User login
Thrombectomy fails to improve PCI outcomes, ups stroke risk
SAN DIEGO – Routine manual thrombectomy before percutaneous coronary intervention did not improve 180-day outcomes and was linked with an increased risk of stroke in patients with acute ST-segment elevation MI in the TOTAL trial.
Routine thrombectomy had no effect on the primary outcome of cardiovascular death, MI, cardiogenic shock, or New York Heart Association class IV heart failure, occurring in 6.9% of thrombectomy patients and 7% of PCI-only patients.
However, the study’s primary safety endpoint of stroke at 30 days doubled in patients undergoing routine thrombectomy before PCI to 33 events (0.7%), compared with those who had PCI with only bailout thrombectomy (16 events [0.3%]; P = .015).
The same pattern was observed with stroke or transient ischemic attack within 30 days (42 vs. 19 events; hazard ratio, 2.21; P = .003) and continued for stroke within 180 days (52 vs. 25 events; HR, 2.08; P = .002).
“The stroke findings are unexpected and we believe require confirmation in other datasets. A detailed case-by-case review is underway to help us understand the etiology and the relationship with the procedure,” lead author Dr. Sanjit S. Jolly said at the annual meeting of the American College of Cardiology.
Enthusiasm for manual thrombus aspiration was sparked by a survival benefit observed in the single-center, prospective TAPAS trial in ST-segment elevation MI patients (STEMI), and the procedure was widely adopted.
The more recent, multicenter TASTE trial, however, reported that routine thrombectomy before PCI failed to significantly reduce 30-day mortality in 7,244 STEMI patients, though there were trends toward reductions in stent thrombosis and hospitalization for recurrent MI.
TOTAL (Manual Aspiration Thrombectomy Plus PCI vs. PCI Alone in STEMI) randomly assigned 10,063 patients within 12 hours of STEMI symptoms to primary PCI either with upfront manual thrombectomy or only bailout thrombectomy if the PCI strategy failed.
The lack of significant differences between groups in the primary outcome was also true in all the components of the primary outcome. Furthermore, there was no effect on the primary outcome based on thrombotic burden, a question that remained unanswered after TASTE, Dr. Jolly reported. The TOTAL results were published online simultaneously with his report (N. Engl. J. Med. 2015 March 16 [doi:10.1056/NEJMoa1415098]).
“TOTAL and TASTE emphasize the need to conduct large randomized trials of common interventions, even when small trials appear positive,” Dr. Jolly said.
Discussant Dr. Steven Nissen, chair of cardiovascular medicine at Cleveland Clinic, described the routine use of thrombectomy as “a sad story about device regulation in the United States” in that the evidence level needed to get a medical device on the market is so far below that required for drug approval that patients undergo procedures without good randomized trial evidence to show they even work.
“We dodged a bullet recently with renal denervation when everyone thought it would work, and when you finally tested it, it didn’t,” Dr. Nissen said. “Let this be a lesson to us: We need to have more rigorous studies of medical devices before they get to market and get used in very large numbers of people.”
Currently, aspiration thrombectomy carries a IIa recommendation for use with PCI in the most recent ACC/American Heart Association guidelines for the management of patients with STEMI (J. Am. Coll. Cardiol. 2009;54:2205-41).
When asked whether the guidelines should change based on the TOTAL and TASTE results, Dr. Jolly said there should be a clear recommendation that routine thrombus aspiration should not be the appropriate approach, while the issue of bailout aspiration may be left to clinician judgment.
The finding of late strokes is difficult to understand and should be interpreted with caution because of the small number of strokes occurring between 30 and 180 days, he said. Detailed analysis of all strokes will be presented at a later meeting, but Rankin Scale scores show several strokes were “very debilitating.” There is a consistency in the data, as a meta-analysis of smaller trials also identified an increased stroke risk with adjunctive thrombectomy.
Discussant Dr. Gregg W. Stone, director of cardiovascular research and education at Columbia University Medical Center in New York, said a mechanism for periprocedural stroke with aspiration can be envisioned, but that understanding the risk of ongoing, late stroke is more difficult.
As for why thrombectomy didn’t work, “aspiration is incredibly inefficient, thromboemboli still occur before, during, and after aspiration, the timing of aspiration is often too late to benefit most patients,” and other mechanisms of myonecrosis may predominate, such as reperfusion injury, he observed.
Dr. Stone said the TOTAL results should change practice and that the guideline recommendation should be downgraded to IIb.
“There are some patients who have a very large thrombus burden who have trouble dealing with all that thrombus in the cath lab who might benefit, and it is impossible to design randomized trials for small sections and groups of patients,” he said. “I wouldn’t make it class III by any means, but I think it’ll take a long time for that reduction in use to actually transmit through clinical practice, because I must say interventional cardiologists love the idea of simply removing thrombus with a relatively easy-to-use device.”
Dr. David Kandzari, director of interventional cardiology at the Piedmont Heart Center in Atlanta, said in an interview that TOTAL will make operators much more selective and cautious in their performance of thrombectomy until further insights into the stroke issue are available. Thrombectomy should be reserved for bailout instances and not as a front-line therapy, he said.
On the other hand, the stroke rate in the early phase was not significantly different between groups in an as-treated analysis, and an opportunity exists to investigate potential differences between stroke and nonstroke patients to determine whether other comorbidities rather than thrombectomy per se may account for the stroke signal, Dr. Kandzari observed.
TOTAL was funded by the Canadian Institutes of Health Research, Canadian Network and Centre for Trials Internationally, and Medtronic. Dr. Jolly disclosed receiving consulting fees and honoraria from AstraZeneca, speaking fees for St. Jude, and research grants from Medtronic. Dr. Nissen has received research support from and is a consultant/adviser to numerous pharmaceutical companies; all honoraria or consulting fees go directly to charity so that he receives neither income nor a tax deduction. Dr. Stone reported consulting honoraria from Guided Delivery Systems, Miracor, and Reva, and ownership interest or partnership in Arstasis, Caliber, VNT, Micardia, Biostar family funds, and Medfocus family funds. Dr. Kandzari reported research and grant support from Medtronic, Biotronic, Abbott Vascular, and Boston Scientific.
SAN DIEGO – Routine manual thrombectomy before percutaneous coronary intervention did not improve 180-day outcomes and was linked with an increased risk of stroke in patients with acute ST-segment elevation MI in the TOTAL trial.
Routine thrombectomy had no effect on the primary outcome of cardiovascular death, MI, cardiogenic shock, or New York Heart Association class IV heart failure, occurring in 6.9% of thrombectomy patients and 7% of PCI-only patients.
However, the study’s primary safety endpoint of stroke at 30 days doubled in patients undergoing routine thrombectomy before PCI to 33 events (0.7%), compared with those who had PCI with only bailout thrombectomy (16 events [0.3%]; P = .015).
The same pattern was observed with stroke or transient ischemic attack within 30 days (42 vs. 19 events; hazard ratio, 2.21; P = .003) and continued for stroke within 180 days (52 vs. 25 events; HR, 2.08; P = .002).
“The stroke findings are unexpected and we believe require confirmation in other datasets. A detailed case-by-case review is underway to help us understand the etiology and the relationship with the procedure,” lead author Dr. Sanjit S. Jolly said at the annual meeting of the American College of Cardiology.
Enthusiasm for manual thrombus aspiration was sparked by a survival benefit observed in the single-center, prospective TAPAS trial in ST-segment elevation MI patients (STEMI), and the procedure was widely adopted.
The more recent, multicenter TASTE trial, however, reported that routine thrombectomy before PCI failed to significantly reduce 30-day mortality in 7,244 STEMI patients, though there were trends toward reductions in stent thrombosis and hospitalization for recurrent MI.
TOTAL (Manual Aspiration Thrombectomy Plus PCI vs. PCI Alone in STEMI) randomly assigned 10,063 patients within 12 hours of STEMI symptoms to primary PCI either with upfront manual thrombectomy or only bailout thrombectomy if the PCI strategy failed.
The lack of significant differences between groups in the primary outcome was also true in all the components of the primary outcome. Furthermore, there was no effect on the primary outcome based on thrombotic burden, a question that remained unanswered after TASTE, Dr. Jolly reported. The TOTAL results were published online simultaneously with his report (N. Engl. J. Med. 2015 March 16 [doi:10.1056/NEJMoa1415098]).
“TOTAL and TASTE emphasize the need to conduct large randomized trials of common interventions, even when small trials appear positive,” Dr. Jolly said.
Discussant Dr. Steven Nissen, chair of cardiovascular medicine at Cleveland Clinic, described the routine use of thrombectomy as “a sad story about device regulation in the United States” in that the evidence level needed to get a medical device on the market is so far below that required for drug approval that patients undergo procedures without good randomized trial evidence to show they even work.
“We dodged a bullet recently with renal denervation when everyone thought it would work, and when you finally tested it, it didn’t,” Dr. Nissen said. “Let this be a lesson to us: We need to have more rigorous studies of medical devices before they get to market and get used in very large numbers of people.”
Currently, aspiration thrombectomy carries a IIa recommendation for use with PCI in the most recent ACC/American Heart Association guidelines for the management of patients with STEMI (J. Am. Coll. Cardiol. 2009;54:2205-41).
When asked whether the guidelines should change based on the TOTAL and TASTE results, Dr. Jolly said there should be a clear recommendation that routine thrombus aspiration should not be the appropriate approach, while the issue of bailout aspiration may be left to clinician judgment.
The finding of late strokes is difficult to understand and should be interpreted with caution because of the small number of strokes occurring between 30 and 180 days, he said. Detailed analysis of all strokes will be presented at a later meeting, but Rankin Scale scores show several strokes were “very debilitating.” There is a consistency in the data, as a meta-analysis of smaller trials also identified an increased stroke risk with adjunctive thrombectomy.
Discussant Dr. Gregg W. Stone, director of cardiovascular research and education at Columbia University Medical Center in New York, said a mechanism for periprocedural stroke with aspiration can be envisioned, but that understanding the risk of ongoing, late stroke is more difficult.
As for why thrombectomy didn’t work, “aspiration is incredibly inefficient, thromboemboli still occur before, during, and after aspiration, the timing of aspiration is often too late to benefit most patients,” and other mechanisms of myonecrosis may predominate, such as reperfusion injury, he observed.
Dr. Stone said the TOTAL results should change practice and that the guideline recommendation should be downgraded to IIb.
“There are some patients who have a very large thrombus burden who have trouble dealing with all that thrombus in the cath lab who might benefit, and it is impossible to design randomized trials for small sections and groups of patients,” he said. “I wouldn’t make it class III by any means, but I think it’ll take a long time for that reduction in use to actually transmit through clinical practice, because I must say interventional cardiologists love the idea of simply removing thrombus with a relatively easy-to-use device.”
Dr. David Kandzari, director of interventional cardiology at the Piedmont Heart Center in Atlanta, said in an interview that TOTAL will make operators much more selective and cautious in their performance of thrombectomy until further insights into the stroke issue are available. Thrombectomy should be reserved for bailout instances and not as a front-line therapy, he said.
On the other hand, the stroke rate in the early phase was not significantly different between groups in an as-treated analysis, and an opportunity exists to investigate potential differences between stroke and nonstroke patients to determine whether other comorbidities rather than thrombectomy per se may account for the stroke signal, Dr. Kandzari observed.
TOTAL was funded by the Canadian Institutes of Health Research, Canadian Network and Centre for Trials Internationally, and Medtronic. Dr. Jolly disclosed receiving consulting fees and honoraria from AstraZeneca, speaking fees for St. Jude, and research grants from Medtronic. Dr. Nissen has received research support from and is a consultant/adviser to numerous pharmaceutical companies; all honoraria or consulting fees go directly to charity so that he receives neither income nor a tax deduction. Dr. Stone reported consulting honoraria from Guided Delivery Systems, Miracor, and Reva, and ownership interest or partnership in Arstasis, Caliber, VNT, Micardia, Biostar family funds, and Medfocus family funds. Dr. Kandzari reported research and grant support from Medtronic, Biotronic, Abbott Vascular, and Boston Scientific.
SAN DIEGO – Routine manual thrombectomy before percutaneous coronary intervention did not improve 180-day outcomes and was linked with an increased risk of stroke in patients with acute ST-segment elevation MI in the TOTAL trial.
Routine thrombectomy had no effect on the primary outcome of cardiovascular death, MI, cardiogenic shock, or New York Heart Association class IV heart failure, occurring in 6.9% of thrombectomy patients and 7% of PCI-only patients.
However, the study’s primary safety endpoint of stroke at 30 days doubled in patients undergoing routine thrombectomy before PCI to 33 events (0.7%), compared with those who had PCI with only bailout thrombectomy (16 events [0.3%]; P = .015).
The same pattern was observed with stroke or transient ischemic attack within 30 days (42 vs. 19 events; hazard ratio, 2.21; P = .003) and continued for stroke within 180 days (52 vs. 25 events; HR, 2.08; P = .002).
“The stroke findings are unexpected and we believe require confirmation in other datasets. A detailed case-by-case review is underway to help us understand the etiology and the relationship with the procedure,” lead author Dr. Sanjit S. Jolly said at the annual meeting of the American College of Cardiology.
Enthusiasm for manual thrombus aspiration was sparked by a survival benefit observed in the single-center, prospective TAPAS trial in ST-segment elevation MI patients (STEMI), and the procedure was widely adopted.
The more recent, multicenter TASTE trial, however, reported that routine thrombectomy before PCI failed to significantly reduce 30-day mortality in 7,244 STEMI patients, though there were trends toward reductions in stent thrombosis and hospitalization for recurrent MI.
TOTAL (Manual Aspiration Thrombectomy Plus PCI vs. PCI Alone in STEMI) randomly assigned 10,063 patients within 12 hours of STEMI symptoms to primary PCI either with upfront manual thrombectomy or only bailout thrombectomy if the PCI strategy failed.
The lack of significant differences between groups in the primary outcome was also true in all the components of the primary outcome. Furthermore, there was no effect on the primary outcome based on thrombotic burden, a question that remained unanswered after TASTE, Dr. Jolly reported. The TOTAL results were published online simultaneously with his report (N. Engl. J. Med. 2015 March 16 [doi:10.1056/NEJMoa1415098]).
“TOTAL and TASTE emphasize the need to conduct large randomized trials of common interventions, even when small trials appear positive,” Dr. Jolly said.
Discussant Dr. Steven Nissen, chair of cardiovascular medicine at Cleveland Clinic, described the routine use of thrombectomy as “a sad story about device regulation in the United States” in that the evidence level needed to get a medical device on the market is so far below that required for drug approval that patients undergo procedures without good randomized trial evidence to show they even work.
“We dodged a bullet recently with renal denervation when everyone thought it would work, and when you finally tested it, it didn’t,” Dr. Nissen said. “Let this be a lesson to us: We need to have more rigorous studies of medical devices before they get to market and get used in very large numbers of people.”
Currently, aspiration thrombectomy carries a IIa recommendation for use with PCI in the most recent ACC/American Heart Association guidelines for the management of patients with STEMI (J. Am. Coll. Cardiol. 2009;54:2205-41).
When asked whether the guidelines should change based on the TOTAL and TASTE results, Dr. Jolly said there should be a clear recommendation that routine thrombus aspiration should not be the appropriate approach, while the issue of bailout aspiration may be left to clinician judgment.
The finding of late strokes is difficult to understand and should be interpreted with caution because of the small number of strokes occurring between 30 and 180 days, he said. Detailed analysis of all strokes will be presented at a later meeting, but Rankin Scale scores show several strokes were “very debilitating.” There is a consistency in the data, as a meta-analysis of smaller trials also identified an increased stroke risk with adjunctive thrombectomy.
Discussant Dr. Gregg W. Stone, director of cardiovascular research and education at Columbia University Medical Center in New York, said a mechanism for periprocedural stroke with aspiration can be envisioned, but that understanding the risk of ongoing, late stroke is more difficult.
As for why thrombectomy didn’t work, “aspiration is incredibly inefficient, thromboemboli still occur before, during, and after aspiration, the timing of aspiration is often too late to benefit most patients,” and other mechanisms of myonecrosis may predominate, such as reperfusion injury, he observed.
Dr. Stone said the TOTAL results should change practice and that the guideline recommendation should be downgraded to IIb.
“There are some patients who have a very large thrombus burden who have trouble dealing with all that thrombus in the cath lab who might benefit, and it is impossible to design randomized trials for small sections and groups of patients,” he said. “I wouldn’t make it class III by any means, but I think it’ll take a long time for that reduction in use to actually transmit through clinical practice, because I must say interventional cardiologists love the idea of simply removing thrombus with a relatively easy-to-use device.”
Dr. David Kandzari, director of interventional cardiology at the Piedmont Heart Center in Atlanta, said in an interview that TOTAL will make operators much more selective and cautious in their performance of thrombectomy until further insights into the stroke issue are available. Thrombectomy should be reserved for bailout instances and not as a front-line therapy, he said.
On the other hand, the stroke rate in the early phase was not significantly different between groups in an as-treated analysis, and an opportunity exists to investigate potential differences between stroke and nonstroke patients to determine whether other comorbidities rather than thrombectomy per se may account for the stroke signal, Dr. Kandzari observed.
TOTAL was funded by the Canadian Institutes of Health Research, Canadian Network and Centre for Trials Internationally, and Medtronic. Dr. Jolly disclosed receiving consulting fees and honoraria from AstraZeneca, speaking fees for St. Jude, and research grants from Medtronic. Dr. Nissen has received research support from and is a consultant/adviser to numerous pharmaceutical companies; all honoraria or consulting fees go directly to charity so that he receives neither income nor a tax deduction. Dr. Stone reported consulting honoraria from Guided Delivery Systems, Miracor, and Reva, and ownership interest or partnership in Arstasis, Caliber, VNT, Micardia, Biostar family funds, and Medfocus family funds. Dr. Kandzari reported research and grant support from Medtronic, Biotronic, Abbott Vascular, and Boston Scientific.
