User login
Richard Franki is the associate editor who writes and creates graphs. He started with the company in 1987, when it was known as the International Medical News Group. In his years as a journalist, Richard has worked for Cap Cities/ABC, Disney, Harcourt, Elsevier, Quadrant, Frontline, and Internet Brands. In the 1990s, he was a contributor to the ill-fated Indications column, predecessor of Livin' on the MDedge.
It’s official: COVID-19 was bad for the health care business
COVID-19 took a huge cut of clinicians’ business in March and April
In the first 2 months of the COVID-19 pandemic, health care professionals experienced sharp drops in both utilization and revenue, according to an analysis of the nation’s largest collection of private health care claims data.
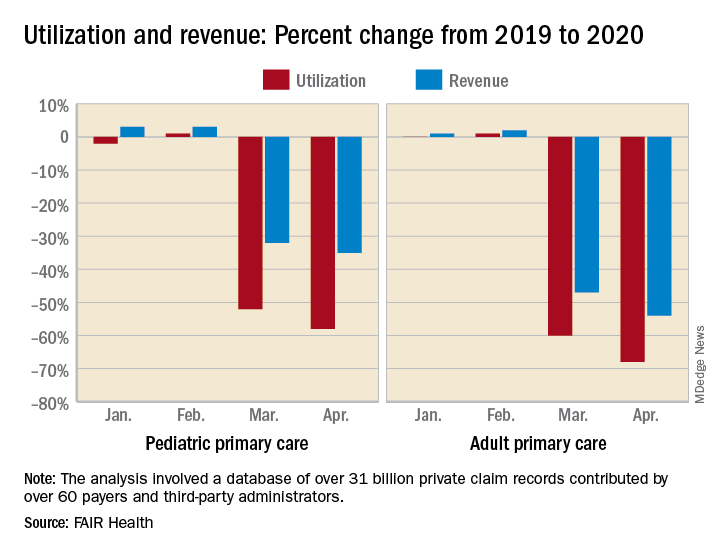
For the months of March and April 2020, use of medical professional services dropped by 65% and 68%, respectively, compared with last year, and estimated revenue fell by 45% and 48%, FAIR Health, a nonprofit organization that manages a database of 31 billion claim records, said in a new report.
For the Northeast states – the epicenter of the pandemic in March and April – patient volume was down by 60% in March and 80% in April, while revenue fell by 55% in March and 79% in April, the organization said.
For this analysis, “a professional service was defined as any service provided by an individual (e.g., physician, nurse, nurse practitioner, physician assistant) instead of being billed by a facility,” FAIR Health noted. Figures for 2019 were adjusted using the Consumer Price Index.
The size of the pandemic-related decreases in utilization and income varied by specialty. Of the seven specialties included in the study, oral surgery was hit the hardest, followed by gastroenterology, cardiology, orthopedics, dermatology, adult primary care, and pediatric primary care, FAIR Health said.
After experiencing a 2% drop in utilization this January and an increase of 4% in February, compared with 2019, gastroenterology saw corresponding drops of 73% in March and 77% in April. Estimated revenue for the specialty was flat in January and rose by 10% in February, but plummeted by 75% in March and 80% in April, the FAIR Health data show.
In cardiology, patient volume from 2019 to 2020 looked like this: Down by 4% in January, up 5% in February, down by 62% in March, and down by 71% in April. The earnings numbers tell a similar story: Down by 2% in January, up by 15% in February, down by 57% in March, and down by 73% in April, the organization reported.
Dermatology did the best among the non–primary care specialties, but that was just a relative success. Utilization still dropped by 62% and 68% in March and April of 2020, compared with last year, and revenue declined by 50% in March and 59% in April, FAIR Health said.
For adult primary care, the utilization numbers were similar, but revenue took a somewhat smaller hit. Patient volume from 2019 to 2020 was fairly steady in January and February, then nosedived in March (down 60%) and April (down 68%). Earnings were up initially, rising 1% in January and 2% in February, but fell 47% in March and 54% in April, FAIR Health said.
Pediatric primary care, it appears, may have been buoyed somewhat by its younger patients. The specialty as a whole saw utilization tumble by 52% in March and 58% in April, but revenue dropped by just 32% and 35%, respectively, according to the report.
A little extra data diving showed that the figures for preventive care visits for patients aged 0-4 years in March and April were –2% and 0% for volume and –2% and 1% for revenue. Meanwhile, the volume of immunizations only dropped by 14% and 10% and vaccine-related revenue slipped by just 7% and 2%, FAIR Health noted.
“Across many specialties from January to April 2020, office or other outpatient [evaluation and management] visits became more common relative to other procedures. ... This may have been due in part to the fact that many of these E&M services could be rendered via telehealth,” FAIR Health said.
Telehealth, however, was no panacea, the report explained: “Even when medical practices have continued to function via telehealth, many have experienced lower reimbursements for telehealth visits than for in-person visits and more time educating patients on how to use the technology.”
COVID-19 took a huge cut of clinicians’ business in March and April
COVID-19 took a huge cut of clinicians’ business in March and April
In the first 2 months of the COVID-19 pandemic, health care professionals experienced sharp drops in both utilization and revenue, according to an analysis of the nation’s largest collection of private health care claims data.
For the months of March and April 2020, use of medical professional services dropped by 65% and 68%, respectively, compared with last year, and estimated revenue fell by 45% and 48%, FAIR Health, a nonprofit organization that manages a database of 31 billion claim records, said in a new report.
For the Northeast states – the epicenter of the pandemic in March and April – patient volume was down by 60% in March and 80% in April, while revenue fell by 55% in March and 79% in April, the organization said.
For this analysis, “a professional service was defined as any service provided by an individual (e.g., physician, nurse, nurse practitioner, physician assistant) instead of being billed by a facility,” FAIR Health noted. Figures for 2019 were adjusted using the Consumer Price Index.
The size of the pandemic-related decreases in utilization and income varied by specialty. Of the seven specialties included in the study, oral surgery was hit the hardest, followed by gastroenterology, cardiology, orthopedics, dermatology, adult primary care, and pediatric primary care, FAIR Health said.
After experiencing a 2% drop in utilization this January and an increase of 4% in February, compared with 2019, gastroenterology saw corresponding drops of 73% in March and 77% in April. Estimated revenue for the specialty was flat in January and rose by 10% in February, but plummeted by 75% in March and 80% in April, the FAIR Health data show.
In cardiology, patient volume from 2019 to 2020 looked like this: Down by 4% in January, up 5% in February, down by 62% in March, and down by 71% in April. The earnings numbers tell a similar story: Down by 2% in January, up by 15% in February, down by 57% in March, and down by 73% in April, the organization reported.
Dermatology did the best among the non–primary care specialties, but that was just a relative success. Utilization still dropped by 62% and 68% in March and April of 2020, compared with last year, and revenue declined by 50% in March and 59% in April, FAIR Health said.
For adult primary care, the utilization numbers were similar, but revenue took a somewhat smaller hit. Patient volume from 2019 to 2020 was fairly steady in January and February, then nosedived in March (down 60%) and April (down 68%). Earnings were up initially, rising 1% in January and 2% in February, but fell 47% in March and 54% in April, FAIR Health said.
Pediatric primary care, it appears, may have been buoyed somewhat by its younger patients. The specialty as a whole saw utilization tumble by 52% in March and 58% in April, but revenue dropped by just 32% and 35%, respectively, according to the report.
A little extra data diving showed that the figures for preventive care visits for patients aged 0-4 years in March and April were –2% and 0% for volume and –2% and 1% for revenue. Meanwhile, the volume of immunizations only dropped by 14% and 10% and vaccine-related revenue slipped by just 7% and 2%, FAIR Health noted.
“Across many specialties from January to April 2020, office or other outpatient [evaluation and management] visits became more common relative to other procedures. ... This may have been due in part to the fact that many of these E&M services could be rendered via telehealth,” FAIR Health said.
Telehealth, however, was no panacea, the report explained: “Even when medical practices have continued to function via telehealth, many have experienced lower reimbursements for telehealth visits than for in-person visits and more time educating patients on how to use the technology.”
In the first 2 months of the COVID-19 pandemic, health care professionals experienced sharp drops in both utilization and revenue, according to an analysis of the nation’s largest collection of private health care claims data.
For the months of March and April 2020, use of medical professional services dropped by 65% and 68%, respectively, compared with last year, and estimated revenue fell by 45% and 48%, FAIR Health, a nonprofit organization that manages a database of 31 billion claim records, said in a new report.
For the Northeast states – the epicenter of the pandemic in March and April – patient volume was down by 60% in March and 80% in April, while revenue fell by 55% in March and 79% in April, the organization said.
For this analysis, “a professional service was defined as any service provided by an individual (e.g., physician, nurse, nurse practitioner, physician assistant) instead of being billed by a facility,” FAIR Health noted. Figures for 2019 were adjusted using the Consumer Price Index.
The size of the pandemic-related decreases in utilization and income varied by specialty. Of the seven specialties included in the study, oral surgery was hit the hardest, followed by gastroenterology, cardiology, orthopedics, dermatology, adult primary care, and pediatric primary care, FAIR Health said.
After experiencing a 2% drop in utilization this January and an increase of 4% in February, compared with 2019, gastroenterology saw corresponding drops of 73% in March and 77% in April. Estimated revenue for the specialty was flat in January and rose by 10% in February, but plummeted by 75% in March and 80% in April, the FAIR Health data show.
In cardiology, patient volume from 2019 to 2020 looked like this: Down by 4% in January, up 5% in February, down by 62% in March, and down by 71% in April. The earnings numbers tell a similar story: Down by 2% in January, up by 15% in February, down by 57% in March, and down by 73% in April, the organization reported.
Dermatology did the best among the non–primary care specialties, but that was just a relative success. Utilization still dropped by 62% and 68% in March and April of 2020, compared with last year, and revenue declined by 50% in March and 59% in April, FAIR Health said.
For adult primary care, the utilization numbers were similar, but revenue took a somewhat smaller hit. Patient volume from 2019 to 2020 was fairly steady in January and February, then nosedived in March (down 60%) and April (down 68%). Earnings were up initially, rising 1% in January and 2% in February, but fell 47% in March and 54% in April, FAIR Health said.
Pediatric primary care, it appears, may have been buoyed somewhat by its younger patients. The specialty as a whole saw utilization tumble by 52% in March and 58% in April, but revenue dropped by just 32% and 35%, respectively, according to the report.
A little extra data diving showed that the figures for preventive care visits for patients aged 0-4 years in March and April were –2% and 0% for volume and –2% and 1% for revenue. Meanwhile, the volume of immunizations only dropped by 14% and 10% and vaccine-related revenue slipped by just 7% and 2%, FAIR Health noted.
