User login
Richard Franki is the associate editor who writes and creates graphs. He started with the company in 1987, when it was known as the International Medical News Group. In his years as a journalist, Richard has worked for Cap Cities/ABC, Disney, Harcourt, Elsevier, Quadrant, Frontline, and Internet Brands. In the 1990s, he was a contributor to the ill-fated Indications column, predecessor of Livin' on the MDedge.
Second-melanoma risk higher with indoor tanning
than those who avoid indoor tanning, according to a retrospective study involving 434 melanoma patients.

The incidence of second melanomas over the entire 16-year course of the study was 25.2% among the tanning-bed users and 18.6% for nonusers. Among these study subjects – 27 with tanning-bed exposure and 61 without – median time to the second tumor was 225 days (0.62 years) for exposed patients and 1,280 days (3.50 years) for those with no exposure, the investigators reported.
This study, they wrote, is the first to show that “patients who had second primary melanoma diagnoses were more likely to have had” exposure to artificial UVR. The increased radiation intensity of tanning beds, “as opposed to UVR from ambient sunlight, in a physiologically vulnerable patient population [fair-skinned persons] at an early age contributes to our findings of decreased tumor lag time.”
SOURCE: Li Y et al. J Am Acad Dermatol. 2018;79(6):1101-8.
than those who avoid indoor tanning, according to a retrospective study involving 434 melanoma patients.

The incidence of second melanomas over the entire 16-year course of the study was 25.2% among the tanning-bed users and 18.6% for nonusers. Among these study subjects – 27 with tanning-bed exposure and 61 without – median time to the second tumor was 225 days (0.62 years) for exposed patients and 1,280 days (3.50 years) for those with no exposure, the investigators reported.
This study, they wrote, is the first to show that “patients who had second primary melanoma diagnoses were more likely to have had” exposure to artificial UVR. The increased radiation intensity of tanning beds, “as opposed to UVR from ambient sunlight, in a physiologically vulnerable patient population [fair-skinned persons] at an early age contributes to our findings of decreased tumor lag time.”
SOURCE: Li Y et al. J Am Acad Dermatol. 2018;79(6):1101-8.
than those who avoid indoor tanning, according to a retrospective study involving 434 melanoma patients.

The incidence of second melanomas over the entire 16-year course of the study was 25.2% among the tanning-bed users and 18.6% for nonusers. Among these study subjects – 27 with tanning-bed exposure and 61 without – median time to the second tumor was 225 days (0.62 years) for exposed patients and 1,280 days (3.50 years) for those with no exposure, the investigators reported.
This study, they wrote, is the first to show that “patients who had second primary melanoma diagnoses were more likely to have had” exposure to artificial UVR. The increased radiation intensity of tanning beds, “as opposed to UVR from ambient sunlight, in a physiologically vulnerable patient population [fair-skinned persons] at an early age contributes to our findings of decreased tumor lag time.”
SOURCE: Li Y et al. J Am Acad Dermatol. 2018;79(6):1101-8.
FROM THE JOURNAL OF THE AMERICAN ACADEMY OF DERMATOLOGY
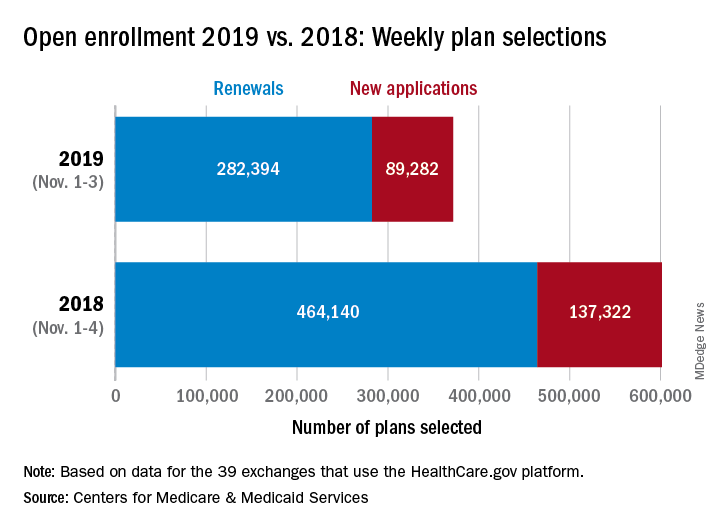
Open enrollment: HealthCare.gov busier in week 2
but the gap has closed since week 1, according to the Centers for Medicare & Medicaid Services.
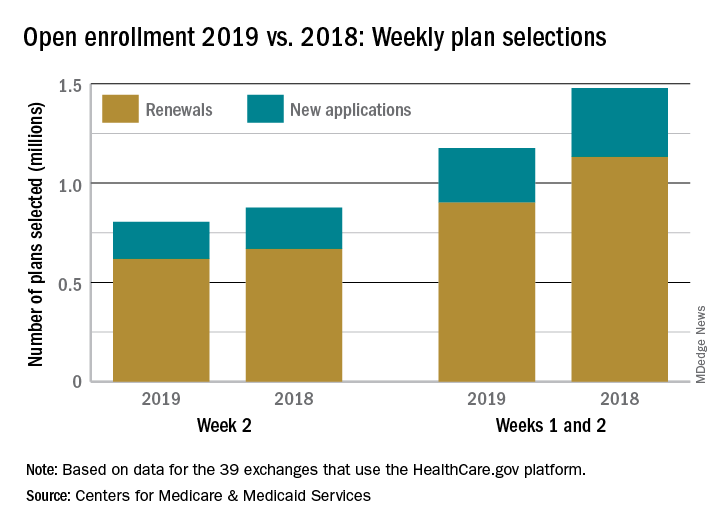
With almost 805,000 plans selected this year during the second week (Nov. 4-10) of open enrollment, the total for the 2019 coverage year stands at nearly 1.18 million for the 39 states that use the HealthCare.gov platform, which is down 20.4% from the 1.48 million plans selected through the first 2 weeks of last year’s enrollment period. After week 1, this year’s total enrollment was down by 38%, compared with last year, CMS data show.
Consumers renewing their insurance plans account for the majority selected for 2019 coverage – 619,000 in week 2 and 901,000 for weeks 1 and 2 (close to 77% in each case) – with the rest coming from new consumers – 186,000 in week 2 and 275,000 overall. The figures reported in the weekly enrollment snapshot could change later since they represent selections only and not “consumers who have paid premiums to effectuate their enrollment,” CMS said.
but the gap has closed since week 1, according to the Centers for Medicare & Medicaid Services.
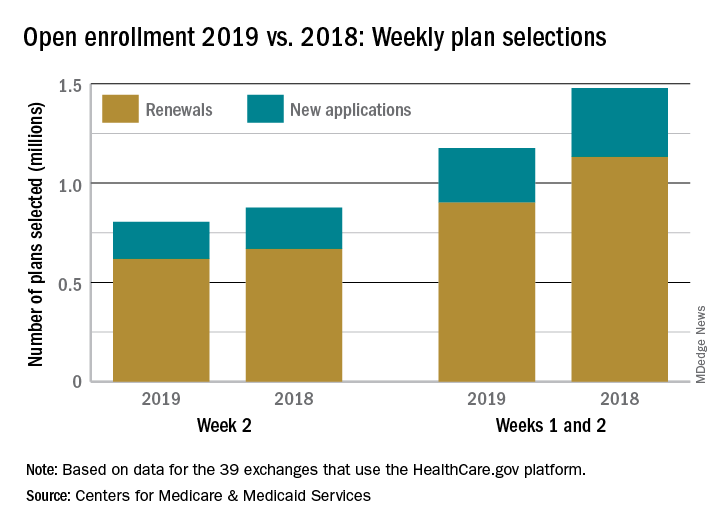
With almost 805,000 plans selected this year during the second week (Nov. 4-10) of open enrollment, the total for the 2019 coverage year stands at nearly 1.18 million for the 39 states that use the HealthCare.gov platform, which is down 20.4% from the 1.48 million plans selected through the first 2 weeks of last year’s enrollment period. After week 1, this year’s total enrollment was down by 38%, compared with last year, CMS data show.
Consumers renewing their insurance plans account for the majority selected for 2019 coverage – 619,000 in week 2 and 901,000 for weeks 1 and 2 (close to 77% in each case) – with the rest coming from new consumers – 186,000 in week 2 and 275,000 overall. The figures reported in the weekly enrollment snapshot could change later since they represent selections only and not “consumers who have paid premiums to effectuate their enrollment,” CMS said.
but the gap has closed since week 1, according to the Centers for Medicare & Medicaid Services.
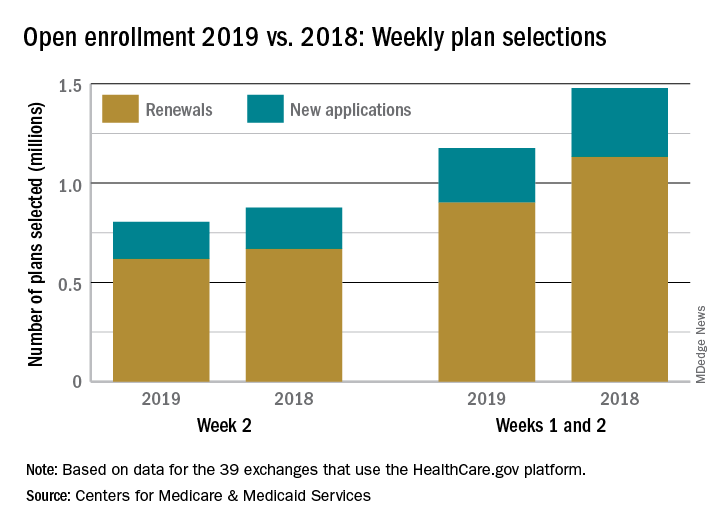
With almost 805,000 plans selected this year during the second week (Nov. 4-10) of open enrollment, the total for the 2019 coverage year stands at nearly 1.18 million for the 39 states that use the HealthCare.gov platform, which is down 20.4% from the 1.48 million plans selected through the first 2 weeks of last year’s enrollment period. After week 1, this year’s total enrollment was down by 38%, compared with last year, CMS data show.
Consumers renewing their insurance plans account for the majority selected for 2019 coverage – 619,000 in week 2 and 901,000 for weeks 1 and 2 (close to 77% in each case) – with the rest coming from new consumers – 186,000 in week 2 and 275,000 overall. The figures reported in the weekly enrollment snapshot could change later since they represent selections only and not “consumers who have paid premiums to effectuate their enrollment,” CMS said.
