User login
-
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]


The new one-percenters: Children with COVID-19
according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
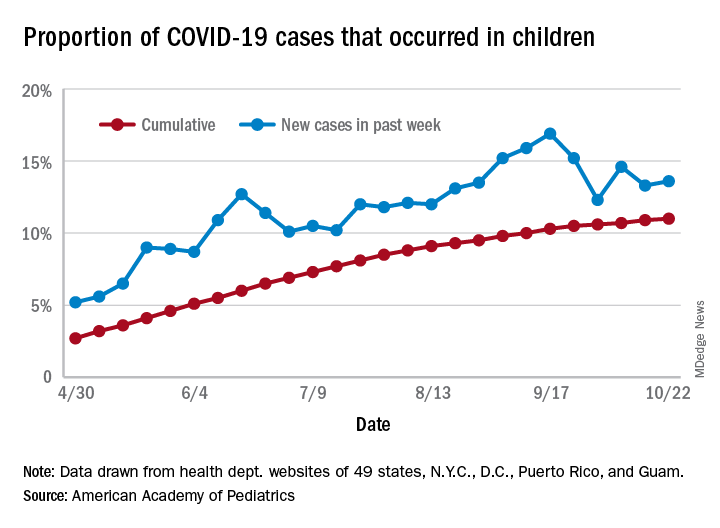
There have been 1,052 cases of COVID-19 per 100,000 children as of Oct. 22, and that works out to 1.05% of all children in the country. The cumulative number of pediatric cases is 792,188, and children now represent 11% of all COVID-19 cases, the AAP and the CHA reported Oct. 26.
There were just over 50,000 new child cases reported in the week ending Oct. 22, which was 13.6% of the national total of almost 370,000. That’s up slightly from the 13.3% the previous week but still down from the spike seen in mid-September, based on the data collected from the websites of 49 state health departments (New York does not report ages), along with the District of Columbia, New York City, Puerto Rico, and Guam.
The state-level data show that California has had more COVID-19 cases in children (92,864) than any other state, although Texas has reported ages for only 7% of its confirmed cases. Illinois is next with 46,006 cases, followed by Florida at 45,575, although Florida is using an age range of 0-14 years to define a child case, the AAP and CHA noted.
Other measures largely put small states at the extremes:
- North Dakota has the highest cumulative rate: 2,954 cases per 100,000 children.
- Vermont has the lowest cumulative rate: 190.5 per 100,000.
- Wyoming has the highest proportion of cases in children: 27.7%.
- New Jersey has the lowest proportion of child cases: 4.6%.
There were no COVID-19–related deaths in children reported the week ending Oct. 22, so the total number remains at 120, which is just 0.06% of the total for all ages, based on data from 42 states and New York City. Hospitalization figures put admissions at almost 5,600 in children, or 1.7% of all hospitalizations, although those data come from just 24 states and New York City, the AAP and CHA said.
according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
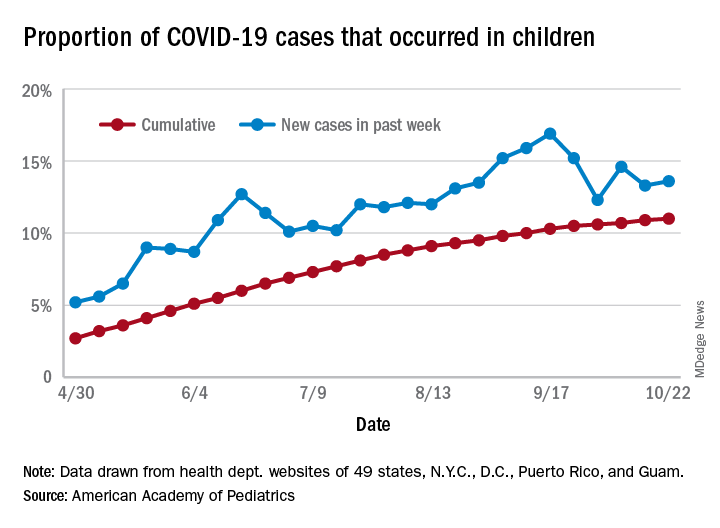
There have been 1,052 cases of COVID-19 per 100,000 children as of Oct. 22, and that works out to 1.05% of all children in the country. The cumulative number of pediatric cases is 792,188, and children now represent 11% of all COVID-19 cases, the AAP and the CHA reported Oct. 26.
There were just over 50,000 new child cases reported in the week ending Oct. 22, which was 13.6% of the national total of almost 370,000. That’s up slightly from the 13.3% the previous week but still down from the spike seen in mid-September, based on the data collected from the websites of 49 state health departments (New York does not report ages), along with the District of Columbia, New York City, Puerto Rico, and Guam.
The state-level data show that California has had more COVID-19 cases in children (92,864) than any other state, although Texas has reported ages for only 7% of its confirmed cases. Illinois is next with 46,006 cases, followed by Florida at 45,575, although Florida is using an age range of 0-14 years to define a child case, the AAP and CHA noted.
Other measures largely put small states at the extremes:
- North Dakota has the highest cumulative rate: 2,954 cases per 100,000 children.
- Vermont has the lowest cumulative rate: 190.5 per 100,000.
- Wyoming has the highest proportion of cases in children: 27.7%.
- New Jersey has the lowest proportion of child cases: 4.6%.
There were no COVID-19–related deaths in children reported the week ending Oct. 22, so the total number remains at 120, which is just 0.06% of the total for all ages, based on data from 42 states and New York City. Hospitalization figures put admissions at almost 5,600 in children, or 1.7% of all hospitalizations, although those data come from just 24 states and New York City, the AAP and CHA said.
according to a report from the American Academy of Pediatrics and the Children’s Hospital Association.
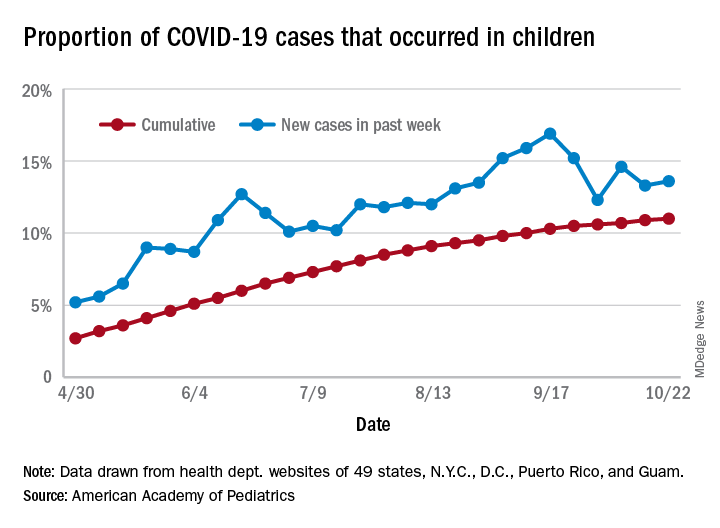
There have been 1,052 cases of COVID-19 per 100,000 children as of Oct. 22, and that works out to 1.05% of all children in the country. The cumulative number of pediatric cases is 792,188, and children now represent 11% of all COVID-19 cases, the AAP and the CHA reported Oct. 26.
There were just over 50,000 new child cases reported in the week ending Oct. 22, which was 13.6% of the national total of almost 370,000. That’s up slightly from the 13.3% the previous week but still down from the spike seen in mid-September, based on the data collected from the websites of 49 state health departments (New York does not report ages), along with the District of Columbia, New York City, Puerto Rico, and Guam.
The state-level data show that California has had more COVID-19 cases in children (92,864) than any other state, although Texas has reported ages for only 7% of its confirmed cases. Illinois is next with 46,006 cases, followed by Florida at 45,575, although Florida is using an age range of 0-14 years to define a child case, the AAP and CHA noted.
Other measures largely put small states at the extremes:
- North Dakota has the highest cumulative rate: 2,954 cases per 100,000 children.
- Vermont has the lowest cumulative rate: 190.5 per 100,000.
- Wyoming has the highest proportion of cases in children: 27.7%.
- New Jersey has the lowest proportion of child cases: 4.6%.
There were no COVID-19–related deaths in children reported the week ending Oct. 22, so the total number remains at 120, which is just 0.06% of the total for all ages, based on data from 42 states and New York City. Hospitalization figures put admissions at almost 5,600 in children, or 1.7% of all hospitalizations, although those data come from just 24 states and New York City, the AAP and CHA said.
COVID-19: Immunity from antibodies may decline rapidly
Antibody response to the SARS-CoV-2 virus wanes over time, latest research has suggested.
An ongoing study led by Imperial College London (ICL) found that the proportion of people testing positive for COVID-19 antibodies dropped by 26.5% over a 3-month period between June and September.
The findings from a non–peer reviewed preprint suggested that infection with SARS-CoV-2 confers only limited protection against reinfection.
Professor Paul Elliott, director of the REACT-2 programme at ICL, said: “Testing positive for antibodies does not mean you are immune to COVID-19.
“It remains unclear what level of immunity antibodies provide, or for how long this immunity lasts.”
Experts said that, while the findings suggested that immunity might fade over time, the severity of illness from further infections could be reduced.
Antibody prevalence declined in all adults
Results from cross-sectional studies over the 3-month period involved 365,104 adults who self-administered a lateral flow immunoassay test.
There were 17,576 positive tests over the three rounds.
Antibody prevalence, adjusted for test characteristics and weighted to the adult population of England, declined from 6.0% to 4.4%, a reduction of 26.5% over the 3 months.
The decline was seen in all age groups. However, the lowest prevalence of a positive test, and the largest fall, was seen in those aged 75 years and older.
No change was seen in positive antibody tests in health care workers over the 3 months.
The results suggested that people who did not show symptoms of COVID-19 were more likely to lose detectable antibodies sooner than those who did show symptoms.
Prof Helen Ward, one of the lead authors of the report said that, while it was clear that the proportion of people with antibodies was falling over time, “We don’t yet know whether this will leave these people at risk of reinfection with the virus that causes COVID-19, but it is essential that everyone continues to follow guidance to reduce the risk to themselves and others.”
Results ‘weaken argument for herd immunity’
Commenting on the results to the Science Media Centre, Rowland Kao, professor of veterinary epidemiology and data science at the University of Edinburgh, warned that, if the results were correct, “any strategy that relies on ‘herd immunity’ lacks credibility.”
However, he added that, “while the decline is substantial, nevertheless substantial proportions of the population do retain some immune response, over 4 months after the peak of the epidemic”.
Eleanor Riley, professor of immunology and infectious disease, also from the University of Edinburgh, said it was too early to assume that immunity to SARS-CoV-2 did not last because “the study does not look at antibody concentrations, antibody function, or other aspects of immunity such as T-cell immunity and does not look at the trajectory of antibody levels in the same individuals over time”.
However, she said the findings did not mean that a vaccine would be ineffective because vaccines contained adjuvants that could induce durable immune responses, particularly with multiple immunizations.
“What is not clear is how quickly antibody levels would rise again if a person encounters the SARS-CoV-2 virus a second time. It is possible they will still rapidly respond, and either have a milder illness, or remain protected through immune memory,” commented Dr. Alexander Edwards, associate professor in biomedical technology at the University of Reading.
Health Minister Lord Bethell said: “Regardless of the result of an antibody test, everyone must continue to comply with government guidelines including social distancing, self-isolating, and getting a test if you have symptoms, and always remember: hands, face, space.”
This article first appeared on Medscape.com.
Antibody response to the SARS-CoV-2 virus wanes over time, latest research has suggested.
An ongoing study led by Imperial College London (ICL) found that the proportion of people testing positive for COVID-19 antibodies dropped by 26.5% over a 3-month period between June and September.
The findings from a non–peer reviewed preprint suggested that infection with SARS-CoV-2 confers only limited protection against reinfection.
Professor Paul Elliott, director of the REACT-2 programme at ICL, said: “Testing positive for antibodies does not mean you are immune to COVID-19.
“It remains unclear what level of immunity antibodies provide, or for how long this immunity lasts.”
Experts said that, while the findings suggested that immunity might fade over time, the severity of illness from further infections could be reduced.
Antibody prevalence declined in all adults
Results from cross-sectional studies over the 3-month period involved 365,104 adults who self-administered a lateral flow immunoassay test.
There were 17,576 positive tests over the three rounds.
Antibody prevalence, adjusted for test characteristics and weighted to the adult population of England, declined from 6.0% to 4.4%, a reduction of 26.5% over the 3 months.
The decline was seen in all age groups. However, the lowest prevalence of a positive test, and the largest fall, was seen in those aged 75 years and older.
No change was seen in positive antibody tests in health care workers over the 3 months.
The results suggested that people who did not show symptoms of COVID-19 were more likely to lose detectable antibodies sooner than those who did show symptoms.
Prof Helen Ward, one of the lead authors of the report said that, while it was clear that the proportion of people with antibodies was falling over time, “We don’t yet know whether this will leave these people at risk of reinfection with the virus that causes COVID-19, but it is essential that everyone continues to follow guidance to reduce the risk to themselves and others.”
Results ‘weaken argument for herd immunity’
Commenting on the results to the Science Media Centre, Rowland Kao, professor of veterinary epidemiology and data science at the University of Edinburgh, warned that, if the results were correct, “any strategy that relies on ‘herd immunity’ lacks credibility.”
However, he added that, “while the decline is substantial, nevertheless substantial proportions of the population do retain some immune response, over 4 months after the peak of the epidemic”.
Eleanor Riley, professor of immunology and infectious disease, also from the University of Edinburgh, said it was too early to assume that immunity to SARS-CoV-2 did not last because “the study does not look at antibody concentrations, antibody function, or other aspects of immunity such as T-cell immunity and does not look at the trajectory of antibody levels in the same individuals over time”.
However, she said the findings did not mean that a vaccine would be ineffective because vaccines contained adjuvants that could induce durable immune responses, particularly with multiple immunizations.
“What is not clear is how quickly antibody levels would rise again if a person encounters the SARS-CoV-2 virus a second time. It is possible they will still rapidly respond, and either have a milder illness, or remain protected through immune memory,” commented Dr. Alexander Edwards, associate professor in biomedical technology at the University of Reading.
Health Minister Lord Bethell said: “Regardless of the result of an antibody test, everyone must continue to comply with government guidelines including social distancing, self-isolating, and getting a test if you have symptoms, and always remember: hands, face, space.”
This article first appeared on Medscape.com.
Antibody response to the SARS-CoV-2 virus wanes over time, latest research has suggested.
An ongoing study led by Imperial College London (ICL) found that the proportion of people testing positive for COVID-19 antibodies dropped by 26.5% over a 3-month period between June and September.
The findings from a non–peer reviewed preprint suggested that infection with SARS-CoV-2 confers only limited protection against reinfection.
Professor Paul Elliott, director of the REACT-2 programme at ICL, said: “Testing positive for antibodies does not mean you are immune to COVID-19.
“It remains unclear what level of immunity antibodies provide, or for how long this immunity lasts.”
Experts said that, while the findings suggested that immunity might fade over time, the severity of illness from further infections could be reduced.
Antibody prevalence declined in all adults
Results from cross-sectional studies over the 3-month period involved 365,104 adults who self-administered a lateral flow immunoassay test.
There were 17,576 positive tests over the three rounds.
Antibody prevalence, adjusted for test characteristics and weighted to the adult population of England, declined from 6.0% to 4.4%, a reduction of 26.5% over the 3 months.
The decline was seen in all age groups. However, the lowest prevalence of a positive test, and the largest fall, was seen in those aged 75 years and older.
No change was seen in positive antibody tests in health care workers over the 3 months.
The results suggested that people who did not show symptoms of COVID-19 were more likely to lose detectable antibodies sooner than those who did show symptoms.
Prof Helen Ward, one of the lead authors of the report said that, while it was clear that the proportion of people with antibodies was falling over time, “We don’t yet know whether this will leave these people at risk of reinfection with the virus that causes COVID-19, but it is essential that everyone continues to follow guidance to reduce the risk to themselves and others.”
Results ‘weaken argument for herd immunity’
Commenting on the results to the Science Media Centre, Rowland Kao, professor of veterinary epidemiology and data science at the University of Edinburgh, warned that, if the results were correct, “any strategy that relies on ‘herd immunity’ lacks credibility.”
However, he added that, “while the decline is substantial, nevertheless substantial proportions of the population do retain some immune response, over 4 months after the peak of the epidemic”.
Eleanor Riley, professor of immunology and infectious disease, also from the University of Edinburgh, said it was too early to assume that immunity to SARS-CoV-2 did not last because “the study does not look at antibody concentrations, antibody function, or other aspects of immunity such as T-cell immunity and does not look at the trajectory of antibody levels in the same individuals over time”.
However, she said the findings did not mean that a vaccine would be ineffective because vaccines contained adjuvants that could induce durable immune responses, particularly with multiple immunizations.
“What is not clear is how quickly antibody levels would rise again if a person encounters the SARS-CoV-2 virus a second time. It is possible they will still rapidly respond, and either have a milder illness, or remain protected through immune memory,” commented Dr. Alexander Edwards, associate professor in biomedical technology at the University of Reading.
Health Minister Lord Bethell said: “Regardless of the result of an antibody test, everyone must continue to comply with government guidelines including social distancing, self-isolating, and getting a test if you have symptoms, and always remember: hands, face, space.”
This article first appeared on Medscape.com.
Valvular disease and COVID-19 are a deadly mix; don’t delay intervention
Danny Dvir, MD, has a message for physicians who have patients with severe valvular heart disease who are deferring valve replacement or repair until after the COVID-19 pandemic: Urge them not to wait.
Data from the Multicenter International Valve Disease Registry vividly demonstrate that clinical outcomes are poor in patients with uncorrected valve disease who become hospitalized with COVID-19. Indeed, the mortality rate within 30 days after hospital admission in 136 such patients enrolled in the registry from centers in Europe, North America, and Israel was 42%, Dr. Dvir reported at the Transcatheter Cardiovascular Research Therapeutics virtual annual meeting.
“That’s dramatically higher than for an age-matched population infected with COVID-19 without valvular heart disease, which is 10%-15%,” he noted at the meeting sponsored by the Cardiovascular Research Foundation.
The bright spot was that, in the small subgroup of 15 registry participants who underwent transcatheter or, much less frequently, surgical treatment of their failing valve while COVID-19 infected, 30-day mortality was far lower. In fact, it was comparable with the background rate in hospitalized COVID-19 patients without valve disease, according to Dr. Dvir, an interventional cardiologist at Shaare Zedek Medical Center, Hebrew University, Jerusalem.
He personally did several of the transcatheter aortic valve replacements.
“It’s doable. I truly believe that when you get a severe aortic stenosis patient who’s infected with the coronavirus, they get very unstable, but we can treat them. We can treat them even during the infection,” Dr. Dvir said.
The majority of patients in the registry had severe aortic stenosis. In the 42 such patients aged 80 years or more who didn’t undergo transcatheter aortic valve replacement (TAVR) or surgical valve replacement, 30-day mortality was 60%. In contrast, only one of the six patients in this advanced-age category who underwent valve replacement while infected died. Similarly, 30-day mortality was 24% among those younger than age 80 who valve remained untreated, but it dropped to 11% in those who received a prosthetic valve.
“We try our best to protect our patients through social distancing, but we have a treatment that can potentially reduce their mortality risk if they get infected later on. So I say to my patients: ‘Don’t wait at home. Do not wait! If you get infected when you have severe aortic stenosis, the clinical outcome is bad.’ But it seems reasonable that if they get infected when they’ve already been treated for their aortic stenosis or mitral regurgitation, they will do better.”
Dr. Dvir noted that, although the case numbers in the registry series were small and subject to potential bias, the data suggest this treatment approach may be lifesaving.
Session comoderator Timothy D. Henry, MD, commented that this registry study contains a great take-home point: “This is really consistent with what see in a lot of the other areas of COVID, that what we know to be best clinical care, we should do it, with or without the COVID.”
He asked Dr. Dvir about any special measures he takes while doing TAVR in this extreme setting. In the United States, for example, interventionalists are increasingly using transesophageal echocardiography to guide their procedures using conscious sedation, without intubation, noted Dr. Henry, medical director of the Carl and Edyth Lindner Center for Research at the Christ Hospital, Cincinnati.
“We try to minimize the procedure time; that’s one of the important things,” Dr. Dvir replied. “And you need to be protected during the procedure in a very cautious and meticulous way. You need many fans in the room because you sweat a lot.”
Discussant Renu Virmani, MD, president of the CVPath Institute in Gaithersburg, Md., commented: “The main thing I get from this presentation is the need for patients to be educated that if you’ve got valve disease, you’re better off getting it treated before you’ve got COVID. Obviously, try to prevent getting COVID – that’s the best thing you can do – but you can’t always control that.”
Discussant Mamas Mamas, MD, professor of cardiology at Keele University, Staffordshire, England, said deferred treatment of severe valvular heart disease during the pandemic has created a looming public health crisis in the United Kingdom.
“We’ve analyzed the U.K. management of aortic stenosis, and what we’ve found is that during the COVID pandemic there have been 2,500 fewer cases of aortic stenosis that have been treated. We’ve got 2,500 patients on the waiting list, and we’ve got to work out how we’re going to treat them. We estimate with simulations that about 300 of them are going to die before we can get them treated for their aortic stenosis,” according to Dr. Mamas.
Dr. Henry commented that deferral of valve procedures is “really challenging” for a couple of reasons: Not only are patients scared to come into the hospital because they fear getting COVID, but they don’t want to be hospitalized during the pandemic because their family can’t visit them there.
“These patients are mostly over 80 years old. No one wants to come in the hospital when the family won’t be around, especially when you’re 90 years old,” the interventional cardiologist said.
Dr. Dvir reported serving as a consultant to Medtronic, Edwards Lifesciences, Abbott, and Jena.
Danny Dvir, MD, has a message for physicians who have patients with severe valvular heart disease who are deferring valve replacement or repair until after the COVID-19 pandemic: Urge them not to wait.
