User login
-
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]


Parsing the split-decision victory for biologics in COPD
It’s tough to keep up with the proliferation of monoclonal antibodies. Seems every day I’m confronted by a patient who’s using a new drug with a name ending in “mab.” That drug blocks a cellular receptor I haven’t heard of that’s involved in a cascade of interactions I haven’t thought about since medical school. The resulting disruption reduces disease burden, typically at great expense to the medical system, the patient, or both. We’ve truly entered the era of precision medicine. It’s not enough to understand disease; you also must know its heterogeneous expression so that you can prescribe the ‘mab that targets the biology responsible for variants in behavior. All diseases are, in fact, syndromes. This isn’t a bad thing, but it’s a challenge.
A series of ‘mabs have been approved for treating type 2 high (TH2) or eosinophilic asthma. We refer to this group of ‘mabs generically as biologics. The group includes omalizumab, mepolizumab, dupilumab, benralizumab, reslizumab, and tezepelumab. While mechanism of action varies slightly across drugs, the biologics all target a specific arm of the immune system. Efficacy is linearly related to serum eosinophil count and there’s little clinically or pharmacologically to distinguish one from another. Of course, no head-to-head comparisons of efficacy are available and there’s no financial incentive for them to be performed.
Latest research
A new randomized controlled trial (RCT) of dupilumab for chronic obstructive pulmonary disease (COPD) adds to the aforementioned biologic knowledge base. Turns out it works as long as the patients are carefully selected. Researchers enrolled GOLD D (or E depending on which iteration of the GOLD Statement you use) patients on triple inhaler therapy (inhaled corticosteroids [ICS]/long-acting beta-agonist [LABA]/long-acting muscarinic antagonist [LAMA]) with two moderate exacerbations or one exacerbation requiring hospitalization in the past year. Blood eosinophil counts were > 300 cells/mcL and chronic bronchitis was present clinically. The primary and multiple secondary outcomes were improved with dupilumab.
This is welcome news. I’ve treated countless patients with severe COPD who have repeated exacerbations despite my efforts to prevent them. These patients are on ICS/LABA/LAMA and azithromycin or roflumilast, and occasionally both. While every COPD guideline known to man forbids using chronic oral corticosteroids (OCS), I’ve prescribed them repeatedly because the benefits to keeping a recalcitrant, exacerbating patient out of the hospital seem to outweigh OCS risks. It would be nice to have a better option. Although we were taught that they were immutably distinct in medical school, every first-year pulmonary fellow knows that asthma and COPD share more similarities than differences, so it makes sense that proven asthma therapies would work for some patients with COPD.
However, the dupilumab study must be placed in context. Past studies haven’t been as positive. In 2017, two separate RCTs found that mepolizumab reduced the annual rate of moderate to severe exacerbations (primary outcome) in one trial but not the other. Interpretation gets more complicated when broken down by intention to treat (ITT) vs. modified ITT and when secondary outcomes are considered. Sparing you those details, this trial does not instill confidence, leading the Food and Drug Administration to refuse approval for mepolizumab for COPD. A second RCT of benralizumab for COPD was published in 2019. Much less cognitive load was required to interpret this one; it was negative. FDA approval was not requested.
Looking through the trial designs for the three RCTs of biologics for COPD, I couldn’t find major differences that could explain the discordant results. Sample size and enrollment criteria were similar. As stated, I don’t believe that the biologic data in asthma allow for predicting efficacy in one eosinophilic patient vs. another and I assume the same would be true for COPD. All three trials found that eosinophils were eliminated, so responses were biologically equivalent.
Key takeaways
If trial design and pharmacology don’t account for the disparate outcomes, how do we explain them? More important, how do we translate these trials into clinical practice? I looked for a review or editorial by a scientist-clinician smarter than I so I could steal their ideas and express them as pedantic euphemisms here. I found it curious that I was unable to find one. A recent publication in the American Journal of Respiratory and Critical Care Medicine suggests that the answer lies within the complex lattice of eosinophil subtypes, but I’m unqualified to judge the veracity of this “phenotype within a phenotype” theory.
More trials in COPD are being done. We should have results on tezepelumab, that great savior that may cover noneosinophilic asthma phenotypes, within the next few years. Until then, we’re stuck defying guidelines with the anachronistic use of OCS for the COPD patient who exacerbates through ICS/LABA/LAMA, roflumilast, and azithromycin.
Dr. Holley is professor of medicine at Uniformed Services University in Bethesda, Md., and a pulmonary/sleep and critical care medicine physician at MedStar Washington Hospital Center in Washington. He reported receiving income from CHEST College, Metapharm, and WebMD.
A version of this article first appeared on Medscape.com.
It’s tough to keep up with the proliferation of monoclonal antibodies. Seems every day I’m confronted by a patient who’s using a new drug with a name ending in “mab.” That drug blocks a cellular receptor I haven’t heard of that’s involved in a cascade of interactions I haven’t thought about since medical school. The resulting disruption reduces disease burden, typically at great expense to the medical system, the patient, or both. We’ve truly entered the era of precision medicine. It’s not enough to understand disease; you also must know its heterogeneous expression so that you can prescribe the ‘mab that targets the biology responsible for variants in behavior. All diseases are, in fact, syndromes. This isn’t a bad thing, but it’s a challenge.
A series of ‘mabs have been approved for treating type 2 high (TH2) or eosinophilic asthma. We refer to this group of ‘mabs generically as biologics. The group includes omalizumab, mepolizumab, dupilumab, benralizumab, reslizumab, and tezepelumab. While mechanism of action varies slightly across drugs, the biologics all target a specific arm of the immune system. Efficacy is linearly related to serum eosinophil count and there’s little clinically or pharmacologically to distinguish one from another. Of course, no head-to-head comparisons of efficacy are available and there’s no financial incentive for them to be performed.
Latest research
A new randomized controlled trial (RCT) of dupilumab for chronic obstructive pulmonary disease (COPD) adds to the aforementioned biologic knowledge base. Turns out it works as long as the patients are carefully selected. Researchers enrolled GOLD D (or E depending on which iteration of the GOLD Statement you use) patients on triple inhaler therapy (inhaled corticosteroids [ICS]/long-acting beta-agonist [LABA]/long-acting muscarinic antagonist [LAMA]) with two moderate exacerbations or one exacerbation requiring hospitalization in the past year. Blood eosinophil counts were > 300 cells/mcL and chronic bronchitis was present clinically. The primary and multiple secondary outcomes were improved with dupilumab.
This is welcome news. I’ve treated countless patients with severe COPD who have repeated exacerbations despite my efforts to prevent them. These patients are on ICS/LABA/LAMA and azithromycin or roflumilast, and occasionally both. While every COPD guideline known to man forbids using chronic oral corticosteroids (OCS), I’ve prescribed them repeatedly because the benefits to keeping a recalcitrant, exacerbating patient out of the hospital seem to outweigh OCS risks. It would be nice to have a better option. Although we were taught that they were immutably distinct in medical school, every first-year pulmonary fellow knows that asthma and COPD share more similarities than differences, so it makes sense that proven asthma therapies would work for some patients with COPD.
However, the dupilumab study must be placed in context. Past studies haven’t been as positive. In 2017, two separate RCTs found that mepolizumab reduced the annual rate of moderate to severe exacerbations (primary outcome) in one trial but not the other. Interpretation gets more complicated when broken down by intention to treat (ITT) vs. modified ITT and when secondary outcomes are considered. Sparing you those details, this trial does not instill confidence, leading the Food and Drug Administration to refuse approval for mepolizumab for COPD. A second RCT of benralizumab for COPD was published in 2019. Much less cognitive load was required to interpret this one; it was negative. FDA approval was not requested.
Looking through the trial designs for the three RCTs of biologics for COPD, I couldn’t find major differences that could explain the discordant results. Sample size and enrollment criteria were similar. As stated, I don’t believe that the biologic data in asthma allow for predicting efficacy in one eosinophilic patient vs. another and I assume the same would be true for COPD. All three trials found that eosinophils were eliminated, so responses were biologically equivalent.
Key takeaways
If trial design and pharmacology don’t account for the disparate outcomes, how do we explain them? More important, how do we translate these trials into clinical practice? I looked for a review or editorial by a scientist-clinician smarter than I so I could steal their ideas and express them as pedantic euphemisms here. I found it curious that I was unable to find one. A recent publication in the American Journal of Respiratory and Critical Care Medicine suggests that the answer lies within the complex lattice of eosinophil subtypes, but I’m unqualified to judge the veracity of this “phenotype within a phenotype” theory.
More trials in COPD are being done. We should have results on tezepelumab, that great savior that may cover noneosinophilic asthma phenotypes, within the next few years. Until then, we’re stuck defying guidelines with the anachronistic use of OCS for the COPD patient who exacerbates through ICS/LABA/LAMA, roflumilast, and azithromycin.
Dr. Holley is professor of medicine at Uniformed Services University in Bethesda, Md., and a pulmonary/sleep and critical care medicine physician at MedStar Washington Hospital Center in Washington. He reported receiving income from CHEST College, Metapharm, and WebMD.
A version of this article first appeared on Medscape.com.
It’s tough to keep up with the proliferation of monoclonal antibodies. Seems every day I’m confronted by a patient who’s using a new drug with a name ending in “mab.” That drug blocks a cellular receptor I haven’t heard of that’s involved in a cascade of interactions I haven’t thought about since medical school. The resulting disruption reduces disease burden, typically at great expense to the medical system, the patient, or both. We’ve truly entered the era of precision medicine. It’s not enough to understand disease; you also must know its heterogeneous expression so that you can prescribe the ‘mab that targets the biology responsible for variants in behavior. All diseases are, in fact, syndromes. This isn’t a bad thing, but it’s a challenge.
A series of ‘mabs have been approved for treating type 2 high (TH2) or eosinophilic asthma. We refer to this group of ‘mabs generically as biologics. The group includes omalizumab, mepolizumab, dupilumab, benralizumab, reslizumab, and tezepelumab. While mechanism of action varies slightly across drugs, the biologics all target a specific arm of the immune system. Efficacy is linearly related to serum eosinophil count and there’s little clinically or pharmacologically to distinguish one from another. Of course, no head-to-head comparisons of efficacy are available and there’s no financial incentive for them to be performed.
Latest research
A new randomized controlled trial (RCT) of dupilumab for chronic obstructive pulmonary disease (COPD) adds to the aforementioned biologic knowledge base. Turns out it works as long as the patients are carefully selected. Researchers enrolled GOLD D (or E depending on which iteration of the GOLD Statement you use) patients on triple inhaler therapy (inhaled corticosteroids [ICS]/long-acting beta-agonist [LABA]/long-acting muscarinic antagonist [LAMA]) with two moderate exacerbations or one exacerbation requiring hospitalization in the past year. Blood eosinophil counts were > 300 cells/mcL and chronic bronchitis was present clinically. The primary and multiple secondary outcomes were improved with dupilumab.
This is welcome news. I’ve treated countless patients with severe COPD who have repeated exacerbations despite my efforts to prevent them. These patients are on ICS/LABA/LAMA and azithromycin or roflumilast, and occasionally both. While every COPD guideline known to man forbids using chronic oral corticosteroids (OCS), I’ve prescribed them repeatedly because the benefits to keeping a recalcitrant, exacerbating patient out of the hospital seem to outweigh OCS risks. It would be nice to have a better option. Although we were taught that they were immutably distinct in medical school, every first-year pulmonary fellow knows that asthma and COPD share more similarities than differences, so it makes sense that proven asthma therapies would work for some patients with COPD.
However, the dupilumab study must be placed in context. Past studies haven’t been as positive. In 2017, two separate RCTs found that mepolizumab reduced the annual rate of moderate to severe exacerbations (primary outcome) in one trial but not the other. Interpretation gets more complicated when broken down by intention to treat (ITT) vs. modified ITT and when secondary outcomes are considered. Sparing you those details, this trial does not instill confidence, leading the Food and Drug Administration to refuse approval for mepolizumab for COPD. A second RCT of benralizumab for COPD was published in 2019. Much less cognitive load was required to interpret this one; it was negative. FDA approval was not requested.
Looking through the trial designs for the three RCTs of biologics for COPD, I couldn’t find major differences that could explain the discordant results. Sample size and enrollment criteria were similar. As stated, I don’t believe that the biologic data in asthma allow for predicting efficacy in one eosinophilic patient vs. another and I assume the same would be true for COPD. All three trials found that eosinophils were eliminated, so responses were biologically equivalent.
Key takeaways
If trial design and pharmacology don’t account for the disparate outcomes, how do we explain them? More important, how do we translate these trials into clinical practice? I looked for a review or editorial by a scientist-clinician smarter than I so I could steal their ideas and express them as pedantic euphemisms here. I found it curious that I was unable to find one. A recent publication in the American Journal of Respiratory and Critical Care Medicine suggests that the answer lies within the complex lattice of eosinophil subtypes, but I’m unqualified to judge the veracity of this “phenotype within a phenotype” theory.
More trials in COPD are being done. We should have results on tezepelumab, that great savior that may cover noneosinophilic asthma phenotypes, within the next few years. Until then, we’re stuck defying guidelines with the anachronistic use of OCS for the COPD patient who exacerbates through ICS/LABA/LAMA, roflumilast, and azithromycin.
Dr. Holley is professor of medicine at Uniformed Services University in Bethesda, Md., and a pulmonary/sleep and critical care medicine physician at MedStar Washington Hospital Center in Washington. He reported receiving income from CHEST College, Metapharm, and WebMD.
A version of this article first appeared on Medscape.com.
Patient aggression against receptionists demands protocols
“I’ve been hit in the head by a walking stick,” a primary care receptionist reported.
“A mother came in and was screaming and swearing at me because she couldn’t get an appointment for her daughters,” another receptionist reported.
“I’ve had people throw a bag of syringes at me because we don’t accept syringes,” said another.
Reports such as these are part of the literature supporting a review that finds patient aggression against receptionists is a serious safety concern for primary care offices and affects delivery of health care.
The review was published online in the BMJ’s Family Medicine and Community Health journal.
“Receptionists in general practice deserve evidence-based measures to improve their working conditions and well-being,” say the authors, led by Fiona Willer, PhD, of the Centre for Community Health and Wellbeing at the University of Queensland, Brisbane, Australia.
Though the study looked primarily at European and Australian practices, physicians in the United States say the incidences are familiar.
Cause often lack of access
Dr. Willer and colleagues point out that the root cause of patient regression is typically related to operational factors, such as inefficient scheduling or lack of access to the medical providers.
“However, reception staff are placed in the unenviable position of having to deal with the aftermath of the poor function of these systems without having the status or autonomy to overhaul them,” the authors note.
Authors analyzed 20 studies on aggression against receptionists.
Among the findings:
- All studies reported that patient hostility and verbal abuse of receptionists “was a frequent, routine, and relatively unavoidable occurrence in general practice.”
- Nine studies reported acts of physical violence toward receptionists, with all reporting that physical abuse occurred much less frequently than verbal abuse.
- Some acts were very severe, including being hit, shaken, held at gunpoint, stalked, and threatened with a razorblade.
The studies also discussed ways to prevent potential aggression or react to it, including:
- Regular staff training for managing patient aggression.
- Designing clinics with “safe rooms” and “cool down” spaces.
- Providing clear acrylic shields between receptionists and patients.
- Developing formal policy/procedure/protocol/action guides relating to management of patients.
Behavior can interrupt health care delivery
Carrie Janiski, DO, regional medical director at Golden Valley Health Centers in California, who was not part of the review, said she has seen the aggressive behavior the authors document in her practice’s lobby, “including yelling, name-calling, and threatening language or physical behavior.”
The instances disrupt health care delivery to the patient, who is often in crisis, and all patients and staff in the clinic, she said.
“The patient needs help and the aggressive way they are seeking it could cause harm to others or prevent them from receiving all the help they need,” she said.
She says in practices she has worked in, some effective mitigation strategies have included open-access scheduling, increased walk-in availability for appointments, de-escalation training for front-line staff, and office and exam room layout designed for safety.
She added that incident review is important and should include a process for patient dismissal from the practice.
Dustin Arnold, DO, an internal medicine specialist and chief medical officer at UnityPoint Health-St. Luke’s Hospital, Cedar Rapids, IA, said he agrees with the authors on the urgency for action.
“This is an urgent concern for practices across the country. Your receptionist is the face of your practice, and you should invest in them,” said Dr. Arnold, who was not part of the review.
He said he has seen “verbal abuse and generalized incivility” from patients against receptionists in practices where he has worked.
He said the measure the authors list that he thinks is most effective is staff de-escalation training.
“However, the best preventative measure is for the physician to be on time and minimize cancellation of appointments,” he said. “These are the two primary triggers of a patient becoming disruptive.”
He said his practice has installed a panic button at the front desk and built an alert into the electronic health record indicating that a patient has shown disruptive behavior in the past.
The authors conclude: “Staff training and protocols to manage patient aggression and ongoing structured staff support should be considered essential in general practice. Evidence-based strategies to prevent, manage, and mitigate the harms of patient aggression towards general practice reception staff are urgently needed.”
The authors and Dr. Janiski and Dr. Arnold declared no relevant financial relationships.
