User login
Richard Franki is the associate editor who writes and creates graphs. He started with the company in 1987, when it was known as the International Medical News Group. In his years as a journalist, Richard has worked for Cap Cities/ABC, Disney, Harcourt, Elsevier, Quadrant, Frontline, and Internet Brands. In the 1990s, he was a contributor to the ill-fated Indications column, predecessor of Livin' on the MDedge.
Biologic approved for atopic dermatitis in children
The Food and Drug Administration has approved dupilumab for children aged 6-11 years with moderate to severe atopic dermatitis, the manufacturers announced.
The new indication is for children “whose disease is not adequately controlled with topical prescription therapies or when those therapies are not advisable,” Regeneron and Sanofi said in a press release, which points out that this is the first biologic approved for AD in this age group.
For children aged 6-11, the two available dupilumab (Dupixent) doses in prefilled syringes are given based on weight – 300 mg every 4 weeks for children between 15 to 29 kg and 200 mg every 2 weeks for children 30 to 59 kg – following an initial loading dose.
In phase 3 trials, children with severe AD who received dupilumab and topical corticosteroids improved significantly in overall disease severity, skin clearance, and itch, compared with those getting steroids alone. Eczema Area and Severity Index-75, for example, was reached by 75% of patients on either dupilumab dose, compared with 28% and 26% , respectively, for those receiving steroids alone every 4 and every 2 weeks, the statement said.
Over the 16-week treatment period, overall rates of adverse events were 65% for those getting dupilumab every 4 weeks and 61% for every 2 weeks – compared with steroids alone (72% and 75%, respectively), the statement said.
The fully human monoclonal antibody inhibits signaling of the interleukin-4 and interleukin-13 proteins and is already approved as an add-on maintenance treatment in children aged 12 years and older with moderate to severe asthma (eosinophilic phenotype or oral-corticosteroid dependent) and in adults with inadequately controlled chronic rhinosinusitis with nasal polyposis, according to the prescribing information.
The Food and Drug Administration has approved dupilumab for children aged 6-11 years with moderate to severe atopic dermatitis, the manufacturers announced.
The new indication is for children “whose disease is not adequately controlled with topical prescription therapies or when those therapies are not advisable,” Regeneron and Sanofi said in a press release, which points out that this is the first biologic approved for AD in this age group.
For children aged 6-11, the two available dupilumab (Dupixent) doses in prefilled syringes are given based on weight – 300 mg every 4 weeks for children between 15 to 29 kg and 200 mg every 2 weeks for children 30 to 59 kg – following an initial loading dose.
In phase 3 trials, children with severe AD who received dupilumab and topical corticosteroids improved significantly in overall disease severity, skin clearance, and itch, compared with those getting steroids alone. Eczema Area and Severity Index-75, for example, was reached by 75% of patients on either dupilumab dose, compared with 28% and 26% , respectively, for those receiving steroids alone every 4 and every 2 weeks, the statement said.
Over the 16-week treatment period, overall rates of adverse events were 65% for those getting dupilumab every 4 weeks and 61% for every 2 weeks – compared with steroids alone (72% and 75%, respectively), the statement said.
The fully human monoclonal antibody inhibits signaling of the interleukin-4 and interleukin-13 proteins and is already approved as an add-on maintenance treatment in children aged 12 years and older with moderate to severe asthma (eosinophilic phenotype or oral-corticosteroid dependent) and in adults with inadequately controlled chronic rhinosinusitis with nasal polyposis, according to the prescribing information.
The Food and Drug Administration has approved dupilumab for children aged 6-11 years with moderate to severe atopic dermatitis, the manufacturers announced.
The new indication is for children “whose disease is not adequately controlled with topical prescription therapies or when those therapies are not advisable,” Regeneron and Sanofi said in a press release, which points out that this is the first biologic approved for AD in this age group.
For children aged 6-11, the two available dupilumab (Dupixent) doses in prefilled syringes are given based on weight – 300 mg every 4 weeks for children between 15 to 29 kg and 200 mg every 2 weeks for children 30 to 59 kg – following an initial loading dose.
In phase 3 trials, children with severe AD who received dupilumab and topical corticosteroids improved significantly in overall disease severity, skin clearance, and itch, compared with those getting steroids alone. Eczema Area and Severity Index-75, for example, was reached by 75% of patients on either dupilumab dose, compared with 28% and 26% , respectively, for those receiving steroids alone every 4 and every 2 weeks, the statement said.
Over the 16-week treatment period, overall rates of adverse events were 65% for those getting dupilumab every 4 weeks and 61% for every 2 weeks – compared with steroids alone (72% and 75%, respectively), the statement said.
The fully human monoclonal antibody inhibits signaling of the interleukin-4 and interleukin-13 proteins and is already approved as an add-on maintenance treatment in children aged 12 years and older with moderate to severe asthma (eosinophilic phenotype or oral-corticosteroid dependent) and in adults with inadequately controlled chronic rhinosinusitis with nasal polyposis, according to the prescribing information.
Most patients with lichen sclerosus receive appropriate treatment
The claims-based prevalence of 0.05% found in the study is lower than previously reported, and only 16% of the diagnoses were in women aged 18-44 years, Laura E. Melnick, MD, and associates wrote after identifying 10,004 females aged 0-65 years with lichen sclerosus in the IBM MarketScan Commercial Claims and Encounters Databases from 2015 to 2017. The majority (79%) of those diagnosed were aged 45-65 years (average, 50.8 years).
In pediatric patients (up to age 17 years), the low prevalence (0.01%) “may be attributable to several factors including relative rarity, as well as variability in pediatric clinicians’ familiarity with [lichen sclerosus] and in patients’ clinical symptoms,” said Dr. Melnick and associates in the department of dermatology at New York University.
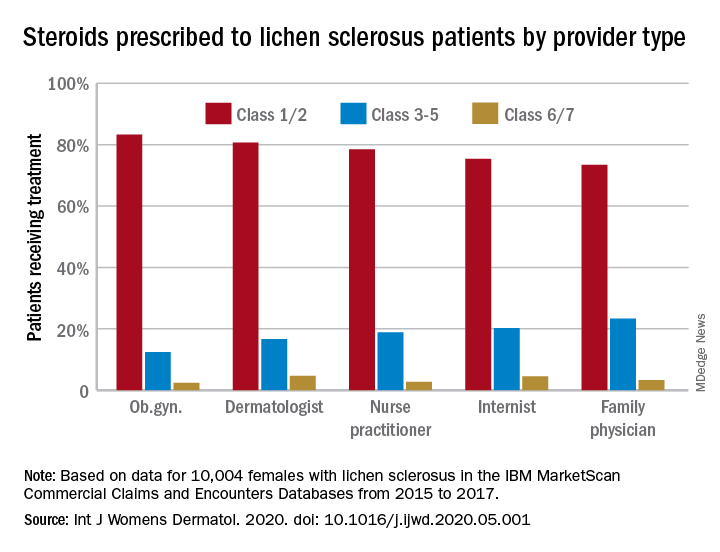
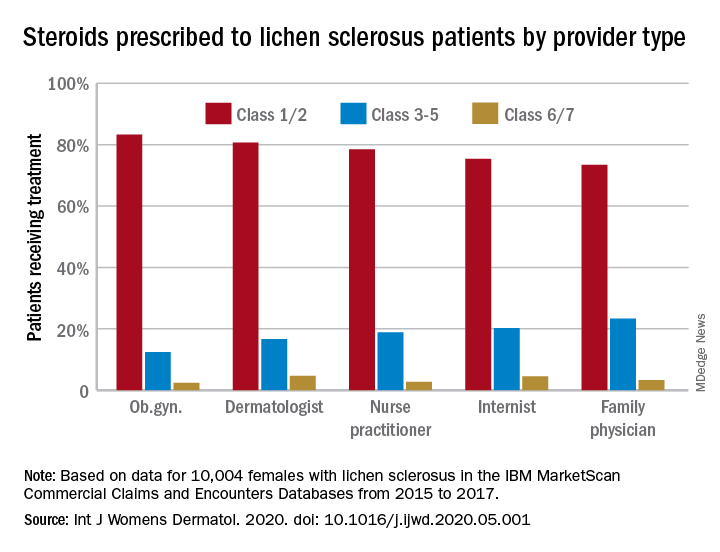
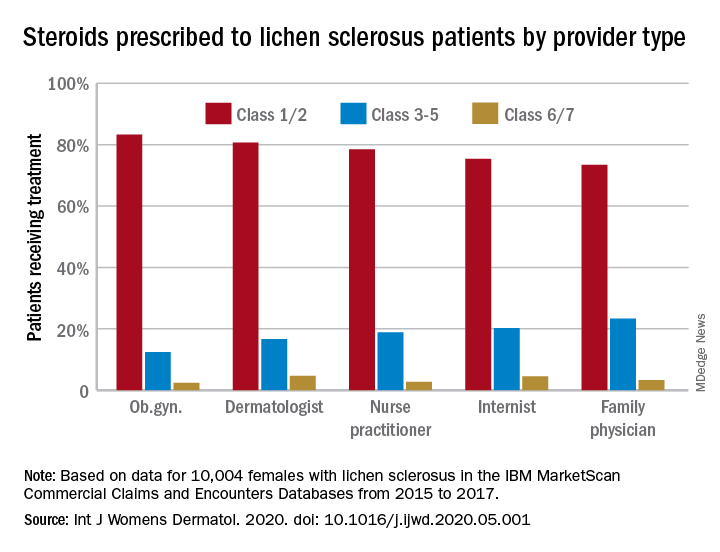
Just over half of all diagnoses (52.4%) were made by ob.gyns., with dermatologists next at 14.5%, followed by family physicians (6.5%), nurse practitioners (2.5%), and internists (0.4%), they reported in the International Journal of Women’s Dermatology.
