User login
‘No justification’ for suicide warning on all antiseizure meds
, new research shows. “There appears to be no justification for the FDA to label every new antiseizure medication with a warning that it may increase risk of suicidality,” said study investigator Michael R. Sperling, MD, professor of neurology, Thomas Jefferson University, Philadelphia.
“How many patients are afraid of their medication and do not take it because of the warning – and are consequently at risk because of that? We do not know, but have anecdotal experience that this is certainly an issue,” Dr. Sperling, who is director of the Jefferson Comprehensive Epilepsy Center, added.
The study was published online August 2 in JAMA Neurology.
Blanket warning
In 2008, the FDA issued an alert stating that antiseizure medications increase suicidality. The alert was based on pooled data from placebo-controlled clinical trials that included 11 antiseizure medications – carbamazepine, felbamate, gabapentin, lamotrigine, levetiracetam, oxcarbazepine, pregabalin, tiagabine, topiramate, valproate, and zonisamide.
The meta-analytic review showed that, compared with placebo, antiseizure medications nearly doubled suicide risk among patients treated for epilepsy, psychiatric disorders, and other diseases. As a result of the FDA study, all antiseizure medications that have been approved since 2008 carry a warning for suicidality.
However, subsequent analyses did not show the same results, Dr. Sperling and colleagues noted.
“Pivotal” antiseizure medication epilepsy trials since 2008 have evaluated suicidality prospectively. Since 2011, trials have included the validated Columbia Suicidality Severity Rating Scale, they noted.
Meta analysis showed no increased risk
Dr. Sperling and colleagues conducted a meta-analysis of 17 randomized placebo-controlled epilepsy trials of five antiseizure medications approved since 2008. These antiseizure medications were eslicarbazepine, perampanel, brivaracetam, cannabidiol, and cenobamate. The trials involved 5,996 patients, including 4,000 who were treated with antiseizure medications and 1,996 who were treated with placebo.
Confining the analysis to epilepsy trials avoids potential confounders, such as possible differences in suicidality risks between different diseases, the researchers noted.
They found no evidence of increased risk for suicidal ideation (overall risk ratio, antiseizure medications vs. placebo: 0.75; 95% confidence interval: 0.35-1.60) or suicide attempt (risk ratio, 0.75; 95% CI: 0.30-1.87) overall or for any individual antiseizure medication.
Suicidal ideation occurred in 12 of 4,000 patients treated with antiseizure medications (0.30%), versus 7 of 1,996 patients treated with placebo (0.35%) (P = .74). Three patients who were treated with antiseizure medications attempted suicide; no patients who were treated with placebo attempted suicide (P = .22). There were no completed suicides.
“There is no current evidence that the five antiseizure medications evaluated in this study increase suicidality in epilepsy and merit a suicidality class warning,” the investigators wrote. When prescribed for epilepsy, “evidence does not support the FDA’s labeling practice of a blanket assumption of increased suicidality,” said Dr. Sperling.
“Our findings indicate the nonspecific suicide warning for all epilepsy drugs is simply not justifiable,” he said. “The results are not surprising. Different drugs affect cells in different ways. So there’s no reason to expect that every drug would increase suicide risk for every patient,” Dr. Sperling said in a statement.
“It’s important to recognize that epilepsy has many causes – perinatal injury, stroke, tumor, head trauma, developmental malformations, genetic causes, and others – and these underlying etiologies may well contribute to the presence of depression and suicidality in this population,” he said in an interview. “Psychodynamic influences also may occur as a consequence of having seizures. This is a complicated area, and drugs are simply one piece of the puzzle,” he added.
Dr. Sperling said the FDA has accomplished “one useful thing with its warning – it highlighted that physicians and other health care providers must pay attention to their patients’ psychological state, ask questions, and treat accordingly.”
The study had no specific funding. Dr. Sperling has received grants from Eisai, Medtronic, Neurelis, SK Life Science, Sunovion, Takeda, Xenon, Cerevel Therapeutics, UCB Pharma, and Engage Pharma; personal fees from Neurelis, Medscape, Neurology Live, International Medical Press, UCB Pharma, Eisai, Oxford University Press, and Projects in Knowledge. He has also consulted for Medtronic outside the submitted work; payments went to Thomas Jefferson University. A complete list of authors’ disclosures is available with the original article.
A version of this article first appeared on Medscape.com.
, new research shows. “There appears to be no justification for the FDA to label every new antiseizure medication with a warning that it may increase risk of suicidality,” said study investigator Michael R. Sperling, MD, professor of neurology, Thomas Jefferson University, Philadelphia.
“How many patients are afraid of their medication and do not take it because of the warning – and are consequently at risk because of that? We do not know, but have anecdotal experience that this is certainly an issue,” Dr. Sperling, who is director of the Jefferson Comprehensive Epilepsy Center, added.
The study was published online August 2 in JAMA Neurology.
Blanket warning
In 2008, the FDA issued an alert stating that antiseizure medications increase suicidality. The alert was based on pooled data from placebo-controlled clinical trials that included 11 antiseizure medications – carbamazepine, felbamate, gabapentin, lamotrigine, levetiracetam, oxcarbazepine, pregabalin, tiagabine, topiramate, valproate, and zonisamide.
The meta-analytic review showed that, compared with placebo, antiseizure medications nearly doubled suicide risk among patients treated for epilepsy, psychiatric disorders, and other diseases. As a result of the FDA study, all antiseizure medications that have been approved since 2008 carry a warning for suicidality.
However, subsequent analyses did not show the same results, Dr. Sperling and colleagues noted.
“Pivotal” antiseizure medication epilepsy trials since 2008 have evaluated suicidality prospectively. Since 2011, trials have included the validated Columbia Suicidality Severity Rating Scale, they noted.
Meta analysis showed no increased risk
Dr. Sperling and colleagues conducted a meta-analysis of 17 randomized placebo-controlled epilepsy trials of five antiseizure medications approved since 2008. These antiseizure medications were eslicarbazepine, perampanel, brivaracetam, cannabidiol, and cenobamate. The trials involved 5,996 patients, including 4,000 who were treated with antiseizure medications and 1,996 who were treated with placebo.
Confining the analysis to epilepsy trials avoids potential confounders, such as possible differences in suicidality risks between different diseases, the researchers noted.
They found no evidence of increased risk for suicidal ideation (overall risk ratio, antiseizure medications vs. placebo: 0.75; 95% confidence interval: 0.35-1.60) or suicide attempt (risk ratio, 0.75; 95% CI: 0.30-1.87) overall or for any individual antiseizure medication.
Suicidal ideation occurred in 12 of 4,000 patients treated with antiseizure medications (0.30%), versus 7 of 1,996 patients treated with placebo (0.35%) (P = .74). Three patients who were treated with antiseizure medications attempted suicide; no patients who were treated with placebo attempted suicide (P = .22). There were no completed suicides.
“There is no current evidence that the five antiseizure medications evaluated in this study increase suicidality in epilepsy and merit a suicidality class warning,” the investigators wrote. When prescribed for epilepsy, “evidence does not support the FDA’s labeling practice of a blanket assumption of increased suicidality,” said Dr. Sperling.
“Our findings indicate the nonspecific suicide warning for all epilepsy drugs is simply not justifiable,” he said. “The results are not surprising. Different drugs affect cells in different ways. So there’s no reason to expect that every drug would increase suicide risk for every patient,” Dr. Sperling said in a statement.
“It’s important to recognize that epilepsy has many causes – perinatal injury, stroke, tumor, head trauma, developmental malformations, genetic causes, and others – and these underlying etiologies may well contribute to the presence of depression and suicidality in this population,” he said in an interview. “Psychodynamic influences also may occur as a consequence of having seizures. This is a complicated area, and drugs are simply one piece of the puzzle,” he added.
Dr. Sperling said the FDA has accomplished “one useful thing with its warning – it highlighted that physicians and other health care providers must pay attention to their patients’ psychological state, ask questions, and treat accordingly.”
The study had no specific funding. Dr. Sperling has received grants from Eisai, Medtronic, Neurelis, SK Life Science, Sunovion, Takeda, Xenon, Cerevel Therapeutics, UCB Pharma, and Engage Pharma; personal fees from Neurelis, Medscape, Neurology Live, International Medical Press, UCB Pharma, Eisai, Oxford University Press, and Projects in Knowledge. He has also consulted for Medtronic outside the submitted work; payments went to Thomas Jefferson University. A complete list of authors’ disclosures is available with the original article.
A version of this article first appeared on Medscape.com.
, new research shows. “There appears to be no justification for the FDA to label every new antiseizure medication with a warning that it may increase risk of suicidality,” said study investigator Michael R. Sperling, MD, professor of neurology, Thomas Jefferson University, Philadelphia.
“How many patients are afraid of their medication and do not take it because of the warning – and are consequently at risk because of that? We do not know, but have anecdotal experience that this is certainly an issue,” Dr. Sperling, who is director of the Jefferson Comprehensive Epilepsy Center, added.
The study was published online August 2 in JAMA Neurology.
Blanket warning
In 2008, the FDA issued an alert stating that antiseizure medications increase suicidality. The alert was based on pooled data from placebo-controlled clinical trials that included 11 antiseizure medications – carbamazepine, felbamate, gabapentin, lamotrigine, levetiracetam, oxcarbazepine, pregabalin, tiagabine, topiramate, valproate, and zonisamide.
The meta-analytic review showed that, compared with placebo, antiseizure medications nearly doubled suicide risk among patients treated for epilepsy, psychiatric disorders, and other diseases. As a result of the FDA study, all antiseizure medications that have been approved since 2008 carry a warning for suicidality.
However, subsequent analyses did not show the same results, Dr. Sperling and colleagues noted.
“Pivotal” antiseizure medication epilepsy trials since 2008 have evaluated suicidality prospectively. Since 2011, trials have included the validated Columbia Suicidality Severity Rating Scale, they noted.
Meta analysis showed no increased risk
Dr. Sperling and colleagues conducted a meta-analysis of 17 randomized placebo-controlled epilepsy trials of five antiseizure medications approved since 2008. These antiseizure medications were eslicarbazepine, perampanel, brivaracetam, cannabidiol, and cenobamate. The trials involved 5,996 patients, including 4,000 who were treated with antiseizure medications and 1,996 who were treated with placebo.
Confining the analysis to epilepsy trials avoids potential confounders, such as possible differences in suicidality risks between different diseases, the researchers noted.
They found no evidence of increased risk for suicidal ideation (overall risk ratio, antiseizure medications vs. placebo: 0.75; 95% confidence interval: 0.35-1.60) or suicide attempt (risk ratio, 0.75; 95% CI: 0.30-1.87) overall or for any individual antiseizure medication.
Suicidal ideation occurred in 12 of 4,000 patients treated with antiseizure medications (0.30%), versus 7 of 1,996 patients treated with placebo (0.35%) (P = .74). Three patients who were treated with antiseizure medications attempted suicide; no patients who were treated with placebo attempted suicide (P = .22). There were no completed suicides.
“There is no current evidence that the five antiseizure medications evaluated in this study increase suicidality in epilepsy and merit a suicidality class warning,” the investigators wrote. When prescribed for epilepsy, “evidence does not support the FDA’s labeling practice of a blanket assumption of increased suicidality,” said Dr. Sperling.
“Our findings indicate the nonspecific suicide warning for all epilepsy drugs is simply not justifiable,” he said. “The results are not surprising. Different drugs affect cells in different ways. So there’s no reason to expect that every drug would increase suicide risk for every patient,” Dr. Sperling said in a statement.
“It’s important to recognize that epilepsy has many causes – perinatal injury, stroke, tumor, head trauma, developmental malformations, genetic causes, and others – and these underlying etiologies may well contribute to the presence of depression and suicidality in this population,” he said in an interview. “Psychodynamic influences also may occur as a consequence of having seizures. This is a complicated area, and drugs are simply one piece of the puzzle,” he added.
Dr. Sperling said the FDA has accomplished “one useful thing with its warning – it highlighted that physicians and other health care providers must pay attention to their patients’ psychological state, ask questions, and treat accordingly.”
The study had no specific funding. Dr. Sperling has received grants from Eisai, Medtronic, Neurelis, SK Life Science, Sunovion, Takeda, Xenon, Cerevel Therapeutics, UCB Pharma, and Engage Pharma; personal fees from Neurelis, Medscape, Neurology Live, International Medical Press, UCB Pharma, Eisai, Oxford University Press, and Projects in Knowledge. He has also consulted for Medtronic outside the submitted work; payments went to Thomas Jefferson University. A complete list of authors’ disclosures is available with the original article.
A version of this article first appeared on Medscape.com.
FROM JAMA NEUROLOGY
CDC officially endorses third dose of mRNA vaccines for immunocompromised
Centers for Disease Control and Prevention Director Rochelle Walensky, MD, has officially signed off on a recommendation by an independent panel of 11 experts to allow people with weakened immune function to get a third dose of certain COVID-19 vaccines.
The decision follows a unanimous vote by the CDC’s Advisory Committee on Immunization Practices (ACIP), which in turn came hours after the U.S. Food and Drug Administration updated its Emergency Use Authorization (EUA) for the Pfizer and Moderna mRNA vaccines.
About 7 million adults in the United States have moderately to severely impaired immune function because of a medical condition they live with or a medication they take to manage a health condition.
People who fall into this category are at higher risk of being hospitalized or dying if they get COVID-19. They are also more likely to transmit the infection. About 40% of vaccinated patients who are hospitalized with breakthrough cases are immunocompromised.
Recent studies have shown that between one-third and one-half of immunocompromised people who didn’t develop antibodies after two doses of a vaccine do get some level of protection after a third dose.
Even then, however, the protection immunocompromised people get from vaccines is not as robust as someone who has healthy immune function, and some panel members were concerned that a third dose might come with a false sense of security.
“My only concern with adding a third dose for the immunocompromised is the impression that our immunocompromised population [will] then be safe,” said ACIP member Helen Talbot, MD, MPH, an associate professor of medicine at Vanderbilt University Medical Center in Nashville, Tenn.
“I think the reality is they’ll be safer but still at incredibly high risk for severe disease and death,” she said.
In updating its EUA, the FDA stressed that, even after a third dose, people who are immunocompromised will still need to wear a mask indoors, socially distance, and avoid large crowds. In addition, family members and other close contacts should be fully vaccinated to protect these vulnerable individuals.
Johnson & Johnson not in the mix
The boosters will be available to children as young as 12 years of age who’ve had a Pfizer vaccine or those ages 18 and older who’ve gotten the Moderna vaccine.
For now, people who’ve had the one-dose Johnson & Johnson vaccine have not been cleared to get a second dose of any vaccine.
FDA experts acknowledged the gap but said that people who had received the Johnson & Johnson vaccine represented a small slice of vaccinated Americans, and said they couldn’t act before the FDA had updated its authorization for that vaccine, which the agency is actively exploring.
“We had to do what we’re doing based on the data we have in hand,” said Peter Marks, MD, director of the Center for Biologics Evaluation and Research at the FDA, the division of the agency that regulates vaccines.
“We think at least there is a solution here for the very large majority of immunocompromised individuals, and we believe we will probably have a solution for the remainder in the not-too-distant future,” Dr. Marks said.
In its updated EUA, the FDA said that the third shots were intended for people who had undergone solid organ transplants or have an “equivalent level of immunocompromise.”
The details
Clinical experts on the CDC panel spent a good deal of time trying to suss out exactly what conditions might fall under the FDA’s umbrella for a third dose.
In a presentation to the committee, Neela Goswami, MD, PhD, an assistant professor of infectious diseases at Emory University School of Medicine and of epidemiology at the Emory Rollins School of Public Health, Atlanta, stressed that the shots are intended for patients who are moderately or severely immunocompromised, in close consultation with their doctors, but that people who should qualify would include those:
- Receiving treatment for solid tumors or blood cancers
- Taking immunosuppressing medications after a solid organ transplant
- Within 2 years of receiving CAR-T therapy or a stem cell transplant
- Who have primary immunodeficiencies – rare genetic disorders that prevent the immune system from working properly
- With advanced or untreated
- Taking high-dose corticosteroids (more than 20 milligrams of or its equivalent daily), alkylating agents, antimetabolites, chemotherapy, TNF blockers, or other immunomodulating or immunosuppressing biologics
- With certain chronic medical conditions, such as or asplenia – living without a spleen
- Receiving dialysis
In discussion, CDC experts clarified that these third doses were not intended for people whose immune function had waned with age, such as elderly residents of long-term care facilities or people with chronic diseases like diabetes.
The idea is to try to get a third dose of the vaccine they’ve already had – Moderna or Pfizer – but if that’s not feasible, it’s fine for the third dose to be different from what someone has had before. The third dose should be given at least 28 days after a second dose, and, ideally, before the initiation of immunosuppressive therapy.
Participants in the meeting said that the CDC would post updated materials on its website to help guide physicians on exactly who should receive third doses.
Ultimately, however, the extra doses will be given on an honor system; no prescriptions or other kinds of clinical documentation will be required for people to get a third dose of these shots.
Tests to measure neutralizing antibodies are also not recommended before the shots are given because of differences in the types of tests used to measure these antibodies and the difficulty in interpreting them. It’s unclear right now what level of neutralizing antibodies is needed for protection.
‘Peace of mind’
In public testimony, Heather Braaten, a 44-year-old being treated for ovarian cancer, said she was grateful to have gotten two shots of the Pfizer vaccine last winter, in between rounds of chemotherapy, but she knew she was probably not well protected. She said she’d become obsessive over the past few months reading medical studies and trying to understand her risk.
“I have felt distraught over the situation. My prognosis is poor. I most likely have about two to three years left to live, so everything counts,” Ms. Braaten said.
She said her life ambitions were humble. She wants to visit with friends and family and not have to worry that she’ll be a breakthrough case. She wants to go grocery shopping again and “not panic and leave the store after five minutes.” She’d love to feel free to travel, she said.
“While I understand I still need to be cautious, I am hopeful for the peace of mind and greater freedom a third shot can provide,” Ms. Braaten said.
More boosters on the way?
In the second half of the meeting, the CDC also signaled that it was considering the use of boosters for people whose immunity might have waned in the months since they had completed their vaccine series, particularly seniors. About 75% of people hospitalized with vaccine breakthrough cases are over age 65, according to CDC data.
