User login
Is mild cognitive impairment reversible?
new research shows.
The investigators found individuals with these factors, which are all markers of cognitive reserve, had a significantly greater chance of reversion from MCI to normal cognition (NC) than progression from MCI to dementia.
In a cohort study of more than 600 women aged 75 years or older, about a third of those with MCI reverted to NC at some point during follow-up, which sends “an encouraging message,” study author Suzanne Tyas, PhD, associate professor, University of Waterloo (Ont.), said in an interview.
“That’s a positive thing for people to keep in mind when they’re thinking about prognosis. Some of these novel characteristics we’ve identified might be useful in thinking about how likely a particular patient might be to improve versus decline cognitively,” Dr. Tyas added.
The findings were published online Feb. 4, 2022, in the journal Neurology.
Highly educated cohort
As the population ages, the number of individuals experiencing age-related conditions, including dementia, increases. There is no cure for most dementia types so prevention is key – and preventing dementia requires understanding its risk factors, Dr. Tyas noted.
The analysis included participants from the Nun Study, a longitudinal study of aging and cognition among members of the School Sisters of Notre Dame in the United States. All were 75 and older at baseline, which was from 1991 to 1993; about 14.5% were older than 90 years.
Participants were generally highly educated, with 84.5% attaining an undergraduate or graduate degree. They also had a similar socioeconomic status, level of social supports, marital and reproductive history, and alcohol and tobacco use.
Researchers examined cognitive function at baseline and then about annually until death or end of the 12th round of assessments. They used five measures from the Consortium to Establish a Registry for Alzheimer’s Disease neuropsychological battery to categorize subjects into NC, MCI, or dementia: Delayed Word Recall, Verbal Fluency, Boston Naming, Constructional Praxis, and the Mini-Mental State Exam.
The current analysis focused on the 619 participants with data on apolipoprotein E (apo E) epsilon-4 genotyping and education. From convent archives, investigators also had access to the nuns’ early high school academic performance in English, Latin, algebra, and geometry.
“Typically we only have data for [overall] education. But I know from teaching that there’s a difference between people who just pass my courses and graduate with a university degree versus those who really excel,” Dr. Tyas said.
The researchers also assessed handwriting samples from before the participants entered the religious order. From these, they scored “idea density,” which is the number of ideas contained in the writing and “grammatical complexity,” which includes structure, use of clauses, subclauses, and so on.
Dementia not inevitable
Results showed 472 of the 619 participants had MCI during the study period. About 30.3% of these showed at least one reverse transition from MCI to NC during a mean follow-up of 8.6 years; 83.9% went on to develop dementia.
This shows converting from MCI to NC occurs relatively frequently, Dr. Tyas noted.
“This is encouraging because some people think that if they have a diagnosis of MCI they are inevitably going to decline to dementia,” she added.
The researchers also used complicated modeling of transition rates over time between NC, MCI, and dementia and adjusted for participants who died. They estimated relative risk of reversion versus progression for age, apo E, and potential cognitive reserve indicators.
Not surprisingly, younger age (90 years or less) and absence of apo E epsilon-4 allele contributed to a significantly higher rate for reversion from MCI to NC versus progression from MCI to dementia.
However, although age and apo E are known risk factors for dementia, these have not been examined in the context of whether individuals with MCI are more likely to improve or decline, said Dr. Tyas.
Higher educational attainment, the traditional indicator of cognitive reserve, was associated with a significantly higher relative risk for reversion from MCI to NC versus progression from MCI to dementia (RR, 2.6) for a bachelor’s degree versus less education.
There was a greater RR for even higher education after adjusting for age and apo E epsilon-4 status.
Language skills key
Interestingly, the investigators also found a significant association with good grades in high school English but not other subjects (RR for higher vs. lower English grades, 1.83; 95% confidence interval, 1.07-3.14).
In addition, they found both characteristics of written language skills (idea density and grammatical complexity) were significant predictors of conversion to NC.
“Those with high levels of idea density were four times more likely to improve to normal cognition than progress to dementia, and the effect was even stronger for grammatical structure. Those individuals with higher levels were almost six times more likely to improve than decline,” Dr. Tyas reported.
The RR for higher versus lower idea density was 3.93 (95% CI, 1.3-11.9) and the RR for higher versus lower grammatical complexity was 5.78 (95% CI, 1.56-21.42).
These new results could be useful when planning future clinical trials, Dr. Tyas noted. “MCI in some people is going to improve even without any treatment, and this should be taken into consideration when recruiting participants to a study and when interpreting the results.
“You don’t want something to look like it’s a benefit of the treatment when in fact these individuals would have just reverted on their own,” she added.
Research implications
Commenting on the findings, Claire Sexton, DPhil, director of scientific programs and outreach at the Alzheimer’s Association, noted that, in “this study of highly educated, older women,” transitions from MCI to NC “were about equally common” as transitions from MCI to dementia.
“As advances are made in early detection of dementia, and treatments are developed and marketed for people living with MCI, this article’s findings are important to inform discussions of prognosis with patients and [to the] design of clinical trials,” Dr. Sexton said.
The study was funded by the Canadian Institutes of Health Research and the Natural Sciences and Engineering Research Council of Canada. Funding for the Nun Study at the University of Kentucky was provided by the U.S. National Institute of Aging and the Kleberg Foundation. Dr. Tyas has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research shows.
The investigators found individuals with these factors, which are all markers of cognitive reserve, had a significantly greater chance of reversion from MCI to normal cognition (NC) than progression from MCI to dementia.
In a cohort study of more than 600 women aged 75 years or older, about a third of those with MCI reverted to NC at some point during follow-up, which sends “an encouraging message,” study author Suzanne Tyas, PhD, associate professor, University of Waterloo (Ont.), said in an interview.
“That’s a positive thing for people to keep in mind when they’re thinking about prognosis. Some of these novel characteristics we’ve identified might be useful in thinking about how likely a particular patient might be to improve versus decline cognitively,” Dr. Tyas added.
The findings were published online Feb. 4, 2022, in the journal Neurology.
Highly educated cohort
As the population ages, the number of individuals experiencing age-related conditions, including dementia, increases. There is no cure for most dementia types so prevention is key – and preventing dementia requires understanding its risk factors, Dr. Tyas noted.
The analysis included participants from the Nun Study, a longitudinal study of aging and cognition among members of the School Sisters of Notre Dame in the United States. All were 75 and older at baseline, which was from 1991 to 1993; about 14.5% were older than 90 years.
Participants were generally highly educated, with 84.5% attaining an undergraduate or graduate degree. They also had a similar socioeconomic status, level of social supports, marital and reproductive history, and alcohol and tobacco use.
Researchers examined cognitive function at baseline and then about annually until death or end of the 12th round of assessments. They used five measures from the Consortium to Establish a Registry for Alzheimer’s Disease neuropsychological battery to categorize subjects into NC, MCI, or dementia: Delayed Word Recall, Verbal Fluency, Boston Naming, Constructional Praxis, and the Mini-Mental State Exam.
The current analysis focused on the 619 participants with data on apolipoprotein E (apo E) epsilon-4 genotyping and education. From convent archives, investigators also had access to the nuns’ early high school academic performance in English, Latin, algebra, and geometry.
“Typically we only have data for [overall] education. But I know from teaching that there’s a difference between people who just pass my courses and graduate with a university degree versus those who really excel,” Dr. Tyas said.
The researchers also assessed handwriting samples from before the participants entered the religious order. From these, they scored “idea density,” which is the number of ideas contained in the writing and “grammatical complexity,” which includes structure, use of clauses, subclauses, and so on.
Dementia not inevitable
Results showed 472 of the 619 participants had MCI during the study period. About 30.3% of these showed at least one reverse transition from MCI to NC during a mean follow-up of 8.6 years; 83.9% went on to develop dementia.
This shows converting from MCI to NC occurs relatively frequently, Dr. Tyas noted.
“This is encouraging because some people think that if they have a diagnosis of MCI they are inevitably going to decline to dementia,” she added.
The researchers also used complicated modeling of transition rates over time between NC, MCI, and dementia and adjusted for participants who died. They estimated relative risk of reversion versus progression for age, apo E, and potential cognitive reserve indicators.
Not surprisingly, younger age (90 years or less) and absence of apo E epsilon-4 allele contributed to a significantly higher rate for reversion from MCI to NC versus progression from MCI to dementia.
However, although age and apo E are known risk factors for dementia, these have not been examined in the context of whether individuals with MCI are more likely to improve or decline, said Dr. Tyas.
Higher educational attainment, the traditional indicator of cognitive reserve, was associated with a significantly higher relative risk for reversion from MCI to NC versus progression from MCI to dementia (RR, 2.6) for a bachelor’s degree versus less education.
There was a greater RR for even higher education after adjusting for age and apo E epsilon-4 status.
Language skills key
Interestingly, the investigators also found a significant association with good grades in high school English but not other subjects (RR for higher vs. lower English grades, 1.83; 95% confidence interval, 1.07-3.14).
In addition, they found both characteristics of written language skills (idea density and grammatical complexity) were significant predictors of conversion to NC.
“Those with high levels of idea density were four times more likely to improve to normal cognition than progress to dementia, and the effect was even stronger for grammatical structure. Those individuals with higher levels were almost six times more likely to improve than decline,” Dr. Tyas reported.
The RR for higher versus lower idea density was 3.93 (95% CI, 1.3-11.9) and the RR for higher versus lower grammatical complexity was 5.78 (95% CI, 1.56-21.42).
These new results could be useful when planning future clinical trials, Dr. Tyas noted. “MCI in some people is going to improve even without any treatment, and this should be taken into consideration when recruiting participants to a study and when interpreting the results.
“You don’t want something to look like it’s a benefit of the treatment when in fact these individuals would have just reverted on their own,” she added.
Research implications
Commenting on the findings, Claire Sexton, DPhil, director of scientific programs and outreach at the Alzheimer’s Association, noted that, in “this study of highly educated, older women,” transitions from MCI to NC “were about equally common” as transitions from MCI to dementia.
“As advances are made in early detection of dementia, and treatments are developed and marketed for people living with MCI, this article’s findings are important to inform discussions of prognosis with patients and [to the] design of clinical trials,” Dr. Sexton said.
The study was funded by the Canadian Institutes of Health Research and the Natural Sciences and Engineering Research Council of Canada. Funding for the Nun Study at the University of Kentucky was provided by the U.S. National Institute of Aging and the Kleberg Foundation. Dr. Tyas has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
new research shows.
The investigators found individuals with these factors, which are all markers of cognitive reserve, had a significantly greater chance of reversion from MCI to normal cognition (NC) than progression from MCI to dementia.
In a cohort study of more than 600 women aged 75 years or older, about a third of those with MCI reverted to NC at some point during follow-up, which sends “an encouraging message,” study author Suzanne Tyas, PhD, associate professor, University of Waterloo (Ont.), said in an interview.
“That’s a positive thing for people to keep in mind when they’re thinking about prognosis. Some of these novel characteristics we’ve identified might be useful in thinking about how likely a particular patient might be to improve versus decline cognitively,” Dr. Tyas added.
The findings were published online Feb. 4, 2022, in the journal Neurology.
Highly educated cohort
As the population ages, the number of individuals experiencing age-related conditions, including dementia, increases. There is no cure for most dementia types so prevention is key – and preventing dementia requires understanding its risk factors, Dr. Tyas noted.
The analysis included participants from the Nun Study, a longitudinal study of aging and cognition among members of the School Sisters of Notre Dame in the United States. All were 75 and older at baseline, which was from 1991 to 1993; about 14.5% were older than 90 years.
Participants were generally highly educated, with 84.5% attaining an undergraduate or graduate degree. They also had a similar socioeconomic status, level of social supports, marital and reproductive history, and alcohol and tobacco use.
Researchers examined cognitive function at baseline and then about annually until death or end of the 12th round of assessments. They used five measures from the Consortium to Establish a Registry for Alzheimer’s Disease neuropsychological battery to categorize subjects into NC, MCI, or dementia: Delayed Word Recall, Verbal Fluency, Boston Naming, Constructional Praxis, and the Mini-Mental State Exam.
The current analysis focused on the 619 participants with data on apolipoprotein E (apo E) epsilon-4 genotyping and education. From convent archives, investigators also had access to the nuns’ early high school academic performance in English, Latin, algebra, and geometry.
“Typically we only have data for [overall] education. But I know from teaching that there’s a difference between people who just pass my courses and graduate with a university degree versus those who really excel,” Dr. Tyas said.
The researchers also assessed handwriting samples from before the participants entered the religious order. From these, they scored “idea density,” which is the number of ideas contained in the writing and “grammatical complexity,” which includes structure, use of clauses, subclauses, and so on.
Dementia not inevitable
Results showed 472 of the 619 participants had MCI during the study period. About 30.3% of these showed at least one reverse transition from MCI to NC during a mean follow-up of 8.6 years; 83.9% went on to develop dementia.
This shows converting from MCI to NC occurs relatively frequently, Dr. Tyas noted.
“This is encouraging because some people think that if they have a diagnosis of MCI they are inevitably going to decline to dementia,” she added.
The researchers also used complicated modeling of transition rates over time between NC, MCI, and dementia and adjusted for participants who died. They estimated relative risk of reversion versus progression for age, apo E, and potential cognitive reserve indicators.
Not surprisingly, younger age (90 years or less) and absence of apo E epsilon-4 allele contributed to a significantly higher rate for reversion from MCI to NC versus progression from MCI to dementia.
However, although age and apo E are known risk factors for dementia, these have not been examined in the context of whether individuals with MCI are more likely to improve or decline, said Dr. Tyas.
Higher educational attainment, the traditional indicator of cognitive reserve, was associated with a significantly higher relative risk for reversion from MCI to NC versus progression from MCI to dementia (RR, 2.6) for a bachelor’s degree versus less education.
There was a greater RR for even higher education after adjusting for age and apo E epsilon-4 status.
Language skills key
Interestingly, the investigators also found a significant association with good grades in high school English but not other subjects (RR for higher vs. lower English grades, 1.83; 95% confidence interval, 1.07-3.14).
In addition, they found both characteristics of written language skills (idea density and grammatical complexity) were significant predictors of conversion to NC.
“Those with high levels of idea density were four times more likely to improve to normal cognition than progress to dementia, and the effect was even stronger for grammatical structure. Those individuals with higher levels were almost six times more likely to improve than decline,” Dr. Tyas reported.
The RR for higher versus lower idea density was 3.93 (95% CI, 1.3-11.9) and the RR for higher versus lower grammatical complexity was 5.78 (95% CI, 1.56-21.42).
These new results could be useful when planning future clinical trials, Dr. Tyas noted. “MCI in some people is going to improve even without any treatment, and this should be taken into consideration when recruiting participants to a study and when interpreting the results.
“You don’t want something to look like it’s a benefit of the treatment when in fact these individuals would have just reverted on their own,” she added.
Research implications
Commenting on the findings, Claire Sexton, DPhil, director of scientific programs and outreach at the Alzheimer’s Association, noted that, in “this study of highly educated, older women,” transitions from MCI to NC “were about equally common” as transitions from MCI to dementia.
“As advances are made in early detection of dementia, and treatments are developed and marketed for people living with MCI, this article’s findings are important to inform discussions of prognosis with patients and [to the] design of clinical trials,” Dr. Sexton said.
The study was funded by the Canadian Institutes of Health Research and the Natural Sciences and Engineering Research Council of Canada. Funding for the Nun Study at the University of Kentucky was provided by the U.S. National Institute of Aging and the Kleberg Foundation. Dr. Tyas has disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
ILAE offers first guide to treating depression in epilepsy
The new guidance highlights the high prevalence of depression among patients with epilepsy while offering the first systematic approach to treatment, reported lead author Marco Mula, MD, PhD, of Atkinson Morley Regional Neuroscience Centre at St George’s University Hospital, London, and colleagues.
“Despite evidence that depression represents a frequently encountered comorbidity [among patients with epilepsy], data on the treatment of depression in epilepsy [are] still limited and recommendations rely mostly on individual clinical experience and expertise,” the investigators wrote in Epilepsia.
Recommendations cover first-line treatment of unipolar depression in epilepsy without other psychiatric disorders.
For patients with mild depression, the guidance supports psychological intervention without pharmacologic therapy; however, if the patient wishes to use medication, has had a positive response to medication in the past, or nonpharmacologic treatments have previously failed or are unavailable, then SSRIs should be considered first-choice therapy. For moderate to severe depression, SSRIs are the first choice, according to Dr. Mula and colleagues.
“It has to be acknowledged that there is considerable debate in the psychiatric literature about the treatment of mild depression in adults,” the investigators noted. “A patient-level meta-analysis pointed out that the magnitude of benefit of antidepressant medications compared with placebo increases with severity of depression symptoms and it may be minimal or nonexistent, on average, in patients with mild or moderate symptoms.”
If a patient does not respond to first-line therapy, then venlafaxine should be considered, according to the guidance. When a patient does respond to therapy, treatment should be continued for at least 6 months, and when residual symptoms persist, treatment should be continued until resolution.
“In people with depression it is established that around two-thirds of patients do not achieve full remission with first-line treatment,” Dr. Mula and colleagues wrote. “In people with epilepsy, current data show that up to 50% of patients do not achieve full remission from depression. For this reason, augmentation strategies are often needed. They should be adopted by psychiatrists, neuropsychiatrists, or mental health professionals familiar with such therapeutic strategies.”
Beyond these key recommendations, the guidance covers a range of additional topics, including other pharmacologic options, medication discontinuation strategies, electroconvulsive therapy, light therapy, exercise training, vagus nerve stimulation, and repetitive transcranial magnetic stimulation.
