User login
Richard Franki is the associate editor who writes and creates graphs. He started with the company in 1987, when it was known as the International Medical News Group. In his years as a journalist, Richard has worked for Cap Cities/ABC, Disney, Harcourt, Elsevier, Quadrant, Frontline, and Internet Brands. In the 1990s, he was a contributor to the ill-fated Indications column, predecessor of Livin' on the MDedge.
Open enrollment 2020: HealthCare.gov activity down from last year
The federal health insurance exchange is now through the first 2 weeks of its 2020 open enrollment on the HealthCare.gov platform, and just over 930,000 plans have been selected, the Centers for Medicare & Medicaid Services reported.
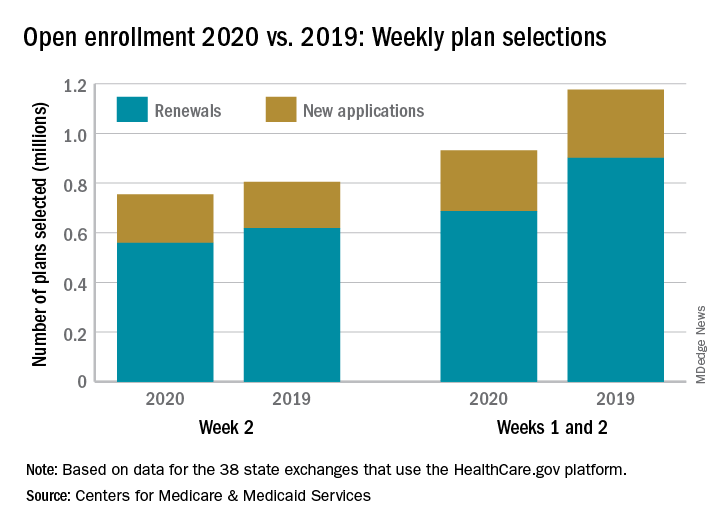
The majority of those selections – almost 690,000 – were made by consumers renewing their existing coverage, with the rest coming from new consumers who did not have exchange coverage for 2019, the CMS said in its weekly enrollment snapshot on Nov. 13.
The total number of plans selected through week 2 is down almost 21% from last year, when selections totaled almost 1.18 million. This year, however, week 1 of open enrollment was only 2 days long (Nov. 1-2), versus 3 days (Nov. 1-3) last year, and last year there were 39 states using HealthCare.gov, compared with 38 this year since Nevada now has its own state-based exchange.
The total number of plans selected during a particular reporting period can change later if plans are modified or canceled, CMS noted, and “the weekly snapshot only reports new plan selections and active plan renewals and does not report the number of consumers who have paid premiums to effectuate their enrollment.”
The federal health insurance exchange is now through the first 2 weeks of its 2020 open enrollment on the HealthCare.gov platform, and just over 930,000 plans have been selected, the Centers for Medicare & Medicaid Services reported.
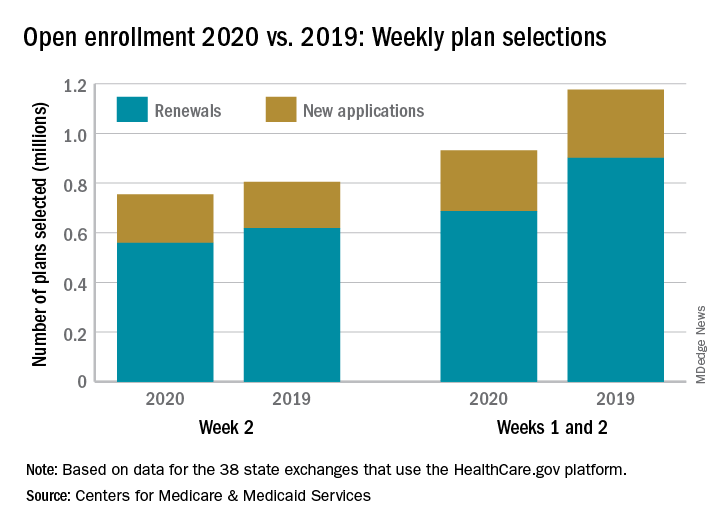
The majority of those selections – almost 690,000 – were made by consumers renewing their existing coverage, with the rest coming from new consumers who did not have exchange coverage for 2019, the CMS said in its weekly enrollment snapshot on Nov. 13.
The total number of plans selected through week 2 is down almost 21% from last year, when selections totaled almost 1.18 million. This year, however, week 1 of open enrollment was only 2 days long (Nov. 1-2), versus 3 days (Nov. 1-3) last year, and last year there were 39 states using HealthCare.gov, compared with 38 this year since Nevada now has its own state-based exchange.
The total number of plans selected during a particular reporting period can change later if plans are modified or canceled, CMS noted, and “the weekly snapshot only reports new plan selections and active plan renewals and does not report the number of consumers who have paid premiums to effectuate their enrollment.”
The federal health insurance exchange is now through the first 2 weeks of its 2020 open enrollment on the HealthCare.gov platform, and just over 930,000 plans have been selected, the Centers for Medicare & Medicaid Services reported.
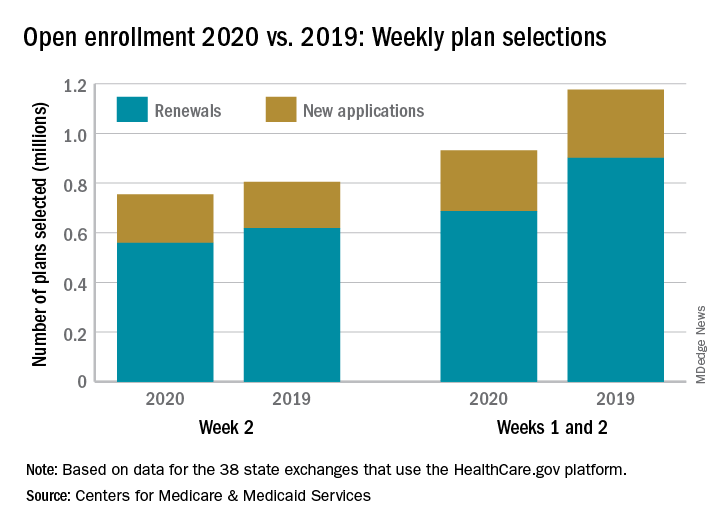
The majority of those selections – almost 690,000 – were made by consumers renewing their existing coverage, with the rest coming from new consumers who did not have exchange coverage for 2019, the CMS said in its weekly enrollment snapshot on Nov. 13.
The total number of plans selected through week 2 is down almost 21% from last year, when selections totaled almost 1.18 million. This year, however, week 1 of open enrollment was only 2 days long (Nov. 1-2), versus 3 days (Nov. 1-3) last year, and last year there were 39 states using HealthCare.gov, compared with 38 this year since Nevada now has its own state-based exchange.
The total number of plans selected during a particular reporting period can change later if plans are modified or canceled, CMS noted, and “the weekly snapshot only reports new plan selections and active plan renewals and does not report the number of consumers who have paid premiums to effectuate their enrollment.”
Spray-painted bandages and pharma sings ‘Dough Canada!’
He’s not quite dead yet!
In 2015, Benjamin Schreiber, an Iowa man convicted of murder and sentenced to life in prison without parole, developed a case of septic poisoning because of large, untreated kidney stones. While at the hospital, his heart stopped several times, requiring resuscitation. After being stabilized, he underwent surgery to remove the kidney stones and was then released back to his prison cell.
Fast forward to 2018. Mr. Schreiber filed for relief from his conviction, arguing that, because he technically died, his life sentence had been served and he should be released. While the logic is impeccable, an Iowa district court didn’t buy it, noting that the fact that Mr. Schreiber was able to submit a petition for his release “confirms the petitioner’s current status as living.”
Sadly for Mr. Schreiber, the Iowa Court of Appeals agreed with the lower court’s decision. In a wonderfully pithy summation of the case, Judge Amanda Potterfield wrote: “Schreiber is either still alive, in which case he must remain in prison, or he is actually dead, in which case this appeal is moot.”
While the Livin’ on the MDedge team is glad that a convicted murderer will not be released back into the public, we salute his devotion to the art of technicality. The judges may not have been convinced, but you’re dead to us, Mr. Schreiber.
Breaking news: Drug companies gouge consumers
Canada. It’s home to many things: Trees, glaciers, beavers, and several people. But we Americans also know it as the home of cheap drugs. It may be borderline illegal, but that’s never stopped America from taking things that don’t belong to us before.
You’d think then that it’d be great being sick in Canada. But it turns out that many of those poor, desperate souls living in the frozen tundra of the north are actually overpaying for drugs just like the rest of us, according to research published in the Canadian Medical Association Journal.
It all comes down to those strange items called drug discount cards. They’re coupons offered by brand-name drug manufacturers to keep patients from switching to cheap generics.
Sounds great, right? Well, while a few patients saw savings, the average cost to patients with public insurance increased by 1.3% over generics. And if you were unfortunate enough to have private insurance, you’d be paying 46% more using the cards rather than generics. In some instances, patients were paying a whole $10 more for a prescription of the name brand, compared with the generic. And we thought Tim Hortons was our northern neighbor’s only company making a lot of dough. Ten loonies more per Rx ain’t Timbits.
So, Canada, how does it feel to have your health care made fun of? U-S-A! U-S-A! Now, if you’ll excuse us, we’re off to pay $1,000 a pill to cure us some hepatitis C. That’s some real red-blooded American price gouging right there.
This looks like a job for vacuum science
The LOTME staff, of course, scans a veritable buffet of sources to come up with the tasty tidbits we present each week to our deliciously wonderful and highly scrumptious readers each week.
One of our favorite sauces … umm, we mean sources, and the home of a tantalizing medical morsel (can you tell it’s almost lunch time?), is the Journal of Vacuum Science and Technology B. That’s B, not A. Anyone, at least anyone who’s serious about vacuum science, will tell you that the Journal of Vacuum Science and Technology A is pretty much a bottomless pit of trolling, political bickering, and popular nonsense. But B, now that’s a different story.
B is where we meet the EStAD (electrostatic and air driven) device. EStAD is a portable device that may someday offer physicians and first responders a way to treat wounds in rural areas where immediate care may not be available, the investigators said.
EStAD, using a process called electrospinning along with a confined electric field, works like a can of spray paint to deposit a fiber mat, which could be a bandage or a drug, onto a wound.
The device is still under development, but the research team reports that it has been successfully tested on a porcine skin incision and a gloved human hand.
The next step in EStAD development is to bring it to Washington, where the investigators will see if spray-on bandages can stand up to the hot air coming out of politicians’ mouths. We’re hoping that they sell tickets.
He’s not quite dead yet!
