User login
Richard Franki is the associate editor who writes and creates graphs. He started with the company in 1987, when it was known as the International Medical News Group. In his years as a journalist, Richard has worked for Cap Cities/ABC, Disney, Harcourt, Elsevier, Quadrant, Frontline, and Internet Brands. In the 1990s, he was a contributor to the ill-fated Indications column, predecessor of Livin' on the MDedge.
With midterm elections near, PhRMA continues to spend
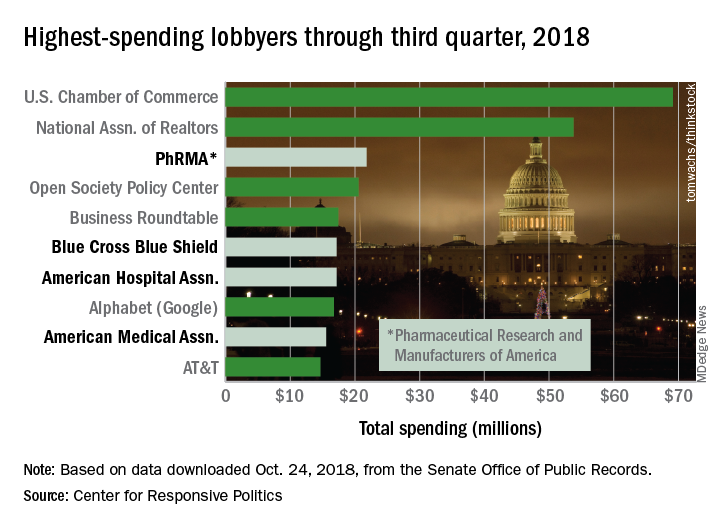
PhRMA’s $21.8 million worth of lobbying through September put it ahead of Blue Cross Blue Shield’s $17.2 million. PhRMA remains on pace to exceed its previous spending high of $27.2 million in 2009, and the health sector as a whole, with a lobbying bill of $421.5 million for three-quarters of 2018, is just slightly ahead of last year’s record of $561.3 million, the center reported on OpenSecrets.org.
PhRMA is third overall in lobbying spending so far this year, behind the U.S. Chamber of Commerce ($69.1 million) and the National Association of Realtors ($53.8 million). Blue Cross Blue Shield is sixth overall, with the American Hospital Association ($17.2 million, seventh) and the American Medical Association ($15.5 million, ninth) also in the top 10, according to the center’s analysis of data from the Senate Office of Public Records.
The pharmaceutical/health product industry leads health-sector lobbying with $216.1 million in spending so far in 2018, followed by hospitals/nursing homes at $73.6 million, health professionals at $68.6 million, and health services/HMOs at $57.5 million.
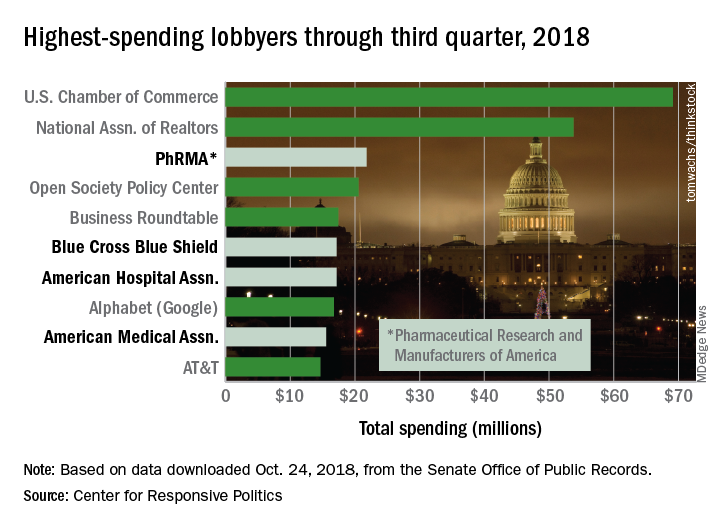
PhRMA’s $21.8 million worth of lobbying through September put it ahead of Blue Cross Blue Shield’s $17.2 million. PhRMA remains on pace to exceed its previous spending high of $27.2 million in 2009, and the health sector as a whole, with a lobbying bill of $421.5 million for three-quarters of 2018, is just slightly ahead of last year’s record of $561.3 million, the center reported on OpenSecrets.org.
PhRMA is third overall in lobbying spending so far this year, behind the U.S. Chamber of Commerce ($69.1 million) and the National Association of Realtors ($53.8 million). Blue Cross Blue Shield is sixth overall, with the American Hospital Association ($17.2 million, seventh) and the American Medical Association ($15.5 million, ninth) also in the top 10, according to the center’s analysis of data from the Senate Office of Public Records.
The pharmaceutical/health product industry leads health-sector lobbying with $216.1 million in spending so far in 2018, followed by hospitals/nursing homes at $73.6 million, health professionals at $68.6 million, and health services/HMOs at $57.5 million.
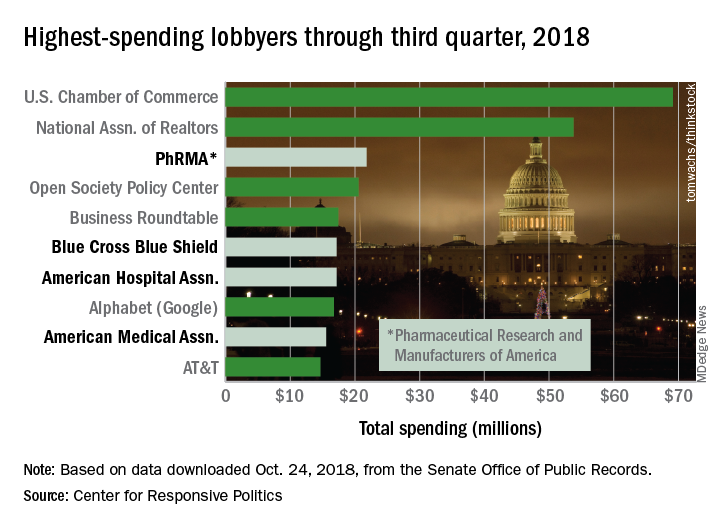
PhRMA’s $21.8 million worth of lobbying through September put it ahead of Blue Cross Blue Shield’s $17.2 million. PhRMA remains on pace to exceed its previous spending high of $27.2 million in 2009, and the health sector as a whole, with a lobbying bill of $421.5 million for three-quarters of 2018, is just slightly ahead of last year’s record of $561.3 million, the center reported on OpenSecrets.org.
PhRMA is third overall in lobbying spending so far this year, behind the U.S. Chamber of Commerce ($69.1 million) and the National Association of Realtors ($53.8 million). Blue Cross Blue Shield is sixth overall, with the American Hospital Association ($17.2 million, seventh) and the American Medical Association ($15.5 million, ninth) also in the top 10, according to the center’s analysis of data from the Senate Office of Public Records.
The pharmaceutical/health product industry leads health-sector lobbying with $216.1 million in spending so far in 2018, followed by hospitals/nursing homes at $73.6 million, health professionals at $68.6 million, and health services/HMOs at $57.5 million.
Kids and guns: Injury costs rose as incidence fell
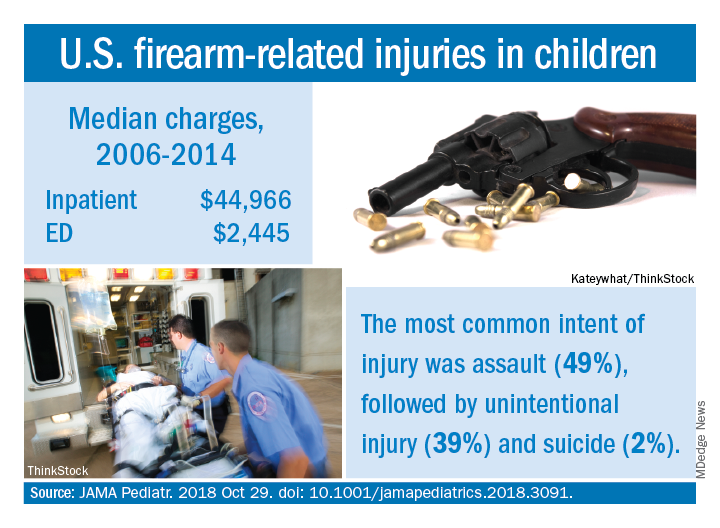
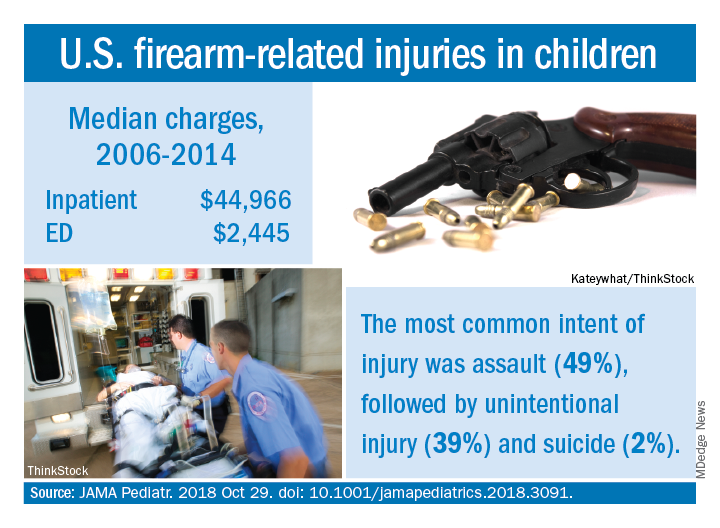
Hospital costs for children with firearm-related injuries rose from 2006 to 2014, while the incidence of emergency department visits declined over the same period, according to the first national study of such visits in children.
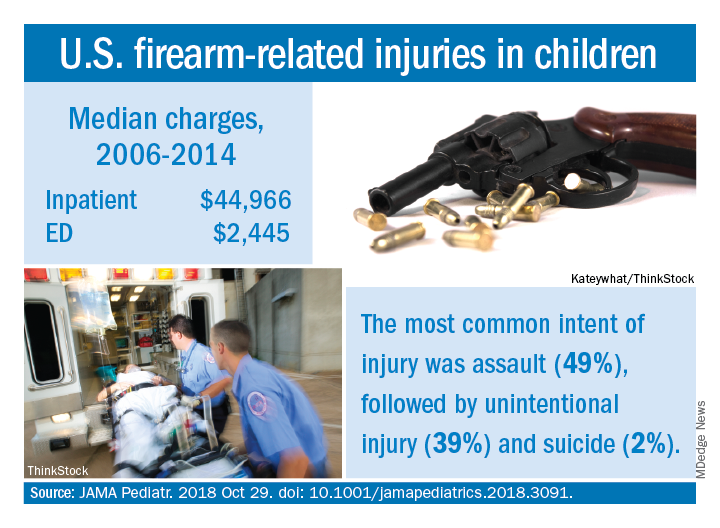
Median charges were $2,445 for an ED visit and $44,966 for inpatient management of individuals under 18 years of age for the entire study period, with both increasing over time and all data adjusted to 2018 dollars. The median charge for an ED visit rose from over $2,100 in 2006 to under $2,900 in 2014, while the inpatient median increased from approximately $43,000 to about $59,000. Total charges for firearm-related injuries in children were $2.5 billion during 2006-2014, with a mean of $270 million a year, Faiz Gani, MBBS, and Joseph K. Canner, MHS, said in JAMA Pediatrics.
The overall incidence of ED visits was 11.3/100,000 children under 18 years of age for the study period, with a steady decline seen from 2006, when incidence was about 15 visits/100,000, to 10/100,000 in 2014. The rate had dropped to about 7.5 visits/100,000 in 2013 before increasing in 2014, Dr. Gani and Mr. Canner of Johns Hopkins University, Baltimore, said based on data for 75,086 visits from the Nationwide Emergency Medicine Sample.
A trend observed throughout the course of the study was the higher incidence of ED visits among males, which was consistently more than five times higher than that of females. The highest incidence by age group was 85.9/100,000 for males aged 15-17 years. The most common intent of injury was assault at 49%, with unintentional injury next at 39% and suicide at 2%, the investigators reported.