“Across many specialties from January to April 2020, office or other outpatient [evaluation and management] visits became more common relative to other procedures. ... This may have been due in part to the fact that many of these E&M services could be rendered via telehealth,” FAIR Health said.
Telehealth, however, was no panacea, the report explained: “Even when medical practices have continued to function via telehealth, many have experienced lower reimbursements for telehealth visits than for in-person visits and more time educating patients on how to use the technology.”
Long-acting insulin analogue approved for type 1 and type 2 diabetes
the Food and Drug Administration announced June 11.
“Long-acting insulin products like insulin glargine play an important role in the treatment of types 1 and 2 diabetes mellitus,” Patrick Archdeacon, MD, acting associate director for therapeutics in the FDA’s Division of Diabetes, Lipid Disorders, and Obesity, said in a written statement via email.
Semglee will be marketed by Mylan Pharmaceuticals and will be available in a multidose 10-mL vial or a single-patient-use 3-mL prefilled pen.
The approval was based primarily on two randomized, confirmatory clinical trials called INSTRIDE1 and INSTRIDE 2, according to a release by Mylan and Biocon Biologic. They compared Semglee (MYL-1501D) to branded insulin glargine (Lantus) in adults and children for 1 year and found no treatment difference.
The FDA noted that, for patients with type 1 diabetes, Semglee must be used along with a short-acting insulin. The recommended starting dose is approximately one-third of the total daily insulin requirement. For those with type 2 diabetes, the starting dose is 0.2 units/kg or up to 10 units once daily, according to the prescribing information.
Semglee is not recommended for treating diabetic ketoacidosis and is contraindicated during episodes of hypoglycemia.
“Today’s approval provides patients with an additional safe and effective treatment option and also expands the number of products that are available to serve as a reference product for a proposed insulin glargine biosimilar or interchangeable biosimilar product now that the biosimilar pathway is available for insulin products following the statutory transition earlier this year,” Dr. Archdeacon said.
the Food and Drug Administration announced June 11.
“Long-acting insulin products like insulin glargine play an important role in the treatment of types 1 and 2 diabetes mellitus,” Patrick Archdeacon, MD, acting associate director for therapeutics in the FDA’s Division of Diabetes, Lipid Disorders, and Obesity, said in a written statement via email.
Semglee will be marketed by Mylan Pharmaceuticals and will be available in a multidose 10-mL vial or a single-patient-use 3-mL prefilled pen.
The approval was based primarily on two randomized, confirmatory clinical trials called INSTRIDE1 and INSTRIDE 2, according to a release by Mylan and Biocon Biologic. They compared Semglee (MYL-1501D) to branded insulin glargine (Lantus) in adults and children for 1 year and found no treatment difference.
The FDA noted that, for patients with type 1 diabetes, Semglee must be used along with a short-acting insulin. The recommended starting dose is approximately one-third of the total daily insulin requirement. For those with type 2 diabetes, the starting dose is 0.2 units/kg or up to 10 units once daily, according to the prescribing information.
Semglee is not recommended for treating diabetic ketoacidosis and is contraindicated during episodes of hypoglycemia.
“Today’s approval provides patients with an additional safe and effective treatment option and also expands the number of products that are available to serve as a reference product for a proposed insulin glargine biosimilar or interchangeable biosimilar product now that the biosimilar pathway is available for insulin products following the statutory transition earlier this year,” Dr. Archdeacon said.
the Food and Drug Administration announced June 11.
“Long-acting insulin products like insulin glargine play an important role in the treatment of types 1 and 2 diabetes mellitus,” Patrick Archdeacon, MD, acting associate director for therapeutics in the FDA’s Division of Diabetes, Lipid Disorders, and Obesity, said in a written statement via email.
Semglee will be marketed by Mylan Pharmaceuticals and will be available in a multidose 10-mL vial or a single-patient-use 3-mL prefilled pen.
The approval was based primarily on two randomized, confirmatory clinical trials called INSTRIDE1 and INSTRIDE 2, according to a release by Mylan and Biocon Biologic. They compared Semglee (MYL-1501D) to branded insulin glargine (Lantus) in adults and children for 1 year and found no treatment difference.
The FDA noted that, for patients with type 1 diabetes, Semglee must be used along with a short-acting insulin. The recommended starting dose is approximately one-third of the total daily insulin requirement. For those with type 2 diabetes, the starting dose is 0.2 units/kg or up to 10 units once daily, according to the prescribing information.
Semglee is not recommended for treating diabetic ketoacidosis and is contraindicated during episodes of hypoglycemia.
“Today’s approval provides patients with an additional safe and effective treatment option and also expands the number of products that are available to serve as a reference product for a proposed insulin glargine biosimilar or interchangeable biosimilar product now that the biosimilar pathway is available for insulin products following the statutory transition earlier this year,” Dr. Archdeacon said.
Racism joins COVID-19 at the primary care table
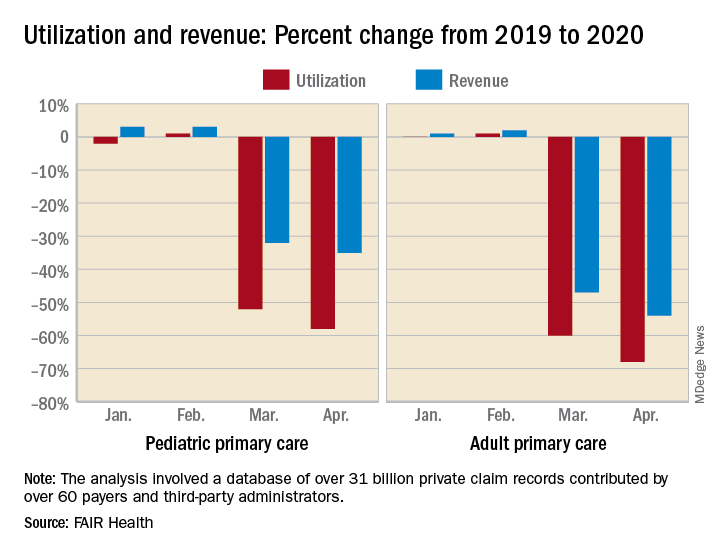
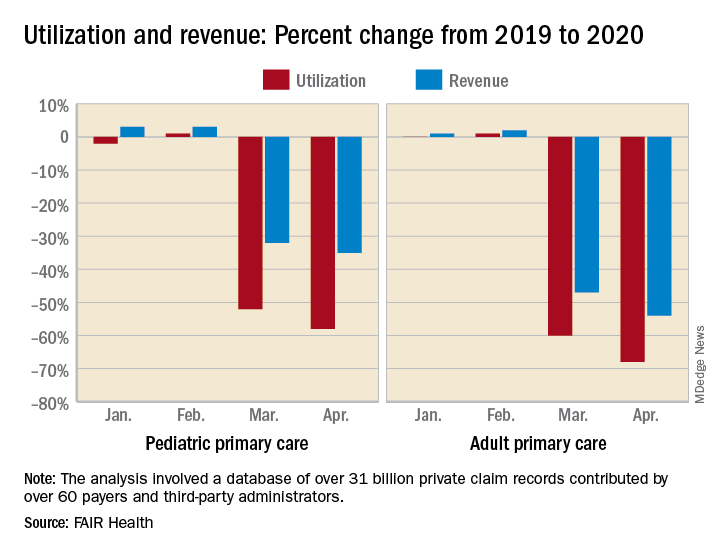
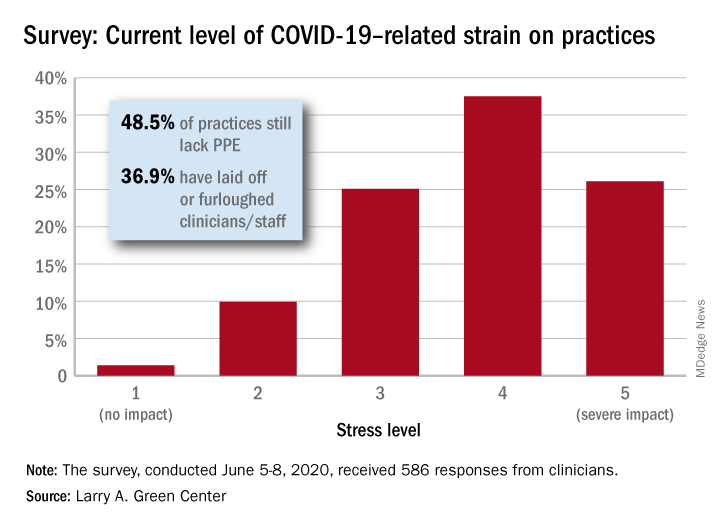
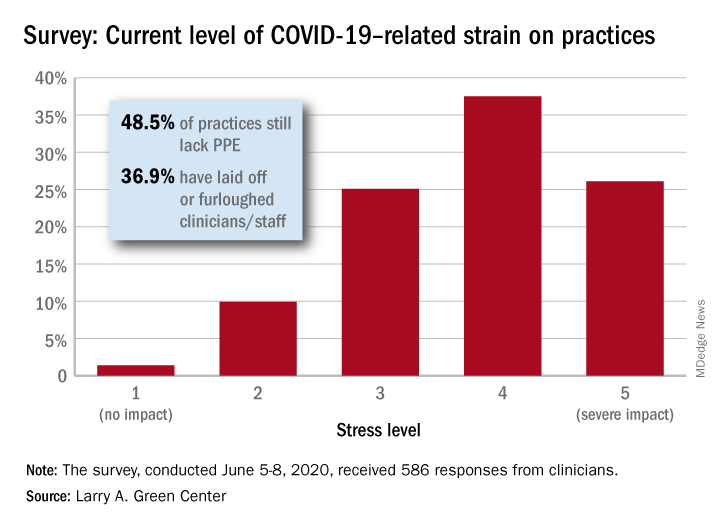
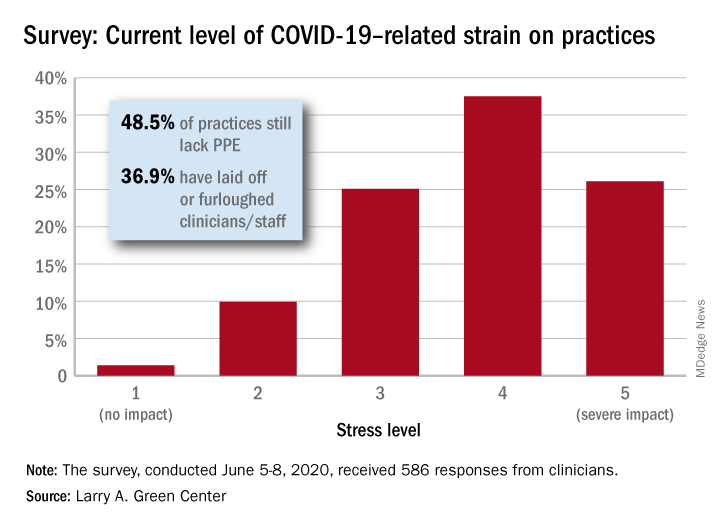
Primary care clinicians, already experiencing all-time high stress levels related to COVID-19, are now struggling to cope with the fallout from racism and the death of George Floyd, according to a survey conducted June 5-8.
