User login
Bringing you the latest news, research and reviews, exclusive interviews, podcasts, quizzes, and more.
div[contains(@class, 'header__large-screen')]
div[contains(@class, 'read-next-article')]
div[contains(@class, 'main-prefix')]
div[contains(@class, 'nav-primary')]
nav[contains(@class, 'nav-primary')]
section[contains(@class, 'footer-nav-section-wrapper')]
footer[@id='footer']
section[contains(@class, 'nav-hidden')]
div[contains(@class, 'ce-card-content')]
nav[contains(@class, 'nav-ce-stack')]
div[contains(@class, 'view-medstat-quiz-listing-panes')]
div[contains(@class, 'pane-article-sidebar-latest-news')]
VTE risk not elevated in AD patients on JAK inhibitors: Study
, according to a new systemic review and meta-analysis, published online in JAMA Dermatology.
“These findings may provide a reference for clinicians in prescribing JAK inhibitors for patients with AD,” Tai-Li Chen, MD, of Taipei (Taiwan) Veterans General Hospital, Taipei, and colleagues wrote in the study.
The results shed some welcome light on treatment for this dermatologic population, for whom enthusiasm about JAK inhibitors was dampened by the addition of a boxed warning to the labels of JAK inhibitors last year, required by the Food and Drug Administration. The warning, which describes an increased risk of “serious heart-related events such as heart attack or stroke, cancer, blood clots, and death” was triggered by results of the ORAL Surveillance study of patients with rheumatoid arthritis (RA) treated with tofacitinib.
The boxed warning is also included in the labels of topical ruxolitinib, a JAK inhibitor approved by the FDA for mild to moderate AD in 2021, and in the labels of two oral JAK inhibitors, upadacitinib and abrocitinib, approved by the FDA for treating moderate to severe AD in January 2022.
Despite the new findings, some dermatologists are still urging caution.
“All the JAK inhibitor trials are short term. I still think the precautionary principle applies and we need to counsel on the risks of JAKs,” tweeted Aaron Drucker, MD, a dermatologist at Women’s College Hospital, and associate professor at the University of Toronto. “It is great to have these as options for our patients. But we need to be aware of the risks associated with this class of medications, counsel patients about them when we are informing them of the risks and benefits of treatment options, and wait for more data specific to this population to make even more informed decisions,” he told this news organization.
The meta-analysis examined both the risk of incident VTE in untreated patients with AD compared with non-AD patients, as well as the risk of VTE in AD patients treated with JAK inhibitors compared with those on either placebo or dupilumab. Four JAK inhibitors were studied: abrocitinib, baricitinib (under FDA review for AD), upadacitinib, and SHR0302 (in clinical trials).
Two studies (458,206 participants) found the overall incidence rate of VTE for patients with AD was 0.23 events per 100 patient-years. The risk was did not differ from that in non-AD patients (pooled hazard ratio [HR], 0.95; 95% confidence interval [CI], 0.62-1.45).
Another 15 studies included 8,787 participants with AD and found no significant differences in the rates of VTE in AD patients treated with JAK inhibitors (0.05%) versus those treated with placebo or dupilumab (0.03%). However “with the increasing applications of JAK inhibitors in AD, more clinical data are needed to identify patients at high risk for VTE,” noted the authors.
“We need more, long-term data,” agreed Dr. Drucker, adding that a major issue is the short-term nature of AD trials to date (generally up to 16 weeks), which “don’t provide adequate reassurance.” He said although the FDA’s boxed warning was prompted by a trial in RA patients treated with tofacitinib (a less selective JAK inhibitor than those approved by the FDA for AD), and the same risks have not been demonstrated specifically for the JAK inhibitors used for a patients with AD, he still remains cautious.
While agreeing on the need for more long-term data, Andrew Blauvelt, MD, MBA, president of Oregon Medical Research Center, Portland, said that the new findings should “provide reassurance” to dermatologists and are “consonant with recent published meta-analyses reporting no increased VTE risk in patients with psoriasis, RA, or inflammatory bowel disease treated with JAK inhibitors” in Arthritis & Rheumatology, and Mayo Clinic Proceedings.
In an interview, Dr. Blauvelt said that safety profiles emerging for the newer JAK inhibitors, which block JAK 1/2, have been overshadowed by the older RA data for tofacitinib – which is a JAK 1/3 inhibitor, “despite emerging long-term, monotherapy, clinical study data for dermatologic diseases showing no or rare risks of developing severe adverse events outlined in the boxed warnings.”
Both Dr. Blauvelt and Dr. Drucker pointed out that people with RA tend to have more comorbidities than those with AD that would predispose them to adverse events. In fact, “approximately 75% of patients in the ORAL Surveillance study were also on concomitant methotrexate and/or prednisone, which can greatly confound safety results,” said Dr. Blauvelt.
The study authors did not report any disclosures. No funding source for the study was provided. Dr. Drucker has no relevant disclosures. Dr. Blauvelt has been a clinical study investigator in trials for AD treatments, including JAK inhibitors; his disclosures include serving as a speaker, scientific adviser, and/or clinical study investigator for multiple companies including AbbVie, Arcutis, Bristol-Myers Squibb, Pfizer, Incyte, Regeneron, Sanofi Genzyme, and UCB Pharma.
, according to a new systemic review and meta-analysis, published online in JAMA Dermatology.
“These findings may provide a reference for clinicians in prescribing JAK inhibitors for patients with AD,” Tai-Li Chen, MD, of Taipei (Taiwan) Veterans General Hospital, Taipei, and colleagues wrote in the study.
The results shed some welcome light on treatment for this dermatologic population, for whom enthusiasm about JAK inhibitors was dampened by the addition of a boxed warning to the labels of JAK inhibitors last year, required by the Food and Drug Administration. The warning, which describes an increased risk of “serious heart-related events such as heart attack or stroke, cancer, blood clots, and death” was triggered by results of the ORAL Surveillance study of patients with rheumatoid arthritis (RA) treated with tofacitinib.
The boxed warning is also included in the labels of topical ruxolitinib, a JAK inhibitor approved by the FDA for mild to moderate AD in 2021, and in the labels of two oral JAK inhibitors, upadacitinib and abrocitinib, approved by the FDA for treating moderate to severe AD in January 2022.
Despite the new findings, some dermatologists are still urging caution.
“All the JAK inhibitor trials are short term. I still think the precautionary principle applies and we need to counsel on the risks of JAKs,” tweeted Aaron Drucker, MD, a dermatologist at Women’s College Hospital, and associate professor at the University of Toronto. “It is great to have these as options for our patients. But we need to be aware of the risks associated with this class of medications, counsel patients about them when we are informing them of the risks and benefits of treatment options, and wait for more data specific to this population to make even more informed decisions,” he told this news organization.
The meta-analysis examined both the risk of incident VTE in untreated patients with AD compared with non-AD patients, as well as the risk of VTE in AD patients treated with JAK inhibitors compared with those on either placebo or dupilumab. Four JAK inhibitors were studied: abrocitinib, baricitinib (under FDA review for AD), upadacitinib, and SHR0302 (in clinical trials).
Two studies (458,206 participants) found the overall incidence rate of VTE for patients with AD was 0.23 events per 100 patient-years. The risk was did not differ from that in non-AD patients (pooled hazard ratio [HR], 0.95; 95% confidence interval [CI], 0.62-1.45).
Another 15 studies included 8,787 participants with AD and found no significant differences in the rates of VTE in AD patients treated with JAK inhibitors (0.05%) versus those treated with placebo or dupilumab (0.03%). However “with the increasing applications of JAK inhibitors in AD, more clinical data are needed to identify patients at high risk for VTE,” noted the authors.
“We need more, long-term data,” agreed Dr. Drucker, adding that a major issue is the short-term nature of AD trials to date (generally up to 16 weeks), which “don’t provide adequate reassurance.” He said although the FDA’s boxed warning was prompted by a trial in RA patients treated with tofacitinib (a less selective JAK inhibitor than those approved by the FDA for AD), and the same risks have not been demonstrated specifically for the JAK inhibitors used for a patients with AD, he still remains cautious.
While agreeing on the need for more long-term data, Andrew Blauvelt, MD, MBA, president of Oregon Medical Research Center, Portland, said that the new findings should “provide reassurance” to dermatologists and are “consonant with recent published meta-analyses reporting no increased VTE risk in patients with psoriasis, RA, or inflammatory bowel disease treated with JAK inhibitors” in Arthritis & Rheumatology, and Mayo Clinic Proceedings.
In an interview, Dr. Blauvelt said that safety profiles emerging for the newer JAK inhibitors, which block JAK 1/2, have been overshadowed by the older RA data for tofacitinib – which is a JAK 1/3 inhibitor, “despite emerging long-term, monotherapy, clinical study data for dermatologic diseases showing no or rare risks of developing severe adverse events outlined in the boxed warnings.”
Both Dr. Blauvelt and Dr. Drucker pointed out that people with RA tend to have more comorbidities than those with AD that would predispose them to adverse events. In fact, “approximately 75% of patients in the ORAL Surveillance study were also on concomitant methotrexate and/or prednisone, which can greatly confound safety results,” said Dr. Blauvelt.
The study authors did not report any disclosures. No funding source for the study was provided. Dr. Drucker has no relevant disclosures. Dr. Blauvelt has been a clinical study investigator in trials for AD treatments, including JAK inhibitors; his disclosures include serving as a speaker, scientific adviser, and/or clinical study investigator for multiple companies including AbbVie, Arcutis, Bristol-Myers Squibb, Pfizer, Incyte, Regeneron, Sanofi Genzyme, and UCB Pharma.
, according to a new systemic review and meta-analysis, published online in JAMA Dermatology.
“These findings may provide a reference for clinicians in prescribing JAK inhibitors for patients with AD,” Tai-Li Chen, MD, of Taipei (Taiwan) Veterans General Hospital, Taipei, and colleagues wrote in the study.
The results shed some welcome light on treatment for this dermatologic population, for whom enthusiasm about JAK inhibitors was dampened by the addition of a boxed warning to the labels of JAK inhibitors last year, required by the Food and Drug Administration. The warning, which describes an increased risk of “serious heart-related events such as heart attack or stroke, cancer, blood clots, and death” was triggered by results of the ORAL Surveillance study of patients with rheumatoid arthritis (RA) treated with tofacitinib.
The boxed warning is also included in the labels of topical ruxolitinib, a JAK inhibitor approved by the FDA for mild to moderate AD in 2021, and in the labels of two oral JAK inhibitors, upadacitinib and abrocitinib, approved by the FDA for treating moderate to severe AD in January 2022.
Despite the new findings, some dermatologists are still urging caution.
“All the JAK inhibitor trials are short term. I still think the precautionary principle applies and we need to counsel on the risks of JAKs,” tweeted Aaron Drucker, MD, a dermatologist at Women’s College Hospital, and associate professor at the University of Toronto. “It is great to have these as options for our patients. But we need to be aware of the risks associated with this class of medications, counsel patients about them when we are informing them of the risks and benefits of treatment options, and wait for more data specific to this population to make even more informed decisions,” he told this news organization.
The meta-analysis examined both the risk of incident VTE in untreated patients with AD compared with non-AD patients, as well as the risk of VTE in AD patients treated with JAK inhibitors compared with those on either placebo or dupilumab. Four JAK inhibitors were studied: abrocitinib, baricitinib (under FDA review for AD), upadacitinib, and SHR0302 (in clinical trials).
Two studies (458,206 participants) found the overall incidence rate of VTE for patients with AD was 0.23 events per 100 patient-years. The risk was did not differ from that in non-AD patients (pooled hazard ratio [HR], 0.95; 95% confidence interval [CI], 0.62-1.45).
Another 15 studies included 8,787 participants with AD and found no significant differences in the rates of VTE in AD patients treated with JAK inhibitors (0.05%) versus those treated with placebo or dupilumab (0.03%). However “with the increasing applications of JAK inhibitors in AD, more clinical data are needed to identify patients at high risk for VTE,” noted the authors.
“We need more, long-term data,” agreed Dr. Drucker, adding that a major issue is the short-term nature of AD trials to date (generally up to 16 weeks), which “don’t provide adequate reassurance.” He said although the FDA’s boxed warning was prompted by a trial in RA patients treated with tofacitinib (a less selective JAK inhibitor than those approved by the FDA for AD), and the same risks have not been demonstrated specifically for the JAK inhibitors used for a patients with AD, he still remains cautious.
While agreeing on the need for more long-term data, Andrew Blauvelt, MD, MBA, president of Oregon Medical Research Center, Portland, said that the new findings should “provide reassurance” to dermatologists and are “consonant with recent published meta-analyses reporting no increased VTE risk in patients with psoriasis, RA, or inflammatory bowel disease treated with JAK inhibitors” in Arthritis & Rheumatology, and Mayo Clinic Proceedings.
In an interview, Dr. Blauvelt said that safety profiles emerging for the newer JAK inhibitors, which block JAK 1/2, have been overshadowed by the older RA data for tofacitinib – which is a JAK 1/3 inhibitor, “despite emerging long-term, monotherapy, clinical study data for dermatologic diseases showing no or rare risks of developing severe adverse events outlined in the boxed warnings.”
Both Dr. Blauvelt and Dr. Drucker pointed out that people with RA tend to have more comorbidities than those with AD that would predispose them to adverse events. In fact, “approximately 75% of patients in the ORAL Surveillance study were also on concomitant methotrexate and/or prednisone, which can greatly confound safety results,” said Dr. Blauvelt.
The study authors did not report any disclosures. No funding source for the study was provided. Dr. Drucker has no relevant disclosures. Dr. Blauvelt has been a clinical study investigator in trials for AD treatments, including JAK inhibitors; his disclosures include serving as a speaker, scientific adviser, and/or clinical study investigator for multiple companies including AbbVie, Arcutis, Bristol-Myers Squibb, Pfizer, Incyte, Regeneron, Sanofi Genzyme, and UCB Pharma.
FROM JAMA DERMATOLOGY
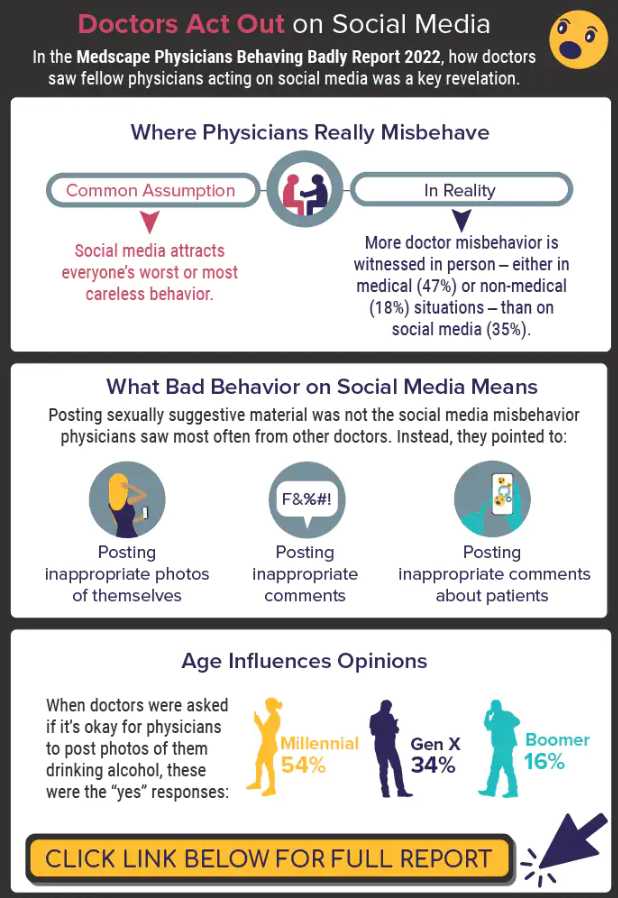
Infographic: Is physician behavior on social media really so bad?
The medical profession is held to a high standard of personal conduct, so physicians keep a sharp eye out for how fellow doctors behave. That goes for social media as well as in-person conduct.
(and it’s not as egregious as you might think). If you’re interested in delving deeper into the data, check out the Medscape Physicians Behaving Badly Report 2022.
A version of this article first appeared on Medscape.com.
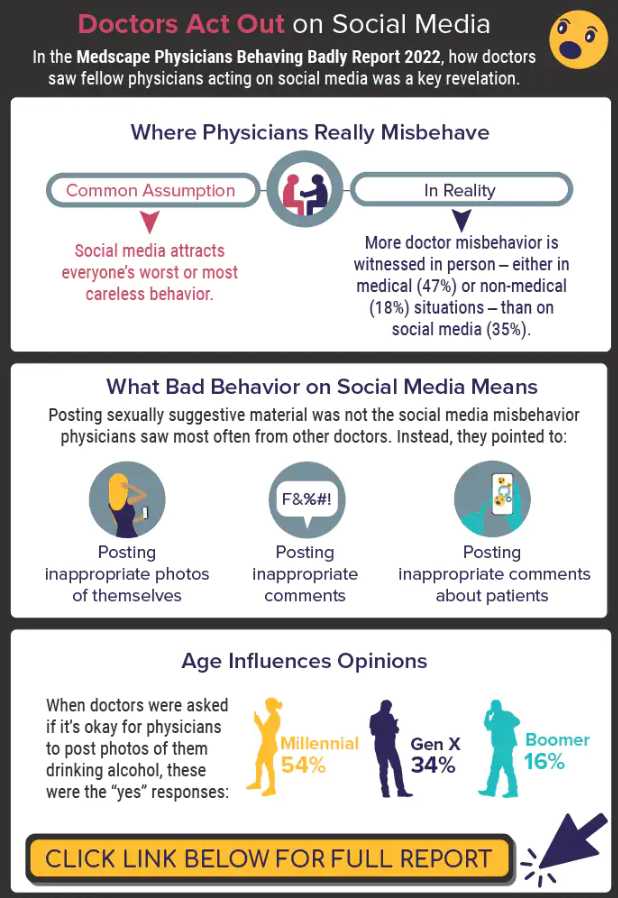
The medical profession is held to a high standard of personal conduct, so physicians keep a sharp eye out for how fellow doctors behave. That goes for social media as well as in-person conduct.
(and it’s not as egregious as you might think). If you’re interested in delving deeper into the data, check out the Medscape Physicians Behaving Badly Report 2022.
A version of this article first appeared on Medscape.com.