Those considerations are becoming more urgent as the Delta variant continues to pummel less vaccinated states and counties.
In its presentation to the ACIP, Heather Scobie, PhD, MPH, a member of the CDC’s COVID Response Team, highlighted data from Canada, Israel, Qatar, and the United Kingdom showing that, while the Pfizer vaccine was still highly effective at preventing hospitalizations and death, it’s far less likely when faced with Delta to prevent an infection that causes symptoms.
In Israel, Pfizer’s vaccine prevented symptoms an average of 41% of the time. In Qatar, which is also using the Moderna vaccine, Pfizer’s prevented symptomatic infections with Delta about 54% of the time compared with 85% with Moderna’s.
Dr. Scobie noted that Pfizer’s waning efficacy may have something to do with the fact that it uses a lower dosage than Moderna’s. Pfizer’s recommended dosing interval is also shorter – 3 weeks compared with 4 weeks for Moderna’s. Stretching the time between shots has been shown to boost vaccine effectiveness, she said.
New data from the Mayo clinic, published ahead of peer review, also suggest that Pfizer’s protection may be fading more quickly than Moderna’s.
In February, both shots were nearly 100% effective at preventing the SARS-CoV-2 infection, but by July, against Delta, Pfizer’s efficacy had dropped to somewhere between 13% and 62%, while Moderna’s was still effective at preventing infection between 58% and 87% of the time.
In July, Pfizer’s was between 24% and 94% effective at preventing hospitalization with a COVID-19 infection and Moderna’s was between 33% and 96% effective at preventing hospitalization.
While that may sound like cause for concern, Dr. Scobie noted that, as of August 2, severe COVD-19 outcomes after vaccination are still very rare. Among 164 million fully vaccinated people in the United States there have been about 7,000 hospitalizations and 1,500 deaths; nearly three out of four of these have been in people over the age of 65.
The ACIP will next meet on August 24 to focus solely on the COVID-19 vaccines.
A version of this article first appeared on Medscape.com.
Centers for Disease Control and Prevention Director Rochelle Walensky, MD, has officially signed off on a recommendation by an independent panel of 11 experts to allow people with weakened immune function to get a third dose of certain COVID-19 vaccines.
The decision follows a unanimous vote by the CDC’s Advisory Committee on Immunization Practices (ACIP), which in turn came hours after the U.S. Food and Drug Administration updated its Emergency Use Authorization (EUA) for the Pfizer and Moderna mRNA vaccines.
About 7 million adults in the United States have moderately to severely impaired immune function because of a medical condition they live with or a medication they take to manage a health condition.
People who fall into this category are at higher risk of being hospitalized or dying if they get COVID-19. They are also more likely to transmit the infection. About 40% of vaccinated patients who are hospitalized with breakthrough cases are immunocompromised.
Recent studies have shown that between one-third and one-half of immunocompromised people who didn’t develop antibodies after two doses of a vaccine do get some level of protection after a third dose.
Even then, however, the protection immunocompromised people get from vaccines is not as robust as someone who has healthy immune function, and some panel members were concerned that a third dose might come with a false sense of security.
“My only concern with adding a third dose for the immunocompromised is the impression that our immunocompromised population [will] then be safe,” said ACIP member Helen Talbot, MD, MPH, an associate professor of medicine at Vanderbilt University Medical Center in Nashville, Tenn.
“I think the reality is they’ll be safer but still at incredibly high risk for severe disease and death,” she said.
In updating its EUA, the FDA stressed that, even after a third dose, people who are immunocompromised will still need to wear a mask indoors, socially distance, and avoid large crowds. In addition, family members and other close contacts should be fully vaccinated to protect these vulnerable individuals.
Johnson & Johnson not in the mix
The boosters will be available to children as young as 12 years of age who’ve had a Pfizer vaccine or those ages 18 and older who’ve gotten the Moderna vaccine.
For now, people who’ve had the one-dose Johnson & Johnson vaccine have not been cleared to get a second dose of any vaccine.
FDA experts acknowledged the gap but said that people who had received the Johnson & Johnson vaccine represented a small slice of vaccinated Americans, and said they couldn’t act before the FDA had updated its authorization for that vaccine, which the agency is actively exploring.
“We had to do what we’re doing based on the data we have in hand,” said Peter Marks, MD, director of the Center for Biologics Evaluation and Research at the FDA, the division of the agency that regulates vaccines.
“We think at least there is a solution here for the very large majority of immunocompromised individuals, and we believe we will probably have a solution for the remainder in the not-too-distant future,” Dr. Marks said.
In its updated EUA, the FDA said that the third shots were intended for people who had undergone solid organ transplants or have an “equivalent level of immunocompromise.”
The details
Clinical experts on the CDC panel spent a good deal of time trying to suss out exactly what conditions might fall under the FDA’s umbrella for a third dose.
In a presentation to the committee, Neela Goswami, MD, PhD, an assistant professor of infectious diseases at Emory University School of Medicine and of epidemiology at the Emory Rollins School of Public Health, Atlanta, stressed that the shots are intended for patients who are moderately or severely immunocompromised, in close consultation with their doctors, but that people who should qualify would include those:
- Receiving treatment for solid tumors or blood cancers
- Taking immunosuppressing medications after a solid organ transplant
- Within 2 years of receiving CAR-T therapy or a stem cell transplant
- Who have primary immunodeficiencies – rare genetic disorders that prevent the immune system from working properly
- With advanced or untreated
- Taking high-dose corticosteroids (more than 20 milligrams of or its equivalent daily), alkylating agents, antimetabolites, chemotherapy, TNF blockers, or other immunomodulating or immunosuppressing biologics
- With certain chronic medical conditions, such as or asplenia – living without a spleen
- Receiving dialysis
In discussion, CDC experts clarified that these third doses were not intended for people whose immune function had waned with age, such as elderly residents of long-term care facilities or people with chronic diseases like diabetes.
The idea is to try to get a third dose of the vaccine they’ve already had – Moderna or Pfizer – but if that’s not feasible, it’s fine for the third dose to be different from what someone has had before. The third dose should be given at least 28 days after a second dose, and, ideally, before the initiation of immunosuppressive therapy.
Participants in the meeting said that the CDC would post updated materials on its website to help guide physicians on exactly who should receive third doses.
Ultimately, however, the extra doses will be given on an honor system; no prescriptions or other kinds of clinical documentation will be required for people to get a third dose of these shots.
Tests to measure neutralizing antibodies are also not recommended before the shots are given because of differences in the types of tests used to measure these antibodies and the difficulty in interpreting them. It’s unclear right now what level of neutralizing antibodies is needed for protection.
‘Peace of mind’
In public testimony, Heather Braaten, a 44-year-old being treated for ovarian cancer, said she was grateful to have gotten two shots of the Pfizer vaccine last winter, in between rounds of chemotherapy, but she knew she was probably not well protected. She said she’d become obsessive over the past few months reading medical studies and trying to understand her risk.
“I have felt distraught over the situation. My prognosis is poor. I most likely have about two to three years left to live, so everything counts,” Ms. Braaten said.
She said her life ambitions were humble. She wants to visit with friends and family and not have to worry that she’ll be a breakthrough case. She wants to go grocery shopping again and “not panic and leave the store after five minutes.” She’d love to feel free to travel, she said.
“While I understand I still need to be cautious, I am hopeful for the peace of mind and greater freedom a third shot can provide,” Ms. Braaten said.
More boosters on the way?
In the second half of the meeting, the CDC also signaled that it was considering the use of boosters for people whose immunity might have waned in the months since they had completed their vaccine series, particularly seniors. About 75% of people hospitalized with vaccine breakthrough cases are over age 65, according to CDC data.
Those considerations are becoming more urgent as the Delta variant continues to pummel less vaccinated states and counties.
In its presentation to the ACIP, Heather Scobie, PhD, MPH, a member of the CDC’s COVID Response Team, highlighted data from Canada, Israel, Qatar, and the United Kingdom showing that, while the Pfizer vaccine was still highly effective at preventing hospitalizations and death, it’s far less likely when faced with Delta to prevent an infection that causes symptoms.
In Israel, Pfizer’s vaccine prevented symptoms an average of 41% of the time. In Qatar, which is also using the Moderna vaccine, Pfizer’s prevented symptomatic infections with Delta about 54% of the time compared with 85% with Moderna’s.
Dr. Scobie noted that Pfizer’s waning efficacy may have something to do with the fact that it uses a lower dosage than Moderna’s. Pfizer’s recommended dosing interval is also shorter – 3 weeks compared with 4 weeks for Moderna’s. Stretching the time between shots has been shown to boost vaccine effectiveness, she said.
New data from the Mayo clinic, published ahead of peer review, also suggest that Pfizer’s protection may be fading more quickly than Moderna’s.
In February, both shots were nearly 100% effective at preventing the SARS-CoV-2 infection, but by July, against Delta, Pfizer’s efficacy had dropped to somewhere between 13% and 62%, while Moderna’s was still effective at preventing infection between 58% and 87% of the time.
In July, Pfizer’s was between 24% and 94% effective at preventing hospitalization with a COVID-19 infection and Moderna’s was between 33% and 96% effective at preventing hospitalization.
While that may sound like cause for concern, Dr. Scobie noted that, as of August 2, severe COVD-19 outcomes after vaccination are still very rare. Among 164 million fully vaccinated people in the United States there have been about 7,000 hospitalizations and 1,500 deaths; nearly three out of four of these have been in people over the age of 65.
The ACIP will next meet on August 24 to focus solely on the COVID-19 vaccines.
A version of this article first appeared on Medscape.com.
Centers for Disease Control and Prevention Director Rochelle Walensky, MD, has officially signed off on a recommendation by an independent panel of 11 experts to allow people with weakened immune function to get a third dose of certain COVID-19 vaccines.
The decision follows a unanimous vote by the CDC’s Advisory Committee on Immunization Practices (ACIP), which in turn came hours after the U.S. Food and Drug Administration updated its Emergency Use Authorization (EUA) for the Pfizer and Moderna mRNA vaccines.
About 7 million adults in the United States have moderately to severely impaired immune function because of a medical condition they live with or a medication they take to manage a health condition.
People who fall into this category are at higher risk of being hospitalized or dying if they get COVID-19. They are also more likely to transmit the infection. About 40% of vaccinated patients who are hospitalized with breakthrough cases are immunocompromised.
Recent studies have shown that between one-third and one-half of immunocompromised people who didn’t develop antibodies after two doses of a vaccine do get some level of protection after a third dose.
Even then, however, the protection immunocompromised people get from vaccines is not as robust as someone who has healthy immune function, and some panel members were concerned that a third dose might come with a false sense of security.
“My only concern with adding a third dose for the immunocompromised is the impression that our immunocompromised population [will] then be safe,” said ACIP member Helen Talbot, MD, MPH, an associate professor of medicine at Vanderbilt University Medical Center in Nashville, Tenn.
“I think the reality is they’ll be safer but still at incredibly high risk for severe disease and death,” she said.
In updating its EUA, the FDA stressed that, even after a third dose, people who are immunocompromised will still need to wear a mask indoors, socially distance, and avoid large crowds. In addition, family members and other close contacts should be fully vaccinated to protect these vulnerable individuals.
Johnson & Johnson not in the mix
The boosters will be available to children as young as 12 years of age who’ve had a Pfizer vaccine or those ages 18 and older who’ve gotten the Moderna vaccine.
For now, people who’ve had the one-dose Johnson & Johnson vaccine have not been cleared to get a second dose of any vaccine.
FDA experts acknowledged the gap but said that people who had received the Johnson & Johnson vaccine represented a small slice of vaccinated Americans, and said they couldn’t act before the FDA had updated its authorization for that vaccine, which the agency is actively exploring.
“We had to do what we’re doing based on the data we have in hand,” said Peter Marks, MD, director of the Center for Biologics Evaluation and Research at the FDA, the division of the agency that regulates vaccines.
“We think at least there is a solution here for the very large majority of immunocompromised individuals, and we believe we will probably have a solution for the remainder in the not-too-distant future,” Dr. Marks said.
In its updated EUA, the FDA said that the third shots were intended for people who had undergone solid organ transplants or have an “equivalent level of immunocompromise.”
The details
Clinical experts on the CDC panel spent a good deal of time trying to suss out exactly what conditions might fall under the FDA’s umbrella for a third dose.
In a presentation to the committee, Neela Goswami, MD, PhD, an assistant professor of infectious diseases at Emory University School of Medicine and of epidemiology at the Emory Rollins School of Public Health, Atlanta, stressed that the shots are intended for patients who are moderately or severely immunocompromised, in close consultation with their doctors, but that people who should qualify would include those:
- Receiving treatment for solid tumors or blood cancers
- Taking immunosuppressing medications after a solid organ transplant
- Within 2 years of receiving CAR-T therapy or a stem cell transplant
- Who have primary immunodeficiencies – rare genetic disorders that prevent the immune system from working properly
- With advanced or untreated
- Taking high-dose corticosteroids (more than 20 milligrams of or its equivalent daily), alkylating agents, antimetabolites, chemotherapy, TNF blockers, or other immunomodulating or immunosuppressing biologics
- With certain chronic medical conditions, such as or asplenia – living without a spleen
- Receiving dialysis
In discussion, CDC experts clarified that these third doses were not intended for people whose immune function had waned with age, such as elderly residents of long-term care facilities or people with chronic diseases like diabetes.
The idea is to try to get a third dose of the vaccine they’ve already had – Moderna or Pfizer – but if that’s not feasible, it’s fine for the third dose to be different from what someone has had before. The third dose should be given at least 28 days after a second dose, and, ideally, before the initiation of immunosuppressive therapy.
Participants in the meeting said that the CDC would post updated materials on its website to help guide physicians on exactly who should receive third doses.
Ultimately, however, the extra doses will be given on an honor system; no prescriptions or other kinds of clinical documentation will be required for people to get a third dose of these shots.
Tests to measure neutralizing antibodies are also not recommended before the shots are given because of differences in the types of tests used to measure these antibodies and the difficulty in interpreting them. It’s unclear right now what level of neutralizing antibodies is needed for protection.
‘Peace of mind’
In public testimony, Heather Braaten, a 44-year-old being treated for ovarian cancer, said she was grateful to have gotten two shots of the Pfizer vaccine last winter, in between rounds of chemotherapy, but she knew she was probably not well protected. She said she’d become obsessive over the past few months reading medical studies and trying to understand her risk.
“I have felt distraught over the situation. My prognosis is poor. I most likely have about two to three years left to live, so everything counts,” Ms. Braaten said.
She said her life ambitions were humble. She wants to visit with friends and family and not have to worry that she’ll be a breakthrough case. She wants to go grocery shopping again and “not panic and leave the store after five minutes.” She’d love to feel free to travel, she said.
“While I understand I still need to be cautious, I am hopeful for the peace of mind and greater freedom a third shot can provide,” Ms. Braaten said.
More boosters on the way?
In the second half of the meeting, the CDC also signaled that it was considering the use of boosters for people whose immunity might have waned in the months since they had completed their vaccine series, particularly seniors. About 75% of people hospitalized with vaccine breakthrough cases are over age 65, according to CDC data.
Those considerations are becoming more urgent as the Delta variant continues to pummel less vaccinated states and counties.
In its presentation to the ACIP, Heather Scobie, PhD, MPH, a member of the CDC’s COVID Response Team, highlighted data from Canada, Israel, Qatar, and the United Kingdom showing that, while the Pfizer vaccine was still highly effective at preventing hospitalizations and death, it’s far less likely when faced with Delta to prevent an infection that causes symptoms.
In Israel, Pfizer’s vaccine prevented symptoms an average of 41% of the time. In Qatar, which is also using the Moderna vaccine, Pfizer’s prevented symptomatic infections with Delta about 54% of the time compared with 85% with Moderna’s.
Dr. Scobie noted that Pfizer’s waning efficacy may have something to do with the fact that it uses a lower dosage than Moderna’s. Pfizer’s recommended dosing interval is also shorter – 3 weeks compared with 4 weeks for Moderna’s. Stretching the time between shots has been shown to boost vaccine effectiveness, she said.
New data from the Mayo clinic, published ahead of peer review, also suggest that Pfizer’s protection may be fading more quickly than Moderna’s.
In February, both shots were nearly 100% effective at preventing the SARS-CoV-2 infection, but by July, against Delta, Pfizer’s efficacy had dropped to somewhere between 13% and 62%, while Moderna’s was still effective at preventing infection between 58% and 87% of the time.
In July, Pfizer’s was between 24% and 94% effective at preventing hospitalization with a COVID-19 infection and Moderna’s was between 33% and 96% effective at preventing hospitalization.
While that may sound like cause for concern, Dr. Scobie noted that, as of August 2, severe COVD-19 outcomes after vaccination are still very rare. Among 164 million fully vaccinated people in the United States there have been about 7,000 hospitalizations and 1,500 deaths; nearly three out of four of these have been in people over the age of 65.
The ACIP will next meet on August 24 to focus solely on the COVID-19 vaccines.
A version of this article first appeared on Medscape.com.
25% of patients with cancer lack immunity against measles
Before the onslaught of COVID-19, researchers at the Fred Hutchinson Cancer Research Center in Seattle had another infectious disease worry: an “unprecedented” outbreak of measles.
“In 2019, we saw the most measles cases in any year since the 1990s,” said Sara Marquis, MPH, a clinical research coordinator at the center. The worry, she says, was that various oncology treatments, such as bone marrow transplantations and assorted biologics, “may leave cancer patients severely immunosuppressed” and thus vulnerable to infectious diseases.
Measles-related illness is typically not severe but can lead to pneumonia, deafness, and death, even in immunocompetent people, Ms. Marquis added.
So in 2019, a team at Fred Hutchinson initiated a study to get a sense of immunity to measles among patients with cancer.
They now report that of a group of 900-plus patients, 25% lacked protective antibodies for measles. That’s “significantly more” than the general population, in which about 8% of people lack these antibodies, Ms. Marquis said.
The study, published online in JAMA Network Open, also found that 38% lacked protection against the less-worrisome infectious disease of mumps, which is more than the 13% found in the general population.
