User login
-
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]


Apatinib plus gefitinib: Better PFS but more toxicity
ACTIVE is the first phase 3 trial of an oral vascular epidermal growth factor receptor–2 (VEGFR2) tyrosine kinase inhibitor (TKI) added to an EGFR-TKI as first-line therapy in this population, according to Li Zhang, MD, of Sun Yat-sen University Cancer Center in Guangzhou, China.
Dr. Zhang presented results from ACTIVE at the European Society for Medical Oncology Virtual Congress 2020.
“This dual oral regimen will provide more convenient treatment for patients who require long-term administration,” Dr. Zhang said. He added that apatinib plus gefitinib “is expected to become a new first-line treatment option for EGFR-mutant NSCLC.”
A discussant for the ACTIVE study was less optimistic, however, noting that the regimen proved tough to tolerate for some patients, and the PFS benefit may not translate to overall survival.
Study rationale and details
Sensitizing EGFR mutations occur in about 10% of White patients and up to 50% of Asian patients, Dr. Zhang noted. Unfortunately, most patients progress after first-line treatment with EGFR-TKIs because of acquired resistance.
Blocking VEGF receptor pathways has been shown to enhance EGFR-TKIs in EGFR-mutated NSCLC, and pilot study results have shown apatinib – an oral VEGFR2–TKI – to be safe and well-tolerated with promising efficacy in combination with gefitinib, Dr. Zhang added.
To expand upon those results, he and his colleagues tested apatinib with gefitinib in the phase 3, double-blind, placebo-controlled ACTIVE trial (CTONG1706).
The trial included 313 patients (median age, 58.5 years) with locally advanced, metastatic, or recurrent nonsquamous NSCLC. All were chemotherapy-naive and EGFR mutation-positive (exon 19 deletion or exon 21 L858R).
Patients were randomized 1:1 to first-line apatinib at 500 mg daily plus gefitinib at 250 mg daily (n = 157) or placebo plus gefitinib at 250 mg daily (n = 156) until progressive disease or unacceptable toxicity.
Efficacy and safety
The primary endpoint was PFS by independent review. The median follow-up was 15.8 months.
The median PFS was 13.7 months in the apatinib group and 10.2 months in the placebo group (hazard ratio, 0.71; P = .0189).
Objective response rates were similar for both groups – 77.1% with apatinib and 73.7% with placebo. However, depth of response ≥30% and depth of response ≥50% both favored the apatinib arm – 89.2% versus 79.5% for ≥ 30% (P = .0209) and 64.3% versus 52.6% for ≥50% (P = .0238).
In addition, the median duration of response was longer for the apatinib group – 12.9 months versus 9.3 months (HR, 0.64; P = .005).
Exploratory biomarker analyses showed the benefit of apatinib was more common in patients with TP53 exon 8 mutations.
The rate of grade 3 or higher treatment-emergent adverse events was 84.1% in the apatinib arm and 37.7% in the placebo arm. Diarrhea (73.2%) and hypertension (68.2%) were the most common treatment-emergent adverse events in the apatinib group.
Dose interruptions were more common in the apatinib group (59.5% vs. 22.7%) as were dose reductions (48.4% vs. 4.5%). However, treatment discontinuations attributable to treatment-emergent adverse events were few in both arms (5.1% in the apatinib arm and 3.2% in the placebo arm).
Cause for hesitation
“VEGFR-TKIs have not yet found a solid home in lung cancer,” said study discussant Lecia V. Sequist, MD, of Massachusetts General Hospital in Boston.
Listing 10 VEGFR-TKIs, Dr. Sequist noted: “None of them have changed practice.”
She added that, while an all-oral regimen is appealing, the benefit of adding apatinib to gefitinib was modest, and the regimen was “fairly difficult” to tolerate. “The PFS with apatinib plus gefitinib is well below what we see with other EGFR/VEGF first-line studies,” she said.
Dr. Sequist also observed that most studies have shown a PFS benefit but no overall survival benefit. “That, in combination with the toxicity, makes me a little hesitant about this regimen. The role of VEGF remains unclear in EGFR mutation–positive lung cancer in 2020,” she concluded.
The ACTIVE study was funded by Jiangsu HengRui Medicine, the Chinese Thoracic Oncology Group, and grants from Sun Yat-sen University and the National Key R&D Program of China. Dr. Zhang disclosed relationships with AstraZeneca, Bristol-Myers Squibb, Eli Lilly, Pfizer, and Roche. Dr. Sequist disclosed relationships with AstraZeneca, Bristol-Myers Squibb, Blueprint Medicines, and many other companies.
SOURCE: Zhang L et al. ESMO 2020, Abstract LBA50.
ACTIVE is the first phase 3 trial of an oral vascular epidermal growth factor receptor–2 (VEGFR2) tyrosine kinase inhibitor (TKI) added to an EGFR-TKI as first-line therapy in this population, according to Li Zhang, MD, of Sun Yat-sen University Cancer Center in Guangzhou, China.
Dr. Zhang presented results from ACTIVE at the European Society for Medical Oncology Virtual Congress 2020.
“This dual oral regimen will provide more convenient treatment for patients who require long-term administration,” Dr. Zhang said. He added that apatinib plus gefitinib “is expected to become a new first-line treatment option for EGFR-mutant NSCLC.”
A discussant for the ACTIVE study was less optimistic, however, noting that the regimen proved tough to tolerate for some patients, and the PFS benefit may not translate to overall survival.
Study rationale and details
Sensitizing EGFR mutations occur in about 10% of White patients and up to 50% of Asian patients, Dr. Zhang noted. Unfortunately, most patients progress after first-line treatment with EGFR-TKIs because of acquired resistance.
Blocking VEGF receptor pathways has been shown to enhance EGFR-TKIs in EGFR-mutated NSCLC, and pilot study results have shown apatinib – an oral VEGFR2–TKI – to be safe and well-tolerated with promising efficacy in combination with gefitinib, Dr. Zhang added.
To expand upon those results, he and his colleagues tested apatinib with gefitinib in the phase 3, double-blind, placebo-controlled ACTIVE trial (CTONG1706).
The trial included 313 patients (median age, 58.5 years) with locally advanced, metastatic, or recurrent nonsquamous NSCLC. All were chemotherapy-naive and EGFR mutation-positive (exon 19 deletion or exon 21 L858R).
Patients were randomized 1:1 to first-line apatinib at 500 mg daily plus gefitinib at 250 mg daily (n = 157) or placebo plus gefitinib at 250 mg daily (n = 156) until progressive disease or unacceptable toxicity.
Efficacy and safety
The primary endpoint was PFS by independent review. The median follow-up was 15.8 months.
The median PFS was 13.7 months in the apatinib group and 10.2 months in the placebo group (hazard ratio, 0.71; P = .0189).
Objective response rates were similar for both groups – 77.1% with apatinib and 73.7% with placebo. However, depth of response ≥30% and depth of response ≥50% both favored the apatinib arm – 89.2% versus 79.5% for ≥ 30% (P = .0209) and 64.3% versus 52.6% for ≥50% (P = .0238).
In addition, the median duration of response was longer for the apatinib group – 12.9 months versus 9.3 months (HR, 0.64; P = .005).
Exploratory biomarker analyses showed the benefit of apatinib was more common in patients with TP53 exon 8 mutations.
The rate of grade 3 or higher treatment-emergent adverse events was 84.1% in the apatinib arm and 37.7% in the placebo arm. Diarrhea (73.2%) and hypertension (68.2%) were the most common treatment-emergent adverse events in the apatinib group.
Dose interruptions were more common in the apatinib group (59.5% vs. 22.7%) as were dose reductions (48.4% vs. 4.5%). However, treatment discontinuations attributable to treatment-emergent adverse events were few in both arms (5.1% in the apatinib arm and 3.2% in the placebo arm).
Cause for hesitation
“VEGFR-TKIs have not yet found a solid home in lung cancer,” said study discussant Lecia V. Sequist, MD, of Massachusetts General Hospital in Boston.
Listing 10 VEGFR-TKIs, Dr. Sequist noted: “None of them have changed practice.”
She added that, while an all-oral regimen is appealing, the benefit of adding apatinib to gefitinib was modest, and the regimen was “fairly difficult” to tolerate. “The PFS with apatinib plus gefitinib is well below what we see with other EGFR/VEGF first-line studies,” she said.
Dr. Sequist also observed that most studies have shown a PFS benefit but no overall survival benefit. “That, in combination with the toxicity, makes me a little hesitant about this regimen. The role of VEGF remains unclear in EGFR mutation–positive lung cancer in 2020,” she concluded.
The ACTIVE study was funded by Jiangsu HengRui Medicine, the Chinese Thoracic Oncology Group, and grants from Sun Yat-sen University and the National Key R&D Program of China. Dr. Zhang disclosed relationships with AstraZeneca, Bristol-Myers Squibb, Eli Lilly, Pfizer, and Roche. Dr. Sequist disclosed relationships with AstraZeneca, Bristol-Myers Squibb, Blueprint Medicines, and many other companies.
SOURCE: Zhang L et al. ESMO 2020, Abstract LBA50.
ACTIVE is the first phase 3 trial of an oral vascular epidermal growth factor receptor–2 (VEGFR2) tyrosine kinase inhibitor (TKI) added to an EGFR-TKI as first-line therapy in this population, according to Li Zhang, MD, of Sun Yat-sen University Cancer Center in Guangzhou, China.
Dr. Zhang presented results from ACTIVE at the European Society for Medical Oncology Virtual Congress 2020.
“This dual oral regimen will provide more convenient treatment for patients who require long-term administration,” Dr. Zhang said. He added that apatinib plus gefitinib “is expected to become a new first-line treatment option for EGFR-mutant NSCLC.”
A discussant for the ACTIVE study was less optimistic, however, noting that the regimen proved tough to tolerate for some patients, and the PFS benefit may not translate to overall survival.
Study rationale and details
Sensitizing EGFR mutations occur in about 10% of White patients and up to 50% of Asian patients, Dr. Zhang noted. Unfortunately, most patients progress after first-line treatment with EGFR-TKIs because of acquired resistance.
Blocking VEGF receptor pathways has been shown to enhance EGFR-TKIs in EGFR-mutated NSCLC, and pilot study results have shown apatinib – an oral VEGFR2–TKI – to be safe and well-tolerated with promising efficacy in combination with gefitinib, Dr. Zhang added.
To expand upon those results, he and his colleagues tested apatinib with gefitinib in the phase 3, double-blind, placebo-controlled ACTIVE trial (CTONG1706).
The trial included 313 patients (median age, 58.5 years) with locally advanced, metastatic, or recurrent nonsquamous NSCLC. All were chemotherapy-naive and EGFR mutation-positive (exon 19 deletion or exon 21 L858R).
Patients were randomized 1:1 to first-line apatinib at 500 mg daily plus gefitinib at 250 mg daily (n = 157) or placebo plus gefitinib at 250 mg daily (n = 156) until progressive disease or unacceptable toxicity.
Efficacy and safety
The primary endpoint was PFS by independent review. The median follow-up was 15.8 months.
The median PFS was 13.7 months in the apatinib group and 10.2 months in the placebo group (hazard ratio, 0.71; P = .0189).
Objective response rates were similar for both groups – 77.1% with apatinib and 73.7% with placebo. However, depth of response ≥30% and depth of response ≥50% both favored the apatinib arm – 89.2% versus 79.5% for ≥ 30% (P = .0209) and 64.3% versus 52.6% for ≥50% (P = .0238).
In addition, the median duration of response was longer for the apatinib group – 12.9 months versus 9.3 months (HR, 0.64; P = .005).
Exploratory biomarker analyses showed the benefit of apatinib was more common in patients with TP53 exon 8 mutations.
The rate of grade 3 or higher treatment-emergent adverse events was 84.1% in the apatinib arm and 37.7% in the placebo arm. Diarrhea (73.2%) and hypertension (68.2%) were the most common treatment-emergent adverse events in the apatinib group.
Dose interruptions were more common in the apatinib group (59.5% vs. 22.7%) as were dose reductions (48.4% vs. 4.5%). However, treatment discontinuations attributable to treatment-emergent adverse events were few in both arms (5.1% in the apatinib arm and 3.2% in the placebo arm).
Cause for hesitation
“VEGFR-TKIs have not yet found a solid home in lung cancer,” said study discussant Lecia V. Sequist, MD, of Massachusetts General Hospital in Boston.
Listing 10 VEGFR-TKIs, Dr. Sequist noted: “None of them have changed practice.”
She added that, while an all-oral regimen is appealing, the benefit of adding apatinib to gefitinib was modest, and the regimen was “fairly difficult” to tolerate. “The PFS with apatinib plus gefitinib is well below what we see with other EGFR/VEGF first-line studies,” she said.
Dr. Sequist also observed that most studies have shown a PFS benefit but no overall survival benefit. “That, in combination with the toxicity, makes me a little hesitant about this regimen. The role of VEGF remains unclear in EGFR mutation–positive lung cancer in 2020,” she concluded.
The ACTIVE study was funded by Jiangsu HengRui Medicine, the Chinese Thoracic Oncology Group, and grants from Sun Yat-sen University and the National Key R&D Program of China. Dr. Zhang disclosed relationships with AstraZeneca, Bristol-Myers Squibb, Eli Lilly, Pfizer, and Roche. Dr. Sequist disclosed relationships with AstraZeneca, Bristol-Myers Squibb, Blueprint Medicines, and many other companies.
SOURCE: Zhang L et al. ESMO 2020, Abstract LBA50.
FROM ESMO 2020
Post-COVID clinics get jump-start from patients with lingering illness
Clarence Troutman survived a 2-month hospital stay with COVID-19, then went home in early June. But he’s far from over the disease, still suffering from limited endurance, shortness of breath and hands that can be stiff and swollen.
“Before COVID, I was a 59-year-old, relatively healthy man,” said the broadband technician from Denver. “If I had to say where I’m at now, I’d say about 50% of where I was, but when I first went home, I was at 20%.”
He credits much of his progress to the “motivation and education” gleaned from a new program for post-COVID patients at the University of Colorado at Denver, Aurora, one of a small but growing number of clinics aimed at treating and studying those who have had the unpredictable coronavirus.
As the election nears, much attention is focused on daily infection numbers or the climbing death toll, but another measure matters: Patients who survive but continue to wrestle with a range of physical or mental effects, including lung damage, heart or neurologic concerns, anxiety, and depression.
“We need to think about how we’re going to provide care for patients who may be recovering for years after the virus,” said Sarah Jolley, MD, a pulmonologist with UCHealth University of Colorado Hospital and director of UCHealth’s Post-Covid Clinic, where Mr. Troutman is seen.
That need has jump-started post-COVID clinics, which bring together a range of specialists into a one-stop shop.
One of the first and largest such clinics is at Mount Sinai in New York City, but programs have also launched at the University of California,San Francisco; Stanford (Calif.) University Medical Center; and the University of Pennsylvania, Philadelphia. The Cleveland Clinic plans to open one early next year. And it’s not just academic medical centers: St. John’s Well Child and Family Center, part of a network of community clinics in south central Los Angeles, said this month it aims to test thousands of its patients who were diagnosed with COVID-19 since March for long-term effects.
Mental health specialists are also involved, along with social workers and pharmacists. Many of the centers also do research studies, aiming to better understand why the virus hits certain patients so hard.
“Some of our patients, even those on a ventilator on death’s door, will come out remarkably unscathed,” said Lekshmi Santhosh, MD, an assistant professor of pulmonary critical care and a leader of the post-COVID program at UCSF, called the OPTIMAL clinic. “Others, even those who were never hospitalized, have disabling fatigue, ongoing chest pain, and shortness of breath, and there’s a whole spectrum in between.”
‘Staggering’ medical need
It’s too early to know how long the persistent medical effects and symptoms will linger, or to make accurate estimates on the percentage of patients affected.
Some early studies are sobering. An Austrian report released this month found that 76 of the first 86 patients studied had evidence of lung damage 6 weeks after hospital discharge, but that dropped to 48 patients at 12 weeks.
Some researchers and clinics say about 10% of U.S. COVID patients they see may have longer-running effects, said Zijian Chen, MD, medical director of the Center for Post-COVID Care at Mount Sinai, which has enrolled 400 patients so far.
If that estimate is correct – and Dr. Chen emphasized that more research is needed to make sure – it translates to patients entering the medical system in droves, often with multiple issues.
How health systems and insurers respond will be key, he said. More than 6.5 million U.S. residents have tested positive for the disease. If fewer than 10% – say 500,000 – already have long-lasting symptoms, “that number is staggering,” Dr. Chen said. “How much medical care will be needed for that?”
Though start-up costs could be a hurdle, the clinics themselves may eventually draw much-needed revenue to medical centers by attracting patients, many of whom have insurance to cover some or all of the cost of repeated visits.
Dr. Chen said the specialized centers can help lower health spending by providing more cost effective, coordinated care that avoids duplicative testing a patient might otherwise undergo.
“We’ve seen patients that when they come in, they’ve already had four MRI or CT scans and a stack of bloodwork,” he said.
The program consolidates those earlier results and determines if any additional testing is needed. Sometimes the answer to what’s causing patients’ long-lasting symptoms remains elusive. One problem for patients seeking help outside of dedicated clinics is that when there is no clear cause for their condition, they may be told the symptoms are imagined.
“I believe in the patients,” said Dr. Chen.
About half the clinic’s patients have received test results showing damage, said Dr. Chen, an endocrinologist and internal medicine physician. For those patients, the clinic can develop a treatment plan. But, frustratingly, the other half have inconclusive test results yet exhibit a range of symptoms.
“That makes it more difficult to treat,” said Dr. Chen.
Experts see parallels to a push in the past decade to establish special clinics to treat patients released from ICU wards, who may have problems related to long-term bed rest or the delirium many experience while hospitalized. Some of the current post-COVID clinics are modeled after the post-ICU clinics or are expanded versions of them.
The ICU Recovery Center at Vanderbilt University Medical Center, Nashville, Tenn., for instance, which opened in 2012, is accepting post-COVID patients.
There are about a dozen post-ICU clinics nationally, some of which are also now working with COVID patients, said James Jackson, director of long-term outcomes at the Vanderbilt center. In addition, he’s heard of at least another dozen post-COVID centers in development.