Treatment for lichen sclerosus, in the form of high-potency topical corticosteroids, was mostly appropriate. Ob.gyns. prescribed class 1/2 steroids to 83% of their patients, tops among all clinicians. Dermatologists were just over 80%, and the other clinician categories were all over 70%, the investigators said.
“Understanding the current management of [lichen sclerosus] is important given that un- or undertreated disease can significantly impact patients’ quality of life, lead to increased lower urinary tract symptoms and irreversible architectural changes, and predispose women to squamous cell carcinoma,” they wrote.
SOURCE: Melnick LE et al. Int J Womens Dermatol. 2020. doi: 10.1016/j.ijwd.2020.05.001.
The claims-based prevalence of 0.05% found in the study is lower than previously reported, and only 16% of the diagnoses were in women aged 18-44 years, Laura E. Melnick, MD, and associates wrote after identifying 10,004 females aged 0-65 years with lichen sclerosus in the IBM MarketScan Commercial Claims and Encounters Databases from 2015 to 2017. The majority (79%) of those diagnosed were aged 45-65 years (average, 50.8 years).
In pediatric patients (up to age 17 years), the low prevalence (0.01%) “may be attributable to several factors including relative rarity, as well as variability in pediatric clinicians’ familiarity with [lichen sclerosus] and in patients’ clinical symptoms,” said Dr. Melnick and associates in the department of dermatology at New York University.
Just over half of all diagnoses (52.4%) were made by ob.gyns., with dermatologists next at 14.5%, followed by family physicians (6.5%), nurse practitioners (2.5%), and internists (0.4%), they reported in the International Journal of Women’s Dermatology.
Treatment for lichen sclerosus, in the form of high-potency topical corticosteroids, was mostly appropriate. Ob.gyns. prescribed class 1/2 steroids to 83% of their patients, tops among all clinicians. Dermatologists were just over 80%, and the other clinician categories were all over 70%, the investigators said.
“Understanding the current management of [lichen sclerosus] is important given that un- or undertreated disease can significantly impact patients’ quality of life, lead to increased lower urinary tract symptoms and irreversible architectural changes, and predispose women to squamous cell carcinoma,” they wrote.
SOURCE: Melnick LE et al. Int J Womens Dermatol. 2020. doi: 10.1016/j.ijwd.2020.05.001.
The claims-based prevalence of 0.05% found in the study is lower than previously reported, and only 16% of the diagnoses were in women aged 18-44 years, Laura E. Melnick, MD, and associates wrote after identifying 10,004 females aged 0-65 years with lichen sclerosus in the IBM MarketScan Commercial Claims and Encounters Databases from 2015 to 2017. The majority (79%) of those diagnosed were aged 45-65 years (average, 50.8 years).
In pediatric patients (up to age 17 years), the low prevalence (0.01%) “may be attributable to several factors including relative rarity, as well as variability in pediatric clinicians’ familiarity with [lichen sclerosus] and in patients’ clinical symptoms,” said Dr. Melnick and associates in the department of dermatology at New York University.
Just over half of all diagnoses (52.4%) were made by ob.gyns., with dermatologists next at 14.5%, followed by family physicians (6.5%), nurse practitioners (2.5%), and internists (0.4%), they reported in the International Journal of Women’s Dermatology.
Treatment for lichen sclerosus, in the form of high-potency topical corticosteroids, was mostly appropriate. Ob.gyns. prescribed class 1/2 steroids to 83% of their patients, tops among all clinicians. Dermatologists were just over 80%, and the other clinician categories were all over 70%, the investigators said.
“Understanding the current management of [lichen sclerosus] is important given that un- or undertreated disease can significantly impact patients’ quality of life, lead to increased lower urinary tract symptoms and irreversible architectural changes, and predispose women to squamous cell carcinoma,” they wrote.
SOURCE: Melnick LE et al. Int J Womens Dermatol. 2020. doi: 10.1016/j.ijwd.2020.05.001.
FROM THE INTERNATIONAL JOURNAL OF WOMEN’S DERMATOLOGY
U.S. fertility rates fall to record lows
and birth rates for women under age 30 fell to record lows, according to the National Center for Health Statistics.
To be exact – at least as exact as is possible from these provisional data – there were 3,745,540 births in the United States last year. That’s down about 1% from 2018 and is the lowest number of births since 1985, Brady E. Hamilton, PhD, and associates at the NCHS said in a rapid release report.
As births go, so goes the general fertility rate. A 2% decrease from 2018 to 2019 left the fertility rate at its lowest point ever: 58.2 births per 1,000 women aged 15-44 years, compared with 59.1 per 1,000 in 2018, the investigators said, based on data from the National Vital Statistics System.
The total fertility rate – defined as “the number of births that a hypothetical group of 1,000 women would have over their lifetimes, based on the age-specific birth rate in a given year” – also reached a record low of 1,705 births per 1,000 women last year after falling 1% from 2018, they reported.
The falling birth rates did not include women over age 35. The birth rate among women aged 40-44 increased by 2% from 2018, as it reached 12.0 births per 1,000 in 2019. “The rate for this age group has risen almost continuously since 1985 by an average of 3% per year,” Dr. Hamilton and associates wrote.
The birth rate for women aged 30-34 years, 98.3 per 1,000, was down 1% from 2018 but was still the highest for any age category. Among younger women, rates all dropped to record lows: 16.6 (ages 15-19), 66.6 (ages 20-24), and 93.7 (ages 25-29), they said.
Preterm birth rates, on the other hand, rose for the fifth year in a row. The rate for 2019, 10.23% of all births, represents an increase of 2% over 2018 and is “the highest level reported in more than a decade,” the investigators noted.
and birth rates for women under age 30 fell to record lows, according to the National Center for Health Statistics.
To be exact – at least as exact as is possible from these provisional data – there were 3,745,540 births in the United States last year. That’s down about 1% from 2018 and is the lowest number of births since 1985, Brady E. Hamilton, PhD, and associates at the NCHS said in a rapid release report.
As births go, so goes the general fertility rate. A 2% decrease from 2018 to 2019 left the fertility rate at its lowest point ever: 58.2 births per 1,000 women aged 15-44 years, compared with 59.1 per 1,000 in 2018, the investigators said, based on data from the National Vital Statistics System.
The total fertility rate – defined as “the number of births that a hypothetical group of 1,000 women would have over their lifetimes, based on the age-specific birth rate in a given year” – also reached a record low of 1,705 births per 1,000 women last year after falling 1% from 2018, they reported.
The falling birth rates did not include women over age 35. The birth rate among women aged 40-44 increased by 2% from 2018, as it reached 12.0 births per 1,000 in 2019. “The rate for this age group has risen almost continuously since 1985 by an average of 3% per year,” Dr. Hamilton and associates wrote.
The birth rate for women aged 30-34 years, 98.3 per 1,000, was down 1% from 2018 but was still the highest for any age category. Among younger women, rates all dropped to record lows: 16.6 (ages 15-19), 66.6 (ages 20-24), and 93.7 (ages 25-29), they said.
Preterm birth rates, on the other hand, rose for the fifth year in a row. The rate for 2019, 10.23% of all births, represents an increase of 2% over 2018 and is “the highest level reported in more than a decade,” the investigators noted.
and birth rates for women under age 30 fell to record lows, according to the National Center for Health Statistics.
To be exact – at least as exact as is possible from these provisional data – there were 3,745,540 births in the United States last year. That’s down about 1% from 2018 and is the lowest number of births since 1985, Brady E. Hamilton, PhD, and associates at the NCHS said in a rapid release report.
As births go, so goes the general fertility rate. A 2% decrease from 2018 to 2019 left the fertility rate at its lowest point ever: 58.2 births per 1,000 women aged 15-44 years, compared with 59.1 per 1,000 in 2018, the investigators said, based on data from the National Vital Statistics System.
The total fertility rate – defined as “the number of births that a hypothetical group of 1,000 women would have over their lifetimes, based on the age-specific birth rate in a given year” – also reached a record low of 1,705 births per 1,000 women last year after falling 1% from 2018, they reported.
The falling birth rates did not include women over age 35. The birth rate among women aged 40-44 increased by 2% from 2018, as it reached 12.0 births per 1,000 in 2019. “The rate for this age group has risen almost continuously since 1985 by an average of 3% per year,” Dr. Hamilton and associates wrote.
The birth rate for women aged 30-34 years, 98.3 per 1,000, was down 1% from 2018 but was still the highest for any age category. Among younger women, rates all dropped to record lows: 16.6 (ages 15-19), 66.6 (ages 20-24), and 93.7 (ages 25-29), they said.
Preterm birth rates, on the other hand, rose for the fifth year in a row. The rate for 2019, 10.23% of all births, represents an increase of 2% over 2018 and is “the highest level reported in more than a decade,” the investigators noted.