“The scary thing about measles is that it is one of the most contagious diseases known,” Ms. Marquis told this news organization, adding that it is about twice as contagious as the COVID-19 Delta variant.
And it’s not just in the state of Washington. “We’re seeing it more and more in the community,” as various outbreaks continue to happen, she said.
“Deficits in protective antibodies underscore patients’ increased risk during outbreaks and emphasize the need for community-based efforts to increase herd immunity to protect this population,” the study authors conclude.
In short, administration of the measles-mumps-rubella (MMR) vaccine, introduced in 1963, must continue universally, they said
“We’ve had so many incredible advances in cancer treatment in recent years. … it would be devastating to see something like measles, which is a vaccine-preventable disease, come through and negate those efforts,” said study coauthor Elizabeth Krantz, MS, a biostatistician at Fred Hutchinson.
The health care teams and family caregivers of patients with cancer should also make sure they are vaccinated, said Ms. Marquis. However, some patients may not be able to get a measles booster vaccine because it is a live vaccine or because they cannot generate enough antibodies for it to be protective, she explained.
Three subgroups more likely to have deficits
The new study, which is one of the first to measure measles and mumps seroprevalence among patients with cancer in the modern era of cancer treatment, also identified three subgroups that more commonly had immunity deficits: those aged 30-59 years; those with hematologic malignant neoplasms, and those who had received a hematopoietic cell transplant.
In the study, residual clinical plasma samples were obtained from 959 consecutive patients with cancer at Seattle Cancer Care Alliance and Fred Hutchinson in August 2019. These samples were tested for measles and mumps IgG by using a commercial enzyme-linked immunosorbent assay. In all, 60% of patients had a solid tumor and 40% had a blood cancer.
As noted above, the seroprevalence of measles antibodies was 0.75 and the seroprevalence of mumps antibodies was 0.62.
A study author explained why the study included mumps, a less threatening infection.
“We assessed mumps in this study out of interest to compare response in the MMR vaccine component – particularly as we could assess a potent vaccine (measles) versus one that has a weaker immunologic response (mumps). We remain worried about outbreaks of mumps as MMR vaccination rates drop across the U.S.,” wrote Steven Pergam, MD, MPH, infectious disease specialist at Fred Hutchinson, in an email.
Vaccination vigilance is one of the study’s messages. “We all need to do our part to make sure we are up to date with our vaccinations so we can make sure we protect those who are vulnerable,” said Ms. Krantz.
The study was funded by the National Cancer Institute and Seattle Cancer Care Alliance. Multiple study authors have ties to pharmaceutical companies.
A version of this article first appeared on Medscape.com.
Before the onslaught of COVID-19, researchers at the Fred Hutchinson Cancer Research Center in Seattle had another infectious disease worry: an “unprecedented” outbreak of measles.
“In 2019, we saw the most measles cases in any year since the 1990s,” said Sara Marquis, MPH, a clinical research coordinator at the center. The worry, she says, was that various oncology treatments, such as bone marrow transplantations and assorted biologics, “may leave cancer patients severely immunosuppressed” and thus vulnerable to infectious diseases.
Measles-related illness is typically not severe but can lead to pneumonia, deafness, and death, even in immunocompetent people, Ms. Marquis added.
So in 2019, a team at Fred Hutchinson initiated a study to get a sense of immunity to measles among patients with cancer.
They now report that of a group of 900-plus patients, 25% lacked protective antibodies for measles. That’s “significantly more” than the general population, in which about 8% of people lack these antibodies, Ms. Marquis said.
The study, published online in JAMA Network Open, also found that 38% lacked protection against the less-worrisome infectious disease of mumps, which is more than the 13% found in the general population.
“The scary thing about measles is that it is one of the most contagious diseases known,” Ms. Marquis told this news organization, adding that it is about twice as contagious as the COVID-19 Delta variant.
And it’s not just in the state of Washington. “We’re seeing it more and more in the community,” as various outbreaks continue to happen, she said.
“Deficits in protective antibodies underscore patients’ increased risk during outbreaks and emphasize the need for community-based efforts to increase herd immunity to protect this population,” the study authors conclude.
In short, administration of the measles-mumps-rubella (MMR) vaccine, introduced in 1963, must continue universally, they said
“We’ve had so many incredible advances in cancer treatment in recent years. … it would be devastating to see something like measles, which is a vaccine-preventable disease, come through and negate those efforts,” said study coauthor Elizabeth Krantz, MS, a biostatistician at Fred Hutchinson.
The health care teams and family caregivers of patients with cancer should also make sure they are vaccinated, said Ms. Marquis. However, some patients may not be able to get a measles booster vaccine because it is a live vaccine or because they cannot generate enough antibodies for it to be protective, she explained.
Three subgroups more likely to have deficits
The new study, which is one of the first to measure measles and mumps seroprevalence among patients with cancer in the modern era of cancer treatment, also identified three subgroups that more commonly had immunity deficits: those aged 30-59 years; those with hematologic malignant neoplasms, and those who had received a hematopoietic cell transplant.
In the study, residual clinical plasma samples were obtained from 959 consecutive patients with cancer at Seattle Cancer Care Alliance and Fred Hutchinson in August 2019. These samples were tested for measles and mumps IgG by using a commercial enzyme-linked immunosorbent assay. In all, 60% of patients had a solid tumor and 40% had a blood cancer.
As noted above, the seroprevalence of measles antibodies was 0.75 and the seroprevalence of mumps antibodies was 0.62.
A study author explained why the study included mumps, a less threatening infection.
“We assessed mumps in this study out of interest to compare response in the MMR vaccine component – particularly as we could assess a potent vaccine (measles) versus one that has a weaker immunologic response (mumps). We remain worried about outbreaks of mumps as MMR vaccination rates drop across the U.S.,” wrote Steven Pergam, MD, MPH, infectious disease specialist at Fred Hutchinson, in an email.
Vaccination vigilance is one of the study’s messages. “We all need to do our part to make sure we are up to date with our vaccinations so we can make sure we protect those who are vulnerable,” said Ms. Krantz.
The study was funded by the National Cancer Institute and Seattle Cancer Care Alliance. Multiple study authors have ties to pharmaceutical companies.
A version of this article first appeared on Medscape.com.
Before the onslaught of COVID-19, researchers at the Fred Hutchinson Cancer Research Center in Seattle had another infectious disease worry: an “unprecedented” outbreak of measles.
“In 2019, we saw the most measles cases in any year since the 1990s,” said Sara Marquis, MPH, a clinical research coordinator at the center. The worry, she says, was that various oncology treatments, such as bone marrow transplantations and assorted biologics, “may leave cancer patients severely immunosuppressed” and thus vulnerable to infectious diseases.
Measles-related illness is typically not severe but can lead to pneumonia, deafness, and death, even in immunocompetent people, Ms. Marquis added.
So in 2019, a team at Fred Hutchinson initiated a study to get a sense of immunity to measles among patients with cancer.
They now report that of a group of 900-plus patients, 25% lacked protective antibodies for measles. That’s “significantly more” than the general population, in which about 8% of people lack these antibodies, Ms. Marquis said.
The study, published online in JAMA Network Open, also found that 38% lacked protection against the less-worrisome infectious disease of mumps, which is more than the 13% found in the general population.
“The scary thing about measles is that it is one of the most contagious diseases known,” Ms. Marquis told this news organization, adding that it is about twice as contagious as the COVID-19 Delta variant.
And it’s not just in the state of Washington. “We’re seeing it more and more in the community,” as various outbreaks continue to happen, she said.
“Deficits in protective antibodies underscore patients’ increased risk during outbreaks and emphasize the need for community-based efforts to increase herd immunity to protect this population,” the study authors conclude.
In short, administration of the measles-mumps-rubella (MMR) vaccine, introduced in 1963, must continue universally, they said
“We’ve had so many incredible advances in cancer treatment in recent years. … it would be devastating to see something like measles, which is a vaccine-preventable disease, come through and negate those efforts,” said study coauthor Elizabeth Krantz, MS, a biostatistician at Fred Hutchinson.
The health care teams and family caregivers of patients with cancer should also make sure they are vaccinated, said Ms. Marquis. However, some patients may not be able to get a measles booster vaccine because it is a live vaccine or because they cannot generate enough antibodies for it to be protective, she explained.
Three subgroups more likely to have deficits
The new study, which is one of the first to measure measles and mumps seroprevalence among patients with cancer in the modern era of cancer treatment, also identified three subgroups that more commonly had immunity deficits: those aged 30-59 years; those with hematologic malignant neoplasms, and those who had received a hematopoietic cell transplant.
In the study, residual clinical plasma samples were obtained from 959 consecutive patients with cancer at Seattle Cancer Care Alliance and Fred Hutchinson in August 2019. These samples were tested for measles and mumps IgG by using a commercial enzyme-linked immunosorbent assay. In all, 60% of patients had a solid tumor and 40% had a blood cancer.
As noted above, the seroprevalence of measles antibodies was 0.75 and the seroprevalence of mumps antibodies was 0.62.
A study author explained why the study included mumps, a less threatening infection.
“We assessed mumps in this study out of interest to compare response in the MMR vaccine component – particularly as we could assess a potent vaccine (measles) versus one that has a weaker immunologic response (mumps). We remain worried about outbreaks of mumps as MMR vaccination rates drop across the U.S.,” wrote Steven Pergam, MD, MPH, infectious disease specialist at Fred Hutchinson, in an email.
Vaccination vigilance is one of the study’s messages. “We all need to do our part to make sure we are up to date with our vaccinations so we can make sure we protect those who are vulnerable,” said Ms. Krantz.
The study was funded by the National Cancer Institute and Seattle Cancer Care Alliance. Multiple study authors have ties to pharmaceutical companies.
A version of this article first appeared on Medscape.com.
Exercise tied to 50% reduction in mortality after stroke
, with a greater than 50% reduction in risk.
Lead study author Raed A. Joundi, MD, DPhil, of the University of Calgary (Alta.), said he expected results to show exercise was beneficial, but was surprised by the magnitude of the association between physical activity and lower mortality risk.
The impact of physical activity also differed significantly by age; those younger than 75 had a 79% reduction in mortality risk, compared with 32% in those age 75 and older.
“This is even after adjusting for factors such heart disease, respiratory conditions, smoking, and other functional limitations,” said Dr. Joundi.
The study was published online Aug. 11 in the journal Neurology.
For this analysis, the researchers used data on a cohort of people across Canada (excluding the province of Quebec) over 3-9 years. The 895 patients with prior stroke averaged 72 years of age, while the 97,805 in the control group had an average age of 63.
Weekly physical activity averages were evaluated using the self-reporting Canadian Community Health Survey, which was linked with administrative databases to evaluate the association of physical activity with long-term risk for mortality among stroke survivors, compared with controls.
Physical activity was measured in metabolic equivalents (METs); meeting minimum physical activity guidelines was defined as 10 MET-hours/week.
During the study period, more stroke patients than controls died (24.7% vs. 5.7%). However, those who met the physical activity guideline recommendations of 10 MET-hours/week had a lower mortality, both in the stroke survivor group (14.6% vs. 33.2%; adjusted hazard ratio, 0.46; 95% confidence interval, 0.29-0.73) and among control participants (3.6% vs. 7.9%; aHR 0.69; 95% CI, 0.62-0.76).
The largest absolute and relative reduction in mortality was among stroke respondents younger than 75 (10.5% vs. 29%; aHR, 0.21; 95% CI, 0.10-0.43), the researchers note.
There was a significant interaction with age for the stroke patients but not the control group.
“The greatest reduction in mortality was seen between 0 and 10 METs per week … so the main point is that something is better than nothing,” said Dr. Joundi.
Exercise guidelines for the future
Although current guidelines recommend physical activity in stroke survivors, investigators noted that these are largely based on studies in the general population. Therefore, the aim of this research was to get a better understanding of the role of physical activity in the health of stroke survivors in the community, which could ultimately be used to design improved public health campaigns and physical activity interventions.
Given that this is a large study of stroke survivors in the community, Dr. Joundi hopes the results will influence future activity guidelines for those who have suffered a stroke.
“We found a log-linear relationship between physical activity and mortality such that 10 MET-hours/week was associated with large reductions in mortality with most benefit achieved by 20 MET-hours/week,” the authors concluded. “These thresholds could be considered for use in future guidelines for stroke.”
Clinical trials are underway to provide evidence for the implementation of exercise programs after stroke, they add, and offering physical activity programs to stroke survivors in the community “is an increasing priority in the U.S., Canada, and Europe.”
“People are at higher risk of death early on after a stroke but also months and years later, so if we can identify a relatively low-cost and easy intervention like physical activity to improve health and reduce the risk of death for stroke survivors it would be important,” Dr. Joundi said.
Key barriers
Paul George, MD, PhD, a stroke and vascular neurologist at Stanford (Calif.) University, said findings such as these further strengthen the argument that physical exercise is important after stroke.
“Because the study looked specifically at stroke patients, it can provide further guidance on physical activity recommendations that we provide to our patients following stroke,” said Dr. George, who was not associated with the study.
Going forward, he said, more research is needed to identify specifically what is preventing stroke patients from exercising more. What is required, he said, is “future research to determine the key barriers to physical activity following stroke and methods to reduce these will also be important to increasing physical activity in stroke survivors.”
Dr. Joundi said determining how to tailor exercise recommendations to meet the wide range of capabilities of stroke survivors will be another key factor.
“Stroke survivors may have some disabilities, so we need to be able to engage them at an [exercise] level that’s possible for them,” he said.
The study did not include stroke survivors living in long-term care homes.
The study had no targeted funding. Coauthor Eric E. Smith, MD, MPH, reports royalties from UpToDate, and consulting fees from Alnylam, Biogen, and Javelin. Dr. Joundi and the other coauthors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, with a greater than 50% reduction in risk.
Lead study author Raed A. Joundi, MD, DPhil, of the University of Calgary (Alta.), said he expected results to show exercise was beneficial, but was surprised by the magnitude of the association between physical activity and lower mortality risk.
The impact of physical activity also differed significantly by age; those younger than 75 had a 79% reduction in mortality risk, compared with 32% in those age 75 and older.
“This is even after adjusting for factors such heart disease, respiratory conditions, smoking, and other functional limitations,” said Dr. Joundi.
The study was published online Aug. 11 in the journal Neurology.
For this analysis, the researchers used data on a cohort of people across Canada (excluding the province of Quebec) over 3-9 years. The 895 patients with prior stroke averaged 72 years of age, while the 97,805 in the control group had an average age of 63.
Weekly physical activity averages were evaluated using the self-reporting Canadian Community Health Survey, which was linked with administrative databases to evaluate the association of physical activity with long-term risk for mortality among stroke survivors, compared with controls.
Physical activity was measured in metabolic equivalents (METs); meeting minimum physical activity guidelines was defined as 10 MET-hours/week.
During the study period, more stroke patients than controls died (24.7% vs. 5.7%). However, those who met the physical activity guideline recommendations of 10 MET-hours/week had a lower mortality, both in the stroke survivor group (14.6% vs. 33.2%; adjusted hazard ratio, 0.46; 95% confidence interval, 0.29-0.73) and among control participants (3.6% vs. 7.9%; aHR 0.69; 95% CI, 0.62-0.76).
The largest absolute and relative reduction in mortality was among stroke respondents younger than 75 (10.5% vs. 29%; aHR, 0.21; 95% CI, 0.10-0.43), the researchers note.
There was a significant interaction with age for the stroke patients but not the control group.
“The greatest reduction in mortality was seen between 0 and 10 METs per week … so the main point is that something is better than nothing,” said Dr. Joundi.
Exercise guidelines for the future
Although current guidelines recommend physical activity in stroke survivors, investigators noted that these are largely based on studies in the general population. Therefore, the aim of this research was to get a better understanding of the role of physical activity in the health of stroke survivors in the community, which could ultimately be used to design improved public health campaigns and physical activity interventions.
Given that this is a large study of stroke survivors in the community, Dr. Joundi hopes the results will influence future activity guidelines for those who have suffered a stroke.
“We found a log-linear relationship between physical activity and mortality such that 10 MET-hours/week was associated with large reductions in mortality with most benefit achieved by 20 MET-hours/week,” the authors concluded. “These thresholds could be considered for use in future guidelines for stroke.”
Clinical trials are underway to provide evidence for the implementation of exercise programs after stroke, they add, and offering physical activity programs to stroke survivors in the community “is an increasing priority in the U.S., Canada, and Europe.”
“People are at higher risk of death early on after a stroke but also months and years later, so if we can identify a relatively low-cost and easy intervention like physical activity to improve health and reduce the risk of death for stroke survivors it would be important,” Dr. Joundi said.
Key barriers
Paul George, MD, PhD, a stroke and vascular neurologist at Stanford (Calif.) University, said findings such as these further strengthen the argument that physical exercise is important after stroke.
“Because the study looked specifically at stroke patients, it can provide further guidance on physical activity recommendations that we provide to our patients following stroke,” said Dr. George, who was not associated with the study.
Going forward, he said, more research is needed to identify specifically what is preventing stroke patients from exercising more. What is required, he said, is “future research to determine the key barriers to physical activity following stroke and methods to reduce these will also be important to increasing physical activity in stroke survivors.”
Dr. Joundi said determining how to tailor exercise recommendations to meet the wide range of capabilities of stroke survivors will be another key factor.
“Stroke survivors may have some disabilities, so we need to be able to engage them at an [exercise] level that’s possible for them,” he said.
The study did not include stroke survivors living in long-term care homes.
The study had no targeted funding. Coauthor Eric E. Smith, MD, MPH, reports royalties from UpToDate, and consulting fees from Alnylam, Biogen, and Javelin. Dr. Joundi and the other coauthors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
, with a greater than 50% reduction in risk.
Lead study author Raed A. Joundi, MD, DPhil, of the University of Calgary (Alta.), said he expected results to show exercise was beneficial, but was surprised by the magnitude of the association between physical activity and lower mortality risk.
The impact of physical activity also differed significantly by age; those younger than 75 had a 79% reduction in mortality risk, compared with 32% in those age 75 and older.
“This is even after adjusting for factors such heart disease, respiratory conditions, smoking, and other functional limitations,” said Dr. Joundi.