Data from the Multicenter International Valve Disease Registry vividly demonstrate that clinical outcomes are poor in patients with uncorrected valve disease who become hospitalized with COVID-19. Indeed, the mortality rate within 30 days after hospital admission in 136 such patients enrolled in the registry from centers in Europe, North America, and Israel was 42%, Dr. Dvir reported at the Transcatheter Cardiovascular Research Therapeutics virtual annual meeting.
“That’s dramatically higher than for an age-matched population infected with COVID-19 without valvular heart disease, which is 10%-15%,” he noted at the meeting sponsored by the Cardiovascular Research Foundation.
The bright spot was that, in the small subgroup of 15 registry participants who underwent transcatheter or, much less frequently, surgical treatment of their failing valve while COVID-19 infected, 30-day mortality was far lower. In fact, it was comparable with the background rate in hospitalized COVID-19 patients without valve disease, according to Dr. Dvir, an interventional cardiologist at Shaare Zedek Medical Center, Hebrew University, Jerusalem.
He personally did several of the transcatheter aortic valve replacements.
“It’s doable. I truly believe that when you get a severe aortic stenosis patient who’s infected with the coronavirus, they get very unstable, but we can treat them. We can treat them even during the infection,” Dr. Dvir said.
The majority of patients in the registry had severe aortic stenosis. In the 42 such patients aged 80 years or more who didn’t undergo transcatheter aortic valve replacement (TAVR) or surgical valve replacement, 30-day mortality was 60%. In contrast, only one of the six patients in this advanced-age category who underwent valve replacement while infected died. Similarly, 30-day mortality was 24% among those younger than age 80 who valve remained untreated, but it dropped to 11% in those who received a prosthetic valve.
“We try our best to protect our patients through social distancing, but we have a treatment that can potentially reduce their mortality risk if they get infected later on. So I say to my patients: ‘Don’t wait at home. Do not wait! If you get infected when you have severe aortic stenosis, the clinical outcome is bad.’ But it seems reasonable that if they get infected when they’ve already been treated for their aortic stenosis or mitral regurgitation, they will do better.”
Dr. Dvir noted that, although the case numbers in the registry series were small and subject to potential bias, the data suggest this treatment approach may be lifesaving.
Session comoderator Timothy D. Henry, MD, commented that this registry study contains a great take-home point: “This is really consistent with what see in a lot of the other areas of COVID, that what we know to be best clinical care, we should do it, with or without the COVID.”
He asked Dr. Dvir about any special measures he takes while doing TAVR in this extreme setting. In the United States, for example, interventionalists are increasingly using transesophageal echocardiography to guide their procedures using conscious sedation, without intubation, noted Dr. Henry, medical director of the Carl and Edyth Lindner Center for Research at the Christ Hospital, Cincinnati.
“We try to minimize the procedure time; that’s one of the important things,” Dr. Dvir replied. “And you need to be protected during the procedure in a very cautious and meticulous way. You need many fans in the room because you sweat a lot.”
Discussant Renu Virmani, MD, president of the CVPath Institute in Gaithersburg, Md., commented: “The main thing I get from this presentation is the need for patients to be educated that if you’ve got valve disease, you’re better off getting it treated before you’ve got COVID. Obviously, try to prevent getting COVID – that’s the best thing you can do – but you can’t always control that.”
Discussant Mamas Mamas, MD, professor of cardiology at Keele University, Staffordshire, England, said deferred treatment of severe valvular heart disease during the pandemic has created a looming public health crisis in the United Kingdom.
“We’ve analyzed the U.K. management of aortic stenosis, and what we’ve found is that during the COVID pandemic there have been 2,500 fewer cases of aortic stenosis that have been treated. We’ve got 2,500 patients on the waiting list, and we’ve got to work out how we’re going to treat them. We estimate with simulations that about 300 of them are going to die before we can get them treated for their aortic stenosis,” according to Dr. Mamas.
Dr. Henry commented that deferral of valve procedures is “really challenging” for a couple of reasons: Not only are patients scared to come into the hospital because they fear getting COVID, but they don’t want to be hospitalized during the pandemic because their family can’t visit them there.
“These patients are mostly over 80 years old. No one wants to come in the hospital when the family won’t be around, especially when you’re 90 years old,” the interventional cardiologist said.
Dr. Dvir reported serving as a consultant to Medtronic, Edwards Lifesciences, Abbott, and Jena.
Danny Dvir, MD, has a message for physicians who have patients with severe valvular heart disease who are deferring valve replacement or repair until after the COVID-19 pandemic: Urge them not to wait.
Data from the Multicenter International Valve Disease Registry vividly demonstrate that clinical outcomes are poor in patients with uncorrected valve disease who become hospitalized with COVID-19. Indeed, the mortality rate within 30 days after hospital admission in 136 such patients enrolled in the registry from centers in Europe, North America, and Israel was 42%, Dr. Dvir reported at the Transcatheter Cardiovascular Research Therapeutics virtual annual meeting.
“That’s dramatically higher than for an age-matched population infected with COVID-19 without valvular heart disease, which is 10%-15%,” he noted at the meeting sponsored by the Cardiovascular Research Foundation.
The bright spot was that, in the small subgroup of 15 registry participants who underwent transcatheter or, much less frequently, surgical treatment of their failing valve while COVID-19 infected, 30-day mortality was far lower. In fact, it was comparable with the background rate in hospitalized COVID-19 patients without valve disease, according to Dr. Dvir, an interventional cardiologist at Shaare Zedek Medical Center, Hebrew University, Jerusalem.
He personally did several of the transcatheter aortic valve replacements.
“It’s doable. I truly believe that when you get a severe aortic stenosis patient who’s infected with the coronavirus, they get very unstable, but we can treat them. We can treat them even during the infection,” Dr. Dvir said.
The majority of patients in the registry had severe aortic stenosis. In the 42 such patients aged 80 years or more who didn’t undergo transcatheter aortic valve replacement (TAVR) or surgical valve replacement, 30-day mortality was 60%. In contrast, only one of the six patients in this advanced-age category who underwent valve replacement while infected died. Similarly, 30-day mortality was 24% among those younger than age 80 who valve remained untreated, but it dropped to 11% in those who received a prosthetic valve.
“We try our best to protect our patients through social distancing, but we have a treatment that can potentially reduce their mortality risk if they get infected later on. So I say to my patients: ‘Don’t wait at home. Do not wait! If you get infected when you have severe aortic stenosis, the clinical outcome is bad.’ But it seems reasonable that if they get infected when they’ve already been treated for their aortic stenosis or mitral regurgitation, they will do better.”
Dr. Dvir noted that, although the case numbers in the registry series were small and subject to potential bias, the data suggest this treatment approach may be lifesaving.
Session comoderator Timothy D. Henry, MD, commented that this registry study contains a great take-home point: “This is really consistent with what see in a lot of the other areas of COVID, that what we know to be best clinical care, we should do it, with or without the COVID.”
He asked Dr. Dvir about any special measures he takes while doing TAVR in this extreme setting. In the United States, for example, interventionalists are increasingly using transesophageal echocardiography to guide their procedures using conscious sedation, without intubation, noted Dr. Henry, medical director of the Carl and Edyth Lindner Center for Research at the Christ Hospital, Cincinnati.
“We try to minimize the procedure time; that’s one of the important things,” Dr. Dvir replied. “And you need to be protected during the procedure in a very cautious and meticulous way. You need many fans in the room because you sweat a lot.”
Discussant Renu Virmani, MD, president of the CVPath Institute in Gaithersburg, Md., commented: “The main thing I get from this presentation is the need for patients to be educated that if you’ve got valve disease, you’re better off getting it treated before you’ve got COVID. Obviously, try to prevent getting COVID – that’s the best thing you can do – but you can’t always control that.”
Discussant Mamas Mamas, MD, professor of cardiology at Keele University, Staffordshire, England, said deferred treatment of severe valvular heart disease during the pandemic has created a looming public health crisis in the United Kingdom.
“We’ve analyzed the U.K. management of aortic stenosis, and what we’ve found is that during the COVID pandemic there have been 2,500 fewer cases of aortic stenosis that have been treated. We’ve got 2,500 patients on the waiting list, and we’ve got to work out how we’re going to treat them. We estimate with simulations that about 300 of them are going to die before we can get them treated for their aortic stenosis,” according to Dr. Mamas.
Dr. Henry commented that deferral of valve procedures is “really challenging” for a couple of reasons: Not only are patients scared to come into the hospital because they fear getting COVID, but they don’t want to be hospitalized during the pandemic because their family can’t visit them there.
“These patients are mostly over 80 years old. No one wants to come in the hospital when the family won’t be around, especially when you’re 90 years old,” the interventional cardiologist said.
Dr. Dvir reported serving as a consultant to Medtronic, Edwards Lifesciences, Abbott, and Jena.
FROM TCT 2020
Few women hospitalized for influenza have been vaccinated
Researchers analyzed data from 9,652 women ages 15-44 who were hospitalized with laboratory-confirmed influenza from October through April during the 2010-2019 influenza seasons. Data were pulled from the U.S. Influenza Hospitalization Surveillance Network (FluSurv-NET).
Of those women, 2,697 (28%) were pregnant. Median age was 28 and median gestational age was 32 weeks. Those studied included 36% who were non-Hispanic White; 29% non-Hispanic Black; and 20% Hispanic women.
Some 89% of the women, pregnant and nonpregnant, received antivirals while in the hospital but only 31% reported they had received the flu vaccine in the current season, despite guideline recommendations citing clear evidence that vaccination is safe for mother and baby.
Rachel Holstein, MPH, an epidemiology and information science fellow at the Centers for Disease Control and Prevention, who presented her team’s work as part of IDWeek 2020, explained that the mother’s vaccination can help protect the baby from flu infection for several months after birth, before the baby can be vaccinated.
She noted that pregnant women are at high risk for influenza-associated hospitalization.
“Changes in the immune system, heart, and lungs during pregnancy make pregnant women, and women up to 2 weeks post partum, more prone to severe illness from flu, including illness resulting in hospitalization,” she said in an interview
“Vaccination has been shown to reduce the risk of flu-associated acute respiratory infection in pregnant women by up to one-half,” she said. “A 2018 study showed that getting a flu shot reduced a pregnant woman’s risk of being hospitalized with flu by an average of 40%.»
FluSurv-NET data show hospitalizations were more common in the third trimester of pregnancy compared with the first and second, Holstein said. The most common underlying conditions among these women were asthma (23%) and obesity (10%), and 12% were current tobacco smokers. Overall, 5% of pregnant women with flu required ICU admission, 2% needed mechanical ventilation, and 6% developed pneumonia.
Vaccine uptake lowest in first two trimesters
Holstein said vaccine coverage was lowest among women in their first or second trimesters for all 9 seasons, and overall vaccination coverage increased significantly over time.
Uptake also differed by age. The data showed coverage was lower among women aged 15-34 years, compared with women 35 years and older (34% vs. 50%).
“It was as low as 15% among pregnant women aged 15-34 years in the 2011-12 season,” she added.
Jeanne Sheffield, MD, director of the division of maternal-fetal medicine at Johns Hopkins Medicine, Baltimore, said in an interview the low uptake of vaccine shown in this study is both familiar and frustrating.
She said education from health care providers has improved, but women are nonetheless frequently fearful. She pointed out the widespread phenomenon of vaccine hesitancy in the general population.
Coverage was 45.3% among adults in the 2018-2019 flu season, 8.2 percentage points higher than coverage during the 2017-18 season (37.1%) according to CDC estimates.
Added to that, she said, is further hesitancy when women believe vaccination could harm the unborn baby, despite “very good data that flu vaccine is safe in pregnancy, acceptable in pregnancy in all trimesters, and is optimal standard of care.”
Holstein added, “We know from past research that a range of factors – including negative attitudes and beliefs about vaccines, less knowledge about and access to vaccines, and a lack of trust in healthcare providers and vaccines – can contribute to lower vaccination rates.”
Healthcare providers play a key role in increasing flu vaccinations among pregnant women, she said.
“A provider recommendation, combined with an offer to administer a flu vaccine at the time of visit, remains one of the best ways to accomplish this,” Holstein said.
Holstein and Sheffield have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Researchers analyzed data from 9,652 women ages 15-44 who were hospitalized with laboratory-confirmed influenza from October through April during the 2010-2019 influenza seasons. Data were pulled from the U.S. Influenza Hospitalization Surveillance Network (FluSurv-NET).
Of those women, 2,697 (28%) were pregnant. Median age was 28 and median gestational age was 32 weeks. Those studied included 36% who were non-Hispanic White; 29% non-Hispanic Black; and 20% Hispanic women.
Some 89% of the women, pregnant and nonpregnant, received antivirals while in the hospital but only 31% reported they had received the flu vaccine in the current season, despite guideline recommendations citing clear evidence that vaccination is safe for mother and baby.
Rachel Holstein, MPH, an epidemiology and information science fellow at the Centers for Disease Control and Prevention, who presented her team’s work as part of IDWeek 2020, explained that the mother’s vaccination can help protect the baby from flu infection for several months after birth, before the baby can be vaccinated.
She noted that pregnant women are at high risk for influenza-associated hospitalization.
“Changes in the immune system, heart, and lungs during pregnancy make pregnant women, and women up to 2 weeks post partum, more prone to severe illness from flu, including illness resulting in hospitalization,” she said in an interview
“Vaccination has been shown to reduce the risk of flu-associated acute respiratory infection in pregnant women by up to one-half,” she said. “A 2018 study showed that getting a flu shot reduced a pregnant woman’s risk of being hospitalized with flu by an average of 40%.»
FluSurv-NET data show hospitalizations were more common in the third trimester of pregnancy compared with the first and second, Holstein said. The most common underlying conditions among these women were asthma (23%) and obesity (10%), and 12% were current tobacco smokers. Overall, 5% of pregnant women with flu required ICU admission, 2% needed mechanical ventilation, and 6% developed pneumonia.
Vaccine uptake lowest in first two trimesters
Holstein said vaccine coverage was lowest among women in their first or second trimesters for all 9 seasons, and overall vaccination coverage increased significantly over time.
Uptake also differed by age. The data showed coverage was lower among women aged 15-34 years, compared with women 35 years and older (34% vs. 50%).
“It was as low as 15% among pregnant women aged 15-34 years in the 2011-12 season,” she added.
Jeanne Sheffield, MD, director of the division of maternal-fetal medicine at Johns Hopkins Medicine, Baltimore, said in an interview the low uptake of vaccine shown in this study is both familiar and frustrating.
She said education from health care providers has improved, but women are nonetheless frequently fearful. She pointed out the widespread phenomenon of vaccine hesitancy in the general population.
Coverage was 45.3% among adults in the 2018-2019 flu season, 8.2 percentage points higher than coverage during the 2017-18 season (37.1%) according to CDC estimates.
Added to that, she said, is further hesitancy when women believe vaccination could harm the unborn baby, despite “very good data that flu vaccine is safe in pregnancy, acceptable in pregnancy in all trimesters, and is optimal standard of care.”
Holstein added, “We know from past research that a range of factors – including negative attitudes and beliefs about vaccines, less knowledge about and access to vaccines, and a lack of trust in healthcare providers and vaccines – can contribute to lower vaccination rates.”
Healthcare providers play a key role in increasing flu vaccinations among pregnant women, she said.
“A provider recommendation, combined with an offer to administer a flu vaccine at the time of visit, remains one of the best ways to accomplish this,” Holstein said.
Holstein and Sheffield have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
Researchers analyzed data from 9,652 women ages 15-44 who were hospitalized with laboratory-confirmed influenza from October through April during the 2010-2019 influenza seasons. Data were pulled from the U.S. Influenza Hospitalization Surveillance Network (FluSurv-NET).
Of those women, 2,697 (28%) were pregnant. Median age was 28 and median gestational age was 32 weeks. Those studied included 36% who were non-Hispanic White; 29% non-Hispanic Black; and 20% Hispanic women.
Some 89% of the women, pregnant and nonpregnant, received antivirals while in the hospital but only 31% reported they had received the flu vaccine in the current season, despite guideline recommendations citing clear evidence that vaccination is safe for mother and baby.
Rachel Holstein, MPH, an epidemiology and information science fellow at the Centers for Disease Control and Prevention, who presented her team’s work as part of IDWeek 2020, explained that the mother’s vaccination can help protect the baby from flu infection for several months after birth, before the baby can be vaccinated.
She noted that pregnant women are at high risk for influenza-associated hospitalization.
“Changes in the immune system, heart, and lungs during pregnancy make pregnant women, and women up to 2 weeks post partum, more prone to severe illness from flu, including illness resulting in hospitalization,” she said in an interview
“Vaccination has been shown to reduce the risk of flu-associated acute respiratory infection in pregnant women by up to one-half,” she said. “A 2018 study showed that getting a flu shot reduced a pregnant woman’s risk of being hospitalized with flu by an average of 40%.»
FluSurv-NET data show hospitalizations were more common in the third trimester of pregnancy compared with the first and second, Holstein said. The most common underlying conditions among these women were asthma (23%) and obesity (10%), and 12% were current tobacco smokers. Overall, 5% of pregnant women with flu required ICU admission, 2% needed mechanical ventilation, and 6% developed pneumonia.
Vaccine uptake lowest in first two trimesters
Holstein said vaccine coverage was lowest among women in their first or second trimesters for all 9 seasons, and overall vaccination coverage increased significantly over time.
Uptake also differed by age. The data showed coverage was lower among women aged 15-34 years, compared with women 35 years and older (34% vs. 50%).
“It was as low as 15% among pregnant women aged 15-34 years in the 2011-12 season,” she added.
Jeanne Sheffield, MD, director of the division of maternal-fetal medicine at Johns Hopkins Medicine, Baltimore, said in an interview the low uptake of vaccine shown in this study is both familiar and frustrating.
She said education from health care providers has improved, but women are nonetheless frequently fearful. She pointed out the widespread phenomenon of vaccine hesitancy in the general population.
Coverage was 45.3% among adults in the 2018-2019 flu season, 8.2 percentage points higher than coverage during the 2017-18 season (37.1%) according to CDC estimates.
Added to that, she said, is further hesitancy when women believe vaccination could harm the unborn baby, despite “very good data that flu vaccine is safe in pregnancy, acceptable in pregnancy in all trimesters, and is optimal standard of care.”
Holstein added, “We know from past research that a range of factors – including negative attitudes and beliefs about vaccines, less knowledge about and access to vaccines, and a lack of trust in healthcare providers and vaccines – can contribute to lower vaccination rates.”
Healthcare providers play a key role in increasing flu vaccinations among pregnant women, she said.
“A provider recommendation, combined with an offer to administer a flu vaccine at the time of visit, remains one of the best ways to accomplish this,” Holstein said.
Holstein and Sheffield have disclosed no relevant financial relationships.
This article first appeared on Medscape.com.
COVID-19: Thromboembolic events high despite prophylaxis
in a new large observational U.S. study.
“Despite very high rate of antithrombotic prophylaxis there were a high rate of thromboembolic events suggesting that we are probably not providing enough thromboprophylaxis,” lead author Gregory Piazza, MD, Brigham and Women’s Hospital, Boston, said in an interview.
“Standard prophylaxis as recommended in the guidelines is a low dose of low-molecular-weight heparin once daily, but these results suggest [patients] probably need higher doses,” he added.
However, Dr. Piazza cautioned that this is an observational study and randomized trials are needed to make changes in treatment strategies. Several such trials are currently underway.
The current study was published online ahead of print in the Nov. 3 issue of the Journal of the American College of Cardiology.
Rates similar to other very sick patients
The study showed that while thromboembolic complications were high, they were not as high as seen in some of the earlier studies from Asia and Europe, Dr. Piazza noted.
“The numbers we were seeing in early reports were so high we couldn’t figure out how that was possible,” he said. “Our study suggests that, in a U.S. population receiving thromboprophylaxis, the rate of thromboembolic complications [are] more in line with what we would expect to see in other very sick patients who end up in ICU.”
He suggested that the very high rates of thromboembolic complications in the early studies from Asia may have been because of the lack of thromboprophylaxis, which is not routine in hospitalized patients there. “Some of the earlier studies also used routine ultrasound and so picked up asymptomatic thrombotic events, which was not the case in our study. So our results are more representative of the U.S. population.”
Dr. Piazza attributed the high rate of thromboembolic complications being reported with COVID-19 to the sheer number of very sick patients being admitted to the hospital.
“We are accustomed to seeing a rare case of thrombosis despite prophylaxis in hospitalized patients, but we are seeing more in COVID patients. This is probably just because we have more critically ill patients,” he said.
“We are seeing an incredible influx of patients to the ICU that we have never experienced before, so the increase in thromboembolic complications is more obvious. In prior years we probably haven’t had enough critically ill patients at any one time to raise the flag about thromboprophylaxis,” he commented.
The study also found a high rate of cardiovascular complications. They are seeing an increase in the risk of MI, which is to be expected in such sick patients, but they also see quite a bit of new atrial fibrillation, myocarditis, and heart failure in patients who don’t always have underlying cardiovascular disease, he said.
“So this virus does appear to have a predilection to causing cardiovascular complications, but this is probably because it is making patients so sick,” Dr. Piazza said. “If flu was this virulent and resulted in such high rates of acute respiratory distress syndrome (ARDS), we would probably see similar cardiovascular complication rates.”
For the current report, the researchers analyzed a retrospective cohort of 1,114 patients with COVID-19 diagnosed through the Mass General Brigham integrated health network. Of these, 170 had been admitted to the ICU, 229 had been hospitalized but not treated in ICU, and 715 were outpatients. In terms of ethnicity, 22% were Hispanic/Latino and 44% were non-White.
Cardiovascular risk factors were common, with 36% of patients having hypertension, 29% hyperlipidemia, and 18% diabetes. Prophylactic anticoagulation was prescribed in 89% of patients with COVID-19 in the intensive care cohort and 85% of those in the hospitalized non–intensive care setting.
Results showed that major arterial or venous thromboembolism (VTE) occurred in 35% of the intensive care cohort, 2.6% of those hospitalized but not treated in ICU, and 0% of outpatients.