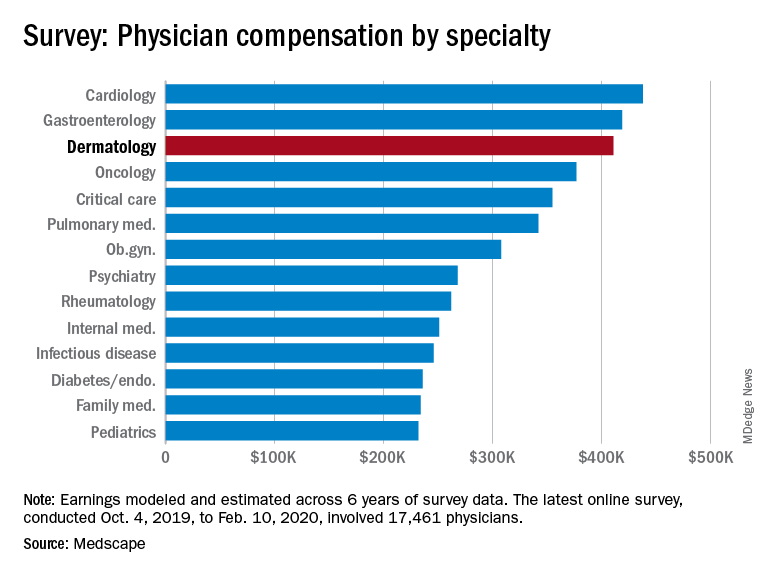
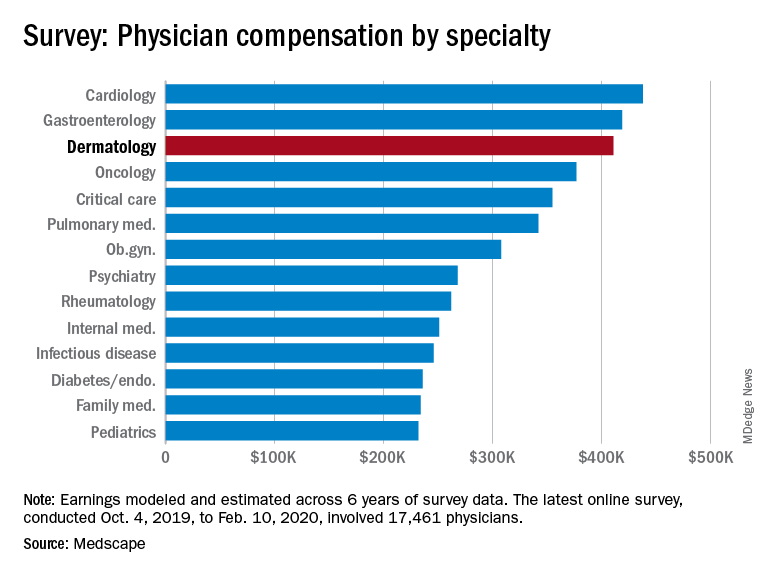
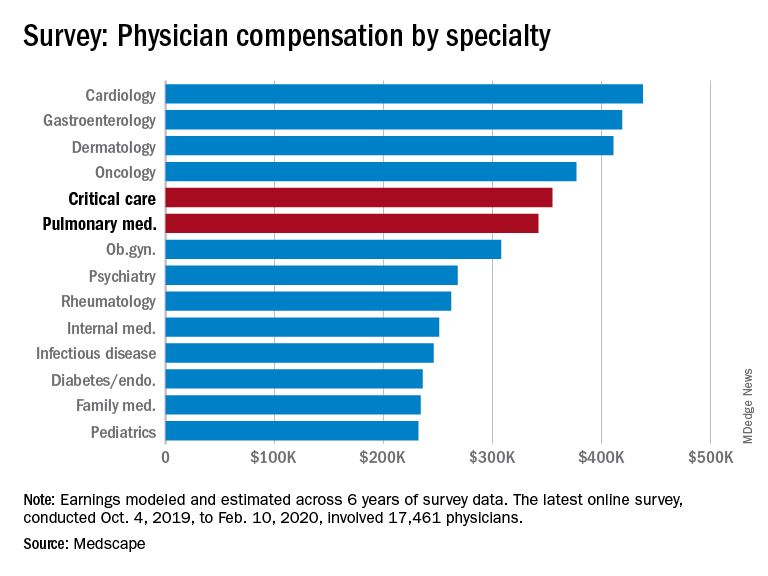
Dermatologists saw small income drop before pandemic
As the COVID spring progresses, the days before the pandemic may seem like a dream: Practices were open, waiting rooms were full of unmasked people, and PPE was plentiful.
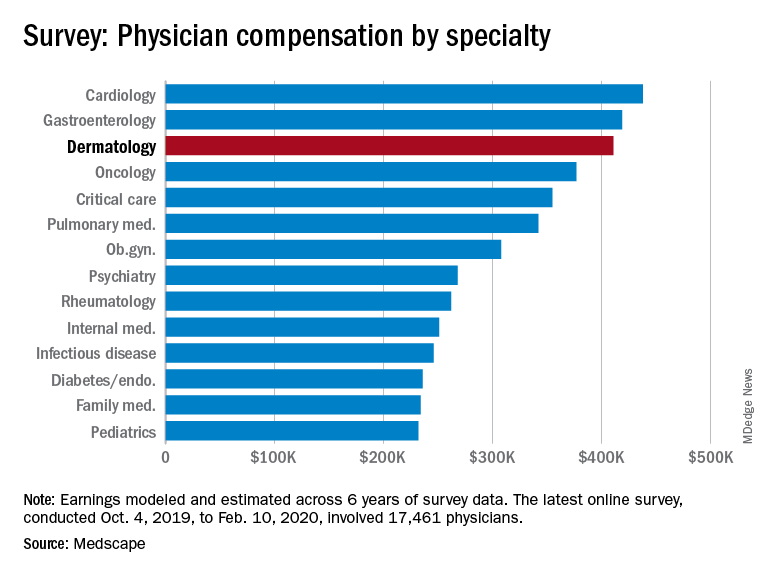
Back then, it turns out, earnings were down. Average compensation reported by dermatologists dropped from $419,000 in 2019 to $411,000 this year, a 1.9% decrease. Average income for all specialists was $346,000 in this year’s survey – 1.5% higher than the $341,000 earned in 2019, Medscape reported.
Prospects for this year of the pandemic are not better. “Specialists are currently having more troubles than [primary care physicians] because they’re dependent on elective cases, which can’t be directly addressed by telemedicine,” Joel Greenwald, MD, the CEO of Greenwald Wealth Management in St. Louis Park, Minn., told Medscape.
Despite the drop in earnings, 65% of dermatologists said that they were fairly compensated, which is more than the 61% who expressed that opinion in 2015 and more than 22 of the 29 specialties included in this year’s survey, Medscape noted.
Dermatologists (76%) were just below the average for all physicians (77%) when asked if they would choose medicine again, but they were near the top when asked if they would choose the same specialty (95%). Only orthopedics (97%) and oncology (96%) were higher, the survey data show.
The biggest problem area for dermatologists, by a small margin, is difficult patients. The most challenging part of their job, according to 24% of those responding, is “dealing with difficult patients,” with 23% choosing “having so many rules and regulations.” Among all physicians, rules/regulations was the leading choice with 27% of the vote, Medscape said.
The survey respondents were Medscape members who had been invited to participate. The sample size was 17,461 physicians, and compensation was modeled and estimated based on a range of variables across 6 years of survey data. The sampling error was ±0.74%.
As the COVID spring progresses, the days before the pandemic may seem like a dream: Practices were open, waiting rooms were full of unmasked people, and PPE was plentiful.
Back then, it turns out, earnings were down. Average compensation reported by dermatologists dropped from $419,000 in 2019 to $411,000 this year, a 1.9% decrease. Average income for all specialists was $346,000 in this year’s survey – 1.5% higher than the $341,000 earned in 2019, Medscape reported.
Prospects for this year of the pandemic are not better. “Specialists are currently having more troubles than [primary care physicians] because they’re dependent on elective cases, which can’t be directly addressed by telemedicine,” Joel Greenwald, MD, the CEO of Greenwald Wealth Management in St. Louis Park, Minn., told Medscape.
Despite the drop in earnings, 65% of dermatologists said that they were fairly compensated, which is more than the 61% who expressed that opinion in 2015 and more than 22 of the 29 specialties included in this year’s survey, Medscape noted.
Dermatologists (76%) were just below the average for all physicians (77%) when asked if they would choose medicine again, but they were near the top when asked if they would choose the same specialty (95%). Only orthopedics (97%) and oncology (96%) were higher, the survey data show.
The biggest problem area for dermatologists, by a small margin, is difficult patients. The most challenging part of their job, according to 24% of those responding, is “dealing with difficult patients,” with 23% choosing “having so many rules and regulations.” Among all physicians, rules/regulations was the leading choice with 27% of the vote, Medscape said.
The survey respondents were Medscape members who had been invited to participate. The sample size was 17,461 physicians, and compensation was modeled and estimated based on a range of variables across 6 years of survey data. The sampling error was ±0.74%.
As the COVID spring progresses, the days before the pandemic may seem like a dream: Practices were open, waiting rooms were full of unmasked people, and PPE was plentiful.
Back then, it turns out, earnings were down. Average compensation reported by dermatologists dropped from $419,000 in 2019 to $411,000 this year, a 1.9% decrease. Average income for all specialists was $346,000 in this year’s survey – 1.5% higher than the $341,000 earned in 2019, Medscape reported.
Prospects for this year of the pandemic are not better. “Specialists are currently having more troubles than [primary care physicians] because they’re dependent on elective cases, which can’t be directly addressed by telemedicine,” Joel Greenwald, MD, the CEO of Greenwald Wealth Management in St. Louis Park, Minn., told Medscape.
Despite the drop in earnings, 65% of dermatologists said that they were fairly compensated, which is more than the 61% who expressed that opinion in 2015 and more than 22 of the 29 specialties included in this year’s survey, Medscape noted.
Dermatologists (76%) were just below the average for all physicians (77%) when asked if they would choose medicine again, but they were near the top when asked if they would choose the same specialty (95%). Only orthopedics (97%) and oncology (96%) were higher, the survey data show.
The biggest problem area for dermatologists, by a small margin, is difficult patients. The most challenging part of their job, according to 24% of those responding, is “dealing with difficult patients,” with 23% choosing “having so many rules and regulations.” Among all physicians, rules/regulations was the leading choice with 27% of the vote, Medscape said.
The survey respondents were Medscape members who had been invited to participate. The sample size was 17,461 physicians, and compensation was modeled and estimated based on a range of variables across 6 years of survey data. The sampling error was ±0.74%.