The study was published online Aug. 11 in the journal Neurology.
For this analysis, the researchers used data on a cohort of people across Canada (excluding the province of Quebec) over 3-9 years. The 895 patients with prior stroke averaged 72 years of age, while the 97,805 in the control group had an average age of 63.
Weekly physical activity averages were evaluated using the self-reporting Canadian Community Health Survey, which was linked with administrative databases to evaluate the association of physical activity with long-term risk for mortality among stroke survivors, compared with controls.
Physical activity was measured in metabolic equivalents (METs); meeting minimum physical activity guidelines was defined as 10 MET-hours/week.
During the study period, more stroke patients than controls died (24.7% vs. 5.7%). However, those who met the physical activity guideline recommendations of 10 MET-hours/week had a lower mortality, both in the stroke survivor group (14.6% vs. 33.2%; adjusted hazard ratio, 0.46; 95% confidence interval, 0.29-0.73) and among control participants (3.6% vs. 7.9%; aHR 0.69; 95% CI, 0.62-0.76).
The largest absolute and relative reduction in mortality was among stroke respondents younger than 75 (10.5% vs. 29%; aHR, 0.21; 95% CI, 0.10-0.43), the researchers note.
There was a significant interaction with age for the stroke patients but not the control group.
“The greatest reduction in mortality was seen between 0 and 10 METs per week … so the main point is that something is better than nothing,” said Dr. Joundi.
Exercise guidelines for the future
Although current guidelines recommend physical activity in stroke survivors, investigators noted that these are largely based on studies in the general population. Therefore, the aim of this research was to get a better understanding of the role of physical activity in the health of stroke survivors in the community, which could ultimately be used to design improved public health campaigns and physical activity interventions.
Given that this is a large study of stroke survivors in the community, Dr. Joundi hopes the results will influence future activity guidelines for those who have suffered a stroke.
“We found a log-linear relationship between physical activity and mortality such that 10 MET-hours/week was associated with large reductions in mortality with most benefit achieved by 20 MET-hours/week,” the authors concluded. “These thresholds could be considered for use in future guidelines for stroke.”
Clinical trials are underway to provide evidence for the implementation of exercise programs after stroke, they add, and offering physical activity programs to stroke survivors in the community “is an increasing priority in the U.S., Canada, and Europe.”
“People are at higher risk of death early on after a stroke but also months and years later, so if we can identify a relatively low-cost and easy intervention like physical activity to improve health and reduce the risk of death for stroke survivors it would be important,” Dr. Joundi said.
Key barriers
Paul George, MD, PhD, a stroke and vascular neurologist at Stanford (Calif.) University, said findings such as these further strengthen the argument that physical exercise is important after stroke.
“Because the study looked specifically at stroke patients, it can provide further guidance on physical activity recommendations that we provide to our patients following stroke,” said Dr. George, who was not associated with the study.
Going forward, he said, more research is needed to identify specifically what is preventing stroke patients from exercising more. What is required, he said, is “future research to determine the key barriers to physical activity following stroke and methods to reduce these will also be important to increasing physical activity in stroke survivors.”
Dr. Joundi said determining how to tailor exercise recommendations to meet the wide range of capabilities of stroke survivors will be another key factor.
“Stroke survivors may have some disabilities, so we need to be able to engage them at an [exercise] level that’s possible for them,” he said.
The study did not include stroke survivors living in long-term care homes.
The study had no targeted funding. Coauthor Eric E. Smith, MD, MPH, reports royalties from UpToDate, and consulting fees from Alnylam, Biogen, and Javelin. Dr. Joundi and the other coauthors have disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Age, distance from dermatology clinic <p>predict number of melanomas diagnosed
Among patients from a single dermatology practice who were diagnosed with two or more melanomas over an 8-year period, 45% lived more than 20 miles away from the practice, and almost 60% were 70 years of age and older, results from single-center study showed.
“Dermatologists have known that many people are underdiagnosed for melanoma, but now our research supports that the problem is especially concentrated among older patients living in remote areas,” corresponding author Rose Parisi, MBA, said in an interview. “With this information, dermatologists should consider identifying and reaching out to their patients in this at-risk subpopulation, increasing the frequency of full-body skin exams, and collaborating with primary care physicians to educate them about melanoma’s dangers.”
In a study published online Aug. 3 in the Journal of the American Academy of Dermatology, Ms. Parisi of Albany Medical College, New York, and colleagues drew from the electronic medical records of a single-specialty private dermatology practice that serves urban, suburban, and rural patient populations to identify 346 melanoma pathology reports from patients cared for between 2012 and 2020. They limited their investigation to those diagnosed with biopsy-confirmed melanoma and analyzed the number of melanomas, Breslow depth, follow-up full-body skin exams, family history of melanoma, gender, insurance, and age (categorized as younger than 70 years and 70 years or older). To determine patient travel distance, they calculated the miles between the ZIP codes of the patient’s residence and the dermatology practice.
Regression analysis revealed that the . Specifically, among patients diagnosed with two or more melanomas, 45.0% lived more than 20 miles away and 21.3% lived less than 15 miles away; 59.6% were age 70 and older, while 40.4% were younger than age 70 (P less than .01).
No statistically significant association was observed between travel distance and Breslow depth or follow-up full-body skin exams within 1 year following diagnosis.
In other findings, among patients who lived more than 20 miles from the practice, those aged 70 and older were diagnosed with 0.56 more melanomas than patients between the ages of 58 and 70 (P = .00003), and 0.31 more melanomas than patients who lived 15-20 miles away (P = .014). No statistically significant differences in the number of melanomas diagnosed were observed between patients in either age group who lived fewer than 15 miles from the office.
“We were surprised that the combination of age and patient distance to diagnosing dermatology provider was such a powerful predictor of the number of diagnosed melanomas,” Ms. Parisi said. “It’s probably due to less mobility among older patients living in more remote areas, and it puts them at higher risk of multiple melanomas. This was something we haven’t seen in the dermatology literature.”
She and her coauthors acknowledged that the limited sampling of patients from a single practice “may not generalize across all urban and rural settings, and results must be considered preliminary,” they wrote. However, “our findings reveal an important vulnerability among older patients in nonurban areas, and efforts to improve access to melanoma diagnosis should be concentrated on this geodemographic segment.”
Nikolai Klebanov, MD, of the department of dermatology at Massachusetts General Hospital, Boston, who was asked to comment on the study, described what was addressed in the study as a “timely and an important topic.”
In an interview, he said, “there is less access to dermatologists and other medical specialists outside of large metropolitan and suburban areas,” and there are other health disparities affecting people living in rural or more underserved areas, which, he added, “also became exacerbated by the COVID-19 pandemic.”
For future studies on this topic, Dr. Klebanov said that he would be interested to see diagnoses measured per person-year rather than the total number of melanomas diagnosed. “More elderly patients may also be those who have ‘stuck with the practice’ for longer, and had a longer follow-up that gives more time to catch more melanomas,” he said.
“Adjusting for median income using ZIP codes could also help adjust for socioeconomic status, which would help with external validity of the study. Income relationships to geography are not the same in all cities; some have wealthy suburbs within 20 miles, while some have more underserved and rural areas at that distance.”
Neither the researchers nor Dr. Klebanov reported having financial disclosures.
Among patients from a single dermatology practice who were diagnosed with two or more melanomas over an 8-year period, 45% lived more than 20 miles away from the practice, and almost 60% were 70 years of age and older, results from single-center study showed.
“Dermatologists have known that many people are underdiagnosed for melanoma, but now our research supports that the problem is especially concentrated among older patients living in remote areas,” corresponding author Rose Parisi, MBA, said in an interview. “With this information, dermatologists should consider identifying and reaching out to their patients in this at-risk subpopulation, increasing the frequency of full-body skin exams, and collaborating with primary care physicians to educate them about melanoma’s dangers.”
In a study published online Aug. 3 in the Journal of the American Academy of Dermatology, Ms. Parisi of Albany Medical College, New York, and colleagues drew from the electronic medical records of a single-specialty private dermatology practice that serves urban, suburban, and rural patient populations to identify 346 melanoma pathology reports from patients cared for between 2012 and 2020. They limited their investigation to those diagnosed with biopsy-confirmed melanoma and analyzed the number of melanomas, Breslow depth, follow-up full-body skin exams, family history of melanoma, gender, insurance, and age (categorized as younger than 70 years and 70 years or older). To determine patient travel distance, they calculated the miles between the ZIP codes of the patient’s residence and the dermatology practice.
Regression analysis revealed that the . Specifically, among patients diagnosed with two or more melanomas, 45.0% lived more than 20 miles away and 21.3% lived less than 15 miles away; 59.6% were age 70 and older, while 40.4% were younger than age 70 (P less than .01).
No statistically significant association was observed between travel distance and Breslow depth or follow-up full-body skin exams within 1 year following diagnosis.
In other findings, among patients who lived more than 20 miles from the practice, those aged 70 and older were diagnosed with 0.56 more melanomas than patients between the ages of 58 and 70 (P = .00003), and 0.31 more melanomas than patients who lived 15-20 miles away (P = .014). No statistically significant differences in the number of melanomas diagnosed were observed between patients in either age group who lived fewer than 15 miles from the office.
“We were surprised that the combination of age and patient distance to diagnosing dermatology provider was such a powerful predictor of the number of diagnosed melanomas,” Ms. Parisi said. “It’s probably due to less mobility among older patients living in more remote areas, and it puts them at higher risk of multiple melanomas. This was something we haven’t seen in the dermatology literature.”
She and her coauthors acknowledged that the limited sampling of patients from a single practice “may not generalize across all urban and rural settings, and results must be considered preliminary,” they wrote. However, “our findings reveal an important vulnerability among older patients in nonurban areas, and efforts to improve access to melanoma diagnosis should be concentrated on this geodemographic segment.”
Nikolai Klebanov, MD, of the department of dermatology at Massachusetts General Hospital, Boston, who was asked to comment on the study, described what was addressed in the study as a “timely and an important topic.”
In an interview, he said, “there is less access to dermatologists and other medical specialists outside of large metropolitan and suburban areas,” and there are other health disparities affecting people living in rural or more underserved areas, which, he added, “also became exacerbated by the COVID-19 pandemic.”
For future studies on this topic, Dr. Klebanov said that he would be interested to see diagnoses measured per person-year rather than the total number of melanomas diagnosed. “More elderly patients may also be those who have ‘stuck with the practice’ for longer, and had a longer follow-up that gives more time to catch more melanomas,” he said.
“Adjusting for median income using ZIP codes could also help adjust for socioeconomic status, which would help with external validity of the study. Income relationships to geography are not the same in all cities; some have wealthy suburbs within 20 miles, while some have more underserved and rural areas at that distance.”
Neither the researchers nor Dr. Klebanov reported having financial disclosures.
Among patients from a single dermatology practice who were diagnosed with two or more melanomas over an 8-year period, 45% lived more than 20 miles away from the practice, and almost 60% were 70 years of age and older, results from single-center study showed.
“Dermatologists have known that many people are underdiagnosed for melanoma, but now our research supports that the problem is especially concentrated among older patients living in remote areas,” corresponding author Rose Parisi, MBA, said in an interview. “With this information, dermatologists should consider identifying and reaching out to their patients in this at-risk subpopulation, increasing the frequency of full-body skin exams, and collaborating with primary care physicians to educate them about melanoma’s dangers.”
In a study published online Aug. 3 in the Journal of the American Academy of Dermatology, Ms. Parisi of Albany Medical College, New York, and colleagues drew from the electronic medical records of a single-specialty private dermatology practice that serves urban, suburban, and rural patient populations to identify 346 melanoma pathology reports from patients cared for between 2012 and 2020. They limited their investigation to those diagnosed with biopsy-confirmed melanoma and analyzed the number of melanomas, Breslow depth, follow-up full-body skin exams, family history of melanoma, gender, insurance, and age (categorized as younger than 70 years and 70 years or older). To determine patient travel distance, they calculated the miles between the ZIP codes of the patient’s residence and the dermatology practice.
Regression analysis revealed that the . Specifically, among patients diagnosed with two or more melanomas, 45.0% lived more than 20 miles away and 21.3% lived less than 15 miles away; 59.6% were age 70 and older, while 40.4% were younger than age 70 (P less than .01).
No statistically significant association was observed between travel distance and Breslow depth or follow-up full-body skin exams within 1 year following diagnosis.
In other findings, among patients who lived more than 20 miles from the practice, those aged 70 and older were diagnosed with 0.56 more melanomas than patients between the ages of 58 and 70 (P = .00003), and 0.31 more melanomas than patients who lived 15-20 miles away (P = .014). No statistically significant differences in the number of melanomas diagnosed were observed between patients in either age group who lived fewer than 15 miles from the office.
“We were surprised that the combination of age and patient distance to diagnosing dermatology provider was such a powerful predictor of the number of diagnosed melanomas,” Ms. Parisi said. “It’s probably due to less mobility among older patients living in more remote areas, and it puts them at higher risk of multiple melanomas. This was something we haven’t seen in the dermatology literature.”
She and her coauthors acknowledged that the limited sampling of patients from a single practice “may not generalize across all urban and rural settings, and results must be considered preliminary,” they wrote. However, “our findings reveal an important vulnerability among older patients in nonurban areas, and efforts to improve access to melanoma diagnosis should be concentrated on this geodemographic segment.”
Nikolai Klebanov, MD, of the department of dermatology at Massachusetts General Hospital, Boston, who was asked to comment on the study, described what was addressed in the study as a “timely and an important topic.”
In an interview, he said, “there is less access to dermatologists and other medical specialists outside of large metropolitan and suburban areas,” and there are other health disparities affecting people living in rural or more underserved areas, which, he added, “also became exacerbated by the COVID-19 pandemic.”
For future studies on this topic, Dr. Klebanov said that he would be interested to see diagnoses measured per person-year rather than the total number of melanomas diagnosed. “More elderly patients may also be those who have ‘stuck with the practice’ for longer, and had a longer follow-up that gives more time to catch more melanomas,” he said.
“Adjusting for median income using ZIP codes could also help adjust for socioeconomic status, which would help with external validity of the study. Income relationships to geography are not the same in all cities; some have wealthy suburbs within 20 miles, while some have more underserved and rural areas at that distance.”
Neither the researchers nor Dr. Klebanov reported having financial disclosures.
FROM JAMA DERMATOLOGY
Flavonoids dietary ‘powerhouses’ for cognitive decline prevention
, new research shows.
Among the different types of flavonoids, flavones (found in some spices and yellow or orange fruits and vegetables) and anthocyanins (found in blueberries, blackberries, and cherries) seem to have most protective effect, the researchers report.
“There is mounting evidence suggesting flavonoids are powerhouses when it comes to preventing your thinking skills from declining as you get older,” study investigator Walter Willett, MD, DrPH, Harvard University, Boston, said in a statement.
“Our results are exciting because they show that making simple changes to your diet could help prevent cognitive decline,” said Dr. Willett.
The study was published online July 28 in the journal Neurology.
Antioxidant punch
Flavonoids, naturally occurring phytochemicals found in plants, are strong antioxidants. Considering the likely role of oxidative stress in age-related cognitive decline, flavonoids have been proposed as a potentially important preventive.
For the study, Dr. Willett and colleagues prospectively examined associations between long-term dietary flavonoids (flavonols, flavones, flavanones, flavan-3-ols, anthocyanins, polymeric flavonoids, and proanthocyanidins) and subjective cognitive decline in 49,493 women from the Nurses’ Health Study (1984-2006) and 27,842 men from the Health Professionals Follow-up Study (1986-2002).
Those in the highest quintile of flavonoid consumption consumed about 600 mg daily on average while those in the lowest quintile got only about 150 mg daily.
After adjusting for age, total energy intake, major nondietary factors, and specific dietary factors, a higher intake of total flavonoids was associated with lower likelihood of self-reported subjective cognitive decline during follow up.
Individuals in the highest quintile of daily consumption had about a 20% lower risk of subjective cognitive decline relative to peers in the lowest quintile (pooled multivariable-adjusted odds ratio: 0.81; 95% confidence interval, 0.76-0.89).
The strongest protective associations were found for flavones (OR, 0.62; 95% confidence interval, 0.57-0.68), flavanones (OR, 0.64; 95% CI, 0.58-0.68), and anthocyanins (OR, 0.76; 95% CI, 0.72-0.84) (P trend < .0001 for all groups).
“The people in our study who did the best over time ate an average of at least half a serving per day of foods like orange juice, oranges, peppers, celery, grapefruits, grapefruit juice, apples, and pears,” Dr. Willett said.
“While it is possible other phytochemicals are at work here, a colorful diet rich in flavonoids – and specifically flavones and anthocyanins – seems to be a good bet for promoting long-term brain health,” he added.
A limitation of the study is that participants reported on their diets and may not recall perfectly what they ate or how much.
Healthy diet best bet for brain health
Reached for comment, Christopher Weber, PhD, director of global science initiatives for the Alzheimer’s Association, said this study “adds to our understanding of which elements of a healthy diet may be important in reducing dementia risk; flavonols may be one of those elements.”
“However, at this point, people should not put too much stock in specific nutrients – including subsets of flavonols – for reducing dementia risk until more research is done. Rather, they should focus on eating an overall healthy diet,” he said.
“It would be wonderful if a particular food or supplement could delay or prevent Alzheimer’s disease, but we do not have scientific evidence to support such claims. Randomized controlled clinical trials are necessary to evaluate whether any food or supplement has a scientifically proven beneficial effect,” Dr. Weber added.
For now, the Alzheimer’s Association “encourages everyone to eat a healthy and balanced diet as a way to help reduce the risk of cognitive decline,” Dr. Weber said.
“With more than 6 million Americans living with Alzheimer’s disease and other dementia today, there is a pressing need to test the effectiveness of a healthy lifestyle regimen to reduce risk of cognitive decline in a large and diverse population,” he added.
The Alzheimer’s Association has launched a 2-year clinical trial, called the U.S. Study to Protect Brain Health Through Lifestyle Intervention to Reduce Risk (U.S. POINTER), to do just that.
“While we research that definitive lifestyle ‘recipe,’ there are things we can do today that may decrease our risk of cognitive decline as we age. Eating a heart-healthy diet, exercising regularly, and staying cognitively engaged are just a few,” Dr. Weber added.