Major adverse cardiovascular events occurred in 46% of the intensive care cohort, 6.1% of those hospitalized but non-ICU, and 0% of outpatients.
Symptomatic VTE occurred in 27% of those admitted to ICU, 2.2% of those hospitalized but non-ICU, and 0% of outpatients.
“We found that outpatients had a very low rate of thromboembolic complications, with the vast majority of the risk being in hospitalized patients, especially those in ICU,” Dr. Piazza said.
“These results suggest that we don’t need routine thromboprophylaxis for all outpatients with COVID-19, but there will probably be some patients who need it – those with risk factors for thromboembolism.”
Catheter- and device-associated deep vein thrombosis accounted for 76.9% of the DVTs observed in the study.
“Our finding of high frequency of catheter-associated DVT supports the judicious use of central venous catheters that have been widely implemented, especially in the ICU, to minimize recurrent health care team exposure and facilitate monitoring,” the researchers wrote.
ARDS biggest risk factor
Of all the markers of disease severity, the presence of ARDS had the strongest association with adverse outcomes, including major arterial or VTE, major adverse cardiovascular events, symptomatic VTE, and death.
“The severe inflammatory state associated with ARDS and other complications of COVID-19 and its resultant hypercoagulability may explain, at least in part, the high frequency of thromboembolic events. Improved risk stratification, utilizing biochemical markers of inflammation and activated coagulation as well as clinical indicators, such as ARDS, may play an important role in the early identification of patients with an increased likelihood of developing symptomatic VTE or arterial thrombosis,” the researchers wrote. “They may benefit from full- or intermediate-intensity antithrombotic therapy rather than prophylactic anticoagulation.”
They point out that this study provides a cross-sectional view of the cardiovascular complications of COVID-19 in a large health care network, consisting of two academic medical centers serving the greater Boston area, several community hospitals, and numerous outpatient care sites.
“The study incorporates a wide scope of clinically meaningful cardiovascular endpoints and utilizes a rigorous process of event adjudication. Although data on patients with COVID-19 in the ICU have been the subject of most reports, our study provides insights into the broad spectrum of all hospitalized and outpatient populations,” the authors noted.
“The high frequency of arterial or venous thromboembolism in hospitalized patients despite routine thromboprophylaxis suggests the need for improved risk stratification and enhanced preventive efforts,” they concluded.
The study is continuing, and the researchers expect to have data on 10,000 patients by the end of winter.
Wait for randomized trials
In an accompanying editorial, Robert McBane, MD, Mayo Clinic, Rochester, Minn., said that these data provide important real-world arterial and venous thrombotic event rates across a large, integrated health care network and an experienced roster of clinician-scientists devoted to thrombosis research.
Noting that whether to interpret these results as alarming or reassuring requires a comparison of expected thromboembolic event rates separate from the pandemic, he pointed out that, while the overall VTE rate among ICU patients was high, the vast majority of these events were attributable to central venous lines, and apart from these, the event rates do not appear inflated relative to prior published incidence rates from the pre–COVID-19 era.
“It is therefore important to resist the urge to overprevent or overtreat patients and expose them to the serious risks of major bleeding,” Dr. McBane wrote, adding that “the systematized approach to delivery of guideline-driven VTE prophylaxis across this large, integrated health network likely contributed to the relatively low rates of serious thrombotic outcomes reported.”
He further noted that, as the majority of VTE events were related to central venous lines in ICU patients, “this underscores the importance of a bundled care approach to central venous line management with daily assessment of the continued necessity of central access.
“A number of important clinical trials aimed at optimizing thromboprophylaxis during hospitalization, following hospital dismissal, and in ambulatory settings are underway. Until available, the lessons of thoughtful anticoagulant prophylaxis and treatment guidelines harvested from years of clinical research appear to apply,” he concluded.
This study was funded, in part, by a research grant from Janssen Pharmaceuticals. Dr. Piazza has received research grant support from EKOS Corporation, Bayer, Bristol-Myers Squibb/Pfizer, Portola Pharmaceuticals, and Janssen Pharmaceuticals; and has received consulting fees from Amgen, Pfizer, Boston Scientific, Agile, and Thrombolex. Dr. McBane reported no relevant disclosures.
A version of this article originally appeared on Medscape.com.
in a new large observational U.S. study.
“Despite very high rate of antithrombotic prophylaxis there were a high rate of thromboembolic events suggesting that we are probably not providing enough thromboprophylaxis,” lead author Gregory Piazza, MD, Brigham and Women’s Hospital, Boston, said in an interview.
“Standard prophylaxis as recommended in the guidelines is a low dose of low-molecular-weight heparin once daily, but these results suggest [patients] probably need higher doses,” he added.
However, Dr. Piazza cautioned that this is an observational study and randomized trials are needed to make changes in treatment strategies. Several such trials are currently underway.
The current study was published online ahead of print in the Nov. 3 issue of the Journal of the American College of Cardiology.
Rates similar to other very sick patients
The study showed that while thromboembolic complications were high, they were not as high as seen in some of the earlier studies from Asia and Europe, Dr. Piazza noted.
“The numbers we were seeing in early reports were so high we couldn’t figure out how that was possible,” he said. “Our study suggests that, in a U.S. population receiving thromboprophylaxis, the rate of thromboembolic complications [are] more in line with what we would expect to see in other very sick patients who end up in ICU.”
He suggested that the very high rates of thromboembolic complications in the early studies from Asia may have been because of the lack of thromboprophylaxis, which is not routine in hospitalized patients there. “Some of the earlier studies also used routine ultrasound and so picked up asymptomatic thrombotic events, which was not the case in our study. So our results are more representative of the U.S. population.”
Dr. Piazza attributed the high rate of thromboembolic complications being reported with COVID-19 to the sheer number of very sick patients being admitted to the hospital.
“We are accustomed to seeing a rare case of thrombosis despite prophylaxis in hospitalized patients, but we are seeing more in COVID patients. This is probably just because we have more critically ill patients,” he said.
“We are seeing an incredible influx of patients to the ICU that we have never experienced before, so the increase in thromboembolic complications is more obvious. In prior years we probably haven’t had enough critically ill patients at any one time to raise the flag about thromboprophylaxis,” he commented.
The study also found a high rate of cardiovascular complications. They are seeing an increase in the risk of MI, which is to be expected in such sick patients, but they also see quite a bit of new atrial fibrillation, myocarditis, and heart failure in patients who don’t always have underlying cardiovascular disease, he said.
“So this virus does appear to have a predilection to causing cardiovascular complications, but this is probably because it is making patients so sick,” Dr. Piazza said. “If flu was this virulent and resulted in such high rates of acute respiratory distress syndrome (ARDS), we would probably see similar cardiovascular complication rates.”
For the current report, the researchers analyzed a retrospective cohort of 1,114 patients with COVID-19 diagnosed through the Mass General Brigham integrated health network. Of these, 170 had been admitted to the ICU, 229 had been hospitalized but not treated in ICU, and 715 were outpatients. In terms of ethnicity, 22% were Hispanic/Latino and 44% were non-White.
Cardiovascular risk factors were common, with 36% of patients having hypertension, 29% hyperlipidemia, and 18% diabetes. Prophylactic anticoagulation was prescribed in 89% of patients with COVID-19 in the intensive care cohort and 85% of those in the hospitalized non–intensive care setting.
Results showed that major arterial or venous thromboembolism (VTE) occurred in 35% of the intensive care cohort, 2.6% of those hospitalized but not treated in ICU, and 0% of outpatients.
Major adverse cardiovascular events occurred in 46% of the intensive care cohort, 6.1% of those hospitalized but non-ICU, and 0% of outpatients.
Symptomatic VTE occurred in 27% of those admitted to ICU, 2.2% of those hospitalized but non-ICU, and 0% of outpatients.
“We found that outpatients had a very low rate of thromboembolic complications, with the vast majority of the risk being in hospitalized patients, especially those in ICU,” Dr. Piazza said.
“These results suggest that we don’t need routine thromboprophylaxis for all outpatients with COVID-19, but there will probably be some patients who need it – those with risk factors for thromboembolism.”
Catheter- and device-associated deep vein thrombosis accounted for 76.9% of the DVTs observed in the study.
“Our finding of high frequency of catheter-associated DVT supports the judicious use of central venous catheters that have been widely implemented, especially in the ICU, to minimize recurrent health care team exposure and facilitate monitoring,” the researchers wrote.
ARDS biggest risk factor
Of all the markers of disease severity, the presence of ARDS had the strongest association with adverse outcomes, including major arterial or VTE, major adverse cardiovascular events, symptomatic VTE, and death.
“The severe inflammatory state associated with ARDS and other complications of COVID-19 and its resultant hypercoagulability may explain, at least in part, the high frequency of thromboembolic events. Improved risk stratification, utilizing biochemical markers of inflammation and activated coagulation as well as clinical indicators, such as ARDS, may play an important role in the early identification of patients with an increased likelihood of developing symptomatic VTE or arterial thrombosis,” the researchers wrote. “They may benefit from full- or intermediate-intensity antithrombotic therapy rather than prophylactic anticoagulation.”
They point out that this study provides a cross-sectional view of the cardiovascular complications of COVID-19 in a large health care network, consisting of two academic medical centers serving the greater Boston area, several community hospitals, and numerous outpatient care sites.
“The study incorporates a wide scope of clinically meaningful cardiovascular endpoints and utilizes a rigorous process of event adjudication. Although data on patients with COVID-19 in the ICU have been the subject of most reports, our study provides insights into the broad spectrum of all hospitalized and outpatient populations,” the authors noted.
“The high frequency of arterial or venous thromboembolism in hospitalized patients despite routine thromboprophylaxis suggests the need for improved risk stratification and enhanced preventive efforts,” they concluded.
The study is continuing, and the researchers expect to have data on 10,000 patients by the end of winter.
Wait for randomized trials
In an accompanying editorial, Robert McBane, MD, Mayo Clinic, Rochester, Minn., said that these data provide important real-world arterial and venous thrombotic event rates across a large, integrated health care network and an experienced roster of clinician-scientists devoted to thrombosis research.
Noting that whether to interpret these results as alarming or reassuring requires a comparison of expected thromboembolic event rates separate from the pandemic, he pointed out that, while the overall VTE rate among ICU patients was high, the vast majority of these events were attributable to central venous lines, and apart from these, the event rates do not appear inflated relative to prior published incidence rates from the pre–COVID-19 era.
“It is therefore important to resist the urge to overprevent or overtreat patients and expose them to the serious risks of major bleeding,” Dr. McBane wrote, adding that “the systematized approach to delivery of guideline-driven VTE prophylaxis across this large, integrated health network likely contributed to the relatively low rates of serious thrombotic outcomes reported.”
He further noted that, as the majority of VTE events were related to central venous lines in ICU patients, “this underscores the importance of a bundled care approach to central venous line management with daily assessment of the continued necessity of central access.
“A number of important clinical trials aimed at optimizing thromboprophylaxis during hospitalization, following hospital dismissal, and in ambulatory settings are underway. Until available, the lessons of thoughtful anticoagulant prophylaxis and treatment guidelines harvested from years of clinical research appear to apply,” he concluded.
This study was funded, in part, by a research grant from Janssen Pharmaceuticals. Dr. Piazza has received research grant support from EKOS Corporation, Bayer, Bristol-Myers Squibb/Pfizer, Portola Pharmaceuticals, and Janssen Pharmaceuticals; and has received consulting fees from Amgen, Pfizer, Boston Scientific, Agile, and Thrombolex. Dr. McBane reported no relevant disclosures.
A version of this article originally appeared on Medscape.com.
in a new large observational U.S. study.
“Despite very high rate of antithrombotic prophylaxis there were a high rate of thromboembolic events suggesting that we are probably not providing enough thromboprophylaxis,” lead author Gregory Piazza, MD, Brigham and Women’s Hospital, Boston, said in an interview.
“Standard prophylaxis as recommended in the guidelines is a low dose of low-molecular-weight heparin once daily, but these results suggest [patients] probably need higher doses,” he added.
However, Dr. Piazza cautioned that this is an observational study and randomized trials are needed to make changes in treatment strategies. Several such trials are currently underway.
The current study was published online ahead of print in the Nov. 3 issue of the Journal of the American College of Cardiology.
Rates similar to other very sick patients
The study showed that while thromboembolic complications were high, they were not as high as seen in some of the earlier studies from Asia and Europe, Dr. Piazza noted.
“The numbers we were seeing in early reports were so high we couldn’t figure out how that was possible,” he said. “Our study suggests that, in a U.S. population receiving thromboprophylaxis, the rate of thromboembolic complications [are] more in line with what we would expect to see in other very sick patients who end up in ICU.”
He suggested that the very high rates of thromboembolic complications in the early studies from Asia may have been because of the lack of thromboprophylaxis, which is not routine in hospitalized patients there. “Some of the earlier studies also used routine ultrasound and so picked up asymptomatic thrombotic events, which was not the case in our study. So our results are more representative of the U.S. population.”
Dr. Piazza attributed the high rate of thromboembolic complications being reported with COVID-19 to the sheer number of very sick patients being admitted to the hospital.
“We are accustomed to seeing a rare case of thrombosis despite prophylaxis in hospitalized patients, but we are seeing more in COVID patients. This is probably just because we have more critically ill patients,” he said.
“We are seeing an incredible influx of patients to the ICU that we have never experienced before, so the increase in thromboembolic complications is more obvious. In prior years we probably haven’t had enough critically ill patients at any one time to raise the flag about thromboprophylaxis,” he commented.
The study also found a high rate of cardiovascular complications. They are seeing an increase in the risk of MI, which is to be expected in such sick patients, but they also see quite a bit of new atrial fibrillation, myocarditis, and heart failure in patients who don’t always have underlying cardiovascular disease, he said.
“So this virus does appear to have a predilection to causing cardiovascular complications, but this is probably because it is making patients so sick,” Dr. Piazza said. “If flu was this virulent and resulted in such high rates of acute respiratory distress syndrome (ARDS), we would probably see similar cardiovascular complication rates.”
For the current report, the researchers analyzed a retrospective cohort of 1,114 patients with COVID-19 diagnosed through the Mass General Brigham integrated health network. Of these, 170 had been admitted to the ICU, 229 had been hospitalized but not treated in ICU, and 715 were outpatients. In terms of ethnicity, 22% were Hispanic/Latino and 44% were non-White.
Cardiovascular risk factors were common, with 36% of patients having hypertension, 29% hyperlipidemia, and 18% diabetes. Prophylactic anticoagulation was prescribed in 89% of patients with COVID-19 in the intensive care cohort and 85% of those in the hospitalized non–intensive care setting.
Results showed that major arterial or venous thromboembolism (VTE) occurred in 35% of the intensive care cohort, 2.6% of those hospitalized but not treated in ICU, and 0% of outpatients.
Major adverse cardiovascular events occurred in 46% of the intensive care cohort, 6.1% of those hospitalized but non-ICU, and 0% of outpatients.
Symptomatic VTE occurred in 27% of those admitted to ICU, 2.2% of those hospitalized but non-ICU, and 0% of outpatients.
“We found that outpatients had a very low rate of thromboembolic complications, with the vast majority of the risk being in hospitalized patients, especially those in ICU,” Dr. Piazza said.
“These results suggest that we don’t need routine thromboprophylaxis for all outpatients with COVID-19, but there will probably be some patients who need it – those with risk factors for thromboembolism.”
Catheter- and device-associated deep vein thrombosis accounted for 76.9% of the DVTs observed in the study.
“Our finding of high frequency of catheter-associated DVT supports the judicious use of central venous catheters that have been widely implemented, especially in the ICU, to minimize recurrent health care team exposure and facilitate monitoring,” the researchers wrote.
ARDS biggest risk factor
Of all the markers of disease severity, the presence of ARDS had the strongest association with adverse outcomes, including major arterial or VTE, major adverse cardiovascular events, symptomatic VTE, and death.
“The severe inflammatory state associated with ARDS and other complications of COVID-19 and its resultant hypercoagulability may explain, at least in part, the high frequency of thromboembolic events. Improved risk stratification, utilizing biochemical markers of inflammation and activated coagulation as well as clinical indicators, such as ARDS, may play an important role in the early identification of patients with an increased likelihood of developing symptomatic VTE or arterial thrombosis,” the researchers wrote. “They may benefit from full- or intermediate-intensity antithrombotic therapy rather than prophylactic anticoagulation.”
They point out that this study provides a cross-sectional view of the cardiovascular complications of COVID-19 in a large health care network, consisting of two academic medical centers serving the greater Boston area, several community hospitals, and numerous outpatient care sites.
“The study incorporates a wide scope of clinically meaningful cardiovascular endpoints and utilizes a rigorous process of event adjudication. Although data on patients with COVID-19 in the ICU have been the subject of most reports, our study provides insights into the broad spectrum of all hospitalized and outpatient populations,” the authors noted.
“The high frequency of arterial or venous thromboembolism in hospitalized patients despite routine thromboprophylaxis suggests the need for improved risk stratification and enhanced preventive efforts,” they concluded.
The study is continuing, and the researchers expect to have data on 10,000 patients by the end of winter.
Wait for randomized trials
In an accompanying editorial, Robert McBane, MD, Mayo Clinic, Rochester, Minn., said that these data provide important real-world arterial and venous thrombotic event rates across a large, integrated health care network and an experienced roster of clinician-scientists devoted to thrombosis research.
Noting that whether to interpret these results as alarming or reassuring requires a comparison of expected thromboembolic event rates separate from the pandemic, he pointed out that, while the overall VTE rate among ICU patients was high, the vast majority of these events were attributable to central venous lines, and apart from these, the event rates do not appear inflated relative to prior published incidence rates from the pre–COVID-19 era.
“It is therefore important to resist the urge to overprevent or overtreat patients and expose them to the serious risks of major bleeding,” Dr. McBane wrote, adding that “the systematized approach to delivery of guideline-driven VTE prophylaxis across this large, integrated health network likely contributed to the relatively low rates of serious thrombotic outcomes reported.”
He further noted that, as the majority of VTE events were related to central venous lines in ICU patients, “this underscores the importance of a bundled care approach to central venous line management with daily assessment of the continued necessity of central access.
“A number of important clinical trials aimed at optimizing thromboprophylaxis during hospitalization, following hospital dismissal, and in ambulatory settings are underway. Until available, the lessons of thoughtful anticoagulant prophylaxis and treatment guidelines harvested from years of clinical research appear to apply,” he concluded.
This study was funded, in part, by a research grant from Janssen Pharmaceuticals. Dr. Piazza has received research grant support from EKOS Corporation, Bayer, Bristol-Myers Squibb/Pfizer, Portola Pharmaceuticals, and Janssen Pharmaceuticals; and has received consulting fees from Amgen, Pfizer, Boston Scientific, Agile, and Thrombolex. Dr. McBane reported no relevant disclosures.
A version of this article originally appeared on Medscape.com.
Sleep-disordered breathing in neuromuscular disease
Sleep-disordered breathing (SDB) is a common sleep disturbance in neuromuscular disease (NMD) affecting 36% to 53% of diagnosed adults (Arens R, et al. Paediatr Respir Rev. 2010;11[1]:24). Disturbances in sleep may serve as the earliest sign of muscle weakness in these patients, at times being detected before their underlying neuromuscular disease is diagnosed. This is of paramount importance to sleep medicine and pulmonary physicians who may be among the first specialists to evaluate these patients and can play a vital role in the recognition and diagnosis of neuromuscular disease. Herein, we will provide a guide to aid the reader in recognizing the early signs and symptoms of NMD as it pertains to sleep, as earlier diagnosis may lead to improved quality of life or possibly even survival, in some cases.
Pathophysiology
To begin, it is important to understand the pathophysiology of NMD and how it is altered during the sleep state. Sleep-related physiologic changes in healthy humans include reduction in upper airway muscle tone, blunting of chemoreceptors associated with pharyngeal dilator augmentation, and sleep stage-specific changes in skeletal muscle tone. In patients with NMD, these changes may not be adequately compensated for, leading to sleep-disordered breathing that can present as sleep apnea, hypoventilation, or hypoxia (Govindarajan R, et al. Sleep Issues in Neuromuscular Disorders: A Clinical Guide. Springer International Publishing AG, Springer Nature 2018).
Central respiratory control
The respiratory centers in the pons and medulla are generally spared from the primary effects of most NMD; however, over time, they may be affected secondarily. Similar to obesity hypoventilation syndrome (OHS), untreated chronic sleep-related hypoventilation from NMD can impair the sensitivity of respiratory chemoreceptors leading to worsening hypoventilation.
Upper airway resistance
Pharyngeal muscle tone is key to maintaining a patent airway during sleep. In some NMD, bulbar muscle weakness with pharyngeal dilator muscle hypotonia leads to increased upper airway resistance, especially during REM sleep, which can result in obstructive sleep apnea (OSA). In addition to weakness affecting the upper airway musculature, anatomical changes may also contribute to sleep-disordered breathing. In Pompe disease, for example, macroglossia and fibro-fatty replacement of tongue muscles may occur, leading to the development of OSA.
Diaphragm weakness
In NMD that affects the diaphragm, there is an increased reliance on the skeletal muscles of respiration to maintain adequate ventilation as the underlying disease progresses. Generally, weakness of the diaphragm will cause disturbances in REM sleep first as, during REM, ventilation predominately depends on the diaphragm and patients lose the assistance of their skeletal muscles. However, over time, the progressive weakening of the diaphragm will progress to involve NREM sleep as well, clinically manifesting with frank sleep apnea, hypoventilation, and, ultimately, chronic hypercapnic respiratory failure.
Inspiratory muscle weakness
As noted above, there are many other muscles used in inspiration in addition to the diaphragm. Other primary muscles include the intercostal and scalene muscles, and accessory muscles include the sternocleidomastoid, pectoralis, latissimus dorsi, erector spinae, and trapezius muscles. While sleep and breathing problems may begin early in the course of a neuromuscular disease, the complex restrictive lung disease pattern that we see in these patients may not develop until the respiratory muscles of the chest wall are involved. This restriction, which corresponds to lower lung volumes, leads to a fall in the caudal traction force of the airways which can lead to reduction in the pharyngeal airway cross section. Because these issues are worsened in the supine position, their pathophysiologic effects on respiration are most notable during sleep, putting patients at higher risk of OSA.
