User login
-
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]


Artificial intelligence: The Netflix of cancer treatment
Chemotherapy, now streaming at just $15.99 a month!
It’s a lazy Sunday and you flip on Netflix, looking for something new to watch. There’s an almost-overwhelming number of shows out there, but right at the top of the recommended list is something that strikes your fancy right away. The algorithm behind the scenes is doing its job well, winnowing the universe of content right down to the few things you’ll find relevant, based on what you’ve watched and liked in the past.
Now, the almighty content algorithm is coming for something a little more useful than binge watching obscure 80s sitcoms: cancer treatment.
By plugging the fully sequenced genomes of nearly 10,000 patients with 33 different types of cancer into an algorithm powered by the same sort of artificial intelligence used by Netflix, researchers from London and San Diego found 21 common faults in the chromosomes of tumors, which they called copy number signatures. While cancer is a complex disease, when faults occur in those copy number signatures, the results were similar across the board. If X genetic defect occurs within a tumor, Y result will happen, even across cancer types. For example, tumors whose chromosomes had shattered and reformed had by far the worst disease outcomes.
The eventual hope is that, just as Netflix can predict what you’ll want to watch based on what you’ve already seen, oncologists will be able to predict the course of a cancer, based on the tumor’s early genetic traits, and get ahead of future genetic degradation to prevent the worst outcomes. A sort of “Oh, your tumor has enjoyed The Office. Might we suggest a treatment of 30 Rock” situation. Further research will be required to determine whether or not the cancer algorithm can get us part 2 of “Stranger Things 4” a week early.
Pay criminals, cut crime?
What is the best method for punishing those who commit wrongdoing? Fines? Jail time? Actually, no. A recent study says that financial compensation works best.
In other words, pay them for their actions. Really.
Psychologist Tage S. Rai, PhD, of the University of California, San Diego, Rady School of Management, found that people who hurt others or commit crimes are actually doing it because they think it’s the right thing to do. The results of this study say play at the angle of their morality. When that’s compromised, the offender is less likely to do it again.
Four different experiments were conducted using an online economics game with nearly 1,500 participants. Dr. Rai found that providing a monetary bonus for inflicting a punishment on a third party within the game cut the participants’ willingness to do it again by 50%.
“People punish others to signal their own goodness and receiving compensation might make it seem as though they’re driven by greed rather than justice,” he said.
The big deterrent, though, was negative judgment from peers. People in the study were even more hesitant to inflict harm and gain a profit if they thought they were going to be judged for it.
So maybe the answer to cutting crime isn’t as simple as slapping on a fine. It’s slapping on shame and paying them for it.
A conspiracy of chronobiologic proportions
The Golden State Warriors just won the NBA championship – that much is true – but we’ve got some news that you didn’t get from ESPN. The kind of news that their “partners” from the NBA didn’t want them to report. Unlike most conspiracy theories, however, this one has some science behind it.
In this case, science in the form of a study published in Frontiers in Physiology says that jet lag had a greater effect on the Boston Celtics than it did on the Warriors.
“Eastward travel – where the destination time is later than the origin time – requires the athlete to shorten their day (known as a phase advance). During phase advance, athletes often struggle to fall asleep at an earlier bedtime, leading to sleep loss and, consequently, potential impaired physiological performance and motivation the next day,” senior author Elise Facer-Childs, PhD, of Monash University, Melbourne, said in written statement.
Dr. Facer-Childs and associates took a very close look at 10 seasons’ worth of NBA games – 11,481 games, to be exact – and found “that eastward (but not westward) jet lag was associated with impaired performance for home (but not away) teams.” The existence of a pro-Western bias against teams that traveled eastward for their home games was clear:
- The chance of winning for eastern teams was reduced by 6.0%.
- They grabbed 1.3 fewer rebounds per game.
- Their field goal percentage was 1.2% lower.
And here’s the final nail in the conspiracy coffin: The NBA knew about the jet lag effect and changed the schedule of the finals in 2014 in a way that makes it worse. Before that, the higher-seeded team got two home games, then the lower-seeded team had three at home, followed by two more at the home of the higher seed. Now it’s a 2-2-1-1-1 arrangement that leads to more travel and, of course, more jet lag.
The study was published during the championship series, so the investigators suggested that the Celtics “might benefit from chronobiology-informed strategies designed to mitigate eastward jet lag symptomatology.”
So there you have it, sports fans/conspiracy theorists: You can’t chase Steph Curry around the court for 48 minutes without the right chronobiology-informed strategy. Everyone knows that.
Being hungry can alter your ‘type’
Fasting and being hungry can be a dangerous mix for becoming “hangry” and irritable, but did you know being hungry can also affect your attraction to other people?
Evidence has shown that being hungry can affect important things such as decision-making, memory, cognition, and function. It might affect decision-making in the sense that those six tacos at Taco Bell might win out over grilled chicken breast and veggies at home, but can hunger make you think that the person you just swiped right on isn’t really your type after all?
We’ll leave that up to Valentina Cazzato of Liverpool (England) John Moores University and associates, whose study involved 44 people, of whom 21 were women in their early 20s. The participants were shown computer-generated images of men and women of different sizes. The same background was used for each picture and all the expressions of the models were neutral. Participants were asked to rate each image on how much they liked it. One study was done on participants who had been fasting for 12 hours, and the second was done on those who had just eaten something.
The subjects generally preferred slim models over more rounded ones, but not after fasting. When they were hungry, they found the round human bodies and faces more attractive. So, yes, it’s definitely possible that hunger can alter your attraction to others.
“Future work might seek to elucidate the relationship between physiological states of hunger and shifts in appreciation of the human bodies and whether this relationship might be mediated by individual traits associated with to beholder’s body adiposity,” said researchers.
Chemotherapy, now streaming at just $15.99 a month!
It’s a lazy Sunday and you flip on Netflix, looking for something new to watch. There’s an almost-overwhelming number of shows out there, but right at the top of the recommended list is something that strikes your fancy right away. The algorithm behind the scenes is doing its job well, winnowing the universe of content right down to the few things you’ll find relevant, based on what you’ve watched and liked in the past.
Now, the almighty content algorithm is coming for something a little more useful than binge watching obscure 80s sitcoms: cancer treatment.
By plugging the fully sequenced genomes of nearly 10,000 patients with 33 different types of cancer into an algorithm powered by the same sort of artificial intelligence used by Netflix, researchers from London and San Diego found 21 common faults in the chromosomes of tumors, which they called copy number signatures. While cancer is a complex disease, when faults occur in those copy number signatures, the results were similar across the board. If X genetic defect occurs within a tumor, Y result will happen, even across cancer types. For example, tumors whose chromosomes had shattered and reformed had by far the worst disease outcomes.
The eventual hope is that, just as Netflix can predict what you’ll want to watch based on what you’ve already seen, oncologists will be able to predict the course of a cancer, based on the tumor’s early genetic traits, and get ahead of future genetic degradation to prevent the worst outcomes. A sort of “Oh, your tumor has enjoyed The Office. Might we suggest a treatment of 30 Rock” situation. Further research will be required to determine whether or not the cancer algorithm can get us part 2 of “Stranger Things 4” a week early.
Pay criminals, cut crime?
What is the best method for punishing those who commit wrongdoing? Fines? Jail time? Actually, no. A recent study says that financial compensation works best.
In other words, pay them for their actions. Really.
Psychologist Tage S. Rai, PhD, of the University of California, San Diego, Rady School of Management, found that people who hurt others or commit crimes are actually doing it because they think it’s the right thing to do. The results of this study say play at the angle of their morality. When that’s compromised, the offender is less likely to do it again.
Four different experiments were conducted using an online economics game with nearly 1,500 participants. Dr. Rai found that providing a monetary bonus for inflicting a punishment on a third party within the game cut the participants’ willingness to do it again by 50%.
“People punish others to signal their own goodness and receiving compensation might make it seem as though they’re driven by greed rather than justice,” he said.
The big deterrent, though, was negative judgment from peers. People in the study were even more hesitant to inflict harm and gain a profit if they thought they were going to be judged for it.
So maybe the answer to cutting crime isn’t as simple as slapping on a fine. It’s slapping on shame and paying them for it.
A conspiracy of chronobiologic proportions
The Golden State Warriors just won the NBA championship – that much is true – but we’ve got some news that you didn’t get from ESPN. The kind of news that their “partners” from the NBA didn’t want them to report. Unlike most conspiracy theories, however, this one has some science behind it.
In this case, science in the form of a study published in Frontiers in Physiology says that jet lag had a greater effect on the Boston Celtics than it did on the Warriors.
“Eastward travel – where the destination time is later than the origin time – requires the athlete to shorten their day (known as a phase advance). During phase advance, athletes often struggle to fall asleep at an earlier bedtime, leading to sleep loss and, consequently, potential impaired physiological performance and motivation the next day,” senior author Elise Facer-Childs, PhD, of Monash University, Melbourne, said in written statement.
Dr. Facer-Childs and associates took a very close look at 10 seasons’ worth of NBA games – 11,481 games, to be exact – and found “that eastward (but not westward) jet lag was associated with impaired performance for home (but not away) teams.” The existence of a pro-Western bias against teams that traveled eastward for their home games was clear:
- The chance of winning for eastern teams was reduced by 6.0%.
- They grabbed 1.3 fewer rebounds per game.
- Their field goal percentage was 1.2% lower.
And here’s the final nail in the conspiracy coffin: The NBA knew about the jet lag effect and changed the schedule of the finals in 2014 in a way that makes it worse. Before that, the higher-seeded team got two home games, then the lower-seeded team had three at home, followed by two more at the home of the higher seed. Now it’s a 2-2-1-1-1 arrangement that leads to more travel and, of course, more jet lag.
The study was published during the championship series, so the investigators suggested that the Celtics “might benefit from chronobiology-informed strategies designed to mitigate eastward jet lag symptomatology.”
So there you have it, sports fans/conspiracy theorists: You can’t chase Steph Curry around the court for 48 minutes without the right chronobiology-informed strategy. Everyone knows that.
Being hungry can alter your ‘type’
Fasting and being hungry can be a dangerous mix for becoming “hangry” and irritable, but did you know being hungry can also affect your attraction to other people?
Evidence has shown that being hungry can affect important things such as decision-making, memory, cognition, and function. It might affect decision-making in the sense that those six tacos at Taco Bell might win out over grilled chicken breast and veggies at home, but can hunger make you think that the person you just swiped right on isn’t really your type after all?
We’ll leave that up to Valentina Cazzato of Liverpool (England) John Moores University and associates, whose study involved 44 people, of whom 21 were women in their early 20s. The participants were shown computer-generated images of men and women of different sizes. The same background was used for each picture and all the expressions of the models were neutral. Participants were asked to rate each image on how much they liked it. One study was done on participants who had been fasting for 12 hours, and the second was done on those who had just eaten something.
The subjects generally preferred slim models over more rounded ones, but not after fasting. When they were hungry, they found the round human bodies and faces more attractive. So, yes, it’s definitely possible that hunger can alter your attraction to others.
“Future work might seek to elucidate the relationship between physiological states of hunger and shifts in appreciation of the human bodies and whether this relationship might be mediated by individual traits associated with to beholder’s body adiposity,” said researchers.
Chemotherapy, now streaming at just $15.99 a month!
It’s a lazy Sunday and you flip on Netflix, looking for something new to watch. There’s an almost-overwhelming number of shows out there, but right at the top of the recommended list is something that strikes your fancy right away. The algorithm behind the scenes is doing its job well, winnowing the universe of content right down to the few things you’ll find relevant, based on what you’ve watched and liked in the past.
Now, the almighty content algorithm is coming for something a little more useful than binge watching obscure 80s sitcoms: cancer treatment.
By plugging the fully sequenced genomes of nearly 10,000 patients with 33 different types of cancer into an algorithm powered by the same sort of artificial intelligence used by Netflix, researchers from London and San Diego found 21 common faults in the chromosomes of tumors, which they called copy number signatures. While cancer is a complex disease, when faults occur in those copy number signatures, the results were similar across the board. If X genetic defect occurs within a tumor, Y result will happen, even across cancer types. For example, tumors whose chromosomes had shattered and reformed had by far the worst disease outcomes.
The eventual hope is that, just as Netflix can predict what you’ll want to watch based on what you’ve already seen, oncologists will be able to predict the course of a cancer, based on the tumor’s early genetic traits, and get ahead of future genetic degradation to prevent the worst outcomes. A sort of “Oh, your tumor has enjoyed The Office. Might we suggest a treatment of 30 Rock” situation. Further research will be required to determine whether or not the cancer algorithm can get us part 2 of “Stranger Things 4” a week early.
Pay criminals, cut crime?
What is the best method for punishing those who commit wrongdoing? Fines? Jail time? Actually, no. A recent study says that financial compensation works best.
In other words, pay them for their actions. Really.
Psychologist Tage S. Rai, PhD, of the University of California, San Diego, Rady School of Management, found that people who hurt others or commit crimes are actually doing it because they think it’s the right thing to do. The results of this study say play at the angle of their morality. When that’s compromised, the offender is less likely to do it again.
Four different experiments were conducted using an online economics game with nearly 1,500 participants. Dr. Rai found that providing a monetary bonus for inflicting a punishment on a third party within the game cut the participants’ willingness to do it again by 50%.
“People punish others to signal their own goodness and receiving compensation might make it seem as though they’re driven by greed rather than justice,” he said.
The big deterrent, though, was negative judgment from peers. People in the study were even more hesitant to inflict harm and gain a profit if they thought they were going to be judged for it.
So maybe the answer to cutting crime isn’t as simple as slapping on a fine. It’s slapping on shame and paying them for it.
A conspiracy of chronobiologic proportions
The Golden State Warriors just won the NBA championship – that much is true – but we’ve got some news that you didn’t get from ESPN. The kind of news that their “partners” from the NBA didn’t want them to report. Unlike most conspiracy theories, however, this one has some science behind it.
In this case, science in the form of a study published in Frontiers in Physiology says that jet lag had a greater effect on the Boston Celtics than it did on the Warriors.
“Eastward travel – where the destination time is later than the origin time – requires the athlete to shorten their day (known as a phase advance). During phase advance, athletes often struggle to fall asleep at an earlier bedtime, leading to sleep loss and, consequently, potential impaired physiological performance and motivation the next day,” senior author Elise Facer-Childs, PhD, of Monash University, Melbourne, said in written statement.
Dr. Facer-Childs and associates took a very close look at 10 seasons’ worth of NBA games – 11,481 games, to be exact – and found “that eastward (but not westward) jet lag was associated with impaired performance for home (but not away) teams.” The existence of a pro-Western bias against teams that traveled eastward for their home games was clear:
- The chance of winning for eastern teams was reduced by 6.0%.
- They grabbed 1.3 fewer rebounds per game.
- Their field goal percentage was 1.2% lower.
And here’s the final nail in the conspiracy coffin: The NBA knew about the jet lag effect and changed the schedule of the finals in 2014 in a way that makes it worse. Before that, the higher-seeded team got two home games, then the lower-seeded team had three at home, followed by two more at the home of the higher seed. Now it’s a 2-2-1-1-1 arrangement that leads to more travel and, of course, more jet lag.
The study was published during the championship series, so the investigators suggested that the Celtics “might benefit from chronobiology-informed strategies designed to mitigate eastward jet lag symptomatology.”
So there you have it, sports fans/conspiracy theorists: You can’t chase Steph Curry around the court for 48 minutes without the right chronobiology-informed strategy. Everyone knows that.
Being hungry can alter your ‘type’
Fasting and being hungry can be a dangerous mix for becoming “hangry” and irritable, but did you know being hungry can also affect your attraction to other people?
Evidence has shown that being hungry can affect important things such as decision-making, memory, cognition, and function. It might affect decision-making in the sense that those six tacos at Taco Bell might win out over grilled chicken breast and veggies at home, but can hunger make you think that the person you just swiped right on isn’t really your type after all?
We’ll leave that up to Valentina Cazzato of Liverpool (England) John Moores University and associates, whose study involved 44 people, of whom 21 were women in their early 20s. The participants were shown computer-generated images of men and women of different sizes. The same background was used for each picture and all the expressions of the models were neutral. Participants were asked to rate each image on how much they liked it. One study was done on participants who had been fasting for 12 hours, and the second was done on those who had just eaten something.