The centers generally do an initial assessment a few weeks after a patient is diagnosed or discharged from the hospital, often by video call. Check-in and repeat visits are scheduled every month or so after that.
“In an ideal world, with these post-COVID clinics, you can identify the patients and get them into rehab,” he said. “Even if the primary thing these clinics did was to say to patients: ‘This is real, it is not all in your head,’ that impact would be important.”
A question of feasibility
Financing is the largest obstacle, program proponents said. Many hospitals lost substantial revenue to canceled elective procedures during stay-at-home periods.
“So, it’s not a great time to be pitching a new activity that requires a start-up subsidy,” said Glenn Melnick, PhD, a professor of health economics at the University of Southern California.
At UCSF, a select group of faculty members staff the post-COVID clinics and some mental health professionals volunteer their time, said Dr. Santhosh.
Dr. Chen said he was able to recruit team members and support staff from the ranks of those whose elective patient caseload had dropped.
Dr. Jackson said unfortunately there’s not been enough research into the cost-and-clinical effectiveness of post-ICU centers.
“In the early days, there may have been questions about how much value does this add,” he noted. “Now, the question is not so much is it a good idea, but is it feasible?”
Right now, the post-COVID centers are foremost a research effort, said Len Nichols, an economist and nonresident fellow at the Urban Institute. “If these guys get good at treating long-term symptoms, that’s good for all of us. There’s not enough patients to make it a business model yet, but if they become the place to go when you get it, it could become a business model for some of the elite institutions.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
Clarence Troutman survived a 2-month hospital stay with COVID-19, then went home in early June. But he’s far from over the disease, still suffering from limited endurance, shortness of breath and hands that can be stiff and swollen.
“Before COVID, I was a 59-year-old, relatively healthy man,” said the broadband technician from Denver. “If I had to say where I’m at now, I’d say about 50% of where I was, but when I first went home, I was at 20%.”
He credits much of his progress to the “motivation and education” gleaned from a new program for post-COVID patients at the University of Colorado at Denver, Aurora, one of a small but growing number of clinics aimed at treating and studying those who have had the unpredictable coronavirus.
As the election nears, much attention is focused on daily infection numbers or the climbing death toll, but another measure matters: Patients who survive but continue to wrestle with a range of physical or mental effects, including lung damage, heart or neurologic concerns, anxiety, and depression.
“We need to think about how we’re going to provide care for patients who may be recovering for years after the virus,” said Sarah Jolley, MD, a pulmonologist with UCHealth University of Colorado Hospital and director of UCHealth’s Post-Covid Clinic, where Mr. Troutman is seen.
That need has jump-started post-COVID clinics, which bring together a range of specialists into a one-stop shop.
One of the first and largest such clinics is at Mount Sinai in New York City, but programs have also launched at the University of California,San Francisco; Stanford (Calif.) University Medical Center; and the University of Pennsylvania, Philadelphia. The Cleveland Clinic plans to open one early next year. And it’s not just academic medical centers: St. John’s Well Child and Family Center, part of a network of community clinics in south central Los Angeles, said this month it aims to test thousands of its patients who were diagnosed with COVID-19 since March for long-term effects.
Mental health specialists are also involved, along with social workers and pharmacists. Many of the centers also do research studies, aiming to better understand why the virus hits certain patients so hard.
“Some of our patients, even those on a ventilator on death’s door, will come out remarkably unscathed,” said Lekshmi Santhosh, MD, an assistant professor of pulmonary critical care and a leader of the post-COVID program at UCSF, called the OPTIMAL clinic. “Others, even those who were never hospitalized, have disabling fatigue, ongoing chest pain, and shortness of breath, and there’s a whole spectrum in between.”
‘Staggering’ medical need
It’s too early to know how long the persistent medical effects and symptoms will linger, or to make accurate estimates on the percentage of patients affected.
Some early studies are sobering. An Austrian report released this month found that 76 of the first 86 patients studied had evidence of lung damage 6 weeks after hospital discharge, but that dropped to 48 patients at 12 weeks.
Some researchers and clinics say about 10% of U.S. COVID patients they see may have longer-running effects, said Zijian Chen, MD, medical director of the Center for Post-COVID Care at Mount Sinai, which has enrolled 400 patients so far.
If that estimate is correct – and Dr. Chen emphasized that more research is needed to make sure – it translates to patients entering the medical system in droves, often with multiple issues.
How health systems and insurers respond will be key, he said. More than 6.5 million U.S. residents have tested positive for the disease. If fewer than 10% – say 500,000 – already have long-lasting symptoms, “that number is staggering,” Dr. Chen said. “How much medical care will be needed for that?”
Though start-up costs could be a hurdle, the clinics themselves may eventually draw much-needed revenue to medical centers by attracting patients, many of whom have insurance to cover some or all of the cost of repeated visits.
Dr. Chen said the specialized centers can help lower health spending by providing more cost effective, coordinated care that avoids duplicative testing a patient might otherwise undergo.
“We’ve seen patients that when they come in, they’ve already had four MRI or CT scans and a stack of bloodwork,” he said.
The program consolidates those earlier results and determines if any additional testing is needed. Sometimes the answer to what’s causing patients’ long-lasting symptoms remains elusive. One problem for patients seeking help outside of dedicated clinics is that when there is no clear cause for their condition, they may be told the symptoms are imagined.
“I believe in the patients,” said Dr. Chen.
About half the clinic’s patients have received test results showing damage, said Dr. Chen, an endocrinologist and internal medicine physician. For those patients, the clinic can develop a treatment plan. But, frustratingly, the other half have inconclusive test results yet exhibit a range of symptoms.
“That makes it more difficult to treat,” said Dr. Chen.
Experts see parallels to a push in the past decade to establish special clinics to treat patients released from ICU wards, who may have problems related to long-term bed rest or the delirium many experience while hospitalized. Some of the current post-COVID clinics are modeled after the post-ICU clinics or are expanded versions of them.
The ICU Recovery Center at Vanderbilt University Medical Center, Nashville, Tenn., for instance, which opened in 2012, is accepting post-COVID patients.
There are about a dozen post-ICU clinics nationally, some of which are also now working with COVID patients, said James Jackson, director of long-term outcomes at the Vanderbilt center. In addition, he’s heard of at least another dozen post-COVID centers in development.
The centers generally do an initial assessment a few weeks after a patient is diagnosed or discharged from the hospital, often by video call. Check-in and repeat visits are scheduled every month or so after that.
“In an ideal world, with these post-COVID clinics, you can identify the patients and get them into rehab,” he said. “Even if the primary thing these clinics did was to say to patients: ‘This is real, it is not all in your head,’ that impact would be important.”
A question of feasibility
Financing is the largest obstacle, program proponents said. Many hospitals lost substantial revenue to canceled elective procedures during stay-at-home periods.
“So, it’s not a great time to be pitching a new activity that requires a start-up subsidy,” said Glenn Melnick, PhD, a professor of health economics at the University of Southern California.
At UCSF, a select group of faculty members staff the post-COVID clinics and some mental health professionals volunteer their time, said Dr. Santhosh.
Dr. Chen said he was able to recruit team members and support staff from the ranks of those whose elective patient caseload had dropped.
Dr. Jackson said unfortunately there’s not been enough research into the cost-and-clinical effectiveness of post-ICU centers.
“In the early days, there may have been questions about how much value does this add,” he noted. “Now, the question is not so much is it a good idea, but is it feasible?”
Right now, the post-COVID centers are foremost a research effort, said Len Nichols, an economist and nonresident fellow at the Urban Institute. “If these guys get good at treating long-term symptoms, that’s good for all of us. There’s not enough patients to make it a business model yet, but if they become the place to go when you get it, it could become a business model for some of the elite institutions.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
Clarence Troutman survived a 2-month hospital stay with COVID-19, then went home in early June. But he’s far from over the disease, still suffering from limited endurance, shortness of breath and hands that can be stiff and swollen.
“Before COVID, I was a 59-year-old, relatively healthy man,” said the broadband technician from Denver. “If I had to say where I’m at now, I’d say about 50% of where I was, but when I first went home, I was at 20%.”
He credits much of his progress to the “motivation and education” gleaned from a new program for post-COVID patients at the University of Colorado at Denver, Aurora, one of a small but growing number of clinics aimed at treating and studying those who have had the unpredictable coronavirus.
As the election nears, much attention is focused on daily infection numbers or the climbing death toll, but another measure matters: Patients who survive but continue to wrestle with a range of physical or mental effects, including lung damage, heart or neurologic concerns, anxiety, and depression.
“We need to think about how we’re going to provide care for patients who may be recovering for years after the virus,” said Sarah Jolley, MD, a pulmonologist with UCHealth University of Colorado Hospital and director of UCHealth’s Post-Covid Clinic, where Mr. Troutman is seen.
That need has jump-started post-COVID clinics, which bring together a range of specialists into a one-stop shop.
One of the first and largest such clinics is at Mount Sinai in New York City, but programs have also launched at the University of California,San Francisco; Stanford (Calif.) University Medical Center; and the University of Pennsylvania, Philadelphia. The Cleveland Clinic plans to open one early next year. And it’s not just academic medical centers: St. John’s Well Child and Family Center, part of a network of community clinics in south central Los Angeles, said this month it aims to test thousands of its patients who were diagnosed with COVID-19 since March for long-term effects.
Mental health specialists are also involved, along with social workers and pharmacists. Many of the centers also do research studies, aiming to better understand why the virus hits certain patients so hard.
“Some of our patients, even those on a ventilator on death’s door, will come out remarkably unscathed,” said Lekshmi Santhosh, MD, an assistant professor of pulmonary critical care and a leader of the post-COVID program at UCSF, called the OPTIMAL clinic. “Others, even those who were never hospitalized, have disabling fatigue, ongoing chest pain, and shortness of breath, and there’s a whole spectrum in between.”
‘Staggering’ medical need
It’s too early to know how long the persistent medical effects and symptoms will linger, or to make accurate estimates on the percentage of patients affected.
Some early studies are sobering. An Austrian report released this month found that 76 of the first 86 patients studied had evidence of lung damage 6 weeks after hospital discharge, but that dropped to 48 patients at 12 weeks.
Some researchers and clinics say about 10% of U.S. COVID patients they see may have longer-running effects, said Zijian Chen, MD, medical director of the Center for Post-COVID Care at Mount Sinai, which has enrolled 400 patients so far.
If that estimate is correct – and Dr. Chen emphasized that more research is needed to make sure – it translates to patients entering the medical system in droves, often with multiple issues.
How health systems and insurers respond will be key, he said. More than 6.5 million U.S. residents have tested positive for the disease. If fewer than 10% – say 500,000 – already have long-lasting symptoms, “that number is staggering,” Dr. Chen said. “How much medical care will be needed for that?”
Though start-up costs could be a hurdle, the clinics themselves may eventually draw much-needed revenue to medical centers by attracting patients, many of whom have insurance to cover some or all of the cost of repeated visits.
Dr. Chen said the specialized centers can help lower health spending by providing more cost effective, coordinated care that avoids duplicative testing a patient might otherwise undergo.
“We’ve seen patients that when they come in, they’ve already had four MRI or CT scans and a stack of bloodwork,” he said.
The program consolidates those earlier results and determines if any additional testing is needed. Sometimes the answer to what’s causing patients’ long-lasting symptoms remains elusive. One problem for patients seeking help outside of dedicated clinics is that when there is no clear cause for their condition, they may be told the symptoms are imagined.
“I believe in the patients,” said Dr. Chen.
About half the clinic’s patients have received test results showing damage, said Dr. Chen, an endocrinologist and internal medicine physician. For those patients, the clinic can develop a treatment plan. But, frustratingly, the other half have inconclusive test results yet exhibit a range of symptoms.
“That makes it more difficult to treat,” said Dr. Chen.
Experts see parallels to a push in the past decade to establish special clinics to treat patients released from ICU wards, who may have problems related to long-term bed rest or the delirium many experience while hospitalized. Some of the current post-COVID clinics are modeled after the post-ICU clinics or are expanded versions of them.
The ICU Recovery Center at Vanderbilt University Medical Center, Nashville, Tenn., for instance, which opened in 2012, is accepting post-COVID patients.
There are about a dozen post-ICU clinics nationally, some of which are also now working with COVID patients, said James Jackson, director of long-term outcomes at the Vanderbilt center. In addition, he’s heard of at least another dozen post-COVID centers in development.
The centers generally do an initial assessment a few weeks after a patient is diagnosed or discharged from the hospital, often by video call. Check-in and repeat visits are scheduled every month or so after that.
“In an ideal world, with these post-COVID clinics, you can identify the patients and get them into rehab,” he said. “Even if the primary thing these clinics did was to say to patients: ‘This is real, it is not all in your head,’ that impact would be important.”
A question of feasibility
Financing is the largest obstacle, program proponents said. Many hospitals lost substantial revenue to canceled elective procedures during stay-at-home periods.
“So, it’s not a great time to be pitching a new activity that requires a start-up subsidy,” said Glenn Melnick, PhD, a professor of health economics at the University of Southern California.
At UCSF, a select group of faculty members staff the post-COVID clinics and some mental health professionals volunteer their time, said Dr. Santhosh.
Dr. Chen said he was able to recruit team members and support staff from the ranks of those whose elective patient caseload had dropped.
Dr. Jackson said unfortunately there’s not been enough research into the cost-and-clinical effectiveness of post-ICU centers.
“In the early days, there may have been questions about how much value does this add,” he noted. “Now, the question is not so much is it a good idea, but is it feasible?”
Right now, the post-COVID centers are foremost a research effort, said Len Nichols, an economist and nonresident fellow at the Urban Institute. “If these guys get good at treating long-term symptoms, that’s good for all of us. There’s not enough patients to make it a business model yet, but if they become the place to go when you get it, it could become a business model for some of the elite institutions.”
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
Screening algorithm safely selects patients for OSA treatment before bariatric surgery
A novel algorithm for selecting patients who require treatment for obstructive sleep apnea (OSA) before undergoing bariatric surgery proved safe in a prospective cohort study of 1,103 patients.
Screening for OSA is recommended before bariatric surgery. OSA has been associated in several meta-analyses with increased risk for postoperative complications – not limited to bariatric surgery – and some studies have suggested that this increased risk may be limited to severe OSA, said Frédéric Series, MD, of Université Laval, Quebec City, at the virtual annual meeting of the Associated Sleep Societies.
The preoperative screening algorithm, which utilizes the results of nocturnal home oximetry and morning capillary gas measurements, effectively stratified patients for the risk of postoperative adverse events and “safely selected patients who don’t need [continuous positive airway pressure] before bariatric surgery,” he said. “The risk of postoperative adverse events following bariatric surgery was not increased in untreated OSA patients with low or moderate risk of severe OSA and hypoventilation.”
The study also demonstrated, he said, that patients with severe OSA with or without hypoventilation, even when correctly treated, remain at higher risk for complications.
The algorithm utilizes an oxygen desaturation index (ODI) corresponding to 3% drops in SaO2 and the percent of the total recording time with an SaO2 below 90%, as well as capillary gas measurements (PCO2). Treatment was initiated for those with severe OSA (ODI ≥ 25/hr, < 10% of recording time with a SaO2 below 90%) or OSA with hypoventilation (PCO2 ≥ 45).
“When the ODI was less than 25 per hour, and when the total recording time spent below 90% SaO2 was less than 10%, with PCO2 < 45 mmHg, we expected no need for CPAP treatment,” Dr. Series said. For analysis, the investigators considered part of the untreated group – those with an ODI < 10/hr (no or mild OSA) – as a control group.
Treated patients underwent CPAP/BiPAP for a mean duration of 1.5 months. Good treatment compliance was mandatory for surgery, and treatment was continued immediately after extubation, in the recovery room, in nearly all patients, Dr. Series reported.
The analysis covered 1,103 patients: 447 controls (40.8%), 358 untreated (32.7%), 289 treated for OSA (26.4%) and 9 (0.8%) treated for OSA + hypoventilation. Patients with OSA, particularly those with severe OSA and those with hypoventilation, were older and heavier and significantly more likely to have hypertension and diabetes than controls.
There were no differences between the four groups in 10-day reoperation or 30-day readmission occurrence, and postoperative complications were “particularly infrequent in the control and OSA-untreated groups, with no differences between these two groups,” Dr. Series said.
Cardiac arrhythmia (mainly atrial fibrillation) occurred more frequently in the OSA-treated group (2.4%) and the OSA/hypoventilation patients (11%) than in the other groups (0.5%-0.6%).
Respiratory failure occurred in about one-third of patients with hypoventilation, and admission to the ICU was “dramatically higher” in patients with hypoventilation (67%), because of respiratory failure, arrhythmia, or other unstable medical conditions, Dr. Series said.
There were no differences between the groups in the duration of surgery or the amount of anesthetic used, but the length of stay in the recovery room was significantly longer in the OSA-treated and hypoventilation groups. The length of hospital stay was also longer in these groups. Sleeve gastrectomy was the most frequent bariatric surgical procedure across all groups, including 100% of patients with hypoventilation, he noted.
Asked to comment on the study, Octavian C. Ioachimescu, MD, PhD, of Emory University in Atlanta and the Atlanta Veterans Affairs Medical Center in Decatur, said the algorithm “clearly deserves further validation in other clinical-based cohorts and longer-term outcome assessment.”
Dr. Series reported that he has no relevant disclosures. Dr. Ioachimescu also said he has no relevant disclosures.
A novel algorithm for selecting patients who require treatment for obstructive sleep apnea (OSA) before undergoing bariatric surgery proved safe in a prospective cohort study of 1,103 patients.
Screening for OSA is recommended before bariatric surgery. OSA has been associated in several meta-analyses with increased risk for postoperative complications – not limited to bariatric surgery – and some studies have suggested that this increased risk may be limited to severe OSA, said Frédéric Series, MD, of Université Laval, Quebec City, at the virtual annual meeting of the Associated Sleep Societies.
The preoperative screening algorithm, which utilizes the results of nocturnal home oximetry and morning capillary gas measurements, effectively stratified patients for the risk of postoperative adverse events and “safely selected patients who don’t need [continuous positive airway pressure] before bariatric surgery,” he said. “The risk of postoperative adverse events following bariatric surgery was not increased in untreated OSA patients with low or moderate risk of severe OSA and hypoventilation.”