Necrotizing lunchitis, pneumonia throwdown, global gamete warming
Global gamete warming
Apparently, increasing deadly wildfires, hurricanes, and global famine aren’t enough. Turns out, climate change has found yet another way to harm its arch nemeses, a.k.a. every single species on the planet. A study originally published in Nature Communications found that rising temperatures also have a significant effect on male (but not female) fertility. Men: so fragile.
Testing fertility in flour beetles, researchers concluded that successive heat waves of 5-7° C above normal for 5 days reduced sperm competitiveness and practically sterilized the males. Inseminated sperm inside females were also not spared the devastating effects of the heat-wave conditions. And, as the icing on the cake, reduced fertility persisted amongst later generations.
Unless we can figure out how robot sperm can deliver DNA, we’re in trouble.
Pneumonia throwdown
Previously, we pitted Clostridium difficile against cockroaches in a battle of toughness. In this week’s edition of Bacteria vs. the World, bacterial pneumonia goes up against another worthy adversary, viral pneumonia.
“We’ve always known pneumonia was a risk factor for a major adverse cardiac event,” said J. Brent Muhlestein, MD, of Intermountain Medical Center in Salt Lake City. “What we didn’t know was which type of pneumonia was more dangerous.”
To find out, he and his associates followed almost 4,800 patients hospitalized with pneumonia and tracked nonfatal heart attacks, stroke, heart failure, or death. Data they presented at the American Heart Association scientific sessions in Chicago show that 34% of patients with bacterial pneumonia had a major cardiovascular event within 90 days, compared with 26% of those diagnosed with viral pneumonia. It is likely “that bacterial pneumonia causes greater inflammation of the arteries compared to viral pneumonia,” Dr. Muhlestein said.
So the bacteria stay undefeated, and somewhere Chuck Norris, who will never have a heart attack – even a heart isn’t foolish enough to attack Chuck Norris – is smiling.
Ch-ch-check it out
Drop the beat! Researchers at the University of California were interested in examining beatboxing processes to explore how the human mind works.
These crazy scientists threw some beatboxers into an MRI for an exclusive performance and studied the movements of their mouth and tongue. Researchers hypothesized that beatboxers base their sounds on already-known speech. But they discovered that these talented virtuosos are creating a whole new language.
“They’re coming up with ways to create these really complex acrobatic sounds by taking approaches drawn from different parts of the mouth that they don’t use in any language, and nobody uses for any language,” according to the lead researcher.
Does that mean beatboxing will be taught in schools as a foreign language? Perhaps. It might be more useful than learning Latin.
Keloid castration
Keloids – those pesky overgrowths of scar tissue – can be mighty hard to treat.
“Virtually every patient says, ‘I want this cut off – I want it gone,’ ” dermatologist Hilary E. Baldwin, MD, said in a presentation at the recent Las Vegas Dermatology Seminar. She responds to patients with reality checks about what’s actually possible in keloid treatment.
But sometimes, they just want to adjust the appearance of their keloids. Like the man who complained that “my keloid looks like my junk.” Dr. Baldwin took a look and had to agree – the keloid on his deltoid was the spitting image of male genitalia. She treated the keloid with the equivalent of castration (removing its “testicles” via surgery) and circumcision of sorts (flattening its “glans penis” via corticosteroids).
“It didn’t look pretty,” she said, as at least one male member of the audience squirmed, “but it no longer looked offensive to him.”
‘Necrotizing lunchitis’
Here at the Bureau of Livin’ on the MDedge, we pride ourselves on having the best words. And being University of Michigan graduates. So, the pain is Likert-scale 10 when Big Ten rivals have better words – and worse office fridges.
Exhibit A: the operative report surgical-taped to a Penn State University call room refrigerator, which general surgery resident and American hero Dr. Cassie Sonntag shared on Twitter. The 18-cubic-foot communal Kenmore’s diagnosis? “Necrotizing lunchitis.”
The grave condition called for immediate intervention by surgeon “Whitt,” with assistance from circulating nurse “Liu.” The surgical team performed “debridement of the upper, middle, and lower compartments of the call room refrigerator with extension into the fridge door, disarticulation and washout of the lower chamber, explantation of necrotic lunches of varying ages.” Complications? “Multiple never-before-seen species of mold casually exterminated.” The patient’s postprocedure condition is “guarded.” The complete report is well worth your review. Even if the Sears appliance’s specimens were “refused by path.”
Global gamete warming
Apparently, increasing deadly wildfires, hurricanes, and global famine aren’t enough. Turns out, climate change has found yet another way to harm its arch nemeses, a.k.a. every single species on the planet. A study originally published in Nature Communications found that rising temperatures also have a significant effect on male (but not female) fertility. Men: so fragile.
Testing fertility in flour beetles, researchers concluded that successive heat waves of 5-7° C above normal for 5 days reduced sperm competitiveness and practically sterilized the males. Inseminated sperm inside females were also not spared the devastating effects of the heat-wave conditions. And, as the icing on the cake, reduced fertility persisted amongst later generations.
Unless we can figure out how robot sperm can deliver DNA, we’re in trouble.
Pneumonia throwdown
Previously, we pitted Clostridium difficile against cockroaches in a battle of toughness. In this week’s edition of Bacteria vs. the World, bacterial pneumonia goes up against another worthy adversary, viral pneumonia.
“We’ve always known pneumonia was a risk factor for a major adverse cardiac event,” said J. Brent Muhlestein, MD, of Intermountain Medical Center in Salt Lake City. “What we didn’t know was which type of pneumonia was more dangerous.”
To find out, he and his associates followed almost 4,800 patients hospitalized with pneumonia and tracked nonfatal heart attacks, stroke, heart failure, or death. Data they presented at the American Heart Association scientific sessions in Chicago show that 34% of patients with bacterial pneumonia had a major cardiovascular event within 90 days, compared with 26% of those diagnosed with viral pneumonia. It is likely “that bacterial pneumonia causes greater inflammation of the arteries compared to viral pneumonia,” Dr. Muhlestein said.
So the bacteria stay undefeated, and somewhere Chuck Norris, who will never have a heart attack – even a heart isn’t foolish enough to attack Chuck Norris – is smiling.
Ch-ch-check it out
Drop the beat! Researchers at the University of California were interested in examining beatboxing processes to explore how the human mind works.
These crazy scientists threw some beatboxers into an MRI for an exclusive performance and studied the movements of their mouth and tongue. Researchers hypothesized that beatboxers base their sounds on already-known speech. But they discovered that these talented virtuosos are creating a whole new language.
“They’re coming up with ways to create these really complex acrobatic sounds by taking approaches drawn from different parts of the mouth that they don’t use in any language, and nobody uses for any language,” according to the lead researcher.
Does that mean beatboxing will be taught in schools as a foreign language? Perhaps. It might be more useful than learning Latin.
Keloid castration
Keloids – those pesky overgrowths of scar tissue – can be mighty hard to treat.
“Virtually every patient says, ‘I want this cut off – I want it gone,’ ” dermatologist Hilary E. Baldwin, MD, said in a presentation at the recent Las Vegas Dermatology Seminar. She responds to patients with reality checks about what’s actually possible in keloid treatment.
But sometimes, they just want to adjust the appearance of their keloids. Like the man who complained that “my keloid looks like my junk.” Dr. Baldwin took a look and had to agree – the keloid on his deltoid was the spitting image of male genitalia. She treated the keloid with the equivalent of castration (removing its “testicles” via surgery) and circumcision of sorts (flattening its “glans penis” via corticosteroids).
“It didn’t look pretty,” she said, as at least one male member of the audience squirmed, “but it no longer looked offensive to him.”
‘Necrotizing lunchitis’
Here at the Bureau of Livin’ on the MDedge, we pride ourselves on having the best words. And being University of Michigan graduates. So, the pain is Likert-scale 10 when Big Ten rivals have better words – and worse office fridges.
Exhibit A: the operative report surgical-taped to a Penn State University call room refrigerator, which general surgery resident and American hero Dr. Cassie Sonntag shared on Twitter. The 18-cubic-foot communal Kenmore’s diagnosis? “Necrotizing lunchitis.”
The grave condition called for immediate intervention by surgeon “Whitt,” with assistance from circulating nurse “Liu.” The surgical team performed “debridement of the upper, middle, and lower compartments of the call room refrigerator with extension into the fridge door, disarticulation and washout of the lower chamber, explantation of necrotic lunches of varying ages.” Complications? “Multiple never-before-seen species of mold casually exterminated.” The patient’s postprocedure condition is “guarded.” The complete report is well worth your review. Even if the Sears appliance’s specimens were “refused by path.”
Global gamete warming
Apparently, increasing deadly wildfires, hurricanes, and global famine aren’t enough. Turns out, climate change has found yet another way to harm its arch nemeses, a.k.a. every single species on the planet. A study originally published in Nature Communications found that rising temperatures also have a significant effect on male (but not female) fertility. Men: so fragile.
Testing fertility in flour beetles, researchers concluded that successive heat waves of 5-7° C above normal for 5 days reduced sperm competitiveness and practically sterilized the males. Inseminated sperm inside females were also not spared the devastating effects of the heat-wave conditions. And, as the icing on the cake, reduced fertility persisted amongst later generations.
Unless we can figure out how robot sperm can deliver DNA, we’re in trouble.
Pneumonia throwdown
Previously, we pitted Clostridium difficile against cockroaches in a battle of toughness. In this week’s edition of Bacteria vs. the World, bacterial pneumonia goes up against another worthy adversary, viral pneumonia.
“We’ve always known pneumonia was a risk factor for a major adverse cardiac event,” said J. Brent Muhlestein, MD, of Intermountain Medical Center in Salt Lake City. “What we didn’t know was which type of pneumonia was more dangerous.”
To find out, he and his associates followed almost 4,800 patients hospitalized with pneumonia and tracked nonfatal heart attacks, stroke, heart failure, or death. Data they presented at the American Heart Association scientific sessions in Chicago show that 34% of patients with bacterial pneumonia had a major cardiovascular event within 90 days, compared with 26% of those diagnosed with viral pneumonia. It is likely “that bacterial pneumonia causes greater inflammation of the arteries compared to viral pneumonia,” Dr. Muhlestein said.