In 2015, Benjamin Schreiber, an Iowa man convicted of murder and sentenced to life in prison without parole, developed a case of septic poisoning because of large, untreated kidney stones. While at the hospital, his heart stopped several times, requiring resuscitation. After being stabilized, he underwent surgery to remove the kidney stones and was then released back to his prison cell.
Fast forward to 2018. Mr. Schreiber filed for relief from his conviction, arguing that, because he technically died, his life sentence had been served and he should be released. While the logic is impeccable, an Iowa district court didn’t buy it, noting that the fact that Mr. Schreiber was able to submit a petition for his release “confirms the petitioner’s current status as living.”
Sadly for Mr. Schreiber, the Iowa Court of Appeals agreed with the lower court’s decision. In a wonderfully pithy summation of the case, Judge Amanda Potterfield wrote: “Schreiber is either still alive, in which case he must remain in prison, or he is actually dead, in which case this appeal is moot.”
While the Livin’ on the MDedge team is glad that a convicted murderer will not be released back into the public, we salute his devotion to the art of technicality. The judges may not have been convinced, but you’re dead to us, Mr. Schreiber.
Breaking news: Drug companies gouge consumers
Canada. It’s home to many things: Trees, glaciers, beavers, and several people. But we Americans also know it as the home of cheap drugs. It may be borderline illegal, but that’s never stopped America from taking things that don’t belong to us before.
You’d think then that it’d be great being sick in Canada. But it turns out that many of those poor, desperate souls living in the frozen tundra of the north are actually overpaying for drugs just like the rest of us, according to research published in the Canadian Medical Association Journal.
It all comes down to those strange items called drug discount cards. They’re coupons offered by brand-name drug manufacturers to keep patients from switching to cheap generics.
Sounds great, right? Well, while a few patients saw savings, the average cost to patients with public insurance increased by 1.3% over generics. And if you were unfortunate enough to have private insurance, you’d be paying 46% more using the cards rather than generics. In some instances, patients were paying a whole $10 more for a prescription of the name brand, compared with the generic. And we thought Tim Hortons was our northern neighbor’s only company making a lot of dough. Ten loonies more per Rx ain’t Timbits.
So, Canada, how does it feel to have your health care made fun of? U-S-A! U-S-A! Now, if you’ll excuse us, we’re off to pay $1,000 a pill to cure us some hepatitis C. That’s some real red-blooded American price gouging right there.
This looks like a job for vacuum science
The LOTME staff, of course, scans a veritable buffet of sources to come up with the tasty tidbits we present each week to our deliciously wonderful and highly scrumptious readers each week.
One of our favorite sauces … umm, we mean sources, and the home of a tantalizing medical morsel (can you tell it’s almost lunch time?), is the Journal of Vacuum Science and Technology B. That’s B, not A. Anyone, at least anyone who’s serious about vacuum science, will tell you that the Journal of Vacuum Science and Technology A is pretty much a bottomless pit of trolling, political bickering, and popular nonsense. But B, now that’s a different story.
B is where we meet the EStAD (electrostatic and air driven) device. EStAD is a portable device that may someday offer physicians and first responders a way to treat wounds in rural areas where immediate care may not be available, the investigators said.
EStAD, using a process called electrospinning along with a confined electric field, works like a can of spray paint to deposit a fiber mat, which could be a bandage or a drug, onto a wound.
The device is still under development, but the research team reports that it has been successfully tested on a porcine skin incision and a gloved human hand.
The next step in EStAD development is to bring it to Washington, where the investigators will see if spray-on bandages can stand up to the hot air coming out of politicians’ mouths. We’re hoping that they sell tickets.
He’s not quite dead yet!
In 2015, Benjamin Schreiber, an Iowa man convicted of murder and sentenced to life in prison without parole, developed a case of septic poisoning because of large, untreated kidney stones. While at the hospital, his heart stopped several times, requiring resuscitation. After being stabilized, he underwent surgery to remove the kidney stones and was then released back to his prison cell.
Fast forward to 2018. Mr. Schreiber filed for relief from his conviction, arguing that, because he technically died, his life sentence had been served and he should be released. While the logic is impeccable, an Iowa district court didn’t buy it, noting that the fact that Mr. Schreiber was able to submit a petition for his release “confirms the petitioner’s current status as living.”
Sadly for Mr. Schreiber, the Iowa Court of Appeals agreed with the lower court’s decision. In a wonderfully pithy summation of the case, Judge Amanda Potterfield wrote: “Schreiber is either still alive, in which case he must remain in prison, or he is actually dead, in which case this appeal is moot.”
While the Livin’ on the MDedge team is glad that a convicted murderer will not be released back into the public, we salute his devotion to the art of technicality. The judges may not have been convinced, but you’re dead to us, Mr. Schreiber.
Breaking news: Drug companies gouge consumers
Canada. It’s home to many things: Trees, glaciers, beavers, and several people. But we Americans also know it as the home of cheap drugs. It may be borderline illegal, but that’s never stopped America from taking things that don’t belong to us before.
You’d think then that it’d be great being sick in Canada. But it turns out that many of those poor, desperate souls living in the frozen tundra of the north are actually overpaying for drugs just like the rest of us, according to research published in the Canadian Medical Association Journal.
It all comes down to those strange items called drug discount cards. They’re coupons offered by brand-name drug manufacturers to keep patients from switching to cheap generics.
Sounds great, right? Well, while a few patients saw savings, the average cost to patients with public insurance increased by 1.3% over generics. And if you were unfortunate enough to have private insurance, you’d be paying 46% more using the cards rather than generics. In some instances, patients were paying a whole $10 more for a prescription of the name brand, compared with the generic. And we thought Tim Hortons was our northern neighbor’s only company making a lot of dough. Ten loonies more per Rx ain’t Timbits.
So, Canada, how does it feel to have your health care made fun of? U-S-A! U-S-A! Now, if you’ll excuse us, we’re off to pay $1,000 a pill to cure us some hepatitis C. That’s some real red-blooded American price gouging right there.
This looks like a job for vacuum science
The LOTME staff, of course, scans a veritable buffet of sources to come up with the tasty tidbits we present each week to our deliciously wonderful and highly scrumptious readers each week.
One of our favorite sauces … umm, we mean sources, and the home of a tantalizing medical morsel (can you tell it’s almost lunch time?), is the Journal of Vacuum Science and Technology B. That’s B, not A. Anyone, at least anyone who’s serious about vacuum science, will tell you that the Journal of Vacuum Science and Technology A is pretty much a bottomless pit of trolling, political bickering, and popular nonsense. But B, now that’s a different story.
B is where we meet the EStAD (electrostatic and air driven) device. EStAD is a portable device that may someday offer physicians and first responders a way to treat wounds in rural areas where immediate care may not be available, the investigators said.
EStAD, using a process called electrospinning along with a confined electric field, works like a can of spray paint to deposit a fiber mat, which could be a bandage or a drug, onto a wound.
The device is still under development, but the research team reports that it has been successfully tested on a porcine skin incision and a gloved human hand.
The next step in EStAD development is to bring it to Washington, where the investigators will see if spray-on bandages can stand up to the hot air coming out of politicians’ mouths. We’re hoping that they sell tickets.
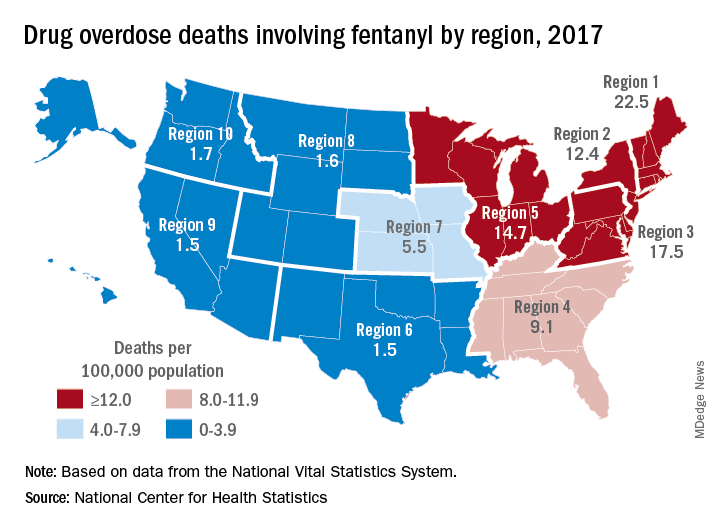
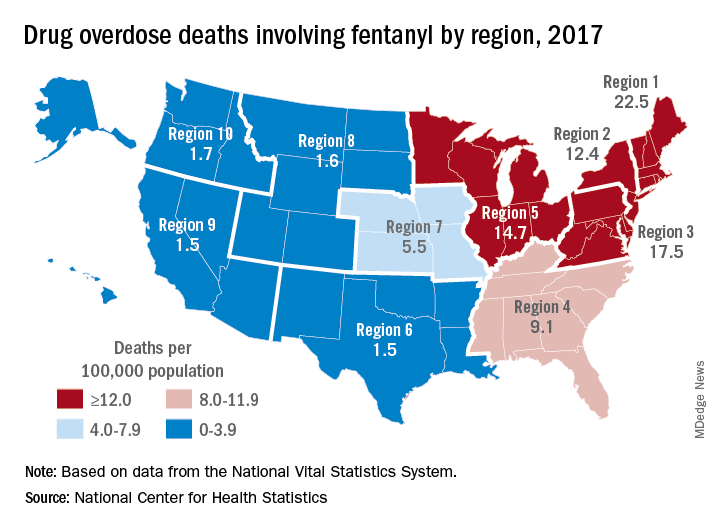
Fentanyl-related deaths show strong regional pattern
Fentanyl was involved in more overdose deaths than any other drug in 2017, and the death rate in New England was 15 times higher than in regions of the Midwest and West, according to the National Center for Health Statistics.
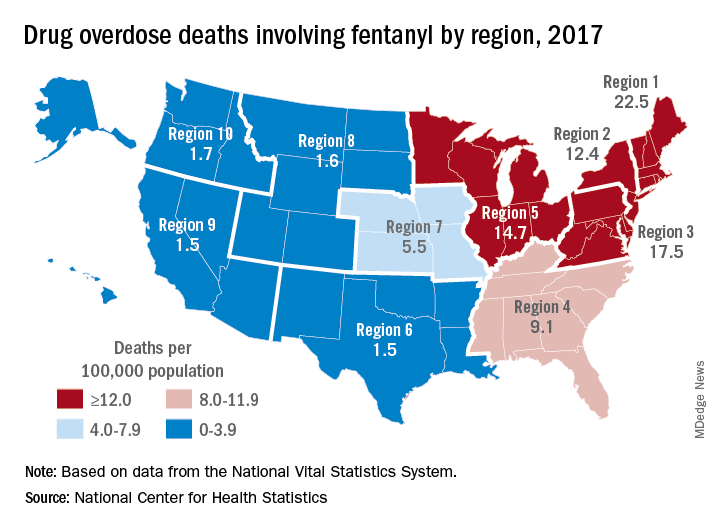
Nationally, fentanyl was involved in 39% of all drug overdose deaths and had an age-adjusted death rate of 8.7/100,000 standard population in 2017. In 2016, when fentanyl also was the most involved drug in the United States, the corresponding figures were 29% and 5.9/100,000, the agency said in a recent report.