The study also demonstrated, he said, that patients with severe OSA with or without hypoventilation, even when correctly treated, remain at higher risk for complications.
The algorithm utilizes an oxygen desaturation index (ODI) corresponding to 3% drops in SaO2 and the percent of the total recording time with an SaO2 below 90%, as well as capillary gas measurements (PCO2). Treatment was initiated for those with severe OSA (ODI ≥ 25/hr, < 10% of recording time with a SaO2 below 90%) or OSA with hypoventilation (PCO2 ≥ 45).
“When the ODI was less than 25 per hour, and when the total recording time spent below 90% SaO2 was less than 10%, with PCO2 < 45 mmHg, we expected no need for CPAP treatment,” Dr. Series said. For analysis, the investigators considered part of the untreated group – those with an ODI < 10/hr (no or mild OSA) – as a control group.
Treated patients underwent CPAP/BiPAP for a mean duration of 1.5 months. Good treatment compliance was mandatory for surgery, and treatment was continued immediately after extubation, in the recovery room, in nearly all patients, Dr. Series reported.
The analysis covered 1,103 patients: 447 controls (40.8%), 358 untreated (32.7%), 289 treated for OSA (26.4%) and 9 (0.8%) treated for OSA + hypoventilation. Patients with OSA, particularly those with severe OSA and those with hypoventilation, were older and heavier and significantly more likely to have hypertension and diabetes than controls.
There were no differences between the four groups in 10-day reoperation or 30-day readmission occurrence, and postoperative complications were “particularly infrequent in the control and OSA-untreated groups, with no differences between these two groups,” Dr. Series said.
Cardiac arrhythmia (mainly atrial fibrillation) occurred more frequently in the OSA-treated group (2.4%) and the OSA/hypoventilation patients (11%) than in the other groups (0.5%-0.6%).
Respiratory failure occurred in about one-third of patients with hypoventilation, and admission to the ICU was “dramatically higher” in patients with hypoventilation (67%), because of respiratory failure, arrhythmia, or other unstable medical conditions, Dr. Series said.
There were no differences between the groups in the duration of surgery or the amount of anesthetic used, but the length of stay in the recovery room was significantly longer in the OSA-treated and hypoventilation groups. The length of hospital stay was also longer in these groups. Sleeve gastrectomy was the most frequent bariatric surgical procedure across all groups, including 100% of patients with hypoventilation, he noted.
Asked to comment on the study, Octavian C. Ioachimescu, MD, PhD, of Emory University in Atlanta and the Atlanta Veterans Affairs Medical Center in Decatur, said the algorithm “clearly deserves further validation in other clinical-based cohorts and longer-term outcome assessment.”
Dr. Series reported that he has no relevant disclosures. Dr. Ioachimescu also said he has no relevant disclosures.
A novel algorithm for selecting patients who require treatment for obstructive sleep apnea (OSA) before undergoing bariatric surgery proved safe in a prospective cohort study of 1,103 patients.
Screening for OSA is recommended before bariatric surgery. OSA has been associated in several meta-analyses with increased risk for postoperative complications – not limited to bariatric surgery – and some studies have suggested that this increased risk may be limited to severe OSA, said Frédéric Series, MD, of Université Laval, Quebec City, at the virtual annual meeting of the Associated Sleep Societies.
The preoperative screening algorithm, which utilizes the results of nocturnal home oximetry and morning capillary gas measurements, effectively stratified patients for the risk of postoperative adverse events and “safely selected patients who don’t need [continuous positive airway pressure] before bariatric surgery,” he said. “The risk of postoperative adverse events following bariatric surgery was not increased in untreated OSA patients with low or moderate risk of severe OSA and hypoventilation.”
The study also demonstrated, he said, that patients with severe OSA with or without hypoventilation, even when correctly treated, remain at higher risk for complications.
The algorithm utilizes an oxygen desaturation index (ODI) corresponding to 3% drops in SaO2 and the percent of the total recording time with an SaO2 below 90%, as well as capillary gas measurements (PCO2). Treatment was initiated for those with severe OSA (ODI ≥ 25/hr, < 10% of recording time with a SaO2 below 90%) or OSA with hypoventilation (PCO2 ≥ 45).
“When the ODI was less than 25 per hour, and when the total recording time spent below 90% SaO2 was less than 10%, with PCO2 < 45 mmHg, we expected no need for CPAP treatment,” Dr. Series said. For analysis, the investigators considered part of the untreated group – those with an ODI < 10/hr (no or mild OSA) – as a control group.
Treated patients underwent CPAP/BiPAP for a mean duration of 1.5 months. Good treatment compliance was mandatory for surgery, and treatment was continued immediately after extubation, in the recovery room, in nearly all patients, Dr. Series reported.
The analysis covered 1,103 patients: 447 controls (40.8%), 358 untreated (32.7%), 289 treated for OSA (26.4%) and 9 (0.8%) treated for OSA + hypoventilation. Patients with OSA, particularly those with severe OSA and those with hypoventilation, were older and heavier and significantly more likely to have hypertension and diabetes than controls.
There were no differences between the four groups in 10-day reoperation or 30-day readmission occurrence, and postoperative complications were “particularly infrequent in the control and OSA-untreated groups, with no differences between these two groups,” Dr. Series said.
Cardiac arrhythmia (mainly atrial fibrillation) occurred more frequently in the OSA-treated group (2.4%) and the OSA/hypoventilation patients (11%) than in the other groups (0.5%-0.6%).
Respiratory failure occurred in about one-third of patients with hypoventilation, and admission to the ICU was “dramatically higher” in patients with hypoventilation (67%), because of respiratory failure, arrhythmia, or other unstable medical conditions, Dr. Series said.
There were no differences between the groups in the duration of surgery or the amount of anesthetic used, but the length of stay in the recovery room was significantly longer in the OSA-treated and hypoventilation groups. The length of hospital stay was also longer in these groups. Sleeve gastrectomy was the most frequent bariatric surgical procedure across all groups, including 100% of patients with hypoventilation, he noted.
Asked to comment on the study, Octavian C. Ioachimescu, MD, PhD, of Emory University in Atlanta and the Atlanta Veterans Affairs Medical Center in Decatur, said the algorithm “clearly deserves further validation in other clinical-based cohorts and longer-term outcome assessment.”
Dr. Series reported that he has no relevant disclosures. Dr. Ioachimescu also said he has no relevant disclosures.
REPORTING FROM SLEEP 2020
Nerve damage linked to prone positioning in COVID-19
A new case series describes peripheral nerve injuries associated with this type of positioning and suggests ways to minimize the potential damage.
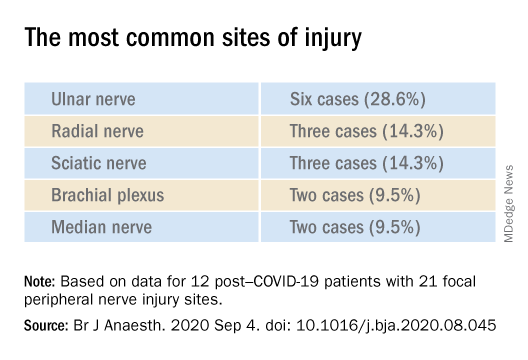
“Physicians should remain aware of increased susceptibility to peripheral nerve damage in patients with severe COVID-19 after prone positioning, since it is surprisingly common among these patients, and should refine standard protocols accordingly to reduce that risk,” said senior author Colin Franz, MD, PhD, director of the Electrodiagnostic Laboratory, Shirley Ryan AbilityLab, Chicago.
The article was published online Sept. 4 in the British Journal of Anaesthesiology.
Unique type of nerve injury
Many patients who are admitted to the intensive care unit with COVID-19 undergo invasive mechanical ventilation because of acute respiratory distress syndrome (ARDS). Clinical guidelines recommend that such patients lie in the prone position 12-16 hours per day.
“Prone positioning for up to 16 hours is a therapy we use for patients with more severe forms of ARDS, and high-level evidence points to mortality benefit in patients with moderate to severe ARDS if [mechanical] ventilation occurs,” said study coauthor James McCauley Walter, MD, of the pulmonary division at Northwestern University, Chicago.
With a “significant number of COVID-19 patients flooding the ICU, we quickly started to prone a lot of them, but if you are in a specific position for multiple hours a day, coupled with the neurotoxic effects of the SARS-CoV-2 virus itself, you may be exposed to a unique type of nerve injury,” he said.
Dr. Walter said that the “incidence of asymmetric neuropathies seems out of proportion to what has been reported in non–COVID-19 settings, which is what caught our attention.”
Many of these patients are discharged to rehabilitation hospitals, and “what we noticed, which was unique about COVID-19 patients coming to our rehab hospital, was that, compared with other patients who had been critically ill with a long hospital stay, there was a significantly higher percentage of COVID-19 patients who had peripheral nerve damage,” Dr. Franz said.
The authors described 12 of these patients who were admitted between April 24 and June 30, 2020 (mean age, 60.3 years; range, 23-80 years). The sample included White, Black, and Hispanic individuals. Eleven of the 12 post–COVID-19 patients with peripheral nerve damage had experienced prone positioning during acute management.
The average number of days patients received mechanical ventilation was 33.6 (range, 12-62 days). The average number of proning sessions was 4.5 (range, 1-16) with an average of 81.2 hours (range, 16-252 hours) spent prone.
A major contributor
Dr. Franz suggested that prone positioning is likely not the only cause of peripheral nerve damage but “may play a big role in these patients who are vulnerable because of viral infection and the critical illness that causes damage and nerve injuries.”
“The first component of lifesaving care for the critically ill in the ICU is intravenous fluids, mechanical ventilation, steroids, and antibiotics for infection,” said Dr. Walter.
“We are trying to come up with ways to place patients in prone position in safer ways, to pay attention to pressure points and areas of injury that we have seen and try to offload them, to see if we can decrease the rate of these injuries,” he added.
The researchers’ article includes a heat map diagram as a “template for where to focus the most efforts, in terms of decreasing pressure,” Dr. Walter said.
“The nerves are accepting too much force for gravely ill COVID-19 patients to handle, so we suggest using the template to determine where extra padding might be needed, or a protocol that might include changes in positioning,” he added.
Dr. Franz described the interventions used for COVID-19 patients with prone positioning–related peripheral nerve damage. “The first step is trying to address the problems one by one, either trying to solve them through exercise or teaching new skills, new ways to compensate, beginning with basic activities, such as getting out of bed and self-care,” he said.
Long-term recovery of nerve injuries depends on how severe the injuries are. Some nerves can slowly regenerate – possibly at the rate of 1 inch per month – which can be a long process, taking between a year and 18 months.
Dr. Franz said that therapies for this condition are “extrapolated from clinical trial work” on promoting nerve regeneration after surgery using electrical stimulation to enable nerves to regrow at a faster rate.
“Regeneration is not only slow, but it may not happen completely, leaving the patient with permanent nerve damage – in fact, based on our experience and what has been reported, the percentage of patients with full recovery is only 10%,” he said.
The most common symptomatic complaint other than lack of movement or feeling is neuropathic pain, “which may require medication to take the edge off the pain,” Dr. Franz added.
Irreversible damage?
Commenting on the study, Tae Chung, MD, of the departments of physical medicine, rehabilitation, and neurology, Johns Hopkins University, Baltimore, said the study “provides one of the first and the largest description of peripheral nerve injury associated with prone positioning for management of ARDS from COVID-19.”
Dr. Chung, who was not involved in the research, noted that “various neurological complications from COVID-19 have been reported, and some of them may result in irreversible neurological damage or delay the recovery from COVID-19 infection,” so “accurate and timely diagnosis of such neurological complications is critical for rehabilitation of the COVID-19 survivors.”
The study received no funding. Dr. Franz, Dr. Walter, study coauthors, and Dr. Chung report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
A new case series describes peripheral nerve injuries associated with this type of positioning and suggests ways to minimize the potential damage.
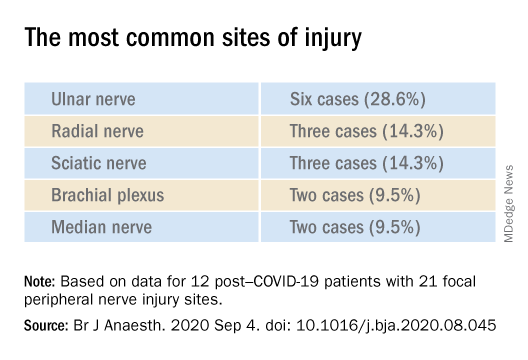
“Physicians should remain aware of increased susceptibility to peripheral nerve damage in patients with severe COVID-19 after prone positioning, since it is surprisingly common among these patients, and should refine standard protocols accordingly to reduce that risk,” said senior author Colin Franz, MD, PhD, director of the Electrodiagnostic Laboratory, Shirley Ryan AbilityLab, Chicago.
The article was published online Sept. 4 in the British Journal of Anaesthesiology.
Unique type of nerve injury
Many patients who are admitted to the intensive care unit with COVID-19 undergo invasive mechanical ventilation because of acute respiratory distress syndrome (ARDS). Clinical guidelines recommend that such patients lie in the prone position 12-16 hours per day.
“Prone positioning for up to 16 hours is a therapy we use for patients with more severe forms of ARDS, and high-level evidence points to mortality benefit in patients with moderate to severe ARDS if [mechanical] ventilation occurs,” said study coauthor James McCauley Walter, MD, of the pulmonary division at Northwestern University, Chicago.
With a “significant number of COVID-19 patients flooding the ICU, we quickly started to prone a lot of them, but if you are in a specific position for multiple hours a day, coupled with the neurotoxic effects of the SARS-CoV-2 virus itself, you may be exposed to a unique type of nerve injury,” he said.
Dr. Walter said that the “incidence of asymmetric neuropathies seems out of proportion to what has been reported in non–COVID-19 settings, which is what caught our attention.”
Many of these patients are discharged to rehabilitation hospitals, and “what we noticed, which was unique about COVID-19 patients coming to our rehab hospital, was that, compared with other patients who had been critically ill with a long hospital stay, there was a significantly higher percentage of COVID-19 patients who had peripheral nerve damage,” Dr. Franz said.
The authors described 12 of these patients who were admitted between April 24 and June 30, 2020 (mean age, 60.3 years; range, 23-80 years). The sample included White, Black, and Hispanic individuals. Eleven of the 12 post–COVID-19 patients with peripheral nerve damage had experienced prone positioning during acute management.
The average number of days patients received mechanical ventilation was 33.6 (range, 12-62 days). The average number of proning sessions was 4.5 (range, 1-16) with an average of 81.2 hours (range, 16-252 hours) spent prone.
A major contributor
Dr. Franz suggested that prone positioning is likely not the only cause of peripheral nerve damage but “may play a big role in these patients who are vulnerable because of viral infection and the critical illness that causes damage and nerve injuries.”
“The first component of lifesaving care for the critically ill in the ICU is intravenous fluids, mechanical ventilation, steroids, and antibiotics for infection,” said Dr. Walter.
“We are trying to come up with ways to place patients in prone position in safer ways, to pay attention to pressure points and areas of injury that we have seen and try to offload them, to see if we can decrease the rate of these injuries,” he added.
The researchers’ article includes a heat map diagram as a “template for where to focus the most efforts, in terms of decreasing pressure,” Dr. Walter said.
“The nerves are accepting too much force for gravely ill COVID-19 patients to handle, so we suggest using the template to determine where extra padding might be needed, or a protocol that might include changes in positioning,” he added.
Dr. Franz described the interventions used for COVID-19 patients with prone positioning–related peripheral nerve damage. “The first step is trying to address the problems one by one, either trying to solve them through exercise or teaching new skills, new ways to compensate, beginning with basic activities, such as getting out of bed and self-care,” he said.
Long-term recovery of nerve injuries depends on how severe the injuries are. Some nerves can slowly regenerate – possibly at the rate of 1 inch per month – which can be a long process, taking between a year and 18 months.
Dr. Franz said that therapies for this condition are “extrapolated from clinical trial work” on promoting nerve regeneration after surgery using electrical stimulation to enable nerves to regrow at a faster rate.
“Regeneration is not only slow, but it may not happen completely, leaving the patient with permanent nerve damage – in fact, based on our experience and what has been reported, the percentage of patients with full recovery is only 10%,” he said.
The most common symptomatic complaint other than lack of movement or feeling is neuropathic pain, “which may require medication to take the edge off the pain,” Dr. Franz added.
Irreversible damage?
Commenting on the study, Tae Chung, MD, of the departments of physical medicine, rehabilitation, and neurology, Johns Hopkins University, Baltimore, said the study “provides one of the first and the largest description of peripheral nerve injury associated with prone positioning for management of ARDS from COVID-19.”
Dr. Chung, who was not involved in the research, noted that “various neurological complications from COVID-19 have been reported, and some of them may result in irreversible neurological damage or delay the recovery from COVID-19 infection,” so “accurate and timely diagnosis of such neurological complications is critical for rehabilitation of the COVID-19 survivors.”
The study received no funding. Dr. Franz, Dr. Walter, study coauthors, and Dr. Chung report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
A new case series describes peripheral nerve injuries associated with this type of positioning and suggests ways to minimize the potential damage.
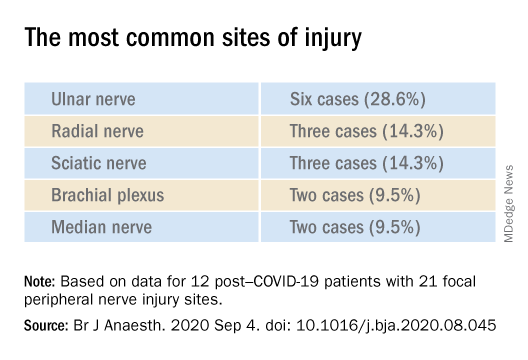
“Physicians should remain aware of increased susceptibility to peripheral nerve damage in patients with severe COVID-19 after prone positioning, since it is surprisingly common among these patients, and should refine standard protocols accordingly to reduce that risk,” said senior author Colin Franz, MD, PhD, director of the Electrodiagnostic Laboratory, Shirley Ryan AbilityLab, Chicago.
The article was published online Sept. 4 in the British Journal of Anaesthesiology.
