User login
CGRPs in real world: Similar efficacy, more AEs
and has found that patients who fail on one of the treatments are likely to fail again if they’re switched to another.
At the virtual annual meeting of the American Headache Society, Larry Robbins, MD, assistant professor of neurology at Chicago Medical School, North Chicago, reported on the results of his postapproval study of 369 migraine patients taking one of the three approved CGRP mAbs. “If patients do not do well on one mAb, it is sometimes worthwhile to switch, but most patients do not do well from the second or third mAb as well,” Dr. Robbins said in an interview. “In addition, there are numerous adverse effects that were not captured in the official phase 3 studies. Efficacy has held up well, but for a number of reasons, the true adverse event profile is often missed.”
Assessing efficacy and adverse events
In evaluating the efficacy of the three approved CGRP mAbs, Dr. Robbins used measures of degree of relief based on percentage decrease of symptoms versus baseline and the number of migraine days, combined with the number of moderate or severe headache days. Most of the patients kept calendars and were interviewed by two headache specialists. The study also utilized a 10-point visual analog scale and averaged relief over 3 months.
Of the patients on erenumab (n = 220), 10% described 95%-100% relief of symptoms, 24% reported 71%-100% relief, 34% described 31%-70% relief, and 43% experienced 0%-30% relief. Adverse events among this group included constipation (20%), nausea (7%), increased headache and fatigue (5% for each), and joint pain and depression (3% for each). Three patients on erenumab experienced unspecified serious adverse reactions.
In the fremanezumab group (n = 79), 8% described 95%-100% relief, 18% had 71%-100% relief, 33% experienced 31%-70% improvement, and 50% had 30% improvement or less. Adverse events in these patients included nausea, constipation, and depression (6% each); increased headache and muscle pain or cramps (5% each); rash, joint pain, anxiety, fatigue, or weight gain (4% for each ); and injection-site reactions, irritability, or alopecia (3% combined).
Patients taking galcanezumab (n = 70) reported the following outcomes: 3% had 95%-100% relief of symptoms, 14% had 71%-100% relief, 46% with 31%-70% relief, and 40% had 0%-30% relief. This group’s adverse events included constipation (10%); depression and increased headache (6% for each); nausea, fatigue, or injection-site reactions (4% each ); and muscle pain or cramps, rash, anxiety, weight gain, or alopecia (3% each).
Dr. Robbins also assessed switching from one CGRP mAb to another for various reasons. “When the reason for switching was poor efficacy, only 27% of patients did well,” he stated in the presentation. “If the reason was adverse events, 33% did well. When insurance/financial reasons alone were the reason, but efficacy was adequate, 58% did well after switching.”
Overall, postapproval efficacy of the medications “held up well,” Dr. Robbins noted. “Efficacy after 2 months somewhat predicted how patients would do after 6 months.” Among the predictors of poor response his study identified were opioid use and moderate or severe refractory chronic migraine at baseline.
However, the rates of adverse events he reported were significantly greater than those reported in the clinical trials, Dr. Robbins said. He noted four reasons to explain this discrepancy: the trials did not use an 18-item supplemental checklist that he has advocated to identify patients at risk of side effects, the trials weren’t powered for adverse events, patients in the trials tended to be less refractory than those in the clinic, and that adverse events tend to be underreported in trials.
“Adverse events become disaggregated, with the same descriptors used for an adverse event,” Dr. Robbins said. “Examples include fatigue, somnolence, and tiredness; all may be 1%, while different patients are describing the same adverse event. It is possible to reaggregate the adverse events after the study, but this is fraught with error.”
Uncovering shortcomings in clinical trials
Emily Rubenstein Engel, MD, director of the Dalessio Headache Center at the Scripps Clinic in La Jolla, Calif., noted that Dr. Robbins’ findings are significant for two reasons. “Dr. Robbins has uncovered a general flaw in clinical trials, whereby the lack of consistency of adverse event terminology as well as the lack of a standardized questionnaire format for adverse events can result in significant under-reporting of adverse events,” she said.
“Specifically for the CGRPs,” Dr. Engel continued, “he has raised awareness that this new class of medication, however promising from an efficacy standpoint, has side effects that are much more frequent and severe than seen in the initial clinical trials.”
Dr. Robbins reported financial relationships with Allergan, Amgen and Teva. Dr. Engel has no financial relationships to disclose.
and has found that patients who fail on one of the treatments are likely to fail again if they’re switched to another.
At the virtual annual meeting of the American Headache Society, Larry Robbins, MD, assistant professor of neurology at Chicago Medical School, North Chicago, reported on the results of his postapproval study of 369 migraine patients taking one of the three approved CGRP mAbs. “If patients do not do well on one mAb, it is sometimes worthwhile to switch, but most patients do not do well from the second or third mAb as well,” Dr. Robbins said in an interview. “In addition, there are numerous adverse effects that were not captured in the official phase 3 studies. Efficacy has held up well, but for a number of reasons, the true adverse event profile is often missed.”
Assessing efficacy and adverse events
In evaluating the efficacy of the three approved CGRP mAbs, Dr. Robbins used measures of degree of relief based on percentage decrease of symptoms versus baseline and the number of migraine days, combined with the number of moderate or severe headache days. Most of the patients kept calendars and were interviewed by two headache specialists. The study also utilized a 10-point visual analog scale and averaged relief over 3 months.
Of the patients on erenumab (n = 220), 10% described 95%-100% relief of symptoms, 24% reported 71%-100% relief, 34% described 31%-70% relief, and 43% experienced 0%-30% relief. Adverse events among this group included constipation (20%), nausea (7%), increased headache and fatigue (5% for each), and joint pain and depression (3% for each). Three patients on erenumab experienced unspecified serious adverse reactions.
In the fremanezumab group (n = 79), 8% described 95%-100% relief, 18% had 71%-100% relief, 33% experienced 31%-70% improvement, and 50% had 30% improvement or less. Adverse events in these patients included nausea, constipation, and depression (6% each); increased headache and muscle pain or cramps (5% each); rash, joint pain, anxiety, fatigue, or weight gain (4% for each ); and injection-site reactions, irritability, or alopecia (3% combined).
Patients taking galcanezumab (n = 70) reported the following outcomes: 3% had 95%-100% relief of symptoms, 14% had 71%-100% relief, 46% with 31%-70% relief, and 40% had 0%-30% relief. This group’s adverse events included constipation (10%); depression and increased headache (6% for each); nausea, fatigue, or injection-site reactions (4% each ); and muscle pain or cramps, rash, anxiety, weight gain, or alopecia (3% each).
Dr. Robbins also assessed switching from one CGRP mAb to another for various reasons. “When the reason for switching was poor efficacy, only 27% of patients did well,” he stated in the presentation. “If the reason was adverse events, 33% did well. When insurance/financial reasons alone were the reason, but efficacy was adequate, 58% did well after switching.”
Overall, postapproval efficacy of the medications “held up well,” Dr. Robbins noted. “Efficacy after 2 months somewhat predicted how patients would do after 6 months.” Among the predictors of poor response his study identified were opioid use and moderate or severe refractory chronic migraine at baseline.
However, the rates of adverse events he reported were significantly greater than those reported in the clinical trials, Dr. Robbins said. He noted four reasons to explain this discrepancy: the trials did not use an 18-item supplemental checklist that he has advocated to identify patients at risk of side effects, the trials weren’t powered for adverse events, patients in the trials tended to be less refractory than those in the clinic, and that adverse events tend to be underreported in trials.
“Adverse events become disaggregated, with the same descriptors used for an adverse event,” Dr. Robbins said. “Examples include fatigue, somnolence, and tiredness; all may be 1%, while different patients are describing the same adverse event. It is possible to reaggregate the adverse events after the study, but this is fraught with error.”
Uncovering shortcomings in clinical trials
Emily Rubenstein Engel, MD, director of the Dalessio Headache Center at the Scripps Clinic in La Jolla, Calif., noted that Dr. Robbins’ findings are significant for two reasons. “Dr. Robbins has uncovered a general flaw in clinical trials, whereby the lack of consistency of adverse event terminology as well as the lack of a standardized questionnaire format for adverse events can result in significant under-reporting of adverse events,” she said.
“Specifically for the CGRPs,” Dr. Engel continued, “he has raised awareness that this new class of medication, however promising from an efficacy standpoint, has side effects that are much more frequent and severe than seen in the initial clinical trials.”
Dr. Robbins reported financial relationships with Allergan, Amgen and Teva. Dr. Engel has no financial relationships to disclose.
and has found that patients who fail on one of the treatments are likely to fail again if they’re switched to another.
At the virtual annual meeting of the American Headache Society, Larry Robbins, MD, assistant professor of neurology at Chicago Medical School, North Chicago, reported on the results of his postapproval study of 369 migraine patients taking one of the three approved CGRP mAbs. “If patients do not do well on one mAb, it is sometimes worthwhile to switch, but most patients do not do well from the second or third mAb as well,” Dr. Robbins said in an interview. “In addition, there are numerous adverse effects that were not captured in the official phase 3 studies. Efficacy has held up well, but for a number of reasons, the true adverse event profile is often missed.”
Assessing efficacy and adverse events
In evaluating the efficacy of the three approved CGRP mAbs, Dr. Robbins used measures of degree of relief based on percentage decrease of symptoms versus baseline and the number of migraine days, combined with the number of moderate or severe headache days. Most of the patients kept calendars and were interviewed by two headache specialists. The study also utilized a 10-point visual analog scale and averaged relief over 3 months.
Of the patients on erenumab (n = 220), 10% described 95%-100% relief of symptoms, 24% reported 71%-100% relief, 34% described 31%-70% relief, and 43% experienced 0%-30% relief. Adverse events among this group included constipation (20%), nausea (7%), increased headache and fatigue (5% for each), and joint pain and depression (3% for each). Three patients on erenumab experienced unspecified serious adverse reactions.
In the fremanezumab group (n = 79), 8% described 95%-100% relief, 18% had 71%-100% relief, 33% experienced 31%-70% improvement, and 50% had 30% improvement or less. Adverse events in these patients included nausea, constipation, and depression (6% each); increased headache and muscle pain or cramps (5% each); rash, joint pain, anxiety, fatigue, or weight gain (4% for each ); and injection-site reactions, irritability, or alopecia (3% combined).
Patients taking galcanezumab (n = 70) reported the following outcomes: 3% had 95%-100% relief of symptoms, 14% had 71%-100% relief, 46% with 31%-70% relief, and 40% had 0%-30% relief. This group’s adverse events included constipation (10%); depression and increased headache (6% for each); nausea, fatigue, or injection-site reactions (4% each ); and muscle pain or cramps, rash, anxiety, weight gain, or alopecia (3% each).
Dr. Robbins also assessed switching from one CGRP mAb to another for various reasons. “When the reason for switching was poor efficacy, only 27% of patients did well,” he stated in the presentation. “If the reason was adverse events, 33% did well. When insurance/financial reasons alone were the reason, but efficacy was adequate, 58% did well after switching.”
Overall, postapproval efficacy of the medications “held up well,” Dr. Robbins noted. “Efficacy after 2 months somewhat predicted how patients would do after 6 months.” Among the predictors of poor response his study identified were opioid use and moderate or severe refractory chronic migraine at baseline.
However, the rates of adverse events he reported were significantly greater than those reported in the clinical trials, Dr. Robbins said. He noted four reasons to explain this discrepancy: the trials did not use an 18-item supplemental checklist that he has advocated to identify patients at risk of side effects, the trials weren’t powered for adverse events, patients in the trials tended to be less refractory than those in the clinic, and that adverse events tend to be underreported in trials.
“Adverse events become disaggregated, with the same descriptors used for an adverse event,” Dr. Robbins said. “Examples include fatigue, somnolence, and tiredness; all may be 1%, while different patients are describing the same adverse event. It is possible to reaggregate the adverse events after the study, but this is fraught with error.”
Uncovering shortcomings in clinical trials
Emily Rubenstein Engel, MD, director of the Dalessio Headache Center at the Scripps Clinic in La Jolla, Calif., noted that Dr. Robbins’ findings are significant for two reasons. “Dr. Robbins has uncovered a general flaw in clinical trials, whereby the lack of consistency of adverse event terminology as well as the lack of a standardized questionnaire format for adverse events can result in significant under-reporting of adverse events,” she said.
“Specifically for the CGRPs,” Dr. Engel continued, “he has raised awareness that this new class of medication, however promising from an efficacy standpoint, has side effects that are much more frequent and severe than seen in the initial clinical trials.”
Dr. Robbins reported financial relationships with Allergan, Amgen and Teva. Dr. Engel has no financial relationships to disclose.
FROM AHS 2020
Population study supports migraine–dementia link
Preliminary results from a population-based cohort study support previous reports that migraine is a midlife risk factor for dementia later in life, but further determined that according to results from a Danish registry presented at the virtual annual meeting of the American Headache Society.
“The findings of this study emphasize the need for studies in the migraine-dementia pathophysiology, in particular in migraine cases with aura,” said Sabrina Islamoska, MSc, PhD, a postdoctoral researcher in the department of public health at the University of Copenhagen. “This study highlights the importance of monitoring severe migraine to potentially prevent dementia.”
A national register-based study
The study used Danish national register–based data from 1988 to 2017 of 1.66 million individuals born between 1935 and 1956, retrieving exposure information until age 59 years and following individuals for dementia after age 60. The matched analysis included 18,135 people registered with migraine before age 59 and 1.38 million without migraine. The matched study population was 62,578.
A diagnosis of dementia or use of dementia medications after age 60 years was the main outcome. Covariates included socioeconomic factors, psychiatric comorbidities and other headache diagnoses.
“To the best of our knowledge, no previous national register–based studies have investigated the risk of dementia among individuals who suffer from migraine with aura,” Dr. Islamoska said.
The preliminary findings revealed that the median age at diagnosis was 49 years and about 70% of the migraine population were women. “There was a 50% higher dementia rate in individuals who had any migraine diagnosis,” Dr. Islamoska said.
“We also found a 20% higher but nonsignificant dementia rate in individuals who had migraine without aura,” she said. However, when the migraine-with-aura population was evaluated, it was found to have a dementia rate two times higher than people with no migraine. “The dementia rate was higher if individuals had more frequent hospital contacts with migraine.”
The findings support the hypothesis that migraine is a midlife risk factor for dementia later in life, she said.
“The findings underline the value of investigating the effect of migraine medications in dementia risk to assess the impact of mild to moderate migraines,” Dr. Islamoska said. “Therefore, the next step is to investigate the risk of dementia among users of migraine medications who are not diagnosed with migraines at hospitals.”
Strengths of the study, Dr. Islamoska noted, were its size and national nature of its population, that it included all migraine diagnoses at hospitals over a 29-year period, that it made adjustments for confounding of well-established dementia risk factors, and that it validated dementia diagnoses after age 60 years.
One limitation was that the study only included hospital-based diagnoses of dementia while 60% of cases in Denmark are undiagnosed, “thus our results only apply to migraine that is severe enough to require a hospital contact,” Dr. Islamoska said, while most migraine cases are treated in the primary care setting.
Also, the young study population may have a lower dementia risk. “We also know that age of migraine registration may not corresponded with the actual onset, since migraine is a complex disorder with individual variation in patient’s burden and course of disease,” Dr. Islamoska said.
“Future studies are needed to understand the pathological mechanisms underlying the relationship between migraine and dementia and to investigate whether proper prophylactic treatment of migraine can potentially prevent dementia,” Dr. Islamoska said. “In addition, when investigating the association between these two prevalent neurological disorders, the timing of migraine diagnosis and dementia onset is important to ensure temporality. We took this into account in our study to strengthen the validity of our results.”
‘Surprising’ findings
Andrew Charles, MD, director of the Goldberg Migraine Program at the University of California, Los Angeles, said the Danish study makes an important contribution to the literature on dementia risk factors. “Vanishingly small amounts of attention have been paid to migraine as a potential risk factor,” he said. However, he called the results “surprising” based on his own clinical experience. “I actually had a sense that migraine was somehow protective against Alzheimer’s or other kinds of dementias.”
He questioned if the migraine-dementia link could be a “reporting artifact” of migraine sufferers merely going to the neurologist, raising the likelihood of a positive migraine diagnosis. Nonetheless, the results are “intriguing” and raise important questions about migraine therapy and dementia risk.
“If it holds up, it really is something that behooves us to understand whether intervening in terms of therapy for migraine has even more consequences beyond just the immediate relief of symptoms,” Dr. Charles said. “It’s something we should be thinking about in terms of preventing longer-term consequences of this disorder.”
Dr. Islamoska disclosed that Veluxfondent funded the study as part of her PhD project. Dr. Charles disclosed he is a consultant to Amgen, Biohaven Pharmaceuticals, Eli Lilly, Lundbeck, and Novartis.
SOURCE: Islamoska S et al. AHS 2020, Submission 846214.
Preliminary results from a population-based cohort study support previous reports that migraine is a midlife risk factor for dementia later in life, but further determined that according to results from a Danish registry presented at the virtual annual meeting of the American Headache Society.
“The findings of this study emphasize the need for studies in the migraine-dementia pathophysiology, in particular in migraine cases with aura,” said Sabrina Islamoska, MSc, PhD, a postdoctoral researcher in the department of public health at the University of Copenhagen. “This study highlights the importance of monitoring severe migraine to potentially prevent dementia.”
A national register-based study
The study used Danish national register–based data from 1988 to 2017 of 1.66 million individuals born between 1935 and 1956, retrieving exposure information until age 59 years and following individuals for dementia after age 60. The matched analysis included 18,135 people registered with migraine before age 59 and 1.38 million without migraine. The matched study population was 62,578.
A diagnosis of dementia or use of dementia medications after age 60 years was the main outcome. Covariates included socioeconomic factors, psychiatric comorbidities and other headache diagnoses.
