User login
Tom Collins is a freelance writer in South Florida who has written about medical topics from nasty infections to ethical dilemmas, runaway tumors to tornado-chasing doctors. He travels the globe gathering conference health news and lives in West Palm Beach.
FDA Investigates Major Bleeding Events in Dabigatran Patients
A little more than a year after the new anticoagulant dabigatran (Pradaxa) was approved for stroke prevention in nonvalvular atrial fibrillation (NVAF) patients, the FDA is evaluating post-marketing reports of serious bleeds in patients taking the drug.
The FDA is trying to determine if patients on Pradaxa are experiencing severe bleeding more than expected based on results of the clinical trial that led to Pradaxa’s approval, according to FDA spokeswoman Sandy Walsh.
“At this time, FDA continues to believe that Pradaxa provides an important health benefit when used as directed and recommends that healthcare professionals who prescribe Pradaxa follow the recommendations in the approved drug label,” Walsh tells The Hospitalist.

—Robert Pendleton, MD, director of the hospitalist program, University of Utah Healthcare; medical director, University Healthcare Thrombosis Service
Patients should not stop taking dabigatran without first talking to their doctors, the FDA announcement cautions. While “serious, even fatal events have been reported,” according to the FDA’s announcement, Walsh says the FDA isn’t prepared to say how many reports of serious bleeding events have been received because they’re still being reviewed.
“We often put out ‘early’ communications when we learn of drug safety issues,” she says. “We want to be transparent and make [the] public [aware of] what we do know, but our analysis is not final. At this point, the FDA is still evaluating this issue.”
Bleeding that leads to serious or fatal outcomes is a well-recognized complication of all anticoagulant therapies.
Dabigatran, a direct thrombin inhibitor, was approved in October 2010, becoming the first new oral anticoagulant approved in 50 years. It was the first approved among several new anti-coagulants that are poised to enter the market and are expected to challenge warfarin (Coumadin), the longtime standard of care.
The new drugs—including rivaroxaban (Xarelto), a Factor Xa-inhibitor that was approved in 2011—have been eagerly anticipated because they don’t require frequent blood draws for monitoring, as warfarin does. Hospitalists are especially interested in the new anticoagulant therapies because they treat numerous patients at an increased risk of clotting.
In the RE-LY trial, the 18,000-patient clinical trial comparing dabigatran and warfarin, major bleeding events occurred at similar rates with the two drugs.
Dabigatran manufacturer Boehringer Ingelheim is working with the FDA to evaluate the major bleeding reports, but spokeswoman Anna Moses says the drug has been performing according to expectations.
“Global data collected to date on major bleeding are consistent with our expectations based on the RE-LY trial and are in alignment with the U.S. Prescribing Information, which clearly state the benefits and risks associated with Pradaxa,” Moses says. “Overall, the positive-benefit-risk ratio of Pradaxa in NVAF remains unchanged.” (Visit the manufacturer website for prescribing information [PDF].)
Robert Pendleton, MD, director of the hospitalist program at the University of Utah Healthcare and Medical Director of the University Healthcare Thrombosis Service, expressed no surprise at the FDA’s statement.
“Although the data with new anticoagulants like Pradaxa is very favorable in a clinical trial setting, there’s great risk of enhanced demonstration of harm in the real-world setting if it’s not used optimally,” Dr. Pendleton says. “There will be more liberal sort of prescribing in a less-pure patient population.
So if people are not particularly cognizant of a patient’s renal function, their body weight, prior history of bleeding, etc., then you’re sort of applying new drugs in patients who are even more prone to bleed.”
Dr. Pendleton notes that in subgroup analyses, the slight benefits of the new drugs have come in patients with poor warfarin control, so if patients with good warfarin control are switched, outcomes could generally be expected not to be better, and could be worse.
“It won’t cause me to take people who I have prescribed Pradaxa and switch them back to warfarin,” he says, “but part of that is [that] here, in our healthcare system, we’re pretty cautious in who gets put on one of the new agents. And so those that do are patients who are most like those in the clinical trial.”
Tom Collins is a freelance writer in Florida.
A little more than a year after the new anticoagulant dabigatran (Pradaxa) was approved for stroke prevention in nonvalvular atrial fibrillation (NVAF) patients, the FDA is evaluating post-marketing reports of serious bleeds in patients taking the drug.
The FDA is trying to determine if patients on Pradaxa are experiencing severe bleeding more than expected based on results of the clinical trial that led to Pradaxa’s approval, according to FDA spokeswoman Sandy Walsh.
“At this time, FDA continues to believe that Pradaxa provides an important health benefit when used as directed and recommends that healthcare professionals who prescribe Pradaxa follow the recommendations in the approved drug label,” Walsh tells The Hospitalist.

—Robert Pendleton, MD, director of the hospitalist program, University of Utah Healthcare; medical director, University Healthcare Thrombosis Service
Patients should not stop taking dabigatran without first talking to their doctors, the FDA announcement cautions. While “serious, even fatal events have been reported,” according to the FDA’s announcement, Walsh says the FDA isn’t prepared to say how many reports of serious bleeding events have been received because they’re still being reviewed.
“We often put out ‘early’ communications when we learn of drug safety issues,” she says. “We want to be transparent and make [the] public [aware of] what we do know, but our analysis is not final. At this point, the FDA is still evaluating this issue.”
Bleeding that leads to serious or fatal outcomes is a well-recognized complication of all anticoagulant therapies.
Dabigatran, a direct thrombin inhibitor, was approved in October 2010, becoming the first new oral anticoagulant approved in 50 years. It was the first approved among several new anti-coagulants that are poised to enter the market and are expected to challenge warfarin (Coumadin), the longtime standard of care.
The new drugs—including rivaroxaban (Xarelto), a Factor Xa-inhibitor that was approved in 2011—have been eagerly anticipated because they don’t require frequent blood draws for monitoring, as warfarin does. Hospitalists are especially interested in the new anticoagulant therapies because they treat numerous patients at an increased risk of clotting.
In the RE-LY trial, the 18,000-patient clinical trial comparing dabigatran and warfarin, major bleeding events occurred at similar rates with the two drugs.
Dabigatran manufacturer Boehringer Ingelheim is working with the FDA to evaluate the major bleeding reports, but spokeswoman Anna Moses says the drug has been performing according to expectations.
“Global data collected to date on major bleeding are consistent with our expectations based on the RE-LY trial and are in alignment with the U.S. Prescribing Information, which clearly state the benefits and risks associated with Pradaxa,” Moses says. “Overall, the positive-benefit-risk ratio of Pradaxa in NVAF remains unchanged.” (Visit the manufacturer website for prescribing information [PDF].)
Robert Pendleton, MD, director of the hospitalist program at the University of Utah Healthcare and Medical Director of the University Healthcare Thrombosis Service, expressed no surprise at the FDA’s statement.
“Although the data with new anticoagulants like Pradaxa is very favorable in a clinical trial setting, there’s great risk of enhanced demonstration of harm in the real-world setting if it’s not used optimally,” Dr. Pendleton says. “There will be more liberal sort of prescribing in a less-pure patient population.
So if people are not particularly cognizant of a patient’s renal function, their body weight, prior history of bleeding, etc., then you’re sort of applying new drugs in patients who are even more prone to bleed.”
Dr. Pendleton notes that in subgroup analyses, the slight benefits of the new drugs have come in patients with poor warfarin control, so if patients with good warfarin control are switched, outcomes could generally be expected not to be better, and could be worse.
“It won’t cause me to take people who I have prescribed Pradaxa and switch them back to warfarin,” he says, “but part of that is [that] here, in our healthcare system, we’re pretty cautious in who gets put on one of the new agents. And so those that do are patients who are most like those in the clinical trial.”
Tom Collins is a freelance writer in Florida.
A little more than a year after the new anticoagulant dabigatran (Pradaxa) was approved for stroke prevention in nonvalvular atrial fibrillation (NVAF) patients, the FDA is evaluating post-marketing reports of serious bleeds in patients taking the drug.
The FDA is trying to determine if patients on Pradaxa are experiencing severe bleeding more than expected based on results of the clinical trial that led to Pradaxa’s approval, according to FDA spokeswoman Sandy Walsh.
“At this time, FDA continues to believe that Pradaxa provides an important health benefit when used as directed and recommends that healthcare professionals who prescribe Pradaxa follow the recommendations in the approved drug label,” Walsh tells The Hospitalist.

—Robert Pendleton, MD, director of the hospitalist program, University of Utah Healthcare; medical director, University Healthcare Thrombosis Service
Patients should not stop taking dabigatran without first talking to their doctors, the FDA announcement cautions. While “serious, even fatal events have been reported,” according to the FDA’s announcement, Walsh says the FDA isn’t prepared to say how many reports of serious bleeding events have been received because they’re still being reviewed.
“We often put out ‘early’ communications when we learn of drug safety issues,” she says. “We want to be transparent and make [the] public [aware of] what we do know, but our analysis is not final. At this point, the FDA is still evaluating this issue.”
Bleeding that leads to serious or fatal outcomes is a well-recognized complication of all anticoagulant therapies.
Dabigatran, a direct thrombin inhibitor, was approved in October 2010, becoming the first new oral anticoagulant approved in 50 years. It was the first approved among several new anti-coagulants that are poised to enter the market and are expected to challenge warfarin (Coumadin), the longtime standard of care.
The new drugs—including rivaroxaban (Xarelto), a Factor Xa-inhibitor that was approved in 2011—have been eagerly anticipated because they don’t require frequent blood draws for monitoring, as warfarin does. Hospitalists are especially interested in the new anticoagulant therapies because they treat numerous patients at an increased risk of clotting.
In the RE-LY trial, the 18,000-patient clinical trial comparing dabigatran and warfarin, major bleeding events occurred at similar rates with the two drugs.
Dabigatran manufacturer Boehringer Ingelheim is working with the FDA to evaluate the major bleeding reports, but spokeswoman Anna Moses says the drug has been performing according to expectations.
“Global data collected to date on major bleeding are consistent with our expectations based on the RE-LY trial and are in alignment with the U.S. Prescribing Information, which clearly state the benefits and risks associated with Pradaxa,” Moses says. “Overall, the positive-benefit-risk ratio of Pradaxa in NVAF remains unchanged.” (Visit the manufacturer website for prescribing information [PDF].)
Robert Pendleton, MD, director of the hospitalist program at the University of Utah Healthcare and Medical Director of the University Healthcare Thrombosis Service, expressed no surprise at the FDA’s statement.
“Although the data with new anticoagulants like Pradaxa is very favorable in a clinical trial setting, there’s great risk of enhanced demonstration of harm in the real-world setting if it’s not used optimally,” Dr. Pendleton says. “There will be more liberal sort of prescribing in a less-pure patient population.
So if people are not particularly cognizant of a patient’s renal function, their body weight, prior history of bleeding, etc., then you’re sort of applying new drugs in patients who are even more prone to bleed.”
Dr. Pendleton notes that in subgroup analyses, the slight benefits of the new drugs have come in patients with poor warfarin control, so if patients with good warfarin control are switched, outcomes could generally be expected not to be better, and could be worse.
“It won’t cause me to take people who I have prescribed Pradaxa and switch them back to warfarin,” he says, “but part of that is [that] here, in our healthcare system, we’re pretty cautious in who gets put on one of the new agents. And so those that do are patients who are most like those in the clinical trial.”
Tom Collins is a freelance writer in Florida.
Are hospitalists taking C. diff seriously enough? Maybe, maybe not
Clostridium difficile has been on the radar of infectious disease (ID) experts for the better part of a decade now. But how mindful are hospitalists of the problem, and how seriously are they taking it?
“I think we’re getting there,” says Danielle Scheurer, MD, MSCR, SFHM, a hospitalist and medical director of quality at the Medical University of South Carolina in Charleston. But she adds, “Because the bugs are invisible, you feel a little bit disconnected from your direct role in all this.”
Stuart Cohen, MD, an ID expert at the University of California Davis and a fellow with the Infectious Diseases Society of America, says not everyone is as concerned about C. diff as they should be.
—Stuart Cohen, MD, infectious disease expert, University of California Davis, fellow, Infectious Diseases Society of America
“I think most people still see C. diff as just basically being a nuisance, and so they don’t really take it quite so seriously. Until somebody sees a patient have to get a colectomy or die from C. diff, I don’t think that there’s necessarily an appreciation to the severity of the illness,” he says. “You don’t really get this sense that it’s anything other than, ‘Well, we’ll just give them some vancomycin or we’ll just give them some metronidazole and we’ll take care of it.’”
Ketino Kobaidze, MD, a hospitalist at Emory University Hospital Midtown in Atlanta, says she thinks hospitalists should be more involved in antibiotic stewardship efforts and in research efforts to combat C. diff.
“I’m sure everybody knows and everybody takes it into consideration,” she says. But she also says not all hospitalists view C. diff as an acute problem that warrants urgent treatment “or we might be in trouble,” she says. “I’m not sure about that.”
Dr. Scheurer says the solution to treating C. diff properly is keeping a mindset on the safety of your patients. “Then it can motivate you and your group,” she says. “Every single number affects a person. It’s not just a rate. Zero is the goal.”
Tom Collins is a freelance medical writer based in Florida.
Clostridium difficile has been on the radar of infectious disease (ID) experts for the better part of a decade now. But how mindful are hospitalists of the problem, and how seriously are they taking it?
“I think we’re getting there,” says Danielle Scheurer, MD, MSCR, SFHM, a hospitalist and medical director of quality at the Medical University of South Carolina in Charleston. But she adds, “Because the bugs are invisible, you feel a little bit disconnected from your direct role in all this.”
Stuart Cohen, MD, an ID expert at the University of California Davis and a fellow with the Infectious Diseases Society of America, says not everyone is as concerned about C. diff as they should be.
—Stuart Cohen, MD, infectious disease expert, University of California Davis, fellow, Infectious Diseases Society of America
“I think most people still see C. diff as just basically being a nuisance, and so they don’t really take it quite so seriously. Until somebody sees a patient have to get a colectomy or die from C. diff, I don’t think that there’s necessarily an appreciation to the severity of the illness,” he says. “You don’t really get this sense that it’s anything other than, ‘Well, we’ll just give them some vancomycin or we’ll just give them some metronidazole and we’ll take care of it.’”
Ketino Kobaidze, MD, a hospitalist at Emory University Hospital Midtown in Atlanta, says she thinks hospitalists should be more involved in antibiotic stewardship efforts and in research efforts to combat C. diff.
“I’m sure everybody knows and everybody takes it into consideration,” she says. But she also says not all hospitalists view C. diff as an acute problem that warrants urgent treatment “or we might be in trouble,” she says. “I’m not sure about that.”
Dr. Scheurer says the solution to treating C. diff properly is keeping a mindset on the safety of your patients. “Then it can motivate you and your group,” she says. “Every single number affects a person. It’s not just a rate. Zero is the goal.”
Tom Collins is a freelance medical writer based in Florida.
Clostridium difficile has been on the radar of infectious disease (ID) experts for the better part of a decade now. But how mindful are hospitalists of the problem, and how seriously are they taking it?
“I think we’re getting there,” says Danielle Scheurer, MD, MSCR, SFHM, a hospitalist and medical director of quality at the Medical University of South Carolina in Charleston. But she adds, “Because the bugs are invisible, you feel a little bit disconnected from your direct role in all this.”
Stuart Cohen, MD, an ID expert at the University of California Davis and a fellow with the Infectious Diseases Society of America, says not everyone is as concerned about C. diff as they should be.
—Stuart Cohen, MD, infectious disease expert, University of California Davis, fellow, Infectious Diseases Society of America
“I think most people still see C. diff as just basically being a nuisance, and so they don’t really take it quite so seriously. Until somebody sees a patient have to get a colectomy or die from C. diff, I don’t think that there’s necessarily an appreciation to the severity of the illness,” he says. “You don’t really get this sense that it’s anything other than, ‘Well, we’ll just give them some vancomycin or we’ll just give them some metronidazole and we’ll take care of it.’”
Ketino Kobaidze, MD, a hospitalist at Emory University Hospital Midtown in Atlanta, says she thinks hospitalists should be more involved in antibiotic stewardship efforts and in research efforts to combat C. diff.
“I’m sure everybody knows and everybody takes it into consideration,” she says. But she also says not all hospitalists view C. diff as an acute problem that warrants urgent treatment “or we might be in trouble,” she says. “I’m not sure about that.”
Dr. Scheurer says the solution to treating C. diff properly is keeping a mindset on the safety of your patients. “Then it can motivate you and your group,” she says. “Every single number affects a person. It’s not just a rate. Zero is the goal.”
Tom Collins is a freelance medical writer based in Florida.
ONLINE EXCLUSIVE: Listen to CDC expert Carolyn Gould and Emory hospitalist Ketino Kobaidze discuss C. diff prevention
Click here to listen to Dr. Gould
Click here to listen to Dr. Kobaidze
Click here to listen to Dr. Gould
Click here to listen to Dr. Kobaidze
Click here to listen to Dr. Gould
Click here to listen to Dr. Kobaidze
Gut Reaction
At 480-bed Emory University Hospital Midtown in Atlanta, the physicians and staff seemingly are doing all the right things to foil one of hospital’s archenemies: Clostridium difficile. The bacteria, better known as C. diff, is responsible for a sharp rise in hospital-acquired infections over the past decade, rivaling even MRSA.
In 2010, Emory Midtown launched a campaign to boost awareness of the importance of hand washing before and after treating patients infected with C. diff and those likely to be infected. They also began using the polymerase-chain-reaction-based assay to detect the bacteria, a test with much higher sensitivity that helps to more efficiently identify those infected so control measures can be more prompt and targeted. They use a hypochlorite mixture to clean the rooms of those infected, which is considered a must. And a committee monitors the use of antibiotics to prevent overuse—often the scapegoat for the rise of the hard-to-kill bacteria.
Still, at Emory, the rate of C. diff is about the same as the national average, says hospitalist Ketino Kobaidze, MD, assistant professor at the Emory University School of Medicine and a member of the antimicrobial stewardship and infectious disease control committees at Midtown. While Dr. Kobaidze says her institution is doing a good job of trying to keep C. diff under control, she thinks hospitalists can do more.
“My feeling is that we are not as involved as we’re supposed to be,” she says. “I think we need to be a little bit more proactive, be involved in committees and research activities across the hospital.”
—Kevin Kavanagh, MD, founder, Health Watch USA
You Are Not Alone
The experience at Emory Midtown is far from unusual—healthcare facilities, and hospitalists, across the country have seen healthcare-related C. diff cases more than double since 2001 to between 400,000 and 500,000 a year, says Carolyn Gould, MD, a medical epidemiologist in the division of healthcare quality promotion at the Centers for Disease Control and Prevention (CDC) in Atlanta.
Hospitalists, whether they realize it or not, are intimately involved in how well the C. diff outbreak is controlled. Infectious-disease (ID) specialists say hospitalists are perfectly situated to make an impact in efforts to help curb the outbreak.
“Hospitalists are critical to this effort,” Dr. Gould says. “They’re in the hospital day in and day out, and they’re constantly interacting with the patients, staff, and administration. They’re often the first on the scene to see a patient who might have suddenly developed diarrhea; they’re the first to react. I think they’re in a prime position to play a leadership role to prevent C. diff infections.”
They’re also situated well to work with infection-control experts on antimicrobial stewardship programs, she says.
“I look at hospitalists just like I would have looked at internists managing their own patients 15 years ago,” says Stuart Cohen, MD, an ID expert with the University of California at Davis and a fellow with the Infectious Diseases Society of America who was lead author of the latest published IDSA guidelines on C. diff treatment. “And so they’re the first-line people.”
continued below...
A Tough Bug
Believed to be aided largely by the use of broad-spectrum antibiotics that knock out the colon’s natural flora, C. diff in the hospital—as well as nursing homes and acute-care facilities—has raged for much of the past decade. Its rise is tied to the emergence of a new hypervirulent strain known as BI/NAP1/027, or NAP1 for short. The strain is highly resistant to fluoroquinolones, such as ciprofloxacin and levofloxacin, which are used often in healthcare settings.
“A fluoroquinolone will wipe out a lot of your normal flora in your gut,” Dr. Gould says. “But it won’t wipe out C. diff, in particular this hypervirulent strain. And so this strain can flourish in the presence of fluoroquinolones.” The strain produces up to 15 to 20 times more toxins than other C. diff strains, according to some data, she adds.
Vancomycin (Vanconin) and metronidazole (Flagyl) are the most common antibiotics used to treat patients infected with C. diff. Mortality rates are higher among the elderly, largely because of their weaker immune system, Dr. Gould says. Studies have generally shown mortality rates of 10% or a bit lower.1
More recent studies have shown that the number of hospital-related C. diff cases might have begun to level off in 2008 and 2009. Dr. Gould says she thinks the leveling off is for real, but there is debate over what the immediate future holds.
“There’s a lot of work and initiatives, especially state-based initiatives, that are being done in hospitals. And there’s reason to believe they’re effective,” she says, adding it’s harder to get a good picture of the problem in long-term care facilities and in the community.
Dr. Cohen with the IDSA says it’s too soon to say whether the problem is hitting a plateau. “CDC data are always a couple of years behind,” he says. “Until you see another data point, you can’t tell whether that’s just a transient flattening and whether it’s going to keep going up or not.”
Kevin Kavanagh, MD, founder of the patient advocacy group Health Watch USA and a retired otolaryngologist in Kentucky who has taken a keen interest in the C. diff problem, says he doesn’t think the end of the tunnel is within view yet.
“I think C. diff is going to get worse before it gets better,” Dr. Kavanagh says. “And that’s not necessarily because the healthcare profession isn’t doing due diligence. This is a tough organism.—it can be tough to treat and can be very tough to kill.”
The Best Defense?
Because C. diff lives within protective spores, sound hand hygiene practices and room-cleaning practices are essential for keeping infections to a minimum. Alcohol-based hand sanitizers, effective against other organisms including MRSA, do not kill C. diff. The bacteria must be mechanically removed through hand washing.
And even hand washing might not be totally effective at getting rid of the spores, which means it’s important for healthcare workers to gown and glove in high-risk rooms.
Sodium hypochlorite solutions, or bleach mixtures, have to be used to clean rooms occupied by patients with C. diff, and the prevailing thought is to clean the rooms of patients suspected of having C. diff, even if those cases might not be confirmed.
Equally important to cleaning and hand washing is systemwide emphasis on antibiotic stewardship. A 2011 study at the State University of New York Buffalo found that the risk of a C. diff infection rose with the number of antibiotics taken.2