AT ACC 2015
Key clinical point: Routine manual thrombectomy did not improve 180-day outcomes and increased the risk of stroke, compared with PCI alone.
Major finding: Thrombectomy plus PCI did not improve the primary outcome vs. PCI alone (6.9% vs. 7%) and doubled the 30-day stroke rate (0.7% vs. 0.3%).
Data source: Prospective study in 10,063 patients with STEMI.
Disclosures: TOTAL was funded by the Canadian Institutes of Health Research, Canadian Network and Centre for Trials Internationally, and Medtronic. Dr. Jolly disclosed receiving consulting fees and honoraria from AstraZeneca, speaking fees for St. Jude, and research grants from Medtronic.
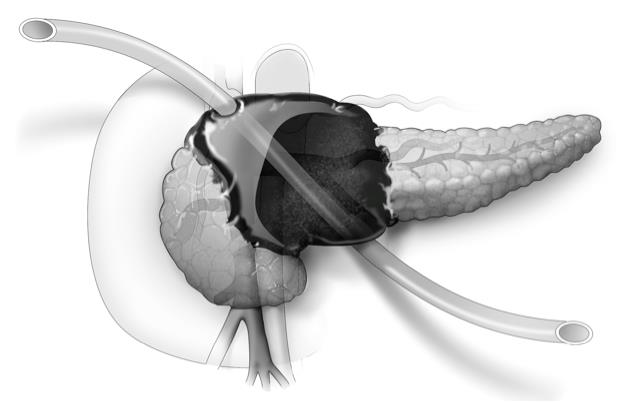
U-tube drainage adds option for necrotizing pancreatitis
CHICAGO – Placement of a U-tube drain provides enhanced percutaneous drainage and minimizes catheter-related complications in patients with complicated or infected necrotizing pancreatitis, new research suggests.
The U-tube method uses a large, 20-French Silastic tube with numerous large holes in the middle. One exit must be anterior through the peritoneal cavity and the other can be posterior in the retroperitoneum, Dr. Daniel E. Abbott said at the annual meeting of the Central Surgical Association.
The novel drainage system allows bidirectional flushing, greater interface with large fluid collections leading to more rapid resolution of retroperitoneal necrosis, and less risk of dislodgement resulting in fewer catheter exchanges or replacements. The system also creates a large-bore fistula tract to fall back on should subsequent fistulojejunostomy be needed, said Dr. Abbott of the University of Cincinnati Medical Center.
He reported on the largest clinical experience with primary U-tube drainage to date, involving 22 patients with necrotizing pancreatitis (NP) treated from 2011 to 2014. In 7 patients, (32%) no surgical procedure was ultimately required.
Of the others, 13 required further surgical intervention for a disrupted duct, and (59%) 2 patients died (9.1% ), Dr. Abbott said. Among eight patients who underwent fistulojejunostomy and five who underwent distal pancreatectomy and/or splenectomy, NP resolved in all but one patient with a recurrent amylase-rich fluid leak.
This compares favorably with a 20% mortality rate and 80% NP resolution among five institutional controls treated with open necrosectomy, he said.
Dr. Abbott acknowledged that the study was limited by small numbers and an insufficient control group for direct comparison.
Other studies have shown mortality rates in NP ranging from 39% with open necrosectomy to 4.5% with focused open necrosectomy, but their median length of stays were 54.5 days and 57 days, respectively. LOS was trimmed to just 19 days in one open necrosectomy study (Ann. Surg. 2008;247:294-9), but mortality was 11.4%, Dr. Abbott observed.
Dr. Abbott’s center is currently placing one to two U-tubes per month in patients with symptomatic NP (nausea, vomiting, weight loss, or infection on radiographic imaging) amenable to drainage and plans to update the analysis with prospectively collected data, including costs, in 2-3 years, he said.
“The U-tube obviously seems to work very well, but ... our radiologists sometimes have a hard time placing just one single tube. That [U-]tube, in particular, has to come anterior and out posterior and other organs can potentially get in the way,” said Dr. Michael Ujiki, director of minimally invasive surgery at NorthShore University Health System, Evanston, Ill.
The morbidity and mortality rates are certainly better, but the improvements could be the result of improved ICU care or getting away from antibiotics, said Dr. Ujiki, a discussant at the meeting.
Dr. Abbott noted that “we are operating on people when they’re generally well instead of operating when they’re generally sick. When you’re doing an open necrosectomy, not only might there be multisystem organ failure, but [patients’] nutritional status is undoubtedly poor as well.”
Radiologists have yet to be unable to place a U-tube, but have delayed placement in stable, normotensive patients until fluid collections get larger to provide a better target, he said. The U-tube also can be placed at separate interventions. The two things patients complain most about are the size of the large tubes and when enzymatic fluid leaks onto their skin if the tube become clogged.
CHICAGO – Placement of a U-tube drain provides enhanced percutaneous drainage and minimizes catheter-related complications in patients with complicated or infected necrotizing pancreatitis, new research suggests.
The U-tube method uses a large, 20-French Silastic tube with numerous large holes in the middle. One exit must be anterior through the peritoneal cavity and the other can be posterior in the retroperitoneum, Dr. Daniel E. Abbott said at the annual meeting of the Central Surgical Association.
The novel drainage system allows bidirectional flushing, greater interface with large fluid collections leading to more rapid resolution of retroperitoneal necrosis, and less risk of dislodgement resulting in fewer catheter exchanges or replacements. The system also creates a large-bore fistula tract to fall back on should subsequent fistulojejunostomy be needed, said Dr. Abbott of the University of Cincinnati Medical Center.
He reported on the largest clinical experience with primary U-tube drainage to date, involving 22 patients with necrotizing pancreatitis (NP) treated from 2011 to 2014. In 7 patients, (32%) no surgical procedure was ultimately required.
Of the others, 13 required further surgical intervention for a disrupted duct, and (59%) 2 patients died (9.1% ), Dr. Abbott said. Among eight patients who underwent fistulojejunostomy and five who underwent distal pancreatectomy and/or splenectomy, NP resolved in all but one patient with a recurrent amylase-rich fluid leak.
This compares favorably with a 20% mortality rate and 80% NP resolution among five institutional controls treated with open necrosectomy, he said.
Dr. Abbott acknowledged that the study was limited by small numbers and an insufficient control group for direct comparison.
Other studies have shown mortality rates in NP ranging from 39% with open necrosectomy to 4.5% with focused open necrosectomy, but their median length of stays were 54.5 days and 57 days, respectively. LOS was trimmed to just 19 days in one open necrosectomy study (Ann. Surg. 2008;247:294-9), but mortality was 11.4%, Dr. Abbott observed.
Dr. Abbott’s center is currently placing one to two U-tubes per month in patients with symptomatic NP (nausea, vomiting, weight loss, or infection on radiographic imaging) amenable to drainage and plans to update the analysis with prospectively collected data, including costs, in 2-3 years, he said.
“The U-tube obviously seems to work very well, but ... our radiologists sometimes have a hard time placing just one single tube. That [U-]tube, in particular, has to come anterior and out posterior and other organs can potentially get in the way,” said Dr. Michael Ujiki, director of minimally invasive surgery at NorthShore University Health System, Evanston, Ill.
The morbidity and mortality rates are certainly better, but the improvements could be the result of improved ICU care or getting away from antibiotics, said Dr. Ujiki, a discussant at the meeting.
Dr. Abbott noted that “we are operating on people when they’re generally well instead of operating when they’re generally sick. When you’re doing an open necrosectomy, not only might there be multisystem organ failure, but [patients’] nutritional status is undoubtedly poor as well.”
Radiologists have yet to be unable to place a U-tube, but have delayed placement in stable, normotensive patients until fluid collections get larger to provide a better target, he said. The U-tube also can be placed at separate interventions. The two things patients complain most about are the size of the large tubes and when enzymatic fluid leaks onto their skin if the tube become clogged.
CHICAGO – Placement of a U-tube drain provides enhanced percutaneous drainage and minimizes catheter-related complications in patients with complicated or infected necrotizing pancreatitis, new research suggests.
The U-tube method uses a large, 20-French Silastic tube with numerous large holes in the middle. One exit must be anterior through the peritoneal cavity and the other can be posterior in the retroperitoneum, Dr. Daniel E. Abbott said at the annual meeting of the Central Surgical Association.
The novel drainage system allows bidirectional flushing, greater interface with large fluid collections leading to more rapid resolution of retroperitoneal necrosis, and less risk of dislodgement resulting in fewer catheter exchanges or replacements. The system also creates a large-bore fistula tract to fall back on should subsequent fistulojejunostomy be needed, said Dr. Abbott of the University of Cincinnati Medical Center.
He reported on the largest clinical experience with primary U-tube drainage to date, involving 22 patients with necrotizing pancreatitis (NP) treated from 2011 to 2014. In 7 patients, (32%) no surgical procedure was ultimately required.
Of the others, 13 required further surgical intervention for a disrupted duct, and (59%) 2 patients died (9.1% ), Dr. Abbott said. Among eight patients who underwent fistulojejunostomy and five who underwent distal pancreatectomy and/or splenectomy, NP resolved in all but one patient with a recurrent amylase-rich fluid leak.
This compares favorably with a 20% mortality rate and 80% NP resolution among five institutional controls treated with open necrosectomy, he said.
Dr. Abbott acknowledged that the study was limited by small numbers and an insufficient control group for direct comparison.
Other studies have shown mortality rates in NP ranging from 39% with open necrosectomy to 4.5% with focused open necrosectomy, but their median length of stays were 54.5 days and 57 days, respectively. LOS was trimmed to just 19 days in one open necrosectomy study (Ann. Surg. 2008;247:294-9), but mortality was 11.4%, Dr. Abbott observed.
Dr. Abbott’s center is currently placing one to two U-tubes per month in patients with symptomatic NP (nausea, vomiting, weight loss, or infection on radiographic imaging) amenable to drainage and plans to update the analysis with prospectively collected data, including costs, in 2-3 years, he said.
“The U-tube obviously seems to work very well, but ... our radiologists sometimes have a hard time placing just one single tube. That [U-]tube, in particular, has to come anterior and out posterior and other organs can potentially get in the way,” said Dr. Michael Ujiki, director of minimally invasive surgery at NorthShore University Health System, Evanston, Ill.
The morbidity and mortality rates are certainly better, but the improvements could be the result of improved ICU care or getting away from antibiotics, said Dr. Ujiki, a discussant at the meeting.
Dr. Abbott noted that “we are operating on people when they’re generally well instead of operating when they’re generally sick. When you’re doing an open necrosectomy, not only might there be multisystem organ failure, but [patients’] nutritional status is undoubtedly poor as well.”
Radiologists have yet to be unable to place a U-tube, but have delayed placement in stable, normotensive patients until fluid collections get larger to provide a better target, he said. The U-tube also can be placed at separate interventions. The two things patients complain most about are the size of the large tubes and when enzymatic fluid leaks onto their skin if the tube become clogged.
AT THE ANNUAL MEETING OF THE CENTRAL SURGICAL ASSOCIATION
Key clinical point: U-tube drainage may eliminate the need for surgery in severe necrotizing pancreatitis.
Major finding: Disease-specific mortality occurred in 2 of 22 patients.
Data source: Retrospective study of 22 patients with symptomatic and/or infected necrotizing pancreatitis.
Disclosures: The researchers reported having no financial conflicts.
Smaller tubes take bite out of blood draws in critically ill
CHICAGO – Switching from conventional to small-volume phlebotomy tubes is an easy step toward reducing iatrogenic blood loss in critically ill adults, a new study suggests.
“We were looking at the amount of blood we were drawing off these patients and when we asked the nurses, the numbers were crazy. It could be as high as 20 mL per time that they drew off the patient and we felt we had to do better. The common sense dictum is the more blood you draw off, the more harm you are causing the patient,” principal investigator Dr. Heather Dolman from Detroit Receiving Hospital, Wayne State University, said in an interview.
For patients staying only a day or 2 at the hospital, the type of blood tube used may not make a difference. But for the critically ill, who studies suggest can have an average of 5 to more than 24 samples drawn a day, the cumulative blood loss over an extended stay can be sizable.
Clinicians are also inclined to order more diagnostic tests as the severity of illness increases, thus putting their sickest patients at the greatest risk of iatrogenic anemia and transfusion. Anemia secondary to phlebotomy accounts for up to 40% of packed red blood cells transfused, Dr. Dolman noted at the annual meeting of the Central Surgical Association.
The process of blood sampling itself also involves a fair amount of waste. Conventional arterial line systems require that an initial blood sample be removed to “clear the line.” This typically results in 2-10 mL of blood being discarded before a second sample of undiluted blood can be obtained.
Some hospitals have turned to closed blood sampling devices that avoid the need for a second sample. The impact of blood-conserving devices on transfusion rates has been underwhelming, with only one study showing a positive impact leading to reduced blood product use.
As part of their blood-conserving strategy, Dr. Dolman and her colleagues asked the hospital to invest in small-volume phlebotomy tubes (SVTs), which are sized somewhere between a conventional-volume tube (CVT) and a pediatric blood tube.
SVTs reduce the amount of blood needed from 8.5 mL with a conventional tube to 5.0 mL for a basic metabolic panel, from 6.0 mL to 2.0 mL for a complete blood count (CBC) or cross-matching, and from 2.7 mL to 1.8 mL for a prothrombin time /internationalized ratio/partial thromboplastin time, Dr. Dolman said. The cost of an SVT is the same as a CVT, as is the cost of the machinery needed to analyze the samples.
“Everyone is worried about missing out on data, but if you look at the research on the amount of blood the machine really needs, it is only 0.1 mL, that’s less than a cc,” she said. “The technology has been there for a while, I just think the common sense aspect of all this, no one has ever thought of.”
The investigators then retrospectively compared 248 critically ill patients in the ICU, of whom 116 had blood drawn with an SVT and 132 with a CVT. The two groups were well matched with respect to age (55 years vs. 57 years), admission to the emergency surgery/trauma service (63% vs. 64%), and mean APACHE II scores (14.1 vs. 12.7).
Transfusion was at the discretion of the primary team using a restrictive hemoglobin threshold of < 7.0 gm/dL, unless hemodynamic instability or active bleeding were present.
Utilizing an SVT significantly reduced daily blood loss from phlebotomy from 31.7 mL with a CVT to 22.5 mL (P < .0001) and overall phlebotomy blood loss from 299 mL to 174 mL (P < .001), Dr. Dolman reported.
This translated into a nonsignificant trend for fewer units of packed red blood cells transfused in the SVT group (mean 4.4 vs. 6.0; P = .16).
The same pattern was observed in the 158 patients admitted to the emergency surgery/trauma service, with SVT also leading to significantly fewer episodes of severe anemia (6 vs. 20; P = .01) and a trend toward shorter ICU stays (9.2 days vs. 10.6 days; P = .46), she said.
Patients with an APACHE score of at least 20, a group one would anticipate to derive greater advantage from a blood-conserving strategy, did not benefit from use of an SVT vs. a CVT, but the number of patients was very low at just 27 and 19, respectively, Dr. Dolman noted.
Anemia, however, had a profound impact on the critically ill cohort. Patients with severe anemia were significantly more likely than those with a hemoglobin level of at least 7 gm/dL to have longer ICU stays (16 days vs. 7.7 days; P < .001), longer hospital stays (23.3 days vs. 13.6 days; P < .001), and to die in the hospital (29% vs. 13%; P = .01).
Using a small-volume tube cut the number of patients with more than one episode of severe anemia from 22 to 11 (P = .01) and those with more than two episodes from 6 to 4 (P = .53).
“Anemia in the critically ill is a significant problem,” Dr. Dolman said. “Phlebotomy waste contributes to anemia and should be recorded to decrease this hidden loss.”
The impact of transfusion vs. no transfusion was less pronounced with respect to ICU stay (12 days vs. 6 days; P < .001), hospital stay (19 days vs. 11 days; P = .44), and in-hospital mortality (17% vs. 15%; P = .60), but can lead to other negative sequelae such as increased risk of infection, circulatory overload transfusion reactions, and immune modulation, she added.
Detroit Receiving Hospital continues to use conventional tubes in its ICU and other units, although a switch to small-volume tubes is expected to be considered following peer review of the full results, Dr. Dolman said.
Dr. Dolman reported having no financial disclosures.
On Twitter @pwendl
“This is something that should be replicated at institutions across the country,” discussant William C. Cirocco said in an interview. “Why not? It may not have clinical implications for the patient who is only in the hospital for 2 or 3 days, but for the ICU patient, it will have big impact. It’s a no-brainer.”
Dr. William C. Cirocco is a professor of surgery at Ohio State University in Columbus. He reported no relevant conflicts of interest.
“This is something that should be replicated at institutions across the country,” discussant William C. Cirocco said in an interview. “Why not? It may not have clinical implications for the patient who is only in the hospital for 2 or 3 days, but for the ICU patient, it will have big impact. It’s a no-brainer.”
Dr. William C. Cirocco is a professor of surgery at Ohio State University in Columbus. He reported no relevant conflicts of interest.
“This is something that should be replicated at institutions across the country,” discussant William C. Cirocco said in an interview. “Why not? It may not have clinical implications for the patient who is only in the hospital for 2 or 3 days, but for the ICU patient, it will have big impact. It’s a no-brainer.”
Dr. William C. Cirocco is a professor of surgery at Ohio State University in Columbus. He reported no relevant conflicts of interest.
CHICAGO – Switching from conventional to small-volume phlebotomy tubes is an easy step toward reducing iatrogenic blood loss in critically ill adults, a new study suggests.
“We were looking at the amount of blood we were drawing off these patients and when we asked the nurses, the numbers were crazy. It could be as high as 20 mL per time that they drew off the patient and we felt we had to do better. The common sense dictum is the more blood you draw off, the more harm you are causing the patient,” principal investigator Dr. Heather Dolman from Detroit Receiving Hospital, Wayne State University, said in an interview.