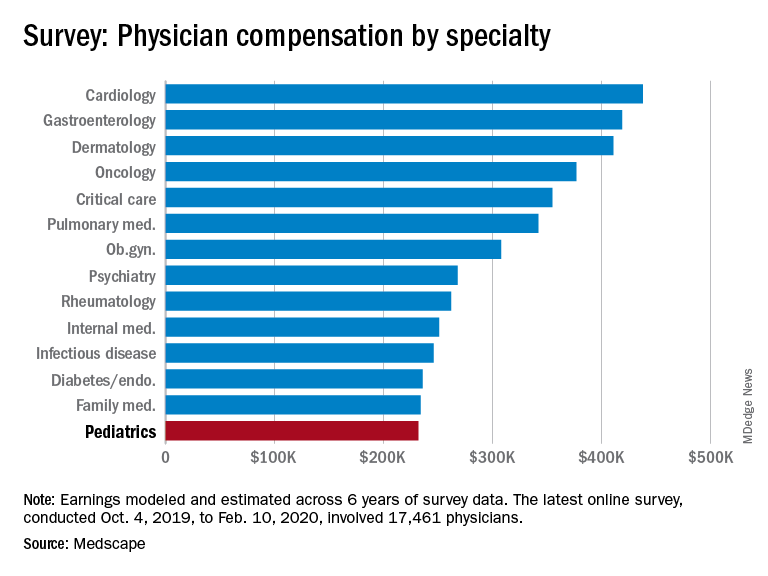
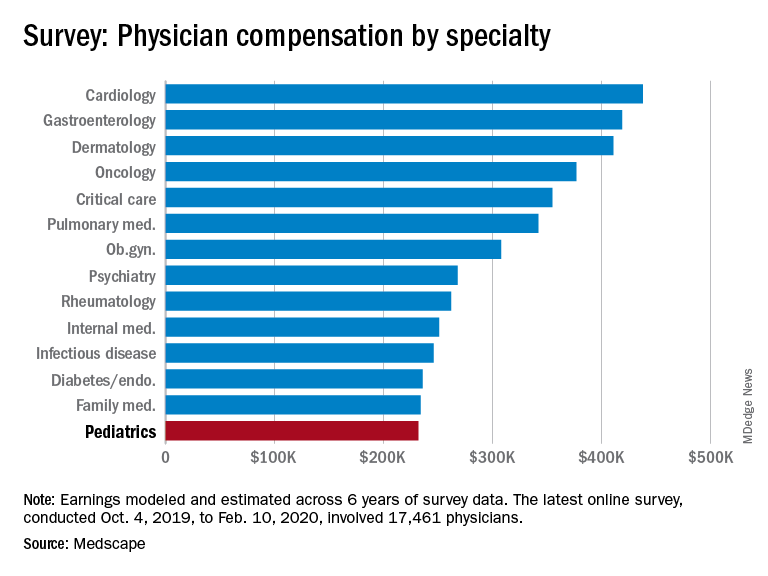
Pediatrics earnings were on the upswing before pandemic
As the COVID-19 spring progresses, the days before the pandemic may seem like a dream: Practices were open, waiting rooms were full of unmasked people, and personal protective equipment was plentiful.
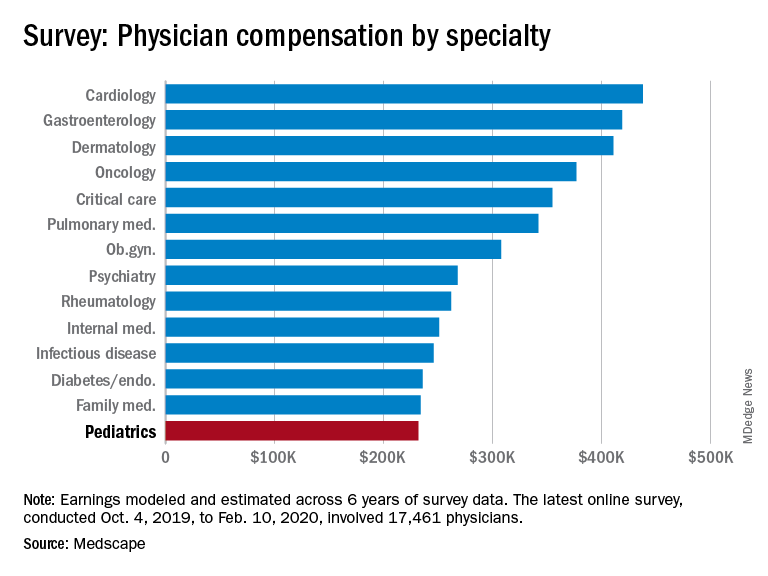
Medscape’s latest physician survey, conducted from Oct. 4, 2019, to Feb. 10, 2020, shows what pediatrics looked like just before the coronavirus arrived.
Back then, earnings were up. Average income for all primary care physicians was $243,000 in this year’s survey – 2.5% higher than the $237,000 earned in 2019, Medscape reported.
Prospects for the next year, however, are grim. “We found out that we have a 10% salary decrease effective May 2 to Dec. 25. Our bonus will be based on clinical productivity, and since our numbers are down, that is likely to go away,” a pediatric emergency physician told Medscape.
Before the pandemic, 53% of pediatricians said that they were fairly compensated, right between internists at 52% and family physicians at 54% and in the middle of the overall specialty pack, which ranged from nephrology at 44% to oncology, emergency medicine, and radiology at 67%, the survey data show.
Primary care physicians and specialists were nearly equal in hours spent seeing patients each week – 37.6 for primary care and 38.0 for specialists – but family physicians and internists both averaged more hours than pediatricians doing paperwork and administration each week, at 15.9 and 18.5 versus 14.7, respectively, Medscape said.
Pediatricians (38%) were more likely than the average physician (27%) to say that “gratitude/relationships with patients” was the most rewarding part of their job, and less likely to say that “having so many rules and regulations” was the most challenging part (22% vs. 26%), according to the survey.
When asked if they would choose medicine again, 78% of pediatricians said yes, just above the 77% for all physicians. Pediatricians, however, were much more likely (83%) to say they would choose the same specialty, compared with family physicians (70%) and internists (66%), Medscape found.
The survey respondents were Medscape members who had been invited to participate. The sample size was 17,461 physicians, and compensation was modeled and estimated based on a range of variables across 6 years of survey data. The sampling error was ±0.74%.
As the COVID-19 spring progresses, the days before the pandemic may seem like a dream: Practices were open, waiting rooms were full of unmasked people, and personal protective equipment was plentiful.
Medscape’s latest physician survey, conducted from Oct. 4, 2019, to Feb. 10, 2020, shows what pediatrics looked like just before the coronavirus arrived.
Back then, earnings were up. Average income for all primary care physicians was $243,000 in this year’s survey – 2.5% higher than the $237,000 earned in 2019, Medscape reported.
Prospects for the next year, however, are grim. “We found out that we have a 10% salary decrease effective May 2 to Dec. 25. Our bonus will be based on clinical productivity, and since our numbers are down, that is likely to go away,” a pediatric emergency physician told Medscape.
Before the pandemic, 53% of pediatricians said that they were fairly compensated, right between internists at 52% and family physicians at 54% and in the middle of the overall specialty pack, which ranged from nephrology at 44% to oncology, emergency medicine, and radiology at 67%, the survey data show.
Primary care physicians and specialists were nearly equal in hours spent seeing patients each week – 37.6 for primary care and 38.0 for specialists – but family physicians and internists both averaged more hours than pediatricians doing paperwork and administration each week, at 15.9 and 18.5 versus 14.7, respectively, Medscape said.
Pediatricians (38%) were more likely than the average physician (27%) to say that “gratitude/relationships with patients” was the most rewarding part of their job, and less likely to say that “having so many rules and regulations” was the most challenging part (22% vs. 26%), according to the survey.
When asked if they would choose medicine again, 78% of pediatricians said yes, just above the 77% for all physicians. Pediatricians, however, were much more likely (83%) to say they would choose the same specialty, compared with family physicians (70%) and internists (66%), Medscape found.
The survey respondents were Medscape members who had been invited to participate. The sample size was 17,461 physicians, and compensation was modeled and estimated based on a range of variables across 6 years of survey data. The sampling error was ±0.74%.
As the COVID-19 spring progresses, the days before the pandemic may seem like a dream: Practices were open, waiting rooms were full of unmasked people, and personal protective equipment was plentiful.
Medscape’s latest physician survey, conducted from Oct. 4, 2019, to Feb. 10, 2020, shows what pediatrics looked like just before the coronavirus arrived.
Back then, earnings were up. Average income for all primary care physicians was $243,000 in this year’s survey – 2.5% higher than the $237,000 earned in 2019, Medscape reported.
Prospects for the next year, however, are grim. “We found out that we have a 10% salary decrease effective May 2 to Dec. 25. Our bonus will be based on clinical productivity, and since our numbers are down, that is likely to go away,” a pediatric emergency physician told Medscape.
Before the pandemic, 53% of pediatricians said that they were fairly compensated, right between internists at 52% and family physicians at 54% and in the middle of the overall specialty pack, which ranged from nephrology at 44% to oncology, emergency medicine, and radiology at 67%, the survey data show.
Primary care physicians and specialists were nearly equal in hours spent seeing patients each week – 37.6 for primary care and 38.0 for specialists – but family physicians and internists both averaged more hours than pediatricians doing paperwork and administration each week, at 15.9 and 18.5 versus 14.7, respectively, Medscape said.
Pediatricians (38%) were more likely than the average physician (27%) to say that “gratitude/relationships with patients” was the most rewarding part of their job, and less likely to say that “having so many rules and regulations” was the most challenging part (22% vs. 26%), according to the survey.
When asked if they would choose medicine again, 78% of pediatricians said yes, just above the 77% for all physicians. Pediatricians, however, were much more likely (83%) to say they would choose the same specialty, compared with family physicians (70%) and internists (66%), Medscape found.
The survey respondents were Medscape members who had been invited to participate. The sample size was 17,461 physicians, and compensation was modeled and estimated based on a range of variables across 6 years of survey data. The sampling error was ±0.74%.