Fentanyl was the most involved drug in overdose deaths for 6 of the country’s 10 public health regions in 2017, with a clear pattern of decreasing use from east to west. The highest death rate (22.5/100,000) occurred in Region 1 (New England) and the lowest rates (1.5/100,000) came in Region 6 (Arkansas, Louisiana, New Mexico, Oklahoma, and Texas) and Region 9 (Arizona, California, Hawaii, and Nevada), the researchers said.
A somewhat similar pattern was seen for heroin, which was second nationally on the list of drugs most frequently involved in overdose deaths (23%), except that New England was somewhat below three other regions in the East and upper Midwest. The highest heroin death rate (8.6/100,000) was seen in Region 2 (New Jersey and New York) and the lowest (2.2) occurred in Region 9, they said, based on data from the National Vital Statistics System’s mortality files.
The fentanyl pattern was even more closely repeated with cocaine, third in involvement nationally at 21% of overdose deaths in 2017. The high in overdose deaths (9.5/100,000) came in Region 1 again, and the low in Region 9 (1.3), along with Region 7 (Iowa, Kansas, Missouri, and Nebraska) and Region 10 (Alaska, Idaho, Oregon, and Washington), the report showed.
The regional pattern of overdose deaths for methamphetamine, which was fourth nationally in involvement (13.3%), basically reversed the other three drugs: highest in the West and lowest in the Northeast. Region 9 had the highest death rate (5.2/100,000) and Region 2 the lowest (0.4), with Region 1 just ahead at 0.6.
Fentanyl was involved in more overdose deaths than any other drug in 2017, and the death rate in New England was 15 times higher than in regions of the Midwest and West, according to the National Center for Health Statistics.
Nationally, fentanyl was involved in 39% of all drug overdose deaths and had an age-adjusted death rate of 8.7/100,000 standard population in 2017. In 2016, when fentanyl also was the most involved drug in the United States, the corresponding figures were 29% and 5.9/100,000, the agency said in a recent report.
Fentanyl was the most involved drug in overdose deaths for 6 of the country’s 10 public health regions in 2017, with a clear pattern of decreasing use from east to west. The highest death rate (22.5/100,000) occurred in Region 1 (New England) and the lowest rates (1.5/100,000) came in Region 6 (Arkansas, Louisiana, New Mexico, Oklahoma, and Texas) and Region 9 (Arizona, California, Hawaii, and Nevada), the researchers said.
A somewhat similar pattern was seen for heroin, which was second nationally on the list of drugs most frequently involved in overdose deaths (23%), except that New England was somewhat below three other regions in the East and upper Midwest. The highest heroin death rate (8.6/100,000) was seen in Region 2 (New Jersey and New York) and the lowest (2.2) occurred in Region 9, they said, based on data from the National Vital Statistics System’s mortality files.
The fentanyl pattern was even more closely repeated with cocaine, third in involvement nationally at 21% of overdose deaths in 2017. The high in overdose deaths (9.5/100,000) came in Region 1 again, and the low in Region 9 (1.3), along with Region 7 (Iowa, Kansas, Missouri, and Nebraska) and Region 10 (Alaska, Idaho, Oregon, and Washington), the report showed.
The regional pattern of overdose deaths for methamphetamine, which was fourth nationally in involvement (13.3%), basically reversed the other three drugs: highest in the West and lowest in the Northeast. Region 9 had the highest death rate (5.2/100,000) and Region 2 the lowest (0.4), with Region 1 just ahead at 0.6.
Fentanyl was involved in more overdose deaths than any other drug in 2017, and the death rate in New England was 15 times higher than in regions of the Midwest and West, according to the National Center for Health Statistics.
Nationally, fentanyl was involved in 39% of all drug overdose deaths and had an age-adjusted death rate of 8.7/100,000 standard population in 2017. In 2016, when fentanyl also was the most involved drug in the United States, the corresponding figures were 29% and 5.9/100,000, the agency said in a recent report.
Fentanyl was the most involved drug in overdose deaths for 6 of the country’s 10 public health regions in 2017, with a clear pattern of decreasing use from east to west. The highest death rate (22.5/100,000) occurred in Region 1 (New England) and the lowest rates (1.5/100,000) came in Region 6 (Arkansas, Louisiana, New Mexico, Oklahoma, and Texas) and Region 9 (Arizona, California, Hawaii, and Nevada), the researchers said.
A somewhat similar pattern was seen for heroin, which was second nationally on the list of drugs most frequently involved in overdose deaths (23%), except that New England was somewhat below three other regions in the East and upper Midwest. The highest heroin death rate (8.6/100,000) was seen in Region 2 (New Jersey and New York) and the lowest (2.2) occurred in Region 9, they said, based on data from the National Vital Statistics System’s mortality files.
The fentanyl pattern was even more closely repeated with cocaine, third in involvement nationally at 21% of overdose deaths in 2017. The high in overdose deaths (9.5/100,000) came in Region 1 again, and the low in Region 9 (1.3), along with Region 7 (Iowa, Kansas, Missouri, and Nebraska) and Region 10 (Alaska, Idaho, Oregon, and Washington), the report showed.
The regional pattern of overdose deaths for methamphetamine, which was fourth nationally in involvement (13.3%), basically reversed the other three drugs: highest in the West and lowest in the Northeast. Region 9 had the highest death rate (5.2/100,000) and Region 2 the lowest (0.4), with Region 1 just ahead at 0.6.
Medicare beneficiaries pay most for Alzheimer’s
according to the Kaiser Family Foundation.
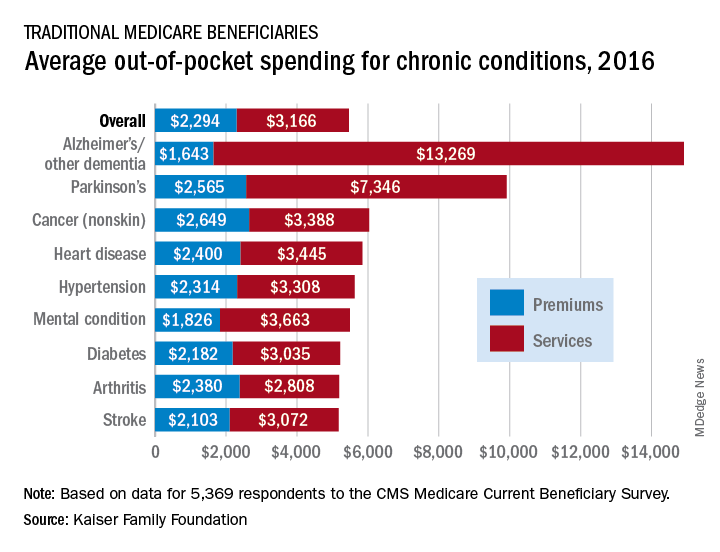
Out-of-pocket spending for Alzheimer’s disease or other dementia was higher than any other chronic condition, averaging $14,913 in 2016 (the latest year for which data are available), compared with $5,460 for all beneficiaries in traditional Medicare, Kaiser investigators said in a recent report based on data for 5,369 respondents to the Medicare Current Beneficiary Survey.
Those totals were divided between services – including long-term care facilities, medical providers and supplies, and prescription drugs – and premiums for Medicare and other types of supplemental insurance. The premium associated with Alzheimer’s, $1,643, was the lowest of any major chronic condition, but the average cost for services, $13,269, was almost twice as high as the next most expensive condition, Parkinson’s disease, and more than four times higher than the overall Medicare average, Juliette Cubanski, PhD, and associates said.
Out-of-pocket costs are higher for patients with Alzheimer’s and Parkinson’s because “these beneficiaries are more likely to reside in a long-term care facility than those with other conditions,” they said. In 2016, out-of-pocket spending on long-term care facility services averaged over $27,000 for Medicare beneficiaries with Alzheimer’s and other dementia and over $28,000 for those with Parkinson’s disease. For all traditional Medicare beneficiaries, average out-of-pocket spending on such services was $1,014.
“The fact that traditional Medicare does not have an annual out-of-pocket limit and does not cover certain services that older adults are more likely to need may undermine the financial security that Medicare provides, especially for people with significant needs and limited incomes. Addressing these gaps would help to alleviate the financial burden of health care for people with Medicare, although doing so would also increase federal spending and taxes,” Dr. Cubanski and associates wrote.
according to the Kaiser Family Foundation.
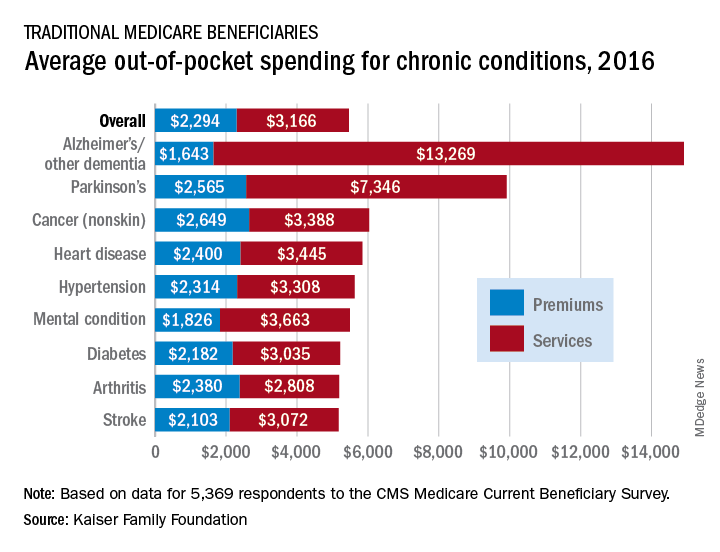
Out-of-pocket spending for Alzheimer’s disease or other dementia was higher than any other chronic condition, averaging $14,913 in 2016 (the latest year for which data are available), compared with $5,460 for all beneficiaries in traditional Medicare, Kaiser investigators said in a recent report based on data for 5,369 respondents to the Medicare Current Beneficiary Survey.
Those totals were divided between services – including long-term care facilities, medical providers and supplies, and prescription drugs – and premiums for Medicare and other types of supplemental insurance. The premium associated with Alzheimer’s, $1,643, was the lowest of any major chronic condition, but the average cost for services, $13,269, was almost twice as high as the next most expensive condition, Parkinson’s disease, and more than four times higher than the overall Medicare average, Juliette Cubanski, PhD, and associates said.