“To the best of our knowledge, no previous national register–based studies have investigated the risk of dementia among individuals who suffer from migraine with aura,” Dr. Islamoska said.
The preliminary findings revealed that the median age at diagnosis was 49 years and about 70% of the migraine population were women. “There was a 50% higher dementia rate in individuals who had any migraine diagnosis,” Dr. Islamoska said.
“We also found a 20% higher but nonsignificant dementia rate in individuals who had migraine without aura,” she said. However, when the migraine-with-aura population was evaluated, it was found to have a dementia rate two times higher than people with no migraine. “The dementia rate was higher if individuals had more frequent hospital contacts with migraine.”
The findings support the hypothesis that migraine is a midlife risk factor for dementia later in life, she said.
“The findings underline the value of investigating the effect of migraine medications in dementia risk to assess the impact of mild to moderate migraines,” Dr. Islamoska said. “Therefore, the next step is to investigate the risk of dementia among users of migraine medications who are not diagnosed with migraines at hospitals.”
Strengths of the study, Dr. Islamoska noted, were its size and national nature of its population, that it included all migraine diagnoses at hospitals over a 29-year period, that it made adjustments for confounding of well-established dementia risk factors, and that it validated dementia diagnoses after age 60 years.
One limitation was that the study only included hospital-based diagnoses of dementia while 60% of cases in Denmark are undiagnosed, “thus our results only apply to migraine that is severe enough to require a hospital contact,” Dr. Islamoska said, while most migraine cases are treated in the primary care setting.
Also, the young study population may have a lower dementia risk. “We also know that age of migraine registration may not corresponded with the actual onset, since migraine is a complex disorder with individual variation in patient’s burden and course of disease,” Dr. Islamoska said.
“Future studies are needed to understand the pathological mechanisms underlying the relationship between migraine and dementia and to investigate whether proper prophylactic treatment of migraine can potentially prevent dementia,” Dr. Islamoska said. “In addition, when investigating the association between these two prevalent neurological disorders, the timing of migraine diagnosis and dementia onset is important to ensure temporality. We took this into account in our study to strengthen the validity of our results.”
‘Surprising’ findings
Andrew Charles, MD, director of the Goldberg Migraine Program at the University of California, Los Angeles, said the Danish study makes an important contribution to the literature on dementia risk factors. “Vanishingly small amounts of attention have been paid to migraine as a potential risk factor,” he said. However, he called the results “surprising” based on his own clinical experience. “I actually had a sense that migraine was somehow protective against Alzheimer’s or other kinds of dementias.”
He questioned if the migraine-dementia link could be a “reporting artifact” of migraine sufferers merely going to the neurologist, raising the likelihood of a positive migraine diagnosis. Nonetheless, the results are “intriguing” and raise important questions about migraine therapy and dementia risk.
“If it holds up, it really is something that behooves us to understand whether intervening in terms of therapy for migraine has even more consequences beyond just the immediate relief of symptoms,” Dr. Charles said. “It’s something we should be thinking about in terms of preventing longer-term consequences of this disorder.”
Dr. Islamoska disclosed that Veluxfondent funded the study as part of her PhD project. Dr. Charles disclosed he is a consultant to Amgen, Biohaven Pharmaceuticals, Eli Lilly, Lundbeck, and Novartis.
SOURCE: Islamoska S et al. AHS 2020, Submission 846214.
Preliminary results from a population-based cohort study support previous reports that migraine is a midlife risk factor for dementia later in life, but further determined that according to results from a Danish registry presented at the virtual annual meeting of the American Headache Society.
“The findings of this study emphasize the need for studies in the migraine-dementia pathophysiology, in particular in migraine cases with aura,” said Sabrina Islamoska, MSc, PhD, a postdoctoral researcher in the department of public health at the University of Copenhagen. “This study highlights the importance of monitoring severe migraine to potentially prevent dementia.”
A national register-based study
The study used Danish national register–based data from 1988 to 2017 of 1.66 million individuals born between 1935 and 1956, retrieving exposure information until age 59 years and following individuals for dementia after age 60. The matched analysis included 18,135 people registered with migraine before age 59 and 1.38 million without migraine. The matched study population was 62,578.
A diagnosis of dementia or use of dementia medications after age 60 years was the main outcome. Covariates included socioeconomic factors, psychiatric comorbidities and other headache diagnoses.
“To the best of our knowledge, no previous national register–based studies have investigated the risk of dementia among individuals who suffer from migraine with aura,” Dr. Islamoska said.
The preliminary findings revealed that the median age at diagnosis was 49 years and about 70% of the migraine population were women. “There was a 50% higher dementia rate in individuals who had any migraine diagnosis,” Dr. Islamoska said.
“We also found a 20% higher but nonsignificant dementia rate in individuals who had migraine without aura,” she said. However, when the migraine-with-aura population was evaluated, it was found to have a dementia rate two times higher than people with no migraine. “The dementia rate was higher if individuals had more frequent hospital contacts with migraine.”
The findings support the hypothesis that migraine is a midlife risk factor for dementia later in life, she said.
“The findings underline the value of investigating the effect of migraine medications in dementia risk to assess the impact of mild to moderate migraines,” Dr. Islamoska said. “Therefore, the next step is to investigate the risk of dementia among users of migraine medications who are not diagnosed with migraines at hospitals.”
Strengths of the study, Dr. Islamoska noted, were its size and national nature of its population, that it included all migraine diagnoses at hospitals over a 29-year period, that it made adjustments for confounding of well-established dementia risk factors, and that it validated dementia diagnoses after age 60 years.
One limitation was that the study only included hospital-based diagnoses of dementia while 60% of cases in Denmark are undiagnosed, “thus our results only apply to migraine that is severe enough to require a hospital contact,” Dr. Islamoska said, while most migraine cases are treated in the primary care setting.
Also, the young study population may have a lower dementia risk. “We also know that age of migraine registration may not corresponded with the actual onset, since migraine is a complex disorder with individual variation in patient’s burden and course of disease,” Dr. Islamoska said.
“Future studies are needed to understand the pathological mechanisms underlying the relationship between migraine and dementia and to investigate whether proper prophylactic treatment of migraine can potentially prevent dementia,” Dr. Islamoska said. “In addition, when investigating the association between these two prevalent neurological disorders, the timing of migraine diagnosis and dementia onset is important to ensure temporality. We took this into account in our study to strengthen the validity of our results.”
‘Surprising’ findings
Andrew Charles, MD, director of the Goldberg Migraine Program at the University of California, Los Angeles, said the Danish study makes an important contribution to the literature on dementia risk factors. “Vanishingly small amounts of attention have been paid to migraine as a potential risk factor,” he said. However, he called the results “surprising” based on his own clinical experience. “I actually had a sense that migraine was somehow protective against Alzheimer’s or other kinds of dementias.”
He questioned if the migraine-dementia link could be a “reporting artifact” of migraine sufferers merely going to the neurologist, raising the likelihood of a positive migraine diagnosis. Nonetheless, the results are “intriguing” and raise important questions about migraine therapy and dementia risk.
“If it holds up, it really is something that behooves us to understand whether intervening in terms of therapy for migraine has even more consequences beyond just the immediate relief of symptoms,” Dr. Charles said. “It’s something we should be thinking about in terms of preventing longer-term consequences of this disorder.”
Dr. Islamoska disclosed that Veluxfondent funded the study as part of her PhD project. Dr. Charles disclosed he is a consultant to Amgen, Biohaven Pharmaceuticals, Eli Lilly, Lundbeck, and Novartis.
SOURCE: Islamoska S et al. AHS 2020, Submission 846214.
FROM AHS 2020
COVID-19 guideline update: Wear N95 masks during endoscopy
Nausea, vomiting, and diarrhea are gastrointestinal symptoms that COVID-19 patients have had, and up to 30% have been reported to have liver symptoms. Because patients with these symptoms may require endoscopy, the American Gastroenterological Association has issued a rapid recommendation document that advises physicians and health care workers to use N95 masks, double gloves, and negative pressure rooms when performing GI procedures during the COVID-19 pandemic.
The recommendations, published in Gastroenterology (2020. doi: 10.1053/j.gastro.2020.03.072), also cover non-COVID-19 patients and situations where N95 masks should be used, offer guidelines for triaging patients for endoscopy and timing of nonurgent procedures, and evaluate the latest evidence in the incidence of GI and liver manifestations of COVID-19. The guideline panel met in March.
The document includes seven recommendations for use of personal protective equipment by physicians and nurses performing GI procedures. The recommendations and the level of evidence supporting them fall under four categories:
1. Masks, comprising four recommendations: N95 masks for upper and lower GI procedures regardless of a patient’s COVID-19 status; no surgical masks only in confirmed COVID-19 patients or suspected cases; and reused N95 masks when fresh ones aren’t available instead of using a surgical mask only (very low to moderate level of evidence depending on the recommendation).
2. Double-gloving when performing any GI procedure regardless of the patient’s COVID-19 status (moderate quality evidence).
3. When available, a negative-pressure room should be used for any COVID-19 patient or suspect rather than a regular endoscopy room (very low certainty of evidence).
4. Continue to practice standard cleaning, endoscopic disinfection, and reprocessing protocols regardless of a patient’s COVID-19 status (good practice statement).
For decontamination, the panel noted that commonly used biocidal agents, such as hydrogen peroxide, alcohols, sodium hypochlorite, or benzalkonium chloride have proved effective for decontaminating of coronavirus.
For implementing the PPE recommendations, the panel stated that personnel still need to practice don and doff standard protocols, and that N95 masks should be fitted for each individual.
Other steps include banning personal belongings in the procedure area, minimizing the number of personnel in the room, avoiding change of personnel and keeping nonprocedural personnel out during the procedure, considering using nursing teams that follow the patient through preprocedure, procedure, and recovery, and considering having endoscopy teams remain together during the day to minimize exposure.
The triage recommendations stated that “trained medical personnel” should review all procedures and categorize them as time-sensitive or not time-sensitive, based on a framework the recommendation includes. In “an open-access endoscopy system” when there isn’t enough information to determine timing for the procedure, the recommendation provides a three-step approach: a phone consult with the referring physician, a telehealth visit with the patient, or a multidisciplinary team approach or virtual disease/tumor board.
“The proposed framework of separating procedures into time-sensitive and non–time-sensitive cases may be useful in determining which procedures if delayed may negatively impact on patient-important outcomes,” wrote Shahnaz Sultan, MD, AGAF, of the University of Minnesota, Minneapolis, and colleagues. The panel noted decision-making should focus on “patient-important outcomes.”
For nonurgent procedures, the panel arrived at a consensus that 8 weeks was an appropriate window for reassessment of deferred procedures, depending on the availability of resources and if the time sensitivity of the procedure changes.
The panel also attempted to determine the likelihood of GI and liver manifestations of COVID-19 by evaluating published cohort studies. They found that 2%-13.8% of patients had diarrhea, 1%-10.1% had nausea or vomiting, and one study reported 2% had abdominal pain (Am J Gastroenterol. 2020 May;115[5]766-73). What’s more, some studies have shown stool samples positive for SARS-CoV-2 RNA even after respiratory samples were negative.
The evidence on liver manifestations isn’t as robust, but one study reported that 20%-30% of patients had liver injury upon diagnosis of COVID-19 (Gastroenterology. 2020;158:1518-9), and that severe hepatitis has been reported but liver failure seems rare (Lancet. 2020 Feb 15;395[10223]:507-13). “The pattern of liver injury appears to be predominantly hepatocellular, and the etiology remains uncertain but may represent a secondary effect of the systemic inflammatory response observed with COVID-19 disease, although direct viral infection and drug-induced liver injury cannot be excluded,” Dr. Sultan and colleagues noted.
There were no relevant author conflicts of interest. The American Gastroenterological Association (AGA) Institute funded the study.
SOURCE: Sultan S et al. Gastroenterology. 2020. doi: 10.1053/j.gastro.2020.03.072.
Nausea, vomiting, and diarrhea are gastrointestinal symptoms that COVID-19 patients have had, and up to 30% have been reported to have liver symptoms. Because patients with these symptoms may require endoscopy, the American Gastroenterological Association has issued a rapid recommendation document that advises physicians and health care workers to use N95 masks, double gloves, and negative pressure rooms when performing GI procedures during the COVID-19 pandemic.
The recommendations, published in Gastroenterology (2020. doi: 10.1053/j.gastro.2020.03.072), also cover non-COVID-19 patients and situations where N95 masks should be used, offer guidelines for triaging patients for endoscopy and timing of nonurgent procedures, and evaluate the latest evidence in the incidence of GI and liver manifestations of COVID-19. The guideline panel met in March.
The document includes seven recommendations for use of personal protective equipment by physicians and nurses performing GI procedures. The recommendations and the level of evidence supporting them fall under four categories:
1. Masks, comprising four recommendations: N95 masks for upper and lower GI procedures regardless of a patient’s COVID-19 status; no surgical masks only in confirmed COVID-19 patients or suspected cases; and reused N95 masks when fresh ones aren’t available instead of using a surgical mask only (very low to moderate level of evidence depending on the recommendation).
2. Double-gloving when performing any GI procedure regardless of the patient’s COVID-19 status (moderate quality evidence).
3. When available, a negative-pressure room should be used for any COVID-19 patient or suspect rather than a regular endoscopy room (very low certainty of evidence).
4. Continue to practice standard cleaning, endoscopic disinfection, and reprocessing protocols regardless of a patient’s COVID-19 status (good practice statement).
For decontamination, the panel noted that commonly used biocidal agents, such as hydrogen peroxide, alcohols, sodium hypochlorite, or benzalkonium chloride have proved effective for decontaminating of coronavirus.
For implementing the PPE recommendations, the panel stated that personnel still need to practice don and doff standard protocols, and that N95 masks should be fitted for each individual.
Other steps include banning personal belongings in the procedure area, minimizing the number of personnel in the room, avoiding change of personnel and keeping nonprocedural personnel out during the procedure, considering using nursing teams that follow the patient through preprocedure, procedure, and recovery, and considering having endoscopy teams remain together during the day to minimize exposure.
The triage recommendations stated that “trained medical personnel” should review all procedures and categorize them as time-sensitive or not time-sensitive, based on a framework the recommendation includes. In “an open-access endoscopy system” when there isn’t enough information to determine timing for the procedure, the recommendation provides a three-step approach: a phone consult with the referring physician, a telehealth visit with the patient, or a multidisciplinary team approach or virtual disease/tumor board.
“The proposed framework of separating procedures into time-sensitive and non–time-sensitive cases may be useful in determining which procedures if delayed may negatively impact on patient-important outcomes,” wrote Shahnaz Sultan, MD, AGAF, of the University of Minnesota, Minneapolis, and colleagues. The panel noted decision-making should focus on “patient-important outcomes.”
For nonurgent procedures, the panel arrived at a consensus that 8 weeks was an appropriate window for reassessment of deferred procedures, depending on the availability of resources and if the time sensitivity of the procedure changes.
The panel also attempted to determine the likelihood of GI and liver manifestations of COVID-19 by evaluating published cohort studies. They found that 2%-13.8% of patients had diarrhea, 1%-10.1% had nausea or vomiting, and one study reported 2% had abdominal pain (Am J Gastroenterol. 2020 May;115[5]766-73). What’s more, some studies have shown stool samples positive for SARS-CoV-2 RNA even after respiratory samples were negative.
The evidence on liver manifestations isn’t as robust, but one study reported that 20%-30% of patients had liver injury upon diagnosis of COVID-19 (Gastroenterology. 2020;158:1518-9), and that severe hepatitis has been reported but liver failure seems rare (Lancet. 2020 Feb 15;395[10223]:507-13). “The pattern of liver injury appears to be predominantly hepatocellular, and the etiology remains uncertain but may represent a secondary effect of the systemic inflammatory response observed with COVID-19 disease, although direct viral infection and drug-induced liver injury cannot be excluded,” Dr. Sultan and colleagues noted.
There were no relevant author conflicts of interest. The American Gastroenterological Association (AGA) Institute funded the study.
SOURCE: Sultan S et al. Gastroenterology. 2020. doi: 10.1053/j.gastro.2020.03.072.
Nausea, vomiting, and diarrhea are gastrointestinal symptoms that COVID-19 patients have had, and up to 30% have been reported to have liver symptoms. Because patients with these symptoms may require endoscopy, the American Gastroenterological Association has issued a rapid recommendation document that advises physicians and health care workers to use N95 masks, double gloves, and negative pressure rooms when performing GI procedures during the COVID-19 pandemic.
The recommendations, published in Gastroenterology (2020. doi: 10.1053/j.gastro.2020.03.072), also cover non-COVID-19 patients and situations where N95 masks should be used, offer guidelines for triaging patients for endoscopy and timing of nonurgent procedures, and evaluate the latest evidence in the incidence of GI and liver manifestations of COVID-19. The guideline panel met in March.
The document includes seven recommendations for use of personal protective equipment by physicians and nurses performing GI procedures. The recommendations and the level of evidence supporting them fall under four categories:
1. Masks, comprising four recommendations: N95 masks for upper and lower GI procedures regardless of a patient’s COVID-19 status; no surgical masks only in confirmed COVID-19 patients or suspected cases; and reused N95 masks when fresh ones aren’t available instead of using a surgical mask only (very low to moderate level of evidence depending on the recommendation).
2. Double-gloving when performing any GI procedure regardless of the patient’s COVID-19 status (moderate quality evidence).
3. When available, a negative-pressure room should be used for any COVID-19 patient or suspect rather than a regular endoscopy room (very low certainty of evidence).
4. Continue to practice standard cleaning, endoscopic disinfection, and reprocessing protocols regardless of a patient’s COVID-19 status (good practice statement).