“I’ve been hit in the head by a walking stick,” a primary care receptionist reported.
“A mother came in and was screaming and swearing at me because she couldn’t get an appointment for her daughters,” another receptionist reported.
“I’ve had people throw a bag of syringes at me because we don’t accept syringes,” said another.
Reports such as these are part of the literature supporting a review that finds patient aggression against receptionists is a serious safety concern for primary care offices and affects delivery of health care.
The review was published online in the BMJ’s Family Medicine and Community Health journal.
“Receptionists in general practice deserve evidence-based measures to improve their working conditions and well-being,” say the authors, led by Fiona Willer, PhD, of the Centre for Community Health and Wellbeing at the University of Queensland, Brisbane, Australia.
Though the study looked primarily at European and Australian practices, physicians in the United States say the incidences are familiar.
Cause often lack of access
Dr. Willer and colleagues point out that the root cause of patient regression is typically related to operational factors, such as inefficient scheduling or lack of access to the medical providers.
“However, reception staff are placed in the unenviable position of having to deal with the aftermath of the poor function of these systems without having the status or autonomy to overhaul them,” the authors note.
Authors analyzed 20 studies on aggression against receptionists.
Among the findings:
- All studies reported that patient hostility and verbal abuse of receptionists “was a frequent, routine, and relatively unavoidable occurrence in general practice.”
- Nine studies reported acts of physical violence toward receptionists, with all reporting that physical abuse occurred much less frequently than verbal abuse.
- Some acts were very severe, including being hit, shaken, held at gunpoint, stalked, and threatened with a razorblade.
The studies also discussed ways to prevent potential aggression or react to it, including:
- Regular staff training for managing patient aggression.
- Designing clinics with “safe rooms” and “cool down” spaces.
- Providing clear acrylic shields between receptionists and patients.
- Developing formal policy/procedure/protocol/action guides relating to management of patients.
Behavior can interrupt health care delivery
Carrie Janiski, DO, regional medical director at Golden Valley Health Centers in California, who was not part of the review, said she has seen the aggressive behavior the authors document in her practice’s lobby, “including yelling, name-calling, and threatening language or physical behavior.”
The instances disrupt health care delivery to the patient, who is often in crisis, and all patients and staff in the clinic, she said.
“The patient needs help and the aggressive way they are seeking it could cause harm to others or prevent them from receiving all the help they need,” she said.
She says in practices she has worked in, some effective mitigation strategies have included open-access scheduling, increased walk-in availability for appointments, de-escalation training for front-line staff, and office and exam room layout designed for safety.
She added that incident review is important and should include a process for patient dismissal from the practice.
Dustin Arnold, DO, an internal medicine specialist and chief medical officer at UnityPoint Health-St. Luke’s Hospital, Cedar Rapids, IA, said he agrees with the authors on the urgency for action.
“This is an urgent concern for practices across the country. Your receptionist is the face of your practice, and you should invest in them,” said Dr. Arnold, who was not part of the review.
He said he has seen “verbal abuse and generalized incivility” from patients against receptionists in practices where he has worked.
He said the measure the authors list that he thinks is most effective is staff de-escalation training.
“However, the best preventative measure is for the physician to be on time and minimize cancellation of appointments,” he said. “These are the two primary triggers of a patient becoming disruptive.”
He said his practice has installed a panic button at the front desk and built an alert into the electronic health record indicating that a patient has shown disruptive behavior in the past.
The authors conclude: “Staff training and protocols to manage patient aggression and ongoing structured staff support should be considered essential in general practice. Evidence-based strategies to prevent, manage, and mitigate the harms of patient aggression towards general practice reception staff are urgently needed.”
The authors and Dr. Janiski and Dr. Arnold declared no relevant financial relationships.
“I’ve been hit in the head by a walking stick,” a primary care receptionist reported.
“A mother came in and was screaming and swearing at me because she couldn’t get an appointment for her daughters,” another receptionist reported.
“I’ve had people throw a bag of syringes at me because we don’t accept syringes,” said another.
Reports such as these are part of the literature supporting a review that finds patient aggression against receptionists is a serious safety concern for primary care offices and affects delivery of health care.
The review was published online in the BMJ’s Family Medicine and Community Health journal.
“Receptionists in general practice deserve evidence-based measures to improve their working conditions and well-being,” say the authors, led by Fiona Willer, PhD, of the Centre for Community Health and Wellbeing at the University of Queensland, Brisbane, Australia.
Though the study looked primarily at European and Australian practices, physicians in the United States say the incidences are familiar.
Cause often lack of access
Dr. Willer and colleagues point out that the root cause of patient regression is typically related to operational factors, such as inefficient scheduling or lack of access to the medical providers.
“However, reception staff are placed in the unenviable position of having to deal with the aftermath of the poor function of these systems without having the status or autonomy to overhaul them,” the authors note.
Authors analyzed 20 studies on aggression against receptionists.
Among the findings:
- All studies reported that patient hostility and verbal abuse of receptionists “was a frequent, routine, and relatively unavoidable occurrence in general practice.”
- Nine studies reported acts of physical violence toward receptionists, with all reporting that physical abuse occurred much less frequently than verbal abuse.
- Some acts were very severe, including being hit, shaken, held at gunpoint, stalked, and threatened with a razorblade.
The studies also discussed ways to prevent potential aggression or react to it, including:
- Regular staff training for managing patient aggression.
- Designing clinics with “safe rooms” and “cool down” spaces.
- Providing clear acrylic shields between receptionists and patients.
- Developing formal policy/procedure/protocol/action guides relating to management of patients.
Behavior can interrupt health care delivery
Carrie Janiski, DO, regional medical director at Golden Valley Health Centers in California, who was not part of the review, said she has seen the aggressive behavior the authors document in her practice’s lobby, “including yelling, name-calling, and threatening language or physical behavior.”
The instances disrupt health care delivery to the patient, who is often in crisis, and all patients and staff in the clinic, she said.
“The patient needs help and the aggressive way they are seeking it could cause harm to others or prevent them from receiving all the help they need,” she said.
She says in practices she has worked in, some effective mitigation strategies have included open-access scheduling, increased walk-in availability for appointments, de-escalation training for front-line staff, and office and exam room layout designed for safety.
She added that incident review is important and should include a process for patient dismissal from the practice.
Dustin Arnold, DO, an internal medicine specialist and chief medical officer at UnityPoint Health-St. Luke’s Hospital, Cedar Rapids, IA, said he agrees with the authors on the urgency for action.
“This is an urgent concern for practices across the country. Your receptionist is the face of your practice, and you should invest in them,” said Dr. Arnold, who was not part of the review.
He said he has seen “verbal abuse and generalized incivility” from patients against receptionists in practices where he has worked.
He said the measure the authors list that he thinks is most effective is staff de-escalation training.
“However, the best preventative measure is for the physician to be on time and minimize cancellation of appointments,” he said. “These are the two primary triggers of a patient becoming disruptive.”
He said his practice has installed a panic button at the front desk and built an alert into the electronic health record indicating that a patient has shown disruptive behavior in the past.
The authors conclude: “Staff training and protocols to manage patient aggression and ongoing structured staff support should be considered essential in general practice. Evidence-based strategies to prevent, manage, and mitigate the harms of patient aggression towards general practice reception staff are urgently needed.”
The authors and Dr. Janiski and Dr. Arnold declared no relevant financial relationships.
FROM FAMILY MEDICINE AND COMMUNITY HEALTH
PCPs key to heart failure care after discharge
Madeline Sterling, MD, knew something was wrong when she heard her patient’s voice on the phone. The patient was breathing too fast and sounded fatigued. Like many people with heart failure, this patient had several comorbidities: diabetes, high blood pressure, and cancer, which was in remission.
The patient had been in and out of the hospital several times and was afraid of going back, but Dr. Sterling, a primary care physician, advised her that it was the safe thing to do.
During the woman’s stay, the inpatient cardiology team called Dr. Sterling to provide status updates and ask for input. When the patient was discharged, Dr. Sterling received information on what medicines had been changed and scheduled follow-up care within 10 days. Dr. Sterling, who’d cared for the woman for many years, called her family, her home health aide, and another caregiver to discuss the plan.
“When you know these patients really well, it’s helpful,” Dr. Sterling, a professor of medicine at Weill Cornell Medicine, New York, said. Primary care clinicians have “an appreciation for how all these conditions fit together, how the medicines fit together, and how to put that patient’s priorities at the front of the equation.”
Research has shown that follow-up care within 7-10 days after discharge, especially for patients with heart failure, can prevent hospital readmissions. Patients’ health can change rapidly following discharge: They may start retaining fluid or may not know how to maintain a low-sodium diet, or they might have trouble obtaining medication. Primary care clinicians spot these early warning signs in follow-up visits.
Heart failure affects more than 6 million adults in the United States, according to the Centers for Disease Control and Prevention. The condition is a common cause of hospital readmissions within 30 days of discharge, according to research published by the American Heart Association.
Patients with heart failure are particularly challenging to care for because of comorbidities.
“They’re a very, very sick group of patients that are very difficult to manage,” said Noah Moss, MD, an advanced heart failure and transplant cardiologist at Mount Sinai Hospital, New York.
But patients do not always receive the follow-up care they need, some studies have found.
Right drugs at the right time
Kelly Axsom, MD, a cardiologist at the Columbia University Medical Center, New York, and director of the centralized heart failure management program at the New York–Presbyterian Hospital System, called the primary care clinician the “captain of the ship,” ensuring that medications are reconciled and providing education about what to eat after discharge.
“It’s actually pretty complicated to go from being in the hospital to being at home,” Dr. Axsom said. “There are often many medication changes, there are lots of instructions that are told to you as a patient that are hard to remember.”
A patient’s weight might fluctuate in the days following discharge because the dose of diuretics might be too low or too high and need to be adjusted, according to Ishani Ganguli, MD, MPH, an assistant professor of medicine and a general internist in the Division of General Internal Medicine and Primary Care at Harvard Medical School and Brigham and Women’s Hospital, Boston.
K. Melissa Hayes, DNP, ANP-BC, CHFN, an assistant professor in the adult gerontology primary care program at the Vanderbilt University School of Nursing, Nashville, Tenn., recalled one patient who was given a months’ worth of medications following his discharge from the hospital.
“He was given expensive medications he couldn’t afford and not any refills or how to get those medications,” Dr. Hayes said.
Sometimes patients have no way to get to the pharmacy, or their pharmacy doesn’t have the medication they need, or their insurance doesn’t cover the drugs.
“The average patient is on at least six medications for heart failure, maybe even seven, and then that’s not including all their other medications,” Dr. Hayes said. “That can be a lot for people to keep up with.”
Dr. Hayes talks to her patients with heart failure about what drugs they have been prescribed and what medications they require more of, and she deprescribes any that are duplicative.
Helping patients understand why they are taking each drug encourages them to stick to the regimen. Diuretics, for example, can lead to frequent urination. If patients are unable to take regular bathroom breaks, they may be tempted to stop using the medication – a potentially catastrophic mistake.
“Often I have patients say, ‘Nobody ever explained it to me that way,’ ” Dr. Hayes said. “Someone can have a PhD but not understand their medications.”
Clinicians also can alert patients to commonly used medications that can worsen heart failure, such as diabetes drugs and over-the-counter medications such as ibuprofen.
Patients should be prescribed a combination of four recommended medications. But several studies have found that clinicians often fail to achieve the target doses for those medications. The use of guideline-directed medications reduces mortality and hospitalization rates, according to multiple clinical trials.
Eyes and ears on the patient
Once home, patients must stick to the right diet, weigh themselves every day, and monitor their blood pressure. But changing behaviors can be a struggle.
“Being seen quickly within a couple of days of discharge, you can catch things,” said Dr. Hayes, who has edited a book on managing patients with heart failure in primary care.
“It’s an opportunity to see how they’re doing at home, make sure they have their medications, make sure there’s been no misunderstanding or miscommunication about what they’re supposed to be doing at home,” says Marc Itskowitz, MD, a primary care physician affiliated with Allegheny General Hospital, Pittsburgh.
Ideally, a record that readily integrates information from wearables – such as blood pressure and weight – would make it easier to spot abnormalities, Dr. Itskowtiz said. “I think we’re still in the infancy of the electronic health record,” he said.
Ensuring that follow-up visits are as accessible as possible for patients is also important. Telehealth makes it easier for patients after they return home from the hospital, Dr. Itskowitz said.
More infrastructure
Another challenge of providing follow-up care for patients with heart failure is completing all the tasks a clinician must do within a 20-minute visit: an examination; education on the condition and medications; counseling on diet and exercise; coordination of medical equipment, such as a blood pressure cuff for home use; and making appointments with specialists.
“In the current system, additional support for primary care is needed so we can do all this,” Dr. Sterling said.
Staff at primary care clinics should be trained to answer calls from patients when they experience changes in their weight or are worried about other potential problems. “A lot of primary care practices are bare bones,” Dr. Hayes said, meaning they might not have the staff to field those calls. Educating patients as to when they should call their physician, especially after experiencing worsening symptoms, is also important.
Dr. Hayes suggests setting aside time in the schedule each week to see patients who have been recently discharged from the hospital. In the Cardiology and Vascular Clinic at Nashville General Hospital, Tenn., where she spends half a day each week, Dr. Hayes requests 30 minutes to see patients who have recently been discharged from hospital.
Even when the process goes smoothly, some patients will return to the hospital because of the progressive nature of heart failure, according to Dr. Hayes. Improving care following their hospitalization can keep these people from rapidly declining.
“Most patients with heart failure want to be taking care of the grandchildren or be able to enjoy family dinners together,” Dr. Axsom said. “I think anything we can do to help improve their quality of life is really important.”
Take-home
- See heart failure patients early after their discharge from hospital, ideally within 7-10 days.
- Make sure patients have access to the right medications at the right dosages and that they know why they’re taking them.
- Educate patients about the diet they should be following.
- Have a system to monitor patients’ symptoms and let them know when they should call.
A version of this article first appeared on Medscape.com.
Madeline Sterling, MD, knew something was wrong when she heard her patient’s voice on the phone. The patient was breathing too fast and sounded fatigued. Like many people with heart failure, this patient had several comorbidities: diabetes, high blood pressure, and cancer, which was in remission.
The patient had been in and out of the hospital several times and was afraid of going back, but Dr. Sterling, a primary care physician, advised her that it was the safe thing to do.
During the woman’s stay, the inpatient cardiology team called Dr. Sterling to provide status updates and ask for input. When the patient was discharged, Dr. Sterling received information on what medicines had been changed and scheduled follow-up care within 10 days. Dr. Sterling, who’d cared for the woman for many years, called her family, her home health aide, and another caregiver to discuss the plan.
“When you know these patients really well, it’s helpful,” Dr. Sterling, a professor of medicine at Weill Cornell Medicine, New York, said. Primary care clinicians have “an appreciation for how all these conditions fit together, how the medicines fit together, and how to put that patient’s priorities at the front of the equation.”
Research has shown that follow-up care within 7-10 days after discharge, especially for patients with heart failure, can prevent hospital readmissions. Patients’ health can change rapidly following discharge: They may start retaining fluid or may not know how to maintain a low-sodium diet, or they might have trouble obtaining medication. Primary care clinicians spot these early warning signs in follow-up visits.
Heart failure affects more than 6 million adults in the United States, according to the Centers for Disease Control and Prevention. The condition is a common cause of hospital readmissions within 30 days of discharge, according to research published by the American Heart Association.
Patients with heart failure are particularly challenging to care for because of comorbidities.
“They’re a very, very sick group of patients that are very difficult to manage,” said Noah Moss, MD, an advanced heart failure and transplant cardiologist at Mount Sinai Hospital, New York.
But patients do not always receive the follow-up care they need, some studies have found.
Right drugs at the right time
Kelly Axsom, MD, a cardiologist at the Columbia University Medical Center, New York, and director of the centralized heart failure management program at the New York–Presbyterian Hospital System, called the primary care clinician the “captain of the ship,” ensuring that medications are reconciled and providing education about what to eat after discharge.
“It’s actually pretty complicated to go from being in the hospital to being at home,” Dr. Axsom said. “There are often many medication changes, there are lots of instructions that are told to you as a patient that are hard to remember.”
A patient’s weight might fluctuate in the days following discharge because the dose of diuretics might be too low or too high and need to be adjusted, according to Ishani Ganguli, MD, MPH, an assistant professor of medicine and a general internist in the Division of General Internal Medicine and Primary Care at Harvard Medical School and Brigham and Women’s Hospital, Boston.
K. Melissa Hayes, DNP, ANP-BC, CHFN, an assistant professor in the adult gerontology primary care program at the Vanderbilt University School of Nursing, Nashville, Tenn., recalled one patient who was given a months’ worth of medications following his discharge from the hospital.
“He was given expensive medications he couldn’t afford and not any refills or how to get those medications,” Dr. Hayes said.
Sometimes patients have no way to get to the pharmacy, or their pharmacy doesn’t have the medication they need, or their insurance doesn’t cover the drugs.
“The average patient is on at least six medications for heart failure, maybe even seven, and then that’s not including all their other medications,” Dr. Hayes said. “That can be a lot for people to keep up with.”
