User login
Dietary supplements hyped as LDL cholesterol lowering are a bust: SPORT
in a randomized trial of adults without cardiovascular disease but at increased cardiovascular risk.
In contrast, those who took the low dose of a high-potency statin in the eight-arm comparative study showed a significant 38% drop in LDL cholesterol levels over 28 days, a performance that blew away the six supplements containing fish oil, cinnamon, garlic, turmeric, plant sterols, or red yeast rice.
The supplements showed little or no effect on any measured lipid biomarkers, which also included total cholesterol and triglycerides, or C-reactive protein (CRP), which reflects systemic inflammation.
The findings undercut the widespread heart-health marketing claims for such supplements and could potentially restore faith in statins for the many patients looking for alternatives, researchers say.
“We all see patients that have their medication lists littered with dietary supplements,” observed Luke J. Laffin, MD, of the Cleveland Clinic Foundation. And it’s more than just heart patients who use them.
Almost $50 billion is spent on dietary supplements annually in the United States, and recent data suggest that more than three-fourths of the population use them, 18% of those based on specious heart-health claims, Dr. Laffin said in a Nov. 6 presentation at the American Heart Association scientific sessions.
The findings of the Supplements, Placebo, or Rosuvastatin Study (SPORT) and how they are framed for the public “are important for public health,” he said.
“As cardiologists, primary care doctors, and others, we really should use these results to have evidence-based discussions with patients” regarding the value of even low-dose statins and the supplements’ “lack of benefit,” said Dr. Laffin, lead author on the SPORT publication, which was published the same day in the Journal of the American College of Cardiology.
Patients assigned to low-dose rosuvastatin showed a mean 24.4% drop in total cholesterol levels over 28 days, the study’s primary endpoint. That differed from the placebo group and those for each supplement at P < .001.
They also averaged a 19.2% decrease in serum triglycerides, P < .05 for all group comparisons. None of the six supplements was significantly different from placebo for change in levels of either total cholesterol or triglycerides.
Nor were there significant differences in adverse events across the groups; there were no adverse changes in liver or kidney function tests or glucose levels; and there were no signs of musculoskeletal symptoms, the published report notes.
How to message the results
The SPORT trial is valuable for “addressing the void of data on supplements and cardiovascular health,” Chiadi E. Ndumele, MD, PhD, Johns Hopkins University, Baltimore, said as the invited discussant following Dr. Laffin’s presentation.
But they also send a reassuring message about statins, he noted. In a recent study of statin-nonadherent patients, 80% “were worried about statin side effects as the primary reason for not taking their statin, and 72% preferred using natural supplements instead of taking their prescription therapy,” Dr. Ndumele said. “The reason for this is clearly mistrust, misinformation, and a lack of evidence.”
The next step, he proposed, should be to get the study’s positive message about statins to the public, and especially patients “who are hesitant about statin use.” The current study “underscores the fact that using a low dose of a high-potency statin is associated with a very, very low risk of side effects.”
At a media briefing on SPORT, Amit Khera, MD, agreed the randomized trial provides some needed evidence that can be discussed with patients. “If someone’s coming to see me for cholesterol, we can say definitively now, at least there is data that these [supplements] don’t help your cholesterol and statins do.” Dr. Khera directs the preventive cardiology program at University of Texas Southwestern Medical Center, Dallas.
“I think for those who are there very specifically to lower their cholesterol, hopefully this will resonate,” he said.
“I personally didn’t see a lot of harms in using these supplements. But I also didn’t see any benefits,” Dr. Khera told this news organization.
“Now, if you’re taking them for other reasons, so be it. But if you need to lower your cholesterol for cardiovascular health reasons,” he said, “you need to know that they are minimally to not effective at all.”
But such supplements still “are not without harm,” Dr. Laffin proposed at the press conference. For example, they have potential for drug-drug interactions, “not only with cardiovascular medicines, but those taken for other reasons,” he said. “There are 90,000 supplements on the market in the United States today, and there are all kinds of potential safety issues associated with them.”
In patient discussions, Dr. Laffin said, “I do not think it’s good enough to say, you can waste your money [on supplements] as long as you’re taking your statin. These can actually be harmful in certain situations.”
SPORT, described as a single-center study, randomly assigned 199 participants from “throughout the Cleveland Clinic Health System in northeast Ohio” to one of the eight treatment groups. The investigators were blinded to treatment assignments, Dr. Laffin reported.
High adherence
Entry criteria included age 40 to 75 years with no history of cardiovascular disease, LDL-cholesterol from 70 to 189 mg/dL, and a 5%-20% 10-year risk of atherosclerotic cardiovascular disease by the pooled cohort equations. The predominantly White cohort averaged 64.4 years in age and 59% were women.
They were assigned to receive rosuvastatin 5 mg daily, placebo, or daily doses of supplements, with 25 patients per group, except the fish-oil group, which comprised 24 patients.
The daily supplement dosages were 2,400 mg for fish oil (Nature Made); 2,400 mg for cinnamon (NutriFlair), 5,000 mcg allicin for the garlic (Garlique), 4,500 mg for turmeric curcumin (BioSchwartz), 1,600 mg plant sterols (CholestOff Plus, Nature Made), and 2,400 mg red yeast rice (Arazo Nutrition).
Adherence to the assigned regimens was high, Dr. Laffin said, given that only four participants took less than 70% of their assigned doses.
Levels of LDL cholesterol in the statin group fell by 37.9% in 28 days, and by 35.2% relative to the placebo group (P < .001 for both differences), whereas any changes in LDL cholesterol among patients taking the most supplements were not significantly different from the placebo group. Of note, LDL cholesterol levels rose 7.8% (P = .01) compared with placebo among the group assigned to the garlic supplement.
Rosuvastatin had no apparent effect on HDL cholesterol levels, nor did most of the supplements; but such levels in patients taking the plant sterol supplement decreased by 7.1% (P = .02) compared to placebo and by 4% (P = .01) compared to the statin group.
None of the noncontrol groups, including those assigned to rosuvastatin, showed significant changes in high-sensitivity CRP levels compared with the placebo group. The lack of rosuvastatin effect on the inflammatory biomarker, the researchers speculated, is probably explained by the statins’ low dose as well as the limited size of the trial population.
There were two serious adverse events, including one deep venous thrombosis in the placebo group and a liver adenocarcinoma in a patient assigned to fish oil who “had not yet taken any of the study drug at the time of the serious adverse event,” the published report notes.
It remains open whether any of the assigned regimens could show different results over the long term, Dr. Laffin said. The SPORT trial’s 28-day duration, he said, “may not have fully captured the impact of supplements on lipid and inflammatory biomarkers.”
Nor is it known whether the supplements can potentially affect clinical outcomes. But “you could make an argument that it would be unethical” to randomize similar patients to a placebo-controlled, cardiovascular outcomes trial comparing the same six supplements and a statin.
Dr. Laffin has disclosed consulting or serving on a steering committee for Medtronic, Lilly, Mineralys Therapeutics, AstraZeneca, and Crispr Therapeutics; receiving research funding from AstraZeneca; and having ownership interest in LucidAct Health and Gordy Health. Dr. Ndumele and Dr. Khera have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
in a randomized trial of adults without cardiovascular disease but at increased cardiovascular risk.
In contrast, those who took the low dose of a high-potency statin in the eight-arm comparative study showed a significant 38% drop in LDL cholesterol levels over 28 days, a performance that blew away the six supplements containing fish oil, cinnamon, garlic, turmeric, plant sterols, or red yeast rice.
The supplements showed little or no effect on any measured lipid biomarkers, which also included total cholesterol and triglycerides, or C-reactive protein (CRP), which reflects systemic inflammation.
The findings undercut the widespread heart-health marketing claims for such supplements and could potentially restore faith in statins for the many patients looking for alternatives, researchers say.
“We all see patients that have their medication lists littered with dietary supplements,” observed Luke J. Laffin, MD, of the Cleveland Clinic Foundation. And it’s more than just heart patients who use them.
Almost $50 billion is spent on dietary supplements annually in the United States, and recent data suggest that more than three-fourths of the population use them, 18% of those based on specious heart-health claims, Dr. Laffin said in a Nov. 6 presentation at the American Heart Association scientific sessions.
The findings of the Supplements, Placebo, or Rosuvastatin Study (SPORT) and how they are framed for the public “are important for public health,” he said.
“As cardiologists, primary care doctors, and others, we really should use these results to have evidence-based discussions with patients” regarding the value of even low-dose statins and the supplements’ “lack of benefit,” said Dr. Laffin, lead author on the SPORT publication, which was published the same day in the Journal of the American College of Cardiology.
Patients assigned to low-dose rosuvastatin showed a mean 24.4% drop in total cholesterol levels over 28 days, the study’s primary endpoint. That differed from the placebo group and those for each supplement at P < .001.
They also averaged a 19.2% decrease in serum triglycerides, P < .05 for all group comparisons. None of the six supplements was significantly different from placebo for change in levels of either total cholesterol or triglycerides.
Nor were there significant differences in adverse events across the groups; there were no adverse changes in liver or kidney function tests or glucose levels; and there were no signs of musculoskeletal symptoms, the published report notes.
How to message the results
The SPORT trial is valuable for “addressing the void of data on supplements and cardiovascular health,” Chiadi E. Ndumele, MD, PhD, Johns Hopkins University, Baltimore, said as the invited discussant following Dr. Laffin’s presentation.
But they also send a reassuring message about statins, he noted. In a recent study of statin-nonadherent patients, 80% “were worried about statin side effects as the primary reason for not taking their statin, and 72% preferred using natural supplements instead of taking their prescription therapy,” Dr. Ndumele said. “The reason for this is clearly mistrust, misinformation, and a lack of evidence.”
The next step, he proposed, should be to get the study’s positive message about statins to the public, and especially patients “who are hesitant about statin use.” The current study “underscores the fact that using a low dose of a high-potency statin is associated with a very, very low risk of side effects.”
At a media briefing on SPORT, Amit Khera, MD, agreed the randomized trial provides some needed evidence that can be discussed with patients. “If someone’s coming to see me for cholesterol, we can say definitively now, at least there is data that these [supplements] don’t help your cholesterol and statins do.” Dr. Khera directs the preventive cardiology program at University of Texas Southwestern Medical Center, Dallas.
“I think for those who are there very specifically to lower their cholesterol, hopefully this will resonate,” he said.
“I personally didn’t see a lot of harms in using these supplements. But I also didn’t see any benefits,” Dr. Khera told this news organization.
“Now, if you’re taking them for other reasons, so be it. But if you need to lower your cholesterol for cardiovascular health reasons,” he said, “you need to know that they are minimally to not effective at all.”
But such supplements still “are not without harm,” Dr. Laffin proposed at the press conference. For example, they have potential for drug-drug interactions, “not only with cardiovascular medicines, but those taken for other reasons,” he said. “There are 90,000 supplements on the market in the United States today, and there are all kinds of potential safety issues associated with them.”
In patient discussions, Dr. Laffin said, “I do not think it’s good enough to say, you can waste your money [on supplements] as long as you’re taking your statin. These can actually be harmful in certain situations.”
SPORT, described as a single-center study, randomly assigned 199 participants from “throughout the Cleveland Clinic Health System in northeast Ohio” to one of the eight treatment groups. The investigators were blinded to treatment assignments, Dr. Laffin reported.
High adherence
Entry criteria included age 40 to 75 years with no history of cardiovascular disease, LDL-cholesterol from 70 to 189 mg/dL, and a 5%-20% 10-year risk of atherosclerotic cardiovascular disease by the pooled cohort equations. The predominantly White cohort averaged 64.4 years in age and 59% were women.
They were assigned to receive rosuvastatin 5 mg daily, placebo, or daily doses of supplements, with 25 patients per group, except the fish-oil group, which comprised 24 patients.
The daily supplement dosages were 2,400 mg for fish oil (Nature Made); 2,400 mg for cinnamon (NutriFlair), 5,000 mcg allicin for the garlic (Garlique), 4,500 mg for turmeric curcumin (BioSchwartz), 1,600 mg plant sterols (CholestOff Plus, Nature Made), and 2,400 mg red yeast rice (Arazo Nutrition).
Adherence to the assigned regimens was high, Dr. Laffin said, given that only four participants took less than 70% of their assigned doses.
Levels of LDL cholesterol in the statin group fell by 37.9% in 28 days, and by 35.2% relative to the placebo group (P < .001 for both differences), whereas any changes in LDL cholesterol among patients taking the most supplements were not significantly different from the placebo group. Of note, LDL cholesterol levels rose 7.8% (P = .01) compared with placebo among the group assigned to the garlic supplement.
Rosuvastatin had no apparent effect on HDL cholesterol levels, nor did most of the supplements; but such levels in patients taking the plant sterol supplement decreased by 7.1% (P = .02) compared to placebo and by 4% (P = .01) compared to the statin group.
None of the noncontrol groups, including those assigned to rosuvastatin, showed significant changes in high-sensitivity CRP levels compared with the placebo group. The lack of rosuvastatin effect on the inflammatory biomarker, the researchers speculated, is probably explained by the statins’ low dose as well as the limited size of the trial population.
There were two serious adverse events, including one deep venous thrombosis in the placebo group and a liver adenocarcinoma in a patient assigned to fish oil who “had not yet taken any of the study drug at the time of the serious adverse event,” the published report notes.
It remains open whether any of the assigned regimens could show different results over the long term, Dr. Laffin said. The SPORT trial’s 28-day duration, he said, “may not have fully captured the impact of supplements on lipid and inflammatory biomarkers.”
Nor is it known whether the supplements can potentially affect clinical outcomes. But “you could make an argument that it would be unethical” to randomize similar patients to a placebo-controlled, cardiovascular outcomes trial comparing the same six supplements and a statin.
Dr. Laffin has disclosed consulting or serving on a steering committee for Medtronic, Lilly, Mineralys Therapeutics, AstraZeneca, and Crispr Therapeutics; receiving research funding from AstraZeneca; and having ownership interest in LucidAct Health and Gordy Health. Dr. Ndumele and Dr. Khera have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
in a randomized trial of adults without cardiovascular disease but at increased cardiovascular risk.
In contrast, those who took the low dose of a high-potency statin in the eight-arm comparative study showed a significant 38% drop in LDL cholesterol levels over 28 days, a performance that blew away the six supplements containing fish oil, cinnamon, garlic, turmeric, plant sterols, or red yeast rice.
The supplements showed little or no effect on any measured lipid biomarkers, which also included total cholesterol and triglycerides, or C-reactive protein (CRP), which reflects systemic inflammation.
The findings undercut the widespread heart-health marketing claims for such supplements and could potentially restore faith in statins for the many patients looking for alternatives, researchers say.
“We all see patients that have their medication lists littered with dietary supplements,” observed Luke J. Laffin, MD, of the Cleveland Clinic Foundation. And it’s more than just heart patients who use them.
Almost $50 billion is spent on dietary supplements annually in the United States, and recent data suggest that more than three-fourths of the population use them, 18% of those based on specious heart-health claims, Dr. Laffin said in a Nov. 6 presentation at the American Heart Association scientific sessions.
The findings of the Supplements, Placebo, or Rosuvastatin Study (SPORT) and how they are framed for the public “are important for public health,” he said.
“As cardiologists, primary care doctors, and others, we really should use these results to have evidence-based discussions with patients” regarding the value of even low-dose statins and the supplements’ “lack of benefit,” said Dr. Laffin, lead author on the SPORT publication, which was published the same day in the Journal of the American College of Cardiology.
Patients assigned to low-dose rosuvastatin showed a mean 24.4% drop in total cholesterol levels over 28 days, the study’s primary endpoint. That differed from the placebo group and those for each supplement at P < .001.
They also averaged a 19.2% decrease in serum triglycerides, P < .05 for all group comparisons. None of the six supplements was significantly different from placebo for change in levels of either total cholesterol or triglycerides.
Nor were there significant differences in adverse events across the groups; there were no adverse changes in liver or kidney function tests or glucose levels; and there were no signs of musculoskeletal symptoms, the published report notes.
How to message the results
The SPORT trial is valuable for “addressing the void of data on supplements and cardiovascular health,” Chiadi E. Ndumele, MD, PhD, Johns Hopkins University, Baltimore, said as the invited discussant following Dr. Laffin’s presentation.
But they also send a reassuring message about statins, he noted. In a recent study of statin-nonadherent patients, 80% “were worried about statin side effects as the primary reason for not taking their statin, and 72% preferred using natural supplements instead of taking their prescription therapy,” Dr. Ndumele said. “The reason for this is clearly mistrust, misinformation, and a lack of evidence.”
The next step, he proposed, should be to get the study’s positive message about statins to the public, and especially patients “who are hesitant about statin use.” The current study “underscores the fact that using a low dose of a high-potency statin is associated with a very, very low risk of side effects.”
At a media briefing on SPORT, Amit Khera, MD, agreed the randomized trial provides some needed evidence that can be discussed with patients. “If someone’s coming to see me for cholesterol, we can say definitively now, at least there is data that these [supplements] don’t help your cholesterol and statins do.” Dr. Khera directs the preventive cardiology program at University of Texas Southwestern Medical Center, Dallas.
“I think for those who are there very specifically to lower their cholesterol, hopefully this will resonate,” he said.
“I personally didn’t see a lot of harms in using these supplements. But I also didn’t see any benefits,” Dr. Khera told this news organization.
“Now, if you’re taking them for other reasons, so be it. But if you need to lower your cholesterol for cardiovascular health reasons,” he said, “you need to know that they are minimally to not effective at all.”
But such supplements still “are not without harm,” Dr. Laffin proposed at the press conference. For example, they have potential for drug-drug interactions, “not only with cardiovascular medicines, but those taken for other reasons,” he said. “There are 90,000 supplements on the market in the United States today, and there are all kinds of potential safety issues associated with them.”
In patient discussions, Dr. Laffin said, “I do not think it’s good enough to say, you can waste your money [on supplements] as long as you’re taking your statin. These can actually be harmful in certain situations.”
SPORT, described as a single-center study, randomly assigned 199 participants from “throughout the Cleveland Clinic Health System in northeast Ohio” to one of the eight treatment groups. The investigators were blinded to treatment assignments, Dr. Laffin reported.
High adherence
Entry criteria included age 40 to 75 years with no history of cardiovascular disease, LDL-cholesterol from 70 to 189 mg/dL, and a 5%-20% 10-year risk of atherosclerotic cardiovascular disease by the pooled cohort equations. The predominantly White cohort averaged 64.4 years in age and 59% were women.