When asked how the situation has affected their practices, two-thirds of the survey’s 586 respondents said that George Floyd’s death and related events had been the subject of practice conversations and 12% “drew clear connections between the current racial unrest and the health of their patients,” the Larry A. Green Center said in a recent statement.
One-third of the clinicians also said that recent racism-related events have had a negative effect on their own well-being, and that connection was expressed even more strongly in a related survey of 1,111 patients that was conducted June 8.
In that survey, about 65% of patients said that racism affected emotional, psychological, and behavioral health, and 40% noted that George Floyd’s death had a negative impact on the well-being of friends, the Larry A. Green Center said in partnership with the Primary Care Collaborative and 3rd Conversation.
“The fact that so many patients and clinicians agree that racism is a driver of health points to the incredible role primary care plays in creating safe spaces to process deep societal and personal issues,” said Christine Bechtel, cofounder of 3rd Conversation, a community of patients and providers.
COVID-19, in the meantime, is still doing its thing. Almost two-thirds (63%) of respondents to the clinician survey said that stress levels at their practices had reached all-time-high levels in the last 4 weeks.
Just 1.4% of the primary care clinicians said that the pandemic had put no strain on their practices (see graph), and just 10% rated that strain as a 2 on a scale of 1-5, the center said. Among the stressors:
About 49% continue to lack PPE.
About 40% still have no or limited ability for testing.
About 37% of practice settings still report layoffs and furloughs.
About 31% report that clinician salaries are still being skipped or deferred.
“Both public and private policy makers must take immediate steps to stabilize primary care,” said Ann Greiner, president and CEO of the Primary Care Collaborative. “This financial support is necessary but not sufficient. Instead, we need wholesale reform of payment in order to achieve the kind of high-performing primary care that truly meets patient needs.”
Primary care clinicians, already experiencing all-time high stress levels related to COVID-19, are now struggling to cope with the fallout from racism and the death of George Floyd, according to a survey conducted June 5-8.
When asked how the situation has affected their practices, two-thirds of the survey’s 586 respondents said that George Floyd’s death and related events had been the subject of practice conversations and 12% “drew clear connections between the current racial unrest and the health of their patients,” the Larry A. Green Center said in a recent statement.
One-third of the clinicians also said that recent racism-related events have had a negative effect on their own well-being, and that connection was expressed even more strongly in a related survey of 1,111 patients that was conducted June 8.
In that survey, about 65% of patients said that racism affected emotional, psychological, and behavioral health, and 40% noted that George Floyd’s death had a negative impact on the well-being of friends, the Larry A. Green Center said in partnership with the Primary Care Collaborative and 3rd Conversation.
“The fact that so many patients and clinicians agree that racism is a driver of health points to the incredible role primary care plays in creating safe spaces to process deep societal and personal issues,” said Christine Bechtel, cofounder of 3rd Conversation, a community of patients and providers.
COVID-19, in the meantime, is still doing its thing. Almost two-thirds (63%) of respondents to the clinician survey said that stress levels at their practices had reached all-time-high levels in the last 4 weeks.
Just 1.4% of the primary care clinicians said that the pandemic had put no strain on their practices (see graph), and just 10% rated that strain as a 2 on a scale of 1-5, the center said. Among the stressors:
About 49% continue to lack PPE.
About 40% still have no or limited ability for testing.
About 37% of practice settings still report layoffs and furloughs.
About 31% report that clinician salaries are still being skipped or deferred.
“Both public and private policy makers must take immediate steps to stabilize primary care,” said Ann Greiner, president and CEO of the Primary Care Collaborative. “This financial support is necessary but not sufficient. Instead, we need wholesale reform of payment in order to achieve the kind of high-performing primary care that truly meets patient needs.”
Primary care clinicians, already experiencing all-time high stress levels related to COVID-19, are now struggling to cope with the fallout from racism and the death of George Floyd, according to a survey conducted June 5-8.
When asked how the situation has affected their practices, two-thirds of the survey’s 586 respondents said that George Floyd’s death and related events had been the subject of practice conversations and 12% “drew clear connections between the current racial unrest and the health of their patients,” the Larry A. Green Center said in a recent statement.
One-third of the clinicians also said that recent racism-related events have had a negative effect on their own well-being, and that connection was expressed even more strongly in a related survey of 1,111 patients that was conducted June 8.
In that survey, about 65% of patients said that racism affected emotional, psychological, and behavioral health, and 40% noted that George Floyd’s death had a negative impact on the well-being of friends, the Larry A. Green Center said in partnership with the Primary Care Collaborative and 3rd Conversation.
“The fact that so many patients and clinicians agree that racism is a driver of health points to the incredible role primary care plays in creating safe spaces to process deep societal and personal issues,” said Christine Bechtel, cofounder of 3rd Conversation, a community of patients and providers.
COVID-19, in the meantime, is still doing its thing. Almost two-thirds (63%) of respondents to the clinician survey said that stress levels at their practices had reached all-time-high levels in the last 4 weeks.
Just 1.4% of the primary care clinicians said that the pandemic had put no strain on their practices (see graph), and just 10% rated that strain as a 2 on a scale of 1-5, the center said. Among the stressors:
About 49% continue to lack PPE.
About 40% still have no or limited ability for testing.
About 37% of practice settings still report layoffs and furloughs.
About 31% report that clinician salaries are still being skipped or deferred.
“Both public and private policy makers must take immediate steps to stabilize primary care,” said Ann Greiner, president and CEO of the Primary Care Collaborative. “This financial support is necessary but not sufficient. Instead, we need wholesale reform of payment in order to achieve the kind of high-performing primary care that truly meets patient needs.”
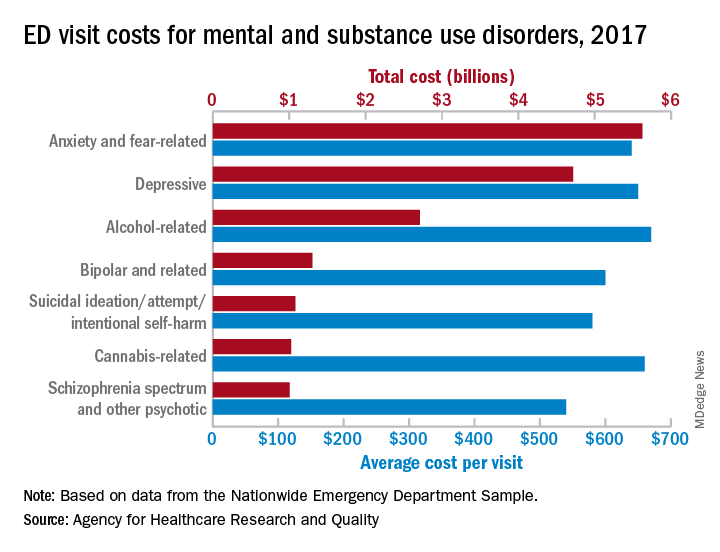
Mental health visits account for 19% of ED costs
Emergency department visits for mental and substance use disorders (MUSDs) cost $14.6 billion in 2017, representing 19% of the total for all ED visits that year, according to the Agency for Healthcare Quality and Research.
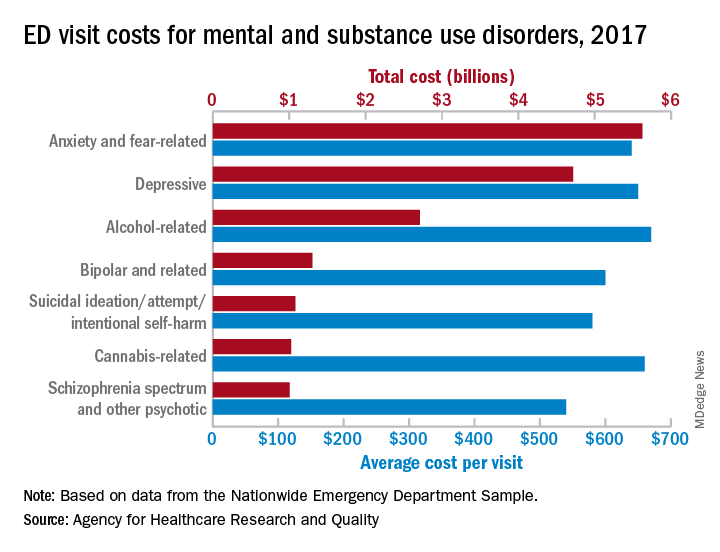
In terms of the total number of visits for MUSDs, 23.1 million, the proportion was slightly lower: 16% of all ED visits for the year, Zeynal Karaca, PhD, a senior economist with AHRQ, and Brian J. Moore, PhD, a senior research leader at IBM Watson Health, said in a recent statistical brief.
Put those figures together and the average visit for an MUSD diagnosis cost $630 and that is 19% higher than the average of $530 for all 145 million ED visits, they reported based on data from the Nationwide Emergency Department Sample.
The most costly MUSD diagnosis in 2017 was anxiety and fear-related disorders, with a total of $5.6 billion for ED visits, followed by depressive disorders at $4.7 billion and alcohol-related disorders at $2.7 billion. Some ED visits may involve more than one MUSD diagnosis, so the sum of all the individual diagnoses does not agree with the total for the entire MUSD category, the researchers noted.
On a per-visit basis, in 2017. [It was not included in the graph because it was 13th.] Other disorders with high per-visit costs were alcohol-related ($670), cannabis-related ($660), and depressive and stimulant-related (both with $650), Dr. Karaca and Dr. Moore said.
Patients with MUSDs who were routinely discharged after an ED visit in 2017 represented a much lower share of the total MUSD cost (68.0%), compared with the overall group of ED visitors (81.4%), but MUSD visits resulting in an inpatient admission made up a larger proportion of costs (19.0%), compared with all visits (9.5%), they said.
Costs between MUSD visits and all ED visits also differed by patient age. Visits by patients aged 0-9 years represented only 0.7% of MUSD-related ED costs but 5.6% of the overall cost, but the respective figures for those aged 45-64 were 36.2% for MUSD costs and 28.5% for the total ED cost, they reported.
SOURCE: Karaca Z and Moore BJ. HCUP Statistical Brief #257. May 12, 2020.