So the bacteria stay undefeated, and somewhere Chuck Norris, who will never have a heart attack – even a heart isn’t foolish enough to attack Chuck Norris – is smiling.
Ch-ch-check it out
Drop the beat! Researchers at the University of California were interested in examining beatboxing processes to explore how the human mind works.
These crazy scientists threw some beatboxers into an MRI for an exclusive performance and studied the movements of their mouth and tongue. Researchers hypothesized that beatboxers base their sounds on already-known speech. But they discovered that these talented virtuosos are creating a whole new language.
“They’re coming up with ways to create these really complex acrobatic sounds by taking approaches drawn from different parts of the mouth that they don’t use in any language, and nobody uses for any language,” according to the lead researcher.
Does that mean beatboxing will be taught in schools as a foreign language? Perhaps. It might be more useful than learning Latin.
Keloid castration
Keloids – those pesky overgrowths of scar tissue – can be mighty hard to treat.
“Virtually every patient says, ‘I want this cut off – I want it gone,’ ” dermatologist Hilary E. Baldwin, MD, said in a presentation at the recent Las Vegas Dermatology Seminar. She responds to patients with reality checks about what’s actually possible in keloid treatment.
But sometimes, they just want to adjust the appearance of their keloids. Like the man who complained that “my keloid looks like my junk.” Dr. Baldwin took a look and had to agree – the keloid on his deltoid was the spitting image of male genitalia. She treated the keloid with the equivalent of castration (removing its “testicles” via surgery) and circumcision of sorts (flattening its “glans penis” via corticosteroids).
“It didn’t look pretty,” she said, as at least one male member of the audience squirmed, “but it no longer looked offensive to him.”
‘Necrotizing lunchitis’
Here at the Bureau of Livin’ on the MDedge, we pride ourselves on having the best words. And being University of Michigan graduates. So, the pain is Likert-scale 10 when Big Ten rivals have better words – and worse office fridges.
Exhibit A: the operative report surgical-taped to a Penn State University call room refrigerator, which general surgery resident and American hero Dr. Cassie Sonntag shared on Twitter. The 18-cubic-foot communal Kenmore’s diagnosis? “Necrotizing lunchitis.”
The grave condition called for immediate intervention by surgeon “Whitt,” with assistance from circulating nurse “Liu.” The surgical team performed “debridement of the upper, middle, and lower compartments of the call room refrigerator with extension into the fridge door, disarticulation and washout of the lower chamber, explantation of necrotic lunches of varying ages.” Complications? “Multiple never-before-seen species of mold casually exterminated.” The patient’s postprocedure condition is “guarded.” The complete report is well worth your review. Even if the Sears appliance’s specimens were “refused by path.”
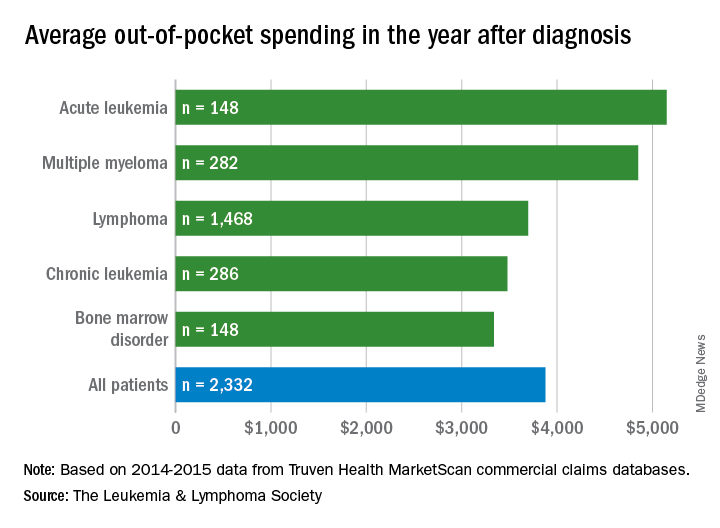
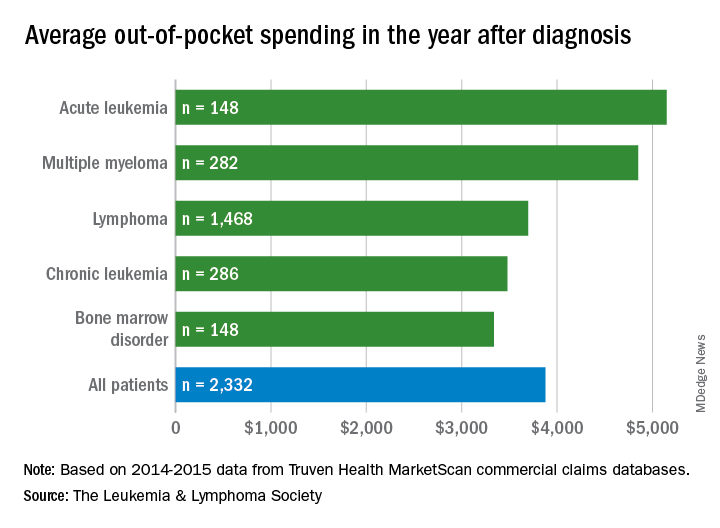
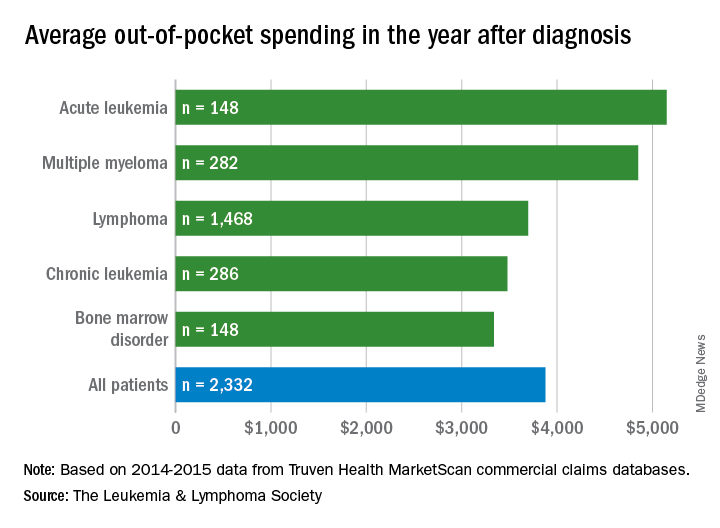
Financial burden of blood cancers in the U.S.
An analysis of more than 2,000 U.S. patients with blood cancers revealed an average healthcare cost of almost $157,000 in the first year after diagnosis.
Costs were highest for acute leukemia patients—almost triple the average for all blood cancers.
Out-of-pocket (OOP) costs were initially highest for acute leukemia patients. However, over time, OOP costs became highest for patients with multiple myeloma.
These results are included in a report commissioned by the Leukemia & Lymphoma Society and prepared by the actuarial firm Milliman.
The report is based on data from the Truven Health MarketScan commercial claims databases.
The cost figures are drawn from data for 2,332 patients, ages 18 to 64, who were diagnosed with blood cancer in 2014 and followed through 2016. This includes the following:
- 1,468 patients with lymphoma
- 286 with chronic leukemia
- 282 with multiple myeloma
- 148 with acute leukemia
- 148 with bone marrow disorders (myelodysplastic syndromes).
The average allowed spending—the amount paid by the payer and patient combined—in the first 12 months after diagnosis was:
- $156,845 overall
- $463,414 for acute leukemia
- $213,879 for multiple myeloma
- $133,744 for bone marrow disorders
- $130,545 for lymphoma
- $88,913 for chronic leukemia.
Differences in OOP costs were smaller, although OOP spending was 32% higher for acute leukemia patients than the overall average.
Average OOP costs—which include coinsurance, copay, and deductible—in the first 12 months after diagnosis were:
- $3,877 overall
- $5,147 for acute leukemia
- $4,849 for multiple myeloma
- $3,695 for lymphoma
- $3,480 for chronic leukemia
- $3,336 for bone marrow disorders.
Although OOP costs were initially highest for acute leukemia patients, over time, costs for multiple myeloma patients became the highest.
The average OOP costs in the month of diagnosis were $1,637 for acute leukemia patients and $1,210 for multiple myeloma patients.
The total accumulated OOP costs 3 years after diagnosis were $8,797 for acute leukemia and $9,127 for multiple myeloma. For the other blood cancers, the average 3-year accumulated OOP costs were under $7,800.
The Leukemia & Lymphoma Society received support from Pfizer, Genentech, and Amgen for this work.
An analysis of more than 2,000 U.S. patients with blood cancers revealed an average healthcare cost of almost $157,000 in the first year after diagnosis.
Costs were highest for acute leukemia patients—almost triple the average for all blood cancers.
Out-of-pocket (OOP) costs were initially highest for acute leukemia patients. However, over time, OOP costs became highest for patients with multiple myeloma.
These results are included in a report commissioned by the Leukemia & Lymphoma Society and prepared by the actuarial firm Milliman.
The report is based on data from the Truven Health MarketScan commercial claims databases.
The cost figures are drawn from data for 2,332 patients, ages 18 to 64, who were diagnosed with blood cancer in 2014 and followed through 2016. This includes the following:
- 1,468 patients with lymphoma
- 286 with chronic leukemia
- 282 with multiple myeloma
- 148 with acute leukemia
- 148 with bone marrow disorders (myelodysplastic syndromes).
The average allowed spending—the amount paid by the payer and patient combined—in the first 12 months after diagnosis was:
- $156,845 overall
- $463,414 for acute leukemia
- $213,879 for multiple myeloma
- $133,744 for bone marrow disorders
- $130,545 for lymphoma
- $88,913 for chronic leukemia.
Differences in OOP costs were smaller, although OOP spending was 32% higher for acute leukemia patients than the overall average.
Average OOP costs—which include coinsurance, copay, and deductible—in the first 12 months after diagnosis were:
- $3,877 overall
- $5,147 for acute leukemia
- $4,849 for multiple myeloma
- $3,695 for lymphoma
- $3,480 for chronic leukemia
- $3,336 for bone marrow disorders.
Although OOP costs were initially highest for acute leukemia patients, over time, costs for multiple myeloma patients became the highest.
The average OOP costs in the month of diagnosis were $1,637 for acute leukemia patients and $1,210 for multiple myeloma patients.
The total accumulated OOP costs 3 years after diagnosis were $8,797 for acute leukemia and $9,127 for multiple myeloma. For the other blood cancers, the average 3-year accumulated OOP costs were under $7,800.