Cardiac abnormalities
Lastly, it should be noted that diseases such as the muscular dystrophies, myotonic dystrophy, mitochondriopathies, and nemaline myopathy can be associated with a cardiomyopathy ,which can lead to central sleep apnea in the form of Cheyne-Stokes breathing.
Sleep-disordered breathing in specific NMDs
In amyotrophic lateral sclerosis (ALS), up to 75% of patients may have SDB, the majority of which is central sleep apnea (CSA) and hypoventilation although they still have a higher prevalence of obstructive sleep apnea (OSA) than the general population. Whether the diaphragm or the pharyngeal muscles are predominantly affected may have something to do with the type of apnea a patient experiences; however, studies have shown that even in bulbar ALS, CSA is most common. It should be noted, that this is not Cheyne-Stokes CSA, but rather lack of chest wall and abdominal movement due to weakness. (David WS, et al. J Neurol Sci. 1997;152[suppl 1]:S29-35).
In myasthenia gravis (MG), about 40% to 60% of patients have SDB, and about 30% develop overt respiratory weakness, generally late in the course of their disease. Many of these patients report excessive daytime sleepiness, often attributed to myasthenic fatigue requiring treatment with corticosteroids. It is important to evaluate for sleep apnea, given that if diagnosed and treated, their generalized fatigue may improve and the need for steroids may be reduced or eliminated altogether. It is also important to note that the respiratory and sleep issues MG patients face may not correlate with the severity of their overall disease, such that patients well-controlled on medications from a generalized weakness standpoint may still require home noninvasive ventilation (NIV) for chronic respiratory failure due to weakness of the respiratory system muscles.
Duchenne muscular dystrophy (DMD), an X-linked disease associated with dysfunction of dystrophin synthesis, is often diagnosed in early childhood and gradually progresses over years. Their initial sleep and respiratory symptoms can be subtle and may start with increased nighttime awakenings and daytime somnolence. Generally, these patients will develop OSA in the first decade of life and progress to hypoventilation in their second decade and beyond. These patients are especially important to recognize, as studies have shown appropriate NIV therapy may significantly prolong their life (Finder JD, et al; American Thoracic Society. Am J Respir Crit Care Med. 2004(Aug 15);170[4]:456-465).
In addition to the well-known motor neuron and neuromuscular diseases mentioned above, neuropathic diseases can lead to sleep disturbances, as well. In Charcot-Marie-Tooth (CMT), pharyngeal and laryngeal neuropathy, as well as hypoglossal nerve dysfunction, lead to OSA. Similar to ALS and MG, there is a significant amount of CSA and hypoventilation, likely related to phrenic neuropathy. In contrast to MG, in CMT, the severity of neuropathic disease does correlate to the severity of sleep apnea.
Testing
Testing can range from overnight oximetry to polysomnogram (PSG) with CO2 monitoring. Generally, all patients with a rapidly progressive neuromuscular disease should get pulmonary function testing (PFT) (upright and supine) to evaluate forced vital capacity (FVC) every 3 to 6 months to monitor for respiratory failure. Laboratory studies that can be helpful in assessing for SDB are the PaCO2 (> 45 mm Hg) measured on an arterial blood gas and serum bicarbonate levels (>27 mmol/L or a base excess >4 mmol/L). Patients can qualify for NIV with an overnight SaO2 less than or equal to 88% for greater than or equal to 5 minutes in a 2-hour recording period, PaCO2 greater than or equal to 45 mm Hg, forced vital capacity (FVC) < 50% of predicted, or maximal inspiratory pressure (MIP) <60 cm H2O. For ALS specifically, sniff nasal pressure < 40 cm H2O and orthopnea are additional criteria that can be used. It is worth noting that a PSG is not required for NIV qualification in neuromuscular respiratory insufficiency. However, PSG is beneficial in patients with preserved PFTs but suspected of having early nocturnal respiratory impairment.
Therapy
NIV is the mainstay of therapy for SDB in patients with NMD and has been associated with a slower decline in FVC and improved survival in some cases, as demonstrated in studies of patients with DMD or ALS. Generally, a bi-level PAP mode is preferred; the expiratory positive airway pressure prevents micro-atelectasis and improves V/Q matching and the inspiratory positive airway pressure reduces inspiratory muscle load and optimizes ventilation. As weakness progresses, patients may have difficulty creating enough negative force to initiate a spontaneous breath, thus a mode with a set respiratory rate is preferred that can be implemented in bi-level PAP or more advanced modes such as volume-assured pressure support (VAPS) modality. For patients who are unable to tolerate NIV, particularly those with severe bulbar disease and difficult to manage respiratory secretions, tracheostomy with mechanical ventilation may ultimately be needed. This decision should be made as part of a multidisciplinary shared decision-making conversation with the patient, their family, and their team of providers.
Summary
Sleep is a particularly vulnerable state for patients with NMD, and in many patients, disturbances in sleep may be the first clue to their ultimate diagnosis. It is important that sleep medicine and pulmonary specialists understand the pathophysiology and management of NMD as they can play a vital role in the interdisciplinary care of these patients.
Dr. Greer is a Sleep Medicine Fellow, Division of Pulmonary, Allergy, Critical Care, and Sleep Medicine; Dr. Collop is Professor of Medicine and Neurology, Director, Emory Sleep Center; Emory University, Atlanta, Georgia.
Sleep-disordered breathing (SDB) is a common sleep disturbance in neuromuscular disease (NMD) affecting 36% to 53% of diagnosed adults (Arens R, et al. Paediatr Respir Rev. 2010;11[1]:24). Disturbances in sleep may serve as the earliest sign of muscle weakness in these patients, at times being detected before their underlying neuromuscular disease is diagnosed. This is of paramount importance to sleep medicine and pulmonary physicians who may be among the first specialists to evaluate these patients and can play a vital role in the recognition and diagnosis of neuromuscular disease. Herein, we will provide a guide to aid the reader in recognizing the early signs and symptoms of NMD as it pertains to sleep, as earlier diagnosis may lead to improved quality of life or possibly even survival, in some cases.
Pathophysiology
To begin, it is important to understand the pathophysiology of NMD and how it is altered during the sleep state. Sleep-related physiologic changes in healthy humans include reduction in upper airway muscle tone, blunting of chemoreceptors associated with pharyngeal dilator augmentation, and sleep stage-specific changes in skeletal muscle tone. In patients with NMD, these changes may not be adequately compensated for, leading to sleep-disordered breathing that can present as sleep apnea, hypoventilation, or hypoxia (Govindarajan R, et al. Sleep Issues in Neuromuscular Disorders: A Clinical Guide. Springer International Publishing AG, Springer Nature 2018).
Central respiratory control
The respiratory centers in the pons and medulla are generally spared from the primary effects of most NMD; however, over time, they may be affected secondarily. Similar to obesity hypoventilation syndrome (OHS), untreated chronic sleep-related hypoventilation from NMD can impair the sensitivity of respiratory chemoreceptors leading to worsening hypoventilation.
Upper airway resistance
Pharyngeal muscle tone is key to maintaining a patent airway during sleep. In some NMD, bulbar muscle weakness with pharyngeal dilator muscle hypotonia leads to increased upper airway resistance, especially during REM sleep, which can result in obstructive sleep apnea (OSA). In addition to weakness affecting the upper airway musculature, anatomical changes may also contribute to sleep-disordered breathing. In Pompe disease, for example, macroglossia and fibro-fatty replacement of tongue muscles may occur, leading to the development of OSA.
Diaphragm weakness
In NMD that affects the diaphragm, there is an increased reliance on the skeletal muscles of respiration to maintain adequate ventilation as the underlying disease progresses. Generally, weakness of the diaphragm will cause disturbances in REM sleep first as, during REM, ventilation predominately depends on the diaphragm and patients lose the assistance of their skeletal muscles. However, over time, the progressive weakening of the diaphragm will progress to involve NREM sleep as well, clinically manifesting with frank sleep apnea, hypoventilation, and, ultimately, chronic hypercapnic respiratory failure.
Inspiratory muscle weakness
As noted above, there are many other muscles used in inspiration in addition to the diaphragm. Other primary muscles include the intercostal and scalene muscles, and accessory muscles include the sternocleidomastoid, pectoralis, latissimus dorsi, erector spinae, and trapezius muscles. While sleep and breathing problems may begin early in the course of a neuromuscular disease, the complex restrictive lung disease pattern that we see in these patients may not develop until the respiratory muscles of the chest wall are involved. This restriction, which corresponds to lower lung volumes, leads to a fall in the caudal traction force of the airways which can lead to reduction in the pharyngeal airway cross section. Because these issues are worsened in the supine position, their pathophysiologic effects on respiration are most notable during sleep, putting patients at higher risk of OSA.
Cardiac abnormalities
Lastly, it should be noted that diseases such as the muscular dystrophies, myotonic dystrophy, mitochondriopathies, and nemaline myopathy can be associated with a cardiomyopathy ,which can lead to central sleep apnea in the form of Cheyne-Stokes breathing.
Sleep-disordered breathing in specific NMDs
In amyotrophic lateral sclerosis (ALS), up to 75% of patients may have SDB, the majority of which is central sleep apnea (CSA) and hypoventilation although they still have a higher prevalence of obstructive sleep apnea (OSA) than the general population. Whether the diaphragm or the pharyngeal muscles are predominantly affected may have something to do with the type of apnea a patient experiences; however, studies have shown that even in bulbar ALS, CSA is most common. It should be noted, that this is not Cheyne-Stokes CSA, but rather lack of chest wall and abdominal movement due to weakness. (David WS, et al. J Neurol Sci. 1997;152[suppl 1]:S29-35).
In myasthenia gravis (MG), about 40% to 60% of patients have SDB, and about 30% develop overt respiratory weakness, generally late in the course of their disease. Many of these patients report excessive daytime sleepiness, often attributed to myasthenic fatigue requiring treatment with corticosteroids. It is important to evaluate for sleep apnea, given that if diagnosed and treated, their generalized fatigue may improve and the need for steroids may be reduced or eliminated altogether. It is also important to note that the respiratory and sleep issues MG patients face may not correlate with the severity of their overall disease, such that patients well-controlled on medications from a generalized weakness standpoint may still require home noninvasive ventilation (NIV) for chronic respiratory failure due to weakness of the respiratory system muscles.
Duchenne muscular dystrophy (DMD), an X-linked disease associated with dysfunction of dystrophin synthesis, is often diagnosed in early childhood and gradually progresses over years. Their initial sleep and respiratory symptoms can be subtle and may start with increased nighttime awakenings and daytime somnolence. Generally, these patients will develop OSA in the first decade of life and progress to hypoventilation in their second decade and beyond. These patients are especially important to recognize, as studies have shown appropriate NIV therapy may significantly prolong their life (Finder JD, et al; American Thoracic Society. Am J Respir Crit Care Med. 2004(Aug 15);170[4]:456-465).
In addition to the well-known motor neuron and neuromuscular diseases mentioned above, neuropathic diseases can lead to sleep disturbances, as well. In Charcot-Marie-Tooth (CMT), pharyngeal and laryngeal neuropathy, as well as hypoglossal nerve dysfunction, lead to OSA. Similar to ALS and MG, there is a significant amount of CSA and hypoventilation, likely related to phrenic neuropathy. In contrast to MG, in CMT, the severity of neuropathic disease does correlate to the severity of sleep apnea.
Testing
Testing can range from overnight oximetry to polysomnogram (PSG) with CO2 monitoring. Generally, all patients with a rapidly progressive neuromuscular disease should get pulmonary function testing (PFT) (upright and supine) to evaluate forced vital capacity (FVC) every 3 to 6 months to monitor for respiratory failure. Laboratory studies that can be helpful in assessing for SDB are the PaCO2 (> 45 mm Hg) measured on an arterial blood gas and serum bicarbonate levels (>27 mmol/L or a base excess >4 mmol/L). Patients can qualify for NIV with an overnight SaO2 less than or equal to 88% for greater than or equal to 5 minutes in a 2-hour recording period, PaCO2 greater than or equal to 45 mm Hg, forced vital capacity (FVC) < 50% of predicted, or maximal inspiratory pressure (MIP) <60 cm H2O. For ALS specifically, sniff nasal pressure < 40 cm H2O and orthopnea are additional criteria that can be used. It is worth noting that a PSG is not required for NIV qualification in neuromuscular respiratory insufficiency. However, PSG is beneficial in patients with preserved PFTs but suspected of having early nocturnal respiratory impairment.
Therapy
NIV is the mainstay of therapy for SDB in patients with NMD and has been associated with a slower decline in FVC and improved survival in some cases, as demonstrated in studies of patients with DMD or ALS. Generally, a bi-level PAP mode is preferred; the expiratory positive airway pressure prevents micro-atelectasis and improves V/Q matching and the inspiratory positive airway pressure reduces inspiratory muscle load and optimizes ventilation. As weakness progresses, patients may have difficulty creating enough negative force to initiate a spontaneous breath, thus a mode with a set respiratory rate is preferred that can be implemented in bi-level PAP or more advanced modes such as volume-assured pressure support (VAPS) modality. For patients who are unable to tolerate NIV, particularly those with severe bulbar disease and difficult to manage respiratory secretions, tracheostomy with mechanical ventilation may ultimately be needed. This decision should be made as part of a multidisciplinary shared decision-making conversation with the patient, their family, and their team of providers.
Summary
Sleep is a particularly vulnerable state for patients with NMD, and in many patients, disturbances in sleep may be the first clue to their ultimate diagnosis. It is important that sleep medicine and pulmonary specialists understand the pathophysiology and management of NMD as they can play a vital role in the interdisciplinary care of these patients.
Dr. Greer is a Sleep Medicine Fellow, Division of Pulmonary, Allergy, Critical Care, and Sleep Medicine; Dr. Collop is Professor of Medicine and Neurology, Director, Emory Sleep Center; Emory University, Atlanta, Georgia.
Sleep-disordered breathing (SDB) is a common sleep disturbance in neuromuscular disease (NMD) affecting 36% to 53% of diagnosed adults (Arens R, et al. Paediatr Respir Rev. 2010;11[1]:24). Disturbances in sleep may serve as the earliest sign of muscle weakness in these patients, at times being detected before their underlying neuromuscular disease is diagnosed. This is of paramount importance to sleep medicine and pulmonary physicians who may be among the first specialists to evaluate these patients and can play a vital role in the recognition and diagnosis of neuromuscular disease. Herein, we will provide a guide to aid the reader in recognizing the early signs and symptoms of NMD as it pertains to sleep, as earlier diagnosis may lead to improved quality of life or possibly even survival, in some cases.
Pathophysiology
To begin, it is important to understand the pathophysiology of NMD and how it is altered during the sleep state. Sleep-related physiologic changes in healthy humans include reduction in upper airway muscle tone, blunting of chemoreceptors associated with pharyngeal dilator augmentation, and sleep stage-specific changes in skeletal muscle tone. In patients with NMD, these changes may not be adequately compensated for, leading to sleep-disordered breathing that can present as sleep apnea, hypoventilation, or hypoxia (Govindarajan R, et al. Sleep Issues in Neuromuscular Disorders: A Clinical Guide. Springer International Publishing AG, Springer Nature 2018).
Central respiratory control
The respiratory centers in the pons and medulla are generally spared from the primary effects of most NMD; however, over time, they may be affected secondarily. Similar to obesity hypoventilation syndrome (OHS), untreated chronic sleep-related hypoventilation from NMD can impair the sensitivity of respiratory chemoreceptors leading to worsening hypoventilation.
Upper airway resistance
Pharyngeal muscle tone is key to maintaining a patent airway during sleep. In some NMD, bulbar muscle weakness with pharyngeal dilator muscle hypotonia leads to increased upper airway resistance, especially during REM sleep, which can result in obstructive sleep apnea (OSA). In addition to weakness affecting the upper airway musculature, anatomical changes may also contribute to sleep-disordered breathing. In Pompe disease, for example, macroglossia and fibro-fatty replacement of tongue muscles may occur, leading to the development of OSA.
Diaphragm weakness
In NMD that affects the diaphragm, there is an increased reliance on the skeletal muscles of respiration to maintain adequate ventilation as the underlying disease progresses. Generally, weakness of the diaphragm will cause disturbances in REM sleep first as, during REM, ventilation predominately depends on the diaphragm and patients lose the assistance of their skeletal muscles. However, over time, the progressive weakening of the diaphragm will progress to involve NREM sleep as well, clinically manifesting with frank sleep apnea, hypoventilation, and, ultimately, chronic hypercapnic respiratory failure.
Inspiratory muscle weakness
As noted above, there are many other muscles used in inspiration in addition to the diaphragm. Other primary muscles include the intercostal and scalene muscles, and accessory muscles include the sternocleidomastoid, pectoralis, latissimus dorsi, erector spinae, and trapezius muscles. While sleep and breathing problems may begin early in the course of a neuromuscular disease, the complex restrictive lung disease pattern that we see in these patients may not develop until the respiratory muscles of the chest wall are involved. This restriction, which corresponds to lower lung volumes, leads to a fall in the caudal traction force of the airways which can lead to reduction in the pharyngeal airway cross section. Because these issues are worsened in the supine position, their pathophysiologic effects on respiration are most notable during sleep, putting patients at higher risk of OSA.
Cardiac abnormalities
Lastly, it should be noted that diseases such as the muscular dystrophies, myotonic dystrophy, mitochondriopathies, and nemaline myopathy can be associated with a cardiomyopathy ,which can lead to central sleep apnea in the form of Cheyne-Stokes breathing.
Sleep-disordered breathing in specific NMDs
In amyotrophic lateral sclerosis (ALS), up to 75% of patients may have SDB, the majority of which is central sleep apnea (CSA) and hypoventilation although they still have a higher prevalence of obstructive sleep apnea (OSA) than the general population. Whether the diaphragm or the pharyngeal muscles are predominantly affected may have something to do with the type of apnea a patient experiences; however, studies have shown that even in bulbar ALS, CSA is most common. It should be noted, that this is not Cheyne-Stokes CSA, but rather lack of chest wall and abdominal movement due to weakness. (David WS, et al. J Neurol Sci. 1997;152[suppl 1]:S29-35).
In myasthenia gravis (MG), about 40% to 60% of patients have SDB, and about 30% develop overt respiratory weakness, generally late in the course of their disease. Many of these patients report excessive daytime sleepiness, often attributed to myasthenic fatigue requiring treatment with corticosteroids. It is important to evaluate for sleep apnea, given that if diagnosed and treated, their generalized fatigue may improve and the need for steroids may be reduced or eliminated altogether. It is also important to note that the respiratory and sleep issues MG patients face may not correlate with the severity of their overall disease, such that patients well-controlled on medications from a generalized weakness standpoint may still require home noninvasive ventilation (NIV) for chronic respiratory failure due to weakness of the respiratory system muscles.
Duchenne muscular dystrophy (DMD), an X-linked disease associated with dysfunction of dystrophin synthesis, is often diagnosed in early childhood and gradually progresses over years. Their initial sleep and respiratory symptoms can be subtle and may start with increased nighttime awakenings and daytime somnolence. Generally, these patients will develop OSA in the first decade of life and progress to hypoventilation in their second decade and beyond. These patients are especially important to recognize, as studies have shown appropriate NIV therapy may significantly prolong their life (Finder JD, et al; American Thoracic Society. Am J Respir Crit Care Med. 2004(Aug 15);170[4]:456-465).
In addition to the well-known motor neuron and neuromuscular diseases mentioned above, neuropathic diseases can lead to sleep disturbances, as well. In Charcot-Marie-Tooth (CMT), pharyngeal and laryngeal neuropathy, as well as hypoglossal nerve dysfunction, lead to OSA. Similar to ALS and MG, there is a significant amount of CSA and hypoventilation, likely related to phrenic neuropathy. In contrast to MG, in CMT, the severity of neuropathic disease does correlate to the severity of sleep apnea.
Testing
Testing can range from overnight oximetry to polysomnogram (PSG) with CO2 monitoring. Generally, all patients with a rapidly progressive neuromuscular disease should get pulmonary function testing (PFT) (upright and supine) to evaluate forced vital capacity (FVC) every 3 to 6 months to monitor for respiratory failure. Laboratory studies that can be helpful in assessing for SDB are the PaCO2 (> 45 mm Hg) measured on an arterial blood gas and serum bicarbonate levels (>27 mmol/L or a base excess >4 mmol/L). Patients can qualify for NIV with an overnight SaO2 less than or equal to 88% for greater than or equal to 5 minutes in a 2-hour recording period, PaCO2 greater than or equal to 45 mm Hg, forced vital capacity (FVC) < 50% of predicted, or maximal inspiratory pressure (MIP) <60 cm H2O. For ALS specifically, sniff nasal pressure < 40 cm H2O and orthopnea are additional criteria that can be used. It is worth noting that a PSG is not required for NIV qualification in neuromuscular respiratory insufficiency. However, PSG is beneficial in patients with preserved PFTs but suspected of having early nocturnal respiratory impairment.
Therapy
NIV is the mainstay of therapy for SDB in patients with NMD and has been associated with a slower decline in FVC and improved survival in some cases, as demonstrated in studies of patients with DMD or ALS. Generally, a bi-level PAP mode is preferred; the expiratory positive airway pressure prevents micro-atelectasis and improves V/Q matching and the inspiratory positive airway pressure reduces inspiratory muscle load and optimizes ventilation. As weakness progresses, patients may have difficulty creating enough negative force to initiate a spontaneous breath, thus a mode with a set respiratory rate is preferred that can be implemented in bi-level PAP or more advanced modes such as volume-assured pressure support (VAPS) modality. For patients who are unable to tolerate NIV, particularly those with severe bulbar disease and difficult to manage respiratory secretions, tracheostomy with mechanical ventilation may ultimately be needed. This decision should be made as part of a multidisciplinary shared decision-making conversation with the patient, their family, and their team of providers.