—Carolyn Gould, MD, medical epidemiologist, division of healthcare quality promotion, Centers of Disease Control and Prevention, Atlanta
While a broad-spectrum antibiotic might be necessary at first, once the results of cultures are received, the treatment should be finely tailored to kill only the problem bacteria so that the body’s natural defenses aren’t broken down, Dr. Gould explains.
“If someone is very sick and you’re not sure what is going on, it’s very reasonable to treat them empirically with broad-spectrum antibiotics,” she says. “The important thing is that you send the appropriate cultures before so that you know what you’re treating and you can optimize those antibiotics with daily assessments.”
It’s clear why an overreliance on broad-spectrum drugs prevails in U.S. health settings, Dr. Cohen acknowledges. Recent literature suggests treating critically ill patients with wide-ranging antimicrobials as the mortality rate can be twice as high with narrower options. “I think people have gotten very quick to give broad-spectrum therapy,” he says.
continued below...
National Response, Localized Attention
Dr. Kavanagh of Health Watch USA says that more information about C. diff is needed, particularly publicly available numbers of infections at hospitals. Some states require those figures to be reported, but most don’t. And there is no current federal mandate on reporting of C. diff cases, although acute-care hospitals will be required to report C. diff infection rates starting in 2013.
“We really have scant data,” he says. “There is not a lot of reporting if you look at the nation on a whole. And I think that underscores one of the reasons why you need to have data for action. You need to have reporting of these organisms to the National Healthcare Safety Network so that the CDC can monitor and can make plans and can do effective interventions.
“You want to know where the areas of highest infection are,” he adds. “You want to know what interventions work and don’t work. If you don’t have a national coordinated reporting system, it really makes it difficult to address the problem. C. diff is going to be much harder to control than MRSA or other bacteria because it changes into a hard-to-kill dormant spore stage and then re-occurs at some point.”
The Centers for Medicare & Medicaid Services (CMS) has proposed adding C. diff infections to the list of hospital-acquired conditions that will not be reimbursable. It is widely hoped that such a measure will go a long way toward stamping out the problem.
Dr. Kobaidze of Emory notes that C. diff is a dynamic problem, always adapting and posing new challenges. And hospitalists should be more involved in answering these questions through research. One recent question, she points out, is whether proton pump inhibitor use is related to the rise of C. diff.
Ultimately, though, controlling C. diff in hospitals might come down to what is done day to day inside the hospital. And hospitalists can play a big role.
Danielle Scheurer, MD, MSCR, SFHM, a hospitalist and medical director of quality at the Medical University of South Carolina in Charleston, says that a full-time pharmacist on the hospital’s antimicrobial stewardship committee is always reviewing antibiotic prescriptions and is prepared to flag cases in which a broad-spectrum is used when one with a more narrow scope might be more appropriate.
The hospital has done its best, as part of its “renovation cycle,” to standardize the layouts of rooms “so that the second you open the door you know exactly where the alcohol gel is and where the soap and the sink is going to be.” The idea is to make compliance as “mindless” as possible. Such efforts can be hampered by structural limitations though, she says.
HM group leaders, she suggests, can play an important part simply by being good role models—gowning and gloving without complaint before entering high-risk rooms and reinforcing the message that such efforts have real effects on patient safety.
But she also acknowledges that “it always sounds easy....There has to be some level of redundancy built into the hospital system. This is more of a system thing than the individual hospitalist.”
One level of redundancy at MUSC that has been particularly effective, she says, are “secret shoppers” who keep an eye out for medical teams that might not be washing their hands as they go in and out of high-risk rooms. Each unit is responsible for their hand hygiene numbers—which include both self-reported figures and those obtained by the secret onlookers—and those numbers are made available to the hospital.
Those units with the best numbers are sometimes given a reward, such as a pizza party, but it’s colleagues’ knowledge of the numbers that matters most, she says.
“That, in and of itself, is a powerful motivator,” Dr. Scheurer says. “We bring it to all of our quality operations meetings, all the administrators, the CEO, the CMO. It’s very motivating for every unit. They don’t want to be the trailing unit.”
Tom Collins is a freelance medical writer based in Miami.
References
- Orenstein R, Aronhalt KC, McManus JE Jr., Fedraw LA. A targeted strategy to wipe out Clostridium difficile. Infect Control Hosp Epidemiol. 2011;32(11):1137-1139.
- Stevens V, Dumyati G, Fine LS, Fisher SG, van Wijngaarden E. Cumulative antibiotic exposures over time and the risk of Clostridium difficile infection. Clin Infect Dis. 2011;53(1):42-48.
At 480-bed Emory University Hospital Midtown in Atlanta, the physicians and staff seemingly are doing all the right things to foil one of hospital’s archenemies: Clostridium difficile. The bacteria, better known as C. diff, is responsible for a sharp rise in hospital-acquired infections over the past decade, rivaling even MRSA.
In 2010, Emory Midtown launched a campaign to boost awareness of the importance of hand washing before and after treating patients infected with C. diff and those likely to be infected. They also began using the polymerase-chain-reaction-based assay to detect the bacteria, a test with much higher sensitivity that helps to more efficiently identify those infected so control measures can be more prompt and targeted. They use a hypochlorite mixture to clean the rooms of those infected, which is considered a must. And a committee monitors the use of antibiotics to prevent overuse—often the scapegoat for the rise of the hard-to-kill bacteria.
Still, at Emory, the rate of C. diff is about the same as the national average, says hospitalist Ketino Kobaidze, MD, assistant professor at the Emory University School of Medicine and a member of the antimicrobial stewardship and infectious disease control committees at Midtown. While Dr. Kobaidze says her institution is doing a good job of trying to keep C. diff under control, she thinks hospitalists can do more.
“My feeling is that we are not as involved as we’re supposed to be,” she says. “I think we need to be a little bit more proactive, be involved in committees and research activities across the hospital.”
—Kevin Kavanagh, MD, founder, Health Watch USA
You Are Not Alone
The experience at Emory Midtown is far from unusual—healthcare facilities, and hospitalists, across the country have seen healthcare-related C. diff cases more than double since 2001 to between 400,000 and 500,000 a year, says Carolyn Gould, MD, a medical epidemiologist in the division of healthcare quality promotion at the Centers for Disease Control and Prevention (CDC) in Atlanta.
Hospitalists, whether they realize it or not, are intimately involved in how well the C. diff outbreak is controlled. Infectious-disease (ID) specialists say hospitalists are perfectly situated to make an impact in efforts to help curb the outbreak.
“Hospitalists are critical to this effort,” Dr. Gould says. “They’re in the hospital day in and day out, and they’re constantly interacting with the patients, staff, and administration. They’re often the first on the scene to see a patient who might have suddenly developed diarrhea; they’re the first to react. I think they’re in a prime position to play a leadership role to prevent C. diff infections.”
They’re also situated well to work with infection-control experts on antimicrobial stewardship programs, she says.
“I look at hospitalists just like I would have looked at internists managing their own patients 15 years ago,” says Stuart Cohen, MD, an ID expert with the University of California at Davis and a fellow with the Infectious Diseases Society of America who was lead author of the latest published IDSA guidelines on C. diff treatment. “And so they’re the first-line people.”
continued below...
A Tough Bug
Believed to be aided largely by the use of broad-spectrum antibiotics that knock out the colon’s natural flora, C. diff in the hospital—as well as nursing homes and acute-care facilities—has raged for much of the past decade. Its rise is tied to the emergence of a new hypervirulent strain known as BI/NAP1/027, or NAP1 for short. The strain is highly resistant to fluoroquinolones, such as ciprofloxacin and levofloxacin, which are used often in healthcare settings.
“A fluoroquinolone will wipe out a lot of your normal flora in your gut,” Dr. Gould says. “But it won’t wipe out C. diff, in particular this hypervirulent strain. And so this strain can flourish in the presence of fluoroquinolones.” The strain produces up to 15 to 20 times more toxins than other C. diff strains, according to some data, she adds.
Vancomycin (Vanconin) and metronidazole (Flagyl) are the most common antibiotics used to treat patients infected with C. diff. Mortality rates are higher among the elderly, largely because of their weaker immune system, Dr. Gould says. Studies have generally shown mortality rates of 10% or a bit lower.1
More recent studies have shown that the number of hospital-related C. diff cases might have begun to level off in 2008 and 2009. Dr. Gould says she thinks the leveling off is for real, but there is debate over what the immediate future holds.
“There’s a lot of work and initiatives, especially state-based initiatives, that are being done in hospitals. And there’s reason to believe they’re effective,” she says, adding it’s harder to get a good picture of the problem in long-term care facilities and in the community.
Dr. Cohen with the IDSA says it’s too soon to say whether the problem is hitting a plateau. “CDC data are always a couple of years behind,” he says. “Until you see another data point, you can’t tell whether that’s just a transient flattening and whether it’s going to keep going up or not.”
Kevin Kavanagh, MD, founder of the patient advocacy group Health Watch USA and a retired otolaryngologist in Kentucky who has taken a keen interest in the C. diff problem, says he doesn’t think the end of the tunnel is within view yet.
“I think C. diff is going to get worse before it gets better,” Dr. Kavanagh says. “And that’s not necessarily because the healthcare profession isn’t doing due diligence. This is a tough organism.—it can be tough to treat and can be very tough to kill.”
The Best Defense?
Because C. diff lives within protective spores, sound hand hygiene practices and room-cleaning practices are essential for keeping infections to a minimum. Alcohol-based hand sanitizers, effective against other organisms including MRSA, do not kill C. diff. The bacteria must be mechanically removed through hand washing.
And even hand washing might not be totally effective at getting rid of the spores, which means it’s important for healthcare workers to gown and glove in high-risk rooms.
Sodium hypochlorite solutions, or bleach mixtures, have to be used to clean rooms occupied by patients with C. diff, and the prevailing thought is to clean the rooms of patients suspected of having C. diff, even if those cases might not be confirmed.
Equally important to cleaning and hand washing is systemwide emphasis on antibiotic stewardship. A 2011 study at the State University of New York Buffalo found that the risk of a C. diff infection rose with the number of antibiotics taken.2

—Carolyn Gould, MD, medical epidemiologist, division of healthcare quality promotion, Centers of Disease Control and Prevention, Atlanta
While a broad-spectrum antibiotic might be necessary at first, once the results of cultures are received, the treatment should be finely tailored to kill only the problem bacteria so that the body’s natural defenses aren’t broken down, Dr. Gould explains.
“If someone is very sick and you’re not sure what is going on, it’s very reasonable to treat them empirically with broad-spectrum antibiotics,” she says. “The important thing is that you send the appropriate cultures before so that you know what you’re treating and you can optimize those antibiotics with daily assessments.”
It’s clear why an overreliance on broad-spectrum drugs prevails in U.S. health settings, Dr. Cohen acknowledges. Recent literature suggests treating critically ill patients with wide-ranging antimicrobials as the mortality rate can be twice as high with narrower options. “I think people have gotten very quick to give broad-spectrum therapy,” he says.
continued below...
National Response, Localized Attention
Dr. Kavanagh of Health Watch USA says that more information about C. diff is needed, particularly publicly available numbers of infections at hospitals. Some states require those figures to be reported, but most don’t. And there is no current federal mandate on reporting of C. diff cases, although acute-care hospitals will be required to report C. diff infection rates starting in 2013.
“We really have scant data,” he says. “There is not a lot of reporting if you look at the nation on a whole. And I think that underscores one of the reasons why you need to have data for action. You need to have reporting of these organisms to the National Healthcare Safety Network so that the CDC can monitor and can make plans and can do effective interventions.
“You want to know where the areas of highest infection are,” he adds. “You want to know what interventions work and don’t work. If you don’t have a national coordinated reporting system, it really makes it difficult to address the problem. C. diff is going to be much harder to control than MRSA or other bacteria because it changes into a hard-to-kill dormant spore stage and then re-occurs at some point.”
The Centers for Medicare & Medicaid Services (CMS) has proposed adding C. diff infections to the list of hospital-acquired conditions that will not be reimbursable. It is widely hoped that such a measure will go a long way toward stamping out the problem.
Dr. Kobaidze of Emory notes that C. diff is a dynamic problem, always adapting and posing new challenges. And hospitalists should be more involved in answering these questions through research. One recent question, she points out, is whether proton pump inhibitor use is related to the rise of C. diff.
Ultimately, though, controlling C. diff in hospitals might come down to what is done day to day inside the hospital. And hospitalists can play a big role.
Danielle Scheurer, MD, MSCR, SFHM, a hospitalist and medical director of quality at the Medical University of South Carolina in Charleston, says that a full-time pharmacist on the hospital’s antimicrobial stewardship committee is always reviewing antibiotic prescriptions and is prepared to flag cases in which a broad-spectrum is used when one with a more narrow scope might be more appropriate.
The hospital has done its best, as part of its “renovation cycle,” to standardize the layouts of rooms “so that the second you open the door you know exactly where the alcohol gel is and where the soap and the sink is going to be.” The idea is to make compliance as “mindless” as possible. Such efforts can be hampered by structural limitations though, she says.
HM group leaders, she suggests, can play an important part simply by being good role models—gowning and gloving without complaint before entering high-risk rooms and reinforcing the message that such efforts have real effects on patient safety.
But she also acknowledges that “it always sounds easy....There has to be some level of redundancy built into the hospital system. This is more of a system thing than the individual hospitalist.”
One level of redundancy at MUSC that has been particularly effective, she says, are “secret shoppers” who keep an eye out for medical teams that might not be washing their hands as they go in and out of high-risk rooms. Each unit is responsible for their hand hygiene numbers—which include both self-reported figures and those obtained by the secret onlookers—and those numbers are made available to the hospital.
Those units with the best numbers are sometimes given a reward, such as a pizza party, but it’s colleagues’ knowledge of the numbers that matters most, she says.
“That, in and of itself, is a powerful motivator,” Dr. Scheurer says. “We bring it to all of our quality operations meetings, all the administrators, the CEO, the CMO. It’s very motivating for every unit. They don’t want to be the trailing unit.”
Tom Collins is a freelance medical writer based in Miami.
References
- Orenstein R, Aronhalt KC, McManus JE Jr., Fedraw LA. A targeted strategy to wipe out Clostridium difficile. Infect Control Hosp Epidemiol. 2011;32(11):1137-1139.
- Stevens V, Dumyati G, Fine LS, Fisher SG, van Wijngaarden E. Cumulative antibiotic exposures over time and the risk of Clostridium difficile infection. Clin Infect Dis. 2011;53(1):42-48.
At 480-bed Emory University Hospital Midtown in Atlanta, the physicians and staff seemingly are doing all the right things to foil one of hospital’s archenemies: Clostridium difficile. The bacteria, better known as C. diff, is responsible for a sharp rise in hospital-acquired infections over the past decade, rivaling even MRSA.
In 2010, Emory Midtown launched a campaign to boost awareness of the importance of hand washing before and after treating patients infected with C. diff and those likely to be infected. They also began using the polymerase-chain-reaction-based assay to detect the bacteria, a test with much higher sensitivity that helps to more efficiently identify those infected so control measures can be more prompt and targeted. They use a hypochlorite mixture to clean the rooms of those infected, which is considered a must. And a committee monitors the use of antibiotics to prevent overuse—often the scapegoat for the rise of the hard-to-kill bacteria.
Still, at Emory, the rate of C. diff is about the same as the national average, says hospitalist Ketino Kobaidze, MD, assistant professor at the Emory University School of Medicine and a member of the antimicrobial stewardship and infectious disease control committees at Midtown. While Dr. Kobaidze says her institution is doing a good job of trying to keep C. diff under control, she thinks hospitalists can do more.
“My feeling is that we are not as involved as we’re supposed to be,” she says. “I think we need to be a little bit more proactive, be involved in committees and research activities across the hospital.”
—Kevin Kavanagh, MD, founder, Health Watch USA
You Are Not Alone
The experience at Emory Midtown is far from unusual—healthcare facilities, and hospitalists, across the country have seen healthcare-related C. diff cases more than double since 2001 to between 400,000 and 500,000 a year, says Carolyn Gould, MD, a medical epidemiologist in the division of healthcare quality promotion at the Centers for Disease Control and Prevention (CDC) in Atlanta.
Hospitalists, whether they realize it or not, are intimately involved in how well the C. diff outbreak is controlled. Infectious-disease (ID) specialists say hospitalists are perfectly situated to make an impact in efforts to help curb the outbreak.
“Hospitalists are critical to this effort,” Dr. Gould says. “They’re in the hospital day in and day out, and they’re constantly interacting with the patients, staff, and administration. They’re often the first on the scene to see a patient who might have suddenly developed diarrhea; they’re the first to react. I think they’re in a prime position to play a leadership role to prevent C. diff infections.”
They’re also situated well to work with infection-control experts on antimicrobial stewardship programs, she says.
“I look at hospitalists just like I would have looked at internists managing their own patients 15 years ago,” says Stuart Cohen, MD, an ID expert with the University of California at Davis and a fellow with the Infectious Diseases Society of America who was lead author of the latest published IDSA guidelines on C. diff treatment. “And so they’re the first-line people.”
continued below...
A Tough Bug
Believed to be aided largely by the use of broad-spectrum antibiotics that knock out the colon’s natural flora, C. diff in the hospital—as well as nursing homes and acute-care facilities—has raged for much of the past decade. Its rise is tied to the emergence of a new hypervirulent strain known as BI/NAP1/027, or NAP1 for short. The strain is highly resistant to fluoroquinolones, such as ciprofloxacin and levofloxacin, which are used often in healthcare settings.
“A fluoroquinolone will wipe out a lot of your normal flora in your gut,” Dr. Gould says. “But it won’t wipe out C. diff, in particular this hypervirulent strain. And so this strain can flourish in the presence of fluoroquinolones.” The strain produces up to 15 to 20 times more toxins than other C. diff strains, according to some data, she adds.
Vancomycin (Vanconin) and metronidazole (Flagyl) are the most common antibiotics used to treat patients infected with C. diff. Mortality rates are higher among the elderly, largely because of their weaker immune system, Dr. Gould says. Studies have generally shown mortality rates of 10% or a bit lower.1
More recent studies have shown that the number of hospital-related C. diff cases might have begun to level off in 2008 and 2009. Dr. Gould says she thinks the leveling off is for real, but there is debate over what the immediate future holds.
“There’s a lot of work and initiatives, especially state-based initiatives, that are being done in hospitals. And there’s reason to believe they’re effective,” she says, adding it’s harder to get a good picture of the problem in long-term care facilities and in the community.
Dr. Cohen with the IDSA says it’s too soon to say whether the problem is hitting a plateau. “CDC data are always a couple of years behind,” he says. “Until you see another data point, you can’t tell whether that’s just a transient flattening and whether it’s going to keep going up or not.”
Kevin Kavanagh, MD, founder of the patient advocacy group Health Watch USA and a retired otolaryngologist in Kentucky who has taken a keen interest in the C. diff problem, says he doesn’t think the end of the tunnel is within view yet.
“I think C. diff is going to get worse before it gets better,” Dr. Kavanagh says. “And that’s not necessarily because the healthcare profession isn’t doing due diligence. This is a tough organism.—it can be tough to treat and can be very tough to kill.”
The Best Defense?
Because C. diff lives within protective spores, sound hand hygiene practices and room-cleaning practices are essential for keeping infections to a minimum. Alcohol-based hand sanitizers, effective against other organisms including MRSA, do not kill C. diff. The bacteria must be mechanically removed through hand washing.
And even hand washing might not be totally effective at getting rid of the spores, which means it’s important for healthcare workers to gown and glove in high-risk rooms.
Sodium hypochlorite solutions, or bleach mixtures, have to be used to clean rooms occupied by patients with C. diff, and the prevailing thought is to clean the rooms of patients suspected of having C. diff, even if those cases might not be confirmed.
Equally important to cleaning and hand washing is systemwide emphasis on antibiotic stewardship. A 2011 study at the State University of New York Buffalo found that the risk of a C. diff infection rose with the number of antibiotics taken.2