Emergency department visits for mental and substance use disorders (MUSDs) cost $14.6 billion in 2017, representing 19% of the total for all ED visits that year, according to the Agency for Healthcare Quality and Research.
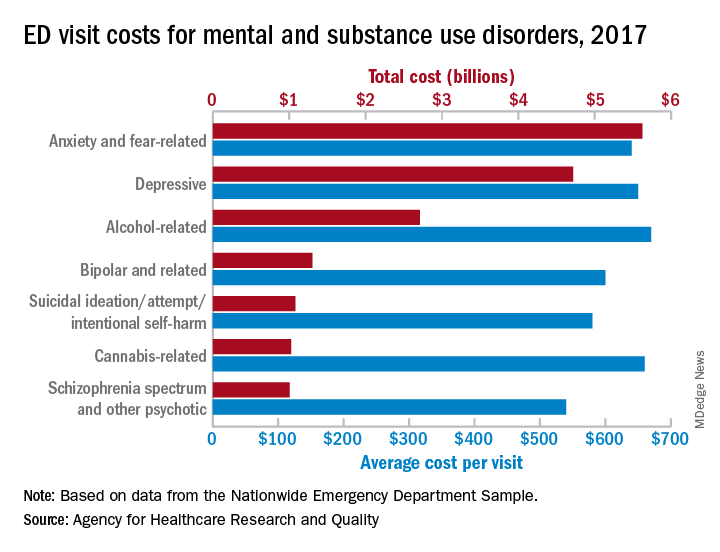
In terms of the total number of visits for MUSDs, 23.1 million, the proportion was slightly lower: 16% of all ED visits for the year, Zeynal Karaca, PhD, a senior economist with AHRQ, and Brian J. Moore, PhD, a senior research leader at IBM Watson Health, said in a recent statistical brief.
Put those figures together and the average visit for an MUSD diagnosis cost $630 and that is 19% higher than the average of $530 for all 145 million ED visits, they reported based on data from the Nationwide Emergency Department Sample.
The most costly MUSD diagnosis in 2017 was anxiety and fear-related disorders, with a total of $5.6 billion for ED visits, followed by depressive disorders at $4.7 billion and alcohol-related disorders at $2.7 billion. Some ED visits may involve more than one MUSD diagnosis, so the sum of all the individual diagnoses does not agree with the total for the entire MUSD category, the researchers noted.
On a per-visit basis, in 2017. [It was not included in the graph because it was 13th.] Other disorders with high per-visit costs were alcohol-related ($670), cannabis-related ($660), and depressive and stimulant-related (both with $650), Dr. Karaca and Dr. Moore said.
Patients with MUSDs who were routinely discharged after an ED visit in 2017 represented a much lower share of the total MUSD cost (68.0%), compared with the overall group of ED visitors (81.4%), but MUSD visits resulting in an inpatient admission made up a larger proportion of costs (19.0%), compared with all visits (9.5%), they said.
Costs between MUSD visits and all ED visits also differed by patient age. Visits by patients aged 0-9 years represented only 0.7% of MUSD-related ED costs but 5.6% of the overall cost, but the respective figures for those aged 45-64 were 36.2% for MUSD costs and 28.5% for the total ED cost, they reported.
SOURCE: Karaca Z and Moore BJ. HCUP Statistical Brief #257. May 12, 2020.
Emergency department visits for mental and substance use disorders (MUSDs) cost $14.6 billion in 2017, representing 19% of the total for all ED visits that year, according to the Agency for Healthcare Quality and Research.
In terms of the total number of visits for MUSDs, 23.1 million, the proportion was slightly lower: 16% of all ED visits for the year, Zeynal Karaca, PhD, a senior economist with AHRQ, and Brian J. Moore, PhD, a senior research leader at IBM Watson Health, said in a recent statistical brief.
Put those figures together and the average visit for an MUSD diagnosis cost $630 and that is 19% higher than the average of $530 for all 145 million ED visits, they reported based on data from the Nationwide Emergency Department Sample.
The most costly MUSD diagnosis in 2017 was anxiety and fear-related disorders, with a total of $5.6 billion for ED visits, followed by depressive disorders at $4.7 billion and alcohol-related disorders at $2.7 billion. Some ED visits may involve more than one MUSD diagnosis, so the sum of all the individual diagnoses does not agree with the total for the entire MUSD category, the researchers noted.
On a per-visit basis, in 2017. [It was not included in the graph because it was 13th.] Other disorders with high per-visit costs were alcohol-related ($670), cannabis-related ($660), and depressive and stimulant-related (both with $650), Dr. Karaca and Dr. Moore said.
Patients with MUSDs who were routinely discharged after an ED visit in 2017 represented a much lower share of the total MUSD cost (68.0%), compared with the overall group of ED visitors (81.4%), but MUSD visits resulting in an inpatient admission made up a larger proportion of costs (19.0%), compared with all visits (9.5%), they said.
Costs between MUSD visits and all ED visits also differed by patient age. Visits by patients aged 0-9 years represented only 0.7% of MUSD-related ED costs but 5.6% of the overall cost, but the respective figures for those aged 45-64 were 36.2% for MUSD costs and 28.5% for the total ED cost, they reported.
SOURCE: Karaca Z and Moore BJ. HCUP Statistical Brief #257. May 12, 2020.
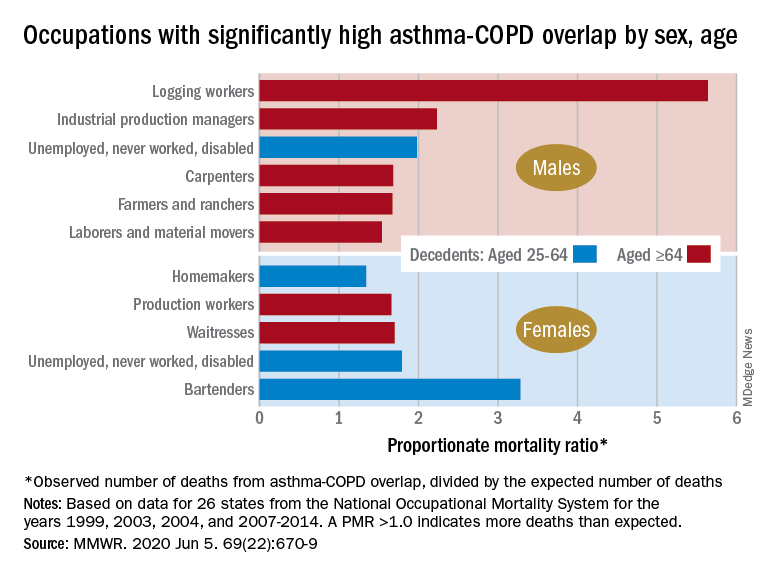
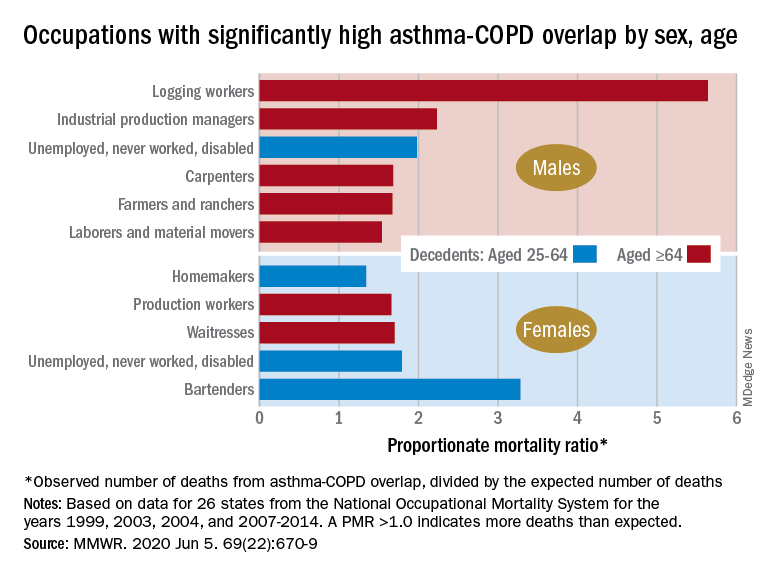
By the numbers: Asthma-COPD overlap deaths
Death rates for combined asthma and chronic obstructive pulmonary disease declined during 1999-2016, but the risk remains higher among women, compared with men, and in certain occupations, according to a recent report from the Centers for Disease Control and Prevention.
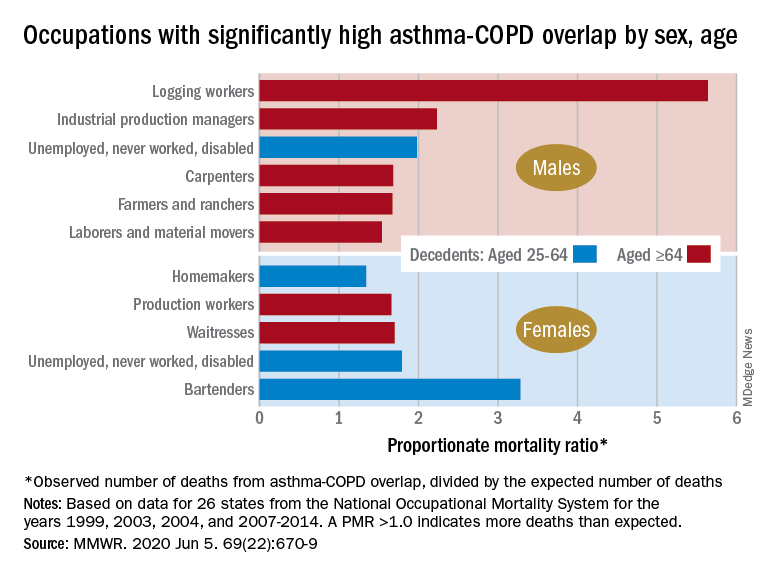
There is also an association between mortality and nonworking status among adults aged 25-64 years, which “suggests that asthma-COPD overlap might be associated with substantial morbidity,” Katelynn E. Dodd, MPH, and associates at the CDC’s National Institute for Occupational Safety and Health said in the Morbidity and Mortality Weekly Report. “These patients have been reported to have worse health outcomes than do those with asthma or COPD alone.”
For females with asthma-COPD overlap, the age-adjusted death rate among adults aged 25 years and older dropped from 7.71 per million in 1999 to 4.01 in 2016, with corresponding rates of 6.70 and 3.01 per million for males, they reported.
In 1999-2016, a total of 18,766 U.S. decedents aged ≥25 years had both asthma and COPD assigned as the underlying or contributing cause of death (12,028 women and 6,738 men), for an overall death rate of 5.03 per million persons (women, 5.59; men, 4.30), data from the National Vital Statistics System show.