This “first and largest nationally representative study” demonstrates the “substantial clinical and financial burden associated with firearm-related injuries among pediatric patients. Moving forward, additional resources and funds should be allocated to the study of firearm-related injuries. Only through further understanding of the social, political, and health-related risk factors for these injuries can we develop and implement effective policies to address this public health concern, wrote Dr. Gani and Mr. Canner, who reported no conflicts of interest.
SOURCE: JAMA Pediatr. 2018 Oct 29. doi: 10.1001/jamapediatrics.2018.3091.
Hospital costs for children with firearm-related injuries rose from 2006 to 2014, while the incidence of emergency department visits declined over the same period, according to the first national study of such visits in children.
Median charges were $2,445 for an ED visit and $44,966 for inpatient management of individuals under 18 years of age for the entire study period, with both increasing over time and all data adjusted to 2018 dollars. The median charge for an ED visit rose from over $2,100 in 2006 to under $2,900 in 2014, while the inpatient median increased from approximately $43,000 to about $59,000. Total charges for firearm-related injuries in children were $2.5 billion during 2006-2014, with a mean of $270 million a year, Faiz Gani, MBBS, and Joseph K. Canner, MHS, said in JAMA Pediatrics.
The overall incidence of ED visits was 11.3/100,000 children under 18 years of age for the study period, with a steady decline seen from 2006, when incidence was about 15 visits/100,000, to 10/100,000 in 2014. The rate had dropped to about 7.5 visits/100,000 in 2013 before increasing in 2014, Dr. Gani and Mr. Canner of Johns Hopkins University, Baltimore, said based on data for 75,086 visits from the Nationwide Emergency Medicine Sample.
A trend observed throughout the course of the study was the higher incidence of ED visits among males, which was consistently more than five times higher than that of females. The highest incidence by age group was 85.9/100,000 for males aged 15-17 years. The most common intent of injury was assault at 49%, with unintentional injury next at 39% and suicide at 2%, the investigators reported.
This “first and largest nationally representative study” demonstrates the “substantial clinical and financial burden associated with firearm-related injuries among pediatric patients. Moving forward, additional resources and funds should be allocated to the study of firearm-related injuries. Only through further understanding of the social, political, and health-related risk factors for these injuries can we develop and implement effective policies to address this public health concern, wrote Dr. Gani and Mr. Canner, who reported no conflicts of interest.
SOURCE: JAMA Pediatr. 2018 Oct 29. doi: 10.1001/jamapediatrics.2018.3091.
Hospital costs for children with firearm-related injuries rose from 2006 to 2014, while the incidence of emergency department visits declined over the same period, according to the first national study of such visits in children.
Median charges were $2,445 for an ED visit and $44,966 for inpatient management of individuals under 18 years of age for the entire study period, with both increasing over time and all data adjusted to 2018 dollars. The median charge for an ED visit rose from over $2,100 in 2006 to under $2,900 in 2014, while the inpatient median increased from approximately $43,000 to about $59,000. Total charges for firearm-related injuries in children were $2.5 billion during 2006-2014, with a mean of $270 million a year, Faiz Gani, MBBS, and Joseph K. Canner, MHS, said in JAMA Pediatrics.
The overall incidence of ED visits was 11.3/100,000 children under 18 years of age for the study period, with a steady decline seen from 2006, when incidence was about 15 visits/100,000, to 10/100,000 in 2014. The rate had dropped to about 7.5 visits/100,000 in 2013 before increasing in 2014, Dr. Gani and Mr. Canner of Johns Hopkins University, Baltimore, said based on data for 75,086 visits from the Nationwide Emergency Medicine Sample.
A trend observed throughout the course of the study was the higher incidence of ED visits among males, which was consistently more than five times higher than that of females. The highest incidence by age group was 85.9/100,000 for males aged 15-17 years. The most common intent of injury was assault at 49%, with unintentional injury next at 39% and suicide at 2%, the investigators reported.
This “first and largest nationally representative study” demonstrates the “substantial clinical and financial burden associated with firearm-related injuries among pediatric patients. Moving forward, additional resources and funds should be allocated to the study of firearm-related injuries. Only through further understanding of the social, political, and health-related risk factors for these injuries can we develop and implement effective policies to address this public health concern, wrote Dr. Gani and Mr. Canner, who reported no conflicts of interest.
SOURCE: JAMA Pediatr. 2018 Oct 29. doi: 10.1001/jamapediatrics.2018.3091.
FROM JAMA PEDIATRICS
‘Woeful lack of awareness’ leads to delayed diagnoses for women with ovarian cancer
Lack of knowledge about ovarian cancer prevents many women from seeking medical attention, which delays diagnosis and treatment and may prove increasingly dangerous as incidence rises by an expected 55% over the next 2 decades, according to the World Ovarian Cancer Coalition.
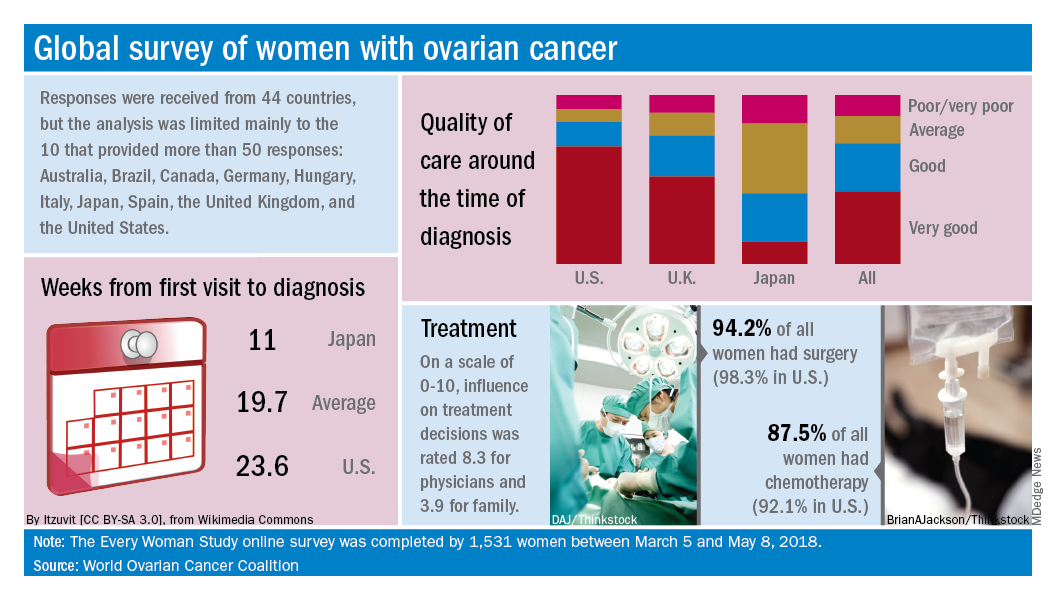
Data from the coalition’s 2018 survey of women with ovarian cancer show that 18% had never heard of the disease before their diagnosis and 51% had heard of it but did not know anything about it. The Every Women Study survey, completed by 1,531 women in 44 countries, also reveals that nine out of ten had experienced symptoms prior to diagnosis but fewer than half saw a physician within a month of noticing those symptoms, the coalition said.
“This study, for the first time, provides powerful evidence of the challenges faced by women diagnosed with ovarian cancer across the world and sets an agenda for global change. We were especially shocked by the widespread, woeful lack of awareness of ovarian cancer,” Annwen Jones, coalition vice-chair and cochair of the study, said in a separate written statement.
Results varied considerably by country, and only 10 countries provided enough responses to allow comparisons: Australia (120), Brazil (52), Canada (167), Germany (141), Hungary (58), Italy (92), Japan (250), Spain (70), the United Kingdom (176), and the United States (248).
Among those comparisons, women in Germany (5.5 weeks) and Spain (7.9 weeks) were the first to visit a physician after first experiencing symptoms, while those in Italy (15.2 weeks) and the United States (12.9 weeks) were last. The United States was also longest in time from first visit to diagnosis (23.6 weeks), and Japan was the shortest (11 weeks). Despite that world-longest time to diagnosis, however, over 69% of U.S. women said that their care around the time of diagnosis was very good, which was higher than any other country, the coalition reported.
Surgery statistics were closer among countries, with an average of 94% of all women undergoing surgery to treat their ovarian cancer. The United States, at 98.3%, was second to Spain’s 98.5%, and Hungary was the largest outlier on the low side at 59%. Over 87% of all women reported having chemotherapy to treat or control their cancer, and 9.8% of women said that they had received intraperitoneal chemotherapy. In the United States, 22.5% of women received intraperitoneal therapy, compared with 0.7% for the United Kingdom.
“No one country has all the answers, and whilst there is still an urgent need for a step-change in the level of investment in research for better treatments and tools for early diagnosis, there are significant opportunities to improve survival and quality of life for women in the immediate and short term to make a series of marginal gains if these variations are addressed by individual countries,” the coalition said in the report.
Lack of knowledge about ovarian cancer prevents many women from seeking medical attention, which delays diagnosis and treatment and may prove increasingly dangerous as incidence rises by an expected 55% over the next 2 decades, according to the World Ovarian Cancer Coalition.
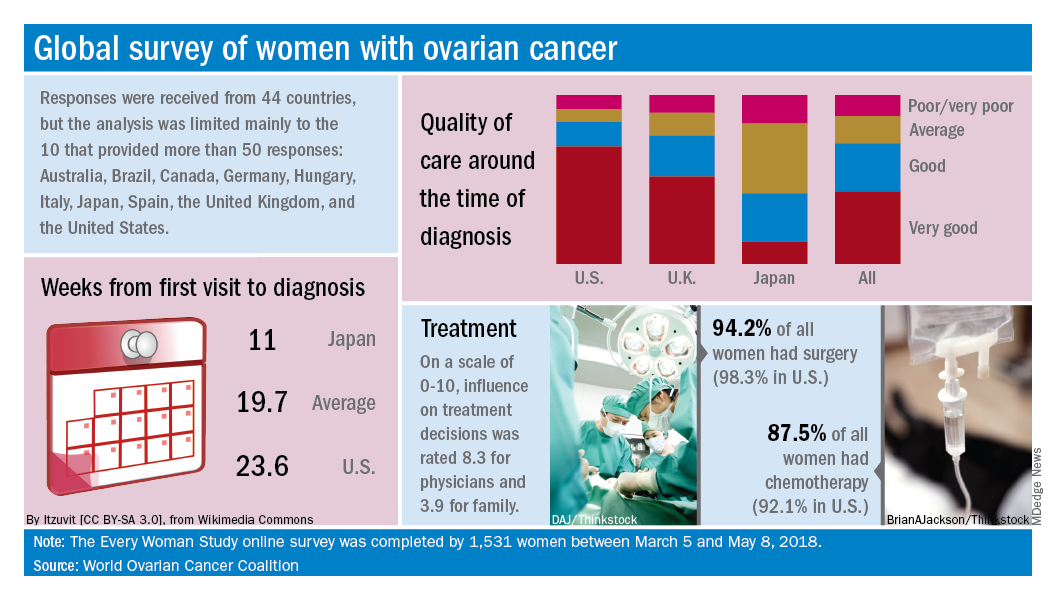
Data from the coalition’s 2018 survey of women with ovarian cancer show that 18% had never heard of the disease before their diagnosis and 51% had heard of it but did not know anything about it. The Every Women Study survey, completed by 1,531 women in 44 countries, also reveals that nine out of ten had experienced symptoms prior to diagnosis but fewer than half saw a physician within a month of noticing those symptoms, the coalition said.
“This study, for the first time, provides powerful evidence of the challenges faced by women diagnosed with ovarian cancer across the world and sets an agenda for global change. We were especially shocked by the widespread, woeful lack of awareness of ovarian cancer,” Annwen Jones, coalition vice-chair and cochair of the study, said in a separate written statement.
Results varied considerably by country, and only 10 countries provided enough responses to allow comparisons: Australia (120), Brazil (52), Canada (167), Germany (141), Hungary (58), Italy (92), Japan (250), Spain (70), the United Kingdom (176), and the United States (248).
Among those comparisons, women in Germany (5.5 weeks) and Spain (7.9 weeks) were the first to visit a physician after first experiencing symptoms, while those in Italy (15.2 weeks) and the United States (12.9 weeks) were last. The United States was also longest in time from first visit to diagnosis (23.6 weeks), and Japan was the shortest (11 weeks). Despite that world-longest time to diagnosis, however, over 69% of U.S. women said that their care around the time of diagnosis was very good, which was higher than any other country, the coalition reported.