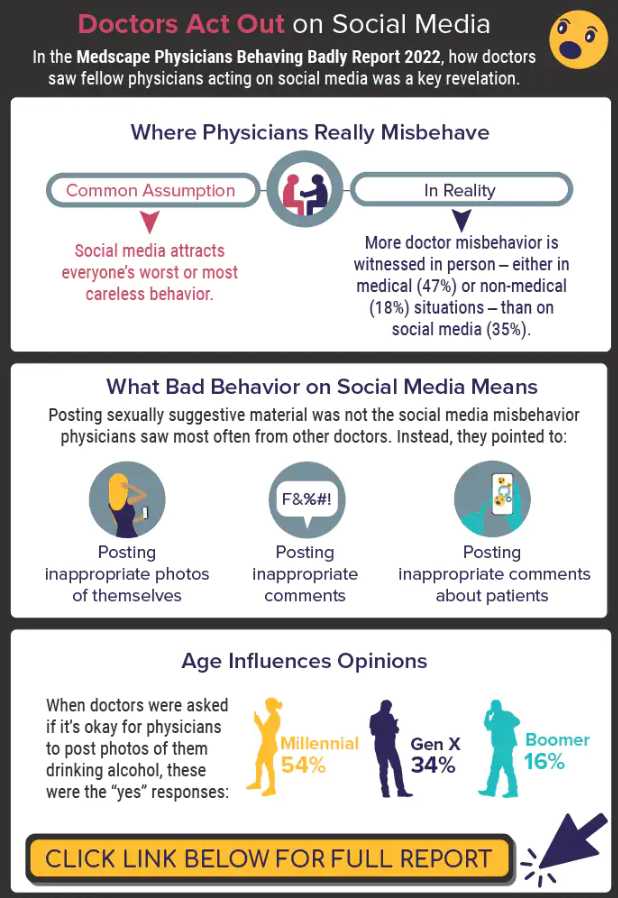
The medical profession is held to a high standard of personal conduct, so physicians keep a sharp eye out for how fellow doctors behave. That goes for social media as well as in-person conduct.
(and it’s not as egregious as you might think). If you’re interested in delving deeper into the data, check out the Medscape Physicians Behaving Badly Report 2022.
A version of this article first appeared on Medscape.com.
Paxlovid reduces risk of COVID death by 79% in older adults
The antiviral drug Paxlovid appears to reduce the risk of dying from COVID-19 by 79% and decrease hospitalizations by 73% in at-risk patients who are ages 65 and older, according to a new study published in The New England Journal of Medicine.
The pill, which is a combination of the drugs nirmatrelvir and ritonavir, received FDA emergency use authorization in December 2021 to treat mild to moderate disease in ages 12 and older who face high risks for having severe COVID-19, hospitalization, and death.
“The results of the study show unequivocally that treatment with Paxlovid significantly reduces the risk of hospitalization and death from COVID-19,” Doron Netzer, MD, the senior study author and a researcher with Clalit Health Services, Tel Aviv, told The Jerusalem Post.
“We are the country’s leader in the provision of giving Paxlovid to relevant patients,” he said. “It was given to patients all over the country, with medical teams monitoring the patients who took the pills.”
, the news outlet reported. The research team analyzed information from Clalit’s electronic medical records. The health care organization covers about 52% of the Israeli population and almost two-thirds of older adults. More than 30,000 COVID-19 patients in Israel have been treated with the drug so far.
Dr. Netzer and colleagues looked at hospitalization and death data for at-risk COVID-19 patients ages 40 and older between Jan. 9 and March 31, when the original Omicron variant was the dominant strain in Israel. During that time, more than 1.1 million Clalit patients were infected with COVID-19, 109,000 patients were considered at-risk, and 3,900 patients received the drug.
The average age of the patients was 60, and 39% of the patients were 65 and older. Overall, 78% of the patients had previous COVID-19 immunity due to vaccination, prior infection, or both.
Among ages 65 and older, the rate of COVID-19 hospitalization was 14.7 cases per 100,000 person-days among treated patients, compared with 58.9 cases per 100,000 person-days among untreated patients. This represented a 73% lower chance of being hospitalized.
Among ages 40-64, the rate of hospitalization due to COVID-19 was 15.2 cases per 100,000 person-days among treated patients, compared with 15.8 cases per 100,000 person-days among untreated patients. The risk of hospitalization wasn’t significantly lower for this age group.
Among ages 65 and older, there were two deaths from COVID-19 in 2,484 treated patients, compared with 158 in the 40,337 untreated patients. This represented a 79% lower chance of dying from COVID-19.
Among ages 40-64, there was one death from COVID-19 in 1,418 treated patients, compared with 16 in the 65,015 untreated patients. The risk of death wasn’t significantly lower for this age group.
For both age groups, a lack of previous COVID-19 immunity and a previous hospitalization were most strongly linked to high rates of hospitalization during the Omicron wave.
The researchers noted that they didn’t break down the data on ages 40-64 who had cancer and other severe conditions that weaken the immune system. These patients may be more likely to benefit from Paxlovid, they said, though future studies will need to analyze the data.
The study didn’t receive any financial or in-kind support, the authors said.
A version of this article first appeared on WebMD.com.
The antiviral drug Paxlovid appears to reduce the risk of dying from COVID-19 by 79% and decrease hospitalizations by 73% in at-risk patients who are ages 65 and older, according to a new study published in The New England Journal of Medicine.
The pill, which is a combination of the drugs nirmatrelvir and ritonavir, received FDA emergency use authorization in December 2021 to treat mild to moderate disease in ages 12 and older who face high risks for having severe COVID-19, hospitalization, and death.
“The results of the study show unequivocally that treatment with Paxlovid significantly reduces the risk of hospitalization and death from COVID-19,” Doron Netzer, MD, the senior study author and a researcher with Clalit Health Services, Tel Aviv, told The Jerusalem Post.
“We are the country’s leader in the provision of giving Paxlovid to relevant patients,” he said. “It was given to patients all over the country, with medical teams monitoring the patients who took the pills.”
, the news outlet reported. The research team analyzed information from Clalit’s electronic medical records. The health care organization covers about 52% of the Israeli population and almost two-thirds of older adults. More than 30,000 COVID-19 patients in Israel have been treated with the drug so far.
Dr. Netzer and colleagues looked at hospitalization and death data for at-risk COVID-19 patients ages 40 and older between Jan. 9 and March 31, when the original Omicron variant was the dominant strain in Israel. During that time, more than 1.1 million Clalit patients were infected with COVID-19, 109,000 patients were considered at-risk, and 3,900 patients received the drug.
The average age of the patients was 60, and 39% of the patients were 65 and older. Overall, 78% of the patients had previous COVID-19 immunity due to vaccination, prior infection, or both.
Among ages 65 and older, the rate of COVID-19 hospitalization was 14.7 cases per 100,000 person-days among treated patients, compared with 58.9 cases per 100,000 person-days among untreated patients. This represented a 73% lower chance of being hospitalized.
Among ages 40-64, the rate of hospitalization due to COVID-19 was 15.2 cases per 100,000 person-days among treated patients, compared with 15.8 cases per 100,000 person-days among untreated patients. The risk of hospitalization wasn’t significantly lower for this age group.
Among ages 65 and older, there were two deaths from COVID-19 in 2,484 treated patients, compared with 158 in the 40,337 untreated patients. This represented a 79% lower chance of dying from COVID-19.
Among ages 40-64, there was one death from COVID-19 in 1,418 treated patients, compared with 16 in the 65,015 untreated patients. The risk of death wasn’t significantly lower for this age group.
For both age groups, a lack of previous COVID-19 immunity and a previous hospitalization were most strongly linked to high rates of hospitalization during the Omicron wave.
The researchers noted that they didn’t break down the data on ages 40-64 who had cancer and other severe conditions that weaken the immune system. These patients may be more likely to benefit from Paxlovid, they said, though future studies will need to analyze the data.
The study didn’t receive any financial or in-kind support, the authors said.
A version of this article first appeared on WebMD.com.
The antiviral drug Paxlovid appears to reduce the risk of dying from COVID-19 by 79% and decrease hospitalizations by 73% in at-risk patients who are ages 65 and older, according to a new study published in The New England Journal of Medicine.
The pill, which is a combination of the drugs nirmatrelvir and ritonavir, received FDA emergency use authorization in December 2021 to treat mild to moderate disease in ages 12 and older who face high risks for having severe COVID-19, hospitalization, and death.
“The results of the study show unequivocally that treatment with Paxlovid significantly reduces the risk of hospitalization and death from COVID-19,” Doron Netzer, MD, the senior study author and a researcher with Clalit Health Services, Tel Aviv, told The Jerusalem Post.
“We are the country’s leader in the provision of giving Paxlovid to relevant patients,” he said. “It was given to patients all over the country, with medical teams monitoring the patients who took the pills.”
, the news outlet reported. The research team analyzed information from Clalit’s electronic medical records. The health care organization covers about 52% of the Israeli population and almost two-thirds of older adults. More than 30,000 COVID-19 patients in Israel have been treated with the drug so far.
Dr. Netzer and colleagues looked at hospitalization and death data for at-risk COVID-19 patients ages 40 and older between Jan. 9 and March 31, when the original Omicron variant was the dominant strain in Israel. During that time, more than 1.1 million Clalit patients were infected with COVID-19, 109,000 patients were considered at-risk, and 3,900 patients received the drug.
The average age of the patients was 60, and 39% of the patients were 65 and older. Overall, 78% of the patients had previous COVID-19 immunity due to vaccination, prior infection, or both.
Among ages 65 and older, the rate of COVID-19 hospitalization was 14.7 cases per 100,000 person-days among treated patients, compared with 58.9 cases per 100,000 person-days among untreated patients. This represented a 73% lower chance of being hospitalized.
Among ages 40-64, the rate of hospitalization due to COVID-19 was 15.2 cases per 100,000 person-days among treated patients, compared with 15.8 cases per 100,000 person-days among untreated patients. The risk of hospitalization wasn’t significantly lower for this age group.
Among ages 65 and older, there were two deaths from COVID-19 in 2,484 treated patients, compared with 158 in the 40,337 untreated patients. This represented a 79% lower chance of dying from COVID-19.
Among ages 40-64, there was one death from COVID-19 in 1,418 treated patients, compared with 16 in the 65,015 untreated patients. The risk of death wasn’t significantly lower for this age group.
For both age groups, a lack of previous COVID-19 immunity and a previous hospitalization were most strongly linked to high rates of hospitalization during the Omicron wave.
The researchers noted that they didn’t break down the data on ages 40-64 who had cancer and other severe conditions that weaken the immune system. These patients may be more likely to benefit from Paxlovid, they said, though future studies will need to analyze the data.
The study didn’t receive any financial or in-kind support, the authors said.
A version of this article first appeared on WebMD.com.
FROM THE NEW ENGLAND JOURNAL OF MEDICINE
ACC fills gaps on guidance for nonstatin therapies for LDL-C lowering
To address current gaps in expert guidance on newer nonstatin agents, the American College of Cardiology has issued an expert consensus decision pathway on the role of nonstatin therapies in LDL cholesterol lowering for risk reduction in atherosclerotic cardiovascular disease (ASCVD).
Since the publication of the most recent AHA/ACC cholesterol guidelines in 2018, a number of newer nonstatin medications have become available for management of lipid-associated risk, including bempedoic acid, inclisiran, evinacumab, and icosapent ethyl.
These medications were not addressed in the 2018 AHA/ACC Guideline on the Management of Blood Cholesterol.
The 53-page document – 2022 ACC Expert Consensus Decision Pathway on the Role of Nonstatin Therapies for LDL-Cholesterol Lowering in the Management of Atherosclerotic Cardiovascular Disease Risk – was published online in the Journal of the American College of Cardiology.
The new expert consensus document provides guidance for clinicians until the next formal guidelines are produced, Donald Lloyd-Jones, MD, chair of the writing committee, told this news organization.
The writing group focused on three key areas regarding the use of nonstatin therapies where recent scientific evidence is still under review and clinical trials are still underway:
- In what patient populations should newer nonstatin therapies be considered?
- In what situations should newer nonstatin therapies be considered?
- If newer nonstatin therapies are to be added, which therapies should be considered and in what order to maximize patient benefit and preference?
The document provides algorithms that endorse the four evidence-based patient groups identified in the 2018 guidelines and assumes that the patient is currently taking or has attempted to take a statin, given that that is the most effective initial therapy, the writing group says.
“The algorithms have been streamlined for ease of use by clinicians to help them identify who may need adjunctive nonstatin medications, to provide thresholds for consideration of those medications, and to provide a prioritization of those medications based on the strength of available evidence of efficacy,” said Dr. Lloyd-Jones, chair of the department of preventive medicine at Northwestern University’s Feinberg School of Medicine, Chicago.
“We hope that these pathways will assist the decision-making process for clinicians and patients,” he added.
He also noted that statins remain the “most important first-line therapy for reducing ASCVD risk, because of their efficacy, safety, and low cost. However, for some patients, there are now options if statins do not fully achieve the goals for reducing ASCVD risk or if statins are not tolerated at effective doses.”
“The new expert consensus document highlights that higher-risk patients should be considered more often for adjunctive therapy and provides user-friendly decision pathways to assist in considering the reasonable choices available under different clinical scenarios,” Dr. Lloyd-Jones said.
The document has been endorsed by the National Lipid Association.
This research had no commercial funding. Dr. Lloyd-Jones has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
To address current gaps in expert guidance on newer nonstatin agents, the American College of Cardiology has issued an expert consensus decision pathway on the role of nonstatin therapies in LDL cholesterol lowering for risk reduction in atherosclerotic cardiovascular disease (ASCVD).
Since the publication of the most recent AHA/ACC cholesterol guidelines in 2018, a number of newer nonstatin medications have become available for management of lipid-associated risk, including bempedoic acid, inclisiran, evinacumab, and icosapent ethyl.
These medications were not addressed in the 2018 AHA/ACC Guideline on the Management of Blood Cholesterol.
The 53-page document – 2022 ACC Expert Consensus Decision Pathway on the Role of Nonstatin Therapies for LDL-Cholesterol Lowering in the Management of Atherosclerotic Cardiovascular Disease Risk – was published online in the Journal of the American College of Cardiology.
The new expert consensus document provides guidance for clinicians until the next formal guidelines are produced, Donald Lloyd-Jones, MD, chair of the writing committee, told this news organization.
The writing group focused on three key areas regarding the use of nonstatin therapies where recent scientific evidence is still under review and clinical trials are still underway:
- In what patient populations should newer nonstatin therapies be considered?
- In what situations should newer nonstatin therapies be considered?
- If newer nonstatin therapies are to be added, which therapies should be considered and in what order to maximize patient benefit and preference?
The document provides algorithms that endorse the four evidence-based patient groups identified in the 2018 guidelines and assumes that the patient is currently taking or has attempted to take a statin, given that that is the most effective initial therapy, the writing group says.
“The algorithms have been streamlined for ease of use by clinicians to help them identify who may need adjunctive nonstatin medications, to provide thresholds for consideration of those medications, and to provide a prioritization of those medications based on the strength of available evidence of efficacy,” said Dr. Lloyd-Jones, chair of the department of preventive medicine at Northwestern University’s Feinberg School of Medicine, Chicago.
“We hope that these pathways will assist the decision-making process for clinicians and patients,” he added.
He also noted that statins remain the “most important first-line therapy for reducing ASCVD risk, because of their efficacy, safety, and low cost. However, for some patients, there are now options if statins do not fully achieve the goals for reducing ASCVD risk or if statins are not tolerated at effective doses.”
“The new expert consensus document highlights that higher-risk patients should be considered more often for adjunctive therapy and provides user-friendly decision pathways to assist in considering the reasonable choices available under different clinical scenarios,” Dr. Lloyd-Jones said.
The document has been endorsed by the National Lipid Association.
This research had no commercial funding. Dr. Lloyd-Jones has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
To address current gaps in expert guidance on newer nonstatin agents, the American College of Cardiology has issued an expert consensus decision pathway on the role of nonstatin therapies in LDL cholesterol lowering for risk reduction in atherosclerotic cardiovascular disease (ASCVD).
Since the publication of the most recent AHA/ACC cholesterol guidelines in 2018, a number of newer nonstatin medications have become available for management of lipid-associated risk, including bempedoic acid, inclisiran, evinacumab, and icosapent ethyl.
These medications were not addressed in the 2018 AHA/ACC Guideline on the Management of Blood Cholesterol.
The 53-page document – 2022 ACC Expert Consensus Decision Pathway on the Role of Nonstatin Therapies for LDL-Cholesterol Lowering in the Management of Atherosclerotic Cardiovascular Disease Risk – was published online in the Journal of the American College of Cardiology.
The new expert consensus document provides guidance for clinicians until the next formal guidelines are produced, Donald Lloyd-Jones, MD, chair of the writing committee, told this news organization.
The writing group focused on three key areas regarding the use of nonstatin therapies where recent scientific evidence is still under review and clinical trials are still underway:
- In what patient populations should newer nonstatin therapies be considered?
- In what situations should newer nonstatin therapies be considered?
- If newer nonstatin therapies are to be added, which therapies should be considered and in what order to maximize patient benefit and preference?
The document provides algorithms that endorse the four evidence-based patient groups identified in the 2018 guidelines and assumes that the patient is currently taking or has attempted to take a statin, given that that is the most effective initial therapy, the writing group says.
“The algorithms have been streamlined for ease of use by clinicians to help them identify who may need adjunctive nonstatin medications, to provide thresholds for consideration of those medications, and to provide a prioritization of those medications based on the strength of available evidence of efficacy,” said Dr. Lloyd-Jones, chair of the department of preventive medicine at Northwestern University’s Feinberg School of Medicine, Chicago.
“We hope that these pathways will assist the decision-making process for clinicians and patients,” he added.
He also noted that statins remain the “most important first-line therapy for reducing ASCVD risk, because of their efficacy, safety, and low cost. However, for some patients, there are now options if statins do not fully achieve the goals for reducing ASCVD risk or if statins are not tolerated at effective doses.”
“The new expert consensus document highlights that higher-risk patients should be considered more often for adjunctive therapy and provides user-friendly decision pathways to assist in considering the reasonable choices available under different clinical scenarios,” Dr. Lloyd-Jones said.
The document has been endorsed by the National Lipid Association.
This research had no commercial funding. Dr. Lloyd-Jones has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
No benefit of routine stress test POST-PCI in high-risk patients
New randomized trial results show no benefit in clinical outcomes from active surveillance using functional testing over usual care among high-risk patients with previous percutaneous coronary intervention (PCI).
At 2 years, there was no difference in a composite outcome of death from any cause, MI, or hospitalization for unstable angina between patients who had routine functional testing at 1 year and patients receiving standard care in the POST-PCI trial.
“Our trial does not support active surveillance with routine functional testing for follow-up strategy in high-risk patients who undergo PCI,” first author Duk-Woo Park, MD, division of cardiology, Asan Medical Center, University of Ulsan, Seoul, South Korea, said in an interview.
The researchers said their results should be interpreted in the context of previous findings from the ISCHEMIA trial that showed no difference in death or ischemic events with an initial invasive versus an initial conservative approach in patients with stable coronary artery disease and moderate to severe ischemia on stress testing.
“Both the ISCHEMIA and POST-PCI trials show the benefits of a ‘less is more’ concept (i.e., if more invasive strategies or testing are performed less frequently, it will result in better patient outcomes),” the authors wrote. Although characteristics of the patients in these trials “were quite different, a more invasive therapeutic approach (in the ISCHEMIA trial) as well as a more aggressive follow-up approach (in the POST-PCI trial) did not provide an additional treatment effect beyond a conservative strategy on the basis of guideline-directed medical therapy.”
Results were presented at the annual congress of the European Society of Cardiology and published online simultaneously in the New England Journal of Medicine.
‘Compelling new evidence’
In an editorial accompanying the publication, Jacqueline E. Tamis-Holland, MD, Icahn School of Medicine at Mount Sinai, Mount Sinai Morningside Hospital, New York, also agreed that this new result “builds on the findings” from the ISCHEMIA trial. “Collectively, these trials highlight the lack of benefit of routine stress testing in asymptomatic patients.”