The Leukemia & Lymphoma Society received support from Pfizer, Genentech, and Amgen for this work.
An analysis of more than 2,000 U.S. patients with blood cancers revealed an average healthcare cost of almost $157,000 in the first year after diagnosis.
Costs were highest for acute leukemia patients—almost triple the average for all blood cancers.
Out-of-pocket (OOP) costs were initially highest for acute leukemia patients. However, over time, OOP costs became highest for patients with multiple myeloma.
These results are included in a report commissioned by the Leukemia & Lymphoma Society and prepared by the actuarial firm Milliman.
The report is based on data from the Truven Health MarketScan commercial claims databases.
The cost figures are drawn from data for 2,332 patients, ages 18 to 64, who were diagnosed with blood cancer in 2014 and followed through 2016. This includes the following:
- 1,468 patients with lymphoma
- 286 with chronic leukemia
- 282 with multiple myeloma
- 148 with acute leukemia
- 148 with bone marrow disorders (myelodysplastic syndromes).
The average allowed spending—the amount paid by the payer and patient combined—in the first 12 months after diagnosis was:
- $156,845 overall
- $463,414 for acute leukemia
- $213,879 for multiple myeloma
- $133,744 for bone marrow disorders
- $130,545 for lymphoma
- $88,913 for chronic leukemia.
Differences in OOP costs were smaller, although OOP spending was 32% higher for acute leukemia patients than the overall average.
Average OOP costs—which include coinsurance, copay, and deductible—in the first 12 months after diagnosis were:
- $3,877 overall
- $5,147 for acute leukemia
- $4,849 for multiple myeloma
- $3,695 for lymphoma
- $3,480 for chronic leukemia
- $3,336 for bone marrow disorders.
Although OOP costs were initially highest for acute leukemia patients, over time, costs for multiple myeloma patients became the highest.
The average OOP costs in the month of diagnosis were $1,637 for acute leukemia patients and $1,210 for multiple myeloma patients.
The total accumulated OOP costs 3 years after diagnosis were $8,797 for acute leukemia and $9,127 for multiple myeloma. For the other blood cancers, the average 3-year accumulated OOP costs were under $7,800.
The Leukemia & Lymphoma Society received support from Pfizer, Genentech, and Amgen for this work.
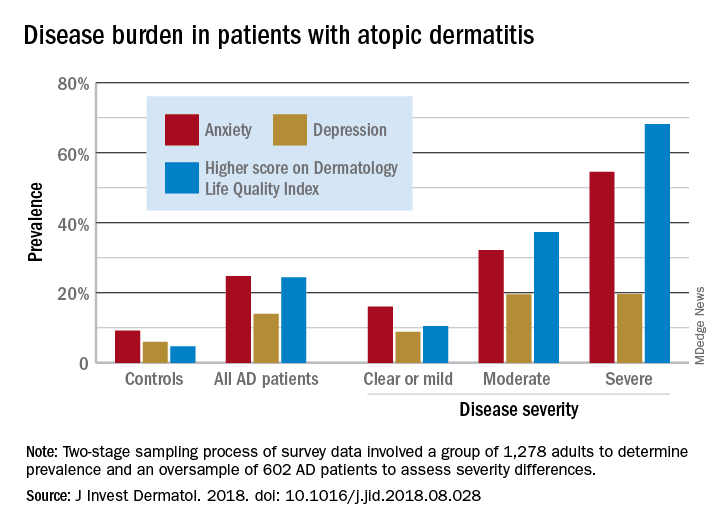
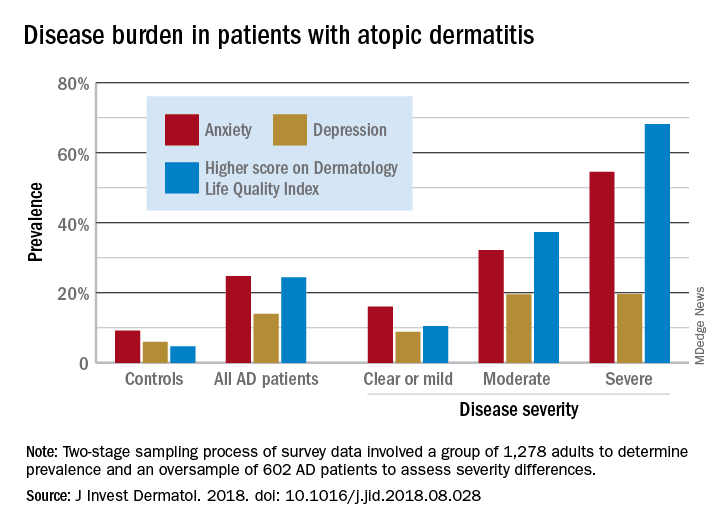
Atopic dermatitis hits mental health, quality of life
Atopic dermatitis (AD) places a considerable burden on mental health and quality of life for patients with disease of even moderate severity, according to a cross-sectional study of data from the Atopic Dermatitis in America survey.
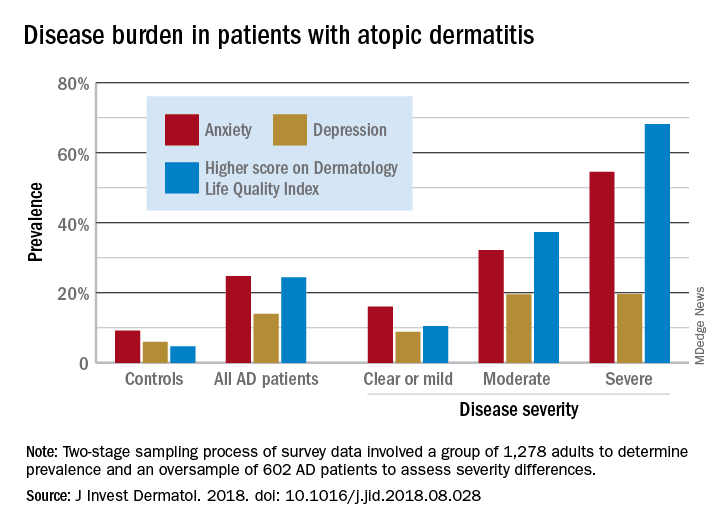
Among adults with severe AD, the mean score on the Dermatology Life Quality Index was 11.4, with a score of 6-30 representing a moderate to large effect on quality of life. The mean for those with moderate disease, 5.9, was just below that range, but 37% of that group did have scores between 6 and 30, Zelma C. Chiesa Fuxench, MD, of the University of Pennsylvania, Philadelphia, and her associates said in the Journal of Investigative Dermatology.
The mean on the Dermatology Life Quality Index for all AD patients was 4.1, with 24% falling into the moderate to large effect range, compared with 1% and 5% for controls. Results were similar on the mental health measure used, the Hospital Anxiety and Depression Scale (HADS). Mean HADS-anxiety scores were 7.0 for all AD patients and 4.7 for controls, and HADS-depression means were 5.8 for AD patients and 3.6 for controls, the investigators reported.
Analysis by disease severity found that 32% of those with moderate AD and almost 56% with severe AD had clinical anxiety (HADS-A score of 11-21), while somewhat lower prevalences were seen for clinical depression (HADS-D score of 11-21): 19.5% for those with moderate AD and 19.7% for patients with severe AD, Dr. Chiesa Fuxench and her associates said.
“An increasing number of studies provide evidence that AD is associated with marked [quality of life] impairment and increased health care costs with higher burden and costs in those with more severe disease. Additional studies should center on exploring those factors associated with AD, and AD disease severity, which lead to increased disease burden in this population,” they wrote.
Respondents to the Atopic Dermatitis in America survey were part of the GfK Knowledge Panel. The study involved a two-stage sampling process: one group of 1,278 adults determined prevalence ,and an oversample of 602 AD patients assessed severity differences.
Dr. Chiesa Fuxench has received research grants from Regeneron, Sanofi, Tioga, and Vanda for work related to atopic dermatitis and has received honoraria for CME work in atopic dermatitis sponsored by educational grants from Regeneron and Sanofi.
SOURCE: J Invest Dermatol. 2018. doi: 10.1016/j.jid.2018.08.028.
Atopic dermatitis (AD) places a considerable burden on mental health and quality of life for patients with disease of even moderate severity, according to a cross-sectional study of data from the Atopic Dermatitis in America survey.
Among adults with severe AD, the mean score on the Dermatology Life Quality Index was 11.4, with a score of 6-30 representing a moderate to large effect on quality of life. The mean for those with moderate disease, 5.9, was just below that range, but 37% of that group did have scores between 6 and 30, Zelma C. Chiesa Fuxench, MD, of the University of Pennsylvania, Philadelphia, and her associates said in the Journal of Investigative Dermatology.
The mean on the Dermatology Life Quality Index for all AD patients was 4.1, with 24% falling into the moderate to large effect range, compared with 1% and 5% for controls. Results were similar on the mental health measure used, the Hospital Anxiety and Depression Scale (HADS). Mean HADS-anxiety scores were 7.0 for all AD patients and 4.7 for controls, and HADS-depression means were 5.8 for AD patients and 3.6 for controls, the investigators reported.
Analysis by disease severity found that 32% of those with moderate AD and almost 56% with severe AD had clinical anxiety (HADS-A score of 11-21), while somewhat lower prevalences were seen for clinical depression (HADS-D score of 11-21): 19.5% for those with moderate AD and 19.7% for patients with severe AD, Dr. Chiesa Fuxench and her associates said.
“An increasing number of studies provide evidence that AD is associated with marked [quality of life] impairment and increased health care costs with higher burden and costs in those with more severe disease. Additional studies should center on exploring those factors associated with AD, and AD disease severity, which lead to increased disease burden in this population,” they wrote.
Respondents to the Atopic Dermatitis in America survey were part of the GfK Knowledge Panel. The study involved a two-stage sampling process: one group of 1,278 adults determined prevalence ,and an oversample of 602 AD patients assessed severity differences.
Dr. Chiesa Fuxench has received research grants from Regeneron, Sanofi, Tioga, and Vanda for work related to atopic dermatitis and has received honoraria for CME work in atopic dermatitis sponsored by educational grants from Regeneron and Sanofi.
SOURCE: J Invest Dermatol. 2018. doi: 10.1016/j.jid.2018.08.028.