They were assigned to receive rosuvastatin 5 mg daily, placebo, or daily doses of supplements, with 25 patients per group, except the fish-oil group, which comprised 24 patients.
The daily supplement dosages were 2,400 mg for fish oil (Nature Made); 2,400 mg for cinnamon (NutriFlair), 5,000 mcg allicin for the garlic (Garlique), 4,500 mg for turmeric curcumin (BioSchwartz), 1,600 mg plant sterols (CholestOff Plus, Nature Made), and 2,400 mg red yeast rice (Arazo Nutrition).
Adherence to the assigned regimens was high, Dr. Laffin said, given that only four participants took less than 70% of their assigned doses.
Levels of LDL cholesterol in the statin group fell by 37.9% in 28 days, and by 35.2% relative to the placebo group (P < .001 for both differences), whereas any changes in LDL cholesterol among patients taking the most supplements were not significantly different from the placebo group. Of note, LDL cholesterol levels rose 7.8% (P = .01) compared with placebo among the group assigned to the garlic supplement.
Rosuvastatin had no apparent effect on HDL cholesterol levels, nor did most of the supplements; but such levels in patients taking the plant sterol supplement decreased by 7.1% (P = .02) compared to placebo and by 4% (P = .01) compared to the statin group.
None of the noncontrol groups, including those assigned to rosuvastatin, showed significant changes in high-sensitivity CRP levels compared with the placebo group. The lack of rosuvastatin effect on the inflammatory biomarker, the researchers speculated, is probably explained by the statins’ low dose as well as the limited size of the trial population.
There were two serious adverse events, including one deep venous thrombosis in the placebo group and a liver adenocarcinoma in a patient assigned to fish oil who “had not yet taken any of the study drug at the time of the serious adverse event,” the published report notes.
It remains open whether any of the assigned regimens could show different results over the long term, Dr. Laffin said. The SPORT trial’s 28-day duration, he said, “may not have fully captured the impact of supplements on lipid and inflammatory biomarkers.”
Nor is it known whether the supplements can potentially affect clinical outcomes. But “you could make an argument that it would be unethical” to randomize similar patients to a placebo-controlled, cardiovascular outcomes trial comparing the same six supplements and a statin.
Dr. Laffin has disclosed consulting or serving on a steering committee for Medtronic, Lilly, Mineralys Therapeutics, AstraZeneca, and Crispr Therapeutics; receiving research funding from AstraZeneca; and having ownership interest in LucidAct Health and Gordy Health. Dr. Ndumele and Dr. Khera have reported no relevant financial relationships.
A version of this article first appeared on Medscape.com.
AT AHA 2022
Avoid routine early ECMO in severe cardiogenic shock: ECMO-CS
CHICAGO – Routine early, expeditious use of extracorporeal membrane oxygenation (ECMO) is a common strategy in patients with severe cardiogenic shock, but a less aggressive initial approach may be just as effective, a randomized trial suggests.
In the study that assigned patients with “rapidly deteriorating or severe” cardiogenic shock to one or the other approach, clinical outcomes were no better for those who received immediate ECMO than for those initially managed with inotropes and vasopressors, researchers said.
The conservative strategy, importantly, allowed for downstream ECMO in the event of hemodynamic deterioration, which occurred in a substantial 39% of cases, observed Petr Ostadal, MD, PhD, when presenting the results at the American Heart Association scientific sessions.
Dr. Ostadal of Na Homolce Hospital, Prague, is also first author on the published report of the study, called Extracorporeal Membrane Oxygenation in the Therapy of Cardiogenic Shock (ECMO-CS), which was published the same day in Circulation.
The trial makes a firm case for preferring the conservative initial approach over routine early ECMO in the kind of patients it entered, Larry A. Allen, MD, MHS, University of Coloradoat Denver, Aurora, told this news organization.
More than 60% of the trial’s 117 patients had shock secondary to an acute coronary syndrome; another 23% were in heart failure decompensation.
A preference for the conservative initial approach would be welcome, he said. The early aggressive ECMO approach is resource intensive and carries some important risks, such as stroke or coagulopathy, said Dr. Allen, who is not connected with ECMO-CS. Yet it is increasingly the go-to approach in such patients, based primarily on observational data.
Although early ECMO apparently didn’t benefit patients in this study in their specific stage of cardiogenic shock, Dr. Allen observed, it would presumably help some, but identifying them in practice presents challenges. “Defining where people are in the spectrum of early versus middle versus late cardiogenic shock is actually very tricky.”
It will therefore be important, he said, to identify ways to predict which conservatively managed patients do well with the strategy, and which are most at risk for hemodynamic deterioration and for whom ECMO should be readily available.
“I think part of what ECMO-CS tells us is that, if a patient is stable on intravenous inotropic and vasopressor support, you can defer ECMO while you’re thinking about the patient – about their larger context and the right medical decision-making for them.”
The trial randomly assigned 122 patients with rapidly deteriorating or severe cardiogenic shock to the immediate-ECMO or the conservative strategy at four centers in the Czech Republic. The 117 patients for whom informed consent could be obtained were included in the analysis, 58 and 59 patients, respectively. Their mean age was about 65 years and three-fourths were male.
The primary endpoint, the only endpoint for which the study was powered, consisted of death from any cause, resuscitated circulatory arrest, or use of a different form of mechanical circulatory support (MCS) by 30 days.
It occurred in 63.8% of patients assigned to immediate ECMO and 71.2% of those in the conservative strategy group, for a hazard ratio of 0.72 (95% confidence interval, 0.46-1.12; P = .21).
As individual endpoints, rates of death from any cause and resuscitated arrest did not significantly differ between the groups, but conservatively managed patients more often used another form of MCS. The HRs were 1.11 (95% CI, 0.66-1.87) for death from any cause, 0.79 (95% CI, 0.27-2.28) for resuscitated cardiac arrest, and 0.38 (95% CI, 0.18-0.79) for use of another MCS device.
The rates for serious adverse events – including bleeding, ischemia, stroke, pneumonia, or sepsis – were similar at 60.3% in the early-ECMO group and 61% in group with conservative initial management, Dr. Ostadal reported.
Other than the 23 patients in the conservative initial strategy group who went on to receive ECMO (1.9 days after randomization, on average), 1 went on to undergo implantation with a HeartMate (Abbott) ventricular assist device and 3 received an Impella pump (Abiomed).
Six patients in the early-ECMO group were already receiving intra-aortic balloon pump (IABP) support at randomization, two underwent temporary implantation with a Centrimag device (Abbott), and three went on to receive a HeartMate device, the published report notes.
ECMO is the optimal first choice for MCS in such patients with cardiogenic shock who need a circulatory support device, especially because it also oxygenates the blood, Dr. Ostadal told this news organization.
But ECMO doesn’t help with ventricular unloading. Indeed, it can sometimes reduce ventricular preload, especially if right-heart pressures are low. So MCS devices that unload the ventricle, typically an IABP, can complement ECMO.
Dr. Ostadal speculates, however, that there may be a better pairing option. “Impella plus ECMO, I think, is the combination which has a future,” he said, for patients in cardiogenic shock who need a short-term percutaneous hemodynamic support device. Impella “supports the whole circulation” and unloads the left ventricle.
“A balloon pump in combination with ECMO is still not a bad choice. It’s very cheap in comparison with Impella.” But in his opinion, Dr. Ostadal said, “The combination of Impella plus ECMO is more efficient from a hemodynamic point of view.”
As the published report notes, ongoing randomized trials looking at ECMO plus other MCS devices in cardiogenic shock include ECLS-SHOCK, with a projected enrollment of 420 patients, and EURO-SHOCK, aiming for a similar number of patients; both compare routine ECMO to conservative management.
In addition, ANCHOR, in which ECMO is combined with IABP, and DanShock, which looks at early use of Impella rather than ECMO, are enrolling patients with shock secondary to acute coronary syndromes.
Dr. Ostadal disclosed consulting for Getinge, Edwards, Medtronic, Biomedica, and Xenios/Fresenius, and receiving research support from Xenios/Fresenius. Dr. Allen disclosed modest or significant relationships with ACI Clinical, Novartis, UpToDate, Boston Scientific, and Cytokinetics.
A version of this article first appeared on Medscape.com.
CHICAGO – Routine early, expeditious use of extracorporeal membrane oxygenation (ECMO) is a common strategy in patients with severe cardiogenic shock, but a less aggressive initial approach may be just as effective, a randomized trial suggests.
In the study that assigned patients with “rapidly deteriorating or severe” cardiogenic shock to one or the other approach, clinical outcomes were no better for those who received immediate ECMO than for those initially managed with inotropes and vasopressors, researchers said.
The conservative strategy, importantly, allowed for downstream ECMO in the event of hemodynamic deterioration, which occurred in a substantial 39% of cases, observed Petr Ostadal, MD, PhD, when presenting the results at the American Heart Association scientific sessions.
Dr. Ostadal of Na Homolce Hospital, Prague, is also first author on the published report of the study, called Extracorporeal Membrane Oxygenation in the Therapy of Cardiogenic Shock (ECMO-CS), which was published the same day in Circulation.
The trial makes a firm case for preferring the conservative initial approach over routine early ECMO in the kind of patients it entered, Larry A. Allen, MD, MHS, University of Coloradoat Denver, Aurora, told this news organization.
More than 60% of the trial’s 117 patients had shock secondary to an acute coronary syndrome; another 23% were in heart failure decompensation.
A preference for the conservative initial approach would be welcome, he said. The early aggressive ECMO approach is resource intensive and carries some important risks, such as stroke or coagulopathy, said Dr. Allen, who is not connected with ECMO-CS. Yet it is increasingly the go-to approach in such patients, based primarily on observational data.
Although early ECMO apparently didn’t benefit patients in this study in their specific stage of cardiogenic shock, Dr. Allen observed, it would presumably help some, but identifying them in practice presents challenges. “Defining where people are in the spectrum of early versus middle versus late cardiogenic shock is actually very tricky.”
It will therefore be important, he said, to identify ways to predict which conservatively managed patients do well with the strategy, and which are most at risk for hemodynamic deterioration and for whom ECMO should be readily available.
“I think part of what ECMO-CS tells us is that, if a patient is stable on intravenous inotropic and vasopressor support, you can defer ECMO while you’re thinking about the patient – about their larger context and the right medical decision-making for them.”
The trial randomly assigned 122 patients with rapidly deteriorating or severe cardiogenic shock to the immediate-ECMO or the conservative strategy at four centers in the Czech Republic. The 117 patients for whom informed consent could be obtained were included in the analysis, 58 and 59 patients, respectively. Their mean age was about 65 years and three-fourths were male.
The primary endpoint, the only endpoint for which the study was powered, consisted of death from any cause, resuscitated circulatory arrest, or use of a different form of mechanical circulatory support (MCS) by 30 days.
It occurred in 63.8% of patients assigned to immediate ECMO and 71.2% of those in the conservative strategy group, for a hazard ratio of 0.72 (95% confidence interval, 0.46-1.12; P = .21).
As individual endpoints, rates of death from any cause and resuscitated arrest did not significantly differ between the groups, but conservatively managed patients more often used another form of MCS. The HRs were 1.11 (95% CI, 0.66-1.87) for death from any cause, 0.79 (95% CI, 0.27-2.28) for resuscitated cardiac arrest, and 0.38 (95% CI, 0.18-0.79) for use of another MCS device.
The rates for serious adverse events – including bleeding, ischemia, stroke, pneumonia, or sepsis – were similar at 60.3% in the early-ECMO group and 61% in group with conservative initial management, Dr. Ostadal reported.
Other than the 23 patients in the conservative initial strategy group who went on to receive ECMO (1.9 days after randomization, on average), 1 went on to undergo implantation with a HeartMate (Abbott) ventricular assist device and 3 received an Impella pump (Abiomed).
Six patients in the early-ECMO group were already receiving intra-aortic balloon pump (IABP) support at randomization, two underwent temporary implantation with a Centrimag device (Abbott), and three went on to receive a HeartMate device, the published report notes.
ECMO is the optimal first choice for MCS in such patients with cardiogenic shock who need a circulatory support device, especially because it also oxygenates the blood, Dr. Ostadal told this news organization.
But ECMO doesn’t help with ventricular unloading. Indeed, it can sometimes reduce ventricular preload, especially if right-heart pressures are low. So MCS devices that unload the ventricle, typically an IABP, can complement ECMO.
Dr. Ostadal speculates, however, that there may be a better pairing option. “Impella plus ECMO, I think, is the combination which has a future,” he said, for patients in cardiogenic shock who need a short-term percutaneous hemodynamic support device. Impella “supports the whole circulation” and unloads the left ventricle.
“A balloon pump in combination with ECMO is still not a bad choice. It’s very cheap in comparison with Impella.” But in his opinion, Dr. Ostadal said, “The combination of Impella plus ECMO is more efficient from a hemodynamic point of view.”
As the published report notes, ongoing randomized trials looking at ECMO plus other MCS devices in cardiogenic shock include ECLS-SHOCK, with a projected enrollment of 420 patients, and EURO-SHOCK, aiming for a similar number of patients; both compare routine ECMO to conservative management.
In addition, ANCHOR, in which ECMO is combined with IABP, and DanShock, which looks at early use of Impella rather than ECMO, are enrolling patients with shock secondary to acute coronary syndromes.
Dr. Ostadal disclosed consulting for Getinge, Edwards, Medtronic, Biomedica, and Xenios/Fresenius, and receiving research support from Xenios/Fresenius. Dr. Allen disclosed modest or significant relationships with ACI Clinical, Novartis, UpToDate, Boston Scientific, and Cytokinetics.
A version of this article first appeared on Medscape.com.
CHICAGO – Routine early, expeditious use of extracorporeal membrane oxygenation (ECMO) is a common strategy in patients with severe cardiogenic shock, but a less aggressive initial approach may be just as effective, a randomized trial suggests.
In the study that assigned patients with “rapidly deteriorating or severe” cardiogenic shock to one or the other approach, clinical outcomes were no better for those who received immediate ECMO than for those initially managed with inotropes and vasopressors, researchers said.
The conservative strategy, importantly, allowed for downstream ECMO in the event of hemodynamic deterioration, which occurred in a substantial 39% of cases, observed Petr Ostadal, MD, PhD, when presenting the results at the American Heart Association scientific sessions.
Dr. Ostadal of Na Homolce Hospital, Prague, is also first author on the published report of the study, called Extracorporeal Membrane Oxygenation in the Therapy of Cardiogenic Shock (ECMO-CS), which was published the same day in Circulation.
The trial makes a firm case for preferring the conservative initial approach over routine early ECMO in the kind of patients it entered, Larry A. Allen, MD, MHS, University of Coloradoat Denver, Aurora, told this news organization.
More than 60% of the trial’s 117 patients had shock secondary to an acute coronary syndrome; another 23% were in heart failure decompensation.
A preference for the conservative initial approach would be welcome, he said. The early aggressive ECMO approach is resource intensive and carries some important risks, such as stroke or coagulopathy, said Dr. Allen, who is not connected with ECMO-CS. Yet it is increasingly the go-to approach in such patients, based primarily on observational data.
Although early ECMO apparently didn’t benefit patients in this study in their specific stage of cardiogenic shock, Dr. Allen observed, it would presumably help some, but identifying them in practice presents challenges. “Defining where people are in the spectrum of early versus middle versus late cardiogenic shock is actually very tricky.”
It will therefore be important, he said, to identify ways to predict which conservatively managed patients do well with the strategy, and which are most at risk for hemodynamic deterioration and for whom ECMO should be readily available.
“I think part of what ECMO-CS tells us is that, if a patient is stable on intravenous inotropic and vasopressor support, you can defer ECMO while you’re thinking about the patient – about their larger context and the right medical decision-making for them.”
The trial randomly assigned 122 patients with rapidly deteriorating or severe cardiogenic shock to the immediate-ECMO or the conservative strategy at four centers in the Czech Republic. The 117 patients for whom informed consent could be obtained were included in the analysis, 58 and 59 patients, respectively. Their mean age was about 65 years and three-fourths were male.
The primary endpoint, the only endpoint for which the study was powered, consisted of death from any cause, resuscitated circulatory arrest, or use of a different form of mechanical circulatory support (MCS) by 30 days.
It occurred in 63.8% of patients assigned to immediate ECMO and 71.2% of those in the conservative strategy group, for a hazard ratio of 0.72 (95% confidence interval, 0.46-1.12; P = .21).
As individual endpoints, rates of death from any cause and resuscitated arrest did not significantly differ between the groups, but conservatively managed patients more often used another form of MCS. The HRs were 1.11 (95% CI, 0.66-1.87) for death from any cause, 0.79 (95% CI, 0.27-2.28) for resuscitated cardiac arrest, and 0.38 (95% CI, 0.18-0.79) for use of another MCS device.
The rates for serious adverse events – including bleeding, ischemia, stroke, pneumonia, or sepsis – were similar at 60.3% in the early-ECMO group and 61% in group with conservative initial management, Dr. Ostadal reported.
Other than the 23 patients in the conservative initial strategy group who went on to receive ECMO (1.9 days after randomization, on average), 1 went on to undergo implantation with a HeartMate (Abbott) ventricular assist device and 3 received an Impella pump (Abiomed).
Six patients in the early-ECMO group were already receiving intra-aortic balloon pump (IABP) support at randomization, two underwent temporary implantation with a Centrimag device (Abbott), and three went on to receive a HeartMate device, the published report notes.
ECMO is the optimal first choice for MCS in such patients with cardiogenic shock who need a circulatory support device, especially because it also oxygenates the blood, Dr. Ostadal told this news organization.
But ECMO doesn’t help with ventricular unloading. Indeed, it can sometimes reduce ventricular preload, especially if right-heart pressures are low. So MCS devices that unload the ventricle, typically an IABP, can complement ECMO.
Dr. Ostadal speculates, however, that there may be a better pairing option. “Impella plus ECMO, I think, is the combination which has a future,” he said, for patients in cardiogenic shock who need a short-term percutaneous hemodynamic support device. Impella “supports the whole circulation” and unloads the left ventricle.
“A balloon pump in combination with ECMO is still not a bad choice. It’s very cheap in comparison with Impella.” But in his opinion, Dr. Ostadal said, “The combination of Impella plus ECMO is more efficient from a hemodynamic point of view.”