Unique type of nerve injury
Many patients who are admitted to the intensive care unit with COVID-19 undergo invasive mechanical ventilation because of acute respiratory distress syndrome (ARDS). Clinical guidelines recommend that such patients lie in the prone position 12-16 hours per day.
“Prone positioning for up to 16 hours is a therapy we use for patients with more severe forms of ARDS, and high-level evidence points to mortality benefit in patients with moderate to severe ARDS if [mechanical] ventilation occurs,” said study coauthor James McCauley Walter, MD, of the pulmonary division at Northwestern University, Chicago.
With a “significant number of COVID-19 patients flooding the ICU, we quickly started to prone a lot of them, but if you are in a specific position for multiple hours a day, coupled with the neurotoxic effects of the SARS-CoV-2 virus itself, you may be exposed to a unique type of nerve injury,” he said.
Dr. Walter said that the “incidence of asymmetric neuropathies seems out of proportion to what has been reported in non–COVID-19 settings, which is what caught our attention.”
Many of these patients are discharged to rehabilitation hospitals, and “what we noticed, which was unique about COVID-19 patients coming to our rehab hospital, was that, compared with other patients who had been critically ill with a long hospital stay, there was a significantly higher percentage of COVID-19 patients who had peripheral nerve damage,” Dr. Franz said.
The authors described 12 of these patients who were admitted between April 24 and June 30, 2020 (mean age, 60.3 years; range, 23-80 years). The sample included White, Black, and Hispanic individuals. Eleven of the 12 post–COVID-19 patients with peripheral nerve damage had experienced prone positioning during acute management.
The average number of days patients received mechanical ventilation was 33.6 (range, 12-62 days). The average number of proning sessions was 4.5 (range, 1-16) with an average of 81.2 hours (range, 16-252 hours) spent prone.
A major contributor
Dr. Franz suggested that prone positioning is likely not the only cause of peripheral nerve damage but “may play a big role in these patients who are vulnerable because of viral infection and the critical illness that causes damage and nerve injuries.”
“The first component of lifesaving care for the critically ill in the ICU is intravenous fluids, mechanical ventilation, steroids, and antibiotics for infection,” said Dr. Walter.
“We are trying to come up with ways to place patients in prone position in safer ways, to pay attention to pressure points and areas of injury that we have seen and try to offload them, to see if we can decrease the rate of these injuries,” he added.
The researchers’ article includes a heat map diagram as a “template for where to focus the most efforts, in terms of decreasing pressure,” Dr. Walter said.
“The nerves are accepting too much force for gravely ill COVID-19 patients to handle, so we suggest using the template to determine where extra padding might be needed, or a protocol that might include changes in positioning,” he added.
Dr. Franz described the interventions used for COVID-19 patients with prone positioning–related peripheral nerve damage. “The first step is trying to address the problems one by one, either trying to solve them through exercise or teaching new skills, new ways to compensate, beginning with basic activities, such as getting out of bed and self-care,” he said.
Long-term recovery of nerve injuries depends on how severe the injuries are. Some nerves can slowly regenerate – possibly at the rate of 1 inch per month – which can be a long process, taking between a year and 18 months.
Dr. Franz said that therapies for this condition are “extrapolated from clinical trial work” on promoting nerve regeneration after surgery using electrical stimulation to enable nerves to regrow at a faster rate.
“Regeneration is not only slow, but it may not happen completely, leaving the patient with permanent nerve damage – in fact, based on our experience and what has been reported, the percentage of patients with full recovery is only 10%,” he said.
The most common symptomatic complaint other than lack of movement or feeling is neuropathic pain, “which may require medication to take the edge off the pain,” Dr. Franz added.
Irreversible damage?
Commenting on the study, Tae Chung, MD, of the departments of physical medicine, rehabilitation, and neurology, Johns Hopkins University, Baltimore, said the study “provides one of the first and the largest description of peripheral nerve injury associated with prone positioning for management of ARDS from COVID-19.”
Dr. Chung, who was not involved in the research, noted that “various neurological complications from COVID-19 have been reported, and some of them may result in irreversible neurological damage or delay the recovery from COVID-19 infection,” so “accurate and timely diagnosis of such neurological complications is critical for rehabilitation of the COVID-19 survivors.”
The study received no funding. Dr. Franz, Dr. Walter, study coauthors, and Dr. Chung report no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
FROM THE BRITISH JOURNAL OF ANAESTHESIOLOGY
Trump signs Medicare loan relief bill delaying repayments
President Trump on Oct. 1 signed a bill to keep the federal government running through December 11. This “continuing resolution” (CR), which was approved by the Senate Wednesday on an 84-10 vote, according to The New York Times, includes provisions to delay repayment by physicians of pandemic-related Medicare loans and to reduce the loans’ interest rate.
In an earlier news release, the American Medical Association reported that Congress and the White House had agreed to include the provisions on Medicare loans in the CR.
Under the Medicare Accelerated and Advance Payments (AAP) program, the Centers for Medicare & Medicaid Services advanced money to physicians who were financially impacted by the pandemic. The program, created in March, was suspended in late April.
Physicians who received the Medicare loans were supposed to start paying them back 120 days after they were made. CMS planned to recoup the advances by offsetting them against Medicare claims payments due to physicians. Practices had up to 210 days (7 months) to repay the loans through this process before being asked to repay them directly with interest of 10.25%.
For the practices that received these advances, that meant their Medicare cash flow was scheduled to dry up, starting in August. However, CMS quietly abstained from collecting these payments when they came due, according to Modern Healthcare.
New terms
The amount to be recouped from each claim is reduced from 100% to 25% of the claim for the first 11 months and to 50% of claims withheld for an additional 6 months. If the loan is not repaid in full by then, the provider must pay the balance with interest of 4%.
More than 80% of the $100 billion that CMS loaned to healthcare providers through May 2 went to hospitals, Modern Healthcare calculated. Of the remainder, specialty or multispecialty practices received $3.5 billion, internal medicine specialists got $24 million, family physicians were loaned $15 million, and federally qualified health centers received $20 million.
In the AMA’s news release, AMA President Susan Bailey, MD, who assumed the post in June, called the original loan repayment plan an “economic sword hanging over physician practices.”
This article first appeared on Medscape.com.
President Trump on Oct. 1 signed a bill to keep the federal government running through December 11. This “continuing resolution” (CR), which was approved by the Senate Wednesday on an 84-10 vote, according to The New York Times, includes provisions to delay repayment by physicians of pandemic-related Medicare loans and to reduce the loans’ interest rate.
In an earlier news release, the American Medical Association reported that Congress and the White House had agreed to include the provisions on Medicare loans in the CR.
Under the Medicare Accelerated and Advance Payments (AAP) program, the Centers for Medicare & Medicaid Services advanced money to physicians who were financially impacted by the pandemic. The program, created in March, was suspended in late April.
Physicians who received the Medicare loans were supposed to start paying them back 120 days after they were made. CMS planned to recoup the advances by offsetting them against Medicare claims payments due to physicians. Practices had up to 210 days (7 months) to repay the loans through this process before being asked to repay them directly with interest of 10.25%.
For the practices that received these advances, that meant their Medicare cash flow was scheduled to dry up, starting in August. However, CMS quietly abstained from collecting these payments when they came due, according to Modern Healthcare.
New terms
The amount to be recouped from each claim is reduced from 100% to 25% of the claim for the first 11 months and to 50% of claims withheld for an additional 6 months. If the loan is not repaid in full by then, the provider must pay the balance with interest of 4%.
More than 80% of the $100 billion that CMS loaned to healthcare providers through May 2 went to hospitals, Modern Healthcare calculated. Of the remainder, specialty or multispecialty practices received $3.5 billion, internal medicine specialists got $24 million, family physicians were loaned $15 million, and federally qualified health centers received $20 million.
In the AMA’s news release, AMA President Susan Bailey, MD, who assumed the post in June, called the original loan repayment plan an “economic sword hanging over physician practices.”
This article first appeared on Medscape.com.
President Trump on Oct. 1 signed a bill to keep the federal government running through December 11. This “continuing resolution” (CR), which was approved by the Senate Wednesday on an 84-10 vote, according to The New York Times, includes provisions to delay repayment by physicians of pandemic-related Medicare loans and to reduce the loans’ interest rate.
In an earlier news release, the American Medical Association reported that Congress and the White House had agreed to include the provisions on Medicare loans in the CR.
Under the Medicare Accelerated and Advance Payments (AAP) program, the Centers for Medicare & Medicaid Services advanced money to physicians who were financially impacted by the pandemic. The program, created in March, was suspended in late April.
Physicians who received the Medicare loans were supposed to start paying them back 120 days after they were made. CMS planned to recoup the advances by offsetting them against Medicare claims payments due to physicians. Practices had up to 210 days (7 months) to repay the loans through this process before being asked to repay them directly with interest of 10.25%.
For the practices that received these advances, that meant their Medicare cash flow was scheduled to dry up, starting in August. However, CMS quietly abstained from collecting these payments when they came due, according to Modern Healthcare.
New terms
The amount to be recouped from each claim is reduced from 100% to 25% of the claim for the first 11 months and to 50% of claims withheld for an additional 6 months. If the loan is not repaid in full by then, the provider must pay the balance with interest of 4%.
More than 80% of the $100 billion that CMS loaned to healthcare providers through May 2 went to hospitals, Modern Healthcare calculated. Of the remainder, specialty or multispecialty practices received $3.5 billion, internal medicine specialists got $24 million, family physicians were loaned $15 million, and federally qualified health centers received $20 million.
In the AMA’s news release, AMA President Susan Bailey, MD, who assumed the post in June, called the original loan repayment plan an “economic sword hanging over physician practices.”
This article first appeared on Medscape.com.
Geriatric patients: My three rules for them
I have been in practice for 31 years, so many of my patients are now in their 80s and 90s. Practices age with us, and I have been seeing many of these patients for 25-30 years.
Absolutely, positively make sure you move!
Our older patients often have many reasons not to move, including pain from arthritis, deconditioning, muscle weakness, fatigue, and depression. “Keeping moving” is probably the most important thing a patient can do for their health.
Holme and Anderssen studied a large cohort of men for cardiovascular risk in 1972 and again in 2000. The surviving men were followed over an additional 12 years.1 They found that 30 minutes of physical activity 6 days a week was associated with a 40% reduction in mortality. Sedentary men had a reduced life expectancy of about 5 years, compared with men who were moderately to vigorously physically active.
Stewart etal. studied the benefit of physical activity in people with stable coronary disease.2 They concluded that, in patients with stable coronary heart disease, more physical activity was associated with lower mortality, and the largest benefit occurred in the sedentary patient groups and the highest cardiac risk groups.
Saint-Maurice et al. studied the effects of total daily step count and step intensity on mortality risk.3 They found that the risk of all-cause mortality decreases as the total number of daily steps increases, but that the speed of those steps did not make a difference. This is very encouraging data for our elderly patients. Moving is the secret, even if it may not be moving at a fast pace!
Never, ever get on a ladder!
This one should be part of every geriatric’s assessment and every Medicare wellness exam. I first experienced the horror of what can happen when elderly people climb when a 96-year-old healthy patient of mine fell off his roof and died. I never thought to tell him climbing on the roof was an awful idea.
Akland et al. looked at the epidemiology and outcomes of ladder-related falls that required ICU admission.4 Hospital mortality was 26%, and almost all of the mortalities occurred in older males in domestic falls, who died as a result of traumatic brain injury. Fewer than half of the survivors were living independently 1 year after the fall.
Valmuur et al. studied ladder related falls in Australia.5 They found that rates of ladder related falls requiring hospitalization rose from about 20/100,000 for men ages 15-29 years to 78/100,000 for men aged over 60 years. Of those who died from fall-related injury, 82% were over the age of 60, with more than 70% dying from head injuries.
Schaffarczyk et al. looked at the impact of nonoccupational falls from ladders in men aged over 50 years.6 The mean age of the patients in the study was 64 years (range, 50-85), with 27% suffering severe trauma. There was a striking impact on long-term function occurring in over half the study patients. The authors did interviews with patients in follow-up long after the falls and found that most never thought of themselves at risk for a fall, and after the experience of a bad fall, would never consider going on a ladder again. I think it is important for health care professionals to discuss the dangers of ladder use with our older patients, pointing out the higher risk of falling and the potential for the fall to be a life-changing or life-ending event.
Let them eat!
Many patients have a reduced appetite as they age. We work hard with our patients to choose a healthy diet throughout their lives, to help ward off obesity, treat hypertension, prevent or control diabetes, or provide heart health. Many patients just stop being interested in food, reduce intake, and may lose weight and muscle mass. When my patients pass the age of 85, I change my focus to encouraging them to eat for calories, socialization, and joy. I think the marginal benefits of more restrictive diets are small, compared with the benefits of helping your patients enjoy eating again. I ask patients what their very favorite foods are and encourage them to have them.
Pearl
Keep your patients eating and moving, except not onto a ladder!
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. Holme I, Anderssen SA. Increases in physical activity is as important as smoking cessation for reduction in total mortality in elderly men: 12 years of follow-up of the Oslo II study. Br J Sports Med. 2015; 49:743-8.
2. Stewart RAH et al. Physical activity and mortality in patients with stable coronary heart disease. J Am Coll Cardiol. 2017 Oct 3;70(14):1689-1700..
3. Saint-Maurice PF et al. Association of daily step count and step intensity with mortality among U.S. adults. JAMA 2020;323:1151-60.
4. Ackland HM et al. Danger at every rung: Epidemiology and outcomes of ICU-admitted ladder-related trauma. Injury. 2016;47:1109-117.
5. Vallmuur K et al. Falls from ladders in Australia: comparing occupational and nonoccupational injuries across age groups. Aust N Z J Public Health. 2016 Dec;40(6):559-63.
6. Schaffarczyk K et al. Nonoccupational falls from ladders in men 50 years and over: Contributing factors and impact. Injury. 2020 Aug;51(8):1798-1804.
I have been in practice for 31 years, so many of my patients are now in their 80s and 90s. Practices age with us, and I have been seeing many of these patients for 25-30 years.
Absolutely, positively make sure you move!
Our older patients often have many reasons not to move, including pain from arthritis, deconditioning, muscle weakness, fatigue, and depression. “Keeping moving” is probably the most important thing a patient can do for their health.
Holme and Anderssen studied a large cohort of men for cardiovascular risk in 1972 and again in 2000. The surviving men were followed over an additional 12 years.1 They found that 30 minutes of physical activity 6 days a week was associated with a 40% reduction in mortality. Sedentary men had a reduced life expectancy of about 5 years, compared with men who were moderately to vigorously physically active.
Stewart etal. studied the benefit of physical activity in people with stable coronary disease.2 They concluded that, in patients with stable coronary heart disease, more physical activity was associated with lower mortality, and the largest benefit occurred in the sedentary patient groups and the highest cardiac risk groups.
Saint-Maurice et al. studied the effects of total daily step count and step intensity on mortality risk.3 They found that the risk of all-cause mortality decreases as the total number of daily steps increases, but that the speed of those steps did not make a difference. This is very encouraging data for our elderly patients. Moving is the secret, even if it may not be moving at a fast pace!
Never, ever get on a ladder!
This one should be part of every geriatric’s assessment and every Medicare wellness exam. I first experienced the horror of what can happen when elderly people climb when a 96-year-old healthy patient of mine fell off his roof and died. I never thought to tell him climbing on the roof was an awful idea.
Akland et al. looked at the epidemiology and outcomes of ladder-related falls that required ICU admission.4 Hospital mortality was 26%, and almost all of the mortalities occurred in older males in domestic falls, who died as a result of traumatic brain injury. Fewer than half of the survivors were living independently 1 year after the fall.
Valmuur et al. studied ladder related falls in Australia.5 They found that rates of ladder related falls requiring hospitalization rose from about 20/100,000 for men ages 15-29 years to 78/100,000 for men aged over 60 years. Of those who died from fall-related injury, 82% were over the age of 60, with more than 70% dying from head injuries.
Schaffarczyk et al. looked at the impact of nonoccupational falls from ladders in men aged over 50 years.6 The mean age of the patients in the study was 64 years (range, 50-85), with 27% suffering severe trauma. There was a striking impact on long-term function occurring in over half the study patients. The authors did interviews with patients in follow-up long after the falls and found that most never thought of themselves at risk for a fall, and after the experience of a bad fall, would never consider going on a ladder again. I think it is important for health care professionals to discuss the dangers of ladder use with our older patients, pointing out the higher risk of falling and the potential for the fall to be a life-changing or life-ending event.
Let them eat!
Many patients have a reduced appetite as they age. We work hard with our patients to choose a healthy diet throughout their lives, to help ward off obesity, treat hypertension, prevent or control diabetes, or provide heart health. Many patients just stop being interested in food, reduce intake, and may lose weight and muscle mass. When my patients pass the age of 85, I change my focus to encouraging them to eat for calories, socialization, and joy. I think the marginal benefits of more restrictive diets are small, compared with the benefits of helping your patients enjoy eating again. I ask patients what their very favorite foods are and encourage them to have them.
Pearl
Keep your patients eating and moving, except not onto a ladder!
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. Holme I, Anderssen SA. Increases in physical activity is as important as smoking cessation for reduction in total mortality in elderly men: 12 years of follow-up of the Oslo II study. Br J Sports Med. 2015; 49:743-8.
2. Stewart RAH et al. Physical activity and mortality in patients with stable coronary heart disease. J Am Coll Cardiol. 2017 Oct 3;70(14):1689-1700..
3. Saint-Maurice PF et al. Association of daily step count and step intensity with mortality among U.S. adults. JAMA 2020;323:1151-60.
4. Ackland HM et al. Danger at every rung: Epidemiology and outcomes of ICU-admitted ladder-related trauma. Injury. 2016;47:1109-117.
5. Vallmuur K et al. Falls from ladders in Australia: comparing occupational and nonoccupational injuries across age groups. Aust N Z J Public Health. 2016 Dec;40(6):559-63.
6. Schaffarczyk K et al. Nonoccupational falls from ladders in men 50 years and over: Contributing factors and impact. Injury. 2020 Aug;51(8):1798-1804.
I have been in practice for 31 years, so many of my patients are now in their 80s and 90s. Practices age with us, and I have been seeing many of these patients for 25-30 years.
Absolutely, positively make sure you move!