Dr. Tamis-Holland pointed out that many of the deaths in this trial occurred before the 1-year stress test, possibly related to stent thrombosis, and therefore would not have been prevented by routine testing at 1 year. And overall, event rates were “quite low, and most likely reflect adherence to guideline recommendations” in the trial. For example, 99% of patients were receiving statins, and 74% of the procedures used intravascular imaging for the PCI procedures, “a much greater proportion of use than most centers in the United States,” she noted.
“The POST-PCI trial provides compelling new evidence for a future class III recommendation for routine surveillance testing after PCI,” Dr. Tamis-Holland concluded “Until then, we must refrain from prescribing surveillance stress testing to our patients after PCI, in the absence of other clinical signs or symptoms suggestive of stent failure.”
Commenting on the results, B. Hadley Wilson, MD, executive vice chair of the Sanger Heart & Vascular Institute/Atrium Health, clinical professor of medicine at University of North Carolina at Chapel Hill, and vice president of the American College of Cardiology, said that for decades it’s been thought that patients who had high-risk PCI needed to be followed more closely for potential future events.
“And it actually turned out there was no difference in outcomes between the groups,” he said in an interview.
“So, I think it’s a good study – well conducted, good numbers – that answers the question that routine functional stress testing, even for high-risk PCI patients, is not effective or cost effective or beneficial on a yearly basis,” he said. “I think it will help frame care that patients will just be followed with best medical therapy and then if they have recurrence of symptoms they would be considered for further evaluation, either with stress testing or angiography.”
High-risk characteristics
Current guidelines do not advocate the use of routine stress testing after revascularization, the authors wrote in their paper. “However, surveillance with the use of imaging-based stress testing may be considered in high-risk patients at 6 months after a revascularization procedure (class IIb recommendation), and routine imaging-based stress testing may be considered at 1 year after PCI and more than 5 years after CABG [coronary artery bypass graft] (class IIb recommendation).”
But in real-world clinical practice, Dr. Park said, “follow-up strategy for patients who underwent PCI or CABG is still undetermined.” Particularly, “it could be more problematic in high-risk PCI patients with high-risk anatomical or clinical characteristics. Thus, we performed this POST-PCI trial comparing routine stress testing follow-up strategy versus standard-care follow-up strategy in high-risk PCI patients.”
The researchers randomly assigned 1,706 patients with high-risk anatomical or clinical characteristics who had undergone PCI to a follow-up strategy of routine functional testing, including nuclear stress testing, exercise electrocardiography, or stress echocardiography at 1 year, or to standard care alone.
High-risk anatomical features included left main or bifurcation disease; restenotic or long, diffuse lesions; or bypass graft disease. High-risk clinical characteristics included diabetes mellitus, chronic kidney disease, or enzyme-positive acute coronary syndrome.
Mean age of the patients was 64.7 years; 21.0% had left main disease, 43.5% had bifurcation disease, 69.8% had multivessel disease, 70.1% had diffuse long lesions, 38.7% had diabetes, and 96.4% had been treated with drug-eluting stents.
At 2 years, a primary-outcome event had occurred in 46 of 849 patients (Kaplan-Meier estimate, 5.5%) in the functional-testing group and in 51 of 857 (Kaplan-Meier estimate, 6.0%) in the standard-care group (hazard ratio, 0.90; 95% confidence interval, 0.61-1.35; P = .62). There were no between-group differences in the components of the primary outcome.
Secondary endpoints included invasive coronary angiography or repeat revascularization. At 2 years, 12.3% of the patients in the functional-testing group and 9.3% in the standard-care group had undergone invasive coronary angiography (difference, 2.99 percentage points; 95% CI, −0.01 to 5.99 percentage points), and 8.1% and 5.8% of patients, respectively, had a repeat revascularization procedure (difference, 2.23 percentage points; 95% CI, −0.22 to 4.68 percentage points).
Positive results on stress tests were more common with nuclear imaging than with exercise ECG or stress echocardiography, the authors noted. Subsequent coronary angiography and repeat revascularization were more common in patients with positive results on nuclear stress imaging and exercise ECG than in those with discordant results between nuclear imaging and exercise ECG.
POST-PCI was funded by the CardioVascular Research Foundation and Daewoong Pharmaceutical Company. Dr. Park reported grants from the Cardiovascular Research Foundation and Daewoong Pharmaceutical Company. Dr. Tamis-Holland reported “other” funding from Pfizer outside the submitted work. Dr. Wilson reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
New randomized trial results show no benefit in clinical outcomes from active surveillance using functional testing over usual care among high-risk patients with previous percutaneous coronary intervention (PCI).
At 2 years, there was no difference in a composite outcome of death from any cause, MI, or hospitalization for unstable angina between patients who had routine functional testing at 1 year and patients receiving standard care in the POST-PCI trial.
“Our trial does not support active surveillance with routine functional testing for follow-up strategy in high-risk patients who undergo PCI,” first author Duk-Woo Park, MD, division of cardiology, Asan Medical Center, University of Ulsan, Seoul, South Korea, said in an interview.
The researchers said their results should be interpreted in the context of previous findings from the ISCHEMIA trial that showed no difference in death or ischemic events with an initial invasive versus an initial conservative approach in patients with stable coronary artery disease and moderate to severe ischemia on stress testing.
“Both the ISCHEMIA and POST-PCI trials show the benefits of a ‘less is more’ concept (i.e., if more invasive strategies or testing are performed less frequently, it will result in better patient outcomes),” the authors wrote. Although characteristics of the patients in these trials “were quite different, a more invasive therapeutic approach (in the ISCHEMIA trial) as well as a more aggressive follow-up approach (in the POST-PCI trial) did not provide an additional treatment effect beyond a conservative strategy on the basis of guideline-directed medical therapy.”
Results were presented at the annual congress of the European Society of Cardiology and published online simultaneously in the New England Journal of Medicine.
‘Compelling new evidence’
In an editorial accompanying the publication, Jacqueline E. Tamis-Holland, MD, Icahn School of Medicine at Mount Sinai, Mount Sinai Morningside Hospital, New York, also agreed that this new result “builds on the findings” from the ISCHEMIA trial. “Collectively, these trials highlight the lack of benefit of routine stress testing in asymptomatic patients.”
Dr. Tamis-Holland pointed out that many of the deaths in this trial occurred before the 1-year stress test, possibly related to stent thrombosis, and therefore would not have been prevented by routine testing at 1 year. And overall, event rates were “quite low, and most likely reflect adherence to guideline recommendations” in the trial. For example, 99% of patients were receiving statins, and 74% of the procedures used intravascular imaging for the PCI procedures, “a much greater proportion of use than most centers in the United States,” she noted.
“The POST-PCI trial provides compelling new evidence for a future class III recommendation for routine surveillance testing after PCI,” Dr. Tamis-Holland concluded “Until then, we must refrain from prescribing surveillance stress testing to our patients after PCI, in the absence of other clinical signs or symptoms suggestive of stent failure.”
Commenting on the results, B. Hadley Wilson, MD, executive vice chair of the Sanger Heart & Vascular Institute/Atrium Health, clinical professor of medicine at University of North Carolina at Chapel Hill, and vice president of the American College of Cardiology, said that for decades it’s been thought that patients who had high-risk PCI needed to be followed more closely for potential future events.
“And it actually turned out there was no difference in outcomes between the groups,” he said in an interview.
“So, I think it’s a good study – well conducted, good numbers – that answers the question that routine functional stress testing, even for high-risk PCI patients, is not effective or cost effective or beneficial on a yearly basis,” he said. “I think it will help frame care that patients will just be followed with best medical therapy and then if they have recurrence of symptoms they would be considered for further evaluation, either with stress testing or angiography.”
High-risk characteristics
Current guidelines do not advocate the use of routine stress testing after revascularization, the authors wrote in their paper. “However, surveillance with the use of imaging-based stress testing may be considered in high-risk patients at 6 months after a revascularization procedure (class IIb recommendation), and routine imaging-based stress testing may be considered at 1 year after PCI and more than 5 years after CABG [coronary artery bypass graft] (class IIb recommendation).”
But in real-world clinical practice, Dr. Park said, “follow-up strategy for patients who underwent PCI or CABG is still undetermined.” Particularly, “it could be more problematic in high-risk PCI patients with high-risk anatomical or clinical characteristics. Thus, we performed this POST-PCI trial comparing routine stress testing follow-up strategy versus standard-care follow-up strategy in high-risk PCI patients.”
The researchers randomly assigned 1,706 patients with high-risk anatomical or clinical characteristics who had undergone PCI to a follow-up strategy of routine functional testing, including nuclear stress testing, exercise electrocardiography, or stress echocardiography at 1 year, or to standard care alone.
High-risk anatomical features included left main or bifurcation disease; restenotic or long, diffuse lesions; or bypass graft disease. High-risk clinical characteristics included diabetes mellitus, chronic kidney disease, or enzyme-positive acute coronary syndrome.
Mean age of the patients was 64.7 years; 21.0% had left main disease, 43.5% had bifurcation disease, 69.8% had multivessel disease, 70.1% had diffuse long lesions, 38.7% had diabetes, and 96.4% had been treated with drug-eluting stents.
At 2 years, a primary-outcome event had occurred in 46 of 849 patients (Kaplan-Meier estimate, 5.5%) in the functional-testing group and in 51 of 857 (Kaplan-Meier estimate, 6.0%) in the standard-care group (hazard ratio, 0.90; 95% confidence interval, 0.61-1.35; P = .62). There were no between-group differences in the components of the primary outcome.
Secondary endpoints included invasive coronary angiography or repeat revascularization. At 2 years, 12.3% of the patients in the functional-testing group and 9.3% in the standard-care group had undergone invasive coronary angiography (difference, 2.99 percentage points; 95% CI, −0.01 to 5.99 percentage points), and 8.1% and 5.8% of patients, respectively, had a repeat revascularization procedure (difference, 2.23 percentage points; 95% CI, −0.22 to 4.68 percentage points).
Positive results on stress tests were more common with nuclear imaging than with exercise ECG or stress echocardiography, the authors noted. Subsequent coronary angiography and repeat revascularization were more common in patients with positive results on nuclear stress imaging and exercise ECG than in those with discordant results between nuclear imaging and exercise ECG.
POST-PCI was funded by the CardioVascular Research Foundation and Daewoong Pharmaceutical Company. Dr. Park reported grants from the Cardiovascular Research Foundation and Daewoong Pharmaceutical Company. Dr. Tamis-Holland reported “other” funding from Pfizer outside the submitted work. Dr. Wilson reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
New randomized trial results show no benefit in clinical outcomes from active surveillance using functional testing over usual care among high-risk patients with previous percutaneous coronary intervention (PCI).
At 2 years, there was no difference in a composite outcome of death from any cause, MI, or hospitalization for unstable angina between patients who had routine functional testing at 1 year and patients receiving standard care in the POST-PCI trial.
“Our trial does not support active surveillance with routine functional testing for follow-up strategy in high-risk patients who undergo PCI,” first author Duk-Woo Park, MD, division of cardiology, Asan Medical Center, University of Ulsan, Seoul, South Korea, said in an interview.
The researchers said their results should be interpreted in the context of previous findings from the ISCHEMIA trial that showed no difference in death or ischemic events with an initial invasive versus an initial conservative approach in patients with stable coronary artery disease and moderate to severe ischemia on stress testing.
“Both the ISCHEMIA and POST-PCI trials show the benefits of a ‘less is more’ concept (i.e., if more invasive strategies or testing are performed less frequently, it will result in better patient outcomes),” the authors wrote. Although characteristics of the patients in these trials “were quite different, a more invasive therapeutic approach (in the ISCHEMIA trial) as well as a more aggressive follow-up approach (in the POST-PCI trial) did not provide an additional treatment effect beyond a conservative strategy on the basis of guideline-directed medical therapy.”
Results were presented at the annual congress of the European Society of Cardiology and published online simultaneously in the New England Journal of Medicine.
‘Compelling new evidence’
In an editorial accompanying the publication, Jacqueline E. Tamis-Holland, MD, Icahn School of Medicine at Mount Sinai, Mount Sinai Morningside Hospital, New York, also agreed that this new result “builds on the findings” from the ISCHEMIA trial. “Collectively, these trials highlight the lack of benefit of routine stress testing in asymptomatic patients.”
Dr. Tamis-Holland pointed out that many of the deaths in this trial occurred before the 1-year stress test, possibly related to stent thrombosis, and therefore would not have been prevented by routine testing at 1 year. And overall, event rates were “quite low, and most likely reflect adherence to guideline recommendations” in the trial. For example, 99% of patients were receiving statins, and 74% of the procedures used intravascular imaging for the PCI procedures, “a much greater proportion of use than most centers in the United States,” she noted.
“The POST-PCI trial provides compelling new evidence for a future class III recommendation for routine surveillance testing after PCI,” Dr. Tamis-Holland concluded “Until then, we must refrain from prescribing surveillance stress testing to our patients after PCI, in the absence of other clinical signs or symptoms suggestive of stent failure.”
Commenting on the results, B. Hadley Wilson, MD, executive vice chair of the Sanger Heart & Vascular Institute/Atrium Health, clinical professor of medicine at University of North Carolina at Chapel Hill, and vice president of the American College of Cardiology, said that for decades it’s been thought that patients who had high-risk PCI needed to be followed more closely for potential future events.
“And it actually turned out there was no difference in outcomes between the groups,” he said in an interview.
“So, I think it’s a good study – well conducted, good numbers – that answers the question that routine functional stress testing, even for high-risk PCI patients, is not effective or cost effective or beneficial on a yearly basis,” he said. “I think it will help frame care that patients will just be followed with best medical therapy and then if they have recurrence of symptoms they would be considered for further evaluation, either with stress testing or angiography.”
High-risk characteristics
Current guidelines do not advocate the use of routine stress testing after revascularization, the authors wrote in their paper. “However, surveillance with the use of imaging-based stress testing may be considered in high-risk patients at 6 months after a revascularization procedure (class IIb recommendation), and routine imaging-based stress testing may be considered at 1 year after PCI and more than 5 years after CABG [coronary artery bypass graft] (class IIb recommendation).”
But in real-world clinical practice, Dr. Park said, “follow-up strategy for patients who underwent PCI or CABG is still undetermined.” Particularly, “it could be more problematic in high-risk PCI patients with high-risk anatomical or clinical characteristics. Thus, we performed this POST-PCI trial comparing routine stress testing follow-up strategy versus standard-care follow-up strategy in high-risk PCI patients.”
The researchers randomly assigned 1,706 patients with high-risk anatomical or clinical characteristics who had undergone PCI to a follow-up strategy of routine functional testing, including nuclear stress testing, exercise electrocardiography, or stress echocardiography at 1 year, or to standard care alone.
High-risk anatomical features included left main or bifurcation disease; restenotic or long, diffuse lesions; or bypass graft disease. High-risk clinical characteristics included diabetes mellitus, chronic kidney disease, or enzyme-positive acute coronary syndrome.
Mean age of the patients was 64.7 years; 21.0% had left main disease, 43.5% had bifurcation disease, 69.8% had multivessel disease, 70.1% had diffuse long lesions, 38.7% had diabetes, and 96.4% had been treated with drug-eluting stents.
At 2 years, a primary-outcome event had occurred in 46 of 849 patients (Kaplan-Meier estimate, 5.5%) in the functional-testing group and in 51 of 857 (Kaplan-Meier estimate, 6.0%) in the standard-care group (hazard ratio, 0.90; 95% confidence interval, 0.61-1.35; P = .62). There were no between-group differences in the components of the primary outcome.
Secondary endpoints included invasive coronary angiography or repeat revascularization. At 2 years, 12.3% of the patients in the functional-testing group and 9.3% in the standard-care group had undergone invasive coronary angiography (difference, 2.99 percentage points; 95% CI, −0.01 to 5.99 percentage points), and 8.1% and 5.8% of patients, respectively, had a repeat revascularization procedure (difference, 2.23 percentage points; 95% CI, −0.22 to 4.68 percentage points).
Positive results on stress tests were more common with nuclear imaging than with exercise ECG or stress echocardiography, the authors noted. Subsequent coronary angiography and repeat revascularization were more common in patients with positive results on nuclear stress imaging and exercise ECG than in those with discordant results between nuclear imaging and exercise ECG.
POST-PCI was funded by the CardioVascular Research Foundation and Daewoong Pharmaceutical Company. Dr. Park reported grants from the Cardiovascular Research Foundation and Daewoong Pharmaceutical Company. Dr. Tamis-Holland reported “other” funding from Pfizer outside the submitted work. Dr. Wilson reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM ESC CONGRESS 2022
Rivaroxaban outmatched by VKAs for AFib in rheumatic heart disease
Contrary to expectations, vitamin K antagonists (VKAs) reduced the risk for ischemic stroke and death, compared with the factor Xa inhibitor rivaroxaban, (Xarelto, Janssen) in patients with rheumatic heart disease and atrial fibrillation (AFib), in the INVICTUS trial.
Patients receiving a VKA, typically warfarin, had a 25% lower risk for the primary outcome – a composite of stroke, systemic embolism, myocardial infarction, or death from vascular or unknown causes outcome – than receiving rivaroxaban (hazard ratio, 1.25; 95% confidence interval, 1.10-1.41).
This difference was driven primarily by a significant reduction in the risk for death in the VKA group, and without a significant increase in major bleeding, reported Ganesan Karthikeyan, MD, from the All India Institute of Medical Sciences in New Delhi.
“VKA should remain the standard of care for patients with rheumatic heart disease and atrial fibrillation,” he concluded in a hotline session at the annual congress of the European Society of Cardiology.
The study, simultaneously published in the New England Journal of Medicine, is the first randomized controlled trial to assess anticoagulant therapy in patients with rheumatic heart disease and AFib.
“Who could have possibly guessed these results? Certainly not me,” said invited discussant Renato D. Lopes, MD, MHS, PhD, Duke Clinical Research Institute, Durham, N.C. “To me, this is one more classical example of why we need to do randomized trials, since they are the only reliable way to determine treatment effects and drive clinical practice.”
Evidence gap
Rheumatic heart disease affects over 40 million people, mainly living in low- and low- to middle-income countries. About 20% of symptomatic patients have AF and an elevated stroke risk, but previous AFib trials excluded these patients, Dr. Karthikeyan noted.
INVICTUS was led by the Population Health Research Institute in Hamilton, Ont., and enrolled 4,565 patients from 24 countries in Africa, Asia, and Latin America who had rheumatic heart disease, AFib or atrial flutter, and an increased stroke risk caused by any of the following: CHA2DS2VASc score of 2 or more, moderate to severe mitral stenosis (valve area ≤ 2.0 cm2), left atrial spontaneous echo contrast, or left atrial thrombus.
Participants were randomly assigned to receive rivaroxaban, 20 mg once daily (15 mg/d if creatinine clearance was 15-49 mL/min), or a VKA titrated to an international normalized ratio (INR) of 2.0-3.0.
Warfarin was used in 79%-85% of patients assigned to VKA, with the percentage varying between visits. The INR was in therapeutic range in 33.2% of patients at baseline, 65.1% at 3 years, and 64.1% at 4 years.