As the published report notes, ongoing randomized trials looking at ECMO plus other MCS devices in cardiogenic shock include ECLS-SHOCK, with a projected enrollment of 420 patients, and EURO-SHOCK, aiming for a similar number of patients; both compare routine ECMO to conservative management.
In addition, ANCHOR, in which ECMO is combined with IABP, and DanShock, which looks at early use of Impella rather than ECMO, are enrolling patients with shock secondary to acute coronary syndromes.
Dr. Ostadal disclosed consulting for Getinge, Edwards, Medtronic, Biomedica, and Xenios/Fresenius, and receiving research support from Xenios/Fresenius. Dr. Allen disclosed modest or significant relationships with ACI Clinical, Novartis, UpToDate, Boston Scientific, and Cytokinetics.
A version of this article first appeared on Medscape.com.
AT AHA 2022
No survival advantage for either torsemide or furosemide in HF: TRANSFORM-HF
CHICAGO – The choice of loop diuretic for decongestion in patients hospitalized with heart failure (HF) may make little difference to survival or readmission risk over the next year, at least when deciding between furosemide or torsemide, a randomized trial suggests.
Both drugs are old and widely used, but differences between the two loop diuretics in bioavailability, effects on potassium levels, and other features have led some clinicians to sometimes prefer torsemide. Until now, however, no randomized HF trials have compared the two drugs.
The new findings suggest clinicians can continue starting such patients with HF on either agent, at their discretion, without concern that the choice may compromise outcomes, say researchers from the TRANSFORM-HF trial, which compared furosemide-first and torsemide-first diuretic strategies in a diverse population of patients with HF.
Given that the two strategies were similarly effective for survival and rehospitalization, clinicians caring for patients with HF can focus more on “getting patients on the right dose for their loop diuretic, and prioritizing those therapies proven to improve clinical outcomes,” said Robert J. Mentz, MD, of Duke University Clinical Research Institute, Durham, N.C.
Dr. Mentz, a TRANSFORM-HF principal investigator, presented the primary results November 5 at the American Heart Association scientific sessions.
The trial had randomly assigned 2,859 patients hospitalized with HF and with a plan for oral loop diuretic therapy to initiate treatment with furosemide or torsemide. Clinicians were encouraged to maintain patients on the assigned diuretic, but crossovers to the other drug or other diuretic changes were allowed.
Rates of death from any cause, the primary endpoint, were about 26% in both groups over a median 17-month follow-up, regardless of ejection fraction (EF).
The composite rates of all-cause death or hospitalization at 12 months were also not significantly different, about 49% for those started on furosemide and about 47% for patients initially prescribed torsemide.
As a pragmatic comparative effectiveness trial, TRANSFORM-HF entered diverse patients with HF, broadly representative of actual clinical practice, who were managed according to routine practice and a streamlined study protocol at more than 60 U.S. centers, Dr. Mentz observed.
One of the pragmatic design’s advantages, he told this news organization, was “how efficient it was” as a randomized comparison of treatment strategies for clinical outcomes. It was “relatively low cost” and recruited patients quickly, compared with conventional randomized trials, “and we answered the question clearly.” The trial’s results, Dr. Mentz said, reflect “what happens in the real world.”
When might torsemide have the edge?
Although furosemide is the most commonly used loop diuretic in HF, and there are others besides it and torsemide, the latter has both known and theoretical advantages that set it apart. Torsemide is more than twice as potent as furosemide and more bioavailable, and its treatment effect lasts longer, the TRANSFORM-HF investigators have noted.
In addition, preclinical and small clinical studies suggest torsemide may have pleiotropic effects that might be theoretical advantages for patients with HF. For example, it appears to downregulate the renin-angiotensin-aldosterone system (RAAS) and reduce myocardial fibrosis and promote reverse ventricular remodeling, the group writes.
In practice, therefore, torsemide may be preferred in patients with furosemide resistance or “challenges with bioavailability, especially those with very advanced heart failure with congestion who may have gut edema, where oral furosemide and other loop diuretics are not effectively absorbed,” Biykem Bozkurt, MD, PhD, Baylor College of Medicine, Houston, told this news organization.
In such patients, she said, torsemide “is considered to be a better choice for individuals who have diuretic resistance with advanced congestion.”
The drug’s apparent pleiotropic effects, such as RAAS inhibition, may have less relevance to the TRANSFORM-HF primary endpoint of all-cause mortality than to clinical outcomes more likely associated with successful decongestion, such as HF hospitalization, Dr. Bozkurt proposed.
The trial’s pragmatic design, however, made it more feasible to focus on all-cause mortality and less practical to use measures of successful decongestion, such as volume loss or reduction in natriuretic peptide levels, she observed. Those are endpoints of special interest when diuretics are compared, “especially for the subgroup of patients who are diuretic resistant.”
Over the last 20 years or so, “we’ve learned that hospitalized heart failure is a very different disease process with a different natural history,” observed Clyde W. Yancy, MD, MSc, Northwestern University, Chicago, who was not part of the current study.
“So, the idea that something as nuanced as choice of one loop diuretic over the other, in that setting, would be sufficient to change the natural history, may be still a high bar for us,” he said in an interview.
“Based on these data, one would have to argue that whichever loop diuretic you select for the hospitalized patient – and a lot of that is driven by market exigencies right now – it turns out that the response is indistinguishable,” Dr. Yancy said. “That means if your hospital happens to have furosemide on the formulary, use it. If furosemide is not available but torsemide is available, use it.”
Dr. Yancy said he’d like to see a trial similar to TRANSFORM-HF but in outpatients receiving today’s guideline-directed medical therapy, which includes the sodium-glucose cotransporter 2 (SGLT2) inhibitors, drugs that increase the fractional excretion of sodium and have a “diureticlike” effect.
Such a trial, he said, would explore “the combination of not one, or two, but three agents with a diuretic effect – a loop diuretic, a mineralocorticoid antagonist, and an SGLT2 inhibitor – in ambulatory, optimized patients. It might make a difference.”
HF regardless of EF
The trial enrolled patients hospitalized with worsening or new-onset HF with a plan for long-term loop diuretic therapy who had either an EF of 40% or lower or, regardless of EF, elevated natriuretic peptide levels when hospitalized.
Of the 2,859 participants, whose mean age was about 65 years, about 36% were women and 34% African American. Overall, 1,428 were assigned to receive furosemide as their initial oral diuretic and 1,431 patients were assigned to the torsemide-first strategy.
The rate of death from any cause in both groups was 17 per 100 patient-years at a median of 17.4 months. The hazard ratio for torsemide vs. furosemide was 1.02 (95% confidence interval, 0.89-1.18; P = .77).
The corresponding HR at 12 months for all-cause death or hospitalization was 0.92 (95% CI, 0.83-1.02; P = .11). The relative risk for any hospitalization was 0.94 (95% CI, 0.84-1.07).
Pragmatic design: Other implications
Dosing was left to clinician discretion in the open-label study, as was whether patients maintained their assigned drug or switched over to the other agent. Indeed, 5.4% of patients crossed over to the other loop diuretic, and 2.8% went off loop diuretics entirely between in-hospital randomization and discharge, Dr. Mentz reported. By day 30, 6.7% had crossed over, and 7% had stopped taking loop diuretics.
The diuretic crossovers and discontinuations, Dr. Mentz said, likely biased the trial’s outcomes, such that the two strategies performed about equally well. Efforts were made, however, to at least partially overcome that limitation.
“We put measures in place to support adherence – sending letters to their primary doctors, giving them a wallet card so they would know which therapy they were on, having conversations about the importance of trying to stay on the randomized therapy,” Dr. Mentz said in an interview. Still, some clinicians saw differences between the two agents that prompted them, at some point, to switch patients from one loop diuretic to the other.
But interestingly, Dr. Mentz reported, the two strategies did not significantly differ in all-cause mortality or the composite of all-cause mortality or hospitalization in analysis by intention to treat.
Dr. Mentz discloses receiving honoraria from AstraZeneca, Bayer/Merck, Boehringer Ingelheim/Lilly, Cytokinetics, Pharmacosmos, Respicardia, Windtree Therapeutics, and Zoll; and research grants from American Regent and Novartis. Dr. Bozkurt discloses receiving honoraria from AstraZeneca, Baxter Health Care, and Sanofi Aventis and having other relationships with Renovacor, Respicardia, Abbott Vascular, Liva Nova, Vifor, and Cardurion. Dr. Yancy discloses a modest relationship with Abbott.
A version of this article first appeared on Medscape.com.
CHICAGO – The choice of loop diuretic for decongestion in patients hospitalized with heart failure (HF) may make little difference to survival or readmission risk over the next year, at least when deciding between furosemide or torsemide, a randomized trial suggests.
Both drugs are old and widely used, but differences between the two loop diuretics in bioavailability, effects on potassium levels, and other features have led some clinicians to sometimes prefer torsemide. Until now, however, no randomized HF trials have compared the two drugs.
The new findings suggest clinicians can continue starting such patients with HF on either agent, at their discretion, without concern that the choice may compromise outcomes, say researchers from the TRANSFORM-HF trial, which compared furosemide-first and torsemide-first diuretic strategies in a diverse population of patients with HF.
Given that the two strategies were similarly effective for survival and rehospitalization, clinicians caring for patients with HF can focus more on “getting patients on the right dose for their loop diuretic, and prioritizing those therapies proven to improve clinical outcomes,” said Robert J. Mentz, MD, of Duke University Clinical Research Institute, Durham, N.C.
Dr. Mentz, a TRANSFORM-HF principal investigator, presented the primary results November 5 at the American Heart Association scientific sessions.
The trial had randomly assigned 2,859 patients hospitalized with HF and with a plan for oral loop diuretic therapy to initiate treatment with furosemide or torsemide. Clinicians were encouraged to maintain patients on the assigned diuretic, but crossovers to the other drug or other diuretic changes were allowed.
Rates of death from any cause, the primary endpoint, were about 26% in both groups over a median 17-month follow-up, regardless of ejection fraction (EF).
The composite rates of all-cause death or hospitalization at 12 months were also not significantly different, about 49% for those started on furosemide and about 47% for patients initially prescribed torsemide.
As a pragmatic comparative effectiveness trial, TRANSFORM-HF entered diverse patients with HF, broadly representative of actual clinical practice, who were managed according to routine practice and a streamlined study protocol at more than 60 U.S. centers, Dr. Mentz observed.
One of the pragmatic design’s advantages, he told this news organization, was “how efficient it was” as a randomized comparison of treatment strategies for clinical outcomes. It was “relatively low cost” and recruited patients quickly, compared with conventional randomized trials, “and we answered the question clearly.” The trial’s results, Dr. Mentz said, reflect “what happens in the real world.”
When might torsemide have the edge?
Although furosemide is the most commonly used loop diuretic in HF, and there are others besides it and torsemide, the latter has both known and theoretical advantages that set it apart. Torsemide is more than twice as potent as furosemide and more bioavailable, and its treatment effect lasts longer, the TRANSFORM-HF investigators have noted.
In addition, preclinical and small clinical studies suggest torsemide may have pleiotropic effects that might be theoretical advantages for patients with HF. For example, it appears to downregulate the renin-angiotensin-aldosterone system (RAAS) and reduce myocardial fibrosis and promote reverse ventricular remodeling, the group writes.
In practice, therefore, torsemide may be preferred in patients with furosemide resistance or “challenges with bioavailability, especially those with very advanced heart failure with congestion who may have gut edema, where oral furosemide and other loop diuretics are not effectively absorbed,” Biykem Bozkurt, MD, PhD, Baylor College of Medicine, Houston, told this news organization.
In such patients, she said, torsemide “is considered to be a better choice for individuals who have diuretic resistance with advanced congestion.”
The drug’s apparent pleiotropic effects, such as RAAS inhibition, may have less relevance to the TRANSFORM-HF primary endpoint of all-cause mortality than to clinical outcomes more likely associated with successful decongestion, such as HF hospitalization, Dr. Bozkurt proposed.
The trial’s pragmatic design, however, made it more feasible to focus on all-cause mortality and less practical to use measures of successful decongestion, such as volume loss or reduction in natriuretic peptide levels, she observed. Those are endpoints of special interest when diuretics are compared, “especially for the subgroup of patients who are diuretic resistant.”
Over the last 20 years or so, “we’ve learned that hospitalized heart failure is a very different disease process with a different natural history,” observed Clyde W. Yancy, MD, MSc, Northwestern University, Chicago, who was not part of the current study.
“So, the idea that something as nuanced as choice of one loop diuretic over the other, in that setting, would be sufficient to change the natural history, may be still a high bar for us,” he said in an interview.
“Based on these data, one would have to argue that whichever loop diuretic you select for the hospitalized patient – and a lot of that is driven by market exigencies right now – it turns out that the response is indistinguishable,” Dr. Yancy said. “That means if your hospital happens to have furosemide on the formulary, use it. If furosemide is not available but torsemide is available, use it.”
Dr. Yancy said he’d like to see a trial similar to TRANSFORM-HF but in outpatients receiving today’s guideline-directed medical therapy, which includes the sodium-glucose cotransporter 2 (SGLT2) inhibitors, drugs that increase the fractional excretion of sodium and have a “diureticlike” effect.
Such a trial, he said, would explore “the combination of not one, or two, but three agents with a diuretic effect – a loop diuretic, a mineralocorticoid antagonist, and an SGLT2 inhibitor – in ambulatory, optimized patients. It might make a difference.”
HF regardless of EF
The trial enrolled patients hospitalized with worsening or new-onset HF with a plan for long-term loop diuretic therapy who had either an EF of 40% or lower or, regardless of EF, elevated natriuretic peptide levels when hospitalized.
Of the 2,859 participants, whose mean age was about 65 years, about 36% were women and 34% African American. Overall, 1,428 were assigned to receive furosemide as their initial oral diuretic and 1,431 patients were assigned to the torsemide-first strategy.
The rate of death from any cause in both groups was 17 per 100 patient-years at a median of 17.4 months. The hazard ratio for torsemide vs. furosemide was 1.02 (95% confidence interval, 0.89-1.18; P = .77).
The corresponding HR at 12 months for all-cause death or hospitalization was 0.92 (95% CI, 0.83-1.02; P = .11). The relative risk for any hospitalization was 0.94 (95% CI, 0.84-1.07).
Pragmatic design: Other implications
Dosing was left to clinician discretion in the open-label study, as was whether patients maintained their assigned drug or switched over to the other agent. Indeed, 5.4% of patients crossed over to the other loop diuretic, and 2.8% went off loop diuretics entirely between in-hospital randomization and discharge, Dr. Mentz reported. By day 30, 6.7% had crossed over, and 7% had stopped taking loop diuretics.
The diuretic crossovers and discontinuations, Dr. Mentz said, likely biased the trial’s outcomes, such that the two strategies performed about equally well. Efforts were made, however, to at least partially overcome that limitation.
“We put measures in place to support adherence – sending letters to their primary doctors, giving them a wallet card so they would know which therapy they were on, having conversations about the importance of trying to stay on the randomized therapy,” Dr. Mentz said in an interview. Still, some clinicians saw differences between the two agents that prompted them, at some point, to switch patients from one loop diuretic to the other.
But interestingly, Dr. Mentz reported, the two strategies did not significantly differ in all-cause mortality or the composite of all-cause mortality or hospitalization in analysis by intention to treat.
Dr. Mentz discloses receiving honoraria from AstraZeneca, Bayer/Merck, Boehringer Ingelheim/Lilly, Cytokinetics, Pharmacosmos, Respicardia, Windtree Therapeutics, and Zoll; and research grants from American Regent and Novartis. Dr. Bozkurt discloses receiving honoraria from AstraZeneca, Baxter Health Care, and Sanofi Aventis and having other relationships with Renovacor, Respicardia, Abbott Vascular, Liva Nova, Vifor, and Cardurion. Dr. Yancy discloses a modest relationship with Abbott.
A version of this article first appeared on Medscape.com.
CHICAGO – The choice of loop diuretic for decongestion in patients hospitalized with heart failure (HF) may make little difference to survival or readmission risk over the next year, at least when deciding between furosemide or torsemide, a randomized trial suggests.
Both drugs are old and widely used, but differences between the two loop diuretics in bioavailability, effects on potassium levels, and other features have led some clinicians to sometimes prefer torsemide. Until now, however, no randomized HF trials have compared the two drugs.
The new findings suggest clinicians can continue starting such patients with HF on either agent, at their discretion, without concern that the choice may compromise outcomes, say researchers from the TRANSFORM-HF trial, which compared furosemide-first and torsemide-first diuretic strategies in a diverse population of patients with HF.
Given that the two strategies were similarly effective for survival and rehospitalization, clinicians caring for patients with HF can focus more on “getting patients on the right dose for their loop diuretic, and prioritizing those therapies proven to improve clinical outcomes,” said Robert J. Mentz, MD, of Duke University Clinical Research Institute, Durham, N.C.
Dr. Mentz, a TRANSFORM-HF principal investigator, presented the primary results November 5 at the American Heart Association scientific sessions.
The trial had randomly assigned 2,859 patients hospitalized with HF and with a plan for oral loop diuretic therapy to initiate treatment with furosemide or torsemide. Clinicians were encouraged to maintain patients on the assigned diuretic, but crossovers to the other drug or other diuretic changes were allowed.
Rates of death from any cause, the primary endpoint, were about 26% in both groups over a median 17-month follow-up, regardless of ejection fraction (EF).
The composite rates of all-cause death or hospitalization at 12 months were also not significantly different, about 49% for those started on furosemide and about 47% for patients initially prescribed torsemide.
As a pragmatic comparative effectiveness trial, TRANSFORM-HF entered diverse patients with HF, broadly representative of actual clinical practice, who were managed according to routine practice and a streamlined study protocol at more than 60 U.S. centers, Dr. Mentz observed.
One of the pragmatic design’s advantages, he told this news organization, was “how efficient it was” as a randomized comparison of treatment strategies for clinical outcomes. It was “relatively low cost” and recruited patients quickly, compared with conventional randomized trials, “and we answered the question clearly.” The trial’s results, Dr. Mentz said, reflect “what happens in the real world.”
When might torsemide have the edge?
Although furosemide is the most commonly used loop diuretic in HF, and there are others besides it and torsemide, the latter has both known and theoretical advantages that set it apart. Torsemide is more than twice as potent as furosemide and more bioavailable, and its treatment effect lasts longer, the TRANSFORM-HF investigators have noted.