Our older patients often have many reasons not to move, including pain from arthritis, deconditioning, muscle weakness, fatigue, and depression. “Keeping moving” is probably the most important thing a patient can do for their health.
Holme and Anderssen studied a large cohort of men for cardiovascular risk in 1972 and again in 2000. The surviving men were followed over an additional 12 years.1 They found that 30 minutes of physical activity 6 days a week was associated with a 40% reduction in mortality. Sedentary men had a reduced life expectancy of about 5 years, compared with men who were moderately to vigorously physically active.
Stewart etal. studied the benefit of physical activity in people with stable coronary disease.2 They concluded that, in patients with stable coronary heart disease, more physical activity was associated with lower mortality, and the largest benefit occurred in the sedentary patient groups and the highest cardiac risk groups.
Saint-Maurice et al. studied the effects of total daily step count and step intensity on mortality risk.3 They found that the risk of all-cause mortality decreases as the total number of daily steps increases, but that the speed of those steps did not make a difference. This is very encouraging data for our elderly patients. Moving is the secret, even if it may not be moving at a fast pace!
Never, ever get on a ladder!
This one should be part of every geriatric’s assessment and every Medicare wellness exam. I first experienced the horror of what can happen when elderly people climb when a 96-year-old healthy patient of mine fell off his roof and died. I never thought to tell him climbing on the roof was an awful idea.
Akland et al. looked at the epidemiology and outcomes of ladder-related falls that required ICU admission.4 Hospital mortality was 26%, and almost all of the mortalities occurred in older males in domestic falls, who died as a result of traumatic brain injury. Fewer than half of the survivors were living independently 1 year after the fall.
Valmuur et al. studied ladder related falls in Australia.5 They found that rates of ladder related falls requiring hospitalization rose from about 20/100,000 for men ages 15-29 years to 78/100,000 for men aged over 60 years. Of those who died from fall-related injury, 82% were over the age of 60, with more than 70% dying from head injuries.
Schaffarczyk et al. looked at the impact of nonoccupational falls from ladders in men aged over 50 years.6 The mean age of the patients in the study was 64 years (range, 50-85), with 27% suffering severe trauma. There was a striking impact on long-term function occurring in over half the study patients. The authors did interviews with patients in follow-up long after the falls and found that most never thought of themselves at risk for a fall, and after the experience of a bad fall, would never consider going on a ladder again. I think it is important for health care professionals to discuss the dangers of ladder use with our older patients, pointing out the higher risk of falling and the potential for the fall to be a life-changing or life-ending event.
Let them eat!
Many patients have a reduced appetite as they age. We work hard with our patients to choose a healthy diet throughout their lives, to help ward off obesity, treat hypertension, prevent or control diabetes, or provide heart health. Many patients just stop being interested in food, reduce intake, and may lose weight and muscle mass. When my patients pass the age of 85, I change my focus to encouraging them to eat for calories, socialization, and joy. I think the marginal benefits of more restrictive diets are small, compared with the benefits of helping your patients enjoy eating again. I ask patients what their very favorite foods are and encourage them to have them.
Pearl
Keep your patients eating and moving, except not onto a ladder!
Dr. Paauw is professor of medicine in the division of general internal medicine at the University of Washington, Seattle, and serves as third-year medical student clerkship director at the University of Washington. He is a member of the editorial advisory board of Internal Medicine News. Dr. Paauw has no conflicts to disclose. Contact him at [email protected].
References
1. Holme I, Anderssen SA. Increases in physical activity is as important as smoking cessation for reduction in total mortality in elderly men: 12 years of follow-up of the Oslo II study. Br J Sports Med. 2015; 49:743-8.
2. Stewart RAH et al. Physical activity and mortality in patients with stable coronary heart disease. J Am Coll Cardiol. 2017 Oct 3;70(14):1689-1700..
3. Saint-Maurice PF et al. Association of daily step count and step intensity with mortality among U.S. adults. JAMA 2020;323:1151-60.
4. Ackland HM et al. Danger at every rung: Epidemiology and outcomes of ICU-admitted ladder-related trauma. Injury. 2016;47:1109-117.
5. Vallmuur K et al. Falls from ladders in Australia: comparing occupational and nonoccupational injuries across age groups. Aust N Z J Public Health. 2016 Dec;40(6):559-63.
6. Schaffarczyk K et al. Nonoccupational falls from ladders in men 50 years and over: Contributing factors and impact. Injury. 2020 Aug;51(8):1798-1804.
Children’s share of new COVID-19 cases is on the rise
The cumulative percentage of COVID-19 cases reported in children continues to climb, but “the history behind that cumulative number shows substantial change,” according to a new analysis of state health department data.
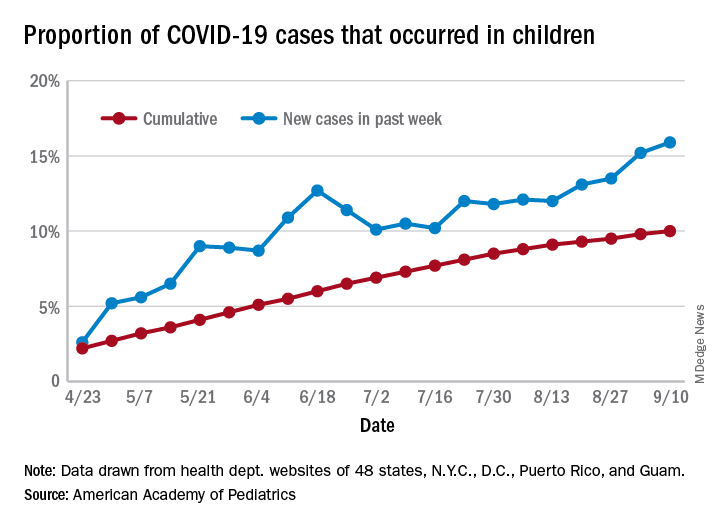
As of Sept. 10, the 549,432 cases in children represented 10.0% of all reported COVID-19 cases in the United States following a substantial rise over the course of the pandemic – the figure was 7.7% on July 16 and 3.2% on May 7, Blake Sisk, PhD, of the American Academy of Pediatrics and associates reported Sept. 29 in Pediatrics.
Unlike the cumulative number, the weekly proportion of cases in children fell early in the summer but then started climbing again in late July. Dr. Sisk and associates wrote.
Despite the increase, however, the proportion of pediatric COVID-19 cases is still well below children’s share of the overall population (22.6%). Also, “it is unclear how much of the increase in child cases is due to increased testing capacity, although CDC data from public and commercial laboratories show the share of all tests administered to children ages 0-17 has remained stable at 5%-7% since late April,” they said.
Data for the current report were drawn from 49 state health department websites (New York state does not report ages for COVID-19 cases), along with New York City, the District of Columbia, Puerto Rico, and Guam. Alabama changed its definition of a child case in August and was not included in the trend analysis (see graph), the investigators explained.
Those data show “substantial variation in case growth by region: in April, a preponderance of cases was in the Northeast. In June, cases surged in the South and West, followed by mid-July increases in the Midwest,” Dr. Sisk and associates said.
The increase among children in Midwest states is ongoing with the number of new cases reaching its highest level yet during the week ending Sept. 10, they reported.
SOURCE: Sisk B et al. Pediatrics. 2020 Sep 29. doi: 10.1542/peds.2020-027425.
The cumulative percentage of COVID-19 cases reported in children continues to climb, but “the history behind that cumulative number shows substantial change,” according to a new analysis of state health department data.
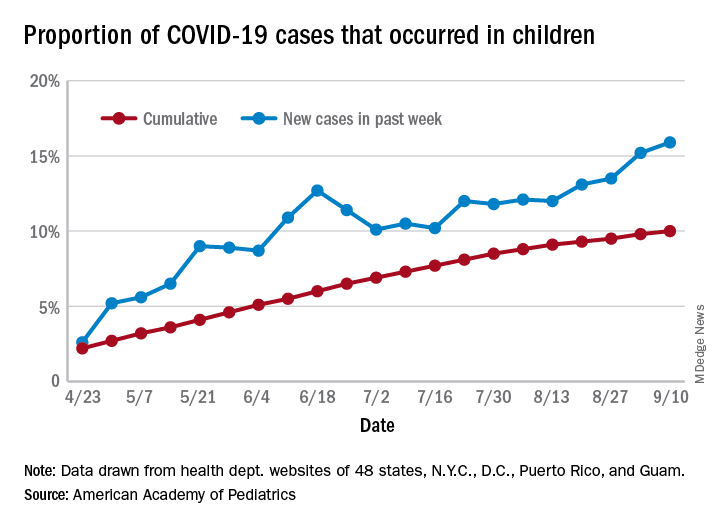
As of Sept. 10, the 549,432 cases in children represented 10.0% of all reported COVID-19 cases in the United States following a substantial rise over the course of the pandemic – the figure was 7.7% on July 16 and 3.2% on May 7, Blake Sisk, PhD, of the American Academy of Pediatrics and associates reported Sept. 29 in Pediatrics.
Unlike the cumulative number, the weekly proportion of cases in children fell early in the summer but then started climbing again in late July. Dr. Sisk and associates wrote.
Despite the increase, however, the proportion of pediatric COVID-19 cases is still well below children’s share of the overall population (22.6%). Also, “it is unclear how much of the increase in child cases is due to increased testing capacity, although CDC data from public and commercial laboratories show the share of all tests administered to children ages 0-17 has remained stable at 5%-7% since late April,” they said.
Data for the current report were drawn from 49 state health department websites (New York state does not report ages for COVID-19 cases), along with New York City, the District of Columbia, Puerto Rico, and Guam. Alabama changed its definition of a child case in August and was not included in the trend analysis (see graph), the investigators explained.
Those data show “substantial variation in case growth by region: in April, a preponderance of cases was in the Northeast. In June, cases surged in the South and West, followed by mid-July increases in the Midwest,” Dr. Sisk and associates said.
The increase among children in Midwest states is ongoing with the number of new cases reaching its highest level yet during the week ending Sept. 10, they reported.
SOURCE: Sisk B et al. Pediatrics. 2020 Sep 29. doi: 10.1542/peds.2020-027425.
The cumulative percentage of COVID-19 cases reported in children continues to climb, but “the history behind that cumulative number shows substantial change,” according to a new analysis of state health department data.
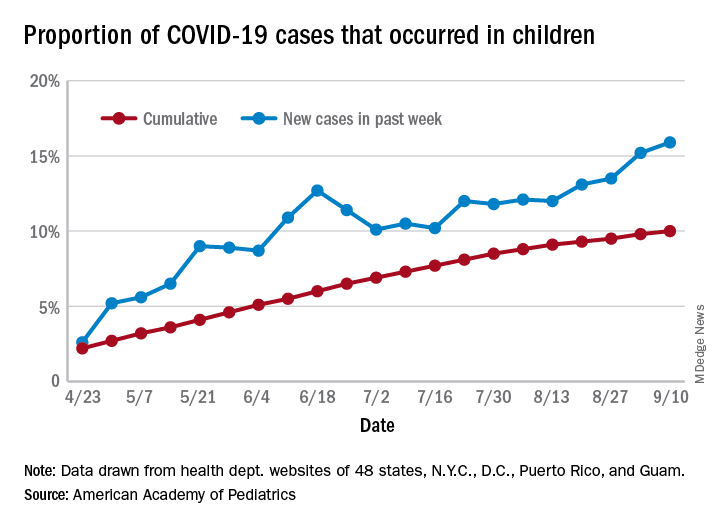
As of Sept. 10, the 549,432 cases in children represented 10.0% of all reported COVID-19 cases in the United States following a substantial rise over the course of the pandemic – the figure was 7.7% on July 16 and 3.2% on May 7, Blake Sisk, PhD, of the American Academy of Pediatrics and associates reported Sept. 29 in Pediatrics.
Unlike the cumulative number, the weekly proportion of cases in children fell early in the summer but then started climbing again in late July. Dr. Sisk and associates wrote.
Despite the increase, however, the proportion of pediatric COVID-19 cases is still well below children’s share of the overall population (22.6%). Also, “it is unclear how much of the increase in child cases is due to increased testing capacity, although CDC data from public and commercial laboratories show the share of all tests administered to children ages 0-17 has remained stable at 5%-7% since late April,” they said.
Data for the current report were drawn from 49 state health department websites (New York state does not report ages for COVID-19 cases), along with New York City, the District of Columbia, Puerto Rico, and Guam. Alabama changed its definition of a child case in August and was not included in the trend analysis (see graph), the investigators explained.
Those data show “substantial variation in case growth by region: in April, a preponderance of cases was in the Northeast. In June, cases surged in the South and West, followed by mid-July increases in the Midwest,” Dr. Sisk and associates said.
The increase among children in Midwest states is ongoing with the number of new cases reaching its highest level yet during the week ending Sept. 10, they reported.
SOURCE: Sisk B et al. Pediatrics. 2020 Sep 29. doi: 10.1542/peds.2020-027425.
FROM PEDIATRICS
Pandemic poses new challenges for rural doctors
These include struggling with seeing patients virtually and treating patients who have politicized the virus. Additionally, the pandemic has exposed rural practices to greater financial difficulties.
Before the pandemic some rurally based primary care physicians were already working through big challenges, such as having few local medical colleagues to consult and working in small practices with lean budgets. In fact, data gathered by the National Rural Health Association showed that there are only 40 primary care physicians per 100,000 patients in rural regions, compared with 53 in urban areas – and the number of physicians overall is 13 per 10,000 in rural areas, compared with 31 in cities.
In the prepandemic world, for some doctors, the challenges were balanced by the benefits of practicing in these sparsely populated communities with scenic, low-traffic roads. Some perks of practicing in rural areas touted by doctors included having a fast commute, being able to swim in a lake near the office before work, having a low cost of living, and feeling like they are making a difference in their communities as they treat generations of the families they see around town.
But today, new hurdles to practicing medicine in rural America created by the COVID-19 pandemic have caused the hardships to feel heavier than the joys at times for some physicians interviewed by MDedge.
Many independent rural practices in need of assistance were not able to get much from the federal Provider Relief Funds, said John M. Westfall, MD, who is director of the Robert Graham Center for Policy Studies in Family Medicine and Primary Care, in an interview.
“Rural primary care doctors function independently or in smaller critical access hospitals and community health centers,” said Dr. Westfall, who previously practiced family medicine in a small town in Colorado. “Many of these have much less financial reserves so are at risk of cutbacks and closure.”
Jacqueline W. Fincher, MD, an internist based in a tiny Georgia community along the highway between Atlanta and Augusta, said her small practice works on really thin margins and doesn’t have much cushion. At the beginning of the pandemic, all visits were down, and her practice operated at a loss. To help, Dr. Fincher and her colleagues applied for funding from the Small Business Administration’s Paycheck Protection Program (PPP) through the CARES Act.
“COVID-19 has had a tremendous impact especially on primary care practices. We live and die by volume. … Our volume in mid-March to mid-May really dropped dramatically,” explained Dr. Fincher, who is also president of the American College of Physicians. “The PPP sustained us for 2 months, enabling us to pay our staff and to remain open and get us up and running on telehealth.”
Starting up telemedicine
Experiencing spotty or no access to broadband Internet is nothing new to rural physicians, but having this problem interfere with their ability to provide care to patients is.
As much of the American health system rapidly embraced telehealth during the pandemic, obtaining access to high-speed Internet has been a major challenge for rural patients, noted Dr. Westfall.
“Some practices were able to quickly adopt some telehealth capacity with phone and video. Changes in payment for telehealth helped. But in some rural communities there was not adequate Internet bandwidth for quality video connections. And some patients did not have the means for high-speed video connections,” Dr. Westfall said.
Indeed, according to a 2019 Pew Research Center survey, 63% of rural Americans say they can access the Internet through a broadband connection at home, compared with 75% and 79% in suburban and urban areas, respectively.
In the Appalachian town of Zanesville, Ohio, for example, family physician Shelly L. Dunmyer, MD, and her colleagues discovered that many patients don’t have Internet access at home. Dr. Fincher has to go to the office to conduct telehealth visits because her own Internet access at home is unpredictable. As for patients, it may take 15 minutes for them to work out technical glitches and find good Internet reception, said Dr. Fincher. For internist Y. Ki Shin, MD, who practices in the coastal town of Montesano in Washington state, about 25% of his practice’s telehealth visits must be conducted by phone because of limitations on video, such as lack of high-speed access.
But telephone visits are often insufficient replacements for appointments via video, according to several rural physicians interviewed for this piece.
“Telehealth can be frustrating at times due to connectivity issues which can be difficult at times in the rural areas,” said Dr. Fincher. “In order for telehealth to be reasonably helpful to patients and physicians to care for people with chronic problems, the patients must have things like blood pressure monitors, glucometers, and scales to address problems like hypertension, diabetes myelitis, and congestive heart failure.”
“If you have the audio and video and the data from these devices, you’re good. If you don’t have these data, and/or don’t have the video you just can’t provide good care,” she explained.
Dr. Dunmyer and her colleagues at Medical Home Primary Care Center in Zanesville, Ohio, found a way to get around the problem of patients not being able to access Internet to participate in video visits from their homes. This involved having her patients drive into her practice’s parking lot to participate in modified telehealth visits. Staffers gave iPads to patients in their cars, and Dr. Dunmyer conducted visits from her office, about 50 yards away.
“We were even doing Medicare wellness visits: Instead of asking them to get up and move around the room, we would sit at the window and wave at them, ask them to get out, walk around the car. We were able to check mobility and all kinds of things that we’d normally do in the office,” Dr. Dunmyer explained in an interview.
The family physician noted that her practice is now conducting fewer parking lot visits since her office is allowing in-person appointments, but that they’re still an option for her patients.
Treating political adversaries
Some rural physicians have experienced strained relationships with patients for reasons other than technology – stark differences in opinion over the pandemic itself. Certain patients are following President Trump’s lead and questioning everything from the pandemic death toll to preventive measures recommended by scientists and medical experts, physicians interviewed by MDedge said.
Patients everywhere share these viewpoints, of course, but research and election results confirm that rural areas are more receptive to conservative viewpoints. In 2018, a Pew Research Center survey reported that rural and urban areas are “becoming more polarized politically,” and “rural areas tend to have a higher concentration of Republicans and Republican-leaning independents.” For example, 40% of rural respondents reported “very warm” or “somewhat warm” feelings toward Donald Trump, compared with just 19% in urban areas.