For patients staying only a day or 2 at the hospital, the type of blood tube used may not make a difference. But for the critically ill, who studies suggest can have an average of 5 to more than 24 samples drawn a day, the cumulative blood loss over an extended stay can be sizable.
Clinicians are also inclined to order more diagnostic tests as the severity of illness increases, thus putting their sickest patients at the greatest risk of iatrogenic anemia and transfusion. Anemia secondary to phlebotomy accounts for up to 40% of packed red blood cells transfused, Dr. Dolman noted at the annual meeting of the Central Surgical Association.
The process of blood sampling itself also involves a fair amount of waste. Conventional arterial line systems require that an initial blood sample be removed to “clear the line.” This typically results in 2-10 mL of blood being discarded before a second sample of undiluted blood can be obtained.
Some hospitals have turned to closed blood sampling devices that avoid the need for a second sample. The impact of blood-conserving devices on transfusion rates has been underwhelming, with only one study showing a positive impact leading to reduced blood product use.
As part of their blood-conserving strategy, Dr. Dolman and her colleagues asked the hospital to invest in small-volume phlebotomy tubes (SVTs), which are sized somewhere between a conventional-volume tube (CVT) and a pediatric blood tube.
SVTs reduce the amount of blood needed from 8.5 mL with a conventional tube to 5.0 mL for a basic metabolic panel, from 6.0 mL to 2.0 mL for a complete blood count (CBC) or cross-matching, and from 2.7 mL to 1.8 mL for a prothrombin time /internationalized ratio/partial thromboplastin time, Dr. Dolman said. The cost of an SVT is the same as a CVT, as is the cost of the machinery needed to analyze the samples.
“Everyone is worried about missing out on data, but if you look at the research on the amount of blood the machine really needs, it is only 0.1 mL, that’s less than a cc,” she said. “The technology has been there for a while, I just think the common sense aspect of all this, no one has ever thought of.”
The investigators then retrospectively compared 248 critically ill patients in the ICU, of whom 116 had blood drawn with an SVT and 132 with a CVT. The two groups were well matched with respect to age (55 years vs. 57 years), admission to the emergency surgery/trauma service (63% vs. 64%), and mean APACHE II scores (14.1 vs. 12.7).
Transfusion was at the discretion of the primary team using a restrictive hemoglobin threshold of < 7.0 gm/dL, unless hemodynamic instability or active bleeding were present.
Utilizing an SVT significantly reduced daily blood loss from phlebotomy from 31.7 mL with a CVT to 22.5 mL (P < .0001) and overall phlebotomy blood loss from 299 mL to 174 mL (P < .001), Dr. Dolman reported.
This translated into a nonsignificant trend for fewer units of packed red blood cells transfused in the SVT group (mean 4.4 vs. 6.0; P = .16).
The same pattern was observed in the 158 patients admitted to the emergency surgery/trauma service, with SVT also leading to significantly fewer episodes of severe anemia (6 vs. 20; P = .01) and a trend toward shorter ICU stays (9.2 days vs. 10.6 days; P = .46), she said.
Patients with an APACHE score of at least 20, a group one would anticipate to derive greater advantage from a blood-conserving strategy, did not benefit from use of an SVT vs. a CVT, but the number of patients was very low at just 27 and 19, respectively, Dr. Dolman noted.
Anemia, however, had a profound impact on the critically ill cohort. Patients with severe anemia were significantly more likely than those with a hemoglobin level of at least 7 gm/dL to have longer ICU stays (16 days vs. 7.7 days; P < .001), longer hospital stays (23.3 days vs. 13.6 days; P < .001), and to die in the hospital (29% vs. 13%; P = .01).
Using a small-volume tube cut the number of patients with more than one episode of severe anemia from 22 to 11 (P = .01) and those with more than two episodes from 6 to 4 (P = .53).
“Anemia in the critically ill is a significant problem,” Dr. Dolman said. “Phlebotomy waste contributes to anemia and should be recorded to decrease this hidden loss.”
The impact of transfusion vs. no transfusion was less pronounced with respect to ICU stay (12 days vs. 6 days; P < .001), hospital stay (19 days vs. 11 days; P = .44), and in-hospital mortality (17% vs. 15%; P = .60), but can lead to other negative sequelae such as increased risk of infection, circulatory overload transfusion reactions, and immune modulation, she added.
Detroit Receiving Hospital continues to use conventional tubes in its ICU and other units, although a switch to small-volume tubes is expected to be considered following peer review of the full results, Dr. Dolman said.
Dr. Dolman reported having no financial disclosures.
On Twitter @pwendl
CHICAGO – Switching from conventional to small-volume phlebotomy tubes is an easy step toward reducing iatrogenic blood loss in critically ill adults, a new study suggests.
“We were looking at the amount of blood we were drawing off these patients and when we asked the nurses, the numbers were crazy. It could be as high as 20 mL per time that they drew off the patient and we felt we had to do better. The common sense dictum is the more blood you draw off, the more harm you are causing the patient,” principal investigator Dr. Heather Dolman from Detroit Receiving Hospital, Wayne State University, said in an interview.
For patients staying only a day or 2 at the hospital, the type of blood tube used may not make a difference. But for the critically ill, who studies suggest can have an average of 5 to more than 24 samples drawn a day, the cumulative blood loss over an extended stay can be sizable.
Clinicians are also inclined to order more diagnostic tests as the severity of illness increases, thus putting their sickest patients at the greatest risk of iatrogenic anemia and transfusion. Anemia secondary to phlebotomy accounts for up to 40% of packed red blood cells transfused, Dr. Dolman noted at the annual meeting of the Central Surgical Association.
The process of blood sampling itself also involves a fair amount of waste. Conventional arterial line systems require that an initial blood sample be removed to “clear the line.” This typically results in 2-10 mL of blood being discarded before a second sample of undiluted blood can be obtained.
Some hospitals have turned to closed blood sampling devices that avoid the need for a second sample. The impact of blood-conserving devices on transfusion rates has been underwhelming, with only one study showing a positive impact leading to reduced blood product use.
As part of their blood-conserving strategy, Dr. Dolman and her colleagues asked the hospital to invest in small-volume phlebotomy tubes (SVTs), which are sized somewhere between a conventional-volume tube (CVT) and a pediatric blood tube.
SVTs reduce the amount of blood needed from 8.5 mL with a conventional tube to 5.0 mL for a basic metabolic panel, from 6.0 mL to 2.0 mL for a complete blood count (CBC) or cross-matching, and from 2.7 mL to 1.8 mL for a prothrombin time /internationalized ratio/partial thromboplastin time, Dr. Dolman said. The cost of an SVT is the same as a CVT, as is the cost of the machinery needed to analyze the samples.
“Everyone is worried about missing out on data, but if you look at the research on the amount of blood the machine really needs, it is only 0.1 mL, that’s less than a cc,” she said. “The technology has been there for a while, I just think the common sense aspect of all this, no one has ever thought of.”
The investigators then retrospectively compared 248 critically ill patients in the ICU, of whom 116 had blood drawn with an SVT and 132 with a CVT. The two groups were well matched with respect to age (55 years vs. 57 years), admission to the emergency surgery/trauma service (63% vs. 64%), and mean APACHE II scores (14.1 vs. 12.7).
Transfusion was at the discretion of the primary team using a restrictive hemoglobin threshold of < 7.0 gm/dL, unless hemodynamic instability or active bleeding were present.
Utilizing an SVT significantly reduced daily blood loss from phlebotomy from 31.7 mL with a CVT to 22.5 mL (P < .0001) and overall phlebotomy blood loss from 299 mL to 174 mL (P < .001), Dr. Dolman reported.
This translated into a nonsignificant trend for fewer units of packed red blood cells transfused in the SVT group (mean 4.4 vs. 6.0; P = .16).
The same pattern was observed in the 158 patients admitted to the emergency surgery/trauma service, with SVT also leading to significantly fewer episodes of severe anemia (6 vs. 20; P = .01) and a trend toward shorter ICU stays (9.2 days vs. 10.6 days; P = .46), she said.
Patients with an APACHE score of at least 20, a group one would anticipate to derive greater advantage from a blood-conserving strategy, did not benefit from use of an SVT vs. a CVT, but the number of patients was very low at just 27 and 19, respectively, Dr. Dolman noted.
Anemia, however, had a profound impact on the critically ill cohort. Patients with severe anemia were significantly more likely than those with a hemoglobin level of at least 7 gm/dL to have longer ICU stays (16 days vs. 7.7 days; P < .001), longer hospital stays (23.3 days vs. 13.6 days; P < .001), and to die in the hospital (29% vs. 13%; P = .01).
Using a small-volume tube cut the number of patients with more than one episode of severe anemia from 22 to 11 (P = .01) and those with more than two episodes from 6 to 4 (P = .53).
“Anemia in the critically ill is a significant problem,” Dr. Dolman said. “Phlebotomy waste contributes to anemia and should be recorded to decrease this hidden loss.”
The impact of transfusion vs. no transfusion was less pronounced with respect to ICU stay (12 days vs. 6 days; P < .001), hospital stay (19 days vs. 11 days; P = .44), and in-hospital mortality (17% vs. 15%; P = .60), but can lead to other negative sequelae such as increased risk of infection, circulatory overload transfusion reactions, and immune modulation, she added.
Detroit Receiving Hospital continues to use conventional tubes in its ICU and other units, although a switch to small-volume tubes is expected to be considered following peer review of the full results, Dr. Dolman said.
Dr. Dolman reported having no financial disclosures.
On Twitter @pwendl
AT THE ANNUAL MEETING OF THE CENTRAL SURGICAL ASSOCIATION
Key clinical point: Utilizing small-volume phlebotomy tubes minimizes diagnostic blood loss in the critically ill.
Major finding: Small tubes vs. conventional tubes reduced overall phlebotomy blood loss (174 mL vs. 299 mL; P < .001) and transfused packed RBCs (mean 4.4 units vs. 6.0 units; P = .16).
Data source: Retrospective case cohort in 248 critically ill patients.
Disclosures: Dr. Dolman reported having no financial disclosures.
Lateral neck dissection morbidity high, but transient
CHICAGO – Lateral neck dissection for thyroid cancer is associated with significant early postoperative morbidity of 20%, even in the hands of experienced endocrine surgeons at a high-volume medical center.
Among 99 procedures, 20 patients had 26 complications, including surgical site infection in 10, chyle leak in 7, spinal accessory nerve dysfunction in 7, and seroma in 2.
Long-term complications were rare, however, occurring in just one patient with a spinal accessory nerve injury, Dr. Jason A. Glenn said at the annual meeting of the Central Surgical Association.
Using a prospectively collected thyroid database, the investigators reviewed 96 patients who underwent lateral neck dissection (LND) for suspicion of initial or recurrent lateral neck metastases by one of four experienced endocrine surgeons at the Medical College of Wisconsin in Milwaukee.
Three patients had reoperations during the study period of February 2009 and June 2014, resulting in 99 procedures and 198 lateral necks evaluated preoperatively. Most patients were women (73%) and their median age was 45 years.
LND was performed on 127 necks and metastatic disease was confirmed in 111 (87%). This included all 82 patients who had positive preoperative fine needle aspiration (FNA), 25 of 37 patients operated on without FNA, and 4 of 8 patients with a negative or nondiagnostic FNA, Dr. Glenn said.
The median number of lymph nodes excised was 22 (range 1-122), with a median of 3 (range 0-39) malignant nodes per lateral neck.
“FNA is an important adjunct in the preoperative evaluation, especially when it returns a positive result,” he said. “However, when FNA is negative, not available, or not performed, you really must consider the entire clinical picture, as 64% of these patients were found to have lymph node metastases in our study.”
Surgical drains were placed in 94% of the 127 lateral neck dissections and remained in place for a median of 6 days. The median length of stay was 1 day.
There was no association between drain duration and surgical site infection, although chyle leak was associated with a significantly longer median drain duration (12 days vs. 6 days; P value < .01), Dr. Glenn said.
Two of the seven patients with chyle leak, defined by drain output that was milky white and/or exceeded 1,000 cc in 24 hours, underwent reoperation with ligation of the cervical thoracic duct and fibrin sealant application. Both leaks resolved and patients were discharge on postoperative day 2.
“Surgical drains allow for early leak recognition and monitoring of leak resolution,” he said. “Most of these complications were diagnosed and managed on an outpatient basis, highlighting the importance of continuity of care between the inpatient and outpatient setting for the treatment of thyroid cancer.”
Discussant Janice L. Pasieka, head of general surgery and a clinical professor of surgery and oncology at the University of Calgary (Alberta), said the retrospective review is a very valuable contribution to the literature because of its comprehensive follow-up.
“Today, most patients with this type of procedure are discharged within the 23 hours, and as such, complications such as nerve palsies, chyle leaks, and surgical site infections are not apparent for the majority of patients during their hospital stay,” Dr. Pasieka said. “Many times, the true incidences are lost unless the patient re-presents to the health care system, thus introducing your bias of only those significant enough to require intervention.”
Dr. Glenn and his coauthors reported no financial disclosures.
CHICAGO – Lateral neck dissection for thyroid cancer is associated with significant early postoperative morbidity of 20%, even in the hands of experienced endocrine surgeons at a high-volume medical center.
Among 99 procedures, 20 patients had 26 complications, including surgical site infection in 10, chyle leak in 7, spinal accessory nerve dysfunction in 7, and seroma in 2.
Long-term complications were rare, however, occurring in just one patient with a spinal accessory nerve injury, Dr. Jason A. Glenn said at the annual meeting of the Central Surgical Association.
Using a prospectively collected thyroid database, the investigators reviewed 96 patients who underwent lateral neck dissection (LND) for suspicion of initial or recurrent lateral neck metastases by one of four experienced endocrine surgeons at the Medical College of Wisconsin in Milwaukee.
Three patients had reoperations during the study period of February 2009 and June 2014, resulting in 99 procedures and 198 lateral necks evaluated preoperatively. Most patients were women (73%) and their median age was 45 years.
LND was performed on 127 necks and metastatic disease was confirmed in 111 (87%). This included all 82 patients who had positive preoperative fine needle aspiration (FNA), 25 of 37 patients operated on without FNA, and 4 of 8 patients with a negative or nondiagnostic FNA, Dr. Glenn said.
The median number of lymph nodes excised was 22 (range 1-122), with a median of 3 (range 0-39) malignant nodes per lateral neck.
“FNA is an important adjunct in the preoperative evaluation, especially when it returns a positive result,” he said. “However, when FNA is negative, not available, or not performed, you really must consider the entire clinical picture, as 64% of these patients were found to have lymph node metastases in our study.”
Surgical drains were placed in 94% of the 127 lateral neck dissections and remained in place for a median of 6 days. The median length of stay was 1 day.
There was no association between drain duration and surgical site infection, although chyle leak was associated with a significantly longer median drain duration (12 days vs. 6 days; P value < .01), Dr. Glenn said.
Two of the seven patients with chyle leak, defined by drain output that was milky white and/or exceeded 1,000 cc in 24 hours, underwent reoperation with ligation of the cervical thoracic duct and fibrin sealant application. Both leaks resolved and patients were discharge on postoperative day 2.
“Surgical drains allow for early leak recognition and monitoring of leak resolution,” he said. “Most of these complications were diagnosed and managed on an outpatient basis, highlighting the importance of continuity of care between the inpatient and outpatient setting for the treatment of thyroid cancer.”
Discussant Janice L. Pasieka, head of general surgery and a clinical professor of surgery and oncology at the University of Calgary (Alberta), said the retrospective review is a very valuable contribution to the literature because of its comprehensive follow-up.
“Today, most patients with this type of procedure are discharged within the 23 hours, and as such, complications such as nerve palsies, chyle leaks, and surgical site infections are not apparent for the majority of patients during their hospital stay,” Dr. Pasieka said. “Many times, the true incidences are lost unless the patient re-presents to the health care system, thus introducing your bias of only those significant enough to require intervention.”
Dr. Glenn and his coauthors reported no financial disclosures.
CHICAGO – Lateral neck dissection for thyroid cancer is associated with significant early postoperative morbidity of 20%, even in the hands of experienced endocrine surgeons at a high-volume medical center.
Among 99 procedures, 20 patients had 26 complications, including surgical site infection in 10, chyle leak in 7, spinal accessory nerve dysfunction in 7, and seroma in 2.
Long-term complications were rare, however, occurring in just one patient with a spinal accessory nerve injury, Dr. Jason A. Glenn said at the annual meeting of the Central Surgical Association.
Using a prospectively collected thyroid database, the investigators reviewed 96 patients who underwent lateral neck dissection (LND) for suspicion of initial or recurrent lateral neck metastases by one of four experienced endocrine surgeons at the Medical College of Wisconsin in Milwaukee.
Three patients had reoperations during the study period of February 2009 and June 2014, resulting in 99 procedures and 198 lateral necks evaluated preoperatively. Most patients were women (73%) and their median age was 45 years.
LND was performed on 127 necks and metastatic disease was confirmed in 111 (87%). This included all 82 patients who had positive preoperative fine needle aspiration (FNA), 25 of 37 patients operated on without FNA, and 4 of 8 patients with a negative or nondiagnostic FNA, Dr. Glenn said.
The median number of lymph nodes excised was 22 (range 1-122), with a median of 3 (range 0-39) malignant nodes per lateral neck.
“FNA is an important adjunct in the preoperative evaluation, especially when it returns a positive result,” he said. “However, when FNA is negative, not available, or not performed, you really must consider the entire clinical picture, as 64% of these patients were found to have lymph node metastases in our study.”
Surgical drains were placed in 94% of the 127 lateral neck dissections and remained in place for a median of 6 days. The median length of stay was 1 day.
There was no association between drain duration and surgical site infection, although chyle leak was associated with a significantly longer median drain duration (12 days vs. 6 days; P value < .01), Dr. Glenn said.
Two of the seven patients with chyle leak, defined by drain output that was milky white and/or exceeded 1,000 cc in 24 hours, underwent reoperation with ligation of the cervical thoracic duct and fibrin sealant application. Both leaks resolved and patients were discharge on postoperative day 2.