Also weighing in, Taylor Wallace, PhD, adjunct professor, department of nutrition and food studies, George Mason University, Fairfax, Va., said the study results are not surprising.
“Scientific data on the ability of flavonoids to prevent age-related chronic diseases, including cognitive decline, has accumulated immensely over the last decade. This epidemiological study reinforces findings from smaller shorter-duration clinical trials and mechanistic studies,” said Dr. Wallace, who was not involved in the study.
“Flavonoids show great potential in reducing inflammation and oxidative stress in the body. They are also vasodilators that help improve blood flow, which is important for the cardiovascular and cerebrovascular systems,” he noted.
“Typically, foods rich in flavonoids are also nutrient-dense in vitamins, minerals, and dietary fiber (eg, fruits and vegetables). Anthocyanins in blueberries have long been known to prevent cognitive decline with age,” Dr. Wallace said.
Dr. Wallace was part of a 14-member panel of nutrition scientists who recently reviewed available evidence around fruit and vegetable intake and health.
“Our findings are consistent with this study in regard to cognitive decline and other disease states. Cruciferous vegetables, dark-green leafy vegetables, citrus fruits, and dark-colored berries seem to have superior effects on health promotion and disease prevention in general,” said Dr. Wallace.
This work was supported by grants from the National Institutes of Health. The authors have disclosed no relevant financial relationships. Dr. Weber has no relevant disclosures. Dr. Wallace is principal and chief executive officer of the Think Healthy Group; editor of the Journal of Dietary Supplements; and deputy editor-in-chief of the Journal of the American College of Nutrition.
A version of this article first appeared on Medscape.com.
, new research shows.
Among the different types of flavonoids, flavones (found in some spices and yellow or orange fruits and vegetables) and anthocyanins (found in blueberries, blackberries, and cherries) seem to have most protective effect, the researchers report.
“There is mounting evidence suggesting flavonoids are powerhouses when it comes to preventing your thinking skills from declining as you get older,” study investigator Walter Willett, MD, DrPH, Harvard University, Boston, said in a statement.
“Our results are exciting because they show that making simple changes to your diet could help prevent cognitive decline,” said Dr. Willett.
The study was published online July 28 in the journal Neurology.
Antioxidant punch
Flavonoids, naturally occurring phytochemicals found in plants, are strong antioxidants. Considering the likely role of oxidative stress in age-related cognitive decline, flavonoids have been proposed as a potentially important preventive.
For the study, Dr. Willett and colleagues prospectively examined associations between long-term dietary flavonoids (flavonols, flavones, flavanones, flavan-3-ols, anthocyanins, polymeric flavonoids, and proanthocyanidins) and subjective cognitive decline in 49,493 women from the Nurses’ Health Study (1984-2006) and 27,842 men from the Health Professionals Follow-up Study (1986-2002).
Those in the highest quintile of flavonoid consumption consumed about 600 mg daily on average while those in the lowest quintile got only about 150 mg daily.
After adjusting for age, total energy intake, major nondietary factors, and specific dietary factors, a higher intake of total flavonoids was associated with lower likelihood of self-reported subjective cognitive decline during follow up.
Individuals in the highest quintile of daily consumption had about a 20% lower risk of subjective cognitive decline relative to peers in the lowest quintile (pooled multivariable-adjusted odds ratio: 0.81; 95% confidence interval, 0.76-0.89).
The strongest protective associations were found for flavones (OR, 0.62; 95% confidence interval, 0.57-0.68), flavanones (OR, 0.64; 95% CI, 0.58-0.68), and anthocyanins (OR, 0.76; 95% CI, 0.72-0.84) (P trend < .0001 for all groups).
“The people in our study who did the best over time ate an average of at least half a serving per day of foods like orange juice, oranges, peppers, celery, grapefruits, grapefruit juice, apples, and pears,” Dr. Willett said.
“While it is possible other phytochemicals are at work here, a colorful diet rich in flavonoids – and specifically flavones and anthocyanins – seems to be a good bet for promoting long-term brain health,” he added.
A limitation of the study is that participants reported on their diets and may not recall perfectly what they ate or how much.
Healthy diet best bet for brain health
Reached for comment, Christopher Weber, PhD, director of global science initiatives for the Alzheimer’s Association, said this study “adds to our understanding of which elements of a healthy diet may be important in reducing dementia risk; flavonols may be one of those elements.”
“However, at this point, people should not put too much stock in specific nutrients – including subsets of flavonols – for reducing dementia risk until more research is done. Rather, they should focus on eating an overall healthy diet,” he said.
“It would be wonderful if a particular food or supplement could delay or prevent Alzheimer’s disease, but we do not have scientific evidence to support such claims. Randomized controlled clinical trials are necessary to evaluate whether any food or supplement has a scientifically proven beneficial effect,” Dr. Weber added.
For now, the Alzheimer’s Association “encourages everyone to eat a healthy and balanced diet as a way to help reduce the risk of cognitive decline,” Dr. Weber said.
“With more than 6 million Americans living with Alzheimer’s disease and other dementia today, there is a pressing need to test the effectiveness of a healthy lifestyle regimen to reduce risk of cognitive decline in a large and diverse population,” he added.
The Alzheimer’s Association has launched a 2-year clinical trial, called the U.S. Study to Protect Brain Health Through Lifestyle Intervention to Reduce Risk (U.S. POINTER), to do just that.
“While we research that definitive lifestyle ‘recipe,’ there are things we can do today that may decrease our risk of cognitive decline as we age. Eating a heart-healthy diet, exercising regularly, and staying cognitively engaged are just a few,” Dr. Weber added.
Also weighing in, Taylor Wallace, PhD, adjunct professor, department of nutrition and food studies, George Mason University, Fairfax, Va., said the study results are not surprising.
“Scientific data on the ability of flavonoids to prevent age-related chronic diseases, including cognitive decline, has accumulated immensely over the last decade. This epidemiological study reinforces findings from smaller shorter-duration clinical trials and mechanistic studies,” said Dr. Wallace, who was not involved in the study.
“Flavonoids show great potential in reducing inflammation and oxidative stress in the body. They are also vasodilators that help improve blood flow, which is important for the cardiovascular and cerebrovascular systems,” he noted.
“Typically, foods rich in flavonoids are also nutrient-dense in vitamins, minerals, and dietary fiber (eg, fruits and vegetables). Anthocyanins in blueberries have long been known to prevent cognitive decline with age,” Dr. Wallace said.
Dr. Wallace was part of a 14-member panel of nutrition scientists who recently reviewed available evidence around fruit and vegetable intake and health.
“Our findings are consistent with this study in regard to cognitive decline and other disease states. Cruciferous vegetables, dark-green leafy vegetables, citrus fruits, and dark-colored berries seem to have superior effects on health promotion and disease prevention in general,” said Dr. Wallace.
This work was supported by grants from the National Institutes of Health. The authors have disclosed no relevant financial relationships. Dr. Weber has no relevant disclosures. Dr. Wallace is principal and chief executive officer of the Think Healthy Group; editor of the Journal of Dietary Supplements; and deputy editor-in-chief of the Journal of the American College of Nutrition.
A version of this article first appeared on Medscape.com.
, new research shows.
Among the different types of flavonoids, flavones (found in some spices and yellow or orange fruits and vegetables) and anthocyanins (found in blueberries, blackberries, and cherries) seem to have most protective effect, the researchers report.
“There is mounting evidence suggesting flavonoids are powerhouses when it comes to preventing your thinking skills from declining as you get older,” study investigator Walter Willett, MD, DrPH, Harvard University, Boston, said in a statement.
“Our results are exciting because they show that making simple changes to your diet could help prevent cognitive decline,” said Dr. Willett.
The study was published online July 28 in the journal Neurology.
Antioxidant punch
Flavonoids, naturally occurring phytochemicals found in plants, are strong antioxidants. Considering the likely role of oxidative stress in age-related cognitive decline, flavonoids have been proposed as a potentially important preventive.
For the study, Dr. Willett and colleagues prospectively examined associations between long-term dietary flavonoids (flavonols, flavones, flavanones, flavan-3-ols, anthocyanins, polymeric flavonoids, and proanthocyanidins) and subjective cognitive decline in 49,493 women from the Nurses’ Health Study (1984-2006) and 27,842 men from the Health Professionals Follow-up Study (1986-2002).
Those in the highest quintile of flavonoid consumption consumed about 600 mg daily on average while those in the lowest quintile got only about 150 mg daily.
After adjusting for age, total energy intake, major nondietary factors, and specific dietary factors, a higher intake of total flavonoids was associated with lower likelihood of self-reported subjective cognitive decline during follow up.
Individuals in the highest quintile of daily consumption had about a 20% lower risk of subjective cognitive decline relative to peers in the lowest quintile (pooled multivariable-adjusted odds ratio: 0.81; 95% confidence interval, 0.76-0.89).
The strongest protective associations were found for flavones (OR, 0.62; 95% confidence interval, 0.57-0.68), flavanones (OR, 0.64; 95% CI, 0.58-0.68), and anthocyanins (OR, 0.76; 95% CI, 0.72-0.84) (P trend < .0001 for all groups).
“The people in our study who did the best over time ate an average of at least half a serving per day of foods like orange juice, oranges, peppers, celery, grapefruits, grapefruit juice, apples, and pears,” Dr. Willett said.
“While it is possible other phytochemicals are at work here, a colorful diet rich in flavonoids – and specifically flavones and anthocyanins – seems to be a good bet for promoting long-term brain health,” he added.
A limitation of the study is that participants reported on their diets and may not recall perfectly what they ate or how much.
Healthy diet best bet for brain health
Reached for comment, Christopher Weber, PhD, director of global science initiatives for the Alzheimer’s Association, said this study “adds to our understanding of which elements of a healthy diet may be important in reducing dementia risk; flavonols may be one of those elements.”
“However, at this point, people should not put too much stock in specific nutrients – including subsets of flavonols – for reducing dementia risk until more research is done. Rather, they should focus on eating an overall healthy diet,” he said.
“It would be wonderful if a particular food or supplement could delay or prevent Alzheimer’s disease, but we do not have scientific evidence to support such claims. Randomized controlled clinical trials are necessary to evaluate whether any food or supplement has a scientifically proven beneficial effect,” Dr. Weber added.
For now, the Alzheimer’s Association “encourages everyone to eat a healthy and balanced diet as a way to help reduce the risk of cognitive decline,” Dr. Weber said.
“With more than 6 million Americans living with Alzheimer’s disease and other dementia today, there is a pressing need to test the effectiveness of a healthy lifestyle regimen to reduce risk of cognitive decline in a large and diverse population,” he added.
The Alzheimer’s Association has launched a 2-year clinical trial, called the U.S. Study to Protect Brain Health Through Lifestyle Intervention to Reduce Risk (U.S. POINTER), to do just that.
“While we research that definitive lifestyle ‘recipe,’ there are things we can do today that may decrease our risk of cognitive decline as we age. Eating a heart-healthy diet, exercising regularly, and staying cognitively engaged are just a few,” Dr. Weber added.
Also weighing in, Taylor Wallace, PhD, adjunct professor, department of nutrition and food studies, George Mason University, Fairfax, Va., said the study results are not surprising.
“Scientific data on the ability of flavonoids to prevent age-related chronic diseases, including cognitive decline, has accumulated immensely over the last decade. This epidemiological study reinforces findings from smaller shorter-duration clinical trials and mechanistic studies,” said Dr. Wallace, who was not involved in the study.
“Flavonoids show great potential in reducing inflammation and oxidative stress in the body. They are also vasodilators that help improve blood flow, which is important for the cardiovascular and cerebrovascular systems,” he noted.
“Typically, foods rich in flavonoids are also nutrient-dense in vitamins, minerals, and dietary fiber (eg, fruits and vegetables). Anthocyanins in blueberries have long been known to prevent cognitive decline with age,” Dr. Wallace said.
Dr. Wallace was part of a 14-member panel of nutrition scientists who recently reviewed available evidence around fruit and vegetable intake and health.
“Our findings are consistent with this study in regard to cognitive decline and other disease states. Cruciferous vegetables, dark-green leafy vegetables, citrus fruits, and dark-colored berries seem to have superior effects on health promotion and disease prevention in general,” said Dr. Wallace.
This work was supported by grants from the National Institutes of Health. The authors have disclosed no relevant financial relationships. Dr. Weber has no relevant disclosures. Dr. Wallace is principal and chief executive officer of the Think Healthy Group; editor of the Journal of Dietary Supplements; and deputy editor-in-chief of the Journal of the American College of Nutrition.
A version of this article first appeared on Medscape.com.
FROM NEUROLOGY
‘Routine’ use of focal therapy for prostate cancer in next 5 years
They maintain that focal therapy (FT) offers a “middle ground” between two extremes: Treating the whole gland with radical prostatectomy or radiotherapy and not treating immediately via active surveillance or watchful waiting.
Focal therapy typically treats the primary lesion within the prostate, while leaving the rest of the gland intact. Most often performed with cryoablation or high-intensity focused ultrasound (HIFU), it can also be carried out with a variety of technologies, including transurethral ultrasound ablation and focal laser ablation.
The shift to focal therapy will coincide with maturing, long-term data from studies with various technologies, predict the authors, led by Amir Lebastchi, MD, a urologist at the University of Southern California.
“Standard adoption of focal therapy is ultimately dependent on the availability of robust level I evidence, which in turn will drive medical societies and payees,” the authors also write.
But payees are already making changes, even without such data, they add.
For example, in January the American Medical Association announced a new code for high-intensity focal ultrasound (HIFU): This approach now has a Current Procedural Terminology (CPT) code from the U.S. Centers for Medicare & Medicaid Services
This news organization reached out to Matthew Cooperberg, MD, MPH, a urologist at the University of California, San Francisco (UCSF), for comments about the essay’s optimism; he has questioned focal therapy in the past because of a lack of strong supporting evidence.
“While ‘routine’ is a bit of a vague term, now that HIFU has a CPT code, I do expect its use will in fact increase in the next 5 years,” Dr. Cooperberg wrote in an email. “The question is whether its use will increase appropriately.”
The challenge with focal therapy – regardless of energy modality – remains patient selection and accurate ablation zone definition, he added.
Notably, UCSF has launched a new HIFU program – and Dr. Cooperberg has referred selected patients. “I’m both enthusiastic and cautious about the future, and we need to track our outcomes very closely across various practice settings,” he said.
While waiting for CHRONOS, select wisely
The goal of focal therapy is to treat only the area with the most aggressive tumor, known as the index tumor, while leaving the remaining gland and its surrounding structures alone, according to Derek Lomas, MD, PharmD, a urologist at the Mayo Clinic in Rochester, Minn., in an explanatory article. “This approach is widely accepted in other types of cancer. For example, we commonly treat kidney cancers by removing or ablating only the tumor while leaving the rest of the kidney intact.”
However, some focal therapies also include approaches known as hemiablations, in which a full half of the prostate is destroyed, and approaches that leave very little of the gland behind.
Each of the modalities used for focal therapy has “unique indications, risks, and benefits and uses a different energy source for ablation,” Dr. Lebastchi and colleagues write in their essay.
They assert that focal therapy can provide oncological efficacy similar to radical prostatectomy or radiotherapy “while considerably reducing or even eliminating functional morbidities, such as incontinence and erectile dysfunction.”
Overall, they say focal therapy offers an opportunity for improved care because there is “an increasing body of emerging evidence demonstrating a favorable adverse effect profile with oncological control similar to whole-gland treatment options.”
What is that evidence?
In the essay, Dr. Lebastchi and colleagues point to a number of single-arm studies with encouraging efficacy and safety results. They also highlight a phase 3, randomized trial that they were involved in: This compared focal therapy (partial gland ablation with vascular-targeted photodynamic therapy) with active surveillance in early-stage disease and uniformly showed better post-treatment biopsy (disease/no disease) and conversion-to-prostatectomy results with the focal therapy out to 4 years (J Urol. 2018;200:786-793).
However, that study did not have an active treatment comparator. For that gold standard, there is now anticipation for results from the CHRONOS trial in the United Kingdom, especially part A of the trial, which compares radical therapy to focal therapy (HIFU or cryotherapy), with 5-year progression-free survival as the primary outcome. That trial is slated for completion in 2027.
Until then, the lack of prospective randomized clinical trials and long-term follow-up “hinders acceptance [of focal therapy] in the urology community,” the essay authors comment.
Meanwhile, careful patient selection is very important, they say.
The latest relevant guidelines state that appropriate candidates are men with a solitary, well-defined index lesion; patients with bilateral multifocal lesions; or very advanced tumors that are not appropriate for the focal approach.
A multidisciplinary international expert panel recently convened to establish guidance for clinicians offering focal therapies and then published a consensus statement to advise practitioners and researchers.
UCSF’s Dr. Cooperberg sees plenty of room for improvement among focal therapy practitioners and investigators. “From an outcomes standpoint, follow-up protocols and definitions of success remain inconsistent. I believe we’re making progress in all these areas, but we’re not there yet,” he says.
To date, some patients have been managed poorly, Dr. Cooperberg added. “We certainly see many patients who have been inadequately counseled as to HIFU’s advantages and disadvantages, with sometimes disastrous results.”
Some of those unfortunate results may have arisen from the U.S. Food and Drug Administration’s initial approval of HIFU in 2015, which was for use in ablating prostate tissue in general and not cancer specifically. This approval generated confusion, one expert commented at the time: “The FDA doesn’t specify whether it’s for benign or malignant disease; it’s a bit vague, like saying you can drive this car, but we’re not going to tell you how to drive it,” said Manoj Monga, MD, from the Cleveland Clinic.
Dr. Lebastchi has disclosed no relevant financial relationships; co-author Inderbir Gill, MD, is an unpaid consultant for Steba Biotech, and co-author Andre Luis Abreu, MD, is a consultant for Koelis and was a proctor in training for Steba Biotech. Dr. Cooperberg is a consultant for Alessa Therapeutics.
A version of this article first appeared on Medscape.com.
They maintain that focal therapy (FT) offers a “middle ground” between two extremes: Treating the whole gland with radical prostatectomy or radiotherapy and not treating immediately via active surveillance or watchful waiting.
