreaks are known.
“We are doing this with the goal of slowing the introduction of this new virus into the U.S. and buying us more time to prepare,” Dr. Messonnier said, noting the containment strategies have been largely successful, though it will be more difficult as more countries experience community spread of the virus.
Dr. Messonnier also reiterated that at this time there are no vaccines and no medicines to treat the coronavirus. She stressed the need to adhere to nonpharmaceutical interventions (NPIs), as they will be “the most important tools in our response to this virus.”
She said the NPIs will vary based on the severity of the outbreak in any given local community and include personal protective measures that individuals can take every day (many of which mirror the recommendations for preventing the spread of the seasonal flu virus), community NPIs that involve social distancing measures designed to keep people away from others, and environmental NPIs such as surface cleaning measures.
CDC’s latest warning comes as parent agency the Department of Health & Human Services is seeking $2.5 billion in funds from Congress to address the coronavirus outbreak.
During a separate press conference on the same day, HHS Secretary Alex Azar noted that there are five major priorities related to those funds, which would be used in the current year, including expansion of surveillance work within the influenza surveillance network; supporting public health preparedness and response for state and local governments; support the development of therapeutics and the development of vaccines; and the purchase of personal protective equipment for national stockpiles.
Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Disease at the National Institutes of Health, added during the press conference that vaccine work is in progress and could be ready for phase 1 testing within a month and a half. If all goes well, it would still be at least 12 - 18 months following the completion of a phase 2 trial before it could be produced for mass consumption.
“It is certainly conceivable that this issue with this coronavirus will go well beyond this season into next season,” Dr. Fauci said. “So a vaccine may not solve the problems of the next couple of months, but it certainly would be an important tool that we would have and we will keep you posted on that.”
He also mentioned that NIAID is looking at a number of candidates for therapeutic treatment of coronavirus. He highlighted Gilead’s remdesivir, a nucleotide analog, as one which undergoing two trials – a randomized controlled trial in China and a copy of that trial in Nebraska among patients with the coronavirus who were taken from the Diamond Princess cruise line in Japan.
“I am optimistic that we will at least get an answer if we do have do have a therapy that really is a gamechanger because then we could do something from the standpoint of intervention for those who are sick,” Dr. Fauci said.
UPDATE: This story was updated 2/25 at 4:51 p.m. ET
“We have for many weeks been saying that, while we hope this is not going to be severe, we are planning as if it is,” Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the CDC, said during a Feb. 25, 2020, telebriefing with reporters. “The data over the last week and the spread in other countries has certainly raised our level of concern and raised our level expectation that we are going to have community spread here.”
Dr. Messonnier noted that the coronavirus is now showing signs of community spread without a known source of exposure in a number of countries, including in Hong Kong, Iran, Italy, Japan, Singapore, South Korea, Taiwan, and Thailand. This has now raised the belief that there will be more widespread outbreaks in the United States.
“What we still don’t know is what that will look like,” she said. “As many of you know, we can have community spread in the United States and have it be reasonably mild. We can have community spread in the U.S. and have it be very severe. That is what we don’t completely know yet and we certainly also don’t exactly know when it is going to happen.”
She reiterated the number of actions being taken to slow the potential spread in the United States, including detecting, tracking, and isolating all cases, as well as restricting travel into the United States and issuing travel advisories for countries where coronavirus outbreaks are known.
“We are doing this with the goal of slowing the introduction of this new virus into the U.S. and buying us more time to prepare,” Dr. Messonnier said, noting the containment strategies have been largely successful, though it will be more difficult as more countries experience community spread of the virus.
Dr. Messonnier also reiterated that at this time there are no vaccines and no medicines to treat the coronavirus. She stressed the need to adhere to nonpharmaceutical interventions (NPIs), as they will be “the most important tools in our response to this virus.”
She said the NPIs will vary based on the severity of the outbreak in any given local community and include personal protective measures that individuals can take every day (many of which mirror the recommendations for preventing the spread of the seasonal flu virus), community NPIs that involve social distancing measures designed to keep people away from others, and environmental NPIs such as surface cleaning measures.
CDC’s latest warning comes as parent agency the Department of Health & Human Services is seeking $2.5 billion in funds from Congress to address the coronavirus outbreak.
During a separate press conference on the same day, HHS Secretary Alex Azar noted that there are five major priorities related to those funds, which would be used in the current year, including expansion of surveillance work within the influenza surveillance network; supporting public health preparedness and response for state and local governments; support the development of therapeutics and the development of vaccines; and the purchase of personal protective equipment for national stockpiles.
Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Disease at the National Institutes of Health, added during the press conference that vaccine work is in progress and could be ready for phase 1 testing within a month and a half. If all goes well, it would still be at least 12 - 18 months following the completion of a phase 2 trial before it could be produced for mass consumption.
“It is certainly conceivable that this issue with this coronavirus will go well beyond this season into next season,” Dr. Fauci said. “So a vaccine may not solve the problems of the next couple of months, but it certainly would be an important tool that we would have and we will keep you posted on that.”
He also mentioned that NIAID is looking at a number of candidates for therapeutic treatment of coronavirus. He highlighted Gilead’s remdesivir, a nucleotide analog, as one which undergoing two trials – a randomized controlled trial in China and a copy of that trial in Nebraska among patients with the coronavirus who were taken from the Diamond Princess cruise line in Japan.
“I am optimistic that we will at least get an answer if we do have do have a therapy that really is a gamechanger because then we could do something from the standpoint of intervention for those who are sick,” Dr. Fauci said.
UPDATE: This story was updated 2/25 at 4:51 p.m. ET
“We have for many weeks been saying that, while we hope this is not going to be severe, we are planning as if it is,” Nancy Messonnier, MD, director of the National Center for Immunization and Respiratory Diseases at the CDC, said during a Feb. 25, 2020, telebriefing with reporters. “The data over the last week and the spread in other countries has certainly raised our level of concern and raised our level expectation that we are going to have community spread here.”
Dr. Messonnier noted that the coronavirus is now showing signs of community spread without a known source of exposure in a number of countries, including in Hong Kong, Iran, Italy, Japan, Singapore, South Korea, Taiwan, and Thailand. This has now raised the belief that there will be more widespread outbreaks in the United States.
“What we still don’t know is what that will look like,” she said. “As many of you know, we can have community spread in the United States and have it be reasonably mild. We can have community spread in the U.S. and have it be very severe. That is what we don’t completely know yet and we certainly also don’t exactly know when it is going to happen.”
She reiterated the number of actions being taken to slow the potential spread in the United States, including detecting, tracking, and isolating all cases, as well as restricting travel into the United States and issuing travel advisories for countries where coronavirus outbreaks are known.
“We are doing this with the goal of slowing the introduction of this new virus into the U.S. and buying us more time to prepare,” Dr. Messonnier said, noting the containment strategies have been largely successful, though it will be more difficult as more countries experience community spread of the virus.
Dr. Messonnier also reiterated that at this time there are no vaccines and no medicines to treat the coronavirus. She stressed the need to adhere to nonpharmaceutical interventions (NPIs), as they will be “the most important tools in our response to this virus.”
She said the NPIs will vary based on the severity of the outbreak in any given local community and include personal protective measures that individuals can take every day (many of which mirror the recommendations for preventing the spread of the seasonal flu virus), community NPIs that involve social distancing measures designed to keep people away from others, and environmental NPIs such as surface cleaning measures.
CDC’s latest warning comes as parent agency the Department of Health & Human Services is seeking $2.5 billion in funds from Congress to address the coronavirus outbreak.
During a separate press conference on the same day, HHS Secretary Alex Azar noted that there are five major priorities related to those funds, which would be used in the current year, including expansion of surveillance work within the influenza surveillance network; supporting public health preparedness and response for state and local governments; support the development of therapeutics and the development of vaccines; and the purchase of personal protective equipment for national stockpiles.
Anthony S. Fauci, MD, director of the National Institute of Allergy and Infectious Disease at the National Institutes of Health, added during the press conference that vaccine work is in progress and could be ready for phase 1 testing within a month and a half. If all goes well, it would still be at least 12 - 18 months following the completion of a phase 2 trial before it could be produced for mass consumption.
“It is certainly conceivable that this issue with this coronavirus will go well beyond this season into next season,” Dr. Fauci said. “So a vaccine may not solve the problems of the next couple of months, but it certainly would be an important tool that we would have and we will keep you posted on that.”
