User login
-
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]


TB treatment can be shortened for most children: study
The World Health Organization is expected to recommend truncating treatment of children with mild tuberculosis by 2 months – from 6 months to 4 – after a randomized trial found similar outcomes with the shorter regimen.
An international team of investigators found the abbreviated course of antibiotics was no less effective or safe than conventional treatment and saved an average of $17.34 per child – money that could be used to mitigate the toll of TB, which is estimated to sicken 1.1 million children worldwide each year.
The findings come as deaths from TB are rising as a result of the COVID-19 pandemic, which has hindered efforts to find and treat patients. In 2020, according to the WHO, an estimated 1.5 million people died from TB, the first year-over-year increase in such deaths since 2005.
Nearly a quarter of children with TB die, primarily because they go undiagnosed, according to the researchers, who published the study in the New England Journal of Medicine. Shorter treatment “translates into very large cost savings that could be used to improve screening and diagnosis to address the current case detection gap,” first author Anna Turkova, MD, of University College London, told this news organization.
The standard TB regimen is based on trials in adults with severe respiratory disease. However, about two-thirds of children have nonsevere infections.
For the study, Dr. Turkova and colleagues assigned 1,204 children with TB in four countries – Uganda, Zambia, South Africa, and India – to either a 4- or 6-month regimen with first-line medications rifampin, isoniazid, pyrazinamide, and ethambutol. Participants were aged 2 months to 15 years and had symptomatic nonsevere lung or lymph node infections with a negative test on a sputum smear microscopy. Eleven percent also had HIV.
After 18 months, 16 participants in the group that received the shortened treatment and 18 in the standard treatment group had experienced an unfavorable outcome – defined as treatment failure, recurrence of TB, loss to follow-up, or death (adjusted difference, -0.4 percentage points; 95% confidence interval, -2.2 to 1.5).
Similar numbers – 47 in the 4-month group and 48 in the 6-month group – experienced severe or life-threatening adverse events, most commonly chest infections, such as pneumonia, and liver problems, during treatment or up to 30 days after the last dose.
New guidelines coming soon
The WHO plans to issue new guidelines and a handbook for TB management in children and adolescents on March 24, World Tuberculosis Day, a spokesman for the agency told Medscape.
Anna Mandalakas, MD, PhD, director of the Global Tuberculosis Program at Baylor College of Medicine, department of pediatrics, Houston, said the shorter regimen should enable more children to successfully complete TB treatment.
“It can be challenging to convince young children to take medications on a regular basis for 6 months,” Dr. Mandalakas, a member of a WHO guidelines development group that reviewed the study, told this news organization. “Despite best intentions, parents often become fatigued and give up the medicine battle.”
Leo Martinez, PhD, an epidemiologist at Boston University School of Public Health who studies pediatric TB, noted that study’s cost-effectiveness analysis applies only to health care costs. Families often suffer financially through lost wages, transportation to health care facilities, and lost employment, fueling a cycle of poverty and disease in low-income countries, he said.
A WHO statement noted that long treatment regimens can add toxicity and risk of drug interactions for children with HIV.
Separate efforts have been underway to hasten TB treatment in different groups of patients. A study published in NEJM showed that 4 months of the potent antibiotic rifapentine, along with another antibiotic, moxifloxacin, was non-inferior to the standard 6-month regimen in patients aged 12 and older. According to the editorial accompanying that study, the research illustrated the potential for shorter treatment courses that would be cheaper and less cumbersome, although that particular combination poses hurdles such as adherence issues and potential bacterial resistance.
Experts agreed that improved diagnostic procedures are critical to significantly reducing TB pediatric deaths – an issue that Dr. Turkova said will be addressed in WHO’s forthcoming handbook.
Because no gold-standard test exists for TB, and symptoms often overlap with other infections, widespread screening of children in households where adults have been diagnosed with TB has been found to improve detection of the disease. “Training of health care workers, easy-to-implement diagnostic algorithms, and widely accessible training materials on chest radiography in childhood TB should also improve case finding and treatment initiation,” she said.
The trial was supported by U.K. government and charitable research funders. Dr. Turkova and Dr. Martinez reported no financial disclosures. Dr. Mandalakas reported honoraria from WHO to support the preparation of diagnostics and treatment chapters in the operational handbook, for providing lectures for Medscape, and for serving on a data safety monitoring board for Janssen Pharmaceuticals.
A version of this article first appeared on Medscape.com.
The World Health Organization is expected to recommend truncating treatment of children with mild tuberculosis by 2 months – from 6 months to 4 – after a randomized trial found similar outcomes with the shorter regimen.
An international team of investigators found the abbreviated course of antibiotics was no less effective or safe than conventional treatment and saved an average of $17.34 per child – money that could be used to mitigate the toll of TB, which is estimated to sicken 1.1 million children worldwide each year.
The findings come as deaths from TB are rising as a result of the COVID-19 pandemic, which has hindered efforts to find and treat patients. In 2020, according to the WHO, an estimated 1.5 million people died from TB, the first year-over-year increase in such deaths since 2005.
Nearly a quarter of children with TB die, primarily because they go undiagnosed, according to the researchers, who published the study in the New England Journal of Medicine. Shorter treatment “translates into very large cost savings that could be used to improve screening and diagnosis to address the current case detection gap,” first author Anna Turkova, MD, of University College London, told this news organization.
The standard TB regimen is based on trials in adults with severe respiratory disease. However, about two-thirds of children have nonsevere infections.
For the study, Dr. Turkova and colleagues assigned 1,204 children with TB in four countries – Uganda, Zambia, South Africa, and India – to either a 4- or 6-month regimen with first-line medications rifampin, isoniazid, pyrazinamide, and ethambutol. Participants were aged 2 months to 15 years and had symptomatic nonsevere lung or lymph node infections with a negative test on a sputum smear microscopy. Eleven percent also had HIV.
After 18 months, 16 participants in the group that received the shortened treatment and 18 in the standard treatment group had experienced an unfavorable outcome – defined as treatment failure, recurrence of TB, loss to follow-up, or death (adjusted difference, -0.4 percentage points; 95% confidence interval, -2.2 to 1.5).
Similar numbers – 47 in the 4-month group and 48 in the 6-month group – experienced severe or life-threatening adverse events, most commonly chest infections, such as pneumonia, and liver problems, during treatment or up to 30 days after the last dose.
New guidelines coming soon
The WHO plans to issue new guidelines and a handbook for TB management in children and adolescents on March 24, World Tuberculosis Day, a spokesman for the agency told Medscape.
Anna Mandalakas, MD, PhD, director of the Global Tuberculosis Program at Baylor College of Medicine, department of pediatrics, Houston, said the shorter regimen should enable more children to successfully complete TB treatment.
“It can be challenging to convince young children to take medications on a regular basis for 6 months,” Dr. Mandalakas, a member of a WHO guidelines development group that reviewed the study, told this news organization. “Despite best intentions, parents often become fatigued and give up the medicine battle.”
Leo Martinez, PhD, an epidemiologist at Boston University School of Public Health who studies pediatric TB, noted that study’s cost-effectiveness analysis applies only to health care costs. Families often suffer financially through lost wages, transportation to health care facilities, and lost employment, fueling a cycle of poverty and disease in low-income countries, he said.
A WHO statement noted that long treatment regimens can add toxicity and risk of drug interactions for children with HIV.
Separate efforts have been underway to hasten TB treatment in different groups of patients. A study published in NEJM showed that 4 months of the potent antibiotic rifapentine, along with another antibiotic, moxifloxacin, was non-inferior to the standard 6-month regimen in patients aged 12 and older. According to the editorial accompanying that study, the research illustrated the potential for shorter treatment courses that would be cheaper and less cumbersome, although that particular combination poses hurdles such as adherence issues and potential bacterial resistance.
Experts agreed that improved diagnostic procedures are critical to significantly reducing TB pediatric deaths – an issue that Dr. Turkova said will be addressed in WHO’s forthcoming handbook.
Because no gold-standard test exists for TB, and symptoms often overlap with other infections, widespread screening of children in households where adults have been diagnosed with TB has been found to improve detection of the disease. “Training of health care workers, easy-to-implement diagnostic algorithms, and widely accessible training materials on chest radiography in childhood TB should also improve case finding and treatment initiation,” she said.
The trial was supported by U.K. government and charitable research funders. Dr. Turkova and Dr. Martinez reported no financial disclosures. Dr. Mandalakas reported honoraria from WHO to support the preparation of diagnostics and treatment chapters in the operational handbook, for providing lectures for Medscape, and for serving on a data safety monitoring board for Janssen Pharmaceuticals.
A version of this article first appeared on Medscape.com.
The World Health Organization is expected to recommend truncating treatment of children with mild tuberculosis by 2 months – from 6 months to 4 – after a randomized trial found similar outcomes with the shorter regimen.
An international team of investigators found the abbreviated course of antibiotics was no less effective or safe than conventional treatment and saved an average of $17.34 per child – money that could be used to mitigate the toll of TB, which is estimated to sicken 1.1 million children worldwide each year.
The findings come as deaths from TB are rising as a result of the COVID-19 pandemic, which has hindered efforts to find and treat patients. In 2020, according to the WHO, an estimated 1.5 million people died from TB, the first year-over-year increase in such deaths since 2005.
Nearly a quarter of children with TB die, primarily because they go undiagnosed, according to the researchers, who published the study in the New England Journal of Medicine. Shorter treatment “translates into very large cost savings that could be used to improve screening and diagnosis to address the current case detection gap,” first author Anna Turkova, MD, of University College London, told this news organization.
The standard TB regimen is based on trials in adults with severe respiratory disease. However, about two-thirds of children have nonsevere infections.
For the study, Dr. Turkova and colleagues assigned 1,204 children with TB in four countries – Uganda, Zambia, South Africa, and India – to either a 4- or 6-month regimen with first-line medications rifampin, isoniazid, pyrazinamide, and ethambutol. Participants were aged 2 months to 15 years and had symptomatic nonsevere lung or lymph node infections with a negative test on a sputum smear microscopy. Eleven percent also had HIV.
After 18 months, 16 participants in the group that received the shortened treatment and 18 in the standard treatment group had experienced an unfavorable outcome – defined as treatment failure, recurrence of TB, loss to follow-up, or death (adjusted difference, -0.4 percentage points; 95% confidence interval, -2.2 to 1.5).
Similar numbers – 47 in the 4-month group and 48 in the 6-month group – experienced severe or life-threatening adverse events, most commonly chest infections, such as pneumonia, and liver problems, during treatment or up to 30 days after the last dose.
New guidelines coming soon
The WHO plans to issue new guidelines and a handbook for TB management in children and adolescents on March 24, World Tuberculosis Day, a spokesman for the agency told Medscape.
Anna Mandalakas, MD, PhD, director of the Global Tuberculosis Program at Baylor College of Medicine, department of pediatrics, Houston, said the shorter regimen should enable more children to successfully complete TB treatment.
“It can be challenging to convince young children to take medications on a regular basis for 6 months,” Dr. Mandalakas, a member of a WHO guidelines development group that reviewed the study, told this news organization. “Despite best intentions, parents often become fatigued and give up the medicine battle.”
Leo Martinez, PhD, an epidemiologist at Boston University School of Public Health who studies pediatric TB, noted that study’s cost-effectiveness analysis applies only to health care costs. Families often suffer financially through lost wages, transportation to health care facilities, and lost employment, fueling a cycle of poverty and disease in low-income countries, he said.
A WHO statement noted that long treatment regimens can add toxicity and risk of drug interactions for children with HIV.
Separate efforts have been underway to hasten TB treatment in different groups of patients. A study published in NEJM showed that 4 months of the potent antibiotic rifapentine, along with another antibiotic, moxifloxacin, was non-inferior to the standard 6-month regimen in patients aged 12 and older. According to the editorial accompanying that study, the research illustrated the potential for shorter treatment courses that would be cheaper and less cumbersome, although that particular combination poses hurdles such as adherence issues and potential bacterial resistance.
Experts agreed that improved diagnostic procedures are critical to significantly reducing TB pediatric deaths – an issue that Dr. Turkova said will be addressed in WHO’s forthcoming handbook.
Because no gold-standard test exists for TB, and symptoms often overlap with other infections, widespread screening of children in households where adults have been diagnosed with TB has been found to improve detection of the disease. “Training of health care workers, easy-to-implement diagnostic algorithms, and widely accessible training materials on chest radiography in childhood TB should also improve case finding and treatment initiation,” she said.
The trial was supported by U.K. government and charitable research funders. Dr. Turkova and Dr. Martinez reported no financial disclosures. Dr. Mandalakas reported honoraria from WHO to support the preparation of diagnostics and treatment chapters in the operational handbook, for providing lectures for Medscape, and for serving on a data safety monitoring board for Janssen Pharmaceuticals.
A version of this article first appeared on Medscape.com.
Children and COVID: Decline in new cases reaches 7th week
New cases of COVID-19 in U.S. children have fallen to their lowest level since the beginning of the Delta surge in July of 2021, according to the American Academy of Pediatrics and the Children’s Hospital Association.
. Over those 7 weeks, new cases dropped over 96% from the 1.15 million reported for Jan. 14-20, based on data collected by the AAP and CHA from state and territorial health departments.
The last time that the weekly count was below 42,000 was July 16-22, 2021, when almost 39,000 cases were reported in the midst of the Delta upsurge. That was shortly after cases had reached their lowest point, 8,447, since the early stages of the pandemic in 2020, the AAP/CHA data show.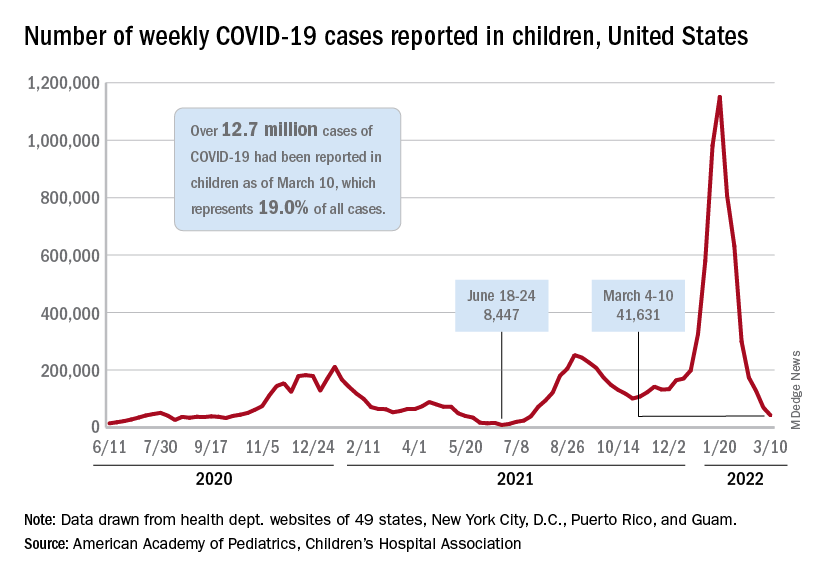
The cumulative number of pediatric cases is now up to 12.7 million, while the overall proportion of cases occurring in children held steady at 19.0% for the 4th week in a row, the AAP and CHA said in their weekly COVID-19 report. The Centers for Disease Control and Prevention, using an age range of 0-18 versus the states’ variety of ages, puts total cases at 11.7 million and deaths at 1,656 as of March 14.
Data from the CDC’s COVID-19–Associated Hospitalization Surveillance Network show that hospitalizations with laboratory-confirmed infection were down by 50% in children aged 0-4 years, by 63% among 5- to 11-year-olds, and by 58% in those aged 12-17 years for the week of Feb. 27 to March 5, compared with the week before.
The pace of vaccination continues to follow a similar trend, as the declines seen through February have continued into March. Cumulatively, 33.7% of children aged 5-11 have received at least one dose, and 26.8% are fully vaccinated, with corresponding numbers of 68.0% and 58.0% for children aged 12-17, the CDC reported on its COVID Data Tracker.
State-level data show that children aged 5-11 in Vermont, with a rate of 65%, are the most likely to have received at least one dose of COVID vaccine, while just 15% of 5- to 11-year-olds in Alabama, Louisiana, and Mississippi have gotten their first dose. Among children aged 12-17, that rate ranges from 40% in Wyoming to 94% in Hawaii, Massachusetts, and Rhode Island, the AAP said in a separate report based on CDC data.
In a recent report involving 1,364 children aged 5-15 years, two doses of the COVID-19 vaccine reduced the risk of infection from the Omicron variant by 31% in children aged 5-11 years and by 59% among children aged 12-15 years, said Ashley L. Fowlkes, ScD, of the CDC’s COVID-19 Emergency Response Team, and associates (MMWR 2022 Mar 11;71).
New cases of COVID-19 in U.S. children have fallen to their lowest level since the beginning of the Delta surge in July of 2021, according to the American Academy of Pediatrics and the Children’s Hospital Association.
. Over those 7 weeks, new cases dropped over 96% from the 1.15 million reported for Jan. 14-20, based on data collected by the AAP and CHA from state and territorial health departments.
The last time that the weekly count was below 42,000 was July 16-22, 2021, when almost 39,000 cases were reported in the midst of the Delta upsurge. That was shortly after cases had reached their lowest point, 8,447, since the early stages of the pandemic in 2020, the AAP/CHA data show.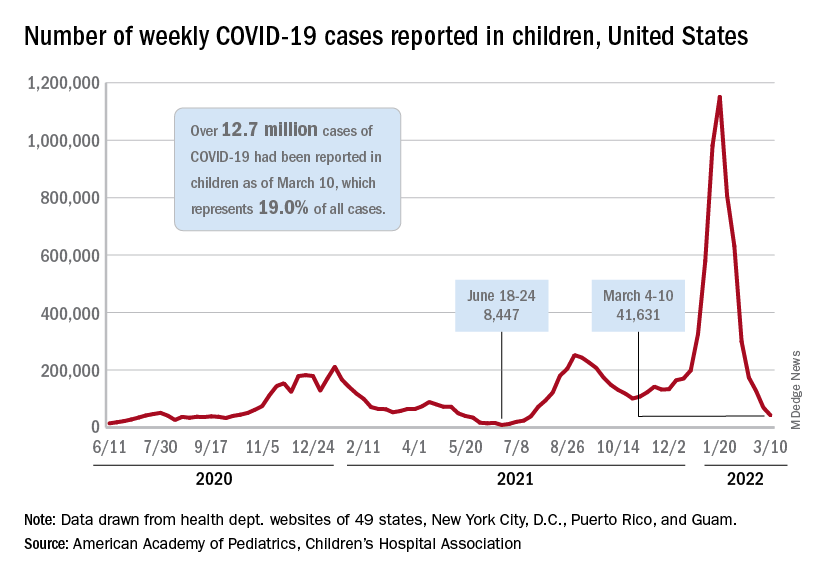
The cumulative number of pediatric cases is now up to 12.7 million, while the overall proportion of cases occurring in children held steady at 19.0% for the 4th week in a row, the AAP and CHA said in their weekly COVID-19 report. The Centers for Disease Control and Prevention, using an age range of 0-18 versus the states’ variety of ages, puts total cases at 11.7 million and deaths at 1,656 as of March 14.
Data from the CDC’s COVID-19–Associated Hospitalization Surveillance Network show that hospitalizations with laboratory-confirmed infection were down by 50% in children aged 0-4 years, by 63% among 5- to 11-year-olds, and by 58% in those aged 12-17 years for the week of Feb. 27 to March 5, compared with the week before.