Useful advice that counters common misconceptions
According to Jacqueline A. French, MD, a professor at NYU Langone Medical Center, Dr. Mula and colleagues are “top notch,” and their recommendations “hit every nail on the head.”
Dr. French, chief medical officer of The Epilepsy Foundation, emphasized the importance of the publication, which addresses two common misconceptions within the medical community: First, that standard antidepressants are insufficient to treat depression in patients with epilepsy, and second, that antidepressants may trigger seizures.
“The first purpose [of the publication] is to say, yes, these antidepressants do work,” Dr. French said, “and no, they don’t worsen seizures, and you can use them safely, and they are appropriate to use.”
Dr. French explained that managing depression remains a practice gap among epileptologists and neurologists because it is a diagnosis that doesn’t traditionally fall into their purview, yet many patients with epilepsy forgo visiting their primary care providers, who more frequently diagnose and manage depression. Dr. French agreed with the guidance that epilepsy specialists should fill this gap.
“We need to at least be able to take people through their first antidepressant, even though we were not trained to be psychiatrists,” Dr. French said. “That’s part of the best care of our patients.”
Imad Najm, MD, director of the Charles Shor Epilepsy Center, Cleveland Clinic, said the recommendations are a step forward in the field, as they are supported by clinical data, instead of just clinical experience and expertise.
Still, Dr. Najm noted that more work is needed to stratify risk of depression in epilepsy and evaluate a possible causal relationship between epilepsy therapies and depression.
He went on to emphasizes the scale of issue at hand, and the stakes involved.
“Depression, anxiety, and psychosis affect a large number of patients with epilepsy,” Dr. Najm said. “Clinical screening and recognition of these comorbidities leads to the institution of treatment options and significant improvement in quality of life. Mental health professionals should be an integral part of any comprehensive epilepsy center.”
The investigators disclosed relationships with Esai, UCB, Elsevier, and others. Dr. French is indirectly involved with multiple pharmaceutical companies developing epilepsy drugs through her role as director of The Epilepsy Study Consortium, a nonprofit organization. Dr. Najm reported no conflicts of interest.
The new guidance highlights the high prevalence of depression among patients with epilepsy while offering the first systematic approach to treatment, reported lead author Marco Mula, MD, PhD, of Atkinson Morley Regional Neuroscience Centre at St George’s University Hospital, London, and colleagues.
“Despite evidence that depression represents a frequently encountered comorbidity [among patients with epilepsy], data on the treatment of depression in epilepsy [are] still limited and recommendations rely mostly on individual clinical experience and expertise,” the investigators wrote in Epilepsia.
Recommendations cover first-line treatment of unipolar depression in epilepsy without other psychiatric disorders.
For patients with mild depression, the guidance supports psychological intervention without pharmacologic therapy; however, if the patient wishes to use medication, has had a positive response to medication in the past, or nonpharmacologic treatments have previously failed or are unavailable, then SSRIs should be considered first-choice therapy. For moderate to severe depression, SSRIs are the first choice, according to Dr. Mula and colleagues.
“It has to be acknowledged that there is considerable debate in the psychiatric literature about the treatment of mild depression in adults,” the investigators noted. “A patient-level meta-analysis pointed out that the magnitude of benefit of antidepressant medications compared with placebo increases with severity of depression symptoms and it may be minimal or nonexistent, on average, in patients with mild or moderate symptoms.”
If a patient does not respond to first-line therapy, then venlafaxine should be considered, according to the guidance. When a patient does respond to therapy, treatment should be continued for at least 6 months, and when residual symptoms persist, treatment should be continued until resolution.
“In people with depression it is established that around two-thirds of patients do not achieve full remission with first-line treatment,” Dr. Mula and colleagues wrote. “In people with epilepsy, current data show that up to 50% of patients do not achieve full remission from depression. For this reason, augmentation strategies are often needed. They should be adopted by psychiatrists, neuropsychiatrists, or mental health professionals familiar with such therapeutic strategies.”
Beyond these key recommendations, the guidance covers a range of additional topics, including other pharmacologic options, medication discontinuation strategies, electroconvulsive therapy, light therapy, exercise training, vagus nerve stimulation, and repetitive transcranial magnetic stimulation.
Useful advice that counters common misconceptions
According to Jacqueline A. French, MD, a professor at NYU Langone Medical Center, Dr. Mula and colleagues are “top notch,” and their recommendations “hit every nail on the head.”
Dr. French, chief medical officer of The Epilepsy Foundation, emphasized the importance of the publication, which addresses two common misconceptions within the medical community: First, that standard antidepressants are insufficient to treat depression in patients with epilepsy, and second, that antidepressants may trigger seizures.
“The first purpose [of the publication] is to say, yes, these antidepressants do work,” Dr. French said, “and no, they don’t worsen seizures, and you can use them safely, and they are appropriate to use.”
Dr. French explained that managing depression remains a practice gap among epileptologists and neurologists because it is a diagnosis that doesn’t traditionally fall into their purview, yet many patients with epilepsy forgo visiting their primary care providers, who more frequently diagnose and manage depression. Dr. French agreed with the guidance that epilepsy specialists should fill this gap.
“We need to at least be able to take people through their first antidepressant, even though we were not trained to be psychiatrists,” Dr. French said. “That’s part of the best care of our patients.”
Imad Najm, MD, director of the Charles Shor Epilepsy Center, Cleveland Clinic, said the recommendations are a step forward in the field, as they are supported by clinical data, instead of just clinical experience and expertise.
Still, Dr. Najm noted that more work is needed to stratify risk of depression in epilepsy and evaluate a possible causal relationship between epilepsy therapies and depression.
He went on to emphasizes the scale of issue at hand, and the stakes involved.
“Depression, anxiety, and psychosis affect a large number of patients with epilepsy,” Dr. Najm said. “Clinical screening and recognition of these comorbidities leads to the institution of treatment options and significant improvement in quality of life. Mental health professionals should be an integral part of any comprehensive epilepsy center.”
The investigators disclosed relationships with Esai, UCB, Elsevier, and others. Dr. French is indirectly involved with multiple pharmaceutical companies developing epilepsy drugs through her role as director of The Epilepsy Study Consortium, a nonprofit organization. Dr. Najm reported no conflicts of interest.
The new guidance highlights the high prevalence of depression among patients with epilepsy while offering the first systematic approach to treatment, reported lead author Marco Mula, MD, PhD, of Atkinson Morley Regional Neuroscience Centre at St George’s University Hospital, London, and colleagues.
“Despite evidence that depression represents a frequently encountered comorbidity [among patients with epilepsy], data on the treatment of depression in epilepsy [are] still limited and recommendations rely mostly on individual clinical experience and expertise,” the investigators wrote in Epilepsia.
Recommendations cover first-line treatment of unipolar depression in epilepsy without other psychiatric disorders.
For patients with mild depression, the guidance supports psychological intervention without pharmacologic therapy; however, if the patient wishes to use medication, has had a positive response to medication in the past, or nonpharmacologic treatments have previously failed or are unavailable, then SSRIs should be considered first-choice therapy. For moderate to severe depression, SSRIs are the first choice, according to Dr. Mula and colleagues.
“It has to be acknowledged that there is considerable debate in the psychiatric literature about the treatment of mild depression in adults,” the investigators noted. “A patient-level meta-analysis pointed out that the magnitude of benefit of antidepressant medications compared with placebo increases with severity of depression symptoms and it may be minimal or nonexistent, on average, in patients with mild or moderate symptoms.”
If a patient does not respond to first-line therapy, then venlafaxine should be considered, according to the guidance. When a patient does respond to therapy, treatment should be continued for at least 6 months, and when residual symptoms persist, treatment should be continued until resolution.
“In people with depression it is established that around two-thirds of patients do not achieve full remission with first-line treatment,” Dr. Mula and colleagues wrote. “In people with epilepsy, current data show that up to 50% of patients do not achieve full remission from depression. For this reason, augmentation strategies are often needed. They should be adopted by psychiatrists, neuropsychiatrists, or mental health professionals familiar with such therapeutic strategies.”
Beyond these key recommendations, the guidance covers a range of additional topics, including other pharmacologic options, medication discontinuation strategies, electroconvulsive therapy, light therapy, exercise training, vagus nerve stimulation, and repetitive transcranial magnetic stimulation.
Useful advice that counters common misconceptions
According to Jacqueline A. French, MD, a professor at NYU Langone Medical Center, Dr. Mula and colleagues are “top notch,” and their recommendations “hit every nail on the head.”
Dr. French, chief medical officer of The Epilepsy Foundation, emphasized the importance of the publication, which addresses two common misconceptions within the medical community: First, that standard antidepressants are insufficient to treat depression in patients with epilepsy, and second, that antidepressants may trigger seizures.
“The first purpose [of the publication] is to say, yes, these antidepressants do work,” Dr. French said, “and no, they don’t worsen seizures, and you can use them safely, and they are appropriate to use.”
Dr. French explained that managing depression remains a practice gap among epileptologists and neurologists because it is a diagnosis that doesn’t traditionally fall into their purview, yet many patients with epilepsy forgo visiting their primary care providers, who more frequently diagnose and manage depression. Dr. French agreed with the guidance that epilepsy specialists should fill this gap.
“We need to at least be able to take people through their first antidepressant, even though we were not trained to be psychiatrists,” Dr. French said. “That’s part of the best care of our patients.”
Imad Najm, MD, director of the Charles Shor Epilepsy Center, Cleveland Clinic, said the recommendations are a step forward in the field, as they are supported by clinical data, instead of just clinical experience and expertise.
Still, Dr. Najm noted that more work is needed to stratify risk of depression in epilepsy and evaluate a possible causal relationship between epilepsy therapies and depression.
He went on to emphasizes the scale of issue at hand, and the stakes involved.
“Depression, anxiety, and psychosis affect a large number of patients with epilepsy,” Dr. Najm said. “Clinical screening and recognition of these comorbidities leads to the institution of treatment options and significant improvement in quality of life. Mental health professionals should be an integral part of any comprehensive epilepsy center.”
The investigators disclosed relationships with Esai, UCB, Elsevier, and others. Dr. French is indirectly involved with multiple pharmaceutical companies developing epilepsy drugs through her role as director of The Epilepsy Study Consortium, a nonprofit organization. Dr. Najm reported no conflicts of interest.
FROM EPILEPSIA
PACAP38- and VIP-induced cluster headache attacks do not appear to alter CGRP levels
such as tryptase and histamine, a new study has found.
“Whether cluster headache attacks provoked by CGRP and PACAP38/VIP are mediated by distinct signaling pathways will be worth investigating in forthcoming studies,” wrote Lanfranco Pellesi, MD, of the Danish Headache Center at the University of Copenhagen, and his coauthors. The study was published in Cephalalgia.
To assess how these biochemical variables might contribute to cluster headache attacks, the researchers launched a randomized, double-blind trial of data from 44 Danish participants with cluster headache. The average age of the patients was 38 years; 14 had active episodic cluster headache, 15 had episodic cluster headache in remission, and 15 had chronic cluster headache.
All patients received a continuous infusion of either PACAP38 (10 pmol/kg per minute) or VIP (8 pmol/kg per minute) over a 20-minute period, using a time- and volume-controlled infusion pump. Blood was collected for analysis at fixed time points, including at baseline, at the end of the infusion, 10 minutes after the infusion, and 70 minutes after the infusion. Technical problems led to missing values in 285 out of 1,144 planned plasma samples.
PACAP38 infusion resulted in a cluster headache attack in 13 of the 44 participants and VIP induced an attack in 12 of the 44. No differences in plasma CGRP (P = .7074), tryptase (P = .6673), and histamine (P = .4792) levels were found between patients who developed attacks and those who did not, and the plasma concentrations did not differ among the various blood-drawing time points.
There was also no difference in plasma CGRP levels between patients with active episodic cluster headache, those with episodic cluster headache in remission, and those with chronic cluster headache. After post hoc analysis, plasma tryptase and plasma histamine levels were similar among the three cluster headache patient groups.
The final link to the cluster headache puzzle has not yet been found
“We know a lot about cluster headache: how it presents, how we can stop it acutely, and how we can stop it preventively. But we don’t know everything about all the neurotransmitters involved, the triggers that start an attack, or the causes of pain,” Alan Rapoport, MD, professor of neurology at the University of California, Los Angeles (UCLA), and past president of the International Headache Society, said in an interview. “This study was performed to find the answer to a small piece of the puzzle. Is CGRP the missing link for patients who begin a cluster attack, or should we be looking elsewhere?
“I would be cautious and say it appears that it doesn’t seem to be related, but further studies may show something different,” he added. “The reason for my qualification: There is a monoclonal antibody [galcanezumab], which grabs CGRP and prevents it from docking on its receptor, that has been approved for preventive treatment of episodic cluster headache. When you have episodic cluster, go into a cluster period, and take galcanezumab, it could and should decrease the number of attacks that you would ordinarily have had. That means it is related somewhat. But it certainly doesn’t work for everyone, so more investigations like this are needed.”
“What’s important about this study is that it opens up the possibility that there is another way into the cluster attack that could be operationalized for therapeutic purposes,” Peter Goadsby, MD, PhD, professor of neurology at UCLA and president of the American Headache Society, said in an interview.
When asked about the authors’ stated interest in investigating “if monoclonal antibodies targeting the CGRP pathway prevent PACAP38- or VIP-induced cluster headache attacks” as a follow-up, Dr. Goadsby strongly backed the idea. “If I sound excited about actually exploring whether that was a useful treatment or not, it’s because cluster headache is a dreadful condition. And the sooner you could work out whether it was useful or put the money into something else, well, that’s where I’d go.
“I think the principle here of doing experimental medicine, getting into human work with targets like this at the earliest possible time, is something that is not done as often as would be appropriate,” he added. “There is not enough investment, in my view, in early phase experimental work, which really just gets to that next step. Broadly speaking, the encouragement and support of experimental medicine is crucial to developing new therapies.”
The authors recognized their study’s potential limitations, including it’s being an exploratory study with results that should be interpreted cautiously. They acknowledged discrepancies with previous studies of plasma CGRP during cluster headache attacks, offering “different methodologies, including intra-assay differences and the location of blood sampling” as a possible reason. They also explained that some of the data are missing “completely at random” due to their policy of discarding all observations with incomplete laboratory measurements, adding that the impact on their sample size was “only modest.”
“In spite of these limitations,” Dr. Rapoport said, “this is an excellent study that shows us that PACAP38- and VIP-induced cluster headache attacks are not associated with alterations in plasma CGRP or in histamine and tryptase.”
Regarding potential conflicts of interest, one author reported being employed at the testing lab where the histamine measurements were conducted, as did another author who serves as the lab’s scientific adviser. A third author reported receiving personal fees from various pharmaceutical companies.
such as tryptase and histamine, a new study has found.
“Whether cluster headache attacks provoked by CGRP and PACAP38/VIP are mediated by distinct signaling pathways will be worth investigating in forthcoming studies,” wrote Lanfranco Pellesi, MD, of the Danish Headache Center at the University of Copenhagen, and his coauthors. The study was published in Cephalalgia.
To assess how these biochemical variables might contribute to cluster headache attacks, the researchers launched a randomized, double-blind trial of data from 44 Danish participants with cluster headache. The average age of the patients was 38 years; 14 had active episodic cluster headache, 15 had episodic cluster headache in remission, and 15 had chronic cluster headache.
All patients received a continuous infusion of either PACAP38 (10 pmol/kg per minute) or VIP (8 pmol/kg per minute) over a 20-minute period, using a time- and volume-controlled infusion pump. Blood was collected for analysis at fixed time points, including at baseline, at the end of the infusion, 10 minutes after the infusion, and 70 minutes after the infusion. Technical problems led to missing values in 285 out of 1,144 planned plasma samples.
PACAP38 infusion resulted in a cluster headache attack in 13 of the 44 participants and VIP induced an attack in 12 of the 44. No differences in plasma CGRP (P = .7074), tryptase (P = .6673), and histamine (P = .4792) levels were found between patients who developed attacks and those who did not, and the plasma concentrations did not differ among the various blood-drawing time points.
There was also no difference in plasma CGRP levels between patients with active episodic cluster headache, those with episodic cluster headache in remission, and those with chronic cluster headache. After post hoc analysis, plasma tryptase and plasma histamine levels were similar among the three cluster headache patient groups.
The final link to the cluster headache puzzle has not yet been found
“We know a lot about cluster headache: how it presents, how we can stop it acutely, and how we can stop it preventively. But we don’t know everything about all the neurotransmitters involved, the triggers that start an attack, or the causes of pain,” Alan Rapoport, MD, professor of neurology at the University of California, Los Angeles (UCLA), and past president of the International Headache Society, said in an interview. “This study was performed to find the answer to a small piece of the puzzle. Is CGRP the missing link for patients who begin a cluster attack, or should we be looking elsewhere?
“I would be cautious and say it appears that it doesn’t seem to be related, but further studies may show something different,” he added. “The reason for my qualification: There is a monoclonal antibody [galcanezumab], which grabs CGRP and prevents it from docking on its receptor, that has been approved for preventive treatment of episodic cluster headache. When you have episodic cluster, go into a cluster period, and take galcanezumab, it could and should decrease the number of attacks that you would ordinarily have had. That means it is related somewhat. But it certainly doesn’t work for everyone, so more investigations like this are needed.”
“What’s important about this study is that it opens up the possibility that there is another way into the cluster attack that could be operationalized for therapeutic purposes,” Peter Goadsby, MD, PhD, professor of neurology at UCLA and president of the American Headache Society, said in an interview.
When asked about the authors’ stated interest in investigating “if monoclonal antibodies targeting the CGRP pathway prevent PACAP38- or VIP-induced cluster headache attacks” as a follow-up, Dr. Goadsby strongly backed the idea. “If I sound excited about actually exploring whether that was a useful treatment or not, it’s because cluster headache is a dreadful condition. And the sooner you could work out whether it was useful or put the money into something else, well, that’s where I’d go.