—Carolyn Gould, MD, medical epidemiologist, division of healthcare quality promotion, Centers of Disease Control and Prevention, Atlanta
While a broad-spectrum antibiotic might be necessary at first, once the results of cultures are received, the treatment should be finely tailored to kill only the problem bacteria so that the body’s natural defenses aren’t broken down, Dr. Gould explains.
“If someone is very sick and you’re not sure what is going on, it’s very reasonable to treat them empirically with broad-spectrum antibiotics,” she says. “The important thing is that you send the appropriate cultures before so that you know what you’re treating and you can optimize those antibiotics with daily assessments.”
It’s clear why an overreliance on broad-spectrum drugs prevails in U.S. health settings, Dr. Cohen acknowledges. Recent literature suggests treating critically ill patients with wide-ranging antimicrobials as the mortality rate can be twice as high with narrower options. “I think people have gotten very quick to give broad-spectrum therapy,” he says.
continued below...
National Response, Localized Attention
Dr. Kavanagh of Health Watch USA says that more information about C. diff is needed, particularly publicly available numbers of infections at hospitals. Some states require those figures to be reported, but most don’t. And there is no current federal mandate on reporting of C. diff cases, although acute-care hospitals will be required to report C. diff infection rates starting in 2013.
“We really have scant data,” he says. “There is not a lot of reporting if you look at the nation on a whole. And I think that underscores one of the reasons why you need to have data for action. You need to have reporting of these organisms to the National Healthcare Safety Network so that the CDC can monitor and can make plans and can do effective interventions.
“You want to know where the areas of highest infection are,” he adds. “You want to know what interventions work and don’t work. If you don’t have a national coordinated reporting system, it really makes it difficult to address the problem. C. diff is going to be much harder to control than MRSA or other bacteria because it changes into a hard-to-kill dormant spore stage and then re-occurs at some point.”
The Centers for Medicare & Medicaid Services (CMS) has proposed adding C. diff infections to the list of hospital-acquired conditions that will not be reimbursable. It is widely hoped that such a measure will go a long way toward stamping out the problem.
Dr. Kobaidze of Emory notes that C. diff is a dynamic problem, always adapting and posing new challenges. And hospitalists should be more involved in answering these questions through research. One recent question, she points out, is whether proton pump inhibitor use is related to the rise of C. diff.
Ultimately, though, controlling C. diff in hospitals might come down to what is done day to day inside the hospital. And hospitalists can play a big role.
Danielle Scheurer, MD, MSCR, SFHM, a hospitalist and medical director of quality at the Medical University of South Carolina in Charleston, says that a full-time pharmacist on the hospital’s antimicrobial stewardship committee is always reviewing antibiotic prescriptions and is prepared to flag cases in which a broad-spectrum is used when one with a more narrow scope might be more appropriate.
The hospital has done its best, as part of its “renovation cycle,” to standardize the layouts of rooms “so that the second you open the door you know exactly where the alcohol gel is and where the soap and the sink is going to be.” The idea is to make compliance as “mindless” as possible. Such efforts can be hampered by structural limitations though, she says.
HM group leaders, she suggests, can play an important part simply by being good role models—gowning and gloving without complaint before entering high-risk rooms and reinforcing the message that such efforts have real effects on patient safety.
But she also acknowledges that “it always sounds easy....There has to be some level of redundancy built into the hospital system. This is more of a system thing than the individual hospitalist.”
One level of redundancy at MUSC that has been particularly effective, she says, are “secret shoppers” who keep an eye out for medical teams that might not be washing their hands as they go in and out of high-risk rooms. Each unit is responsible for their hand hygiene numbers—which include both self-reported figures and those obtained by the secret onlookers—and those numbers are made available to the hospital.
Those units with the best numbers are sometimes given a reward, such as a pizza party, but it’s colleagues’ knowledge of the numbers that matters most, she says.
“That, in and of itself, is a powerful motivator,” Dr. Scheurer says. “We bring it to all of our quality operations meetings, all the administrators, the CEO, the CMO. It’s very motivating for every unit. They don’t want to be the trailing unit.”
Tom Collins is a freelance medical writer based in Miami.
References
- Orenstein R, Aronhalt KC, McManus JE Jr., Fedraw LA. A targeted strategy to wipe out Clostridium difficile. Infect Control Hosp Epidemiol. 2011;32(11):1137-1139.
- Stevens V, Dumyati G, Fine LS, Fisher SG, van Wijngaarden E. Cumulative antibiotic exposures over time and the risk of Clostridium difficile infection. Clin Infect Dis. 2011;53(1):42-48.
Business Drivers
MIAMI BEACH, Fla.—Muralidharan Reddy, MD, had just finished a five-hour class on the business concepts behind running a hospital and how a hospital CEO thinks—part of the entry-level curriculum at SHM’s Leadership Academy. As he stood up from the round table in a room still buzzing with conversation, he was glad he had signed up—in fact, he had been one of the first to arrive for the 7:30 a.m. session at the Fontainebleau resort.
“It improves my CV, number one,” says Dr. Reddy, a hospitalist at New England Baptist Hospital in Boston. “And it’s not just the CV, but I need the experience to guide me to work as a leader in a hospital group, or even plan on starting a group, or things like that. If I’m going to be a hospitalist, I have to work on trying to get those skills.”
A big plus, he adds, is “you get to learn from experts.”
The four-day academy provides hospitalists an intense learning experience. “Some of these skills, people learn it on the job or you get it through Academy,” Dr. Reddy says. “So I do both.”
Hospitalists who participate in the session repeatedly express concerns that if they don’t hone their understanding of the business aspects of the hospital and refine their skills in interacting with colleagues, they could be left behind in a fast-moving environment.
“I think it’s important,” said Mana Goshtasbi, MD, a hospitalist with Cogent HMG who has worked for two years at St. Joseph’s Hospital in Tampa, Fla. “I think that’s the direction. I think you have to know this stuff because of all the changes.”
Leadership Academy courses come in three levels, which build on one another: Foundations for Effective Leadership, Personal Leadership Excellence, and Strengthening Your Organization. Those who have completed the three levels can apply for certification, which requires completion of a pre-approved leadership project.
Know Your Value, Know Your Customers
In his first-level session, instructor Michael Guthrie, MD, MBA, executive in residence and adjunct professor at the University of Colorado Denver School of Business’ program in health administration, spent most of his presentation on his feet, wending his way among the tables, challenging the physician-students to think differently from the ways they’ve been trained to think about healthcare. That starts with stepping outside of themselves and taking a look at how they are viewed in terms of the hospital they’re working with as hospitalists, says Dr. Guthrie, former CEO of the Good Samaritan Health System in San Jose, Calif., and former COO for the Penrose-St. Francis Healthcare System in Colorado.
“What’s affecting the organization that you operate in, and what does that mean about the kinds of demands that are being made of you and requests that are being made of you?” he asks the attendees. “What does it mean about the value that’s received from the work that you do in that organization?”
A hospitalists’ value is a common theme. “What is it that you offer as hospitalists that has created a group of enthusiasts?” he asks. “What is it that you offer to any customer that’s of value to them that they would give up their hard-earned money in exchange for it? Who are your customers?”
A key “customer” group is primary-care physicians (PCPs) whose patients end up under a hospitalist’s care, he explains. They get value from the hospitalist in a variety of ways.
“That’s a more effective way for them to spend their life [at their own clinic],” he says. “They get to manage their schedule differently, they don’t have to drive. They are all exchange values. … There’s a very definite exchange going on here. If you fail in that exchange, we all know what would happen, right? They’d stop sending you patients.”
A physician chimes in: “If you’re the only hospitalist there, they don’t have a choice.”
Dr. Guthrie, quick to seize upon what he sees as a teaching moment, tells the group to “be careful.”
“In the short term, that’s absolutely true,” he says. “In the long term, there are a lot of other alternatives. And if there aren’t, someone will invent one. You see that’s the thing about our society—if there’s an opportunity with a whole, big, dissatisfied customer segment, somebody will notice and invent the way to satisfy their needs. That’s called capitalism.”
It’s what happened with the late Steve Jobs and the iPod, when he realized customers needed a way to easily access their music collections, Dr. Guthrie points out.
“He understood the dissatisfactions of the market,” he continues. “Before that, they didn’t have any choices.
“Healthcare is the same. But it’s a little more difficult to develop those choices. It’s hard to build a new hospital right in the middle of someplace where there’s only one hospital. So they invent other ways to do it, ways to get their patients taken care of: They travel.”
About 700,000 people flew to Southeast Asia last year for medical procedures, he says, making the point that American patients have options.
“Somewhat difficult, but they do have alternatives,” he says. “Customers will, when pushed hard enough, if dissatisfied enough, leave you, even when you think you have them trapped.”
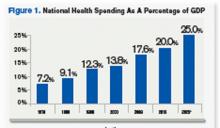
Source: Hartman, M: Martin, A; McDonnell, P et al. (2009). National Helath Spending In 2007: Slower Drug Spending Contributes To Lowest Rate Of Overall Growth Since 1998. Health Affairs, Jan/Feb., p 247. www.healthaffairs.org). See also, Orzag, Peter; Congressional Budget Office (2008). Growth in Health Care Costs, testimony before the Sentae Budget Committee, Jan. 31, p.1. (www.cbo.gov/doc.cfm?index-8948). Center for Medicare & Medicaid Services, January 2011.
Think Tanks
A key part of the session is time set aside for group work, in which Dr. Guthrie gives the class an assignment and attendees tackle it at their tables as a unit. The first task is to identify business drivers at hospitals, what the objectives of the hospital should be in response to those things, and how those objectives affect the work of hospitalists.
Then the groups go to work. A few minutes later, though, Dr. Guthrie speaks up through the chatter.
“Let’s stop for a minute. I want to tell you that most of you are on completely the wrong track,” he says, drawing chuckles. “But this is part of the reason we do it this way. The idea here is to get outside of your head.”
One group lists “profit” as a business driver.
“Profit is not a business driver,” he says. “I know you’re sort of raised to think that way. It isn’t. It’s a measurement. It’s like blood pressure. So it is not a business driver. We use it as a measurement of the success with which we’re synthesizing the business drivers and the environment and meeting the objectives of those drivers, or those trends.”
Business drivers are more along the lines of government mandates and an aging population, which some of the groups had mentioned. “That’s the level of abstraction I want you get to,” he says. “Think out in the marketplace.”
When it comes down to it, Dr. Guthrie explains, the hospitalist plays a role in just about every measurement used to determine excellence at a hospital—from quality to customer loyalty, from retention of patients to productivity.
He also emphasizes the difference between how a doctor has been trained essentially to be an individual expert—patient presents a problem, doctor presents a solution—and how those trained to be managers and leaders operate through other people.
Leaders of the Future
Daniel Duzan, MD, a hospitalist for TeamHealth at Fort Loudoun Medical Center in Lenoir City, Tenn., southwest of Knoxville, says doctors he knows recommended the academy. He says it made sense to him because he’s “migrating toward a leadership role in my own hospital.”
“My goal for coming was to kind of lay some foundation for skills and requirements that it takes to kind of migrate from just being a regular hospitalist to being one that’s got some extra responsibility,” Dr. Duzan says.
He was happy to learn more about “some of the jargon, lingo, that’s getting pushed our direction in terms of business drivers and the objectives” as well as “what would it be like to be the CEO, etc., and kind of putting us in their shoes, hearing things, seeing things and how they think about things, then developing plans.”
Jeet Gujral, MD, a hospitalist at Southside Hospital on Long Island, N.Y., says her motivation to learn about practice management is due in part to the new demands she is feeling because of the business considerations of the hospital. Talking with other hospitalists about their experiences was a big help, she says. In fact, she adds, that was probably even more helpful than the actual content of the session.
“I think what I’m getting more out of it [is that] there are several who are feeling the same heat,” she says. “It’s nice not feeling alone.”
Tom Collins is a freelance writer based in Florida.
MIAMI BEACH, Fla.—Muralidharan Reddy, MD, had just finished a five-hour class on the business concepts behind running a hospital and how a hospital CEO thinks—part of the entry-level curriculum at SHM’s Leadership Academy. As he stood up from the round table in a room still buzzing with conversation, he was glad he had signed up—in fact, he had been one of the first to arrive for the 7:30 a.m. session at the Fontainebleau resort.
“It improves my CV, number one,” says Dr. Reddy, a hospitalist at New England Baptist Hospital in Boston. “And it’s not just the CV, but I need the experience to guide me to work as a leader in a hospital group, or even plan on starting a group, or things like that. If I’m going to be a hospitalist, I have to work on trying to get those skills.”
A big plus, he adds, is “you get to learn from experts.”
The four-day academy provides hospitalists an intense learning experience. “Some of these skills, people learn it on the job or you get it through Academy,” Dr. Reddy says. “So I do both.”
Hospitalists who participate in the session repeatedly express concerns that if they don’t hone their understanding of the business aspects of the hospital and refine their skills in interacting with colleagues, they could be left behind in a fast-moving environment.
“I think it’s important,” said Mana Goshtasbi, MD, a hospitalist with Cogent HMG who has worked for two years at St. Joseph’s Hospital in Tampa, Fla. “I think that’s the direction. I think you have to know this stuff because of all the changes.”
Leadership Academy courses come in three levels, which build on one another: Foundations for Effective Leadership, Personal Leadership Excellence, and Strengthening Your Organization. Those who have completed the three levels can apply for certification, which requires completion of a pre-approved leadership project.
Know Your Value, Know Your Customers
In his first-level session, instructor Michael Guthrie, MD, MBA, executive in residence and adjunct professor at the University of Colorado Denver School of Business’ program in health administration, spent most of his presentation on his feet, wending his way among the tables, challenging the physician-students to think differently from the ways they’ve been trained to think about healthcare. That starts with stepping outside of themselves and taking a look at how they are viewed in terms of the hospital they’re working with as hospitalists, says Dr. Guthrie, former CEO of the Good Samaritan Health System in San Jose, Calif., and former COO for the Penrose-St. Francis Healthcare System in Colorado.
“What’s affecting the organization that you operate in, and what does that mean about the kinds of demands that are being made of you and requests that are being made of you?” he asks the attendees. “What does it mean about the value that’s received from the work that you do in that organization?”
A hospitalists’ value is a common theme. “What is it that you offer as hospitalists that has created a group of enthusiasts?” he asks. “What is it that you offer to any customer that’s of value to them that they would give up their hard-earned money in exchange for it? Who are your customers?”
A key “customer” group is primary-care physicians (PCPs) whose patients end up under a hospitalist’s care, he explains. They get value from the hospitalist in a variety of ways.
“That’s a more effective way for them to spend their life [at their own clinic],” he says. “They get to manage their schedule differently, they don’t have to drive. They are all exchange values. … There’s a very definite exchange going on here. If you fail in that exchange, we all know what would happen, right? They’d stop sending you patients.”
A physician chimes in: “If you’re the only hospitalist there, they don’t have a choice.”
Dr. Guthrie, quick to seize upon what he sees as a teaching moment, tells the group to “be careful.”
“In the short term, that’s absolutely true,” he says. “In the long term, there are a lot of other alternatives. And if there aren’t, someone will invent one. You see that’s the thing about our society—if there’s an opportunity with a whole, big, dissatisfied customer segment, somebody will notice and invent the way to satisfy their needs. That’s called capitalism.”
It’s what happened with the late Steve Jobs and the iPod, when he realized customers needed a way to easily access their music collections, Dr. Guthrie points out.
“He understood the dissatisfactions of the market,” he continues. “Before that, they didn’t have any choices.
“Healthcare is the same. But it’s a little more difficult to develop those choices. It’s hard to build a new hospital right in the middle of someplace where there’s only one hospital. So they invent other ways to do it, ways to get their patients taken care of: They travel.”
About 700,000 people flew to Southeast Asia last year for medical procedures, he says, making the point that American patients have options.
“Somewhat difficult, but they do have alternatives,” he says. “Customers will, when pushed hard enough, if dissatisfied enough, leave you, even when you think you have them trapped.”
Source: Hartman, M: Martin, A; McDonnell, P et al. (2009). National Helath Spending In 2007: Slower Drug Spending Contributes To Lowest Rate Of Overall Growth Since 1998. Health Affairs, Jan/Feb., p 247. www.healthaffairs.org). See also, Orzag, Peter; Congressional Budget Office (2008). Growth in Health Care Costs, testimony before the Sentae Budget Committee, Jan. 31, p.1. (www.cbo.gov/doc.cfm?index-8948). Center for Medicare & Medicaid Services, January 2011.
Think Tanks
A key part of the session is time set aside for group work, in which Dr. Guthrie gives the class an assignment and attendees tackle it at their tables as a unit. The first task is to identify business drivers at hospitals, what the objectives of the hospital should be in response to those things, and how those objectives affect the work of hospitalists.
Then the groups go to work. A few minutes later, though, Dr. Guthrie speaks up through the chatter.
“Let’s stop for a minute. I want to tell you that most of you are on completely the wrong track,” he says, drawing chuckles. “But this is part of the reason we do it this way. The idea here is to get outside of your head.”
One group lists “profit” as a business driver.
“Profit is not a business driver,” he says. “I know you’re sort of raised to think that way. It isn’t. It’s a measurement. It’s like blood pressure. So it is not a business driver. We use it as a measurement of the success with which we’re synthesizing the business drivers and the environment and meeting the objectives of those drivers, or those trends.”
Business drivers are more along the lines of government mandates and an aging population, which some of the groups had mentioned. “That’s the level of abstraction I want you get to,” he says. “Think out in the marketplace.”
When it comes down to it, Dr. Guthrie explains, the hospitalist plays a role in just about every measurement used to determine excellence at a hospital—from quality to customer loyalty, from retention of patients to productivity.
He also emphasizes the difference between how a doctor has been trained essentially to be an individual expert—patient presents a problem, doctor presents a solution—and how those trained to be managers and leaders operate through other people.
Leaders of the Future
Daniel Duzan, MD, a hospitalist for TeamHealth at Fort Loudoun Medical Center in Lenoir City, Tenn., southwest of Knoxville, says doctors he knows recommended the academy. He says it made sense to him because he’s “migrating toward a leadership role in my own hospital.”
“My goal for coming was to kind of lay some foundation for skills and requirements that it takes to kind of migrate from just being a regular hospitalist to being one that’s got some extra responsibility,” Dr. Duzan says.
He was happy to learn more about “some of the jargon, lingo, that’s getting pushed our direction in terms of business drivers and the objectives” as well as “what would it be like to be the CEO, etc., and kind of putting us in their shoes, hearing things, seeing things and how they think about things, then developing plans.”
Jeet Gujral, MD, a hospitalist at Southside Hospital on Long Island, N.Y., says her motivation to learn about practice management is due in part to the new demands she is feeling because of the business considerations of the hospital. Talking with other hospitalists about their experiences was a big help, she says. In fact, she adds, that was probably even more helpful than the actual content of the session.
“I think what I’m getting more out of it [is that] there are several who are feeling the same heat,” she says. “It’s nice not feeling alone.”
Tom Collins is a freelance writer based in Florida.
MIAMI BEACH, Fla.—Muralidharan Reddy, MD, had just finished a five-hour class on the business concepts behind running a hospital and how a hospital CEO thinks—part of the entry-level curriculum at SHM’s Leadership Academy. As he stood up from the round table in a room still buzzing with conversation, he was glad he had signed up—in fact, he had been one of the first to arrive for the 7:30 a.m. session at the Fontainebleau resort.
“It improves my CV, number one,” says Dr. Reddy, a hospitalist at New England Baptist Hospital in Boston. “And it’s not just the CV, but I need the experience to guide me to work as a leader in a hospital group, or even plan on starting a group, or things like that. If I’m going to be a hospitalist, I have to work on trying to get those skills.”
A big plus, he adds, is “you get to learn from experts.”
The four-day academy provides hospitalists an intense learning experience. “Some of these skills, people learn it on the job or you get it through Academy,” Dr. Reddy says. “So I do both.”
Hospitalists who participate in the session repeatedly express concerns that if they don’t hone their understanding of the business aspects of the hospital and refine their skills in interacting with colleagues, they could be left behind in a fast-moving environment.
“I think it’s important,” said Mana Goshtasbi, MD, a hospitalist with Cogent HMG who has worked for two years at St. Joseph’s Hospital in Tampa, Fla. “I think that’s the direction. I think you have to know this stuff because of all the changes.”
Leadership Academy courses come in three levels, which build on one another: Foundations for Effective Leadership, Personal Leadership Excellence, and Strengthening Your Organization. Those who have completed the three levels can apply for certification, which requires completion of a pre-approved leadership project.
Know Your Value, Know Your Customers
In his first-level session, instructor Michael Guthrie, MD, MBA, executive in residence and adjunct professor at the University of Colorado Denver School of Business’ program in health administration, spent most of his presentation on his feet, wending his way among the tables, challenging the physician-students to think differently from the ways they’ve been trained to think about healthcare. That starts with stepping outside of themselves and taking a look at how they are viewed in terms of the hospital they’re working with as hospitalists, says Dr. Guthrie, former CEO of the Good Samaritan Health System in San Jose, Calif., and former COO for the Penrose-St. Francis Healthcare System in Colorado.
“What’s affecting the organization that you operate in, and what does that mean about the kinds of demands that are being made of you and requests that are being made of you?” he asks the attendees. “What does it mean about the value that’s received from the work that you do in that organization?”
A hospitalists’ value is a common theme. “What is it that you offer as hospitalists that has created a group of enthusiasts?” he asks. “What is it that you offer to any customer that’s of value to them that they would give up their hard-earned money in exchange for it? Who are your customers?”
A key “customer” group is primary-care physicians (PCPs) whose patients end up under a hospitalist’s care, he explains. They get value from the hospitalist in a variety of ways.
“That’s a more effective way for them to spend their life [at their own clinic],” he says. “They get to manage their schedule differently, they don’t have to drive. They are all exchange values. … There’s a very definite exchange going on here. If you fail in that exchange, we all know what would happen, right? They’d stop sending you patients.”
A physician chimes in: “If you’re the only hospitalist there, they don’t have a choice.”
Dr. Guthrie, quick to seize upon what he sees as a teaching moment, tells the group to “be careful.”
“In the short term, that’s absolutely true,” he says. “In the long term, there are a lot of other alternatives. And if there aren’t, someone will invent one. You see that’s the thing about our society—if there’s an opportunity with a whole, big, dissatisfied customer segment, somebody will notice and invent the way to satisfy their needs. That’s called capitalism.”
It’s what happened with the late Steve Jobs and the iPod, when he realized customers needed a way to easily access their music collections, Dr. Guthrie points out.
“He understood the dissatisfactions of the market,” he continues. “Before that, they didn’t have any choices.
“Healthcare is the same. But it’s a little more difficult to develop those choices. It’s hard to build a new hospital right in the middle of someplace where there’s only one hospital. So they invent other ways to do it, ways to get their patients taken care of: They travel.”
About 700,000 people flew to Southeast Asia last year for medical procedures, he says, making the point that American patients have options.
“Somewhat difficult, but they do have alternatives,” he says. “Customers will, when pushed hard enough, if dissatisfied enough, leave you, even when you think you have them trapped.”
Source: Hartman, M: Martin, A; McDonnell, P et al. (2009). National Helath Spending In 2007: Slower Drug Spending Contributes To Lowest Rate Of Overall Growth Since 1998. Health Affairs, Jan/Feb., p 247. www.healthaffairs.org). See also, Orzag, Peter; Congressional Budget Office (2008). Growth in Health Care Costs, testimony before the Sentae Budget Committee, Jan. 31, p.1. (www.cbo.gov/doc.cfm?index-8948). Center for Medicare & Medicaid Services, January 2011.
Think Tanks
A key part of the session is time set aside for group work, in which Dr. Guthrie gives the class an assignment and attendees tackle it at their tables as a unit. The first task is to identify business drivers at hospitals, what the objectives of the hospital should be in response to those things, and how those objectives affect the work of hospitalists.
Then the groups go to work. A few minutes later, though, Dr. Guthrie speaks up through the chatter.
“Let’s stop for a minute. I want to tell you that most of you are on completely the wrong track,” he says, drawing chuckles. “But this is part of the reason we do it this way. The idea here is to get outside of your head.”
One group lists “profit” as a business driver.
“Profit is not a business driver,” he says. “I know you’re sort of raised to think that way. It isn’t. It’s a measurement. It’s like blood pressure. So it is not a business driver. We use it as a measurement of the success with which we’re synthesizing the business drivers and the environment and meeting the objectives of those drivers, or those trends.”
Business drivers are more along the lines of government mandates and an aging population, which some of the groups had mentioned. “That’s the level of abstraction I want you get to,” he says. “Think out in the marketplace.”
When it comes down to it, Dr. Guthrie explains, the hospitalist plays a role in just about every measurement used to determine excellence at a hospital—from quality to customer loyalty, from retention of patients to productivity.
He also emphasizes the difference between how a doctor has been trained essentially to be an individual expert—patient presents a problem, doctor presents a solution—and how those trained to be managers and leaders operate through other people.
Leaders of the Future
Daniel Duzan, MD, a hospitalist for TeamHealth at Fort Loudoun Medical Center in Lenoir City, Tenn., southwest of Knoxville, says doctors he knows recommended the academy. He says it made sense to him because he’s “migrating toward a leadership role in my own hospital.”
“My goal for coming was to kind of lay some foundation for skills and requirements that it takes to kind of migrate from just being a regular hospitalist to being one that’s got some extra responsibility,” Dr. Duzan says.
He was happy to learn more about “some of the jargon, lingo, that’s getting pushed our direction in terms of business drivers and the objectives” as well as “what would it be like to be the CEO, etc., and kind of putting us in their shoes, hearing things, seeing things and how they think about things, then developing plans.”
Jeet Gujral, MD, a hospitalist at Southside Hospital on Long Island, N.Y., says her motivation to learn about practice management is due in part to the new demands she is feeling because of the business considerations of the hospital. Talking with other hospitalists about their experiences was a big help, she says. In fact, she adds, that was probably even more helpful than the actual content of the session.
“I think what I’m getting more out of it [is that] there are several who are feeling the same heat,” she says. “It’s nice not feeling alone.”
Tom Collins is a freelance writer based in Florida.
Help Wanted
SHM’s Leadership Academies have been well received, with at least 1,200 having taken the courses so far. Some of those participants, though, craved something more—some recognition for the ways those lessons are being incorporated on the job in their hospitals.
So this year, for the first time, SHM is offering something beyond the third level of the Leadership Academies. Those who have completed all three levels in the academy can now seek Leadership Certification, based mainly on completion of a project to make a positive change at their hospitals.
Rusty Holman, MD, MHM, director of the academy program and chief clinical officer at Cogent HMG, says the impetus came from past participants.
“Those who have attended the Leadership Academies came forward and said, ‘You know, we’re doing some really important coursework, we’re investing in ourselves in both our knowledge and our skills as leaders. We are furthermore involved in a lot of change efforts within the hospital and improvement efforts—whether it’s related to quality or it’s related to some business function or it’s related to education and training. And wrapping all that together, wouldn’t it be nice if we had some certificate or something from the medical society saying that, yes, we completed this coursework and we have achieved a certain level of recognition and have that recognition come directly from the professional medical society?’”
The project for certification has to be approved, and a performance and growth evaluation has to be completed. Once a project is approved, participants will be connected with advisors to help them along. Those taking the Leadership Academy coursework will have five years to apply that coursework to the certification process. But to be fair to those who have already gone through the academy and may already be near the time limit, anyone can apply their coursework through January 2013.
SHM expects that the certification will take an average of 18 months to complete, but it can be completed in as little as one year or as many as five years.