He also mentioned that NIAID is looking at a number of candidates for therapeutic treatment of coronavirus. He highlighted Gilead’s remdesivir, a nucleotide analog, as one which undergoing two trials – a randomized controlled trial in China and a copy of that trial in Nebraska among patients with the coronavirus who were taken from the Diamond Princess cruise line in Japan.
“I am optimistic that we will at least get an answer if we do have do have a therapy that really is a gamechanger because then we could do something from the standpoint of intervention for those who are sick,” Dr. Fauci said.
UPDATE: This story was updated 2/25 at 4:51 p.m. ET
ID Blog: SARS-CoV-2 – What’s in a name?
Coming up with a moniker for the new coronavirus shows the perils of naming names.
There is no Baby Book of Names or hurricane alphabet to readily name diseases and their causal entities. Throughout history and even in the modern era, a host of considerations have intruded on the decision as to what to call these blights upon humanity. Names have varied from inflammatory to misleading, from colloquial to scientific. And when it concerns a new epidemiological entity such as the latest coronavirus outbreak originating in China, health organizations, media, politicians, scientific taxonomy commissions, and the public at large all have a stake in the naming.
From “Wuhan virus” to “novel coronavirus-2019” to “COVID-19 virus,” the name of the new coronavirus that first appeared in China has been evolving to its now official designation: SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2). But where did the final name come from, how does such a name become official, and who makes it so?
Virus taxonomy
The Coronavirus Study Group (CSG) of the International Committee on Taxonomy of Viruses (ICTV) named the new coronavirus SARS-CoV-2 based upon its genetic relationship to the original SARS-CoV that caused an outbreak of disease in 2002–2003.
According to the ICTV website, the first internationally organized attempts to introduce order into the bewildering variety of viruses took place at the International Congress of Microbiology held in Moscow in 1966 where a committee was created that later became the ICTV and was given the task of developing a single, universal taxonomic scheme for all the viruses infecting animals, plants, fungi, bacteria, and archaea. The ICTV was created as a committee of the virology division of the International Union of Microbiological Societies and is governed by statutes approved by the virology division. Virus classification and nomenclature are subject to rules set out in an International Code.
These designate that: “The universal virus classification system shall employ the hierarchical levels of realm, subrealm, kingdom, subkingdom, phylum, subphylum, class, subclass, order, suborder, family, subfamily, genus, subgenus and species.”
Many of the topmost areas of classification are based on whether the viruses are DNA or RNA, single or double stranded, and have a simple protein shell or a complex lipoprotein envelope. Other levels of classification include host species, type of replication, and type of diseases they cause, the later exemplified in the SARS designation for this virus.
There are 98 international study groups (SGs) covering all major virus orders, families, and genera that are part of the ICTV, and it was the one dedicated to the single-stranded RNA coronaviruses, the CSG, that came up with the SARS-CoV-2 name and first referenced it in their Feb 11 publication in the Cold Springs Harbor preprint journal bioRxiv.
“Based on phylogeny, taxonomy and established practice, the CSG formally recognizes this virus as a sister to severe acute respiratory syndrome coronaviruses (SARS-CoVs) of the species severe acute respiratory syndrome–related coronavirus and designates it as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2),” they wrote.
According to the National Center for Biotechnology Information Taxonomy Browser, with respect to the original SARS CoV virus, of which this is a relative, the full taxonomic designation is: Viruses, Riboviria, Nidovirales, Cornidovirineae, Coronaviridae, Orthocoronavirinae, Betacoronavirus, Sarbecovirus.
The problem with naming names
The World Health Organization currently is not using the official scientific name of the virus, but rather is merely labeling it with regard to the disease: COVID-19, which simply refers to coronavirus disease 2019.
They are following a modern standard by which disease names avoid inflammatory connotations with people and places. Too often in the past from syphilis as the “French pox,” the 1918 influenza as the “Spanish flu,” AIDS as the “gay plague,” Middle East Respiratory Syndrome (MERS), and the currently named “WuFlu,” which made an appearance early in the new outbreak and which is symbolic of a sudden wave of anti-Asian, and specifically Chinese, prejudice.
Chinatown districts even in the United States are being affected economically through unwarranted fear associated with the virus. And there have been equivalently virulent outbreaks of hate speech against Asian individuals in places untouched by the new virus.
However, although SARS-CoV-2 as a name avoids such problems, different considerations led the WHO to reject it in its discussions, determining that its use ties it to tightly to the much more deadly SARS-CoV-1 virus in the public mind, risking greater fear and panic, especially in Asia, where SARS-CoV-1 had the biggest impact.
Back in 1896, William Sykes, MD, writing in the first flush of the triumph of germ theory in modern medicine, attempted to give some guidance to how medical science should best come up with new names of diseases by merging the demands of common parlance with those of taxonomic legitimacy. His “On the Origin and History of Disease-Names,” published in the Lancet, had clearcut advice: “It is vain to attempt to replace a folk name or one widely adopted by the people by a new one deliberately coined by scholars, and this for the following reasons: first, whatever names may be accepted by medical men must be translated by them into the vernacular of their patients, and by a resulting reaction the vernacular name comes to be the commoner one with themselves; and, secondly, there is no continuity or unchangeableness in the terms invented by savants, which are amended, improved upon, and displaced by the next writer on the subject, or, even more absurdly still, by the very inventors themselves in a subsequent publication.”
This is the reason that virus taxonomy provides names based upon unchangeable scientific descriptors of the actual disease causing entity, as illustrated by the decisions of the ICTV. In addition, the genomic sequences being provided by the scientific community are all being organized under the SARS-CoV-2 name and thus are cementing that moniker as the only acceptable scientific one.
Whether the rest of the world universally adopts SARS-CoV-2 as a name is still in question. If the outbreak spreads significantly beyond its current limits, fear and confusion – and simply the need for a more familiar-sounding label – may lead the general public to adopt more colloquial designations than those that science attempts to impose, as Dr. Sykes suggested back in 1896. That remains to be seen.
[email protected]
Mark Lesney is the managing editor of MDedge.com/IDPractioner. He has a PhD in plant virology and a PhD in the history of science, with a focus on the history of biotechnology and medicine. He has served as an adjunct assistant professor of the department of biochemistry and molecular & cellular biology at Georgetown University, Washington.
Coming up with a moniker for the new coronavirus shows the perils of naming names.
Coming up with a moniker for the new coronavirus shows the perils of naming names.
There is no Baby Book of Names or hurricane alphabet to readily name diseases and their causal entities. Throughout history and even in the modern era, a host of considerations have intruded on the decision as to what to call these blights upon humanity. Names have varied from inflammatory to misleading, from colloquial to scientific. And when it concerns a new epidemiological entity such as the latest coronavirus outbreak originating in China, health organizations, media, politicians, scientific taxonomy commissions, and the public at large all have a stake in the naming.
From “Wuhan virus” to “novel coronavirus-2019” to “COVID-19 virus,” the name of the new coronavirus that first appeared in China has been evolving to its now official designation: SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2). But where did the final name come from, how does such a name become official, and who makes it so?
Virus taxonomy
The Coronavirus Study Group (CSG) of the International Committee on Taxonomy of Viruses (ICTV) named the new coronavirus SARS-CoV-2 based upon its genetic relationship to the original SARS-CoV that caused an outbreak of disease in 2002–2003.
According to the ICTV website, the first internationally organized attempts to introduce order into the bewildering variety of viruses took place at the International Congress of Microbiology held in Moscow in 1966 where a committee was created that later became the ICTV and was given the task of developing a single, universal taxonomic scheme for all the viruses infecting animals, plants, fungi, bacteria, and archaea. The ICTV was created as a committee of the virology division of the International Union of Microbiological Societies and is governed by statutes approved by the virology division. Virus classification and nomenclature are subject to rules set out in an International Code.
These designate that: “The universal virus classification system shall employ the hierarchical levels of realm, subrealm, kingdom, subkingdom, phylum, subphylum, class, subclass, order, suborder, family, subfamily, genus, subgenus and species.”
Many of the topmost areas of classification are based on whether the viruses are DNA or RNA, single or double stranded, and have a simple protein shell or a complex lipoprotein envelope. Other levels of classification include host species, type of replication, and type of diseases they cause, the later exemplified in the SARS designation for this virus.