“I think the principle here of doing experimental medicine, getting into human work with targets like this at the earliest possible time, is something that is not done as often as would be appropriate,” he added. “There is not enough investment, in my view, in early phase experimental work, which really just gets to that next step. Broadly speaking, the encouragement and support of experimental medicine is crucial to developing new therapies.”
The authors recognized their study’s potential limitations, including it’s being an exploratory study with results that should be interpreted cautiously. They acknowledged discrepancies with previous studies of plasma CGRP during cluster headache attacks, offering “different methodologies, including intra-assay differences and the location of blood sampling” as a possible reason. They also explained that some of the data are missing “completely at random” due to their policy of discarding all observations with incomplete laboratory measurements, adding that the impact on their sample size was “only modest.”
“In spite of these limitations,” Dr. Rapoport said, “this is an excellent study that shows us that PACAP38- and VIP-induced cluster headache attacks are not associated with alterations in plasma CGRP or in histamine and tryptase.”
Regarding potential conflicts of interest, one author reported being employed at the testing lab where the histamine measurements were conducted, as did another author who serves as the lab’s scientific adviser. A third author reported receiving personal fees from various pharmaceutical companies.
such as tryptase and histamine, a new study has found.
“Whether cluster headache attacks provoked by CGRP and PACAP38/VIP are mediated by distinct signaling pathways will be worth investigating in forthcoming studies,” wrote Lanfranco Pellesi, MD, of the Danish Headache Center at the University of Copenhagen, and his coauthors. The study was published in Cephalalgia.
To assess how these biochemical variables might contribute to cluster headache attacks, the researchers launched a randomized, double-blind trial of data from 44 Danish participants with cluster headache. The average age of the patients was 38 years; 14 had active episodic cluster headache, 15 had episodic cluster headache in remission, and 15 had chronic cluster headache.
All patients received a continuous infusion of either PACAP38 (10 pmol/kg per minute) or VIP (8 pmol/kg per minute) over a 20-minute period, using a time- and volume-controlled infusion pump. Blood was collected for analysis at fixed time points, including at baseline, at the end of the infusion, 10 minutes after the infusion, and 70 minutes after the infusion. Technical problems led to missing values in 285 out of 1,144 planned plasma samples.
PACAP38 infusion resulted in a cluster headache attack in 13 of the 44 participants and VIP induced an attack in 12 of the 44. No differences in plasma CGRP (P = .7074), tryptase (P = .6673), and histamine (P = .4792) levels were found between patients who developed attacks and those who did not, and the plasma concentrations did not differ among the various blood-drawing time points.
There was also no difference in plasma CGRP levels between patients with active episodic cluster headache, those with episodic cluster headache in remission, and those with chronic cluster headache. After post hoc analysis, plasma tryptase and plasma histamine levels were similar among the three cluster headache patient groups.
The final link to the cluster headache puzzle has not yet been found
“We know a lot about cluster headache: how it presents, how we can stop it acutely, and how we can stop it preventively. But we don’t know everything about all the neurotransmitters involved, the triggers that start an attack, or the causes of pain,” Alan Rapoport, MD, professor of neurology at the University of California, Los Angeles (UCLA), and past president of the International Headache Society, said in an interview. “This study was performed to find the answer to a small piece of the puzzle. Is CGRP the missing link for patients who begin a cluster attack, or should we be looking elsewhere?
“I would be cautious and say it appears that it doesn’t seem to be related, but further studies may show something different,” he added. “The reason for my qualification: There is a monoclonal antibody [galcanezumab], which grabs CGRP and prevents it from docking on its receptor, that has been approved for preventive treatment of episodic cluster headache. When you have episodic cluster, go into a cluster period, and take galcanezumab, it could and should decrease the number of attacks that you would ordinarily have had. That means it is related somewhat. But it certainly doesn’t work for everyone, so more investigations like this are needed.”
“What’s important about this study is that it opens up the possibility that there is another way into the cluster attack that could be operationalized for therapeutic purposes,” Peter Goadsby, MD, PhD, professor of neurology at UCLA and president of the American Headache Society, said in an interview.
When asked about the authors’ stated interest in investigating “if monoclonal antibodies targeting the CGRP pathway prevent PACAP38- or VIP-induced cluster headache attacks” as a follow-up, Dr. Goadsby strongly backed the idea. “If I sound excited about actually exploring whether that was a useful treatment or not, it’s because cluster headache is a dreadful condition. And the sooner you could work out whether it was useful or put the money into something else, well, that’s where I’d go.
“I think the principle here of doing experimental medicine, getting into human work with targets like this at the earliest possible time, is something that is not done as often as would be appropriate,” he added. “There is not enough investment, in my view, in early phase experimental work, which really just gets to that next step. Broadly speaking, the encouragement and support of experimental medicine is crucial to developing new therapies.”
The authors recognized their study’s potential limitations, including it’s being an exploratory study with results that should be interpreted cautiously. They acknowledged discrepancies with previous studies of plasma CGRP during cluster headache attacks, offering “different methodologies, including intra-assay differences and the location of blood sampling” as a possible reason. They also explained that some of the data are missing “completely at random” due to their policy of discarding all observations with incomplete laboratory measurements, adding that the impact on their sample size was “only modest.”
“In spite of these limitations,” Dr. Rapoport said, “this is an excellent study that shows us that PACAP38- and VIP-induced cluster headache attacks are not associated with alterations in plasma CGRP or in histamine and tryptase.”
Regarding potential conflicts of interest, one author reported being employed at the testing lab where the histamine measurements were conducted, as did another author who serves as the lab’s scientific adviser. A third author reported receiving personal fees from various pharmaceutical companies.
FROM CEPHALALGIA
Perinatal deaths from COVID show ‘extensive’ placental damage
Recent evidence has shown that women who contract COVID-19 during pregnancy are at increased risk for pregnancy loss and neonatal death. Now, an analysis of pathology data from dozens of perinatal deaths shows how.
Unlike numerous pathogens that kill the fetus by infecting it directly, SARS-CoV-2 causes “widespread and severe” destruction of the placenta that deprives the fetus of oxygen, a team of 44 researchers in 12 countries concluded after examining 64 stillbirths and four neonatal deaths in which the placentas were infected with the virus. They noted that such damage occurs in a small percentage of pregnant women with COVID and that all the women in the study had not been vaccinated against the disease.
The findings were published online Feb. 10 in the Archives of Pathology & Laboratory Medicine.
Nearly all placentas had each of three features that pathologists have dubbed SARS-CoV-2 placentitis: large deposits of fibrin, a clotting protein that obstructs the flow of blood, death of cells in the trophoblast, and an unusual form of inflammation called chronic histiocytic intervillositis. Some had other abnormalities that could have exacerbated the condition.
The researchers called the extent of damage “striking,” affecting 77.7% of the placenta on average. The virus did not appear to harm fetal tissue, but placental damage “was extensive and highly destructive,” they write. Notably, none of the women in the analysis were known to have severe COVID.
Virus seen ‘chewing up the placenta’
David Schwartz, MD, a pathologist in Atlanta, and the lead author of the study, said COVID appears to be unique in destroying the placenta.
“I don’t know of any infection that does that to this degree or with this uniformity,” Dr. Schwartz told this news organization. “The simple message is that this infection is chewing up the placenta and destroying its capability to oxygenate the fetus.”
In November, the Centers for Disease Control and Prevention reported that maternal COVID increases the risk of losing a pregnancy. From March 2020 to September 2021, 8,154 stillbirths were reported, affecting 0.65% of births by women without COVID and 1.26% of births by women with COVID, for a relative risk of 1.90 (95% confidence interval, 1.69-2.15).
Delta, the variant that dominated in mid-2021, appears to have been particularly harmful. The CDC reported that the relative risk for stillbirth for mothers with COVID-19 during that period increased to 4.04 (95% CI, 3.28-4.97). Many cases in the new analysis coincided with Delta.
Dr. Schwartz and his colleagues said immunization, along with antiviral therapy, might reduce the chance of SARS-CoV-2 infecting the placenta. None of the mothers in the analysis was vaccinated, and Dr. Schwartz said he is not aware of a single case in a vaccinated woman.
The analysis comes on the heels of a study from the National Institutes of Health linking severe to moderate COVID infection to greater risk of other pregnancy complications: cesarean and preterm delivery, death during childbirth, postpartum hemorrhaging, and non-COVID infections.
Diana Bianchi, MD, director of NIH’s Eunice Kennedy Shriver National Institute of Child Health and Human Development, said those findings underscore the need for pregnant women to be vaccinated. (The shots have been shown to be safe for pregnant women.)
Denise Jamieson, MD, MPH, chair of the department of gynecology and obstetrics at Emory University, Atlanta, who was not involved in the new analysis, said the findings may have important clinical implications. In addition to ensuring that pregnant patients are fully vaccinated, she said “there may be opportunities to more closely monitor the placenta during pregnancy using imaging modalities such as ultrasound.”
Even in the presence of severe abnormalities, a fetus that has reached a viable gestational age could potentially be delivered prior to stillbirth, Dr. Jamieson said. The 64 stillbirths in the analysis ranged from 15 to 39.2 weeks of gestation, with an average of 30 weeks. Eight were delivered at full term.
However, additional studies are needed to support monitoring of placental changes, she said: “It is not ready for prime time now.”
Christopher Zahn, MD, vice president of practice activities the American College of Obstetricians and Gynecologists, cautioned that data on COVID and pregnancy complications remain limited.
The findings in this analysis “do not prove the association between COVID-19 infection and neonatal outcomes,” Dr. Zahn said. “While stillbirth could potentially be another adverse outcome for pregnant people who contract COVID-19, currently we don’t have enough data to confirm that a COVID-19 infection at any point in pregnancy indicates increased risk of stillbirth.”
He added that ACOG continues to strongly recommend vaccination against COVID for women who are pregnant, recently pregnant, or planning to be pregnant.
Dr. Schwartz and Dr. Jamieson have disclosed no relevant financial relationships. One author reported receiving financial support from the Slovak Research and Development Agency. Another reported funding from the Belgian Fund for Scientific Research and the Fetus for Life charity.
A version of this article first appeared on Medscape.com.
Recent evidence has shown that women who contract COVID-19 during pregnancy are at increased risk for pregnancy loss and neonatal death. Now, an analysis of pathology data from dozens of perinatal deaths shows how.
Unlike numerous pathogens that kill the fetus by infecting it directly, SARS-CoV-2 causes “widespread and severe” destruction of the placenta that deprives the fetus of oxygen, a team of 44 researchers in 12 countries concluded after examining 64 stillbirths and four neonatal deaths in which the placentas were infected with the virus. They noted that such damage occurs in a small percentage of pregnant women with COVID and that all the women in the study had not been vaccinated against the disease.
The findings were published online Feb. 10 in the Archives of Pathology & Laboratory Medicine.
Nearly all placentas had each of three features that pathologists have dubbed SARS-CoV-2 placentitis: large deposits of fibrin, a clotting protein that obstructs the flow of blood, death of cells in the trophoblast, and an unusual form of inflammation called chronic histiocytic intervillositis. Some had other abnormalities that could have exacerbated the condition.
The researchers called the extent of damage “striking,” affecting 77.7% of the placenta on average. The virus did not appear to harm fetal tissue, but placental damage “was extensive and highly destructive,” they write. Notably, none of the women in the analysis were known to have severe COVID.
Virus seen ‘chewing up the placenta’
David Schwartz, MD, a pathologist in Atlanta, and the lead author of the study, said COVID appears to be unique in destroying the placenta.
“I don’t know of any infection that does that to this degree or with this uniformity,” Dr. Schwartz told this news organization. “The simple message is that this infection is chewing up the placenta and destroying its capability to oxygenate the fetus.”
In November, the Centers for Disease Control and Prevention reported that maternal COVID increases the risk of losing a pregnancy. From March 2020 to September 2021, 8,154 stillbirths were reported, affecting 0.65% of births by women without COVID and 1.26% of births by women with COVID, for a relative risk of 1.90 (95% confidence interval, 1.69-2.15).
Delta, the variant that dominated in mid-2021, appears to have been particularly harmful. The CDC reported that the relative risk for stillbirth for mothers with COVID-19 during that period increased to 4.04 (95% CI, 3.28-4.97). Many cases in the new analysis coincided with Delta.
Dr. Schwartz and his colleagues said immunization, along with antiviral therapy, might reduce the chance of SARS-CoV-2 infecting the placenta. None of the mothers in the analysis was vaccinated, and Dr. Schwartz said he is not aware of a single case in a vaccinated woman.
The analysis comes on the heels of a study from the National Institutes of Health linking severe to moderate COVID infection to greater risk of other pregnancy complications: cesarean and preterm delivery, death during childbirth, postpartum hemorrhaging, and non-COVID infections.
Diana Bianchi, MD, director of NIH’s Eunice Kennedy Shriver National Institute of Child Health and Human Development, said those findings underscore the need for pregnant women to be vaccinated. (The shots have been shown to be safe for pregnant women.)
Denise Jamieson, MD, MPH, chair of the department of gynecology and obstetrics at Emory University, Atlanta, who was not involved in the new analysis, said the findings may have important clinical implications. In addition to ensuring that pregnant patients are fully vaccinated, she said “there may be opportunities to more closely monitor the placenta during pregnancy using imaging modalities such as ultrasound.”
Even in the presence of severe abnormalities, a fetus that has reached a viable gestational age could potentially be delivered prior to stillbirth, Dr. Jamieson said. The 64 stillbirths in the analysis ranged from 15 to 39.2 weeks of gestation, with an average of 30 weeks. Eight were delivered at full term.
However, additional studies are needed to support monitoring of placental changes, she said: “It is not ready for prime time now.”
Christopher Zahn, MD, vice president of practice activities the American College of Obstetricians and Gynecologists, cautioned that data on COVID and pregnancy complications remain limited.
The findings in this analysis “do not prove the association between COVID-19 infection and neonatal outcomes,” Dr. Zahn said. “While stillbirth could potentially be another adverse outcome for pregnant people who contract COVID-19, currently we don’t have enough data to confirm that a COVID-19 infection at any point in pregnancy indicates increased risk of stillbirth.”
He added that ACOG continues to strongly recommend vaccination against COVID for women who are pregnant, recently pregnant, or planning to be pregnant.
Dr. Schwartz and Dr. Jamieson have disclosed no relevant financial relationships. One author reported receiving financial support from the Slovak Research and Development Agency. Another reported funding from the Belgian Fund for Scientific Research and the Fetus for Life charity.
A version of this article first appeared on Medscape.com.
Recent evidence has shown that women who contract COVID-19 during pregnancy are at increased risk for pregnancy loss and neonatal death. Now, an analysis of pathology data from dozens of perinatal deaths shows how.
Unlike numerous pathogens that kill the fetus by infecting it directly, SARS-CoV-2 causes “widespread and severe” destruction of the placenta that deprives the fetus of oxygen, a team of 44 researchers in 12 countries concluded after examining 64 stillbirths and four neonatal deaths in which the placentas were infected with the virus. They noted that such damage occurs in a small percentage of pregnant women with COVID and that all the women in the study had not been vaccinated against the disease.
The findings were published online Feb. 10 in the Archives of Pathology & Laboratory Medicine.
Nearly all placentas had each of three features that pathologists have dubbed SARS-CoV-2 placentitis: large deposits of fibrin, a clotting protein that obstructs the flow of blood, death of cells in the trophoblast, and an unusual form of inflammation called chronic histiocytic intervillositis. Some had other abnormalities that could have exacerbated the condition.
The researchers called the extent of damage “striking,” affecting 77.7% of the placenta on average. The virus did not appear to harm fetal tissue, but placental damage “was extensive and highly destructive,” they write. Notably, none of the women in the analysis were known to have severe COVID.
Virus seen ‘chewing up the placenta’
David Schwartz, MD, a pathologist in Atlanta, and the lead author of the study, said COVID appears to be unique in destroying the placenta.
“I don’t know of any infection that does that to this degree or with this uniformity,” Dr. Schwartz told this news organization. “The simple message is that this infection is chewing up the placenta and destroying its capability to oxygenate the fetus.”
In November, the Centers for Disease Control and Prevention reported that maternal COVID increases the risk of losing a pregnancy. From March 2020 to September 2021, 8,154 stillbirths were reported, affecting 0.65% of births by women without COVID and 1.26% of births by women with COVID, for a relative risk of 1.90 (95% confidence interval, 1.69-2.15).
Delta, the variant that dominated in mid-2021, appears to have been particularly harmful. The CDC reported that the relative risk for stillbirth for mothers with COVID-19 during that period increased to 4.04 (95% CI, 3.28-4.97). Many cases in the new analysis coincided with Delta.
Dr. Schwartz and his colleagues said immunization, along with antiviral therapy, might reduce the chance of SARS-CoV-2 infecting the placenta. None of the mothers in the analysis was vaccinated, and Dr. Schwartz said he is not aware of a single case in a vaccinated woman.
The analysis comes on the heels of a study from the National Institutes of Health linking severe to moderate COVID infection to greater risk of other pregnancy complications: cesarean and preterm delivery, death during childbirth, postpartum hemorrhaging, and non-COVID infections.
Diana Bianchi, MD, director of NIH’s Eunice Kennedy Shriver National Institute of Child Health and Human Development, said those findings underscore the need for pregnant women to be vaccinated. (The shots have been shown to be safe for pregnant women.)
Denise Jamieson, MD, MPH, chair of the department of gynecology and obstetrics at Emory University, Atlanta, who was not involved in the new analysis, said the findings may have important clinical implications. In addition to ensuring that pregnant patients are fully vaccinated, she said “there may be opportunities to more closely monitor the placenta during pregnancy using imaging modalities such as ultrasound.”
