User login
-
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]


COVID-19 vaccine mandates are working, public health experts say
Some organizations have reported vaccination rates that jumped from less than 50% to more than 90%, according to ABC News. Workplace mandates have especially encouraged employees who were on the fence to get a shot.
“In general, vaccine mandates work,” James Colgrove, a public health professor at Columbia University’s Mailman School of Public Health, told ABC News.
For decades, the United States has monitored the effectiveness of vaccine mandates in schools, he noted, which have successfully required shots against measles, mumps, and other illnesses that used to be widespread. Certain employees, such as hospital workers, must take vaccines for their jobs, he said, and those requirements have also been effective over the years.
“The more normalized it becomes, the more people [know] someone else who is vaccinated, the more people will comply,” he said. “With any vaccine, the longer it’s been around, the more people get with it.”
With the widespread and contagious nature of COVID-19, workplaces have been forced to consider vaccine mandates to protect their employees and prevent worker shortages, Dr. Colgrove said.
Some companies began to issue vaccine rules this summer as the Delta variant caused a jump in cases, hospitalizations, and deaths. Major companies, including Google, Tyson Foods, United Airlines, and the Walt Disney Company, required in-person employees to get a shot. So far, the results from those mandates have been strong, ABC News reported.
For instance, Tyson announced a mandate in August, when less than half of its 140,000 employees were vaccinated. When the deadline came at the end of October, more than 60,000 additional employees had been vaccinated, and the vaccination rate was 96%.
“Has this made a difference in the health and safety of our team members? Absolutely. We’ve seen a significant decline in the number of active cases companywide,” Donnie King, CEO and president of Tyson Foods, said in a statement.
United Airlines has also shared that 99.7% of its 67,000 employees are vaccinated. Within 48 hours of announcing its mandate, the number of unvaccinated staffers fell from 593 to 320 people, ABC News reported.
Vaccine mandates appear to be working in the public sector as well. State health department officials in Washington told ABC News that the percentage of public employees who were vaccinated jumped from 49% in September to 96% by the vaccine mandate deadline in October.
Vaccination rates have also increased in New York City, where some employees in the fire, police, and sanitation departments protested the mandate. By the deadline, vaccination rates shifted from less than 75% to 82% in the fire department, 86% in the police department, and 91% of EMS personnel, ABC News reported.
Overall, vaccine mandates tend to reach groups who aren’t completely against the vaccine, medical experts told the news outlet. A small percentage of the population truly opposes the shot, and in most cases, unvaccinated people are on the fence or haven’t seen good enough messaging for it.
“When you look at vaccine resistance, the people who are the most opposed often make a very large amount of noise that is at odds with the actual numbers who are against vaccination,” Dr. Colgrove said.
A version of this article first appeared on WebMD.com.
Some organizations have reported vaccination rates that jumped from less than 50% to more than 90%, according to ABC News. Workplace mandates have especially encouraged employees who were on the fence to get a shot.
“In general, vaccine mandates work,” James Colgrove, a public health professor at Columbia University’s Mailman School of Public Health, told ABC News.
For decades, the United States has monitored the effectiveness of vaccine mandates in schools, he noted, which have successfully required shots against measles, mumps, and other illnesses that used to be widespread. Certain employees, such as hospital workers, must take vaccines for their jobs, he said, and those requirements have also been effective over the years.
“The more normalized it becomes, the more people [know] someone else who is vaccinated, the more people will comply,” he said. “With any vaccine, the longer it’s been around, the more people get with it.”
With the widespread and contagious nature of COVID-19, workplaces have been forced to consider vaccine mandates to protect their employees and prevent worker shortages, Dr. Colgrove said.
Some companies began to issue vaccine rules this summer as the Delta variant caused a jump in cases, hospitalizations, and deaths. Major companies, including Google, Tyson Foods, United Airlines, and the Walt Disney Company, required in-person employees to get a shot. So far, the results from those mandates have been strong, ABC News reported.
For instance, Tyson announced a mandate in August, when less than half of its 140,000 employees were vaccinated. When the deadline came at the end of October, more than 60,000 additional employees had been vaccinated, and the vaccination rate was 96%.
“Has this made a difference in the health and safety of our team members? Absolutely. We’ve seen a significant decline in the number of active cases companywide,” Donnie King, CEO and president of Tyson Foods, said in a statement.
United Airlines has also shared that 99.7% of its 67,000 employees are vaccinated. Within 48 hours of announcing its mandate, the number of unvaccinated staffers fell from 593 to 320 people, ABC News reported.
Vaccine mandates appear to be working in the public sector as well. State health department officials in Washington told ABC News that the percentage of public employees who were vaccinated jumped from 49% in September to 96% by the vaccine mandate deadline in October.
Vaccination rates have also increased in New York City, where some employees in the fire, police, and sanitation departments protested the mandate. By the deadline, vaccination rates shifted from less than 75% to 82% in the fire department, 86% in the police department, and 91% of EMS personnel, ABC News reported.
Overall, vaccine mandates tend to reach groups who aren’t completely against the vaccine, medical experts told the news outlet. A small percentage of the population truly opposes the shot, and in most cases, unvaccinated people are on the fence or haven’t seen good enough messaging for it.
“When you look at vaccine resistance, the people who are the most opposed often make a very large amount of noise that is at odds with the actual numbers who are against vaccination,” Dr. Colgrove said.
A version of this article first appeared on WebMD.com.
Some organizations have reported vaccination rates that jumped from less than 50% to more than 90%, according to ABC News. Workplace mandates have especially encouraged employees who were on the fence to get a shot.
“In general, vaccine mandates work,” James Colgrove, a public health professor at Columbia University’s Mailman School of Public Health, told ABC News.
For decades, the United States has monitored the effectiveness of vaccine mandates in schools, he noted, which have successfully required shots against measles, mumps, and other illnesses that used to be widespread. Certain employees, such as hospital workers, must take vaccines for their jobs, he said, and those requirements have also been effective over the years.
“The more normalized it becomes, the more people [know] someone else who is vaccinated, the more people will comply,” he said. “With any vaccine, the longer it’s been around, the more people get with it.”
With the widespread and contagious nature of COVID-19, workplaces have been forced to consider vaccine mandates to protect their employees and prevent worker shortages, Dr. Colgrove said.
Some companies began to issue vaccine rules this summer as the Delta variant caused a jump in cases, hospitalizations, and deaths. Major companies, including Google, Tyson Foods, United Airlines, and the Walt Disney Company, required in-person employees to get a shot. So far, the results from those mandates have been strong, ABC News reported.
For instance, Tyson announced a mandate in August, when less than half of its 140,000 employees were vaccinated. When the deadline came at the end of October, more than 60,000 additional employees had been vaccinated, and the vaccination rate was 96%.
“Has this made a difference in the health and safety of our team members? Absolutely. We’ve seen a significant decline in the number of active cases companywide,” Donnie King, CEO and president of Tyson Foods, said in a statement.
United Airlines has also shared that 99.7% of its 67,000 employees are vaccinated. Within 48 hours of announcing its mandate, the number of unvaccinated staffers fell from 593 to 320 people, ABC News reported.
Vaccine mandates appear to be working in the public sector as well. State health department officials in Washington told ABC News that the percentage of public employees who were vaccinated jumped from 49% in September to 96% by the vaccine mandate deadline in October.
Vaccination rates have also increased in New York City, where some employees in the fire, police, and sanitation departments protested the mandate. By the deadline, vaccination rates shifted from less than 75% to 82% in the fire department, 86% in the police department, and 91% of EMS personnel, ABC News reported.
Overall, vaccine mandates tend to reach groups who aren’t completely against the vaccine, medical experts told the news outlet. A small percentage of the population truly opposes the shot, and in most cases, unvaccinated people are on the fence or haven’t seen good enough messaging for it.
“When you look at vaccine resistance, the people who are the most opposed often make a very large amount of noise that is at odds with the actual numbers who are against vaccination,” Dr. Colgrove said.
A version of this article first appeared on WebMD.com.
Genomic classifier is one piece of the ILD diagnosis puzzle
Although genomic testing is useful when an interstitial lung disease diagnosis is uncertain, the testing results themselves aren’t sufficient to make the diagnosis, Daniel Dilling, MD, FCCP, said in a presentation at the annual meeting of the American College of Chest Physicians, which was held virtually.
The genomic classifier (Envisia, Veracyte) helps differentiate idiopathic pulmonary fibrosis (IPF) by detecting usual interstitial pneumonia (UIP), the hallmark pattern of this interstitial lung disease.
However, UIP is just one piece of the larger diagnostic puzzle, according to Dr. Dilling, professor of medicine in the interstitial lung disease program at Loyola University Medical Center in Maywood, Ill.
“Remember, it’s just a pattern, and not a diagnosis of IPF,” Dr. Dilling said in his presentation.
Genomic classifier results correlate well with both histologic and radiographic UIP pattern, studies show.
However, Dr. Dilling said the value of the genomic classifier is not in isolation.
“We don’t use this in a vacuum,” he said. “It increases our confidence and consensus, but it has to be incorporated into a multidisciplinary discussion group.”
Part of the diagnostic pathway
Dr. Dilling said the genomic classifier should be considered part of a diagnostic pathway in uncertain cases, particularly when the risk of surgical lung biopsy is high.
Current clinical practice guidelines recommend surgical lung biopsy for histopathologic diagnosis when clinical and radiologic findings are not definitive for IPF, the speaker said.
However, surgical lung biopsy carries some risk, and sometimes it can’t be done, he added.
In his presentation, Dr. Dilling cited a systematic review and meta-analysis of 23 studies looking at surgical lung biopsy for the diagnosis of interstitial lung diseases.
The postoperative mortality rate was 3.6% in that meta-analysis, published in 2015 in the Journal of Thoracic and Cardiovascular Surgery.
“The final decision regarding whether or not to perform a [surgical lung biopsy] must be based on the balance between benefits to establish a secure diagnosis and the potential risks,” authors wrote at the time.
Mortality risk is higher in immunocompromised and acutely ill patient populations, according to Dr. Dilling, who added that as many of 19% of patients will have complications from surgical lung biopsy.
Genomic classifier studies
In a proof-of-principle study, published in 2017 in the Annals of the American Thoracic Society, authors described how they used machine learning to train an algorithm to distinguish UIP from non-UIP pattern in tissue obtained by transbronchial biopsy (TBB).
The top-performing algorithm distinguished UIP from non-UIP conditions in single TBB samples with specificity of 86% and sensitivity of 63%, according to investigators, who said at the time that independent validation would be needed before the genomic classifier could be applied in clinical settings.
In a prospective validation study, published in 2019 in The Lancet Respiratory Medicine, the genomic classifier identified UIP in TBB samples from 49 patients with a specificity of 88% and sensitivity of 70%.
Excluding patients with definite or probable UIP as shown on high-resolution computed tomography, results show that the classifier had a sensitivity of 76%, specificity of 88%, and positive predictive value of 81%.
“The performance of the test is good, even in that scenario,” Dr. Dilling said.
Real-world results
Dr. Dilling also highlighted a “real-world” study, published earlier in 2021, demonstrating that UIP pattern recognized by a genomic classifier had encouraging sensitivity and specificity when combined with high-resolution CT and clinical factors.
That study included 96 patients who had both diagnostic lung pathology and a transbronchial lung biopsy for molecular testing with the classifier.
The classifier had a sensitivity of 60.3% and a specificity of 92.1% for histology-proven UIP pattern, investigators said in their report, which appears in the American Journal of Respiratory and Critical Care Medicine.
Local radiologists identified UIP with a sensitivity of 34.0% and specificity of 96.9%. But adding genomic classifier testing to local radiology testing increased the diagnostic yield, investigators said, with a sensitivity of 79.2% and specificity of 90.6%.
“This might suggest that the implementation of this into a local [multidisciplinary discussion] with your local radiology expertise might really improve your recognition of UIP,” Dr. Dilling said.
Dr. Dilling reported disclosures related to Bellerophon, Boehringer Ingelheim, Genentech, Nitto Denko, and Lung Bioengineering.
Although genomic testing is useful when an interstitial lung disease diagnosis is uncertain, the testing results themselves aren’t sufficient to make the diagnosis, Daniel Dilling, MD, FCCP, said in a presentation at the annual meeting of the American College of Chest Physicians, which was held virtually.
The genomic classifier (Envisia, Veracyte) helps differentiate idiopathic pulmonary fibrosis (IPF) by detecting usual interstitial pneumonia (UIP), the hallmark pattern of this interstitial lung disease.
However, UIP is just one piece of the larger diagnostic puzzle, according to Dr. Dilling, professor of medicine in the interstitial lung disease program at Loyola University Medical Center in Maywood, Ill.
“Remember, it’s just a pattern, and not a diagnosis of IPF,” Dr. Dilling said in his presentation.
Genomic classifier results correlate well with both histologic and radiographic UIP pattern, studies show.
However, Dr. Dilling said the value of the genomic classifier is not in isolation.
“We don’t use this in a vacuum,” he said. “It increases our confidence and consensus, but it has to be incorporated into a multidisciplinary discussion group.”
Part of the diagnostic pathway
Dr. Dilling said the genomic classifier should be considered part of a diagnostic pathway in uncertain cases, particularly when the risk of surgical lung biopsy is high.
Current clinical practice guidelines recommend surgical lung biopsy for histopathologic diagnosis when clinical and radiologic findings are not definitive for IPF, the speaker said.
However, surgical lung biopsy carries some risk, and sometimes it can’t be done, he added.
In his presentation, Dr. Dilling cited a systematic review and meta-analysis of 23 studies looking at surgical lung biopsy for the diagnosis of interstitial lung diseases.
The postoperative mortality rate was 3.6% in that meta-analysis, published in 2015 in the Journal of Thoracic and Cardiovascular Surgery.
“The final decision regarding whether or not to perform a [surgical lung biopsy] must be based on the balance between benefits to establish a secure diagnosis and the potential risks,” authors wrote at the time.
Mortality risk is higher in immunocompromised and acutely ill patient populations, according to Dr. Dilling, who added that as many of 19% of patients will have complications from surgical lung biopsy.
Genomic classifier studies
In a proof-of-principle study, published in 2017 in the Annals of the American Thoracic Society, authors described how they used machine learning to train an algorithm to distinguish UIP from non-UIP pattern in tissue obtained by transbronchial biopsy (TBB).
The top-performing algorithm distinguished UIP from non-UIP conditions in single TBB samples with specificity of 86% and sensitivity of 63%, according to investigators, who said at the time that independent validation would be needed before the genomic classifier could be applied in clinical settings.
In a prospective validation study, published in 2019 in The Lancet Respiratory Medicine, the genomic classifier identified UIP in TBB samples from 49 patients with a specificity of 88% and sensitivity of 70%.
Excluding patients with definite or probable UIP as shown on high-resolution computed tomography, results show that the classifier had a sensitivity of 76%, specificity of 88%, and positive predictive value of 81%.