For decontamination, the panel noted that commonly used biocidal agents, such as hydrogen peroxide, alcohols, sodium hypochlorite, or benzalkonium chloride have proved effective for decontaminating of coronavirus.
For implementing the PPE recommendations, the panel stated that personnel still need to practice don and doff standard protocols, and that N95 masks should be fitted for each individual.
Other steps include banning personal belongings in the procedure area, minimizing the number of personnel in the room, avoiding change of personnel and keeping nonprocedural personnel out during the procedure, considering using nursing teams that follow the patient through preprocedure, procedure, and recovery, and considering having endoscopy teams remain together during the day to minimize exposure.
The triage recommendations stated that “trained medical personnel” should review all procedures and categorize them as time-sensitive or not time-sensitive, based on a framework the recommendation includes. In “an open-access endoscopy system” when there isn’t enough information to determine timing for the procedure, the recommendation provides a three-step approach: a phone consult with the referring physician, a telehealth visit with the patient, or a multidisciplinary team approach or virtual disease/tumor board.
“The proposed framework of separating procedures into time-sensitive and non–time-sensitive cases may be useful in determining which procedures if delayed may negatively impact on patient-important outcomes,” wrote Shahnaz Sultan, MD, AGAF, of the University of Minnesota, Minneapolis, and colleagues. The panel noted decision-making should focus on “patient-important outcomes.”
For nonurgent procedures, the panel arrived at a consensus that 8 weeks was an appropriate window for reassessment of deferred procedures, depending on the availability of resources and if the time sensitivity of the procedure changes.
The panel also attempted to determine the likelihood of GI and liver manifestations of COVID-19 by evaluating published cohort studies. They found that 2%-13.8% of patients had diarrhea, 1%-10.1% had nausea or vomiting, and one study reported 2% had abdominal pain (Am J Gastroenterol. 2020 May;115[5]766-73). What’s more, some studies have shown stool samples positive for SARS-CoV-2 RNA even after respiratory samples were negative.
The evidence on liver manifestations isn’t as robust, but one study reported that 20%-30% of patients had liver injury upon diagnosis of COVID-19 (Gastroenterology. 2020;158:1518-9), and that severe hepatitis has been reported but liver failure seems rare (Lancet. 2020 Feb 15;395[10223]:507-13). “The pattern of liver injury appears to be predominantly hepatocellular, and the etiology remains uncertain but may represent a secondary effect of the systemic inflammatory response observed with COVID-19 disease, although direct viral infection and drug-induced liver injury cannot be excluded,” Dr. Sultan and colleagues noted.
There were no relevant author conflicts of interest. The American Gastroenterological Association (AGA) Institute funded the study.
SOURCE: Sultan S et al. Gastroenterology. 2020. doi: 10.1053/j.gastro.2020.03.072.
FROM GASTROENTEROLOGY
AGA Clinical practice update: Maintain IBD remission during pandemic
Inflammatory bowel disease (IBD) does not seem to make patients any more likely to contract SARS-COV-2 or develop COVID-19, but a rapid review commissioned by the American Gastroenterological Association acknowledges that determination is based on limited evidence and IBD patients should nonetheless maintain remission to reduce their risk of relapse or hospitalization during the COVID-19 pandemic.
The AGA has published a clinical practice update based on that rapid review online in Gastroenterology (2020. doi: 10.1053/j.gastro.2020.04.012).
Because of the widespread use of immunosuppressive or immune-modifying drugs, “It is understandable why patients with Crohn’s disease and ulcerative colitis have specific concerns and potential for increased risk of infection with SARS-CoV-2,” wrote David T. Rubin, MD, AGAF, of the University of Chicago and colleagues in the expert commentary.
They noted that, while association between GI symptoms and COVID-19 RNA in stool samples isn’t clear, given the reports of GI symptoms in COVID-19 patients – ranging from 10% (JAMA. 2020:323:1061-9) to half of patients (Am J Gastroenterol. 2020;115:766-73) – “the clinical implications of this are quite important.” In IBD patients, changes in digestive symptoms without accompanying fever or respiratory symptoms can be monitored for symptoms that could merit testing for the virus as well as “trigger additional treatment adjustments.”
In accordance with the IOIBD (International Organization for the Study of Inflammatory Bowel Disease) consensus, the update noted that IBD patients should continue going to infusion centers for therapies, provided that the centers use a COVID-19 screening protocol.
Patients with IBD who contract COVID-19 seem more likely to be hospitalized for one or the other disease, but that’s based on data from the international SECURE-IBD registry that had 164 patients as of the writing of the update. The update provides guidance for three scenarios for IBD patients during the pandemic:
- Patients not infected with SARS-CoV-2 should maintain their IBD therapies to sustain remission and avoid relapses. “Aside from the obvious negative consequences of a relapse, relapsing IBD will strain available medical resources, may require steroid therapy or necessitate hospitalization, outcomes that are all much worse than the known risks of existing IBD therapies,” Dr. Rubin and colleagues noted.
- Patients who are infected but have no symptoms of COVID-19 should have their dosing of prednisone adjusted to less than 20 mg/day or switched to budesonide; suspend thiopurines, methotrexate, and tofacitinib; and delay dosing of monoclonal antibodies (anti–tumor necrosis factor [anti-TNF] drugs, ustekinumab, or vedolizumab) for 2 weeks while their symptoms for COVID-19 are monitored. “Restarting therapy after 2 weeks if the patient has not developed manifestations of COVID-19 is reasonable,” wrote Dr. Rubin and colleagues. Emerging serial testing should indicate antibody status, but the effectiveness of stool testing for SARS-CoV-2 in these cases “remains to be seen.”
- In the patient with confirmed COVID-19, adjustment of IBD therapy “is appropriate, based on the understanding of the immune activity of the therapy and whether that therapy may worsen outcomes with COVID-19,” the update stated. Therapy adjustment should focus on reducing immune suppression during the active viral infection. Some studies are evaluating anticytokine-based therapies as COVID-19 treatments, so continued anti-TNF therapies might prevent acute respiratory distress syndrome and multiorgan failure, Dr. Rubin and colleagues wrote. “However, in the absence of those data, guidance is currently based on deciding whether to hold or to continue specific IBD therapies.”
The update considers most IBD therapies, specifically aminosalicylates, topical rectal therapy, dietary management, and antibiotics “safe and may be continued,” and oral budesonide can be continued if it’s needed for ongoing IBD control. However, corticosteroids “should be avoided and discontinued quickly.”
Likewise, during the acute stage of COVID-19, thiopurines, methotrexate, and tofacitinib should be discontinued, and anti-TNF drugs and ustekinumab should be stopped during viral illness. Holding vedolizumab during viral illness is also appropriate, according to the update, although the IOIBD group was uncertain if doing so was necessary.
If the IBD patient has digestive symptoms with COVID-19, ongoing supportive care of the COVID-19 is “reasonable,” but investigating the causes of the digestive symptoms “is critically important.” That should include ruling out enteric infections and confirming active inflammation with nonendoscopic testing. Endoscopy should be relegated to only urgent and emergent cases.
Management of IBD in COVID-19 patients also depends on disease severity. Safer therapies are indicated for mild disease, but withholding IBD therapy in moderate to severe cases may not be practical. “In this setting, the risks and benefits of escalating IBD therapy must be carefully weighed against the severity of the COVID-19,” Dr. Rubin and colleagues noted.
In hospitalized patients with severe COVID-19 and poor prognoses, “IBD therapy will likely take a back seat,” the update stated, although COVID-19 therapies should take the concomitant IBD into account. In patients with milder cases of COVID-19, IBD management should focus on acute manifestations, but intravenous steroid therapy shouldn’t exceed 3 days. The update urged providers to submit cases of IBD and confirmed COVID-19 to the SECURE-IBD registry at COVIDIBD.org.
Dr. Rubin disclosed financial relationships with AbbVie, Boehringer Ingelheim, Bristol-Myers Squibb, Celgene/Syneos, Gilead Sciences, Takeda, and many other pharmaceutical companies. Coauthors disclosed relationships with those companies and Medimmune, Novus Therapeutics, Osiris Therapeutics, RedHill Biopharma, Sanofi-Aventis, UCB Pharma, and multiple other pharmaceutical companies.
SOURCE: Rubin DT, et al. Gastroenterology. 2020: doi: 10.1053/j.gastro.2020.04.012
Inflammatory bowel disease (IBD) does not seem to make patients any more likely to contract SARS-COV-2 or develop COVID-19, but a rapid review commissioned by the American Gastroenterological Association acknowledges that determination is based on limited evidence and IBD patients should nonetheless maintain remission to reduce their risk of relapse or hospitalization during the COVID-19 pandemic.
The AGA has published a clinical practice update based on that rapid review online in Gastroenterology (2020. doi: 10.1053/j.gastro.2020.04.012).
Because of the widespread use of immunosuppressive or immune-modifying drugs, “It is understandable why patients with Crohn’s disease and ulcerative colitis have specific concerns and potential for increased risk of infection with SARS-CoV-2,” wrote David T. Rubin, MD, AGAF, of the University of Chicago and colleagues in the expert commentary.
They noted that, while association between GI symptoms and COVID-19 RNA in stool samples isn’t clear, given the reports of GI symptoms in COVID-19 patients – ranging from 10% (JAMA. 2020:323:1061-9) to half of patients (Am J Gastroenterol. 2020;115:766-73) – “the clinical implications of this are quite important.” In IBD patients, changes in digestive symptoms without accompanying fever or respiratory symptoms can be monitored for symptoms that could merit testing for the virus as well as “trigger additional treatment adjustments.”
In accordance with the IOIBD (International Organization for the Study of Inflammatory Bowel Disease) consensus, the update noted that IBD patients should continue going to infusion centers for therapies, provided that the centers use a COVID-19 screening protocol.
Patients with IBD who contract COVID-19 seem more likely to be hospitalized for one or the other disease, but that’s based on data from the international SECURE-IBD registry that had 164 patients as of the writing of the update. The update provides guidance for three scenarios for IBD patients during the pandemic:
- Patients not infected with SARS-CoV-2 should maintain their IBD therapies to sustain remission and avoid relapses. “Aside from the obvious negative consequences of a relapse, relapsing IBD will strain available medical resources, may require steroid therapy or necessitate hospitalization, outcomes that are all much worse than the known risks of existing IBD therapies,” Dr. Rubin and colleagues noted.
- Patients who are infected but have no symptoms of COVID-19 should have their dosing of prednisone adjusted to less than 20 mg/day or switched to budesonide; suspend thiopurines, methotrexate, and tofacitinib; and delay dosing of monoclonal antibodies (anti–tumor necrosis factor [anti-TNF] drugs, ustekinumab, or vedolizumab) for 2 weeks while their symptoms for COVID-19 are monitored. “Restarting therapy after 2 weeks if the patient has not developed manifestations of COVID-19 is reasonable,” wrote Dr. Rubin and colleagues. Emerging serial testing should indicate antibody status, but the effectiveness of stool testing for SARS-CoV-2 in these cases “remains to be seen.”
- In the patient with confirmed COVID-19, adjustment of IBD therapy “is appropriate, based on the understanding of the immune activity of the therapy and whether that therapy may worsen outcomes with COVID-19,” the update stated. Therapy adjustment should focus on reducing immune suppression during the active viral infection. Some studies are evaluating anticytokine-based therapies as COVID-19 treatments, so continued anti-TNF therapies might prevent acute respiratory distress syndrome and multiorgan failure, Dr. Rubin and colleagues wrote. “However, in the absence of those data, guidance is currently based on deciding whether to hold or to continue specific IBD therapies.”
The update considers most IBD therapies, specifically aminosalicylates, topical rectal therapy, dietary management, and antibiotics “safe and may be continued,” and oral budesonide can be continued if it’s needed for ongoing IBD control. However, corticosteroids “should be avoided and discontinued quickly.”
Likewise, during the acute stage of COVID-19, thiopurines, methotrexate, and tofacitinib should be discontinued, and anti-TNF drugs and ustekinumab should be stopped during viral illness. Holding vedolizumab during viral illness is also appropriate, according to the update, although the IOIBD group was uncertain if doing so was necessary.
If the IBD patient has digestive symptoms with COVID-19, ongoing supportive care of the COVID-19 is “reasonable,” but investigating the causes of the digestive symptoms “is critically important.” That should include ruling out enteric infections and confirming active inflammation with nonendoscopic testing. Endoscopy should be relegated to only urgent and emergent cases.
Management of IBD in COVID-19 patients also depends on disease severity. Safer therapies are indicated for mild disease, but withholding IBD therapy in moderate to severe cases may not be practical. “In this setting, the risks and benefits of escalating IBD therapy must be carefully weighed against the severity of the COVID-19,” Dr. Rubin and colleagues noted.
In hospitalized patients with severe COVID-19 and poor prognoses, “IBD therapy will likely take a back seat,” the update stated, although COVID-19 therapies should take the concomitant IBD into account. In patients with milder cases of COVID-19, IBD management should focus on acute manifestations, but intravenous steroid therapy shouldn’t exceed 3 days. The update urged providers to submit cases of IBD and confirmed COVID-19 to the SECURE-IBD registry at COVIDIBD.org.
Dr. Rubin disclosed financial relationships with AbbVie, Boehringer Ingelheim, Bristol-Myers Squibb, Celgene/Syneos, Gilead Sciences, Takeda, and many other pharmaceutical companies. Coauthors disclosed relationships with those companies and Medimmune, Novus Therapeutics, Osiris Therapeutics, RedHill Biopharma, Sanofi-Aventis, UCB Pharma, and multiple other pharmaceutical companies.
SOURCE: Rubin DT, et al. Gastroenterology. 2020: doi: 10.1053/j.gastro.2020.04.012
Inflammatory bowel disease (IBD) does not seem to make patients any more likely to contract SARS-COV-2 or develop COVID-19, but a rapid review commissioned by the American Gastroenterological Association acknowledges that determination is based on limited evidence and IBD patients should nonetheless maintain remission to reduce their risk of relapse or hospitalization during the COVID-19 pandemic.
The AGA has published a clinical practice update based on that rapid review online in Gastroenterology (2020. doi: 10.1053/j.gastro.2020.04.012).
Because of the widespread use of immunosuppressive or immune-modifying drugs, “It is understandable why patients with Crohn’s disease and ulcerative colitis have specific concerns and potential for increased risk of infection with SARS-CoV-2,” wrote David T. Rubin, MD, AGAF, of the University of Chicago and colleagues in the expert commentary.
They noted that, while association between GI symptoms and COVID-19 RNA in stool samples isn’t clear, given the reports of GI symptoms in COVID-19 patients – ranging from 10% (JAMA. 2020:323:1061-9) to half of patients (Am J Gastroenterol. 2020;115:766-73) – “the clinical implications of this are quite important.” In IBD patients, changes in digestive symptoms without accompanying fever or respiratory symptoms can be monitored for symptoms that could merit testing for the virus as well as “trigger additional treatment adjustments.”
In accordance with the IOIBD (International Organization for the Study of Inflammatory Bowel Disease) consensus, the update noted that IBD patients should continue going to infusion centers for therapies, provided that the centers use a COVID-19 screening protocol.
Patients with IBD who contract COVID-19 seem more likely to be hospitalized for one or the other disease, but that’s based on data from the international SECURE-IBD registry that had 164 patients as of the writing of the update. The update provides guidance for three scenarios for IBD patients during the pandemic:
- Patients not infected with SARS-CoV-2 should maintain their IBD therapies to sustain remission and avoid relapses. “Aside from the obvious negative consequences of a relapse, relapsing IBD will strain available medical resources, may require steroid therapy or necessitate hospitalization, outcomes that are all much worse than the known risks of existing IBD therapies,” Dr. Rubin and colleagues noted.
- Patients who are infected but have no symptoms of COVID-19 should have their dosing of prednisone adjusted to less than 20 mg/day or switched to budesonide; suspend thiopurines, methotrexate, and tofacitinib; and delay dosing of monoclonal antibodies (anti–tumor necrosis factor [anti-TNF] drugs, ustekinumab, or vedolizumab) for 2 weeks while their symptoms for COVID-19 are monitored. “Restarting therapy after 2 weeks if the patient has not developed manifestations of COVID-19 is reasonable,” wrote Dr. Rubin and colleagues. Emerging serial testing should indicate antibody status, but the effectiveness of stool testing for SARS-CoV-2 in these cases “remains to be seen.”
- In the patient with confirmed COVID-19, adjustment of IBD therapy “is appropriate, based on the understanding of the immune activity of the therapy and whether that therapy may worsen outcomes with COVID-19,” the update stated. Therapy adjustment should focus on reducing immune suppression during the active viral infection. Some studies are evaluating anticytokine-based therapies as COVID-19 treatments, so continued anti-TNF therapies might prevent acute respiratory distress syndrome and multiorgan failure, Dr. Rubin and colleagues wrote. “However, in the absence of those data, guidance is currently based on deciding whether to hold or to continue specific IBD therapies.”
The update considers most IBD therapies, specifically aminosalicylates, topical rectal therapy, dietary management, and antibiotics “safe and may be continued,” and oral budesonide can be continued if it’s needed for ongoing IBD control. However, corticosteroids “should be avoided and discontinued quickly.”
Likewise, during the acute stage of COVID-19, thiopurines, methotrexate, and tofacitinib should be discontinued, and anti-TNF drugs and ustekinumab should be stopped during viral illness. Holding vedolizumab during viral illness is also appropriate, according to the update, although the IOIBD group was uncertain if doing so was necessary.
If the IBD patient has digestive symptoms with COVID-19, ongoing supportive care of the COVID-19 is “reasonable,” but investigating the causes of the digestive symptoms “is critically important.” That should include ruling out enteric infections and confirming active inflammation with nonendoscopic testing. Endoscopy should be relegated to only urgent and emergent cases.