The subjects generally preferred slim models over more rounded ones, but not after fasting. When they were hungry, they found the round human bodies and faces more attractive. So, yes, it’s definitely possible that hunger can alter your attraction to others.
“Future work might seek to elucidate the relationship between physiological states of hunger and shifts in appreciation of the human bodies and whether this relationship might be mediated by individual traits associated with to beholder’s body adiposity,” said researchers.
Children and COVID: Vaccines now available to all ages
The COVID-19 prevention effort in children enters its next phase as June draws to a close, while new pediatric cases continued on a downward trend and hospitalizations continued to rise.
The COVID-19 vaccines from Pfizer-BioNTech and Moderna were approved for use in children as young as 6 months, the Centers for Disease Control and Prevention announced on June 18.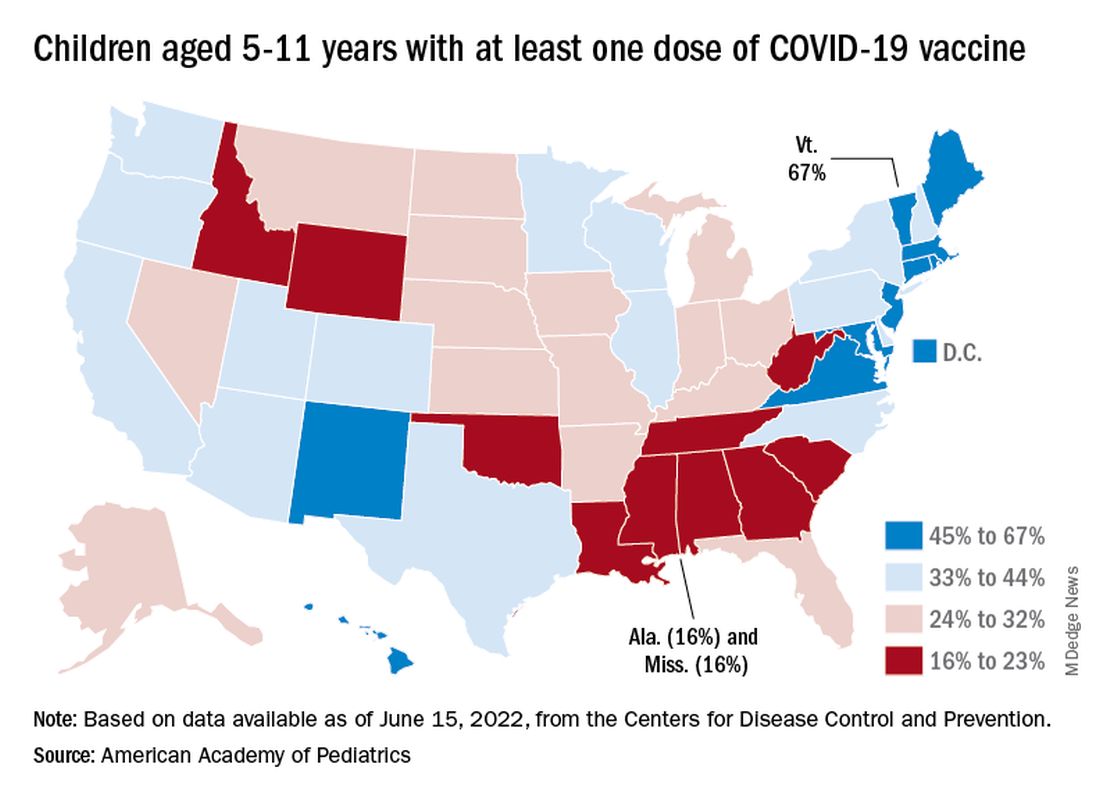
“We know millions of parents and caregivers are eager to get their young children vaccinated. ... I encourage parents and caregivers with questions to talk to their doctor, nurse, or local pharmacist to learn more about the benefits of vaccinations,” CDC Director Rochelle P. Walensky, MD, MPH, said in a written statement.
There are, however, indications that many parents are not that eager. Another 11% said “they will only do so if they are required,” Kaiser noted.
The vaccination experience with children aged 5-11 years seems to agree with those numbers. As of June 16, more than 7 months after the vaccine became available, just over 36% had received at least one dose and about 30% were fully vaccinated, CDC data show.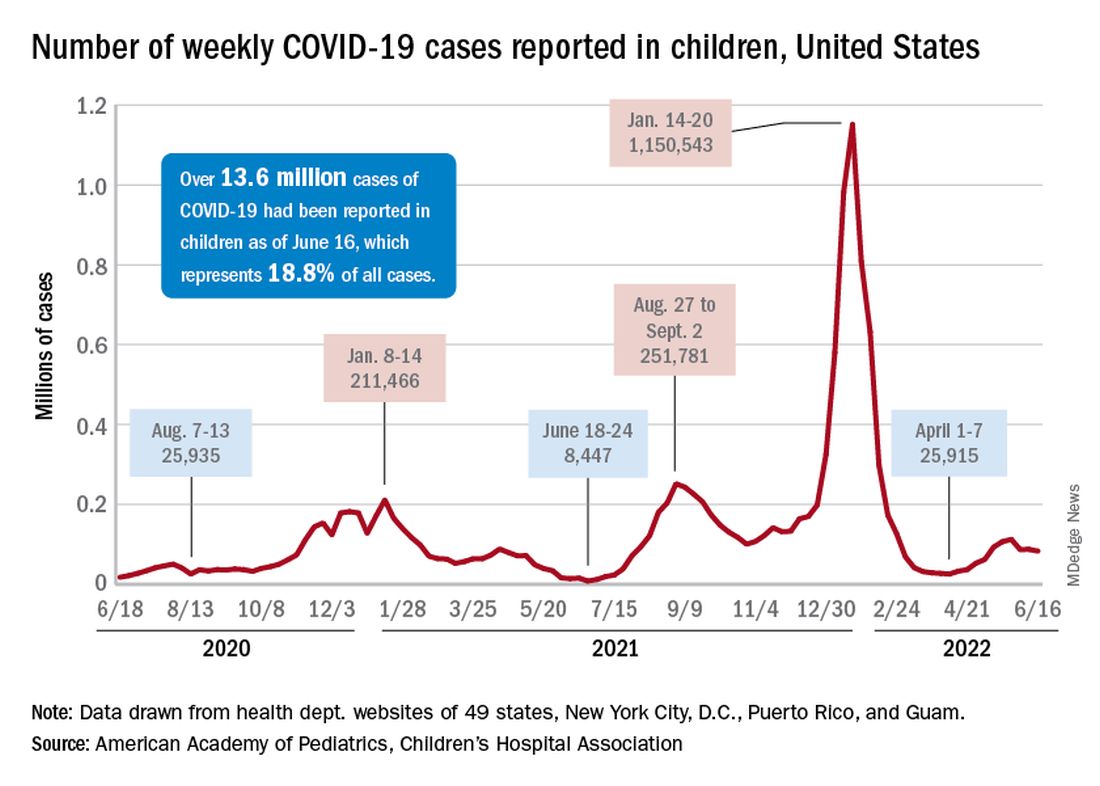
There are, according to the American Academy of Pediatrics, still five states where less than 20% of eligible 5- to 11-year-olds have received an initial vaccination. Among children aged 12-17, uptake has been much higher: 70% have received at least one dose and 60% are fully vaccinated, the CDC said.
Trends for new cases, hospitalizations diverging
COVID incidence in children, meanwhile, dropped for the second time in 3 weeks. There were 83,000 new cases reported during June 10-16, a decline of 4.8% from the previous week, according to the AAP and the Children’s Hospital Association.
New cases had risen by a very slight 0.31% during the week of June 3-9 after dropping 22% the week before (May 27 to June 2). Total cases in children have surpassed 13.6 million, which represents 18.8% of cases in all ages since the start of the pandemic, the AAP and CHA said in their weekly COVID report.
New admissions of children with confirmed COVID-19, however, have continued to climb since early to mid April. On June 16, the rate for children aged 0-17 years was up to 0.31 per 100,000, compared with the 0.13 per 100,000 recorded as late as April 11, the CDC said on its COVID Data Tracker.
The COVID-19 prevention effort in children enters its next phase as June draws to a close, while new pediatric cases continued on a downward trend and hospitalizations continued to rise.
The COVID-19 vaccines from Pfizer-BioNTech and Moderna were approved for use in children as young as 6 months, the Centers for Disease Control and Prevention announced on June 18.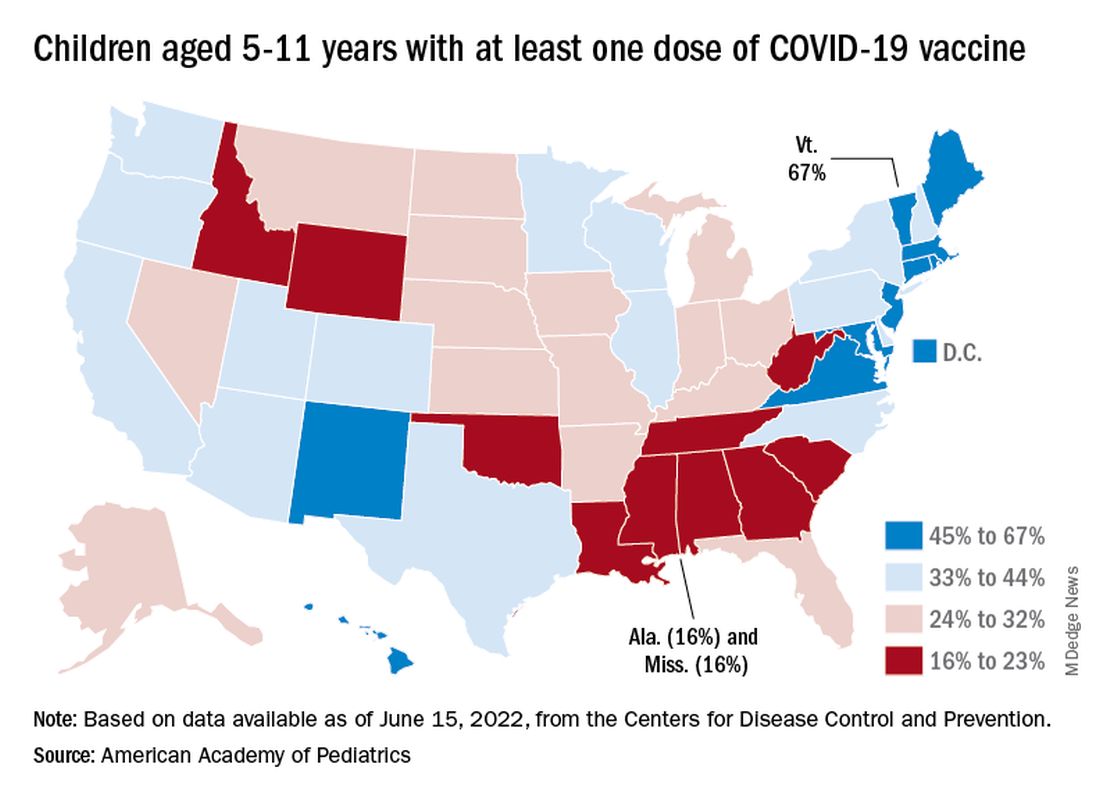
“We know millions of parents and caregivers are eager to get their young children vaccinated. ... I encourage parents and caregivers with questions to talk to their doctor, nurse, or local pharmacist to learn more about the benefits of vaccinations,” CDC Director Rochelle P. Walensky, MD, MPH, said in a written statement.
There are, however, indications that many parents are not that eager. Another 11% said “they will only do so if they are required,” Kaiser noted.
The vaccination experience with children aged 5-11 years seems to agree with those numbers. As of June 16, more than 7 months after the vaccine became available, just over 36% had received at least one dose and about 30% were fully vaccinated, CDC data show.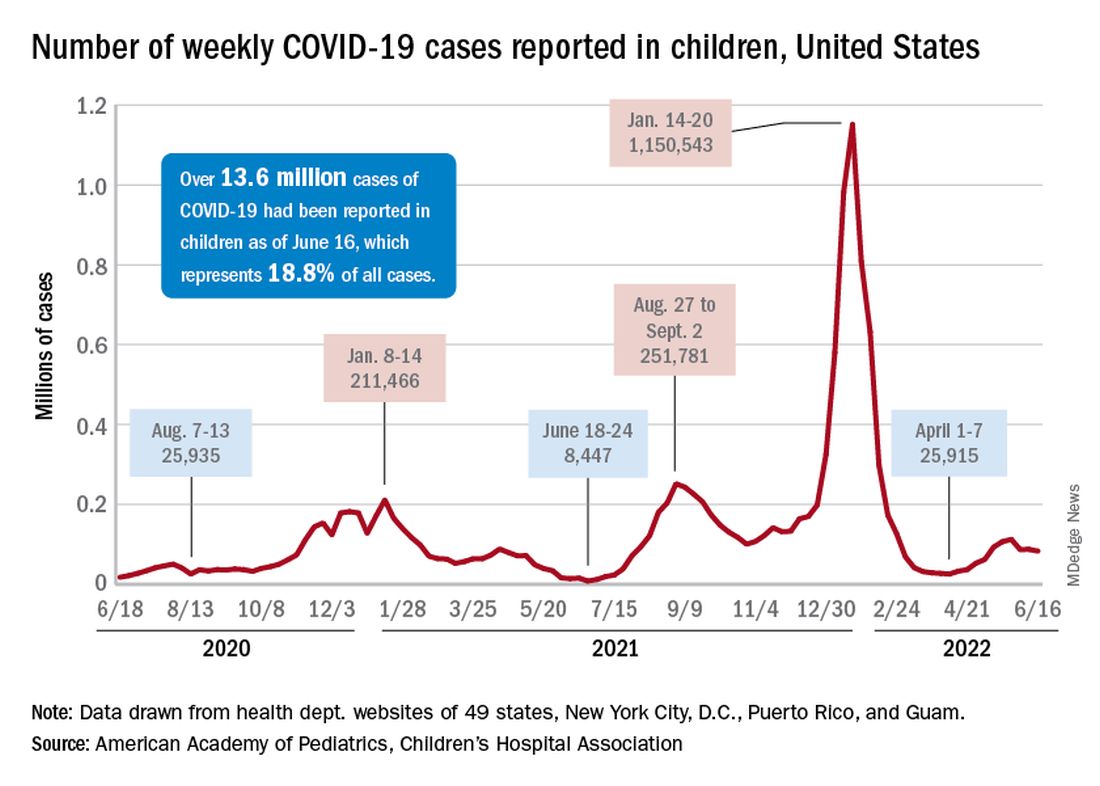
There are, according to the American Academy of Pediatrics, still five states where less than 20% of eligible 5- to 11-year-olds have received an initial vaccination. Among children aged 12-17, uptake has been much higher: 70% have received at least one dose and 60% are fully vaccinated, the CDC said.
Trends for new cases, hospitalizations diverging
COVID incidence in children, meanwhile, dropped for the second time in 3 weeks. There were 83,000 new cases reported during June 10-16, a decline of 4.8% from the previous week, according to the AAP and the Children’s Hospital Association.
New cases had risen by a very slight 0.31% during the week of June 3-9 after dropping 22% the week before (May 27 to June 2). Total cases in children have surpassed 13.6 million, which represents 18.8% of cases in all ages since the start of the pandemic, the AAP and CHA said in their weekly COVID report.
New admissions of children with confirmed COVID-19, however, have continued to climb since early to mid April. On June 16, the rate for children aged 0-17 years was up to 0.31 per 100,000, compared with the 0.13 per 100,000 recorded as late as April 11, the CDC said on its COVID Data Tracker.
The COVID-19 prevention effort in children enters its next phase as June draws to a close, while new pediatric cases continued on a downward trend and hospitalizations continued to rise.