“The performance of the test is good, even in that scenario,” Dr. Dilling said.
Real-world results
Dr. Dilling also highlighted a “real-world” study, published earlier in 2021, demonstrating that UIP pattern recognized by a genomic classifier had encouraging sensitivity and specificity when combined with high-resolution CT and clinical factors.
That study included 96 patients who had both diagnostic lung pathology and a transbronchial lung biopsy for molecular testing with the classifier.
The classifier had a sensitivity of 60.3% and a specificity of 92.1% for histology-proven UIP pattern, investigators said in their report, which appears in the American Journal of Respiratory and Critical Care Medicine.
Local radiologists identified UIP with a sensitivity of 34.0% and specificity of 96.9%. But adding genomic classifier testing to local radiology testing increased the diagnostic yield, investigators said, with a sensitivity of 79.2% and specificity of 90.6%.
“This might suggest that the implementation of this into a local [multidisciplinary discussion] with your local radiology expertise might really improve your recognition of UIP,” Dr. Dilling said.
Dr. Dilling reported disclosures related to Bellerophon, Boehringer Ingelheim, Genentech, Nitto Denko, and Lung Bioengineering.
Although genomic testing is useful when an interstitial lung disease diagnosis is uncertain, the testing results themselves aren’t sufficient to make the diagnosis, Daniel Dilling, MD, FCCP, said in a presentation at the annual meeting of the American College of Chest Physicians, which was held virtually.
The genomic classifier (Envisia, Veracyte) helps differentiate idiopathic pulmonary fibrosis (IPF) by detecting usual interstitial pneumonia (UIP), the hallmark pattern of this interstitial lung disease.
However, UIP is just one piece of the larger diagnostic puzzle, according to Dr. Dilling, professor of medicine in the interstitial lung disease program at Loyola University Medical Center in Maywood, Ill.
“Remember, it’s just a pattern, and not a diagnosis of IPF,” Dr. Dilling said in his presentation.
Genomic classifier results correlate well with both histologic and radiographic UIP pattern, studies show.
However, Dr. Dilling said the value of the genomic classifier is not in isolation.
“We don’t use this in a vacuum,” he said. “It increases our confidence and consensus, but it has to be incorporated into a multidisciplinary discussion group.”
Part of the diagnostic pathway
Dr. Dilling said the genomic classifier should be considered part of a diagnostic pathway in uncertain cases, particularly when the risk of surgical lung biopsy is high.
Current clinical practice guidelines recommend surgical lung biopsy for histopathologic diagnosis when clinical and radiologic findings are not definitive for IPF, the speaker said.
However, surgical lung biopsy carries some risk, and sometimes it can’t be done, he added.
In his presentation, Dr. Dilling cited a systematic review and meta-analysis of 23 studies looking at surgical lung biopsy for the diagnosis of interstitial lung diseases.
The postoperative mortality rate was 3.6% in that meta-analysis, published in 2015 in the Journal of Thoracic and Cardiovascular Surgery.
“The final decision regarding whether or not to perform a [surgical lung biopsy] must be based on the balance between benefits to establish a secure diagnosis and the potential risks,” authors wrote at the time.
Mortality risk is higher in immunocompromised and acutely ill patient populations, according to Dr. Dilling, who added that as many of 19% of patients will have complications from surgical lung biopsy.
Genomic classifier studies
In a proof-of-principle study, published in 2017 in the Annals of the American Thoracic Society, authors described how they used machine learning to train an algorithm to distinguish UIP from non-UIP pattern in tissue obtained by transbronchial biopsy (TBB).
The top-performing algorithm distinguished UIP from non-UIP conditions in single TBB samples with specificity of 86% and sensitivity of 63%, according to investigators, who said at the time that independent validation would be needed before the genomic classifier could be applied in clinical settings.
In a prospective validation study, published in 2019 in The Lancet Respiratory Medicine, the genomic classifier identified UIP in TBB samples from 49 patients with a specificity of 88% and sensitivity of 70%.
Excluding patients with definite or probable UIP as shown on high-resolution computed tomography, results show that the classifier had a sensitivity of 76%, specificity of 88%, and positive predictive value of 81%.
“The performance of the test is good, even in that scenario,” Dr. Dilling said.
Real-world results
Dr. Dilling also highlighted a “real-world” study, published earlier in 2021, demonstrating that UIP pattern recognized by a genomic classifier had encouraging sensitivity and specificity when combined with high-resolution CT and clinical factors.
That study included 96 patients who had both diagnostic lung pathology and a transbronchial lung biopsy for molecular testing with the classifier.
The classifier had a sensitivity of 60.3% and a specificity of 92.1% for histology-proven UIP pattern, investigators said in their report, which appears in the American Journal of Respiratory and Critical Care Medicine.
Local radiologists identified UIP with a sensitivity of 34.0% and specificity of 96.9%. But adding genomic classifier testing to local radiology testing increased the diagnostic yield, investigators said, with a sensitivity of 79.2% and specificity of 90.6%.
“This might suggest that the implementation of this into a local [multidisciplinary discussion] with your local radiology expertise might really improve your recognition of UIP,” Dr. Dilling said.
Dr. Dilling reported disclosures related to Bellerophon, Boehringer Ingelheim, Genentech, Nitto Denko, and Lung Bioengineering.
FROM CHEST 2021
Should you tell your doctor that you’re a doctor?
The question drew spirited debate when urologist Ashley Winter, MD, made a simple, straightforward request on Twitter: “If you are a doctor & you come to an appointment please tell me you are a doctor, not because I will treat you differently but because it’s easier to speak in jargon.”
She later added, “This doesn’t’ mean I would be less patient-focused or emotional with a physician or other [healthcare worker]. Just means that, instead of saying ‘you will have a catheter draining your urine to a bag,’ I can say, ‘you will have a Foley.’ ”
The Tweet followed an encounter with a patient who told Dr. Winter that he was a doctor only after she had gone to some length explaining a surgical procedure in lay terms.
“I explained the surgery, obviously assuming he was an intelligent adult, but using fully layman’s terms,” she said in an interview. The patient then told her that he was a doctor. “I guess I felt this embarrassment — I wouldn’t have treated him differently, but I just could have discussed the procedure with him in more professional terms.”
“To some extent, it was my own fault,” she commented in an interview. “I didn’t take the time to ask [about his work] at the beginning of the consultation, but that’s a fine line, also,” added Dr. Winter, a urologist and sexual medicine physician in Portland, Ore.
“You know that patient is there because they want care from you and it’s not necessarily always at the forefront of importance to be asking them what they do for their work, but alternatively, if you don’t ask then you put them in this position where they have to find a way to go ahead and tell you.”
Several people chimed in on the thread to voice their thoughts on the matter. Some commiserated with Dr. Winter’s experience:
“I took care of a retired cardiologist in the hospital as a second-year resident and honest to god he let me ramble on ‘explaining’ his echo result and never told me. I found out a couple days later and wanted to die,” posted @MaddyAndrewsMD.
Another recalled a similarly embarrassing experience when she “went on and on” discussing headaches with a patient whose husband “was in the corner smirking.”
“They told my attending later [that the] husband was a retired FM doc who practiced medicine longer than I’ve been alive. I wanted to die,” posted @JSinghDO.
Many on the thread, though, were doctors and other healthcare professionals speaking as patients. Some said they didn’t want to disclose their status as a healthcare provider because they felt it affected the care they received.
For example, @drhelenrainford commented: “In my experience my care is less ‘caring’ when they know I am a [doctor]. I get spoken to like they are discussing a patient with me — no empathy just facts and difficult results just blurted out without consideration. Awful awful time as an inpatient …but that’s another story!”
@Dr_B_Ring said: “Nope – You and I speak different jargon – I would want you to speak to me like a human that doesn’t know your jargon. My ego would get in the way of asking about the acronyms I don’t know if you knew I was a fellow physician.”
Conversely, @lozzlemcfozzle said: “Honestly I prefer not to tell my Doctors — I’ve found people skip explanations assuming I ‘know,’ or seem a little nervous when I tell them!”
Others said they felt uncomfortable — pretentious, even — in announcing their status, or worried that they might come across as expecting special care.
“It’s such a tough needle to thread. Want to tell people early but not come off as demanding special treatment, but don’t want to wait too long and it seems like a trap,” said @MDaware.
Twitter user @MsBabyCatcher wrote: “I have a hard time doing this because I don’t want people to think I’m being pretentious or going to micromanage/dictate care.”
Replying to @MsBabyCatcher, @RedStethoscope wrote: “I used to think this too until I got [very poor] care a few times, and was advised by other doctor moms to ‘play the doctor card.’ I have gotten better/more compassionate care by making sure it’s clear that I’m a physician (which is junk, but here we are).”
Several of those responding used the words “tricky” and “awkward,” suggesting a common theme for doctors presenting as patients.
“I struggle with this. My 5-year-old broke her arm this weekend, we spent hours in the ED, of my own hospital, I never mentioned it because I didn’t want to get preferential care. But as they were explaining her type of fracture, it felt awkward and inefficient,” said @lindsay_petty.
To avoid the awkwardness, a number of respondents said they purposefully use medical jargon to open up a conversation rather than just offering up the information that they are a doctor.
Still others offered suggestions on how to broach the subject more directly when presenting as a patient:
‘”Just FYI I’m a X doc but I’m here because I really want your help and advice!” That’s what I usually do,” wrote @drcakefm.
@BeeSting14618 Tweeted: “I usually say ‘I know some of this but I’m here because I want YOUR guidance. Also I may ask dumb questions, and I’ll tell you if a question is asking your opinion or making a request.’”
A few others injected a bit of humor: “I just do the 14-part handshake that only doctors know. Is that not customary?” quipped @Branmiz25.
“Ah yes, that transmits the entire [history of present illness],” replied Dr. Winter.
Jokes aside, the topic is obviously one that touched on a shared experience among healthcare providers, Dr. Winter commented. The Twitter thread she started just “blew up.”
That’s typically a sign that the Tweet is relatable for a lot of people, she said.
“It’s definitely something that all of us as care providers and as patients understand. It’s a funny, awkward thing that can really change an interaction, so we probably all feel pretty strongly about our experiences related to that,” she added.
The debate begs the question: Is there a duty or ethical reason to disclose?
“I definitely think it is very reasonable to disclose that one is a medical professional to another doctor,” medical ethicist Charlotte Blease, PhD, said in an interview. “There are good reasons to believe doing so might make a difference to the quality of communication and transparency.”
If the ability to use medical terminology or jargon more freely improves patient understanding, autonomy, and shared decision-making, then it may be of benefit, said Dr. Blease, a Keane OpenNotes Scholar at Beth Israel Deaconess Medical Center in Boston.
“Since doctors should strive to communicate effectively with every patient and to respect their unique needs and level of understanding, then I see no reason to deny that one is a medic,” she added.”
Knowing how to share the information is another story.
“This is something that affects all of us as physicians — we’re going to be patients at some point, right?” Dr. Winter commented. “But I don’t think how to disclose that is something that was ever brought up in my medical training.”
“Maybe there should just be a discussion of this one day when people are in medical school — maybe in a professionalism course — to broach this topic or look at if there’s any literature on outcomes related to disclosure of status or what are best practices,” she suggested.
A version of this article first appeared on Medscape.com.
The question drew spirited debate when urologist Ashley Winter, MD, made a simple, straightforward request on Twitter: “If you are a doctor & you come to an appointment please tell me you are a doctor, not because I will treat you differently but because it’s easier to speak in jargon.”
She later added, “This doesn’t’ mean I would be less patient-focused or emotional with a physician or other [healthcare worker]. Just means that, instead of saying ‘you will have a catheter draining your urine to a bag,’ I can say, ‘you will have a Foley.’ ”
The Tweet followed an encounter with a patient who told Dr. Winter that he was a doctor only after she had gone to some length explaining a surgical procedure in lay terms.
“I explained the surgery, obviously assuming he was an intelligent adult, but using fully layman’s terms,” she said in an interview. The patient then told her that he was a doctor. “I guess I felt this embarrassment — I wouldn’t have treated him differently, but I just could have discussed the procedure with him in more professional terms.”
“To some extent, it was my own fault,” she commented in an interview. “I didn’t take the time to ask [about his work] at the beginning of the consultation, but that’s a fine line, also,” added Dr. Winter, a urologist and sexual medicine physician in Portland, Ore.
“You know that patient is there because they want care from you and it’s not necessarily always at the forefront of importance to be asking them what they do for their work, but alternatively, if you don’t ask then you put them in this position where they have to find a way to go ahead and tell you.”
Several people chimed in on the thread to voice their thoughts on the matter. Some commiserated with Dr. Winter’s experience:
“I took care of a retired cardiologist in the hospital as a second-year resident and honest to god he let me ramble on ‘explaining’ his echo result and never told me. I found out a couple days later and wanted to die,” posted @MaddyAndrewsMD.
Another recalled a similarly embarrassing experience when she “went on and on” discussing headaches with a patient whose husband “was in the corner smirking.”
“They told my attending later [that the] husband was a retired FM doc who practiced medicine longer than I’ve been alive. I wanted to die,” posted @JSinghDO.
Many on the thread, though, were doctors and other healthcare professionals speaking as patients. Some said they didn’t want to disclose their status as a healthcare provider because they felt it affected the care they received.
For example, @drhelenrainford commented: “In my experience my care is less ‘caring’ when they know I am a [doctor]. I get spoken to like they are discussing a patient with me — no empathy just facts and difficult results just blurted out without consideration. Awful awful time as an inpatient …but that’s another story!”
@Dr_B_Ring said: “Nope – You and I speak different jargon – I would want you to speak to me like a human that doesn’t know your jargon. My ego would get in the way of asking about the acronyms I don’t know if you knew I was a fellow physician.”
Conversely, @lozzlemcfozzle said: “Honestly I prefer not to tell my Doctors — I’ve found people skip explanations assuming I ‘know,’ or seem a little nervous when I tell them!”
Others said they felt uncomfortable — pretentious, even — in announcing their status, or worried that they might come across as expecting special care.
“It’s such a tough needle to thread. Want to tell people early but not come off as demanding special treatment, but don’t want to wait too long and it seems like a trap,” said @MDaware.
Twitter user @MsBabyCatcher wrote: “I have a hard time doing this because I don’t want people to think I’m being pretentious or going to micromanage/dictate care.”
Replying to @MsBabyCatcher, @RedStethoscope wrote: “I used to think this too until I got [very poor] care a few times, and was advised by other doctor moms to ‘play the doctor card.’ I have gotten better/more compassionate care by making sure it’s clear that I’m a physician (which is junk, but here we are).”
Several of those responding used the words “tricky” and “awkward,” suggesting a common theme for doctors presenting as patients.
“I struggle with this. My 5-year-old broke her arm this weekend, we spent hours in the ED, of my own hospital, I never mentioned it because I didn’t want to get preferential care. But as they were explaining her type of fracture, it felt awkward and inefficient,” said @lindsay_petty.