Atopic dermatitis (AD) places a considerable burden on mental health and quality of life for patients with disease of even moderate severity, according to a cross-sectional study of data from the Atopic Dermatitis in America survey.
Among adults with severe AD, the mean score on the Dermatology Life Quality Index was 11.4, with a score of 6-30 representing a moderate to large effect on quality of life. The mean for those with moderate disease, 5.9, was just below that range, but 37% of that group did have scores between 6 and 30, Zelma C. Chiesa Fuxench, MD, of the University of Pennsylvania, Philadelphia, and her associates said in the Journal of Investigative Dermatology.
The mean on the Dermatology Life Quality Index for all AD patients was 4.1, with 24% falling into the moderate to large effect range, compared with 1% and 5% for controls. Results were similar on the mental health measure used, the Hospital Anxiety and Depression Scale (HADS). Mean HADS-anxiety scores were 7.0 for all AD patients and 4.7 for controls, and HADS-depression means were 5.8 for AD patients and 3.6 for controls, the investigators reported.
Analysis by disease severity found that 32% of those with moderate AD and almost 56% with severe AD had clinical anxiety (HADS-A score of 11-21), while somewhat lower prevalences were seen for clinical depression (HADS-D score of 11-21): 19.5% for those with moderate AD and 19.7% for patients with severe AD, Dr. Chiesa Fuxench and her associates said.
“An increasing number of studies provide evidence that AD is associated with marked [quality of life] impairment and increased health care costs with higher burden and costs in those with more severe disease. Additional studies should center on exploring those factors associated with AD, and AD disease severity, which lead to increased disease burden in this population,” they wrote.
Respondents to the Atopic Dermatitis in America survey were part of the GfK Knowledge Panel. The study involved a two-stage sampling process: one group of 1,278 adults determined prevalence ,and an oversample of 602 AD patients assessed severity differences.
Dr. Chiesa Fuxench has received research grants from Regeneron, Sanofi, Tioga, and Vanda for work related to atopic dermatitis and has received honoraria for CME work in atopic dermatitis sponsored by educational grants from Regeneron and Sanofi.
SOURCE: J Invest Dermatol. 2018. doi: 10.1016/j.jid.2018.08.028.
FROM THE JOURNAL OF INVESTIGATIVE DERMATOLOGY
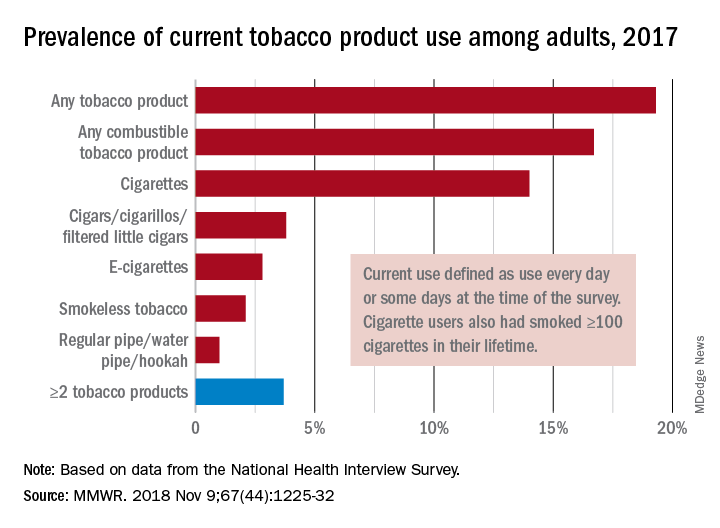
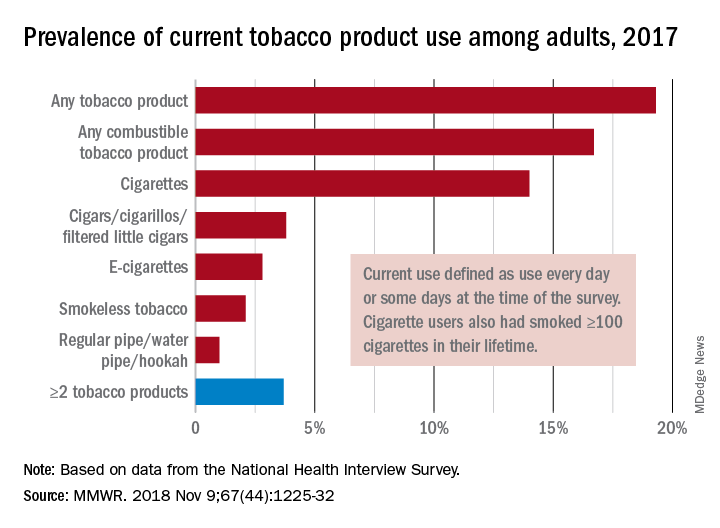
Cigarette smoking at lowest level ever
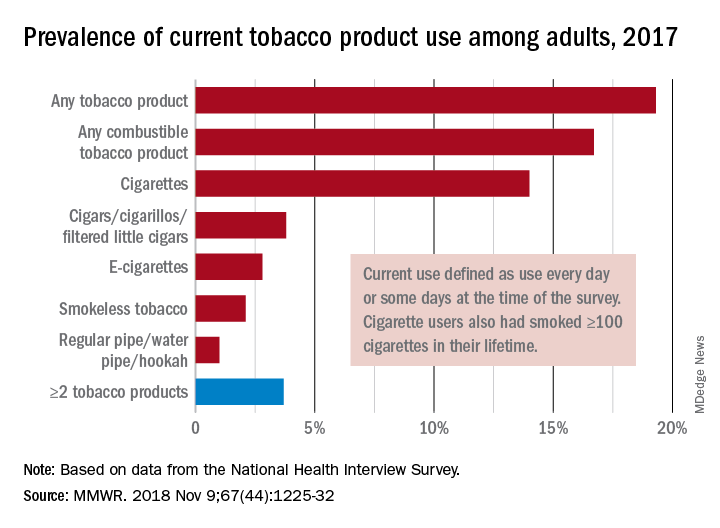
“This new all-time low in cigarette smoking among U.S. adults is a tremendous public health accomplishment, and it demonstrates the importance of continued proven strategies to reduce smoking,” CDC Director Robert Redfield said in a written statement.
In 2017, 19.3% of adults aged 18 years and older – approximately 47.4 million Americans – reported current use of some type of tobacco product, and current use of combustible tobacco was 16.7%, Teresa W. Wang, PhD, of the CDC’s National Center for Chronic Disease Prevention and Health Promotion, Atlanta, and her associates reported in the Morbidity and Mortality Weekly Report. Current use was defined as use every day or some days, with an added requirement of at least 100 cigarettes in a lifetime added for cigarette smokers.
Data from the National Health Interview Survey showed that from 2016 to 2017, current use declined for any tobacco product, any combustible tobacco product, cigarettes, smokeless tobacco, and the combination of two or more tobacco products. The most common combination in 2017 was cigarettes and e-cigarettes, which was reported by 30.1% of the 9 million adults who used more than one product, Dr. Wang and her associates said.
Prevalence of current tobacco use was higher among men than women (24.8% vs. 14.2%), and adults aged 25-44 years (22.5%) had the highest level by age, followed by those aged 45-64 years (21.3%), 18-24 years (18.3%), and 65 years or older (11%). Use by race/ethnicity was highest among American Indian/Alaska Natives (29.8%), with the Midwest putting up the highest prevalence by region at 23.5%, they said.
“Although cigarette smoking among U.S. adults has declined considerably, tobacco products have evolved in recent years to include various combustible, noncombustible, and electronic products,” Dr. Wang and her associates wrote. “Implementation of evidence-based tobacco control interventions that address the diversity of tobacco products used by U.S. adults, in coordination with regulation of tobacco product manufacturing, marketing, and sales, can reduce tobacco-related disease and death in the United States.”
SOURCE: Wang TW et al. MMWR. 2018 Nov 9;67[44]:1225-32.
“This new all-time low in cigarette smoking among U.S. adults is a tremendous public health accomplishment, and it demonstrates the importance of continued proven strategies to reduce smoking,” CDC Director Robert Redfield said in a written statement.
In 2017, 19.3% of adults aged 18 years and older – approximately 47.4 million Americans – reported current use of some type of tobacco product, and current use of combustible tobacco was 16.7%, Teresa W. Wang, PhD, of the CDC’s National Center for Chronic Disease Prevention and Health Promotion, Atlanta, and her associates reported in the Morbidity and Mortality Weekly Report. Current use was defined as use every day or some days, with an added requirement of at least 100 cigarettes in a lifetime added for cigarette smokers.
Data from the National Health Interview Survey showed that from 2016 to 2017, current use declined for any tobacco product, any combustible tobacco product, cigarettes, smokeless tobacco, and the combination of two or more tobacco products. The most common combination in 2017 was cigarettes and e-cigarettes, which was reported by 30.1% of the 9 million adults who used more than one product, Dr. Wang and her associates said.
Prevalence of current tobacco use was higher among men than women (24.8% vs. 14.2%), and adults aged 25-44 years (22.5%) had the highest level by age, followed by those aged 45-64 years (21.3%), 18-24 years (18.3%), and 65 years or older (11%). Use by race/ethnicity was highest among American Indian/Alaska Natives (29.8%), with the Midwest putting up the highest prevalence by region at 23.5%, they said.
“Although cigarette smoking among U.S. adults has declined considerably, tobacco products have evolved in recent years to include various combustible, noncombustible, and electronic products,” Dr. Wang and her associates wrote. “Implementation of evidence-based tobacco control interventions that address the diversity of tobacco products used by U.S. adults, in coordination with regulation of tobacco product manufacturing, marketing, and sales, can reduce tobacco-related disease and death in the United States.”
SOURCE: Wang TW et al. MMWR. 2018 Nov 9;67[44]:1225-32.
“This new all-time low in cigarette smoking among U.S. adults is a tremendous public health accomplishment, and it demonstrates the importance of continued proven strategies to reduce smoking,” CDC Director Robert Redfield said in a written statement.
In 2017, 19.3% of adults aged 18 years and older – approximately 47.4 million Americans – reported current use of some type of tobacco product, and current use of combustible tobacco was 16.7%, Teresa W. Wang, PhD, of the CDC’s National Center for Chronic Disease Prevention and Health Promotion, Atlanta, and her associates reported in the Morbidity and Mortality Weekly Report. Current use was defined as use every day or some days, with an added requirement of at least 100 cigarettes in a lifetime added for cigarette smokers.