Dr. Hayes talks to her patients with heart failure about what drugs they have been prescribed and what medications they require more of, and she deprescribes any that are duplicative.
Helping patients understand why they are taking each drug encourages them to stick to the regimen. Diuretics, for example, can lead to frequent urination. If patients are unable to take regular bathroom breaks, they may be tempted to stop using the medication – a potentially catastrophic mistake.
“Often I have patients say, ‘Nobody ever explained it to me that way,’ ” Dr. Hayes said. “Someone can have a PhD but not understand their medications.”
Clinicians also can alert patients to commonly used medications that can worsen heart failure, such as diabetes drugs and over-the-counter medications such as ibuprofen.
Patients should be prescribed a combination of four recommended medications. But several studies have found that clinicians often fail to achieve the target doses for those medications. The use of guideline-directed medications reduces mortality and hospitalization rates, according to multiple clinical trials.
Eyes and ears on the patient
Once home, patients must stick to the right diet, weigh themselves every day, and monitor their blood pressure. But changing behaviors can be a struggle.
“Being seen quickly within a couple of days of discharge, you can catch things,” said Dr. Hayes, who has edited a book on managing patients with heart failure in primary care.
“It’s an opportunity to see how they’re doing at home, make sure they have their medications, make sure there’s been no misunderstanding or miscommunication about what they’re supposed to be doing at home,” says Marc Itskowitz, MD, a primary care physician affiliated with Allegheny General Hospital, Pittsburgh.
Ideally, a record that readily integrates information from wearables – such as blood pressure and weight – would make it easier to spot abnormalities, Dr. Itskowtiz said. “I think we’re still in the infancy of the electronic health record,” he said.
Ensuring that follow-up visits are as accessible as possible for patients is also important. Telehealth makes it easier for patients after they return home from the hospital, Dr. Itskowitz said.
More infrastructure
Another challenge of providing follow-up care for patients with heart failure is completing all the tasks a clinician must do within a 20-minute visit: an examination; education on the condition and medications; counseling on diet and exercise; coordination of medical equipment, such as a blood pressure cuff for home use; and making appointments with specialists.
“In the current system, additional support for primary care is needed so we can do all this,” Dr. Sterling said.
Staff at primary care clinics should be trained to answer calls from patients when they experience changes in their weight or are worried about other potential problems. “A lot of primary care practices are bare bones,” Dr. Hayes said, meaning they might not have the staff to field those calls. Educating patients as to when they should call their physician, especially after experiencing worsening symptoms, is also important.
Dr. Hayes suggests setting aside time in the schedule each week to see patients who have been recently discharged from the hospital. In the Cardiology and Vascular Clinic at Nashville General Hospital, Tenn., where she spends half a day each week, Dr. Hayes requests 30 minutes to see patients who have recently been discharged from hospital.
Even when the process goes smoothly, some patients will return to the hospital because of the progressive nature of heart failure, according to Dr. Hayes. Improving care following their hospitalization can keep these people from rapidly declining.
“Most patients with heart failure want to be taking care of the grandchildren or be able to enjoy family dinners together,” Dr. Axsom said. “I think anything we can do to help improve their quality of life is really important.”
Take-home
- See heart failure patients early after their discharge from hospital, ideally within 7-10 days.
- Make sure patients have access to the right medications at the right dosages and that they know why they’re taking them.
- Educate patients about the diet they should be following.
- Have a system to monitor patients’ symptoms and let them know when they should call.
A version of this article first appeared on Medscape.com.
Madeline Sterling, MD, knew something was wrong when she heard her patient’s voice on the phone. The patient was breathing too fast and sounded fatigued. Like many people with heart failure, this patient had several comorbidities: diabetes, high blood pressure, and cancer, which was in remission.
The patient had been in and out of the hospital several times and was afraid of going back, but Dr. Sterling, a primary care physician, advised her that it was the safe thing to do.
During the woman’s stay, the inpatient cardiology team called Dr. Sterling to provide status updates and ask for input. When the patient was discharged, Dr. Sterling received information on what medicines had been changed and scheduled follow-up care within 10 days. Dr. Sterling, who’d cared for the woman for many years, called her family, her home health aide, and another caregiver to discuss the plan.
“When you know these patients really well, it’s helpful,” Dr. Sterling, a professor of medicine at Weill Cornell Medicine, New York, said. Primary care clinicians have “an appreciation for how all these conditions fit together, how the medicines fit together, and how to put that patient’s priorities at the front of the equation.”
Research has shown that follow-up care within 7-10 days after discharge, especially for patients with heart failure, can prevent hospital readmissions. Patients’ health can change rapidly following discharge: They may start retaining fluid or may not know how to maintain a low-sodium diet, or they might have trouble obtaining medication. Primary care clinicians spot these early warning signs in follow-up visits.
Heart failure affects more than 6 million adults in the United States, according to the Centers for Disease Control and Prevention. The condition is a common cause of hospital readmissions within 30 days of discharge, according to research published by the American Heart Association.
Patients with heart failure are particularly challenging to care for because of comorbidities.
“They’re a very, very sick group of patients that are very difficult to manage,” said Noah Moss, MD, an advanced heart failure and transplant cardiologist at Mount Sinai Hospital, New York.
But patients do not always receive the follow-up care they need, some studies have found.
Right drugs at the right time
Kelly Axsom, MD, a cardiologist at the Columbia University Medical Center, New York, and director of the centralized heart failure management program at the New York–Presbyterian Hospital System, called the primary care clinician the “captain of the ship,” ensuring that medications are reconciled and providing education about what to eat after discharge.
“It’s actually pretty complicated to go from being in the hospital to being at home,” Dr. Axsom said. “There are often many medication changes, there are lots of instructions that are told to you as a patient that are hard to remember.”
A patient’s weight might fluctuate in the days following discharge because the dose of diuretics might be too low or too high and need to be adjusted, according to Ishani Ganguli, MD, MPH, an assistant professor of medicine and a general internist in the Division of General Internal Medicine and Primary Care at Harvard Medical School and Brigham and Women’s Hospital, Boston.
K. Melissa Hayes, DNP, ANP-BC, CHFN, an assistant professor in the adult gerontology primary care program at the Vanderbilt University School of Nursing, Nashville, Tenn., recalled one patient who was given a months’ worth of medications following his discharge from the hospital.
“He was given expensive medications he couldn’t afford and not any refills or how to get those medications,” Dr. Hayes said.
Sometimes patients have no way to get to the pharmacy, or their pharmacy doesn’t have the medication they need, or their insurance doesn’t cover the drugs.
“The average patient is on at least six medications for heart failure, maybe even seven, and then that’s not including all their other medications,” Dr. Hayes said. “That can be a lot for people to keep up with.”
Dr. Hayes talks to her patients with heart failure about what drugs they have been prescribed and what medications they require more of, and she deprescribes any that are duplicative.
Helping patients understand why they are taking each drug encourages them to stick to the regimen. Diuretics, for example, can lead to frequent urination. If patients are unable to take regular bathroom breaks, they may be tempted to stop using the medication – a potentially catastrophic mistake.
“Often I have patients say, ‘Nobody ever explained it to me that way,’ ” Dr. Hayes said. “Someone can have a PhD but not understand their medications.”
Clinicians also can alert patients to commonly used medications that can worsen heart failure, such as diabetes drugs and over-the-counter medications such as ibuprofen.
Patients should be prescribed a combination of four recommended medications. But several studies have found that clinicians often fail to achieve the target doses for those medications. The use of guideline-directed medications reduces mortality and hospitalization rates, according to multiple clinical trials.
Eyes and ears on the patient
Once home, patients must stick to the right diet, weigh themselves every day, and monitor their blood pressure. But changing behaviors can be a struggle.
“Being seen quickly within a couple of days of discharge, you can catch things,” said Dr. Hayes, who has edited a book on managing patients with heart failure in primary care.
“It’s an opportunity to see how they’re doing at home, make sure they have their medications, make sure there’s been no misunderstanding or miscommunication about what they’re supposed to be doing at home,” says Marc Itskowitz, MD, a primary care physician affiliated with Allegheny General Hospital, Pittsburgh.
Ideally, a record that readily integrates information from wearables – such as blood pressure and weight – would make it easier to spot abnormalities, Dr. Itskowtiz said. “I think we’re still in the infancy of the electronic health record,” he said.
Ensuring that follow-up visits are as accessible as possible for patients is also important. Telehealth makes it easier for patients after they return home from the hospital, Dr. Itskowitz said.
More infrastructure
Another challenge of providing follow-up care for patients with heart failure is completing all the tasks a clinician must do within a 20-minute visit: an examination; education on the condition and medications; counseling on diet and exercise; coordination of medical equipment, such as a blood pressure cuff for home use; and making appointments with specialists.
“In the current system, additional support for primary care is needed so we can do all this,” Dr. Sterling said.
Staff at primary care clinics should be trained to answer calls from patients when they experience changes in their weight or are worried about other potential problems. “A lot of primary care practices are bare bones,” Dr. Hayes said, meaning they might not have the staff to field those calls. Educating patients as to when they should call their physician, especially after experiencing worsening symptoms, is also important.
Dr. Hayes suggests setting aside time in the schedule each week to see patients who have been recently discharged from the hospital. In the Cardiology and Vascular Clinic at Nashville General Hospital, Tenn., where she spends half a day each week, Dr. Hayes requests 30 minutes to see patients who have recently been discharged from hospital.
Even when the process goes smoothly, some patients will return to the hospital because of the progressive nature of heart failure, according to Dr. Hayes. Improving care following their hospitalization can keep these people from rapidly declining.
“Most patients with heart failure want to be taking care of the grandchildren or be able to enjoy family dinners together,” Dr. Axsom said. “I think anything we can do to help improve their quality of life is really important.”
Take-home
- See heart failure patients early after their discharge from hospital, ideally within 7-10 days.
- Make sure patients have access to the right medications at the right dosages and that they know why they’re taking them.
- Educate patients about the diet they should be following.
- Have a system to monitor patients’ symptoms and let them know when they should call.
A version of this article first appeared on Medscape.com.
Geriatric care principles should apply to ICUs as well
Baseball legend Leroy “Satchel” Paige famously said that “age is a question of mind over matter: If you don’t mind, it doesn’t matter.”
But even the strongest and most supple minds can’t avoid the effects of advanced age and accompanying physical frailty, and for community-dwelling elderly with pulmonary diseases frailty is a predictor of both hospitalization and death, investigators have found.
For example, among 1,188 community-dwelling older adults enrolled in the Toledo (Spain) Study for Healthy Aging, declining pulmonary function measured by forced expiratory volume in 1 second (FEV1) and forced vital capacity (FVC) was associated with increased risk for frailty and hospitalization, and a more than twofold greater risk for death in participants both with and without respiratory diseases. These findings were reported by Walter Sepulveda-Loyola, PT, MSC, PhD, from the Faculty of Health and Social Sciences at Universidad de Las Americas in Santiago, Chile, and colleagues in the journal Heart & Lung.
Similarly, results of a meta-analysis performed by investigators at Jiangsu (China) University showed that among 13,203 patients with chronic obstructive pulmonary disease (COPD), frailty was associated with a more than 2.6-fold relative increase in risk for death from any cause, and “prefrailty,” an intermediate state between frailty and “robustness,” was associated with a 48% relative increase in all-cause mortality. Frailty was also associated with a 2.2-fold risk for COPD exacerbations of any severity, the authors reported in JAMDA: The Journal of Post-Acute and Long-Term Care Medicine.
The good (old) USA
In June 2023 the U.S. Census Bureau announced that the median age of the U.S. population is now 38.9 years, and according to a 2016 Census Bureau report funded by the National Institutes of Health, “America’s 65-and-over population is projected to nearly double over the next three decades, from 48 million to 88 million by 2050.”
With the graying of the U.S. population the burden on pulmonary and critical care experts will almost inevitably increase, as evidenced by research from Julien Cobert, MD, from the University of California, San Francisco, and colleagues.
The investigators looked at trends over time in older adults admitted to ICUs from 1988 through 2015 using data from the Health and Retirement Study (HRS), a nationally representative, longitudinal study of older adults. They found that rates of preexisting frailty, disability, and multimorbidity increased over the study period.
“Our findings suggest a growing prevalence of geriatric conditions among older adults admitted to the ICU, suggesting a pressing need to integrate geriatric principles into critical care medicine. Further research could examine if early interventions emphasizing physical, cognitive, mental health, delirium prevention, advance care planning, and rehabilitation individualized to critically ill elderly patients with preexisting geriatric conditions could improve ICU outcomes and post-ICU recovery,” they wrote in a study published in the journal CHEST.
In an editorial accompanying the study by Dr. Cobert and colleagues, Nathan E. Brummel, MD, from The Ohio State University College of Medicine and Davis Heart and Lung Research Institute in Columbus, said “the finding that nearly 30% of overall HRS participants were admitted to the ICU provides novel data about the extent to which older Americans are affected by critical illness. Because the number of older Americans is projected to continue to increase for the next 30 years or more, these data make clear the ongoing importance of aging-focused research and clinical care.”
Dr. Brummel also noted that older adults who are admitted to the ICU today are at greater risk for poor outcomes than those admitted in prior years, as evidenced by the increased prevalence of disability, frailty, and multimorbidity.
“Moreover, because the average age of those admitted to the ICU only changed by 1 year during the study, these data show that increases in vulnerability are not simply due to chronological age, and they suggest that to identify those with greater baseline vulnerability, screening for geriatric syndromes at ICU admission may be warranted,” he wrote.
Geriatric principles in the ICU
“I think what’s most important is that we think about patients from a geriatric principles standpoint, not just when they’re admitted to the hospital but especially when they’re admitted to the ICU,” Dr. Cobert said in an interview.
“The first step is ensuring that we’re asking questions about their underlying comorbidities, especially around frailty, hearing, vision loss, falls, multimorbidities, polypharmacy – things that are primarily done on the outpatient side in geriatric clinics, but things that we should probably be a little bit more cognizant of, given that we’re starting to see higher rates of patients coming in with these issues,” he said.
Critical care specialists need to take a more holistic approach and try to understand as best they can each patients’ goals and then determine whether the ICU staff are acting in concordance with those goals, he emphasized.
For example, ICU clinicians should try to understand whether patients were losing function or having mobility difficulties before hospital and ICU admission, and what they hope to retain when or if they are discharged. ICU staff can then try as much as reasonably possible to minimize interventions that could contribute to impairment after discharge.
Frailty and COPD in the ICU
There are special considerations for frail elderly with obstructive airway disease, Dr. Cobert noted.
Patients with advanced COPD, for example, are likely to be on home oxygen.
“Home oxygen is a big deal,” he said. “It can definitely help with functioning and there’s potentially a mortality benefit in certain populations. But that said, it’s a flammable object that they have to carry around and lug with them all the time. It contributes to falls, it’s tethering, it’s life-limiting in many ways.”
In addition, many patients with COPD have multiple re-hospitalizations, and for clinicians the challenge is “understanding what their goals are, what their motivations are, especially when they live with dyspnea, with advanced lung disease. Is intubation within their goals of care? Has their functional status been declining over time? Are there things that we can optimize holistically and globally as their COPD advances over time?”
Another important component of critical care for the frail elderly is consideration of patients’ palliative care needs and what their symptoms and symptom burdens were like prior to hospitalizations.
“The ICU experience and the critical illness experience may serve as an inflexion point – more likely a downward inflection point – whereby their needs increase, their symptoms can worsen, and their health, especially their global health, worsens. Their preexisting geriatric conditions might be a moving target after another hit and another traumatic stressor like the ICU setting,” Dr. Cobert said.
The study by Dr. Cobert and colleagues was supported by the National Institute on Aging. Dr. Cobert had no reported conflicts of interest.
Baseball legend Leroy “Satchel” Paige famously said that “age is a question of mind over matter: If you don’t mind, it doesn’t matter.”
But even the strongest and most supple minds can’t avoid the effects of advanced age and accompanying physical frailty, and for community-dwelling elderly with pulmonary diseases frailty is a predictor of both hospitalization and death, investigators have found.
For example, among 1,188 community-dwelling older adults enrolled in the Toledo (Spain) Study for Healthy Aging, declining pulmonary function measured by forced expiratory volume in 1 second (FEV1) and forced vital capacity (FVC) was associated with increased risk for frailty and hospitalization, and a more than twofold greater risk for death in participants both with and without respiratory diseases. These findings were reported by Walter Sepulveda-Loyola, PT, MSC, PhD, from the Faculty of Health and Social Sciences at Universidad de Las Americas in Santiago, Chile, and colleagues in the journal Heart & Lung.
Similarly, results of a meta-analysis performed by investigators at Jiangsu (China) University showed that among 13,203 patients with chronic obstructive pulmonary disease (COPD), frailty was associated with a more than 2.6-fold relative increase in risk for death from any cause, and “prefrailty,” an intermediate state between frailty and “robustness,” was associated with a 48% relative increase in all-cause mortality. Frailty was also associated with a 2.2-fold risk for COPD exacerbations of any severity, the authors reported in JAMDA: The Journal of Post-Acute and Long-Term Care Medicine.
The good (old) USA
In June 2023 the U.S. Census Bureau announced that the median age of the U.S. population is now 38.9 years, and according to a 2016 Census Bureau report funded by the National Institutes of Health, “America’s 65-and-over population is projected to nearly double over the next three decades, from 48 million to 88 million by 2050.”