There are 98 international study groups (SGs) covering all major virus orders, families, and genera that are part of the ICTV, and it was the one dedicated to the single-stranded RNA coronaviruses, the CSG, that came up with the SARS-CoV-2 name and first referenced it in their Feb 11 publication in the Cold Springs Harbor preprint journal bioRxiv.
“Based on phylogeny, taxonomy and established practice, the CSG formally recognizes this virus as a sister to severe acute respiratory syndrome coronaviruses (SARS-CoVs) of the species severe acute respiratory syndrome–related coronavirus and designates it as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2),” they wrote.
According to the National Center for Biotechnology Information Taxonomy Browser, with respect to the original SARS CoV virus, of which this is a relative, the full taxonomic designation is: Viruses, Riboviria, Nidovirales, Cornidovirineae, Coronaviridae, Orthocoronavirinae, Betacoronavirus, Sarbecovirus.
The problem with naming names
The World Health Organization currently is not using the official scientific name of the virus, but rather is merely labeling it with regard to the disease: COVID-19, which simply refers to coronavirus disease 2019.
They are following a modern standard by which disease names avoid inflammatory connotations with people and places. Too often in the past from syphilis as the “French pox,” the 1918 influenza as the “Spanish flu,” AIDS as the “gay plague,” Middle East Respiratory Syndrome (MERS), and the currently named “WuFlu,” which made an appearance early in the new outbreak and which is symbolic of a sudden wave of anti-Asian, and specifically Chinese, prejudice.
Chinatown districts even in the United States are being affected economically through unwarranted fear associated with the virus. And there have been equivalently virulent outbreaks of hate speech against Asian individuals in places untouched by the new virus.
However, although SARS-CoV-2 as a name avoids such problems, different considerations led the WHO to reject it in its discussions, determining that its use ties it to tightly to the much more deadly SARS-CoV-1 virus in the public mind, risking greater fear and panic, especially in Asia, where SARS-CoV-1 had the biggest impact.
Back in 1896, William Sykes, MD, writing in the first flush of the triumph of germ theory in modern medicine, attempted to give some guidance to how medical science should best come up with new names of diseases by merging the demands of common parlance with those of taxonomic legitimacy. His “On the Origin and History of Disease-Names,” published in the Lancet, had clearcut advice: “It is vain to attempt to replace a folk name or one widely adopted by the people by a new one deliberately coined by scholars, and this for the following reasons: first, whatever names may be accepted by medical men must be translated by them into the vernacular of their patients, and by a resulting reaction the vernacular name comes to be the commoner one with themselves; and, secondly, there is no continuity or unchangeableness in the terms invented by savants, which are amended, improved upon, and displaced by the next writer on the subject, or, even more absurdly still, by the very inventors themselves in a subsequent publication.”
This is the reason that virus taxonomy provides names based upon unchangeable scientific descriptors of the actual disease causing entity, as illustrated by the decisions of the ICTV. In addition, the genomic sequences being provided by the scientific community are all being organized under the SARS-CoV-2 name and thus are cementing that moniker as the only acceptable scientific one.
Whether the rest of the world universally adopts SARS-CoV-2 as a name is still in question. If the outbreak spreads significantly beyond its current limits, fear and confusion – and simply the need for a more familiar-sounding label – may lead the general public to adopt more colloquial designations than those that science attempts to impose, as Dr. Sykes suggested back in 1896. That remains to be seen.
[email protected]
Mark Lesney is the managing editor of MDedge.com/IDPractioner. He has a PhD in plant virology and a PhD in the history of science, with a focus on the history of biotechnology and medicine. He has served as an adjunct assistant professor of the department of biochemistry and molecular & cellular biology at Georgetown University, Washington.
There is no Baby Book of Names or hurricane alphabet to readily name diseases and their causal entities. Throughout history and even in the modern era, a host of considerations have intruded on the decision as to what to call these blights upon humanity. Names have varied from inflammatory to misleading, from colloquial to scientific. And when it concerns a new epidemiological entity such as the latest coronavirus outbreak originating in China, health organizations, media, politicians, scientific taxonomy commissions, and the public at large all have a stake in the naming.
From “Wuhan virus” to “novel coronavirus-2019” to “COVID-19 virus,” the name of the new coronavirus that first appeared in China has been evolving to its now official designation: SARS-CoV-2 (severe acute respiratory syndrome coronavirus 2). But where did the final name come from, how does such a name become official, and who makes it so?
Virus taxonomy
The Coronavirus Study Group (CSG) of the International Committee on Taxonomy of Viruses (ICTV) named the new coronavirus SARS-CoV-2 based upon its genetic relationship to the original SARS-CoV that caused an outbreak of disease in 2002–2003.
According to the ICTV website, the first internationally organized attempts to introduce order into the bewildering variety of viruses took place at the International Congress of Microbiology held in Moscow in 1966 where a committee was created that later became the ICTV and was given the task of developing a single, universal taxonomic scheme for all the viruses infecting animals, plants, fungi, bacteria, and archaea. The ICTV was created as a committee of the virology division of the International Union of Microbiological Societies and is governed by statutes approved by the virology division. Virus classification and nomenclature are subject to rules set out in an International Code.
These designate that: “The universal virus classification system shall employ the hierarchical levels of realm, subrealm, kingdom, subkingdom, phylum, subphylum, class, subclass, order, suborder, family, subfamily, genus, subgenus and species.”
Many of the topmost areas of classification are based on whether the viruses are DNA or RNA, single or double stranded, and have a simple protein shell or a complex lipoprotein envelope. Other levels of classification include host species, type of replication, and type of diseases they cause, the later exemplified in the SARS designation for this virus.
There are 98 international study groups (SGs) covering all major virus orders, families, and genera that are part of the ICTV, and it was the one dedicated to the single-stranded RNA coronaviruses, the CSG, that came up with the SARS-CoV-2 name and first referenced it in their Feb 11 publication in the Cold Springs Harbor preprint journal bioRxiv.
“Based on phylogeny, taxonomy and established practice, the CSG formally recognizes this virus as a sister to severe acute respiratory syndrome coronaviruses (SARS-CoVs) of the species severe acute respiratory syndrome–related coronavirus and designates it as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2),” they wrote.
According to the National Center for Biotechnology Information Taxonomy Browser, with respect to the original SARS CoV virus, of which this is a relative, the full taxonomic designation is: Viruses, Riboviria, Nidovirales, Cornidovirineae, Coronaviridae, Orthocoronavirinae, Betacoronavirus, Sarbecovirus.
The problem with naming names
The World Health Organization currently is not using the official scientific name of the virus, but rather is merely labeling it with regard to the disease: COVID-19, which simply refers to coronavirus disease 2019.
They are following a modern standard by which disease names avoid inflammatory connotations with people and places. Too often in the past from syphilis as the “French pox,” the 1918 influenza as the “Spanish flu,” AIDS as the “gay plague,” Middle East Respiratory Syndrome (MERS), and the currently named “WuFlu,” which made an appearance early in the new outbreak and which is symbolic of a sudden wave of anti-Asian, and specifically Chinese, prejudice.
Chinatown districts even in the United States are being affected economically through unwarranted fear associated with the virus. And there have been equivalently virulent outbreaks of hate speech against Asian individuals in places untouched by the new virus.
However, although SARS-CoV-2 as a name avoids such problems, different considerations led the WHO to reject it in its discussions, determining that its use ties it to tightly to the much more deadly SARS-CoV-1 virus in the public mind, risking greater fear and panic, especially in Asia, where SARS-CoV-1 had the biggest impact.
Back in 1896, William Sykes, MD, writing in the first flush of the triumph of germ theory in modern medicine, attempted to give some guidance to how medical science should best come up with new names of diseases by merging the demands of common parlance with those of taxonomic legitimacy. His “On the Origin and History of Disease-Names,” published in the Lancet, had clearcut advice: “It is vain to attempt to replace a folk name or one widely adopted by the people by a new one deliberately coined by scholars, and this for the following reasons: first, whatever names may be accepted by medical men must be translated by them into the vernacular of their patients, and by a resulting reaction the vernacular name comes to be the commoner one with themselves; and, secondly, there is no continuity or unchangeableness in the terms invented by savants, which are amended, improved upon, and displaced by the next writer on the subject, or, even more absurdly still, by the very inventors themselves in a subsequent publication.”