Even in the presence of severe abnormalities, a fetus that has reached a viable gestational age could potentially be delivered prior to stillbirth, Dr. Jamieson said. The 64 stillbirths in the analysis ranged from 15 to 39.2 weeks of gestation, with an average of 30 weeks. Eight were delivered at full term.
However, additional studies are needed to support monitoring of placental changes, she said: “It is not ready for prime time now.”
Christopher Zahn, MD, vice president of practice activities the American College of Obstetricians and Gynecologists, cautioned that data on COVID and pregnancy complications remain limited.
The findings in this analysis “do not prove the association between COVID-19 infection and neonatal outcomes,” Dr. Zahn said. “While stillbirth could potentially be another adverse outcome for pregnant people who contract COVID-19, currently we don’t have enough data to confirm that a COVID-19 infection at any point in pregnancy indicates increased risk of stillbirth.”
He added that ACOG continues to strongly recommend vaccination against COVID for women who are pregnant, recently pregnant, or planning to be pregnant.
Dr. Schwartz and Dr. Jamieson have disclosed no relevant financial relationships. One author reported receiving financial support from the Slovak Research and Development Agency. Another reported funding from the Belgian Fund for Scientific Research and the Fetus for Life charity.
A version of this article first appeared on Medscape.com.
Stopping venetoclax treatment early reduces CLL survival outcomes
“There’s not a lot of awareness about the fact that you’re probably better off not permanently discontinuing treatment,” Anthony R. Mato, first author of the research published in Haematologica, said in an interview.
“Instead, attempting dose reductions with later resumption to complete the planned schedule for treatment probably could improve outcomes,” said Dr. Mato, who is director of the CLL Program at Memorial Sloan Kettering Cancer Center in New York.
Venetoclax, a potent B-cell lymphoma-2 (BCL2) inhibitor, provides a novel, chemotherapy-free treatment option for first-line and r/r CLL. While its safety profile is manageable, treatment interruptions are very common, and premature discontinuations are reported in about a third of patients, often because of adverse events.
Lacking data on the effects of those interruptions on survival outcomes, Dr. Mato and colleagues conducted a post hoc analysis of the phase 3 MURANO trial. In this open-label study, treatment with six cycles of venetoclax in combination with rituximab followed by venetoclax once daily for a total of 2 years showed superior progression-free survival, compared with six cycles of bendamustine plus rituximab in patients with r/r CLL (P < .0001).
The current analysis involved 194 intention-to-treat patients from the trial’s venetoclax arm, among whom 140 (72%) completed 2 years of therapy, and 54 (28%) prematurely discontinued treatment. The most common reasons for discontinuation were adverse events (53.7%) and disease progression (22.2%).
Among those with early discontinuation for any reason except disease progression, the rate of progression-free survival was significantly inferior, compared with those who completed the treatment (hazard ratio, 5.98; P < .0001), as was the rate or discontinuation caused specifically by adverse events, which most commonly involved neutropenia or thrombocytopenia (HR, 5.82; P < .0001).
Those who discontinued had a mean duration of venetoclax therapy of 11.3 months, compared with 24.4 months for all patients. For each additional month of venetoclax therapy, there was a significantly lower risk of a progression-free survival event (P = .0263) and of an overall survival event (P < .0001).
The treatment interruption rate was much higher, at 69% (134), involving neutropenia in 43% (84) of instances and requiring dose reductions in 23% (45) of cases.
However, in contrast to permanent discontinuations, the temporary interruptions and dose reductions had no significant effect on progression-free or overall survival, regardless of the duration.
“Improved progression-free and overall survival were associated with greater cumulative venetoclax treatment exposure,” the authors wrote.
“The results of these analyses highlight the importance of appropriately managing treatment modifications to ensure optimal outcomes for patients receiving targeted treatment for CLL,” they said.
Key measures including “better supportive care, use of growth factors, and more aggressive strategies for dose reduction could potentially help to improve or decrease the number of patients discontinuing due to an adverse event,” Dr. Mato added.“We can’t say definitively because this is not a randomized study – it’s a retrospective analysis from a randomized study – but those measures likely could have a positive impact on patient outcomes.”
The study received support from Genentech and AbbVie. Dr. Mato reported consulting or other relationships with AbbVie, AstraZeneca, Celgene, DTRM, Genentech, Janssen, Loxo, PCYC, Sunesis, and TG Therapeutics.
“There’s not a lot of awareness about the fact that you’re probably better off not permanently discontinuing treatment,” Anthony R. Mato, first author of the research published in Haematologica, said in an interview.
“Instead, attempting dose reductions with later resumption to complete the planned schedule for treatment probably could improve outcomes,” said Dr. Mato, who is director of the CLL Program at Memorial Sloan Kettering Cancer Center in New York.
Venetoclax, a potent B-cell lymphoma-2 (BCL2) inhibitor, provides a novel, chemotherapy-free treatment option for first-line and r/r CLL. While its safety profile is manageable, treatment interruptions are very common, and premature discontinuations are reported in about a third of patients, often because of adverse events.
Lacking data on the effects of those interruptions on survival outcomes, Dr. Mato and colleagues conducted a post hoc analysis of the phase 3 MURANO trial. In this open-label study, treatment with six cycles of venetoclax in combination with rituximab followed by venetoclax once daily for a total of 2 years showed superior progression-free survival, compared with six cycles of bendamustine plus rituximab in patients with r/r CLL (P < .0001).
The current analysis involved 194 intention-to-treat patients from the trial’s venetoclax arm, among whom 140 (72%) completed 2 years of therapy, and 54 (28%) prematurely discontinued treatment. The most common reasons for discontinuation were adverse events (53.7%) and disease progression (22.2%).
Among those with early discontinuation for any reason except disease progression, the rate of progression-free survival was significantly inferior, compared with those who completed the treatment (hazard ratio, 5.98; P < .0001), as was the rate or discontinuation caused specifically by adverse events, which most commonly involved neutropenia or thrombocytopenia (HR, 5.82; P < .0001).
Those who discontinued had a mean duration of venetoclax therapy of 11.3 months, compared with 24.4 months for all patients. For each additional month of venetoclax therapy, there was a significantly lower risk of a progression-free survival event (P = .0263) and of an overall survival event (P < .0001).
The treatment interruption rate was much higher, at 69% (134), involving neutropenia in 43% (84) of instances and requiring dose reductions in 23% (45) of cases.
However, in contrast to permanent discontinuations, the temporary interruptions and dose reductions had no significant effect on progression-free or overall survival, regardless of the duration.
“Improved progression-free and overall survival were associated with greater cumulative venetoclax treatment exposure,” the authors wrote.
“The results of these analyses highlight the importance of appropriately managing treatment modifications to ensure optimal outcomes for patients receiving targeted treatment for CLL,” they said.
Key measures including “better supportive care, use of growth factors, and more aggressive strategies for dose reduction could potentially help to improve or decrease the number of patients discontinuing due to an adverse event,” Dr. Mato added.“We can’t say definitively because this is not a randomized study – it’s a retrospective analysis from a randomized study – but those measures likely could have a positive impact on patient outcomes.”
The study received support from Genentech and AbbVie. Dr. Mato reported consulting or other relationships with AbbVie, AstraZeneca, Celgene, DTRM, Genentech, Janssen, Loxo, PCYC, Sunesis, and TG Therapeutics.
“There’s not a lot of awareness about the fact that you’re probably better off not permanently discontinuing treatment,” Anthony R. Mato, first author of the research published in Haematologica, said in an interview.
“Instead, attempting dose reductions with later resumption to complete the planned schedule for treatment probably could improve outcomes,” said Dr. Mato, who is director of the CLL Program at Memorial Sloan Kettering Cancer Center in New York.
Venetoclax, a potent B-cell lymphoma-2 (BCL2) inhibitor, provides a novel, chemotherapy-free treatment option for first-line and r/r CLL. While its safety profile is manageable, treatment interruptions are very common, and premature discontinuations are reported in about a third of patients, often because of adverse events.
Lacking data on the effects of those interruptions on survival outcomes, Dr. Mato and colleagues conducted a post hoc analysis of the phase 3 MURANO trial. In this open-label study, treatment with six cycles of venetoclax in combination with rituximab followed by venetoclax once daily for a total of 2 years showed superior progression-free survival, compared with six cycles of bendamustine plus rituximab in patients with r/r CLL (P < .0001).
The current analysis involved 194 intention-to-treat patients from the trial’s venetoclax arm, among whom 140 (72%) completed 2 years of therapy, and 54 (28%) prematurely discontinued treatment. The most common reasons for discontinuation were adverse events (53.7%) and disease progression (22.2%).
Among those with early discontinuation for any reason except disease progression, the rate of progression-free survival was significantly inferior, compared with those who completed the treatment (hazard ratio, 5.98; P < .0001), as was the rate or discontinuation caused specifically by adverse events, which most commonly involved neutropenia or thrombocytopenia (HR, 5.82; P < .0001).
Those who discontinued had a mean duration of venetoclax therapy of 11.3 months, compared with 24.4 months for all patients. For each additional month of venetoclax therapy, there was a significantly lower risk of a progression-free survival event (P = .0263) and of an overall survival event (P < .0001).
The treatment interruption rate was much higher, at 69% (134), involving neutropenia in 43% (84) of instances and requiring dose reductions in 23% (45) of cases.
However, in contrast to permanent discontinuations, the temporary interruptions and dose reductions had no significant effect on progression-free or overall survival, regardless of the duration.
“Improved progression-free and overall survival were associated with greater cumulative venetoclax treatment exposure,” the authors wrote.
“The results of these analyses highlight the importance of appropriately managing treatment modifications to ensure optimal outcomes for patients receiving targeted treatment for CLL,” they said.
Key measures including “better supportive care, use of growth factors, and more aggressive strategies for dose reduction could potentially help to improve or decrease the number of patients discontinuing due to an adverse event,” Dr. Mato added.“We can’t say definitively because this is not a randomized study – it’s a retrospective analysis from a randomized study – but those measures likely could have a positive impact on patient outcomes.”
The study received support from Genentech and AbbVie. Dr. Mato reported consulting or other relationships with AbbVie, AstraZeneca, Celgene, DTRM, Genentech, Janssen, Loxo, PCYC, Sunesis, and TG Therapeutics.
Agreement reached for research definition of ‘long COVID’ in children and young people
Long COVID can affect adults, young people, and children, and now for the first time, in a landmark study accepted for publication in the Archives of Disease in Childhood, formal agreement has been made on a research definition for post–acute COVID-19, or “long COVID” as it is commonly known, in children and young people.
The researchers charged themselves with a single objective – to derive a research definition for long COVID (post–acute COVID-19) in children and young people to allow comparisons between research studies. Specifically, so studies on prevalence, course, and outcome of long COVID in this age group can be reliably compared, because to date there has been no consensus. In fact, the authors pointed out how the “slew of definitions” currently used all differ in number, type, and duration of symptoms, which hampers research efforts. In addition, the lack of definition consensus has contributed to very wide reported variations in the estimated prevalence of long COVID in children of 1%-51%, with the authors saying that a “consistently applied definition of long COVID will help reduce the variability of prevalence estimates.”
Statements sequentially whittled down
“Using robust consensus methodology,” the authors said, “we derived a research definition for long COVID in children and young people.”
To achieve the definition consensus, a three-phase online Delphi process was used, followed by a virtual consensus meeting. The 123 participants registered to take part in the study included 23 people (19%) in a lived experience panel, 50 (42%) in the researcher or researcher/service delivery combined panel and 47 (39%) in the service delivery panel. Of 120 registered participants, 105 (88%) completed phase 1, 86 eligible participants (82% of those completing phase 1) completed phase 2 and 77 eligible participants (90% of those completing phase 2) completed phase 3. Seventeen participants attended and voted at the consensus meeting – 4 (23%) from the service delivery panel, 11 (65%) from the researcher panel, and 2 (12%) from the lived experience panel.
Presented with 49 statements in each phase, participants scored these from 1-9 based on how important they were perceived to be with regards inclusion in the research definition of long COVID in children and young people. Having been sequentially whittled down in three phases, 10 statements were discussed at the consensus meeting, and a panel of eight 11- to 17-year-olds affected by long COVID also reviewed the statements to reach a final agreement.
Five of the statements were agreed to be included in the definition, which stated that long COVID in children and young people is a condition in which a child or young person has symptoms (at least one of which is a physical symptom) that have continued or developed after a diagnosis of COVID-19 (confirmed with one or more positive COVID tests); impact their physical, mental, or social well-being; are interfering with some aspect of daily living (for example, school, work, home, or relationships); and persist for a minimum duration of 12 weeks after initial testing for COVID-19 (even if symptoms have waxed and waned over that period).
David Strain, MBChB, MD, chair of the BMA board of science and clinical senior lecturer and honorary consultant, University of Exeter (England), told the Science Media Centre: “A Delphi study builds a consensus from the world’s experts by presenting a series of statements and continuing to refine them until there is agreement as to what the definition of pediatric long COVID should be.” He added: “This is vitally important in order to align the global research effort into long COVID.”
Reassuringly similar
From the agreed five statements, a further research definition was proposed to align with the World Health Organization definition for adults: “Post–COVID-19 condition occurs in young people with a history of confirmed SARS CoV-2 infection, with at least one persisting physical symptom for a minimum duration of 12 weeks after initial testing that cannot be explained by an alternative diagnosis. The symptoms have an impact on everyday functioning, may continue or develop after COVID-19 infection, and may fluctuate or relapse over time.”
The authors concluded: “This is the first research definition of long COVID (post–COVID-19 condition) in children and young people and complements the clinical case definition in adults proposed by WHO,” adding that the two definitions are “reassuringly similar.”
They reiterated how widespread adoption of this definition would allow comparisons between studies such that a core outcome set can be developed and the prevalence, course and outcome of long COVID in children and young people can be reliably evaluated, which “will substantially help strengthen the evidence base on this debilitating condition.”
In addition, the authors said that a consistently applied definition of long COVID will help to provide a “more accurate picture on the true impact of the condition.”
The researchers emphasized the need to differentiate between a clinical case definition and a research definition of long COVID and explained: “It is understandable that the patient groups representing people with long COVID are concerned about a definition that could restrict access to services that are needed.”
They went on to say that in their view the decision whether a child or young person can see a health care professional, access any support needed, or be referred, investigated, or treated for long COVID should be a “shared decision involving the young person, their carers, and clinicians.”
Dr. Strain reinforced that it was important that the definition was a research one and not a clinical one, pointing out that the 12-week period in the research definition “does not necessarily mean that a child or young person should need to wait 3 months before being offered help or assistance from their health care team, indeed a 3-month delay in offering support to a child or young person, at this vitally important period of their educational development, could have lasting long-term impacts.”
A version of this article first appeared on Medscape.co.uk.
Long COVID can affect adults, young people, and children, and now for the first time, in a landmark study accepted for publication in the Archives of Disease in Childhood, formal agreement has been made on a research definition for post–acute COVID-19, or “long COVID” as it is commonly known, in children and young people.
The researchers charged themselves with a single objective – to derive a research definition for long COVID (post–acute COVID-19) in children and young people to allow comparisons between research studies. Specifically, so studies on prevalence, course, and outcome of long COVID in this age group can be reliably compared, because to date there has been no consensus. In fact, the authors pointed out how the “slew of definitions” currently used all differ in number, type, and duration of symptoms, which hampers research efforts. In addition, the lack of definition consensus has contributed to very wide reported variations in the estimated prevalence of long COVID in children of 1%-51%, with the authors saying that a “consistently applied definition of long COVID will help reduce the variability of prevalence estimates.”
Statements sequentially whittled down
“Using robust consensus methodology,” the authors said, “we derived a research definition for long COVID in children and young people.”
To achieve the definition consensus, a three-phase online Delphi process was used, followed by a virtual consensus meeting. The 123 participants registered to take part in the study included 23 people (19%) in a lived experience panel, 50 (42%) in the researcher or researcher/service delivery combined panel and 47 (39%) in the service delivery panel. Of 120 registered participants, 105 (88%) completed phase 1, 86 eligible participants (82% of those completing phase 1) completed phase 2 and 77 eligible participants (90% of those completing phase 2) completed phase 3. Seventeen participants attended and voted at the consensus meeting – 4 (23%) from the service delivery panel, 11 (65%) from the researcher panel, and 2 (12%) from the lived experience panel.
Presented with 49 statements in each phase, participants scored these from 1-9 based on how important they were perceived to be with regards inclusion in the research definition of long COVID in children and young people. Having been sequentially whittled down in three phases, 10 statements were discussed at the consensus meeting, and a panel of eight 11- to 17-year-olds affected by long COVID also reviewed the statements to reach a final agreement.
Five of the statements were agreed to be included in the definition, which stated that long COVID in children and young people is a condition in which a child or young person has symptoms (at least one of which is a physical symptom) that have continued or developed after a diagnosis of COVID-19 (confirmed with one or more positive COVID tests); impact their physical, mental, or social well-being; are interfering with some aspect of daily living (for example, school, work, home, or relationships); and persist for a minimum duration of 12 weeks after initial testing for COVID-19 (even if symptoms have waxed and waned over that period).
David Strain, MBChB, MD, chair of the BMA board of science and clinical senior lecturer and honorary consultant, University of Exeter (England), told the Science Media Centre: “A Delphi study builds a consensus from the world’s experts by presenting a series of statements and continuing to refine them until there is agreement as to what the definition of pediatric long COVID should be.” He added: “This is vitally important in order to align the global research effort into long COVID.”