Additional analysis, based on the calculation of proportionate mortality ratios (PMRs), also showed that mortality varied by occupational status and age for both males and females, the investigators said, noting that workplace exposures, such as dusts and secondhand smoke, are known to cause both asthma and COPD.
The PMR represents the observed number of deaths from asthma-COPD overlap in a specified industry or occupation, divided by the expected number of deaths, so a value over 1.0 indicates that there were more deaths associated with the condition than expected, Ms. Dodd and her associates explained.
Among female decedents, the occupation with the highest PMR that was statistically significant was bartending at 3.28. For men, the highest significant PMR, 5.64, occurred in logging workers. Those rates, however, only applied to one of the two age groups: 25-64 years in women and ≥65 in men, based on data from the National Occupational Mortality Surveillance, which included information from 26 states for the years 1999, 2003, 2004, and 2007-2014.
Occupationally speaking, the one area of common ground between males and females was lack of occupation. PMRs for those aged 25-64 years “were significantly elevated among men (1.98) and women (1.79) who were unemployed, never worked, or were disabled workers,” they said. PMRs were elevated for nonworking older males and females but were not significant.
The elevated PMRs suggest “that asthma-COPD overlap might be associated with substantial morbidity resulting in loss of employment [because] retired and unemployed persons might have left the workforce because of severe asthma or COPD,” the investigators wrote.
SOURCE: Dodd KE et al. MMWR. 2020 Jun 5. 69(22):670-9.
Death rates for combined asthma and chronic obstructive pulmonary disease declined during 1999-2016, but the risk remains higher among women, compared with men, and in certain occupations, according to a recent report from the Centers for Disease Control and Prevention.
There is also an association between mortality and nonworking status among adults aged 25-64 years, which “suggests that asthma-COPD overlap might be associated with substantial morbidity,” Katelynn E. Dodd, MPH, and associates at the CDC’s National Institute for Occupational Safety and Health said in the Morbidity and Mortality Weekly Report. “These patients have been reported to have worse health outcomes than do those with asthma or COPD alone.”
For females with asthma-COPD overlap, the age-adjusted death rate among adults aged 25 years and older dropped from 7.71 per million in 1999 to 4.01 in 2016, with corresponding rates of 6.70 and 3.01 per million for males, they reported.
In 1999-2016, a total of 18,766 U.S. decedents aged ≥25 years had both asthma and COPD assigned as the underlying or contributing cause of death (12,028 women and 6,738 men), for an overall death rate of 5.03 per million persons (women, 5.59; men, 4.30), data from the National Vital Statistics System show.
Additional analysis, based on the calculation of proportionate mortality ratios (PMRs), also showed that mortality varied by occupational status and age for both males and females, the investigators said, noting that workplace exposures, such as dusts and secondhand smoke, are known to cause both asthma and COPD.
The PMR represents the observed number of deaths from asthma-COPD overlap in a specified industry or occupation, divided by the expected number of deaths, so a value over 1.0 indicates that there were more deaths associated with the condition than expected, Ms. Dodd and her associates explained.
Among female decedents, the occupation with the highest PMR that was statistically significant was bartending at 3.28. For men, the highest significant PMR, 5.64, occurred in logging workers. Those rates, however, only applied to one of the two age groups: 25-64 years in women and ≥65 in men, based on data from the National Occupational Mortality Surveillance, which included information from 26 states for the years 1999, 2003, 2004, and 2007-2014.
Occupationally speaking, the one area of common ground between males and females was lack of occupation. PMRs for those aged 25-64 years “were significantly elevated among men (1.98) and women (1.79) who were unemployed, never worked, or were disabled workers,” they said. PMRs were elevated for nonworking older males and females but were not significant.
The elevated PMRs suggest “that asthma-COPD overlap might be associated with substantial morbidity resulting in loss of employment [because] retired and unemployed persons might have left the workforce because of severe asthma or COPD,” the investigators wrote.
SOURCE: Dodd KE et al. MMWR. 2020 Jun 5. 69(22):670-9.
Death rates for combined asthma and chronic obstructive pulmonary disease declined during 1999-2016, but the risk remains higher among women, compared with men, and in certain occupations, according to a recent report from the Centers for Disease Control and Prevention.
There is also an association between mortality and nonworking status among adults aged 25-64 years, which “suggests that asthma-COPD overlap might be associated with substantial morbidity,” Katelynn E. Dodd, MPH, and associates at the CDC’s National Institute for Occupational Safety and Health said in the Morbidity and Mortality Weekly Report. “These patients have been reported to have worse health outcomes than do those with asthma or COPD alone.”
For females with asthma-COPD overlap, the age-adjusted death rate among adults aged 25 years and older dropped from 7.71 per million in 1999 to 4.01 in 2016, with corresponding rates of 6.70 and 3.01 per million for males, they reported.
In 1999-2016, a total of 18,766 U.S. decedents aged ≥25 years had both asthma and COPD assigned as the underlying or contributing cause of death (12,028 women and 6,738 men), for an overall death rate of 5.03 per million persons (women, 5.59; men, 4.30), data from the National Vital Statistics System show.
Additional analysis, based on the calculation of proportionate mortality ratios (PMRs), also showed that mortality varied by occupational status and age for both males and females, the investigators said, noting that workplace exposures, such as dusts and secondhand smoke, are known to cause both asthma and COPD.
The PMR represents the observed number of deaths from asthma-COPD overlap in a specified industry or occupation, divided by the expected number of deaths, so a value over 1.0 indicates that there were more deaths associated with the condition than expected, Ms. Dodd and her associates explained.
Among female decedents, the occupation with the highest PMR that was statistically significant was bartending at 3.28. For men, the highest significant PMR, 5.64, occurred in logging workers. Those rates, however, only applied to one of the two age groups: 25-64 years in women and ≥65 in men, based on data from the National Occupational Mortality Surveillance, which included information from 26 states for the years 1999, 2003, 2004, and 2007-2014.
Occupationally speaking, the one area of common ground between males and females was lack of occupation. PMRs for those aged 25-64 years “were significantly elevated among men (1.98) and women (1.79) who were unemployed, never worked, or were disabled workers,” they said. PMRs were elevated for nonworking older males and females but were not significant.
The elevated PMRs suggest “that asthma-COPD overlap might be associated with substantial morbidity resulting in loss of employment [because] retired and unemployed persons might have left the workforce because of severe asthma or COPD,” the investigators wrote.
SOURCE: Dodd KE et al. MMWR. 2020 Jun 5. 69(22):670-9.
FROM MMWR
Americans avoided emergency departments early in the pandemic
compared with the corresponding period in 2019, according to a report from the Centers for Disease Control and Prevention.
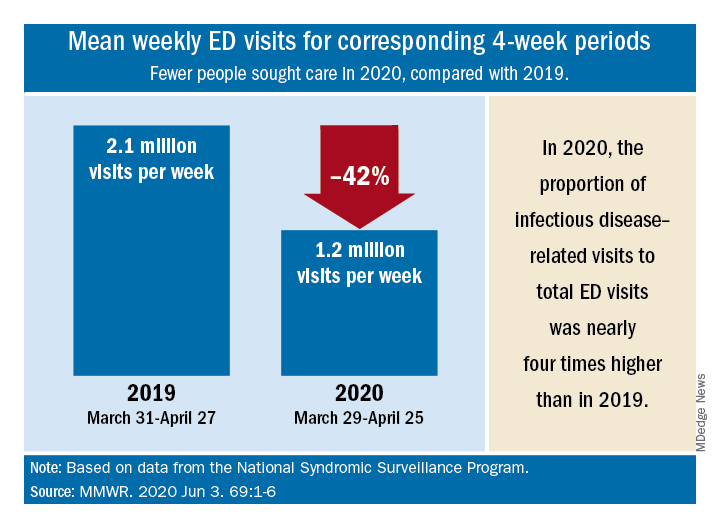
“The striking decline in ED visits nationwide … suggests that the pandemic has altered the use of the ED by the public,” Kathleen P. Hartnett, PhD, and associates at the CDC said June 3 in the Mortality and Morbidity Weekly Report.
The weekly mean was just over 1.2 million ED visits for the 4 weeks from March 29 to April 25, 2020, compared with the nearly 2.2 million visits per week recorded from March 31 to April 27, 2019 – a drop of 42%, based on an analysis of data from the National Syndromic Surveillance Program.
Despite that drop, ED visits for infectious disease–related reasons, taken as a proportion of all 1.2 ED visits during the early pandemic period, were 3.8 times higher than the comparison period in 2019, the investigators reported.
ED visits also were higher in 2020 for specified and unspecified lower respiratory disease not including influenza, pneumonia, asthma, or bronchitis (prevalence ratio of 1.99, compared with 2019), cardiac arrest and ventricular fibrillation (PR, 1.98), and pneumonia not caused by tuberculosis (PR, 1.91), Dr. Hartnett and associates said.
Prevalence ratios for the early pandemic period were down for most other conditions, with some of the largest decreases seen for influenza (PR, 0.16), otitis media (PR, 0.35), and neoplasm-related encounters (PR, 0.40), they said.
Visits have increased each week since reaching their lowest point during April 12-18, but the number for the most recent full week, May 24-30, which was not included in the analysis, was still 26% lower than the corresponding week in 2019, the CDC team pointed out.
“Some persons could be delaying care for conditions that might result in additional mortality if left untreated,” the investigators noted, and those “who use the ED as a safety net because they lack access to primary care and telemedicine might be disproportionately affected if they avoid seeking care because of concerns about the infection risk in the ED.”
SOURCE: Hartnett KP et al. MMWR. 2020 Jun 3. 69:1-6.
compared with the corresponding period in 2019, according to a report from the Centers for Disease Control and Prevention.
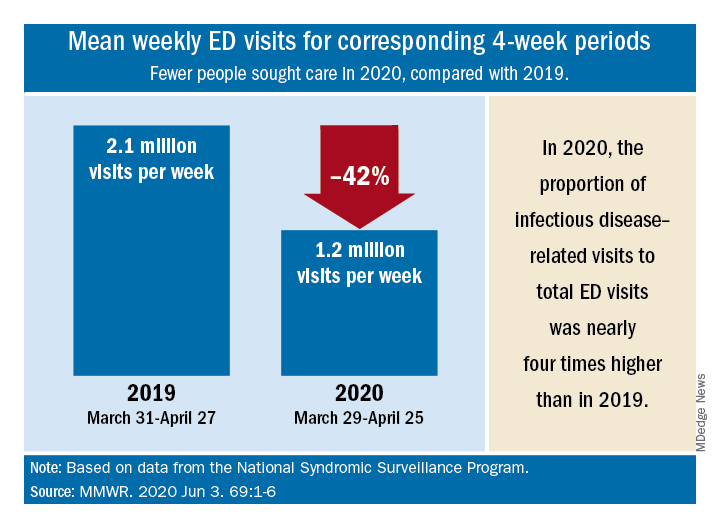
“The striking decline in ED visits nationwide … suggests that the pandemic has altered the use of the ED by the public,” Kathleen P. Hartnett, PhD, and associates at the CDC said June 3 in the Mortality and Morbidity Weekly Report.