Out-of-pocket costs are higher for patients with Alzheimer’s and Parkinson’s because “these beneficiaries are more likely to reside in a long-term care facility than those with other conditions,” they said. In 2016, out-of-pocket spending on long-term care facility services averaged over $27,000 for Medicare beneficiaries with Alzheimer’s and other dementia and over $28,000 for those with Parkinson’s disease. For all traditional Medicare beneficiaries, average out-of-pocket spending on such services was $1,014.
“The fact that traditional Medicare does not have an annual out-of-pocket limit and does not cover certain services that older adults are more likely to need may undermine the financial security that Medicare provides, especially for people with significant needs and limited incomes. Addressing these gaps would help to alleviate the financial burden of health care for people with Medicare, although doing so would also increase federal spending and taxes,” Dr. Cubanski and associates wrote.
according to the Kaiser Family Foundation.
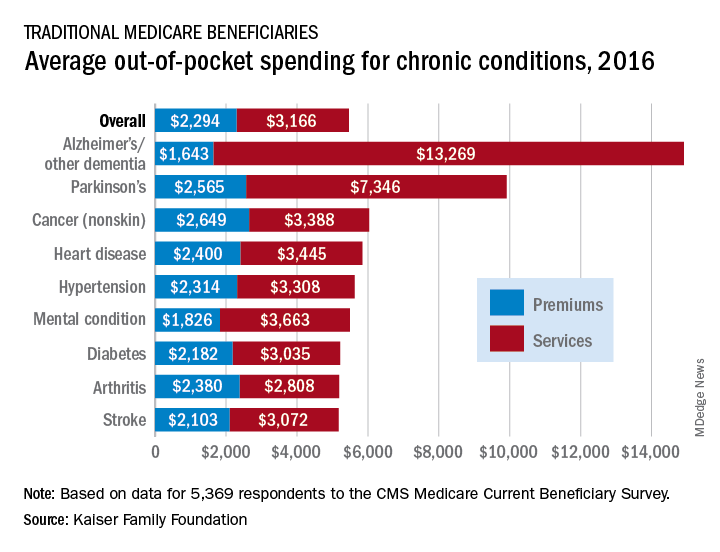
Out-of-pocket spending for Alzheimer’s disease or other dementia was higher than any other chronic condition, averaging $14,913 in 2016 (the latest year for which data are available), compared with $5,460 for all beneficiaries in traditional Medicare, Kaiser investigators said in a recent report based on data for 5,369 respondents to the Medicare Current Beneficiary Survey.
Those totals were divided between services – including long-term care facilities, medical providers and supplies, and prescription drugs – and premiums for Medicare and other types of supplemental insurance. The premium associated with Alzheimer’s, $1,643, was the lowest of any major chronic condition, but the average cost for services, $13,269, was almost twice as high as the next most expensive condition, Parkinson’s disease, and more than four times higher than the overall Medicare average, Juliette Cubanski, PhD, and associates said.
Out-of-pocket costs are higher for patients with Alzheimer’s and Parkinson’s because “these beneficiaries are more likely to reside in a long-term care facility than those with other conditions,” they said. In 2016, out-of-pocket spending on long-term care facility services averaged over $27,000 for Medicare beneficiaries with Alzheimer’s and other dementia and over $28,000 for those with Parkinson’s disease. For all traditional Medicare beneficiaries, average out-of-pocket spending on such services was $1,014.
“The fact that traditional Medicare does not have an annual out-of-pocket limit and does not cover certain services that older adults are more likely to need may undermine the financial security that Medicare provides, especially for people with significant needs and limited incomes. Addressing these gaps would help to alleviate the financial burden of health care for people with Medicare, although doing so would also increase federal spending and taxes,” Dr. Cubanski and associates wrote.
Sleep vs. Netflix, and grape juice BPAP
Sleep vs. Netflix: the eternal struggle
Ladies and gentlemen, welcome to Livin’ on the MDedge World Championship Boxing! Tonight, we bring you a classic match-up in the endless battle for your valuable time.
In the red corner, weighing in at a muscular 8 hours, is the defending champion: a good night’s sleep! And now for the challenger in the blue corner, coming in at a strong “just one more episode, I promise,” it’s binge watching!
Oh, sleep opens the match strong: According to a survey from the American Academy of Sleep Medicine, U.S. adults rank sleep as their second-most important priority, with only family beating it out. My goodness, that is a strong opening offensive.
But wait, binge watching is countering! According to the very same survey, 88% of Americans have admitted that they’d lost sleep because they’d stayed up late to watch extra episodes of a TV show or streaming series, a rate that rises to 95% in people aged 18-44 years. Oh dear, sleep looks like it’s in trouble.
Hang on, what’s binge watching doing? It’s unleashing a quick barrage of attacks: 72% of men aged 18-34 reported delaying sleep for video games, two-thirds of U.S. adults reported losing sleep to read a book, and nearly 60% of adults delayed sleep to watch sports. We feel slightly conflicted about our metaphor choice now.
And with a final haymaker from “guess I’ll watch ‘The Office’ for a sixth time,” binge watching has defeated the defending champion! Be sure to tune in next week, when alcohol takes on common sense. A true fight for the ages there.
Lead us not into temptation
Can anyone resist the temptation of binge watching? Can no one swim against the sleep-depriving, show-streaming current? Is resistance to an “Orange Is the New Black” bender futile?
University of Wyoming researchers say there’s hope. Those who would sleep svelte and sound in a world of streaming services and Krispy Kreme must plan ahead to tame temptation.
Proactive temptation management begins long before those chocolate iced glazed with sprinkles appear at the nurses’ station. Planning your response ahead of time increases the odds that the first episode of “Stranger Things” is also the evening’s last episode.
Using psychology’s human lab mice – undergraduate students – the researchers tested five temptation-proofing self-control strategies.
The first strategy: situation selection. If “Game of Thrones” is on in the den, avoid the room as if it were an unmucked House Lannister horse stall. Second: situation modification. Is your spouse hotboxing GoT on an iPad next to you in the bed? Politely suggest that GoT is even better when viewed on the living room sofa.
The third strategy: distraction. Enjoy the wholesome snap of a Finn Crisp while your coworkers destroy those Krispy Kremes like Daenerys leveling King’s Landing. Fourth: reappraisal. Tell yourself that season 2 of “Ozark” can’t surpass season 1, and will simply swindle you of your precious time. And fifth, the Nancy-Reagan, temptation-resistance classic: response inhibition. When offered the narcotic that is “Breaking Bad,” just say no!
Which temptation strategies worked best?
Planning ahead with one through four led fewer Cowboy State undergrads into temptation.
As for responding in the moment? Well, the Krispy Kremes would’ve never lasted past season 2 of “The Great British Baking Show.”
Stuck between a tongue and a hard place
There once was a 7-year-old boy who loved grape juice. He loved grape juice so much that he didn’t want to waste any after drinking a bottle of the stuff.
To get every last drop, he tried to use his tongue to lick the inside of a grape juice bottle. One particular bottle, however, was evil and had other plans. It grabbed his tongue and wouldn’t let go, even after his mother tried to help him.
She took him to the great healing wizards at Auf der Bult Children’s Hospital in Hannover, Germany – which is quite surprising, because they live in New Jersey. [Just kidding, they’re from Hannover – just checking to see if you’re paying attention.]
When their magic wands didn’t work, doctors at the hospital mildly sedated the boy with midazolam and esketamine and then advanced a 70-mm plastic button cannula between the neck of the bottle and his tongue, hoping to release the presumed vacuum. No such luck.
It was at that point that the greatest of all the wizards, Dr. Christoph Eich, a pediatric anesthesiologist at the hospital, remembered having a similar problem with a particularly villainous bottle of “grape juice” during his magical training days some 20 years earlier.
The solution then, he discovered, was to connect the cannula to a syringe and inject air into the bottle to produce positive pressure and force out the foreign object.
Dr. Eich’s reinvention of BPAP (bottle positive airway pressure) worked on the child, who, once the purple discoloration of his tongue faded after 3 days, was none the worse for wear and lived happily ever after.
We’re just wondering if the good doctor told the child’s mother that the original situation involved a bottle of wine that couldn’t be opened because no one had a corkscrew. Well, maybe she reads the European Journal of Anaesthesiology.
Sleep vs. Netflix: the eternal struggle
Ladies and gentlemen, welcome to Livin’ on the MDedge World Championship Boxing! Tonight, we bring you a classic match-up in the endless battle for your valuable time.
In the red corner, weighing in at a muscular 8 hours, is the defending champion: a good night’s sleep! And now for the challenger in the blue corner, coming in at a strong “just one more episode, I promise,” it’s binge watching!
Oh, sleep opens the match strong: According to a survey from the American Academy of Sleep Medicine, U.S. adults rank sleep as their second-most important priority, with only family beating it out. My goodness, that is a strong opening offensive.
But wait, binge watching is countering! According to the very same survey, 88% of Americans have admitted that they’d lost sleep because they’d stayed up late to watch extra episodes of a TV show or streaming series, a rate that rises to 95% in people aged 18-44 years. Oh dear, sleep looks like it’s in trouble.
Hang on, what’s binge watching doing? It’s unleashing a quick barrage of attacks: 72% of men aged 18-34 reported delaying sleep for video games, two-thirds of U.S. adults reported losing sleep to read a book, and nearly 60% of adults delayed sleep to watch sports. We feel slightly conflicted about our metaphor choice now.
And with a final haymaker from “guess I’ll watch ‘The Office’ for a sixth time,” binge watching has defeated the defending champion! Be sure to tune in next week, when alcohol takes on common sense. A true fight for the ages there.
Lead us not into temptation
Can anyone resist the temptation of binge watching? Can no one swim against the sleep-depriving, show-streaming current? Is resistance to an “Orange Is the New Black” bender futile?
University of Wyoming researchers say there’s hope. Those who would sleep svelte and sound in a world of streaming services and Krispy Kreme must plan ahead to tame temptation.
Proactive temptation management begins long before those chocolate iced glazed with sprinkles appear at the nurses’ station. Planning your response ahead of time increases the odds that the first episode of “Stranger Things” is also the evening’s last episode.
Using psychology’s human lab mice – undergraduate students – the researchers tested five temptation-proofing self-control strategies.
The first strategy: situation selection. If “Game of Thrones” is on in the den, avoid the room as if it were an unmucked House Lannister horse stall. Second: situation modification. Is your spouse hotboxing GoT on an iPad next to you in the bed? Politely suggest that GoT is even better when viewed on the living room sofa.
The third strategy: distraction. Enjoy the wholesome snap of a Finn Crisp while your coworkers destroy those Krispy Kremes like Daenerys leveling King’s Landing. Fourth: reappraisal. Tell yourself that season 2 of “Ozark” can’t surpass season 1, and will simply swindle you of your precious time. And fifth, the Nancy-Reagan, temptation-resistance classic: response inhibition. When offered the narcotic that is “Breaking Bad,” just say no!
Which temptation strategies worked best?
Planning ahead with one through four led fewer Cowboy State undergrads into temptation.