During an average follow-up of 3.1 years, the primary outcome occurred in 446 patients in the VKA group (6.49% per year) and 560 patients in the rivaroxaban group (8.21% per year). The restricted mean survival time for the primary outcome was 1,675 vs. 1,599 days, respectively (difference, –76 days; 95% CI, –121 to –31 days; P for superiority < .001).
The rate of stroke or systemic embolism was similar between the VKA and rivaroxaban groups (75 vs. 94 events), although ischemic strokes were significantly lower with VKA (48 vs. 74 events).
No easy explanation
Deaths were significantly lower with VKA than rivaroxaban, at 442 versus 552 (restricted mean survival time for death, 1,608 vs. 1,587 days; difference, −72 days; 95% CI, –117 to –28 days).
“This reduction is not easily explained,” Dr. Karthikeyan acknowledged. “We cannot explain this reduction by the reduction in stroke that we saw because the number of deaths that are prevented by VKA are far larger than the number of strokes that are prevented. Moreover, the number of deaths were mainly heart failure or sudden deaths.”
Numbers of patients with major bleeding were also similar in the VKA and rivaroxaban groups (56 vs. 40 patients; P = .18), although numbers with fatal bleeding were lower with rivaroxaban (15 vs. 4, respectively).
By design, there were more physician interactions for monthly monitoring of INR in the VKA group, “but we do not believe such a large reduction can be explained entirely by increased health care contact,” he said. Moreover, there was no significant between-group difference in heart failure medications or hospitalizations or the need for valve replacement.
Almost a quarter (23%) of patients in the rivaroxaban group permanently discontinued the study drug versus just 6% in the VKA group.
Importantly, the mortality benefit emerged much later than in other trials and coincided with the time when the INR became therapeutic at about 3 years, Dr. Karthikeyan said. But it is unknown whether this is because of the INR or an unrelated effect.
More physician contact
Following the presentation, session cochair C. Michael Gibson, MD, Baim Institute for Clinical Research, Harvard Medical School, Boston, questioned the 23% discontinuation rate for rivaroxaban. “Is this really a superiority of warfarin or is this superiority of having someone come in and see their physician for a lot of checks on their INR?”
In response, Dr. Karthikeyan said that permanent discontinuation rates were about 20%-25% in shorter-duration direct oral anticoagulant trials, such as RELY, ROCKET-AF, and ARISTOLE, and exceeded 30% in ENGAGE-AF with 2.8 years’ follow-up.
“So, this is not new,” he said, adding that 31.4% of rivaroxaban patients did so for valve replacement surgery and subsequently received nonstudy VKA.
Dr. Lopes said it is important to keep in mind that INVICTUS enrolled a “very different population” that was younger (mean age, 50.5 years), was much more often female (72.3%), and had fewer comorbidities than patients with AFib who did not have rheumatic heart disease in the pivotal trials.
“It will be interesting to see the treatment effect according to mitral stenosis severity, since we had about 30% with mild mitral stenosis and additionally 18% of patients without mitral stenosis,” he added.
Co–principal investigator Stuart J. Connolly, MD, from the Population Health Research Institute, said physician contacts may be a factor but that the mortality difference was clear, highly significant, and sufficiently powered.
“What’s amazing is that what we’re seeing here is something that hasn’t been previously described with VKA or warfarin, which is that it reduces mortality,” he said in an interview.
Rivaroxaban has never been shown to reduce mortality in any particular condition, and a meta-analysis of other novel oral anticoagulants shows only a small reduction in mortality, caused almost completely by less intracranial hemorrhage than warfarin, he added. “So, we don’t think this is a problem with rivaroxaban. In some ways, rivaroxaban is an innocent bystander to a trial of warfarin in patients with rheumatic heart disease and atrial fibrillation.”
Dr. Connolly said more work is needed to explain the findings and analyses are planned to see which patients are at highest risk for death as well as looking at the relationship between INR control and outcomes.
“We need to do more research on what it is about VKA that could explain this,” he said. “Is it affecting the myocardium in some way, is it preventing fibrosis, is there some off target effect, not on the anticoagulation system, that could explain this?”
Athena Poppas, MD, chief of cardiology at Brown University, Providence, R.I., and past president of the American College of Cardiology, said “INVICTUS is an incredibly important study that needed to be done.”
“The results – though disappointing and surprising in some ways – I don’t think we can explain them away and change what we are doing right now,” she said in an interview.
Although warfarin is a cheap drug, Dr. Poppas said, it would be tremendously helpful to have an alternative treatment for these patients. Mechanistic studies are needed to understand the observed mortality advantage and low bleeding rates but that trials of other novel anticoagulants are also needed.
“But I’m not sure that will happen,” she added. “It’s unlikely to be industry sponsored, so it would be a very expensive lift with a low likelihood of success.”
In an editorial accompanying the paper, Gregory Y.H. Lip, MD, University of Liverpool (England), pointed out that observational data show similar or even higher risks for major bleeding with rivaroxaban than with warfarin. “To improve outcomes in these patients, we therefore need to look beyond anticoagulation alone or beyond a type of anticoagulation drug per se. Indeed, a one-size-fits-all approach may not be appropriate.”
The study was funded by an unrestricted grant from Bayer. Dr. Karthikeyan and Dr. Poppas reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Contrary to expectations, vitamin K antagonists (VKAs) reduced the risk for ischemic stroke and death, compared with the factor Xa inhibitor rivaroxaban, (Xarelto, Janssen) in patients with rheumatic heart disease and atrial fibrillation (AFib), in the INVICTUS trial.
Patients receiving a VKA, typically warfarin, had a 25% lower risk for the primary outcome – a composite of stroke, systemic embolism, myocardial infarction, or death from vascular or unknown causes outcome – than receiving rivaroxaban (hazard ratio, 1.25; 95% confidence interval, 1.10-1.41).
This difference was driven primarily by a significant reduction in the risk for death in the VKA group, and without a significant increase in major bleeding, reported Ganesan Karthikeyan, MD, from the All India Institute of Medical Sciences in New Delhi.
“VKA should remain the standard of care for patients with rheumatic heart disease and atrial fibrillation,” he concluded in a hotline session at the annual congress of the European Society of Cardiology.
The study, simultaneously published in the New England Journal of Medicine, is the first randomized controlled trial to assess anticoagulant therapy in patients with rheumatic heart disease and AFib.
“Who could have possibly guessed these results? Certainly not me,” said invited discussant Renato D. Lopes, MD, MHS, PhD, Duke Clinical Research Institute, Durham, N.C. “To me, this is one more classical example of why we need to do randomized trials, since they are the only reliable way to determine treatment effects and drive clinical practice.”
Evidence gap
Rheumatic heart disease affects over 40 million people, mainly living in low- and low- to middle-income countries. About 20% of symptomatic patients have AF and an elevated stroke risk, but previous AFib trials excluded these patients, Dr. Karthikeyan noted.
INVICTUS was led by the Population Health Research Institute in Hamilton, Ont., and enrolled 4,565 patients from 24 countries in Africa, Asia, and Latin America who had rheumatic heart disease, AFib or atrial flutter, and an increased stroke risk caused by any of the following: CHA2DS2VASc score of 2 or more, moderate to severe mitral stenosis (valve area ≤ 2.0 cm2), left atrial spontaneous echo contrast, or left atrial thrombus.
Participants were randomly assigned to receive rivaroxaban, 20 mg once daily (15 mg/d if creatinine clearance was 15-49 mL/min), or a VKA titrated to an international normalized ratio (INR) of 2.0-3.0.
Warfarin was used in 79%-85% of patients assigned to VKA, with the percentage varying between visits. The INR was in therapeutic range in 33.2% of patients at baseline, 65.1% at 3 years, and 64.1% at 4 years.
During an average follow-up of 3.1 years, the primary outcome occurred in 446 patients in the VKA group (6.49% per year) and 560 patients in the rivaroxaban group (8.21% per year). The restricted mean survival time for the primary outcome was 1,675 vs. 1,599 days, respectively (difference, –76 days; 95% CI, –121 to –31 days; P for superiority < .001).
The rate of stroke or systemic embolism was similar between the VKA and rivaroxaban groups (75 vs. 94 events), although ischemic strokes were significantly lower with VKA (48 vs. 74 events).
No easy explanation
Deaths were significantly lower with VKA than rivaroxaban, at 442 versus 552 (restricted mean survival time for death, 1,608 vs. 1,587 days; difference, −72 days; 95% CI, –117 to –28 days).
“This reduction is not easily explained,” Dr. Karthikeyan acknowledged. “We cannot explain this reduction by the reduction in stroke that we saw because the number of deaths that are prevented by VKA are far larger than the number of strokes that are prevented. Moreover, the number of deaths were mainly heart failure or sudden deaths.”
Numbers of patients with major bleeding were also similar in the VKA and rivaroxaban groups (56 vs. 40 patients; P = .18), although numbers with fatal bleeding were lower with rivaroxaban (15 vs. 4, respectively).
By design, there were more physician interactions for monthly monitoring of INR in the VKA group, “but we do not believe such a large reduction can be explained entirely by increased health care contact,” he said. Moreover, there was no significant between-group difference in heart failure medications or hospitalizations or the need for valve replacement.
Almost a quarter (23%) of patients in the rivaroxaban group permanently discontinued the study drug versus just 6% in the VKA group.
Importantly, the mortality benefit emerged much later than in other trials and coincided with the time when the INR became therapeutic at about 3 years, Dr. Karthikeyan said. But it is unknown whether this is because of the INR or an unrelated effect.
More physician contact
Following the presentation, session cochair C. Michael Gibson, MD, Baim Institute for Clinical Research, Harvard Medical School, Boston, questioned the 23% discontinuation rate for rivaroxaban. “Is this really a superiority of warfarin or is this superiority of having someone come in and see their physician for a lot of checks on their INR?”
In response, Dr. Karthikeyan said that permanent discontinuation rates were about 20%-25% in shorter-duration direct oral anticoagulant trials, such as RELY, ROCKET-AF, and ARISTOLE, and exceeded 30% in ENGAGE-AF with 2.8 years’ follow-up.
“So, this is not new,” he said, adding that 31.4% of rivaroxaban patients did so for valve replacement surgery and subsequently received nonstudy VKA.
Dr. Lopes said it is important to keep in mind that INVICTUS enrolled a “very different population” that was younger (mean age, 50.5 years), was much more often female (72.3%), and had fewer comorbidities than patients with AFib who did not have rheumatic heart disease in the pivotal trials.
“It will be interesting to see the treatment effect according to mitral stenosis severity, since we had about 30% with mild mitral stenosis and additionally 18% of patients without mitral stenosis,” he added.
Co–principal investigator Stuart J. Connolly, MD, from the Population Health Research Institute, said physician contacts may be a factor but that the mortality difference was clear, highly significant, and sufficiently powered.
“What’s amazing is that what we’re seeing here is something that hasn’t been previously described with VKA or warfarin, which is that it reduces mortality,” he said in an interview.
Rivaroxaban has never been shown to reduce mortality in any particular condition, and a meta-analysis of other novel oral anticoagulants shows only a small reduction in mortality, caused almost completely by less intracranial hemorrhage than warfarin, he added. “So, we don’t think this is a problem with rivaroxaban. In some ways, rivaroxaban is an innocent bystander to a trial of warfarin in patients with rheumatic heart disease and atrial fibrillation.”
Dr. Connolly said more work is needed to explain the findings and analyses are planned to see which patients are at highest risk for death as well as looking at the relationship between INR control and outcomes.
“We need to do more research on what it is about VKA that could explain this,” he said. “Is it affecting the myocardium in some way, is it preventing fibrosis, is there some off target effect, not on the anticoagulation system, that could explain this?”
Athena Poppas, MD, chief of cardiology at Brown University, Providence, R.I., and past president of the American College of Cardiology, said “INVICTUS is an incredibly important study that needed to be done.”
“The results – though disappointing and surprising in some ways – I don’t think we can explain them away and change what we are doing right now,” she said in an interview.
Although warfarin is a cheap drug, Dr. Poppas said, it would be tremendously helpful to have an alternative treatment for these patients. Mechanistic studies are needed to understand the observed mortality advantage and low bleeding rates but that trials of other novel anticoagulants are also needed.
“But I’m not sure that will happen,” she added. “It’s unlikely to be industry sponsored, so it would be a very expensive lift with a low likelihood of success.”
In an editorial accompanying the paper, Gregory Y.H. Lip, MD, University of Liverpool (England), pointed out that observational data show similar or even higher risks for major bleeding with rivaroxaban than with warfarin. “To improve outcomes in these patients, we therefore need to look beyond anticoagulation alone or beyond a type of anticoagulation drug per se. Indeed, a one-size-fits-all approach may not be appropriate.”
The study was funded by an unrestricted grant from Bayer. Dr. Karthikeyan and Dr. Poppas reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
Contrary to expectations, vitamin K antagonists (VKAs) reduced the risk for ischemic stroke and death, compared with the factor Xa inhibitor rivaroxaban, (Xarelto, Janssen) in patients with rheumatic heart disease and atrial fibrillation (AFib), in the INVICTUS trial.
Patients receiving a VKA, typically warfarin, had a 25% lower risk for the primary outcome – a composite of stroke, systemic embolism, myocardial infarction, or death from vascular or unknown causes outcome – than receiving rivaroxaban (hazard ratio, 1.25; 95% confidence interval, 1.10-1.41).
This difference was driven primarily by a significant reduction in the risk for death in the VKA group, and without a significant increase in major bleeding, reported Ganesan Karthikeyan, MD, from the All India Institute of Medical Sciences in New Delhi.
“VKA should remain the standard of care for patients with rheumatic heart disease and atrial fibrillation,” he concluded in a hotline session at the annual congress of the European Society of Cardiology.
The study, simultaneously published in the New England Journal of Medicine, is the first randomized controlled trial to assess anticoagulant therapy in patients with rheumatic heart disease and AFib.
“Who could have possibly guessed these results? Certainly not me,” said invited discussant Renato D. Lopes, MD, MHS, PhD, Duke Clinical Research Institute, Durham, N.C. “To me, this is one more classical example of why we need to do randomized trials, since they are the only reliable way to determine treatment effects and drive clinical practice.”
Evidence gap
Rheumatic heart disease affects over 40 million people, mainly living in low- and low- to middle-income countries. About 20% of symptomatic patients have AF and an elevated stroke risk, but previous AFib trials excluded these patients, Dr. Karthikeyan noted.
INVICTUS was led by the Population Health Research Institute in Hamilton, Ont., and enrolled 4,565 patients from 24 countries in Africa, Asia, and Latin America who had rheumatic heart disease, AFib or atrial flutter, and an increased stroke risk caused by any of the following: CHA2DS2VASc score of 2 or more, moderate to severe mitral stenosis (valve area ≤ 2.0 cm2), left atrial spontaneous echo contrast, or left atrial thrombus.
Participants were randomly assigned to receive rivaroxaban, 20 mg once daily (15 mg/d if creatinine clearance was 15-49 mL/min), or a VKA titrated to an international normalized ratio (INR) of 2.0-3.0.
Warfarin was used in 79%-85% of patients assigned to VKA, with the percentage varying between visits. The INR was in therapeutic range in 33.2% of patients at baseline, 65.1% at 3 years, and 64.1% at 4 years.
During an average follow-up of 3.1 years, the primary outcome occurred in 446 patients in the VKA group (6.49% per year) and 560 patients in the rivaroxaban group (8.21% per year). The restricted mean survival time for the primary outcome was 1,675 vs. 1,599 days, respectively (difference, –76 days; 95% CI, –121 to –31 days; P for superiority < .001).
The rate of stroke or systemic embolism was similar between the VKA and rivaroxaban groups (75 vs. 94 events), although ischemic strokes were significantly lower with VKA (48 vs. 74 events).
No easy explanation
Deaths were significantly lower with VKA than rivaroxaban, at 442 versus 552 (restricted mean survival time for death, 1,608 vs. 1,587 days; difference, −72 days; 95% CI, –117 to –28 days).
“This reduction is not easily explained,” Dr. Karthikeyan acknowledged. “We cannot explain this reduction by the reduction in stroke that we saw because the number of deaths that are prevented by VKA are far larger than the number of strokes that are prevented. Moreover, the number of deaths were mainly heart failure or sudden deaths.”
Numbers of patients with major bleeding were also similar in the VKA and rivaroxaban groups (56 vs. 40 patients; P = .18), although numbers with fatal bleeding were lower with rivaroxaban (15 vs. 4, respectively).
By design, there were more physician interactions for monthly monitoring of INR in the VKA group, “but we do not believe such a large reduction can be explained entirely by increased health care contact,” he said. Moreover, there was no significant between-group difference in heart failure medications or hospitalizations or the need for valve replacement.
Almost a quarter (23%) of patients in the rivaroxaban group permanently discontinued the study drug versus just 6% in the VKA group.
Importantly, the mortality benefit emerged much later than in other trials and coincided with the time when the INR became therapeutic at about 3 years, Dr. Karthikeyan said. But it is unknown whether this is because of the INR or an unrelated effect.
More physician contact
Following the presentation, session cochair C. Michael Gibson, MD, Baim Institute for Clinical Research, Harvard Medical School, Boston, questioned the 23% discontinuation rate for rivaroxaban. “Is this really a superiority of warfarin or is this superiority of having someone come in and see their physician for a lot of checks on their INR?”
In response, Dr. Karthikeyan said that permanent discontinuation rates were about 20%-25% in shorter-duration direct oral anticoagulant trials, such as RELY, ROCKET-AF, and ARISTOLE, and exceeded 30% in ENGAGE-AF with 2.8 years’ follow-up.
“So, this is not new,” he said, adding that 31.4% of rivaroxaban patients did so for valve replacement surgery and subsequently received nonstudy VKA.
Dr. Lopes said it is important to keep in mind that INVICTUS enrolled a “very different population” that was younger (mean age, 50.5 years), was much more often female (72.3%), and had fewer comorbidities than patients with AFib who did not have rheumatic heart disease in the pivotal trials.
“It will be interesting to see the treatment effect according to mitral stenosis severity, since we had about 30% with mild mitral stenosis and additionally 18% of patients without mitral stenosis,” he added.
Co–principal investigator Stuart J. Connolly, MD, from the Population Health Research Institute, said physician contacts may be a factor but that the mortality difference was clear, highly significant, and sufficiently powered.
“What’s amazing is that what we’re seeing here is something that hasn’t been previously described with VKA or warfarin, which is that it reduces mortality,” he said in an interview.
Rivaroxaban has never been shown to reduce mortality in any particular condition, and a meta-analysis of other novel oral anticoagulants shows only a small reduction in mortality, caused almost completely by less intracranial hemorrhage than warfarin, he added. “So, we don’t think this is a problem with rivaroxaban. In some ways, rivaroxaban is an innocent bystander to a trial of warfarin in patients with rheumatic heart disease and atrial fibrillation.”
Dr. Connolly said more work is needed to explain the findings and analyses are planned to see which patients are at highest risk for death as well as looking at the relationship between INR control and outcomes.
“We need to do more research on what it is about VKA that could explain this,” he said. “Is it affecting the myocardium in some way, is it preventing fibrosis, is there some off target effect, not on the anticoagulation system, that could explain this?”