Reassuringly similar
From the agreed five statements, a further research definition was proposed to align with the World Health Organization definition for adults: “Post–COVID-19 condition occurs in young people with a history of confirmed SARS CoV-2 infection, with at least one persisting physical symptom for a minimum duration of 12 weeks after initial testing that cannot be explained by an alternative diagnosis. The symptoms have an impact on everyday functioning, may continue or develop after COVID-19 infection, and may fluctuate or relapse over time.”
The authors concluded: “This is the first research definition of long COVID (post–COVID-19 condition) in children and young people and complements the clinical case definition in adults proposed by WHO,” adding that the two definitions are “reassuringly similar.”
They reiterated how widespread adoption of this definition would allow comparisons between studies such that a core outcome set can be developed and the prevalence, course and outcome of long COVID in children and young people can be reliably evaluated, which “will substantially help strengthen the evidence base on this debilitating condition.”
In addition, the authors said that a consistently applied definition of long COVID will help to provide a “more accurate picture on the true impact of the condition.”
The researchers emphasized the need to differentiate between a clinical case definition and a research definition of long COVID and explained: “It is understandable that the patient groups representing people with long COVID are concerned about a definition that could restrict access to services that are needed.”
They went on to say that in their view the decision whether a child or young person can see a health care professional, access any support needed, or be referred, investigated, or treated for long COVID should be a “shared decision involving the young person, their carers, and clinicians.”
Dr. Strain reinforced that it was important that the definition was a research one and not a clinical one, pointing out that the 12-week period in the research definition “does not necessarily mean that a child or young person should need to wait 3 months before being offered help or assistance from their health care team, indeed a 3-month delay in offering support to a child or young person, at this vitally important period of their educational development, could have lasting long-term impacts.”
A version of this article first appeared on Medscape.co.uk.
Long COVID can affect adults, young people, and children, and now for the first time, in a landmark study accepted for publication in the Archives of Disease in Childhood, formal agreement has been made on a research definition for post–acute COVID-19, or “long COVID” as it is commonly known, in children and young people.
The researchers charged themselves with a single objective – to derive a research definition for long COVID (post–acute COVID-19) in children and young people to allow comparisons between research studies. Specifically, so studies on prevalence, course, and outcome of long COVID in this age group can be reliably compared, because to date there has been no consensus. In fact, the authors pointed out how the “slew of definitions” currently used all differ in number, type, and duration of symptoms, which hampers research efforts. In addition, the lack of definition consensus has contributed to very wide reported variations in the estimated prevalence of long COVID in children of 1%-51%, with the authors saying that a “consistently applied definition of long COVID will help reduce the variability of prevalence estimates.”
Statements sequentially whittled down
“Using robust consensus methodology,” the authors said, “we derived a research definition for long COVID in children and young people.”
To achieve the definition consensus, a three-phase online Delphi process was used, followed by a virtual consensus meeting. The 123 participants registered to take part in the study included 23 people (19%) in a lived experience panel, 50 (42%) in the researcher or researcher/service delivery combined panel and 47 (39%) in the service delivery panel. Of 120 registered participants, 105 (88%) completed phase 1, 86 eligible participants (82% of those completing phase 1) completed phase 2 and 77 eligible participants (90% of those completing phase 2) completed phase 3. Seventeen participants attended and voted at the consensus meeting – 4 (23%) from the service delivery panel, 11 (65%) from the researcher panel, and 2 (12%) from the lived experience panel.
Presented with 49 statements in each phase, participants scored these from 1-9 based on how important they were perceived to be with regards inclusion in the research definition of long COVID in children and young people. Having been sequentially whittled down in three phases, 10 statements were discussed at the consensus meeting, and a panel of eight 11- to 17-year-olds affected by long COVID also reviewed the statements to reach a final agreement.
Five of the statements were agreed to be included in the definition, which stated that long COVID in children and young people is a condition in which a child or young person has symptoms (at least one of which is a physical symptom) that have continued or developed after a diagnosis of COVID-19 (confirmed with one or more positive COVID tests); impact their physical, mental, or social well-being; are interfering with some aspect of daily living (for example, school, work, home, or relationships); and persist for a minimum duration of 12 weeks after initial testing for COVID-19 (even if symptoms have waxed and waned over that period).
David Strain, MBChB, MD, chair of the BMA board of science and clinical senior lecturer and honorary consultant, University of Exeter (England), told the Science Media Centre: “A Delphi study builds a consensus from the world’s experts by presenting a series of statements and continuing to refine them until there is agreement as to what the definition of pediatric long COVID should be.” He added: “This is vitally important in order to align the global research effort into long COVID.”
Reassuringly similar
From the agreed five statements, a further research definition was proposed to align with the World Health Organization definition for adults: “Post–COVID-19 condition occurs in young people with a history of confirmed SARS CoV-2 infection, with at least one persisting physical symptom for a minimum duration of 12 weeks after initial testing that cannot be explained by an alternative diagnosis. The symptoms have an impact on everyday functioning, may continue or develop after COVID-19 infection, and may fluctuate or relapse over time.”
The authors concluded: “This is the first research definition of long COVID (post–COVID-19 condition) in children and young people and complements the clinical case definition in adults proposed by WHO,” adding that the two definitions are “reassuringly similar.”
They reiterated how widespread adoption of this definition would allow comparisons between studies such that a core outcome set can be developed and the prevalence, course and outcome of long COVID in children and young people can be reliably evaluated, which “will substantially help strengthen the evidence base on this debilitating condition.”
In addition, the authors said that a consistently applied definition of long COVID will help to provide a “more accurate picture on the true impact of the condition.”
The researchers emphasized the need to differentiate between a clinical case definition and a research definition of long COVID and explained: “It is understandable that the patient groups representing people with long COVID are concerned about a definition that could restrict access to services that are needed.”
They went on to say that in their view the decision whether a child or young person can see a health care professional, access any support needed, or be referred, investigated, or treated for long COVID should be a “shared decision involving the young person, their carers, and clinicians.”
Dr. Strain reinforced that it was important that the definition was a research one and not a clinical one, pointing out that the 12-week period in the research definition “does not necessarily mean that a child or young person should need to wait 3 months before being offered help or assistance from their health care team, indeed a 3-month delay in offering support to a child or young person, at this vitally important period of their educational development, could have lasting long-term impacts.”
A version of this article first appeared on Medscape.co.uk.
FROM THE ARCHIVES OF DISEASE IN CHILDHOOD
Improved follow-up needed to find late-stage pancreatic cancers
A relatively large number of late-stage pancreatic ductal adenocarcinomas (PDACs) are detected during follow-up surveillance, yet no single patient- or protocol-specific factor appears to be significantly associated with detecting late-stage disease during this period, according to a new systematic literature review and meta-analysis.
The researchers, led by Ankit Chhoda, MD, of Yale University, New Haven, Conn., wrote in Gastroenterology that interval progression in high-risk individuals “highlights the need for improved follow-up methodology with higher accuracy to detect prognostically significant and treatable lesions.”
Individuals at high risk for PDAC are encouraged to undergo routine surveillance for the disease because early detection and resection of T1N0M0 PDAC and high-grade precursors may improve survival outcomes. According to Dr. Chhoda and colleagues, challenges of interval progression of cancers during the surveillance period for gastrointestinal malignancies have been well described in the general and at-risk patient populations. Previous studies, the authors explained, have not scrutinized the issues associated with late-stage PDACs detected during follow-up surveillance.
“Late-stage PDACs necessitate critical appraisal of current follow-up strategies to detect successful targets and perform timely resections,” the authors wrote. The researchers added that the diagnosis of late-stage PDACs during follow-up emphasizes the need for implementing “quality measures to avoid preventable causes, including surveillance adherence and diagnostic errors.”
To understand the incidence rates of late-stage PDACs during follow-up in high-risk individuals, Dr. Chhoda and researchers performed a systematic literature review and meta-analysis of data that included follow-up strategies for early PDAC detection among a high-risk population.
Outcomes of interest for the analysis included the overall diagnosis of advanced neoplasia as well as surveillance-detected/interval late-stage PDACs (T2–4N0M0/metastatic stage PDAC) during follow-up. The investigators defined surveillance-detected and interval late-stage PDACs as late-stage PDACs that were detected during surveillance and as those presenting symptomatically between visits, respectively.
The researchers also performed metaregression of the incidence rates of late-stage PDACs to examine the relationship with clinicoradiologic features in high-risk individuals.
A total of 13 studies on surveillance in 2,169 high-risk individuals were included in the systematic review, while 12 studies were included in the meta-analysis. Across studies, high-risk individuals were followed for over 7,302.72 patient-years for the purposes of detecting incident lesions or progression of preexisting pancreatic abnormalities.
In all high-risk individuals who underwent follow-up, the investigators identified a total yield of advanced neoplasia of 53. This total yield consisted of 7 high-grade pancreatic intraepithelial neoplasms, 7 high-grade intraductal papillary mucinous neoplasms, and 39 PDACs. According to the meta-analysis, the cumulative incidence of advanced neoplasia was 3.3 (95% confidence interval, 0.6-7.4; P < .001) per 1,000 patient-years. During follow-up, the cumulative incidence of surveillance-detected/interval late-stage PDACs was 1.7 per 1,000 patient-years (95% CI, 0.2-4.0; P = .03).
In a separate analysis, the investigators sought to identify the relationship between the modality of follow-up imaging and late-stage PDAC incidence. Imaging modalities used during follow-up were mostly cross-sectional imaging, such as computed tomography or magnetic resonance imaging with cholangiopancreatography (n = 4) or endoscopic ultrasound and cross-sectional modalities (n = 8).
The investigators found no significant associations between late-stage PDACs and surveillance imaging, baseline pancreatic morphology, study location, genetic background, gender, or age. Incidence of late-stage PDACs in studies with mostly cross-sectional imaging was 0.7 per 1,000 patient-years (95% CI, 0.0-8.0). This incidence rate was lower than that reported with EUS and cross-sectional modalities (2.5 per 1,000 patient-years; 95% CI, 0.6-5.4), but this difference was not statistically significant (P = .2).
No significant difference was found during follow-up in the incidence of late-stage PDACs between high-risk individuals with baseline pancreatic abnormalities (0.0 no significant difference; 95% CI, 0.0-0.3) vs. high-risk individuals with normal baseline (0.9 per 1,000 patient-years; 95% CI, 0.0-2.8) (P = .9).
Most studies included in the analysis did not report on diagnostic errors and surveillance adherence, the researchers wrote. Nonadherence to surveillance as well as delays in surveillance accounted for four late-stage PDACs, and surveillance cessation and/or delays were reported in 4 out of 19 high-risk individuals. There was limited information on symptoms, presentation timing, site of lesion, and surveillance adherence, which the investigators indicated prevented a formal meta-analysis.
In their summary, the study authors noted that in clinical practice there is a need for improved quality measures and adherence to surveillance programs to reduce the risk of diagnostic errors. The authors stated that evidence on the impact of these quality measures “on surveillance outcomes will not only improve quality of surveillance practices, but also enrich our communication with patients who undergo surveillance.”
The researchers reported no conflicts of interest with the pharmaceutical industry, and the study did not receive any funding.
A relatively large number of late-stage pancreatic ductal adenocarcinomas (PDACs) are detected during follow-up surveillance, yet no single patient- or protocol-specific factor appears to be significantly associated with detecting late-stage disease during this period, according to a new systematic literature review and meta-analysis.
The researchers, led by Ankit Chhoda, MD, of Yale University, New Haven, Conn., wrote in Gastroenterology that interval progression in high-risk individuals “highlights the need for improved follow-up methodology with higher accuracy to detect prognostically significant and treatable lesions.”
Individuals at high risk for PDAC are encouraged to undergo routine surveillance for the disease because early detection and resection of T1N0M0 PDAC and high-grade precursors may improve survival outcomes. According to Dr. Chhoda and colleagues, challenges of interval progression of cancers during the surveillance period for gastrointestinal malignancies have been well described in the general and at-risk patient populations. Previous studies, the authors explained, have not scrutinized the issues associated with late-stage PDACs detected during follow-up surveillance.
“Late-stage PDACs necessitate critical appraisal of current follow-up strategies to detect successful targets and perform timely resections,” the authors wrote. The researchers added that the diagnosis of late-stage PDACs during follow-up emphasizes the need for implementing “quality measures to avoid preventable causes, including surveillance adherence and diagnostic errors.”
To understand the incidence rates of late-stage PDACs during follow-up in high-risk individuals, Dr. Chhoda and researchers performed a systematic literature review and meta-analysis of data that included follow-up strategies for early PDAC detection among a high-risk population.
Outcomes of interest for the analysis included the overall diagnosis of advanced neoplasia as well as surveillance-detected/interval late-stage PDACs (T2–4N0M0/metastatic stage PDAC) during follow-up. The investigators defined surveillance-detected and interval late-stage PDACs as late-stage PDACs that were detected during surveillance and as those presenting symptomatically between visits, respectively.
The researchers also performed metaregression of the incidence rates of late-stage PDACs to examine the relationship with clinicoradiologic features in high-risk individuals.
A total of 13 studies on surveillance in 2,169 high-risk individuals were included in the systematic review, while 12 studies were included in the meta-analysis. Across studies, high-risk individuals were followed for over 7,302.72 patient-years for the purposes of detecting incident lesions or progression of preexisting pancreatic abnormalities.
In all high-risk individuals who underwent follow-up, the investigators identified a total yield of advanced neoplasia of 53. This total yield consisted of 7 high-grade pancreatic intraepithelial neoplasms, 7 high-grade intraductal papillary mucinous neoplasms, and 39 PDACs. According to the meta-analysis, the cumulative incidence of advanced neoplasia was 3.3 (95% confidence interval, 0.6-7.4; P < .001) per 1,000 patient-years. During follow-up, the cumulative incidence of surveillance-detected/interval late-stage PDACs was 1.7 per 1,000 patient-years (95% CI, 0.2-4.0; P = .03).
In a separate analysis, the investigators sought to identify the relationship between the modality of follow-up imaging and late-stage PDAC incidence. Imaging modalities used during follow-up were mostly cross-sectional imaging, such as computed tomography or magnetic resonance imaging with cholangiopancreatography (n = 4) or endoscopic ultrasound and cross-sectional modalities (n = 8).
The investigators found no significant associations between late-stage PDACs and surveillance imaging, baseline pancreatic morphology, study location, genetic background, gender, or age. Incidence of late-stage PDACs in studies with mostly cross-sectional imaging was 0.7 per 1,000 patient-years (95% CI, 0.0-8.0). This incidence rate was lower than that reported with EUS and cross-sectional modalities (2.5 per 1,000 patient-years; 95% CI, 0.6-5.4), but this difference was not statistically significant (P = .2).
No significant difference was found during follow-up in the incidence of late-stage PDACs between high-risk individuals with baseline pancreatic abnormalities (0.0 no significant difference; 95% CI, 0.0-0.3) vs. high-risk individuals with normal baseline (0.9 per 1,000 patient-years; 95% CI, 0.0-2.8) (P = .9).
Most studies included in the analysis did not report on diagnostic errors and surveillance adherence, the researchers wrote. Nonadherence to surveillance as well as delays in surveillance accounted for four late-stage PDACs, and surveillance cessation and/or delays were reported in 4 out of 19 high-risk individuals. There was limited information on symptoms, presentation timing, site of lesion, and surveillance adherence, which the investigators indicated prevented a formal meta-analysis.
In their summary, the study authors noted that in clinical practice there is a need for improved quality measures and adherence to surveillance programs to reduce the risk of diagnostic errors. The authors stated that evidence on the impact of these quality measures “on surveillance outcomes will not only improve quality of surveillance practices, but also enrich our communication with patients who undergo surveillance.”
The researchers reported no conflicts of interest with the pharmaceutical industry, and the study did not receive any funding.
A relatively large number of late-stage pancreatic ductal adenocarcinomas (PDACs) are detected during follow-up surveillance, yet no single patient- or protocol-specific factor appears to be significantly associated with detecting late-stage disease during this period, according to a new systematic literature review and meta-analysis.
The researchers, led by Ankit Chhoda, MD, of Yale University, New Haven, Conn., wrote in Gastroenterology that interval progression in high-risk individuals “highlights the need for improved follow-up methodology with higher accuracy to detect prognostically significant and treatable lesions.”
Individuals at high risk for PDAC are encouraged to undergo routine surveillance for the disease because early detection and resection of T1N0M0 PDAC and high-grade precursors may improve survival outcomes. According to Dr. Chhoda and colleagues, challenges of interval progression of cancers during the surveillance period for gastrointestinal malignancies have been well described in the general and at-risk patient populations. Previous studies, the authors explained, have not scrutinized the issues associated with late-stage PDACs detected during follow-up surveillance.
“Late-stage PDACs necessitate critical appraisal of current follow-up strategies to detect successful targets and perform timely resections,” the authors wrote. The researchers added that the diagnosis of late-stage PDACs during follow-up emphasizes the need for implementing “quality measures to avoid preventable causes, including surveillance adherence and diagnostic errors.”
To understand the incidence rates of late-stage PDACs during follow-up in high-risk individuals, Dr. Chhoda and researchers performed a systematic literature review and meta-analysis of data that included follow-up strategies for early PDAC detection among a high-risk population.
Outcomes of interest for the analysis included the overall diagnosis of advanced neoplasia as well as surveillance-detected/interval late-stage PDACs (T2–4N0M0/metastatic stage PDAC) during follow-up. The investigators defined surveillance-detected and interval late-stage PDACs as late-stage PDACs that were detected during surveillance and as those presenting symptomatically between visits, respectively.
The researchers also performed metaregression of the incidence rates of late-stage PDACs to examine the relationship with clinicoradiologic features in high-risk individuals.