—Rusty Holman, MD, MHM, chief clinical officer, Cogent HMG, director, Leadership Academy, former SHM president
Tina Budnitz, MPH, senior advisor to the CEO of SHM and a chief designer of the Leadership Certification program, says the main idea was to make it relevant and meaningful.
The program was crafted “with adult education principles in mind,” she says. “You get to design a project that’s going to be meaningful for you. We’re also trying to put you into small, networked groups of networked faculty and peers that can provide support for you along the way.”
When participants submit their projects, they’ll get “very detailed feedback” from experts on potential problems and will be directed to resources. If someone proposes a project on deep vein thrombosis (DVT) prevention, for example, they might be directed to webinars on the topic or other hospitals in their area where DVT prevention programs have been implemented so that the participants can contact them if they choose.
Budnitz says Leadership Certification is meant to plug a gap in leadership curriculum at business schools and in coursework in programs like the American College of Physician Executives.
“What they aren’t able to do is provide education in the context of hospital medicine,” she says.
The cost of the program is $2,500. That is in addition to the cost to participate in Leadership Academies, which range from $1,800 to $2,000 each.
One of the first to sign up for the program, Darlene Tad-y, MD, a hospitalist and assistant professor at the University of Colorado Denver, says she already has noticed that she has been able to apply concepts she has learned in the academies to work situations: supervising residents, interns, and medical students as the attending physician, serving on hospital committees, and taking a leadership role within her hospitalist group.
She says the Leadership Certification program makes sense for her because she isn’t sure she wants to pursue an MBA but still wants to refine certain skills.
She said that in her project, she will attempt to improve transitions of care, looking specifically at communication at the time of discharge. The project is one that she likely would have undertaken anyway because it’s important to her institution and patient care, but doing it as part of the certification program gives her more resources, along with the chance to earn the certificate.

—Darlene Tad-y, MD, assistant professor, University of Colorado Denver
The skills learned through certification would be helpful to anyone, regardless of their supervisory role, she notes.
“I’m not the division head, I’m not the chief, but I don’t think that leadership necessarily is bestowed by a title,” she says. “I think it’s what you’re doing. It’s the actions that you’re taking and the way that you’re approaching things. And it’s a skill set that I feel like you need to work on and develop. And I think that’s what the certification will help me [with].”
Ilan Alhadeff, MD, FHM, program medical director with Cogent HMG who works at Hackensack University Medical Center in New Jersey, says his project will involve techniques to increase patient satisfaction scores, focusing largely on the communication that drives those scores.
He is taking leadership in the field seriously, particularly because the demands of hospitalists will be heightened amid healthcare reform efforts.
The importance of quality markers and patient experience will only grow, and hospitalists are positioned to have a big impact on them, he says.
“Hospitals are at big financial risk, which could result in further consolidation of healthcare institutions,” Dr. Alhadeff says. “We’re poised to have the biggest impact on those numbers, [moreso] than any individual primary-care doctor.”
Dr. Alhadeff says it might not be easy to fit the project in, considering all the demands on his time already, but it’s something he feels compelled to do.
“I would [call it akin] to telling a patient they need to find time to exercise,” he says. “There’s no time, but we just have to make time and we have to do it.”
Dr. Holman says the important thing is the learning that takes place while participants are involved in the projects, not necessarily the projects’ results. In a project that aims to reduce 30-day readmission rates, for example, a lot can be learned even if the effort fails.
“In fact, in that scenario, we would expect that the lessons learned would be very robust, would be very rich,” says Dr. Holman, a former SHM president. “And the focus would be on both, perhaps technical reasons why readmission rates went up, but [also] a very significant focus on lessons learned about what things undermined the effort or made the effort less than successful. And it’s those lessons learned that help us grow as leaders, and tying it back to things that we learned in the Leadership Academies and applying it to a real-life scenario.”
The academy and the certification program, Dr. Holman says, will create a “self-sustaining” environment in which people may be more likely to participate in the academy if they know they can use their coursework to vault to the next step later, should they choose to do so.
It’s an important time for a new layer of leadership training, he adds, because of all of the challenges facing hospital medicine and healthcare at large. “There’s an age-old question: Are leaders born, or are they made?” he says. “And to me, the answer to that question doesn’t matter. There will never be enough natural-born leaders to get all of this done. So we have to develop people who have the interest and have the potential. We would be squandering a huge opportunity if we didn’t undertake that ourselves.”
Tom Collins is a freelance writer based in Miami.
SHM’s Leadership Academies have been well received, with at least 1,200 having taken the courses so far. Some of those participants, though, craved something more—some recognition for the ways those lessons are being incorporated on the job in their hospitals.
So this year, for the first time, SHM is offering something beyond the third level of the Leadership Academies. Those who have completed all three levels in the academy can now seek Leadership Certification, based mainly on completion of a project to make a positive change at their hospitals.
Rusty Holman, MD, MHM, director of the academy program and chief clinical officer at Cogent HMG, says the impetus came from past participants.
“Those who have attended the Leadership Academies came forward and said, ‘You know, we’re doing some really important coursework, we’re investing in ourselves in both our knowledge and our skills as leaders. We are furthermore involved in a lot of change efforts within the hospital and improvement efforts—whether it’s related to quality or it’s related to some business function or it’s related to education and training. And wrapping all that together, wouldn’t it be nice if we had some certificate or something from the medical society saying that, yes, we completed this coursework and we have achieved a certain level of recognition and have that recognition come directly from the professional medical society?’”
The project for certification has to be approved, and a performance and growth evaluation has to be completed. Once a project is approved, participants will be connected with advisors to help them along. Those taking the Leadership Academy coursework will have five years to apply that coursework to the certification process. But to be fair to those who have already gone through the academy and may already be near the time limit, anyone can apply their coursework through January 2013.
SHM expects that the certification will take an average of 18 months to complete, but it can be completed in as little as one year or as many as five years.

—Rusty Holman, MD, MHM, chief clinical officer, Cogent HMG, director, Leadership Academy, former SHM president
Tina Budnitz, MPH, senior advisor to the CEO of SHM and a chief designer of the Leadership Certification program, says the main idea was to make it relevant and meaningful.
The program was crafted “with adult education principles in mind,” she says. “You get to design a project that’s going to be meaningful for you. We’re also trying to put you into small, networked groups of networked faculty and peers that can provide support for you along the way.”
When participants submit their projects, they’ll get “very detailed feedback” from experts on potential problems and will be directed to resources. If someone proposes a project on deep vein thrombosis (DVT) prevention, for example, they might be directed to webinars on the topic or other hospitals in their area where DVT prevention programs have been implemented so that the participants can contact them if they choose.
Budnitz says Leadership Certification is meant to plug a gap in leadership curriculum at business schools and in coursework in programs like the American College of Physician Executives.
“What they aren’t able to do is provide education in the context of hospital medicine,” she says.
The cost of the program is $2,500. That is in addition to the cost to participate in Leadership Academies, which range from $1,800 to $2,000 each.
One of the first to sign up for the program, Darlene Tad-y, MD, a hospitalist and assistant professor at the University of Colorado Denver, says she already has noticed that she has been able to apply concepts she has learned in the academies to work situations: supervising residents, interns, and medical students as the attending physician, serving on hospital committees, and taking a leadership role within her hospitalist group.
She says the Leadership Certification program makes sense for her because she isn’t sure she wants to pursue an MBA but still wants to refine certain skills.
She said that in her project, she will attempt to improve transitions of care, looking specifically at communication at the time of discharge. The project is one that she likely would have undertaken anyway because it’s important to her institution and patient care, but doing it as part of the certification program gives her more resources, along with the chance to earn the certificate.