Management of IBD in COVID-19 patients also depends on disease severity. Safer therapies are indicated for mild disease, but withholding IBD therapy in moderate to severe cases may not be practical. “In this setting, the risks and benefits of escalating IBD therapy must be carefully weighed against the severity of the COVID-19,” Dr. Rubin and colleagues noted.
In hospitalized patients with severe COVID-19 and poor prognoses, “IBD therapy will likely take a back seat,” the update stated, although COVID-19 therapies should take the concomitant IBD into account. In patients with milder cases of COVID-19, IBD management should focus on acute manifestations, but intravenous steroid therapy shouldn’t exceed 3 days. The update urged providers to submit cases of IBD and confirmed COVID-19 to the SECURE-IBD registry at COVIDIBD.org.
Dr. Rubin disclosed financial relationships with AbbVie, Boehringer Ingelheim, Bristol-Myers Squibb, Celgene/Syneos, Gilead Sciences, Takeda, and many other pharmaceutical companies. Coauthors disclosed relationships with those companies and Medimmune, Novus Therapeutics, Osiris Therapeutics, RedHill Biopharma, Sanofi-Aventis, UCB Pharma, and multiple other pharmaceutical companies.
SOURCE: Rubin DT, et al. Gastroenterology. 2020: doi: 10.1053/j.gastro.2020.04.012
FROM GASTROENTEROLOGY
GI cancer death disproportional to incidence rates
Cancers of the gastrointestinal tract represented about one in four cancer cases in 2018 but more than one in three cancer-related deaths, underscoring the importance of preventive measures, according to an analysis of global cancer datasets that identified trends in five major GI cancer types – esophageal, stomach, colorectal, liver, and pancreatic – published in Gastroenterology.
“Although the incidence of some GI cancer types has decreased, this group of malignancies continues to pose major challenges to public health,” wrote Melina Arnold, PhD, of the International for Research on Cancer in Lyon, France, and colleagues. “Primary and secondary prevention measures are important for controlling these malignancies – most importantly, reducing consumption of tobacco and alcohol, obesity control, immunizing populations against hepatitis B virus infection, and screening for colorectal cancer.”
For example, the study found that the proportion of GI cancer deaths in Asia exceeds that of new cases, with the greatest disparity in China, while the opposite can be said of GI cancer trends in Europe and North America.
The study reported 4.8 million new cases of GI cancer and 3.4 million deaths worldwide in 2018. GI cancers accounted for 26% of the global cancer burden but 35% of cancer-related deaths. Incidence-to-death disparities were greatest for Africa, accounting for 4% of new cases and 5% of deaths; and Asia, with about 63% of new cases but 65% of deaths. The disparity was even wider in China, which accounted for 38% of worldwide cases but 41% of the deaths. Europe and North America, on the other hand, accounted for 26% of global cases but 23% of deaths. High death rates of these cancers are associated with late detection, Dr. Arnold and colleagues noted.
Regarding the five different types of GI cancer, the study reported the following:
- Esophageal cancer accounted for 572,000 new cases and 508,000 deaths in 2018, making it the sixth-most-deadly cancer worldwide. Rates in men are two to three times higher than in women. Eastern Asia has the highest rates, 12.2 per 100,000 person-years, followed by eastern Africa (8.3) and southern Africa (7.4). China alone accounts for 54% of the global burden. A large percentage of these cancers in developing countries are squamous cell carcinoma, the most common form of esophageal cancer globally, which has been linked to tobacco use, heavy alcohol consumption, opium intake, air pollution, and diet.
- Gastric cancer accounted for more than 1 million new cases and nearly 800,000 deaths in 2018. Again, the incidence is twice as high in men as in women, and eastern Asia has the highest rates of 22 per 100,000 vs. < 5 in Africa, North America, and northern Europe. Cardia gastric cancer (CGC), associated with obesity and gastroesophageal reflux disease, is more prevalent in Western countries, while noncardia gastric cancer (CG) is more prevalent in countries with higher rates of Helicobacter pylori infection. In the United States specifically, CGC is more common in non-Hispanic whites than other ethnic groups. Gastric cancer rates have been declining in recent years, although trends of CGC and cancer of the gastric corpus, which the study terms “a noncardia subsite,” among younger people “may lead to a deceleration or a reversal” of declining gastric cancer rates, stated Dr. Arnold and colleagues.
- Colorectal cancer remained the most commonly diagnosed GI cancer in 2018, accounting for 1.8 million cases and 881,000 deaths, which represents 1 in 10 cancer deaths. The highest incidence was found in Australia/New Zealand, the lowest in south and central Asia. Colorectal cancers are in “transition” from infection-related cancers to those related to “rapid societal and economic change.” Dr. Arnold and colleagues attributed these changes to higher dietary intake of fats, sugar, and animal-source foods and increases in sedentary behavior and obesity. Despite advances in cures for colorectal cancer, disparities continue, even in high-income countries, and screening programs have been limited, according to the study. Colorectal cancer will be “one of the main contributors” to the doubling of cancer rates in older adults by 2035.
- Liver cancer comprised 841,000 cases and 782,000 deaths in 2018, making it the sixth-most-diagnosed cancer but the fourth most deadly. “Transitioning countries” in eastern Asia, Micronesia, and northern Africa have the highest rates. In eastern Asia, hepatitis B infections and aflatoxins are the primary risk factors for hepatocellular carcinoma, while in Japan and Europe hepatitis C is the main cause for hepatocellular carcinoma. Decreases in both infections and aflatoxins may explain declines in liver cancer rates in those regions. Whereas in lower-risk areas, increasing liver cancer rates caused by more widespread obesity and diabetes may be offsetting declines in HBV and HCV rates.
- Pancreatic cancer was the 12th-most-common cancer but the seventh leading cause of cancer death, with 432,000 cases and 459,000 deaths in 2018. Wealthy countries have incidence and death rates three to four times higher than do less-developed countries, with rates highest in Europe, North America, and Australia/New Zealand. Because pancreatic cancer isn’t typically diagnosed until it is in the metastatic or locally advanced state, curative surgery isn’t feasible, Dr. Arnold and colleagues stated. Population aging and growth, along with advances in treating other types of cancers, mean that pancreatic cancer “has become or is set out to become one of the leading causes of cancer-related death in many countries,” Dr. Arnold and colleagues stated. They added that, in the European Union, pancreatic cancer is already the third-leading cause of cancer death after lung and colorectal cancer.
The findings, Dr. Arnold and colleagues wrote, underscore the shift of the cancer burden toward transitioning countries, “which are less equipped to manage this increasing burden.” In the United States, the rates of all five GI cancers in young adults (aged 25-49 years) have increased.
GI cancers, with the exception of colorectal cancers, also contribute disproportionately to cancer-related death rates, mostly because all but colorectal cancers are difficult to diagnose.
However, early detection and screening programs for gastric cancer in Japan and Korea, and esophageal cancer in China “have shown promising results,” Dr. Arnold and colleagues said. “Pancreatic cancer, on the other hand, is becoming a more important contributor to cancer-related mortality as a consequence of improved diagnosis and management of the historically most common forms of cancer death,” they wrote.
Prevention remains key, and lifestyle choices like smoking, alcohol intake, and physical activity are all drivers of GI cancer burden. “Primary and secondary prevention measures remain the most important tools to control this group of malignancies, particularly in light of their preventability and often dreadful prognosis,” Dr. Arnold and colleagues wrote.
Dr. Arnold and colleagues have no financial relationships to disclose.
SOURCE: Arnold M et al. Gastroenterology. 2020 Apr 2;S0016-5085(20)30452-2. doi: 10.1053/j.gastro.2020.02.068.
Cancers of the gastrointestinal tract represented about one in four cancer cases in 2018 but more than one in three cancer-related deaths, underscoring the importance of preventive measures, according to an analysis of global cancer datasets that identified trends in five major GI cancer types – esophageal, stomach, colorectal, liver, and pancreatic – published in Gastroenterology.
“Although the incidence of some GI cancer types has decreased, this group of malignancies continues to pose major challenges to public health,” wrote Melina Arnold, PhD, of the International for Research on Cancer in Lyon, France, and colleagues. “Primary and secondary prevention measures are important for controlling these malignancies – most importantly, reducing consumption of tobacco and alcohol, obesity control, immunizing populations against hepatitis B virus infection, and screening for colorectal cancer.”
For example, the study found that the proportion of GI cancer deaths in Asia exceeds that of new cases, with the greatest disparity in China, while the opposite can be said of GI cancer trends in Europe and North America.
The study reported 4.8 million new cases of GI cancer and 3.4 million deaths worldwide in 2018. GI cancers accounted for 26% of the global cancer burden but 35% of cancer-related deaths. Incidence-to-death disparities were greatest for Africa, accounting for 4% of new cases and 5% of deaths; and Asia, with about 63% of new cases but 65% of deaths. The disparity was even wider in China, which accounted for 38% of worldwide cases but 41% of the deaths. Europe and North America, on the other hand, accounted for 26% of global cases but 23% of deaths. High death rates of these cancers are associated with late detection, Dr. Arnold and colleagues noted.
Regarding the five different types of GI cancer, the study reported the following:
- Esophageal cancer accounted for 572,000 new cases and 508,000 deaths in 2018, making it the sixth-most-deadly cancer worldwide. Rates in men are two to three times higher than in women. Eastern Asia has the highest rates, 12.2 per 100,000 person-years, followed by eastern Africa (8.3) and southern Africa (7.4). China alone accounts for 54% of the global burden. A large percentage of these cancers in developing countries are squamous cell carcinoma, the most common form of esophageal cancer globally, which has been linked to tobacco use, heavy alcohol consumption, opium intake, air pollution, and diet.
- Gastric cancer accounted for more than 1 million new cases and nearly 800,000 deaths in 2018. Again, the incidence is twice as high in men as in women, and eastern Asia has the highest rates of 22 per 100,000 vs. < 5 in Africa, North America, and northern Europe. Cardia gastric cancer (CGC), associated with obesity and gastroesophageal reflux disease, is more prevalent in Western countries, while noncardia gastric cancer (CG) is more prevalent in countries with higher rates of Helicobacter pylori infection. In the United States specifically, CGC is more common in non-Hispanic whites than other ethnic groups. Gastric cancer rates have been declining in recent years, although trends of CGC and cancer of the gastric corpus, which the study terms “a noncardia subsite,” among younger people “may lead to a deceleration or a reversal” of declining gastric cancer rates, stated Dr. Arnold and colleagues.
- Colorectal cancer remained the most commonly diagnosed GI cancer in 2018, accounting for 1.8 million cases and 881,000 deaths, which represents 1 in 10 cancer deaths. The highest incidence was found in Australia/New Zealand, the lowest in south and central Asia. Colorectal cancers are in “transition” from infection-related cancers to those related to “rapid societal and economic change.” Dr. Arnold and colleagues attributed these changes to higher dietary intake of fats, sugar, and animal-source foods and increases in sedentary behavior and obesity. Despite advances in cures for colorectal cancer, disparities continue, even in high-income countries, and screening programs have been limited, according to the study. Colorectal cancer will be “one of the main contributors” to the doubling of cancer rates in older adults by 2035.
- Liver cancer comprised 841,000 cases and 782,000 deaths in 2018, making it the sixth-most-diagnosed cancer but the fourth most deadly. “Transitioning countries” in eastern Asia, Micronesia, and northern Africa have the highest rates. In eastern Asia, hepatitis B infections and aflatoxins are the primary risk factors for hepatocellular carcinoma, while in Japan and Europe hepatitis C is the main cause for hepatocellular carcinoma. Decreases in both infections and aflatoxins may explain declines in liver cancer rates in those regions. Whereas in lower-risk areas, increasing liver cancer rates caused by more widespread obesity and diabetes may be offsetting declines in HBV and HCV rates.
- Pancreatic cancer was the 12th-most-common cancer but the seventh leading cause of cancer death, with 432,000 cases and 459,000 deaths in 2018. Wealthy countries have incidence and death rates three to four times higher than do less-developed countries, with rates highest in Europe, North America, and Australia/New Zealand. Because pancreatic cancer isn’t typically diagnosed until it is in the metastatic or locally advanced state, curative surgery isn’t feasible, Dr. Arnold and colleagues stated. Population aging and growth, along with advances in treating other types of cancers, mean that pancreatic cancer “has become or is set out to become one of the leading causes of cancer-related death in many countries,” Dr. Arnold and colleagues stated. They added that, in the European Union, pancreatic cancer is already the third-leading cause of cancer death after lung and colorectal cancer.
The findings, Dr. Arnold and colleagues wrote, underscore the shift of the cancer burden toward transitioning countries, “which are less equipped to manage this increasing burden.” In the United States, the rates of all five GI cancers in young adults (aged 25-49 years) have increased.
GI cancers, with the exception of colorectal cancers, also contribute disproportionately to cancer-related death rates, mostly because all but colorectal cancers are difficult to diagnose.
However, early detection and screening programs for gastric cancer in Japan and Korea, and esophageal cancer in China “have shown promising results,” Dr. Arnold and colleagues said. “Pancreatic cancer, on the other hand, is becoming a more important contributor to cancer-related mortality as a consequence of improved diagnosis and management of the historically most common forms of cancer death,” they wrote.
Prevention remains key, and lifestyle choices like smoking, alcohol intake, and physical activity are all drivers of GI cancer burden. “Primary and secondary prevention measures remain the most important tools to control this group of malignancies, particularly in light of their preventability and often dreadful prognosis,” Dr. Arnold and colleagues wrote.
Dr. Arnold and colleagues have no financial relationships to disclose.
SOURCE: Arnold M et al. Gastroenterology. 2020 Apr 2;S0016-5085(20)30452-2. doi: 10.1053/j.gastro.2020.02.068.
Cancers of the gastrointestinal tract represented about one in four cancer cases in 2018 but more than one in three cancer-related deaths, underscoring the importance of preventive measures, according to an analysis of global cancer datasets that identified trends in five major GI cancer types – esophageal, stomach, colorectal, liver, and pancreatic – published in Gastroenterology.
“Although the incidence of some GI cancer types has decreased, this group of malignancies continues to pose major challenges to public health,” wrote Melina Arnold, PhD, of the International for Research on Cancer in Lyon, France, and colleagues. “Primary and secondary prevention measures are important for controlling these malignancies – most importantly, reducing consumption of tobacco and alcohol, obesity control, immunizing populations against hepatitis B virus infection, and screening for colorectal cancer.”
For example, the study found that the proportion of GI cancer deaths in Asia exceeds that of new cases, with the greatest disparity in China, while the opposite can be said of GI cancer trends in Europe and North America.
The study reported 4.8 million new cases of GI cancer and 3.4 million deaths worldwide in 2018. GI cancers accounted for 26% of the global cancer burden but 35% of cancer-related deaths. Incidence-to-death disparities were greatest for Africa, accounting for 4% of new cases and 5% of deaths; and Asia, with about 63% of new cases but 65% of deaths. The disparity was even wider in China, which accounted for 38% of worldwide cases but 41% of the deaths. Europe and North America, on the other hand, accounted for 26% of global cases but 23% of deaths. High death rates of these cancers are associated with late detection, Dr. Arnold and colleagues noted.
Regarding the five different types of GI cancer, the study reported the following:
- Esophageal cancer accounted for 572,000 new cases and 508,000 deaths in 2018, making it the sixth-most-deadly cancer worldwide. Rates in men are two to three times higher than in women. Eastern Asia has the highest rates, 12.2 per 100,000 person-years, followed by eastern Africa (8.3) and southern Africa (7.4). China alone accounts for 54% of the global burden. A large percentage of these cancers in developing countries are squamous cell carcinoma, the most common form of esophageal cancer globally, which has been linked to tobacco use, heavy alcohol consumption, opium intake, air pollution, and diet.
- Gastric cancer accounted for more than 1 million new cases and nearly 800,000 deaths in 2018. Again, the incidence is twice as high in men as in women, and eastern Asia has the highest rates of 22 per 100,000 vs. < 5 in Africa, North America, and northern Europe. Cardia gastric cancer (CGC), associated with obesity and gastroesophageal reflux disease, is more prevalent in Western countries, while noncardia gastric cancer (CG) is more prevalent in countries with higher rates of Helicobacter pylori infection. In the United States specifically, CGC is more common in non-Hispanic whites than other ethnic groups. Gastric cancer rates have been declining in recent years, although trends of CGC and cancer of the gastric corpus, which the study terms “a noncardia subsite,” among younger people “may lead to a deceleration or a reversal” of declining gastric cancer rates, stated Dr. Arnold and colleagues.
- Colorectal cancer remained the most commonly diagnosed GI cancer in 2018, accounting for 1.8 million cases and 881,000 deaths, which represents 1 in 10 cancer deaths. The highest incidence was found in Australia/New Zealand, the lowest in south and central Asia. Colorectal cancers are in “transition” from infection-related cancers to those related to “rapid societal and economic change.” Dr. Arnold and colleagues attributed these changes to higher dietary intake of fats, sugar, and animal-source foods and increases in sedentary behavior and obesity. Despite advances in cures for colorectal cancer, disparities continue, even in high-income countries, and screening programs have been limited, according to the study. Colorectal cancer will be “one of the main contributors” to the doubling of cancer rates in older adults by 2035.
- Liver cancer comprised 841,000 cases and 782,000 deaths in 2018, making it the sixth-most-diagnosed cancer but the fourth most deadly. “Transitioning countries” in eastern Asia, Micronesia, and northern Africa have the highest rates. In eastern Asia, hepatitis B infections and aflatoxins are the primary risk factors for hepatocellular carcinoma, while in Japan and Europe hepatitis C is the main cause for hepatocellular carcinoma. Decreases in both infections and aflatoxins may explain declines in liver cancer rates in those regions. Whereas in lower-risk areas, increasing liver cancer rates caused by more widespread obesity and diabetes may be offsetting declines in HBV and HCV rates.