The pace of vaccination continues to follow a similar trend, as the declines seen through February have continued into March. Cumulatively, 33.7% of children aged 5-11 have received at least one dose, and 26.8% are fully vaccinated, with corresponding numbers of 68.0% and 58.0% for children aged 12-17, the CDC reported on its COVID Data Tracker.
State-level data show that children aged 5-11 in Vermont, with a rate of 65%, are the most likely to have received at least one dose of COVID vaccine, while just 15% of 5- to 11-year-olds in Alabama, Louisiana, and Mississippi have gotten their first dose. Among children aged 12-17, that rate ranges from 40% in Wyoming to 94% in Hawaii, Massachusetts, and Rhode Island, the AAP said in a separate report based on CDC data.
In a recent report involving 1,364 children aged 5-15 years, two doses of the COVID-19 vaccine reduced the risk of infection from the Omicron variant by 31% in children aged 5-11 years and by 59% among children aged 12-15 years, said Ashley L. Fowlkes, ScD, of the CDC’s COVID-19 Emergency Response Team, and associates (MMWR 2022 Mar 11;71).
New cases of COVID-19 in U.S. children have fallen to their lowest level since the beginning of the Delta surge in July of 2021, according to the American Academy of Pediatrics and the Children’s Hospital Association.
. Over those 7 weeks, new cases dropped over 96% from the 1.15 million reported for Jan. 14-20, based on data collected by the AAP and CHA from state and territorial health departments.
The last time that the weekly count was below 42,000 was July 16-22, 2021, when almost 39,000 cases were reported in the midst of the Delta upsurge. That was shortly after cases had reached their lowest point, 8,447, since the early stages of the pandemic in 2020, the AAP/CHA data show.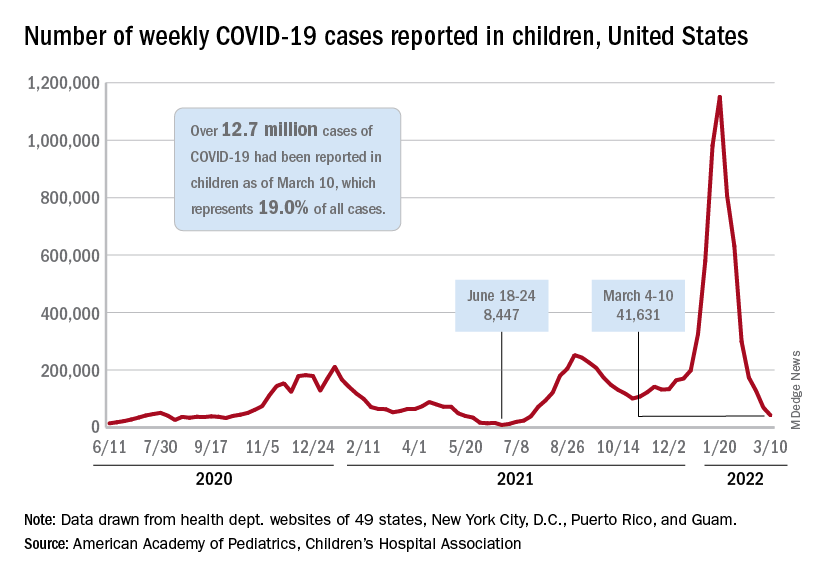
The cumulative number of pediatric cases is now up to 12.7 million, while the overall proportion of cases occurring in children held steady at 19.0% for the 4th week in a row, the AAP and CHA said in their weekly COVID-19 report. The Centers for Disease Control and Prevention, using an age range of 0-18 versus the states’ variety of ages, puts total cases at 11.7 million and deaths at 1,656 as of March 14.
Data from the CDC’s COVID-19–Associated Hospitalization Surveillance Network show that hospitalizations with laboratory-confirmed infection were down by 50% in children aged 0-4 years, by 63% among 5- to 11-year-olds, and by 58% in those aged 12-17 years for the week of Feb. 27 to March 5, compared with the week before.
The pace of vaccination continues to follow a similar trend, as the declines seen through February have continued into March. Cumulatively, 33.7% of children aged 5-11 have received at least one dose, and 26.8% are fully vaccinated, with corresponding numbers of 68.0% and 58.0% for children aged 12-17, the CDC reported on its COVID Data Tracker.
State-level data show that children aged 5-11 in Vermont, with a rate of 65%, are the most likely to have received at least one dose of COVID vaccine, while just 15% of 5- to 11-year-olds in Alabama, Louisiana, and Mississippi have gotten their first dose. Among children aged 12-17, that rate ranges from 40% in Wyoming to 94% in Hawaii, Massachusetts, and Rhode Island, the AAP said in a separate report based on CDC data.
In a recent report involving 1,364 children aged 5-15 years, two doses of the COVID-19 vaccine reduced the risk of infection from the Omicron variant by 31% in children aged 5-11 years and by 59% among children aged 12-15 years, said Ashley L. Fowlkes, ScD, of the CDC’s COVID-19 Emergency Response Team, and associates (MMWR 2022 Mar 11;71).
Death of pig heart transplant patient is more a beginning than an end
The genetically altered pig’s heart “worked like a rock star, beautifully functioning,” the surgeon who performed the pioneering Jan. 7 xenotransplant procedure said in a press statement on the death of the patient, David Bennett Sr.
“He wasn’t able to overcome what turned out to be devastating – the debilitation from his previous period of heart failure, which was extreme,” said Bartley P. Griffith, MD, clinical director of the cardiac xenotransplantation program at the University of Maryland, Baltimore.
Representatives of the institution aren’t offering many details on the cause of Mr. Bennett’s death on March 8, 60 days after his operation, but said they will elaborate when their findings are formally published. But their comments seem to downplay the unique nature of the implanted heart itself as a culprit and instead implicate the patient’s diminished overall clinical condition and what grew into an ongoing battle with infections.
The 57-year-old Bennett, bedridden with end-stage heart failure, judged a poor candidate for a ventricular assist device, and on extracorporeal membrane oxygenation (ECMO), reportedly was offered the extraordinary surgery after being turned down for a conventional transplant at several major centers.
“Until day 45 or 50, he was doing very well,” Muhammad M. Mohiuddin, MD, the xenotransplantation program’s scientific director, observed in the statement. But infections soon took advantage of his hobbled immune system.
Given his “preexisting condition and how frail his body was,” Dr. Mohiuddin said, “we were having difficulty maintaining a balance between his immunosuppression and controlling his infection.” Mr. Bennett went into multiple organ failure and “I think that resulted in his passing away.”
Beyond wildest dreams
The surgeons confidently framed Mr. Bennett’s experience as a milestone for heart xenotransplantation. “The demonstration that it was possible, beyond the wildest dreams of most people in the field, even, at this point – that we were able to take a genetically engineered organ and watch it function flawlessly for 9 weeks – is pretty positive in terms of the potential of this therapy,” Dr. Griffith said.
But enough questions linger that others were more circumspect, even as they praised the accomplishment. “There’s no question that this is a historic event,” Mandeep R. Mehra, MD, of Harvard Medical School, and director of the Center for Advanced Heart Disease at Brigham and Women’s Hospital, both in Boston, said in an interview.
Still, “I don’t think we should just conclude that it was the patient’s frailty or death from infection,” Dr. Mehra said. With so few details available, “I would be very careful in prematurely concluding that the problem did not reside with the heart but with the patient. We cannot be sure.”
For example, he noted, “6 to 8 weeks is right around the time when some cardiac complications, like accelerated forms of vasculopathy, could become evident.” Immune-mediated cardiac allograft vasculopathy is a common cause of heart transplant failure.
Or, “it could as easily have been the fact that immunosuppression was modified at 6 to 7 weeks in response to potential infection, which could have led to a cardiac compromise,” Dr. Mehra said. “We just don’t know.”
“It’s really important that this be reported in a scientifically accurate way, because we will all learn from this,” Lori J. West, MD, DPhil, said in an interview.
Little seems to be known for sure about the actual cause of death, “but the fact there was not hyperacute rejection is itself a big step forward. And we know, at least from the limited information we have, that it did not occur,” observed Dr. West, who directs the Alberta Transplant Institute, Edmonton, and the Canadian Donation and Transplantation Research Program. She is a professor of pediatrics with adjunct positions in the departments of surgery and microbiology/immunology.
Dr. West also sees Mr. Bennett’s struggle with infections and adjustments to his unique immunosuppressive regimen, at least as characterized by his care team, as in line with the experience of many heart transplant recipients facing the same threat.
“We already walk this tightrope with every transplant patient,” she said. Typically, they’re put on a somewhat standardized immunosuppressant regimen, “and then we modify it a bit, either increasing or decreasing it, depending on the posttransplant course.” The regimen can become especially intense in response to new signs of rejection, “and you know that that’s going to have an impact on susceptibility to all kinds of infections.”
Full circle
The porcine heart was protected along two fronts against assault from Mr. Bennett’s immune system and other inhospitable aspects of his physiology, either of which could also have been obstacles to success: Genetic modification (Revivicor) of the pig that provided the heart, and a singularly aggressive antirejection drug regimen for the patient.
The knockout of three genes targeting specific porcine cell-surface carbohydrates that provoke a strong human antibody response reportedly averted a hyperacute rejection response that would have caused the graft to fail almost immediately.
Other genetic manipulations, some using CRISPR technology, silenced genes encoded for porcine endogenous retroviruses. Others were aimed at controlling myocardial growth and stemming graft microangiopathy.
Mr. Bennett himself was treated with powerful immunosuppressants, including an investigational anti-CD40 monoclonal antibody (KPL-404, Kiniksa Pharmaceuticals) that, according to UMSOM, inhibits a well-recognized pathway critical to B-cell proliferation, T-cell activation, and antibody production.
“I suspect the patient may not have had rejection, but unfortunately, that intense immunosuppression really set him up – even if he had been half that age – for a very difficult time,” David A. Baran, MD, a cardiologist from Sentara Advanced Heart Failure Center, Norfolk, Va., who studies transplant immunology, said in an interview.
“This is in some ways like the original heart transplant in 1967, when the ability to do the surgery evolved before understanding of the immunosuppression needed. Four or 5 years later, heart transplantation almost died out, before the development of better immunosuppressants like cyclosporine and later tacrolimus,” Dr. Baran said.
“The current age, when we use less immunosuppression than ever, is based on 30 years of progressive success,” he noted. This landmark xenotransplantation “basically turns back the clock to a time when the intensity of immunosuppression by definition had to be extremely high, because we really didn’t know what to expect.”
Emerging role of xeno-organs
Xenotransplantation has been touted as potential strategy for expanding the pool of organs available for transplantation. Mr. Bennett’s “breakthrough surgery” takes the world “one step closer to solving the organ shortage crisis,” his surgeon, Dr. Griffith, announced soon after the procedure. “There are simply not enough donor human hearts available to meet the long list of potential recipients.”
But it’s not the only proposed approach. Measures could be taken, for example, to make more efficient use of the human organs that become available, partly by opening the field to additional less-than-ideal hearts and loosening regulatory mandates for projected graft survival.
“Every year, more than two-thirds of donor organs in the United States are discarded. So it’s not actually that we don’t have enough organs, it’s that we don’t have enough organs that people are willing to take,” Dr. Baran said. Still, it’s important to pursue all promising avenues, and “the genetic manipulation pathway is remarkable.”
But “honestly, organs such as kidneys probably make the most sense” for early study of xenotransplantation from pigs, he said. “The waiting list for kidneys is also very long, but if the kidney graft were to fail, the patient wouldn’t die. It would allow us to work out the immunosuppression without putting patients’ lives at risk.”
Often overlooked in assessments of organ demand, Dr. West said, is that “a lot of patients who could benefit from a transplant will never even be listed for a transplant.” It’s not clear why; perhaps they have multiple comorbidities, live too far from a transplant center, “or they’re too big or too small. Even if there were unlimited organs, you could never meet the needs of people who could benefit from transplantation.”
So even if more available donor organs were used, she said, there would still be a gap that xenotransplantation could help fill. “I’m very much in favor of research that allows us to continue to try to find a pathway to xenotransplantation. I think it’s critically important.”
Unquestionably, “we now need to have a dialogue to entertain how a technology like this, using modern medicine with gene editing, is really going to be utilized,” Dr. Mehra said. The Bennett case “does open up the field, but it also raises caution.” There should be broad participation to move the field forward, “coordinated through either societies or nationally allocated advisory committees that oversee the movement of this technology, to the next step.”
Ideally, that next step “would be to do a safety clinical trial in the right patient,” he said. “And the right patient, by definition, would be one who does not have a life-prolonging option, either mechanical circulatory support or allograft transplantation. That would be the goal.”
Dr. Mehra has reported receiving payments to his institution from Abbott for consulting; consulting fees from Janssen, Mesoblast, Broadview Ventures, Natera, Paragonix, Moderna, and the Baim Institute for Clinical Research; and serving on a scientific advisory board NuPulseCV, Leviticus, and FineHeart. Dr. Baran disclosed consulting for Getinge and LivaNova; speaking for Pfizer; and serving on trial steering committees for CareDx and Procyrion, all unrelated to xenotransplantation. Dr. West has declared no relevant conflicts.
A version of this article first appeared on Medscape.com.
The genetically altered pig’s heart “worked like a rock star, beautifully functioning,” the surgeon who performed the pioneering Jan. 7 xenotransplant procedure said in a press statement on the death of the patient, David Bennett Sr.
“He wasn’t able to overcome what turned out to be devastating – the debilitation from his previous period of heart failure, which was extreme,” said Bartley P. Griffith, MD, clinical director of the cardiac xenotransplantation program at the University of Maryland, Baltimore.
Representatives of the institution aren’t offering many details on the cause of Mr. Bennett’s death on March 8, 60 days after his operation, but said they will elaborate when their findings are formally published. But their comments seem to downplay the unique nature of the implanted heart itself as a culprit and instead implicate the patient’s diminished overall clinical condition and what grew into an ongoing battle with infections.
The 57-year-old Bennett, bedridden with end-stage heart failure, judged a poor candidate for a ventricular assist device, and on extracorporeal membrane oxygenation (ECMO), reportedly was offered the extraordinary surgery after being turned down for a conventional transplant at several major centers.
“Until day 45 or 50, he was doing very well,” Muhammad M. Mohiuddin, MD, the xenotransplantation program’s scientific director, observed in the statement. But infections soon took advantage of his hobbled immune system.
Given his “preexisting condition and how frail his body was,” Dr. Mohiuddin said, “we were having difficulty maintaining a balance between his immunosuppression and controlling his infection.” Mr. Bennett went into multiple organ failure and “I think that resulted in his passing away.”
Beyond wildest dreams
The surgeons confidently framed Mr. Bennett’s experience as a milestone for heart xenotransplantation. “The demonstration that it was possible, beyond the wildest dreams of most people in the field, even, at this point – that we were able to take a genetically engineered organ and watch it function flawlessly for 9 weeks – is pretty positive in terms of the potential of this therapy,” Dr. Griffith said.
But enough questions linger that others were more circumspect, even as they praised the accomplishment. “There’s no question that this is a historic event,” Mandeep R. Mehra, MD, of Harvard Medical School, and director of the Center for Advanced Heart Disease at Brigham and Women’s Hospital, both in Boston, said in an interview.
Still, “I don’t think we should just conclude that it was the patient’s frailty or death from infection,” Dr. Mehra said. With so few details available, “I would be very careful in prematurely concluding that the problem did not reside with the heart but with the patient. We cannot be sure.”
For example, he noted, “6 to 8 weeks is right around the time when some cardiac complications, like accelerated forms of vasculopathy, could become evident.” Immune-mediated cardiac allograft vasculopathy is a common cause of heart transplant failure.
Or, “it could as easily have been the fact that immunosuppression was modified at 6 to 7 weeks in response to potential infection, which could have led to a cardiac compromise,” Dr. Mehra said. “We just don’t know.”
“It’s really important that this be reported in a scientifically accurate way, because we will all learn from this,” Lori J. West, MD, DPhil, said in an interview.
Little seems to be known for sure about the actual cause of death, “but the fact there was not hyperacute rejection is itself a big step forward. And we know, at least from the limited information we have, that it did not occur,” observed Dr. West, who directs the Alberta Transplant Institute, Edmonton, and the Canadian Donation and Transplantation Research Program. She is a professor of pediatrics with adjunct positions in the departments of surgery and microbiology/immunology.
Dr. West also sees Mr. Bennett’s struggle with infections and adjustments to his unique immunosuppressive regimen, at least as characterized by his care team, as in line with the experience of many heart transplant recipients facing the same threat.
“We already walk this tightrope with every transplant patient,” she said. Typically, they’re put on a somewhat standardized immunosuppressant regimen, “and then we modify it a bit, either increasing or decreasing it, depending on the posttransplant course.” The regimen can become especially intense in response to new signs of rejection, “and you know that that’s going to have an impact on susceptibility to all kinds of infections.”
Full circle
The porcine heart was protected along two fronts against assault from Mr. Bennett’s immune system and other inhospitable aspects of his physiology, either of which could also have been obstacles to success: Genetic modification (Revivicor) of the pig that provided the heart, and a singularly aggressive antirejection drug regimen for the patient.
The knockout of three genes targeting specific porcine cell-surface carbohydrates that provoke a strong human antibody response reportedly averted a hyperacute rejection response that would have caused the graft to fail almost immediately.
Other genetic manipulations, some using CRISPR technology, silenced genes encoded for porcine endogenous retroviruses. Others were aimed at controlling myocardial growth and stemming graft microangiopathy.
Mr. Bennett himself was treated with powerful immunosuppressants, including an investigational anti-CD40 monoclonal antibody (KPL-404, Kiniksa Pharmaceuticals) that, according to UMSOM, inhibits a well-recognized pathway critical to B-cell proliferation, T-cell activation, and antibody production.
“I suspect the patient may not have had rejection, but unfortunately, that intense immunosuppression really set him up – even if he had been half that age – for a very difficult time,” David A. Baran, MD, a cardiologist from Sentara Advanced Heart Failure Center, Norfolk, Va., who studies transplant immunology, said in an interview.
“This is in some ways like the original heart transplant in 1967, when the ability to do the surgery evolved before understanding of the immunosuppression needed. Four or 5 years later, heart transplantation almost died out, before the development of better immunosuppressants like cyclosporine and later tacrolimus,” Dr. Baran said.
“The current age, when we use less immunosuppression than ever, is based on 30 years of progressive success,” he noted. This landmark xenotransplantation “basically turns back the clock to a time when the intensity of immunosuppression by definition had to be extremely high, because we really didn’t know what to expect.”
Emerging role of xeno-organs
Xenotransplantation has been touted as potential strategy for expanding the pool of organs available for transplantation. Mr. Bennett’s “breakthrough surgery” takes the world “one step closer to solving the organ shortage crisis,” his surgeon, Dr. Griffith, announced soon after the procedure. “There are simply not enough donor human hearts available to meet the long list of potential recipients.”
But it’s not the only proposed approach. Measures could be taken, for example, to make more efficient use of the human organs that become available, partly by opening the field to additional less-than-ideal hearts and loosening regulatory mandates for projected graft survival.
“Every year, more than two-thirds of donor organs in the United States are discarded. So it’s not actually that we don’t have enough organs, it’s that we don’t have enough organs that people are willing to take,” Dr. Baran said. Still, it’s important to pursue all promising avenues, and “the genetic manipulation pathway is remarkable.”