Surgery statistics were closer among countries, with an average of 94% of all women undergoing surgery to treat their ovarian cancer. The United States, at 98.3%, was second to Spain’s 98.5%, and Hungary was the largest outlier on the low side at 59%. Over 87% of all women reported having chemotherapy to treat or control their cancer, and 9.8% of women said that they had received intraperitoneal chemotherapy. In the United States, 22.5% of women received intraperitoneal therapy, compared with 0.7% for the United Kingdom.
“No one country has all the answers, and whilst there is still an urgent need for a step-change in the level of investment in research for better treatments and tools for early diagnosis, there are significant opportunities to improve survival and quality of life for women in the immediate and short term to make a series of marginal gains if these variations are addressed by individual countries,” the coalition said in the report.
Lack of knowledge about ovarian cancer prevents many women from seeking medical attention, which delays diagnosis and treatment and may prove increasingly dangerous as incidence rises by an expected 55% over the next 2 decades, according to the World Ovarian Cancer Coalition.
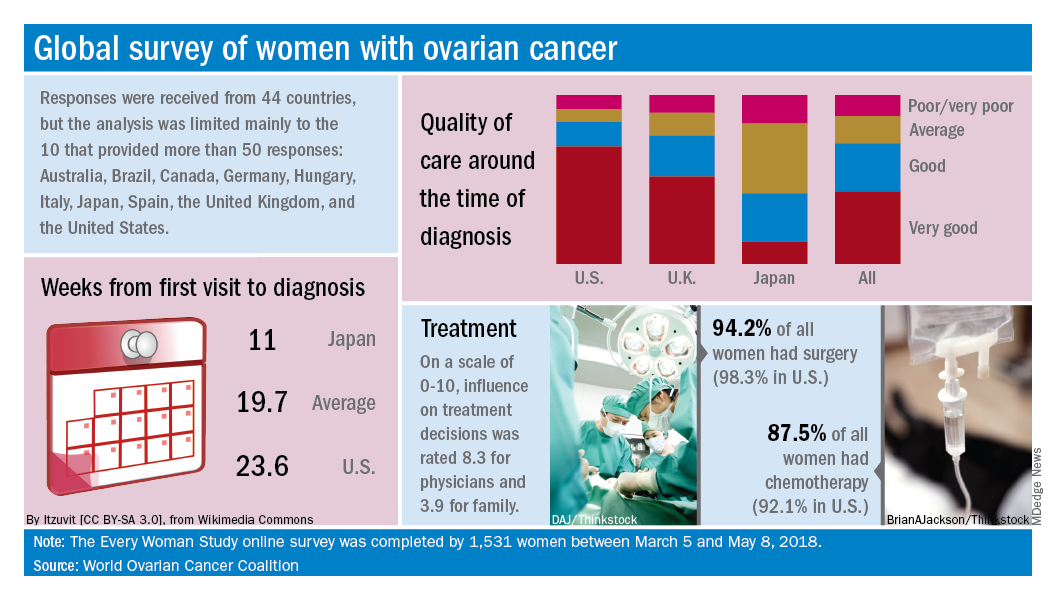
Data from the coalition’s 2018 survey of women with ovarian cancer show that 18% had never heard of the disease before their diagnosis and 51% had heard of it but did not know anything about it. The Every Women Study survey, completed by 1,531 women in 44 countries, also reveals that nine out of ten had experienced symptoms prior to diagnosis but fewer than half saw a physician within a month of noticing those symptoms, the coalition said.
“This study, for the first time, provides powerful evidence of the challenges faced by women diagnosed with ovarian cancer across the world and sets an agenda for global change. We were especially shocked by the widespread, woeful lack of awareness of ovarian cancer,” Annwen Jones, coalition vice-chair and cochair of the study, said in a separate written statement.
Results varied considerably by country, and only 10 countries provided enough responses to allow comparisons: Australia (120), Brazil (52), Canada (167), Germany (141), Hungary (58), Italy (92), Japan (250), Spain (70), the United Kingdom (176), and the United States (248).
Among those comparisons, women in Germany (5.5 weeks) and Spain (7.9 weeks) were the first to visit a physician after first experiencing symptoms, while those in Italy (15.2 weeks) and the United States (12.9 weeks) were last. The United States was also longest in time from first visit to diagnosis (23.6 weeks), and Japan was the shortest (11 weeks). Despite that world-longest time to diagnosis, however, over 69% of U.S. women said that their care around the time of diagnosis was very good, which was higher than any other country, the coalition reported.
Surgery statistics were closer among countries, with an average of 94% of all women undergoing surgery to treat their ovarian cancer. The United States, at 98.3%, was second to Spain’s 98.5%, and Hungary was the largest outlier on the low side at 59%. Over 87% of all women reported having chemotherapy to treat or control their cancer, and 9.8% of women said that they had received intraperitoneal chemotherapy. In the United States, 22.5% of women received intraperitoneal therapy, compared with 0.7% for the United Kingdom.
“No one country has all the answers, and whilst there is still an urgent need for a step-change in the level of investment in research for better treatments and tools for early diagnosis, there are significant opportunities to improve survival and quality of life for women in the immediate and short term to make a series of marginal gains if these variations are addressed by individual countries,” the coalition said in the report.
Drug overdose deaths down since late 2017
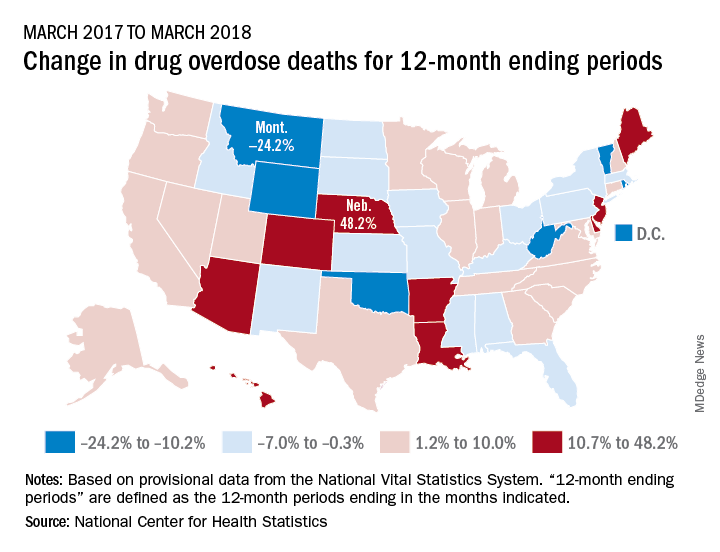
Longer-term data, however, show an increase over the year from March 2017 to March 2018, as the short-term decrease was not enough to overcome the previous year’s increase. The provisional 12-month ending count – deaths during the 12-month period ending in the month indicated – went from 66,859 in March 2017 to 68,690 in March 2018, an increase of 2.7%, the NCHS reported.
That year-long increase was not spread evenly among the states. Nebraska’s 12-month ending count jumped over 48% from March 2017 to March 2018, more than twice as much as second-place Hawaii’s 20.9%. Montana had the largest drop over that year, –24.2%, with Wyoming next at –20.7% and the District of Columbia third at –14.8%, data from the National Vital Statistics System show.
“Provisional drug overdose death data are often incomplete,” the NCHS noted, “and the degree of completeness varies by jurisdiction and 12-month ending period. Consequently, the numbers of drug overdose deaths are underestimated, based on provisional data relative to final data and are subject to random variation.”
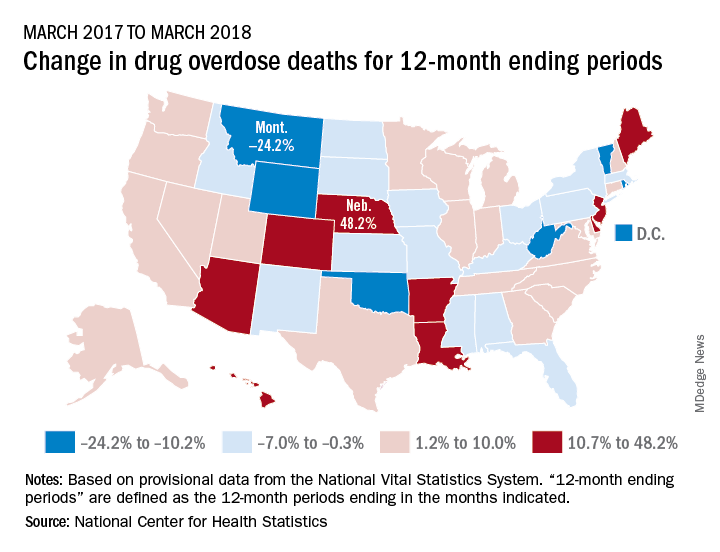
Longer-term data, however, show an increase over the year from March 2017 to March 2018, as the short-term decrease was not enough to overcome the previous year’s increase. The provisional 12-month ending count – deaths during the 12-month period ending in the month indicated – went from 66,859 in March 2017 to 68,690 in March 2018, an increase of 2.7%, the NCHS reported.
That year-long increase was not spread evenly among the states. Nebraska’s 12-month ending count jumped over 48% from March 2017 to March 2018, more than twice as much as second-place Hawaii’s 20.9%. Montana had the largest drop over that year, –24.2%, with Wyoming next at –20.7% and the District of Columbia third at –14.8%, data from the National Vital Statistics System show.
“Provisional drug overdose death data are often incomplete,” the NCHS noted, “and the degree of completeness varies by jurisdiction and 12-month ending period. Consequently, the numbers of drug overdose deaths are underestimated, based on provisional data relative to final data and are subject to random variation.”
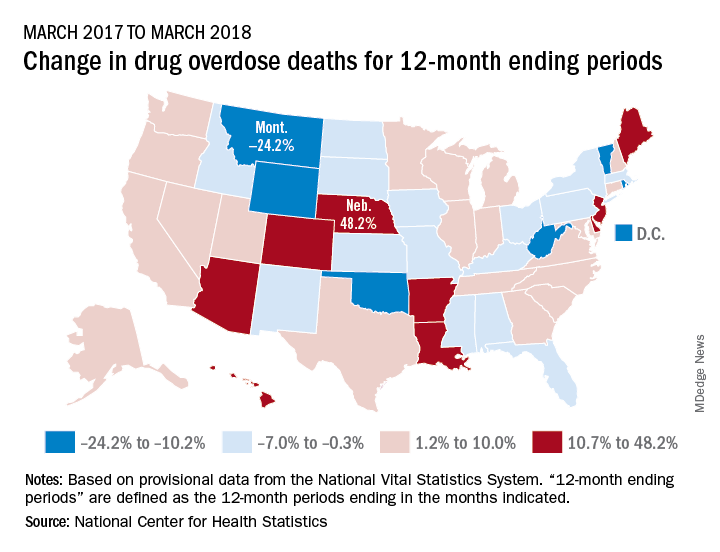
Longer-term data, however, show an increase over the year from March 2017 to March 2018, as the short-term decrease was not enough to overcome the previous year’s increase. The provisional 12-month ending count – deaths during the 12-month period ending in the month indicated – went from 66,859 in March 2017 to 68,690 in March 2018, an increase of 2.7%, the NCHS reported.
That year-long increase was not spread evenly among the states. Nebraska’s 12-month ending count jumped over 48% from March 2017 to March 2018, more than twice as much as second-place Hawaii’s 20.9%. Montana had the largest drop over that year, –24.2%, with Wyoming next at –20.7% and the District of Columbia third at –14.8%, data from the National Vital Statistics System show.
“Provisional drug overdose death data are often incomplete,” the NCHS noted, “and the degree of completeness varies by jurisdiction and 12-month ending period. Consequently, the numbers of drug overdose deaths are underestimated, based on provisional data relative to final data and are subject to random variation.”
Robot sperm, CRISPR-Cas9 parenting, eavesdropping on brains
Life (and mice) find a way
Apparently we have learned nothing from “Jurassic Park.” This time, though, we might get a world overrun by ... mice? Researchers in China have utilized the complex science of gene editing to help same-sex mice couples bear offspring. This is the first time both female-female and male-male pairs have produced pups (previously, only the female pairs were able to carry to full term) using CRISPR-Cas9. The experiment also served as a study in the relative uselessness of males: All the pups born of male pairs died shortly after birth. Researchers are hopeful to move on to bigger mammals including monkeys, which could eventually turn this “Jurassic Park” adventure into a full-on “Planet of the Apes” nightmare. Best of luck to them!