Dr. Shin has struggled to cope with patients who want to argue about pandemic safety precautions like wearing masks and seem to question whether systemic racism exists.
“We are seeing a lot more people who feel that this pandemic is not real, that it’s a political and not-true infection,” he said in an interview. “We’ve had patients who were angry at us because we made them wear masks, and some were demanding hydroxychloroquine and wanted to have an argument because we’re not going to prescribe it for them.”
In one situation, which he found especially disturbing, Dr. Shin had to leave the exam room because a patient wouldn’t stop challenging him regarding the pandemic. Things have gotten so bad that Dr. Shin has even questioned whether he wants to continue his long career in his small town because of local political attitudes such as opposition to mask-wearing and social distancing.
“Mr. Trump’s misinformation on this pandemic made my job much more difficult. As a minority, I feel less safe in my community than ever,” said Dr. Shin, who described himself as Asian American.
Despite these new stressors, Dr. Shin has experienced some joyful moments while practicing medicine in the pandemic.
He said a recent home visit to a patient who had been hospitalized for over 3 months and nearly died helped him put political disputes with his patients into perspective.
“He was discharged home but is bedbound. He had gangrene on his toes, and I could not fully examine him using video,” Dr. Shin recalled. “It was tricky to find the house, but a very large Trump sign was very helpful in locating it. It was a good visit: He was happy to see me, and I was happy to see that he was doing okay at home.”
“I need to remind myself that supporting Mr. Trump does not always mean that my patient supports Mr. Trump’s view on the pandemic and the race issues in our country,” Dr. Shin added.
The Washington-based internist said he also tells himself that, even if his patients refuse to follow his strong advice regarding pandemic precautions, it does not mean he has failed as a doctor.
“I need to continue to educate patients about the dangers of COVID infection but cannot be angry if they don’t choose to follow my recommendations,” he noted.
Dr. Fincher says her close connection with patients has allowed her to smooth over politically charged claims about the pandemic in the town of Thomson, Georgia, with a population 6,800.
“I have a sense that, even though we may differ in our understanding of some basic facts, they appreciate what I say since we have a long-term relationship built on trust,” she said. This kind of trust, Dr. Fincher suggested, may be more common than in urban areas where there’s a larger supply of physicians, and patients don’t see the same doctors for long periods of time.
“It’s more meaningful when it comes from me, rather than doctors who are [new to patients] every year when their employer changes their insurance,” she noted.
These include struggling with seeing patients virtually and treating patients who have politicized the virus. Additionally, the pandemic has exposed rural practices to greater financial difficulties.
Before the pandemic some rurally based primary care physicians were already working through big challenges, such as having few local medical colleagues to consult and working in small practices with lean budgets. In fact, data gathered by the National Rural Health Association showed that there are only 40 primary care physicians per 100,000 patients in rural regions, compared with 53 in urban areas – and the number of physicians overall is 13 per 10,000 in rural areas, compared with 31 in cities.
In the prepandemic world, for some doctors, the challenges were balanced by the benefits of practicing in these sparsely populated communities with scenic, low-traffic roads. Some perks of practicing in rural areas touted by doctors included having a fast commute, being able to swim in a lake near the office before work, having a low cost of living, and feeling like they are making a difference in their communities as they treat generations of the families they see around town.
But today, new hurdles to practicing medicine in rural America created by the COVID-19 pandemic have caused the hardships to feel heavier than the joys at times for some physicians interviewed by MDedge.
Many independent rural practices in need of assistance were not able to get much from the federal Provider Relief Funds, said John M. Westfall, MD, who is director of the Robert Graham Center for Policy Studies in Family Medicine and Primary Care, in an interview.
“Rural primary care doctors function independently or in smaller critical access hospitals and community health centers,” said Dr. Westfall, who previously practiced family medicine in a small town in Colorado. “Many of these have much less financial reserves so are at risk of cutbacks and closure.”
Jacqueline W. Fincher, MD, an internist based in a tiny Georgia community along the highway between Atlanta and Augusta, said her small practice works on really thin margins and doesn’t have much cushion. At the beginning of the pandemic, all visits were down, and her practice operated at a loss. To help, Dr. Fincher and her colleagues applied for funding from the Small Business Administration’s Paycheck Protection Program (PPP) through the CARES Act.
“COVID-19 has had a tremendous impact especially on primary care practices. We live and die by volume. … Our volume in mid-March to mid-May really dropped dramatically,” explained Dr. Fincher, who is also president of the American College of Physicians. “The PPP sustained us for 2 months, enabling us to pay our staff and to remain open and get us up and running on telehealth.”
Starting up telemedicine
Experiencing spotty or no access to broadband Internet is nothing new to rural physicians, but having this problem interfere with their ability to provide care to patients is.
As much of the American health system rapidly embraced telehealth during the pandemic, obtaining access to high-speed Internet has been a major challenge for rural patients, noted Dr. Westfall.
“Some practices were able to quickly adopt some telehealth capacity with phone and video. Changes in payment for telehealth helped. But in some rural communities there was not adequate Internet bandwidth for quality video connections. And some patients did not have the means for high-speed video connections,” Dr. Westfall said.
Indeed, according to a 2019 Pew Research Center survey, 63% of rural Americans say they can access the Internet through a broadband connection at home, compared with 75% and 79% in suburban and urban areas, respectively.
In the Appalachian town of Zanesville, Ohio, for example, family physician Shelly L. Dunmyer, MD, and her colleagues discovered that many patients don’t have Internet access at home. Dr. Fincher has to go to the office to conduct telehealth visits because her own Internet access at home is unpredictable. As for patients, it may take 15 minutes for them to work out technical glitches and find good Internet reception, said Dr. Fincher. For internist Y. Ki Shin, MD, who practices in the coastal town of Montesano in Washington state, about 25% of his practice’s telehealth visits must be conducted by phone because of limitations on video, such as lack of high-speed access.
But telephone visits are often insufficient replacements for appointments via video, according to several rural physicians interviewed for this piece.
“Telehealth can be frustrating at times due to connectivity issues which can be difficult at times in the rural areas,” said Dr. Fincher. “In order for telehealth to be reasonably helpful to patients and physicians to care for people with chronic problems, the patients must have things like blood pressure monitors, glucometers, and scales to address problems like hypertension, diabetes myelitis, and congestive heart failure.”
“If you have the audio and video and the data from these devices, you’re good. If you don’t have these data, and/or don’t have the video you just can’t provide good care,” she explained.
Dr. Dunmyer and her colleagues at Medical Home Primary Care Center in Zanesville, Ohio, found a way to get around the problem of patients not being able to access Internet to participate in video visits from their homes. This involved having her patients drive into her practice’s parking lot to participate in modified telehealth visits. Staffers gave iPads to patients in their cars, and Dr. Dunmyer conducted visits from her office, about 50 yards away.
“We were even doing Medicare wellness visits: Instead of asking them to get up and move around the room, we would sit at the window and wave at them, ask them to get out, walk around the car. We were able to check mobility and all kinds of things that we’d normally do in the office,” Dr. Dunmyer explained in an interview.
The family physician noted that her practice is now conducting fewer parking lot visits since her office is allowing in-person appointments, but that they’re still an option for her patients.
Treating political adversaries
Some rural physicians have experienced strained relationships with patients for reasons other than technology – stark differences in opinion over the pandemic itself. Certain patients are following President Trump’s lead and questioning everything from the pandemic death toll to preventive measures recommended by scientists and medical experts, physicians interviewed by MDedge said.
Patients everywhere share these viewpoints, of course, but research and election results confirm that rural areas are more receptive to conservative viewpoints. In 2018, a Pew Research Center survey reported that rural and urban areas are “becoming more polarized politically,” and “rural areas tend to have a higher concentration of Republicans and Republican-leaning independents.” For example, 40% of rural respondents reported “very warm” or “somewhat warm” feelings toward Donald Trump, compared with just 19% in urban areas.
Dr. Shin has struggled to cope with patients who want to argue about pandemic safety precautions like wearing masks and seem to question whether systemic racism exists.
“We are seeing a lot more people who feel that this pandemic is not real, that it’s a political and not-true infection,” he said in an interview. “We’ve had patients who were angry at us because we made them wear masks, and some were demanding hydroxychloroquine and wanted to have an argument because we’re not going to prescribe it for them.”
In one situation, which he found especially disturbing, Dr. Shin had to leave the exam room because a patient wouldn’t stop challenging him regarding the pandemic. Things have gotten so bad that Dr. Shin has even questioned whether he wants to continue his long career in his small town because of local political attitudes such as opposition to mask-wearing and social distancing.
“Mr. Trump’s misinformation on this pandemic made my job much more difficult. As a minority, I feel less safe in my community than ever,” said Dr. Shin, who described himself as Asian American.
Despite these new stressors, Dr. Shin has experienced some joyful moments while practicing medicine in the pandemic.
He said a recent home visit to a patient who had been hospitalized for over 3 months and nearly died helped him put political disputes with his patients into perspective.
“He was discharged home but is bedbound. He had gangrene on his toes, and I could not fully examine him using video,” Dr. Shin recalled. “It was tricky to find the house, but a very large Trump sign was very helpful in locating it. It was a good visit: He was happy to see me, and I was happy to see that he was doing okay at home.”
“I need to remind myself that supporting Mr. Trump does not always mean that my patient supports Mr. Trump’s view on the pandemic and the race issues in our country,” Dr. Shin added.
The Washington-based internist said he also tells himself that, even if his patients refuse to follow his strong advice regarding pandemic precautions, it does not mean he has failed as a doctor.
“I need to continue to educate patients about the dangers of COVID infection but cannot be angry if they don’t choose to follow my recommendations,” he noted.
Dr. Fincher says her close connection with patients has allowed her to smooth over politically charged claims about the pandemic in the town of Thomson, Georgia, with a population 6,800.
“I have a sense that, even though we may differ in our understanding of some basic facts, they appreciate what I say since we have a long-term relationship built on trust,” she said. This kind of trust, Dr. Fincher suggested, may be more common than in urban areas where there’s a larger supply of physicians, and patients don’t see the same doctors for long periods of time.
“It’s more meaningful when it comes from me, rather than doctors who are [new to patients] every year when their employer changes their insurance,” she noted.
These include struggling with seeing patients virtually and treating patients who have politicized the virus. Additionally, the pandemic has exposed rural practices to greater financial difficulties.
Before the pandemic some rurally based primary care physicians were already working through big challenges, such as having few local medical colleagues to consult and working in small practices with lean budgets. In fact, data gathered by the National Rural Health Association showed that there are only 40 primary care physicians per 100,000 patients in rural regions, compared with 53 in urban areas – and the number of physicians overall is 13 per 10,000 in rural areas, compared with 31 in cities.
In the prepandemic world, for some doctors, the challenges were balanced by the benefits of practicing in these sparsely populated communities with scenic, low-traffic roads. Some perks of practicing in rural areas touted by doctors included having a fast commute, being able to swim in a lake near the office before work, having a low cost of living, and feeling like they are making a difference in their communities as they treat generations of the families they see around town.
But today, new hurdles to practicing medicine in rural America created by the COVID-19 pandemic have caused the hardships to feel heavier than the joys at times for some physicians interviewed by MDedge.
Many independent rural practices in need of assistance were not able to get much from the federal Provider Relief Funds, said John M. Westfall, MD, who is director of the Robert Graham Center for Policy Studies in Family Medicine and Primary Care, in an interview.
“Rural primary care doctors function independently or in smaller critical access hospitals and community health centers,” said Dr. Westfall, who previously practiced family medicine in a small town in Colorado. “Many of these have much less financial reserves so are at risk of cutbacks and closure.”
Jacqueline W. Fincher, MD, an internist based in a tiny Georgia community along the highway between Atlanta and Augusta, said her small practice works on really thin margins and doesn’t have much cushion. At the beginning of the pandemic, all visits were down, and her practice operated at a loss. To help, Dr. Fincher and her colleagues applied for funding from the Small Business Administration’s Paycheck Protection Program (PPP) through the CARES Act.
“COVID-19 has had a tremendous impact especially on primary care practices. We live and die by volume. … Our volume in mid-March to mid-May really dropped dramatically,” explained Dr. Fincher, who is also president of the American College of Physicians. “The PPP sustained us for 2 months, enabling us to pay our staff and to remain open and get us up and running on telehealth.”
Starting up telemedicine
Experiencing spotty or no access to broadband Internet is nothing new to rural physicians, but having this problem interfere with their ability to provide care to patients is.
As much of the American health system rapidly embraced telehealth during the pandemic, obtaining access to high-speed Internet has been a major challenge for rural patients, noted Dr. Westfall.
“Some practices were able to quickly adopt some telehealth capacity with phone and video. Changes in payment for telehealth helped. But in some rural communities there was not adequate Internet bandwidth for quality video connections. And some patients did not have the means for high-speed video connections,” Dr. Westfall said.
Indeed, according to a 2019 Pew Research Center survey, 63% of rural Americans say they can access the Internet through a broadband connection at home, compared with 75% and 79% in suburban and urban areas, respectively.
In the Appalachian town of Zanesville, Ohio, for example, family physician Shelly L. Dunmyer, MD, and her colleagues discovered that many patients don’t have Internet access at home. Dr. Fincher has to go to the office to conduct telehealth visits because her own Internet access at home is unpredictable. As for patients, it may take 15 minutes for them to work out technical glitches and find good Internet reception, said Dr. Fincher. For internist Y. Ki Shin, MD, who practices in the coastal town of Montesano in Washington state, about 25% of his practice’s telehealth visits must be conducted by phone because of limitations on video, such as lack of high-speed access.
But telephone visits are often insufficient replacements for appointments via video, according to several rural physicians interviewed for this piece.
“Telehealth can be frustrating at times due to connectivity issues which can be difficult at times in the rural areas,” said Dr. Fincher. “In order for telehealth to be reasonably helpful to patients and physicians to care for people with chronic problems, the patients must have things like blood pressure monitors, glucometers, and scales to address problems like hypertension, diabetes myelitis, and congestive heart failure.”
“If you have the audio and video and the data from these devices, you’re good. If you don’t have these data, and/or don’t have the video you just can’t provide good care,” she explained.
Dr. Dunmyer and her colleagues at Medical Home Primary Care Center in Zanesville, Ohio, found a way to get around the problem of patients not being able to access Internet to participate in video visits from their homes. This involved having her patients drive into her practice’s parking lot to participate in modified telehealth visits. Staffers gave iPads to patients in their cars, and Dr. Dunmyer conducted visits from her office, about 50 yards away.
“We were even doing Medicare wellness visits: Instead of asking them to get up and move around the room, we would sit at the window and wave at them, ask them to get out, walk around the car. We were able to check mobility and all kinds of things that we’d normally do in the office,” Dr. Dunmyer explained in an interview.
The family physician noted that her practice is now conducting fewer parking lot visits since her office is allowing in-person appointments, but that they’re still an option for her patients.
Treating political adversaries
Some rural physicians have experienced strained relationships with patients for reasons other than technology – stark differences in opinion over the pandemic itself. Certain patients are following President Trump’s lead and questioning everything from the pandemic death toll to preventive measures recommended by scientists and medical experts, physicians interviewed by MDedge said.
Patients everywhere share these viewpoints, of course, but research and election results confirm that rural areas are more receptive to conservative viewpoints. In 2018, a Pew Research Center survey reported that rural and urban areas are “becoming more polarized politically,” and “rural areas tend to have a higher concentration of Republicans and Republican-leaning independents.” For example, 40% of rural respondents reported “very warm” or “somewhat warm” feelings toward Donald Trump, compared with just 19% in urban areas.
Dr. Shin has struggled to cope with patients who want to argue about pandemic safety precautions like wearing masks and seem to question whether systemic racism exists.
“We are seeing a lot more people who feel that this pandemic is not real, that it’s a political and not-true infection,” he said in an interview. “We’ve had patients who were angry at us because we made them wear masks, and some were demanding hydroxychloroquine and wanted to have an argument because we’re not going to prescribe it for them.”
In one situation, which he found especially disturbing, Dr. Shin had to leave the exam room because a patient wouldn’t stop challenging him regarding the pandemic. Things have gotten so bad that Dr. Shin has even questioned whether he wants to continue his long career in his small town because of local political attitudes such as opposition to mask-wearing and social distancing.
“Mr. Trump’s misinformation on this pandemic made my job much more difficult. As a minority, I feel less safe in my community than ever,” said Dr. Shin, who described himself as Asian American.
Despite these new stressors, Dr. Shin has experienced some joyful moments while practicing medicine in the pandemic.
He said a recent home visit to a patient who had been hospitalized for over 3 months and nearly died helped him put political disputes with his patients into perspective.
“He was discharged home but is bedbound. He had gangrene on his toes, and I could not fully examine him using video,” Dr. Shin recalled. “It was tricky to find the house, but a very large Trump sign was very helpful in locating it. It was a good visit: He was happy to see me, and I was happy to see that he was doing okay at home.”
“I need to remind myself that supporting Mr. Trump does not always mean that my patient supports Mr. Trump’s view on the pandemic and the race issues in our country,” Dr. Shin added.
The Washington-based internist said he also tells himself that, even if his patients refuse to follow his strong advice regarding pandemic precautions, it does not mean he has failed as a doctor.
“I need to continue to educate patients about the dangers of COVID infection but cannot be angry if they don’t choose to follow my recommendations,” he noted.
Dr. Fincher says her close connection with patients has allowed her to smooth over politically charged claims about the pandemic in the town of Thomson, Georgia, with a population 6,800.
“I have a sense that, even though we may differ in our understanding of some basic facts, they appreciate what I say since we have a long-term relationship built on trust,” she said. This kind of trust, Dr. Fincher suggested, may be more common than in urban areas where there’s a larger supply of physicians, and patients don’t see the same doctors for long periods of time.
“It’s more meaningful when it comes from me, rather than doctors who are [new to patients] every year when their employer changes their insurance,” she noted.
Revamping mentorship in medicine
Why the current system fails underrepresented physicians — and tips to improve it
Mentoring is often promoted as an organizational practice to promote diversity and inclusion. New or established group members who want to further their careers look for a mentor to guide them toward success within a system by amplifying their strengths and accomplishments and defending and promoting them when necessary. But how can mentoring work if there isn’t a mentor?