But “honestly, organs such as kidneys probably make the most sense” for early study of xenotransplantation from pigs, he said. “The waiting list for kidneys is also very long, but if the kidney graft were to fail, the patient wouldn’t die. It would allow us to work out the immunosuppression without putting patients’ lives at risk.”
Often overlooked in assessments of organ demand, Dr. West said, is that “a lot of patients who could benefit from a transplant will never even be listed for a transplant.” It’s not clear why; perhaps they have multiple comorbidities, live too far from a transplant center, “or they’re too big or too small. Even if there were unlimited organs, you could never meet the needs of people who could benefit from transplantation.”
So even if more available donor organs were used, she said, there would still be a gap that xenotransplantation could help fill. “I’m very much in favor of research that allows us to continue to try to find a pathway to xenotransplantation. I think it’s critically important.”
Unquestionably, “we now need to have a dialogue to entertain how a technology like this, using modern medicine with gene editing, is really going to be utilized,” Dr. Mehra said. The Bennett case “does open up the field, but it also raises caution.” There should be broad participation to move the field forward, “coordinated through either societies or nationally allocated advisory committees that oversee the movement of this technology, to the next step.”
Ideally, that next step “would be to do a safety clinical trial in the right patient,” he said. “And the right patient, by definition, would be one who does not have a life-prolonging option, either mechanical circulatory support or allograft transplantation. That would be the goal.”
Dr. Mehra has reported receiving payments to his institution from Abbott for consulting; consulting fees from Janssen, Mesoblast, Broadview Ventures, Natera, Paragonix, Moderna, and the Baim Institute for Clinical Research; and serving on a scientific advisory board NuPulseCV, Leviticus, and FineHeart. Dr. Baran disclosed consulting for Getinge and LivaNova; speaking for Pfizer; and serving on trial steering committees for CareDx and Procyrion, all unrelated to xenotransplantation. Dr. West has declared no relevant conflicts.
A version of this article first appeared on Medscape.com.
The genetically altered pig’s heart “worked like a rock star, beautifully functioning,” the surgeon who performed the pioneering Jan. 7 xenotransplant procedure said in a press statement on the death of the patient, David Bennett Sr.
“He wasn’t able to overcome what turned out to be devastating – the debilitation from his previous period of heart failure, which was extreme,” said Bartley P. Griffith, MD, clinical director of the cardiac xenotransplantation program at the University of Maryland, Baltimore.
Representatives of the institution aren’t offering many details on the cause of Mr. Bennett’s death on March 8, 60 days after his operation, but said they will elaborate when their findings are formally published. But their comments seem to downplay the unique nature of the implanted heart itself as a culprit and instead implicate the patient’s diminished overall clinical condition and what grew into an ongoing battle with infections.
The 57-year-old Bennett, bedridden with end-stage heart failure, judged a poor candidate for a ventricular assist device, and on extracorporeal membrane oxygenation (ECMO), reportedly was offered the extraordinary surgery after being turned down for a conventional transplant at several major centers.
“Until day 45 or 50, he was doing very well,” Muhammad M. Mohiuddin, MD, the xenotransplantation program’s scientific director, observed in the statement. But infections soon took advantage of his hobbled immune system.
Given his “preexisting condition and how frail his body was,” Dr. Mohiuddin said, “we were having difficulty maintaining a balance between his immunosuppression and controlling his infection.” Mr. Bennett went into multiple organ failure and “I think that resulted in his passing away.”
Beyond wildest dreams
The surgeons confidently framed Mr. Bennett’s experience as a milestone for heart xenotransplantation. “The demonstration that it was possible, beyond the wildest dreams of most people in the field, even, at this point – that we were able to take a genetically engineered organ and watch it function flawlessly for 9 weeks – is pretty positive in terms of the potential of this therapy,” Dr. Griffith said.
But enough questions linger that others were more circumspect, even as they praised the accomplishment. “There’s no question that this is a historic event,” Mandeep R. Mehra, MD, of Harvard Medical School, and director of the Center for Advanced Heart Disease at Brigham and Women’s Hospital, both in Boston, said in an interview.
Still, “I don’t think we should just conclude that it was the patient’s frailty or death from infection,” Dr. Mehra said. With so few details available, “I would be very careful in prematurely concluding that the problem did not reside with the heart but with the patient. We cannot be sure.”
For example, he noted, “6 to 8 weeks is right around the time when some cardiac complications, like accelerated forms of vasculopathy, could become evident.” Immune-mediated cardiac allograft vasculopathy is a common cause of heart transplant failure.
Or, “it could as easily have been the fact that immunosuppression was modified at 6 to 7 weeks in response to potential infection, which could have led to a cardiac compromise,” Dr. Mehra said. “We just don’t know.”
“It’s really important that this be reported in a scientifically accurate way, because we will all learn from this,” Lori J. West, MD, DPhil, said in an interview.
Little seems to be known for sure about the actual cause of death, “but the fact there was not hyperacute rejection is itself a big step forward. And we know, at least from the limited information we have, that it did not occur,” observed Dr. West, who directs the Alberta Transplant Institute, Edmonton, and the Canadian Donation and Transplantation Research Program. She is a professor of pediatrics with adjunct positions in the departments of surgery and microbiology/immunology.
Dr. West also sees Mr. Bennett’s struggle with infections and adjustments to his unique immunosuppressive regimen, at least as characterized by his care team, as in line with the experience of many heart transplant recipients facing the same threat.
“We already walk this tightrope with every transplant patient,” she said. Typically, they’re put on a somewhat standardized immunosuppressant regimen, “and then we modify it a bit, either increasing or decreasing it, depending on the posttransplant course.” The regimen can become especially intense in response to new signs of rejection, “and you know that that’s going to have an impact on susceptibility to all kinds of infections.”
Full circle
The porcine heart was protected along two fronts against assault from Mr. Bennett’s immune system and other inhospitable aspects of his physiology, either of which could also have been obstacles to success: Genetic modification (Revivicor) of the pig that provided the heart, and a singularly aggressive antirejection drug regimen for the patient.
The knockout of three genes targeting specific porcine cell-surface carbohydrates that provoke a strong human antibody response reportedly averted a hyperacute rejection response that would have caused the graft to fail almost immediately.
Other genetic manipulations, some using CRISPR technology, silenced genes encoded for porcine endogenous retroviruses. Others were aimed at controlling myocardial growth and stemming graft microangiopathy.
Mr. Bennett himself was treated with powerful immunosuppressants, including an investigational anti-CD40 monoclonal antibody (KPL-404, Kiniksa Pharmaceuticals) that, according to UMSOM, inhibits a well-recognized pathway critical to B-cell proliferation, T-cell activation, and antibody production.
“I suspect the patient may not have had rejection, but unfortunately, that intense immunosuppression really set him up – even if he had been half that age – for a very difficult time,” David A. Baran, MD, a cardiologist from Sentara Advanced Heart Failure Center, Norfolk, Va., who studies transplant immunology, said in an interview.
“This is in some ways like the original heart transplant in 1967, when the ability to do the surgery evolved before understanding of the immunosuppression needed. Four or 5 years later, heart transplantation almost died out, before the development of better immunosuppressants like cyclosporine and later tacrolimus,” Dr. Baran said.
“The current age, when we use less immunosuppression than ever, is based on 30 years of progressive success,” he noted. This landmark xenotransplantation “basically turns back the clock to a time when the intensity of immunosuppression by definition had to be extremely high, because we really didn’t know what to expect.”
Emerging role of xeno-organs
Xenotransplantation has been touted as potential strategy for expanding the pool of organs available for transplantation. Mr. Bennett’s “breakthrough surgery” takes the world “one step closer to solving the organ shortage crisis,” his surgeon, Dr. Griffith, announced soon after the procedure. “There are simply not enough donor human hearts available to meet the long list of potential recipients.”
But it’s not the only proposed approach. Measures could be taken, for example, to make more efficient use of the human organs that become available, partly by opening the field to additional less-than-ideal hearts and loosening regulatory mandates for projected graft survival.
“Every year, more than two-thirds of donor organs in the United States are discarded. So it’s not actually that we don’t have enough organs, it’s that we don’t have enough organs that people are willing to take,” Dr. Baran said. Still, it’s important to pursue all promising avenues, and “the genetic manipulation pathway is remarkable.”
But “honestly, organs such as kidneys probably make the most sense” for early study of xenotransplantation from pigs, he said. “The waiting list for kidneys is also very long, but if the kidney graft were to fail, the patient wouldn’t die. It would allow us to work out the immunosuppression without putting patients’ lives at risk.”
Often overlooked in assessments of organ demand, Dr. West said, is that “a lot of patients who could benefit from a transplant will never even be listed for a transplant.” It’s not clear why; perhaps they have multiple comorbidities, live too far from a transplant center, “or they’re too big or too small. Even if there were unlimited organs, you could never meet the needs of people who could benefit from transplantation.”
So even if more available donor organs were used, she said, there would still be a gap that xenotransplantation could help fill. “I’m very much in favor of research that allows us to continue to try to find a pathway to xenotransplantation. I think it’s critically important.”
Unquestionably, “we now need to have a dialogue to entertain how a technology like this, using modern medicine with gene editing, is really going to be utilized,” Dr. Mehra said. The Bennett case “does open up the field, but it also raises caution.” There should be broad participation to move the field forward, “coordinated through either societies or nationally allocated advisory committees that oversee the movement of this technology, to the next step.”
Ideally, that next step “would be to do a safety clinical trial in the right patient,” he said. “And the right patient, by definition, would be one who does not have a life-prolonging option, either mechanical circulatory support or allograft transplantation. That would be the goal.”
Dr. Mehra has reported receiving payments to his institution from Abbott for consulting; consulting fees from Janssen, Mesoblast, Broadview Ventures, Natera, Paragonix, Moderna, and the Baim Institute for Clinical Research; and serving on a scientific advisory board NuPulseCV, Leviticus, and FineHeart. Dr. Baran disclosed consulting for Getinge and LivaNova; speaking for Pfizer; and serving on trial steering committees for CareDx and Procyrion, all unrelated to xenotransplantation. Dr. West has declared no relevant conflicts.
A version of this article first appeared on Medscape.com.
Lung cancer with ILD patients fare poorly after thoracic radiotherapy
Most lung cancer patients with interstitial lung disease will not benefit from thoracic radiotherapy, based on data from a systematic review of 24 studies.
Thoracic radiotherapy remains a key part of lung cancer treatment for early and metastatic disease. However, patients with both small cell lung cancer (SCLC) and non–small cell lung cancer (NSCLC) associated with interstitial lung disease (ILD) fare worse than do those without ILD, often because of acute exacerbation of ILD and severe or fatal pneumonitis, wrote Animesh Saha, MD, of Apollo Multi-Specialty Hospitals, Kolkata, India, and colleagues. Consequently, clinicians may hesitate to offer radiotherapy to these patients.
In a review published in Clinical Oncology, the researchers identified 24 studies, including phase II and phase III randomized or nonrandomized trials, as well as prospective, observational studies and retrospective real-world studies. The goal of the review was to report the incidence and predictors of radiation pneumonitis associated with different types of thoracic radiotherapy for lung cancer patients with ILD, the researchers said. Treatment types included curative-intent fractionated radiotherapy or chemoradiotherapy or moderately hypofractionated (nonstereotactic ablative radiotherapy [SABR]) and hyperfractionated radiotherapy as well as particle beam therapies.
The studies included patients with SCLC or NSCLC and any form of ILD, including subclinical, radiologically diagnosed, or symptomatic, the researchers said.
Overall, the median incidence of grade 3 or higher radiation pneumonitis was 19.7%; the median incidence in patients treated with conventional radical radiotherapy, SABR, and particle beam therapy was 31.8%, 11.9%, and 20.25%, respectively.
Eighteen studies reported grade 5 radiation pneumonitis; the overall median incidence was 6%, but as high as 60% in some studies. When separated by treatment type, the median incidence was 2.7%, 6.25%, and 6.25%, respectively, in patients treated with radical radiotherapy (non-SABR), SABR, and particle beam therapy.
Independent predictors of severe radiation pneumonitis (grade 2 or higher and grade 3 or higher) included subclinical or radiological ILD, the researchers said. Among ILD subtypes, studies have shown increased risk for severe radiation pneumonitis among those with non-IPF or non-UIP pattern fibrosis.
In addition, patient-related factors of low forced vital capacity (FVC) and low forced expiratory volume in 1 second (FEV1), have been associated with severe radiation pneumonitis, the researchers said. They also found increased risk for patients with lower lobe tumor location compared to other lobes.
As for treatment-related factors, a history of gemcitabine chemotherapy was associated with an increased risk of grade 3 or higher radiation pneumonitis.
“There is always concern about using thoracic radiotherapy in lung cancer patients with coexisting ILD in view of the risks involved,” the researchers wrote in their discussion of the findings. “Although thoracic radiotherapy is expected to produce similar local control, overall survival is worse in lung cancer patients with ILD than without, probably due to the poor prognosis associated with ILD and associated treatment-related mortality,” they said.
The findings were limited by several factors including the heterogeneity of the studies and study population and the retrospective design of most of the studies, the researchers noted.
However, the results highlight the increased risk of severe and fatal radiation pneumonitis in lung cancer patients with ILD and the need for careful patient selection and counseling if thoracic radiotherapy is to be considered, they concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
Most lung cancer patients with interstitial lung disease will not benefit from thoracic radiotherapy, based on data from a systematic review of 24 studies.
Thoracic radiotherapy remains a key part of lung cancer treatment for early and metastatic disease. However, patients with both small cell lung cancer (SCLC) and non–small cell lung cancer (NSCLC) associated with interstitial lung disease (ILD) fare worse than do those without ILD, often because of acute exacerbation of ILD and severe or fatal pneumonitis, wrote Animesh Saha, MD, of Apollo Multi-Specialty Hospitals, Kolkata, India, and colleagues. Consequently, clinicians may hesitate to offer radiotherapy to these patients.
In a review published in Clinical Oncology, the researchers identified 24 studies, including phase II and phase III randomized or nonrandomized trials, as well as prospective, observational studies and retrospective real-world studies. The goal of the review was to report the incidence and predictors of radiation pneumonitis associated with different types of thoracic radiotherapy for lung cancer patients with ILD, the researchers said. Treatment types included curative-intent fractionated radiotherapy or chemoradiotherapy or moderately hypofractionated (nonstereotactic ablative radiotherapy [SABR]) and hyperfractionated radiotherapy as well as particle beam therapies.
The studies included patients with SCLC or NSCLC and any form of ILD, including subclinical, radiologically diagnosed, or symptomatic, the researchers said.
Overall, the median incidence of grade 3 or higher radiation pneumonitis was 19.7%; the median incidence in patients treated with conventional radical radiotherapy, SABR, and particle beam therapy was 31.8%, 11.9%, and 20.25%, respectively.
Eighteen studies reported grade 5 radiation pneumonitis; the overall median incidence was 6%, but as high as 60% in some studies. When separated by treatment type, the median incidence was 2.7%, 6.25%, and 6.25%, respectively, in patients treated with radical radiotherapy (non-SABR), SABR, and particle beam therapy.
Independent predictors of severe radiation pneumonitis (grade 2 or higher and grade 3 or higher) included subclinical or radiological ILD, the researchers said. Among ILD subtypes, studies have shown increased risk for severe radiation pneumonitis among those with non-IPF or non-UIP pattern fibrosis.
In addition, patient-related factors of low forced vital capacity (FVC) and low forced expiratory volume in 1 second (FEV1), have been associated with severe radiation pneumonitis, the researchers said. They also found increased risk for patients with lower lobe tumor location compared to other lobes.
As for treatment-related factors, a history of gemcitabine chemotherapy was associated with an increased risk of grade 3 or higher radiation pneumonitis.
“There is always concern about using thoracic radiotherapy in lung cancer patients with coexisting ILD in view of the risks involved,” the researchers wrote in their discussion of the findings. “Although thoracic radiotherapy is expected to produce similar local control, overall survival is worse in lung cancer patients with ILD than without, probably due to the poor prognosis associated with ILD and associated treatment-related mortality,” they said.
The findings were limited by several factors including the heterogeneity of the studies and study population and the retrospective design of most of the studies, the researchers noted.
However, the results highlight the increased risk of severe and fatal radiation pneumonitis in lung cancer patients with ILD and the need for careful patient selection and counseling if thoracic radiotherapy is to be considered, they concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
Most lung cancer patients with interstitial lung disease will not benefit from thoracic radiotherapy, based on data from a systematic review of 24 studies.
Thoracic radiotherapy remains a key part of lung cancer treatment for early and metastatic disease. However, patients with both small cell lung cancer (SCLC) and non–small cell lung cancer (NSCLC) associated with interstitial lung disease (ILD) fare worse than do those without ILD, often because of acute exacerbation of ILD and severe or fatal pneumonitis, wrote Animesh Saha, MD, of Apollo Multi-Specialty Hospitals, Kolkata, India, and colleagues. Consequently, clinicians may hesitate to offer radiotherapy to these patients.
In a review published in Clinical Oncology, the researchers identified 24 studies, including phase II and phase III randomized or nonrandomized trials, as well as prospective, observational studies and retrospective real-world studies. The goal of the review was to report the incidence and predictors of radiation pneumonitis associated with different types of thoracic radiotherapy for lung cancer patients with ILD, the researchers said. Treatment types included curative-intent fractionated radiotherapy or chemoradiotherapy or moderately hypofractionated (nonstereotactic ablative radiotherapy [SABR]) and hyperfractionated radiotherapy as well as particle beam therapies.
The studies included patients with SCLC or NSCLC and any form of ILD, including subclinical, radiologically diagnosed, or symptomatic, the researchers said.
Overall, the median incidence of grade 3 or higher radiation pneumonitis was 19.7%; the median incidence in patients treated with conventional radical radiotherapy, SABR, and particle beam therapy was 31.8%, 11.9%, and 20.25%, respectively.
Eighteen studies reported grade 5 radiation pneumonitis; the overall median incidence was 6%, but as high as 60% in some studies. When separated by treatment type, the median incidence was 2.7%, 6.25%, and 6.25%, respectively, in patients treated with radical radiotherapy (non-SABR), SABR, and particle beam therapy.
Independent predictors of severe radiation pneumonitis (grade 2 or higher and grade 3 or higher) included subclinical or radiological ILD, the researchers said. Among ILD subtypes, studies have shown increased risk for severe radiation pneumonitis among those with non-IPF or non-UIP pattern fibrosis.
In addition, patient-related factors of low forced vital capacity (FVC) and low forced expiratory volume in 1 second (FEV1), have been associated with severe radiation pneumonitis, the researchers said. They also found increased risk for patients with lower lobe tumor location compared to other lobes.
As for treatment-related factors, a history of gemcitabine chemotherapy was associated with an increased risk of grade 3 or higher radiation pneumonitis.
“There is always concern about using thoracic radiotherapy in lung cancer patients with coexisting ILD in view of the risks involved,” the researchers wrote in their discussion of the findings. “Although thoracic radiotherapy is expected to produce similar local control, overall survival is worse in lung cancer patients with ILD than without, probably due to the poor prognosis associated with ILD and associated treatment-related mortality,” they said.
The findings were limited by several factors including the heterogeneity of the studies and study population and the retrospective design of most of the studies, the researchers noted.