Hold me closer, tiny robot
Gentleman, we’ve all been put on notice. A team from the University of Exeter in England has taken the next step toward redundancy for the male of the species: robot sperm. Now that we’ve got your attention, take a deep breath and relax. It’s not that bad. The idea is for the robot sperm, or “torque-driven ferromagnetic swimmers,” to be used to deliver drugs, not DNA, the investigators explained. Each millimeter-long device consists “of a magnetic head and flexible tail that allows them to ‘swim’ to a specific location when activated by a magnetic field,” they said. “Developing this technology could radically change the way we do medicine. The swimmers could one day be used to direct drugs to the right areas of the body by swimming through blood vessels,” senior investigator Feodor Ogrin said. So, it looks like it’s going to be okay for men after all. Still, we have to wonder, how long will it be before Siri and Alexa try to make a withdrawal from the robot sperm bank?
Eavesdropping on the brain
Does this count as mind reading? A team of scientists and clinicians from the University of Cambridge has created a new method of testing brain function after tumor removal. The current method of running through cognitive tests while a patient is awake and the brain is exposed is painless (albeit objectively horrifying) but can be risky, and the current cognitive tests can be limited. This new approach is much safer – everyone wears protective gloves and gently massages the brain while singing “Kumbaya” ... Just kidding. Clinicians actually use MRI to examine the brain before surgery and determine how different regions of that ball of gray matter communicate with each other. A 3D-printed model of the patient’s brain is also provided, both as a handy 3D map and a fun souvenir! Because that’s what the world of medicine is missing: a gift shop.
Cannabinoids. Period.
When other medical news columns go high, we go low. How anatomically low? “Cannabis-infused vaginal suppositories.” Those of you about to be made reproductively moot by robot sperm and CRISPR-Cas9 should stop with the junior-high smirking. Because our more mature readers may be interested in an upcoming study. Foria Wellness is ready to put its cannabinoid-infused menstrual pain relief product, Foria Relief, to the test this fall in an observational study of 400 women. The suppositories deliver 60 mg of tetrahydrocannabinol and 10 mg of cannabidiol to their target. The company claims it’s a natural, side-effect–free analgesic alternative to hormonal birth control, ibuprofen, and opioids. And unlike unsuppositoried cannabinoid pain products that waft from place to place around a user’s system, Foria Relief promises sustained focus on its specific task. A quality that smirking junior-high types often lack.
Life (and mice) find a way
Apparently we have learned nothing from “Jurassic Park.” This time, though, we might get a world overrun by ... mice? Researchers in China have utilized the complex science of gene editing to help same-sex mice couples bear offspring. This is the first time both female-female and male-male pairs have produced pups (previously, only the female pairs were able to carry to full term) using CRISPR-Cas9. The experiment also served as a study in the relative uselessness of males: All the pups born of male pairs died shortly after birth. Researchers are hopeful to move on to bigger mammals including monkeys, which could eventually turn this “Jurassic Park” adventure into a full-on “Planet of the Apes” nightmare. Best of luck to them!
Hold me closer, tiny robot
Gentleman, we’ve all been put on notice. A team from the University of Exeter in England has taken the next step toward redundancy for the male of the species: robot sperm. Now that we’ve got your attention, take a deep breath and relax. It’s not that bad. The idea is for the robot sperm, or “torque-driven ferromagnetic swimmers,” to be used to deliver drugs, not DNA, the investigators explained. Each millimeter-long device consists “of a magnetic head and flexible tail that allows them to ‘swim’ to a specific location when activated by a magnetic field,” they said. “Developing this technology could radically change the way we do medicine. The swimmers could one day be used to direct drugs to the right areas of the body by swimming through blood vessels,” senior investigator Feodor Ogrin said. So, it looks like it’s going to be okay for men after all. Still, we have to wonder, how long will it be before Siri and Alexa try to make a withdrawal from the robot sperm bank?
Eavesdropping on the brain
Does this count as mind reading? A team of scientists and clinicians from the University of Cambridge has created a new method of testing brain function after tumor removal. The current method of running through cognitive tests while a patient is awake and the brain is exposed is painless (albeit objectively horrifying) but can be risky, and the current cognitive tests can be limited. This new approach is much safer – everyone wears protective gloves and gently massages the brain while singing “Kumbaya” ... Just kidding. Clinicians actually use MRI to examine the brain before surgery and determine how different regions of that ball of gray matter communicate with each other. A 3D-printed model of the patient’s brain is also provided, both as a handy 3D map and a fun souvenir! Because that’s what the world of medicine is missing: a gift shop.
Cannabinoids. Period.
When other medical news columns go high, we go low. How anatomically low? “Cannabis-infused vaginal suppositories.” Those of you about to be made reproductively moot by robot sperm and CRISPR-Cas9 should stop with the junior-high smirking. Because our more mature readers may be interested in an upcoming study. Foria Wellness is ready to put its cannabinoid-infused menstrual pain relief product, Foria Relief, to the test this fall in an observational study of 400 women. The suppositories deliver 60 mg of tetrahydrocannabinol and 10 mg of cannabidiol to their target. The company claims it’s a natural, side-effect–free analgesic alternative to hormonal birth control, ibuprofen, and opioids. And unlike unsuppositoried cannabinoid pain products that waft from place to place around a user’s system, Foria Relief promises sustained focus on its specific task. A quality that smirking junior-high types often lack.
Life (and mice) find a way
Apparently we have learned nothing from “Jurassic Park.” This time, though, we might get a world overrun by ... mice? Researchers in China have utilized the complex science of gene editing to help same-sex mice couples bear offspring. This is the first time both female-female and male-male pairs have produced pups (previously, only the female pairs were able to carry to full term) using CRISPR-Cas9. The experiment also served as a study in the relative uselessness of males: All the pups born of male pairs died shortly after birth. Researchers are hopeful to move on to bigger mammals including monkeys, which could eventually turn this “Jurassic Park” adventure into a full-on “Planet of the Apes” nightmare. Best of luck to them!
Hold me closer, tiny robot
Gentleman, we’ve all been put on notice. A team from the University of Exeter in England has taken the next step toward redundancy for the male of the species: robot sperm. Now that we’ve got your attention, take a deep breath and relax. It’s not that bad. The idea is for the robot sperm, or “torque-driven ferromagnetic swimmers,” to be used to deliver drugs, not DNA, the investigators explained. Each millimeter-long device consists “of a magnetic head and flexible tail that allows them to ‘swim’ to a specific location when activated by a magnetic field,” they said. “Developing this technology could radically change the way we do medicine. The swimmers could one day be used to direct drugs to the right areas of the body by swimming through blood vessels,” senior investigator Feodor Ogrin said. So, it looks like it’s going to be okay for men after all. Still, we have to wonder, how long will it be before Siri and Alexa try to make a withdrawal from the robot sperm bank?
Eavesdropping on the brain
Does this count as mind reading? A team of scientists and clinicians from the University of Cambridge has created a new method of testing brain function after tumor removal. The current method of running through cognitive tests while a patient is awake and the brain is exposed is painless (albeit objectively horrifying) but can be risky, and the current cognitive tests can be limited. This new approach is much safer – everyone wears protective gloves and gently massages the brain while singing “Kumbaya” ... Just kidding. Clinicians actually use MRI to examine the brain before surgery and determine how different regions of that ball of gray matter communicate with each other. A 3D-printed model of the patient’s brain is also provided, both as a handy 3D map and a fun souvenir! Because that’s what the world of medicine is missing: a gift shop.
Cannabinoids. Period.
When other medical news columns go high, we go low. How anatomically low? “Cannabis-infused vaginal suppositories.” Those of you about to be made reproductively moot by robot sperm and CRISPR-Cas9 should stop with the junior-high smirking. Because our more mature readers may be interested in an upcoming study. Foria Wellness is ready to put its cannabinoid-infused menstrual pain relief product, Foria Relief, to the test this fall in an observational study of 400 women. The suppositories deliver 60 mg of tetrahydrocannabinol and 10 mg of cannabidiol to their target. The company claims it’s a natural, side-effect–free analgesic alternative to hormonal birth control, ibuprofen, and opioids. And unlike unsuppositoried cannabinoid pain products that waft from place to place around a user’s system, Foria Relief promises sustained focus on its specific task. A quality that smirking junior-high types often lack.
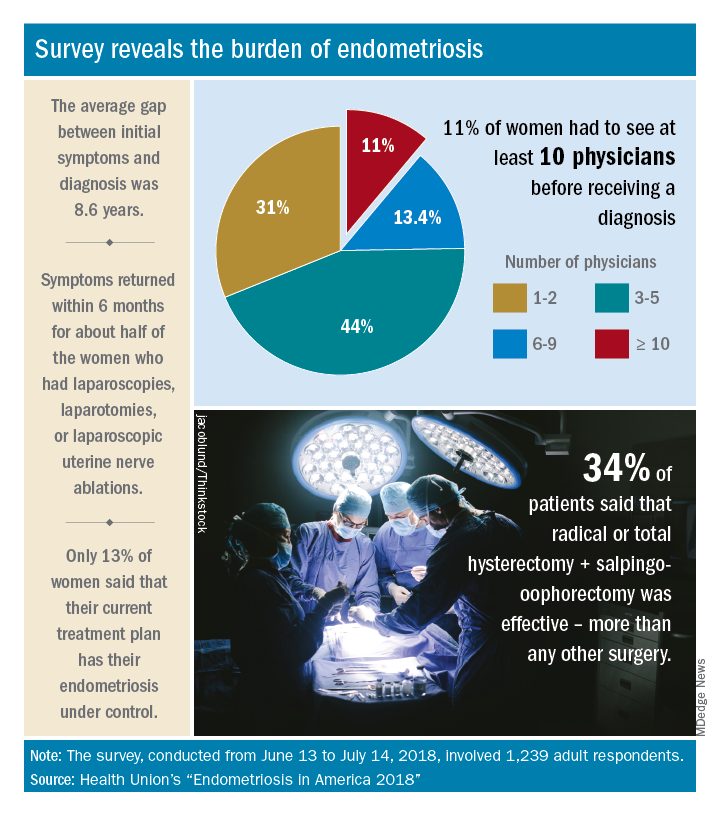
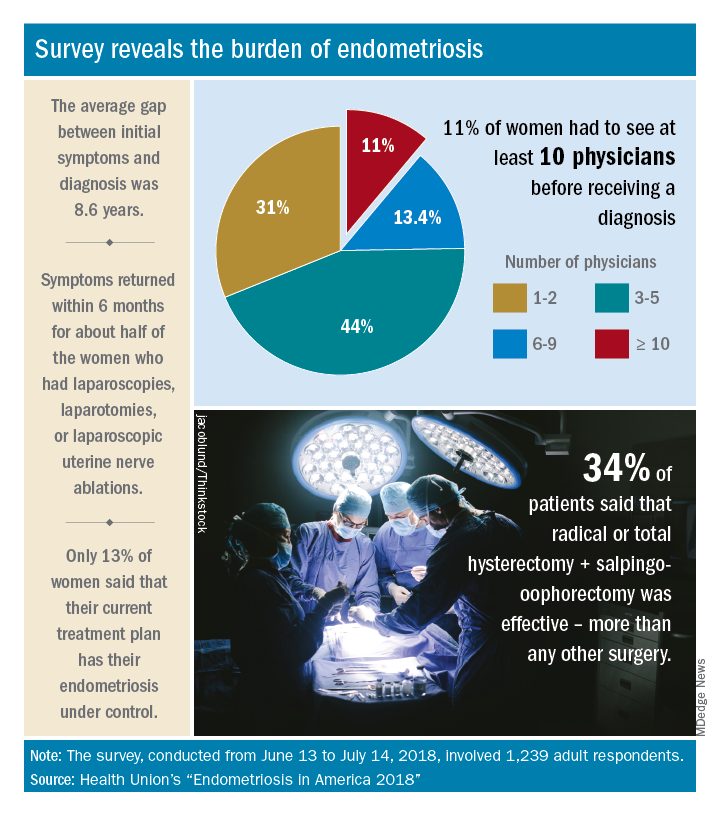
Diagnosis is an ongoing concern in endometriosis
according to a new survey by Health Union, a family of online health communities.