Data from the National Health Interview Survey showed that from 2016 to 2017, current use declined for any tobacco product, any combustible tobacco product, cigarettes, smokeless tobacco, and the combination of two or more tobacco products. The most common combination in 2017 was cigarettes and e-cigarettes, which was reported by 30.1% of the 9 million adults who used more than one product, Dr. Wang and her associates said.
Prevalence of current tobacco use was higher among men than women (24.8% vs. 14.2%), and adults aged 25-44 years (22.5%) had the highest level by age, followed by those aged 45-64 years (21.3%), 18-24 years (18.3%), and 65 years or older (11%). Use by race/ethnicity was highest among American Indian/Alaska Natives (29.8%), with the Midwest putting up the highest prevalence by region at 23.5%, they said.
“Although cigarette smoking among U.S. adults has declined considerably, tobacco products have evolved in recent years to include various combustible, noncombustible, and electronic products,” Dr. Wang and her associates wrote. “Implementation of evidence-based tobacco control interventions that address the diversity of tobacco products used by U.S. adults, in coordination with regulation of tobacco product manufacturing, marketing, and sales, can reduce tobacco-related disease and death in the United States.”
SOURCE: Wang TW et al. MMWR. 2018 Nov 9;67[44]:1225-32.
FROM MMWR
Report details financial burden of blood cancers
with costs for acute leukemia almost tripling that amount, according to a new report from the Leukemia & Lymphoma Society (LLS).
Total allowed cost – the average amount paid by the insurer and patient combined – for acute leukemia was more than $463,000 for the 12 months after initial diagnosis. Averages for the other four cancers included in the analysis came in at $214,000 for multiple myeloma, $134,000 for bone marrow disorders, $131,000 for lymphoma, and $89,000 for chronic leukemia, the LLS said.
The cost figures are drawn from claims data for 2,332 patients diagnosed in 2014.
Differences in out-of-pocket (OOP) costs were smaller, with the average for all patients at almost $3,900 in the year after diagnosis and acute leukemia coming in the highest at $5,100. Over time, however, OOP costs for multiple myeloma patients became the highest, totaling $9,100 for the 3 years after diagnosis, compared with $8,800 for acute leukemia and an average of less than $7,800 for the other blood cancers, the LLS said in the report, which was prepared by the actuarial firm Milliman.
OOP costs also varied by the type of plan. Patients in high-deductible plans averaged nearly $5,400 for the first year after diagnosis, compared with $3,300 for those with traditional insurance, the LLS noted. For acute leukemia, the OOP costs of high-deductible plans were more than twice as high as those of traditional plans.
The study was based on data for adults aged 18-64 years from the Truven Health MarketScan commercial claims databases for the years from 2013 to 2016. The LLS received support for the study from Pfizer, Genentech, and Amgen.
with costs for acute leukemia almost tripling that amount, according to a new report from the Leukemia & Lymphoma Society (LLS).
Total allowed cost – the average amount paid by the insurer and patient combined – for acute leukemia was more than $463,000 for the 12 months after initial diagnosis. Averages for the other four cancers included in the analysis came in at $214,000 for multiple myeloma, $134,000 for bone marrow disorders, $131,000 for lymphoma, and $89,000 for chronic leukemia, the LLS said.
The cost figures are drawn from claims data for 2,332 patients diagnosed in 2014.
Differences in out-of-pocket (OOP) costs were smaller, with the average for all patients at almost $3,900 in the year after diagnosis and acute leukemia coming in the highest at $5,100. Over time, however, OOP costs for multiple myeloma patients became the highest, totaling $9,100 for the 3 years after diagnosis, compared with $8,800 for acute leukemia and an average of less than $7,800 for the other blood cancers, the LLS said in the report, which was prepared by the actuarial firm Milliman.
OOP costs also varied by the type of plan. Patients in high-deductible plans averaged nearly $5,400 for the first year after diagnosis, compared with $3,300 for those with traditional insurance, the LLS noted. For acute leukemia, the OOP costs of high-deductible plans were more than twice as high as those of traditional plans.
The study was based on data for adults aged 18-64 years from the Truven Health MarketScan commercial claims databases for the years from 2013 to 2016. The LLS received support for the study from Pfizer, Genentech, and Amgen.
with costs for acute leukemia almost tripling that amount, according to a new report from the Leukemia & Lymphoma Society (LLS).
Total allowed cost – the average amount paid by the insurer and patient combined – for acute leukemia was more than $463,000 for the 12 months after initial diagnosis. Averages for the other four cancers included in the analysis came in at $214,000 for multiple myeloma, $134,000 for bone marrow disorders, $131,000 for lymphoma, and $89,000 for chronic leukemia, the LLS said.
The cost figures are drawn from claims data for 2,332 patients diagnosed in 2014.
Differences in out-of-pocket (OOP) costs were smaller, with the average for all patients at almost $3,900 in the year after diagnosis and acute leukemia coming in the highest at $5,100. Over time, however, OOP costs for multiple myeloma patients became the highest, totaling $9,100 for the 3 years after diagnosis, compared with $8,800 for acute leukemia and an average of less than $7,800 for the other blood cancers, the LLS said in the report, which was prepared by the actuarial firm Milliman.
OOP costs also varied by the type of plan. Patients in high-deductible plans averaged nearly $5,400 for the first year after diagnosis, compared with $3,300 for those with traditional insurance, the LLS noted. For acute leukemia, the OOP costs of high-deductible plans were more than twice as high as those of traditional plans.
The study was based on data for adults aged 18-64 years from the Truven Health MarketScan commercial claims databases for the years from 2013 to 2016. The LLS received support for the study from Pfizer, Genentech, and Amgen.
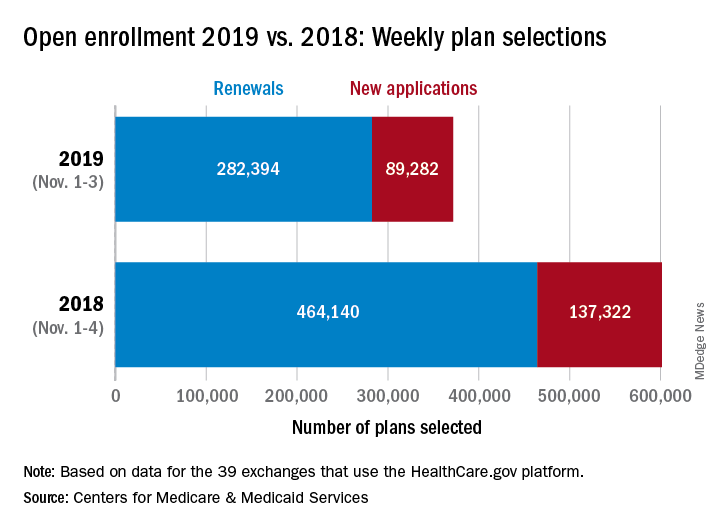
Open enrollment: Slow first week at HealthCare.gov
About 372,000 people selected a health insurance plan during the first week of Affordable Care Act open enrollment for 2019, according to the Centers for Medicare & Medicaid Services. The first week was short, with only 3 days to select coverage.
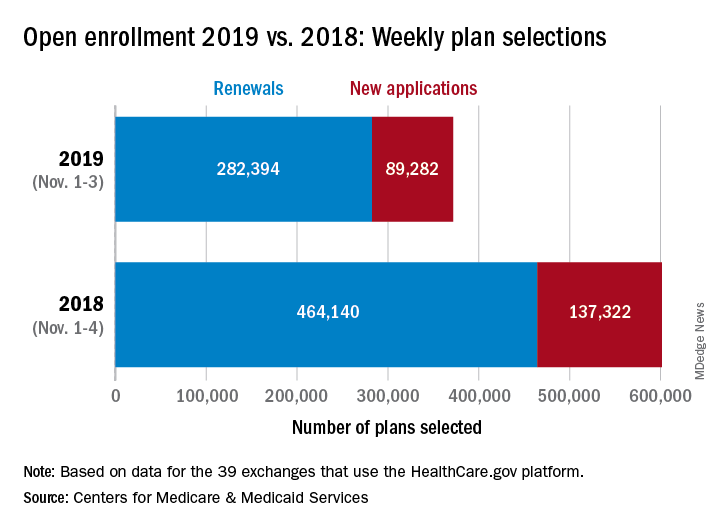
For Nov. 1-3, the exact number of plans selected was 371,676, which is about 38% less than last year’s first week, which was 4 days long, so the average number of plans selected per day was down by a little less than 18%, CMS data show.
“The final number of plan selections associated with enrollment activity during a reporting period may change due to plan modifications or cancellations,” CMS officials said, adding that the weekly data release “only reports new plan selections and active plan renewals and does not report the number of consumers who have paid premiums to effectuate their enrollment.”
Open enrollment will continue for another 6 weeks, with Dec. 15 being the final day to enroll for 2019 coverage on the 39 state exchanges that use the HealthCare.gov platform.
About 372,000 people selected a health insurance plan during the first week of Affordable Care Act open enrollment for 2019, according to the Centers for Medicare & Medicaid Services. The first week was short, with only 3 days to select coverage.
For Nov. 1-3, the exact number of plans selected was 371,676, which is about 38% less than last year’s first week, which was 4 days long, so the average number of plans selected per day was down by a little less than 18%, CMS data show.
“The final number of plan selections associated with enrollment activity during a reporting period may change due to plan modifications or cancellations,” CMS officials said, adding that the weekly data release “only reports new plan selections and active plan renewals and does not report the number of consumers who have paid premiums to effectuate their enrollment.”
Open enrollment will continue for another 6 weeks, with Dec. 15 being the final day to enroll for 2019 coverage on the 39 state exchanges that use the HealthCare.gov platform.
About 372,000 people selected a health insurance plan during the first week of Affordable Care Act open enrollment for 2019, according to the Centers for Medicare & Medicaid Services. The first week was short, with only 3 days to select coverage.
For Nov. 1-3, the exact number of plans selected was 371,676, which is about 38% less than last year’s first week, which was 4 days long, so the average number of plans selected per day was down by a little less than 18%, CMS data show.
“The final number of plan selections associated with enrollment activity during a reporting period may change due to plan modifications or cancellations,” CMS officials said, adding that the weekly data release “only reports new plan selections and active plan renewals and does not report the number of consumers who have paid premiums to effectuate their enrollment.”