“Surgical drains allow for early leak recognition and monitoring of leak resolution,” he said. “Most of these complications were diagnosed and managed on an outpatient basis, highlighting the importance of continuity of care between the inpatient and outpatient setting for the treatment of thyroid cancer.”
Discussant Janice L. Pasieka, head of general surgery and a clinical professor of surgery and oncology at the University of Calgary (Alberta), said the retrospective review is a very valuable contribution to the literature because of its comprehensive follow-up.
“Today, most patients with this type of procedure are discharged within the 23 hours, and as such, complications such as nerve palsies, chyle leaks, and surgical site infections are not apparent for the majority of patients during their hospital stay,” Dr. Pasieka said. “Many times, the true incidences are lost unless the patient re-presents to the health care system, thus introducing your bias of only those significant enough to require intervention.”
Dr. Glenn and his coauthors reported no financial disclosures.
AT THE ANNUAL MEETING OF THE CENTRAL SURGICAL ASSOCIATION
Key clinical point: Lateral neck dissections for thyroid cancer are associated with high early morbidity but few long-term complications.
Major finding: The overall complication rate was 20%, however, most were transient.
Data source: Retrospective observational series of 96 patients undergoing lateral neck dissection.
Disclosures: Dr. Glenn and his coauthors reported no financial disclosures.
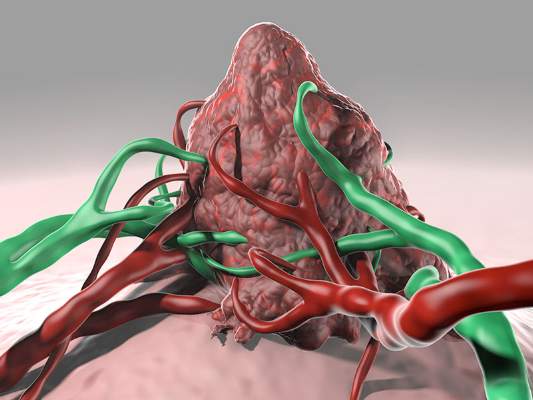
Personalized Melanoma Vaccine Evokes Immune Response
A customized vaccine targeting patient-specific, tumor neoantigens evoked an immune response in three adults with advanced cutaneous melanoma in a proof-of-principle study that paves the way for a phase I trial.
The data are “too premature to conclude that the treatment had any therapeutic benefit to the patients,” Dr. Gerald P. Linette of Washington University in St. Louis, Mo., said in a teleconference. However, he noted that a phase I trial would likely begin within the next 9-12 months.
“Our primary goal was to see if this was safe, and if we could elicit an immune response,” Dr. Linette said.
Vaccination not only augmented T-cell immunity directed against naturally occurring, dominant tumor neoantigens, but also expanded the breadth of the immune response by revealing additional subdominant neoantigens, lead author Beatriz M. Carreno, Ph.D., of Washington University in St. Louis and her associates reported online April 2 in Science (doi:10.1126/science.aaa3828).
All three patients had stage IIIC, resected, cutaneous melanoma and had failed prior therapy with ipilimumab (Yervoy).
Some melanoma patients harbor tumor missense mutations, translated into amino acid substitutions (AAS). These mutations are thought to produce antigens that the immune system perceives as foreign, prompting a tumor-specific T-cell response. Heretofore, there has been no systematic evaluation of these neoantigens or whether vaccination can enhance these responses.
The aim of the current study was to determine the safety, tolerability, and immunologic responses to AAS peptides inside a modified dendritic cell vaccine. Seven AAS peptide candidates were selected among validated HLA-A*02:01 binders, along with the melanoma peptides G209-2M and G280-9V as positive controls for vaccination.
In each patient, T cell immunity to one AAS peptide was detected in prevaccine peripheral blood mononuclear cell samples.
The treatment differs from other personalized cancer vaccines in two key ways, Dr. Carreno said in the teleconference.
“We mature the [dendritic] cells before we give them back to the patients; the cells make growth factors that we have previously shown are important to the generation of the immune response,” she said. In addition, the vaccine was given as an infusion, rather than an injection, she noted.
Vaccination augmented the T-cell response to the three neoantigens – TMEM48 F169L, SEC24A P469, EXOC8 Q656P – with observed frequencies of 23%, 64%, and 89%, respectively.
Immune monitoring also detected T-cell immunity to two additional neoantigens per patient, Dr. Carreno and her associates reported.
Robust immune responses were detected as early as week 2 and peaked at weeks 8-9 after the initial dose. Each patient received three vaccine doses, without side effects or toxicity.
“Vaccination against tumor antigens appears safe as all three patients are alive and well, with no autoimmune adverse events,” the researchers wrote. Post vaccine restaging CT revealed stable disease in a 54-year-old man with BRAF V6003 mutation-positive melanoma. A second man, who had achieved a complete response to ipilimumab for BRAF V6003-positive disease, remains in complete remission after receiving the vaccine in the adjuvant setting.
The vaccine induced 30% tumor reduction in a woman with extensive skin metastases and 5-12 mm lung nodules after ipilimumab and vemurafenib (Zelboraf), but tumor size returned back to baseline dimensions 12 weeks later with no new disease sites. Her disease has remained stable for the past 8 months, the researchers said.
However, it is too soon to attribute a clinical benefit to the observed immune response to the vaccine, Dr. Linette emphasized. “I would be speculating if I said the vaccine had any benefit to the patients,” he said.
Vaccination increased the frequency of most existing prevaccine T-cell receptor-beta (TCR-beta) clonotypes and revealed new clonotypes for 6 neoantigens.
For both dominant and subdominant neoantigens, the TCR-beta repertoire was increased significantly after vaccination. For example, 84 clonotypes representing 19 TCR-beta families were detected for TKT R438W, 61 clonotypes representing 12 TCR-beta families were detected for SEC24A P469L, and 12 clonotypes representing 8 TCR-beta families were detected for EXOC8 Q656P.
“The revelation of a highly diverse TCR-beta repertoire specific for dominant and subdominant neoantigens was surprising and points to a potentially rich pool of naive tumor-specific T cells that remain ignorant unless activated by vaccination,” the researchers wrote.
Recent data indicate that CTLA-4 monoclonal antibody use can alter TCR repertoire diversity in patients, suggesting a potential strategy of combination checkpoint inhibitors, including ipilimumab, and neoantigen vaccines. The novel vaccine strategy also could be used to treat other malignancies with high mutational burdens such as lung, bladder, and colorectal cancers, while other genomic alterations may generate potential neoantigens relevant in low–mutational burden cancers such as leukemia, the authors suggest.
Although the cells in this study were grown in a specialized laboratory, “as the technology improves, I think this [strategy] will become reproducible and available at other medical centers,” Dr. Linette said.
This work was supported by Barnes-Jewish Hospital Foundation, Siteman Cancer Frontier Fund, Our Mark on Melanoma (MOM) Foundation, Come Out Swinging (COS) Foundation, Blackout Melanoma Foundation and the National Cancer Institute.
Heidi Splete contributed to this story.
A customized vaccine targeting patient-specific, tumor neoantigens evoked an immune response in three adults with advanced cutaneous melanoma in a proof-of-principle study that paves the way for a phase I trial.
The data are “too premature to conclude that the treatment had any therapeutic benefit to the patients,” Dr. Gerald P. Linette of Washington University in St. Louis, Mo., said in a teleconference. However, he noted that a phase I trial would likely begin within the next 9-12 months.
“Our primary goal was to see if this was safe, and if we could elicit an immune response,” Dr. Linette said.
Vaccination not only augmented T-cell immunity directed against naturally occurring, dominant tumor neoantigens, but also expanded the breadth of the immune response by revealing additional subdominant neoantigens, lead author Beatriz M. Carreno, Ph.D., of Washington University in St. Louis and her associates reported online April 2 in Science (doi:10.1126/science.aaa3828).
All three patients had stage IIIC, resected, cutaneous melanoma and had failed prior therapy with ipilimumab (Yervoy).
Some melanoma patients harbor tumor missense mutations, translated into amino acid substitutions (AAS). These mutations are thought to produce antigens that the immune system perceives as foreign, prompting a tumor-specific T-cell response. Heretofore, there has been no systematic evaluation of these neoantigens or whether vaccination can enhance these responses.
The aim of the current study was to determine the safety, tolerability, and immunologic responses to AAS peptides inside a modified dendritic cell vaccine. Seven AAS peptide candidates were selected among validated HLA-A*02:01 binders, along with the melanoma peptides G209-2M and G280-9V as positive controls for vaccination.
In each patient, T cell immunity to one AAS peptide was detected in prevaccine peripheral blood mononuclear cell samples.
The treatment differs from other personalized cancer vaccines in two key ways, Dr. Carreno said in the teleconference.
“We mature the [dendritic] cells before we give them back to the patients; the cells make growth factors that we have previously shown are important to the generation of the immune response,” she said. In addition, the vaccine was given as an infusion, rather than an injection, she noted.
Vaccination augmented the T-cell response to the three neoantigens – TMEM48 F169L, SEC24A P469, EXOC8 Q656P – with observed frequencies of 23%, 64%, and 89%, respectively.
Immune monitoring also detected T-cell immunity to two additional neoantigens per patient, Dr. Carreno and her associates reported.
Robust immune responses were detected as early as week 2 and peaked at weeks 8-9 after the initial dose. Each patient received three vaccine doses, without side effects or toxicity.
“Vaccination against tumor antigens appears safe as all three patients are alive and well, with no autoimmune adverse events,” the researchers wrote. Post vaccine restaging CT revealed stable disease in a 54-year-old man with BRAF V6003 mutation-positive melanoma. A second man, who had achieved a complete response to ipilimumab for BRAF V6003-positive disease, remains in complete remission after receiving the vaccine in the adjuvant setting.
The vaccine induced 30% tumor reduction in a woman with extensive skin metastases and 5-12 mm lung nodules after ipilimumab and vemurafenib (Zelboraf), but tumor size returned back to baseline dimensions 12 weeks later with no new disease sites. Her disease has remained stable for the past 8 months, the researchers said.
However, it is too soon to attribute a clinical benefit to the observed immune response to the vaccine, Dr. Linette emphasized. “I would be speculating if I said the vaccine had any benefit to the patients,” he said.
Vaccination increased the frequency of most existing prevaccine T-cell receptor-beta (TCR-beta) clonotypes and revealed new clonotypes for 6 neoantigens.
For both dominant and subdominant neoantigens, the TCR-beta repertoire was increased significantly after vaccination. For example, 84 clonotypes representing 19 TCR-beta families were detected for TKT R438W, 61 clonotypes representing 12 TCR-beta families were detected for SEC24A P469L, and 12 clonotypes representing 8 TCR-beta families were detected for EXOC8 Q656P.
“The revelation of a highly diverse TCR-beta repertoire specific for dominant and subdominant neoantigens was surprising and points to a potentially rich pool of naive tumor-specific T cells that remain ignorant unless activated by vaccination,” the researchers wrote.
Recent data indicate that CTLA-4 monoclonal antibody use can alter TCR repertoire diversity in patients, suggesting a potential strategy of combination checkpoint inhibitors, including ipilimumab, and neoantigen vaccines. The novel vaccine strategy also could be used to treat other malignancies with high mutational burdens such as lung, bladder, and colorectal cancers, while other genomic alterations may generate potential neoantigens relevant in low–mutational burden cancers such as leukemia, the authors suggest.
Although the cells in this study were grown in a specialized laboratory, “as the technology improves, I think this [strategy] will become reproducible and available at other medical centers,” Dr. Linette said.
This work was supported by Barnes-Jewish Hospital Foundation, Siteman Cancer Frontier Fund, Our Mark on Melanoma (MOM) Foundation, Come Out Swinging (COS) Foundation, Blackout Melanoma Foundation and the National Cancer Institute.
Heidi Splete contributed to this story.
A customized vaccine targeting patient-specific, tumor neoantigens evoked an immune response in three adults with advanced cutaneous melanoma in a proof-of-principle study that paves the way for a phase I trial.
The data are “too premature to conclude that the treatment had any therapeutic benefit to the patients,” Dr. Gerald P. Linette of Washington University in St. Louis, Mo., said in a teleconference. However, he noted that a phase I trial would likely begin within the next 9-12 months.
“Our primary goal was to see if this was safe, and if we could elicit an immune response,” Dr. Linette said.
Vaccination not only augmented T-cell immunity directed against naturally occurring, dominant tumor neoantigens, but also expanded the breadth of the immune response by revealing additional subdominant neoantigens, lead author Beatriz M. Carreno, Ph.D., of Washington University in St. Louis and her associates reported online April 2 in Science (doi:10.1126/science.aaa3828).
All three patients had stage IIIC, resected, cutaneous melanoma and had failed prior therapy with ipilimumab (Yervoy).
Some melanoma patients harbor tumor missense mutations, translated into amino acid substitutions (AAS). These mutations are thought to produce antigens that the immune system perceives as foreign, prompting a tumor-specific T-cell response. Heretofore, there has been no systematic evaluation of these neoantigens or whether vaccination can enhance these responses.
The aim of the current study was to determine the safety, tolerability, and immunologic responses to AAS peptides inside a modified dendritic cell vaccine. Seven AAS peptide candidates were selected among validated HLA-A*02:01 binders, along with the melanoma peptides G209-2M and G280-9V as positive controls for vaccination.
In each patient, T cell immunity to one AAS peptide was detected in prevaccine peripheral blood mononuclear cell samples.
The treatment differs from other personalized cancer vaccines in two key ways, Dr. Carreno said in the teleconference.
“We mature the [dendritic] cells before we give them back to the patients; the cells make growth factors that we have previously shown are important to the generation of the immune response,” she said. In addition, the vaccine was given as an infusion, rather than an injection, she noted.
Vaccination augmented the T-cell response to the three neoantigens – TMEM48 F169L, SEC24A P469, EXOC8 Q656P – with observed frequencies of 23%, 64%, and 89%, respectively.
Immune monitoring also detected T-cell immunity to two additional neoantigens per patient, Dr. Carreno and her associates reported.
Robust immune responses were detected as early as week 2 and peaked at weeks 8-9 after the initial dose. Each patient received three vaccine doses, without side effects or toxicity.
“Vaccination against tumor antigens appears safe as all three patients are alive and well, with no autoimmune adverse events,” the researchers wrote. Post vaccine restaging CT revealed stable disease in a 54-year-old man with BRAF V6003 mutation-positive melanoma. A second man, who had achieved a complete response to ipilimumab for BRAF V6003-positive disease, remains in complete remission after receiving the vaccine in the adjuvant setting.
The vaccine induced 30% tumor reduction in a woman with extensive skin metastases and 5-12 mm lung nodules after ipilimumab and vemurafenib (Zelboraf), but tumor size returned back to baseline dimensions 12 weeks later with no new disease sites. Her disease has remained stable for the past 8 months, the researchers said.
However, it is too soon to attribute a clinical benefit to the observed immune response to the vaccine, Dr. Linette emphasized. “I would be speculating if I said the vaccine had any benefit to the patients,” he said.
Vaccination increased the frequency of most existing prevaccine T-cell receptor-beta (TCR-beta) clonotypes and revealed new clonotypes for 6 neoantigens.
For both dominant and subdominant neoantigens, the TCR-beta repertoire was increased significantly after vaccination. For example, 84 clonotypes representing 19 TCR-beta families were detected for TKT R438W, 61 clonotypes representing 12 TCR-beta families were detected for SEC24A P469L, and 12 clonotypes representing 8 TCR-beta families were detected for EXOC8 Q656P.
“The revelation of a highly diverse TCR-beta repertoire specific for dominant and subdominant neoantigens was surprising and points to a potentially rich pool of naive tumor-specific T cells that remain ignorant unless activated by vaccination,” the researchers wrote.
Recent data indicate that CTLA-4 monoclonal antibody use can alter TCR repertoire diversity in patients, suggesting a potential strategy of combination checkpoint inhibitors, including ipilimumab, and neoantigen vaccines. The novel vaccine strategy also could be used to treat other malignancies with high mutational burdens such as lung, bladder, and colorectal cancers, while other genomic alterations may generate potential neoantigens relevant in low–mutational burden cancers such as leukemia, the authors suggest.
Although the cells in this study were grown in a specialized laboratory, “as the technology improves, I think this [strategy] will become reproducible and available at other medical centers,” Dr. Linette said.
This work was supported by Barnes-Jewish Hospital Foundation, Siteman Cancer Frontier Fund, Our Mark on Melanoma (MOM) Foundation, Come Out Swinging (COS) Foundation, Blackout Melanoma Foundation and the National Cancer Institute.
Heidi Splete contributed to this story.
FROM SCIENCE
Personalized melanoma vaccine evokes immune response
A customized vaccine targeting patient-specific, tumor neoantigens evoked an immune response in three adults with advanced cutaneous melanoma in a proof-of-principle study that paves the way for a phase I trial.
The data are “too premature to conclude that the treatment had any therapeutic benefit to the patients,” Dr. Gerald P. Linette of Washington University in St. Louis, Mo., said in a teleconference. However, he noted that a phase I trial would likely begin within the next 9-12 months.
“Our primary goal was to see if this was safe, and if we could elicit an immune response,” Dr. Linette said.
Vaccination not only augmented T-cell immunity directed against naturally occurring, dominant tumor neoantigens, but also expanded the breadth of the immune response by revealing additional subdominant neoantigens, lead author Beatriz M. Carreno, Ph.D., of Washington University in St. Louis and her associates reported online April 2 in Science (doi:10.1126/science.aaa3828).
All three patients had stage IIIC, resected, cutaneous melanoma and had failed prior therapy with ipilimumab (Yervoy).
Some melanoma patients harbor tumor missense mutations, translated into amino acid substitutions (AAS). These mutations are thought to produce antigens that the immune system perceives as foreign, prompting a tumor-specific T-cell response. Heretofore, there has been no systematic evaluation of these neoantigens or whether vaccination can enhance these responses.