However, the results highlight the increased risk of severe and fatal radiation pneumonitis in lung cancer patients with ILD and the need for careful patient selection and counseling if thoracic radiotherapy is to be considered, they concluded.
The study received no outside funding. The researchers had no financial conflicts to disclose.
FROM CLINICAL ONCOLOGY
Air trapping common in patients with long COVID
, according to a prospective study that compared 100 COVID-19 survivors who had persistent symptoms and 106 healthy control persons.
“Something is going on in the distal airways related to either inflammation or fibrosis that is giving us a signal of air trapping,” noted senior author Alejandro P. Comellas, MD, in a press release. The study was stimulated by reports from University of Iowa clinicians noting that many patients with initial SARS-CoV-2 infection who were either hospitalized or were treated in the ambulatory setting later reported shortness of breath and other respiratory symptoms indicative of chronic lung disease.
Study results
Investigators classified patients (mean age, 48 years; 66 women) with post-acute sequelae of COVID-19 according to whether they were ambulatory (67%), hospitalized (17%), or required treatment in the intensive care unit (16%). They then compared CT findings of patients who had COVID-19 and persistent symptoms with those of a healthy control group.
COVID-19 severity did not affect the percentage of cases of lung with air trapping among these patients. Air trapping occurred at rates of 25.4% among ambulatory patients, 34.6% in hospitalized patients, and in 27.3% of those requiring intensive care (P = .10). The percentage of lungs affected by air trapping in ambulatory participants was sharply and significantly higher than in healthy controls (25.4% vs. 7.2%; P < .001). Also, air trapping persisted; it was still present in 8 of 9 participants who underwent imaging more than 200 days post diagnosis.
Qualitative analysis of chest CT images showed that the most common imaging abnormality was air trapping (58%); ground glass opacities (GGOs) were found in 51% (46/91), note Dr. Comellas and coauthors. This suggests ongoing lung inflammation, edema, or fibrosis. These symptoms are often observed during acute COVID-19, frequently in an organizing pneumonia pattern, and have been shown to persist for months after infection in survivors of severe disease. The mean percentage of total lung classified as having regional GGOs on chest CT scans was 13.2% and 28.7%, respectively, in the hospitalized and ICU groups, both very much higher than in the ambulatory group, at 3.7% (P < .001 for both). Among healthy controls, the GGO rate on chest CT was only 0.06% (P < .001).
In addition, air trapping correlated with the ratio of residual volume to total lung capacity (r = 0.6; P < .001) but not with spirometry results. In fact, the investigators did not observe airflow obstruction by spirometry in any group, suggesting that air trapping in these patients involves only small rather than large airways and that these small airways contribute little to total airway resistance. Only when a large percentage, perhaps 75% or more, of all small airways are obstructed will spirometry pick up small airways disease, the authors observe.
Continuing disease
The findings taken together suggest that functional small airways disease and air trapping are a consequence of SARS-CoV-2 infection, according to Dr. Comellas. “If a portion of patients continues to have small airways disease, then we need to think about the mechanisms behind it,” he said. “It could be something related to inflammation that’s reversible, or it may be something related to a scar that is irreversible, and then we need to look at ways to prevent further progression of the disease.” Furthermore, “studies aimed at determining the natural history of functional small airways disease in patients with post-acute sequelae of COVID-19 and the biological mechanisms that underlie these findings are urgently needed to identify therapeutic and preventative interventions,” Dr. Comellas, professor of internal medicine at Carver College of Medicine, University of Iowa, Iowa City, concluded.
The study limitations, the authors state, include the fact that theirs was a single-center study that enrolled participants infected early during the COVID-19 pandemic and did not include patients with Delta or Omicron variants, thus limiting the generalizability of the findings.
The study was published in Radiology.
The reported findings “indicate a long-term impact on bronchiolar obstruction,” states Brett M. Elicker, MD, professor of clinical radiology, University of California, San Francisco, in an accompanying editorial . Because collagen may be absorbed for months after an acute insult, it is not entirely clear whether the abnormalities seen in the current study will be permanent. He said further, “the presence of ground glass opacity and/or fibrosis on CT were most common in the patients admitted to the ICU and likely correspond to post-organizing pneumonia and/or post-diffuse alveolar damage fibrosis.”
Dr. Elicker also pointed out that organizing pneumonia is especially common among patients with COVID-19 and is usually highly steroid-responsive. The opacities improve or resolve with treatment, but sometimes residual fibrosis occurs. “Longer-term studies assessing the clinical and imaging manifestations 1-2 years after the initial infection are needed to fully ascertain the permanent manifestations of post-COVID fibrosis.”
The study was supported by grants from the National Institutes of Health. The authors and Dr. Elicker have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, according to a prospective study that compared 100 COVID-19 survivors who had persistent symptoms and 106 healthy control persons.
“Something is going on in the distal airways related to either inflammation or fibrosis that is giving us a signal of air trapping,” noted senior author Alejandro P. Comellas, MD, in a press release. The study was stimulated by reports from University of Iowa clinicians noting that many patients with initial SARS-CoV-2 infection who were either hospitalized or were treated in the ambulatory setting later reported shortness of breath and other respiratory symptoms indicative of chronic lung disease.
Study results
Investigators classified patients (mean age, 48 years; 66 women) with post-acute sequelae of COVID-19 according to whether they were ambulatory (67%), hospitalized (17%), or required treatment in the intensive care unit (16%). They then compared CT findings of patients who had COVID-19 and persistent symptoms with those of a healthy control group.
COVID-19 severity did not affect the percentage of cases of lung with air trapping among these patients. Air trapping occurred at rates of 25.4% among ambulatory patients, 34.6% in hospitalized patients, and in 27.3% of those requiring intensive care (P = .10). The percentage of lungs affected by air trapping in ambulatory participants was sharply and significantly higher than in healthy controls (25.4% vs. 7.2%; P < .001). Also, air trapping persisted; it was still present in 8 of 9 participants who underwent imaging more than 200 days post diagnosis.
Qualitative analysis of chest CT images showed that the most common imaging abnormality was air trapping (58%); ground glass opacities (GGOs) were found in 51% (46/91), note Dr. Comellas and coauthors. This suggests ongoing lung inflammation, edema, or fibrosis. These symptoms are often observed during acute COVID-19, frequently in an organizing pneumonia pattern, and have been shown to persist for months after infection in survivors of severe disease. The mean percentage of total lung classified as having regional GGOs on chest CT scans was 13.2% and 28.7%, respectively, in the hospitalized and ICU groups, both very much higher than in the ambulatory group, at 3.7% (P < .001 for both). Among healthy controls, the GGO rate on chest CT was only 0.06% (P < .001).
In addition, air trapping correlated with the ratio of residual volume to total lung capacity (r = 0.6; P < .001) but not with spirometry results. In fact, the investigators did not observe airflow obstruction by spirometry in any group, suggesting that air trapping in these patients involves only small rather than large airways and that these small airways contribute little to total airway resistance. Only when a large percentage, perhaps 75% or more, of all small airways are obstructed will spirometry pick up small airways disease, the authors observe.
Continuing disease
The findings taken together suggest that functional small airways disease and air trapping are a consequence of SARS-CoV-2 infection, according to Dr. Comellas. “If a portion of patients continues to have small airways disease, then we need to think about the mechanisms behind it,” he said. “It could be something related to inflammation that’s reversible, or it may be something related to a scar that is irreversible, and then we need to look at ways to prevent further progression of the disease.” Furthermore, “studies aimed at determining the natural history of functional small airways disease in patients with post-acute sequelae of COVID-19 and the biological mechanisms that underlie these findings are urgently needed to identify therapeutic and preventative interventions,” Dr. Comellas, professor of internal medicine at Carver College of Medicine, University of Iowa, Iowa City, concluded.
The study limitations, the authors state, include the fact that theirs was a single-center study that enrolled participants infected early during the COVID-19 pandemic and did not include patients with Delta or Omicron variants, thus limiting the generalizability of the findings.
The study was published in Radiology.
The reported findings “indicate a long-term impact on bronchiolar obstruction,” states Brett M. Elicker, MD, professor of clinical radiology, University of California, San Francisco, in an accompanying editorial . Because collagen may be absorbed for months after an acute insult, it is not entirely clear whether the abnormalities seen in the current study will be permanent. He said further, “the presence of ground glass opacity and/or fibrosis on CT were most common in the patients admitted to the ICU and likely correspond to post-organizing pneumonia and/or post-diffuse alveolar damage fibrosis.”
Dr. Elicker also pointed out that organizing pneumonia is especially common among patients with COVID-19 and is usually highly steroid-responsive. The opacities improve or resolve with treatment, but sometimes residual fibrosis occurs. “Longer-term studies assessing the clinical and imaging manifestations 1-2 years after the initial infection are needed to fully ascertain the permanent manifestations of post-COVID fibrosis.”
The study was supported by grants from the National Institutes of Health. The authors and Dr. Elicker have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, according to a prospective study that compared 100 COVID-19 survivors who had persistent symptoms and 106 healthy control persons.
“Something is going on in the distal airways related to either inflammation or fibrosis that is giving us a signal of air trapping,” noted senior author Alejandro P. Comellas, MD, in a press release. The study was stimulated by reports from University of Iowa clinicians noting that many patients with initial SARS-CoV-2 infection who were either hospitalized or were treated in the ambulatory setting later reported shortness of breath and other respiratory symptoms indicative of chronic lung disease.
Study results
Investigators classified patients (mean age, 48 years; 66 women) with post-acute sequelae of COVID-19 according to whether they were ambulatory (67%), hospitalized (17%), or required treatment in the intensive care unit (16%). They then compared CT findings of patients who had COVID-19 and persistent symptoms with those of a healthy control group.
COVID-19 severity did not affect the percentage of cases of lung with air trapping among these patients. Air trapping occurred at rates of 25.4% among ambulatory patients, 34.6% in hospitalized patients, and in 27.3% of those requiring intensive care (P = .10). The percentage of lungs affected by air trapping in ambulatory participants was sharply and significantly higher than in healthy controls (25.4% vs. 7.2%; P < .001). Also, air trapping persisted; it was still present in 8 of 9 participants who underwent imaging more than 200 days post diagnosis.
Qualitative analysis of chest CT images showed that the most common imaging abnormality was air trapping (58%); ground glass opacities (GGOs) were found in 51% (46/91), note Dr. Comellas and coauthors. This suggests ongoing lung inflammation, edema, or fibrosis. These symptoms are often observed during acute COVID-19, frequently in an organizing pneumonia pattern, and have been shown to persist for months after infection in survivors of severe disease. The mean percentage of total lung classified as having regional GGOs on chest CT scans was 13.2% and 28.7%, respectively, in the hospitalized and ICU groups, both very much higher than in the ambulatory group, at 3.7% (P < .001 for both). Among healthy controls, the GGO rate on chest CT was only 0.06% (P < .001).
In addition, air trapping correlated with the ratio of residual volume to total lung capacity (r = 0.6; P < .001) but not with spirometry results. In fact, the investigators did not observe airflow obstruction by spirometry in any group, suggesting that air trapping in these patients involves only small rather than large airways and that these small airways contribute little to total airway resistance. Only when a large percentage, perhaps 75% or more, of all small airways are obstructed will spirometry pick up small airways disease, the authors observe.
Continuing disease
The findings taken together suggest that functional small airways disease and air trapping are a consequence of SARS-CoV-2 infection, according to Dr. Comellas. “If a portion of patients continues to have small airways disease, then we need to think about the mechanisms behind it,” he said. “It could be something related to inflammation that’s reversible, or it may be something related to a scar that is irreversible, and then we need to look at ways to prevent further progression of the disease.” Furthermore, “studies aimed at determining the natural history of functional small airways disease in patients with post-acute sequelae of COVID-19 and the biological mechanisms that underlie these findings are urgently needed to identify therapeutic and preventative interventions,” Dr. Comellas, professor of internal medicine at Carver College of Medicine, University of Iowa, Iowa City, concluded.
The study limitations, the authors state, include the fact that theirs was a single-center study that enrolled participants infected early during the COVID-19 pandemic and did not include patients with Delta or Omicron variants, thus limiting the generalizability of the findings.
The study was published in Radiology.
The reported findings “indicate a long-term impact on bronchiolar obstruction,” states Brett M. Elicker, MD, professor of clinical radiology, University of California, San Francisco, in an accompanying editorial . Because collagen may be absorbed for months after an acute insult, it is not entirely clear whether the abnormalities seen in the current study will be permanent. He said further, “the presence of ground glass opacity and/or fibrosis on CT were most common in the patients admitted to the ICU and likely correspond to post-organizing pneumonia and/or post-diffuse alveolar damage fibrosis.”
Dr. Elicker also pointed out that organizing pneumonia is especially common among patients with COVID-19 and is usually highly steroid-responsive. The opacities improve or resolve with treatment, but sometimes residual fibrosis occurs. “Longer-term studies assessing the clinical and imaging manifestations 1-2 years after the initial infection are needed to fully ascertain the permanent manifestations of post-COVID fibrosis.”
The study was supported by grants from the National Institutes of Health. The authors and Dr. Elicker have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM RADIOLOGY
CPAP has only small effect on metabolic syndrome
Continuous positive airway pressure (CPAP) may be only modestly effective for ameliorating metabolic syndrome in patients with moderate to severe obstructive sleep apnea (OSA).
That conclusion comes from investigators in a randomized controlled, trial, who found that, among 100 patients with OSA and a recent diagnosis of metabolic syndrome (MS), 18% of those assigned to use CPAP at night had a reversal of MS at 6 months of follow-up, compared with 4% of controls who were assigned to use nasal strips at night (P = .04).
The majority of patients assigned to CPAP still retained their MS diagnoses at 6 months, and CPAP did not significantly reduce individual components of the syndrome. Use of CPAP was, however, associated with small reductions in visceral fat and improvement in endothelial function, reported Sara Q.C. Giampa, PhD, from the University of São Paulo, and colleagues.
“Despite a significant rate of MS reversibility after CPAP therapy, most of the patients maintained the MS diagnosis. The modest effects of CPAP on MS reversibility underscore the need for combined therapy with CPAP, aiming to maximize metabolic syndrome recovery in parallel with improvements in OSA severity and related symptoms,” according to their study, reported in the journal CHEST®.
Asked whether he still recommends CPAP to patients with OSA and the metabolic syndrome, given the findings, corresponding author Luciano F. Drager, MD, PhD, replied “yes, definitely.”
“Despite the modest rate in reversing metabolic syndrome after CPAP, the rate was 5-fold higher than non-effective treatment (18% vs. 4%),” he said in an interview.
Dr. Drager noted that studies of other single interventions such as physical exercise to reverse MS in patients with OSA also had modest results.
A researcher who studies the relationship between sleep, circadian rhythms, and metabolism commented that, although the patients in the CPAP group were compliant with the assigned equipment and had both reductions in apneic events and improvement in oxygen saturation, the effect of CPAP on the metabolic syndrome was rather small.
“The CPAP was doing what we thought it was supposed to do, but it didn’t have the magnitude of effect on the metabolic syndrome as I expected or I think as the authors expected,” said Deanna Arble, PhD, assistant professor of biological science at Marquette University, Milwaukee.
She noted that the study also failed to detect a significant improvement in the blood pressure component of metabolic syndrome.
“In my experience and my review of the literature, blood pressure tends to be the one that’s improved most dramatically with CPAP,” she said.
Dr. Arble was not involved in the study.
Study details
In the trial, titled TREATOSA-MS, the investigators enrolled 100 patients with a recent diagnosis of metabolic syndrome and moderate to severe OSA, defined as 15 or more apnea-hypopnea index events per hour. The patients were stratified by body mass index and then randomized to undergo therapeutic CPAP or to use nasal strips for 6 months.
At baseline and at the end of each intervention investigators measured anthropometric variables, blood pressure, glucose, and lipid profiles. They also leptin and adiponectin, body composition, food intake, physical activity, subcutaneous and abdominal fat (visceral and hepatic), and endothelial function to control for potential confounders.
As noted previously, they found that after 6 months “most patients with OSA randomized to CPAP retained the MS diagnosis, but the rate of MS reversibility was higher than observed in the placebo group.” The difference in metabolic syndrome reversal, 18% with CPAP versus 4% with nasal strips, translated into a hazard ratio favoring CPAP of 5.27 (P = .04).
Also as noted, in analyses adjusted for baseline values, CPAP did not significantly improve either weight, liver fat, lip profiles, or the adiposity biomarkers leptin and adiponectin, but did have “very modest” influence on reducing visceral fat and improving endothelial function.
Rigorous study
Dr. Arble said that most studies of the association between OSA and metabolic syndrome have focused on only one or two of the parameters that were included in the TREATOSA-MS study, giving the findings additional weight.
“This could potentially be a very good, carefully controlled first insight into how obstructive sleep apnea is related to the metabolic syndrome,” she said.
The study was funded by grants Fundação de Amparo Q22 à Pesquisa do Estado de São Paulo and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior. The authors and Dr. Arble reported having no conflicts of interest to disclose.
Continuous positive airway pressure (CPAP) may be only modestly effective for ameliorating metabolic syndrome in patients with moderate to severe obstructive sleep apnea (OSA).
That conclusion comes from investigators in a randomized controlled, trial, who found that, among 100 patients with OSA and a recent diagnosis of metabolic syndrome (MS), 18% of those assigned to use CPAP at night had a reversal of MS at 6 months of follow-up, compared with 4% of controls who were assigned to use nasal strips at night (P = .04).
The majority of patients assigned to CPAP still retained their MS diagnoses at 6 months, and CPAP did not significantly reduce individual components of the syndrome. Use of CPAP was, however, associated with small reductions in visceral fat and improvement in endothelial function, reported Sara Q.C. Giampa, PhD, from the University of São Paulo, and colleagues.
“Despite a significant rate of MS reversibility after CPAP therapy, most of the patients maintained the MS diagnosis. The modest effects of CPAP on MS reversibility underscore the need for combined therapy with CPAP, aiming to maximize metabolic syndrome recovery in parallel with improvements in OSA severity and related symptoms,” according to their study, reported in the journal CHEST®.
Asked whether he still recommends CPAP to patients with OSA and the metabolic syndrome, given the findings, corresponding author Luciano F. Drager, MD, PhD, replied “yes, definitely.”
“Despite the modest rate in reversing metabolic syndrome after CPAP, the rate was 5-fold higher than non-effective treatment (18% vs. 4%),” he said in an interview.
Dr. Drager noted that studies of other single interventions such as physical exercise to reverse MS in patients with OSA also had modest results.
A researcher who studies the relationship between sleep, circadian rhythms, and metabolism commented that, although the patients in the CPAP group were compliant with the assigned equipment and had both reductions in apneic events and improvement in oxygen saturation, the effect of CPAP on the metabolic syndrome was rather small.
“The CPAP was doing what we thought it was supposed to do, but it didn’t have the magnitude of effect on the metabolic syndrome as I expected or I think as the authors expected,” said Deanna Arble, PhD, assistant professor of biological science at Marquette University, Milwaukee.
She noted that the study also failed to detect a significant improvement in the blood pressure component of metabolic syndrome.
“In my experience and my review of the literature, blood pressure tends to be the one that’s improved most dramatically with CPAP,” she said.
Dr. Arble was not involved in the study.