Athena Poppas, MD, chief of cardiology at Brown University, Providence, R.I., and past president of the American College of Cardiology, said “INVICTUS is an incredibly important study that needed to be done.”
“The results – though disappointing and surprising in some ways – I don’t think we can explain them away and change what we are doing right now,” she said in an interview.
Although warfarin is a cheap drug, Dr. Poppas said, it would be tremendously helpful to have an alternative treatment for these patients. Mechanistic studies are needed to understand the observed mortality advantage and low bleeding rates but that trials of other novel anticoagulants are also needed.
“But I’m not sure that will happen,” she added. “It’s unlikely to be industry sponsored, so it would be a very expensive lift with a low likelihood of success.”
In an editorial accompanying the paper, Gregory Y.H. Lip, MD, University of Liverpool (England), pointed out that observational data show similar or even higher risks for major bleeding with rivaroxaban than with warfarin. “To improve outcomes in these patients, we therefore need to look beyond anticoagulation alone or beyond a type of anticoagulation drug per se. Indeed, a one-size-fits-all approach may not be appropriate.”
The study was funded by an unrestricted grant from Bayer. Dr. Karthikeyan and Dr. Poppas reported no relevant conflicts of interest.
A version of this article first appeared on Medscape.com.
FROM ESC CONGRESS 2022
COVID-19 vaccine safe in patients with heart failure
Patients with heart failure (HF) who received two doses of COVID mRNA vaccines were not more likely to have worsening disease, venous thromboembolism, or myocarditis within 90 days than similar unvaccinated patients, in a case-control study in Denmark.
Moreover, in the 90 days after receiving the second shot, vaccinated patients were less likely to die of any cause, compared with unvaccinated patients during a similar 90-day period.
Caroline Sindet-Pedersen, PhD, Herlev and Gentofte Hospital, Hellerup, Denmark, and colleagues presented these findings at the annual congress of the European Society of Cardiology.
Major risk is not receiving vaccine
These results “confirm that the major risk for patients with HF is not receiving vaccination for COVID-19,” Marco Metra, MD, who was not involved with this research, said in an interview.
Dr. Metra was coauthor of an ESC guidance for the diagnosis and management of cardiovascular disease during the COVID-19 pandemic, published online ahead of print November 2021 in the European Heart Journal.
The guidance explains that patients with HF are at increased risk for hospitalization, need for mechanical ventilation, and death because of COVID-19, and that vaccination reduces the risk for serious illness from COVID-19, Dr. Sindet-Pedersen and colleagues explained in a press release from the ESC.
However, “concerns remain,” they added, “about the safety of the SARS-CoV-2 mRNA vaccines in heart failure patients, due to a perceived increased risk of cardiovascular side effects.”
The study findings suggest that “there should be no concern about cardiovascular side effects from mRNA vaccines in heart failure patients,” Dr. Sindet-Pedersen and colleagues summarized.
The results also “point to a beneficial effect of vaccination on mortality” and “indicate that patients with HF should be prioritized for COVID-19 vaccinations and boosters,” they added.
“There are ongoing concerns about the safety of COVID-19 vaccination in fragile patients and patients with heart failure,” said Dr. Metra, professor of cardiology and director of the Institute of Cardiology of the Civil Hospital and University of Brescia (Italy).
“These concerns are not based on evidence but just on reports of rare side effects (namely, myocarditis and pericarditis) in vaccinated people,” he added.
Dr. Metra also coauthored a position paper on COVID-19 vaccination in patients with HF from the Heart Failure Association of the ESC, which was published online October 2021 in the European Journal of Heart Failure.
“The current study,” he summarized, “shows a lower risk of mortality among patients vaccinated, compared with those not vaccinated.
“It has limitations,” he cautioned, “as it is not a prospective randomized study, but [rather] an observational one with comparison between vaccinated and not vaccinated patients with similar characteristics.
“However, it was done in a large population,” he noted, “and its results confirm that the major risk for patients with HF is not receiving vaccination for COVID-19.”
95% of patients with HF in Denmark double vaccinated
The group did not analyze the types of all-cause death in their study, Dr. Sindet-Pedersen clarified in an interview.
Other studies have shown that vaccines are associated with improved survival, she noted. For example, bacillus Calmette-Guérin vaccines and the measles vaccines have been linked with a decreased risk for nonspecific mortality in children, and influenza vaccines are associated with decreased all-cause mortality in patients with HF.
The rates of vaccination in this study were much higher than those for patients with HF in the United States.
In a study of 7,094 patients with HF seen at the Mount Sinai Health System between January 2021 and January 2022, 31% of patients were fully vaccinated with two doses and 14.8% had also received a booster, as per Centers for Disease Control and Prevention guidance. However, another 9.1% of patients were only partially vaccinated with one dose, and 45% remained unvaccinated by January 2022,
In the current study, “the uptake was very high,” Dr. Sindet-Pedersen noted, that is, “95% of the prevalent heart failure patients in 2021 received a vaccine.”
“It might be that the last 5% of the patients that did not receive a vaccine were too ill [terminal] to receive the vaccine,” she speculated, “or that was due to personal reasons.”
The researchers identified 50,893 patients with HF who were double vaccinated in 2021 and they matched them with 50,893 unvaccinated patients with HF in 2019 (prepandemic), with the same age, sex, HF duration, use of HF medications, ischemic heart disease, cancer, diabetes, atrial fibrillation, and admission with HF within 90 days.
Almost all patients in the vaccinated group received the Pfizer/BioNTech mRNA vaccine (92%) and the rest received the Moderna mRNA vaccine (8%), in 2021.
The patients had a mean age of 74, and 64% were men. They had HF for a median of 4.1 years.
During the 90-day follow-up, 1,311 patients in the unvaccinated cohort (2.56%) and 1,113 patients in the vaccinated cohort (2.23%) died; there was a significantly lower risk for all-cause death in the vaccinated cohort versus the unvaccinated cohort (–0.33 percentage points; 95% CI, –0.52 to –0.15 percentage points).
The risk for worsening heart failure was 1.1% in each group; myocarditis and venous thromboembolism were extremely rare, and risks for these conditions were not significantly different in the two groups.
The researchers and Dr. Metra declared they have no relevant financial disclosures. Dr. Metra is editor-in-chief of the European Journal of Heart Failure and senior consulting editor of the European Heart Journal.
A version of this article first appeared on Medscape.com.
Patients with heart failure (HF) who received two doses of COVID mRNA vaccines were not more likely to have worsening disease, venous thromboembolism, or myocarditis within 90 days than similar unvaccinated patients, in a case-control study in Denmark.
Moreover, in the 90 days after receiving the second shot, vaccinated patients were less likely to die of any cause, compared with unvaccinated patients during a similar 90-day period.
Caroline Sindet-Pedersen, PhD, Herlev and Gentofte Hospital, Hellerup, Denmark, and colleagues presented these findings at the annual congress of the European Society of Cardiology.
Major risk is not receiving vaccine
These results “confirm that the major risk for patients with HF is not receiving vaccination for COVID-19,” Marco Metra, MD, who was not involved with this research, said in an interview.
Dr. Metra was coauthor of an ESC guidance for the diagnosis and management of cardiovascular disease during the COVID-19 pandemic, published online ahead of print November 2021 in the European Heart Journal.
The guidance explains that patients with HF are at increased risk for hospitalization, need for mechanical ventilation, and death because of COVID-19, and that vaccination reduces the risk for serious illness from COVID-19, Dr. Sindet-Pedersen and colleagues explained in a press release from the ESC.
However, “concerns remain,” they added, “about the safety of the SARS-CoV-2 mRNA vaccines in heart failure patients, due to a perceived increased risk of cardiovascular side effects.”
The study findings suggest that “there should be no concern about cardiovascular side effects from mRNA vaccines in heart failure patients,” Dr. Sindet-Pedersen and colleagues summarized.
The results also “point to a beneficial effect of vaccination on mortality” and “indicate that patients with HF should be prioritized for COVID-19 vaccinations and boosters,” they added.
“There are ongoing concerns about the safety of COVID-19 vaccination in fragile patients and patients with heart failure,” said Dr. Metra, professor of cardiology and director of the Institute of Cardiology of the Civil Hospital and University of Brescia (Italy).
“These concerns are not based on evidence but just on reports of rare side effects (namely, myocarditis and pericarditis) in vaccinated people,” he added.
Dr. Metra also coauthored a position paper on COVID-19 vaccination in patients with HF from the Heart Failure Association of the ESC, which was published online October 2021 in the European Journal of Heart Failure.
“The current study,” he summarized, “shows a lower risk of mortality among patients vaccinated, compared with those not vaccinated.
“It has limitations,” he cautioned, “as it is not a prospective randomized study, but [rather] an observational one with comparison between vaccinated and not vaccinated patients with similar characteristics.
“However, it was done in a large population,” he noted, “and its results confirm that the major risk for patients with HF is not receiving vaccination for COVID-19.”
95% of patients with HF in Denmark double vaccinated
The group did not analyze the types of all-cause death in their study, Dr. Sindet-Pedersen clarified in an interview.
Other studies have shown that vaccines are associated with improved survival, she noted. For example, bacillus Calmette-Guérin vaccines and the measles vaccines have been linked with a decreased risk for nonspecific mortality in children, and influenza vaccines are associated with decreased all-cause mortality in patients with HF.
The rates of vaccination in this study were much higher than those for patients with HF in the United States.
In a study of 7,094 patients with HF seen at the Mount Sinai Health System between January 2021 and January 2022, 31% of patients were fully vaccinated with two doses and 14.8% had also received a booster, as per Centers for Disease Control and Prevention guidance. However, another 9.1% of patients were only partially vaccinated with one dose, and 45% remained unvaccinated by January 2022,
In the current study, “the uptake was very high,” Dr. Sindet-Pedersen noted, that is, “95% of the prevalent heart failure patients in 2021 received a vaccine.”
“It might be that the last 5% of the patients that did not receive a vaccine were too ill [terminal] to receive the vaccine,” she speculated, “or that was due to personal reasons.”
The researchers identified 50,893 patients with HF who were double vaccinated in 2021 and they matched them with 50,893 unvaccinated patients with HF in 2019 (prepandemic), with the same age, sex, HF duration, use of HF medications, ischemic heart disease, cancer, diabetes, atrial fibrillation, and admission with HF within 90 days.
Almost all patients in the vaccinated group received the Pfizer/BioNTech mRNA vaccine (92%) and the rest received the Moderna mRNA vaccine (8%), in 2021.
The patients had a mean age of 74, and 64% were men. They had HF for a median of 4.1 years.
During the 90-day follow-up, 1,311 patients in the unvaccinated cohort (2.56%) and 1,113 patients in the vaccinated cohort (2.23%) died; there was a significantly lower risk for all-cause death in the vaccinated cohort versus the unvaccinated cohort (–0.33 percentage points; 95% CI, –0.52 to –0.15 percentage points).
The risk for worsening heart failure was 1.1% in each group; myocarditis and venous thromboembolism were extremely rare, and risks for these conditions were not significantly different in the two groups.
The researchers and Dr. Metra declared they have no relevant financial disclosures. Dr. Metra is editor-in-chief of the European Journal of Heart Failure and senior consulting editor of the European Heart Journal.
A version of this article first appeared on Medscape.com.
Patients with heart failure (HF) who received two doses of COVID mRNA vaccines were not more likely to have worsening disease, venous thromboembolism, or myocarditis within 90 days than similar unvaccinated patients, in a case-control study in Denmark.
Moreover, in the 90 days after receiving the second shot, vaccinated patients were less likely to die of any cause, compared with unvaccinated patients during a similar 90-day period.
Caroline Sindet-Pedersen, PhD, Herlev and Gentofte Hospital, Hellerup, Denmark, and colleagues presented these findings at the annual congress of the European Society of Cardiology.
Major risk is not receiving vaccine
These results “confirm that the major risk for patients with HF is not receiving vaccination for COVID-19,” Marco Metra, MD, who was not involved with this research, said in an interview.
Dr. Metra was coauthor of an ESC guidance for the diagnosis and management of cardiovascular disease during the COVID-19 pandemic, published online ahead of print November 2021 in the European Heart Journal.
The guidance explains that patients with HF are at increased risk for hospitalization, need for mechanical ventilation, and death because of COVID-19, and that vaccination reduces the risk for serious illness from COVID-19, Dr. Sindet-Pedersen and colleagues explained in a press release from the ESC.
However, “concerns remain,” they added, “about the safety of the SARS-CoV-2 mRNA vaccines in heart failure patients, due to a perceived increased risk of cardiovascular side effects.”
The study findings suggest that “there should be no concern about cardiovascular side effects from mRNA vaccines in heart failure patients,” Dr. Sindet-Pedersen and colleagues summarized.
The results also “point to a beneficial effect of vaccination on mortality” and “indicate that patients with HF should be prioritized for COVID-19 vaccinations and boosters,” they added.
“There are ongoing concerns about the safety of COVID-19 vaccination in fragile patients and patients with heart failure,” said Dr. Metra, professor of cardiology and director of the Institute of Cardiology of the Civil Hospital and University of Brescia (Italy).
“These concerns are not based on evidence but just on reports of rare side effects (namely, myocarditis and pericarditis) in vaccinated people,” he added.
Dr. Metra also coauthored a position paper on COVID-19 vaccination in patients with HF from the Heart Failure Association of the ESC, which was published online October 2021 in the European Journal of Heart Failure.
“The current study,” he summarized, “shows a lower risk of mortality among patients vaccinated, compared with those not vaccinated.
“It has limitations,” he cautioned, “as it is not a prospective randomized study, but [rather] an observational one with comparison between vaccinated and not vaccinated patients with similar characteristics.
“However, it was done in a large population,” he noted, “and its results confirm that the major risk for patients with HF is not receiving vaccination for COVID-19.”
95% of patients with HF in Denmark double vaccinated
The group did not analyze the types of all-cause death in their study, Dr. Sindet-Pedersen clarified in an interview.
Other studies have shown that vaccines are associated with improved survival, she noted. For example, bacillus Calmette-Guérin vaccines and the measles vaccines have been linked with a decreased risk for nonspecific mortality in children, and influenza vaccines are associated with decreased all-cause mortality in patients with HF.
The rates of vaccination in this study were much higher than those for patients with HF in the United States.
In a study of 7,094 patients with HF seen at the Mount Sinai Health System between January 2021 and January 2022, 31% of patients were fully vaccinated with two doses and 14.8% had also received a booster, as per Centers for Disease Control and Prevention guidance. However, another 9.1% of patients were only partially vaccinated with one dose, and 45% remained unvaccinated by January 2022,
In the current study, “the uptake was very high,” Dr. Sindet-Pedersen noted, that is, “95% of the prevalent heart failure patients in 2021 received a vaccine.”
“It might be that the last 5% of the patients that did not receive a vaccine were too ill [terminal] to receive the vaccine,” she speculated, “or that was due to personal reasons.”
The researchers identified 50,893 patients with HF who were double vaccinated in 2021 and they matched them with 50,893 unvaccinated patients with HF in 2019 (prepandemic), with the same age, sex, HF duration, use of HF medications, ischemic heart disease, cancer, diabetes, atrial fibrillation, and admission with HF within 90 days.
Almost all patients in the vaccinated group received the Pfizer/BioNTech mRNA vaccine (92%) and the rest received the Moderna mRNA vaccine (8%), in 2021.
The patients had a mean age of 74, and 64% were men. They had HF for a median of 4.1 years.
During the 90-day follow-up, 1,311 patients in the unvaccinated cohort (2.56%) and 1,113 patients in the vaccinated cohort (2.23%) died; there was a significantly lower risk for all-cause death in the vaccinated cohort versus the unvaccinated cohort (–0.33 percentage points; 95% CI, –0.52 to –0.15 percentage points).
The risk for worsening heart failure was 1.1% in each group; myocarditis and venous thromboembolism were extremely rare, and risks for these conditions were not significantly different in the two groups.
The researchers and Dr. Metra declared they have no relevant financial disclosures. Dr. Metra is editor-in-chief of the European Journal of Heart Failure and senior consulting editor of the European Heart Journal.
A version of this article first appeared on Medscape.com.
FROM ESC CONGRESS 2022
AXIOMATIC-SSP: Cautious optimism on factor XI inhibitor in stroke
The new factor XI inhibitor antithrombotic, milvexian (Bristol-Myers Squibb/Janssen), has shown promising results in a dose-finding phase 2 trial in patients with acute ischemic stroke or transient ischemic attack (TIA), when given in addition to dual antiplatelet therapy.
Although there was no significant reduction in the primary composite endpoint of ischemic stroke or incident infarct on brain MRI at 90 days with milvexian versus placebo in the AXIOMATIC-SSP study, with no apparent dose response, the drug numerically reduced the risk for symptomatic ischemic stroke at most doses. And doses from 25 mg to 100 mg twice daily showed an approximately 30% relative risk reduction in symptomatic ischemic stroke versus placebo.
Milvexian at 25 mg once and twice daily was associated with a low incidence of major bleeding; a moderate increase in bleeding was seen with higher doses.
There was no increase in severe bleeding, compared with placebo, and no fatal bleeding occurred any study group.
“Based on the observed efficacy signal for ischemic stroke, the bleeding profile, and the overall safety and tolerability, milvexian will be further studied in a phase 3 trial in a similar stroke population,” concluded lead investigator, Mukul Sharma, MD, associate professor of medicine at McMaster University, Hamilton, Ont.
Dr. Sharma presented the AXIOMATIC-SSP study results at the annual congress of the European Society of Cardiology.
New generation
Dr. Sharma explained that factor XI inhibitors represent the latest hope for a new generation of antithrombotic drugs with a low bleeding risk.
This has come about after observations that individuals born with factor XI deficiency have lower rates of ischemic stroke and thromboembolism than matched controls, without an offsetting increase in cerebral hemorrhage. In addition, spontaneous bleeding in these individuals is uncommon, and it is thought that factor XI is a strong driver of thrombus growth but plays a less important role in hemostasis, he noted.
“I think there is a tremendous niche for these drugs in stroke prevention,” Dr. Sharma said in an interview. “There is a huge unmet need in stroke patients for something other than aspirin over the long term which is effective but doesn’t cause hemorrhage.”
Dr. Sharma reported that antithrombotic efficacy of milvexian has already been demonstrated in a study of patients undergoing knee replacement in which the drug showed similar or increased efficacy in reducing thromboembolism, compared with enoxaparin, 40 mg, without an increase in major bleeding.
The aim of the current AXIOMATIC-SSP study was to find a dose suitable for use in the treatment of patients with acute stroke or TIA.
Patients with an acute ischemic stroke or TIA are at a high risk for another stroke in the first few months. Although antiplatelet drugs have reduced this event rate, there is still a significant residual risk for ischemic stroke, and the potential for major bleeding with additional antithrombotic therapies has limited the effectiveness of these options, Dr. Sharma explained. Currently, no anticoagulants are approved for noncardioembolic ischemic stroke prevention in the early phase.
The AXIOMATIC-SSP study included 2,366 patients within 48 hours of onset of a mild to moderate acute nonlacunar ischemic stroke. All patients had visible atherosclerotic plaque in a vessel supplying the affected brain region, and they all received background treatment with open-label aspirin and clopidogrel for 21 days, followed by open-label aspirin alone from days 22 to 90.