Summary
Sleep is a particularly vulnerable state for patients with NMD, and in many patients, disturbances in sleep may be the first clue to their ultimate diagnosis. It is important that sleep medicine and pulmonary specialists understand the pathophysiology and management of NMD as they can play a vital role in the interdisciplinary care of these patients.
Dr. Greer is a Sleep Medicine Fellow, Division of Pulmonary, Allergy, Critical Care, and Sleep Medicine; Dr. Collop is Professor of Medicine and Neurology, Director, Emory Sleep Center; Emory University, Atlanta, Georgia.
President’s final report
As I am writing my final presidential report, my presidential year is coming to a close. It was certainly not what I could have anticipated, but an incredible opportunity for my personal and professional growth, and a year in which CHEST adapted and grew, as well. We accomplished a great deal during this unprecedented year, and I will take this opportunity for a year-in-review!
In the winter, As COVID-19 appeared across the globe, we established a COVID-19 Task Force led by then incoming President, Dr. Steve Simpson, with the goal of keeping our members updated on the latest research and clinical management of COVID-19 illness, as well as distilling and delivering the latest COVID-19 related information quickly to those on the front lines. We have held weekly COVID-19 webinars, disseminated infographics, and developed an interactive COVID-19 quiz. CHEST also published several COVID-19-related guideline statements and expert panel reports on bronchoscopy, tracheostomy, lung nodule management, and venous thromboembolism in the setting of COVID-19.
Knowing the stress that our health-care workers were under, we also established a CHEST Wellness Center. This longitudinal, webinar-based curriculum, led by Dr. Alex Niven, had its impetus with COVID-19 but will continue and be extended to general wellness topics.
In March, we joined forces with NAMDRC, under the CHEST umbrella and a combination of our board members and their former board members now make up our Health Policy and Advocacy Committee (HPAC), led by Drs. Neil Freedman and Jim Lamberti, with CHEST Past-President, Dr. John Studdard, also actively involved. Our HPAC is already focusing on home ventilation and competitive bidding, oxygen prescribing, education and access, pulmonary rehabilitation, and tobacco and vaping. The monthly Washington Watchline online publication features the latest on advocacy-related issues of interest to our membership. Last month, the HPAC held a multiorganizational technical expert panel meeting on nocturnal noninvasive ventilation, with plans to submit a manuscript on outcomes from the meeting to the journal CHEST®. These activities are an answer to our member’s requests and needs in the areas of advocacy.
With the onset of the pandemic, we pivoted the delivery of our signature education to virtual platforms beginning with a successful global congress in Bologna in June with 3,500 registered attendees. This was a wonderful way to provide education to our global audience. I want to thank co-chairs Dr. Bill Kelly and Dr. Girolamo Pelaia, and Dr. Francesco de Blasio from our Italian Delegation for their innovative leadership. In August, we held our first virtual Board Review Courses in Pulmonary Medicine, Critical Care Medicine, and Pediatric Pulmonary Medicine, attended by 775 registered attendees complete with didactic sessions, audience response sessions, SEEK sessions and live Q&A with the faculty. The on-demand versions of these courses are also available.
The CHEST® journal, in its second year with Dr. Peter Mazzone at the helm, continues to be a leading source of clinically relevant research and patient management guidance for pulmonary, critical care, and sleep medicine clinicians worldwide. The year 2020 has been a year like no other -- submission rates have doubled since the start of the pandemic, with nearly 5,000 manuscript submissions so far, this year. The journal has rapidly built a robust and growing COVID-19 topic collection, with relevant original research, guidelines, commentaries, and more, published online, within days of acceptance. The journal will continue to seek innovative ways to meet the needs of its readers and contributors during this time when our members and their patients urgently need current and high-quality information.
This year, CHEST hit a publishing milestone, with the publication of SEEK Critical Care 30, and the SEEK program is celebrating 30 years! Those who registered for CHEST 2020 by October 15 received the announcement regarding the commemorative “30 years of SEEK” collection.
Our Guidelines Oversight Committee has continued to publish evidence-based guidelines in the areas of cough and cryobiopsy, with a guideline on hypersensitivity pneumonitis and updated guidelines in our core topics of lung cancer and venous thromboembolism in the works.
Under the leadership of Dr. Aneesa Das, the NetWorks Task Force started work to accomplish the goal of increasing member engagement and reach by developing pilot projects focusing on infographics interviews with key opinion leaders and social media communications. Additionally, the Digital Strategy Task Force launched a redesigned website for the Foundation, which you can see at chestfoundation.org, and look for exciting changes coming to the CHEST website in the very near future.
We have continued our collaborative partnerships with our sister societies. We established the volunteer clinician matching program with the American Thoracic Society (ATS) to send clinicians to areas of need during the pandemic, and partnered on other COVID-19 related activities. We held a virtual fellow’s graduation with ATS and the Association of Pulmonary and Critical Care Medicine Program Directors. CHEST leadership attended the Asian Pacific Respiratory Society in Vietnam in November, the Society of Critical Care Medicine, and Forum of International Respiratory Societies in February and the recent virtual meetings of ATS, European Respiratory Society, and the Brazilian Thoracic Society.
The CHEST Foundation has continued on their mission to champion lung health and make a difference through their successful fundraising. This was highlighted with a tremendous foundation gala in San Antonio in December, The Golden Era of Erin Popovich, attended by more than 500 people. Since COVID-19, the Foundation held several creative virtual fundraising events ranging from wine tastings to poker night to bingo night to a recent trivia night, as well as actively participating in COVID-19-related campaigns, such as the partnership with ATS for COVID-19 public service announcements directed to those affected by COVID-19, and other fundraising campaigns, such as the Buy-a-Mask Give-a-Mask campaign. In addition, the Foundation has continued with their support for clinical research grants, community service grants, and patient education resources and toolkits. For example, they have developed an oxygen tool kit to provide access and empowerment to patients in need.
Thank you to all our donors for continuing to support these CHEST Foundation initiatives. The Foundation couldn’t continue to do this amazing work to create an impact and raise awareness for lung health without you.
As the movement to combat racism and racial disparity swept across our nation, we issued a statement of equity in early June. In September, the CHEST Foundation launched the first of a series of Listening Tours to hear from community needs in the areas of trust, access, and equity. Information from these tours will be used to launch a designated fund to have the power to transform these needs into action. CHEST is now actively developing a strategic plan focusing on how CHEST can make an impactful difference in this arena. We want to ensure we take this essential time to listen, reflect, and make appropriate plans for ways we can truly make a difference. Expect more to come on this in the coming year.
The year concluded with CHEST 2020. CHEST 2020 had the highest number of case reports and abstracts ever submitted to a CHEST Annual meeting, and a total registration of more than 4,000. At CHEST 2020, you had an opportunity to see a reimagined virtual annual meeting with combinations of interactive live and prerecorded didactic sessions, audience response sessions, live Q&A with the faculty, educational games at the CHEST Gaming Hub, CHEST Challenge Championship, networking opportunities, narrated abstracts, case reports, original research presentations, COVID-19 update sessions, industry-sponsored programs, a virtual exhibit hall, and surprises, to deliver the in–person CHEST experience virtually. In addition, this came with the greatest number of CME/MOC credits we have ever offered! And, CHEST 2020 education will continue throughout the year with ongoing postgraduate courses creating the ultimate longitudinal educational experience. While nothing can replace the opportunity to connect with our community in person, I hope you found that this year’s meeting provided a wealth of learning, connection, and fun.
My sincere thanks to the CHEST 2020 Program Chair, Dr. Victor Test, to the entire Scientific Program Committee, and to our incredible CHEST staff, for the immense amount of hard work over the past year to reimagine CHEST 2020 and make it a reality. Little did Victor know that he would be planning three meetings, a live meeting, a hybrid meeting, and, ultimately, a virtual meeting. Thank you for all you did to make CHEST 2020 a meeting to remember. We plan to continue our efforts to maintain and grow educational innovation year-round through more e-learning, virtual learning, and, hopefully soon, live learning, both locally, nationally, and internationally.
As my year closes, you are in excellent hands with Dr. Steven Simpson, your 83rd President, who will lead the organization forward. You will hear more from him, but you are in the hands of a thoughtful and dedicated leader with a long history of CHEST experience, strong expertise in critical care, and a thought leader in the COVID-19 pandemic, including serving on the NIH COVID-19 Treatment Guidelines Panel.
There are so many people to thank! I want to thank my family, my husband and children, and my work family, the faculty and fellows of my division, for their unwavering support. I also want to thank my Co-President lineage group for their counsel and wisdom, several Past Presidents who I have called on over this past year for advice, Drs. John Studdard, Gerard Silvestri, and Darcy Marciniuk among others, the Board (who I only saw face-to-face once!), our CHEST leadership and educators, and the incredible CHEST staff, the Executive Leadership Team, and our superb, hard-working CEO/EVP Bob Musacchio. Last, and most importantly, I would like to thank our members for being in the trenches this year as we all dealt with COVID-19. You are the heroes! At the beginning of my term last year, I told you that my goal was to be “the welcoming home” for interprofessional health-care team members seeking to obtain the best possible educational experiences and patient outcomes. I had no idea how absolutely needed this would be for our chest medicine family this year. CHEST has always been your connection to relevant clinical information and late-breaking updates in our field – but this year, our CHEST community has been even more than that. Through this year of crisis and change, you all have shown resilience; a resilience molded by being flexible. Not only have you embodied flexibility at your home institutions, you’ve embodied flexibility in your learning, teaching, and connecting. You’ve joined us as we’ve reimagined what learning at CHEST is all about – I sincerely thank you for that!
As I am writing my final presidential report, my presidential year is coming to a close. It was certainly not what I could have anticipated, but an incredible opportunity for my personal and professional growth, and a year in which CHEST adapted and grew, as well. We accomplished a great deal during this unprecedented year, and I will take this opportunity for a year-in-review!
In the winter, As COVID-19 appeared across the globe, we established a COVID-19 Task Force led by then incoming President, Dr. Steve Simpson, with the goal of keeping our members updated on the latest research and clinical management of COVID-19 illness, as well as distilling and delivering the latest COVID-19 related information quickly to those on the front lines. We have held weekly COVID-19 webinars, disseminated infographics, and developed an interactive COVID-19 quiz. CHEST also published several COVID-19-related guideline statements and expert panel reports on bronchoscopy, tracheostomy, lung nodule management, and venous thromboembolism in the setting of COVID-19.
Knowing the stress that our health-care workers were under, we also established a CHEST Wellness Center. This longitudinal, webinar-based curriculum, led by Dr. Alex Niven, had its impetus with COVID-19 but will continue and be extended to general wellness topics.
In March, we joined forces with NAMDRC, under the CHEST umbrella and a combination of our board members and their former board members now make up our Health Policy and Advocacy Committee (HPAC), led by Drs. Neil Freedman and Jim Lamberti, with CHEST Past-President, Dr. John Studdard, also actively involved. Our HPAC is already focusing on home ventilation and competitive bidding, oxygen prescribing, education and access, pulmonary rehabilitation, and tobacco and vaping. The monthly Washington Watchline online publication features the latest on advocacy-related issues of interest to our membership. Last month, the HPAC held a multiorganizational technical expert panel meeting on nocturnal noninvasive ventilation, with plans to submit a manuscript on outcomes from the meeting to the journal CHEST®. These activities are an answer to our member’s requests and needs in the areas of advocacy.
With the onset of the pandemic, we pivoted the delivery of our signature education to virtual platforms beginning with a successful global congress in Bologna in June with 3,500 registered attendees. This was a wonderful way to provide education to our global audience. I want to thank co-chairs Dr. Bill Kelly and Dr. Girolamo Pelaia, and Dr. Francesco de Blasio from our Italian Delegation for their innovative leadership. In August, we held our first virtual Board Review Courses in Pulmonary Medicine, Critical Care Medicine, and Pediatric Pulmonary Medicine, attended by 775 registered attendees complete with didactic sessions, audience response sessions, SEEK sessions and live Q&A with the faculty. The on-demand versions of these courses are also available.
The CHEST® journal, in its second year with Dr. Peter Mazzone at the helm, continues to be a leading source of clinically relevant research and patient management guidance for pulmonary, critical care, and sleep medicine clinicians worldwide. The year 2020 has been a year like no other -- submission rates have doubled since the start of the pandemic, with nearly 5,000 manuscript submissions so far, this year. The journal has rapidly built a robust and growing COVID-19 topic collection, with relevant original research, guidelines, commentaries, and more, published online, within days of acceptance. The journal will continue to seek innovative ways to meet the needs of its readers and contributors during this time when our members and their patients urgently need current and high-quality information.
This year, CHEST hit a publishing milestone, with the publication of SEEK Critical Care 30, and the SEEK program is celebrating 30 years! Those who registered for CHEST 2020 by October 15 received the announcement regarding the commemorative “30 years of SEEK” collection.
Our Guidelines Oversight Committee has continued to publish evidence-based guidelines in the areas of cough and cryobiopsy, with a guideline on hypersensitivity pneumonitis and updated guidelines in our core topics of lung cancer and venous thromboembolism in the works.
Under the leadership of Dr. Aneesa Das, the NetWorks Task Force started work to accomplish the goal of increasing member engagement and reach by developing pilot projects focusing on infographics interviews with key opinion leaders and social media communications. Additionally, the Digital Strategy Task Force launched a redesigned website for the Foundation, which you can see at chestfoundation.org, and look for exciting changes coming to the CHEST website in the very near future.
We have continued our collaborative partnerships with our sister societies. We established the volunteer clinician matching program with the American Thoracic Society (ATS) to send clinicians to areas of need during the pandemic, and partnered on other COVID-19 related activities. We held a virtual fellow’s graduation with ATS and the Association of Pulmonary and Critical Care Medicine Program Directors. CHEST leadership attended the Asian Pacific Respiratory Society in Vietnam in November, the Society of Critical Care Medicine, and Forum of International Respiratory Societies in February and the recent virtual meetings of ATS, European Respiratory Society, and the Brazilian Thoracic Society.
The CHEST Foundation has continued on their mission to champion lung health and make a difference through their successful fundraising. This was highlighted with a tremendous foundation gala in San Antonio in December, The Golden Era of Erin Popovich, attended by more than 500 people. Since COVID-19, the Foundation held several creative virtual fundraising events ranging from wine tastings to poker night to bingo night to a recent trivia night, as well as actively participating in COVID-19-related campaigns, such as the partnership with ATS for COVID-19 public service announcements directed to those affected by COVID-19, and other fundraising campaigns, such as the Buy-a-Mask Give-a-Mask campaign. In addition, the Foundation has continued with their support for clinical research grants, community service grants, and patient education resources and toolkits. For example, they have developed an oxygen tool kit to provide access and empowerment to patients in need.
Thank you to all our donors for continuing to support these CHEST Foundation initiatives. The Foundation couldn’t continue to do this amazing work to create an impact and raise awareness for lung health without you.
As the movement to combat racism and racial disparity swept across our nation, we issued a statement of equity in early June. In September, the CHEST Foundation launched the first of a series of Listening Tours to hear from community needs in the areas of trust, access, and equity. Information from these tours will be used to launch a designated fund to have the power to transform these needs into action. CHEST is now actively developing a strategic plan focusing on how CHEST can make an impactful difference in this arena. We want to ensure we take this essential time to listen, reflect, and make appropriate plans for ways we can truly make a difference. Expect more to come on this in the coming year.
The year concluded with CHEST 2020. CHEST 2020 had the highest number of case reports and abstracts ever submitted to a CHEST Annual meeting, and a total registration of more than 4,000. At CHEST 2020, you had an opportunity to see a reimagined virtual annual meeting with combinations of interactive live and prerecorded didactic sessions, audience response sessions, live Q&A with the faculty, educational games at the CHEST Gaming Hub, CHEST Challenge Championship, networking opportunities, narrated abstracts, case reports, original research presentations, COVID-19 update sessions, industry-sponsored programs, a virtual exhibit hall, and surprises, to deliver the in–person CHEST experience virtually. In addition, this came with the greatest number of CME/MOC credits we have ever offered! And, CHEST 2020 education will continue throughout the year with ongoing postgraduate courses creating the ultimate longitudinal educational experience. While nothing can replace the opportunity to connect with our community in person, I hope you found that this year’s meeting provided a wealth of learning, connection, and fun.
My sincere thanks to the CHEST 2020 Program Chair, Dr. Victor Test, to the entire Scientific Program Committee, and to our incredible CHEST staff, for the immense amount of hard work over the past year to reimagine CHEST 2020 and make it a reality. Little did Victor know that he would be planning three meetings, a live meeting, a hybrid meeting, and, ultimately, a virtual meeting. Thank you for all you did to make CHEST 2020 a meeting to remember. We plan to continue our efforts to maintain and grow educational innovation year-round through more e-learning, virtual learning, and, hopefully soon, live learning, both locally, nationally, and internationally.
As my year closes, you are in excellent hands with Dr. Steven Simpson, your 83rd President, who will lead the organization forward. You will hear more from him, but you are in the hands of a thoughtful and dedicated leader with a long history of CHEST experience, strong expertise in critical care, and a thought leader in the COVID-19 pandemic, including serving on the NIH COVID-19 Treatment Guidelines Panel.
There are so many people to thank! I want to thank my family, my husband and children, and my work family, the faculty and fellows of my division, for their unwavering support. I also want to thank my Co-President lineage group for their counsel and wisdom, several Past Presidents who I have called on over this past year for advice, Drs. John Studdard, Gerard Silvestri, and Darcy Marciniuk among others, the Board (who I only saw face-to-face once!), our CHEST leadership and educators, and the incredible CHEST staff, the Executive Leadership Team, and our superb, hard-working CEO/EVP Bob Musacchio. Last, and most importantly, I would like to thank our members for being in the trenches this year as we all dealt with COVID-19. You are the heroes! At the beginning of my term last year, I told you that my goal was to be “the welcoming home” for interprofessional health-care team members seeking to obtain the best possible educational experiences and patient outcomes. I had no idea how absolutely needed this would be for our chest medicine family this year. CHEST has always been your connection to relevant clinical information and late-breaking updates in our field – but this year, our CHEST community has been even more than that. Through this year of crisis and change, you all have shown resilience; a resilience molded by being flexible. Not only have you embodied flexibility at your home institutions, you’ve embodied flexibility in your learning, teaching, and connecting. You’ve joined us as we’ve reimagined what learning at CHEST is all about – I sincerely thank you for that!
As I am writing my final presidential report, my presidential year is coming to a close. It was certainly not what I could have anticipated, but an incredible opportunity for my personal and professional growth, and a year in which CHEST adapted and grew, as well. We accomplished a great deal during this unprecedented year, and I will take this opportunity for a year-in-review!
In the winter, As COVID-19 appeared across the globe, we established a COVID-19 Task Force led by then incoming President, Dr. Steve Simpson, with the goal of keeping our members updated on the latest research and clinical management of COVID-19 illness, as well as distilling and delivering the latest COVID-19 related information quickly to those on the front lines. We have held weekly COVID-19 webinars, disseminated infographics, and developed an interactive COVID-19 quiz. CHEST also published several COVID-19-related guideline statements and expert panel reports on bronchoscopy, tracheostomy, lung nodule management, and venous thromboembolism in the setting of COVID-19.
Knowing the stress that our health-care workers were under, we also established a CHEST Wellness Center. This longitudinal, webinar-based curriculum, led by Dr. Alex Niven, had its impetus with COVID-19 but will continue and be extended to general wellness topics.
In March, we joined forces with NAMDRC, under the CHEST umbrella and a combination of our board members and their former board members now make up our Health Policy and Advocacy Committee (HPAC), led by Drs. Neil Freedman and Jim Lamberti, with CHEST Past-President, Dr. John Studdard, also actively involved. Our HPAC is already focusing on home ventilation and competitive bidding, oxygen prescribing, education and access, pulmonary rehabilitation, and tobacco and vaping. The monthly Washington Watchline online publication features the latest on advocacy-related issues of interest to our membership. Last month, the HPAC held a multiorganizational technical expert panel meeting on nocturnal noninvasive ventilation, with plans to submit a manuscript on outcomes from the meeting to the journal CHEST®. These activities are an answer to our member’s requests and needs in the areas of advocacy.
With the onset of the pandemic, we pivoted the delivery of our signature education to virtual platforms beginning with a successful global congress in Bologna in June with 3,500 registered attendees. This was a wonderful way to provide education to our global audience. I want to thank co-chairs Dr. Bill Kelly and Dr. Girolamo Pelaia, and Dr. Francesco de Blasio from our Italian Delegation for their innovative leadership. In August, we held our first virtual Board Review Courses in Pulmonary Medicine, Critical Care Medicine, and Pediatric Pulmonary Medicine, attended by 775 registered attendees complete with didactic sessions, audience response sessions, SEEK sessions and live Q&A with the faculty. The on-demand versions of these courses are also available.
The CHEST® journal, in its second year with Dr. Peter Mazzone at the helm, continues to be a leading source of clinically relevant research and patient management guidance for pulmonary, critical care, and sleep medicine clinicians worldwide. The year 2020 has been a year like no other -- submission rates have doubled since the start of the pandemic, with nearly 5,000 manuscript submissions so far, this year. The journal has rapidly built a robust and growing COVID-19 topic collection, with relevant original research, guidelines, commentaries, and more, published online, within days of acceptance. The journal will continue to seek innovative ways to meet the needs of its readers and contributors during this time when our members and their patients urgently need current and high-quality information.
This year, CHEST hit a publishing milestone, with the publication of SEEK Critical Care 30, and the SEEK program is celebrating 30 years! Those who registered for CHEST 2020 by October 15 received the announcement regarding the commemorative “30 years of SEEK” collection.
Our Guidelines Oversight Committee has continued to publish evidence-based guidelines in the areas of cough and cryobiopsy, with a guideline on hypersensitivity pneumonitis and updated guidelines in our core topics of lung cancer and venous thromboembolism in the works.