In addition, preclinical and small clinical studies suggest torsemide may have pleiotropic effects that might be theoretical advantages for patients with HF. For example, it appears to downregulate the renin-angiotensin-aldosterone system (RAAS) and reduce myocardial fibrosis and promote reverse ventricular remodeling, the group writes.
In practice, therefore, torsemide may be preferred in patients with furosemide resistance or “challenges with bioavailability, especially those with very advanced heart failure with congestion who may have gut edema, where oral furosemide and other loop diuretics are not effectively absorbed,” Biykem Bozkurt, MD, PhD, Baylor College of Medicine, Houston, told this news organization.
In such patients, she said, torsemide “is considered to be a better choice for individuals who have diuretic resistance with advanced congestion.”
The drug’s apparent pleiotropic effects, such as RAAS inhibition, may have less relevance to the TRANSFORM-HF primary endpoint of all-cause mortality than to clinical outcomes more likely associated with successful decongestion, such as HF hospitalization, Dr. Bozkurt proposed.
The trial’s pragmatic design, however, made it more feasible to focus on all-cause mortality and less practical to use measures of successful decongestion, such as volume loss or reduction in natriuretic peptide levels, she observed. Those are endpoints of special interest when diuretics are compared, “especially for the subgroup of patients who are diuretic resistant.”
Over the last 20 years or so, “we’ve learned that hospitalized heart failure is a very different disease process with a different natural history,” observed Clyde W. Yancy, MD, MSc, Northwestern University, Chicago, who was not part of the current study.
“So, the idea that something as nuanced as choice of one loop diuretic over the other, in that setting, would be sufficient to change the natural history, may be still a high bar for us,” he said in an interview.
“Based on these data, one would have to argue that whichever loop diuretic you select for the hospitalized patient – and a lot of that is driven by market exigencies right now – it turns out that the response is indistinguishable,” Dr. Yancy said. “That means if your hospital happens to have furosemide on the formulary, use it. If furosemide is not available but torsemide is available, use it.”
Dr. Yancy said he’d like to see a trial similar to TRANSFORM-HF but in outpatients receiving today’s guideline-directed medical therapy, which includes the sodium-glucose cotransporter 2 (SGLT2) inhibitors, drugs that increase the fractional excretion of sodium and have a “diureticlike” effect.
Such a trial, he said, would explore “the combination of not one, or two, but three agents with a diuretic effect – a loop diuretic, a mineralocorticoid antagonist, and an SGLT2 inhibitor – in ambulatory, optimized patients. It might make a difference.”
HF regardless of EF
The trial enrolled patients hospitalized with worsening or new-onset HF with a plan for long-term loop diuretic therapy who had either an EF of 40% or lower or, regardless of EF, elevated natriuretic peptide levels when hospitalized.
Of the 2,859 participants, whose mean age was about 65 years, about 36% were women and 34% African American. Overall, 1,428 were assigned to receive furosemide as their initial oral diuretic and 1,431 patients were assigned to the torsemide-first strategy.
The rate of death from any cause in both groups was 17 per 100 patient-years at a median of 17.4 months. The hazard ratio for torsemide vs. furosemide was 1.02 (95% confidence interval, 0.89-1.18; P = .77).
The corresponding HR at 12 months for all-cause death or hospitalization was 0.92 (95% CI, 0.83-1.02; P = .11). The relative risk for any hospitalization was 0.94 (95% CI, 0.84-1.07).
Pragmatic design: Other implications
Dosing was left to clinician discretion in the open-label study, as was whether patients maintained their assigned drug or switched over to the other agent. Indeed, 5.4% of patients crossed over to the other loop diuretic, and 2.8% went off loop diuretics entirely between in-hospital randomization and discharge, Dr. Mentz reported. By day 30, 6.7% had crossed over, and 7% had stopped taking loop diuretics.
The diuretic crossovers and discontinuations, Dr. Mentz said, likely biased the trial’s outcomes, such that the two strategies performed about equally well. Efforts were made, however, to at least partially overcome that limitation.
“We put measures in place to support adherence – sending letters to their primary doctors, giving them a wallet card so they would know which therapy they were on, having conversations about the importance of trying to stay on the randomized therapy,” Dr. Mentz said in an interview. Still, some clinicians saw differences between the two agents that prompted them, at some point, to switch patients from one loop diuretic to the other.
But interestingly, Dr. Mentz reported, the two strategies did not significantly differ in all-cause mortality or the composite of all-cause mortality or hospitalization in analysis by intention to treat.
Dr. Mentz discloses receiving honoraria from AstraZeneca, Bayer/Merck, Boehringer Ingelheim/Lilly, Cytokinetics, Pharmacosmos, Respicardia, Windtree Therapeutics, and Zoll; and research grants from American Regent and Novartis. Dr. Bozkurt discloses receiving honoraria from AstraZeneca, Baxter Health Care, and Sanofi Aventis and having other relationships with Renovacor, Respicardia, Abbott Vascular, Liva Nova, Vifor, and Cardurion. Dr. Yancy discloses a modest relationship with Abbott.
A version of this article first appeared on Medscape.com.
AT AHA 2022
AHA 2022 to recapture in-person vibe but preserve global reach
That a bustling medical conference can have global reach as it unfolds is one of the COVID pandemic’s many lessons for science. Hybrid meetings such as the American Heart Association scientific sessions, getting underway Nov. 5 in Chicago and cyberspace, are one of its legacies.
The conference is set to recapture the magic of the in-person Scientific Sessions last experienced in Philadelphia in 2019. But planners are mindful of a special responsibility to younger clinicians and scientists who entered the field knowing only the virtual format and who may not know “what it’s like in a room when major science is presented or to present posters and have people come by for conversations,” Manesh R. Patel, MD, chair of the AHA 2022 Scientific Sessions program committee, told this news organization.
Still, the pandemic has underlined the value of live streaming for the great many who can’t attend in person, Dr. Patel said. At AHA 2022, virtual access doesn’t mean only late breaking and featured presentations; more than 70 full sessions will be streamed from Friday through Monday.
Overall, the conference has more than 800 sessions on the schedule, about a third are panels or invited lectures and two-thirds are original reports on the latest research. At the core of the research offerings, 78 studies and analyses are slated across 18 Late-Breaking Science (LBS) and Featured Science (FS) sessions from Saturday through Monday. At least 30 presentations and abstracts will enter the peer-reviewed literature right away with their simultaneous online publication, Dr. Patel said.
More a meet-and-greet than a presentation, the Puppy Snuggles Booth will make a return appearance in Chicago after earning rave reviews at the 2019 Sessions in Philadelphia. All are invited to take a breather from their schedules to pet, cuddle, and play with a passel of pups, all in need of homes and available for adoption. The experience’s favorable effect on blood pressure is almost guaranteed.
LBS and FS highlights
“It’s an amazing year for Late Breaking Science and Featured Science at the Scientific Sessions,” Dr. Patel said of the presentations selected for special attention after a rigorous review process. “We have science that is as broad and as deep as we’ve seen in years.”
Saturday’s two LBS sessions kick off the series with studies looking at agents long available in heart failure and hypertension but lacking solid supporting evidence, “pretty large randomized trials that are, we think, going to affect clinical practice as soon as they are presented,” Dr. Patel said.
They include TRANSFORM-HF, a comparison of the loop diuretics furosemide and torsemide in patients hospitalized with heart failure. And the Diuretic Comparison Project (DCP), with more than 13,000 patients with hypertension assigned to the diuretics chlorthalidone or hydrochlorothiazide, “is going to immediately impact how people think about blood pressure management,” Dr. Patel said.
Other highlights in the hypertension arena include the CRHCP trial, the MB-BP study, the Rich Life Project, and the polypill efficacy and safety trial QUARTET-USA, all in Sunday’s LBS-4; and the FRESH, PRECISION, and BrigHTN trials, all in LBS-9 on Monday.
Other heart failure trials joining TRANSFORM-HF in the line-up include IRONMAN, which revisited IV iron therapy in iron-deficient patients, in LBS-2 on Saturday and, in FS-4 on Monday, BETA3LVH and STRONG-HF, the latter a timely randomized test of pre- and post-discharge biomarker-driven uptitration of guideline-directed heart failure meds.
STRONG-HF was halted early, the trial’s nonprofit sponsor announced only weeks ago, after patients following the intensive uptitration strategy versus usual care showed a reduced risk of death or heart failure readmission; few other details were given.
Several sessions will be devoted to a rare breed of randomized trial, one that tests the efficacy of traditional herbal meds or nonprescription supplements against proven medications. “These are going to get a lot of people’s interest, one can imagine, because they are on common questions that patients bring to the clinic every day,” Dr. Patel said.
Such studies include CTS-AMI, which explored the traditional Chinese herbal medicine tongxinluo in ST-segment elevation myocardial infarction, in LBS-3 on Sunday, and SPORT in Sunday’s LBS-5, a small randomized comparison of low-dose rosuvastatin, cinnamon, garlic, turmeric, an omega-3 fish-oil supplement, a plant sterol, red yeast rice, and placebo for any effects on LDL-C levels.
Other novel approaches to dyslipidemia management are to be covered in RESPECT-EPA and OCEAN(a)-DOSE, both in LBS-5 on Sunday, and all five presentations in Monday’s FS-9, including ARCHES-2, SHASTA-2, FOURIER-OLE, and ORION-3.
The interplay of antiplatelets and coronary interventions will be explored in presentations called OPTION, in LBS-6 on Sunday, and HOST-EXAM and TWILIGHT, in FS-6 on Monday.
Coronary and peripheral-vascular interventions are center stage in reports on RAPCO in LBS-3 and BRIGHT-4 in LBS-6, both on Sunday, and BEST-CLI in LBS-7 and the After-80 Study in FS-6, both on Monday.
Several Monday reports will cover comorbidities and complications associated with COVID-19, including PREVENT-HD in LBS-7, and PANAMO, FERMIN, COVID-NET, and a secondary analysis of the DELIVER trial in FS-5.
Rebroadcasts for the Pacific Rim
The sessions will also feature several evening rebroadcasts of earlier LBS sessions that meeting planners scored highly for scientific merit and potential clinical impact but also for their “regional pull,” primarily for our colleagues in Asia, Dr. Patel said.
The first two LBS sessions presented live during the day in Chicago will be rebroadcast that evening as, for example, Sunday morning and afternoon fare in Tokyo and Singapore. And LBS-5 live Sunday afternoon will rebroadcast that night as a Monday mid-morning session in, say, Hong Kong or Seoul.
This year’s AHA meeting spans the range of cardiovascular care, from precision therapies, such as gene editing or specific drugs, to broad strategies that consider, for example, social determinants of health, Dr. Patel said. “I think people, when they leave the Scientific Sessions, will feel very engaged in the larger conversation about how you impact very common conditions globally.”
A version of this article first appeared on Medscape.com.
That a bustling medical conference can have global reach as it unfolds is one of the COVID pandemic’s many lessons for science. Hybrid meetings such as the American Heart Association scientific sessions, getting underway Nov. 5 in Chicago and cyberspace, are one of its legacies.
The conference is set to recapture the magic of the in-person Scientific Sessions last experienced in Philadelphia in 2019. But planners are mindful of a special responsibility to younger clinicians and scientists who entered the field knowing only the virtual format and who may not know “what it’s like in a room when major science is presented or to present posters and have people come by for conversations,” Manesh R. Patel, MD, chair of the AHA 2022 Scientific Sessions program committee, told this news organization.
Still, the pandemic has underlined the value of live streaming for the great many who can’t attend in person, Dr. Patel said. At AHA 2022, virtual access doesn’t mean only late breaking and featured presentations; more than 70 full sessions will be streamed from Friday through Monday.
Overall, the conference has more than 800 sessions on the schedule, about a third are panels or invited lectures and two-thirds are original reports on the latest research. At the core of the research offerings, 78 studies and analyses are slated across 18 Late-Breaking Science (LBS) and Featured Science (FS) sessions from Saturday through Monday. At least 30 presentations and abstracts will enter the peer-reviewed literature right away with their simultaneous online publication, Dr. Patel said.
More a meet-and-greet than a presentation, the Puppy Snuggles Booth will make a return appearance in Chicago after earning rave reviews at the 2019 Sessions in Philadelphia. All are invited to take a breather from their schedules to pet, cuddle, and play with a passel of pups, all in need of homes and available for adoption. The experience’s favorable effect on blood pressure is almost guaranteed.
LBS and FS highlights
“It’s an amazing year for Late Breaking Science and Featured Science at the Scientific Sessions,” Dr. Patel said of the presentations selected for special attention after a rigorous review process. “We have science that is as broad and as deep as we’ve seen in years.”
Saturday’s two LBS sessions kick off the series with studies looking at agents long available in heart failure and hypertension but lacking solid supporting evidence, “pretty large randomized trials that are, we think, going to affect clinical practice as soon as they are presented,” Dr. Patel said.
They include TRANSFORM-HF, a comparison of the loop diuretics furosemide and torsemide in patients hospitalized with heart failure. And the Diuretic Comparison Project (DCP), with more than 13,000 patients with hypertension assigned to the diuretics chlorthalidone or hydrochlorothiazide, “is going to immediately impact how people think about blood pressure management,” Dr. Patel said.
Other highlights in the hypertension arena include the CRHCP trial, the MB-BP study, the Rich Life Project, and the polypill efficacy and safety trial QUARTET-USA, all in Sunday’s LBS-4; and the FRESH, PRECISION, and BrigHTN trials, all in LBS-9 on Monday.
Other heart failure trials joining TRANSFORM-HF in the line-up include IRONMAN, which revisited IV iron therapy in iron-deficient patients, in LBS-2 on Saturday and, in FS-4 on Monday, BETA3LVH and STRONG-HF, the latter a timely randomized test of pre- and post-discharge biomarker-driven uptitration of guideline-directed heart failure meds.
STRONG-HF was halted early, the trial’s nonprofit sponsor announced only weeks ago, after patients following the intensive uptitration strategy versus usual care showed a reduced risk of death or heart failure readmission; few other details were given.
Several sessions will be devoted to a rare breed of randomized trial, one that tests the efficacy of traditional herbal meds or nonprescription supplements against proven medications. “These are going to get a lot of people’s interest, one can imagine, because they are on common questions that patients bring to the clinic every day,” Dr. Patel said.
Such studies include CTS-AMI, which explored the traditional Chinese herbal medicine tongxinluo in ST-segment elevation myocardial infarction, in LBS-3 on Sunday, and SPORT in Sunday’s LBS-5, a small randomized comparison of low-dose rosuvastatin, cinnamon, garlic, turmeric, an omega-3 fish-oil supplement, a plant sterol, red yeast rice, and placebo for any effects on LDL-C levels.
Other novel approaches to dyslipidemia management are to be covered in RESPECT-EPA and OCEAN(a)-DOSE, both in LBS-5 on Sunday, and all five presentations in Monday’s FS-9, including ARCHES-2, SHASTA-2, FOURIER-OLE, and ORION-3.
The interplay of antiplatelets and coronary interventions will be explored in presentations called OPTION, in LBS-6 on Sunday, and HOST-EXAM and TWILIGHT, in FS-6 on Monday.
Coronary and peripheral-vascular interventions are center stage in reports on RAPCO in LBS-3 and BRIGHT-4 in LBS-6, both on Sunday, and BEST-CLI in LBS-7 and the After-80 Study in FS-6, both on Monday.
Several Monday reports will cover comorbidities and complications associated with COVID-19, including PREVENT-HD in LBS-7, and PANAMO, FERMIN, COVID-NET, and a secondary analysis of the DELIVER trial in FS-5.
Rebroadcasts for the Pacific Rim
The sessions will also feature several evening rebroadcasts of earlier LBS sessions that meeting planners scored highly for scientific merit and potential clinical impact but also for their “regional pull,” primarily for our colleagues in Asia, Dr. Patel said.
The first two LBS sessions presented live during the day in Chicago will be rebroadcast that evening as, for example, Sunday morning and afternoon fare in Tokyo and Singapore. And LBS-5 live Sunday afternoon will rebroadcast that night as a Monday mid-morning session in, say, Hong Kong or Seoul.
This year’s AHA meeting spans the range of cardiovascular care, from precision therapies, such as gene editing or specific drugs, to broad strategies that consider, for example, social determinants of health, Dr. Patel said. “I think people, when they leave the Scientific Sessions, will feel very engaged in the larger conversation about how you impact very common conditions globally.”
A version of this article first appeared on Medscape.com.
That a bustling medical conference can have global reach as it unfolds is one of the COVID pandemic’s many lessons for science. Hybrid meetings such as the American Heart Association scientific sessions, getting underway Nov. 5 in Chicago and cyberspace, are one of its legacies.
The conference is set to recapture the magic of the in-person Scientific Sessions last experienced in Philadelphia in 2019. But planners are mindful of a special responsibility to younger clinicians and scientists who entered the field knowing only the virtual format and who may not know “what it’s like in a room when major science is presented or to present posters and have people come by for conversations,” Manesh R. Patel, MD, chair of the AHA 2022 Scientific Sessions program committee, told this news organization.
Still, the pandemic has underlined the value of live streaming for the great many who can’t attend in person, Dr. Patel said. At AHA 2022, virtual access doesn’t mean only late breaking and featured presentations; more than 70 full sessions will be streamed from Friday through Monday.
Overall, the conference has more than 800 sessions on the schedule, about a third are panels or invited lectures and two-thirds are original reports on the latest research. At the core of the research offerings, 78 studies and analyses are slated across 18 Late-Breaking Science (LBS) and Featured Science (FS) sessions from Saturday through Monday. At least 30 presentations and abstracts will enter the peer-reviewed literature right away with their simultaneous online publication, Dr. Patel said.
More a meet-and-greet than a presentation, the Puppy Snuggles Booth will make a return appearance in Chicago after earning rave reviews at the 2019 Sessions in Philadelphia. All are invited to take a breather from their schedules to pet, cuddle, and play with a passel of pups, all in need of homes and available for adoption. The experience’s favorable effect on blood pressure is almost guaranteed.
LBS and FS highlights
“It’s an amazing year for Late Breaking Science and Featured Science at the Scientific Sessions,” Dr. Patel said of the presentations selected for special attention after a rigorous review process. “We have science that is as broad and as deep as we’ve seen in years.”