- Pancreatic cancer was the 12th-most-common cancer but the seventh leading cause of cancer death, with 432,000 cases and 459,000 deaths in 2018. Wealthy countries have incidence and death rates three to four times higher than do less-developed countries, with rates highest in Europe, North America, and Australia/New Zealand. Because pancreatic cancer isn’t typically diagnosed until it is in the metastatic or locally advanced state, curative surgery isn’t feasible, Dr. Arnold and colleagues stated. Population aging and growth, along with advances in treating other types of cancers, mean that pancreatic cancer “has become or is set out to become one of the leading causes of cancer-related death in many countries,” Dr. Arnold and colleagues stated. They added that, in the European Union, pancreatic cancer is already the third-leading cause of cancer death after lung and colorectal cancer.
The findings, Dr. Arnold and colleagues wrote, underscore the shift of the cancer burden toward transitioning countries, “which are less equipped to manage this increasing burden.” In the United States, the rates of all five GI cancers in young adults (aged 25-49 years) have increased.
GI cancers, with the exception of colorectal cancers, also contribute disproportionately to cancer-related death rates, mostly because all but colorectal cancers are difficult to diagnose.
However, early detection and screening programs for gastric cancer in Japan and Korea, and esophageal cancer in China “have shown promising results,” Dr. Arnold and colleagues said. “Pancreatic cancer, on the other hand, is becoming a more important contributor to cancer-related mortality as a consequence of improved diagnosis and management of the historically most common forms of cancer death,” they wrote.
Prevention remains key, and lifestyle choices like smoking, alcohol intake, and physical activity are all drivers of GI cancer burden. “Primary and secondary prevention measures remain the most important tools to control this group of malignancies, particularly in light of their preventability and often dreadful prognosis,” Dr. Arnold and colleagues wrote.
Dr. Arnold and colleagues have no financial relationships to disclose.
SOURCE: Arnold M et al. Gastroenterology. 2020 Apr 2;S0016-5085(20)30452-2. doi: 10.1053/j.gastro.2020.02.068.
FROM GASTROENTEROLOGY
AGA clinical practice update: Pancreatic cancer screening
Individuals at high risk for pancreatic cancer should at least be considered for screening for the disease, states a new clinical practice update from the American Gastroenterological Association that further defines what constitutes high risk for pancreatic cancer, when and how screenings should occur, and the role of genetic testing and counseling (Gastroenterology. 2020. doi: 10.1053/j.gastro.2020.03.088).
Individuals who have a first-degree relative with two or more genetically related relatives with pancreatic cancer should be considered for screening, as should people with Peutz-Jeghers syndrome, a CDKN2A gene mutation, one or more first-degree relatives with pancreatic cancer with Lynch syndrome and mutations in the BRCA1, BRCA2, PALB2, and ATM genes, the clinical update stated. Screening in high-risk individuals should begin at age 50, but some groups should start having screening earlier: age 40 in carriers of the CKDN2A and PRSS1 mutations with hereditary pancreatitis; and age 35 in those with Peutz-Jeghers syndrome.
“Studies to date have demonstrated variability regarding definitions of high-risk groups and the age at which screening should be initiated,” wrote Harry R. Aslanian, MD, AGAF, of Yale New Haven (Conn.) Hospital, and coauthors. “The genetic basis of much of the inherited susceptibility to pancreas cancer remains unexplained (in approximately 90% of cases) and familial history is important in risk stratification.”
Genetic testing and counseling should be considered for any familial pancreas cancer relative – that is, a person with two or more first-degree relatives with pancreas cancer that’s outside the definition of other hereditary cancers. “A positive germline mutation is associated with an increased risk of neoplastic progression and may also lead to screening for other relevant associated cancers,” wrote Dr. Aslanian and coauthors.
The screening itself should consist of MRI and endoscopic ultrasonography (EUS) in combination, the clinical practice update states. It defines detectable targets as stage 1 pancreatic ductal adenocarcinoma and high-risk neoplasms such as intraductal papillary mucinous neoplasms with high-grade dysplasia and some enlarged pancreatic intraepithelial neoplasms.
High-risk patients having screening should also be enrolled in a registry and referred to a pancreas center of excellence.
The update suggests screening every 12 months when the baseline screening is negative for any suspect lesions, with shorter intervals for EUS when suspected lesions are found: 6-12 months for low-risk lesions; 3-6 months for intermediate lesions; and 3 months for high-risk lesions if the patient hasn’t had surgery to remove the lesions.
Regarding management of positive screening results, a multidisciplinary team should confer with the individual and family to determine therapy. If surgery is indicated, it should be done at a high-volume center.
The update also provides guidance for two scenarios when patients shouldn’t undergo screening: those at average risk; and those at high-risk more likely to die from another cause. Of course, the physician should review the limitations and risk of screening with patients beforehand.
Dr. Aslanian and coauthors noted that a number of areas require further study, including defining the highest-risk groups and refining screening tests with high sensitivity and specificity to detect high-grade precursors, along with more data on risks of precursor lesions themselves.
They also acknowledged the need for more study into the effectiveness of pancreatic cancer screening, although a randomized clinical trial comparing screening vs. no screening “might be challenging to conduct given implementation of clinical screening as standard of care in some practices.” Blood tests for pancreatic cancer screening in high-risk patients also need more study, they stated.
The authors did not report any funding sources or conflicts of interest.
SOURCE: Aslanian HR et al. Gastroenterology. 2020. doi: 10.1053/j.gastro.2020.03.088.
Individuals at high risk for pancreatic cancer should at least be considered for screening for the disease, states a new clinical practice update from the American Gastroenterological Association that further defines what constitutes high risk for pancreatic cancer, when and how screenings should occur, and the role of genetic testing and counseling (Gastroenterology. 2020. doi: 10.1053/j.gastro.2020.03.088).
Individuals who have a first-degree relative with two or more genetically related relatives with pancreatic cancer should be considered for screening, as should people with Peutz-Jeghers syndrome, a CDKN2A gene mutation, one or more first-degree relatives with pancreatic cancer with Lynch syndrome and mutations in the BRCA1, BRCA2, PALB2, and ATM genes, the clinical update stated. Screening in high-risk individuals should begin at age 50, but some groups should start having screening earlier: age 40 in carriers of the CKDN2A and PRSS1 mutations with hereditary pancreatitis; and age 35 in those with Peutz-Jeghers syndrome.
“Studies to date have demonstrated variability regarding definitions of high-risk groups and the age at which screening should be initiated,” wrote Harry R. Aslanian, MD, AGAF, of Yale New Haven (Conn.) Hospital, and coauthors. “The genetic basis of much of the inherited susceptibility to pancreas cancer remains unexplained (in approximately 90% of cases) and familial history is important in risk stratification.”
Genetic testing and counseling should be considered for any familial pancreas cancer relative – that is, a person with two or more first-degree relatives with pancreas cancer that’s outside the definition of other hereditary cancers. “A positive germline mutation is associated with an increased risk of neoplastic progression and may also lead to screening for other relevant associated cancers,” wrote Dr. Aslanian and coauthors.
The screening itself should consist of MRI and endoscopic ultrasonography (EUS) in combination, the clinical practice update states. It defines detectable targets as stage 1 pancreatic ductal adenocarcinoma and high-risk neoplasms such as intraductal papillary mucinous neoplasms with high-grade dysplasia and some enlarged pancreatic intraepithelial neoplasms.
High-risk patients having screening should also be enrolled in a registry and referred to a pancreas center of excellence.
The update suggests screening every 12 months when the baseline screening is negative for any suspect lesions, with shorter intervals for EUS when suspected lesions are found: 6-12 months for low-risk lesions; 3-6 months for intermediate lesions; and 3 months for high-risk lesions if the patient hasn’t had surgery to remove the lesions.
Regarding management of positive screening results, a multidisciplinary team should confer with the individual and family to determine therapy. If surgery is indicated, it should be done at a high-volume center.
The update also provides guidance for two scenarios when patients shouldn’t undergo screening: those at average risk; and those at high-risk more likely to die from another cause. Of course, the physician should review the limitations and risk of screening with patients beforehand.
Dr. Aslanian and coauthors noted that a number of areas require further study, including defining the highest-risk groups and refining screening tests with high sensitivity and specificity to detect high-grade precursors, along with more data on risks of precursor lesions themselves.
They also acknowledged the need for more study into the effectiveness of pancreatic cancer screening, although a randomized clinical trial comparing screening vs. no screening “might be challenging to conduct given implementation of clinical screening as standard of care in some practices.” Blood tests for pancreatic cancer screening in high-risk patients also need more study, they stated.
The authors did not report any funding sources or conflicts of interest.
SOURCE: Aslanian HR et al. Gastroenterology. 2020. doi: 10.1053/j.gastro.2020.03.088.
Individuals at high risk for pancreatic cancer should at least be considered for screening for the disease, states a new clinical practice update from the American Gastroenterological Association that further defines what constitutes high risk for pancreatic cancer, when and how screenings should occur, and the role of genetic testing and counseling (Gastroenterology. 2020. doi: 10.1053/j.gastro.2020.03.088).
Individuals who have a first-degree relative with two or more genetically related relatives with pancreatic cancer should be considered for screening, as should people with Peutz-Jeghers syndrome, a CDKN2A gene mutation, one or more first-degree relatives with pancreatic cancer with Lynch syndrome and mutations in the BRCA1, BRCA2, PALB2, and ATM genes, the clinical update stated. Screening in high-risk individuals should begin at age 50, but some groups should start having screening earlier: age 40 in carriers of the CKDN2A and PRSS1 mutations with hereditary pancreatitis; and age 35 in those with Peutz-Jeghers syndrome.
“Studies to date have demonstrated variability regarding definitions of high-risk groups and the age at which screening should be initiated,” wrote Harry R. Aslanian, MD, AGAF, of Yale New Haven (Conn.) Hospital, and coauthors. “The genetic basis of much of the inherited susceptibility to pancreas cancer remains unexplained (in approximately 90% of cases) and familial history is important in risk stratification.”
Genetic testing and counseling should be considered for any familial pancreas cancer relative – that is, a person with two or more first-degree relatives with pancreas cancer that’s outside the definition of other hereditary cancers. “A positive germline mutation is associated with an increased risk of neoplastic progression and may also lead to screening for other relevant associated cancers,” wrote Dr. Aslanian and coauthors.
The screening itself should consist of MRI and endoscopic ultrasonography (EUS) in combination, the clinical practice update states. It defines detectable targets as stage 1 pancreatic ductal adenocarcinoma and high-risk neoplasms such as intraductal papillary mucinous neoplasms with high-grade dysplasia and some enlarged pancreatic intraepithelial neoplasms.
High-risk patients having screening should also be enrolled in a registry and referred to a pancreas center of excellence.
The update suggests screening every 12 months when the baseline screening is negative for any suspect lesions, with shorter intervals for EUS when suspected lesions are found: 6-12 months for low-risk lesions; 3-6 months for intermediate lesions; and 3 months for high-risk lesions if the patient hasn’t had surgery to remove the lesions.
Regarding management of positive screening results, a multidisciplinary team should confer with the individual and family to determine therapy. If surgery is indicated, it should be done at a high-volume center.
The update also provides guidance for two scenarios when patients shouldn’t undergo screening: those at average risk; and those at high-risk more likely to die from another cause. Of course, the physician should review the limitations and risk of screening with patients beforehand.
Dr. Aslanian and coauthors noted that a number of areas require further study, including defining the highest-risk groups and refining screening tests with high sensitivity and specificity to detect high-grade precursors, along with more data on risks of precursor lesions themselves.
They also acknowledged the need for more study into the effectiveness of pancreatic cancer screening, although a randomized clinical trial comparing screening vs. no screening “might be challenging to conduct given implementation of clinical screening as standard of care in some practices.” Blood tests for pancreatic cancer screening in high-risk patients also need more study, they stated.
The authors did not report any funding sources or conflicts of interest.
SOURCE: Aslanian HR et al. Gastroenterology. 2020. doi: 10.1053/j.gastro.2020.03.088.
RA raises cardiac risk even without CAD
In patients with rheumatoid arthritis (RA), strategies to prevent cardiovascular events, such as treating hypertension, encouraging patients to stop smoking, and reinforcing statin therapy, may be especially important, regardless of whether they have a history of coronary artery disease because their risk for adverse cardiovascular outcomes is significantly greater than for patients who have neither RA nor coronary artery disease (CAD), a large population-based study from Denmark suggests.
“Among patients with RA, risk stratification by presence or absence of documented CAD may allow for screening and personalized treatment strategies,” wrote Brian B. Løgstrup, MD, PhD, DMSc, of Aarhus (Denmark) University Hospital, and his colleagues.
The study, published in Annals of the Rheumatic Diseases, analyzed 125,331 patients with and without CAD in the Western Denmark Heart Registry who had coronary angiography from 2003 through 2016. The cohort included 671 RA patients with no confirmed CAD and 1,061 RA patients who had CAD.
The study makes a significant contribution to the literature in reporting on the additive risk of RA and CAD, said Christie M. Bartels, MD, associate professor in the division of rheumatology at the University of Wisconsin, Madison. “Even among patients with both conditions [RA and CVD], they were less likely to get statin therapy,” she said, noting that the 82.6% of study patients with both CAD and RA were on statins vs. 86.5% of those with CAD alone, while the former had significantly higher rates of hypertension – 64.3% vs. 58.8%. “We’re doing a less effective job on secondary prevention,” she said. The anti-inflammatory properties of statins can also have an additive benefit in RA, she noted.
“This study shows that the rheumatologist can play a role in reinforcing the importance of primary and secondary cardiovascular disease prevention – meaning hypertension control, counseling patients to stop smoking and following up on statin therapy in RA,” Dr. Bartels added.
The study presents two novel findings, Dr. Løgstrup and colleagues noted:
- That RA confers a statistically significant, “but numerically marginally,” heightened risk of cardiovascular events other than stroke.
- Among patients with CAD, RA confers an increased risk of cardiac and all-cause death as well as MI and major adverse cardiovascular events (MACE).
“These finding indicate that RA may have a potential impact for precipitating cardiovascular events beyond CAD and, even more importantly, that RA seems to exacerbate the clinical risk of cardiovascular events in the presence of CAD,” Dr. Løgstrup and colleagues wrote.
The study found that patients with neither RA nor CAD had the lowest 10-year rates of MI (2.7%), ischemic stroke (2.9%), all-cause death (21.6%), cardiac death (2.3%), and MACE (7.3%).
By comparison, those with RA but no CAD had 10-year rates of 3.8% for MI, 5.5% for stroke, 35.6% for all-cause death, 3% for cardiac death, and 11.5% for MACE. Rates for those outcomes for people with CAD but no RA were 9.9% for MI, 4.6% for stroke, 33.3% for all-cause death, 7% for cardiac death, and 19.1% for MACE.
For patients with both RA and CAD, 10-year rates were 12.2% for MI, 4.4% for stroke, 49% for all-cause death, 10.9% for cardiac death, and 24.3% for MACE.
The researchers also performed a risk adjustment analysis based on potential confounding variables across the different groups, such as age, gender, comorbidities including diabetes and hypertension, active smoking status, and anticoagulant, antiplatelet, and statin therapy. The adjusted analysis revealed that patients with RA alone had a 63% greater risk of MI, 68% greater risk for stroke, 42% greater risk for all-cause death, 25% greater risk for cardiac death, and 60% greater risk for MACE than did people who had neither RA nor CAD.
For people with both RA and CAD, the adjusted risks were significantly higher when compared to people with neither: more than four times greater for MI and MACE, 55% greater for stroke, almost double for all-cause death, and 3.7 times greater for cardiac death. People with CAD but no RA also had higher adjusted risk rates compared to people with neither, but had variable rates when compared to people with RA but no CAD, and significantly lower adjusted rates compared to people with both.
The nature of CAD was also a factor, Dr. Løgstrup and colleagues noted. “We found more non-obstructive CAD but no increased incidence of one-vessel, two-vessel, and three-vessel disease in patients with RA than in patients without RA,” they wrote. That’s in line with other published studies (Semin Arthritis Rheum. 2010;40[3]:215–21 and J Rheumatol. 2007;34[5]:937–42), but counter to a study that found increased plaque burden and higher rates of multivessel disease among people with RA (Ann Rheum Dis. 2014;73:1797–804). Differences in methodology, vessel disease definitions, and study population may explain these deviations.
The study authors did not declare any outside source of funding or any competing interests.
Dr. Bartels disclosed receiving institutional grant funding through Pfizer.
SOURCE: Løgstrup BB et al. Ann Rheum Dis. 2020 May 29. doi: 10.1136/annrheumdis-2020-217154.
In patients with rheumatoid arthritis (RA), strategies to prevent cardiovascular events, such as treating hypertension, encouraging patients to stop smoking, and reinforcing statin therapy, may be especially important, regardless of whether they have a history of coronary artery disease because their risk for adverse cardiovascular outcomes is significantly greater than for patients who have neither RA nor coronary artery disease (CAD), a large population-based study from Denmark suggests.
“Among patients with RA, risk stratification by presence or absence of documented CAD may allow for screening and personalized treatment strategies,” wrote Brian B. Løgstrup, MD, PhD, DMSc, of Aarhus (Denmark) University Hospital, and his colleagues.
The study, published in Annals of the Rheumatic Diseases, analyzed 125,331 patients with and without CAD in the Western Denmark Heart Registry who had coronary angiography from 2003 through 2016. The cohort included 671 RA patients with no confirmed CAD and 1,061 RA patients who had CAD.