This is the reason that virus taxonomy provides names based upon unchangeable scientific descriptors of the actual disease causing entity, as illustrated by the decisions of the ICTV. In addition, the genomic sequences being provided by the scientific community are all being organized under the SARS-CoV-2 name and thus are cementing that moniker as the only acceptable scientific one.
Whether the rest of the world universally adopts SARS-CoV-2 as a name is still in question. If the outbreak spreads significantly beyond its current limits, fear and confusion – and simply the need for a more familiar-sounding label – may lead the general public to adopt more colloquial designations than those that science attempts to impose, as Dr. Sykes suggested back in 1896. That remains to be seen.
[email protected]
Mark Lesney is the managing editor of MDedge.com/IDPractioner. He has a PhD in plant virology and a PhD in the history of science, with a focus on the history of biotechnology and medicine. He has served as an adjunct assistant professor of the department of biochemistry and molecular & cellular biology at Georgetown University, Washington.
China’s health authorities release large coronavirus case series
The Chinese Center for Disease Control and Prevention has released the largest case series to date for novel coronavirus 2019 (COVID-19), and a summary of key findings appears in JAMA.
- The virus, which spread from a single city to a whole country in only 30 days, has so far has caused over 72,314 cases as of Feb. 11, 2020, and 1,023 fatalities (2.3%) overall.
- The age distribution shows that most of the cases (87%) occurred in patients aged 30-79 years, while 10% were in patients 29 years and younger and 3% at 80 years and older.
- Following the SARS outbreak in 2002-2003, the Chinese government adjusted its epidemic response protocol. For example, according to the summary, while there were 300 cases and 5 deaths with SARS before the Chinese government reported it to the World Health Organization, there were only 27 cases and no deaths with COVID-19 before it was reported to that agency.
- A major goal, the authors wrote, is to buy enough time for scientific research, hopefully before the disease has become too widespread.
The summary argues that, while some measures the Chinese government has taken could be seen as extreme, the overall benefits and lives saved outweigh the potential infringement on civil liberties. It also suggests that countries need to work together in situations like this because disease pathogens do not respect geopolitical borders.
SOURCE: Wu Z, McGoogan JM. JAMA. 2020 Feb 24. doi: 10.1001/jama.2020.2648.
The Chinese Center for Disease Control and Prevention has released the largest case series to date for novel coronavirus 2019 (COVID-19), and a summary of key findings appears in JAMA.
- The virus, which spread from a single city to a whole country in only 30 days, has so far has caused over 72,314 cases as of Feb. 11, 2020, and 1,023 fatalities (2.3%) overall.
- The age distribution shows that most of the cases (87%) occurred in patients aged 30-79 years, while 10% were in patients 29 years and younger and 3% at 80 years and older.
- Following the SARS outbreak in 2002-2003, the Chinese government adjusted its epidemic response protocol. For example, according to the summary, while there were 300 cases and 5 deaths with SARS before the Chinese government reported it to the World Health Organization, there were only 27 cases and no deaths with COVID-19 before it was reported to that agency.
- A major goal, the authors wrote, is to buy enough time for scientific research, hopefully before the disease has become too widespread.
The summary argues that, while some measures the Chinese government has taken could be seen as extreme, the overall benefits and lives saved outweigh the potential infringement on civil liberties. It also suggests that countries need to work together in situations like this because disease pathogens do not respect geopolitical borders.
SOURCE: Wu Z, McGoogan JM. JAMA. 2020 Feb 24. doi: 10.1001/jama.2020.2648.
The Chinese Center for Disease Control and Prevention has released the largest case series to date for novel coronavirus 2019 (COVID-19), and a summary of key findings appears in JAMA.
- The virus, which spread from a single city to a whole country in only 30 days, has so far has caused over 72,314 cases as of Feb. 11, 2020, and 1,023 fatalities (2.3%) overall.
- The age distribution shows that most of the cases (87%) occurred in patients aged 30-79 years, while 10% were in patients 29 years and younger and 3% at 80 years and older.
- Following the SARS outbreak in 2002-2003, the Chinese government adjusted its epidemic response protocol. For example, according to the summary, while there were 300 cases and 5 deaths with SARS before the Chinese government reported it to the World Health Organization, there were only 27 cases and no deaths with COVID-19 before it was reported to that agency.
- A major goal, the authors wrote, is to buy enough time for scientific research, hopefully before the disease has become too widespread.
The summary argues that, while some measures the Chinese government has taken could be seen as extreme, the overall benefits and lives saved outweigh the potential infringement on civil liberties. It also suggests that countries need to work together in situations like this because disease pathogens do not respect geopolitical borders.
SOURCE: Wu Z, McGoogan JM. JAMA. 2020 Feb 24. doi: 10.1001/jama.2020.2648.
FROM JAMA
Lipidologists welcome bempedoic acid as new lipid-lowering option
Bempedoic acid, the first agent in a new class of drugs that reduce LDL cholesterol, received Food and Drug Administration approval on Feb. 21 for treating selected hypercholesterolemic patients and is a welcome addition to the medicine cabinet, say lipid experts.
However, it is a tertiary option at least until results from a 14,000 patient clinical-outcome trial of bempedoic acid come out, likely in 2022, they agreed.
“I’m excited to have a new tool in the toolkit for treating high-risk patients, but I will always reach first for the drugs proven to reduce clinical outcomes,” said Erin D. Michos, MD, director of Women’s Cardiovascular Health and associate director of Preventive Cardiology at Johns Hopkins Medicine in Baltimore. That sentiment, shared by other experts, should for the time being relegate bempedoic acid (Nexletol) to a backup role behind statins, ezetimibe, and the PCSK9 inhibitor antibodies that are all now on the U.S. market and all buttressed with evidence of their ability to cut cardiovascular disease death and other CVD outcomes from large outcome studies.
The existing evidence base for bempedoic acid rests primarily two multicenter, randomized, placebo-controlled clinical trials of bempedoic acid in patients with LDL levels above 70 mg/dL while on maximally tolerated lipid-lowering therapy. In CLEAR Harmony, results showed that treatment with bempedoic acid cut LDL-cholesterol levels by an average of 18% more compared with placebo (N Engl J Med 2019;380:1022-32). In CLEAR Wisdom, bempedoic acid reduced LDL cholesterol levels by 17% (JAMA. 2019;322[18]:1780-8).
While those two trials proved the drug’s ability to lower levels of LDL cholesterol, they lacked the power to address whether this effect cut the incidence of CVD events, a question that the CLEAR Outcomes trial aims to answer.
“I believe in the lipid hypothesis, but the main thing we need to see is whether bempedoic acid leads to a meaningful reduction in CVD events. The window for bempedoic acid will remain narrow until we see the outcomes results,” Dr. Michos said in an interview.
Bempedoic acid is a prodrug that’s activated in liver and targets the same cholesterol synthesis pathway as statins by inhibition of ATP-citrate lyase, an enzyme that’s upstream of HMG-CoA reductase, thereby enhancing LDL cholesterol clearance via up-regulation of LDL receptors
.
“,” said Jennifer G. Robinson, MD, professor of epidemiology and medicine and director of the Prevention Intervention Center of the University of Iowa in Iowa City. That would be just a portion of the newly labeled target population. The FDA’s approved label for bempedoic acid cites the drug as an “adjunct to diet and maximally tolerated statin therapy for the treatment of adults with heterozygous familial hypercholesterolemia (HeFH) or established atherosclerotic cardiovascular disease (ASCVD) who require additional lowering of LDL-C.”
The current lack of outcomes evidence for bempedoic acid was not an issue for Robert H. Eckel, MD, an endocrinologist and lipid management specialist at the University of Colorado at Denver in Aurora. Having results from CLEAR Outcomes “may be helpful, but LDL cholesterol lowering in the range where the FDA has indicated using bempedoic acid seems all we need for now,” he said in an interview. Viewing bempedoic acid as potentially useful for both HeFH and ASCVD patients, Dr. Eckel particularly cited the possibility of using the new drug in combination with ezetimibe, another oral, once-daily agent with a moderate but additive effect for cutting LDL cholesterol.
Combined treatment with bempedoic acid and ezetimibe “may be successful in avoiding [using] a PCSK9 inhibitor in some patients, and in particular patients with HeFH or those who are statin intolerant.” But like his colleagues, Dr. Eckel agreed that, for the moment, ezetimibe has an edge over bempedoic acid because of its more extensive evidence base. “If the combination of bempedoic acid and ezetimibe is not needed, the decision [of which one of these to use] needs to depend on the outcome trial results for ezetimibe,” he said. Other factors clinicians could apply if faced with choosing between these two agents include the significant reduction in high-sensitivity C-reactive protein that bempedoic acid produces; the downside that bempedoic acid can cause in some patients an early and persistent rise in serum uric acid levels that can trigger gout flares in patients with a history of gout or at risk for gout; and cost, he said.