The COVID-19 vaccines from Pfizer-BioNTech and Moderna were approved for use in children as young as 6 months, the Centers for Disease Control and Prevention announced on June 18.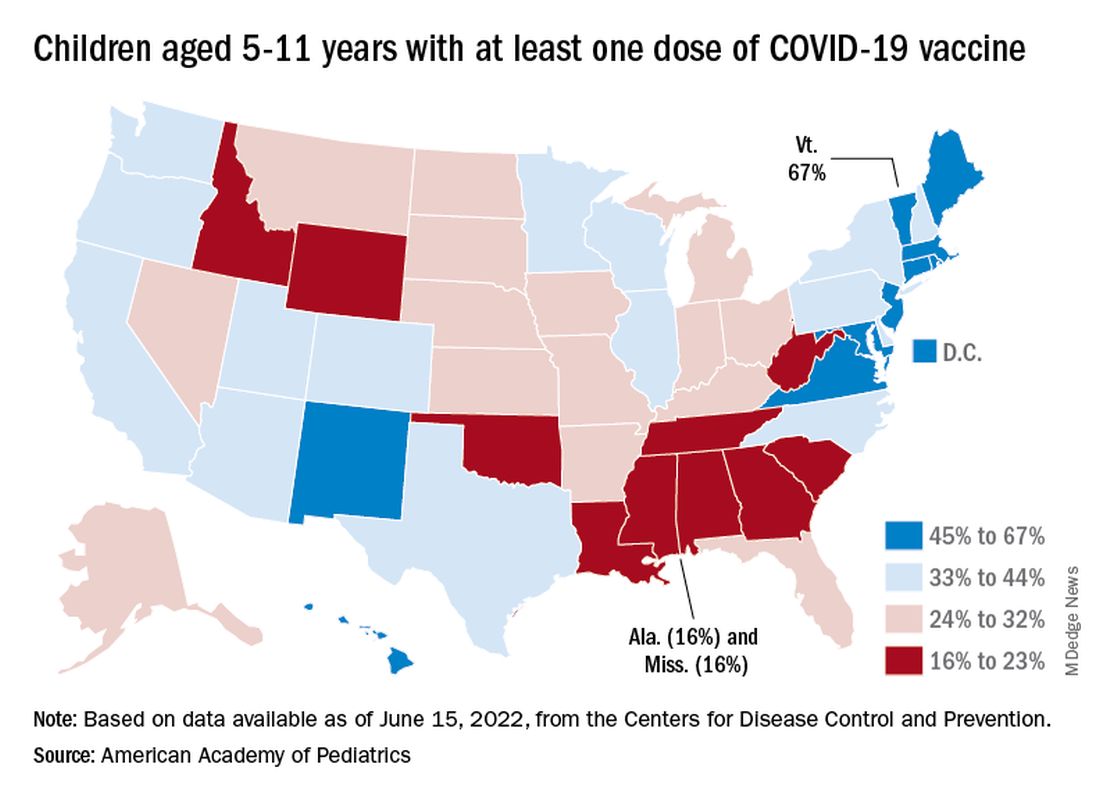
“We know millions of parents and caregivers are eager to get their young children vaccinated. ... I encourage parents and caregivers with questions to talk to their doctor, nurse, or local pharmacist to learn more about the benefits of vaccinations,” CDC Director Rochelle P. Walensky, MD, MPH, said in a written statement.
There are, however, indications that many parents are not that eager. Another 11% said “they will only do so if they are required,” Kaiser noted.
The vaccination experience with children aged 5-11 years seems to agree with those numbers. As of June 16, more than 7 months after the vaccine became available, just over 36% had received at least one dose and about 30% were fully vaccinated, CDC data show.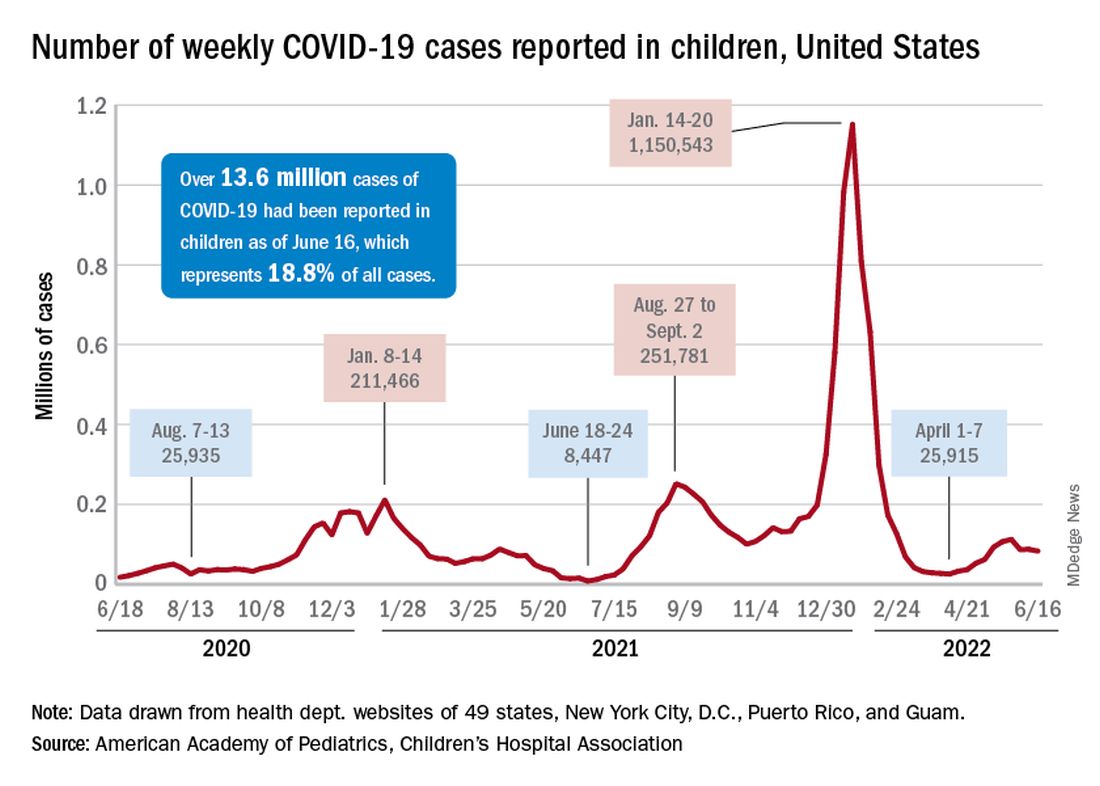
There are, according to the American Academy of Pediatrics, still five states where less than 20% of eligible 5- to 11-year-olds have received an initial vaccination. Among children aged 12-17, uptake has been much higher: 70% have received at least one dose and 60% are fully vaccinated, the CDC said.
Trends for new cases, hospitalizations diverging
COVID incidence in children, meanwhile, dropped for the second time in 3 weeks. There were 83,000 new cases reported during June 10-16, a decline of 4.8% from the previous week, according to the AAP and the Children’s Hospital Association.
New cases had risen by a very slight 0.31% during the week of June 3-9 after dropping 22% the week before (May 27 to June 2). Total cases in children have surpassed 13.6 million, which represents 18.8% of cases in all ages since the start of the pandemic, the AAP and CHA said in their weekly COVID report.
New admissions of children with confirmed COVID-19, however, have continued to climb since early to mid April. On June 16, the rate for children aged 0-17 years was up to 0.31 per 100,000, compared with the 0.13 per 100,000 recorded as late as April 11, the CDC said on its COVID Data Tracker.
New saliva-based COVID-19 test provides rapid results
A rapid, saliva-based test for COVID-19 could enable testing, diagnosis, and prescribing to take place in a single office visit by immediately confirming whether a patient has the infection and needs to be treated, researchers say. The test has sparked commercial interest and earned additional funding from the Canadian government.
The test uses a DNA aptamer – a short, synthetic oligonucleotide that binds to a specific molecular target – that shows high affinity for the SARS-CoV-2 spike protein and its variants. The approach “can be rapidly adapted to different threats,” as well, Leyla Soleymani, PhD, an associate professor of engineering physics at McMaster University, Hamilton, Ontario, Canada, told this news organization. Her team invented the approach.
Adaptable to other pathogens
Current gold-standard COVID-19 tests are based on reverse transcription-polymerase chain reaction (RT-PCR), which are sensitive but costly, complicated, and require waiting at least a couple of days for results, according to Dr. Soleymani and colleagues. Rapid nucleic acid and antigen tests have only “moderate” sensitivity and specificity, particularly when viral loads are low. None have been shown to work well with saliva samples.
By contrast, the new test “uses a reader and test cartridges, similar to the glucose reader,” said Dr. Soleymani, who is also Canada Research chair in Miniaturized Biomedical Devices. A small sample of saliva is added to a chemical reagent and inserted into the reader, which is attached to a smartphone. Once commercialized, the point-of-care test is expected to be performed quickly in a physician’s office or in a clinic.
“The same reader can be applied to a variety of infectious diseases or infection panels by developing new cartridges,” Dr. Soleymani explained. “Noroviruses and bacteria such as C. difficile are on our list” to examine next.What’s more, she added, “this test is ideally positioned for settings where access to centralized labs is not possible, such as less developed countries.”
The team’s recent studies seem to support the promise. A study published last year in the international edition of Angewandte Chemie documents the development of the test, which at that point could detect wild-type SARS-CoV-2 and its Alpha and Delta variants in unprocessed saliva samples in 10 minutes with 80.5% sensitivity and 100% specificity.
This study was followed in January 2022 by a paper in Chemistry showing that the device also detected Alpha, Gamma, Epsilon, Kappa, and Omicron variants, demonstrating its potential for recognizing rapidly evolving targets such as those found in SARS-CoV-2.
In another demonstration of its versatility, the technology was recently adapted and successfully detected animal viruses from saliva samples.
Commercial and government funding
The findings prompted Zentek, an intellectual property development and commercialization company in Guelph, Ont., to license the technology, with plans to invest more than $1 million in the next 5 years to scale up production of the test components and adapt the technology for other forms of infection.
Furthermore, the collaborative efforts required to develop the test and move it forward gained funding from Canada’s Natural Sciences and Engineering Research Council, which is investing nearly $1.5 million in the form of two grants: $1 million to further streamline the technology development in preparation for the next pandemic and $488,440 (including $140,000 from Zentek) to get the current test to market as quickly as possible.
Meanwhile, Dr. Soleymani is urging clinicians “to be open to nontraditional diagnostic approaches even if the traditional tests do the job. Such tests are more rapid and can be used to enable personalized medicine. Our success relies on collaboration and support from clinicians.”
Further validation needed
Daniel Kuritzkes, MD, chief of infectious diseases at Brigham and Women’s Hospital and the Harriet Ryan Albee Professor of Medicine at Harvard Medical School, Boston, commented on the study in response to a request from this news organization.
While “it’s always good to have more testing options available,” he said, “we don’t yet have very much information about performance characteristics of the test – that is, its sensitivity and specificity. I’d like to see the performance characteristics of this test compared to PCR tests and to the current rapid antigen tests using a large number of patient samples with currently circulating variants, and tests over time to see how soon tests become positive after symptom onset and for how long they remain positive.”
“Further validation studies and emergency use authorization or approval by regulatory authorities are needed before we will see this test implemented in the field,” Dr. Kuritzkes concluded.
A version of this article first appeared on Medscape.com.
A rapid, saliva-based test for COVID-19 could enable testing, diagnosis, and prescribing to take place in a single office visit by immediately confirming whether a patient has the infection and needs to be treated, researchers say. The test has sparked commercial interest and earned additional funding from the Canadian government.
The test uses a DNA aptamer – a short, synthetic oligonucleotide that binds to a specific molecular target – that shows high affinity for the SARS-CoV-2 spike protein and its variants. The approach “can be rapidly adapted to different threats,” as well, Leyla Soleymani, PhD, an associate professor of engineering physics at McMaster University, Hamilton, Ontario, Canada, told this news organization. Her team invented the approach.
Adaptable to other pathogens
Current gold-standard COVID-19 tests are based on reverse transcription-polymerase chain reaction (RT-PCR), which are sensitive but costly, complicated, and require waiting at least a couple of days for results, according to Dr. Soleymani and colleagues. Rapid nucleic acid and antigen tests have only “moderate” sensitivity and specificity, particularly when viral loads are low. None have been shown to work well with saliva samples.
By contrast, the new test “uses a reader and test cartridges, similar to the glucose reader,” said Dr. Soleymani, who is also Canada Research chair in Miniaturized Biomedical Devices. A small sample of saliva is added to a chemical reagent and inserted into the reader, which is attached to a smartphone. Once commercialized, the point-of-care test is expected to be performed quickly in a physician’s office or in a clinic.
“The same reader can be applied to a variety of infectious diseases or infection panels by developing new cartridges,” Dr. Soleymani explained. “Noroviruses and bacteria such as C. difficile are on our list” to examine next.What’s more, she added, “this test is ideally positioned for settings where access to centralized labs is not possible, such as less developed countries.”
The team’s recent studies seem to support the promise. A study published last year in the international edition of Angewandte Chemie documents the development of the test, which at that point could detect wild-type SARS-CoV-2 and its Alpha and Delta variants in unprocessed saliva samples in 10 minutes with 80.5% sensitivity and 100% specificity.
This study was followed in January 2022 by a paper in Chemistry showing that the device also detected Alpha, Gamma, Epsilon, Kappa, and Omicron variants, demonstrating its potential for recognizing rapidly evolving targets such as those found in SARS-CoV-2.
In another demonstration of its versatility, the technology was recently adapted and successfully detected animal viruses from saliva samples.
Commercial and government funding
The findings prompted Zentek, an intellectual property development and commercialization company in Guelph, Ont., to license the technology, with plans to invest more than $1 million in the next 5 years to scale up production of the test components and adapt the technology for other forms of infection.
Furthermore, the collaborative efforts required to develop the test and move it forward gained funding from Canada’s Natural Sciences and Engineering Research Council, which is investing nearly $1.5 million in the form of two grants: $1 million to further streamline the technology development in preparation for the next pandemic and $488,440 (including $140,000 from Zentek) to get the current test to market as quickly as possible.
Meanwhile, Dr. Soleymani is urging clinicians “to be open to nontraditional diagnostic approaches even if the traditional tests do the job. Such tests are more rapid and can be used to enable personalized medicine. Our success relies on collaboration and support from clinicians.”
Further validation needed
Daniel Kuritzkes, MD, chief of infectious diseases at Brigham and Women’s Hospital and the Harriet Ryan Albee Professor of Medicine at Harvard Medical School, Boston, commented on the study in response to a request from this news organization.
While “it’s always good to have more testing options available,” he said, “we don’t yet have very much information about performance characteristics of the test – that is, its sensitivity and specificity. I’d like to see the performance characteristics of this test compared to PCR tests and to the current rapid antigen tests using a large number of patient samples with currently circulating variants, and tests over time to see how soon tests become positive after symptom onset and for how long they remain positive.”
“Further validation studies and emergency use authorization or approval by regulatory authorities are needed before we will see this test implemented in the field,” Dr. Kuritzkes concluded.
A version of this article first appeared on Medscape.com.
A rapid, saliva-based test for COVID-19 could enable testing, diagnosis, and prescribing to take place in a single office visit by immediately confirming whether a patient has the infection and needs to be treated, researchers say. The test has sparked commercial interest and earned additional funding from the Canadian government.
The test uses a DNA aptamer – a short, synthetic oligonucleotide that binds to a specific molecular target – that shows high affinity for the SARS-CoV-2 spike protein and its variants. The approach “can be rapidly adapted to different threats,” as well, Leyla Soleymani, PhD, an associate professor of engineering physics at McMaster University, Hamilton, Ontario, Canada, told this news organization. Her team invented the approach.
Adaptable to other pathogens
Current gold-standard COVID-19 tests are based on reverse transcription-polymerase chain reaction (RT-PCR), which are sensitive but costly, complicated, and require waiting at least a couple of days for results, according to Dr. Soleymani and colleagues. Rapid nucleic acid and antigen tests have only “moderate” sensitivity and specificity, particularly when viral loads are low. None have been shown to work well with saliva samples.