To avoid the awkwardness, a number of respondents said they purposefully use medical jargon to open up a conversation rather than just offering up the information that they are a doctor.
Still others offered suggestions on how to broach the subject more directly when presenting as a patient:
‘”Just FYI I’m a X doc but I’m here because I really want your help and advice!” That’s what I usually do,” wrote @drcakefm.
@BeeSting14618 Tweeted: “I usually say ‘I know some of this but I’m here because I want YOUR guidance. Also I may ask dumb questions, and I’ll tell you if a question is asking your opinion or making a request.’”
A few others injected a bit of humor: “I just do the 14-part handshake that only doctors know. Is that not customary?” quipped @Branmiz25.
“Ah yes, that transmits the entire [history of present illness],” replied Dr. Winter.
Jokes aside, the topic is obviously one that touched on a shared experience among healthcare providers, Dr. Winter commented. The Twitter thread she started just “blew up.”
That’s typically a sign that the Tweet is relatable for a lot of people, she said.
“It’s definitely something that all of us as care providers and as patients understand. It’s a funny, awkward thing that can really change an interaction, so we probably all feel pretty strongly about our experiences related to that,” she added.
The debate begs the question: Is there a duty or ethical reason to disclose?
“I definitely think it is very reasonable to disclose that one is a medical professional to another doctor,” medical ethicist Charlotte Blease, PhD, said in an interview. “There are good reasons to believe doing so might make a difference to the quality of communication and transparency.”
If the ability to use medical terminology or jargon more freely improves patient understanding, autonomy, and shared decision-making, then it may be of benefit, said Dr. Blease, a Keane OpenNotes Scholar at Beth Israel Deaconess Medical Center in Boston.
“Since doctors should strive to communicate effectively with every patient and to respect their unique needs and level of understanding, then I see no reason to deny that one is a medic,” she added.”
Knowing how to share the information is another story.
“This is something that affects all of us as physicians — we’re going to be patients at some point, right?” Dr. Winter commented. “But I don’t think how to disclose that is something that was ever brought up in my medical training.”
“Maybe there should just be a discussion of this one day when people are in medical school — maybe in a professionalism course — to broach this topic or look at if there’s any literature on outcomes related to disclosure of status or what are best practices,” she suggested.
A version of this article first appeared on Medscape.com.
The question drew spirited debate when urologist Ashley Winter, MD, made a simple, straightforward request on Twitter: “If you are a doctor & you come to an appointment please tell me you are a doctor, not because I will treat you differently but because it’s easier to speak in jargon.”
She later added, “This doesn’t’ mean I would be less patient-focused or emotional with a physician or other [healthcare worker]. Just means that, instead of saying ‘you will have a catheter draining your urine to a bag,’ I can say, ‘you will have a Foley.’ ”
The Tweet followed an encounter with a patient who told Dr. Winter that he was a doctor only after she had gone to some length explaining a surgical procedure in lay terms.
“I explained the surgery, obviously assuming he was an intelligent adult, but using fully layman’s terms,” she said in an interview. The patient then told her that he was a doctor. “I guess I felt this embarrassment — I wouldn’t have treated him differently, but I just could have discussed the procedure with him in more professional terms.”
“To some extent, it was my own fault,” she commented in an interview. “I didn’t take the time to ask [about his work] at the beginning of the consultation, but that’s a fine line, also,” added Dr. Winter, a urologist and sexual medicine physician in Portland, Ore.
“You know that patient is there because they want care from you and it’s not necessarily always at the forefront of importance to be asking them what they do for their work, but alternatively, if you don’t ask then you put them in this position where they have to find a way to go ahead and tell you.”
Several people chimed in on the thread to voice their thoughts on the matter. Some commiserated with Dr. Winter’s experience:
“I took care of a retired cardiologist in the hospital as a second-year resident and honest to god he let me ramble on ‘explaining’ his echo result and never told me. I found out a couple days later and wanted to die,” posted @MaddyAndrewsMD.
Another recalled a similarly embarrassing experience when she “went on and on” discussing headaches with a patient whose husband “was in the corner smirking.”
“They told my attending later [that the] husband was a retired FM doc who practiced medicine longer than I’ve been alive. I wanted to die,” posted @JSinghDO.
Many on the thread, though, were doctors and other healthcare professionals speaking as patients. Some said they didn’t want to disclose their status as a healthcare provider because they felt it affected the care they received.
For example, @drhelenrainford commented: “In my experience my care is less ‘caring’ when they know I am a [doctor]. I get spoken to like they are discussing a patient with me — no empathy just facts and difficult results just blurted out without consideration. Awful awful time as an inpatient …but that’s another story!”
@Dr_B_Ring said: “Nope – You and I speak different jargon – I would want you to speak to me like a human that doesn’t know your jargon. My ego would get in the way of asking about the acronyms I don’t know if you knew I was a fellow physician.”
Conversely, @lozzlemcfozzle said: “Honestly I prefer not to tell my Doctors — I’ve found people skip explanations assuming I ‘know,’ or seem a little nervous when I tell them!”
Others said they felt uncomfortable — pretentious, even — in announcing their status, or worried that they might come across as expecting special care.
“It’s such a tough needle to thread. Want to tell people early but not come off as demanding special treatment, but don’t want to wait too long and it seems like a trap,” said @MDaware.
Twitter user @MsBabyCatcher wrote: “I have a hard time doing this because I don’t want people to think I’m being pretentious or going to micromanage/dictate care.”
Replying to @MsBabyCatcher, @RedStethoscope wrote: “I used to think this too until I got [very poor] care a few times, and was advised by other doctor moms to ‘play the doctor card.’ I have gotten better/more compassionate care by making sure it’s clear that I’m a physician (which is junk, but here we are).”
Several of those responding used the words “tricky” and “awkward,” suggesting a common theme for doctors presenting as patients.
“I struggle with this. My 5-year-old broke her arm this weekend, we spent hours in the ED, of my own hospital, I never mentioned it because I didn’t want to get preferential care. But as they were explaining her type of fracture, it felt awkward and inefficient,” said @lindsay_petty.
To avoid the awkwardness, a number of respondents said they purposefully use medical jargon to open up a conversation rather than just offering up the information that they are a doctor.
Still others offered suggestions on how to broach the subject more directly when presenting as a patient:
‘”Just FYI I’m a X doc but I’m here because I really want your help and advice!” That’s what I usually do,” wrote @drcakefm.
@BeeSting14618 Tweeted: “I usually say ‘I know some of this but I’m here because I want YOUR guidance. Also I may ask dumb questions, and I’ll tell you if a question is asking your opinion or making a request.’”
A few others injected a bit of humor: “I just do the 14-part handshake that only doctors know. Is that not customary?” quipped @Branmiz25.
“Ah yes, that transmits the entire [history of present illness],” replied Dr. Winter.
Jokes aside, the topic is obviously one that touched on a shared experience among healthcare providers, Dr. Winter commented. The Twitter thread she started just “blew up.”
That’s typically a sign that the Tweet is relatable for a lot of people, she said.
“It’s definitely something that all of us as care providers and as patients understand. It’s a funny, awkward thing that can really change an interaction, so we probably all feel pretty strongly about our experiences related to that,” she added.
The debate begs the question: Is there a duty or ethical reason to disclose?
“I definitely think it is very reasonable to disclose that one is a medical professional to another doctor,” medical ethicist Charlotte Blease, PhD, said in an interview. “There are good reasons to believe doing so might make a difference to the quality of communication and transparency.”
If the ability to use medical terminology or jargon more freely improves patient understanding, autonomy, and shared decision-making, then it may be of benefit, said Dr. Blease, a Keane OpenNotes Scholar at Beth Israel Deaconess Medical Center in Boston.
“Since doctors should strive to communicate effectively with every patient and to respect their unique needs and level of understanding, then I see no reason to deny that one is a medic,” she added.”
Knowing how to share the information is another story.
“This is something that affects all of us as physicians — we’re going to be patients at some point, right?” Dr. Winter commented. “But I don’t think how to disclose that is something that was ever brought up in my medical training.”
“Maybe there should just be a discussion of this one day when people are in medical school — maybe in a professionalism course — to broach this topic or look at if there’s any literature on outcomes related to disclosure of status or what are best practices,” she suggested.
A version of this article first appeared on Medscape.com.
Unvaccinated people 20 times more likely to die from COVID: Texas study
During the month of September, , according to a new study from the Texas Department of State Health Services.
The data also showed that unvaccinated people were 13 times more likely to test positive for COVID-19 than people who were fully vaccinated.
“This analysis quantifies what we’ve known for months,” Jennifer Shuford, MD, the state’s chief epidemiologist, told The Dallas Morning News.
“The COVID-19 vaccines are doing an excellent job of protecting people from getting sick and from dying from COVID-19,” she said. “Vaccination remains the best way to keep yourself and the people close to you safe from this deadly disease.”
As part of the study, researchers analyzed electronic lab reports, death certificates, and state immunization records, with a particular focus on September when the contagious Delta variant surged across Texas. The research marks the state’s first statistical analysis of COVID-19 vaccinations in Texas and the effects, the newspaper reported.
The protective effect of vaccination was most noticeable among younger groups. During September, the risk of COVID-19 death was 23 times higher in unvaccinated people in their 30s and 55 times higher for unvaccinated people in their 40s.
In addition, there were fewer than 10 COVID-19 deaths in September among fully vaccinated people between ages 18-29, as compared with 339 deaths among unvaccinated people in the same age group.
Then, looking at a longer time period -- from Jan. 15 to Oct. 1 -- the researchers found that unvaccinated people were 45 times more likely to contract COVID-19 than fully vaccinated people. The protective effect of vaccination against infection was strong across all adult age groups but greatest among ages 12-17.
“All authorized COVID-19 vaccines in the United States are highly effective at protecting people from getting sick or severely ill with COVID-19, including those infected with Delta and other known variants,” the study authors wrote. “Real world data from Texas clearly shows these benefits.”
About 15.6 million people in Texas have been fully vaccinated against COVID-19 in a state of about 29 million residents, according to state data. About 66% of the population has received at least one dose, while 58% is fully vaccinated.
A version of this article first appeared on WebMD.com.
During the month of September, , according to a new study from the Texas Department of State Health Services.
The data also showed that unvaccinated people were 13 times more likely to test positive for COVID-19 than people who were fully vaccinated.
“This analysis quantifies what we’ve known for months,” Jennifer Shuford, MD, the state’s chief epidemiologist, told The Dallas Morning News.
“The COVID-19 vaccines are doing an excellent job of protecting people from getting sick and from dying from COVID-19,” she said. “Vaccination remains the best way to keep yourself and the people close to you safe from this deadly disease.”
As part of the study, researchers analyzed electronic lab reports, death certificates, and state immunization records, with a particular focus on September when the contagious Delta variant surged across Texas. The research marks the state’s first statistical analysis of COVID-19 vaccinations in Texas and the effects, the newspaper reported.
The protective effect of vaccination was most noticeable among younger groups. During September, the risk of COVID-19 death was 23 times higher in unvaccinated people in their 30s and 55 times higher for unvaccinated people in their 40s.
In addition, there were fewer than 10 COVID-19 deaths in September among fully vaccinated people between ages 18-29, as compared with 339 deaths among unvaccinated people in the same age group.
Then, looking at a longer time period -- from Jan. 15 to Oct. 1 -- the researchers found that unvaccinated people were 45 times more likely to contract COVID-19 than fully vaccinated people. The protective effect of vaccination against infection was strong across all adult age groups but greatest among ages 12-17.
“All authorized COVID-19 vaccines in the United States are highly effective at protecting people from getting sick or severely ill with COVID-19, including those infected with Delta and other known variants,” the study authors wrote. “Real world data from Texas clearly shows these benefits.”
About 15.6 million people in Texas have been fully vaccinated against COVID-19 in a state of about 29 million residents, according to state data. About 66% of the population has received at least one dose, while 58% is fully vaccinated.
A version of this article first appeared on WebMD.com.
During the month of September, , according to a new study from the Texas Department of State Health Services.
The data also showed that unvaccinated people were 13 times more likely to test positive for COVID-19 than people who were fully vaccinated.
“This analysis quantifies what we’ve known for months,” Jennifer Shuford, MD, the state’s chief epidemiologist, told The Dallas Morning News.
“The COVID-19 vaccines are doing an excellent job of protecting people from getting sick and from dying from COVID-19,” she said. “Vaccination remains the best way to keep yourself and the people close to you safe from this deadly disease.”
As part of the study, researchers analyzed electronic lab reports, death certificates, and state immunization records, with a particular focus on September when the contagious Delta variant surged across Texas. The research marks the state’s first statistical analysis of COVID-19 vaccinations in Texas and the effects, the newspaper reported.
The protective effect of vaccination was most noticeable among younger groups. During September, the risk of COVID-19 death was 23 times higher in unvaccinated people in their 30s and 55 times higher for unvaccinated people in their 40s.
In addition, there were fewer than 10 COVID-19 deaths in September among fully vaccinated people between ages 18-29, as compared with 339 deaths among unvaccinated people in the same age group.
Then, looking at a longer time period -- from Jan. 15 to Oct. 1 -- the researchers found that unvaccinated people were 45 times more likely to contract COVID-19 than fully vaccinated people. The protective effect of vaccination against infection was strong across all adult age groups but greatest among ages 12-17.
“All authorized COVID-19 vaccines in the United States are highly effective at protecting people from getting sick or severely ill with COVID-19, including those infected with Delta and other known variants,” the study authors wrote. “Real world data from Texas clearly shows these benefits.”
About 15.6 million people in Texas have been fully vaccinated against COVID-19 in a state of about 29 million residents, according to state data. About 66% of the population has received at least one dose, while 58% is fully vaccinated.
A version of this article first appeared on WebMD.com.
Essential Updates on Lung Cancer Biomarkers From CHEST 2021
Dr Nichole Tanner, associate professor at the University of South Carolina, discusses new data on lung cancer biomarker testing from CHEST 2021.
First, Dr Tanner shares two abstracts that discuss how endobronchial ultrasound (EBUS) demonstrated high-success yields in next-generation sequencing. One of the abstracts looked at EBUS transbronchial needle aspiration in patients with lung cancer, whereas the other examined EBUS-guided fine needle aspiration in patients with nonsquamous non–small cell lung cancer.
Next, she discusses a small study that demonstrated the ability of the Percepta Genomic Sequencing Classifier to successfully reclassify patients in whom bronchoscopy was nondiagnostic. About half of the patients were either down-classified to low risk, which can help to avoid additional invasive procedures, or up-classified to high risk, which can inform next steps for intervention.
Dr Tanner concludes by reviewing a retrospective analysis of the PANOPTIC clinical trial, which used the Nodify CDT test to evaluate a panel of seven lung cancer–associated autoantibodies in study patients who had incidentally discovered indeterminate pulmonary nodules. The autoantibodies were able to detect likely malignant nodules regardless of lung cancer type, histology, or stage.