With the graying of the U.S. population the burden on pulmonary and critical care experts will almost inevitably increase, as evidenced by research from Julien Cobert, MD, from the University of California, San Francisco, and colleagues.
The investigators looked at trends over time in older adults admitted to ICUs from 1988 through 2015 using data from the Health and Retirement Study (HRS), a nationally representative, longitudinal study of older adults. They found that rates of preexisting frailty, disability, and multimorbidity increased over the study period.
“Our findings suggest a growing prevalence of geriatric conditions among older adults admitted to the ICU, suggesting a pressing need to integrate geriatric principles into critical care medicine. Further research could examine if early interventions emphasizing physical, cognitive, mental health, delirium prevention, advance care planning, and rehabilitation individualized to critically ill elderly patients with preexisting geriatric conditions could improve ICU outcomes and post-ICU recovery,” they wrote in a study published in the journal CHEST.
In an editorial accompanying the study by Dr. Cobert and colleagues, Nathan E. Brummel, MD, from The Ohio State University College of Medicine and Davis Heart and Lung Research Institute in Columbus, said “the finding that nearly 30% of overall HRS participants were admitted to the ICU provides novel data about the extent to which older Americans are affected by critical illness. Because the number of older Americans is projected to continue to increase for the next 30 years or more, these data make clear the ongoing importance of aging-focused research and clinical care.”
Dr. Brummel also noted that older adults who are admitted to the ICU today are at greater risk for poor outcomes than those admitted in prior years, as evidenced by the increased prevalence of disability, frailty, and multimorbidity.
“Moreover, because the average age of those admitted to the ICU only changed by 1 year during the study, these data show that increases in vulnerability are not simply due to chronological age, and they suggest that to identify those with greater baseline vulnerability, screening for geriatric syndromes at ICU admission may be warranted,” he wrote.
Geriatric principles in the ICU
“I think what’s most important is that we think about patients from a geriatric principles standpoint, not just when they’re admitted to the hospital but especially when they’re admitted to the ICU,” Dr. Cobert said in an interview.
“The first step is ensuring that we’re asking questions about their underlying comorbidities, especially around frailty, hearing, vision loss, falls, multimorbidities, polypharmacy – things that are primarily done on the outpatient side in geriatric clinics, but things that we should probably be a little bit more cognizant of, given that we’re starting to see higher rates of patients coming in with these issues,” he said.
Critical care specialists need to take a more holistic approach and try to understand as best they can each patients’ goals and then determine whether the ICU staff are acting in concordance with those goals, he emphasized.
For example, ICU clinicians should try to understand whether patients were losing function or having mobility difficulties before hospital and ICU admission, and what they hope to retain when or if they are discharged. ICU staff can then try as much as reasonably possible to minimize interventions that could contribute to impairment after discharge.
Frailty and COPD in the ICU
There are special considerations for frail elderly with obstructive airway disease, Dr. Cobert noted.
Patients with advanced COPD, for example, are likely to be on home oxygen.
“Home oxygen is a big deal,” he said. “It can definitely help with functioning and there’s potentially a mortality benefit in certain populations. But that said, it’s a flammable object that they have to carry around and lug with them all the time. It contributes to falls, it’s tethering, it’s life-limiting in many ways.”
In addition, many patients with COPD have multiple re-hospitalizations, and for clinicians the challenge is “understanding what their goals are, what their motivations are, especially when they live with dyspnea, with advanced lung disease. Is intubation within their goals of care? Has their functional status been declining over time? Are there things that we can optimize holistically and globally as their COPD advances over time?”
Another important component of critical care for the frail elderly is consideration of patients’ palliative care needs and what their symptoms and symptom burdens were like prior to hospitalizations.
“The ICU experience and the critical illness experience may serve as an inflexion point – more likely a downward inflection point – whereby their needs increase, their symptoms can worsen, and their health, especially their global health, worsens. Their preexisting geriatric conditions might be a moving target after another hit and another traumatic stressor like the ICU setting,” Dr. Cobert said.
The study by Dr. Cobert and colleagues was supported by the National Institute on Aging. Dr. Cobert had no reported conflicts of interest.
Baseball legend Leroy “Satchel” Paige famously said that “age is a question of mind over matter: If you don’t mind, it doesn’t matter.”
But even the strongest and most supple minds can’t avoid the effects of advanced age and accompanying physical frailty, and for community-dwelling elderly with pulmonary diseases frailty is a predictor of both hospitalization and death, investigators have found.
For example, among 1,188 community-dwelling older adults enrolled in the Toledo (Spain) Study for Healthy Aging, declining pulmonary function measured by forced expiratory volume in 1 second (FEV1) and forced vital capacity (FVC) was associated with increased risk for frailty and hospitalization, and a more than twofold greater risk for death in participants both with and without respiratory diseases. These findings were reported by Walter Sepulveda-Loyola, PT, MSC, PhD, from the Faculty of Health and Social Sciences at Universidad de Las Americas in Santiago, Chile, and colleagues in the journal Heart & Lung.
Similarly, results of a meta-analysis performed by investigators at Jiangsu (China) University showed that among 13,203 patients with chronic obstructive pulmonary disease (COPD), frailty was associated with a more than 2.6-fold relative increase in risk for death from any cause, and “prefrailty,” an intermediate state between frailty and “robustness,” was associated with a 48% relative increase in all-cause mortality. Frailty was also associated with a 2.2-fold risk for COPD exacerbations of any severity, the authors reported in JAMDA: The Journal of Post-Acute and Long-Term Care Medicine.
The good (old) USA
In June 2023 the U.S. Census Bureau announced that the median age of the U.S. population is now 38.9 years, and according to a 2016 Census Bureau report funded by the National Institutes of Health, “America’s 65-and-over population is projected to nearly double over the next three decades, from 48 million to 88 million by 2050.”
With the graying of the U.S. population the burden on pulmonary and critical care experts will almost inevitably increase, as evidenced by research from Julien Cobert, MD, from the University of California, San Francisco, and colleagues.
The investigators looked at trends over time in older adults admitted to ICUs from 1988 through 2015 using data from the Health and Retirement Study (HRS), a nationally representative, longitudinal study of older adults. They found that rates of preexisting frailty, disability, and multimorbidity increased over the study period.
“Our findings suggest a growing prevalence of geriatric conditions among older adults admitted to the ICU, suggesting a pressing need to integrate geriatric principles into critical care medicine. Further research could examine if early interventions emphasizing physical, cognitive, mental health, delirium prevention, advance care planning, and rehabilitation individualized to critically ill elderly patients with preexisting geriatric conditions could improve ICU outcomes and post-ICU recovery,” they wrote in a study published in the journal CHEST.
In an editorial accompanying the study by Dr. Cobert and colleagues, Nathan E. Brummel, MD, from The Ohio State University College of Medicine and Davis Heart and Lung Research Institute in Columbus, said “the finding that nearly 30% of overall HRS participants were admitted to the ICU provides novel data about the extent to which older Americans are affected by critical illness. Because the number of older Americans is projected to continue to increase for the next 30 years or more, these data make clear the ongoing importance of aging-focused research and clinical care.”
Dr. Brummel also noted that older adults who are admitted to the ICU today are at greater risk for poor outcomes than those admitted in prior years, as evidenced by the increased prevalence of disability, frailty, and multimorbidity.
“Moreover, because the average age of those admitted to the ICU only changed by 1 year during the study, these data show that increases in vulnerability are not simply due to chronological age, and they suggest that to identify those with greater baseline vulnerability, screening for geriatric syndromes at ICU admission may be warranted,” he wrote.
Geriatric principles in the ICU
“I think what’s most important is that we think about patients from a geriatric principles standpoint, not just when they’re admitted to the hospital but especially when they’re admitted to the ICU,” Dr. Cobert said in an interview.
“The first step is ensuring that we’re asking questions about their underlying comorbidities, especially around frailty, hearing, vision loss, falls, multimorbidities, polypharmacy – things that are primarily done on the outpatient side in geriatric clinics, but things that we should probably be a little bit more cognizant of, given that we’re starting to see higher rates of patients coming in with these issues,” he said.
Critical care specialists need to take a more holistic approach and try to understand as best they can each patients’ goals and then determine whether the ICU staff are acting in concordance with those goals, he emphasized.
For example, ICU clinicians should try to understand whether patients were losing function or having mobility difficulties before hospital and ICU admission, and what they hope to retain when or if they are discharged. ICU staff can then try as much as reasonably possible to minimize interventions that could contribute to impairment after discharge.
Frailty and COPD in the ICU
There are special considerations for frail elderly with obstructive airway disease, Dr. Cobert noted.
Patients with advanced COPD, for example, are likely to be on home oxygen.
“Home oxygen is a big deal,” he said. “It can definitely help with functioning and there’s potentially a mortality benefit in certain populations. But that said, it’s a flammable object that they have to carry around and lug with them all the time. It contributes to falls, it’s tethering, it’s life-limiting in many ways.”
In addition, many patients with COPD have multiple re-hospitalizations, and for clinicians the challenge is “understanding what their goals are, what their motivations are, especially when they live with dyspnea, with advanced lung disease. Is intubation within their goals of care? Has their functional status been declining over time? Are there things that we can optimize holistically and globally as their COPD advances over time?”
Another important component of critical care for the frail elderly is consideration of patients’ palliative care needs and what their symptoms and symptom burdens were like prior to hospitalizations.
“The ICU experience and the critical illness experience may serve as an inflexion point – more likely a downward inflection point – whereby their needs increase, their symptoms can worsen, and their health, especially their global health, worsens. Their preexisting geriatric conditions might be a moving target after another hit and another traumatic stressor like the ICU setting,” Dr. Cobert said.
The study by Dr. Cobert and colleagues was supported by the National Institute on Aging. Dr. Cobert had no reported conflicts of interest.
Long COVID ‘brain fog’ confounds doctors, but new research offers hope
Kate Whitley was petrified of COVID-19 from the beginning of the pandemic because she has Hashimoto disease, an autoimmune disorder that she knew put her at high risk for complications.
She was right to be worried. Two months after contracting the infection in September 2022, the 42-year-old Nashville resident was diagnosed with long COVID. For Ms. Whitley, the resulting brain fog has been the most challenging factor. She is the owner of a successful paper goods store, and she can’t remember basic aspects of her job. She can’t tolerate loud noises and gets so distracted that she has trouble remembering what she was doing.
Ms. Whitley doesn’t like the term “brain fog” because it doesn’t begin to describe the dramatic disruption to her life over the past 7 months.
Brain fog is among the most common symptoms of long COVID, and also one of the most poorly understood. A reported 46% of those diagnosed with long COVID complain of brain fog or a loss of memory. Many clinicians agree that the term is vague and often doesn’t truly represent the condition. That, in turn, makes it harder for doctors to diagnose and treat it. There are no standard tests for it, nor are there guidelines for symptom management or treatment.
“There’s a lot of imprecision in the term because it might mean different things to different patients,” said James C. Jackson, PsyD, a neuropsychiatrist at Vanderbilt University, Nashville, Tenn., and author of a new book, “Clearing the Fog: From Surviving to Thriving With Long COVID – A Practical Guide.”
Dr. Jackson, who began treating Ms. Whitley in February 2023, said that it makes more sense to call brain fog a brain impairment or an acquired brain injury (ABI) because it doesn’t occur gradually. COVID damages the brain and causes injury. For those with long COVID who were previously in the intensive care unit and may have undergone ventilation, hypoxic brain injury may result from the lack of oxygen to the brain.
Even among those with milder cases of acute COVID, there’s some evidence that persistent neuroinflammation in the brain caused by an activated immune system may also cause damage.
In both cases, the results can be debilitating. Ms. Whitley also has dysautonomia – a disorder of the autonomic nervous system that can cause dizziness, sweating, and headaches along with fatigue and heart palpitations.
She said that she’s so forgetful that when she sees people socially, she’s nervous of what she’ll say. “I feel like I’m constantly sticking my foot in my mouth because I can’t remember details of other people’s lives,” she said.
Although brain disorders such as Alzheimer’s disease and other forms of dementia are marked by a slow decline, ABI occurs more suddenly and may include a loss of executive function and attention.
“With a brain injury, you’re doing fine, and then some event happens (in this case COVID), and immediately after that, your cognitive function is different,” said Dr. Jackson.
Additionally, ABI is an actual diagnosis, whereas brain fog is not.
“With a brain injury, there’s a treatment pathway for cognitive rehabilitation,” said Dr. Jackson.
Treatments may include speech, cognitive, and occupational therapy as well as meeting with a neuropsychiatrist for treatment of the mental and behavioral disorders that may result. Dr. Jackson said that while many patients aren’t functioning cognitively or physically at 100%, they can make enough strides that they don’t have to give up things such as driving and, in some cases, their jobs.
Other experts agree that long COVID may damage the brain. An April 2022 study published in the journal Nature found strong evidence that SARS-CoV-2 infection may cause brain-related abnormalities, for example, a reduction in gray matter in certain parts of the brain, including the prefrontal cortex, hypothalamus, and amygdala.
Additionally, white matter, which is found deeper in the brain and is responsible for the exchange of information between different parts of the brain, may also be at risk of damage as a result of the virus, according to a November 2022 study published in the journal SN Comprehensive Clinical Medicine.
Calling it a “fog” makes it easier for clinicians and the general public to dismiss its severity, said Tyler Reed Bell, PhD, a researcher who specializes in viruses that cause brain injury. He is a fellow in the department of psychiatry at the University of California, San Diego. Brain fog can make driving and returning to work especially dangerous. Because of difficulty focusing, patients are much more likely to make mistakes that cause accidents.
“The COVID virus is very invasive to the brain,” Dr. Bell said.
Others contend this may be a rush to judgment. Karla L. Thompson, PhD, lead neuropsychologist at the University of North Carolina at Chapel Hill’s COVID Recovery Clinic, agrees that in more serious cases of COVID that cause a lack of oxygen to the brain, it’s reasonable to call it a brain injury. But brain fog can also be associated with other long COVID symptoms, not just damage to the brain.
Chronic fatigue and poor sleep are both commonly reported symptoms of long COVID that negatively affect brain function, she said. Sleep disturbances, cardiac problems, dysautonomia, and emotional distress could also affect the way the brain functions post COVID. Finding the right treatment requires identifying all the factors contributing to cognitive impairment.
Part of the problem in treating long COVID brain fog is that diagnostic technology is not sensitive enough to detect inflammation that could be causing damage.
Grace McComsey, MD, who leads the long COVID RECOVER study at University Hospitals Health System in Cleveland, said her team is working on identifying biomarkers that could detect brain inflammation in a way similar to the manner researchers have identified biomarkers to help diagnose chronic fatigue syndrome. Additionally, a new study published last month in JAMA for the first time clearly defined 12 symptoms of long COVID, and brain fog was listed among them. All of this contributes to the development of clear diagnostic criteria.
“It will make a big difference once we have some consistency among clinicians in diagnosing the condition,” said Dr. McComsey.
Ms. Whitley is thankful for the treatment that she’s received thus far. She’s seeing a cognitive rehabilitation therapist, who assesses her memory, cognition, and attention span and gives her tools to break up simple tasks, such as driving, so that they don’t feel overwhelming. She’s back behind the wheel and back to work.
But perhaps most importantly, Ms. Whitley joined a support group, led by Dr. Jackson, that includes other people experiencing the same symptoms she is. When she was at her darkest, they understood.
“Talking to other survivors has been the only solace in all this,” Ms. Whitley said. “Together, we grieve all that’s been lost.”
A version of this article first appeared on Medscape.com.
Kate Whitley was petrified of COVID-19 from the beginning of the pandemic because she has Hashimoto disease, an autoimmune disorder that she knew put her at high risk for complications.
She was right to be worried. Two months after contracting the infection in September 2022, the 42-year-old Nashville resident was diagnosed with long COVID. For Ms. Whitley, the resulting brain fog has been the most challenging factor. She is the owner of a successful paper goods store, and she can’t remember basic aspects of her job. She can’t tolerate loud noises and gets so distracted that she has trouble remembering what she was doing.
Ms. Whitley doesn’t like the term “brain fog” because it doesn’t begin to describe the dramatic disruption to her life over the past 7 months.
Brain fog is among the most common symptoms of long COVID, and also one of the most poorly understood. A reported 46% of those diagnosed with long COVID complain of brain fog or a loss of memory. Many clinicians agree that the term is vague and often doesn’t truly represent the condition. That, in turn, makes it harder for doctors to diagnose and treat it. There are no standard tests for it, nor are there guidelines for symptom management or treatment.
“There’s a lot of imprecision in the term because it might mean different things to different patients,” said James C. Jackson, PsyD, a neuropsychiatrist at Vanderbilt University, Nashville, Tenn., and author of a new book, “Clearing the Fog: From Surviving to Thriving With Long COVID – A Practical Guide.”
Dr. Jackson, who began treating Ms. Whitley in February 2023, said that it makes more sense to call brain fog a brain impairment or an acquired brain injury (ABI) because it doesn’t occur gradually. COVID damages the brain and causes injury. For those with long COVID who were previously in the intensive care unit and may have undergone ventilation, hypoxic brain injury may result from the lack of oxygen to the brain.