By contrast, the new test “uses a reader and test cartridges, similar to the glucose reader,” said Dr. Soleymani, who is also Canada Research chair in Miniaturized Biomedical Devices. A small sample of saliva is added to a chemical reagent and inserted into the reader, which is attached to a smartphone. Once commercialized, the point-of-care test is expected to be performed quickly in a physician’s office or in a clinic.
“The same reader can be applied to a variety of infectious diseases or infection panels by developing new cartridges,” Dr. Soleymani explained. “Noroviruses and bacteria such as C. difficile are on our list” to examine next.What’s more, she added, “this test is ideally positioned for settings where access to centralized labs is not possible, such as less developed countries.”
The team’s recent studies seem to support the promise. A study published last year in the international edition of Angewandte Chemie documents the development of the test, which at that point could detect wild-type SARS-CoV-2 and its Alpha and Delta variants in unprocessed saliva samples in 10 minutes with 80.5% sensitivity and 100% specificity.
This study was followed in January 2022 by a paper in Chemistry showing that the device also detected Alpha, Gamma, Epsilon, Kappa, and Omicron variants, demonstrating its potential for recognizing rapidly evolving targets such as those found in SARS-CoV-2.
In another demonstration of its versatility, the technology was recently adapted and successfully detected animal viruses from saliva samples.
Commercial and government funding
The findings prompted Zentek, an intellectual property development and commercialization company in Guelph, Ont., to license the technology, with plans to invest more than $1 million in the next 5 years to scale up production of the test components and adapt the technology for other forms of infection.
Furthermore, the collaborative efforts required to develop the test and move it forward gained funding from Canada’s Natural Sciences and Engineering Research Council, which is investing nearly $1.5 million in the form of two grants: $1 million to further streamline the technology development in preparation for the next pandemic and $488,440 (including $140,000 from Zentek) to get the current test to market as quickly as possible.
Meanwhile, Dr. Soleymani is urging clinicians “to be open to nontraditional diagnostic approaches even if the traditional tests do the job. Such tests are more rapid and can be used to enable personalized medicine. Our success relies on collaboration and support from clinicians.”
Further validation needed
Daniel Kuritzkes, MD, chief of infectious diseases at Brigham and Women’s Hospital and the Harriet Ryan Albee Professor of Medicine at Harvard Medical School, Boston, commented on the study in response to a request from this news organization.
While “it’s always good to have more testing options available,” he said, “we don’t yet have very much information about performance characteristics of the test – that is, its sensitivity and specificity. I’d like to see the performance characteristics of this test compared to PCR tests and to the current rapid antigen tests using a large number of patient samples with currently circulating variants, and tests over time to see how soon tests become positive after symptom onset and for how long they remain positive.”
“Further validation studies and emergency use authorization or approval by regulatory authorities are needed before we will see this test implemented in the field,” Dr. Kuritzkes concluded.
A version of this article first appeared on Medscape.com.
Biden moves to limit nicotine levels in cigarettes
The Department of Health and Human Services posted a notice that details plans for a new rule to create a maximum allowed amount of nicotine in certain tobacco products. The Food and Drug Administration would take the action, the notice said, “to reduce addictiveness to certain tobacco products, thus giving addicted users a greater ability to quit.” The product standard would also help keep nonsmokers interested in trying tobacco, mainly youth, from starting to smoke and become regulars.
“Lowering nicotine levels to minimally addictive or non-addictive levels would decrease the likelihood that future generations of young people become addicted to cigarettes and help more currently addicted smokers to quit,” FDA Commissioner Robert Califf, MD, said in a statement.
The FDA, in charge of regulating cigarettes, issues a proposed rule when changes are discussed. That would be followed by a period for public comments before a final rule could be issued.
The proposed rule was first reported by The Washington Post.
The FDA in 2018 published a study in the New England Journal of Medicine that estimated that a potential limit on nicotine in cigarettes could, by the year 2100, prevent more than 33 million people from becoming regular smokers, and prevent the deaths of more than 8 million people from tobacco-related illnesses.
The action to reduce nicotine levels would fit in with President Joe Biden’s goal of reducing cancer death rates by half over 25 years. Each year, according to the American Cancer Society, about 480,000 deaths (about 1 in 5) are related to smoking. Currently, about 34 million American adults still smoke cigarettes.
Matthew Myers, president of the Campaign for Tobacco-Free Kids, called the proposed rule a “truly game-changing proposal.”
“There is no other single action our country can take that would prevent more young people from becoming addicted to tobacco or have a greater impact on reducing deaths from cancer, cardiovascular disease and respiratory disease,” Mr. Myers said in a statement.
However, he said, “these gains will only be realized if the administration and the FDA demonstrate a full-throated commitment to finalizing and implementing this proposal.”
The FDA proposed the nicotine reduction strategy in talks with the White House and the Department of Health and Human Services early in 2021, according to the Post.
Earlier this year, the FDA issued a proposed rule to ban menthol flavoring in cigarettes. The agency is accepting public comments though July 5.
The action of reducing nicotine levels would likely take years to complete, Mitch Zeller, JD, recently retired director of the FDA Center for Tobacco Products, told the Post.
In 2018, the FDA issued a proposed ruling to set a standard for maximum nicotine levels in cigarettes.
Advocates say the action of slashing nicotine, the active – and addictive – ingredient in cigarettes, would save millions of lives for generations to come. Opponents liken it to the prohibition of alcohol in the 1920s and predict the action will fail.
Others say that if limits are put on nicotine levels, adults should have greater access to noncombustible alternatives.
A version of this article first appeared on WebMD.com.
The Department of Health and Human Services posted a notice that details plans for a new rule to create a maximum allowed amount of nicotine in certain tobacco products. The Food and Drug Administration would take the action, the notice said, “to reduce addictiveness to certain tobacco products, thus giving addicted users a greater ability to quit.” The product standard would also help keep nonsmokers interested in trying tobacco, mainly youth, from starting to smoke and become regulars.
“Lowering nicotine levels to minimally addictive or non-addictive levels would decrease the likelihood that future generations of young people become addicted to cigarettes and help more currently addicted smokers to quit,” FDA Commissioner Robert Califf, MD, said in a statement.
The FDA, in charge of regulating cigarettes, issues a proposed rule when changes are discussed. That would be followed by a period for public comments before a final rule could be issued.
The proposed rule was first reported by The Washington Post.
The FDA in 2018 published a study in the New England Journal of Medicine that estimated that a potential limit on nicotine in cigarettes could, by the year 2100, prevent more than 33 million people from becoming regular smokers, and prevent the deaths of more than 8 million people from tobacco-related illnesses.
The action to reduce nicotine levels would fit in with President Joe Biden’s goal of reducing cancer death rates by half over 25 years. Each year, according to the American Cancer Society, about 480,000 deaths (about 1 in 5) are related to smoking. Currently, about 34 million American adults still smoke cigarettes.
Matthew Myers, president of the Campaign for Tobacco-Free Kids, called the proposed rule a “truly game-changing proposal.”
“There is no other single action our country can take that would prevent more young people from becoming addicted to tobacco or have a greater impact on reducing deaths from cancer, cardiovascular disease and respiratory disease,” Mr. Myers said in a statement.
However, he said, “these gains will only be realized if the administration and the FDA demonstrate a full-throated commitment to finalizing and implementing this proposal.”
The FDA proposed the nicotine reduction strategy in talks with the White House and the Department of Health and Human Services early in 2021, according to the Post.
Earlier this year, the FDA issued a proposed rule to ban menthol flavoring in cigarettes. The agency is accepting public comments though July 5.
The action of reducing nicotine levels would likely take years to complete, Mitch Zeller, JD, recently retired director of the FDA Center for Tobacco Products, told the Post.
In 2018, the FDA issued a proposed ruling to set a standard for maximum nicotine levels in cigarettes.
Advocates say the action of slashing nicotine, the active – and addictive – ingredient in cigarettes, would save millions of lives for generations to come. Opponents liken it to the prohibition of alcohol in the 1920s and predict the action will fail.
Others say that if limits are put on nicotine levels, adults should have greater access to noncombustible alternatives.
A version of this article first appeared on WebMD.com.
The Department of Health and Human Services posted a notice that details plans for a new rule to create a maximum allowed amount of nicotine in certain tobacco products. The Food and Drug Administration would take the action, the notice said, “to reduce addictiveness to certain tobacco products, thus giving addicted users a greater ability to quit.” The product standard would also help keep nonsmokers interested in trying tobacco, mainly youth, from starting to smoke and become regulars.
“Lowering nicotine levels to minimally addictive or non-addictive levels would decrease the likelihood that future generations of young people become addicted to cigarettes and help more currently addicted smokers to quit,” FDA Commissioner Robert Califf, MD, said in a statement.
The FDA, in charge of regulating cigarettes, issues a proposed rule when changes are discussed. That would be followed by a period for public comments before a final rule could be issued.
The proposed rule was first reported by The Washington Post.
The FDA in 2018 published a study in the New England Journal of Medicine that estimated that a potential limit on nicotine in cigarettes could, by the year 2100, prevent more than 33 million people from becoming regular smokers, and prevent the deaths of more than 8 million people from tobacco-related illnesses.
The action to reduce nicotine levels would fit in with President Joe Biden’s goal of reducing cancer death rates by half over 25 years. Each year, according to the American Cancer Society, about 480,000 deaths (about 1 in 5) are related to smoking. Currently, about 34 million American adults still smoke cigarettes.
Matthew Myers, president of the Campaign for Tobacco-Free Kids, called the proposed rule a “truly game-changing proposal.”
“There is no other single action our country can take that would prevent more young people from becoming addicted to tobacco or have a greater impact on reducing deaths from cancer, cardiovascular disease and respiratory disease,” Mr. Myers said in a statement.
However, he said, “these gains will only be realized if the administration and the FDA demonstrate a full-throated commitment to finalizing and implementing this proposal.”
The FDA proposed the nicotine reduction strategy in talks with the White House and the Department of Health and Human Services early in 2021, according to the Post.
Earlier this year, the FDA issued a proposed rule to ban menthol flavoring in cigarettes. The agency is accepting public comments though July 5.
The action of reducing nicotine levels would likely take years to complete, Mitch Zeller, JD, recently retired director of the FDA Center for Tobacco Products, told the Post.
In 2018, the FDA issued a proposed ruling to set a standard for maximum nicotine levels in cigarettes.
Advocates say the action of slashing nicotine, the active – and addictive – ingredient in cigarettes, would save millions of lives for generations to come. Opponents liken it to the prohibition of alcohol in the 1920s and predict the action will fail.
Others say that if limits are put on nicotine levels, adults should have greater access to noncombustible alternatives.
A version of this article first appeared on WebMD.com.
Vaping safety views shifted following lung injury reports
Adults in the United States increasingly perceive electronic cigarettes, or e-cigarettes, as “more harmful” than traditional cigarettes, according to a new study published in the American Journal of Preventive Medicine.
In addition, the percentage of people who exclusively used traditional cigarettes almost doubled between 2019 and 2020 among those who perceived e-cigarettes as more harmful, jumping from 8.4% in 2019 to 16.3% in 2020.
“We were able to show that these changes in perception potentially changed behaviors on a population level,” said Priti Bandi, PhD, principal scientist at the American Cancer Society in Atlanta and lead author of the study.
Since e-cigarettes entered the U.S. market in 2006, public health experts have questioned claims from manufacturers that the products work as a harm reduction tool to help traditional cigarette smokers to quit. Public perceptions have generally been that e-cigarettes are safer for a person’s health. While the research is still emerging on the long-term health outcomes of users, public opinion has shifted since the introduction of the devices.
The new study showed a sharp change in public perception of e-cigarettes following media coverage of cases of users who presented to emergency rooms with mysterious lung symptoms in 2019. The Centers for Disease Control and Prevention eventually found that what are now called e-cigarette or vaping product use–associated lung injuries were linked to vitamin E acetate, an additive to tetrahydrocannabinol-containing products but not nicotine.
The last update from the CDC came in February 2020, shortly before the COVID-19 pandemic swept through the United States, prompting a sharp shift to investigate the new virus among both health care providers and researchers.
Dr. Bandi and colleagues gathered 2018-2020 data from a National Institutes of Health database called the Health Information National Trends Survey, a mail-based, nationally representative, cross-sectional survey of U.S. adults and their attitudes of cancer and health-related information. More than 3,000 people each year responded to questions about e-cigarettes.
The study found that the percentage of people who believed e-cigarettes to be more harmful than traditional cigarettes more than tripled from 6.8% in 2018 to 28.3% in 2020. Fewer people also viewed e-cigarettes as less harmful than traditional cigarettes, falling from 17.6% in 2018 to 11.4% in 2020. Fewer people also said they were unsure about which product was more harmful.
Among those who believed e-cigarettes were “relatively” less harmful than traditional cigarettes, use of e-cigarettes jumped from 15.3% in 2019 to 26.7% in 2020.
The implications
The main finding that people started smoking cigarettes when they thought e-cigarettes were more harmful should be a wake-up to public health officials and doctors who communicate health risks to patients, according to Dr. Bandi and other experts.
Messaging should be more nuanced, Dr. Bandi said. Many adults use e-cigarettes as a cessation tool, and she and other experts point to research that shows the products are, at least in the short-term, less harmful especially as a smoking cessation tool. Vapes are among the most popular tools people use when they want to quit smoking – with the majority of U.S. adults using vapes either partially or fully to quit, according to the CDC.
Some countries, such as England, are moving to allow doctors to prescribe e-cigarettes to help reduce smoking rates. United Kingdom regulatory authorities in 2021 said they’re considering allowing licensing the devices for use in smoking cessation.
“There is an absolute need for ongoing, accurate communication from public health authorities targeted toward the appropriate audiences,” Bandi said.
Ashley Brooks-Russell, PhD, MPH, associate professor at the University of Colorado at Denver, Aurora, said the finding that perceptions can change behavior is good news. However, the bad news is that adults overcorrected and switched to cigarettes, which are proven to cause cancer and other health conditions.
“We’re good in public health about messaging that cigarettes are bad, that tobacco is broadly harmful,” Dr. Brooks-Russell said in an interview. “We’re really bad at talking about lesser options, like if you’re going to smoke, e-cigarettes are less harmful.”
But other health leaders warn that e-cigarettes might produce the same adverse health outcomes, or worse, as cigarettes. The only way researchers will gain a conclusive answer is decades into a patient’s life. Until then, it’s not clear if any potential benefit from smoking cessation will outweigh the risks.
“This research should remind healthcare providers to find out what products patients are using, how much, and if those patients experience health issues later on,” said Kevin McQueen, MHA, lead respiratory director at University of Colorado Health System and president of the Colorado Respiratory Care Society.
“My concern is that while people are starting to think e-cigarettes are more dangerous, some people still think they are safe – and we don’t know how much safer they are,” he said. “And we aren’t going to know until 10, 15, 20 years from now.”
All authors were employed by the American Cancer Society at the time of the study, which receives grants from private and corporate foundations, including foundations associated with companies in the health sector for research outside of the submitted work. The authors are not funded by or key personnel for any of these grants, and their salaries are solely funded through American Cancer Society funds. No other financial disclosures were reported.
A version of this article first appeared on Medscape.com.
Adults in the United States increasingly perceive electronic cigarettes, or e-cigarettes, as “more harmful” than traditional cigarettes, according to a new study published in the American Journal of Preventive Medicine.
In addition, the percentage of people who exclusively used traditional cigarettes almost doubled between 2019 and 2020 among those who perceived e-cigarettes as more harmful, jumping from 8.4% in 2019 to 16.3% in 2020.
“We were able to show that these changes in perception potentially changed behaviors on a population level,” said Priti Bandi, PhD, principal scientist at the American Cancer Society in Atlanta and lead author of the study.
Since e-cigarettes entered the U.S. market in 2006, public health experts have questioned claims from manufacturers that the products work as a harm reduction tool to help traditional cigarette smokers to quit. Public perceptions have generally been that e-cigarettes are safer for a person’s health. While the research is still emerging on the long-term health outcomes of users, public opinion has shifted since the introduction of the devices.