Open enrollment will continue for another 6 weeks, with Dec. 15 being the final day to enroll for 2019 coverage on the 39 state exchanges that use the HealthCare.gov platform.
Dark-roast dementia, cocktail dermatitis, and violent good guys
Dark roast has the most
The most … best chance … dark-roast coffee may protect your brain against Parkinson’s disease, okay? Rhyming can be hard. A Canadian study recently found that the compounds in brewed coffee, called phenylindanes, may have neuroprotective effects by inhibiting amyloid-beta, tau, or alpha-synuclein. Researchers examined light roast, dark roast, and decaf dark roast and concluded that the dark roast contains stronger inhibitors. We always figured those ridiculous light-roast coffees were for the weak, but now we have proof.
Researchers also looked at the effect of caffeine. Sweet, sweet caffeine. While a potent psychoactive component, pure caffeine appeared to have no effect on amyloid-beta, tau, or alpha-synuclein aggregation. Does this mean coffee is the cure for Parkinson’s disease? Not quite yet, but keep on chuggin’. And while you’re at it, have some pomegranate, too.
Cocktail dermatitis
Dermatologist Vincent DeLeo, MD, isn’t a psychic or a seer. But he plays one in the examination room. Every now and then, a patient walks in with noninflammatory blisters or hyperpigmentation, often on their hands. Dr. DeLeo takes a look and asks if the patient was enjoying some gin and tonics the previous weekend. “They think you’re God because of course they were,” he told an audience at the recent Coastal Dermatology Symposium.
The culprit? An allergy to the dark green skin of limes, a.k.a. “margarita photodermatitis.” Dr. DeLeo says it may take a few days for the blisters to appear. And he advised colleagues to not photo test the patient because it could make things worse. As for treatment, steroids can help. So can switching to Scotch and soda.
The animals are getting high
Australian animals are getting a contact high, according to a research team that studied stream invertebrates around Melbourne. When we consume pharmaceuticals, our bodies do not totally absorb them. Now, evidence shows that the residual drugs that leave our system are ending up in waterways. What does that mean? It means animals are getting free drugs, and that’s just not fair.
The water-dwelling invertebrates are also passing on these residual compounds to other animals, like spiders who eat invertebrate larvae. Researchers also predicted that platypuses in particular might soon be exposed to high levels of antidepressants. At least the platypuses will be happy.
Health care goes to the movies
Science, as many of those involved in the time-honored but often misunderstood pursuit of truthiness would agree, is a strange, wonderful, yet fickle mistress. One day, she’ll have you comparing the quantity and quality of infant stools or shoving whooping cough bacteria up people’s noses. And the next day, she’ll invite you to join her at the local mega-movie multiplex for the latest Hollywood blockbuster.
Just ask Robert Olympia, MD, of Penn State University, Hershey, and his associates, who watched 10 superhero-based films from 2015 and 2016 and counted the violent acts committed by “good guys” and “bad guys.” Their analysis, presented at the annual meeting of the American Academy of Pediatrics in Orlando, shows that good guys committed 23 violent acts per hour, compared with 18 per hour for the bad guys. Young people who watch these movies “may be influenced by their portrayal of risk-taking behaviors and acts of violence. … Pediatric health care providers should educate families about the violence depicted in this genre of film and the potential dangers that may occur when children attempt to emulate these perceived heroes,” said Dr. Olympia.
Of course, his own superhero-ready name suggests that he may be battling – in a nonviolent way, we’re sure – Bleeding Ulcer, The Bowel Movement, Anal Fissure, Migraineur, and/or The Endoscopist in the next Avengers movie.
Dark roast has the most
The most … best chance … dark-roast coffee may protect your brain against Parkinson’s disease, okay? Rhyming can be hard. A Canadian study recently found that the compounds in brewed coffee, called phenylindanes, may have neuroprotective effects by inhibiting amyloid-beta, tau, or alpha-synuclein. Researchers examined light roast, dark roast, and decaf dark roast and concluded that the dark roast contains stronger inhibitors. We always figured those ridiculous light-roast coffees were for the weak, but now we have proof.
Researchers also looked at the effect of caffeine. Sweet, sweet caffeine. While a potent psychoactive component, pure caffeine appeared to have no effect on amyloid-beta, tau, or alpha-synuclein aggregation. Does this mean coffee is the cure for Parkinson’s disease? Not quite yet, but keep on chuggin’. And while you’re at it, have some pomegranate, too.
Cocktail dermatitis
Dermatologist Vincent DeLeo, MD, isn’t a psychic or a seer. But he plays one in the examination room. Every now and then, a patient walks in with noninflammatory blisters or hyperpigmentation, often on their hands. Dr. DeLeo takes a look and asks if the patient was enjoying some gin and tonics the previous weekend. “They think you’re God because of course they were,” he told an audience at the recent Coastal Dermatology Symposium.
The culprit? An allergy to the dark green skin of limes, a.k.a. “margarita photodermatitis.” Dr. DeLeo says it may take a few days for the blisters to appear. And he advised colleagues to not photo test the patient because it could make things worse. As for treatment, steroids can help. So can switching to Scotch and soda.
The animals are getting high
Australian animals are getting a contact high, according to a research team that studied stream invertebrates around Melbourne. When we consume pharmaceuticals, our bodies do not totally absorb them. Now, evidence shows that the residual drugs that leave our system are ending up in waterways. What does that mean? It means animals are getting free drugs, and that’s just not fair.
The water-dwelling invertebrates are also passing on these residual compounds to other animals, like spiders who eat invertebrate larvae. Researchers also predicted that platypuses in particular might soon be exposed to high levels of antidepressants. At least the platypuses will be happy.
Health care goes to the movies
Science, as many of those involved in the time-honored but often misunderstood pursuit of truthiness would agree, is a strange, wonderful, yet fickle mistress. One day, she’ll have you comparing the quantity and quality of infant stools or shoving whooping cough bacteria up people’s noses. And the next day, she’ll invite you to join her at the local mega-movie multiplex for the latest Hollywood blockbuster.
Just ask Robert Olympia, MD, of Penn State University, Hershey, and his associates, who watched 10 superhero-based films from 2015 and 2016 and counted the violent acts committed by “good guys” and “bad guys.” Their analysis, presented at the annual meeting of the American Academy of Pediatrics in Orlando, shows that good guys committed 23 violent acts per hour, compared with 18 per hour for the bad guys. Young people who watch these movies “may be influenced by their portrayal of risk-taking behaviors and acts of violence. … Pediatric health care providers should educate families about the violence depicted in this genre of film and the potential dangers that may occur when children attempt to emulate these perceived heroes,” said Dr. Olympia.
Of course, his own superhero-ready name suggests that he may be battling – in a nonviolent way, we’re sure – Bleeding Ulcer, The Bowel Movement, Anal Fissure, Migraineur, and/or The Endoscopist in the next Avengers movie.
Dark roast has the most
The most … best chance … dark-roast coffee may protect your brain against Parkinson’s disease, okay? Rhyming can be hard. A Canadian study recently found that the compounds in brewed coffee, called phenylindanes, may have neuroprotective effects by inhibiting amyloid-beta, tau, or alpha-synuclein. Researchers examined light roast, dark roast, and decaf dark roast and concluded that the dark roast contains stronger inhibitors. We always figured those ridiculous light-roast coffees were for the weak, but now we have proof.
Researchers also looked at the effect of caffeine. Sweet, sweet caffeine. While a potent psychoactive component, pure caffeine appeared to have no effect on amyloid-beta, tau, or alpha-synuclein aggregation. Does this mean coffee is the cure for Parkinson’s disease? Not quite yet, but keep on chuggin’. And while you’re at it, have some pomegranate, too.
Cocktail dermatitis
Dermatologist Vincent DeLeo, MD, isn’t a psychic or a seer. But he plays one in the examination room. Every now and then, a patient walks in with noninflammatory blisters or hyperpigmentation, often on their hands. Dr. DeLeo takes a look and asks if the patient was enjoying some gin and tonics the previous weekend. “They think you’re God because of course they were,” he told an audience at the recent Coastal Dermatology Symposium.
The culprit? An allergy to the dark green skin of limes, a.k.a. “margarita photodermatitis.” Dr. DeLeo says it may take a few days for the blisters to appear. And he advised colleagues to not photo test the patient because it could make things worse. As for treatment, steroids can help. So can switching to Scotch and soda.
The animals are getting high
Australian animals are getting a contact high, according to a research team that studied stream invertebrates around Melbourne. When we consume pharmaceuticals, our bodies do not totally absorb them. Now, evidence shows that the residual drugs that leave our system are ending up in waterways. What does that mean? It means animals are getting free drugs, and that’s just not fair.
The water-dwelling invertebrates are also passing on these residual compounds to other animals, like spiders who eat invertebrate larvae. Researchers also predicted that platypuses in particular might soon be exposed to high levels of antidepressants. At least the platypuses will be happy.
Health care goes to the movies
Science, as many of those involved in the time-honored but often misunderstood pursuit of truthiness would agree, is a strange, wonderful, yet fickle mistress. One day, she’ll have you comparing the quantity and quality of infant stools or shoving whooping cough bacteria up people’s noses. And the next day, she’ll invite you to join her at the local mega-movie multiplex for the latest Hollywood blockbuster.
Just ask Robert Olympia, MD, of Penn State University, Hershey, and his associates, who watched 10 superhero-based films from 2015 and 2016 and counted the violent acts committed by “good guys” and “bad guys.” Their analysis, presented at the annual meeting of the American Academy of Pediatrics in Orlando, shows that good guys committed 23 violent acts per hour, compared with 18 per hour for the bad guys. Young people who watch these movies “may be influenced by their portrayal of risk-taking behaviors and acts of violence. … Pediatric health care providers should educate families about the violence depicted in this genre of film and the potential dangers that may occur when children attempt to emulate these perceived heroes,” said Dr. Olympia.
Of course, his own superhero-ready name suggests that he may be battling – in a nonviolent way, we’re sure – Bleeding Ulcer, The Bowel Movement, Anal Fissure, Migraineur, and/or The Endoscopist in the next Avengers movie.
Ecstasy for PTSD, cockroach-tough C. diff, cardio-friendly queso
Rolling in ecstasy
Treating post-traumatic stress disorder could now be as simple as hitting the club. Not really, but in the longest and largest study of its kind, researchers looked at the effects of MDMA on patients with chronic PTSD.