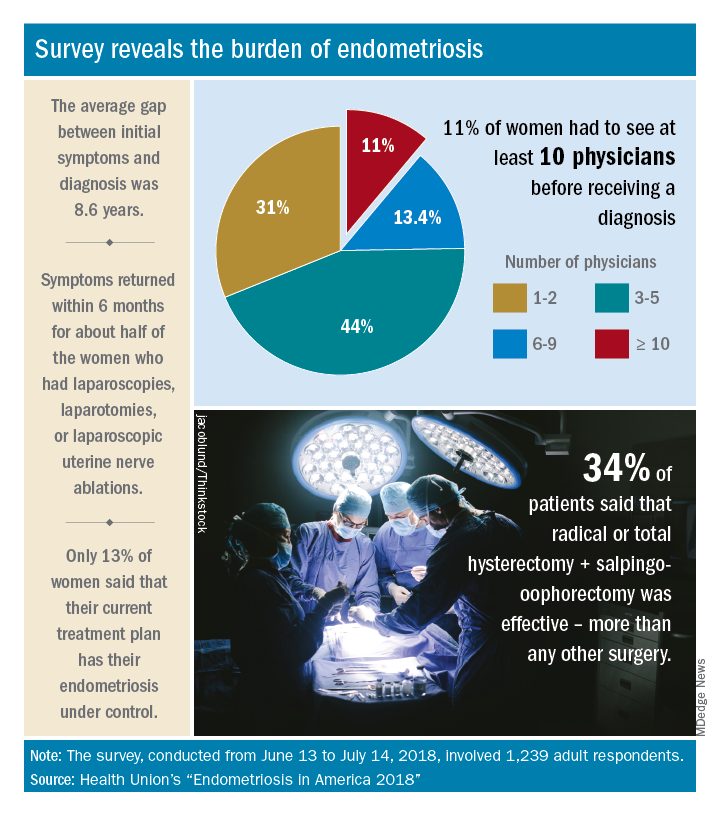
Advances in support and understanding have been made through research and dissemination of information via the Internet, but complete control of endometriosis remains elusive, as only 13% of the 1,239 women surveyed from June 13 to July 14, 2018, said that their condition was under control with their current treatment plan.
Before control, of course, comes diagnosis, and the average gap between onset of symptoms and diagnosis was 8.6 years. Such a gap “can lead to delayed treatment and a potentially negative impact on quality of life,” Health Union said in a written statement. Those years of delays often involved visits to multiple physicians: 44% of respondents saw 3-5 physicians before receiving a diagnosis and 11% had to see 10 or more physicians.
“When comparing differences between symptom onset-to-diagnosis groups, there are some significant findings that suggest a fair amount of progress has been made, for the better,” Health Union said, noting that women who received a diagnosis in less than 5 years “were significantly less likely to think their symptoms were related to their menstrual cycles than those with a longer symptoms-to-diagnosis gap.” Respondents who had a gap of less than 2 years “were more likely to seek medical care as soon as possible” and to have used hormone therapies than those with longer gaps, the group said.
The most common diagnostic tests were laparoscopy, reported by 85% of respondents, and pelvic/transvaginal ultrasound, reported by 46%. Of the women who did not have a laparoscopy, 43% were undergoing a surgical procedure for another condition when their endometriosis was discovered. Laparoscopy also was by far the most common surgery to treat endometriosis, with a 79% prevalence among respondents, compared with 16% for laparotomy and 12% for oophorectomy, Health Union reported in Endometriosis in America 2018.
Common nonsurgical tactics to improve symptoms included increased water intake (79%), use of a heating pad (75%), and increased fresh fruit (64%) or green vegetables (62%) in the diet. Three-quarters of respondents also tried alternative and complementary therapies such as vitamins, exercise, and acupuncture, the report showed.
“Living with endometriosis is much easier now than it was not even a decade ago, as the Internet and social media have definitely increased knowledge about the disease,” said Endometriosis.net (one of the Health Union online communities) patient advocate Laura Kiesel. “When I first suspected I had the disease, in the mid-90s, hardly anyone had heard about it, and those aware of it didn’t think it was very serious. All these years later, I get a lot more sympathy and support – both online and in person – and people understand how serious, painful, and life altering it could be.”
according to a new survey by Health Union, a family of online health communities.
Advances in support and understanding have been made through research and dissemination of information via the Internet, but complete control of endometriosis remains elusive, as only 13% of the 1,239 women surveyed from June 13 to July 14, 2018, said that their condition was under control with their current treatment plan.
Before control, of course, comes diagnosis, and the average gap between onset of symptoms and diagnosis was 8.6 years. Such a gap “can lead to delayed treatment and a potentially negative impact on quality of life,” Health Union said in a written statement. Those years of delays often involved visits to multiple physicians: 44% of respondents saw 3-5 physicians before receiving a diagnosis and 11% had to see 10 or more physicians.
“When comparing differences between symptom onset-to-diagnosis groups, there are some significant findings that suggest a fair amount of progress has been made, for the better,” Health Union said, noting that women who received a diagnosis in less than 5 years “were significantly less likely to think their symptoms were related to their menstrual cycles than those with a longer symptoms-to-diagnosis gap.” Respondents who had a gap of less than 2 years “were more likely to seek medical care as soon as possible” and to have used hormone therapies than those with longer gaps, the group said.
The most common diagnostic tests were laparoscopy, reported by 85% of respondents, and pelvic/transvaginal ultrasound, reported by 46%. Of the women who did not have a laparoscopy, 43% were undergoing a surgical procedure for another condition when their endometriosis was discovered. Laparoscopy also was by far the most common surgery to treat endometriosis, with a 79% prevalence among respondents, compared with 16% for laparotomy and 12% for oophorectomy, Health Union reported in Endometriosis in America 2018.
Common nonsurgical tactics to improve symptoms included increased water intake (79%), use of a heating pad (75%), and increased fresh fruit (64%) or green vegetables (62%) in the diet. Three-quarters of respondents also tried alternative and complementary therapies such as vitamins, exercise, and acupuncture, the report showed.
“Living with endometriosis is much easier now than it was not even a decade ago, as the Internet and social media have definitely increased knowledge about the disease,” said Endometriosis.net (one of the Health Union online communities) patient advocate Laura Kiesel. “When I first suspected I had the disease, in the mid-90s, hardly anyone had heard about it, and those aware of it didn’t think it was very serious. All these years later, I get a lot more sympathy and support – both online and in person – and people understand how serious, painful, and life altering it could be.”
according to a new survey by Health Union, a family of online health communities.
Advances in support and understanding have been made through research and dissemination of information via the Internet, but complete control of endometriosis remains elusive, as only 13% of the 1,239 women surveyed from June 13 to July 14, 2018, said that their condition was under control with their current treatment plan.
Before control, of course, comes diagnosis, and the average gap between onset of symptoms and diagnosis was 8.6 years. Such a gap “can lead to delayed treatment and a potentially negative impact on quality of life,” Health Union said in a written statement. Those years of delays often involved visits to multiple physicians: 44% of respondents saw 3-5 physicians before receiving a diagnosis and 11% had to see 10 or more physicians.
“When comparing differences between symptom onset-to-diagnosis groups, there are some significant findings that suggest a fair amount of progress has been made, for the better,” Health Union said, noting that women who received a diagnosis in less than 5 years “were significantly less likely to think their symptoms were related to their menstrual cycles than those with a longer symptoms-to-diagnosis gap.” Respondents who had a gap of less than 2 years “were more likely to seek medical care as soon as possible” and to have used hormone therapies than those with longer gaps, the group said.
The most common diagnostic tests were laparoscopy, reported by 85% of respondents, and pelvic/transvaginal ultrasound, reported by 46%. Of the women who did not have a laparoscopy, 43% were undergoing a surgical procedure for another condition when their endometriosis was discovered. Laparoscopy also was by far the most common surgery to treat endometriosis, with a 79% prevalence among respondents, compared with 16% for laparotomy and 12% for oophorectomy, Health Union reported in Endometriosis in America 2018.
Common nonsurgical tactics to improve symptoms included increased water intake (79%), use of a heating pad (75%), and increased fresh fruit (64%) or green vegetables (62%) in the diet. Three-quarters of respondents also tried alternative and complementary therapies such as vitamins, exercise, and acupuncture, the report showed.
“Living with endometriosis is much easier now than it was not even a decade ago, as the Internet and social media have definitely increased knowledge about the disease,” said Endometriosis.net (one of the Health Union online communities) patient advocate Laura Kiesel. “When I first suspected I had the disease, in the mid-90s, hardly anyone had heard about it, and those aware of it didn’t think it was very serious. All these years later, I get a lot more sympathy and support – both online and in person – and people understand how serious, painful, and life altering it could be.”
Snake bite detox, kidney stone coaster cure, soporific speakers
At least opioids don’t bite
Remember that song about the old lady who “swallowed” a fly? Well, what if the fly were actually a poisonous snake? And what if she didn’t really swallow it? And what if we stopped asking so many questions? A 33-year-old Indian man who was addicted to alcohol, tobacco, and opioids in the form of raw opium and “puppy husk” (we’re thinking it’s poppy husk, but the case report clearly said “puppy”) heard about something new: letting a poisonous snake bite you on the tongue.
He found some nomadic snake charmers to provide the snake (possibly a cobra, but he’s not sure), and the snake’s bite provides him with an hour of jerky body movements, blurred vision, and unresponsiveness, followed by 3-4 weeks of heightened arousal and a sense of well-being that is “more intense tha[n] the state of high experienced … with any dose of alcohol or opioids,” according to the Indian Journal of Psychological Medicine (2018;40[3]:269-71). Plus, he doesn’t use nearly as much alcohol and opium. (Yes, he has done this more than once. You’re rude to ask.)
The old lady in the song, of course, dies after “swallowing” a horse. Fortunately for this guy, there’s no such thing as a poisonous horse.
Ride out the kidney stones
Disney World, the happiest place on earth – unless you’re a kidney stone. A professor from the College of Osteopathic Medicine at Michigan State University, East Lansing, was inspired when one of his patients told him a recent trip to the Magic Kingdom had successfully dislodged a kidney stone. Armed with a silicone model of the renal system, David Wartinger, DO, spent many grueling hours atop various theme park rides. And, one can only assume, many more grueling hours exploring Cinderella’s Castle.
Dr. Wartinger discovered that the Big Thunder Mountain Railroad was more effective than Space Mountain or the Rock ‘n’ Roller Coaster at rattling around the rider and thus shaking out those kidney stones.
The brave professor’s tireless work has earned him one of 2018’s Ig Nobel prizes. We salute you.
In Russia, bear cures YOU
They do things a bit differently in Russia. Who else but a group of Russians would stare a freshly caught and presumably very angry Siberian brown bear in the mouth and think, “Hmm, yes – the perfect source for new and exciting antibiotics!”
Somehow, they managed to make it work. In an article published in Proceedings of the National Academy of Sciences, Russian scientists demonstrated a new technology that rapidly tests the microbiota within bear saliva for potential antibiotics to use against antibiotic-resistant infections such as Staphylococcus aureus. In one of the thousands of samples taken, all introduced S. aureus bacteria had been eliminated, and further analysis showed the presence of amicoumacin, a previously known antibiotic.
And this is just one bear. Who knows what new and exciting goodies lie in the mouths of other bears? Now, we feel it’s important to note that the saliva of any sufficiently wild animal would have sufficed. But when in Russia, if you can think of an excuse to catch a bear, then by God you had better go catch a bear. Anything less would be an insult to the Motherland!
I need a hug
Don’t we all. A new study from the department of psychology at Carnegie Mellon University in Pittsburgh examined whether hugs actually do anything to improve a bad mood. Unverified rumors purport that the study was commissioned by a cuddly red monster named Elmo.
Researchers concluded that consensual hugs are beneficial after some sort of conflict or negative event during the day and that they positively affect the hug-receiver. Researchers also concluded that hugs given by teddy bears or red pandas are the most beneficial, but human hugs will do if those aren’t available. Despite their bactericidal qualities, hugs from Russian bears aren’t encouraged.
Next slide, pleazzzzzzz
Picture a world in which your smartwatch counted backward. In which the room WiFi is a black hole. In which space-time’s zipper seems hopelessly stuck, with a loose string – or, in fact, PowerPoint slide #14 – wedged into its interlocking teeth. That’s right: You’re in a session at a medical conference.