The new study showed a sharp change in public perception of e-cigarettes following media coverage of cases of users who presented to emergency rooms with mysterious lung symptoms in 2019. The Centers for Disease Control and Prevention eventually found that what are now called e-cigarette or vaping product use–associated lung injuries were linked to vitamin E acetate, an additive to tetrahydrocannabinol-containing products but not nicotine.
The last update from the CDC came in February 2020, shortly before the COVID-19 pandemic swept through the United States, prompting a sharp shift to investigate the new virus among both health care providers and researchers.
Dr. Bandi and colleagues gathered 2018-2020 data from a National Institutes of Health database called the Health Information National Trends Survey, a mail-based, nationally representative, cross-sectional survey of U.S. adults and their attitudes of cancer and health-related information. More than 3,000 people each year responded to questions about e-cigarettes.
The study found that the percentage of people who believed e-cigarettes to be more harmful than traditional cigarettes more than tripled from 6.8% in 2018 to 28.3% in 2020. Fewer people also viewed e-cigarettes as less harmful than traditional cigarettes, falling from 17.6% in 2018 to 11.4% in 2020. Fewer people also said they were unsure about which product was more harmful.
Among those who believed e-cigarettes were “relatively” less harmful than traditional cigarettes, use of e-cigarettes jumped from 15.3% in 2019 to 26.7% in 2020.
The implications
The main finding that people started smoking cigarettes when they thought e-cigarettes were more harmful should be a wake-up to public health officials and doctors who communicate health risks to patients, according to Dr. Bandi and other experts.
Messaging should be more nuanced, Dr. Bandi said. Many adults use e-cigarettes as a cessation tool, and she and other experts point to research that shows the products are, at least in the short-term, less harmful especially as a smoking cessation tool. Vapes are among the most popular tools people use when they want to quit smoking – with the majority of U.S. adults using vapes either partially or fully to quit, according to the CDC.
Some countries, such as England, are moving to allow doctors to prescribe e-cigarettes to help reduce smoking rates. United Kingdom regulatory authorities in 2021 said they’re considering allowing licensing the devices for use in smoking cessation.
“There is an absolute need for ongoing, accurate communication from public health authorities targeted toward the appropriate audiences,” Bandi said.
Ashley Brooks-Russell, PhD, MPH, associate professor at the University of Colorado at Denver, Aurora, said the finding that perceptions can change behavior is good news. However, the bad news is that adults overcorrected and switched to cigarettes, which are proven to cause cancer and other health conditions.
“We’re good in public health about messaging that cigarettes are bad, that tobacco is broadly harmful,” Dr. Brooks-Russell said in an interview. “We’re really bad at talking about lesser options, like if you’re going to smoke, e-cigarettes are less harmful.”
But other health leaders warn that e-cigarettes might produce the same adverse health outcomes, or worse, as cigarettes. The only way researchers will gain a conclusive answer is decades into a patient’s life. Until then, it’s not clear if any potential benefit from smoking cessation will outweigh the risks.
“This research should remind healthcare providers to find out what products patients are using, how much, and if those patients experience health issues later on,” said Kevin McQueen, MHA, lead respiratory director at University of Colorado Health System and president of the Colorado Respiratory Care Society.
“My concern is that while people are starting to think e-cigarettes are more dangerous, some people still think they are safe – and we don’t know how much safer they are,” he said. “And we aren’t going to know until 10, 15, 20 years from now.”
All authors were employed by the American Cancer Society at the time of the study, which receives grants from private and corporate foundations, including foundations associated with companies in the health sector for research outside of the submitted work. The authors are not funded by or key personnel for any of these grants, and their salaries are solely funded through American Cancer Society funds. No other financial disclosures were reported.
A version of this article first appeared on Medscape.com.
Adults in the United States increasingly perceive electronic cigarettes, or e-cigarettes, as “more harmful” than traditional cigarettes, according to a new study published in the American Journal of Preventive Medicine.
In addition, the percentage of people who exclusively used traditional cigarettes almost doubled between 2019 and 2020 among those who perceived e-cigarettes as more harmful, jumping from 8.4% in 2019 to 16.3% in 2020.
“We were able to show that these changes in perception potentially changed behaviors on a population level,” said Priti Bandi, PhD, principal scientist at the American Cancer Society in Atlanta and lead author of the study.
Since e-cigarettes entered the U.S. market in 2006, public health experts have questioned claims from manufacturers that the products work as a harm reduction tool to help traditional cigarette smokers to quit. Public perceptions have generally been that e-cigarettes are safer for a person’s health. While the research is still emerging on the long-term health outcomes of users, public opinion has shifted since the introduction of the devices.
The new study showed a sharp change in public perception of e-cigarettes following media coverage of cases of users who presented to emergency rooms with mysterious lung symptoms in 2019. The Centers for Disease Control and Prevention eventually found that what are now called e-cigarette or vaping product use–associated lung injuries were linked to vitamin E acetate, an additive to tetrahydrocannabinol-containing products but not nicotine.
The last update from the CDC came in February 2020, shortly before the COVID-19 pandemic swept through the United States, prompting a sharp shift to investigate the new virus among both health care providers and researchers.
Dr. Bandi and colleagues gathered 2018-2020 data from a National Institutes of Health database called the Health Information National Trends Survey, a mail-based, nationally representative, cross-sectional survey of U.S. adults and their attitudes of cancer and health-related information. More than 3,000 people each year responded to questions about e-cigarettes.
The study found that the percentage of people who believed e-cigarettes to be more harmful than traditional cigarettes more than tripled from 6.8% in 2018 to 28.3% in 2020. Fewer people also viewed e-cigarettes as less harmful than traditional cigarettes, falling from 17.6% in 2018 to 11.4% in 2020. Fewer people also said they were unsure about which product was more harmful.
Among those who believed e-cigarettes were “relatively” less harmful than traditional cigarettes, use of e-cigarettes jumped from 15.3% in 2019 to 26.7% in 2020.
The implications
The main finding that people started smoking cigarettes when they thought e-cigarettes were more harmful should be a wake-up to public health officials and doctors who communicate health risks to patients, according to Dr. Bandi and other experts.
Messaging should be more nuanced, Dr. Bandi said. Many adults use e-cigarettes as a cessation tool, and she and other experts point to research that shows the products are, at least in the short-term, less harmful especially as a smoking cessation tool. Vapes are among the most popular tools people use when they want to quit smoking – with the majority of U.S. adults using vapes either partially or fully to quit, according to the CDC.
Some countries, such as England, are moving to allow doctors to prescribe e-cigarettes to help reduce smoking rates. United Kingdom regulatory authorities in 2021 said they’re considering allowing licensing the devices for use in smoking cessation.
“There is an absolute need for ongoing, accurate communication from public health authorities targeted toward the appropriate audiences,” Bandi said.
Ashley Brooks-Russell, PhD, MPH, associate professor at the University of Colorado at Denver, Aurora, said the finding that perceptions can change behavior is good news. However, the bad news is that adults overcorrected and switched to cigarettes, which are proven to cause cancer and other health conditions.
“We’re good in public health about messaging that cigarettes are bad, that tobacco is broadly harmful,” Dr. Brooks-Russell said in an interview. “We’re really bad at talking about lesser options, like if you’re going to smoke, e-cigarettes are less harmful.”
But other health leaders warn that e-cigarettes might produce the same adverse health outcomes, or worse, as cigarettes. The only way researchers will gain a conclusive answer is decades into a patient’s life. Until then, it’s not clear if any potential benefit from smoking cessation will outweigh the risks.
“This research should remind healthcare providers to find out what products patients are using, how much, and if those patients experience health issues later on,” said Kevin McQueen, MHA, lead respiratory director at University of Colorado Health System and president of the Colorado Respiratory Care Society.
“My concern is that while people are starting to think e-cigarettes are more dangerous, some people still think they are safe – and we don’t know how much safer they are,” he said. “And we aren’t going to know until 10, 15, 20 years from now.”
All authors were employed by the American Cancer Society at the time of the study, which receives grants from private and corporate foundations, including foundations associated with companies in the health sector for research outside of the submitted work. The authors are not funded by or key personnel for any of these grants, and their salaries are solely funded through American Cancer Society funds. No other financial disclosures were reported.
A version of this article first appeared on Medscape.com.
FROM THE AMERICAN JOURNAL OF PREVENTIVE MEDICINE
What are the signs of post–acute infection syndromes?
The long-term health consequences of COVID-19 have refocused our attention on post–acute infection syndromes (PAIS), starting a discussion on the need for a complete understanding of multisystemic pathophysiology, clinical indicators, and the epidemiology of these syndromes, representing a significant blind spot in the field of medicine. A better understanding of these persistent symptom profiles, not only for post-acute sequelae of SARS-CoV-2 infection (PASC), better known as long COVID, but also for other diseases with unexplainable post-acute sequelae, would allow doctors to fine tune the diagnostic criteria. Having a clear definition and better understanding of post–acute infection symptoms is a necessary step toward developing an evidence-based, multidisciplinary management approach.
PAIS, PASC, or long COVID
The observation of unexplained chronic sequelae after SARS-CoV-2 is known as PASC or long COVID.
Long COVID has been reported as a syndrome in survivors of serious and critical disease, but the effects also persist over time for subjects who experienced a mild infection that did not require admission to hospital. This means that PASC, especially when occurring after a mild or moderate COVID-19 infection, shares many of the same characteristics as chronic diseases triggered by other pathogenic organisms, many of which have not been sufficiently clarified.
PAIS are characterized by a set of core symptoms centering on the following:
- Exertion intolerance
- Disproportionate levels of fatigue
- Neurocognitive and sensory impairment
- Flu-like symptoms
- Unrefreshing sleep
- Myalgia/arthralgia
A plethora of nonspecific symptoms are often present to various degrees.
These similarities suggest a unifying pathophysiology that needs to be elucidated to properly understand and manage postinfectious chronic disability.
Overview of PAIS
A detailed revision on what is currently known about PAIS was published in Nature Medicine. It provided various useful pieces of information to assist with the poor recognition of these conditions in clinical practice, a result of which is that patients might experience delayed or a complete lack of clinical care.
The following consolidated postinfection sequelae are mentioned:
- Q fever fatigue syndrome, which follows infection by the intracellular bacterium Coxiella burnetii
- Post-dengue fatigue syndrome, which can follow infection by the mosquito-borne dengue virus
- Fatiguing and rheumatic symptoms in a subset of individuals infected with chikungunya virus, a mosquito-borne virus that causes fever and joint pain in the acute phase
- Post-polio syndrome, which can emerge as many as 15-40 years after an initial poliomyelitis attack (similarly, some other neurotropic microbes, such as West Nile virus, might lead to persistent effects)
- Prolonged, debilitating, chronic symptoms have long been reported in a subset of patients after common and typically nonserious infections. For example, after mononucleosis, a condition generally caused by Epstein-Barr virus (EBV), and after an outbreak of Giardia lamblia, an intestinal parasite that usually causes acute intestinal illness. In fact, several studies identified the association of this outbreak of giardiasis with chronic fatigue, irritable bowel syndrome (IBS), and fibromyalgia persisting for many years.
- Views expressed in the literature regarding the frequency and the validity of posttreatment Lyme disease syndrome are divided. Although substantial evidence points to persistence of arthralgia, fatigue, and subjective neurocognitive impairments in a minority of patients with Lyme disease after the recommended antibiotic treatment, some of the early studies have failed to characterize the initial Lyme disease episode with sufficient rigor.
Symptoms and signs
The symptoms and signs which, based on the evidence available, are seen more frequently in health care checks may be characterized as the following:
- Exertion intolerance, fatigue
- Flu-like and ‘sickness behavior’ symptoms: fever, feverishness, muscle pain, feeling sick, malaise, sweating, irritability
- Neurological/neurocognitive symptoms: brain fog, impaired concentration or memory, trouble finding words
- Rheumatologic symptoms: chronic or recurrent joint pain
- Trigger-specific symptoms: for example, eye problems post Ebola, IBS post Giardia, anosmia and ageusia post COVID-19, motor disturbances post polio and post West Nile virus
Myalgic encephalomyelitis/chronic fatigue syndrome
Patients with this disorder experience worsening of symptoms following physical, cognitive, or emotional exertion above their (very low) tolerated limit. Other prominent features frequently observed in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) are neurocognitive impairments (colloquially referred to as brain fog), unrefreshing sleep, pain, sensory disturbances, gastrointestinal issues, and various forms of dysautonomia. Up to 75% of ME/CFS cases report an infection-like episode preceding the onset of their illness. Postinfectious and postviral fatigue syndromes were originally postulated as subsets of chronic fatigue syndrome. However, there appears to be no clear consensus at present about whether these terms should be considered synonymous to the ME/CFS label or any of its subsets, or include a wider range of postinfectious fatigue conditions.
Practical diagnostic criteria
From a revision of the available criteria, it emerges that the diagnostic criteria for a PAIS should include not only the presence of symptoms, but ideally also the intensity, course, and constellation of symptoms within an individual, as the individual symptoms and symptom trajectories of PAIS vary over time, rendering a mere comparison of symptom presence at a single time point misleading. Furthermore, when a diagnosis of ME/CFS is made, attention should be given to the choice of diagnostic criteria, with preference given to the more conservative criteria, so as not to run the risk of overestimating the syndrome.
Asthenia is the cornerstone symptom for most epidemiological studies on PAIS, but it would be reductive to concentrate only on this rather than the other characteristics, such as the exacerbation of symptoms following exertion, together with other characteristic symptoms and signs that may allow for better identification of the overall, observable clinical picture in these postinfection syndromes, which have significant impacts on a patient’s quality of life.
This article was translated from Univadis Italy. A version of this article appeared on Medscape.com.
The long-term health consequences of COVID-19 have refocused our attention on post–acute infection syndromes (PAIS), starting a discussion on the need for a complete understanding of multisystemic pathophysiology, clinical indicators, and the epidemiology of these syndromes, representing a significant blind spot in the field of medicine. A better understanding of these persistent symptom profiles, not only for post-acute sequelae of SARS-CoV-2 infection (PASC), better known as long COVID, but also for other diseases with unexplainable post-acute sequelae, would allow doctors to fine tune the diagnostic criteria. Having a clear definition and better understanding of post–acute infection symptoms is a necessary step toward developing an evidence-based, multidisciplinary management approach.
PAIS, PASC, or long COVID
The observation of unexplained chronic sequelae after SARS-CoV-2 is known as PASC or long COVID.
Long COVID has been reported as a syndrome in survivors of serious and critical disease, but the effects also persist over time for subjects who experienced a mild infection that did not require admission to hospital. This means that PASC, especially when occurring after a mild or moderate COVID-19 infection, shares many of the same characteristics as chronic diseases triggered by other pathogenic organisms, many of which have not been sufficiently clarified.
PAIS are characterized by a set of core symptoms centering on the following:
- Exertion intolerance
- Disproportionate levels of fatigue
- Neurocognitive and sensory impairment
- Flu-like symptoms
- Unrefreshing sleep
- Myalgia/arthralgia
A plethora of nonspecific symptoms are often present to various degrees.
These similarities suggest a unifying pathophysiology that needs to be elucidated to properly understand and manage postinfectious chronic disability.
Overview of PAIS
A detailed revision on what is currently known about PAIS was published in Nature Medicine. It provided various useful pieces of information to assist with the poor recognition of these conditions in clinical practice, a result of which is that patients might experience delayed or a complete lack of clinical care.
The following consolidated postinfection sequelae are mentioned:
- Q fever fatigue syndrome, which follows infection by the intracellular bacterium Coxiella burnetii
- Post-dengue fatigue syndrome, which can follow infection by the mosquito-borne dengue virus
- Fatiguing and rheumatic symptoms in a subset of individuals infected with chikungunya virus, a mosquito-borne virus that causes fever and joint pain in the acute phase
- Post-polio syndrome, which can emerge as many as 15-40 years after an initial poliomyelitis attack (similarly, some other neurotropic microbes, such as West Nile virus, might lead to persistent effects)
- Prolonged, debilitating, chronic symptoms have long been reported in a subset of patients after common and typically nonserious infections. For example, after mononucleosis, a condition generally caused by Epstein-Barr virus (EBV), and after an outbreak of Giardia lamblia, an intestinal parasite that usually causes acute intestinal illness. In fact, several studies identified the association of this outbreak of giardiasis with chronic fatigue, irritable bowel syndrome (IBS), and fibromyalgia persisting for many years.