Saturday’s two LBS sessions kick off the series with studies looking at agents long available in heart failure and hypertension but lacking solid supporting evidence, “pretty large randomized trials that are, we think, going to affect clinical practice as soon as they are presented,” Dr. Patel said.
They include TRANSFORM-HF, a comparison of the loop diuretics furosemide and torsemide in patients hospitalized with heart failure. And the Diuretic Comparison Project (DCP), with more than 13,000 patients with hypertension assigned to the diuretics chlorthalidone or hydrochlorothiazide, “is going to immediately impact how people think about blood pressure management,” Dr. Patel said.
Other highlights in the hypertension arena include the CRHCP trial, the MB-BP study, the Rich Life Project, and the polypill efficacy and safety trial QUARTET-USA, all in Sunday’s LBS-4; and the FRESH, PRECISION, and BrigHTN trials, all in LBS-9 on Monday.
Other heart failure trials joining TRANSFORM-HF in the line-up include IRONMAN, which revisited IV iron therapy in iron-deficient patients, in LBS-2 on Saturday and, in FS-4 on Monday, BETA3LVH and STRONG-HF, the latter a timely randomized test of pre- and post-discharge biomarker-driven uptitration of guideline-directed heart failure meds.
STRONG-HF was halted early, the trial’s nonprofit sponsor announced only weeks ago, after patients following the intensive uptitration strategy versus usual care showed a reduced risk of death or heart failure readmission; few other details were given.
Several sessions will be devoted to a rare breed of randomized trial, one that tests the efficacy of traditional herbal meds or nonprescription supplements against proven medications. “These are going to get a lot of people’s interest, one can imagine, because they are on common questions that patients bring to the clinic every day,” Dr. Patel said.
Such studies include CTS-AMI, which explored the traditional Chinese herbal medicine tongxinluo in ST-segment elevation myocardial infarction, in LBS-3 on Sunday, and SPORT in Sunday’s LBS-5, a small randomized comparison of low-dose rosuvastatin, cinnamon, garlic, turmeric, an omega-3 fish-oil supplement, a plant sterol, red yeast rice, and placebo for any effects on LDL-C levels.
Other novel approaches to dyslipidemia management are to be covered in RESPECT-EPA and OCEAN(a)-DOSE, both in LBS-5 on Sunday, and all five presentations in Monday’s FS-9, including ARCHES-2, SHASTA-2, FOURIER-OLE, and ORION-3.
The interplay of antiplatelets and coronary interventions will be explored in presentations called OPTION, in LBS-6 on Sunday, and HOST-EXAM and TWILIGHT, in FS-6 on Monday.
Coronary and peripheral-vascular interventions are center stage in reports on RAPCO in LBS-3 and BRIGHT-4 in LBS-6, both on Sunday, and BEST-CLI in LBS-7 and the After-80 Study in FS-6, both on Monday.
Several Monday reports will cover comorbidities and complications associated with COVID-19, including PREVENT-HD in LBS-7, and PANAMO, FERMIN, COVID-NET, and a secondary analysis of the DELIVER trial in FS-5.
Rebroadcasts for the Pacific Rim
The sessions will also feature several evening rebroadcasts of earlier LBS sessions that meeting planners scored highly for scientific merit and potential clinical impact but also for their “regional pull,” primarily for our colleagues in Asia, Dr. Patel said.
The first two LBS sessions presented live during the day in Chicago will be rebroadcast that evening as, for example, Sunday morning and afternoon fare in Tokyo and Singapore. And LBS-5 live Sunday afternoon will rebroadcast that night as a Monday mid-morning session in, say, Hong Kong or Seoul.
This year’s AHA meeting spans the range of cardiovascular care, from precision therapies, such as gene editing or specific drugs, to broad strategies that consider, for example, social determinants of health, Dr. Patel said. “I think people, when they leave the Scientific Sessions, will feel very engaged in the larger conversation about how you impact very common conditions globally.”
A version of this article first appeared on Medscape.com.
FDA OKs Medtronic lead for left bundle branch pacing
Labeling for a Medtronic pacing lead, already indicated for stimulation of the His bundle, has been expanded to include the left bundle branch (LBB), the company announced on Oct. 17.
The U.S. Food and Drug Administration previously expanded the Medtronic SelectSecure MRI SureScan Model 3830 lead’s approval in 2018 to include His-bundle pacing. “Now this cardiac lead is approved for pacing and sensing at the bundle of His or in the left bundle branch area as an alternative to apical pacing in the right ventricle in a single- or dual-chamber pacing system,” Medtronic states in a press release.
The Model 3830 lead was initially approved for atrial or right ventricular pacing and sensing, the announcement says, and now “has more than 20 years of proven performance and reliability.”
The newly expanded conduction system pacing indication is “based on evidence from multiple sources spanning more than 20,000 treated patients,” for which the company cited “Medtronic data on file.”
A version of this article first appeared on Medscape.com.
Labeling for a Medtronic pacing lead, already indicated for stimulation of the His bundle, has been expanded to include the left bundle branch (LBB), the company announced on Oct. 17.
The U.S. Food and Drug Administration previously expanded the Medtronic SelectSecure MRI SureScan Model 3830 lead’s approval in 2018 to include His-bundle pacing. “Now this cardiac lead is approved for pacing and sensing at the bundle of His or in the left bundle branch area as an alternative to apical pacing in the right ventricle in a single- or dual-chamber pacing system,” Medtronic states in a press release.
The Model 3830 lead was initially approved for atrial or right ventricular pacing and sensing, the announcement says, and now “has more than 20 years of proven performance and reliability.”
The newly expanded conduction system pacing indication is “based on evidence from multiple sources spanning more than 20,000 treated patients,” for which the company cited “Medtronic data on file.”
A version of this article first appeared on Medscape.com.
Labeling for a Medtronic pacing lead, already indicated for stimulation of the His bundle, has been expanded to include the left bundle branch (LBB), the company announced on Oct. 17.
The U.S. Food and Drug Administration previously expanded the Medtronic SelectSecure MRI SureScan Model 3830 lead’s approval in 2018 to include His-bundle pacing. “Now this cardiac lead is approved for pacing and sensing at the bundle of His or in the left bundle branch area as an alternative to apical pacing in the right ventricle in a single- or dual-chamber pacing system,” Medtronic states in a press release.
The Model 3830 lead was initially approved for atrial or right ventricular pacing and sensing, the announcement says, and now “has more than 20 years of proven performance and reliability.”
The newly expanded conduction system pacing indication is “based on evidence from multiple sources spanning more than 20,000 treated patients,” for which the company cited “Medtronic data on file.”
A version of this article first appeared on Medscape.com.
Trial of early intensive meds at HF discharge halted for benefit: STRONG-HF
A “high-intensity-care” strategy based on early and rapid uptitration of guideline-directed meds improves postdischarge clinical outcomes for patients hospitalized with decompensated heart failure (HF), suggest topline results from a randomized trial.
The STRONG-HF study was halted early on recommendation from its data safety monitoring board after an interim analysis suggested the high-intensity-care strategy significantly cut risk of death or HF readmission, compared with a standard-of-care approach.
The trial termination was announced in a press release from one of its sponsors, The Heart Initiative, a nonprofit organization. STRONG-HF was also supported by Roche Diagnostics.
The early termination was based on interim data from the approximately 1,000 patients, out of an estimated planned enrollment of 1,800, who had been followed for at least 90 days. The study’s actual primary endpoint had been defined by death or HF readmission at 6 months.
The announcement did not include outcomes data or P values, or any other indication of the magnitude of benefit from the high-intensity-care approach.
Patients in STRONG-HF who had been assigned to a high-intensity-care strategy had been started in-hospital on a beta blocker, a renin-angiotensin system inhibitor (RASi), and a mineralocorticoid receptor blocker (MRA) with dosages uptitrated at least halfway by the time of discharge.
The meds were uptitrated fully within 2 weeks of discharge guided by clinical and biomarker assessments, especially natriuretic peptides, at frequent postdischarge visits, the press release states.
Patients conducted “safety visits 1 week after any uptitration and follow-up visits at 6 weeks and 3 months,” the announcement notes. “At each visit, patients were assessed by physical examination for congestion and blood tests, including NT-proBNP measurements.”
The “full STRONG-HF trial results” are scheduled for presentation at the American Heart Association annual scientific sessions, the announcement states.
STRONG-HF is sponsored by The Heart Initiative and Roche Diagnostics.
A version of this article first appeared on Medscape.com.
A “high-intensity-care” strategy based on early and rapid uptitration of guideline-directed meds improves postdischarge clinical outcomes for patients hospitalized with decompensated heart failure (HF), suggest topline results from a randomized trial.
The STRONG-HF study was halted early on recommendation from its data safety monitoring board after an interim analysis suggested the high-intensity-care strategy significantly cut risk of death or HF readmission, compared with a standard-of-care approach.
The trial termination was announced in a press release from one of its sponsors, The Heart Initiative, a nonprofit organization. STRONG-HF was also supported by Roche Diagnostics.
The early termination was based on interim data from the approximately 1,000 patients, out of an estimated planned enrollment of 1,800, who had been followed for at least 90 days. The study’s actual primary endpoint had been defined by death or HF readmission at 6 months.
The announcement did not include outcomes data or P values, or any other indication of the magnitude of benefit from the high-intensity-care approach.
Patients in STRONG-HF who had been assigned to a high-intensity-care strategy had been started in-hospital on a beta blocker, a renin-angiotensin system inhibitor (RASi), and a mineralocorticoid receptor blocker (MRA) with dosages uptitrated at least halfway by the time of discharge.
The meds were uptitrated fully within 2 weeks of discharge guided by clinical and biomarker assessments, especially natriuretic peptides, at frequent postdischarge visits, the press release states.
Patients conducted “safety visits 1 week after any uptitration and follow-up visits at 6 weeks and 3 months,” the announcement notes. “At each visit, patients were assessed by physical examination for congestion and blood tests, including NT-proBNP measurements.”
The “full STRONG-HF trial results” are scheduled for presentation at the American Heart Association annual scientific sessions, the announcement states.
STRONG-HF is sponsored by The Heart Initiative and Roche Diagnostics.
A version of this article first appeared on Medscape.com.
A “high-intensity-care” strategy based on early and rapid uptitration of guideline-directed meds improves postdischarge clinical outcomes for patients hospitalized with decompensated heart failure (HF), suggest topline results from a randomized trial.
The STRONG-HF study was halted early on recommendation from its data safety monitoring board after an interim analysis suggested the high-intensity-care strategy significantly cut risk of death or HF readmission, compared with a standard-of-care approach.
The trial termination was announced in a press release from one of its sponsors, The Heart Initiative, a nonprofit organization. STRONG-HF was also supported by Roche Diagnostics.
The early termination was based on interim data from the approximately 1,000 patients, out of an estimated planned enrollment of 1,800, who had been followed for at least 90 days. The study’s actual primary endpoint had been defined by death or HF readmission at 6 months.
The announcement did not include outcomes data or P values, or any other indication of the magnitude of benefit from the high-intensity-care approach.
Patients in STRONG-HF who had been assigned to a high-intensity-care strategy had been started in-hospital on a beta blocker, a renin-angiotensin system inhibitor (RASi), and a mineralocorticoid receptor blocker (MRA) with dosages uptitrated at least halfway by the time of discharge.
The meds were uptitrated fully within 2 weeks of discharge guided by clinical and biomarker assessments, especially natriuretic peptides, at frequent postdischarge visits, the press release states.
Patients conducted “safety visits 1 week after any uptitration and follow-up visits at 6 weeks and 3 months,” the announcement notes. “At each visit, patients were assessed by physical examination for congestion and blood tests, including NT-proBNP measurements.”
The “full STRONG-HF trial results” are scheduled for presentation at the American Heart Association annual scientific sessions, the announcement states.
STRONG-HF is sponsored by The Heart Initiative and Roche Diagnostics.
A version of this article first appeared on Medscape.com.
FDA approves self-administered, SubQ furosemide preparation
The Food and Drug Administration has approved a furosemide preparation (Furoscix, scPharmaceuticals) intended for subcutaneous self-administration by outpatients with chronic heart failure and volume overload, the company has announced.
The product is indicated for use with a SmartDose On-Body Infuser (West Pharmaceutical Services) single-use subcutaneous administration device, which affixes to the abdomen.
The infuser is loaded by the patient or caregiver with a prefilled cartridge and is programmed to deliver Furoscix 30 mg over 1 hour followed by a 4-hour infusion at 12.5 mg/h, for a total fixed dose of 80 mg, scPharmaceuticals said in a press release on the drug approval.
Furosemide, a loop diuretic and one of the world’s most frequently used drugs, is conventionally given intravenously in the hospital or orally on an outpatient basis.
The company describes its furosemide preparation, used with the infuser, as “the first and only FDA-approved subcutaneous loop diuretic that delivers [intravenous]-equivalent diuresis at home.” It has been shown to “produce similar diuresis and natriuresis compared to intravenous furosemide.”
“This marks a tremendous opportunity to improve the at-home management of worsening congestion in patients with heart failure who display reduced responsiveness to oral diuretics and require administration of [intravenous] diuretics, which typically requires admission to the hospital,” William T. Abraham, MD, said in the press release.
The FDA approval “is significant and will allow patients to be treated outside of the hospital setting,” said Dr. Abraham, of Ohio State University, Columbus, and an scPharmaceuticals board member.
The Furoscix indication doesn’t cover emergent use or use in acute pulmonary edema, nor is it meant to be used chronically “and should be replaced with oral diuretics as soon as practical,” the company states.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved a furosemide preparation (Furoscix, scPharmaceuticals) intended for subcutaneous self-administration by outpatients with chronic heart failure and volume overload, the company has announced.
The product is indicated for use with a SmartDose On-Body Infuser (West Pharmaceutical Services) single-use subcutaneous administration device, which affixes to the abdomen.
The infuser is loaded by the patient or caregiver with a prefilled cartridge and is programmed to deliver Furoscix 30 mg over 1 hour followed by a 4-hour infusion at 12.5 mg/h, for a total fixed dose of 80 mg, scPharmaceuticals said in a press release on the drug approval.
Furosemide, a loop diuretic and one of the world’s most frequently used drugs, is conventionally given intravenously in the hospital or orally on an outpatient basis.
The company describes its furosemide preparation, used with the infuser, as “the first and only FDA-approved subcutaneous loop diuretic that delivers [intravenous]-equivalent diuresis at home.” It has been shown to “produce similar diuresis and natriuresis compared to intravenous furosemide.”
“This marks a tremendous opportunity to improve the at-home management of worsening congestion in patients with heart failure who display reduced responsiveness to oral diuretics and require administration of [intravenous] diuretics, which typically requires admission to the hospital,” William T. Abraham, MD, said in the press release.
The FDA approval “is significant and will allow patients to be treated outside of the hospital setting,” said Dr. Abraham, of Ohio State University, Columbus, and an scPharmaceuticals board member.
The Furoscix indication doesn’t cover emergent use or use in acute pulmonary edema, nor is it meant to be used chronically “and should be replaced with oral diuretics as soon as practical,” the company states.
A version of this article first appeared on Medscape.com.
The Food and Drug Administration has approved a furosemide preparation (Furoscix, scPharmaceuticals) intended for subcutaneous self-administration by outpatients with chronic heart failure and volume overload, the company has announced.
The product is indicated for use with a SmartDose On-Body Infuser (West Pharmaceutical Services) single-use subcutaneous administration device, which affixes to the abdomen.
The infuser is loaded by the patient or caregiver with a prefilled cartridge and is programmed to deliver Furoscix 30 mg over 1 hour followed by a 4-hour infusion at 12.5 mg/h, for a total fixed dose of 80 mg, scPharmaceuticals said in a press release on the drug approval.
Furosemide, a loop diuretic and one of the world’s most frequently used drugs, is conventionally given intravenously in the hospital or orally on an outpatient basis.
The company describes its furosemide preparation, used with the infuser, as “the first and only FDA-approved subcutaneous loop diuretic that delivers [intravenous]-equivalent diuresis at home.” It has been shown to “produce similar diuresis and natriuresis compared to intravenous furosemide.”
“This marks a tremendous opportunity to improve the at-home management of worsening congestion in patients with heart failure who display reduced responsiveness to oral diuretics and require administration of [intravenous] diuretics, which typically requires admission to the hospital,” William T. Abraham, MD, said in the press release.
The FDA approval “is significant and will allow patients to be treated outside of the hospital setting,” said Dr. Abraham, of Ohio State University, Columbus, and an scPharmaceuticals board member.
The Furoscix indication doesn’t cover emergent use or use in acute pulmonary edema, nor is it meant to be used chronically “and should be replaced with oral diuretics as soon as practical,” the company states.
A version of this article first appeared on Medscape.com.
Dapagliflozin DELIVERs regardless of systolic pressure in HFpEF
Whatever the mechanism of benefit from dapagliflozin (Farxiga) in patients with heart failure (HF) – and potentially also other sodium-glucose cotransporter 2 (SGLT2) inhibitors – its blood pressure lowering effects aren’t likely to contribute much.
Indeed, at least in patients with HF and non-reduced ejection fractions, dapagliflozin has only a modest BP-lowering effect and cuts cardiovascular (CV) risk regardless of baseline pressure or change in systolic BP, suggests a secondary analysis from the large placebo-controlled DELIVER trial.
Systolic BP fell over 1 month by just under 2 mmHg, on average, in trial patients with either mildly reduced or preserved ejection fraction (HFmrEF or HFpEF, respectively) assigned to take dapagliflozin versus placebo.
The effect was achieved without increasing the risk for adverse events from dapagliflozin, even among patients with the lowest baseline systolic pressures. Adverse outcomes overall, however, were more common at the lowest systolic BP level than at higher pressures, researchers reported.
They say the findings should help alleviate long-standing concerns that initiating SGLT2 inhibitors, with their recognized diuretic effects, might present a hazard in patients with HF and low systolic BP.
“It is a consistent theme in heart failure trials that the blood pressure–lowering effect of SGLT2 inhibitors is more modest than it is in non–heart-failure populations,” Senthil Selvaraj, MD, Duke University, Durham, N.C., told this news organization.
Changes to antihypertensive drug therapy throughout the trial, which presumably enhanced BP responses and “might occur more frequently in the placebo group,” Dr. Selvaraj said, “might explain why the blood pressure effect is a little bit more modest in this population.”