A total of 13 studies on surveillance in 2,169 high-risk individuals were included in the systematic review, while 12 studies were included in the meta-analysis. Across studies, high-risk individuals were followed for over 7,302.72 patient-years for the purposes of detecting incident lesions or progression of preexisting pancreatic abnormalities.
In all high-risk individuals who underwent follow-up, the investigators identified a total yield of advanced neoplasia of 53. This total yield consisted of 7 high-grade pancreatic intraepithelial neoplasms, 7 high-grade intraductal papillary mucinous neoplasms, and 39 PDACs. According to the meta-analysis, the cumulative incidence of advanced neoplasia was 3.3 (95% confidence interval, 0.6-7.4; P < .001) per 1,000 patient-years. During follow-up, the cumulative incidence of surveillance-detected/interval late-stage PDACs was 1.7 per 1,000 patient-years (95% CI, 0.2-4.0; P = .03).
In a separate analysis, the investigators sought to identify the relationship between the modality of follow-up imaging and late-stage PDAC incidence. Imaging modalities used during follow-up were mostly cross-sectional imaging, such as computed tomography or magnetic resonance imaging with cholangiopancreatography (n = 4) or endoscopic ultrasound and cross-sectional modalities (n = 8).
The investigators found no significant associations between late-stage PDACs and surveillance imaging, baseline pancreatic morphology, study location, genetic background, gender, or age. Incidence of late-stage PDACs in studies with mostly cross-sectional imaging was 0.7 per 1,000 patient-years (95% CI, 0.0-8.0). This incidence rate was lower than that reported with EUS and cross-sectional modalities (2.5 per 1,000 patient-years; 95% CI, 0.6-5.4), but this difference was not statistically significant (P = .2).
No significant difference was found during follow-up in the incidence of late-stage PDACs between high-risk individuals with baseline pancreatic abnormalities (0.0 no significant difference; 95% CI, 0.0-0.3) vs. high-risk individuals with normal baseline (0.9 per 1,000 patient-years; 95% CI, 0.0-2.8) (P = .9).
Most studies included in the analysis did not report on diagnostic errors and surveillance adherence, the researchers wrote. Nonadherence to surveillance as well as delays in surveillance accounted for four late-stage PDACs, and surveillance cessation and/or delays were reported in 4 out of 19 high-risk individuals. There was limited information on symptoms, presentation timing, site of lesion, and surveillance adherence, which the investigators indicated prevented a formal meta-analysis.
In their summary, the study authors noted that in clinical practice there is a need for improved quality measures and adherence to surveillance programs to reduce the risk of diagnostic errors. The authors stated that evidence on the impact of these quality measures “on surveillance outcomes will not only improve quality of surveillance practices, but also enrich our communication with patients who undergo surveillance.”
The researchers reported no conflicts of interest with the pharmaceutical industry, and the study did not receive any funding.
FROM GASTROENTEROLOGY
Oncologists in malpractice suits: Less than other specialties
, notes the latest Medscape Malpractice Report.
Over a third (39%) of oncologists who were surveyed said that they had been named in at least one malpractice suit, according to the Medscape Oncologist Malpractice Report 2021.
This number is considerably lower than that reported by physicians across all specialties (51%), and it is also much lower than that reported by oncologists in past years. In the 2019 report, 54% of oncologists surveyed said they had been named in a malpractice suit, while in the 2017 report, the figure was 53%.
The dramatic decline in malpractice suits may have much to do with the COVID-19 pandemic, when oncology care was in a state of flux.
“Fewer people were seeking cancer care during the COVID pandemic, which might have impacted the number of lawsuits brought against oncologists,” says Paul Walker, a New York–based malpractice attorney at Walker Medical Law, who represents physicians and other healthcare professionals.
“Additionally, a fair number of people who died of COVID were also older,” he pointed out, and it is often older people who get cancer, so there were fewer older people who consulted an oncologist or were treated by one, he added.
However, the pandemic may be storing up trouble for future years. “Patient fears of contracting COVID-19 have led many to avoid seeking or resuming care, so delays in diagnosing new cancer cases could mean that more patients are diagnosed at a later stage of their disease, leading to potential adverse events and malpractice claims,” commented David L. Feldman, MD, MBA, chief medical officer of The Doctors Company Group.
This latest 2021 Medscape Malpractice Report was compiled from an online survey that included more than 4,300 physicians from 29 specialties. It included 106 oncologists. More than half of respondents (56%) had been in practice for more than 25 years, and 54% were aged 60 years or older. The survey was available from May 21 to August 28, 2021.
Similar to findings in previous years, complications from treatment/surgery were the most common reason for the lawsuits (31%). Failure to make a correct diagnosis or a delay in diagnosis was the second most common reason (23%), while 20% of patients sued because of a poor outcome or disease progression.
Surprise at being sued
Among the oncologists who reported involvement in a lawsuit in 2021, the majority (86%) said they were “very surprised” or “somewhat surprised” by the malpractice suit, which is similar to that of other physicians surveyed. However, fewer were surprised this year as compared to 2019 and 2017 (90% and 94%).
One reason for the surprise over the litigation was that it concerned a patient who had been treated a long time ago. One oncologist wrote that “the patient had not seen me for over 7 years and during that time, he did not call me with his new symptomatology. I was only named in the suit because I had previously been involved.”
Another common scenario reported by oncologists was being named in a lawsuit which was brought by another clinician’s patient. “I was the chairperson of the department, and one of the doctors in the practice was involved in the suit,” wrote one respondent. “I was named as an accomplice.”
More than half of surveyed oncologists said that they were able to identify the patient who bought the suit, and these figures are again comparable to those of other physicians. One oncologist commented that in the case he was involved with, the family did not understand or accept the nature of cancer and the different ways that a patient could die of complications. This patient had died of sepsis and pneumonia related to decubitus ulcers that were completely unrelated to her radiation therapy.
As in the case above, sometimes it is the family who filed the lawsuit, not the patient.
“The patient may even recognize that you did your best and be grateful for your skill and efforts, but the family can’t accept that grandma died of cancer and brings a lawsuit,” said Dennis Hursh, an attorney with Physicians Agreement Health Law in Pennsylvania.
When looking at outcomes of the lawsuit, 40% of oncologists were dismissed from the suit within the first few months, or the case was settled before going to trial. This trend is also consistent with the results from the 2019 and 2017 surveys. When the case did go to trial, 10% received a favorable verdict, which was the same in 2019.
“It seems that most of my clients end up being released from lawsuits, and many lawsuits are dismissed prior to proceeding to trial,” Mr. Hursh commented.
Murdering psychopath
Some oncologists weighed in on what they felt was the worst experience of being sued.
“Mental anguish, knowing that I did nothing wrong,” said one physician. Another reported that it was a feeling of being “inadequate and totally alone.”
Another oncologist commented that the “depositions from lawyers implied that I was worse than a murdering psychopath. My reputation was permanently damaged.”
However, the vast majority of oncologists (88%) did not believe that the lawsuit negatively affected their career, which was similar to physicians in general. That said, many did complain about the ongoing requirement to report the lawsuit to the credentialing committee, even if it was dismissed, and then having to pay increased malpractice premiums. “I still need to document this episode every single time I apply for any medical position, even more than 29 years after I was dismissed from the case,” said one respondent.
When asked if they would do anything differently, many oncologists (42%) said no, they would not have done anything differently. This is similar to the responses from physicians in general and with 2019 responses from oncologists. However, 15% of the respondents said that in retrospect, they would not have taken on that patient to begin with.
Some oncologists noted that they would have been more conscientious in relaying the information to the referring physician. Evan Lyman, an associate attorney at Voute, Lohrfink, McAndrew, Meisner & Roberts, LLP, in White Plains, N.Y., pointed out that a common reason for lawsuits is a slip-up of communication between the specialist and the referring physician.
Oncologists who had been sued have some insights to offer to colleagues, should they find themselves in a similar situation.
“Only answer with short and precise statements,” wrote one oncologist. “Attend all the depositions as much as you can; they are more likely to fabricate or exaggerate if you are not sitting in the room.”
Another physician said to base “everything on the medical record and do not answer hypothetical questions.”
“Document all interactions with patients as if a jury will be reading them, word by word,” said one respondent.
As for the public or patients, oncologists had this message: “malpractice suits should be rarely launched and only when gross errors can be absolutely proven.”
Another oncologist pointed out that communication is key. “Speak to the physicians against whom you have distrust. Lots of things could be cleared by good communication.”
A version of this article first appeared on Medscape.com.
, notes the latest Medscape Malpractice Report.
Over a third (39%) of oncologists who were surveyed said that they had been named in at least one malpractice suit, according to the Medscape Oncologist Malpractice Report 2021.
This number is considerably lower than that reported by physicians across all specialties (51%), and it is also much lower than that reported by oncologists in past years. In the 2019 report, 54% of oncologists surveyed said they had been named in a malpractice suit, while in the 2017 report, the figure was 53%.
The dramatic decline in malpractice suits may have much to do with the COVID-19 pandemic, when oncology care was in a state of flux.
“Fewer people were seeking cancer care during the COVID pandemic, which might have impacted the number of lawsuits brought against oncologists,” says Paul Walker, a New York–based malpractice attorney at Walker Medical Law, who represents physicians and other healthcare professionals.
“Additionally, a fair number of people who died of COVID were also older,” he pointed out, and it is often older people who get cancer, so there were fewer older people who consulted an oncologist or were treated by one, he added.
However, the pandemic may be storing up trouble for future years. “Patient fears of contracting COVID-19 have led many to avoid seeking or resuming care, so delays in diagnosing new cancer cases could mean that more patients are diagnosed at a later stage of their disease, leading to potential adverse events and malpractice claims,” commented David L. Feldman, MD, MBA, chief medical officer of The Doctors Company Group.
This latest 2021 Medscape Malpractice Report was compiled from an online survey that included more than 4,300 physicians from 29 specialties. It included 106 oncologists. More than half of respondents (56%) had been in practice for more than 25 years, and 54% were aged 60 years or older. The survey was available from May 21 to August 28, 2021.
Similar to findings in previous years, complications from treatment/surgery were the most common reason for the lawsuits (31%). Failure to make a correct diagnosis or a delay in diagnosis was the second most common reason (23%), while 20% of patients sued because of a poor outcome or disease progression.
Surprise at being sued
Among the oncologists who reported involvement in a lawsuit in 2021, the majority (86%) said they were “very surprised” or “somewhat surprised” by the malpractice suit, which is similar to that of other physicians surveyed. However, fewer were surprised this year as compared to 2019 and 2017 (90% and 94%).
One reason for the surprise over the litigation was that it concerned a patient who had been treated a long time ago. One oncologist wrote that “the patient had not seen me for over 7 years and during that time, he did not call me with his new symptomatology. I was only named in the suit because I had previously been involved.”
Another common scenario reported by oncologists was being named in a lawsuit which was brought by another clinician’s patient. “I was the chairperson of the department, and one of the doctors in the practice was involved in the suit,” wrote one respondent. “I was named as an accomplice.”
More than half of surveyed oncologists said that they were able to identify the patient who bought the suit, and these figures are again comparable to those of other physicians. One oncologist commented that in the case he was involved with, the family did not understand or accept the nature of cancer and the different ways that a patient could die of complications. This patient had died of sepsis and pneumonia related to decubitus ulcers that were completely unrelated to her radiation therapy.
As in the case above, sometimes it is the family who filed the lawsuit, not the patient.
“The patient may even recognize that you did your best and be grateful for your skill and efforts, but the family can’t accept that grandma died of cancer and brings a lawsuit,” said Dennis Hursh, an attorney with Physicians Agreement Health Law in Pennsylvania.
When looking at outcomes of the lawsuit, 40% of oncologists were dismissed from the suit within the first few months, or the case was settled before going to trial. This trend is also consistent with the results from the 2019 and 2017 surveys. When the case did go to trial, 10% received a favorable verdict, which was the same in 2019.
“It seems that most of my clients end up being released from lawsuits, and many lawsuits are dismissed prior to proceeding to trial,” Mr. Hursh commented.
Murdering psychopath
Some oncologists weighed in on what they felt was the worst experience of being sued.
“Mental anguish, knowing that I did nothing wrong,” said one physician. Another reported that it was a feeling of being “inadequate and totally alone.”
Another oncologist commented that the “depositions from lawyers implied that I was worse than a murdering psychopath. My reputation was permanently damaged.”
However, the vast majority of oncologists (88%) did not believe that the lawsuit negatively affected their career, which was similar to physicians in general. That said, many did complain about the ongoing requirement to report the lawsuit to the credentialing committee, even if it was dismissed, and then having to pay increased malpractice premiums. “I still need to document this episode every single time I apply for any medical position, even more than 29 years after I was dismissed from the case,” said one respondent.
When asked if they would do anything differently, many oncologists (42%) said no, they would not have done anything differently. This is similar to the responses from physicians in general and with 2019 responses from oncologists. However, 15% of the respondents said that in retrospect, they would not have taken on that patient to begin with.
Some oncologists noted that they would have been more conscientious in relaying the information to the referring physician. Evan Lyman, an associate attorney at Voute, Lohrfink, McAndrew, Meisner & Roberts, LLP, in White Plains, N.Y., pointed out that a common reason for lawsuits is a slip-up of communication between the specialist and the referring physician.
Oncologists who had been sued have some insights to offer to colleagues, should they find themselves in a similar situation.
“Only answer with short and precise statements,” wrote one oncologist. “Attend all the depositions as much as you can; they are more likely to fabricate or exaggerate if you are not sitting in the room.”
Another physician said to base “everything on the medical record and do not answer hypothetical questions.”
“Document all interactions with patients as if a jury will be reading them, word by word,” said one respondent.
As for the public or patients, oncologists had this message: “malpractice suits should be rarely launched and only when gross errors can be absolutely proven.”
Another oncologist pointed out that communication is key. “Speak to the physicians against whom you have distrust. Lots of things could be cleared by good communication.”
A version of this article first appeared on Medscape.com.
, notes the latest Medscape Malpractice Report.
Over a third (39%) of oncologists who were surveyed said that they had been named in at least one malpractice suit, according to the Medscape Oncologist Malpractice Report 2021.
This number is considerably lower than that reported by physicians across all specialties (51%), and it is also much lower than that reported by oncologists in past years. In the 2019 report, 54% of oncologists surveyed said they had been named in a malpractice suit, while in the 2017 report, the figure was 53%.
The dramatic decline in malpractice suits may have much to do with the COVID-19 pandemic, when oncology care was in a state of flux.
“Fewer people were seeking cancer care during the COVID pandemic, which might have impacted the number of lawsuits brought against oncologists,” says Paul Walker, a New York–based malpractice attorney at Walker Medical Law, who represents physicians and other healthcare professionals.
“Additionally, a fair number of people who died of COVID were also older,” he pointed out, and it is often older people who get cancer, so there were fewer older people who consulted an oncologist or were treated by one, he added.
However, the pandemic may be storing up trouble for future years. “Patient fears of contracting COVID-19 have led many to avoid seeking or resuming care, so delays in diagnosing new cancer cases could mean that more patients are diagnosed at a later stage of their disease, leading to potential adverse events and malpractice claims,” commented David L. Feldman, MD, MBA, chief medical officer of The Doctors Company Group.
This latest 2021 Medscape Malpractice Report was compiled from an online survey that included more than 4,300 physicians from 29 specialties. It included 106 oncologists. More than half of respondents (56%) had been in practice for more than 25 years, and 54% were aged 60 years or older. The survey was available from May 21 to August 28, 2021.
Similar to findings in previous years, complications from treatment/surgery were the most common reason for the lawsuits (31%). Failure to make a correct diagnosis or a delay in diagnosis was the second most common reason (23%), while 20% of patients sued because of a poor outcome or disease progression.
Surprise at being sued
Among the oncologists who reported involvement in a lawsuit in 2021, the majority (86%) said they were “very surprised” or “somewhat surprised” by the malpractice suit, which is similar to that of other physicians surveyed. However, fewer were surprised this year as compared to 2019 and 2017 (90% and 94%).
One reason for the surprise over the litigation was that it concerned a patient who had been treated a long time ago. One oncologist wrote that “the patient had not seen me for over 7 years and during that time, he did not call me with his new symptomatology. I was only named in the suit because I had previously been involved.”
Another common scenario reported by oncologists was being named in a lawsuit which was brought by another clinician’s patient. “I was the chairperson of the department, and one of the doctors in the practice was involved in the suit,” wrote one respondent. “I was named as an accomplice.”
More than half of surveyed oncologists said that they were able to identify the patient who bought the suit, and these figures are again comparable to those of other physicians. One oncologist commented that in the case he was involved with, the family did not understand or accept the nature of cancer and the different ways that a patient could die of complications. This patient had died of sepsis and pneumonia related to decubitus ulcers that were completely unrelated to her radiation therapy.
As in the case above, sometimes it is the family who filed the lawsuit, not the patient.
“The patient may even recognize that you did your best and be grateful for your skill and efforts, but the family can’t accept that grandma died of cancer and brings a lawsuit,” said Dennis Hursh, an attorney with Physicians Agreement Health Law in Pennsylvania.
When looking at outcomes of the lawsuit, 40% of oncologists were dismissed from the suit within the first few months, or the case was settled before going to trial. This trend is also consistent with the results from the 2019 and 2017 surveys. When the case did go to trial, 10% received a favorable verdict, which was the same in 2019.
“It seems that most of my clients end up being released from lawsuits, and many lawsuits are dismissed prior to proceeding to trial,” Mr. Hursh commented.
Murdering psychopath
Some oncologists weighed in on what they felt was the worst experience of being sued.
“Mental anguish, knowing that I did nothing wrong,” said one physician. Another reported that it was a feeling of being “inadequate and totally alone.”