- Views expressed in the literature regarding the frequency and the validity of posttreatment Lyme disease syndrome are divided. Although substantial evidence points to persistence of arthralgia, fatigue, and subjective neurocognitive impairments in a minority of patients with Lyme disease after the recommended antibiotic treatment, some of the early studies have failed to characterize the initial Lyme disease episode with sufficient rigor.
Symptoms and signs
The symptoms and signs which, based on the evidence available, are seen more frequently in health care checks may be characterized as the following:
- Exertion intolerance, fatigue
- Flu-like and ‘sickness behavior’ symptoms: fever, feverishness, muscle pain, feeling sick, malaise, sweating, irritability
- Neurological/neurocognitive symptoms: brain fog, impaired concentration or memory, trouble finding words
- Rheumatologic symptoms: chronic or recurrent joint pain
- Trigger-specific symptoms: for example, eye problems post Ebola, IBS post Giardia, anosmia and ageusia post COVID-19, motor disturbances post polio and post West Nile virus
Myalgic encephalomyelitis/chronic fatigue syndrome
Patients with this disorder experience worsening of symptoms following physical, cognitive, or emotional exertion above their (very low) tolerated limit. Other prominent features frequently observed in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) are neurocognitive impairments (colloquially referred to as brain fog), unrefreshing sleep, pain, sensory disturbances, gastrointestinal issues, and various forms of dysautonomia. Up to 75% of ME/CFS cases report an infection-like episode preceding the onset of their illness. Postinfectious and postviral fatigue syndromes were originally postulated as subsets of chronic fatigue syndrome. However, there appears to be no clear consensus at present about whether these terms should be considered synonymous to the ME/CFS label or any of its subsets, or include a wider range of postinfectious fatigue conditions.
Practical diagnostic criteria
From a revision of the available criteria, it emerges that the diagnostic criteria for a PAIS should include not only the presence of symptoms, but ideally also the intensity, course, and constellation of symptoms within an individual, as the individual symptoms and symptom trajectories of PAIS vary over time, rendering a mere comparison of symptom presence at a single time point misleading. Furthermore, when a diagnosis of ME/CFS is made, attention should be given to the choice of diagnostic criteria, with preference given to the more conservative criteria, so as not to run the risk of overestimating the syndrome.
Asthenia is the cornerstone symptom for most epidemiological studies on PAIS, but it would be reductive to concentrate only on this rather than the other characteristics, such as the exacerbation of symptoms following exertion, together with other characteristic symptoms and signs that may allow for better identification of the overall, observable clinical picture in these postinfection syndromes, which have significant impacts on a patient’s quality of life.
This article was translated from Univadis Italy. A version of this article appeared on Medscape.com.
The long-term health consequences of COVID-19 have refocused our attention on post–acute infection syndromes (PAIS), starting a discussion on the need for a complete understanding of multisystemic pathophysiology, clinical indicators, and the epidemiology of these syndromes, representing a significant blind spot in the field of medicine. A better understanding of these persistent symptom profiles, not only for post-acute sequelae of SARS-CoV-2 infection (PASC), better known as long COVID, but also for other diseases with unexplainable post-acute sequelae, would allow doctors to fine tune the diagnostic criteria. Having a clear definition and better understanding of post–acute infection symptoms is a necessary step toward developing an evidence-based, multidisciplinary management approach.
PAIS, PASC, or long COVID
The observation of unexplained chronic sequelae after SARS-CoV-2 is known as PASC or long COVID.
Long COVID has been reported as a syndrome in survivors of serious and critical disease, but the effects also persist over time for subjects who experienced a mild infection that did not require admission to hospital. This means that PASC, especially when occurring after a mild or moderate COVID-19 infection, shares many of the same characteristics as chronic diseases triggered by other pathogenic organisms, many of which have not been sufficiently clarified.
PAIS are characterized by a set of core symptoms centering on the following:
- Exertion intolerance
- Disproportionate levels of fatigue
- Neurocognitive and sensory impairment
- Flu-like symptoms
- Unrefreshing sleep
- Myalgia/arthralgia
A plethora of nonspecific symptoms are often present to various degrees.
These similarities suggest a unifying pathophysiology that needs to be elucidated to properly understand and manage postinfectious chronic disability.
Overview of PAIS
A detailed revision on what is currently known about PAIS was published in Nature Medicine. It provided various useful pieces of information to assist with the poor recognition of these conditions in clinical practice, a result of which is that patients might experience delayed or a complete lack of clinical care.
The following consolidated postinfection sequelae are mentioned:
- Q fever fatigue syndrome, which follows infection by the intracellular bacterium Coxiella burnetii
- Post-dengue fatigue syndrome, which can follow infection by the mosquito-borne dengue virus
- Fatiguing and rheumatic symptoms in a subset of individuals infected with chikungunya virus, a mosquito-borne virus that causes fever and joint pain in the acute phase
- Post-polio syndrome, which can emerge as many as 15-40 years after an initial poliomyelitis attack (similarly, some other neurotropic microbes, such as West Nile virus, might lead to persistent effects)
- Prolonged, debilitating, chronic symptoms have long been reported in a subset of patients after common and typically nonserious infections. For example, after mononucleosis, a condition generally caused by Epstein-Barr virus (EBV), and after an outbreak of Giardia lamblia, an intestinal parasite that usually causes acute intestinal illness. In fact, several studies identified the association of this outbreak of giardiasis with chronic fatigue, irritable bowel syndrome (IBS), and fibromyalgia persisting for many years.
- Views expressed in the literature regarding the frequency and the validity of posttreatment Lyme disease syndrome are divided. Although substantial evidence points to persistence of arthralgia, fatigue, and subjective neurocognitive impairments in a minority of patients with Lyme disease after the recommended antibiotic treatment, some of the early studies have failed to characterize the initial Lyme disease episode with sufficient rigor.
Symptoms and signs
The symptoms and signs which, based on the evidence available, are seen more frequently in health care checks may be characterized as the following:
- Exertion intolerance, fatigue
- Flu-like and ‘sickness behavior’ symptoms: fever, feverishness, muscle pain, feeling sick, malaise, sweating, irritability
- Neurological/neurocognitive symptoms: brain fog, impaired concentration or memory, trouble finding words
- Rheumatologic symptoms: chronic or recurrent joint pain
- Trigger-specific symptoms: for example, eye problems post Ebola, IBS post Giardia, anosmia and ageusia post COVID-19, motor disturbances post polio and post West Nile virus
Myalgic encephalomyelitis/chronic fatigue syndrome
Patients with this disorder experience worsening of symptoms following physical, cognitive, or emotional exertion above their (very low) tolerated limit. Other prominent features frequently observed in myalgic encephalomyelitis/chronic fatigue syndrome (ME/CFS) are neurocognitive impairments (colloquially referred to as brain fog), unrefreshing sleep, pain, sensory disturbances, gastrointestinal issues, and various forms of dysautonomia. Up to 75% of ME/CFS cases report an infection-like episode preceding the onset of their illness. Postinfectious and postviral fatigue syndromes were originally postulated as subsets of chronic fatigue syndrome. However, there appears to be no clear consensus at present about whether these terms should be considered synonymous to the ME/CFS label or any of its subsets, or include a wider range of postinfectious fatigue conditions.
Practical diagnostic criteria
From a revision of the available criteria, it emerges that the diagnostic criteria for a PAIS should include not only the presence of symptoms, but ideally also the intensity, course, and constellation of symptoms within an individual, as the individual symptoms and symptom trajectories of PAIS vary over time, rendering a mere comparison of symptom presence at a single time point misleading. Furthermore, when a diagnosis of ME/CFS is made, attention should be given to the choice of diagnostic criteria, with preference given to the more conservative criteria, so as not to run the risk of overestimating the syndrome.
Asthenia is the cornerstone symptom for most epidemiological studies on PAIS, but it would be reductive to concentrate only on this rather than the other characteristics, such as the exacerbation of symptoms following exertion, together with other characteristic symptoms and signs that may allow for better identification of the overall, observable clinical picture in these postinfection syndromes, which have significant impacts on a patient’s quality of life.
This article was translated from Univadis Italy. A version of this article appeared on Medscape.com.
IL-6 antibody mitigates mucus hypersecretion in COPD
Treatment with an interleukin-6 neutralizing antibody significantly reduced airway mucus hypersecretion (AMH) in chronic obstructive pulmonary disease (COPD), based on data from human and mouse cells in a human organoid model.
AMH plays a large part in aggravating airway obstruction in patients with COPD, Yuan-Yuan Wei, MD, of First Affiliated Hospital of Anhui Medical University, Hefei, China, and colleagues wrote.
Current pharmacotherapies relieve COPD symptoms and improve exercise tolerance, but have not proven effective for relieving the airflow limitations caused by mucus accumulation that “leads to irreversible structural damage and an unfavorable prognosis,” the researchers said. Although reducing AMH could help manage COPD, the molecular mechanisms of action have not been fully explored.
In a study published in Biomedicine & Pharmacotherapy , the researchers examined the relationship between IL-6 and AMH. Since IL-6 has been shown to cause overexpression of the mucin-type protein known as Muc5ac, they hypothesized that IL-6 antibodies (IL-6Ab) might block this protein elevation.
The researchers recruited 30 adults with COPD and 30 controls from a single center. Bronchial epithelial cells were isolated from the participants and measured the levels of Muc5ac protein and mRNA in the lung tissue. Compared with controls, COPD patients had elevated Muc5ac positively correlated with IL-6.
The researchers then created an organoid model of a trachea for COPD patients and controls. In the model, Muc5ac was similarly elevated in COPD patients, compared with controls. “Furthermore, IL-6 significantly induced excessive secretion of mucus in the organoid model of trachea in COPD patients as observed under electron microscope, and IL-6Ab attenuated these effects,” they noted.
IL-6 significantly increased both Muc5ac mRNA and protein expression in the organoid model of trachea (P < .0001 and P < .005, respectively), but both of these significantly decreased when treated with IL-6Ab (P < .0001 and P < .05, respectively).
The researchers also examined human and mouse cells to explore the mechanism of action of IL-6Ab. Using high-throughput sequencing, they found that the IL-6Ab induced nuclear translocation of the Nrt2 gene in COPD patients, and that this action promoted the effect of IL-6Ab on excessive mucus secretion.
The study findings were limited by the relatively small study population from a single center, the researchers noted.
However, the results support the potential of IL-6Ab as “a novel therapeutic strategy in the treatment of IL-6–induced hypersecretion of airway mucus so as to improve airflow limitations in COPD,” they concluded.
The study was supported by supported by the National Natural Science Foundation of China and the Scientific Research Project of Education Department of Anhui Province. The researchers had no financial conflicts to disclose.
Treatment with an interleukin-6 neutralizing antibody significantly reduced airway mucus hypersecretion (AMH) in chronic obstructive pulmonary disease (COPD), based on data from human and mouse cells in a human organoid model.
AMH plays a large part in aggravating airway obstruction in patients with COPD, Yuan-Yuan Wei, MD, of First Affiliated Hospital of Anhui Medical University, Hefei, China, and colleagues wrote.
Current pharmacotherapies relieve COPD symptoms and improve exercise tolerance, but have not proven effective for relieving the airflow limitations caused by mucus accumulation that “leads to irreversible structural damage and an unfavorable prognosis,” the researchers said. Although reducing AMH could help manage COPD, the molecular mechanisms of action have not been fully explored.
In a study published in Biomedicine & Pharmacotherapy , the researchers examined the relationship between IL-6 and AMH. Since IL-6 has been shown to cause overexpression of the mucin-type protein known as Muc5ac, they hypothesized that IL-6 antibodies (IL-6Ab) might block this protein elevation.
The researchers recruited 30 adults with COPD and 30 controls from a single center. Bronchial epithelial cells were isolated from the participants and measured the levels of Muc5ac protein and mRNA in the lung tissue. Compared with controls, COPD patients had elevated Muc5ac positively correlated with IL-6.
The researchers then created an organoid model of a trachea for COPD patients and controls. In the model, Muc5ac was similarly elevated in COPD patients, compared with controls. “Furthermore, IL-6 significantly induced excessive secretion of mucus in the organoid model of trachea in COPD patients as observed under electron microscope, and IL-6Ab attenuated these effects,” they noted.
IL-6 significantly increased both Muc5ac mRNA and protein expression in the organoid model of trachea (P < .0001 and P < .005, respectively), but both of these significantly decreased when treated with IL-6Ab (P < .0001 and P < .05, respectively).
The researchers also examined human and mouse cells to explore the mechanism of action of IL-6Ab. Using high-throughput sequencing, they found that the IL-6Ab induced nuclear translocation of the Nrt2 gene in COPD patients, and that this action promoted the effect of IL-6Ab on excessive mucus secretion.
The study findings were limited by the relatively small study population from a single center, the researchers noted.
However, the results support the potential of IL-6Ab as “a novel therapeutic strategy in the treatment of IL-6–induced hypersecretion of airway mucus so as to improve airflow limitations in COPD,” they concluded.
The study was supported by supported by the National Natural Science Foundation of China and the Scientific Research Project of Education Department of Anhui Province. The researchers had no financial conflicts to disclose.
Treatment with an interleukin-6 neutralizing antibody significantly reduced airway mucus hypersecretion (AMH) in chronic obstructive pulmonary disease (COPD), based on data from human and mouse cells in a human organoid model.
AMH plays a large part in aggravating airway obstruction in patients with COPD, Yuan-Yuan Wei, MD, of First Affiliated Hospital of Anhui Medical University, Hefei, China, and colleagues wrote.
Current pharmacotherapies relieve COPD symptoms and improve exercise tolerance, but have not proven effective for relieving the airflow limitations caused by mucus accumulation that “leads to irreversible structural damage and an unfavorable prognosis,” the researchers said. Although reducing AMH could help manage COPD, the molecular mechanisms of action have not been fully explored.
In a study published in Biomedicine & Pharmacotherapy , the researchers examined the relationship between IL-6 and AMH. Since IL-6 has been shown to cause overexpression of the mucin-type protein known as Muc5ac, they hypothesized that IL-6 antibodies (IL-6Ab) might block this protein elevation.
The researchers recruited 30 adults with COPD and 30 controls from a single center. Bronchial epithelial cells were isolated from the participants and measured the levels of Muc5ac protein and mRNA in the lung tissue. Compared with controls, COPD patients had elevated Muc5ac positively correlated with IL-6.
The researchers then created an organoid model of a trachea for COPD patients and controls. In the model, Muc5ac was similarly elevated in COPD patients, compared with controls. “Furthermore, IL-6 significantly induced excessive secretion of mucus in the organoid model of trachea in COPD patients as observed under electron microscope, and IL-6Ab attenuated these effects,” they noted.
IL-6 significantly increased both Muc5ac mRNA and protein expression in the organoid model of trachea (P < .0001 and P < .005, respectively), but both of these significantly decreased when treated with IL-6Ab (P < .0001 and P < .05, respectively).
The researchers also examined human and mouse cells to explore the mechanism of action of IL-6Ab. Using high-throughput sequencing, they found that the IL-6Ab induced nuclear translocation of the Nrt2 gene in COPD patients, and that this action promoted the effect of IL-6Ab on excessive mucus secretion.
The study findings were limited by the relatively small study population from a single center, the researchers noted.
However, the results support the potential of IL-6Ab as “a novel therapeutic strategy in the treatment of IL-6–induced hypersecretion of airway mucus so as to improve airflow limitations in COPD,” they concluded.
The study was supported by supported by the National Natural Science Foundation of China and the Scientific Research Project of Education Department of Anhui Province. The researchers had no financial conflicts to disclose.
FROM BIOMEDICINE & PHARMACOTHERAPY
Children with autism experience more severe sleep apnea
Symptoms of obstructive sleep apnea (OSA) were significantly more common in children with autism spectrum disorder (ASD), compared with controls, based on data from 166 individuals up to age 18 years.