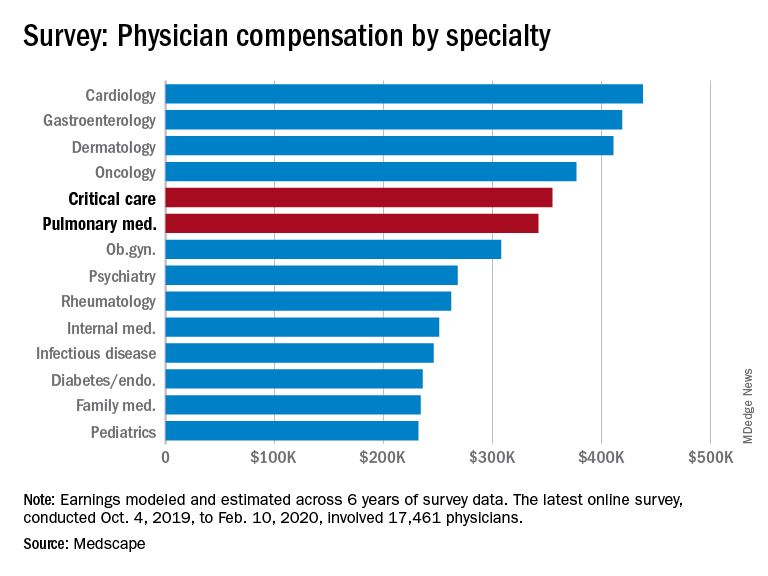
Pulmonology, critical care earnings on the upswing before pandemic
As the COVID spring progresses, the days before the pandemic may seem like a dream: Practices were open, waiting rooms were full of unmasked people, and PPE was plentiful.
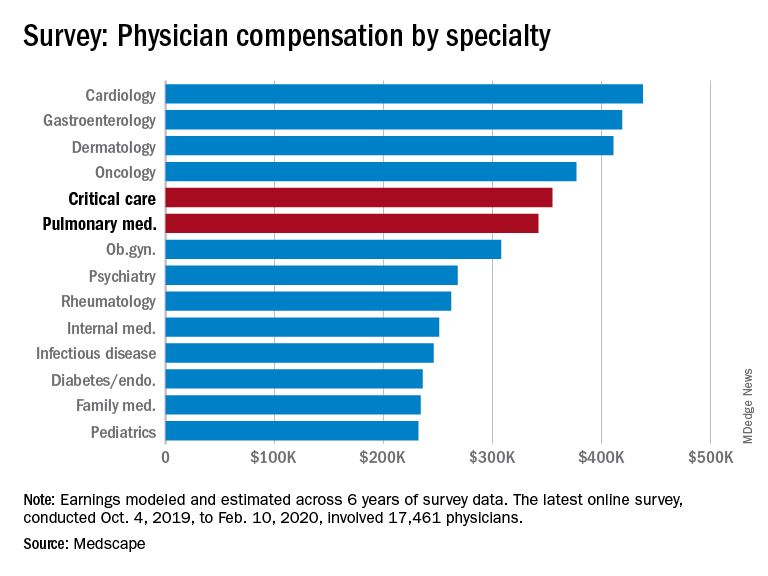
Medscape’s latest physician survey, conducted from Oct. 4, 2019, to Feb. 10, 2020, shows what pulmonology and critical care looked like just before the coronavirus arrived.
Back then, earnings were up. Average compensation reported by pulmonologists was up from $331,000 in 2019 to $342,000 this year, a 3.3% increase. For intensivists, earnings rose from $349,000 to $355,000, or 1.7%. Average income for all specialists was $346,000 in this year’s survey – 1.5% higher than the $341,000 earned in 2019, Medscape reported.
Prospects for the next year, however, are grim. “We found out that we have a 10% salary decrease effective May 2 to Dec. 25. Our bonus will be based on clinical productivity, and since our numbers are down, that is likely to go away,” a pediatric emergency physician told Medscape.
One problem area for intensivists, even before the pandemic, was paperwork and administration. Of the 26 specialties for which data are available, critical care was highest for amount of time spent on paperwork, at 19.1 hours per week. Those in pulmonary medicine spent 15.6 hours per week, which also happened to be the average for all specialists, the survey data show.
Both specialties also ranked high in denied/resubmitted claims: Intensivists were fourth among the 27 types of specialists with reliable data, with 20% of claims denied, and pulmonologists were tied for eighth at 18%, Medscape said.
Only 50% of pulmonologists surveyed said that they were being fairly compensated, putting them 26th among the 29 specialties on that list. Those in critical care medicine were 13th, with a 59% positive response, Medscape reported.
In the end, though, it looks like you can’t keep a good pulmonologist or intensivist down. When asked if they would choose medicine again, 83% of pulmonologists said yes, just one percentage point behind a three-way tie for first. Intensivists were just a little further down the list at 81%, according to the survey.
The respondents were Medscape members who had been invited to participate. The sample size was 17,461 physicians, and compensation was modeled and estimated based on a range of variables across 6 years of survey data. The sampling error was ±0.74%.
As the COVID spring progresses, the days before the pandemic may seem like a dream: Practices were open, waiting rooms were full of unmasked people, and PPE was plentiful.
Medscape’s latest physician survey, conducted from Oct. 4, 2019, to Feb. 10, 2020, shows what pulmonology and critical care looked like just before the coronavirus arrived.
Back then, earnings were up. Average compensation reported by pulmonologists was up from $331,000 in 2019 to $342,000 this year, a 3.3% increase. For intensivists, earnings rose from $349,000 to $355,000, or 1.7%. Average income for all specialists was $346,000 in this year’s survey – 1.5% higher than the $341,000 earned in 2019, Medscape reported.
Prospects for the next year, however, are grim. “We found out that we have a 10% salary decrease effective May 2 to Dec. 25. Our bonus will be based on clinical productivity, and since our numbers are down, that is likely to go away,” a pediatric emergency physician told Medscape.
One problem area for intensivists, even before the pandemic, was paperwork and administration. Of the 26 specialties for which data are available, critical care was highest for amount of time spent on paperwork, at 19.1 hours per week. Those in pulmonary medicine spent 15.6 hours per week, which also happened to be the average for all specialists, the survey data show.
Both specialties also ranked high in denied/resubmitted claims: Intensivists were fourth among the 27 types of specialists with reliable data, with 20% of claims denied, and pulmonologists were tied for eighth at 18%, Medscape said.
Only 50% of pulmonologists surveyed said that they were being fairly compensated, putting them 26th among the 29 specialties on that list. Those in critical care medicine were 13th, with a 59% positive response, Medscape reported.
In the end, though, it looks like you can’t keep a good pulmonologist or intensivist down. When asked if they would choose medicine again, 83% of pulmonologists said yes, just one percentage point behind a three-way tie for first. Intensivists were just a little further down the list at 81%, according to the survey.
The respondents were Medscape members who had been invited to participate. The sample size was 17,461 physicians, and compensation was modeled and estimated based on a range of variables across 6 years of survey data. The sampling error was ±0.74%.
As the COVID spring progresses, the days before the pandemic may seem like a dream: Practices were open, waiting rooms were full of unmasked people, and PPE was plentiful.
Medscape’s latest physician survey, conducted from Oct. 4, 2019, to Feb. 10, 2020, shows what pulmonology and critical care looked like just before the coronavirus arrived.
Back then, earnings were up. Average compensation reported by pulmonologists was up from $331,000 in 2019 to $342,000 this year, a 3.3% increase. For intensivists, earnings rose from $349,000 to $355,000, or 1.7%. Average income for all specialists was $346,000 in this year’s survey – 1.5% higher than the $341,000 earned in 2019, Medscape reported.
Prospects for the next year, however, are grim. “We found out that we have a 10% salary decrease effective May 2 to Dec. 25. Our bonus will be based on clinical productivity, and since our numbers are down, that is likely to go away,” a pediatric emergency physician told Medscape.
One problem area for intensivists, even before the pandemic, was paperwork and administration. Of the 26 specialties for which data are available, critical care was highest for amount of time spent on paperwork, at 19.1 hours per week. Those in pulmonary medicine spent 15.6 hours per week, which also happened to be the average for all specialists, the survey data show.
Both specialties also ranked high in denied/resubmitted claims: Intensivists were fourth among the 27 types of specialists with reliable data, with 20% of claims denied, and pulmonologists were tied for eighth at 18%, Medscape said.
Only 50% of pulmonologists surveyed said that they were being fairly compensated, putting them 26th among the 29 specialties on that list. Those in critical care medicine were 13th, with a 59% positive response, Medscape reported.
In the end, though, it looks like you can’t keep a good pulmonologist or intensivist down. When asked if they would choose medicine again, 83% of pulmonologists said yes, just one percentage point behind a three-way tie for first. Intensivists were just a little further down the list at 81%, according to the survey.
The respondents were Medscape members who had been invited to participate. The sample size was 17,461 physicians, and compensation was modeled and estimated based on a range of variables across 6 years of survey data. The sampling error was ±0.74%.