Another oncologist commented that the “depositions from lawyers implied that I was worse than a murdering psychopath. My reputation was permanently damaged.”
However, the vast majority of oncologists (88%) did not believe that the lawsuit negatively affected their career, which was similar to physicians in general. That said, many did complain about the ongoing requirement to report the lawsuit to the credentialing committee, even if it was dismissed, and then having to pay increased malpractice premiums. “I still need to document this episode every single time I apply for any medical position, even more than 29 years after I was dismissed from the case,” said one respondent.
When asked if they would do anything differently, many oncologists (42%) said no, they would not have done anything differently. This is similar to the responses from physicians in general and with 2019 responses from oncologists. However, 15% of the respondents said that in retrospect, they would not have taken on that patient to begin with.
Some oncologists noted that they would have been more conscientious in relaying the information to the referring physician. Evan Lyman, an associate attorney at Voute, Lohrfink, McAndrew, Meisner & Roberts, LLP, in White Plains, N.Y., pointed out that a common reason for lawsuits is a slip-up of communication between the specialist and the referring physician.
Oncologists who had been sued have some insights to offer to colleagues, should they find themselves in a similar situation.
“Only answer with short and precise statements,” wrote one oncologist. “Attend all the depositions as much as you can; they are more likely to fabricate or exaggerate if you are not sitting in the room.”
Another physician said to base “everything on the medical record and do not answer hypothetical questions.”
“Document all interactions with patients as if a jury will be reading them, word by word,” said one respondent.
As for the public or patients, oncologists had this message: “malpractice suits should be rarely launched and only when gross errors can be absolutely proven.”
Another oncologist pointed out that communication is key. “Speak to the physicians against whom you have distrust. Lots of things could be cleared by good communication.”
A version of this article first appeared on Medscape.com.
FDA investigates possible increased risk of death with lymphoma drug
The FDA granted accelerated approval to umbralisib in February 2021 for patients with two types of lymphoma: Adults with relapsed or refractory marginal zone lymphoma who received at least one prior therapy, and those with relapsed or refractory follicular lymphoma who received at least three prior therapies.
According to the FDA, the possible increased risk of death arose from early findings in a phase 3 trial evaluating the drug in a related type of cancer: chronic lymphocytic leukemia.
“Because of the seriousness of this safety concern and the similarities between the two types of cancer for which this drug is approved and the type of cancer that was studied in the clinical trial, we are alerting patients and health care professionals that we are reevaluating this risk against the benefits of Ukoniq [umbralisib] for its approved uses,” the FDA safety communication states.
The FDA said it performed an initial review of data from the phase 3, randomized controlled UNITY trial, which is evaluating the efficacy of umbralisib plus a monoclonal antibody in patients with chronic lymphocytic leukemia.
“The results showed a possible increased risk of death in patients receiving the combination of Ukoniq [umbralisib] and the monoclonal antibody compared to the control arm,” according to the FDA. “Those receiving the combination of Ukoniq [umbralisib] and the monoclonal antibody also experienced more serious adverse events than those in the control arm.”
Although the drug has not been approved for patients with chronic lymphocytic leukemia, the FDA believes the findings could “have implications for its approved uses” in marginal zone lymphoma and follicular lymphoma.
However, the phase 2 trial that led to February 2021 approvals found the drug’s safety profile to be “manageable,” with serious adverse reactions reported in 18% of patients receiving the dual oral inhibitor of phosphoinositide 3 kinase delta and casein kinase 1 epsilon. These adverse reactions included diarrhea-colitis (4%), pneumonia (3%), sepsis (2%), and urinary tract infection (2%); however, no elevated risk of death was indicated in that analysis.
The FDA noted it will continue to evaluate the results from the phase 3 UNITY trial in chronic lymphocytic leukemia and has suspended enrollment of new patients in other ongoing clinical trials of the drug.
The FDA stated that it would communicate its “final conclusions and recommendations when we have completed our review.” In the meantime, the agency asks health care professionals to review how patients receiving umbralisib are faring and discuss “the risks and benefits of continuing” versus switching to other treatments.
The FDA also asks clinicians and patients to report side effects involving the drug to the FDA MedWatch program.
A version of this article first appeared on Medscape.com.
The FDA granted accelerated approval to umbralisib in February 2021 for patients with two types of lymphoma: Adults with relapsed or refractory marginal zone lymphoma who received at least one prior therapy, and those with relapsed or refractory follicular lymphoma who received at least three prior therapies.
According to the FDA, the possible increased risk of death arose from early findings in a phase 3 trial evaluating the drug in a related type of cancer: chronic lymphocytic leukemia.
“Because of the seriousness of this safety concern and the similarities between the two types of cancer for which this drug is approved and the type of cancer that was studied in the clinical trial, we are alerting patients and health care professionals that we are reevaluating this risk against the benefits of Ukoniq [umbralisib] for its approved uses,” the FDA safety communication states.
The FDA said it performed an initial review of data from the phase 3, randomized controlled UNITY trial, which is evaluating the efficacy of umbralisib plus a monoclonal antibody in patients with chronic lymphocytic leukemia.
“The results showed a possible increased risk of death in patients receiving the combination of Ukoniq [umbralisib] and the monoclonal antibody compared to the control arm,” according to the FDA. “Those receiving the combination of Ukoniq [umbralisib] and the monoclonal antibody also experienced more serious adverse events than those in the control arm.”
Although the drug has not been approved for patients with chronic lymphocytic leukemia, the FDA believes the findings could “have implications for its approved uses” in marginal zone lymphoma and follicular lymphoma.
However, the phase 2 trial that led to February 2021 approvals found the drug’s safety profile to be “manageable,” with serious adverse reactions reported in 18% of patients receiving the dual oral inhibitor of phosphoinositide 3 kinase delta and casein kinase 1 epsilon. These adverse reactions included diarrhea-colitis (4%), pneumonia (3%), sepsis (2%), and urinary tract infection (2%); however, no elevated risk of death was indicated in that analysis.
The FDA noted it will continue to evaluate the results from the phase 3 UNITY trial in chronic lymphocytic leukemia and has suspended enrollment of new patients in other ongoing clinical trials of the drug.
The FDA stated that it would communicate its “final conclusions and recommendations when we have completed our review.” In the meantime, the agency asks health care professionals to review how patients receiving umbralisib are faring and discuss “the risks and benefits of continuing” versus switching to other treatments.
The FDA also asks clinicians and patients to report side effects involving the drug to the FDA MedWatch program.
A version of this article first appeared on Medscape.com.
The FDA granted accelerated approval to umbralisib in February 2021 for patients with two types of lymphoma: Adults with relapsed or refractory marginal zone lymphoma who received at least one prior therapy, and those with relapsed or refractory follicular lymphoma who received at least three prior therapies.
According to the FDA, the possible increased risk of death arose from early findings in a phase 3 trial evaluating the drug in a related type of cancer: chronic lymphocytic leukemia.
“Because of the seriousness of this safety concern and the similarities between the two types of cancer for which this drug is approved and the type of cancer that was studied in the clinical trial, we are alerting patients and health care professionals that we are reevaluating this risk against the benefits of Ukoniq [umbralisib] for its approved uses,” the FDA safety communication states.
The FDA said it performed an initial review of data from the phase 3, randomized controlled UNITY trial, which is evaluating the efficacy of umbralisib plus a monoclonal antibody in patients with chronic lymphocytic leukemia.
“The results showed a possible increased risk of death in patients receiving the combination of Ukoniq [umbralisib] and the monoclonal antibody compared to the control arm,” according to the FDA. “Those receiving the combination of Ukoniq [umbralisib] and the monoclonal antibody also experienced more serious adverse events than those in the control arm.”
Although the drug has not been approved for patients with chronic lymphocytic leukemia, the FDA believes the findings could “have implications for its approved uses” in marginal zone lymphoma and follicular lymphoma.
However, the phase 2 trial that led to February 2021 approvals found the drug’s safety profile to be “manageable,” with serious adverse reactions reported in 18% of patients receiving the dual oral inhibitor of phosphoinositide 3 kinase delta and casein kinase 1 epsilon. These adverse reactions included diarrhea-colitis (4%), pneumonia (3%), sepsis (2%), and urinary tract infection (2%); however, no elevated risk of death was indicated in that analysis.
The FDA noted it will continue to evaluate the results from the phase 3 UNITY trial in chronic lymphocytic leukemia and has suspended enrollment of new patients in other ongoing clinical trials of the drug.
The FDA stated that it would communicate its “final conclusions and recommendations when we have completed our review.” In the meantime, the agency asks health care professionals to review how patients receiving umbralisib are faring and discuss “the risks and benefits of continuing” versus switching to other treatments.
The FDA also asks clinicians and patients to report side effects involving the drug to the FDA MedWatch program.
A version of this article first appeared on Medscape.com.
Guttate Psoriasis Following COVID-19 Infection
Psoriasis is an inflammatory skin condition affecting 1% to 5% of the world population. 1 Guttate psoriasis is a subgroup of psoriasis that most commonly presents as raindroplike, erythematous, silvery, scaly papules. There have been limited reports of guttate psoriasis caused by rhinovirus and COVID-19 infection, but a PubMed search of articles indexed for MEDLINE using the term COVID-19 guttate psoriasis yielded only 3 documented cases of a psoriatic flare secondary to SARS-CoV-2 infection. 1-4 Herein, we detail a case in which a patient with mild SARS-CoV-2 infection who did not have a personal or family history of psoriasis experienced a moderate psoriatic flare 3 weeks after diagnosis of COVID-19.
Case Report
A 55-year-old woman was diagnosed with COVID-19 after SARS-CoV-2 RNA was detected from a nasopharyngeal swab. She reported moderate fatigue but no other symptoms. At the time of infection, she was not taking medications and reported neither a personal nor family history of psoriasis.
Three weeks after the COVID-19 diagnosis, she reported erythematous scaly papules only on the trunk and backs of the legs. Two months after the COVID-19 diagnosis, she was evaluated in our practice and diagnosed with guttate psoriasis. The patient refused biopsy. Physical examination revealed that the affected body surface area had increased to 5%; erythematous, silvery, scaly papules were found on the trunk, anterior and posterior legs, and lateral thighs (Figure). At the time of evaluation, she did not report joint pain or nail changes.
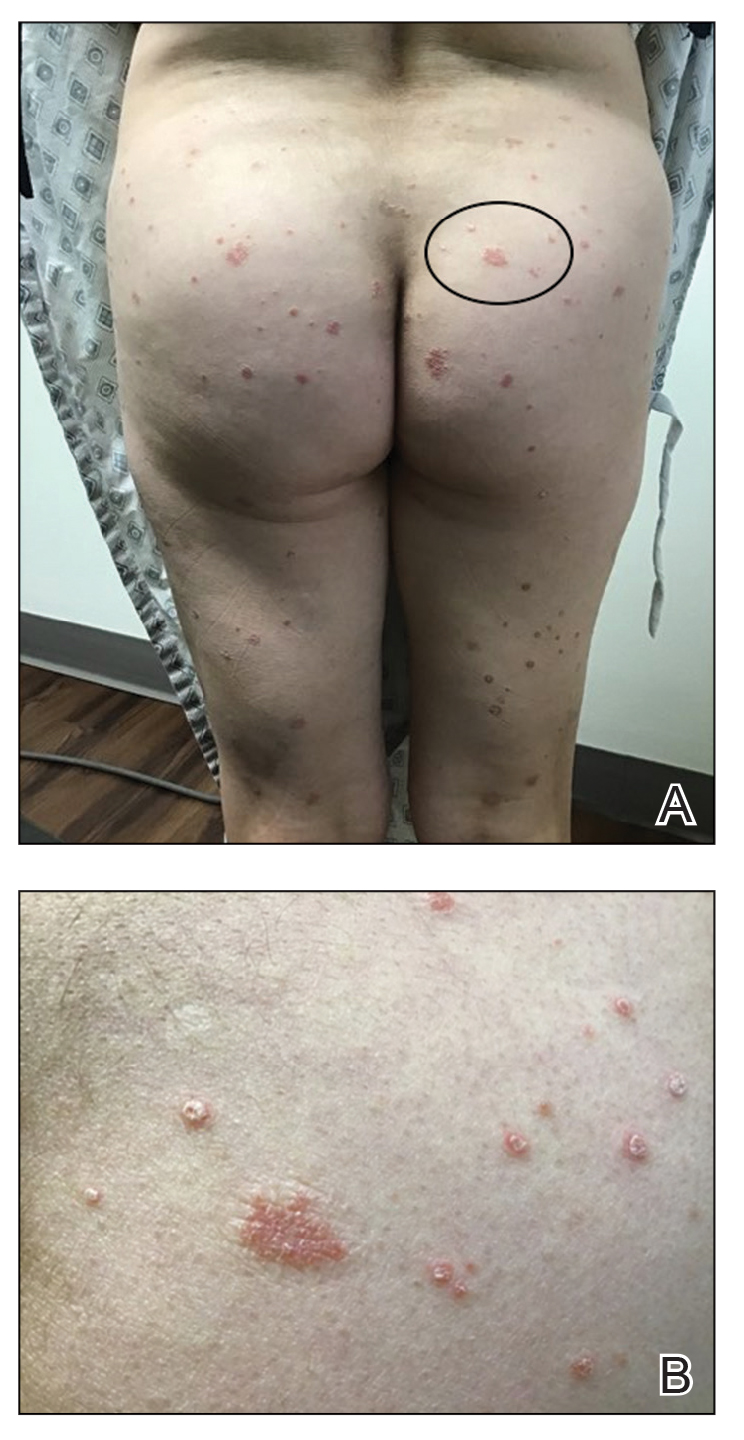
The patient was treated with triamcinolone acetonide cream 0.1% twice daily for 2 to 4 weeks. The guttate psoriasis resolved.
Comment
A sudden psoriatic flare can be linked to dysregulation of the innate immune response. Guttate psoriasis and generalized plaque-type psoriasis are postulated to have similar pathogenetic mechanisms, but guttate psoriasis is the only type of psoriasis that originates from viral infection. Initially, viral RNA will stimulate the toll-like receptor 3 protein, leading to increased production of the pathogenic cytokine IL-36γ and pathogenic chemokine CXCL8 (also known as IL-8), both of which are biomarkers for psoriasis.1 Specifically, IL-36γ and CXCL8 are known to further stimulate the proinflammatory cascade during the innate immune response displayed in guttate psoriasis.5,6
Our patient had a mild case of COVID-19, and she first reported the erythematous and scaly papules 3 weeks after infection. Dysregulation of proinflammatory cytokines must have started in the initial stages—within 7 days—of the viral infection. Guttate psoriasis arises within 3 weeks of infection with other viral and bacterial triggers, most commonly with streptococcal infections.1
Rodríguez et al7 described a phenomenon in which both SARS-CoV-2 and Middle East respiratory syndrome, both caused by a coronavirus, can lead to a reduction of type I interferon, which in turn leads to failure of control of viral replication during initial stages of a viral infection. This triggers an increase in proinflammatory cytokines and chemokines, including IL‐36γ and CXCL8. This pathologic mechanism might apply to SARS-CoV-2, as demonstrated in our patient’s sudden psoriatic flare 3 weeks after the COVID-19 diagnosis. However, further investigation and quantification of the putatively involved cytokines is necessary for confirmation.
Conclusion
Psoriasis, a chronic inflammatory skin condition, has been linked predominantly to genetic and environmental factors. Guttate psoriasis as a secondary reaction after streptococcal tonsillar and respiratory infections has been reported.1
Our case is the fourth documented case of guttate psoriasis secondary to COVID-19 infection.2-4 However, it is the second documented case of a patient with a diagnosis of guttate psoriasis secondary to COVID-19 infection who had neither a personal nor family history of psoriasis.
Because SARS-CoV-2 is a novel virus, the long-term effects of COVID-19 remain unclear. We report this case and its findings to introduce a novel clinical manifestation of SARS-CoV-2 infection.
- Sbidian E, Madrange M, Viguier M, et al. Respiratory virus infection triggers acute psoriasis flares across different clinical subtypes and genetic backgrounds. Br J Dermatol. 2019;181:1304-1306. doi:10.1111/bjd.18203
- Gananandan K, Sacks B, Ewing I. Guttate psoriasis secondary to COVID-19. BMJ Case Rep. 2020;13:e237367. doi:10.1136/bcr-2020-237367
- Rouai M, Rabhi F, Mansouri N, et al. New-onset guttate psoriasis secondary to COVID-19. Clin Case Rep. 2021;9:e04542. doi:10.1002/ccr3.4542
- Agarwal A, Tripathy T, Kar BR. Guttate flare in a patient with chronic plaque psoriasis following COVID-19 infection: a case report. J Cosmet Dermatol. 2021;20:3064-3065. doi:10.1111/jocd.14396
- Madonna S, Girolomoni G, Dinarello CA, et al. The significance of IL-36 hyperactivation and IL-36R targeting in psoriasis. Int J Mol Sci. 2019;20:3318. doi:10.3390/ijms20133318
- Nedoszytko B, Sokołowska-Wojdyło M, Ruckemann-Dziurdzin´ska K, et al. Chemokines and cytokines network in the pathogenesis of the inflammatory skin diseases: atopic dermatitis, psoriasis and skin mastocytosis. Postepy Dermatol Alergol. 2014;31:84-91. doi:10.5114/pdia.2014.40920
- Rodríguez Y, Novelli L, Rojas M, et al. Autoinflammatory and autoimmune conditions at the crossroad of COVID-19. J Autoimmun. 2020;114:102506. doi:10.1016/j.jaut.2020.102506
Psoriasis is an inflammatory skin condition affecting 1% to 5% of the world population. 1 Guttate psoriasis is a subgroup of psoriasis that most commonly presents as raindroplike, erythematous, silvery, scaly papules. There have been limited reports of guttate psoriasis caused by rhinovirus and COVID-19 infection, but a PubMed search of articles indexed for MEDLINE using the term COVID-19 guttate psoriasis yielded only 3 documented cases of a psoriatic flare secondary to SARS-CoV-2 infection. 1-4 Herein, we detail a case in which a patient with mild SARS-CoV-2 infection who did not have a personal or family history of psoriasis experienced a moderate psoriatic flare 3 weeks after diagnosis of COVID-19.