The aim of the current study was to determine the safety, tolerability, and immunologic responses to AAS peptides inside a modified dendritic cell vaccine. Seven AAS peptide candidates were selected among validated HLA-A*02:01 binders, along with the melanoma peptides G209-2M and G280-9V as positive controls for vaccination.
In each patient, T cell immunity to one AAS peptide was detected in prevaccine peripheral blood mononuclear cell samples.
The treatment differs from other personalized cancer vaccines in two key ways, Dr. Carreno said in the teleconference.
“We mature the [dendritic] cells before we give them back to the patients; the cells make growth factors that we have previously shown are important to the generation of the immune response,” she said. In addition, the vaccine was given as an infusion, rather than an injection, she noted.
Vaccination augmented the T-cell response to the three neoantigens – TMEM48 F169L, SEC24A P469, EXOC8 Q656P – with observed frequencies of 23%, 64%, and 89%, respectively.
Immune monitoring also detected T-cell immunity to two additional neoantigens per patient, Dr. Carreno and her associates reported.
Robust immune responses were detected as early as week 2 and peaked at weeks 8-9 after the initial dose. Each patient received three vaccine doses, without side effects or toxicity.
“Vaccination against tumor antigens appears safe as all three patients are alive and well, with no autoimmune adverse events,” the researchers wrote. Post vaccine restaging CT revealed stable disease in a 54-year-old man with BRAF V6003 mutation-positive melanoma. A second man, who had achieved a complete response to ipilimumab for BRAF V6003-positive disease, remains in complete remission after receiving the vaccine in the adjuvant setting.
The vaccine induced 30% tumor reduction in a woman with extensive skin metastases and 5-12 mm lung nodules after ipilimumab and vemurafenib (Zelboraf), but tumor size returned back to baseline dimensions 12 weeks later with no new disease sites. Her disease has remained stable for the past 8 months, the researchers said.
However, it is too soon to attribute a clinical benefit to the observed immune response to the vaccine, Dr. Linette emphasized. “I would be speculating if I said the vaccine had any benefit to the patients,” he said.
Vaccination increased the frequency of most existing prevaccine T-cell receptor-beta (TCR-beta) clonotypes and revealed new clonotypes for 6 neoantigens.
For both dominant and subdominant neoantigens, the TCR-beta repertoire was increased significantly after vaccination. For example, 84 clonotypes representing 19 TCR-beta families were detected for TKT R438W, 61 clonotypes representing 12 TCR-beta families were detected for SEC24A P469L, and 12 clonotypes representing 8 TCR-beta families were detected for EXOC8 Q656P.
“The revelation of a highly diverse TCR-beta repertoire specific for dominant and subdominant neoantigens was surprising and points to a potentially rich pool of naive tumor-specific T cells that remain ignorant unless activated by vaccination,” the researchers wrote.
Recent data indicate that CTLA-4 monoclonal antibody use can alter TCR repertoire diversity in patients, suggesting a potential strategy of combination checkpoint inhibitors, including ipilimumab, and neoantigen vaccines. The novel vaccine strategy also could be used to treat other malignancies with high mutational burdens such as lung, bladder, and colorectal cancers, while other genomic alterations may generate potential neoantigens relevant in low–mutational burden cancers such as leukemia, the authors suggest.
Although the cells in this study were grown in a specialized laboratory, “as the technology improves, I think this [strategy] will become reproducible and available at other medical centers,” Dr. Linette said.
This work was supported by Barnes-Jewish Hospital Foundation, Siteman Cancer Frontier Fund, Our Mark on Melanoma (MOM) Foundation, Come Out Swinging (COS) Foundation, Blackout Melanoma Foundation and the National Cancer Institute.
Heidi Splete contributed to this story.
A customized vaccine targeting patient-specific, tumor neoantigens evoked an immune response in three adults with advanced cutaneous melanoma in a proof-of-principle study that paves the way for a phase I trial.
The data are “too premature to conclude that the treatment had any therapeutic benefit to the patients,” Dr. Gerald P. Linette of Washington University in St. Louis, Mo., said in a teleconference. However, he noted that a phase I trial would likely begin within the next 9-12 months.
“Our primary goal was to see if this was safe, and if we could elicit an immune response,” Dr. Linette said.
Vaccination not only augmented T-cell immunity directed against naturally occurring, dominant tumor neoantigens, but also expanded the breadth of the immune response by revealing additional subdominant neoantigens, lead author Beatriz M. Carreno, Ph.D., of Washington University in St. Louis and her associates reported online April 2 in Science (doi:10.1126/science.aaa3828).
All three patients had stage IIIC, resected, cutaneous melanoma and had failed prior therapy with ipilimumab (Yervoy).
Some melanoma patients harbor tumor missense mutations, translated into amino acid substitutions (AAS). These mutations are thought to produce antigens that the immune system perceives as foreign, prompting a tumor-specific T-cell response. Heretofore, there has been no systematic evaluation of these neoantigens or whether vaccination can enhance these responses.
The aim of the current study was to determine the safety, tolerability, and immunologic responses to AAS peptides inside a modified dendritic cell vaccine. Seven AAS peptide candidates were selected among validated HLA-A*02:01 binders, along with the melanoma peptides G209-2M and G280-9V as positive controls for vaccination.
In each patient, T cell immunity to one AAS peptide was detected in prevaccine peripheral blood mononuclear cell samples.
The treatment differs from other personalized cancer vaccines in two key ways, Dr. Carreno said in the teleconference.
“We mature the [dendritic] cells before we give them back to the patients; the cells make growth factors that we have previously shown are important to the generation of the immune response,” she said. In addition, the vaccine was given as an infusion, rather than an injection, she noted.
Vaccination augmented the T-cell response to the three neoantigens – TMEM48 F169L, SEC24A P469, EXOC8 Q656P – with observed frequencies of 23%, 64%, and 89%, respectively.
Immune monitoring also detected T-cell immunity to two additional neoantigens per patient, Dr. Carreno and her associates reported.
Robust immune responses were detected as early as week 2 and peaked at weeks 8-9 after the initial dose. Each patient received three vaccine doses, without side effects or toxicity.
“Vaccination against tumor antigens appears safe as all three patients are alive and well, with no autoimmune adverse events,” the researchers wrote. Post vaccine restaging CT revealed stable disease in a 54-year-old man with BRAF V6003 mutation-positive melanoma. A second man, who had achieved a complete response to ipilimumab for BRAF V6003-positive disease, remains in complete remission after receiving the vaccine in the adjuvant setting.
The vaccine induced 30% tumor reduction in a woman with extensive skin metastases and 5-12 mm lung nodules after ipilimumab and vemurafenib (Zelboraf), but tumor size returned back to baseline dimensions 12 weeks later with no new disease sites. Her disease has remained stable for the past 8 months, the researchers said.
However, it is too soon to attribute a clinical benefit to the observed immune response to the vaccine, Dr. Linette emphasized. “I would be speculating if I said the vaccine had any benefit to the patients,” he said.
Vaccination increased the frequency of most existing prevaccine T-cell receptor-beta (TCR-beta) clonotypes and revealed new clonotypes for 6 neoantigens.
For both dominant and subdominant neoantigens, the TCR-beta repertoire was increased significantly after vaccination. For example, 84 clonotypes representing 19 TCR-beta families were detected for TKT R438W, 61 clonotypes representing 12 TCR-beta families were detected for SEC24A P469L, and 12 clonotypes representing 8 TCR-beta families were detected for EXOC8 Q656P.
“The revelation of a highly diverse TCR-beta repertoire specific for dominant and subdominant neoantigens was surprising and points to a potentially rich pool of naive tumor-specific T cells that remain ignorant unless activated by vaccination,” the researchers wrote.
Recent data indicate that CTLA-4 monoclonal antibody use can alter TCR repertoire diversity in patients, suggesting a potential strategy of combination checkpoint inhibitors, including ipilimumab, and neoantigen vaccines. The novel vaccine strategy also could be used to treat other malignancies with high mutational burdens such as lung, bladder, and colorectal cancers, while other genomic alterations may generate potential neoantigens relevant in low–mutational burden cancers such as leukemia, the authors suggest.
Although the cells in this study were grown in a specialized laboratory, “as the technology improves, I think this [strategy] will become reproducible and available at other medical centers,” Dr. Linette said.
This work was supported by Barnes-Jewish Hospital Foundation, Siteman Cancer Frontier Fund, Our Mark on Melanoma (MOM) Foundation, Come Out Swinging (COS) Foundation, Blackout Melanoma Foundation and the National Cancer Institute.
Heidi Splete contributed to this story.
A customized vaccine targeting patient-specific, tumor neoantigens evoked an immune response in three adults with advanced cutaneous melanoma in a proof-of-principle study that paves the way for a phase I trial.
The data are “too premature to conclude that the treatment had any therapeutic benefit to the patients,” Dr. Gerald P. Linette of Washington University in St. Louis, Mo., said in a teleconference. However, he noted that a phase I trial would likely begin within the next 9-12 months.
“Our primary goal was to see if this was safe, and if we could elicit an immune response,” Dr. Linette said.
Vaccination not only augmented T-cell immunity directed against naturally occurring, dominant tumor neoantigens, but also expanded the breadth of the immune response by revealing additional subdominant neoantigens, lead author Beatriz M. Carreno, Ph.D., of Washington University in St. Louis and her associates reported online April 2 in Science (doi:10.1126/science.aaa3828).
All three patients had stage IIIC, resected, cutaneous melanoma and had failed prior therapy with ipilimumab (Yervoy).
Some melanoma patients harbor tumor missense mutations, translated into amino acid substitutions (AAS). These mutations are thought to produce antigens that the immune system perceives as foreign, prompting a tumor-specific T-cell response. Heretofore, there has been no systematic evaluation of these neoantigens or whether vaccination can enhance these responses.
The aim of the current study was to determine the safety, tolerability, and immunologic responses to AAS peptides inside a modified dendritic cell vaccine. Seven AAS peptide candidates were selected among validated HLA-A*02:01 binders, along with the melanoma peptides G209-2M and G280-9V as positive controls for vaccination.
In each patient, T cell immunity to one AAS peptide was detected in prevaccine peripheral blood mononuclear cell samples.
The treatment differs from other personalized cancer vaccines in two key ways, Dr. Carreno said in the teleconference.
“We mature the [dendritic] cells before we give them back to the patients; the cells make growth factors that we have previously shown are important to the generation of the immune response,” she said. In addition, the vaccine was given as an infusion, rather than an injection, she noted.
Vaccination augmented the T-cell response to the three neoantigens – TMEM48 F169L, SEC24A P469, EXOC8 Q656P – with observed frequencies of 23%, 64%, and 89%, respectively.
Immune monitoring also detected T-cell immunity to two additional neoantigens per patient, Dr. Carreno and her associates reported.
Robust immune responses were detected as early as week 2 and peaked at weeks 8-9 after the initial dose. Each patient received three vaccine doses, without side effects or toxicity.
“Vaccination against tumor antigens appears safe as all three patients are alive and well, with no autoimmune adverse events,” the researchers wrote. Post vaccine restaging CT revealed stable disease in a 54-year-old man with BRAF V6003 mutation-positive melanoma. A second man, who had achieved a complete response to ipilimumab for BRAF V6003-positive disease, remains in complete remission after receiving the vaccine in the adjuvant setting.
The vaccine induced 30% tumor reduction in a woman with extensive skin metastases and 5-12 mm lung nodules after ipilimumab and vemurafenib (Zelboraf), but tumor size returned back to baseline dimensions 12 weeks later with no new disease sites. Her disease has remained stable for the past 8 months, the researchers said.
However, it is too soon to attribute a clinical benefit to the observed immune response to the vaccine, Dr. Linette emphasized. “I would be speculating if I said the vaccine had any benefit to the patients,” he said.
Vaccination increased the frequency of most existing prevaccine T-cell receptor-beta (TCR-beta) clonotypes and revealed new clonotypes for 6 neoantigens.
For both dominant and subdominant neoantigens, the TCR-beta repertoire was increased significantly after vaccination. For example, 84 clonotypes representing 19 TCR-beta families were detected for TKT R438W, 61 clonotypes representing 12 TCR-beta families were detected for SEC24A P469L, and 12 clonotypes representing 8 TCR-beta families were detected for EXOC8 Q656P.
“The revelation of a highly diverse TCR-beta repertoire specific for dominant and subdominant neoantigens was surprising and points to a potentially rich pool of naive tumor-specific T cells that remain ignorant unless activated by vaccination,” the researchers wrote.
Recent data indicate that CTLA-4 monoclonal antibody use can alter TCR repertoire diversity in patients, suggesting a potential strategy of combination checkpoint inhibitors, including ipilimumab, and neoantigen vaccines. The novel vaccine strategy also could be used to treat other malignancies with high mutational burdens such as lung, bladder, and colorectal cancers, while other genomic alterations may generate potential neoantigens relevant in low–mutational burden cancers such as leukemia, the authors suggest.
Although the cells in this study were grown in a specialized laboratory, “as the technology improves, I think this [strategy] will become reproducible and available at other medical centers,” Dr. Linette said.
This work was supported by Barnes-Jewish Hospital Foundation, Siteman Cancer Frontier Fund, Our Mark on Melanoma (MOM) Foundation, Come Out Swinging (COS) Foundation, Blackout Melanoma Foundation and the National Cancer Institute.
Heidi Splete contributed to this story.
FROM SCIENCE
Key clinical point: Vaccination against patient-specific tumor neoantigens may represent a novel therapeutic strategy in melanoma and other malignancies.
Major finding: The vaccine enhanced T-cell immunity to naturally occurring neoantigens and revealed two additional neoantigens per patient.
Data source: Proof-of-principle study of three patients with resected, cutaneous melanoma.
Disclosures: This work was supported by Barnes-Jewish Hospital Foundation, Siteman Cancer Frontier Fund, Our Mark on Melanoma (MOM) Foundation, Come Out Swinging (COS) Foundation, Blackout Melanoma Foundation and the National Cancer Institute.
Advanced age no barrier to aggressive heart attack treatment
SAN DIEGO – Patients aged 80 years and older benefit from more invasive early treatment after non-ST-elevation myocardial infarction or unstable angina, the After Eighty Trial showed.
After a median follow-up of 1.5 years, an invasive strategy that included coronary angiography significantly reduced the primary endpoint of myocardial infarction (MI), need for urgent revascularization, stroke, and death from 61% with optimal medical treatment to 41% (risk ratio, 0.48; P value < .00001).
That drop was driven primarily by significantly fewer MIs (17% vs. 30%; RR, 0.50; P = .0003) and urgent revascularizations (2% vs. 11%; RR, 0.19; P = .0001), lead author Dr. Nicolai Tegn reported at the American College of Cardiology/Cardiovascular Research Foundation Innovation in Intervention Summit.
There were no significant differences between the invasive and conservative strategy groups in rates of stroke (3% vs. 6%; RR, 0.61; P = .26) or all-cause death (25% vs. 27%; RR, 0.87; P = .53).
The composite of death and MI, however, significantly favored the invasive group (35% vs. 48%; RR, 0.54; P < .0001), he said during a latebreaking clinical trial session.
After Eighty randomly assigned 457 patients, aged 80 years or older, to either optimal medical therapy with no invasive treatments or coronary angiography at a percutaneous coronary intervention (PCI) center the day after inclusion, plus optimal medical therapy after about 4-5 hours if PCI was not performed or about 6-18 hours if it was. Of the 225 patients receiving angiography, 48% went on to balloon angioplasty and/or coronary stenting, and 3% had bypass surgery.
Patients 80 years or older account for roughly one-third of all patients with non-STEMI and unstable angina, but they are underrepresented in clinical trials. As a result, the role of an early invasive strategy, and even an invasive strategy at all, in those elderly patients is still a subject of debate, observed Dr. Tegn, a cardiologist from Rikshospitalet, Oslo University Hospital, Oslo.
The study demonstrated that an invasive strategy is superior to a conservative strategy in patients at least 80 years with NSTEMI or unstable angina, he concluded.
After Eighty is a welcome study because of the under-representation of the elderly in clinical trials, Dr. David Kandzari, director of interventional cardiology at the Piedmont Heart Center in Atlanta, said during a press briefing at the meeting. But it raises the challenge of identifying patients in clinical practice with the same qualifying characteristics, he added, given that the study population represents only 10% of the entire screened population,
There was also a fairly high prevalence of patients who angiographically did not have significant coronary artery disease, yet MI and stroke rates were quite considerable.
That said, “the study in other ways reminds us that the coronary anatomy does not know the age of the patient, meaning that the findings of a benefit of an early invasive strategy seem consistent with previous studies we know across the management of patients with acute coronary syndromes,” Dr. Kandzari said.
After Eighty investigators screened 4,187 elderly patients presenting at 17 community hospitals in Norway with non-STEMI or unstable angina, with or without ST-segment depression in ECG, and normal or elevated troponin T or I levels. Patients had to have no chest pain or other ischemic symptoms after medical treatment and mobilization.
In all, 3,730 patients were excluded for life expectancy less than 12 months because of a serious comorbidity; ongoing or recent bleeding; inability to comply with protocol; clinically unstable including ongoing ischemia; refusal to participate; logistic reasons; or other reasons.
The average age was 84.7 years in the invasive group (range 80-93 years) and 84.9 years in the conservative group (range 80-94 years).
Medical treatment during the index admission included 75 mg aspirin in 97% of both the invasive and conservative groups, clopidogrel (85% vs. 82%), ticagrelor (both 5%), angiotensin-converting enzyme (ACE) inhibitor/angiotensin receptor blockers (ARB) (43% vs. 50%), beta blocker (83% vs. 85%), statins (90% vs. 85%), loop or thiazide diuretics (41% vs. 33%), calcium channel blocker (20% vs. 21%), nitrates (45% vs. 55%), warfarin (17% vs. 9%), low molecular-weight heparin (both 76% ), and dabigatran in one patient in each group.