Under the leadership of Dr. Aneesa Das, the NetWorks Task Force started work to accomplish the goal of increasing member engagement and reach by developing pilot projects focusing on infographics interviews with key opinion leaders and social media communications. Additionally, the Digital Strategy Task Force launched a redesigned website for the Foundation, which you can see at chestfoundation.org, and look for exciting changes coming to the CHEST website in the very near future.
We have continued our collaborative partnerships with our sister societies. We established the volunteer clinician matching program with the American Thoracic Society (ATS) to send clinicians to areas of need during the pandemic, and partnered on other COVID-19 related activities. We held a virtual fellow’s graduation with ATS and the Association of Pulmonary and Critical Care Medicine Program Directors. CHEST leadership attended the Asian Pacific Respiratory Society in Vietnam in November, the Society of Critical Care Medicine, and Forum of International Respiratory Societies in February and the recent virtual meetings of ATS, European Respiratory Society, and the Brazilian Thoracic Society.
The CHEST Foundation has continued on their mission to champion lung health and make a difference through their successful fundraising. This was highlighted with a tremendous foundation gala in San Antonio in December, The Golden Era of Erin Popovich, attended by more than 500 people. Since COVID-19, the Foundation held several creative virtual fundraising events ranging from wine tastings to poker night to bingo night to a recent trivia night, as well as actively participating in COVID-19-related campaigns, such as the partnership with ATS for COVID-19 public service announcements directed to those affected by COVID-19, and other fundraising campaigns, such as the Buy-a-Mask Give-a-Mask campaign. In addition, the Foundation has continued with their support for clinical research grants, community service grants, and patient education resources and toolkits. For example, they have developed an oxygen tool kit to provide access and empowerment to patients in need.
Thank you to all our donors for continuing to support these CHEST Foundation initiatives. The Foundation couldn’t continue to do this amazing work to create an impact and raise awareness for lung health without you.
As the movement to combat racism and racial disparity swept across our nation, we issued a statement of equity in early June. In September, the CHEST Foundation launched the first of a series of Listening Tours to hear from community needs in the areas of trust, access, and equity. Information from these tours will be used to launch a designated fund to have the power to transform these needs into action. CHEST is now actively developing a strategic plan focusing on how CHEST can make an impactful difference in this arena. We want to ensure we take this essential time to listen, reflect, and make appropriate plans for ways we can truly make a difference. Expect more to come on this in the coming year.
The year concluded with CHEST 2020. CHEST 2020 had the highest number of case reports and abstracts ever submitted to a CHEST Annual meeting, and a total registration of more than 4,000. At CHEST 2020, you had an opportunity to see a reimagined virtual annual meeting with combinations of interactive live and prerecorded didactic sessions, audience response sessions, live Q&A with the faculty, educational games at the CHEST Gaming Hub, CHEST Challenge Championship, networking opportunities, narrated abstracts, case reports, original research presentations, COVID-19 update sessions, industry-sponsored programs, a virtual exhibit hall, and surprises, to deliver the in–person CHEST experience virtually. In addition, this came with the greatest number of CME/MOC credits we have ever offered! And, CHEST 2020 education will continue throughout the year with ongoing postgraduate courses creating the ultimate longitudinal educational experience. While nothing can replace the opportunity to connect with our community in person, I hope you found that this year’s meeting provided a wealth of learning, connection, and fun.
My sincere thanks to the CHEST 2020 Program Chair, Dr. Victor Test, to the entire Scientific Program Committee, and to our incredible CHEST staff, for the immense amount of hard work over the past year to reimagine CHEST 2020 and make it a reality. Little did Victor know that he would be planning three meetings, a live meeting, a hybrid meeting, and, ultimately, a virtual meeting. Thank you for all you did to make CHEST 2020 a meeting to remember. We plan to continue our efforts to maintain and grow educational innovation year-round through more e-learning, virtual learning, and, hopefully soon, live learning, both locally, nationally, and internationally.
As my year closes, you are in excellent hands with Dr. Steven Simpson, your 83rd President, who will lead the organization forward. You will hear more from him, but you are in the hands of a thoughtful and dedicated leader with a long history of CHEST experience, strong expertise in critical care, and a thought leader in the COVID-19 pandemic, including serving on the NIH COVID-19 Treatment Guidelines Panel.
There are so many people to thank! I want to thank my family, my husband and children, and my work family, the faculty and fellows of my division, for their unwavering support. I also want to thank my Co-President lineage group for their counsel and wisdom, several Past Presidents who I have called on over this past year for advice, Drs. John Studdard, Gerard Silvestri, and Darcy Marciniuk among others, the Board (who I only saw face-to-face once!), our CHEST leadership and educators, and the incredible CHEST staff, the Executive Leadership Team, and our superb, hard-working CEO/EVP Bob Musacchio. Last, and most importantly, I would like to thank our members for being in the trenches this year as we all dealt with COVID-19. You are the heroes! At the beginning of my term last year, I told you that my goal was to be “the welcoming home” for interprofessional health-care team members seeking to obtain the best possible educational experiences and patient outcomes. I had no idea how absolutely needed this would be for our chest medicine family this year. CHEST has always been your connection to relevant clinical information and late-breaking updates in our field – but this year, our CHEST community has been even more than that. Through this year of crisis and change, you all have shown resilience; a resilience molded by being flexible. Not only have you embodied flexibility at your home institutions, you’ve embodied flexibility in your learning, teaching, and connecting. You’ve joined us as we’ve reimagined what learning at CHEST is all about – I sincerely thank you for that!
OSA diagnoses not carried forward to the inpatient setting
Obstructive sleep apnea diagnoses may not be carried over to the inpatient setting, with potentially negative consequences for clinical outcomes, quality of life, and health care costs, an investigator said at the virtual meeting of the American College of Chest Physicians.
In a retrospective, single-center study, nearly 40% of patients with obstructive sleep apnea (OSA) diagnosed in the outpatient setting did not have a corresponding diagnosis during hospitalization, according to researcher Nitasa Sahu, MD.*
The missed OSA diagnoses could have especially negative implications for patients who don’t continue on positive airway pressure (PAP) therapy during the hospital stay, said Dr. Sahu, a fellow in pulmonary/critical care at St. Luke’s University Health Network in Bethlehem, Pa.
The finding indicates a large-magnitude opportunity to improve health care through better communication and optimized care, according to the researcher.
“Obstructive sleep apnea is underrecognized, it’s underdiagnosed, and it has a lot of implications for a patient’s hospitalization,” she said in interview
Clinical pathways should be set up to ensure that patients with OSA are properly identified and use their prescribed treatment, according to Dr. Sahu.
“I think that should, and would, reduce overall health care costs, with better outcomes as well,” she said.
Pulmonologist Saadia A. Faiz, MD, FCCP, said she hoped this study, presented at a late-breaking abstract at the virtual meeting, would highlight the importance of OSA screening and call attention to barriers to screening that may be in place in the inpatient setting.
That’s especially important because, after admission, the focus is often on the cause of admission rather than underlying comorbidities such as OSA, said Dr. Faiz, professor in the department of pulmonary medicine at the University of Texas MD Anderson Cancer Center in Houston.
“Working in a cancer hospital, the focus is always on the cancer, so sometimes even the patient will dismiss issues with their sleep,” Dr. Faiz said of her own experience in an interview.
“Often with sleep apnea, for people in the general population, the reason they seek medical attention is because their spouse notices that they’re snoring, so it is something that is not as emphasized,” added Dr. Faiz, who was not involved in the study.
In their study, Dr. Sahu and coauthors reviewed electronic health record data for adults hospitalized on the general internal medicine service at Penn State Hershey Medical Center from January 2017 through 2018. They restricted their search to first admissions.
The researchers looked for ICD-9 codes indicating an OSA diagnosis during their inpatient admission. They looked for the same codes in the preceding 5 years to see if the patients had a prior outpatient OSA diagnosis.
The inpatient cohort included 13,067 patients, of whom 53% were male, 87% were White, and 77% were over 50 years of age. Comorbidities included hypertension in 42%, atrial fibrillation in 21%, type 2 diabetes mellitus in 14%, congestive heart failure in 15%, and prior stroke in 0.5%.
A total of 991 individuals in the inpatient cohort had a prior outpatient OSA diagnosis. Of that group, 376 patients (38%) did not have an inpatient OSA diagnosis on inpatient record, according to the reported study data.
That large proportion of discordant diagnoses suggests a lot of missed opportunities to provide OSA therapy in the inpatient setting and to reinforce chronic disease state management, according to Dr. Sahu and colleagues.
How those discordant OSA diagnoses impact length of stay, cost of care, and readmissions are unanswered questions that deserve further study, Dr. Sahu said.
Among patients who did not have outpatient OSA diagnoses, another 804 patients, or about 6%, ended up with an inpatient diagnosis during their hospitalization, the researchers also reported.
While a number of those inpatient OSA diagnoses could have been coded in error, it’s also possible that they were indeed cases of OSA that went unrecognized until the individuals were hospitalized, Dr. Sahu said.
Dr. Sahu had no relevant relationships to report related to the study. One of four study coauthors reported relationships with Boehringer-Ingelheim, Nitto Denko, and Galapagos.
SOURCE: Sahu N. CHEST 2020. Abstract.
*Correction, 11/3/20: An earlier version of this article misstated the name of Nitasa Sahu, MD.
Obstructive sleep apnea diagnoses may not be carried over to the inpatient setting, with potentially negative consequences for clinical outcomes, quality of life, and health care costs, an investigator said at the virtual meeting of the American College of Chest Physicians.
In a retrospective, single-center study, nearly 40% of patients with obstructive sleep apnea (OSA) diagnosed in the outpatient setting did not have a corresponding diagnosis during hospitalization, according to researcher Nitasa Sahu, MD.*
The missed OSA diagnoses could have especially negative implications for patients who don’t continue on positive airway pressure (PAP) therapy during the hospital stay, said Dr. Sahu, a fellow in pulmonary/critical care at St. Luke’s University Health Network in Bethlehem, Pa.
The finding indicates a large-magnitude opportunity to improve health care through better communication and optimized care, according to the researcher.
“Obstructive sleep apnea is underrecognized, it’s underdiagnosed, and it has a lot of implications for a patient’s hospitalization,” she said in interview
Clinical pathways should be set up to ensure that patients with OSA are properly identified and use their prescribed treatment, according to Dr. Sahu.
“I think that should, and would, reduce overall health care costs, with better outcomes as well,” she said.
Pulmonologist Saadia A. Faiz, MD, FCCP, said she hoped this study, presented at a late-breaking abstract at the virtual meeting, would highlight the importance of OSA screening and call attention to barriers to screening that may be in place in the inpatient setting.
That’s especially important because, after admission, the focus is often on the cause of admission rather than underlying comorbidities such as OSA, said Dr. Faiz, professor in the department of pulmonary medicine at the University of Texas MD Anderson Cancer Center in Houston.
“Working in a cancer hospital, the focus is always on the cancer, so sometimes even the patient will dismiss issues with their sleep,” Dr. Faiz said of her own experience in an interview.
“Often with sleep apnea, for people in the general population, the reason they seek medical attention is because their spouse notices that they’re snoring, so it is something that is not as emphasized,” added Dr. Faiz, who was not involved in the study.
In their study, Dr. Sahu and coauthors reviewed electronic health record data for adults hospitalized on the general internal medicine service at Penn State Hershey Medical Center from January 2017 through 2018. They restricted their search to first admissions.
The researchers looked for ICD-9 codes indicating an OSA diagnosis during their inpatient admission. They looked for the same codes in the preceding 5 years to see if the patients had a prior outpatient OSA diagnosis.
The inpatient cohort included 13,067 patients, of whom 53% were male, 87% were White, and 77% were over 50 years of age. Comorbidities included hypertension in 42%, atrial fibrillation in 21%, type 2 diabetes mellitus in 14%, congestive heart failure in 15%, and prior stroke in 0.5%.
A total of 991 individuals in the inpatient cohort had a prior outpatient OSA diagnosis. Of that group, 376 patients (38%) did not have an inpatient OSA diagnosis on inpatient record, according to the reported study data.
That large proportion of discordant diagnoses suggests a lot of missed opportunities to provide OSA therapy in the inpatient setting and to reinforce chronic disease state management, according to Dr. Sahu and colleagues.
How those discordant OSA diagnoses impact length of stay, cost of care, and readmissions are unanswered questions that deserve further study, Dr. Sahu said.
Among patients who did not have outpatient OSA diagnoses, another 804 patients, or about 6%, ended up with an inpatient diagnosis during their hospitalization, the researchers also reported.
While a number of those inpatient OSA diagnoses could have been coded in error, it’s also possible that they were indeed cases of OSA that went unrecognized until the individuals were hospitalized, Dr. Sahu said.
Dr. Sahu had no relevant relationships to report related to the study. One of four study coauthors reported relationships with Boehringer-Ingelheim, Nitto Denko, and Galapagos.
SOURCE: Sahu N. CHEST 2020. Abstract.
*Correction, 11/3/20: An earlier version of this article misstated the name of Nitasa Sahu, MD.
Obstructive sleep apnea diagnoses may not be carried over to the inpatient setting, with potentially negative consequences for clinical outcomes, quality of life, and health care costs, an investigator said at the virtual meeting of the American College of Chest Physicians.
In a retrospective, single-center study, nearly 40% of patients with obstructive sleep apnea (OSA) diagnosed in the outpatient setting did not have a corresponding diagnosis during hospitalization, according to researcher Nitasa Sahu, MD.*
The missed OSA diagnoses could have especially negative implications for patients who don’t continue on positive airway pressure (PAP) therapy during the hospital stay, said Dr. Sahu, a fellow in pulmonary/critical care at St. Luke’s University Health Network in Bethlehem, Pa.
The finding indicates a large-magnitude opportunity to improve health care through better communication and optimized care, according to the researcher.
“Obstructive sleep apnea is underrecognized, it’s underdiagnosed, and it has a lot of implications for a patient’s hospitalization,” she said in interview
Clinical pathways should be set up to ensure that patients with OSA are properly identified and use their prescribed treatment, according to Dr. Sahu.
“I think that should, and would, reduce overall health care costs, with better outcomes as well,” she said.
Pulmonologist Saadia A. Faiz, MD, FCCP, said she hoped this study, presented at a late-breaking abstract at the virtual meeting, would highlight the importance of OSA screening and call attention to barriers to screening that may be in place in the inpatient setting.
That’s especially important because, after admission, the focus is often on the cause of admission rather than underlying comorbidities such as OSA, said Dr. Faiz, professor in the department of pulmonary medicine at the University of Texas MD Anderson Cancer Center in Houston.
“Working in a cancer hospital, the focus is always on the cancer, so sometimes even the patient will dismiss issues with their sleep,” Dr. Faiz said of her own experience in an interview.
“Often with sleep apnea, for people in the general population, the reason they seek medical attention is because their spouse notices that they’re snoring, so it is something that is not as emphasized,” added Dr. Faiz, who was not involved in the study.
In their study, Dr. Sahu and coauthors reviewed electronic health record data for adults hospitalized on the general internal medicine service at Penn State Hershey Medical Center from January 2017 through 2018. They restricted their search to first admissions.
The researchers looked for ICD-9 codes indicating an OSA diagnosis during their inpatient admission. They looked for the same codes in the preceding 5 years to see if the patients had a prior outpatient OSA diagnosis.
The inpatient cohort included 13,067 patients, of whom 53% were male, 87% were White, and 77% were over 50 years of age. Comorbidities included hypertension in 42%, atrial fibrillation in 21%, type 2 diabetes mellitus in 14%, congestive heart failure in 15%, and prior stroke in 0.5%.
A total of 991 individuals in the inpatient cohort had a prior outpatient OSA diagnosis. Of that group, 376 patients (38%) did not have an inpatient OSA diagnosis on inpatient record, according to the reported study data.
That large proportion of discordant diagnoses suggests a lot of missed opportunities to provide OSA therapy in the inpatient setting and to reinforce chronic disease state management, according to Dr. Sahu and colleagues.
How those discordant OSA diagnoses impact length of stay, cost of care, and readmissions are unanswered questions that deserve further study, Dr. Sahu said.
Among patients who did not have outpatient OSA diagnoses, another 804 patients, or about 6%, ended up with an inpatient diagnosis during their hospitalization, the researchers also reported.
While a number of those inpatient OSA diagnoses could have been coded in error, it’s also possible that they were indeed cases of OSA that went unrecognized until the individuals were hospitalized, Dr. Sahu said.
Dr. Sahu had no relevant relationships to report related to the study. One of four study coauthors reported relationships with Boehringer-Ingelheim, Nitto Denko, and Galapagos.
SOURCE: Sahu N. CHEST 2020. Abstract.
*Correction, 11/3/20: An earlier version of this article misstated the name of Nitasa Sahu, MD.
FROM CHEST 2020
Health care workers implore OSHA for more oversight on COVID-19 safety
Last spring, when Cliff Willmeng, RN, was working at United Hospital in St. Paul, Minnesota, he’d take off his personal protective equipment (PPE) in the same hallway where children were transported from ambulances to the neighboring Children’s Hospital emergency department. Stretchers would roll across red tape on the floor that designated the area as a “hot zone.” The door from a break room was about 10 feet away.
Willmeng has been a union activist all his life, but he’d never filed a complaint with the Occupational Safety and Health Administration (OSHA) until the COVID-19 pandemic hit.
Concerned about the inadequate space for doffing PPE and other situations in which the spread of SARS-CoV-2 seemed possible, Willmeng and other colleagues filed multiple OSHA complaints with the Minnesota Department of Labor in March and April. Willmeng was also worried about bringing SARS-CoV-2 on his scrubs home to his wife and kids, and he started wearing hospital-supplied scrubs that were meant for doctors and that were washed on site, which was against hospital policy. The hospital fired Willmeng on May 8, citing code of conduct and respectful workplace violations arising from the uniform dispute.
In August, the state agency issued Willmeng’s hospital a $2,100 fine for failure to comply with guidance regarding “respiratory protection” in response to worker complaints over the fact that they were instructed to restaple elastic bands on N95 masks early in the pandemic. In a statement, United Hospital said it contested the citation, and it is in discussions with Minnesota OSHA. “We have and continue to instruct employees not to alter N95 respirators or reuse damaged or soiled N95 respirators,” such as when the straps are broken, the statement says.
Minnesota OSHA has received three times as many emails and phone calls from workers and employers requesting information and assistance during the pandemic, compared with last year, said spokesperson James Honerman. “If Minnesota OSHA is made aware of a workplace safety or health issue, it assesses the situation and determines how best to respond, including conducting a workplace investigation.”
But Willmeng, who has been out of work since he was fired, says that without a receipt or confirmation from OSHA, he has no way of knowing whether there has been any follow-up regarding his complaints. Minnesota OSHA said workers should receive a letter once a case is resolved.
Like Willmeng’s case, none of the more than 10,000 COVID-related complaints the federal OSHA office has received from across the country have resulted in meaningful sanctions. Unions have picketed local OSHA offices and publicized complaints on behalf of their members to protest what they see as a lack of oversight. Legislators have called on US Department of Labor Secretary Eugene Scalia to step up enforcement.
For many health care workers, complaining to OSHA is a last resort after failing to get satisfactory responses from supervisors and appealing to unions for help. But with such minimal oversight from OSHA, some union leaders and legislators say it’s actually more dangerous than not having workplace safety enforcement at all. Lack of directives from the Trump administration has left the agency without the teeth it has cut under previous administrations, and recent changes to the agency’s rules raise questions about whether companies are ever required to report workers’ hospitalizations due to COVID-19.
“It’s so ineffective that it’s more dangerous to workers,” said Kim Cordova, president of United Food and Commercial Workers (UFCW) Local 7, which represents 22,000 health care and other workers in Colorado and Wyoming. “Employers only do what they’re forced to do.” Instead of deterring a multi-billion-dollar company, she said, such low fines signal that a company doesn’t need to worry about COVID-related safety.
“OSHA is doing a lamentably poor job protecting workers during the pandemic,” said James Brudney, JD, a professor at Fordham Law School, in New York, and former chief counsel of the U.S. Senate Subcommittee on Labor. “I’m not alone in saying that the agency has performed so badly.”
Former government officials writing in JAMA were similarly critical: “In the face of the greatest worker health crisis in recent history, OSHA, the lead government agency responsible for worker health and safety, has not fulfilled its responsibilities.”
What could have been
There were early signs that the agency wouldn’t be heavy-handed about COVID-19 safety concerns, Brudney said.
The agency could have issued Emergency Temporary Standards, rules it can put in place during pandemics that address specific short-term concerns. These rules could have required employers to take infection-control measures to protect workers, including mask wearing, providing proper PPE, and screening for COVID-19 symptoms. “That’s what the agency is supposed to do. They’re supposed to respond to an emergency with emergency measures,” Brudney said.
But despite legislative pressure and a court case, Secretary of Labor Eugene Scalia has declined to do so, saying that the agency would instead rely on its regular general duty clause, which is always in place to keep workplaces free from hazards that “cause death or serious physical harm.” The agency invoked the general duty clause for COVID-19–related violations for the first time in September to levy modest fines.
In response to a request for an interview, a Department of Labor spokesperson said that preexisting OSHA requirements apply to workers during the pandemic, including providing PPE for workers and assessing sanitation and cleanliness standards. The agency has issued specific guidance to companies on pandemic preparedness, she said, and that it responds to all complaints. Additionally, she cited whistleblower laws that make it illegal for employers to retaliate against employees for making safety and health complaints.
The federal OSHA office received 10,868 COVID-related complaints from Feb. 1 through Oct. 20, citing issues ranging from failure to provide proper PPE to not informing workers about exposures. As of Oct. 22, a total of 2,349 of the complaints involved healthcare workers. This count doesn’t include the untold number of “informal” complaints handled by state OSHA offices.
In a recent JAMA opinion piece, two former government officials agreed that “the federal government has not fully utilized OSHA’s public safety authority” and called the issuing of an Emergency Temporary Standard that would require employers to develop and implement infection control plans “the most important action the federal government could take” to protect workers.