Now, one meeting attendee has boldly researched what many an attendee has wondered before: Do boring speakers really talk for longer? Taking one for all humanity, that intrepid time traveler endured an inhumane, institutional review board–unapproved study design of 50 12-minute meeting sessions. After 4 minutes, he determined whether the speaker was, scientifically speaking, “boring” or “not boring.” He then clocked the time each speaker took to wrap it up.
Spoiler alert: “Not boring” also meant “done sooner” – in a mean time of 11 minutes and 42 seconds versus 13 minutes and 12 seconds for those oscillating in the dullness duality’s boring state. So, if the 4-minute marker heralds a soporific session? There’s more schwag and better WiFi in the exhibit hall.
At least opioids don’t bite
Remember that song about the old lady who “swallowed” a fly? Well, what if the fly were actually a poisonous snake? And what if she didn’t really swallow it? And what if we stopped asking so many questions? A 33-year-old Indian man who was addicted to alcohol, tobacco, and opioids in the form of raw opium and “puppy husk” (we’re thinking it’s poppy husk, but the case report clearly said “puppy”) heard about something new: letting a poisonous snake bite you on the tongue.
He found some nomadic snake charmers to provide the snake (possibly a cobra, but he’s not sure), and the snake’s bite provides him with an hour of jerky body movements, blurred vision, and unresponsiveness, followed by 3-4 weeks of heightened arousal and a sense of well-being that is “more intense tha[n] the state of high experienced … with any dose of alcohol or opioids,” according to the Indian Journal of Psychological Medicine (2018;40[3]:269-71). Plus, he doesn’t use nearly as much alcohol and opium. (Yes, he has done this more than once. You’re rude to ask.)
The old lady in the song, of course, dies after “swallowing” a horse. Fortunately for this guy, there’s no such thing as a poisonous horse.
Ride out the kidney stones
Disney World, the happiest place on earth – unless you’re a kidney stone. A professor from the College of Osteopathic Medicine at Michigan State University, East Lansing, was inspired when one of his patients told him a recent trip to the Magic Kingdom had successfully dislodged a kidney stone. Armed with a silicone model of the renal system, David Wartinger, DO, spent many grueling hours atop various theme park rides. And, one can only assume, many more grueling hours exploring Cinderella’s Castle.
Dr. Wartinger discovered that the Big Thunder Mountain Railroad was more effective than Space Mountain or the Rock ‘n’ Roller Coaster at rattling around the rider and thus shaking out those kidney stones.
The brave professor’s tireless work has earned him one of 2018’s Ig Nobel prizes. We salute you.
In Russia, bear cures YOU
They do things a bit differently in Russia. Who else but a group of Russians would stare a freshly caught and presumably very angry Siberian brown bear in the mouth and think, “Hmm, yes – the perfect source for new and exciting antibiotics!”
Somehow, they managed to make it work. In an article published in Proceedings of the National Academy of Sciences, Russian scientists demonstrated a new technology that rapidly tests the microbiota within bear saliva for potential antibiotics to use against antibiotic-resistant infections such as Staphylococcus aureus. In one of the thousands of samples taken, all introduced S. aureus bacteria had been eliminated, and further analysis showed the presence of amicoumacin, a previously known antibiotic.
And this is just one bear. Who knows what new and exciting goodies lie in the mouths of other bears? Now, we feel it’s important to note that the saliva of any sufficiently wild animal would have sufficed. But when in Russia, if you can think of an excuse to catch a bear, then by God you had better go catch a bear. Anything less would be an insult to the Motherland!
I need a hug
Don’t we all. A new study from the department of psychology at Carnegie Mellon University in Pittsburgh examined whether hugs actually do anything to improve a bad mood. Unverified rumors purport that the study was commissioned by a cuddly red monster named Elmo.
Researchers concluded that consensual hugs are beneficial after some sort of conflict or negative event during the day and that they positively affect the hug-receiver. Researchers also concluded that hugs given by teddy bears or red pandas are the most beneficial, but human hugs will do if those aren’t available. Despite their bactericidal qualities, hugs from Russian bears aren’t encouraged.
Next slide, pleazzzzzzz
Picture a world in which your smartwatch counted backward. In which the room WiFi is a black hole. In which space-time’s zipper seems hopelessly stuck, with a loose string – or, in fact, PowerPoint slide #14 – wedged into its interlocking teeth. That’s right: You’re in a session at a medical conference.
Now, one meeting attendee has boldly researched what many an attendee has wondered before: Do boring speakers really talk for longer? Taking one for all humanity, that intrepid time traveler endured an inhumane, institutional review board–unapproved study design of 50 12-minute meeting sessions. After 4 minutes, he determined whether the speaker was, scientifically speaking, “boring” or “not boring.” He then clocked the time each speaker took to wrap it up.
Spoiler alert: “Not boring” also meant “done sooner” – in a mean time of 11 minutes and 42 seconds versus 13 minutes and 12 seconds for those oscillating in the dullness duality’s boring state. So, if the 4-minute marker heralds a soporific session? There’s more schwag and better WiFi in the exhibit hall.
At least opioids don’t bite
Remember that song about the old lady who “swallowed” a fly? Well, what if the fly were actually a poisonous snake? And what if she didn’t really swallow it? And what if we stopped asking so many questions? A 33-year-old Indian man who was addicted to alcohol, tobacco, and opioids in the form of raw opium and “puppy husk” (we’re thinking it’s poppy husk, but the case report clearly said “puppy”) heard about something new: letting a poisonous snake bite you on the tongue.
He found some nomadic snake charmers to provide the snake (possibly a cobra, but he’s not sure), and the snake’s bite provides him with an hour of jerky body movements, blurred vision, and unresponsiveness, followed by 3-4 weeks of heightened arousal and a sense of well-being that is “more intense tha[n] the state of high experienced … with any dose of alcohol or opioids,” according to the Indian Journal of Psychological Medicine (2018;40[3]:269-71). Plus, he doesn’t use nearly as much alcohol and opium. (Yes, he has done this more than once. You’re rude to ask.)
The old lady in the song, of course, dies after “swallowing” a horse. Fortunately for this guy, there’s no such thing as a poisonous horse.
Ride out the kidney stones
Disney World, the happiest place on earth – unless you’re a kidney stone. A professor from the College of Osteopathic Medicine at Michigan State University, East Lansing, was inspired when one of his patients told him a recent trip to the Magic Kingdom had successfully dislodged a kidney stone. Armed with a silicone model of the renal system, David Wartinger, DO, spent many grueling hours atop various theme park rides. And, one can only assume, many more grueling hours exploring Cinderella’s Castle.
Dr. Wartinger discovered that the Big Thunder Mountain Railroad was more effective than Space Mountain or the Rock ‘n’ Roller Coaster at rattling around the rider and thus shaking out those kidney stones.
The brave professor’s tireless work has earned him one of 2018’s Ig Nobel prizes. We salute you.
In Russia, bear cures YOU
They do things a bit differently in Russia. Who else but a group of Russians would stare a freshly caught and presumably very angry Siberian brown bear in the mouth and think, “Hmm, yes – the perfect source for new and exciting antibiotics!”
Somehow, they managed to make it work. In an article published in Proceedings of the National Academy of Sciences, Russian scientists demonstrated a new technology that rapidly tests the microbiota within bear saliva for potential antibiotics to use against antibiotic-resistant infections such as Staphylococcus aureus. In one of the thousands of samples taken, all introduced S. aureus bacteria had been eliminated, and further analysis showed the presence of amicoumacin, a previously known antibiotic.
And this is just one bear. Who knows what new and exciting goodies lie in the mouths of other bears? Now, we feel it’s important to note that the saliva of any sufficiently wild animal would have sufficed. But when in Russia, if you can think of an excuse to catch a bear, then by God you had better go catch a bear. Anything less would be an insult to the Motherland!
I need a hug
Don’t we all. A new study from the department of psychology at Carnegie Mellon University in Pittsburgh examined whether hugs actually do anything to improve a bad mood. Unverified rumors purport that the study was commissioned by a cuddly red monster named Elmo.
Researchers concluded that consensual hugs are beneficial after some sort of conflict or negative event during the day and that they positively affect the hug-receiver. Researchers also concluded that hugs given by teddy bears or red pandas are the most beneficial, but human hugs will do if those aren’t available. Despite their bactericidal qualities, hugs from Russian bears aren’t encouraged.
Next slide, pleazzzzzzz
Picture a world in which your smartwatch counted backward. In which the room WiFi is a black hole. In which space-time’s zipper seems hopelessly stuck, with a loose string – or, in fact, PowerPoint slide #14 – wedged into its interlocking teeth. That’s right: You’re in a session at a medical conference.
Now, one meeting attendee has boldly researched what many an attendee has wondered before: Do boring speakers really talk for longer? Taking one for all humanity, that intrepid time traveler endured an inhumane, institutional review board–unapproved study design of 50 12-minute meeting sessions. After 4 minutes, he determined whether the speaker was, scientifically speaking, “boring” or “not boring.” He then clocked the time each speaker took to wrap it up.
Spoiler alert: “Not boring” also meant “done sooner” – in a mean time of 11 minutes and 42 seconds versus 13 minutes and 12 seconds for those oscillating in the dullness duality’s boring state. So, if the 4-minute marker heralds a soporific session? There’s more schwag and better WiFi in the exhibit hall.
Anxiety and depression widespread among arthritis patients
Adults with arthritis are almost twice as likely to have symptoms of anxiety than depression, but the depressed patients are more likely to receive treatment, according to the Centers for Disease Control and Prevention.
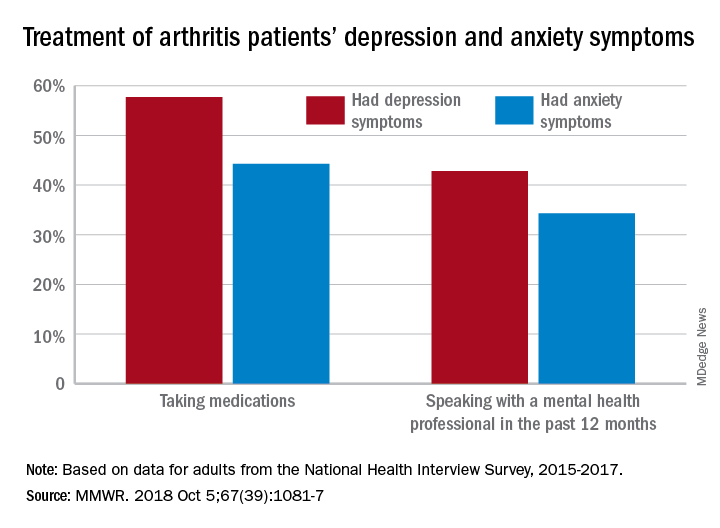
During 2015-2017, the prevalence of anxiety symptoms was 22.5% in adults with arthritis, compared with 12.1% for depression symptoms. Treatment of those symptoms, however, was another story: 57.7% of arthritis patients with depression symptoms were taking medications, versus 44.3% of those with anxiety symptoms, and 42.8% of those with symptoms of depression reported seeing a mental health professional the past 12 months, compared with 34.3% of adults with anxiety, Dana Guglielmo, MPH, of the CDC’s National Center for Chronic Disease Prevention and Health Promotion, Atlanta, and her associates reported in the Morbidity and Mortality Weekly Report.
Prevalences of anxiety and depression symptoms varied considerably by sociodemographic characteristic during 2015-2017. Anxiety and depression were both more common in those aged 18-44 years (28.3% and 13.7%, respectively) than in those aged over 65 (9.7% and 6.2%), and women with arthritis were more likely than were men to experience symptoms of anxiety (26.9% vs. 16%) and depression (14% vs. 9.2%), the investigators said, based on data from the National Health Interview Survey.
Among racial/ethnic groups, the prevalence of anxiety was highest for whites (23.9%) and lowest for Asians (10.6%), who also had lowest depression symptom prevalence at 3.3%, with American Indians/Alaska Natives highest at 15.4%. Adults categorized as other/multiple race, however, were highest in both cases at 32.3% for anxiety and 17.4% for depression, Ms. Guglielmo and her associates said.
The overall prevalence of anxiety and depression symptoms in patients with arthritis was much higher than in those without arthritis – 10.7% for anxiety and 4.7% for depression – which “suggests that all adults with arthritis would benefit from mental health screening,” they noted.