As for responding in the moment? Well, the Krispy Kremes would’ve never lasted past season 2 of “The Great British Baking Show.”
Stuck between a tongue and a hard place
There once was a 7-year-old boy who loved grape juice. He loved grape juice so much that he didn’t want to waste any after drinking a bottle of the stuff.
To get every last drop, he tried to use his tongue to lick the inside of a grape juice bottle. One particular bottle, however, was evil and had other plans. It grabbed his tongue and wouldn’t let go, even after his mother tried to help him.
She took him to the great healing wizards at Auf der Bult Children’s Hospital in Hannover, Germany – which is quite surprising, because they live in New Jersey. [Just kidding, they’re from Hannover – just checking to see if you’re paying attention.]
When their magic wands didn’t work, doctors at the hospital mildly sedated the boy with midazolam and esketamine and then advanced a 70-mm plastic button cannula between the neck of the bottle and his tongue, hoping to release the presumed vacuum. No such luck.
It was at that point that the greatest of all the wizards, Dr. Christoph Eich, a pediatric anesthesiologist at the hospital, remembered having a similar problem with a particularly villainous bottle of “grape juice” during his magical training days some 20 years earlier.
The solution then, he discovered, was to connect the cannula to a syringe and inject air into the bottle to produce positive pressure and force out the foreign object.
Dr. Eich’s reinvention of BPAP (bottle positive airway pressure) worked on the child, who, once the purple discoloration of his tongue faded after 3 days, was none the worse for wear and lived happily ever after.
We’re just wondering if the good doctor told the child’s mother that the original situation involved a bottle of wine that couldn’t be opened because no one had a corkscrew. Well, maybe she reads the European Journal of Anaesthesiology.
Sleep vs. Netflix: the eternal struggle
Ladies and gentlemen, welcome to Livin’ on the MDedge World Championship Boxing! Tonight, we bring you a classic match-up in the endless battle for your valuable time.
In the red corner, weighing in at a muscular 8 hours, is the defending champion: a good night’s sleep! And now for the challenger in the blue corner, coming in at a strong “just one more episode, I promise,” it’s binge watching!
Oh, sleep opens the match strong: According to a survey from the American Academy of Sleep Medicine, U.S. adults rank sleep as their second-most important priority, with only family beating it out. My goodness, that is a strong opening offensive.
But wait, binge watching is countering! According to the very same survey, 88% of Americans have admitted that they’d lost sleep because they’d stayed up late to watch extra episodes of a TV show or streaming series, a rate that rises to 95% in people aged 18-44 years. Oh dear, sleep looks like it’s in trouble.
Hang on, what’s binge watching doing? It’s unleashing a quick barrage of attacks: 72% of men aged 18-34 reported delaying sleep for video games, two-thirds of U.S. adults reported losing sleep to read a book, and nearly 60% of adults delayed sleep to watch sports. We feel slightly conflicted about our metaphor choice now.
And with a final haymaker from “guess I’ll watch ‘The Office’ for a sixth time,” binge watching has defeated the defending champion! Be sure to tune in next week, when alcohol takes on common sense. A true fight for the ages there.
Lead us not into temptation
Can anyone resist the temptation of binge watching? Can no one swim against the sleep-depriving, show-streaming current? Is resistance to an “Orange Is the New Black” bender futile?
University of Wyoming researchers say there’s hope. Those who would sleep svelte and sound in a world of streaming services and Krispy Kreme must plan ahead to tame temptation.
Proactive temptation management begins long before those chocolate iced glazed with sprinkles appear at the nurses’ station. Planning your response ahead of time increases the odds that the first episode of “Stranger Things” is also the evening’s last episode.
Using psychology’s human lab mice – undergraduate students – the researchers tested five temptation-proofing self-control strategies.
The first strategy: situation selection. If “Game of Thrones” is on in the den, avoid the room as if it were an unmucked House Lannister horse stall. Second: situation modification. Is your spouse hotboxing GoT on an iPad next to you in the bed? Politely suggest that GoT is even better when viewed on the living room sofa.
The third strategy: distraction. Enjoy the wholesome snap of a Finn Crisp while your coworkers destroy those Krispy Kremes like Daenerys leveling King’s Landing. Fourth: reappraisal. Tell yourself that season 2 of “Ozark” can’t surpass season 1, and will simply swindle you of your precious time. And fifth, the Nancy-Reagan, temptation-resistance classic: response inhibition. When offered the narcotic that is “Breaking Bad,” just say no!
Which temptation strategies worked best?
Planning ahead with one through four led fewer Cowboy State undergrads into temptation.
As for responding in the moment? Well, the Krispy Kremes would’ve never lasted past season 2 of “The Great British Baking Show.”
Stuck between a tongue and a hard place
There once was a 7-year-old boy who loved grape juice. He loved grape juice so much that he didn’t want to waste any after drinking a bottle of the stuff.
To get every last drop, he tried to use his tongue to lick the inside of a grape juice bottle. One particular bottle, however, was evil and had other plans. It grabbed his tongue and wouldn’t let go, even after his mother tried to help him.
She took him to the great healing wizards at Auf der Bult Children’s Hospital in Hannover, Germany – which is quite surprising, because they live in New Jersey. [Just kidding, they’re from Hannover – just checking to see if you’re paying attention.]
When their magic wands didn’t work, doctors at the hospital mildly sedated the boy with midazolam and esketamine and then advanced a 70-mm plastic button cannula between the neck of the bottle and his tongue, hoping to release the presumed vacuum. No such luck.
It was at that point that the greatest of all the wizards, Dr. Christoph Eich, a pediatric anesthesiologist at the hospital, remembered having a similar problem with a particularly villainous bottle of “grape juice” during his magical training days some 20 years earlier.
The solution then, he discovered, was to connect the cannula to a syringe and inject air into the bottle to produce positive pressure and force out the foreign object.
Dr. Eich’s reinvention of BPAP (bottle positive airway pressure) worked on the child, who, once the purple discoloration of his tongue faded after 3 days, was none the worse for wear and lived happily ever after.
We’re just wondering if the good doctor told the child’s mother that the original situation involved a bottle of wine that couldn’t be opened because no one had a corkscrew. Well, maybe she reads the European Journal of Anaesthesiology.
Student vapers make mint the most popular Juul flavor
according to data from the 2019 Monitoring the Future study.
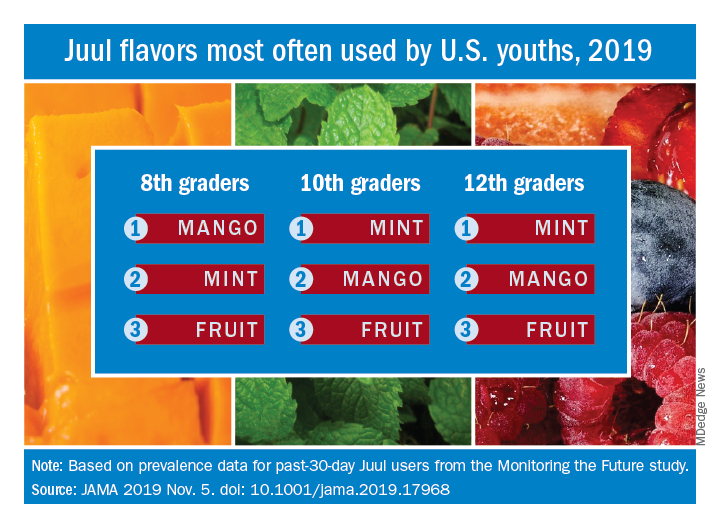
Almost half (47.1%) of the 12th graders who had used Juul e-cigarettes in the past 30 days reported that mint was the flavor they most often used, compared with 23.8% for mango and 8.6% for fruit, which is a combination of flavors, Adam M. Leventhal, PhD, of the University of Southern California, Los Angeles, and associates wrote in JAMA.
Mint was also the flavor most often used by 10th graders (43.5%), with mango again second at 27.3%, and fruit third at 10.8%. Eighth-grade students switched mango (33.5%) and mint (29.2%) but had fruit third again at 16.0%, the investigators reported, based on data for 1,739 respondents to the Monitoring the Future survey who had used a vaping product within the past 30 days.
Juul has suspended sales of four – mango, fruit, creme, and cucumber – of its original eight flavors, Dr. Leventhal and associates noted, and e-cigarette flavors other than tobacco, menthol, and mint have been prohibited by some local municipalities.
“The current findings raise uncertainty whether regulations or sales suspensions that exempt mint flavors are optimal strategies for reducing youth e-cigarette use,” they wrote.
As this article was being written, the Wall Street Journal had just reported that the Food and Drug Administration will ban mint and all other e-cigarette flavors except tobacco and menthol.
SOURCE: Leventhal AM et al. JAMA. 2019 Nov 5. doi: 10.1001/jama.2019.17968.
according to data from the 2019 Monitoring the Future study.
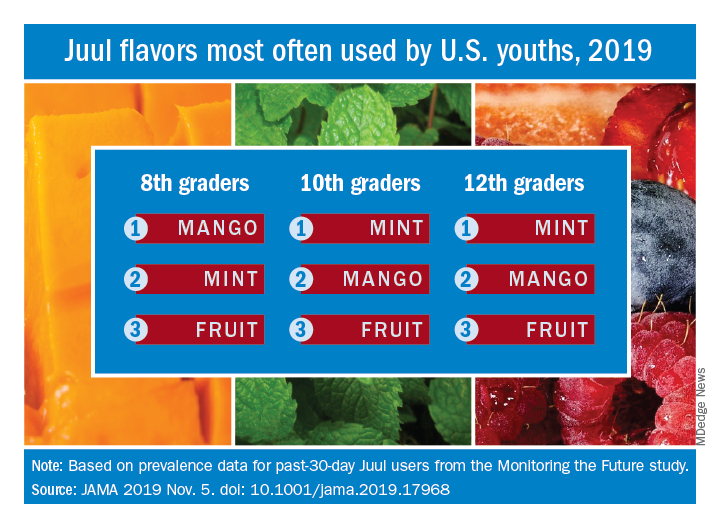
Almost half (47.1%) of the 12th graders who had used Juul e-cigarettes in the past 30 days reported that mint was the flavor they most often used, compared with 23.8% for mango and 8.6% for fruit, which is a combination of flavors, Adam M. Leventhal, PhD, of the University of Southern California, Los Angeles, and associates wrote in JAMA.
Mint was also the flavor most often used by 10th graders (43.5%), with mango again second at 27.3%, and fruit third at 10.8%. Eighth-grade students switched mango (33.5%) and mint (29.2%) but had fruit third again at 16.0%, the investigators reported, based on data for 1,739 respondents to the Monitoring the Future survey who had used a vaping product within the past 30 days.
Juul has suspended sales of four – mango, fruit, creme, and cucumber – of its original eight flavors, Dr. Leventhal and associates noted, and e-cigarette flavors other than tobacco, menthol, and mint have been prohibited by some local municipalities.