--
Nichole T. Tanner, MD, MSCR, FCCP, Associate Professor, Department of Medicine, Medical University of South Carolina, Charleston, South Carolina
Nichole T. Tanner, MD, MSCR, FCCP, has disclosed no relevant financial relationships.
Dr Nichole Tanner, associate professor at the University of South Carolina, discusses new data on lung cancer biomarker testing from CHEST 2021.
First, Dr Tanner shares two abstracts that discuss how endobronchial ultrasound (EBUS) demonstrated high-success yields in next-generation sequencing. One of the abstracts looked at EBUS transbronchial needle aspiration in patients with lung cancer, whereas the other examined EBUS-guided fine needle aspiration in patients with nonsquamous non–small cell lung cancer.
Next, she discusses a small study that demonstrated the ability of the Percepta Genomic Sequencing Classifier to successfully reclassify patients in whom bronchoscopy was nondiagnostic. About half of the patients were either down-classified to low risk, which can help to avoid additional invasive procedures, or up-classified to high risk, which can inform next steps for intervention.
Dr Tanner concludes by reviewing a retrospective analysis of the PANOPTIC clinical trial, which used the Nodify CDT test to evaluate a panel of seven lung cancer–associated autoantibodies in study patients who had incidentally discovered indeterminate pulmonary nodules. The autoantibodies were able to detect likely malignant nodules regardless of lung cancer type, histology, or stage.
--
Nichole T. Tanner, MD, MSCR, FCCP, Associate Professor, Department of Medicine, Medical University of South Carolina, Charleston, South Carolina
Nichole T. Tanner, MD, MSCR, FCCP, has disclosed no relevant financial relationships.
Dr Nichole Tanner, associate professor at the University of South Carolina, discusses new data on lung cancer biomarker testing from CHEST 2021.
First, Dr Tanner shares two abstracts that discuss how endobronchial ultrasound (EBUS) demonstrated high-success yields in next-generation sequencing. One of the abstracts looked at EBUS transbronchial needle aspiration in patients with lung cancer, whereas the other examined EBUS-guided fine needle aspiration in patients with nonsquamous non–small cell lung cancer.
Next, she discusses a small study that demonstrated the ability of the Percepta Genomic Sequencing Classifier to successfully reclassify patients in whom bronchoscopy was nondiagnostic. About half of the patients were either down-classified to low risk, which can help to avoid additional invasive procedures, or up-classified to high risk, which can inform next steps for intervention.
Dr Tanner concludes by reviewing a retrospective analysis of the PANOPTIC clinical trial, which used the Nodify CDT test to evaluate a panel of seven lung cancer–associated autoantibodies in study patients who had incidentally discovered indeterminate pulmonary nodules. The autoantibodies were able to detect likely malignant nodules regardless of lung cancer type, histology, or stage.
--
Nichole T. Tanner, MD, MSCR, FCCP, Associate Professor, Department of Medicine, Medical University of South Carolina, Charleston, South Carolina
Nichole T. Tanner, MD, MSCR, FCCP, has disclosed no relevant financial relationships.
Children and COVID: New cases up again after dropping for 8 weeks
As children aged 5-11 years began to receive the first officially approved doses of COVID-19 vaccine, new pediatric cases increased after 8 consecutive weeks of declines, according to the American Academy of Pediatrics and the Children’s Hospital Association.
Weekly cases peaked at almost 252,000 in early September and then dropped for 8 straight weeks before this latest rise, the AAP and the CHA said in their weekly COVID report, which is based on data reported by 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.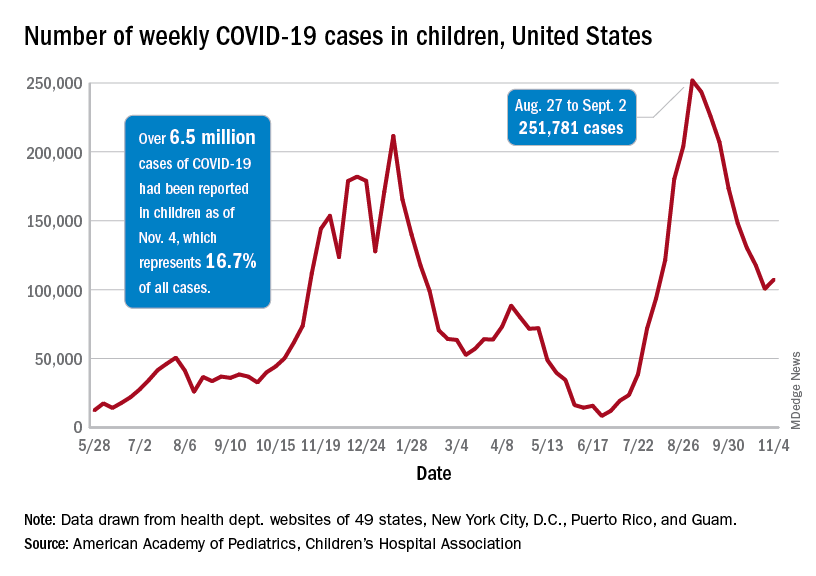
The end of that 8-week drop, unfortunately, allowed another streak to continue: New cases have been above 100,000 for 13 consecutive weeks, the AAP and CHA noted.
The cumulative COVID count in children as of Nov. 4 was 6.5 million, the AAP/CHA said, although that figure does not fully cover Alabama, Nebraska, and Texas, which stopped public reporting over the summer. The Centers for Disease Control and Prevention, with input from all states and territories, puts the total through Nov. 8 at almost 5.7 million cases in children under 18 years of age, while most states define a child as someone aged 0-19 years.
As for the newest group of vaccinees, the CDC said that “updated vaccination data for 5-11 year-olds will be added to COVID Data Tracker later this week,” meaning the week of Nov. 7-13. Currently available data, however, show that almost 157,000 children under age 12 initiated vaccination in the 14 days ending Nov. 8, which was more than those aged 12-15 and 16-17 years combined (127,000).
Among those older groups, the CDC reports that 57.1% of 12- to 15-year-olds have received at least one dose and 47.9% are fully vaccinated, while 64.0% of those aged 16-17 have gotten at least one dose and 55.2% are fully vaccinated. Altogether, about 13.9 million children under age 18 have gotten at least one dose and almost 11.6 million are fully vaccinated, according to the CDC.
As children aged 5-11 years began to receive the first officially approved doses of COVID-19 vaccine, new pediatric cases increased after 8 consecutive weeks of declines, according to the American Academy of Pediatrics and the Children’s Hospital Association.
Weekly cases peaked at almost 252,000 in early September and then dropped for 8 straight weeks before this latest rise, the AAP and the CHA said in their weekly COVID report, which is based on data reported by 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.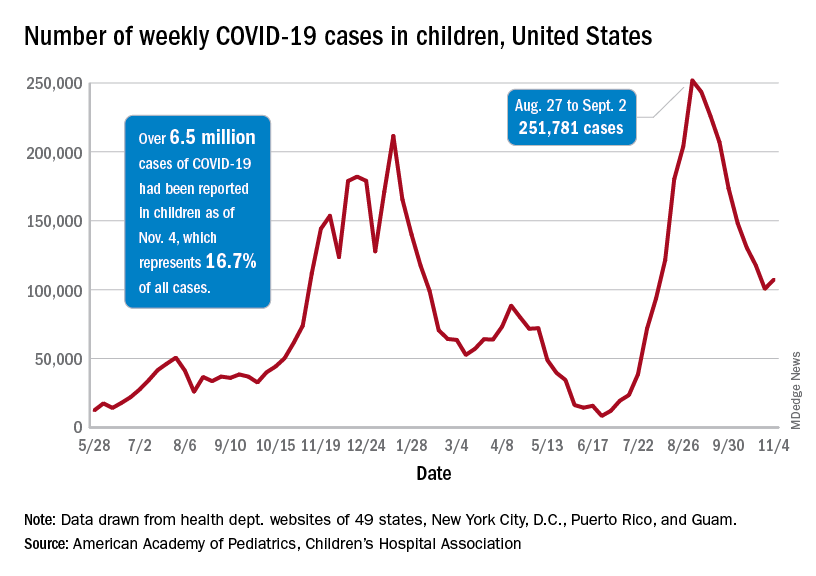
The end of that 8-week drop, unfortunately, allowed another streak to continue: New cases have been above 100,000 for 13 consecutive weeks, the AAP and CHA noted.
The cumulative COVID count in children as of Nov. 4 was 6.5 million, the AAP/CHA said, although that figure does not fully cover Alabama, Nebraska, and Texas, which stopped public reporting over the summer. The Centers for Disease Control and Prevention, with input from all states and territories, puts the total through Nov. 8 at almost 5.7 million cases in children under 18 years of age, while most states define a child as someone aged 0-19 years.
As for the newest group of vaccinees, the CDC said that “updated vaccination data for 5-11 year-olds will be added to COVID Data Tracker later this week,” meaning the week of Nov. 7-13. Currently available data, however, show that almost 157,000 children under age 12 initiated vaccination in the 14 days ending Nov. 8, which was more than those aged 12-15 and 16-17 years combined (127,000).
Among those older groups, the CDC reports that 57.1% of 12- to 15-year-olds have received at least one dose and 47.9% are fully vaccinated, while 64.0% of those aged 16-17 have gotten at least one dose and 55.2% are fully vaccinated. Altogether, about 13.9 million children under age 18 have gotten at least one dose and almost 11.6 million are fully vaccinated, according to the CDC.
As children aged 5-11 years began to receive the first officially approved doses of COVID-19 vaccine, new pediatric cases increased after 8 consecutive weeks of declines, according to the American Academy of Pediatrics and the Children’s Hospital Association.
Weekly cases peaked at almost 252,000 in early September and then dropped for 8 straight weeks before this latest rise, the AAP and the CHA said in their weekly COVID report, which is based on data reported by 49 states (excluding New York), the District of Columbia, New York City, Puerto Rico, and Guam.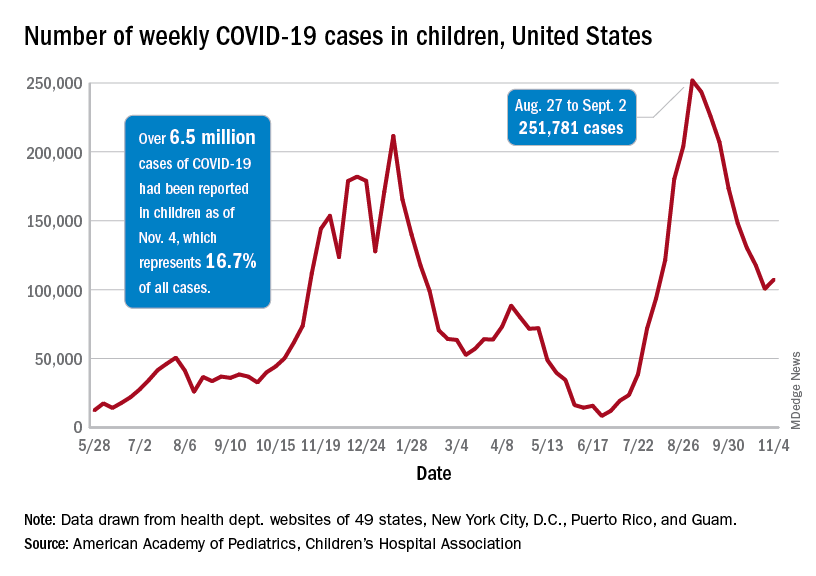
The end of that 8-week drop, unfortunately, allowed another streak to continue: New cases have been above 100,000 for 13 consecutive weeks, the AAP and CHA noted.
The cumulative COVID count in children as of Nov. 4 was 6.5 million, the AAP/CHA said, although that figure does not fully cover Alabama, Nebraska, and Texas, which stopped public reporting over the summer. The Centers for Disease Control and Prevention, with input from all states and territories, puts the total through Nov. 8 at almost 5.7 million cases in children under 18 years of age, while most states define a child as someone aged 0-19 years.
As for the newest group of vaccinees, the CDC said that “updated vaccination data for 5-11 year-olds will be added to COVID Data Tracker later this week,” meaning the week of Nov. 7-13. Currently available data, however, show that almost 157,000 children under age 12 initiated vaccination in the 14 days ending Nov. 8, which was more than those aged 12-15 and 16-17 years combined (127,000).
Among those older groups, the CDC reports that 57.1% of 12- to 15-year-olds have received at least one dose and 47.9% are fully vaccinated, while 64.0% of those aged 16-17 have gotten at least one dose and 55.2% are fully vaccinated. Altogether, about 13.9 million children under age 18 have gotten at least one dose and almost 11.6 million are fully vaccinated, according to the CDC.
Electronic ‘nose’ sniffs out sarcoidosis
An electronic nose (eNose) that measures volatile organic compounds (VOCs) emitted from the lungs successfully distinguished sarcoidosis from interstitial lung disease (ILD) and healthy controls, according to a report in the journal CHEST.
The approach has the potential to generate clinical data that can’t be achieved through other noninvasive means, such as the serum biomarker soluble interleukin-2 receptor (sIL-2R). sIL-2R is often used to track disease activity, but it isn’t specific for diagnosing sarcoidosis, and it isn’t available worldwide.
Sarcoidosis is a granulomatous inflammatory disease with no known cause and can affect most organs, but an estimated 89%-99% of cases affect the lungs. There is no simple noninvasive diagnostic test, leaving physicians to rely on clinical features, biopsies to obtain tissue pathology, and the ruling out of other granulomatous diagnoses.
The challenge is more difficult because sarcoidosis is a heterogeneous disease, with great variation in the number of organs affected, severity, rate of progression, and response to therapy.
Previous researchers have used VOCs in an attempt to diagnose diseases, since the compounds reflect pathophysiological processes. Gas chromatography/mass spectrometry (GCMS) is one method to identify the individual VOCs, but the process is time consuming and complex. Some nevertheless showed potential in sarcoidosis, but failed to reproduce their performance in validation cohorts.
In the new study, a cross-sectional analysis showed that exhaled breath analysis using an eNose had excellent sensitivity and specificity for distinguishing sarcoidosis from ILD and healthy controls, and identified sarcoidosis regardless of pulmonary involvement, pulmonary fibrosis, multiple organ involvement, immunosuppressive treatment, or whether or not pathology supported the diagnosis.
The eNose technology produces a “breath-print” after combining information from a broad range of VOCs. The information originates from an array of metal-oxide semiconductor sensors with partial specificity that artificial intelligence processes to discern patterns. Overall, the system functions similarly to the mammalian olfactory system. The artificial intelligence instead views it as a “breath-print” that it can compare against previously learned patterns.