They were randomly assigned to one of five doses of milvexian (25, 50, 100, or 200 mg twice daily or 25 mg once daily) or placebo daily for 90 days.
The primary efficacy endpoint (symptomatic ischemic stroke or incident infarct on brain MRI) was numerically lower at the 50-mg and 100-mg twice-daily doses, and there was no apparent dose response (placebo, 16.6%; 25 mg once daily, 16.2%; 25 mg twice daily, 18.5%; 50 mg twice daily, 14.1%; 100 mg twice daily, 14.7%; 200 mg twice daily, 16.4%).
However, milvexian was associated with a numerically lower risk for clinical ischemic stroke at all doses except 200 mg twice daily, with doses from 25 to 100 mg twice daily showing an approximately 30% relative risk reduction versus placebo (placebo, 5.5%; 25 mg once daily, 4.6%; 25 mg twice daily, 3.8%; 50 mg twice daily, 4.0%; 100 mg twice daily, 3.5%; 200 mg twice daily, 7.7%).
The main safety endpoint was major bleeding, defined as Bleeding Academic Research Consortium type 3 or 5 bleeding. This was similar to placebo for milvexian 25 mg once daily and twice daily (all 0.6%) but was moderately increased in the 50 mg twice daily (1.5%), 100 mg twice daily (1.6%), and 200 mg twice daily (1.5%) groups.
Most major bleeding episodes were gastrointestinal. There was no increase in severe bleeding or symptomatic intracranial hemorrhage versus placebo, and no fatal bleeding occurred in any arm of the study.
Incremental improvement
On the hope for a class of drugs that reduce ischemic events without increasing bleeding, Dr. Sharma said, “we keep hoping for a home run where there is no increase in bleeding with a new generation of antithrombotic, but what we seem to get is an incremental improvement with each new class.
“Factor Xa inhibitors have a lower rate of bleeding, compared to warfarin. I think we will see another incremental improvement in bleeding with these new factor XI inhibitors and hopefully less of the more serious bleeding,” he said in an interview.
He pointed out that, in this study, milvexian was given on top of dual antiplatelet therapy. “In stroke neurology that sounds very risky as we know that going from a single antiplatelet to two antiplatelet agents increases the risk of bleeding and now we are adding in a third antithrombotic, but we feel comfortable doing it because of what has been observed in patients who have a genetic deficiency of factor XI – very low rates of spontaneous bleeding and they don’t bleed intracranially largely,” he added.
In addition to milvexian, another oral factor XI inhibitor, asundexian (Bayer), is also in development, and similar results were reported in a phase 2 stroke trial (PACIFIC-STROKE) at the same ESC session.
Both drugs are now believed to be going forward into phase 3 trials.
Discussant of the study at the ESC Hotline session, Giovanna Liuzzo, MD, Catholic University of Rome, highlighted the large unmet need for stroke therapies, noting that patients with acute stroke or TIA have a stroke recurrence rate of 5% at 30 days and 17% at 2 years. Although antiplatelet agents are recommended, the use of anticoagulants has been limited by concerns over bleeding risk, and the factor XI inhibitors are promising in that they have the potential for a lower bleeding risk.
She suggested that results from the AXIOMATIC-SSP could point to a dose of milvexian of 25 mg twice daily as a balance between efficacy and bleeding to be taken into larger phase 3 trials
“The jury is still out on the safety and efficacy of milvexian as an adjunct to dual antiplatelet therapy for the prevention of recurrent noncardioembolic stroke,” Dr. Liuzzo concluded. “Only large-scale phase 3 trials will establish the safety and efficacy of factor XI inhibitors in the prevention of venous and arterial thrombosis.”
The AXIOMATIC-SSP study was funded by the Bristol-Myers Squibb/Janssen alliance. Dr. Sharma reported research contracts with Bristol-Myers Squibb, Bayer, and AstraZeneca, and consulting fees from Janssen, Bayer, HLS Therapeutics, and Alexion.
A version of this article first appeared on Medscape.com.
The new factor XI inhibitor antithrombotic, milvexian (Bristol-Myers Squibb/Janssen), has shown promising results in a dose-finding phase 2 trial in patients with acute ischemic stroke or transient ischemic attack (TIA), when given in addition to dual antiplatelet therapy.
Although there was no significant reduction in the primary composite endpoint of ischemic stroke or incident infarct on brain MRI at 90 days with milvexian versus placebo in the AXIOMATIC-SSP study, with no apparent dose response, the drug numerically reduced the risk for symptomatic ischemic stroke at most doses. And doses from 25 mg to 100 mg twice daily showed an approximately 30% relative risk reduction in symptomatic ischemic stroke versus placebo.
Milvexian at 25 mg once and twice daily was associated with a low incidence of major bleeding; a moderate increase in bleeding was seen with higher doses.
There was no increase in severe bleeding, compared with placebo, and no fatal bleeding occurred any study group.
“Based on the observed efficacy signal for ischemic stroke, the bleeding profile, and the overall safety and tolerability, milvexian will be further studied in a phase 3 trial in a similar stroke population,” concluded lead investigator, Mukul Sharma, MD, associate professor of medicine at McMaster University, Hamilton, Ont.
Dr. Sharma presented the AXIOMATIC-SSP study results at the annual congress of the European Society of Cardiology.
New generation
Dr. Sharma explained that factor XI inhibitors represent the latest hope for a new generation of antithrombotic drugs with a low bleeding risk.
This has come about after observations that individuals born with factor XI deficiency have lower rates of ischemic stroke and thromboembolism than matched controls, without an offsetting increase in cerebral hemorrhage. In addition, spontaneous bleeding in these individuals is uncommon, and it is thought that factor XI is a strong driver of thrombus growth but plays a less important role in hemostasis, he noted.
“I think there is a tremendous niche for these drugs in stroke prevention,” Dr. Sharma said in an interview. “There is a huge unmet need in stroke patients for something other than aspirin over the long term which is effective but doesn’t cause hemorrhage.”
Dr. Sharma reported that antithrombotic efficacy of milvexian has already been demonstrated in a study of patients undergoing knee replacement in which the drug showed similar or increased efficacy in reducing thromboembolism, compared with enoxaparin, 40 mg, without an increase in major bleeding.
The aim of the current AXIOMATIC-SSP study was to find a dose suitable for use in the treatment of patients with acute stroke or TIA.
Patients with an acute ischemic stroke or TIA are at a high risk for another stroke in the first few months. Although antiplatelet drugs have reduced this event rate, there is still a significant residual risk for ischemic stroke, and the potential for major bleeding with additional antithrombotic therapies has limited the effectiveness of these options, Dr. Sharma explained. Currently, no anticoagulants are approved for noncardioembolic ischemic stroke prevention in the early phase.
The AXIOMATIC-SSP study included 2,366 patients within 48 hours of onset of a mild to moderate acute nonlacunar ischemic stroke. All patients had visible atherosclerotic plaque in a vessel supplying the affected brain region, and they all received background treatment with open-label aspirin and clopidogrel for 21 days, followed by open-label aspirin alone from days 22 to 90.
They were randomly assigned to one of five doses of milvexian (25, 50, 100, or 200 mg twice daily or 25 mg once daily) or placebo daily for 90 days.
The primary efficacy endpoint (symptomatic ischemic stroke or incident infarct on brain MRI) was numerically lower at the 50-mg and 100-mg twice-daily doses, and there was no apparent dose response (placebo, 16.6%; 25 mg once daily, 16.2%; 25 mg twice daily, 18.5%; 50 mg twice daily, 14.1%; 100 mg twice daily, 14.7%; 200 mg twice daily, 16.4%).
However, milvexian was associated with a numerically lower risk for clinical ischemic stroke at all doses except 200 mg twice daily, with doses from 25 to 100 mg twice daily showing an approximately 30% relative risk reduction versus placebo (placebo, 5.5%; 25 mg once daily, 4.6%; 25 mg twice daily, 3.8%; 50 mg twice daily, 4.0%; 100 mg twice daily, 3.5%; 200 mg twice daily, 7.7%).
The main safety endpoint was major bleeding, defined as Bleeding Academic Research Consortium type 3 or 5 bleeding. This was similar to placebo for milvexian 25 mg once daily and twice daily (all 0.6%) but was moderately increased in the 50 mg twice daily (1.5%), 100 mg twice daily (1.6%), and 200 mg twice daily (1.5%) groups.
Most major bleeding episodes were gastrointestinal. There was no increase in severe bleeding or symptomatic intracranial hemorrhage versus placebo, and no fatal bleeding occurred in any arm of the study.
Incremental improvement
On the hope for a class of drugs that reduce ischemic events without increasing bleeding, Dr. Sharma said, “we keep hoping for a home run where there is no increase in bleeding with a new generation of antithrombotic, but what we seem to get is an incremental improvement with each new class.
“Factor Xa inhibitors have a lower rate of bleeding, compared to warfarin. I think we will see another incremental improvement in bleeding with these new factor XI inhibitors and hopefully less of the more serious bleeding,” he said in an interview.
He pointed out that, in this study, milvexian was given on top of dual antiplatelet therapy. “In stroke neurology that sounds very risky as we know that going from a single antiplatelet to two antiplatelet agents increases the risk of bleeding and now we are adding in a third antithrombotic, but we feel comfortable doing it because of what has been observed in patients who have a genetic deficiency of factor XI – very low rates of spontaneous bleeding and they don’t bleed intracranially largely,” he added.
In addition to milvexian, another oral factor XI inhibitor, asundexian (Bayer), is also in development, and similar results were reported in a phase 2 stroke trial (PACIFIC-STROKE) at the same ESC session.
Both drugs are now believed to be going forward into phase 3 trials.
Discussant of the study at the ESC Hotline session, Giovanna Liuzzo, MD, Catholic University of Rome, highlighted the large unmet need for stroke therapies, noting that patients with acute stroke or TIA have a stroke recurrence rate of 5% at 30 days and 17% at 2 years. Although antiplatelet agents are recommended, the use of anticoagulants has been limited by concerns over bleeding risk, and the factor XI inhibitors are promising in that they have the potential for a lower bleeding risk.
She suggested that results from the AXIOMATIC-SSP could point to a dose of milvexian of 25 mg twice daily as a balance between efficacy and bleeding to be taken into larger phase 3 trials
“The jury is still out on the safety and efficacy of milvexian as an adjunct to dual antiplatelet therapy for the prevention of recurrent noncardioembolic stroke,” Dr. Liuzzo concluded. “Only large-scale phase 3 trials will establish the safety and efficacy of factor XI inhibitors in the prevention of venous and arterial thrombosis.”
The AXIOMATIC-SSP study was funded by the Bristol-Myers Squibb/Janssen alliance. Dr. Sharma reported research contracts with Bristol-Myers Squibb, Bayer, and AstraZeneca, and consulting fees from Janssen, Bayer, HLS Therapeutics, and Alexion.
A version of this article first appeared on Medscape.com.
The new factor XI inhibitor antithrombotic, milvexian (Bristol-Myers Squibb/Janssen), has shown promising results in a dose-finding phase 2 trial in patients with acute ischemic stroke or transient ischemic attack (TIA), when given in addition to dual antiplatelet therapy.
Although there was no significant reduction in the primary composite endpoint of ischemic stroke or incident infarct on brain MRI at 90 days with milvexian versus placebo in the AXIOMATIC-SSP study, with no apparent dose response, the drug numerically reduced the risk for symptomatic ischemic stroke at most doses. And doses from 25 mg to 100 mg twice daily showed an approximately 30% relative risk reduction in symptomatic ischemic stroke versus placebo.
Milvexian at 25 mg once and twice daily was associated with a low incidence of major bleeding; a moderate increase in bleeding was seen with higher doses.
There was no increase in severe bleeding, compared with placebo, and no fatal bleeding occurred any study group.
“Based on the observed efficacy signal for ischemic stroke, the bleeding profile, and the overall safety and tolerability, milvexian will be further studied in a phase 3 trial in a similar stroke population,” concluded lead investigator, Mukul Sharma, MD, associate professor of medicine at McMaster University, Hamilton, Ont.
Dr. Sharma presented the AXIOMATIC-SSP study results at the annual congress of the European Society of Cardiology.
New generation
Dr. Sharma explained that factor XI inhibitors represent the latest hope for a new generation of antithrombotic drugs with a low bleeding risk.
This has come about after observations that individuals born with factor XI deficiency have lower rates of ischemic stroke and thromboembolism than matched controls, without an offsetting increase in cerebral hemorrhage. In addition, spontaneous bleeding in these individuals is uncommon, and it is thought that factor XI is a strong driver of thrombus growth but plays a less important role in hemostasis, he noted.
“I think there is a tremendous niche for these drugs in stroke prevention,” Dr. Sharma said in an interview. “There is a huge unmet need in stroke patients for something other than aspirin over the long term which is effective but doesn’t cause hemorrhage.”
Dr. Sharma reported that antithrombotic efficacy of milvexian has already been demonstrated in a study of patients undergoing knee replacement in which the drug showed similar or increased efficacy in reducing thromboembolism, compared with enoxaparin, 40 mg, without an increase in major bleeding.
The aim of the current AXIOMATIC-SSP study was to find a dose suitable for use in the treatment of patients with acute stroke or TIA.
Patients with an acute ischemic stroke or TIA are at a high risk for another stroke in the first few months. Although antiplatelet drugs have reduced this event rate, there is still a significant residual risk for ischemic stroke, and the potential for major bleeding with additional antithrombotic therapies has limited the effectiveness of these options, Dr. Sharma explained. Currently, no anticoagulants are approved for noncardioembolic ischemic stroke prevention in the early phase.
The AXIOMATIC-SSP study included 2,366 patients within 48 hours of onset of a mild to moderate acute nonlacunar ischemic stroke. All patients had visible atherosclerotic plaque in a vessel supplying the affected brain region, and they all received background treatment with open-label aspirin and clopidogrel for 21 days, followed by open-label aspirin alone from days 22 to 90.
They were randomly assigned to one of five doses of milvexian (25, 50, 100, or 200 mg twice daily or 25 mg once daily) or placebo daily for 90 days.
The primary efficacy endpoint (symptomatic ischemic stroke or incident infarct on brain MRI) was numerically lower at the 50-mg and 100-mg twice-daily doses, and there was no apparent dose response (placebo, 16.6%; 25 mg once daily, 16.2%; 25 mg twice daily, 18.5%; 50 mg twice daily, 14.1%; 100 mg twice daily, 14.7%; 200 mg twice daily, 16.4%).
However, milvexian was associated with a numerically lower risk for clinical ischemic stroke at all doses except 200 mg twice daily, with doses from 25 to 100 mg twice daily showing an approximately 30% relative risk reduction versus placebo (placebo, 5.5%; 25 mg once daily, 4.6%; 25 mg twice daily, 3.8%; 50 mg twice daily, 4.0%; 100 mg twice daily, 3.5%; 200 mg twice daily, 7.7%).
The main safety endpoint was major bleeding, defined as Bleeding Academic Research Consortium type 3 or 5 bleeding. This was similar to placebo for milvexian 25 mg once daily and twice daily (all 0.6%) but was moderately increased in the 50 mg twice daily (1.5%), 100 mg twice daily (1.6%), and 200 mg twice daily (1.5%) groups.
Most major bleeding episodes were gastrointestinal. There was no increase in severe bleeding or symptomatic intracranial hemorrhage versus placebo, and no fatal bleeding occurred in any arm of the study.
Incremental improvement
On the hope for a class of drugs that reduce ischemic events without increasing bleeding, Dr. Sharma said, “we keep hoping for a home run where there is no increase in bleeding with a new generation of antithrombotic, but what we seem to get is an incremental improvement with each new class.
“Factor Xa inhibitors have a lower rate of bleeding, compared to warfarin. I think we will see another incremental improvement in bleeding with these new factor XI inhibitors and hopefully less of the more serious bleeding,” he said in an interview.
He pointed out that, in this study, milvexian was given on top of dual antiplatelet therapy. “In stroke neurology that sounds very risky as we know that going from a single antiplatelet to two antiplatelet agents increases the risk of bleeding and now we are adding in a third antithrombotic, but we feel comfortable doing it because of what has been observed in patients who have a genetic deficiency of factor XI – very low rates of spontaneous bleeding and they don’t bleed intracranially largely,” he added.
In addition to milvexian, another oral factor XI inhibitor, asundexian (Bayer), is also in development, and similar results were reported in a phase 2 stroke trial (PACIFIC-STROKE) at the same ESC session.
Both drugs are now believed to be going forward into phase 3 trials.
Discussant of the study at the ESC Hotline session, Giovanna Liuzzo, MD, Catholic University of Rome, highlighted the large unmet need for stroke therapies, noting that patients with acute stroke or TIA have a stroke recurrence rate of 5% at 30 days and 17% at 2 years. Although antiplatelet agents are recommended, the use of anticoagulants has been limited by concerns over bleeding risk, and the factor XI inhibitors are promising in that they have the potential for a lower bleeding risk.
She suggested that results from the AXIOMATIC-SSP could point to a dose of milvexian of 25 mg twice daily as a balance between efficacy and bleeding to be taken into larger phase 3 trials
“The jury is still out on the safety and efficacy of milvexian as an adjunct to dual antiplatelet therapy for the prevention of recurrent noncardioembolic stroke,” Dr. Liuzzo concluded. “Only large-scale phase 3 trials will establish the safety and efficacy of factor XI inhibitors in the prevention of venous and arterial thrombosis.”
The AXIOMATIC-SSP study was funded by the Bristol-Myers Squibb/Janssen alliance. Dr. Sharma reported research contracts with Bristol-Myers Squibb, Bayer, and AstraZeneca, and consulting fees from Janssen, Bayer, HLS Therapeutics, and Alexion.
A version of this article first appeared on Medscape.com.
FROM ESC CONGRESS 2022
ALL-HEART: No benefit of allopurinol in ischemic heart disease
Allopurinol, a drug commonly used to treat gout, provided no benefit in terms of reducing cardiovascular (CV) events in patients with ischemic heart disease, new randomized trial results show.
Treatment of these patients without gout with 600 mg of allopurinol daily had no effect on composite primary endpoint outcomes, including nonfatal MI, nonfatal stroke, or CV death.
“ALL-HEART is the first large, prospective, randomized trial of the effect of allopurinol on major cardiovascular outcomes in patients with ischemic heart disease and provides robust evidence on the role of allopurinol in these patients,” principal investigator Isla Shelagh Mackenzie, MBChB (Honors), PhD, University of Dundee (Scotland), concluded at a press conference.
Their results suggest allopurinol should not be recommended for secondary prevention of events in this group, Dr. Mackenzie said. Although it remains an important treatment for gout, she added, “other avenues for treatment of ischemic heart disease should be explored in future.”
Results of the ALL-HEART (Allopurinol and Cardiovascular Outcomes in Ischemic Heart Disease) trial were presented at the annual congress of the European Society of Cardiology.
Gout treatment
Allopurinol is a xanthine oxidase inhibitor and acts by reducing serum uric acid levels and oxidative stress. Treatment is generally well tolerated, Dr. Mackenzie noted in her presentation, but some patients develop a rash, which can in some cases be serious or even fatal, progressing to Stevens-Johnson syndrome or toxic epidermal necrolysis, “particularly in certain ethnicities.” If rash develops, the advice is to stop treatment immediately.