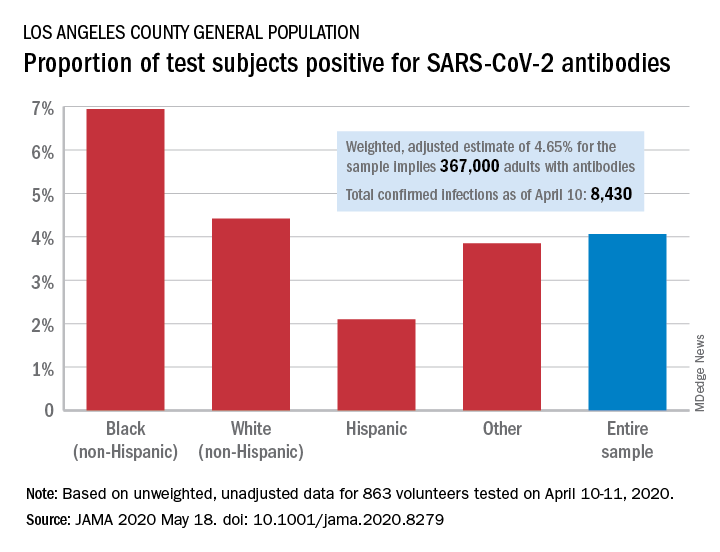
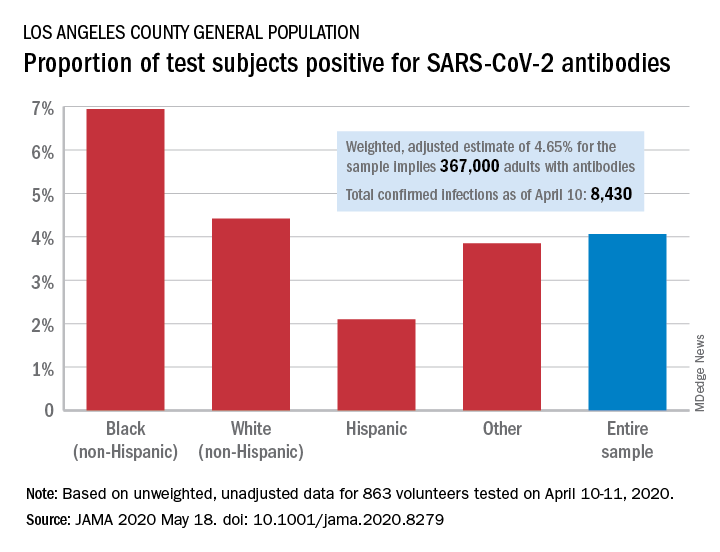
Antibody testing suggests COVID-19 cases are being missed
The number of COVID-19 infections in the community may be “substantially greater” than totals confirmed by authorities, based on SARS-CoV-2 antibody testing among a random sample of adults in Los Angeles County, Calif.
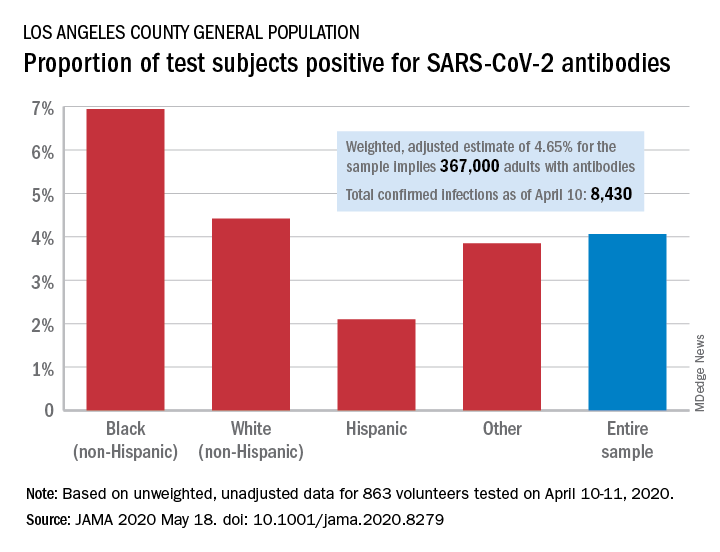
Testing of 863 people on April 10-11 revealed that 35 (4.06%) were positive for SARS-CoV-2–specific antibodies (IgM or IgG), and after adjustment for test sensitivity and specificity, the weighted prevalence for the entire sample was 4.65%, Neeraj Sood, PhD, of the University of Southern California, Los Angeles, and associates wrote in JAMA.
The estimate of 4.65% “implies that approximately 367,000 adults [in Los Angeles County] had SARS-CoV-2 antibodies, which is substantially greater than the 8,430 cumulative number of confirmed infections in the county on April 10,” they wrote.
It also suggests that fatality rates based on the larger number of infections may be lower than rates based on confirmed cases. “In addition, contact tracing methods to limit the spread of infection will face considerable challenges,” Dr. Sood and associates said.
Test positivity varied by race/ethnicity, sex, and income. The proportion of non-Hispanic blacks with a positive result was 6.94%, compared with 4.42% for non-Hispanic whites, 2.10% for Hispanics, and 3.85% for others. Men were much more likely than women to be positive for SARS-CoV-2: 5.18% vs. 3.31%, the investigators said.
Household income favored the middle ground. Those individuals making less than $50,000 a year had a positivity rate of 5.14% and those with an income of $100,000 or more had a rate of 4.90%, but only 1.58% of those making $50,000-$99,999 tested positive, they reported.
The authors reported numerous sources of nonprofit organization support.
SOURCE: Sood N et al. JAMA 2020 May 18. doi: 10.1001/jama.2020.8279.
The number of COVID-19 infections in the community may be “substantially greater” than totals confirmed by authorities, based on SARS-CoV-2 antibody testing among a random sample of adults in Los Angeles County, Calif.
Testing of 863 people on April 10-11 revealed that 35 (4.06%) were positive for SARS-CoV-2–specific antibodies (IgM or IgG), and after adjustment for test sensitivity and specificity, the weighted prevalence for the entire sample was 4.65%, Neeraj Sood, PhD, of the University of Southern California, Los Angeles, and associates wrote in JAMA.
The estimate of 4.65% “implies that approximately 367,000 adults [in Los Angeles County] had SARS-CoV-2 antibodies, which is substantially greater than the 8,430 cumulative number of confirmed infections in the county on April 10,” they wrote.
It also suggests that fatality rates based on the larger number of infections may be lower than rates based on confirmed cases. “In addition, contact tracing methods to limit the spread of infection will face considerable challenges,” Dr. Sood and associates said.
Test positivity varied by race/ethnicity, sex, and income. The proportion of non-Hispanic blacks with a positive result was 6.94%, compared with 4.42% for non-Hispanic whites, 2.10% for Hispanics, and 3.85% for others. Men were much more likely than women to be positive for SARS-CoV-2: 5.18% vs. 3.31%, the investigators said.
Household income favored the middle ground. Those individuals making less than $50,000 a year had a positivity rate of 5.14% and those with an income of $100,000 or more had a rate of 4.90%, but only 1.58% of those making $50,000-$99,999 tested positive, they reported.
The authors reported numerous sources of nonprofit organization support.
SOURCE: Sood N et al. JAMA 2020 May 18. doi: 10.1001/jama.2020.8279.
The number of COVID-19 infections in the community may be “substantially greater” than totals confirmed by authorities, based on SARS-CoV-2 antibody testing among a random sample of adults in Los Angeles County, Calif.
Testing of 863 people on April 10-11 revealed that 35 (4.06%) were positive for SARS-CoV-2–specific antibodies (IgM or IgG), and after adjustment for test sensitivity and specificity, the weighted prevalence for the entire sample was 4.65%, Neeraj Sood, PhD, of the University of Southern California, Los Angeles, and associates wrote in JAMA.
The estimate of 4.65% “implies that approximately 367,000 adults [in Los Angeles County] had SARS-CoV-2 antibodies, which is substantially greater than the 8,430 cumulative number of confirmed infections in the county on April 10,” they wrote.
It also suggests that fatality rates based on the larger number of infections may be lower than rates based on confirmed cases. “In addition, contact tracing methods to limit the spread of infection will face considerable challenges,” Dr. Sood and associates said.
Test positivity varied by race/ethnicity, sex, and income. The proportion of non-Hispanic blacks with a positive result was 6.94%, compared with 4.42% for non-Hispanic whites, 2.10% for Hispanics, and 3.85% for others. Men were much more likely than women to be positive for SARS-CoV-2: 5.18% vs. 3.31%, the investigators said.
Household income favored the middle ground. Those individuals making less than $50,000 a year had a positivity rate of 5.14% and those with an income of $100,000 or more had a rate of 4.90%, but only 1.58% of those making $50,000-$99,999 tested positive, they reported.
The authors reported numerous sources of nonprofit organization support.
SOURCE: Sood N et al. JAMA 2020 May 18. doi: 10.1001/jama.2020.8279.
FROM JAMA
States vary in vulnerability to COVID-19 impact
West Virginia’s large elderly population and high rates of chronic kidney disease, cardiovascular disease, diabetes, and COPD make it the most vulnerable state to the coronavirus, according to a new analysis.

Vulnerability to the virus “isn’t just health related, though, as many people are harmed by the economic effects of the pandemic,” personal finance website WalletHub said May 12.
“It’s important for the U.S. to dedicate a large portion of its resources to providing medical support during the coronavirus pandemic, but we should also support people who don’t have adequate housing or enough money to survive the pandemic,” said WalletHub analyst Jill Gonzalez.
WalletHub graded each state on 28 measures – including share of obese adults, share of homes lacking access to basic hygienic facilities, and biggest increases in unemployment because of COVID-19 – grouped into three dimensions of vulnerability: medical (60% of the total score), housing (15%), and financial (25%).
Using those measures, Louisiana is the most vulnerable state after West Virginia, followed by Mississippi, Arkansas, and Alabama. All 5 states finished in the top 6 for medical vulnerability, and 4 were in the top 10 for financial vulnerability, but only 1 (Arkansas) was in the top 10 for housing vulnerability, WalletHub said.
Among the three vulnerability dimensions, West Virginia was first in medical, Hawaii (33rd overall) was first in housing, and Louisiana was first in financial. Utah is the least vulnerable state, overall, and the least vulnerable states in each dimension are, respectively, Colorado (50th overall), the District of Columbia (29th overall), and Iowa (45th overall), the report showed.
A look at the individual metrics WalletHub used shows some serious disparities:
- New Jersey’s unemployment recipiency rate of 57.2%, the highest in the country, is 6.1 times higher than North Carolina’s 9.3%.
- The highest uninsured rate, 17.4% in Texas, is 6.2 times higher than in Massachusetts, which is the lowest at 2.8%.
- In California, the share of the homeless population that is unsheltered (71.7%) is more than 33 times higher than in North Dakota (2.2%).
“The financial damage caused by COVID-19 is leaving many Americans without the means to pay their bills and purchase necessities. … The U.S. must continue to support its financially vulnerable populations even after the virus has subsided,” Ms. Gonzalez said.