“It is a quite easy, simple, and quick procedure, which is noninvasive. We can collect a lot of data from the VOCs in the exhaled breath because there are several sensors that cross-react. We can create breath profiles and group patients to see if profiles differ. Ultimately, we can use the profiles to diagnose or detect disease in the earlier stage and more accurately,” said Iris van der Sar, MD. Dr. van der Sar is the lead author on the study and a PhD candidate at Erasmus Medical Center in Rotterdam.
The study requires further prospective validation, but the technology could have important clinical benefits, said senior author and principal investigator Marlies Wijsenbeek, MD, PhD, pulmonologist and head of the Interstitial Lung Disease Center at Erasmus Medical Center. “If we in future can avoid a biopsy, that would be most attractive,” said Dr. Wijsenbeek.
“We hope to come to a point-of-care device that can be used to facilitate early diagnosis at low burden for the patient and health care system,” said Karen Moor, MD, PhD, and post-doc on this project. The researchers also hope to determine if the eNose can help evaluate a patient’s response to therapy.
Studies of eNose technology in other chronic diseases have shown promising results, but not all results have been validated yet in independent or external cohorts.
The current study included 569 outpatients, 252 with sarcoidosis and 317 with ILD, along with 48 healthy controls. The researchers constructed a training set using 168 patients with sarcoidosis and 32 healthy controls, and a validation set using 84 patients with sarcoidosis and 16 healthy controls. The eNose differentiated between patients and controls in both groups, with an area under the curve of 1.00 for each regardless of pulmonary involvement or treatment.
It also distinguished those with sarcoidosis and pulmonary involvement from those with ILD, with an AUC of 0.90 (95% confidence interval, 0.87-0.94) in the training set, and an AUC of 0.87 (95% CI, 0.82-0.93) in the validation set.
It differentiated between pulmonary sarcoidosis and hypersensitivity pneumonitis in the training set (AUC 0.95; 95% CI, 0.90-0.99) and the validation set (AUC, 0.88; 95% CI, 0.75-1.00).
The study received no funding. Dr. Wijsenbeek, Dr. van der Sar, and Dr. Moor have no relevant financial disclosures.
An electronic nose (eNose) that measures volatile organic compounds (VOCs) emitted from the lungs successfully distinguished sarcoidosis from interstitial lung disease (ILD) and healthy controls, according to a report in the journal CHEST.
The approach has the potential to generate clinical data that can’t be achieved through other noninvasive means, such as the serum biomarker soluble interleukin-2 receptor (sIL-2R). sIL-2R is often used to track disease activity, but it isn’t specific for diagnosing sarcoidosis, and it isn’t available worldwide.
Sarcoidosis is a granulomatous inflammatory disease with no known cause and can affect most organs, but an estimated 89%-99% of cases affect the lungs. There is no simple noninvasive diagnostic test, leaving physicians to rely on clinical features, biopsies to obtain tissue pathology, and the ruling out of other granulomatous diagnoses.
The challenge is more difficult because sarcoidosis is a heterogeneous disease, with great variation in the number of organs affected, severity, rate of progression, and response to therapy.
Previous researchers have used VOCs in an attempt to diagnose diseases, since the compounds reflect pathophysiological processes. Gas chromatography/mass spectrometry (GCMS) is one method to identify the individual VOCs, but the process is time consuming and complex. Some nevertheless showed potential in sarcoidosis, but failed to reproduce their performance in validation cohorts.
In the new study, a cross-sectional analysis showed that exhaled breath analysis using an eNose had excellent sensitivity and specificity for distinguishing sarcoidosis from ILD and healthy controls, and identified sarcoidosis regardless of pulmonary involvement, pulmonary fibrosis, multiple organ involvement, immunosuppressive treatment, or whether or not pathology supported the diagnosis.
The eNose technology produces a “breath-print” after combining information from a broad range of VOCs. The information originates from an array of metal-oxide semiconductor sensors with partial specificity that artificial intelligence processes to discern patterns. Overall, the system functions similarly to the mammalian olfactory system. The artificial intelligence instead views it as a “breath-print” that it can compare against previously learned patterns.
“It is a quite easy, simple, and quick procedure, which is noninvasive. We can collect a lot of data from the VOCs in the exhaled breath because there are several sensors that cross-react. We can create breath profiles and group patients to see if profiles differ. Ultimately, we can use the profiles to diagnose or detect disease in the earlier stage and more accurately,” said Iris van der Sar, MD. Dr. van der Sar is the lead author on the study and a PhD candidate at Erasmus Medical Center in Rotterdam.
The study requires further prospective validation, but the technology could have important clinical benefits, said senior author and principal investigator Marlies Wijsenbeek, MD, PhD, pulmonologist and head of the Interstitial Lung Disease Center at Erasmus Medical Center. “If we in future can avoid a biopsy, that would be most attractive,” said Dr. Wijsenbeek.
“We hope to come to a point-of-care device that can be used to facilitate early diagnosis at low burden for the patient and health care system,” said Karen Moor, MD, PhD, and post-doc on this project. The researchers also hope to determine if the eNose can help evaluate a patient’s response to therapy.
Studies of eNose technology in other chronic diseases have shown promising results, but not all results have been validated yet in independent or external cohorts.
The current study included 569 outpatients, 252 with sarcoidosis and 317 with ILD, along with 48 healthy controls. The researchers constructed a training set using 168 patients with sarcoidosis and 32 healthy controls, and a validation set using 84 patients with sarcoidosis and 16 healthy controls. The eNose differentiated between patients and controls in both groups, with an area under the curve of 1.00 for each regardless of pulmonary involvement or treatment.
It also distinguished those with sarcoidosis and pulmonary involvement from those with ILD, with an AUC of 0.90 (95% confidence interval, 0.87-0.94) in the training set, and an AUC of 0.87 (95% CI, 0.82-0.93) in the validation set.
It differentiated between pulmonary sarcoidosis and hypersensitivity pneumonitis in the training set (AUC 0.95; 95% CI, 0.90-0.99) and the validation set (AUC, 0.88; 95% CI, 0.75-1.00).
The study received no funding. Dr. Wijsenbeek, Dr. van der Sar, and Dr. Moor have no relevant financial disclosures.
An electronic nose (eNose) that measures volatile organic compounds (VOCs) emitted from the lungs successfully distinguished sarcoidosis from interstitial lung disease (ILD) and healthy controls, according to a report in the journal CHEST.
The approach has the potential to generate clinical data that can’t be achieved through other noninvasive means, such as the serum biomarker soluble interleukin-2 receptor (sIL-2R). sIL-2R is often used to track disease activity, but it isn’t specific for diagnosing sarcoidosis, and it isn’t available worldwide.
Sarcoidosis is a granulomatous inflammatory disease with no known cause and can affect most organs, but an estimated 89%-99% of cases affect the lungs. There is no simple noninvasive diagnostic test, leaving physicians to rely on clinical features, biopsies to obtain tissue pathology, and the ruling out of other granulomatous diagnoses.
The challenge is more difficult because sarcoidosis is a heterogeneous disease, with great variation in the number of organs affected, severity, rate of progression, and response to therapy.
Previous researchers have used VOCs in an attempt to diagnose diseases, since the compounds reflect pathophysiological processes. Gas chromatography/mass spectrometry (GCMS) is one method to identify the individual VOCs, but the process is time consuming and complex. Some nevertheless showed potential in sarcoidosis, but failed to reproduce their performance in validation cohorts.
In the new study, a cross-sectional analysis showed that exhaled breath analysis using an eNose had excellent sensitivity and specificity for distinguishing sarcoidosis from ILD and healthy controls, and identified sarcoidosis regardless of pulmonary involvement, pulmonary fibrosis, multiple organ involvement, immunosuppressive treatment, or whether or not pathology supported the diagnosis.
The eNose technology produces a “breath-print” after combining information from a broad range of VOCs. The information originates from an array of metal-oxide semiconductor sensors with partial specificity that artificial intelligence processes to discern patterns. Overall, the system functions similarly to the mammalian olfactory system. The artificial intelligence instead views it as a “breath-print” that it can compare against previously learned patterns.
“It is a quite easy, simple, and quick procedure, which is noninvasive. We can collect a lot of data from the VOCs in the exhaled breath because there are several sensors that cross-react. We can create breath profiles and group patients to see if profiles differ. Ultimately, we can use the profiles to diagnose or detect disease in the earlier stage and more accurately,” said Iris van der Sar, MD. Dr. van der Sar is the lead author on the study and a PhD candidate at Erasmus Medical Center in Rotterdam.
The study requires further prospective validation, but the technology could have important clinical benefits, said senior author and principal investigator Marlies Wijsenbeek, MD, PhD, pulmonologist and head of the Interstitial Lung Disease Center at Erasmus Medical Center. “If we in future can avoid a biopsy, that would be most attractive,” said Dr. Wijsenbeek.
“We hope to come to a point-of-care device that can be used to facilitate early diagnosis at low burden for the patient and health care system,” said Karen Moor, MD, PhD, and post-doc on this project. The researchers also hope to determine if the eNose can help evaluate a patient’s response to therapy.
Studies of eNose technology in other chronic diseases have shown promising results, but not all results have been validated yet in independent or external cohorts.
The current study included 569 outpatients, 252 with sarcoidosis and 317 with ILD, along with 48 healthy controls. The researchers constructed a training set using 168 patients with sarcoidosis and 32 healthy controls, and a validation set using 84 patients with sarcoidosis and 16 healthy controls. The eNose differentiated between patients and controls in both groups, with an area under the curve of 1.00 for each regardless of pulmonary involvement or treatment.
It also distinguished those with sarcoidosis and pulmonary involvement from those with ILD, with an AUC of 0.90 (95% confidence interval, 0.87-0.94) in the training set, and an AUC of 0.87 (95% CI, 0.82-0.93) in the validation set.
It differentiated between pulmonary sarcoidosis and hypersensitivity pneumonitis in the training set (AUC 0.95; 95% CI, 0.90-0.99) and the validation set (AUC, 0.88; 95% CI, 0.75-1.00).
The study received no funding. Dr. Wijsenbeek, Dr. van der Sar, and Dr. Moor have no relevant financial disclosures.
FROM CHEST
Early trials underway to test mushrooms as COVID treatment
The U.S. Food and Drug Administration (FDA) approved the MACH-19 trials (the acronym for Mushrooms and Chinese Herbs for COVID-19) after researchers applied for approval in April.
The first two phase 1 randomized, double-blind, placebo-controlled trials have begun at UCLA and the University of California San Diego to treat COVID-19 patients quarantining at home with mild to moderate symptoms. A third trial is investigating the use of medicinal mushrooms as an adjuvant to COVID-19 vaccines.
The researchers have also launched a fourth trial testing the mushrooms against placebo as an adjunct to a COVID booster shot. It looks at the effect in people who have comorbidities that would reduce their vaccine response. An article in JAMA described the trials.
The two mushroom varieties being tested — turkey tail and agarikon — are available as over-the-counter supplements, according to the report. They are a separate class from hallucinogenic or “magic” mushrooms being tested for other uses in medicine.
“They are not even as psychoactive as a cup of tea,” Gordon Saxe, MD, PhD, MPH, principal investigator for the MACH-19 trials, told this news organization.
For each of the MACH-19 treatment trials, researchers plan to recruit 66 people who are quarantined at home with mild to moderate COVID-19 symptoms. Participants will be randomly assigned either to receive the mushroom combination, the Chinese herbs, or a placebo for 2 weeks, according to the JAMA paper.
D. Craig Hopp, PhD, deputy director of the division of extramural research at the National Center for Complementary and Integrative Health (NCCIH), told JAMA in an interview that he was “mildly concerned” about using mushrooms to treat people with active SARS-CoV-2 infection.
“We know that a cytokine storm poses the greatest risk of COVID mortality, not the virus itself,” Dr. Hopp said. “The danger is that an immune-stimulating agent like mushrooms might supercharge an individual’s immune response, leading to a cytokine storm.”
Stephen Wilson, PhD, an immunologist who consulted on the trials when he was chief operating officer of the La Jolla Institute for Immunology, says in the JAMA article that a cytokine storm is unlikely for these patients because the mushroom components “don’t mimic inflammatory cytokines.” Dr. Wilson is now chief innovations officer at Statera Biopharma.
“We think the mushrooms increase the number of immunologic opportunities to better see and respond to a specific threat. In the doses used, the mushrooms perturb the immune system in a good way but fall far short of driving hyper or sustained inflammation,” Dr. Wilson said.
Dr. Saxe said the FDA process was extensive and rigorous and FDA investigators also asked about potential cytokine storms before approving the trials. Cytokine storm is not an issue with a healthy response, Dr. Saxe pointed out. It’s a response that’s not balanced or modulated.
“Mushrooms are immunomodulatory,” he said. “In some ways they very specifically enhance immunity. In other ways they calm down overimmunity.” Dr. Saxe noted that they did a sentinel study for the storm potential “and we didn’t see any evidence for it.”
“Not a crazy concept”
Dr. Saxe pointed out that one of the mushrooms in the combo they use — agarikon — was used to treat pulmonary infections 2,300 years ago.
“Hippocrates, the father of western medicine, used mushrooms,” he said. “Penicillin comes from fungi. It’s not a crazy concept. Most people who oppose this or are skeptics — to some extent, it’s a lack of information.”
Dr. Saxe explained that there are receptors on human cells that bind specific mushroom polysaccharides.
“There’s a hand-in-glove fit there,” Dr. Saxe said, and that’s one way mushrooms can modulate immune cell behavior, which could have an effect against SARS-CoV-2.
Daniel Kuritzkes, MD, chief of the division of infectious diseases at Brigham and Women’s Hospital in Boston, who was not part of the study, told this news organization that he wasn’t surprised the FDA approved moving forward with the trials.
“As long as you can demonstrate that there is a rationale for doing the trial and that you have some safety data or a plan to collect safety data, they are fairly liberal about doing early-phase studies. It would be a much different issue, I think, if they were proposing to do a study for actual licensing or approval of a drug,” Dr. Kuritzkes said.
As yet unanswered, he noted, is which component of the mushrooms or herbs is having the effect. It will be a challenge, he said, to know from one batch of the compound to the next that you have the same amount of material and that it’s going to have the same potency among lots.
Another challenge is how the mushrooms and herbs might interact with other therapies, Dr. Kuritzkes said.
He gave the example of St. John’s Wort, which has been problematic in HIV treatment.
“If someone is on certain HIV medicines and they also are taking St. John’s Wort, they basically are causing the liver to eat up the HIV drug and they don’t get adequate levels of the drug,” he said.
Though there are many challenges ahead, Dr. Kuritzkes acknowledged, but added that “this is a great starting point.”
He, too, pointed out that many traditional medicines were discovered from plants.
“The most famous of these is quinine, which came from cinchona bark that was used to treat malaria.” Dr. Kuritzkes said. Digitalis, often used to treat heart failure, comes from the fox glove plant, he added.
He said it’s important to remember that “people shouldn’t be seeking experimental therapies in place of proven therapies, they should be thinking of them in addition to proven therapies.»