The weekly mean was just over 1.2 million ED visits for the 4 weeks from March 29 to April 25, 2020, compared with the nearly 2.2 million visits per week recorded from March 31 to April 27, 2019 – a drop of 42%, based on an analysis of data from the National Syndromic Surveillance Program.
Despite that drop, ED visits for infectious disease–related reasons, taken as a proportion of all 1.2 ED visits during the early pandemic period, were 3.8 times higher than the comparison period in 2019, the investigators reported.
ED visits also were higher in 2020 for specified and unspecified lower respiratory disease not including influenza, pneumonia, asthma, or bronchitis (prevalence ratio of 1.99, compared with 2019), cardiac arrest and ventricular fibrillation (PR, 1.98), and pneumonia not caused by tuberculosis (PR, 1.91), Dr. Hartnett and associates said.
Prevalence ratios for the early pandemic period were down for most other conditions, with some of the largest decreases seen for influenza (PR, 0.16), otitis media (PR, 0.35), and neoplasm-related encounters (PR, 0.40), they said.
Visits have increased each week since reaching their lowest point during April 12-18, but the number for the most recent full week, May 24-30, which was not included in the analysis, was still 26% lower than the corresponding week in 2019, the CDC team pointed out.
“Some persons could be delaying care for conditions that might result in additional mortality if left untreated,” the investigators noted, and those “who use the ED as a safety net because they lack access to primary care and telemedicine might be disproportionately affected if they avoid seeking care because of concerns about the infection risk in the ED.”
SOURCE: Hartnett KP et al. MMWR. 2020 Jun 3. 69:1-6.
compared with the corresponding period in 2019, according to a report from the Centers for Disease Control and Prevention.
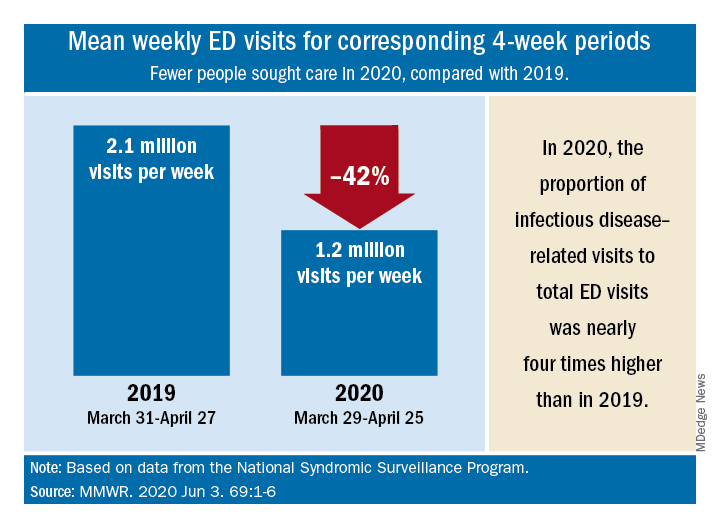
“The striking decline in ED visits nationwide … suggests that the pandemic has altered the use of the ED by the public,” Kathleen P. Hartnett, PhD, and associates at the CDC said June 3 in the Mortality and Morbidity Weekly Report.
The weekly mean was just over 1.2 million ED visits for the 4 weeks from March 29 to April 25, 2020, compared with the nearly 2.2 million visits per week recorded from March 31 to April 27, 2019 – a drop of 42%, based on an analysis of data from the National Syndromic Surveillance Program.
Despite that drop, ED visits for infectious disease–related reasons, taken as a proportion of all 1.2 ED visits during the early pandemic period, were 3.8 times higher than the comparison period in 2019, the investigators reported.
ED visits also were higher in 2020 for specified and unspecified lower respiratory disease not including influenza, pneumonia, asthma, or bronchitis (prevalence ratio of 1.99, compared with 2019), cardiac arrest and ventricular fibrillation (PR, 1.98), and pneumonia not caused by tuberculosis (PR, 1.91), Dr. Hartnett and associates said.
Prevalence ratios for the early pandemic period were down for most other conditions, with some of the largest decreases seen for influenza (PR, 0.16), otitis media (PR, 0.35), and neoplasm-related encounters (PR, 0.40), they said.
Visits have increased each week since reaching their lowest point during April 12-18, but the number for the most recent full week, May 24-30, which was not included in the analysis, was still 26% lower than the corresponding week in 2019, the CDC team pointed out.
“Some persons could be delaying care for conditions that might result in additional mortality if left untreated,” the investigators noted, and those “who use the ED as a safety net because they lack access to primary care and telemedicine might be disproportionately affected if they avoid seeking care because of concerns about the infection risk in the ED.”
SOURCE: Hartnett KP et al. MMWR. 2020 Jun 3. 69:1-6.
FROM MMWR
COVID-19 effect: Prescription fills mostly down for leading drugs
Prescription fills for hydroxychloroquine/chloroquine spiked right after COVID-19 was declared a national emergency in March, but use of the drugs still remains well above 2019 levels, based on data from more than 58,000 U.S. pharmacies.
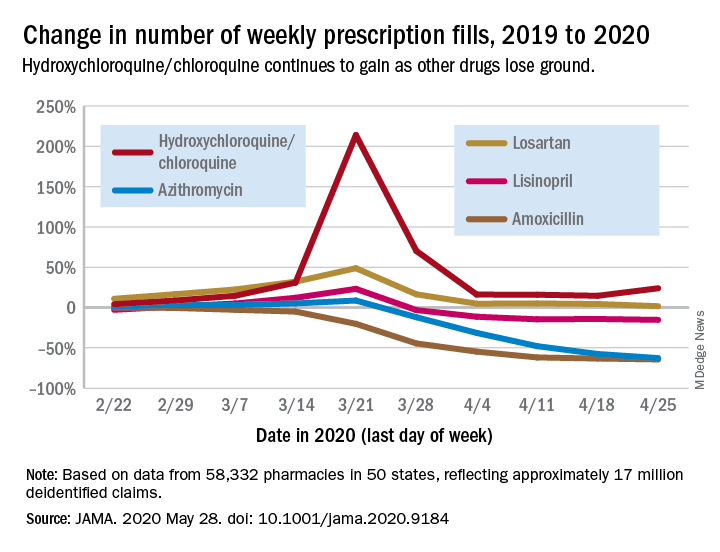
Hydroxychloroquine/chloroquine are also doing better than any of the prescription drugs in the top 10 based on total claims in 2019, Muthiah Vaduganathan, MD, MPH, of Brigham and Women’s Hospital, Boston, and associates reported May 28 in a research letter in JAMA.
Prescription fills for hydroxychloroquine/chloroquine have been above 2019 levels every week since the national emergency was declared on March 13, with the high occurring during the week of March 15-21, when fills were 214% higher than the corresponding week in 2019. The lowest level in that time came during the week of April 12-18, with growth of 14.6% over 2019, the investigators said.
The drugs occupying the top 10 – amlodipine, amoxicillin, atorvastatin, gabapentin, hydrocodone-acetaminophen, levothyroxine, lisinopril, losartan, omeprazole, and sertraline – have not done as well. Losartan, the only one that hasn’t lost ground in any week since March 13, rose by almost 49% during March 15-21, but was down to a 1.7% rise by the end of the study period, they reported.
Meanwhile, the other drug touted as a treatment for COVID-19, azithromycin, has fallen farther than most of the top 10. By April 19-25, the last week of the study period, fills for the antibiotic were down 62.7%, compared with last year, the analysis showed. Only amoxicillin had dropped more (64.4%).
“The modest decline for most common long-term therapies after peak could represent reduced contact with prescribing clinicians, restricted access to pharmacies, pharmacist rationing, loss of insurance from unemployment, or replete supplies from early stockpiling,” Dr. Vaduganathan and associates wrote.
The investigators “used all-payer U.S. pharmacy data from 58,332 chain, independent, and mail-order pharmacies across 14,421 zip codes in 50 states, reflecting approximately 17 million deidentified claims,” to estimate national prescription fills, they explained.
SOURCE: Vaduganathan M et al. JAMA 2020 May 28. doi: 10.1001/jama.2020.9184.
Prescription fills for hydroxychloroquine/chloroquine spiked right after COVID-19 was declared a national emergency in March, but use of the drugs still remains well above 2019 levels, based on data from more than 58,000 U.S. pharmacies.
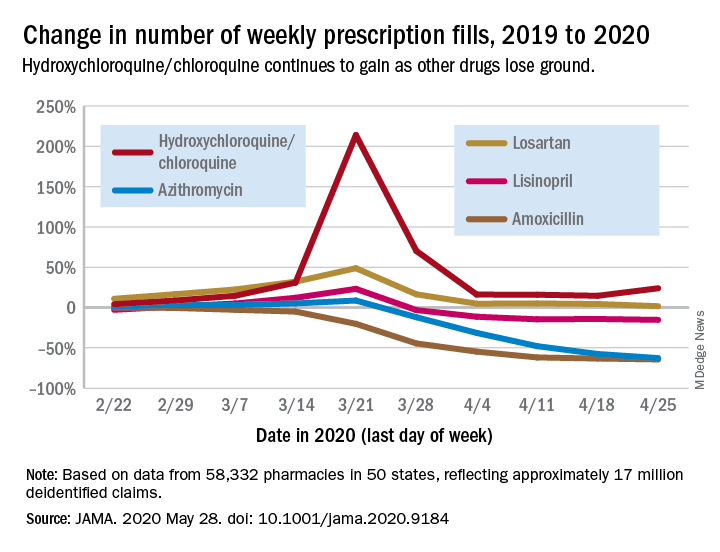
Hydroxychloroquine/chloroquine are also doing better than any of the prescription drugs in the top 10 based on total claims in 2019, Muthiah Vaduganathan, MD, MPH, of Brigham and Women’s Hospital, Boston, and associates reported May 28 in a research letter in JAMA.
Prescription fills for hydroxychloroquine/chloroquine have been above 2019 levels every week since the national emergency was declared on March 13, with the high occurring during the week of March 15-21, when fills were 214% higher than the corresponding week in 2019. The lowest level in that time came during the week of April 12-18, with growth of 14.6% over 2019, the investigators said.
The drugs occupying the top 10 – amlodipine, amoxicillin, atorvastatin, gabapentin, hydrocodone-acetaminophen, levothyroxine, lisinopril, losartan, omeprazole, and sertraline – have not done as well. Losartan, the only one that hasn’t lost ground in any week since March 13, rose by almost 49% during March 15-21, but was down to a 1.7% rise by the end of the study period, they reported.