“Employers are more likely to implement these controls if they are mandated by a government agency that has adequate enforcement tools to ensure compliance,” wrote former Assistant Secretary of Labor David Michaels, PhD, MPH, now at the Milken Institute School of Public Health of the George Washington University, Washington, and Gregory Wagner, MD, a former senior adviser at the National Institute for Occupational Safety and Health at the Centers for Disease Control and Prevention, now at the Harvard T.H. Chan School of Public Health, Boston.
They cited the success of a standard that OSHA issued in 1991 in response to the HIV/AIDS crisis. “The bloodborne pathogens standard has contributed to a substantial decline in health care worker risk for bloodborne diseases like HIV and hepatitis B and C,” they wrote. In a new report for the Century Foundation, the pair offered recommendations to the federal government for controlling the spread of the disease by ramping up OSHA’s role.
OSHA did issue a response plan that requires employers to report in regard to employees who experienced workplace exposures to SARS-CoV-2 and who were hospitalized with COVID-19 or died of the disease within certain time frames, but recent changes to these rules make experts question whether companies are in fact required to report hospitalizations.
In its second revision of guidelines, added to its FAQ page on Sept. 30, the agency said that, in order to be reportable, “an in-patient hospitalization due to COVID-19 must occur within 24 hours of an exposure to SARS-CoV-2 at work” and that the employer must report the hospitalization within 24 hours of learning both that the employee has been hospitalized and that the reason for the hospitalization was a work-related case of COVID-19. Previously, the 24-hour hospitalization window started at the time of diagnosis of the disease, rather than the work-related exposure.
The agency subsequently dropped the first citation it had issued for a COVID-related violation, even though the company, a nursing home, had already agreed to pay $3,904 for reporting employee hospitalizations late.
“It’s a step backwards from an important workplace and public health function that OSHA should be doing,” said Wagner, coauthor of the JAMA opinion piece.
Even without issuing Emergency Temporary Standards, critics say OSHA could have acted much earlier. OSHA issued its first COVID-related federal citation, the one against the nursing home that was dropped, in May for events that occurred in mid-April. The second COVID-related federal citation came in July.
The agency could also charge much more substantial fines for the citations it has issued. If a medical facility was cited for a PPE violation, such as the Minnesota hospital where workers were told to restaple the elastic bands on N95s, the agency could have cited the hospital for one violation per employee. Such fines based on multiple violations could add up to the hundreds of thousands to millions of dollars.
“It would send a signal to the highest-risk employers that these are violations that need to be addressed immediately,” Brudney said.
Many of the 22 state OSHA offices appear to be more responsive to COVID-related complaints than the federal agency, creating a system in which health care workers have substantially different rights from one state to the next. The governor of California, for example, recently authorized California’s OSHA division to consider COVID-19 an imminent hazard, to prohibit workers from entering areas where the hazard exists, and to require employers to disclose exposures. The state also recently issued large fines for COVID safety issues: $222,075 to frozen food manufacturer Overhill Farms and $214,080 to employment agency Jobsource North America.
Elsewhere, state laws such as New Jersey’s Conscientious Employee Protection Act give workers the right to refuse to work in unsafe situations, Brudney said. “A lot more action is going on at the state level because so little is being done at the federal level,” he said. “Some of it is governors committed to protecting essential workers and their families.”
Unions call for sanctions
Unions are both decrying the lack of enforcement thus far and seeking more oversight going forward.
In August, the National Nurses’ United (NNU) union filed a complaint to implore OSHA to investigate the country’s biggest hospital systems, HCA Healthcare, which operates 184 hospitals and about 2,000 other care sites in 21 states and the United Kingdom. The union describes how, throughout HCA hospitals, there is an environment conducive to the spread of coronavirus. Nurses share space and equipment, such as computers, desks, phones, bathrooms, and break rooms, where staff take off masks to eat and drink. The complaint also describes how there is resistance to testing nurses and a lack of communication about infections among colleagues.
“When they have total disregard for safety, they should be punished to the utmost,” said Markowitz, noting that HCA Healthcare is worth $40 billion. “They can penalize them, but if it’s unsafe conditions for RNs and healthcare workers, we know it’s unsafe for the patients. There needs to be drastic measures to prevent hospital corporations from behaving that way.”
In a statement, HCA spokesman Harlow Sumerford said the company has followed CDC guidance for protecting frontline caregivers. “We’re proud of our response and the significant resources we’ve deployed to help protect our colleagues. Meanwhile, the NNU has chosen to use this pandemic as an opportunity to gain publicity by attacking hospitals across the country,” Sumerford said.
Members of the union recently protested in front of the federal OSHA offices in Denver.
After several months, OSHA finally penalized a meat packing plant where eight workers (six union members) had died of COVID-19 last spring. But the amount – $15,615 – was so low that Cordova worries it will actually have a worse impact than no fine.
“It’s more dangerous to workers because now employers know [they won’t be punished meaningfully],” she said. “During the pandemic, OSHA has been absolutely absent.”
Thus, the recent picketing outside the offices in Denver. But, Cordova noted, it’s unlikely OSHA employees saw them. Their own offices were deemed too risky to stay open during the pandemic. They were vacant.
A version of this article originally appeared on Medscape.com.
Last spring, when Cliff Willmeng, RN, was working at United Hospital in St. Paul, Minnesota, he’d take off his personal protective equipment (PPE) in the same hallway where children were transported from ambulances to the neighboring Children’s Hospital emergency department. Stretchers would roll across red tape on the floor that designated the area as a “hot zone.” The door from a break room was about 10 feet away.
Willmeng has been a union activist all his life, but he’d never filed a complaint with the Occupational Safety and Health Administration (OSHA) until the COVID-19 pandemic hit.
Concerned about the inadequate space for doffing PPE and other situations in which the spread of SARS-CoV-2 seemed possible, Willmeng and other colleagues filed multiple OSHA complaints with the Minnesota Department of Labor in March and April. Willmeng was also worried about bringing SARS-CoV-2 on his scrubs home to his wife and kids, and he started wearing hospital-supplied scrubs that were meant for doctors and that were washed on site, which was against hospital policy. The hospital fired Willmeng on May 8, citing code of conduct and respectful workplace violations arising from the uniform dispute.
In August, the state agency issued Willmeng’s hospital a $2,100 fine for failure to comply with guidance regarding “respiratory protection” in response to worker complaints over the fact that they were instructed to restaple elastic bands on N95 masks early in the pandemic. In a statement, United Hospital said it contested the citation, and it is in discussions with Minnesota OSHA. “We have and continue to instruct employees not to alter N95 respirators or reuse damaged or soiled N95 respirators,” such as when the straps are broken, the statement says.
Minnesota OSHA has received three times as many emails and phone calls from workers and employers requesting information and assistance during the pandemic, compared with last year, said spokesperson James Honerman. “If Minnesota OSHA is made aware of a workplace safety or health issue, it assesses the situation and determines how best to respond, including conducting a workplace investigation.”
But Willmeng, who has been out of work since he was fired, says that without a receipt or confirmation from OSHA, he has no way of knowing whether there has been any follow-up regarding his complaints. Minnesota OSHA said workers should receive a letter once a case is resolved.
Like Willmeng’s case, none of the more than 10,000 COVID-related complaints the federal OSHA office has received from across the country have resulted in meaningful sanctions. Unions have picketed local OSHA offices and publicized complaints on behalf of their members to protest what they see as a lack of oversight. Legislators have called on US Department of Labor Secretary Eugene Scalia to step up enforcement.
For many health care workers, complaining to OSHA is a last resort after failing to get satisfactory responses from supervisors and appealing to unions for help. But with such minimal oversight from OSHA, some union leaders and legislators say it’s actually more dangerous than not having workplace safety enforcement at all. Lack of directives from the Trump administration has left the agency without the teeth it has cut under previous administrations, and recent changes to the agency’s rules raise questions about whether companies are ever required to report workers’ hospitalizations due to COVID-19.
“It’s so ineffective that it’s more dangerous to workers,” said Kim Cordova, president of United Food and Commercial Workers (UFCW) Local 7, which represents 22,000 health care and other workers in Colorado and Wyoming. “Employers only do what they’re forced to do.” Instead of deterring a multi-billion-dollar company, she said, such low fines signal that a company doesn’t need to worry about COVID-related safety.
“OSHA is doing a lamentably poor job protecting workers during the pandemic,” said James Brudney, JD, a professor at Fordham Law School, in New York, and former chief counsel of the U.S. Senate Subcommittee on Labor. “I’m not alone in saying that the agency has performed so badly.”
Former government officials writing in JAMA were similarly critical: “In the face of the greatest worker health crisis in recent history, OSHA, the lead government agency responsible for worker health and safety, has not fulfilled its responsibilities.”
What could have been
There were early signs that the agency wouldn’t be heavy-handed about COVID-19 safety concerns, Brudney said.
The agency could have issued Emergency Temporary Standards, rules it can put in place during pandemics that address specific short-term concerns. These rules could have required employers to take infection-control measures to protect workers, including mask wearing, providing proper PPE, and screening for COVID-19 symptoms. “That’s what the agency is supposed to do. They’re supposed to respond to an emergency with emergency measures,” Brudney said.
But despite legislative pressure and a court case, Secretary of Labor Eugene Scalia has declined to do so, saying that the agency would instead rely on its regular general duty clause, which is always in place to keep workplaces free from hazards that “cause death or serious physical harm.” The agency invoked the general duty clause for COVID-19–related violations for the first time in September to levy modest fines.
In response to a request for an interview, a Department of Labor spokesperson said that preexisting OSHA requirements apply to workers during the pandemic, including providing PPE for workers and assessing sanitation and cleanliness standards. The agency has issued specific guidance to companies on pandemic preparedness, she said, and that it responds to all complaints. Additionally, she cited whistleblower laws that make it illegal for employers to retaliate against employees for making safety and health complaints.
The federal OSHA office received 10,868 COVID-related complaints from Feb. 1 through Oct. 20, citing issues ranging from failure to provide proper PPE to not informing workers about exposures. As of Oct. 22, a total of 2,349 of the complaints involved healthcare workers. This count doesn’t include the untold number of “informal” complaints handled by state OSHA offices.
In a recent JAMA opinion piece, two former government officials agreed that “the federal government has not fully utilized OSHA’s public safety authority” and called the issuing of an Emergency Temporary Standard that would require employers to develop and implement infection control plans “the most important action the federal government could take” to protect workers.
“Employers are more likely to implement these controls if they are mandated by a government agency that has adequate enforcement tools to ensure compliance,” wrote former Assistant Secretary of Labor David Michaels, PhD, MPH, now at the Milken Institute School of Public Health of the George Washington University, Washington, and Gregory Wagner, MD, a former senior adviser at the National Institute for Occupational Safety and Health at the Centers for Disease Control and Prevention, now at the Harvard T.H. Chan School of Public Health, Boston.
They cited the success of a standard that OSHA issued in 1991 in response to the HIV/AIDS crisis. “The bloodborne pathogens standard has contributed to a substantial decline in health care worker risk for bloodborne diseases like HIV and hepatitis B and C,” they wrote. In a new report for the Century Foundation, the pair offered recommendations to the federal government for controlling the spread of the disease by ramping up OSHA’s role.
OSHA did issue a response plan that requires employers to report in regard to employees who experienced workplace exposures to SARS-CoV-2 and who were hospitalized with COVID-19 or died of the disease within certain time frames, but recent changes to these rules make experts question whether companies are in fact required to report hospitalizations.
In its second revision of guidelines, added to its FAQ page on Sept. 30, the agency said that, in order to be reportable, “an in-patient hospitalization due to COVID-19 must occur within 24 hours of an exposure to SARS-CoV-2 at work” and that the employer must report the hospitalization within 24 hours of learning both that the employee has been hospitalized and that the reason for the hospitalization was a work-related case of COVID-19. Previously, the 24-hour hospitalization window started at the time of diagnosis of the disease, rather than the work-related exposure.
The agency subsequently dropped the first citation it had issued for a COVID-related violation, even though the company, a nursing home, had already agreed to pay $3,904 for reporting employee hospitalizations late.
“It’s a step backwards from an important workplace and public health function that OSHA should be doing,” said Wagner, coauthor of the JAMA opinion piece.
Even without issuing Emergency Temporary Standards, critics say OSHA could have acted much earlier. OSHA issued its first COVID-related federal citation, the one against the nursing home that was dropped, in May for events that occurred in mid-April. The second COVID-related federal citation came in July.
The agency could also charge much more substantial fines for the citations it has issued. If a medical facility was cited for a PPE violation, such as the Minnesota hospital where workers were told to restaple the elastic bands on N95s, the agency could have cited the hospital for one violation per employee. Such fines based on multiple violations could add up to the hundreds of thousands to millions of dollars.
“It would send a signal to the highest-risk employers that these are violations that need to be addressed immediately,” Brudney said.
Many of the 22 state OSHA offices appear to be more responsive to COVID-related complaints than the federal agency, creating a system in which health care workers have substantially different rights from one state to the next. The governor of California, for example, recently authorized California’s OSHA division to consider COVID-19 an imminent hazard, to prohibit workers from entering areas where the hazard exists, and to require employers to disclose exposures. The state also recently issued large fines for COVID safety issues: $222,075 to frozen food manufacturer Overhill Farms and $214,080 to employment agency Jobsource North America.
Elsewhere, state laws such as New Jersey’s Conscientious Employee Protection Act give workers the right to refuse to work in unsafe situations, Brudney said. “A lot more action is going on at the state level because so little is being done at the federal level,” he said. “Some of it is governors committed to protecting essential workers and their families.”
Unions call for sanctions
Unions are both decrying the lack of enforcement thus far and seeking more oversight going forward.
In August, the National Nurses’ United (NNU) union filed a complaint to implore OSHA to investigate the country’s biggest hospital systems, HCA Healthcare, which operates 184 hospitals and about 2,000 other care sites in 21 states and the United Kingdom. The union describes how, throughout HCA hospitals, there is an environment conducive to the spread of coronavirus. Nurses share space and equipment, such as computers, desks, phones, bathrooms, and break rooms, where staff take off masks to eat and drink. The complaint also describes how there is resistance to testing nurses and a lack of communication about infections among colleagues.
“When they have total disregard for safety, they should be punished to the utmost,” said Markowitz, noting that HCA Healthcare is worth $40 billion. “They can penalize them, but if it’s unsafe conditions for RNs and healthcare workers, we know it’s unsafe for the patients. There needs to be drastic measures to prevent hospital corporations from behaving that way.”
In a statement, HCA spokesman Harlow Sumerford said the company has followed CDC guidance for protecting frontline caregivers. “We’re proud of our response and the significant resources we’ve deployed to help protect our colleagues. Meanwhile, the NNU has chosen to use this pandemic as an opportunity to gain publicity by attacking hospitals across the country,” Sumerford said.
Members of the union recently protested in front of the federal OSHA offices in Denver.
After several months, OSHA finally penalized a meat packing plant where eight workers (six union members) had died of COVID-19 last spring. But the amount – $15,615 – was so low that Cordova worries it will actually have a worse impact than no fine.
“It’s more dangerous to workers because now employers know [they won’t be punished meaningfully],” she said. “During the pandemic, OSHA has been absolutely absent.”
Thus, the recent picketing outside the offices in Denver. But, Cordova noted, it’s unlikely OSHA employees saw them. Their own offices were deemed too risky to stay open during the pandemic. They were vacant.
A version of this article originally appeared on Medscape.com.
Last spring, when Cliff Willmeng, RN, was working at United Hospital in St. Paul, Minnesota, he’d take off his personal protective equipment (PPE) in the same hallway where children were transported from ambulances to the neighboring Children’s Hospital emergency department. Stretchers would roll across red tape on the floor that designated the area as a “hot zone.” The door from a break room was about 10 feet away.
Willmeng has been a union activist all his life, but he’d never filed a complaint with the Occupational Safety and Health Administration (OSHA) until the COVID-19 pandemic hit.
Concerned about the inadequate space for doffing PPE and other situations in which the spread of SARS-CoV-2 seemed possible, Willmeng and other colleagues filed multiple OSHA complaints with the Minnesota Department of Labor in March and April. Willmeng was also worried about bringing SARS-CoV-2 on his scrubs home to his wife and kids, and he started wearing hospital-supplied scrubs that were meant for doctors and that were washed on site, which was against hospital policy. The hospital fired Willmeng on May 8, citing code of conduct and respectful workplace violations arising from the uniform dispute.
In August, the state agency issued Willmeng’s hospital a $2,100 fine for failure to comply with guidance regarding “respiratory protection” in response to worker complaints over the fact that they were instructed to restaple elastic bands on N95 masks early in the pandemic. In a statement, United Hospital said it contested the citation, and it is in discussions with Minnesota OSHA. “We have and continue to instruct employees not to alter N95 respirators or reuse damaged or soiled N95 respirators,” such as when the straps are broken, the statement says.
Minnesota OSHA has received three times as many emails and phone calls from workers and employers requesting information and assistance during the pandemic, compared with last year, said spokesperson James Honerman. “If Minnesota OSHA is made aware of a workplace safety or health issue, it assesses the situation and determines how best to respond, including conducting a workplace investigation.”
But Willmeng, who has been out of work since he was fired, says that without a receipt or confirmation from OSHA, he has no way of knowing whether there has been any follow-up regarding his complaints. Minnesota OSHA said workers should receive a letter once a case is resolved.
Like Willmeng’s case, none of the more than 10,000 COVID-related complaints the federal OSHA office has received from across the country have resulted in meaningful sanctions. Unions have picketed local OSHA offices and publicized complaints on behalf of their members to protest what they see as a lack of oversight. Legislators have called on US Department of Labor Secretary Eugene Scalia to step up enforcement.
For many health care workers, complaining to OSHA is a last resort after failing to get satisfactory responses from supervisors and appealing to unions for help. But with such minimal oversight from OSHA, some union leaders and legislators say it’s actually more dangerous than not having workplace safety enforcement at all. Lack of directives from the Trump administration has left the agency without the teeth it has cut under previous administrations, and recent changes to the agency’s rules raise questions about whether companies are ever required to report workers’ hospitalizations due to COVID-19.
“It’s so ineffective that it’s more dangerous to workers,” said Kim Cordova, president of United Food and Commercial Workers (UFCW) Local 7, which represents 22,000 health care and other workers in Colorado and Wyoming. “Employers only do what they’re forced to do.” Instead of deterring a multi-billion-dollar company, she said, such low fines signal that a company doesn’t need to worry about COVID-related safety.
“OSHA is doing a lamentably poor job protecting workers during the pandemic,” said James Brudney, JD, a professor at Fordham Law School, in New York, and former chief counsel of the U.S. Senate Subcommittee on Labor. “I’m not alone in saying that the agency has performed so badly.”
Former government officials writing in JAMA were similarly critical: “In the face of the greatest worker health crisis in recent history, OSHA, the lead government agency responsible for worker health and safety, has not fulfilled its responsibilities.”
What could have been
There were early signs that the agency wouldn’t be heavy-handed about COVID-19 safety concerns, Brudney said.
The agency could have issued Emergency Temporary Standards, rules it can put in place during pandemics that address specific short-term concerns. These rules could have required employers to take infection-control measures to protect workers, including mask wearing, providing proper PPE, and screening for COVID-19 symptoms. “That’s what the agency is supposed to do. They’re supposed to respond to an emergency with emergency measures,” Brudney said.
But despite legislative pressure and a court case, Secretary of Labor Eugene Scalia has declined to do so, saying that the agency would instead rely on its regular general duty clause, which is always in place to keep workplaces free from hazards that “cause death or serious physical harm.” The agency invoked the general duty clause for COVID-19–related violations for the first time in September to levy modest fines.
In response to a request for an interview, a Department of Labor spokesperson said that preexisting OSHA requirements apply to workers during the pandemic, including providing PPE for workers and assessing sanitation and cleanliness standards. The agency has issued specific guidance to companies on pandemic preparedness, she said, and that it responds to all complaints. Additionally, she cited whistleblower laws that make it illegal for employers to retaliate against employees for making safety and health complaints.
The federal OSHA office received 10,868 COVID-related complaints from Feb. 1 through Oct. 20, citing issues ranging from failure to provide proper PPE to not informing workers about exposures. As of Oct. 22, a total of 2,349 of the complaints involved healthcare workers. This count doesn’t include the untold number of “informal” complaints handled by state OSHA offices.
In a recent JAMA opinion piece, two former government officials agreed that “the federal government has not fully utilized OSHA’s public safety authority” and called the issuing of an Emergency Temporary Standard that would require employers to develop and implement infection control plans “the most important action the federal government could take” to protect workers.
“Employers are more likely to implement these controls if they are mandated by a government agency that has adequate enforcement tools to ensure compliance,” wrote former Assistant Secretary of Labor David Michaels, PhD, MPH, now at the Milken Institute School of Public Health of the George Washington University, Washington, and Gregory Wagner, MD, a former senior adviser at the National Institute for Occupational Safety and Health at the Centers for Disease Control and Prevention, now at the Harvard T.H. Chan School of Public Health, Boston.
They cited the success of a standard that OSHA issued in 1991 in response to the HIV/AIDS crisis. “The bloodborne pathogens standard has contributed to a substantial decline in health care worker risk for bloodborne diseases like HIV and hepatitis B and C,” they wrote. In a new report for the Century Foundation, the pair offered recommendations to the federal government for controlling the spread of the disease by ramping up OSHA’s role.
OSHA did issue a response plan that requires employers to report in regard to employees who experienced workplace exposures to SARS-CoV-2 and who were hospitalized with COVID-19 or died of the disease within certain time frames, but recent changes to these rules make experts question whether companies are in fact required to report hospitalizations.
In its second revision of guidelines, added to its FAQ page on Sept. 30, the agency said that, in order to be reportable, “an in-patient hospitalization due to COVID-19 must occur within 24 hours of an exposure to SARS-CoV-2 at work” and that the employer must report the hospitalization within 24 hours of learning both that the employee has been hospitalized and that the reason for the hospitalization was a work-related case of COVID-19. Previously, the 24-hour hospitalization window started at the time of diagnosis of the disease, rather than the work-related exposure.
