User login
A customized vaccine targeting patient-specific, tumor neoantigens evoked an immune response in three adults with advanced cutaneous melanoma in a proof-of-principle study that paves the way for a phase I trial.
The data are “too premature to conclude that the treatment had any therapeutic benefit to the patients,” Dr. Gerald P. Linette of Washington University in St. Louis, Mo., said in a teleconference. However, he noted that a phase I trial would likely begin within the next 9-12 months.
“Our primary goal was to see if this was safe, and if we could elicit an immune response,” Dr. Linette said.
Vaccination not only augmented T-cell immunity directed against naturally occurring, dominant tumor neoantigens, but also expanded the breadth of the immune response by revealing additional subdominant neoantigens, lead author Beatriz M. Carreno, Ph.D., of Washington University in St. Louis and her associates reported online April 2 in Science (doi:10.1126/science.aaa3828).
All three patients had stage IIIC, resected, cutaneous melanoma and had failed prior therapy with ipilimumab (Yervoy).
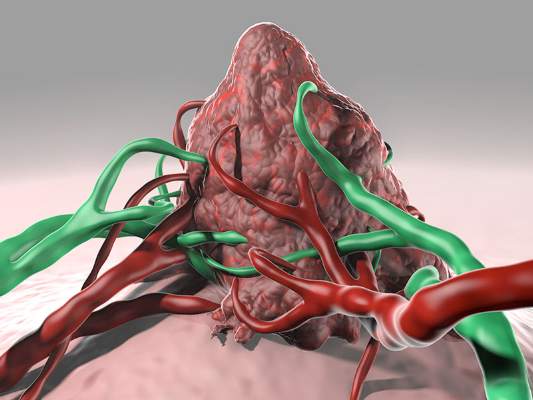
Some melanoma patients harbor tumor missense mutations, translated into amino acid substitutions (AAS). These mutations are thought to produce antigens that the immune system perceives as foreign, prompting a tumor-specific T-cell response. Heretofore, there has been no systematic evaluation of these neoantigens or whether vaccination can enhance these responses.
The aim of the current study was to determine the safety, tolerability, and immunologic responses to AAS peptides inside a modified dendritic cell vaccine. Seven AAS peptide candidates were selected among validated HLA-A*02:01 binders, along with the melanoma peptides G209-2M and G280-9V as positive controls for vaccination.
In each patient, T cell immunity to one AAS peptide was detected in prevaccine peripheral blood mononuclear cell samples.
The treatment differs from other personalized cancer vaccines in two key ways, Dr. Carreno said in the teleconference.
“We mature the [dendritic] cells before we give them back to the patients; the cells make growth factors that we have previously shown are important to the generation of the immune response,” she said. In addition, the vaccine was given as an infusion, rather than an injection, she noted.
Vaccination augmented the T-cell response to the three neoantigens – TMEM48 F169L, SEC24A P469, EXOC8 Q656P – with observed frequencies of 23%, 64%, and 89%, respectively.
Immune monitoring also detected T-cell immunity to two additional neoantigens per patient, Dr. Carreno and her associates reported.
Robust immune responses were detected as early as week 2 and peaked at weeks 8-9 after the initial dose. Each patient received three vaccine doses, without side effects or toxicity.
“Vaccination against tumor antigens appears safe as all three patients are alive and well, with no autoimmune adverse events,” the researchers wrote. Post vaccine restaging CT revealed stable disease in a 54-year-old man with BRAF V6003 mutation-positive melanoma. A second man, who had achieved a complete response to ipilimumab for BRAF V6003-positive disease, remains in complete remission after receiving the vaccine in the adjuvant setting.
The vaccine induced 30% tumor reduction in a woman with extensive skin metastases and 5-12 mm lung nodules after ipilimumab and vemurafenib (Zelboraf), but tumor size returned back to baseline dimensions 12 weeks later with no new disease sites. Her disease has remained stable for the past 8 months, the researchers said.
However, it is too soon to attribute a clinical benefit to the observed immune response to the vaccine, Dr. Linette emphasized. “I would be speculating if I said the vaccine had any benefit to the patients,” he said.