Medical therapy at discharge in the invasive and conservative groups was aspirin (both 93%), clopidogrel (both 72%), ticagrelor (both 4%), ACE inhibitor/ARB (52% vs. 54%), beta blockers (both 84%), statins (90% vs. 86%), diuretics (45% vs. 38%), calcium channel blocker (24% vs. 23%), nitrates (34% vs. 48%), warfarin (21% vs. 14%), rivaroxaban (three patients in both groups), and dabigatran (one patient vs. six patients).
There were no differences in bleeding rates between the two groups, Dr. Tegn said. Four major bleeding events were reported in both groups, while 23 patients in the invasive group and 16 patients in the conservative group had minor bleeds.
The Norwegian Health Association sponsored the study. Dr. Tegn reported nothing to disclose. Dr. Kandazari reported research and grant support from Abbott Vascular, Biotronic, Boston Scientific, and Medtronic, and minor consulting honoraria from Boston Scientific and Medtronic.
SAN DIEGO – Patients aged 80 years and older benefit from more invasive early treatment after non-ST-elevation myocardial infarction or unstable angina, the After Eighty Trial showed.
After a median follow-up of 1.5 years, an invasive strategy that included coronary angiography significantly reduced the primary endpoint of myocardial infarction (MI), need for urgent revascularization, stroke, and death from 61% with optimal medical treatment to 41% (risk ratio, 0.48; P value < .00001).
That drop was driven primarily by significantly fewer MIs (17% vs. 30%; RR, 0.50; P = .0003) and urgent revascularizations (2% vs. 11%; RR, 0.19; P = .0001), lead author Dr. Nicolai Tegn reported at the American College of Cardiology/Cardiovascular Research Foundation Innovation in Intervention Summit.
There were no significant differences between the invasive and conservative strategy groups in rates of stroke (3% vs. 6%; RR, 0.61; P = .26) or all-cause death (25% vs. 27%; RR, 0.87; P = .53).
The composite of death and MI, however, significantly favored the invasive group (35% vs. 48%; RR, 0.54; P < .0001), he said during a latebreaking clinical trial session.
After Eighty randomly assigned 457 patients, aged 80 years or older, to either optimal medical therapy with no invasive treatments or coronary angiography at a percutaneous coronary intervention (PCI) center the day after inclusion, plus optimal medical therapy after about 4-5 hours if PCI was not performed or about 6-18 hours if it was. Of the 225 patients receiving angiography, 48% went on to balloon angioplasty and/or coronary stenting, and 3% had bypass surgery.
Patients 80 years or older account for roughly one-third of all patients with non-STEMI and unstable angina, but they are underrepresented in clinical trials. As a result, the role of an early invasive strategy, and even an invasive strategy at all, in those elderly patients is still a subject of debate, observed Dr. Tegn, a cardiologist from Rikshospitalet, Oslo University Hospital, Oslo.
The study demonstrated that an invasive strategy is superior to a conservative strategy in patients at least 80 years with NSTEMI or unstable angina, he concluded.
After Eighty is a welcome study because of the under-representation of the elderly in clinical trials, Dr. David Kandzari, director of interventional cardiology at the Piedmont Heart Center in Atlanta, said during a press briefing at the meeting. But it raises the challenge of identifying patients in clinical practice with the same qualifying characteristics, he added, given that the study population represents only 10% of the entire screened population,
There was also a fairly high prevalence of patients who angiographically did not have significant coronary artery disease, yet MI and stroke rates were quite considerable.
That said, “the study in other ways reminds us that the coronary anatomy does not know the age of the patient, meaning that the findings of a benefit of an early invasive strategy seem consistent with previous studies we know across the management of patients with acute coronary syndromes,” Dr. Kandzari said.
After Eighty investigators screened 4,187 elderly patients presenting at 17 community hospitals in Norway with non-STEMI or unstable angina, with or without ST-segment depression in ECG, and normal or elevated troponin T or I levels. Patients had to have no chest pain or other ischemic symptoms after medical treatment and mobilization.
In all, 3,730 patients were excluded for life expectancy less than 12 months because of a serious comorbidity; ongoing or recent bleeding; inability to comply with protocol; clinically unstable including ongoing ischemia; refusal to participate; logistic reasons; or other reasons.
The average age was 84.7 years in the invasive group (range 80-93 years) and 84.9 years in the conservative group (range 80-94 years).
Medical treatment during the index admission included 75 mg aspirin in 97% of both the invasive and conservative groups, clopidogrel (85% vs. 82%), ticagrelor (both 5%), angiotensin-converting enzyme (ACE) inhibitor/angiotensin receptor blockers (ARB) (43% vs. 50%), beta blocker (83% vs. 85%), statins (90% vs. 85%), loop or thiazide diuretics (41% vs. 33%), calcium channel blocker (20% vs. 21%), nitrates (45% vs. 55%), warfarin (17% vs. 9%), low molecular-weight heparin (both 76% ), and dabigatran in one patient in each group.
Medical therapy at discharge in the invasive and conservative groups was aspirin (both 93%), clopidogrel (both 72%), ticagrelor (both 4%), ACE inhibitor/ARB (52% vs. 54%), beta blockers (both 84%), statins (90% vs. 86%), diuretics (45% vs. 38%), calcium channel blocker (24% vs. 23%), nitrates (34% vs. 48%), warfarin (21% vs. 14%), rivaroxaban (three patients in both groups), and dabigatran (one patient vs. six patients).
There were no differences in bleeding rates between the two groups, Dr. Tegn said. Four major bleeding events were reported in both groups, while 23 patients in the invasive group and 16 patients in the conservative group had minor bleeds.
The Norwegian Health Association sponsored the study. Dr. Tegn reported nothing to disclose. Dr. Kandazari reported research and grant support from Abbott Vascular, Biotronic, Boston Scientific, and Medtronic, and minor consulting honoraria from Boston Scientific and Medtronic.
SAN DIEGO – Patients aged 80 years and older benefit from more invasive early treatment after non-ST-elevation myocardial infarction or unstable angina, the After Eighty Trial showed.
After a median follow-up of 1.5 years, an invasive strategy that included coronary angiography significantly reduced the primary endpoint of myocardial infarction (MI), need for urgent revascularization, stroke, and death from 61% with optimal medical treatment to 41% (risk ratio, 0.48; P value < .00001).
That drop was driven primarily by significantly fewer MIs (17% vs. 30%; RR, 0.50; P = .0003) and urgent revascularizations (2% vs. 11%; RR, 0.19; P = .0001), lead author Dr. Nicolai Tegn reported at the American College of Cardiology/Cardiovascular Research Foundation Innovation in Intervention Summit.
There were no significant differences between the invasive and conservative strategy groups in rates of stroke (3% vs. 6%; RR, 0.61; P = .26) or all-cause death (25% vs. 27%; RR, 0.87; P = .53).
The composite of death and MI, however, significantly favored the invasive group (35% vs. 48%; RR, 0.54; P < .0001), he said during a latebreaking clinical trial session.
After Eighty randomly assigned 457 patients, aged 80 years or older, to either optimal medical therapy with no invasive treatments or coronary angiography at a percutaneous coronary intervention (PCI) center the day after inclusion, plus optimal medical therapy after about 4-5 hours if PCI was not performed or about 6-18 hours if it was. Of the 225 patients receiving angiography, 48% went on to balloon angioplasty and/or coronary stenting, and 3% had bypass surgery.
Patients 80 years or older account for roughly one-third of all patients with non-STEMI and unstable angina, but they are underrepresented in clinical trials. As a result, the role of an early invasive strategy, and even an invasive strategy at all, in those elderly patients is still a subject of debate, observed Dr. Tegn, a cardiologist from Rikshospitalet, Oslo University Hospital, Oslo.
The study demonstrated that an invasive strategy is superior to a conservative strategy in patients at least 80 years with NSTEMI or unstable angina, he concluded.
After Eighty is a welcome study because of the under-representation of the elderly in clinical trials, Dr. David Kandzari, director of interventional cardiology at the Piedmont Heart Center in Atlanta, said during a press briefing at the meeting. But it raises the challenge of identifying patients in clinical practice with the same qualifying characteristics, he added, given that the study population represents only 10% of the entire screened population,
There was also a fairly high prevalence of patients who angiographically did not have significant coronary artery disease, yet MI and stroke rates were quite considerable.
That said, “the study in other ways reminds us that the coronary anatomy does not know the age of the patient, meaning that the findings of a benefit of an early invasive strategy seem consistent with previous studies we know across the management of patients with acute coronary syndromes,” Dr. Kandzari said.
After Eighty investigators screened 4,187 elderly patients presenting at 17 community hospitals in Norway with non-STEMI or unstable angina, with or without ST-segment depression in ECG, and normal or elevated troponin T or I levels. Patients had to have no chest pain or other ischemic symptoms after medical treatment and mobilization.
In all, 3,730 patients were excluded for life expectancy less than 12 months because of a serious comorbidity; ongoing or recent bleeding; inability to comply with protocol; clinically unstable including ongoing ischemia; refusal to participate; logistic reasons; or other reasons.
The average age was 84.7 years in the invasive group (range 80-93 years) and 84.9 years in the conservative group (range 80-94 years).
Medical treatment during the index admission included 75 mg aspirin in 97% of both the invasive and conservative groups, clopidogrel (85% vs. 82%), ticagrelor (both 5%), angiotensin-converting enzyme (ACE) inhibitor/angiotensin receptor blockers (ARB) (43% vs. 50%), beta blocker (83% vs. 85%), statins (90% vs. 85%), loop or thiazide diuretics (41% vs. 33%), calcium channel blocker (20% vs. 21%), nitrates (45% vs. 55%), warfarin (17% vs. 9%), low molecular-weight heparin (both 76% ), and dabigatran in one patient in each group.
Medical therapy at discharge in the invasive and conservative groups was aspirin (both 93%), clopidogrel (both 72%), ticagrelor (both 4%), ACE inhibitor/ARB (52% vs. 54%), beta blockers (both 84%), statins (90% vs. 86%), diuretics (45% vs. 38%), calcium channel blocker (24% vs. 23%), nitrates (34% vs. 48%), warfarin (21% vs. 14%), rivaroxaban (three patients in both groups), and dabigatran (one patient vs. six patients).
There were no differences in bleeding rates between the two groups, Dr. Tegn said. Four major bleeding events were reported in both groups, while 23 patients in the invasive group and 16 patients in the conservative group had minor bleeds.
The Norwegian Health Association sponsored the study. Dr. Tegn reported nothing to disclose. Dr. Kandazari reported research and grant support from Abbott Vascular, Biotronic, Boston Scientific, and Medtronic, and minor consulting honoraria from Boston Scientific and Medtronic.
AT ACC/CRF i2 SUMMIT
Key clinical point: An early invasive treatment strategy improved most outcomes in patients aged 80 years and older with acute coronary syndromes.
Major finding: Myocardial infarction, need for urgent revascularization, stroke, and death were significantly lower with invasive vs. conservative care (41% vs. 61%; risk ratio, 0.48; P < .00001).
Data source: Randomized study in 457 patients aged 80 years or older with non-STEMI or unstable angina.
Disclosures: The Norwegian Health Association sponsored the study. Dr. Tegn reported nothing to disclose. Dr. Kandzari reported research and grant support from Abbott Vascular, Biotronic, Boston Scientific, and Medtronic, and minor consulting honoraria from Boston Scientific and Medtronic.
Mesenteric stenting: an evolving therapy
CHICAGO – Mesenteric stenting has replaced open surgery as first-line treatment for chronic mesenteric ischemia, but it is still a therapy in flux.
Controversy exists over single- versus multivessel revascularization when both the celiac artery (CA) and superior mesenteric artery (SMA) are diseased and symptoms are consistent with chronic mesenteric ischemia (CMI), Dr. Jean Panneton said at a symposium on vascular surgery sponsored by Northwestern University.
Some vascular specialists argue that complete revascularization provides better protection when one vessel occludes, while those favoring single-vessel revascularization contend that bypassing only the most problematic vessel avoids a longer, more complex operation in these typically fragile patients.
The data on single- versus multivessel mesenteric bypass is mixed, he said. Some studies have found that two-vessel bypass results in less symptom recurrence, improved patency, and fewer reinterventions than single-vessel bypass. Other studies, however, have found no difference in 1-year patency or freedom from symptom recurrence between the two treatments.
Regardless of the number of vessels treated, no consensus exists as to which artery responds best to stenting, Dr. Panneton, from Eastern Virginia Medical School in Norfolk, said. In their own review of 121 consecutive patients over a 7-year period, there was a major discrepancy between SMA and CA stenting in 1-year primary patency (55% vs. 18%) and 6-month clinical patency (86% vs. 67%).
“In our experience, celiac stenting had much worse ISR [in-stent restenosis] and clinical patency rates than SMA stenting, which questions its utility,” he said.
In the celiac group, stents with a diameter < 6 mm were significantly more likely than larger-caliber stents to lose primary patency, defined as peak systolic velocity < 350 cm/sec.
Interestingly, a subset analysis of patients undergoing two-vessel stenting of the CA and SMA revealed no significant differences in ISR rates or survival free from symptom recurrence, compared with single SMA stenting (J. Vasc. Surg. 2013;57:1062-6).
Surveillance after mesenteric stenting is another area in flux. Duplex ultrasound (DUS) has been validated as an accurate modality for determining native mesenteric artery stenosis, but no firm DUS criteria exist for diagnosing ISR, Dr. Panneton said. Several studies have reported that DUS velocity criteria for native mesenteric stenosis overestimates the percentage of stenosis of stented arteries.
A receiver operator curve (ROC) analysis by Dr. Panneton and his colleagues demonstrated that an SMA peak systolic velocity (PSV) of 445 cm/sec had the highest sensitivity (96%), but only 43% specificity for predicting ISR.
Further prospective validation is needed, although a similar ROC analysis reported 100% sensitivity and 95% sensitivity using a PSV of 412 cm/sec to identify SMA > 70% ISR (J. Vasc. Surg. 2012;55:730-8), he noted.
Intravascular ultrasound (IVUS) is useful as an adjunct to DUS and angiography for the detection of ISR of mesenteric arteries, but isn’t practical for routine surveillance. There is also a dearth of data on outcomes when IVUS is used with other imaging modalities, Dr. Panneton added.
What is clear is that a paradigm shift has occurred in the treatment of CMI, reflected in a threefold increase in the number of mesenteric revascularizations performed in the U.S. during the last 10 years. Still, 5-year survival rates are nearly identical between open surgery and mesenteric stenting, despite primary, secondary, and clinical patency rates seeming to favor open mesenteric bypass.
“Future technology will address the higher ISR and reintervention rates associated with mesenteric stenting and likely improve outcomes,” Dr. Panneton said.
Mesenteric stenting can still be useful, even after bypass, he said, highlighting a 78-year-old woman with a history of aortobifemoral bypass who required endovascular rescue of an SMA graft thrombosis after presenting with acute mesenteric ischemia.
“We were able with a guidewire, to get through the reversed C-loop graft that came from the iliac to the SMA and get into the distal SMA vessel,” he said. “We also used pharmacomechanical thrombectomy to really declot the graft and place a stent at the proximal anastomosis of the iliac-SMA Dacron graft.”
The team has also done mesenteric stenting using a retrograde open mesenteric stenting technique.
“It’s quite useful in acute mesenteric ischemia, but we’ve also used it more recently even in chronic mesenteric ischemia for patients who did not tolerate aortic cross-clamping or did not have any good aorta,” he said. “An example of that would be a porcelain aorta where we don’t want to clamp anything.”
Dr. Panneton is a consultant and serves on the speaker’s bureau for Medtronic.
CHICAGO – Mesenteric stenting has replaced open surgery as first-line treatment for chronic mesenteric ischemia, but it is still a therapy in flux.
Controversy exists over single- versus multivessel revascularization when both the celiac artery (CA) and superior mesenteric artery (SMA) are diseased and symptoms are consistent with chronic mesenteric ischemia (CMI), Dr. Jean Panneton said at a symposium on vascular surgery sponsored by Northwestern University.
Some vascular specialists argue that complete revascularization provides better protection when one vessel occludes, while those favoring single-vessel revascularization contend that bypassing only the most problematic vessel avoids a longer, more complex operation in these typically fragile patients.
The data on single- versus multivessel mesenteric bypass is mixed, he said. Some studies have found that two-vessel bypass results in less symptom recurrence, improved patency, and fewer reinterventions than single-vessel bypass. Other studies, however, have found no difference in 1-year patency or freedom from symptom recurrence between the two treatments.
Regardless of the number of vessels treated, no consensus exists as to which artery responds best to stenting, Dr. Panneton, from Eastern Virginia Medical School in Norfolk, said. In their own review of 121 consecutive patients over a 7-year period, there was a major discrepancy between SMA and CA stenting in 1-year primary patency (55% vs. 18%) and 6-month clinical patency (86% vs. 67%).
“In our experience, celiac stenting had much worse ISR [in-stent restenosis] and clinical patency rates than SMA stenting, which questions its utility,” he said.
In the celiac group, stents with a diameter < 6 mm were significantly more likely than larger-caliber stents to lose primary patency, defined as peak systolic velocity < 350 cm/sec.
Interestingly, a subset analysis of patients undergoing two-vessel stenting of the CA and SMA revealed no significant differences in ISR rates or survival free from symptom recurrence, compared with single SMA stenting (J. Vasc. Surg. 2013;57:1062-6).
Surveillance after mesenteric stenting is another area in flux. Duplex ultrasound (DUS) has been validated as an accurate modality for determining native mesenteric artery stenosis, but no firm DUS criteria exist for diagnosing ISR, Dr. Panneton said. Several studies have reported that DUS velocity criteria for native mesenteric stenosis overestimates the percentage of stenosis of stented arteries.
A receiver operator curve (ROC) analysis by Dr. Panneton and his colleagues demonstrated that an SMA peak systolic velocity (PSV) of 445 cm/sec had the highest sensitivity (96%), but only 43% specificity for predicting ISR.