Focal therapy typically treats the primary lesion within the prostate, while leaving the rest of the gland intact. Most often performed with cryoablation or high-intensity focused ultrasound (HIFU), it can also be carried out with a variety of technologies, including transurethral ultrasound ablation and focal laser ablation.
The shift to focal therapy will coincide with maturing, long-term data from studies with various technologies, predict the authors, led by Amir Lebastchi, MD, a urologist at the University of Southern California.
“Standard adoption of focal therapy is ultimately dependent on the availability of robust level I evidence, which in turn will drive medical societies and payees,” the authors also write.
But payees are already making changes, even without such data, they add.
For example, in January the American Medical Association announced a new code for high-intensity focal ultrasound (HIFU): This approach now has a Current Procedural Terminology (CPT) code from the U.S. Centers for Medicare & Medicaid Services
This news organization reached out to Matthew Cooperberg, MD, MPH, a urologist at the University of California, San Francisco (UCSF), for comments about the essay’s optimism; he has questioned focal therapy in the past because of a lack of strong supporting evidence.
“While ‘routine’ is a bit of a vague term, now that HIFU has a CPT code, I do expect its use will in fact increase in the next 5 years,” Dr. Cooperberg wrote in an email. “The question is whether its use will increase appropriately.”
The challenge with focal therapy – regardless of energy modality – remains patient selection and accurate ablation zone definition, he added.
Notably, UCSF has launched a new HIFU program – and Dr. Cooperberg has referred selected patients. “I’m both enthusiastic and cautious about the future, and we need to track our outcomes very closely across various practice settings,” he said.
While waiting for CHRONOS, select wisely
The goal of focal therapy is to treat only the area with the most aggressive tumor, known as the index tumor, while leaving the remaining gland and its surrounding structures alone, according to Derek Lomas, MD, PharmD, a urologist at the Mayo Clinic in Rochester, Minn., in an explanatory article. “This approach is widely accepted in other types of cancer. For example, we commonly treat kidney cancers by removing or ablating only the tumor while leaving the rest of the kidney intact.”
However, some focal therapies also include approaches known as hemiablations, in which a full half of the prostate is destroyed, and approaches that leave very little of the gland behind.
Each of the modalities used for focal therapy has “unique indications, risks, and benefits and uses a different energy source for ablation,” Dr. Lebastchi and colleagues write in their essay.
They assert that focal therapy can provide oncological efficacy similar to radical prostatectomy or radiotherapy “while considerably reducing or even eliminating functional morbidities, such as incontinence and erectile dysfunction.”
Overall, they say focal therapy offers an opportunity for improved care because there is “an increasing body of emerging evidence demonstrating a favorable adverse effect profile with oncological control similar to whole-gland treatment options.”
What is that evidence?
In the essay, Dr. Lebastchi and colleagues point to a number of single-arm studies with encouraging efficacy and safety results. They also highlight a phase 3, randomized trial that they were involved in: This compared focal therapy (partial gland ablation with vascular-targeted photodynamic therapy) with active surveillance in early-stage disease and uniformly showed better post-treatment biopsy (disease/no disease) and conversion-to-prostatectomy results with the focal therapy out to 4 years (J Urol. 2018;200:786-793).
However, that study did not have an active treatment comparator. For that gold standard, there is now anticipation for results from the CHRONOS trial in the United Kingdom, especially part A of the trial, which compares radical therapy to focal therapy (HIFU or cryotherapy), with 5-year progression-free survival as the primary outcome. That trial is slated for completion in 2027.
Until then, the lack of prospective randomized clinical trials and long-term follow-up “hinders acceptance [of focal therapy] in the urology community,” the essay authors comment.
Meanwhile, careful patient selection is very important, they say.
The latest relevant guidelines state that appropriate candidates are men with a solitary, well-defined index lesion; patients with bilateral multifocal lesions; or very advanced tumors that are not appropriate for the focal approach.
A multidisciplinary international expert panel recently convened to establish guidance for clinicians offering focal therapies and then published a consensus statement to advise practitioners and researchers.
UCSF’s Dr. Cooperberg sees plenty of room for improvement among focal therapy practitioners and investigators. “From an outcomes standpoint, follow-up protocols and definitions of success remain inconsistent. I believe we’re making progress in all these areas, but we’re not there yet,” he says.
To date, some patients have been managed poorly, Dr. Cooperberg added. “We certainly see many patients who have been inadequately counseled as to HIFU’s advantages and disadvantages, with sometimes disastrous results.”
Some of those unfortunate results may have arisen from the U.S. Food and Drug Administration’s initial approval of HIFU in 2015, which was for use in ablating prostate tissue in general and not cancer specifically. This approval generated confusion, one expert commented at the time: “The FDA doesn’t specify whether it’s for benign or malignant disease; it’s a bit vague, like saying you can drive this car, but we’re not going to tell you how to drive it,” said Manoj Monga, MD, from the Cleveland Clinic.
Dr. Lebastchi has disclosed no relevant financial relationships; co-author Inderbir Gill, MD, is an unpaid consultant for Steba Biotech, and co-author Andre Luis Abreu, MD, is a consultant for Koelis and was a proctor in training for Steba Biotech. Dr. Cooperberg is a consultant for Alessa Therapeutics.
A version of this article first appeared on Medscape.com.
They maintain that focal therapy (FT) offers a “middle ground” between two extremes: Treating the whole gland with radical prostatectomy or radiotherapy and not treating immediately via active surveillance or watchful waiting.
Focal therapy typically treats the primary lesion within the prostate, while leaving the rest of the gland intact. Most often performed with cryoablation or high-intensity focused ultrasound (HIFU), it can also be carried out with a variety of technologies, including transurethral ultrasound ablation and focal laser ablation.
The shift to focal therapy will coincide with maturing, long-term data from studies with various technologies, predict the authors, led by Amir Lebastchi, MD, a urologist at the University of Southern California.
“Standard adoption of focal therapy is ultimately dependent on the availability of robust level I evidence, which in turn will drive medical societies and payees,” the authors also write.
But payees are already making changes, even without such data, they add.
For example, in January the American Medical Association announced a new code for high-intensity focal ultrasound (HIFU): This approach now has a Current Procedural Terminology (CPT) code from the U.S. Centers for Medicare & Medicaid Services
This news organization reached out to Matthew Cooperberg, MD, MPH, a urologist at the University of California, San Francisco (UCSF), for comments about the essay’s optimism; he has questioned focal therapy in the past because of a lack of strong supporting evidence.
“While ‘routine’ is a bit of a vague term, now that HIFU has a CPT code, I do expect its use will in fact increase in the next 5 years,” Dr. Cooperberg wrote in an email. “The question is whether its use will increase appropriately.”
The challenge with focal therapy – regardless of energy modality – remains patient selection and accurate ablation zone definition, he added.
Notably, UCSF has launched a new HIFU program – and Dr. Cooperberg has referred selected patients. “I’m both enthusiastic and cautious about the future, and we need to track our outcomes very closely across various practice settings,” he said.
While waiting for CHRONOS, select wisely
The goal of focal therapy is to treat only the area with the most aggressive tumor, known as the index tumor, while leaving the remaining gland and its surrounding structures alone, according to Derek Lomas, MD, PharmD, a urologist at the Mayo Clinic in Rochester, Minn., in an explanatory article. “This approach is widely accepted in other types of cancer. For example, we commonly treat kidney cancers by removing or ablating only the tumor while leaving the rest of the kidney intact.”
However, some focal therapies also include approaches known as hemiablations, in which a full half of the prostate is destroyed, and approaches that leave very little of the gland behind.
Each of the modalities used for focal therapy has “unique indications, risks, and benefits and uses a different energy source for ablation,” Dr. Lebastchi and colleagues write in their essay.
They assert that focal therapy can provide oncological efficacy similar to radical prostatectomy or radiotherapy “while considerably reducing or even eliminating functional morbidities, such as incontinence and erectile dysfunction.”
Overall, they say focal therapy offers an opportunity for improved care because there is “an increasing body of emerging evidence demonstrating a favorable adverse effect profile with oncological control similar to whole-gland treatment options.”
What is that evidence?
In the essay, Dr. Lebastchi and colleagues point to a number of single-arm studies with encouraging efficacy and safety results. They also highlight a phase 3, randomized trial that they were involved in: This compared focal therapy (partial gland ablation with vascular-targeted photodynamic therapy) with active surveillance in early-stage disease and uniformly showed better post-treatment biopsy (disease/no disease) and conversion-to-prostatectomy results with the focal therapy out to 4 years (J Urol. 2018;200:786-793).
However, that study did not have an active treatment comparator. For that gold standard, there is now anticipation for results from the CHRONOS trial in the United Kingdom, especially part A of the trial, which compares radical therapy to focal therapy (HIFU or cryotherapy), with 5-year progression-free survival as the primary outcome. That trial is slated for completion in 2027.
Until then, the lack of prospective randomized clinical trials and long-term follow-up “hinders acceptance [of focal therapy] in the urology community,” the essay authors comment.
Meanwhile, careful patient selection is very important, they say.
The latest relevant guidelines state that appropriate candidates are men with a solitary, well-defined index lesion; patients with bilateral multifocal lesions; or very advanced tumors that are not appropriate for the focal approach.
A multidisciplinary international expert panel recently convened to establish guidance for clinicians offering focal therapies and then published a consensus statement to advise practitioners and researchers.
UCSF’s Dr. Cooperberg sees plenty of room for improvement among focal therapy practitioners and investigators. “From an outcomes standpoint, follow-up protocols and definitions of success remain inconsistent. I believe we’re making progress in all these areas, but we’re not there yet,” he says.
To date, some patients have been managed poorly, Dr. Cooperberg added. “We certainly see many patients who have been inadequately counseled as to HIFU’s advantages and disadvantages, with sometimes disastrous results.”
Some of those unfortunate results may have arisen from the U.S. Food and Drug Administration’s initial approval of HIFU in 2015, which was for use in ablating prostate tissue in general and not cancer specifically. This approval generated confusion, one expert commented at the time: “The FDA doesn’t specify whether it’s for benign or malignant disease; it’s a bit vague, like saying you can drive this car, but we’re not going to tell you how to drive it,” said Manoj Monga, MD, from the Cleveland Clinic.
Dr. Lebastchi has disclosed no relevant financial relationships; co-author Inderbir Gill, MD, is an unpaid consultant for Steba Biotech, and co-author Andre Luis Abreu, MD, is a consultant for Koelis and was a proctor in training for Steba Biotech. Dr. Cooperberg is a consultant for Alessa Therapeutics.
A version of this article first appeared on Medscape.com.
Short-term approach is best for seizure prevention after intracerebral hemorrhage
(sICH), new research shows.
Investigators created a model that simulated common clinical scenarios to compare four antiseizure drug strategies – conservative, moderate, aggressive, and risk-guided. They used the 2HELPS2B score as a risk stratification tool to guide clinical decisions.
The investigators found that the short-term, early-seizure prophylaxis strategies “dominated” long-term therapy under most clinical scenarios, underscoring the importance of early discontinuation of antiseizure drug therapy.
“The main message here was that strategies that involved long-term antiseizure drug prescription (moderate and aggressive) fail to provide better outcomes in most clinical scenarios, when compared with strategies using short-term prophylaxis (conservative and risk-guided),” senior investigator Lidia M.V.R. Moura, MD, MPH, assistant professor of neurology, Harvard Medical School, Boston, said in an interview.
The study was published online July 26 in JAMA Neurology.
Common complication
“Acute asymptomatic seizures [early seizures ≤7 days after stroke] are a common complication of sICH,” the authors noted.
Potential safety concerns have prompted recommendations against the use of antiseizure medications for primary prophylaxis. However, approximately 40% of U.S. patients with sICH do receive prophylactic levetiracetam before seizure development. For these patients, the duration of prophylaxis varies widely.
“Because seizure risk is a key determinant of which patient groups might benefit most from different prophylaxis strategies, validated tools for predicting early ... and late ... seizure risks could aid physicians in treatment decisions. However, no clinical trials or prospective studies have evaluated the net benefit of various strategies after sICH,” the investigators noted.
“Our patients who were survivors of an intracerebral hemorrhage motivated us to conduct the study,” said Dr. Moura, who is also director of the MGH NeuroValue Laboratory. “Some would come to the clinic with a long list of medications; some of them were taking antiseizure drugs for many years, but they never had a documented seizure.” These patients did not know why they had been taking an antiseizure drug for so long.
“In these conversations, we noted so much variability in indications and variability in patient access to specialty care to make treatment decisions. We noted that the evidence behind our current guidelines on seizure management was limited,” she added.
Dr. Moura and colleagues were “committed to improve outcome for people with neurological conditions by leveraging research methods that can help guide providers and systems, especially when data from clinical trials is lacking,” so they “decided to compare different strategies head to head using available data and generate evidence that could be used in situations with many trade-offs in risks and benefits.”
To investigate, the researchers used a simulation model and decision analysis to compare four treatment strategies on the basis of type of therapy (primary vs. secondary prophylaxis), timing of event (early vs. late seizures), and duration of therapy (1-week [short-term] versus indefinite [long-term] therapy).
These four strategies were as follows:
- Conservative: short-term (7-day) secondary early-seizure prophylaxis with long-term therapy after late seizure
- Moderate: long-term secondary early-seizure prophylaxis or late-seizure therapy
- Aggressive: long-term primary prophylaxis
- Risk-guided: short-term secondary early-seizure prophylaxis among low-risk patients (2HELPS2b score, 0), short-term primary prophylaxis among patients at higher risk (2HELPS2B score ≥1), and long-term secondary therapy for late seizure
The decision tree’s outcome measure was the number of expected quality-adjusted life-years.
Primary prophylaxis was defined as “treatment initiated immediately on hospital admission.” Secondary prophylaxis was defined as “treatment started after a seizure” and was subdivided into secondary early-seizure prophylaxis, defined as treatment started after a seizure occurring in the first 7 days after the stroke, or secondary late-seizure therapy, defined as treatment started or restarted after a seizure occurring after the first poststroke week.
Incorporate early-risk stratification tool
The researchers created four common clinical scenarios and then applied the decision-making model to each. They found that the preferred strategies differed, depending on the particular scenario.
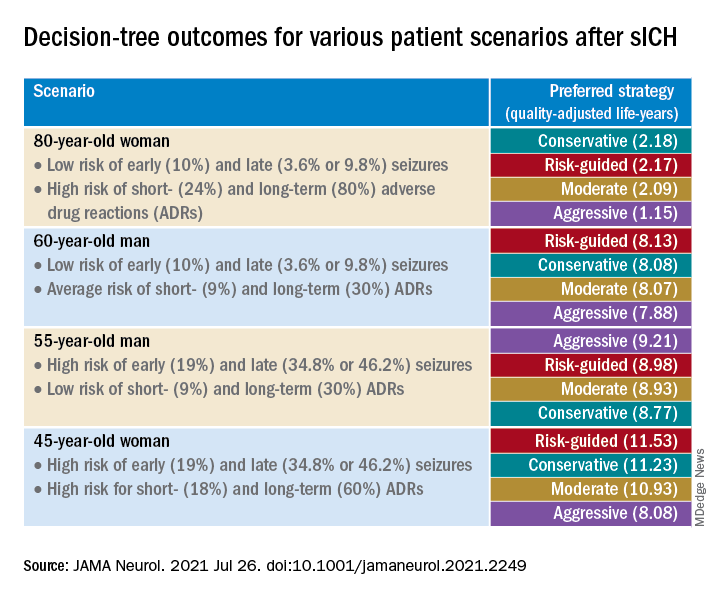
Sensitivity analyses revealed that short-term strategies, including the conservative and risk-guided approaches, were preferable in most cases, with the risk-guided strategy performing comparably or even better than alternative strategies in most cases.
“Our findings suggest that a strategy that incorporates an early-seizure risk stratification tool [2HELPS2B] is favored over alternative strategies in most settings,” Dr. Moura commented.
“Current services with rapidly available EEG may consider using a 1-hour screening with EEG upon admission for all patients presenting with sICH to risk-stratify those patients, using the 2HELPS2B tool,” she continued. “If EEG is unavailable for early-seizure risk stratification, the conservative strategy seems most reasonable.”
‘Potential fallacies’
Commenting on the study, José Biller, MD, professor and chairman, department of neurology, Loyola University Chicago, Maywood, Ill., called it a “well-written and intriguing contribution [to the field], with potential fallacies.”
The bottom line, he said, is that only a randomized, long-term, prospective, multicenter, high-quality study with larger cohorts can prove or disprove the investigators’ assumption.
The authors acknowledged that a limitation of the study was the use of published literature to obtain data to estimate model parameters and that they did not account for other possible factors that might modify some parameter estimates.
Nevertheless, Dr. Moura said the findings have important practical implications because they “highlight the importance of discontinuing antiseizure medications that were started during a hospitalization for sICH in patients that only had an early seizure.”
It is “of great importance for all providers to reassess the indication of antiseizure medications. Those drugs are not free of risks and can impact the patient’s health and quality of life,” she added.
The study was supported by grants from the National Institutes of Health. Dr. Moura reported receiving funding from the Centers for Disease Control and Prevention, the NIH, and the Epilepsy Foundation of America (Epilepsy Learning Healthcare System) as the director of the data coordinating center. Dr. Biller is the editor-in-chief of the Journal of Stroke and Cerebrovascular Diseases and a section editor of UpToDate.
A version of this article first appeared on Medscape.com.
(sICH), new research shows.
Investigators created a model that simulated common clinical scenarios to compare four antiseizure drug strategies – conservative, moderate, aggressive, and risk-guided. They used the 2HELPS2B score as a risk stratification tool to guide clinical decisions.
The investigators found that the short-term, early-seizure prophylaxis strategies “dominated” long-term therapy under most clinical scenarios, underscoring the importance of early discontinuation of antiseizure drug therapy.
“The main message here was that strategies that involved long-term antiseizure drug prescription (moderate and aggressive) fail to provide better outcomes in most clinical scenarios, when compared with strategies using short-term prophylaxis (conservative and risk-guided),” senior investigator Lidia M.V.R. Moura, MD, MPH, assistant professor of neurology, Harvard Medical School, Boston, said in an interview.