“The importance of serum uric acid levels in cardiovascular disease is controversial, and there have been different reports over the years of how important they may be,” Dr. Mackenzie explained.
Observational studies have shown variable results, whereas intervention trials, most with fewer than 100 participants, have suggested potential improvements in factors such as blood pressure, endothelial function, left ventricular hypertrophy, or carotid intima-media thickness. Some have reported benefits in acute coronary syndrome and coronary artery bypass grafting, but others have not, she said. A previous study by their own group suggested an improvement in chest pain and exercise time in patients with chronic stable angina and documented coronary artery disease (CAD).
“So, until now, there have been no large prospective randomized trials of the effects of allopurinol on major cardiovascular outcomes in patients with ischemic heart disease,” Dr. Mackenzie said, and this was the aim of ALL-HEART.
ALL-HEART was a prospective, randomized, open-label, blinded-endpoint, multicenter trial. Patients with ischemia heart disease but no history of gout were recruited from 424 general practices across the United Kingdom, starting in February 2014 and with follow-up ending in September 2021. Participants were randomly assigned 1:1 to receive 600 mg of allopurinol daily or usual care.
“It was a decentralized trial, so the follow-up was largely remote after the first 6 weeks, and that included using record linkage data collected from centralized NHS [National Health Service] databases for hospitalizations and deaths in Scotland and England,” she said. The average follow-up was 4.8 years.
During that time, 258 (9.0%) participants in the allopurinol group and 76 (2.6%) in usual care withdrew from follow-up. By the end of the trial, 57.4% of patients in the allopurinol arm withdrew from randomized treatment.
Mean serum uric acid levels dropped from 0.34 mmol/L at baseline to 0.18 mmol/L at 6 weeks of treatment, “so we can see that the treatment was effective at lowering uric acid,” she noted.
In total, there were 5,721 patients in the final intention-to-treat analysis, and 639 patients had a first primary event.
For the primary outcome of nonfatal MI, nonfatal stroke, and cardiovascular death, there was no difference between the groups, the researchers reported, with a hazard ratio of 1.04 (95% confidence interval, 0.89-1.21; P = .65). Similarly, in secondary analyses, there were no differences in any of the component endpoints making up the primary outcome (nonfatal MI: HR, 0.97; 95% CI, 0.78-1.21; P = .81; nonfatal stroke: HR, 1.20; 95% CI, 0.89-1.60; P = .23; cardiovascular death: HR, 1.10; 95% CI, 0.85-1.43; P = .48), or in all-cause mortality (HR, 1.02; 95% CI, 0.87-1.20; P = .77), between the two groups, Dr. Mackenzie noted, “so a definitively neutral trial all round.”
In addition, no differences were seen in prespecified subgroups, including age, sex, estimated glomerular filtration rate, or diabetes, MI, heart failure, peripheral arterial disease, stroke, and stroke or transient ischemic attack at baseline.
There were also no significant effects on quality of life outcomes. Cost-effectiveness analyses are ongoing, although no differences are expected there, Dr. Mackenzie noted.
In terms of safety, incident cancers and all-cause mortality did not differ between groups. Serious adverse events were also similar between groups, Dr. Mackenzie said, “and there were no fatal treatment-related SAEs [serious adverse events] in the study.”
Another negative antioxidant trial
Invited discussant for the presentation, Leslie Cho, MD, of the Cleveland Clinic said that ALL-HEART, while an excellent trial with a pragmatic design, constitutes yet another negative antioxidant trial.
She pointed to three problems with this study and antioxidant trials in general. “First, the problem is with the antioxidant,” a xanthine oxidase inhibitor. “Xanthine oxidase is not a major trigger of oxidative stress. In a field of major players,” including nitric oxide, uncoupled endothelial nitric oxide synthase, and mitochondria myeloperoxidase, Dr. Cho said, “xanthine oxidase is a minor player.”
“Moreover, 57% of the patients stopped taking allopurinol, and rightfully so,” she said. Patients were receiving optimal medical therapies, many of which are also antioxidants, including statins, ACE inhibitors, angiotensin receptor blockers, and beta-blockers.
Second, the patient population was older, with an average age of 72 years. “This makes the ALL-HEART study a chronic angina study, chronic CAD study, one of the oldest modern day CAD trials. If you look at LoDoCo or ISCHEMIA trials, the average age is 63.” Patients also had established disease, many with previous revascularization.
The final issue seen with this trial, and all antioxidant trials, is that patient selection is not based on oxidative stress or antioxidant level. “The antioxidant trials have been disappointing at best. There is clear and convincing evidence that oxidative stress is involved in the pathogenesis of atherosclerosis, and yet study after study of antioxidant trials have been negative,” she said.
“Currently, there is no reliable measurement of global level of oxidative stress,” Dr. Cho noted. “Moreover, dose response was not tested, and if we cannot test the baseline antioxidant stress level of patients, we also cannot measure the effect of treatment on the global oxidative stress.”
So, “is there no hope for antioxidant trials?” she asked. Three factors will be required for future success, she said. “No. 1, selecting the right patient at the right time. No. 2, a reliable biomarker to measure oxidative stress to guide who should get therapy, and if the therapy is working. And lastly, targeted therapies that work on major triggers of oxidative stress.”
Also commenting on the results, B. Hadley Wilson, MD, executive vice chair of the Sanger Heart & Vascular Institute/Atrium Health, clinical professor of medicine at the University of North Carolina at Chapel Hill, and vice president of the American College of Cardiology, called ALL-HEART “an important and interesting study.”
“For years, cardiologists and others have been interested in allopurinol as an anti-inflammatory, xanthine oxidase inhibitor ... to prevent coronary ischemic events,” he said in an interview.
But this was a well-designed, well-conducted study, and “unfortunately there was no improvement in the primary outcome, no reduction in major cardiovascular events like myocardial infarction or stroke or cardiovascular death,” Dr. Wilson said. “So, it’s a bit of a disappointment that it’s not there as an important medication to help us with these patients with ischemic heart disease, but it’s also an important question answered — that we need to look at treatments for ischemic heart disease other than allopurinol.”
The trial was supported by the National Institute for Health and Care Research Health Technology Assessment Program in the United Kingdom. Dr. Mackenzie reported research contracts to her institution from NIHR HTA for this work, and other disclosures related to other work. Dr. Cho and Dr. Wilson reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
Allopurinol, a drug commonly used to treat gout, provided no benefit in terms of reducing cardiovascular (CV) events in patients with ischemic heart disease, new randomized trial results show.
Treatment of these patients without gout with 600 mg of allopurinol daily had no effect on composite primary endpoint outcomes, including nonfatal MI, nonfatal stroke, or CV death.
“ALL-HEART is the first large, prospective, randomized trial of the effect of allopurinol on major cardiovascular outcomes in patients with ischemic heart disease and provides robust evidence on the role of allopurinol in these patients,” principal investigator Isla Shelagh Mackenzie, MBChB (Honors), PhD, University of Dundee (Scotland), concluded at a press conference.
Their results suggest allopurinol should not be recommended for secondary prevention of events in this group, Dr. Mackenzie said. Although it remains an important treatment for gout, she added, “other avenues for treatment of ischemic heart disease should be explored in future.”
Results of the ALL-HEART (Allopurinol and Cardiovascular Outcomes in Ischemic Heart Disease) trial were presented at the annual congress of the European Society of Cardiology.
Gout treatment
Allopurinol is a xanthine oxidase inhibitor and acts by reducing serum uric acid levels and oxidative stress. Treatment is generally well tolerated, Dr. Mackenzie noted in her presentation, but some patients develop a rash, which can in some cases be serious or even fatal, progressing to Stevens-Johnson syndrome or toxic epidermal necrolysis, “particularly in certain ethnicities.” If rash develops, the advice is to stop treatment immediately.
“The importance of serum uric acid levels in cardiovascular disease is controversial, and there have been different reports over the years of how important they may be,” Dr. Mackenzie explained.
Observational studies have shown variable results, whereas intervention trials, most with fewer than 100 participants, have suggested potential improvements in factors such as blood pressure, endothelial function, left ventricular hypertrophy, or carotid intima-media thickness. Some have reported benefits in acute coronary syndrome and coronary artery bypass grafting, but others have not, she said. A previous study by their own group suggested an improvement in chest pain and exercise time in patients with chronic stable angina and documented coronary artery disease (CAD).
“So, until now, there have been no large prospective randomized trials of the effects of allopurinol on major cardiovascular outcomes in patients with ischemic heart disease,” Dr. Mackenzie said, and this was the aim of ALL-HEART.
ALL-HEART was a prospective, randomized, open-label, blinded-endpoint, multicenter trial. Patients with ischemia heart disease but no history of gout were recruited from 424 general practices across the United Kingdom, starting in February 2014 and with follow-up ending in September 2021. Participants were randomly assigned 1:1 to receive 600 mg of allopurinol daily or usual care.
“It was a decentralized trial, so the follow-up was largely remote after the first 6 weeks, and that included using record linkage data collected from centralized NHS [National Health Service] databases for hospitalizations and deaths in Scotland and England,” she said. The average follow-up was 4.8 years.
During that time, 258 (9.0%) participants in the allopurinol group and 76 (2.6%) in usual care withdrew from follow-up. By the end of the trial, 57.4% of patients in the allopurinol arm withdrew from randomized treatment.
Mean serum uric acid levels dropped from 0.34 mmol/L at baseline to 0.18 mmol/L at 6 weeks of treatment, “so we can see that the treatment was effective at lowering uric acid,” she noted.
In total, there were 5,721 patients in the final intention-to-treat analysis, and 639 patients had a first primary event.
For the primary outcome of nonfatal MI, nonfatal stroke, and cardiovascular death, there was no difference between the groups, the researchers reported, with a hazard ratio of 1.04 (95% confidence interval, 0.89-1.21; P = .65). Similarly, in secondary analyses, there were no differences in any of the component endpoints making up the primary outcome (nonfatal MI: HR, 0.97; 95% CI, 0.78-1.21; P = .81; nonfatal stroke: HR, 1.20; 95% CI, 0.89-1.60; P = .23; cardiovascular death: HR, 1.10; 95% CI, 0.85-1.43; P = .48), or in all-cause mortality (HR, 1.02; 95% CI, 0.87-1.20; P = .77), between the two groups, Dr. Mackenzie noted, “so a definitively neutral trial all round.”
In addition, no differences were seen in prespecified subgroups, including age, sex, estimated glomerular filtration rate, or diabetes, MI, heart failure, peripheral arterial disease, stroke, and stroke or transient ischemic attack at baseline.
There were also no significant effects on quality of life outcomes. Cost-effectiveness analyses are ongoing, although no differences are expected there, Dr. Mackenzie noted.
In terms of safety, incident cancers and all-cause mortality did not differ between groups. Serious adverse events were also similar between groups, Dr. Mackenzie said, “and there were no fatal treatment-related SAEs [serious adverse events] in the study.”
Another negative antioxidant trial
Invited discussant for the presentation, Leslie Cho, MD, of the Cleveland Clinic said that ALL-HEART, while an excellent trial with a pragmatic design, constitutes yet another negative antioxidant trial.
She pointed to three problems with this study and antioxidant trials in general. “First, the problem is with the antioxidant,” a xanthine oxidase inhibitor. “Xanthine oxidase is not a major trigger of oxidative stress. In a field of major players,” including nitric oxide, uncoupled endothelial nitric oxide synthase, and mitochondria myeloperoxidase, Dr. Cho said, “xanthine oxidase is a minor player.”
“Moreover, 57% of the patients stopped taking allopurinol, and rightfully so,” she said. Patients were receiving optimal medical therapies, many of which are also antioxidants, including statins, ACE inhibitors, angiotensin receptor blockers, and beta-blockers.
Second, the patient population was older, with an average age of 72 years. “This makes the ALL-HEART study a chronic angina study, chronic CAD study, one of the oldest modern day CAD trials. If you look at LoDoCo or ISCHEMIA trials, the average age is 63.” Patients also had established disease, many with previous revascularization.
The final issue seen with this trial, and all antioxidant trials, is that patient selection is not based on oxidative stress or antioxidant level. “The antioxidant trials have been disappointing at best. There is clear and convincing evidence that oxidative stress is involved in the pathogenesis of atherosclerosis, and yet study after study of antioxidant trials have been negative,” she said.
“Currently, there is no reliable measurement of global level of oxidative stress,” Dr. Cho noted. “Moreover, dose response was not tested, and if we cannot test the baseline antioxidant stress level of patients, we also cannot measure the effect of treatment on the global oxidative stress.”
So, “is there no hope for antioxidant trials?” she asked. Three factors will be required for future success, she said. “No. 1, selecting the right patient at the right time. No. 2, a reliable biomarker to measure oxidative stress to guide who should get therapy, and if the therapy is working. And lastly, targeted therapies that work on major triggers of oxidative stress.”
Also commenting on the results, B. Hadley Wilson, MD, executive vice chair of the Sanger Heart & Vascular Institute/Atrium Health, clinical professor of medicine at the University of North Carolina at Chapel Hill, and vice president of the American College of Cardiology, called ALL-HEART “an important and interesting study.”
“For years, cardiologists and others have been interested in allopurinol as an anti-inflammatory, xanthine oxidase inhibitor ... to prevent coronary ischemic events,” he said in an interview.
But this was a well-designed, well-conducted study, and “unfortunately there was no improvement in the primary outcome, no reduction in major cardiovascular events like myocardial infarction or stroke or cardiovascular death,” Dr. Wilson said. “So, it’s a bit of a disappointment that it’s not there as an important medication to help us with these patients with ischemic heart disease, but it’s also an important question answered — that we need to look at treatments for ischemic heart disease other than allopurinol.”
The trial was supported by the National Institute for Health and Care Research Health Technology Assessment Program in the United Kingdom. Dr. Mackenzie reported research contracts to her institution from NIHR HTA for this work, and other disclosures related to other work. Dr. Cho and Dr. Wilson reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
Allopurinol, a drug commonly used to treat gout, provided no benefit in terms of reducing cardiovascular (CV) events in patients with ischemic heart disease, new randomized trial results show.
Treatment of these patients without gout with 600 mg of allopurinol daily had no effect on composite primary endpoint outcomes, including nonfatal MI, nonfatal stroke, or CV death.
“ALL-HEART is the first large, prospective, randomized trial of the effect of allopurinol on major cardiovascular outcomes in patients with ischemic heart disease and provides robust evidence on the role of allopurinol in these patients,” principal investigator Isla Shelagh Mackenzie, MBChB (Honors), PhD, University of Dundee (Scotland), concluded at a press conference.
Their results suggest allopurinol should not be recommended for secondary prevention of events in this group, Dr. Mackenzie said. Although it remains an important treatment for gout, she added, “other avenues for treatment of ischemic heart disease should be explored in future.”
Results of the ALL-HEART (Allopurinol and Cardiovascular Outcomes in Ischemic Heart Disease) trial were presented at the annual congress of the European Society of Cardiology.
Gout treatment
Allopurinol is a xanthine oxidase inhibitor and acts by reducing serum uric acid levels and oxidative stress. Treatment is generally well tolerated, Dr. Mackenzie noted in her presentation, but some patients develop a rash, which can in some cases be serious or even fatal, progressing to Stevens-Johnson syndrome or toxic epidermal necrolysis, “particularly in certain ethnicities.” If rash develops, the advice is to stop treatment immediately.
“The importance of serum uric acid levels in cardiovascular disease is controversial, and there have been different reports over the years of how important they may be,” Dr. Mackenzie explained.
Observational studies have shown variable results, whereas intervention trials, most with fewer than 100 participants, have suggested potential improvements in factors such as blood pressure, endothelial function, left ventricular hypertrophy, or carotid intima-media thickness. Some have reported benefits in acute coronary syndrome and coronary artery bypass grafting, but others have not, she said. A previous study by their own group suggested an improvement in chest pain and exercise time in patients with chronic stable angina and documented coronary artery disease (CAD).
“So, until now, there have been no large prospective randomized trials of the effects of allopurinol on major cardiovascular outcomes in patients with ischemic heart disease,” Dr. Mackenzie said, and this was the aim of ALL-HEART.
ALL-HEART was a prospective, randomized, open-label, blinded-endpoint, multicenter trial. Patients with ischemia heart disease but no history of gout were recruited from 424 general practices across the United Kingdom, starting in February 2014 and with follow-up ending in September 2021. Participants were randomly assigned 1:1 to receive 600 mg of allopurinol daily or usual care.
“It was a decentralized trial, so the follow-up was largely remote after the first 6 weeks, and that included using record linkage data collected from centralized NHS [National Health Service] databases for hospitalizations and deaths in Scotland and England,” she said. The average follow-up was 4.8 years.
During that time, 258 (9.0%) participants in the allopurinol group and 76 (2.6%) in usual care withdrew from follow-up. By the end of the trial, 57.4% of patients in the allopurinol arm withdrew from randomized treatment.
Mean serum uric acid levels dropped from 0.34 mmol/L at baseline to 0.18 mmol/L at 6 weeks of treatment, “so we can see that the treatment was effective at lowering uric acid,” she noted.
In total, there were 5,721 patients in the final intention-to-treat analysis, and 639 patients had a first primary event.
For the primary outcome of nonfatal MI, nonfatal stroke, and cardiovascular death, there was no difference between the groups, the researchers reported, with a hazard ratio of 1.04 (95% confidence interval, 0.89-1.21; P = .65). Similarly, in secondary analyses, there were no differences in any of the component endpoints making up the primary outcome (nonfatal MI: HR, 0.97; 95% CI, 0.78-1.21; P = .81; nonfatal stroke: HR, 1.20; 95% CI, 0.89-1.60; P = .23; cardiovascular death: HR, 1.10; 95% CI, 0.85-1.43; P = .48), or in all-cause mortality (HR, 1.02; 95% CI, 0.87-1.20; P = .77), between the two groups, Dr. Mackenzie noted, “so a definitively neutral trial all round.”
In addition, no differences were seen in prespecified subgroups, including age, sex, estimated glomerular filtration rate, or diabetes, MI, heart failure, peripheral arterial disease, stroke, and stroke or transient ischemic attack at baseline.
There were also no significant effects on quality of life outcomes. Cost-effectiveness analyses are ongoing, although no differences are expected there, Dr. Mackenzie noted.
In terms of safety, incident cancers and all-cause mortality did not differ between groups. Serious adverse events were also similar between groups, Dr. Mackenzie said, “and there were no fatal treatment-related SAEs [serious adverse events] in the study.”
Another negative antioxidant trial
Invited discussant for the presentation, Leslie Cho, MD, of the Cleveland Clinic said that ALL-HEART, while an excellent trial with a pragmatic design, constitutes yet another negative antioxidant trial.
She pointed to three problems with this study and antioxidant trials in general. “First, the problem is with the antioxidant,” a xanthine oxidase inhibitor. “Xanthine oxidase is not a major trigger of oxidative stress. In a field of major players,” including nitric oxide, uncoupled endothelial nitric oxide synthase, and mitochondria myeloperoxidase, Dr. Cho said, “xanthine oxidase is a minor player.”