A co-author reports an investment in the dietary supplement company Mycomedica Life Sciences, for which he also serves as an unpaid scientific adviser. Another co-author is a medical consultant for Evergreen Herbs and Medical Supplies. Dr. Hopp, Dr. Saxe, and Dr. Wilson have disclosed no relevant financial relationships. Dr. Kuritzkes consults for Merck, Gilead, and GlaxoSmithKline.
The U.S. Food and Drug Administration (FDA) approved the MACH-19 trials (the acronym for Mushrooms and Chinese Herbs for COVID-19) after researchers applied for approval in April.
The first two phase 1 randomized, double-blind, placebo-controlled trials have begun at UCLA and the University of California San Diego to treat COVID-19 patients quarantining at home with mild to moderate symptoms. A third trial is investigating the use of medicinal mushrooms as an adjuvant to COVID-19 vaccines.
The researchers have also launched a fourth trial testing the mushrooms against placebo as an adjunct to a COVID booster shot. It looks at the effect in people who have comorbidities that would reduce their vaccine response. An article in JAMA described the trials.
The two mushroom varieties being tested — turkey tail and agarikon — are available as over-the-counter supplements, according to the report. They are a separate class from hallucinogenic or “magic” mushrooms being tested for other uses in medicine.
“They are not even as psychoactive as a cup of tea,” Gordon Saxe, MD, PhD, MPH, principal investigator for the MACH-19 trials, told this news organization.
For each of the MACH-19 treatment trials, researchers plan to recruit 66 people who are quarantined at home with mild to moderate COVID-19 symptoms. Participants will be randomly assigned either to receive the mushroom combination, the Chinese herbs, or a placebo for 2 weeks, according to the JAMA paper.
D. Craig Hopp, PhD, deputy director of the division of extramural research at the National Center for Complementary and Integrative Health (NCCIH), told JAMA in an interview that he was “mildly concerned” about using mushrooms to treat people with active SARS-CoV-2 infection.
“We know that a cytokine storm poses the greatest risk of COVID mortality, not the virus itself,” Dr. Hopp said. “The danger is that an immune-stimulating agent like mushrooms might supercharge an individual’s immune response, leading to a cytokine storm.”
Stephen Wilson, PhD, an immunologist who consulted on the trials when he was chief operating officer of the La Jolla Institute for Immunology, says in the JAMA article that a cytokine storm is unlikely for these patients because the mushroom components “don’t mimic inflammatory cytokines.” Dr. Wilson is now chief innovations officer at Statera Biopharma.
“We think the mushrooms increase the number of immunologic opportunities to better see and respond to a specific threat. In the doses used, the mushrooms perturb the immune system in a good way but fall far short of driving hyper or sustained inflammation,” Dr. Wilson said.
Dr. Saxe said the FDA process was extensive and rigorous and FDA investigators also asked about potential cytokine storms before approving the trials. Cytokine storm is not an issue with a healthy response, Dr. Saxe pointed out. It’s a response that’s not balanced or modulated.
“Mushrooms are immunomodulatory,” he said. “In some ways they very specifically enhance immunity. In other ways they calm down overimmunity.” Dr. Saxe noted that they did a sentinel study for the storm potential “and we didn’t see any evidence for it.”
“Not a crazy concept”
Dr. Saxe pointed out that one of the mushrooms in the combo they use — agarikon — was used to treat pulmonary infections 2,300 years ago.
“Hippocrates, the father of western medicine, used mushrooms,” he said. “Penicillin comes from fungi. It’s not a crazy concept. Most people who oppose this or are skeptics — to some extent, it’s a lack of information.”
Dr. Saxe explained that there are receptors on human cells that bind specific mushroom polysaccharides.
“There’s a hand-in-glove fit there,” Dr. Saxe said, and that’s one way mushrooms can modulate immune cell behavior, which could have an effect against SARS-CoV-2.
Daniel Kuritzkes, MD, chief of the division of infectious diseases at Brigham and Women’s Hospital in Boston, who was not part of the study, told this news organization that he wasn’t surprised the FDA approved moving forward with the trials.
“As long as you can demonstrate that there is a rationale for doing the trial and that you have some safety data or a plan to collect safety data, they are fairly liberal about doing early-phase studies. It would be a much different issue, I think, if they were proposing to do a study for actual licensing or approval of a drug,” Dr. Kuritzkes said.
As yet unanswered, he noted, is which component of the mushrooms or herbs is having the effect. It will be a challenge, he said, to know from one batch of the compound to the next that you have the same amount of material and that it’s going to have the same potency among lots.
Another challenge is how the mushrooms and herbs might interact with other therapies, Dr. Kuritzkes said.
He gave the example of St. John’s Wort, which has been problematic in HIV treatment.
“If someone is on certain HIV medicines and they also are taking St. John’s Wort, they basically are causing the liver to eat up the HIV drug and they don’t get adequate levels of the drug,” he said.
Though there are many challenges ahead, Dr. Kuritzkes acknowledged, but added that “this is a great starting point.”
He, too, pointed out that many traditional medicines were discovered from plants.
“The most famous of these is quinine, which came from cinchona bark that was used to treat malaria.” Dr. Kuritzkes said. Digitalis, often used to treat heart failure, comes from the fox glove plant, he added.
He said it’s important to remember that “people shouldn’t be seeking experimental therapies in place of proven therapies, they should be thinking of them in addition to proven therapies.»
A co-author reports an investment in the dietary supplement company Mycomedica Life Sciences, for which he also serves as an unpaid scientific adviser. Another co-author is a medical consultant for Evergreen Herbs and Medical Supplies. Dr. Hopp, Dr. Saxe, and Dr. Wilson have disclosed no relevant financial relationships. Dr. Kuritzkes consults for Merck, Gilead, and GlaxoSmithKline.
The U.S. Food and Drug Administration (FDA) approved the MACH-19 trials (the acronym for Mushrooms and Chinese Herbs for COVID-19) after researchers applied for approval in April.
The first two phase 1 randomized, double-blind, placebo-controlled trials have begun at UCLA and the University of California San Diego to treat COVID-19 patients quarantining at home with mild to moderate symptoms. A third trial is investigating the use of medicinal mushrooms as an adjuvant to COVID-19 vaccines.
The researchers have also launched a fourth trial testing the mushrooms against placebo as an adjunct to a COVID booster shot. It looks at the effect in people who have comorbidities that would reduce their vaccine response. An article in JAMA described the trials.
The two mushroom varieties being tested — turkey tail and agarikon — are available as over-the-counter supplements, according to the report. They are a separate class from hallucinogenic or “magic” mushrooms being tested for other uses in medicine.
“They are not even as psychoactive as a cup of tea,” Gordon Saxe, MD, PhD, MPH, principal investigator for the MACH-19 trials, told this news organization.
For each of the MACH-19 treatment trials, researchers plan to recruit 66 people who are quarantined at home with mild to moderate COVID-19 symptoms. Participants will be randomly assigned either to receive the mushroom combination, the Chinese herbs, or a placebo for 2 weeks, according to the JAMA paper.
D. Craig Hopp, PhD, deputy director of the division of extramural research at the National Center for Complementary and Integrative Health (NCCIH), told JAMA in an interview that he was “mildly concerned” about using mushrooms to treat people with active SARS-CoV-2 infection.
“We know that a cytokine storm poses the greatest risk of COVID mortality, not the virus itself,” Dr. Hopp said. “The danger is that an immune-stimulating agent like mushrooms might supercharge an individual’s immune response, leading to a cytokine storm.”
Stephen Wilson, PhD, an immunologist who consulted on the trials when he was chief operating officer of the La Jolla Institute for Immunology, says in the JAMA article that a cytokine storm is unlikely for these patients because the mushroom components “don’t mimic inflammatory cytokines.” Dr. Wilson is now chief innovations officer at Statera Biopharma.
“We think the mushrooms increase the number of immunologic opportunities to better see and respond to a specific threat. In the doses used, the mushrooms perturb the immune system in a good way but fall far short of driving hyper or sustained inflammation,” Dr. Wilson said.
Dr. Saxe said the FDA process was extensive and rigorous and FDA investigators also asked about potential cytokine storms before approving the trials. Cytokine storm is not an issue with a healthy response, Dr. Saxe pointed out. It’s a response that’s not balanced or modulated.
“Mushrooms are immunomodulatory,” he said. “In some ways they very specifically enhance immunity. In other ways they calm down overimmunity.” Dr. Saxe noted that they did a sentinel study for the storm potential “and we didn’t see any evidence for it.”
“Not a crazy concept”
Dr. Saxe pointed out that one of the mushrooms in the combo they use — agarikon — was used to treat pulmonary infections 2,300 years ago.
“Hippocrates, the father of western medicine, used mushrooms,” he said. “Penicillin comes from fungi. It’s not a crazy concept. Most people who oppose this or are skeptics — to some extent, it’s a lack of information.”
Dr. Saxe explained that there are receptors on human cells that bind specific mushroom polysaccharides.
“There’s a hand-in-glove fit there,” Dr. Saxe said, and that’s one way mushrooms can modulate immune cell behavior, which could have an effect against SARS-CoV-2.
Daniel Kuritzkes, MD, chief of the division of infectious diseases at Brigham and Women’s Hospital in Boston, who was not part of the study, told this news organization that he wasn’t surprised the FDA approved moving forward with the trials.
“As long as you can demonstrate that there is a rationale for doing the trial and that you have some safety data or a plan to collect safety data, they are fairly liberal about doing early-phase studies. It would be a much different issue, I think, if they were proposing to do a study for actual licensing or approval of a drug,” Dr. Kuritzkes said.
As yet unanswered, he noted, is which component of the mushrooms or herbs is having the effect. It will be a challenge, he said, to know from one batch of the compound to the next that you have the same amount of material and that it’s going to have the same potency among lots.
Another challenge is how the mushrooms and herbs might interact with other therapies, Dr. Kuritzkes said.
He gave the example of St. John’s Wort, which has been problematic in HIV treatment.
“If someone is on certain HIV medicines and they also are taking St. John’s Wort, they basically are causing the liver to eat up the HIV drug and they don’t get adequate levels of the drug,” he said.
Though there are many challenges ahead, Dr. Kuritzkes acknowledged, but added that “this is a great starting point.”
He, too, pointed out that many traditional medicines were discovered from plants.
“The most famous of these is quinine, which came from cinchona bark that was used to treat malaria.” Dr. Kuritzkes said. Digitalis, often used to treat heart failure, comes from the fox glove plant, he added.
He said it’s important to remember that “people shouldn’t be seeking experimental therapies in place of proven therapies, they should be thinking of them in addition to proven therapies.»
A co-author reports an investment in the dietary supplement company Mycomedica Life Sciences, for which he also serves as an unpaid scientific adviser. Another co-author is a medical consultant for Evergreen Herbs and Medical Supplies. Dr. Hopp, Dr. Saxe, and Dr. Wilson have disclosed no relevant financial relationships. Dr. Kuritzkes consults for Merck, Gilead, and GlaxoSmithKline.
FROM JAMA
As constituents clamor for ivermectin, Republican politicians embrace the cause
When state senators in South Carolina held two hearings in September about COVID-19 treatments, they got an earful on the benefits of ivermectin — which many of the lawmakers echoed, sharing experiences of their own loved ones.
The demands for access to the drug were loud and insistent, despite federal regulators’ recent warning against using the drug to treat COVID.
Ivermectin is a generic drug that has been used for decades to treat river blindness, scabies, and even head lice. Veterinarians also use it, in different formulations and dosages, to treat animals for parasites like worms.
At one of the South Carolina hearings, Pressley Stutts III reminded the panel that his father, a prominent GOP leader in the state, had died of COVID a month earlier. He believed ivermectin could have helped him. But doctors at the hospital wouldn’t discuss it.
“I went every bit as far as I could without getting myself thrown in jail trying to save my father’s life,” he told the panel, as lawmakers offered condolences.
“What is going on here?” he asked, with the passion in his voice growing. “My dad’s dead!”
After the pandemic began, scientists launched clinical trials to see if ivermectin could help as a treatment for COVID. Some are still ongoing. But providers in mainstream medicine have rejected it as a COVID treatment, citing the poor quality of the studies to date, and two notorious “preprint” studies that were circulated before they were peer-reviewed, and later taken off the internet because of inaccurate and flawed data.
On Aug. 26, the Centers for Disease Control and Prevention advised clinicians not to use ivermectin, citing insufficient evidence of benefit and pointing out that unauthorized use had led to accidental poisonings. Vaccination, the CDC reiterated, is still the best way to avoid serious illness and death from the coronavirus.
But many Americans remain convinced ivermectin could be beneficial, and some politicians appear to be listening to them.
“If we have medications out here that are working — or seem to be working — I think it’s absolutely horrible that we’re not trying them,” said Republican state Sen. Tom Corbin in South Carolina. He questioned doctors who had come to the Statehouse to counter efforts to move ivermectin into mainstream use.
The doctors challenged the implied insult that they weren’t following best practices: “Any implication that any of us would do anything to withhold effective treatments from our patients is really insulting to our profession,” said Dr. Annie Andrews, a professor at the Medical University of South Carolina who has cared for COVID patients throughout the pandemic.
Instead of listening to the medical consensus, some politicians in states like South Carolina seem to be taking cues from doctors on the fringe. During one September hearing, state senators patched in a call from Dr. Pierre Kory.
Last year, Dr. Kory started a nonprofit called the Front Line COVID-19 Critical Care Alliance, which promotes ivermectin. He said he’s not making money by prescribing the drug, though the nonprofit does solicit donations and has not yet filed required financial documents with the IRS.
Dr. Kory acknowledged his medical opinions have landed him on “an island.”
He first testified about ivermectin to a U.S. Senate committee in December. That video went viral. Although it was taken down by YouTube, his Senate testimony prompted patients across the country to ask for ivermectin when they fell ill.
By late August, outpatient prescriptions had jumped 24-fold. Calls to poison control hotlines had tripled, mostly related to people taking ivermectin formulations meant for livestock.
Dr. Kory said he has effectively lost two jobs over his views on ivermectin. At his current hospital in Wisconsin, where he runs the intensive care unit two weeks a month, managers called him to a meeting in September, where he was informed he could no longer prescribe ivermectin. He’d been giving it to “every patient with COVID,” he said.
“After the pharma-geddon that was unleashed, yeah, they shut it down,” he told the South Carolina lawmakers. “And I will tell you that many hospitals across the country had already shut it down months ago.”
Framing the ivermectin fight as a battle against faceless federal agencies and big pharmaceutical corporations appealed to Americans already suspicious of the science behind the pandemic and the approved COVID vaccines.
Dr. Kory suggests success stories with COVID treatments in other parts of the world have been suppressed to instead promote the vaccines.
In an interview with NPR, Dr. Kory said he regrets the flashpoint he helped ignite.
“I feel really bad for the patients, and I feel really bad for the doctors,” he told NPR. “Both of them — both the patients and doctors — are trapped.”