Cost is the room-dwelling elephant that colors many decisions about which lipid-lowering drug to use for patients, with options running the price gamut from the generic and uniformly affordable statins and ezetimibe, to the notoriously pricey PCSK9 inhibitors that remain for many patients either prohibitively expensive or hard to get covered by some insurers. Bempedoic acid seems on track to fall somewhere between these two poles, although staff members from Esperion, the company that developed and will market bempedoic acid as Nexletol starting on March 30, declared in a conference call on Feb. 24 that “cost will not be an issue,” for indicated patients prescribed the drug. Company representatives cited a program of coupons, discounts, and rebates they have planned that they anticipate will allow patients who meet the labeled indications to have an out-of-pocket cost for bempedoic acid of “as low as” $10 for a 90-pill supply. They also noted their goal of getting bempedoic acid onto the lowest tier of the Medicare formulary.
How these steps actually play out in the fun house of U.S. prescription drug pricing and preauthorizations remains to be seen. “Out-of-pocket costs are not the real drivers” of drug access, noted Dr. Robinson. “Insurers will likely start with restricted access and prior authorization requirements, just as they did with ezetimibe when it was on patent and prior to having the results from a CVD outcomes trial.” For the time being, bempedoic acid can generally be seen as “expensive ezetimibe,” summed up Dr. Robinson.
Despite that somewhat dismissive characterization, experts are intrigued by the possibility of combining two moderately potent, oral, and safe lipid-lowering drugs in selected patients as a potential alternative to the still financially challenging PCSK9 inhibitors. Combining bempedoic acid and ezetimibe “has a lot of appeal,” said Dr. Michos. “Even though preauthorization has gotten better, it’s still a challenge to get a PCSK9 inhibitor approved.”
Much of her enthusiasm stems from a study reported last year that randomized 301 patients to treatment with bempedoic acid, ezetimibe, or both. The results showed that combined treatment has a similar safety profile to treatment with either drug alone, and produced a cut in LDL cholesterol that was roughly additive for the reductions produced by each drug by itself: Ezetimibe alone cut LDL by about 23%, bempedoic acid alone by about 17%, and the two dosed together once daily resulted in an average 36% drop (Eur J Prev Cardiol. 2019 Jul 29. doi: 10.1177/2047487319864671). The results showed that, “in patients requiring intensive LDL cholesterol lowering, who cannot afford PCSK9 inhibitors, or have statin intolerance, bempedoic acid and ezetimibe are stronger together and can serve as an alternative approach for lipid management in ASCVD prevention,” wrote Dr. Michos and a coauthor in a commentary that appeared with the study results (Eur J Prev Cardiol. 2019 Jul 29. doi: 10.1177/2047487319864672).
The concept of combined bempedoic acid and ezetimibe treatment is so appealing that the bempedoic acid manufacturer, Esperion, has already developed a single-pill formulation of the two drugs that received FDA marketing approval on February 26. A company statement said that marketing of this combined formulation, Nexlizet, will start in July 2020.
Although interest in bempedoic acid seems running high for patients included in the new FDA indication, Dr. Michos and others see possibly greater potential for what would now be off-label use for primary prevention in high-risk patients without HeFH, patients who generally don’t qualify for insurance coverage of a PCSK9 inhibitor.
“Use in primary prevention in [non-HeFH] patients with insufficient lowering of LDL cholesterol wouldn’t surprise me,” but a big concern will be out-of-pocket cost when off-label use precludes insurance coverage or discount eligibility, noted Dr. Eckel. An Esperion spokesperson said that the undiscounted, wholesale acquisition cost for bempedoic acid is expected to be roughly $10/pill, or about $300 for a 30-day supply, positioning it more or less midway between generic statins and ezetimibe and the list price for a PCSk9 inhibitor of roughly $500/month.
“I’m most excited about bempedoic acid in the off-label space, for patients who can’t get approved for a PCSK9 inhibitor, for treating patients with subclinical ASCVD, or really high-risk patients with multiple risk factors including diabetes,” especially when these patients are intolerant of a high-intensity statin regimen, said Dr. Michos. “I have a clinic full of patients” who can’t take their full, indicated dosage of a high-intensity statin, and when those patients also can’t get on treatment with a PCSK9 inhibitor then bempedoic acid will be an important part of their alternative regimen, she explained.
Dr. Michos had no disclosures. Dr. Robinson has received research funding from Esperion and from several other companies, and she has been a consultant to Amgen, Merck, Novartis, Novo Nordisk, Pfizer, Regeneron, and Sanofi. Dr. Eckel has received honoraria from Kowa, Merck, Novo Nordisk, and Sanofi/Regeneron.
This article was updated 2/27/20.
Bempedoic acid, the first agent in a new class of drugs that reduce LDL cholesterol, received Food and Drug Administration approval on Feb. 21 for treating selected hypercholesterolemic patients and is a welcome addition to the medicine cabinet, say lipid experts.
However, it is a tertiary option at least until results from a 14,000 patient clinical-outcome trial of bempedoic acid come out, likely in 2022, they agreed.
“I’m excited to have a new tool in the toolkit for treating high-risk patients, but I will always reach first for the drugs proven to reduce clinical outcomes,” said Erin D. Michos, MD, director of Women’s Cardiovascular Health and associate director of Preventive Cardiology at Johns Hopkins Medicine in Baltimore. That sentiment, shared by other experts, should for the time being relegate bempedoic acid (Nexletol) to a backup role behind statins, ezetimibe, and the PCSK9 inhibitor antibodies that are all now on the U.S. market and all buttressed with evidence of their ability to cut cardiovascular disease death and other CVD outcomes from large outcome studies.
The existing evidence base for bempedoic acid rests primarily two multicenter, randomized, placebo-controlled clinical trials of bempedoic acid in patients with LDL levels above 70 mg/dL while on maximally tolerated lipid-lowering therapy. In CLEAR Harmony, results showed that treatment with bempedoic acid cut LDL-cholesterol levels by an average of 18% more compared with placebo (N Engl J Med 2019;380:1022-32). In CLEAR Wisdom, bempedoic acid reduced LDL cholesterol levels by 17% (JAMA. 2019;322[18]:1780-8).
While those two trials proved the drug’s ability to lower levels of LDL cholesterol, they lacked the power to address whether this effect cut the incidence of CVD events, a question that the CLEAR Outcomes trial aims to answer.
“I believe in the lipid hypothesis, but the main thing we need to see is whether bempedoic acid leads to a meaningful reduction in CVD events. The window for bempedoic acid will remain narrow until we see the outcomes results,” Dr. Michos said in an interview.
Bempedoic acid is a prodrug that’s activated in liver and targets the same cholesterol synthesis pathway as statins by inhibition of ATP-citrate lyase, an enzyme that’s upstream of HMG-CoA reductase, thereby enhancing LDL cholesterol clearance via up-regulation of LDL receptors
.
“,” said Jennifer G. Robinson, MD, professor of epidemiology and medicine and director of the Prevention Intervention Center of the University of Iowa in Iowa City. That would be just a portion of the newly labeled target population. The FDA’s approved label for bempedoic acid cites the drug as an “adjunct to diet and maximally tolerated statin therapy for the treatment of adults with heterozygous familial hypercholesterolemia (HeFH) or established atherosclerotic cardiovascular disease (ASCVD) who require additional lowering of LDL-C.”
The current lack of outcomes evidence for bempedoic acid was not an issue for Robert H. Eckel, MD, an endocrinologist and lipid management specialist at the University of Colorado at Denver in Aurora. Having results from CLEAR Outcomes “may be helpful, but LDL cholesterol lowering in the range where the FDA has indicated using bempedoic acid seems all we need for now,” he said in an interview. Viewing bempedoic acid as potentially useful for both HeFH and ASCVD patients, Dr. Eckel particularly cited the possibility of using the new drug in combination with ezetimibe, another oral, once-daily agent with a moderate but additive effect for cutting LDL cholesterol.