Dr. Selvaraj presented the analysis at the Annual Scientific Meeting of the Heart Failure Society of America, held in National Harbor, Md., and is lead author on its same-day publication in JACC: Heart Failure.
The findings “reinforce the clinical benefits of SGLT2 inhibitors in patients with heart failure across the full spectrum of ejection fractions and large range of systolic blood pressures,” said Gregg C. Fonarow, MD, University of California, Los Angeles Medical Center, who was not part of the DELIVER analysis.
The study’s greater adjusted risks for CV and all-cause mortality risks at the lowest baseline systolic pressures “parallels a series of observational analyses from registries, including OPTIMIZE-HF,” Dr. Fonarow observed.
In those prior studies of patients with established HFpEF, “systolic BP less than 120 mmHg or even 130 mmHg was associated with worse outcomes than those with higher systolic BP.”
The current findings, therefore, “highlight how optimal blood pressure targets in patients with established heart failure have not been well established,” Dr. Fonarow said.
The analysis included all 6,263 participants in DELIVER, outpatients or patients hospitalized for worsening HF who were in NYHA class 2-4 with a left ventricular ejection fraction (LVEF) greater than 40%. They averaged 72 in age, and 44% were women. Their mean baseline systolic BP was 128 mmHg.
After 1 month, mean systolic BP had fallen by 1.8 mmHg (P < .001) in patients who had been randomly assigned to dapagliflozin versus placebo. The effect was consistent (interaction P = .16) across all systolic BP categories (less than 120 mmHg, 120-129 mmHg, 130-139 mmHg, and 140 mmHg or higher).
The effect was similarly independent of estimated glomerular filtration rate (eGFR) and LVEF (interaction P = .30 and P = .33, respectively), Dr. Selvaraj reported.
In an analysis adjusted for both baseline and 1-month change in systolic BP, the effect of dapagliflozin on the primary endpoint was “minimally attenuated,” compared with the primary analysis, he said. That suggests the clinical benefits “did not significantly relate to the blood pressure–lowering effect” of the SGLT2 inhibitor.
In that analysis, the hazard ratio for CV death or worsening HF for dapagliflozin versus placebo was 0.85 (95% confidence interval, 0.75-0.96; P = .010). The HR had been 0.82 (95% CI, 0.73-0.92; P < .001) overall in the DELIVER primary analysis.
The current study doesn’t shed further light on the main SGLT2 inhibitor mechanism of clinical benefit in nondiabetics with HF, which remains a mystery.
“There is a diuretic effect, but it’s not incredibly robust,” Dr. Selvaraj observed. It may contribute to the drugs’ benefits, “but it’s definitely more than that – a lot more than that.”
DELIVER was funded by AstraZeneca. Dr. Selvaraj reported no relevant conflicts. Disclosures for the other authors are in the report. Dr. Fonarow has reported receiving personal fees from Abbott, Amgen, AstraZeneca, Bayer, Cytokinetics, Edwards, Janssen, Medtronic, Merck, and Novartis.
A version of this article first appeared on Medscape.com.
Whatever the mechanism of benefit from dapagliflozin (Farxiga) in patients with heart failure (HF) – and potentially also other sodium-glucose cotransporter 2 (SGLT2) inhibitors – its blood pressure lowering effects aren’t likely to contribute much.
Indeed, at least in patients with HF and non-reduced ejection fractions, dapagliflozin has only a modest BP-lowering effect and cuts cardiovascular (CV) risk regardless of baseline pressure or change in systolic BP, suggests a secondary analysis from the large placebo-controlled DELIVER trial.
Systolic BP fell over 1 month by just under 2 mmHg, on average, in trial patients with either mildly reduced or preserved ejection fraction (HFmrEF or HFpEF, respectively) assigned to take dapagliflozin versus placebo.
The effect was achieved without increasing the risk for adverse events from dapagliflozin, even among patients with the lowest baseline systolic pressures. Adverse outcomes overall, however, were more common at the lowest systolic BP level than at higher pressures, researchers reported.
They say the findings should help alleviate long-standing concerns that initiating SGLT2 inhibitors, with their recognized diuretic effects, might present a hazard in patients with HF and low systolic BP.
“It is a consistent theme in heart failure trials that the blood pressure–lowering effect of SGLT2 inhibitors is more modest than it is in non–heart-failure populations,” Senthil Selvaraj, MD, Duke University, Durham, N.C., told this news organization.
Changes to antihypertensive drug therapy throughout the trial, which presumably enhanced BP responses and “might occur more frequently in the placebo group,” Dr. Selvaraj said, “might explain why the blood pressure effect is a little bit more modest in this population.”
Dr. Selvaraj presented the analysis at the Annual Scientific Meeting of the Heart Failure Society of America, held in National Harbor, Md., and is lead author on its same-day publication in JACC: Heart Failure.
The findings “reinforce the clinical benefits of SGLT2 inhibitors in patients with heart failure across the full spectrum of ejection fractions and large range of systolic blood pressures,” said Gregg C. Fonarow, MD, University of California, Los Angeles Medical Center, who was not part of the DELIVER analysis.
The study’s greater adjusted risks for CV and all-cause mortality risks at the lowest baseline systolic pressures “parallels a series of observational analyses from registries, including OPTIMIZE-HF,” Dr. Fonarow observed.
In those prior studies of patients with established HFpEF, “systolic BP less than 120 mmHg or even 130 mmHg was associated with worse outcomes than those with higher systolic BP.”
The current findings, therefore, “highlight how optimal blood pressure targets in patients with established heart failure have not been well established,” Dr. Fonarow said.
The analysis included all 6,263 participants in DELIVER, outpatients or patients hospitalized for worsening HF who were in NYHA class 2-4 with a left ventricular ejection fraction (LVEF) greater than 40%. They averaged 72 in age, and 44% were women. Their mean baseline systolic BP was 128 mmHg.
After 1 month, mean systolic BP had fallen by 1.8 mmHg (P < .001) in patients who had been randomly assigned to dapagliflozin versus placebo. The effect was consistent (interaction P = .16) across all systolic BP categories (less than 120 mmHg, 120-129 mmHg, 130-139 mmHg, and 140 mmHg or higher).
The effect was similarly independent of estimated glomerular filtration rate (eGFR) and LVEF (interaction P = .30 and P = .33, respectively), Dr. Selvaraj reported.
In an analysis adjusted for both baseline and 1-month change in systolic BP, the effect of dapagliflozin on the primary endpoint was “minimally attenuated,” compared with the primary analysis, he said. That suggests the clinical benefits “did not significantly relate to the blood pressure–lowering effect” of the SGLT2 inhibitor.
In that analysis, the hazard ratio for CV death or worsening HF for dapagliflozin versus placebo was 0.85 (95% confidence interval, 0.75-0.96; P = .010). The HR had been 0.82 (95% CI, 0.73-0.92; P < .001) overall in the DELIVER primary analysis.
The current study doesn’t shed further light on the main SGLT2 inhibitor mechanism of clinical benefit in nondiabetics with HF, which remains a mystery.
“There is a diuretic effect, but it’s not incredibly robust,” Dr. Selvaraj observed. It may contribute to the drugs’ benefits, “but it’s definitely more than that – a lot more than that.”
DELIVER was funded by AstraZeneca. Dr. Selvaraj reported no relevant conflicts. Disclosures for the other authors are in the report. Dr. Fonarow has reported receiving personal fees from Abbott, Amgen, AstraZeneca, Bayer, Cytokinetics, Edwards, Janssen, Medtronic, Merck, and Novartis.
A version of this article first appeared on Medscape.com.
Whatever the mechanism of benefit from dapagliflozin (Farxiga) in patients with heart failure (HF) – and potentially also other sodium-glucose cotransporter 2 (SGLT2) inhibitors – its blood pressure lowering effects aren’t likely to contribute much.
Indeed, at least in patients with HF and non-reduced ejection fractions, dapagliflozin has only a modest BP-lowering effect and cuts cardiovascular (CV) risk regardless of baseline pressure or change in systolic BP, suggests a secondary analysis from the large placebo-controlled DELIVER trial.
Systolic BP fell over 1 month by just under 2 mmHg, on average, in trial patients with either mildly reduced or preserved ejection fraction (HFmrEF or HFpEF, respectively) assigned to take dapagliflozin versus placebo.
The effect was achieved without increasing the risk for adverse events from dapagliflozin, even among patients with the lowest baseline systolic pressures. Adverse outcomes overall, however, were more common at the lowest systolic BP level than at higher pressures, researchers reported.
They say the findings should help alleviate long-standing concerns that initiating SGLT2 inhibitors, with their recognized diuretic effects, might present a hazard in patients with HF and low systolic BP.
“It is a consistent theme in heart failure trials that the blood pressure–lowering effect of SGLT2 inhibitors is more modest than it is in non–heart-failure populations,” Senthil Selvaraj, MD, Duke University, Durham, N.C., told this news organization.
Changes to antihypertensive drug therapy throughout the trial, which presumably enhanced BP responses and “might occur more frequently in the placebo group,” Dr. Selvaraj said, “might explain why the blood pressure effect is a little bit more modest in this population.”
Dr. Selvaraj presented the analysis at the Annual Scientific Meeting of the Heart Failure Society of America, held in National Harbor, Md., and is lead author on its same-day publication in JACC: Heart Failure.
The findings “reinforce the clinical benefits of SGLT2 inhibitors in patients with heart failure across the full spectrum of ejection fractions and large range of systolic blood pressures,” said Gregg C. Fonarow, MD, University of California, Los Angeles Medical Center, who was not part of the DELIVER analysis.
The study’s greater adjusted risks for CV and all-cause mortality risks at the lowest baseline systolic pressures “parallels a series of observational analyses from registries, including OPTIMIZE-HF,” Dr. Fonarow observed.
In those prior studies of patients with established HFpEF, “systolic BP less than 120 mmHg or even 130 mmHg was associated with worse outcomes than those with higher systolic BP.”
The current findings, therefore, “highlight how optimal blood pressure targets in patients with established heart failure have not been well established,” Dr. Fonarow said.
The analysis included all 6,263 participants in DELIVER, outpatients or patients hospitalized for worsening HF who were in NYHA class 2-4 with a left ventricular ejection fraction (LVEF) greater than 40%. They averaged 72 in age, and 44% were women. Their mean baseline systolic BP was 128 mmHg.
After 1 month, mean systolic BP had fallen by 1.8 mmHg (P < .001) in patients who had been randomly assigned to dapagliflozin versus placebo. The effect was consistent (interaction P = .16) across all systolic BP categories (less than 120 mmHg, 120-129 mmHg, 130-139 mmHg, and 140 mmHg or higher).
The effect was similarly independent of estimated glomerular filtration rate (eGFR) and LVEF (interaction P = .30 and P = .33, respectively), Dr. Selvaraj reported.
In an analysis adjusted for both baseline and 1-month change in systolic BP, the effect of dapagliflozin on the primary endpoint was “minimally attenuated,” compared with the primary analysis, he said. That suggests the clinical benefits “did not significantly relate to the blood pressure–lowering effect” of the SGLT2 inhibitor.
In that analysis, the hazard ratio for CV death or worsening HF for dapagliflozin versus placebo was 0.85 (95% confidence interval, 0.75-0.96; P = .010). The HR had been 0.82 (95% CI, 0.73-0.92; P < .001) overall in the DELIVER primary analysis.
The current study doesn’t shed further light on the main SGLT2 inhibitor mechanism of clinical benefit in nondiabetics with HF, which remains a mystery.
“There is a diuretic effect, but it’s not incredibly robust,” Dr. Selvaraj observed. It may contribute to the drugs’ benefits, “but it’s definitely more than that – a lot more than that.”
DELIVER was funded by AstraZeneca. Dr. Selvaraj reported no relevant conflicts. Disclosures for the other authors are in the report. Dr. Fonarow has reported receiving personal fees from Abbott, Amgen, AstraZeneca, Bayer, Cytokinetics, Edwards, Janssen, Medtronic, Merck, and Novartis.
A version of this article first appeared on Medscape.com.
Salt pills for patients with acute decompensated heart failure?
Restriction of dietary salt to alleviate or prevent volume overload in patients with acute decompensated heart failure (ADHF) is common hospital practice, but without a solid evidence base. A trial testing whether taking salt pills might have benefits for patients with ADHF undergoing intensive diuresis, therefore, may seem a bit counterintuitive.
In just such a randomized, placebo-controlled trial, the approach made no difference to weight loss on diuresis, a proxy for volume reduction, or to serum creatinine levels in ADHF patients receiving high-dose intravenous diuretic therapy.
The patients consumed the extra salt during their intravenous therapy in the form of tablets providing 6 g sodium chloride daily on top of their hospital-provided, low-sodium meals.
During that time, serum sodium levels remained stable for the 34 patients assigned to the salt tablets but dropped significantly in the 31 given placebo pills.
They lost about the same weight, averages of 4 kg and 4.6 kg (8.8-10 lb), respectively, and their urine output was also similar. Patients who took the salt tablets showed less of an increase in blood urea nitrogen (BUN) at both 96 hours and at discharge.
The findings “challenge the routine practice of sodium chloride restriction in acute heart failure, something done thousands of times a day, millions of times a year,” Robert A. Montgomery, MD, Cleveland Clinic, said when presenting the study at the annual scientific meeting of the Heart Failure Society of America.
The trial, called OSPREY-AHF (Oral Sodium to Preserve Renal Efficiency in Acute Heart Failure), also may encourage a shift in ADHF management from a preoccupation with salt restriction to focus more on fighting fluid retention.
OSPREY-HF took on “an established practice that doesn’t have much high-quality evidentiary support,” one guided primarily by consensus and observational data, Montgomery said in an interview.
There are also potential downsides to dietary sodium restriction, including some that may complicate or block ADHF therapies.
“Low-sodium diets can be associated with decreased caloric intake and nutritional quality,” Dr. Montgomery observed. And observational studies suggest that “patients who are on a low sodium diet can develop increased neurohormonal activation. The kidney is not sensing salt, and so starts ramping up the hormones,” which promotes diuretic resistance.
But emerging evidence also suggests “that giving sodium chloride in the form of hypertonic saline can help patients who are diuretic resistant.” The intervention, which appears to attenuate the neurohormonal activation associated with high-dose intravenous diuretics, Dr. Montgomery noted, helped inspire the design of OSPREY-AHF.
Edema consists of “a gallon of water and a pinch of salt, so we really should stop being so salt-centric and think much more about water as the problem in decompensated heart failure,” said John G.F. Cleland, MD, PhD, during the question-and-answer period after Montgomery’s presentation. Dr. Cleland, of the University of Glasgow Institute of Health and Wellbeing, is not connected to OSPREY-AHF.
“I think that maybe we overinterpret how important salt is” as a focus of volume management in ADHF, offered David Lanfear, MD, Henry Ford Health System, Detroit, who is also not part of the study.
OSPREY-AHF was well conducted but applies to a “very specific” clinical setting, Dr. Lanfear said in an interview. “These people are getting aggressive diuresis, a big dose and continuous infusion. It’s not everybody that has heart failure.”
Although the study was small, “I think it will fuel interest in this area and, probably, further investigation,” he said. The trial on its own won’t change practice, “but it will raise some eyebrows.”
The trial included patients with ADHF who have been “admitted to a cardiovascular medicine floor, not the intensive care unit” and were receiving at least 10 mg per hour of furosemide. It excluded any who were “hypernatremic or severely hyponatremic,” said Dr. Montgomery when presenting the study. They were required to have an initial estimated glomerular filtration rate (eGFR) of at least 15 mL/min per 1.73 m2.
The patients were randomly assigned double blind at a single center to receive tablets providing 2 g sodium chloride or placebo pills – 34 and 31 patients, respectively – three times daily during intravenous diuresis.
At 96 hours, the two groups showed no difference in change in creatinine levels or change in weight, both primary endpoints. Nor did they differ in urine output or change in eGFR. But serum sodium levels fell further, and BUN levels went up more in those given placebo.
The two groups showed no differences in hospital length of stay, use of renal replacement therapy at 90 days, ICU time during the index hospitalization, 30-day readmission, or 90-day mortality – although the trial wasn’t powered for clinical outcomes, Dr. Montgomery reported.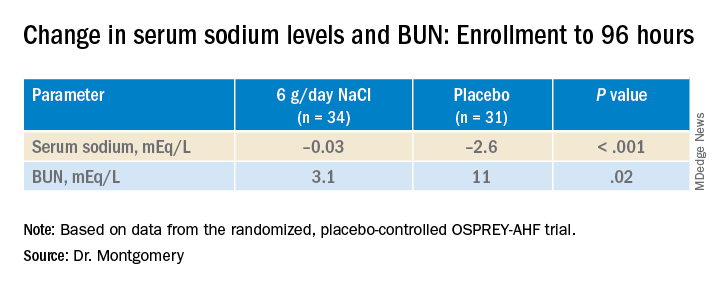
"We have patients who complain about their sodium-restricted diet, we have patients that have cachexia, who have a lot of complaints about provider-ordered meals and recommendations,” Dr. Montgomery explained in an interview.
Clinicians provide education and invest a lot of effort into getting patients with heart failure to start and maintain a low-sodium diet, he said. “But a low-sodium diet, in prior studies – and our study adds to this – is not a lever that actually seems to positively or adversely affect patients.”
Dr. Montgomery pointed to the recently published SODIUM-HF trial comparing low-sodium and unrestricted-sodium diets in outpatients with heart failure. It saw no clinical benefit from the low-sodium intervention.
Until studies show, potentially, that sodium restriction in hospitalized patients with heart failure makes a clinical difference, Dr. Montgomery said, “I’d say we should invest our time in things that we know are the most helpful, like getting them on guideline-directed medical therapy, when instead we spend an enormous amount of time counseling on and enforcing dietary restriction.”
Support for this study was provided by Cleveland Clinic Heart Vascular and Thoracic Institute’s Wilson Grant and Kaufman Center for Heart Failure Treatment and Recovery Grant. Dr. Lanfear disclosed research support from SomaLogic and Lilly; consulting for Abbott Laboratories, AstraZeneca, Janssen, Martin Pharmaceuticals, and Amgen; and serving on advisory panels for Illumina and Cytokinetics. Dr. Montgomery and Dr. Cleland disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Restriction of dietary salt to alleviate or prevent volume overload in patients with acute decompensated heart failure (ADHF) is common hospital practice, but without a solid evidence base. A trial testing whether taking salt pills might have benefits for patients with ADHF undergoing intensive diuresis, therefore, may seem a bit counterintuitive.