—Darlene Tad-y, MD, assistant professor, University of Colorado Denver
The skills learned through certification would be helpful to anyone, regardless of their supervisory role, she notes.
“I’m not the division head, I’m not the chief, but I don’t think that leadership necessarily is bestowed by a title,” she says. “I think it’s what you’re doing. It’s the actions that you’re taking and the way that you’re approaching things. And it’s a skill set that I feel like you need to work on and develop. And I think that’s what the certification will help me [with].”
Ilan Alhadeff, MD, FHM, program medical director with Cogent HMG who works at Hackensack University Medical Center in New Jersey, says his project will involve techniques to increase patient satisfaction scores, focusing largely on the communication that drives those scores.
He is taking leadership in the field seriously, particularly because the demands of hospitalists will be heightened amid healthcare reform efforts.
The importance of quality markers and patient experience will only grow, and hospitalists are positioned to have a big impact on them, he says.
“Hospitals are at big financial risk, which could result in further consolidation of healthcare institutions,” Dr. Alhadeff says. “We’re poised to have the biggest impact on those numbers, [moreso] than any individual primary-care doctor.”
Dr. Alhadeff says it might not be easy to fit the project in, considering all the demands on his time already, but it’s something he feels compelled to do.
“I would [call it akin] to telling a patient they need to find time to exercise,” he says. “There’s no time, but we just have to make time and we have to do it.”
Dr. Holman says the important thing is the learning that takes place while participants are involved in the projects, not necessarily the projects’ results. In a project that aims to reduce 30-day readmission rates, for example, a lot can be learned even if the effort fails.
“In fact, in that scenario, we would expect that the lessons learned would be very robust, would be very rich,” says Dr. Holman, a former SHM president. “And the focus would be on both, perhaps technical reasons why readmission rates went up, but [also] a very significant focus on lessons learned about what things undermined the effort or made the effort less than successful. And it’s those lessons learned that help us grow as leaders, and tying it back to things that we learned in the Leadership Academies and applying it to a real-life scenario.”
The academy and the certification program, Dr. Holman says, will create a “self-sustaining” environment in which people may be more likely to participate in the academy if they know they can use their coursework to vault to the next step later, should they choose to do so.
It’s an important time for a new layer of leadership training, he adds, because of all of the challenges facing hospital medicine and healthcare at large. “There’s an age-old question: Are leaders born, or are they made?” he says. “And to me, the answer to that question doesn’t matter. There will never be enough natural-born leaders to get all of this done. So we have to develop people who have the interest and have the potential. We would be squandering a huge opportunity if we didn’t undertake that ourselves.”
Tom Collins is a freelance writer based in Miami.
SHM’s Leadership Academies have been well received, with at least 1,200 having taken the courses so far. Some of those participants, though, craved something more—some recognition for the ways those lessons are being incorporated on the job in their hospitals.
So this year, for the first time, SHM is offering something beyond the third level of the Leadership Academies. Those who have completed all three levels in the academy can now seek Leadership Certification, based mainly on completion of a project to make a positive change at their hospitals.
Rusty Holman, MD, MHM, director of the academy program and chief clinical officer at Cogent HMG, says the impetus came from past participants.
“Those who have attended the Leadership Academies came forward and said, ‘You know, we’re doing some really important coursework, we’re investing in ourselves in both our knowledge and our skills as leaders. We are furthermore involved in a lot of change efforts within the hospital and improvement efforts—whether it’s related to quality or it’s related to some business function or it’s related to education and training. And wrapping all that together, wouldn’t it be nice if we had some certificate or something from the medical society saying that, yes, we completed this coursework and we have achieved a certain level of recognition and have that recognition come directly from the professional medical society?’”
The project for certification has to be approved, and a performance and growth evaluation has to be completed. Once a project is approved, participants will be connected with advisors to help them along. Those taking the Leadership Academy coursework will have five years to apply that coursework to the certification process. But to be fair to those who have already gone through the academy and may already be near the time limit, anyone can apply their coursework through January 2013.
SHM expects that the certification will take an average of 18 months to complete, but it can be completed in as little as one year or as many as five years.

—Rusty Holman, MD, MHM, chief clinical officer, Cogent HMG, director, Leadership Academy, former SHM president
Tina Budnitz, MPH, senior advisor to the CEO of SHM and a chief designer of the Leadership Certification program, says the main idea was to make it relevant and meaningful.
The program was crafted “with adult education principles in mind,” she says. “You get to design a project that’s going to be meaningful for you. We’re also trying to put you into small, networked groups of networked faculty and peers that can provide support for you along the way.”
When participants submit their projects, they’ll get “very detailed feedback” from experts on potential problems and will be directed to resources. If someone proposes a project on deep vein thrombosis (DVT) prevention, for example, they might be directed to webinars on the topic or other hospitals in their area where DVT prevention programs have been implemented so that the participants can contact them if they choose.
Budnitz says Leadership Certification is meant to plug a gap in leadership curriculum at business schools and in coursework in programs like the American College of Physician Executives.
“What they aren’t able to do is provide education in the context of hospital medicine,” she says.
The cost of the program is $2,500. That is in addition to the cost to participate in Leadership Academies, which range from $1,800 to $2,000 each.
One of the first to sign up for the program, Darlene Tad-y, MD, a hospitalist and assistant professor at the University of Colorado Denver, says she already has noticed that she has been able to apply concepts she has learned in the academies to work situations: supervising residents, interns, and medical students as the attending physician, serving on hospital committees, and taking a leadership role within her hospitalist group.
She says the Leadership Certification program makes sense for her because she isn’t sure she wants to pursue an MBA but still wants to refine certain skills.
She said that in her project, she will attempt to improve transitions of care, looking specifically at communication at the time of discharge. The project is one that she likely would have undertaken anyway because it’s important to her institution and patient care, but doing it as part of the certification program gives her more resources, along with the chance to earn the certificate.