Study details
In the trial, titled TREATOSA-MS, the investigators enrolled 100 patients with a recent diagnosis of metabolic syndrome and moderate to severe OSA, defined as 15 or more apnea-hypopnea index events per hour. The patients were stratified by body mass index and then randomized to undergo therapeutic CPAP or to use nasal strips for 6 months.
At baseline and at the end of each intervention investigators measured anthropometric variables, blood pressure, glucose, and lipid profiles. They also leptin and adiponectin, body composition, food intake, physical activity, subcutaneous and abdominal fat (visceral and hepatic), and endothelial function to control for potential confounders.
As noted previously, they found that after 6 months “most patients with OSA randomized to CPAP retained the MS diagnosis, but the rate of MS reversibility was higher than observed in the placebo group.” The difference in metabolic syndrome reversal, 18% with CPAP versus 4% with nasal strips, translated into a hazard ratio favoring CPAP of 5.27 (P = .04).
Also as noted, in analyses adjusted for baseline values, CPAP did not significantly improve either weight, liver fat, lip profiles, or the adiposity biomarkers leptin and adiponectin, but did have “very modest” influence on reducing visceral fat and improving endothelial function.
Rigorous study
Dr. Arble said that most studies of the association between OSA and metabolic syndrome have focused on only one or two of the parameters that were included in the TREATOSA-MS study, giving the findings additional weight.
“This could potentially be a very good, carefully controlled first insight into how obstructive sleep apnea is related to the metabolic syndrome,” she said.
The study was funded by grants Fundação de Amparo Q22 à Pesquisa do Estado de São Paulo and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior. The authors and Dr. Arble reported having no conflicts of interest to disclose.
Continuous positive airway pressure (CPAP) may be only modestly effective for ameliorating metabolic syndrome in patients with moderate to severe obstructive sleep apnea (OSA).
That conclusion comes from investigators in a randomized controlled, trial, who found that, among 100 patients with OSA and a recent diagnosis of metabolic syndrome (MS), 18% of those assigned to use CPAP at night had a reversal of MS at 6 months of follow-up, compared with 4% of controls who were assigned to use nasal strips at night (P = .04).
The majority of patients assigned to CPAP still retained their MS diagnoses at 6 months, and CPAP did not significantly reduce individual components of the syndrome. Use of CPAP was, however, associated with small reductions in visceral fat and improvement in endothelial function, reported Sara Q.C. Giampa, PhD, from the University of São Paulo, and colleagues.
“Despite a significant rate of MS reversibility after CPAP therapy, most of the patients maintained the MS diagnosis. The modest effects of CPAP on MS reversibility underscore the need for combined therapy with CPAP, aiming to maximize metabolic syndrome recovery in parallel with improvements in OSA severity and related symptoms,” according to their study, reported in the journal CHEST®.
Asked whether he still recommends CPAP to patients with OSA and the metabolic syndrome, given the findings, corresponding author Luciano F. Drager, MD, PhD, replied “yes, definitely.”
“Despite the modest rate in reversing metabolic syndrome after CPAP, the rate was 5-fold higher than non-effective treatment (18% vs. 4%),” he said in an interview.
Dr. Drager noted that studies of other single interventions such as physical exercise to reverse MS in patients with OSA also had modest results.
A researcher who studies the relationship between sleep, circadian rhythms, and metabolism commented that, although the patients in the CPAP group were compliant with the assigned equipment and had both reductions in apneic events and improvement in oxygen saturation, the effect of CPAP on the metabolic syndrome was rather small.
“The CPAP was doing what we thought it was supposed to do, but it didn’t have the magnitude of effect on the metabolic syndrome as I expected or I think as the authors expected,” said Deanna Arble, PhD, assistant professor of biological science at Marquette University, Milwaukee.
She noted that the study also failed to detect a significant improvement in the blood pressure component of metabolic syndrome.
“In my experience and my review of the literature, blood pressure tends to be the one that’s improved most dramatically with CPAP,” she said.
Dr. Arble was not involved in the study.
Study details
In the trial, titled TREATOSA-MS, the investigators enrolled 100 patients with a recent diagnosis of metabolic syndrome and moderate to severe OSA, defined as 15 or more apnea-hypopnea index events per hour. The patients were stratified by body mass index and then randomized to undergo therapeutic CPAP or to use nasal strips for 6 months.
At baseline and at the end of each intervention investigators measured anthropometric variables, blood pressure, glucose, and lipid profiles. They also leptin and adiponectin, body composition, food intake, physical activity, subcutaneous and abdominal fat (visceral and hepatic), and endothelial function to control for potential confounders.
As noted previously, they found that after 6 months “most patients with OSA randomized to CPAP retained the MS diagnosis, but the rate of MS reversibility was higher than observed in the placebo group.” The difference in metabolic syndrome reversal, 18% with CPAP versus 4% with nasal strips, translated into a hazard ratio favoring CPAP of 5.27 (P = .04).
Also as noted, in analyses adjusted for baseline values, CPAP did not significantly improve either weight, liver fat, lip profiles, or the adiposity biomarkers leptin and adiponectin, but did have “very modest” influence on reducing visceral fat and improving endothelial function.
Rigorous study
Dr. Arble said that most studies of the association between OSA and metabolic syndrome have focused on only one or two of the parameters that were included in the TREATOSA-MS study, giving the findings additional weight.
“This could potentially be a very good, carefully controlled first insight into how obstructive sleep apnea is related to the metabolic syndrome,” she said.
The study was funded by grants Fundação de Amparo Q22 à Pesquisa do Estado de São Paulo and Coordenação de Aperfeiçoamento de Pessoal de Nível Superior. The authors and Dr. Arble reported having no conflicts of interest to disclose.
FROM CHEST
Digital monitors can relieve asthma burden by boosting medication adherence and inhaler technique
PHOENIX – Before considering oral steroids or biologic therapies, many people with difficult-to-control asthma can reduce symptoms by addressing medication adherence and inhaler technique – and digital monitoring devices can play a key role.
Often physicians “will approach a patient about a biologic if they’re not responding to standard therapy. But we need to sometimes go back to those basic building blocks, like, are you taking the standard therapy?” William C. Anderson, MD, codirector of the multidisciplinary asthma clinic at Children’s Hospital Colorado, Aurora, said in an interview.
At the annual meeting of the American Academy of Allergy, Asthma, and Immunology, he and others presented data highlighting the diagnostic and therapeutic potential of digital monitoring devices for difficult-to-control asthma, the theme of the 2022s meeting.
The Global Initiative for Asthma (GINA) defines asthma as “difficult to control” if it remains uncontrolled despite medium- or high-dose inhaled corticosteroids with a second controller or with maintenance oral steroids, or if the asthma requires high-dose treatment to curb symptoms and exacerbations. About 17% of adult asthma patients have difficult-to-control asthma, according to the 2021 GINA report.
However, correcting for inhaling technique and adherence cuts the 17% down to just 3.7%, Giselle Mosnaim, MD, an allergist at NorthShore University HealthSystem outside Chicago and AAAAI immediate past president, told attendees at a Feb. 25 session on digital technologies for asthma management.
The CRITIKAL study, which reviewed data from more than 5,000 asthma patients, “showed that, if you have critical errors in inhaler technique, this leads to worse asthma outcomes and increased asthma exacerbations,” Dr. Mosnaim said. Sadly, it also shows that, from 1975 to 2014, despite new devices and new technologies, “we still have poor inhaler technique.”
As for ways to measure adherence, physician judgments tend to be inaccurate, patient self-reporting has proved unreliable, and prescription refill data doesn’t indicate whether patients actually used the medications. “The ideal measure of adherence should be objective, accurate and unobtrusive to minimize impact on patient behavior and allow reliable data collection in real-world settings,” Dr. Mosnaim said. “So electronic medication monitors are the gold standard.”
Tracking adherence
A closing afternoon session featured three presentations on research tracking adherence and outcomes in difficult-to-treat asthma patients – two pediatric cohorts and one across all ages. All studies used the Propeller Health sensor, a Food and Drug Administration–cleared device that attaches to the patient’s inhaler and automatically collects information on where, when, and how often they use their medication. The sensor then sends that information to a data cloud accessible to the patient and their health care professional.
Dr. Anderson’s team scoured a nationwide Propeller Health database for 8,000 patients using the digital monitors with controller therapies for asthma or chronic obstructive pulmonary disease (COPD). The study explored whether adherence differed for once-daily versus twice-daily medications, and if adherence differed based on patient age (4-60+ years).
For both asthma and COPD patients, those on once-daily regimens had higher medication adherence, compared with those who were prescribed twice-daily therapies. Plus, a greater proportion of once-daily patients met the prespecified 80% adherence threshold.
Looking across ages, medication use in the youngest group (aged 4-11 years) looked comparable with 30-somethings, “probably because parents are the ones giving the drug,” Dr. Anderson said. Mirroring patterns from other studies, adherence levels dipped in adolescents and young adults, relative to other age subsets.
Since this population-level analysis didn’t include individualized data on exacerbations or asthma control, “we can’t relate this to outcomes,” Dr. Anderson noted. But he said the data correlating medication use with adherence suggest that once-daily formulations may be the better option.
In one of the two pediatric studies, Matt McCulloch, MD, an allergy and immunology fellow working with Dr. Anderson, and colleagues reviewed charts of 40 children who received care at the Colorado Children’s multidisciplinary asthma clinic between 2018 and 2021. Half of these patients used Propeller Health sensors with their daily inhaled controller; the other patients were matched for age, ethnicity, sex, medication level, and disease control and severity – but had no electronic monitoring device.
On the whole, children who used digital monitoring for 12 months did not fare much better than matched controls on lung function (judged by forced expiratory volume) or asthma control (measured by Asthma Control Test scores).
However, within the digital monitoring group, patients who stayed on the Propeller system for 12 months did have better asthma control, fewer exacerbations, and improved asthma severity scores (measured by the Composite Asthma Severity Index), compared with when they first began digital monitoring. These children had all received care at the clinic for a while before their families opted for the electronic sensor, so “the effect wouldn’t have just been from starting in the clinic,” Dr. McCulloch said in an interview.
The gains came despite waning medication adherence. Similar to other digital monitoring studies, use of daily controller therapies in this retrospective analysis began at 50%-80% but dropped considerably during the first 4-5 months before settling into the 20%-30% range by 1 year.
Rachelle Ramsey, PhD, a pediatric research psychologist at Cincinnati Children’s Hospital Medical Center, presented data from 20 children with difficult-to-treat asthma who received 8 weeks of a digital adherence intervention during a 12-month treatment period. They analyzed three subsets – each with interventions based on how well the patients were managing daily controller therapy at baseline.
One patient with high (>80%) baseline adherence just received digital monitoring. The seven patients who began the study with intermediate (50%-80%) adherence received digital monitoring plus prescriptive text messaging. And the 12 children with poorest (<50%) baseline adherence received digital monitoring and a telehealth session in which a behavioral health specialist helped them set goals and create strategies to overcome barriers – for example, keeping the inhaler near their toothbrush in order to pair medication use with a daily habit.
“Overall, we found that matching Propeller with a behavioral intervention really improved adherence,” Dr. Ramsey said in an interview. While patients were receiving the intervention, adherence averaged across all groups increased from 39% to 76%. However, once the intervention period ended, the group’s adherence regressed toward baseline (36%).
Although adherence did not associate with clinical gains in this small study, the use of digital monitoring to improve medication adherence has translated to better outcomes in other recent efforts.
Remote monitoring
In a quality improvement project in the United Kingdom, nurses asked difficult-to-control asthma patients if they understood how to use their corticosteroid/long-acting beta2-agonist (LABA) inhalers and if they were adhering to treatment guidelines.
Those who answered yes to these questions were invited to a 28-day study that involved swapping their steroid/LABA inhalers for a different controller/bronchodilator (fluticasone/salmeterol) with INCA (Inhaler Compliance Assessment), a device that not only tracks adherence but also uses acoustics to gauge inhaler technique.
Among the 23 patients who participated, many had better clinical outcomes after 28 days of INCA monitoring. As Dr. Mosnaim told attendees, “what was amazing is so many of the patients that had been these difficult-to-control asthmatics who would have gone on to oral steroids or perhaps a biologic – lo and behold, you put them on a digital inhaler, and what do you see?” In two-thirds of the patients, “you see FeNo [a test that measures airway inflammation by detecting nitric oxide in exhalations] goes down. You see spirometry improve. You see the asthma control questionnaire improve. You see blood eosinophils go down.”
And in a 2020 randomized trial, Dr. Mosnaim and colleagues recruited 100 adults with uncontrolled asthma who had prescriptions for a daily inhaled corticosteroid and a short-acting beta-agonist (SABA) inhaler. Participants received Propeller sensors for their steroid and SABA inhalers. After a 2-week run-in period to calculate baseline corticosteroid adherence and SABA use for all participants, half the participants were randomly assigned to the control group, which had the app and sensor in silent mode, merely to collect data on medication use – whereas the treatment group received reminders, alerts, and monthly phone calls from providers who gave feedback on adherence and technique.
After 3 months of digital monitoring, patients didn’t use their rescue medication quite as often – as judged by a rise in the percentage of SABA-free days, compared with when they began the study. But the change in SABA-free days relative to baseline was more pronounced in the treatment group (19%) than in the control group (6%).
As seen in the other digital monitoring studies, adherence to daily corticosteroids fell with time, but the drop was milder in treated participants (2%) versus the control group (17%). So in this study, digital monitoring plus mobile app reminders and clinician feedback “prevented against fall in adherence to inhaled steroids over time,” Dr. Mosnaim said.
These results are “very encouraging” and offer “proof of concept that this type of remote monitoring could work,” Thanai Pongdee, MD, an allergist-immunologist with the Mayo Clinic in Rochester, Minn., said in an interview. One limitation was that the study was too short to measure exacerbation rates. A yearlong analysis would be “really fascinating because you’d catch all the seasons of the year – all the pollen seasons, all these things that could exacerbate you. Some people’s asthma can be quite seasonal.”
More important, the clinical utility of digital sensors will depend on how physicians choose to use them. If the doctor puts out a “blanket recommendation for using it but doesn’t ask you about it or doesn’t use the data to inform your care, then I think people just lose engagement and lose excitement over it,” Dr. Ramsey said. But if the health care team “asks you about the data or looks at the data with you or shows you how valuable this can be to your care, then I think that changes things.”
Building these analyses and interactions into the clinic workflow isn’t trivial. “If you have this wealth of data coming in, how are you going to look at it? Are you going to have an individual person assigned to this role? How are you going to respond to alerts?” Dr. Anderson asked.
In addition, because some digital monitors issue alerts when a patient’s asthma is not well controlled, some providers worry about liability if “something bad were to happen if you had that data but didn’t act upon it,” he said. Yet he noted that remote data monitoring is already used routinely in other areas of medicine, such as managing diabetes and heart conditions, “and it’s not like people are getting dinged for that stuff.”
Another issue is cost. Insurance only covers digital monitors in select cases, but it’s a bit of a catch-22. Insurers “don’t want to cover it until they get the data, but you can’t get the data until insurance covers it,” said Dr. Anderson, who added that “this year we finally got CPT reimbursement codes for monitoring devices.”
On the whole, studies of digital medication monitors suggest that better outcomes require “a good partnership between the health care provider and the patient,” Dr. Pongdee said. “It wasn’t like you could just put these things on and expect them to help. You still need that personal relationship to get the optimal results. We can have all this technology, but you still can’t take the people out of it.”
Dr. Mosnaim reported receiving current research grant support from GlaxoSmithKline, Novartis, Sanofi-Regeneron, and Teva; and past research grant support from AstraZeneca, Alk-Abello, and Genentech. She is immediate past president of the AAAAI, and directs the board of directors for the American Board of Allergy and Immunology. Dr. Anderson has served as a consultant for Regeneron, GlaxoSmithKline, and AstraZeneca, and has received research support from Colorado Medicaid. Dr. McCulloch and Dr. Ramsey disclosed no relevant financial relationships. Dr. Pongdee serves as an at-large director on the American Academy of Allergy, Asthma and Immunology board of directors. He receives grant funding from GlaxoSmithKline, and the Mayo Clinic is a trial site for GlaxoSmithKline and AstraZeneca.
A version of this article first appeared on Medscape.com.
PHOENIX – Before considering oral steroids or biologic therapies, many people with difficult-to-control asthma can reduce symptoms by addressing medication adherence and inhaler technique – and digital monitoring devices can play a key role.
Often physicians “will approach a patient about a biologic if they’re not responding to standard therapy. But we need to sometimes go back to those basic building blocks, like, are you taking the standard therapy?” William C. Anderson, MD, codirector of the multidisciplinary asthma clinic at Children’s Hospital Colorado, Aurora, said in an interview.
At the annual meeting of the American Academy of Allergy, Asthma, and Immunology, he and others presented data highlighting the diagnostic and therapeutic potential of digital monitoring devices for difficult-to-control asthma, the theme of the 2022s meeting.
The Global Initiative for Asthma (GINA) defines asthma as “difficult to control” if it remains uncontrolled despite medium- or high-dose inhaled corticosteroids with a second controller or with maintenance oral steroids, or if the asthma requires high-dose treatment to curb symptoms and exacerbations. About 17% of adult asthma patients have difficult-to-control asthma, according to the 2021 GINA report.
However, correcting for inhaling technique and adherence cuts the 17% down to just 3.7%, Giselle Mosnaim, MD, an allergist at NorthShore University HealthSystem outside Chicago and AAAAI immediate past president, told attendees at a Feb. 25 session on digital technologies for asthma management.
The CRITIKAL study, which reviewed data from more than 5,000 asthma patients, “showed that, if you have critical errors in inhaler technique, this leads to worse asthma outcomes and increased asthma exacerbations,” Dr. Mosnaim said. Sadly, it also shows that, from 1975 to 2014, despite new devices and new technologies, “we still have poor inhaler technique.”
As for ways to measure adherence, physician judgments tend to be inaccurate, patient self-reporting has proved unreliable, and prescription refill data doesn’t indicate whether patients actually used the medications. “The ideal measure of adherence should be objective, accurate and unobtrusive to minimize impact on patient behavior and allow reliable data collection in real-world settings,” Dr. Mosnaim said. “So electronic medication monitors are the gold standard.”
Tracking adherence
A closing afternoon session featured three presentations on research tracking adherence and outcomes in difficult-to-treat asthma patients – two pediatric cohorts and one across all ages. All studies used the Propeller Health sensor, a Food and Drug Administration–cleared device that attaches to the patient’s inhaler and automatically collects information on where, when, and how often they use their medication. The sensor then sends that information to a data cloud accessible to the patient and their health care professional.
Dr. Anderson’s team scoured a nationwide Propeller Health database for 8,000 patients using the digital monitors with controller therapies for asthma or chronic obstructive pulmonary disease (COPD). The study explored whether adherence differed for once-daily versus twice-daily medications, and if adherence differed based on patient age (4-60+ years).
For both asthma and COPD patients, those on once-daily regimens had higher medication adherence, compared with those who were prescribed twice-daily therapies. Plus, a greater proportion of once-daily patients met the prespecified 80% adherence threshold.
Looking across ages, medication use in the youngest group (aged 4-11 years) looked comparable with 30-somethings, “probably because parents are the ones giving the drug,” Dr. Anderson said. Mirroring patterns from other studies, adherence levels dipped in adolescents and young adults, relative to other age subsets.
Since this population-level analysis didn’t include individualized data on exacerbations or asthma control, “we can’t relate this to outcomes,” Dr. Anderson noted. But he said the data correlating medication use with adherence suggest that once-daily formulations may be the better option.