In just such a randomized, placebo-controlled trial, the approach made no difference to weight loss on diuresis, a proxy for volume reduction, or to serum creatinine levels in ADHF patients receiving high-dose intravenous diuretic therapy.
The patients consumed the extra salt during their intravenous therapy in the form of tablets providing 6 g sodium chloride daily on top of their hospital-provided, low-sodium meals.
During that time, serum sodium levels remained stable for the 34 patients assigned to the salt tablets but dropped significantly in the 31 given placebo pills.
They lost about the same weight, averages of 4 kg and 4.6 kg (8.8-10 lb), respectively, and their urine output was also similar. Patients who took the salt tablets showed less of an increase in blood urea nitrogen (BUN) at both 96 hours and at discharge.
The findings “challenge the routine practice of sodium chloride restriction in acute heart failure, something done thousands of times a day, millions of times a year,” Robert A. Montgomery, MD, Cleveland Clinic, said when presenting the study at the annual scientific meeting of the Heart Failure Society of America.
The trial, called OSPREY-AHF (Oral Sodium to Preserve Renal Efficiency in Acute Heart Failure), also may encourage a shift in ADHF management from a preoccupation with salt restriction to focus more on fighting fluid retention.
OSPREY-HF took on “an established practice that doesn’t have much high-quality evidentiary support,” one guided primarily by consensus and observational data, Montgomery said in an interview.
There are also potential downsides to dietary sodium restriction, including some that may complicate or block ADHF therapies.
“Low-sodium diets can be associated with decreased caloric intake and nutritional quality,” Dr. Montgomery observed. And observational studies suggest that “patients who are on a low sodium diet can develop increased neurohormonal activation. The kidney is not sensing salt, and so starts ramping up the hormones,” which promotes diuretic resistance.
But emerging evidence also suggests “that giving sodium chloride in the form of hypertonic saline can help patients who are diuretic resistant.” The intervention, which appears to attenuate the neurohormonal activation associated with high-dose intravenous diuretics, Dr. Montgomery noted, helped inspire the design of OSPREY-AHF.
Edema consists of “a gallon of water and a pinch of salt, so we really should stop being so salt-centric and think much more about water as the problem in decompensated heart failure,” said John G.F. Cleland, MD, PhD, during the question-and-answer period after Montgomery’s presentation. Dr. Cleland, of the University of Glasgow Institute of Health and Wellbeing, is not connected to OSPREY-AHF.
“I think that maybe we overinterpret how important salt is” as a focus of volume management in ADHF, offered David Lanfear, MD, Henry Ford Health System, Detroit, who is also not part of the study.
OSPREY-AHF was well conducted but applies to a “very specific” clinical setting, Dr. Lanfear said in an interview. “These people are getting aggressive diuresis, a big dose and continuous infusion. It’s not everybody that has heart failure.”
Although the study was small, “I think it will fuel interest in this area and, probably, further investigation,” he said. The trial on its own won’t change practice, “but it will raise some eyebrows.”
The trial included patients with ADHF who have been “admitted to a cardiovascular medicine floor, not the intensive care unit” and were receiving at least 10 mg per hour of furosemide. It excluded any who were “hypernatremic or severely hyponatremic,” said Dr. Montgomery when presenting the study. They were required to have an initial estimated glomerular filtration rate (eGFR) of at least 15 mL/min per 1.73 m2.
The patients were randomly assigned double blind at a single center to receive tablets providing 2 g sodium chloride or placebo pills – 34 and 31 patients, respectively – three times daily during intravenous diuresis.
At 96 hours, the two groups showed no difference in change in creatinine levels or change in weight, both primary endpoints. Nor did they differ in urine output or change in eGFR. But serum sodium levels fell further, and BUN levels went up more in those given placebo.
The two groups showed no differences in hospital length of stay, use of renal replacement therapy at 90 days, ICU time during the index hospitalization, 30-day readmission, or 90-day mortality – although the trial wasn’t powered for clinical outcomes, Dr. Montgomery reported.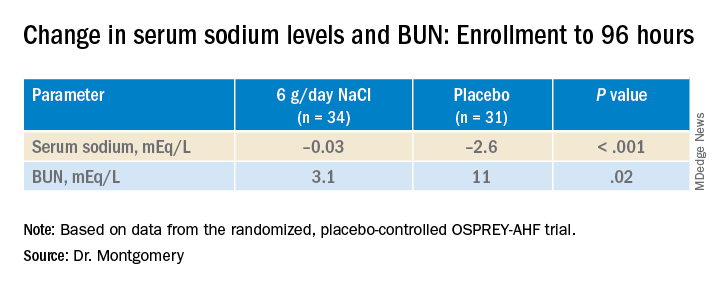
"We have patients who complain about their sodium-restricted diet, we have patients that have cachexia, who have a lot of complaints about provider-ordered meals and recommendations,” Dr. Montgomery explained in an interview.
Clinicians provide education and invest a lot of effort into getting patients with heart failure to start and maintain a low-sodium diet, he said. “But a low-sodium diet, in prior studies – and our study adds to this – is not a lever that actually seems to positively or adversely affect patients.”
Dr. Montgomery pointed to the recently published SODIUM-HF trial comparing low-sodium and unrestricted-sodium diets in outpatients with heart failure. It saw no clinical benefit from the low-sodium intervention.
Until studies show, potentially, that sodium restriction in hospitalized patients with heart failure makes a clinical difference, Dr. Montgomery said, “I’d say we should invest our time in things that we know are the most helpful, like getting them on guideline-directed medical therapy, when instead we spend an enormous amount of time counseling on and enforcing dietary restriction.”
Support for this study was provided by Cleveland Clinic Heart Vascular and Thoracic Institute’s Wilson Grant and Kaufman Center for Heart Failure Treatment and Recovery Grant. Dr. Lanfear disclosed research support from SomaLogic and Lilly; consulting for Abbott Laboratories, AstraZeneca, Janssen, Martin Pharmaceuticals, and Amgen; and serving on advisory panels for Illumina and Cytokinetics. Dr. Montgomery and Dr. Cleland disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
Restriction of dietary salt to alleviate or prevent volume overload in patients with acute decompensated heart failure (ADHF) is common hospital practice, but without a solid evidence base. A trial testing whether taking salt pills might have benefits for patients with ADHF undergoing intensive diuresis, therefore, may seem a bit counterintuitive.
In just such a randomized, placebo-controlled trial, the approach made no difference to weight loss on diuresis, a proxy for volume reduction, or to serum creatinine levels in ADHF patients receiving high-dose intravenous diuretic therapy.
The patients consumed the extra salt during their intravenous therapy in the form of tablets providing 6 g sodium chloride daily on top of their hospital-provided, low-sodium meals.
During that time, serum sodium levels remained stable for the 34 patients assigned to the salt tablets but dropped significantly in the 31 given placebo pills.
They lost about the same weight, averages of 4 kg and 4.6 kg (8.8-10 lb), respectively, and their urine output was also similar. Patients who took the salt tablets showed less of an increase in blood urea nitrogen (BUN) at both 96 hours and at discharge.
The findings “challenge the routine practice of sodium chloride restriction in acute heart failure, something done thousands of times a day, millions of times a year,” Robert A. Montgomery, MD, Cleveland Clinic, said when presenting the study at the annual scientific meeting of the Heart Failure Society of America.
The trial, called OSPREY-AHF (Oral Sodium to Preserve Renal Efficiency in Acute Heart Failure), also may encourage a shift in ADHF management from a preoccupation with salt restriction to focus more on fighting fluid retention.
OSPREY-HF took on “an established practice that doesn’t have much high-quality evidentiary support,” one guided primarily by consensus and observational data, Montgomery said in an interview.
There are also potential downsides to dietary sodium restriction, including some that may complicate or block ADHF therapies.
“Low-sodium diets can be associated with decreased caloric intake and nutritional quality,” Dr. Montgomery observed. And observational studies suggest that “patients who are on a low sodium diet can develop increased neurohormonal activation. The kidney is not sensing salt, and so starts ramping up the hormones,” which promotes diuretic resistance.
But emerging evidence also suggests “that giving sodium chloride in the form of hypertonic saline can help patients who are diuretic resistant.” The intervention, which appears to attenuate the neurohormonal activation associated with high-dose intravenous diuretics, Dr. Montgomery noted, helped inspire the design of OSPREY-AHF.
Edema consists of “a gallon of water and a pinch of salt, so we really should stop being so salt-centric and think much more about water as the problem in decompensated heart failure,” said John G.F. Cleland, MD, PhD, during the question-and-answer period after Montgomery’s presentation. Dr. Cleland, of the University of Glasgow Institute of Health and Wellbeing, is not connected to OSPREY-AHF.
“I think that maybe we overinterpret how important salt is” as a focus of volume management in ADHF, offered David Lanfear, MD, Henry Ford Health System, Detroit, who is also not part of the study.
OSPREY-AHF was well conducted but applies to a “very specific” clinical setting, Dr. Lanfear said in an interview. “These people are getting aggressive diuresis, a big dose and continuous infusion. It’s not everybody that has heart failure.”
Although the study was small, “I think it will fuel interest in this area and, probably, further investigation,” he said. The trial on its own won’t change practice, “but it will raise some eyebrows.”
The trial included patients with ADHF who have been “admitted to a cardiovascular medicine floor, not the intensive care unit” and were receiving at least 10 mg per hour of furosemide. It excluded any who were “hypernatremic or severely hyponatremic,” said Dr. Montgomery when presenting the study. They were required to have an initial estimated glomerular filtration rate (eGFR) of at least 15 mL/min per 1.73 m2.
The patients were randomly assigned double blind at a single center to receive tablets providing 2 g sodium chloride or placebo pills – 34 and 31 patients, respectively – three times daily during intravenous diuresis.
At 96 hours, the two groups showed no difference in change in creatinine levels or change in weight, both primary endpoints. Nor did they differ in urine output or change in eGFR. But serum sodium levels fell further, and BUN levels went up more in those given placebo.
The two groups showed no differences in hospital length of stay, use of renal replacement therapy at 90 days, ICU time during the index hospitalization, 30-day readmission, or 90-day mortality – although the trial wasn’t powered for clinical outcomes, Dr. Montgomery reported.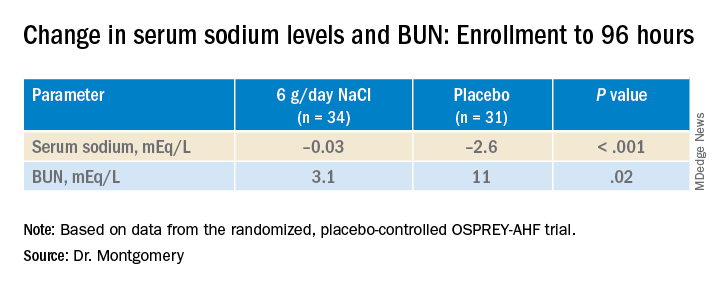
"We have patients who complain about their sodium-restricted diet, we have patients that have cachexia, who have a lot of complaints about provider-ordered meals and recommendations,” Dr. Montgomery explained in an interview.
Clinicians provide education and invest a lot of effort into getting patients with heart failure to start and maintain a low-sodium diet, he said. “But a low-sodium diet, in prior studies – and our study adds to this – is not a lever that actually seems to positively or adversely affect patients.”
Dr. Montgomery pointed to the recently published SODIUM-HF trial comparing low-sodium and unrestricted-sodium diets in outpatients with heart failure. It saw no clinical benefit from the low-sodium intervention.
Until studies show, potentially, that sodium restriction in hospitalized patients with heart failure makes a clinical difference, Dr. Montgomery said, “I’d say we should invest our time in things that we know are the most helpful, like getting them on guideline-directed medical therapy, when instead we spend an enormous amount of time counseling on and enforcing dietary restriction.”
Support for this study was provided by Cleveland Clinic Heart Vascular and Thoracic Institute’s Wilson Grant and Kaufman Center for Heart Failure Treatment and Recovery Grant. Dr. Lanfear disclosed research support from SomaLogic and Lilly; consulting for Abbott Laboratories, AstraZeneca, Janssen, Martin Pharmaceuticals, and Amgen; and serving on advisory panels for Illumina and Cytokinetics. Dr. Montgomery and Dr. Cleland disclosed no relevant financial relationships.
A version of this article first appeared on Medscape.com.
FROM HFSA 2022
Add PCSK9 inhibitor to high-intensity statin at primary PCI, proposes sham-controlled EPIC-STEMI
It’s best to have patients on aggressive lipid-lowering therapy before discharge after an acute ST-segment elevation myocardial infarction (STEMI), so why not start it right away – even in the cath lab – using some of the most potent LDL cholesterol–lowering agents available?
That was a main idea behind the randomized, sham-controlled EPIC-STEMI trial, in which STEMI patients were started on a PCSK9 (proprotein convertase subtilisin/kexin type 9) inhibitor immediately before direct percutaneous coronary intervention (PCI) and on top of high-intensity statins.
Those in the trial getting the active agent showed a 22% drop in LDL cholesterol levels by 6 weeks, compared with the control group given a sham injection along with high-intensity statins. They were also more likely to meet LDL cholesterol goals specified in some guidelines, including reduction by at least 50%. And those outcomes were achieved regardless of baseline LDL cholesterol levels or prior statin use.
Adoption of the trial’s early, aggressive LDL cholesterolreduction strategy in practice “has the potential to substantially reduce morbidity and mortality” in such cases “by further reducing LDL beyond statins in a much greater number of high-risk patients than are currently being treated with these agents,” suggested principal investigator Shamir R. Mehta, MD, MSc, when presenting the findings at the Transcatheter Cardiovascular Therapeutics annual meeting, sponsored by the Cardiovascular Research Foundation.
Adherence to secondary prevention measures in patients with acute coronary syndromes (ACS) is much better if they are started before hospital discharge, explained Dr. Mehta, senior scientist with Population Health Research Institute and professor of medicine at McMaster University, Hamilton, Ont. But “as soon as the patient has left the hospital, it is much more difficult to get these therapies on board.”
Routine adoption of such aggressive in-hospital, lipid-lowering therapy for the vast population with ACS would likely mean far fewer deaths and cardiovascular events “across a broader patient population.”
EPIC-STEMI is among the first studies to explore the strategy. “I think that’s the point of the trial that we wanted to make, that we don’t yet have data on this. We’re treading very carefully with PCSK9 inhibitors, and it’s just inching forward in populations. And I think we need a bold trial to see whether or not this changes things.”
The PCSK9 inhibitor alirocumab (Praluent) was used in EPIC-STEMI, which was published in EuroIntervention, with Dr. Mehta as lead author, the same day as his presentation. The drug and its sham injection were given on top of either atorvastatin 40-80 mg or rosuvastatin 40 mg.
Early initiation of statins in patients with acute STEMI has become standard, but there’s good evidence from intracoronary imaging studies suggesting that the addition of PCSK9 inhibitors might promote further stabilization of plaques that could potentially cause recurrent ischemic events.
Treatment with the injectable drugs plus statins led to significant coronary lesion regression in the GLAGOV trial of patients with stable coronary disease. And initiation of PCSK9 inhibitors with high-intensity statins soon after PCI for ACS improved atheroma shrinkage in non–infarct-related arteries over 1 year in the recent, placebo-controlled PACMAN-AMI trial.
Dr. Mehta pointed out that LDL reductions on PCSK9 inhibition, compared with the sham control, weren’t necessarily as impressive as might be expected from the major trials of long-term therapy with the drugs.
“You need longer [therapy] in order to see a difference in LDL levels when you use a PCSK9 inhibitor acutely. This is shown also on measures of infarct size.” There was no difference between treatment groups in infarct size as measured by levels of the MB fraction of creatine kinase, he reported.
“What this is telling us is that the acute use of a PCSK9 inhibitor did not modify the size or the severity of the baseline STEMI event.”
And EPIC-STEMI was too small and never intended to assess clinical outcomes; it was more about feasibility and what degree of LDL cholesterol lowering might be expected.
The trial was needed, Dr. Mehta said, because the PCSK9 inhibitors haven’t been extensively adopted into clinical practice and are not getting to the patients who could most benefit. One of the reasons for that is quite clear to him. “We are missing the high-risk patients because we are not treating them acutely,” Dr. Mehta said in an interview.
The strategy “has not yet been evaluated, and there have been barriers,” he observed. “Cost has been a barrier. Access to the drug has been a barrier. But in terms of the science, in terms of reducing cardiovascular events, this is a strategy that has to be tested.”
The aggressive, early LDL cholesterol reduction strategy should be evaluated for its effect on long-term outcomes, “especially knowing that in the first 30 days to 6 months post STEMI there’s a tremendous uptick in ischemic events, including recurrent myocardial infarction,” Roxana Mehran, MD, said at a media briefing on EPIC-STEMI held before Dr. Mehta’s formal presentation.
The “fantastic reduction acutely” with a PCSK9 inhibitor on top of statins, “hopefully reducing inflammation” similarly to what’s been observed in past trials, “absolutely warrants” a STEMI clinical outcomes trial, said Dr. Mehran, Icahn School of Medicine at Mount Sinai, New York, who isn’t connected with EPIC-STEMI.
If better post-discharge medication adherence is one of the acute strategy’s goals, it will be important to consider the potential influence of prescribing a periodically injected drug, proposed Eric A. Cohen, MD, Sunnybrook Health Sciences Center, Toronto, at the press conference.
“Keep in mind that STEMI patients typically come to the hospital on zero medications and leave 2 days later on five medications,” Dr. Cohen observed. “I’m curious whether having one of those as a sub-Q injection every 2 weeks, and reducing the pill burden, will help or deter adherence to therapy. I think it’s worth studying.”
The trial originally included 97 patients undergoing PCI for STEMI who were randomly assigned to receive the PCSK9 inhibitor or a sham injection on top of high-intensity statins, without regard to LDL cholesterol levels. Randomization took place after diagnostic angiography but before PCI.
The analysis, however, subsequently excluded 29 patients who could not continue with the study, “mainly because of hospital research clinic closure due to the COVID-19 pandemic,” the published report states.