—Darlene Tad-y, MD, assistant professor, University of Colorado Denver
The skills learned through certification would be helpful to anyone, regardless of their supervisory role, she notes.
“I’m not the division head, I’m not the chief, but I don’t think that leadership necessarily is bestowed by a title,” she says. “I think it’s what you’re doing. It’s the actions that you’re taking and the way that you’re approaching things. And it’s a skill set that I feel like you need to work on and develop. And I think that’s what the certification will help me [with].”
Ilan Alhadeff, MD, FHM, program medical director with Cogent HMG who works at Hackensack University Medical Center in New Jersey, says his project will involve techniques to increase patient satisfaction scores, focusing largely on the communication that drives those scores.
He is taking leadership in the field seriously, particularly because the demands of hospitalists will be heightened amid healthcare reform efforts.
The importance of quality markers and patient experience will only grow, and hospitalists are positioned to have a big impact on them, he says.
“Hospitals are at big financial risk, which could result in further consolidation of healthcare institutions,” Dr. Alhadeff says. “We’re poised to have the biggest impact on those numbers, [moreso] than any individual primary-care doctor.”
Dr. Alhadeff says it might not be easy to fit the project in, considering all the demands on his time already, but it’s something he feels compelled to do.
“I would [call it akin] to telling a patient they need to find time to exercise,” he says. “There’s no time, but we just have to make time and we have to do it.”
Dr. Holman says the important thing is the learning that takes place while participants are involved in the projects, not necessarily the projects’ results. In a project that aims to reduce 30-day readmission rates, for example, a lot can be learned even if the effort fails.
“In fact, in that scenario, we would expect that the lessons learned would be very robust, would be very rich,” says Dr. Holman, a former SHM president. “And the focus would be on both, perhaps technical reasons why readmission rates went up, but [also] a very significant focus on lessons learned about what things undermined the effort or made the effort less than successful. And it’s those lessons learned that help us grow as leaders, and tying it back to things that we learned in the Leadership Academies and applying it to a real-life scenario.”
The academy and the certification program, Dr. Holman says, will create a “self-sustaining” environment in which people may be more likely to participate in the academy if they know they can use their coursework to vault to the next step later, should they choose to do so.
It’s an important time for a new layer of leadership training, he adds, because of all of the challenges facing hospital medicine and healthcare at large. “There’s an age-old question: Are leaders born, or are they made?” he says. “And to me, the answer to that question doesn’t matter. There will never be enough natural-born leaders to get all of this done. So we have to develop people who have the interest and have the potential. We would be squandering a huge opportunity if we didn’t undertake that ourselves.”
Tom Collins is a freelance writer based in Miami.
HM@15 - Myriad Points of View
HM’s evolution the past 15 years has helped to reshape patient care in the hospital. Hospitalists near and far, young and old, are most proud of their work.
But how do others view hospitalists? What do nurses, pharmacists, and surgical specialists—professionals who work with hospitalists on a daily basis—say about hospitalists and their daily contributions to medicine and the U.S. healthcare system?
The Hospitalist talked with an array of medical professionals to develop a 360-degree sense of how HM is regarded in the medical community, speaking with sources affiliated with organizations as those sources are inclined to have a more panoramic understanding of how their field views hospitalists. The views presented are those of the individuals and do not necessarily represent the stances of their organizations.
Pharmacy
Stan Kent, president of the American Society of Health-System Pharmacists, says he always thought that the idea of having doctors who worked exclusively in the hospital would be good idea—even before there was such a thing as a hospitalist.
“I witnessed the movement of internists and surgeons transformed from being hospital-based to more office-based,” says Kent, who also is an assistant vice president at Northshore University Health System in Evanston, Ill., where he oversees pharmacy services. “I always wished that there could be more consistency on the part of those physicians in taking care of the patients in the hospital.”
Once hospitalists became a fixture in hospitals, their familiarity with the hospital and knowledge helped pharmacists do their jobs better, according to Kent. With hospitals becoming more and more complex, with electronic medical records and the handling of cases that are more and more difficult, doctors generally are less efficient if they’re not intimately involved in the system.
Kristi Killelea, an inpatient pharmacist at Northshore, says that it’s easier to develop working relationships with hospitalists whom you frequently see in the hospital.
“From the inpatient perspective, I think the nice part about hospitalists is they are more familiar with inpatient medicine, which typically involves more intravenous-type medications,” she says. “It just makes it easier to deal with them because they see that a little bit more frequently.”
There are times when the gap between inpatient care and outpatient care shows, she notes, but that is uncommon. “Sometimes, if you’re looking for historical knowledge about the patient, about why they are doing what they’re doing with the medication, [hospitalists] can’t always contribute that because they’re not following the patient in their office,” she says. “But I think that’s more rare than the norm.”
Even as medication reconciliation continues to be an issue throughout the healthcare landscape, Kent and Killelea agree it’s not due to hospitalists. “Sometimes patients tell their PCP that they’re taking Lipitor, for example, but they don’t give them the strength and they don’t tell them how many times they’re taking it. Those instances become more cumbersome from a medication reconciliation standpoint,” Kent says. “Whereas if this information is gathered by the hospitalist, they are more accurate and complete, I think, in getting that history, and then doing the reconciliation.”
Quality Control
To date, there is no definitive data to show what effect hospitalists have on the quality of care at hospitals, says Robert Wise, MD, medical advisor to the Joint Commission’s Division of Healthcare Quality Evaluation in Washington, D.C.
He says a hospitalist can’t be judged on his or her own but has to be seen in the context of the system in which he or she is working. Hospitalists have in-depth knowledge of the complex processes and technology special to hospital care, but their work is only part of the entire “episode of care” for a patient.
“While the physician in the hospital is highly trained to deal with the unique clinical needs of that patient, it is also important that the team treating the patient has all relevant information from all clinicians who may have treated the patient prior to the acute episode,” he says.
“It is also critical that when the patient is discharged that there is as seamless transition back to the system that will continue to care for that patient. Those handoffs may or may not be working well.”
The handoff, to and from the hospital, is one of the most risk-fraught areas for patients. So what is gained from the specialized skills of hospitalists might be lost if transitions from the hospital are not done well, Dr. Wise explains. “The hospitalist concept, while adding a new level of expertise, also increases the fragmentation of care and, therefore, can lead to some increased risk,” he says. “That risk is mitigated by well-functioning systems that can both initiate and accept the transfers.”
The use and mastery of the electronic medical record is crucial to the successful handoff, he adds.
“Another issue that is often discussed is whether, as the number of [hospital]-employed physicians increase, that will impact the medical staff’s freedom to constructively challenge hospital administration or the board concerning issues of quality and safety,” Dr. Wise says. “While this remains a theoretical issue, as the number of medical staff members employed by the hospital increase, [it is important] that their voices on the issues of quality and safety of medical care remain unimpeded.”
He also says that the speed of the growth of the hospitalist field comes with a certain amount of risk.
“The current hospitalist system attempts to assure that seriously ill patients are being treated by physicians who are current and competent in the complicated, high-tech environment of the 21st-century hospital,” he explains. “It will take time to develop a number of the supporting systems. If the speed of growth is very rapid, it is possible that the supporting systems, both inside and outside of the hospital, will not be able to keep up. None of these possible problems are insurmountable, but all will take a significant amount of attention and resources to support this method to deliver care.”
—Robert Wise, MD, medical advisor, Division of Healthcare Quality Evaluation, The Joint Commission, Washington, D.C.
Orthopedic Surgery
Older orthopedic patients are at serious risk after surgery, but their chances are improved by the work of hospitalists, says Alexandra Page, MD, a member of the American Academy of Orthopaedic Surgeons’ National Health Care Systems Committee and a surgeon with Kaiser Permanente in La Jolla, Calif., who works with geriatric patients.
A major role of hospitalists in support of orthopedic surgeons is to help patients be “as tuned up as they can be prior to surgery,” she says.
For octogenarians, there is a 25% mortality rate in the year after a hip fracture. For a nonagenarian, the one-year mortality rate is 50%.
“That’s a real high risk, and we don’t even in orthopedics have a good sense of what those factors are that make them so high-risk,” says Dr. Page, adding that it is known that optimal levels of glycemic control can minimize perioperative complications like infection.
That makes it all the more important for hospitalists to get patients into the best shape possible. After the operation, hospitalists help control blood pressure and blood sugar, and take steps to minimize post-operative delirium.
“It doesn’t affect our ability to perform the surgery at a technical level, but ultimately it gives our patients better outcomes,” Dr. Page says. “That’s really what it’s all about.”
Dr. Page’s role as an examiner for the orthopedic boards gives her insight into how different hospital systems work. She says she hopes there can be more consistency in the role that hospitalists have in helping with orthopedic surgery patients, with patients being routinely admitted through the hospitalist service. “I think there’s still a lot of variability, in terms of who’s managing these patients,” she says.
Continued below...
Family Medicine
When one of his patients is admitted to the hospital and comes under the care of a hospitalist, his involvement doesn’t end, says Glen Stream, MD, president-elect of the American Academy of Family Physicians, who works with Rockwood Clinic in Spokane, Wash.
Dr. Stream continues to keep in touch with patients, and that has made for a good working relationship with hospitalists. It helps put patients at ease and helps with handoffs to and from the hospital, he says. “I don’t think you can overcommunicate in either direction,” he says. “The most complete medical information enables the best-informed decision-making for treatment decisions.” Such levels of involvement usually are welcomed by hospitalists, he says, adding “I’ve been able to be the hospital physician’s advocate.”
Meanwhile, HM has made his office-based practice more flexible and more accessible. “In my medical group, a number of my partners actually start seeing patients [in the office] as early as seven in the morning,” Dr. Stream says. “They can commit to being there for patients at that early hour.”
He points out that handoffs to and from primary-care doctors and hospitalists has improved, but it’s still a work in progress. “I think it’s gotten better over time,” he says. “I think there’s recognition—on both sides of those handoffs—that things could be improved. I think the commitment is there both for the ambulatory physicians, the primary-care doctor, the family doctor, and the hospitalist taking care of them.”
Although hospitalists generally are better compensation than family doctors, Dr. Stream says he isn’t aware of “any friction” from family physicians. “Our academy, our members, family physicians, believe that the work that [we] do is undervalued in our current healthcare system. But that doesn’t mean that we have to compare ourselves to hospitalists,” he says.
Nursing
Even as fragmentation of medical care has increased, the emergence of the hospitalist has helped to streamline care, says Joanne Disch, PhD, RN, president-elect of the American Academy of Nursing and clinical professor at the University of Minnesota School of Nursing in Minneapolis.
“There has become such increasing fragmentation of who is the team around the patient,” she says. But, she notes, “the hospitalist really provided a mechanism to promote continuity of care.”
Nurses, she says, have found hospitalists to be “somebody who can cover your back.” “When the system works right, the nurses do not have to seek out a physician and hope that they can either grab somebody or somebody makes rounds,” Disch says, noting a general frustration amongst her peers as to a lack of clarity in regard to who’s in charge. “What hospitalists inherently do, structurally, is provide a main physician who will be the accountable one in the hospital setting. You have a named person that the nurse knows, ‘Ah, this is who I need to go to.’ ”
Although most nurses welcomed hospitalists from the very beginning, she continues, the addition of MDs into the hospital setting did cause confusion, most notably over the roles of PCPs, referring physicians, and hospitalists.
“It wasn’t clear the extent of this individual’s responsibility and how to use them effectively, but over time my sense is that people … really find this helpful,” she says.
An area that might have room for improvement is hospitalist-nurse communication, with more “huddling” and discussions at shift change. Better communication with patients’ families also could be improved, she says. “[It] gets a little confusing sometimes,” she says. “Either everybody, or nobody, is talking with the patient and the family.”
Hospital Administration
The reaction of Craig Becker, a member of the American Hospital Association board and president of the Tennessee Hospital Association, was, at first, fairly dismissive. An idea being discussed in the industry—inpatient physicians working full-time in hospitals—would not be worth it, he thought. He couldn’t get past the notion that such an arrangement would be “a waste of money,” and that if someone tried it, it would just be in the clinical-care units.
Once a couple of hospitals started hospitalist services, he was more inclined to listen. “I was getting feedback from them, and they were saying: ‘Boy, this has made a big difference, both in patient care and financially,’ ” Becker explains. Once he noticed HM programs popping up in small, rural hospitals, Becker knew “this was a movement whose time had come.”
In Tennessee, where hospitalists were almost unheard of a decade ago, hospitalists now work in every shape and size of hospital, some with fewer than 100 beds. At one hospital that employs its own hospitalist, there are just 58 beds and an attached nursing home, Becker says.
Showing that hospitalists have been worth the cost is really as simple as looking at the length of stay, he says. “If you can knock six-tenths of a day off a stay, that’s pretty significant savings,” Becker says.
Becker notes other positives the HM model has brought to Tennessee hospitals: They make the jobs of hospital administrators easier because specialists and referring physicians are happier.
“They can spend more time doing whatever they want to do on a personal basis or in their offices,” he says. “So I think just in terms of improving relationships with the medical staffs, hospitalists have been a real plus.”
Tom Collins is a freelance writer based in Florida.
HM’s evolution the past 15 years has helped to reshape patient care in the hospital. Hospitalists near and far, young and old, are most proud of their work.
But how do others view hospitalists? What do nurses, pharmacists, and surgical specialists—professionals who work with hospitalists on a daily basis—say about hospitalists and their daily contributions to medicine and the U.S. healthcare system?
The Hospitalist talked with an array of medical professionals to develop a 360-degree sense of how HM is regarded in the medical community, speaking with sources affiliated with organizations as those sources are inclined to have a more panoramic understanding of how their field views hospitalists. The views presented are those of the individuals and do not necessarily represent the stances of their organizations.
Pharmacy
Stan Kent, president of the American Society of Health-System Pharmacists, says he always thought that the idea of having doctors who worked exclusively in the hospital would be good idea—even before there was such a thing as a hospitalist.
“I witnessed the movement of internists and surgeons transformed from being hospital-based to more office-based,” says Kent, who also is an assistant vice president at Northshore University Health System in Evanston, Ill., where he oversees pharmacy services. “I always wished that there could be more consistency on the part of those physicians in taking care of the patients in the hospital.”
Once hospitalists became a fixture in hospitals, their familiarity with the hospital and knowledge helped pharmacists do their jobs better, according to Kent. With hospitals becoming more and more complex, with electronic medical records and the handling of cases that are more and more difficult, doctors generally are less efficient if they’re not intimately involved in the system.
Kristi Killelea, an inpatient pharmacist at Northshore, says that it’s easier to develop working relationships with hospitalists whom you frequently see in the hospital.
“From the inpatient perspective, I think the nice part about hospitalists is they are more familiar with inpatient medicine, which typically involves more intravenous-type medications,” she says. “It just makes it easier to deal with them because they see that a little bit more frequently.”
There are times when the gap between inpatient care and outpatient care shows, she notes, but that is uncommon. “Sometimes, if you’re looking for historical knowledge about the patient, about why they are doing what they’re doing with the medication, [hospitalists] can’t always contribute that because they’re not following the patient in their office,” she says. “But I think that’s more rare than the norm.”
Even as medication reconciliation continues to be an issue throughout the healthcare landscape, Kent and Killelea agree it’s not due to hospitalists. “Sometimes patients tell their PCP that they’re taking Lipitor, for example, but they don’t give them the strength and they don’t tell them how many times they’re taking it. Those instances become more cumbersome from a medication reconciliation standpoint,” Kent says. “Whereas if this information is gathered by the hospitalist, they are more accurate and complete, I think, in getting that history, and then doing the reconciliation.”
Quality Control
To date, there is no definitive data to show what effect hospitalists have on the quality of care at hospitals, says Robert Wise, MD, medical advisor to the Joint Commission’s Division of Healthcare Quality Evaluation in Washington, D.C.
He says a hospitalist can’t be judged on his or her own but has to be seen in the context of the system in which he or she is working. Hospitalists have in-depth knowledge of the complex processes and technology special to hospital care, but their work is only part of the entire “episode of care” for a patient.
“While the physician in the hospital is highly trained to deal with the unique clinical needs of that patient, it is also important that the team treating the patient has all relevant information from all clinicians who may have treated the patient prior to the acute episode,” he says.
“It is also critical that when the patient is discharged that there is as seamless transition back to the system that will continue to care for that patient. Those handoffs may or may not be working well.”
The handoff, to and from the hospital, is one of the most risk-fraught areas for patients. So what is gained from the specialized skills of hospitalists might be lost if transitions from the hospital are not done well, Dr. Wise explains. “The hospitalist concept, while adding a new level of expertise, also increases the fragmentation of care and, therefore, can lead to some increased risk,” he says. “That risk is mitigated by well-functioning systems that can both initiate and accept the transfers.”
The use and mastery of the electronic medical record is crucial to the successful handoff, he adds.
“Another issue that is often discussed is whether, as the number of [hospital]-employed physicians increase, that will impact the medical staff’s freedom to constructively challenge hospital administration or the board concerning issues of quality and safety,” Dr. Wise says. “While this remains a theoretical issue, as the number of medical staff members employed by the hospital increase, [it is important] that their voices on the issues of quality and safety of medical care remain unimpeded.”
He also says that the speed of the growth of the hospitalist field comes with a certain amount of risk.
“The current hospitalist system attempts to assure that seriously ill patients are being treated by physicians who are current and competent in the complicated, high-tech environment of the 21st-century hospital,” he explains. “It will take time to develop a number of the supporting systems. If the speed of growth is very rapid, it is possible that the supporting systems, both inside and outside of the hospital, will not be able to keep up. None of these possible problems are insurmountable, but all will take a significant amount of attention and resources to support this method to deliver care.”
—Robert Wise, MD, medical advisor, Division of Healthcare Quality Evaluation, The Joint Commission, Washington, D.C.
Orthopedic Surgery
Older orthopedic patients are at serious risk after surgery, but their chances are improved by the work of hospitalists, says Alexandra Page, MD, a member of the American Academy of Orthopaedic Surgeons’ National Health Care Systems Committee and a surgeon with Kaiser Permanente in La Jolla, Calif., who works with geriatric patients.
A major role of hospitalists in support of orthopedic surgeons is to help patients be “as tuned up as they can be prior to surgery,” she says.
For octogenarians, there is a 25% mortality rate in the year after a hip fracture. For a nonagenarian, the one-year mortality rate is 50%.
“That’s a real high risk, and we don’t even in orthopedics have a good sense of what those factors are that make them so high-risk,” says Dr. Page, adding that it is known that optimal levels of glycemic control can minimize perioperative complications like infection.
That makes it all the more important for hospitalists to get patients into the best shape possible. After the operation, hospitalists help control blood pressure and blood sugar, and take steps to minimize post-operative delirium.
“It doesn’t affect our ability to perform the surgery at a technical level, but ultimately it gives our patients better outcomes,” Dr. Page says. “That’s really what it’s all about.”
Dr. Page’s role as an examiner for the orthopedic boards gives her insight into how different hospital systems work. She says she hopes there can be more consistency in the role that hospitalists have in helping with orthopedic surgery patients, with patients being routinely admitted through the hospitalist service. “I think there’s still a lot of variability, in terms of who’s managing these patients,” she says.
Continued below...
Family Medicine
When one of his patients is admitted to the hospital and comes under the care of a hospitalist, his involvement doesn’t end, says Glen Stream, MD, president-elect of the American Academy of Family Physicians, who works with Rockwood Clinic in Spokane, Wash.
Dr. Stream continues to keep in touch with patients, and that has made for a good working relationship with hospitalists. It helps put patients at ease and helps with handoffs to and from the hospital, he says. “I don’t think you can overcommunicate in either direction,” he says. “The most complete medical information enables the best-informed decision-making for treatment decisions.” Such levels of involvement usually are welcomed by hospitalists, he says, adding “I’ve been able to be the hospital physician’s advocate.”
Meanwhile, HM has made his office-based practice more flexible and more accessible. “In my medical group, a number of my partners actually start seeing patients [in the office] as early as seven in the morning,” Dr. Stream says. “They can commit to being there for patients at that early hour.”
He points out that handoffs to and from primary-care doctors and hospitalists has improved, but it’s still a work in progress. “I think it’s gotten better over time,” he says. “I think there’s recognition—on both sides of those handoffs—that things could be improved. I think the commitment is there both for the ambulatory physicians, the primary-care doctor, the family doctor, and the hospitalist taking care of them.”
Although hospitalists generally are better compensation than family doctors, Dr. Stream says he isn’t aware of “any friction” from family physicians. “Our academy, our members, family physicians, believe that the work that [we] do is undervalued in our current healthcare system. But that doesn’t mean that we have to compare ourselves to hospitalists,” he says.
Nursing
Even as fragmentation of medical care has increased, the emergence of the hospitalist has helped to streamline care, says Joanne Disch, PhD, RN, president-elect of the American Academy of Nursing and clinical professor at the University of Minnesota School of Nursing in Minneapolis.
“There has become such increasing fragmentation of who is the team around the patient,” she says. But, she notes, “the hospitalist really provided a mechanism to promote continuity of care.”
Nurses, she says, have found hospitalists to be “somebody who can cover your back.” “When the system works right, the nurses do not have to seek out a physician and hope that they can either grab somebody or somebody makes rounds,” Disch says, noting a general frustration amongst her peers as to a lack of clarity in regard to who’s in charge. “What hospitalists inherently do, structurally, is provide a main physician who will be the accountable one in the hospital setting. You have a named person that the nurse knows, ‘Ah, this is who I need to go to.’ ”
Although most nurses welcomed hospitalists from the very beginning, she continues, the addition of MDs into the hospital setting did cause confusion, most notably over the roles of PCPs, referring physicians, and hospitalists.
“It wasn’t clear the extent of this individual’s responsibility and how to use them effectively, but over time my sense is that people … really find this helpful,” she says.
An area that might have room for improvement is hospitalist-nurse communication, with more “huddling” and discussions at shift change. Better communication with patients’ families also could be improved, she says. “[It] gets a little confusing sometimes,” she says. “Either everybody, or nobody, is talking with the patient and the family.”
Hospital Administration
The reaction of Craig Becker, a member of the American Hospital Association board and president of the Tennessee Hospital Association, was, at first, fairly dismissive. An idea being discussed in the industry—inpatient physicians working full-time in hospitals—would not be worth it, he thought. He couldn’t get past the notion that such an arrangement would be “a waste of money,” and that if someone tried it, it would just be in the clinical-care units.
Once a couple of hospitals started hospitalist services, he was more inclined to listen. “I was getting feedback from them, and they were saying: ‘Boy, this has made a big difference, both in patient care and financially,’ ” Becker explains. Once he noticed HM programs popping up in small, rural hospitals, Becker knew “this was a movement whose time had come.”
In Tennessee, where hospitalists were almost unheard of a decade ago, hospitalists now work in every shape and size of hospital, some with fewer than 100 beds. At one hospital that employs its own hospitalist, there are just 58 beds and an attached nursing home, Becker says.
Showing that hospitalists have been worth the cost is really as simple as looking at the length of stay, he says. “If you can knock six-tenths of a day off a stay, that’s pretty significant savings,” Becker says.
Becker notes other positives the HM model has brought to Tennessee hospitals: They make the jobs of hospital administrators easier because specialists and referring physicians are happier.
“They can spend more time doing whatever they want to do on a personal basis or in their offices,” he says. “So I think just in terms of improving relationships with the medical staffs, hospitalists have been a real plus.”
Tom Collins is a freelance writer based in Florida.
HM’s evolution the past 15 years has helped to reshape patient care in the hospital. Hospitalists near and far, young and old, are most proud of their work.
But how do others view hospitalists? What do nurses, pharmacists, and surgical specialists—professionals who work with hospitalists on a daily basis—say about hospitalists and their daily contributions to medicine and the U.S. healthcare system?
The Hospitalist talked with an array of medical professionals to develop a 360-degree sense of how HM is regarded in the medical community, speaking with sources affiliated with organizations as those sources are inclined to have a more panoramic understanding of how their field views hospitalists. The views presented are those of the individuals and do not necessarily represent the stances of their organizations.
Pharmacy
Stan Kent, president of the American Society of Health-System Pharmacists, says he always thought that the idea of having doctors who worked exclusively in the hospital would be good idea—even before there was such a thing as a hospitalist.
“I witnessed the movement of internists and surgeons transformed from being hospital-based to more office-based,” says Kent, who also is an assistant vice president at Northshore University Health System in Evanston, Ill., where he oversees pharmacy services. “I always wished that there could be more consistency on the part of those physicians in taking care of the patients in the hospital.”
Once hospitalists became a fixture in hospitals, their familiarity with the hospital and knowledge helped pharmacists do their jobs better, according to Kent. With hospitals becoming more and more complex, with electronic medical records and the handling of cases that are more and more difficult, doctors generally are less efficient if they’re not intimately involved in the system.
Kristi Killelea, an inpatient pharmacist at Northshore, says that it’s easier to develop working relationships with hospitalists whom you frequently see in the hospital.
“From the inpatient perspective, I think the nice part about hospitalists is they are more familiar with inpatient medicine, which typically involves more intravenous-type medications,” she says. “It just makes it easier to deal with them because they see that a little bit more frequently.”
There are times when the gap between inpatient care and outpatient care shows, she notes, but that is uncommon. “Sometimes, if you’re looking for historical knowledge about the patient, about why they are doing what they’re doing with the medication, [hospitalists] can’t always contribute that because they’re not following the patient in their office,” she says. “But I think that’s more rare than the norm.”
Even as medication reconciliation continues to be an issue throughout the healthcare landscape, Kent and Killelea agree it’s not due to hospitalists. “Sometimes patients tell their PCP that they’re taking Lipitor, for example, but they don’t give them the strength and they don’t tell them how many times they’re taking it. Those instances become more cumbersome from a medication reconciliation standpoint,” Kent says. “Whereas if this information is gathered by the hospitalist, they are more accurate and complete, I think, in getting that history, and then doing the reconciliation.”
Quality Control
To date, there is no definitive data to show what effect hospitalists have on the quality of care at hospitals, says Robert Wise, MD, medical advisor to the Joint Commission’s Division of Healthcare Quality Evaluation in Washington, D.C.
He says a hospitalist can’t be judged on his or her own but has to be seen in the context of the system in which he or she is working. Hospitalists have in-depth knowledge of the complex processes and technology special to hospital care, but their work is only part of the entire “episode of care” for a patient.
“While the physician in the hospital is highly trained to deal with the unique clinical needs of that patient, it is also important that the team treating the patient has all relevant information from all clinicians who may have treated the patient prior to the acute episode,” he says.
“It is also critical that when the patient is discharged that there is as seamless transition back to the system that will continue to care for that patient. Those handoffs may or may not be working well.”
The handoff, to and from the hospital, is one of the most risk-fraught areas for patients. So what is gained from the specialized skills of hospitalists might be lost if transitions from the hospital are not done well, Dr. Wise explains. “The hospitalist concept, while adding a new level of expertise, also increases the fragmentation of care and, therefore, can lead to some increased risk,” he says. “That risk is mitigated by well-functioning systems that can both initiate and accept the transfers.”
The use and mastery of the electronic medical record is crucial to the successful handoff, he adds.
“Another issue that is often discussed is whether, as the number of [hospital]-employed physicians increase, that will impact the medical staff’s freedom to constructively challenge hospital administration or the board concerning issues of quality and safety,” Dr. Wise says. “While this remains a theoretical issue, as the number of medical staff members employed by the hospital increase, [it is important] that their voices on the issues of quality and safety of medical care remain unimpeded.”
He also says that the speed of the growth of the hospitalist field comes with a certain amount of risk.
“The current hospitalist system attempts to assure that seriously ill patients are being treated by physicians who are current and competent in the complicated, high-tech environment of the 21st-century hospital,” he explains. “It will take time to develop a number of the supporting systems. If the speed of growth is very rapid, it is possible that the supporting systems, both inside and outside of the hospital, will not be able to keep up. None of these possible problems are insurmountable, but all will take a significant amount of attention and resources to support this method to deliver care.”
—Robert Wise, MD, medical advisor, Division of Healthcare Quality Evaluation, The Joint Commission, Washington, D.C.
Orthopedic Surgery
Older orthopedic patients are at serious risk after surgery, but their chances are improved by the work of hospitalists, says Alexandra Page, MD, a member of the American Academy of Orthopaedic Surgeons’ National Health Care Systems Committee and a surgeon with Kaiser Permanente in La Jolla, Calif., who works with geriatric patients.
A major role of hospitalists in support of orthopedic surgeons is to help patients be “as tuned up as they can be prior to surgery,” she says.
For octogenarians, there is a 25% mortality rate in the year after a hip fracture. For a nonagenarian, the one-year mortality rate is 50%.
“That’s a real high risk, and we don’t even in orthopedics have a good sense of what those factors are that make them so high-risk,” says Dr. Page, adding that it is known that optimal levels of glycemic control can minimize perioperative complications like infection.
That makes it all the more important for hospitalists to get patients into the best shape possible. After the operation, hospitalists help control blood pressure and blood sugar, and take steps to minimize post-operative delirium.
“It doesn’t affect our ability to perform the surgery at a technical level, but ultimately it gives our patients better outcomes,” Dr. Page says. “That’s really what it’s all about.”
Dr. Page’s role as an examiner for the orthopedic boards gives her insight into how different hospital systems work. She says she hopes there can be more consistency in the role that hospitalists have in helping with orthopedic surgery patients, with patients being routinely admitted through the hospitalist service. “I think there’s still a lot of variability, in terms of who’s managing these patients,” she says.
Continued below...
Family Medicine
When one of his patients is admitted to the hospital and comes under the care of a hospitalist, his involvement doesn’t end, says Glen Stream, MD, president-elect of the American Academy of Family Physicians, who works with Rockwood Clinic in Spokane, Wash.
Dr. Stream continues to keep in touch with patients, and that has made for a good working relationship with hospitalists. It helps put patients at ease and helps with handoffs to and from the hospital, he says. “I don’t think you can overcommunicate in either direction,” he says. “The most complete medical information enables the best-informed decision-making for treatment decisions.” Such levels of involvement usually are welcomed by hospitalists, he says, adding “I’ve been able to be the hospital physician’s advocate.”
Meanwhile, HM has made his office-based practice more flexible and more accessible. “In my medical group, a number of my partners actually start seeing patients [in the office] as early as seven in the morning,” Dr. Stream says. “They can commit to being there for patients at that early hour.”
He points out that handoffs to and from primary-care doctors and hospitalists has improved, but it’s still a work in progress. “I think it’s gotten better over time,” he says. “I think there’s recognition—on both sides of those handoffs—that things could be improved. I think the commitment is there both for the ambulatory physicians, the primary-care doctor, the family doctor, and the hospitalist taking care of them.”
Although hospitalists generally are better compensation than family doctors, Dr. Stream says he isn’t aware of “any friction” from family physicians. “Our academy, our members, family physicians, believe that the work that [we] do is undervalued in our current healthcare system. But that doesn’t mean that we have to compare ourselves to hospitalists,” he says.
Nursing
Even as fragmentation of medical care has increased, the emergence of the hospitalist has helped to streamline care, says Joanne Disch, PhD, RN, president-elect of the American Academy of Nursing and clinical professor at the University of Minnesota School of Nursing in Minneapolis.
“There has become such increasing fragmentation of who is the team around the patient,” she says. But, she notes, “the hospitalist really provided a mechanism to promote continuity of care.”
Nurses, she says, have found hospitalists to be “somebody who can cover your back.” “When the system works right, the nurses do not have to seek out a physician and hope that they can either grab somebody or somebody makes rounds,” Disch says, noting a general frustration amongst her peers as to a lack of clarity in regard to who’s in charge. “What hospitalists inherently do, structurally, is provide a main physician who will be the accountable one in the hospital setting. You have a named person that the nurse knows, ‘Ah, this is who I need to go to.’ ”
Although most nurses welcomed hospitalists from the very beginning, she continues, the addition of MDs into the hospital setting did cause confusion, most notably over the roles of PCPs, referring physicians, and hospitalists.
“It wasn’t clear the extent of this individual’s responsibility and how to use them effectively, but over time my sense is that people … really find this helpful,” she says.
An area that might have room for improvement is hospitalist-nurse communication, with more “huddling” and discussions at shift change. Better communication with patients’ families also could be improved, she says. “[It] gets a little confusing sometimes,” she says. “Either everybody, or nobody, is talking with the patient and the family.”
Hospital Administration
The reaction of Craig Becker, a member of the American Hospital Association board and president of the Tennessee Hospital Association, was, at first, fairly dismissive. An idea being discussed in the industry—inpatient physicians working full-time in hospitals—would not be worth it, he thought. He couldn’t get past the notion that such an arrangement would be “a waste of money,” and that if someone tried it, it would just be in the clinical-care units.
Once a couple of hospitals started hospitalist services, he was more inclined to listen. “I was getting feedback from them, and they were saying: ‘Boy, this has made a big difference, both in patient care and financially,’ ” Becker explains. Once he noticed HM programs popping up in small, rural hospitals, Becker knew “this was a movement whose time had come.”
In Tennessee, where hospitalists were almost unheard of a decade ago, hospitalists now work in every shape and size of hospital, some with fewer than 100 beds. At one hospital that employs its own hospitalist, there are just 58 beds and an attached nursing home, Becker says.
Showing that hospitalists have been worth the cost is really as simple as looking at the length of stay, he says. “If you can knock six-tenths of a day off a stay, that’s pretty significant savings,” Becker says.
Becker notes other positives the HM model has brought to Tennessee hospitals: They make the jobs of hospital administrators easier because specialists and referring physicians are happier.
“They can spend more time doing whatever they want to do on a personal basis or in their offices,” he says. “So I think just in terms of improving relationships with the medical staffs, hospitalists have been a real plus.”
Tom Collins is a freelance writer based in Florida.
Anticoagulant Rivaroxaban Clears FDA Panel Hurdle
An FDA advisory panel has recommended the approval of rivaroxaban (Xarelto) for stroke prevention in patients with non-valvular atrial fibrillation, but the panelists raised questions about the methodology of the trial that compared the drug to the gold standard, warfarin (Coumadin).
A final decision on the drug is expected in November.
Rivaroxaban has been developed as a once-a-day oral medication that prevents clotting by inhibiting factor Xa, a key component in the generation of thrombin. It is one medication in a line of drugs trying to position themselves to replace warfarin, which has many contraindications and requires frequent blood draws for monitoring; the new drugs would not require frequent blood draws.
Panelists questioned whether ROCKET-AF—the trial that compared rivaroxaban to warfarin—was sufficient to show noninferiority, as only 55% of the patients on warfarin had international normalized ratio (INR) levels needed for stroke prevention.
Ian Jenkins, MD, assistant professor in the division of hospital medicine at the University of California at San Diego, says that rivaroxaban “will be an option for AF, but probably not my first choice.”
Another oral warfarin alternative—dabigatran, which inhibits thrombin—is already available, he notes. And dabigatran was found to be superior to warfarin, while rivaroxaban was only found to be noninferior. But Dr. Jenkins also notes that dabigatran and rivaroxaban have not been compared head-to-head.
“The low percent of therapeutic INRs in ROCKET-AF does concern me,” Dr. Jenkins adds, “but we have to remember that the patients who will benefit the most from these medications are the ones with difficult-to-control INRs anyway.”
He also explains that patients now doing well on warfarin don’t have a “great reason” to boost their costs by trying another drug.
An FDA advisory panel has recommended the approval of rivaroxaban (Xarelto) for stroke prevention in patients with non-valvular atrial fibrillation, but the panelists raised questions about the methodology of the trial that compared the drug to the gold standard, warfarin (Coumadin).
A final decision on the drug is expected in November.
Rivaroxaban has been developed as a once-a-day oral medication that prevents clotting by inhibiting factor Xa, a key component in the generation of thrombin. It is one medication in a line of drugs trying to position themselves to replace warfarin, which has many contraindications and requires frequent blood draws for monitoring; the new drugs would not require frequent blood draws.
Panelists questioned whether ROCKET-AF—the trial that compared rivaroxaban to warfarin—was sufficient to show noninferiority, as only 55% of the patients on warfarin had international normalized ratio (INR) levels needed for stroke prevention.
Ian Jenkins, MD, assistant professor in the division of hospital medicine at the University of California at San Diego, says that rivaroxaban “will be an option for AF, but probably not my first choice.”
Another oral warfarin alternative—dabigatran, which inhibits thrombin—is already available, he notes. And dabigatran was found to be superior to warfarin, while rivaroxaban was only found to be noninferior. But Dr. Jenkins also notes that dabigatran and rivaroxaban have not been compared head-to-head.
“The low percent of therapeutic INRs in ROCKET-AF does concern me,” Dr. Jenkins adds, “but we have to remember that the patients who will benefit the most from these medications are the ones with difficult-to-control INRs anyway.”
He also explains that patients now doing well on warfarin don’t have a “great reason” to boost their costs by trying another drug.
An FDA advisory panel has recommended the approval of rivaroxaban (Xarelto) for stroke prevention in patients with non-valvular atrial fibrillation, but the panelists raised questions about the methodology of the trial that compared the drug to the gold standard, warfarin (Coumadin).
A final decision on the drug is expected in November.
Rivaroxaban has been developed as a once-a-day oral medication that prevents clotting by inhibiting factor Xa, a key component in the generation of thrombin. It is one medication in a line of drugs trying to position themselves to replace warfarin, which has many contraindications and requires frequent blood draws for monitoring; the new drugs would not require frequent blood draws.
Panelists questioned whether ROCKET-AF—the trial that compared rivaroxaban to warfarin—was sufficient to show noninferiority, as only 55% of the patients on warfarin had international normalized ratio (INR) levels needed for stroke prevention.
Ian Jenkins, MD, assistant professor in the division of hospital medicine at the University of California at San Diego, says that rivaroxaban “will be an option for AF, but probably not my first choice.”
Another oral warfarin alternative—dabigatran, which inhibits thrombin—is already available, he notes. And dabigatran was found to be superior to warfarin, while rivaroxaban was only found to be noninferior. But Dr. Jenkins also notes that dabigatran and rivaroxaban have not been compared head-to-head.
“The low percent of therapeutic INRs in ROCKET-AF does concern me,” Dr. Jenkins adds, “but we have to remember that the patients who will benefit the most from these medications are the ones with difficult-to-control INRs anyway.”
He also explains that patients now doing well on warfarin don’t have a “great reason” to boost their costs by trying another drug.
Conglomerate HM?
William Geers, MD, finished up his residency in 2007, then went to work for a close-knit emergency-medicine group of about 25 doctors in Daytona Beach, Fla.
“Everybody was pretty tight,” he says of his first job.
He had met his wife in residency in Daytona, but after a while, they figured it was time for a change. “We’d been in Daytona for about six years and were ready to go try someplace different,” Dr. Geers says. “Tallahassee seemed like a good match because that’s kind of right in between our families.”
He soon landed a hospitalist job at Capital Regional Medical Center, and he suddenly was a part of EmCare, one of the biggest corporations in the emergency-medicine field and, more recently, in the field of hospital medicine. EmCare provides doctors to about 400 hospitals nationwide.
Dr. Geers said the corporate affiliation didn’t factor into his decision, adding that he took more of a traditional approach when choosing a new job.
“At the time, this program was a little bit smaller, which I liked,” says Dr. Geers, who also looked at the city’s other hospital, Tallahassee Memorial. “I met some of the physicians over here. I liked them.”
But he has noticed perks.
“I think we have some advantages working with EmCare in that we do have a pretty big group that’s backing us,” he explains. “I feel a little more secure with issues like malpractice. If things like that ever come up, I really feel like I have a lot of support with EmCare.”
With the corporate presence on the rise in HM, more and more hospitalists are entering the ranks of large companies. Some are doing so straight out of residency. Some are giving up their private practices and selling them to corporations looking to expand.
Corporations that provide hospitalists to hospitals are getting ever bigger, using sophisticated infrastructure and economies of scale, they say, to make life easier for the people who work for them, allowing the hospitalists to focus on patient care. Their efficiencies are attractive to hospitals looking to simplify.
Three years ago, North Hollywood, Calif.-based IPC: The Hospitalist Company became a publicly traded company. Its stock price has more than doubled since then.
In July, Eagle Hospital Physicians acquired North Carolina-based PrimeDoc and its 100 doctors covering seven hospitals. Similar acquisitions by larger corporations have become almost weekly news.
And, probably most significantly, Cogent Healthcare recently completed a merger with Hospitalists Management Group, a union of two of the biggest hospitalist companies in the U.S. The new company, Cogent HMG, now includes a corps of 1,000 doctors, nurses, and physician assistants (PAs), with client hospitals in 28 states.
Cogent had clients that were medium to large in size, generally in more urban areas but scattered geographically. HMG mostly served small- to medium-sized hospitals with densities in certain regions. With the merger came a recognition that the larger a company becomes, the greater the opportunity for efficiency and better services, says Rusty Holman, MD, MHM, chief clinical officer of the new company.
“The real value out of bringing these two companies together is bringing the best of different worlds together, creating new products and services for hospitals that don’t exist today, and to be able to serve a broader customer base,” says Dr. Holman, a former SHM president. “It’s also to leverage some of the infrastructure that has been built over a greater number of programs and hospitals to gain efficiency and scale that way. So that is the primary focus of the integration today.”
Cogent HMG CEO Steve Houff, MD, says the merger will mean investment in clinical support, physician recruiting, and technology, and will benefit patients and hospital partners alike.
“Both Cogent and HMG have a track record for delivering improvements in clinical quality and patient satisfaction at each of the hospitals we serve. The plan is for that to continue on a broader scale,” he wrote in an email to The Hospitalist.