Even among those with milder cases of acute COVID, there’s some evidence that persistent neuroinflammation in the brain caused by an activated immune system may also cause damage.
In both cases, the results can be debilitating. Ms. Whitley also has dysautonomia – a disorder of the autonomic nervous system that can cause dizziness, sweating, and headaches along with fatigue and heart palpitations.
She said that she’s so forgetful that when she sees people socially, she’s nervous of what she’ll say. “I feel like I’m constantly sticking my foot in my mouth because I can’t remember details of other people’s lives,” she said.
Although brain disorders such as Alzheimer’s disease and other forms of dementia are marked by a slow decline, ABI occurs more suddenly and may include a loss of executive function and attention.
“With a brain injury, you’re doing fine, and then some event happens (in this case COVID), and immediately after that, your cognitive function is different,” said Dr. Jackson.
Additionally, ABI is an actual diagnosis, whereas brain fog is not.
“With a brain injury, there’s a treatment pathway for cognitive rehabilitation,” said Dr. Jackson.
Treatments may include speech, cognitive, and occupational therapy as well as meeting with a neuropsychiatrist for treatment of the mental and behavioral disorders that may result. Dr. Jackson said that while many patients aren’t functioning cognitively or physically at 100%, they can make enough strides that they don’t have to give up things such as driving and, in some cases, their jobs.
Other experts agree that long COVID may damage the brain. An April 2022 study published in the journal Nature found strong evidence that SARS-CoV-2 infection may cause brain-related abnormalities, for example, a reduction in gray matter in certain parts of the brain, including the prefrontal cortex, hypothalamus, and amygdala.
Additionally, white matter, which is found deeper in the brain and is responsible for the exchange of information between different parts of the brain, may also be at risk of damage as a result of the virus, according to a November 2022 study published in the journal SN Comprehensive Clinical Medicine.
Calling it a “fog” makes it easier for clinicians and the general public to dismiss its severity, said Tyler Reed Bell, PhD, a researcher who specializes in viruses that cause brain injury. He is a fellow in the department of psychiatry at the University of California, San Diego. Brain fog can make driving and returning to work especially dangerous. Because of difficulty focusing, patients are much more likely to make mistakes that cause accidents.
“The COVID virus is very invasive to the brain,” Dr. Bell said.
Others contend this may be a rush to judgment. Karla L. Thompson, PhD, lead neuropsychologist at the University of North Carolina at Chapel Hill’s COVID Recovery Clinic, agrees that in more serious cases of COVID that cause a lack of oxygen to the brain, it’s reasonable to call it a brain injury. But brain fog can also be associated with other long COVID symptoms, not just damage to the brain.
Chronic fatigue and poor sleep are both commonly reported symptoms of long COVID that negatively affect brain function, she said. Sleep disturbances, cardiac problems, dysautonomia, and emotional distress could also affect the way the brain functions post COVID. Finding the right treatment requires identifying all the factors contributing to cognitive impairment.
Part of the problem in treating long COVID brain fog is that diagnostic technology is not sensitive enough to detect inflammation that could be causing damage.
Grace McComsey, MD, who leads the long COVID RECOVER study at University Hospitals Health System in Cleveland, said her team is working on identifying biomarkers that could detect brain inflammation in a way similar to the manner researchers have identified biomarkers to help diagnose chronic fatigue syndrome. Additionally, a new study published last month in JAMA for the first time clearly defined 12 symptoms of long COVID, and brain fog was listed among them. All of this contributes to the development of clear diagnostic criteria.
“It will make a big difference once we have some consistency among clinicians in diagnosing the condition,” said Dr. McComsey.
Ms. Whitley is thankful for the treatment that she’s received thus far. She’s seeing a cognitive rehabilitation therapist, who assesses her memory, cognition, and attention span and gives her tools to break up simple tasks, such as driving, so that they don’t feel overwhelming. She’s back behind the wheel and back to work.
But perhaps most importantly, Ms. Whitley joined a support group, led by Dr. Jackson, that includes other people experiencing the same symptoms she is. When she was at her darkest, they understood.
“Talking to other survivors has been the only solace in all this,” Ms. Whitley said. “Together, we grieve all that’s been lost.”
A version of this article first appeared on Medscape.com.
Kate Whitley was petrified of COVID-19 from the beginning of the pandemic because she has Hashimoto disease, an autoimmune disorder that she knew put her at high risk for complications.
She was right to be worried. Two months after contracting the infection in September 2022, the 42-year-old Nashville resident was diagnosed with long COVID. For Ms. Whitley, the resulting brain fog has been the most challenging factor. She is the owner of a successful paper goods store, and she can’t remember basic aspects of her job. She can’t tolerate loud noises and gets so distracted that she has trouble remembering what she was doing.
Ms. Whitley doesn’t like the term “brain fog” because it doesn’t begin to describe the dramatic disruption to her life over the past 7 months.
Brain fog is among the most common symptoms of long COVID, and also one of the most poorly understood. A reported 46% of those diagnosed with long COVID complain of brain fog or a loss of memory. Many clinicians agree that the term is vague and often doesn’t truly represent the condition. That, in turn, makes it harder for doctors to diagnose and treat it. There are no standard tests for it, nor are there guidelines for symptom management or treatment.
“There’s a lot of imprecision in the term because it might mean different things to different patients,” said James C. Jackson, PsyD, a neuropsychiatrist at Vanderbilt University, Nashville, Tenn., and author of a new book, “Clearing the Fog: From Surviving to Thriving With Long COVID – A Practical Guide.”
Dr. Jackson, who began treating Ms. Whitley in February 2023, said that it makes more sense to call brain fog a brain impairment or an acquired brain injury (ABI) because it doesn’t occur gradually. COVID damages the brain and causes injury. For those with long COVID who were previously in the intensive care unit and may have undergone ventilation, hypoxic brain injury may result from the lack of oxygen to the brain.
Even among those with milder cases of acute COVID, there’s some evidence that persistent neuroinflammation in the brain caused by an activated immune system may also cause damage.
In both cases, the results can be debilitating. Ms. Whitley also has dysautonomia – a disorder of the autonomic nervous system that can cause dizziness, sweating, and headaches along with fatigue and heart palpitations.
She said that she’s so forgetful that when she sees people socially, she’s nervous of what she’ll say. “I feel like I’m constantly sticking my foot in my mouth because I can’t remember details of other people’s lives,” she said.
Although brain disorders such as Alzheimer’s disease and other forms of dementia are marked by a slow decline, ABI occurs more suddenly and may include a loss of executive function and attention.
“With a brain injury, you’re doing fine, and then some event happens (in this case COVID), and immediately after that, your cognitive function is different,” said Dr. Jackson.
Additionally, ABI is an actual diagnosis, whereas brain fog is not.
“With a brain injury, there’s a treatment pathway for cognitive rehabilitation,” said Dr. Jackson.
Treatments may include speech, cognitive, and occupational therapy as well as meeting with a neuropsychiatrist for treatment of the mental and behavioral disorders that may result. Dr. Jackson said that while many patients aren’t functioning cognitively or physically at 100%, they can make enough strides that they don’t have to give up things such as driving and, in some cases, their jobs.
Other experts agree that long COVID may damage the brain. An April 2022 study published in the journal Nature found strong evidence that SARS-CoV-2 infection may cause brain-related abnormalities, for example, a reduction in gray matter in certain parts of the brain, including the prefrontal cortex, hypothalamus, and amygdala.
Additionally, white matter, which is found deeper in the brain and is responsible for the exchange of information between different parts of the brain, may also be at risk of damage as a result of the virus, according to a November 2022 study published in the journal SN Comprehensive Clinical Medicine.
Calling it a “fog” makes it easier for clinicians and the general public to dismiss its severity, said Tyler Reed Bell, PhD, a researcher who specializes in viruses that cause brain injury. He is a fellow in the department of psychiatry at the University of California, San Diego. Brain fog can make driving and returning to work especially dangerous. Because of difficulty focusing, patients are much more likely to make mistakes that cause accidents.
“The COVID virus is very invasive to the brain,” Dr. Bell said.
Others contend this may be a rush to judgment. Karla L. Thompson, PhD, lead neuropsychologist at the University of North Carolina at Chapel Hill’s COVID Recovery Clinic, agrees that in more serious cases of COVID that cause a lack of oxygen to the brain, it’s reasonable to call it a brain injury. But brain fog can also be associated with other long COVID symptoms, not just damage to the brain.
Chronic fatigue and poor sleep are both commonly reported symptoms of long COVID that negatively affect brain function, she said. Sleep disturbances, cardiac problems, dysautonomia, and emotional distress could also affect the way the brain functions post COVID. Finding the right treatment requires identifying all the factors contributing to cognitive impairment.
Part of the problem in treating long COVID brain fog is that diagnostic technology is not sensitive enough to detect inflammation that could be causing damage.
Grace McComsey, MD, who leads the long COVID RECOVER study at University Hospitals Health System in Cleveland, said her team is working on identifying biomarkers that could detect brain inflammation in a way similar to the manner researchers have identified biomarkers to help diagnose chronic fatigue syndrome. Additionally, a new study published last month in JAMA for the first time clearly defined 12 symptoms of long COVID, and brain fog was listed among them. All of this contributes to the development of clear diagnostic criteria.
“It will make a big difference once we have some consistency among clinicians in diagnosing the condition,” said Dr. McComsey.
Ms. Whitley is thankful for the treatment that she’s received thus far. She’s seeing a cognitive rehabilitation therapist, who assesses her memory, cognition, and attention span and gives her tools to break up simple tasks, such as driving, so that they don’t feel overwhelming. She’s back behind the wheel and back to work.
But perhaps most importantly, Ms. Whitley joined a support group, led by Dr. Jackson, that includes other people experiencing the same symptoms she is. When she was at her darkest, they understood.
“Talking to other survivors has been the only solace in all this,” Ms. Whitley said. “Together, we grieve all that’s been lost.”
A version of this article first appeared on Medscape.com.
Postacute effects of COVID on par with those of sepsis, flu
A large observational study examined population-wide data for 13 postacute conditions in patients who had been hospitalized with a COVID-19 infection and found that all but one of these conditions, venous thromboembolism, occurred at comparable rates in those hospitalized for sepsis and influenza.
“For us, the main takeaway was that patients hospitalized for severe illness in general really require ongoing treatment and support after they’re discharged. That type of care is often very challenging to coordinate for people in a sometimes siloed and fragmented health care system,” study author Kieran Quinn, MD, PhD, a clinician at Sinai Health in Toronto, and assistant professor at the University of Toronto, said in an interview.
The study was published in JAMA Internal Medicine.
Postacute effects
The investigators compared clinical and health administrative data from 26,499 Ontarians hospitalized with COVID-19 with data from three additional cohorts who had been hospitalized with influenza (17,516 patients) and sepsis. The sepsis cohort was divided into two groups, those hospitalized during the COVID-19 pandemic (52,878 patients) and a historical control population (282,473 patients).
These comparators allowed the researchers to compare COVID-19 with other severe infectious illnesses and control for any changes in health care delivery that may have occurred during the pandemic. The addition of sepsis cohorts was needed for the latter purpose, since influenza rates dropped significantly after the onset of the pandemic.
The study outcomes (including cardiovascular, neurological, and mental health conditions and rheumatoid arthritis) were selected based on previous associations with COVID-19 infections, as well as their availability in the data, according to Dr. Quinn. The investigators used diagnostic codes recorded in Ontario’s Institute for Clinical Evaluative Sciences database. The investigators observed some of the studied conditions in their own patients. “Many of us on the research team are practicing clinicians who care for people living with long COVID,” said Dr. Quinn.
Compared with cohorts with other serious infections, those hospitalized with COVID-19 were not at increased risk for selected cardiovascular or neurological disorders, rheumatoid arthritis, or mental health conditions within 1 year following hospitalization. Incident venous thromboembolic disease, however, was more common after hospitalization for COVID-19 than after hospitalization for influenza (adjusted hazard ratio, 1.77).
The study results corroborate previous findings that influenza and sepsis can have serious long-term health effects, such as heart failure, dementia, and depression, and found that the same was true for COVID-19 infections. For all three infections, patients at high risk require additional support after their initial discharge.
Defining long COVID
Although there was no increased risk with COVID-19 for most conditions, these results do not mean that the postacute effects of the infection, often called “long COVID,” are not significant, Dr. Quinn emphasized. The researcher believes that it’s important to listen to the many patients reporting symptoms and validate their experiences.
There needs to be greater consensus among the global health community on what constitutes long COVID. While the research led by Dr. Quinn focuses on postacute health conditions, some definitions of long COVID, such as that of the World Health Organization, refer only to ongoing symptoms of the original infection.
While there is now a diagnostic code for treating long COVID in Ontario, the data available to the researchers did not include information on some common symptoms of post-COVID condition, like chronic fatigue. In the data used, there was not an accurate way to identify patients who had developed conditions like myalgic encephalomyelitis/chronic fatigue syndrome and postural orthostatic tachycardia syndrome, said Dr. Quinn.
In addition to creating clear definitions and determining the best treatments, prevention is essential, said Dr. Quinn. Prior studies have shown that vaccination helps prevent ICU admission for COVID-19.
‘Important questions remain’
Commenting on the finding, Aravind Ganesh, MD, DPhil, a neurologist at the University of Calgary (Alta.), said that by including control populations, the study addressed an important limitation of previous research. Dr. Ganesh, who was not involved in the study, said that the controls help to determine the cause of associations found in other studies, including his own research on long-term symptoms following outpatient care for COVID-19.
“I think what this tells us is that maybe a lot of the issues that we’ve been seeing as complications attributable to COVID are, in fact, complications attributable to serious illness,” said Dr. Ganesh. He also found the association with venous thromboembolism interesting because the condition is recognized as a key risk factor for COVID-19 outcomes.
Compared with smaller randomized control trials, the population-level data provided a much larger sample size for the study. However, this design comes with limitations as well, Dr. Ganesh noted. The study relies on the administrative data of diagnostic codes and misses symptoms that aren’t associated with a diagnosis. In addition, because the cohorts were not assigned randomly, it may not account for preexisting risk factors.
While the study demonstrates associations with physical and mental health conditions, the cause of postacute effects from COVID-19, influenza, and sepsis is still unclear. “Important questions remain,” said Dr. Ganesh. “Why is it that these patients are experiencing these symptoms?”
The study was supported by ICES and the Canadian Institutes of Health Research. Dr. Quinn reported part-time employment at Public Health Ontario and stock in Pfizer and BioNTech. Dr. Ganesh reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A large observational study examined population-wide data for 13 postacute conditions in patients who had been hospitalized with a COVID-19 infection and found that all but one of these conditions, venous thromboembolism, occurred at comparable rates in those hospitalized for sepsis and influenza.
“For us, the main takeaway was that patients hospitalized for severe illness in general really require ongoing treatment and support after they’re discharged. That type of care is often very challenging to coordinate for people in a sometimes siloed and fragmented health care system,” study author Kieran Quinn, MD, PhD, a clinician at Sinai Health in Toronto, and assistant professor at the University of Toronto, said in an interview.
The study was published in JAMA Internal Medicine.
Postacute effects
The investigators compared clinical and health administrative data from 26,499 Ontarians hospitalized with COVID-19 with data from three additional cohorts who had been hospitalized with influenza (17,516 patients) and sepsis. The sepsis cohort was divided into two groups, those hospitalized during the COVID-19 pandemic (52,878 patients) and a historical control population (282,473 patients).
These comparators allowed the researchers to compare COVID-19 with other severe infectious illnesses and control for any changes in health care delivery that may have occurred during the pandemic. The addition of sepsis cohorts was needed for the latter purpose, since influenza rates dropped significantly after the onset of the pandemic.
The study outcomes (including cardiovascular, neurological, and mental health conditions and rheumatoid arthritis) were selected based on previous associations with COVID-19 infections, as well as their availability in the data, according to Dr. Quinn. The investigators used diagnostic codes recorded in Ontario’s Institute for Clinical Evaluative Sciences database. The investigators observed some of the studied conditions in their own patients. “Many of us on the research team are practicing clinicians who care for people living with long COVID,” said Dr. Quinn.
Compared with cohorts with other serious infections, those hospitalized with COVID-19 were not at increased risk for selected cardiovascular or neurological disorders, rheumatoid arthritis, or mental health conditions within 1 year following hospitalization. Incident venous thromboembolic disease, however, was more common after hospitalization for COVID-19 than after hospitalization for influenza (adjusted hazard ratio, 1.77).
The study results corroborate previous findings that influenza and sepsis can have serious long-term health effects, such as heart failure, dementia, and depression, and found that the same was true for COVID-19 infections. For all three infections, patients at high risk require additional support after their initial discharge.
Defining long COVID
Although there was no increased risk with COVID-19 for most conditions, these results do not mean that the postacute effects of the infection, often called “long COVID,” are not significant, Dr. Quinn emphasized. The researcher believes that it’s important to listen to the many patients reporting symptoms and validate their experiences.
There needs to be greater consensus among the global health community on what constitutes long COVID. While the research led by Dr. Quinn focuses on postacute health conditions, some definitions of long COVID, such as that of the World Health Organization, refer only to ongoing symptoms of the original infection.