In one of the two pediatric studies, Matt McCulloch, MD, an allergy and immunology fellow working with Dr. Anderson, and colleagues reviewed charts of 40 children who received care at the Colorado Children’s multidisciplinary asthma clinic between 2018 and 2021. Half of these patients used Propeller Health sensors with their daily inhaled controller; the other patients were matched for age, ethnicity, sex, medication level, and disease control and severity – but had no electronic monitoring device.
On the whole, children who used digital monitoring for 12 months did not fare much better than matched controls on lung function (judged by forced expiratory volume) or asthma control (measured by Asthma Control Test scores).
However, within the digital monitoring group, patients who stayed on the Propeller system for 12 months did have better asthma control, fewer exacerbations, and improved asthma severity scores (measured by the Composite Asthma Severity Index), compared with when they first began digital monitoring. These children had all received care at the clinic for a while before their families opted for the electronic sensor, so “the effect wouldn’t have just been from starting in the clinic,” Dr. McCulloch said in an interview.
The gains came despite waning medication adherence. Similar to other digital monitoring studies, use of daily controller therapies in this retrospective analysis began at 50%-80% but dropped considerably during the first 4-5 months before settling into the 20%-30% range by 1 year.
Rachelle Ramsey, PhD, a pediatric research psychologist at Cincinnati Children’s Hospital Medical Center, presented data from 20 children with difficult-to-treat asthma who received 8 weeks of a digital adherence intervention during a 12-month treatment period. They analyzed three subsets – each with interventions based on how well the patients were managing daily controller therapy at baseline.
One patient with high (>80%) baseline adherence just received digital monitoring. The seven patients who began the study with intermediate (50%-80%) adherence received digital monitoring plus prescriptive text messaging. And the 12 children with poorest (<50%) baseline adherence received digital monitoring and a telehealth session in which a behavioral health specialist helped them set goals and create strategies to overcome barriers – for example, keeping the inhaler near their toothbrush in order to pair medication use with a daily habit.
“Overall, we found that matching Propeller with a behavioral intervention really improved adherence,” Dr. Ramsey said in an interview. While patients were receiving the intervention, adherence averaged across all groups increased from 39% to 76%. However, once the intervention period ended, the group’s adherence regressed toward baseline (36%).
Although adherence did not associate with clinical gains in this small study, the use of digital monitoring to improve medication adherence has translated to better outcomes in other recent efforts.
Remote monitoring
In a quality improvement project in the United Kingdom, nurses asked difficult-to-control asthma patients if they understood how to use their corticosteroid/long-acting beta2-agonist (LABA) inhalers and if they were adhering to treatment guidelines.
Those who answered yes to these questions were invited to a 28-day study that involved swapping their steroid/LABA inhalers for a different controller/bronchodilator (fluticasone/salmeterol) with INCA (Inhaler Compliance Assessment), a device that not only tracks adherence but also uses acoustics to gauge inhaler technique.
Among the 23 patients who participated, many had better clinical outcomes after 28 days of INCA monitoring. As Dr. Mosnaim told attendees, “what was amazing is so many of the patients that had been these difficult-to-control asthmatics who would have gone on to oral steroids or perhaps a biologic – lo and behold, you put them on a digital inhaler, and what do you see?” In two-thirds of the patients, “you see FeNo [a test that measures airway inflammation by detecting nitric oxide in exhalations] goes down. You see spirometry improve. You see the asthma control questionnaire improve. You see blood eosinophils go down.”
And in a 2020 randomized trial, Dr. Mosnaim and colleagues recruited 100 adults with uncontrolled asthma who had prescriptions for a daily inhaled corticosteroid and a short-acting beta-agonist (SABA) inhaler. Participants received Propeller sensors for their steroid and SABA inhalers. After a 2-week run-in period to calculate baseline corticosteroid adherence and SABA use for all participants, half the participants were randomly assigned to the control group, which had the app and sensor in silent mode, merely to collect data on medication use – whereas the treatment group received reminders, alerts, and monthly phone calls from providers who gave feedback on adherence and technique.
After 3 months of digital monitoring, patients didn’t use their rescue medication quite as often – as judged by a rise in the percentage of SABA-free days, compared with when they began the study. But the change in SABA-free days relative to baseline was more pronounced in the treatment group (19%) than in the control group (6%).
As seen in the other digital monitoring studies, adherence to daily corticosteroids fell with time, but the drop was milder in treated participants (2%) versus the control group (17%). So in this study, digital monitoring plus mobile app reminders and clinician feedback “prevented against fall in adherence to inhaled steroids over time,” Dr. Mosnaim said.
These results are “very encouraging” and offer “proof of concept that this type of remote monitoring could work,” Thanai Pongdee, MD, an allergist-immunologist with the Mayo Clinic in Rochester, Minn., said in an interview. One limitation was that the study was too short to measure exacerbation rates. A yearlong analysis would be “really fascinating because you’d catch all the seasons of the year – all the pollen seasons, all these things that could exacerbate you. Some people’s asthma can be quite seasonal.”
More important, the clinical utility of digital sensors will depend on how physicians choose to use them. If the doctor puts out a “blanket recommendation for using it but doesn’t ask you about it or doesn’t use the data to inform your care, then I think people just lose engagement and lose excitement over it,” Dr. Ramsey said. But if the health care team “asks you about the data or looks at the data with you or shows you how valuable this can be to your care, then I think that changes things.”
Building these analyses and interactions into the clinic workflow isn’t trivial. “If you have this wealth of data coming in, how are you going to look at it? Are you going to have an individual person assigned to this role? How are you going to respond to alerts?” Dr. Anderson asked.
In addition, because some digital monitors issue alerts when a patient’s asthma is not well controlled, some providers worry about liability if “something bad were to happen if you had that data but didn’t act upon it,” he said. Yet he noted that remote data monitoring is already used routinely in other areas of medicine, such as managing diabetes and heart conditions, “and it’s not like people are getting dinged for that stuff.”
Another issue is cost. Insurance only covers digital monitors in select cases, but it’s a bit of a catch-22. Insurers “don’t want to cover it until they get the data, but you can’t get the data until insurance covers it,” said Dr. Anderson, who added that “this year we finally got CPT reimbursement codes for monitoring devices.”
On the whole, studies of digital medication monitors suggest that better outcomes require “a good partnership between the health care provider and the patient,” Dr. Pongdee said. “It wasn’t like you could just put these things on and expect them to help. You still need that personal relationship to get the optimal results. We can have all this technology, but you still can’t take the people out of it.”
Dr. Mosnaim reported receiving current research grant support from GlaxoSmithKline, Novartis, Sanofi-Regeneron, and Teva; and past research grant support from AstraZeneca, Alk-Abello, and Genentech. She is immediate past president of the AAAAI, and directs the board of directors for the American Board of Allergy and Immunology. Dr. Anderson has served as a consultant for Regeneron, GlaxoSmithKline, and AstraZeneca, and has received research support from Colorado Medicaid. Dr. McCulloch and Dr. Ramsey disclosed no relevant financial relationships. Dr. Pongdee serves as an at-large director on the American Academy of Allergy, Asthma and Immunology board of directors. He receives grant funding from GlaxoSmithKline, and the Mayo Clinic is a trial site for GlaxoSmithKline and AstraZeneca.
A version of this article first appeared on Medscape.com.
PHOENIX – Before considering oral steroids or biologic therapies, many people with difficult-to-control asthma can reduce symptoms by addressing medication adherence and inhaler technique – and digital monitoring devices can play a key role.
Often physicians “will approach a patient about a biologic if they’re not responding to standard therapy. But we need to sometimes go back to those basic building blocks, like, are you taking the standard therapy?” William C. Anderson, MD, codirector of the multidisciplinary asthma clinic at Children’s Hospital Colorado, Aurora, said in an interview.
At the annual meeting of the American Academy of Allergy, Asthma, and Immunology, he and others presented data highlighting the diagnostic and therapeutic potential of digital monitoring devices for difficult-to-control asthma, the theme of the 2022s meeting.
The Global Initiative for Asthma (GINA) defines asthma as “difficult to control” if it remains uncontrolled despite medium- or high-dose inhaled corticosteroids with a second controller or with maintenance oral steroids, or if the asthma requires high-dose treatment to curb symptoms and exacerbations. About 17% of adult asthma patients have difficult-to-control asthma, according to the 2021 GINA report.
However, correcting for inhaling technique and adherence cuts the 17% down to just 3.7%, Giselle Mosnaim, MD, an allergist at NorthShore University HealthSystem outside Chicago and AAAAI immediate past president, told attendees at a Feb. 25 session on digital technologies for asthma management.
The CRITIKAL study, which reviewed data from more than 5,000 asthma patients, “showed that, if you have critical errors in inhaler technique, this leads to worse asthma outcomes and increased asthma exacerbations,” Dr. Mosnaim said. Sadly, it also shows that, from 1975 to 2014, despite new devices and new technologies, “we still have poor inhaler technique.”
As for ways to measure adherence, physician judgments tend to be inaccurate, patient self-reporting has proved unreliable, and prescription refill data doesn’t indicate whether patients actually used the medications. “The ideal measure of adherence should be objective, accurate and unobtrusive to minimize impact on patient behavior and allow reliable data collection in real-world settings,” Dr. Mosnaim said. “So electronic medication monitors are the gold standard.”
Tracking adherence
A closing afternoon session featured three presentations on research tracking adherence and outcomes in difficult-to-treat asthma patients – two pediatric cohorts and one across all ages. All studies used the Propeller Health sensor, a Food and Drug Administration–cleared device that attaches to the patient’s inhaler and automatically collects information on where, when, and how often they use their medication. The sensor then sends that information to a data cloud accessible to the patient and their health care professional.
Dr. Anderson’s team scoured a nationwide Propeller Health database for 8,000 patients using the digital monitors with controller therapies for asthma or chronic obstructive pulmonary disease (COPD). The study explored whether adherence differed for once-daily versus twice-daily medications, and if adherence differed based on patient age (4-60+ years).
For both asthma and COPD patients, those on once-daily regimens had higher medication adherence, compared with those who were prescribed twice-daily therapies. Plus, a greater proportion of once-daily patients met the prespecified 80% adherence threshold.
Looking across ages, medication use in the youngest group (aged 4-11 years) looked comparable with 30-somethings, “probably because parents are the ones giving the drug,” Dr. Anderson said. Mirroring patterns from other studies, adherence levels dipped in adolescents and young adults, relative to other age subsets.
Since this population-level analysis didn’t include individualized data on exacerbations or asthma control, “we can’t relate this to outcomes,” Dr. Anderson noted. But he said the data correlating medication use with adherence suggest that once-daily formulations may be the better option.
In one of the two pediatric studies, Matt McCulloch, MD, an allergy and immunology fellow working with Dr. Anderson, and colleagues reviewed charts of 40 children who received care at the Colorado Children’s multidisciplinary asthma clinic between 2018 and 2021. Half of these patients used Propeller Health sensors with their daily inhaled controller; the other patients were matched for age, ethnicity, sex, medication level, and disease control and severity – but had no electronic monitoring device.
On the whole, children who used digital monitoring for 12 months did not fare much better than matched controls on lung function (judged by forced expiratory volume) or asthma control (measured by Asthma Control Test scores).
However, within the digital monitoring group, patients who stayed on the Propeller system for 12 months did have better asthma control, fewer exacerbations, and improved asthma severity scores (measured by the Composite Asthma Severity Index), compared with when they first began digital monitoring. These children had all received care at the clinic for a while before their families opted for the electronic sensor, so “the effect wouldn’t have just been from starting in the clinic,” Dr. McCulloch said in an interview.
The gains came despite waning medication adherence. Similar to other digital monitoring studies, use of daily controller therapies in this retrospective analysis began at 50%-80% but dropped considerably during the first 4-5 months before settling into the 20%-30% range by 1 year.
Rachelle Ramsey, PhD, a pediatric research psychologist at Cincinnati Children’s Hospital Medical Center, presented data from 20 children with difficult-to-treat asthma who received 8 weeks of a digital adherence intervention during a 12-month treatment period. They analyzed three subsets – each with interventions based on how well the patients were managing daily controller therapy at baseline.
One patient with high (>80%) baseline adherence just received digital monitoring. The seven patients who began the study with intermediate (50%-80%) adherence received digital monitoring plus prescriptive text messaging. And the 12 children with poorest (<50%) baseline adherence received digital monitoring and a telehealth session in which a behavioral health specialist helped them set goals and create strategies to overcome barriers – for example, keeping the inhaler near their toothbrush in order to pair medication use with a daily habit.
“Overall, we found that matching Propeller with a behavioral intervention really improved adherence,” Dr. Ramsey said in an interview. While patients were receiving the intervention, adherence averaged across all groups increased from 39% to 76%. However, once the intervention period ended, the group’s adherence regressed toward baseline (36%).
Although adherence did not associate with clinical gains in this small study, the use of digital monitoring to improve medication adherence has translated to better outcomes in other recent efforts.
Remote monitoring
In a quality improvement project in the United Kingdom, nurses asked difficult-to-control asthma patients if they understood how to use their corticosteroid/long-acting beta2-agonist (LABA) inhalers and if they were adhering to treatment guidelines.
Those who answered yes to these questions were invited to a 28-day study that involved swapping their steroid/LABA inhalers for a different controller/bronchodilator (fluticasone/salmeterol) with INCA (Inhaler Compliance Assessment), a device that not only tracks adherence but also uses acoustics to gauge inhaler technique.
Among the 23 patients who participated, many had better clinical outcomes after 28 days of INCA monitoring. As Dr. Mosnaim told attendees, “what was amazing is so many of the patients that had been these difficult-to-control asthmatics who would have gone on to oral steroids or perhaps a biologic – lo and behold, you put them on a digital inhaler, and what do you see?” In two-thirds of the patients, “you see FeNo [a test that measures airway inflammation by detecting nitric oxide in exhalations] goes down. You see spirometry improve. You see the asthma control questionnaire improve. You see blood eosinophils go down.”
And in a 2020 randomized trial, Dr. Mosnaim and colleagues recruited 100 adults with uncontrolled asthma who had prescriptions for a daily inhaled corticosteroid and a short-acting beta-agonist (SABA) inhaler. Participants received Propeller sensors for their steroid and SABA inhalers. After a 2-week run-in period to calculate baseline corticosteroid adherence and SABA use for all participants, half the participants were randomly assigned to the control group, which had the app and sensor in silent mode, merely to collect data on medication use – whereas the treatment group received reminders, alerts, and monthly phone calls from providers who gave feedback on adherence and technique.
After 3 months of digital monitoring, patients didn’t use their rescue medication quite as often – as judged by a rise in the percentage of SABA-free days, compared with when they began the study. But the change in SABA-free days relative to baseline was more pronounced in the treatment group (19%) than in the control group (6%).
As seen in the other digital monitoring studies, adherence to daily corticosteroids fell with time, but the drop was milder in treated participants (2%) versus the control group (17%). So in this study, digital monitoring plus mobile app reminders and clinician feedback “prevented against fall in adherence to inhaled steroids over time,” Dr. Mosnaim said.
These results are “very encouraging” and offer “proof of concept that this type of remote monitoring could work,” Thanai Pongdee, MD, an allergist-immunologist with the Mayo Clinic in Rochester, Minn., said in an interview. One limitation was that the study was too short to measure exacerbation rates. A yearlong analysis would be “really fascinating because you’d catch all the seasons of the year – all the pollen seasons, all these things that could exacerbate you. Some people’s asthma can be quite seasonal.”
More important, the clinical utility of digital sensors will depend on how physicians choose to use them. If the doctor puts out a “blanket recommendation for using it but doesn’t ask you about it or doesn’t use the data to inform your care, then I think people just lose engagement and lose excitement over it,” Dr. Ramsey said. But if the health care team “asks you about the data or looks at the data with you or shows you how valuable this can be to your care, then I think that changes things.”
Building these analyses and interactions into the clinic workflow isn’t trivial. “If you have this wealth of data coming in, how are you going to look at it? Are you going to have an individual person assigned to this role? How are you going to respond to alerts?” Dr. Anderson asked.
In addition, because some digital monitors issue alerts when a patient’s asthma is not well controlled, some providers worry about liability if “something bad were to happen if you had that data but didn’t act upon it,” he said. Yet he noted that remote data monitoring is already used routinely in other areas of medicine, such as managing diabetes and heart conditions, “and it’s not like people are getting dinged for that stuff.”
Another issue is cost. Insurance only covers digital monitors in select cases, but it’s a bit of a catch-22. Insurers “don’t want to cover it until they get the data, but you can’t get the data until insurance covers it,” said Dr. Anderson, who added that “this year we finally got CPT reimbursement codes for monitoring devices.”
On the whole, studies of digital medication monitors suggest that better outcomes require “a good partnership between the health care provider and the patient,” Dr. Pongdee said. “It wasn’t like you could just put these things on and expect them to help. You still need that personal relationship to get the optimal results. We can have all this technology, but you still can’t take the people out of it.”
Dr. Mosnaim reported receiving current research grant support from GlaxoSmithKline, Novartis, Sanofi-Regeneron, and Teva; and past research grant support from AstraZeneca, Alk-Abello, and Genentech. She is immediate past president of the AAAAI, and directs the board of directors for the American Board of Allergy and Immunology. Dr. Anderson has served as a consultant for Regeneron, GlaxoSmithKline, and AstraZeneca, and has received research support from Colorado Medicaid. Dr. McCulloch and Dr. Ramsey disclosed no relevant financial relationships. Dr. Pongdee serves as an at-large director on the American Academy of Allergy, Asthma and Immunology board of directors. He receives grant funding from GlaxoSmithKline, and the Mayo Clinic is a trial site for GlaxoSmithKline and AstraZeneca.
A version of this article first appeared on Medscape.com.
AT AAAAI
New 3D printable stent holds promise for tracheal tumors
Airflow obstruction caused by a malignant tracheal tumor may be managed with a uniquely designed, 3-dimensional (3D) drug-eluting tracheal stent that, at least in animal models so far, works well and may soon be ready for human trials, Chinese investigators are reporting.
The research was published online Jan. 29 in Materials Today Chemistry.
The problems with currently available stents used to treat airflow obstruction are considerable, corresponding author Shengrong Guo, PhD, professor of pharmaceutics, Shanghai Jiao Tong University, China, and colleagues observe. “Tracheal stents physically open up stenosis, recover airway patency, and promptly relieve symptoms, but [they] cannot treat the tumor,” they explain.
“Thus, tracheal restenosis always occurs soon [after], due to progressive tumor growth after stent placement,” they add. Moreover, implanted stents cover the entire tracheal mucosa, thus preventing mucus and sputum discharge, causing airway blockage, the investigators also note. Compounding these flaws is the unalterable fact that delivery of chemotherapy to a malignant tracheal tumor is inefficient, and systemic chemotherapy is always associated with systemic side effects.
All of these issues make it very challenging to treat these tumors, Dr. Guo noted. On the other hand, if there were a means to deliver a chemotherapeutic agent more directly to the disease site – as is done with drug-eluting beads, for example, in other tumor types – then at least drug delivery would be much more efficient. “In this study, a novel tracheal stent was designed with features of a C-shaped and trilayered wall,” the researchers explain.