Patients are still demanding the treatment, but doctors sympathetic to their wishes are being told by their health systems not to try it.
Now conservatives in elected office are sensing political payoff if they step in to help patients get the drug. State legislatures, including those in Tennessee and Alaska, are debating various ways to increase access to ivermectin — with proposals such as shielding doctors from repercussions for prescribing it, or forcing pharmacists to fill questionable prescriptions.
The Montana State News Bureau reported that the state’s Republican attorney general dispatched a state trooper to a hospital in Helena where a politically connected patient was dying of COVID. Her family was asking for ivermectin.
In a statement, St. Peter’s Hospital said doctors and nurses were “harassed and threatened by three public officials.”
“These officials have no medical training or experience, yet they were insisting our providers give treatments for COVID-19 that are not authorized, clinically approved, or within the guidelines established by the FDA and the CDC,” the statement added.
On Oct. 14, the Republican attorney general in Nebraska addressed the controversy, issuing a nearly 50-page legal opinion arguing that doctors who consider the “off-label” use of ivermectin and hydroxychloroquine for COVID are acting within the parameters of their state medical licenses, as long as the physician obtains appropriate informed consent from a patient.
Some patients have filed lawsuits to obtain ivermectin, with mixed success. A patient in Illinois was denied. But other hospitals, including one in Ohio, have been forced to administer the drug against the objections of their physicians.
Even as they gain powerful political supporters, some ivermectin fans say they’re now avoiding the health care system — because they’ve lost faith in it.
Lesa Berry, of Richmond, Va., had a friend who died earlier this year of COVID. The doctors refused to use ivermectin, despite requests from Ms. Berry and the patient’s daughter.
They know better now, she said.
“My first attempt would have been to keep her out of the hospital,” Ms. Berry said. “Because right now when you go to the hospital, they only give you what’s on the CDC protocol.”
Ms. Berry and her husband have purchased their own supply of ivermectin, which they keep at home.
This story is from a partnership that includes NPR, Nashville Public Radio and KHN. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
When state senators in South Carolina held two hearings in September about COVID-19 treatments, they got an earful on the benefits of ivermectin — which many of the lawmakers echoed, sharing experiences of their own loved ones.
The demands for access to the drug were loud and insistent, despite federal regulators’ recent warning against using the drug to treat COVID.
Ivermectin is a generic drug that has been used for decades to treat river blindness, scabies, and even head lice. Veterinarians also use it, in different formulations and dosages, to treat animals for parasites like worms.
At one of the South Carolina hearings, Pressley Stutts III reminded the panel that his father, a prominent GOP leader in the state, had died of COVID a month earlier. He believed ivermectin could have helped him. But doctors at the hospital wouldn’t discuss it.
“I went every bit as far as I could without getting myself thrown in jail trying to save my father’s life,” he told the panel, as lawmakers offered condolences.
“What is going on here?” he asked, with the passion in his voice growing. “My dad’s dead!”
After the pandemic began, scientists launched clinical trials to see if ivermectin could help as a treatment for COVID. Some are still ongoing. But providers in mainstream medicine have rejected it as a COVID treatment, citing the poor quality of the studies to date, and two notorious “preprint” studies that were circulated before they were peer-reviewed, and later taken off the internet because of inaccurate and flawed data.
On Aug. 26, the Centers for Disease Control and Prevention advised clinicians not to use ivermectin, citing insufficient evidence of benefit and pointing out that unauthorized use had led to accidental poisonings. Vaccination, the CDC reiterated, is still the best way to avoid serious illness and death from the coronavirus.
But many Americans remain convinced ivermectin could be beneficial, and some politicians appear to be listening to them.
“If we have medications out here that are working — or seem to be working — I think it’s absolutely horrible that we’re not trying them,” said Republican state Sen. Tom Corbin in South Carolina. He questioned doctors who had come to the Statehouse to counter efforts to move ivermectin into mainstream use.
The doctors challenged the implied insult that they weren’t following best practices: “Any implication that any of us would do anything to withhold effective treatments from our patients is really insulting to our profession,” said Dr. Annie Andrews, a professor at the Medical University of South Carolina who has cared for COVID patients throughout the pandemic.
Instead of listening to the medical consensus, some politicians in states like South Carolina seem to be taking cues from doctors on the fringe. During one September hearing, state senators patched in a call from Dr. Pierre Kory.
Last year, Dr. Kory started a nonprofit called the Front Line COVID-19 Critical Care Alliance, which promotes ivermectin. He said he’s not making money by prescribing the drug, though the nonprofit does solicit donations and has not yet filed required financial documents with the IRS.
Dr. Kory acknowledged his medical opinions have landed him on “an island.”
He first testified about ivermectin to a U.S. Senate committee in December. That video went viral. Although it was taken down by YouTube, his Senate testimony prompted patients across the country to ask for ivermectin when they fell ill.
By late August, outpatient prescriptions had jumped 24-fold. Calls to poison control hotlines had tripled, mostly related to people taking ivermectin formulations meant for livestock.
Dr. Kory said he has effectively lost two jobs over his views on ivermectin. At his current hospital in Wisconsin, where he runs the intensive care unit two weeks a month, managers called him to a meeting in September, where he was informed he could no longer prescribe ivermectin. He’d been giving it to “every patient with COVID,” he said.
“After the pharma-geddon that was unleashed, yeah, they shut it down,” he told the South Carolina lawmakers. “And I will tell you that many hospitals across the country had already shut it down months ago.”
Framing the ivermectin fight as a battle against faceless federal agencies and big pharmaceutical corporations appealed to Americans already suspicious of the science behind the pandemic and the approved COVID vaccines.
Dr. Kory suggests success stories with COVID treatments in other parts of the world have been suppressed to instead promote the vaccines.
In an interview with NPR, Dr. Kory said he regrets the flashpoint he helped ignite.
“I feel really bad for the patients, and I feel really bad for the doctors,” he told NPR. “Both of them — both the patients and doctors — are trapped.”
Patients are still demanding the treatment, but doctors sympathetic to their wishes are being told by their health systems not to try it.
Now conservatives in elected office are sensing political payoff if they step in to help patients get the drug. State legislatures, including those in Tennessee and Alaska, are debating various ways to increase access to ivermectin — with proposals such as shielding doctors from repercussions for prescribing it, or forcing pharmacists to fill questionable prescriptions.
The Montana State News Bureau reported that the state’s Republican attorney general dispatched a state trooper to a hospital in Helena where a politically connected patient was dying of COVID. Her family was asking for ivermectin.
In a statement, St. Peter’s Hospital said doctors and nurses were “harassed and threatened by three public officials.”
“These officials have no medical training or experience, yet they were insisting our providers give treatments for COVID-19 that are not authorized, clinically approved, or within the guidelines established by the FDA and the CDC,” the statement added.
On Oct. 14, the Republican attorney general in Nebraska addressed the controversy, issuing a nearly 50-page legal opinion arguing that doctors who consider the “off-label” use of ivermectin and hydroxychloroquine for COVID are acting within the parameters of their state medical licenses, as long as the physician obtains appropriate informed consent from a patient.
Some patients have filed lawsuits to obtain ivermectin, with mixed success. A patient in Illinois was denied. But other hospitals, including one in Ohio, have been forced to administer the drug against the objections of their physicians.
Even as they gain powerful political supporters, some ivermectin fans say they’re now avoiding the health care system — because they’ve lost faith in it.
Lesa Berry, of Richmond, Va., had a friend who died earlier this year of COVID. The doctors refused to use ivermectin, despite requests from Ms. Berry and the patient’s daughter.
They know better now, she said.
“My first attempt would have been to keep her out of the hospital,” Ms. Berry said. “Because right now when you go to the hospital, they only give you what’s on the CDC protocol.”
Ms. Berry and her husband have purchased their own supply of ivermectin, which they keep at home.
This story is from a partnership that includes NPR, Nashville Public Radio and KHN. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
When state senators in South Carolina held two hearings in September about COVID-19 treatments, they got an earful on the benefits of ivermectin — which many of the lawmakers echoed, sharing experiences of their own loved ones.
The demands for access to the drug were loud and insistent, despite federal regulators’ recent warning against using the drug to treat COVID.
Ivermectin is a generic drug that has been used for decades to treat river blindness, scabies, and even head lice. Veterinarians also use it, in different formulations and dosages, to treat animals for parasites like worms.
At one of the South Carolina hearings, Pressley Stutts III reminded the panel that his father, a prominent GOP leader in the state, had died of COVID a month earlier. He believed ivermectin could have helped him. But doctors at the hospital wouldn’t discuss it.
“I went every bit as far as I could without getting myself thrown in jail trying to save my father’s life,” he told the panel, as lawmakers offered condolences.
“What is going on here?” he asked, with the passion in his voice growing. “My dad’s dead!”
After the pandemic began, scientists launched clinical trials to see if ivermectin could help as a treatment for COVID. Some are still ongoing. But providers in mainstream medicine have rejected it as a COVID treatment, citing the poor quality of the studies to date, and two notorious “preprint” studies that were circulated before they were peer-reviewed, and later taken off the internet because of inaccurate and flawed data.
On Aug. 26, the Centers for Disease Control and Prevention advised clinicians not to use ivermectin, citing insufficient evidence of benefit and pointing out that unauthorized use had led to accidental poisonings. Vaccination, the CDC reiterated, is still the best way to avoid serious illness and death from the coronavirus.
But many Americans remain convinced ivermectin could be beneficial, and some politicians appear to be listening to them.
“If we have medications out here that are working — or seem to be working — I think it’s absolutely horrible that we’re not trying them,” said Republican state Sen. Tom Corbin in South Carolina. He questioned doctors who had come to the Statehouse to counter efforts to move ivermectin into mainstream use.
The doctors challenged the implied insult that they weren’t following best practices: “Any implication that any of us would do anything to withhold effective treatments from our patients is really insulting to our profession,” said Dr. Annie Andrews, a professor at the Medical University of South Carolina who has cared for COVID patients throughout the pandemic.
Instead of listening to the medical consensus, some politicians in states like South Carolina seem to be taking cues from doctors on the fringe. During one September hearing, state senators patched in a call from Dr. Pierre Kory.
Last year, Dr. Kory started a nonprofit called the Front Line COVID-19 Critical Care Alliance, which promotes ivermectin. He said he’s not making money by prescribing the drug, though the nonprofit does solicit donations and has not yet filed required financial documents with the IRS.
Dr. Kory acknowledged his medical opinions have landed him on “an island.”
He first testified about ivermectin to a U.S. Senate committee in December. That video went viral. Although it was taken down by YouTube, his Senate testimony prompted patients across the country to ask for ivermectin when they fell ill.
By late August, outpatient prescriptions had jumped 24-fold. Calls to poison control hotlines had tripled, mostly related to people taking ivermectin formulations meant for livestock.
Dr. Kory said he has effectively lost two jobs over his views on ivermectin. At his current hospital in Wisconsin, where he runs the intensive care unit two weeks a month, managers called him to a meeting in September, where he was informed he could no longer prescribe ivermectin. He’d been giving it to “every patient with COVID,” he said.
“After the pharma-geddon that was unleashed, yeah, they shut it down,” he told the South Carolina lawmakers. “And I will tell you that many hospitals across the country had already shut it down months ago.”
Framing the ivermectin fight as a battle against faceless federal agencies and big pharmaceutical corporations appealed to Americans already suspicious of the science behind the pandemic and the approved COVID vaccines.
Dr. Kory suggests success stories with COVID treatments in other parts of the world have been suppressed to instead promote the vaccines.
In an interview with NPR, Dr. Kory said he regrets the flashpoint he helped ignite.
“I feel really bad for the patients, and I feel really bad for the doctors,” he told NPR. “Both of them — both the patients and doctors — are trapped.”
Patients are still demanding the treatment, but doctors sympathetic to their wishes are being told by their health systems not to try it.
Now conservatives in elected office are sensing political payoff if they step in to help patients get the drug. State legislatures, including those in Tennessee and Alaska, are debating various ways to increase access to ivermectin — with proposals such as shielding doctors from repercussions for prescribing it, or forcing pharmacists to fill questionable prescriptions.
The Montana State News Bureau reported that the state’s Republican attorney general dispatched a state trooper to a hospital in Helena where a politically connected patient was dying of COVID. Her family was asking for ivermectin.
In a statement, St. Peter’s Hospital said doctors and nurses were “harassed and threatened by three public officials.”
“These officials have no medical training or experience, yet they were insisting our providers give treatments for COVID-19 that are not authorized, clinically approved, or within the guidelines established by the FDA and the CDC,” the statement added.
On Oct. 14, the Republican attorney general in Nebraska addressed the controversy, issuing a nearly 50-page legal opinion arguing that doctors who consider the “off-label” use of ivermectin and hydroxychloroquine for COVID are acting within the parameters of their state medical licenses, as long as the physician obtains appropriate informed consent from a patient.
Some patients have filed lawsuits to obtain ivermectin, with mixed success. A patient in Illinois was denied. But other hospitals, including one in Ohio, have been forced to administer the drug against the objections of their physicians.
Even as they gain powerful political supporters, some ivermectin fans say they’re now avoiding the health care system — because they’ve lost faith in it.
Lesa Berry, of Richmond, Va., had a friend who died earlier this year of COVID. The doctors refused to use ivermectin, despite requests from Ms. Berry and the patient’s daughter.
They know better now, she said.
“My first attempt would have been to keep her out of the hospital,” Ms. Berry said. “Because right now when you go to the hospital, they only give you what’s on the CDC protocol.”
Ms. Berry and her husband have purchased their own supply of ivermectin, which they keep at home.
This story is from a partnership that includes NPR, Nashville Public Radio and KHN. KHN (Kaiser Health News) is a national newsroom that produces in-depth journalism about health issues. Together with Policy Analysis and Polling, KHN is one of the three major operating programs at KFF (Kaiser Family Foundation). KFF is an endowed nonprofit organization providing information on health issues to the nation.
Does zinc really help treat colds?
A new study published in BMJ Open adds to the evidence that zinc is effective against viral respiratory infections, such as colds.
Jennifer Hunter, PhD, BMed, of Western Sydney University’s NICM Health Research Institute, New South Wales, Australia, and colleagues conducted a meta-analysis of 28 randomized controlled trials (RCTs). They searched 17 English and Chinese databases to identify the trials and then used the Cochrane rapid review technique for the analysis.
The trials included 5,446 adults who had received zinc in a variety of formulations and routes — oral, sublingual, and nasal spray. The researchers separately analyzed whether zinc prevented or treated respiratory tract infections (RTIs)
Oral or intranasal zinc prevented five RTIs per 100 person-months (95% CI, 1 – 8; numbers needed to treat, 20). There was a 32% lower relative risk (RR) of developing mild to moderate symptoms consistent with a viral RTI.