“The current findings raise uncertainty whether regulations or sales suspensions that exempt mint flavors are optimal strategies for reducing youth e-cigarette use,” they wrote.
As this article was being written, the Wall Street Journal had just reported that the Food and Drug Administration will ban mint and all other e-cigarette flavors except tobacco and menthol.
SOURCE: Leventhal AM et al. JAMA. 2019 Nov 5. doi: 10.1001/jama.2019.17968.
according to data from the 2019 Monitoring the Future study.
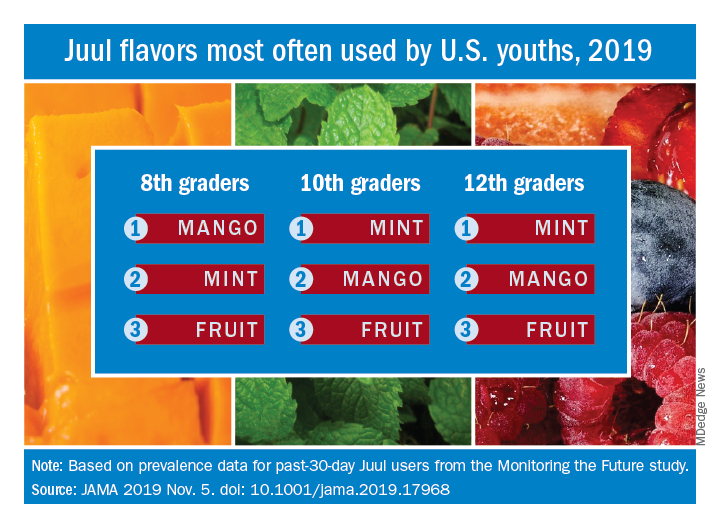
Almost half (47.1%) of the 12th graders who had used Juul e-cigarettes in the past 30 days reported that mint was the flavor they most often used, compared with 23.8% for mango and 8.6% for fruit, which is a combination of flavors, Adam M. Leventhal, PhD, of the University of Southern California, Los Angeles, and associates wrote in JAMA.
Mint was also the flavor most often used by 10th graders (43.5%), with mango again second at 27.3%, and fruit third at 10.8%. Eighth-grade students switched mango (33.5%) and mint (29.2%) but had fruit third again at 16.0%, the investigators reported, based on data for 1,739 respondents to the Monitoring the Future survey who had used a vaping product within the past 30 days.
Juul has suspended sales of four – mango, fruit, creme, and cucumber – of its original eight flavors, Dr. Leventhal and associates noted, and e-cigarette flavors other than tobacco, menthol, and mint have been prohibited by some local municipalities.
“The current findings raise uncertainty whether regulations or sales suspensions that exempt mint flavors are optimal strategies for reducing youth e-cigarette use,” they wrote.
As this article was being written, the Wall Street Journal had just reported that the Food and Drug Administration will ban mint and all other e-cigarette flavors except tobacco and menthol.
SOURCE: Leventhal AM et al. JAMA. 2019 Nov 5. doi: 10.1001/jama.2019.17968.
FROM JAMA
Premiums down slightly for 2020 plans on HealthCare.gov
The average family of four will see a 4% drop in its premium for a benchmark plan on the HealthCare.gov Marketplace in 2020, compared with 2019, according to the Centers for Medicare & Medicaid Services.
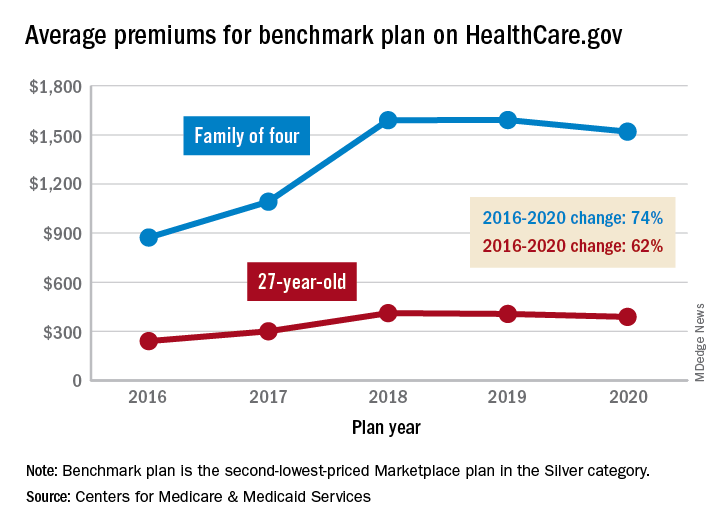
That family’s $1,520 premium for coverage next year will, however, be 74% higher than the average of $873 for the same plan in 2016. The situation is similar for a single person with a benchmark plan – defined as the second-lowest-priced Marketplace health insurance plan in the Silver category. The average premium for a 27-year-old, $388, for coverage in 2020 also will be 4% lower than in 2019, but that’s still 62% higher than in 2016, CMS said in a recent report.
The 4% average reductions for 2020 follow a 1% decrease for a 27-year-old on the benchmark plan and a $1 increase for a family of four between 2018 and 2019. “We have been committed to taking every step possible to lower premiums and provide more choices. A second year of declining premiums and expanding choice is proof that our actions to promote more stability are working. But premiums are still too high for people without subsidies,” CMS Administrator Seema Verma said in a statement.
Consumers looking for health care coverage on 1 of the 38 state exchanges during the upcoming open enrollment period (Nov. 1 to Dec. 15) also will have more choices. The average number of qualified health plans available to enrollees will be 37.9 for the 2020 plan year, compared with 25.9 for 2019 and 24.8 in 2018. The number of companies issuing those plans also rose for the second consecutive year, going from 132 for the 2018 plan year to 155 in 2019 and 175 in 2020, CMS reported.
The average family of four will see a 4% drop in its premium for a benchmark plan on the HealthCare.gov Marketplace in 2020, compared with 2019, according to the Centers for Medicare & Medicaid Services.
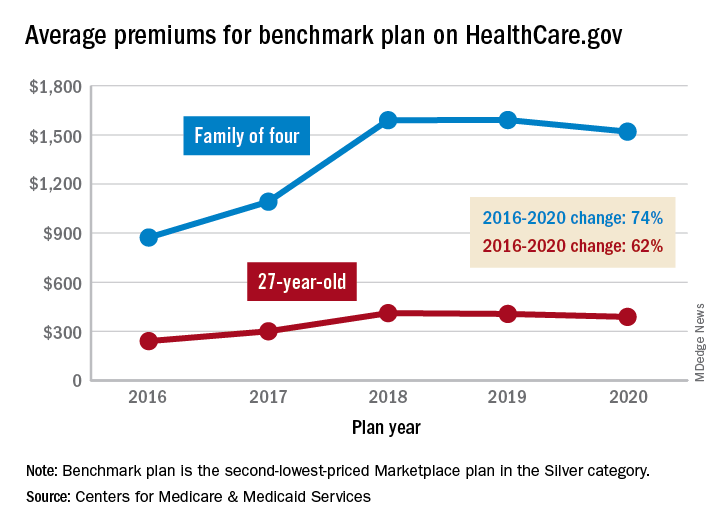
That family’s $1,520 premium for coverage next year will, however, be 74% higher than the average of $873 for the same plan in 2016. The situation is similar for a single person with a benchmark plan – defined as the second-lowest-priced Marketplace health insurance plan in the Silver category. The average premium for a 27-year-old, $388, for coverage in 2020 also will be 4% lower than in 2019, but that’s still 62% higher than in 2016, CMS said in a recent report.
The 4% average reductions for 2020 follow a 1% decrease for a 27-year-old on the benchmark plan and a $1 increase for a family of four between 2018 and 2019. “We have been committed to taking every step possible to lower premiums and provide more choices. A second year of declining premiums and expanding choice is proof that our actions to promote more stability are working. But premiums are still too high for people without subsidies,” CMS Administrator Seema Verma said in a statement.
Consumers looking for health care coverage on 1 of the 38 state exchanges during the upcoming open enrollment period (Nov. 1 to Dec. 15) also will have more choices. The average number of qualified health plans available to enrollees will be 37.9 for the 2020 plan year, compared with 25.9 for 2019 and 24.8 in 2018. The number of companies issuing those plans also rose for the second consecutive year, going from 132 for the 2018 plan year to 155 in 2019 and 175 in 2020, CMS reported.
The average family of four will see a 4% drop in its premium for a benchmark plan on the HealthCare.gov Marketplace in 2020, compared with 2019, according to the Centers for Medicare & Medicaid Services.
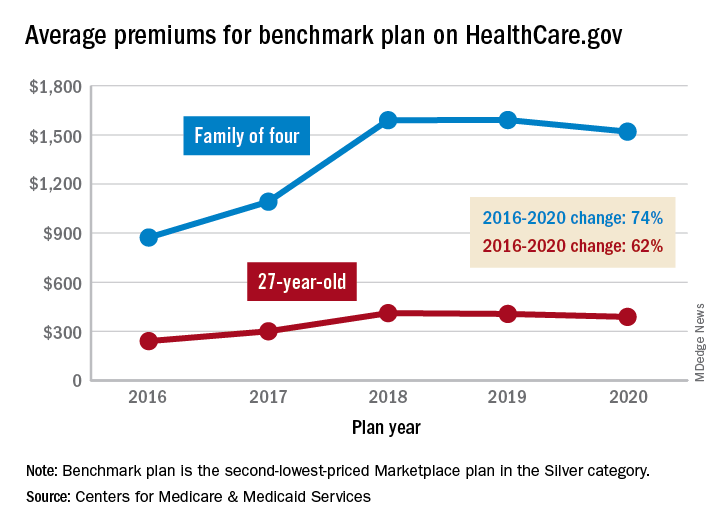
That family’s $1,520 premium for coverage next year will, however, be 74% higher than the average of $873 for the same plan in 2016. The situation is similar for a single person with a benchmark plan – defined as the second-lowest-priced Marketplace health insurance plan in the Silver category. The average premium for a 27-year-old, $388, for coverage in 2020 also will be 4% lower than in 2019, but that’s still 62% higher than in 2016, CMS said in a recent report.
The 4% average reductions for 2020 follow a 1% decrease for a 27-year-old on the benchmark plan and a $1 increase for a family of four between 2018 and 2019. “We have been committed to taking every step possible to lower premiums and provide more choices. A second year of declining premiums and expanding choice is proof that our actions to promote more stability are working. But premiums are still too high for people without subsidies,” CMS Administrator Seema Verma said in a statement.
Consumers looking for health care coverage on 1 of the 38 state exchanges during the upcoming open enrollment period (Nov. 1 to Dec. 15) also will have more choices. The average number of qualified health plans available to enrollees will be 37.9 for the 2020 plan year, compared with 25.9 for 2019 and 24.8 in 2018. The number of companies issuing those plans also rose for the second consecutive year, going from 132 for the 2018 plan year to 155 in 2019 and 175 in 2020, CMS reported.