The study was published online July 26 in JAMA Neurology.
Common complication
“Acute asymptomatic seizures [early seizures ≤7 days after stroke] are a common complication of sICH,” the authors noted.
Potential safety concerns have prompted recommendations against the use of antiseizure medications for primary prophylaxis. However, approximately 40% of U.S. patients with sICH do receive prophylactic levetiracetam before seizure development. For these patients, the duration of prophylaxis varies widely.
“Because seizure risk is a key determinant of which patient groups might benefit most from different prophylaxis strategies, validated tools for predicting early ... and late ... seizure risks could aid physicians in treatment decisions. However, no clinical trials or prospective studies have evaluated the net benefit of various strategies after sICH,” the investigators noted.
“Our patients who were survivors of an intracerebral hemorrhage motivated us to conduct the study,” said Dr. Moura, who is also director of the MGH NeuroValue Laboratory. “Some would come to the clinic with a long list of medications; some of them were taking antiseizure drugs for many years, but they never had a documented seizure.” These patients did not know why they had been taking an antiseizure drug for so long.
“In these conversations, we noted so much variability in indications and variability in patient access to specialty care to make treatment decisions. We noted that the evidence behind our current guidelines on seizure management was limited,” she added.
Dr. Moura and colleagues were “committed to improve outcome for people with neurological conditions by leveraging research methods that can help guide providers and systems, especially when data from clinical trials is lacking,” so they “decided to compare different strategies head to head using available data and generate evidence that could be used in situations with many trade-offs in risks and benefits.”
To investigate, the researchers used a simulation model and decision analysis to compare four treatment strategies on the basis of type of therapy (primary vs. secondary prophylaxis), timing of event (early vs. late seizures), and duration of therapy (1-week [short-term] versus indefinite [long-term] therapy).
These four strategies were as follows:
- Conservative: short-term (7-day) secondary early-seizure prophylaxis with long-term therapy after late seizure
- Moderate: long-term secondary early-seizure prophylaxis or late-seizure therapy
- Aggressive: long-term primary prophylaxis
- Risk-guided: short-term secondary early-seizure prophylaxis among low-risk patients (2HELPS2b score, 0), short-term primary prophylaxis among patients at higher risk (2HELPS2B score ≥1), and long-term secondary therapy for late seizure
The decision tree’s outcome measure was the number of expected quality-adjusted life-years.
Primary prophylaxis was defined as “treatment initiated immediately on hospital admission.” Secondary prophylaxis was defined as “treatment started after a seizure” and was subdivided into secondary early-seizure prophylaxis, defined as treatment started after a seizure occurring in the first 7 days after the stroke, or secondary late-seizure therapy, defined as treatment started or restarted after a seizure occurring after the first poststroke week.
Incorporate early-risk stratification tool
The researchers created four common clinical scenarios and then applied the decision-making model to each. They found that the preferred strategies differed, depending on the particular scenario.
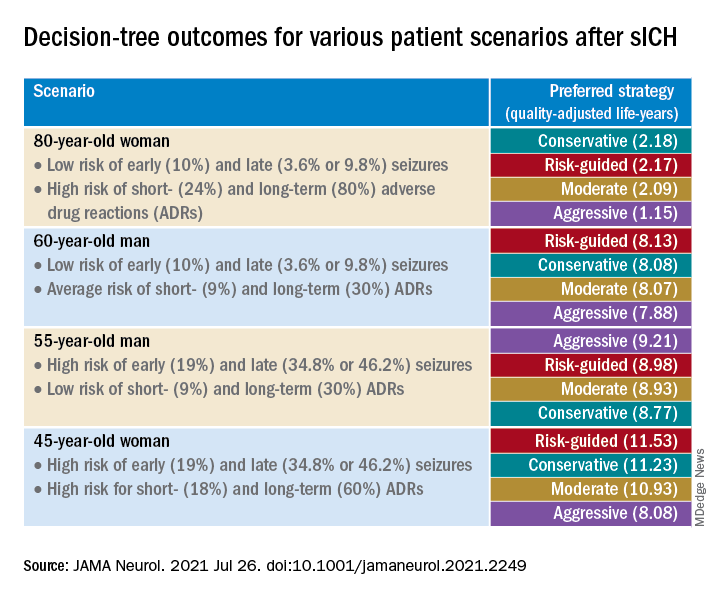
Sensitivity analyses revealed that short-term strategies, including the conservative and risk-guided approaches, were preferable in most cases, with the risk-guided strategy performing comparably or even better than alternative strategies in most cases.
“Our findings suggest that a strategy that incorporates an early-seizure risk stratification tool [2HELPS2B] is favored over alternative strategies in most settings,” Dr. Moura commented.
“Current services with rapidly available EEG may consider using a 1-hour screening with EEG upon admission for all patients presenting with sICH to risk-stratify those patients, using the 2HELPS2B tool,” she continued. “If EEG is unavailable for early-seizure risk stratification, the conservative strategy seems most reasonable.”
‘Potential fallacies’
Commenting on the study, José Biller, MD, professor and chairman, department of neurology, Loyola University Chicago, Maywood, Ill., called it a “well-written and intriguing contribution [to the field], with potential fallacies.”
The bottom line, he said, is that only a randomized, long-term, prospective, multicenter, high-quality study with larger cohorts can prove or disprove the investigators’ assumption.
The authors acknowledged that a limitation of the study was the use of published literature to obtain data to estimate model parameters and that they did not account for other possible factors that might modify some parameter estimates.
Nevertheless, Dr. Moura said the findings have important practical implications because they “highlight the importance of discontinuing antiseizure medications that were started during a hospitalization for sICH in patients that only had an early seizure.”
It is “of great importance for all providers to reassess the indication of antiseizure medications. Those drugs are not free of risks and can impact the patient’s health and quality of life,” she added.
The study was supported by grants from the National Institutes of Health. Dr. Moura reported receiving funding from the Centers for Disease Control and Prevention, the NIH, and the Epilepsy Foundation of America (Epilepsy Learning Healthcare System) as the director of the data coordinating center. Dr. Biller is the editor-in-chief of the Journal of Stroke and Cerebrovascular Diseases and a section editor of UpToDate.
A version of this article first appeared on Medscape.com.
(sICH), new research shows.
Investigators created a model that simulated common clinical scenarios to compare four antiseizure drug strategies – conservative, moderate, aggressive, and risk-guided. They used the 2HELPS2B score as a risk stratification tool to guide clinical decisions.
The investigators found that the short-term, early-seizure prophylaxis strategies “dominated” long-term therapy under most clinical scenarios, underscoring the importance of early discontinuation of antiseizure drug therapy.
“The main message here was that strategies that involved long-term antiseizure drug prescription (moderate and aggressive) fail to provide better outcomes in most clinical scenarios, when compared with strategies using short-term prophylaxis (conservative and risk-guided),” senior investigator Lidia M.V.R. Moura, MD, MPH, assistant professor of neurology, Harvard Medical School, Boston, said in an interview.
The study was published online July 26 in JAMA Neurology.
Common complication
“Acute asymptomatic seizures [early seizures ≤7 days after stroke] are a common complication of sICH,” the authors noted.
Potential safety concerns have prompted recommendations against the use of antiseizure medications for primary prophylaxis. However, approximately 40% of U.S. patients with sICH do receive prophylactic levetiracetam before seizure development. For these patients, the duration of prophylaxis varies widely.
“Because seizure risk is a key determinant of which patient groups might benefit most from different prophylaxis strategies, validated tools for predicting early ... and late ... seizure risks could aid physicians in treatment decisions. However, no clinical trials or prospective studies have evaluated the net benefit of various strategies after sICH,” the investigators noted.
“Our patients who were survivors of an intracerebral hemorrhage motivated us to conduct the study,” said Dr. Moura, who is also director of the MGH NeuroValue Laboratory. “Some would come to the clinic with a long list of medications; some of them were taking antiseizure drugs for many years, but they never had a documented seizure.” These patients did not know why they had been taking an antiseizure drug for so long.
“In these conversations, we noted so much variability in indications and variability in patient access to specialty care to make treatment decisions. We noted that the evidence behind our current guidelines on seizure management was limited,” she added.
Dr. Moura and colleagues were “committed to improve outcome for people with neurological conditions by leveraging research methods that can help guide providers and systems, especially when data from clinical trials is lacking,” so they “decided to compare different strategies head to head using available data and generate evidence that could be used in situations with many trade-offs in risks and benefits.”
To investigate, the researchers used a simulation model and decision analysis to compare four treatment strategies on the basis of type of therapy (primary vs. secondary prophylaxis), timing of event (early vs. late seizures), and duration of therapy (1-week [short-term] versus indefinite [long-term] therapy).
These four strategies were as follows:
- Conservative: short-term (7-day) secondary early-seizure prophylaxis with long-term therapy after late seizure
- Moderate: long-term secondary early-seizure prophylaxis or late-seizure therapy
- Aggressive: long-term primary prophylaxis
- Risk-guided: short-term secondary early-seizure prophylaxis among low-risk patients (2HELPS2b score, 0), short-term primary prophylaxis among patients at higher risk (2HELPS2B score ≥1), and long-term secondary therapy for late seizure
The decision tree’s outcome measure was the number of expected quality-adjusted life-years.
Primary prophylaxis was defined as “treatment initiated immediately on hospital admission.” Secondary prophylaxis was defined as “treatment started after a seizure” and was subdivided into secondary early-seizure prophylaxis, defined as treatment started after a seizure occurring in the first 7 days after the stroke, or secondary late-seizure therapy, defined as treatment started or restarted after a seizure occurring after the first poststroke week.
Incorporate early-risk stratification tool
The researchers created four common clinical scenarios and then applied the decision-making model to each. They found that the preferred strategies differed, depending on the particular scenario.
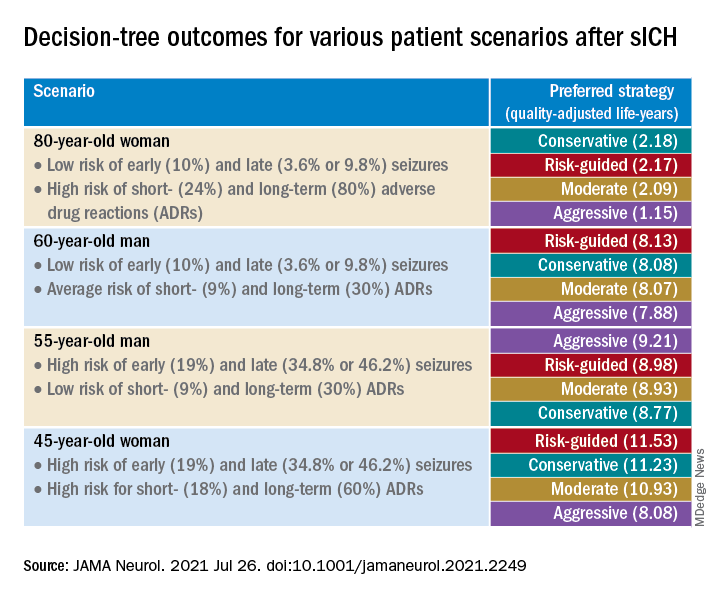
Sensitivity analyses revealed that short-term strategies, including the conservative and risk-guided approaches, were preferable in most cases, with the risk-guided strategy performing comparably or even better than alternative strategies in most cases.
“Our findings suggest that a strategy that incorporates an early-seizure risk stratification tool [2HELPS2B] is favored over alternative strategies in most settings,” Dr. Moura commented.
“Current services with rapidly available EEG may consider using a 1-hour screening with EEG upon admission for all patients presenting with sICH to risk-stratify those patients, using the 2HELPS2B tool,” she continued. “If EEG is unavailable for early-seizure risk stratification, the conservative strategy seems most reasonable.”
‘Potential fallacies’
Commenting on the study, José Biller, MD, professor and chairman, department of neurology, Loyola University Chicago, Maywood, Ill., called it a “well-written and intriguing contribution [to the field], with potential fallacies.”
The bottom line, he said, is that only a randomized, long-term, prospective, multicenter, high-quality study with larger cohorts can prove or disprove the investigators’ assumption.
The authors acknowledged that a limitation of the study was the use of published literature to obtain data to estimate model parameters and that they did not account for other possible factors that might modify some parameter estimates.
Nevertheless, Dr. Moura said the findings have important practical implications because they “highlight the importance of discontinuing antiseizure medications that were started during a hospitalization for sICH in patients that only had an early seizure.”
It is “of great importance for all providers to reassess the indication of antiseizure medications. Those drugs are not free of risks and can impact the patient’s health and quality of life,” she added.
The study was supported by grants from the National Institutes of Health. Dr. Moura reported receiving funding from the Centers for Disease Control and Prevention, the NIH, and the Epilepsy Foundation of America (Epilepsy Learning Healthcare System) as the director of the data coordinating center. Dr. Biller is the editor-in-chief of the Journal of Stroke and Cerebrovascular Diseases and a section editor of UpToDate.
A version of this article first appeared on Medscape.com.
Virtual roller-coaster may explain the ups and downs of migraine
and may explain the mechanisms underlying common symptoms and increased activity in certain brain regions in migraine patients.
In a new study, the prevalence of dizziness was 65% among patients with migraine who underwent a virtual roller-coaster ride versus 30% among those without migraine. In addition, imaging showed greater neuronal activity after the simulation in those with migraine.
“Migraine patients reported more dizziness and motion sickness, as well as longer symptom duration and intensity, in a virtual roller-coaster ride,” even though the videos and timing were identical for both groups, said study investigator Arne May, MD, PhD, professor of neurology at the University of Hamburg (Germany).
“We found differences not just in behavioral results but also in specific activations of areas within the cerebellum and the frontal gyrus. Migraine patients process such visual input differently from controls and activate a specific brain network to do so,” he added.
The findings were published online July 21, 2021, in Neurology.
The brain’s response
Nausea, which is among the diagnostic criteria for migraine, is the main symptom of motion sickness. Vestibular symptoms such as dizziness are also components of migraine.
Previous research has examined how the brain processes visual and motion stimuli in migraine, but the reasons patients with migraine are susceptible to motion sickness and dizziness remain unclear.
The researchers used a simulated roller-coaster ride to study the clinical and brain responses to motion among participants with and participants without migraine. They enrolled 20 consecutive patients with migraine who presented to a tertiary headache clinic between January and March 2020 and enrolled 20 healthy participants from a university hospital and the community. The average age of the study population was 30 years, and more than 80% were women.
In response to a questionnaire, participants provided information about demographics and headache features, including onset, frequency, and intensity. They also provided information about their status within the migraine phase and about vestibular symptoms experienced in daily life.
While undergoing functional MRI (fMRI), all participants watched two short videos that provided a first-person perspective of a roller-coaster ride. During the videos, they wore ear buds that conveyed the sound of a car riding over the rails.
The first video included more horizontal perspectives, and the second had more vertical perspectives. Each video was shown three times in random order.
During fMRI, participants reported intensity of nausea and vestibular symptoms using an 11-point Likert scale. After the experiment, they responded to a questionnaire that evaluated intensity and duration of nausea, dizziness, and vertigo experienced during the videos.
Participants also were given the Simulator Sickness Questionnaire (SSQ), which assessed motion sickness. A 100-point visual analog scale (VAS) was used to rate how realistic the roller-coaster experience had been.
There were no differences in sex or age between the migraine group and the healthy control group. Half of the patients with migraine reported aura. The mean number of migraine attacks within the previous month was 3.7. The mean Migraine Disability Assessment score was 21.5, which indicates severe disability.
Nausea, dizziness often neglected
Baseline prevalence of vestibular symptoms was 75% in the migraine group and 5% in the control group (P < .0001). These symptoms included dizziness (60% and 5%, respectively; P < .0001) and postural symptoms (40% and 0%, respectively; P = .003).
At baseline, vestibular symptoms were more frequent (P = .001), more intense (P < .0001), and were associated with greater disability (P = .001) in patients with migraine, compared with participants without migraine. The patients with migraine were also more susceptible to motion sickness (P = .02) and had higher depression scores (P = .001).
During the roller-coaster simulation, dizziness was more prevalent among patients with migraine than among those without migraine (65% vs. 30%; P = .03). Patients with migraine also reported more motion sickness (SSQ score, 47.3 vs. 24.3; P = .004), longer symptom duration (1:19 minutes vs. 00:27 minutes; P = .03), and symptoms of greater intensity (VAS, 22.0 vs. 9.9; P = .03).
Brain activity also differed between groups. Among patients with migraine, neuronal activity was greater in clusters within the right superior and left inferior occipital gyrus, the left pontine nuclei, and the left cerebellar lobules V and VI.
There was a moderately negative correlation of activation of the inferior occipital gyrus with migraine disability (r = –0.46; P = .04). Activation within the pontine nuclei correlated positively with motion sickness scores (r = 0.32; P = .04).
In addition, among patients with migraine, activity in the cerebellar lobule VIIb and in the left middle frontal gyrus was decreased in comparison with persons without migraine. Also among patients with migraine, there was enhanced connectivity between the pontine nuclei, cerebellar areas V and VI, and the interior and superior occipital gyrus and numerous cortical areas.
Clinicians often neglect to treat dizziness and nausea in patients with migraine, said Dr. May. However, these symptoms are part of migraine, even when attacks are not occurring.
“I have learned that if we can explain such symptoms, they are better accepted,” said Dr. May. “We need more and better basic research because we need to understand before we treat.”
Toward faster, more effective treatment
Commenting on the study, Erik Viirre, MD, PhD, professor in the department of neurosciences, University of California, San Diego, said, “we can be excited and celebrate that these researchers are using these news tools to investigate the operation of the migraine brain.
“That will combine with the new therapies and the genomics to give us a powerful approach to this particular condition,” said Dr. Viirre, who was not involved with the research.
The findings provide significant detail about the interconnections between the various brain regions affected by migraine, he noted. These regions include not just the sensory centers but also areas involved in higher executive function and emotional responses.
By identifying these regions, the findings show “some of the underlying mechanisms of these clinically relevant features,” said Dr. Viirre, who is also director of UCSD’s Arthur C. Clarke Center for Human Imagination.