Use of zinc was also associated with an 87% lower risk of developing moderately severe symptoms (incidence rate ratio, 0.13; 95% CI, 0.04 – 0.38) and a 28% lower risk of developing milder symptoms. The largest reductions in RR were for moderately severe symptoms consistent with an influenza-like illness.
Symptoms resolved 2 days earlier with sublingual or intranasal zinc compared with placebo (95% CI, 0.61 – 3.50; very low-certainty quality of evidence). There were clinically significant reductions in day 3 symptom severity scores (mean difference, -1.20 points; 95% CI, -0.66 to -1.74; low-certainty quality of evidence) but not in overall symptom severity. Participants who used sublingual or topical nasal zinc early in the course of illness were 1.8 times more likely to recover before those who used a placebo.
However, the investigators found no benefit of zinc when patients were inoculated with rhinovirus; there was no reduction in the risk of developing a cold. Asked about this disparity, Dr. Hunter said, “It might well be that when inoculating people to make sure they get infected, you give them a really high dose of the virus. [This] doesn’t really mimic what happens in the real world.”
On the downside of supplemental zinc, there were more side effects among those who used zinc, including nausea or gastrointestinal discomfort, mouth irritation, or soreness from sublingual lozenges (RR, 1.41; 95% CI, 1.17 – 1.69; number needed to harm, 7; moderate-certainty quality of evidence). The risk for a serious adverse event, such as loss of smell or copper deficiency, was low. Although not found in these studies, postmarketing studies have found that there is a risk for severe and in some cases permanent loss of smell associated with the use of nasal gels or sprays containing zinc. Three such products were recalled from the market.
The trial could not provide answers about the comparative efficacy of different types of zinc formulations, nor could the investigators recommend specific doses. The trial was not designed to assess zinc for the prevention or treatment of COVID-19.
Asked for independent comment, pediatrician Aamer Imdad, MBBS, assistant professor at the State University of New York Upstate Medical University, Syracuse, told this news organization, “It’s a very comprehensive review for zinc-related studies in adults” but was challenging because of the “significant clinical heterogeneity in the population.”
Dr. Imdad explained that zinc has “absolutely” been shown to be effective for children with diarrhea. The World Health Organization has recommended it since 2004. “The way it works in diarrhea is that it helps with the regeneration of the epithelium.... It also improves the immunity itself, especially the cell-mediated immunity.” He raised the question of whether it might work similarly in the respiratory tract. Dr. Imdad has a long-standing interest in the use of zinc for pediatric infections. Regarding this study, he concluded, “I think we still need to know the nuts and bolts of this intervention before we can recommend it more specifically.”
Dr. Hunter said, “We don’t have any high-quality studies that have evaluated zinc orally as treatment once you’re actually infected and have symptoms of the cold or influenza, or COVID.”
Asked about zinc’s possible role, Dr. Hunter said, “So I do think it gives us a viable alternative. More people are going, ‘What can I do?’ And you know as well as I do people come to you, and [they say], ‘Well, just give me something. Even if it’s a day or a little bit of symptom relief, anything to make me feel better that isn’t going to hurt me and doesn’t have any major risks.’ So I think in the short term, clinicians and consumers can consider trying it.”
Dr. Hunter was not keen on giving zinc to family members after they develop an RTI: “Consider it. But I don’t think we have enough evidence to say definitely yes.” But she does see a potential role for “people who are at risk of suboptimal zinc absorption, like people who are taking a variety of pharmaceuticals [notably proton pump inhibitors] that block or reduce the absorption of zinc, people with a whole lot of the chronic diseases that we know are associated with an increased risk of worse outcomes from respiratory viral infections, and older adults. Yes, I think [for] those high-risk groups, you could consider using zinc, either in a moderate dose longer term or in a higher dose for very short bursts of, like, 1 to 2 weeks.”
Dr. Hunter concluded, “Up until now, we all commonly thought that zinc’s role was only for people who were zinc deficient, and now we’ve got some signals pointing towards its potential role as an anti-infective and anti-inflammatory agent in people who don’t have zinc deficiency.”
But both Dr. Hunter and Dr. Imdad emphasized that zinc is not a game changer. There is a hint that it produces a small benefit in prevention and may slightly shorten the duration of RTIs. More research is needed.
Dr. Hunter has received payment for providing expert advice about traditional, complementary, and integrative medicine, including nutraceuticals, to industry, government bodies, and nongovernmental organizations and has spoken at workshops, seminars, and conferences for which registration, travel, and/or accommodation has been paid for by the organizers. Dr. Imdad has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new study published in BMJ Open adds to the evidence that zinc is effective against viral respiratory infections, such as colds.
Jennifer Hunter, PhD, BMed, of Western Sydney University’s NICM Health Research Institute, New South Wales, Australia, and colleagues conducted a meta-analysis of 28 randomized controlled trials (RCTs). They searched 17 English and Chinese databases to identify the trials and then used the Cochrane rapid review technique for the analysis.
The trials included 5,446 adults who had received zinc in a variety of formulations and routes — oral, sublingual, and nasal spray. The researchers separately analyzed whether zinc prevented or treated respiratory tract infections (RTIs)
Oral or intranasal zinc prevented five RTIs per 100 person-months (95% CI, 1 – 8; numbers needed to treat, 20). There was a 32% lower relative risk (RR) of developing mild to moderate symptoms consistent with a viral RTI.
Use of zinc was also associated with an 87% lower risk of developing moderately severe symptoms (incidence rate ratio, 0.13; 95% CI, 0.04 – 0.38) and a 28% lower risk of developing milder symptoms. The largest reductions in RR were for moderately severe symptoms consistent with an influenza-like illness.
Symptoms resolved 2 days earlier with sublingual or intranasal zinc compared with placebo (95% CI, 0.61 – 3.50; very low-certainty quality of evidence). There were clinically significant reductions in day 3 symptom severity scores (mean difference, -1.20 points; 95% CI, -0.66 to -1.74; low-certainty quality of evidence) but not in overall symptom severity. Participants who used sublingual or topical nasal zinc early in the course of illness were 1.8 times more likely to recover before those who used a placebo.
However, the investigators found no benefit of zinc when patients were inoculated with rhinovirus; there was no reduction in the risk of developing a cold. Asked about this disparity, Dr. Hunter said, “It might well be that when inoculating people to make sure they get infected, you give them a really high dose of the virus. [This] doesn’t really mimic what happens in the real world.”
On the downside of supplemental zinc, there were more side effects among those who used zinc, including nausea or gastrointestinal discomfort, mouth irritation, or soreness from sublingual lozenges (RR, 1.41; 95% CI, 1.17 – 1.69; number needed to harm, 7; moderate-certainty quality of evidence). The risk for a serious adverse event, such as loss of smell or copper deficiency, was low. Although not found in these studies, postmarketing studies have found that there is a risk for severe and in some cases permanent loss of smell associated with the use of nasal gels or sprays containing zinc. Three such products were recalled from the market.
The trial could not provide answers about the comparative efficacy of different types of zinc formulations, nor could the investigators recommend specific doses. The trial was not designed to assess zinc for the prevention or treatment of COVID-19.
Asked for independent comment, pediatrician Aamer Imdad, MBBS, assistant professor at the State University of New York Upstate Medical University, Syracuse, told this news organization, “It’s a very comprehensive review for zinc-related studies in adults” but was challenging because of the “significant clinical heterogeneity in the population.”
Dr. Imdad explained that zinc has “absolutely” been shown to be effective for children with diarrhea. The World Health Organization has recommended it since 2004. “The way it works in diarrhea is that it helps with the regeneration of the epithelium.... It also improves the immunity itself, especially the cell-mediated immunity.” He raised the question of whether it might work similarly in the respiratory tract. Dr. Imdad has a long-standing interest in the use of zinc for pediatric infections. Regarding this study, he concluded, “I think we still need to know the nuts and bolts of this intervention before we can recommend it more specifically.”
Dr. Hunter said, “We don’t have any high-quality studies that have evaluated zinc orally as treatment once you’re actually infected and have symptoms of the cold or influenza, or COVID.”
Asked about zinc’s possible role, Dr. Hunter said, “So I do think it gives us a viable alternative. More people are going, ‘What can I do?’ And you know as well as I do people come to you, and [they say], ‘Well, just give me something. Even if it’s a day or a little bit of symptom relief, anything to make me feel better that isn’t going to hurt me and doesn’t have any major risks.’ So I think in the short term, clinicians and consumers can consider trying it.”
Dr. Hunter was not keen on giving zinc to family members after they develop an RTI: “Consider it. But I don’t think we have enough evidence to say definitely yes.” But she does see a potential role for “people who are at risk of suboptimal zinc absorption, like people who are taking a variety of pharmaceuticals [notably proton pump inhibitors] that block or reduce the absorption of zinc, people with a whole lot of the chronic diseases that we know are associated with an increased risk of worse outcomes from respiratory viral infections, and older adults. Yes, I think [for] those high-risk groups, you could consider using zinc, either in a moderate dose longer term or in a higher dose for very short bursts of, like, 1 to 2 weeks.”
Dr. Hunter concluded, “Up until now, we all commonly thought that zinc’s role was only for people who were zinc deficient, and now we’ve got some signals pointing towards its potential role as an anti-infective and anti-inflammatory agent in people who don’t have zinc deficiency.”
But both Dr. Hunter and Dr. Imdad emphasized that zinc is not a game changer. There is a hint that it produces a small benefit in prevention and may slightly shorten the duration of RTIs. More research is needed.
Dr. Hunter has received payment for providing expert advice about traditional, complementary, and integrative medicine, including nutraceuticals, to industry, government bodies, and nongovernmental organizations and has spoken at workshops, seminars, and conferences for which registration, travel, and/or accommodation has been paid for by the organizers. Dr. Imdad has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A new study published in BMJ Open adds to the evidence that zinc is effective against viral respiratory infections, such as colds.
Jennifer Hunter, PhD, BMed, of Western Sydney University’s NICM Health Research Institute, New South Wales, Australia, and colleagues conducted a meta-analysis of 28 randomized controlled trials (RCTs). They searched 17 English and Chinese databases to identify the trials and then used the Cochrane rapid review technique for the analysis.
The trials included 5,446 adults who had received zinc in a variety of formulations and routes — oral, sublingual, and nasal spray. The researchers separately analyzed whether zinc prevented or treated respiratory tract infections (RTIs)
Oral or intranasal zinc prevented five RTIs per 100 person-months (95% CI, 1 – 8; numbers needed to treat, 20). There was a 32% lower relative risk (RR) of developing mild to moderate symptoms consistent with a viral RTI.
Use of zinc was also associated with an 87% lower risk of developing moderately severe symptoms (incidence rate ratio, 0.13; 95% CI, 0.04 – 0.38) and a 28% lower risk of developing milder symptoms. The largest reductions in RR were for moderately severe symptoms consistent with an influenza-like illness.
Symptoms resolved 2 days earlier with sublingual or intranasal zinc compared with placebo (95% CI, 0.61 – 3.50; very low-certainty quality of evidence). There were clinically significant reductions in day 3 symptom severity scores (mean difference, -1.20 points; 95% CI, -0.66 to -1.74; low-certainty quality of evidence) but not in overall symptom severity. Participants who used sublingual or topical nasal zinc early in the course of illness were 1.8 times more likely to recover before those who used a placebo.
However, the investigators found no benefit of zinc when patients were inoculated with rhinovirus; there was no reduction in the risk of developing a cold. Asked about this disparity, Dr. Hunter said, “It might well be that when inoculating people to make sure they get infected, you give them a really high dose of the virus. [This] doesn’t really mimic what happens in the real world.”
On the downside of supplemental zinc, there were more side effects among those who used zinc, including nausea or gastrointestinal discomfort, mouth irritation, or soreness from sublingual lozenges (RR, 1.41; 95% CI, 1.17 – 1.69; number needed to harm, 7; moderate-certainty quality of evidence). The risk for a serious adverse event, such as loss of smell or copper deficiency, was low. Although not found in these studies, postmarketing studies have found that there is a risk for severe and in some cases permanent loss of smell associated with the use of nasal gels or sprays containing zinc. Three such products were recalled from the market.
The trial could not provide answers about the comparative efficacy of different types of zinc formulations, nor could the investigators recommend specific doses. The trial was not designed to assess zinc for the prevention or treatment of COVID-19.
Asked for independent comment, pediatrician Aamer Imdad, MBBS, assistant professor at the State University of New York Upstate Medical University, Syracuse, told this news organization, “It’s a very comprehensive review for zinc-related studies in adults” but was challenging because of the “significant clinical heterogeneity in the population.”
Dr. Imdad explained that zinc has “absolutely” been shown to be effective for children with diarrhea. The World Health Organization has recommended it since 2004. “The way it works in diarrhea is that it helps with the regeneration of the epithelium.... It also improves the immunity itself, especially the cell-mediated immunity.” He raised the question of whether it might work similarly in the respiratory tract. Dr. Imdad has a long-standing interest in the use of zinc for pediatric infections. Regarding this study, he concluded, “I think we still need to know the nuts and bolts of this intervention before we can recommend it more specifically.”
Dr. Hunter said, “We don’t have any high-quality studies that have evaluated zinc orally as treatment once you’re actually infected and have symptoms of the cold or influenza, or COVID.”
Asked about zinc’s possible role, Dr. Hunter said, “So I do think it gives us a viable alternative. More people are going, ‘What can I do?’ And you know as well as I do people come to you, and [they say], ‘Well, just give me something. Even if it’s a day or a little bit of symptom relief, anything to make me feel better that isn’t going to hurt me and doesn’t have any major risks.’ So I think in the short term, clinicians and consumers can consider trying it.”
Dr. Hunter was not keen on giving zinc to family members after they develop an RTI: “Consider it. But I don’t think we have enough evidence to say definitely yes.” But she does see a potential role for “people who are at risk of suboptimal zinc absorption, like people who are taking a variety of pharmaceuticals [notably proton pump inhibitors] that block or reduce the absorption of zinc, people with a whole lot of the chronic diseases that we know are associated with an increased risk of worse outcomes from respiratory viral infections, and older adults. Yes, I think [for] those high-risk groups, you could consider using zinc, either in a moderate dose longer term or in a higher dose for very short bursts of, like, 1 to 2 weeks.”
Dr. Hunter concluded, “Up until now, we all commonly thought that zinc’s role was only for people who were zinc deficient, and now we’ve got some signals pointing towards its potential role as an anti-infective and anti-inflammatory agent in people who don’t have zinc deficiency.”
But both Dr. Hunter and Dr. Imdad emphasized that zinc is not a game changer. There is a hint that it produces a small benefit in prevention and may slightly shorten the duration of RTIs. More research is needed.
Dr. Hunter has received payment for providing expert advice about traditional, complementary, and integrative medicine, including nutraceuticals, to industry, government bodies, and nongovernmental organizations and has spoken at workshops, seminars, and conferences for which registration, travel, and/or accommodation has been paid for by the organizers. Dr. Imdad has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM BMJ OPEN