West Virginia’s large elderly population and high rates of chronic kidney disease, cardiovascular disease, diabetes, and COPD make it the most vulnerable state to the coronavirus, according to a new analysis.

Vulnerability to the virus “isn’t just health related, though, as many people are harmed by the economic effects of the pandemic,” personal finance website WalletHub said May 12.
“It’s important for the U.S. to dedicate a large portion of its resources to providing medical support during the coronavirus pandemic, but we should also support people who don’t have adequate housing or enough money to survive the pandemic,” said WalletHub analyst Jill Gonzalez.
WalletHub graded each state on 28 measures – including share of obese adults, share of homes lacking access to basic hygienic facilities, and biggest increases in unemployment because of COVID-19 – grouped into three dimensions of vulnerability: medical (60% of the total score), housing (15%), and financial (25%).
Using those measures, Louisiana is the most vulnerable state after West Virginia, followed by Mississippi, Arkansas, and Alabama. All 5 states finished in the top 6 for medical vulnerability, and 4 were in the top 10 for financial vulnerability, but only 1 (Arkansas) was in the top 10 for housing vulnerability, WalletHub said.
Among the three vulnerability dimensions, West Virginia was first in medical, Hawaii (33rd overall) was first in housing, and Louisiana was first in financial. Utah is the least vulnerable state, overall, and the least vulnerable states in each dimension are, respectively, Colorado (50th overall), the District of Columbia (29th overall), and Iowa (45th overall), the report showed.
A look at the individual metrics WalletHub used shows some serious disparities:
- New Jersey’s unemployment recipiency rate of 57.2%, the highest in the country, is 6.1 times higher than North Carolina’s 9.3%.
- The highest uninsured rate, 17.4% in Texas, is 6.2 times higher than in Massachusetts, which is the lowest at 2.8%.
- In California, the share of the homeless population that is unsheltered (71.7%) is more than 33 times higher than in North Dakota (2.2%).
“The financial damage caused by COVID-19 is leaving many Americans without the means to pay their bills and purchase necessities. … The U.S. must continue to support its financially vulnerable populations even after the virus has subsided,” Ms. Gonzalez said.
West Virginia’s large elderly population and high rates of chronic kidney disease, cardiovascular disease, diabetes, and COPD make it the most vulnerable state to the coronavirus, according to a new analysis.

Vulnerability to the virus “isn’t just health related, though, as many people are harmed by the economic effects of the pandemic,” personal finance website WalletHub said May 12.
“It’s important for the U.S. to dedicate a large portion of its resources to providing medical support during the coronavirus pandemic, but we should also support people who don’t have adequate housing or enough money to survive the pandemic,” said WalletHub analyst Jill Gonzalez.
WalletHub graded each state on 28 measures – including share of obese adults, share of homes lacking access to basic hygienic facilities, and biggest increases in unemployment because of COVID-19 – grouped into three dimensions of vulnerability: medical (60% of the total score), housing (15%), and financial (25%).
Using those measures, Louisiana is the most vulnerable state after West Virginia, followed by Mississippi, Arkansas, and Alabama. All 5 states finished in the top 6 for medical vulnerability, and 4 were in the top 10 for financial vulnerability, but only 1 (Arkansas) was in the top 10 for housing vulnerability, WalletHub said.
Among the three vulnerability dimensions, West Virginia was first in medical, Hawaii (33rd overall) was first in housing, and Louisiana was first in financial. Utah is the least vulnerable state, overall, and the least vulnerable states in each dimension are, respectively, Colorado (50th overall), the District of Columbia (29th overall), and Iowa (45th overall), the report showed.
A look at the individual metrics WalletHub used shows some serious disparities:
- New Jersey’s unemployment recipiency rate of 57.2%, the highest in the country, is 6.1 times higher than North Carolina’s 9.3%.
- The highest uninsured rate, 17.4% in Texas, is 6.2 times higher than in Massachusetts, which is the lowest at 2.8%.
- In California, the share of the homeless population that is unsheltered (71.7%) is more than 33 times higher than in North Dakota (2.2%).
“The financial damage caused by COVID-19 is leaving many Americans without the means to pay their bills and purchase necessities. … The U.S. must continue to support its financially vulnerable populations even after the virus has subsided,” Ms. Gonzalez said.
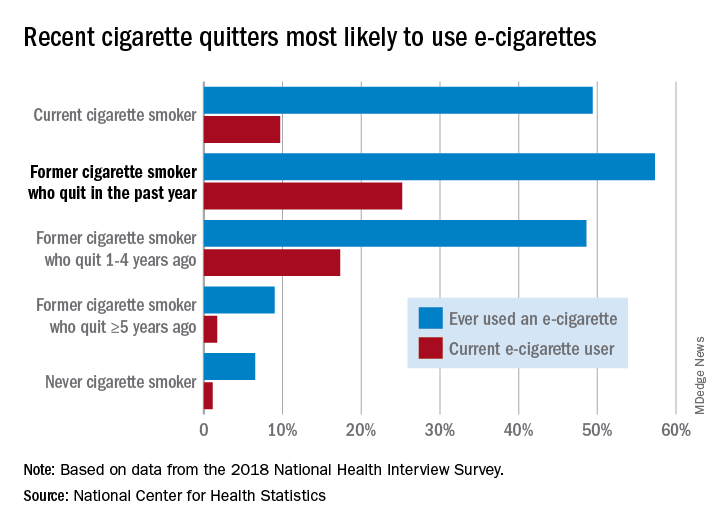
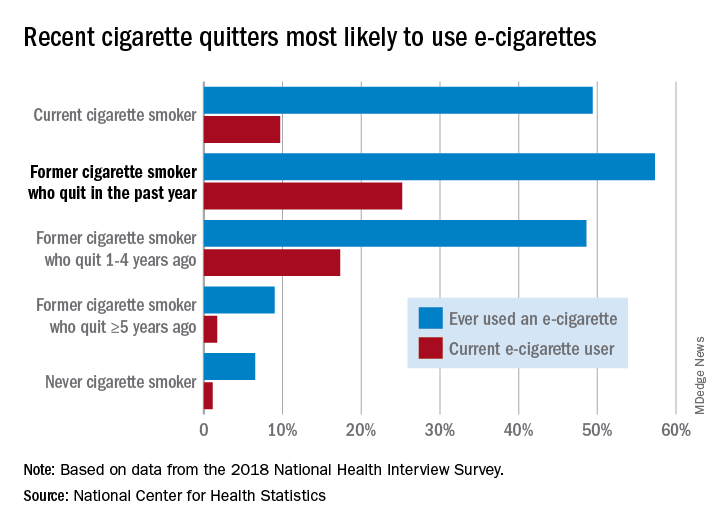
E-cigarette users topped 8 million in 2018
according to a report from the National Center for Health Statistics.
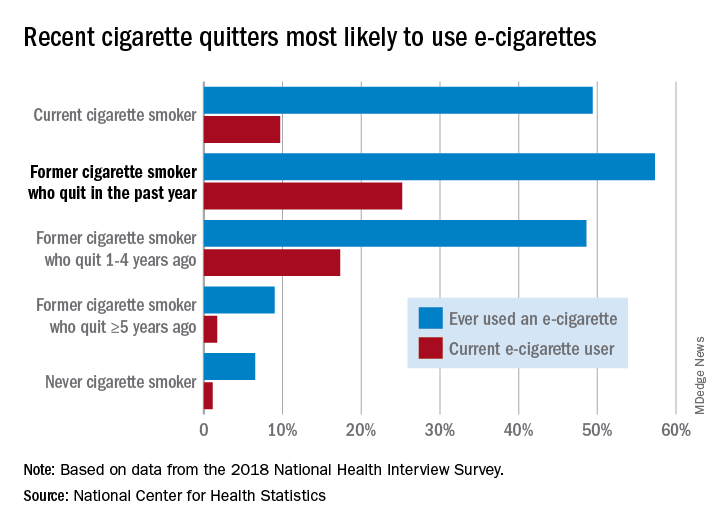
Those 8.1 million individuals who were using e-cigarettes either every day or some days represented 3.2% of the total adult population, based on data from the 2018 National Health Interview Survey. An even larger proportion, 14.9%, said that they had at least tried an e-cigarette, Maria A. Villarroel, PhD, and associates at the NCHS said in a recent data brief.
Most cigarette smokers, both current and former, were even more likely to use e-cigarettes, they noted.
Former cigarette smokers who had quit within the last year were the most likely to use e-cigarettes – 57.3% had ever used one and 25.2% were current users – while current cigarette users (49.4% ever use and 9.7% current use) and former smokers who had quit 1-5 years before (48.6% ever use, 17.3% current) also were above-average e-cigarette consumers, they reported.
Use was significantly lower, however, among former cigarette smokers who had quit 5 or more years earlier (9.0% and 1.7%, respectively) and those who had never smoked (6.5% and 1.1%), the NCHS investigators said.
The survey data also showed much variation among the sociodemographic subgroups:
- E-cigarette ever/current use was significantly higher in men (17.9% and 4.2%) than women (12.3% and 2.3%).
- Whites were significantly more likely to use e-cigarettes (16.9% and 3.7%), compared with Hispanic (11.5% and 2.5%), black (10.0% and 1.6%), and Asian (10.2% and 2.2%) adults.
- There was significant trend of decreasing use from age 18-24 years (25.8% and 7.6%) to 65 years and older (4.7% and 0.8%).
SOURCE: Villarroel MA et al. NCHS Data Brief No. 365, April 2020.
according to a report from the National Center for Health Statistics.
Those 8.1 million individuals who were using e-cigarettes either every day or some days represented 3.2% of the total adult population, based on data from the 2018 National Health Interview Survey. An even larger proportion, 14.9%, said that they had at least tried an e-cigarette, Maria A. Villarroel, PhD, and associates at the NCHS said in a recent data brief.
Most cigarette smokers, both current and former, were even more likely to use e-cigarettes, they noted.