Further prospective validation is needed, although a similar ROC analysis reported 100% sensitivity and 95% sensitivity using a PSV of 412 cm/sec to identify SMA > 70% ISR (J. Vasc. Surg. 2012;55:730-8), he noted.
Intravascular ultrasound (IVUS) is useful as an adjunct to DUS and angiography for the detection of ISR of mesenteric arteries, but isn’t practical for routine surveillance. There is also a dearth of data on outcomes when IVUS is used with other imaging modalities, Dr. Panneton added.
What is clear is that a paradigm shift has occurred in the treatment of CMI, reflected in a threefold increase in the number of mesenteric revascularizations performed in the U.S. during the last 10 years. Still, 5-year survival rates are nearly identical between open surgery and mesenteric stenting, despite primary, secondary, and clinical patency rates seeming to favor open mesenteric bypass.
“Future technology will address the higher ISR and reintervention rates associated with mesenteric stenting and likely improve outcomes,” Dr. Panneton said.
Mesenteric stenting can still be useful, even after bypass, he said, highlighting a 78-year-old woman with a history of aortobifemoral bypass who required endovascular rescue of an SMA graft thrombosis after presenting with acute mesenteric ischemia.
“We were able with a guidewire, to get through the reversed C-loop graft that came from the iliac to the SMA and get into the distal SMA vessel,” he said. “We also used pharmacomechanical thrombectomy to really declot the graft and place a stent at the proximal anastomosis of the iliac-SMA Dacron graft.”
The team has also done mesenteric stenting using a retrograde open mesenteric stenting technique.
“It’s quite useful in acute mesenteric ischemia, but we’ve also used it more recently even in chronic mesenteric ischemia for patients who did not tolerate aortic cross-clamping or did not have any good aorta,” he said. “An example of that would be a porcelain aorta where we don’t want to clamp anything.”
Dr. Panneton is a consultant and serves on the speaker’s bureau for Medtronic.
CHICAGO – Mesenteric stenting has replaced open surgery as first-line treatment for chronic mesenteric ischemia, but it is still a therapy in flux.
Controversy exists over single- versus multivessel revascularization when both the celiac artery (CA) and superior mesenteric artery (SMA) are diseased and symptoms are consistent with chronic mesenteric ischemia (CMI), Dr. Jean Panneton said at a symposium on vascular surgery sponsored by Northwestern University.
Some vascular specialists argue that complete revascularization provides better protection when one vessel occludes, while those favoring single-vessel revascularization contend that bypassing only the most problematic vessel avoids a longer, more complex operation in these typically fragile patients.
The data on single- versus multivessel mesenteric bypass is mixed, he said. Some studies have found that two-vessel bypass results in less symptom recurrence, improved patency, and fewer reinterventions than single-vessel bypass. Other studies, however, have found no difference in 1-year patency or freedom from symptom recurrence between the two treatments.
Regardless of the number of vessels treated, no consensus exists as to which artery responds best to stenting, Dr. Panneton, from Eastern Virginia Medical School in Norfolk, said. In their own review of 121 consecutive patients over a 7-year period, there was a major discrepancy between SMA and CA stenting in 1-year primary patency (55% vs. 18%) and 6-month clinical patency (86% vs. 67%).
“In our experience, celiac stenting had much worse ISR [in-stent restenosis] and clinical patency rates than SMA stenting, which questions its utility,” he said.
In the celiac group, stents with a diameter < 6 mm were significantly more likely than larger-caliber stents to lose primary patency, defined as peak systolic velocity < 350 cm/sec.
Interestingly, a subset analysis of patients undergoing two-vessel stenting of the CA and SMA revealed no significant differences in ISR rates or survival free from symptom recurrence, compared with single SMA stenting (J. Vasc. Surg. 2013;57:1062-6).
Surveillance after mesenteric stenting is another area in flux. Duplex ultrasound (DUS) has been validated as an accurate modality for determining native mesenteric artery stenosis, but no firm DUS criteria exist for diagnosing ISR, Dr. Panneton said. Several studies have reported that DUS velocity criteria for native mesenteric stenosis overestimates the percentage of stenosis of stented arteries.
A receiver operator curve (ROC) analysis by Dr. Panneton and his colleagues demonstrated that an SMA peak systolic velocity (PSV) of 445 cm/sec had the highest sensitivity (96%), but only 43% specificity for predicting ISR.
Further prospective validation is needed, although a similar ROC analysis reported 100% sensitivity and 95% sensitivity using a PSV of 412 cm/sec to identify SMA > 70% ISR (J. Vasc. Surg. 2012;55:730-8), he noted.
Intravascular ultrasound (IVUS) is useful as an adjunct to DUS and angiography for the detection of ISR of mesenteric arteries, but isn’t practical for routine surveillance. There is also a dearth of data on outcomes when IVUS is used with other imaging modalities, Dr. Panneton added.
What is clear is that a paradigm shift has occurred in the treatment of CMI, reflected in a threefold increase in the number of mesenteric revascularizations performed in the U.S. during the last 10 years. Still, 5-year survival rates are nearly identical between open surgery and mesenteric stenting, despite primary, secondary, and clinical patency rates seeming to favor open mesenteric bypass.
“Future technology will address the higher ISR and reintervention rates associated with mesenteric stenting and likely improve outcomes,” Dr. Panneton said.
Mesenteric stenting can still be useful, even after bypass, he said, highlighting a 78-year-old woman with a history of aortobifemoral bypass who required endovascular rescue of an SMA graft thrombosis after presenting with acute mesenteric ischemia.
“We were able with a guidewire, to get through the reversed C-loop graft that came from the iliac to the SMA and get into the distal SMA vessel,” he said. “We also used pharmacomechanical thrombectomy to really declot the graft and place a stent at the proximal anastomosis of the iliac-SMA Dacron graft.”
The team has also done mesenteric stenting using a retrograde open mesenteric stenting technique.
“It’s quite useful in acute mesenteric ischemia, but we’ve also used it more recently even in chronic mesenteric ischemia for patients who did not tolerate aortic cross-clamping or did not have any good aorta,” he said. “An example of that would be a porcelain aorta where we don’t want to clamp anything.”
Dr. Panneton is a consultant and serves on the speaker’s bureau for Medtronic.
EXPERT ANALYSIS FROM THE NORTHWESTERN VASCULAR SYMPOSIUM
Private-academic surgeon salary gap raises concerns Lifestyle choice important Not just the money
LAKE BUENA VISTA, FLA. – Academic surgeons earn an average of 10% or $1.3 million less in gross income across their lifetime than surgeons in private practice, an analysis shows.
Some surgical specialties fare better than others, with academic neurosurgeons having the largest reduction in gross income at $4.2 million (–24.2%), while academic pediatric surgeons earn $238,376 more (1.53%) than their private practice counterparts. They were the only ones to do so.
Several academic surgical specialties did not make the 10% average, including trauma surgeons whose lifetime earnings were down 12% or $2.4 million, vascular surgeons at 13.8% or $1.7 million, and surgical oncologists at 12.2% or $1.3 million.
“The concern that we have is that the academic surgeons are where the education of the future lies,” lead study author Dr. Joseph Martin Lopez said at the annual scientific assembly of the Eastern Association for the Surgery of Trauma (EAST).
Every year a new class of surgeons is faced with the question of academic practice or private practice, but they are also struggling with increasing student loan debt and longer training as more surgical residents elect to enter fellowship rather than general practice.
This growing financial liability coupled with declining physician reimbursement could rapidly shift physician practices and thus threaten the fiscal viability of certain surgical fields or academic surgical careers.
“The more financially irresponsible you make it to become an academic surgeon, the more we put at risk our current mode of training,” Dr. Lopez of Wake Forest University in Winston-Salem, N.C., said.
To account for additional factors outside gross income, the investigators ran the numbers using a second analysis, a net present value calculation, however, and came up with roughly the same salary gap to contend with.
Net present value (NPV) calculations are commonly used in business to calculate the profitability of an investment and also have been used in the medical field to gauge return on investment for various careers. The NPV calculation accounts for positive and negative cash flows over the entire length of a career, using in this case, a 5% discount rate and adjusting for inflation, Dr. Lopez explained.
Both the lifetime gross income and 5% NPV calculation used data from the Medical Group Management Association’s 2012 physician salary report, the 2012 Association of American Medical Colleges physician salary report, and the AAMC database for residency and fellow salary.
The NPV assumed a career length of 37-39 years, based on a retirement age of 65 years for all specialties. Positive cash flows included annual salary less federal income tax. Negative cash flows included the average principal for student loans, according to the AAMC, and interest at 5%, the average for the three largest student loan lenders in 2014, he said. Student loan repayment was calculated for a fixed-rate loan to be paid over 25 years beginning after residency or any required fellowship.
The average reduction in 5% NPV across surgical specialties for an academic surgeon versus a privately employed surgeon was 12.8% or $246,499, Dr. Lopez said.
Once again, academic neurosurgeons had the largest reduction in 5% NPV at 25.5% or a loss of $619,681, followed closely by trauma surgeons (23% or $381,179) and surgical oncologists (16.3% or $256,373). Academic pediatric surgeons had the smallest reduction in 5% NPV at 4.2% or $88,827.
During a discussion of the provocative poster, attendees questioned whether it was fair to say that private surgeons make more money without acknowledging the risk they face, compared with surgeons employed in an academic setting.
Dr. Lopez countered that, increasingly, even private surgeons are no longer truly private surgeons.
“More and more surgical groups are being bought up by hospitals, and even the private surgical groups are being bought up by hospitals, which does stabilize your income to some extent,” he said.
“We all still have [relative value unit] goals to meet and RVU incentives that make it so you can get paid a little more, but it’s something that’s a consideration. It is a risk-reward to be a private surgeon. Depending on how your contract is structured or how your group decides to pay the partners, it may be that if you don’t take very much call or take that many cases, you’ll end up on the short end of the stick.”
Dr. Ben L. Zarzaur, a general surgeon at Indiana University in Indianapolis who comoderated the poster discussion, pointed out that market pressures unaccounted for in the model can dramatically influence a surgeon’s salary over a lifetime.
Dr. Lopez agreed, citing how the increasing number of stent placements by cardiologists, for example, has impacted the bottom line of cardiothoracic surgeons. The NPV calculation was specifically used, however, because it gets at market forces such as inflation and return on investment, not addressed by gross income figures alone.
Finally, Dr. Zarzaur turned and asked the relatively young crowd what they would do if offered $600,000 a year, but had to work 110 hours a week or could get $250,000 and work only 40 hours a week.
Most responded that they’d choose the former to repay their student loans and then switch to the lower-paying position.
Responders made much of job satisfaction, work-life balance, and the ability of surgeons in academic practice to take time away from clinical work to conduct research, their ready access to continuing medical education, and their ability to educate the next generation of surgeons.
“Any time we see this academic-private disparity, you have to think about these secondary gains,” Dr. Zarzaur said.
“This is really interesting work. It gets into why we choose what we do, why we’d take $600,000, work 110 hours a week, and get our rear ends kicked. The flip side is, if I saw this, why would you ever go into academics? But people still choose to do it. I’m in academics so there’s a bias, but we choose to do it anyway up to a point. I don’t know where that point is, but up to a point we do.”
Not just the money

|
| Dr. Laura Drudi |
In the United States, academic vascular surgeons earn 13.8% or $1.7 million less than private vascular surgeons. This financial incentive may influence graduating residents and fellows to enter into private practice. This article indicates that this financial disparity may cost academic institutions the expertise needed to train future physicians. Unfortunately, I believe this analysis falls into one of the many myths between academic and private practice; that is, it’s not only about making the most money possible.
The ongoing debate of academic versus private practice shouldn’t really be a debate at all. It is all about personal choices concerning research, education, work-life balance, and finances to name a few. In the end, anyone can shape the ideal practice they want to have. There are many private practices that are involved in resident education, publish extensively and present at national and international meetings. No job is weaved perfectly, but there will usually be a job that fits an individual’s specific goals and desires.
Dr. Laura Drudi is the resident medical editor for Vascular Specialist.
Lifestyle choice important
The basic finding of the disparity is in fact true leaving aside the flawed methodology of too many assumptions by including all academic ranks, practitioners of different durations in practice, difference in benefits, tuition assistance, and assuming student loans for all surgeons plus a risk free rate that is too high.
Our analysis of both vascular and general surgeon compensation points to a larger disparity at junior academic ranks over the last decade. With our own studies showing a shortage of vascular surgeons, retention of practitioners is paramount for all health systems. Academic centers rely on faculty giving up a percentage of their compensation for the pleasure of teaching, research and intellectual stimulation. The unanswered question is: How much of a disparity will junior academic surgeons tolerate, and how do they value lifestyle against additional compensation? Time will tell.
Dr. Bhagwan Satiani is a professor of vascular surgery at the Wexner Medical Center, Ohio State University.
Not just the money

|
| Dr. Laura Drudi |
In the United States, academic vascular surgeons earn 13.8% or $1.7 million less than private vascular surgeons. This financial incentive may influence graduating residents and fellows to enter into private practice. This article indicates that this financial disparity may cost academic institutions the expertise needed to train future physicians. Unfortunately, I believe this analysis falls into one of the many myths between academic and private practice; that is, it’s not only about making the most money possible.
The ongoing debate of academic versus private practice shouldn’t really be a debate at all. It is all about personal choices concerning research, education, work-life balance, and finances to name a few. In the end, anyone can shape the ideal practice they want to have. There are many private practices that are involved in resident education, publish extensively and present at national and international meetings. No job is weaved perfectly, but there will usually be a job that fits an individual’s specific goals and desires.
Dr. Laura Drudi is the resident medical editor for Vascular Specialist.
Lifestyle choice important
The basic finding of the disparity is in fact true leaving aside the flawed methodology of too many assumptions by including all academic ranks, practitioners of different durations in practice, difference in benefits, tuition assistance, and assuming student loans for all surgeons plus a risk free rate that is too high.
Our analysis of both vascular and general surgeon compensation points to a larger disparity at junior academic ranks over the last decade. With our own studies showing a shortage of vascular surgeons, retention of practitioners is paramount for all health systems. Academic centers rely on faculty giving up a percentage of their compensation for the pleasure of teaching, research and intellectual stimulation. The unanswered question is: How much of a disparity will junior academic surgeons tolerate, and how do they value lifestyle against additional compensation? Time will tell.
Dr. Bhagwan Satiani is a professor of vascular surgery at the Wexner Medical Center, Ohio State University.
Not just the money

|
| Dr. Laura Drudi |
In the United States, academic vascular surgeons earn 13.8% or $1.7 million less than private vascular surgeons. This financial incentive may influence graduating residents and fellows to enter into private practice. This article indicates that this financial disparity may cost academic institutions the expertise needed to train future physicians. Unfortunately, I believe this analysis falls into one of the many myths between academic and private practice; that is, it’s not only about making the most money possible.
The ongoing debate of academic versus private practice shouldn’t really be a debate at all. It is all about personal choices concerning research, education, work-life balance, and finances to name a few. In the end, anyone can shape the ideal practice they want to have. There are many private practices that are involved in resident education, publish extensively and present at national and international meetings. No job is weaved perfectly, but there will usually be a job that fits an individual’s specific goals and desires.
Dr. Laura Drudi is the resident medical editor for Vascular Specialist.
Lifestyle choice important
The basic finding of the disparity is in fact true leaving aside the flawed methodology of too many assumptions by including all academic ranks, practitioners of different durations in practice, difference in benefits, tuition assistance, and assuming student loans for all surgeons plus a risk free rate that is too high.
Our analysis of both vascular and general surgeon compensation points to a larger disparity at junior academic ranks over the last decade. With our own studies showing a shortage of vascular surgeons, retention of practitioners is paramount for all health systems. Academic centers rely on faculty giving up a percentage of their compensation for the pleasure of teaching, research and intellectual stimulation. The unanswered question is: How much of a disparity will junior academic surgeons tolerate, and how do they value lifestyle against additional compensation? Time will tell.
Dr. Bhagwan Satiani is a professor of vascular surgery at the Wexner Medical Center, Ohio State University.
LAKE BUENA VISTA, FLA. – Academic surgeons earn an average of 10% or $1.3 million less in gross income across their lifetime than surgeons in private practice, an analysis shows.
Some surgical specialties fare better than others, with academic neurosurgeons having the largest reduction in gross income at $4.2 million (–24.2%), while academic pediatric surgeons earn $238,376 more (1.53%) than their private practice counterparts. They were the only ones to do so.
Several academic surgical specialties did not make the 10% average, including trauma surgeons whose lifetime earnings were down 12% or $2.4 million, vascular surgeons at 13.8% or $1.7 million, and surgical oncologists at 12.2% or $1.3 million.
“The concern that we have is that the academic surgeons are where the education of the future lies,” lead study author Dr. Joseph Martin Lopez said at the annual scientific assembly of the Eastern Association for the Surgery of Trauma (EAST).
Every year a new class of surgeons is faced with the question of academic practice or private practice, but they are also struggling with increasing student loan debt and longer training as more surgical residents elect to enter fellowship rather than general practice.
This growing financial liability coupled with declining physician reimbursement could rapidly shift physician practices and thus threaten the fiscal viability of certain surgical fields or academic surgical careers.
“The more financially irresponsible you make it to become an academic surgeon, the more we put at risk our current mode of training,” Dr. Lopez of Wake Forest University in Winston-Salem, N.C., said.
To account for additional factors outside gross income, the investigators ran the numbers using a second analysis, a net present value calculation, however, and came up with roughly the same salary gap to contend with.
Net present value (NPV) calculations are commonly used in business to calculate the profitability of an investment and also have been used in the medical field to gauge return on investment for various careers. The NPV calculation accounts for positive and negative cash flows over the entire length of a career, using in this case, a 5% discount rate and adjusting for inflation, Dr. Lopez explained.