Vaccination increased the frequency of most existing prevaccine T-cell receptor-beta (TCR-beta) clonotypes and revealed new clonotypes for 6 neoantigens.
For both dominant and subdominant neoantigens, the TCR-beta repertoire was increased significantly after vaccination. For example, 84 clonotypes representing 19 TCR-beta families were detected for TKT R438W, 61 clonotypes representing 12 TCR-beta families were detected for SEC24A P469L, and 12 clonotypes representing 8 TCR-beta families were detected for EXOC8 Q656P.
“The revelation of a highly diverse TCR-beta repertoire specific for dominant and subdominant neoantigens was surprising and points to a potentially rich pool of naive tumor-specific T cells that remain ignorant unless activated by vaccination,” the researchers wrote.
Recent data indicate that CTLA-4 monoclonal antibody use can alter TCR repertoire diversity in patients, suggesting a potential strategy of combination checkpoint inhibitors, including ipilimumab, and neoantigen vaccines. The novel vaccine strategy also could be used to treat other malignancies with high mutational burdens such as lung, bladder, and colorectal cancers, while other genomic alterations may generate potential neoantigens relevant in low–mutational burden cancers such as leukemia, the authors suggest.
Although the cells in this study were grown in a specialized laboratory, “as the technology improves, I think this [strategy] will become reproducible and available at other medical centers,” Dr. Linette said.
This work was supported by Barnes-Jewish Hospital Foundation, Siteman Cancer Frontier Fund, Our Mark on Melanoma (MOM) Foundation, Come Out Swinging (COS) Foundation, Blackout Melanoma Foundation and the National Cancer Institute.
Heidi Splete contributed to this story.
A customized vaccine targeting patient-specific, tumor neoantigens evoked an immune response in three adults with advanced cutaneous melanoma in a proof-of-principle study that paves the way for a phase I trial.
The data are “too premature to conclude that the treatment had any therapeutic benefit to the patients,” Dr. Gerald P. Linette of Washington University in St. Louis, Mo., said in a teleconference. However, he noted that a phase I trial would likely begin within the next 9-12 months.
“Our primary goal was to see if this was safe, and if we could elicit an immune response,” Dr. Linette said.
Vaccination not only augmented T-cell immunity directed against naturally occurring, dominant tumor neoantigens, but also expanded the breadth of the immune response by revealing additional subdominant neoantigens, lead author Beatriz M. Carreno, Ph.D., of Washington University in St. Louis and her associates reported online April 2 in Science (doi:10.1126/science.aaa3828).
All three patients had stage IIIC, resected, cutaneous melanoma and had failed prior therapy with ipilimumab (Yervoy).
Some melanoma patients harbor tumor missense mutations, translated into amino acid substitutions (AAS). These mutations are thought to produce antigens that the immune system perceives as foreign, prompting a tumor-specific T-cell response. Heretofore, there has been no systematic evaluation of these neoantigens or whether vaccination can enhance these responses.
The aim of the current study was to determine the safety, tolerability, and immunologic responses to AAS peptides inside a modified dendritic cell vaccine. Seven AAS peptide candidates were selected among validated HLA-A*02:01 binders, along with the melanoma peptides G209-2M and G280-9V as positive controls for vaccination.
In each patient, T cell immunity to one AAS peptide was detected in prevaccine peripheral blood mononuclear cell samples.
The treatment differs from other personalized cancer vaccines in two key ways, Dr. Carreno said in the teleconference.
“We mature the [dendritic] cells before we give them back to the patients; the cells make growth factors that we have previously shown are important to the generation of the immune response,” she said. In addition, the vaccine was given as an infusion, rather than an injection, she noted.
Vaccination augmented the T-cell response to the three neoantigens – TMEM48 F169L, SEC24A P469, EXOC8 Q656P – with observed frequencies of 23%, 64%, and 89%, respectively.
Immune monitoring also detected T-cell immunity to two additional neoantigens per patient, Dr. Carreno and her associates reported.
Robust immune responses were detected as early as week 2 and peaked at weeks 8-9 after the initial dose. Each patient received three vaccine doses, without side effects or toxicity.