, and encouraging physical activity, which is an effective nonpharmacologic strategy that can help reduce the symptoms of anxiety and depression, improve arthritis symptoms, and promote better quality of life,” the investigators wrote.
SOURCE: Guglielmo D et al. MMWR. 2018 Oct 5;67(39):1081-7.
Adults with arthritis are almost twice as likely to have symptoms of anxiety than depression, but the depressed patients are more likely to receive treatment, according to the Centers for Disease Control and Prevention.
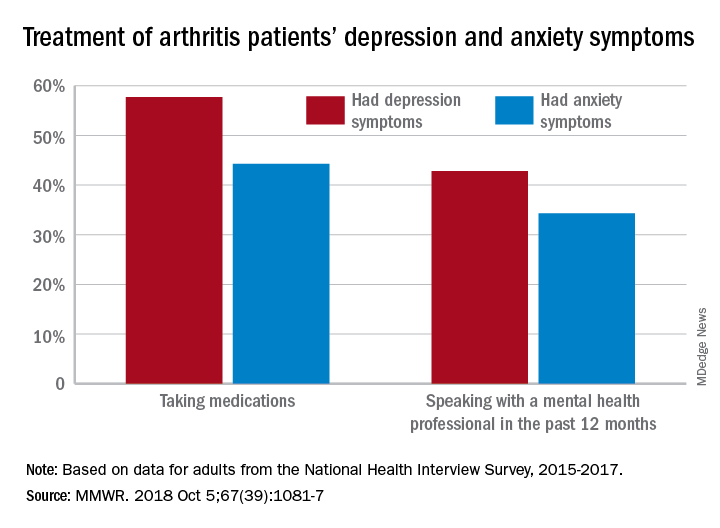
During 2015-2017, the prevalence of anxiety symptoms was 22.5% in adults with arthritis, compared with 12.1% for depression symptoms. Treatment of those symptoms, however, was another story: 57.7% of arthritis patients with depression symptoms were taking medications, versus 44.3% of those with anxiety symptoms, and 42.8% of those with symptoms of depression reported seeing a mental health professional the past 12 months, compared with 34.3% of adults with anxiety, Dana Guglielmo, MPH, of the CDC’s National Center for Chronic Disease Prevention and Health Promotion, Atlanta, and her associates reported in the Morbidity and Mortality Weekly Report.
Prevalences of anxiety and depression symptoms varied considerably by sociodemographic characteristic during 2015-2017. Anxiety and depression were both more common in those aged 18-44 years (28.3% and 13.7%, respectively) than in those aged over 65 (9.7% and 6.2%), and women with arthritis were more likely than were men to experience symptoms of anxiety (26.9% vs. 16%) and depression (14% vs. 9.2%), the investigators said, based on data from the National Health Interview Survey.
Among racial/ethnic groups, the prevalence of anxiety was highest for whites (23.9%) and lowest for Asians (10.6%), who also had lowest depression symptom prevalence at 3.3%, with American Indians/Alaska Natives highest at 15.4%. Adults categorized as other/multiple race, however, were highest in both cases at 32.3% for anxiety and 17.4% for depression, Ms. Guglielmo and her associates said.
The overall prevalence of anxiety and depression symptoms in patients with arthritis was much higher than in those without arthritis – 10.7% for anxiety and 4.7% for depression – which “suggests that all adults with arthritis would benefit from mental health screening,” they noted.
, and encouraging physical activity, which is an effective nonpharmacologic strategy that can help reduce the symptoms of anxiety and depression, improve arthritis symptoms, and promote better quality of life,” the investigators wrote.
SOURCE: Guglielmo D et al. MMWR. 2018 Oct 5;67(39):1081-7.
Adults with arthritis are almost twice as likely to have symptoms of anxiety than depression, but the depressed patients are more likely to receive treatment, according to the Centers for Disease Control and Prevention.
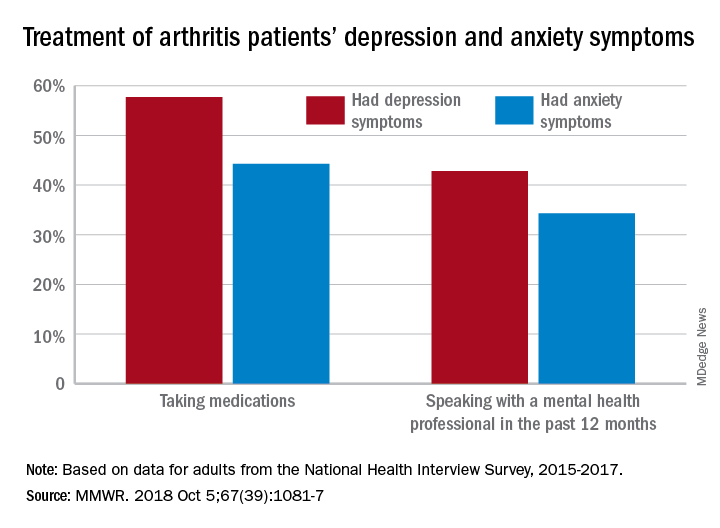
During 2015-2017, the prevalence of anxiety symptoms was 22.5% in adults with arthritis, compared with 12.1% for depression symptoms. Treatment of those symptoms, however, was another story: 57.7% of arthritis patients with depression symptoms were taking medications, versus 44.3% of those with anxiety symptoms, and 42.8% of those with symptoms of depression reported seeing a mental health professional the past 12 months, compared with 34.3% of adults with anxiety, Dana Guglielmo, MPH, of the CDC’s National Center for Chronic Disease Prevention and Health Promotion, Atlanta, and her associates reported in the Morbidity and Mortality Weekly Report.
Prevalences of anxiety and depression symptoms varied considerably by sociodemographic characteristic during 2015-2017. Anxiety and depression were both more common in those aged 18-44 years (28.3% and 13.7%, respectively) than in those aged over 65 (9.7% and 6.2%), and women with arthritis were more likely than were men to experience symptoms of anxiety (26.9% vs. 16%) and depression (14% vs. 9.2%), the investigators said, based on data from the National Health Interview Survey.
Among racial/ethnic groups, the prevalence of anxiety was highest for whites (23.9%) and lowest for Asians (10.6%), who also had lowest depression symptom prevalence at 3.3%, with American Indians/Alaska Natives highest at 15.4%. Adults categorized as other/multiple race, however, were highest in both cases at 32.3% for anxiety and 17.4% for depression, Ms. Guglielmo and her associates said.
The overall prevalence of anxiety and depression symptoms in patients with arthritis was much higher than in those without arthritis – 10.7% for anxiety and 4.7% for depression – which “suggests that all adults with arthritis would benefit from mental health screening,” they noted.
, and encouraging physical activity, which is an effective nonpharmacologic strategy that can help reduce the symptoms of anxiety and depression, improve arthritis symptoms, and promote better quality of life,” the investigators wrote.
SOURCE: Guglielmo D et al. MMWR. 2018 Oct 5;67(39):1081-7.
FROM MMWR
U.S. vs. Europe: Costs of cardiac implant devices compared
Prices that hospitals pay for cardiac implant devices are two to six times higher in the United States than in Europe, according to analysis of a large hospital panel survey.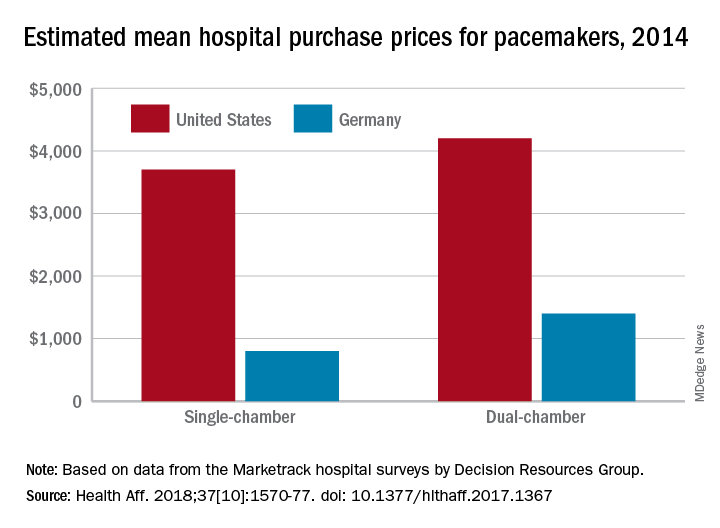
U.S. hospitals had an estimated mean cost of $670 for a bare-metal stent in 2014, compared with $120 in Germany, and the mean costs for dual-chamber pacemakers that year were $4,200 in the United States and $1,400 in Germany, which had lower costs for cardiac devices than the other three European countries – United Kingdom, France, and Italy – included in the study, Martin Wenzl, MSc, and Elias Mossialos, MD, PhD, reported in Health Affairs.
France generally had the highest costs among the European countries, with Italy next and then the United Kingdom. The estimated cost of bare-metal stents was actually higher for French hospitals ($750) than for those in the United States, and Italy had mean prices similar to the United Sates for dual-chamber implantable cardioverter-defibrillators. The prices of implantable cardioverter-defibrillators and cardiac resynchronization devices with defibrillating function were the other exceptions, with the United Kingdom similar to or higher than the United States, said Mr. Wenzl and Dr. Mossialos, both of the London School of Economics and Political Science.
The analysis of data from Decision Resources Group’s Marketrack hospital surveys also showed significant variation between the hospitals in each country, with the exception of France, where payments are based on the specific device rather than the procedure and the system “creates weak incentives for hospitals to negotiate lower prices,” they said. In most of the device categories, “variation between hospitals in each country was similar to variation between countries,” they wrote, adding that prices in general “were only weakly correlated with volumes purchased by hospitals.”
The study was supported by a grant from the Commonwealth Fund. The investigators did not disclose any possible conflicts of interest.
SOURCE: Wenzi M, Mossialos E. Health Aff. 2018;37[10]:1570-77. doi: 10.1377/hlthaff.2017.1367.
Prices that hospitals pay for cardiac implant devices are two to six times higher in the United States than in Europe, according to analysis of a large hospital panel survey.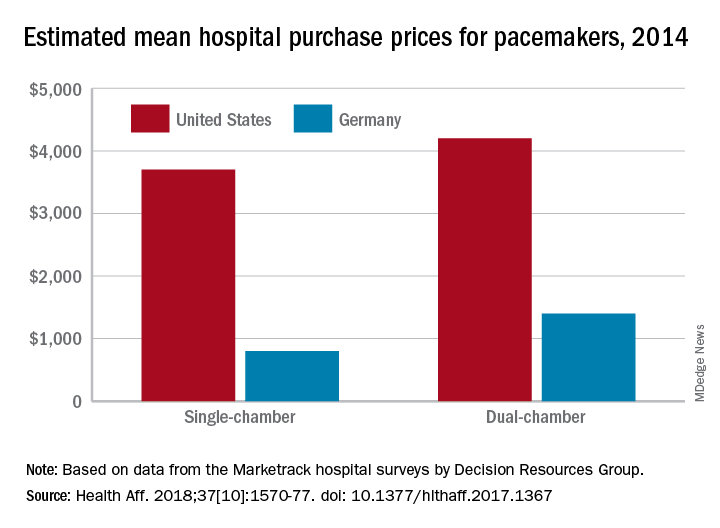
U.S. hospitals had an estimated mean cost of $670 for a bare-metal stent in 2014, compared with $120 in Germany, and the mean costs for dual-chamber pacemakers that year were $4,200 in the United States and $1,400 in Germany, which had lower costs for cardiac devices than the other three European countries – United Kingdom, France, and Italy – included in the study, Martin Wenzl, MSc, and Elias Mossialos, MD, PhD, reported in Health Affairs.
France generally had the highest costs among the European countries, with Italy next and then the United Kingdom. The estimated cost of bare-metal stents was actually higher for French hospitals ($750) than for those in the United States, and Italy had mean prices similar to the United Sates for dual-chamber implantable cardioverter-defibrillators. The prices of implantable cardioverter-defibrillators and cardiac resynchronization devices with defibrillating function were the other exceptions, with the United Kingdom similar to or higher than the United States, said Mr. Wenzl and Dr. Mossialos, both of the London School of Economics and Political Science.