Meanwhile, the other drug touted as a treatment for COVID-19, azithromycin, has fallen farther than most of the top 10. By April 19-25, the last week of the study period, fills for the antibiotic were down 62.7%, compared with last year, the analysis showed. Only amoxicillin had dropped more (64.4%).
“The modest decline for most common long-term therapies after peak could represent reduced contact with prescribing clinicians, restricted access to pharmacies, pharmacist rationing, loss of insurance from unemployment, or replete supplies from early stockpiling,” Dr. Vaduganathan and associates wrote.
The investigators “used all-payer U.S. pharmacy data from 58,332 chain, independent, and mail-order pharmacies across 14,421 zip codes in 50 states, reflecting approximately 17 million deidentified claims,” to estimate national prescription fills, they explained.
SOURCE: Vaduganathan M et al. JAMA 2020 May 28. doi: 10.1001/jama.2020.9184.
Prescription fills for hydroxychloroquine/chloroquine spiked right after COVID-19 was declared a national emergency in March, but use of the drugs still remains well above 2019 levels, based on data from more than 58,000 U.S. pharmacies.
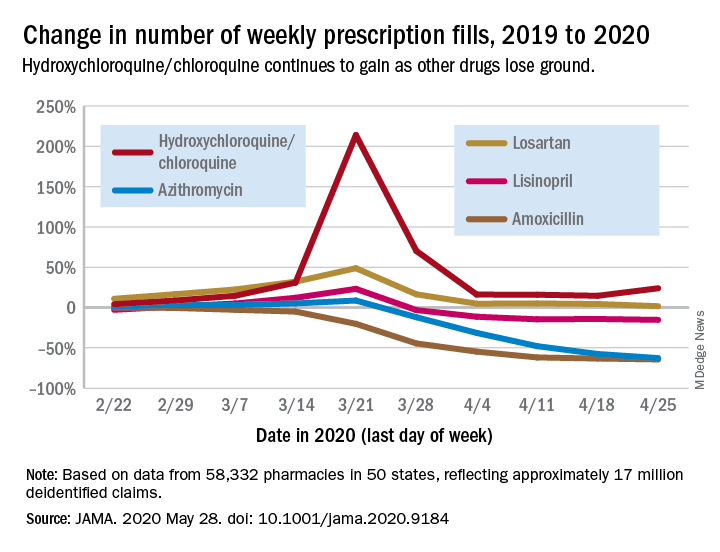
Hydroxychloroquine/chloroquine are also doing better than any of the prescription drugs in the top 10 based on total claims in 2019, Muthiah Vaduganathan, MD, MPH, of Brigham and Women’s Hospital, Boston, and associates reported May 28 in a research letter in JAMA.
Prescription fills for hydroxychloroquine/chloroquine have been above 2019 levels every week since the national emergency was declared on March 13, with the high occurring during the week of March 15-21, when fills were 214% higher than the corresponding week in 2019. The lowest level in that time came during the week of April 12-18, with growth of 14.6% over 2019, the investigators said.
The drugs occupying the top 10 – amlodipine, amoxicillin, atorvastatin, gabapentin, hydrocodone-acetaminophen, levothyroxine, lisinopril, losartan, omeprazole, and sertraline – have not done as well. Losartan, the only one that hasn’t lost ground in any week since March 13, rose by almost 49% during March 15-21, but was down to a 1.7% rise by the end of the study period, they reported.
Meanwhile, the other drug touted as a treatment for COVID-19, azithromycin, has fallen farther than most of the top 10. By April 19-25, the last week of the study period, fills for the antibiotic were down 62.7%, compared with last year, the analysis showed. Only amoxicillin had dropped more (64.4%).
“The modest decline for most common long-term therapies after peak could represent reduced contact with prescribing clinicians, restricted access to pharmacies, pharmacist rationing, loss of insurance from unemployment, or replete supplies from early stockpiling,” Dr. Vaduganathan and associates wrote.
The investigators “used all-payer U.S. pharmacy data from 58,332 chain, independent, and mail-order pharmacies across 14,421 zip codes in 50 states, reflecting approximately 17 million deidentified claims,” to estimate national prescription fills, they explained.
SOURCE: Vaduganathan M et al. JAMA 2020 May 28. doi: 10.1001/jama.2020.9184.
FROM JAMA
COVID-19: Putting distance between projection and reality
When it comes to COVID-19, studies show that social distancing flattened the curve.
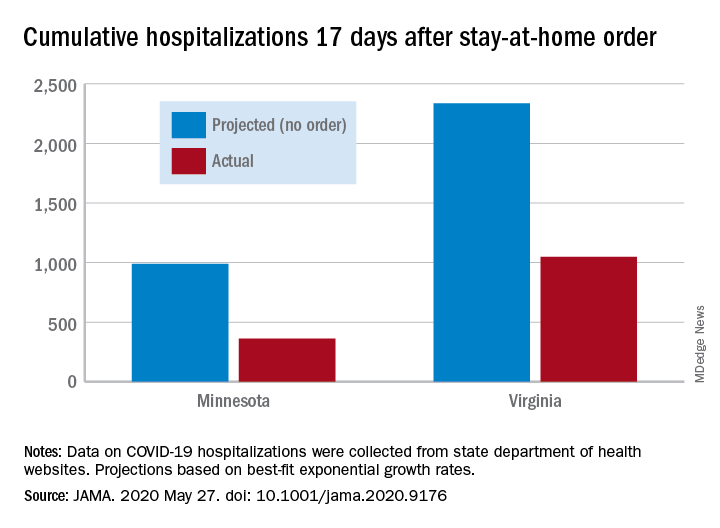
Cumulative hospitalizations in four states with stay-at-home orders were well short of the projected exponential growth curves, Soumya Sen, PhD, of the University of Minnesota, Minneapolis, and associates reported May 27 in a research letter in JAMA. All states were observed through April 28.
The deviations between observed cases and worst-case projections in the four states – Colorado, Minnesota, Ohio, and Virginia – all began within 8-10 days of the stay-at-home orders. In Minnesota, 17 days after the order, there were 361 cumulative hospitalizations, compared with a projection of 988 had no such action been taken. In Virginia, the corresponding numbers were 1,048 observed and 2,335 projected, they reported.
“Observed hospitalizations consistently fell outside of the 95% prediction bands of the projected exponential growth curve,” Dr. Sen and associates noted.
In a separate Canadian study measuring COVID-19 patients occupying ICU beds in Ontario and deaths among those cases, hospitals “would have rapidly exceeded ICU capacity and observed substantially higher mortality” without any physical distancing intervention, Ashleigh R. Tuite, PhD, MPH, of the University of Toronto and associates wrote May 27 in a letter in Annals of Internal Medicine.
Their model, based on a 70% reduction in physical contacts for March 19–May 3, projected 2.0 cases per 100,000 population with physical distancing and 37.4 per 100,000 without. Deaths among those ICU patients were projected at 2.5 per 100,000 with distancing and 12.7 per 100,000 without intervention, they reported.
“Our modeling also shows the challenges associated with relaxation of physical distancing measures without a concomitant increase in other public health measures. Specifically, when the number of contacts between persons returns to more than 50% of normal, we expect disease activity to resurge rapidly and ICUs to quickly reach capacity,” they wrote.
The study published in JAMA used publicly available data from the University of Minnesota COVID-19 Hospitalization Project, which is partially funded by the University of Minnesota Office of Academic Clinical Affairs and United Health Foundation.
SOURCES: Sen S et al. JAMA. 2020 May 27. doi: 10.1001/jama.2020.9176; Tuite AR et al. Ann Intern Med. 2020 May 27. doi: 10.7326/M20-2945.
When it comes to COVID-19, studies show that social distancing flattened the curve.
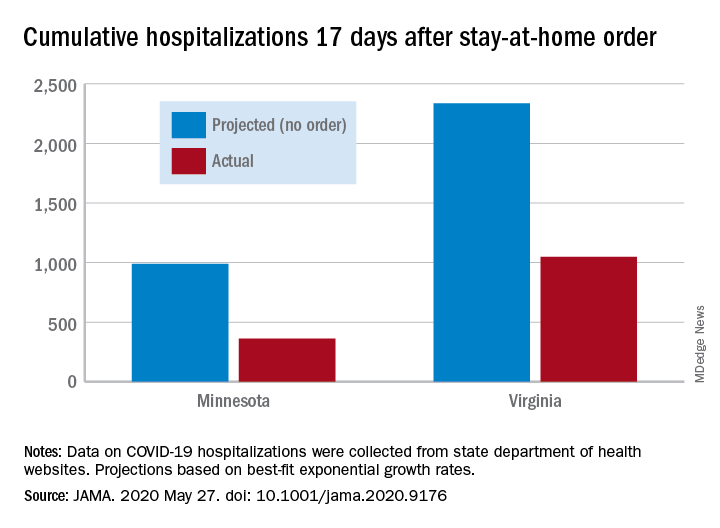
Cumulative hospitalizations in four states with stay-at-home orders were well short of the projected exponential growth curves, Soumya Sen, PhD, of the University of Minnesota, Minneapolis, and associates reported May 27 in a research letter in JAMA. All states were observed through April 28.
The deviations between observed cases and worst-case projections in the four states – Colorado, Minnesota, Ohio, and Virginia – all began within 8-10 days of the stay-at-home orders. In Minnesota, 17 days after the order, there were 361 cumulative hospitalizations, compared with a projection of 988 had no such action been taken. In Virginia, the corresponding numbers were 1,048 observed and 2,335 projected, they reported.
“Observed hospitalizations consistently fell outside of the 95% prediction bands of the projected exponential growth curve,” Dr. Sen and associates noted.
In a separate Canadian study measuring COVID-19 patients occupying ICU beds in Ontario and deaths among those cases, hospitals “would have rapidly exceeded ICU capacity and observed substantially higher mortality” without any physical distancing intervention, Ashleigh R. Tuite, PhD, MPH, of the University of Toronto and associates wrote May 27 in a letter in Annals of Internal Medicine.
Their model, based on a 70% reduction in physical contacts for March 19–May 3, projected 2.0 cases per 100,000 population with physical distancing and 37.4 per 100,000 without. Deaths among those ICU patients were projected at 2.5 per 100,000 with distancing and 12.7 per 100,000 without intervention, they reported.
“Our modeling also shows the challenges associated with relaxation of physical distancing measures without a concomitant increase in other public health measures. Specifically, when the number of contacts between persons returns to more than 50% of normal, we expect disease activity to resurge rapidly and ICUs to quickly reach capacity,” they wrote.