The gap angle of the newly developed stent is 72°; the inner diameter is 0.5 cm, and it is 2.0 cm in length. The trilayered wall consists of an inner layer of poly (ε-caprolactone) (PCL), which is a biodegradable and implantable material used alone or compounded with other ingredients to print implants. The middle layer consists of magnetic nanoparticle (MNP)–loaded PCL. The authors explain that MNPs have been approved in the U.S. as contrast agents in MRI.
Combined with temperature-responsive materials, MNPs can serve as a source of magnetic thermotherapy as well, which can be used to control drug release and facilitate drug penetration into deeper tissues. The outer layer of the stent contains a paclitaxel-loaded ethylene-vinyl acetate copolymer layer.
“The C-shaped tracheal stents are easily fabricated on a roller by using a self-made specific three-dimensional printer,” the authors explain. They point out that the C-shaped tracheal stents do not cover the entire tracheal wall, and the uncovered gap in that wall allows for normal mucus and sputum discharge.
In vivo evaluation
Once the stents were printed, the researchers evaluated the biosafety and applicability of their C-shaped tracheal stents. Small rabbits weighing 2.5 to 3.0 kg were used as experimental models and were prepared for surgery. The stent was implanted in the rabbits’ tracheas through the use of a simple stent delivery device. During follow-up, the rabbits recovered well without any sign of infection or respiratory complications.
The animals were also eating well within about 5 days of the surgery, and their weight gradually increased, suggesting that the implantation of a stent with intermittent magnetic heating did not lead to any prominent systemic toxicities. “All rabbits were [euthanized] 30 days after the placement of the tracheal stents” and the stent was removed from the rabbits’ trachea, the researchers report.
Close observation of the trachea indicated that the gap left by the C-shaped stent could keep the airway patent without blocking either mucus or sputum discharge. “The stents have good biosafety in rabbits and keep airway patency for 1 month without the occurrence of mucus/sputum blockage after implantation in rabbit trachea,” Dr. Guo and colleagues conclude.
“These results provide a scientific basis for the development of novel self-expandable C-shaped tracheal stents with combinatorial tracheal support and local chemotherapy,” they affirm.
Pediatric airway obstruction
Thus far, the role of 3D printing seems to be most prominent in the treatment of pediatric airway obstruction, where it is used in the surgical planning stages and to create the implant itself. In a systematic review of its use for this, Joshua Stramiello, MD, University of California, San Diego, and colleagues identified 37 original articles, 11 of which discussed 3D printing for surgical planning, and 26 of which discussed 3D printing implants for interventions.
“3D printing for surgical planning not only improves preoperative assessment of surgical approach and stent customization but also helps facilitate patient/family education,” the authors observe. Most of the research so far has been focused on bioresorbable external airway splints and biological grafts, they add – “with both animal studies and human case reports showing good results in improving symptoms.” One clinical series focused on the use of a 3D-printed, patient-specific, bioresorbable airway splint in a cohort of critically ill children with severe tracheobronchomalacia. (Tracheobronchomalacia is the abnormal collapse of the windpipe).
When reported, 29 splints had been implanted in 15 children with intrathoracic tracheobronchomalacia. At a median follow-up of 8.5 months, 12 children were long-term survivors, and all but one lived at home. As recently discussed by George Cheng, MD, cofounder of restor3D, a Duke University startup that created the first 3D-printed airway stent using a compressible biocompatible material with properties similar to that of silicone, personalized airway stents have the potential for advance customization, minimize pressure points, and improve airflow dynamics to increase mucus clearance.
In fact, the U.S. Food and Drug Administration has already cleared patient-specific airway stents developed by Thomas Gildea, MD, of the Cleveland Clinic. Both the Duke University and Cleveland Clinic stents have been used in patients, with promising outcomes, Dr. Cheng noted.
The authors and Dr. Stramiello and colleagues have disclosed no relevant financial relationships. Dr. Cheng is the cofounder of restor3D.
A version of this article first appeared on Medscape.com.
Airflow obstruction caused by a malignant tracheal tumor may be managed with a uniquely designed, 3-dimensional (3D) drug-eluting tracheal stent that, at least in animal models so far, works well and may soon be ready for human trials, Chinese investigators are reporting.
The research was published online Jan. 29 in Materials Today Chemistry.
The problems with currently available stents used to treat airflow obstruction are considerable, corresponding author Shengrong Guo, PhD, professor of pharmaceutics, Shanghai Jiao Tong University, China, and colleagues observe. “Tracheal stents physically open up stenosis, recover airway patency, and promptly relieve symptoms, but [they] cannot treat the tumor,” they explain.
“Thus, tracheal restenosis always occurs soon [after], due to progressive tumor growth after stent placement,” they add. Moreover, implanted stents cover the entire tracheal mucosa, thus preventing mucus and sputum discharge, causing airway blockage, the investigators also note. Compounding these flaws is the unalterable fact that delivery of chemotherapy to a malignant tracheal tumor is inefficient, and systemic chemotherapy is always associated with systemic side effects.
All of these issues make it very challenging to treat these tumors, Dr. Guo noted. On the other hand, if there were a means to deliver a chemotherapeutic agent more directly to the disease site – as is done with drug-eluting beads, for example, in other tumor types – then at least drug delivery would be much more efficient. “In this study, a novel tracheal stent was designed with features of a C-shaped and trilayered wall,” the researchers explain.
The gap angle of the newly developed stent is 72°; the inner diameter is 0.5 cm, and it is 2.0 cm in length. The trilayered wall consists of an inner layer of poly (ε-caprolactone) (PCL), which is a biodegradable and implantable material used alone or compounded with other ingredients to print implants. The middle layer consists of magnetic nanoparticle (MNP)–loaded PCL. The authors explain that MNPs have been approved in the U.S. as contrast agents in MRI.
Combined with temperature-responsive materials, MNPs can serve as a source of magnetic thermotherapy as well, which can be used to control drug release and facilitate drug penetration into deeper tissues. The outer layer of the stent contains a paclitaxel-loaded ethylene-vinyl acetate copolymer layer.
“The C-shaped tracheal stents are easily fabricated on a roller by using a self-made specific three-dimensional printer,” the authors explain. They point out that the C-shaped tracheal stents do not cover the entire tracheal wall, and the uncovered gap in that wall allows for normal mucus and sputum discharge.
In vivo evaluation
Once the stents were printed, the researchers evaluated the biosafety and applicability of their C-shaped tracheal stents. Small rabbits weighing 2.5 to 3.0 kg were used as experimental models and were prepared for surgery. The stent was implanted in the rabbits’ tracheas through the use of a simple stent delivery device. During follow-up, the rabbits recovered well without any sign of infection or respiratory complications.
The animals were also eating well within about 5 days of the surgery, and their weight gradually increased, suggesting that the implantation of a stent with intermittent magnetic heating did not lead to any prominent systemic toxicities. “All rabbits were [euthanized] 30 days after the placement of the tracheal stents” and the stent was removed from the rabbits’ trachea, the researchers report.
Close observation of the trachea indicated that the gap left by the C-shaped stent could keep the airway patent without blocking either mucus or sputum discharge. “The stents have good biosafety in rabbits and keep airway patency for 1 month without the occurrence of mucus/sputum blockage after implantation in rabbit trachea,” Dr. Guo and colleagues conclude.
“These results provide a scientific basis for the development of novel self-expandable C-shaped tracheal stents with combinatorial tracheal support and local chemotherapy,” they affirm.
Pediatric airway obstruction
Thus far, the role of 3D printing seems to be most prominent in the treatment of pediatric airway obstruction, where it is used in the surgical planning stages and to create the implant itself. In a systematic review of its use for this, Joshua Stramiello, MD, University of California, San Diego, and colleagues identified 37 original articles, 11 of which discussed 3D printing for surgical planning, and 26 of which discussed 3D printing implants for interventions.
“3D printing for surgical planning not only improves preoperative assessment of surgical approach and stent customization but also helps facilitate patient/family education,” the authors observe. Most of the research so far has been focused on bioresorbable external airway splints and biological grafts, they add – “with both animal studies and human case reports showing good results in improving symptoms.” One clinical series focused on the use of a 3D-printed, patient-specific, bioresorbable airway splint in a cohort of critically ill children with severe tracheobronchomalacia. (Tracheobronchomalacia is the abnormal collapse of the windpipe).
When reported, 29 splints had been implanted in 15 children with intrathoracic tracheobronchomalacia. At a median follow-up of 8.5 months, 12 children were long-term survivors, and all but one lived at home. As recently discussed by George Cheng, MD, cofounder of restor3D, a Duke University startup that created the first 3D-printed airway stent using a compressible biocompatible material with properties similar to that of silicone, personalized airway stents have the potential for advance customization, minimize pressure points, and improve airflow dynamics to increase mucus clearance.
In fact, the U.S. Food and Drug Administration has already cleared patient-specific airway stents developed by Thomas Gildea, MD, of the Cleveland Clinic. Both the Duke University and Cleveland Clinic stents have been used in patients, with promising outcomes, Dr. Cheng noted.
The authors and Dr. Stramiello and colleagues have disclosed no relevant financial relationships. Dr. Cheng is the cofounder of restor3D.
A version of this article first appeared on Medscape.com.
Airflow obstruction caused by a malignant tracheal tumor may be managed with a uniquely designed, 3-dimensional (3D) drug-eluting tracheal stent that, at least in animal models so far, works well and may soon be ready for human trials, Chinese investigators are reporting.
The research was published online Jan. 29 in Materials Today Chemistry.
The problems with currently available stents used to treat airflow obstruction are considerable, corresponding author Shengrong Guo, PhD, professor of pharmaceutics, Shanghai Jiao Tong University, China, and colleagues observe. “Tracheal stents physically open up stenosis, recover airway patency, and promptly relieve symptoms, but [they] cannot treat the tumor,” they explain.
“Thus, tracheal restenosis always occurs soon [after], due to progressive tumor growth after stent placement,” they add. Moreover, implanted stents cover the entire tracheal mucosa, thus preventing mucus and sputum discharge, causing airway blockage, the investigators also note. Compounding these flaws is the unalterable fact that delivery of chemotherapy to a malignant tracheal tumor is inefficient, and systemic chemotherapy is always associated with systemic side effects.
All of these issues make it very challenging to treat these tumors, Dr. Guo noted. On the other hand, if there were a means to deliver a chemotherapeutic agent more directly to the disease site – as is done with drug-eluting beads, for example, in other tumor types – then at least drug delivery would be much more efficient. “In this study, a novel tracheal stent was designed with features of a C-shaped and trilayered wall,” the researchers explain.
The gap angle of the newly developed stent is 72°; the inner diameter is 0.5 cm, and it is 2.0 cm in length. The trilayered wall consists of an inner layer of poly (ε-caprolactone) (PCL), which is a biodegradable and implantable material used alone or compounded with other ingredients to print implants. The middle layer consists of magnetic nanoparticle (MNP)–loaded PCL. The authors explain that MNPs have been approved in the U.S. as contrast agents in MRI.
Combined with temperature-responsive materials, MNPs can serve as a source of magnetic thermotherapy as well, which can be used to control drug release and facilitate drug penetration into deeper tissues. The outer layer of the stent contains a paclitaxel-loaded ethylene-vinyl acetate copolymer layer.
“The C-shaped tracheal stents are easily fabricated on a roller by using a self-made specific three-dimensional printer,” the authors explain. They point out that the C-shaped tracheal stents do not cover the entire tracheal wall, and the uncovered gap in that wall allows for normal mucus and sputum discharge.
In vivo evaluation
Once the stents were printed, the researchers evaluated the biosafety and applicability of their C-shaped tracheal stents. Small rabbits weighing 2.5 to 3.0 kg were used as experimental models and were prepared for surgery. The stent was implanted in the rabbits’ tracheas through the use of a simple stent delivery device. During follow-up, the rabbits recovered well without any sign of infection or respiratory complications.
The animals were also eating well within about 5 days of the surgery, and their weight gradually increased, suggesting that the implantation of a stent with intermittent magnetic heating did not lead to any prominent systemic toxicities. “All rabbits were [euthanized] 30 days after the placement of the tracheal stents” and the stent was removed from the rabbits’ trachea, the researchers report.
Close observation of the trachea indicated that the gap left by the C-shaped stent could keep the airway patent without blocking either mucus or sputum discharge. “The stents have good biosafety in rabbits and keep airway patency for 1 month without the occurrence of mucus/sputum blockage after implantation in rabbit trachea,” Dr. Guo and colleagues conclude.
“These results provide a scientific basis for the development of novel self-expandable C-shaped tracheal stents with combinatorial tracheal support and local chemotherapy,” they affirm.
Pediatric airway obstruction
Thus far, the role of 3D printing seems to be most prominent in the treatment of pediatric airway obstruction, where it is used in the surgical planning stages and to create the implant itself. In a systematic review of its use for this, Joshua Stramiello, MD, University of California, San Diego, and colleagues identified 37 original articles, 11 of which discussed 3D printing for surgical planning, and 26 of which discussed 3D printing implants for interventions.
“3D printing for surgical planning not only improves preoperative assessment of surgical approach and stent customization but also helps facilitate patient/family education,” the authors observe. Most of the research so far has been focused on bioresorbable external airway splints and biological grafts, they add – “with both animal studies and human case reports showing good results in improving symptoms.” One clinical series focused on the use of a 3D-printed, patient-specific, bioresorbable airway splint in a cohort of critically ill children with severe tracheobronchomalacia. (Tracheobronchomalacia is the abnormal collapse of the windpipe).
When reported, 29 splints had been implanted in 15 children with intrathoracic tracheobronchomalacia. At a median follow-up of 8.5 months, 12 children were long-term survivors, and all but one lived at home. As recently discussed by George Cheng, MD, cofounder of restor3D, a Duke University startup that created the first 3D-printed airway stent using a compressible biocompatible material with properties similar to that of silicone, personalized airway stents have the potential for advance customization, minimize pressure points, and improve airflow dynamics to increase mucus clearance.
In fact, the U.S. Food and Drug Administration has already cleared patient-specific airway stents developed by Thomas Gildea, MD, of the Cleveland Clinic. Both the Duke University and Cleveland Clinic stents have been used in patients, with promising outcomes, Dr. Cheng noted.
The authors and Dr. Stramiello and colleagues have disclosed no relevant financial relationships. Dr. Cheng is the cofounder of restor3D.
A version of this article first appeared on Medscape.com.
Resistance exercise may be best workout for a good night’s sleep
CHICAGO – A randomized trial suggests resistance exercise promotes better sleep than other workouts among inactive adults, particularly those who are poor sleepers.
“We thought resistance exercise would be somewhere in the same neighborhood as aerobic exercise or that maybe combined exercise would be a little bit better but, no, it was consistently resistance exercise, on its own, that seemed to show the most benefits across the board,” Angelique Brellenthin, PhD, told this news organization.
The results were presented at the recent Epidemiology, Prevention/Lifestyle & Cardiometabolic Health meeting sponsored by the American Heart Association.
Even before the pandemic and bedtime “doom scrolling” took hold, research showed that a third of Americans regularly get less than 7 hours of sleep. The AHA recommends aerobic exercise to improve sleep and promote cardiovascular health, yet little is known on how it compares with other types of exercise in the general population, she said.
Dr. Brellenthin and coinvestigator Duck-chul Lee, PhD, both of Iowa State University in Ames, recruited 406 inactive adults, aged 35-70 years, who had obesity or overweight (mean body mass index, 31.2 kg/m2) and had elevated or stage 1 hypertension and randomly assigned them to no exercise or 60 minutes of supervised aerobic, resistance, or combination exercise three times per week for 12 months.
The aerobic exercise group could choose among treadmills, upright or recumbent bikes, and ellipticals, and the participants had their heart rate monitored to ensure they were continuously getting moderate- to vigorous-intensity exercise.
The resistance exercise group performed three sets of 8-16 repetitions at 50%-80% of their one-rep maximum on 12 resistance machines: a leg press, chest press, lat pulldown, leg curl, leg extension, biceps curl, triceps pushdown, shoulder press, abdominal crunch, lower back extension, torso rotation, and hip abduction.
The combination group did 30 minutes of aerobic exercise at moderate to vigorous intensity, and then two sets of 8-16 repetitions of resistance exercise on 9 machines instead of 12.
Exercise adherence over the year was 84%, 77%, and 85%, respectively.
Participants also completed the Pittsburgh Sleep Quality Index (PSQI) at baseline and 12 months. Among the 386 participants (53% women) with evaluable data, 35% had poor-quality sleep, as indicated by a global PSQI score of more than 5, and 42% regularly slept less than 7 hours per night.
In adjusted analyses, sleep duration at 12 months, on average, increased by 13 minutes in the resistance-exercise group (P = .009), decreased by 0.6 minute in the aerobic-exercise group, and increased by 2 minutes in the combined-exercise group and by 4 minutes in the control group.
Among participants who got less than 7 hours of sleep at baseline, however, sleep duration increased by 40 minutes (P < .0001), compared with increases of 23 minutes in the aerobic group, 17 minutes in the combined group, and 15 minutes in the control group.
Overall sleep efficiency, or the ratio of total sleep time to time in bed, improved in the resistance (P = .0005) and combined (P = .03) exercise groups, but not in the aerobic or control groups.
Sleep latency, or the time needed to fall asleep, decreased by 3 minutes in the resistance-exercise group, with no notable changes in the other groups.
Sleep quality and the number of sleep disturbances improved in all groups, including the control group. This could be due to simply being part of a health intervention, which included a month of lifestyle education classes, Dr. Brellenthin suggested.
It’s unclear why the aerobic-exercise group didn’t show greater gains, given the wealth of research showing it improves sleep, she said, but it had fewer poor sleepers at baseline than the resistance group (33% vs. 42%). “So it may be that people who were already getting good sleep didn’t have much room to improve.”
Among the poor-quality sleepers at baseline, resistance exercise significantly improved sleep quality (-2.4 vs. -1.0 points; P = .009) and duration (+36 vs. +3 minutes; P = .02), compared with the control group. It also improved sleep efficiency by 9.0%, compared with 0.9% in the control group (P = .002) and 8.0% for the combined-exercise group (P = .01).
“For a lot of people who know their sleep could be a bit better, this could be a place to start without resorting to medications, if they wanted to focus on a lifestyle intervention,” Dr. Brellenthin said.
It’s not fully understood how resistance exercise improves sleep, but it might contribute to better overall mental health and it might enhance the synthesis and release of certain hormones, such as testosterone and human growth hormone, which are associated with better sleep, Dr. Brellenthin said. Another hypothesis is that it causes direct microscopic damage to muscle tissue, forcing that tissue to adapt and grow over time. “So potentially that microscopic damage could provide that extra signal boost to the brain to replenish and repair, and get this person sleep.”
The study was limited by the use of self-reported sleep outcomes and a lack of detailed information on sleep medications, although 81% of participants reported taking no such medications.
The research was supported by a National Institutes of Health/National Heart, Lung, and Blood Institute grant to Dr. Lee. Dr. Brellenthin reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
CHICAGO – A randomized trial suggests resistance exercise promotes better sleep than other workouts among inactive adults, particularly those who are poor sleepers.
“We thought resistance exercise would be somewhere in the same neighborhood as aerobic exercise or that maybe combined exercise would be a little bit better but, no, it was consistently resistance exercise, on its own, that seemed to show the most benefits across the board,” Angelique Brellenthin, PhD, told this news organization.
The results were presented at the recent Epidemiology, Prevention/Lifestyle & Cardiometabolic Health meeting sponsored by the American Heart Association.