The analysis of data from Decision Resources Group’s Marketrack hospital surveys also showed significant variation between the hospitals in each country, with the exception of France, where payments are based on the specific device rather than the procedure and the system “creates weak incentives for hospitals to negotiate lower prices,” they said. In most of the device categories, “variation between hospitals in each country was similar to variation between countries,” they wrote, adding that prices in general “were only weakly correlated with volumes purchased by hospitals.”
The study was supported by a grant from the Commonwealth Fund. The investigators did not disclose any possible conflicts of interest.
SOURCE: Wenzi M, Mossialos E. Health Aff. 2018;37[10]:1570-77. doi: 10.1377/hlthaff.2017.1367.
Prices that hospitals pay for cardiac implant devices are two to six times higher in the United States than in Europe, according to analysis of a large hospital panel survey.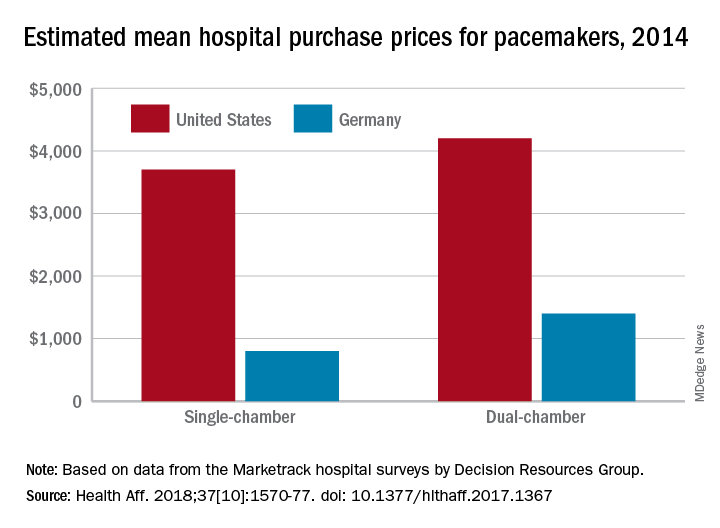
U.S. hospitals had an estimated mean cost of $670 for a bare-metal stent in 2014, compared with $120 in Germany, and the mean costs for dual-chamber pacemakers that year were $4,200 in the United States and $1,400 in Germany, which had lower costs for cardiac devices than the other three European countries – United Kingdom, France, and Italy – included in the study, Martin Wenzl, MSc, and Elias Mossialos, MD, PhD, reported in Health Affairs.
France generally had the highest costs among the European countries, with Italy next and then the United Kingdom. The estimated cost of bare-metal stents was actually higher for French hospitals ($750) than for those in the United States, and Italy had mean prices similar to the United Sates for dual-chamber implantable cardioverter-defibrillators. The prices of implantable cardioverter-defibrillators and cardiac resynchronization devices with defibrillating function were the other exceptions, with the United Kingdom similar to or higher than the United States, said Mr. Wenzl and Dr. Mossialos, both of the London School of Economics and Political Science.
The analysis of data from Decision Resources Group’s Marketrack hospital surveys also showed significant variation between the hospitals in each country, with the exception of France, where payments are based on the specific device rather than the procedure and the system “creates weak incentives for hospitals to negotiate lower prices,” they said. In most of the device categories, “variation between hospitals in each country was similar to variation between countries,” they wrote, adding that prices in general “were only weakly correlated with volumes purchased by hospitals.”
The study was supported by a grant from the Commonwealth Fund. The investigators did not disclose any possible conflicts of interest.
SOURCE: Wenzi M, Mossialos E. Health Aff. 2018;37[10]:1570-77. doi: 10.1377/hlthaff.2017.1367.
FROM HEALTH AFFAIRS
U.S. obesity continues to advance
The prevalence of adult obesity was at or above 35% for seven states in 2017, which is up from five states in 2016 and no states in 2012, according to the Centers for Disease Control and Prevention.
Iowa and Oklahoma, the two newest states with prevalences at or exceeding 35%, joined Alabama, Arkansas, Louisiana, Mississippi, and West Virginia, which has the country’s highest rate of adult obesity at 38.1%. Colorado’s 22.6% rate is the lowest prevalence among all states. The District of Columbia and Hawaii also have prevalences under 25%; previously, Massachusetts also was in this group, but its prevalence went up to 25.9% last year, the CDC reported.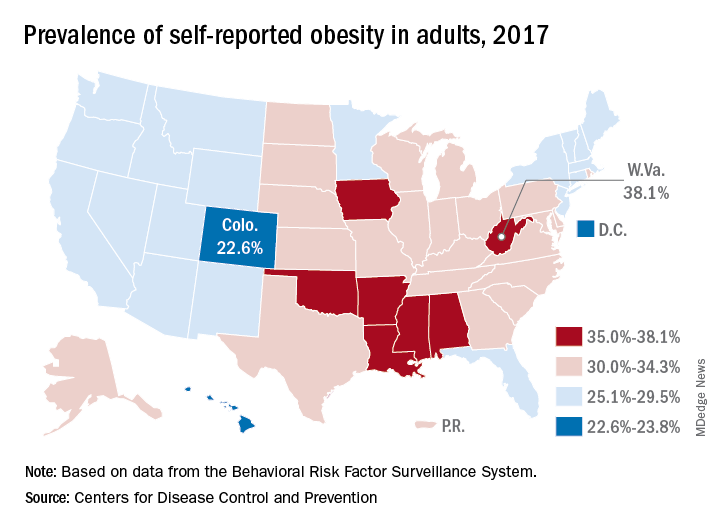
Regional disparities in self-reported adult obesity put the South (32.4%) and the Midwest (32.3%) well ahead of the Northeast (27.7%) and the West (26.1%) in 2017. Racial and ethnic disparities also were seen, with large gaps between blacks, who had a prevalence of 39%, and Hispanics (32.4%) and whites (29.3%). Obesity prevalence was 35% or higher among black adults in 31 states and D.C., while this was true among Hispanics in eight states and among whites in one (West Virginia), although the prevalence was at or above 35% for multiple racial groups in some of these states, the CDC reported based on data from the Behavioral Risk Factor Surveillance System.
“Obesity costs the United States health care system over $147 billion a year [and] research has shown that obesity affects work productivity and military readiness,” the CDC said in a written statement. “To protect the health of the next generation, support for healthy behaviors such as healthy eating, better sleep, stress management, and physical activity should start early and expand to reach Americans across the lifespan in the communities where they live, learn, work, and play.”
The AGA Obesity Practice Guide provides physicians with a comprehensive, multi-disciplinary process to guide and personalize innovative obesity care for safe and effective weight management. Learn more at http://ow.ly/p1Fh30lOXYD
The prevalence of adult obesity was at or above 35% for seven states in 2017, which is up from five states in 2016 and no states in 2012, according to the Centers for Disease Control and Prevention.
Iowa and Oklahoma, the two newest states with prevalences at or exceeding 35%, joined Alabama, Arkansas, Louisiana, Mississippi, and West Virginia, which has the country’s highest rate of adult obesity at 38.1%. Colorado’s 22.6% rate is the lowest prevalence among all states. The District of Columbia and Hawaii also have prevalences under 25%; previously, Massachusetts also was in this group, but its prevalence went up to 25.9% last year, the CDC reported.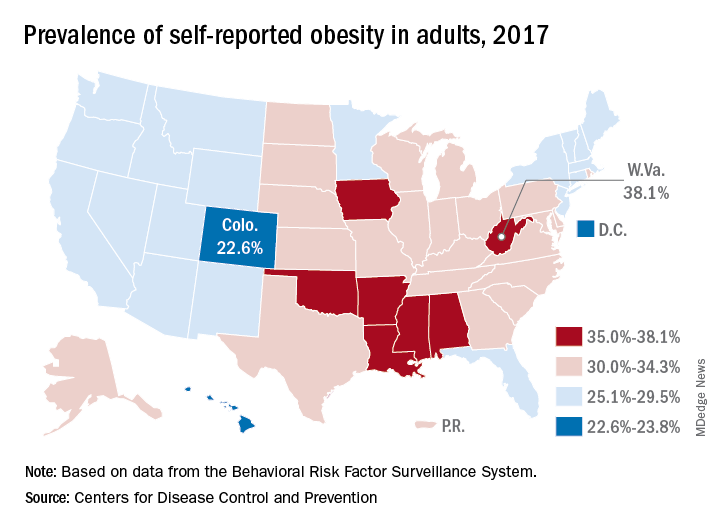
Regional disparities in self-reported adult obesity put the South (32.4%) and the Midwest (32.3%) well ahead of the Northeast (27.7%) and the West (26.1%) in 2017. Racial and ethnic disparities also were seen, with large gaps between blacks, who had a prevalence of 39%, and Hispanics (32.4%) and whites (29.3%). Obesity prevalence was 35% or higher among black adults in 31 states and D.C., while this was true among Hispanics in eight states and among whites in one (West Virginia), although the prevalence was at or above 35% for multiple racial groups in some of these states, the CDC reported based on data from the Behavioral Risk Factor Surveillance System.
“Obesity costs the United States health care system over $147 billion a year [and] research has shown that obesity affects work productivity and military readiness,” the CDC said in a written statement. “To protect the health of the next generation, support for healthy behaviors such as healthy eating, better sleep, stress management, and physical activity should start early and expand to reach Americans across the lifespan in the communities where they live, learn, work, and play.”
The AGA Obesity Practice Guide provides physicians with a comprehensive, multi-disciplinary process to guide and personalize innovative obesity care for safe and effective weight management. Learn more at http://ow.ly/p1Fh30lOXYD
The prevalence of adult obesity was at or above 35% for seven states in 2017, which is up from five states in 2016 and no states in 2012, according to the Centers for Disease Control and Prevention.
Iowa and Oklahoma, the two newest states with prevalences at or exceeding 35%, joined Alabama, Arkansas, Louisiana, Mississippi, and West Virginia, which has the country’s highest rate of adult obesity at 38.1%. Colorado’s 22.6% rate is the lowest prevalence among all states. The District of Columbia and Hawaii also have prevalences under 25%; previously, Massachusetts also was in this group, but its prevalence went up to 25.9% last year, the CDC reported.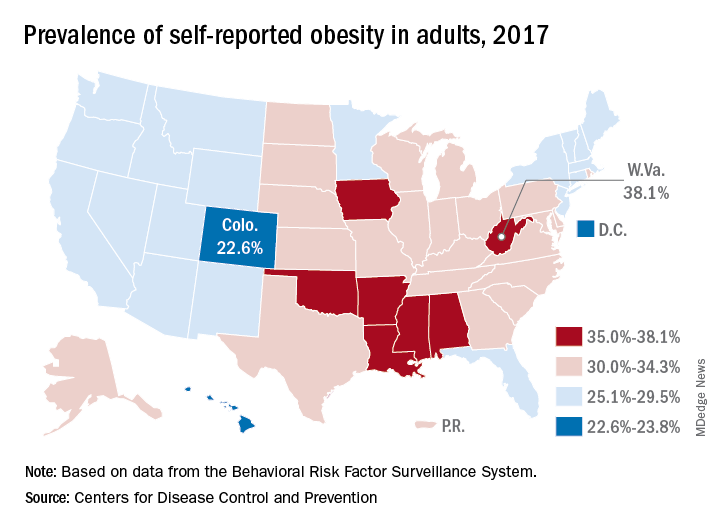
Regional disparities in self-reported adult obesity put the South (32.4%) and the Midwest (32.3%) well ahead of the Northeast (27.7%) and the West (26.1%) in 2017. Racial and ethnic disparities also were seen, with large gaps between blacks, who had a prevalence of 39%, and Hispanics (32.4%) and whites (29.3%). Obesity prevalence was 35% or higher among black adults in 31 states and D.C., while this was true among Hispanics in eight states and among whites in one (West Virginia), although the prevalence was at or above 35% for multiple racial groups in some of these states, the CDC reported based on data from the Behavioral Risk Factor Surveillance System.
“Obesity costs the United States health care system over $147 billion a year [and] research has shown that obesity affects work productivity and military readiness,” the CDC said in a written statement. “To protect the health of the next generation, support for healthy behaviors such as healthy eating, better sleep, stress management, and physical activity should start early and expand to reach Americans across the lifespan in the communities where they live, learn, work, and play.”
The AGA Obesity Practice Guide provides physicians with a comprehensive, multi-disciplinary process to guide and personalize innovative obesity care for safe and effective weight management. Learn more at http://ow.ly/p1Fh30lOXYD