“Vaccination against tumor antigens appears safe as all three patients are alive and well, with no autoimmune adverse events,” the researchers wrote. Post vaccine restaging CT revealed stable disease in a 54-year-old man with BRAF V6003 mutation-positive melanoma. A second man, who had achieved a complete response to ipilimumab for BRAF V6003-positive disease, remains in complete remission after receiving the vaccine in the adjuvant setting.
The vaccine induced 30% tumor reduction in a woman with extensive skin metastases and 5-12 mm lung nodules after ipilimumab and vemurafenib (Zelboraf), but tumor size returned back to baseline dimensions 12 weeks later with no new disease sites. Her disease has remained stable for the past 8 months, the researchers said.
However, it is too soon to attribute a clinical benefit to the observed immune response to the vaccine, Dr. Linette emphasized. “I would be speculating if I said the vaccine had any benefit to the patients,” he said.
Vaccination increased the frequency of most existing prevaccine T-cell receptor-beta (TCR-beta) clonotypes and revealed new clonotypes for 6 neoantigens.
For both dominant and subdominant neoantigens, the TCR-beta repertoire was increased significantly after vaccination. For example, 84 clonotypes representing 19 TCR-beta families were detected for TKT R438W, 61 clonotypes representing 12 TCR-beta families were detected for SEC24A P469L, and 12 clonotypes representing 8 TCR-beta families were detected for EXOC8 Q656P.
“The revelation of a highly diverse TCR-beta repertoire specific for dominant and subdominant neoantigens was surprising and points to a potentially rich pool of naive tumor-specific T cells that remain ignorant unless activated by vaccination,” the researchers wrote.
Recent data indicate that CTLA-4 monoclonal antibody use can alter TCR repertoire diversity in patients, suggesting a potential strategy of combination checkpoint inhibitors, including ipilimumab, and neoantigen vaccines. The novel vaccine strategy also could be used to treat other malignancies with high mutational burdens such as lung, bladder, and colorectal cancers, while other genomic alterations may generate potential neoantigens relevant in low–mutational burden cancers such as leukemia, the authors suggest.
Although the cells in this study were grown in a specialized laboratory, “as the technology improves, I think this [strategy] will become reproducible and available at other medical centers,” Dr. Linette said.
This work was supported by Barnes-Jewish Hospital Foundation, Siteman Cancer Frontier Fund, Our Mark on Melanoma (MOM) Foundation, Come Out Swinging (COS) Foundation, Blackout Melanoma Foundation and the National Cancer Institute.
Heidi Splete contributed to this story.
A customized vaccine targeting patient-specific, tumor neoantigens evoked an immune response in three adults with advanced cutaneous melanoma in a proof-of-principle study that paves the way for a phase I trial.
The data are “too premature to conclude that the treatment had any therapeutic benefit to the patients,” Dr. Gerald P. Linette of Washington University in St. Louis, Mo., said in a teleconference. However, he noted that a phase I trial would likely begin within the next 9-12 months.
“Our primary goal was to see if this was safe, and if we could elicit an immune response,” Dr. Linette said.
Vaccination not only augmented T-cell immunity directed against naturally occurring, dominant tumor neoantigens, but also expanded the breadth of the immune response by revealing additional subdominant neoantigens, lead author Beatriz M. Carreno, Ph.D., of Washington University in St. Louis and her associates reported online April 2 in Science (doi:10.1126/science.aaa3828).
All three patients had stage IIIC, resected, cutaneous melanoma and had failed prior therapy with ipilimumab (Yervoy).
Some melanoma patients harbor tumor missense mutations, translated into amino acid substitutions (AAS). These mutations are thought to produce antigens that the immune system perceives as foreign, prompting a tumor-specific T-cell response. Heretofore, there has been no systematic evaluation of these neoantigens or whether vaccination can enhance these responses.
The aim of the current study was to determine the safety, tolerability, and immunologic responses to AAS peptides inside a modified dendritic cell vaccine. Seven AAS peptide candidates were selected among validated HLA-A*02:01 binders, along with the melanoma peptides G209-2M and G280-9V as positive controls for vaccination.