Werewolves of Vallejo and a haunted-house doctor’s note
A crappy excuse of a database
Have you ever been so impressed with your bowel movement that you’ve been compelled to record the incident for posterity? No? Just us? Well, you may want to reconsider, because a pair of AI tech companies are looking for a few good poop pictures.
It’s all part of the “Give a S--t” (you can probably guess what we’ve censored out) campaign, a joint venture from Auggi, a gut health start-up, and Seed Health. The companies hope to use photos sent in by regular people to build an app that would help people with chronic gut problems automatically track their own bowel movements. In addition, the photo library could also be used for research into gut-related diseases such as irritable bowl syndrome.
The two companies hope to collect 100,000 photos for their library, which is an absolutely prodigious amount of poop to sort through. But hey, that’s what the AI is for. They already know the AI works, as Auggi created a proof-of-concept library of 36,000 images of faux feces made from blue Play-Doh. The AI was able to recognize consistency according to the Bristol scale basically 100% of the time.
If you’ve been inspired, you can submit your lovely poop pictures here. Seed and Auggi expect contributers to send only one image each, but multiple submissions are welcome. They’ve already received a dozen from LOTME world headquarters. We love a good bowel movement here.
Criminal moon
“The Wolf Man.” “An American Werewolf in London.” “The Howling.” “Teen Wolf.” All terrifying Hollywood tales of bloodthirsty behavior and sanguinary slaughter. (Michael J. Fox as a hirsute homicidal lycan? Okay, maybe not “Teen Wolf.”)
And the propellant igniting all that criminal lycanthropy? The full moon.
Any teacher will swear a full moon portends the kind of student behavior that an entire pot of teachers’ lounge coffee can’t counter. And every cop knows it’s going to be a “Training Day” shift when the lunar light shines brightest.
But is the Thin Blue Line truly stretched to snapping during a full moon? New York University’s BetaGov research team looked at the purported “lunar effect” linking crime and the full moon. A lit review revealed mixed findings for and against a criminal lunar effect. The team then collaborated with the Vallejo, Calif., police department to match the moon’s phases with the city’s crime events. They did the same with departments in Canada and Mexico.
The results? A full moon had no effect on Vallejo’s crime rate, or anywhere else in North America.
While the finding eviscerates the moon-induced mayhem hypothesis, cops walking a full-moonlit beat can at least take comfort in this fact: Unlike London, Vallejo is clearly free of American werewolves.
A doctor’s note … of terror
With Halloween upon us, here’s a veddy scary riddle: When is a sports physical not a sports physical?
When it’s a haunted house physical.
Specifically, when the haunted house is McKamey Manor in Summertown, Tenn. … and in Huntsville, Ala. That’s right, it can be in two places at the same time. Terrifying.
McKamey Manor is considered by many to be the most terrifying haunted house in the United States, and by some to be a “torture chamber under disguise.”
The “Surivial [we think they misspelled it on purpose to make it even scarier] Horror Challenge” is so terrifying that management requires all participants to have a “completed ‘sports physical’ and doctor’s letter stating you are physically and mentally cleared,” as well as proof of medical insurance. Each paying customer also has to “pass a portable drug test on the day of the show,” according to the McKamey Manor website.
The manor also happens to be the subject of a petition, which currently has over 58,000 signatures, asking state officials in Alabama and Tennessee to shut it down because “some people have had to seek professional psychiatric help and medical care for extensive injuries.”
Ironically, we hear that some of the most traumatized customers have been actual physicians who succumbed to the horrors of Prior Approval Asylum, the EHR Torment Room, and the River of the Damned Maintenance of Certification.
A crappy excuse of a database
Have you ever been so impressed with your bowel movement that you’ve been compelled to record the incident for posterity? No? Just us? Well, you may want to reconsider, because a pair of AI tech companies are looking for a few good poop pictures.
It’s all part of the “Give a S--t” (you can probably guess what we’ve censored out) campaign, a joint venture from Auggi, a gut health start-up, and Seed Health. The companies hope to use photos sent in by regular people to build an app that would help people with chronic gut problems automatically track their own bowel movements. In addition, the photo library could also be used for research into gut-related diseases such as irritable bowl syndrome.
The two companies hope to collect 100,000 photos for their library, which is an absolutely prodigious amount of poop to sort through. But hey, that’s what the AI is for. They already know the AI works, as Auggi created a proof-of-concept library of 36,000 images of faux feces made from blue Play-Doh. The AI was able to recognize consistency according to the Bristol scale basically 100% of the time.
If you’ve been inspired, you can submit your lovely poop pictures here. Seed and Auggi expect contributers to send only one image each, but multiple submissions are welcome. They’ve already received a dozen from LOTME world headquarters. We love a good bowel movement here.
Criminal moon
“The Wolf Man.” “An American Werewolf in London.” “The Howling.” “Teen Wolf.” All terrifying Hollywood tales of bloodthirsty behavior and sanguinary slaughter. (Michael J. Fox as a hirsute homicidal lycan? Okay, maybe not “Teen Wolf.”)
And the propellant igniting all that criminal lycanthropy? The full moon.
Any teacher will swear a full moon portends the kind of student behavior that an entire pot of teachers’ lounge coffee can’t counter. And every cop knows it’s going to be a “Training Day” shift when the lunar light shines brightest.
But is the Thin Blue Line truly stretched to snapping during a full moon? New York University’s BetaGov research team looked at the purported “lunar effect” linking crime and the full moon. A lit review revealed mixed findings for and against a criminal lunar effect. The team then collaborated with the Vallejo, Calif., police department to match the moon’s phases with the city’s crime events. They did the same with departments in Canada and Mexico.
The results? A full moon had no effect on Vallejo’s crime rate, or anywhere else in North America.
While the finding eviscerates the moon-induced mayhem hypothesis, cops walking a full-moonlit beat can at least take comfort in this fact: Unlike London, Vallejo is clearly free of American werewolves.
A doctor’s note … of terror
With Halloween upon us, here’s a veddy scary riddle: When is a sports physical not a sports physical?
When it’s a haunted house physical.
Specifically, when the haunted house is McKamey Manor in Summertown, Tenn. … and in Huntsville, Ala. That’s right, it can be in two places at the same time. Terrifying.
McKamey Manor is considered by many to be the most terrifying haunted house in the United States, and by some to be a “torture chamber under disguise.”
The “Surivial [we think they misspelled it on purpose to make it even scarier] Horror Challenge” is so terrifying that management requires all participants to have a “completed ‘sports physical’ and doctor’s letter stating you are physically and mentally cleared,” as well as proof of medical insurance. Each paying customer also has to “pass a portable drug test on the day of the show,” according to the McKamey Manor website.
The manor also happens to be the subject of a petition, which currently has over 58,000 signatures, asking state officials in Alabama and Tennessee to shut it down because “some people have had to seek professional psychiatric help and medical care for extensive injuries.”
Ironically, we hear that some of the most traumatized customers have been actual physicians who succumbed to the horrors of Prior Approval Asylum, the EHR Torment Room, and the River of the Damned Maintenance of Certification.
A crappy excuse of a database
Have you ever been so impressed with your bowel movement that you’ve been compelled to record the incident for posterity? No? Just us? Well, you may want to reconsider, because a pair of AI tech companies are looking for a few good poop pictures.
It’s all part of the “Give a S--t” (you can probably guess what we’ve censored out) campaign, a joint venture from Auggi, a gut health start-up, and Seed Health. The companies hope to use photos sent in by regular people to build an app that would help people with chronic gut problems automatically track their own bowel movements. In addition, the photo library could also be used for research into gut-related diseases such as irritable bowl syndrome.
The two companies hope to collect 100,000 photos for their library, which is an absolutely prodigious amount of poop to sort through. But hey, that’s what the AI is for. They already know the AI works, as Auggi created a proof-of-concept library of 36,000 images of faux feces made from blue Play-Doh. The AI was able to recognize consistency according to the Bristol scale basically 100% of the time.
If you’ve been inspired, you can submit your lovely poop pictures here. Seed and Auggi expect contributers to send only one image each, but multiple submissions are welcome. They’ve already received a dozen from LOTME world headquarters. We love a good bowel movement here.
Criminal moon
“The Wolf Man.” “An American Werewolf in London.” “The Howling.” “Teen Wolf.” All terrifying Hollywood tales of bloodthirsty behavior and sanguinary slaughter. (Michael J. Fox as a hirsute homicidal lycan? Okay, maybe not “Teen Wolf.”)
And the propellant igniting all that criminal lycanthropy? The full moon.
Any teacher will swear a full moon portends the kind of student behavior that an entire pot of teachers’ lounge coffee can’t counter. And every cop knows it’s going to be a “Training Day” shift when the lunar light shines brightest.
But is the Thin Blue Line truly stretched to snapping during a full moon? New York University’s BetaGov research team looked at the purported “lunar effect” linking crime and the full moon. A lit review revealed mixed findings for and against a criminal lunar effect. The team then collaborated with the Vallejo, Calif., police department to match the moon’s phases with the city’s crime events. They did the same with departments in Canada and Mexico.
The results? A full moon had no effect on Vallejo’s crime rate, or anywhere else in North America.
While the finding eviscerates the moon-induced mayhem hypothesis, cops walking a full-moonlit beat can at least take comfort in this fact: Unlike London, Vallejo is clearly free of American werewolves.
A doctor’s note … of terror
With Halloween upon us, here’s a veddy scary riddle: When is a sports physical not a sports physical?
When it’s a haunted house physical.
Specifically, when the haunted house is McKamey Manor in Summertown, Tenn. … and in Huntsville, Ala. That’s right, it can be in two places at the same time. Terrifying.
McKamey Manor is considered by many to be the most terrifying haunted house in the United States, and by some to be a “torture chamber under disguise.”
The “Surivial [we think they misspelled it on purpose to make it even scarier] Horror Challenge” is so terrifying that management requires all participants to have a “completed ‘sports physical’ and doctor’s letter stating you are physically and mentally cleared,” as well as proof of medical insurance. Each paying customer also has to “pass a portable drug test on the day of the show,” according to the McKamey Manor website.
The manor also happens to be the subject of a petition, which currently has over 58,000 signatures, asking state officials in Alabama and Tennessee to shut it down because “some people have had to seek professional psychiatric help and medical care for extensive injuries.”
Ironically, we hear that some of the most traumatized customers have been actual physicians who succumbed to the horrors of Prior Approval Asylum, the EHR Torment Room, and the River of the Damned Maintenance of Certification.
THC use reported in majority of vaping-related illnesses
(EVALI), according to the Centers for Disease Control and Prevention.