While there is now a diagnostic code for treating long COVID in Ontario, the data available to the researchers did not include information on some common symptoms of post-COVID condition, like chronic fatigue. In the data used, there was not an accurate way to identify patients who had developed conditions like myalgic encephalomyelitis/chronic fatigue syndrome and postural orthostatic tachycardia syndrome, said Dr. Quinn.
In addition to creating clear definitions and determining the best treatments, prevention is essential, said Dr. Quinn. Prior studies have shown that vaccination helps prevent ICU admission for COVID-19.
‘Important questions remain’
Commenting on the finding, Aravind Ganesh, MD, DPhil, a neurologist at the University of Calgary (Alta.), said that by including control populations, the study addressed an important limitation of previous research. Dr. Ganesh, who was not involved in the study, said that the controls help to determine the cause of associations found in other studies, including his own research on long-term symptoms following outpatient care for COVID-19.
“I think what this tells us is that maybe a lot of the issues that we’ve been seeing as complications attributable to COVID are, in fact, complications attributable to serious illness,” said Dr. Ganesh. He also found the association with venous thromboembolism interesting because the condition is recognized as a key risk factor for COVID-19 outcomes.
Compared with smaller randomized control trials, the population-level data provided a much larger sample size for the study. However, this design comes with limitations as well, Dr. Ganesh noted. The study relies on the administrative data of diagnostic codes and misses symptoms that aren’t associated with a diagnosis. In addition, because the cohorts were not assigned randomly, it may not account for preexisting risk factors.
While the study demonstrates associations with physical and mental health conditions, the cause of postacute effects from COVID-19, influenza, and sepsis is still unclear. “Important questions remain,” said Dr. Ganesh. “Why is it that these patients are experiencing these symptoms?”
The study was supported by ICES and the Canadian Institutes of Health Research. Dr. Quinn reported part-time employment at Public Health Ontario and stock in Pfizer and BioNTech. Dr. Ganesh reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
A large observational study examined population-wide data for 13 postacute conditions in patients who had been hospitalized with a COVID-19 infection and found that all but one of these conditions, venous thromboembolism, occurred at comparable rates in those hospitalized for sepsis and influenza.
“For us, the main takeaway was that patients hospitalized for severe illness in general really require ongoing treatment and support after they’re discharged. That type of care is often very challenging to coordinate for people in a sometimes siloed and fragmented health care system,” study author Kieran Quinn, MD, PhD, a clinician at Sinai Health in Toronto, and assistant professor at the University of Toronto, said in an interview.
The study was published in JAMA Internal Medicine.
Postacute effects
The investigators compared clinical and health administrative data from 26,499 Ontarians hospitalized with COVID-19 with data from three additional cohorts who had been hospitalized with influenza (17,516 patients) and sepsis. The sepsis cohort was divided into two groups, those hospitalized during the COVID-19 pandemic (52,878 patients) and a historical control population (282,473 patients).
These comparators allowed the researchers to compare COVID-19 with other severe infectious illnesses and control for any changes in health care delivery that may have occurred during the pandemic. The addition of sepsis cohorts was needed for the latter purpose, since influenza rates dropped significantly after the onset of the pandemic.
The study outcomes (including cardiovascular, neurological, and mental health conditions and rheumatoid arthritis) were selected based on previous associations with COVID-19 infections, as well as their availability in the data, according to Dr. Quinn. The investigators used diagnostic codes recorded in Ontario’s Institute for Clinical Evaluative Sciences database. The investigators observed some of the studied conditions in their own patients. “Many of us on the research team are practicing clinicians who care for people living with long COVID,” said Dr. Quinn.
Compared with cohorts with other serious infections, those hospitalized with COVID-19 were not at increased risk for selected cardiovascular or neurological disorders, rheumatoid arthritis, or mental health conditions within 1 year following hospitalization. Incident venous thromboembolic disease, however, was more common after hospitalization for COVID-19 than after hospitalization for influenza (adjusted hazard ratio, 1.77).
The study results corroborate previous findings that influenza and sepsis can have serious long-term health effects, such as heart failure, dementia, and depression, and found that the same was true for COVID-19 infections. For all three infections, patients at high risk require additional support after their initial discharge.
Defining long COVID
Although there was no increased risk with COVID-19 for most conditions, these results do not mean that the postacute effects of the infection, often called “long COVID,” are not significant, Dr. Quinn emphasized. The researcher believes that it’s important to listen to the many patients reporting symptoms and validate their experiences.
There needs to be greater consensus among the global health community on what constitutes long COVID. While the research led by Dr. Quinn focuses on postacute health conditions, some definitions of long COVID, such as that of the World Health Organization, refer only to ongoing symptoms of the original infection.
While there is now a diagnostic code for treating long COVID in Ontario, the data available to the researchers did not include information on some common symptoms of post-COVID condition, like chronic fatigue. In the data used, there was not an accurate way to identify patients who had developed conditions like myalgic encephalomyelitis/chronic fatigue syndrome and postural orthostatic tachycardia syndrome, said Dr. Quinn.
In addition to creating clear definitions and determining the best treatments, prevention is essential, said Dr. Quinn. Prior studies have shown that vaccination helps prevent ICU admission for COVID-19.
‘Important questions remain’
Commenting on the finding, Aravind Ganesh, MD, DPhil, a neurologist at the University of Calgary (Alta.), said that by including control populations, the study addressed an important limitation of previous research. Dr. Ganesh, who was not involved in the study, said that the controls help to determine the cause of associations found in other studies, including his own research on long-term symptoms following outpatient care for COVID-19.
“I think what this tells us is that maybe a lot of the issues that we’ve been seeing as complications attributable to COVID are, in fact, complications attributable to serious illness,” said Dr. Ganesh. He also found the association with venous thromboembolism interesting because the condition is recognized as a key risk factor for COVID-19 outcomes.
Compared with smaller randomized control trials, the population-level data provided a much larger sample size for the study. However, this design comes with limitations as well, Dr. Ganesh noted. The study relies on the administrative data of diagnostic codes and misses symptoms that aren’t associated with a diagnosis. In addition, because the cohorts were not assigned randomly, it may not account for preexisting risk factors.
While the study demonstrates associations with physical and mental health conditions, the cause of postacute effects from COVID-19, influenza, and sepsis is still unclear. “Important questions remain,” said Dr. Ganesh. “Why is it that these patients are experiencing these symptoms?”
The study was supported by ICES and the Canadian Institutes of Health Research. Dr. Quinn reported part-time employment at Public Health Ontario and stock in Pfizer and BioNTech. Dr. Ganesh reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM JAMA INTERNAL MEDICINE
Diabetes may short circuit pembrolizumab benefits in NSCLC
TOPLINE:
METHODOLOGY:
- Investigators reviewed the medical records of 203 consecutive patients with metastatic NSCLC who received first-line pembrolizumab either alone or in combination with chemotherapy at a single tertiary center in Israel.
- Overall, 1 in 4 patients (n = 51) had diabetes mellitus; most (n = 42) were being treated with oral hypoglycemic agents, frequently metformin, and 7 were taking insulin.
- Rates of tumors with PD‐L1 expression above 50% were not significantly different among patients with diabetes and those without.
TAKEAWAY:
- Overall, among patients with diabetes, median progression-free survival (PFS) was significantly shorter than among patients without diabetes (5.9 vs. 7.1 months), as was overall survival (12 vs. 21 months).
- Shorter overall survival was more pronounced among those with diabetes who received pembrolizumab alone (12 vs. 27 months) in comparison with patients who received pembrolizumab plus chemotherapy (14.3 vs. 19.4 months).
- After adjusting for potential confounders, multivariate analysis confirmed that diabetes was an independent risk factor for shorter PFS (hazard ratio, 1.67) and shorter overall survival (HR, 1.73) for patients with NSCLC.
- In a validation cohort of 452 patients with metastatic NSCLC, only 19.6% of those with diabetes continued to take pembrolizumab at 12 months versus 31.7% of those without diabetes.
IN PRACTICE:
“As NSCLC patients with [diabetes] constitute a significant subgroup, there is an urgent need to validate our findings and explore whether outcomes in these patients can be improved by better glycemic control,” the authors said, adding that “chemotherapy may offset some of the deleterious effects” of diabetes.
SOURCE:
The study was led by Yasmin Leshem, MD, PhD, of the Tel Aviv Sourasky Medical Center, and was published in Cancer.
LIMITATIONS:
- Without access to blood test results outside the hospital, the researchers could not determine whether better glycemic control might have improved outcomes.
- The incidence of type 1 or 2 diabetes was not well documented.
DISCLOSURES:
- No funding source was reported.
- Two investigators reported receiving consulting and/or other fees from Bristol-Myers Squibb, Roche, Merck, Novartis, and Merck Sharp and Dohme.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Investigators reviewed the medical records of 203 consecutive patients with metastatic NSCLC who received first-line pembrolizumab either alone or in combination with chemotherapy at a single tertiary center in Israel.
- Overall, 1 in 4 patients (n = 51) had diabetes mellitus; most (n = 42) were being treated with oral hypoglycemic agents, frequently metformin, and 7 were taking insulin.
- Rates of tumors with PD‐L1 expression above 50% were not significantly different among patients with diabetes and those without.
TAKEAWAY:
- Overall, among patients with diabetes, median progression-free survival (PFS) was significantly shorter than among patients without diabetes (5.9 vs. 7.1 months), as was overall survival (12 vs. 21 months).
- Shorter overall survival was more pronounced among those with diabetes who received pembrolizumab alone (12 vs. 27 months) in comparison with patients who received pembrolizumab plus chemotherapy (14.3 vs. 19.4 months).
- After adjusting for potential confounders, multivariate analysis confirmed that diabetes was an independent risk factor for shorter PFS (hazard ratio, 1.67) and shorter overall survival (HR, 1.73) for patients with NSCLC.
- In a validation cohort of 452 patients with metastatic NSCLC, only 19.6% of those with diabetes continued to take pembrolizumab at 12 months versus 31.7% of those without diabetes.
IN PRACTICE:
“As NSCLC patients with [diabetes] constitute a significant subgroup, there is an urgent need to validate our findings and explore whether outcomes in these patients can be improved by better glycemic control,” the authors said, adding that “chemotherapy may offset some of the deleterious effects” of diabetes.
SOURCE:
The study was led by Yasmin Leshem, MD, PhD, of the Tel Aviv Sourasky Medical Center, and was published in Cancer.
LIMITATIONS:
- Without access to blood test results outside the hospital, the researchers could not determine whether better glycemic control might have improved outcomes.
- The incidence of type 1 or 2 diabetes was not well documented.
DISCLOSURES:
- No funding source was reported.
- Two investigators reported receiving consulting and/or other fees from Bristol-Myers Squibb, Roche, Merck, Novartis, and Merck Sharp and Dohme.
A version of this article first appeared on Medscape.com.
TOPLINE:
METHODOLOGY:
- Investigators reviewed the medical records of 203 consecutive patients with metastatic NSCLC who received first-line pembrolizumab either alone or in combination with chemotherapy at a single tertiary center in Israel.
- Overall, 1 in 4 patients (n = 51) had diabetes mellitus; most (n = 42) were being treated with oral hypoglycemic agents, frequently metformin, and 7 were taking insulin.
- Rates of tumors with PD‐L1 expression above 50% were not significantly different among patients with diabetes and those without.
TAKEAWAY:
- Overall, among patients with diabetes, median progression-free survival (PFS) was significantly shorter than among patients without diabetes (5.9 vs. 7.1 months), as was overall survival (12 vs. 21 months).
- Shorter overall survival was more pronounced among those with diabetes who received pembrolizumab alone (12 vs. 27 months) in comparison with patients who received pembrolizumab plus chemotherapy (14.3 vs. 19.4 months).
- After adjusting for potential confounders, multivariate analysis confirmed that diabetes was an independent risk factor for shorter PFS (hazard ratio, 1.67) and shorter overall survival (HR, 1.73) for patients with NSCLC.
- In a validation cohort of 452 patients with metastatic NSCLC, only 19.6% of those with diabetes continued to take pembrolizumab at 12 months versus 31.7% of those without diabetes.
IN PRACTICE:
“As NSCLC patients with [diabetes] constitute a significant subgroup, there is an urgent need to validate our findings and explore whether outcomes in these patients can be improved by better glycemic control,” the authors said, adding that “chemotherapy may offset some of the deleterious effects” of diabetes.
SOURCE:
The study was led by Yasmin Leshem, MD, PhD, of the Tel Aviv Sourasky Medical Center, and was published in Cancer.
LIMITATIONS:
- Without access to blood test results outside the hospital, the researchers could not determine whether better glycemic control might have improved outcomes.
- The incidence of type 1 or 2 diabetes was not well documented.
DISCLOSURES:
- No funding source was reported.
- Two investigators reported receiving consulting and/or other fees from Bristol-Myers Squibb, Roche, Merck, Novartis, and Merck Sharp and Dohme.
A version of this article first appeared on Medscape.com.
New definition for iron deficiency in CV disease proposed
with implications that may extend to cardiovascular disease in general.
In the study involving more than 900 patients with PH, investigators at seven U.S. centers determined the prevalence of iron deficiency by two separate definitions and assessed its associations with functional measures and quality of life (QoL) scores.
An iron deficiency definition used conventionally in heart failure (HF) – ferritin less than 100 g/mL or 100-299 ng/mL with transferrin saturation (TSAT) less than 20% – failed to discriminate patients with reduced peak oxygen consumption (peakVO2), 6-minute walk test (6MWT) results, and QoL scores on the 36-item Short Form Survey (SF-36).
But an alternative definition for iron deficiency, simply a TSAT less than 21%, did predict such patients with reduced peakVO2, 6MWT, and QoL. It was also associated with an increased mortality risk. The study was published in the European Heart Journal.
“A low TSAT, less than 21%, is key in the pathophysiology of iron deficiency in pulmonary hypertension” and is associated with those important clinical and functional characteristics, lead author Pieter Martens MD, PhD, said in an interview. The study “underscores the importance of these criteria in future intervention studies in the field of pulmonary hypertension testing iron therapies.”
A broader implication is that “we should revise how we define iron deficiency in heart failure and cardiovascular disease in general and how we select patients for iron therapies,” said Dr. Martens, of the Heart, Vascular & Thoracic Institute of the Cleveland Clinic.
Iron’s role in pulmonary vascular disease
“Iron deficiency is associated with an energetic deficit, especially in high energy–demanding tissue, leading to early skeletal muscle acidification and diminished left and right ventricular (RV) contractile reserve during exercise,” the published report states. It can lead to “maladaptive RV remodeling,” which is a “hallmark feature” predictive of morbidity and mortality in patients with pulmonary vascular disease (PVD).
Some studies have suggested that iron deficiency is a common comorbidity in patients with PVD, their estimates of its prevalence ranging widely due in part to the “absence of a uniform definition,” write the authors.
Dr. Martens said the current study was conducted partly in response to the increasingly common observation that the HF-associated definition of iron deficiency “has limitations.” Yet, “without validation in the field of pulmonary hypertension, the 2022 pulmonary hypertension guidelines endorse this definition.”
As iron deficiency is a causal risk factor for HF progression, Dr. Martens added, the HF field has “taught us the importance of using validated definitions for iron deficiency when selecting patients for iron treatment in randomized controlled trials.”
Moreover, some evidence suggests that iron deficiency by some definitions may be associated with diminished exercise capacity and QoL in patients with PVD, which are associations that have not been confirmed in large studies, the report notes.
Therefore, it continues, the study sought to “determine and validate” the optimal definition of iron deficiency in patients with PVD; document its prevalence; and explore associations between iron deficiency and exercise capacity, QoL, and cardiac and pulmonary vascular remodeling.
Evaluating definitions of iron deficiency
The prospective study, called PVDOMICS, entered 1,195 subjects with available iron levels. After exclusion of 38 patients with sarcoidosis, myeloproliferative disease, or hemoglobinopathy, there remained 693 patients with “overt” PH, 225 with a milder form of PH who served as PVD comparators, and 90 age-, sex-, race/ethnicity- matched “healthy” adults who served as controls.
According to the conventional HF definition of iron deficiency – that is, ferritin 100-299 ng/mL and TSAT less than 20% – the prevalences were 74% in patients with overt PH and 72% of those “across the PVD spectrum.”
But by that definition, iron deficient and non-iron deficient patients didn’t differ significantly in peakVO2, 6MWT distance, or SF-36 physical component scores.