The study published in JAMA used publicly available data from the University of Minnesota COVID-19 Hospitalization Project, which is partially funded by the University of Minnesota Office of Academic Clinical Affairs and United Health Foundation.
SOURCES: Sen S et al. JAMA. 2020 May 27. doi: 10.1001/jama.2020.9176; Tuite AR et al. Ann Intern Med. 2020 May 27. doi: 10.7326/M20-2945.
When it comes to COVID-19, studies show that social distancing flattened the curve.
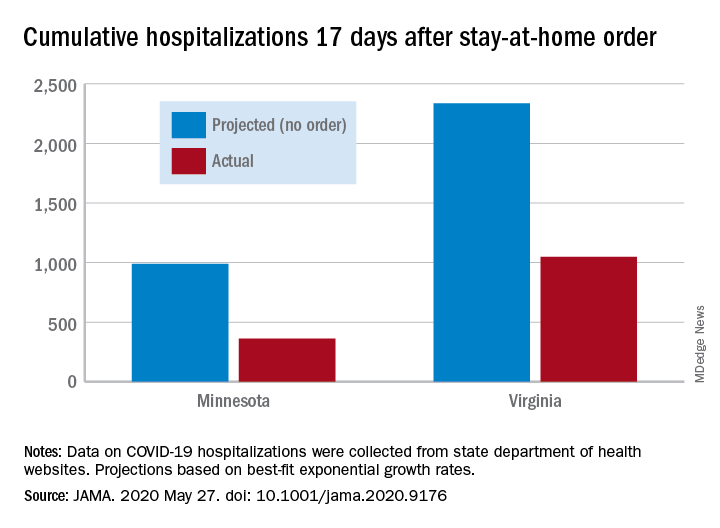
Cumulative hospitalizations in four states with stay-at-home orders were well short of the projected exponential growth curves, Soumya Sen, PhD, of the University of Minnesota, Minneapolis, and associates reported May 27 in a research letter in JAMA. All states were observed through April 28.
The deviations between observed cases and worst-case projections in the four states – Colorado, Minnesota, Ohio, and Virginia – all began within 8-10 days of the stay-at-home orders. In Minnesota, 17 days after the order, there were 361 cumulative hospitalizations, compared with a projection of 988 had no such action been taken. In Virginia, the corresponding numbers were 1,048 observed and 2,335 projected, they reported.
“Observed hospitalizations consistently fell outside of the 95% prediction bands of the projected exponential growth curve,” Dr. Sen and associates noted.
In a separate Canadian study measuring COVID-19 patients occupying ICU beds in Ontario and deaths among those cases, hospitals “would have rapidly exceeded ICU capacity and observed substantially higher mortality” without any physical distancing intervention, Ashleigh R. Tuite, PhD, MPH, of the University of Toronto and associates wrote May 27 in a letter in Annals of Internal Medicine.
Their model, based on a 70% reduction in physical contacts for March 19–May 3, projected 2.0 cases per 100,000 population with physical distancing and 37.4 per 100,000 without. Deaths among those ICU patients were projected at 2.5 per 100,000 with distancing and 12.7 per 100,000 without intervention, they reported.
“Our modeling also shows the challenges associated with relaxation of physical distancing measures without a concomitant increase in other public health measures. Specifically, when the number of contacts between persons returns to more than 50% of normal, we expect disease activity to resurge rapidly and ICUs to quickly reach capacity,” they wrote.
The study published in JAMA used publicly available data from the University of Minnesota COVID-19 Hospitalization Project, which is partially funded by the University of Minnesota Office of Academic Clinical Affairs and United Health Foundation.
SOURCES: Sen S et al. JAMA. 2020 May 27. doi: 10.1001/jama.2020.9176; Tuite AR et al. Ann Intern Med. 2020 May 27. doi: 10.7326/M20-2945.
New crayons reflect the global palette of skin tones
After more than 8 months of development,
“With the world growing more diverse than ever before, Crayola hopes our new Colors of the World crayons will increase representation and foster a greater sense of belonging and acceptance,” CEO Rich Wuerthele said in a written statement.
The company partnered with a cosmetic industry foundation-color expert to create “colors that step down from light to deep shades across rose, almond, and golden undertones, resulting in a 24 global shade palette that authentically reflects the full spectrum of human complexions,” according to Crayola’s statement. The 24- and 32-count Colors of the World packs will start reaching stores in July. The pack of 32 crayons includes the 24 skin colors along with 4 hair and 4 eye colors.
After more than 8 months of development,
“With the world growing more diverse than ever before, Crayola hopes our new Colors of the World crayons will increase representation and foster a greater sense of belonging and acceptance,” CEO Rich Wuerthele said in a written statement.
The company partnered with a cosmetic industry foundation-color expert to create “colors that step down from light to deep shades across rose, almond, and golden undertones, resulting in a 24 global shade palette that authentically reflects the full spectrum of human complexions,” according to Crayola’s statement. The 24- and 32-count Colors of the World packs will start reaching stores in July. The pack of 32 crayons includes the 24 skin colors along with 4 hair and 4 eye colors.
After more than 8 months of development,
“With the world growing more diverse than ever before, Crayola hopes our new Colors of the World crayons will increase representation and foster a greater sense of belonging and acceptance,” CEO Rich Wuerthele said in a written statement.
The company partnered with a cosmetic industry foundation-color expert to create “colors that step down from light to deep shades across rose, almond, and golden undertones, resulting in a 24 global shade palette that authentically reflects the full spectrum of human complexions,” according to Crayola’s statement. The 24- and 32-count Colors of the World packs will start reaching stores in July. The pack of 32 crayons includes the 24 skin colors along with 4 hair and 4 eye colors.
Suicide often associated with bullying in LGBTQ youth
based on analysis of a national database.

Among suicide decedents aged 10-19 years who were classified as LGBTQ, 21% had been bullied, compared with 4% of non-LGBTQ youths, and the discrepancy increased among younger individuals, Kirsty A. Clark, PhD, of Yale University, New Haven, Conn., and associates wrote in JAMA Pediatrics.
Here’s how the presence of bullying broke down by age group by LGBTQ/non-LGBTQ status: 68%/15% among 10- to 13-year-olds, 28%/7% for 14- to-16-year-olds, and 7%/2% among 17- to 19-year-olds, based on data for 2003-2017 from the National Violent Death Reporting System.
Postmortem records from that reporting system include “two narratives summarizing the coroner or medical examiner records and law enforcement reports describing suicide antecedents as reported by the decedent’s family or friends; the decedent’s diary, social media, and text or email messages; and any suicide note,” the investigators noted.
Although prevalence of bullying was higher among LGBTQ youth, non-LGBTQ individuals represented 97% of the 9,884 suicide decedents and 86% of the 490 bullying-associated deaths in the study, they wrote.
Other suicide antecedents also were more prevalent in the LGBTQ group: depressed mood (46% vs. 35%), suicide-thought history (37% vs. 21%), suicide-attempt history (28% vs. 21%), and school-related problem (27% vs. 18%), Dr. Clark and associates reported.
“Bullying can be a deadly antecedent to suicide, especially among LGBTQ youth,” the investigators wrote. “Pediatricians can help to reduce this risk through adopting clinical practice approaches sensitive to the vulnerabilities of LGBTQ youth.”
SOURCE: Clark KA et al. JAMA Pediatr. 2020 May 26. doi: 10.1001/jamapediatrics.2020.0940.
based on analysis of a national database.

Among suicide decedents aged 10-19 years who were classified as LGBTQ, 21% had been bullied, compared with 4% of non-LGBTQ youths, and the discrepancy increased among younger individuals, Kirsty A. Clark, PhD, of Yale University, New Haven, Conn., and associates wrote in JAMA Pediatrics.
Here’s how the presence of bullying broke down by age group by LGBTQ/non-LGBTQ status: 68%/15% among 10- to 13-year-olds, 28%/7% for 14- to-16-year-olds, and 7%/2% among 17- to 19-year-olds, based on data for 2003-2017 from the National Violent Death Reporting System.
Postmortem records from that reporting system include “two narratives summarizing the coroner or medical examiner records and law enforcement reports describing suicide antecedents as reported by the decedent’s family or friends; the decedent’s diary, social media, and text or email messages; and any suicide note,” the investigators noted.
Although prevalence of bullying was higher among LGBTQ youth, non-LGBTQ individuals represented 97% of the 9,884 suicide decedents and 86% of the 490 bullying-associated deaths in the study, they wrote.
Other suicide antecedents also were more prevalent in the LGBTQ group: depressed mood (46% vs. 35%), suicide-thought history (37% vs. 21%), suicide-attempt history (28% vs. 21%), and school-related problem (27% vs. 18%), Dr. Clark and associates reported.
“Bullying can be a deadly antecedent to suicide, especially among LGBTQ youth,” the investigators wrote. “Pediatricians can help to reduce this risk through adopting clinical practice approaches sensitive to the vulnerabilities of LGBTQ youth.”
SOURCE: Clark KA et al. JAMA Pediatr. 2020 May 26. doi: 10.1001/jamapediatrics.2020.0940.
based on analysis of a national database.

Among suicide decedents aged 10-19 years who were classified as LGBTQ, 21% had been bullied, compared with 4% of non-LGBTQ youths, and the discrepancy increased among younger individuals, Kirsty A. Clark, PhD, of Yale University, New Haven, Conn., and associates wrote in JAMA Pediatrics.
Here’s how the presence of bullying broke down by age group by LGBTQ/non-LGBTQ status: 68%/15% among 10- to 13-year-olds, 28%/7% for 14- to-16-year-olds, and 7%/2% among 17- to 19-year-olds, based on data for 2003-2017 from the National Violent Death Reporting System.
Postmortem records from that reporting system include “two narratives summarizing the coroner or medical examiner records and law enforcement reports describing suicide antecedents as reported by the decedent’s family or friends; the decedent’s diary, social media, and text or email messages; and any suicide note,” the investigators noted.
Although prevalence of bullying was higher among LGBTQ youth, non-LGBTQ individuals represented 97% of the 9,884 suicide decedents and 86% of the 490 bullying-associated deaths in the study, they wrote.
Other suicide antecedents also were more prevalent in the LGBTQ group: depressed mood (46% vs. 35%), suicide-thought history (37% vs. 21%), suicide-attempt history (28% vs. 21%), and school-related problem (27% vs. 18%), Dr. Clark and associates reported.
“Bullying can be a deadly antecedent to suicide, especially among LGBTQ youth,” the investigators wrote. “Pediatricians can help to reduce this risk through adopting clinical practice approaches sensitive to the vulnerabilities of LGBTQ youth.”
SOURCE: Clark KA et al. JAMA Pediatr. 2020 May 26. doi: 10.1001/jamapediatrics.2020.0940.
FROM JAMA PEDIATRICS