After three sessions of taking MDMA (in a controlled environment, not in a warehouse in Brooklyn), 76% of study participants no longer met the criteria for PTSD. This is excellent news for those who suffer from PTSD – and the latest breakthrough in a significant shift toward accepting hallucinogenic drugs as possible treatments for mental health issues. Who knows, perhaps medicinal molly cards could soon be appearing.
And what next after that? Ketamine? Oh wait.
Infection is its own reward
Cockroaches are tough. Really tough. Survive compression forces of 300 times their body weight tough. Live without a head for a week tough. Laugh off a nuclear Armageddon tough. Can anything be tougher than that? Researchers at De Montfort University in Leicester, England, have a possible candidate, and it’s not Chuck Norris (Infect Control Hosp Epidemiol. 2018 Oct 16:1-6. doi: 10.1017/ice.2018.255).
They took cotton bed sheets contaminated with Clostridium difficile and put them “through a simulated washer extractor cycle using an industrial bleach detergent with sodium hypochlorite 15% and peracetic acid sour 14%.” Other contaminated sheets went to a commercial laundry service, “where they were washed in a washer extractor (infected linen wash) with industrial detergent, pressed, dried, and finished according to the current National Health Service in the United Kingdom’s health care laundry policy,” they said in a separate written statement. The result of all that effort? The average C. difficile spore load was reduced by 40%. In other words, most of the spores survived.
That not-so-comforting outcome does, however, leave us with a slightly comforting bit of conjecture: Those super tough cockroaches – the ones that survive the apocalypse that wipes out humans – will probably have diarrhea.
More cheese, please
The healing powers of cheese are now backed with science. A study from the University of Eastern Finland examined the incidence of coronary heart disease in men who ate a lot of fermented dairy (cheese, yogurt, kefir) and men who did not.
Researchers divided 2,000 men into four groups based on fermented dairy consumption and found that the men in the highest-consumption group had a 26% lower risk of incident coronary heart disease. Unfortunately for the “Got Milk?” ad campaign, researchers also discovered that men who consumed high levels of non-fermented dairy had a higher risk of coronary heart disease.
Next time your doctor asks about your cheese consumption, you can show them this study as proof that cheese helps the heart and the soul.
The new math, health care edition
You may think that 2 plus 2 always equals 4, but health care billing has taken another route. Here’s a seemingly simple equation, as reported by Kaiser Health News: One patient with a rash that got worse when she used her antifungal cream plus one allergy skin-patch test (okay, so it involved 119 allergens – we’ll give you that) at Stanford (Calif.) Health Care equals one bill … for $48,329.
The patient, Janet Winston of Eureka, Calif., said, “I was grateful I had such wonderful care at Stanford, but I was pretty outraged they could charge that. … No one cut into me. No one gave me anesthesia.” Her insurer paid its negotiated share of $11,376.47, and Ms. Winston’s 20% share of that came to $3,103.73, which she bargained down to $1,561.86.
For insurers, large health systems like Stanford may be too big to fight, suggested Harvard University health care economist Leemore Dafny, who told KHN that “everyone wants to point fingers at the providers, but … a lot of times [insurers] roll over and pay the rates.”
In the end, though, Stanford received less than $13,000 of its original charge, so maybe 2 plus 2 only equals 3. A tough pill to swallow, perhaps, but the whole situation has a kind of chilling Donnie-and-Marie quality to it: a little bit new math, and a little bit “1984.”
Rolling in ecstasy
Treating post-traumatic stress disorder could now be as simple as hitting the club. Not really, but in the longest and largest study of its kind, researchers looked at the effects of MDMA on patients with chronic PTSD.
After three sessions of taking MDMA (in a controlled environment, not in a warehouse in Brooklyn), 76% of study participants no longer met the criteria for PTSD. This is excellent news for those who suffer from PTSD – and the latest breakthrough in a significant shift toward accepting hallucinogenic drugs as possible treatments for mental health issues. Who knows, perhaps medicinal molly cards could soon be appearing.
And what next after that? Ketamine? Oh wait.
Infection is its own reward
Cockroaches are tough. Really tough. Survive compression forces of 300 times their body weight tough. Live without a head for a week tough. Laugh off a nuclear Armageddon tough. Can anything be tougher than that? Researchers at De Montfort University in Leicester, England, have a possible candidate, and it’s not Chuck Norris (Infect Control Hosp Epidemiol. 2018 Oct 16:1-6. doi: 10.1017/ice.2018.255).
They took cotton bed sheets contaminated with Clostridium difficile and put them “through a simulated washer extractor cycle using an industrial bleach detergent with sodium hypochlorite 15% and peracetic acid sour 14%.” Other contaminated sheets went to a commercial laundry service, “where they were washed in a washer extractor (infected linen wash) with industrial detergent, pressed, dried, and finished according to the current National Health Service in the United Kingdom’s health care laundry policy,” they said in a separate written statement. The result of all that effort? The average C. difficile spore load was reduced by 40%. In other words, most of the spores survived.
That not-so-comforting outcome does, however, leave us with a slightly comforting bit of conjecture: Those super tough cockroaches – the ones that survive the apocalypse that wipes out humans – will probably have diarrhea.
More cheese, please
The healing powers of cheese are now backed with science. A study from the University of Eastern Finland examined the incidence of coronary heart disease in men who ate a lot of fermented dairy (cheese, yogurt, kefir) and men who did not.
Researchers divided 2,000 men into four groups based on fermented dairy consumption and found that the men in the highest-consumption group had a 26% lower risk of incident coronary heart disease. Unfortunately for the “Got Milk?” ad campaign, researchers also discovered that men who consumed high levels of non-fermented dairy had a higher risk of coronary heart disease.
Next time your doctor asks about your cheese consumption, you can show them this study as proof that cheese helps the heart and the soul.
The new math, health care edition
You may think that 2 plus 2 always equals 4, but health care billing has taken another route. Here’s a seemingly simple equation, as reported by Kaiser Health News: One patient with a rash that got worse when she used her antifungal cream plus one allergy skin-patch test (okay, so it involved 119 allergens – we’ll give you that) at Stanford (Calif.) Health Care equals one bill … for $48,329.
The patient, Janet Winston of Eureka, Calif., said, “I was grateful I had such wonderful care at Stanford, but I was pretty outraged they could charge that. … No one cut into me. No one gave me anesthesia.” Her insurer paid its negotiated share of $11,376.47, and Ms. Winston’s 20% share of that came to $3,103.73, which she bargained down to $1,561.86.
For insurers, large health systems like Stanford may be too big to fight, suggested Harvard University health care economist Leemore Dafny, who told KHN that “everyone wants to point fingers at the providers, but … a lot of times [insurers] roll over and pay the rates.”
In the end, though, Stanford received less than $13,000 of its original charge, so maybe 2 plus 2 only equals 3. A tough pill to swallow, perhaps, but the whole situation has a kind of chilling Donnie-and-Marie quality to it: a little bit new math, and a little bit “1984.”
Rolling in ecstasy
Treating post-traumatic stress disorder could now be as simple as hitting the club. Not really, but in the longest and largest study of its kind, researchers looked at the effects of MDMA on patients with chronic PTSD.
After three sessions of taking MDMA (in a controlled environment, not in a warehouse in Brooklyn), 76% of study participants no longer met the criteria for PTSD. This is excellent news for those who suffer from PTSD – and the latest breakthrough in a significant shift toward accepting hallucinogenic drugs as possible treatments for mental health issues. Who knows, perhaps medicinal molly cards could soon be appearing.
And what next after that? Ketamine? Oh wait.
Infection is its own reward
Cockroaches are tough. Really tough. Survive compression forces of 300 times their body weight tough. Live without a head for a week tough. Laugh off a nuclear Armageddon tough. Can anything be tougher than that? Researchers at De Montfort University in Leicester, England, have a possible candidate, and it’s not Chuck Norris (Infect Control Hosp Epidemiol. 2018 Oct 16:1-6. doi: 10.1017/ice.2018.255).
They took cotton bed sheets contaminated with Clostridium difficile and put them “through a simulated washer extractor cycle using an industrial bleach detergent with sodium hypochlorite 15% and peracetic acid sour 14%.” Other contaminated sheets went to a commercial laundry service, “where they were washed in a washer extractor (infected linen wash) with industrial detergent, pressed, dried, and finished according to the current National Health Service in the United Kingdom’s health care laundry policy,” they said in a separate written statement. The result of all that effort? The average C. difficile spore load was reduced by 40%. In other words, most of the spores survived.
That not-so-comforting outcome does, however, leave us with a slightly comforting bit of conjecture: Those super tough cockroaches – the ones that survive the apocalypse that wipes out humans – will probably have diarrhea.
More cheese, please
The healing powers of cheese are now backed with science. A study from the University of Eastern Finland examined the incidence of coronary heart disease in men who ate a lot of fermented dairy (cheese, yogurt, kefir) and men who did not.
Researchers divided 2,000 men into four groups based on fermented dairy consumption and found that the men in the highest-consumption group had a 26% lower risk of incident coronary heart disease. Unfortunately for the “Got Milk?” ad campaign, researchers also discovered that men who consumed high levels of non-fermented dairy had a higher risk of coronary heart disease.
Next time your doctor asks about your cheese consumption, you can show them this study as proof that cheese helps the heart and the soul.
The new math, health care edition
You may think that 2 plus 2 always equals 4, but health care billing has taken another route. Here’s a seemingly simple equation, as reported by Kaiser Health News: One patient with a rash that got worse when she used her antifungal cream plus one allergy skin-patch test (okay, so it involved 119 allergens – we’ll give you that) at Stanford (Calif.) Health Care equals one bill … for $48,329.
The patient, Janet Winston of Eureka, Calif., said, “I was grateful I had such wonderful care at Stanford, but I was pretty outraged they could charge that. … No one cut into me. No one gave me anesthesia.” Her insurer paid its negotiated share of $11,376.47, and Ms. Winston’s 20% share of that came to $3,103.73, which she bargained down to $1,561.86.
For insurers, large health systems like Stanford may be too big to fight, suggested Harvard University health care economist Leemore Dafny, who told KHN that “everyone wants to point fingers at the providers, but … a lot of times [insurers] roll over and pay the rates.”
In the end, though, Stanford received less than $13,000 of its original charge, so maybe 2 plus 2 only equals 3. A tough pill to swallow, perhaps, but the whole situation has a kind of chilling Donnie-and-Marie quality to it: a little bit new math, and a little bit “1984.”