Case Report
A 55-year-old woman was diagnosed with COVID-19 after SARS-CoV-2 RNA was detected from a nasopharyngeal swab. She reported moderate fatigue but no other symptoms. At the time of infection, she was not taking medications and reported neither a personal nor family history of psoriasis.
Three weeks after the COVID-19 diagnosis, she reported erythematous scaly papules only on the trunk and backs of the legs. Two months after the COVID-19 diagnosis, she was evaluated in our practice and diagnosed with guttate psoriasis. The patient refused biopsy. Physical examination revealed that the affected body surface area had increased to 5%; erythematous, silvery, scaly papules were found on the trunk, anterior and posterior legs, and lateral thighs (Figure). At the time of evaluation, she did not report joint pain or nail changes.
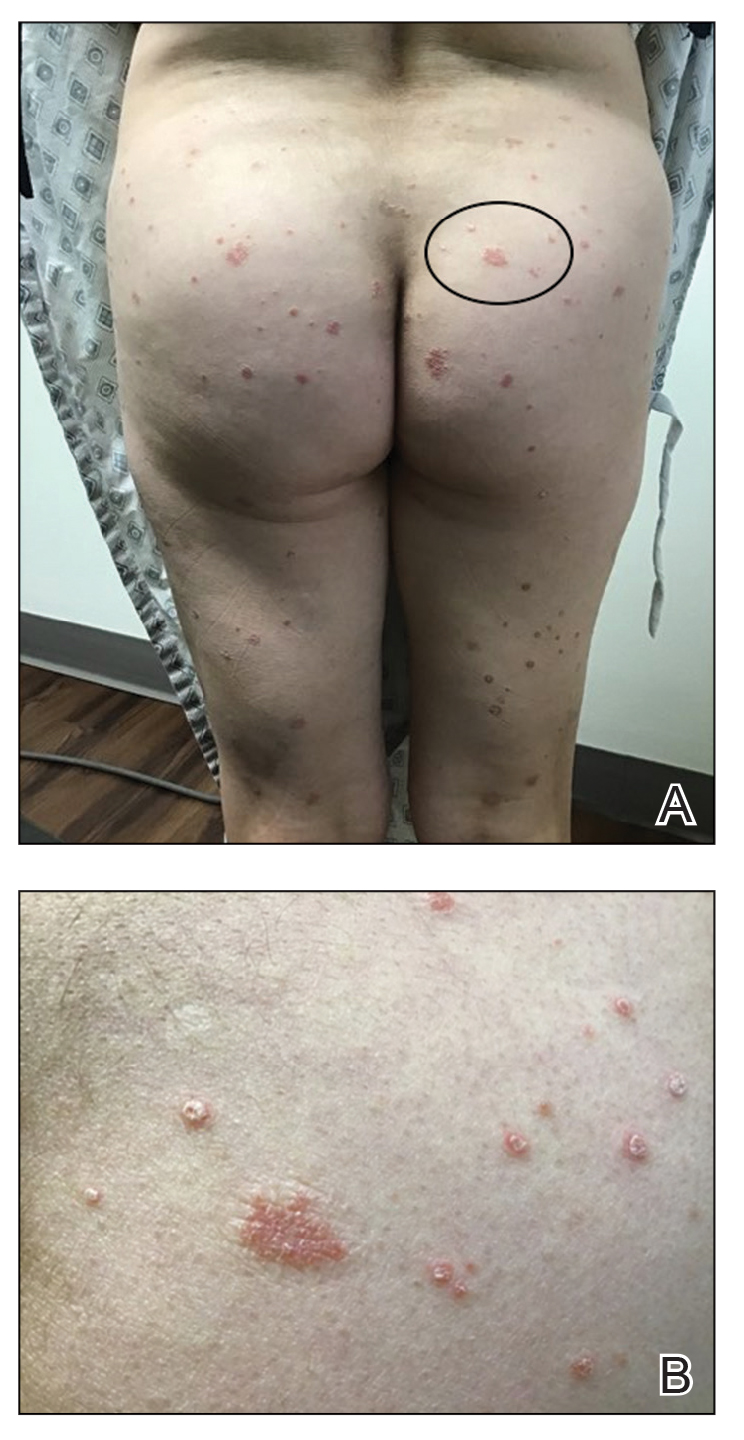
The patient was treated with triamcinolone acetonide cream 0.1% twice daily for 2 to 4 weeks. The guttate psoriasis resolved.
Comment
A sudden psoriatic flare can be linked to dysregulation of the innate immune response. Guttate psoriasis and generalized plaque-type psoriasis are postulated to have similar pathogenetic mechanisms, but guttate psoriasis is the only type of psoriasis that originates from viral infection. Initially, viral RNA will stimulate the toll-like receptor 3 protein, leading to increased production of the pathogenic cytokine IL-36γ and pathogenic chemokine CXCL8 (also known as IL-8), both of which are biomarkers for psoriasis.1 Specifically, IL-36γ and CXCL8 are known to further stimulate the proinflammatory cascade during the innate immune response displayed in guttate psoriasis.5,6
Our patient had a mild case of COVID-19, and she first reported the erythematous and scaly papules 3 weeks after infection. Dysregulation of proinflammatory cytokines must have started in the initial stages—within 7 days—of the viral infection. Guttate psoriasis arises within 3 weeks of infection with other viral and bacterial triggers, most commonly with streptococcal infections.1
Rodríguez et al7 described a phenomenon in which both SARS-CoV-2 and Middle East respiratory syndrome, both caused by a coronavirus, can lead to a reduction of type I interferon, which in turn leads to failure of control of viral replication during initial stages of a viral infection. This triggers an increase in proinflammatory cytokines and chemokines, including IL‐36γ and CXCL8. This pathologic mechanism might apply to SARS-CoV-2, as demonstrated in our patient’s sudden psoriatic flare 3 weeks after the COVID-19 diagnosis. However, further investigation and quantification of the putatively involved cytokines is necessary for confirmation.
Conclusion
Psoriasis, a chronic inflammatory skin condition, has been linked predominantly to genetic and environmental factors. Guttate psoriasis as a secondary reaction after streptococcal tonsillar and respiratory infections has been reported.1
Our case is the fourth documented case of guttate psoriasis secondary to COVID-19 infection.2-4 However, it is the second documented case of a patient with a diagnosis of guttate psoriasis secondary to COVID-19 infection who had neither a personal nor family history of psoriasis.
Because SARS-CoV-2 is a novel virus, the long-term effects of COVID-19 remain unclear. We report this case and its findings to introduce a novel clinical manifestation of SARS-CoV-2 infection.
Psoriasis is an inflammatory skin condition affecting 1% to 5% of the world population. 1 Guttate psoriasis is a subgroup of psoriasis that most commonly presents as raindroplike, erythematous, silvery, scaly papules. There have been limited reports of guttate psoriasis caused by rhinovirus and COVID-19 infection, but a PubMed search of articles indexed for MEDLINE using the term COVID-19 guttate psoriasis yielded only 3 documented cases of a psoriatic flare secondary to SARS-CoV-2 infection. 1-4 Herein, we detail a case in which a patient with mild SARS-CoV-2 infection who did not have a personal or family history of psoriasis experienced a moderate psoriatic flare 3 weeks after diagnosis of COVID-19.
Case Report
A 55-year-old woman was diagnosed with COVID-19 after SARS-CoV-2 RNA was detected from a nasopharyngeal swab. She reported moderate fatigue but no other symptoms. At the time of infection, she was not taking medications and reported neither a personal nor family history of psoriasis.
Three weeks after the COVID-19 diagnosis, she reported erythematous scaly papules only on the trunk and backs of the legs. Two months after the COVID-19 diagnosis, she was evaluated in our practice and diagnosed with guttate psoriasis. The patient refused biopsy. Physical examination revealed that the affected body surface area had increased to 5%; erythematous, silvery, scaly papules were found on the trunk, anterior and posterior legs, and lateral thighs (Figure). At the time of evaluation, she did not report joint pain or nail changes.
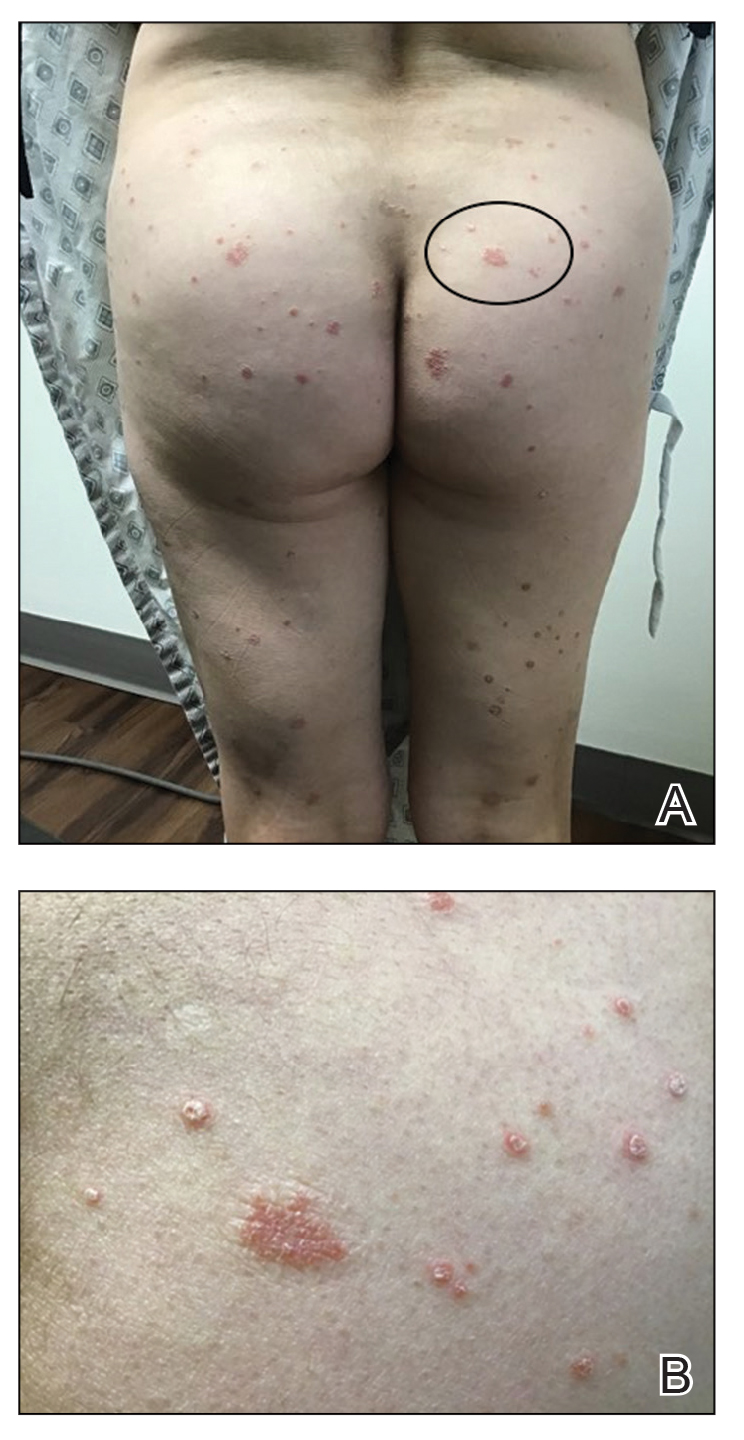
The patient was treated with triamcinolone acetonide cream 0.1% twice daily for 2 to 4 weeks. The guttate psoriasis resolved.
Comment
A sudden psoriatic flare can be linked to dysregulation of the innate immune response. Guttate psoriasis and generalized plaque-type psoriasis are postulated to have similar pathogenetic mechanisms, but guttate psoriasis is the only type of psoriasis that originates from viral infection. Initially, viral RNA will stimulate the toll-like receptor 3 protein, leading to increased production of the pathogenic cytokine IL-36γ and pathogenic chemokine CXCL8 (also known as IL-8), both of which are biomarkers for psoriasis.1 Specifically, IL-36γ and CXCL8 are known to further stimulate the proinflammatory cascade during the innate immune response displayed in guttate psoriasis.5,6
Our patient had a mild case of COVID-19, and she first reported the erythematous and scaly papules 3 weeks after infection. Dysregulation of proinflammatory cytokines must have started in the initial stages—within 7 days—of the viral infection. Guttate psoriasis arises within 3 weeks of infection with other viral and bacterial triggers, most commonly with streptococcal infections.1
Rodríguez et al7 described a phenomenon in which both SARS-CoV-2 and Middle East respiratory syndrome, both caused by a coronavirus, can lead to a reduction of type I interferon, which in turn leads to failure of control of viral replication during initial stages of a viral infection. This triggers an increase in proinflammatory cytokines and chemokines, including IL‐36γ and CXCL8. This pathologic mechanism might apply to SARS-CoV-2, as demonstrated in our patient’s sudden psoriatic flare 3 weeks after the COVID-19 diagnosis. However, further investigation and quantification of the putatively involved cytokines is necessary for confirmation.
Conclusion
Psoriasis, a chronic inflammatory skin condition, has been linked predominantly to genetic and environmental factors. Guttate psoriasis as a secondary reaction after streptococcal tonsillar and respiratory infections has been reported.1
Our case is the fourth documented case of guttate psoriasis secondary to COVID-19 infection.2-4 However, it is the second documented case of a patient with a diagnosis of guttate psoriasis secondary to COVID-19 infection who had neither a personal nor family history of psoriasis.
Because SARS-CoV-2 is a novel virus, the long-term effects of COVID-19 remain unclear. We report this case and its findings to introduce a novel clinical manifestation of SARS-CoV-2 infection.
- Sbidian E, Madrange M, Viguier M, et al. Respiratory virus infection triggers acute psoriasis flares across different clinical subtypes and genetic backgrounds. Br J Dermatol. 2019;181:1304-1306. doi:10.1111/bjd.18203
- Gananandan K, Sacks B, Ewing I. Guttate psoriasis secondary to COVID-19. BMJ Case Rep. 2020;13:e237367. doi:10.1136/bcr-2020-237367
- Rouai M, Rabhi F, Mansouri N, et al. New-onset guttate psoriasis secondary to COVID-19. Clin Case Rep. 2021;9:e04542. doi:10.1002/ccr3.4542
- Agarwal A, Tripathy T, Kar BR. Guttate flare in a patient with chronic plaque psoriasis following COVID-19 infection: a case report. J Cosmet Dermatol. 2021;20:3064-3065. doi:10.1111/jocd.14396
- Madonna S, Girolomoni G, Dinarello CA, et al. The significance of IL-36 hyperactivation and IL-36R targeting in psoriasis. Int J Mol Sci. 2019;20:3318. doi:10.3390/ijms20133318
- Nedoszytko B, Sokołowska-Wojdyło M, Ruckemann-Dziurdzin´ska K, et al. Chemokines and cytokines network in the pathogenesis of the inflammatory skin diseases: atopic dermatitis, psoriasis and skin mastocytosis. Postepy Dermatol Alergol. 2014;31:84-91. doi:10.5114/pdia.2014.40920
- Rodríguez Y, Novelli L, Rojas M, et al. Autoinflammatory and autoimmune conditions at the crossroad of COVID-19. J Autoimmun. 2020;114:102506. doi:10.1016/j.jaut.2020.102506
- Sbidian E, Madrange M, Viguier M, et al. Respiratory virus infection triggers acute psoriasis flares across different clinical subtypes and genetic backgrounds. Br J Dermatol. 2019;181:1304-1306. doi:10.1111/bjd.18203
- Gananandan K, Sacks B, Ewing I. Guttate psoriasis secondary to COVID-19. BMJ Case Rep. 2020;13:e237367. doi:10.1136/bcr-2020-237367
- Rouai M, Rabhi F, Mansouri N, et al. New-onset guttate psoriasis secondary to COVID-19. Clin Case Rep. 2021;9:e04542. doi:10.1002/ccr3.4542
- Agarwal A, Tripathy T, Kar BR. Guttate flare in a patient with chronic plaque psoriasis following COVID-19 infection: a case report. J Cosmet Dermatol. 2021;20:3064-3065. doi:10.1111/jocd.14396
- Madonna S, Girolomoni G, Dinarello CA, et al. The significance of IL-36 hyperactivation and IL-36R targeting in psoriasis. Int J Mol Sci. 2019;20:3318. doi:10.3390/ijms20133318
- Nedoszytko B, Sokołowska-Wojdyło M, Ruckemann-Dziurdzin´ska K, et al. Chemokines and cytokines network in the pathogenesis of the inflammatory skin diseases: atopic dermatitis, psoriasis and skin mastocytosis. Postepy Dermatol Alergol. 2014;31:84-91. doi:10.5114/pdia.2014.40920
- Rodríguez Y, Novelli L, Rojas M, et al. Autoinflammatory and autoimmune conditions at the crossroad of COVID-19. J Autoimmun. 2020;114:102506. doi:10.1016/j.jaut.2020.102506
Practice Points
- Guttate psoriasis is the only type of psoriasis that originates from viral infection.
- Dysregulation of proinflammatory cytokines during COVID-19 infection in our patient led to development of guttate psoriasis 3 weeks later.