The study makes a significant contribution to the literature in reporting on the additive risk of RA and CAD, said Christie M. Bartels, MD, associate professor in the division of rheumatology at the University of Wisconsin, Madison. “Even among patients with both conditions [RA and CVD], they were less likely to get statin therapy,” she said, noting that the 82.6% of study patients with both CAD and RA were on statins vs. 86.5% of those with CAD alone, while the former had significantly higher rates of hypertension – 64.3% vs. 58.8%. “We’re doing a less effective job on secondary prevention,” she said. The anti-inflammatory properties of statins can also have an additive benefit in RA, she noted.
“This study shows that the rheumatologist can play a role in reinforcing the importance of primary and secondary cardiovascular disease prevention – meaning hypertension control, counseling patients to stop smoking and following up on statin therapy in RA,” Dr. Bartels added.
The study presents two novel findings, Dr. Løgstrup and colleagues noted:
- That RA confers a statistically significant, “but numerically marginally,” heightened risk of cardiovascular events other than stroke.
- Among patients with CAD, RA confers an increased risk of cardiac and all-cause death as well as MI and major adverse cardiovascular events (MACE).
“These finding indicate that RA may have a potential impact for precipitating cardiovascular events beyond CAD and, even more importantly, that RA seems to exacerbate the clinical risk of cardiovascular events in the presence of CAD,” Dr. Løgstrup and colleagues wrote.
The study found that patients with neither RA nor CAD had the lowest 10-year rates of MI (2.7%), ischemic stroke (2.9%), all-cause death (21.6%), cardiac death (2.3%), and MACE (7.3%).
By comparison, those with RA but no CAD had 10-year rates of 3.8% for MI, 5.5% for stroke, 35.6% for all-cause death, 3% for cardiac death, and 11.5% for MACE. Rates for those outcomes for people with CAD but no RA were 9.9% for MI, 4.6% for stroke, 33.3% for all-cause death, 7% for cardiac death, and 19.1% for MACE.
For patients with both RA and CAD, 10-year rates were 12.2% for MI, 4.4% for stroke, 49% for all-cause death, 10.9% for cardiac death, and 24.3% for MACE.
The researchers also performed a risk adjustment analysis based on potential confounding variables across the different groups, such as age, gender, comorbidities including diabetes and hypertension, active smoking status, and anticoagulant, antiplatelet, and statin therapy. The adjusted analysis revealed that patients with RA alone had a 63% greater risk of MI, 68% greater risk for stroke, 42% greater risk for all-cause death, 25% greater risk for cardiac death, and 60% greater risk for MACE than did people who had neither RA nor CAD.
For people with both RA and CAD, the adjusted risks were significantly higher when compared to people with neither: more than four times greater for MI and MACE, 55% greater for stroke, almost double for all-cause death, and 3.7 times greater for cardiac death. People with CAD but no RA also had higher adjusted risk rates compared to people with neither, but had variable rates when compared to people with RA but no CAD, and significantly lower adjusted rates compared to people with both.
The nature of CAD was also a factor, Dr. Løgstrup and colleagues noted. “We found more non-obstructive CAD but no increased incidence of one-vessel, two-vessel, and three-vessel disease in patients with RA than in patients without RA,” they wrote. That’s in line with other published studies (Semin Arthritis Rheum. 2010;40[3]:215–21 and J Rheumatol. 2007;34[5]:937–42), but counter to a study that found increased plaque burden and higher rates of multivessel disease among people with RA (Ann Rheum Dis. 2014;73:1797–804). Differences in methodology, vessel disease definitions, and study population may explain these deviations.
The study authors did not declare any outside source of funding or any competing interests.
Dr. Bartels disclosed receiving institutional grant funding through Pfizer.
SOURCE: Løgstrup BB et al. Ann Rheum Dis. 2020 May 29. doi: 10.1136/annrheumdis-2020-217154.
In patients with rheumatoid arthritis (RA), strategies to prevent cardiovascular events, such as treating hypertension, encouraging patients to stop smoking, and reinforcing statin therapy, may be especially important, regardless of whether they have a history of coronary artery disease because their risk for adverse cardiovascular outcomes is significantly greater than for patients who have neither RA nor coronary artery disease (CAD), a large population-based study from Denmark suggests.
“Among patients with RA, risk stratification by presence or absence of documented CAD may allow for screening and personalized treatment strategies,” wrote Brian B. Løgstrup, MD, PhD, DMSc, of Aarhus (Denmark) University Hospital, and his colleagues.
The study, published in Annals of the Rheumatic Diseases, analyzed 125,331 patients with and without CAD in the Western Denmark Heart Registry who had coronary angiography from 2003 through 2016. The cohort included 671 RA patients with no confirmed CAD and 1,061 RA patients who had CAD.
The study makes a significant contribution to the literature in reporting on the additive risk of RA and CAD, said Christie M. Bartels, MD, associate professor in the division of rheumatology at the University of Wisconsin, Madison. “Even among patients with both conditions [RA and CVD], they were less likely to get statin therapy,” she said, noting that the 82.6% of study patients with both CAD and RA were on statins vs. 86.5% of those with CAD alone, while the former had significantly higher rates of hypertension – 64.3% vs. 58.8%. “We’re doing a less effective job on secondary prevention,” she said. The anti-inflammatory properties of statins can also have an additive benefit in RA, she noted.
“This study shows that the rheumatologist can play a role in reinforcing the importance of primary and secondary cardiovascular disease prevention – meaning hypertension control, counseling patients to stop smoking and following up on statin therapy in RA,” Dr. Bartels added.
The study presents two novel findings, Dr. Løgstrup and colleagues noted:
- That RA confers a statistically significant, “but numerically marginally,” heightened risk of cardiovascular events other than stroke.
- Among patients with CAD, RA confers an increased risk of cardiac and all-cause death as well as MI and major adverse cardiovascular events (MACE).
“These finding indicate that RA may have a potential impact for precipitating cardiovascular events beyond CAD and, even more importantly, that RA seems to exacerbate the clinical risk of cardiovascular events in the presence of CAD,” Dr. Løgstrup and colleagues wrote.
The study found that patients with neither RA nor CAD had the lowest 10-year rates of MI (2.7%), ischemic stroke (2.9%), all-cause death (21.6%), cardiac death (2.3%), and MACE (7.3%).
By comparison, those with RA but no CAD had 10-year rates of 3.8% for MI, 5.5% for stroke, 35.6% for all-cause death, 3% for cardiac death, and 11.5% for MACE. Rates for those outcomes for people with CAD but no RA were 9.9% for MI, 4.6% for stroke, 33.3% for all-cause death, 7% for cardiac death, and 19.1% for MACE.
For patients with both RA and CAD, 10-year rates were 12.2% for MI, 4.4% for stroke, 49% for all-cause death, 10.9% for cardiac death, and 24.3% for MACE.
The researchers also performed a risk adjustment analysis based on potential confounding variables across the different groups, such as age, gender, comorbidities including diabetes and hypertension, active smoking status, and anticoagulant, antiplatelet, and statin therapy. The adjusted analysis revealed that patients with RA alone had a 63% greater risk of MI, 68% greater risk for stroke, 42% greater risk for all-cause death, 25% greater risk for cardiac death, and 60% greater risk for MACE than did people who had neither RA nor CAD.
For people with both RA and CAD, the adjusted risks were significantly higher when compared to people with neither: more than four times greater for MI and MACE, 55% greater for stroke, almost double for all-cause death, and 3.7 times greater for cardiac death. People with CAD but no RA also had higher adjusted risk rates compared to people with neither, but had variable rates when compared to people with RA but no CAD, and significantly lower adjusted rates compared to people with both.
The nature of CAD was also a factor, Dr. Løgstrup and colleagues noted. “We found more non-obstructive CAD but no increased incidence of one-vessel, two-vessel, and three-vessel disease in patients with RA than in patients without RA,” they wrote. That’s in line with other published studies (Semin Arthritis Rheum. 2010;40[3]:215–21 and J Rheumatol. 2007;34[5]:937–42), but counter to a study that found increased plaque burden and higher rates of multivessel disease among people with RA (Ann Rheum Dis. 2014;73:1797–804). Differences in methodology, vessel disease definitions, and study population may explain these deviations.
The study authors did not declare any outside source of funding or any competing interests.
Dr. Bartels disclosed receiving institutional grant funding through Pfizer.
SOURCE: Løgstrup BB et al. Ann Rheum Dis. 2020 May 29. doi: 10.1136/annrheumdis-2020-217154.
FROM ANNALS OF THE RHEUMATIC DISEASES
FLU/SAL inhalers for COPD carry greater pneumonia risk
For well over a decade the elevated risk of pneumonia from inhaled corticosteroids for moderate to very severe COPD has been well documented, although the pneumonia risks from different types of ICSs have not been well understood.
Researchers from Taiwan have taken a step in to investigate this question with a nationwide cohort study that reported inhalers with budesonide and beclomethasone may have a lower pneumonia risk than that of fluticasone propionate/salmeterol inhalers (CHEST. 2020;157:117-29).
The study is the first to include beclomethasone-containing inhalers in a comparison of ICS/long-acting beta2-agonist (LABA) fixed combinations to evaluate pneumonia risk, along with dose and drug properties, wrote Ting-Yu Chang, MS, of the Graduate Institute of Clinical Pharmacology at the College of Medicine, National Taiwan University in Taipei, and colleagues.
The study evaluated 42,393 people with COPD in the National Health Insurance Research Database who got at least two continuous prescriptions for three different types of inhalers:
- Budesonide/formoterol (BUD/FOR).
- Beclomethasone/formoterol (BEC/FOR).
- Fluticasone propionate/salmeterol (FLU/SAL).
The study included patients aged 40 years and older who used a metered-dose inhaler (MDI) or dry-powder inhaler (DPI) between January 2011 and June 2015.
Patient experience with adverse events (AEs) was a factor in risk stratification, Mr. Chang and colleagues noted. “For the comparison between the BEC/FOR MDI and FLU/SAL MDI, the lower risk associated with the BEC/FOR MDI was more prominent in patients without severe AE in the past year,” they wrote.
The study found that BUD/FOR DPI users had a 17% lower risk of severe pneumonia and a 12% lower risk of severe AEs than that of FLU/SAL DPI users. The risk difference in pneumonia remained significant after adjustment for the ICS-equivalent daily dose, but the spread for AEs didn’t.
BEC/FOR MDI users were 31% less likely to get severe pneumonia and 18% less likely to have severe AEs than were FLU/SAL MDI users, but that difference declined and became nonsignificant after adjustment for the ICS-equivalent daily dose.
The study also found that a high average daily dose (> 500 mcg/d) of FLU/SAL MDI carried a 66% greater risk of severe pneumonia, compared with that of low-dose users. Also, medium-dose BEC/FOR MDI users (FLU equivalent 299-499 mcg/d) had a 38% greater risk of severe pneumonia than low-dose (< 200 mcg/d) users.
The variable pneumonia risks may be linked to each ICS’s pharmacokinetics, specifically their distinct lipophilic properties, Mr. Chang and colleagues wrote. Fluticasone propionate is known to be more lipophilic than budesonide, and while beclomethasone is more lipophilic than both, as a prodrug it rapidly converts to lower lipophilicity upon contact with bronchial secretions. “In general, a lipophilic ICS has a longer retention time within the airway or lung tissue to exert local immunosuppression and reduce inflammation,” Mr. Chang and colleagues stated.
The Taiwan Ministry of Science and Technology provided partial support for the study. Mr. Chang and colleagues have no relationships to disclose.
SOURCE: Chang TY et al. CHEST. 2020;157:117-29.
For well over a decade the elevated risk of pneumonia from inhaled corticosteroids for moderate to very severe COPD has been well documented, although the pneumonia risks from different types of ICSs have not been well understood.
Researchers from Taiwan have taken a step in to investigate this question with a nationwide cohort study that reported inhalers with budesonide and beclomethasone may have a lower pneumonia risk than that of fluticasone propionate/salmeterol inhalers (CHEST. 2020;157:117-29).
The study is the first to include beclomethasone-containing inhalers in a comparison of ICS/long-acting beta2-agonist (LABA) fixed combinations to evaluate pneumonia risk, along with dose and drug properties, wrote Ting-Yu Chang, MS, of the Graduate Institute of Clinical Pharmacology at the College of Medicine, National Taiwan University in Taipei, and colleagues.
The study evaluated 42,393 people with COPD in the National Health Insurance Research Database who got at least two continuous prescriptions for three different types of inhalers:
- Budesonide/formoterol (BUD/FOR).
- Beclomethasone/formoterol (BEC/FOR).
- Fluticasone propionate/salmeterol (FLU/SAL).
The study included patients aged 40 years and older who used a metered-dose inhaler (MDI) or dry-powder inhaler (DPI) between January 2011 and June 2015.
Patient experience with adverse events (AEs) was a factor in risk stratification, Mr. Chang and colleagues noted. “For the comparison between the BEC/FOR MDI and FLU/SAL MDI, the lower risk associated with the BEC/FOR MDI was more prominent in patients without severe AE in the past year,” they wrote.
The study found that BUD/FOR DPI users had a 17% lower risk of severe pneumonia and a 12% lower risk of severe AEs than that of FLU/SAL DPI users. The risk difference in pneumonia remained significant after adjustment for the ICS-equivalent daily dose, but the spread for AEs didn’t.
BEC/FOR MDI users were 31% less likely to get severe pneumonia and 18% less likely to have severe AEs than were FLU/SAL MDI users, but that difference declined and became nonsignificant after adjustment for the ICS-equivalent daily dose.
The study also found that a high average daily dose (> 500 mcg/d) of FLU/SAL MDI carried a 66% greater risk of severe pneumonia, compared with that of low-dose users. Also, medium-dose BEC/FOR MDI users (FLU equivalent 299-499 mcg/d) had a 38% greater risk of severe pneumonia than low-dose (< 200 mcg/d) users.
The variable pneumonia risks may be linked to each ICS’s pharmacokinetics, specifically their distinct lipophilic properties, Mr. Chang and colleagues wrote. Fluticasone propionate is known to be more lipophilic than budesonide, and while beclomethasone is more lipophilic than both, as a prodrug it rapidly converts to lower lipophilicity upon contact with bronchial secretions. “In general, a lipophilic ICS has a longer retention time within the airway or lung tissue to exert local immunosuppression and reduce inflammation,” Mr. Chang and colleagues stated.
The Taiwan Ministry of Science and Technology provided partial support for the study. Mr. Chang and colleagues have no relationships to disclose.
SOURCE: Chang TY et al. CHEST. 2020;157:117-29.
For well over a decade the elevated risk of pneumonia from inhaled corticosteroids for moderate to very severe COPD has been well documented, although the pneumonia risks from different types of ICSs have not been well understood.
Researchers from Taiwan have taken a step in to investigate this question with a nationwide cohort study that reported inhalers with budesonide and beclomethasone may have a lower pneumonia risk than that of fluticasone propionate/salmeterol inhalers (CHEST. 2020;157:117-29).
The study is the first to include beclomethasone-containing inhalers in a comparison of ICS/long-acting beta2-agonist (LABA) fixed combinations to evaluate pneumonia risk, along with dose and drug properties, wrote Ting-Yu Chang, MS, of the Graduate Institute of Clinical Pharmacology at the College of Medicine, National Taiwan University in Taipei, and colleagues.
The study evaluated 42,393 people with COPD in the National Health Insurance Research Database who got at least two continuous prescriptions for three different types of inhalers:
- Budesonide/formoterol (BUD/FOR).
- Beclomethasone/formoterol (BEC/FOR).
- Fluticasone propionate/salmeterol (FLU/SAL).
The study included patients aged 40 years and older who used a metered-dose inhaler (MDI) or dry-powder inhaler (DPI) between January 2011 and June 2015.
Patient experience with adverse events (AEs) was a factor in risk stratification, Mr. Chang and colleagues noted. “For the comparison between the BEC/FOR MDI and FLU/SAL MDI, the lower risk associated with the BEC/FOR MDI was more prominent in patients without severe AE in the past year,” they wrote.
The study found that BUD/FOR DPI users had a 17% lower risk of severe pneumonia and a 12% lower risk of severe AEs than that of FLU/SAL DPI users. The risk difference in pneumonia remained significant after adjustment for the ICS-equivalent daily dose, but the spread for AEs didn’t.
BEC/FOR MDI users were 31% less likely to get severe pneumonia and 18% less likely to have severe AEs than were FLU/SAL MDI users, but that difference declined and became nonsignificant after adjustment for the ICS-equivalent daily dose.
The study also found that a high average daily dose (> 500 mcg/d) of FLU/SAL MDI carried a 66% greater risk of severe pneumonia, compared with that of low-dose users. Also, medium-dose BEC/FOR MDI users (FLU equivalent 299-499 mcg/d) had a 38% greater risk of severe pneumonia than low-dose (< 200 mcg/d) users.
The variable pneumonia risks may be linked to each ICS’s pharmacokinetics, specifically their distinct lipophilic properties, Mr. Chang and colleagues wrote. Fluticasone propionate is known to be more lipophilic than budesonide, and while beclomethasone is more lipophilic than both, as a prodrug it rapidly converts to lower lipophilicity upon contact with bronchial secretions. “In general, a lipophilic ICS has a longer retention time within the airway or lung tissue to exert local immunosuppression and reduce inflammation,” Mr. Chang and colleagues stated.
The Taiwan Ministry of Science and Technology provided partial support for the study. Mr. Chang and colleagues have no relationships to disclose.
SOURCE: Chang TY et al. CHEST. 2020;157:117-29.
FROM CHEST
Working group proposes MRI definitions of structural lesions indicative of axial spondyloarthritis
What constitutes a structural lesion of the sacroiliac joints on MRI that’s indicative of axial spondyloarthritis (axSpA) has long been a matter of conjecture, but the Assessment of SpondyloArthritis International Society (ASAS) MRI Working Group has developed new definitions that showed a high degree of specificity in identifying such lesions in the disease.