In contrast, patients meeting the alternative definition of iron deficiency of TSAT less than 21% showed significantly reduced functional and QoL measures, compared with those with TSAT greater than or equal to 21%.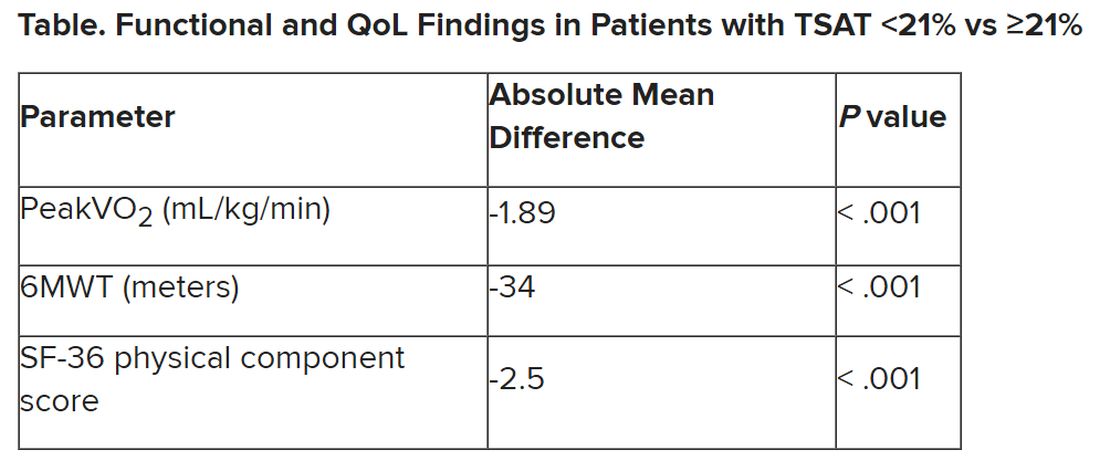
The group with TSAT less than 21% also showed significantly more RV remodeling at cardiac MRI, compared with those who had TSAT greater than or equal to 21%, but their invasively measured pulmonary vascular resistance was comparable.
Of note, those with TSAT less than 21% also showed significantly increased all-cause mortality (hazard ratio, 1.63; 95% confidence interval, 1.13-2.34; P = .009) after adjustment for age, sex, hemoglobin, and natriuretic peptide levels.
“Proper validation of the definition of iron deficiency is important for prognostication,” the published report states, “but also for providing a working definition that can be used to identify suitable patients for inclusion in randomized controlled trials” of drugs for iron deficiency.
Additionally, the finding that TSAT less than 21% points to patients with diminished functional and exercise capacity is “consistent with more recent studies in the field of heart failure” that suggest “functional abnormalities and adverse cardiac remodeling are worse in patients with a low TSAT.” Indeed, the report states, such treatment effects have been “the most convincing” in HF trials.
Broader implications
An accompanying editorial agrees that the study’s implications apply well beyond PH. It highlights that iron deficiency is common in PH, while such PH is “not substantially different from the problem in patients with heart failure, chronic kidney disease, and cardiovascular disease in general,” lead editorialist John G.F. Cleland, MD, PhD, University of Glasgow, said in an interview. “It’s also common as people get older, even in those without these diseases.”
Dr. Cleland said the anemia definition currently used in cardiovascular research and practice is based on a hemoglobin concentration below the 5th percentile of age and sex in primarily young, healthy people, and not on its association with clinical outcomes.
“We recently analyzed data on a large population in the United Kingdom with a broad range of cardiovascular diseases and found that unless anemia is severe, [other] markers of iron deficiency are usually not measured,” he said. A low hemoglobin and TSAT, but not low ferritin levels, are associated with worse prognosis.
Dr. Cleland agreed that the HF-oriented definition is “poor,” with profound implications for the conduct of clinical trials. “If the definition of iron deficiency lacks specificity, then clinical trials will include many patients without iron deficiency who are unlikely to benefit from and might be harmed by IV iron.” Inclusion of such patients may also “dilute” any benefit that might emerge and render the outcome inaccurate.
But if the definition of iron deficiency lacks sensitivity, “then in clinical practice, many patients with iron deficiency may be denied a simple and effective treatment.”
Measuring serum iron could potentially be useful, but it’s usually not done in randomized trials “especially since taking an iron tablet can give a temporary ‘blip’ in serum iron,” Dr. Cleland said. “So TSAT is a reasonable compromise.” He said he “looks forward” to any further data on serum iron as a way of assessing iron deficiency and anemia.
Half full vs. half empty
Dr. Cleland likened the question of whom to treat with iron supplementation as a “glass half full versus half empty” clinical dilemma. “One approach is to give iron to everyone unless there’s evidence that they’re overloaded,” he said, “while the other is to withhold iron from everyone unless there’s evidence that they’re iron depleted.”
Recent evidence from the IRONMAN trial suggested that its patients with HF who received intravenous iron were less likely to be hospitalized for infections, particularly COVID-19, than a usual-care group. The treatment may also help reduce frailty.
“So should we be offering IV iron specifically to people considered iron deficient, or should we be ensuring that everyone over age 70 get iron supplements?” Dr. Cleland mused rhetorically. On a cautionary note, he added, perhaps iron supplementation will be harmful if it’s not necessary.
Dr. Cleland proposed “focusing for the moment on people who are iron deficient but investigating the possibility that we are being overly restrictive and should be giving iron to a much broader population.” That course, however, would require large population-based studies.
“We need more experience,” Dr. Cleland said, “to make sure that the benefits outweigh any risks before we can just give iron to everyone.”
Dr. Martens has received consultancy fees from AstraZeneca, Abbott, Bayer, Boehringer Ingelheim, Daiichi Sankyo, Novartis, Novo Nordisk, and Vifor Pharma. Dr. Cleland declares grant support, support for travel, and personal honoraria from Pharmacosmos and Vifor. Disclosures for other authors are in the published report and editorial.
A version of this article first appeared on Medscape.com.
with implications that may extend to cardiovascular disease in general.
In the study involving more than 900 patients with PH, investigators at seven U.S. centers determined the prevalence of iron deficiency by two separate definitions and assessed its associations with functional measures and quality of life (QoL) scores.
An iron deficiency definition used conventionally in heart failure (HF) – ferritin less than 100 g/mL or 100-299 ng/mL with transferrin saturation (TSAT) less than 20% – failed to discriminate patients with reduced peak oxygen consumption (peakVO2), 6-minute walk test (6MWT) results, and QoL scores on the 36-item Short Form Survey (SF-36).
But an alternative definition for iron deficiency, simply a TSAT less than 21%, did predict such patients with reduced peakVO2, 6MWT, and QoL. It was also associated with an increased mortality risk. The study was published in the European Heart Journal.
“A low TSAT, less than 21%, is key in the pathophysiology of iron deficiency in pulmonary hypertension” and is associated with those important clinical and functional characteristics, lead author Pieter Martens MD, PhD, said in an interview. The study “underscores the importance of these criteria in future intervention studies in the field of pulmonary hypertension testing iron therapies.”
A broader implication is that “we should revise how we define iron deficiency in heart failure and cardiovascular disease in general and how we select patients for iron therapies,” said Dr. Martens, of the Heart, Vascular & Thoracic Institute of the Cleveland Clinic.
Iron’s role in pulmonary vascular disease
“Iron deficiency is associated with an energetic deficit, especially in high energy–demanding tissue, leading to early skeletal muscle acidification and diminished left and right ventricular (RV) contractile reserve during exercise,” the published report states. It can lead to “maladaptive RV remodeling,” which is a “hallmark feature” predictive of morbidity and mortality in patients with pulmonary vascular disease (PVD).
Some studies have suggested that iron deficiency is a common comorbidity in patients with PVD, their estimates of its prevalence ranging widely due in part to the “absence of a uniform definition,” write the authors.
Dr. Martens said the current study was conducted partly in response to the increasingly common observation that the HF-associated definition of iron deficiency “has limitations.” Yet, “without validation in the field of pulmonary hypertension, the 2022 pulmonary hypertension guidelines endorse this definition.”
As iron deficiency is a causal risk factor for HF progression, Dr. Martens added, the HF field has “taught us the importance of using validated definitions for iron deficiency when selecting patients for iron treatment in randomized controlled trials.”
Moreover, some evidence suggests that iron deficiency by some definitions may be associated with diminished exercise capacity and QoL in patients with PVD, which are associations that have not been confirmed in large studies, the report notes.
Therefore, it continues, the study sought to “determine and validate” the optimal definition of iron deficiency in patients with PVD; document its prevalence; and explore associations between iron deficiency and exercise capacity, QoL, and cardiac and pulmonary vascular remodeling.
Evaluating definitions of iron deficiency
The prospective study, called PVDOMICS, entered 1,195 subjects with available iron levels. After exclusion of 38 patients with sarcoidosis, myeloproliferative disease, or hemoglobinopathy, there remained 693 patients with “overt” PH, 225 with a milder form of PH who served as PVD comparators, and 90 age-, sex-, race/ethnicity- matched “healthy” adults who served as controls.
According to the conventional HF definition of iron deficiency – that is, ferritin 100-299 ng/mL and TSAT less than 20% – the prevalences were 74% in patients with overt PH and 72% of those “across the PVD spectrum.”
But by that definition, iron deficient and non-iron deficient patients didn’t differ significantly in peakVO2, 6MWT distance, or SF-36 physical component scores.
In contrast, patients meeting the alternative definition of iron deficiency of TSAT less than 21% showed significantly reduced functional and QoL measures, compared with those with TSAT greater than or equal to 21%.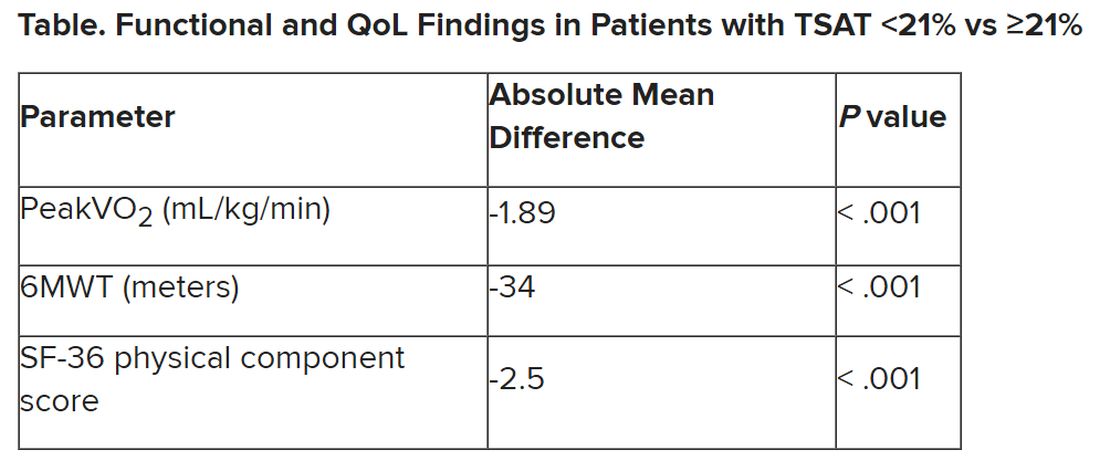
The group with TSAT less than 21% also showed significantly more RV remodeling at cardiac MRI, compared with those who had TSAT greater than or equal to 21%, but their invasively measured pulmonary vascular resistance was comparable.
Of note, those with TSAT less than 21% also showed significantly increased all-cause mortality (hazard ratio, 1.63; 95% confidence interval, 1.13-2.34; P = .009) after adjustment for age, sex, hemoglobin, and natriuretic peptide levels.
“Proper validation of the definition of iron deficiency is important for prognostication,” the published report states, “but also for providing a working definition that can be used to identify suitable patients for inclusion in randomized controlled trials” of drugs for iron deficiency.
Additionally, the finding that TSAT less than 21% points to patients with diminished functional and exercise capacity is “consistent with more recent studies in the field of heart failure” that suggest “functional abnormalities and adverse cardiac remodeling are worse in patients with a low TSAT.” Indeed, the report states, such treatment effects have been “the most convincing” in HF trials.
Broader implications
An accompanying editorial agrees that the study’s implications apply well beyond PH. It highlights that iron deficiency is common in PH, while such PH is “not substantially different from the problem in patients with heart failure, chronic kidney disease, and cardiovascular disease in general,” lead editorialist John G.F. Cleland, MD, PhD, University of Glasgow, said in an interview. “It’s also common as people get older, even in those without these diseases.”
Dr. Cleland said the anemia definition currently used in cardiovascular research and practice is based on a hemoglobin concentration below the 5th percentile of age and sex in primarily young, healthy people, and not on its association with clinical outcomes.
“We recently analyzed data on a large population in the United Kingdom with a broad range of cardiovascular diseases and found that unless anemia is severe, [other] markers of iron deficiency are usually not measured,” he said. A low hemoglobin and TSAT, but not low ferritin levels, are associated with worse prognosis.
Dr. Cleland agreed that the HF-oriented definition is “poor,” with profound implications for the conduct of clinical trials. “If the definition of iron deficiency lacks specificity, then clinical trials will include many patients without iron deficiency who are unlikely to benefit from and might be harmed by IV iron.” Inclusion of such patients may also “dilute” any benefit that might emerge and render the outcome inaccurate.
But if the definition of iron deficiency lacks sensitivity, “then in clinical practice, many patients with iron deficiency may be denied a simple and effective treatment.”
Measuring serum iron could potentially be useful, but it’s usually not done in randomized trials “especially since taking an iron tablet can give a temporary ‘blip’ in serum iron,” Dr. Cleland said. “So TSAT is a reasonable compromise.” He said he “looks forward” to any further data on serum iron as a way of assessing iron deficiency and anemia.
Half full vs. half empty
Dr. Cleland likened the question of whom to treat with iron supplementation as a “glass half full versus half empty” clinical dilemma. “One approach is to give iron to everyone unless there’s evidence that they’re overloaded,” he said, “while the other is to withhold iron from everyone unless there’s evidence that they’re iron depleted.”
Recent evidence from the IRONMAN trial suggested that its patients with HF who received intravenous iron were less likely to be hospitalized for infections, particularly COVID-19, than a usual-care group. The treatment may also help reduce frailty.
“So should we be offering IV iron specifically to people considered iron deficient, or should we be ensuring that everyone over age 70 get iron supplements?” Dr. Cleland mused rhetorically. On a cautionary note, he added, perhaps iron supplementation will be harmful if it’s not necessary.
Dr. Cleland proposed “focusing for the moment on people who are iron deficient but investigating the possibility that we are being overly restrictive and should be giving iron to a much broader population.” That course, however, would require large population-based studies.
“We need more experience,” Dr. Cleland said, “to make sure that the benefits outweigh any risks before we can just give iron to everyone.”
Dr. Martens has received consultancy fees from AstraZeneca, Abbott, Bayer, Boehringer Ingelheim, Daiichi Sankyo, Novartis, Novo Nordisk, and Vifor Pharma. Dr. Cleland declares grant support, support for travel, and personal honoraria from Pharmacosmos and Vifor. Disclosures for other authors are in the published report and editorial.
A version of this article first appeared on Medscape.com.
with implications that may extend to cardiovascular disease in general.
In the study involving more than 900 patients with PH, investigators at seven U.S. centers determined the prevalence of iron deficiency by two separate definitions and assessed its associations with functional measures and quality of life (QoL) scores.
An iron deficiency definition used conventionally in heart failure (HF) – ferritin less than 100 g/mL or 100-299 ng/mL with transferrin saturation (TSAT) less than 20% – failed to discriminate patients with reduced peak oxygen consumption (peakVO2), 6-minute walk test (6MWT) results, and QoL scores on the 36-item Short Form Survey (SF-36).
But an alternative definition for iron deficiency, simply a TSAT less than 21%, did predict such patients with reduced peakVO2, 6MWT, and QoL. It was also associated with an increased mortality risk. The study was published in the European Heart Journal.
“A low TSAT, less than 21%, is key in the pathophysiology of iron deficiency in pulmonary hypertension” and is associated with those important clinical and functional characteristics, lead author Pieter Martens MD, PhD, said in an interview. The study “underscores the importance of these criteria in future intervention studies in the field of pulmonary hypertension testing iron therapies.”
A broader implication is that “we should revise how we define iron deficiency in heart failure and cardiovascular disease in general and how we select patients for iron therapies,” said Dr. Martens, of the Heart, Vascular & Thoracic Institute of the Cleveland Clinic.
Iron’s role in pulmonary vascular disease
“Iron deficiency is associated with an energetic deficit, especially in high energy–demanding tissue, leading to early skeletal muscle acidification and diminished left and right ventricular (RV) contractile reserve during exercise,” the published report states. It can lead to “maladaptive RV remodeling,” which is a “hallmark feature” predictive of morbidity and mortality in patients with pulmonary vascular disease (PVD).
Some studies have suggested that iron deficiency is a common comorbidity in patients with PVD, their estimates of its prevalence ranging widely due in part to the “absence of a uniform definition,” write the authors.
Dr. Martens said the current study was conducted partly in response to the increasingly common observation that the HF-associated definition of iron deficiency “has limitations.” Yet, “without validation in the field of pulmonary hypertension, the 2022 pulmonary hypertension guidelines endorse this definition.”
As iron deficiency is a causal risk factor for HF progression, Dr. Martens added, the HF field has “taught us the importance of using validated definitions for iron deficiency when selecting patients for iron treatment in randomized controlled trials.”
Moreover, some evidence suggests that iron deficiency by some definitions may be associated with diminished exercise capacity and QoL in patients with PVD, which are associations that have not been confirmed in large studies, the report notes.
Therefore, it continues, the study sought to “determine and validate” the optimal definition of iron deficiency in patients with PVD; document its prevalence; and explore associations between iron deficiency and exercise capacity, QoL, and cardiac and pulmonary vascular remodeling.