For underrepresented groups or marginalized physicians, it too often looks as if there are no mentors who understand the struggles of being a racial or ethnic minority group member or mentors who are even cognizant of those struggles. Mentoring is a practice that occurs within the overarching systems of practice groups, academic departments, hospitals, medicine, and society at large. These systems frequently carry the legacies of bias, discrimination, and exclusion. The mentoring itself that takes place within a biased system risks perpetuating institutional bias, exclusion, or a sense of unworthiness in the mentee. It is stressful for any person with a minority background or even a minority interest to feel that there’s no one to emulate in their immediate working environment. When that is the case, a natural question follows: “Do I even belong here?”
Before departments and psychiatric practices turn to old, surface-level solutions like using mentorship to appear more welcoming to underrepresented groups, leaders must explicitly evaluate their track record of mentorship within their system and determine whether mentorship has been used to protect the status quo or move the culture forward. As mentorship is inherently an imbalanced relationship, there must be department- or group-level reflection about the diversity of mentors and also their examinations of mentors’ own preconceived notions of who will make a “good” mentee.
At the most basic level, leaders can examine whether there are gaps in who is mentored and who is not. Other parts of mentoring relationships should also be examined: a) How can mentoring happen if there is a dearth of underrepresented groups in the department? b) What type of mentoring style is favored? Do departments/groups look for a natural fit between mentor and mentee or are they matched based on interests, ideals, and goals? and c) How is the worthiness for mentorship determined?
One example is the fraught process of evaluating “worthiness” among residents. Prospective mentors frequently divide trainees unofficially into a top-tier candidates, middle-tier performers who may be overlooked, and a bottom tier who are avoided when it comes to mentorship. Because this division is informal and usually based on extremely early perceptions of trainees’ aptitude and openness, the process can be subject to an individual mentor’s conscious and unconscious bias, which then plays a large role in perpetuating systemic racism. When it comes to these informal but often rigid divisions, it can be hard to fall from the top when mentees are buoyed by good will, frequent opportunities to shine, and the mentor’s reputation. Likewise,
Below are three recommendations to consider for improving mentorship within departments:
1) Consider opportunities for senior mentors and potential mentees to interact with one another outside of assigned duties so that some mentorship relationships can be formed organically.
2) Review when mentorship relationships have been ineffective or unsuccessful versus productive and useful for both participants.
3) Increase opportunities for adjunct or former faculty who remain connected to the institution to also be mentors. This approach would open up more possibilities and could increase the diversity of available mentors.
If mentorship is to be part of the armamentarium for promoting equity within academia and workplaces alike, it must be examined and changed to meet the new reality.
Dr. Posada is assistant clinical professor, department of psychiatry and behavioral sciences at George Washington University in Washington. She also serves as staff physician at George Washington Medical Faculty Associates, also in Washington. She disclosed no relevant financial relationships. Dr. Forrester is consultation-liaison psychiatry fellowship training director at the University of Maryland, Baltimore. She disclosed no relevant financial relationships.
Why the current system fails underrepresented physicians — and tips to improve it
Why the current system fails underrepresented physicians — and tips to improve it
Mentoring is often promoted as an organizational practice to promote diversity and inclusion. New or established group members who want to further their careers look for a mentor to guide them toward success within a system by amplifying their strengths and accomplishments and defending and promoting them when necessary. But how can mentoring work if there isn’t a mentor?
For underrepresented groups or marginalized physicians, it too often looks as if there are no mentors who understand the struggles of being a racial or ethnic minority group member or mentors who are even cognizant of those struggles. Mentoring is a practice that occurs within the overarching systems of practice groups, academic departments, hospitals, medicine, and society at large. These systems frequently carry the legacies of bias, discrimination, and exclusion. The mentoring itself that takes place within a biased system risks perpetuating institutional bias, exclusion, or a sense of unworthiness in the mentee. It is stressful for any person with a minority background or even a minority interest to feel that there’s no one to emulate in their immediate working environment. When that is the case, a natural question follows: “Do I even belong here?”
Before departments and psychiatric practices turn to old, surface-level solutions like using mentorship to appear more welcoming to underrepresented groups, leaders must explicitly evaluate their track record of mentorship within their system and determine whether mentorship has been used to protect the status quo or move the culture forward. As mentorship is inherently an imbalanced relationship, there must be department- or group-level reflection about the diversity of mentors and also their examinations of mentors’ own preconceived notions of who will make a “good” mentee.
At the most basic level, leaders can examine whether there are gaps in who is mentored and who is not. Other parts of mentoring relationships should also be examined: a) How can mentoring happen if there is a dearth of underrepresented groups in the department? b) What type of mentoring style is favored? Do departments/groups look for a natural fit between mentor and mentee or are they matched based on interests, ideals, and goals? and c) How is the worthiness for mentorship determined?
One example is the fraught process of evaluating “worthiness” among residents. Prospective mentors frequently divide trainees unofficially into a top-tier candidates, middle-tier performers who may be overlooked, and a bottom tier who are avoided when it comes to mentorship. Because this division is informal and usually based on extremely early perceptions of trainees’ aptitude and openness, the process can be subject to an individual mentor’s conscious and unconscious bias, which then plays a large role in perpetuating systemic racism. When it comes to these informal but often rigid divisions, it can be hard to fall from the top when mentees are buoyed by good will, frequent opportunities to shine, and the mentor’s reputation. Likewise,
Below are three recommendations to consider for improving mentorship within departments:
1) Consider opportunities for senior mentors and potential mentees to interact with one another outside of assigned duties so that some mentorship relationships can be formed organically.
2) Review when mentorship relationships have been ineffective or unsuccessful versus productive and useful for both participants.
3) Increase opportunities for adjunct or former faculty who remain connected to the institution to also be mentors. This approach would open up more possibilities and could increase the diversity of available mentors.
If mentorship is to be part of the armamentarium for promoting equity within academia and workplaces alike, it must be examined and changed to meet the new reality.
Dr. Posada is assistant clinical professor, department of psychiatry and behavioral sciences at George Washington University in Washington. She also serves as staff physician at George Washington Medical Faculty Associates, also in Washington. She disclosed no relevant financial relationships. Dr. Forrester is consultation-liaison psychiatry fellowship training director at the University of Maryland, Baltimore. She disclosed no relevant financial relationships.
Mentoring is often promoted as an organizational practice to promote diversity and inclusion. New or established group members who want to further their careers look for a mentor to guide them toward success within a system by amplifying their strengths and accomplishments and defending and promoting them when necessary. But how can mentoring work if there isn’t a mentor?
For underrepresented groups or marginalized physicians, it too often looks as if there are no mentors who understand the struggles of being a racial or ethnic minority group member or mentors who are even cognizant of those struggles. Mentoring is a practice that occurs within the overarching systems of practice groups, academic departments, hospitals, medicine, and society at large. These systems frequently carry the legacies of bias, discrimination, and exclusion. The mentoring itself that takes place within a biased system risks perpetuating institutional bias, exclusion, or a sense of unworthiness in the mentee. It is stressful for any person with a minority background or even a minority interest to feel that there’s no one to emulate in their immediate working environment. When that is the case, a natural question follows: “Do I even belong here?”
Before departments and psychiatric practices turn to old, surface-level solutions like using mentorship to appear more welcoming to underrepresented groups, leaders must explicitly evaluate their track record of mentorship within their system and determine whether mentorship has been used to protect the status quo or move the culture forward. As mentorship is inherently an imbalanced relationship, there must be department- or group-level reflection about the diversity of mentors and also their examinations of mentors’ own preconceived notions of who will make a “good” mentee.
At the most basic level, leaders can examine whether there are gaps in who is mentored and who is not. Other parts of mentoring relationships should also be examined: a) How can mentoring happen if there is a dearth of underrepresented groups in the department? b) What type of mentoring style is favored? Do departments/groups look for a natural fit between mentor and mentee or are they matched based on interests, ideals, and goals? and c) How is the worthiness for mentorship determined?
One example is the fraught process of evaluating “worthiness” among residents. Prospective mentors frequently divide trainees unofficially into a top-tier candidates, middle-tier performers who may be overlooked, and a bottom tier who are avoided when it comes to mentorship. Because this division is informal and usually based on extremely early perceptions of trainees’ aptitude and openness, the process can be subject to an individual mentor’s conscious and unconscious bias, which then plays a large role in perpetuating systemic racism. When it comes to these informal but often rigid divisions, it can be hard to fall from the top when mentees are buoyed by good will, frequent opportunities to shine, and the mentor’s reputation. Likewise,
Below are three recommendations to consider for improving mentorship within departments:
1) Consider opportunities for senior mentors and potential mentees to interact with one another outside of assigned duties so that some mentorship relationships can be formed organically.
2) Review when mentorship relationships have been ineffective or unsuccessful versus productive and useful for both participants.
3) Increase opportunities for adjunct or former faculty who remain connected to the institution to also be mentors. This approach would open up more possibilities and could increase the diversity of available mentors.
If mentorship is to be part of the armamentarium for promoting equity within academia and workplaces alike, it must be examined and changed to meet the new reality.
Dr. Posada is assistant clinical professor, department of psychiatry and behavioral sciences at George Washington University in Washington. She also serves as staff physician at George Washington Medical Faculty Associates, also in Washington. She disclosed no relevant financial relationships. Dr. Forrester is consultation-liaison psychiatry fellowship training director at the University of Maryland, Baltimore. She disclosed no relevant financial relationships.
COVID-19 airway management: Expert tips on infection control
As continue to evolve, practicing vigilant transmission-based infection control precautions remains essential.
This starts with observing droplet precautions to prevent exposure to droplets larger than 5 microns in size, Charles Griffis, PhD, CRNA, said at a Society for Critical Care Medicine virtual meeting: COVID-19: What’s Next. “These are particles exhaled from infected persons and which fall within around 6 feet and involve an exposure time of 15 or more minutes of contact,” said Dr. Griffis, of the department of anesthesiology at the University of Southern California, Los Angeles. “We will always observe standard precautions, which include hand hygiene, gloves, hair and eye cover, medical mask, and face shield. We will observe these at all times for all patients and layer our transmission-based precautions on top.”
During aerosol-producing procedures such as airway management maneuvers, tracheostomies, and bronchoscopies, very fine microscopic particles less than 5 microns in size are produced, which remain airborne for potentially many hours and travel long distances. “We will add an N95 mask or a powered air-purifying respirator (PAPR) device to filter out tiny particles in addition to our ever-present standard precautions,” he said. “Contact precautions are indicated for direct contact with patient saliva, blood, urine, and stool. In addition to standard precautions, we’re going to add an impermeable gown and we’ll continue with gloves, eye protection, and shoe covers. The message is to all of us. We have to observe all of the infection precautions that all of us have learned and trained in to avoid exposure.”
In terms of airway management for infected patients for elective procedures and surgery, recommendations based on current and previous coronavirus outbreaks suggest that all patients get polymerase chain reaction (PCR) tested within 24-48 hours of elective procedures or surgeries. If positive, they should be quarantined for 10-14 days and then, if asymptomatic, these patients may be retested or they can be regarded as negative. “Patients who are PCR positive with active infection and active symptoms receive only urgent or emergent care in most settings,” said Dr. Griffis, a member of the American Association of Nurse Anesthetists Infection Control Advisory Panel. “The care provided to our patients, whether they’re positive or not, is individualized per patient needs and institutional policy. Some folks have made the decision to treat all patients as infected and to use airborne precautions for all aerosol-producing procedures for all patients all the time.”
When a COVID-19 patient requires emergent or urgent airway management because of respiratory failure or some other surgical or procedural intervention necessitating airway management, preprocedural planning is key, he continued. This means establishing the steps in airway management scenarios for infected patients and rehearsing those steps in each ICU setting with key personnel such as nurses, respiratory therapists, and medical staff. “You want to make sure that the PPE is readily available and determine and limit the number of personnel that are going to enter the patient’s room or area for airway management,” Dr. Griffis said. “Have all the airway equipment and drugs immediately available. Perhaps you could organize them in a cart which is decontaminated after every use.”
He also recommends forming an intubation team for ICUs and perhaps even for ORs, where the most experienced clinicians perform airway management. “This helps to avoid unnecessary airway manipulation and minimizes personnel exposure and time to airway establishment,” he said.
Always attempt to house the infected patient in an airborne isolation, negative-pressure room, with a minimum of 12 exchanges per hour and which will take 35 minutes for 99.99% removal of airborne contaminants after airway management. “These numbers are important to remember for room turnover safety,” he said.
Patient factors to review during airway management include assessing the past medical history, inspecting the airway and considering the patient’s current physiological status as time permits. Previously in the pandemic, intubation was used earlier in the disease course, but now data suggest that patients do better without intubation if possible (Am J Trop Med Hyg. 2020;102[6]. doi: 10.4269/aitmh.20-0283). “This is because the pathophysiology of COVID-19 is such that the lung tissue is predisposed to iatrogenic barotrauma damage from positive-pressure ventilation,” Dr. Griffis said. “In addition, COVID patients appear to tolerate significant hypoxemia without distress in many cases. Therefore, many clinicians now hold off on intubation until the hypoxemic patient begins exhibiting signs and symptoms of respiratory distress.”
Options for delivering noninvasive airway support for COVID-19 patients include high-flow nasal cannula and noninvasive positive-pressure ventilation via CPAP or BiPAP. To mitigate the associated aerosol production, consider applying a surgical mask, helmet, or face mask over the airway device/patient’s face. “Another measure that has proven helpful in general respiratory support is to actually put the patient in a prone position to help redistribute ventilation throughout the lungs,” Dr. Griffis said (see Resp Care. 2015;60[11]:1660-87).
To prepare for the actual intubation procedure, gather two expert intubators who are going to be entering the patient’s room. The team should perform hand hygiene and don full PPE prior to entry. “It’s recommended that you consider wearing double gloves for the intubation,” he said. “Have the airway equipment easily accessible in a central location on a cart or in a kit, and use disposable, single-use equipment if possible. All of the usual intubation equipment to maintain a clear airway and give positive pressure ventilation should be arranged for easy access. A video laryngoscope should be used, if possible, for greater accuracy and reduced procedure time. Ready access to sedation and muscle relaxant drugs must be assured at all times.”
For the intubation procedure itself, Dr. Griffis recommends ensuring that an oxygen source, positive-pressure ventilation, and suction and resuscitation drugs and equipment are available per institutional protocol. Assign one person outside the room to coordinate supplies and assistance. “Preoxygenate the patient as permitted by clinical status,” he said. “A nonrebreathing oxygen mask can be used if sufficient spontaneous ventilation is present. Assess the airway, check and arrange equipment for easy access, and develop the safest airway management plan. Consider a rapid sequence induction and intubation as the first option.” Avoid positive-pressure ventilation or awake fiber optic intubation unless absolutely necessary, thus avoiding aerosol production. “Only ventilate the patient after the endotracheal tube cuff is inflated, to avoid aerosol release,” he said.
For intubation, administer airway procedural drugs and insert the laryngoscope – ideally a video laryngoscope if available. Intubate the trachea under direct vision, inflate the cuff, and remove outer gloves. Then attach the Ambu bag with a 99% filtration efficiency, heat-and-moisture exchange filter; and proceed to ventilate the patient, checking for chest rise, breath sounds, and CO2 production. “Discard contaminated equipment in designated bins and secure the tube,” Dr. Griffis advised. “Attach the ventilator with an HMEF filter to protect the ventilator circuit and inner parts of the machine. Recheck your breath sounds, CO2 production, and oxygen saturation, and adjust your vent settings as indicated.”
For post intubation, Dr. Griffis recommends securing contaminated discardable equipment in biohazard-labeled bins or bags, safely doffing your PPE, and retaining your N95 mask in the room. Remove your inner gloves, perform hand hygiene with soap and water if available, with alcohol-based hand rub if not, then don clean gloves. Exit the room, safely transporting any contaminated equipment that will be reused such as a cart or video laryngoscope to decontamination areas for processing. “Once clear of the room, order your chest x-ray to confirm your tube position per institutional protocol, understanding that radiology techs are all going to be following infection control procedures and wearing their PPE,” he said.
For extubation, Dr. Griffis recommends excusing all nonessential personnel from the patient room and assigning an assistant outside the room for necessary help. An experienced airway management expert should evaluate the patient wearing full PPE and be double-gloved. “If the extubation criteria are met, suction the pharynx and extubate,” he said. “Remove outer gloves and apply desired oxygen delivery equipment to the patient and assess respiratory status and vital signs for stability.” Next, discard all contaminated equipment in designated bins, doff contaminated PPE, and retain your N95 mask. Doff inner gloves, perform hand hygiene, and don clean gloves. “Exit the room, hand off contaminated equipment that is reusable, doff your gloves outside, do hand hygiene, then proceed to change your scrubs and complete your own personal hygiene measures,” he said.
Dr. Griffis reported having no financial disclosures.
“While the PPE used for intubation of a coronavirus patient is certainly more than the typical droplet precautions observed when intubating any other patient, the process and best practices aren’t terribly different from usual standard of care: Ensuring all necessary equipment is readily available with backup plans should the airway be difficult,” said Megan Conroy, MD, assistant professor of clinical medicine at The Ohio State University.
“We’ve been streamlining the team that’s present in the room for intubations of COVID patients, but I’m always amazed at the team members that stand at the ready to lend additional assistance just from the other side of the door. So while fewer personnel may be exposed, I wouldn’t consider the team needed for intubation to actually be much smaller, we’re just functioning differently.
In my practice the decision of when to intubate, clinically, doesn’t vary too much from any other form of severe ARDS. We may tolerate higher FiO2 requirements on heated high-flow nasal cannula if the patient exhibits acceptable work of breathing, but I wouldn’t advise allowing a patient to remain hypoxemic with oxygen needs unmet by noninvasive methods out of fear of intubation or ventilator management. In my opinion, this simply delays a necessary therapy and only makes for a higher risk intubation. Certainly, the decision to intubate is never based on only one single data point, but takes an expert assessment of the whole clinical picture.
I’d assert that it’s true in every disease that patients do better if it’s possible to avoid intubation – but I would argue that the ability to avoid intubation is determined primarily by the disease course and clinical scenario, and not by whether the physician wishes to avoid intubation or not. If I can safely manage a patient off of a ventilator, I will always do so, COVID or otherwise. I think in this phase of the pandemic, patients ‘do better without intubation’ because those who didn’t require intubation were inherently doing better!”