The agency subsequently dropped the first citation it had issued for a COVID-related violation, even though the company, a nursing home, had already agreed to pay $3,904 for reporting employee hospitalizations late.
“It’s a step backwards from an important workplace and public health function that OSHA should be doing,” said Wagner, coauthor of the JAMA opinion piece.
Even without issuing Emergency Temporary Standards, critics say OSHA could have acted much earlier. OSHA issued its first COVID-related federal citation, the one against the nursing home that was dropped, in May for events that occurred in mid-April. The second COVID-related federal citation came in July.
The agency could also charge much more substantial fines for the citations it has issued. If a medical facility was cited for a PPE violation, such as the Minnesota hospital where workers were told to restaple the elastic bands on N95s, the agency could have cited the hospital for one violation per employee. Such fines based on multiple violations could add up to the hundreds of thousands to millions of dollars.
“It would send a signal to the highest-risk employers that these are violations that need to be addressed immediately,” Brudney said.
Many of the 22 state OSHA offices appear to be more responsive to COVID-related complaints than the federal agency, creating a system in which health care workers have substantially different rights from one state to the next. The governor of California, for example, recently authorized California’s OSHA division to consider COVID-19 an imminent hazard, to prohibit workers from entering areas where the hazard exists, and to require employers to disclose exposures. The state also recently issued large fines for COVID safety issues: $222,075 to frozen food manufacturer Overhill Farms and $214,080 to employment agency Jobsource North America.
Elsewhere, state laws such as New Jersey’s Conscientious Employee Protection Act give workers the right to refuse to work in unsafe situations, Brudney said. “A lot more action is going on at the state level because so little is being done at the federal level,” he said. “Some of it is governors committed to protecting essential workers and their families.”
Unions call for sanctions
Unions are both decrying the lack of enforcement thus far and seeking more oversight going forward.
In August, the National Nurses’ United (NNU) union filed a complaint to implore OSHA to investigate the country’s biggest hospital systems, HCA Healthcare, which operates 184 hospitals and about 2,000 other care sites in 21 states and the United Kingdom. The union describes how, throughout HCA hospitals, there is an environment conducive to the spread of coronavirus. Nurses share space and equipment, such as computers, desks, phones, bathrooms, and break rooms, where staff take off masks to eat and drink. The complaint also describes how there is resistance to testing nurses and a lack of communication about infections among colleagues.
“When they have total disregard for safety, they should be punished to the utmost,” said Markowitz, noting that HCA Healthcare is worth $40 billion. “They can penalize them, but if it’s unsafe conditions for RNs and healthcare workers, we know it’s unsafe for the patients. There needs to be drastic measures to prevent hospital corporations from behaving that way.”
In a statement, HCA spokesman Harlow Sumerford said the company has followed CDC guidance for protecting frontline caregivers. “We’re proud of our response and the significant resources we’ve deployed to help protect our colleagues. Meanwhile, the NNU has chosen to use this pandemic as an opportunity to gain publicity by attacking hospitals across the country,” Sumerford said.
Members of the union recently protested in front of the federal OSHA offices in Denver.
After several months, OSHA finally penalized a meat packing plant where eight workers (six union members) had died of COVID-19 last spring. But the amount – $15,615 – was so low that Cordova worries it will actually have a worse impact than no fine.
“It’s more dangerous to workers because now employers know [they won’t be punished meaningfully],” she said. “During the pandemic, OSHA has been absolutely absent.”
Thus, the recent picketing outside the offices in Denver. But, Cordova noted, it’s unlikely OSHA employees saw them. Their own offices were deemed too risky to stay open during the pandemic. They were vacant.
A version of this article originally appeared on Medscape.com.
COVID spikes exacerbate health worker shortages in Rocky Mountains, Great Plains
In Montana, pandemic-induced staffing shortages have shuttered a clinic in the state’s capital, led a northwestern regional hospital to ask employees exposed to COVID-19 to continue to work and emptied a health department 400 miles to the east.
“Just one more person out and we wouldn’t be able to keep the surgeries going,” said Dr. Shelly Harkins, MD, chief medical officer of St. Peter’s Health in Helena, a city of roughly 32,000 where cases continue to spread. “When the virus is just all around you, it’s almost impossible to not be deemed a contact at some point. One case can take out a whole team of people in a blink of an eye.”
In North Dakota, where cases per resident are growing faster than any other state, hospitals may once again curtail elective surgeries and possibly seek government aid to hire more nurses if the situation gets worse, North Dakota Hospital Association President Tim Blasl said.
“How long can we run at this rate with the workforce that we have?” Blasl said. “You can have all the licensed beds you want, but if you don’t have anybody to staff those beds, it doesn’t do you any good.”
The northern Rocky Mountains, Great Plains and Upper Midwest are seeing the highest surge of COVID-19 cases in the nation, as some residents have ignored recommendations for curtailing the virus, such as wearing masks and avoiding large gatherings. Montana, Idaho, Utah, Wyoming, North Dakota, South Dakota, Nebraska, Iowa, and Wisconsin have recently ranked among the top 10 U.S. states in confirmed cases per 100,000 residents over a 7-day period, according to an analysis by the New York Times.
Such coronavirus infections – and the quarantines that occur because of them – are exacerbating the health care worker shortage that existed in these states well before the pandemic. Unlike in the nation’s metropolitan hubs, these outbreaks are scattered across hundreds of miles. And even in these states’ biggest cities, the ranks of medical professionals are in short supply. Specialists and registered nurses are sometimes harder to track down than ventilators, N95 masks or hospital beds. Without enough care providers, patients may not be able to get the medical attention they need.
Hospitals have asked staffers to cover extra shifts and learn new skills. They have brought in temporary workers from other parts of the country and transferred some patients to less-crowded hospitals. But, at St. Peter’s Health, if the hospital’s one kidney doctor gets sick or is told to quarantine, Dr. Harkins doesn’t expect to find a backup.
“We make a point to not have excessive staff because we have an obligation to keep the cost of health care down for a community – we just don’t have a lot of slack in our rope,” Dr. Harkins said. “What we don’t account for is a mass exodus of staff for 14 days.”
Some hospitals are already at patient capacity or are nearly there. That’s not just because of the growing number of COVID-19 patients. Elective surgeries have resumed, and medical emergencies don’t pause for a pandemic.
Some Montana hospitals formed agreements with local affiliates early in the pandemic to share staff if one came up short. But now that the disease is spreading fast – and widely – the hope is that their needs don’t peak all at once.
Montana state officials keep a list of primarily in-state volunteer workers ready to travel to towns with shortages of contact tracers, nurses and more. But during a press conference on Oct. 15, Democratic Gov. Steve Bullock said the state had exhausted that database, and its nationwide request for National Guard medical staffing hadn’t brought in new workers.
“If you are a registered nurse, licensed practical nurse, paramedic, EMT, CNA or contact tracer, and are able to join our workforce, please do consider joining our team,” Gov. Bullock said.
This month, Kalispell Regional Medical Center in northwestern Montana even stopped quarantining COVID-exposed staff who remain asymptomatic, a change allowed by Centers for Disease Control and Prevention guidelines for health facilities facing staffing shortages.
“That’s very telling for what staffing is going through right now,” said Andrea Lueck, a registered nurse at the center. “We’re so tight that employees are called off of quarantine.”
Financial pressure early in the pandemic led the hospital to furlough staff, but it had to bring most of them back to work because it needs those bodies more than ever. The regional hub is based in Flathead County, which has recorded the state’s second-highest number of active COVID-19 cases.
Mellody Sharpton, a hospital spokesperson, said hospital workers who are exposed to someone infected with the virus are tested within three to five days and monitored for symptoms. The hospital is also pulling in new workers, with 25 traveling health professionals on hand and another 25 temporary ones on the way.
But Ms. Sharpton said the best way to conserve the hospital’s workforce is to stop the disease surge in the community.
Earlier in the pandemic, Central Montana Medical Center in Lewistown, a town of fewer than 6,000, experienced an exodus of part-time workers or those close to retirement who decided their jobs weren’t worth the risk. The facility recently secured two traveling workers, but both backed out because they couldn’t find housing. And, so far, roughly 40 of the hospital’s 322 employees have missed work for reasons connected to COVID-19.
“We’re at a critical staffing shortage and have been since the beginning of COVID,” said Joanie Slaybaugh, Central Montana Medical Center’s director of human resources. “We’re small enough, everybody feels an obligation to protect themselves and to protect each other. But it doesn’t take much to take out our staff.”
Roosevelt County, where roughly 11,000 live on the northeastern edge of Montana, had one of the nation’s highest rates of new cases as of Oct. 15. But by the end of the month, the county health department will lose half of its registered nurses as one person is about to retire and another was hired through a grant that’s ending. That leaves only one registered nurse aside from its director, Patty Presser. The health department already had to close earlier during the pandemic because of COVID exposure and not enough staffers to cover the gap. Now, if Ms. Presser can’t find nurse replacements in time, she hopes volunteers will step in, though she added they typically stay for only a few weeks.
“I need someone to do immunizations for my community, and you don’t become an immunization nurse in 14 days,” she said. “We don’t have the workforce here to deal with this virus, not even right now, and then I’m going to have my best two people go.”
Back in Helena, Dr. Harkins said St. Peter’s Health had to close a specialty outpatient clinic that treats chronic diseases for two weeks at the end of September because the entire staff had to quarantine.
Now the hospital is considering having doctors take turns spending a week working from home, so that if another wave of quarantines hits in the hospital, at least one untainted person can be brought back to work. But that won’t help for some specialties, like the hospital’s sole kidney doctor.
Every time Dr. Harkins’ phone rings, she said, she takes a breath and hopes it’s not another case that will force a whole division to close.
“Because I think immediately of the hundreds of people that need that service and won’t have it for 14 days,” she said.
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
In Montana, pandemic-induced staffing shortages have shuttered a clinic in the state’s capital, led a northwestern regional hospital to ask employees exposed to COVID-19 to continue to work and emptied a health department 400 miles to the east.
“Just one more person out and we wouldn’t be able to keep the surgeries going,” said Dr. Shelly Harkins, MD, chief medical officer of St. Peter’s Health in Helena, a city of roughly 32,000 where cases continue to spread. “When the virus is just all around you, it’s almost impossible to not be deemed a contact at some point. One case can take out a whole team of people in a blink of an eye.”
In North Dakota, where cases per resident are growing faster than any other state, hospitals may once again curtail elective surgeries and possibly seek government aid to hire more nurses if the situation gets worse, North Dakota Hospital Association President Tim Blasl said.
“How long can we run at this rate with the workforce that we have?” Blasl said. “You can have all the licensed beds you want, but if you don’t have anybody to staff those beds, it doesn’t do you any good.”
The northern Rocky Mountains, Great Plains and Upper Midwest are seeing the highest surge of COVID-19 cases in the nation, as some residents have ignored recommendations for curtailing the virus, such as wearing masks and avoiding large gatherings. Montana, Idaho, Utah, Wyoming, North Dakota, South Dakota, Nebraska, Iowa, and Wisconsin have recently ranked among the top 10 U.S. states in confirmed cases per 100,000 residents over a 7-day period, according to an analysis by the New York Times.
Such coronavirus infections – and the quarantines that occur because of them – are exacerbating the health care worker shortage that existed in these states well before the pandemic. Unlike in the nation’s metropolitan hubs, these outbreaks are scattered across hundreds of miles. And even in these states’ biggest cities, the ranks of medical professionals are in short supply. Specialists and registered nurses are sometimes harder to track down than ventilators, N95 masks or hospital beds. Without enough care providers, patients may not be able to get the medical attention they need.
Hospitals have asked staffers to cover extra shifts and learn new skills. They have brought in temporary workers from other parts of the country and transferred some patients to less-crowded hospitals. But, at St. Peter’s Health, if the hospital’s one kidney doctor gets sick or is told to quarantine, Dr. Harkins doesn’t expect to find a backup.
“We make a point to not have excessive staff because we have an obligation to keep the cost of health care down for a community – we just don’t have a lot of slack in our rope,” Dr. Harkins said. “What we don’t account for is a mass exodus of staff for 14 days.”
Some hospitals are already at patient capacity or are nearly there. That’s not just because of the growing number of COVID-19 patients. Elective surgeries have resumed, and medical emergencies don’t pause for a pandemic.
Some Montana hospitals formed agreements with local affiliates early in the pandemic to share staff if one came up short. But now that the disease is spreading fast – and widely – the hope is that their needs don’t peak all at once.
Montana state officials keep a list of primarily in-state volunteer workers ready to travel to towns with shortages of contact tracers, nurses and more. But during a press conference on Oct. 15, Democratic Gov. Steve Bullock said the state had exhausted that database, and its nationwide request for National Guard medical staffing hadn’t brought in new workers.
“If you are a registered nurse, licensed practical nurse, paramedic, EMT, CNA or contact tracer, and are able to join our workforce, please do consider joining our team,” Gov. Bullock said.
This month, Kalispell Regional Medical Center in northwestern Montana even stopped quarantining COVID-exposed staff who remain asymptomatic, a change allowed by Centers for Disease Control and Prevention guidelines for health facilities facing staffing shortages.
“That’s very telling for what staffing is going through right now,” said Andrea Lueck, a registered nurse at the center. “We’re so tight that employees are called off of quarantine.”
Financial pressure early in the pandemic led the hospital to furlough staff, but it had to bring most of them back to work because it needs those bodies more than ever. The regional hub is based in Flathead County, which has recorded the state’s second-highest number of active COVID-19 cases.
Mellody Sharpton, a hospital spokesperson, said hospital workers who are exposed to someone infected with the virus are tested within three to five days and monitored for symptoms. The hospital is also pulling in new workers, with 25 traveling health professionals on hand and another 25 temporary ones on the way.
But Ms. Sharpton said the best way to conserve the hospital’s workforce is to stop the disease surge in the community.
Earlier in the pandemic, Central Montana Medical Center in Lewistown, a town of fewer than 6,000, experienced an exodus of part-time workers or those close to retirement who decided their jobs weren’t worth the risk. The facility recently secured two traveling workers, but both backed out because they couldn’t find housing. And, so far, roughly 40 of the hospital’s 322 employees have missed work for reasons connected to COVID-19.
“We’re at a critical staffing shortage and have been since the beginning of COVID,” said Joanie Slaybaugh, Central Montana Medical Center’s director of human resources. “We’re small enough, everybody feels an obligation to protect themselves and to protect each other. But it doesn’t take much to take out our staff.”
Roosevelt County, where roughly 11,000 live on the northeastern edge of Montana, had one of the nation’s highest rates of new cases as of Oct. 15. But by the end of the month, the county health department will lose half of its registered nurses as one person is about to retire and another was hired through a grant that’s ending. That leaves only one registered nurse aside from its director, Patty Presser. The health department already had to close earlier during the pandemic because of COVID exposure and not enough staffers to cover the gap. Now, if Ms. Presser can’t find nurse replacements in time, she hopes volunteers will step in, though she added they typically stay for only a few weeks.
“I need someone to do immunizations for my community, and you don’t become an immunization nurse in 14 days,” she said. “We don’t have the workforce here to deal with this virus, not even right now, and then I’m going to have my best two people go.”
Back in Helena, Dr. Harkins said St. Peter’s Health had to close a specialty outpatient clinic that treats chronic diseases for two weeks at the end of September because the entire staff had to quarantine.
Now the hospital is considering having doctors take turns spending a week working from home, so that if another wave of quarantines hits in the hospital, at least one untainted person can be brought back to work. But that won’t help for some specialties, like the hospital’s sole kidney doctor.
Every time Dr. Harkins’ phone rings, she said, she takes a breath and hopes it’s not another case that will force a whole division to close.
“Because I think immediately of the hundreds of people that need that service and won’t have it for 14 days,” she said.
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.
In Montana, pandemic-induced staffing shortages have shuttered a clinic in the state’s capital, led a northwestern regional hospital to ask employees exposed to COVID-19 to continue to work and emptied a health department 400 miles to the east.
“Just one more person out and we wouldn’t be able to keep the surgeries going,” said Dr. Shelly Harkins, MD, chief medical officer of St. Peter’s Health in Helena, a city of roughly 32,000 where cases continue to spread. “When the virus is just all around you, it’s almost impossible to not be deemed a contact at some point. One case can take out a whole team of people in a blink of an eye.”
In North Dakota, where cases per resident are growing faster than any other state, hospitals may once again curtail elective surgeries and possibly seek government aid to hire more nurses if the situation gets worse, North Dakota Hospital Association President Tim Blasl said.
“How long can we run at this rate with the workforce that we have?” Blasl said. “You can have all the licensed beds you want, but if you don’t have anybody to staff those beds, it doesn’t do you any good.”
The northern Rocky Mountains, Great Plains and Upper Midwest are seeing the highest surge of COVID-19 cases in the nation, as some residents have ignored recommendations for curtailing the virus, such as wearing masks and avoiding large gatherings. Montana, Idaho, Utah, Wyoming, North Dakota, South Dakota, Nebraska, Iowa, and Wisconsin have recently ranked among the top 10 U.S. states in confirmed cases per 100,000 residents over a 7-day period, according to an analysis by the New York Times.
Such coronavirus infections – and the quarantines that occur because of them – are exacerbating the health care worker shortage that existed in these states well before the pandemic. Unlike in the nation’s metropolitan hubs, these outbreaks are scattered across hundreds of miles. And even in these states’ biggest cities, the ranks of medical professionals are in short supply. Specialists and registered nurses are sometimes harder to track down than ventilators, N95 masks or hospital beds. Without enough care providers, patients may not be able to get the medical attention they need.
Hospitals have asked staffers to cover extra shifts and learn new skills. They have brought in temporary workers from other parts of the country and transferred some patients to less-crowded hospitals. But, at St. Peter’s Health, if the hospital’s one kidney doctor gets sick or is told to quarantine, Dr. Harkins doesn’t expect to find a backup.
“We make a point to not have excessive staff because we have an obligation to keep the cost of health care down for a community – we just don’t have a lot of slack in our rope,” Dr. Harkins said. “What we don’t account for is a mass exodus of staff for 14 days.”
Some hospitals are already at patient capacity or are nearly there. That’s not just because of the growing number of COVID-19 patients. Elective surgeries have resumed, and medical emergencies don’t pause for a pandemic.
Some Montana hospitals formed agreements with local affiliates early in the pandemic to share staff if one came up short. But now that the disease is spreading fast – and widely – the hope is that their needs don’t peak all at once.
Montana state officials keep a list of primarily in-state volunteer workers ready to travel to towns with shortages of contact tracers, nurses and more. But during a press conference on Oct. 15, Democratic Gov. Steve Bullock said the state had exhausted that database, and its nationwide request for National Guard medical staffing hadn’t brought in new workers.
“If you are a registered nurse, licensed practical nurse, paramedic, EMT, CNA or contact tracer, and are able to join our workforce, please do consider joining our team,” Gov. Bullock said.
This month, Kalispell Regional Medical Center in northwestern Montana even stopped quarantining COVID-exposed staff who remain asymptomatic, a change allowed by Centers for Disease Control and Prevention guidelines for health facilities facing staffing shortages.
“That’s very telling for what staffing is going through right now,” said Andrea Lueck, a registered nurse at the center. “We’re so tight that employees are called off of quarantine.”
Financial pressure early in the pandemic led the hospital to furlough staff, but it had to bring most of them back to work because it needs those bodies more than ever. The regional hub is based in Flathead County, which has recorded the state’s second-highest number of active COVID-19 cases.
Mellody Sharpton, a hospital spokesperson, said hospital workers who are exposed to someone infected with the virus are tested within three to five days and monitored for symptoms. The hospital is also pulling in new workers, with 25 traveling health professionals on hand and another 25 temporary ones on the way.
But Ms. Sharpton said the best way to conserve the hospital’s workforce is to stop the disease surge in the community.
Earlier in the pandemic, Central Montana Medical Center in Lewistown, a town of fewer than 6,000, experienced an exodus of part-time workers or those close to retirement who decided their jobs weren’t worth the risk. The facility recently secured two traveling workers, but both backed out because they couldn’t find housing. And, so far, roughly 40 of the hospital’s 322 employees have missed work for reasons connected to COVID-19.
“We’re at a critical staffing shortage and have been since the beginning of COVID,” said Joanie Slaybaugh, Central Montana Medical Center’s director of human resources. “We’re small enough, everybody feels an obligation to protect themselves and to protect each other. But it doesn’t take much to take out our staff.”
Roosevelt County, where roughly 11,000 live on the northeastern edge of Montana, had one of the nation’s highest rates of new cases as of Oct. 15. But by the end of the month, the county health department will lose half of its registered nurses as one person is about to retire and another was hired through a grant that’s ending. That leaves only one registered nurse aside from its director, Patty Presser. The health department already had to close earlier during the pandemic because of COVID exposure and not enough staffers to cover the gap. Now, if Ms. Presser can’t find nurse replacements in time, she hopes volunteers will step in, though she added they typically stay for only a few weeks.
“I need someone to do immunizations for my community, and you don’t become an immunization nurse in 14 days,” she said. “We don’t have the workforce here to deal with this virus, not even right now, and then I’m going to have my best two people go.”
Back in Helena, Dr. Harkins said St. Peter’s Health had to close a specialty outpatient clinic that treats chronic diseases for two weeks at the end of September because the entire staff had to quarantine.
Now the hospital is considering having doctors take turns spending a week working from home, so that if another wave of quarantines hits in the hospital, at least one untainted person can be brought back to work. But that won’t help for some specialties, like the hospital’s sole kidney doctor.
Every time Dr. Harkins’ phone rings, she said, she takes a breath and hopes it’s not another case that will force a whole division to close.
“Because I think immediately of the hundreds of people that need that service and won’t have it for 14 days,” she said.
Kaiser Health News is a nonprofit news service covering health issues. It is an editorially independent program of KFF (Kaiser Family Foundation), which is not affiliated with Kaiser Permanente.