Both the lifetime gross income and 5% NPV calculation used data from the Medical Group Management Association’s 2012 physician salary report, the 2012 Association of American Medical Colleges physician salary report, and the AAMC database for residency and fellow salary.
The NPV assumed a career length of 37-39 years, based on a retirement age of 65 years for all specialties. Positive cash flows included annual salary less federal income tax. Negative cash flows included the average principal for student loans, according to the AAMC, and interest at 5%, the average for the three largest student loan lenders in 2014, he said. Student loan repayment was calculated for a fixed-rate loan to be paid over 25 years beginning after residency or any required fellowship.
The average reduction in 5% NPV across surgical specialties for an academic surgeon versus a privately employed surgeon was 12.8% or $246,499, Dr. Lopez said.
Once again, academic neurosurgeons had the largest reduction in 5% NPV at 25.5% or a loss of $619,681, followed closely by trauma surgeons (23% or $381,179) and surgical oncologists (16.3% or $256,373). Academic pediatric surgeons had the smallest reduction in 5% NPV at 4.2% or $88,827.
During a discussion of the provocative poster, attendees questioned whether it was fair to say that private surgeons make more money without acknowledging the risk they face, compared with surgeons employed in an academic setting.
Dr. Lopez countered that, increasingly, even private surgeons are no longer truly private surgeons.
“More and more surgical groups are being bought up by hospitals, and even the private surgical groups are being bought up by hospitals, which does stabilize your income to some extent,” he said.
“We all still have [relative value unit] goals to meet and RVU incentives that make it so you can get paid a little more, but it’s something that’s a consideration. It is a risk-reward to be a private surgeon. Depending on how your contract is structured or how your group decides to pay the partners, it may be that if you don’t take very much call or take that many cases, you’ll end up on the short end of the stick.”
Dr. Ben L. Zarzaur, a general surgeon at Indiana University in Indianapolis who comoderated the poster discussion, pointed out that market pressures unaccounted for in the model can dramatically influence a surgeon’s salary over a lifetime.
Dr. Lopez agreed, citing how the increasing number of stent placements by cardiologists, for example, has impacted the bottom line of cardiothoracic surgeons. The NPV calculation was specifically used, however, because it gets at market forces such as inflation and return on investment, not addressed by gross income figures alone.
Finally, Dr. Zarzaur turned and asked the relatively young crowd what they would do if offered $600,000 a year, but had to work 110 hours a week or could get $250,000 and work only 40 hours a week.
Most responded that they’d choose the former to repay their student loans and then switch to the lower-paying position.
Responders made much of job satisfaction, work-life balance, and the ability of surgeons in academic practice to take time away from clinical work to conduct research, their ready access to continuing medical education, and their ability to educate the next generation of surgeons.
“Any time we see this academic-private disparity, you have to think about these secondary gains,” Dr. Zarzaur said.
“This is really interesting work. It gets into why we choose what we do, why we’d take $600,000, work 110 hours a week, and get our rear ends kicked. The flip side is, if I saw this, why would you ever go into academics? But people still choose to do it. I’m in academics so there’s a bias, but we choose to do it anyway up to a point. I don’t know where that point is, but up to a point we do.”
LAKE BUENA VISTA, FLA. – Academic surgeons earn an average of 10% or $1.3 million less in gross income across their lifetime than surgeons in private practice, an analysis shows.
Some surgical specialties fare better than others, with academic neurosurgeons having the largest reduction in gross income at $4.2 million (–24.2%), while academic pediatric surgeons earn $238,376 more (1.53%) than their private practice counterparts. They were the only ones to do so.
Several academic surgical specialties did not make the 10% average, including trauma surgeons whose lifetime earnings were down 12% or $2.4 million, vascular surgeons at 13.8% or $1.7 million, and surgical oncologists at 12.2% or $1.3 million.
“The concern that we have is that the academic surgeons are where the education of the future lies,” lead study author Dr. Joseph Martin Lopez said at the annual scientific assembly of the Eastern Association for the Surgery of Trauma (EAST).
Every year a new class of surgeons is faced with the question of academic practice or private practice, but they are also struggling with increasing student loan debt and longer training as more surgical residents elect to enter fellowship rather than general practice.
This growing financial liability coupled with declining physician reimbursement could rapidly shift physician practices and thus threaten the fiscal viability of certain surgical fields or academic surgical careers.
“The more financially irresponsible you make it to become an academic surgeon, the more we put at risk our current mode of training,” Dr. Lopez of Wake Forest University in Winston-Salem, N.C., said.
To account for additional factors outside gross income, the investigators ran the numbers using a second analysis, a net present value calculation, however, and came up with roughly the same salary gap to contend with.
Net present value (NPV) calculations are commonly used in business to calculate the profitability of an investment and also have been used in the medical field to gauge return on investment for various careers. The NPV calculation accounts for positive and negative cash flows over the entire length of a career, using in this case, a 5% discount rate and adjusting for inflation, Dr. Lopez explained.
Both the lifetime gross income and 5% NPV calculation used data from the Medical Group Management Association’s 2012 physician salary report, the 2012 Association of American Medical Colleges physician salary report, and the AAMC database for residency and fellow salary.
The NPV assumed a career length of 37-39 years, based on a retirement age of 65 years for all specialties. Positive cash flows included annual salary less federal income tax. Negative cash flows included the average principal for student loans, according to the AAMC, and interest at 5%, the average for the three largest student loan lenders in 2014, he said. Student loan repayment was calculated for a fixed-rate loan to be paid over 25 years beginning after residency or any required fellowship.
The average reduction in 5% NPV across surgical specialties for an academic surgeon versus a privately employed surgeon was 12.8% or $246,499, Dr. Lopez said.
Once again, academic neurosurgeons had the largest reduction in 5% NPV at 25.5% or a loss of $619,681, followed closely by trauma surgeons (23% or $381,179) and surgical oncologists (16.3% or $256,373). Academic pediatric surgeons had the smallest reduction in 5% NPV at 4.2% or $88,827.
During a discussion of the provocative poster, attendees questioned whether it was fair to say that private surgeons make more money without acknowledging the risk they face, compared with surgeons employed in an academic setting.
Dr. Lopez countered that, increasingly, even private surgeons are no longer truly private surgeons.
“More and more surgical groups are being bought up by hospitals, and even the private surgical groups are being bought up by hospitals, which does stabilize your income to some extent,” he said.
“We all still have [relative value unit] goals to meet and RVU incentives that make it so you can get paid a little more, but it’s something that’s a consideration. It is a risk-reward to be a private surgeon. Depending on how your contract is structured or how your group decides to pay the partners, it may be that if you don’t take very much call or take that many cases, you’ll end up on the short end of the stick.”
Dr. Ben L. Zarzaur, a general surgeon at Indiana University in Indianapolis who comoderated the poster discussion, pointed out that market pressures unaccounted for in the model can dramatically influence a surgeon’s salary over a lifetime.
Dr. Lopez agreed, citing how the increasing number of stent placements by cardiologists, for example, has impacted the bottom line of cardiothoracic surgeons. The NPV calculation was specifically used, however, because it gets at market forces such as inflation and return on investment, not addressed by gross income figures alone.
Finally, Dr. Zarzaur turned and asked the relatively young crowd what they would do if offered $600,000 a year, but had to work 110 hours a week or could get $250,000 and work only 40 hours a week.
Most responded that they’d choose the former to repay their student loans and then switch to the lower-paying position.
Responders made much of job satisfaction, work-life balance, and the ability of surgeons in academic practice to take time away from clinical work to conduct research, their ready access to continuing medical education, and their ability to educate the next generation of surgeons.
“Any time we see this academic-private disparity, you have to think about these secondary gains,” Dr. Zarzaur said.
“This is really interesting work. It gets into why we choose what we do, why we’d take $600,000, work 110 hours a week, and get our rear ends kicked. The flip side is, if I saw this, why would you ever go into academics? But people still choose to do it. I’m in academics so there’s a bias, but we choose to do it anyway up to a point. I don’t know where that point is, but up to a point we do.”
HALS and LAP colectomy each offer unique benefits
CHICAGO – A nationwide analysis comparing straight versus hand-assisted laparoscopic colectomy appears to have resulted in a draw.
Despite being used more commonly in patients with higher body mass index and comorbidities, hand-assisted laparoscopic surgery (HALS) resulted in a significantly shorter operative time than did straight laparoscopic surgery (LAP) (171 minutes vs. 178.8 minutes; P < .001).
On the other hand, LAP was associated with a significantly shorter length of stay (5.9 days vs. 6.0 days; P < .001), fewer complications (15.9% vs. 18.2%; P = .006), fewer specifically superficial skin infections (4.1% vs. 5.4%; P = .007), and less prolonged postoperative ileus (7.5% vs. 9.1%; P = .01).
The differences were statistically significant likely because of the high volume of patients in each group, but are unlikely to be clinically significant in terms of patient care, senior study author Dr. I. Emre Gorgun said at the annual meeting of the Central Surgical Association.
CSA incoming president Dr. Scott A. Gruber, chief of staff at the John D. Dingell VA Medical Center in Detroit, agreed. “There were very, very small differences. I think they were trying to show that the two [approaches] are virtually equivalent,” he said in an interview. “Each has its advantages and disadvantages, but the HALS technique was used in more complex, more high-risk patients,” Dr. Gruber said.
HALS bridges the learning gap between open and straight laparoscopic surgery, which has been slow to gain adoption in colorectal surgery because it is technically demanding and has a steep learning curve, said Dr. Gorgun, a colorectal surgeon at the Cleveland Clinic. HALS allows surgeons to regain tactile sensation and manual retraction, enabling them to perform even more complex operations more effectively.
Studies also suggest that HALS reduces conversion rates and preserves the short-term benefits of LAP, though a nationwide comparison of short-term outcomes using the two techniques has been absent.
To fill this knowledge gap, the investigators used the 2012 colectomy-targeted American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP
At baseline, the HALS group was significantly older than the LAP group (61.5 years vs. 60 years), had a higher body mass index (28.6 kg/m2 vs. 28 kg/m2), was more likely to be hypertensive (49.8% vs. 45.1%), and to be American Society of Anesthesiologists class III (42% vs. 37.4%) and class IV (2.8% vs. 2.7%). Steroid use for inflammatory bowel disease was significantly higher in the LAP group (6.5% vs. 5.4%).
Mortality rates were similar in the LAP and HALS groups (0.52% vs. 0.50%; P = .94), Dr. Gorgun reported.
Multivariate logistic regression adjusted for comorbid conditions lessened the degree of differences between the two groups, but continued to favor HALS for shorter operative time (odds ratio, 0.94) and favor LAP for shorter hospital stays (OR, 1.05) and less superficial surgical site infections (OR, 1.31), less prolonged post-operative ileus (OR, 1.25), and overall morbidity (OR, 1.16).
“Both LAP and HALS approaches are used in minimally invasive colorectal surgery based on their respective contributions and complement each other,” Dr. Gorgun concluded. “Implementing the best approach to decrease postoperative complication rates and increase use of MIS [minimally invasive surgery] will play a role in improving patient care and overall quality of health care.”
Dr. Gorgun, his coauthors, and Dr. Gruber reported having no financial conflicts
CHICAGO – A nationwide analysis comparing straight versus hand-assisted laparoscopic colectomy appears to have resulted in a draw.
Despite being used more commonly in patients with higher body mass index and comorbidities, hand-assisted laparoscopic surgery (HALS) resulted in a significantly shorter operative time than did straight laparoscopic surgery (LAP) (171 minutes vs. 178.8 minutes; P < .001).
On the other hand, LAP was associated with a significantly shorter length of stay (5.9 days vs. 6.0 days; P < .001), fewer complications (15.9% vs. 18.2%; P = .006), fewer specifically superficial skin infections (4.1% vs. 5.4%; P = .007), and less prolonged postoperative ileus (7.5% vs. 9.1%; P = .01).
The differences were statistically significant likely because of the high volume of patients in each group, but are unlikely to be clinically significant in terms of patient care, senior study author Dr. I. Emre Gorgun said at the annual meeting of the Central Surgical Association.
CSA incoming president Dr. Scott A. Gruber, chief of staff at the John D. Dingell VA Medical Center in Detroit, agreed. “There were very, very small differences. I think they were trying to show that the two [approaches] are virtually equivalent,” he said in an interview. “Each has its advantages and disadvantages, but the HALS technique was used in more complex, more high-risk patients,” Dr. Gruber said.
HALS bridges the learning gap between open and straight laparoscopic surgery, which has been slow to gain adoption in colorectal surgery because it is technically demanding and has a steep learning curve, said Dr. Gorgun, a colorectal surgeon at the Cleveland Clinic. HALS allows surgeons to regain tactile sensation and manual retraction, enabling them to perform even more complex operations more effectively.
Studies also suggest that HALS reduces conversion rates and preserves the short-term benefits of LAP, though a nationwide comparison of short-term outcomes using the two techniques has been absent.
To fill this knowledge gap, the investigators used the 2012 colectomy-targeted American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP
At baseline, the HALS group was significantly older than the LAP group (61.5 years vs. 60 years), had a higher body mass index (28.6 kg/m2 vs. 28 kg/m2), was more likely to be hypertensive (49.8% vs. 45.1%), and to be American Society of Anesthesiologists class III (42% vs. 37.4%) and class IV (2.8% vs. 2.7%). Steroid use for inflammatory bowel disease was significantly higher in the LAP group (6.5% vs. 5.4%).
Mortality rates were similar in the LAP and HALS groups (0.52% vs. 0.50%; P = .94), Dr. Gorgun reported.
Multivariate logistic regression adjusted for comorbid conditions lessened the degree of differences between the two groups, but continued to favor HALS for shorter operative time (odds ratio, 0.94) and favor LAP for shorter hospital stays (OR, 1.05) and less superficial surgical site infections (OR, 1.31), less prolonged post-operative ileus (OR, 1.25), and overall morbidity (OR, 1.16).
“Both LAP and HALS approaches are used in minimally invasive colorectal surgery based on their respective contributions and complement each other,” Dr. Gorgun concluded. “Implementing the best approach to decrease postoperative complication rates and increase use of MIS [minimally invasive surgery] will play a role in improving patient care and overall quality of health care.”
Dr. Gorgun, his coauthors, and Dr. Gruber reported having no financial conflicts
CHICAGO – A nationwide analysis comparing straight versus hand-assisted laparoscopic colectomy appears to have resulted in a draw.
Despite being used more commonly in patients with higher body mass index and comorbidities, hand-assisted laparoscopic surgery (HALS) resulted in a significantly shorter operative time than did straight laparoscopic surgery (LAP) (171 minutes vs. 178.8 minutes; P < .001).
On the other hand, LAP was associated with a significantly shorter length of stay (5.9 days vs. 6.0 days; P < .001), fewer complications (15.9% vs. 18.2%; P = .006), fewer specifically superficial skin infections (4.1% vs. 5.4%; P = .007), and less prolonged postoperative ileus (7.5% vs. 9.1%; P = .01).
The differences were statistically significant likely because of the high volume of patients in each group, but are unlikely to be clinically significant in terms of patient care, senior study author Dr. I. Emre Gorgun said at the annual meeting of the Central Surgical Association.
CSA incoming president Dr. Scott A. Gruber, chief of staff at the John D. Dingell VA Medical Center in Detroit, agreed. “There were very, very small differences. I think they were trying to show that the two [approaches] are virtually equivalent,” he said in an interview. “Each has its advantages and disadvantages, but the HALS technique was used in more complex, more high-risk patients,” Dr. Gruber said.
HALS bridges the learning gap between open and straight laparoscopic surgery, which has been slow to gain adoption in colorectal surgery because it is technically demanding and has a steep learning curve, said Dr. Gorgun, a colorectal surgeon at the Cleveland Clinic. HALS allows surgeons to regain tactile sensation and manual retraction, enabling them to perform even more complex operations more effectively.
Studies also suggest that HALS reduces conversion rates and preserves the short-term benefits of LAP, though a nationwide comparison of short-term outcomes using the two techniques has been absent.
To fill this knowledge gap, the investigators used the 2012 colectomy-targeted American College of Surgeons National Surgical Quality Improvement Program (ACS NSQIP
At baseline, the HALS group was significantly older than the LAP group (61.5 years vs. 60 years), had a higher body mass index (28.6 kg/m2 vs. 28 kg/m2), was more likely to be hypertensive (49.8% vs. 45.1%), and to be American Society of Anesthesiologists class III (42% vs. 37.4%) and class IV (2.8% vs. 2.7%). Steroid use for inflammatory bowel disease was significantly higher in the LAP group (6.5% vs. 5.4%).
Mortality rates were similar in the LAP and HALS groups (0.52% vs. 0.50%; P = .94), Dr. Gorgun reported.
Multivariate logistic regression adjusted for comorbid conditions lessened the degree of differences between the two groups, but continued to favor HALS for shorter operative time (odds ratio, 0.94) and favor LAP for shorter hospital stays (OR, 1.05) and less superficial surgical site infections (OR, 1.31), less prolonged post-operative ileus (OR, 1.25), and overall morbidity (OR, 1.16).
“Both LAP and HALS approaches are used in minimally invasive colorectal surgery based on their respective contributions and complement each other,” Dr. Gorgun concluded. “Implementing the best approach to decrease postoperative complication rates and increase use of MIS [minimally invasive surgery] will play a role in improving patient care and overall quality of health care.”
Dr. Gorgun, his coauthors, and Dr. Gruber reported having no financial conflicts
AT THE ANNUAL MEETING OF THE CENTRAL SURGICAL ASSOCIATION
Key clinical point: Straight and hand-assisted laparoscopic colectomy offer unique benefits, and HALS is a good option in more complex patients.
Major finding: Surgery was 7 minutes shorter with HALS, while complications were down 2.3% with LAP.
Data source: Retrospective study of 7,843 patients undergoing colectomy in the ACS NSQIP database.
Disclosures: Dr. Gorgun, his coauthors, and Dr. Gruber reported having no financial conflicts.