Former cigarette smokers who had quit within the last year were the most likely to use e-cigarettes – 57.3% had ever used one and 25.2% were current users – while current cigarette users (49.4% ever use and 9.7% current use) and former smokers who had quit 1-5 years before (48.6% ever use, 17.3% current) also were above-average e-cigarette consumers, they reported.
Use was significantly lower, however, among former cigarette smokers who had quit 5 or more years earlier (9.0% and 1.7%, respectively) and those who had never smoked (6.5% and 1.1%), the NCHS investigators said.
The survey data also showed much variation among the sociodemographic subgroups:
- E-cigarette ever/current use was significantly higher in men (17.9% and 4.2%) than women (12.3% and 2.3%).
- Whites were significantly more likely to use e-cigarettes (16.9% and 3.7%), compared with Hispanic (11.5% and 2.5%), black (10.0% and 1.6%), and Asian (10.2% and 2.2%) adults.
- There was significant trend of decreasing use from age 18-24 years (25.8% and 7.6%) to 65 years and older (4.7% and 0.8%).
SOURCE: Villarroel MA et al. NCHS Data Brief No. 365, April 2020.
according to a report from the National Center for Health Statistics.
Those 8.1 million individuals who were using e-cigarettes either every day or some days represented 3.2% of the total adult population, based on data from the 2018 National Health Interview Survey. An even larger proportion, 14.9%, said that they had at least tried an e-cigarette, Maria A. Villarroel, PhD, and associates at the NCHS said in a recent data brief.
Most cigarette smokers, both current and former, were even more likely to use e-cigarettes, they noted.
Former cigarette smokers who had quit within the last year were the most likely to use e-cigarettes – 57.3% had ever used one and 25.2% were current users – while current cigarette users (49.4% ever use and 9.7% current use) and former smokers who had quit 1-5 years before (48.6% ever use, 17.3% current) also were above-average e-cigarette consumers, they reported.
Use was significantly lower, however, among former cigarette smokers who had quit 5 or more years earlier (9.0% and 1.7%, respectively) and those who had never smoked (6.5% and 1.1%), the NCHS investigators said.
The survey data also showed much variation among the sociodemographic subgroups:
- E-cigarette ever/current use was significantly higher in men (17.9% and 4.2%) than women (12.3% and 2.3%).
- Whites were significantly more likely to use e-cigarettes (16.9% and 3.7%), compared with Hispanic (11.5% and 2.5%), black (10.0% and 1.6%), and Asian (10.2% and 2.2%) adults.
- There was significant trend of decreasing use from age 18-24 years (25.8% and 7.6%) to 65 years and older (4.7% and 0.8%).
SOURCE: Villarroel MA et al. NCHS Data Brief No. 365, April 2020.
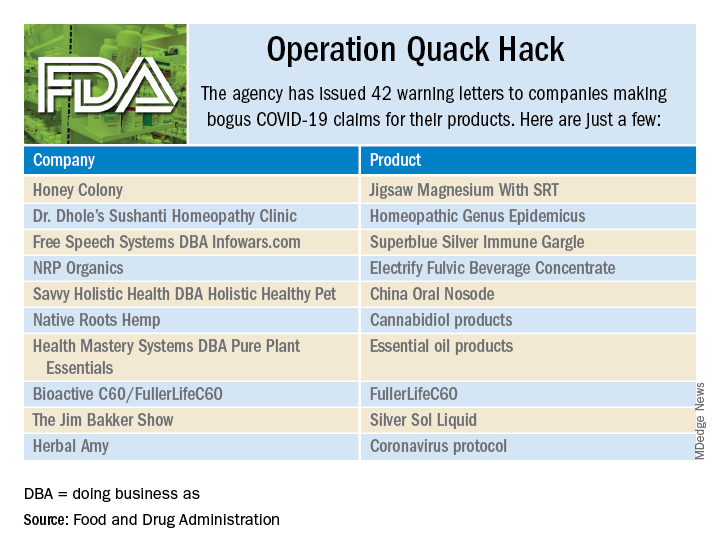
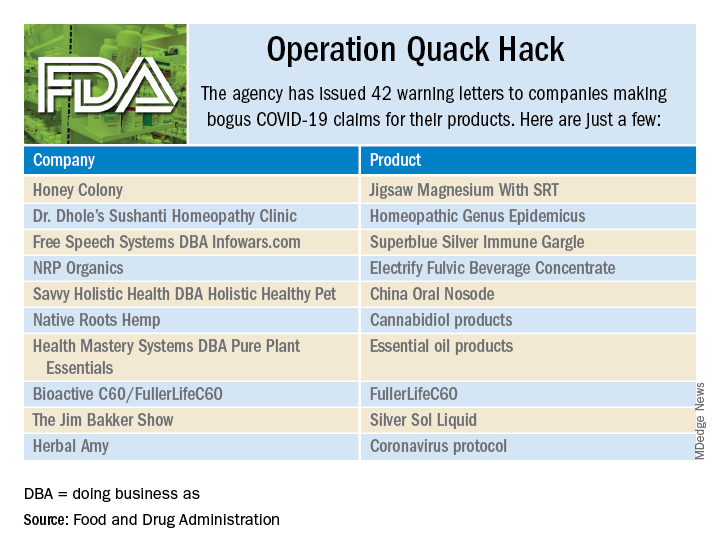
Operation Quack Hack: FDA moves to stop fraudulent COVID-19 products
No form of human misery can be allowed to go unexploited, and the pandemic, it seems, is no exception.
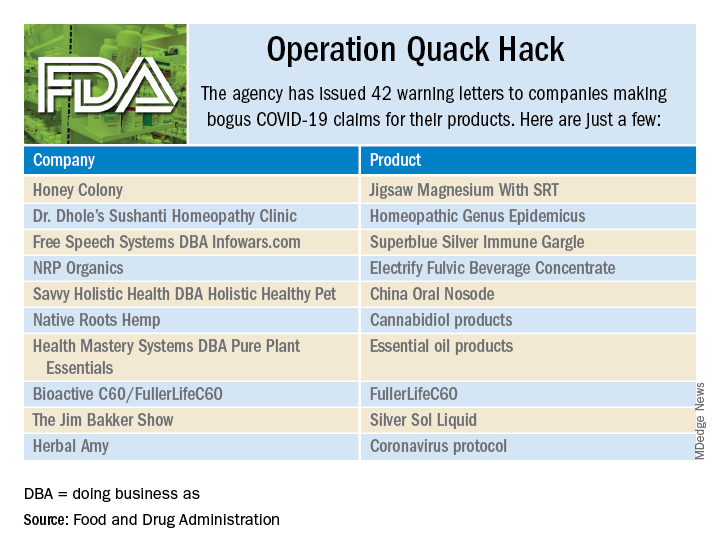
As part of Operation Quack Hack, the Food and Drug Administration has stepped up its investigation and enforcement efforts against companies and individuals that are “taking advantage of widespread fear among consumers during the COVID-19 pandemic” by selling fake products and treatments for coronavirus.
As of May 7, 2020, the agency had issued 42 warning letters to companies that were “selling unapproved products that fraudulently claim to mitigate, prevent, treat, diagnose or cure COVID-19,” the FDA announced in a written statement. Of those 42 products, 29 are no longer being sold with any sort of COVID-19 claim.
Since the beginning of the pandemic, Operation Quack Hack has uncovered hundreds of such products – drugs, testing kits, and personal protective equipment – being sold online, and complaints were sent to domain-name registrars and Internet marketplaces that have, in most cases, removed the postings, the FDA said.
“We will continue to monitor the online ecosystem for fraudulent products peddled by bad actors seeking to profit from this global pandemic. We encourage anyone aware of suspected fraudulent medical products for COVID-19 to report them to the FDA,” the statement said.
No form of human misery can be allowed to go unexploited, and the pandemic, it seems, is no exception.
As part of Operation Quack Hack, the Food and Drug Administration has stepped up its investigation and enforcement efforts against companies and individuals that are “taking advantage of widespread fear among consumers during the COVID-19 pandemic” by selling fake products and treatments for coronavirus.
As of May 7, 2020, the agency had issued 42 warning letters to companies that were “selling unapproved products that fraudulently claim to mitigate, prevent, treat, diagnose or cure COVID-19,” the FDA announced in a written statement. Of those 42 products, 29 are no longer being sold with any sort of COVID-19 claim.
Since the beginning of the pandemic, Operation Quack Hack has uncovered hundreds of such products – drugs, testing kits, and personal protective equipment – being sold online, and complaints were sent to domain-name registrars and Internet marketplaces that have, in most cases, removed the postings, the FDA said.
“We will continue to monitor the online ecosystem for fraudulent products peddled by bad actors seeking to profit from this global pandemic. We encourage anyone aware of suspected fraudulent medical products for COVID-19 to report them to the FDA,” the statement said.
No form of human misery can be allowed to go unexploited, and the pandemic, it seems, is no exception.
As part of Operation Quack Hack, the Food and Drug Administration has stepped up its investigation and enforcement efforts against companies and individuals that are “taking advantage of widespread fear among consumers during the COVID-19 pandemic” by selling fake products and treatments for coronavirus.
As of May 7, 2020, the agency had issued 42 warning letters to companies that were “selling unapproved products that fraudulently claim to mitigate, prevent, treat, diagnose or cure COVID-19,” the FDA announced in a written statement. Of those 42 products, 29 are no longer being sold with any sort of COVID-19 claim.
Since the beginning of the pandemic, Operation Quack Hack has uncovered hundreds of such products – drugs, testing kits, and personal protective equipment – being sold online, and complaints were sent to domain-name registrars and Internet marketplaces that have, in most cases, removed the postings, the FDA said.
“We will continue to monitor the online ecosystem for fraudulent products peddled by bad actors seeking to profit from this global pandemic. We encourage anyone aware of suspected fraudulent medical products for COVID-19 to report them to the FDA,” the statement said.