The investigators set up the motion simulation well and used sound fMRI methodology, he added. However, imaging studies of the brain’s response to motion pose several challenges.
“The biggest challenge in any of these circumstances is that you can’t put an actual fMRI scanner on a roller-coaster,” said Dr. Viirre. “The actual acceleration and gravitational sensations delivered by a roller-coaster and gravity, of course, do not occur when you’re lying still in an MRI scanner.” Nevertheless, the pseudoacceleration produced by a visual stimulus is a reasonable proxy.
The findings also suggest that researchers in the future could examine whether any new therapeutic interventions for migraine modulate the brain functions differently for individuals with migraine than for those without migraine, he noted.
“That’s going to lead us to a faster, more effective, more reliable suite of migraine therapies,” said Dr. Viirre.
The study also reminds clinicians to take a broader approach to patients with migraine, and it underscores the value of strategies such as self-calming techniques, which can reduce the number and intensity of headaches, he said.
“Literally demonstrating these functional differences in the migraine brain is a hugely important message of advocacy for people with migraine,” Dr. Viirre concluded.
The study was funded by the German Research Foundation. Drs. May and Viirre have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
and may explain the mechanisms underlying common symptoms and increased activity in certain brain regions in migraine patients.
In a new study, the prevalence of dizziness was 65% among patients with migraine who underwent a virtual roller-coaster ride versus 30% among those without migraine. In addition, imaging showed greater neuronal activity after the simulation in those with migraine.
“Migraine patients reported more dizziness and motion sickness, as well as longer symptom duration and intensity, in a virtual roller-coaster ride,” even though the videos and timing were identical for both groups, said study investigator Arne May, MD, PhD, professor of neurology at the University of Hamburg (Germany).
“We found differences not just in behavioral results but also in specific activations of areas within the cerebellum and the frontal gyrus. Migraine patients process such visual input differently from controls and activate a specific brain network to do so,” he added.
The findings were published online July 21, 2021, in Neurology.
The brain’s response
Nausea, which is among the diagnostic criteria for migraine, is the main symptom of motion sickness. Vestibular symptoms such as dizziness are also components of migraine.
Previous research has examined how the brain processes visual and motion stimuli in migraine, but the reasons patients with migraine are susceptible to motion sickness and dizziness remain unclear.
The researchers used a simulated roller-coaster ride to study the clinical and brain responses to motion among participants with and participants without migraine. They enrolled 20 consecutive patients with migraine who presented to a tertiary headache clinic between January and March 2020 and enrolled 20 healthy participants from a university hospital and the community. The average age of the study population was 30 years, and more than 80% were women.
In response to a questionnaire, participants provided information about demographics and headache features, including onset, frequency, and intensity. They also provided information about their status within the migraine phase and about vestibular symptoms experienced in daily life.
While undergoing functional MRI (fMRI), all participants watched two short videos that provided a first-person perspective of a roller-coaster ride. During the videos, they wore ear buds that conveyed the sound of a car riding over the rails.
The first video included more horizontal perspectives, and the second had more vertical perspectives. Each video was shown three times in random order.
During fMRI, participants reported intensity of nausea and vestibular symptoms using an 11-point Likert scale. After the experiment, they responded to a questionnaire that evaluated intensity and duration of nausea, dizziness, and vertigo experienced during the videos.
Participants also were given the Simulator Sickness Questionnaire (SSQ), which assessed motion sickness. A 100-point visual analog scale (VAS) was used to rate how realistic the roller-coaster experience had been.
There were no differences in sex or age between the migraine group and the healthy control group. Half of the patients with migraine reported aura. The mean number of migraine attacks within the previous month was 3.7. The mean Migraine Disability Assessment score was 21.5, which indicates severe disability.
Nausea, dizziness often neglected
Baseline prevalence of vestibular symptoms was 75% in the migraine group and 5% in the control group (P < .0001). These symptoms included dizziness (60% and 5%, respectively; P < .0001) and postural symptoms (40% and 0%, respectively; P = .003).
At baseline, vestibular symptoms were more frequent (P = .001), more intense (P < .0001), and were associated with greater disability (P = .001) in patients with migraine, compared with participants without migraine. The patients with migraine were also more susceptible to motion sickness (P = .02) and had higher depression scores (P = .001).
During the roller-coaster simulation, dizziness was more prevalent among patients with migraine than among those without migraine (65% vs. 30%; P = .03). Patients with migraine also reported more motion sickness (SSQ score, 47.3 vs. 24.3; P = .004), longer symptom duration (1:19 minutes vs. 00:27 minutes; P = .03), and symptoms of greater intensity (VAS, 22.0 vs. 9.9; P = .03).
Brain activity also differed between groups. Among patients with migraine, neuronal activity was greater in clusters within the right superior and left inferior occipital gyrus, the left pontine nuclei, and the left cerebellar lobules V and VI.
There was a moderately negative correlation of activation of the inferior occipital gyrus with migraine disability (r = –0.46; P = .04). Activation within the pontine nuclei correlated positively with motion sickness scores (r = 0.32; P = .04).
In addition, among patients with migraine, activity in the cerebellar lobule VIIb and in the left middle frontal gyrus was decreased in comparison with persons without migraine. Also among patients with migraine, there was enhanced connectivity between the pontine nuclei, cerebellar areas V and VI, and the interior and superior occipital gyrus and numerous cortical areas.
Clinicians often neglect to treat dizziness and nausea in patients with migraine, said Dr. May. However, these symptoms are part of migraine, even when attacks are not occurring.
“I have learned that if we can explain such symptoms, they are better accepted,” said Dr. May. “We need more and better basic research because we need to understand before we treat.”
Toward faster, more effective treatment
Commenting on the study, Erik Viirre, MD, PhD, professor in the department of neurosciences, University of California, San Diego, said, “we can be excited and celebrate that these researchers are using these news tools to investigate the operation of the migraine brain.
“That will combine with the new therapies and the genomics to give us a powerful approach to this particular condition,” said Dr. Viirre, who was not involved with the research.
The findings provide significant detail about the interconnections between the various brain regions affected by migraine, he noted. These regions include not just the sensory centers but also areas involved in higher executive function and emotional responses.
By identifying these regions, the findings show “some of the underlying mechanisms of these clinically relevant features,” said Dr. Viirre, who is also director of UCSD’s Arthur C. Clarke Center for Human Imagination.
The investigators set up the motion simulation well and used sound fMRI methodology, he added. However, imaging studies of the brain’s response to motion pose several challenges.
“The biggest challenge in any of these circumstances is that you can’t put an actual fMRI scanner on a roller-coaster,” said Dr. Viirre. “The actual acceleration and gravitational sensations delivered by a roller-coaster and gravity, of course, do not occur when you’re lying still in an MRI scanner.” Nevertheless, the pseudoacceleration produced by a visual stimulus is a reasonable proxy.
The findings also suggest that researchers in the future could examine whether any new therapeutic interventions for migraine modulate the brain functions differently for individuals with migraine than for those without migraine, he noted.
“That’s going to lead us to a faster, more effective, more reliable suite of migraine therapies,” said Dr. Viirre.
The study also reminds clinicians to take a broader approach to patients with migraine, and it underscores the value of strategies such as self-calming techniques, which can reduce the number and intensity of headaches, he said.
“Literally demonstrating these functional differences in the migraine brain is a hugely important message of advocacy for people with migraine,” Dr. Viirre concluded.
The study was funded by the German Research Foundation. Drs. May and Viirre have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
and may explain the mechanisms underlying common symptoms and increased activity in certain brain regions in migraine patients.
In a new study, the prevalence of dizziness was 65% among patients with migraine who underwent a virtual roller-coaster ride versus 30% among those without migraine. In addition, imaging showed greater neuronal activity after the simulation in those with migraine.
“Migraine patients reported more dizziness and motion sickness, as well as longer symptom duration and intensity, in a virtual roller-coaster ride,” even though the videos and timing were identical for both groups, said study investigator Arne May, MD, PhD, professor of neurology at the University of Hamburg (Germany).
“We found differences not just in behavioral results but also in specific activations of areas within the cerebellum and the frontal gyrus. Migraine patients process such visual input differently from controls and activate a specific brain network to do so,” he added.
The findings were published online July 21, 2021, in Neurology.
The brain’s response
Nausea, which is among the diagnostic criteria for migraine, is the main symptom of motion sickness. Vestibular symptoms such as dizziness are also components of migraine.
Previous research has examined how the brain processes visual and motion stimuli in migraine, but the reasons patients with migraine are susceptible to motion sickness and dizziness remain unclear.
The researchers used a simulated roller-coaster ride to study the clinical and brain responses to motion among participants with and participants without migraine. They enrolled 20 consecutive patients with migraine who presented to a tertiary headache clinic between January and March 2020 and enrolled 20 healthy participants from a university hospital and the community. The average age of the study population was 30 years, and more than 80% were women.
In response to a questionnaire, participants provided information about demographics and headache features, including onset, frequency, and intensity. They also provided information about their status within the migraine phase and about vestibular symptoms experienced in daily life.
While undergoing functional MRI (fMRI), all participants watched two short videos that provided a first-person perspective of a roller-coaster ride. During the videos, they wore ear buds that conveyed the sound of a car riding over the rails.
The first video included more horizontal perspectives, and the second had more vertical perspectives. Each video was shown three times in random order.
During fMRI, participants reported intensity of nausea and vestibular symptoms using an 11-point Likert scale. After the experiment, they responded to a questionnaire that evaluated intensity and duration of nausea, dizziness, and vertigo experienced during the videos.
Participants also were given the Simulator Sickness Questionnaire (SSQ), which assessed motion sickness. A 100-point visual analog scale (VAS) was used to rate how realistic the roller-coaster experience had been.
There were no differences in sex or age between the migraine group and the healthy control group. Half of the patients with migraine reported aura. The mean number of migraine attacks within the previous month was 3.7. The mean Migraine Disability Assessment score was 21.5, which indicates severe disability.
Nausea, dizziness often neglected
Baseline prevalence of vestibular symptoms was 75% in the migraine group and 5% in the control group (P < .0001). These symptoms included dizziness (60% and 5%, respectively; P < .0001) and postural symptoms (40% and 0%, respectively; P = .003).
At baseline, vestibular symptoms were more frequent (P = .001), more intense (P < .0001), and were associated with greater disability (P = .001) in patients with migraine, compared with participants without migraine. The patients with migraine were also more susceptible to motion sickness (P = .02) and had higher depression scores (P = .001).
During the roller-coaster simulation, dizziness was more prevalent among patients with migraine than among those without migraine (65% vs. 30%; P = .03). Patients with migraine also reported more motion sickness (SSQ score, 47.3 vs. 24.3; P = .004), longer symptom duration (1:19 minutes vs. 00:27 minutes; P = .03), and symptoms of greater intensity (VAS, 22.0 vs. 9.9; P = .03).
Brain activity also differed between groups. Among patients with migraine, neuronal activity was greater in clusters within the right superior and left inferior occipital gyrus, the left pontine nuclei, and the left cerebellar lobules V and VI.
There was a moderately negative correlation of activation of the inferior occipital gyrus with migraine disability (r = –0.46; P = .04). Activation within the pontine nuclei correlated positively with motion sickness scores (r = 0.32; P = .04).
In addition, among patients with migraine, activity in the cerebellar lobule VIIb and in the left middle frontal gyrus was decreased in comparison with persons without migraine. Also among patients with migraine, there was enhanced connectivity between the pontine nuclei, cerebellar areas V and VI, and the interior and superior occipital gyrus and numerous cortical areas.
Clinicians often neglect to treat dizziness and nausea in patients with migraine, said Dr. May. However, these symptoms are part of migraine, even when attacks are not occurring.
“I have learned that if we can explain such symptoms, they are better accepted,” said Dr. May. “We need more and better basic research because we need to understand before we treat.”
Toward faster, more effective treatment
Commenting on the study, Erik Viirre, MD, PhD, professor in the department of neurosciences, University of California, San Diego, said, “we can be excited and celebrate that these researchers are using these news tools to investigate the operation of the migraine brain.
“That will combine with the new therapies and the genomics to give us a powerful approach to this particular condition,” said Dr. Viirre, who was not involved with the research.
The findings provide significant detail about the interconnections between the various brain regions affected by migraine, he noted. These regions include not just the sensory centers but also areas involved in higher executive function and emotional responses.
By identifying these regions, the findings show “some of the underlying mechanisms of these clinically relevant features,” said Dr. Viirre, who is also director of UCSD’s Arthur C. Clarke Center for Human Imagination.
The investigators set up the motion simulation well and used sound fMRI methodology, he added. However, imaging studies of the brain’s response to motion pose several challenges.
“The biggest challenge in any of these circumstances is that you can’t put an actual fMRI scanner on a roller-coaster,” said Dr. Viirre. “The actual acceleration and gravitational sensations delivered by a roller-coaster and gravity, of course, do not occur when you’re lying still in an MRI scanner.” Nevertheless, the pseudoacceleration produced by a visual stimulus is a reasonable proxy.
The findings also suggest that researchers in the future could examine whether any new therapeutic interventions for migraine modulate the brain functions differently for individuals with migraine than for those without migraine, he noted.
“That’s going to lead us to a faster, more effective, more reliable suite of migraine therapies,” said Dr. Viirre.
The study also reminds clinicians to take a broader approach to patients with migraine, and it underscores the value of strategies such as self-calming techniques, which can reduce the number and intensity of headaches, he said.
“Literally demonstrating these functional differences in the migraine brain is a hugely important message of advocacy for people with migraine,” Dr. Viirre concluded.
The study was funded by the German Research Foundation. Drs. May and Viirre have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Infusion shown effective for acquired von Willebrand disease
Acquired von Willebrand disease (aVWD) is a rare and serious condition associated with lymphoproliferative disorders, malignancy, autoimmune disorders, and cardiovascular disease. It is most commonly caused by monoclonal gammopathy of undetermined significance (MGUS), which acts to clear von Willebrand factor from the patient’s bloodstream. However, a continuous-infusion of plasma-derived von Willebrand factor (VWF) concentrate provided adequate hemostasis in aVWD resulting from MGUS, according to Kathryn E. Dane, PharmD, of Johns Hopkins University, Baltimore, and colleagues.
The infusion rapidly achieved target ristocetin cofactor activity with or without intravenous immunoglobulin in three patients, as detailed in the report published online in Blood Advances.
The three consecutive patients with aVWD were treated with plasma-derived VWF concentrate administered for periprocedural optimization (patient 1, an 85-year old woman) or to treat bleeding episodes (patient 2, an 88-year-old man; and patient 3, a 53-year-old woman). Factor VIII activity was measured via a 1-stage clotting test and von Willebrand factor activity was measured with a ristocetin cofactor assay.
Promising results
All three patients demonstrated increased VWF ristocetin cofactor and factor VIII activities within hours of initiation of the continuous infusion concentrate, according to the report.
“We hypothesize that the efficacy of CI VWF concentrate in aVWD may be related to continuous provision of VWF, allowing binding and neutralization of anti-VWF IgG antibodies, and providing adequate circulating unbound VWF for appropriate hemostatic efficacy,” the researchers concluded.
The authors reported that they had no competing financial interests.
Acquired von Willebrand disease (aVWD) is a rare and serious condition associated with lymphoproliferative disorders, malignancy, autoimmune disorders, and cardiovascular disease. It is most commonly caused by monoclonal gammopathy of undetermined significance (MGUS), which acts to clear von Willebrand factor from the patient’s bloodstream. However, a continuous-infusion of plasma-derived von Willebrand factor (VWF) concentrate provided adequate hemostasis in aVWD resulting from MGUS, according to Kathryn E. Dane, PharmD, of Johns Hopkins University, Baltimore, and colleagues.
The infusion rapidly achieved target ristocetin cofactor activity with or without intravenous immunoglobulin in three patients, as detailed in the report published online in Blood Advances.
The three consecutive patients with aVWD were treated with plasma-derived VWF concentrate administered for periprocedural optimization (patient 1, an 85-year old woman) or to treat bleeding episodes (patient 2, an 88-year-old man; and patient 3, a 53-year-old woman). Factor VIII activity was measured via a 1-stage clotting test and von Willebrand factor activity was measured with a ristocetin cofactor assay.
Promising results
All three patients demonstrated increased VWF ristocetin cofactor and factor VIII activities within hours of initiation of the continuous infusion concentrate, according to the report.
“We hypothesize that the efficacy of CI VWF concentrate in aVWD may be related to continuous provision of VWF, allowing binding and neutralization of anti-VWF IgG antibodies, and providing adequate circulating unbound VWF for appropriate hemostatic efficacy,” the researchers concluded.
The authors reported that they had no competing financial interests.
Acquired von Willebrand disease (aVWD) is a rare and serious condition associated with lymphoproliferative disorders, malignancy, autoimmune disorders, and cardiovascular disease. It is most commonly caused by monoclonal gammopathy of undetermined significance (MGUS), which acts to clear von Willebrand factor from the patient’s bloodstream. However, a continuous-infusion of plasma-derived von Willebrand factor (VWF) concentrate provided adequate hemostasis in aVWD resulting from MGUS, according to Kathryn E. Dane, PharmD, of Johns Hopkins University, Baltimore, and colleagues.
The infusion rapidly achieved target ristocetin cofactor activity with or without intravenous immunoglobulin in three patients, as detailed in the report published online in Blood Advances.
The three consecutive patients with aVWD were treated with plasma-derived VWF concentrate administered for periprocedural optimization (patient 1, an 85-year old woman) or to treat bleeding episodes (patient 2, an 88-year-old man; and patient 3, a 53-year-old woman). Factor VIII activity was measured via a 1-stage clotting test and von Willebrand factor activity was measured with a ristocetin cofactor assay.
Promising results
All three patients demonstrated increased VWF ristocetin cofactor and factor VIII activities within hours of initiation of the continuous infusion concentrate, according to the report.
“We hypothesize that the efficacy of CI VWF concentrate in aVWD may be related to continuous provision of VWF, allowing binding and neutralization of anti-VWF IgG antibodies, and providing adequate circulating unbound VWF for appropriate hemostatic efficacy,” the researchers concluded.
The authors reported that they had no competing financial interests.
FROM BLOOD ADVANCES