Evaluating definitions of iron deficiency
The prospective study, called PVDOMICS, entered 1,195 subjects with available iron levels. After exclusion of 38 patients with sarcoidosis, myeloproliferative disease, or hemoglobinopathy, there remained 693 patients with “overt” PH, 225 with a milder form of PH who served as PVD comparators, and 90 age-, sex-, race/ethnicity- matched “healthy” adults who served as controls.
According to the conventional HF definition of iron deficiency – that is, ferritin 100-299 ng/mL and TSAT less than 20% – the prevalences were 74% in patients with overt PH and 72% of those “across the PVD spectrum.”
But by that definition, iron deficient and non-iron deficient patients didn’t differ significantly in peakVO2, 6MWT distance, or SF-36 physical component scores.
In contrast, patients meeting the alternative definition of iron deficiency of TSAT less than 21% showed significantly reduced functional and QoL measures, compared with those with TSAT greater than or equal to 21%.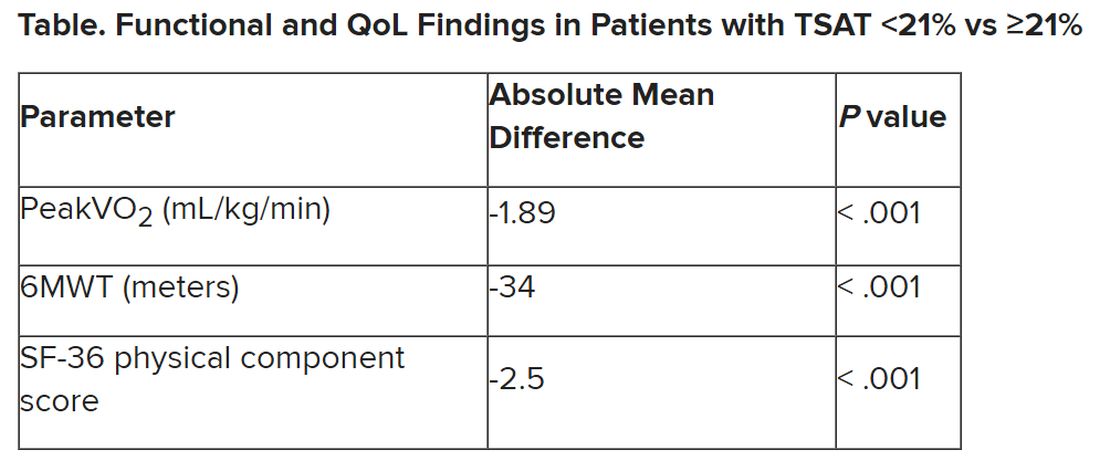
The group with TSAT less than 21% also showed significantly more RV remodeling at cardiac MRI, compared with those who had TSAT greater than or equal to 21%, but their invasively measured pulmonary vascular resistance was comparable.
Of note, those with TSAT less than 21% also showed significantly increased all-cause mortality (hazard ratio, 1.63; 95% confidence interval, 1.13-2.34; P = .009) after adjustment for age, sex, hemoglobin, and natriuretic peptide levels.
“Proper validation of the definition of iron deficiency is important for prognostication,” the published report states, “but also for providing a working definition that can be used to identify suitable patients for inclusion in randomized controlled trials” of drugs for iron deficiency.
Additionally, the finding that TSAT less than 21% points to patients with diminished functional and exercise capacity is “consistent with more recent studies in the field of heart failure” that suggest “functional abnormalities and adverse cardiac remodeling are worse in patients with a low TSAT.” Indeed, the report states, such treatment effects have been “the most convincing” in HF trials.
Broader implications
An accompanying editorial agrees that the study’s implications apply well beyond PH. It highlights that iron deficiency is common in PH, while such PH is “not substantially different from the problem in patients with heart failure, chronic kidney disease, and cardiovascular disease in general,” lead editorialist John G.F. Cleland, MD, PhD, University of Glasgow, said in an interview. “It’s also common as people get older, even in those without these diseases.”
Dr. Cleland said the anemia definition currently used in cardiovascular research and practice is based on a hemoglobin concentration below the 5th percentile of age and sex in primarily young, healthy people, and not on its association with clinical outcomes.
“We recently analyzed data on a large population in the United Kingdom with a broad range of cardiovascular diseases and found that unless anemia is severe, [other] markers of iron deficiency are usually not measured,” he said. A low hemoglobin and TSAT, but not low ferritin levels, are associated with worse prognosis.
Dr. Cleland agreed that the HF-oriented definition is “poor,” with profound implications for the conduct of clinical trials. “If the definition of iron deficiency lacks specificity, then clinical trials will include many patients without iron deficiency who are unlikely to benefit from and might be harmed by IV iron.” Inclusion of such patients may also “dilute” any benefit that might emerge and render the outcome inaccurate.
But if the definition of iron deficiency lacks sensitivity, “then in clinical practice, many patients with iron deficiency may be denied a simple and effective treatment.”
Measuring serum iron could potentially be useful, but it’s usually not done in randomized trials “especially since taking an iron tablet can give a temporary ‘blip’ in serum iron,” Dr. Cleland said. “So TSAT is a reasonable compromise.” He said he “looks forward” to any further data on serum iron as a way of assessing iron deficiency and anemia.
Half full vs. half empty
Dr. Cleland likened the question of whom to treat with iron supplementation as a “glass half full versus half empty” clinical dilemma. “One approach is to give iron to everyone unless there’s evidence that they’re overloaded,” he said, “while the other is to withhold iron from everyone unless there’s evidence that they’re iron depleted.”
Recent evidence from the IRONMAN trial suggested that its patients with HF who received intravenous iron were less likely to be hospitalized for infections, particularly COVID-19, than a usual-care group. The treatment may also help reduce frailty.
“So should we be offering IV iron specifically to people considered iron deficient, or should we be ensuring that everyone over age 70 get iron supplements?” Dr. Cleland mused rhetorically. On a cautionary note, he added, perhaps iron supplementation will be harmful if it’s not necessary.
Dr. Cleland proposed “focusing for the moment on people who are iron deficient but investigating the possibility that we are being overly restrictive and should be giving iron to a much broader population.” That course, however, would require large population-based studies.
“We need more experience,” Dr. Cleland said, “to make sure that the benefits outweigh any risks before we can just give iron to everyone.”
Dr. Martens has received consultancy fees from AstraZeneca, Abbott, Bayer, Boehringer Ingelheim, Daiichi Sankyo, Novartis, Novo Nordisk, and Vifor Pharma. Dr. Cleland declares grant support, support for travel, and personal honoraria from Pharmacosmos and Vifor. Disclosures for other authors are in the published report and editorial.
A version of this article first appeared on Medscape.com.
FROM EUROPEAN HEART JOURNAL
Nebulized amphotericin B does not affect aspergillosis exacerbation-free status at 1 year
Topline
Nebulized amphotericin B does not improve exacerbation-free status at 1 year for patients with bronchopulmonary aspergillosis, though it may delay onset and incidence.
Methodology
Investigators searched PubMed and Embase databases for studies that included at least five patients with allergic bronchopulmonary aspergillosis who were managed with nebulized amphotericin B.
They included five studies, two of which were randomized controlled trials (RCTs), and three were observational studies; there was a total of 188 patients.
The primary objective of this systematic review and meta-analysis was to determine the frequency of patients remaining exacerbation free 1 year after initiating treatment with nebulized amphotericin B.
Takeaway
From the studies (one observational, two RCTs; n = 84) with exacerbation data at 1 or 2 years, the pooled proportion of patients who remained exacerbation free with nebulized amphotericin B at 1 year was 76% (I2 = 64.6%).
The pooled difference in risk with the two RCTs that assessed exacerbation-free status at 1 year was 0.33 and was not significantly different between the nebulized amphotericin B and control arms, which received nebulized saline.
Two RCTs provided the time to first exacerbation, which was significantly longer with nebulized amphotericin B than with nebulized saline (337 vs. 177 days; P = .004; I2 = 82%).
The proportion of patients who experienced two or more exacerbations was significantly lower with nebulized amphotericin B than with nebulized saline (9/33 [27.3%] vs 20/38 [52.6%]; P = .03).
In practice
Also, the proportion of subjects experiencing ≥ 2 exacerbations was also lesser with NAB than in the control,” concluded Valliappan Muthu, MD, and colleagues. However, “the ideal duration and optimal dose of LAMB for nebulization are unclear.”
Study details
“Nebulized amphotericin B for preventing exacerbations in allergic bronchopulmonary aspergillosis: A systematic review and meta-analysis” was published online in Pulmonary Pharmacology and Therapeutics.
Limitations
The current review is limited by the small number of included trials and may have a high risk of bias. Therefore, more evidence is required for the use of nebulized amphotericin B in routine care. The authors have disclosed no conflicts of interest.
A version of this article originally appeared on Medscape.com.
Topline
Nebulized amphotericin B does not improve exacerbation-free status at 1 year for patients with bronchopulmonary aspergillosis, though it may delay onset and incidence.
Methodology
Investigators searched PubMed and Embase databases for studies that included at least five patients with allergic bronchopulmonary aspergillosis who were managed with nebulized amphotericin B.
They included five studies, two of which were randomized controlled trials (RCTs), and three were observational studies; there was a total of 188 patients.
The primary objective of this systematic review and meta-analysis was to determine the frequency of patients remaining exacerbation free 1 year after initiating treatment with nebulized amphotericin B.
Takeaway
From the studies (one observational, two RCTs; n = 84) with exacerbation data at 1 or 2 years, the pooled proportion of patients who remained exacerbation free with nebulized amphotericin B at 1 year was 76% (I2 = 64.6%).
The pooled difference in risk with the two RCTs that assessed exacerbation-free status at 1 year was 0.33 and was not significantly different between the nebulized amphotericin B and control arms, which received nebulized saline.
Two RCTs provided the time to first exacerbation, which was significantly longer with nebulized amphotericin B than with nebulized saline (337 vs. 177 days; P = .004; I2 = 82%).
The proportion of patients who experienced two or more exacerbations was significantly lower with nebulized amphotericin B than with nebulized saline (9/33 [27.3%] vs 20/38 [52.6%]; P = .03).
In practice
Also, the proportion of subjects experiencing ≥ 2 exacerbations was also lesser with NAB than in the control,” concluded Valliappan Muthu, MD, and colleagues. However, “the ideal duration and optimal dose of LAMB for nebulization are unclear.”
Study details
“Nebulized amphotericin B for preventing exacerbations in allergic bronchopulmonary aspergillosis: A systematic review and meta-analysis” was published online in Pulmonary Pharmacology and Therapeutics.
Limitations
The current review is limited by the small number of included trials and may have a high risk of bias. Therefore, more evidence is required for the use of nebulized amphotericin B in routine care. The authors have disclosed no conflicts of interest.
A version of this article originally appeared on Medscape.com.
Topline
Nebulized amphotericin B does not improve exacerbation-free status at 1 year for patients with bronchopulmonary aspergillosis, though it may delay onset and incidence.
Methodology
Investigators searched PubMed and Embase databases for studies that included at least five patients with allergic bronchopulmonary aspergillosis who were managed with nebulized amphotericin B.
They included five studies, two of which were randomized controlled trials (RCTs), and three were observational studies; there was a total of 188 patients.
The primary objective of this systematic review and meta-analysis was to determine the frequency of patients remaining exacerbation free 1 year after initiating treatment with nebulized amphotericin B.
Takeaway
From the studies (one observational, two RCTs; n = 84) with exacerbation data at 1 or 2 years, the pooled proportion of patients who remained exacerbation free with nebulized amphotericin B at 1 year was 76% (I2 = 64.6%).
The pooled difference in risk with the two RCTs that assessed exacerbation-free status at 1 year was 0.33 and was not significantly different between the nebulized amphotericin B and control arms, which received nebulized saline.
Two RCTs provided the time to first exacerbation, which was significantly longer with nebulized amphotericin B than with nebulized saline (337 vs. 177 days; P = .004; I2 = 82%).
The proportion of patients who experienced two or more exacerbations was significantly lower with nebulized amphotericin B than with nebulized saline (9/33 [27.3%] vs 20/38 [52.6%]; P = .03).
In practice
Also, the proportion of subjects experiencing ≥ 2 exacerbations was also lesser with NAB than in the control,” concluded Valliappan Muthu, MD, and colleagues. However, “the ideal duration and optimal dose of LAMB for nebulization are unclear.”
Study details
“Nebulized amphotericin B for preventing exacerbations in allergic bronchopulmonary aspergillosis: A systematic review and meta-analysis” was published online in Pulmonary Pharmacology and Therapeutics.
Limitations
The current review is limited by the small number of included trials and may have a high risk of bias. Therefore, more evidence is required for the use of nebulized amphotericin B in routine care. The authors have disclosed no conflicts of interest.
A version of this article originally appeared on Medscape.com.
Pulmonary embolism confers higher mortality long term
Topline
Long-term mortality rates among individuals who have had a pulmonary embolism are significantly higher than rates in the general population.
Methodology
Researchers investigated long-term outcomes of patients with pulmonary embolism in a single-center registry.
They followed 896 patients for up to 14 years.
Data were from consecutive cases treated between May 2005 and December 2017.
Takeaway
The total follow-up time was 3,908 patient-years (median, 3.1 years).
One-year and five-year mortality rates were 19.7% (95% confidence interval, 17.2%-22.4%) and 37.1% (95% CI, 33.6%-40.5%), respectively, for patients with pulmonary embolism.
The most frequent causes of death were cancer (28.5%), pulmonary embolism (19.4%), infections (13.9%), and cardiovascular events (11.6%).
Late mortality (>30 days) was more frequent than in the general population for patients with cancer (5-year standardized mortality ratio, 2.77; 95% CI, 2.41-3.16) and for patients without cancer (1.80; 95% CI, 1.50-2.14), compared with expected rates.
In practice
stated Johannes Eckelt, Clinic of Cardiology and Pneumology, University Medical Center Göttingen (Germany).
Source
“Long-term Mortality in Pulmonary Embolism: Results in a Single-Center Registry,” by Mr. Eckelt and colleagues was published in Research and Practice in Thrombosis and Haemostasis.
Limitations
Owing to the single-center study design, selection bias cannot be excluded, limiting the generalizability of the study findings, the authors stated.
Disclosures
The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Topline
Long-term mortality rates among individuals who have had a pulmonary embolism are significantly higher than rates in the general population.
Methodology
Researchers investigated long-term outcomes of patients with pulmonary embolism in a single-center registry.
They followed 896 patients for up to 14 years.
Data were from consecutive cases treated between May 2005 and December 2017.
Takeaway
The total follow-up time was 3,908 patient-years (median, 3.1 years).
One-year and five-year mortality rates were 19.7% (95% confidence interval, 17.2%-22.4%) and 37.1% (95% CI, 33.6%-40.5%), respectively, for patients with pulmonary embolism.
The most frequent causes of death were cancer (28.5%), pulmonary embolism (19.4%), infections (13.9%), and cardiovascular events (11.6%).
Late mortality (>30 days) was more frequent than in the general population for patients with cancer (5-year standardized mortality ratio, 2.77; 95% CI, 2.41-3.16) and for patients without cancer (1.80; 95% CI, 1.50-2.14), compared with expected rates.
In practice
stated Johannes Eckelt, Clinic of Cardiology and Pneumology, University Medical Center Göttingen (Germany).
Source
“Long-term Mortality in Pulmonary Embolism: Results in a Single-Center Registry,” by Mr. Eckelt and colleagues was published in Research and Practice in Thrombosis and Haemostasis.
Limitations
Owing to the single-center study design, selection bias cannot be excluded, limiting the generalizability of the study findings, the authors stated.
Disclosures
The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.
Topline
Long-term mortality rates among individuals who have had a pulmonary embolism are significantly higher than rates in the general population.
Methodology
Researchers investigated long-term outcomes of patients with pulmonary embolism in a single-center registry.
They followed 896 patients for up to 14 years.
Data were from consecutive cases treated between May 2005 and December 2017.
Takeaway
The total follow-up time was 3,908 patient-years (median, 3.1 years).
One-year and five-year mortality rates were 19.7% (95% confidence interval, 17.2%-22.4%) and 37.1% (95% CI, 33.6%-40.5%), respectively, for patients with pulmonary embolism.
The most frequent causes of death were cancer (28.5%), pulmonary embolism (19.4%), infections (13.9%), and cardiovascular events (11.6%).
Late mortality (>30 days) was more frequent than in the general population for patients with cancer (5-year standardized mortality ratio, 2.77; 95% CI, 2.41-3.16) and for patients without cancer (1.80; 95% CI, 1.50-2.14), compared with expected rates.
In practice
stated Johannes Eckelt, Clinic of Cardiology and Pneumology, University Medical Center Göttingen (Germany).
Source
“Long-term Mortality in Pulmonary Embolism: Results in a Single-Center Registry,” by Mr. Eckelt and colleagues was published in Research and Practice in Thrombosis and Haemostasis.
Limitations
Owing to the single-center study design, selection bias cannot be excluded, limiting the generalizability of the study findings, the authors stated.
Disclosures
The authors have disclosed no relevant financial relationships.
A version of this article originally appeared on Medscape.com.