“There is a lack of consensus as to what defines a structural lesion on MRI of the sacroiliac joint [SIJ] typical of axial spondyloarthritis. Previous studies have described structural lesions in different ways, precluding meaningful comparisons between studies. The ASAS MRI group has generated updated consensus lesion definitions that describe each of the MRI lesions in the sacroiliac joint. These definitions have been validated by seven expert readers from the ASAS MRI group on MRI images from the ASAS classification cohort,” Walter P. Maksymowych, MD, said at the annual European Congress of Rheumatology, held online this year due to COVID-19.
Making a definitive diagnosis of axSpA can be difficult because MRI can show a variety of SIJ abnormalities in healthy people as well as those with axSpA, said Dr. Maksymowych, chief medical officer of CARE Arthritis and professor in rheumatology at the University of Alberta in Edmonton, said in an interview prior to his presentation at the e-congress. “People who evaluate MRI scans are looking for clues as to what types of lesions they can be confident are indicative of axSpA.”
That started a process by the ASAS MRI group to evaluate scans from the landmark ASAS Classification Cohort study (Ann Rheum Dis. 2019;78:1550-8). “But,” said Dr. Maksymowych, “the MRI scans from that study were never evaluated.” So that work was handed off to the working group, whose 25 members included 7 expert image readers who evaluated the MRI scans.
The group adopted a standardized approach for evaluating MRIs of the SIJ in 148 cases, dividing each SIJ into quadrants and then evaluating consecutive MRI slices. The readers first documented whether they observed a definite structural lesion on the scan, which they then used as an external reference standard. They then analyzed which lesion, and in how many SIJ quadrants or slices, best reflected this external standard.
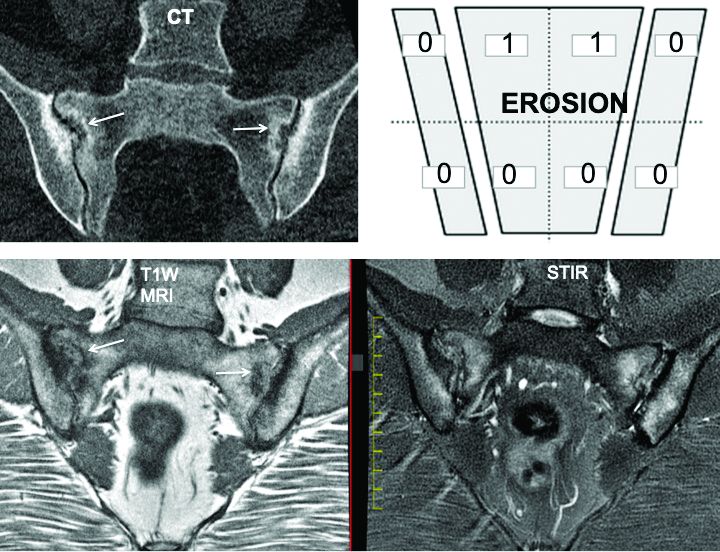
The investigators defined an erosion as “a defect in subchondral bone associated with full-thickness loss of a dark appearance of the subchondral cortex at its expected location, with loss of signal on a T1-weighted, non–fat-suppressed sequence, compared with the normal bright appearance of adjacent bone marrow.” They defined a fat lesion or fat metaplasia as a “bright signal seen on a T1-weighted, non–fat-suppressed sequence that is brighter than normal bone marrow which meets the following requirements: It is homogeneously bright, located in a typical anatomical area (specifically subchondral bone), and has a sharply defined border along its nonarticular border with normal bone marrow.”
An erosion in one quadrant isn’t sufficient to define a scan as positive for a definite structural lesion, said Dr. Maksymowych; but an erosion in three quadrants or in two or more consecutive slices meets the group’s designation of a definite structural lesion. “This showed over a 95% specificity for being associated with a definite structural lesion as defined by a majority of the seven experts,” he said.
The group also determined that a fat lesion typical of axSpA has a homogeneous white appearance on T1-weighted scans with a sharply defined border. The group also determined that such a fat lesion with at least 1-cm horizontal depth from the joint margin in at least one SIJ quadrant is strongly indicative of axSpA.
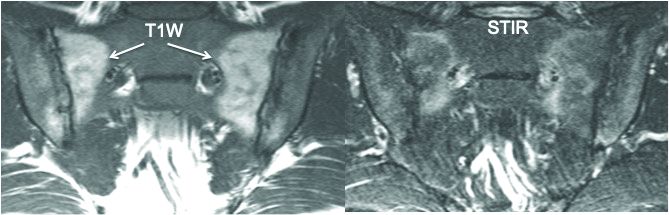
“So we now have definitions for two structural lesions, erosion and fat lesions, that reflect what a majority of experts consider to be a definite structural lesion according to at least 95% specificity,” he said. Sensitivity values were 90% for erosion in three quadrants and 83% for erosions in two or more consecutive slices. and 59% for a fat lesion with at least 1-cm horizontal depth from the joint margin in at least one SIJ quadrant.
The second part of the analysis evaluated the predictive capacity of these lesion definitions for a rheumatologic diagnosis of axSpA at 4.4 years of follow-up. “These lesions predicted SpA with over 95% positive predictive value,” he said. “In other words, if you see them at baseline they’re going to predict SpA with high certainty at follow-up after 4.4 years.”
Three aspects of this study design are unique, Dr. Maksymowych noted. First is the high number of expert MRI readers who evaluated the scans. “There aren’t really too many studies I can think of that used more than two or three expert MRI readers,” he said.
Second is the way in which the study “very precisely and in a very standardized way” applied all the consensus-based ASAS definitions of structural SIJ lesions. “In the past, a variety of ways were used to define these lesions,” he said. “A good example would be the different ways in which erosions have been defined.”
The third novel aspect of the study is that the expert readers’ assessment of what constitutes a definite structural lesion was used as an external reference standard. For example, the study calculated sensitivity and specificity for numbers of SIJ quadrants and consecutive slices with erosion, sclerosis, and fat lesions where a majority of readers agreed on the presence of a structural lesion typical of axSpA with high confidence (3 or greater on a scale of 1-4). “The reason this was put in place is because we recognize sometimes lesions are very subtle and you can’t be certain that they’re reflecting SpA,” he said.
The investigators disclosed relationships with AbbVie, Amgen, Astellas, AstraZeneca, Bristol-Myers Squibb, Boehringer Ingelheim, Celgene, Eli Lilly, Galapagos, Janssen, Merck, Novo Nordisk, Novartis, Orion, Pfizer, Regeneron, Roche, Sandoz, Sanofi, and UCB.
Maksymowych WP et al. Ann Rheum Dis, 2020;79[suppl 1]:53. Abstract OP0079.
What constitutes a structural lesion of the sacroiliac joints on MRI that’s indicative of axial spondyloarthritis (axSpA) has long been a matter of conjecture, but the Assessment of SpondyloArthritis International Society (ASAS) MRI Working Group has developed new definitions that showed a high degree of specificity in identifying such lesions in the disease.
“There is a lack of consensus as to what defines a structural lesion on MRI of the sacroiliac joint [SIJ] typical of axial spondyloarthritis. Previous studies have described structural lesions in different ways, precluding meaningful comparisons between studies. The ASAS MRI group has generated updated consensus lesion definitions that describe each of the MRI lesions in the sacroiliac joint. These definitions have been validated by seven expert readers from the ASAS MRI group on MRI images from the ASAS classification cohort,” Walter P. Maksymowych, MD, said at the annual European Congress of Rheumatology, held online this year due to COVID-19.
Making a definitive diagnosis of axSpA can be difficult because MRI can show a variety of SIJ abnormalities in healthy people as well as those with axSpA, said Dr. Maksymowych, chief medical officer of CARE Arthritis and professor in rheumatology at the University of Alberta in Edmonton, said in an interview prior to his presentation at the e-congress. “People who evaluate MRI scans are looking for clues as to what types of lesions they can be confident are indicative of axSpA.”
That started a process by the ASAS MRI group to evaluate scans from the landmark ASAS Classification Cohort study (Ann Rheum Dis. 2019;78:1550-8). “But,” said Dr. Maksymowych, “the MRI scans from that study were never evaluated.” So that work was handed off to the working group, whose 25 members included 7 expert image readers who evaluated the MRI scans.
The group adopted a standardized approach for evaluating MRIs of the SIJ in 148 cases, dividing each SIJ into quadrants and then evaluating consecutive MRI slices. The readers first documented whether they observed a definite structural lesion on the scan, which they then used as an external reference standard. They then analyzed which lesion, and in how many SIJ quadrants or slices, best reflected this external standard.
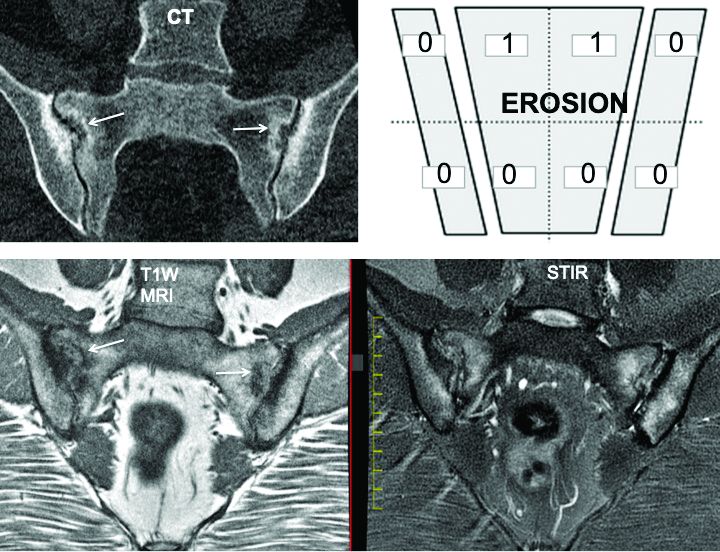
The investigators defined an erosion as “a defect in subchondral bone associated with full-thickness loss of a dark appearance of the subchondral cortex at its expected location, with loss of signal on a T1-weighted, non–fat-suppressed sequence, compared with the normal bright appearance of adjacent bone marrow.” They defined a fat lesion or fat metaplasia as a “bright signal seen on a T1-weighted, non–fat-suppressed sequence that is brighter than normal bone marrow which meets the following requirements: It is homogeneously bright, located in a typical anatomical area (specifically subchondral bone), and has a sharply defined border along its nonarticular border with normal bone marrow.”
An erosion in one quadrant isn’t sufficient to define a scan as positive for a definite structural lesion, said Dr. Maksymowych; but an erosion in three quadrants or in two or more consecutive slices meets the group’s designation of a definite structural lesion. “This showed over a 95% specificity for being associated with a definite structural lesion as defined by a majority of the seven experts,” he said.
The group also determined that a fat lesion typical of axSpA has a homogeneous white appearance on T1-weighted scans with a sharply defined border. The group also determined that such a fat lesion with at least 1-cm horizontal depth from the joint margin in at least one SIJ quadrant is strongly indicative of axSpA.
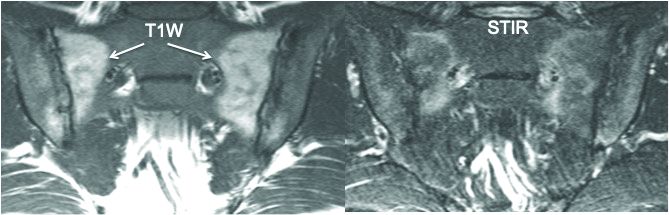
“So we now have definitions for two structural lesions, erosion and fat lesions, that reflect what a majority of experts consider to be a definite structural lesion according to at least 95% specificity,” he said. Sensitivity values were 90% for erosion in three quadrants and 83% for erosions in two or more consecutive slices. and 59% for a fat lesion with at least 1-cm horizontal depth from the joint margin in at least one SIJ quadrant.
The second part of the analysis evaluated the predictive capacity of these lesion definitions for a rheumatologic diagnosis of axSpA at 4.4 years of follow-up. “These lesions predicted SpA with over 95% positive predictive value,” he said. “In other words, if you see them at baseline they’re going to predict SpA with high certainty at follow-up after 4.4 years.”
Three aspects of this study design are unique, Dr. Maksymowych noted. First is the high number of expert MRI readers who evaluated the scans. “There aren’t really too many studies I can think of that used more than two or three expert MRI readers,” he said.
Second is the way in which the study “very precisely and in a very standardized way” applied all the consensus-based ASAS definitions of structural SIJ lesions. “In the past, a variety of ways were used to define these lesions,” he said. “A good example would be the different ways in which erosions have been defined.”
The third novel aspect of the study is that the expert readers’ assessment of what constitutes a definite structural lesion was used as an external reference standard. For example, the study calculated sensitivity and specificity for numbers of SIJ quadrants and consecutive slices with erosion, sclerosis, and fat lesions where a majority of readers agreed on the presence of a structural lesion typical of axSpA with high confidence (3 or greater on a scale of 1-4). “The reason this was put in place is because we recognize sometimes lesions are very subtle and you can’t be certain that they’re reflecting SpA,” he said.
The investigators disclosed relationships with AbbVie, Amgen, Astellas, AstraZeneca, Bristol-Myers Squibb, Boehringer Ingelheim, Celgene, Eli Lilly, Galapagos, Janssen, Merck, Novo Nordisk, Novartis, Orion, Pfizer, Regeneron, Roche, Sandoz, Sanofi, and UCB.
Maksymowych WP et al. Ann Rheum Dis, 2020;79[suppl 1]:53. Abstract OP0079.
What constitutes a structural lesion of the sacroiliac joints on MRI that’s indicative of axial spondyloarthritis (axSpA) has long been a matter of conjecture, but the Assessment of SpondyloArthritis International Society (ASAS) MRI Working Group has developed new definitions that showed a high degree of specificity in identifying such lesions in the disease.
“There is a lack of consensus as to what defines a structural lesion on MRI of the sacroiliac joint [SIJ] typical of axial spondyloarthritis. Previous studies have described structural lesions in different ways, precluding meaningful comparisons between studies. The ASAS MRI group has generated updated consensus lesion definitions that describe each of the MRI lesions in the sacroiliac joint. These definitions have been validated by seven expert readers from the ASAS MRI group on MRI images from the ASAS classification cohort,” Walter P. Maksymowych, MD, said at the annual European Congress of Rheumatology, held online this year due to COVID-19.
Making a definitive diagnosis of axSpA can be difficult because MRI can show a variety of SIJ abnormalities in healthy people as well as those with axSpA, said Dr. Maksymowych, chief medical officer of CARE Arthritis and professor in rheumatology at the University of Alberta in Edmonton, said in an interview prior to his presentation at the e-congress. “People who evaluate MRI scans are looking for clues as to what types of lesions they can be confident are indicative of axSpA.”
That started a process by the ASAS MRI group to evaluate scans from the landmark ASAS Classification Cohort study (Ann Rheum Dis. 2019;78:1550-8). “But,” said Dr. Maksymowych, “the MRI scans from that study were never evaluated.” So that work was handed off to the working group, whose 25 members included 7 expert image readers who evaluated the MRI scans.
The group adopted a standardized approach for evaluating MRIs of the SIJ in 148 cases, dividing each SIJ into quadrants and then evaluating consecutive MRI slices. The readers first documented whether they observed a definite structural lesion on the scan, which they then used as an external reference standard. They then analyzed which lesion, and in how many SIJ quadrants or slices, best reflected this external standard.
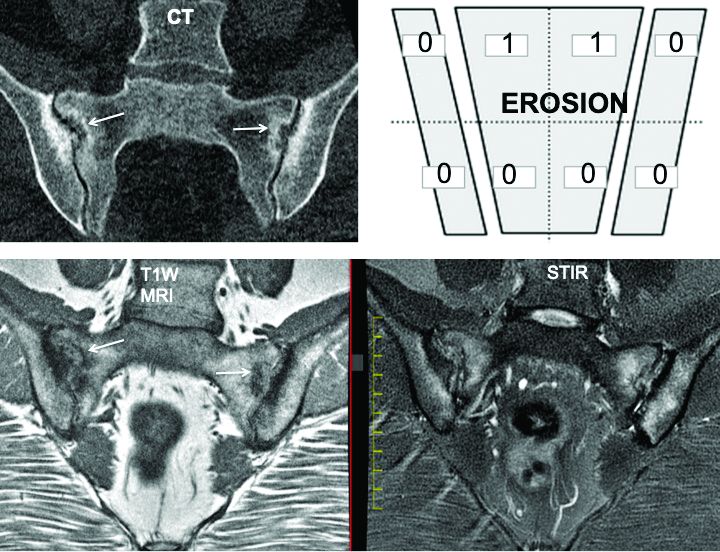
The investigators defined an erosion as “a defect in subchondral bone associated with full-thickness loss of a dark appearance of the subchondral cortex at its expected location, with loss of signal on a T1-weighted, non–fat-suppressed sequence, compared with the normal bright appearance of adjacent bone marrow.” They defined a fat lesion or fat metaplasia as a “bright signal seen on a T1-weighted, non–fat-suppressed sequence that is brighter than normal bone marrow which meets the following requirements: It is homogeneously bright, located in a typical anatomical area (specifically subchondral bone), and has a sharply defined border along its nonarticular border with normal bone marrow.”
An erosion in one quadrant isn’t sufficient to define a scan as positive for a definite structural lesion, said Dr. Maksymowych; but an erosion in three quadrants or in two or more consecutive slices meets the group’s designation of a definite structural lesion. “This showed over a 95% specificity for being associated with a definite structural lesion as defined by a majority of the seven experts,” he said.