Combined treatment with bempedoic acid and ezetimibe “may be successful in avoiding [using] a PCSK9 inhibitor in some patients, and in particular patients with HeFH or those who are statin intolerant.” But like his colleagues, Dr. Eckel agreed that, for the moment, ezetimibe has an edge over bempedoic acid because of its more extensive evidence base. “If the combination of bempedoic acid and ezetimibe is not needed, the decision [of which one of these to use] needs to depend on the outcome trial results for ezetimibe,” he said. Other factors clinicians could apply if faced with choosing between these two agents include the significant reduction in high-sensitivity C-reactive protein that bempedoic acid produces; the downside that bempedoic acid can cause in some patients an early and persistent rise in serum uric acid levels that can trigger gout flares in patients with a history of gout or at risk for gout; and cost, he said.
Cost is the room-dwelling elephant that colors many decisions about which lipid-lowering drug to use for patients, with options running the price gamut from the generic and uniformly affordable statins and ezetimibe, to the notoriously pricey PCSK9 inhibitors that remain for many patients either prohibitively expensive or hard to get covered by some insurers. Bempedoic acid seems on track to fall somewhere between these two poles, although staff members from Esperion, the company that developed and will market bempedoic acid as Nexletol starting on March 30, declared in a conference call on Feb. 24 that “cost will not be an issue,” for indicated patients prescribed the drug. Company representatives cited a program of coupons, discounts, and rebates they have planned that they anticipate will allow patients who meet the labeled indications to have an out-of-pocket cost for bempedoic acid of “as low as” $10 for a 90-pill supply. They also noted their goal of getting bempedoic acid onto the lowest tier of the Medicare formulary.
How these steps actually play out in the fun house of U.S. prescription drug pricing and preauthorizations remains to be seen. “Out-of-pocket costs are not the real drivers” of drug access, noted Dr. Robinson. “Insurers will likely start with restricted access and prior authorization requirements, just as they did with ezetimibe when it was on patent and prior to having the results from a CVD outcomes trial.” For the time being, bempedoic acid can generally be seen as “expensive ezetimibe,” summed up Dr. Robinson.
Despite that somewhat dismissive characterization, experts are intrigued by the possibility of combining two moderately potent, oral, and safe lipid-lowering drugs in selected patients as a potential alternative to the still financially challenging PCSK9 inhibitors. Combining bempedoic acid and ezetimibe “has a lot of appeal,” said Dr. Michos. “Even though preauthorization has gotten better, it’s still a challenge to get a PCSK9 inhibitor approved.”
Much of her enthusiasm stems from a study reported last year that randomized 301 patients to treatment with bempedoic acid, ezetimibe, or both. The results showed that combined treatment has a similar safety profile to treatment with either drug alone, and produced a cut in LDL cholesterol that was roughly additive for the reductions produced by each drug by itself: Ezetimibe alone cut LDL by about 23%, bempedoic acid alone by about 17%, and the two dosed together once daily resulted in an average 36% drop (Eur J Prev Cardiol. 2019 Jul 29. doi: 10.1177/2047487319864671). The results showed that, “in patients requiring intensive LDL cholesterol lowering, who cannot afford PCSK9 inhibitors, or have statin intolerance, bempedoic acid and ezetimibe are stronger together and can serve as an alternative approach for lipid management in ASCVD prevention,” wrote Dr. Michos and a coauthor in a commentary that appeared with the study results (Eur J Prev Cardiol. 2019 Jul 29. doi: 10.1177/2047487319864672).
The concept of combined bempedoic acid and ezetimibe treatment is so appealing that the bempedoic acid manufacturer, Esperion, has already developed a single-pill formulation of the two drugs that received FDA marketing approval on February 26. A company statement said that marketing of this combined formulation, Nexlizet, will start in July 2020.
Although interest in bempedoic acid seems running high for patients included in the new FDA indication, Dr. Michos and others see possibly greater potential for what would now be off-label use for primary prevention in high-risk patients without HeFH, patients who generally don’t qualify for insurance coverage of a PCSK9 inhibitor.
“Use in primary prevention in [non-HeFH] patients with insufficient lowering of LDL cholesterol wouldn’t surprise me,” but a big concern will be out-of-pocket cost when off-label use precludes insurance coverage or discount eligibility, noted Dr. Eckel. An Esperion spokesperson said that the undiscounted, wholesale acquisition cost for bempedoic acid is expected to be roughly $10/pill, or about $300 for a 30-day supply, positioning it more or less midway between generic statins and ezetimibe and the list price for a PCSk9 inhibitor of roughly $500/month.
“I’m most excited about bempedoic acid in the off-label space, for patients who can’t get approved for a PCSK9 inhibitor, for treating patients with subclinical ASCVD, or really high-risk patients with multiple risk factors including diabetes,” especially when these patients are intolerant of a high-intensity statin regimen, said Dr. Michos. “I have a clinic full of patients” who can’t take their full, indicated dosage of a high-intensity statin, and when those patients also can’t get on treatment with a PCSK9 inhibitor then bempedoic acid will be an important part of their alternative regimen, she explained.
Dr. Michos had no disclosures. Dr. Robinson has received research funding from Esperion and from several other companies, and she has been a consultant to Amgen, Merck, Novartis, Novo Nordisk, Pfizer, Regeneron, and Sanofi. Dr. Eckel has received honoraria from Kowa, Merck, Novo Nordisk, and Sanofi/Regeneron.
This article was updated 2/27/20.
Bempedoic acid, the first agent in a new class of drugs that reduce LDL cholesterol, received Food and Drug Administration approval on Feb. 21 for treating selected hypercholesterolemic patients and is a welcome addition to the medicine cabinet, say lipid experts.
However, it is a tertiary option at least until results from a 14,000 patient clinical-outcome trial of bempedoic acid come out, likely in 2022, they agreed.
“I’m excited to have a new tool in the toolkit for treating high-risk patients, but I will always reach first for the drugs proven to reduce clinical outcomes,” said Erin D. Michos, MD, director of Women’s Cardiovascular Health and associate director of Preventive Cardiology at Johns Hopkins Medicine in Baltimore. That sentiment, shared by other experts, should for the time being relegate bempedoic acid (Nexletol) to a backup role behind statins, ezetimibe, and the PCSK9 inhibitor antibodies that are all now on the U.S. market and all buttressed with evidence of their ability to cut cardiovascular disease death and other CVD outcomes from large outcome studies.
The existing evidence base for bempedoic acid rests primarily two multicenter, randomized, placebo-controlled clinical trials of bempedoic acid in patients with LDL levels above 70 mg/dL while on maximally tolerated lipid-lowering therapy. In CLEAR Harmony, results showed that treatment with bempedoic acid cut LDL-cholesterol levels by an average of 18% more compared with placebo (N Engl J Med 2019;380:1022-32). In CLEAR Wisdom, bempedoic acid reduced LDL cholesterol levels by 17% (JAMA. 2019;322[18]:1780-8).
While those two trials proved the drug’s ability to lower levels of LDL cholesterol, they lacked the power to address whether this effect cut the incidence of CVD events, a question that the CLEAR Outcomes trial aims to answer.
“I believe in the lipid hypothesis, but the main thing we need to see is whether bempedoic acid leads to a meaningful reduction in CVD events. The window for bempedoic acid will remain narrow until we see the outcomes results,” Dr. Michos said in an interview.
Bempedoic acid is a prodrug that’s activated in liver and targets the same cholesterol synthesis pathway as statins by inhibition of ATP-citrate lyase, an enzyme that’s upstream of HMG-CoA reductase, thereby enhancing LDL cholesterol clearance via up-regulation of LDL receptors
.
“,” said Jennifer G. Robinson, MD, professor of epidemiology and medicine and director of the Prevention Intervention Center of the University of Iowa in Iowa City. That would be just a portion of the newly labeled target population. The FDA’s approved label for bempedoic acid cites the drug as an “adjunct to diet and maximally tolerated statin therapy for the treatment of adults with heterozygous familial hypercholesterolemia (HeFH) or established atherosclerotic cardiovascular disease (ASCVD) who require additional lowering of LDL-C.”
The current lack of outcomes evidence for bempedoic acid was not an issue for Robert H. Eckel, MD, an endocrinologist and lipid management specialist at the University of Colorado at Denver in Aurora. Having results from CLEAR Outcomes “may be helpful, but LDL cholesterol lowering in the range where the FDA has indicated using bempedoic acid seems all we need for now,” he said in an interview. Viewing bempedoic acid as potentially useful for both HeFH and ASCVD patients, Dr. Eckel particularly cited the possibility of using the new drug in combination with ezetimibe, another oral, once-daily agent with a moderate but additive effect for cutting LDL cholesterol.