Autism spectrum disorder affects approximately 1 in 54 children in the United States, and recent studies have shown an increased risk of obstructive sleep apnea in this population, compared with the general pediatric population, wrote Pooja Santapuram, MD, of Vanderbilt University, Nashville, Tenn., and colleagues.
In a study published in the International Journal of Pediatric Ototrhinolaryngology , the researchers reviewed data from 166 children and adolescents up to 18 years of age with OSA who underwent adenotonsillectomy at a single center between 2019 and 2021. The primary objective was to assess OSA symptoms in children with and without ASD. The study population included 75 children with ASD and 91 controls. The average age of both the ASD group and control group was approximately 73 months.
OSA meets ASD
Obstructive sleep apnea is common in autism spectrum disorder. Children with OSA can present with a range of symptoms, including loud snoring, excessive daytime sleepiness, and changes in cognitive function. Some of these symptoms can overlap with and exacerbate symptoms of ASD, potentially delaying OSA diagnosis in children with both conditions. The primary objective of this study was to assess between-group difference in OSA symptomatology and age at OSA diagnosis in children with and without ASD. To do so, a retrospective chart review was conducted on the 166 pediatric patients.
Overall, significantly more OSA symptoms were reported in children with ASD, compared with controls (P < .001).
Lower autism severity was associated with an increased number of reported OSA symptoms (P = .006). There was not a significant between-group difference in age at OSA diagnosis (P = .999); however, lower autism severity was also associated with an increased age at diagnosis (P = .002). These findings suggest that OSA may present with a higher symptom burden in children with ASD, and children with lower ASD severity often experience delays in OSA diagnosis.
Interestingly, despite the known associations between obesity and OSA, children with an increased body mass index were not diagnosed with OSA at an earlier age in this sample population, the researchers indicated.
Because the current study revealed that children with less severe ASD are more likely to report an increased number of OSA symptoms and be diagnosed at a later age than children without ASD, clinicians should have a heightened sense for OSA evaluation in children with ASD, particularly in children with a lower severity of ASD and an increased BMI, the researchers concluded.
The research study was not externally funded, and the researchers reported that they had no conflicts of interest.
Symptoms of obstructive sleep apnea (OSA) were significantly more common in children with autism spectrum disorder (ASD), compared with controls, based on data from 166 individuals up to age 18 years.
Autism spectrum disorder affects approximately 1 in 54 children in the United States, and recent studies have shown an increased risk of obstructive sleep apnea in this population, compared with the general pediatric population, wrote Pooja Santapuram, MD, of Vanderbilt University, Nashville, Tenn., and colleagues.
In a study published in the International Journal of Pediatric Ototrhinolaryngology , the researchers reviewed data from 166 children and adolescents up to 18 years of age with OSA who underwent adenotonsillectomy at a single center between 2019 and 2021. The primary objective was to assess OSA symptoms in children with and without ASD. The study population included 75 children with ASD and 91 controls. The average age of both the ASD group and control group was approximately 73 months.
OSA meets ASD
Obstructive sleep apnea is common in autism spectrum disorder. Children with OSA can present with a range of symptoms, including loud snoring, excessive daytime sleepiness, and changes in cognitive function. Some of these symptoms can overlap with and exacerbate symptoms of ASD, potentially delaying OSA diagnosis in children with both conditions. The primary objective of this study was to assess between-group difference in OSA symptomatology and age at OSA diagnosis in children with and without ASD. To do so, a retrospective chart review was conducted on the 166 pediatric patients.
Overall, significantly more OSA symptoms were reported in children with ASD, compared with controls (P < .001).
Lower autism severity was associated with an increased number of reported OSA symptoms (P = .006). There was not a significant between-group difference in age at OSA diagnosis (P = .999); however, lower autism severity was also associated with an increased age at diagnosis (P = .002). These findings suggest that OSA may present with a higher symptom burden in children with ASD, and children with lower ASD severity often experience delays in OSA diagnosis.
Interestingly, despite the known associations between obesity and OSA, children with an increased body mass index were not diagnosed with OSA at an earlier age in this sample population, the researchers indicated.
Because the current study revealed that children with less severe ASD are more likely to report an increased number of OSA symptoms and be diagnosed at a later age than children without ASD, clinicians should have a heightened sense for OSA evaluation in children with ASD, particularly in children with a lower severity of ASD and an increased BMI, the researchers concluded.
The research study was not externally funded, and the researchers reported that they had no conflicts of interest.
Symptoms of obstructive sleep apnea (OSA) were significantly more common in children with autism spectrum disorder (ASD), compared with controls, based on data from 166 individuals up to age 18 years.
Autism spectrum disorder affects approximately 1 in 54 children in the United States, and recent studies have shown an increased risk of obstructive sleep apnea in this population, compared with the general pediatric population, wrote Pooja Santapuram, MD, of Vanderbilt University, Nashville, Tenn., and colleagues.
In a study published in the International Journal of Pediatric Ototrhinolaryngology , the researchers reviewed data from 166 children and adolescents up to 18 years of age with OSA who underwent adenotonsillectomy at a single center between 2019 and 2021. The primary objective was to assess OSA symptoms in children with and without ASD. The study population included 75 children with ASD and 91 controls. The average age of both the ASD group and control group was approximately 73 months.
OSA meets ASD
Obstructive sleep apnea is common in autism spectrum disorder. Children with OSA can present with a range of symptoms, including loud snoring, excessive daytime sleepiness, and changes in cognitive function. Some of these symptoms can overlap with and exacerbate symptoms of ASD, potentially delaying OSA diagnosis in children with both conditions. The primary objective of this study was to assess between-group difference in OSA symptomatology and age at OSA diagnosis in children with and without ASD. To do so, a retrospective chart review was conducted on the 166 pediatric patients.
Overall, significantly more OSA symptoms were reported in children with ASD, compared with controls (P < .001).
Lower autism severity was associated with an increased number of reported OSA symptoms (P = .006). There was not a significant between-group difference in age at OSA diagnosis (P = .999); however, lower autism severity was also associated with an increased age at diagnosis (P = .002). These findings suggest that OSA may present with a higher symptom burden in children with ASD, and children with lower ASD severity often experience delays in OSA diagnosis.
Interestingly, despite the known associations between obesity and OSA, children with an increased body mass index were not diagnosed with OSA at an earlier age in this sample population, the researchers indicated.
Because the current study revealed that children with less severe ASD are more likely to report an increased number of OSA symptoms and be diagnosed at a later age than children without ASD, clinicians should have a heightened sense for OSA evaluation in children with ASD, particularly in children with a lower severity of ASD and an increased BMI, the researchers concluded.
The research study was not externally funded, and the researchers reported that they had no conflicts of interest.
FROM THE INTERNATIONAL JOURNAL OF PEDIATRIC OTORHINOLARYNGOLOGY
Disturbed sleep drives poor PrEP adherence in young Black sexual-minority men
Young Black sexual-minority men (YBSMM) who experience sleep disturbance at least 3-4 times a week are much more likely to miss HIV pre-exposure prophylaxis (PrEP) doses than those who rarely report sleep disturbance, according to a new study published online in the journal AIDS and Behavior.
Sleep disturbance, poor cognitive processing, and memory function deficits go hand in hand, especially among people living with HIV.
Data have suggested that poor sleep might be an important factor in common neurocognitive complaints and overall health outcomes, especially among older adults with HIV. But few studies have examined the role that sleep quality might play in driving health behaviors around prevention and PrEP adherence, especially among YBSMM, who are at highest risk for acquiring new HIV infections.
Commonly cited reasons for suboptimal HIV prevention efforts within this population often include stigma, mistrust of the medical system, and a lack of culturally appropriate care.
“We make a lot of assumptions about young people and their brains and their ability to remember things, namely [that] they should be better than older adults at remembering to take medications,” lead study investigator Jade Pagkas-Bather, MD, an infectious disease specialist at University of Chicago Medicine, told this news organization.
“In reality, many young people are not used to taking medications, [especially] for a disease that they do not have.”
Too many pills, too little sleep
The researchers examined data collected from participants in the Neighborhoods and Networks Cohort Study, Chicago, which looked at the role of social, contextual, network, and geospatial factors influencing HIV prevention and care in HIV-negative, cisgender YBSMM between 2018 and 2019.
The investigators included 70 YBSMM participants who reported current PrEP use in the analysis. All were between the ages of 16 and 24 years, self-identified as African American or Black, were assigned male at birth, and reported at least one sexual encounter with a man or transgender woman in the previous 12 months.
Sleep was measured using the Patient Health Questionnaire-9 (PHQ-9) which includes a question on frequency of sleep disturbance (that is, trouble falling asleep, staying asleep, or sleeping too much) categorized as follows: less than 1 day (rarely or none of the time), 1-2 days (some or a little of the time), 3-4 days (occasionally or a moderate amount of time), or 5-7 days (all of the time).
Almost half (47.1%) of participants self-reported some or moderate sleep disturbance, with 8.6% having sleep disturbance all of the time.
“One of the main findings was that poor sleep and having too many pills impacts people’s ability to remember to take their PrEP or is associated with missing PrEP doses,” explained Dr. Pagkas-Bather.
In adjusted models, YBSMM who reported moderate sleep disturbances cited having too many pills to take as the reason for missing or forgetting PrEP doses (adjusted odds ratio, 7.59; 95% confidence interval, 1.05-54.57), compared with peers who did not have sleep issues.
Depression was likewise an important factor. Participants who reported experiencing sleep disturbance all of the time and missing PrEP doses were also highly likely to be depressed (aOR, 11.30; 95% CI, 1.19-107.53).
“The PHQ-9 is a widely accepted measure looking at depression – and sleep as one symptom of depression,” explained Brooke Genkin Rogers, Ph.D., M.P.H., a research scientist and assistant professor of psychiatry and human behavior at the Warren Alpert Medical School of Brown University, Providence, R.I.
Dr. Rogers, who was not involved in the study, noted, “Sleep disturbance is a sign of poor physical or mental health, particularly in an otherwise younger, healthier population.” But Dr. Rogers also had questions about sleep duration (that is, too short or too long) and whether or not it also played a role in poor adherence, information that was not pursued within the study.
“As a clinician, I see quite a few people who are young Black sexual minority men who are on PrEP, or on the converse side, people living with HIV and taking medications for HIV treatment. I would posit a guess that it’s not that people are necessarily sleeping too much, but there are other sorts of factors that interfere with being able to get 8 hours of sleep a night,” explained Dr. Pagkas-Bather.
They include structural issues like greater exposure to housing instability and neighborhood safety.
However, Dr. Pagkas-Bather pointed to an even more critical factor influencing PrEP usage and adherence, one that she refers to as “Trickle Up HIV Care.”
“We can’t just come up with interventions, drugs, and studies and say, we have all of these options, anyone who wants them, come and get them,” she said. “We really need to work very hard at educating and encouraging populations who have no high-level need for prevention and treatment.”
As a clinician who works closely with the YBSMM population, Dr. Pagkas-Bather also shared that her patients have told her that they’ve asked for PrEP and have had providers turn them down because they weren’t comfortable prescribing PrEP or made assumptions about the kind of people who are on PrEP.
“There are sometimes assumptions made about Black men and sexual promiscuity. And the data doesn’t bear that out. It’s not that Black men are having more sex than White men or any other man; it’s that the prevalence of HIV in the Black community is higher overall relative to the population,” noted Dr. Pagkas-Bather.
“We need a nuanced approach to examining these issues ... to take a look at multiple levels of influence on folks’ health and HIV risk,” said Dr. Rogers.
Both clinicians acknowledged that creative solutions have not been exhausted.
“There’s a lot of opportunity if we sit down with communities and share in decisions around HIV treatment and prevention ... if we tap into the wealth and knowledge of the Black communities to prevent HIV,” concluded Dr. Pagkas-Bather.
Dr. Pagkas-Bather reports that she is a Gilead Sciences HIV Research Scholar awardee. Dr. Rogers reports receiving a scientific research grant from Gilead Sciences.
A version of this article first appeared on Medscape.com.
Young Black sexual-minority men (YBSMM) who experience sleep disturbance at least 3-4 times a week are much more likely to miss HIV pre-exposure prophylaxis (PrEP) doses than those who rarely report sleep disturbance, according to a new study published online in the journal AIDS and Behavior.
Sleep disturbance, poor cognitive processing, and memory function deficits go hand in hand, especially among people living with HIV.
Data have suggested that poor sleep might be an important factor in common neurocognitive complaints and overall health outcomes, especially among older adults with HIV. But few studies have examined the role that sleep quality might play in driving health behaviors around prevention and PrEP adherence, especially among YBSMM, who are at highest risk for acquiring new HIV infections.
Commonly cited reasons for suboptimal HIV prevention efforts within this population often include stigma, mistrust of the medical system, and a lack of culturally appropriate care.
“We make a lot of assumptions about young people and their brains and their ability to remember things, namely [that] they should be better than older adults at remembering to take medications,” lead study investigator Jade Pagkas-Bather, MD, an infectious disease specialist at University of Chicago Medicine, told this news organization.
“In reality, many young people are not used to taking medications, [especially] for a disease that they do not have.”
Too many pills, too little sleep
The researchers examined data collected from participants in the Neighborhoods and Networks Cohort Study, Chicago, which looked at the role of social, contextual, network, and geospatial factors influencing HIV prevention and care in HIV-negative, cisgender YBSMM between 2018 and 2019.
The investigators included 70 YBSMM participants who reported current PrEP use in the analysis. All were between the ages of 16 and 24 years, self-identified as African American or Black, were assigned male at birth, and reported at least one sexual encounter with a man or transgender woman in the previous 12 months.
Sleep was measured using the Patient Health Questionnaire-9 (PHQ-9) which includes a question on frequency of sleep disturbance (that is, trouble falling asleep, staying asleep, or sleeping too much) categorized as follows: less than 1 day (rarely or none of the time), 1-2 days (some or a little of the time), 3-4 days (occasionally or a moderate amount of time), or 5-7 days (all of the time).
Almost half (47.1%) of participants self-reported some or moderate sleep disturbance, with 8.6% having sleep disturbance all of the time.
“One of the main findings was that poor sleep and having too many pills impacts people’s ability to remember to take their PrEP or is associated with missing PrEP doses,” explained Dr. Pagkas-Bather.
In adjusted models, YBSMM who reported moderate sleep disturbances cited having too many pills to take as the reason for missing or forgetting PrEP doses (adjusted odds ratio, 7.59; 95% confidence interval, 1.05-54.57), compared with peers who did not have sleep issues.
Depression was likewise an important factor. Participants who reported experiencing sleep disturbance all of the time and missing PrEP doses were also highly likely to be depressed (aOR, 11.30; 95% CI, 1.19-107.53).
“The PHQ-9 is a widely accepted measure looking at depression – and sleep as one symptom of depression,” explained Brooke Genkin Rogers, Ph.D., M.P.H., a research scientist and assistant professor of psychiatry and human behavior at the Warren Alpert Medical School of Brown University, Providence, R.I.
Dr. Rogers, who was not involved in the study, noted, “Sleep disturbance is a sign of poor physical or mental health, particularly in an otherwise younger, healthier population.” But Dr. Rogers also had questions about sleep duration (that is, too short or too long) and whether or not it also played a role in poor adherence, information that was not pursued within the study.
“As a clinician, I see quite a few people who are young Black sexual minority men who are on PrEP, or on the converse side, people living with HIV and taking medications for HIV treatment. I would posit a guess that it’s not that people are necessarily sleeping too much, but there are other sorts of factors that interfere with being able to get 8 hours of sleep a night,” explained Dr. Pagkas-Bather.
They include structural issues like greater exposure to housing instability and neighborhood safety.
However, Dr. Pagkas-Bather pointed to an even more critical factor influencing PrEP usage and adherence, one that she refers to as “Trickle Up HIV Care.”
“We can’t just come up with interventions, drugs, and studies and say, we have all of these options, anyone who wants them, come and get them,” she said. “We really need to work very hard at educating and encouraging populations who have no high-level need for prevention and treatment.”
As a clinician who works closely with the YBSMM population, Dr. Pagkas-Bather also shared that her patients have told her that they’ve asked for PrEP and have had providers turn them down because they weren’t comfortable prescribing PrEP or made assumptions about the kind of people who are on PrEP.