The group also determined that a fat lesion typical of axSpA has a homogeneous white appearance on T1-weighted scans with a sharply defined border. The group also determined that such a fat lesion with at least 1-cm horizontal depth from the joint margin in at least one SIJ quadrant is strongly indicative of axSpA.
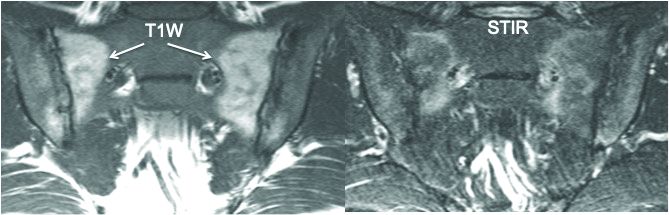
“So we now have definitions for two structural lesions, erosion and fat lesions, that reflect what a majority of experts consider to be a definite structural lesion according to at least 95% specificity,” he said. Sensitivity values were 90% for erosion in three quadrants and 83% for erosions in two or more consecutive slices. and 59% for a fat lesion with at least 1-cm horizontal depth from the joint margin in at least one SIJ quadrant.
The second part of the analysis evaluated the predictive capacity of these lesion definitions for a rheumatologic diagnosis of axSpA at 4.4 years of follow-up. “These lesions predicted SpA with over 95% positive predictive value,” he said. “In other words, if you see them at baseline they’re going to predict SpA with high certainty at follow-up after 4.4 years.”
Three aspects of this study design are unique, Dr. Maksymowych noted. First is the high number of expert MRI readers who evaluated the scans. “There aren’t really too many studies I can think of that used more than two or three expert MRI readers,” he said.
Second is the way in which the study “very precisely and in a very standardized way” applied all the consensus-based ASAS definitions of structural SIJ lesions. “In the past, a variety of ways were used to define these lesions,” he said. “A good example would be the different ways in which erosions have been defined.”
The third novel aspect of the study is that the expert readers’ assessment of what constitutes a definite structural lesion was used as an external reference standard. For example, the study calculated sensitivity and specificity for numbers of SIJ quadrants and consecutive slices with erosion, sclerosis, and fat lesions where a majority of readers agreed on the presence of a structural lesion typical of axSpA with high confidence (3 or greater on a scale of 1-4). “The reason this was put in place is because we recognize sometimes lesions are very subtle and you can’t be certain that they’re reflecting SpA,” he said.
The investigators disclosed relationships with AbbVie, Amgen, Astellas, AstraZeneca, Bristol-Myers Squibb, Boehringer Ingelheim, Celgene, Eli Lilly, Galapagos, Janssen, Merck, Novo Nordisk, Novartis, Orion, Pfizer, Regeneron, Roche, Sandoz, Sanofi, and UCB.
Maksymowych WP et al. Ann Rheum Dis, 2020;79[suppl 1]:53. Abstract OP0079.
FROM EULAR 2020 E-CONGRESS
Distancing works, N95 respirators work better
A study that claims to be the first review of all the available evidence of the effectiveness of physical distancing, face masks, and eye protection to prevent spread of COVID-19 and other respiratory diseases has quantified the effectiveness of these protective measures. The study found that greater physical distancing from an exposed person significantly reduces risk of transmission and that N95 masks, particularly for health care workers, are more effective than other face coverings.
The meta-analysis, published online in The Lancet (2020 Jun 2; doi.org/10.1016/ S0140-6736(20)31142-9) also marks the first evaluation of these protective measures in both community and health care settings for COVID-19, the study authors stated.
“The risk for infection is highly dependent on distance to the individual infected and the type of face mask and eye protection worn,” wrote Derek K. Chu, MD, PhD, of McMaster University in Hamilton, Ont., and colleagues, reporting on behalf of the COVID-19 Systematic Urgent Review Group Effort, or SURGE.
The study reported that physical distancing of at least 1 meter, or about a yard, “seems to be strongly associated with a large protective effect,” but that distancing of 2 meters or about 6 feet could be more effective.
The study involved a systematic review of 172 observational studies across six continents that evaluated distance measures, face masks, and eye protection to prevent transmission between patients with confirmed or probable COVID-19, other severe acute respiratory syndrome (SARS) disease, and Middle East respiratory syndrome (MERS), and their family members, caregivers and health care workers up to May 3, 2020. The meta-analysis involved pooled estimates from 44 comparative studies with 25,697 participants, including seven studies of COVID-19 with 6,674 participants. None of the studies included in the meta-analysis were randomized clinical trials.
A subanalysis of 29 unadjusted and 9 adjusted studies found that the absolute risk of infection in proximity to an exposed individual was 12.8% at 1 m and 2.6% at 2 m. The risk remained constant even when the six COVID-19 studies in this subanalysis were isolated and regardless of being in a health care or non–health-care setting. Each meter of increased distance resulted in a doubling in the change in relative risk (P = .041).
The study also identified what Dr. Chu and colleagues characterized as a “large reduction” in infection risk with the use of both N95 or similar respirators or face masks, with an adjusted risk of infection of 3.1% with a face covering vs. a 17.4% without. The researchers also found a stronger association in health care settings vs. non–health care settings, with a relative risk of 0.3 vs. 0.56, respectively (P = .049). The protective effect of N95 or similar respirators was greater than other masks, with adjusted odds ratios of 0.04 vs. 0.33 (P = .09).
Eye protection was found to reduce the risk of infection to 5.5% vs. 16% without eye protection.
The study also identified potential barriers to social distancing and use of masks and eye protection: discomfort, resource use “linked with potentially decreased equity,” less clear communication, and a perceived lack of empathy on the part of providers toward patients.
Dr. Chu and colleagues wrote that more “high-quality” research, including randomized trials of the optimal physical distance and evaluation of different mask types in non–health care settings “is urgently needed.” They added, “Policymakers at all levels should, therefore, strive to address equity implications for groups with currently limited access to face masks and eye protection.”
The goal of this study was to “inform WHO guidance documents,” the study noted. “Governments and the public health community can use our results to give clear advice for community settings and healthcare workers on these protective measures to reduce infection risk,” said study co-leader Holger Schünemann, MD, MSc, PhD, of McMaster University.
Prof. Raina MacIntyre, MBBS, PhD, head of the biosecurity research program at the Kirby Institute at the University of New South Wales in Sydney, who authored the comment that accompanied the article, said that this study provides evidence for stronger PPE guidelines.
“The Centers for Disease Control and Prevention initially recommended N95s for health workers treating COVID-19 patients, but later downgraded this to surgical masks and even cloth masks and bandannas when there was a supply shortage,” she said. “This study shows that N95s are superior masks and should prompt a review of guidelines that recommend anything less for health workers.”
Recommending anything less than N95 masks for health workers is like sending troops into battle “unarmed or with bows and arrows against a fully armed enemy,” she said. “We are not talking about a device that costs hundreds or thousands of dollars; a N95 costs less than a dollar to produce. All that is needed to address the supply shortage is political will.”
While the study has some shortcomings – namely that it didn’t provide a breakdown of positive tests among COVID-19 participants – it does provide important insight for physicians, Sachin Gupta, MD, a pulmonary and critical care specialist in San Francisco, said in an interview. “The strength of a meta-analysis is that you’re able to get a composite idea; that’s one up side to this,” he said. “They’re confirming what we knew: that distance matters; that more protective masks reduce risk of infection; and that eye protection has an important role.”
Dr. Chu and colleagues have no relevant financial relationships to disclose. One member of SURGE is participating in a clinical trial comparing medical masks and N95 respirators. The World Health Organization provided partial funding for the study.
SOURCE: Chu DK et al. Lancet. 2020 Jun 2; doi.org/10.1016/ S0140-6736(20)31142-9 .
A study that claims to be the first review of all the available evidence of the effectiveness of physical distancing, face masks, and eye protection to prevent spread of COVID-19 and other respiratory diseases has quantified the effectiveness of these protective measures. The study found that greater physical distancing from an exposed person significantly reduces risk of transmission and that N95 masks, particularly for health care workers, are more effective than other face coverings.
The meta-analysis, published online in The Lancet (2020 Jun 2; doi.org/10.1016/ S0140-6736(20)31142-9) also marks the first evaluation of these protective measures in both community and health care settings for COVID-19, the study authors stated.
“The risk for infection is highly dependent on distance to the individual infected and the type of face mask and eye protection worn,” wrote Derek K. Chu, MD, PhD, of McMaster University in Hamilton, Ont., and colleagues, reporting on behalf of the COVID-19 Systematic Urgent Review Group Effort, or SURGE.
The study reported that physical distancing of at least 1 meter, or about a yard, “seems to be strongly associated with a large protective effect,” but that distancing of 2 meters or about 6 feet could be more effective.
The study involved a systematic review of 172 observational studies across six continents that evaluated distance measures, face masks, and eye protection to prevent transmission between patients with confirmed or probable COVID-19, other severe acute respiratory syndrome (SARS) disease, and Middle East respiratory syndrome (MERS), and their family members, caregivers and health care workers up to May 3, 2020. The meta-analysis involved pooled estimates from 44 comparative studies with 25,697 participants, including seven studies of COVID-19 with 6,674 participants. None of the studies included in the meta-analysis were randomized clinical trials.
A subanalysis of 29 unadjusted and 9 adjusted studies found that the absolute risk of infection in proximity to an exposed individual was 12.8% at 1 m and 2.6% at 2 m. The risk remained constant even when the six COVID-19 studies in this subanalysis were isolated and regardless of being in a health care or non–health-care setting. Each meter of increased distance resulted in a doubling in the change in relative risk (P = .041).
The study also identified what Dr. Chu and colleagues characterized as a “large reduction” in infection risk with the use of both N95 or similar respirators or face masks, with an adjusted risk of infection of 3.1% with a face covering vs. a 17.4% without. The researchers also found a stronger association in health care settings vs. non–health care settings, with a relative risk of 0.3 vs. 0.56, respectively (P = .049). The protective effect of N95 or similar respirators was greater than other masks, with adjusted odds ratios of 0.04 vs. 0.33 (P = .09).
Eye protection was found to reduce the risk of infection to 5.5% vs. 16% without eye protection.
The study also identified potential barriers to social distancing and use of masks and eye protection: discomfort, resource use “linked with potentially decreased equity,” less clear communication, and a perceived lack of empathy on the part of providers toward patients.
Dr. Chu and colleagues wrote that more “high-quality” research, including randomized trials of the optimal physical distance and evaluation of different mask types in non–health care settings “is urgently needed.” They added, “Policymakers at all levels should, therefore, strive to address equity implications for groups with currently limited access to face masks and eye protection.”
The goal of this study was to “inform WHO guidance documents,” the study noted. “Governments and the public health community can use our results to give clear advice for community settings and healthcare workers on these protective measures to reduce infection risk,” said study co-leader Holger Schünemann, MD, MSc, PhD, of McMaster University.
Prof. Raina MacIntyre, MBBS, PhD, head of the biosecurity research program at the Kirby Institute at the University of New South Wales in Sydney, who authored the comment that accompanied the article, said that this study provides evidence for stronger PPE guidelines.
“The Centers for Disease Control and Prevention initially recommended N95s for health workers treating COVID-19 patients, but later downgraded this to surgical masks and even cloth masks and bandannas when there was a supply shortage,” she said. “This study shows that N95s are superior masks and should prompt a review of guidelines that recommend anything less for health workers.”
Recommending anything less than N95 masks for health workers is like sending troops into battle “unarmed or with bows and arrows against a fully armed enemy,” she said. “We are not talking about a device that costs hundreds or thousands of dollars; a N95 costs less than a dollar to produce. All that is needed to address the supply shortage is political will.”
While the study has some shortcomings – namely that it didn’t provide a breakdown of positive tests among COVID-19 participants – it does provide important insight for physicians, Sachin Gupta, MD, a pulmonary and critical care specialist in San Francisco, said in an interview. “The strength of a meta-analysis is that you’re able to get a composite idea; that’s one up side to this,” he said. “They’re confirming what we knew: that distance matters; that more protective masks reduce risk of infection; and that eye protection has an important role.”
Dr. Chu and colleagues have no relevant financial relationships to disclose. One member of SURGE is participating in a clinical trial comparing medical masks and N95 respirators. The World Health Organization provided partial funding for the study.
SOURCE: Chu DK et al. Lancet. 2020 Jun 2; doi.org/10.1016/ S0140-6736(20)31142-9 .
A study that claims to be the first review of all the available evidence of the effectiveness of physical distancing, face masks, and eye protection to prevent spread of COVID-19 and other respiratory diseases has quantified the effectiveness of these protective measures. The study found that greater physical distancing from an exposed person significantly reduces risk of transmission and that N95 masks, particularly for health care workers, are more effective than other face coverings.
The meta-analysis, published online in The Lancet (2020 Jun 2; doi.org/10.1016/ S0140-6736(20)31142-9) also marks the first evaluation of these protective measures in both community and health care settings for COVID-19, the study authors stated.
“The risk for infection is highly dependent on distance to the individual infected and the type of face mask and eye protection worn,” wrote Derek K. Chu, MD, PhD, of McMaster University in Hamilton, Ont., and colleagues, reporting on behalf of the COVID-19 Systematic Urgent Review Group Effort, or SURGE.
The study reported that physical distancing of at least 1 meter, or about a yard, “seems to be strongly associated with a large protective effect,” but that distancing of 2 meters or about 6 feet could be more effective.
The study involved a systematic review of 172 observational studies across six continents that evaluated distance measures, face masks, and eye protection to prevent transmission between patients with confirmed or probable COVID-19, other severe acute respiratory syndrome (SARS) disease, and Middle East respiratory syndrome (MERS), and their family members, caregivers and health care workers up to May 3, 2020. The meta-analysis involved pooled estimates from 44 comparative studies with 25,697 participants, including seven studies of COVID-19 with 6,674 participants. None of the studies included in the meta-analysis were randomized clinical trials.
A subanalysis of 29 unadjusted and 9 adjusted studies found that the absolute risk of infection in proximity to an exposed individual was 12.8% at 1 m and 2.6% at 2 m. The risk remained constant even when the six COVID-19 studies in this subanalysis were isolated and regardless of being in a health care or non–health-care setting. Each meter of increased distance resulted in a doubling in the change in relative risk (P = .041).
The study also identified what Dr. Chu and colleagues characterized as a “large reduction” in infection risk with the use of both N95 or similar respirators or face masks, with an adjusted risk of infection of 3.1% with a face covering vs. a 17.4% without. The researchers also found a stronger association in health care settings vs. non–health care settings, with a relative risk of 0.3 vs. 0.56, respectively (P = .049). The protective effect of N95 or similar respirators was greater than other masks, with adjusted odds ratios of 0.04 vs. 0.33 (P = .09).
Eye protection was found to reduce the risk of infection to 5.5% vs. 16% without eye protection.
The study also identified potential barriers to social distancing and use of masks and eye protection: discomfort, resource use “linked with potentially decreased equity,” less clear communication, and a perceived lack of empathy on the part of providers toward patients.
Dr. Chu and colleagues wrote that more “high-quality” research, including randomized trials of the optimal physical distance and evaluation of different mask types in non–health care settings “is urgently needed.” They added, “Policymakers at all levels should, therefore, strive to address equity implications for groups with currently limited access to face masks and eye protection.”
The goal of this study was to “inform WHO guidance documents,” the study noted. “Governments and the public health community can use our results to give clear advice for community settings and healthcare workers on these protective measures to reduce infection risk,” said study co-leader Holger Schünemann, MD, MSc, PhD, of McMaster University.
Prof. Raina MacIntyre, MBBS, PhD, head of the biosecurity research program at the Kirby Institute at the University of New South Wales in Sydney, who authored the comment that accompanied the article, said that this study provides evidence for stronger PPE guidelines.
“The Centers for Disease Control and Prevention initially recommended N95s for health workers treating COVID-19 patients, but later downgraded this to surgical masks and even cloth masks and bandannas when there was a supply shortage,” she said. “This study shows that N95s are superior masks and should prompt a review of guidelines that recommend anything less for health workers.”
Recommending anything less than N95 masks for health workers is like sending troops into battle “unarmed or with bows and arrows against a fully armed enemy,” she said. “We are not talking about a device that costs hundreds or thousands of dollars; a N95 costs less than a dollar to produce. All that is needed to address the supply shortage is political will.”
While the study has some shortcomings – namely that it didn’t provide a breakdown of positive tests among COVID-19 participants – it does provide important insight for physicians, Sachin Gupta, MD, a pulmonary and critical care specialist in San Francisco, said in an interview. “The strength of a meta-analysis is that you’re able to get a composite idea; that’s one up side to this,” he said. “They’re confirming what we knew: that distance matters; that more protective masks reduce risk of infection; and that eye protection has an important role.”
Dr. Chu and colleagues have no relevant financial relationships to disclose. One member of SURGE is participating in a clinical trial comparing medical masks and N95 respirators. The World Health Organization provided partial funding for the study.
SOURCE: Chu DK et al. Lancet. 2020 Jun 2; doi.org/10.1016/ S0140-6736(20)31142-9 .
FROM THE LANCET
Key clinical point: Meta-analysis confirms protective measures reduce risk of spread of COVID-19.
Major finding: Adjusted risk of infection was 3.1% with a face covering vs. 17.4% without.
Study details: Systematic review and meta-analysis of 172 observational studies with 25,697 participants assessing measures to prevent spread of respiratory disease up to May 3, 2020.
Disclosures: Dr. Chu and colleagues have no relevant financial relationships to disclose. One member of SURGE is participating in a clinical trial comparing medical masks and N95 respirators. The study was in part funded by the World Health Organization.
Source: Chu DK et al. Lancet. 2020 Jun 1. doi. org/10.1016/ S0140-6736(20)31142-9.