Combined treatment with bempedoic acid and ezetimibe “may be successful in avoiding [using] a PCSK9 inhibitor in some patients, and in particular patients with HeFH or those who are statin intolerant.” But like his colleagues, Dr. Eckel agreed that, for the moment, ezetimibe has an edge over bempedoic acid because of its more extensive evidence base. “If the combination of bempedoic acid and ezetimibe is not needed, the decision [of which one of these to use] needs to depend on the outcome trial results for ezetimibe,” he said. Other factors clinicians could apply if faced with choosing between these two agents include the significant reduction in high-sensitivity C-reactive protein that bempedoic acid produces; the downside that bempedoic acid can cause in some patients an early and persistent rise in serum uric acid levels that can trigger gout flares in patients with a history of gout or at risk for gout; and cost, he said.
Cost is the room-dwelling elephant that colors many decisions about which lipid-lowering drug to use for patients, with options running the price gamut from the generic and uniformly affordable statins and ezetimibe, to the notoriously pricey PCSK9 inhibitors that remain for many patients either prohibitively expensive or hard to get covered by some insurers. Bempedoic acid seems on track to fall somewhere between these two poles, although staff members from Esperion, the company that developed and will market bempedoic acid as Nexletol starting on March 30, declared in a conference call on Feb. 24 that “cost will not be an issue,” for indicated patients prescribed the drug. Company representatives cited a program of coupons, discounts, and rebates they have planned that they anticipate will allow patients who meet the labeled indications to have an out-of-pocket cost for bempedoic acid of “as low as” $10 for a 90-pill supply. They also noted their goal of getting bempedoic acid onto the lowest tier of the Medicare formulary.
How these steps actually play out in the fun house of U.S. prescription drug pricing and preauthorizations remains to be seen. “Out-of-pocket costs are not the real drivers” of drug access, noted Dr. Robinson. “Insurers will likely start with restricted access and prior authorization requirements, just as they did with ezetimibe when it was on patent and prior to having the results from a CVD outcomes trial.” For the time being, bempedoic acid can generally be seen as “expensive ezetimibe,” summed up Dr. Robinson.
Despite that somewhat dismissive characterization, experts are intrigued by the possibility of combining two moderately potent, oral, and safe lipid-lowering drugs in selected patients as a potential alternative to the still financially challenging PCSK9 inhibitors. Combining bempedoic acid and ezetimibe “has a lot of appeal,” said Dr. Michos. “Even though preauthorization has gotten better, it’s still a challenge to get a PCSK9 inhibitor approved.”
Much of her enthusiasm stems from a study reported last year that randomized 301 patients to treatment with bempedoic acid, ezetimibe, or both. The results showed that combined treatment has a similar safety profile to treatment with either drug alone, and produced a cut in LDL cholesterol that was roughly additive for the reductions produced by each drug by itself: Ezetimibe alone cut LDL by about 23%, bempedoic acid alone by about 17%, and the two dosed together once daily resulted in an average 36% drop (Eur J Prev Cardiol. 2019 Jul 29. doi: 10.1177/2047487319864671). The results showed that, “in patients requiring intensive LDL cholesterol lowering, who cannot afford PCSK9 inhibitors, or have statin intolerance, bempedoic acid and ezetimibe are stronger together and can serve as an alternative approach for lipid management in ASCVD prevention,” wrote Dr. Michos and a coauthor in a commentary that appeared with the study results (Eur J Prev Cardiol. 2019 Jul 29. doi: 10.1177/2047487319864672).
The concept of combined bempedoic acid and ezetimibe treatment is so appealing that the bempedoic acid manufacturer, Esperion, has already developed a single-pill formulation of the two drugs that received FDA marketing approval on February 26. A company statement said that marketing of this combined formulation, Nexlizet, will start in July 2020.
Although interest in bempedoic acid seems running high for patients included in the new FDA indication, Dr. Michos and others see possibly greater potential for what would now be off-label use for primary prevention in high-risk patients without HeFH, patients who generally don’t qualify for insurance coverage of a PCSK9 inhibitor.
“Use in primary prevention in [non-HeFH] patients with insufficient lowering of LDL cholesterol wouldn’t surprise me,” but a big concern will be out-of-pocket cost when off-label use precludes insurance coverage or discount eligibility, noted Dr. Eckel. An Esperion spokesperson said that the undiscounted, wholesale acquisition cost for bempedoic acid is expected to be roughly $10/pill, or about $300 for a 30-day supply, positioning it more or less midway between generic statins and ezetimibe and the list price for a PCSk9 inhibitor of roughly $500/month.
“I’m most excited about bempedoic acid in the off-label space, for patients who can’t get approved for a PCSK9 inhibitor, for treating patients with subclinical ASCVD, or really high-risk patients with multiple risk factors including diabetes,” especially when these patients are intolerant of a high-intensity statin regimen, said Dr. Michos. “I have a clinic full of patients” who can’t take their full, indicated dosage of a high-intensity statin, and when those patients also can’t get on treatment with a PCSK9 inhibitor then bempedoic acid will be an important part of their alternative regimen, she explained.
Dr. Michos had no disclosures. Dr. Robinson has received research funding from Esperion and from several other companies, and she has been a consultant to Amgen, Merck, Novartis, Novo Nordisk, Pfizer, Regeneron, and Sanofi. Dr. Eckel has received honoraria from Kowa, Merck, Novo Nordisk, and Sanofi/Regeneron.
This article was updated 2/27/20.
Study implicates gut bacteria in PAH
Model finds microbiota highly predictive
A unique collection of bacteria in the gut may have a strong association with pulmonary arterial hypertension and could be highly predictive of the disease in undiagnosed patients, according to a study published in the journal Hypertension.
This is the first study to show that people with PAH have a common specific gut microbiota profile, wrote lead study author Mohan Raizada, PhD, distinguished professor in the department of physiology and functional genomics at the University of Florida, Gainesville.
The findings have the potential to change how cardiologists diagnose and treat PAH, he added. “While current PAH treatments focus on the lungs, looking at the lung/gut axis could open the door to new therapies centered in the digestive system,” Dr. Raizada said.
The researchers developed a model that found the specific microbiota profile was 83% accurate in predicting the presence or absence of PAH. If a larger study can validate the findings, the researchers wrote, this could lead to a new test for diagnosing PAH that’s less invasive than cardiac catheterization. It could also lead to new treatments that target the gut microbiome.
Study investigators collected stool samples from 18 PAH patients and 12 people without a history of cardiopulmonary disease. The microbiota DNA from the stool samples were isolated and sequenced. The analysis revealed that PAH patients had reduced richness and evenness of the gut bacteria, known as alpha diversity. They had increased levels of bacteria associated with atherosclerosis, and healthy patients had increased levels of bacteria that produced short-chain fatty acids.
Although recent studies have begun to show potential associations between the gut microbiome and cardiovascular diseases, this research is in its infancy, Mariell Jessup, MD, commented. “Even though the study by Dr. Raizada and colleagues predicted pulmonary arterial hypertension based on an individual’s microbiome with some accuracy, it is an observational study, so it does not prove cause and effect. Many other factors, especially diet, affect the gut microbiome,” added Dr. Jessup, Chief Science and Medical Officer for the American Heart Association.
She stressed that, “In addition, even if studies confirm an association between the gut microbiome and cardiovascular diseases such as PAH, more research is needed to determine if improving gut microbiota could directly impact PAH or other cardiovascular diseases. The findings of this study will not impact clinical practice.”
Dr. Raizada and his coinvestigators offered two possible mechanisms through which the gut microbiome influences pulmonary physiology. One is that lower levels of bacteria that produce the short-chain fatty acid butyrate, such as Coprococcus, Butyrivibrio, Lachnospiraceae, and Eubacterium, along with Clostridia in the gut of PAH patients, may increase gut permeability. Reduced butyrate weakens gut barrier function and can induce inflammation and leakage. This can allow microbial metabolites to enter the circulatory system, disrupting metabolism and immunity and affecting pulmonary vessels.