—R. Jeffrey Taylor, president, chief operating officer, IPC: The Hospitalist Company, North Hollywood, Calif.
The Good, the Bad, the Oligopoly
The average size of a hospitalist group in the U.S. is about 10 full-time equivalents, according to recent survey data from SHM and MGMA. With the swelling of the size of HM’s biggest corporate players comes the question of how far the coalescing will go: Will most patient care eventually be provided by only a few groups?
R. Jeffrey Taylor, IPC’s president and chief operating officer, says the mergers and acquisitions will continue, but he doesn’t see a day when there will be just a few titans ruling all.
“I do think there will be more consolidation going forward than there is now, but I don’t see a future in which there are, you know, two or three groups that completely dominate the landscape,” he says. “There’s always that concern that that’s going to happen in the hospital industry, or that’s going to happen with payors. And there are always new entrants.”
For all the movement toward bigger companies, “this is still an unconsolidated industry,” and new physician practices will always continue to be formed, he says.
“We’re the largest group, and we’re maybe 3 1/2 percent of all the hospitals in the country. I wouldn’t consider this, today, a terribly consolidated industry,” he adds. “I do think it will move in that direction. I just don’t think it will get all the way there, because of the sort of private, entrepreneurial, independent spirit that’s common among physicians.”
Mike Tarwater, a board member of the American Hospital Association, says private hospitalist providers will only be an alternative to—and not a replacement provider for—large, self-contained systems like the Carolinas Medical Center (CMC), for which he serves as CEO. The health system has a wide spectrum of facilities—from large, urban academic centers like the 874-bed medical center in Charlotte, N.C., to 52-bed Anson Community Hospital in Wadesboro, N.C., population 5,780.
“As a system, we have the wherewithal and the recruiting expertise, and, with 1,700 physician associates across the system, we’ve kind of got critical mass,” Tarwater says. “So we will be an alternative to that in our region.”
Frank Michota, MD, FHM, director of academic affairs in the Department of Hospital Medicine at The Cleveland Clinic, says that the extensive training programs of many of the larger hospitalist groups (e.g. Cogent Academy, IPC’s extensive onboarding process and leadership conferences) could be a very good thing for the field.
“I have always thought that companies like Cogent did a very nice job in orienting their hospitalists to the patient-care goals and the process variables that were being measured,” Dr. Michota says. “I think that by making an even larger group, they have the opportunity to continue to standardize the approach to hospital care so that one hospitalist equals one hospitalist equals one hospitalist. I think that’s a positive.”
The flip side, though, is that anything that might be done wrong would be magnified in such a system.
“I think that there are some dangers in how these large companies will incentivize their hospitalists,” he adds. “If they are consistent from hospitalist to hospitalist, but if there’s a perverse adverse effect from one of their financial incentives, it will be carried out across a lot of hospitals all at the same time. “But I think it’s a little early to tell what the impact of this might be. But, at least for right now, it’s actually a positive thing because it standardizes the hospitalist.”
Tarwater says that even when larger corporations buy smaller practices, familiarity tends to remain.
“Most of what I have seen are existing groups that join through merger or acquisition, and so we already have experience with the doctors, we already have long-standing relationships with the doctors,” he says. “I think any health system or hospital would be reticent to sign up with somebody that they’ve never heard of, that doesn’t have a track record, or that they don’t know already at least some of the players.” Hospitals looking to hire a private company have to exercise caution, particularly if the company is trying to break into a new region where it isn’t known.
“Those hospitals and healthcare systems just have to be really careful who they’re signing contracts with,” he said. “It’s no different than anything else we do. You just have to know who your partners are, and what drives them and where they stand on important issues.”
Executives say patient care is not at risk, even as consolidation continues. “With or without competition, we are relentlessly trying to improve our approach to patient care, our performance, and our hospital partnerships,” Cogent HMG’s Dr. Houff says.
Money Talks
It doesn’t appear that more hospitalist companies are planning to go public—at least for now.
The largest privately held company, Cogent HMG, is not planning an initial public offering anytime soon, Dr. Houff says. The company’s goal is to “continue investing in smart growth to capture more of the hospital medicine market, expand offerings to our existing hospital clients, and provide additional support to our clinical teams on the ground,” he says. “We have a strong capital partner to help us in that effort and are not looking at the public markets at this time.”
Taking on stockholders is a tricky business—one that requires careful planning and a willingness from practice leaders and administrators to relinquish some autonomy to outside interests. And then there are the financial requirements.
“They’ve really got to be able to produce some serious revenue in order for somebody to be willing to put some money into them,” says Mark Hamm, CEO of EmCare Inpatient Services.
The lure of working for a private hospitalist company promises to continue to be an attractive one. Some are drawn by the leadership possibilities—those who “aspire to be the true alpha doctor,” as IPC’s Taylor puts it. Others are drawn by the stability of a larger company.
There also is flexibility in location, Dr. Holman notes.
“Now, with Cogent HMG, [hospitalists] have even more choices in terms of relocating within the same company,” he says. “So they can keep all of the benefits, keep all of the knowledge and familiarity of the system and philosophy of care that we employ, and just be able to transfer.”
continued below...
Dr. Houff says the majority of newly recruited physicians are coming out of residency but that the company is attracting physicians in the middle of their careers, along with physicians having backgrounds beyond internal medicine.
In Tallahassee at Capital Regional, Dr. Geers says that he feels there is support from the company that can protect his job quality, with “a little bit more room to negotiate with the hospital if the hospital wants us to take on new responsibilities.
“Whereas if we worked directly for the hospital, I don’t think we’d have much say in the matter,” he says.
He also says he is happy with the predictable schedule; he’s responsible for 7 a.m. to 7 p.m. and nothing more.
“If you’re finished rounding and you’ve seen all your patients and tied up all your loose ends, you’re not always there till 7 p.m.,” he points out. “Sometimes you can leave a little early....Once 7 p.m. comes, you’re not going to get paged in the middle of the night.”
Thomas R. Collins is a freelance medical writer based in Florida.
William Geers, MD, finished up his residency in 2007, then went to work for a close-knit emergency-medicine group of about 25 doctors in Daytona Beach, Fla.
“Everybody was pretty tight,” he says of his first job.
He had met his wife in residency in Daytona, but after a while, they figured it was time for a change. “We’d been in Daytona for about six years and were ready to go try someplace different,” Dr. Geers says. “Tallahassee seemed like a good match because that’s kind of right in between our families.”
He soon landed a hospitalist job at Capital Regional Medical Center, and he suddenly was a part of EmCare, one of the biggest corporations in the emergency-medicine field and, more recently, in the field of hospital medicine. EmCare provides doctors to about 400 hospitals nationwide.
Dr. Geers said the corporate affiliation didn’t factor into his decision, adding that he took more of a traditional approach when choosing a new job.
“At the time, this program was a little bit smaller, which I liked,” says Dr. Geers, who also looked at the city’s other hospital, Tallahassee Memorial. “I met some of the physicians over here. I liked them.”
But he has noticed perks.
“I think we have some advantages working with EmCare in that we do have a pretty big group that’s backing us,” he explains. “I feel a little more secure with issues like malpractice. If things like that ever come up, I really feel like I have a lot of support with EmCare.”
With the corporate presence on the rise in HM, more and more hospitalists are entering the ranks of large companies. Some are doing so straight out of residency. Some are giving up their private practices and selling them to corporations looking to expand.
Corporations that provide hospitalists to hospitals are getting ever bigger, using sophisticated infrastructure and economies of scale, they say, to make life easier for the people who work for them, allowing the hospitalists to focus on patient care. Their efficiencies are attractive to hospitals looking to simplify.
Three years ago, North Hollywood, Calif.-based IPC: The Hospitalist Company became a publicly traded company. Its stock price has more than doubled since then.
In July, Eagle Hospital Physicians acquired North Carolina-based PrimeDoc and its 100 doctors covering seven hospitals. Similar acquisitions by larger corporations have become almost weekly news.
And, probably most significantly, Cogent Healthcare recently completed a merger with Hospitalists Management Group, a union of two of the biggest hospitalist companies in the U.S. The new company, Cogent HMG, now includes a corps of 1,000 doctors, nurses, and physician assistants (PAs), with client hospitals in 28 states.
Cogent had clients that were medium to large in size, generally in more urban areas but scattered geographically. HMG mostly served small- to medium-sized hospitals with densities in certain regions. With the merger came a recognition that the larger a company becomes, the greater the opportunity for efficiency and better services, says Rusty Holman, MD, MHM, chief clinical officer of the new company.
“The real value out of bringing these two companies together is bringing the best of different worlds together, creating new products and services for hospitals that don’t exist today, and to be able to serve a broader customer base,” says Dr. Holman, a former SHM president. “It’s also to leverage some of the infrastructure that has been built over a greater number of programs and hospitals to gain efficiency and scale that way. So that is the primary focus of the integration today.”
Cogent HMG CEO Steve Houff, MD, says the merger will mean investment in clinical support, physician recruiting, and technology, and will benefit patients and hospital partners alike.
“Both Cogent and HMG have a track record for delivering improvements in clinical quality and patient satisfaction at each of the hospitals we serve. The plan is for that to continue on a broader scale,” he wrote in an email to The Hospitalist.