As continue to evolve, practicing vigilant transmission-based infection control precautions remains essential.
This starts with observing droplet precautions to prevent exposure to droplets larger than 5 microns in size, Charles Griffis, PhD, CRNA, said at a Society for Critical Care Medicine virtual meeting: COVID-19: What’s Next. “These are particles exhaled from infected persons and which fall within around 6 feet and involve an exposure time of 15 or more minutes of contact,” said Dr. Griffis, of the department of anesthesiology at the University of Southern California, Los Angeles. “We will always observe standard precautions, which include hand hygiene, gloves, hair and eye cover, medical mask, and face shield. We will observe these at all times for all patients and layer our transmission-based precautions on top.”
During aerosol-producing procedures such as airway management maneuvers, tracheostomies, and bronchoscopies, very fine microscopic particles less than 5 microns in size are produced, which remain airborne for potentially many hours and travel long distances. “We will add an N95 mask or a powered air-purifying respirator (PAPR) device to filter out tiny particles in addition to our ever-present standard precautions,” he said. “Contact precautions are indicated for direct contact with patient saliva, blood, urine, and stool. In addition to standard precautions, we’re going to add an impermeable gown and we’ll continue with gloves, eye protection, and shoe covers. The message is to all of us. We have to observe all of the infection precautions that all of us have learned and trained in to avoid exposure.”
In terms of airway management for infected patients for elective procedures and surgery, recommendations based on current and previous coronavirus outbreaks suggest that all patients get polymerase chain reaction (PCR) tested within 24-48 hours of elective procedures or surgeries. If positive, they should be quarantined for 10-14 days and then, if asymptomatic, these patients may be retested or they can be regarded as negative. “Patients who are PCR positive with active infection and active symptoms receive only urgent or emergent care in most settings,” said Dr. Griffis, a member of the American Association of Nurse Anesthetists Infection Control Advisory Panel. “The care provided to our patients, whether they’re positive or not, is individualized per patient needs and institutional policy. Some folks have made the decision to treat all patients as infected and to use airborne precautions for all aerosol-producing procedures for all patients all the time.”
When a COVID-19 patient requires emergent or urgent airway management because of respiratory failure or some other surgical or procedural intervention necessitating airway management, preprocedural planning is key, he continued. This means establishing the steps in airway management scenarios for infected patients and rehearsing those steps in each ICU setting with key personnel such as nurses, respiratory therapists, and medical staff. “You want to make sure that the PPE is readily available and determine and limit the number of personnel that are going to enter the patient’s room or area for airway management,” Dr. Griffis said. “Have all the airway equipment and drugs immediately available. Perhaps you could organize them in a cart which is decontaminated after every use.”
He also recommends forming an intubation team for ICUs and perhaps even for ORs, where the most experienced clinicians perform airway management. “This helps to avoid unnecessary airway manipulation and minimizes personnel exposure and time to airway establishment,” he said.
Always attempt to house the infected patient in an airborne isolation, negative-pressure room, with a minimum of 12 exchanges per hour and which will take 35 minutes for 99.99% removal of airborne contaminants after airway management. “These numbers are important to remember for room turnover safety,” he said.
Patient factors to review during airway management include assessing the past medical history, inspecting the airway and considering the patient’s current physiological status as time permits. Previously in the pandemic, intubation was used earlier in the disease course, but now data suggest that patients do better without intubation if possible (Am J Trop Med Hyg. 2020;102[6]. doi: 10.4269/aitmh.20-0283). “This is because the pathophysiology of COVID-19 is such that the lung tissue is predisposed to iatrogenic barotrauma damage from positive-pressure ventilation,” Dr. Griffis said. “In addition, COVID patients appear to tolerate significant hypoxemia without distress in many cases. Therefore, many clinicians now hold off on intubation until the hypoxemic patient begins exhibiting signs and symptoms of respiratory distress.”
Options for delivering noninvasive airway support for COVID-19 patients include high-flow nasal cannula and noninvasive positive-pressure ventilation via CPAP or BiPAP. To mitigate the associated aerosol production, consider applying a surgical mask, helmet, or face mask over the airway device/patient’s face. “Another measure that has proven helpful in general respiratory support is to actually put the patient in a prone position to help redistribute ventilation throughout the lungs,” Dr. Griffis said (see Resp Care. 2015;60[11]:1660-87).
To prepare for the actual intubation procedure, gather two expert intubators who are going to be entering the patient’s room. The team should perform hand hygiene and don full PPE prior to entry. “It’s recommended that you consider wearing double gloves for the intubation,” he said. “Have the airway equipment easily accessible in a central location on a cart or in a kit, and use disposable, single-use equipment if possible. All of the usual intubation equipment to maintain a clear airway and give positive pressure ventilation should be arranged for easy access. A video laryngoscope should be used, if possible, for greater accuracy and reduced procedure time. Ready access to sedation and muscle relaxant drugs must be assured at all times.”
For the intubation procedure itself, Dr. Griffis recommends ensuring that an oxygen source, positive-pressure ventilation, and suction and resuscitation drugs and equipment are available per institutional protocol. Assign one person outside the room to coordinate supplies and assistance. “Preoxygenate the patient as permitted by clinical status,” he said. “A nonrebreathing oxygen mask can be used if sufficient spontaneous ventilation is present. Assess the airway, check and arrange equipment for easy access, and develop the safest airway management plan. Consider a rapid sequence induction and intubation as the first option.” Avoid positive-pressure ventilation or awake fiber optic intubation unless absolutely necessary, thus avoiding aerosol production. “Only ventilate the patient after the endotracheal tube cuff is inflated, to avoid aerosol release,” he said.
For intubation, administer airway procedural drugs and insert the laryngoscope – ideally a video laryngoscope if available. Intubate the trachea under direct vision, inflate the cuff, and remove outer gloves. Then attach the Ambu bag with a 99% filtration efficiency, heat-and-moisture exchange filter; and proceed to ventilate the patient, checking for chest rise, breath sounds, and CO2 production. “Discard contaminated equipment in designated bins and secure the tube,” Dr. Griffis advised. “Attach the ventilator with an HMEF filter to protect the ventilator circuit and inner parts of the machine. Recheck your breath sounds, CO2 production, and oxygen saturation, and adjust your vent settings as indicated.”
For post intubation, Dr. Griffis recommends securing contaminated discardable equipment in biohazard-labeled bins or bags, safely doffing your PPE, and retaining your N95 mask in the room. Remove your inner gloves, perform hand hygiene with soap and water if available, with alcohol-based hand rub if not, then don clean gloves. Exit the room, safely transporting any contaminated equipment that will be reused such as a cart or video laryngoscope to decontamination areas for processing. “Once clear of the room, order your chest x-ray to confirm your tube position per institutional protocol, understanding that radiology techs are all going to be following infection control procedures and wearing their PPE,” he said.
For extubation, Dr. Griffis recommends excusing all nonessential personnel from the patient room and assigning an assistant outside the room for necessary help. An experienced airway management expert should evaluate the patient wearing full PPE and be double-gloved. “If the extubation criteria are met, suction the pharynx and extubate,” he said. “Remove outer gloves and apply desired oxygen delivery equipment to the patient and assess respiratory status and vital signs for stability.” Next, discard all contaminated equipment in designated bins, doff contaminated PPE, and retain your N95 mask. Doff inner gloves, perform hand hygiene, and don clean gloves. “Exit the room, hand off contaminated equipment that is reusable, doff your gloves outside, do hand hygiene, then proceed to change your scrubs and complete your own personal hygiene measures,” he said.
Dr. Griffis reported having no financial disclosures.
“While the PPE used for intubation of a coronavirus patient is certainly more than the typical droplet precautions observed when intubating any other patient, the process and best practices aren’t terribly different from usual standard of care: Ensuring all necessary equipment is readily available with backup plans should the airway be difficult,” said Megan Conroy, MD, assistant professor of clinical medicine at The Ohio State University.
“We’ve been streamlining the team that’s present in the room for intubations of COVID patients, but I’m always amazed at the team members that stand at the ready to lend additional assistance just from the other side of the door. So while fewer personnel may be exposed, I wouldn’t consider the team needed for intubation to actually be much smaller, we’re just functioning differently.
In my practice the decision of when to intubate, clinically, doesn’t vary too much from any other form of severe ARDS. We may tolerate higher FiO2 requirements on heated high-flow nasal cannula if the patient exhibits acceptable work of breathing, but I wouldn’t advise allowing a patient to remain hypoxemic with oxygen needs unmet by noninvasive methods out of fear of intubation or ventilator management. In my opinion, this simply delays a necessary therapy and only makes for a higher risk intubation. Certainly, the decision to intubate is never based on only one single data point, but takes an expert assessment of the whole clinical picture.
I’d assert that it’s true in every disease that patients do better if it’s possible to avoid intubation – but I would argue that the ability to avoid intubation is determined primarily by the disease course and clinical scenario, and not by whether the physician wishes to avoid intubation or not. If I can safely manage a patient off of a ventilator, I will always do so, COVID or otherwise. I think in this phase of the pandemic, patients ‘do better without intubation’ because those who didn’t require intubation were inherently doing better!”
As continue to evolve, practicing vigilant transmission-based infection control precautions remains essential.
This starts with observing droplet precautions to prevent exposure to droplets larger than 5 microns in size, Charles Griffis, PhD, CRNA, said at a Society for Critical Care Medicine virtual meeting: COVID-19: What’s Next. “These are particles exhaled from infected persons and which fall within around 6 feet and involve an exposure time of 15 or more minutes of contact,” said Dr. Griffis, of the department of anesthesiology at the University of Southern California, Los Angeles. “We will always observe standard precautions, which include hand hygiene, gloves, hair and eye cover, medical mask, and face shield. We will observe these at all times for all patients and layer our transmission-based precautions on top.”
During aerosol-producing procedures such as airway management maneuvers, tracheostomies, and bronchoscopies, very fine microscopic particles less than 5 microns in size are produced, which remain airborne for potentially many hours and travel long distances. “We will add an N95 mask or a powered air-purifying respirator (PAPR) device to filter out tiny particles in addition to our ever-present standard precautions,” he said. “Contact precautions are indicated for direct contact with patient saliva, blood, urine, and stool. In addition to standard precautions, we’re going to add an impermeable gown and we’ll continue with gloves, eye protection, and shoe covers. The message is to all of us. We have to observe all of the infection precautions that all of us have learned and trained in to avoid exposure.”
In terms of airway management for infected patients for elective procedures and surgery, recommendations based on current and previous coronavirus outbreaks suggest that all patients get polymerase chain reaction (PCR) tested within 24-48 hours of elective procedures or surgeries. If positive, they should be quarantined for 10-14 days and then, if asymptomatic, these patients may be retested or they can be regarded as negative. “Patients who are PCR positive with active infection and active symptoms receive only urgent or emergent care in most settings,” said Dr. Griffis, a member of the American Association of Nurse Anesthetists Infection Control Advisory Panel. “The care provided to our patients, whether they’re positive or not, is individualized per patient needs and institutional policy. Some folks have made the decision to treat all patients as infected and to use airborne precautions for all aerosol-producing procedures for all patients all the time.”
When a COVID-19 patient requires emergent or urgent airway management because of respiratory failure or some other surgical or procedural intervention necessitating airway management, preprocedural planning is key, he continued. This means establishing the steps in airway management scenarios for infected patients and rehearsing those steps in each ICU setting with key personnel such as nurses, respiratory therapists, and medical staff. “You want to make sure that the PPE is readily available and determine and limit the number of personnel that are going to enter the patient’s room or area for airway management,” Dr. Griffis said. “Have all the airway equipment and drugs immediately available. Perhaps you could organize them in a cart which is decontaminated after every use.”
He also recommends forming an intubation team for ICUs and perhaps even for ORs, where the most experienced clinicians perform airway management. “This helps to avoid unnecessary airway manipulation and minimizes personnel exposure and time to airway establishment,” he said.
Always attempt to house the infected patient in an airborne isolation, negative-pressure room, with a minimum of 12 exchanges per hour and which will take 35 minutes for 99.99% removal of airborne contaminants after airway management. “These numbers are important to remember for room turnover safety,” he said.
Patient factors to review during airway management include assessing the past medical history, inspecting the airway and considering the patient’s current physiological status as time permits. Previously in the pandemic, intubation was used earlier in the disease course, but now data suggest that patients do better without intubation if possible (Am J Trop Med Hyg. 2020;102[6]. doi: 10.4269/aitmh.20-0283). “This is because the pathophysiology of COVID-19 is such that the lung tissue is predisposed to iatrogenic barotrauma damage from positive-pressure ventilation,” Dr. Griffis said. “In addition, COVID patients appear to tolerate significant hypoxemia without distress in many cases. Therefore, many clinicians now hold off on intubation until the hypoxemic patient begins exhibiting signs and symptoms of respiratory distress.”
Options for delivering noninvasive airway support for COVID-19 patients include high-flow nasal cannula and noninvasive positive-pressure ventilation via CPAP or BiPAP. To mitigate the associated aerosol production, consider applying a surgical mask, helmet, or face mask over the airway device/patient’s face. “Another measure that has proven helpful in general respiratory support is to actually put the patient in a prone position to help redistribute ventilation throughout the lungs,” Dr. Griffis said (see Resp Care. 2015;60[11]:1660-87).
To prepare for the actual intubation procedure, gather two expert intubators who are going to be entering the patient’s room. The team should perform hand hygiene and don full PPE prior to entry. “It’s recommended that you consider wearing double gloves for the intubation,” he said. “Have the airway equipment easily accessible in a central location on a cart or in a kit, and use disposable, single-use equipment if possible. All of the usual intubation equipment to maintain a clear airway and give positive pressure ventilation should be arranged for easy access. A video laryngoscope should be used, if possible, for greater accuracy and reduced procedure time. Ready access to sedation and muscle relaxant drugs must be assured at all times.”
For the intubation procedure itself, Dr. Griffis recommends ensuring that an oxygen source, positive-pressure ventilation, and suction and resuscitation drugs and equipment are available per institutional protocol. Assign one person outside the room to coordinate supplies and assistance. “Preoxygenate the patient as permitted by clinical status,” he said. “A nonrebreathing oxygen mask can be used if sufficient spontaneous ventilation is present. Assess the airway, check and arrange equipment for easy access, and develop the safest airway management plan. Consider a rapid sequence induction and intubation as the first option.” Avoid positive-pressure ventilation or awake fiber optic intubation unless absolutely necessary, thus avoiding aerosol production. “Only ventilate the patient after the endotracheal tube cuff is inflated, to avoid aerosol release,” he said.
For intubation, administer airway procedural drugs and insert the laryngoscope – ideally a video laryngoscope if available. Intubate the trachea under direct vision, inflate the cuff, and remove outer gloves. Then attach the Ambu bag with a 99% filtration efficiency, heat-and-moisture exchange filter; and proceed to ventilate the patient, checking for chest rise, breath sounds, and CO2 production. “Discard contaminated equipment in designated bins and secure the tube,” Dr. Griffis advised. “Attach the ventilator with an HMEF filter to protect the ventilator circuit and inner parts of the machine. Recheck your breath sounds, CO2 production, and oxygen saturation, and adjust your vent settings as indicated.”
For post intubation, Dr. Griffis recommends securing contaminated discardable equipment in biohazard-labeled bins or bags, safely doffing your PPE, and retaining your N95 mask in the room. Remove your inner gloves, perform hand hygiene with soap and water if available, with alcohol-based hand rub if not, then don clean gloves. Exit the room, safely transporting any contaminated equipment that will be reused such as a cart or video laryngoscope to decontamination areas for processing. “Once clear of the room, order your chest x-ray to confirm your tube position per institutional protocol, understanding that radiology techs are all going to be following infection control procedures and wearing their PPE,” he said.
For extubation, Dr. Griffis recommends excusing all nonessential personnel from the patient room and assigning an assistant outside the room for necessary help. An experienced airway management expert should evaluate the patient wearing full PPE and be double-gloved. “If the extubation criteria are met, suction the pharynx and extubate,” he said. “Remove outer gloves and apply desired oxygen delivery equipment to the patient and assess respiratory status and vital signs for stability.” Next, discard all contaminated equipment in designated bins, doff contaminated PPE, and retain your N95 mask. Doff inner gloves, perform hand hygiene, and don clean gloves. “Exit the room, hand off contaminated equipment that is reusable, doff your gloves outside, do hand hygiene, then proceed to change your scrubs and complete your own personal hygiene measures,” he said.
Dr. Griffis reported having no financial disclosures.
“While the PPE used for intubation of a coronavirus patient is certainly more than the typical droplet precautions observed when intubating any other patient, the process and best practices aren’t terribly different from usual standard of care: Ensuring all necessary equipment is readily available with backup plans should the airway be difficult,” said Megan Conroy, MD, assistant professor of clinical medicine at The Ohio State University.
“We’ve been streamlining the team that’s present in the room for intubations of COVID patients, but I’m always amazed at the team members that stand at the ready to lend additional assistance just from the other side of the door. So while fewer personnel may be exposed, I wouldn’t consider the team needed for intubation to actually be much smaller, we’re just functioning differently.
In my practice the decision of when to intubate, clinically, doesn’t vary too much from any other form of severe ARDS. We may tolerate higher FiO2 requirements on heated high-flow nasal cannula if the patient exhibits acceptable work of breathing, but I wouldn’t advise allowing a patient to remain hypoxemic with oxygen needs unmet by noninvasive methods out of fear of intubation or ventilator management. In my opinion, this simply delays a necessary therapy and only makes for a higher risk intubation. Certainly, the decision to intubate is never based on only one single data point, but takes an expert assessment of the whole clinical picture.
I’d assert that it’s true in every disease that patients do better if it’s possible to avoid intubation – but I would argue that the ability to avoid intubation is determined primarily by the disease course and clinical scenario, and not by whether the physician wishes to avoid intubation or not. If I can safely manage a patient off of a ventilator, I will always do so, COVID or otherwise. I think in this phase of the pandemic, patients ‘do better without intubation’ because those who didn’t require intubation were inherently doing better!”
FROM AN SCCM VIRTUAL MEETING