The second potential mechanism is that increased Collinsella in the PAH cohort may be the culprit that increases gut permeability, resulting in the ensuing gut barrier dysfunction and inflammation. The study noted Collinsella contributed most of the increased genes for the biosynthesis on the amino acid proline in these patients, and that a previous study implicated Collinsella and its parent, Cariobacteriales, in trimethylamine/trimethylamine N-oxide production (TMA/TMAO) in atherosclerosis (Cell. 2015;163[7]:1585-95). The non-PAH patients had higher levels of bacteria that had a low correlation with TMA/TMAO.
“We were very surprised to see such an association within a small group of study subjects,” wrote Dr. Raizada and associates. “It usually requires hundreds of patients to achieve such significance.”
More research is needed to determine if the specific microbiota associated with PAH causes the disease or is a result of it, they concluded.
The study was funded by grants from the National Institutes of Health, the NIH National Center for Research Resources, and the U.S. Department of Defense. Dr. Raizada and coauthors reported no relevant financial relationships.
SOURCE: Raizada MK et al. Hypertension. 2020. doi: 10.1161/HYPERTENSIONAHA.119.14294.
Model finds microbiota highly predictive
Model finds microbiota highly predictive
A unique collection of bacteria in the gut may have a strong association with pulmonary arterial hypertension and could be highly predictive of the disease in undiagnosed patients, according to a study published in the journal Hypertension.
This is the first study to show that people with PAH have a common specific gut microbiota profile, wrote lead study author Mohan Raizada, PhD, distinguished professor in the department of physiology and functional genomics at the University of Florida, Gainesville.
The findings have the potential to change how cardiologists diagnose and treat PAH, he added. “While current PAH treatments focus on the lungs, looking at the lung/gut axis could open the door to new therapies centered in the digestive system,” Dr. Raizada said.
The researchers developed a model that found the specific microbiota profile was 83% accurate in predicting the presence or absence of PAH. If a larger study can validate the findings, the researchers wrote, this could lead to a new test for diagnosing PAH that’s less invasive than cardiac catheterization. It could also lead to new treatments that target the gut microbiome.
Study investigators collected stool samples from 18 PAH patients and 12 people without a history of cardiopulmonary disease. The microbiota DNA from the stool samples were isolated and sequenced. The analysis revealed that PAH patients had reduced richness and evenness of the gut bacteria, known as alpha diversity. They had increased levels of bacteria associated with atherosclerosis, and healthy patients had increased levels of bacteria that produced short-chain fatty acids.
Although recent studies have begun to show potential associations between the gut microbiome and cardiovascular diseases, this research is in its infancy, Mariell Jessup, MD, commented. “Even though the study by Dr. Raizada and colleagues predicted pulmonary arterial hypertension based on an individual’s microbiome with some accuracy, it is an observational study, so it does not prove cause and effect. Many other factors, especially diet, affect the gut microbiome,” added Dr. Jessup, Chief Science and Medical Officer for the American Heart Association.
She stressed that, “In addition, even if studies confirm an association between the gut microbiome and cardiovascular diseases such as PAH, more research is needed to determine if improving gut microbiota could directly impact PAH or other cardiovascular diseases. The findings of this study will not impact clinical practice.”
Dr. Raizada and his coinvestigators offered two possible mechanisms through which the gut microbiome influences pulmonary physiology. One is that lower levels of bacteria that produce the short-chain fatty acid butyrate, such as Coprococcus, Butyrivibrio, Lachnospiraceae, and Eubacterium, along with Clostridia in the gut of PAH patients, may increase gut permeability. Reduced butyrate weakens gut barrier function and can induce inflammation and leakage. This can allow microbial metabolites to enter the circulatory system, disrupting metabolism and immunity and affecting pulmonary vessels.
The second potential mechanism is that increased Collinsella in the PAH cohort may be the culprit that increases gut permeability, resulting in the ensuing gut barrier dysfunction and inflammation. The study noted Collinsella contributed most of the increased genes for the biosynthesis on the amino acid proline in these patients, and that a previous study implicated Collinsella and its parent, Cariobacteriales, in trimethylamine/trimethylamine N-oxide production (TMA/TMAO) in atherosclerosis (Cell. 2015;163[7]:1585-95). The non-PAH patients had higher levels of bacteria that had a low correlation with TMA/TMAO.
“We were very surprised to see such an association within a small group of study subjects,” wrote Dr. Raizada and associates. “It usually requires hundreds of patients to achieve such significance.”
More research is needed to determine if the specific microbiota associated with PAH causes the disease or is a result of it, they concluded.
The study was funded by grants from the National Institutes of Health, the NIH National Center for Research Resources, and the U.S. Department of Defense. Dr. Raizada and coauthors reported no relevant financial relationships.
SOURCE: Raizada MK et al. Hypertension. 2020. doi: 10.1161/HYPERTENSIONAHA.119.14294.
A unique collection of bacteria in the gut may have a strong association with pulmonary arterial hypertension and could be highly predictive of the disease in undiagnosed patients, according to a study published in the journal Hypertension.
This is the first study to show that people with PAH have a common specific gut microbiota profile, wrote lead study author Mohan Raizada, PhD, distinguished professor in the department of physiology and functional genomics at the University of Florida, Gainesville.
The findings have the potential to change how cardiologists diagnose and treat PAH, he added. “While current PAH treatments focus on the lungs, looking at the lung/gut axis could open the door to new therapies centered in the digestive system,” Dr. Raizada said.
The researchers developed a model that found the specific microbiota profile was 83% accurate in predicting the presence or absence of PAH. If a larger study can validate the findings, the researchers wrote, this could lead to a new test for diagnosing PAH that’s less invasive than cardiac catheterization. It could also lead to new treatments that target the gut microbiome.
Study investigators collected stool samples from 18 PAH patients and 12 people without a history of cardiopulmonary disease. The microbiota DNA from the stool samples were isolated and sequenced. The analysis revealed that PAH patients had reduced richness and evenness of the gut bacteria, known as alpha diversity. They had increased levels of bacteria associated with atherosclerosis, and healthy patients had increased levels of bacteria that produced short-chain fatty acids.
Although recent studies have begun to show potential associations between the gut microbiome and cardiovascular diseases, this research is in its infancy, Mariell Jessup, MD, commented. “Even though the study by Dr. Raizada and colleagues predicted pulmonary arterial hypertension based on an individual’s microbiome with some accuracy, it is an observational study, so it does not prove cause and effect. Many other factors, especially diet, affect the gut microbiome,” added Dr. Jessup, Chief Science and Medical Officer for the American Heart Association.
She stressed that, “In addition, even if studies confirm an association between the gut microbiome and cardiovascular diseases such as PAH, more research is needed to determine if improving gut microbiota could directly impact PAH or other cardiovascular diseases. The findings of this study will not impact clinical practice.”
Dr. Raizada and his coinvestigators offered two possible mechanisms through which the gut microbiome influences pulmonary physiology. One is that lower levels of bacteria that produce the short-chain fatty acid butyrate, such as Coprococcus, Butyrivibrio, Lachnospiraceae, and Eubacterium, along with Clostridia in the gut of PAH patients, may increase gut permeability. Reduced butyrate weakens gut barrier function and can induce inflammation and leakage. This can allow microbial metabolites to enter the circulatory system, disrupting metabolism and immunity and affecting pulmonary vessels.
The second potential mechanism is that increased Collinsella in the PAH cohort may be the culprit that increases gut permeability, resulting in the ensuing gut barrier dysfunction and inflammation. The study noted Collinsella contributed most of the increased genes for the biosynthesis on the amino acid proline in these patients, and that a previous study implicated Collinsella and its parent, Cariobacteriales, in trimethylamine/trimethylamine N-oxide production (TMA/TMAO) in atherosclerosis (Cell. 2015;163[7]:1585-95). The non-PAH patients had higher levels of bacteria that had a low correlation with TMA/TMAO.
“We were very surprised to see such an association within a small group of study subjects,” wrote Dr. Raizada and associates. “It usually requires hundreds of patients to achieve such significance.”
More research is needed to determine if the specific microbiota associated with PAH causes the disease or is a result of it, they concluded.
The study was funded by grants from the National Institutes of Health, the NIH National Center for Research Resources, and the U.S. Department of Defense. Dr. Raizada and coauthors reported no relevant financial relationships.
SOURCE: Raizada MK et al. Hypertension. 2020. doi: 10.1161/HYPERTENSIONAHA.119.14294.
FROM HYPERTENSION