Even before the pandemic and bedtime “doom scrolling” took hold, research showed that a third of Americans regularly get less than 7 hours of sleep. The AHA recommends aerobic exercise to improve sleep and promote cardiovascular health, yet little is known on how it compares with other types of exercise in the general population, she said.
Dr. Brellenthin and coinvestigator Duck-chul Lee, PhD, both of Iowa State University in Ames, recruited 406 inactive adults, aged 35-70 years, who had obesity or overweight (mean body mass index, 31.2 kg/m2) and had elevated or stage 1 hypertension and randomly assigned them to no exercise or 60 minutes of supervised aerobic, resistance, or combination exercise three times per week for 12 months.
The aerobic exercise group could choose among treadmills, upright or recumbent bikes, and ellipticals, and the participants had their heart rate monitored to ensure they were continuously getting moderate- to vigorous-intensity exercise.
The resistance exercise group performed three sets of 8-16 repetitions at 50%-80% of their one-rep maximum on 12 resistance machines: a leg press, chest press, lat pulldown, leg curl, leg extension, biceps curl, triceps pushdown, shoulder press, abdominal crunch, lower back extension, torso rotation, and hip abduction.
The combination group did 30 minutes of aerobic exercise at moderate to vigorous intensity, and then two sets of 8-16 repetitions of resistance exercise on 9 machines instead of 12.
Exercise adherence over the year was 84%, 77%, and 85%, respectively.
Participants also completed the Pittsburgh Sleep Quality Index (PSQI) at baseline and 12 months. Among the 386 participants (53% women) with evaluable data, 35% had poor-quality sleep, as indicated by a global PSQI score of more than 5, and 42% regularly slept less than 7 hours per night.
In adjusted analyses, sleep duration at 12 months, on average, increased by 13 minutes in the resistance-exercise group (P = .009), decreased by 0.6 minute in the aerobic-exercise group, and increased by 2 minutes in the combined-exercise group and by 4 minutes in the control group.
Among participants who got less than 7 hours of sleep at baseline, however, sleep duration increased by 40 minutes (P < .0001), compared with increases of 23 minutes in the aerobic group, 17 minutes in the combined group, and 15 minutes in the control group.
Overall sleep efficiency, or the ratio of total sleep time to time in bed, improved in the resistance (P = .0005) and combined (P = .03) exercise groups, but not in the aerobic or control groups.
Sleep latency, or the time needed to fall asleep, decreased by 3 minutes in the resistance-exercise group, with no notable changes in the other groups.
Sleep quality and the number of sleep disturbances improved in all groups, including the control group. This could be due to simply being part of a health intervention, which included a month of lifestyle education classes, Dr. Brellenthin suggested.
It’s unclear why the aerobic-exercise group didn’t show greater gains, given the wealth of research showing it improves sleep, she said, but it had fewer poor sleepers at baseline than the resistance group (33% vs. 42%). “So it may be that people who were already getting good sleep didn’t have much room to improve.”
Among the poor-quality sleepers at baseline, resistance exercise significantly improved sleep quality (-2.4 vs. -1.0 points; P = .009) and duration (+36 vs. +3 minutes; P = .02), compared with the control group. It also improved sleep efficiency by 9.0%, compared with 0.9% in the control group (P = .002) and 8.0% for the combined-exercise group (P = .01).
“For a lot of people who know their sleep could be a bit better, this could be a place to start without resorting to medications, if they wanted to focus on a lifestyle intervention,” Dr. Brellenthin said.
It’s not fully understood how resistance exercise improves sleep, but it might contribute to better overall mental health and it might enhance the synthesis and release of certain hormones, such as testosterone and human growth hormone, which are associated with better sleep, Dr. Brellenthin said. Another hypothesis is that it causes direct microscopic damage to muscle tissue, forcing that tissue to adapt and grow over time. “So potentially that microscopic damage could provide that extra signal boost to the brain to replenish and repair, and get this person sleep.”
The study was limited by the use of self-reported sleep outcomes and a lack of detailed information on sleep medications, although 81% of participants reported taking no such medications.
The research was supported by a National Institutes of Health/National Heart, Lung, and Blood Institute grant to Dr. Lee. Dr. Brellenthin reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
CHICAGO – A randomized trial suggests resistance exercise promotes better sleep than other workouts among inactive adults, particularly those who are poor sleepers.
“We thought resistance exercise would be somewhere in the same neighborhood as aerobic exercise or that maybe combined exercise would be a little bit better but, no, it was consistently resistance exercise, on its own, that seemed to show the most benefits across the board,” Angelique Brellenthin, PhD, told this news organization.
The results were presented at the recent Epidemiology, Prevention/Lifestyle & Cardiometabolic Health meeting sponsored by the American Heart Association.
Even before the pandemic and bedtime “doom scrolling” took hold, research showed that a third of Americans regularly get less than 7 hours of sleep. The AHA recommends aerobic exercise to improve sleep and promote cardiovascular health, yet little is known on how it compares with other types of exercise in the general population, she said.
Dr. Brellenthin and coinvestigator Duck-chul Lee, PhD, both of Iowa State University in Ames, recruited 406 inactive adults, aged 35-70 years, who had obesity or overweight (mean body mass index, 31.2 kg/m2) and had elevated or stage 1 hypertension and randomly assigned them to no exercise or 60 minutes of supervised aerobic, resistance, or combination exercise three times per week for 12 months.
The aerobic exercise group could choose among treadmills, upright or recumbent bikes, and ellipticals, and the participants had their heart rate monitored to ensure they were continuously getting moderate- to vigorous-intensity exercise.
The resistance exercise group performed three sets of 8-16 repetitions at 50%-80% of their one-rep maximum on 12 resistance machines: a leg press, chest press, lat pulldown, leg curl, leg extension, biceps curl, triceps pushdown, shoulder press, abdominal crunch, lower back extension, torso rotation, and hip abduction.
The combination group did 30 minutes of aerobic exercise at moderate to vigorous intensity, and then two sets of 8-16 repetitions of resistance exercise on 9 machines instead of 12.
Exercise adherence over the year was 84%, 77%, and 85%, respectively.
Participants also completed the Pittsburgh Sleep Quality Index (PSQI) at baseline and 12 months. Among the 386 participants (53% women) with evaluable data, 35% had poor-quality sleep, as indicated by a global PSQI score of more than 5, and 42% regularly slept less than 7 hours per night.
In adjusted analyses, sleep duration at 12 months, on average, increased by 13 minutes in the resistance-exercise group (P = .009), decreased by 0.6 minute in the aerobic-exercise group, and increased by 2 minutes in the combined-exercise group and by 4 minutes in the control group.
Among participants who got less than 7 hours of sleep at baseline, however, sleep duration increased by 40 minutes (P < .0001), compared with increases of 23 minutes in the aerobic group, 17 minutes in the combined group, and 15 minutes in the control group.
Overall sleep efficiency, or the ratio of total sleep time to time in bed, improved in the resistance (P = .0005) and combined (P = .03) exercise groups, but not in the aerobic or control groups.
Sleep latency, or the time needed to fall asleep, decreased by 3 minutes in the resistance-exercise group, with no notable changes in the other groups.
Sleep quality and the number of sleep disturbances improved in all groups, including the control group. This could be due to simply being part of a health intervention, which included a month of lifestyle education classes, Dr. Brellenthin suggested.
It’s unclear why the aerobic-exercise group didn’t show greater gains, given the wealth of research showing it improves sleep, she said, but it had fewer poor sleepers at baseline than the resistance group (33% vs. 42%). “So it may be that people who were already getting good sleep didn’t have much room to improve.”
Among the poor-quality sleepers at baseline, resistance exercise significantly improved sleep quality (-2.4 vs. -1.0 points; P = .009) and duration (+36 vs. +3 minutes; P = .02), compared with the control group. It also improved sleep efficiency by 9.0%, compared with 0.9% in the control group (P = .002) and 8.0% for the combined-exercise group (P = .01).
“For a lot of people who know their sleep could be a bit better, this could be a place to start without resorting to medications, if they wanted to focus on a lifestyle intervention,” Dr. Brellenthin said.
It’s not fully understood how resistance exercise improves sleep, but it might contribute to better overall mental health and it might enhance the synthesis and release of certain hormones, such as testosterone and human growth hormone, which are associated with better sleep, Dr. Brellenthin said. Another hypothesis is that it causes direct microscopic damage to muscle tissue, forcing that tissue to adapt and grow over time. “So potentially that microscopic damage could provide that extra signal boost to the brain to replenish and repair, and get this person sleep.”
The study was limited by the use of self-reported sleep outcomes and a lack of detailed information on sleep medications, although 81% of participants reported taking no such medications.
The research was supported by a National Institutes of Health/National Heart, Lung, and Blood Institute grant to Dr. Lee. Dr. Brellenthin reports no relevant financial relationships.
A version of this article first appeared on Medscape.com.
REPORTING FROM EPI/LIFESTYLE 2022
‘Overwhelming’ need to study COVID vaccine–associated tinnitus
It’s now known that tinnitus may be an unexpected side effect of SARS-CoV-2 vaccination, and there is an urgent need to understand the precise mechanisms and best treatment for vaccine-associated tinnitus, researchers say.
As of mid-September 2021, 12,247 cases of tinnitus, or ringing in the ears, following COVID-19 vaccination had been reported to the Vaccine Adverse Event Reporting System of the U.S. Centers for Disease Control and Prevention.
“Despite several cases of tinnitus being reported following SARS-CoV-2 vaccination, the precise pathophysiology is still not clear,” write Syed Hassan Ahmed, 3rd-year MBBS student, Dow University of Health Sciences, Karachi, Pakistan, and coauthors.
The researchers review what is known and unknown about SARS-CoV-2 vaccine-associated tinnitus in an article published online Feb. 11 in Annals of Medicine and Surgery.
Molecular mimicry?
The researchers say cross-reactivity between anti-spike SARS-CoV-2 antibodies and otologic antigens is one possibility, based on the mechanisms behind other COVID-19 vaccine–induced disorders and the phenomenon of molecular mimicry.
“The heptapeptide resemblance between coronavirus spike glycoprotein and numerous human proteins further supports molecular mimicry as a potential mechanism behind such vaccine-induced disorders,” they write.
Anti-spike antibodies may react with antigens anywhere along the auditory pathway and fuel an inflammatory reaction, they point out.
“Therefore, understanding the phenomenon of cross-reactivity and molecular mimicry may be helpful in postulating potential treatment behind not only tinnitus but also the rare events of vaccination associated hearing loss and other otologic manifestations,” the authors say.
Genetic predispositions and associated conditions may also play a significant role in determining whether an individual develops vaccine-induced tinnitus.
Stress and anxiety following COVID vaccination may also play a role, inasmuch as anxiety-related adverse events following vaccination have been reported. Vaccine-related anxiety as a potential cause of tinnitus developing after vaccination needs to be explored, they write.
Jury out on best management
How best to manage COVID vaccine-associated tinnitus also remains unclear, but it starts with a well-established diagnosis, the authors say.
A well-focused and detailed history and examination are essential, with particular emphasis placed on preexisting health conditions, specifically, autoimmune diseases, such as Hashimoto thyroiditis; otologic conditions, such as sensorineural hearing loss; glaucoma; and psychological well-being. According to the review, patients often present with a history of one or more of these disorders.
“However, any such association has not yet been established and requires further investigation to be concluded as potential risk factors for vaccine-induced tinnitus,” they caution.
Routine cranial nerve examination, otoscopy, Weber test, and Rinne test, which are used for tinnitus diagnosis in general, may be helpful for confirmation of vaccine-associated tinnitus.
Owing to the significant association between tinnitus and hearing impairment, audiology should also performed, the authors say.
Although treatments for non–vaccine-induced tinnitus vary significantly, corticosteroids are the top treatment choice for SARS-CoV-2 vaccine-induced tinnitus reported in the literature.
Trials of other drug and nondrug interventions that may uniquely help with vaccine-associated tinnitus are urgently needed, the authors say.
Summing up, the reviewers say, “Although the incidence of COVID-19 vaccine-associated tinnitus is rare, there is an overwhelming need to discern the precise pathophysiology and clinical management as a better understanding of adverse events may help in encountering vaccine hesitancy and hence fostering the COVID-19 global vaccination program.
“Despite the incidence of adverse events, the benefits of the SARS-CoV-2 vaccine in reducing hospitalization and deaths continue to outweigh the rare ramifications,” they conclude.
The research had no specific funding. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
It’s now known that tinnitus may be an unexpected side effect of SARS-CoV-2 vaccination, and there is an urgent need to understand the precise mechanisms and best treatment for vaccine-associated tinnitus, researchers say.
As of mid-September 2021, 12,247 cases of tinnitus, or ringing in the ears, following COVID-19 vaccination had been reported to the Vaccine Adverse Event Reporting System of the U.S. Centers for Disease Control and Prevention.
“Despite several cases of tinnitus being reported following SARS-CoV-2 vaccination, the precise pathophysiology is still not clear,” write Syed Hassan Ahmed, 3rd-year MBBS student, Dow University of Health Sciences, Karachi, Pakistan, and coauthors.
The researchers review what is known and unknown about SARS-CoV-2 vaccine-associated tinnitus in an article published online Feb. 11 in Annals of Medicine and Surgery.
Molecular mimicry?
The researchers say cross-reactivity between anti-spike SARS-CoV-2 antibodies and otologic antigens is one possibility, based on the mechanisms behind other COVID-19 vaccine–induced disorders and the phenomenon of molecular mimicry.
“The heptapeptide resemblance between coronavirus spike glycoprotein and numerous human proteins further supports molecular mimicry as a potential mechanism behind such vaccine-induced disorders,” they write.
Anti-spike antibodies may react with antigens anywhere along the auditory pathway and fuel an inflammatory reaction, they point out.
“Therefore, understanding the phenomenon of cross-reactivity and molecular mimicry may be helpful in postulating potential treatment behind not only tinnitus but also the rare events of vaccination associated hearing loss and other otologic manifestations,” the authors say.
Genetic predispositions and associated conditions may also play a significant role in determining whether an individual develops vaccine-induced tinnitus.
Stress and anxiety following COVID vaccination may also play a role, inasmuch as anxiety-related adverse events following vaccination have been reported. Vaccine-related anxiety as a potential cause of tinnitus developing after vaccination needs to be explored, they write.
Jury out on best management
How best to manage COVID vaccine-associated tinnitus also remains unclear, but it starts with a well-established diagnosis, the authors say.
A well-focused and detailed history and examination are essential, with particular emphasis placed on preexisting health conditions, specifically, autoimmune diseases, such as Hashimoto thyroiditis; otologic conditions, such as sensorineural hearing loss; glaucoma; and psychological well-being. According to the review, patients often present with a history of one or more of these disorders.
“However, any such association has not yet been established and requires further investigation to be concluded as potential risk factors for vaccine-induced tinnitus,” they caution.
Routine cranial nerve examination, otoscopy, Weber test, and Rinne test, which are used for tinnitus diagnosis in general, may be helpful for confirmation of vaccine-associated tinnitus.
Owing to the significant association between tinnitus and hearing impairment, audiology should also performed, the authors say.
Although treatments for non–vaccine-induced tinnitus vary significantly, corticosteroids are the top treatment choice for SARS-CoV-2 vaccine-induced tinnitus reported in the literature.
Trials of other drug and nondrug interventions that may uniquely help with vaccine-associated tinnitus are urgently needed, the authors say.
Summing up, the reviewers say, “Although the incidence of COVID-19 vaccine-associated tinnitus is rare, there is an overwhelming need to discern the precise pathophysiology and clinical management as a better understanding of adverse events may help in encountering vaccine hesitancy and hence fostering the COVID-19 global vaccination program.
“Despite the incidence of adverse events, the benefits of the SARS-CoV-2 vaccine in reducing hospitalization and deaths continue to outweigh the rare ramifications,” they conclude.
The research had no specific funding. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
It’s now known that tinnitus may be an unexpected side effect of SARS-CoV-2 vaccination, and there is an urgent need to understand the precise mechanisms and best treatment for vaccine-associated tinnitus, researchers say.
As of mid-September 2021, 12,247 cases of tinnitus, or ringing in the ears, following COVID-19 vaccination had been reported to the Vaccine Adverse Event Reporting System of the U.S. Centers for Disease Control and Prevention.
“Despite several cases of tinnitus being reported following SARS-CoV-2 vaccination, the precise pathophysiology is still not clear,” write Syed Hassan Ahmed, 3rd-year MBBS student, Dow University of Health Sciences, Karachi, Pakistan, and coauthors.
The researchers review what is known and unknown about SARS-CoV-2 vaccine-associated tinnitus in an article published online Feb. 11 in Annals of Medicine and Surgery.
Molecular mimicry?
The researchers say cross-reactivity between anti-spike SARS-CoV-2 antibodies and otologic antigens is one possibility, based on the mechanisms behind other COVID-19 vaccine–induced disorders and the phenomenon of molecular mimicry.
“The heptapeptide resemblance between coronavirus spike glycoprotein and numerous human proteins further supports molecular mimicry as a potential mechanism behind such vaccine-induced disorders,” they write.
Anti-spike antibodies may react with antigens anywhere along the auditory pathway and fuel an inflammatory reaction, they point out.
“Therefore, understanding the phenomenon of cross-reactivity and molecular mimicry may be helpful in postulating potential treatment behind not only tinnitus but also the rare events of vaccination associated hearing loss and other otologic manifestations,” the authors say.
Genetic predispositions and associated conditions may also play a significant role in determining whether an individual develops vaccine-induced tinnitus.
Stress and anxiety following COVID vaccination may also play a role, inasmuch as anxiety-related adverse events following vaccination have been reported. Vaccine-related anxiety as a potential cause of tinnitus developing after vaccination needs to be explored, they write.
Jury out on best management
How best to manage COVID vaccine-associated tinnitus also remains unclear, but it starts with a well-established diagnosis, the authors say.
A well-focused and detailed history and examination are essential, with particular emphasis placed on preexisting health conditions, specifically, autoimmune diseases, such as Hashimoto thyroiditis; otologic conditions, such as sensorineural hearing loss; glaucoma; and psychological well-being. According to the review, patients often present with a history of one or more of these disorders.
“However, any such association has not yet been established and requires further investigation to be concluded as potential risk factors for vaccine-induced tinnitus,” they caution.
Routine cranial nerve examination, otoscopy, Weber test, and Rinne test, which are used for tinnitus diagnosis in general, may be helpful for confirmation of vaccine-associated tinnitus.
Owing to the significant association between tinnitus and hearing impairment, audiology should also performed, the authors say.
Although treatments for non–vaccine-induced tinnitus vary significantly, corticosteroids are the top treatment choice for SARS-CoV-2 vaccine-induced tinnitus reported in the literature.
Trials of other drug and nondrug interventions that may uniquely help with vaccine-associated tinnitus are urgently needed, the authors say.
Summing up, the reviewers say, “Although the incidence of COVID-19 vaccine-associated tinnitus is rare, there is an overwhelming need to discern the precise pathophysiology and clinical management as a better understanding of adverse events may help in encountering vaccine hesitancy and hence fostering the COVID-19 global vaccination program.
“Despite the incidence of adverse events, the benefits of the SARS-CoV-2 vaccine in reducing hospitalization and deaths continue to outweigh the rare ramifications,” they conclude.
The research had no specific funding. The authors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM ANNALS OF MEDICINE AND SURGERY