“There are sometimes assumptions made about Black men and sexual promiscuity. And the data doesn’t bear that out. It’s not that Black men are having more sex than White men or any other man; it’s that the prevalence of HIV in the Black community is higher overall relative to the population,” noted Dr. Pagkas-Bather.
“We need a nuanced approach to examining these issues ... to take a look at multiple levels of influence on folks’ health and HIV risk,” said Dr. Rogers.
Both clinicians acknowledged that creative solutions have not been exhausted.
“There’s a lot of opportunity if we sit down with communities and share in decisions around HIV treatment and prevention ... if we tap into the wealth and knowledge of the Black communities to prevent HIV,” concluded Dr. Pagkas-Bather.
Dr. Pagkas-Bather reports that she is a Gilead Sciences HIV Research Scholar awardee. Dr. Rogers reports receiving a scientific research grant from Gilead Sciences.
A version of this article first appeared on Medscape.com.
Young Black sexual-minority men (YBSMM) who experience sleep disturbance at least 3-4 times a week are much more likely to miss HIV pre-exposure prophylaxis (PrEP) doses than those who rarely report sleep disturbance, according to a new study published online in the journal AIDS and Behavior.
Sleep disturbance, poor cognitive processing, and memory function deficits go hand in hand, especially among people living with HIV.
Data have suggested that poor sleep might be an important factor in common neurocognitive complaints and overall health outcomes, especially among older adults with HIV. But few studies have examined the role that sleep quality might play in driving health behaviors around prevention and PrEP adherence, especially among YBSMM, who are at highest risk for acquiring new HIV infections.
Commonly cited reasons for suboptimal HIV prevention efforts within this population often include stigma, mistrust of the medical system, and a lack of culturally appropriate care.
“We make a lot of assumptions about young people and their brains and their ability to remember things, namely [that] they should be better than older adults at remembering to take medications,” lead study investigator Jade Pagkas-Bather, MD, an infectious disease specialist at University of Chicago Medicine, told this news organization.
“In reality, many young people are not used to taking medications, [especially] for a disease that they do not have.”
Too many pills, too little sleep
The researchers examined data collected from participants in the Neighborhoods and Networks Cohort Study, Chicago, which looked at the role of social, contextual, network, and geospatial factors influencing HIV prevention and care in HIV-negative, cisgender YBSMM between 2018 and 2019.
The investigators included 70 YBSMM participants who reported current PrEP use in the analysis. All were between the ages of 16 and 24 years, self-identified as African American or Black, were assigned male at birth, and reported at least one sexual encounter with a man or transgender woman in the previous 12 months.
Sleep was measured using the Patient Health Questionnaire-9 (PHQ-9) which includes a question on frequency of sleep disturbance (that is, trouble falling asleep, staying asleep, or sleeping too much) categorized as follows: less than 1 day (rarely or none of the time), 1-2 days (some or a little of the time), 3-4 days (occasionally or a moderate amount of time), or 5-7 days (all of the time).
Almost half (47.1%) of participants self-reported some or moderate sleep disturbance, with 8.6% having sleep disturbance all of the time.
“One of the main findings was that poor sleep and having too many pills impacts people’s ability to remember to take their PrEP or is associated with missing PrEP doses,” explained Dr. Pagkas-Bather.
In adjusted models, YBSMM who reported moderate sleep disturbances cited having too many pills to take as the reason for missing or forgetting PrEP doses (adjusted odds ratio, 7.59; 95% confidence interval, 1.05-54.57), compared with peers who did not have sleep issues.
Depression was likewise an important factor. Participants who reported experiencing sleep disturbance all of the time and missing PrEP doses were also highly likely to be depressed (aOR, 11.30; 95% CI, 1.19-107.53).
“The PHQ-9 is a widely accepted measure looking at depression – and sleep as one symptom of depression,” explained Brooke Genkin Rogers, Ph.D., M.P.H., a research scientist and assistant professor of psychiatry and human behavior at the Warren Alpert Medical School of Brown University, Providence, R.I.
Dr. Rogers, who was not involved in the study, noted, “Sleep disturbance is a sign of poor physical or mental health, particularly in an otherwise younger, healthier population.” But Dr. Rogers also had questions about sleep duration (that is, too short or too long) and whether or not it also played a role in poor adherence, information that was not pursued within the study.
“As a clinician, I see quite a few people who are young Black sexual minority men who are on PrEP, or on the converse side, people living with HIV and taking medications for HIV treatment. I would posit a guess that it’s not that people are necessarily sleeping too much, but there are other sorts of factors that interfere with being able to get 8 hours of sleep a night,” explained Dr. Pagkas-Bather.
They include structural issues like greater exposure to housing instability and neighborhood safety.
However, Dr. Pagkas-Bather pointed to an even more critical factor influencing PrEP usage and adherence, one that she refers to as “Trickle Up HIV Care.”
“We can’t just come up with interventions, drugs, and studies and say, we have all of these options, anyone who wants them, come and get them,” she said. “We really need to work very hard at educating and encouraging populations who have no high-level need for prevention and treatment.”
As a clinician who works closely with the YBSMM population, Dr. Pagkas-Bather also shared that her patients have told her that they’ve asked for PrEP and have had providers turn them down because they weren’t comfortable prescribing PrEP or made assumptions about the kind of people who are on PrEP.
“There are sometimes assumptions made about Black men and sexual promiscuity. And the data doesn’t bear that out. It’s not that Black men are having more sex than White men or any other man; it’s that the prevalence of HIV in the Black community is higher overall relative to the population,” noted Dr. Pagkas-Bather.
“We need a nuanced approach to examining these issues ... to take a look at multiple levels of influence on folks’ health and HIV risk,” said Dr. Rogers.
Both clinicians acknowledged that creative solutions have not been exhausted.
“There’s a lot of opportunity if we sit down with communities and share in decisions around HIV treatment and prevention ... if we tap into the wealth and knowledge of the Black communities to prevent HIV,” concluded Dr. Pagkas-Bather.
Dr. Pagkas-Bather reports that she is a Gilead Sciences HIV Research Scholar awardee. Dr. Rogers reports receiving a scientific research grant from Gilead Sciences.
A version of this article first appeared on Medscape.com.
Diabetes tied to risk of long COVID, too
Individuals with diabetes who experience COVID-19 are at increased risk for long COVID compared to individuals without diabetes, according to data from a literature review of seven studies.
Diabetes remains a risk factor for severe COVID-19, but whether it is a risk factor for postacute sequelae of COVID-19 (PASC), also known as long COVID, remains unclear, Jessica L. Harding, PhD, of Emory University, said in a late-breaking poster session at the annual scientific sessions of the American Diabetes Association.
Long COVID is generally defined as “sequelae that extend beyond the 4 weeks after initial infection” and may include a range of symptoms that affect multiple organs, Dr. Harding said. A study conducted in January of 2022 suggested that type 2 diabetes was one of several strong risk factors for long COVID, she noted.
Dr. Harding and colleagues reviewed data from seven studies published from Jan. 1, 2020, to Jan. 27, 2022, on the risk of PASC in people with and without diabetes. The studies included patients with a minimum of 4 weeks’ follow-up after COVID-19 diagnosis. All seven studies had a longitudinal cohort design, and included adults from high-income countries, with study populations ranging from 104 to 4,182.
Across the studies, long COVID definitions varied, but included ongoing symptoms of fatigue, cough, and dyspnea, with follow-up periods of 4 weeks to 7 months.
Overall, three of the seven studies indicated that diabetes was a risk factor for long COVID (odds ratio [OR] greater than 4 for all) and four studies indicated that diabetes was not a risk factor for long COVID (OR, 0.5-2.2).
One of the three studies showing increased risk included 2,334 individuals hospitalized with COVID-19; of these about 5% had diabetes. The odds ratio for PASC for individuals with diabetes was 4.18. In another study of 209 persons with COVID-19, of whom 22% had diabetes, diabetes was significantly correlated with respiratory viral disease (meaning at least two respiratory symptoms). The third study showing an increased risk of long COVID in diabetes patients included 104 kidney transplant patients, of whom 20% had diabetes; the odds ratio for PASC was 4.42.
The findings were limited by several factors, including the relatively small number of studies and the heterogeneity of studies regarding definitions of long COVID, specific populations at risk, follow-up times, and risk adjustment, Dr. Harding noted.
More high-quality studies across multiple populations and settings are needed to determine if diabetes is indeed a risk factor for long COVID, she said.
In the meantime, “careful monitoring of people with diabetes for development of PASC may be advised,” Dr. Harding concluded.
Findings support need for screening
“Given the devastating impact of COVID on people with diabetes, it’s important to know what data has been accumulated on long COVID for future research and discoveries in this area,” Robert A. Gabbay, MD, chief science and medical officer for the American Diabetes Association, said in an interview. “The more information we have, the better we can understand the implications.”
Dr. Gabbay said he was surprised by the current study findings. “We know very little on this subject, so yes, I am surprised to see just how significant the risk of long COVID for people with diabetes seems to be, but clearly, more research needs to be done to understand long COVID,” he emphasized.
The take-home message for clinicians is the importance of screening patients for PASC; also “ask your patients if they had COVID, to better understand any symptoms they might have that could be related to PACS,” he noted.
“It is crucial that we confirm these results and then look at risk factors in people with diabetes that might explain who is at highest risk and ultimately understand the causes and potential cure,” Dr. Gabbay added.
The study was supported by the National Heart, Lung, and Blood Institute. Dr. Harding and Dr. Gabbay had no financial conflicts to disclose.
Individuals with diabetes who experience COVID-19 are at increased risk for long COVID compared to individuals without diabetes, according to data from a literature review of seven studies.
Diabetes remains a risk factor for severe COVID-19, but whether it is a risk factor for postacute sequelae of COVID-19 (PASC), also known as long COVID, remains unclear, Jessica L. Harding, PhD, of Emory University, said in a late-breaking poster session at the annual scientific sessions of the American Diabetes Association.
Long COVID is generally defined as “sequelae that extend beyond the 4 weeks after initial infection” and may include a range of symptoms that affect multiple organs, Dr. Harding said. A study conducted in January of 2022 suggested that type 2 diabetes was one of several strong risk factors for long COVID, she noted.
Dr. Harding and colleagues reviewed data from seven studies published from Jan. 1, 2020, to Jan. 27, 2022, on the risk of PASC in people with and without diabetes. The studies included patients with a minimum of 4 weeks’ follow-up after COVID-19 diagnosis. All seven studies had a longitudinal cohort design, and included adults from high-income countries, with study populations ranging from 104 to 4,182.
Across the studies, long COVID definitions varied, but included ongoing symptoms of fatigue, cough, and dyspnea, with follow-up periods of 4 weeks to 7 months.
Overall, three of the seven studies indicated that diabetes was a risk factor for long COVID (odds ratio [OR] greater than 4 for all) and four studies indicated that diabetes was not a risk factor for long COVID (OR, 0.5-2.2).
One of the three studies showing increased risk included 2,334 individuals hospitalized with COVID-19; of these about 5% had diabetes. The odds ratio for PASC for individuals with diabetes was 4.18. In another study of 209 persons with COVID-19, of whom 22% had diabetes, diabetes was significantly correlated with respiratory viral disease (meaning at least two respiratory symptoms). The third study showing an increased risk of long COVID in diabetes patients included 104 kidney transplant patients, of whom 20% had diabetes; the odds ratio for PASC was 4.42.
The findings were limited by several factors, including the relatively small number of studies and the heterogeneity of studies regarding definitions of long COVID, specific populations at risk, follow-up times, and risk adjustment, Dr. Harding noted.
More high-quality studies across multiple populations and settings are needed to determine if diabetes is indeed a risk factor for long COVID, she said.
In the meantime, “careful monitoring of people with diabetes for development of PASC may be advised,” Dr. Harding concluded.
Findings support need for screening
“Given the devastating impact of COVID on people with diabetes, it’s important to know what data has been accumulated on long COVID for future research and discoveries in this area,” Robert A. Gabbay, MD, chief science and medical officer for the American Diabetes Association, said in an interview. “The more information we have, the better we can understand the implications.”
Dr. Gabbay said he was surprised by the current study findings. “We know very little on this subject, so yes, I am surprised to see just how significant the risk of long COVID for people with diabetes seems to be, but clearly, more research needs to be done to understand long COVID,” he emphasized.
The take-home message for clinicians is the importance of screening patients for PASC; also “ask your patients if they had COVID, to better understand any symptoms they might have that could be related to PACS,” he noted.
“It is crucial that we confirm these results and then look at risk factors in people with diabetes that might explain who is at highest risk and ultimately understand the causes and potential cure,” Dr. Gabbay added.
The study was supported by the National Heart, Lung, and Blood Institute. Dr. Harding and Dr. Gabbay had no financial conflicts to disclose.
Individuals with diabetes who experience COVID-19 are at increased risk for long COVID compared to individuals without diabetes, according to data from a literature review of seven studies.
Diabetes remains a risk factor for severe COVID-19, but whether it is a risk factor for postacute sequelae of COVID-19 (PASC), also known as long COVID, remains unclear, Jessica L. Harding, PhD, of Emory University, said in a late-breaking poster session at the annual scientific sessions of the American Diabetes Association.
Long COVID is generally defined as “sequelae that extend beyond the 4 weeks after initial infection” and may include a range of symptoms that affect multiple organs, Dr. Harding said. A study conducted in January of 2022 suggested that type 2 diabetes was one of several strong risk factors for long COVID, she noted.
Dr. Harding and colleagues reviewed data from seven studies published from Jan. 1, 2020, to Jan. 27, 2022, on the risk of PASC in people with and without diabetes. The studies included patients with a minimum of 4 weeks’ follow-up after COVID-19 diagnosis. All seven studies had a longitudinal cohort design, and included adults from high-income countries, with study populations ranging from 104 to 4,182.
Across the studies, long COVID definitions varied, but included ongoing symptoms of fatigue, cough, and dyspnea, with follow-up periods of 4 weeks to 7 months.
Overall, three of the seven studies indicated that diabetes was a risk factor for long COVID (odds ratio [OR] greater than 4 for all) and four studies indicated that diabetes was not a risk factor for long COVID (OR, 0.5-2.2).
One of the three studies showing increased risk included 2,334 individuals hospitalized with COVID-19; of these about 5% had diabetes. The odds ratio for PASC for individuals with diabetes was 4.18. In another study of 209 persons with COVID-19, of whom 22% had diabetes, diabetes was significantly correlated with respiratory viral disease (meaning at least two respiratory symptoms). The third study showing an increased risk of long COVID in diabetes patients included 104 kidney transplant patients, of whom 20% had diabetes; the odds ratio for PASC was 4.42.
The findings were limited by several factors, including the relatively small number of studies and the heterogeneity of studies regarding definitions of long COVID, specific populations at risk, follow-up times, and risk adjustment, Dr. Harding noted.
More high-quality studies across multiple populations and settings are needed to determine if diabetes is indeed a risk factor for long COVID, she said.
In the meantime, “careful monitoring of people with diabetes for development of PASC may be advised,” Dr. Harding concluded.
Findings support need for screening
“Given the devastating impact of COVID on people with diabetes, it’s important to know what data has been accumulated on long COVID for future research and discoveries in this area,” Robert A. Gabbay, MD, chief science and medical officer for the American Diabetes Association, said in an interview. “The more information we have, the better we can understand the implications.”
Dr. Gabbay said he was surprised by the current study findings. “We know very little on this subject, so yes, I am surprised to see just how significant the risk of long COVID for people with diabetes seems to be, but clearly, more research needs to be done to understand long COVID,” he emphasized.
The take-home message for clinicians is the importance of screening patients for PASC; also “ask your patients if they had COVID, to better understand any symptoms they might have that could be related to PACS,” he noted.
“It is crucial that we confirm these results and then look at risk factors in people with diabetes that might explain who is at highest risk and ultimately understand the causes and potential cure,” Dr. Gabbay added.
The study was supported by the National Heart, Lung, and Blood Institute. Dr. Harding and Dr. Gabbay had no financial conflicts to disclose.
FROM ADA 2022