In the largest analysis to date, exclusive use of THC-containing products was reported for 34% of the 1,378 patients with confirmed or probable EVALI as of Oct. 15, 2019. Among those who died, 63% had been using THC exclusively during the 3 months preceding symptom onset, Erin D. Moritz, PhD, and associates said Oct. 28 in the Morbidity and Mortality Weekly Report.
Almost two-thirds (64%) of all EVALI patients had used nicotine-containing products at some time in the 3 months before symptom onset, and nicotine use was exclusive for 11%. Any nicotine use was reported for 37% of EVALI-related deaths, with exclusive use at 16%, the investigators reported.
“The data presented here suggest that THC-containing products are playing an important role in this outbreak,” they wrote, but “to date, no single compound or ingredient has emerged as the cause of EVALI, and there might be more than one cause.”
Dr. Moritz and associates also noted that many “patients likely did not know the content of the e-cigarette, or vaping, products they used,” which may have led to misclassification of substances.
SOURCE: Moritz ED et al. MMWR. Morbidity and mortality weekly report 2019 Oct 28;68(early release):1-4.
(EVALI), according to the Centers for Disease Control and Prevention.

In the largest analysis to date, exclusive use of THC-containing products was reported for 34% of the 1,378 patients with confirmed or probable EVALI as of Oct. 15, 2019. Among those who died, 63% had been using THC exclusively during the 3 months preceding symptom onset, Erin D. Moritz, PhD, and associates said Oct. 28 in the Morbidity and Mortality Weekly Report.
Almost two-thirds (64%) of all EVALI patients had used nicotine-containing products at some time in the 3 months before symptom onset, and nicotine use was exclusive for 11%. Any nicotine use was reported for 37% of EVALI-related deaths, with exclusive use at 16%, the investigators reported.
“The data presented here suggest that THC-containing products are playing an important role in this outbreak,” they wrote, but “to date, no single compound or ingredient has emerged as the cause of EVALI, and there might be more than one cause.”
Dr. Moritz and associates also noted that many “patients likely did not know the content of the e-cigarette, or vaping, products they used,” which may have led to misclassification of substances.
SOURCE: Moritz ED et al. MMWR. Morbidity and mortality weekly report 2019 Oct 28;68(early release):1-4.
(EVALI), according to the Centers for Disease Control and Prevention.

In the largest analysis to date, exclusive use of THC-containing products was reported for 34% of the 1,378 patients with confirmed or probable EVALI as of Oct. 15, 2019. Among those who died, 63% had been using THC exclusively during the 3 months preceding symptom onset, Erin D. Moritz, PhD, and associates said Oct. 28 in the Morbidity and Mortality Weekly Report.
Almost two-thirds (64%) of all EVALI patients had used nicotine-containing products at some time in the 3 months before symptom onset, and nicotine use was exclusive for 11%. Any nicotine use was reported for 37% of EVALI-related deaths, with exclusive use at 16%, the investigators reported.
“The data presented here suggest that THC-containing products are playing an important role in this outbreak,” they wrote, but “to date, no single compound or ingredient has emerged as the cause of EVALI, and there might be more than one cause.”
Dr. Moritz and associates also noted that many “patients likely did not know the content of the e-cigarette, or vaping, products they used,” which may have led to misclassification of substances.
SOURCE: Moritz ED et al. MMWR. Morbidity and mortality weekly report 2019 Oct 28;68(early release):1-4.
FROM MMWR
Suicide deaths rising in children aged 10-19 years
according to the National Center for Health Statistics.
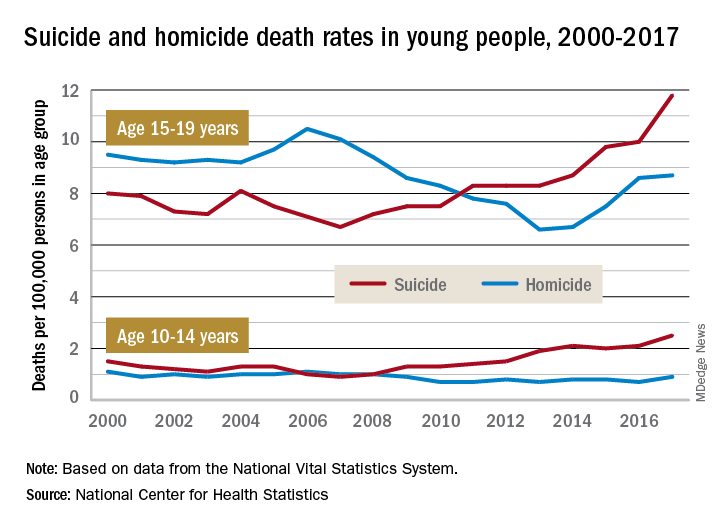
Death rates from suicide for children aged 10-14 years jumped by 178% from 2007 to 2017, while teenagers aged 15-19 years experienced a 76% increase over that period, with both changes reaching significance, the NCHS said in a recent data brief based on data from the National Vital Statistics System.
The actual rate for teens was higher to begin with, however, so in absolute terms the increase is larger for the older group. In 2007, deaths from suicide occurred at a rate of 6.7 per 100,000 persons for persons aged 15-19 years, and by 2017 that rate was up significantly to 11.8 per 100,000. Among children aged 10-14 years, the suicide-related death rate climbed from 0.9 per 100,000 in 2007 to 2.5 in 2014, the NCHS investigators reported.
The news was somewhat better on the other side of the violent death coin. Homicides are down by a significant 18% since 2000 among children aged 10-14 years, as the rate dropped from 1.1 per 100,000 in 2000 to 0.9 in 2017. The homicide rate since 2000 is down slightly for teens aged 15-19 years, but it has risen 32% in recent years, going from 6.6 deaths per 100,000 in 2013 to 8.7 in 2017, they said.
Suicide was the second-leading cause of death in both age groups in 2017, and homicide was third for those aged 15-19 and fifth among 10- to 14-year-olds, the investigators noted.
according to the National Center for Health Statistics.
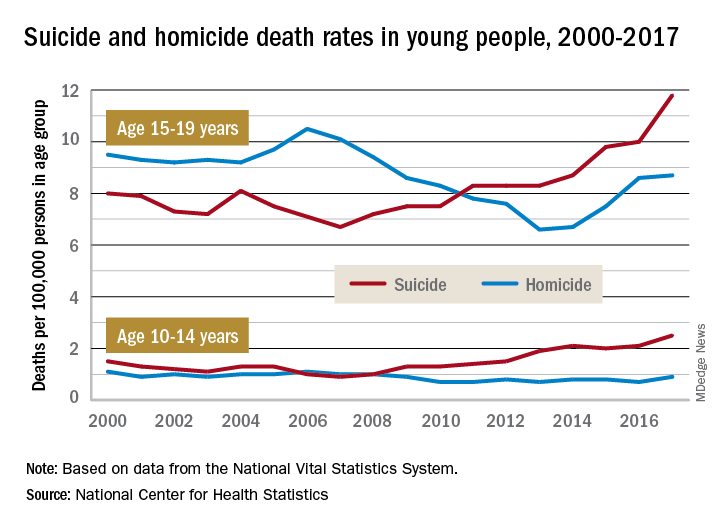
Death rates from suicide for children aged 10-14 years jumped by 178% from 2007 to 2017, while teenagers aged 15-19 years experienced a 76% increase over that period, with both changes reaching significance, the NCHS said in a recent data brief based on data from the National Vital Statistics System.
The actual rate for teens was higher to begin with, however, so in absolute terms the increase is larger for the older group. In 2007, deaths from suicide occurred at a rate of 6.7 per 100,000 persons for persons aged 15-19 years, and by 2017 that rate was up significantly to 11.8 per 100,000. Among children aged 10-14 years, the suicide-related death rate climbed from 0.9 per 100,000 in 2007 to 2.5 in 2014, the NCHS investigators reported.
The news was somewhat better on the other side of the violent death coin. Homicides are down by a significant 18% since 2000 among children aged 10-14 years, as the rate dropped from 1.1 per 100,000 in 2000 to 0.9 in 2017. The homicide rate since 2000 is down slightly for teens aged 15-19 years, but it has risen 32% in recent years, going from 6.6 deaths per 100,000 in 2013 to 8.7 in 2017, they said.
Suicide was the second-leading cause of death in both age groups in 2017, and homicide was third for those aged 15-19 and fifth among 10- to 14-year-olds, the investigators noted.
according to the National Center for Health Statistics.
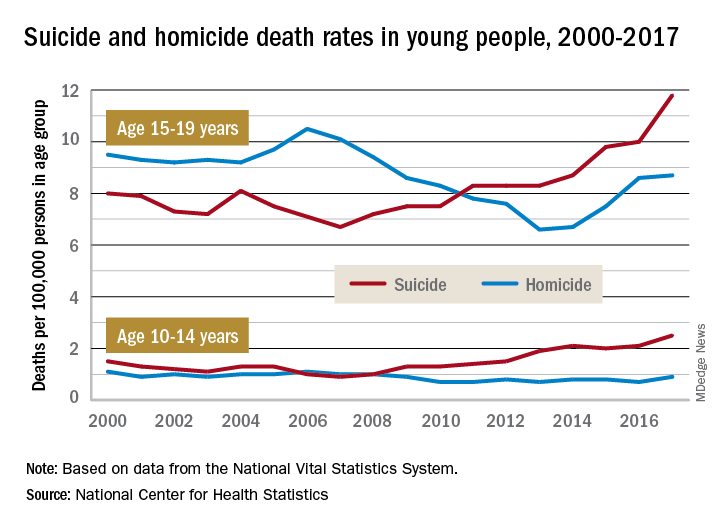
Death rates from suicide for children aged 10-14 years jumped by 178% from 2007 to 2017, while teenagers aged 15-19 years experienced a 76% increase over that period, with both changes reaching significance, the NCHS said in a recent data brief based on data from the National Vital Statistics System.
The actual rate for teens was higher to begin with, however, so in absolute terms the increase is larger for the older group. In 2007, deaths from suicide occurred at a rate of 6.7 per 100,000 persons for persons aged 15-19 years, and by 2017 that rate was up significantly to 11.8 per 100,000. Among children aged 10-14 years, the suicide-related death rate climbed from 0.9 per 100,000 in 2007 to 2.5 in 2014, the NCHS investigators reported.
The news was somewhat better on the other side of the violent death coin. Homicides are down by a significant 18% since 2000 among children aged 10-14 years, as the rate dropped from 1.1 per 100,000 in 2000 to 0.9 in 2017. The homicide rate since 2000 is down slightly for teens aged 15-19 years, but it has risen 32% in recent years, going from 6.6 deaths per 100,000 in 2013 to 8.7 in 2017, they said.
Suicide was the second-leading cause of death in both age groups in 2017, and homicide was third for those aged 15-19 and fifth among 10- to 14-year-olds, the investigators noted.