—R. Jeffrey Taylor, president, chief operating officer, IPC: The Hospitalist Company, North Hollywood, Calif.
The Good, the Bad, the Oligopoly
The average size of a hospitalist group in the U.S. is about 10 full-time equivalents, according to recent survey data from SHM and MGMA. With the swelling of the size of HM’s biggest corporate players comes the question of how far the coalescing will go: Will most patient care eventually be provided by only a few groups?
R. Jeffrey Taylor, IPC’s president and chief operating officer, says the mergers and acquisitions will continue, but he doesn’t see a day when there will be just a few titans ruling all.
“I do think there will be more consolidation going forward than there is now, but I don’t see a future in which there are, you know, two or three groups that completely dominate the landscape,” he says. “There’s always that concern that that’s going to happen in the hospital industry, or that’s going to happen with payors. And there are always new entrants.”
For all the movement toward bigger companies, “this is still an unconsolidated industry,” and new physician practices will always continue to be formed, he says.
“We’re the largest group, and we’re maybe 3 1/2 percent of all the hospitals in the country. I wouldn’t consider this, today, a terribly consolidated industry,” he adds. “I do think it will move in that direction. I just don’t think it will get all the way there, because of the sort of private, entrepreneurial, independent spirit that’s common among physicians.”
Mike Tarwater, a board member of the American Hospital Association, says private hospitalist providers will only be an alternative to—and not a replacement provider for—large, self-contained systems like the Carolinas Medical Center (CMC), for which he serves as CEO. The health system has a wide spectrum of facilities—from large, urban academic centers like the 874-bed medical center in Charlotte, N.C., to 52-bed Anson Community Hospital in Wadesboro, N.C., population 5,780.
“As a system, we have the wherewithal and the recruiting expertise, and, with 1,700 physician associates across the system, we’ve kind of got critical mass,” Tarwater says. “So we will be an alternative to that in our region.”
Frank Michota, MD, FHM, director of academic affairs in the Department of Hospital Medicine at The Cleveland Clinic, says that the extensive training programs of many of the larger hospitalist groups (e.g. Cogent Academy, IPC’s extensive onboarding process and leadership conferences) could be a very good thing for the field.
“I have always thought that companies like Cogent did a very nice job in orienting their hospitalists to the patient-care goals and the process variables that were being measured,” Dr. Michota says. “I think that by making an even larger group, they have the opportunity to continue to standardize the approach to hospital care so that one hospitalist equals one hospitalist equals one hospitalist. I think that’s a positive.”
The flip side, though, is that anything that might be done wrong would be magnified in such a system.
“I think that there are some dangers in how these large companies will incentivize their hospitalists,” he adds. “If they are consistent from hospitalist to hospitalist, but if there’s a perverse adverse effect from one of their financial incentives, it will be carried out across a lot of hospitals all at the same time. “But I think it’s a little early to tell what the impact of this might be. But, at least for right now, it’s actually a positive thing because it standardizes the hospitalist.”
Tarwater says that even when larger corporations buy smaller practices, familiarity tends to remain.
“Most of what I have seen are existing groups that join through merger or acquisition, and so we already have experience with the doctors, we already have long-standing relationships with the doctors,” he says. “I think any health system or hospital would be reticent to sign up with somebody that they’ve never heard of, that doesn’t have a track record, or that they don’t know already at least some of the players.” Hospitals looking to hire a private company have to exercise caution, particularly if the company is trying to break into a new region where it isn’t known.
“Those hospitals and healthcare systems just have to be really careful who they’re signing contracts with,” he said. “It’s no different than anything else we do. You just have to know who your partners are, and what drives them and where they stand on important issues.”
Executives say patient care is not at risk, even as consolidation continues. “With or without competition, we are relentlessly trying to improve our approach to patient care, our performance, and our hospital partnerships,” Cogent HMG’s Dr. Houff says.
Money Talks
It doesn’t appear that more hospitalist companies are planning to go public—at least for now.
The largest privately held company, Cogent HMG, is not planning an initial public offering anytime soon, Dr. Houff says. The company’s goal is to “continue investing in smart growth to capture more of the hospital medicine market, expand offerings to our existing hospital clients, and provide additional support to our clinical teams on the ground,” he says. “We have a strong capital partner to help us in that effort and are not looking at the public markets at this time.”
Taking on stockholders is a tricky business—one that requires careful planning and a willingness from practice leaders and administrators to relinquish some autonomy to outside interests. And then there are the financial requirements.
“They’ve really got to be able to produce some serious revenue in order for somebody to be willing to put some money into them,” says Mark Hamm, CEO of EmCare Inpatient Services.
The lure of working for a private hospitalist company promises to continue to be an attractive one. Some are drawn by the leadership possibilities—those who “aspire to be the true alpha doctor,” as IPC’s Taylor puts it. Others are drawn by the stability of a larger company.
There also is flexibility in location, Dr. Holman notes.
“Now, with Cogent HMG, [hospitalists] have even more choices in terms of relocating within the same company,” he says. “So they can keep all of the benefits, keep all of the knowledge and familiarity of the system and philosophy of care that we employ, and just be able to transfer.”
continued below...
Dr. Houff says the majority of newly recruited physicians are coming out of residency but that the company is attracting physicians in the middle of their careers, along with physicians having backgrounds beyond internal medicine.
In Tallahassee at Capital Regional, Dr. Geers says that he feels there is support from the company that can protect his job quality, with “a little bit more room to negotiate with the hospital if the hospital wants us to take on new responsibilities.
“Whereas if we worked directly for the hospital, I don’t think we’d have much say in the matter,” he says.
He also says he is happy with the predictable schedule; he’s responsible for 7 a.m. to 7 p.m. and nothing more.
“If you’re finished rounding and you’ve seen all your patients and tied up all your loose ends, you’re not always there till 7 p.m.,” he points out. “Sometimes you can leave a little early....Once 7 p.m. comes, you’re not going to get paged in the middle of the night.”
Thomas R. Collins is a freelance medical writer based in Florida.
William Geers, MD, finished up his residency in 2007, then went to work for a close-knit emergency-medicine group of about 25 doctors in Daytona Beach, Fla.
“Everybody was pretty tight,” he says of his first job.
He had met his wife in residency in Daytona, but after a while, they figured it was time for a change. “We’d been in Daytona for about six years and were ready to go try someplace different,” Dr. Geers says. “Tallahassee seemed like a good match because that’s kind of right in between our families.”
He soon landed a hospitalist job at Capital Regional Medical Center, and he suddenly was a part of EmCare, one of the biggest corporations in the emergency-medicine field and, more recently, in the field of hospital medicine. EmCare provides doctors to about 400 hospitals nationwide.
Dr. Geers said the corporate affiliation didn’t factor into his decision, adding that he took more of a traditional approach when choosing a new job.
“At the time, this program was a little bit smaller, which I liked,” says Dr. Geers, who also looked at the city’s other hospital, Tallahassee Memorial. “I met some of the physicians over here. I liked them.”
But he has noticed perks.
“I think we have some advantages working with EmCare in that we do have a pretty big group that’s backing us,” he explains. “I feel a little more secure with issues like malpractice. If things like that ever come up, I really feel like I have a lot of support with EmCare.”
With the corporate presence on the rise in HM, more and more hospitalists are entering the ranks of large companies. Some are doing so straight out of residency. Some are giving up their private practices and selling them to corporations looking to expand.
Corporations that provide hospitalists to hospitals are getting ever bigger, using sophisticated infrastructure and economies of scale, they say, to make life easier for the people who work for them, allowing the hospitalists to focus on patient care. Their efficiencies are attractive to hospitals looking to simplify.
Three years ago, North Hollywood, Calif.-based IPC: The Hospitalist Company became a publicly traded company. Its stock price has more than doubled since then.
In July, Eagle Hospital Physicians acquired North Carolina-based PrimeDoc and its 100 doctors covering seven hospitals. Similar acquisitions by larger corporations have become almost weekly news.
And, probably most significantly, Cogent Healthcare recently completed a merger with Hospitalists Management Group, a union of two of the biggest hospitalist companies in the U.S. The new company, Cogent HMG, now includes a corps of 1,000 doctors, nurses, and physician assistants (PAs), with client hospitals in 28 states.
Cogent had clients that were medium to large in size, generally in more urban areas but scattered geographically. HMG mostly served small- to medium-sized hospitals with densities in certain regions. With the merger came a recognition that the larger a company becomes, the greater the opportunity for efficiency and better services, says Rusty Holman, MD, MHM, chief clinical officer of the new company.
“The real value out of bringing these two companies together is bringing the best of different worlds together, creating new products and services for hospitals that don’t exist today, and to be able to serve a broader customer base,” says Dr. Holman, a former SHM president. “It’s also to leverage some of the infrastructure that has been built over a greater number of programs and hospitals to gain efficiency and scale that way. So that is the primary focus of the integration today.”
Cogent HMG CEO Steve Houff, MD, says the merger will mean investment in clinical support, physician recruiting, and technology, and will benefit patients and hospital partners alike.
“Both Cogent and HMG have a track record for delivering improvements in clinical quality and patient satisfaction at each of the hospitals we serve. The plan is for that to continue on a broader scale,” he wrote in an email to The Hospitalist.

—R. Jeffrey Taylor, president, chief operating officer, IPC: The Hospitalist Company, North Hollywood, Calif.
The Good, the Bad, the Oligopoly
The average size of a hospitalist group in the U.S. is about 10 full-time equivalents, according to recent survey data from SHM and MGMA. With the swelling of the size of HM’s biggest corporate players comes the question of how far the coalescing will go: Will most patient care eventually be provided by only a few groups?
R. Jeffrey Taylor, IPC’s president and chief operating officer, says the mergers and acquisitions will continue, but he doesn’t see a day when there will be just a few titans ruling all.
“I do think there will be more consolidation going forward than there is now, but I don’t see a future in which there are, you know, two or three groups that completely dominate the landscape,” he says. “There’s always that concern that that’s going to happen in the hospital industry, or that’s going to happen with payors. And there are always new entrants.”
For all the movement toward bigger companies, “this is still an unconsolidated industry,” and new physician practices will always continue to be formed, he says.
“We’re the largest group, and we’re maybe 3 1/2 percent of all the hospitals in the country. I wouldn’t consider this, today, a terribly consolidated industry,” he adds. “I do think it will move in that direction. I just don’t think it will get all the way there, because of the sort of private, entrepreneurial, independent spirit that’s common among physicians.”
Mike Tarwater, a board member of the American Hospital Association, says private hospitalist providers will only be an alternative to—and not a replacement provider for—large, self-contained systems like the Carolinas Medical Center (CMC), for which he serves as CEO. The health system has a wide spectrum of facilities—from large, urban academic centers like the 874-bed medical center in Charlotte, N.C., to 52-bed Anson Community Hospital in Wadesboro, N.C., population 5,780.
“As a system, we have the wherewithal and the recruiting expertise, and, with 1,700 physician associates across the system, we’ve kind of got critical mass,” Tarwater says. “So we will be an alternative to that in our region.”
Frank Michota, MD, FHM, director of academic affairs in the Department of Hospital Medicine at The Cleveland Clinic, says that the extensive training programs of many of the larger hospitalist groups (e.g. Cogent Academy, IPC’s extensive onboarding process and leadership conferences) could be a very good thing for the field.
“I have always thought that companies like Cogent did a very nice job in orienting their hospitalists to the patient-care goals and the process variables that were being measured,” Dr. Michota says. “I think that by making an even larger group, they have the opportunity to continue to standardize the approach to hospital care so that one hospitalist equals one hospitalist equals one hospitalist. I think that’s a positive.”
The flip side, though, is that anything that might be done wrong would be magnified in such a system.
“I think that there are some dangers in how these large companies will incentivize their hospitalists,” he adds. “If they are consistent from hospitalist to hospitalist, but if there’s a perverse adverse effect from one of their financial incentives, it will be carried out across a lot of hospitals all at the same time. “But I think it’s a little early to tell what the impact of this might be. But, at least for right now, it’s actually a positive thing because it standardizes the hospitalist.”
Tarwater says that even when larger corporations buy smaller practices, familiarity tends to remain.
“Most of what I have seen are existing groups that join through merger or acquisition, and so we already have experience with the doctors, we already have long-standing relationships with the doctors,” he says. “I think any health system or hospital would be reticent to sign up with somebody that they’ve never heard of, that doesn’t have a track record, or that they don’t know already at least some of the players.” Hospitals looking to hire a private company have to exercise caution, particularly if the company is trying to break into a new region where it isn’t known.
“Those hospitals and healthcare systems just have to be really careful who they’re signing contracts with,” he said. “It’s no different than anything else we do. You just have to know who your partners are, and what drives them and where they stand on important issues.”
Executives say patient care is not at risk, even as consolidation continues. “With or without competition, we are relentlessly trying to improve our approach to patient care, our performance, and our hospital partnerships,” Cogent HMG’s Dr. Houff says.
Money Talks
It doesn’t appear that more hospitalist companies are planning to go public—at least for now.
The largest privately held company, Cogent HMG, is not planning an initial public offering anytime soon, Dr. Houff says. The company’s goal is to “continue investing in smart growth to capture more of the hospital medicine market, expand offerings to our existing hospital clients, and provide additional support to our clinical teams on the ground,” he says. “We have a strong capital partner to help us in that effort and are not looking at the public markets at this time.”
Taking on stockholders is a tricky business—one that requires careful planning and a willingness from practice leaders and administrators to relinquish some autonomy to outside interests. And then there are the financial requirements.
“They’ve really got to be able to produce some serious revenue in order for somebody to be willing to put some money into them,” says Mark Hamm, CEO of EmCare Inpatient Services.
The lure of working for a private hospitalist company promises to continue to be an attractive one. Some are drawn by the leadership possibilities—those who “aspire to be the true alpha doctor,” as IPC’s Taylor puts it. Others are drawn by the stability of a larger company.
There also is flexibility in location, Dr. Holman notes.
“Now, with Cogent HMG, [hospitalists] have even more choices in terms of relocating within the same company,” he says. “So they can keep all of the benefits, keep all of the knowledge and familiarity of the system and philosophy of care that we employ, and just be able to transfer.”
continued below...
Dr. Houff says the majority of newly recruited physicians are coming out of residency but that the company is attracting physicians in the middle of their careers, along with physicians having backgrounds beyond internal medicine.
In Tallahassee at Capital Regional, Dr. Geers says that he feels there is support from the company that can protect his job quality, with “a little bit more room to negotiate with the hospital if the hospital wants us to take on new responsibilities.
“Whereas if we worked directly for the hospital, I don’t think we’d have much say in the matter,” he says.
He also says he is happy with the predictable schedule; he’s responsible for 7 a.m. to 7 p.m. and nothing more.
“If you’re finished rounding and you’ve seen all your patients and tied up all your loose ends, you’re not always there till 7 p.m.,” he points out. “Sometimes you can leave a little early....Once 7 p.m. comes, you’re not going to get paged in the middle of the night.”
Thomas R. Collins is a freelance medical writer based in Florida.
ONLINE EXCLUSIVE: Emergency Medicine Companies Venture into Hospital Medicine
Hollywood, Fla.-based Hospital Physician Partners (HPP) was an ED business when opportunity came knocking: Hospital administrators started asking, “Can you provide us with some hospitalists to go with our emergency-room doctors?”
Today, HPP is firmly in the HM business—and all signs point toward more hospitals hiring companies to handle both emergency care and inpatient care.
“In many ways, we expanded our efforts into hospitalist medicine as a result of requests from our hospital partners,” says Ed Weinberg, HPP’s chief operating officer. “Their needs were such that they asked us to provide hospital medicine services. So from that, it became clear that it was an area that was really growing. And that is something we are pursuing as vigorously as we are emergency medicine.”
HPP handling both emergency care and hospital medicine can help with the transition of patients from the ED to a hospital bed upstairs, he says.
“That’s where our efficiencies are, because we have physicians working who are carrying out the same philosophy,” he says.
Out of HPP’s 120 contracts, 15 are in hospital medicine. But the HM contract numbers are growing quickly, Weinberg notes.
EmCare has about 400 emergency-medicine programs and more than 50 HM programs, according to Mark Hamm, CEO of EmCare Inpatient Services. He says that it can be much more cost effective to contract with one company for both hospitalist and ED services, something hospitals find attractive.
EmCare service agreements range from completely separate emergency and HM staffs to small, rural hospitals where ED physicians also do rounds. Some hospitals “just don’t have the money for a full-time hospitalist and don’t really need one,” Hamm says.
The patient transitions tend to go more smoothly when both types of care are provided by EmCare, he adds. If they’re not, there can be slowdowns.
“Our goal is to quickly and appropriately move patients through the system,” he says. “If we have a hospitalist provider that’s not really on the same page, that can create bottlenecks. But it’s a blip. Our goal is to sit down, even if it’s not an EmCare hospitalist, to sit down with that director and say, ‘Hey look, let’s be the leader here, let’s work together and appropriately expedite these patients.’ We do the same thing on the hospitalist side.”
Inpatient care promises to be a big part of their future business, the executives agreed.
“Hospital medicine,” Weinberg says, “is growing by leaps and bounds.”
Hollywood, Fla.-based Hospital Physician Partners (HPP) was an ED business when opportunity came knocking: Hospital administrators started asking, “Can you provide us with some hospitalists to go with our emergency-room doctors?”
Today, HPP is firmly in the HM business—and all signs point toward more hospitals hiring companies to handle both emergency care and inpatient care.
“In many ways, we expanded our efforts into hospitalist medicine as a result of requests from our hospital partners,” says Ed Weinberg, HPP’s chief operating officer. “Their needs were such that they asked us to provide hospital medicine services. So from that, it became clear that it was an area that was really growing. And that is something we are pursuing as vigorously as we are emergency medicine.”
HPP handling both emergency care and hospital medicine can help with the transition of patients from the ED to a hospital bed upstairs, he says.
“That’s where our efficiencies are, because we have physicians working who are carrying out the same philosophy,” he says.
Out of HPP’s 120 contracts, 15 are in hospital medicine. But the HM contract numbers are growing quickly, Weinberg notes.
EmCare has about 400 emergency-medicine programs and more than 50 HM programs, according to Mark Hamm, CEO of EmCare Inpatient Services. He says that it can be much more cost effective to contract with one company for both hospitalist and ED services, something hospitals find attractive.
EmCare service agreements range from completely separate emergency and HM staffs to small, rural hospitals where ED physicians also do rounds. Some hospitals “just don’t have the money for a full-time hospitalist and don’t really need one,” Hamm says.
The patient transitions tend to go more smoothly when both types of care are provided by EmCare, he adds. If they’re not, there can be slowdowns.
“Our goal is to quickly and appropriately move patients through the system,” he says. “If we have a hospitalist provider that’s not really on the same page, that can create bottlenecks. But it’s a blip. Our goal is to sit down, even if it’s not an EmCare hospitalist, to sit down with that director and say, ‘Hey look, let’s be the leader here, let’s work together and appropriately expedite these patients.’ We do the same thing on the hospitalist side.”
Inpatient care promises to be a big part of their future business, the executives agreed.
“Hospital medicine,” Weinberg says, “is growing by leaps and bounds.”
Hollywood, Fla.-based Hospital Physician Partners (HPP) was an ED business when opportunity came knocking: Hospital administrators started asking, “Can you provide us with some hospitalists to go with our emergency-room doctors?”
Today, HPP is firmly in the HM business—and all signs point toward more hospitals hiring companies to handle both emergency care and inpatient care.
“In many ways, we expanded our efforts into hospitalist medicine as a result of requests from our hospital partners,” says Ed Weinberg, HPP’s chief operating officer. “Their needs were such that they asked us to provide hospital medicine services. So from that, it became clear that it was an area that was really growing. And that is something we are pursuing as vigorously as we are emergency medicine.”
HPP handling both emergency care and hospital medicine can help with the transition of patients from the ED to a hospital bed upstairs, he says.
“That’s where our efficiencies are, because we have physicians working who are carrying out the same philosophy,” he says.
Out of HPP’s 120 contracts, 15 are in hospital medicine. But the HM contract numbers are growing quickly, Weinberg notes.
EmCare has about 400 emergency-medicine programs and more than 50 HM programs, according to Mark Hamm, CEO of EmCare Inpatient Services. He says that it can be much more cost effective to contract with one company for both hospitalist and ED services, something hospitals find attractive.
EmCare service agreements range from completely separate emergency and HM staffs to small, rural hospitals where ED physicians also do rounds. Some hospitals “just don’t have the money for a full-time hospitalist and don’t really need one,” Hamm says.
The patient transitions tend to go more smoothly when both types of care are provided by EmCare, he adds. If they’re not, there can be slowdowns.
“Our goal is to quickly and appropriately move patients through the system,” he says. “If we have a hospitalist provider that’s not really on the same page, that can create bottlenecks. But it’s a blip. Our goal is to sit down, even if it’s not an EmCare hospitalist, to sit down with that director and say, ‘Hey look, let’s be the leader here, let’s work together and appropriately expedite these patients.’ We do the same thing on the hospitalist side.”
Inpatient care promises to be a big part of their future business, the executives agreed.
“Hospital medicine,” Weinberg says, “is growing by leaps and bounds.”