In each patient, T cell immunity to one AAS peptide was detected in prevaccine peripheral blood mononuclear cell samples.
The treatment differs from other personalized cancer vaccines in two key ways, Dr. Carreno said in the teleconference.
“We mature the [dendritic] cells before we give them back to the patients; the cells make growth factors that we have previously shown are important to the generation of the immune response,” she said. In addition, the vaccine was given as an infusion, rather than an injection, she noted.
Vaccination augmented the T-cell response to the three neoantigens – TMEM48 F169L, SEC24A P469, EXOC8 Q656P – with observed frequencies of 23%, 64%, and 89%, respectively.
Immune monitoring also detected T-cell immunity to two additional neoantigens per patient, Dr. Carreno and her associates reported.
Robust immune responses were detected as early as week 2 and peaked at weeks 8-9 after the initial dose. Each patient received three vaccine doses, without side effects or toxicity.
“Vaccination against tumor antigens appears safe as all three patients are alive and well, with no autoimmune adverse events,” the researchers wrote. Post vaccine restaging CT revealed stable disease in a 54-year-old man with BRAF V6003 mutation-positive melanoma. A second man, who had achieved a complete response to ipilimumab for BRAF V6003-positive disease, remains in complete remission after receiving the vaccine in the adjuvant setting.
The vaccine induced 30% tumor reduction in a woman with extensive skin metastases and 5-12 mm lung nodules after ipilimumab and vemurafenib (Zelboraf), but tumor size returned back to baseline dimensions 12 weeks later with no new disease sites. Her disease has remained stable for the past 8 months, the researchers said.
However, it is too soon to attribute a clinical benefit to the observed immune response to the vaccine, Dr. Linette emphasized. “I would be speculating if I said the vaccine had any benefit to the patients,” he said.
Vaccination increased the frequency of most existing prevaccine T-cell receptor-beta (TCR-beta) clonotypes and revealed new clonotypes for 6 neoantigens.
For both dominant and subdominant neoantigens, the TCR-beta repertoire was increased significantly after vaccination. For example, 84 clonotypes representing 19 TCR-beta families were detected for TKT R438W, 61 clonotypes representing 12 TCR-beta families were detected for SEC24A P469L, and 12 clonotypes representing 8 TCR-beta families were detected for EXOC8 Q656P.
“The revelation of a highly diverse TCR-beta repertoire specific for dominant and subdominant neoantigens was surprising and points to a potentially rich pool of naive tumor-specific T cells that remain ignorant unless activated by vaccination,” the researchers wrote.
Recent data indicate that CTLA-4 monoclonal antibody use can alter TCR repertoire diversity in patients, suggesting a potential strategy of combination checkpoint inhibitors, including ipilimumab, and neoantigen vaccines. The novel vaccine strategy also could be used to treat other malignancies with high mutational burdens such as lung, bladder, and colorectal cancers, while other genomic alterations may generate potential neoantigens relevant in low–mutational burden cancers such as leukemia, the authors suggest.
Although the cells in this study were grown in a specialized laboratory, “as the technology improves, I think this [strategy] will become reproducible and available at other medical centers,” Dr. Linette said.
This work was supported by Barnes-Jewish Hospital Foundation, Siteman Cancer Frontier Fund, Our Mark on Melanoma (MOM) Foundation, Come Out Swinging (COS) Foundation, Blackout Melanoma Foundation and the National Cancer Institute.
Heidi Splete contributed to this story.
FROM SCIENCE
Key clinical point: Vaccination against patient-specific tumor neoantigens may represent a novel therapeutic strategy in melanoma and other malignancies.
Major finding: The vaccine enhanced T-cell immunity to naturally occurring neoantigens and revealed two additional neoantigens per patient.
Data source: Proof-of-principle study of three patients with resected, cutaneous melanoma.
Disclosures: This work was supported by Barnes-Jewish Hospital Foundation, Siteman Cancer Frontier Fund, Our Mark on Melanoma (MOM) Foundation, Come Out Swinging (COS) Foundation, Blackout Melanoma Foundation and the National Cancer Institute.