“Moreover, 57% of the patients stopped taking allopurinol, and rightfully so,” she said. Patients were receiving optimal medical therapies, many of which are also antioxidants, including statins, ACE inhibitors, angiotensin receptor blockers, and beta-blockers.
Second, the patient population was older, with an average age of 72 years. “This makes the ALL-HEART study a chronic angina study, chronic CAD study, one of the oldest modern day CAD trials. If you look at LoDoCo or ISCHEMIA trials, the average age is 63.” Patients also had established disease, many with previous revascularization.
The final issue seen with this trial, and all antioxidant trials, is that patient selection is not based on oxidative stress or antioxidant level. “The antioxidant trials have been disappointing at best. There is clear and convincing evidence that oxidative stress is involved in the pathogenesis of atherosclerosis, and yet study after study of antioxidant trials have been negative,” she said.
“Currently, there is no reliable measurement of global level of oxidative stress,” Dr. Cho noted. “Moreover, dose response was not tested, and if we cannot test the baseline antioxidant stress level of patients, we also cannot measure the effect of treatment on the global oxidative stress.”
So, “is there no hope for antioxidant trials?” she asked. Three factors will be required for future success, she said. “No. 1, selecting the right patient at the right time. No. 2, a reliable biomarker to measure oxidative stress to guide who should get therapy, and if the therapy is working. And lastly, targeted therapies that work on major triggers of oxidative stress.”
Also commenting on the results, B. Hadley Wilson, MD, executive vice chair of the Sanger Heart & Vascular Institute/Atrium Health, clinical professor of medicine at the University of North Carolina at Chapel Hill, and vice president of the American College of Cardiology, called ALL-HEART “an important and interesting study.”
“For years, cardiologists and others have been interested in allopurinol as an anti-inflammatory, xanthine oxidase inhibitor ... to prevent coronary ischemic events,” he said in an interview.
But this was a well-designed, well-conducted study, and “unfortunately there was no improvement in the primary outcome, no reduction in major cardiovascular events like myocardial infarction or stroke or cardiovascular death,” Dr. Wilson said. “So, it’s a bit of a disappointment that it’s not there as an important medication to help us with these patients with ischemic heart disease, but it’s also an important question answered — that we need to look at treatments for ischemic heart disease other than allopurinol.”
The trial was supported by the National Institute for Health and Care Research Health Technology Assessment Program in the United Kingdom. Dr. Mackenzie reported research contracts to her institution from NIHR HTA for this work, and other disclosures related to other work. Dr. Cho and Dr. Wilson reported no relevant disclosures.
A version of this article first appeared on Medscape.com.
FROM ESC CONGRESS 2022
Artificial intelligence poised to change paradigm of CV risk prevention
Causal-based algorithm personalizes strategies
Typically, artificial intelligence (AI) is applied to analyze a complex set of variables to make correlations not readily made by unassisted observation. But an AI offshoot, sometimes referred to as causal AI, incorporates causation not just association, and it appears capable of changing the paradigm for preventing cardiovascular (CV) events.
“Causal AI is a new generation of AI algorithms that empowers AI to move beyond prediction to help guide clinical decision-making for each individual,” reported Brian A. Ference, MD, director of research in translational therapeutics, University of Cambridge (England).
In a novel study testing this premise, called CAUSAL AI, this approach was explored with two major risk factors, elevated LDL cholesterol (LDL-C) and elevated systolic BP (SBP). Based on a deep learning algorithm that studied the impact of these risk factors on the biology of atherosclerosis, causal effects of these risk factors were assessed and then embedded in risk estimation.
Causal AI can predict treatment effect
The study showed that the accuracy of risk prediction can be improved markedly with causal AI, but, more importantly, it suggests that causal AI can predict the impact of specific actions to reduce this risk in the context of the patient’s trajectory toward CV events.
“Risk-estimating algorithms are used to select patients at high risk who may benefit from interventions to reduce risk, but they do not include the causal effects of changes in LDL-C and SBP,” Dr. Ference explained.
As a result, they “may not accurately estimate the baseline risk of cardiovascular events caused by a person’s LDL-C or SBP level or the benefit of treating these risk factors,” he added.
In the CAUSAL AI study, presented at the annual congress of the European Society of Cardiology, risk prediction embedded with causal AI demonstrated the ability to match predicted events with actual events in several large sets of patient data.
“Embedding causal effects into risk-estimating algorithms accurately estimates baseline cardiovascular risk caused by LDL and SBP and the benefit of lowering LDL, SBP, or both beginning at any age and extending for any duration,” Dr. Ference said.
Deep-learning AI evaluated more than 300 gene variants
The deep-learning AI was based on Mendelian randomization studies evaluating 140 gene variants associated with LDL-C and 202 variants associated with SBP.
In one test of the predictive impact of causal AI, risk prediction was first conducted in 445,771 participants in the UK Biobank with the Joint British Societies (JBS3) risk calculator. Relative to actual events in this population, the JBS3 alone “consistently underestimated the increased risk caused by elevated LDL, blood pressure, or both” over the lifetime of the patient, according to Dr. Ference.
It also systematically overestimated the risk of cardiovascular events among participants with lower LDL-C, blood pressure, or both.
However, after embedding the causal effect of LDL and blood pressure, “the same algorithm was able to precisely predict the risk of cardiovascular events,” Dr. Ference said. The improved accuracy resulted in “nearly superimposable observed and predicted event curves over time.”
Embedded causal effects precisely predicts outcomes
Causal AI, embedded into risk analyses, was also able to correct for inaccurate risk benefit derived from short-term clinical trials. These also “systematically underestimate the benefit of lowering LDL, blood pressure, or both,” according to Dr. Ference.
“By contrast, after embedding causal effects of LDL and blood pressure into the algorithm, the same algorithm precisely predicted the benefit of lowering LDL, blood pressure, or both at every age, once again producing superimposable observed and predicted event curves.
In another evaluation conducted by Dr. Ference and coinvestigators, the JBS3 algorithm was applied to several major trials, such as the Heart Protection Trial and HOPE-3. By itself, the JBS3 algorithm predicted less benefit than actually observed.
“After embedding causal effects of LDL and blood pressure, the same algorithm was able to precisely predict the benefit of lowering LDL, blood pressure, or both observed in the trials after 3-5 years,” Dr. Ference reported.
In a sensitivity analysis, the accuracy of the prediction remained largely similar across stratifications by risk factors, such as male sex, presence of diabetes, family history of cardiovascular disease, and other variables. It was also similar across participant age prior to a cardiovascular event and all durations of follow-up.
The data presented by Dr. Ference provides compelling evidence that JBS3, which is widely used in the United Kingdom for risk estimates, does not accurately estimate the risk of cardiovascular disease caused by elevated LDL or SBP. It also fails to estimate the benefit of treating these risk factors.
“Therefore, they cannot be used to determine the optimal timing, intensity, and duration of therapies to prevent cardiovascular events,” Dr. Ference said.
By embedding the causal effects of LDL-C and blood pressure through an AI-based algorithm, the benefit of treatment can be estimated accurately “beginning at any age and lasting for any duration, thus providing the essential information to inform individual treatment decisions about ultimate timing, intensity, and duration,” according to Dr. Ference.
Routine application awaits further steps
Despite the promise of this concept, there are many steps to be taken before it is introduced into the clinic, asserted designated discussant Folkert Asselbergs, MD, PhD. In addition to testing the accuracy in multiple populations, “we have to do the trials as well,” meaning prospective evaluations to validate the concept is meaningful for improving outcomes.
However, he does not doubt that the concept of causal AI is promising and likely to have a meaningful impact on cardiology after further validation.
“Causal AI is a crucial step that we need to take for more efficient health care,” he said. One reason he expressed caution is that several risk scores enhanced by AI, although not necessarily causal AI, have shown only “modest predictive value” in several studies that he cited.
“Hopefully the data presented from the CAUSAL AI study will really help us take a step up in the discussion to see how we can really benefit by including genetic information in an AI framework to include causality in predicting risk and predicting benefit of treatment,” said Dr. Asselbergs, professor of precision medicine, University of Utrecht (the Netherlands) Medical Center.
Dr. Ference reported financial relationships with more than 15 pharmaceutical companies. Dr. Asselbergs reported no potential conflicts of interest.
Causal-based algorithm personalizes strategies
Causal-based algorithm personalizes strategies
Typically, artificial intelligence (AI) is applied to analyze a complex set of variables to make correlations not readily made by unassisted observation. But an AI offshoot, sometimes referred to as causal AI, incorporates causation not just association, and it appears capable of changing the paradigm for preventing cardiovascular (CV) events.
“Causal AI is a new generation of AI algorithms that empowers AI to move beyond prediction to help guide clinical decision-making for each individual,” reported Brian A. Ference, MD, director of research in translational therapeutics, University of Cambridge (England).
In a novel study testing this premise, called CAUSAL AI, this approach was explored with two major risk factors, elevated LDL cholesterol (LDL-C) and elevated systolic BP (SBP). Based on a deep learning algorithm that studied the impact of these risk factors on the biology of atherosclerosis, causal effects of these risk factors were assessed and then embedded in risk estimation.
Causal AI can predict treatment effect
The study showed that the accuracy of risk prediction can be improved markedly with causal AI, but, more importantly, it suggests that causal AI can predict the impact of specific actions to reduce this risk in the context of the patient’s trajectory toward CV events.
“Risk-estimating algorithms are used to select patients at high risk who may benefit from interventions to reduce risk, but they do not include the causal effects of changes in LDL-C and SBP,” Dr. Ference explained.
As a result, they “may not accurately estimate the baseline risk of cardiovascular events caused by a person’s LDL-C or SBP level or the benefit of treating these risk factors,” he added.
In the CAUSAL AI study, presented at the annual congress of the European Society of Cardiology, risk prediction embedded with causal AI demonstrated the ability to match predicted events with actual events in several large sets of patient data.
“Embedding causal effects into risk-estimating algorithms accurately estimates baseline cardiovascular risk caused by LDL and SBP and the benefit of lowering LDL, SBP, or both beginning at any age and extending for any duration,” Dr. Ference said.
Deep-learning AI evaluated more than 300 gene variants
The deep-learning AI was based on Mendelian randomization studies evaluating 140 gene variants associated with LDL-C and 202 variants associated with SBP.
In one test of the predictive impact of causal AI, risk prediction was first conducted in 445,771 participants in the UK Biobank with the Joint British Societies (JBS3) risk calculator. Relative to actual events in this population, the JBS3 alone “consistently underestimated the increased risk caused by elevated LDL, blood pressure, or both” over the lifetime of the patient, according to Dr. Ference.
It also systematically overestimated the risk of cardiovascular events among participants with lower LDL-C, blood pressure, or both.
However, after embedding the causal effect of LDL and blood pressure, “the same algorithm was able to precisely predict the risk of cardiovascular events,” Dr. Ference said. The improved accuracy resulted in “nearly superimposable observed and predicted event curves over time.”
Embedded causal effects precisely predicts outcomes
Causal AI, embedded into risk analyses, was also able to correct for inaccurate risk benefit derived from short-term clinical trials. These also “systematically underestimate the benefit of lowering LDL, blood pressure, or both,” according to Dr. Ference.
“By contrast, after embedding causal effects of LDL and blood pressure into the algorithm, the same algorithm precisely predicted the benefit of lowering LDL, blood pressure, or both at every age, once again producing superimposable observed and predicted event curves.
In another evaluation conducted by Dr. Ference and coinvestigators, the JBS3 algorithm was applied to several major trials, such as the Heart Protection Trial and HOPE-3. By itself, the JBS3 algorithm predicted less benefit than actually observed.
“After embedding causal effects of LDL and blood pressure, the same algorithm was able to precisely predict the benefit of lowering LDL, blood pressure, or both observed in the trials after 3-5 years,” Dr. Ference reported.
In a sensitivity analysis, the accuracy of the prediction remained largely similar across stratifications by risk factors, such as male sex, presence of diabetes, family history of cardiovascular disease, and other variables. It was also similar across participant age prior to a cardiovascular event and all durations of follow-up.
The data presented by Dr. Ference provides compelling evidence that JBS3, which is widely used in the United Kingdom for risk estimates, does not accurately estimate the risk of cardiovascular disease caused by elevated LDL or SBP. It also fails to estimate the benefit of treating these risk factors.
“Therefore, they cannot be used to determine the optimal timing, intensity, and duration of therapies to prevent cardiovascular events,” Dr. Ference said.
By embedding the causal effects of LDL-C and blood pressure through an AI-based algorithm, the benefit of treatment can be estimated accurately “beginning at any age and lasting for any duration, thus providing the essential information to inform individual treatment decisions about ultimate timing, intensity, and duration,” according to Dr. Ference.
Routine application awaits further steps
Despite the promise of this concept, there are many steps to be taken before it is introduced into the clinic, asserted designated discussant Folkert Asselbergs, MD, PhD. In addition to testing the accuracy in multiple populations, “we have to do the trials as well,” meaning prospective evaluations to validate the concept is meaningful for improving outcomes.
However, he does not doubt that the concept of causal AI is promising and likely to have a meaningful impact on cardiology after further validation.
“Causal AI is a crucial step that we need to take for more efficient health care,” he said. One reason he expressed caution is that several risk scores enhanced by AI, although not necessarily causal AI, have shown only “modest predictive value” in several studies that he cited.
“Hopefully the data presented from the CAUSAL AI study will really help us take a step up in the discussion to see how we can really benefit by including genetic information in an AI framework to include causality in predicting risk and predicting benefit of treatment,” said Dr. Asselbergs, professor of precision medicine, University of Utrecht (the Netherlands) Medical Center.
Dr. Ference reported financial relationships with more than 15 pharmaceutical companies. Dr. Asselbergs reported no potential conflicts of interest.
Typically, artificial intelligence (AI) is applied to analyze a complex set of variables to make correlations not readily made by unassisted observation. But an AI offshoot, sometimes referred to as causal AI, incorporates causation not just association, and it appears capable of changing the paradigm for preventing cardiovascular (CV) events.
“Causal AI is a new generation of AI algorithms that empowers AI to move beyond prediction to help guide clinical decision-making for each individual,” reported Brian A. Ference, MD, director of research in translational therapeutics, University of Cambridge (England).
In a novel study testing this premise, called CAUSAL AI, this approach was explored with two major risk factors, elevated LDL cholesterol (LDL-C) and elevated systolic BP (SBP). Based on a deep learning algorithm that studied the impact of these risk factors on the biology of atherosclerosis, causal effects of these risk factors were assessed and then embedded in risk estimation.
Causal AI can predict treatment effect
The study showed that the accuracy of risk prediction can be improved markedly with causal AI, but, more importantly, it suggests that causal AI can predict the impact of specific actions to reduce this risk in the context of the patient’s trajectory toward CV events.
“Risk-estimating algorithms are used to select patients at high risk who may benefit from interventions to reduce risk, but they do not include the causal effects of changes in LDL-C and SBP,” Dr. Ference explained.
As a result, they “may not accurately estimate the baseline risk of cardiovascular events caused by a person’s LDL-C or SBP level or the benefit of treating these risk factors,” he added.
In the CAUSAL AI study, presented at the annual congress of the European Society of Cardiology, risk prediction embedded with causal AI demonstrated the ability to match predicted events with actual events in several large sets of patient data.
“Embedding causal effects into risk-estimating algorithms accurately estimates baseline cardiovascular risk caused by LDL and SBP and the benefit of lowering LDL, SBP, or both beginning at any age and extending for any duration,” Dr. Ference said.
Deep-learning AI evaluated more than 300 gene variants
The deep-learning AI was based on Mendelian randomization studies evaluating 140 gene variants associated with LDL-C and 202 variants associated with SBP.
In one test of the predictive impact of causal AI, risk prediction was first conducted in 445,771 participants in the UK Biobank with the Joint British Societies (JBS3) risk calculator. Relative to actual events in this population, the JBS3 alone “consistently underestimated the increased risk caused by elevated LDL, blood pressure, or both” over the lifetime of the patient, according to Dr. Ference.
It also systematically overestimated the risk of cardiovascular events among participants with lower LDL-C, blood pressure, or both.
However, after embedding the causal effect of LDL and blood pressure, “the same algorithm was able to precisely predict the risk of cardiovascular events,” Dr. Ference said. The improved accuracy resulted in “nearly superimposable observed and predicted event curves over time.”
Embedded causal effects precisely predicts outcomes
Causal AI, embedded into risk analyses, was also able to correct for inaccurate risk benefit derived from short-term clinical trials. These also “systematically underestimate the benefit of lowering LDL, blood pressure, or both,” according to Dr. Ference.
“By contrast, after embedding causal effects of LDL and blood pressure into the algorithm, the same algorithm precisely predicted the benefit of lowering LDL, blood pressure, or both at every age, once again producing superimposable observed and predicted event curves.
In another evaluation conducted by Dr. Ference and coinvestigators, the JBS3 algorithm was applied to several major trials, such as the Heart Protection Trial and HOPE-3. By itself, the JBS3 algorithm predicted less benefit than actually observed.
“After embedding causal effects of LDL and blood pressure, the same algorithm was able to precisely predict the benefit of lowering LDL, blood pressure, or both observed in the trials after 3-5 years,” Dr. Ference reported.
In a sensitivity analysis, the accuracy of the prediction remained largely similar across stratifications by risk factors, such as male sex, presence of diabetes, family history of cardiovascular disease, and other variables. It was also similar across participant age prior to a cardiovascular event and all durations of follow-up.
The data presented by Dr. Ference provides compelling evidence that JBS3, which is widely used in the United Kingdom for risk estimates, does not accurately estimate the risk of cardiovascular disease caused by elevated LDL or SBP. It also fails to estimate the benefit of treating these risk factors.
“Therefore, they cannot be used to determine the optimal timing, intensity, and duration of therapies to prevent cardiovascular events,” Dr. Ference said.
By embedding the causal effects of LDL-C and blood pressure through an AI-based algorithm, the benefit of treatment can be estimated accurately “beginning at any age and lasting for any duration, thus providing the essential information to inform individual treatment decisions about ultimate timing, intensity, and duration,” according to Dr. Ference.
Routine application awaits further steps
Despite the promise of this concept, there are many steps to be taken before it is introduced into the clinic, asserted designated discussant Folkert Asselbergs, MD, PhD. In addition to testing the accuracy in multiple populations, “we have to do the trials as well,” meaning prospective evaluations to validate the concept is meaningful for improving outcomes.
However, he does not doubt that the concept of causal AI is promising and likely to have a meaningful impact on cardiology after further validation.
“Causal AI is a crucial step that we need to take for more efficient health care,” he said. One reason he expressed caution is that several risk scores enhanced by AI, although not necessarily causal AI, have shown only “modest predictive value” in several studies that he cited.
“Hopefully the data presented from the CAUSAL AI study will really help us take a step up in the discussion to see how we can really benefit by including genetic information in an AI framework to include causality in predicting risk and predicting benefit of treatment,” said Dr. Asselbergs, professor of precision medicine, University of Utrecht (the Netherlands) Medical Center.
Dr. Ference reported financial relationships with more than 15 pharmaceutical companies. Dr. Asselbergs reported no potential conflicts of interest.
FROM ESC CONGRESS 2022