That left 68 patients who had received at least one dose of PCSK9 inhibitor, alirocumab 150 mg subcutaneously, or the sham injection, and had at least one blood draw for LDL cholesterol response which, Dr. Mehta said, still left adequate statistical power for the LDL cholesterol–based primary endpoint.
By 6 weeks, LDL cholesterol levels had fallen 72.9% in the active-therapy group and by 48.1% in the control group (P < .001). Also, 92.1% and 56.7% of patients, respectively (P = .002), had achieved levels below the 1.4 mmol/L (54 mg/dL) goal in the European guidelines, Dr. Mehta reported.
Levels fell more than 50% compared with baseline in 89.5% of alirocumab patients and 60% (P = .007) of controls, respectively.
There was no significant difference in rates of attaining LDL cholesterol levels below the 70 mg/dL (1.8 mmol/L) threshold specified in U.S. guidelines for very high-risk patients: 94.7% of alirocumab patients and 83.4% of controls (P = .26).
Nor did the groups differ significantly in natriuretic peptide levels, which reflect ventricular remodeling; or in 6-week change in the inflammatory biomarker high-sensitivity C-reactive protein.
An open-label, randomized trial scheduled to launch before the end of 2022 will explore similarly early initiation of a PCSK9 inhibitor, compared with standard lipid management, in an estimated 4,000 patients hospitalized with STEMI or non-STEMI.
The EVOLVE MI trial is looking at the monoclonal antibody evolocumab (Repatha) for its effect on the primary endpoint of myocardial infarction, ischemic stroke, arterial revascularization, or death from any cause over an expected 3-4 years.
EPIC-STEMI was supported in part by Sanofi. Dr. Mehta reported an unrestricted grant from Sanofi to Hamilton Health Sciences for the present study and consulting fees from Amgen, Sanofi, and Novartis. Dr. Cohen disclosed receiving grant support from and holding research contracts with Abbott Vascular; and receiving fees for consulting, honoraria, or serving on a speaker’s bureau for Abbott Vascular, Medtronic, and Baylis. Dr. Mehran disclosed receiving grants or research support from numerous pharmaceutical companies; receiving consultant fee or honoraria or serving on a speaker’s bureau for Novartis, Abbott Vascular, Janssen, Medtronic, Medscape/WebMD, and Cine-Med Research; and holding equity, stock, or stock options with Control Rad, Applied Therapeutics, and Elixir Medical.
A version of this article first appeared on Medscape.com.
It’s best to have patients on aggressive lipid-lowering therapy before discharge after an acute ST-segment elevation myocardial infarction (STEMI), so why not start it right away – even in the cath lab – using some of the most potent LDL cholesterol–lowering agents available?
That was a main idea behind the randomized, sham-controlled EPIC-STEMI trial, in which STEMI patients were started on a PCSK9 (proprotein convertase subtilisin/kexin type 9) inhibitor immediately before direct percutaneous coronary intervention (PCI) and on top of high-intensity statins.
Those in the trial getting the active agent showed a 22% drop in LDL cholesterol levels by 6 weeks, compared with the control group given a sham injection along with high-intensity statins. They were also more likely to meet LDL cholesterol goals specified in some guidelines, including reduction by at least 50%. And those outcomes were achieved regardless of baseline LDL cholesterol levels or prior statin use.
Adoption of the trial’s early, aggressive LDL cholesterolreduction strategy in practice “has the potential to substantially reduce morbidity and mortality” in such cases “by further reducing LDL beyond statins in a much greater number of high-risk patients than are currently being treated with these agents,” suggested principal investigator Shamir R. Mehta, MD, MSc, when presenting the findings at the Transcatheter Cardiovascular Therapeutics annual meeting, sponsored by the Cardiovascular Research Foundation.
Adherence to secondary prevention measures in patients with acute coronary syndromes (ACS) is much better if they are started before hospital discharge, explained Dr. Mehta, senior scientist with Population Health Research Institute and professor of medicine at McMaster University, Hamilton, Ont. But “as soon as the patient has left the hospital, it is much more difficult to get these therapies on board.”
Routine adoption of such aggressive in-hospital, lipid-lowering therapy for the vast population with ACS would likely mean far fewer deaths and cardiovascular events “across a broader patient population.”
EPIC-STEMI is among the first studies to explore the strategy. “I think that’s the point of the trial that we wanted to make, that we don’t yet have data on this. We’re treading very carefully with PCSK9 inhibitors, and it’s just inching forward in populations. And I think we need a bold trial to see whether or not this changes things.”
The PCSK9 inhibitor alirocumab (Praluent) was used in EPIC-STEMI, which was published in EuroIntervention, with Dr. Mehta as lead author, the same day as his presentation. The drug and its sham injection were given on top of either atorvastatin 40-80 mg or rosuvastatin 40 mg.
Early initiation of statins in patients with acute STEMI has become standard, but there’s good evidence from intracoronary imaging studies suggesting that the addition of PCSK9 inhibitors might promote further stabilization of plaques that could potentially cause recurrent ischemic events.
Treatment with the injectable drugs plus statins led to significant coronary lesion regression in the GLAGOV trial of patients with stable coronary disease. And initiation of PCSK9 inhibitors with high-intensity statins soon after PCI for ACS improved atheroma shrinkage in non–infarct-related arteries over 1 year in the recent, placebo-controlled PACMAN-AMI trial.
Dr. Mehta pointed out that LDL reductions on PCSK9 inhibition, compared with the sham control, weren’t necessarily as impressive as might be expected from the major trials of long-term therapy with the drugs.
“You need longer [therapy] in order to see a difference in LDL levels when you use a PCSK9 inhibitor acutely. This is shown also on measures of infarct size.” There was no difference between treatment groups in infarct size as measured by levels of the MB fraction of creatine kinase, he reported.
“What this is telling us is that the acute use of a PCSK9 inhibitor did not modify the size or the severity of the baseline STEMI event.”
And EPIC-STEMI was too small and never intended to assess clinical outcomes; it was more about feasibility and what degree of LDL cholesterol lowering might be expected.
The trial was needed, Dr. Mehta said, because the PCSK9 inhibitors haven’t been extensively adopted into clinical practice and are not getting to the patients who could most benefit. One of the reasons for that is quite clear to him. “We are missing the high-risk patients because we are not treating them acutely,” Dr. Mehta said in an interview.
The strategy “has not yet been evaluated, and there have been barriers,” he observed. “Cost has been a barrier. Access to the drug has been a barrier. But in terms of the science, in terms of reducing cardiovascular events, this is a strategy that has to be tested.”
The aggressive, early LDL cholesterol reduction strategy should be evaluated for its effect on long-term outcomes, “especially knowing that in the first 30 days to 6 months post STEMI there’s a tremendous uptick in ischemic events, including recurrent myocardial infarction,” Roxana Mehran, MD, said at a media briefing on EPIC-STEMI held before Dr. Mehta’s formal presentation.
The “fantastic reduction acutely” with a PCSK9 inhibitor on top of statins, “hopefully reducing inflammation” similarly to what’s been observed in past trials, “absolutely warrants” a STEMI clinical outcomes trial, said Dr. Mehran, Icahn School of Medicine at Mount Sinai, New York, who isn’t connected with EPIC-STEMI.
If better post-discharge medication adherence is one of the acute strategy’s goals, it will be important to consider the potential influence of prescribing a periodically injected drug, proposed Eric A. Cohen, MD, Sunnybrook Health Sciences Center, Toronto, at the press conference.
“Keep in mind that STEMI patients typically come to the hospital on zero medications and leave 2 days later on five medications,” Dr. Cohen observed. “I’m curious whether having one of those as a sub-Q injection every 2 weeks, and reducing the pill burden, will help or deter adherence to therapy. I think it’s worth studying.”
The trial originally included 97 patients undergoing PCI for STEMI who were randomly assigned to receive the PCSK9 inhibitor or a sham injection on top of high-intensity statins, without regard to LDL cholesterol levels. Randomization took place after diagnostic angiography but before PCI.
The analysis, however, subsequently excluded 29 patients who could not continue with the study, “mainly because of hospital research clinic closure due to the COVID-19 pandemic,” the published report states.
That left 68 patients who had received at least one dose of PCSK9 inhibitor, alirocumab 150 mg subcutaneously, or the sham injection, and had at least one blood draw for LDL cholesterol response which, Dr. Mehta said, still left adequate statistical power for the LDL cholesterol–based primary endpoint.
By 6 weeks, LDL cholesterol levels had fallen 72.9% in the active-therapy group and by 48.1% in the control group (P < .001). Also, 92.1% and 56.7% of patients, respectively (P = .002), had achieved levels below the 1.4 mmol/L (54 mg/dL) goal in the European guidelines, Dr. Mehta reported.
Levels fell more than 50% compared with baseline in 89.5% of alirocumab patients and 60% (P = .007) of controls, respectively.
There was no significant difference in rates of attaining LDL cholesterol levels below the 70 mg/dL (1.8 mmol/L) threshold specified in U.S. guidelines for very high-risk patients: 94.7% of alirocumab patients and 83.4% of controls (P = .26).
Nor did the groups differ significantly in natriuretic peptide levels, which reflect ventricular remodeling; or in 6-week change in the inflammatory biomarker high-sensitivity C-reactive protein.
An open-label, randomized trial scheduled to launch before the end of 2022 will explore similarly early initiation of a PCSK9 inhibitor, compared with standard lipid management, in an estimated 4,000 patients hospitalized with STEMI or non-STEMI.
The EVOLVE MI trial is looking at the monoclonal antibody evolocumab (Repatha) for its effect on the primary endpoint of myocardial infarction, ischemic stroke, arterial revascularization, or death from any cause over an expected 3-4 years.
EPIC-STEMI was supported in part by Sanofi. Dr. Mehta reported an unrestricted grant from Sanofi to Hamilton Health Sciences for the present study and consulting fees from Amgen, Sanofi, and Novartis. Dr. Cohen disclosed receiving grant support from and holding research contracts with Abbott Vascular; and receiving fees for consulting, honoraria, or serving on a speaker’s bureau for Abbott Vascular, Medtronic, and Baylis. Dr. Mehran disclosed receiving grants or research support from numerous pharmaceutical companies; receiving consultant fee or honoraria or serving on a speaker’s bureau for Novartis, Abbott Vascular, Janssen, Medtronic, Medscape/WebMD, and Cine-Med Research; and holding equity, stock, or stock options with Control Rad, Applied Therapeutics, and Elixir Medical.
A version of this article first appeared on Medscape.com.
It’s best to have patients on aggressive lipid-lowering therapy before discharge after an acute ST-segment elevation myocardial infarction (STEMI), so why not start it right away – even in the cath lab – using some of the most potent LDL cholesterol–lowering agents available?
That was a main idea behind the randomized, sham-controlled EPIC-STEMI trial, in which STEMI patients were started on a PCSK9 (proprotein convertase subtilisin/kexin type 9) inhibitor immediately before direct percutaneous coronary intervention (PCI) and on top of high-intensity statins.
Those in the trial getting the active agent showed a 22% drop in LDL cholesterol levels by 6 weeks, compared with the control group given a sham injection along with high-intensity statins. They were also more likely to meet LDL cholesterol goals specified in some guidelines, including reduction by at least 50%. And those outcomes were achieved regardless of baseline LDL cholesterol levels or prior statin use.
Adoption of the trial’s early, aggressive LDL cholesterolreduction strategy in practice “has the potential to substantially reduce morbidity and mortality” in such cases “by further reducing LDL beyond statins in a much greater number of high-risk patients than are currently being treated with these agents,” suggested principal investigator Shamir R. Mehta, MD, MSc, when presenting the findings at the Transcatheter Cardiovascular Therapeutics annual meeting, sponsored by the Cardiovascular Research Foundation.
Adherence to secondary prevention measures in patients with acute coronary syndromes (ACS) is much better if they are started before hospital discharge, explained Dr. Mehta, senior scientist with Population Health Research Institute and professor of medicine at McMaster University, Hamilton, Ont. But “as soon as the patient has left the hospital, it is much more difficult to get these therapies on board.”
Routine adoption of such aggressive in-hospital, lipid-lowering therapy for the vast population with ACS would likely mean far fewer deaths and cardiovascular events “across a broader patient population.”
EPIC-STEMI is among the first studies to explore the strategy. “I think that’s the point of the trial that we wanted to make, that we don’t yet have data on this. We’re treading very carefully with PCSK9 inhibitors, and it’s just inching forward in populations. And I think we need a bold trial to see whether or not this changes things.”
The PCSK9 inhibitor alirocumab (Praluent) was used in EPIC-STEMI, which was published in EuroIntervention, with Dr. Mehta as lead author, the same day as his presentation. The drug and its sham injection were given on top of either atorvastatin 40-80 mg or rosuvastatin 40 mg.
Early initiation of statins in patients with acute STEMI has become standard, but there’s good evidence from intracoronary imaging studies suggesting that the addition of PCSK9 inhibitors might promote further stabilization of plaques that could potentially cause recurrent ischemic events.
Treatment with the injectable drugs plus statins led to significant coronary lesion regression in the GLAGOV trial of patients with stable coronary disease. And initiation of PCSK9 inhibitors with high-intensity statins soon after PCI for ACS improved atheroma shrinkage in non–infarct-related arteries over 1 year in the recent, placebo-controlled PACMAN-AMI trial.
Dr. Mehta pointed out that LDL reductions on PCSK9 inhibition, compared with the sham control, weren’t necessarily as impressive as might be expected from the major trials of long-term therapy with the drugs.
“You need longer [therapy] in order to see a difference in LDL levels when you use a PCSK9 inhibitor acutely. This is shown also on measures of infarct size.” There was no difference between treatment groups in infarct size as measured by levels of the MB fraction of creatine kinase, he reported.
“What this is telling us is that the acute use of a PCSK9 inhibitor did not modify the size or the severity of the baseline STEMI event.”
And EPIC-STEMI was too small and never intended to assess clinical outcomes; it was more about feasibility and what degree of LDL cholesterol lowering might be expected.
The trial was needed, Dr. Mehta said, because the PCSK9 inhibitors haven’t been extensively adopted into clinical practice and are not getting to the patients who could most benefit. One of the reasons for that is quite clear to him. “We are missing the high-risk patients because we are not treating them acutely,” Dr. Mehta said in an interview.
The strategy “has not yet been evaluated, and there have been barriers,” he observed. “Cost has been a barrier. Access to the drug has been a barrier. But in terms of the science, in terms of reducing cardiovascular events, this is a strategy that has to be tested.”
The aggressive, early LDL cholesterol reduction strategy should be evaluated for its effect on long-term outcomes, “especially knowing that in the first 30 days to 6 months post STEMI there’s a tremendous uptick in ischemic events, including recurrent myocardial infarction,” Roxana Mehran, MD, said at a media briefing on EPIC-STEMI held before Dr. Mehta’s formal presentation.
The “fantastic reduction acutely” with a PCSK9 inhibitor on top of statins, “hopefully reducing inflammation” similarly to what’s been observed in past trials, “absolutely warrants” a STEMI clinical outcomes trial, said Dr. Mehran, Icahn School of Medicine at Mount Sinai, New York, who isn’t connected with EPIC-STEMI.
If better post-discharge medication adherence is one of the acute strategy’s goals, it will be important to consider the potential influence of prescribing a periodically injected drug, proposed Eric A. Cohen, MD, Sunnybrook Health Sciences Center, Toronto, at the press conference.
“Keep in mind that STEMI patients typically come to the hospital on zero medications and leave 2 days later on five medications,” Dr. Cohen observed. “I’m curious whether having one of those as a sub-Q injection every 2 weeks, and reducing the pill burden, will help or deter adherence to therapy. I think it’s worth studying.”
The trial originally included 97 patients undergoing PCI for STEMI who were randomly assigned to receive the PCSK9 inhibitor or a sham injection on top of high-intensity statins, without regard to LDL cholesterol levels. Randomization took place after diagnostic angiography but before PCI.
The analysis, however, subsequently excluded 29 patients who could not continue with the study, “mainly because of hospital research clinic closure due to the COVID-19 pandemic,” the published report states.
That left 68 patients who had received at least one dose of PCSK9 inhibitor, alirocumab 150 mg subcutaneously, or the sham injection, and had at least one blood draw for LDL cholesterol response which, Dr. Mehta said, still left adequate statistical power for the LDL cholesterol–based primary endpoint.
By 6 weeks, LDL cholesterol levels had fallen 72.9% in the active-therapy group and by 48.1% in the control group (P < .001). Also, 92.1% and 56.7% of patients, respectively (P = .002), had achieved levels below the 1.4 mmol/L (54 mg/dL) goal in the European guidelines, Dr. Mehta reported.
Levels fell more than 50% compared with baseline in 89.5% of alirocumab patients and 60% (P = .007) of controls, respectively.
There was no significant difference in rates of attaining LDL cholesterol levels below the 70 mg/dL (1.8 mmol/L) threshold specified in U.S. guidelines for very high-risk patients: 94.7% of alirocumab patients and 83.4% of controls (P = .26).
Nor did the groups differ significantly in natriuretic peptide levels, which reflect ventricular remodeling; or in 6-week change in the inflammatory biomarker high-sensitivity C-reactive protein.
An open-label, randomized trial scheduled to launch before the end of 2022 will explore similarly early initiation of a PCSK9 inhibitor, compared with standard lipid management, in an estimated 4,000 patients hospitalized with STEMI or non-STEMI.
The EVOLVE MI trial is looking at the monoclonal antibody evolocumab (Repatha) for its effect on the primary endpoint of myocardial infarction, ischemic stroke, arterial revascularization, or death from any cause over an expected 3-4 years.
EPIC-STEMI was supported in part by Sanofi. Dr. Mehta reported an unrestricted grant from Sanofi to Hamilton Health Sciences for the present study and consulting fees from Amgen, Sanofi, and Novartis. Dr. Cohen disclosed receiving grant support from and holding research contracts with Abbott Vascular; and receiving fees for consulting, honoraria, or serving on a speaker’s bureau for Abbott Vascular, Medtronic, and Baylis. Dr. Mehran disclosed receiving grants or research support from numerous pharmaceutical companies; receiving consultant fee or honoraria or serving on a speaker’s bureau for Novartis, Abbott Vascular, Janssen, Medtronic, Medscape/WebMD, and Cine-Med Research; and holding equity, stock, or stock options with Control Rad, Applied Therapeutics, and Elixir Medical.
A version of this article first appeared on Medscape.com.
FROM TCT 2022